February 2022
◆
Volume 105, Number 2 www.aafp.org/afp American Family Physician 191
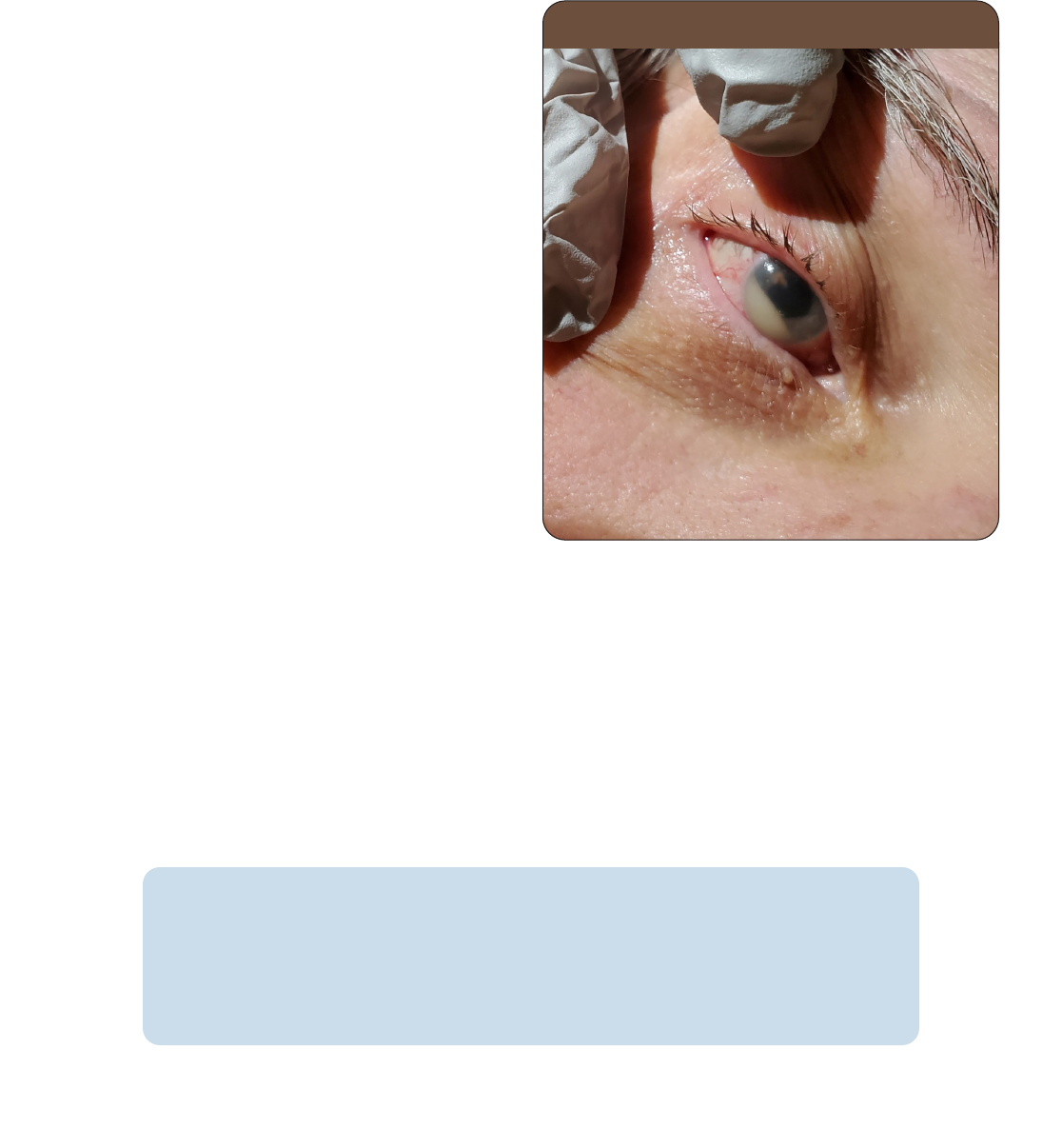
A 65-year-old man presented with three days of
pain and pressure in his right eye, accompanied
by blurred vision and photosensitivity. He did
not have pain with eye movement. He had a fever
and chills. He had a history of poorly controlled
diabetes mellitus and a urinary tract infection a
week earlier that was treated with ciprooxacin.
Physical examination revealed a mildly dilated
right pupil, with incomplete constriction to light,
compared with the le pupil. A small collection
of white uid was observed in the anterior cham-
ber of the right eye (Figure 1).
Question
Based on the patient’s history and physical
examination findings, which one of the follow-
ing is the most likely diagnosis?
l A. Acute glaucoma.
l B. Behçet syndrome.
l C. Corneal ulcer.
l D. Endogenous bacterial endophthalmitis.
l E. Pseudohypopyon.
See the following page for discussion.
The editors of AFP welcome submissions for Photo Quiz. Guidelines for preparing and submitting a
Photo Quiz manuscript can be found in the Authors’ Guide at https:// www.aafp.org/afp/photoquizinfo.
To be considered for publication, submissions must meet these guidelines. Email submissions to
afpphoto@ aafp.org.
This series is coordinated by John E. Delzell Jr., MD, MSPH, associate medical editor.
A collection of Photo Quiz published in AFP is available at https:// www.aafp.org/afp/photoquiz.
Author disclosure: No relevant financial aliations.
Photo Quiz
Inflammation of the Eye
Richard M. Rubin, MD, and Ayodeji Alaketu, MD, Travis Air Force Base, California
FIGURE 1
Downloaded from the American Family Physician website at www.aafp.org/afp. Copyright © 2022 American Academy of Family Physicians. For the private, non-
commercial use of one individual user of the website. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.
Downloaded from the American Family Physician website at www.aafp.org/afp. Copyright © 2022 American Academy of Family Physicians. For the private, non-
commercial use of one individual user of the website. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.
192 American Family Physician www.aafp.org/afp Volume 105, Number 2
◆
February 2022
PHOTO QUIZ
Discussion
e answer is D: endogenous bacterial endophthal-
mitis, an intraocular infection caused by hematog-
enous spread of organisms from an extraocular
location.
1
Findings include decreased vision, eyelid
edema, pupillary abnormalities, hypopyon, and
conjunctival injection. Diagnosis is based on phys-
ical examination and blood culture ndings. Intra-
ocular uid culture from the anterior chamber and
vitreous may be needed to conrm the diagnosis if
blood culture results are negative.
1
is patient was
found to have group B streptococcus bacteremia,
conrmed with vitreous culture.
Treatment of endogenous bacterial endoph-
thalmitis includes intravenous antibiotics to
manage the systemic infection. e ocular infec-
tion may be managed with pars plana vitrectomy,
intravitreal antibiotics, and steroids, and the intraocular
infection managed with topical steroids, antibiotics, and
cycloplegics.
2
e prognosis for visual improvement is poor
despite treatment. Patients with a history of alcoholism, car-
diovascular disease, and diabetes mellitus are at increased
risk of endogenous bacterial endophthalmitis.
3
Patients with
endogenous bacterial endophthalmitis should be evaluated
for endocarditis. e hypopyon in this patient indicates leu-
kocytes within the anterior chamber of the eye, which war-
rants emergent evaluation by an ophthalmologist.
4
Acute glaucoma is an ocular emergency. It presents with
a mid-dilated xed pupil with severe eye pain and a prom-
inent ciliary ush. Patients also report nausea, vomiting,
cloudy vision, seeing rings around lights, and headache.
Acute glaucoma is caused by anterior chamber angle clo-
sure in the aected eye, leading to an increased intraocular
pressure of more than 40 mm Hg. Hypopyon is not seen
in patients with glaucoma. Patients should be emergently
referred to an ophthalmologist. Patients should not receive
topical steroids or antibiotics because these treatments may
lead to infection or corneal ulceration.
5
Behçet syndrome is a multisystem inammatory disor-
der. e classic presentation is painful mucocutaneous sores
in the mouth, anterior uveitis, genital sores, and pathergy
(skin rashes resistant to healing). e cause is unknown but
may be genetic. Diagnosis is based on the presence of recur-
rent oral ulcers and at least two of the other classic ndings.
Hypopyon may occur in 10% to 30% of patients who have
Behçet syndrome with anterior uveitis. Behçet syndrome is
treated with immunomodulatory therapy and systemic cor-
ticosteroids if the patient reports vision changes.
6
Most corneal ulcers are caused by direct minor trauma to
the eye, such as from contact lenses. e area may become
infected with bacteria, viruses, or fungi, usually secondary to
the breakdown of the protective epithelial barrier of the eye.
Patients with corneal ulcers present with decreased
visual
acuity, photophobia, and conjunctival injection. Patients
should be referred to an ophthalmologist. If consultation or
referral is not available within hours, it is reasonable to obtain
cultures and start ophthalmic antibiotics immediately.
7
Pseudohypopyon is the accumulation of neoplastic cells
in the anterior chamber of the eye that usually occurs in
patients with lymphoma, leukemia, or retinoblastoma. It
may be the only presenting feature of recurrent lymphoma,
even in the setting of negative imaging and cerebrospinal
uid ndings. Diagnosis can be conrmed with ow cytom-
etry of an anterior chamber aspirate. Patients with bilateral
pseudohypopyon have a poor prognosis.
8
The opinions and assertions contained herein are the private
views of the authors and are not to be construed as ocial or as
reflecting the views of the U.S. Air Force Medical Department or
the U.S. Air Force at large.
Address correspondence to Ayodeji Alaketu, MD, at ayodeji.f.
alaketu.mil@ mail.mil. Reprints are not available from the authors.
References
1. Jackson TL, Paraskevopoulos T, Georgalas I. Systematic review of 342
cases of endogenous bacterial endophthalmitis. Surv Ophthalmol.
2014; 59(6): 627-635.
2. Jenkins TL, Talcott KE, Matsunaga DR, et al. Endogenous bacterial
endophthalmitis. Ocul Immunol Inflamm. 2020; 28(6): 975-983.
3. Nishida T, Ishida K, Niwa Y, et al. An eleven-year retrospective study of
endogenous bacterial endophthalmitis [published online January 31,
2015]. J Ophthalmol. Accessed August 4, 2020. https:// www.hindawi.
com/journals/joph/2015/261310/
4. Huang JJ, Gaudio PA, eds. Ocular Inflammatory Disease and Uveitis:
Diagnosis and Treatment. Lippincott Williams & Wilkins; 2010.
5. Goroll AH, Mulley AG, eds. Primary Care Medicine: Oce Evaluation and
Management of the Adult Patient. 7th ed. Wolters Kluwer Health; 2014.
6. Harman LE, Margo CE, Roetzheim RG. Uveitis. Am Fam Physician.
2014; 90(10): 711-716. Accessed January 6, 2022. https:// www.aafp.org/
afp/2014/1115/p711.html
7. Domino FJ, ed. 5-Minute Clinical Consult. 21st ed. Lippincott Williams
& Wilkins; 2013.
8. Dorrepaal SJ, Margolin EA, Wang C. Bilateral pseudohypopyon as
a presenting feature of recurrent diuse large B-cell lymphoma. J Neu-
roophthalmol. 2010; 30(1): 67-69. ■
SUMMARY TABLE
Condition Characteristics
Acute glaucoma Severe eye pain and prominent ciliary flush; nausea,
vomiting, cloudy vision, rings around lights, headache
Behçet
syndrome
Classically presents with recurrent painful mucocu-
taneous sores in the mouth, anterior uveitis, genital
sores, and pathergy
Corneal ulcer Infection of cornea usually secondary to minor
trauma such as from contact lenses; decreased visual
acuity, photophobia, conjunctival injection
Endogenous
bacterial
endophthalmitis
History of recent bacteremia; decreased vision,
eyelid edema, pupillary abnormalities, hypopyon,
conjunctival injection
Pseudohypopyon Accumulation of neoplastic cells in the anterior
chamber of the eye; usually occurs in patients with
lymphoma, leukemia, or retinoblastoma
