Pain Management Network
aci.health.nsw.gov.au
Ophthalmology Network
Eye Emergency Manual
An illustrated guide
aci.health.nsw.gov.au
THIRD EDITION, DECEMBER 2023
This information is not a substitute for healthcare providers’ professional judgement.
Agency for Clinical Innovation aci.health.nsw.gov.au
Agency for Clinical Innovation
1 Reserve Road, St Leonards NSW 2065
Locked Bag 2030, St Leonards NSW 1590
Phone: +61 2 9464 4666 | Email: aci-info@health.nsw.gov.au | Web: aci.health.nsw.gov.au
Further copies of this publication can be obtained from the Agency for Clinical Innovation website at aci.health.nsw.gov.au
Disclaimer: the content within this publication was accurate at the time of publication.
© State of New South Wales (Agency for Clinical Innovation) 2023. Creative Commons Attribution-No Derivatives
4.0 licence. For current information go to: aci.health.nsw.gov.au. The ACI logo and cover image are excluded from
the Creative Commons licence and may only be used with express permission.
Title Eye Emergency Manual, 3rd Edition
Published December 2023
Next review 2028
Produced by ACI Ophthalmology Network
Preferred citation
NSW Agency for Clinical Innovation. Eye Emergency Manual, 3rd Edition.
Sydney: ACI; 2023.
TRIM ACI/D23/169 SHPN (ACI) 230806 ISBN 978-1-76023-644-1
ACI_8666 [11/23]
Agency for Clinical Innovation aci.health.nsw.gov.au
Eye Emergency Manual December 2023
Background 1
Introduction 3
Anatomy 4
Anatomy terms 5
Eye assessments 6
History to ascertain 7
Assessing the severely injured patient 15
Paediatric assessment 16
Examinations 18
Examination essentials 18
General inspection and assessment
of periocular and globe trauma 20
Visual acuity 23
Pupil examination 27
Visual field, eye movements
andeyelid examination 29
Eyelid eversion 33
Special eye examinations 34
Direct ophthalmoscope 34
Checking intraocular pressure 35
Slit lamp 37
Eye referrals and discharge advice 40
Traumacommunication checklist 40
Acute visual disturbance
communication checklist 40
Red eye or eyelid
communication checklist 40
Visual requirements for driving 41
Prevention of visual impairment 42
Eye trauma 43
Blunt ocular trauma 44
Chemical burns 46
Closed globe injury 49
Flash burns 51
Lid laceration 52
Non-accidental injury (NAI) 54
Open globe injury
(penetratingeye injury) 55
Orbital fracture 57
Retrobulbar haemorrhage
(orbital compartment syndrome) 59
Acute visual disturbance 61
Third (3rd) cranial nerve palsy 62
Fourth (4th) cranial nerve palsy 63
Sixth (6th) cranial nerve palsy 65
Central retinal artery occlusion (CRAO) 66
Central retinal vein occlusion (CRVO) 68
Central serous chorioretinopathy 69
Dry eye/exposure keratopathy 70
Giant cell arteritis (GCA)/anterior
ischaemic optic neuropathy (AION) 72
Idiopathic intracranial hypertension (IIH):
transientvisual obscuration 73
Intermittent angle closure/
acuteangle closure 75
Lens subluxation 76
Contents
Agency for Clinical Innovation aci.health.nsw.gov.au
Eye Emergency Manual December 2023
Macular haemorrhage in wet
age-related macular degeneration 77
Macular pathology 78
Migraine 78
Myasthenia gravis 79
Optic neuritis 80
Posterior vitreous detachment (PVD) 8 1
Retinal tear or detachment 83
Thyroid eye disease 84
Transient ischaemic attack
(amaurosis fugax) or retinal emboli 85
Visual pathway lesion 87
Vitreous haemorrhage 87
Acute red eye or eyelid 89
Acute red eye overview 90
Acute angle closure crisis 91
Acute blepharitis 93
Allergic conjunctivitis 94
Iritis (anterior uveitis or an anterior
chamber inflammation) 95
Bacterial or acanthamoebal ulcer 96
Bacterial conjunctivitis 97
Chalazion/stye 98
Corneal or conjunctival foreignbody/
corneal abrasion 100
Ectropion 103
Entropion 104
Episcleritis 105
Eyelid lesion 106
Herpes simplex virus keratitis
(HSV/HSK) 106
Herpes zoster ophthalmicus (HZO)/
shingles 108
Hyphaema 109
Hypopyon 111
Marginal keratitis 112
Neovascular glaucoma 113
Ophthalmia neonatorum
(neonatal conjunctivitis) 114
Preseptal cellulitis
(periorbital cellulitis) 116
Pterygium 118
Scleritis 119
Subconjunctival haemorrhage 121
Trichiasis 122
Viral conjunctivitis 123
Treatments 125
Ocular drugs 126
How to put in eye drops 130
References 131
Appendix: Evidence base 133
PubMed search terms 133
Google search terms 133
Inclusion and exclusion criteria 133
Bibliography 133
Glossary 135

Eye Emergency Manual December 2023
Agency for Clinical Innovation 1 aci.health.nsw.gov.au
Background
The Eye Emergency Manual (EEM) is designed for medical, nursing and alliedhealth
staff in emergency departments and critical care, and for rural general practitioners.
The EEM has not undergone a formal process ofevidence-based clinical practice guideline development;
however, it is the result of consensus opinion determined by relevant experts. The EEM is not a denitive
statement on correct procedures; rather, it is a general guide to be followed subject to clinical judgement.
The EEM is based on the best information available at the time of writing.
The EEM was rst released in 2007 and last updated in 2009. The current review was undertaken by the ACI
Ophthalmology Network with oversight by a clinical working group led by Dr Parth Shah.
Method
The EEM was reviewed formally by members
of a working group, including clinicians in
ophthalmology, optometry, orthoptics, emergency
and critical care, and rural general practice
across NSW. Data for theEEM were drawn from
a literature search, consensus expert opinion of
the working group and consultation.
Rapid, targeted literature searches of PubMed
were conducted in June and July 2023. Searches
were related to: eye diseases OR eye injuries
AND emergency treatment AND guidelines
OR principles.
Grey literature searches were completed using
Google and Google Scholar.
Refer to "Appendix: Evidence base" for search
terms and reference list.
Consultation
The following groups were consulted for this
revision:
• Members of the working group
(as listed under ‘Acknowledgements’ below)
• ACI Networks
• Survey respondents
The Eye Emergency Manual is endorsed by the
Australian College of Emergency Nursing and
the Save Sight Institute, University of Sydney.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 2 aci.health.nsw.gov.au
Acknowledgements
Parth Shah, Ophthalmologist, Prince of Wales
Hospital and Sydney Children’s Hospital
Claire Cuppitt, General Practitioner
Lin Davis, Nurse Educator, Rural Critical Care,
Hunter New England LHD
Michael Golding, Emergency Physician,
Prince of Wales Hospital
Paula Katalinic, Optometrist and Professional
Services and Advocacy Manager, Optometry
NSW/ACT
Yves Kerdraon, Ophthalmologist, Sydney
Hospital/ Sydney Eye Hospital and
ConcordHospital
Kerrie Martin, Ophthalmology Network and
Clinical Genetics Network Manager, Agency for
Clinical Innovation
Erin McArthur, Project Ofcer, Agency for
Clinical Innovation
Peter McCluskey, Professor and Chair of
Ophthalmology, University of Sydney and
Director, Save Sight Institute
Joanna McCulloch, Clinical Nurse Consultant
Ophthalmology, Sydney Hospital/Sydney
Eye Hospital
Danielle Morgan, Acting Deputy Head of
Orthoptic Department, Sydney Hospital/Sydney
Eye Hospital
David Murphy, Director of Emergency Medicine,
Prince of Wales Hospital

Eye Emergency Manual December 2023
Agency for Clinical Innovation 3 aci.health.nsw.gov.au
Introduction
The EEM is designed to provide a
quick and simple guide to recognising
important signs and symptoms, and
assisting with the management of
common eye emergencies. The EEM
will also assist with triaging patients
to appropriate care.
How to use this resource
For ease of use, the EEM has a large
amount of graphic content and is divided
into basic ophthalmic diagnostic
techniques/treatment and management
of common eye presentations.
Each condition includes
information about:
• immediate action (if any)
• history
• examination
• treatment
• communication checklist(s).
Each condition has red ags used
to increase the triage weighting or
indicate urgent ophthalmic referral
with an explanation of relevance.

Anatomy
Agency for Clinical Innovation 4 aci.health.nsw.gov.au
Eye Emergency Manual November 2023

Eye Emergency Manual December 2023
Agency for Clinical Innovation 5 aci.health.nsw.gov.au
Anatomy
Anatomy terms
Useful terms when describing an
eye lesion
• Right vs. left
• Globe vs. eyelids vs. periocular region
• Nasal (medial) vs. temporal (lateral)
• Superior vs. inferior (relative to the pupil)
• Corneal clock hours (as seen by the examiner,
e.g. 3 o’clock is the temporal limbus of the
left eye)
• Surface area of the cornea, e.g. 30% ulcer
Useful pathological terms
• Ulcer (loss of epithelium from the cornea,
conjunctiva or eyelid skin)
• White dot on the cornea or opacication: try to
differentiate between inltrate (abscess/
infection), long-standing scar, foreign body or
hazy cornea
• Redness on the conjunctiva: try to differentiate
between conjunctival injection, subconjunctival
haemorrhage and inamed conjunctival lesion,
e.g. pterygium or pingueculum
• Laceration (partial- or full-thickness if involving
the cornea, conjunctiva, sclera or eyelid)
• Blunt or sharp eye injury (depending on the
object used)
• Penetrating wound (which enters the full
thickness of the cornea or sclera)
• Leaking or sealed wound: use Seidel test to
determine if a penetrating wound is
actively leaking

Eye assessments
Agency for Clinical Innovation 6 aci.health.nsw.gov.au
Eye Emergency Manual November 2023
Eye Emergency Manual December 2023
Agency for Clinical Innovation 7 aci.health.nsw.gov.au
Eye assessments
History to ascertain
Basics
• Age
• Allergies
Reason for presentation
• Visual loss
• Eye pain
• Eye redness
• Trauma
• Foreign body
• Chemical injury
• Flashes/oaters
• Diplopia (double vision)
If a chemical injury is
suspected, postpone
further history-taking or
examination and
immediately begin
irrigation of the eye(s).
Mode of presentation
• Post trauma
• Self-presenting due to symptoms
• Via general practitioner (GP)
or optometrist
Past medical history
• Including microvascular
risk factors
• Social history
• Medications
Ophthalmic background
• Glasses: distance/reading/
bifocals/multifocals
• Contact lenses
• Eye surgery (when was it done,
where and by whom)
• Eye laser (what was it for)
• Eye drops (prescribed or
over-the-counter)
• Whether the patient is known to
anophthalmologist or
ophthalmology department
• When, where and who last saw the
patient and what problems were
being managed
Eye Emergency Manual December 2023
Agency for Clinical Innovation 8 aci.health.nsw.gov.au
Consider the following when conducting an
eye assessment:
• Demographics are crucial to the diagnosis of
many ophthalmic conditions. An ophthalmologist
will often ask you to go back and clarify a
patient’s age before moving on to the details of
the presentation.
• The most common reasons for patients to
present with ophthalmic problems are listed
above. Determining which of these is relevant to
the patient will focus your clinical assessment
and discussion with the ophthalmologist. Be
aware that this is a simplied approach and
there may be multiple reasons, such as visual
loss following trauma, or there may be
another symptom.
• Patients often confuse optometry and
ophthalmology, so be careful to make this
distinction yourself. If the patient refers to
advice given by their ‘eye doctor’ clarify exactly
who they mean and what advice was given.
Take note of drops that may have been
prescribed by a GP or an optometrist in the
recent past. Steroid drops are occasionally
prescribed for red eyes but can cause
blinding complications when used
inappropriately. Steroid eye drops should
only be prescribed following a
comprehensive ophthalmic examination
and in situations where close ophthalmic
follow-up can be provided.
• Ask if the patient drives and in what capacity.
• Ask if the patient is a carer for someone else, or
if they are cared for themselves.
Notes
You must specically ask if the patient has
had any eye surgery, laser or injections.
Remember that the patient may not volunteer
the information because they may not deem
it relevant, but it may be crucial to diagnosis.
Because many ophthalmic procedures are
done on an outpatient or day surgery basis,
with regional anaesthetic, and can be very
rapid, patients may omit to mention them
simply because they have forgotten. This is
particularly the case if the procedure was
performed many years ago
without complication.
Intravitreal injections are the modern
standard of care for certain types of
macular degeneration, diabetic
macular oedema and other
ophthalmic conditions, and hence are
very common. This treatment entails
regular injections, sometimes
monthly, and prevents blindness in
many thousands of patients. It also
exposes patients to the rare but
devastating complication of
intraocular infection
(endophthalmitis) following injection.
Any patient presenting with
ophthalmic symptoms following an
intravitreal injection requires urgent
ophthalmic review.
Although the most common ophthalmic
operation is cataract surgery, there are many
different operations that a patient may have
had, including retinal detachment surgery,
surgery for glaucoma or corneal
transplantation. It is very helpful if the
patient can tell you what they have had, so
try to elicit these details.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 9 aci.health.nsw.gov.au
Visual loss
• When it occurred
• What the patient was doing
• What has happened since the visual loss
Ask the patient to describe the following:
• Total ‘black out’ or ‘blurry’
• Intermittent or constant
• Whole or part of the visual eld
• One or both eyes
• If the eyes are painful or painless
• Are the eyes red or white
• Preceding ashes/oaters OR brief
episodes of visual loss
• Any similar previous episodes
Consider whether the patient has associated
symptoms, such as:
• Headache
• Nausea or vomiting
Notes
Visual loss is potentially very serious
and should be accorded an
appropriate level of concern.
Of the numerous potential causes of visual
loss, some can be elucidated with the above
questions.
For example:
• Rapid, painful visual loss in a red eye with
associated headache and vomiting may be
due to an angle closure crisis (angle
closure glaucoma).
• Sudden vision loss in one eye that was
preceded by intermittent episodes in the
hours or days prior may be amaurosis
fugax, heralding an impending
cerebrovascular accident or anterior
ischaemic optic neuropathy due to giant
cell arteritis (GCA).
• Visual loss in one or both eyes that is
accompanied by headache may be due to
GCA or elevated intracranial pressure.
• Visual loss preceded by ashes/oaters
may be due to a retinal detachment.
If you are concerned about a neurological
cause for visual loss, it is reasonable to
proceed with appropriate neuroimaging prior
to contacting an ophthalmologist. An
ophthalmologist may help with the diagnosis
of some neurosurgical emergencies but
cannot treat them.
Flashes/oaters are a common reason for
presentation and may indicate the presence
of a retinal tear or may be innocuous. There is
no way to make this distinction from the
patient’s history. Therefore, a patient with
ashes/oaters should be regarded as
having a retinal tear until proven otherwise.
This requires a detailed examination of the
peripheral retina by an ophthalmologist with
specialised equipment and is beyond the
scope of an emergency department
(ED) assessment.
Patients may not notice loss of vision in one
eye and only come to realise this sometime
later when the good eye is covered for
another reason. This is not common, but can
occur once other causes of acute visual loss
have been excluded.
Abrupt vision loss in any patient over
50 years of age mandates
consideration of giant cell arteritis
(GCA) (see next).
Eye Emergency Manual December 2023
Agency for Clinical Innovation 10 aci.health.nsw.gov.au
Double vision (diplopia)
• Double vision (diplopia) can be a confusing
symptom for both the patient and the doctor.
Keep it simple by working through the
following questions:
• Is it only present with both eyes open?
• Is it present if one eye is closed? If so,
which eye?
If double vision is only present with both eyes open,
consider whether:
• the two images are side-by-side, on top of each
other, or vertically displaced
• the double vision resolves if the patient looks in
a particular direction
• the double vision gets worse (greater separation
between the images) in another direction.
Notes
• Consider whether it is truly double vision,
as opposed to one eye’s blurred image
superimposed on the other eye’s clear
image. This would suggest that visual loss
or blurring is the real issue.
• Binocular diplopia occurs if the double
vision is only seen with both eyes open.
This usually means that the eyes are
misaligned due to an imbalance of the
extraocular muscles.
Binocular diplopia is an emergency
as it may indicate a cranial nerve
palsy due to intracranial pathology,
for example, a third cranial nerve
palsy caused by an aneurysm of the
posterior communicating artery. Pay
close attention to the presence of
eyelid ptosis, pupil changes,
concurrent headache and other
neurological symptoms, and proceed
with urgent neuroimaging if you
deem it appropriate.
Binocular diplopia in any patient over
50 years of age mandates
consideration of giant cell arteritis
(GCA) (see next).
Other common causes of diplopia are other
cranial nerve palsies, myasthenia gravis,
thyroid eye disease and periorbital fractures,
so look for the clinical signs associated with
these disorders.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 11 aci.health.nsw.gov.au
Painful or red eyes
Ask the patient the following questions:
• Has the patient had recent intraocular
surgery, laser or intraocular injections?
• Does the patient wear contact lenses?
If so, has the patient been swimming with,
sleeping with or overwearing the
contact lenses?
• Does the patient have decreased vision?
• Did the patient experience any prior
trauma, foreign body or ash from welding?
• What is the duration of symptoms?
• Does it affect one or both eyes? One eye
then the other?
• Are the eyes itchy?
• Is there discharge?
• Do family members or other contacts of the
patient have a red eye?
• Has the patient experienced any prior
similar episodes? If so, were they
investigated and what was the cause,
if known?
• Has the patient had prior herpetic
eye disease?
• Does the patient have any cold sores or
need for prior acyclovir?
• Does the patient have any systemic
symptoms such as rash, arthritis
or urethritis?
Notes
An urgent ophthalmic referral is
mandatory if a patient presents with
symptoms following a recent
ophthalmic procedure, especially any
eye surgery or intravitreal injection
(injection into the eye).
Similarly, any contact lens wearer
with red or painful eyes (or visual
changes) warrants an urgent
ophthalmic review.
Discharging, red eyes in a neonate
within one month of birth is an
ophthalmic emergency and requires
immediate input from ophthalmology,
paediatrics and infectious diseases.
• Red, painful eye(s) associated with visual
loss may be due to acute angle closure
crisis, corneal infection, severe
intraocular inammation, (e.g. iritis) or
intraocular infection (endophthalmitis).
• The presence of discharge usually
indicates a viral, bacterial or
allergic conjunctivitis.
• Herpetic eye disease tends to be
recurrent and can be associated with
signicant corneal scarring and visual
impairment. Patients may be aware of the
presence of corneal scars or that they
needed topical (or systemic) antivirals in
the past. Patients with herpetic eye
disease often need chronic low-dose
topical steroids or prophylactic systemic
antivirals, which may be a clue to
their diagnosis.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 12 aci.health.nsw.gov.au
Trauma or chemical injury
If a chemical injury is suspected, postpone
further history-taking or examination and
immediately begin irrigation of the eye(s).
Ask the patient the following questions:
• What time did the trauma/chemical
injury happen?
• Where did it happen?
• What was the mechanism?
• If a chemical injury is suspected, what was
the chemical?
• If a foreign body is suspected, what does
the patient think it might be?
• Was the patient doing any grinding or other
industrial activities before eye symptoms?
• Was any plant or organic material involved?
• Were the patient’s glasses or any protective
eyewear worn?
• How has vision been affected since
the injury?
Figure 1. White blow-out fracture.
Notes
Ophthalmic trauma and chemical injuries are
potentially blinding. Because of this, the
normal sequence of history and examination
is sometimes suspended.
In the case of a chemical injury,
check the pH and immediately begin
copious irrigation until the pH is
normal. This is one situation in which
you do not need to check visual
acuity in the acute stage. Find out
what the chemical was, whether it
was acid or alkali and liaise with the
Poisons Information Centre (131 126)
for further information.
Globe ruptures can occur following
serious or seemingly innocuous
injuries and from both blunt or
penetrating trauma. If you suspect a
globe rupture, stop examining the
patient and immediately apply a clear
shield over the eye. Do not clean the
eye or perform any manipulation, as
this can worsen the injury. However,
you must still check the visual acuity.
Retrobulbar haemorrhage is usually
dramatic and readily apparent from
an examination. It is a clinical
diagnosis, and you must check visual
acuity. If suspected, liaise urgently
with an ophthalmologist who can
perform emergency lateral
canthotomy and lower lid
cantholysis. This can sometimes also
be performed by plastic and
maxillofacial surgeons or ED
physicians, depending upon the skill
set possessed.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 13 aci.health.nsw.gov.au
• If the eye has been scratched, determine
whether organic material was involved as
this increases the risk of infection,
especially fungal keratitis.
• Always document the mechanism of any
eye injury carefully, as it may have
medicolegal implications. If there is a
chemical injury, document whether the
exposure happened at work or in
the home.
• Be specic about the type of eye
protection worn at the time of injury,
including the patient’s own glasses,
specialised protective spectacles or
protective goggles.
• Glasses worn at the time of trauma can
shatter and pieces of the lens or frame
may contribute to ocular injury. Maintain a
low threshold of suspicion for penetrating
eye injury and, if possible, ask to examine
the glasses that may have been brought to
hospital with the patient.
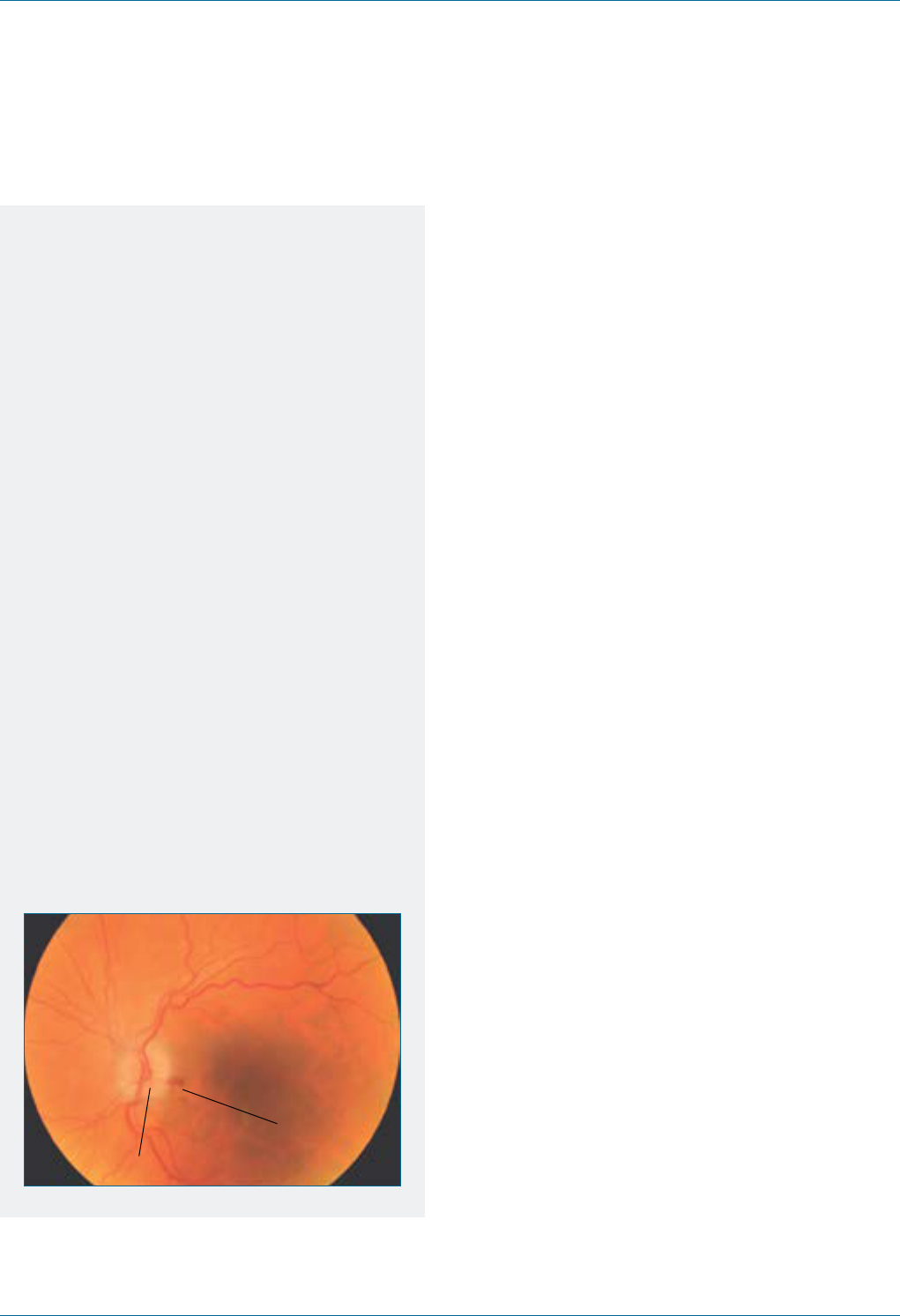
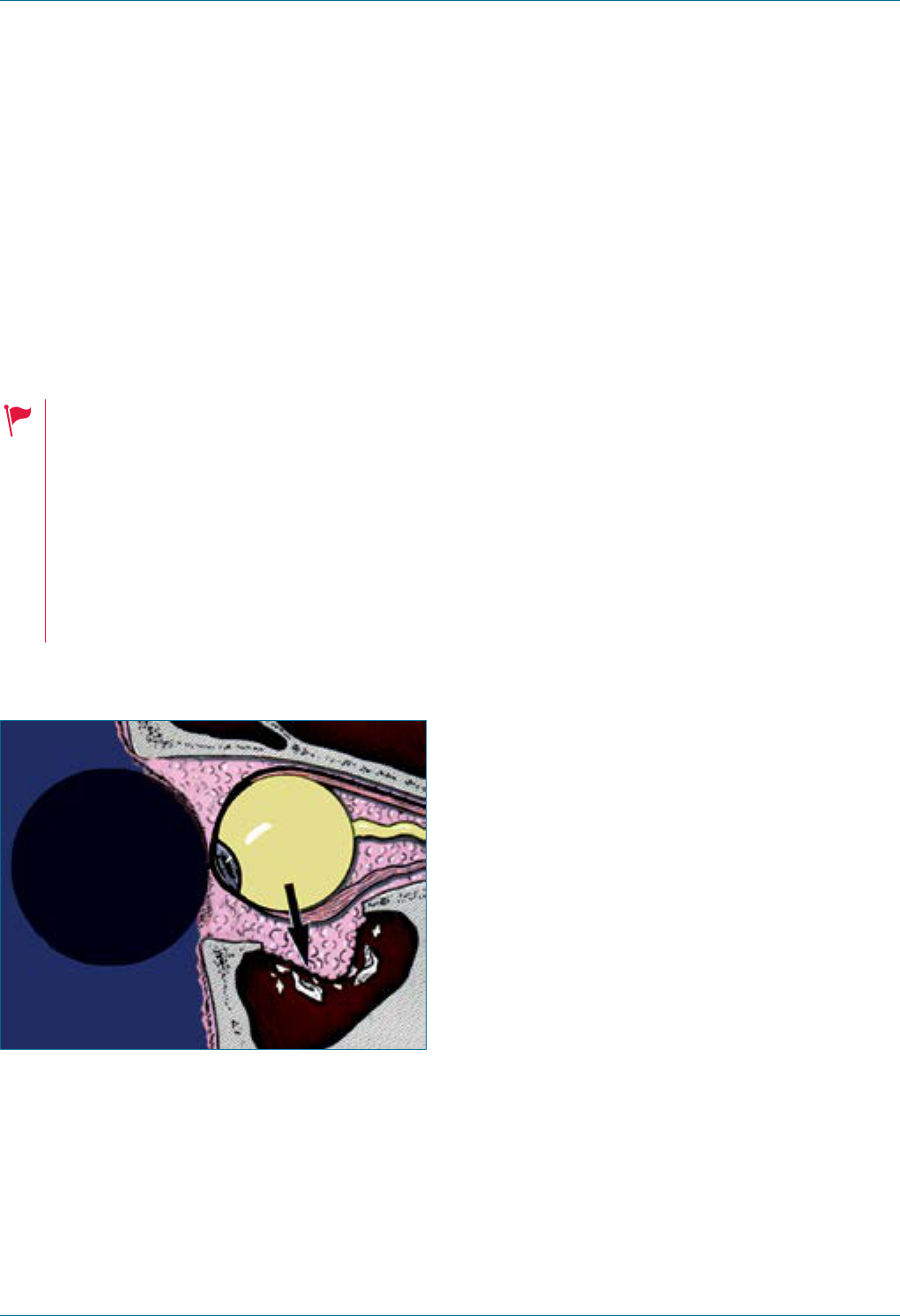
Figure 2. Swollen optic disc and
haemorrhage.
Haemorrhage
Swollen optic disc
Eye Emergency Manual December 2023
Agency for Clinical Innovation 14 aci.health.nsw.gov.au
AION due to giant cell arteritis
Consider the following in determining if the patient
has giant cell arteritis (GCA):
• Abrupt, painless loss of vision in one or
both eyes
• Brief, transient visual loss in hours or days prior
• Double vision
• Headache (classically frontotemporal)
• Jaw or tongue claudication
(worse with chewing or talking)
• Discomfort on brushing hair over one or
both temples
• Weight loss
• Anorexia
• Polymyalgia rheumatica symptoms (pain and
stiffness in pelvic or shoulder girdles)
Notes
Suspect giant cell arteritis (GCA)
inany patient over 50 who presents
with visual changes or a cranial
nerve palsy.
• You may have already considered GCA if
the patient has visual loss or diplopia, but
take the opportunity to consider the
diagnosis again prior to contacting
an ophthalmologist.
• GCA can present insidiously and rapidly
progress to bilateral complete blindness,
in some cases despite
adequate treatment.
• The diagnosis of GCA is largely clinical, i.e.
it is based on history and supplemented
with inammatory markers, and only later
by a temporal artery biopsy. Treatment is
usually undertaken in the presence of
compelling history, regardless of
inammatory markers.
• If you suspect GCA, liaise urgently
with an ophthalmologist. Referrals to
endocrinology or rheumatology may also
be appropriate in certain
clinical scenarios.
• Jaw (or tongue) claudication can be
differentiated from other causes of dental
or temporomandibular pain by determining
that (as with all claudication) there is no
pain at the beginning of mastication, and
that pain develops after a specic amount
of time, abates after cessation of chewing
and recurs upon resumption.
• Document symptoms specically and in
point form, (e.g. ‘no headache, no jaw
claudication, no tongue claudication’)
rather than simply writing ‘no GCA
symptoms’ as this might be
challenged subsequently.
• The relevant clinical signs to elicit on
examination in suspected GCA are:
tenderness over the supercial temporal
arteries or paucity of pulsation on one or
the other side and the presence of a
relative afferent pupillary defect (RAPD).
In acute GCA, the optic disc may be pale
and swollen, and while an effort may be
made to visualise the optic disc, this is
normally outside the scope of an
ED examination.

Eye Emergency Manual December 2023
Agency for Clinical Innovation 15 aci.health.nsw.gov.au
Assessing the severely
injured patient
Although life-threatening injuries take priority over
the assessment of the eye, it is not acceptable for
severe ocular injury to go unrecognised in a multi-
trauma patient once life-threatening issues have
been stabilised.
There are two main reasons for including an eye
assessment in the assessment of relevant
trauma patients:
• Firstly, damage to the eye can become the
dening injury for a patient who has survived
severe trauma, irrespective of the other injuries
they sustained. Hence, it is important to be
aware of these injuries early so that they can be
addressed appropriately.
• Secondly, although rare, some ocular injuries are
amenable to timely intervention that can
sometimes restore vision, e.g. retrobulbar
haemorrhage and chemical injury. Missing these
entities can contribute signicantly to a
patient’s morbidity.
Technique
Checking visual acuity in recumbent or restrained
patients or those in cervical collars can be difcult,
but this is vital if an ophthalmic injury is suspected.
Strategies include the following:
• Use another staff member to occlude the other
eye or hold a pinhole.
• Lower the patient’s bed without compromising
immobilisation of the spine.
• Hold a 3m chart above the patient’s bed. Ensure
your safety rst and foremost and adhere to
work health and safety regulations.
• Permanently tape a 3m or 6m chart to the
ceiling after measuring the distance between
the bed (putative position of the eyes) and the
ceiling. The acuity readings can be calibrated
based on the distance you have measured, e.g.
an eye that just sees the largest ‘E’ on a 6m
chart (labelled ‘60’) from a 2m distance should
be recorded as ‘2/60’.
While it is not possible to check visual acuity in
obtunded or intubated patients, you must still
undertake the following:
1. Perform a general inspection of the globe:
− check the integrity of the globe for rupture
− examine without putting pressure on the eye
− check for retrobulbar haemorrhage
− check for a bulging, tense, proptotic eye with
an inability to close the eyelids
− check for periocular and eyelid lacerations.
2. Check pupillary reactions for:
− direct and consensual pupil reaction
− RAPD and pupil size
This is the most important source of information in
obtunded patients (remember that the room must
be temporarily darkened to assess this).

Eye Emergency Manual December 2023
Agency for Clinical Innovation 16 aci.health.nsw.gov.au
Paediatric assessment
Paediatric assessment can be very difcult,
particularly if the child is injured or distressed. Do
not delegate the task of assessing a child to a junior
or an inexperienced member of the ED team and do
not separate the child from their parent(s) during
the assessment.
History
• Find out the child’s age, vaccination and
fasting status.
• Obtain a detailed history from an adult witness.
• A lot of information can be gathered by simply
observing the child while you take their history.
• Assess visual acuity for each eye based on the
patient’s age and ability to interact. Although
this can be difcult, it is vitally important and
cannot be deferred. Enlist the parent’s help for
an explanation, covering an eye or holding a
visual target. Check visual acuity before the
child becomes distressed, as may happen when
you examine them.
• Check visual acuity as appropriate for each
age group.
Babies
Assess the ability to x and follow light and
blink in response to bright lights (use a target
with a central, steady and maintained gaze). A
small child will x and reach for a bright object.
Toddlers
Assess the ability to identify and reach for a
small coloured target (e.g. single 100s and
1,000s sprinkles or similarly sized rolled up
piece of paper). Sprinkles (e.g. 100s and
1,000s) are commonly used to test ne vision
in children.
Infants
Assess visual acuity using a shape (or Snellen)
chart using a matching board (‘tumbling-E’s).
Age 5 or older
Assess using Snellen acuity test. Check pupils
and for an RAPD.
Some eyedrops will sting upon instillation.
Topical anaesthetic, although initially painful,
can be very useful as it will relieve pain for
about 20 minutes and may allow the child to
spontaneously open their eye after a
few minutes.
It may be necessary to gently restrain a child
to facilitate examination, or it may be feasible
to sedate the child in the ED, provided staff
with the appropriate training are available. In
some cases, it is necessary to plan an
examination under anaesthesia to complete
the assessment.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 17 aci.health.nsw.gov.au
Notes
If a history is unavailable, always suspect an
injury or foreign body as a cause for a red or
painful eye in a child. If you suspect non-
accidental injury (NAI), contact the relevant
child protection service in your area.
Periorbital cellulitis can be more aggressive in
children than in adults. It is normally treated by
admitting the child and placing them on
intravenous antibiotics under ophthalmology
and paediatric care.
Conjunctivitis in any child within one month of
birth is a medical emergency and requires input
from ophthalmology, infectious diseases and
potentially the child protection unit.
As is true for adult patients, do not put any
pressure on an eye that you suspect may be
ruptured. This is particularly an issue in children
where examination can be difcult. If you
suspect a globe rupture, put a shield on the eye,
fast the child and contact ophthalmology.
Orbital oor fractures in children are more
likely to adopt a greenstick conguration and
entrap part of the inferior rectus without
signicant external signs of injury. Be wary of
the classic presentation of the white-eye
blow-out fracture – a child presenting following
blunt periocular injury with an uninamed white
eye and inability to look up. They may be quite
unwell if they have a concurrent oculocardiac
reex (which is more common in children) and
this can provoke nausea, vomiting and
fatal bradyarrhythmias.
A child presenting at any age with no red reex
is said to have leukocoria. This may be noticed
by the parents, following a photograph that has
been taken, or by an optometrist. Several very
serious pathologies must be excluded in this
situation, chiey retinoblastoma. Leukocoria
requires urgent ophthalmic assessment.
As discussed in the visual acuity section,
amblyopia is a common cause of reduced vision
in adulthood. It occurs due to some sort of
visual impairment in children and cannot be
treated beyond approximately 10 years of age.
Ifyou discover unequal vision in a child whose
vision you have checked, the child may have
amblyopia that is still amenable to treatment.
Contact ophthalmology to arrange an
examination within 1–2 weeks.

Eye Emergency Manual December 2023
Agency for Clinical Innovation 18 aci.health.nsw.gov.au
Examinations
Examination essentials
Assessment of ophthalmology patients follows the same basic pattern of history and examination as in every
other area of medicine.
Below is a brief checklist for history and examination that should be used when assessing patients with
ophthalmic complaints. Please refer to it before contacting an ophthalmologist to ensure you have addressed
all the major points. The subsequent sections provide more information on each specic area.
Key points
Consider the following in examining patients:
• Take a history, check visual acuity, perform a
general inspection at arm’s length and look for
an RAPD for all patients.
• Selected other examinations may
be appropriate.
• It is usually not necessary to dilate pupils in ED.
Only dilate a patient’s pupils after you have
spoken with an ophthalmologist (and in cases of
trauma, the neurosurgery team).
History
• Age
• Basic demographics
• Medical history
Reasons for presentation
• Visual loss
• Diplopia (double vision)
• Painful or red eyes
• Trauma or foreign body
• Flashes and oaters
• Glasses/contact lenses/eye drops
• Prior or recent eye surgery/laser/injections
Examination
Essential
1. Visual acuity
− Without and with a pinhole for each eye
− 6/5 to 6/60, counting ngers (CF), hand
movements (HM), perception of light (PL)
orno perception of light (NPL)
Figure 3.
Snellen chart
using 6m eye
chart (visual
acuity ratio
inred).
6/60
6/36
6/24
6/18
6/12
6/9
6/6
6/5
6/4
2. General inspection
− Periocular injuries or injury to the globe
− Eye red or white
− Ptosis, proptosis or obvious misalignment
of the eye
− Gross surface anatomy of the orbit, lids,
lashes and eye

Eye Emergency Manual December 2023
Agency for Clinical Innovation 19 aci.health.nsw.gov.au
3. Pupils
− RAPD
− Direct and consensual response for each eye
− Size, shape and reactivity to light
4. Red reex with a direct ophthalmoscope
Essential in patients with visual loss or change or
neurological complaints
5. Visual elds
6. Eye movements
7. Cranial nerve examination
Additional
8. Slit lamp examination
9. Examination with direct ophthalmoscope
Contact an ophthalmologist immediately
after your assessment if you suspect
these conditions:
• Giant cell arteritis (GCA)
• Endophthalmitis
• Penetrating eye injury
• Retrobulbar haemorrhage
• Severe chemical injury
• Ophthalmia neonatorum
• Acute angle closure glaucoma
• Pain, redness or decreased vision in an
eye after any intraocular procedure
(surgery or injection) or in a contact
lens wearer
• Ophthalmic symptoms in any patient
withonly one eye (includes prosthetic
eye or long-standing poor vision in the
other eye)
Until proven otherwise
• Flashes and oaters = retinal tear
• Visual loss, visual change and diplopia in a
patient >50 years of age = GCA
• Serious periocular trauma = ruptured or
penetrated globe
• Serious periocular trauma = associated
intracranial injury
• Periocular lacerations contain a foreign body
• Eyelid lacerations are full thickness and involve
the globe
Reasons to defer visual acuity testing
• Chemical injury
• Obtunded, intubated or unconscious patient
• Severe life-threatening injury or
neurological concern
Diagnoses of exclusion
• Poor vision due to amblyopia
• Poor vision due to prior visual loss that has only
just become apparent to the patient
Reasons not to dilate a pupil
• Will not allow subsequent assessment for
an RAPD
• May precipitate angle closure
• Situations of head injury (will obviate pupil
measurements if the patient needs
neurological observations)
Eye Emergency Manual December 2023
Agency for Clinical Innovation 20 aci.health.nsw.gov.au
General inspection and assessment
of periocular and globe trauma
A general inspection provides a wealth of
information on all patients, particularly after trauma.
Most external eye ndings can be seen with a bright
pen torch or direct ophthalmoscope. Examine the
eye in an orderly fashion, i.e. lids, conjunctiva,
cornea, iris, pupil, anterior chamber, lens.
Address the following questions:
• Is the eye red or white?
• Is the globe ruptured or penetrated?
• Are there signs of
retrobulbar haemorrhage?
• Are there periocular lacerations
and ecchymoses?
• Are there signs of cranial nerve palsy?
• Is there cellulitis or swelling of the eyelids
or skin around the eye?
• Is there a foreign body in the lids, eye
or orbit?
Remember that in all serious trauma to the eye, a
penetrating eye injury and concurrent intracranial
injury must be excluded.
1. Is the globe intact?
Always begin with observation (see
questions above) and check visual acuity,
eye movements and pupils.
If you suspect globe rupture or penetrating
eye injury, examine with the utmost care.
Do not put any pressure on the eye. Gently
distract the eyelids by pressing ONLY on
the orbital margins.
External clues:
• Missile protruding from the eye: do not
remove it or touch it
• Swollen, haemorrhagic eyelids
• Obvious prolapse of uveal contents
• Distortion of the cornea or the globe
• Circumferential conjunctival swelling
and haemorrhage
• Complete ‘8-ball’ hyphaema
If you conrm globe rupture, do not
examine any further. Put a clear plastic
shield (or other makeshift mechanical
protection) over the eye, avoiding pads or
anything that might come in contact with
the eye. Contact ophthalmologist. Any
pressure put on the eye will exacerbate
the injury.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 21 aci.health.nsw.gov.au
2. Is there a retrobulbar
haemorrhage?
External clues:
• Bulging, tense or proptotic eye with an
inability to close the eyelids following
blunt trauma
Check visual acuity and for an RAPD. The
presence of a periorbital fracture does
NOTpreclude a retrobulbar haemorrhage.
Retrobulbar haemorrhage is a clinical
diagnosis and does not need imaging for
conrmation. If you suspect it is present,
liaise urgently with an ophthalmologist,
emergency physician or a plastic or
maxillofacial surgeon to perform
canthotomy and lower lid cantholysis.
3. Are there periocular ecchymoses
(‘black eye’) and inammation?
External clues:
• Document presence and extent
Take note of any localised eyelid swellings which
may indicate abscesses or chalazia.
Bilateral periocular ecchymoses in a head trauma
patient is suggestive of a base of skull fracture.
4. Are there periocular and
eyelid lacerations?
External clues:
• Document number, size, location and depth
• All periocular lacerations must be assumed to
have a foreign body until proven otherwise
For eyelid lacerations, document which eyelid and
location (medial, middle or lateral third). Eyelid
lacerations must be assumed to be full-thickness,
(i.e. through-and-through) until proven otherwise.
Severe eyelid lacerations may result in the
inability to close the eye and protect the
ocular surface. In such situations blinding
corneal exposure can rapidly occur.
Notes
• Lacerations involving the eyelid margin
need specialised repair.
• Lacerations involving the medial-most
portion of the eyelid may also involve the
lacrimal canaliculus and need
specialised repair.
• Periorbital cellulitis may complicate
lacerations, in this case, document the
extent of erythema.
5. Documentation
For external clues, draw a diagram and provide
accurate measurements at the initial assessment.
Note whether any lacerations have been sutured
prior to your assessment. Facial scarring can be
very disguring and patients may not be aware that
scarring will result, so it is important to explain this
and document that you have had this discussion.
In accordance with NSW Health policy, in
emergency situations a personal device can be
used to capture and store relevant clinical images
due to the urgent need for care, treatment or
advice. Images should be transferred to the local
health records management system as soon as
practical and the image permanently deleted from
the personal device.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 22 aci.health.nsw.gov.au
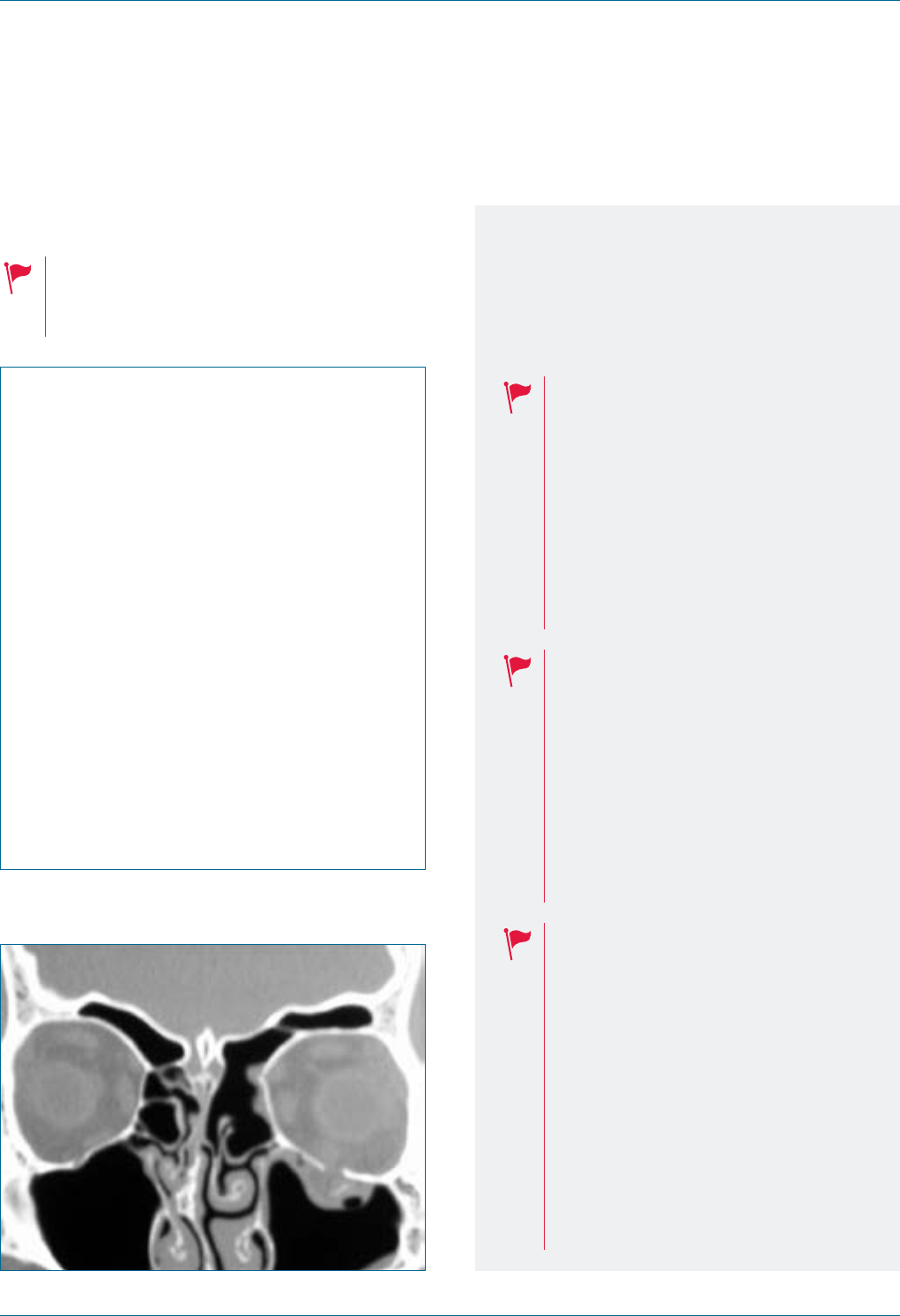
6. Imaging
Imaging is very important following periocular
trauma for the diagnosis of periorbital fractures
and to dene globe and soft tissue injuries.
Computed tomography (CT) imaging is often the
preferred modality in orbital pathology.
If a periorbital fracture is present with
entrapment of extraocular muscles, be
alert to the possibility of the oculocardiac
reex which can cause
life-threatening bradyarrhythmias.
In all serious periocular trauma, consider
that the patient may also have intracranial
trauma. Examine, image and liaise with
other specialties accordingly.
Figure 4. Orbital oor fracture.
7. Cranial nerve palsies
Consider the following:
• Perform a cranial nerve exam as you
would normally.
• See the relevant sections for specic
assessment of pupils, visual eld (for second
cranial nerve/optic nerve) and ocular movements
for third (3rd) and sixth (6th) cranial nerves.
• Signs of a 3rd cranial nerve palsy include ptosis
on one side, an eye that is misaligned downward
and laterally, and a dilated pupil.
• Signs of a unilateral or bilateral 6th cranial
nerve palsy include misalignment of the eye(s)
medially, in addition to the inability to abduct
the eye(s).
• Signs of a seventh (7th) cranial nerve palsy
include the inability to close the eye and
drooping of the lower eyelid and corner of
the mouth.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 23 aci.health.nsw.gov.au
Visual acuity
Visual acuity provides the most important
information about how an eye is functioning and is
the basic means of examining an ophthalmology
patient. It is analogous to blood pressure
measurement or an electrocardiogram (ECG).
Visual acuity must be checked in any patient with
an ophthalmic complaint or periocular injury.
Visual acuity assessment is not complete
unless the following are performed:
• Checked in each eye separately
• With the patient’s distance correction
(distance glasses)
• Without then with a pinhole
• Documented in notes
Technique
Visual acuity assessment can be confusing, so
keep it simple.
1. Sit the patient 6m away from the chart or 3m
away from a mirror that is reecting a chart
positioned above their head, thus creating an
optical 6m. Make sure that the chart is
illuminated (either room lights are on, or the
globe is turned on behind the chart if it is a
retro-illuminated chart).
2. Ask the patient to put on their distance glasses
(the glasses they use for driving, not reading). If
you are unsure, try with and without; distance
glasses will improve the patient’s
distance vision.
3. Use a solid object to occlude one eye. If the
patient is using their hand, ask them to hold the
palm of their hand gently up against their eye,
rather than their ngers, as it is possible to
peek through ngers.
Options to ensure the eye is fully occluded:
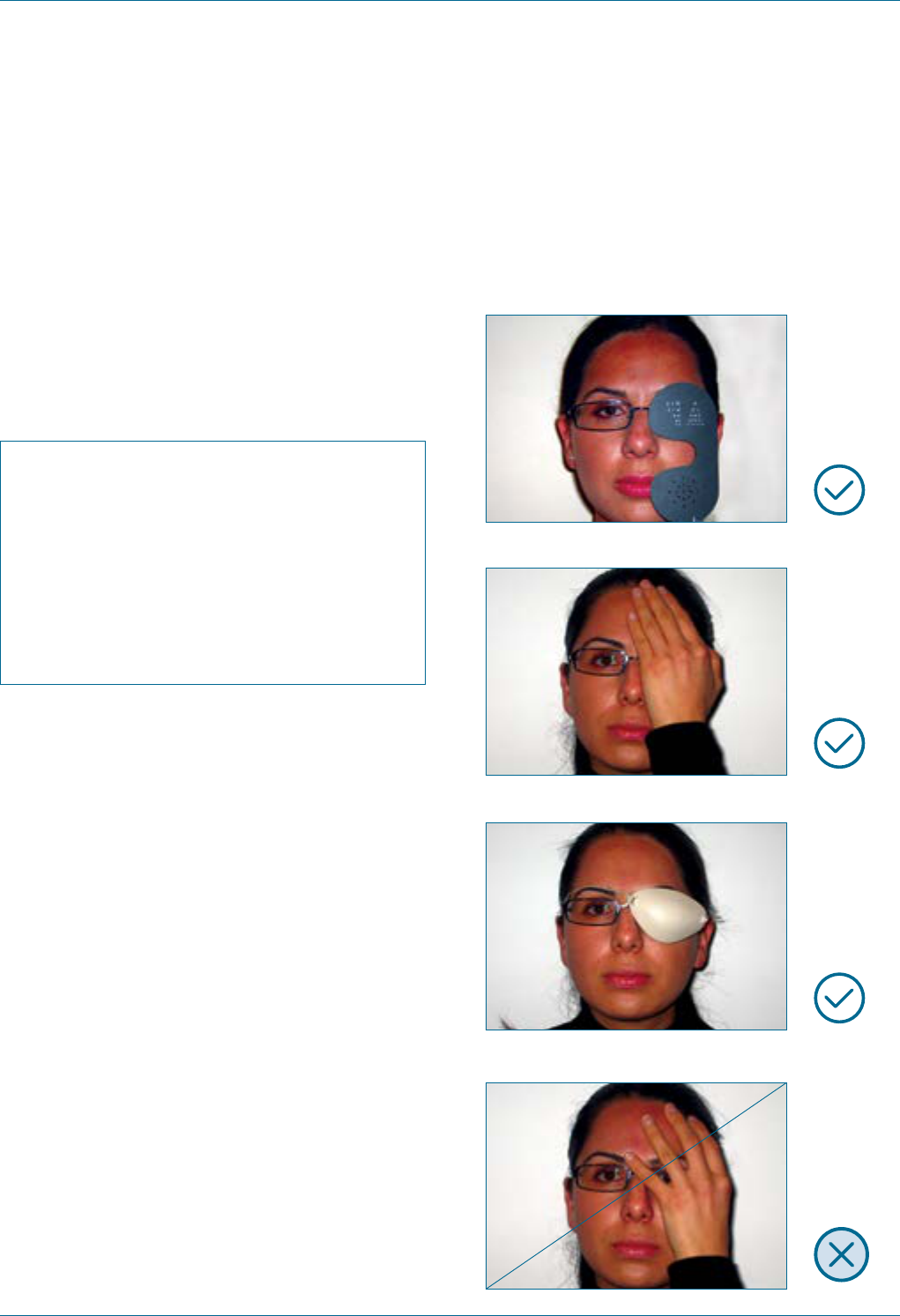
Figure 5. Correct.
Figure 6. Correct.
Figure 7. Correct.
Figure 8. Incorrect: beware of peeking!
Eye Emergency Manual December 2023
Agency for Clinical Innovation 24 aci.health.nsw.gov.au
4. Ask the patient to read as low down on the chart
as they can. Don’t correct the patient if they
make a mistake. Provide encouragement
irrespective of whether they are correct or
incorrect. Don’t let the patient give up once
things become blurry, instead encourage them
to keep going. It is not uncommon for patients
to give up several lines above their actual acuity
because it is blurry. Push them to get as low as
possible on the chart. A patient’s visual acuity is
dened as the line where they correctly guess
≥50% of the letters, whether they appear blurry
or not.
5. Document as you go, using the following
convention: the number ‘6’ over the number of
the lowest line that the patient can read (that is,
60, 36, 24, 18, 12, 9, 6, 5), giving you the familiar
fraction (6/60, 6/36, 6/24, 6/18, 6/12, 6/9, 6/6,
6/5). ‘RVA with glasses + pinhole is 6/18’ is
equivalent to saying that your patient, with
distance glasses and a superimposed pinhole,
can see at 6m what a normal person can see at
18m (6/18, which is a fraction less than 1, can be
thought of as less than normal vision). The top
number refers to the testing distance, (e.g. 6)
and the bottom number refers to the size of the
letters the patient sees (e.g. 6, 9, 12, 18, 24, 60).
6. Now test the eye looking through a pinhole. Use
an occluder with a pinhole, or, if not available,
poke a hole in a piece of paper with a 19G
needle (or even the tip of a pen). Look through it
yourself before giving it to the patient to ensure
that the aperture is clear. You may be surprised
to note that your vision improves as well. Do
NOT attempt to make a pinhole while the
patient is holding the paper over their eye. Ask
the patient to read the chart again and record
the pinhole acuity as above.
7. If the patient cannot read the largest line on the
chart, test if they can count how many ngers
you are holding up in front of their eye. Test
progressively at 30cm, 1m, 2m and 3m. If
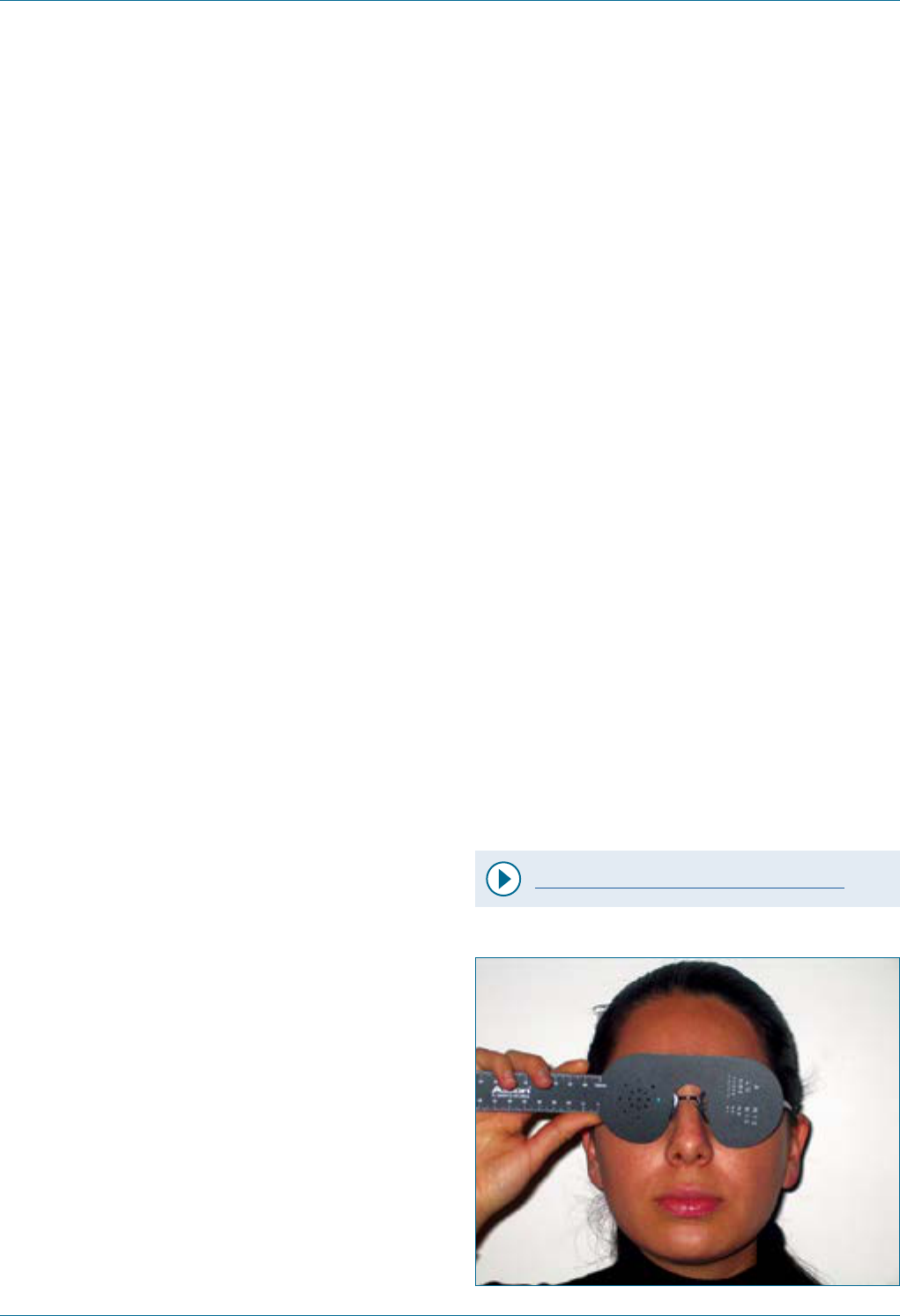
Figure 9. Pinhole occluder.
possible, record vision as CF and the distance at
which you measured.
8. If the patient cannot count ngers, assess
whether that eye can see your hand moving.
Wave your hand back and forth in front of their
eye at 30cm or more. If you are too close, they
may perceive light ickering, feel the air
movement on their face or hear your bracelets,
rather than see your hand moving. Ask the
patient to either describe the direction your
hand is moving or mirror the movement with
their hand. If possible, record vision as HM.
9. If the patient cannot perceive hand movements,
darken the room lights, ensure the other eye is
completely occluded and shine a bright light
into the eye from about 10cm. Ask if they can
see it. Shine the light on and off the eye
repeatedly and ask the patient to identify when
the light is on their eye. If they can, vision can be
recorded as light perception (LP or PL). If they
cannot, it is recorded as no light perception
(NLP or NPL).
10. Repeat the same process with the other eye.
Video - How to measure visual acuity
Eye Emergency Manual December 2023
Agency for Clinical Innovation 25 aci.health.nsw.gov.au
Notes
Visual acuity must be checked for every patient
with an ophthalmic complaint or periocular
injury. It is of vital importance for assessment
and prognosis. There are instances in which
visual acuity assessment can be deferred, e.g.
acute chemical injury, where irrigation takes
priority, or in severe life-threatening trauma
where attending to life-threatening injuries
takes priority. However, in both cases, visual
acuity must still be assessed at some stage to
ensure severe eye injuries are not missed.
Visual acuity must be documented in your
notes. Avoid writing ‘normal visual acuity’ or
‘blind’ as this does not provide any objective
information. Instead, record the specic acuity
in each eye without, then with, a pinhole. If this
is omitted, or the specic acuity is not
documented, the statement ‘normal visual
acuity’ can subsequently be challenged. This is
particularly an issue during handover in EDs,
where a colleague may have claimed to check
visual acuity but not recorded it.
It is unacceptable to say that a patient has
‘normal’ or ‘6/6’ vision because they can read
newspaper print, the writing on an IV bag, the
lowest line on a handheld chart or anything
other than the 6/6 line on a Snellen chart that is
6m away. Similarly, documenting vision as
counting ngers because that is all you have
checked and you do not have an acuity chart
means that the patient’s vision has not been
examined. It may be tempting to do these things
because measuring visual acuity using a chart
can be inconvenient, but it means visual acuity
has not been correctly checked, and there can
potentially be serious medical and
medicolegal repercussions.
A vision of 6/6 does not preclude serious
ocular pathology.
Test the eye that you suspect to have poorer
vision rst, to lessen the chance that the patient
will remember the letters when you test the
other eye. Observe the patient carefully during
the test to ensure that they are not looking
around the occluder or their hand or peeking in
another way. Visual acuity testing is an
objective test and the patient can either read
the letters or not, irrespective of whether they
are subjectively blurry or clear.
A patient must get at least 50% of the letters
correct on each line to be credited with that
acuity. It is possible to record mistaken letters
(on a line that was achieved) with a superscript
of -1, -2 or -3, or extra correct letters on the next
line (if the whole line was not achieved) with a
superscript of +1, +2 or +3 next to the visual
acuity. For example, you may record the acuity
as 6/12-1.
Patients may not know which glasses you mean
when you ask them to put on their ‘distance
glasses’. You can be more specic by asking
which glasses they use to drive or watch TV. If
there is still confusion, simply test the vision
with and without each pair. Multifocal glasses
provide distance correction when looking
through the top segment and near correction
when looking through the lower segment.
Ensure that the occluder used for the other eye
is not pushing multifocal glasses up the
patient’s nose, causing them to look through
the glasses’ reading segment.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 26 aci.health.nsw.gov.au
A pinhole works by eliminating spherical
aberration, or the poorly focused rays of light
that are refracted at the periphery of a lens (in
this case, the eye’s tear lm, cornea and lens). A
pinhole eliminates most refractive error and
approximates a ‘universal’ lens, and this gives
vital information about an eye’s best possible
vision. Visual acuity testing is not complete until
pinhole acuity for each eye is tested and
recorded. Remember that visual acuity testing
should be done with glasses and then with a
pinhole as well. It is a common misconception
that testing with glasses and with a pinhole are
mutually exclusive. If a patient’s distance
glasses have not been updated for some time,
they may have signicantly better acuity when
tested with a pinhole as well.
‘Normal’ visual acuity or 6/6 means that the
patient can see at 6m the same target that a
person with normal vision can see at 6m. As the
denominator increases, the visual acuity
decreases, so a vision of 6/60 means that while
a person with normal vision could see the target
at 60m, the patient can only see it at 6m.
Similarly, 6/36 vision means that while a person
with normal vision could see the target at 36m,
the patient can only see it at 6m.
The distance to the chart is of paramount
importance. If the chart is closer, it will give an
inaccurate visual acuity. While it is possible to
mathematically adjust the ratio to reect a
shorter viewing distance, this adds an
unnecessary level of complexity to an ED
assessment. Keep it simple and check at 6m
(either directly or reected in a mirror).
Near acuity (or reading vision) as checked with a
handheld chart or a mobile phone app is an
alternate means of checking acuity but is NOT
readily interchangeable with distance acuity.
Snellen distance acuity is the standard method
of measuring a patient’s acuity and has the
most clinical relevance. It can create confusion
if a different method is used, particularly when
the acuity on presentation in ED is needed for
comparison at later stages in the
patient’s assessment.
An alternative to using a wall-mounted chart is
a scaled, handheld paper chart that is held at
3m. This is particularly useful for examining
bed-bound or recumbent patients. However, it is
more prone to inaccuracy as it is difcult to
calibrate exactly 3m from the patient’s eye and
charts that have been photocopied suffer a
degradation in contrast which can also
articially degrade visual acuity. Many of these
charts are also inaccurately labelled
concerning the visual acuity corresponding to
each line.
Patients who do not recognise the common
Snellen letters can be tested with the
‘tumbling-E’ chart. This replaces Snellen letters
with the letter ‘E’ in four different orientations:
up, down, left or right. The patient is asked to
point in the direction that the ‘E’ is pointing on
the chart.
If a patient is in pain, it is reasonable to instil a
drop of local anaesthetic to facilitate checking
visual acuity. Give the patient a few minutes
after anaesthetic instillation for the eyelid
spasm to subside.
Although amblyopia is a common cause of
unilateral poor vision in adults, do not attribute
reduced vision in ED to amblyopia. It is a
diagnosis of exclusion. Amblyopic eyes are as
prone to pathology as non-amblyopic eyes, and,
Eye Emergency Manual December 2023
Agency for Clinical Innovation 27 aci.health.nsw.gov.au
in some cases, more likely to be injured. Be
especially attentive if a patient describes
further worsening of vision in an eye that
was suspected to be amblyopic.
A vision of NLP has an extremely poor
prognosis and tends only to occur in the
very end stage of diseases such as
glaucoma, retinal detachment, injury to the
optic nerve or following serious injury. While
you may encounter patients in whom an eye
has been NLP for some years, if an eye
suddenly becomes NLP, then very serious
pathology is present. In patients over 50
years old, abrupt loss of vision to NLP
means GCA until proven otherwise. Liaise
with an ophthalmologist and commence
treatment to prevent a similar occurrence in
the other eye.
Common pathologies such as
cataracts, vitreous haemorrhage
and amblyopia do not cause vision
of NLP. The instances in which an
eye recovers some vision after
having been NLP are very rare.
Pupil examination
Pupil examination is a vital part of both the
ophthalmic and neurological assessment. It must
be done in all patients. In obtunded or severely
injured patients it may be the only type of
examination possible other than general inspection
and fundoscopy.
Pupil examination is not complete unless you have
assessed for an RAPD.
If a pupil abnormality is detected, you must also
examine the patient’s eye movements, eyelids and
visual eld.
Key aspects of pupil examination are size, shape
and reactivity. In ambient light, both pupils should
be of equal size and shape. Physiological anisocoria
is present in up to 15% of the population and does
not imply an RAPD.
Technique
Pupil examination technique requires the following:
1. Observe pupil size in the light. Ask the patient
to look at a target behind you, so that there is no
accommodation on a near target which will
inuence the size of the pupils. Look for a
difference in pupil size (anisocoria), difference
in iris colour (heterochromia) or irregularity of
the normally round shape.
2. Darken the room and check pupil size again.
Note whether any difference in pupil size is
more pronounced in the light or the dark.
3. Shine a bright light into one pupil and observe it
constricting to assess the direct pupil response
on that side.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 28 aci.health.nsw.gov.au
4. Check that the other eye also constricts to
assess the consensual light reex. Repeat this
process by shining the light into the other eye.
5. Check for an RAPD. Shine a bright light into one
pupil for 2–3 seconds, then rapidly ick the
light across to the other side, and hold it for the
same duration. An RAPD is present if the pupil
initially dilates (instead of initially constricting)
when icking across from the other side. You
can go back and forth several times until
convinced of the ndings, provided that the
time over each eye is the same and the time in
between the eyes is very short.
Video - How to examine an RAPD
Notes
Although an RAPD may be subtle in some
cases, it is a vitally important clinical sign to
elicit in situations of sudden visual loss and
ophthalmic trauma.
When pupils have been pharmacologically
dilated, it is not possible to test for an RAPD.
This is one of the principal reasons that
pupils are not dilated in ED prior to
ophthalmic assessment.
The key to detecting an RAPD reliably is to
ensure that each eye is exposed to the same
amount of bright light for the same amount of
time, with the briefest possible transit
between each eye. It is possible to mistakenly
give the impression of an RAPD if the light
intensity or the time over each eye varies.
The principle behind an RAPD is that by
alternately presenting each eye with a
symmetrical, intense light source, a subtle
unilateral optic nerve defect will be exposed.
If the optic nerve is damaged on one side,
when the light icks to that eye, the direct
response is less than the consensual
response from the recent contralateral light
stimulation, and so the pupil is observed to
dilate. It should be noted that this
observation is based on the direct and
consensual pupillary reexes being equal
in amplitude.
Vision loss in giant cell arteritis (GCA)
(or any other cause of optic neuropathy)
is associated with a relative afferent
pupillary defect (RAPD).
It may be hard to assess pupil size in the dark
if the patient has a dark-coloured iris.
Experiment with using a diffuse light shone
from above or below that allows you to see
the pupil without inuencing its size or with a
single-ash camera.
Remember that a unilaterally dilated
pupil on one side may indicate an
acute third (3rd) cranial nerve palsy
and urgent neuroimaging and liaison
with a neurosurgical service is
required if detected.
There are many situations in which pupils
may be abnormally shaped, including
intraocular inammation, prior surgery or
accidental trauma.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 29 aci.health.nsw.gov.au
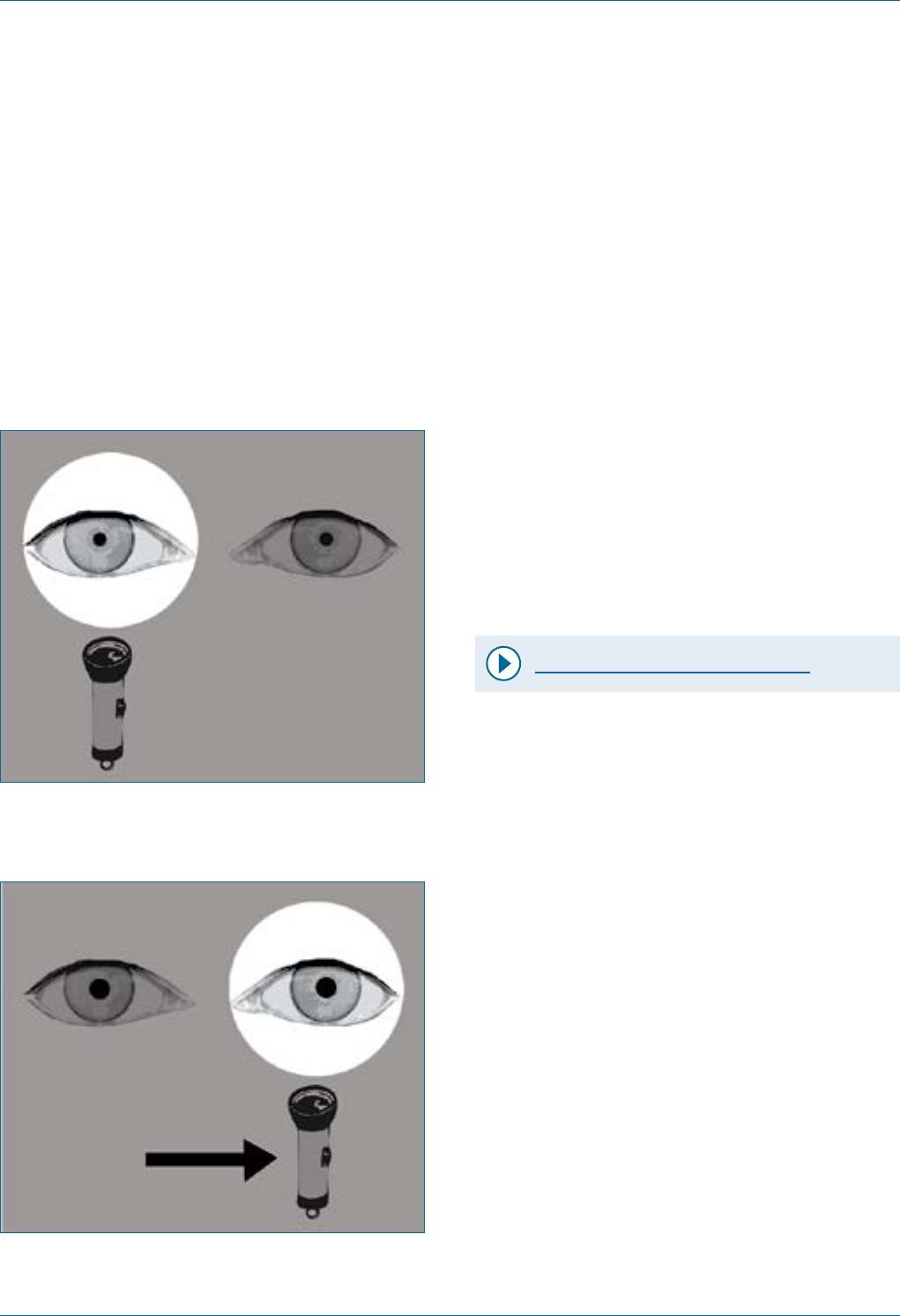
Swinging torch test
This involves demonstrating a left relative afferent
pupillary defect where the left pupil dilates after
prior consensual constriction with direct light
stimulation of the right eye.
Figure 10. Swinging torch test
(consensual constriction).
Figure 11. Swinging torch test (left pupil
apparent dilation).
Visual eld, eye movements
andeyelid examination
Visual eld, eye movement testing and eyelid
examination are not mandatory in all ophthalmic
patients (for example, a simple foreign body) but
must be tested in anyone with visual changes or
suspected optic nerve, orbital or neurological
pathology. If a patient has a pupil abnormality,
these three examinations must be performed.
Given how rapidly and easily it can be done, have a
low threshold for testing it if you think it might
be relevant.
Technique for visual eld
Video - Technique for visual eld
1. Begin by explaining what you are going to do.
Telling the patient that you are testing their
‘peripheral vision’ can make it easier for the
patient to follow your instructions.
2. Ask the patient to remove their glasses so that
the rims do notinterfere with the assessment.
3. Sit opposite the patient with your eyes at the
same height, about 50cm away from their face.
4. Place a hand over one of your eyes and ask the
patient to mirror you, e.g. if you cover your left
eye, they cover their right eye.
5. Ask the patient to keep their eye covered, to
look directly at your eye with their uncovered
eye, and not to look away.
6. Clench the st of your free hand and hold it in a
reasonably peripheral position in one quadrant
of your peripheral vision.

Eye Emergency Manual December 2023
Agency for Clinical Innovation 30 aci.health.nsw.gov.au
7. Ask the patient how many ngers they see
and hold up a random number. Look at the
patient’s eye to ensure that they do not look at
your hand.
8. Test in all four quadrants in the same manner
and repeat the process on the other side.
9. Test for a scotoma by slowly moving your
nger from an area where the patient cannot
see to where they can. Repeat until you have
mapped the scotoma to your satisfaction.
Notes
Visual eld testing to confrontation is
unlikely to allow you to detect subtle or
small visual eld defects but larger defects
can be detected.
As you are sitting opposite the patient, your
visual eld is a reasonable approximation of
theirs. It is important to hold your hands in
the same coronal plane in each position and
equidistant from you and the patient.
Neglecting to do this distorts the eld that
you are assessing.
You can use the hand that was covering your
eye, provided you keep that eye closed and
remember the position of that monocular
visual eld with your hand in place. This
makes the examination more uid.
Alternatively, you can switch hands.
You can hold up several nger combinations
in each quadrant to ensure that the patient
can see them.
It is not uncommon for patients to
inadvertently look at your hand when they
realise your ngers are moving. The most
important thing is to recognise when this
happens, remind the patient to look at your
eye instead and repeat the step with a
different number of ngers.
A patient’s visual acuity must be at least
counting ngers to allow you to test their
eld to confrontation.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 31 aci.health.nsw.gov.au
Technique for eye movements
Eye movement examination must be performed
in any patient with diplopia (double vision), pupil
or eyelid abnormalities.
Eye movement examination technique requires
the following:
1. Explain what you are going to do by asking
the patient to keep their head still and follow
your nger with their eyes.
2. Hold your index nger up in front of the
patient, then trace an ‘H’ pattern in a coronal
plane in front of them.
3. Ask the patient to tell you if they have double
vision, (e.g. ‘see two ngers’) in any position
of the ‘H’.
4. Following this, assess each eye separately by
asking the patient to cover one eye and
testing the movements of the other side.
5. Switch over so that both eyes are assessed in
this way. If the patient is experiencing
binocular diplopia, they will not experience
diplopia when one eye is covered.
Notes
When testing eye movements, it may help to
gently place a nger on the patient’s chin or
forehead to remind them not to follow with
their head.
If a patient has an eye movement disorder
you must check their pupils, eyelid and
visual eld.
In a sixth (6th) cranial nerve palsy, the
patient may not be able to abduct their eye.
In a third (3rd) cranial nerve palsy, the
patient may not be able to elevate, depress
or adduct the eye, and you may notice
associated pupil and eyelid changes.
In an orbital wall fracture, the patient may
not be able to move the eye in the opposite
direction, especially if there is associated
entrapment of the extraocular muscles
(e.g. inability to elevate the eye in an orbital
oor fracture).
Eye Emergency Manual December 2023
Agency for Clinical Innovation 32 aci.health.nsw.gov.au
Eyelid examination
Eyelid examination must be performed in any
patient with diplopia (double vision), pupil
abnormalities or eye movement disorder and
requires the following:
• Observe for ptosis (drooping of the upper
eyelid over the eye, which may be unilateral or
bilateral). Compare the position of the upper
eyelid on one side with the other. This can be
done by simply judging the relation of the
upper eyelid to the top of the pupil or more
accurately by measuring the vertical height of
the palpebral aperture with a ruler.
• Ask the patient to close their eyes. Determine
whether there is any weakness in this action by
rst observing and then gently trying to part
the eyelids.
Notes
Opening the eye relies upon the third
(oculomotor) cranial nerve and the
sympathetic bres. Therefore, a lesion of the
oculomotor nerve causes ptosis, and if severe
enough, inability to open the eye. A lesion of
the sympathetic bres causes Horner
syndrome and less ptosis.
Other causes of ptosis include trauma,
swelling of the upper eyelid or age-related
degeneration of eyelid tissue.
Closing the eye relies upon the seventh (7th or
facial) cranial nerve. Lesion of the facial nerve
can result in an inability to close the eye, in
addition to drooping of the lower eyelid and
the corner of the mouth. Testing for eyelid
closure in this manner is the same manoeuvre
used in checking facial nerve function.
Inability to close the eye is called
lagophthalmos and, if severe, can
lead rapidly (within hours) to corneal
exposure, irreversible scarring
and blindness.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 33 aci.health.nsw.gov.au
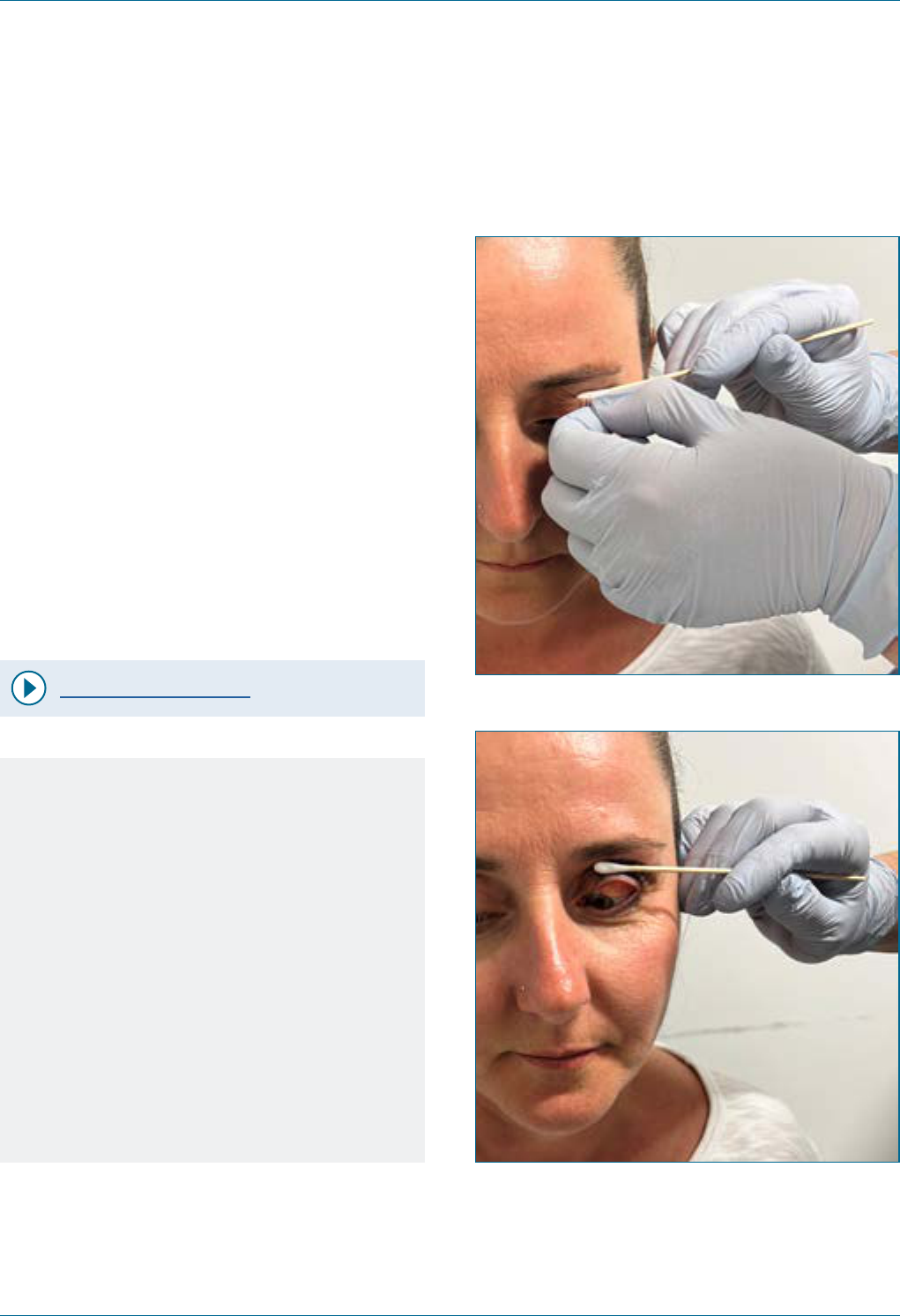
Eyelid eversion
Eyelids must be everted to exclude a subtarsal
foreign body.
Technique
1. Ask the patient to look down.
2. Gently pull the upper eyelid down and away
from the globe using the eyelashes.
3. Place a cotton bud at the midpoint on top of
the eyelid, then bend the eyelid up over the
cotton bud.
4. Slide the cotton bud out and either replace it
on the lid margin to hold the lid in position or
use your nger to do so.
Video - Eyelid eversion
Notes
It is most efcient to evert an eyelid at the
slit lamp, as your view of any potential
subtarsal foreign bodies will be better.
These may be gently removed with a moist
cotton bud.
Patients are often quite averse to having
their eyelids everted. Explain what you are
going to do, and that while it may feel
unusual, it should not be uncomfortable.
It may be easier to grip the edge of the
eyelid and eyelashes if you wear a glove.
Figure 12. Everting eyelid.
Figure 13. Everting eyelid.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 34 aci.health.nsw.gov.au
Special eye examinations
Direct ophthalmoscope
It is not necessary to perform a detailed
examination with a direct ophthalmoscope for an
ED ophthalmology assessment, although it is very
helpful if you use it to determine whether the
patient has a red reex or not. Examination with a
direct ophthalmoscope does not take priority over
the simple assessment of visual acuity, pupils and
general inspection.
Do not dilate a patient’s pupils until you have
spoken with an ophthalmologist as it means that an
RAPD cannot be assessed and the patient cannot
have pupil observations for several hours.
Technique
Video -
Direct ophthalmoscope examination
1. Watch the video of direct
ophthalmoscope examination.
2. Darken the room and ask the patient to look at a
target behind you on the wall.
3. Adjust the dioptric correction to zero. Turn the
ophthalmoscope light on.
4. Use the same eye as the one you are examining
on the patient, i.e. your right eye for the
patient’s right eye.
5. Standing back from the patient, look through
the viewing aperture and shine the light into the
patient’s pupil. You should see a red reection
(‘red reex’).
6. If necessary, adjust the dioptric correction to
improve the clarity of the image.
7. To examine the retina, move in closer, keeping
the light focused on the red reex. You must get
very close to the patient (within 5cm).
8. When you are close enough you will see some
retinal detail, usually a retinal blood vessel.
Follow this vessel until you can see the
optic disc.
Notes
The direct ophthalmoscope provides a
highly magnied, narrow angle view of the
fundus. It cannot reliably be used to
examine the retina in sufcient detail to
exclude pathology. For this reason, patients
with suspected posterior segment
pathology such as optic disc swelling or
retinal tears need to be examined by
an ophthalmologist.
Other tools may be available in your ED also,
including a pan ophthalmoscope or a
non-mydriatic fundus camera. Acquiring one
of these is highly recommended.
Loss of the red reex occurs in several
conditions (such as retinoblastoma,
cataract, vitreous haemorrhage or retinal
detachment) and this information can assist
greatly with triaging ophthalmic referrals.
It is much easier to examine the retina if the
patient’s pupil is pharmacologically dilated.
However, pupil dilation prevents subsequent
assessment for an RAPD, can rarely
precipitate acute angle closure in some
patients and obscures neurological
observations in patients with a head injury.
For these reasons, pupil dilation should only
be undertaken after discussion with an
ophthalmologist (and, in some cases,
a neurosurgeon).
Eye Emergency Manual December 2023
Agency for Clinical Innovation 35 aci.health.nsw.gov.au
Checking intraocular pressure
Although not available in every ED, several
handheld devices can be used to measure
intraocular pressure.
Never check intraocular pressure if you suspect
that a globe may be ruptured.
Applanation tonometers (e.g. Tono-pen)
Video - Tono-pen technique
1. Explain what you are going to do to the patient.
Position the patient upright, looking in a
horizontal direction.
2. Administer topical anaesthetic (tetracaine or
plain lignocaine).
3. Place a disposable rubber shield over the
tonometer probe. Use a different shield for
each patient.
4. Turn the tonometer on using the button on the
top of the device. Wait for it to beep and for the
display to come on.
5. Holding the tonometer horizontally, gently tap
the probe against the centre of the cornea
several times. You may need to gently hold the
patient’s eyelids open to achieve this.
6. The tonometer will make ten recordings in quick
succession and then beep loudly, displaying the
average intraocular pressure on the screen.
Notes
Patients can be quite anxious about having
their pressures checked, as many have
unpleasant recollections of the ‘puff’
tonometers that are commonly used by
optometrists. You can reassure the patient
that this is a different technique and that
while it may feel unusual, it will not be
uncomfortable (apart from the
topical anaesthetic).
If holding the patient’s eyelids with your
ngers, make sure you are not pressing on
the globe itself as this will cause an
inaccurately high pressure reading. Restrain
the eyelids by tethering them to the bony
orbital margins.
Always store the tonometer with a cardboard
sleeve over the probe, as this part of the
device can be very easily damaged.
As with any test, it is possible to get
erroneous measurements. If you doubt the
reading, repeat the examination.
Troubleshooting tips are to ensure the sleeve
is taut across the tip of the device, and that
measurements are taken from the central
cornea, holding the tonometer in a horizontal
position. If you are having difculty getting
ten readings (which should be very rapid),
make sure that the tonometer is in contact
with the cornea and make very small to-and-
fro movements with your hand.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 36 aci.health.nsw.gov.au
Rebound tonometer (e.g. iCare)
Video - iCare tonometer technique
1. Tell the patient what you are going to do.
2. Turn the device on. It will prompt you to insert a
small, disposable, round-ended pin-like probe.
Once inserted, the probe will shudder back-
and-forth for a moment as the device conrms
its position.
3. Hold the device vertically just in front of the
eye. The probe should be horizontal, only a few
millimetres away from the eye and pointing at
the central cornea.
4. Press the button. The probe will gently rebound
off the cornea and then return to position,
usually quicker than the patient can blink.
5. Press four more times. The machine will collect
ve readings and then display the
intraocular pressure.
Notes
Explain to the patient that this device is
different to the puff tonometry they may
have experienced before and that this will
not cause any discomfort.
Unlike applanation tonometers, you do
not need topical anaesthetic to check the
intraocular pressure with a rebound tonometer.
The patient may feel the contact with their
cornea, but the sensation is remarkably light
and, in some cases is only barely noticed.
Because rebound tonometers are so fast, you
often do not need to hold the patient’s
eyelids. However, the rapid succession of
beeps and barely appreciated sensations on
the cornea can be bewildering. It often helps
to pick your moment and time each
measurement between blinks. Speaking
calmly to the patient and reassuring them is
very important.
A rebound tonometer may be superior for
checking intraocular pressure in children
because it is so rapid and does not need
topical anaesthetic or pressure on the eyelids.
Some rebound tonometers can be held at
orientations other than vertical, making
them more useful for recumbent and
bed-bound patients.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 37 aci.health.nsw.gov.au
Slit lamp
A slit lamp is a binocular microscope with an
adjustable, confocal light source that enables the
ophthalmologist to examine the eye in detail, from
the eyelids to the retina. Although a slit lamp
examination is often not wholly necessary for the
basic assessment of an ophthalmology patient, it is
certainly preferable and remains vital for such
conditions as corneal foreign bodies and corneal
epithelial defects.
Technique (e.g. Haag-Streit slit lamps)
Video - How to use a slit lamp in 5 minutes
Video - Slit lamp basic examination
1. Ensure that both you and the patient are sitting
on height-adjustable chairs. Bring both chairs
close to the slit lamp.
2. Adjust the table height so that the patient can
place their chin on the chin rest and their
forehead can touch the headrest.
3. Adjust the height of the chin rest so that the
patient’s lateral canthus is aligned with the
black grooved line on the vertical support.
4. Adjust the eyepieces so that they are both at
‘zero’. If you have a refractive error, it is best to
wear your own spectacles. While it is possible to
adjust the optics of the slit lamp to compensate,
this can create unnecessary confusion.
5. Turn the lter selection switch to the left-most
(or second from left-most) position. This is the
brightest setting and will allow you to see more
of the eye. While it is bright, the patient’s
perception of brightness comes mostly from
the width of the beam.
6. Adjust the aperture height knob to create a
maximally tall beam (8mm) and the aperture
width knob to create a very narrow beam
(<0.5mm). This gives the best viewing
characteristics. A beam that is too wide will
make it harder for you to appreciate depth and
be uncomfortable for the patient.
7. Turn the illumination arm to the same side as
the eye that you are examining and angle it
between 30° and 60° from the midline. Ask the
patient to look at your opposite ear with their
other eye. Switch the arrangement when you
switch eyes.
8. Turn the slit lamp on and adjust the
characteristics of the light beam if needed.
9. Begin by coarse-focusing. Do not look through
the microscope initially, but instead look beside
it at the light shining on the patient’s face. Move
the whole slit lamp base to bring the light into
sharp focus on the patient’s eye. You can then
look through the microscope.
10. Adjust the width of the eyepieces as you would
on a pair of binoculars.
11. Fine-focus moving the joystick backwards and
forwards. There is nothing else you need to do
to focus. Experiment by moving backwards and
forwards and observing the effect it has on
what you can see. You can move the beam up
and down by turning the joystick.
12. When focused on the eye, examine the
periocular skin, lids, eyelashes, cornea, iris and
lens in an anteroposterior systematic fashion.
Note the location, size and apparent
composition of any foreign bodies.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 38 aci.health.nsw.gov.au
13. To search for a corneal epithelial defect,
administer a drop of uorescein and examine
with the cobalt blue light. This is obtained by
turning the height aperture knob beyond 8mm
until a stop with a blue dot appears. The beam
will turn blue. Widen your beam to the
maximum, as you will usually want to scan the
ocular surface for uorescein staining.
14. When nished, turn the slit lamp off and ask the
patient to sit back. Do not leave the patient
stranded or trapped behind the slit lamp or with
their feet elevated off the ground.
Notes
Patients sometimes lean back during the
examination, pulling their forehead away from
the headrest and causing the eye to go out of
focus. Check the patient’s position periodically
and remind them to come forward again if they
have drifted away. Checking head position is
essential during foreign body
removal procedures.
Ergonomics are important. Adjust the height of
your chairs and that of the table to ensure
comfort. Apart from causing injury, if the
patient is uncomfortable, they are more likely to
drift away, and if you are uncomfortable, you
are less likely to examine them thoroughly.
The cobalt blue light is obtained by turning the
height aperture knob one click beyond 8mm.
The green lter (on the lter selection switch) is
commonly mistaken for the cobalt blue light but
it has different optical characteristics. If you are
looking for an epithelial defect with a green
light, then stop, turn the lter selection switch
back to the left and adjust the height knob until
it stops at the blue light.
Use the terms ‘corneal epithelial defect’ or
‘punctate epithelial erosions’ when describing
what you see with uorescein and the cobalt
blue light. ‘Diffuse uorescein uptake’ is not a
useful descriptive term, and usually means that
the slit lamp was out of focus, that the green
light was used instead of the blue or that the
examiner put too much uorescein into the eye
and did not wait for it to disperse.
The technique for looking for cells is to darken
the room, adjust the height and width apertures
to produce a 1mm x 1mm beam, and direct it
from 45° across the patient’s pupil while
focusing on the middle of the anterior chamber.
Increase the magnication by switching the
lever beneath the eyepieces. Cells will be
illuminated against the dark backdrop of the
pupil as they traverse the light beam, like dust
particles in a sunbeam. While this is a good
thing to test for, it is not considered a standard
part of the ED assessment.
Video - Slit lamp examination
for cells and are
As mentioned above, you can adjust the
magnication by switching the lever beneath
the eyepieces. This can be useful in certain
situations, but in general, keep the slit lamp on
the lower magnication. This makes it easier to
focus and the more zoomed-out view will give
you a better appreciation of normal anatomy
and pathology.
Turn the slit lamp off when you are nished
examining and clean its surfaces
between patients.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 39 aci.health.nsw.gov.au
Troubleshooting
If there is no light when you turn the slit lamp on,
check that:
• it is plugged in and turned on at the power point
• the LED light next to the ON switch is illuminated
• the width and height apertures are open.
Notes
If the width aperture is closed no light will
appear. This is a common reason for no light to
appear. Simply widen the beam to x this.
Similarly, if the height aperture or one of the
lters is turned halfway between stops, light
may not appear. Turn all the way to a stop to
x this.
Does the bulb need to be replaced?
If these simple points are addressed and there
is still no light, this may be the case.
Emergency departments usually have spare
bulbs, but only someone who has experience
replacing a bulb should do so. Ensure that the
slit lamp is turned off and unplugged before
proceeding. If the bulb housing is screwed
down too tightly, or the bulb is not aligned
properly in the socket, it may not work until
these issues have been corrected.
If the view is blurry, try:
• wearing your own glasses
• ensuring the eyepieces are fully pushed in
and dialled to 'zero'
• going through the same process of coarse-
and then ne-focus.
The eyepieces (or oculars) can be adjusted to
account for your refractive error or induced
instrument myopia. However, it is simpler to
wear your own spectacles and keep the
oculars on ‘zero’ (align the little mark opposite
‘0’). The eyepieces can also be removed (for
cleaning) and occasionally you will encounter
slit lamps in which the oculars have been
inadvertently left partially out. Push them in to
make your view clearer.
If you are seeing clearly but not with both
eyes, try:
• adjusting the interpupillary distance by
altering the width between the eyepieces
just like a pair of binoculars
• moving the light column slightly to one side
or the other (sometimes the light column
can obstruct the view through
one eyepiece).

Eye Emergency Manual December 2023
Agency for Clinical Innovation 40 aci.health.nsw.gov.au
Eye referrals and discharge advice
Traumacommunication
checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?
Acute visual disturbance
communication checklist
Consider the following in the presenting patient:
; Presenting complaint: timing,
worsening/improving, monocular/binocular
; Past ocular/medical history
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination (anisocoria and presence
of an RAPD)
; Red reex
; Dilated retinal examination
Red eye or eyelid
communication checklist
Consider the following in the presenting patient:
; What was the onset and duration
of symptoms?
; Is the eye painful or not painful?
; What is the distribution of redness? Is it
localised or diffuse? Does it involve the
tarsal conjunctiva?
; Is the condition purely unilateral or are
there contralateral symptoms?
; What is the best (pinhole) visual acuity of
each eye?
; Are the eyelids involved? Are they red
or swollen?
; Is the cornea normal? Are cloudiness,
opacities or uorescein staining visible?
; Is the anterior chamber normal? Is it deep?
Presence of anterior chamber cells, blood
or hypopyon?
; Is the iris normal? Round, equal, reactive
pupils? Are the normal iris details visible?
; Are the red reexes equal?

Eye Emergency Manual December 2023
Agency for Clinical Innovation 41 aci.health.nsw.gov.au
Visual requirements for driving
Be aware of driving requirements when assessing a
patient with an ophthalmic complaint. Visual
requirements differ depending on whether
someone is a private or commercial driver. A
commercial driver is anyone who drives during their
occupation other than to and from work (such as
bus, truck and taxi drivers, and most couriers) and
there are more stringent licensing requirements
than for private vehicle driving.
Private vehicle licence: visual acuity of 6/12 or
better with both eyes open or in the better eye.
Commercial vehicle licence: visual acuity of 6/9 or
better in the better eye AND 6/18 or better in the
poorer eye.
For drivers in NSW, further information is available
from Transport for NSW.
A person with only one eye (monocular) cannot hold
an unconditional private or commercial driver’s
licence. A conditional licence may be considered by
the driver licensing authority subject to 2-yearly
review, considering the nature of the driving task
and information provided by the treating
optometrist or ophthalmologist. Specic visual
standards must be met that differ for private versus
commercial drivers.
A period of adaptation is required (usually 3
months) after someone is rendered monocular
before they can resume driving. This is because it
takes time to compensate for the loss of
binocularity and peripheral eld and become
familiar with the monocular cues that can provide a
simulacrum of binocular viewing.
Patients with symptomatic diplopia (double vision)
are not permitted to drive. While wearing a patch (or
occluder) over one eye can abolish binocular
diplopia, it also renders the patient monocular and
hence the 3-month adaptation period applies.
A visual eld with both eyes open of 110°
horizontally and 20° vertically (at least 10° above
and below the horizontal midline) without any
signicant eld loss within the central 20° is
required for private driving licences. A commercial
driver is not t to hold an unconditional licence if
they have a visual eld defect. A conditional licence
may be considered if the binocular visual eld is
static, has an extent of at least 140° within 10°
above and below the horizontal midline and no
signicant eld loss is likely to impede driving
performance. A homonymous quadrantanopia or
hemianopia is considered inadequate peripheral
vision. Formal visual eld assessment (perimetry) is
done by an optometrist or ophthalmologist.
If a patient has a visual acuity or eld defect that
violates these requirements, it is your responsibility
to inform the patient that they cannot drive and
document this discussion. In some Australian
states, it is also mandatory for the doctor to
contact the licensing authority to inform them that
the patient’s licence must be suspended.
The Austroads national driver medical standards
Assessing Fitness to Drive set out the
considerations and medical criteria for safe driving.

Eye Emergency Manual December 2023
Agency for Clinical Innovation 42 aci.health.nsw.gov.au
Prevention of visual impairment
The main causes of visual impairment in Australia
are cataracts, macular degeneration and glaucoma,
with the common main risk factor of age. With an
ageing population, the prevalence of visual
impairment is expected to rise.
Diabetic retinopathy
Diabetic retinopathy is the main cause of blindness
among the Australian working population. It is well
established that the microvascular complications
of diabetes, such as retinopathy, can be prevented
by tight glycaemic control. Health professionals
have the important responsibility of educating
patients, including promoting lifestyle changes
such as smoking cessation, exercising regularly
and maintaining a healthy, well-balanced diet.
These not only improve glycaemic control but also
lower blood pressure and reduce the risk of
developing other eye conditions such as macular
degeneration and glaucoma.
Children
Children under the age of 8 are a unique group
where any signicant ocular pathology must be
addressed during this ‘critical period’ of visual
development. Prolonged visual deprivation,
strabismus or refractive errors lead to amblyopia,
which means that the affected eye will have poorer
acuity even if the visual pathway is later optimised.
Therefore, the importance of screening children on
more than one occasion during this ‘critical period’
cannot be overemphasised.
Ocular trauma is a major preventable cause of
visual impairment, with several studies suggesting
that 90% of cases are avoidable. For reasons that
remain unclear, children are overrepresented in this
group. Education, such as the EYEPLAYSAFE
online modules, aims to increase awareness of
potential hazards in school, at home and in outdoor
environments that may lead to ocular injury.
Work injuries
In the adult population, those who work with any
form of metal, particularly using powered hand
tools, are at increased risk of penetrating eye
injuries. Globe rupture tends to occur more
frequently in the older population, with the
combination of falls and a weakened globe, (e.g.
from previous cataract surgery) placing them at
particular risk.
The mandatory use of safety eyewear in the
workplace that complies with Australian Standards
and recommends the use of protection at home
when performing do-it-yourself activities should be
reinforced. Patients who present with a supercial
foreign body should be counselled about these
risks. Furthermore, patients who have intraocular
surgery should be counselled about the risk of
globe rupture in the future, even with only minor
trauma, which usually has a very poor
visual outcome.
These statistics highlight the importance of
implementing prevention strategies to reduce the
burden of disease caused by visual impairment
within Australia, and primary care health
professionals are perhaps in the best position to
promote these.
NSW public specialist
outpatient services
This information is designed as a guide only and
does not replace clinician judgment.
Use the link below for statewide referral criteria
(SRC) for ophthalmology.
https://www.health.nsw.gov.au/outpatients/
referrals

Eye trauma
Agency for Clinical Innovation 43 aci.health.nsw.gov.au
Eye Emergency Manual November 2023
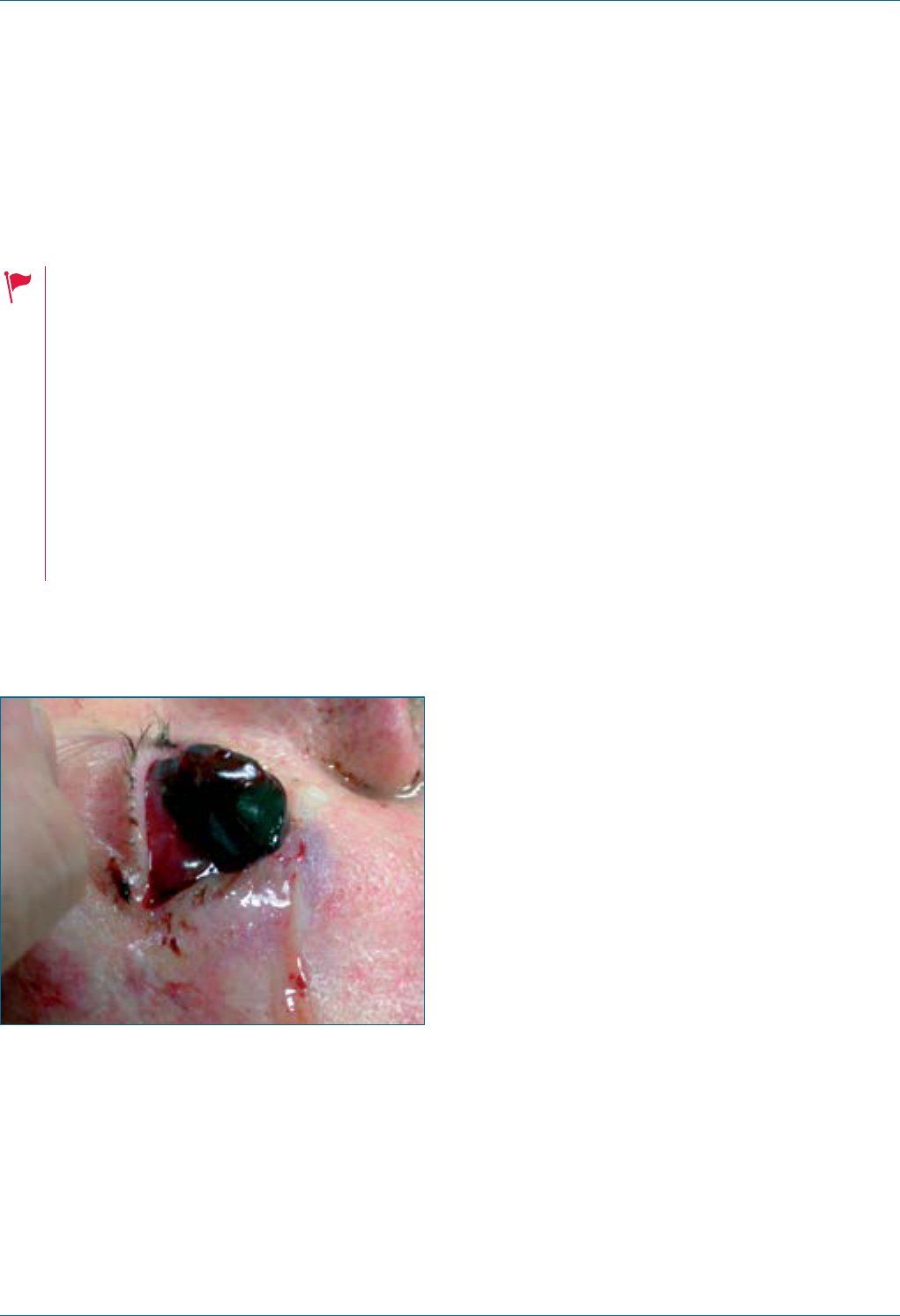
Eye Emergency Manual December 2023
Agency for Clinical Innovation 44 aci.health.nsw.gov.au
Eye trauma
Blunt ocular trauma
Consider the following for blunt eye trauma:
• Difculty opening eyelids and a very tense
orbit suggest retrobulbar haemorrhage.
• Exclude serious head injury depending
on the mechanism of injury and consider
a brain CT.
• Previous eye surgery increases the risk
of open globe injury.
• Small projectiles at high velocities
increase the likelihood of
penetrating trauma.
Figure 14. Ruptured globe with the expulsion of
ocular tissues.
History ndings
• Mechanism of injury: if applicable, the type of
projectile and velocity should be documented
• Flashes and/or oaters: suggest retinal injury
• Double vision: suggests muscle injury or
nerve palsy
• Previous eye surgery or injury increases the risk
of open globe injury
• Eye protection worn does NOT exclude open
globe injury
Examination ndings
• Gently open lids: exclude obvious open globe
injury or retrobulbar haemorrhage (topical
anaesthetic may facilitate this)
• Visual acuity
• Relative afferent pupillary defect (RAPD)
• Red reex
• Ocular motility (ask the patient about double
vision or pain)
• Check heart rate (oculocardiac reex from
muscle entrapment: bradycardia)
• Palpate for orbital rim tenderness (infraorbital
nerve involvement is suggested by abnormal
sensation over the cheek, upper lip or teeth)
• Orbital retropulsion but DO NOT test if open eye
injury is suspected
• Supercial ocular examination with a slit lamp
(or some magnication) to assess for corneal/
conjunctival laceration or penetration
• Further ocular examination, including dilated
fundus examination, as determined by history
and examination ndings
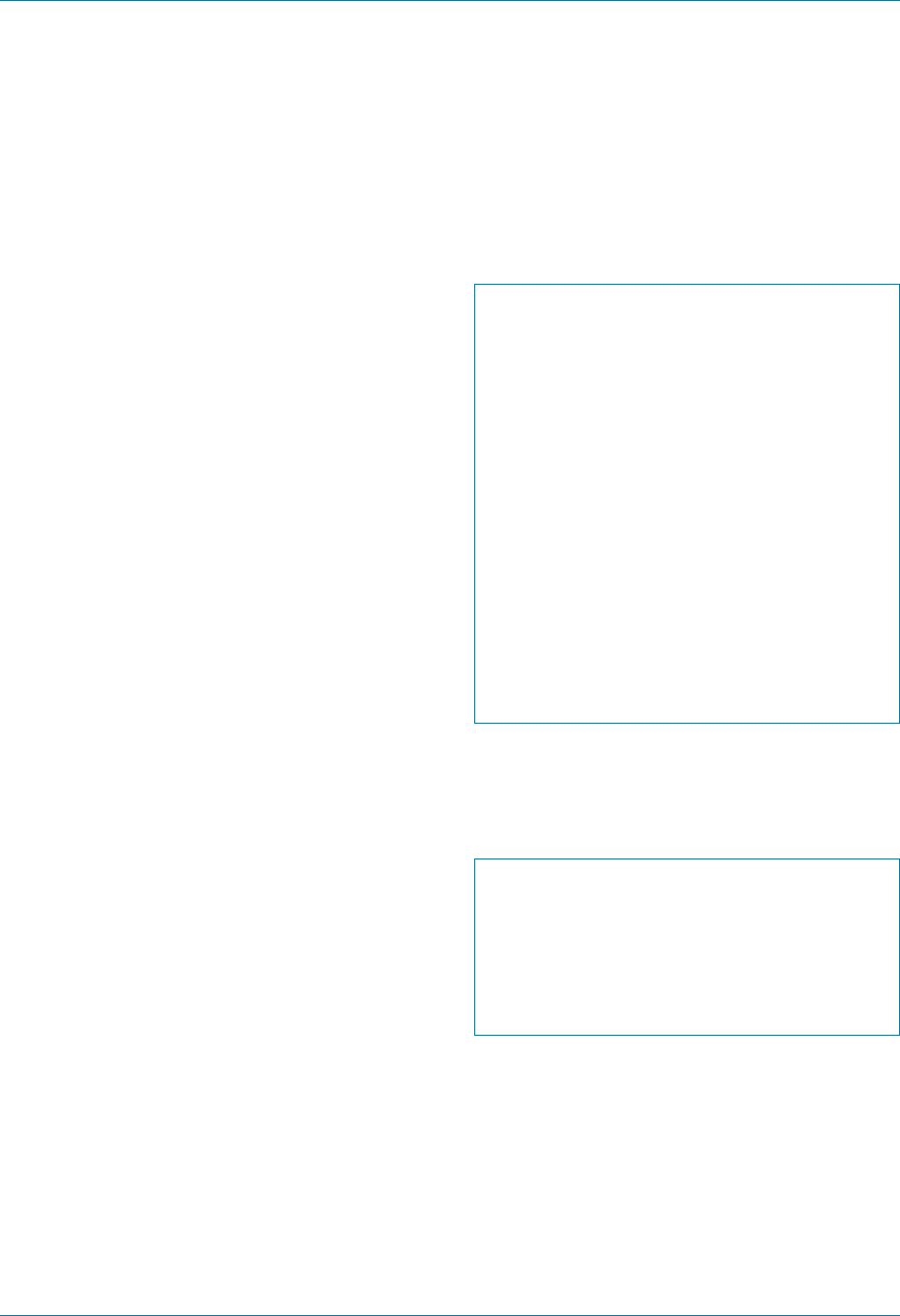
Eye Emergency Manual December 2023
Agency for Clinical Innovation 45 aci.health.nsw.gov.au
Investigations
• CT orbits: look closely at the coronal and
axial sections in soft tissue and bony
windows for fracture, globe integrity or
retrobulbar haemorrhage
Important differentials
• Open globe injury
• Orbit fracture
• Closed globe injury: anterior = hyphaema or
lens dislocation
• Closed globe injury: posterior = retinal tear/
detachment, vitreous haemorrhage or
choroidal rupture
Initial treatment
• Trauma assessment: exclude
life-threatening injuries
• Assume an open globe injury until
proven otherwise
• Analgesia and antiemesis (vomiting and
other Valsalva may cause loss of intraocular
contents in an open globe injury)
Eye traumacommunication checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?
Specic communication checklist
Consider the following:
; Why do you think this is an open/closed
globe injury?
; Is the patient ready for operating theatres
(considering general health, other injuries
and fasting status)?
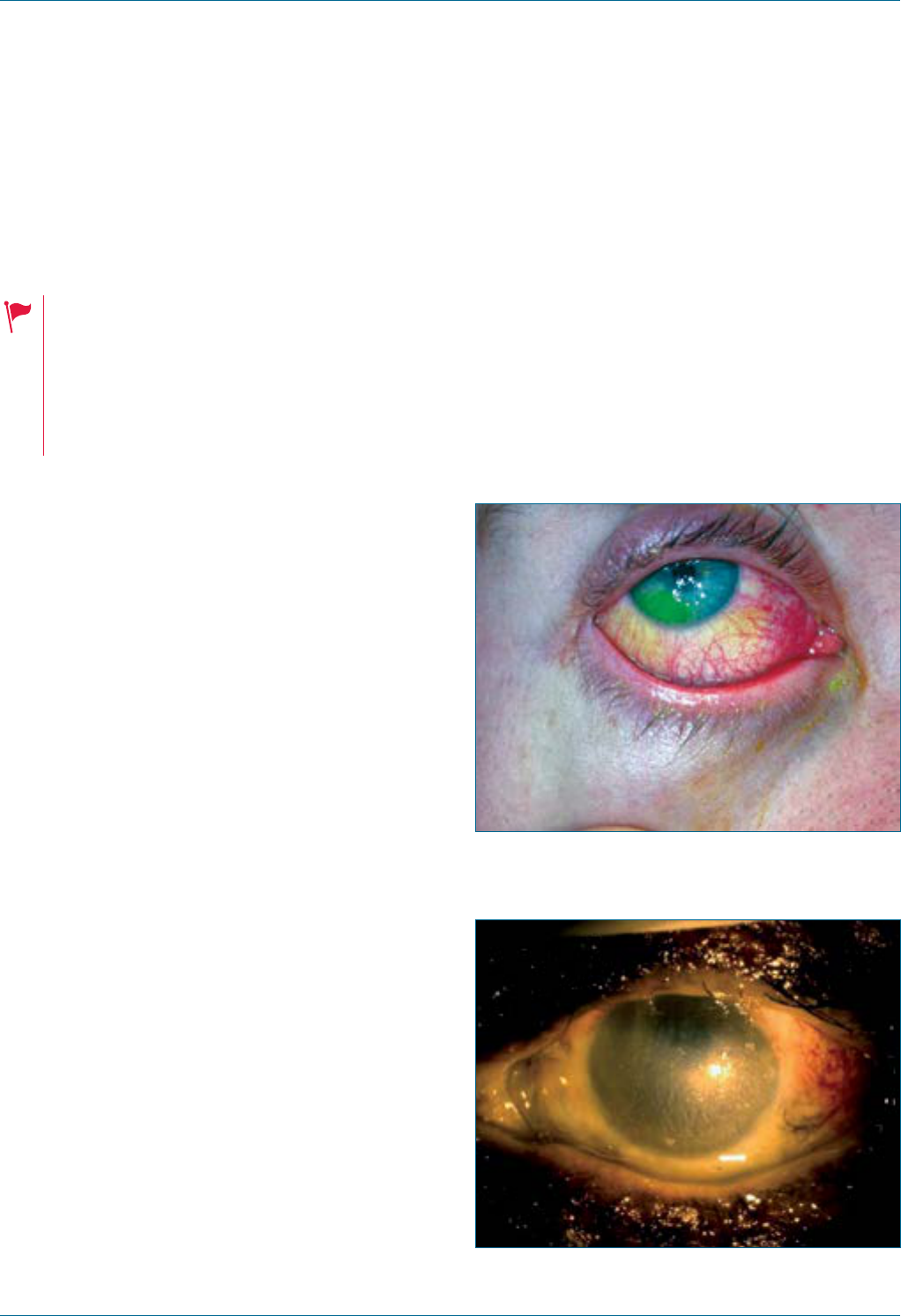
Eye Emergency Manual December 2023
Agency for Clinical Innovation 46 aci.health.nsw.gov.au
Chemical burns
Immediate referral to an ophthalmologist.
Ensure the following:
• Once a chemical injury is suspected, you
must commence irrigation before further
history or examination
• Exclude an open globe injury if the
mechanism is suspicious, (e.g. an explosion)
History ndings
• Time when the burn occurred
• Nature of chemical, i.e. acid/alkali (note alkalis
are more harmful to the eye)
• Any rst aid administered and when that was
done after the incident
Examination ndings
• Consider the following:
• Use topical anaesthesia if necessary
• Trichiasis (inturned eyelashes which may rub on
the cornea)
• Visual acuity
• Fluorescein staining (corneal and conjunctival)
• Cornea clear or cloudy (note iris detail visibility)
• Degree of vascular blanching, particularly at the
limbus, is proportional to the severity of the
chemical burn (see Figure 15, Figure 16 and
Figure 19 for comparison)
• Evert eyelids and note any retained
particulate matter
Investigations
• Measure pH for both eyes using universal
indicator paper in the conjunctival fornix (or a
cut-off urine dipstick if unavailable)
• Repeat pH testing after every second litre
of uids
Important differentials
• Retained particulate chemical
• Thermal injury
• Exclude open globe injury, penetrating or mixed
mechanism injuries, (e.g. explosions)
Figure 15. Acute alkali chemical injury
(mild/moderate).
Figure 16. Acute alkali chemical injury (severe).
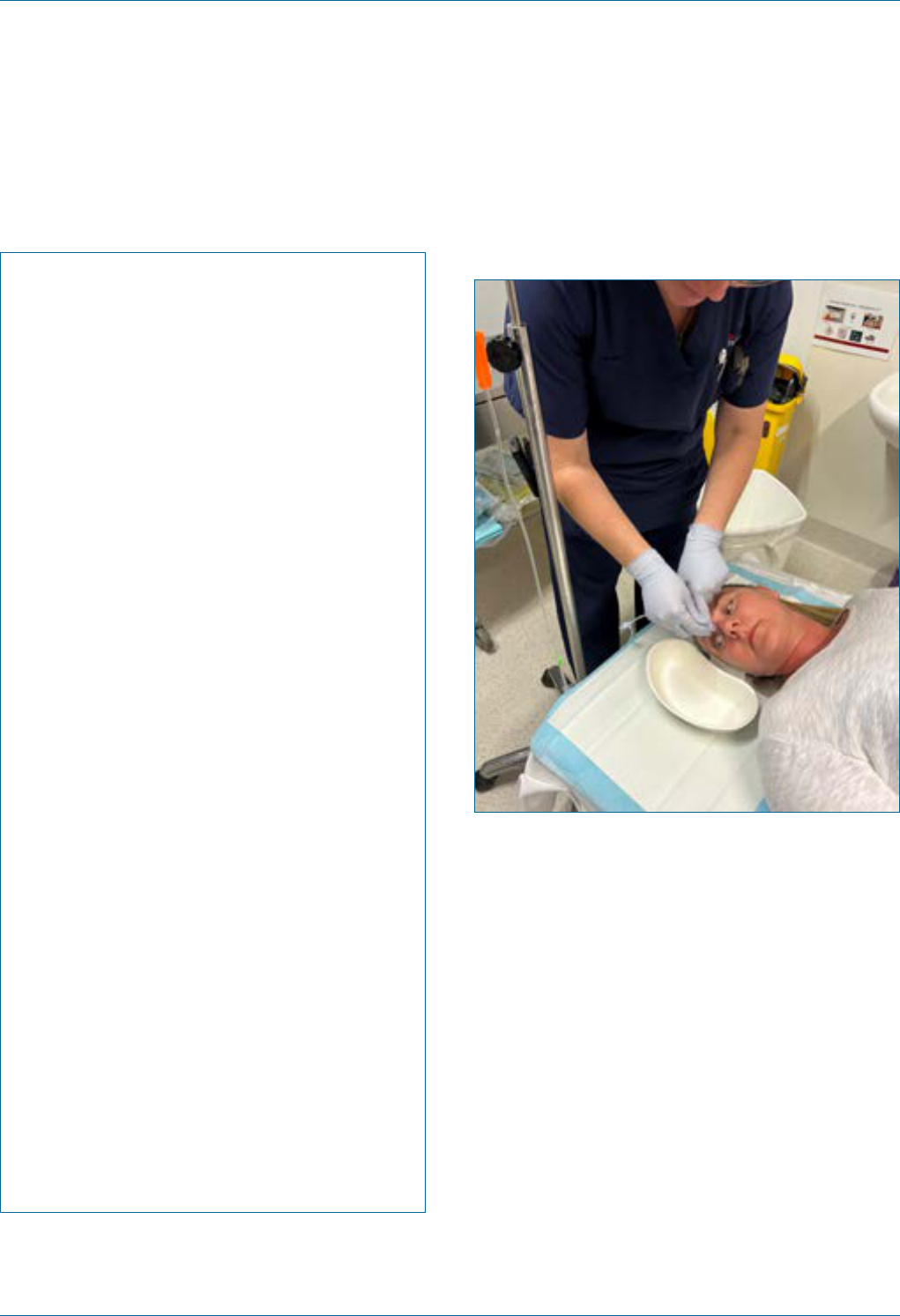
Eye Emergency Manual December 2023
Agency for Clinical Innovation 47 aci.health.nsw.gov.au
Initial treatment
Immediate:
Eye irrigation for chemical burns
1. Administer local anaesthetic drops to the
affected eye/eyes.
2. Commence irrigation with 1L of a neutral
solution, e.g. Hartmann’s, normal saline
(0.9%) in an IV giving set on full ow.
3. Evert the eyelid and clear the eye of any
debris or foreign body that may be present
by sweeping the conjunctival fornices with
a moistened cotton bud.
4. Irrigate from 3–5cm above the ocular
surface. Ask the patient to look left, right,
up and down whilst irrigating.
5. Use nitrous oxide/ketamine if necessary
for irrigation.
6. Review the patient’s pain level every 10
minutes and instill another drop of local
anaesthetic as required.
7. Review after 1L of irrigation administered.
8. Wait 5 minutes after ceasing the irrigation
uid then check the pH in BOTH eyes
(acceptable pH range 6.5–8.5). Compare
with unaffected eye’s pH if
unilateral injury.
9. Consult with the senior medical ofcer or
ophthalmologist and recommence
irrigation if necessary.
10. Severe burns and alkalis usually require
continuous irrigation for at least 30
minutes with 3L of uid.
Figure 17. Irrigation with the eyelid everted.
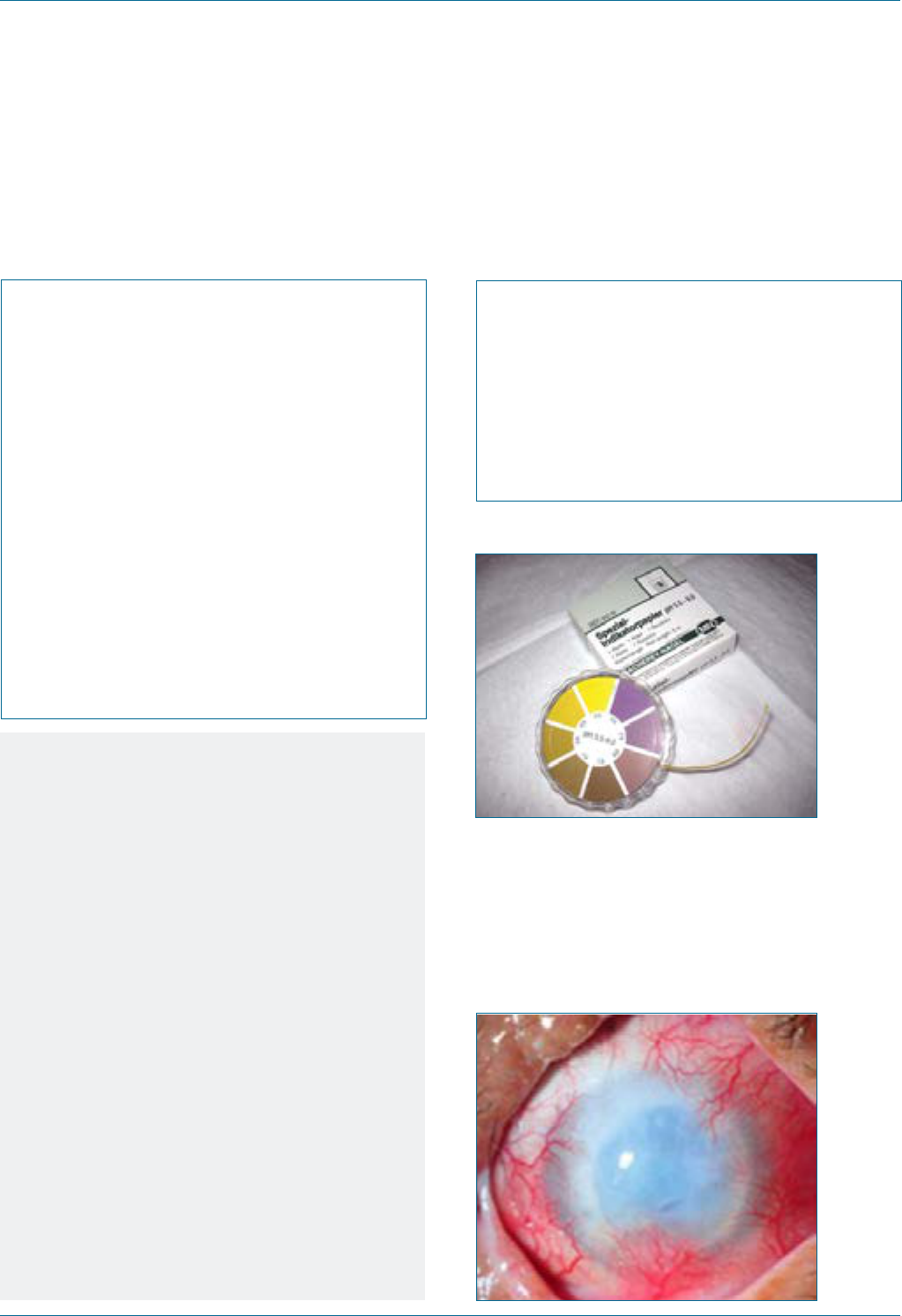
Eye Emergency Manual December 2023
Agency for Clinical Innovation 48 aci.health.nsw.gov.au
Eye traumacommunication checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?
Specic communication checklist
Consider the following:
; What chemical was involved?
; What irrigation has already
been administered?
; Have you everted the upper and
lower eyelids?
; What is the pH?
Notes
• The emergency treatment of a chemical
injury has far greater impact on the nal
ocular outcome than any other factor.
Prompt and thorough irrigation is critical to
avoiding a painful, permanently blind eye in
these patients.
• Examples of acids include toilet cleaner, car
battery uid and pool cleaner.
• Examples of alkalis include bleach, lime/
cement, mortar and plaster, drain cleaner,
oven cleaner and ammonia.
• Alkalis saponify ocular tissues and continue
to burn deeper into the eye, hence they
require more irrigation.
• For medicolegal reasons, it is important to
document when and how the injury
occurred, whether eye protection was
present and whether on-site rst aid
was given.
Figure 18. Universal indicator paper.
Figure 19. Typical long-term outcome of a severe
chemical ocular injury. While a corneal transplant
has been attempted, this has failed and become
opacied and vascularised. Limbal stem cell
damage by chemical injury results in a very poor
long-term visual prognosis.
1
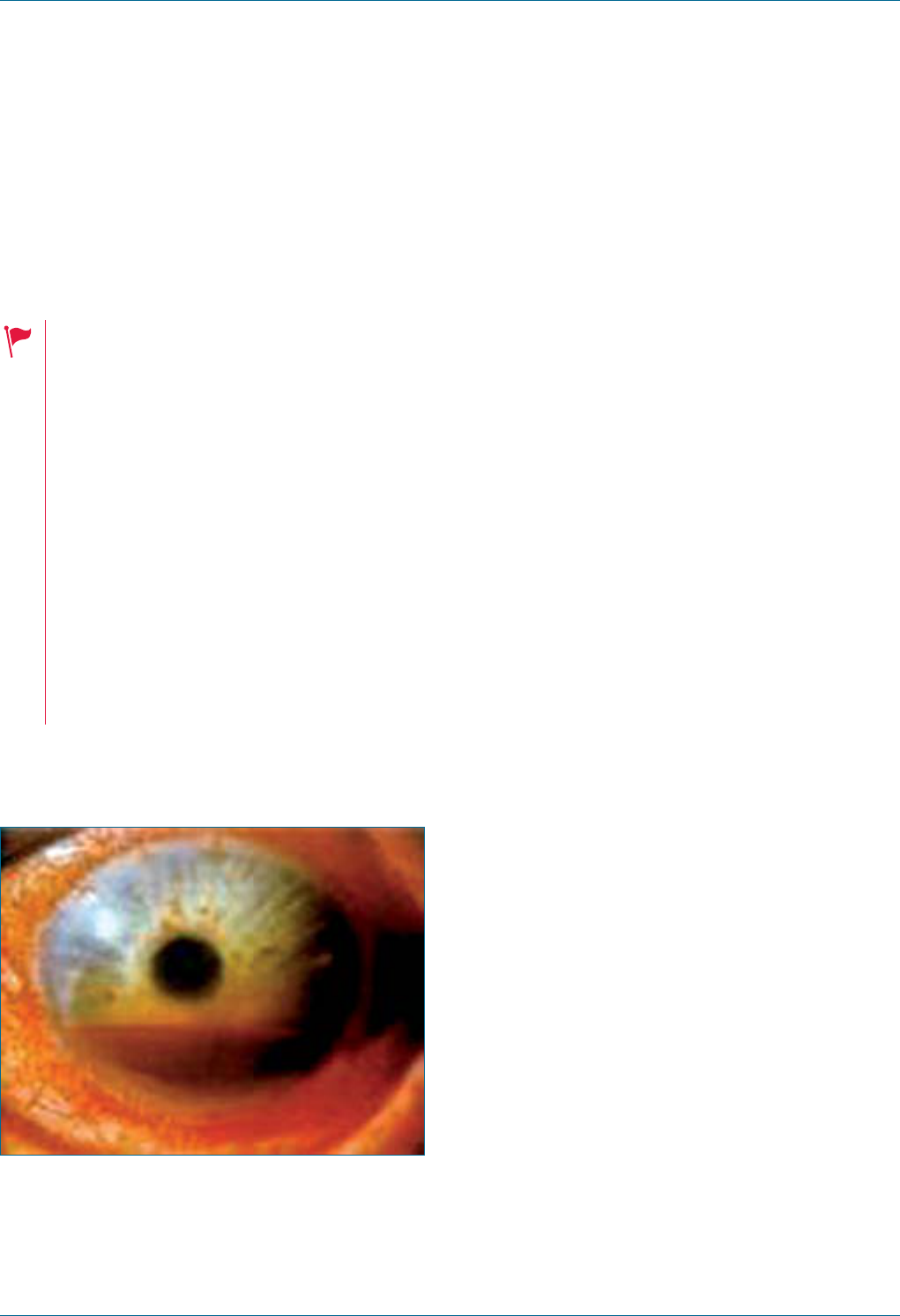
Eye Emergency Manual December 2023
Agency for Clinical Innovation 49 aci.health.nsw.gov.au
Closed globe injury
Urgent referral to an ophthalmologist
required<24hrs.
• History of eye surgery (assume the
patient has an open globe injury until
proven otherwise)
• Reduced visual acuity, not improved
by pinhole
• RAPD
• Loss of red reex
• Photophobia
• Photopsia (ashing lights like a camera
ash) or oaters suggesting
retinal injury
• Irregular pupil
• Difculty opening eyelids and a tense
orbit suggest retrobulbar haemorrhage
Figure 20. Hyphaema: blood in the
anterior chamber.
Important ndings
• Hyphaema
• Traumatic mydriasis
• Lens dislocation
• Loss of red reex with vitreous haemorrhage
• Retinal detachment
History ndings
• Mechanism of injury
• Timing of visual loss after injury
(immediate/delayed, stable/progressive)
• Quality of visual loss: blurring, oaters, curtain,
greying or total blackness, scotoma
• Any previous ocular surgery (this increases the
risk of open globe injury)
• Double vision: suggests muscle injury or
nerve palsy
Examination ndings
• Visual acuity
• Slit lamp examination with uorescein
• Shallow or deep anterior chamber
and hyphaema
• Red reex
• Check pupils for an RAPD and anisocoria
• Visual elds by confrontation
• Extraocular movement
• Fundus examination
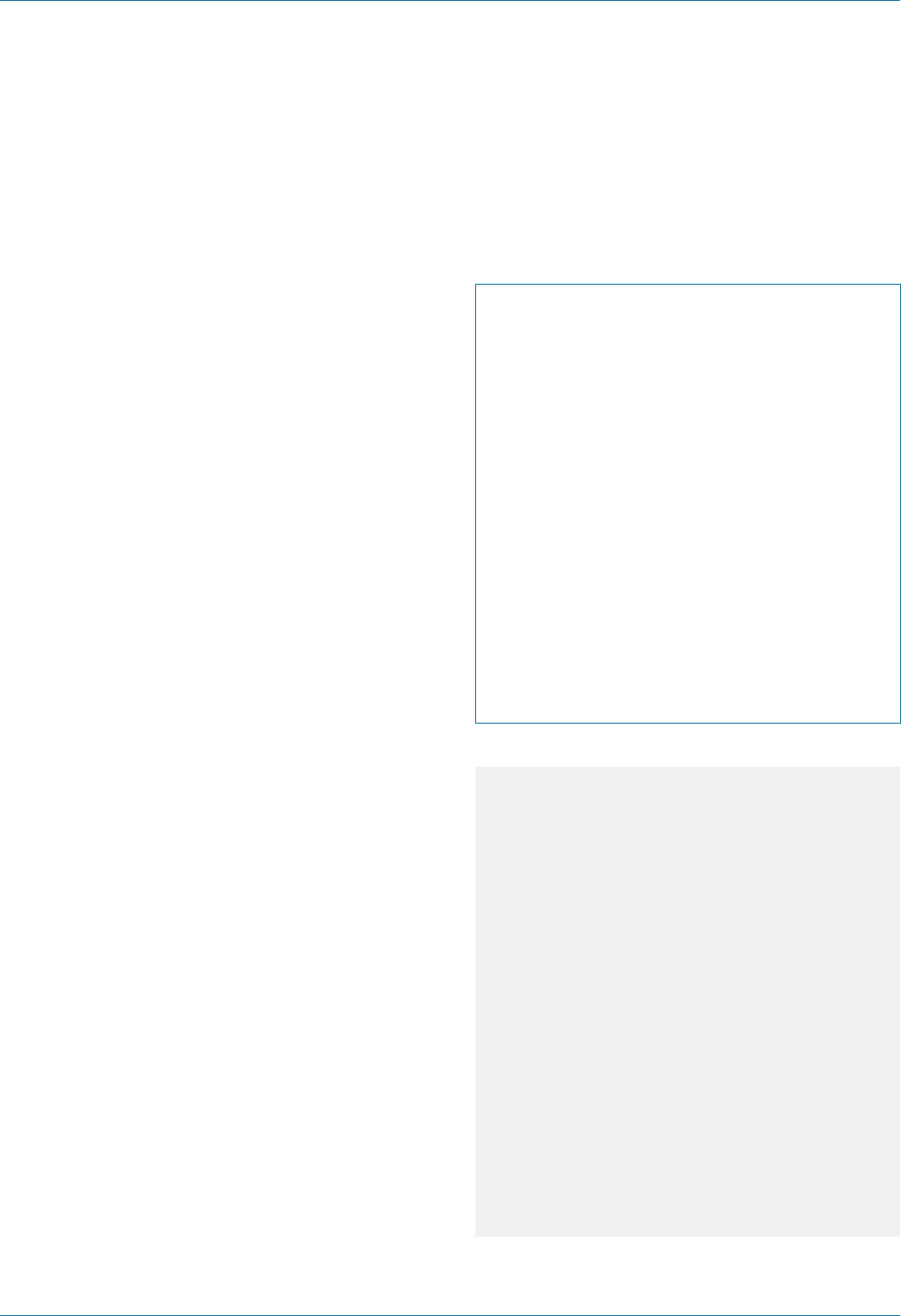
Eye Emergency Manual December 2023
Agency for Clinical Innovation 50 aci.health.nsw.gov.au
Investigations
• Check intraocular pressure (only if open
globe injury has rst been excluded)
Important differentials
• Open globe injury
• Head injury or fracture
• Orbital fracture or retrobulbar haemorrhage
• Closed globe injury: anterior = corneal
abrasion, hyphaema and lens dislocation
• Closed globe injury: posterior = retinal
detachment, vitreous haemorrhage and
choroidal rupture
Initial treatment
• Rest at 45°
• Shield the eye (do not pad)
Eye trauma communication checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?
Notes
Blunt trauma to the eye may result in
considerable damage to the intraocular
contents. Fracture of the orbital wall may
occur due to the transfer of mechanical
energy to the relatively thin orbital bone.
Slit lamp examination must include uorescein
to look for leaking aqueous in open
globe injury.
Is the anterior chamber shallow or deep?
Angle a tall and thin light beam at 45º to
assess anterior chamber depth.
Consider globe ultrasound if loss of red reex
or poor visual acuity (only if open globe injury
has been excluded rst).

Eye Emergency Manual December 2023
Agency for Clinical Innovation 51 aci.health.nsw.gov.au
Flash burns
History ndings
• Mechanism (electric arc welding or UV light,
e.g. sh tank, sun lamp or skiing without
eye protection)
• Symptoms typically appear within
several hours
• Symptoms are usually intense pain, red eye,
photophobia, blepharospasm and tearing
Examination ndings
Consider the following:
• Use topical anaesthesia in the examination
(it will usually relieve pain completely) or
small amounts of analgesia, e.g. IV opioid
or methoxyurane.
• Visual acuity: often mildly decreased (repeat
+/- pinhole after local anaesthesia).
• Slit lamp: conjunctival injection, widespread
supercial punctate epithelial defects
staining with uorescein (often bilateral).
Investigations
• Not required
Important differentials
• Chemical injury
• Corneal foreign body
Initial treatment
• Topical antibiotic drops of preservative-free
articial tears q1–2hr prn (ointment may be
soothing especially overnight)
• Cycloplegic, (e.g. cyclopentolate 1% bd) for
comfort for 2 days
• Oral analgesia as required (stronger
than paracetamol)
• Inform patients to re-present if symptoms have
not improved appreciably after 24 hours
Eye trauma communication checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?

Eye Emergency Manual December 2023
Agency for Clinical Innovation 52 aci.health.nsw.gov.au
Lid laceration
Immediate referral to an ophthalmologist.
An eyelid laceration is a
potential penetrating eye injury
until proven otherwise.
Figure 21. Exploration of an extensive
lid laceration.
Questions to ask the patient:
• Which eye is injured?
• How did it happen? Was there any
possibility of penetration into
the eye/orbit/brain?
• When did it happen?
• What are the symptoms,
(e.g. blurred vision, watery eye or red eye)?
Figure 22. Torn eyelid with avulsed lower
lacrimal canaliculus from a dog bite injury.
Examination ndings
• Wound examination (size and depth, tissues
visualised, e.g. skin, muscle or septum)
• Visual acuity
• Supercial ocular examination with a slit lamp
(or some magnication) and uorescein to
assess for any corneal/conjunctival laceration
or penetration
• Further ocular examination including the extent
of lid closure, eye movements and dilated
fundus examination as determined by history
and examination ndings
• Always consider the possibility of a retained
foreign body
Investigations
• Orbital CT if suspicious for foreign bodies or
orbital fracture (plain X-ray has poor sensitivity)

Eye Emergency Manual December 2023
Agency for Clinical Innovation 53 aci.health.nsw.gov.au
Important differentials
• An eyelid laceration is a potential penetrating
eye injury until proven otherwise.
• Note the extension of injury to surrounding
tissues (globe, orbit, lacrimal drainage
apparatus, paranasal sinuses and brain).
Initial treatment
• Any laceration other than supercial skin will
need an ophthalmic referral
• Involvement of the medial eyelid (where the
lacrimal drainage apparatus resides) or of the
eyelid margin requires ophthalmic referral within
48 hours for repair
• Check for tetanus immunisation status
Treatment if supercial laceration does not involve
the lid margin or lacrimal drainage apparatus:
1. Clean the area and surrounding skin with
antiseptic such as Betadine.
2. Subcutaneous anaesthetic with a
vasoconstrictor (2% lignocaine with adrenaline).
3. Irrigate and debride the wound thoroughly
with saline.
4. Remove foreign bodies if applicable.
5. Suture with a 6/0 non-absorbable suture.
6. Remove sutures within 5 days.
Eye trauma communication checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?
Specic communication checklist
Consider the following:
; Where is the laceration?
; Is it full thickness (involving the lid margin)
or medial to the puncta?
Notes
Eyelid lacerations can cause visual loss from
corneal scarring and permanent discomfort
from poorly functioning eyelids, or recurrent
infection and watering if there is damage to
the lacrimal drainage system.
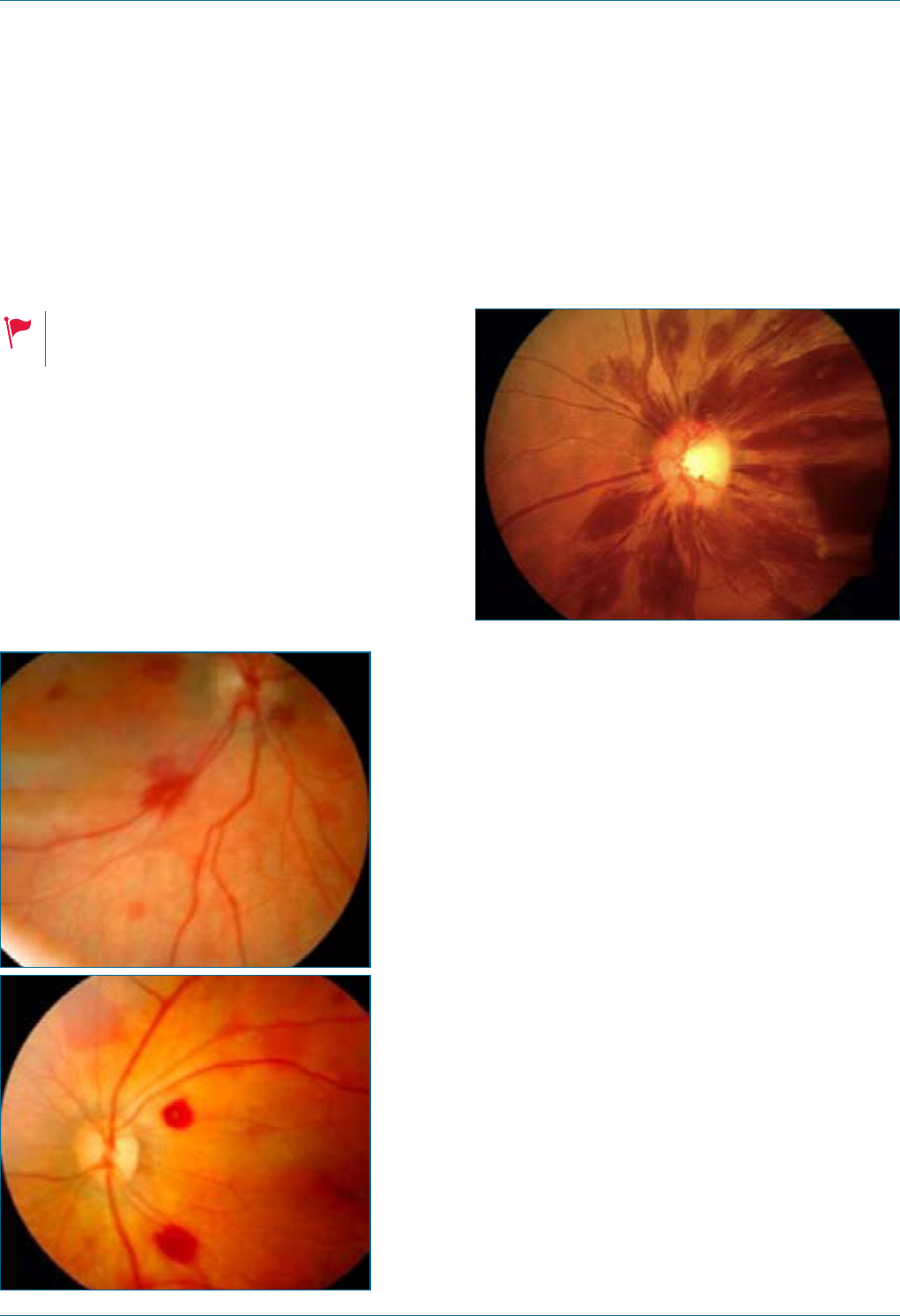
Eye Emergency Manual December 2023
Agency for Clinical Innovation 54 aci.health.nsw.gov.au
Non-accidental injury (NAI)
Seek immediate referral to the
ophthalmologiston the same day.
Referral urgency: immediate to
the child protection unit.
History ndings
• The stated mechanism of injury is
inconsistent with examination ndings
• Changing history of injury
• Recurrent or delayed hospital presentations
Figure 23. Fundus photographs of retinal
haemorrhages in neonates with a history of
birth asphyxia and amniotic uid aspiration.
2
Figure 24. Peripapillary white-centred
retinal haemorrhages.
3
Initial treatment
In a suspected NAI in a child, ensure:
• urgent referral to an appropriate paediatric team
and child protection unit for multi-disciplinary
assessment and management
• an ophthalmologist review for fundoscopic signs
of trauma is required as part of the work-up.
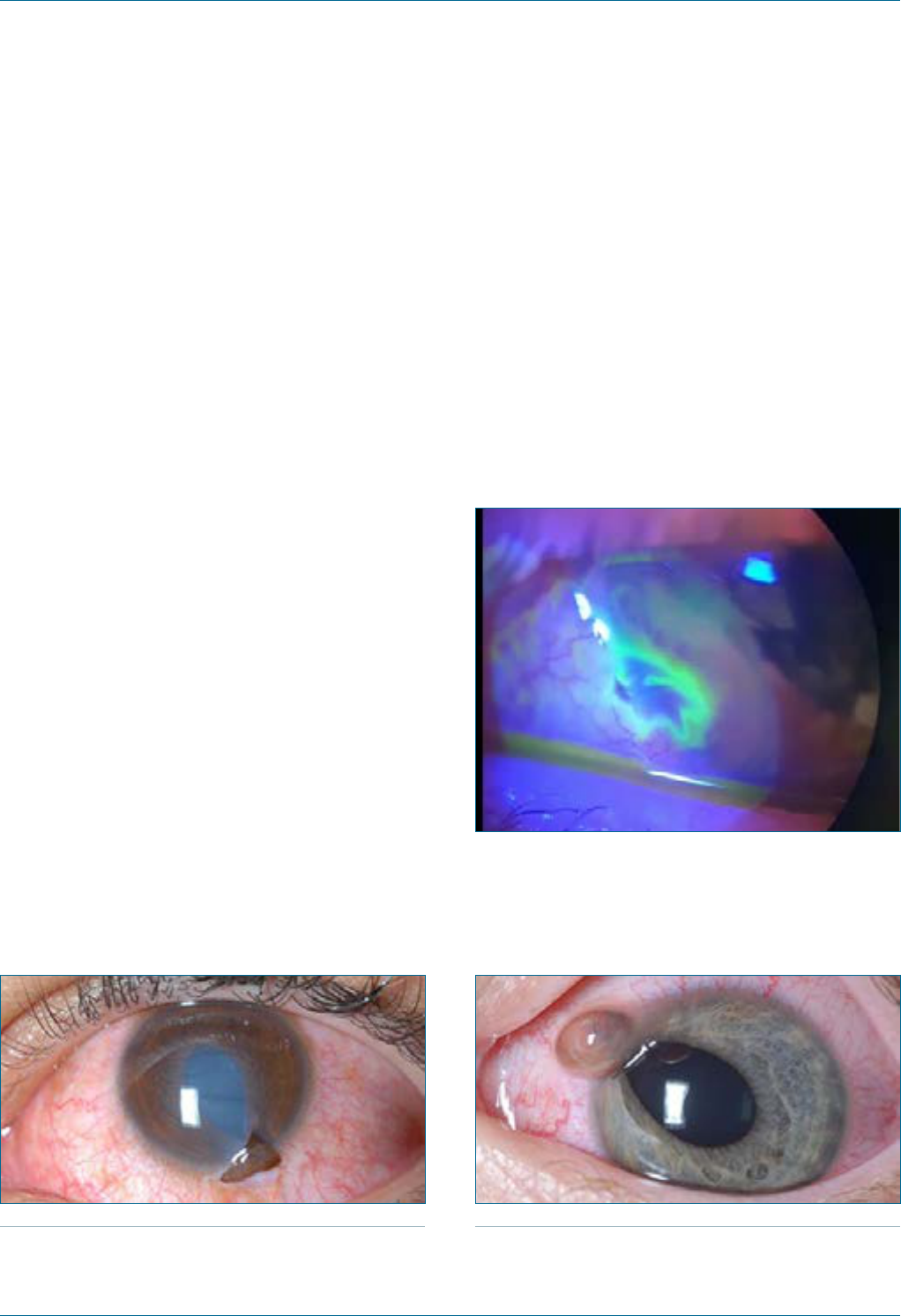
Eye Emergency Manual December 2023
Agency for Clinical Innovation 55 aci.health.nsw.gov.au
Open globe injury
(penetratingeye injury)
Seek an immediate referral to an ophthalmologist.
History ndings
• Mechanism (small objects moving fast are more
likely to cause a penetrating eye injury)
• Timing of visual disturbance after the injury
Examination ndings
• Examination may only need to be cursory if the
trauma is obvious
• Visual acuity and RAPD
• Direct ophthalmoscopy (loss of red reex may
suggest retinal trauma or detachment)
• Slit lamp with uorescein (looking for distorted
anterior chamber structures, corneal/scleral
breaks and Seidel test)
Figure 25. Penetrating eye injury, with a small
amount of iris tissue extruding through the
corneal wound. Also note the teardrop-shaped
pupil and the lens opacication.
Photograph courtesy of Lawrence B. Stack, MD, Professor of
Emergency Medicine and Paediatrics, Vanderbilt University Medical
Center, Nashville, Tennessee, USA.
Figure 26. Seidel test positive: the observation of
the ocular surface stained with 2% uorescein
under diffuse, bright cobalt blue light reveals a
waterfall-like effect as clear aqueous exudes
through a penetrating corneal wound and
displaces the uorescein-stained tear lm.
4
Figure 27. Penetrating eye injury, with iris tissue
extruding through the corneal wound. Note the
tear-drop pupil. The eye is otherwise uninamed,
with the cornea and lens both clear.
Photograph courtesy of Lawrence B. Stack, MD, Professor of
Emergency Medicine and Paediatrics, Vanderbilt University Medical
Center, Nashville, Tennessee, USA.
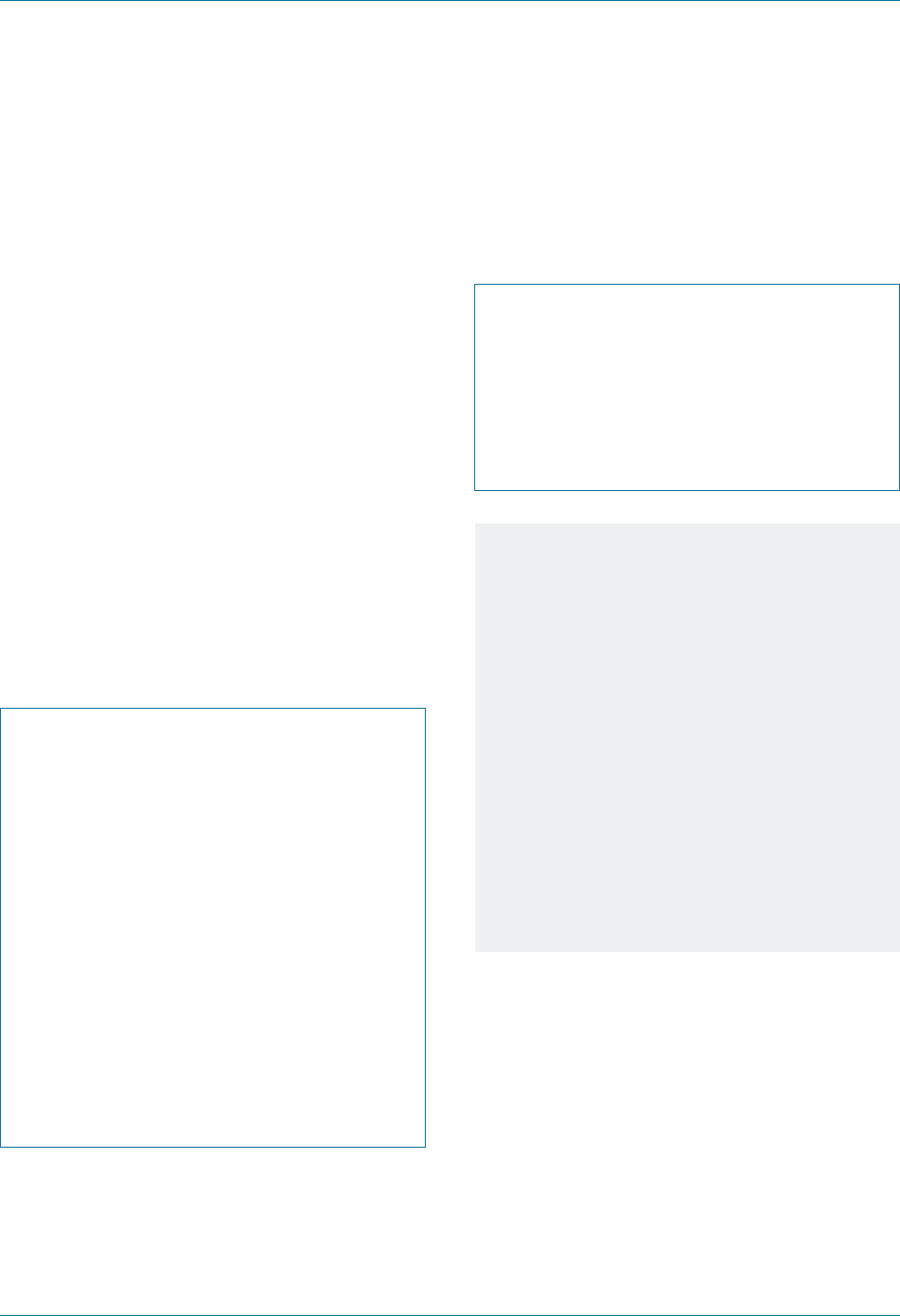
Eye Emergency Manual December 2023
Agency for Clinical Innovation 56 aci.health.nsw.gov.au
Initial treatment
• Shield the eye (do not use a pad) to avoid
inadvertent pressure on the globe
• Antiemetic to avoid expulsion of ocular contents
• Analgesia if required
• IV antibiotics (broad spectrum)
• Tetanus prophylaxis
• Keep nil by mouth, strict bedrest and prepare
for theatre
• No ointment for penetrating eye injury
• Consider a ne-cut orbital CT scan to look for a
foreign body
Eye trauma communication checklist
Follow ISBAR:
; What is the mechanism of trauma?
; Are you concerned about an open
globe injury?
; Is there a history of previous eye surgery
or injury?
; What is the visual acuity (including with
pinhole if not 6/6)?
; Is there an RAPD?
; What are the ndings on slit lamp
examination with uorescein?
; Does the patient have other injuries?
; What treatment has been commenced?
Specic communication checklist
Consider the following:
; What was the likely cause?
; Is there a positive Seidel test?
; Is there a retained foreign body/bodies
clinically or on CT?
; When has the patient fasted from?
Notes
• The pupil may point towards a corneal
perforation or be irregular.
• There may be an iris defect or early lens
opacication visible when examining the
red reex carefully.
• Fluorescein will light up in a waterfall-like
appearance from a leaking corneal wound
(Seidel sign). An entry wound may not be
obvious and may be hidden by conjunctival
tissue or subconjunctival haemorrhage.
• The anterior chamber may be shallow for
anterior injuries or very deep for posterior
injuries (compare with the other eye).

Eye Emergency Manual December 2023
Agency for Clinical Innovation 57 aci.health.nsw.gov.au
Orbital fracture
Immediate referral (phone) if reduced
vision, reduced heart rate (or vomiting)
on up-gaze, evidence of retrobulbar
haemorrhage.
Seek an urgent referral to an
ophthalmologist <24hr.
Refer to plastic surgery or maxillofacial
surgery for consideration of orbital
fracture repair.
Important ndings
• Poor visual acuity
• Difculty opening eyelids (retrobulbar
haemorrhage)
• Haemodynamic instability or vasovagal
syndrome (entrapment of extraocular muscle,
usually inferior rectus)
• Exclude head/intracranial injury
History ndings
• Mechanism of trauma, including the possible
presence of a foreign body, visual disturbance or
any diplopia (double vision)
• Photopsia (light ashes) or oaters (suggestive
of retinal injury)
• Any previous eye surgery (this increases the risk
of an open globe injury)
Examination ndings
• Gently open lids to exclude obvious open globe
injury or retrobulbar haemorrhage
• Visual acuity (also test with pinhole if not 6/6)
• RAPD
• Red reex
• Ocular motility (ask the patient about double
vision or pain)
• Check heart rate (oculocardiac reex)
• Palpate orbital rim tenderness (infraorbital
nerve involvement is suggested by abnormal
sensation over the cheek, upper lip or teeth)
• Retropulsion if open globe injury has
been excluded
• Supercial ocular examination with a slit lamp
(or some magnication) to assess for any
corneal or conjunctival laceration or penetration
• Intraocular pressure check if open globe injury
has been excluded
• Fundus examination (do not dilate until
intracranial injury is excluded and visual acuity
and RAPD are checked)
Investigations
• CT orbits and ne brain slices: look closely at
the coronal and axial sections in soft tissue
windows for fracture, globe integrity or
retrobulbar haemorrhage
Important differentials
• Retrobulbar haemorrhage
• Open globe injury
• Associated closed globe injury
(up to 30% of cases)
Initial treatment
• Analgesia
• No nose blowing (cough/sneeze with open
mouth to avoid an increase in sinus pressure,
which may displace non-sterile material through
fracture and into orbit)
• Broad-spectrum IV antibiotics (see next)
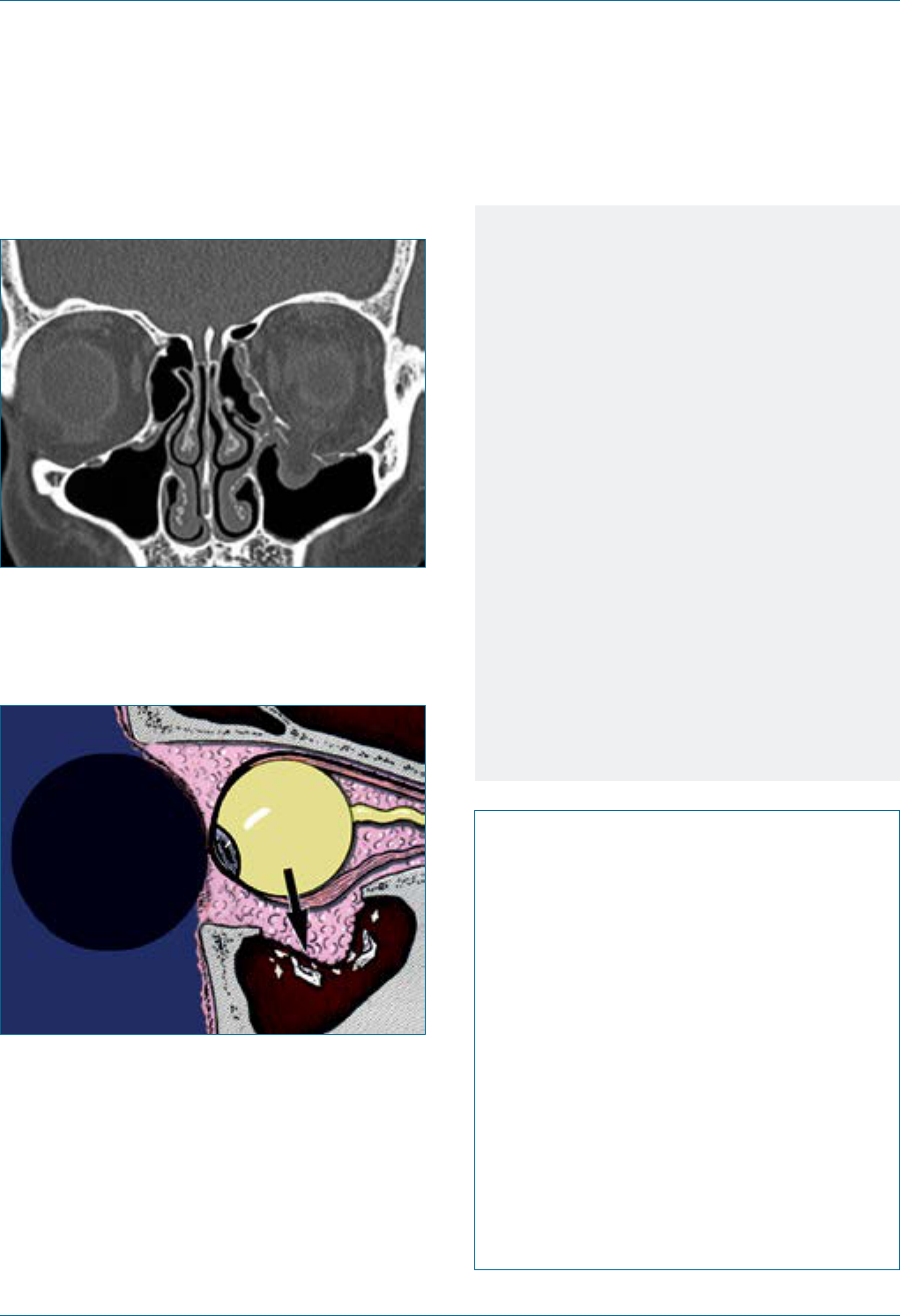
Eye Emergency Manual December 2023
Agency for Clinical Innovation 58 aci.health.nsw.gov.au
Figure 28. Coronal CT scan: left blow-out fracture.
Figure 29. Blow-out fracture: squash ball hit to
the eye.
Notes
• Discharge on oral antibiotics,
(e.g. Augmentin Duo bd for 7 days) and
nasal decongestant spray.
• Gentle ice pack to the orbit for
24–48 hours.
• Surgical repair, if necessary, is usually
performed 7 to 14 days after trauma.
Indications for surgical repair of orbital
oor fracture:
• Immediate repair: oculocardiac reex
in a young patient with white-eyed
blow-out (greenstick) fracture and
entrapped muscle.
• Early repair (<2/52): persistent diplopia,
enophthalmos and hypoglobus.
• Observation only: minimal diplopia
(especially if limited to up-gaze).
Things to consider:
• The force required to cause orbital
fracture is often signicant enough to also
cause closed-eye injuries. Perform an
adequate ocular examination, including
intraocular pressure.
• The medial wall is thinnest and tends to
blow out rst but rarely requires
surgical intervention.
• The orbital oor is the second most
common and can often disturb eye position
and movements.
• The lateral wall and roof are more robust
and tend to fracture only in
higher-force injuries.
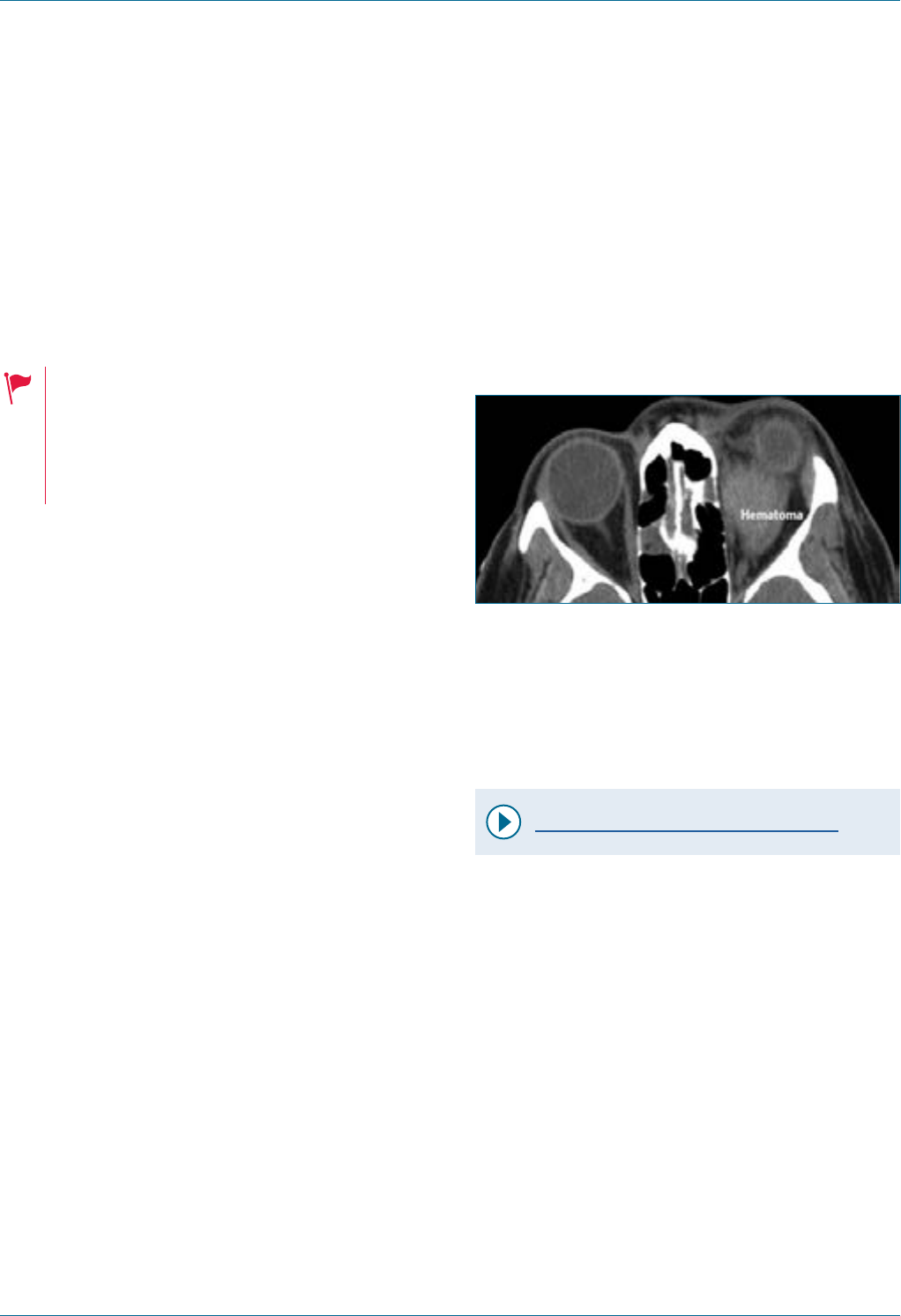
Eye Emergency Manual December 2023
Agency for Clinical Innovation 59 aci.health.nsw.gov.au
Retrobulbar haemorrhage
(orbital compartment syndrome)
Seek an immediate referral to an ophthalmologist.
Consider the following:
• Are there systemic or
intracranial injuries?
• Is the patient on anticoagulants? If so,
this increases the likely need
for intervention.
Examination ndings
• Tense orbit: difculty opening eyelids with
your ngers
• Haemorrhage conned to the orbital rim
• Chemosis (conjunctival swelling)
• Raised intraocular pressure and resistance to
retropulsion: press your index nger against
each globe through the closed lids
• Limited ocular motility, i.e. pain or diplopia
(double vision)
• Reduced vision: if severely reduced vision,
consider immediate treatment
• RAPD: if present, consider immediate treatment
• Progression in any of the above ndings
over time
Investigations
• Intraocular pressure: check with a tonometer
if available
CT orbits and brain: do not delay intervention for CT
if clinically suggestive of vision-threatening
retrobulbar haemorrhage.
Figure 30. Retrobulbar haematoma causing globe
proptosis. The involved globe appears smaller
because it has been pushed superiorly or
inferiorly out of the CT slice.
5
Important differentials
• Open globe injury
Initial treatment
Video - Canthotomy and cantholysis
1. Topical anaesthetic drops: repeat until no sting
on instillation.
2. Subcutaneous local anaesthetic with
adrenaline, (e.g. 2% lignocaine with adrenaline)
to lateral upper and lower eyelid insertions,
deeply to reach the inner aspect of the lateral
orbital rim and subconjunctivally if possible.
Always point away from the globe.
3. Use artery clamp to clamp over lateral canthus
(extending along the eyelid in a ‘Cleopatra line’)
for several seconds.
4. Use sharp-tipped scissors to cut laterally for
1–2cm along the clamped line.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 60 aci.health.nsw.gov.au
5. Hold the lower lid taught with forceps and blunt
dissect between the orbicularis oculi muscle
and lateral canthal tendon.
6. Strum the closed scissors over the tendon
(anteroposterior). When the lateral canthal
tendon has been identied, place each blade of
the scissors on either side, (i.e. one in the
conjunctival fornix and the other in the pocket
between orbicularis and tendon) aiming
inferiorly and cut.
7. Ensure the lower lid is lax with eyelids
readily openable.
8. Apply Chlorsig ointment and an
absorbent dressing.
9. Continue pupil and hourly vision observations.
Specic communication checklist
Consider the following:
; When did the injury occur?
; Are there other systemic or head injuries?
; Is the patient on anticoagulants?
; Do/did you need to perform canthotomy
and cantholysis IMMEDIATELY (dependent
on examination ndings as above)?
Notes
Consider the following:
• Visual outcomes are better in some case
series if canthotomy and cantholysis are
performed within 2 hours of injury.
• When examining a CT of the orbits, check
both the axial and coronal slices using soft
tissue windows. Hyperdensity around the
optic nerve, with proptosis, is suggestive of
retrobulbar haemorrhage.
• Orbital compartment syndrome may be
worse if there are any minimally displaced
orbital fractures. A signicant ‘blow-out’
fracture will usually decompress the orbit.
• The main indication for a canthotomy and
cantholysis is evidence of end-organ
compromise, e.g. reduced visual acuity, an
RAPD or evolving motility disturbance.

Acute visual
disturbance
Agency for Clinical Innovation 61 aci.health.nsw.gov.au
Eye Emergency Manual November 2023
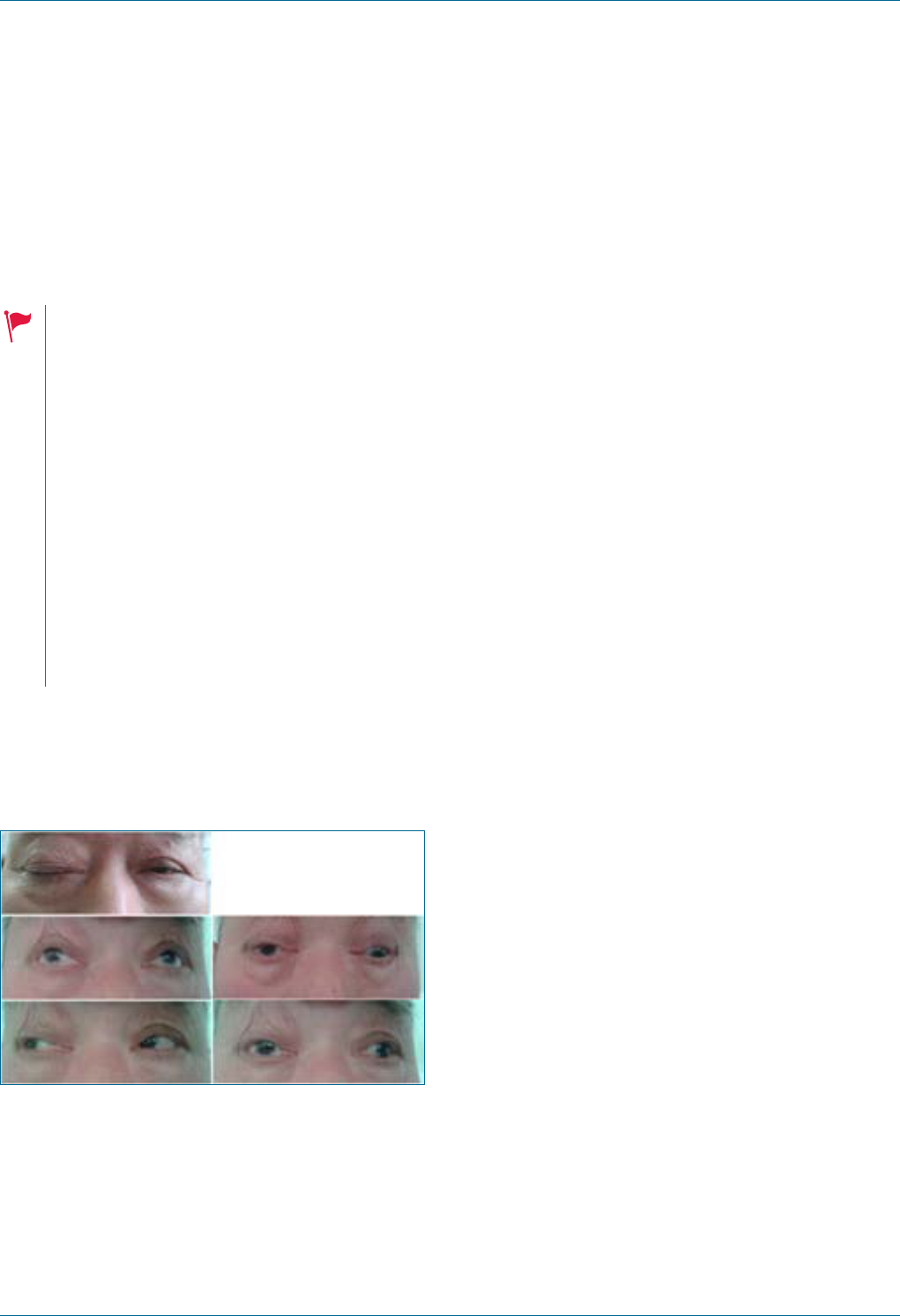
Eye Emergency Manual December 2023
Agency for Clinical Innovation 62 aci.health.nsw.gov.au
Acute visual disturbance
Third (3rd) cranial nerve palsy
Seek an urgent referral to an ophthalmologist <24hr.
Giant cell arteritis (GCA) is a cause of an
isolated 3rd cranial nerve palsy and, if
missed, can lead to irreversible blindness in
one or both eyes. You must specically ask
the patient about GCA symptoms and
document this in the medical record.
A 3rd cranial nerve palsy can be a sign of
raised intracranial pressure. You must ask
about headache symptoms and examine
the optic disc for signs of optic
disc swelling.
Don’t forget to check the other cranial
nerves and ask and look for any other
neurological decits.
Figure 31. Images show right ptosis and 3rd
cranial nerve palsy. The right eyelid is being
pulled up.
6
History ndings
• Vertical and horizontal diplopia (double vision):
note patient may not experience any double
vision if they are experiencing complete ptosis
• Complete/partial ptosis
• May have headache and pain
• In patients >60 years, enquire specically about
GCA symptoms
Examination ndings
• Ptosis (complete/partial)
• Pupil (may or may not be dilated)
• Ocular motility: the eye looks down and out in
primary gaze suggests ophthalmoplegia except
for abduction and intorsion
• Examine the remainder of cranial nerves to
determine if isolated 3rd cranial nerve palsy or
part of multiple cranial nerve palsies
Investigations
• Cardiovascular risk factor work-up
• Fine-cut CTA of Circle of Willis, looking for
aneurysm with pupil involvement
Important differentials
• Pituitary apoplexy
• Posterior communicating artery aneurysm
• Vasculitis
• Thyroid eye disease
• Myasthenia gravis
• Horner’s syndrome (partial ptosis and
normal motility)
• Compression neoplasm
Eye Emergency Manual December 2023
Agency for Clinical Innovation 63 aci.health.nsw.gov.au
Initial treatment
• Liaise with neurology
• Inform the patient that it is illegal to drive while
experiencing diplopia
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history
; Visual acuity (with pinhole if not 6/6)
; Visual elds (by confrontation)
; Pupil examination: anisocoria and relative
afferent pupillary defect (RAPD)
; Red reex
; Dilated retinal examination
; Eyelid examination ndings
(complete/partial ptosis)
; Ocular motility ndings
Fourth (4th) cranial nerve palsy
Seek an urgent referral to an ophthalmologist <24hr.
Giant cell arteritis (GCA) is a cause of an
isolated 4th cranial nerve palsy and, if
missed, can lead to irreversible blindness in
one or both eyes. You must specically ask
the patient about GCA symptoms and
document this in their medical record.
A 4th cranial nerve palsy can be a sign of
raised intracranial pressure. You must ask
about headache symptoms and examine
the optic disc for signs of optic
disc swelling.
Don’t forget to check the other cranial
nerves and ask and look for any other
neurological decits.
History ndings
Consider the following:
• Vertical and/or torsional diplopia: the patient
may describe that images appear tilted/objects
appear in their vision and as leaning to one side.
• Ask about the onset, duration and
improvement/worsening.
• Ask about a history of trauma, head injury
and falls.
• Ask about cardiovascular risk factors,
particularly diabetes.
• Ask about the presence of any GCA symptoms.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 64 aci.health.nsw.gov.au
Examination ndings
• Visual acuity
• Check for RAPD (or RAPD with orbital apex/
cavernous sinus lesion)
• Evidence of head tilt (consider posture and
compare with old photos to
determine chronicity)
• Extraocular movement examination
• Examine the remainder of cranial nerves to
determine if isolated 4th nerve palsy or part of
multiple cranial nerve palsies
Investigations
• Cardiovascular risk factor work-up
• Neuroimaging (CT brain)
Important differentials
• GCA
• Thyroid eye disease
• Myasthenia gravis
• Microvascular
• Trauma
• Congenital
Initial treatment
• Depends on the underlying cause
• Liaise with neurology
• Inform the patient that it is illegal to drive while
experiencing diplopia
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes and how well it has
been managed)
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination (anisocoria or presence
of RAPD)
; Red reex
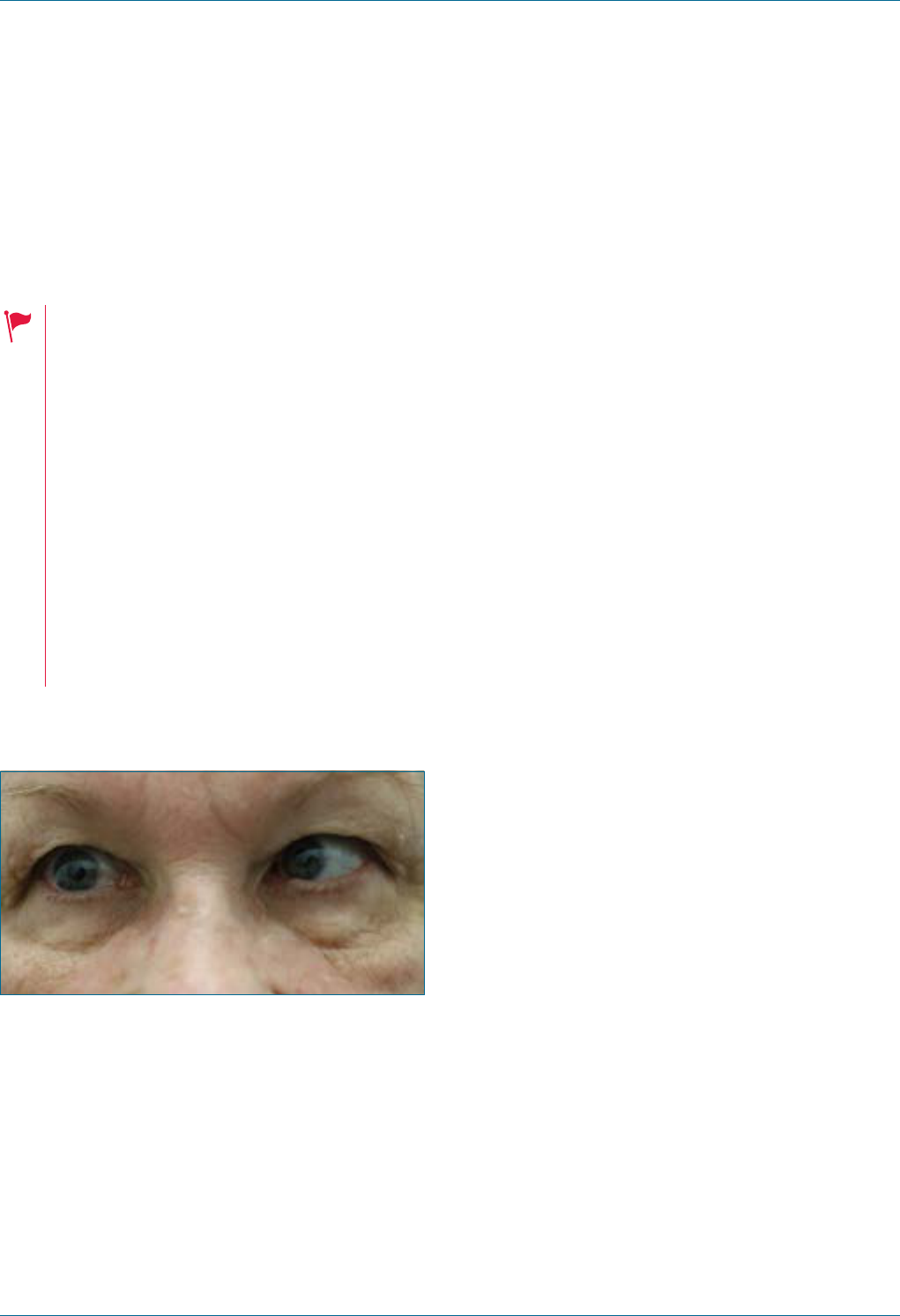
Eye Emergency Manual December 2023
Agency for Clinical Innovation 65 aci.health.nsw.gov.au
Sixth (6th) cranial nerve palsy
Seek an urgent referral to an ophthalmologist <24hr.
Giant cell arteritis (GCA) is a cause of an
isolated 6th cranial nerve palsy and if
missed can lead to irreversible blindness in
one or both eyes. You must specically ask
the patient about GCA symptoms and
document this in their medical record.
A 6th cranial nerve palsy can be a sign of
raised intracranial pressure. You must ask
about headache symptoms and examine
the optic disc for signs of optic
disc swelling.
Don’t forget to check the other cranial
nerves and ask and look for any other
neurological decits.
Figure 32. Patient with 6th cranial nerve palsy.
7
History ndings
Consider the following:
• Horizontal diplopia (double vision) presents as
worse for distance than near, and worse looking
towards the affected side. The patient may
describe double vision whilst driving, watching
television or looking out the window.
• Assess for any headache, morning nausea or
vomiting (raised intracranial pressure).
• Assess for any GCA symptoms.
Examination ndings
• Visual acuity
• Extraocular movements: check for limited
abduction and other directions of gaze
• Pupils normal/not normal: anisocoria or RAPD
• Eyelid positions (no ptosis)
• Exclude swollen optic discs (6th cranial nerve
palsy may be caused by raised intracranial
pressure)
• Examine the remainder of cranial nerves to
determine if isolated 6th cranial nerve palsy or
part of multiple cranial nerve palsies
Investigations
• Cardiovascular risk factor work-up
• CT brain
• Urgent ESR and CRP blood tests if GCA
is suspected
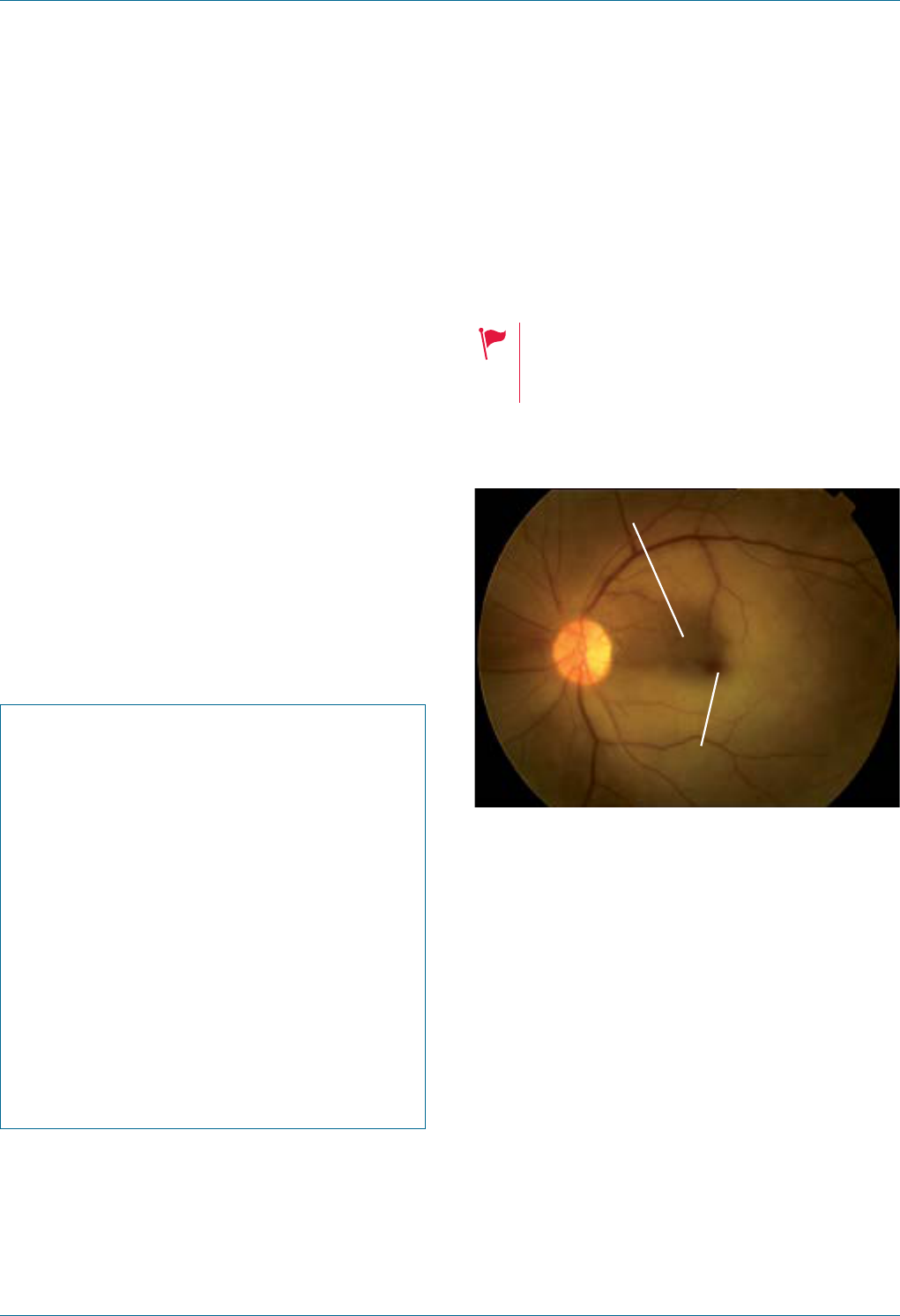
Eye Emergency Manual December 2023
Agency for Clinical Innovation 66 aci.health.nsw.gov.au
Important differentials
• GCA
• Raised intracranial pressure
(e.g., space-occupying lesions)
• Myasthenia gravis
• Trauma
Initial treatment
• Depends on the underlying cause
• Liaise with neurology
• Inform the patient that it is illegal to drive while
experiencing diplopia
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history
(particularly diabetes and how well
it has been managed)
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Ocular motility looking for difculty
abducting the eye, (i.e. looking away from
the nose)
Central retinal artery occlusion
(CRAO)
Seek an immediate referral to an ophthalmologist.
If the patient has giant cell arteritis (GCA)
symptoms, urgent blood tests including
ESR and CRP should be ordered.
Figure 33. Area of cilioretinal sparing (top line)
and ‘cherry red spot’ (lower line).
Area of cilioretinal sparing
"Cherry red spot"
History ndings
• Sudden, painless and persistent loss of vision
• GCA symptoms if >50 years of age
• Cardiovascular risk factors
Examination ndings
• Poor acuity (may have central sparing)
• Marked RAPD
• Fundus examination: may have minimal signs
on fundoscopy
• Pale retina with a cherry red spot and arteriolar
and venular narrowing
• Abnormal temporal artery (if suspected GCA)
Eye Emergency Manual December 2023
Agency for Clinical Innovation 67 aci.health.nsw.gov.au
Investigations
• GCA may cause CRAO: check ESR, CRP and FBC
• Cardiovascular risk factor work-up
• Important differentials
• GCA may co-exist with CRAO
Initial treatment
• Urgent discussion with the ophthalmology team,
especially within 4 hours of the onset of
symptoms, as certain sight-saving treatments
may be attempted
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
GCA symptom list
• Polymyalgia rheumatica
• New onset headache (often temporal)
• Scalp tenderness
• Jaw claudication
• Tongue claudication
• Fever and night sweats
• Loss of weight
• Generalised muscle pain and weakness
• Possible diplopia (double vision) or transient
visual loss
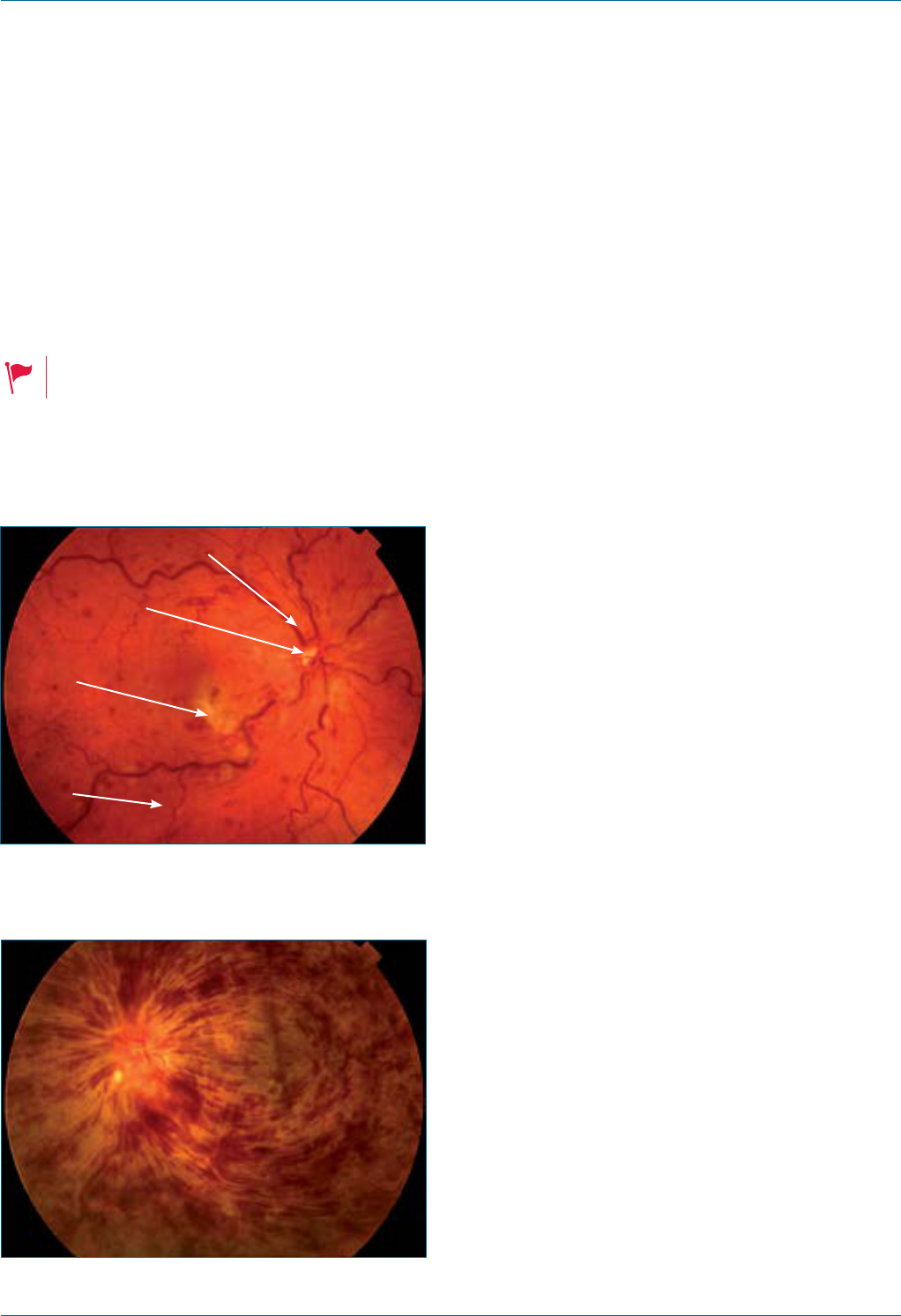
Eye Emergency Manual December 2023
Agency for Clinical Innovation 68 aci.health.nsw.gov.au
Central retinal vein occlusion
(CRVO)
Seek immediate referral by phone to
an ophthalmologist.
Check for high blood pressure.
Figure 34. From top to bottom: dilated tortuous
veins; disc swelling; cotton wool spots; intra-
retinal haemorrhage (visible in all four quadrants).
Dilated tortuous veins
Cotton wool
spots
Disc
swelling
Intra retinal
haemorrhage
(visible in all four
quadrants)
Figure 35. Severe CRVO: haemorrhages obscure
much of fundus detail.
History ndings
• Sudden and painless loss of vision
• Cardiovascular risk factors
• Increasing age
• Glaucoma
Examination ndings
• Visual acuity
• Pupil examination: important prognostic factor
(RAPD)
• May see prominent iris vessels and red eye
(if long-standing)
• Fundus examination shows multiple areas
of haemorrhage
• Intraocular pressure
• Blood pressure
Investigations
• Blood glucose
• Lipids
Important differentials
• Vitreous haemorrhage
• Central retinal artery occlusion
• Giant cell arteritis (GCA)
• Malignant hypertension
(preeclampsia in gravid women)
Initial treatment
• Discuss the case with the ophthalmology team
for referral urgency
• Screen for diabetes and hypertension
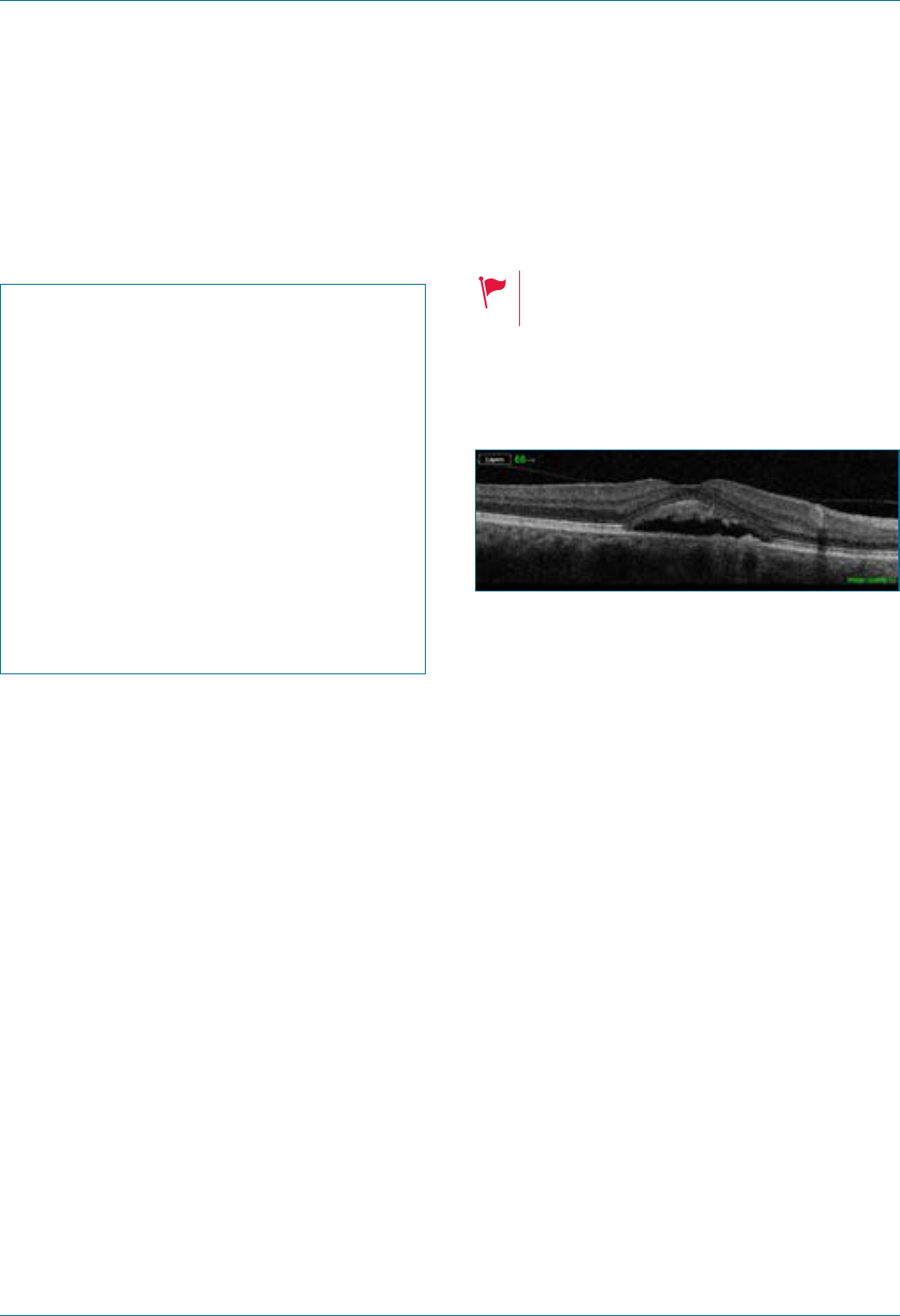
Eye Emergency Manual December 2023
Agency for Clinical Innovation 69 aci.health.nsw.gov.au
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination
; Intraocular pressure
Central serous chorioretinopathy
Consider other diagnoses if signicantly
reduced vision or an elderly patient.
Figure 36. Central serous retinopathy in a retina,
imaged using optical coherence tomography
(OCT; vitreous side is at top of image).
8
History ndings
• Usually young men with a Type A personality
• Central scotoma, metamorphopsia
• May have had a previous episode
• Corticosteroid (any form) use, including topical
or inhaled
Examination ndings
• Reduced visual acuity to around 6/9 or 6/12,
improving a little with pinhole (Amsler grid
shows a relative scotoma or distortion of lines)
• May present with hyperopic refractive shift/
trouble reading, micropsia and colour
vision changes
• Ocular examination otherwise normal
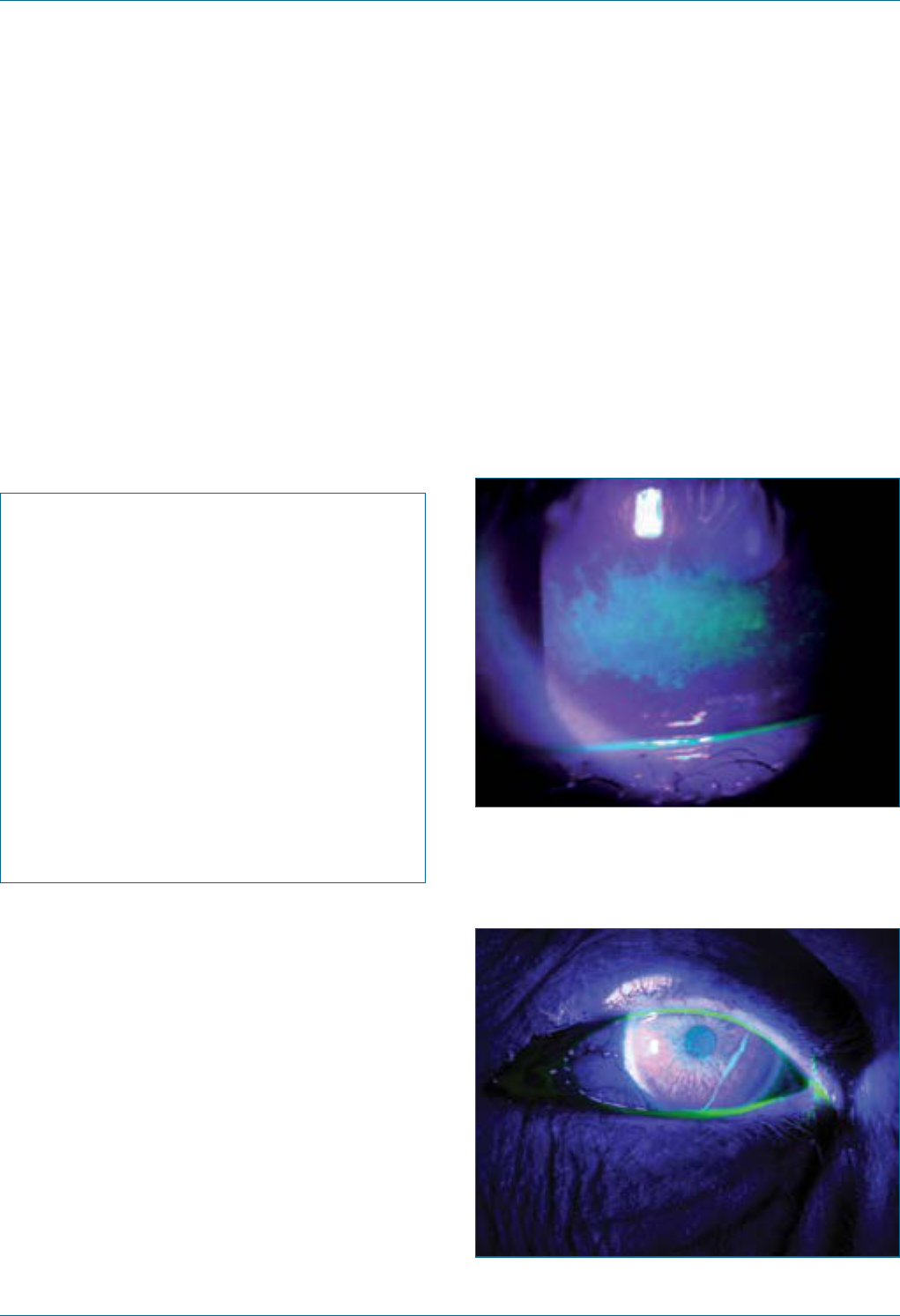
Eye Emergency Manual December 2023
Agency for Clinical Innovation 70 aci.health.nsw.gov.au
Important differentials
• Malignant hypertension
• Choroidal neovascularisation
• Macular haemorrhage
• Macula-off retinal detachment
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination if instructed
; Amsler grid nding
Dry eye/exposure keratopathy
Dry eye is a common chronic ocular condition that
is often caused by, or coexists with, other ocular
diseases. Dry eye may cause temporary, reversible
and minor acute visual disturbance.
Figure 37. Dry eye showing diffuse punctate
staining with uorescein.
Figure 38. Mucus strand is also visible across
thecornea.
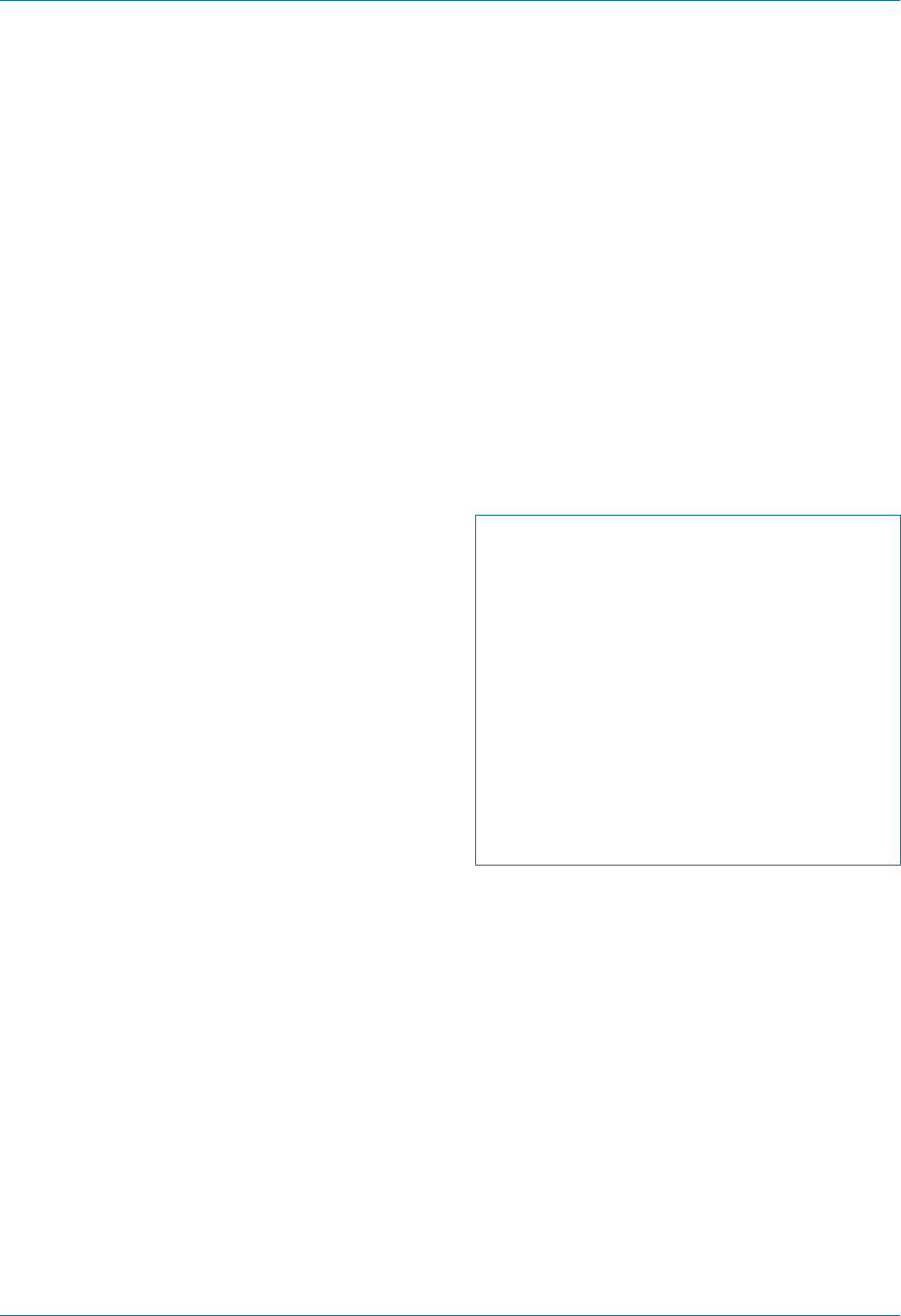
Eye Emergency Manual December 2023
Agency for Clinical Innovation 71 aci.health.nsw.gov.au
History ndings
• Sensation of dry eye, eye pain and intermittent
blurred vision that improves with blinking or
lubricating drops
• Symptoms often worsen in the evening, in
air-conditioned or windy environments, and with
tasks requiring prolonged concentration (with
reduced blink rate)
• Usually bilateral
Examination ndings
Consider the following:
• Visual acuity may be slightly reduced (6/6–6/12)
and may improve with lubricating drops.
• Punctate uorescein staining in interpalpebral
ssure (lower third of cornea). Staining may vary
from no staining or a few punctate erosions, to
severe diffuse corneal and conjunctival staining.
• Coexisting posterior blepharitis is often present.
Important differentials
• Chemical burn
• Eyedrop toxicity (especially preserved drops)
• Contact lens-related problem (overwear or
solution sensitivity)
• Exposure keratopathy
• Flash burn
• Microbial keratitis
Initial treatment
• Lubricating drops, gels or ointments prn
(preserved or preservative-free)
• Reduce exposure to drying conditions (see
History section above)
• Treat any co-existing blepharitis
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination
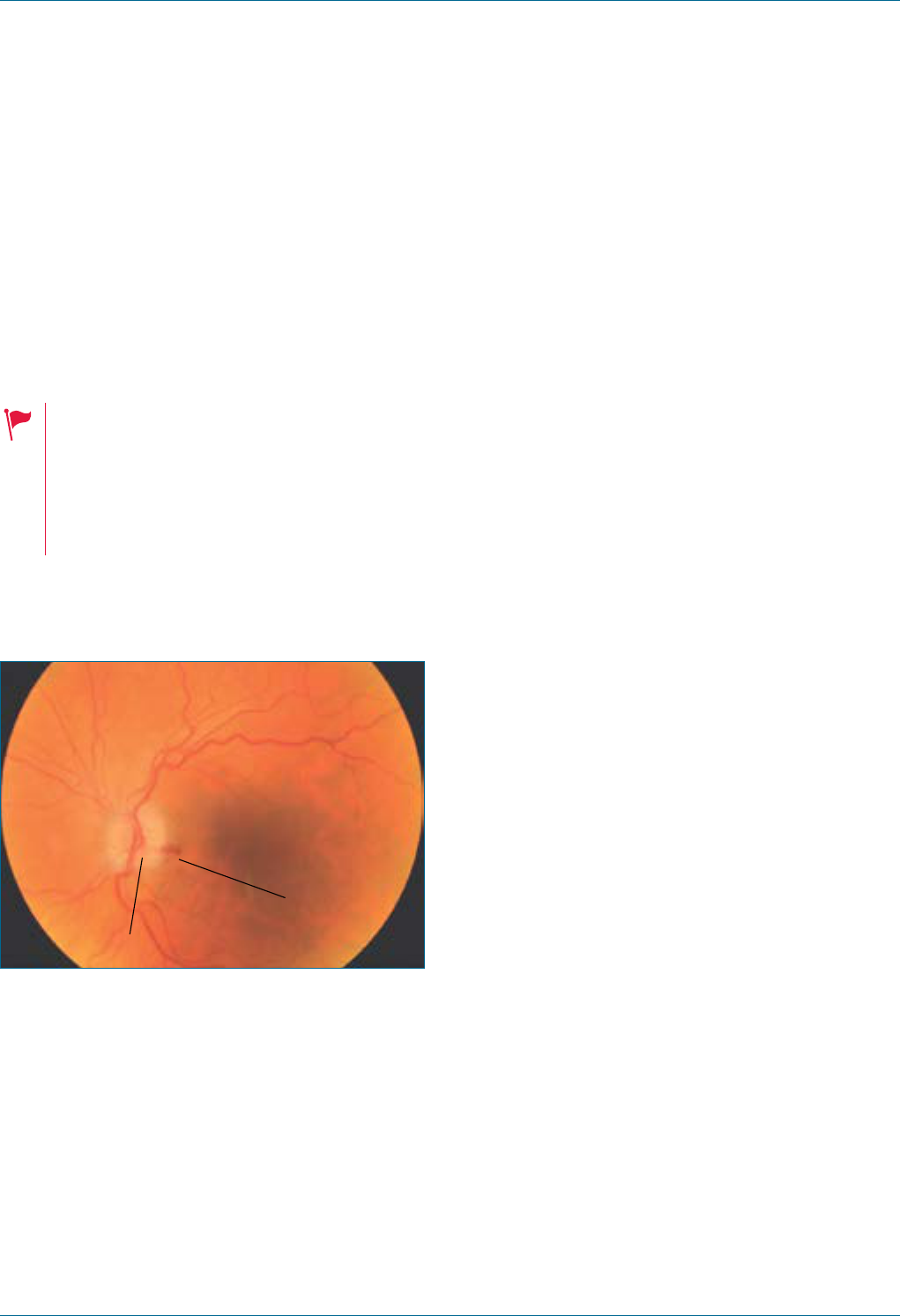
Eye Emergency Manual December 2023
Agency for Clinical Innovation 72 aci.health.nsw.gov.au
Giant cell arteritis (GCA)/
anteriorischaemic optic
neuropathy (AION)
Seek immediate referral by phone to
an ophthalmologist.
• Sudden profound loss of vision
• Constitutional symptoms of giant cell
arteritis (GCA)
• History of intermittent visual loss
• Age >50yrs
Figure 39. Swollen and pale optic disc (shown left)
with a disc margin haemorrhage (shown right).
Haemorrhage
Swollen optic disc
History ndings
• Affects patients older than 50 years of age
• May have polymyalgia rheumatica
• New onset headache (often temporal)
• Scalp tenderness
• Jaw claudication
• Tongue claudication
• Fever and night sweats
• Weight loss
• May have diplopia (double vision) or
transient visual loss
Examination ndings
May include any or all of the following:
• RAPD
• Poor visual acuity, often counting ngers or light
perception (may also be normal)
• Tender and non-pulsatile temporal artery
• Swollen pale optic disc
Investigations
• Immediate ESR and CRP (both/either may
be elevated)
• FBC (high platelet count), EUC, LFT and BSL
(in planning for steroid treatment)
• Plan for temporal artery biopsy (within 1 week)
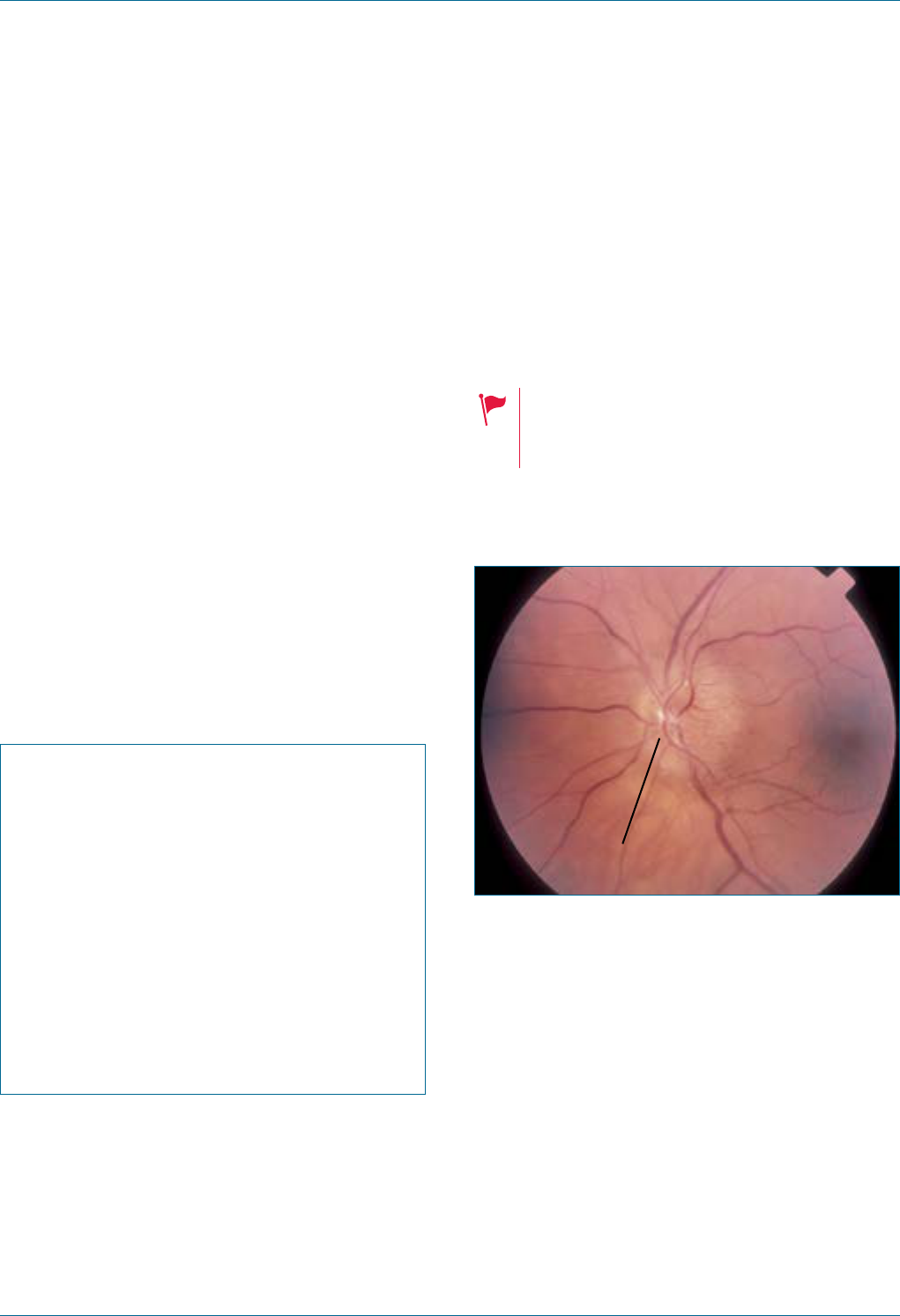
Eye Emergency Manual December 2023
Agency for Clinical Innovation 73 aci.health.nsw.gov.au
Important differentials
• Central retinal artery occlusion (CRAO)
• Non-arteritic anterior ischaemic optic
neuropathy (AION)
Initial treatment
Due to the potential risk of severe and irreversible
blindness, urgent intravenous corticosteroids
should be considered if the diagnosis is likely,
especially if the patient has visual symptoms or a
demonstrated loss of vision.
Urgent referral is required to a rheumatologist and
an ophthalmologist (especially if any visual
symptoms or visual loss).
Specic communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Ask the patient about GCA symptoms
; Past ocular/medical history (particularly
diabetes and how well it has been managed)
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
Idiopathic intracranial
hypertension (IIH):
transientvisual obscuration
Seek immediate referral by phone to an
ophthalmologist < 24hr.
May lead to permanent loss of vision,
severe headache, neurological signs
and drowsiness.
Figure 40. Optic disc swelling (note blurred
disc margins).
Swollen optic disc
History ndings
• Headache, worse in the morning or lying supine
• Transient visual obscuration (seconds)
• Pulsatile tinnitus
• Medication such as oral contraceptive pills,
vitamin A derivatives and tetracyclines
• Most commonly affects young,
overweight females
Eye Emergency Manual December 2023
Agency for Clinical Innovation 74 aci.health.nsw.gov.au
Examination ndings
• Visual acuity is often normal unless advanced
• Visual eld testing (by confrontation) and needs
automated perimetry in private rooms, public
hospital or other eye service
• Pupil examination (RAPD may be absent if
symmetrical optic nerve damage)
• Extraocular movement (may have 6th cranial
nerve palsy or palsies)
• Increased body mass index (weigh the patient)
• Swollen optic disc/s
Investigations
• Blood pressure
• Brain MRI/MRV diagnostics
• Lumbar puncture to check opening pressure
Important differentials
• Venous sinus thrombosis
• Intracranial space-occupying lesion
• Thyroid eye disease
• Lymphoma
• Giant cell arteritis (GCA) if >50 years old
Initial treatment
• Liaise with the ophthalmology team urgently if
the optic nerve is compromised (reduced vision,
RAPD or colour vision change)
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation) and also
need automated perimetry at private
rooms, public hospital or other eye service
; Pupil examination: anisocoria or RAPD
; Red reex
Specic communication checklist
Consider the following:
; Field loss
; Optic disc appearances
; Weight and BMI
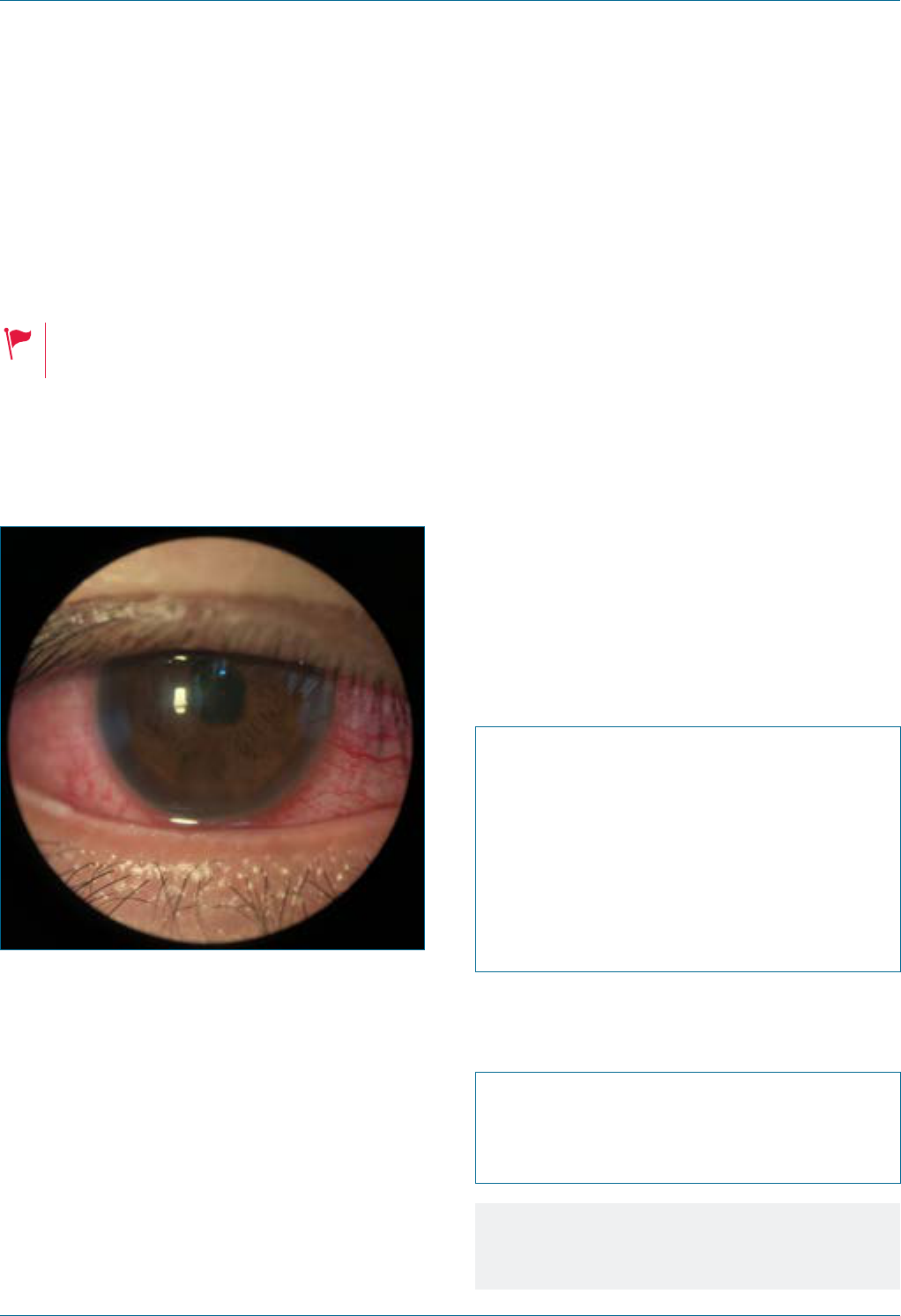
Eye Emergency Manual December 2023
Agency for Clinical Innovation 75 aci.health.nsw.gov.au
Intermittent angle closure/
acuteangle closure
Seek an immediate referral to an ophthalmologist.
Reduced vision and unwell, (e.g. nausea
and vomiting).
Figure 41. Conjunctival vessels dilated at the
corneal edge (ciliary ush and circumcorneal
ush) and hazy cornea characteristic of acute
angle closure, where intermittent is a variant.
9
History ndings
• Usually South East Asian background
• May have signicant glare, a history of eye pain
or blurry vision in dim light
• Uncommon in patients who have had
cataract surgery
Examination ndings
Consider the following:
• Reduced visual acuity, abnormal red reex,
+/- RAPD (if developed retinal complications)
• May also have xed and dilated pupil
• The cornea appears cloudy
• Raised intraocular pressure (if it can be
measured) and the globe may feel rm
on palpation.
Initial treatment
• Liaise with an ophthalmologist
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
Specic communication checklist
Consider the following:
; Slit lamp examination
; Check for a sulphur allergy if treatment
with acetazolamide (diamox) is considered
Notes
Avoid dilating patients with suspected
narrow angles.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 76 aci.health.nsw.gov.au
Lens subluxation
History of ocular trauma and systemic
associations, such as Marfan syndrome.
History ndings
• Reduced vision
• Monocular diplopia (double vision)
• History of eye/head trauma
• Pseudoexfoliation syndrome
• Ocular surgery
• Medical history (Marfan syndrome
or homocystinuria)
Examination ndings
• Visual acuity
• Check intraocular pressure if possible:
RAPD should be absent
• Dilated examination, if instructed by the
ophthalmology team, shows a subluxed lens
or intraocular lens implant
• Assess for associated ocular injury if caused
by trauma
• Physical examination to check features of
Marfan syndrome
Investigations
• Marfan syndrome or homocystinuria work up
if suspected clinically
Important differentials
• Acute angle closure crisis
• Uveitic glaucoma
• Eccentric pupil
• Penetrating eye injury
Initial treatment
• Consult the ophthalmology team to establish the
diagnosis, underlying cause and management
Specic communication checklist
Consider the following:
; Medical history
; Ocular history
; Visual acuity
; Pupil assessment
; Anterior segment ndings (dilated
examination if instructed by the
ophthalmology team) and intraocular
pressure if able to obtain
; Physical examination to look for Marfan
syndrome features
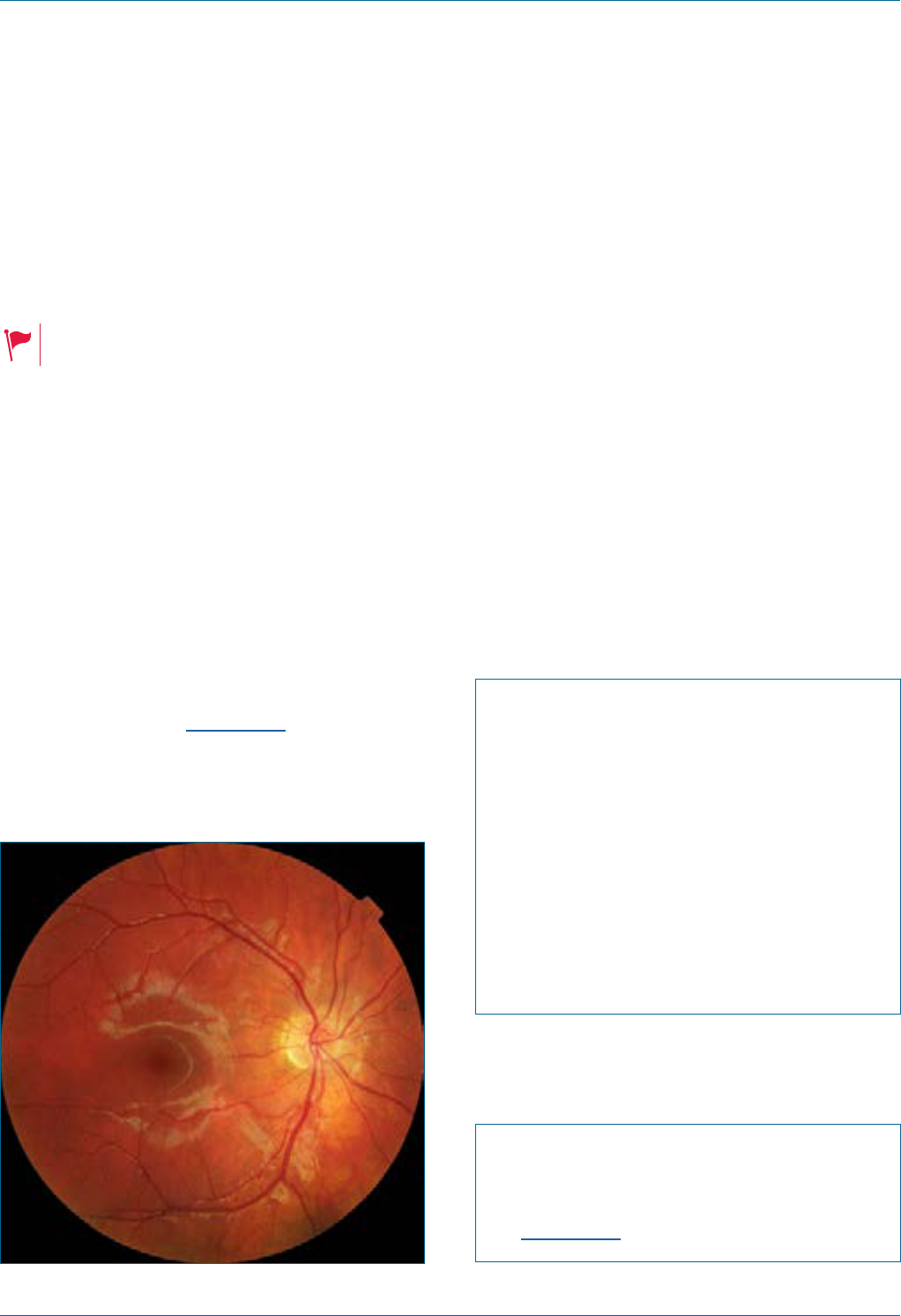
Eye Emergency Manual December 2023
Agency for Clinical Innovation 77 aci.health.nsw.gov.au
Macular haemorrhage in wet
age-related macular degeneration
Seek an immediate referral to an ophthalmologist.
History of age-related macular degeneration.
History ndings
• Sudden, persistent, unilateral, painless loss of
central vision
• History of macular degeneration (may be on
intravitreal anti-VEGF injections)
• May be on anticoagulants
Examination ndings
• Reduced visual acuity with relatively intact or
unaffected peripheral vision
• Central scotoma on Amsler grid
• Pupil examination: RAPD may be present
Figure 42. Central scotoma on Amsler grid.
Important differentials
• Central retinal vein occlusion
• Central retinal artery occlusion
• Haematological malignancy
• Diabetic retinopathy
• Other macular pathology
Initial treatment
• Contact an ophthalmologist to establish
the diagnosis
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination
Specic communication checklist
Consider the following:
; Medical history: anticoagulant use
; Peripheral vision
; Amsler grid nding
Eye Emergency Manual December 2023
Agency for Clinical Innovation 78 aci.health.nsw.gov.au
Macular pathology
The macula is the central region of the retina
and is responsible for central vision. People with
macular conditions are usually symptomatic,
often with reduced visual acuity on Snellen
chart testing. The onset can be acute or chronic.
A detailed posterior segment examination,
including dilation of the pupils and, often, the
use of imaging techniques such as optical
coherence tomography, will aid the diagnosis of
the specic type of macular pathology.
Conditions to consider include macular
haemorrhage, macular hole, epiretinal
membrane, dry age related macular
degeneration, central serous retinopathy,
macular oedema due to diabetic retinopathy and
post-operative macular oedema.
Migraine
Poor vision, neurological symptoms, age>50
and visual disturbance of more than 1 hour.
History ndings
• Headache (unilateral)/throbbing headache
• Nausea and vomiting
• Visual aura (typically precedes migraine onset
and lasts 15–20 minutes)
• Flashes after visual aura
• Central scotoma
• Other neurological symptoms
Examination ndings
• Normal ocular examination
• May present with a scotoma on visual eld
assessment whilst experiencing a
migrainous aura
Important differentials
• Acute angle closure
• Malignant hypertension
• Raised intracranial pressure
• Meningitis
• Central nervous system lesion
Initial treatment
• Consult neurology team
Specic communication checklist
Consider the following:
; Headache
; Medical history and neurological symptoms
; Visual acuity, RAPD and red reex
; Ocular movement
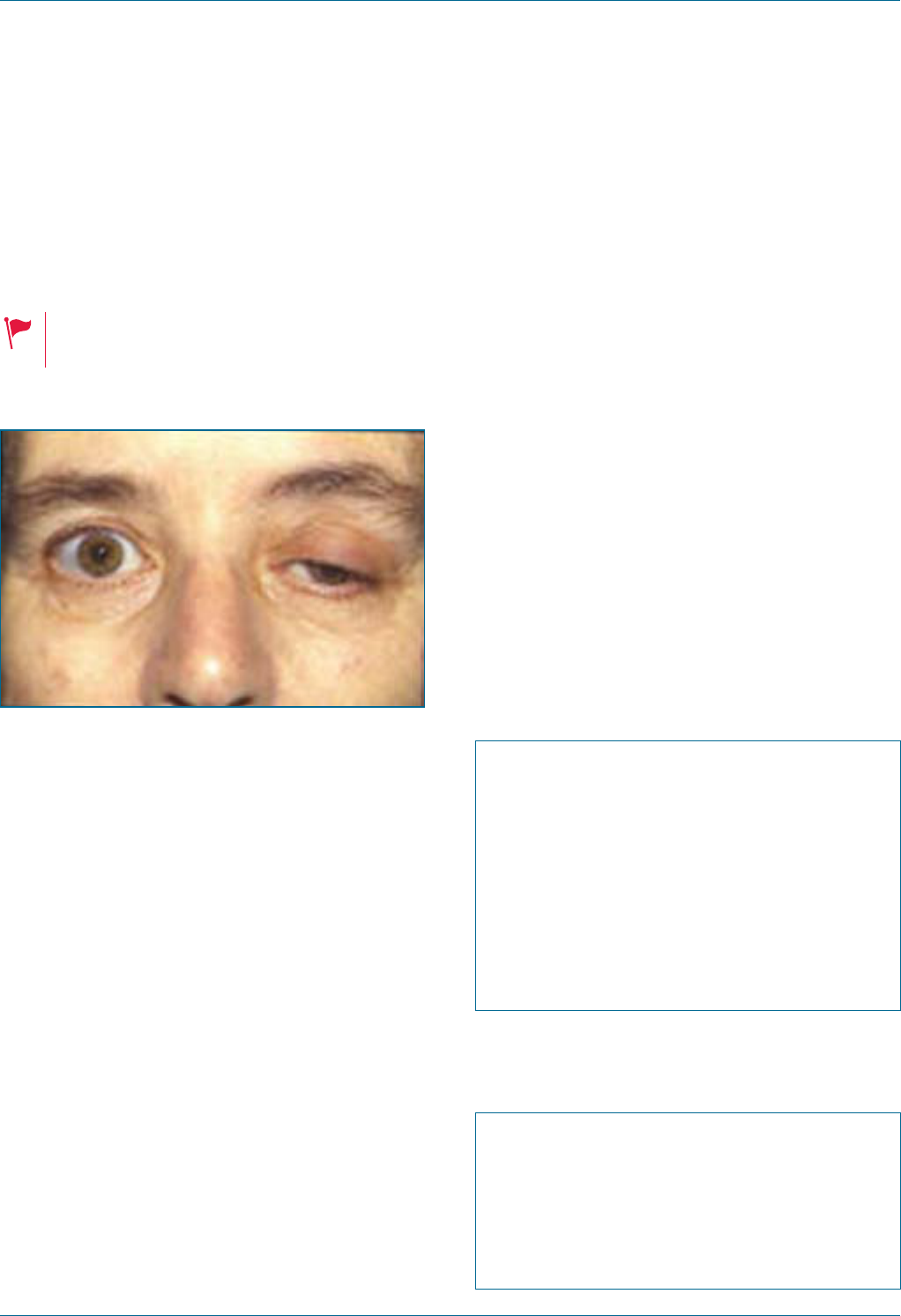
Eye Emergency Manual December 2023
Agency for Clinical Innovation 79 aci.health.nsw.gov.au
Myasthenia gravis
Seek immediate referral by phone to an
ophthalmologist < 24hr.
May be associated with respiratory
distress or difculty swallowing.
Figure 43. Patient with ocular myasthenia gravis.
10
History ndings
• Double vision and ptosis
• Variability of symptoms (worse towards the end
of the day)
• Systemic symptoms (dysphagia, limb weakness
and difculty breathing)
• Fatigability (particularly of the eyelids causing
variable ptosis)
Examination ndings
• Ptosis
• Ocular motility is abnormal, but not 3rd, 4th or
6th cranial nerve palsy pattern (although
myasthenia gravis can mimic these)
• Ice test
• Pupil examination (should be normal; consider
another diagnosis if not)
• Fatigability of lids with sustained up-gaze
(1–2 minutes)
Investigations
• Anti-Ach receptor (AChR) antibody
• Anti-MuSK antibody (muscle-specic kinase)
• Thyroid function tests
Important differentials
• Thyroid eye disease
• Other cranial nerve palsies
• Orbital lesions
Initial treatment
• Discuss with neurology
• Ophthalmology consultation regarding diplopia
(double vision) and ptosis management
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
Specic communication checklist
Consider the following:
; Medical, ocular history (especially any
variability of symptoms and fatigability)
; Pupil assessment
; Extraocular movement assessment
; Ptosis measurement

Eye Emergency Manual December 2023
Agency for Clinical Innovation 80 aci.health.nsw.gov.au
Optic neuritis
Seek an immediate referral by phone to an
ophthalmologist < 24hr.
Atypical optic neuritis features (consider
other diagnoses): bilateral, rapid onset,
systemic symptoms, male, Southeast
Asian background, age >50 (consider
giant cell arteritis (GCA) and profound
visual loss).
Figure 44. Optic neuritis shows a swollen optic
disc and blurred disc margins.
Swollen optic disc
History ndings
• Painless vision loss over hours to days
• Vision loss can be subtle or profound (atypical)
• Reduced visual acuity (blurring), reduced colour
vision and contrast vision
• Usually unilateral but may rarely be bilateral
• Often affects females aged 18–45 years old
• Retrobulbar pain is usually associated with eye
movement and can occur before visual loss
• May have other focal neurological symptoms
relating to demyelination
Examination ndings
• Decreased visual acuity (test with pinhole if
not 6/6)
• Pupil examination (RAPD) tested prior to dilation
• Decreased colour vision
• Possible patchy scotoma but any eld defect is
possible and may be difcult to elicit
on confrontation
• Other focal neurological signs relating to
demyelination are possible
• Check blood pressure
Investigation
• Discussion with neurology if medical imaging
is needed
• Further investigations as per the neurology team
• Consider inammatory and infective causes of
optic neuritis
Important differentials
Consider the following:
• Neuromyelitis optica (in Asian populations with
profound visual loss and bilateral involvement).
• GCA is possible (in older patients).
• Vasculitis is possible.
• Other causes of swollen optic disc, (e.g. GCA,
raised intracranial pressure, idiopathic
intracranial hypertension, systemic
hypertension, central retinal vein occlusion,
thyroid eye disease and diabetic papillitis).
Initial treatment
• Discuss with the neurology team for
further investigations
Eye Emergency Manual December 2023
Agency for Clinical Innovation 81 aci.health.nsw.gov.au
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination if instructed
Specic communication checklist
Consider the following:
; Neurological examination
; Extraocular movements
; Appearance of optic disc
Posterior vitreous detachment
(PVD)
Seek an immediate referral by phone to an
ophthalmologist < 24hr.
Consider other diagnoses if there is visual
acuity loss or visual eld loss.
History ndings
Consider the following:
• Peripheral ashes (usually temporal) and
differentiate from migraine ‘ashes’, which last
several minutes, tend to scintillate, spread
across the visual eld, may be multi-coloured
and are often associated with an adjacent
scotoma or blurring of vision.
• Patients often cannot discern whether
monocular or binocular in origin. Migraines
sometimes do not have associated headaches,
nausea or vomiting.
• The presence of oaters.
• PVD is usually unilateral and painless. Possible
precipitating mild head or eye trauma.
• No neurological symptoms.
Examination ndings
• Visual acuity
• Check red reex (vitreous blood may be seen
oating behind the lens; retinal detachment can
cause loss of the red reex)
• Visual elds (by confrontation)
• Pupil examination: RAPD should not be present
• Dilated retinal examination
Eye Emergency Manual December 2023
Agency for Clinical Innovation 82 aci.health.nsw.gov.au
Important differentials
• Retinal tear/break
• Retinal detachment
Initial treatment
• Liaise with an ophthalmologist
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history (particularly
diabetes) and how well it has been managed
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination if instructed
Specic communication checklist
Consider the following:
; History: peripheral ashes and/or oater/s
; RAPD or red reex
; No other neurological symptoms
Notes
• This is a common condition caused by
liquefaction of vitreous with age. It tends to
occur in 50–60-year olds.
• The ‘ashes’ symptom reects active
vitreous traction on the retina.
• Complete vitreous detachment can take up
to 6 weeks to occur.
• The majority of patients have no long-term
consequences from PVD. A small
percentage may develop a retinal
detachment. Consequently, patients with
new onset of ashes or oaters should be
examined by an ophthalmologist within
24–48 hours. If there is reduced visual
acuity, visual eld loss, blood visible in the
vitreous or other suspicious ndings on
history/examination, please liaise with an
ophthalmologist as more urgent review
may be required.
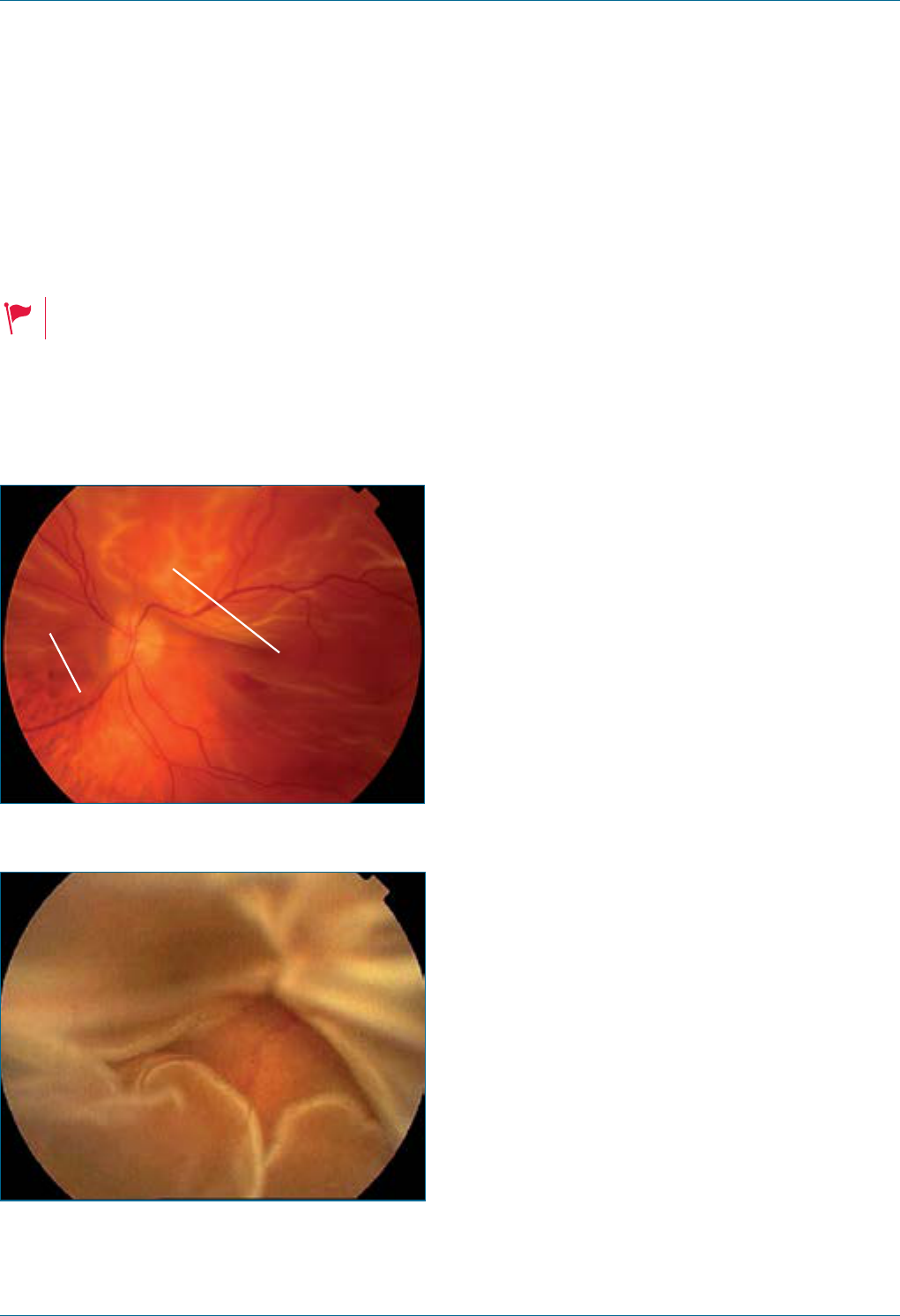
Eye Emergency Manual December 2023
Agency for Clinical Innovation 83 aci.health.nsw.gov.au
Retinal tear or detachment
Seek an immediate referral to an ophthalmologist.
Curtaining and loss of vision.
Figure 45. Retinal detachment (macula off).
The lower end of the lines delineates the inferior
edge of the retinal detachment. The macula is
justinvolved.
Area of attached
retina - choroidal
detail still visible
Detached
retina-loss
of transparency
Figure 46. Subtotal retinal detachment.
History ndings
Consider the following:
• Painless loss of vision: the patient may have a
recent history of increased number of visual
oaters and/or visual ashes.
• There may be a ‘dark shadow’ in the peripheral
visual eld of the affected eye.
• High-risk groups are patients who are myopic
(short-sighted), who have had blunt eye/head
trauma and who have a history of retinal
detachment or eye procedures
Examination ndings
Consider the following:
• Reduced visual acuity if the macula is detached.
If not involved (‘macula on’), the vision is often
6/6. This is a more urgent condition as the
macula can be saved with early surgery.
• Loss of red reex: a mobile detached retina may
be visible on ophthalmoscopy
• Pupil examination is required for RAPD
• Visual eld defects that correspond to the area
of the detached retina can usually be elicited by
confrontation testing
• Often normal anterior segment slit lamp
examination
• Dilated retinal examination: it is generally safe to
dilate these patients once the above
examination has been completed

Eye Emergency Manual December 2023
Agency for Clinical Innovation 84 aci.health.nsw.gov.au
Important differentials
• Posterior vitreous detachment
• Retinal vein or artery occlusion
• Stroke
• Giant cell arteritis (GCA)
• Optic neuritis
• Diabetic retinopathy (tractional detachment or
vitreous haemorrhage)
Initial treatment
• Liaise with ophthalmologist
• Keep the patient nil by mouth for
the possibility of emergency surgery
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination
Specic communication checklist
Consider the following:
; History and risk factors
; Prior cataract or other eye surgery
; Onset of symptoms
; Fasting time
Thyroid eye disease
Loss of vision or incomplete eyelid
closure should prompt an urgent referral
to an ophthalmologist.
Figure 47. Bilateral proptosis (exophthalmos), as
well as asymmetrical eye alignment indicative of
eye muscle neuromuscular involvement.
11
History ndings
• Known Graves’ disease
• Diplopia (double vision), red eye or painful eye
• Blurred vision
• Systemic symptoms of hyperthyroidism
• Smoking history
Examination ndings
• Visual acuity
• Proptosis
• Incomplete lid closure
• Strabismus
• Compressive optic neuropathy
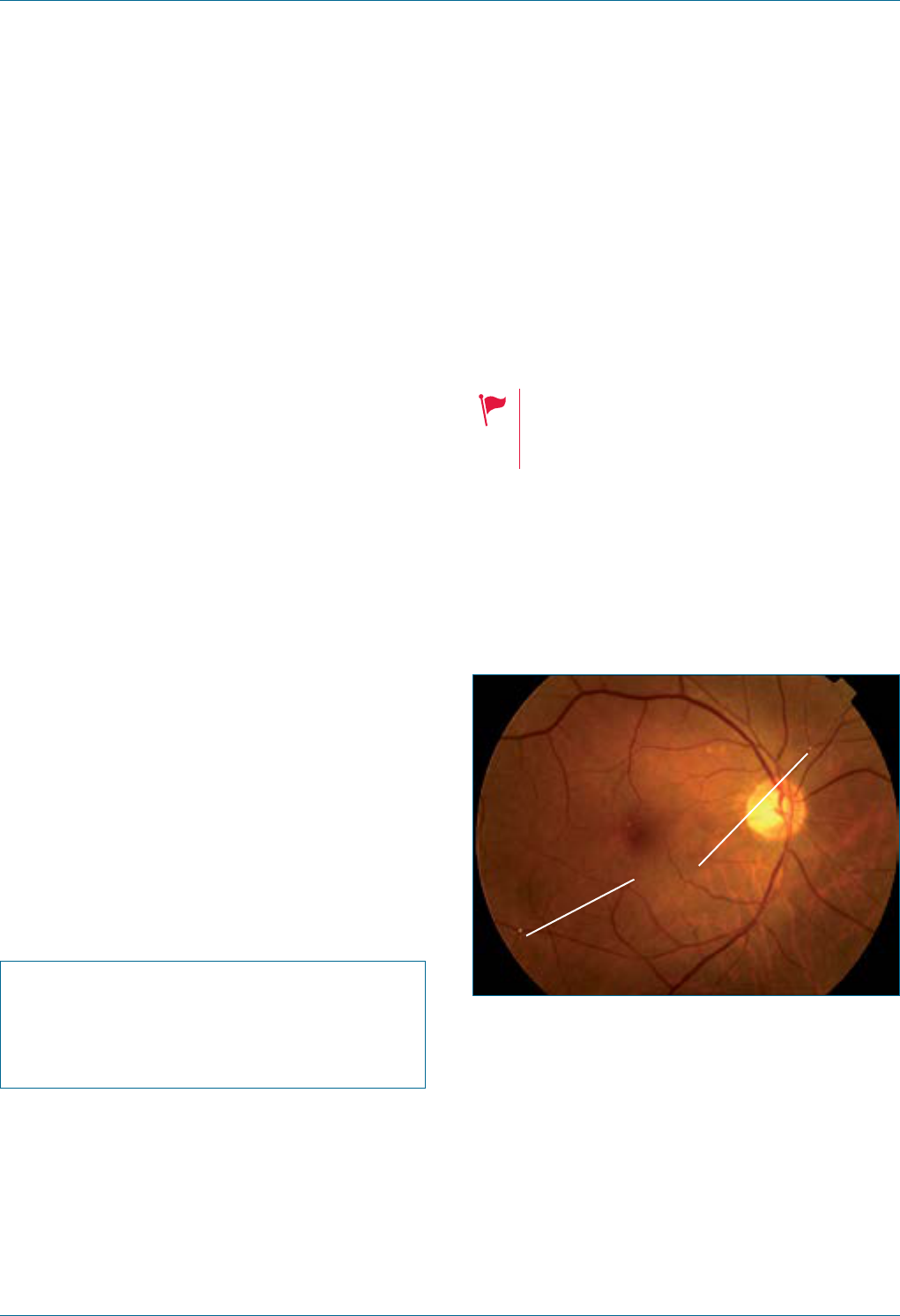
Eye Emergency Manual December 2023
Agency for Clinical Innovation 85 aci.health.nsw.gov.au
• Possible corneal ulcer from exposure of the
cornea from incomplete eyelid closure
• Optic nerve function assessment
• RAPD
• Extraocular muscle palsy
Investigations
• Thyroid function test
• CT orbit if proptosis, red eye
• FBC, LFT, EUC and BSL blood tests in planning
for corticosteroid treatment
Important differentials
• Orbital cellulitis or trauma
• Orbital tumour
Initial treatment
• Immediate ophthalmology consultation is
required if reduced vision (to assess for
compressive optic neuropathy) and for urgent
treatment (if corneal ulcers present)
Specic communication checklist
Consider the following:
; Medical, ocular history
; Visual acuity, red reex, RAPD and
ocular motility
Transient ischaemic attack
(amaurosis fugax) or
retinal emboli
Seek an urgent referral to an
ophthalmologist<24hrs.
Giant cell arteritis (GCA) symptoms,
neurological symptoms and
recurrent episodes.
Referral to neurology/cardiology or vascular
surgery as appropriate. Patients with recurrent
episodes of amaurosis fugax require immediate
diagnostic and therapeutic intervention.
Figure 48. Transient ischaemic attack.
Lines point to visible emboli.
Emboli
History ndings
• Painless, monocular visual loss lasting less than
30 minutes before returning to normal
• Cardiovascular risk factors, including smoking
• History of clotting disorder
• Other neurological symptoms
• History of cardiac arrhythmia
• Anticoagulation therapy
Eye Emergency Manual December 2023
Agency for Clinical Innovation 86 aci.health.nsw.gov.au
Examination ndings
• Usually normal ocular examination ndings:
fundoscopy may reveal small emboli at the
bifurcations of retinal arterioles
• Visual eld assessment, (e.g. may have a visual
eld defect)
• Extraocular movements
• Pupil examination should be normal
• Neurological examination
Investigations
• Assessment of cardiovascular risk factors and
guided by a neurologist
• Blood count, electrolytes, lipids and fasting
blood glucose
• Investigation for thrombophilia and
hypercoagulable state: discuss with
haematology (consider if age <50 or
relevant history)
• Echocardiogram
• Carotid doppler studies
Important differentials
• GCA
• Vasculitis
• Transient visual obscuration
• Transient blurring of vision: dry eye and
vitreous oaters
Initial treatment
• Liaise with physicians
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving and monocular/binocular
; Past ocular/medical history
; Visual acuity
; Visual elds (by confrontation)
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination
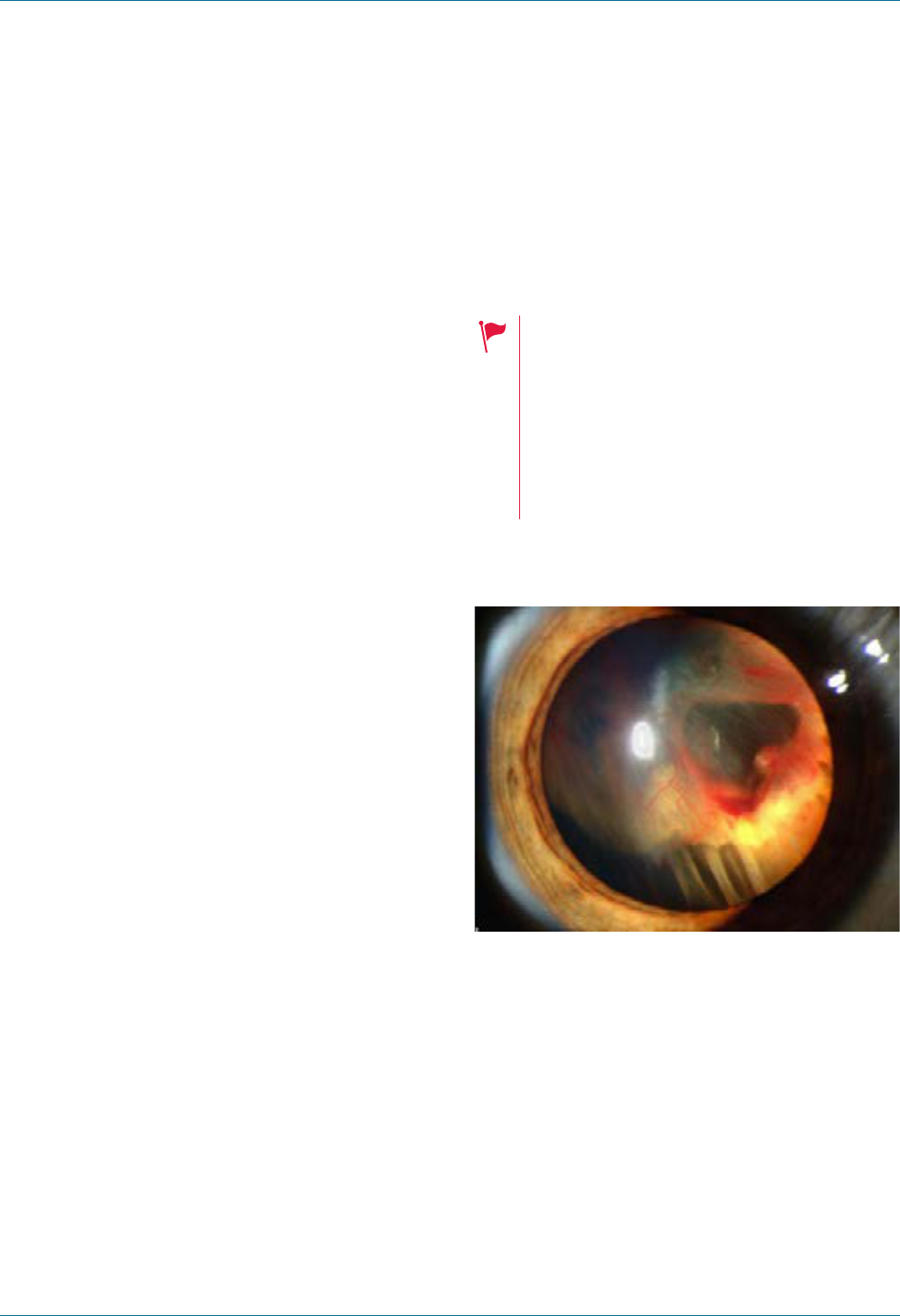
Eye Emergency Manual December 2023
Agency for Clinical Innovation 87 aci.health.nsw.gov.au
Visual pathway lesion
Visual pathway pathology
Patients can present with visual complaints
secondary to non-ocular causes. A thorough
history and neurological assessment should be
performed to consider neuroimaging.
Examples of visual pathway pathologies include:
• Optic neuritis
• Traumatic optic neuropathy
• Giant cell arteritis (GCA)
• Non-arteritic ischaemic optic neuropathy
• Chiasmal lesion
• Pituitary tumour or disease
• Bitemporal hemianopia
Cortical blindness
• Lesions affecting the occipital lobe or other
parts of visual pathway
• Diagnoses of exclusion are necessary and
require a formal ophthalmology assessment
Amblyopia
Amblyopia, or reduced visual acuity, results from
deprivation of optimal visual experience during
early childhood. Patients are usually aware of a
history of amblyopia or ‘lazy eye’.
Functional visual loss
Functional vision loss is a decrease in visual acuity
that cannot be accounted for by anatomical or
physiological ndings. The objective assessments
should demonstrate a visual acuity better than
subjective visual acuity.
Vitreous haemorrhage
Seek an urgent referral to an
ophthalmologist<24hrs.
• Flashes
• Floaters with reduced vision
• Presence of RAPD
• Diabetes
• Age-related macular degeneration
(ARMD)
• History of trauma
Figure 49. Slit lamp photograph shows retinal
detachment with visible vitreous.
12
History ndings
• Sudden loss of vision or ashes/oaters
• May be on anticoagulants
• History of trauma or diabetes
Examination ndings
• Reduced visual acuity: check for RAPD (if
developed retinal complications)
• Anterior vitreous red blood cells (visible on slit
lamp examination)
Eye Emergency Manual December 2023
Agency for Clinical Innovation 88 aci.health.nsw.gov.au
Investigations
• Diabetic work up
• Trauma work up (if applicable)
Important differentials
• Retinal detachment
• Retinal tear
• Posterior vitreous detachment
• Proliferative diabetic retinopathy
Initial treatment
• Discussion with ophthalmologist
Section communication checklist
Consider the following:
; Presenting complaint: timing, worsening/
improving or monocular/binocular
; Past ocular/medical history
; Visual acuity (with pinhole if not 6/6)
; Visual elds by confrontation
; Pupil examination: anisocoria and RAPD
; Red reex
; Dilated retinal examination

Acute red eye
or eyelid
Agency for Clinical Innovation 89 aci.health.nsw.gov.au
Eye Emergency Manual November 2023
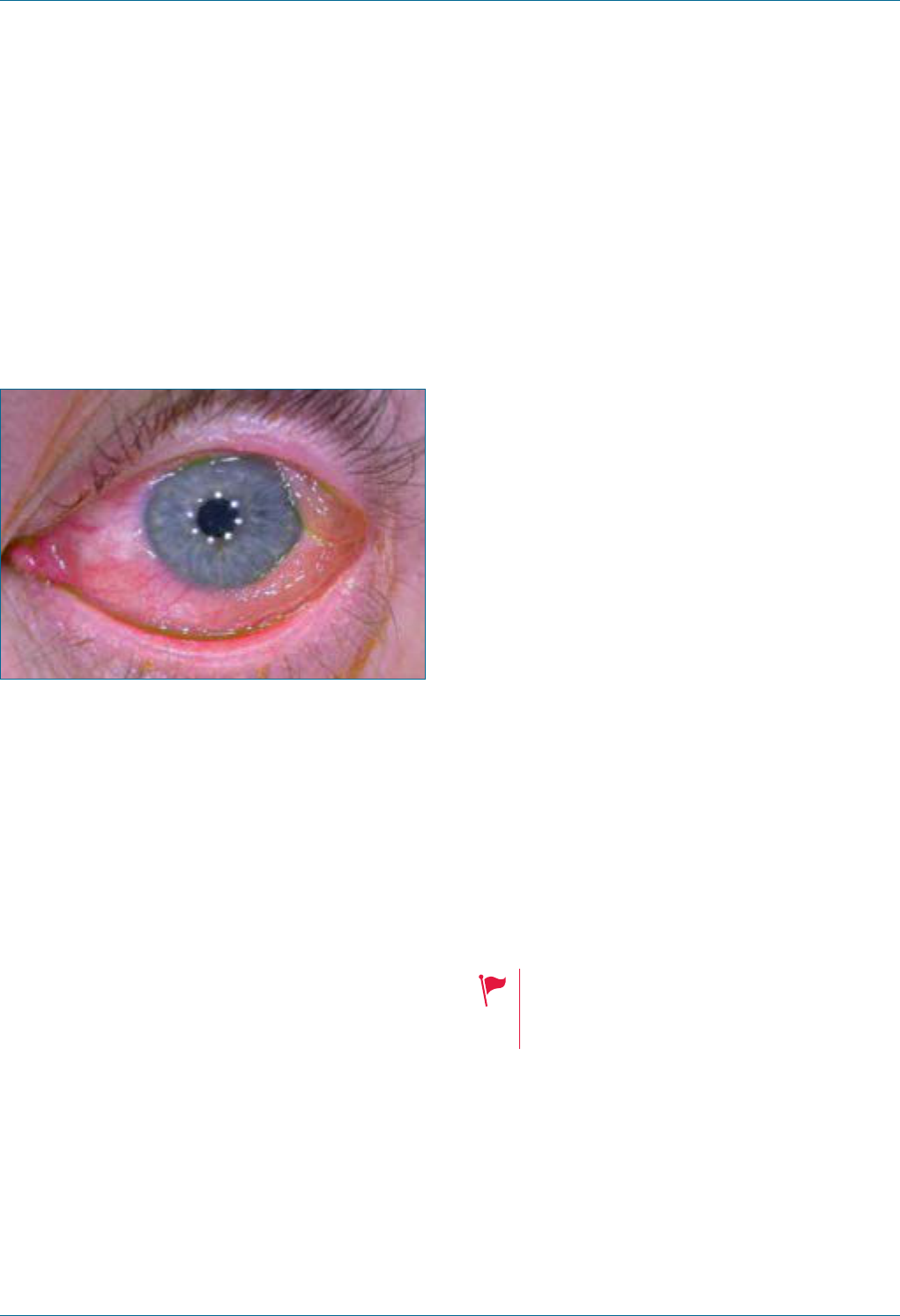
Eye Emergency Manual December 2023
Agency for Clinical Innovation 90 aci.health.nsw.gov.au
Acute red eye or eyelid
Acute red eye overview
Many conditions can lead to a patient presenting
with a red eye. Many of these are self-limiting or
will respond to simple treatment.
Figure 50. Acute red eye.
Indicators of more serious pathology
• Pain (as opposed to irritation) and/or
reduced vision
• Contact lens use
• Foreign body exposure history (in particular any
possibility of penetrating injury)
• Known connective tissue disorders, e.g. risk of
keratitis, iritis/uveitis, epi/scleritis and giant cell
arteritis (GCA)
Indicators of less serious pathology
• Bilateral red eye, especially in the context of
other viral or allergic symptoms (and in the
absence of any of the above indicators)
Additional useful distinctions
Assess pain relief after topical anaesthetic drop. If
total, this suggests conjunctival irritation or if only
partial, consider the ocular disease process.
The presence of corneal epithelial damage
(uorescein uptake) or any loss of corneal clarity.
Conditions are grouped below as disorders,
primarily of:
• eyelid and associated structures
• conjunctiva and cornea
• anterior chamber
• globe and orbit
Urgency
Triage urgency is guided by the Department of
Health’s Summary of ophthalmic emergency
predictors (OEP) for the Australasian Triage Scale.
The urgency of ophthalmology review following ED
assessment is indicated where relevant.
It is rare for a painless red eye to require an urgent
ophthalmological assessment, particularly if vision
is normal.
Beware of making the diagnosis of
monocular conjunctivitis until more serious
eye disease is excluded.
Conjunctival redness can be diffuse or localised.
Use uorescein to ascertain the nature of any
epithelial defect.
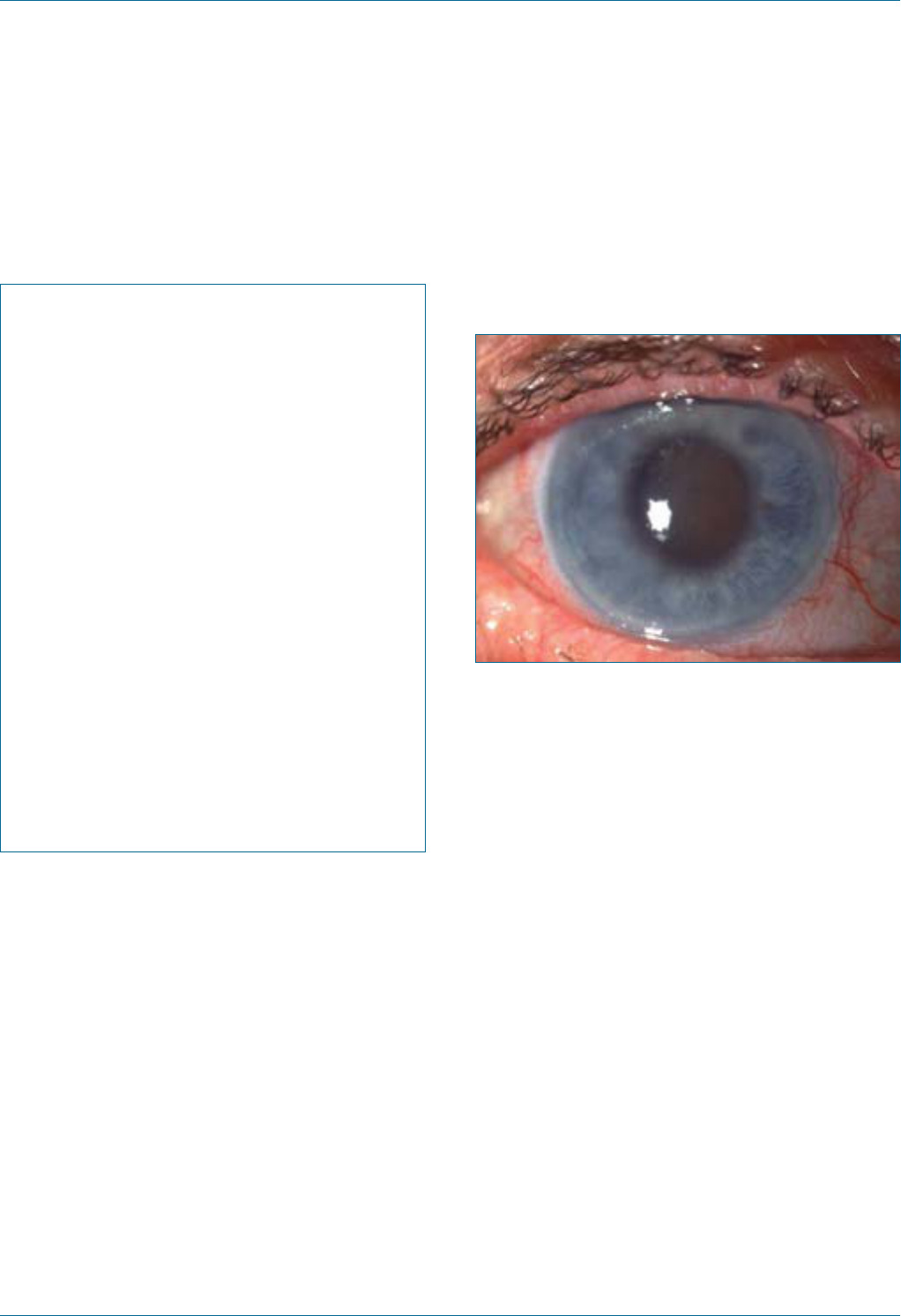
Eye Emergency Manual December 2023
Agency for Clinical Innovation 91 aci.health.nsw.gov.au
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal, i.e.
deep, presence of anterior chamber cells,
blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Acute angle closure crisis
Figure 51. Acute angle crisis, with cloudy cornea,
loss of iris detail, and a xed mid-dilated pupil.
History ndings
• Ocular symptoms include eye ache/pain, cloudy/
loss of vision and red eye
• Systemic symptoms include headache, nausea
and vomiting
Examination ndings
Consider the following:
• The cornea usually has a hazy appearance. The
iris details may be difcult to see due to
corneal oedema.
• The anterior chamber is shallow. Use a ne slit
at 45° on the slit lamp, or shine a torch from the
side for irregular semi-dilated pupils.
• The affected eye is very tender and tense
to palpation.
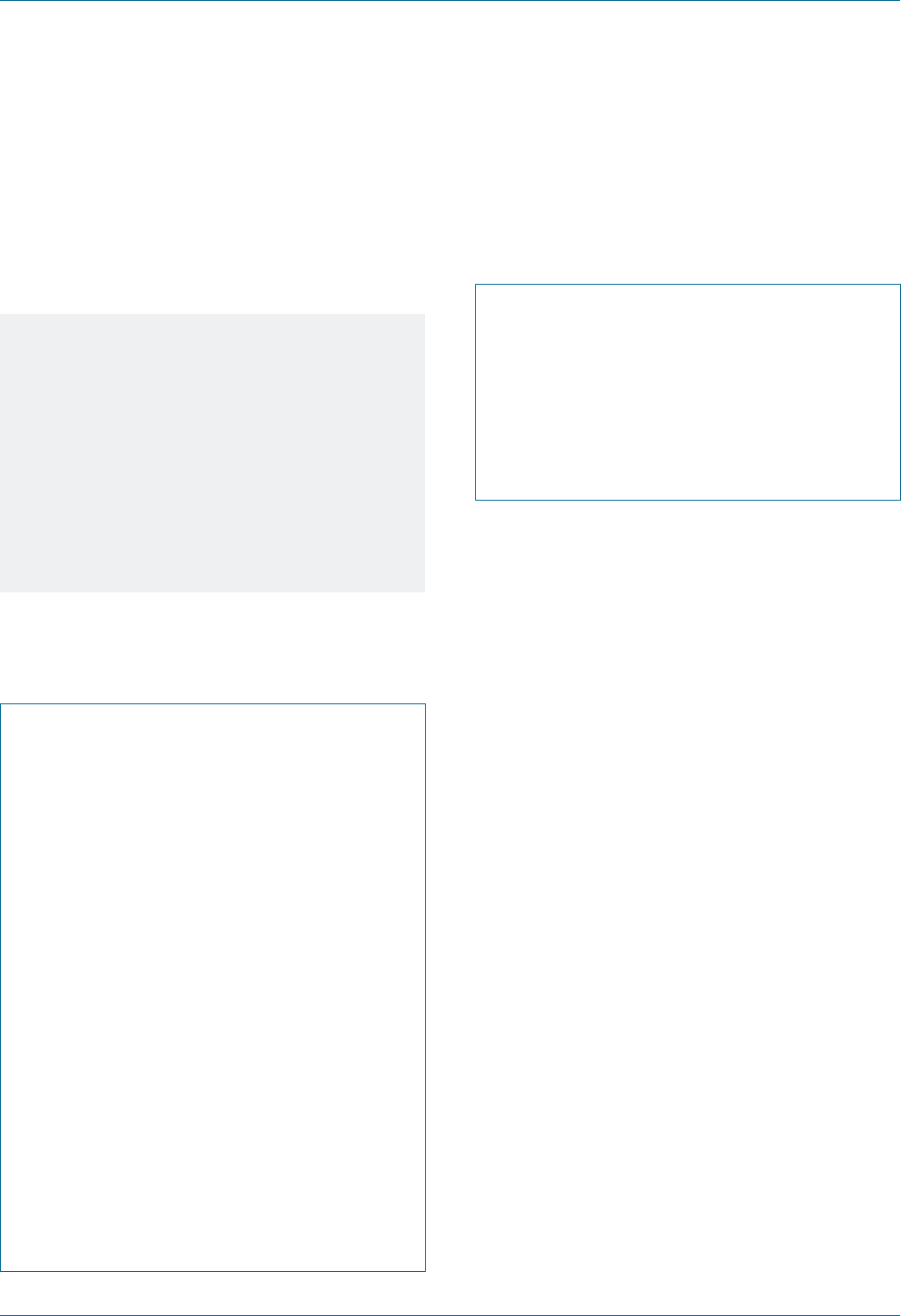
Eye Emergency Manual December 2023
Agency for Clinical Innovation 92 aci.health.nsw.gov.au
Initial treatment
• May require anti-glaucoma drops (see ocular
drug section) and an urgent laser procedure
Notes
Digital palpation tonometry can be
performed. Using both index ngers to
‘ballot’ the eyeball under gently-closed
eyelids, it is possible to compare the
‘hardness’ of the eyeball from one eye to the
other. If the affected eye has elevated
intraocular pressure, then it will feel very
hard and rm to palpation (more like a golf
ball than a gelatinous ball).
Specic communication checklist
Consider the following:
; Symptoms are often triggered by dark
lighting conditions
; Has the patient had cataract surgery
before? If so, then it is extremely unlikely to
be angle closure crisis
; How rm the globe feels on palpation
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal, i.e.
deep, presence of anterior chamber cells,
blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
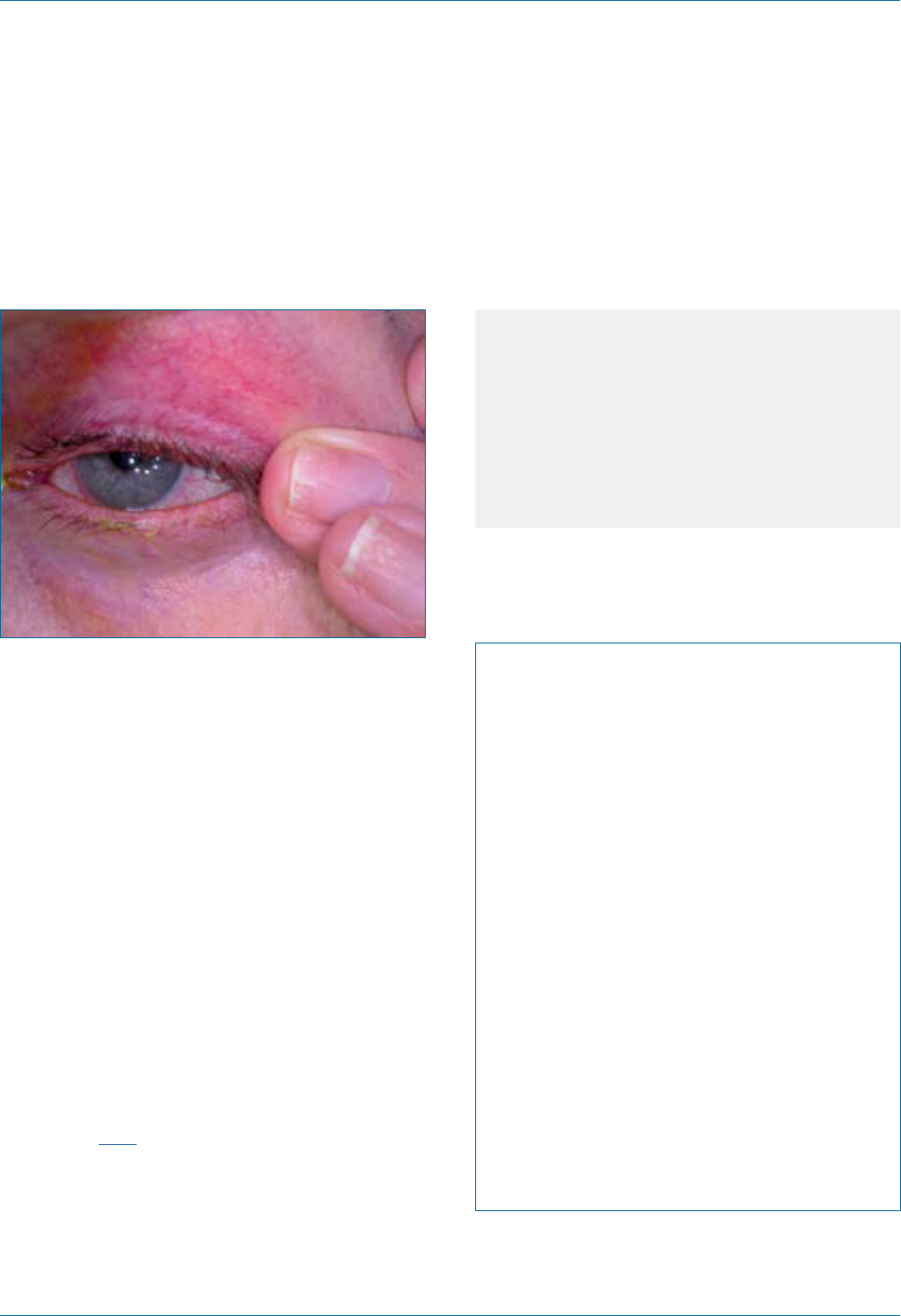
Eye Emergency Manual December 2023
Agency for Clinical Innovation 93 aci.health.nsw.gov.au
Acute blepharitis
Figure 52. Blepharitis.
History ndings
• Foreign body sensation, tearing and crusting
around the eyes and worse in the morning
• Dry eye symptoms with reading and other tasks
and in air-conditioning
Examination ndings
• Crusty, red and thickened eyelid margin
• Closer inspection may reveal ne telangiectatic
vessels at the lid margin and blocked
Meibomian glands
Initial treatment
Consider the following:
• Treat with daily eyelid hygiene and lubrication as
required. Instructions for bathing the eyelids are
available here.
• Treat with antibiotic ointment if indicated, at
night, for 1 month.
• Ophthalmology referral is normally only
indicated if associated ocular damage,
(e.g. from rubbing or trichiasis).
Notes
• Acute blepharitis may be associated with
marginal keratitis, chalazion or dry eyes.
• Blepharitis is localised eyelid margin
inammation, usually with minimal
ocular involvement.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal, i.e.
deep, presence of anterior chamber cells,
blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
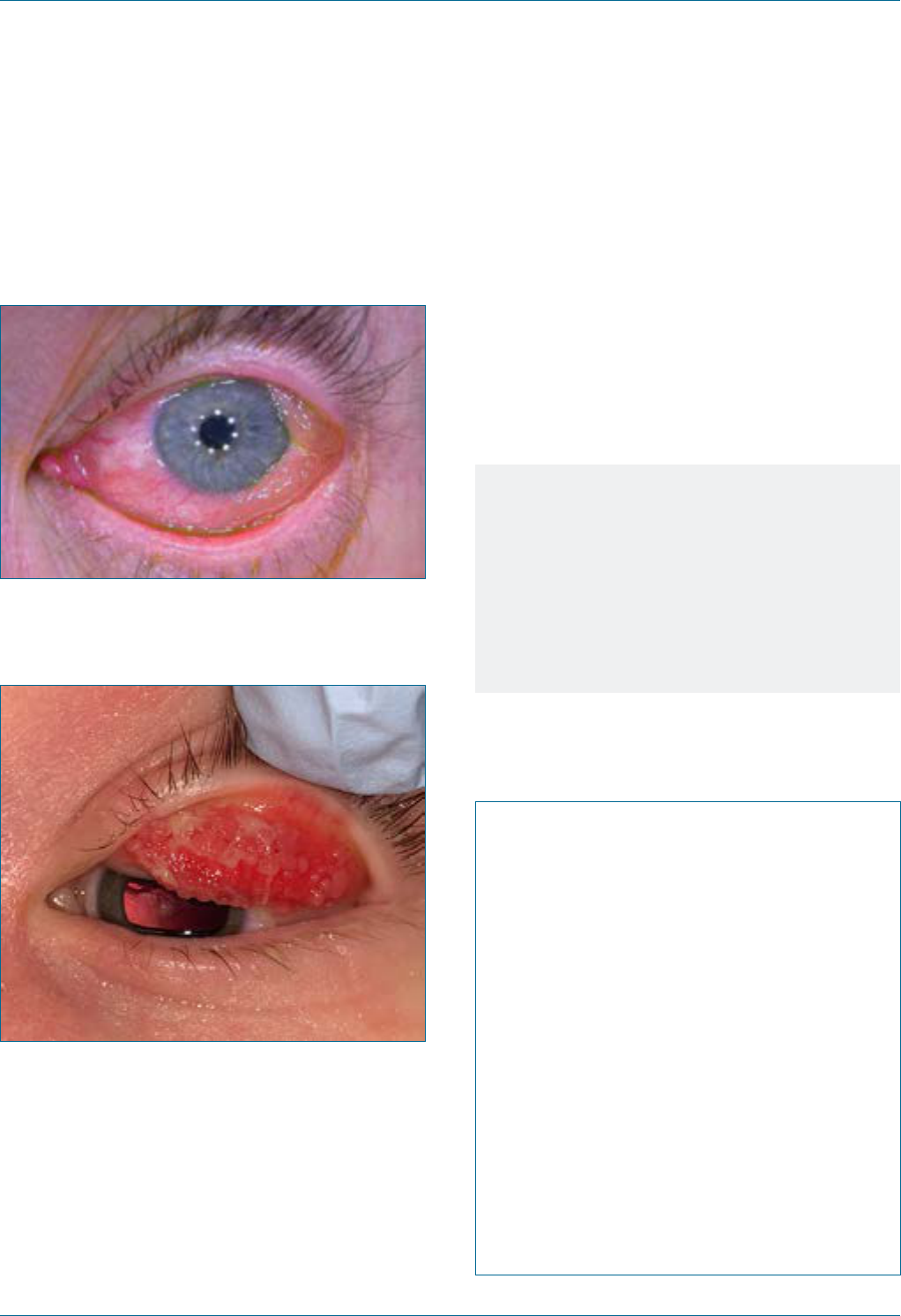
Eye Emergency Manual December 2023
Agency for Clinical Innovation 94 aci.health.nsw.gov.au
Allergic conjunctivitis
Figure 53. Allergic conjunctivitis.
Figure 54. Vernal keratoconjunctivitis:
giant papillae of the upper tarsal conjunctiva.
13
History ndings
• Itchiness is the hallmark symptom
• Watery, red eyes may be a symptom
• Atopic history (asthma, eczema, allergic rhinitis
and conjunctivitis) and these are often
exacerbated together
Initial treatment
• Cool compresses as required
• Ocular lubricating drops, gels or ointments
(preservative free) qid available over the counter
• Consider systemic antihistamine or topical
antihistamine/mast-cell stabiliser
Notes
Allergic conjunctivitis may be severe and
long-standing, and occasionally results in
corneal ulcers and scarring.
If symptoms are not adequately treated with
the above treatment, consider a non-urgent
referral to an ophthalmologist.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
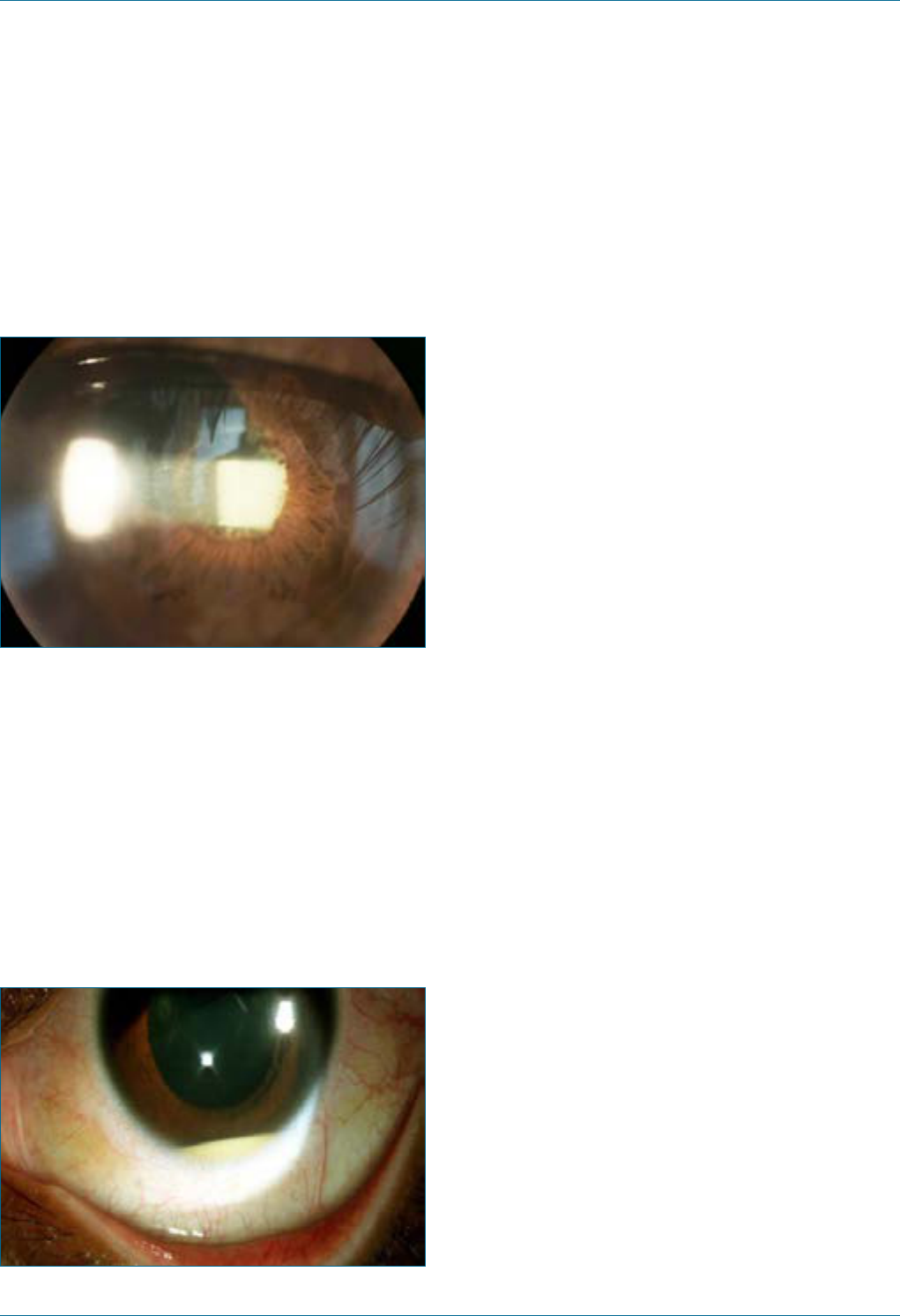
Eye Emergency Manual December 2023
Agency for Clinical Innovation 95 aci.health.nsw.gov.au
Iritis (anterior uveitis or an
anterior chamber inammation)
Figure 55. Anterior uveitis.
14
History ndings
• Red eye
• Pain (usually a deep ache)
• Photophobia
• Timing of onset of symptoms
• If recent intraocular surgery, (e.g. cataract or
injections), consider endophthalmitis
• History of autoimmune disease,
e.g. vasculitis or rheumatoid arthritis
Figure 56. Slit lamp photograph of hypopyon uveitis.
15
Examination ndings
Consider the following:
• Visual acuity may be decreased.
• The eye will often appear diffusely red, although
often more marked near the limbus.
• The pupil may be smaller than the contralateral
pupil, due to iris spasm. It may be irregular and
unreactive to light due to adhesions.
• The anterior chamber may appear cloudy from
suspended white blood cells and are. Look
closely for a hypopyon. Assess the cornea for
white cell inltrates (small white opacities
indicating bacterial infection).
• Check for uorescein staining.
• Check intraocular pressure.
Important differentials
• Endophthalmitis
• Uveitis (iritis)
• Severe corneal inammation from bacterial or
viral infection, or chemical burn
• Intraocular foreign body
Initial treatment
Consider the following:
• It is important to differentiate between the
possible diagnoses to determine the urgency of
referral. Endophthalmitis requires immediate
phone referral, as do most corneal conditions.
• Iritis can be a difcult diagnosis to make, so it is
best to refer early.
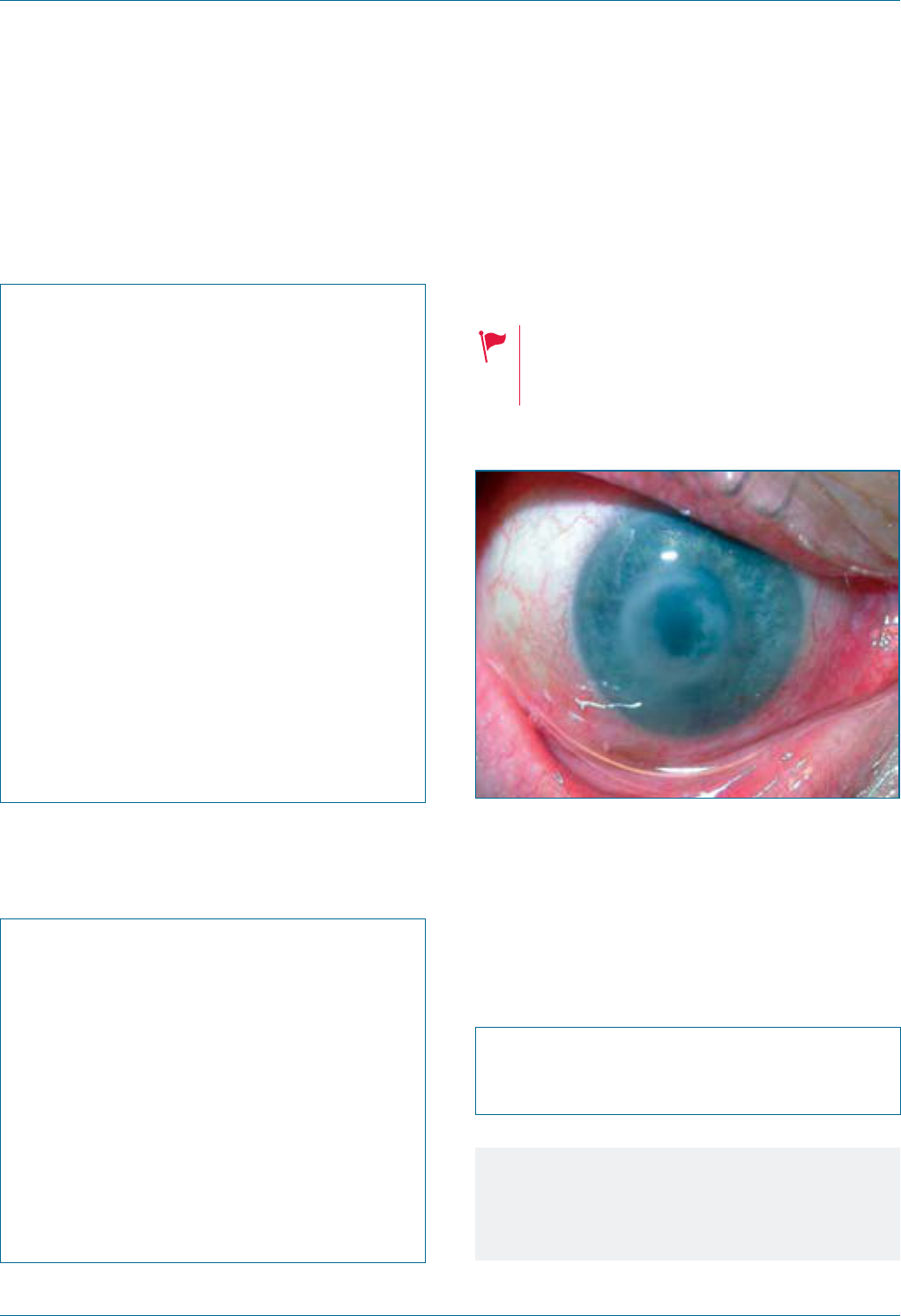
Eye Emergency Manual December 2023
Agency for Clinical Innovation 96 aci.health.nsw.gov.au
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Specic communication checklist
Consider the following:
; Recent intraocular surgery,
(e.g. cataract, injections)
; History of autoimmune disease
; Contralateral symptoms or a purely
unilateral process
; Visual acuity
; Presence of hypopyon
; Anterior chamber cells can be seen on
slit lamp
; Cornea appears normal
Bacterial or acanthamoebal ulcer
Seek an urgent referral to an ophthalmologist.
Seek an immediate consultation by phone.
May require admission for
microbiological investigation and
intensive antibiotic treatment.
Figure 57. Bacterial ulcer.
History ndings
• Often a history of contact lens wear
Specic communication checklist
Consider the following:
; History of contact lens wear and poor
lens hygiene
Notes
• Epithelial defect with an opacied base
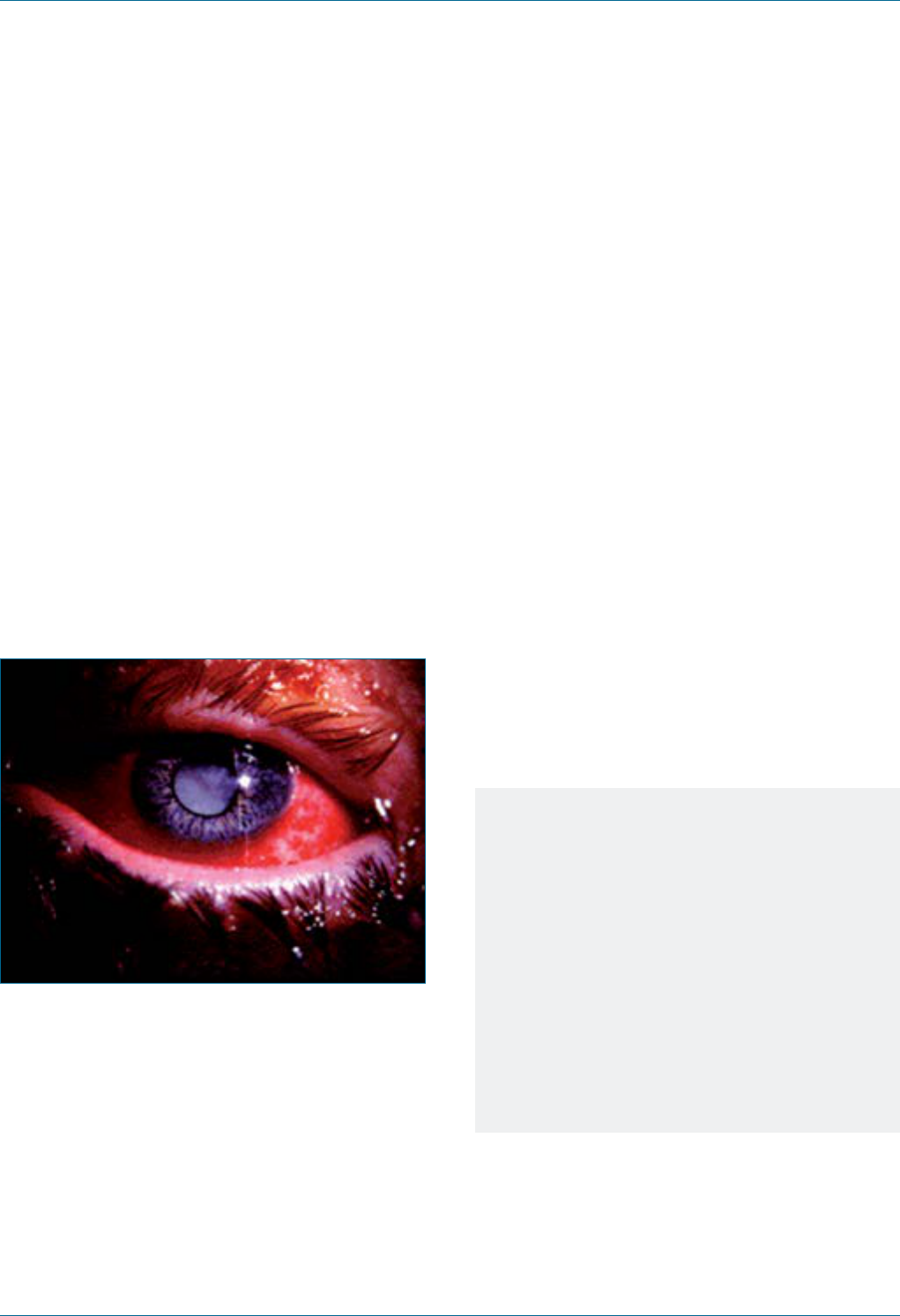
Eye Emergency Manual December 2023
Agency for Clinical Innovation 97 aci.health.nsw.gov.au
Bacterial conjunctivitis
Referral is required if:
• vision is affected
• the condition does not improve with treatment
after 2 days, or worsens
• the condition persists after 5 days of treatment.
Ophthalmia neonatorum, dened as conjunctivitis
within the rst 30 days of life, requires immediate
specialist input and treatment. It should be
considered a separate entity from the bacterial
conjunctivitis that affects older children and adults.
Figure 58. Bacterial conjunctivitis. Tender
inamed conjunctiva with purulent discharge
from the conjunctival sac.
History ndings
Consider the following:
• Bacterial conjunctivitis features no corneal or
anterior chamber involvement unless
gonococcal conjunctivitis is suspected.
• It is essential to administer uorescein to
exclude corneal ulcers.
• A patient with bacterial conjunctivitis presents
systemically well. The condition is common in
the elderly and children.
Initial treatment
• Regular hygiene to minimise secretion buildup
• Wash hands and use separate tissues to avoid
infection of the other eye or other people
• Topical antibiotics qid for 5 days
Notes
Non-gonococcal bacterial conjunctivitis
presents with bulbar conjunctival injection
and purulent or mucopurulent discharge.
Gonococcal bacterial conjunctivitis has
marked bulbar conjunctival and periocular
erythema and oedema.
It is important to exclude corneal inltrate or
ulcers that can lead to a sight-threatening
perforation, usually superiorly.
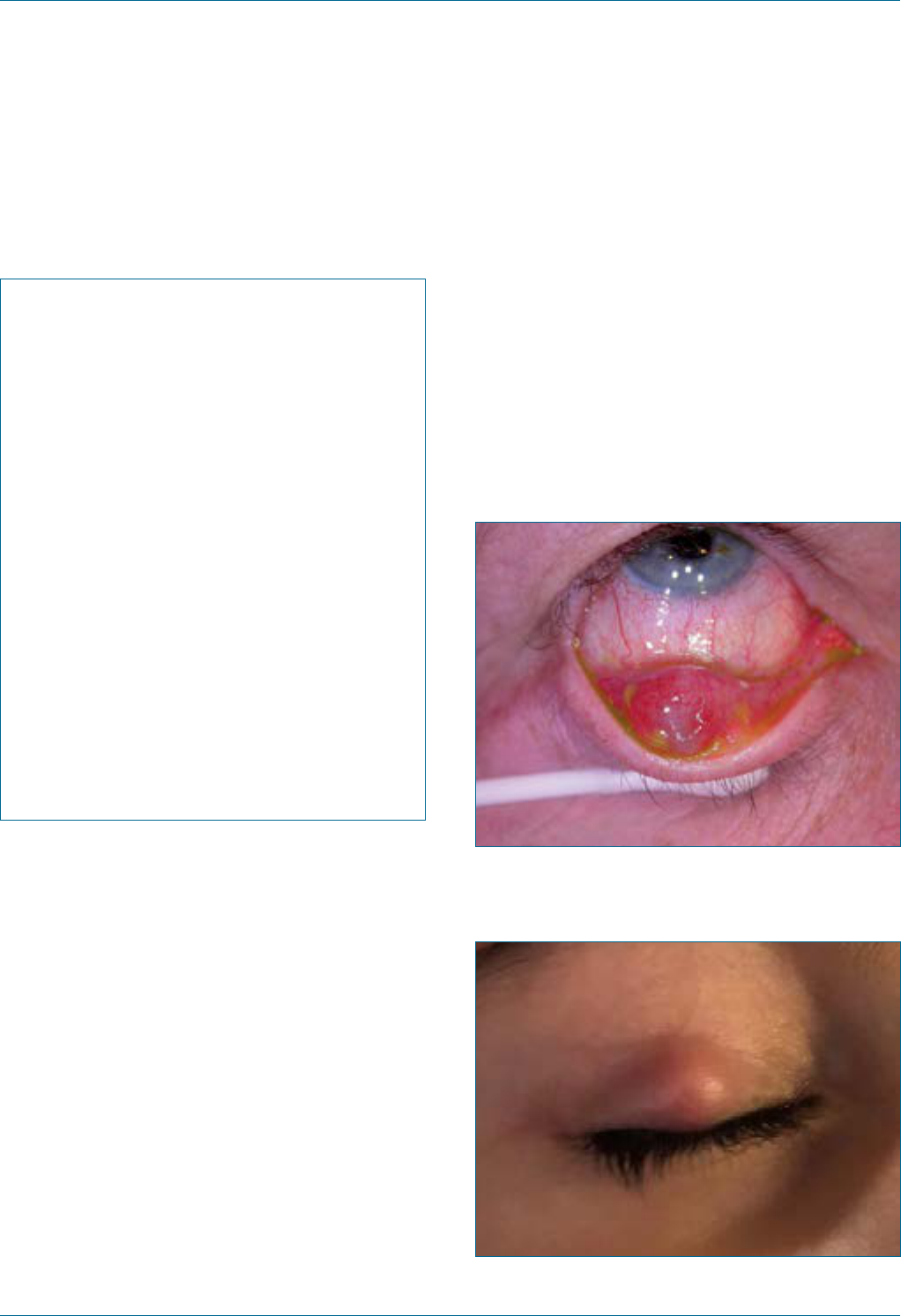
Eye Emergency Manual December 2023
Agency for Clinical Innovation 98 aci.health.nsw.gov.au
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Chalazion/stye
A chalazion swelling is due to a blocked sebaceous
gland. The lid margin is not involved unless a
secondary infection occurs.
A stye is an acute bacterial infection close to/
involving the lid margin. It is associated with lash
follicles and is painful.
Figure 59. Chalazion as seen from the tarsal
conjunctival side.
Figure 60. Chalazion in the upper eyelid, seen
from the skin side.
16
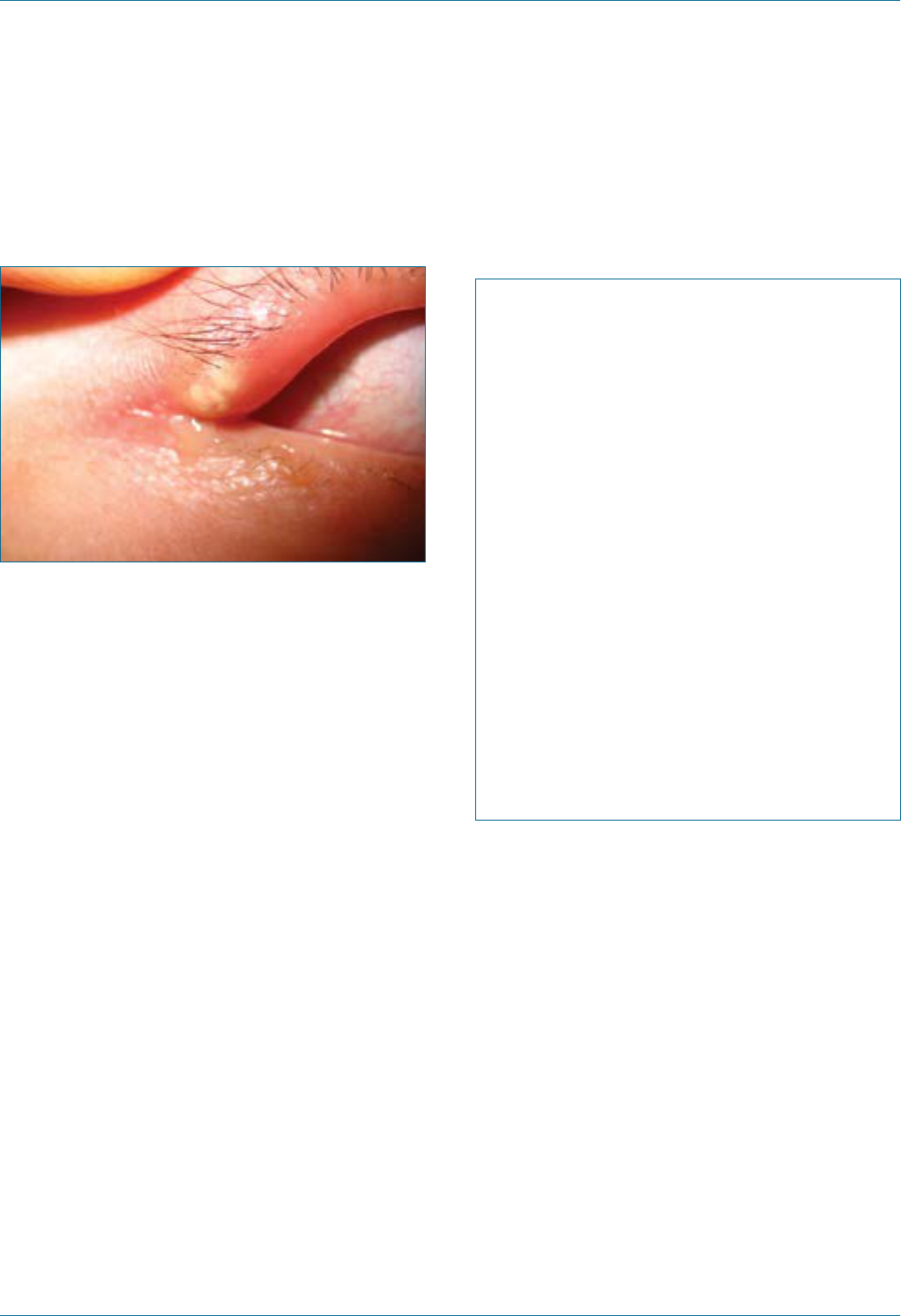
Eye Emergency Manual December 2023
Agency for Clinical Innovation 99 aci.health.nsw.gov.au
Figure 61. Stye in the upper eyelid, at the outer
canthus.
Initial treatment
Consider the following:
• Eyelid hygiene: the eyelid lump will often
disappear after several months of eyelid
hygiene. If bothersome, it may instead be incised
by an ophthalmologist.
• If acutely inamed with surrounding eyelid
inammation, treat as for preseptal cellulitis
with oral antibiotics (dosage as per preseptal
cellulitis) and warm compresses (twice daily)
and ensure ophthalmology follow-up.
Important differentials
Other eyelid lumps, including squamous cell
carcinoma or basal cell carcinoma.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
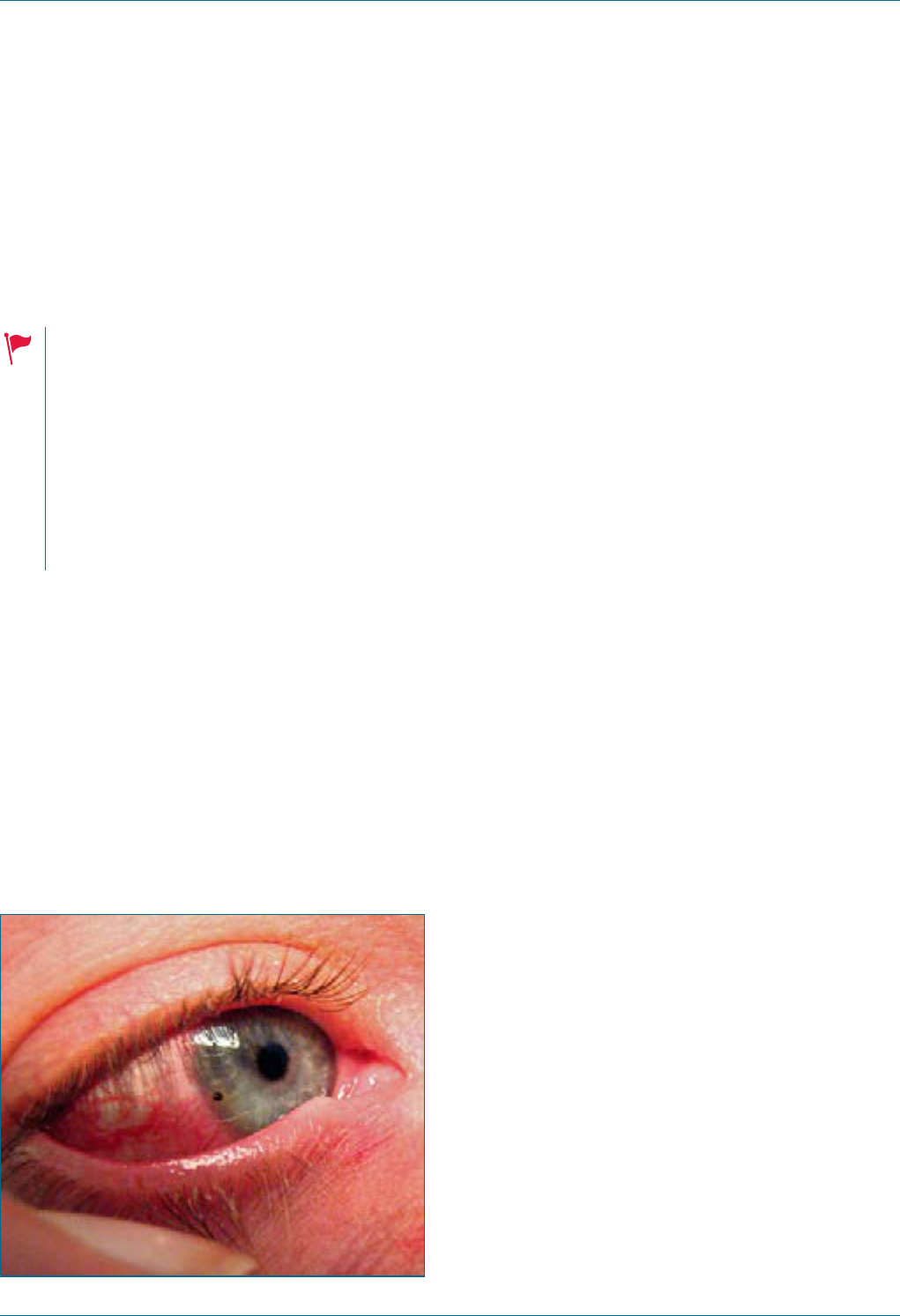
Eye Emergency Manual December 2023
Agency for Clinical Innovation 100 aci.health.nsw.gov.au
Corneal or conjunctival
foreignbody/corneal abrasion
Consider the following:
• Exclude a penetrating eye injury.
• Any foreign body penetration of the
cornea or retained foreign body
requires an urgent referral to an
ophthalmologist for immediate
consultation by phone.
• Discuss with senior staff if the
foreign body is centrally located on
the cornea (over the visual axis).
History ndings
Consider:
• what material the foreign body likely consists of,
e.g. dirt, glass, metal or organic
• the mechanism of impact (hitting metal on metal
is highly likely to cause a penetrating injury,
whereas grinding or welding rarely do so).
Figure 62. A small piece of iron has lodged in the
corneal periphery. Some rust can already be seen.
17
Examination ndings
1. Visual acuity: if not 6/6 then check with
a pinhole.
2. Slit lamp: assess for the size, site/s and nature
of foreign body and the depth of penetration.
3. Examine the cornea, anterior chamber, iris,
pupil and lens for any distortion that may
indicate ocular penetration and require urgent
referral to an ophthalmologist.
4. Evert the eyelids to exclude retained subtarsal
foreign bodies and remove them if appropriate.
5. Use uorescein to exclude Seidel-positive
corneal perforation and measure the size of the
epithelial defect.
Important differentials
Penetrating eye injury: partial thickness corneal
lacerations or full thickness corneal perforations.
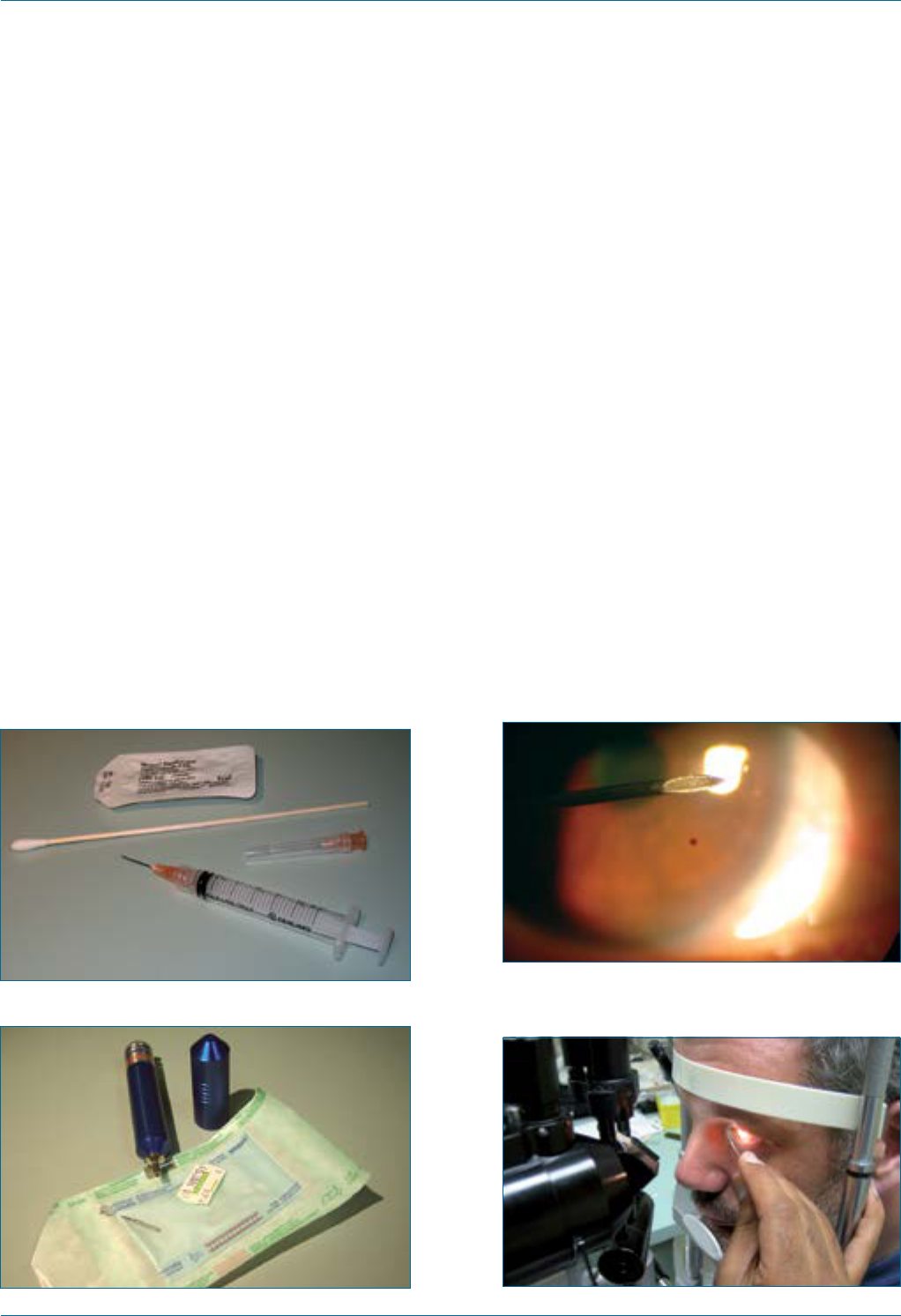
Eye Emergency Manual December 2023
Agency for Clinical Innovation 101 aci.health.nsw.gov.au
Initial treatment
Instruments
• Gloves
• Cotton bud (see Figure 63)
• 21–25g needle (see Figure 65)
• Optional: motorised dental burr (see Figure 64)
Bend the needle tip to 45° from the shaft. Use the
bevelled surface of the instrument angled away
from the patient’s eye. The patient’s forehead
should rest against the slit lamp (see Figure 66).
A motorised dental burr is ONLY for use outside
the central 5mm of the cornea. Always obtain
supervision if you are unfamiliar with
the procedure.
Figure 63. Eye drops, cotton bud and 21-25g
needle.
Figure 64. Motorised dental burr.
Procedure
1. Apply topical anaesthetic agents such as
Amethocaine 1%. Repeat every 30 seconds until
no further discomfort on instillation.
2. Position the patient at slit lamp. Strap or hold
the patient’s head with the help of a colleague
and ask the patient to focus on your ear.
3. Focus the slit lamp.
4. Use an oblique approach tangential to the
cornea. This is very important to reduce the risk
of corneal perforation (see Figure 65 and
Figure 66).
5. Angling a narrow slit beam to 45° can help
identify the depth of the foreign body and
ensure the safety of further removal attempts.
Figure 65. 25G needle angled away from
thepatient.
Figure 66. Corneal foreign body removal with
25Gneedle.
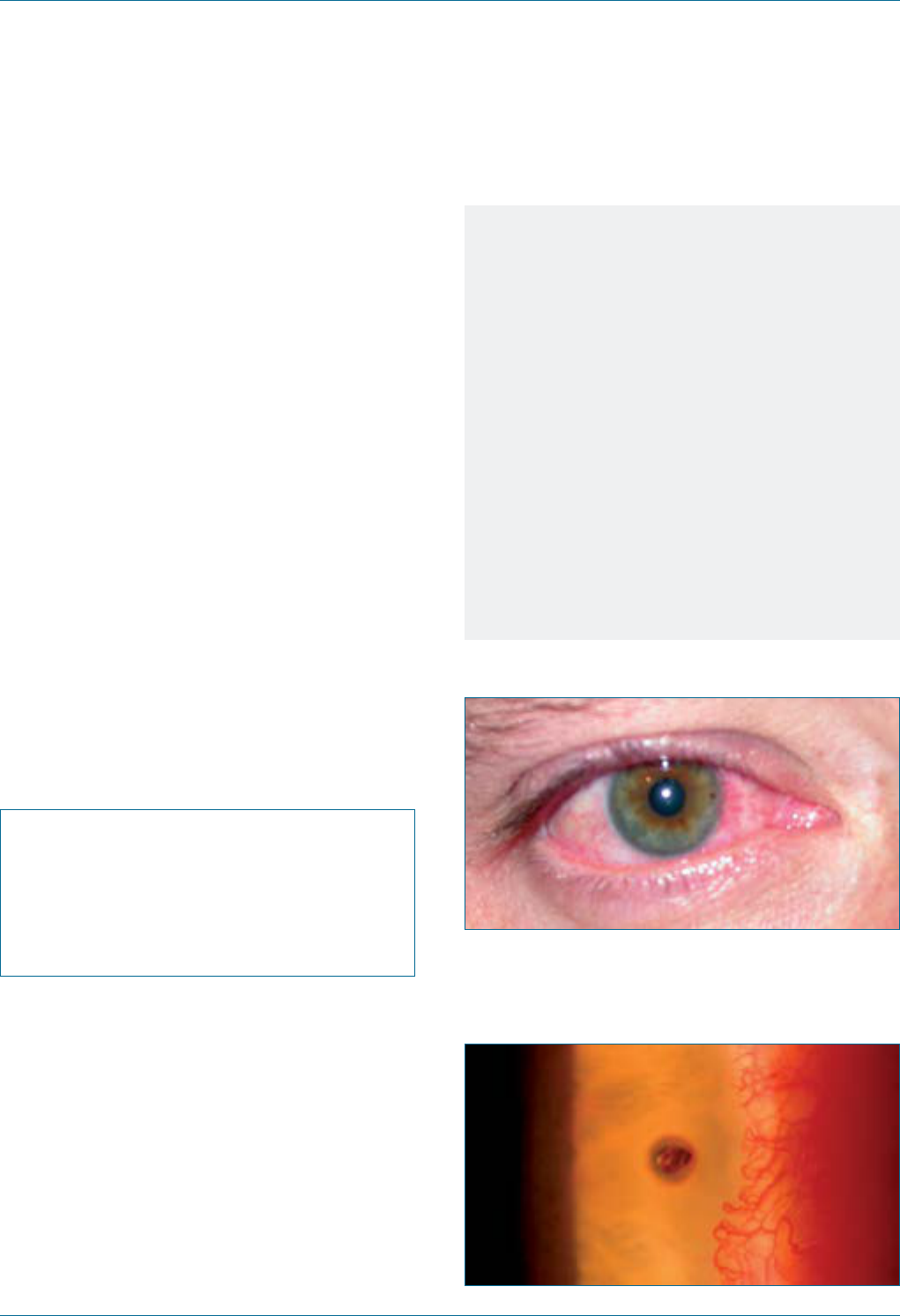
Eye Emergency Manual December 2023
Agency for Clinical Innovation 102 aci.health.nsw.gov.au
After removal
Consider the following:
• Use topical antibiotic (qid) and a cycloplegic
agent, (e.g. cyclopentolate 1% bd) for comfort.
Drops are often preferred and are equally as
effective as an ointment in healing a corneal
wound. Administer oral analgesia as required.
• It is not necessary to pad an eye. The
advantage of not padding is that the patient
can see with both eyes.
• The continued use of anaesthetic drops
is contraindicated.
• Assess daily visual acuity and slit lamp review
until complete healing of the defect. The
defect should be measured (see the section on
slit lamp examination) and compared with
previous ndings.
Specic communication checklist
Consider the following:
; Mechanism and likely type of foreign body
; Location of the foreign body on the cornea
; Presence of a residual foreign body or
rust ring
Notes
• Visual acuity may be reduced in a simple
corneal foreign body due to patient
discomfort or refractive errors. Administer
topical local anaesthetic, (e.g. Amethocaine),
darken the room and repeat using a pinhole.
• Retained organic material may lead to
infection; retained metallic foreign bodies may
lead to the formation of rust rings that produce
scarring and corneal epithelial defects.
• Rust rings in the visual axis should be
removed by an ophthalmologist or suitably
experienced emergency physician.
• Protective eyewear is useful but does not
exclude an open globe injury.
Figure 67. Corneal foreign body (macro).
Figure 68. Corneal foreign body (micro). A small
piece of iron has lodged near the margin of the
cornea. Some rust can already be seen.
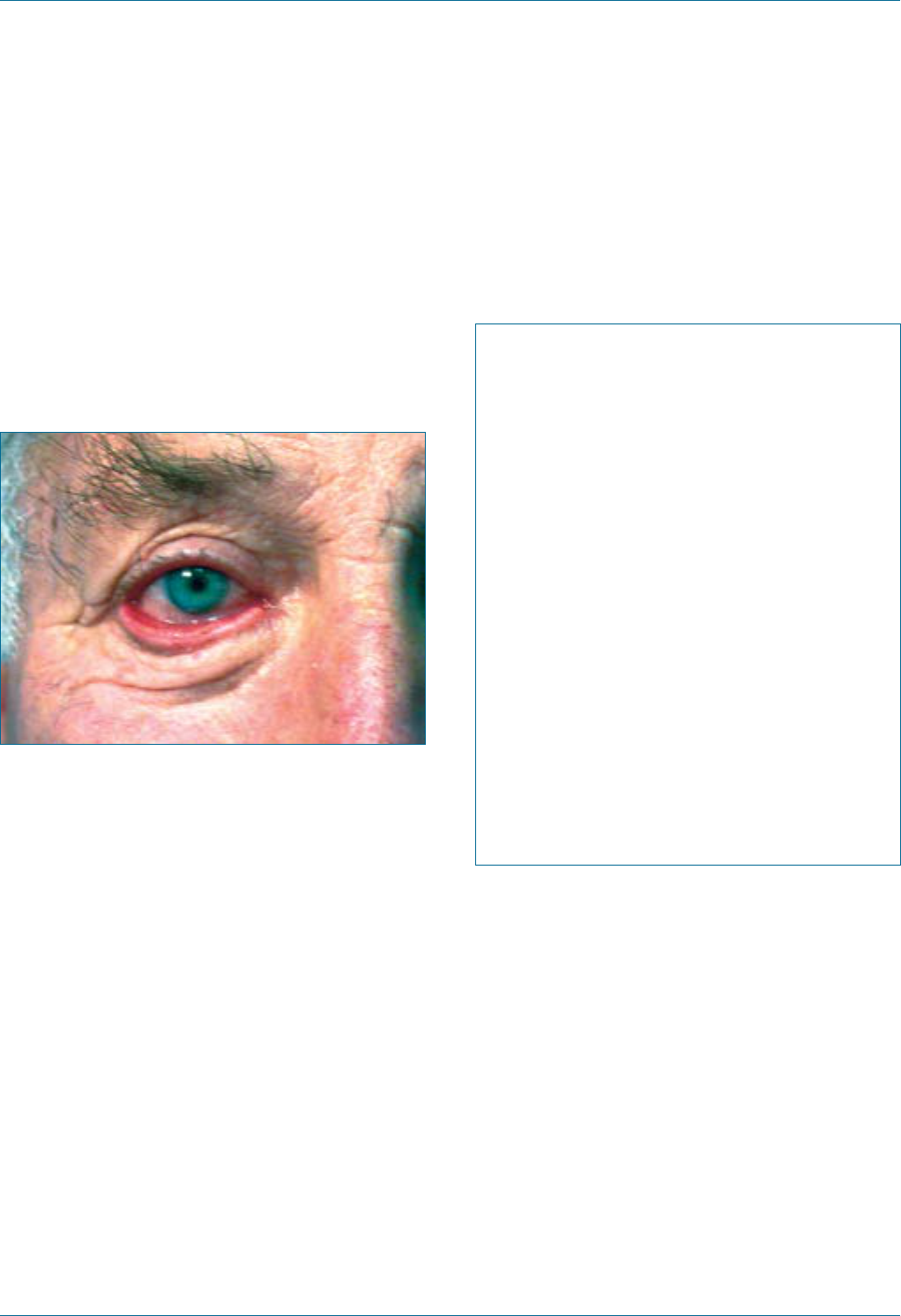
Eye Emergency Manual December 2023
Agency for Clinical Innovation 103 aci.health.nsw.gov.au
Ectropion
Ectropion is a lower eyelid turning outwards with
exposure of the tarsal conjunctiva. It is usually
age-related but may be caused by Bell’s palsy or
contracting scars on the skin of the lower eyelid
and cheek.
Figure 69. Ectropion.
Examination ndings
Consider the following:
• The lower eyelid is loose and can easily be
pulled millimetres from the globe. The tarsal
conjunctiva faces outward and often appears
red due to chronic exposure.
• The eye itself is white. Slit lamp examination
with uorescein may reveal some inferior
punctate erosions due to chronic exposure of
the inferior cornea and conjunctiva.
• The visual acuity is usually normal.
Initial treatment
• Topical lubrication, including night-time ointment
• Refer to an ophthalmologist for non-urgent
surgical management
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
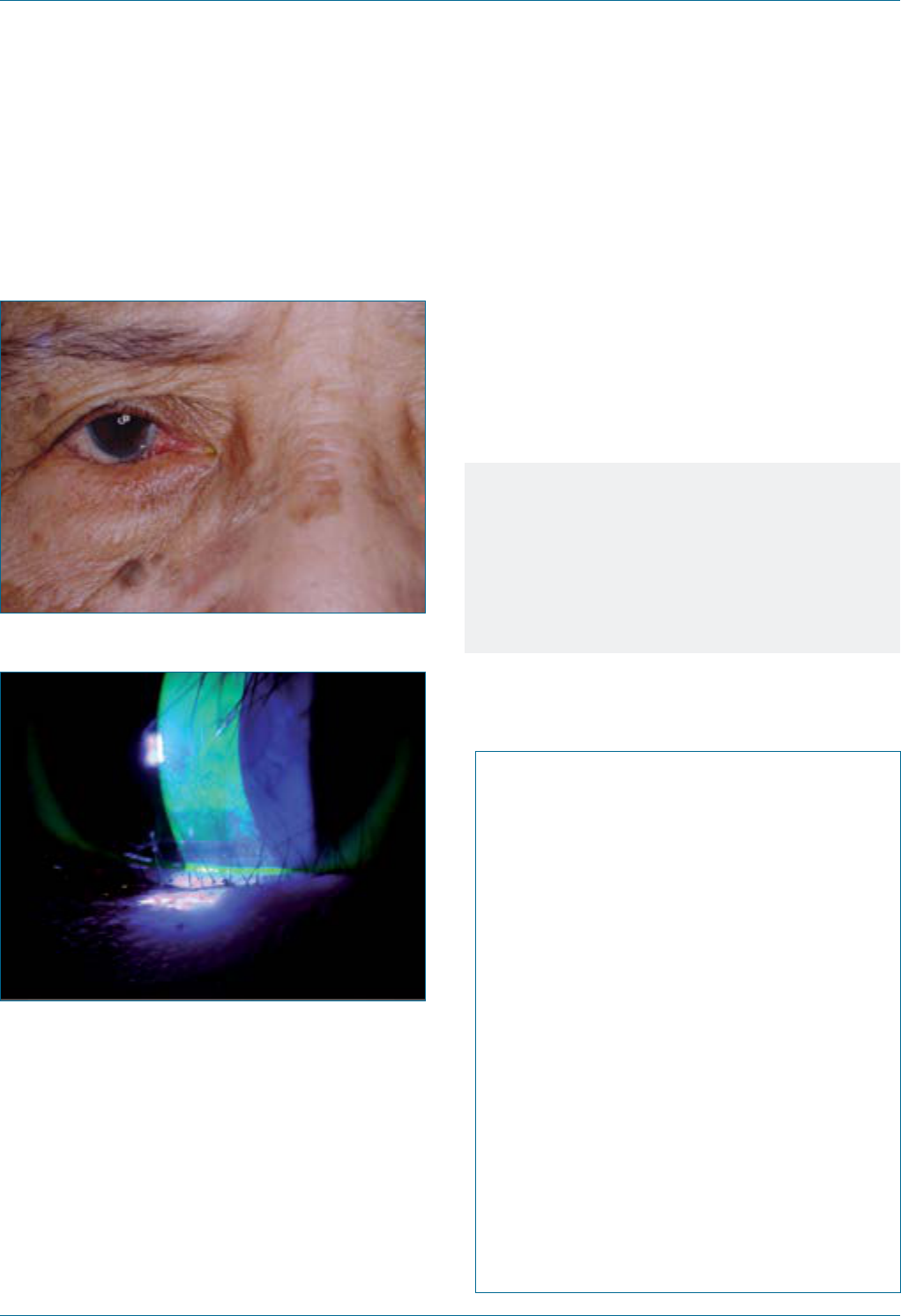
Eye Emergency Manual December 2023
Agency for Clinical Innovation 104 aci.health.nsw.gov.au
Entropion
Figure 70. Entropion.
Figure 71. Corneal abrasion.
History ndings
• Ocular irritation, foreign body sensation
or tearing
Examination ndings
Check the condition of the cornea with a slit lamp
and under blue light with uorescein:
• an intact cornea requires lubrication with a non-
urgent referral
• a corneal ulcer requires taping back the eyelid
away from the cornea, management as for a
corneal foreign body and an ophthalmology
follow-up
• a corneal infection (corneal white opacity and
ulcer) requires urgent referral to
an ophthalmologist.
Notes
Entropion may be age-related, or due to
conjunctival scarring from previous chemical
injury, trauma, surgery or systemic conditions
such as Stevens-Johnson syndrome. Surgery
may be required to reposition the eyelid.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
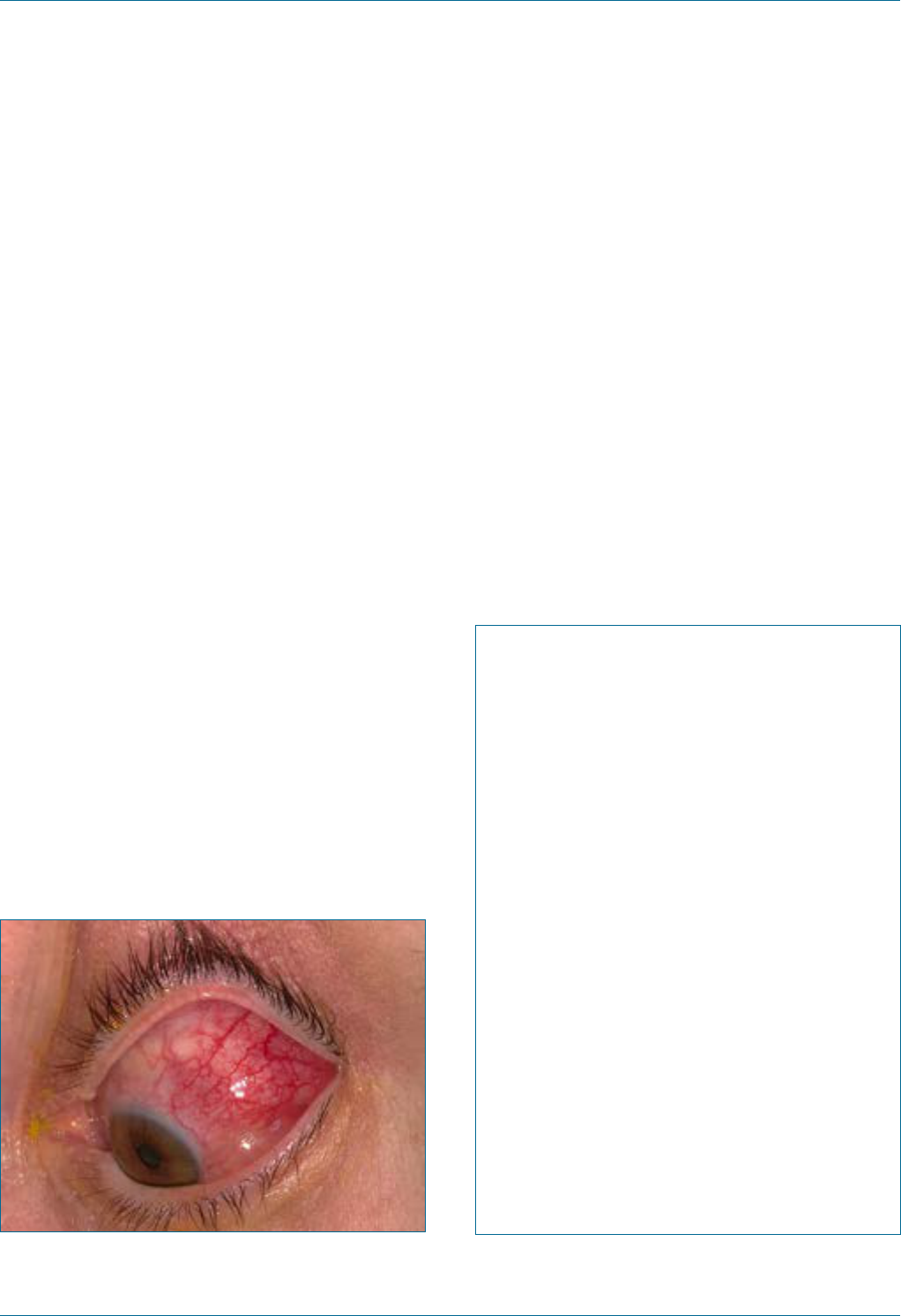
Eye Emergency Manual December 2023
Agency for Clinical Innovation 105 aci.health.nsw.gov.au
Episcleritis
Episcleritis is the inammation of the connective
tissue overlying the sclera.
History ndings
• Acute onset redness and discomfort, usually
focal
• May be unilateral or bilateral
• Vision is unaffected
Important differentials
Consider the following:
• Scleritis: pain wakes the patient from sleep and
the globe is tender to gentle pressure through
the closed eyelid
• Conjunctivitis: redness tends to be more
generalised and the tarsal conjunctiva (evert the
lower eyelid) is involved
• Pterygium (when inamed): raised nasal
pterygium, with localised redness, possibly with
some punctate conjunctival staining
with uorescein
Figure 72. Episcleritis of the eyeball.
18
Initial treatment
• Try frequent (hourly) preservative-free
lubricating drops or gels/ointments
• Minimise exposure to sun, wind
and air-conditioning
• Oral NSAIDs may be helpful
• Non-urgent referral to an ophthalmologist if
recurrent or concerns regarding
possible scleritis
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
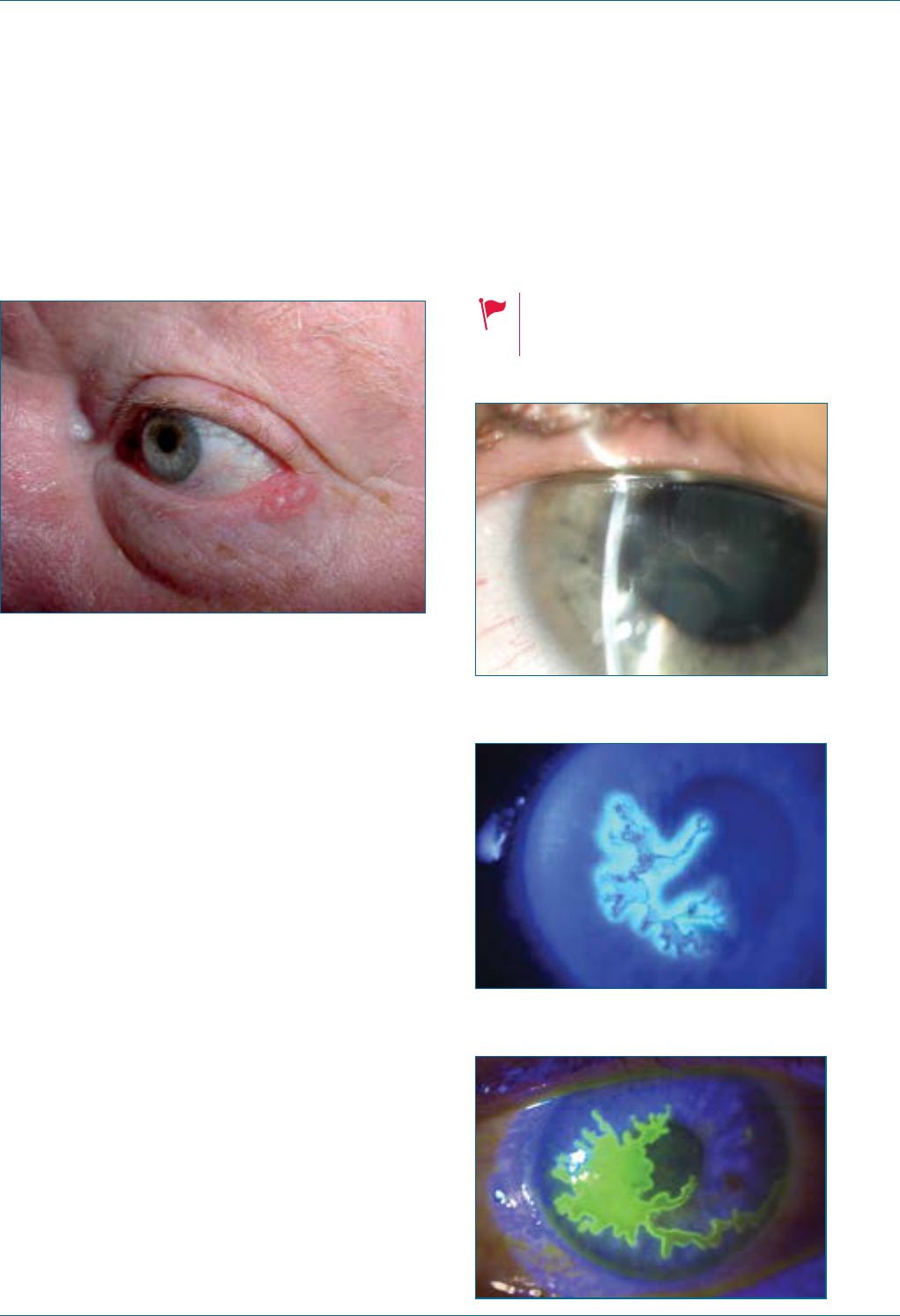
Eye Emergency Manual December 2023
Agency for Clinical Innovation 106 aci.health.nsw.gov.au
Eyelid lesion
Figure 73. Lesion of left lower eyelid.
Initial treatment
Provided there is no overt eyelid infection/
inammation and no ocular involvement, non-
urgent referral is required. Consider
topical antibiotics.
Herpes simplex virus keratitis
(HSV/HSK)
• Herpetic blepharoconjunctivitis
• Ophthalmia neonatorum
Figure 74. Herpes simplex keratitis.
Figure 75. Herpes simplex keratitis
dendritic ulcer with terminal bulbs.
Figure 76. Herpes simplex keratitis
with steroid complication.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 107 aci.health.nsw.gov.au
History ndings
• Unilateral red eye
• Mild blurring of vision
• May have a history of similar episodes in the
same eye or of cold sores
• Ask about possible systemic
immunosuppression
• Topical steroid use will signicantly worsen
this condition
Examination ndings
Consider the following:
• Use uorescein to ascertain the nature of any
epithelial defect.
• Check for dendritic ulcer/s, which are
usually unilateral.
• Multiple previous episodes may have also led
to cornea stromal scarring and
decreased vision.
• A dendritic ulcer (affecting the corneal
epithelium) may also be complicated by
inammation of the deeper corneal layers,
which, if left untreated, can sometimes lead
to perforation. Look for corneal opacication,
loss of iris detail through a cloudy cornea and
reduced vision.
Initial treatment
• Treat with topical acyclovir
• Avoid topical steroid
• Refer to an ophthalmologist within 1–2 days
Specic communication checklist
Consider the following:
; History of cold sores
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or diffuse/
involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber cells,
blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Notes
• Stain with uorescein as the cornea may
develop microdendrites or ulceration.
• Atopic patients will often have more
severe disease.
• Children may develop blepharoconjunctivitis
in primary herpes simplex infection. It may be
bilateral or unilateral, with periocular
vesicles or conjunctivitis.
• Herpes simplex virus keratitis may also be
associated with eczema in children.
• Children will often require admission and
systemic antivirals.
• See the section on ophthalmia neonatorum if
HSV ocular disease in the rst month of life
is suspected.
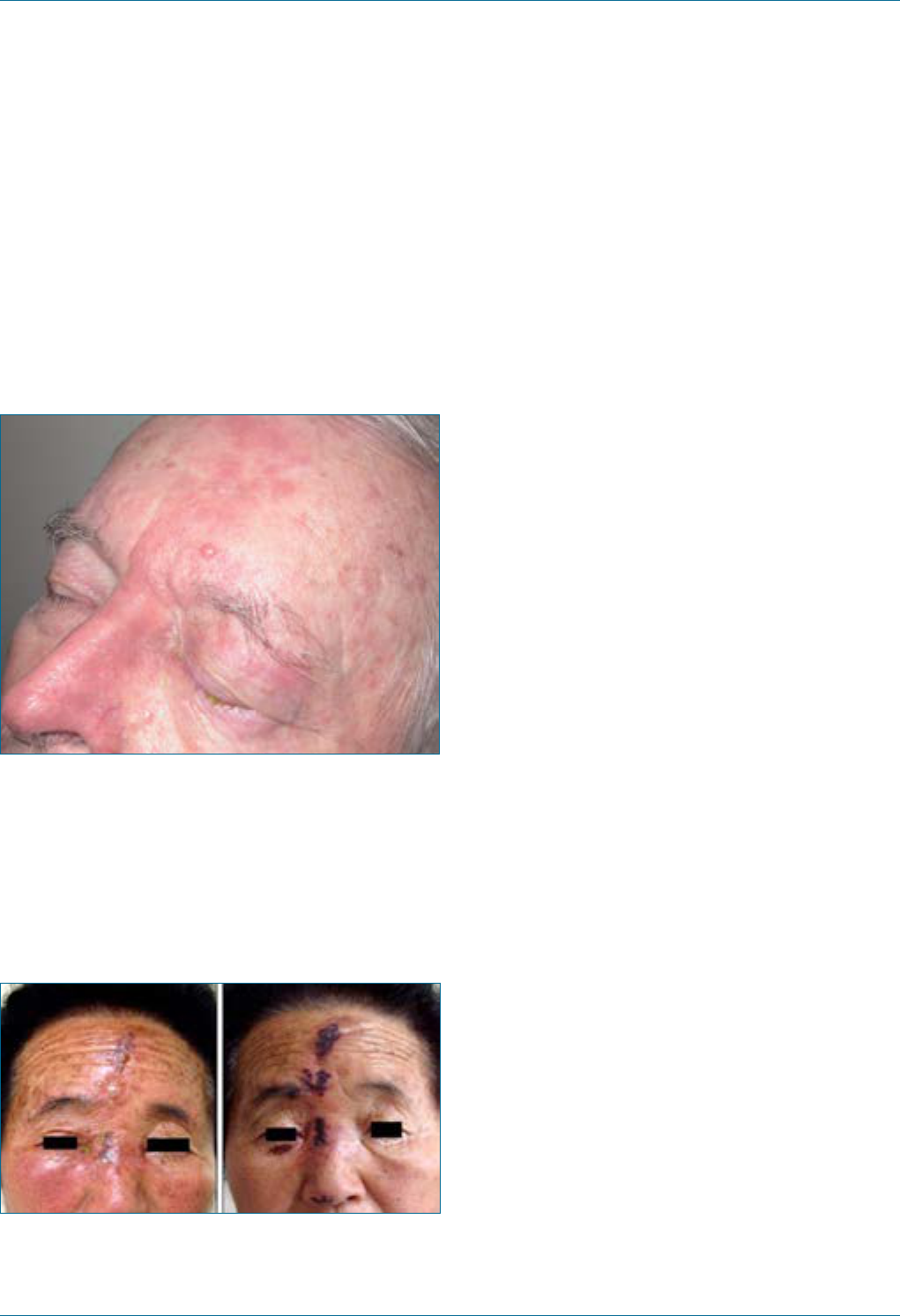
Eye Emergency Manual December 2023
Agency for Clinical Innovation 108 aci.health.nsw.gov.au
Herpes zoster ophthalmicus
(HZO)/shingles
Seek an urgent referral to an ophthalmologist.
Contact an ophthalmologist on the same day if
ocularinvolvement is suspected.
Figure 77. Herpes zoster.
Figure 78. Erythema, oedema, vesiculobullous
eruptions and crusted erosions were present on the
right side of the forehead and yellowish lacrimation
was noted from the right orbital area in the rst
image. Second image shows improvement after 7
days of treatment. Note the vesicles and crusts on
the top and side of the nose (Hutchinson’s sign).
19
Herpes zoster ophthalmicus is shingles affecting
the ophthalmic branch of the trigeminal nerve
(V1). It may or may not involve the eye, which also
has sensory innervation from V1.
History ndings
• Unilateral vesicles over the forehead, scalp
and eyelid
• Often associated with severe pain
• Ask about systemic immunosuppression,
(e.g. drugs, HIV and cancer)
Examination ndings
Consider the following:
• Check visual acuity, extraocular movements,
intraocular pressure and pupils, including
checking for relative afferent pupillary
defect (RAPD).
• A general inspection will reveal a vesicular
rash, which is usually unilateral and does not
cross the midline. Lesions will crust after a
few days.
• Ocular ndings may include blepharitis (lid
vesicle and redness), conjunctivitis, corneal
ulcers (pseudodendrites), viral keratitis
(corneal opacities or clouding and oedema),
signs of iritis, retinitis and optic disc swelling.
Initial treatment
Oral antivirals should ideally be commenced
within 72 hours of the appearance of the rash.
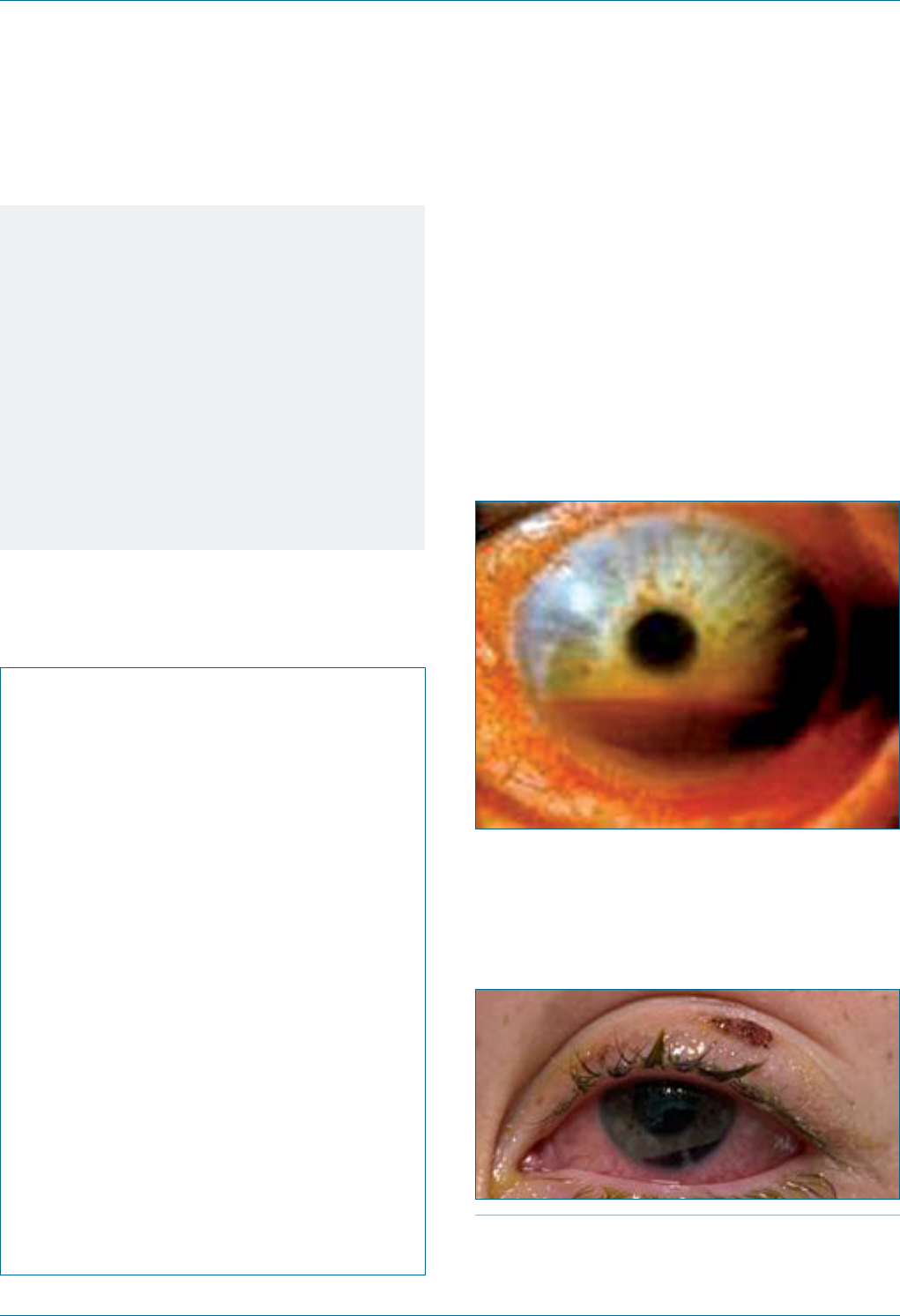
Eye Emergency Manual December 2023
Agency for Clinical Innovation 109 aci.health.nsw.gov.au
Notes
• If the tip of the nose is involved
(Hutchinson’s sign), there is a higher risk
of ocular involvement.
• Always suspect ocular involvement if the
eye is red, vision is reduced or uorescein
staining is present.
• Ocular involvement should prompt
ophthalmic referral within 24 hours, or
earlier if the vision is affected or there are
abnormalities on fundoscopy.
Section communication checklist
Consider the following:
; History of cold sores often exists
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some contralateral
symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Hyphaema
Seek urgent ophthalmology referral and immediate
consultation by phone.
Hyphaema is the presence of blood in the anterior
chamber. It may present as a ne suspension of red
blood cells in aqueous (micro-hyphaema) or as a
blood-aqueous uid level (macro-hyphaema) as
shown in Figure 79 and Figure 80).
Figure 79. Hyphaema.
Figure 80. A 2mm macro-hyphaema, as measured
from the inferior limbus. Note the pupil is dilated
inferiorly. This may signify a focal traumatic
mydriasis, which is often present in a blunt (closed-
eye) injury.
Photograph courtesy of Lawrence B. Stack, MD, Professor of
Emergency Medicine and Paediatrics, Vanderbilt University Medical
Center, Nashville, Tennessee, USA.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 110 aci.health.nsw.gov.au
History ndings
• Usually trauma-related
• Consider non-accidental injury in children and
blood dyscrasias
Examination ndings
• Check visual acuity and pupils
• Check intraocular pressure as this is often
acutely elevated
• Check for other evidence of blunt eye injury and
orbital fracture
Initial treatment
• Protect the eye with a shield
• Avoid pressure on the eye
• Bed rest
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal,
i.e. cloudy, opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Notes
• Permanent vision loss may be caused by
elevated intraocular pressure, cornea blood
staining with prolonged hyphaemia and
associated ocular blunt eye injuries,
(e.g. retinal detachment).
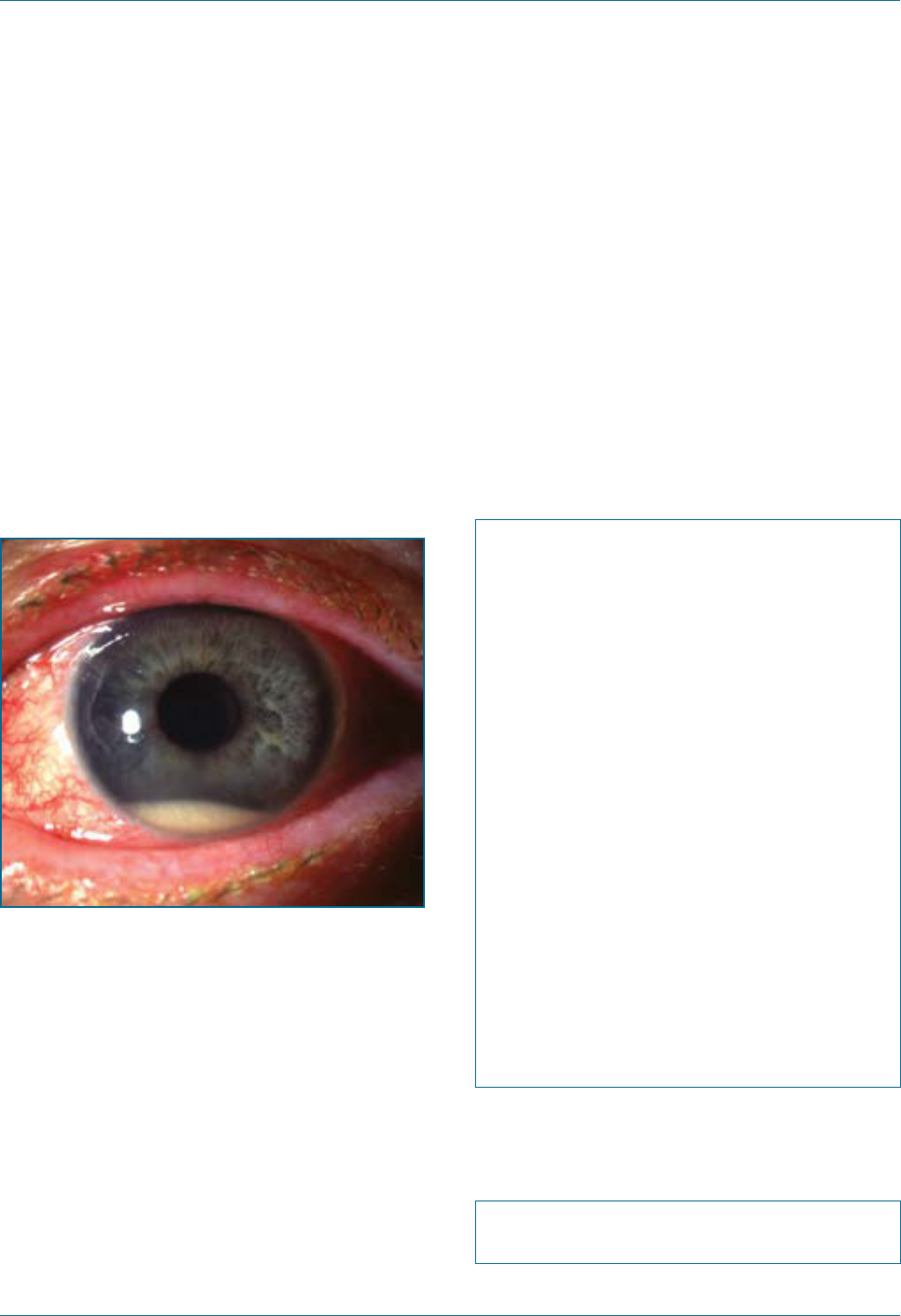
Eye Emergency Manual December 2023
Agency for Clinical Innovation 111 aci.health.nsw.gov.au
Hypopyon
Seek urgent ophthalmology referral and immediate
consultation by phone.
Hypopyon is the presence of pus in the anterior
chamber. It is a sinister sign and is usually
associated with orid intraocular infection
(endophthalmitis), requiring immediate referral to
an ophthalmologist.
Figure 81. Hypopyon with a visible accumulation
of white cells inferiorly seen in severe uveitis.
History ndings
• History of intraocular injection, cataract,
glaucoma or other ocular surgery
• History of eye trauma, intraocular foreign body
or contact lens wear
• Pain, redness or blurring/loss of vision
• Current eyedrops used
Examination ndings
• Visual acuity and pupils
• Slit lamp examination looking for a leaking open
wound (Seidel’s test)
• Check intraocular pressure
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some contralateral
symptoms
; Best (pinhole) visual acuity of each eye
; Eyelid involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Specic communication checklist
Consider the following:
; Recent ocular surgery or trauma
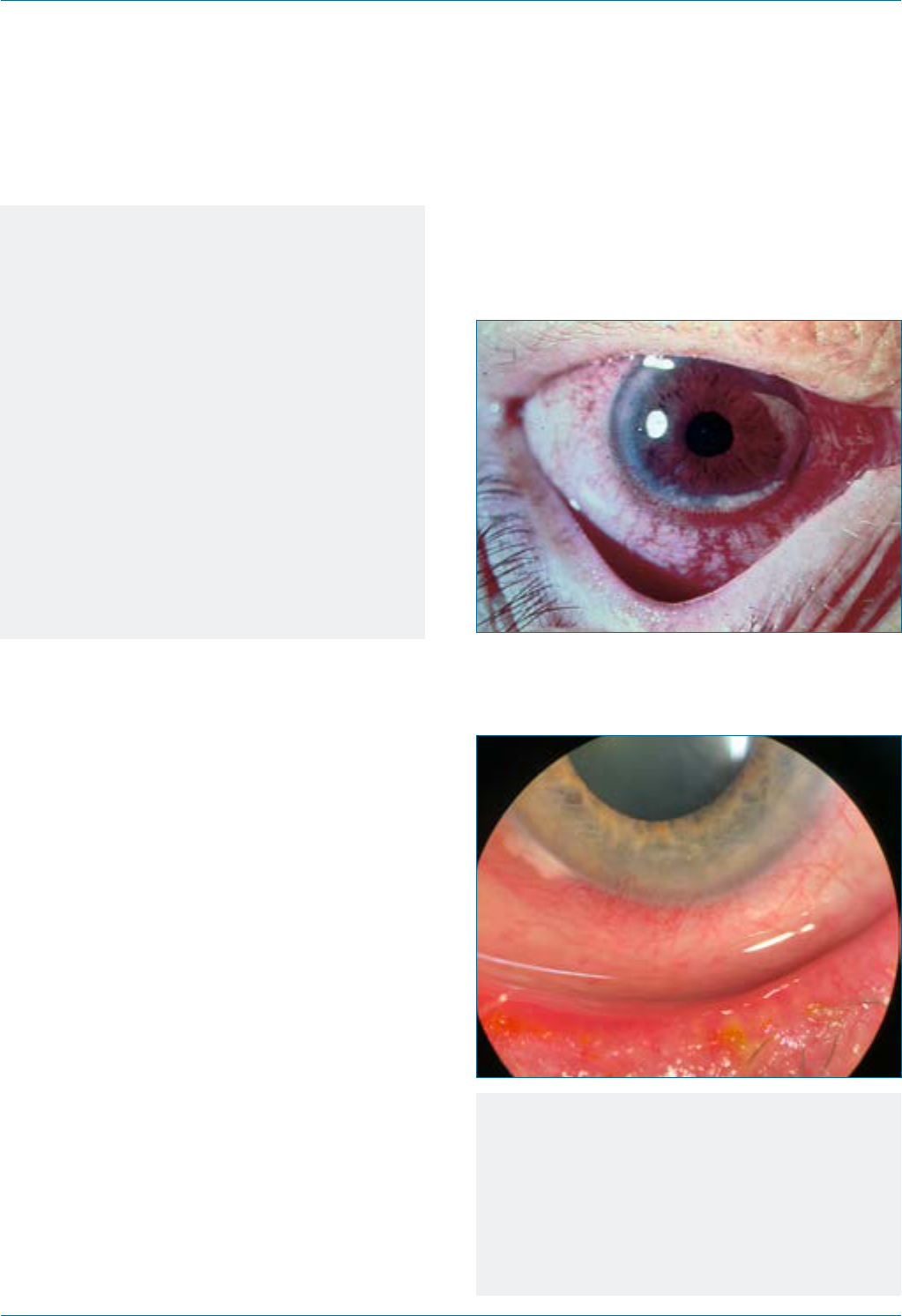
Eye Emergency Manual December 2023
Agency for Clinical Innovation 112 aci.health.nsw.gov.au
Notes
Hypopyon is a sign that there is severe anterior
chamber inammation. This may be due to
endophthalmitis, a severe corneal infection, or
orid uveitis. It should be urgently managed as
endophthalmitis until proven otherwise.
Intravitreal injection (for macular
degeneration) or cataract surgery in the past
1–2 weeks accounts for most cases
of endophthalmitis.
Treatment is immediate intravitreal antibiotics
administered by the ophthalmologist. Failure
to institute prompt treatment often leads to
permanent loss of vision or the eye.
Marginal keratitis
Seek immediate referral to an ophthalmologist.
Figure 82. Marginal keratitis.
Figure 83. Slit lamp photograph of the right eye
with marginal keratitis between 12 o’clock to 2
o’clock positions along with a pannus.
20
Notes
Marginal keratitis:
• is secondary to blepharitis
• features ulcers situated at the
corneal periphery
• requires discussion with an ophthalmologist.
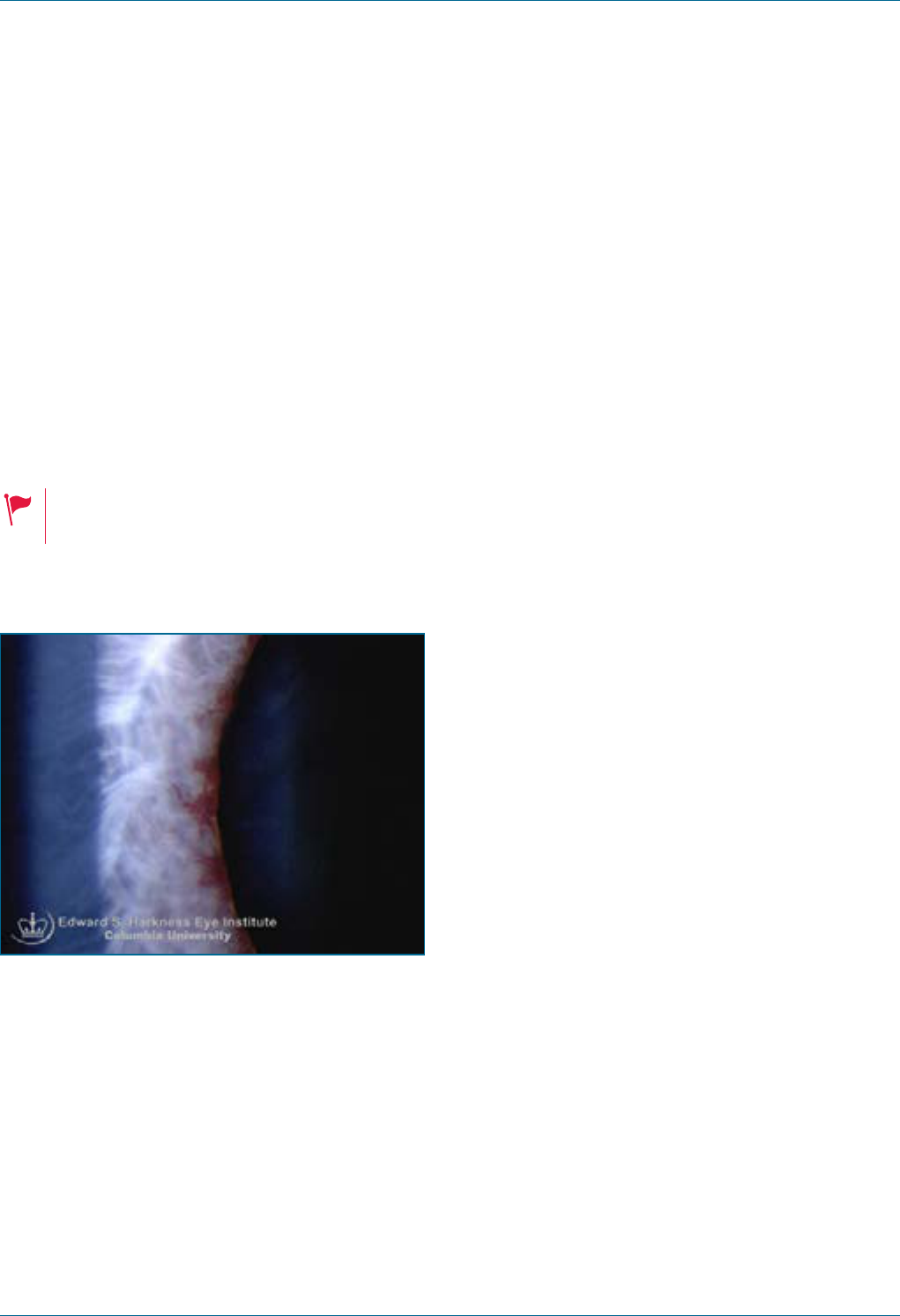
Eye Emergency Manual December 2023
Agency for Clinical Innovation 113 aci.health.nsw.gov.au
Neovascular glaucoma
Seek an urgent referral to an ophthalmologist (<24hr).
Neovascular glaucoma is a type of glaucoma that is
caused by vascular injury to the eye, including
diabetic retinopathy, central retinal vein occlusion,
central retinal artery occlusion and ocular
ischaemic syndrome. The intraocular pressure is
often >35mmHg, and it is a difcult condition
to treat.
Poor vision and high intraocular pressure
(cloudy cornea, nausea or vomiting).
Figure 84. Tufts of neovascularisation at the
peripupillary margin.
21
History ndings
Pain, red eye, photophobia and reduced vision. May
have a history of sudden and persistent visual loss
and/or multiple cardiovascular risk factors.
Examination ndings
• Vision may be reduced due to the underlying
cause of ocular ischaemia
• Iris neovascularisation and conjunctival erythema
• Cloudy cornea if intraocular pressure is raised
• Pupils may be xed, dilated or show an RAPD
• Fundus examination may show retinal pathology
resulting in ischaemia, e.g. diabetic retinopathy
or central retinal vein occlusion (CRVO)
Investigations
• Cardiovascular risk factor work up
Important differentials
• Acute angle closure or uveitic glaucoma
Initial treatment
• Consult the ophthalmology team to establish a
diagnosis and underlying cause
• Address cardiovascular risk factors
Eye Emergency Manual December 2023
Agency for Clinical Innovation 114 aci.health.nsw.gov.au
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Specic communication checklist
Consider the following:
; Medical history and ocular history
; Cardiovascular risk factors
; Visual acuity, pupil assessment, anterior
segment ndings and intraocular pressure
if able to obtain
Ophthalmia neonatorum
(neonatal conjunctivitis)
Seek an urgent referral to an ophthalmologist,
paediatrician and infectious diseases specialist.
This condition often requires admission to
hospital for investigation and treatment.
Ophthalmia neonatorum is an acute purulent
conjunctival infection in the rst weeks of life.
Organisms of concern include Neisseria
gonorrhoeae (N.gonorrhoeae) (especially within
the rst 5 days), Chlamydia trachomatis (C.
trachomatis) (up to 60 days) or HSV. Scarring or
perforation can occur and any signs of
gonococcal sepsis should be elicited. Gonococcal
ophthalmia presents with orid swelling.
Chlamydial ophthalmia usually presents with
milder chemosis. HSV is seen within 2 weeks after
birth and may have typical vesicles on the eyelid
margin. Exclude corneal dendrite with
uorescein staining.
Ophthalmia neonatorum is a serious
infection due to the lack of immunity in
the neonate. Systemic complications
include meningitis, sepsis, arthritis
and pneumonia.
Sight-threatening ocular complications
include corneal ulcer and perforation.
History ndings
• Previous or current sexually transmitted
maternal infection
• Vaginal delivery
• Occurs in the rst month of life
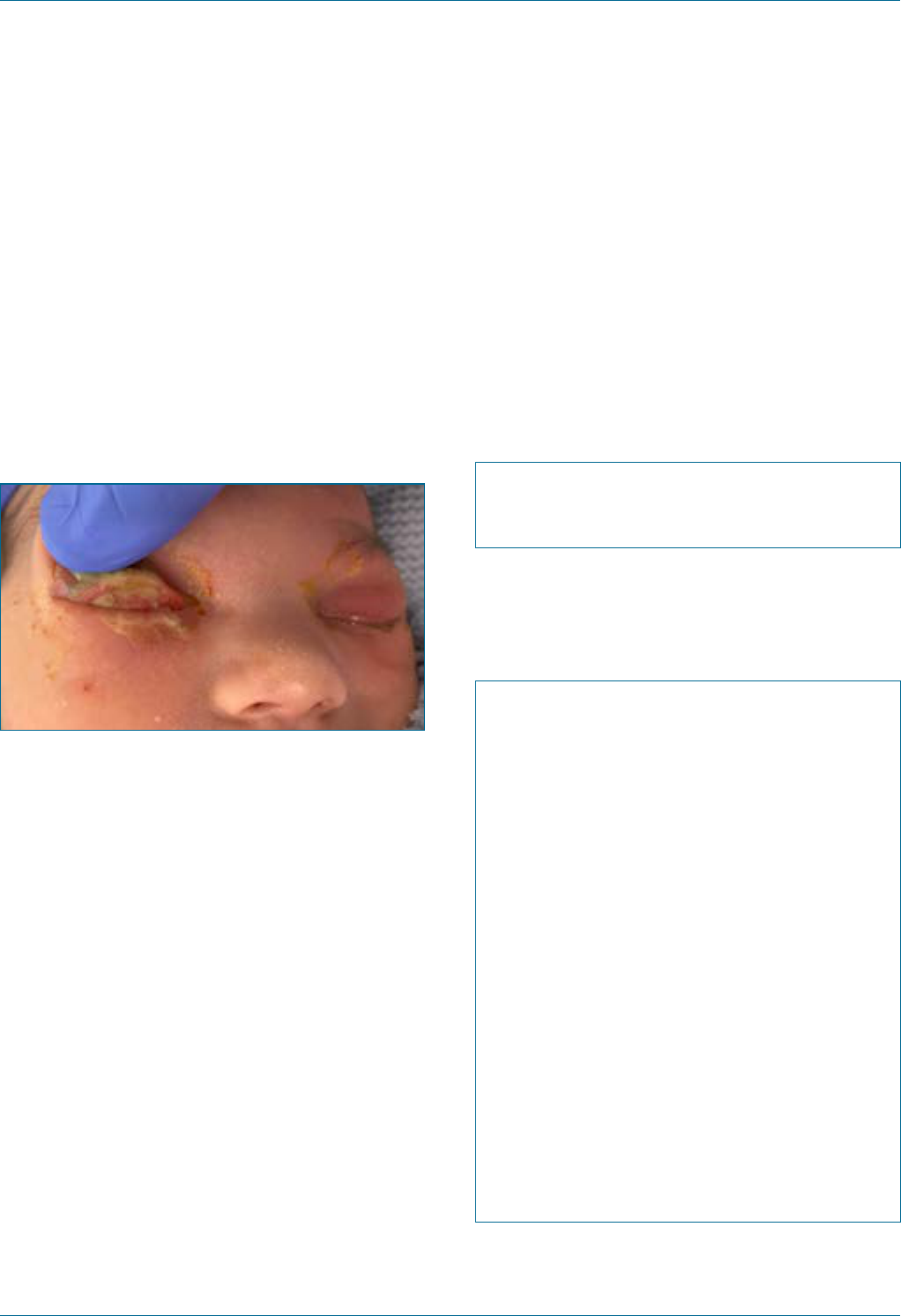
Eye Emergency Manual December 2023
Agency for Clinical Innovation 115 aci.health.nsw.gov.au
Examination ndings
• Bilateral mucopurulent discharge typically
• Red eyes and diffuse conjunctival injection
• Perform uorescein staining to exclude corneal
ulcers or dendrites
Figure 85. Newborn with gonococcal ophthalmia
neonatorum caused by a maternally transmitted
gonococcal infection.
22
Investigations
• Swab for urgent microscopy and culture
• Consider blood cultures to exclude sepsis or
gonococcal infection concerns
Important differentials
Consider the following:
• Dacryocystitis presents with swelling and
erythema just below the inner canthus, but the
eye appears white.
• Nasolacrimal duct obstruction involves high
tear lm and reux of mucopurulent material
from the punctum when pressure is applied
over the lacrimal sac. The eye is white. Symptoms
usually appear in the rst 1–2 months of life.
Initial treatment
• Urgent systemic and topical antibiotic treatment
• Referral to a sexual health clinic for treatment of
parents and contact tracing
Specic communication checklist
Consider the following:
; Ask parents about sexually transmitted
infections
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some contralateral
symptoms
; Best (pinhole) visual acuity of each eye
; Eyelid involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
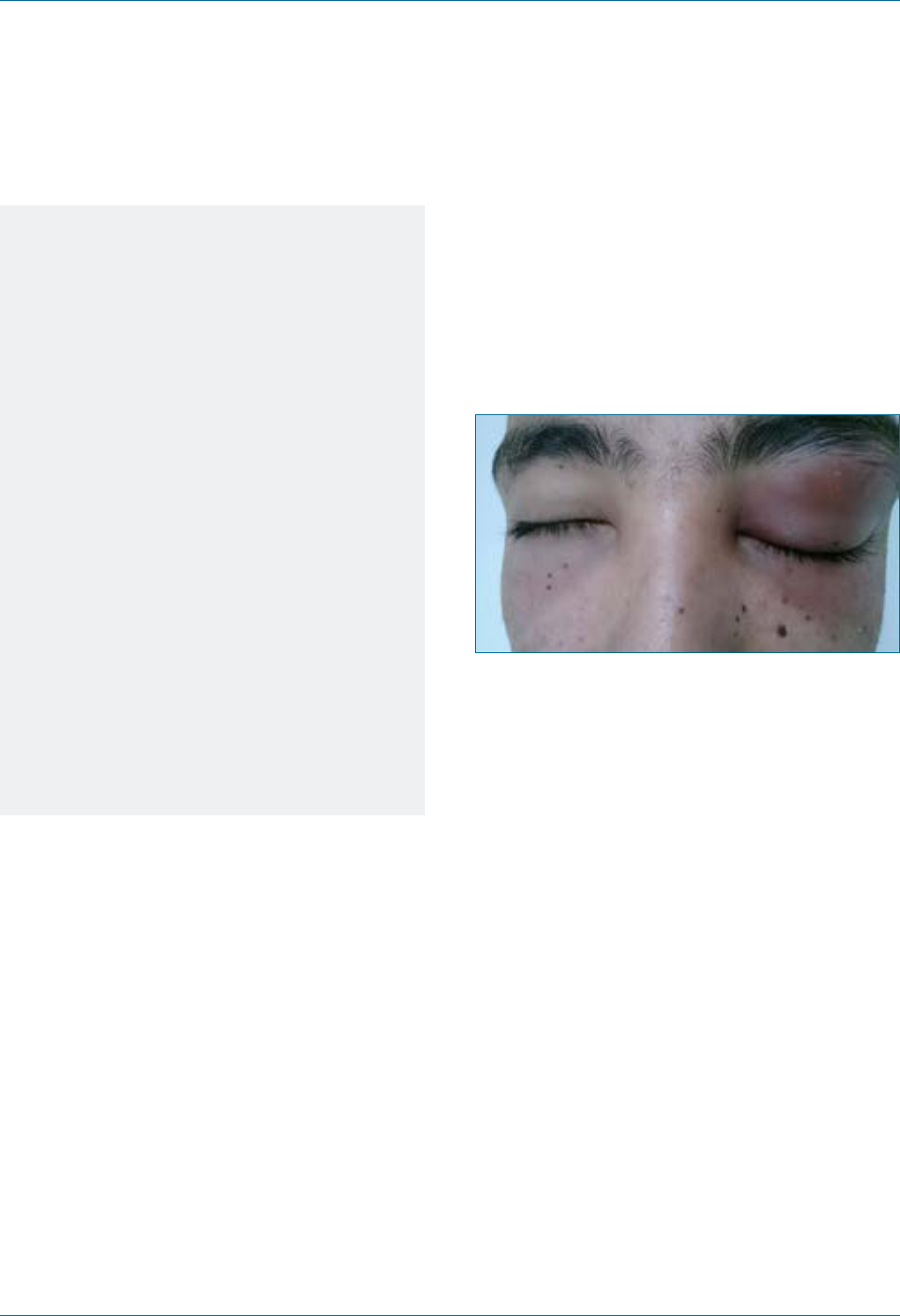
Eye Emergency Manual December 2023
Agency for Clinical Innovation 116 aci.health.nsw.gov.au
Notes
Consider the following:
• As a notiable disease, parents must be
investigated and treated. Seek a referral to
a sexual health clinic.
• Causes include gonorrhoea, chlamydia or
HSV infections.
• A gonorrhoeal infection is usually seen
within 3–4 days after birth, with severe
chemosis and copious discharge. Urgent
systemic treatment is required, as delays
may lead to corneal perforation.
• Chlamydia is the most common causative
infection and is usually seen within the rst
week after birth with mild swelling and
chemosis.
• HSV is seen within 2 weeks after birth and
may present as typical vesicles on the
eyelid margin. Exclude corneal dendrite
with uorescein staining.
Preseptal cellulitis
(periorbital cellulitis)
Seek an urgent referral to an ophthalmologist
(<24 hours).
Figure 86. Periorbital cellulitis in a 20-year-old
man.
23
History ndings
• Trivial trauma may precede cellulitis, including
an insect bite, chalazion or skin trauma
Examination ndings
• Check for proptosis (should be absent but do not
confuse with lid swelling) and extraocular
movements (should be normal)
• Visual acuity and optic nerve function testing
should be normal
• The eye should appear white
• Usually features unilateral eyelid erythema,
tenderness and warmth
• Usually features minimal conjunctival injection
and no pain with eye movements
Eye Emergency Manual December 2023
Agency for Clinical Innovation 117 aci.health.nsw.gov.au
Important differentials
Consider the following:
• Orbital cellulitis: optic nerve function and
vision may be affected, as well as ocular
motility. Proptosis and painful eye movements
may also occur.
• Chalazion: a blocked Meibomian gland may
initially present with diffuse inammation of
the preseptal tissues. This often cannot be
differentiated from preseptal cellulitis
clinically and should therefore be treated as
such. Within a few days, however, a distinct
eyelid lump can be felt and seen, pointing to
the diagnosis of chalazion.
Initial treatment
If the eye is unable to be visualised, or the child is
febrile or unwell or less than 2 years old, then
they must be urgently referred to exclude and
treat possible orbital cellulitis.
Children older than 2 years with non-severe
preseptal infection, who are afebrile and
systemically well, may be treated with broad-
spectrum oral antibiotics and daily review.
Seek a same day referral by phone to
the ophthalmologist.
Section communication checklist
Consider the following:
Specic communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
; History of recent viral URTI or
sinus infection
; Ask for a history of recent skin infection
or trauma
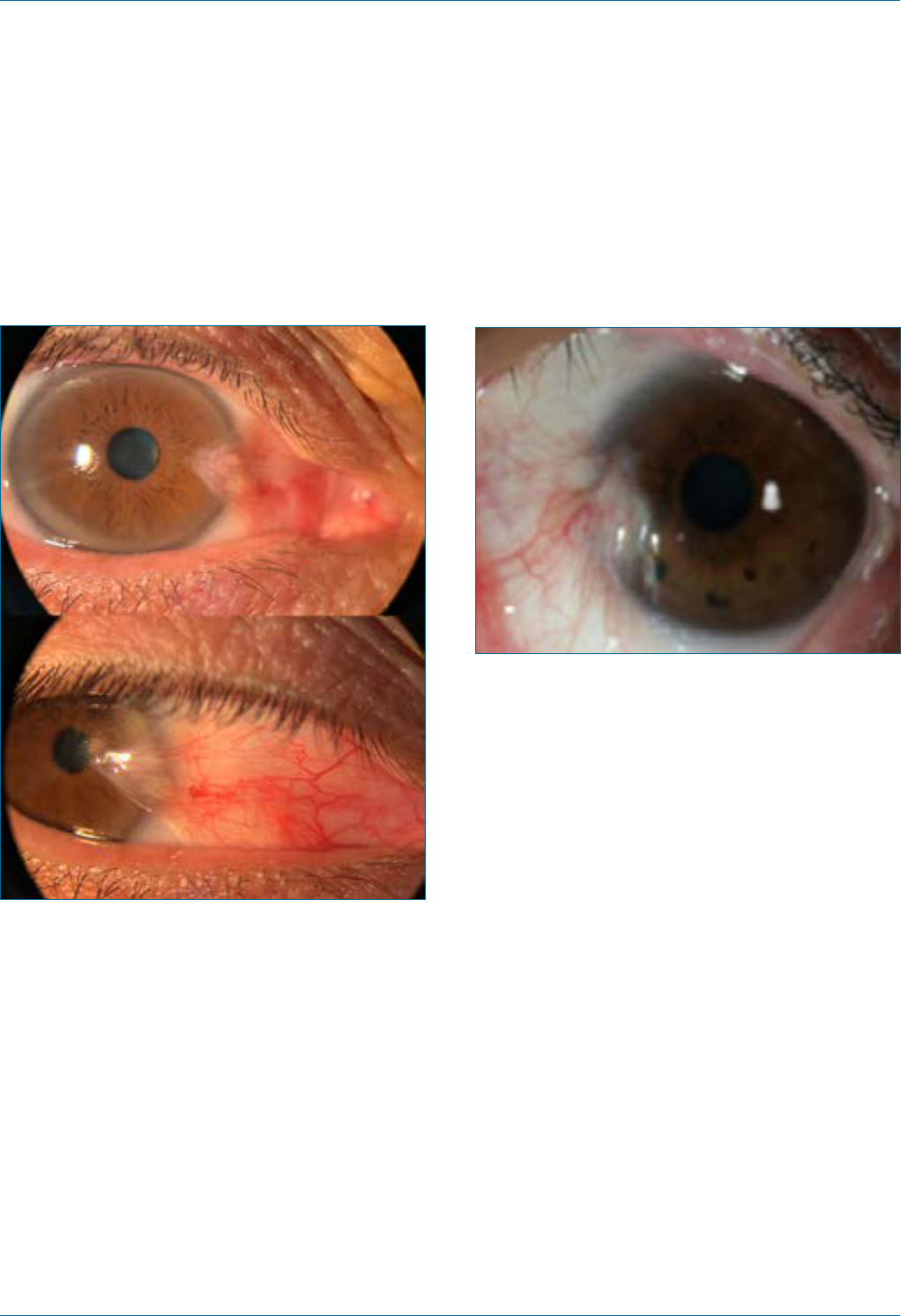
Eye Emergency Manual December 2023
Agency for Clinical Innovation 118 aci.health.nsw.gov.au
Pterygium
Figure 87. Right nasal pterygium. The eye is
looking to the right.
Pterygium is a raised, yellowish eshy lesion at the
limbus that may become painful and red if inamed.
It is usually on the nasal side and is often bilateral.
History ndings
Consider the following:
• A white lesion, often there for many years, which
occasionally becomes red and painful, particularly
following prolonged exposure to dry air and wind,
(e.g. long plane ights or air-conditioning). Once
inamed, it may require several days to settle.
• Check for a history of sun exposure or an
outdoor occupation.
Figure 88. Anterior segment image of pterygium
case. The surface vascularity is scored as +++.
24
Examination ndings
Consider the following:
• Visual acuity may be decreased, but not
acutely, as the presence of the pterygium can
cause optical distortion (astigmatism). This can
be somewhat corrected with glasses or a
pinhole on testing.
• There may be mild punctate staining on
uorescein testing over the pterygium or
adjacent cornea.
Important differentials
• Conjunctival dysplastic lesions look more
eshy, raised and vascular, and are often
rapidly growing
• If in doubt, refer to the ophthalmologist
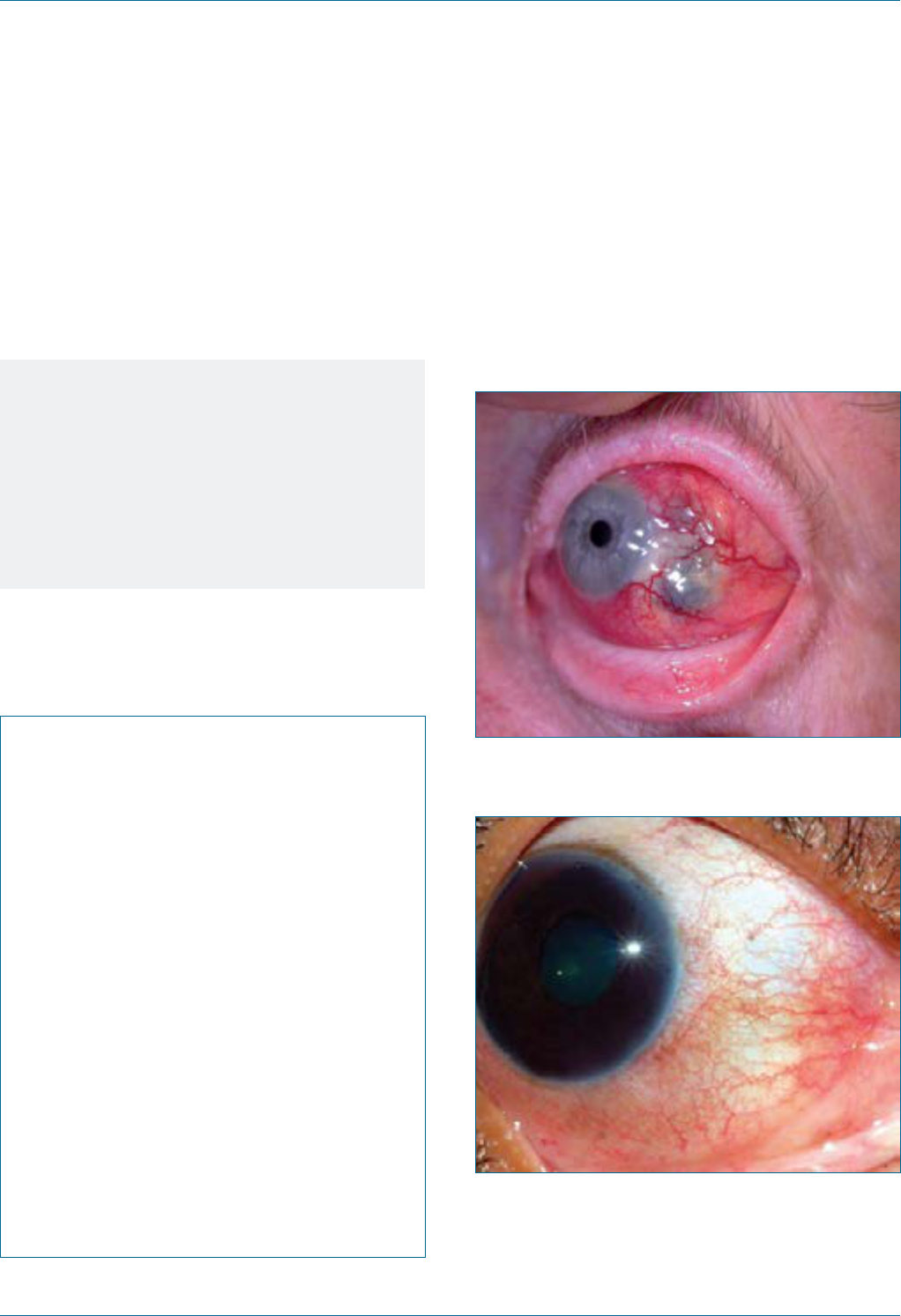
Eye Emergency Manual December 2023
Agency for Clinical Innovation 119 aci.health.nsw.gov.au
Initial treatment
• Lubricating eye drops hourly (preservative-free
drops or gel)
• Wrap-around sunglasses when outdoors
Notes
• Pterygium typically has a long duration and
affects the nasal conjunctivae
more frequently.
• It may be surgically excised by an
ophthalmologist if frequently inamed
or vision-threatening.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Scleritis
Seek an urgent referral to an ophthalmologist
(<24 hours).
Figure 89. Scleritis with scleral thinning and dark
choroidal show.
Figure 90. Inferior scleritis.
25
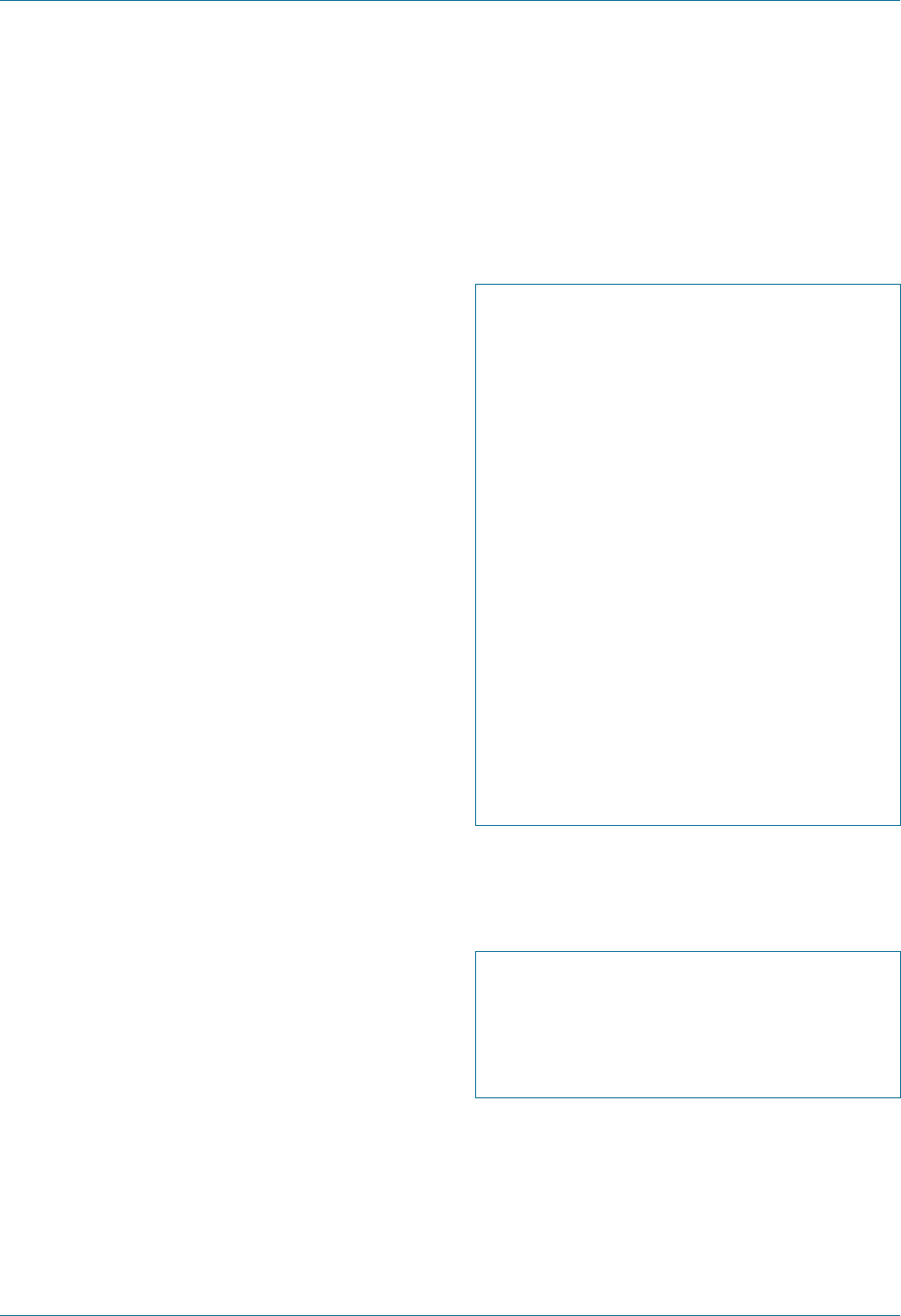
Eye Emergency Manual December 2023
Agency for Clinical Innovation 120 aci.health.nsw.gov.au
History ndings
• Painful and red eye
• Pain is a ‘deep ache’ and often wakes the patient
from sleep
• Redness, usually unilateral, and may be
localised to the involved area or diffuse
• History of life-threatening vasculitis or
connective tissue disease, especially
rheumatoid arthritis
Examination ndings
• Visual acuity may be reduced
• Globe is tender to palpation through the
closed eyelid
• Sclera is thickened and discoloured
• If the sclera is thinned from ongoing
inammation, there may be a dark discolouration
which is the pigmented choroid showing through
(Figure 89); if there is severe thinning, consider
globe perforation
Important differentials
Consider the following:
• Episcleritis occurs when layers supercial to the
sclera are inamed. This may be autoimmune-
related or exposure-related, (e.g. wind while
cycling or air-conditioning on an aeroplane).
• Conjunctivitis is more diffuse and involves the
tarsal conjunctiva.
Initial treatment
• Consult an ophthalmologist
• Consider vasculitis and autoimmune screen
• May consider systemic NSAIDs and steroids on
consultation with an ophthalmologist
and rheumatologist
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Specic communication checklist
Consider the following:
; Ask about pain waking the patient
from sleep
; Systems review, especially for
autoimmune disease
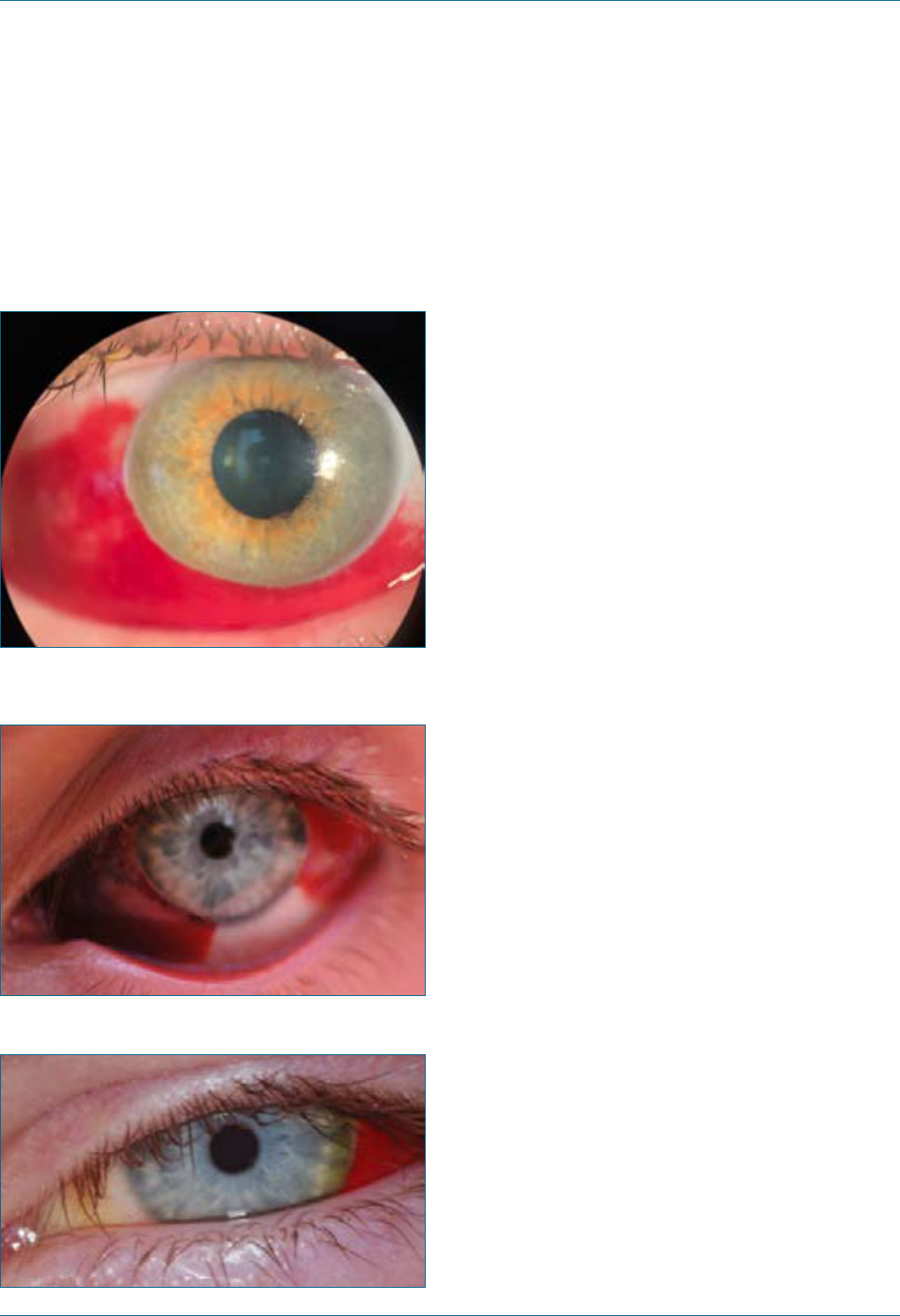
Eye Emergency Manual December 2023
Agency for Clinical Innovation 121 aci.health.nsw.gov.au
Subconjunctival haemorrhage
Figure 91. Subconjunctival haemorrhage of the
temporal bulbar conjunctiva.
26
Figure 92. Subconjunctival haemorrhage after
one week, extending nasally and temporally.
27
Figure 93. Four weeks after haemorrhage.
28
History ndings
Consider the following:
• A subconjunctival haemorrhage is discovered on
waking when looking in the mirror, as it is
otherwise largely asymptomatic.
• It may be associated with mild grittiness or
dryness of the eye if the haemorrhage is raised
and causes adjacent corneal drying.
• It is possibly associated with minor injuries
including eye-rubbing, foreign body
and Valsalva.
• It is common with the use of antiplatelet agents
and anticoagulants.
Examination ndings
• Supercial blood under the conjunctivae
• Unilateral, localised and sharply circumscribed
at the limbus
• Underlying sclera is not visible
• No inammation, pain or discharge
• Vision is unchanged
Important differentials
Consider the following:
• Open-globe injury (penetrating eye injury): a
subconjunctival haemorrhage that is large,
extends posteriorly or with a suspicious history
of penetrating eye injury (involving a sharp
object), ruptured globe (from severe blunt
trauma) or intraocular foreign body should be
examined thoroughly, as the haemorrhage may
mask an underlying scleral wound.
• Examine the visual acuity, pupil shape and
reactions, extraocular movements, anterior
segment on the slit lamp, red reex
and fundoscopy.
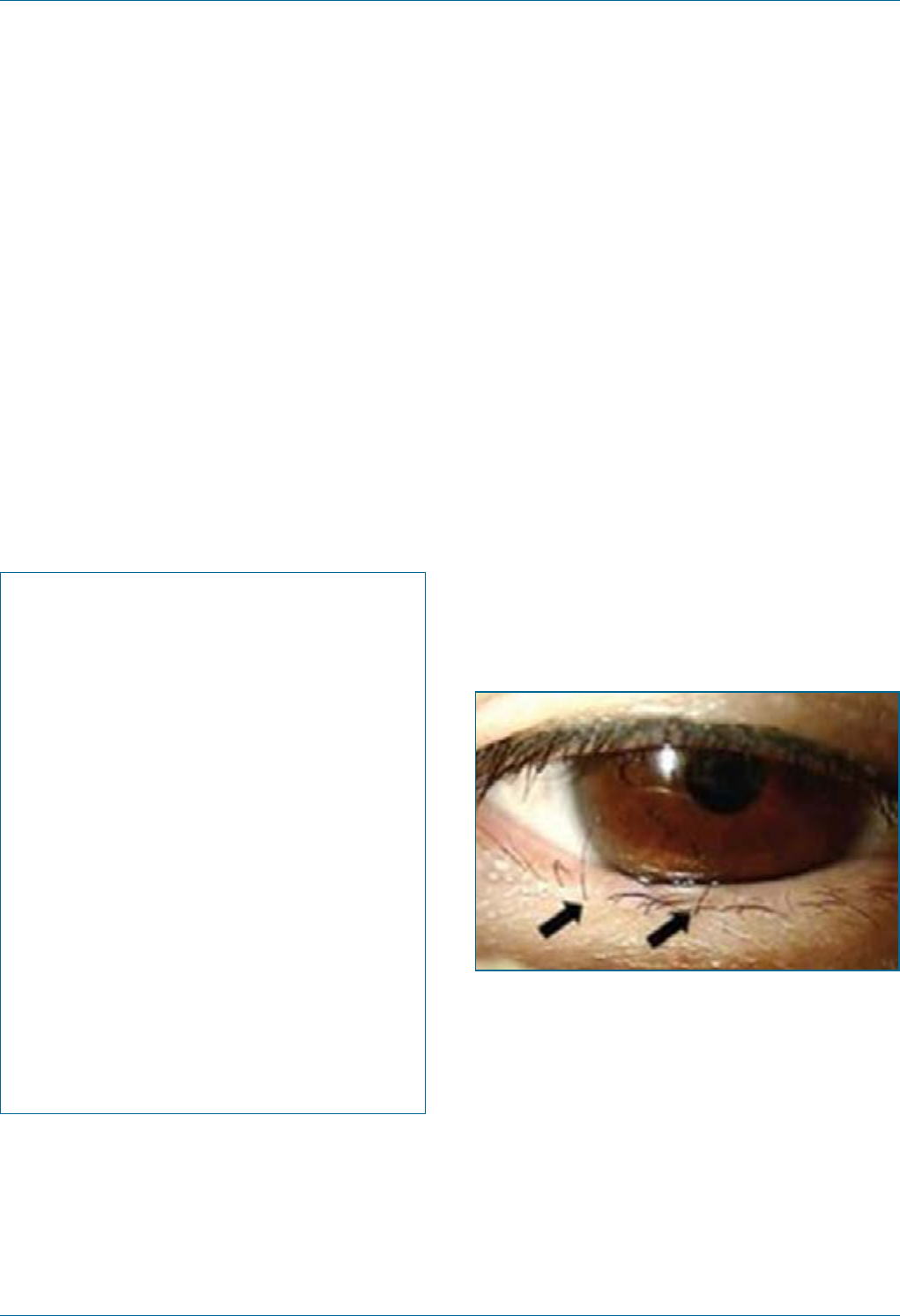
Eye Emergency Manual December 2023
Agency for Clinical Innovation 122 aci.health.nsw.gov.au
Initial treatment
• Check and manage blood pressure
• For patients on Warfarin, check INR and
manage accordingly
• Use lubricating drops if gritty or dry eye
symptoms present
• Refer to an ophthalmologist if the condition
worsens or pain develops
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Trichiasis
A condition where eyelashes (not eyelids) are
abnormally turned in towards the eye.
History ndings
• Ocular irritation, foreign body sensation
and tearing
Examination ndings
• Inturned eyelashes which may rub on the cornea
with blinking
• Corneal staining close to the lash location
(punctate erosions or a frank corneal ulcer)
Figure 94. An image of the preoperative
eyelashes.
29
Initial treatment
• Epilate offending lashes
• Lubricate every 2–3 hours using
preservative-free lubricant
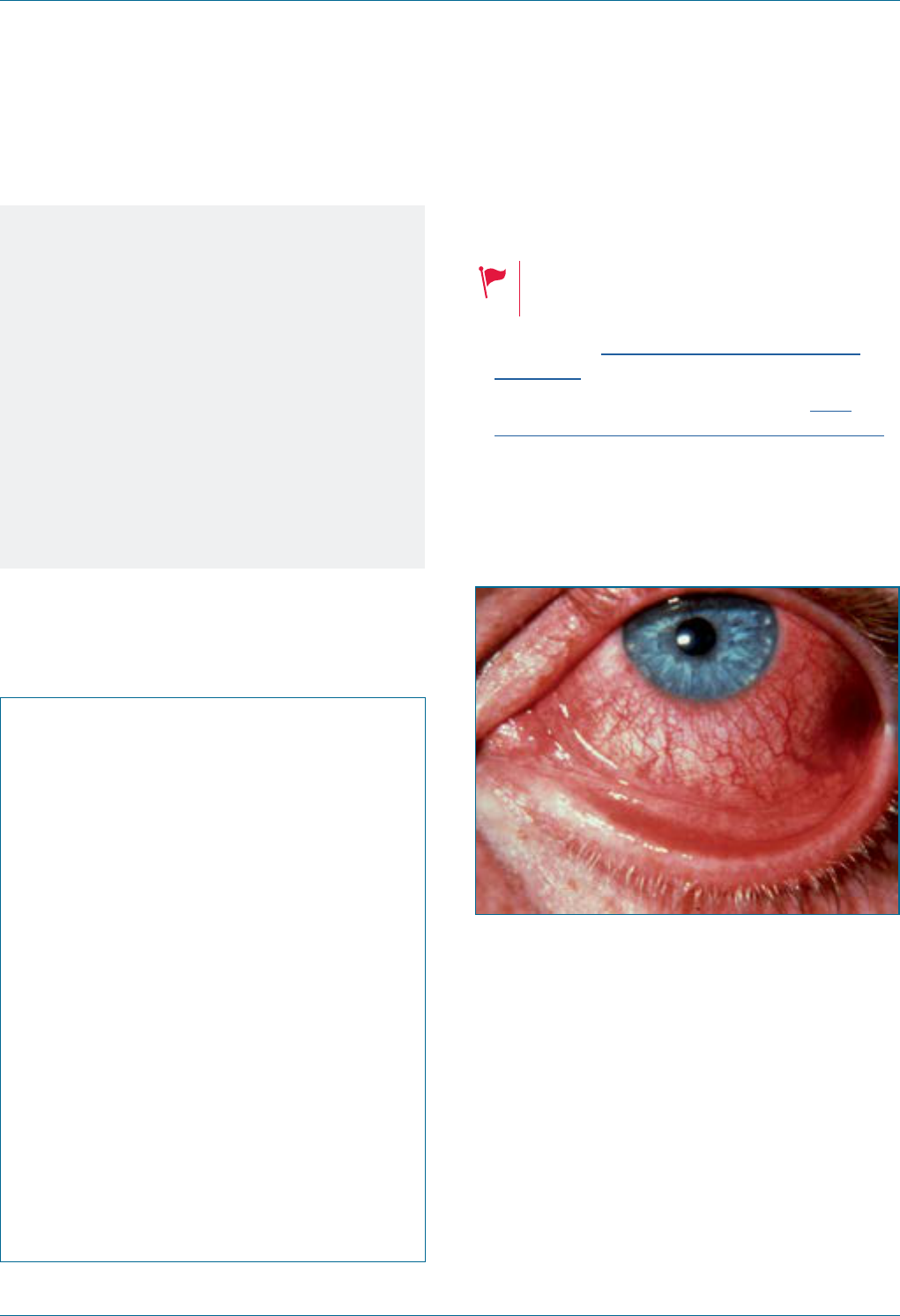
Eye Emergency Manual December 2023
Agency for Clinical Innovation 123 aci.health.nsw.gov.au
Notes
Consider the following:
• Trichiasis often arises from years of
blepharitis, resulting in a distortion of the
eyelid margin.
• Epilated lashes will often grow back after 6
weeks. More permanent treatment (laser,
freezing or electrolysis of lash follicle) may
be performed by an ophthalmologist.
Ophthalmology referral is indicated if
concerns for cornea, e.g. recurrent abrasions.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelids involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes
Viral conjunctivitis
Highly contagious. Observe
Standard Precautions.
• NSW Health Epidemic Keratoconjunctivitis
fact sheet
• RANZCO Infection Control Guidelines Fact
Sheet for Epidemic Keratoconjunctivitis (EKC)
• Viral conjunctivitis is most commonly caused by
adenovirus; however, HSV and VZV, (e.g. part of
V1 shingles) should be considered as causes
Figure 95. Viral conjunctivitis.
History ndings
Consider the following:
• Undertake a contact history with person/s
affected with red eye(s) or upper respiratory
tract infection symptoms (especially children).
• Viral conjunctivitis involves a burning sensation
and watery discharge (different from purulent
exudate in bacterial infections).
• It classically begins in one eye with spread to
the other after 3 days.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 124 aci.health.nsw.gov.au
Examination ndings
• Unilateral or bilateral red eye with involvement
of the whole conjunctiva, including tarsal
conjunctiva on eyelid eversion (use gloves for
infection control)
• Lid eversion may also reveal follicles (small pale
raised lumps of 0.5–1mm between the
injected vessels)
• Preauricular lymphadenopathy
• Visual acuity is usually mostly normal (6/9
or better)
• Check pupils for anisocoria (consider iritis as a
differential diagnosis if miosis is present)
Initial treatment
Consider the following:
• Limit transmission: perform frequent
handwashing, use separate tissues, avoid
contact with others while infectious (about 10–12
days from onset of symptoms), disinfect
surfaces, (e.g. handles and light switches) and
avoid sharing of towels and pillows.
• Provide symptomatic relief using cool
compresses and preservative-free lubricating
drops, gels or ointments every 1¬2 hours.
• Administer antibiotic drops if ulcers are present
as prophylaxis.
• Avoid steroids.
• Seek a more urgent ophthalmology referral
(within 24 hours) if photophobia occurs and
there is a marked decrease in visual acuity.
Notes
• Resolution may take several weeks.
• If it lasts longer than 3 weeks, consider
other diagnoses, including chlamydia
conjunctivitis and other diagnoses, (e.g.
episcleritis, scleritis, iritis and
HSV keratitis).
• Consider other diagnoses if presented with
a unilateral red eye of >3 days duration.
Section communication checklist
Consider the following:
; Onset and duration of symptoms
; Painful/not painful
; Distribution of redness (localised or
diffuse/involving tarsal conjunctiva)
; Purely unilateral, or some
contralateral symptoms
; Best (pinhole) visual acuity of each eye
; Eyelid involvement (red or swollen)
; Cornea normal or not normal, i.e. cloudy,
opacities or uorescein staining
; Anterior chamber normal or not normal,
i.e. deep, presence of anterior chamber
cells, blood or hypopyon
; Iris normal, i.e. round, equal, reactive pupils
with normal iris detail visible
; Equal red reexes

Treatments
Agency for Clinical Innovation 125 aci.health.nsw.gov.au
Eye Emergency Manual November 2023
Eye Emergency Manual December 2023
Agency for Clinical Innovation 126 aci.health.nsw.gov.au
Treatments
Ocular drugs
For detailed information on ocular drugs, refer to
the Sydney Eye Hospital’s Ophthalmic
Pharmacopoeia App.
Eye drops
Eye drops can get washed out if they are instilled in
quick succession. Therefore, wait at least 5–10
minutes between eye drop instillation for maximum
effect.
Many eye drops are available as commercially
prepared Minims that can look indistinguishable
from each other. Check carefully as you prepare an
eye drop, then double-check immediately
before instillation.
In the rare situation that you need to prepare the
periocular skin prior to a procedure, you can use
dilute Betadine with an equal amount of saline (to
give Betadine 5%) or aqueous chlorhexidine (do
NOT use the chlorhexidine, which comes mixed
with alcohol). A drop of either of these substances
can go into the eye, provided there is a topical
anaesthetic already in place and the eye is irrigated
thoroughly afterwards.
Topical anaesthetic
Topical anaesthetic is used to improve patient
comfort and as an aid to examination. Anaesthetic
effects last between 10 and 20 minutes, so warn
the patient that the relief they feel will be
temporary. Ensure that topical anaesthetic is
instilled before irrigating for chemical injuries.
It is not standard practice to prescribe topical
anaesthetic for patients to take home as its safety
has not been established and it may either cause or
mask the development of complications.
Common anaesthetics include Amethocaine 0.1%
(tetracaine) and benoxinate 0.4%, which are usually
available in commercially prepared Minims. It is
also possible to use drops of lignocaine 1–2%
(preferably without adrenaline), identical to the
subcutaneous preparation.
Using topical anaesthetic to treat
epithelial defects
The regular use of topical anaesthetic to improve
comfort while simple corneal epithelial defects
heal is controversial. Studies have shown that
topical anaesthetic is toxic to corneal epithelial and
stromal cells with prolonged use. Several case
series have not demonstrated any adverse effects;
however, safety has not been adequately
established. At the time of writing the issue
remains unresolved.
If you are considering prescribing topical
anaesthetic to improve a patient’s comfort while an
epithelial defect heals, please remember that
safety has not been established. While corneal
epithelial defects are very painful, they will usually
heal within a few days.
Fluorescein
Fluorescein is used to diagnose corneal epithelial
defects. It is generally available in Minims at 2%
concentration (orange), at 0.2% concentration
combined with lignocaine anaesthetic (yellow) or in
uorescein strips moistened with normal saline,
then touched against the conjunctiva or in the
fornix (NOT the cornea itself).
The optical properties of uorescein are that it
absorbs blue light and reects green light. The
chemical properties of uorescein are that it binds

Eye Emergency Manual December 2023
Agency for Clinical Innovation 127 aci.health.nsw.gov.au
to denuded areas of epithelium, and elsewhere is
washed away by the tear lm. This is the basis for
its use: to detect corneal epithelial defects (hence
the importance of using blue light and not green). It
also binds to mucus strands, which can be
differentiated from epithelial defects by their
movement on blinking.
Orange-coloured 2% uorescein does not
uoresce because it is too concentrated. It is used
to detect corneal leaks, which is done by instilling it
at full concentration on the eye and then examining
it under cobalt blue light at the slit lamp. At the
point of the corneal wound, aqueous leaking out
will dilute the uorescein and it will uoresce
(appearing as a green rivulet trickling down through
the orange uorescein in the tear lm). This is
known as a Seidel test, and a leaking wound is
termed ‘Seidel positive’.
For the same reason, if you administer a large drop
of orange 2% uorescein into the eye looking for an
epithelial defect, you will probably not be able to
see one for several minutes, and in that time the
orange uorescein will stain the cornea and leak
into the anterior chamber, rendering further
examination of the anterior chamber more difcult.
The key to using it is to administer a very small drop
into the eye and use the patient’s tear lm to
disperse and dilute it. Also be aware that
uorescein stains contact lenses, skin and clothing
(albeit temporarily), so be careful using it.
Mydriatic drops
Dilating the patient’s pupil allows fundus
examination and is also used in situations of
intraocular inammation to paralyse and enlarge
the pupil. As mentioned elsewhere, it is not
appropriate to dilate a patient’s eyes in the ED
before speaking with an ophthalmologist (or, in
some cases, a neurosurgeon). It usually takes 15 to
20 minutes for the drops to work and vision is
affected for several hours, so patients are not
permitted to drive following dilation.
Commonly available mydriatic drops are
tropicamide 1%, phenylephrine at 2.5% and 10%,
cyclopentolate 1% (or 0.5%) and atropine 1% (one
drop has an effect for 7–10 days), in both Minims
and bottles. Many textbooks will refer to
homatropine, which is a drop that is no longer
manufactured but can generally be replaced
by cyclopentolate.
Topical antibiotics
These are used both as prophylaxis and treatment
for microbial infections and commonly available
preparations include chloramphenicol, ooxacin,
ciprooxacin, gentamicin and tobramycin. Some
are available as drops, others as ointments and
some as both. In certain situations, other antibiotics
can be compounded by pharmacies for use as an
eye drop.
The most common topical antiviral is acyclovir
ointment, which is used for herpetic epithelial
keratitis. This condition requires specialist
ophthalmology management.
Ocular lubricating drops
Lubricating drops are used to treat dry eye, which is
very common. Lubricating drops are generally
available in two forms – preserved (in bottles) and
non-preserved (in Minims, or similar ampoules) –
and can be purchased over the counter from the
chemist. If a patient requires lubricating drops
more than four to six times a day, they should use
non-preserved drops to lower the risk of toxicity
from preservatives. Lubricating gels and ointments
are an alternative. They are effective, longer lasting
and most applicable for nocturnal use but can blur
vision if used during the day.
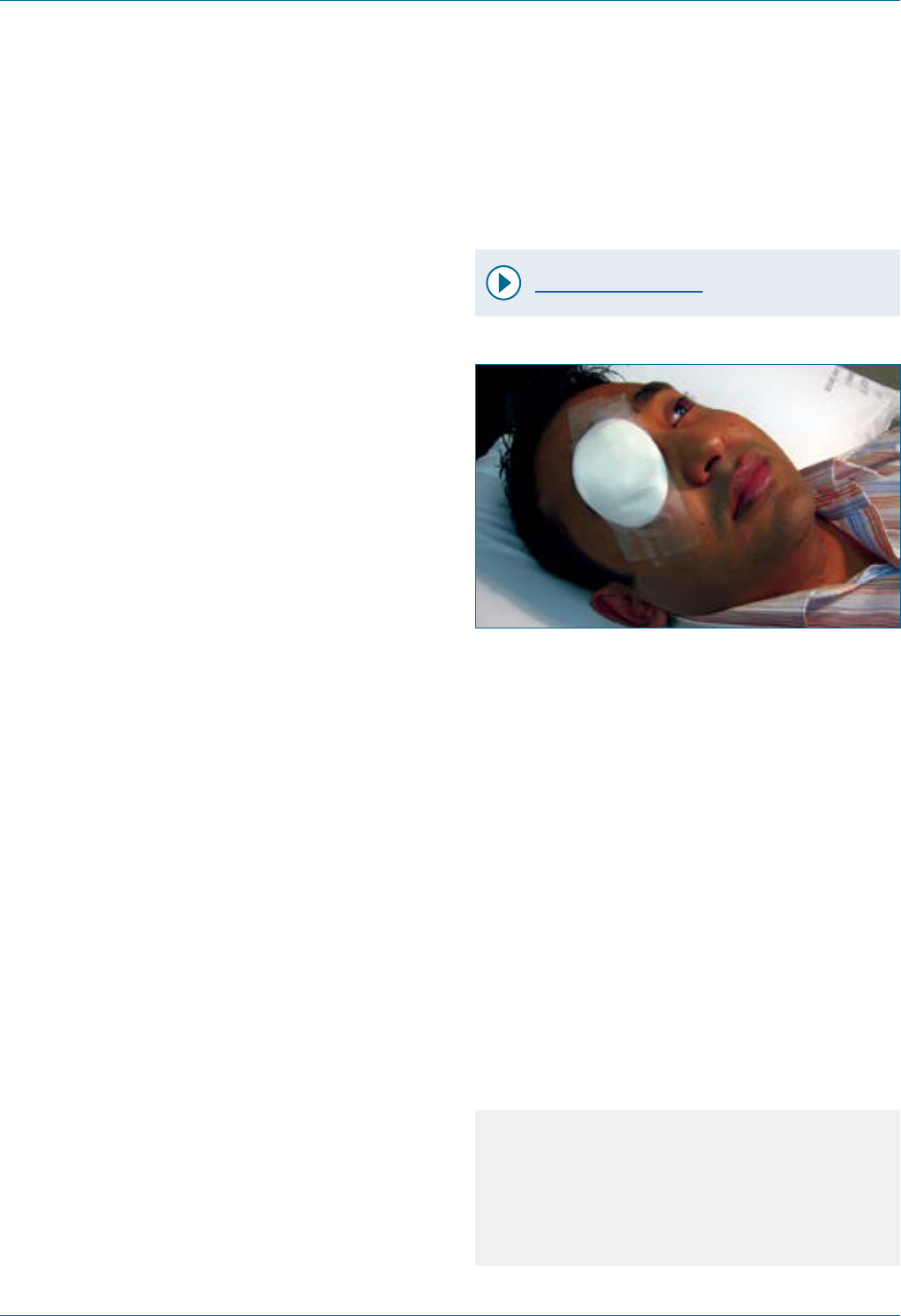
Eye Emergency Manual December 2023
Agency for Clinical Innovation 128 aci.health.nsw.gov.au
Topical steroids
Topical steroids are used to treat ocular surface
and intraocular inammation and should only be
prescribed by an ophthalmologist due to the
substantial risk of complications, including
glaucoma, microbial keratitis and cataracts.
Ocular antihypertensives
(glaucoma drops)
Ocular antihypertensives are used to lower
intraocular pressure in the treatment of glaucoma.
Many patients are on these medications because
glaucoma is such a common disease. There are a
multitude of different drops and drop combinations
across four major drug classes. If required for the
treatment of acutely elevated pressure, refer to
specic advice provided by an ophthalmologist.
Eye pad and shield
It is not wise to pad an eye with minor corneal or
conjunctival trauma. A pad placed inappropriately
may exacerbate injury while the cornea is
anaesthetised, or if the patient is already in pain
due to an existing corneal injury. While a pad may
be placed in specic situations, always discuss it
with an ophthalmologist before doing so. A patient
cannot drive with a pad on one eye as it reduces
depth perception.
It can be tempting to prescribe a topical
anaesthetic to patients with corneal epithelial
defects to improve comfort during healing. Please
be aware that the safety of doing this has not been
established and it remains controversial.
Technique for eye pad
Video - Eye Padding
Figure 96. Single eye pad.
1. Use one or two pads (stacked on top of
each other).
2. Prepare three pieces of tape in advance and
have them on hand.
3. Ask the patient to close their eyes, then place
the pad on rmly so that the eye remains
closed. Tape rmly in place.
4. When applied correctly, the patient’s padded
eye should remain closed when they open the
other eye.
5. The tape should angle away from the mouth. To
ensure that the tape is compact on the eye,
place the pieces parallel to each other.
6. It may help to put chloramphenicol ointment in
the eye prior to applying the pad or use a small
piece of Jelonet between the pad and the
closed eyelid.
Notes
If the eye opens underneath the eye pad, it
may not be noticed by the patient and they can
sustain signicant corneal injury by the time
the pad is removed.
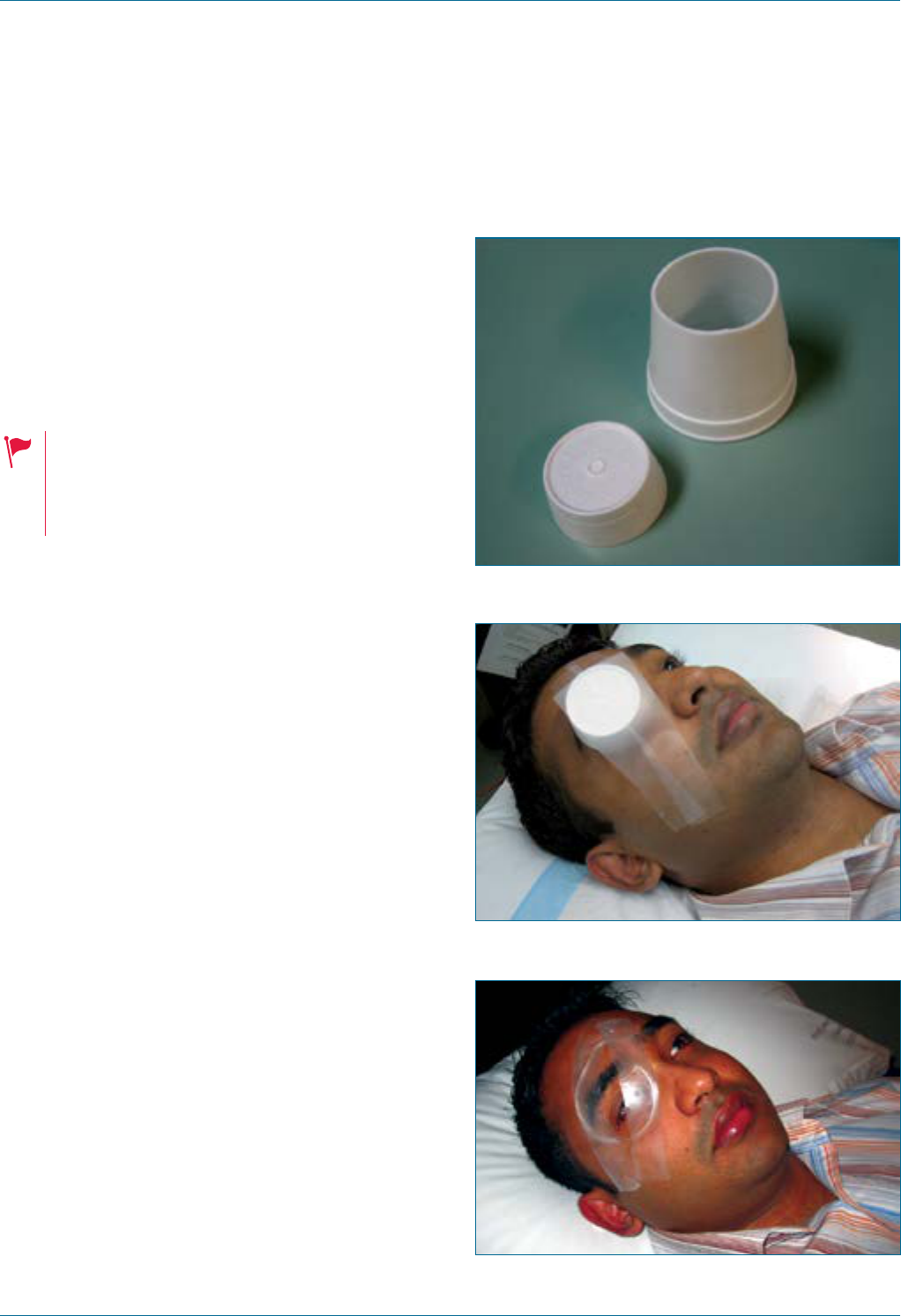
Eye Emergency Manual December 2023
Agency for Clinical Innovation 129 aci.health.nsw.gov.au
Technique for an eye shield
1. Use either a clear plastic shield or a truncated
disposable cup.
2. Place it over the eye without putting any
pressure on the orbit. Make sure the rim of the
shield or the cup is resting on the bony
orbital margin.
In situations of globe rupture do NOT put
anything underneath the shield in contact
with the eye as the goal is to avoid any
pressure on the globe whatsoever.
Figure 97. Shield made from a disposable cup.
Figure 98. Disposable cup.
Figure 99. Eye shield.
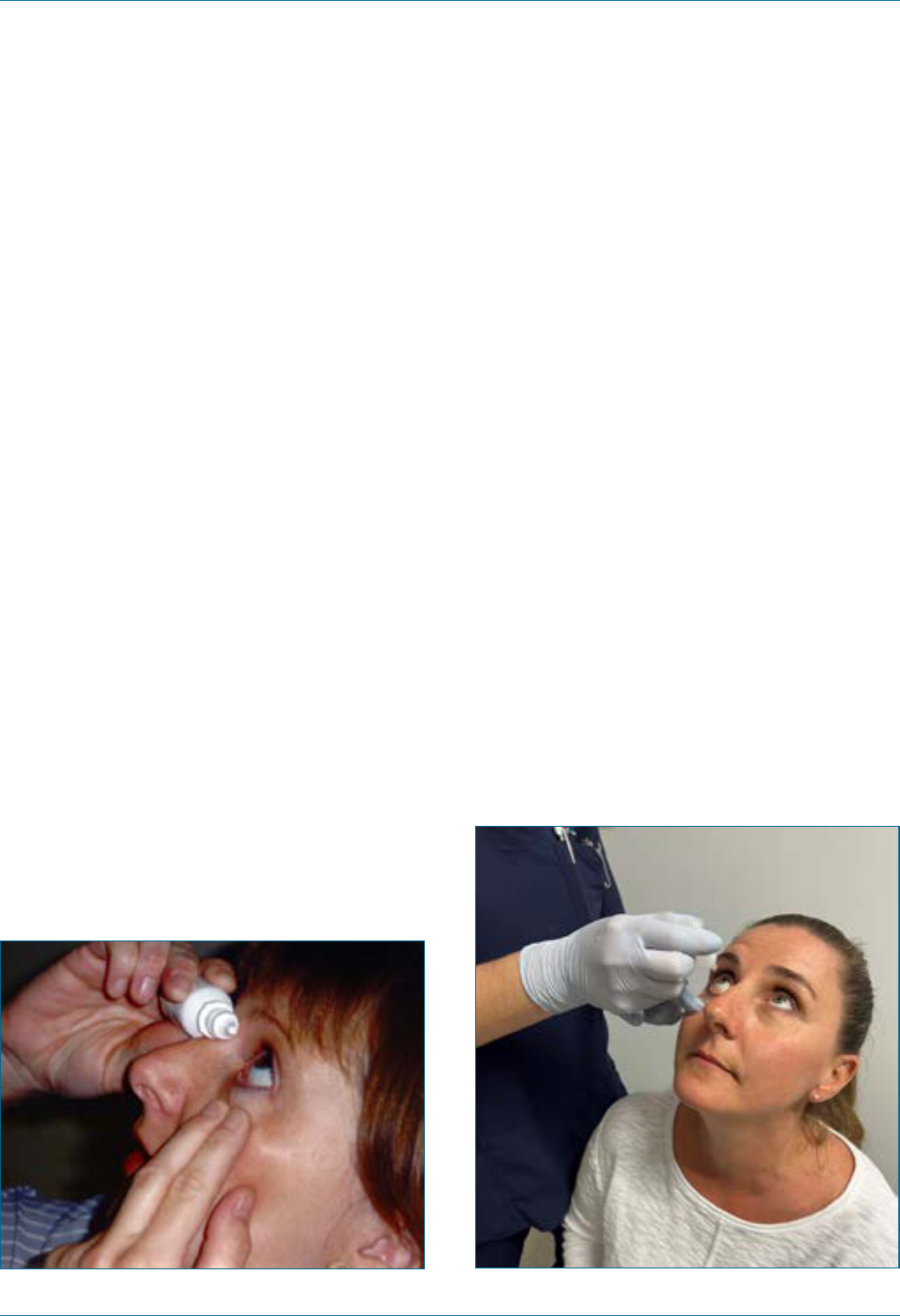
Eye Emergency Manual December 2023
Agency for Clinical Innovation 130 aci.health.nsw.gov.au
How to put in eye drops
Self-instillation
1. Wash hands.
2. Uncap the bottle/tube.
3. Tilt your head up.
4. Use the hand on the opposite side to hold the
bottle resting on the bridge of the nose, taking
care not to touch any surfaces with the
bottle tip.
5. Pull down the lower lid with the ngers of the
same side so that a visible pocket forms in the
space behind the lid.
6. Gently squeeze the bottle to deliver 1 or 2 drops.
7. Shut the eyelid for approximately 1 minute.
8. Wipe away excess drops/ointment from
your face.
9. Re-cap the bottle.
10. Wash hands.
Figure 100. Self-instillation of eye drops.
Assisted instillation
1. Wash hands.
2. Uncap the container or twist off the tab.
3. Pull the lower eyelid gently down with
forenger to form a pocket.
4. Tilt the head slightly back and look up.
5. Hold the bottle gently between the thumb and
forenger and gently squeeze the
recommended number of drops into the
pocket formed.
6. Do not touch the eye with bottle tip.
7. Shut the eye and move the eyeball from side to
side to spread the medication.
8. Wash hands.
Figure 101. Drops administered by a healthcare
worker or family member.
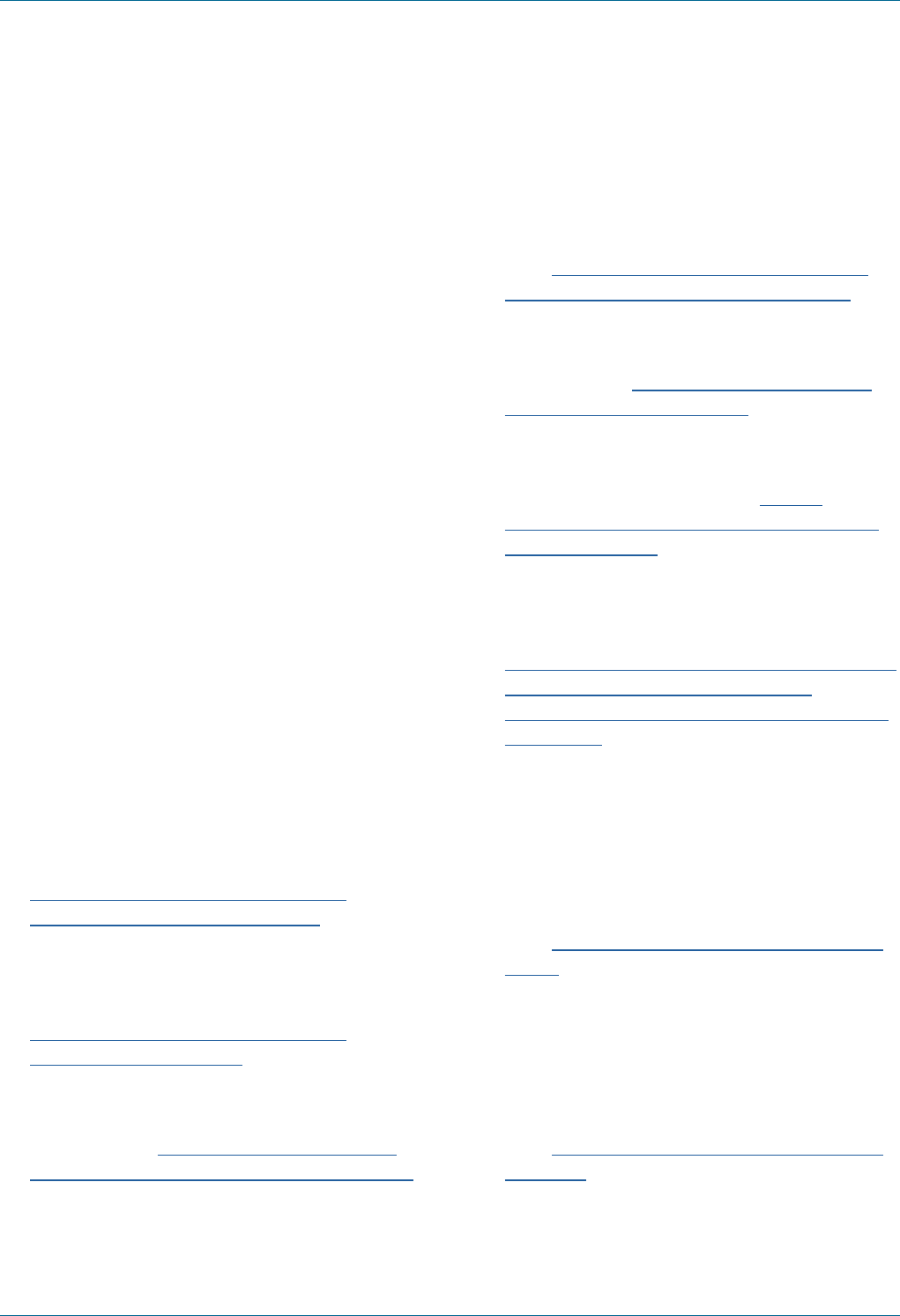
Eye Emergency Manual December 2023
Agency for Clinical Innovation 131 aci.health.nsw.gov.au
References
1. Prabhasawat P, Ekpo P, Uiprasertkul M, et al.
Efcacy of cultivated corneal epithelial stem
cells for ocular surface reconstruction. Clin
Ophthalmol. 2012;6:1483-92. DOI: 10.2147/
OPTH.S33951.
2. Choi YJ, Jung MS, Kim SY. Retinal hemorrhage
associated with perinatal distress in newborns.
Korean J Ophthalmol. 2011 Oct;25(5):311-6. DOI:
10.3341/kjo.2011.25.5.311.
3. Zehetner C, Bechrakis NE. White centered
retinal hemorrhages in vitamin b(12) deciency
anemia. Case Rep Ophthalmol. 2011 May;2(2):140-
4. DOI: 10.1159/000328123.
4. Vijaya L, Manish P, Ronnie G, et al. Management
of complications in glaucoma surgery. Indian J
Ophthalmol. 2011 Jan;59 Suppl(Suppl1):S131-40.
DOI: 10.4103/0301-4738.73689.
5. Thompson D, Stanescu C, Pryor P, et al.
Retrobulbar hematoma from warfarin toxicity
and the limitations of bedside ocular sonography.
West J Emerg Med. 2010 May;11(2):208-10.
6. Wang Y, Wang XH, Tian MM, Xie CJ, Liu Y, Pan
QQ, Lu YN, CC BY 4.0, via Wikimedia Commons
(accessed October 2023). Available from:
https://commons.wikimedia.org/wiki/
File:Oculomotor_nerve_palsy.png
7. Mohammad T Masoud, Ajmal Rehman and Yusuf
Shaikh, CC BY 2.0, via Wikimedia Commons
(accessed October 2023). Available from:
https://commons.wikimedia.org/wiki/
File:Abducens_palsy.jpg
8. Russell Neches (Rneches), CC BY-SA 3.0, via
Wikimedia Commons (accessed October 2023).
Available from: https://commons.wikimedia.
org/wiki/File:Central_serous_retinopathy.jpg
9. Jonathan Trobe, M.D., CC BY 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://commons.wikimedia.org/wiki/
File:Acute_Angle_Closure-glaucoma.jpg
10. Cumulus at Dutch Wikipedia, CC BY-SA 3.0, via
Wikimedia Commons (accessed October 2023).
Available from: https://commons.wikimedia.
org/wiki/File:Myasthenia.jpg
11. CDC/Dr. Sellers/Emory University, Public
domain, via Wikimedia Commons (accessed
October 2023). Available from: https://
commons.wikimedia.org/wiki/File:Bilateral_
exophthalmos.jpg
12. National Eye Institute/National Institutes of
Health, Public domain, via Wikimedia Commons
(accessed October 2023). Available from:
https://commons.wikimedia.org/wiki/File:Slit_
lamp_photograph_showing_retinal_
detachment_in_Von_Hippel-Lindau_disease_
EDA08.JPG
13. La Rosa M, Lionetti E, Reibaldi M, et al. Allergic
conjunctivitis: a comprehensive review of the
literature. Ital J Pediatr. 2013 Mar 14;39:18. doi:
10.1186/1824-7288-39-18.
14. Jonathan Trobe, M.D., CC BY 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://creativecommons.org/licenses/
by/3.0
15. London NJ, Garg SJ, Moorthy RS, et al. Drug-
induced uveitis. J Ophthalmic Inamm Infect.
2013 Mar 25;3(1):43. DOI: 10.1186/1869-5760-3-43.
16. Grook Da Oger, CC BY-SA 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://creativecommons.org/licenses/
by-sa/3.0

Eye Emergency Manual December 2023
Agency for Clinical Innovation 132 aci.health.nsw.gov.au
17. E van Herk, CC BY-SA 3.0, E van Herk, CC BY-SA
3.0, via Wikimedia Commons (accessed October
2023). Available from: https://creativecommons.
org/licenses/by-sa/3.0
18. Asagan, CC BY-SA 3.0, via Wikimedia Commons
(accessed October 2023). Available from:
https://creativecommons.org/licenses/by-
sa/3.0
19. Seo KS, Lee HM, Shin HJ, et al. Coinfection with
herpes zoster ophthalmicus and oriental eye
worm in a rural woman: the rst report of an
unusual case. Ann Dermatol. 2014 Feb;26(1):125-
6. DOI: 10.5021/ad.2014.26.1.125.
20. Babu K, Maralihalli RE. Insect wing tarsal
foreign body causing conjunctival granuloma
and marginal keratitis. Indian J Ophthalmol.
2009 Nov-Dec;57(6):473-4.
DOI: 10.4103/0301-4738.57154.
21. Columbia University Irving Medical Center.
Neovascular glaucoma. New York, USA:
Columbia University; 2023 (accessed October
2023). Available from: https://www.vagelos.
columbia.edu/departments-centers/
ophthalmology/education/digital-reference-
ophthalmology/glaucoma/angle-closure-
glaucoma/neovascular-glaucoma
22. CDC/ J. Pledger, Public domain, via Wikimedia
Commons (accessed October 2023). Available
from: https://commons.wikimedia.org/wiki/
File:Gonococcal_ophthalmia_neonatorum.jpg
23. Afrodriguezg, CC BY-SA 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://commons.wikimedia.org/wiki/
File:Celulitis_Periorbitaria_(Preseptal).JPG
24. Park CY, Choi JS, Lee SJ, et al. Cyclooxygenase-
2-expressing macrophages in human pterygium
co-express vascular endothelial growth factor.
Mol Vis. 2011;17:3468-80.
25. Kamath YS, Rathinam SR, Kawali A. Ocular
toxoplasmosis associated with scleritis. Indian J
Ophthalmol. 2013 Jun;61(6):295-7. DOI:
10.4103/0301-4738.111130.
26. Daniel Flather, CC BY-SA 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://commons.wikimedia.org/wiki/
File:Subconjunctival_hemorrhage_eye.JPG
27. Therealbs 2002, CC BY-SA 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://commons.wikimedia.org/wiki/
File:Subconjunctival_hemorrhage_before_
after_(cropped).jpg
28. Therealbs 2002, CC BY-SA 3.0, via Wikimedia
Commons (accessed October 2023). Available
from: https://commons.wikimedia.org/wiki/
File:Subconjunctival_hemorrhage_before_
after_(cropped4weeks).jpg
29. Kim GN, Yoo WS, Kim SJ, et al. The effect of
0.02% mitomycin C injection into the hair follicle
with radiofrequency ablation in trichiasis
patients. Korean J Ophthalmol. 2014
Feb;28(1):12-8. DOI: 10.3341/kjo.2014.28.1.12.

Eye Emergency Manual December 2023
Agency for Clinical Innovation 133 aci.health.nsw.gov.au
PubMed search terms
((("Eye Diseases"[Mesh] OR "Eye Injuries"[Mesh] OR "eye disease*"[Title] OR "eye injur*"[Title]) AND
("Emergency Treatment"[Mesh] OR ("emergenc*"[Title] AND "treat*"[Title])) OR ("ocular emergenc*"[Title] OR
"eye emergenc*"[Title])) AND ("Guideline" [Publication Type] OR "Practice Guideline" [Publication Type] OR
"guideline*"[Title] OR "principle*"[Title] OR "procedure*"[Title] OR "diagnos*"[Title] OR "management"[Title]))
NOT ("COVID"[Title/Abstract]) AND (english[Filter]) AND (2009:2023[pdat])
Google search terms
eye injury OR eye disease OR eye emergency AND guidelines OR management
Inclusion and exclusion criteria
Inclusion Exclusion
• Published in English
• Studies reporting empirical data, including
modelling studies, and systematic review articles
• Published between 2009 and present
• Letters, comments, editorials, study protocols, case
reports or conference abstracts
• Abstract only
• Studies or results related to COVID-19
Bibliography
Appendix: Evidence base
• Al-Dhibi HA, Al-Mahmood AM, Arevalo JF. A
systematic approach to emergencies in uveitis.
Middle East Afr J Ophthalmol. 2014 Jul-
Sep;21(3):251-8. DOI: 10.4103/0974-9233.134687
Biousse V, Nahab F, Newman NJ. Management of
Acute Retinal Ischemia: Follow the Guidelines!
Ophthalmology. 2018 Oct;125(10):1597-607. DOI:
10.1016/j.ophtha.2018.03.054
• Chou HD, Chen KJ, Kang EY, et al. Eye irrigation
as a rst-line treatment and diagnostic method
for emergency department patients who
complain of ocular foreign bodies. Sci Rep. 2021
Dec 3;11(1):23386. DOI: 10.1038/s41598-021-
02989-3
• Cugati S, Varma DD, Chen CS, et al. Treatment
options for central retinal artery occlusion. Curr
Treat Options Neurol. 2013 Feb;15(1):63-77. DOI:
10.1007/s11940-012-0202-9
• Dasgupta B. Concise guidance: diagnosis and
management of giant cell arteritis. Clin Med
(Lond). 2010 Aug;10(4):381-6. DOI: 10.7861/
clinmedicine.10-4-381
• Department of Health and Aged Care. Summary
of ophthalmic emergency predictors (OEP) for
the ATS [Internet]. Australia: Department of
Health and Aged Care; 2013 Jan 21 [cited 2023
July 13]. Available from: https://www1.health.
gov.au/internet/publications/publishing.nsf/
Content/triageqrg~triageqrg-eye.
• Dua HS, Ting DSJ, Al Saadi A, et al. Chemical eye
injury: pathophysiology, assessment and
management. Eye (Lond). 2020 Nov;34(11):2001-
19. DOI: 10.1038/s41433-020-1026-6
• Eslani M, Baradaran-Rai A, Movahedan A, et al.
The ocular surface chemical burns. J Ophthalmol.
2014;2014:196827. DOI: 10.1155/2014/196827
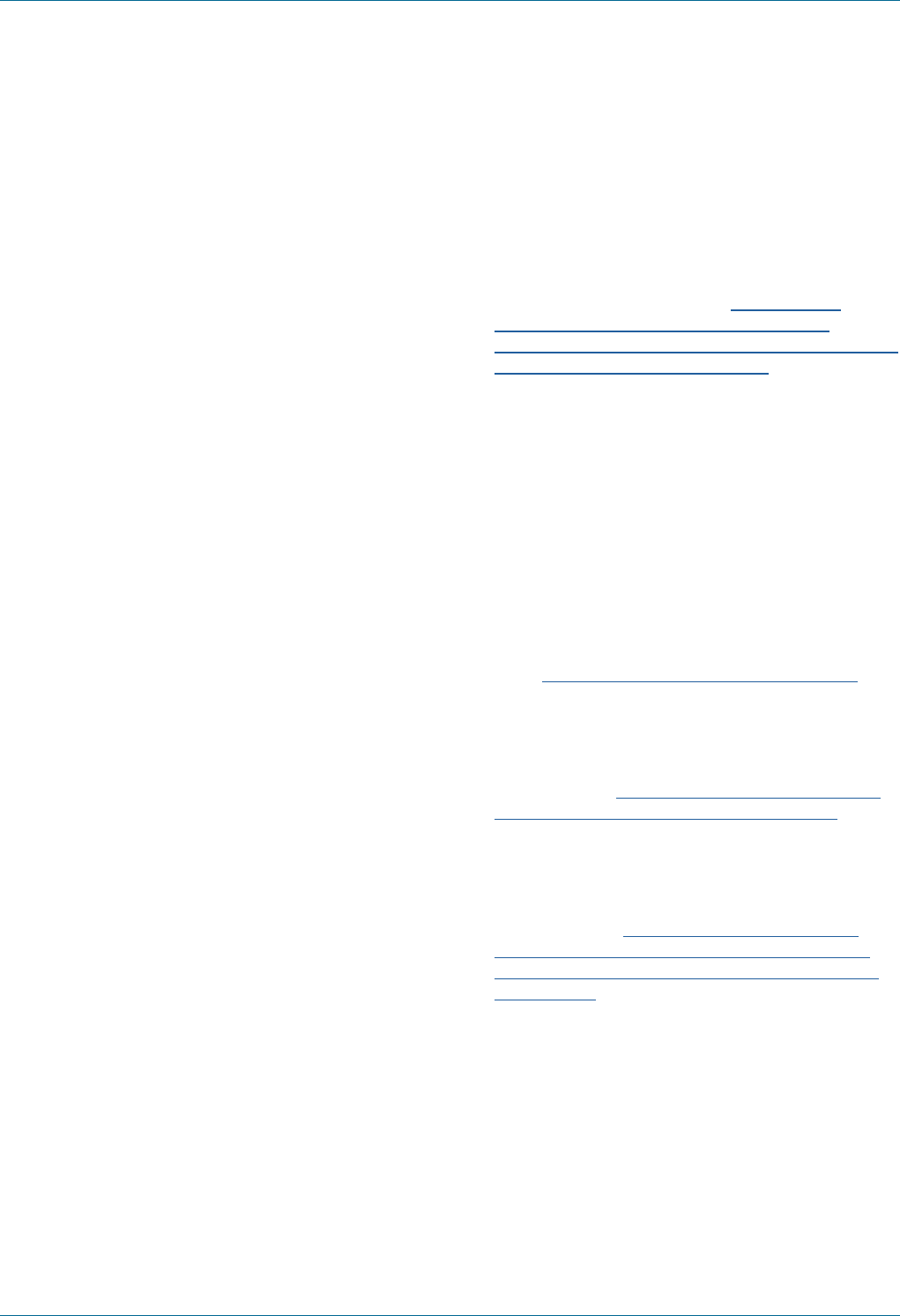
Eye Emergency Manual December 2023
Agency for Clinical Innovation 134 aci.health.nsw.gov.au
• Hayreh SS. Management of ischemic optic
neuropathies. Indian J Ophthalmol. 2011 Mar-
Apr;59(2):123-36. DOI: 10.4103/0301-4738.77024
• Heath Jeffery R, Dobes J, Chen F. Eye injuries:
Understanding ocular trauma. Australian Journal
for General Practitioners. 2022 07/01;51:476-82.
• Hodge C, Lawless M. Ocular emergencies. Aust
Fam Physician. 2008 Jul;37(7):506-9.
• Lindeld D, Das-Bhaumik R. Emergency
department management of penetrating eye
injuries. Int Emerg Nurs. 2009 Jul;17(3):155-60.
DOI: 10.1016/j.ienj.2009.01.003
• Mac Grory B, Schrag M, Biousse V, et al.
Management of Central Retinal Artery
Occlusion: A Scientic Statement From the
American Heart Association. Stroke. 2021
Jun;52(6):e282-e94. DOI: 10.1161/
str.0000000000000366
• Mbonde AA, O'Carroll CB, Dulamea OA, et al.
Current Guidelines on Management of
Amaurosis Fugax and Transient Ischemic
Attacks. Asia Pac J Ophthalmol (Phila). 2022
Mar-Apr 01;11(2):168-76.
DOI: 10.1097/apo.0000000000000511
• Michels TC, Ivan O. Glaucoma: Diagnosis and
Management. Am Fam Physician.
2023 Mar;107(3):253-62.
• Miller SC, Fliotsos MJ, Justin GA, et al. Global
Current Practice Patterns for the Management
of Open Globe Injuries. Am J Ophthalmol. 2022
Feb;234:259-73. DOI: 10.1016/j.ajo.2021.08.003
• Nuzzi R, Buschini E, Actis AG. Ophthalmic
evaluation and management of traumatic
accidents associated with retinal breaks and
detachment: a retrospective study. Eur J
Ophthalmol. 2012 Jul-Aug;22(4):641-6.
DOI: 10.5301/ejo.5000088
• O'Connor PM, Crock CT, Dhillon RS, et al.
Resources for the management of ocular
emergencies in Australia. Emerg Med Australas.
2011 Jun;23(3):331-6.
DOI: 10.1111/j.1742-6723.2011.01411.x
• Optometry Australia. Clinical practice guide for
the diagnosis, treatment and management of
anterior eye conditions [Internet]. Melbourne,
Australia: Optometry Australia; 2018 Apr [cited
2023 Jul 13]. Available from: https://www.
optometry.org.au/wp-content/uploads/
Professional_support/Guidelines/anterior_eye_
clinical_practice_guide__2_.pdf.
• Serrano F, Stack LB, Thurman RJ, et al.
Traumatic eye injuries: management principles
for the prehospital setting. Jems. 2013
Dec;38(12):56-62.
• Sethuraman U, Kamat D. The red eye: evaluation
and management. Clin Pediatr (Phila). 2009
Jul;48(6):588-600. DOI:
10.1177/0009922809333094
• The Royal Children's Hospital Melbourne.
Clinical practice guidelines [Internet]. Melbourne,
Australia: The Royal Children's Hospital
Melbourne; 2022 Oct [cited 2023 July 13]. Available
from: https://www.rch.org.au/clinicalguide/.
• The Royal Victorian Eye and Ear Hospital.
Emergency department clinical practice guidelines
[Internet]. Melbourne, Australia: The Royal Victorian
Eye and Ear Hospital; 2023 [cited 2023 July 13].
Available from: https://eyeandear.org.au/health-
professionals/clinical-practice-guidelines/.
• UpToDate. Approach to diagnosis and initial
treatment of eye injuries in the emergency
department [Internet]. Massachusetts, USA:
UpToDate; 2023 Feb 8 [cited 2023 Jul 18].
Available from: https://www.uptodate.com/
contents/approach-to-diagnosis-and-initial-
treatment-of-eye-injuries-in-the-emergency-
department.
• Varma DD, Cugati S, Lee AW, et al. A review of
central retinal artery occlusion: clinical
presentation and management. Eye (Lond). 2013
Jun;27(6):688-97. DOI: 10.1038/eye.2013.25
• Youn TS, Lavin P, Patrylo M, et al. Current
treatment of central retinal artery occlusion: a
national survey. J Neurol. 2018 Feb;265(2):330-5.
DOI: 10.1007/s00415-017-8702-x
Eye Emergency Manual December 2023
Agency for Clinical Innovation 135 aci.health.nsw.gov.au
Glossary
Term Denition
Acute angle closure Acute angle closure glaucoma is caused by a rapid or sudden increase in
intraocular pressure (IOP), the pressure inside the eye. Urgent
ophthalmologist attention is required.
Age-related macular
degeneration (ARMD)
A medical condition that may result in blurred or no vision in the central
eld of vision. ARMD may be asymptomatic initially.
Amblyopia Reduced visual acuity that results from deprivation of optimal visual
experience during early childhood. Patients are usually aware of a history
of amblyopia or ‘lazy eye’.
Amsler grid A tool to detect vision problems resulting from damage to the macular or
optic nerves. The tool can be downloaded via the macular haemorrhage
wARMD page.
Anisocoria Asymmetry in pupil size. The degree of asymmetry can differ in light and
dark conditions, so measure pupil size in both. Anisocoria is a feature of
third cranial nerve palsy (greater difference in dark), Horner syndrome
(greater difference in light) and iris trauma.
Anterior chamber (AC) Anatomy term: the space between the iris and corneal endothelium.
Anterior ischaemic optic
neuropathy (AION)
Optic nerve dysfunction secondary to arterial ischaemia of the prelaminar
optic disc arteriole. Giant cell arteritis (GCA) is the most common cause.
Arteritic anterior ischaemic
optic neuropathy (AAION)
Optic nerve dysfunction secondary to ischaemia of the prelaminar optic
disc arterioles with resulting disc swelling and pallor. Giant cell arteritis
(GCA) is the most common cause.
Australasian Triage Scale
(ATS)
A set of triage categories agreed upon by the Australasian College for
Emergency Medicine (ACEM) for use in Emergency Departments. Category
1: Immediate simultaneous assessment and treatment; Category 2: <10
minutes; Category 3: <30 minutes; Category 4: <60 minutes; Category 5:
<120 minutes.
Avulsion Pathologic condition: tearing or wrenching away of a part, e.g.the optic
nerve from the globe.
Bacterial keratitis A vision-threatening bacterial infection of the cornea that can cause loss
of vision in severe cases. The rate of progression of symptoms is related to
the virulence of the infecting organism. Diagnosis is based on clinical history
and slit lamp examination showing the presence of a corneal inltrate.
Bacterial/
acanthamoebal ulcer
An infective condition of the cornea involving disruption of the epithelial layer
with involvement of the corneal stroma. Caused by Acanthamoeba infection.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 136 aci.health.nsw.gov.au
Term Denition
Blepharitis Blepharitis is a common eyelid inammation that is sometimes associated
with a bacterial eye infection.
Bradyarrhythmia A slow heart rate: dened as a heart rate of <60 beats per minute (BPM)
in adults.
Canthus The outer or inner corner of the eye where the upper and lower lids meet.
Carotid-cavernous
sinus stula (CCF)
An abnormal communication between the internal or external carotid
arteries and the cavernous sinus.
Cataract The clouding of a normal lens. The main symptom is blurry vision. Patients
may describe vision as looking through a cloudy window. Refer to an
ophthalmologist if not already under care.
Central nervous system
(CNS)
The retina is brain tissue and is considered part of the central nervous
system (CNS). It is the only part of the CNS that can be visualised non-
invasively. Seek neurology referral.
Central retinal vein
occlusion (CRVO)
A blockage of the main vein in the retina.
Central serous
chorioretinopathy/
retinopathy
A disease in which a serous detachment of the neurosensory retina occurs
over an area of leakage from the choriocapillaris through the retinal
pigment epithelium.
Cerebrovascular accident (CVA) Stroke: reduced blood ow to the brain.
Chalazion A benign, painless bump or nodule inside the upper or lower eyelid.
Chemosis Pathologic condition: oedema of the conjunctiva.
Chiasmal pathology Pathology at the part of the brain where the optic nerves partially cross.
Choroidal rupture A break in the choroid.
Cicatrix Scarring that causes shortening of tissue.
Closed globe injury An eye wall wound that is not full thickness.
Coloboma A congenital eye development defect. It can be either unilateral or bilateral
and can affect a number of different parts of the eye. The detection of a
coloboma does not mean that there is a hole in the eye, but that certain
structures within the eye are not fully formed.
Conjunctivitis Inammation of the conjunctiva. May be infective or not.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 137 aci.health.nsw.gov.au
Term Denition
Consensual pupil response Pupil constriction when light is shone in the other eye.
Contusion Injury: a bruise or injury without a break in skin/cover.
Cortical blindness Lesions affecting the occipital lobe or other parts of the posterior
visual pathway.
Counting ngers vision (CF) A level of vision where the patient is just able to repeatedly count how many
ngers are held up 30–300cm in front of them with one eye covered and in
good light. The patient is unable to see any letters on the Snellen chart.
Decompensated phoria When the eye moves outward towards the ear or towards the nose or an
eye moves upward as compared to the other eye. It has a gradual onset.
Diplopia (double vision) Symptom/functional defect: double vision.
Direct pupil response Pupil constriction when light is shone in the eye.
Dry eye Inammation of the conjunctiva and cornea of the eye due to inadequate
tear secretion.
Ecchymosis Pathologic condition: bruising.
Ectropion Eyelid is turned outwards away from the eyeball.
Endophthalmitis An intraocular infection and severe inammation of the anterior and/or
posterior chambers of the eye which can occur following surgery,
intraocular injection and trauma.
Entropion When the eyelid is turned towards the eyeball.
Epidemic keratoconjunctivitis
(EKC)
Viral conjunctivitis. Please see advice from NSW Health Infectious
Diseases web page.
Episcleritis A benign, inammatory disease affecting the episclera.
Erosions Pathologic condition: destruction/eating away/loss of corneal epithelium.
Exposure keratopathy Dryness of the cornea caused by incomplete eyelid closure. Consider
causes such as seventh (7th) cranial nerve palsy and Bell's palsy, eyelid
ectropion or eyelid scars. Other contributing factors include: Sjögren's
syndrome (aqueous tear underproduction), blepharitis (evaporative dry
eye), or neurotropic cornea and ulceration, (e.g. HSV or CNS palsy).
Eyelid hygiene This is an important part of treatment and prevention of blepharitis. Daily
routines involve warmth, massage and cleaning the area.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 138 aci.health.nsw.gov.au
Term Denition
Eyelid margin The portion located at the edge of the eyelid.
Flashes Flashes are a form of photopsia, a visual phenomenon referring to the
perception of light in the absence of external light stimuli. Photopsias
generated in the eye result from mechanical stimulation of the retina by
vitreoretinal traction. These can be triggered by eye movement and are
usually in the temporal visual eld.
Fluorescein An orange dye that is used in conjunction with a blue light to detect foreign
bodies in the eye.
Floaters The perception of dark spots caused by opacities in the vitreous that are
secondary to degenerative vitreous changes. Patients may describe
oaters as ‘cobwebs’ and 'ies' that are more evident with uniform light
backgrounds, (e.g. blue sky).
Fornix/fornices Potential space between the ocular surface and the conjunctival space of
the eyelid.
Fourth (4th) cranial
nerve palsy
Causes the inability to depress the eye and classically presents as a
vertical or torsional binocular diplopia. Because the fourth cranial nerve
innervates the superior oblique, which has a less well-dened pattern of
action than the rectus muscles, it can be hard to discern an eye movement
disorder. As it has the longest intracranial course of all the cranial nerves,
the fourth nerve is particularly vulnerable to trauma, but palsy can also be
caused by giant cell arteritis (GCA) or compression by a tumour.
Functional visual loss A decrease in visual acuity that cannot be accounted for by anatomical or
physiological ndings. Objective assessments should demonstrate a visual
acuity better than subjective visual acuity.
Giant cell arteritis (GCA) A systemic vasculitis affecting medium and large vessels and also known
as temporal arteritis. GCA is an eye emergency that commonly presents as
anterior ischaemic optic neuropathy (AION). Symptoms include
polymyalgia rheumatica, new onset headache (often temporal), scalp
tenderness, jaw claudication, tongue claudication, fever and night sweats,
loss of weight, generalised muscle pain and weakness and diplopia or
transient visual loss.
Glaucoma A group of eye diseases in which the neurons of the optic nerve at the back
of the eye are slowly destroyed.
Globe The eyeball.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 139 aci.health.nsw.gov.au
Term Denition
Hand movements vision (HM) A level of vision that the patient is just able to repeatedly determine when a
hand is held up 30–100cm in front is moving side to side with one eye
covered and in good light. The patient is unable to count ngers.
Herpes simplex A viral disease caused by the herpes simplex virus.
Herpes zoster This virus commonly affects the ophthalmic branch of the trigeminal nerve
(V1). It is also known as shingles. It may or may not involve the eye, which
also has sensory innervation from V1. Ophthalmic manifestations include
conjunctivitis, scleritis, episcleritis, keratitis iridocyclitis, Argyll Robertson
pupil, glaucoma, retinitis, choroiditis, optic neuritis, optic atrophy,
retrobulbar neuritis, exophthalmos, lid retraction, ptosis and extraocular
muscle palsies.
Heterochromia A difference in iris colour. It can occur due to congenital Horner syndrome,
chronic intraocular inammation or prolonged use of some glaucoma drops.
Horner syndrome Caused by a disruption of the sympathetic nervous system. It can cause
minor upper lid ptosis, anisocoria (affected pupil smaller), less sweating on
the affected side of the face (anhidrosis) and a lighter-coloured pupil on
that side (heterochromia) if long-standing or congenital.
Hyperaemia Clinical sign: increased blood ow. Congestion of conjunctival blood vessels.
Hypopyon A visible collection of inammatory cells in the anterior chamber of the eye.
Ice test Myasthenia gravis (MG) diagnostic test: an ice pack is applied to a droopy
eyelid for 2–5 minutes and then the eyelid is examined for improvement
of ptosis.
Identify, Situation,
Background,Assessment
and Recommendation (ISBAR)
A tool to improve patient safety by standardising communication and the
transfer of critical information.
Idiopathic intracranial
hypertension (IIH)
A neurological disorder that is characterised by increased intracranial
pressure in the absence of a tumour or other disease. Commonly also
called pseudotumour cerebri.
Idiopathic orbital
inammatory disease
An inammation of soft tissue involving any area of the orbit.
Inltrate A corneal inltrate is an aggregate of white blood cells located within the
corneal stroma. It usually suggests active bacterial keratitis. There is often
an overlying corneal ulcer, which stains with uorescein.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 140 aci.health.nsw.gov.au
Term Denition
Intermediate/posterior uveitis Uveitis is the inammation of the uvea. Intermediate uveitis (also known as
pars planitis or cyclitis) is the inammation of tissues in the area just
behind the iris and lens of the eye. Posterior uveitis (also known as
choroiditis) refers to inammation of the choroid (back part of the uvea).
Posterior uveitis may affect the retina and/or the optic nerve and may lead
to permanent loss of vision. It is rare.
Intermittent angle closure Intermittent episodes of angle closure glaucoma that resolve between
attacks. Symptoms include headache, eye pain or occasional halos around
lights. Over time, these episodes result in peripheral anterior synechiae
(PAS), which can cause permanent elevation of intraocular pressure (IOP)
(chronic angle closure glaucoma).
Intraocular pressure (IOP) Fluid pressure inside the eye.
Iridoschisis Pathologic condition: splitting of the iris/structural formation of a hole in
the iris.
Iritis Inammation that affects the iris. The iris is a part of the middle layer of
the eye (uvea), so iritis is a type of uveitis, more accurately termed
anterior uveitis.
Ischaemia Pathological condition: localised ischaemia caused by arterial constriction.
Keratitis Infection or inammation of the cornea.
Lacrimal drainage apparatus The system containing the orbital structures for tear production
and drainage.
Lagophthalmos Inability to close the eye. Classically caused by seventh nerve palsy but
can also occur due to traumatic disruption of the eyelids. If severe, it can
lead rapidly (within hours) to corneal exposure, irreversible scarring and
blindness.
Lens dislocation A lens that has moved out of position because some or all of the supporting
ligaments have broken.
Leukocoria A white, rather than red, reex when the retina is illuminated from a
distance. A red reex is normally assessed with a direct ophthalmoscope
shining a light into both eyes from a distance – a reected red glow is
normally observed – but can also be observed from camera ashes. The
life-threatening cause that must urgently be excluded is retinoblastoma, a
cancer of the retina that usually occurs in children.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 141 aci.health.nsw.gov.au
Term Denition
Light perception
(PL or LP)
A level of vision where, with one eye completely covered, the patient is
repeatedly able to determine when a very bright light is shone on their eye
from about 10cm away. Ensure there are no auditory cues, (e.g. clicking of
light switches). The patient is unable to see hand movements.
Limbus The corneal limbus is the border between the cornea and the sclera.
Macular pathology,
(e.g.macular haemorrhage)
The macula is the central region of the retina and is situated at the
posterior pole of the eye. It is the part of the retina that produces central
vision. Pathology or disease in this area are varied and include oedema and
macular haemorrhage, both of which can be caused by age-related
macular degeneration and central serous chorioretinopathy. Seek
ophthalmologist referral.
Migraine A primary headache disorder characterised by recurrent headaches that
are moderate to severe and typically unilateral. Migraine is the most
common reason for aura.
Miosis The excessive constriction of the pupil of the eye relative to the amount of
light the pupil receives. Causes can include drugs, (e.g. opioids, nicotine
products, antipsychotics, imidazolines and antiemetics) or disease.
Myasthenia gravis
(MG)
Ocular myasthenia gravis is a form of myasthenia gravis in which the
muscles that move the eyes and control the eyelids are weakened, causing
double vision and/or drooping eyelids. Symptoms tend to be worse at the
end of the day.
Mydriasis The dilation of the pupil of the eye.
Myopic Short-sighted.
Neoplasm
(orbital, intracranial)
An abnormal growth of tissue that can be benign or malignant. Also
called tumour.
Neovascular glaucoma
(NVG)
Classied as a secondary glaucoma. Delayed diagnosis or poor
management can result in complete loss of vision or even the loss of the
globe itself. Patients may present with severe pain. Seek urgent referral to
an ophthalmologist.
No perception of light
(NPL)
A level of vision where, with one eye covered, the patient is unable to
reliably perceive light. Compare light perception.
Non-accidental injury
(NAI)
A non-accidental injury (NAI) is dened as any abuse purposefully inicted
on a person.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 142 aci.health.nsw.gov.au
Term Denition
Non-arteritic anterior
ischaemic optic
neuropathy (NAION)
Optic nerve dysfunction secondary to ischaemia with resulting disc
swelling and subsequent pallor. It is not associated with vasculitis such as
giant cell arteritis (GCA). It is associated with cardiovascular risk factors,
especially hypertension.
Occipital lobe lesions The occipital lobes are one of four main lobes of the cerebral cortex.
Lesions in this area can affect visual perception, colour recognition,
reading and reading comprehension, as well as depth and the movement of
objects. If severe, can cause cortical blindness.
Oculocardiac reex A potentially fatal reex that occurs due to stimulation of the trigeminal
nerve. The resultant massive parasympathetic outow mediated by the
vagus nerve can cause bradycardia, hypotension and life-threatening
arrhythmias. Entrapment of extraocular muscles by periorbital fractures
can cause oculocardiac reex.
Open globe injury A full thickness injury to the cornea, sclera or both.
Ophthalmia neonatorum Neonatal conjunctivitis contracted by newborns during delivery through an
infected birth canal.
Ophthalmoplegia Weakness or paralysis of one of the extraocular muscles that control eye
movement and keep the eye in place.
Optic nerve dysfunction Optic nerve function can be tested by combining examination of the
various modalities: visual acuity, pupil function, peripheral elds, colour
vision and colour saturation.
Optic neuritis A demyelinating inammation of the optic nerve.
Orbital cellulitis Inammation of eye tissues behind the orbital septum. It most commonly
refers to an acute spread of infection into the eye socket from either the
adjacent sinuses or through the blood.
Palpebral ssure Space between the upper and lower eyelid edges.
Penetrating eye injury When an object penetrates through the globe with no exit wound.
Periorbital cellulitis Inammation and infection of the eyelid and portions of skin around the
eye, anterior to the orbital septum. Also known as preseptal cellulitis.
Photopsia Perceived ashes of light. Associated with posterior vitreous detachment,
migraine with aura without headache and retinal break or detachment.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 143 aci.health.nsw.gov.au
Term Denition
Pingueculum A yellowish patch or bump on the conjunctiva, near the cornea. This is a
fatty degeneration of the conjunctiva overlying the inner or (less
commonly) outer part of the white of the eye. This is a benign condition,
usually requiring no treatment. Articial tears may help to relieve discomfort.
Posterior synechiae Pathological condition: adhesion of the iris to the cornea/lens.
Posterior vitreous
detachment (PVD)
A condition of the eye in which the vitreous membrane separates from the
retina. It refers to the separation of the posterior hyaloid membrane from
the retina anywhere posterior to the vitreous base.
Presbyopia Loss of near vision caused by the loss of elasticity of the lens of the eye,
occurring typically in middle and old age.
Preseptal cellulitis Inammation and infection of the eyelid and portions of skin around the
eye, anterior to the orbital septum. Also known as periorbital cellulitis.
Primary gaze Gaze position determines the effect of extraocular muscle contractions on
the rotation of the eye. Primary gaze is when the eyes look straight ahead.
Prolapse Pathologic condition: slip/falling out of place of a part, e.g. iris may fall
through a wound.
Proptosis Protrusion of the eyeball. Also known as exophthalmos and is usually used
when describing proptosis due to Graves’ disease.
Pterygium A brovascular overgrowth of the conjunctiva onto the cornea.
Ptosis Drooping of the upper eyelid, indicative of third nerve palsy, Horner
syndrome, injury or swelling of the eyelid.
Ptosis measurement Lid crease height, margin reex distance (MRD) and levator function
measurements are needed. Ensure the patient's head in a normal position
with eyebrows relaxed.
Red reex The red reection seen through the pupil from the retina. This is similar to
‘red eye’ in ash photography. The reex is missing if there is an opacity at
the cornea, anterior chamber, lens and vitreous or if the retina is detached.
Reduced vision/
decrease in vision acuity
A decreased capacity of vision that is not corrected by glasses.
Relative afferent pupillary
defect (RAPD)
A pattern of pupil abnormality which is tested by the ‘swinging torch test’.
Also known as Marcus Gunn pupil. Abnormal pupillary response in which
the pupil initially dilates in response to bright light after bright light has
been shone in the contralateral (normal) eye.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 144 aci.health.nsw.gov.au
Term Denition
Retinal tear/detachment
(RD)
A disorder of the eye in which the retina peels away from its underlying
layer of support tissue.
Retrobulbar haemorrhage A rare, rapidly progressive, sight-threatening emergency that results in an
accumulation of blood in the retrobulbar space. It can occur due to orbital
trauma, complications of eyelid or orbital surgery or any process that can
affect the blood supply to the eye. Immediate referral to an
ophthalmologist is needed.
Retropulsion A push back of the eye. Used in eye examination to detect the level of
resistance and orbit mobility.
Scleritis Inammation of the sclera.
Scotoma Blind spot in an otherwise normal vision eld.
Seidel test A test used to reveal ocular leaks from the cornea, sclera or conjunctiva
following an injury.
Seventh (7th) cranial
nerve palsy
Can cause paralysis of facial muscles on that side and may result in the
inability to close the eye (lagophthalmos). This leads to exposure of the
corneal surface, which can rapidly cause irreversible corneal damage and
blindness. Seek immediate referral to an ophthalmologist.
Sixth (6th) cranial nerve palsy Causes the inability to abduct the eye. The patient will classically describe
horizontal binocular diplopia that is worse on looking to the affected side,
and either less marked (or resolved) on looking in the opposite direction or
at a near target. Causes that must be excluded include giant cell arteritis
(GCA), compression by a tumour and trauma. Bilateral sixth nerve palsy
can occur if there is elevated intracranial pressure.
Stroke A medical emergency when blood ow to the brain is blocked. Seek
neurological referral.
Stye An infection of an oil gland in the eyelid. Also known as hordeolum.
Subconjunctival haemorrhage Bleeding underneath the conjunctiva.
Subtarsal foreign body Usually in the upper eyelid. Symptoms include a foreign body sensation,
watering and pain.
Supercial punctate
epithelial defect
Damage of the epithelium of the cornea in a pinpoint pattern under a slit
lamp. Symptoms are nonspecic, including red eye, tearing, foreign body
sensation, photophobia and burning. The eye may appear red with a visible
foreign body or linear corneal abrasion.
Eye Emergency Manual December 2023
Agency for Clinical Innovation 145 aci.health.nsw.gov.au
Term Denition
Symblepharon Pathologic condition: adhesion of the eyelid conjunctiva to the conjunctiva
of the globe.
Tarsal conjunctival The part of the conjunctiva that lines the inside surface of the eyelid.
Temporal arteritis See giant cell arteritis (GCA).
Third (3rd) cranial nerve palsy Classically causes upper lid ptosis, anisocoria (pupil larger on affected
side), downwards and lateral deviation of the affected eye and an inability
to adduct or elevate the eye. Lesser degrees of palsy can result in a minor
ptosis or only partial movement decits. Causes that must be excluded are
an aneurysm of the posterior communicating artery compressing the third
cranial nerve, another intracranial mass or pathology in the cavernous
sinus, giant cell arteritis (GCA) and trauma.
Thyroid eye disease
(TED)
An autoimmune disease that causes inammation of the eye muscles and
fatty tissue behind the eyes. This can cause the eyes to be pushed forward
so the eyes ‘bulge’. Associated with Graves' disease.
Transient visual obscuration Temporary or momentary loss of vision in one or both eyes. May be a
symptom of a number of conditions depending on its clinical features.
Trichiasis A condition (such as entropion) resulting in the eyelashes rubbing against
the cornea causing discomfort and the potential for ulceration.
Ulceration Pathologic condition: loss of substance in skin/mucous tissue due to
gradual necrosis of the tissue.
Uvea Term used to describe the ‘middle’ layer of the eye’s internal structure,
between the retina and the sclera. It comprises the choroid, ciliary body
and iris. Visible uveal tissue following trauma indicates that the globe
is ruptured.
Uveal contents The vascular middle layer of the eye constituting the iris, ciliary body and
the choroid.
Uveitis Inammation of the middle layer of tissue of the uvea (eye wall). Symptoms
include eye redness, pain and blurred vision. Can be unilateral or bilateral.
Valsalva retinopathy Valsalva retinopathy is a preretinal haemorrhage caused by a sudden
increase in intrathoracic or intra-abdominal pressure. Seek an urgent
referral to an ophthalmologist.
Vitreous haemorrhage The extravasation or leakage of blood into the areas in and around the
vitreous humour of the eye.
