~ 14 ~
International Journal of Applied Dental Sciences 2018; 4(2): 14-18
ISSN Print: 2394-7489
ISSN Online: 2394-7497
IJADS 2018; 4(2): 14-18
© 2018 IJADS
www.oraljournal.com
Received: 04-02-2018
Accepted: 05-03-2018
Dr. Upendra Prasad
Post-Graduate Student,
Dept. of Periodontics,
Nair Hospital Dental College,
Mumbai, Maharashtra, India
Dr. Praneeta Kamble
Associate Professor,
Dept. of Periodontics,
Nair Hospital Dental College,
Mumbai, Maharashtra, India
Correspondence
Dr. Upendra Prasad
Post-Graduate Student,
Dept. of Periodontics,
Nair Hospital Dental College,
Mumbai, Maharashtra, India
Idiopathic gingival enlargement: A case report
Dr. Upendra Prasad
and
Dr. Praneeta Kamble
Abstract
Idiopathic gingival enlargement is a rare condition characterized by massive enlargement of the gingival
tissue that causes aesthetic and functional problems. Other forms of gingival enlargement also exist such
as genetic, drug induced etc. This case report addresses the diagnosis and treatment of a case of
idiopathic gingival enlargement in a 21-year-old male. The patient presented with generalized diffuse
gingival enlargement involving the maxillary and mandibular arches extending on buccal and
lingual/palatal surfaces and covering incisal/occlusal third of the teeth resulting in difficulty in speech
and mastication since last 10-12 years. Biopsy report confirmed the diagnosis of fibro-epithelial
hyperplasia. Gingivectomy was carried out in all four quadrants.
Keywords: Gingival enlargement, Idiopathic, Gingivectomy, Fibromatosis
Introduction
Idiopathic gingival enlargement (IGE) is a rare condition characterized by massive
enlargement of the gingiva. The enlargement of gingiva is slow and progressive in nature. It is
also known as elephantiasis, idiopathic fibromatosis, gingivomatosis, and hereditary gingival
fibromatosis
[1]
. It may occur as an isolated disorder or may be associated with conditions like
tuberous sclerosis
[2]
and hypertrichosis
[3]
. Various drugs such as calcium channel blockers
[4]
immunosuppressants
[5]
and anticonvulsants
[6]
can lead to massive gingival enlargement. It
may also occur as a part of syndromes like Zimmerman–Laband syndrome
[7]
,
Jones syndrome
[8]
, Murray‑ Peretic‑ Drescher syndrome
[9]
, Cross syndrome
[10]
, Ramon syndrome
[11]
and
Prune belly syndrome
[12]
.
Several ongoing investigations are ongoing to establish the exact genetic linkage and
heterogeneity associated with the disease, however the exact etiology is still not known. IGE is
now an established hereditary gingival enlargement (HGE) and the terms IGE and HGE are
used interchangeably
[13]
. Hereditary gingival enlargement displays both an autosomal
dominant mode of inheritance in some patients and an autosomal recessive in other cases.
Males and females are equally affected in this disease
[14]
.
Clinically IGE is characterized by gingival overgrowth, pink coloured gingiva which is firm in
consistency, and non‑ haemorrhagic
[15]
. IGE can affect both deciduous as well as permanent
dentition, however it has been shown to worsen during adolescence.
This anomaly is classified as two types according to its form. The localized nodular form is
characterized by the presence of multiple enlargements in the gingiva. The most common
symmetric form results in uniform enlargement of the gingiva. Hyperplastic gingival
enlargement may occur during or after the eruption of primary or permanent dentition and
rarely present at birth
[16]
. The most common effect related to gingival enlargement is mal-
positioning of teeth, diastemas, and prolonged retention of primary teeth. In cases of massive
enlargement the teeth are completely submerged, and the enlargement projects into the oral
vestibule resulting in facial disfigurement, difficulty in mastication, and speech.
Treatment of idiopathic gingival enlargement consists of surgical excision of the hyperplastic
tissue to restore gingival contours, but the recurrence rate is very high following surgical
excision
[17]
. Usually, these types of enlargements are associated with minimal local factors
and minimal alveolar bone loss; however, there have been few reports on this rare lesion where
it was associated with aggressive periodontitis.
~ 15 ~
International Journal of Applied Dental Sciences
Case report
A 21-year-old male patient reported to the outpatient
department of Periodontics with a chief complaint of swollen
gums since 10-12 years involving all his teeth. The swelling
was aesthetically unpleasing and also causes problem during
speech, articulation, mastication, and causing inadequate lip
apposition. Patient did not undergo any kind of dental
treatment for the above problem. He did not give any history
of drugs intake, fever, anorexia, weight loss, seizures, hearing
loss, nor having any physical or mental disorder. Also familial
and postnatal history was non-contributory.
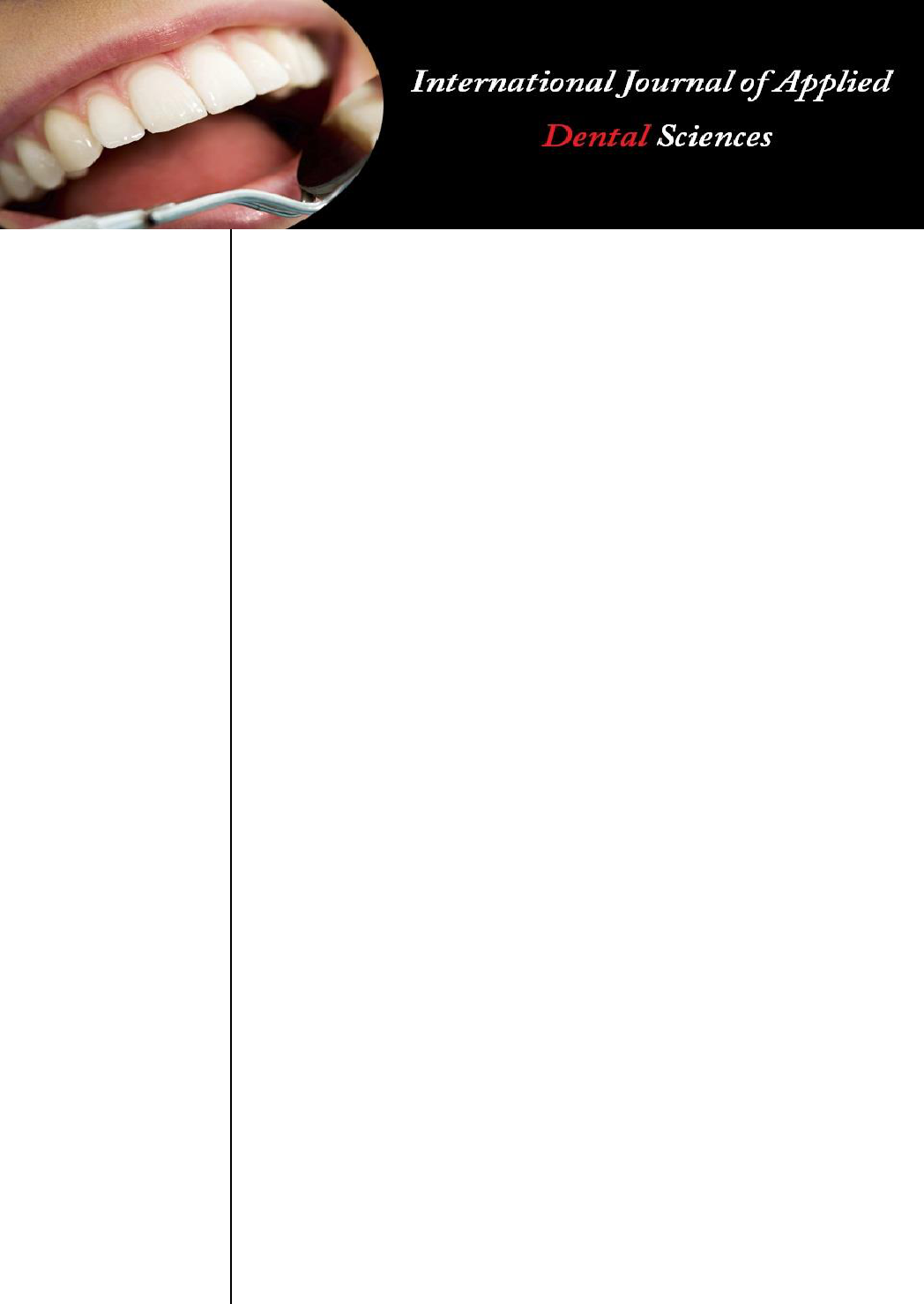
Clinical examination
Extra-oral examination showed that the patient had bilaterally
symmetrical facial profile and lymph nodes were not
palpable, TMJ movements were normal with incompetent lips
and a convex profile. An intraoral examination revealed
generalized, diffuse, nodular enlargement of the gingiva
involving the upper and lower arches, which were pale pink in
colour, and had a firm and fibrous consistency. The two-third
of the teeth surfaces were covered with enlarged gingiva, fig.
1, 2, 3.
Fig 1: Frontal view
Fig 2: Palatal view
Fig 3: Lingual view
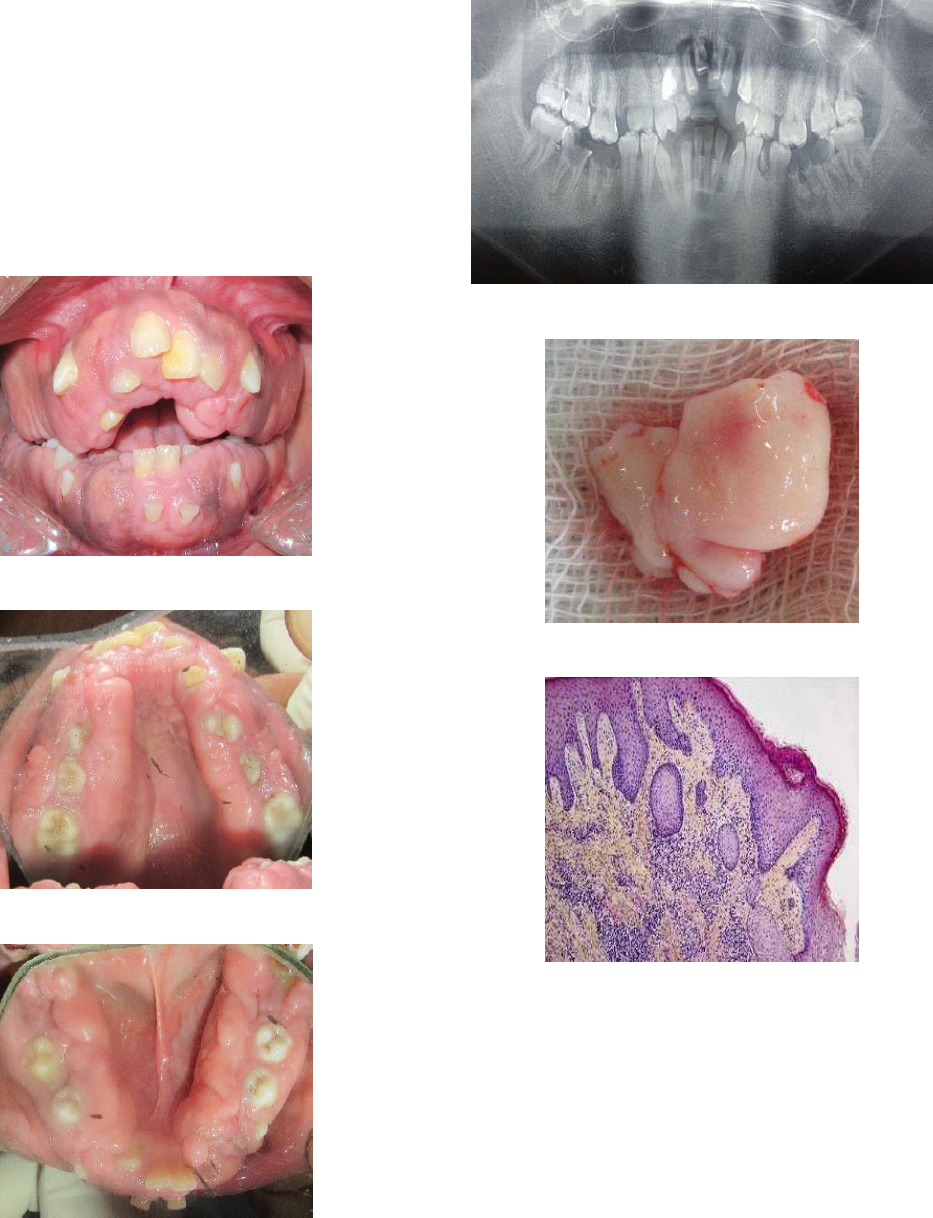
Investigations
Panoramic radiograph showed no bone loss, fig. 4. Carious
lesion were present in 46, 47, 36 and 37. Over-retained
deciduous teeth 53, 71 and 81 were present. Routine blood
investigations were done which was within normal limits.
Excisional biopsy was carried out which was sent for
histopathological evaluation, fig. 5. The Histopathology
revealed the presence of dense connective tissue fibrils and
mild inflammatory cells infiltrates suggestive of fibro-
epithelial hyperplasia, fig. 6.
Fig 4: Panoramic radiograph
Fig 5: Excised
Fig 6: Histopathological slide
Differential diagnosis
Drug-induced enlargement, hereditary gingival enlargement
and idiopathic gingival enlargement.
Diagnosis
The family, medical, and drug histories were non-contributory
in this case; hence it was diagnosed as idiopathic gingival
enlargement.

~ 16 ~
International Journal of Applied Dental Sciences
Treatment
After completion of Phase I treatment, a quadrant-wise
gingivectomy was performed under local anaesthesia using
Kirkland knives for incisions on the facial and lingual
surfaces and Orban periodontal knives were used for
interdental incisions. After achieving haemostasis periodontal
dressing was given in all four quadrants to reduce patient
discomfort, fig. 7-12. Post-operative follow-up was done for
the next 6 months which showed no sign of recurrence
Fig 7: Probing depth.
Fig 8: Gingivectomy with Kirkland knives.
Fig 9: Interdental incision with Orban knives.
Fig 10: Haemostasis achieved
Fig 11: Periodontal dressing

~ 17 ~
International Journal of Applied Dental Sciences
Fig 12: Preoperative and postoperative comparison after six months
Discussion
Gingival fibromatosis may be congenital or hereditary, the
causes of which are not clearly understood. Hence, the terms
idiopathic gingival fibromatosis and hereditary gingival
fibromatosis are often used interchangeably
[14]
.
Fibrotic gingival enlargement can also occur after long
duration therapy with drugs like phenytoin
[6]
cyclosporine
[5]
,
nifedipine
[4]
. Hence use of these drugs should be ruled out.
Gingival fibromatosis may be associated with physical
development, retardation, and hypertrichosis
[3]
. Enlargement
usually begins with the eruption of the permanent dentition
but can develop with the eruption of the deciduous dentition;
rarely it may be present at birth or arise in adulthood
[16]
.
Maximal enlargement occurs either during loss of deciduous
teeth or in the early stages of eruption of permanent teeth and
progresses rapidly during "active" eruption and decreases
with the end of this stage
11
. It has been suggested that gingival
enlargement may be due to nutritional and hormonal factors;
however, these have not been completely substantiated. The
constant increase in the tissue mass can result in delayed
eruption and displacement of teeth, arch deformity, spacing,
and migration of teeth
[12]
. All these features may create
problem in normal mastication and in oral hygiene measures.
Maintaining good oral hygiene is important as the presence of
inflammation and infection can be associated with a risk of
recurrence of the gingival enlargement. However, gingival
fibromatosis recurrence is not only due to the presence of
local factors, but also due to genetic predisposition.
Therefore, it is not possible to predict the long-term results of
gingival fibromatosis treatment even when associated with
good oral hygiene.
Histologically, the gingival fibromatosis is mainly due to an
increase in numbers of fibroblast in the connective tissue
stroma. The nodular appearance can be attributed to the
hyperkeratinized epithelium. The treatment of choice in this
condition was gingivectomy as bony intervention was not
required. Since recurrence can occur within a few months
after surgery and may return to the original condition within
few years, the patient may have to undergo repeated
gingivectomy procedures. However, in this patient there was
no sign of recurrence for the six months follow up period.
Conclusion
Therefore, long-term follow-up is mandatory for maintenance
and to evaluate the predictability of the surgical treatment and
the recurrence of the gingival enlargement. IGE is an
enlargement of genetic predisposition and unknown etiology
and hence the rate of recurrence is very high impending the
normal functions and esthetics of the patient.
References
1. Newman, Takei, Klokkevold, Carranza. Carranza’s
clinical periodontology. Twelfth edition.
2. Thomas D, Rapley J, Strathman R, Parker R. Tuberous
sclerosis with gingival overgrowth. J Periodontol. 1992;
63:713-7.
3. Horning GM, Fisher JG, Barker BF, Killoy WJ, Lowe
JW. Gingival fibromatosis with hypertrichosis: A case
report. J Periodontol. 1985; 56:344-7.
4. Heijl L, Sundin Y. Nitrendipine-induced gingival
overgrowth in dogs. J Periodontol. 1989; 60:104-12.
5. Thomason JM, Seymour RA, Ellis JS, Kelly PJ, Parry G,
Dark J et al. Determinants of gingival overgrowth
severity in organ transplant patients: An examination of
the role of HLA phenotype. J Clin Periodontol. 1996;
23:628-34.
6. Kato T, Okahashi N, Kawai S, Kato T, Inaba H, Morisaki
I et al. Impaired degradation of matrix collagen in human
gingival fibroblasts by the antiepileptic drug phenytoin. J
Periodontol. 2005; 76:941-50.
7. Holzhausen M, Ribeiro FS, Gonçalves D, Correa FO,
Spolidorio LC, Orrico SR. Treatment of gingival
fibromatosis associated with Zimmermann-Laband
syndrome. J Periodontol. 2005; 76:1559-62.
8. Wynne SE, Aldred MJ, Bartold PM. Hereditary gingival
fibromatosis associated with hearing loss and
supernumerary teeth: A new syndrome. J Periodontol.
1995; 66:75-9.
9. Piattelli A, Scarano A, Di Bellucci A, Matarasso S.
Juvenile hyaline fibromatosis of gingiva: A case report. J
Periodontol. 1996; 67:451-3.
10. Cross HE, McKusick VA, Breen W. A new oculocerebral
syndrome with hypopigmentation. J Pediatr. 1967;
70:398-406.
11. Ramon Y, Berman W, Bubis JJ. Gingival fibromatosis
combined with cherubism. Oral Surg Oral Med Oral
Pathol. 1967; 24:435-48.
12. Harrison M, Odell EW, Agrawal M, Saravanamuttu R,
Longhurst P. Gingival fibromatosis with prune‑ belly
syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 1998; 86:304-7.
13. Hart TC, Pallos D, Bozzo L, Almeida OP, Marazita ML,
O’Connell JR, et al. Evidence of genetic heterogeneity
for hereditary gingival fibromatosis. J Dent Res. 2000;
79:1758-64.
14. Arvind Shetty, Neha Gupta, Devanand Shetty, Rukshit
Kadakia. Idiopathic gingival enlargement associated with
generalized aggressive periodontitis in a 19‑ year‑ old
female. Journal of Indian Society of Periodontology.
~ 18 ~
International Journal of Applied Dental Sciences
2014, 18(2).
15. Bittencourt LP, Campos V, Moliterno LF, Ribeiro DP,
Sampaio RK. Hereditary gingival fibromatosis: Review
of the literature and a case report. Quintessence Int. 2000;
31:415-8.
16. Bozzo L, Machado MA, de Almeida OP, Lopes MA,
Coletta RD. Hereditary gingival fibromatosis: Report of
three cases. J Clin Pediatr Dent. 2000; 25:41-6.
17. Danesh-Meyer MJ, Holborow DW. Familial gingival
fibromatosis: A report of two patients. N Z Dent J. 1993;
89:119-22.
