
Medicare Financial Management
Chapter 4 - Debt Collection
Table of Contents
(Rev. 12346, 11-01-23)
Transmittals Issued for this Chapter
10 - Requirements for Collecting Part A and B Provider Non-MSP Overpayments
10.1 - Required Timeframes for Debt Collection Process for Provider Non-MSP Overpayments
20 - Demand Letters
20.1 - Number of Demand Letters
20.2 – Sample Demand Letters All Providers or Suppliers
Exhibit 1 – Initial Demand Letter –Non-935
Exhibit 2 - Initial Demand Letter – 935
Exhibit 3 – Initial Demand Letter- 935
Exhibit 4 – Initial Demand Letter Unfiled Cost Report
Exhibit 5 – Intent to Refer Letter –Non-935
Exhibit 6 – Intent to Refer Letter- 935
Exhibit 7 - Intent to Refer Letter - Unfiled Cost Reports ONLY
30 – Interest Assessment/Payment on Overpayments and Underpayments
30.1 - Final Determination
30.2 – Rates of Interest – FIs and Carriers
30.3 – Interest Accruals
30.4 – Procedures for Applying Interest During Overpayment Recoupment
30.5 – Notification to Providers Regarding Interest Assessment
30.6 – Waiver and Adjustment of Interest Charges
40 – Withholds and Suspensions
40.1 – Recoupment by Withholding Payments
40.2 – Suspension of Payment
50 – Establishing an Extended Repayment Schedule (ERS) - (formerly known as an Extended Repayment
Plan (ERP))
50.1 – ERS Required Documentation --Physician is a Sole Proprietor
50.2 – ERS Required Documentation– Provider is an Entity Other Than a Sole
Proprietor
50.3 – ERS Approval Process
Exhibit 1 – Protocol for Reviewing Extended Repayment Schedule (ERS)
Exhibit 2 – Statement of Source and Application of Funds Period Covered
Exhibit 3 – Cash Flow Statement Period Covered
Exhibit 4 – Projected Cash Flow Statement Cash from Operations (Schedule A) Period Covered
50.4 – Sending the ERS Request to the Regional Office (RO)
50.5 – Monitoring an Approved Extended Repayment Schedule (ERS) and Reporting Requirements
50.6 – Requests From Terminated Providers or Debts that are Pending Referral to Department of
Treasury
60 - Withholding the Federal Share of Payments to Recover Medicare or Medicaid Overpayments - General
60.1 - Withholding the Federal Share of Medicaid Payments to Recover Medicare Overpayments
60.2 – Withholding Medicare Payments to Recover Medicaid Overpayments
70 – Non-Medicare Secondary Payer (Non-MSP Debt Referral Instructions and Debt Collection
Improvement Act of 1996 (DCIA) Activities
70.1 – Background
70.2 – Cross Servicing
70.3 – Treasury Offset program (TOP)
70.4 – Definition of Delinquent Debt
70.5 – Referral Requirements
70.6 – Debt Ineligible for Referral
70.7 – Intent to Refer Letter
70.8 – Response to Intent to Refer Letter
70.9 – Reserved for Future Use
70.10 – Reserved for Future Use
70.11 – Actions Subsequent to Debt Referral
70.12 - Transmission of Debt
70.13 – Updates after Debt Transmission
70.14 – Collections
70.14.1 – Background
70.14.2 – Intra-governmental Payment and Collection (IPAC) System
70.14.3 - CMS Debt Management Collections Interface and Report
70.14.4 - Reserved for Future Use
70.14.5 - Reserved for Future Use
70.14.6 - Extended Repayment Schedule (ERS)
70.14.7 - Excess Collections
70.14.8 - Applying Excess Collections
70.14.8.1 - If the Debtor Has Other Outstanding Debt
70.14.8.2 - If the Debtor Has No Other Outstanding Debt
70.15 – Financial Report for Debt Referred
70.15.1 – Financial Reporting for Non- MSP Debt
70.15.2 – Reserved for Future Use
70.15.3 - Financial Reporting for Collections Received on Debts from Cross Servicing
70.15.4 – Financial Reporting for Debts Returned to Agency (RTA)
70.15.4.1 – Debts RTA for Bankruptcy
70.15.4.2 – RTA and other Debts, Pending Final Disposition
70.15.4.3 – Debts RTA Because Dispute Timer Expired
70.15.4.4 – Debts RTA Paid in Full or Satisfied Payment Agreement or Satisfied
Compromise
70.16 – Debt Close-out
70.17 – Debts Returned to Agency (RTA) by the United States Department of the Treasury
(Treasury)
70.17.1 - Debts RTA by Treasury due to Bankruptcy (RB)
70.17.2 - Debts RTA by Treasury as Uncollectible (RU) or Out of Business (RN)
70.17.3 - Debts RTA by Treasury as Dispute Response not Received Timely (RX)
70.17.4 - Debts RTA by Treasury as a Miscellaneous Dispute, a Manual RTA, Complaint or
as Recall Approved (RD)
70.17.5/Debts RTA by Treasury as paid in Full (RP), Satisfied Payment Agreement (RS) or
Satisfied Compromise (RC)
Exhibit 1 – Intent to Refer (ITR) Letter
Exhibit 5 – Treasury Cross-Servicing Dispute Resolution
80 - Recovery of Non MSP Overpayments from the Beneficiary
80.1 - Reserved for Future Use
80.2 - Immediate Recoupment Requirements for NON-935 Overpayment Recovery from the
Physicians and Other Suppliers
80.3 - Overpayment Recovery from Suppliers of Durable Medical Equipment, Prosthetics, Orthotics,
and Suppliers (DMEPOS)
90 - Physician/Supplier Overpayment Demand Letter - Carrier
90 1 – Part B Overpayment Demand Letters Beneficiaries
90 2 - Part B NON-935 Overpayment Demand Letters to Physicians/Other Suppliers
Exhibit 1 – Initial Demand Letter to Physicians/Suppliers
Exhibit 2 – Follow Up Demand Letter to Physicians/Suppliers
Exhibit 3 – Intent to Refer Letter
Exhibit 4 – Optional Overpayment Customizing Paragraphs
Exhibit 5 – Sample Letter – Check Included for Correct Amount
Exhibit 6 – Sample Letter – Check Included for Wrong Amount (Too Much)
90.3 - Notification to the Beneficiary When Recovery is Sought from the Provider or Physician
90.4 - Sample Letter to Beneficiary Where Recovery is Sought from Provider
110-- Confirmed Identity Theft
110.2-- Seized Monies Received from Law Enforcement
120 – Monitoring Accounts Receivable that are in a Redetermination or Reconsideration Status
130 – Federal Payment Levy Program – IRS Tax Levy Requests
10 - Requirements for Collecting Part A and B Non-MSP Provider Overpayments
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
For purposes of these instructions, the term Provider, Physician and other Supplier will be referred to
as “Provider”.
The following collection activities are the minimum requirements the Medicare contractor (contractor) shall
follow for all Non-MSP provider overpayments. Where additional information is located elsewhere in the
manual chapter, an annotation of the specific section is included. (See Medicare Financial Management
Manual, Publication 100-06, Chapter 3, §40).
1. Initial Demand letter
The contractor shall send an initial demand letter within established timeframes of the identification or
notification of an overpayment. The contractor shall ensure the date of the initial demand letter is the date
the AR is established and the date the letter is mailed. The initial demand letter shall include all required
language and shall meet timeliness standards as outlined in chapter 3 §200 and/or chapter 4 §§20 and 90.
a. Dollar threshold
The threshold amount to send the initial demand letters is $25 (principal). The contractor shall aggregate all
of the overpayments to the provider to meet the threshold amount for the initial demand letter.
b. Undeliverable demand letter
If the contractor receives the initial demand letter back as undeliverable, the contractor shall attempt to reach
the provider by telephone within 10 business days of receiving the undeliverable letter.
If the contractor is unsuccessful at reaching the provider by telephone, the contractor shall at the minimum
attempt to locate the provider through other means including:
• Querying the Provider Enrollment Change of Ownership System (PECOS) to determine if there
is updated contact information (including an email address) for the provide);
• Contacting the medical review staff or fraud and abuse staff for possible updates on the debtor’s
whereabouts;
• Conducting research to see if the provider is in bankruptcy or litigation, and by using the name of
the owners, partners, or the corporation officers;
• Conducting an internet search site, including using Lexis-Nexis® or a similar program;
• Contacting the servicing regional office (RO) for assistance or further guidance, if the contractor
does not have access to a search engine.
The contractor shall document in the case file all attempts to contact the provider.
2. Recoupment
The contractor shall initiate recoupment of the debt, or any remaining balance of the debt, as outlined below,
except when the debt is in the following status: (1) appeal subject to the Limitation on Recoupment
provisions (redetermination/reconsideration), (2) bankruptcy, (3) Extended Repayment Schedule (ERS) or
(4) a pending ERS request.
For Part A (Non-935 Overpayments)
• Recoupment shall begin 16 days from the date of initial demand letter if the debt is not subject to
Limitation on Recoupment provisions of Section 935(f)(2) of the MMA. (See chapter 3, §200)
For Part B (935 and Non-935) and Part A 935 Overpayments
• Recoupment shall begin 41 days from the date of the initial demand letter.
• Recoupment shall continue until the debt is collected in full or is in a status that excludes
recoupment.
3. Interest
If the overpayment is not paid in full 30 days from the date of the initial demand letter, contractors shall
ensure that interest is assessed beginning on day 31. Simple interest shall be charged on the outstanding
principal balance of the debt starting with the date of the initial demand letter and for every 30-day period
thereafter, until the debt is paid in full. Refer to chapter 4, §30 and 42 CFR 405.378 for additional
information.
4. Telephone Contacts:
Contractors shall attempt to contact providers by phone, at least twice, as follows:
a. First telephone contact
• Providers who have been terminated/revoked/ or have withdrawn from the Medicare
program:
o The telephone contact shall be made within 10 business days of the contractor’s notification of
termination/revocation/withdrawal.
• Active Providers:
o The telephone contact shall be made when the debt is at least 60 days delinquent (90 days from the
date of the demand letter) and is not in an appeal, litigation, ERS, or bankruptcy status.
o The telephone contact may be made sooner if the contractor believes that earlier contact may result
in a collection.
o In situations where the provider cannot be reached by telephone the contractor shall leave a
voicemail as needed.
• Successful Phone Contact:
o The contractor shall inform the provider of repayment options (e.g. ERS) and explain that any unpaid
delinquent debt will be referred to Treasury for further collection activity. If the provider has a surety
bond, the contractor shall inform the provider that the debt will be collected through the surety, and
any remaining balance will be referred to Treasury.
o If the first call is successful, (second call would not be necessary) document the contact.
• Unsuccessful Phone Contact
o The contractor shall discontinue telephone efforts when a provider’s number is disconnected.
o The contractor shall at the minimum attempt to locate the provider through other means as listed in
discussion of undeliverable demand letters, section 1(b), above.
b. Second Phone Contact
The second phone call is only necessary if the contractor was unable to directly communicate with the
provider on the first call.
• The contractor shall make a second phone call to the provider at least 7 business days before
referring the debt to Treasury.
• The contractor shall leave a voicemail where the call is directed to voice messaging.
• Leaving the second voicemail message shall be sufficient for attempting to reach the provider by
telephone.
The contractor shall document, in the case file, all attempts to contact the provider.
5. Extended Repayment Schedule (ERS)
If the provider submits an application for an ERS, the contractor shall follow the instructions in
Chapter 4 §50. An ERS application may be requested at any time during the collection process.
6. Intent to Refer (ITR) letter
For providers who have been terminated/revoked or have withdrawn from the Medicare program:
The contractor shall send the ITR letter:
• If the initial demand letter was returned undeliverable and a better address cannot be located (see
below for Instructions Summary for Undeliverable Letters), or
• When the contractor has verified in PECOS or Provider Enrollment that the provider is terminated or
out of business.
o The contractor utilizing HIGLAS shall manually update the accounts receivable (AR)
status code to ‘PROVIDER-TERMINATED’ if the ITR has not been issued and the
contractor learns that the provider is terminated or out of business. HIGLAS will not
allow the AR status code to be updated to ‘PROVIDER-TERMINATED’ if the existing
AR status code is exempt from Treasury referral.
o The contractor utilizing HIGLAS shall manually add a comment to the AR status
indicating that the provider has been terminated or out of business, when a provider has
been terminated or is out of business and has an AR with a status code that is ineligible
for Treasury referral”
o The contractor not utilizing HIGLAS shall manually create the ITR letter and send it as
soon as possible if an ITR letter has not been issued and the contractor learns that the
provider is terminated or out of business.
For active providers:
The contractor shall send the ITR letter when the debt is at least 30 days delinquent (60 days from the
determination date)* and is not in a status excluded from debt referral.
NOTE: In all cases, the contractor shall ensure that the ITR letter is sent in enough time to allow the debtor
60 days’ notice prior to referral to Treasury. In accordance with provisions of the Digital Accountability and
Transparency Act of 2014 (DATA Act) which amended the Debt Collection Improvement Act of 1996
(DCIA), eligible delinquent debts must be referred to Treasury by the 120th day of delinquency. (Refer to
chapter 4, §70 for further detail.)
* The Healthcare Integrated General Ledger Accounting System (HIGLAS) adds an additional 5 grace days
when determining when to generate the ITR letter to allow for interest accruals to appear on the ITR letter;
therefore, the ITR letter will be system generated on day 66.
* Instructions Summary for Undeliverable Letters
1. If the contractor utilizing HIGLAS cannot locate a better address within 10 business days of receipt
of the undeliverable demand letter, the contractor shall manually update the status code to ‘LTR-
UNDL-1ST.’
2. If the contractor locates a better address for the undeliverable initial demand letter, the contractor
shall send the provider a manual undeliverable demand notification letter, with the initial demand
letter attached, to the better address. The original initial demand letter date shall remain in effect.
3. If the contractor not utilizing HIGLAS cannot locate a better address within 10 business days of
receipt of the undeliverable initial demand letter, the contractor shall manually create the ITR letter
immediately and send it as soon as possible.
4. If the ITR letter is returned as undeliverable and a better address cannot be located within 10
business days of receipt, the contractor utilizing HIGLAS shall update the status code to ‘LTR-
UNDL-ITR.’
5. If the contractor locates a better address for the undeliverable ITR letter, the contractor shall send the
provider a manual undeliverable ITR notification letter, with the original ITR letter attached, to the
better address. The original ITR letter date shall remain in effect.
Note: The HIGLAS logic will review the letter history and the debt will become eligible for referral to
Treasury 66 days from the ITR letter date.
7. Surety Bond
Prior to referral to Treasury, DME contractors shall refer to instructions outlined in Medicare Program
Integrity Manual, Publication100-08, chapter 15, §21.7.1.
8. Record Keeping
The contractor shall keep records of all collection activities through all stages of the debt collection process.
This record shall be detailed and include all correspondence and conversations with the provider, checks,
and any other documents associated with debt collection processes.
10.1 - Required Timeframes for Debt Collection Process for Provider Overpayments
(Rev. 259, Issued: 01-15-16 Effective: 02-16-16, Implementation: 02-16-16)

Listed below are the general timeframes for most overpayment debt collection activities. There may
be instances, due to specific circumstances related to the debt, where these timeframes will not apply.
Timeframes (Based on
Date of Demand Letter)
Medicare Contractor
Day 1
The accounts receivable (AR) is created, the
initial demand letter sent. Contractors shall
ensure that the dates for establishing the AR,
creating the demand letter and mailing the letter
are the same.
Day 15
Deadline for provider rebuttal request. A
rebuttal does not delay recoupment.
Day 16
Immediate Recoupment, if requested by the
provider starts by day 16.
Day 16
Recoupment shall begin for overpayments not
subject to Limitation on Recoupment
provisions of Section 935 (f)(2) of the MMA
unless the debt is in an excluded category (ERS
Request, an approved ERS, appeal or
bankruptcy).
Day 31
Interest shall begin to accrue if overpayment is
not paid in full by day 30.
Day 41
If not paid in full by day 40, recoupment begins
for overpayments subject to Limitation on
Recoupment provisions of Section 935(f)(2) of
the MMA unless in an excluded category (ERS
Request, an approved ERS, appeal or
bankruptcy).
Day 90
The contractor shall attempt to contact the
provider by telephone if the debt is 60 days
delinquent and not in a status excluded from
referral to Treasury.
Day 61-90
The contractor shall send the ITR on eligible
delinquent debts.
Day 126-150
Eligible delinquent debt shall be referred to
Treasury.
At least 7 days prior to
referral to Treasury
The contractor shall make a second call to the
provider before the debt is referred to Treasury.
Prior to Referral to
Treasury (DME Only)
The DME contractor shall follow instructions
in IOM Pub. 100-8, Chapter 15, related to
surety bond collection requirements.
20 – Demand Letters
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
There are two overpayment demand letters, an Initial Demand Letter and an Intent to Refer Letter (ITR)
(this does not include notification letters or response letters) used in the debt collection process. The
purpose of an overpayment demand letter is to notify the providers and suppliers of the existence and

amount of an overpayment, and to request repayment. Every demand letter, regardless of the cause of
the overpayment or the status of the provider or supplier, shall meet certain requirements as to form and
content.
Below is a detailed list of the requirements for the basic overpayment demand letters to use in
various overpayment situations (it is not all-inclusive).
Non-Cost Report Overpayment Demand Letters:
The initial demand letter shall be sent to the provider or supplier within 7 calendar days of
the determination of the overpayment.
The letters shall be labeled either Initial Demand Letter or The Intent to Refer Letter (ITR.).
The initial demand letter shall be sent by first class mail, secured email, or fax.
The initial demand letter is an explanation of the nature of the overpayment, how it
was established, a bankruptcy notice, and the amount determined.
The initial demand letter includes language to request the provider or supplier to submit a
refund or arrange for immediate recoupment, or file an appeal (with exception of Requests for
Anticipated Payment (RAP) claims that shall not receive appeal rights, see 100-06 Chapter 3
Section 200.1.2).
The initial demand letter offers the provider or supplier the opportunity to apply for an
Extended Repayment Schedule (ERS) if repayment of the debt will cause financial hardship.
(An ERS shall be analyzed using the criteria set forth in Chapter 4, §50. Any approved ERS
would run from the approval date.)
If payment in full is not received within 30 days, interest will be charged.
The initial demand letter includes Debt Collection Improvement Act (DCIA) Intent Language
for referral to the Treasury Department for cross servicing.
The ITR letter is sent to the provider or supplier at least 60 days after the date of the initial, final
or revised demand letter, if it is not in a status excluded from debt referral, and shall include the
initial demand letter number.
All correspondence, including demand letters, addressed to a provider or supplier in
bankruptcy proceedings, shall be submitted to the Regional Office (RO), which has the lead in
the bankruptcy proceedings, for approval prior to release.
Cost Report Overpayment Demand Letters:
When a provider files a cost report without payment for the amount due from the provider, the
contractor shall send a demand letter to the provider. The demand letter shall inform the provider
that the contractor will recoup (reduce or withhold) Medicare payments if it does not receive the
overpayment amount, or a request for a repayment schedule along with the first month’s payment
within 15 days of the date of the demand letter.
2. In the situation of an unfiled cost report, the cost report reminder letter serves as sufficient notice
that future Medicare payments (interim payments) will be suspended if the overpayment amount is
not received on or before its due date.
3. In addition to the suspension of future Medicare payments for failure to file a cost report,
contractors shall deem all interim and lump-sum payments made for the fiscal period and all
interim and lump-sum payments made in a subsequent period as an overpayment. These
overpayments shall be immediately due and payable to CMS if the cost report is not received
timely.
4. The contractor shall ensure that recoupment of Medicare payments does not start until the cost
report demand letter is generated.
The initial cost report demand letters may be delivered certified mail, electronic mail (e-mail), or
through a secured portal, and shall include a receipt confirmation.
The initial cost report demand letters shall be sent to the provider or supplier on the
7th day after the due date or extended due date of the cost report, if not received.
The initial cost report demand letters shall include the explanation of the overpayment
determination and the amount due or Notice of Program Reimbursement (cost report).
The provider or supplier may submit a cost report, make a refund, arrange for immediate
recoupment, or request an ERS, as applicable.
The percentage of withhold shall be indicated whenever an adjustment (reduction or
suspension) of interim payments has been imposed.
The cost report letters shall offer the provider the opportunity to apply for an ERS if repayment
of the debt will cause financial hardship. (An ERS shall be analyzed using the criteria set forth in
Chapter 4, §50. Any approved ERS would run from the approval date.)
The cost report letters shall include DCIA Intent Language for referral to the Treasury
Department for cross servicing.
The ITR letter shall be mailed to the provider 60 days after the date of the Initial
Demand letter, if it is not in a status excluded from debt referral.
20.1 - Number of Demand Letters
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
In general, the contractor sends one overpayment Initial (1
st
) demand letter to a provider or supplier.
The contractor shall have at all times access to copies of the demand letters generally housed in the case
file, bulk PDF, or in HIGLAS. When the demand letter has been sent and returned as undeliverable, the
contractor shall attempt to locate the provider or supplier (see Chapter 4, §10). If the contractor is
unable to locate the provider or supplier and the overpayment is eligible for referral to the Department of
Treasury, the contractor shall immediately send the ITR demand letter, which shall include the intent to
refer language.
Where a repayment schedule has been established after the Initial (1st) demand letter has been sent
and the provider or supplier defaults on the repayment schedule, the contractor shall count that 1
st
demand letter as one of the two letters (1
st
and ITR) normally sent to an overpaid provider or supplier.
20.2 – Sample Demand Letters All Providers or Suppliers

(Rev. 61, Issued: 12-10-04, Effective: 01-10-05, Implementation: 01-10-05)
It is CMS’ responsibility to protect the Trust Fund and replenish any overpaid funds. In this section,
contractors are given templates to model when sending providers and suppliers a request for payment.
EXHIBIT 1- INITIAL DEMAND LETTER - NON-935–
(Rev .316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
Contractors shall use the appropriate template below:
A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(BPROV1.pdf) Part B Provider/Supplier Initial Demand Letter
2.
(BPROV1VA.pdf) Provider/Supplier Voluntary Returned Check 1st demand letter
3.
(BPROV1N.pdf) Part B Provider/Supplier Notify Initial Demand Letter
4.
(BPROV1V.pdf) Part B Provider/Supplier Voluntary Refund 1
st
Demand Letter
5.
(APROV1.pdf) Part A Aggregate Claims Demand Letter
6.
(APROV-CLA.pdf) Part A No Appeal
B.
Contractors not on HIGLAS and Manual letters shall use this letter as your template.
RE: Initial Demand Letter
Provider/Supplier Name:
Provider/Supplier Number:
&
Overpayment Amount:
&HINVOICE_AMOUNT
Outstanding Balance:
&DEMAND_AMOUNT
C.
Contractors shall use the appropriate first paragraph below:
Dear Sir/Madam:
PART B Provider or Supplier Demand Letter (BPROV1.pdf in HIGLAS)
This is to let you know that you have received a Medicare payment in error, which has resulted in
an overpayment to you of &HINVOICE_AMOUNT. The attached documentation explains how
this happened.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
Or,
PART B Provider or Supplier Notify 1
st
Demand Letter (BPROV1N.pdf in HIGLAS)
We appreciate your recent inquiry regarding a Medicare payment that you believe was paid in error. Our
analysis found that the overpaid amount was &DEMAND_AMOUNT. The attached documentation
explains how this happened. We thank you for bringing this overpayment to our attention.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
Or,

PART B Provider or Supplier Voluntary Returned/Refund 1
st
Demand, (BPROV1VA.pdf in
HIGLAS) or (BPROV1V.pdf in HIGLAS)
We have received your check in the amount of &INVOICE_RECEIPT_AMOUNT. We thank you for
bringing this overpayment to our attention. While we appreciate you submitting payment to us, our
review found that the overpaid amount was &HINVOICE_AMOUNT. The attached documentation
explains how this happened. Please remit the additional &INVOICE_BALANCE_AMOUNT.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please follow
the instructions found at the end of this letter.
Or,
PART A (Non-935) Aggregate Claims Demand Letter (APROV1.pdf in HIGLAS)
Claims adjustments were entered in our system under provider &HPROVIDER_NAME.
Additional adjustments were made to the claims, and a balance in the amount of &DEMAND_
AMOUNT has been outstanding for 60 days. As this amount has not been recouped through claims
submission, the purpose of our letter is to request that this amount be repaid to our office. The attached
documentation explains how this happened.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please follow
the instructions found at the end of this letter.
Or,
PART A No Appeal Claims Demand Letter (APROVNOAPPEAL1.pdf in HIGLAS)
Claims adjustments were entered in our system under provider &HPROVIDER_NAME and a balance in
the amount of &DEMAND_ AMOUNT is due. The purpose of our letter is to request that this amount be
repaid to our office. The attached documentation explains how this happened.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please follow the
instructions found at the end of this letter.
D.
Contractors shall include the following language below in all initial letters after the first
paragraph.
Why you are responsible:
You are responsible for following correct Medicare filing procedures and must use care when billing
and accepting payment. You are responsible for repayment in this matter based upon one or both of the
following criteria:
1.
You billed and/or received payment for services for which you should have known you were
not entitled to receive payment. Therefore, you are not without fault and are responsible for

repaying the overpayment amount.
2.
You received overpayments resulting from retroactive changes in the Medicare Physician
Fee Schedule and/or changes mandated by legislation.
If you dispute this determination, please follow the appropriate appeals process listed below. (Applicable
authorities: § 1870(b) of Social Security Act; sub§ 405.350 - 405.359 of Title 42, sub§ 404.506 - 404.509,
404.510a and 404.512 of Title 20 of the United States Code of Federal Regulations.) [This appeal
paragraph is to be excluded in No-Appeal demand letters.]
Rebuttal Process:
Under our existing regulations 42 CFR § 405.374, providers and suppliers will have 15 days from the
date of this demand letter to submit a statement of rebuttal. The rebuttal process provides the debtor
the opportunity, before the suspension, offset, or recoupment takes effect, to submit any statement (to
include any pertinent information) as to why it should not be put into effect on the date specified in the
notice. A rebuttal is not intended to request a review of supporting medical documentation nor to
express disagreement with the overpayment decision. A rebuttal shall not duplicate the redetermination
process. This is not an appeal of the overpayment determination. Our office will advise you of our
decision 15 days from the mailroom-stamped receipt date of your request.
Interest Assessment:
If you do not refund in 30 days:
In accordance with 42 CFR 405.378, simple interest at the rate of &AR_INTEREST_RATE % will be
charged on the unpaid balance of the overpayment, beginning on the 31st day. Interest is calculated in
30-day periods and is assessed for each full 30-day period that payment is not made on time. Thus, if
payment is received 31 days from the date of final determination, one 30-day period of interest will be
charged. Each payment will be applied first to accrued interest and then to principal. After each
payment, interest will continue to accrue on the remaining principal balance, at the rate of
&AR_INTEREST_RATE %. In addition, please note that Medicare rules require that payment be
either received in our office by &LETTER_DATE_29 (United States Postal Service Postmark) for the
payment to be considered timely. A metered mail postmark received in our office after
&LETTER_DATE_29 will cause an additional month's interest to be assessed on the debt.
Payment by Recoupment:
If payment in full is not received by &LETTER_DATE_40 (&LETTER_DATE_15 for Part A non-
935), payments to you can be recouped (recoupment) until payment in full is received if you haven't
submitted an acceptable ERS request, an immediate recoupment request, and/or a valid and timely
appeal is received.
Make a payment or Arrange for payments:
What you should do:
Please return the overpaid amount to us by &LETTER_DATE_29 and no interest charge will be
assessed. Make the check payable to Medicare Part A and send it with a copy of this letter to:
&CONTRACTOR_NAME
&REVIEW_ADDRESS1

&REVIEW_ADDRESS2
&REVIEW_CITY, &REVIEW_STATE &REVIEW_POSTAL_CODE
In addition, please note that Medicare rules require that payment be either received in our office by,
&LETTER_DATE_29, or United States Postal Service postmark by that date, for the payment to be
considered timely. A metered mail postmark received in our office after &LETTER_DATE_29 will
cause an additional month's interest to be assessed on the debt.
If you are unable to make refund of the entire
amount at this time, advise this office immediately with
a request for an extended repayment schedule (ERS) so that we may determine if you are eligible for
one. Any repayment schedule (where one is approved) would run from the approval date. You can
visit our website at [&CONTRAC TOR_URL] for ERS instructions and forms.
Immediate Recoupment:
If Provider is enrolled in Immediate Recoupment-
NO FURTHER ACTION IS REQUIRED BY YOU. You have previously elected to have your
overpayment(s) repaid through the Immediate Recoupment process. Based on this payments to you will
begin to be recouped on &LETTER_DATE_16 until payment is received in full. If the debt is not
collected in full before day 31, interest will continue to accrue until the debt is collected in full.
If Provider is NOT enrolled in Immediate Recoupment-
TO SIMPLIFY THE REPAYMENT PROCESS, reduce the extra work and cost associated with mailing
your repayment each time, you may elect to have automatic immediate recoupments for ALL overpayments
by requesting the Immediate Recoupment process for All Current and Future Accounts Receivable. This
will automatically begin recoupment starting on day 16 for ALL future accounts receivable. When the initial
request is received after day 16 the debt shall be placed in an immediate recoupment status. If the debt is not
collected in full before day 31, interest will continue to accrue until the debt is collected in full.
You must specify whether you are submitting:
1. A request on the current demanded overpayment (all accounts receivables within this demand letter) and
ALL FUTURE OVERPAYMENTS; or
2. A one-time request on this current demanded overpayment (all accounts receivables) addressed in this
demand letter only.
This process is voluntary and for your convenience.
You can visit our website at {MAC site} for the Immediate Recoupment
Request instructions.
You may contact this office for information on how to fax your request.
You may contact this office for information on how to fax your request. (Immediate recoupment already in
effect for Part A non-935.)
If you wish to appeal this decision: [This appeal paragraph is to be excluded in No-Appeal demand
letters.]
If you disagree with this overpayment decision, you may file an appeal. Please refer to the original
remittance advice for additional instruction. An appeal is a review performed by people independent
of those who have reviewed your claim so far. The first level of appeal is called a redetermination.
You must file your request for a redetermination within 120 days of the date you receive this letter.
Unless you show us otherwise, we assume you received this letter 5 days after the date of this letter.
Please send your request for redetermination to:
&CONTRACTOR_NAME &REVIEW_ADDRESS1 &REVIEW_ADDRESS2
&REVIEW_CITY, &REVIEW_STATE &REVIEW_POSTAL_CODE
Medicaid Offset:
If this matter is not resolved, CMS may instruct the Medicaid State Agency to withhold the Federal
share of any Medicaid payments that may be due you or related facilities until the full amount owed
to Medicare is recouped, Title 42 CFR, § 447.30(g). These recoveries will be in addition to any
recoupments from other Medicare funds due you until the full amount owed to Medicare is
recovered.
Right to Inspect Records Prior to Referral to Treasury:
In the event an ITR letter is sent, you have the right to inspect and copy all records pertaining to your debt.
In order to present evidence or review the CMS records, you must submit a written request to the address
below. Your request must be received within 60 calendar days from the ITR letter date. In response to a
timely request for access to CMS’ records, you will be notified of the location and time when you can
inspect and copy records related to this debt. Interest will continue to accrue during any review period.
Therefore, while review is pending, you will be liable for interest and related late payment charges on
amounts not paid by the due date identified above.
For Individual Debtors Filing a Joint Federal Income Tax Return:
The Treasury Offset Program automatically refers debts to the Internal Revenue Service (IRS) for Offset.
Your Federal income tax refund is subject to offset under this program. If you file a joint income tax
return, you should contact the IRS before filing your tax return to determine the steps to be taken to
protect the share of the refund which may be payable to the non-debtor spouse.
For Debtors that Share a Tax Identification Number(s):
Section 1866(j)(6) of the Social Security Act authorizes the Secretary of Health and Human Services (the
Secretary) to make any necessary adjustments to the payments of an applicable provider or supplier who
shares a TIN with an obligated provider or supplier, one that has an outstanding Medicare overpayment.
The Secretary is authorized to adjust the payments of such a provider or supplier regardless of whether it
has been assigned a different billing number or National Provider Identification Number (NPI) from that
of the provider or supplier with the outstanding Medicare overpayment.
Federal Salary Offset:
If the facility ownership is either a sole proprietorship or partnership, your individual salary(s) may
be offset if you are, or become, a federal employee.
If You Have Filed a Bankruptcy Petition:
If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding, Medicare financial
obligations will be resolved in accordance with the applicable bankruptcy process. Accordingly, we
request that you immediately notify us about this bankruptcy so that we may coordinate with both the
Centers for Medicare & Medicaid Services and the Department of Justice so as to assure that we handle
your situation properly. If possible, when notifying us about the bankruptcy, please include the name
the bankruptcy is filed under and the district where the bankruptcy is filed.
Should you have any questions, please contact your overpayment representative at the following number:
CONTACT_PHONE_NUM_
We look forward to hearing from you shortly.
Sincerely,
Medicare A or B Recovery Unit
Enclosures: How This Overpayment Was Determined
EXHIBIT 2- INITIAL DEMAND LETTER - 935
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(APROV9351.pdf): Part-A Adjustment Initial Claims Demand letter
2.
(BPROV9351.pdf): Part-B 935 Adjustment Initial Claims Demand letter
3.
(APROVAGG9351.pdf): Part-A Aggregate Closure Initial Demand Letter
4.
(BPROVAGG9351.pdf): Part-B Aggregate Closure Initial Demand Letter
5.
(APROVRAC1.pdf): Part-A 935 RAC Adjustment Claims Demand Letter
6.
(BPROVRAC1.pdf): Part-B 935 RAC Adjustment Claims Demand Letter
7.
(APROVRACAGG1.pdf): Part-A 935 RAC Adjustment Claims Initial Demand Letter
8.
(BPROVRACAGG1.pdf): Part-B 935 RAC Adjustment Claims Initial Demand Letter
B.
Contractors not on HIGLAS shall use this letter as your template.
Letter Number: Date:
&HPROVIDER_NAME
&HPROVIDER_ADDRESS1
&HPROVIDER_CITY, &HPROVIDER_STATE
HPROVIDER_POSTAL_CODE
INITIAL REQUEST
[Contractors shall use the appropriate reference below for demanded 935 overpayments.] RE:
MMA 935 –
Overpayment Amount
Dear Sir/Madam,
Contractors shall use the appropriate first paragraph below for all Initial Demands letters except Recovery
Audit Contractors (RAC).
This letter is to inform you that you have received a Medicare payment in error, which has resulted in an
overpayment subject to § 935(f) (2) of the Medicare Modernization Act (MMA), § 1893(f) (2) of the
Social Security Act, Limitation on Recoupment, in the amount & DEMAND_ AMOUNT. The purpose

of this letter is to request that this amount be repaid to our office. The attached explains how this
happened.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
(RAC Demand Letter Language only)
This finding was a result of a Recovery Audit Program review. If you have any questions relating
to this letter or the recoupment process, you should contact us at:
&CONTRACT_STATE_TOLL_FREE_ &CONTRACT_STATE_TOLL_FREE_NUM. If you
have any questions relating to the review rationale or you feel that this finding is in error and
would like to submit additional documentation or discuss the issue further, please contact the
Recovery Auditor.
If you are unable to locate the name and contact information for the Recovery Auditor from
prior correspondence, please contact the Medicare Administrative Contractor, which is located
at the bottom of this page, for further information.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
How This Overpayment Was Determined:
[When applicable on a Manual Letter, include explanation of the overpayment determination.]
[Contractor shall explain the authority for reopening the claims (i.e., consistent with 42 CFR 405.980
and Publication 100-04, Medicare Claims Processing Manual, chapter 34) and explain how the facts of
the case allowed you to reopen within the timeframes established in those sections.]
Why You Are Responsible:
You are responsible for following correct Medicare filing procedures. In this situation, you billed and/or
received payment for services you should have known you were not entitled to. Therefore, you are not
without fault and are responsible for repaying the overpayment amount. If you dispute this
determination, please follow the appropriate appeals process listed below. Applicable authorities: §
1870(b) (c) of the Social Security Act; Sub§ 405.350 - 405.359 of Title 42 CFR, Sub§ 404.506 -
404.509, 404.510a and
404.512 of Title 20 of the United States Code of Federal Regulations.
This amount is subject to § 935(f) (2) of the Medicare Modernization Act (MMA) (section 1893(f) (2) of
the Social Security Act), Limitation on Recoupment (42 CFR 405.379).
Rebuttal Process:
Under our existing regulations at 42 CFR § 405.374, Providers or Suppliers will have 15 days from the
date of this demand letter to have an opportunity for rebuttal by submitting a statement. The rebuttal
process provides the debtor the opportunity, before the suspension of payment, offset, or recoupment
takes effect, to submit any statement (to include any pertinent information) as to why it should not be put
into effect on the date specified in the notice. A rebuttal is not intended as a request for the review
supporting medical documentation nor to express disagreement with the overpayment decision. A
rebuttal shall not duplicate the redetermination process. This is not an appeal of the overpayment
determination. The limitation on recoupment under § 1893 (f) (2) (a) of the Social Security Act does
not apply to rebuttal requests. Our office will advise you of our decision 15 days from the mailroom-
stamped receipt date of your request.
Interest Assessment:
If you do not pay the full amount in 30 days:
In accordance with 42 CFR 405.378, simple interest at the rate of &AR_INTEREST_RATE percent will be
charged on the unpaid balance of the overpayment, beginning on the 31
st
day. Interest is calculated in 30-day
periods and is assessed for each full 30-day period that payment is not made on time.
Thus, if payment is received 31 days from the date of final determination, one 30-day period of interest
will be charged. Each payment will be applied first to accrued interest and then to principal. After each
payment, interest will continue to
accrue on the remaining principal balance, at the rate of
&AR_INTEREST_RATE percent
. A metered mail postmark received in our office after
&LETTER_DATE_29 will cause an additional month's interest to be assessed on the debt.
In addition, please note that
Medicare rules require that payment be either received in our office by
&LETTER_DATE_29 or
United States Postal Service Postmark by that date for the payment to be
considered timely.
Suspended Funds Applied To The Overpayment and Has a Remaining Outstanding Balance:
If the suspended funds are insufficient to fully eliminate any overpayment, and the provider or supplier
meets the requirements of 42 CFR § 405.379 "Limitation on Recoupment" provision under §1893(f) (2) of
the Act, then the provider or supplier is subject to 935 Appeals rights and will be available for offset after
41 days on the remaining balance still owed to CMS. (See 42 CFR § 405.372(e) for more information.)
Payment by Recoupment:
If payment in full is not received by &LETTER_DATE_29 (date of the notification), payments to you can
be recouped (recoupment) until payment in full is received if you haven't submitted an acceptable ERS
request, an immediate recoupment request, and/or a valid and timely appeal is received.
Make a Payment or Arrange for Payments:
What You Should Do:
Please return the overpaid amount to us by &LETTER_DATE_29 and no interest will be
assessed. We request that you refund this amount in full.
Make the check payable to Medicare [Part A] or [Part B] and send it with a copy of this letter to:
&CONTRACTOR_NAME
&CHECK_ADDRESS1
&CHECK_CITY, &CHECK_STATE &CHECK_POSTAL_CODE
If you are unable to make refund of the entire
amount at this time, advise this office immediately
with
a request for an extended repayment schedule (ERS) so that we may determine if you are
eligible for one. Any repayment schedule (where one is approved) would run from the approval
date. You can visit our website at [&CONTRAC TOR_URL] for ERS instructions and
forms.

Immediate Recoupment:
If Provider is enrolled in Immediate Recoupment-
NO FURTHER ACTION IS REQUIRED BY YOU. You have previously elected to have your
overpayment(s) repaid through the Immediate Recoupment process. Based on this payments to you will
begin to be recouped on &LETTER_DATE_16 until payment is received in full. If the debt is not
collected in full before day 31, interest will continue to accrue until the debt is collected in full.
If Provider is NOT enrolled in Immediate Recoupment-
TO SIMPLIFY THE REPAYMENT PROCESS, reduce the extra work and cost associated with mailing
your repayment each time, you may elect to have automatic immediate recoupments for ALL overpayments
by requesting the Immediate Recoupment process for All Current and Future Accounts Receivable. This
will automatically begin recoupment starting on day 16 for ALL future accounts receivable. When the initial
request is received after day 16 the debt shall be placed in an immediate recoupment status. If the debt is not
collected in full before day 31, interest will continue to accrue until the debt is collected in full.
You must specify whether you are submitting:
1. A request on the current demanded overpayment (all accounts receivables within this demand letter) and
ALL FUTURE OVERPAYMENTS; or
2. A one-time request on this current demanded overpayment (all accounts receivables) addressed in this
demand letter only.
This process is voluntary and for your convenience.
You can visit our website at {MAC site} for the Immediate Recoupment
Request instructions.
You may contact this office for information on how to fax your request.
This process is voluntary and for your convenience. Your request must specifically state you understand
you are waiving potential receipt of interest payment pursuant to § 1893(f) (2) for the overpayments.
Note: Such interest may be payable for certain overpayments reversed at the ALJ level or
subsequent levels of appeal.
If You Wish To Appeal This Decision:
If you disagree with this overpayment decision, you may file an appeal. An appeal is a review performed
by people independent of those who have reviewed your claims. The first level of appeal is called a
redetermination. You must file your request for a redetermination 120 days from the date of this letter.
However, if you wish to avoid recoupment from occurring, you need to file your request for
redetermination within 30 days from the date of this letter, as described above. Unless you show us
otherwise, we assume you received this letter within 5 days of the date of this letter.
Please send your request for redetermination to:
&CONTRACTOR_NAME - 935 APPEALS
REDETERMINATION &REVIEW_ADDRESS1
&REVIEW_CITY, &REVIEW_STATE &REVIEW_POSTAL_CODE

How to Stop Recoupment:
Even if the overpayment and any assessed interest has not been paid in full, you can temporarily stop
Medicare from recouping any payments. If you act quickly and decidedly, Medicare will stop
recoupment at two points.
First Opportunity: We must receive a valid and timely request for a redetermination within 30 days
from the date of this letter. We will stop or delay recoupment pending the results of an appeal. To assist
us in expeditiously stopping the recoupment process, we request that you clearly indicate on your appeal
request that this is a 935 overpayment appeal for a redetermination.
Second Opportunity: If the redetermination decision is (1) unfavorable, we will begin to recoup no
earlier than the 60th day from the date of the Medicare redetermination notice (Medicare Appeal
Decision Letter); or (2) if the decision is partially favorable, we will begin to recoup no earlier than the
60th day from the date of the Medicare revised overpayment Notice/Revised Demand Letter. Therefore,
it is important to act quickly and decidedly to limit recoupment by submitting a valid and timely request
for reconsideration within 60 days of the appropriate notice/letter. The address and details on how to
file a request for reconsideration will be included in the Redetermination decision letter.
What Happens Following a Reconsideration By a Qualified Independent Contractor (QIC):
Following a decision or dismissal by the QIC, if the debt has not been paid in full, we will begin or
resume recoupment whether or not you appeal to the next level, Administrative Law Judge (ALJ).
NOTE: Even when recoupment is stopped, interest continues to accrue.
Medicaid Offset:
If this matter is not resolved, CMS may instruct the Medicaid State Agency to withhold the Federal share
of any Medicaid payments that may be due you or related facilities until the full amount owed to
Medicare is recouped; Title 42 CFR, § 447.30(g). These recoveries will be in addition to any
recoupments from other Medicare funds due you until the full amount owed to Medicare is recovered.
Right to Inspect Records Prior to Referral to Treasury:
In the event an Intent to Refer (ITR) letter is sent, you have the right to inspect and copy all records
pertaining to your debt. In order to present evidence or review the CMS records, you must submit a
written request to the address below. Your request must be received within 60 calendar days from the
ITR letter date. In response to a timely request for access to CMS’s records, you will be notified of the
location and time when you can inspect and copy records related to this debt. Interest will continue to
accrue during any review period. Therefore, while review is pending, you will be liable for interest and
related late payment charges on amounts not paid by the due date identified above.
For Individual Debtors Filing a Joint Federal Income Tax Return:
The Treasury Offset Program automatically refers debts to the Internal Revenue
Service (IRS) for Offset. Your Federal income tax refund is subject to offset under this program. If
you file a joint income tax return, you should contact the IRS before filing your tax return to determine the
steps to be taken to protect the share of the refund, which may be payable to the non-debtor spouse.
For Debtors That Share a Tax Identification Number (TIN):

Section 1866(j)(6) of the Social Security Act authorizes the Secretary of Health and Human Services (the
Secretary) to make any necessary adjustments to the payments of an applicable provider or supplier who
shares a TIN with an obligated provider or supplier, one that has an outstanding Medicare overpayment.
The Secretary is authorized to adjust the payments of such a provider or supplier regardless of whether it
has been assigned a different billing number or National Provider Identification Number (NPI) from that
of the provider or supplier with the outstanding Medicare overpayment.
Federal Salary Offset:
If the facility ownership is either a sole proprietorship or partnership, your individual salary(s) may
be offset if you are, or become, a federal employee.
If You Have Filed a Bankruptcy Petition:
If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding, Medicare financial
obligations will be resolved in accordance with the applicable bankruptcy process. Accordingly, we
request that you immediately notify us about this bankruptcy so that we may coordinate with both the
Centers for Medicare & Medicaid Services and the Department of Justice to assure that we handle your
situation properly. If possible, when notifying us about the bankruptcy, please include the name the
bankruptcy is filed under and the district where the bankruptcy is filed.
Should you have any questions, please contact your overpayment consultant at the following:
&BUSINESS_PURPOSE_1
&CONTRACT_CONTACT_PHONE_NUM_
1
We look forward to hearing from you shortly.
Sincerely,
SELECT
Supervisor, Part A Overpayments &CONTRACTOR_NAME
Or,
Medicare Part B Recovery Unit
Enclosures
How This Overpayment Was Determined
EXHIBIT 3- INITIAL DEMAND LETTER- COST REPORTS FILED –
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(APROVCRASF1.pdf): Part-A As-Filed Cost Report Initial Demand letter
2.
(APROVNONCRASF1.pdf): Part A Cost Report Initial Letter – Tentative Settlement
B.
Contractors not on HIGLAS shall use this letter below as your template.
C.
Use the appropriate reference below for the first paragraph.

INITIAL REQUEST
RECEIPT CONFIRMATION REQUESTED
RE: Initial Demand Letter Provider or Supplier Name:
Provider/Supplier Number: &
Overpayment Amount: &HINVOICE_AMOUNT
Outstanding Balance: & DEMAND_AMOUNT
Date:
Dear Mr. Smith:
Contractors shall use the appropriate paragraph for the cost report situation:
(NPR Issued)
On July 26, 20xx, we received your cost report for the fiscal year ending June 30, xxxx. We have fully
reviewed this report, and the results of our review have been incorporated in the enclosed copy of your
Notice of Program Reimbursement (dated August 21, 20xx). As explained in the Notice, we find that
the Valley Convalescent Center has been overpaid $ for the past fiscal year.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
(Tentative Settlement)
On July 26, 20xx, we accepted your cost report for the fiscal year ending June 30, xxxx. We have
completed a preliminary review of this report and have determined that the Valley Convalescent Center
has been overpaid $ for this fiscal year.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
(As Filed Cost Report)
On July 26, 20xx, we received your cost report for the fiscal year ending June 30, xxxx. The cost report,
as filed, reflects an overpayment of $ for this fiscal year. The Provider Reimbursement Manual
(PRM) Part
1, Chapter 24, section 2409.A (2) states that, when a cost report is filed indicating an
overpayment, a full refund shall accompany the cost report submission.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
PLEASE MAIL TO:
&CONTRACTOR_NAME &CHECK_ADDRESS1 &CHECK_ADDRESS2
&CHECK_CITY, &CHECK_STATE &CHECK_POSTAL_CODE
The total of &DEMAND_AMOUNT should immediately be refunded in full. Your facility's check should
include your provider number and be made payable to &CONTRACTOR_NAME.

If payment in full is not received, payments to you will be withheld until payment in full is received or an
acceptable extended repayment request is received. If you have reason to believe that the withhold should
not occur, you must notify [contractor]. We will review your documentation, but will not delay
recoupment.
This is not an appeal of the overpayment determination.
Medicaid Offset
If this matter is not resolved within fifteen (15) days from the date of this letter, CMS may instruct the
Medicaid State Agency to withhold the Federal share of Title XIX of any Medicaid payments that may
be due you or related facilities until the full amount owed Medicare is recouped, Title 42 CFR, §
447.30(g). These recoveries will be in addition to any recoupments from other Medicare funds due you
until the full amount owed to Medicare is recovered. The appeal process is detailed in the Notice of
Program Reimbursement (NPR).
Interest Assessment:
In accordance with 42 CFR 405.378, simple interest at the rate of will be charged on the
unpaid balance of the overpayment beginning on the 31st day. Interest is calculated in 30-day periods
and is assessed for each full 30-day period that payment is not made in full. Thus, if payment is received
31 days from the date of final determination, one 30-day period of interest will be charged and will
continue to be assessed for full 30-day periods on any portion that remains outstanding until the debt is
paid in full.
Each payment will be applied first to accrued interest and then to principal. After each payment,
interest will continue to accrue on the remaining principal balance, at the rate of _.
Extended Repayment Request:
We request that you refund this amount in full. If you are unable to make refund of the entire amount at
this time, advise this office immediately so that we may determine if you are eligible for a repayment
schedule. (Refer to www.Mac.com for details and forms.) Any repayment schedule (where one is
approved) would run from the approval date. If we do not hear from you, your interim payments will be
withheld starting on the 16th day from the date of this letter, and applied towards the outstanding
overpayment balance.
Any amount withheld will not be refunded.
If You Have Filed a Bankruptcy Petition:
If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding, Medicare financial
obligations will be resolved in accordance with the applicable bankruptcy process. Accordingly, we
request that you immediately notify us about this bankruptcy so that we may coordinate with both the
Centers for Medicare & Medicaid Services and the Department of Justice so as to assure that we handle
your situation properly. If possible, when notifying us about the bankruptcy, please include the name
the bankruptcy is filed under and the district where the bankruptcy is filed.
For Debtors That Share a Tax Identification Numbers:
Section 1866(j)(6) of the Social Security Act authorizes the Secretary of Health and Human Services (the
Secretary) to make any necessary adjustments to the payments of an applicable provider or supplier who
shares a TIN with an obligated provider or supplier, one that has an outstanding Medicare overpayment.
The Secretary is authorized to adjust the payments of such a provider or supplier regardless of whether it
has been assigned a different billing number or National Provider Identification Number (NPI) from that
of the provider or supplier with the outstanding Medicare overpayment.

Should you have any questions please contact at . We expect to hear from you
shortly.
Sincerely,
(Name and Title)
Enclosure
(Name and Title)
Enclosure
EXHIBIT 4- INITIAL DEMAND LETTER – UNFILED COST REPORT
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(APROVNONCRASF1.pdf): Part-A Non As-Unfiled Cost Report Initial Demand Letter
B.
Contractors not on HIGLAS shall use this letter as your template.
(Mailed 7 calendar days after cost report was
due.) Date:
INITIAL DEMAND LETTER
[Provider name] [Mail to Name] [Mail to Address 1] [Mail to Address 2] [City} {State} {Zip]
RECEIPT CONFIRMATION REQUESTED
RE: Late Medicare Cost
Report Provider Name: [DBA
Name] Provider Number:
[xxxxxxxx]
Fiscal Year End: [Month, Day, Year]
Dear [Title] [Last Name]
Contractors shall use the appropriate paragraph for the cost report situation:
(Unfiled Cost Report)
We have not received the cost report for [DBA Name], provider number [xxxxxxx] for the period ending
[month/day/year]. Under Title 42 Code of Federal Regulations (CFR), § 413.24, cost reports are due by
the last day of the fifth (5
th
) month following the close of the provider’s cost report year or 30 days after
receipt of valid Provider Statistical and Reimbursement (PS&R) reports from the contractor, whichever
is later. Your report is now late, as it was due [month/day/year].
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
(Home Office Cost Report is Unfiled)
We have not received the home office cost statement from ______. According to our records,
serves as the home office for your facility. Since the home office cost statement remains unfiled, the
amount stated on your filed cost report for the fiscal year ending for home office costs has been
disallowed. This disallowance will continue until the home office submits the home office cost statement.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
Deemed Overpayment:
As a cost report has not been received from your facility, all interim and lump-sum payments made for
the fiscal period noted above are deemed an overpayment. The principal amount of the overpayment
related to this fiscal period is [$ xxxxxx.xx]. If you do not submit a cost report, please be advised that
this letter constitutes Federal Claims Collection Act (FCCA) notification that this amount is now
due and must be remitted to us within thirty (30) days from the date of this letter. Interest will be
assessed on any portion of this amount that is not paid timely in accordance with Title 42 CFR 405.378
(c) (1) (v).
If full payment is not received or arrangements made for an extended repayment schedule, we will take
all action(s) necessary to recover the full amount. You can visit our website at [&CONTRAC
TOR_URL] for ERS instructions and forms.
Suspension:
As your cost report has not been received timely, all payments to your facility have now been suspended
under the authority of Title 42 CFR § 405.371(d). Payments will not be resumed until an acceptable cost
report is received by us.
Interest Charges:
Interest is assessed on late cost reports and late payments under Title 42 CFR 405.378 (c) (1) (v):
1.
Cost reports reflecting an amount due to the Medicare program must include the full amount owed
(including interest) from the day following the date the cost report was due to the date that the cost report
is filed.
2.
If a late cost report reflects that there is an amount due Medicare and the full amount owed (including
interest) is not included with the cost report, interest will continue to accrue on the overpayment until it
is paid in full.
3.
Additionally, when it is determined that an additional overpayment exists on a late-filed cost report,
through interim settlement or NPR, interest will be assessed on the overpayment from the day following
the date the cost report was due to the date the cost report is filed. If the subsequent overpayment is not
paid within thirty (30) days of the date of the first demand letter, additional interest will be assessed from
the date of the subsequent determination until the overpayment is paid in full. If the full amount is not
paid, any partial payments will be applied first to accrued interest and then to principal. After each
partial payment, interest will continue to accrue on the remaining principal balance.
Interest Computation:
The interest rate in effect at the time your cost report was due is [xx.xxx%]. This rate is applicable to any
overpayments related to the untimely filing of your cost report. Under Title 42 CFR § 405.378 (b) (2),

interest charges are assessed in thirty (30)-day periods. Thus, if payment is received 31 days from the date
of final determination, one 30-day period of interest will be assessed and for each full 30-day period until
the debt is paid in full.
Cost Report Submission:
Please attend to this matter immediately by mailing a copy of this letter together with: (1) A completed
cost report, together with any amounts due (principal and interest); (2) A complete refund of all interim
payments, the deemed overpayment (principal and interest), within thirty (30) days of the date of this
letter; or (3) A request for a repayment schedule of all interim payments, the deemed overpayment,
within fifteen (15) days of the date of this letter. Checks are to be made payable to [Contractor]. They
and/or your remittance advice should be annotated with your provider name, number, and cost report year
end that applies to the amount due.
[Prime Contractor] [Division or Group] [Routing, Room Number] [Mail To Address 1] [Mail To
Address 2] [City, State, Zip]
As you are aware, cost reports are subject to further review. There could be additional adjustments
required after completion of a review. Therefore, the records supporting this report are to be retained for
at least three (3) years from the date of the NPR.
For Debtors That Share Tax Identification Numbers:
Section 1866(j)(6) of the Social Security Act authorizes the Secretary of Health and Human Services (the
Secretary) to make any necessary adjustments to the payments of an applicable provider or supplier who
shares a TIN with an obligated provider or supplier, one that has an outstanding Medicare overpayment.
The Secretary is authorized to adjust the payments of such a provider or supplier regardless of whether it
has been assigned a different billing number or National Provider Identification Number (NPI) from that
of the provider or supplier with the outstanding Medicare overpayment.
Medicaid Offset:
If this matter is not resolved within fifteen (15) days from the date of this letter, CMS may instruct the
Medicaid State Agency to withhold the Federal share of any Medicaid payments that may be due you or
related facilities until the full amount owed Medicare is recouped, Title 42 CFR, § 447.30(g). These
recoveries will be in addition to any recoupments from other Medicare funds due you until the full amount
owed to Medicare is recovered.
If You Have Filed a Bankruptcy Petition:
If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding, Medicare financial
obligations will be resolved in accordance with the applicable bankruptcy process. Accordingly, we
request that you immediately notify us about this bankruptcy so that we may coordinate with both the
Centers for Medicare & Medicaid Services and the Department of Justice so as to assure that we handle
your situation properly. If possible, when notifying us about the bankruptcy, please include the name the
bankruptcy is filed under and the district where the bankruptcy is filed.
Termination of Medicare Provider Agreement:
Be advised that under Title XVIII, § 1866(b)(2)(A) of the Social Security Act, continued failure to
submit the required cost report may result in the termination of your Medicare provider agreement.

If you have submitted a cost report and any payment due Medicare, please disregard this letter. If you
have any questions concerning this letter, do not hesitate to call [Title] [Insert full name] at
[(xxx) xxx-xxxx].
Sincerely,
[Title] [Name] [Position Title]
Intent to Refer Letters:
EXHIBIT 5- INTENT TO REFER LETTER- NON-935 –
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
Contractors shall use the appropriate template below:
A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(BPROV3.pdf) Part B Provider Intent to Refer
2.
(APROV3.pdf) Part A Aggregate Claims Intent to Refer
B.
Contractors not on HIGLAS shall use this letter as your template.
Note: Contractors shall use this template for manual letters and shall scan all letters for easy access.
Date: &LETTER
&LETTER_HEADER1 &LETTER_HEADER2
&LETTER_HEADER3 &LETTER_HEADER4
Letter Number: &LETTER_NUMBER
&HPROVIDER_NAME
&HPROVIDER_ADDRESS1
&HPROVIDER_ADDRESS2
&HPROVIDER_CITY, &HPROVIDER_STATE &HPROVIDER_POSTAL_CODE
&HPROVIDER_COUNTRY
RE: Overpayment Amount: &HINVOICE_AMOUNT Outstanding Balance:
&DEMAND_AMOUNT
Provider Number: &HPROVIDER_NUMBER
Notice of Intent to Refer Debt to the Department of Treasury's Debt Collection Center for Cross
Servicing and Offset of Federal Payments and Certain Eligible State Payments
Dear Sir/Madam:
On &DATE_OF_ORIGINAL_DEMAND_LETTER, we sent a letter requesting that you refund an
overpayment made to you in the amount of &HINVOICE_AMOUNT that resulted from claim(s) accounts
receivable(s). As of the date of this letter, we have not yet received payment, an application for an
extended repayment schedule, or have sufficient assigned Medicare claims been submitted for collection of

the balance. The outstanding amount due for this overpayment is &DEMAND_AMOUNT, which includes
a principal amount of &INVOICE_BALANCE_AMOUNT and interest assessed in the amount of
&INTEREST_BALANCE_AMOUNT.
Your debt to the Medicare Program is delinquent and, by way of this letter, we are providing
notice that your debt may be referred to the Department of Treasury's Debt Collection Center
(DCC) for Cross Servicing and Offset of Federal Payments. Your debt may be referred under
provisions of Federal Law, title 31 of the United States Code, § 3720A, which is a provision of the
Debt Collection Improvement Act of 1996.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
Repayment
Your debt will not be referred to the Department of Treasury if you make payment in full. The past due
amount of &DEMAND_AMOUNT owed to the Medicare Program as of &LETTER_DT includes
interest accrued through &LAST_INTEREST_ACCRUAL_DATE. Interest is accrued monthly and is
added to the balance of the debt.
Your check or money order for the amount due should be made payable to Medicare and sent with a
copy of this letter to:
&CONTRACTOR_NAME &CHECK_ADDRESS1 &CHECK_ADDRESS2
&CHECK_CITY, &CHECK_STATE &CHECK_POSTAL_CODE
If you cannot make payment in full, you may be allowed to enter into an extended repayment
agreement if you are eligible under the requirements at 42 C.F.R. 401.607(c)(2). If you are interested
in an extended repayment agreement, please contact this office. Refer to your initial demand letter to
determine your rights to an appeal.
Referral To The U.S. Department of The Treasury for Collection
If your debt remains unpaid 60 days from the date of this letter, your debt will be referred to the United
States Department of the Treasury’s (the Treasury) Debt Management Services for Cross Servicing and
Offset of Federal Payments. Your debt will be referred under 31 U.S.C. 3711(g). The Treasury’s Debt
Management Services will use various tools to collect the debt, including offset of federal payments,
demand letters, phone calls, referral to a private collection agency, and referral to the U.S. Department of
Justice for litigation.
Due Process
You have the right to request an opportunity to inspect and copy records relating to the debt. This request
must be submitted in writing to the address listed below. You have the right to present evidence that all
or part of your debt is not past due or legally enforceable. In order to exercise this right, this office must
receive a copy of the evidence to support your position, along with a copy of this letter. You must submit
any evidence that the debt is not owed or legally enforceable within 60 calendar days of the date of this
letter. If, after sixty (60) calendar days from the date of this letter, we have not received such evidence,
your debt, if it is still outstanding and eligible for referral, may be referred to the Department of Treasury
or its designated Debt Collection Center for cross servicing/offset.
For Individual Debtors Filing a Joint Federal Income Tax Return
The Treasury Offset Program automatically refers debts to the IRS for offset. Your Federal income tax
refund is subject to offset under this program. If you file a joint income tax return, you should contact the
IRS before filing your tax return to determine the steps to be taken to protect the share of the refund, which
may be payable to the non-debtor spouse.
Overpayments from Debtors Who Share Tax Identification Numbers
Section 1866(j)(6) of the Social Security Act authorizes the Secretary of Health and Human Services (the
Secretary) to make any necessary adjustments to the payments of an applicable provider or supplier who
shares a TIN with an obligated provider or supplier, one that has an outstanding Medicare overpayment.
The Secretary is authorized to adjust the payments of such a provider or supplier regardless of whether it
has been assigned a different billing number or National Provider Identification Number (NPI) from that
of the provider or supplier with the outstanding Medicare overpayment.
Federal Salary Offset
If the facility ownership is either a sole proprietorship or partnership, your individual salary(s) may be
offset if you are or become a federal employee.
Medicaid Offset
If this matter is not resolved, CMS may instruct the Medicaid State Agency to withhold the Federal
share of any Medicaid payments that may be due you or related facilities until the full amount owed to
Medicare is recouped, per Title 42 CFR, § 447.30. These recoveries will be in addition to any
recoupment from other Medicare funds due you until the full amount owed to Medicare is recovered.
Bankruptcy
If you have filed bankruptcy and an automatic stay is in effect, you are not subject to offset while the
automatic stay is in effect. Documentation supporting your bankruptcy status, along with a copy of this
notice, must be forwarded to this office at the above address.
Should you have any questions, please contact your overpayment consultant at the following:
&BUSINESS_PURPOSE_1
&CONTRACT_CONTACT_PHONE_NUM_1
&BUSINESS_PURPOSE_2
&CONTRACT_CONTACT_PHONE_NUM_2
&BUSINESS_PURPOSE_3
&CONTRACT_CONTACT_PHONE_NUM_3
&BUSINESS_PURPOSE_4
&CONTRACT_CONTACT_PHONE_NUM_4
&BUSINESS_PURPOSE_5
&CONTRACT_CONTACT_PHONE_NUM_5
We look forward to hearing from you shortly.
Sincerely,
Medicare Recovery Unit
EXHIBIT 6- INTENT TO REFER LETTER - 935 -
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)

A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(APROV9353.pdf) Part A 935 Aggregate & Adjustment Claims Intent to Refer
2.
(APROVRAC2.pdf) Part A 935 RAC Adjustment Claims Intent to Refer
3.
(BPROV9353.pdf) Part B 935 Adjustment Claims Intent to Refer
4.
(BPROVRAC2.pdf) Part B 935 RAC Adjustment Claims Intent to Refer
B.
Contractors shall use the appropriate first paragraph below.
RE: Medicare Overpayment and Notice of Intent to Refer Debt to the Department of Treasury's
Debt Collection Center for Cross Servicing and Offset of Federal Payments and Certain Eligible
State Payments - MMA 935
Provider Name: &HPROVIDER_NAME Provider Number:
&HPROVIDER_NUMBER Outstanding Balance:
&DEMAND_AMOUNT
Dear Sir/Madam:
Part A and B overpayments subject to 935 (excluding RAC overpayments)
On &DATE_OF_ORIGINAL_DEMAND_LETTER, we sent a letter requesting that you refund an
overpayment subject to 935, Limitation on Recoupment. As of this date, we have not yet received
payment, a 935 appeal request, or an application for an extended repayment schedule and insufficient
assigned Medicare claims have been submitted for collection of the balance. The outstanding amount due
for this overpayment is &DEMAND_AMOUNT, which includes a principal amount of
&INVOICE_BALANCE_AMOUNT and interest assessed in the amount of
&INTEREST_BALANCE_AMOUNT.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
Or,
PART A and B 935 RAC Adjustment Claims
On &DATE_OF_ORIGINAL_DEMAND_LETTER, we sent a letter requesting that you refund a
Recovery Auditor-identified overpayment subject to 935, Limitation on Recoupment. As of this date, we
have not yet received payment, a 935 appeal request, or an application for an extended repayment schedule
and insufficient assigned Medicare claims have been submitted for collection of the balance. The
outstanding amount due for this overpayment is &DEMAND_AMOUNT, which includes a principal
amount of &INVOICE_BALANCE_AMOUNT and interest assessed in the amount of
INTEREST_BALANCE_AMOUNT.
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
[Contractors shall include the following language in all ITR-935 letters after the first
paragraph.]
Your debt to the Medicare Program is delinquent and, by this letter, we are providing notice that your debt
will be referred to the Department of Treasury's Debt Collection Center (DCC) for Cross Servicing and
Offset of Federal Payments. This could occur should the amounts recovered through withholding (offset)
of your claims be insufficient to satisfy the monthly amount of your extended repayment schedule or the
amount needed to be current on the extended repayment schedule. Your debt will be referred under
provisions of federal law, title 31 of the United States Code, § 3720A, which is a provision of the Debt
Collection Improvement Act of 1996.
The Debt Collection Improvement Act of 1996 (DCIA) requires Federal agencies to refer delinquent debt
to the Department of Treasury and/or a designated Debt Collection Center (DCC) for collection through
cross servicing and/or the Treasury Offset Program (TOP). Under the offset program, delinquent Federal
debts are collected through offset of other Federal agency payments you may be entitled to, including the
offset of your income tax return through the Internal Revenue Service (IRS). The TOP offsets can also be
taken from eligible state payments you are entitled to.
The DCC shall use various tools to collect the debt, including offset, demand letters, phone calls, referral
to a private collection agency and referral to the Department of Justice for litigation. Other collection
tools available, which may be used, include Federal salary offset and administrative wage garnishment.
If the debt is discharged, it may be reported to the IRS as potential taxable income.
During the collection process, interest shall continue to accrue on the debt and you shall remain
legally responsible for any amount not satisfied through the collection efforts.
For Individual Debtors Filing a Joint Federal Income Tax Return
The Treasury Offset Program automatically refers debt to the IRS for offset. Your Federal income tax
refund is subject to offset under this program. If you file a joint income tax return, you should contact
the IRS before filing your tax return to determine the steps to be taken to protect the share of the refund,
which may be payable to the non-debtor spouse.
Overpayments from Debtors Who Share Tax Identification Numbers
Section 1866(j)(6) of the Social Security Act authorizes the Secretary of Health and Human Services (the
Secretary) to make any necessary adjustments to the payments of an applicable provider or supplier who
shares a TIN with an obligated provider or supplier, one that has an outstanding Medicare overpayment.
The Secretary is authorized to adjust the payments of such a provider or supplier regardless of whether it
has been assigned a different billing number or National Provider Identification Number (NPI) from that
of the provider or supplier with the outstanding Medicare overpayment.
Federal Salary Offset
If the facility ownership is either a sole proprietorship or partnership, your individual salary(s) may
be offset if you are or become a federal employee.
Medicaid Offset
If this matter is not resolved, CMS may instruct the Medicaid State Agency to withhold the
Federal share of any Medicaid payments that may be due you or related facilities until the full amount
owed to Medicare is recouped, Title 42 CFR, § 447.30(g). These recoveries will be in addition to any
recoupment from other Medicare funds due you until the full amount owed to Medicare is recovered.
Please read the following instructions carefully to determine what action you should take to avoid
referral for cross servicing/offset.
Due Process

You have the right to request an opportunity to inspect and copy records relating to the debt. This request
must be submitted in writing to the address listed below. You have a right to present evidence that all or
part of your debt is not past due or legally enforceable. In order to exercise this right, this office must
receive a copy of the evidence to support your position, along with a copy of this letter. You must submit
any evidence that the debt is not owed or legally enforceable within 60 calendar days of the date of this
letter. If, after sixty (60) calendar days from the date of this letter, we have not received such evidence,
your debt, if it is still outstanding and eligible for referral, shall be referred to the Department of Treasury
or its designated DCC for cross servicing/offset.
Repayment
Your debt shall not be referred to the Department of Treasury if you make payment in full. The past due
amount owed to the Medicare Program as of the date of this letter includes current accrued interest.
Interest is accrued monthly and is added to the balance of the debt. Your check or money order for the
amount due should be made payable to:
&CONTRACTOR_NAME &CHECK_ADDRESS1 &CHECK_ADDRESS2
&CHECK_CITY, &CHECK_STATE &CHECK_POSTAL_CODE
Include a copy of this letter with your payment.
If you cannot make payment in full, you may be allowed to enter into an extended repayment
agreement if you are eligible under the extended repayment requirements at 42 C.F.R. 401.607(c)(2). If
you are interested in an extended repayment agreement, please contact this office.
Bankruptcy
If you have filed for bankruptcy and an automatic stay is in effect, you are not subject to offset while
the automatic stay is in effect. Documentation supporting your bankruptcy status, along with a copy
of this notice, must be forwarded to this office at the above address.
We request that you refund this amount in full. If you are unable to make refund of the entire amount at
this time, advise this office immediately so that we may determine if you are eligible for a repayment
schedule. Any repayment schedule (where one is approved) would run from the approval date.
If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding, Medicare financial
obligations will be resolved in accordance with the applicable bankruptcy process. Accordingly, we
request that you immediately notify us about this bankruptcy so that we may coordinate with both the
Centers for Medicare & Medicaid Services and the Department of Justice so as to assure that we handle
your situation properly.
If applicable, we have also initiated a request that your Federal share of Title XIX (Medicaid) payments
be withheld. If this withholding is initiated, it will not be removed until payment in full is received or an
acceptable extended repayment request is received and approved.
Should you have any questions, please contact your overpayment consultant at the following:
&BUSINESS_PURPOSE_1
&CONTRACT_CONTACT_PHONE_NUM_1
&BUSINESS_PURPOSE_2
&CONTRACT_CONTACT_PHONE_NUM_2
&BUSINESS_PURPOSE_3
&CONTRACT_CONTACT_PHONE_NUM_3
&BUSINESS_PURPOSE_4
&CONTRACT_CONTACT_PHONE_NUM_4
&BUSINESS_PURPOSE_5
&CONTRACT_CONTACT_PHONE_NUM_5
We look forward to hearing from you shortly. Sincerely,
Supervisor, Part A Overpayments &CONTRACTOR_NAME
EXHIBIT 7- INTENT TO REFER LETTER - UNFILED COST REPORTS ONLY-
(Rev. 316, Issued: 05-24-19, Effective: 10-01-19, Implementation: 10-07-19)
A.
Contractors on HIGLAS shall use the list below for the appropriate system generated letters.
1.
(APROVCRUNF3.pdf) Part A Unfiled Cost Report Intent to Refer
B.
Contractors not on HIGLAS shall use this letter as your template.
RE: Intent to Refer Letter Provider or Supplier Name: Provider/Supplier Number: &
Overpayment Amount: &HINVOICE_AMOUNT Outstanding
Balance: &DEMAND_AMOUNT
Subject in Bold: Notice of Intent to Refer Unfiled Cost Report Debts to the Department of
Treasury’s Debt Collection Center for Cross Servicing and Offset of Federal Payments
[Insert contractor opening paragraphs concerning the reason for the overpayment, date of
determination and amount due. Refer to previous demand letters or other forms of contact
regarding the debt.]
NOTE: If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding please
follow the instructions found at the end of this letter.
Your unfiled cost report debt to the Medicare Program is delinquent and, by way of this letter, we are
providing notice that your debt may be referred to the Department of Treasury’s Debt Collection Center
(DCC) for Cross Servicing and Offset of Federal Payments. Your debt may be referred under the
provisions of Federal law, Title 31 of the United States Code, § 3720A and the authority of the Debt
Collection Improvement Act of 1996.
The Debt Collection Improvement Act of 1996 (DCIA) requires Federal agencies to refer delinquent debt
to the Department of Treasury and/or a designated Debt Collection Center (DCC) for collection through
cross servicing and/or the Treasury Offset Program. Under the offset program, delinquent Federal debt is
collected through offset of other Federal agency payments you may be entitled to, including the offset of
your income tax return through the Internal Revenue Service (IRS).
The DCC may use various tools to collect the debt, including offset, demand letters, phone calls,
referral to a private collection agency and referral to the Department of Justice for litigation. Other
collection tools available, which may be used, include Federal salary offset and administrative wage
garnishment. If the debt is discharged, it may be reported to the IRS as potential taxable income.
For Individual Debtors Filing a Joint Federal Income Tax Return
The Treasury Offset Program automatically refers debt to the IRS for offset. Your Federal income tax
refund is subject to offset under this program. If you file a joint income tax return, you should contact the
IRS before filing your tax return to determine the steps to be taken to protect the share of the refund, which
may be payable to the non-debtor spouse.
Federal Salary Offset
If the facility ownership is either a sole proprietorship or partnership, your individual salary(s) may be
offset if you are (or become) a federal employee.
Medicaid Offset
As authorized in 42 CFR 447.30, and Section 1914 of the Social Security Act, CMS may instruct the State
Medicaid Agency to offset the Federal share of any Medicaid payments due to you, your agency and/or
related facilities. At that time, the offset shall remain in effect until the Medicare overpayment is paid in
full.
Read the following instructions carefully to determine what action you should take to avoid
referral for cross servicing/offset.
Due Process
You have the right to request an opportunity to inspect and copy records relating to the unfiled cost
report debt. This request must be submitted in writing to the address listed below. You have the right
to present evidence that all or part of your debt is not past due or legally enforceable. In order to
exercise this right, this office must receive a copy of the evidence to support your position, along with a
copy of this letter.
You must submit any evidence that the debt is not owed or legally enforceable within 60 calendar days
of the date of this letter. If, after sixty (60) calendar days from the date of this letter, we have not
received such evidence, your debt, if it is still outstanding and eligible for referral, may be referred to
the Department of Treasury or its designated Debt Collection Center for cross servicing/offset. NOTE:
Unfiled Cost Report debts (including new ones) may be transferred to Treasury for cross
servicing/offset, upon approval from CMS central/regional offices.
Repayment
Your unfiled cost report debt(s) shall not be referred to the Department of Treasury if you submit the
cost report or make the payment in full; otherwise, you will remain legally responsible for any amount
not satisfied through the collection efforts.
Your check or money order for the amount due, made payable to: Medicare
Contractor
Address 000 Street
Anywhere USA 00000-0000
Include a copy of this letter with your payment.
If you cannot make the payment in full, you may be allowed to enter into an extended repayment
agreement.
If you are interested in an extended repayment agreement, please contact this office.
Bankruptcy
If you have filed for bankruptcy and an automatic stay is in effect, you are not subject to offset while the
automatic stay is in effect. You must forward documentation supporting your bankruptcy status, along
with a copy of this notice, to this office at the above address.
If you have any questions concerning this debt, please contact _________________
at __________________________________.
Sincerely,
___________________________
[Signature of Certifying Official]
30 - Interest Assessment/Payment on Overpayments and Underpayments
(Rev. 29, 01-02-04)
The CMS regulations, in accordance with the Federal Claims Collection Act, as amended, the Social
Security Act, and common law establish specific rules for the payment of interest on Medicare
overpayments and underpayments (42 CFR 405.378). As a general rule, interest shall be assessed at the
prevailing rate specified by the Secretary of the Treasury unless the overpayment is recouped or the
underpayment is paid within 30 days of a "final determination."
Interest shall be assessed on overpayments, and shall be paid on underpayments, to providers and suppliers
of services (including physicians and other practitioners), if the overpayment or the underpayment is not
liquidated within 30 days from the date of the final determination.
The provisions of this section may not apply to FI overpayments or underpayments determined as a result of
interim rate and periodic interim payment (PIP) adjustments (See Chapter 3, §60) or utilization reviews.
The basic rules for assessing interest are:
30.1 - Final Determination
(Rev. 29, 01-02-04)
For purposes of this chapter:
A final determination is deemed to occur upon final settlement of a cost report when both an NPR and a
written demand for payment of an overpayment or a written determination of an underpayment is
transmitted to a provider based upon:
• An audited final settlement;
• Final settlement without audit; or
• Reopening for any reason.
In cases in which an NPR is not used as a notice of determination, one of the following determinations is
issued:
• A written determination that an overpayment exists and a written determination for payment;
• A written determination of an underpayment;
• An Administrative Law Judge (ALJ) or hearing officer’s decision that reduces the amount of an
overpayment below the amount that CMS has already collected. A final determination is deemed to
have occurred only when the amount of the overpayment/underpayment has been calculated. This
may be at the decision time and it may be at a later time if recalculations are necessary.
• A written determination that an As Filed Cost Report has been received without payment;
• A written determination that an accelerated payment or advanced payment has occurred and has now
been deemed an overpayment.
A final determination is deemed to occur upon the due date of a timely filed cost report which indicates an
overpayment is due CMS and is not accompanied by payment in full.
A final determination is deemed to occur with respect to a cost report that is not filed on time, from the date
due until such time as the cost report is filed.
30.2 - Rates of Interest - FIs and Carriers
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
The interest rates on overpayments and underpayments is determined in accordance with regulations
promulgated by the Secretary of the Treasury and is the higher of the private consumer rate or the current
value of funds rate prevailing on the date of final determination. Interest accrues from the date of the initial
request for refund and is assessed for each 30-day period, or portion thereof, that payment is delayed after
the initial refund request.
The private consumer rate, historically higher than the current value of funds rate, is subject to quarterly
revision. The Department of the Treasury certifies the revised rate to the Department of Health and Human
Services on a quarterly basis. Medicare contractors will be receiving subsequent quarterly updates of the
new interest rate for Medicare overpayments and underpayments through a recurring update notification.
Interest assessed for both late payments and installment payments is computed as simple interest using a
360-day year. Simple interest is interest that is paid on the original principal balance and after each payment
interest accrues on the remaining unpaid principal balance. Interest charges will not be prorated on a daily
basis for overdue payments received during the month (e.g., 10, 15, or 20 days late). Interest is assessed for
the full 30-day period. The interest rate on each of the final determinations will be the rate in effect on the
date the determination is made.
If periodic but unscheduled payments or credits are made in different calendar quarters, the quarterly rate
prevailing at the time of the final determination is charged and remains the same until the debt is liquidated.
Interest must be recalculated based on the outstanding balance at 30-day intervals from the date of final
determination.
The interest rate charged on overpayments repaid through an approved extended repayment schedule is the
rate that is in effect for the quarter in which the determination was made. The rate remains constant unless
the provider defaults (i.e., misses one consecutive installment payment following a delinquent status) on an
extended repayment agreement. When the provider defaults on such an agreement, interest on the balance of
the debt may be changed to the prevailing rate in effect on the date of the default if that rate is higher than
the rate specified in the agreement.
30.3 - Interest Accruals
(Rev. 41, 04-30-04)
NOTE: Effective October 1, 2004, 42 CFR 405.378 was amended to change how interest is calculated on
Medicare overpayments and underpayments to providers, suppliers, and other health care entities. This
change also applies to Medicare Secondary Payer (MSP) recoveries. Under the new rule, interest is assessed
for each full 30-day period that payment is not made on time. This change applies to Medicare
overpayments and underpayments determined (and MSP debts established) on or after October 1, 2004 (the
effective date of the final rule). Unliquidated debts determined prior to October 1, 2004 will continue to use
the former interest calculation method (a period of less than 30 days is considered to be a full 30-day period)
until paid in full.
Reminder: The date of the demand letter (not the day after) is the first day of the first 30-day period.

A. Accrual of Interest; Timely filed Cost Report/Part B Overpayment Determination
Interest will accrue from the date of the final determination and will either be charged on the overpayment
balance or paid on the underpayment balance for each full 30-day period that complete liquidation is
delayed.
Generally, interest charges on an overpayment begin to accrue on the date the FI issued an NPR and/or the
date the FI or carrier issued a notice of final determination of an overpayment, along with a written demand
for payment. If the overpayment is paid in full within 30 days from the date of determination the interest
accruals are normally waived.
NOTE: The standard systems generally post interest on a monthly basis. Interest is assessed at the end of
30-day periods. If the payment is postmarked on or before the 30
th
day any interest accrual is waived or
zero-balanced in the system.
Cost Report Overpayment-Example of Interest Accrual- The provider with a FYE 08/31/04 submits a cost
report on 01/28/05, showing $10,000 due the program, payment in full accompanies the cost report. On
02/15/05, the intermediary completes the desk review and determines an additional $25,000 overpayment.
On 02/15/05 the first demand letter is sent. The provider does not pay the $25,000 additional overpayment
until 04/03/05 (45 days after the date of the initial demand letter). Interest, therefore, accrues on the $25,000
for one full 30-day period.
Physician/Supplier Overpayment-Example of Interest Accrual- The carrier discovers that an overpayment
for $795.45 exists and sends a demand letter on 12/01/04. The physician/supplier does not remit payment
on the overpayment until 01/15/05 (45 days after the date of the initial demand letter). Therefore, interest
accrues on the $795.45 for one full 30-day period.
Physician/Supplier Overpayment – Example of Interest Accrual Prior to 10/01/2004 –
The carrier discovers that an overpayment for $795.45 exists and sends a demand letter on 09/30/04. (The
determination date of this overpayment is prior to the effective date of the revision to 42 CFR 405.378). The
provider does not remit payment on the overpayment until 11/14/2004 (45 days after the date of the initial
demand letter). Therefore, interest accrues on the $795.45 for two full 30-day periods.
Example of Waiver of Interest- Overpayment Paid in Full within 30 days from the date of determination-
The FI/carrier determines and demands an overpayment on 11/03/04 for $1500.00. The provider remits
payment of $1500.00. The postmark date on the payment is 11/30/04. Any interest accrual is waived since
the overpayment was paid in full within 30 days of the date of determination.
B. Accrual of Interest; Untimely Filed Cost Reports, Regarding Final Determinations at §30.1.
Interest always accrues for any overpayment on a late filed cost report for the period of delinquency when an
overpayment is declared or determined by CMS. The overpayment may appear on the cost report, or may be
determined later (including increases to overpayment, see example 2 below) through desk review or audit.
Interest accrues during the period a cost report remains unfiled beyond the due date. Interest is assessed for
the period of time the cost report was unfiled even if the overpayment is satisfied at the time of the delayed
filing of the cost report. This interest assessment is due and payable following the notice of a final
determination. The interest rate will be the rate in effect as of the day following the due date of the cost
report.
On any subsequent determination that increases the overpayment on a cost report filed untimely, the
additional overpayment is also subject to accrued interest charges for the period the cost report was due until
the date filed. The interest rate will be the rate in effect as of the day following the due date of the cost
report.

Where desk review, audit or reopening determinations increase the originally filed and declared
overpayment, the revised overpayment also is subject to the general provisions governing interest on
overpayments from the date of the new or revised notice of final determination. These interest charges will
be in addition to the interest charges due for the period of time the cost report remained unfiled.
Examples of Application when cost report not filed on time
1. The provider submits its cost report 70 days late and pays the declared overpayment of $50,000 when
filing. Interest at the prevailing rate accrues from the due date until the date filed, or, in this case, two 30-
day periods as only two full 30-day periods have passed. Interest is assessed during the period of
delinquency whether or not payment accompanies the cost report.
The intermediary performs a desk review and determines an additional overpayment of $12,000. Interest, at
the prevailing rate at the time the cost report became overdue is assessed on the $12,000 for the two 30-day
periods of delinquency. In addition, interest accrues at the current prevailing rate on the $12,000 if payment
is not made within 30 days of the date of the initial demand letter.
2. A provider with FYE 6/30/04 has a cost report that is due on 11/30/04. The cost report became overdue
on 12/01/04. On 01/15/05 the cost report was submitted indicating an amount due the program; payment did
not accompany the report. Due to the late submission of the cost report, interest is assessed for one 30-day
period. The interest rate assessed is the rate in effect on the day the cost report became overdue, 12/01/04.
In addition interest, at the rate in effect on the day the cost report became overdue, will accrue on the
declared overpayment from the date the cost report is filed to the date the amount due is paid.
On 03/12/05, the intermediary completes a desk review and determines an additional overpayment, issuing a
NPR and demand letter. Interest will be assessed on this additional amount at the rate in effect on 3/12/05.
In addition interest will be assessed for the period of delinquency at the rate in effect on the day the cost
report became overdue, 12/01/04.
C. Accrual of Interest; Rejected Cost Report
In terms of interest accrual, a rejected cost report is treated like an unfiled cost report. If a cost report is
officially rejected by the contractor, (see Audit and Reimbursement section to determine when to reject a
cost report) interest accrues on the determined overpayment amount from the date the cost report is due until
the date the cost report is resubmitted with payment in full. The determined overpayment amount is the
amount due the program on the accepted cost report. If a cost report is submitted with payment in full and is
later rejected the accrual of interest depends on the determined overpayment amount on the accepted cost
report. If the determined overpayment amount on the accepted cost report was paid in full by the original
submission, no interest accrues. If the determined overpayment amount is different than the overpayment
amount listed on the original rejected cost report, interest will accrue on the difference.
Example of Interest Accrual When the Cost Report is Rejected
1. A provider submits the cost report with payment in full before the due date. Upon review the contractor
rejects the cost report. The provider corrects the cost report and resubmits it. The contractor accepts the
revised cost report. The amount due the program on the revised cost report is equal to the check that
accompanied the original cost report. Since the check fulfilled the determined overpayment on/ before the
due date, there is no interest accrual.
2. A provider submits the cost report with payment in full before the due date. Upon review the contractor
rejects the cost report. The provider corrects the cost report and resubmits it. The contractor accepts the
revised cost report. The amount due the program on the revised cost report is different than the amount of
the check that was submitted with the original cost report. The provider sent in a check for the additional
amount with the revised cost report. Since the check with the original cost report was not the determined

overpayment amount, interest accrues on the difference between the check and the overpayment listed on the
revised cost report. The interest rate is the rate that was in effect on the day the cost report was due.
D. Underpayments
Generally interest charges on an underpayment begin to accrue upon the FI’s or carrier’s issuance of:
• An NPR (FI only) and a notice of final determination of an underpayment under §30.1.
• A notice of final determination of an underpayment under §30.1 when an NPR is not issued.
• An administrative law judge (ALJ) or hearing officer’s decision that reduces the amount of an
overpayment below the amount that CMS has already collected. Interest begins to accrue once
the underpayment amount has been determined. This may be at the decision time if the ALJ
reverses the entire overpayment amount or the ALJ states a principal amount to be paid upon
which interest may be calculated. However, if the ALJ does not specify the overpayment
amount and recalculations are necessary (not including a full reversal of the overpayment
amount) interest will begin to accrue at the time of the recalculations. If the FI/carrier is unsure
when interest should accrue for a particular case, the servicing regional office should be
contacted.
• An Intermediary Hearing or a Provider Reimbursement Review Board (PRRB) decision that
reduces the amount of an overpayment below the amount that CMS has already collected.
However, no interest will be due and payable to a provider if the FI or carrier pays the underpayment within
30 days from the date of notice of final determination of the underpayment. Interest will accrue each 30-day
period on the underpayment balance that has not been satisfied.
30.4 - Procedures for Applying Interest During Overpayment Recoupment
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
A. General
If a provider is unable to satisfy the overpayment within 30 days from the date of final determination and
demand for repayment (§30.1), interest accrues on the unpaid principal balance and is due and payable for
each full 30-day period that an overpayment balance is outstanding. The contractor first applies any
payments received to the accrued interest charges and then to the overpayment principal. If the provider has
more than one overpayment outstanding and a payment is received, the contractor credits the payment to the
oldest overpayment first, unless the provider designates otherwise.
B. Recoupment Through Installment Payments
A provider is expected to repay any overpayment as quickly as possible. If a provider cannot refund the
total amount of the overpayment within 30 days after receiving the first demand letter, it should immediately
request an extended repayment plan. (See Chapter 4, §50 for extended repayment procedures.)
The interest rate to assess on overpayments repaid through an approved extended repayment plan is the rate
in effect for the quarter in which the final determination is issued to the provider.
Interest rates remain constant based upon the initial rate assessed unless the provider defaults, i.e., misses
one consecutive installment payment following a delinquent status of an extended repayment agreement.
Interest on the principal balance of the debt may be changed to the current prevailing rate if (a) the provider
has defaulted on its installment payments and (b) the current prevailing rate in effect on the date the
installment becomes overdue is higher than the rate specified in the agreement. (For FISS and APASS users
only.) Each payment is applied first to accrued interest and then to principal. After each payment interest
will accrue on the remaining unpaid principal balance.
C. Proof of Receipt
The U.S. Postal Service postmark date is controlling in determining the timely receipt of a cost report or
payment of an overpayment. Therefore, the contractor should retain all envelopes in order to have proof of
receipt. If a due date for any payment falls on a holiday or a weekend, the next working day is considered
the official due date for the purpose of applying accrued interest. (FISS and APASS users only.) CMS does
not accept dates imprinted by a provider’s meter postage machine as confirmation of the postmark date. In
these cases, the MAC should use the date the cost report or payment was received, and date stamped. If a
provider utilizes a commercial delivery service the date constituting a timely receipt is the date the
commercial delivery service signs and accepts the package. The date the cost report or payment is received
by the MAC controls if any other mailing service was used.
30.5 - Notification to Providers Regarding Interest Assessment
(Rev. 41, 04-30-04)
A. Cost Report Reminder Letters
The FI is required to issue reminder letters to a provider of the time limitation for filing the cost report when
the institutional provider fails to file by the last day of the fourth month following the end of the cost report
period. In addition to the requirements outlined in Chapter 3, §30 and Chapter 4, §20 the FI must include
the following in a cost report reminder letter:
1. Late Filing Interest- If a cost report is not filed on time and indicates an amount is due CMS,
or if it is subsequently determined that an additional overpayment exists, such as when an NPR is issued,
interest will be assessed on the overpayment from the due date of the cost report to the date the cost report
was filed. This interest assessment is made regardless of whether the overpayment is liquidated within 30
days.
2. Assessed Interest- If a cost report is filed on time and indicates an amount is due CMS,
interest will accrue on that overpayment from the date the cost report is due, unless full payment
accompanies the report or the provider and the contractor agree in writing, in advance, to recoup the amount
of the overpayment from interim payments over the next 30-day period.
B. Notice of Program Reimbursement (NPR)
In addition to the requirements outlined in audit instructions, all NPRs issued after September 3, 1982, must
include the following:
"In accordance with the procedures of 42 CFR 405.378ff interest will be assessed on the
amount due CMS unless full payment is made within 30 days from the date of the Notice.
Interest will be assessed for each full 30-day period that payment is delayed."
C. Overpayment Demand Letters
In addition to the requirements of Chapter 4, §20 and §90 the FI and Carrier’s written demand for repayment
must contain a notice that in accordance with 42 CFR 405.378, interest shall be assessed on all
overpayments at the prevailing rate specified by the Secretary of the Treasury unless repayment is made
within 30 days. Interest shall be assessed for each full 30-day period that payment is delayed and shall
accrue from the date of the final determination. The demand letter shall include the appropriate interest rate
that will be assessed if payment in full is not received within 30 days.

30.6 - Waiver and Adjustment of Interest Charges
(Rev. 41, 04-30-04)
A. Waiver of Interest Charges
Interest charges shall be waived if the overpayment is completely liquidated within 30 days from the date of
final determination, or if the contractor or the RO determines that the administrative cost of collection would
exceed the amount of interest.
For institutional providers serviced by FIs, interest shall not be waived for the period of time during which
the cost report was due but remained unfiled as specified in Chapter 4, §30.1. Also, interest shall not be
waived where a cost report is timely filed indicating an amount due CMS and is not accompanied by
payment in full as specified in Chapter 4, §30.1 unless the provider and the FI agree in advance to liquidate
the overpayment through a reduction in interim payments over the next 30-day period.
For bankrupt providers and interest see Chapter 3, §140.
B. Adjustment of Interest Charges
1. Reopenings-FI
When the FI reopens a final settlement pursuant to 42 CFR 405.1885 - 1887(a) and such reopening reverses
some or all adjustments, whereby the previous overpayment is reduced or eliminated, it makes an
appropriate adjustment to previously assessed and recovered interest to reflect the proper interest chargeable
under 42 CFR 405.378 and the policies set forth.
Should the reopening action establish or increase an overpayment, the rate of interest on the additional or
new overpayment is the rate in effect as of the date of the new notice of final determination.
If the original cost report was not submitted timely, any reopening action, which results in an adjustment to
the previously determined overpayment, shall also include an appropriate adjustment to the late filing
interest assessment.
2. FI and Provider Reimbursement Review Board Hearings - Institutional Providers Serviced by FIs
If an overpayment or underpayment determination is reversed administratively by the FI or by the PRRB,
and the reversal is the final decision in the case, it is necessary to recalculate the correct amount of interest
to be assessed. If any excess interest or principal has been collected, the FI refunds it to the debtor. No
interest accrues on the refunded amount unless payment is not made within 30 days from the date of
notification of the corrected overpayment or underpayment amount.
If the hearing results in an additional overpayment, the FI assesses interest on the additional amount at the
rate in effect on the date of the revised final determination. Interest does not accrue until the FI notifies
the provider of the revised overpayment or underpayment amount.
Example of Application
On 07/18/05, the intermediary completes a final settlement and issues a NPR and a written demand showing
an amount due the program of $16,000. On 09/15/05, the provider pays the $16,000 overpayment plus one
30-day period of accrued interest.
As a result of a hearing on 12/l0/05, the PRRB reverses the intermediary's findings and determines that the
correct amount due the program was $4,000. The excess $12,000 in principal and the accrued interest on
$12000 that was assessed and collected must be returned to the provider.
3. Judicial Review

The policies and procedures of this section do not apply to the time period for which interest is payable
under 42 CFR 413.64(j) because the provider seeks judicial review of an adverse decision by the PRRB or
the decision of the Administrator. Section 1878(f) of the Social Security Act authorizes a court to award
interest in favor of the prevailing party on any amount due as a result of the court’s decision. The interest is
payable for the period beginning on the first day of the first month following the 180-day period which
began on either the date the intermediary made a final determination or the date the intermediary would have
made a final determination had it been done on a timely basis. The interest rate assessed is the rate on
obligations issued for purchase by the Federal Hospital Insurance Trust Fund. This rate of interest can be
found at http://cms.hhs.gov/statistics/trust-fund-interest-rates/. If the FI withheld any portion of the amount
in controversy prior to the date the provider seeks judicial review by a Federal court, and the Medicare
program is the prevailing party, interest is payable by the provider only on the amount not withheld.
Similarly, if the Medicare program seeks to recover amounts previously paid to a provider, and the provider
is the prevailing party, interest on the amounts previously paid to a provider is not payable by the Medicare
program since that amount had been paid and is not due the provider. However, if the Medicare program
had recovered any of the amount in controversy interest would be payable from the time of recovery through
the date of payment.)
40 – Withholds and Suspensions
(Rev. 29, 01-02-04)
In accordance with regulations (42 CFR §405.370), recoupment and suspension are defined as:
Recoupment- The recovery by Medicare of any outstanding Medicare debt by reducing present or future
Medicare payments and applying the amount withheld to the indebtedness.
Suspension of Payment- The withholding of payment by an intermediary or carrier from a provider of an
approved Medicare payment amount before a determination of the amount of the overpayment exists.
40.1 – Recoupment by Withholding Payments
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
A. General
In accordance with regulations (42 CFR §§405.371-372), payments determined to be payable to providers
can be withheld to protect the Medicare program against financial loss if the intermediary has determined
that the provider to whom payments are to be made has been overpaid.
The withholding of interim payments may be partial (for example, a percentage of payments withheld or a
set amount) or complete.
B. Requirements for Withhold
Comply with the following conditions to withhold interim payments:
• Notify the provider in writing through the demand letter or in other correspondence of your intention
to withhold payments, in whole or in part; and
• Give the provider an opportunity to submit a statement (including any evidence) as to why the
withhold shall not be put into effect. Inform the provider it has l5 days following the date of the
notification to submit such a statement.
C. Cost Report Overpayments Percentage of Withhold
Some percentage of withhold shall begin 15 days after the date of the first demand letter (day 16) if the
overpayment has not yet been liquidated or an extended repayment plan has not been requested. The matrix

below shall be utilized to determine the percentage of withhold for an overpayment determined from a cost
report that has been filed (as filed cost report, tentative settlement, or final settlement), a PIP review, or an
interim rate review. See Chapter 3, §30.1 when a cost report remains unfiled.
NOTE: A set amount of withhold may be proposed instead of a percentage. The amount shall not be less
than the appropriate percentage unless specific instructions are received from RO or CO.
D. Physician/Supplier Overpayments- Withhold of Payments
Withhold of all payments shall begin 40 days (41
st
day) after sending the initial overpayment demand letter
unless payment in full has been received or an ERS application has been received. If an ERS application has
Day 16
No word from
provider
100 % withhold
Day 16
Provider has submitted
Extended Repayment
Schedule (ERS)
application
No withhold if provider submitted a good faith
payment along with ERS application. Good faith
payments must continue on a monthly basis until
provider receives written approval or denial of
the ERS request. If good faith payment is not
received with the application request, withhold
shall be initiated at 30%.
Day 16
Provider has submitted
ERS application but it
is incomplete
No withhold as long as provider submitted a first
good faith payment along with ERS application.
If good faith payment is not received with the
application request, withhold shall be initiated at
30%. Once a completed application is
submitted, good faith payments or 30%
withholding must continue on a monthly basis
until provider receives written approval or denial
of the ERS request. If completed information is
not received within an allotted amount of time
(rarely more than 30 days) withhold shall be
initiated at 100%.
Day 16
Provider has said that it
is planning to submit
an ERS application
30% withhold- when ERS application is
received, cease withhold if a good faith payment
accompanies the application request; maintain
30% withhold if payment does not accompany
application.
Day 30
Still no word from
provider
Withhold at 100%.
Day 30+
ERS application is
being reviewed by RO
or CO
No withhold as long as provider continues to
submit appropriate good faith payments on a
monthly basis under the terms of the application
request. If provider did not submit a first good
faith payment or does not submit subsequent
payments, withhold shall be 30% of payments
unless RO or CO gives alternative instructions.
Day 30
Provider said an ERS
application was
forthcoming but has
not been received to
date
Increase withhold to 100%.
If provider calls with an acceptable reason for
the delay, make a judgment call to leave at 30%
until day 45 or refer to RO for direction.
Day 45+
No ERS application
and no payment by
provider
Withhold at 100%
been received and is currently being reviewed by the MAC or CMS RO or CO and the good faith payment
was sent in by the provider with the application, no withhold shall occur. If the good faith payment did not
accompany the ERS application a 30% withhold shall be initiated.
NOTE: Additional Information for MACs
If extenuating circumstances exist and the MAC believe that a higher or lower percentage of withhold is
necessary to protect the Medicare Trust Fund, the MAC shall contact the servicing regional office for
guidance and/or approval. Some examples include knowledge that the provider may file bankruptcy, a
history of non-payment of overpayments, or evidence that the withhold percentage would cause irreparable
harm.
The payment submitted with the ERS application shall be one month’s payment based on the amortization
schedule submitted with the ERS application. The amortization schedule shall not exceed 60 months, shall
include principal and interest and the minimum monthly payment shall not be less than 1/60
th
of the
overpayment. If the provider requests an ERS in excess of 60 months the good faith payment submitted
shall be 1/60
th
of the overpayment. If the good faith payment submitted is not 1/60
th
of the overpayment, the
MAC shall contact the provider (in writing or a documented telephone call with the appropriate personnel at
the provider’s place of business) requesting additional funds. If the provider does not submit additional
funds within 15 days of the date of the request, the MAC shall initiate a 30% withhold.
Until a final decision is made regarding the ERS the provider should submit monthly good faith payments
based on the amortization schedule. If the provider does not continue to submit monthly good faith
payments, the MAC shall contact the provider requesting the payment. If the provider does not submit the
monthly payment within 15 days of the date of the request, the MAC shall initiate a 30% withhold until a
decision is made.
E. Disposition of Withheld Funds
All funds withheld shall be applied towards the outstanding overpayment. The funds shall be applied to the
outstanding and accrued interest first and then to the outstanding principal balance.
F. Duration of Withhold
The withhold shall remain in effect until:
• The overpayment is liquidated;
• You enter into an agreement with the provider for liquidation of the overpayment; or
• On the basis of subsequently acquired evidence, or otherwise, you determine that there is no
overpayment.
40.2 – Suspension of Payment (See Program Integrity Manual)
(Rev. 29, 01-02-04)
Medicare authority to withhold payment in whole or in part for claims otherwise determined to be payable is
found in federal regulations at 42 CFR 405.370-377, which provides for the suspension of payments.
Suspension may be used when the contractor possesses reliable information that:
• Fraud or willful misrepresentation exists;
• An overpayment exists but the amount of the overpayment is not yet determined;
• The payments to be made may not be correct; or

• The provider fails to furnish records and other requested information. (Some examples include cost
reports, credit balance reports, and form CMS-91.)
50 - Establishing an Extended Repayment Schedule (ERS) - (formerly known as an
Extended Repayment Plan (ERP))
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
For purposes of these instructions, the term Provider, Physician and other Supplier will be referred
to as “Provider.”
For purposes of these instructions, the term Medicare Administrative Contractor (MAC) may be
referred to as “Contractor.”
For the purposes of these instructions, the following definitions apply; See 42 C.F.R. §401.607(c)(2)
and (3):
Hardship exists when the total amount of all outstanding overpayments (principal and interest) not included
in an approved, existing repayment schedule is 10 percent or greater than the total Medicare payments made
for: (1) the cost reporting period covered by the most recently submitted cost report; or (2) the previous
calendar year for a non-cost report provider (see below ‘additional factors to consider’ when determining
eligibility).
Extreme Hardship exists when a provider qualifies as being in “hardship” as defined in the previous
paragraph and a 36 month to 60 month extended repayment schedule (ERS) is deemed eligible for approval
consideration by Medicare.
Additional Factors to Consider:
The contractor shall evaluate the request, based on the definitions written above, in conjunction with the
requirements found in sections 50-50.3 of this chapter. For a provider whose situation does not meet the
definitions written above, the contractor shall evaluate the ERS request based on the requirements found in
sections 50-50.3 of this chapter and consider the information in (i) – (iii) below, when deciding whether to
grant an ERS.
The contractor shall determine the number, amount, and frequency of installment payments based on the
information submitted by the debtor and on other factors such as:
(i) Total amount of the claim (overpayment);
(ii) Provider's ability to pay; and
(iii) Cost to CMS of administering an installment agreement.
The contractor shall document evaluation factors, including communication with CMS, used during the
decision-making process.
A provider is expected to repay any overpayment promptly. If repaying an overpayment within 30 days
would constitute a “hardship” on the provider, a request for an ERS should be submitted immediately.
However, if the overpayment is outstanding and not referred to Treasury, the provider shall request an ERS
beyond 30 days, and the contractor shall review that request. Instructions on how to apply for an ERS shall
be available on the contractors’ website for provider reference. Medicare demand letters shall refer
providers to the contractors’ website for detailed ERS instructions. Contractors shall include in the ERS
instructions a form in which the provider can elect to have their underpayments or manual refunds
automatically applied to their overpayment (see section B below). Providers shall be given the option to
request a paper copy.

A. The following steps shall be implemented upon receipt of an ERS:
1. A provider shall submit a signed ERS request which includes:
i. the specific overpayment for which an ERS is being requested;
ii. the number of months requested;
iii. CMS required documents (see sections 50.1-50.2) and a good faith payment equaling one
month’s payment of the providers requested terms with its request (ex. 36 month request =
1/36th minimum). Good faith payments shall not be considered monthly payments for the
MAC approved ERS, but instead, shall be applied to reduce the overall balance of the
overpayment.
This is what constitutes a complete ERS.
2. Contractors shall evaluate all providers’ requests for an extended repayment schedule up to 60
months, and shall only approve/disapprove ERS requests up to 60 months.
3. Contractors should consider ERS requests for 6-15 months on a case-by-case basis. Approval should
only be for cases where it is clear that the debt can be repaid in this short period. Requests for 6 -15
month ERSs do not require submitting financial documentation if the provider meets the hardship
qualifications and does not fall within a scenario found in section 50.3(1).
4. When deemed appropriate, contractors may refer ERS requests that need additional guidance to the
Regional Office (RO), along with a recommendation.
5. The RO will evaluate ERS requests as needed or requested by the contractor for further direction.
(see 42 CFR 401-607(c)(2)(vi)).
6. CMS Central Office (CO) will evaluate ERS requests as needed or requested by the RO.
7. All ERS requests shall be reviewed and evaluated for approval, disapproval, or referral to RO/CO
within 30 calendar days of receipt of the complete request.
8. Providers may request for an ERS under 16 months without submitting financial documentation if
they meet the hardship qualifications and do not fall within a scenario found in section 50.3(1).
9. The Provider shall submit financial documentation for ERS request 16 months or longer.
10. The contractor shall determine eligibility qualifications and the duration of the ERS based on its
review of the provider’s documentation and any other information acquired (such as fraud
information, claims data, overpayment history, etc.).
11. If an ERS is approved and a provider misses one consecutive installment payment following a
delinquent status, the provider is in default. (refer to 42 CFR §401.607(2)(v)). Delinquent loan
status is when a provider misses one installment payment. Default loan status is when a provider
misses one consecutive installment payment, following a delinquent loan status. The contractor
shall send a notice of default to the provider within 5 calendar days, suspend the ERS agreement,
and immediately resume normal debt collection procedures.
12. The contractor shall consider a providers’ request to reinstate the ERS, even after default. If
reinstated, the provider shall be required to submit new documentation to determine eligibility. The
contractor shall determine to reinstate the original ERS agreement or revise the schedule, if
approved. If revised, the contractor shall ensure that the revised terms do not extend the original
and revised schedule beyond 60 months. The ERS will be closed with no reopening, if the provider

were to default again on the reinstated request.
13. The contractor should not grant an ERS to a provider where there is a previously defaulted ERS
that was not resolved (reinstated, paid up to date, or paid in full).
B. The following steps shall be implemented when reviewing and establishing an ERS:
1. If a complete ERS request and a good faith check payment (see note a. below) are received, the
contractor shall start reviewing the request immediately. The contractor shall accept the good faith
payment(s) and suspend any recoupment during the review of the ERS.
2. Contractors shall review the complete ERS package to make a final decision within 30 calendar days
of receipt. If the contractor needs additional time to review an ERS request, it shall work with their
RO to determine a reasonable timeframe to complete.
3. If an ERS request is received with all documentation but no good faith payment, (see note a. below)
the contractor shall immediately place the provider on 30% recoupment during the review of the
ERS.
4. Contractors shall review the ERS documents in detail to determine if there are any other documents
needed. If additional documents are needed the contractors shall request additional documentation.
5. If an incomplete ERS request is received, the contractor shall review the submitted documentation,
determine and request all missing documents. If a good faith payment was not received, the MAC
shall immediately place the provider on no less than 30% recoupment. If the contractor requests
additional documentation and the information is not received by the 16th calendar day after the
contractor’s request, the contractor should close the request and resume normal collect activities.
6. Contractors shall review the ERS documents in detail to determine if there are any other documents
needed. If additional documents are needed the contractors shall request additional documentation.
7. Contractors should extend an additional 15 calendar days to receive the documentation from the
provider before closing the request. Upon receipt, the contractor shall complete its review of the
additional documentation within 5 calendar days.
8. Contractors shall ensure that requesting additional documentation will not unnecessarily extend the
decision-making period.
9. If the contractor needs additional time to conduct the review, they shall work with their RO to
determine a reasonable timeframe to complete.
10. Contractors shall NOT refund any payments received or recouped that occurred while processing
an ERS, but shall apply such amount(s) to the outstanding overpayment(s) (apply to interest first
then principal), unless CMS directs otherwise.
11. If the ERS request is approved, the contractor shall establish an ERS to recover the remaining
balance of an overpayment.
12. Pre-accrued interest shall be recovered first before applying any payments to principal. Pre-
accrued interest can either be recovered in one lump sum or over multiple months (not to exceed 3
months, unless directed by CMS), depending on a provider’s ability to pay in full or over time.
13. Contractors shall ensure that interest continues to accrue on the overpayment until it is paid in full.
While recovering the pre-accrued interest amounts, the contractor shall also recover the interest
that continues to accrue on the outstanding principal balance.
14. Once the pre-accrued interest is paid in full, the ERS (recovering principal and accruing interest)
shall begin.
15. Approved ERS requests will run from the ERS approval date.
16. If the ERS request is denied, the contractor shall continue with normal debt collection activities.
Providers shall be permitted one additional ERS request for an overpayment, where a previous
ERS was denied.
17. If both ERS requests are denied, any additional ERS requests for that overpayment (that a
contractor deems should be considered) shall be forwarded to the RO for review.
18. Contractors shall include in the ERS instructions an option in which the provider can elect to have
all of its underpayments or manual refunds automatically applied to its overpayment. Subject to
section B below, a provider can rescind its consent to automatic recoupment or offset of
underpayments and manual refunds, with further written notice to the contractor.
19. Any underpayments or manual refunds applied to an overpayment shall reduce the term of the
ERS and shall not affect the installment amounts due under any amortization schedule.
20. Unless the provider has submitted a request asking the MAC to automatically
apply underpayments and manual payments to the ERS payments, contractors shall not
automatically apply an underpayment due to a cost report or a manual refund due to over
collection to the ERS overpayment.
21. If the contractor determines a Medicare underpayment or manual refund after establishing an
ERS, the contractor shall notify the provider in writing of the underpayment or manual refund.
22. The contractor shall permit the provider 15 calendar days following the date of notification to
submit a request (with justification) to refund the underpayment.
23. If the provider does not respond in the required timeframe or has not submitted a form asking the
contractor to automatically apply the underpayment or manual refund to the ERS payments, the
contractor shall immediately apply this amount to the ERS payments (with the exception of #20
above).
24. If the provider responds timely, the contractor has 15 calendar days from the receipt date to
determine if the provider’s justification is in the best interest of the Medicare program. The
contractor should either apply the underpayment or refund the amount to the provider.
25. If a provider does not submit such a justification, the contractor shall deny the request and shall
immediately apply this amount to the ERS payments.
26. If the provider fails to provide accurate current financial information, including certifying that
no material change has occurred, the contractor shall apply the underpayment or manual refund
to the ERS.
27. If a refund request is denied, the contractor shall send written notice of the determination to the
provider, explaining the rationale for the determination. The determination is not an initial
determination and is not appealable.

NOTE(S):
a. Good faith payments are monthly payments submitted by the provider while an ERS is in
review. They should equal one (1) month’s payment of the providers requested terms; ex., 36-
month request = 1/36th minimum good faith payment. Payments less than this amount are not
considered a good faith payment. Payments shall continue to be submitted monthly while the
ERS is being reviewed.
b. If under a 935 appeal, the provider shall continue to submit good faith payments or ERS
installment payments. These payments are considered voluntary payments and not 935
recoupments.
50.1 – ERS Required Documentation --Physician is a Sole Proprietor
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
A. The contractor shall require that the provider (physician/sole proprietor) furnish the following
for Extended Repayment Schedule (ERS) request of 15 months or less:
1. Signed Proposed Amortization Schedule – The CMS requires a signed request, including a
proposed monthly term and payment installment schedule, as a provider’s agreement to pay
its overpayment through installment payments. Signatures submitted in electronic form are
permissible.
2. Good Faith Payments – The CMS requires the provider to submit the first good faith
payment (per the proposed amortization schedule) with the ERS application, along with any
future payments due, while under review. Providers shall submit a good faith payment each
month until the ERS review is decided.
B. The contractor shall require that the provider (physician/sole proprietor) furnish the following for an
ERS request of 16 months or more:
1. Signed Proposed Amortization Schedule – The CMS requires a signed request, including a
proposed monthly term and payment installment schedule, as a provider’s agreement to pay
its overpayment through installment payments. Signatures submitted in electronic form are
permissible.
2. Good Faith Payments – The CMS requires the provider to submit the first good faith
payment (per the proposed amortization schedule), along with any future payments due
while under review. Providers shall submit a good faith payment each month until the ERS
review is decided.
3. CMS-379 Form - a completed CMS -379 Form. The information requested on this form is
necessary for the contractor to determine if the physician/sole proprietor will be able to make
installment payments on a claim.
4. Financial Statements - of Debtor.
5. Income Tax Return - a copy of the provider’s income tax filing for the most recent calendar
year.

50.2 - ERS Required Documentation– Provider is an Entity Other Than a Sole
Proprietor
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
A. The contractor shall require that the provider (NOT a physician/sole proprietor) furnish the
following for an Extended Repayment Schedule (ERS) request of 15 months or less:
1. Signed Proposed Amortization Schedule – The CMS requires a signed request, including a
proposed monthly term and payment installment schedule, as a provider’s agreement to pay
its overpayment through installment payments. Signatures submitted in electronic form are
permissible.
2. Good Faith Payments – The CMS requires the provider to submit the first good faith
payment (per the proposed amortization schedule), along with any future payments due while
under review. Providers shall submit a good faith payment each month until the ERS review
is decided.
B. The contractor shall require that the provider (NOT a physician/sole proprietor) furnish the following
for ERS request of 16 months or more:
1. Signed Proposed Amortization Schedule – The CMS requires a signed request, including a
proposed monthly term and payment installment schedule, as a provider’s agreement to pay
its overpayment through installment payments. Signatures submitted in electronic form are
permissible.
2. Good Faith Payments – The CMS requires the provider to submit the first good faith
payment (per the proposed amortization schedule), along with any future payments due
while under review. Providers shall submit a good faith payment each month until the ERS
review is decided.
3. Balance sheets - the provider’s most current balance sheet and the balance sheet for the last
complete Medicare cost reporting period (or the most recent fiscal year).
NOTE:
If the time period between the two balance sheets is less than 6 months (or the provider cannot
submit balance sheets prepared by its accountant), it must submit balance sheets for the last two
complete Medicare cost reporting periods (for providers that file a cost report) or for the last two
complete fiscal years (for providers that don’t file a cost report).
4. Income statements - related to the balance sheets. The CMS requires that both the balance
sheets and income statements include similar agreement language:
MISREPRESENTATION OR FALSIFICATION OF ANY INFORMATION CONTAINED IN
THIS BALANCE SHEET OR INCOME STATEMENT SHALL BE PUNISHABLE BY FINE
AND/OR IMPRISONMENT UNDER FEDERAL LAW.
CERTIFICATION BY OFFICER/ADMINISTRATOR OF PROVIDER(S)
(For physicians/suppliers, “CERTIFICATION BY OFFICER/OWNER OF DEBTOR(S))
I HEREBY CERTIFY that I have examined the balance sheet and income statement prepared
by_______________________ and that, to the best of my knowledge and belief, it is a true,
correct and complete statement from the books and records of the provider.

Signed
Officer/Administrator of Provider(s) Title
(For physicians/suppliers: Officer/Owner of Debtor(s)
Title)
Date
5. Cash flow statements - for the periods covered by the balance sheets (see Exhibit 3 for
recommended format). If the date of the provider’s request for an extended repayment
schedule is more than 3 months after the date of the most recent balance sheet, a cash flow
statement shall be provided for all months between that date and the date of the request.
6. Projected cash flow statement - from the date of the request and covering the remainder of
the fiscal year. If fewer than 6 months remain, the provider shall include a projected cash
flow statement for the following year. (See Exhibit 3 for recommended format.)
7. List of restricted cash funds - by amount as of the date of request and the purpose for
which each fund is to be used (if applicable).
8. List of investments - by type (stock, bond, etc.), amount and current market value as of the
date of the report (if applicable).
9. List of notes and mortgages payable - by amounts as of the date of the report, and their due
dates (if applicable).
10. Schedule showing amounts - due to and from related companies or individuals included in
the balance sheets. The schedule should show the names of related organizations/persons,
TIN and NPI numbers. It shall also show where the amounts appear on the balance sheet--
such as Accounts Receivable, Notes Receivable, etc.
11. Schedule showing types - amounts of expenses (included in the income statements) paid to
related organizations. The schedule shall show names of the related organizations, TIN and
NPI numbers.
12. The percentage of occupancy- by type of patient (e.g., Medicare, Medicaid, private pay)
and total available bed days for the periods the income statements cover.
All financial records must be for the business participating in the program. It should not be for the owner if
the business is a partnership or a corporation. If an outside facility manages the financial aspects of the
business, the provider shall submit individual financial records, as well as the financial records of the outside
facility.
50.3 - ERS Approval Process
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
Contractors shall not approve any Extended Repayment Schedule (ERS) if any of the following apply:
1. When there is reason to suspect that the provider may:
a) file for bankruptcy;
b) cease to do business;
c) discontinue participation in the program; or
d) when there is an indication of fraud or abuse committed against the program.
2. When any of the following is not submitted with request:

a) a signed request agreement;
b) all required documents;
c) a proposed term and installment schedule; and
d) the first installment payment (per the proposed installment schedule).
15 months or less ERS
The contractor shall review and confirm that none of the scenarios listed above apply. The contractor shall
review 12 months of claims and payment history and consider whether it supports full payment of the
overpayment within 15 months or less. Once the contractor determines ability to repay, it shall examine the
status of any outstanding overpayments, cost report settlements, advanced payments and accelerated
payments. In the case any of these overpayments are excessive, in default or delinquent, the contractor shall
determine if an ERS for 15 months or less is appropriate.
16 months or more ERS
The contractor shall review and confirm that none of the scenarios listed in the beginning of this section
apply. The contractor shall analyze the financial data submitted by the provider to determine the availability
of cash, marketable securities, accounts receivable, restricted and unrestricted endowment funds, or special
funds, and considers whether these funds could be used for partial or full payment of the overpayment (see
Exhibits 1-4 below).
The contractor shall review 12 months of claims and payment history, and considers whether it supports full
payment of the overpayment within the requested months. Once the contractor determines ability to repay, it
shall examine the status of any outstanding overpayments, cost report settlements, advanced payments and
accelerated payments. In the case any of these overpayments are excessive, in default or delinquent, the
contractor shall determine if an ERS is appropriate. The contractor shall reference and complete the ERS
protocol sheet (see Exhibit 1) while reviewing and once a decision is made.
The contractor should alter the length of time when approving an ERS request, based on its analysis of the
provider’s submitted documentation. For example, if a provider requests 24 months, but the contractor
determines that 12 months is sufficient, the contractor can deny the 24 month request and extend an offer of
a 12 month repayment plan.
The contractor should request additional financial information from the provider, if needed. It should also
request financial information from the owner if the owner is requesting to submit personal capital to help
repay the Medicare debt.
The contractor shall provide a recommendation to the RO; shall deny or approve for terms under its
authority; or shall request additional information from the provider within 30 days of receipt of the
completed ERS request.
If the provider is unable to furnish all of the required documentation listed in 50.1 and 50.2 of this chapter, a
full explanation shall be provided as to why this is the case. All documentation shall be received within 30
days of the date of the request (see § 50(2) of this chapter). Where the provider’s explanation is reasonable
and the documentation is otherwise acceptable, the contractor shall forward the request for extended
repayment to the RO with its recommendation, within 30 days receipt of the completed request. The
contractor shall comply with Chapter 4 §40 regarding recouping the overpayments pending receipt of the
provider’s documentation and the contractor’s decision on the extended repayment request.
If the provider is able to furnish all of the required documentation listed in 50.1 and 50.2 of this chapter timely,
the contractor shall approve, counter or deny the request within 30 days receipt of the completed request.
If the contractor determines that the provider DOES meet the requirements for an ERS, it shall:
a) notify the provider in writing, within 5 calendar days of making the decision;
b) include the amortization schedule showing principal and interest payment amounts and dates
payments are due; and
c) include approval information on the quarterly report (see § 50.4 of this chapter).
If the contractor determines that the provider DOES NOT meet the requirements for an ERS, it shall:
a) notify the provider in writing, within 5 calendar days of making the decision; and
b) include the denial reason, in the notification.
In the case the provider:
Rejects: If a provider rejects the approved terms, it shall submit a written and signed rejection notice to the
contractor. In this case, the contractor shall close out the request and follow normal recoupment policy and
procedures, at a recoupment rate of 100% of the provider’s payments.
Disagrees: If a provider requests additional month(s) due to hardship, the contractor shall elevate the
request to the RO for further review. When needed, the RO should contact CO for additional guidance.
No Response: If the provider has not responded, the contractor shall proceed with the ERS as outlined in
the approved schedule.
Exhibit I – Protocol for Reviewing Extended Repayment Schedule (ERS)
Provider _______________________________________________________
Provider Number _________________________________
(Part A Only) Cost Report ___________________________
FYE (Part B Only) Date(s) ___________________________
Overpaid Overpayment ______________________________
Amount $ ____________________________________
Date of Demand Letter _________________
No. of Months Requested for ERS ___________
Date of Request Received ___________________
Bankrupt ___ Terminated ___ Suspended ___ Revoked ___ Fraud ___ Documented ____
Decision Date (36 Months or less) _______ (36 or more) ______ # of Mos. Apprvd. ________
Date Referred to RO for Consideration __________________
Name of Contractor ____________________________
Decision Reason __________________________________________________________
Reviewed By ______________________________________________
Contractor Analyst __________________________________________
Supervisor Review __________________________________________
Date _______________________________________
1. Contractor shall summarize the major reasons why the overpayment occurred.
2. Contractor shall review the documentation the provider submits to determine
whether it is complete. (Refer to §50.1 and 50.2 for required documentation.)
Contractor analyzes the financial data submitted (for an ERS over 12 months) to
determine the availability of cash, marketable securities, accounts receivable,
restricted and unrestricted endowment funds, or special funds, and considers
whether these funds could be used for partial or full payment of the overpayment.
3. Contractor shall perform the following calculations by using the most current
financial data that the provider submitted to determine whether the provider qualifies
for an ERS.
(a) Current Ratio
The current ratio relates the dollar value of current assets to the dollar value of
current liabilities in order to evaluate an organization's ability to pay its current
debt. Derived as:
CURRENT ASSETS_______
= CURRENT LIABILITIES
This ratio defines the number of dollars held in current assets per dollar of
current liabilities (e.g., it relates current assets to current liabilities).
Multiple coverage of liabilities is desirable. Generally, high values for the
current ratio imply a good ability to pay short-term obligations and, thus, a
low probability of technical insolvency.
Normally, the contractor considers a current ratio of 2:1 adequate to meet
current liabilities. However, a provider with a current ratio of 2:1 or greater)
can have short-term payment problems if its current assets are not expected to
be in liquid form (cash or short-term investments) in time to meet the expected
payment dates of the current liabilities.
(b) Quick Ratio
A liquidity ratio which measures the number of dollars of liquid assets (cash
plus marketable securities plus accounts receivable) available per dollar of
current liabilities. Derived as:
CASH + MARKETABLE SECURITIES + ACCOUNTS RECEIVABLE
= CURRENT LIABILITIES
This is a more stringent measure of liquidity than the current ratio. The
contractor uses it to determine the adequacy of cash, accounts receivable, and
marketable securities to pay current liabilities.
Normally, the contractor considers a quick ratio of 1.5:1 adequate to meet
current liabilities. However, a provider with a high quick ratio can have short-
term payment problems if it has excessive amounts of slow-paying or doubtful
accounts receivable, which it cannot turn into cash soon enough to meet
maturing current liabilities. Conversely, a low quick ratio might not imply a
future liquidity crisis if current liabilities include terms that will not require
payment from existing current assets.
4. The contractor for institutional providers shall determine whether there are any
settlements (interim rate adjustments or cost report) in process which could be
used to offset the outstanding overpayment.
5. Based upon the previous steps, the contractor shall summarize whether or not it
should approve or deny, or recommend approval of a repayment plan. If it
recommends approval, it indicates the number of months, how it calculated the
monthly payment and the reason(s) for the approval. If it recommends denial, it
indicates the reason(s).

Exhibit 2 - Cash Flow Statement Period Covered
CASH FLOW STATEMENT
FOR THE PERIOD
Cash provided by:
Operations (net) (Schedule A) (See Exhibit 4) $XXXX
Cash donations (unrestricted) XXXX
Long-term borrowing XXXX
Investment earnings (cash dividends, interest) XXXX
Sale of long-term investments XXXX
Sale of equipment XXXX
Issuance of bonds XXXX
Decrease in current assets – other than Accounts
Receivable, Prepaid Expenses, and Inventory XXXX
Increase in current liabilities – other than Accounts
Receivable, Prepaid Expense, and Inventory XXXX
Others XXXX
Total Cash Provided $XXXX

CASH FLOW STATEMENT
FOR THE PERIOD
Cash applied to:
Purchase of equipment $XXXX
Payment of long-term debt XXXX
Purchase of long-term investments
Payment of dividends
Purchase of land and/or building XXXX
(Purchase price less mortgage, capital stock
and non-cash assets given toward purchase)
Increases in current assets - other than XXXX
Accounts Receivable, Prepaid Expenses, and Inventory
Decreases in current liabilities – other than XXXX
Accounts Payable and Prepaid Income
Other XXXX
Total Cash Applied XXXX
Increase (Decrease) in Cash $XXXX
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
- - Cash at end of period (date) $XXXX
Less: Cash at beginning of period (date) XXXX
Increase (Decrease) in Cash XXXX
Exhibit 3 - Projected Cash Flow Statement Cash from Operations
(Schedule A) Period Covered
PROJECTED CASH FLOW
CASH FROM OPERATIONS (SCHEDULE A)
Net Income (or Net Loss)
$XXXX Increases: Depreciation expense
$XXXX
Loss from sale
of equipment
XXXX
Decrease in net Accounts
Receivable XXXX
Decrease in
Prepaid
Expense
XXXX
Decrease in Inventory XXXX
Increase in
Accounts
Payable
XXXX
Increase in Prepaid Income XXXX
Others XXXX
XXXX Gross Cash
from
Operations
Decreases: Gain from sale of equipment $XXXX
Increase in net Accounts Receivable XXXX
Increase in Prepaid Expense XXXX
Increase in Inventory XXXX

Decrease in Accounts Payable XXXX
Decrease in Prepaid Income XXXX
Others XXXX
XXXX Net Cash from Operations
XXXX
$XXXX

Requirements to be Completed Before
Approval or Denial
15 Months or Less
16 Months or More
Received and Reviewed all required
documentation
X
X
Received and Applied
submitted payments while under review
X
X
Complete ERS Protocol
(See Exhibit 1)
X
Analyzed Financial
Statements
X
Reviewed last 12 months Claim
History
X
X
Reviewed last 12
months Payment
History
X
X
Reviewed status of
Additional Outstanding
Overpayments
X
X
Confirmed No Active
Bankruptcy
X
X
Confirmed Enrollment
Status is not– Terminated, Revoked,
Suspended
X
X
Reviewed status of
Outstanding
Advance/Accelerated
Payments
X
X
Part A-
Reviewed status of
Outstanding
Cost Report Settlements
X
X
Confirmed No
Outstanding Fraud
Investigations with CPI Staff
X
X
Sent to RO/CO for opinion
(if needed)
X
X
50.4 – Sending the ERS Request to the Regional Office (RO)
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
After the contractor has reviewed the provider’s supporting documentation and determines that a referral
to the RO is needed, it shall send its recommendation to the RO for consideration of approval. The
contractor shall submit the following:
1. A copy of all information the provider submitted.
2. The date of the initial contact between the contractor and the provider regarding the
overpayment.
3. Copies of all correspondence, including demand letters and the complete Extended Repayment
Schedule (ERS) request. Also include notes of telephone conversations, if any.
4. Part A - The amount of the overpayment; cost report year in which it occurred; dates and
amounts of any repayments; dates and amounts of payments (interim or retroactive) held in
account.
5. Part B - The amount of the overpayment, claim paid date, dates and amounts of any
repayment.
6. Part A - The cost reports in which the overpayments appeared or were found. The contractor
shall furnish any information it has on the financial status of related organizations, as
determined through audits and other sources, such as mercantile reports.
7. Documentation reflecting current enrollment status along with any bankruptcy, fraud and abuse
and other litigation cases.
8. Amount repaid to date on pending ERS request along with current status on any additional
outstanding overpayments.
9. The provider’s proposed repayment plan and rationale.
10. The contractor’s recommendation and supporting rationale including a completed ERS protocol
(See Exhibit 1) and the last 12 months’ claim and payment history.
11. The contractor’s opinion, based on experience, as to the reliability of the financial data.
The RO will grant a provider an ERS of:
(a) Up to 36 months if repaying an overpayment in full will constitute a “hardship,” as defined in
section 50 of this chapter.
(b) 37 months up to 60 months if repaying an overpayment in full will constitute an “extreme
hardship,” as defined in section 50 of this chapter. See also 42 CFR 401-607(c)(2)(vi).
If the contractor receives no response from the RO in 30 days, the contractor shall follow up with the RO
for a status update.
NOTE: An ERS shall be repaid through recoupment, unless a provider supplies a valid reason why the
ERS shall be paid by another method, such as payment by check.
50.5 - Monitoring an Approved Extended Repayment Schedule (ERS) and Reporting
Requirements
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
MACs have access to the CMS HIGLAS ERS Activity dashboard/report in HIGLAS Business Intelligence
(HBI) using the BI Update AR User Responsibility. This report has a comprehensive view of the ERS
portfolio by each MAC jurisdiction. It also helps identify at risk ERS which are delinquent or in default
status by showing risk criteria such as provider average billing and provider non-ERS debt balances. The
data is refreshed daily each morning. MACs can view/search specific ERS data as well as export the
record(s) as required. MACs shall continue to verify the Program Integrity checks in PECOS and with
CPI staff, such as, Terminated/Revoked statuses, before approving an ERS request.
MACs shall provide ERS status updates to CMS upon request using this activity report.
50.6 - Requests from Terminated Providers or Debts that are Pending Referral to
Department of Treasury
(Rev. 12346; Issued:11-01-23; Effective:10-30-23; Implementation:10-30-23)
When approving/denying an Extended Repayment Schedule (ERS) request, the contractor is making a
subjective decision concerning the provider’s ability to repay. All complete ERS requests shall be
reviewed by the contractor. This includes ERS requests from terminated providers and requests received
for debts where the contractor has already sent an Intent to Refer (ITR) letter.
Terminated Providers:
If a terminated provider submits an ERS request, the MAC shall consider the provider’s ability to repay
the debt over time.
The contractor shall refer requests to the RO if it determines that an ERS is in the best interest of the
Medicare program prior to denying the request, based on the requirements in section 50.3. In addition, if
the contractor has a reason to believe that a provider will terminate the program, they should research this
issue and refer the request to the RO for a decision.
Debts that are Pending Referral to Department of Treasury:
If a contractor has sent an ITR letter and the contractor has received an ERS request prior to referral, the
contractor shall review and process the request first to determine eligibility. If the request is approved,
the contractor shall establish the ERS and shall not refer the debt to Treasury. If denying an ERS request
will result in the immediate referral of an active provider to the Department of Treasury, the contractor
shall contact the RO to determine if an alternative exists.
It is preferred to recoup payments from present and future claims payments. If recoupment of payments is
not possible, the contractor shall accept monthly checks in the full amount agreed. If the provider misses

one payment (delinquent loan status), the contractor shall continue with normal debt collection (including
discontinuing the ERS, pursuing the full balance owed, and/or referral to Treasury).
NOTE: The requirements set forth in the Debt Collection Improvement Act of 1996 still apply.
60 - Withholding the Federal Share of Payments to Recover Medicare or Medicaid
Overpayments
(Rev. 29, 01-02-04)
Institutions and persons furnish health care services under both the Medicare and Medicaid programs, and
are reimbursed according to the rules applicable to each program. Overpayments may occur in either
program; at times resulting in a situation where an institution or person that provides services owes a
repayment to one program while being reimbursed from the other.
60.1 - Withholding the Federal Share of Medicaid Payments to Recover Medicare
Overpayments
(Rev. 29, 01-02-04)
Section 1914 of title XIX and 42 CFR §447.30 provide for CMS to withhold the Federal share of
Medicaid payments with respect to Medicaid providers that have, or previously had, a Medicare provider
agreement under §1866, and for physicians when:
• They have received an overpayment of title XVIII funds, and efforts to collect it have been
unsuccessful; or
• Efforts to secure from the provider, the necessary data and information to determine the amount, if
any, of the overpayment have been unsuccessful (i.e., a deemed overpayment because the provider
failed to file a cost report); and
• For physicians or suppliers, they have previously accepted Medicare payment on the basis of an
assignment under section 1842(b)(3)(B)(ii) of the Act, and during the 12 month period preceding
the quarter in which CMS proposes to withhold the Federal share of Medicaid payments for a
Medicare overpayment, submitted no claims under Medicare or submitted claims which total less
than the amount of the overpayment.
The CMS may order the State to withhold the Federal share of Medicaid payments of a provider to
recover Medicare overpayments plus accrued interest.
The FI/carrier shall establish whether or not a provider is subject to these procedures. The FI/carrier must
be sure the provider is participating in title XIX program prior to referring the case to the RO for
withholding. It shall refer only those cases that it is unable to collect through established procedures. The
RO resolves questions with respect to the provider's status in the Medicaid program.
Section 1914(a) of the Act permits, rather than requires, the Secretary to withhold the Federal share of
Medicaid payments to recover Medicare overpayments. To allow flexibility in the administration of this
provision, the ROs routinely determine whether it would be cost effective to withhold the Federal share.
If they determine that it is not feasible, they notify the FI/carrier, citing the reason for not processing the
collection request.
The provider may appeal the FI/carrier’s overpayment determination. The appeal procedures, however,
do not delay the withholding of the Federal share of payments due the Medicaid provider or physician.
If a provider is subject to the procedures for withholding the Federal share of Medicaid payments to
recover the Medicare overpayment and it has not met the conditions in the second demand letter, the
FI/carrier shall contact the RO with a recommendation to initiate withholding action.
If the RO determines that withholding the provider’s federal share of Medicaid payments would be cost
effective, the RO may request copies of the case file, which may include cost reports, demand letters, and
copies of all correspondence and contact with the provider.
To implement the withholding action, the RO notifies the provider and the State Agency (SA) responsible
for the State's title XIX expenditures. The withholding of Federal payments under title XIX remains in
effect until notice is received by the title XIX SA through the RO that:
• The overpayment has been refunded,
• Satisfactory arrangements have been made for repayment, or
• There is no overpayment based upon new evidence or a subsequent audit.
When the withholding of Federal payments under title XIX is no longer necessary, it will be lifted and the
provider again receives Federal title XIX payments for Medicaid services rendered.
The FI/carrier shall notify the RO immediately if the provider submits an acceptable cost report or makes
satisfactory arrangements for the repayment of the overpayment. It includes the date the delinquent cost
report was filed or satisfactory arrangements for the repayment were made. Because the withholding
process is a lengthy one, the RO may revoke a withholding before its effective date if the provider
submits a satisfactory cost report or if it makes satisfactory arrangements for repayment.
The RO monitors the collection and advises the FI/carrier when the overpayment is recovered. If an
excess amount is withheld, it advises the FI/carrier to restore any excess.
60.2 - Withholding Medicare Payments to Recover Medicaid Overpayments
(Rev. 29, 01-02-04)
Section 1885 of title XVIII of the Act and 42 CFR §405.375 provide for CMS to withhold Medicare
payments under both Part A and B to recover Medicaid overpayments that a Medicaid agency has been
unable to collect.
The RO determines if withholding the Medicare payments due the overpaid Medicaid institution is
appropriate. Where it determines that withholding the Medicare payments is proper, it advises the
FI/carrier to withhold the Medicare payments to the institution by the lesser of:
• The amount of the Medicare payments to which the institution would otherwise be entitled;
• The total Medicaid overpayment.
The FI/carrier shall terminate the withholding action if the Medicaid overpayment is recovered or the RO
advises it to do so.
It shall submit to the RO, at least monthly until the overpayment is recovered, the amount of Medicare
payments withheld. If no claims are received in any month, it informs the RO that no payments were
withheld.
The Medicaid agency establishes procedures to assure the return to the institution or person amounts
withheld that are ultimately determined to be in excess of the Medicaid overpayments. The FI/carrier
shall establish internal procedures to account for the Medicare amounts withheld under this section.
70 - Non-Medicare Secondary Payer (Non-MSP) Debt Referral Instructions and Debt
Collection Improvement Act of 1996 (DCIA) Activities
(Rev. 77, Issued: 09-16-05, Effective: 10-17-05, Implementation: 10-17-05)
(MSP Debt Referral Instructions are contained in the Medicare Secondary Payer Manual, Publication
100-05, Chapter 5, Section 60.)
70.1 - Background
(Rev. 77, Issued: 09-16-05, Effective: 10-17-05, Implementation: 10-17-05)
The Debt Collection Improvement Act of 1996 (DCIA) facilitates collections by the Federal Government
and encourages the streamlining of procedures within and among Federal agencies. The DCIA requires
Federal agencies to refer eligible delinquent debt to the Department of Treasury (Treasury) or a Treasury
designated Debt Collection Center (DCC) for cross servicing and/or offset through the Treasury Offset
Program (TOP).
70.2 - Cross Servicing
(Rev. 77, Issued: 09-16-05, Effective: 10-17-05, Implementation: 10-17-05)
Cross servicing is a process whereby Federal agencies refer eligible delinquent debt to Treasury for
collection. The agency referring the debt retains responsibility for reporting the debt on the Treasury
Report on Receivables Due from the Public. The agency is also responsible for removing accounts from
its receivables when Treasury directs it to write off the debt. To effectively collect the debt that agencies
refer, Treasury issues demand letters, conducts telephone follow-up, initiates skip tracing, refers debt for
administrative offset, and refers debt to a private collection agency (PCA). Other collection tools may
include Federal salary offset and administrative wage garnishment. The PCA shall attempt collection of
the debt, using collection tools such as skip tracing, credit report search, demand letters and telephone
calls.
70.3 - Treasury Offset Program (TOP)
(Rev. 136; Issued: 02-15-08; Effective/Implementation Date: 03-17-08)
The TOP is a program that compares Federal payments and eligible state payments with Federal debt.
When a match occurs, the payment is offset to collect the debt. When the Taxpayer Identification
Number (TIN) and name of the debtor match the TIN and name of a payee, the payment to the payee is
offset and monies that would have gone to the payee are sent to the creditor agency to satisfy the debt. A
debt may remain in TOP for offset up to ten years from date of determination. Types of payments that
can be offset may include tax refunds, vendor payments, benefit payments with certain restrictions, and
eligible state payments.
70.4 Definition of Delinquent Debt
(Rev. 77, Issued: 09-16-05, Effective: 10-17-05, Implementation: 10-17-05)
Per DCIA referral criteria, “delinquent” is defined as debt: (1) that has not been paid (in full) by the date
specified in the agency’s initial written notification (i.e., the agency’s first demand letter), unless other
payment arrangements have been made, or (2) that at any time thereafter the debtor defaults on a
repayment agreement.
70.5 - Referral Requirements
(Rev. 259, Issued: 01-15-16 Effective: 02-16-16, Implementation: 02-16-16)
The Centers for Medicare & Medicaid Services (CMS) is mandated to refer all eligible debt, 120 days
delinquent, for cross servicing and/or TOP. Additionally, the CMS has the option of referring such debt
before it is 120 days delinquent.
70.6 - Debt Ineligible for Referral (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Non-MSP debt ineligible for referral include those: (1) in bankruptcy status, (2) in an appeal status
(pending at any level), (3) at the Department of Justice, (4) where the debtor is deceased,
(5) Federal entity debt where the debtor is a Federal agency, (6) where the principal and interest balance is
less than $25, or (7) debt under fraud and abuse investigation where the investigating unit has provided
the contractor with specific instructions not to attempt collection.
Treasury has also approved a waiver for the mandatory referral of unfiled cost report debt for cross
servicing and/or TOP and for debts less than $100 that do not have a TIN.
Contractors shall monitor debt previously ineligible for referral that become eligible for referral. If the
status of the debt changes to an eligible status, contractors shall determine whether an ITR letter has been
sent. If the ITR letter has been sent, and at least 60 days have passed since the date of the ITR letter
(including the ITR letter returned undeliverable), contractors not utilizing HIGLAS shall refer the debt by
utilizing the Debt Referral Form within ten calendar days of the status change making the debt eligible for
referral. If the ITR letter has not been sent, contractors shall send the ITR letter within ten calendar days
of the status change making the debt eligible for referral, and follow the normal debt referral process.
70.7 - Intent to Refer Letter (Rev.11787;
Issued: 01-19-23; Effective: 04-21-23; Implementation: 04-21-23)
To comply with the DCIA requirements to provide specific notice to debtors before referring a debt for
cross servicing and/or TOP, contractors shall send an Intent to Refer (ITR) letter as their final demand
letter for all eligible delinquent debt. The contractor shall send the “final demand letter”, which is defined
as the last letter routinely sent to debtors to request payment, when or before the debt is 30 to 61 days
delinquent (60 to 91 days from the determination date). A sample ITR letter is included in Exhibit 1 of
this section.
The ITR letter shall be sent regardless of previous collections on the debt, unless there is an approved
current extended repayment agreement in effect.
When appropriate, the ITR letter shall include the amount of interest due, along with the date of the last
interest accrual. contractors may add additional wording to this letter that shall provide additional
instructions or clarification regarding the recoupment of the overpayment.
Contractors sending manual ITR letters should use their own language in the opening paragraphs to
explain the reason for the overpayment and the current balance, including interest accrued and the interest
rate.
The ITR letter shall be signed by the contractor official who routinely signs the demand letters.
The language in the ITR letter shall include a sentence that says: “If, after sixty calendar days from the
date of this letter we have not received such evidence, your debt, if it is still outstanding
and eligible for referral, shall be referred to the Department of Treasury or its designated Debt Collection
Center for cross servicing/offset.”
70.8 - Response to Intent to Refer Letter (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Contractors shall respond to any inquiries received as a result of the ITR letter within 15 calendar days of
receipt. If the status of the debt changes based on the communications with the debtor, contractors shall
update all appropriate systems timely.
The ITR letter provides debtors with 60 calendar days to respond. If, by day 61 the debtor has not
responded to the ITR letter, the contractor not utilizing HIGLAS shall refer the debt immediately by using
the Debt Referral Form. For contractors utilizing HIGLAS, the debt will be systematically referred to
Treasury 66 days from the ITR letter date. Debt for which less than full payment was received, or there is
a current repayment agreement that is in default, are eligible for referral for cross servicing and/or TOP.
Where there has been a partial recoupment or collection, but the collection is not the result of a current
extended repayment agreement, the balance (if principal and interest balance is greater than or equal to
$25) shall still be referred for cross servicing and/or TOP. The contractor shall not refer debts to Treasury
that are ineligible for referral or exempt from referral to cross servicing and/or TOP.
Before referring a debt for cross servicing, contractors shall first determine if the debt should be referred
to the Regional Office (RO) for litigation rather than referral to Treasury for cross servicing. If it is
determined that the debt should be litigated, contact the RO for further action.
If the ITR letter is returned as undeliverable, contractors shall follow established procedures to locate a
better address. (See Chapter 4, §§ 10 and 80) If a better address is obtained, the contractor shall send the
provider/supplier a manual ITR notification letter, with the original ITR letter attached, to the better
address. The original ITR letter date shall remain in effect. If the ITR letter is returned as undeliverable
and a better address cannot be located within 10 business days:
• the contractor not utilizing HIGLAS shall refer the debt to Treasury by entering the debt into the
Debt Referral Form 60 calendar days from the date of the original letter.
• the contractor utilizing HIGLAS shall update the status code to ‘LTR-UNDL-ITR.’ HIGLAS will
systematically refer the debt to Treasury 66 days from the ITR letter date.
70.9 - Reserved for Future Use
70.10 - Reserved for Future Use
70.11 - Actions Subsequent to Debt Referral (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Once the debt is referred for cross servicing, active collection efforts by the contractors and/or CMS shall
cease. However, debt referred for cross servicing and/or TOP shall still be maintained in HIGLAS or in
the contractors’ internal systems for financial reporting, interest accrual, and possible internal
recoupment. The contractor not utilizing HIGLAS shall be responsible for updating all the applicable
systems. The contractor shall utilize the Debt Referral Form for the manual change of the status and the
balance of the debt at Treasury.
70.12 - Transmission of Debt
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Prior to the weekly transmission of debts to Treasury, the contractor shall certify its debts by the close of
business on the day before transmission. When CMS transmits debts to Treasury, CMS shall generate an
CMS Debt Management (CMSDM) Outbound Debt Referral Report that will list the debts transmitted
that week. The contractor utilizing HIGLAS shall use the appropriate responsibility to retrieve the report
that will list its debts only. The contractor not utilizing HIGLAS shall update its internal systems with the
debts’ transmission status and send a transmitted debt report to CMS with 15 business days. The
contractors shall review the reports to ensure that debts transmitted remain valid and amounts are
accurate.
70.13 - Update after Debt Transmission (Rev.11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Once a debt has been referred for cross servicing and/or TOP:
The contractors shall update HIGLAS or the Debt Referral Form (contractors not utilizing HIGLAS),
within ten business days of the notification of the change to the debt if the contractors discover an error,
collection (by check or recoupment), or receive information establishing that the debt is ineligible for
cross servicing (i.e., bankruptcy, appeal),
If Treasury or a Private Collection Agency (PCA) discovers an error, collects on the debt, or receives
information, that would render the debt ineligible for cross servicing, Treasury shall notify CMS and its
contractors via the CMS Debt (CMSDM) Management Inbound Acknowledgment, Treasury Dispute
Timer, or Collections Report. The contractor not utilizing HIGLAS shall update its internal records, as
appropriate. The contractor shall return the completed CMSDM Treasury Dispute Timer Reports to CMS
within 30 calendar days.
If Treasury or the PCA receives a dispute from the debtor or obtains additional information regarding the
debt that requires CMS or contractor intervention, a Treasury Cross-Servicing Dispute Resolution Form
shall be sent to CMS. The CMS shall maintain a report of all debt in dispute and forward the information
to the contractors for review and decision. The contractors shall have 30 calendar days to respond to
Treasury and update their internal systems if applicable, and shall copy CMS RO and CO on their
response. The contractor shall recall the debt if it is determined that the dispute is valid.
If Treasury does not receive the response to the dispute timely, the debt may be returned to agency (RTA)
with the reason “dispute timer expired.”
70.14 - Collections
(Rev. 136; Issued: 02-15-08; Effective/Implementation Date: 03-17-08)
70.14.1 – Background (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Collection reports from the Department of the Treasury (Treasury) as a result of cross servicing efforts are
received by CMS central office (CO) through the Intra-governmental Payment and Collection (IPAC)
system multiple times per month. Collections may be received as a result of collection efforts by
Treasury’s Servicing Center or by a Treasury contracted Private Collection Agency (PCA) including
installment payments on Treasury approved extended repayment schedules or from offsets from the TOP.
70.14.2 - Intra-governmental Payment and Collection (IPAC) System (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The collection report generated from the IPAC system includes a break out of principal and interest
collected on individual debts; however, the report does not show the balance and the status of the debt
after the collection. Treasury calculates interest on a daily basis while CMS calculates interest monthly.
Therefore, the amount of interest collected by Treasury or its PCAs may not equal the amount of interest
shown as accrued by the contractors.
70.14.3 - CMS Debt Management Collections Interface and Report (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The CMS Debt Management (CMSDM) Collections Interface reports collections back to HIGLAS on
debts that were referred to Treasury. The contractor shall view its Roundtrip Status Report every Monday
to determine if the CMSDM Treasury Collections Report is available from the Friday HIGLAS cycle.
The contractor shall use the appropriate HIGLAS responsibility to generate the CMSDM Treasury
Collections Report which is the result of processing the interface and is available three times per month.
For each debt listed on the CMSDM Treasury Collections Report, contractors not utilizing HIGLAS shall
apply the collection to principal and interest amounts as indicated. For collection of interest only,
contractors not utilizing HIGLAS shall post the interest as shown on the CMSDM Treasury Collections
Report. An interest adjustment is not required prior to posting the collection. For collection of principal
and interest, contractors not utilizing HIGLAS shall manually adjust the amount of interest accrued in its
internal system to the amount of interest collected as listed on the CMSDM Treasury Collections Report.
This will make the amount of the accrued interest equal to the amount of interest collected which is listed
on the CMSDM Treasury Collections Report. Contractors not utilizing HIGLAS shall then post the
collection. Interest shall continue to accrue on the remaining principal balance. Contractors not utilizing
HIGLAS shall use the current date as the date of collection to post the Treasury collections to their
systems. Contractors not utilizing HIGLAS shall complete and return to CMS the CMSDM Treasury
Collections Report within 15 business days of receipt.
Contractors utilizing HIGLAS shall complete/update their adjustments/refunds within 15 business days of
receipt of the CMSDM Treasury Collections Report. CMS shall run a CMSDM Treasury Collections
Report on day 16 to determine if there are any unapplied debts. If there are any unapplied debts CMS
shall create a report listing those debts and send to the MAC via email. The contractor shall take
immediate corrective action and send an Excel spreadsheet back to CMS showing the updates. If a refund
is not resolved, the contractor shall have an additional 15 business days to resolve the refund.
70.14.4 - Reserved for Future Use
70.14.5 - Reserved for Future Use
70.14.6 - Reserved for Future Use
70.14.7 - Excess Collections (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Amounts collected may exceed the amount of the debt that was referred for cross servicing/TOP. As an
example, an excess collection may result from Treasury and its PCAs receiving a collection and
contractors recouping the same debt by internal withhold.
70.14.8 - Applying Excess Collections (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Contractors shall apply the excess collection to the debt listed on the CMSDM Collection Report in order
to bring the balance to zero. Contractors shall then determine if the debtor has any other outstanding
debts including interest to which the excess collection may be applied.
70.14.8.1 - If the Debtor Has Other Outstanding Debt (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
If the debtor has other outstanding debt, the excess collection shall then be applied to the oldest debt first
(then next oldest), in accordance with established procedures for applying excess collections against a
debtor’s overpayments. The breakout of principal and interest on the CMSDM Treasury Collections
Report does not apply when the excess collection is applied to another outstanding debt.
70.14.8.2 - If the Debtor Has No Other Outstanding Debt (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)

If there are no other outstanding debts, the excess portion of the collection, after bringing the debt listed
on the spreadsheet to a zero balance, shall be refunded. The amount of the refund shall be annotated on
the CMSDM Treasury Collections Report. The contractor shall process the refund within 15 business
days. A copy of the report, with the appropriate annotations regarding the refund, shall be kept in the
debtor file for audit trail purposes. The contractor shall make appropriate adjustments in HIGLAS or its
internal systems, for contractors not utilizing HIGLAS, to reflect the refund activity.
70.15 - Financial Reporting for Debt Referred
(Rev. 77, Issued: 09-16-05, Effective: 10-17-05, Implementation: 10-17-05)
70.15.1 - Financial Reporting for Non-MSP Debt (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The contractor not utilizing HIGLAS shall continue to report the debt at their location for financial
reporting purposes. Debt referred to Treasury for cross servicing shall not be transferred out on the Form
CMS 751 (Status of Accounts Receivable). See Chapter 5 for Financial Reporting instructions.
The contractor not utilizing HIGLAS shall continue to accrue and report interest in its internal systems on
a debt after the debt has been referred for cross servicing.
Contractors shall follow the instructions outlined in Chapter 5, Section 270. The contractors shall report
and post all activities related to these debts according to CMS guidelines and instructions.
70.15.2 - Reserved for Future Use
70.15.3 - Financial Reporting for Collections Received on Debts from Cross Servicing
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Contractors shall follow the instructions outlined in Chapter 5, Section 270. The contractor shall report
and post all activities related to these debts according to CMS guidelines and instructions.
Collections posted to the debts listed on the CMSDM Treasury Collection Report shall be reported in
Section A, Line 4C, Collections Deposited at Other Location, and Section C, Line 4C, Collections
Deposited at Another Location, of Forms CMS H 751. If the debt is in a Currently Not Collectible (CNC)
status, the amounts collected shall be reported in Section A, Line 4A, Re-established as Active A/R, and
Section C, Collections on CNC Debt, of the Forms CMS C 751 and in Section A, Line 6B, Transfers In
From CNC, and Line 4C, Collections Deposited at Other Location on Forms CMS H 751.
The amount of accrued interest that is adjusted in order to equal the amount of interest collected and
posted to the debt shall be reported on Line 5A, Adjusted Amounts, Internal Adjustments, of Forms CMS
H 751 or Line 4E, Other, of Forms CMS C 751, if the debt is in CNC status. Contractors shall separately
track interest adjustment amounts reported on the “Adjusted Amounts” line on Forms CMS H 751 or
reported on the “Other” line on the Forms CMS C 751. The interest adjustment amounts shall be reported
in the “Remarks” section of the Forms CMS 751.
For contractors who have transitioned to the Healthcare Integrated General Ledger Accounting System
(HIGLAS), collections reported and posted to the debts on the CMSDM Treasury Collections Report shall
be reported on the Treasury Report on Receivables and Debt Collection Activities Report (TROR), Part I,
Section A, Line (4)(D), Collections by Treasury through Offset and Cross-Servicing and in Part II,
Section C, Line (1)(G), By Treasury/Designated Debt Collection Center Cross-Servicing. If the debt is in
a Currently Not Collectible (CNC) status, the amounts collected shall be reported in Part I, Section A, on
Line (4) (D), Collections by Treasury Through Offset and Cross-Servicing, and Line (5) (E), Written-Off
Debts Reinstated for Collections and also in Part II, Section C, Line (1) (G), By Treasury/Designated
Debt Collection Center Cross-Servicing.
70.15.4 - Financial Reporting for Debts Returned to Agency (RTA) (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Debts RTA shall be reported in the appropriate line of the CMS Form 751 (contractors not utilizing
HIGLAS) and the Treasury Report of Receivables and Debt Collection Activities (TROR) Reports
(contractors utilizing HIGLAS). Details regarding debts RTA are outlined in Section 70.17 herein.
70.15.4.1 - Debts RTA for Bankruptcy (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Debts RTA for Bankruptcy shall be reported in Bankruptcy status as soon as the contractor has
bankruptcy documentation to support the bankruptcy status.
H751 Reporting
Section B
(4)(B)(1) In Bankruptcy
TROR Reporting
Section B
(1)(D)
70.15.4.2 - RTA and other Debts, Pending Final Disposition (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Debts RTA for the following reasons: uncollectible, out of business, miscellaneous dispute, dispute timer
expired, recall approved, manual RTA, and certain debts that have not been referred to Treasury shall be
reported as follows:
H751Reporting
Section B
4(B)(9) Pending Request Waiver/Compromise – for those debts waiting write off approval.
Section B
(4)(B)(11) Other Exclusions – for those debts not yet eligible for write off due to age or past collections.
Section A
Line 6.A. Amounts Written-Off (Bad Debts) – for those debts approved for Write off Closed.
TROR Reporting
Section B
Line (3)(G) Debt Returned from Cross-Servicing – for those debts not yet eligible for write off due to age or
past collections. The HIGLAS Accounts Receivable status code DR-RTN-CS (Debts Returned from Cross-
Servicing) is mapped to line (3)(G). The receivable balance detail extract can be used to validate the detail of
debts reported to this line.
Part II, Section B, Line (1)(G) – “Other – must footnote” - HIGLAS Accounts Receivable status codes
beginning with “REQ” (request) are mapped to this line. A footnote(s) will be required for all balances
on this line. The footnote(s) should include the dollar amount and number of debts for all debts
containing the “REQ” status codes (i.e. pending ERS request, pending RO WOC approval, etc.)
Section A, Line (6) (B) Written Off and Closed Out – for those debts approved for Write off Closed that
are not in CNC Status. For debts approved for write off closed already in CNC status:
Section D
Line (2) CNC Debts Closed Out During the Current FY
70.15.4.3 - Debts RTA Because Dispute Timer Expired (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Debts to be re-referred to Treasury shall be reported as Referred to Treasury.
H751 Reporting
Section B
4(A) Referred for Cross Servicing OR
Section B
(4)(B)(1)- (11) As appropriate.
TROR Reporting
Section B
Line (3) (J) Debt Referred to Treasury or a Designated Debt Collection Center for Cross-Servicing
– for those debts resubmitted to Treasury. OR
Debts ineligible for referral shall be reported in the appropriate line as an exclusion to debt
referral.
70.15.4.4 - Debts RTA Paid in Full or Satisfied Payment Agreement or Satisfied
Compromise (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Debts in these status codes with other than a zero balance shall be reported as follows until further
instructions are issued:
H751 Reporting
Section B
(4)(B)(11) Other Exclusions.
TROR Reporting
Section B
Line (3)(G) Debt Returned from Cross-Servicing. The HIGLAS Accounts Receivable status code
DR-RTN-CS (Debts Returned from Cross-Servicing) is mapped to line (3)(G). The receivable
balance detail extract can be used to validate the detail of debts reported to this line.
70.16 - Debt Close-Out
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
An agency closes out a debt when it determines that further debt collection actions
are prohibited or the agency does not plan to take any future actions (either active or passive) to try to
collect the debt.
Contractors shall submit the following debts for close-out (termination of collection action).
• Non-MSP provider/supplier debts with a combined principal and interest balance of less than $25.
The HIGLAS Auto Write-Off Program (AWOP) will systematically close-out these particular
debts based on non-excluded transaction types that are 180 days old (from the demand
letter/determination date) with no collections within the last 60 days.
• MSP debt with a combined principal and interest balance of less than $25. The HIGLAS AWOP
will systematically close-out these MSP debts that are at least 120 days old (from the demand
letter/determination date) with no collections within the last 60 days.
• MSP debt where the debtor is deceased. The contractor shall not close-out these debts when the
debtor is deceased and the estate is still open or when the MSP claim arises from a wrongful death,
survival or other cause of action claiming medical damages incurred by the beneficiary where the
settlement, judgment or award is awarded to an individual or entity other than the beneficiary’s
estate. The contractor shall also not terminate collection action or close-out debts that are in
litigation and/or under negotiation by the Office of General Counsel (OGC) or the Department of
Justice (DOJ).
• Non-MSP beneficiary debts with a principal balance less than $50.
• Non-MSP beneficiary debts with principal balance between $50 and $999.99, over 425 days old,
the last payment date is greater than 365 days old, and the contractor has verified there are no
other collections for the same beneficiary.
• Non-MSP beneficiary debts greater than or equal to $1,000, have been referred to the Social
Security Administration (SSA), have no collections, over 425 days old, and the last payment date
is 365 days old.
• Debts greater than six years old that have been returned to agency (RTA) by Treasury and the
contractor has performed the required steps to resolve and/or research the debt to confirm the RTA
status. Debts with a combined principal and interest balance less than $25 do not require any
research. This includes debts that have been returned to agency (RTA’d) with a combined principal and
interest balance less than $25 but later exceeds $25 as a result of accrued interest while awaiting close-
out review.

• Certain debts that have not been referred to Treasury (non-RTA) for various reasons such as
bankruptcy or litigation. The contractor shall submit the justification and supporting
documentation, including OGC correspondence for such debt close-outs.
• Debts, of any amount, regardless of age that cannot be validated, should be recommended for
termination of collection action and close-out. For example, when debts are received as a result of
a contractor transition where no electronic or paper records are available, and other debts where no
records are available to support the balances. The contractor shall make a concerted effort to
validate the debts before selecting this option. A listing of this debt shall be forwarded to the
Office of Financial Management/Financial Services Group/Division of Financials Services and
Debt Management (OFM/FSG/DFSDM) Director for approval. The list should contain the reason
for termination of collection action and close-out recommendation that provides reasonable
evidence to substantiate that the claim is no longer available.
Delegations of Authority for Closing-Out Debts Less Than $25
• CMS has authority to terminate collection action and close-out debts that have a combined principal
and interest balance less than $25.
• The contractor not utilizing HIGLAS shall recommend termination of collection activity of debts, once
the debt is 180 days old (that is, 150 days delinquent) with no collection activity within the past 60 days.
Delegations of Authority for Closing-Out Debt That Was Not Eligible for Referral to Treasury (Non-
RTA) and Non-Uncollectible (RU)/Out of Business (RN) RTA Debt
This delegation of authority only applies to debts not eligible for Treasury referral, such as, bankrupt
issuers/health plans/contributing entities or issuer/health plan/contributing entity debts and debts returned to
agency (RTA) with a code other than RU/RN (non-RU/RN).
• Debts with amounts $100,000 or less (exclusive of interest) may be approved for termination of
collection activity and close-out by CMS.
• Debts with amounts in excess of $100,000 (exclusive of interest) must be referred to the CMS with
the Office of General Counsel (OGC) concurrence for the approval process as described by 42 CFR
401.601(c).
Delegations of Authority for Closing-Out Returned to Agency Debt that is RU/RN
• Returned to Agency Debts classified as RU or RN with amounts of $500,000 or less (exclusive of
interest) may be approved by the CMS without OGC’s concurrence.
• Returned to Agency Debts classified as RU or RN greater than 6 years old and in excess of
$500,000 (exclusive of interest) must be referred to the CMS with OGC concurrence for the approval
process as described by 42 CFR 401.601(c).
Fraud Checks

A fraud check must be completed for ALL providers/suppliers who have a valid National Provider
Identifier (NPI) and has debts submitted for close-out. Before any debts can be submitted to the CO or
RO, the contractor shall submit a fraud check request to the Center for Program Integrity (CPI). Fraud
checks shall be performed through CPI’s Unified Case Management (UCM) system for
providers/suppliers that have an NPI.
The contractor shall use the following instructions for requesting fraud check reports.
1. The contractor shall create an Excel spreadsheet listing the NPIs and names of the
providers/suppliers. The NPIs and provider/supplier names shall be obtained from the related debt
close-out spreadsheet. The contractor shall use the naming format FraudChk_Contractor-
Jurisdiction_Reviewer_Period Ending (example – FraudChk_ABC-J2_RO_FY19Q4) when
naming/saving the file(s).
2. The contractor shall email its fraud check request spreadsheet along with a completed CPI data
request form to [email protected] with the subject line
“Contractor/Jurisdiction Fraud Check Request” (example – ABC/J2 Fraud Check Request).
3. The contractor shall expect to receive the fraud check report from CPI within one week of sending
the fraud check request to CPI. The contractor shall use the fraud check report to determine if the
provider/supplier has an open fraud case. Please note the following:
• The NPI is listed in column A (PRVDR_NPI_NUM).
• Column B (UCM_FRAUD_CHECK) will indicate a “Y” if the NPI was found in UCM.
An “N” in column B will indicate that there are no records listed for the NPI. Therefore, all
other fields will be blank.
• If there is a “Y” in column B, proceed to column P (RFRL_OPEN_IND) to determine if
the case is open or closed. If there is a “Y”, the case is open which means that the
provider’s/supplier’s debts are not eligible for close-out. An “N” indicates that the
provider’s/supplier’s fraud case is closed.
• If there are more than one open and/or closed fraud case for a given provider/supplier,
filter column P with the “Ys” only to get only those providers/suppliers with open fraud
cases. If all entries for a given NPI have an “N” in columns B or P, then the debt is eligible
for RO or CO close-out review/approval. However, if one or more of a given
provider/supplier NPI’s entries has a “Y” in column P, the NPI's debts are not eligible to
be submitted for RO or CO close-out review/approval.
The contractor shall include a copy of the fraud check report for the NPIs that are included on the
particular debt close-out spreadsheet that is sent to the CO or RO.
Debt Close-out Request Submission
The contractor shall submit two separate quarterly debt close-out reports utilizing the Debt Close-Out
Request template/spreadsheet. These reports shall be submitted to CMS no later than the first day of the
second month of each quarter (i.e., November 1, February 1, May 1, and August 1). If this day falls on a
weekend or federal holiday, the next business will be the due date. The contractor utilizing HIGLAS shall
only include new debts with a combined principal and interest balance greater than or equal to $25. The
contractor not utilizing HIGLAS shall include all eligible debts. Each debt shall be considered a separate
identifiable debt and shall not be aggregated with other debts. The contractor shall only include
provider/supplier debt that is associated with a valid National Provider Identifier (NPI).
The contractor shall include in the first report, debts that are not eligible for Treasury referral (e.g.,
beneficiary, deceased provider/supplier), referred to as non-Return to Agency (non-RTA) debts, and non-
RU /RN debts (other than bankruptcy debts) with principal balances up to $100,000 and RU/RN debts
with principal balances up to $500,000. The debts listed on this report will be reviewed and approved by
the RO (CMS CO for Medicare Secondary Payer (MSP) debts).
The contractor shall include in the second report, which is for debts that will be reviewed by OGC, non-
RTA and non-RU/RN debts (other than bankruptcy debts) with a principal balance greater than $100,000
and RU/RN debts with a principal balance greater than $500,000, provided that all categories of debts are
greater than 6 years old.
Debts that will be reviewed by OGC shall also include the following documentation:
Part A Debts
1. Notice of Program Reimbursement (NPR) - (cost report debts only)
2. Initial demand letter
3. Final appeal decision letter sent from contractor’s appeals department to overpayments department
(decision only, exhibits not required)
4. Intent to Refer (ITR) letter
5. Most recent Extended Repayment Schedule (ERS) – (if applicable)
6. A report from PECOS and/or copies of 855 Forms showing:
i. date the debtor’s Medicare enrollment ended; or
ii. identifying information on all owners/managing employees/directors; and
iii. whether there are owners/managing employees/directors of the debtor company who are affiliated
with a provider/supplier that is still operating in the Medicare
program. If so, the MAC shall also include identifying information from PECOS about the
company with which he or she is affiliated, including the interest he or she has in that
company.
Part B and MSP Debts
(Not required if the provider/supplier has more than more than ten debts requested to be closed out during
a quarter. But required for all extrapolated overpayments.)
1. Initial demand letter
2. Intent to Refer (ITR) letter
3. Final appeal decision letter sent from contractor’s appeals department to overpayments department
(decision only, exhibits not required)
4. Most recent Extended Repayment Schedule (ERS) – (if applicable)
5. A report from PECOS and/or copies of 855 Forms showing:
i. date the debtor’s Medicare enrollment ended; or
ii. identifying information on all owners/managing employees/directors; and
iii. whether there are owners/managing employees/directors of the debtor company who are
affiliated with a provider/supplier that is still operating in the Medicare
program. If so, the MAC shall also include identifying information from PECOS about the
company with which he or she is affiliated, including the interest he or she has in that
company.
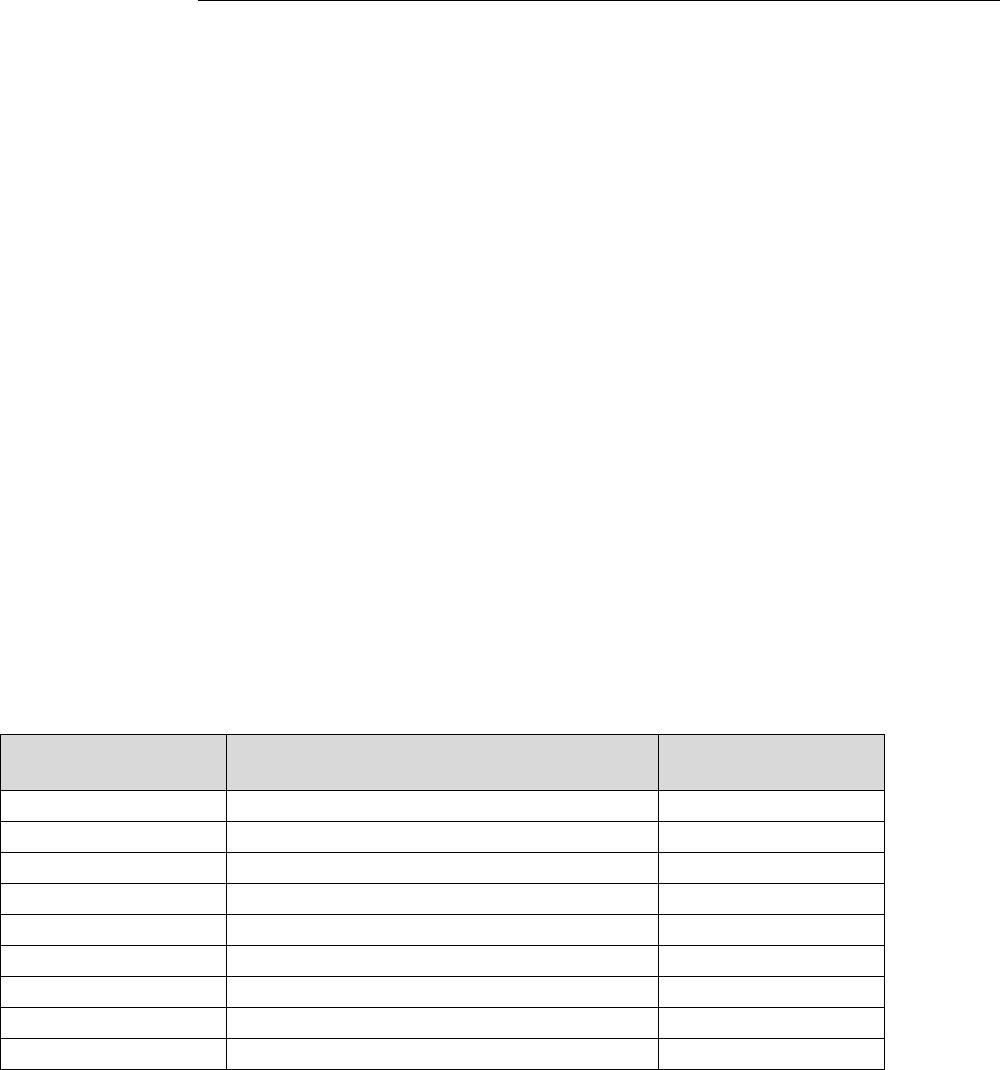
For debts that are submitted to CMS that CMS in turn may forward to OGC with CMS’s
recommendation, the contractor shall provide a separate debt close-out report and certification statement
signed by its Chief Financial Officer in accordance with Financial Management Manual, Ch. 4, § 70.17.2
for the debts serviced by a particular OGC Regional Office (RO). The certification statement must state
that it covers the listed debts and then list: (1) the number of debts; (2) the total principal balance of the
debts; and (3) total interest balance of the debts. The MAC shall use the provider’s/supplier’s address to
determine the OGC RO. Below is the list of the OGC ROs and the states that each RO services. The list
can also be found at https://www.hhs.gov/about/agencies/ogc/key-personnel/regional-offices/index.html.
• Region I (Boston) - Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont
• Region II (New York) - New Jersey, New York, Puerto Rico, Virgin Islands
• Region III (Philadelphia) - Delaware, District of Columbia, Maryland, Pennsylvania, Virginia,
West Virginia
• Region IV (Atlanta) - Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South
Carolina, Tennessee
• Region V (Chicago) - Illinois, Indiana, Michigan, Minnesota, Ohio, Wisconsin
• Region VI (Dallas) - Arkansas, Louisiana, New Mexico, Oklahoma, Texas
• Region VII (Kansas City) - Iowa, Kansas, Missouri, Nebraska
• Region VIII (Denver) - Colorado, Montana, North Dakota, South Dakota, Utah, Wyoming
• Region IX (San Francisco) - American Samoa, Arizona, California, Guam, Hawaii, Nevada
• Region X (Seattle) - Alaska, Idaho, Oregon, Washington
CMS shall respond within 30 days after receipt of the close-out request, except for cases exceeding the
CMS’ delegated authority. For those cases exceeding the CMS authority, the CMS shall forward the case
to the Office of General Counsel (OGC) with the CMS’ recommendation, within 30 days of receipt of the
contractor’s request.
70.17 - Debts Returned to Agency (RTA) by the United States Department of the
Treasury (Treasury) (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The Treasury returns to agency (RTA) debts to the Centers for Medicare & Medicaid Services (CMS)
using the following reasons:
RTA Debt Status
Code
Federal Debt Return Description
(FDRETDSC)
HIGLAS AR Status
Code
RB
In Bankruptcy
RTA-RB
RC
Small Balance
RTA-RC
RC
Account Settled/Compromise
RTA-RC
RC
Satisfied Compromise
RTA-RC
RD
Congressional Dispute
RTA-RD
RD
Debt Amount Incorrect
RTA-RD
RD
Other
RTA-RD
RD
Manual RTA
RTA-RD
RD
Proof of Debt Validated
RTA-RD

RD
Recalled
RTA-RD
RD
Miscellaneous Dispute
RTA-RD
RD
VDPP - Previously Paid
RTA-RD
RD
Complaint
RTA-RD
RD
Wrong Debtor
RTA-RD
RD
Disability/Inability to Pay
RTA-RD
RD
Recall Approved
RTA-RD
RN
Entity Out of Business
RTA-RN
RP
Satisfied Payment Agreement
RTA-RP
RP
Previously Paid
RTA-RP
RP
Paid in Full
RTA-RP
RP
Previously Resolved
RTA-RP
RU
Uncollectible
RTA-RU
RU
Debtor Death
RTA-RU
RU
Inability to Pay
RTA-RU
RX
Claim Not Substantiated
RTA-RX
RX
No Disposition Desc Found
RTA-RX
HIGLAS shall systematically update an RTA debt's AR status code with the appropriate temporary
HIGLAS AR RTA Status Code. The contractor shall use the appropriate HIGLAS responsibility to
generate the weekly RTA report.
The contractor not utilizing HIGLAS shall also download the report, add a column, and indicate what
status the debt was updated to and post in a secure drive where CMS can access the updated
spreadsheet. The contractor shall also add any applicable comments to the spreadsheet.
70.17.1 - Debts RTA by Treasury due to Bankruptcy (RB)
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
Debts in bankruptcy status are ineligible for cross-servicing. The contractors are responsible for obtaining
bankruptcy documentation to support the bankruptcy status code listed on the RTA report. Once the
contractors obtain the documentation, they shall update HIGLAS or their internal records to reflect the
appropriate code for bankruptcy. The contractors shall follow established procedures regarding debts in
bankruptcy status. The contractors shall properly report the status of these debts in their quarterly
financial reports to CMS CO. (See Pub. 100-06, chapter 3, section 140.)
The Treasury no longer routinely sends bankruptcy documents to creditor agencies. Therefore, contractors
shall follow established procedures, including contacting the CMS Regional Office (RO), to obtain
bankruptcy documentation. It is the contractor’s responsibility to obtain the bankruptcy documentation. If
the contractors cannot obtain bankruptcy documentation through established procedures, including asking
the RO for assistance, the contractors may contact Treasury to obtain documentation for RTA debts in
bankruptcy. If the contractors are unable to obtain bankruptcy documentation through established
procedures or through the assistance of the RO, they shall request bankruptcy documentation from
Treasury via email to [email protected]. The subject line of the email request
shall be entitled, “Request for Bankruptcy Information”. If the contractors do not receive a confirmation
from Treasury within 2 business days of the request, the contractor shall re-send the email or make
another request to Treasury via fax number 205-912-6353. The contractors shall include the following
information; the Cross-Servicing Next Generation (CSNG) number, debtor name and the contractor’s
contact information on each request via email or fax.
If the CMS Regional Office of General Counsel (OGC) advises the contractor that debts are not
discharged in bankruptcy and are still eligible for referral, the contractor shall submit a new referral to
Treasury.
70.17.2 - Debts RTA by Treasury as Uncollectible (RU) or Out of Business (RN)
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The temporary HIGLAS RTA Status Code for all debts that are returned to agency as Uncollectible (RU)
or Out of Business (RN) shall be systematically updated, by HIGLAS, to ‘DR-RTN-CS’ (Debt Returned
from Cross-Servicing).
For RU and RN debts with a combined principal and interest balance less than $25:
• Contractors utilizing HIGLAS shall allow the HIGLAS Auto Write-Off Program to identify these
debts and systematically write them off.
• Contractors not utilizing HIGLAS shall submit for close-out review.
The contractors shall use the RTA report to research the RU or RN debts with a combined principal and
interest balance greater than or equal to $25 in order to determine the current status or final disposition.
The debts already in a recalled status are included so that the contractors will know that Treasury
considers the debts uncollectible or out of business.
The contractors shall determine whether collection by litigation is a viable option for debts with a
combined principal and interest balance greater than or equal to $25 showing a status code of RU or RN.
If so, follow established procedures for referring the debts for litigation (See CMS Pub. 100-06, chapter 3,
section 120).
The contractors shall also consider whether all other appropriate actions to collect debts with a combined
principal and interest balance greater than or equal to $25 have been taken before recommending debts for
Write-Off Closed (WOC), including the criteria listed below:
1. Have there been any collections or payments on this debt in the last year? If so, and the contractor
believes further collections are possible, the contractor shall not recommend the debt for WOC,
but shall continue collection efforts for MSP and Non-MSP debts.
2. Has the debtor submitted any Medicare claims in the last 6 months? If so, and the contractor
believes further collections are possible, the contractor shall not recommend the debt for WOC,
but shall continue collections efforts.
3. Is the debtor receiving Medicaid funds? If so, the contractor shall not recommend the debt for
WOC. The contractor shall instead contact the CMS RO to institute an offset, and shall continue
collection efforts.
4. If applicable, did the debtor undergo a Change of Ownership (CHOW) (a new owner who opts to
receive automatic assignment of the old owner’s provider/supplier agreement)?
If so, the contractor shall determine if collection efforts were pursued from the new owner.
(a) If so, the contractor shall recommend for WOC
(b) If not, the contractor shall follow the normal policies and procedures for debts collection.
5. If applicable, did the debtor file any cost reports that the contractor has not yet settled?
If so, the contractor shall not recommend the debt for WOC. Instead, the contractor shall await
settlement of the cost report to determine whether it results in an underpayment. If it does result in
an underpayment, the contractor shall apply any funds due to the provider/supplier to any
outstanding debts first, before releasing any funds to the debtor
6. If applicable, does the debtor have any outstanding unfiled cost reports less than 1 year overdue?
If so, the contractor shall not recommend the debt for WOC. Instead, the contractor shall await
filing and settlement of the cost report to determine whether it results in an underpayment. If it
does result in an underpayment, the contractor shall apply any funds due to outstanding debts first,
before releasing any funds.
7. If applicable, does the debtor have any funds in suspense due to an unfiled cost report? If so, and
the provider/supplier has been terminated from the Medicare Program, the contractor shall apply
the funds in suspense to recover the debt or any other outstanding debts for the provider/supplier.
8. If applicable, does the debtor have any claims or cost reports subject to re-opening?
If so, the contractor shall not recommend the debt for WOC. Instead, the contractor shall wait
until the expiration of the reopening period. If a cost report reopening during this period results in
an underpayment, the contractor shall apply the underpayment to recover the debt or any other
outstanding debts for the debtor, before releasing any funds.
9. Does the debtor have any open appeal(s)? If so, the contractor shall not recommend the debt for
WOC. Instead, the contractor shall await the final determination on the appeal(s), and apply any
funds due from a favorable decision to any outstanding debts first, before releasing any funds.
10. Does the debtor have an active fraud case? If so, the contractor shall not recommend the debt for
WOC. Instead, the contractor shall forward the debt to the appropriate Unified Program Integrity
Contractor (UPIC) or CMS Centers for Program Integrity that has the open fraud case.

If the contractors have considered all of the above criteria above and are recommending the debts for
WOC, the contractors shall submit a request to the CMS RO for approval. The contractor shall submit
these debts as instructed in Chapter 4, § 70.16. The contractor shall include the Contractor Validation
Statement below with each close-out request submission:
Contractor Validation:
We recommend these debts for termination of collection action, close out and write-off-closed.
We considered all criteria in section 70.17.2 in making this recommendation and determined that
these criteria for referral have all been met.
Total debts recommend for Write-Off-Closed:
Number of Debts: _____ Principal Balance: ____________ Interest Balance: ____________
Signature of Medicare Contractor CFO: ________________________
Date: _______________
The debts recommended for WOC that do not meet the above criteria shall remain open until the criteria
for WOC has been met. The contractors shall report these debts on the appropriate line of the CMS
Forms 751 or the Treasury Report on Receivables (TROR) to indicate Treasury has RTA the debts but the
WOC process has not been completed. (See CMS Pub 100-06, chapter 4, section 70.15.4) For all debts
that meet the criteria above, the contractor utilizing HIGLAS shall change the status to the appropriate
Request for Write-Off status code. The contractors shall submit a report of the debts recommended for
WOC to the CMS using established procedures for recommending debts for WOC.
Once CMS approves the debts for WOC, the contractors shall complete the WOC process including
changing the status to the appropriate Write-Off/Approved/Closed status code, making the appropriate
adjustments in HIGLAS or internal system, and making all appropriate adjustments on CMS Form 751 or
the TROR.
70.17.3 - Debts RTA by Treasury as Dispute Response not Received Timely (RX)
(Rev. 11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The Treasury returns debts with this status code because the dispute response was not received timely.
The contractor shall research and resolve the debts in a RX status that have a combined principal and
interest balance greater than or equal to $25 within 30 business days in order to determine the current
status of the debts. No further action is necessary if the debts are already in a recalled status. The
contractors shall add a comment on the HIGLAS comment screen reflecting any action taken, the date of
the RTA report in which the debts appear on and the financial statement reporting quarter in which the
debts were resolved.
RX debts that have a combined principal and interest balance of less than $25
• Contractor Utilizing HIGLAS shall allow HIGLAS to systematically change the status code
to‘DR-RTN-CS’(Debt Returned from Cross-Servicing) which will allow the debt to be identified
and written off by the HIGLAS Auto Write-Off Program.
• Contractors NOT Utilizing HIGLAS shall submit these debts for close-out.
If the debts are still valid and eligible for referral to Treasury, the contractors shall re-refer the debts to
Treasury, even if a response to the disputes were previously submitted to Treasury. The contractors shall
not issue a second Intent to Refer (ITR) letter.
70.17.4 - Debts RTA by Treasury as a Miscellaneous Dispute, a Manual RTA,
Complaint or as Recall Approved (RD) (Rev.
11787; Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
The contractor shall research and resolve debts in a RD RTA status code greater than or equal to $25 and
within 30 calendar days update HIGLAS or its internal system with the final disposition of the debts. If
any debts are still valid and eligible for referral to Treasury, the contractors shall change the status code of
the debts from RD to R-DCS (Debt Resubmitted to Cross-Servicing) to be resubmitted to Treasury. The
contractors shall not issue a second Intent to Refer (ITR) letter for the debts.
RD debts that have a combined principal and interest balance of less than $25
• Contractor Utilizing HIGLAS shall allow HIGLAS to systematically change the status code to
‘DR-RTN-CS’ (Debt Returned from Cross-Servicing) which will allow the debt to be identified
and written off by the HIGLAS Auto Write-Off Program.
• Contractors NOT Utilizing HIGLAS shall submit these debts for close-out.
70.17.5 - Debts RTA by Treasury as Paid in Full (RP), Satisfied Payment Agreement
(RP) or Satisfied Compromise (RC) (Rev. 11787;
Issued:01-19-23; Effective: 04-21-23; Implementation:04-21-23)
• If a debt is returned to agency (RTA) as paid in full (RP), satisfied payment agreement (RP), or
compromise (RC) and a principal balance less than $100 remains after the receipt has been
applied, contractors not utilizing HIGLAS shall adjust down the remaining balance. HIGLAS
shall systematically adjust down these balances to $0.00 for contractors utilizing HIGLAS.
• If a debt is returned to agency (RTA) as paid in full (RP) or satisfied payment agreement (RP),
and a principal balance greater than or equal to $100 remains after the receipt has been applied,
the contractor shall research all activity on the debt to determine if the receipts were
appropriately applied and take any action, if needed. If all receipts were applied appropriately,
the contractor shall then adjust down the remaining balance to $0.00.
• If a debt is returned to agency (RTA) as satisfied compromise (RC) the contractor shall research
all activity on the debt to determine if the receipts were appropriately applied and take any
action, if needed. The contractor shall adjust down the balance to $0.00 using the appropriate
adjustment/write-off code.
If it is determined a refund is valid, the contractors shall follow procedures for applying excess collections
and update HIGLAS or their internal systems to reflect any refund given (see CMS Pub. 100-06, chapter
4, section 70.14.8).

Exhibit 1- Intent to Refer (ITR) Letter
(Rev. 294, Issued: 10-06-17, Effective: 07-03-17, Implementation: 07-03-17)
Intent to Refer Letter
Background
The DCIA requires Federal agencies to refer debt that is 120 days delinquent to the Department of
Treasury or a Treasury designated Debt Collection Center for cross servicing.
Prior to debt transfer, the DCIA requires agencies to inform the debtor of the agency’s intent to refer the
debt, and to provide debtor information regarding the referral process.
Attached are specific paragraphs that explain the process and debtor rights. These paragraphs shall be
included in the intent to refer letter sent to the debtor.
Medicare contractors should use their own language in the opening paragraphs to explain the reason for
the overpayment and the current balance, including interest accrued and the interest rate.
Subject in Bold: Notice of Intent to Refer Debt to the Department of Treasury’s Debt Collection
Center for Cross Servicing and Offset of Federal Payments and Certain Eligible State Payments
Contractor opening paragraphs concerning the reason for the overpayment, date of determination and
amount due. May refer to previous demand letters or other forms of contact regarding the debt.
Your debt to the Medicare Program is delinquent and, by this letter, we are providing notice that your
debt will be referred to the Department of Treasury’s Debt Collection Center (DCC) for Cross Servicing
and Offset of Federal Payments. Your debt will be referred under provisions of Federal law, title 31 of the
United States Code, Section 3720A and the authority of the Debt Collection Improvement Act of 1996.
The Debt Collection Improvement Act of 1996 (DCIA) requires Federal agencies to refer delinquent
debts to the Department of Treasury and/or a designated Debt Collection Center (DCC) for collection
through cross servicing and/or the Treasury Offset Program. Under the offset program, delinquent Federal
debts are collected through offset of other Federal agency payments you may be entitled to, including the
offset of your income tax return through the Internal Revenue Service (IRS). The TOP offsets can also be
taken from eligible state payments to which you are entitled.
The Debt Collection Center will use various tools to collect the debt, including offset, demand letters,
phone calls, referral to a private collection agency and referral to the Department of Justice for litigation.
Other collection tools available, which may be used, include Federal salary offset and administrative
wage garnishment. If the debt is discharged, it may be reported to the IRS as potential taxable income.
During the collection process, interest will continue to accrue on the debt and you will remain legally
responsible for any amount not satisfied through the collection efforts.
For Individual Debtors Filing a Joint Federal Income Tax Return

The Treasury Offset Program automatically refers debts to the IRS for offset. Your Federal income tax
refund is subject to offset under this program. If you file a joint income tax return, you should contact the
IRS before filing your tax return to determine the steps to be taken to protect the share of the refund
which may be payable to the non-debtor spouse.
Federal Salary Offset
If the facility ownership is either a sole proprietorship or partnership, your individual salary(s) may be
offset if you are or become a federal employee.
Medicaid Offset
As authorized at 42 CFR 447.30, (Subsection 1885 of the Social Security Act), CMS may instruct the
State Medicaid Agency to offset the Federal share of any Medicaid payment due you, your agency and/or
related facilities. At that time, the offset will remain in effect until the Medicare overpayment is paid in
full.
Please read the following instructions carefully to determine what action you may take to avoid referral
for cross servicing/offset.
Due Process
You have the right to request an opportunity to inspect and copy records relating to the debt. This request
must be submitted in writing to the address listed below. You have a right to present evidence that all or
part of your debt is not past due or legally enforceable. In order to exercise this right, this office must
receive a copy of the evidence to support your position, along with a copy of this letter. You must submit
any evidence that the debt is not owed or legally enforceable within 60 days of the date of this letter. If,
after sixty days from the date of this letter, we have not received such evidence, your debt, if it is still
outstanding and eligible for referral, will be referred to the Department of Treasury or its designated Debt
Collection Center for cross servicing/offset.
Repayment
Your debt will not be referred to the Department of Treasury if you make payment in full. The past due
amount of $____________owed to the Medicare Program as of _____________ includes interest accrued
through _____________. (Note: Medicare contractors may alter this sentence to read: The past due
amount owed to the Medicare Program as of the date of this letter includes current accrued
interest. This sentence may be omitted for debts that do not accrue interest.) Interest is accrued
monthly and is added to the balance of the debt.
Your check or money order for the amount due should be made payable to:
Medicare
Contractor Address
000 Street
Anywhere, USA 00000-0000.
Include a copy of this letter with your payment.

If you cannot make payment in full, you may be allowed to enter into an extended repayment agreement.
If you are interested in an extended repayment agreement, please contact this office.
Bankruptcy
If you have filed for bankruptcy and an automatic stay is in effect, you are not subject to offset while the
automatic stay is in effect. Documentation supporting your bankruptcy status, along with a copy of this
notice, must be forwarded to this office at the above address.
If you have any questions concerning this debt, please contact ________________
at ________________.
Sincerely,
____________________
Signature of Certifying Official
Official Position
Exhibit 5
(Rev. 315, Issued: 05-17-19, Effective: 06-18- 19, Implementation: 06-18-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare
identification number. For purposes of this manual, Medicare beneficiary identifier references both the
Health Insurance Claim Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new
Medicare card transition period and after for certain business areas that will continue to use the HICN as
part of their processes.
Treasury Cross-Servicing Dispute Resolution
DMS Request Date: Total Number of Pages: _____
SBU
FedDebt Case ID.: Principal Amt: $
Creditor Agency Debt ID: PCA Code:
Debtor:
Program: For CMS Use Only:
Creditor Agency Contact Name: Medicare beneficiary identifier:
Creditor Agency Contact Phone: Beneficiary Name:
Creditor Agency Facsimile:
Dispute Number:
Dispute request reason: Miscellaneous Dispute
Additional comments:

If you have any questions regarding the dispute, please call Valencia Thompson at 205-912-6327.
Creditor Agency must return response to Bosch Stanley via facsimile 205-912-6374 with 60 days of
request date.
Creditor Agency (CA) Dispute Resolution Section:
Please indicate a response by checking one of the following reasons: Please attach supporting
documentation.
DAIC ___ CA agrees. Debt amount is incorrect. Requires financial adjustment.
DACC ___ CA disagrees. Debt amount is correct. Continue collection efforts.
MDAA ___ CA agrees. Miscellaneous dispute, stop collection activity.
MDFF ___ CA agrees. Miscellaneous dispute. Requires financial adjustment, continue
collection efforts.
MDDD ___ CA disagrees. Miscellaneous dispute. Continue collection efforts.
VDWD ___ CA agrees. Wrong debtor, stop collection activity.
VDRD ___ CA disagrees. This is not the wrong debtor, continue collection efforts.
VDPP ___ CA agrees. Previously paid, stop collection activity.
VDNP ___ CA disagrees. Not previously paid, continue collection efforts.
VDPR ___ CA agrees. Previously resolved, stop collection activity.
VDNR ___ CA disagrees. Not previously resolved, continue collection efforts.
Financial Adjustment Information (To Be Completed By Creditor Agency):
Principal Amount $_______________
Interest Amount $_______________
Penalty Amount $_______________
Admin Cost Amount $_______________
Total Balance Owed $_______________
Please check one of the following:
□ Adjustment reflects the total balance currently owed by the debtor, and has been made by our
Agency.
□ Adjustment has not been made in FedDebt by the Agency, and should be made by DMS.
Creditor Agency Response Date: __________ Creditor Agency Response Contact:
__________________
Additional Comments By Creditor Agency:
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
________________________________________________________________________________________________
80 – Recovery of Non MSP Overpayments from the Beneficiary
(Rev. 235, Issued: 05-14-14, Effective: 07-07-14, Implementation: 07-07-14)
80.1 – Reserved for Future Use
(Rev. 235, Issued: 05-14-14, Effective: 07-07-14, Implementation: 07-07-14)
80.2 – Immediate Recoupment Requirements for NON-935 Overpayment Recovery
from the Physicians and Other Suppliers
(Rev. 205; Issued: 02-09-12, Effective: 07-01-12, Implementation: 07-02-12)
Medicare contractors shall offer providers the opportunity to request immediate recoupment.
Providers can elect this process to avoid making payment by check and/or avoid the assessment of interest
if the immediate recoupment pays the debt in full before day 31. If providers request an immediate
recoupment they must understand that it is considered a voluntary repayment.
A. Medicare contractors shall offer two options.
• A one-time request on the specific overpayment and all future overpayments. Or
• A request on the specific overpayment addressed in demand letter.
B. Medicare contractors shall incorporate the following minimum information related to “immediate
recoupment” information on its website:
• This option is for demanded debts only.
• The request must be in writing, and may be submitted using regular mail, facsimile,
or email.
• The request must include the following:
1. Provider Name and contact number
2. Provider’s Medicare Number and/or the National Provider Identification (NPI)
3. Provider’s or the CFO’s signature
4. Letter number
5. Which option the provider is requesting
C. Medicare contractors shall post to the website the language in the demand letter related to the
immediate recoupment option.
D. Medicare contractors shall consider all written requests for an immediate recoupment as a
payment arrangement that constitutes a voluntary payment.
E. Medicare contractors shall inform providers that going through the immediate recoupment process
is considered voluntary payments. Refer to chapter 3 section 200 for overpayments subject to 935.
F. Medicare contractors demand letter and website shall explain, when there is a remaining
principal balance after the initial immediate recoupment you shall continue recoupment and other
collection activities.
G. Medicare contractors’ website shall include instructions for providers currently in an immediate
(offset) arrangement to submit a new request to continue the immediate recoupment process.
H. Medicare contractors shall allow previous immediate offset agreements to continue when
requested awaiting the submission of the new request.
I. Medicare contractors shall update each AR associated to the request within 10 business days
from the mailroom stamped receipt date. Refer to Chapter 4 §90.2.
J. As applicable, Medicare contractors shall use the new functionality in HIGLAS which allows user
to set the flag to immediate recoupment for multiple ARs instead of one AR.
K. Medicare contractors shall update individual or multiple AR’s in the shared systems when a
provider requests the immediate recoupment option.
L. Medicare contractors shall accept a written request to discontinue participation in the immediate
recoupment process at anytime.
M. Medicare contractor shall discontinue the recoupment process per providers’ written request.
• You shall stop this process within 10 business days from the mailroom stamped receipt
date.
80.3 – Overpayment Recovery from Suppliers of Durable Medical Equipment,
Prosthetics, Orthotics, and Supplies (DMEPOS)
(Rev. 208, Issued: 04-20-12, Effective: 05-20-12, Implementation: 05-20-12)
Certain DMEPOS suppliers are required to have surety bonds. Medicare contractors shall follow
instructions in Pub.100-08, chapter 15, §15.21.7.1, related to collecting claims against surety bonds, if
applicable, in addition to normal debt collection activities.
90 – Physician/Supplier Overpayment Demand Letters - Carrier
(Rev. 29, 01-02-04)
When a carrier determines an overpayment for a Part B service the carrier issues a demand letter to the
physician, supplier or beneficiary.
90.1 – Part B Overpayment Demand Letters to Beneficiaries
(Rev. 29, 01-02-04)
See chapter 3, §§100 and110ff
90.2 - Part B NON-935 Overpayment Demand Letters to Physicians/Suppliers
(Rev. 205; Issued: 02-09-12, Effective: 07-01-12, Implementation: 07-02-12)
When a physician/supplier is liable for an overpayment of $10 or more, the carrier shall attempt recovery
through the following procedures. It shall recover an overpayment made to a physician/supplier as an
individual or to a professional corporation (following the procedures described below) only from the party
to whom the overpayment was made. It shall make no attempt to recover an overpayment made to an
individual physician/supplier from a professional corporation with which they may be associated as an
employee or stockholder. Conversely, it shall not attempt recovery from an individual physician/supplier
where the overpayment was made to a professional corporation with which they are, or were, associated.
A. Overpayment Amount Is At Least $10
When the carrier determines an overpayment it shall issue a demand letter that requests the
physician/supplier to pay the debt in full within 30 days, or the amount owed and any assessed interest
will be collected by offset.
B. Overpayment Demand Letter
The purpose of an overpayment demand letter is to notify the physician/supplier of the existence and
amount of an overpayment, and to request repayment. The demand letter shall be written in such a manner
as to fully explain the nature of the overpayment and the amount determined. Each demand letter shall be:
• Sent to the physician/supplier by first class mail; and
• Determined within forty-five (45) calendar days of the discovery of the overpayment and mailed
within seven (7) calendar days of the creation of the accounts receivable and generation of the
demand letter. Longer amounts of time in between discovery and determination must be
supported by additional documentation. In the case of the second request, the letter must be mailed
within 45 days but no earlier than 30 days after the date of the first demand letter.
A. Content of Demand Letters
• Sent to the physician/supplier.
• For a first request, mail within seven (7) calendar days of determination of the overpayment.
• Each demand letter is an explanation of the nature of the overpayment, how it was established, in
addition, the amount determined.
• The Medicare contractor shall include the model immediate recoupment process language within
the content of the Part B non-935 overpayment demand letters to physicians and other suppliers
for the Part B Non-MSP overpayment demand letters.
• The demand letter shall offer the physician and other supplier the opportunity to request an
immediate recoupment. Refer to section 80.2.
• The demand letter shall offer the physician/supplier the opportunity to apply for an extended
repayment plan if immediate repayment of the debt will cause financial hardship. An extended
repayment plan must be approved using the criteria set forth in Chapter 4, §50. Any approved
repayment plan would run from the date of the FIRST REQUEST overpayment demand letter.
• The demand letter constitutes a request to the physician/supplier to refund the overpaid amount.
• The demand letter informs physicians/suppliers that the carrier will recover the overpayment
through the recoupment of current payments due or from future claims submitted unless the carrier
receives repayment or the physician/supplier provides a statement within 15 days of the date of the
letter of why this action should not take place. The demand letter shall also inform
physicians/suppliers that this recoupment will begin on the 41st day from the date of the letter.
• The demand letter informs physicians/suppliers that interest will accrue on the overpayment if
payment in full is not received by the 31st day from the date of the letter. The demand letter shall
also inform physicians/suppliers of the applicable interest rate that will accrue if payment in full is
not received by the 31st day from the date of the letter.
• The demand letter informs physicians/suppliers that they have the right to request a review or
hearing, as appropriate, if they believe the determination is not correct. (See Medicare Claims
Processing, Chapter 29, Appeals of Claims Decisions.) A review is available for disputed
overpayments of any amount, and a carrier fair hearing is available once the review has been
conducted if the amount in dispute is at least $100.
• Bankrupt providers. All correspondence, including demand letters, addressed to a bankrupt
provider must be submitted to the Regional Office who has the lead in the bankruptcy proceedings
for approval prior to release.
The Medicare contractor shall refer to Exhibits I through VI for the standard formats for each demand and
voluntary refund letters to be used in various overpayment situations.
B. Recovery by Recoupment
If, within 15 days of the date of the initial demand letter, the physician/supplier submits a statement
(rebuttal) and/or evidence as to why recoupment should not be effectuated, the carrier shall promptly
evaluate the material. This is different from a request for appeal (see subparagraph F) in that you are
deciding only whether there is a basis to not effectuate recoupment. Any correspondence dealing with the
basis of the overpayment does not affect your decision concerning recoupment. If the carrier determines
that recoupment shall begin, it shall notify the physician/supplier in writing of its determination. It shall
give specific reasons for its decision.
If no such statement (rebuttal) is received or an extended repayment schedule has not been requested, the
contractor shall initiate recovery by recoupment 40 days after the date of the initial demand letter (day
41), unless the physician/supplier refunds the overpaid amount in full. The contractor shall apply any
amounts payable to the physician/supplier by reason of assignment on behalf of any beneficiary to recoup
the overpayment. It shall apply any amount recouped first to the accrued interest and then to the principal.
If it is not possible to make an immediate recoupment, the contractor shall annotate the physician's
account so that the overpayment can be recouped from future Medicare benefits payable. When
recoupment is used, the contractor sends the regular Medicare Summary Notice (MSN) to the beneficiary.
However, it includes with the physician's/supplier's MSN an explanation that the benefits (or a specified
amount of the benefit) are being applied to the overpayment and that the physician may not request the
beneficiary to pay the amount applied to the overpayment.
The contractor shall discontinue recoupment only when the overpayment, plus all accrued interest, is
recovered, it is determined on appeal that the physician/supplier was not overpaid or an acceptable
extended repayment plan request is received (See Chapter 4, §50). After a favorable appeal decision, the
contractor shall refund any excess amount withheld through recoupment. Also, it shall refund any interest
that was collected.
C. Follow-up Request
If the initial demand letter for an overpayment of $10 or more brings no response within 30 days, the
carrier shall send a follow-up letter (enclose a copy of the initial letter to the physician/supplier) within 45
days. If any portion of the overpayment has been recovered, it shall include a statement of that amount.
D. Physician Appeals Within 30 Days of Notification of the Intent to Recoup
If, within 30 days after the date of the initial demand letter informing the physician/supplier of the
intention to recoup, the physician/supplier submits a request for a review or hearing or otherwise protests
the recovery, the carrier shall make every effort to conclude the appeal procedure expediently. However,
it shall begin recoupment 40 days after the initial demand, if payment has not been made, regardless of
the status of any appeal request. (See subparagraph D.)
E. Demand Letter to Physician Returned as Undeliverable
Where a refund letter is returned as undeliverable, the carrier shall attempt to locate the physician/supplier
using such sources as telephone directories, city directories, postmasters, driver's license records,
automobile title records, State and local medical societies, the American Medical Association or its own
Medicare beneficiary records. (See Chapter 4, §80.)
F. Direct Contact with Physician
If attempted recoupment of the overpayment is unsuccessful for 30 days, the carrier shall contact the
physician/supplier by telephone. (See Chapter 4, §80.) Third Demand Letter
If the overpayment has not been recouped and the debt is eligible for referral to the Department of
Treasury an intent to refer letter shall be sent once the overpayment becomes 90 days delinquent. (See CR
1683 or Chapter 4, §70)
EXHIBIT 1- SAMPLE DEMAND LETTERS
Exhibits I through VI include: the initial demand letter with optional opening paragraphs and the follow-
up letter. It also includes a limited set of optional paragraphs to be used in specific situations, e.g.,
medical necessity denials, and installment payments. The carrier shall follow these formats, with the
optional paragraphs, when preparing demand letters.
This section also includes standard letters to be used when the physician/supplier voluntarily submits a
check to the carrier. These letters are optional if the carrier uses the remittance advice to inform
physicians/suppliers of receipt of their refund checks.
EXHIBIT 1 - INITIAL Non-935 DEMAND LETTER TO PHYSICIANS/SUPPLIERS
Dr. Joe Smith
Anywhere St
Anytown, State ZIP Code
Date
Dear Dr. Smith:
Contractors should use the appropriate paragraph:
"This is to let you know that you have received Medicare payment in error which has resulted in an
overpayment to you of $______ for services dated _____ . The following explains how this happened."
or
"We appreciate your recent inquiry regarding Medicare payment that you believe was paid to you in error.
We thank you for bringing this overpayment to our attention."
or
"We have received your check in the amount of $_____. We thank you for bringing this overpayment to
our attention. While we appreciate you submitting payment to us, our review found that the overpaid
amount was $________. Please remit the additional $______."
How this overpayment was determined: NOTE: This paragraph should include a clear explanation of
how the overpayment arose, the amount of the overpayment, how the overpayment was calculated, and
why the original payment was not correct.
Why you are responsible:
NOTE: For medical necessity determinations, the carrier shall insert appropriate paragraphs. It shall be
sure to give an 1879 determination for each claim as well as the regulatory and statutory references for the
1879 determination.
You are responsible for being aware of correct claim filing procedures and must use care when billing and
accepting payment. In this situation you billed and/or received payment for services you should have known
you were not entitled to. Therefore, you are not without fault and are responsible for repaying the
overpayment amount. If you dispute this determination please follow the appropriate appeals process listed
below.
(Applicable Authorities: Section 1870(b) of the Social Security Act; §§ 405.350 - 405.359 of Title 42, §§
404.506 - 404.509, 404.510a and 404.512 of Title 20 of the United States Code of Federal Regulations.)

What you should do:
Please return the overpaid amount to us by __________(date) and no interest charge will be assessed.
Make the check payable to Medicare Part B and send it with a copy of this letter to:
Carrier Name
Address
City, State and Postal ZIP Code
Immediate Recoupment request:
“You may elect to have your overpayment(s) repaid through the “immediate recoupment” process and
avoid paying by check or waiting for the standard recoupment that begins on day 41 from date of the
initial demand letter. A request for immediate recoupment must be received in writing no later than 16
days from the date of initial demand letter. You must specify whether you are submitting:
1. A one-time request for the current overpayment and all future overpayments, or
2. A request for the current overpayment addressed in this demand letter only.
This process is voluntary and for your convenience.
Visit our website at www.______.___ or call (USA MEDICARE CONTRACTOR Name) at (XXX)
XXX-XXXX for additional information and instructions for “Immediate Recoupment”.
You may fax your request to XXX-XXX-XXXX.
If you do not refund in 30 days:
In accordance with 42 CFR 405.378 simple interest at the rate of __ will be charged on the unpaid balance
of the overpayment beginning on the 31st day. Interest is calculated in 30-day periods and is assessed for
each full 30-day period that payment is not made on time. Thus, if payment is received 31 days from the
date of final determination, one 30-day period of interest will be charged. Each payment will be applied
first to accrued interest and then to principal. After each payment interest will continue to accrue on the
remaining principal balance, at the rate of __ .
We request that you refund this amount in full. If you are unable to make refund of the entire amount at
this time, advise this office immediately so that we may determine if you are eligible for a repayment
plan. (See enclosure for details.) Any repayment plan (where one is approved) would run from the date of
this letter.
If payment in full is not received by, (specify a date 40 days from the date of the notification), payments
to you will be withheld until payment in full is received, an acceptable extended repayment request is
received, or a valid and timely appeal is received. If you have reason to believe that the withhold should
not occur on _____ you must notify <contractor> before ___. We will review your documentation.
However, this is not an appeal of the overpayment determination, and it will not delay recoupment.
If you wish to appeal this decision:
If you disagree with this overpayment decision, you may file an appeal. An appeal is a review performed
by people independent of those who have reviewed your claim so far. The first level of appeal is called a
redetermination. You must file your request for a redetermination within 120 days of the date you receive
this letter. Unless you show us otherwise, we assume you received this letter 5 days after the date of this
letter. Please send your request for redetermination to:
Address of Redetermination Department
If you have filed a bankruptcy petition:
If you have filed a bankruptcy petition or are involved in a bankruptcy proceeding, Medicare financial
obligations will be resolved in accordance with the applicable bankruptcy process. Accordingly, we
request that you immediately notify us about this bankruptcy so that we may coordinate with both the
Centers for Medicare & Medicaid Services and the Department of Justice so as to assure that we handle
your situation properly. If possible, when notifying us about the bankruptcy please include the name the
bankruptcy is filed under and the district where the bankruptcy is filed.
Should you have any questions please do not hesitate to contact _______ at __________.
If we can assist you further in the resolution of this matter, we shall be glad to do so. We expect to hear
from you shortly.
Sincerely,
(name and title)
Enclosure
EXHIBIT 2 - FOLLOW UP DEMAND LETTER TO PHYSICIANS/SUPPLIERS
Dr. Joe Smith
Anywhere St
Anytown, State ZIP Code
Dear (Name of Physician/Supplier):
We previously sent you a letter requesting that you refund an overpayment made to you. Enclosed you
will find a copy of the initial letter sent to you which explains how the overpayment was determined and
why you are responsible. As of today, we have not heard from you, either to request an overpayment
appeal or to make payment. The overpaid amount is ______ (principal plus interest) for your claim that
paid on _______. $_______ has been recovered.
As stated in our initial letter, offset of the overpayment amount, plus interest, will be made against any
pending and future assigned Medicare claims.
If you have already sent payment, or our letters have crossed in the mail, we thank you and ask that you
please disregard this letter.
If you have any questions regarding this matter, please contact us at ________.
Sincerely,
(Name of individual)
Enclosure
EXHIBIT 3- INTENT TO REFER LETTER
When an eligible physician/supplier overpayment remains delinquent for 90 or more days, the carrier
shall send an intent to refer letter. (See CR 1683 and Chapter 4, §70 for more information.)
EXHIBIT 4 - OPTIONAL OVERPAYMENT CUSTOMIZING PARAGRAPHS
A1 - The carrier shall include this language in all overpayment letters that involve §1879 medical
necessity denials. It shall place it as the first paragraph under the heading "Why you are responsible."
Based on available information, we have determined that you had or should have had knowledge that the
service(s) were not medically necessary and reasonable because (i.e., pertinent information was available
from the law and regulations [provide a cite, if possible], from [cite name/issue number of your
newsletter], from a meeting you attended on [date], and from your peers in the medical community).
(Applicable Authorities: Section 1879 of the Social Security Act; §§411.404 and 411.406 of Title 42 of
the United States Code of Federal Regulations.)
NOTE: The carrier shall be sure to include the applicable authorities at the end of the §1879 language as
it appears here.
A2 - The carrier shall include this language in all overpayment letters that involve §1879 medical
necessity denials where payment was collected from the beneficiary.
This overpayment is for services that are not medically reasonable and necessary per Medicare standards.
If you collected the amount of the overpayment from the beneficiary, the beneficiary has the right to
request payment from Medicare. Any such indemnification will be recovered from you.
B1 - The carrier shall include the following paragraph in all overpayment letters that involve payment in
excess of the allowed charge.
The overpayment resulted from payment made to you in excess of the allowed charge for services. If you
have collected a coinsurance and/or deductible from the beneficiary based on the incorrect amount, please
be sure to refund the excess amount to the beneficiary.
B2 - The carrier shall include one of the appropriate paragraphs below in all overpayment letters that
involve duplicate payments.
• The overpayment resulted from excess payments caused by multiple processing of the same
charge.
• The overpayment resulted from Medicare payment on an assigned claim for which the beneficiary
also received payment on an itemized bill and turned his payment over to you. Therefore, you are
liable for $________ which represents that portion of the total amount paid in excess of the fee
schedule amount.
• You have mistakenly received duplicate primary payment from both Medicare and another entity
(Specific payer). (Specific payer) is the appropriate payer. As such, you are liable for the portion
of the Medicare payment in excess of the amount Medicare is obligated to pay as secondary payer.
• This overpayment resulted from duplicate Medicare payments to you for services you provided to
(named beneficiary).
NOTE: The above paragraphs are not all-inclusive.
EXHIBIT 5 - SAMPLE LETTER - CHECK INCLUDED FOR CORRECT AMOUNT
Dear (Name of Physician/Supplier):
We appreciate your recent inquiry regarding Medicare payment that you believe was paid to you in error.
We thank you for bringing this overpayment to our attention, thereby protecting the integrity and
resources of the Medicare program.
A review of our records confirms that you have been overpaid. (This paragraph should include a clear
explanation of how the overpayment arose, the amount of the overpayment, how the overpayment was
calculated, and why the original payment was not correct.)
We have received your check in the amount of $_______ and applied it to the overpayment.
Thank you once again for bringing this matter to our attention.
Sincerely,
(Name of individual)
EXHIBIT 6 - SAMPLE LETTER - CHECK INCLUDED BUT WRONG AMOUNT (TOO MUCH)
Dear (Name of Physician/Supplier):
We appreciate your recent inquiry regarding Medicare payment that you believe was paid in error. We
thank you for bringing this overpayment to our attention.
A review of our records confirms that you have been overpaid. (This paragraph should include a clear
explanation of how the overpayment arose, the amount of the overpayment, how the overpayment was
calculated, and why the original payment was not correct.)
We have received your check for $_______. You will notice that the amount of your check exceeds the
overpayment amount. We will send you a check shortly for the excess amount.
Thank you once again for bringing this matter to our attention.
Sincerely,
(Name of individual)
Enclosure
90.3 - Notification to the Beneficiary When Recovery Is Sought from the Provider or
Physician
(Rev. 70, Issued: 05-27-05; Effective and Implementation dates: 06-27-05)
When a claim adjustment creates an overpayment the beneficiary who received the services will normally
receive a Medicare Summary Notice (MSN) notifying the beneficiary about the specifics of the
adjustment and the beneficiary’s appropriate appeal rights. The MSN uses codes with accompanying
descriptions to update the beneficiary. Through a MSN code, the MSN can also be used to inform the
beneficiary that the provider may be requested to repay the difference in the amount paid and the
adjustment to Medicare.
In situations where the claim adjustment creates an overpayment and a MSN is generated, a separate
notice to the beneficiary is not required whenever recovery is sought from the provider.
However, if a MSN is not generated a separate notice to the beneficiary is required whenever recovery is
sought from the provider. Some reasons a MSN may not generate include, but are not limited to, if the
claim has been purged from the system or if the overpayment is because of a mass adjustment. In these
situations a separate notice to the beneficiary is required whenever recovery is sought from the provider.
(See Chapter 3, §§100 & 110ff when recovering from the beneficiary.)
The following instructions apply if a separate notice to the beneficiary is required.
The contractor shall include in the notification to the beneficiary a copy of the letter sent to the provider
unless the letter to the provider mentions more than one beneficiary or deals with overpayments which do
not concern the particular being notified. In such cases, a copy of the initial demand letter sent to the
provider should not be attached to the beneficiary notice.
Where overpayments to a provider have been determined by means of a sample study, the Contractor
shall send a notice only to the beneficiaries identified in the overpayment notice sent to the provider as
individuals on whose behalf the provider was overpaid a specified amount. It shall not send the notice to
the beneficiaries until it has been established that recovery action will be taken.
In all cases the notice to the beneficiary should contain the following:

• The name and address of the provider and dates of service for which the overpayment was
made.
• A clear explanation of why the payment was incorrect.
• A statement that the provider has been requested to refund the overpayment and, if the
provider is liable for medically unnecessary services or (FIs only) custodial care, the
following additional information, as applicable:
• If the error is discovered subsequent to the third calendar year after the year the payment
was approved, and the other conditions described in Chapter 3, §80 apply, the Contractor
shall advise the beneficiary that the provider is prohibited, by law, from requesting
payment for the services; or
• If the beneficiary is determined to be without fault, the Contractor shall state that if the
beneficiary pays for the services, the beneficiary may request that the Contractor
indemnify the beneficiary for such payment. Any indemnification paid to the beneficiary
will be recovered from the provider. (See Medicare Claims Processing Manual, Chapter
30, Financial Liability Protections.)
• In all other cases, Medicare law does not prohibit the provider from requesting the
beneficiary to pay.
An explanation of the beneficiary's appeal rights. (See Medicare Claims Processing Manual, Chapter 29,
Appeals of Claims Decisions.) In the notice to the beneficiary, however, the Contractor shall not mention
waiver since there is no provision for waiver when the physician is liable for the overpayment.
90.4 - Sample Letter to Beneficiary Where Recovery Is Sought From Provider
(Rev. 70, Issued: 05-27-05; Effective and Implementation dates: 06-27-05)
A notice to the beneficiary is required whenever a provider is requested to repay Medicare because of an
overpayment determined as a result of services provided to the beneficiary. If a MSN is generated the
appropriate notice codes shall be utilized informing the beneficiary that the provider may be requested to
repay Medicare. If this occurs no further action needs to be taken. However, if a MSN is not generated
notice shall be sent to the beneficiary. Below is a sample letter to a beneficiary where recovery is sought
from the provider.
Dear ________________:
In (month and year), we made a payment to (provider or physician name and location) on your behalf
for services provided to you (insert dates).
We have reviewed the payment and determined that the services were not covered under the Medicare
program.
(The Contractor shall explain as clearly as possible the reason why all, or part, of the payment was
erroneous.)
It shall use either paragraphs A, B or C below as appropriate:
A - Provider Liable for Medically Unnecessary or Custodial Care Services (Physician
Liable for Medically Unnecessary Services)
(See Medicare Claims Processing, Chapter 30, Financial Liability Protections.)
We have found that you (the beneficiary) did not know or have any way of knowing that the services you
(he/she) received during (dates of services for which beneficiary's liability has been waived) would not
be considered to be reasonable and necessary by Medicare. However, the records show that (physician’s
name) should have known that such services would be considered noncovered. When this situation
occurs, the law requires that the liability for these noncovered services be transferred to the physician.
Therefore, you (the beneficiary) are (is) not responsible for the charges billed by (provider's name)
except for any charges for services or items never covered by Medicare. If you (the beneficiary) have
(has) paid (provider's name) for these services, you may be entitled to a refund. To obtain this refund,
please advise this office and enclose the following documents:
• A copy of this notice;
• The bill you received for the services; and
• The payment receipt from (provider's name), your cancelled check, or any other evidence
showing that you (the beneficiary) have (has) already paid (provider's name) for the services at issue.
You should file your written request for payment within 6 months of the date of this notice.
B. Provider at Fault and Beneficiary Not at Fault for Medically Unnecessary or Custodial Services
and the Overpayment was Discovered Subsequent to the Third Calendar Year After Year Payment
Was Approved
(Provider's name) has been requested to refund this overpayment. Under the Medicare law, (provider's
name) is prohibited from billing you, or any other source, for these noncovered services. If (provider's
name) sends you a bill for these services, send it to us with a copy of this letter.
C. All Other Cases
(Provider's name) has been requested to refund the overpayment. Since the above services are not
covered by Medicare, (Provider's name) may ask you to pay for them. However, if you are billed, this is
a matter between you and (Provider's name) and will not affect your entitlement to future Medicare
benefits in any way.
NOTE: The notification of appeal rights should be in accordance with the reopening rules in Medicare
Claims Processing, Chapter 29, Appeals of Claims Decisions.
110 - Confirmed Identity Theft
(Rev. 336: Issued: 02-07-20: Effective:05-08-20: Implementation; 05-08-20)

The Centers for Medicare & Medicaid Services (CMS) is addressing instances of identity theft confirmed
by the Investigating Unit (IU) through a CMS-approved identity theft victim validation and remediation
process. For purposes of this instruction, the IU is the Unified Program Integrity Contractor (UPIC) and
the CMS Center for Program Integrity (CPI).
When the IU confirms, by letter, to the contractor that a victim’s overpayment(s) resulted from identity
theft:
• The contractor shall immediately discontinue ALL collection efforts on the overpayment(s).
These collection efforts shall include recoupments, sending demand letters, and referring the
overpayment(s) to Treasury.
• Contractors not utilizing the Healthcare Integrated General Ledger Accounting System (HIGLAS)
shall recall the overpayment(s) if it was referred to Treasury.
• The contractor shall update the Shared System, HIGLAS, and ViPS Medicare System (VMS), as
appropriate, for all affected claims and accounts receivables (ARs) within 5 business days from
the confirmation receipt date.
• Contractors utilizing HIGLAS shall adjust down the AR(s) with the “DELETE/ADJ TO ZERO”
activity code and close the AR(s) by changing the AR status code “CLO-ERR.” The
“DELETE/ADJ TO ZERO” activity code will systematically recall the overpayment(s) if it was
referred to Treasury.
• Contractors not utilizing HIGLAS shall adjust down the related AR(s) to $0.00 and change the
status to closed.
• The contractor shall refund any monies within 30 calendar days that were recouped or paid to
satisfy the overpayment(s).
• The contractor shall request CMS to provide a revised (corrected) IRS Form(s) 1099-C if the
original IRS Form(s) 1099-C included the overpayment(s).
o The contractor shall send the request to [email protected] with
"Corrected IRS Form(s) 1099-C Request for Confirmed ID Theft" in the subject field.
o The contractor shall include in its request, a copy of the IU identity theft confirmation
letter and the amount(s) that shall be corrected.
o The contractor shall issue the revised (corrected) IRS Form(s) 1099-C to the victim.
• The contractor shall issue a revised (corrected) IRS Form 1099-MISC if the original IRS Form
1099-MISC issued to the victim contained amounts related to confirmed identity theft.
• The contractor shall notify the victim, by letter, of all activity associated with the overpayment(s)
of the confirmed identity theft case. This activity shall include items such as notice of the
rescission of the overpayment(s), the revision of the IRS Forms 1099-C and/or 1099-MISC, and
the recall of the overpayment(s) from Treasury. The letter shall also include all claim/document
control numbers of all affected claims and all original accounts receivable amounts (principal and
interest) that were adjusted down.
110.2 - Seized Monies Received from Law Enforcement
(Rev. 199, Issued: 11-04-11, Effective: 12-05-11, Implementation: 12-05-11)
The contractor shall apply any seized monies received (e.g., Treasury check) from the perpetrator of the
identity theft to the fraudulent debt in accordance with the Medicare Financial Management Manual,
Publication, 100-06, Chapter 5.
120 – Monitoring Accounts Receivable that are in a Redetermination or
Reconsideration Status
(Rev. 261, Issued: 01-29-16, Effective: 03-01-16, Implementation: 03-01-16)
The MAC shall develop controls to monitor accounts receivable (ARs) that are in the first
(redetermination) or second (reconsideration) level of appeal. ARs that are in either level of appeal are
subject to limitations on recoupment as mandated by Section 935(f)(2)(a) of the Medicare Modernization
Act of 2003. The MAC shall monitor these ARs to make sure the “days in status” are not greater than
120. If the “days in status” are greater than 120, the MAC shall research the appeal to determine the
status/decision of the appeal and update the AR’s status accordingly.
130 –Federal Payment Levy Program – IRS Tax Levy Requests
(Rev. 11462; Issued: 06-23-22; Effective: 07-25-22; Implementation: 07-25-22)
In coordination with the Internal Revenue Services’ Federal Payment Levy Program (FPLP), under Internal
Revenue Manual, Part 5, Chapter 11, Section 7, CMS receives automated Notice of Levy to
collect delinquent debts owed to the federal government. Automated FPLP interfaces with the Bureau of
Fiscal Services’ (BFS) Treasury Offset Program (TOP). CMS shall comply with automated FPLP
requests under 26 U.S.C. §6331(a);(h), which requires:
(1) A Levy shall extend only to property possessed and obligations existing at the time
thereof, in accordance to 26 USC §6331(b);
(2) Any Federal payment owed to the taxpayer shall be levied on a continuous basis, until
such levy is satisfied, as determined by the Secretary of Treasury; 26 USC §6331(h)(1)
(3) Any such levy shall be applied at the rate of 100% for any payment(s) due to a Medicare
provider or supplier under Title XVIII of the Social Security Act. 26 USC §6331(h)(2)
For the purposes of operationalizing the CMS’s obligations under the FPLP, specifically in identifying “an
obligation existing at the time thereof” under 26 USC §6331(a) the Social Security Act, §
1816(c)(3)(A)&(B), and 1842(c)(3)(A)&(B:
(4) “No payment shall be issued, mailed, or otherwise transmitted with respect to any claim
submitted under this title within the applicable number of calendar days after the date
on which the claim is received.” SSA §1816(c)(3)(A)&(B); and
(5) “Applicable number of calendar days” means with respect to claims submitted
electronically as prescribed by the Secretary, 13 days, and with respect to claims
submitted otherwise, 28 days. SSA§ 1842(c)(3)(A)&(B)
The Medicare Claims Processing Manual, Chapter 1, Section 80.2.1.2, Payment Floor Standards,
describe the method of calculation of the applicable calendar days as described in SSA §1816(c)(3) &
§1842(c)(3). For the purpose of implementing this section, the Payment Floor Date, as described in
Chapter 1, Section 80.2.1.2, is the earliest day after receipt of the clean claim that payment may be made.
Any claims payment amounts owed to the provider of services, hospital, or supplier, which are held on the
payment floor, but have not yet reached the Payment Floor Date, regardless of date of
submission, shall be considered “obligation(s) existing at the time thereof” the IRS Levy is received by
CMS.
Under Internal Revenue Manual (IRM) 5.11.6.7.2, and in addition to automatic levies through FPLP,
payments to Medicare providers and suppliers may be general levies, also referred to as paper levies,
received on form 668a.
A. Medicare payment to providers and suppliers are subject to withhold due to receipt of a
general or paper tax levy on form 668a when:
1. A tax levy is served by the Internal Revenue Service (IRS) at the Medicare
Administrative Contractor, or
2. In rare circumstances, received by the CMS.
• CMS as a responsible party shall promptly notify the appropriate MAC if a general or
paper levy is served to the CMS.
B. Once received, the contractor shall implement the general or paper tax levy to recoup funds
against current Medicare claims payments on behalf of the IRS.
C. Contractors shall be responsible to setup the paper levy as a Third-Party Payment (TPP) Debt.
1. Once a paper levy has been end-dated and sufficient paperwork is returned, it is possible for
the provider to receive a new levy for the same provider, with new dates.
2. It is also possible to have more than one paper levy served on a provider (not a duplicate) at the
same time.
• Contractors shall decline the additional 668a tax levy and return it to the IRS with
instruction to resend when the existing debt is finished collecting.
D. General or paper tax levies received on IRS form 668a are not continuous levies.
• If the provider or supplier for whom the paper levy is received is already subject to FPLP, the
paper levy is setup as a TPP and collected according to the HIGLAS hierarchy.
• Any provider claims received after the general or paper levy IRS FORM 668a has been served
shall not be added to the obligated amount due to the provider.
E. Contractors shall follow these steps for general or paper tax levies received on IRS form 668a:
1. The amount shall be held at 100% up to the total amount reflected on the IRS form 668a
general levy;
2. After the claims clear the payment floor, up to the amount of the levy, the amount shall be
transmitted to the Treasury Department as requested; however:
• If the amount due the provider on the day the levy was served, and

• The total amount due the provider for the claims on the floor is not
enough to cover the levy amount (once all the obligated claims clear the
floor, no later than the number of calendar days specified in the IRS
form 668a general levy).
3. The entire amount withheld shall be released to the Treasury Department.
F. Contractors shall have the number of calendar days specified in the IRS form
668a levy to collect funds from the date the third-party transaction is set up.
• Contractors shall add an inactive date to the third-party transaction when the
full amount is not collected in full within the required timeframe.
G. Contractors shall complete the back section on the IRS 668a form as requested by the
IRS.
1. Send back the form to the IRS, after the number of calendar days specified in
the IRS form 668a general levy and the total amount is collected.
2. Report the tax levies as a withholding on the Remittance Advice (RA).
H. Contractors shall setup the TPP offset form for non-tax FPLP withholdings
in the Medicare Provider Payment Offset process which are collected in the
hierarchical order below:
1. Medicare Accounts Receivable debt,
2. FPLP Offsets for Federal Tax debt at 100% maximum of the payable amount,
3. Administrative Offsets for Federal Non-Tax debt at 100% of the payable amount,
and
4. TPP
Refer to https://www.irs.gov/businesses/small-businesses-self-employed/federal-payment-
levy-program
for additional information on the Tax Levy Program.

Transmittals Issued for this Chapter
Rev #
Issue Date
Subject
Impl Date
CR#
R12346FM
11/01/2023
Revisions and Deletions to the Internet Only
Manual (IOM), Publication 100-06, Chapter
4, Debt Collection Related to Extended
Repayment Schedules (ERS) and Debt
Management
10/30/2023
13358
R12323FM
10/20/2023
Revisions and Deletions to the Internet Only
Manual (IOM), Publication 100-06, Chapter
4, Debt Collection Related to Extended
Repayment Schedules (ERS) and Debt
Management- Rescinded and replaced by
Transmittal 12346
10/30/2023
13358
R12262FM
09/28/2023
Revisions and Deletions to the Internet Only
Manual (IOM), Publication 100-06, Chapter
4, Debt Collection Related to Extended
Repayment Schedules (ERS) and Debt
Management - Rescinded and replaced by
Transmittal 12323
10/30/2023
13358
R11787FM
01/19/2023
Publication (Pub.) 100-06, Chapter 4, Section
70 Revision (Removal of Debt Collection
System References and Corresponding
Updates) and Inclusion of Existing Debt
Close-Out (Termination of Collection Action)
Instructions
04/21/2023
12858
R11462FM
06/23/2022
Federal Paper Tax Levy
07/25/2022
12481
R10821FM
05/24/2021
Pub. 100-06, Chapter 4, Section 10 Revision
(New Accounts Receivable (AR) Status
Codes for Undeliverable Initial Demand
Letters and Terminated/Out of Business
Providers
04/26/2021
11832
R10527FM
12/23/2020
Pub. 100-06, Chapter 4, Section 10 Revision
(New Accounts Receivable (AR) Status
Codes for Undeliverable Initial Demand
Letters and Terminated/Out of Business
Providers)- Rescinded and replaced by
Transmittal 10821
04/26/2021
11832
R336FM
02/07/2020
Pub. 100-06, Chapter 4, Section 110
(Confirmed Identity Theft) Revision
05/08/2020
11486
R330FM
11/06/2019
The Medicare Fee-for-Service Recovery
Audit Program
11/04/2019
11464

Rev #
Issue Date
Subject
Impl Date
CR#
R328FM
10/18/2019
Updates to Medicare Financial Management
Manual Chapter 4, Section 50-50.6 Extended
Repayment Schedules
10/07/2019
11128
R326FM
10/04/2019
The Medicare Fee-for-Service Recovery
Audit Program- Rescinded and replaced by
Transmittal 330
11/05/2019
11464
R316FM
05/24/19
Updates to Medicare Financial Management
Manual Chapter 4, Section 20 and 20.1
Demand Letters
10/07/2019
10776
R312FM
04/05/2019
Updates to Medicare Financial Management
Manual Chapter 4, Section 50-50.6 Extended
Repayment Schedules- Rescinded and
replaced by Transmittal 328
10/07/2019
11128
R315FM
05/17/2019
Update to Publication (Pub.) 100-06 to
Provide Language-Only Changes for the New
Medicare Card Project
06/18/2019
11211
R296FM
12/08/2017
Cessation of MAC Validation of Recovery
Audit Program New Issues
01/02/2018
10349
R286FM
06/09/2017
Medicare Financial Management Manual
Chapter 4, Section 20 Demand Letter Updates
07/03/2017
10023
R285FM
06/02/2017
Pub. 100-6, Chapter 3 and 4 Revisions
07/01/2017
10079
R264FM
02/12/2016
Extended Repayment Schedule (ERS)
Manual Updates
03/14/2016
9423
R261FM
01/29/2016
Monitoring Accounts Receivable that are in a
Redetermination or Reconsideration Status
03/01/2016
9470
R259FM
01/15/2016
Internet Only Manual Pub.100-06, Chapter 4
Revisions to Reflect the New Debt Referral
Requirements Mandated by the Digital
Accountability and Transparency Act of 2014
(DATA Act)
02/16/2016
9469
R246FM
11/26/2014
Recovery Auditor Appeal Adjustments with
“RI” Indicator
12/29/2014
8973
R244FM
10/17/2014
Treasury Report on Receivables (TROR)
Reporting
11/18/2014
8936
R241FM
09/26/2014
Recovery Audit Program Tracking Appeals
and Reopenings
10/07/2014
8411

Rev #
Issue Date
Subject
Impl Date
CR#
R235FM
05/14/2014
Revisions and Deletions to the Internet Only
Manual, Publication 100-06, Chapter 4, Debt
Collection (Section 10)
07/07/2014
8315
R233FM
04/04/2014
Revisions and Deletions to the Internet Only
Manual, Publication 100-06, Chapter 4, Debt
Collection (Section 10) – Rescinded and
replaced by Transmittal 235
07/07/2014
8315
R226FM
09/06/2013
Recovery Audit Program Tracking Appeals
and Reopenings – Rescinded and replaced by
Transmittal 241
10/07/2013
8411
R224FM
08/02/2013
Revisions and Deletions to the Internet Only
Manual, Publication 100-06, Chapter 3,
Overpayment (Section 50.3); Chapter 4, Debt
Collection (Section 50 - 50.6 and 100.6.4)
Related to Extended Repayment Schedules
(ERS)
09/03/2013
8347
R210FM
05/18/2012
Validation of Recovery Audit Program New
Issues
06/19/2012
7733
R208FM
04/20/2012
Overpayment Recovery from Suppliers of
Durable Medical Equipment, Prosthetics.
Orthotics and Supplies (DMEPOS)
05/20/2012
7744
R206FM
03/09/2012
Processing of Recovery Audit Program Error
Files
04/09/2012
7724
R205FM
02/09/2012
Immediate Recoupment for Fee For Service
Claims Overpayments
07/02/2012
7688
R204FM
01/27/2012
Immediate Recoupment for Fee For Service
Claims Overpayments – Rescinded and
replaced by Transmittal 205
07/02/2012
7688
R202FM
01/06/2012
Recovery Audit Program MAC-issued
Demand Letters
01/03/2012
7436
R200FM
11/16/2011
Recovery Audit Program Tracking Appeals
and Reopenings
09/27/2011
7458
R199FM
11/04/2011
Instructions for Processing Physicians and
Other Suppliers Debts that Have Been
Confirmed as Identity Theft
12/05/2011
7419
R198FM
10/27/2011
Medicare Financial Management Manual,
Chapter 4-Debts Returned to Agency (RTA)
by Treasury
11/28/2011
7311

Rev #
Issue Date
Subject
Impl Date
CR#
R193FM
08/26/2011
Recovery Audit Program Tracking Appeals
and Reopenings – Rescinded and replaced by
Transmittal 200
09/27/2011
7458
R192FM
07/29/2011
Recovery Audit Program MAC-issued
Demand Letters – Rescinded and replaced by
Transmittal 202
01/03/2012
7436
R189FM
05/06/2011
Recovery Audit Program Tracking
Overpayments Instruction Alteration
06/06/2011
7403
R186FM
03/18/2011
Receivables Initiated by the Recovery
Auditor as Independent Audit Accessible
Information
04/18/2011
7336
R184FM
02/25/2011
Recovery Audit Program Underpayments
Instruction Alteration
03/28/2011
7326
R180FM
12/29/2010
Updated Appeal Reporting Recovery Audit
Contractors (RACs)
01/28/2011
7160
R169FM
04/30/2010
Recovery Audit Contractors (RACs)
06/01/2010
6951
R168FM
04/30/2010
Recovery Audit Contractors (RACs)
06/01/2010
6936
R167FM
03/23/2010
Recovery Audit Contractors (RACs)
05/24/2010
6871
R162FM
10/30/2009
Recovery Audit Contractors (RACs)
12/15/2009
6398
R156FM
08/07/2009
Recovery Audit Contractors
09/08/2009
6582
R152FM
06/12/2009
Recovery Audit Contractors (RACs)
07/13/2009
6384
R148FM
03/06/2009
Recovery Audit Contractors (RACs)
03/13/2009
6273
R145FM
01/09/2009
Recovery Audit Contractors (RACs) –
Rescinded and replaced by Transmittal 148
03/13/2009
6273
R143FM
10/24/2008
Instruction for Monthly Processing of Non-
Medicare Secondary Payer (Non-MSP) Debts
Returned to Agency (RTA) from the
Department of Treasury
01/05/2009
6083
R139FM
07/11/2008
Interaction With Recovery Audit Contractors
(RACs)
08/11/2008
6089
R137FM
02/29/2008
Reporting Costs Directly Associated with the
RAC Program
03/31/2008
5789
R136FM
02/14/2008
Revisions to Debt Referral Instruction
03/17/2008
5875
R124FM
06/29/2007
Treasury Collection on Non-Medicare
Secondary Payer (Non-MSP) Debts
07/30/2007
5631
R109FM
10/27/2006
Claims Accounts Receivable-Clarification to
CR 3963
11/27/2006
5302

Rev #
Issue Date
Subject
Impl Date
CR#
R104FM
08/11/2006
Updated Procedures for AC Communication
with RAC
09/11/2006
5226
R87FM
12/30/2005
Update to Carrier Demand Letter Appeals
Language
01/03/2006
4211
R77FM
09/16/2005
Non-Medicare Secondary Payer (Non-MSP)
Debt Referral and Debt Collection
Improvement Act of 1996 (DCIA) Activities
10/17/2005
3964
R75FM
08/12/2005
New Thresholds for 2nd Demand Letter for
Physicians/Suppliers
09/06/2005
3932
R73FM
08/05/2005
New Thresholds for 2nd Demand Letter for
Physicians/Suppliers - Replaced by Revision
75FM
09/06/2005
3932
R72FM
07/29/2005
Claims Accounts Receivable Update
01/03/2006
3963
R70FM
05/27/2005
Revision to the Beneficiary Notification
Process when Recovery is Sought from the
Provider
06/27/2005
3795
R69FM
05/27/2005
Update to Debt Collection System (DCS)
User Guide
06/27/2005
3868
R68FM
05/20/2005
Instructions for Affiliated Contractors
Involved in the Recovery Audit Contractor
(RAC) Demonstrations
06/20/2005
3773
R61FM
12/10/2004
New Location Code ICC, Status Code AR
and Modified Intent Letter for Unfiled Cost
Reports Only
01/10/2005
3563
R53FM
08/27/2004
Change Request 3367, Debt Collection
System (DCS), replaces Change Request
2952, Debt Collection System (DCS)
09/27/2004
3367
R41FM
04/30/2004
Calculated Interest on Medicare
Overpayments and Underpayments
10/04/2004
3163
R30FM
01/28/2004
Notice of New Interest Rates for Medicare
Overpayments and Underpayments
02/04/2004
2829
R29FM
01/02/2004
Revisions to Chapters 3 and 4
02/06/2004
2911
R19FM
07/25/2003
Intermediary Claims Accounts Receivable
(A/R)
08/08/2003
2753
R13FM
02/03/2003
Termination of Debt Collection Activities
07/01/2003
2436
R04FM
08/30/2002
Initial Publication of Chapter
N/A
N/A
Back to top of Chapter
