Prepared for
the Office of the Assistant Secretary for Planning and Evaluation (ASPE)
at the U.S. Department of Health & Human Services
by
Westat
October 2023
OFFICE OF BEHAVIORAL HEALTH,
DISABILITY, AND AGING POLICY
Addressing Homelessness Among
Older Adults: Final Report
Office of the Assistant Secretary for Planning and Evaluation
The Assistant Secretary for Planning and Evaluation (ASPE) advises the Secretary of the U.S. Department
of Health and Human Services (HHS) on policy development in health, disability, human services, data,
and science; and provides advice and analysis on economic policy. ASPE leads special initiatives;
coordinates the Department's evaluation, research, and demonstration activities; and manages cross-
Department planning activities such as strategic planning, legislative planning, and review of regulations.
Integral to this role, ASPE conducts research and evaluation studies; develops policy analyses; and
estimates the cost and benefits of policy alternatives under consideration by the Department or
Congress.
Office of Behavioral Health, Disability, and Aging Policy
The Office of Behavioral Health, Disability, and Aging Policy (BHDAP) focuses on policies and programs
that support the independence, productivity, health and well-being, and long-term care needs of people
with disabilities, older adults, and people with mental and substance use disorders. Visit BHDAP at
https://aspe.hhs.gov/about/offices/bhdap for all their research activity.
NOTE: BHDAP was previously known as the Office of Disability, Aging, and Long-Term Care Policy
(DALTCP). Only our office name has changed, not our mission, portfolio, or policy focus.
This research was funded by the U.S. Department of Health and Human Services Office of the Assistant
Secretary for Planning and Evaluation under contract and carried out by Westat. Please visit
https://aspe.hhs.gov/topics/homelessness-housing for more information about ASPE research on
homelessness and housing.

ADDRESSING HOMELESSNESS AMONG OLDER ADULTS: FINAL REPORT
Authors
Kathryn A. Henderson, Ph.D.
Nanmathi Manian, Ph.D.
Debra J. Rog, Ph.D.
Evan Robison, MPH
Ethan Jorge
Monirah Al-Abdulmunem, MS
Westat
October 26, 2023
Prepared for
Office of Behavioral Health, Disability, and Aging Policy
Office of the Assistant Secretary for Planning and Evaluation
U.S. Department of Health and Human Services
The opinions and views expressed in this report are those of the authors. They do not reflect the views
of the Department of Health and Human Services, the contractor or any other funding organization. This
report was completed and submitted April 2023.
1
Acknowledgments
The authors would like to acknowledge the contributions of their colleagues, Ilene Rosin, for
assistance with data collection, and Dr. Andreea Balan-Cohen, Dr. Cindy Gruman, and
Dr. Beth Rabinovich for review of this report. We would also like to thank our project officers at
the U.S. Department of Health and Human Services, Office of the Assistant Secretary for
Planning and Evaluation, Lauren Anderson, Emma Nye, and Emily Rosenoff for providing us
guidance and support throughout the project.
We also thank the subject matter experts and service providers we interviewed for this project
for graciously providing us their time and knowledge. Most importantly, we are grateful to the
individuals with lived experience of homelessness in older adulthood who shared with us their
experiences and recommendations.
2
Table of Contents
EXECUTIVE SUMMARY ................................................................................................................................. 4
SECTION 1. INTRODUCTION ....................................................................................................................... 12
Overview of Report .............................................................................................................................. 13
Methodology ........................................................................................................................................ 13
SECTION 2. SIZE, CHARACTERISTICS, AND NEEDS OF THE POPULATION OF OLDER ADULTS
EXPERIENCING HOMELESSNESS ADULTS EXPERIENCING HOMELESSNESS .............................................. 14
Prevalence of Homelessness Among Older Adults .............................................................................. 14
Pathways into Homelessness for Older Adults .................................................................................... 15
Characteristics of Older Adults Experiencing Homelessness ............................................................... 17
Service Needs of Older Adults Experiencing Homelessness ................................................................ 19
SECTION 3. SYSTEMS AND SERVICES AVAILABLE TO SERVE OLDER ADULTS AT RISK OF OR
EXPERIENCING HOMELESSNESS ................................................................................................................. 27
Homelessness Assistance ..................................................................................................................... 28
Housing Programs and Residential Long-Term Care Options .............................................................. 32
Health Care, Long-Term Care, and Behavioral Health Services ........................................................... 39
Income Supports and Other Needs ...................................................................................................... 45
SECTION 4. GAPS AND POTENTIAL STRATEGIES ........................................................................................ 50
Gaps in Service Delivery and Coordination .......................................................................................... 50
Gaps in Knowledge ............................................................................................................................... 53
Potential Strategies .............................................................................................................................. 54
Conclusion ............................................................................................................................................ 56
APPENDIX: OVERVIEW OF METHODOLOGY .............................................................................................. 58
REFERENCES ................................................................................................................................................ 62
ACRONYMS ................................................................................................................................................. 77
3
List of Exhibits
Exhibit 1. Sample Racial/Ethnic Composition for Studies of Older Adults Experiencing
Homelessness ....................................................................................................................... 18
Exhibit 2. Comparison of Characteristics and Needs of Older Adults Experiencing
Homelessness ....................................................................................................................... 20
Exhibit 3. Systems Framework for Addressing Homelessness Among Older Adults ........................... 27
Exhibit 4. Types of Housing Assistance Available for Older Adults Experiencing
Homelessness ....................................................................................................................... 32
Exhibit 5. Types of Residential Long-Term Care Available for Older Adults Experiencing
Homelessness ....................................................................................................................... 36
Exhibit A-1. Key Words and Search Terms Used to Identify Relevant Published and
Unpublished Literature ........................................................................................................ 58
Exhibit A-2. Sources Searched to Identify Relevant Published and Unpublished Literature .................. 59
4
Executive Summary
The number of older adults at risk of and currently experiencing homelessness has increased
rapidly in recent years, a trend that is projected to continue and further accelerate (Culhane et
al., 2013; Culhane et al., 2019). Older adults at risk of or experiencing homelessness have
unique needs compared to other populations experiencing homelessness. As a first step in
understanding how to address the needs of this population, the U.S. Department of Health and
Human Services’ (HHS) Office of the Assistant Secretary for Planning and Evaluation contracted
with Westat to conduct a study of what is known about older adults experiencing
homelessness, including an examination of the size, characteristics, and needs of this
vulnerable population and the services, housing, and supports needed and available to serve
them. The study included an environmental scan of published research, evaluations, and white
papers as well as discussions with subject matter experts, housing and service providers, and
people with lived experience of homelessness as older adults.
This report provides a roadmap for understanding the population of older adults at risk of or
experiencing homelessness and what services and supports are available to serve them. Using
an equity lens, we examine these topics with attention to what is known about racial and ethnic
groups disproportionately impacted by homelessness. We highlight the challenges older adults
face in accessing the assistance available; innovative practices, especially those implemented
during the Novel Coronavirus (COVID-19) pandemic, that could ease these challenges; and
remaining gaps that need to be filled to effectively tackle the problem. We end with
recommendations to better identify and serve older adults at risk of or experiencing
homelessness.
POPULATION OF OLDER ADULTS EXPERIENCING HOMELESSNESS
Older adults are the fastest-growing age group of those experiencing homelessness, composing
nearly half of the homeless population (Kushel, 2022) and their numbers are estimated to triple
by 2030 (Culhane et al., 2019). Older adults are especially vulnerable to homelessness as many
live on fixed incomes insufficient to cover all their expenses, especially housing expenses
(Sermons & Henry, 2010). Half of renters ages 50 and older pay more than 30 percent of their
income on housing (Joint Center for Housing Studies, 2018).
Two trends in the growth of homelessness among older adults are apparent: aging of those
who first experienced homelessness earlier in life and continue to experience homelessness as
older adults and, increasingly, people experiencing homelessness for the first time in older age.
The first group represents a cohort effect: individuals born in the second half of the post-World
War II baby boom (1954-1963) who throughout their lives have had an elevated risk of
homelessness due to limited employment opportunities, coupled with mental health and
substance use disorders. The second group of older adults are experiencing homelessness for
the first time after age 50 after having lived relatively stable lives including long periods of
employment and residential stability. For this group, homelessness is often preceded by

5
stressful life events, such as the death of a spouse or partner, divorce, loss of work, eviction, or
the onset of health problems, coupled with limited or fixed incomes (Cohen, 2004; Crane et al.,
2005).
CHARACTERISTICS OF OLDER ADULTS EXPERIENCING HOMELESSNESS
Older adults with earlier experiences of homelessness have had increased vulnerabilities
throughout their lives, including more adverse childhood experiences, more mental health
conditions, greater alcohol and drug use, higher rates of incarceration, and more
underemployment than those with later entry into homelessness (Brown et al., 2016). In
addition, this group has spent more time homeless both overall and in their current episodes
than those individuals whose first homelessness occurred in older age (Brown et al., 2016).
The few studies that have examined the racial and ethnic composition of older adults
experiencing homelessness are limited in their generalizability due to having small samples
drawn from limited geographic regions. Despite this limitation, their findings are consistent
with national level data in that the percentage of African Americans who are experiencing
homelessness is disproportionately large compared to the overall percentage of African
American older adults (HUD, 2023; Moses, 2019).
SERVICE NEEDS OF OLDER ADULTS EXPERIENCING HOMELESSNESS
Compared to their housed counterparts, older adults experiencing homelessness have higher
rates of health service utilization and more health and health-related concerns, including:
• Significantly shorter life spans (Metraux et al., 2011; Schinka & Byrne, 2018; Brown et al.,
2016; Kushel 2020).
• Higher prevalence and severity of physical and geriatric conditions including memory loss,
falls, difficulty performing activities of daily living (ADLs), cognitive impairment, and
functional impairments (Brown et al., 2011; Brown et al., 2017; Hahn et al., 2006; Hwang et
al., 1997).
• More complex health needs, comparable to housed individuals who are 10-20 years older
(Cohen, 1999; Gelberg et al., 1990; Homelessness Policy Research Institute [HPRI], 2019;
Brown et al., 2016).
• Higher rates of mental health and substance use disorders (Brown et al., 2011; CDC, 2008;
Spinelli et al., 2017).
“Like my body isn't so resilient. When I was younger,
I, mean, I went everywhere and bounced back. And
now it's harder to get up out of the chair, let alone
get up off the sidewalk if you're sleeping outside.”
– Adult currently experiencing homelessness, 59

6
As such, this population has greater need for health care supports, such as access to
medications, durable medical equipment, and assistive technology, as well as assistance with
ADLs, compared to their housed counterparts.
Compared to individuals younger than 50 years who are homeless, older adults experiencing
homelessness have higher rates of chronic illnesses, geriatric conditions, and cognitive
impairments as well as high blood pressure, arthritis, and functional disability (Garibaldi et al.,
2005; Gelberg et al., 1990). Among people experiencing homelessness, older adults and
younger adults have comparable rates of mental health and substance use disorders (DeMallie
et al., 1997; Gelberg et al., 1990; Gordon et al., 2012).
Among older adults experiencing homelessness, older adults who first experienced it earlier in
life have more behavioral health needs and service utilization than those who first experienced
homelessness after age 50. Differences are most pronounced in rates of current mental health
issues, including depressive symptoms, post-traumatic stress disorder, and substance use, as
well as hospitalizations for mental health conditions (Brown et al., 2016).
Finally, food insecurity, lack of transportation, and loss of community surface as additional
challenges for older adults experiencing homelessness. Older adults experiencing homelessness
have rates of food insecurity that are nearly two times higher than estimates among all people
living in poverty (Coleman-Jensen et al., 2016; Tong et al., 2018). Lack of transportation poses a
particularly significant barrier for older adults, who are more likely to have mobility limitations
due to health impairments, including poor eyesight and impaired cognition.
SYSTEMS AND SERVICES AVAILABLE TO SERVE OLDER ADULTS AT RISK OF OR EXPERIENCING
HOMELESSNESS
Homelessness Assistance
Older adults may face unique challenges accessing homelessness assistance, including limited
knowledge about the services available for which they are eligible, heightened anxiety about
and lack of trust in working with providers,
limited access to technology to complete online
applications (National Council on Aging [NCOA],
2022), and difficulty attending scheduled
appointments, providing documentation of
eligibility, or completing the necessary
paperwork (Grenier et al., 2013). As noted by experts, many crisis and interim housing facilities
may not be accessible to older adults with mobility challenges and difficulty performing ADLs or
these facilities may be unable to provide the kind of supports that older adults need. Although
some organizations and municipalities offer programs aimed specifically at older adults, most
communities do not provide this type of assistance.
Homelessness assistance includes
prevention services, identification,
engagement, and assessment services,
as well as crisis or interim housing.
7
Housing Assistance
Access to housing assistance can be difficult
given the current lack of availability and the high
and growing demand among low-income older
adults. Consequently, large numbers of older
adults who are eligible for rental assistance
either have a long wait time for assistance or do
not end up receiving the assistance (Public and
Affordable Housing Research Corporation
[PAHRC], 2020), a finding reflected in our
discussions with people with lived experience.
Experts also noted a lack of residential options
with sufficient support to enable older adults to
age in place.
Health Care, Long-Term Care, and Behavioral
Health Services
Older adults face a number of challenges
receiving the health care they need. Meeting
basic needs such as food and housing often takes
precedence over seeking treatment for physical
and behavioral health needs. Lack of available
providers within communities, limited provider
capacity, a lack of transportation, and mobility
challenges further exacerbate difficulties in
obtaining the health care that older adults experiencing homelessness need (Baggett et al.,
2011; Canham et al., 2020; Kushel et al., 2012; Lee et al., 2020; Ye et al., 2019).
Basic Needs Assistance
Older adults experiencing homelessness often
have difficulty accessing needed assistance.
Individuals without fixed addresses and those
with limited access to technology, as well as
those with health or behavioral health
conditions, may have difficulty establishing
eligibility for assistance or completing their
applications (Tong et al., 2018). Moreover, all of these basic needs programs may be limited in
rural areas.
Housing assistance includes programs
that provide time-limited assistance as
well as a wide range of permanent
subsidized housing options with and
without supportive services. These
include permanent supportive housing,
permanent subsidies, low-income tax
credit housing, and a range of residential
and institutional care settings that may
provide medical management, support
services, and social activities.
Health care, long-term care, and
behavioral health services, including
medications, are available for older
adults through a variety of federal and
state-funded mechanisms including
Medicare, Medicaid, VA benefits (for
eligible veterans), and OAA and SAMHSA
funded programs.
Assistance for basic needs, such as
income, food, transportation, and social
engagement are provided through a
range of federal, state, private, and non-
profit programs.

8
INNOVATIVE PROGRAMS TO SERVE OLDER ADULTS EXPERIENCING HOMELESSNESS
Numerous agencies and municipalities are implementing innovative programs to address the
specific challenges older adults experiencing homelessness face, including with accessing
needed assistance. A sample of the programs is highlighted throughout this report. For
example:
• The Native American Disability Law Center in New Mexico and Arizona creates accounts
for clients in an online benefits application portal to help individuals apply for energy
assistance and other public benefits.
• The Hearth program in Boston, Massachusetts provides outreach to older adults at risk
of or experiencing homelessness to apply for, locate, and move into subsidized housing.
• Serving Seniors in San Diego, California provides transitional housing with facilities
accessible to people with mobility challenges and supportive services focused on the
unique needs of older adults experiencing homelessness.
• The Southern California Clinical and Translational Science Institute in Los Angeles County
is pilot testing the integration of the Community Aging in Place--Advancing Better Living
for Elders (CAPABLE) program with permanent supportive housing to provide home-
based services, such as occupational therapists, nurses, and handypersons, to formerly
homeless older adults who experience difficulties with ADLs.
• St. Paul’s Programs of All-Inclusive Care for the Elderly (PACE) program in San Diego,
California, provides formerly homeless older adults subsidized housing with wrap-
around supportive services, including primary and specialty health services, medication
assistance, mental health services, occupational therapy, and dentistry, as well as meals
and nutrition counseling, social activities,
social services, and transportation
assistance.
Moreover, during the COVID-19 pandemic,
numerous federal, state, and local agencies
provided additional assistance to older adults
experiencing homelessness to access shelter,
housing, and services through increased funding,
policy changes or waivers, and new service
delivery models. Many of these innovations may
be continued or expanded to better serve
vulnerable older adults, especially those who
experience homelessness.
ADDRESSING GAPS IN SERVICE DELIVERY AND COORDINATION
The environmental scan and discussions identified a number of critical gaps in housing and
service availability, accessibility, delivery, and coordination. The following interventions and
Examples of Programs Implemented
During the Pandemic
• Expanded eviction prevention
resources.
• Placement of people experiencing
homelessness into motel rooms.
• Medicare coverage of telehealth
services.
• USDA’s SNAP Online Purchasing Pilot.
9
policy changes offer strategies to enable providers and policymakers to better meet the
housing and support needs of older adults experiencing housing instability and homelessness.
• Identification, outreach, and navigation services particularly targeted to older adults
experiencing homelessness who have specific barriers to receiving assistance, such as
fears of losing their independence or difficulty understanding eligibility requirements
Few non-homelessness providers with whom older adults are connected, such as health
clinics and benefits offices (e.g., Supplemental Nutrition Assistance Program [SNAP]
offices), routinely screen for risk of homelessness. Older adults experiencing
homelessness for the first time may not know what types of assistance are available or
where to go to get it. They may also wait too long to request assistance to maintain
their housing. Older adults experiencing homelessness need resources and assistance to
learn about both the available supports for which they are eligible and the processes of
applying for and accessing these supports.
• Increased access to benefits and services to provide a greater number of older adults at
risk of or experiencing homelessness the assistance they need to address housing, health,
and other challenges. Experts noted that restrictive eligibility criteria such as strict income
and/or asset requirements, age or disability requirements, and other restrictions prevent
or complicate access to key services for older adults experiencing homelessness.
• Crisis and interim housing tailored to older adults. There is a need for emergency
shelter accommodations that include beds that are on the first floor or bottom bunk,
24-hour access to bedrooms and bathrooms, and refrigeration or locked storage for
medications and medical supplies, as well as crisis or interim housing accessible to older
adults with limited mobility, difficulties with ADLs, and needing assistance with limited
health care and medication management.
• Permanent supportive housing tailored to older adults with histories of homelessness.
Older adults with histories of homelessness often have greater functional impairments
and behavioral health challenges, as well as limited connection to their communities.
There is a need for permanent supportive housing with physical accommodations (e.g.,
wheelchair accessible buildings, grab bars in units) to address these needs as well as
access to the types of case management and nursing assistance (e.g., medication
management, wound care) that will allow them to age in place.
• Consistent case management assistance to assist older adults with accessing the
housing and other supports they need.
• Increased capacity of affordable housing. More permanent supportive housing is
needed, as well as a continuum of supports to provide tailored assistance to a diverse
population of individuals, ranging from those who may need only shallow rental
subsidies to those who need intensive medical management and support services.
• Coordination across systems to address the variety and unique needs of older adults
experiencing homelessness. Barriers to coordination include siloed funding streams,
varying eligibility criteria, overburdened staff, and data sharing barriers.
10
GAPS IN KNOWLEDGE
Gaps in knowledge include a lack of:
• Research around equity in services and outcomes.
• Research on the connection between health and homelessness among older adults.
• Documentation of the types of assistance available to older adults and their respective
eligibility criteria and enrollment requirements.
• Additional data on older adults experiencing homelessness.
POTENTIAL STRATEGIES
Through the information identified in this scan, we offer a number of potential strategies for
policymakers and service providers to better identify and serve older adults at risk of or
experiencing homelessness. Strategies for policymakers at federal, state, and local levels to
consider include:
• Additional prevention resources for older adults at risk of homelessness, including
short-term rental assistance, resources to help with property taxes, and assistance with
home maintenance costs.
• Assistance with other costs of living, including food, transportation, and other expenses
that would allow rent-burdened older adults to meet their needs.
• Additional types of affordable housing assistance, such as shallow subsidies and
affordable assisted living.
• Expanded state coverage for home and community-based services (HCBS), such as
assistance with medication management and wound care; assistance with ADLs; and
home management services, to help support individuals as they age.
• Identification of older adults by HUD as a key sub-population in its Annual
Homelessness Assessment Reports to provide more national data on older adults
experiencing homelessness.
• Better cross-system coordination, including through shared goals, flexible or blended
funding streams, better integrated data, and coordination between the No Wrong Door
Initiative with coordinated entry systems.
• Continuation of demonstration projects started during the pandemic, such as the U.S.
Department of Agriculture (USDA)’s SNAP Online Purchasing Pilot, that facilitated
access to services for older adults with limited mobility as well as flexibilities around
Medicaid enrollment and housing vouchers.
Potential strategies for service providers include:
• More proactive identification by service providers, such as health clinics and those
participating in the No Wrong Door Initiative, of older adults who are severely rent-
burdened or otherwise at risk of homelessness.
11
• Better documentation of services and supports available in local communities to enable
older adults at risk of or experiencing homelessness to know what assistance is
available and how they can access it.
• Additional assistance accessing medical equipment, such as eyeglasses and hearing
aids, that may be damaged or lost while people experience homelessness.
• Training for case management staff on issues specific to older adults.
• Improved access to income assistance for eligible individuals through programs such as
Supplemental Security Income (SSI) and Social Security Disability Insurance (SSDI)
Outreach, Access, and Recovery (SOAR) to provide a sustainable source of income for a
larger share of older adults experiencing homelessness.

12
Section 1. Introduction
The number of older adults living in poverty is
increasing (Li & Dalaker, 2021) due in part to the
aging of the United States population overall,
coupled with the growing affordable housing
crisis (Aurand et al., 2021) and the public health
and economic crises that resulted from the
Coronavirus Disease 19 (COVID-19) pandemic.
Older adults are increasingly likely to be housing
cost-burdened (i.e., housing costs require more
than 30 percent of household income) and
severely housing cost-burdened (i.e., housing
costs require more than 50 percent of household
income). In 2019, around 5 million households headed by someone aged 65 or older paid at
least 30 percent of their income on rent, and another 5 million paid at least 50 percent (Joint
Center for Housing Studies, 2019). Not surprisingly, the population of older adults at risk of or
experiencing homelessness is also growing rapidly and is projected to continue to grow over the
next decade (Culhane et al., 2013; Culhane et al., 2019). Until recently, older adults who
experience homelessness have largely struggled with housing issues throughout much of their
adult lives (Culhane et al., 2013), concomitant with other health and life challenges. Yet, recent
research has identified a growing subgroup of older adults who become homeless for the first
time after the age of 50, due largely to economic factors (Brown et al., 2016; Crane et al., 2005;
Shinn et al., 2007).
The growth in this population and the different pathways they follow into homelessness
underscore the critical importance of understanding the needs of this vulnerable population
and what services and housing can best address them. Drawing on published literature and
interviews with researchers, providers, and people experiencing homelessness, this report
provides an overview of the characteristics and needs of older adults at risk of or experiencing
homelessness, differences between individuals who are newly experiencing homelessness in
older age and those who first experienced homelessness earlier in life, and the types of
services, housing, and supports needed to serve them. Using an equity lens, we examine these
topics with attention to what is known about racial and ethnic groups disproportionately
impacted by homelessness. Finally, we add to this summary an exploration of the programs,
policies, services, and supports that exist to prevent and address homelessness across the
systems that serve older adults. Brought together, the research and systems’ offerings provide
a roadmap for determining what is available now to both prevent homelessness among those
at risk as well as what is available to serve those who are experiencing homelessness. We
highlight the challenges older adults face in accessing the assistance they need, innovative
practices, especially those implemented during the COVID-19 pandemic that could ease these
challenges, and remaining gaps that exist that need to be filled to effectively tackle the
problem.
Terminology
Throughout the report, we use the term
“older” adults to refer to people 50
years of age and older, and the term
“senior” to refer to people 62 years of
age and older. We use the term
“elderly” only when referring to specific
eligibility criteria for the various
programs and services discussed.
13
OVERVIEW OF REPORT
Section 2 provides a discussion of the population of older adults experiencing homelessness,
including the prevalence of and pathways into homelessness. We examine the characteristics
and needs of older adults experiencing homelessness, including sociodemographic
characteristics, health and behavioral health conditions, and basic needs. Where possible, we
compare these characteristics and needs to those of housed older adults as well as to younger
adults who are homeless to understand how the characteristics and needs of older adults
experiencing homelessness may be unique. Section 3 addresses the systems and services
available to serve older adults at risk of or experiencing homelessness, including homelessness
and housing supports, health and behavioral health services, income supports, and other basic
needs assistance programs. For each of these service areas, we describe the assistance
available to low-income older adults generally and to older adults experiencing homelessness
specifically. We highlight challenges older adults face in accessing assistance and innovative
programs or strategies available to serve them. We also address changes in policies or practices
during the COVID-19 pandemic to facilitate access to needed services for older adults
experiencing homelessness may be beneficial to continue post-pandemic. In Section 4, we
identify critical gaps in the housing and services available to meet the needs of older adults at
risk of or experiencing homelessness and in existing research. We end with potential strategies
to better identify and serve older adults at risk of or experiencing homelessness.
METHODOLOGY
This report incorporates findings from an environmental scan, including a review and synthesis
of published research, evaluations, and white papers, discussions with subject matter experts
and housing and service providers, and interviews with people with lived experience of
homelessness in older adulthood. Each of these methods is described in further detail in the
Appendix. For the environmental scan, we used a systems approach for identifying key
resources, including focused searches on literature and other resources within the fields of
homelessness and housing, health and behavioral health, and aging. We also conducted
discussions with a diverse set of subject matter experts and housing and service providers.
Throughout the report, these individuals are referred to as experts and providers. We also
collected data through tailored conversations from individuals between the ages of 56 and 74
who were experiencing or had experienced homelessness as older adults. Six people were
currently experiencing homelessness at the time of the discussion and were staying in shelters,
in tents, or on the sidewalk. Eight people were housed, with seven in permanent supportive
housing and one in low-income housing. The goals of these conversations were to learn more
about their experiences accessing the housing, supports they needed, and challenges they
faced.

14
Section 2. Size, Characteristics, and Needs of the Population of Older
Adults Experiencing Homelessness
PREVALENCE OF HOMELESSNESS AMONG OLDER ADULTS
Homelessness among older adults is increasing, with a growing proportion of the population
experiencing homelessness aged 50 and older.
1
People aged 50 and older are the fastest-growing age group of those experiencing
homelessness, and their numbers are estimated to triple by 2030 (Culhane et al., 2019).
According to the U.S. Department of Housing and Urban Development (HUD), in 2021, people
aged 55 and older composed 19.8 percent of the sheltered homeless population (HUD, 2023),
an increase from 17.9 percent in 2020. This rate is even higher when we focus on adult-only
households experiencing homelessness: 28.7 percent in 2021 (HUD, 2023). Among sheltered
homeless adults with chronic patterns of homeless, those aged 55-64 made up the largest share
of people experiencing chronic homelessness (27.0 percent), and a total of 35.7 percent were
aged 55 and older in 2021 (HUD, 2023). The percentage of individuals aged 51 and older in
emergency shelters, transitional housing, and safe havens increased more than 10 percent in a
decade, from 23.0 percent in 2007 to 33.8 percent in 2017
2
(HUD, 2018). Among people
experiencing sheltered homelessness, people ages 55-64 compose a larger proportion (14.7
percent in 2021) than those ages 65 and older (5.1 percent in 2021) (HUD, 2023). In addition,
the percentage of older adults in permanent supportive housing grew during this time from
23.9 percent in 2007 to 38.7 percent in 2017 (HUD, 2018).
Age is the predominant way to define older adults experiencing homelessness, though the
specific age is not universally agreed upon in the literature or in practice.
Most current research on older adults at risk of or experiencing homelessness focuses on those
who are 50 and older. The experts with whom we spoke agreed that defining older adults in
this way makes sense for both research and practical purposes, because the health and mobility
of adults experiencing homelessness at age 50 is similar to that of housed adults who are 15-20
years older. Housing and service providers, on the other hand, noted that they are often
required to define older adults as age 55 and older or 62 and older because of eligibility
restrictions imposed by their programmatic funding sources. For example, Supportive Housing
for the Elderly vouchers provide rental assistance and supportive services to low-income
households that include at least one member who is 62 years or older. Individuals 55 and over
are eligible for other HUD-funded assistance for elderly and disabled households such as
1
In its Annual Homelessness Assessment Reports to Congress, HUD publishes the percentage of people
experiencing unsheltered homelessness only for three age groups: under 18, 18-24, and over 24. Data for older
adults (55-64 and 65 and older) are only available for sheltered populations.
2
In HUD’s Annual Homelessness Assessment Reports to Congress, the age categories for older adults changed in
2017 from 51-62 and 62 and older to 55-64 and 65 and older in 2018. Thus, we cannot measure changes over
time in the size of the population of older adults experiencing sheltered homelessness from before 2017 to
present.
15
Housing Choice Vouchers and public housing. Nutrition assistance, such as Meals on Wheels, is
provided by State Units on Aging and Area Agencies on Aging to adults aged 60 and older. To
provide services to individuals under 55, service providers often must use private funding
sources.
A couple of experts suggested, however, that defining “older adults” among those experiencing
homelessness, especially in relation to determining eligibility for assistance, should be based on
individuals’ health needs or functional limitations rather than age-based criteria alone. They
noted that many adults experiencing homelessness in their 40s and 50s have disabilities
requiring the same level of services and supports typically provided to older adults. Moreover,
due to increased mortality rates among people experiencing homelessness, many of these
individuals never reach “older adult” ages. One provider indicated, however, that there was
insufficient age granularity in data collected on adults experiencing homelessness to best
determine at which ages physical and mental health vulnerabilities are heightened, knowledge
that could help guide the categorization of older adults among those experiencing
homelessness.
PATHWAYS INTO HOMELESSNESS FOR OLDER ADULTS
Income supports for older adults at risk of homelessness are often insufficient to cover their
expenses.
SSI and SSDI are often the primary sources of income for older adults at risk of or experiencing
homelessness, with earned income, panhandling, and monetary assistance from relatives as
supplementary sources (Cohen et al., 1999; Garibaldi et al., 2005; Gonyea et al., 2010). These
income supports are often insufficient to cover the cost of housing and other expenses
(Airgood-Obrycki, 2019). Living on limited, fixed incomes, older adults experience housing cost
burden more frequently than the general population, potentially resulting in housing loss
(Sermons & Henry, 2010). According to the Joint Center on Housing Studies of Harvard
University, people older than age 50 have the highest risk of paying more than 30 percent of
their income on rent or mortgage, with as many as one half of renters ages 50 and older doing
so in 2018 (Joint Center for Housing Studies, 2018). Approximately 10 million households
headed by someone over age 65 pay at least 30 percent of their income on housing, and half of
those pay over 50 percent (Joint Center for Housing Studies, 2019). Nationally, more than 1.7
million extremely low-income renter households with an older adult are severely cost-
burdened, spending more than half their income on rent (Prunhuber & Kwok, 2021). Being cost-
burdened by housing limits resources available for other expenses, including health care,
transportation, and healthy food. With an overwhelming portion of their incomes dedicated to
rent, many severely rent-burdened older adults go without heat, food, or medication to pay
their rent (Prunhuber & Kwok, 2021). Cost-burdened older adults are more likely to report an
inability to fill a prescription or adhere to health care treatments due to cost (Center for
Housing Policy, 2015). Moreover, the challenge of affording housing on limited incomes is
exacerbated for Black and Latinx older renters, who are more likely than White older renters to
16
have insufficient income and few assets as they enter retirement years (Prunhuber & Kwok,
2021).
The population of older homeless adults is comprised of two subgroups with different
trajectories into homelessness.
The growth of homelessness among older adults can be attributed to two trends: aging of those
who first experienced homelessness earlier in life and continue to experience homelessness as
older adults, and those experiencing homelessness for the first time in older age.
Older adults who first experienced homelessness earlier in their lives represent a cohort effect:
individuals born in the second half of the post-World War II baby boom (1954-1963) who have
had an elevated risk of homelessness throughout their lives and have reached aged 50 and
older in the last decade (Culhane et al., 2013). This group of individuals became adults in a time
when there was an oversupply of workers and undersupply of housing, resulting in depressed
wages, high unemployment, and increased rents. These inauspicious circumstances combined
with back-to-back recessions in the late 1970s and early 1980s contributed to intermittent
employment in low-wage jobs and frequent periods of unemployment (Culhane et al., 2013),
and subsequently, increased vulnerability to housing instability and homelessness throughout
their lives. Moreover, this group of older adults experiencing homelessness typically have had
more risk factors (e.g., mental health and substance use disorders) for homelessness
throughout their lives than older adults who first experience homelessness after age 50, thus
increasing their vulnerability to homelessness throughout their lives (Culhane et al., 2013;
Brown et al., 2016). In discussions, experts and providers noted that whereas these individuals
may have initially entered homelessness as younger adults due to economic factors, they often
are unable to regain long-term stability due to physical or behavioral health challenges.
The second group of older adults are people who experience homelessness for the first time
after age 50, largely due to economic instability in their later years. In the Health Outcomes in
People Experiencing Homelessness in Older Middle Age (HOPE HOME) study, almost one-half of
the 350 older adults included in the sample (43 percent) had not experienced homelessness
before age 50 (Brown et al., 2016). In a qualitative study including 79 older adults experiencing
homelessness, Shinn and colleagues (2007) similarly found that over half of the respondents
lived relatively stable lives, typically involving long periods of employment and residential
stability, before becoming homeless at an average age of 59. In an international study of adults
aged 50 and older newly experiencing homelessness in Boston, England, and Melbourne, Crane
and colleagues found that only about one-third of the sample had experienced homelessness
prior to the current episode (Crane et al., 2005). For older adults experiencing homelessness for
the first time, homelessness is often caused by stressful life events, such as the death of a
spouse, divorce, loss of work, eviction, or the onset of health problems, coupled with limited or
fixed incomes (Cohen, 2004; Crane et al., 2005). Seniors and people with disabilities compose
nearly half of renters with extremely low incomes (i.e., at or below the poverty guideline or 30
percent of the area median income) (Aurand et al., 2021), making them vulnerable to
homelessness when stressful events occur (Brown et al., 2016; Kushel, 2020).

17
Experts and providers reinforced these findings: older adults relying on decreased or fixed
incomes often cannot withstand rising housing costs, including increasing rents, increasing
property taxes, and ongoing home maintenance costs. One expert noted that most states do
not have rent control or eviction protection. Another noted that few, if any, tax relief programs
are available nationally for older adults who cannot afford their property taxes, so increasing
house values can lead to financial strain even for those who own their own homes. Additional
factors experts and providers noted that can exacerbate older adults’ risk of homelessness
include financial exploitation, decreased perception of risk that can accompany cognitive aging,
and loss of social supports as family and friends move or pass away. Multiple interviewees
reported that individuals who have been self-reliant for many years often do not reach out for
assistance until their situation is dire due to shame or lack of knowledge about the supports
available offered and how to navigate the system.
These findings also were reflected in the
experiences of the people with lived experience
with whom we spoke. Among the 14 older adults
we engaged in conversation, the majority
indicated they had multiple experiences with
homelessness throughout their lifetimes; two
people experienced homelessness for the first
time as older adults. Both of the newly homeless
individuals reported their homelessness was
caused by changes in their incomes. One individual lost her housing when her rent increased
and her husband’s income declined. Another lost his housing when health problems prevented
him from doing his job. Among those who had previous experiences with homelessness, four
people attributed their recent experiences to mental health issues and substance use disorder,
and two people reported physical injuries led them to lose their jobs and subsequently their
housing. Two people reported having lost their most recent housing when a loved one passed
away and one person reported his house burned down and they had no other place to go. The
remaining three individuals did not cite a cause for their recent homelessness.
CHARACTERISTICS OF OLDER ADULTS EXPERIENCING HOMELESSNESS
Older adults who experienced homelessness earlier in life differ significantly on a range of
characteristics and needs from older adults who first experience homelessness after the age
of 50.
Early evidence suggests that older adults who experienced homelessness earlier in life have had
more vulnerabilities throughout their lives than older adults with later entry into homelessness.
Older adults with earlier experiences of homelessness have more adverse childhood
experiences, chronic medical conditions, drug use, and out-of-home placement during
childhood; more mental health, alcohol and drug use, and incarceration during young
adulthood; and more underemployment, drug use, and traumatic brain injury during middle
adulthood (Brown et al., 2016). In contrast, individuals with later onset homelessness have
“I got peripheral neuropathy in my
hands. My occupation was a ballet
accompanist. When my hands started
getting numb from the peripheral
neuropathy, I could not do that, the line
of work, anymore… That was the first
time that I was not working.” – Male, 65
18
typically been married, held jobs, and maintained housing in the past but experience
homelessness for the first time after age 50 (Brown et al., 2016; Shinn et al., 2007). Although
often living in poverty throughout their adult lives, these individuals have long work histories,
usually in low-paying, physically demanding work.
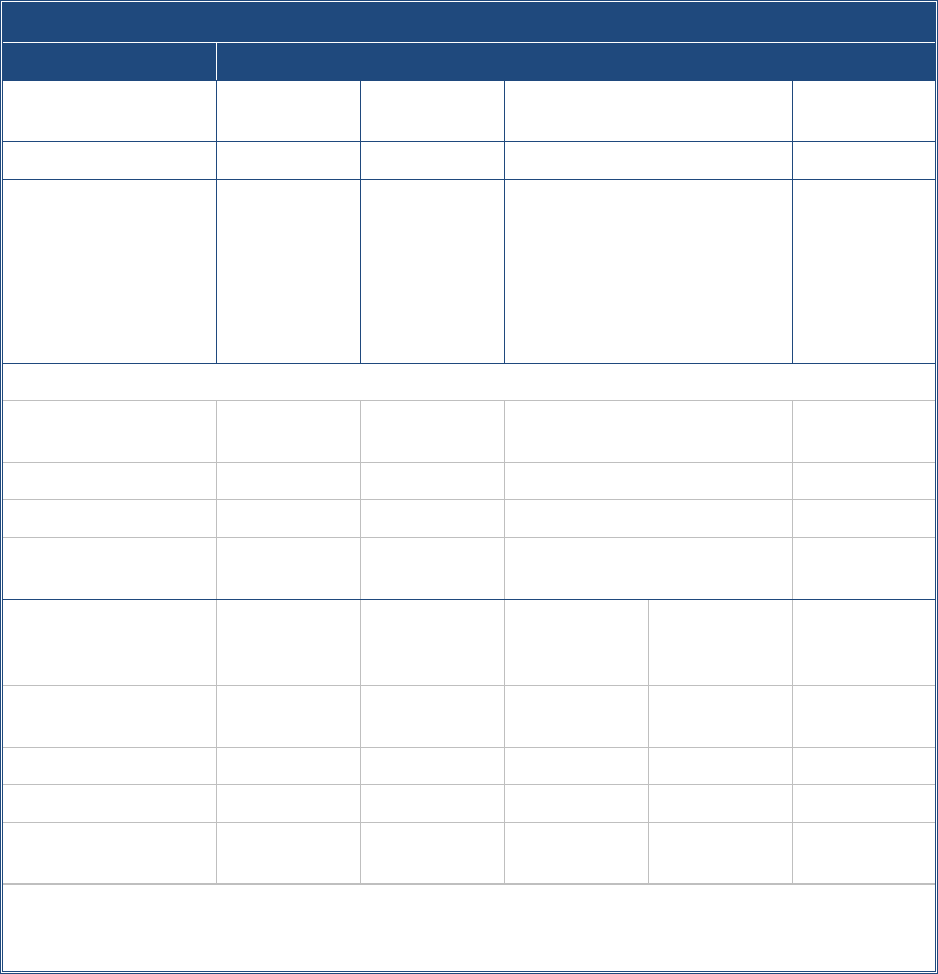
Exhibit 1. Sample Racial/Ethnic Composition for Studies of Older Adults Experiencing Homelessness
Category
Studies of Older Adults Experiencing Homelessness
Study
Brown et al.,
2010
Brown et al.,
2015
Garibaldi et al., 2005
Gordon et al.,
2012
Location
Oakland
Boston
Pittsburgh and Philadelphia
Multi-site
Sample
1
776 older
adult
attendees (50
and older) at
an outreach
event
204 older
adults (50 and
older)
recruited from
emergency
shelters
74 older adults (50 and older)
recruited from unsheltered
enclaves, shelters, and
transitional housing or single-
room occupancy dwellings
408 older
adults (55 and
older)
experiencing
homelessness
with mental
illness
Racial/Ethnic Composition of Sample
2
Black/African
American
54%
40%
81%
28%
White/Caucasian
29%
40%
19%
60%
Latino
8%
10%
--
--
Multiracial/Other
races
9%
9%
--
13%
Racial/Ethnic
Composition of Overall
Population
3
Oakland
Boston
Pittsburgh
Philadelphia
N/A
Black/African
American
22%
24%
23%
41%
White/Caucasian
29%
44%
64%
35%
Latino
27%
20%
4%
15%
Multiracial/Other
races
9%
10%
5%
5%
1
These samples of older adults are often sub-sets of larger samples included in the studies.
2
Terminology reflects that used in the included studies.
3
U.S. Census, 2021.
Those who first experienced homelessness prior to age 50 typically have experienced
homelessness for longer periods of time overall and in their current or recent episodes.
Not surprisingly, older adults who first experienced homelessness prior to age 50 have spent
more time homeless (4.2 years) than those individuals whose first homelessness occurred at
age 50 or older (2.0 years) (Brown et al., 2016). In the HOPE HOME study, the two groups also
19
differed in the length of their current episode of homelessness. Nearly three-fourths (73
percent) of those with first homelessness before age 50 were continuously homeless for one
year or longer in their current episode, compared to 60 percent of those who first experienced
homelessness after the age of 50 (Brown et al., 2016). Those with earlier experiences of
homelessness also spent a greater period of time during the three-year follow-up period living
in unsheltered and institutional settings (shelters, jails, transitional housing), whereas
individuals newly experiencing homelessness as older adults spent greater periods of time
cohabiting or living in rental housing during the follow-up period (Lee et al., 2016).
The limited data available on the racial/ethnic composition of the population of older adults
experiencing homelessness suggests an overrepresentation of people of color.
Data on racial/ethnic composition for this population are available only from a handful of
regional studies. Exhibit 1 provides the racial/ethnic background of each of the study
populations. These studies vary considerably in the geographic area in which they are set and in
the sampling strategies used to identify the population. Despite the differences in how they
were conducted and in their specific findings, each study found a larger percentage of African
Americans experiencing homelessness than the broader population, a finding that is similar to
national data on the overall population of people experiencing homelessness (HUD, 2020;
Moses, 2019).
SERVICE NEEDS OF OLDER ADULTS EXPERIENCING HOMELESSNESS
In this section, we review the service needs of older adults experiencing homelessness and how
they compare to the needs of older housed adults and younger adults experiencing
homelessness. Where available, we include evidence on the differences between the subgroups
of older adults experiencing homelessness for the first time compared to those who have
previously experienced homelessness and between racial/ethnic groups that are
disproportionately likely to experience homelessness.
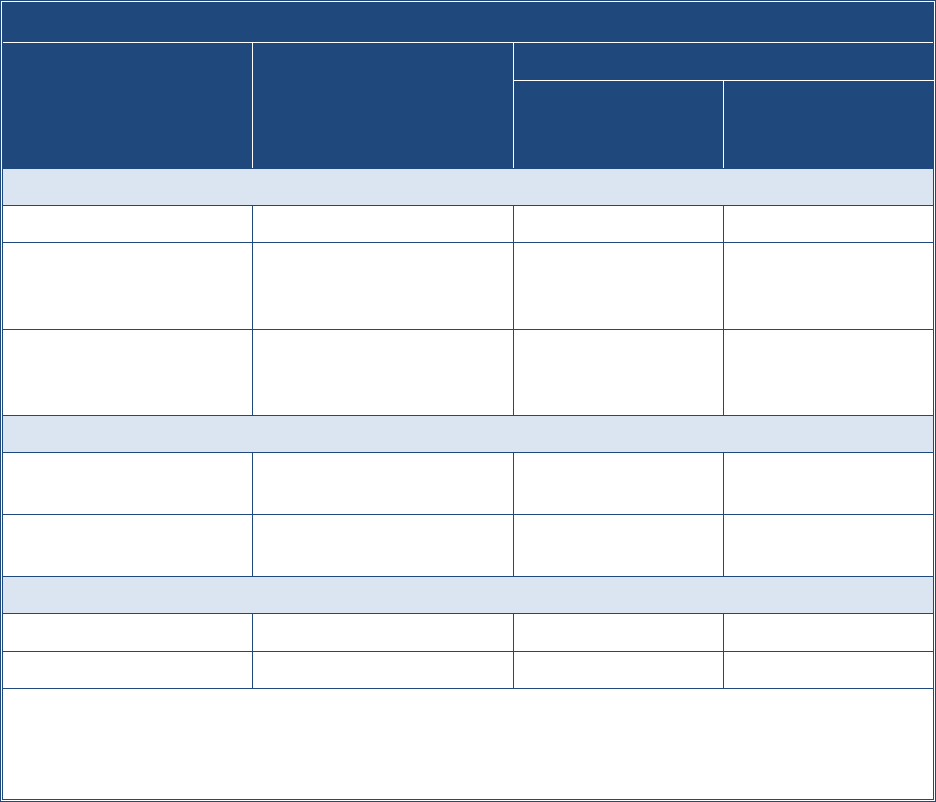
Exhibit 2 provides a summary of the characteristics and service needs of older adults
experiencing homelessness presented here in comparison to older housed adults and younger
homeless adults.
20
Exhibit 2. Comparison of Characteristics and Needs of Older Adults Experiencing Homelessness
Older Adults Experiencing
Homelessness
Finding
Compared to:
Older Housed Adults
Younger Adults
Experiencing
Homelessness
Physical Health Needs
Average life expectancy
64-69 years
Shorter life expectancy
---
Rates of health and
geriatric conditions
30-39% ADL impairment;
21-59% experience
hypertension
Higher rates
Higher rates
Utilization of acute
health care services
43-70% have emergency
department visits;
10-43% have hospitalizations
Higher utilization
Comparable rates
Behavioral Health Needs
Rates of mental health
conditions
~40%
Higher rates
1
No clear patterns
2
Rates of substance use
disorder
26-63%
Higher rates
No clear patterns
Basic Needs
Rates of food insecurity
~55%
Higher rates
3
Higher rates
Lack of transportation
---
---
---
1
As compared to 3 nationally representative samples of older adults.
2
Indicates studies show inconsistent findings on the differences between older and younger adults
experiencing homelessness.
3
As compared to national estimates of population living in poverty.
Physical Health Needs
Older adults experiencing homelessness have significantly shorter life spans than housed
older adults, though they die from similar chronic conditions.
Studies consistently document a shorter life span of older adults experiencing homelessness
despite the range of sub-populations studied, including individuals staying in shelters in New
York City (Metraux et al., 2011); veterans in transitional homeless programs (Schinka et al.,
2017; Schinka & Byrne, 2018); and individuals experiencing homelessness in Oakland, California
(Brown et al., 2016; Kushel, 2020). For example, Metraux and colleagues (2011) matched
administrative records for adults staying in the New York City shelter system with death records
from the Social Security Administration. They found that older adults experiencing
homelessness have a life expectancy of approximately 64 years for men and 69 years for
women (Metraux et al., 2011), compared to national life expectancies of 76 years for men and
81 years for women (Xu et al., 2020). Further, Hwang and colleagues (1997; 2008) found that
both older adults experiencing chronic homelessness and those who first became homeless
later in life had elevated mortality rates. Finally, although the most common causes of death
21
among older homeless adults are similar to housed older adults, for example, cancer and
cardiovascular disease, these illnesses occur approximately 20 years earlier (Kushel, 2020).
Older adults experiencing homelessness have health challenges similar to older adults who
are housed but who are of more advanced ages.
Adults experiencing homelessness between ages 50 and 62 often have health conditions that
are more severe than housed individuals their own age, but similar to those of housed people
who are 10-20 years older (Cohen, 1999; Gelberg et al., 1990; HPRI, 2019; Brown et al., 2016).
Compared to their housed counterparts, older adults experiencing homelessness have a higher
prevalence and severity of physical and geriatric conditions including memory loss, falls,
difficulty performing ADLs, and cognitive impairment (Brown et al., 2011; Brown et al., 2017;
Hahn et al., 2006; Hwang et al., 1997). Moreover, comorbid conditions among older adults
experiencing homelessness are common, including hypertension, arthritis, cognitive
impairment, frailty, hearing difficulty, and urinary incontinence (Kushel, 2020; Brown et al.,
2011, Brown et al., 2016; Brown, 2017; Gelberg et al., 1990). Additionally, in discussions,
experts and providers noted that sleep deprivation resulting from sleeping in unsheltered
locations such as tents or cars or in shelters that were crowded or offered limited hours of
access exacerbated older adults’ physical and mental health challenges and accelerated
cognitive decline.
Older adults have different health conditions than younger adults who are homeless, though
adults of all ages experiencing homelessness have poorer health status than those who are
housed.
Among those experiencing homelessness, older adults compared to younger adults have higher
rates of chronic illnesses such as high blood pressure; geriatric conditions, including arthritis,
and functional disability; and cognitive impairments (Garibaldi et al., 2005; Gelberg et al., 1990).
To illustrate, in a cross-sectional, community-based survey of homeless adults in two United
States cities, older adults were 3.6 times as likely to have a chronic medical condition as those
under age 50 (Garibaldi et al., 2005). Older adults also were more likely to report two or more
medical conditions (59 percent vs 28 percent) compared to the younger adults experiencing
homelessness (Garibaldi et al., 2005). A five-year study of 28,000 adults who received care at
the Boston Health Care for the Homeless Program reported death rates of almost 2.5 times
higher for those ages 45-64 compared to those ages 25-44 (Baggett et al., 2013). When
compared to the general housed population of the same ages, people 25-44 years old
experiencing homelessness had mortality rates 9 times higher, while people 45-64 years old
experiencing homelessness had mortality rates 4.5 times higher (Baggett et al., 2013).
Older adults experiencing homelessness utilize acute health care services at high rates and
significantly more than the general population of older adults.
Older adults experiencing homelessness use acute health care services at high rates, with rates
across studies ranging from 43 percent to 70 percent for emergency department visits and 10-
43 percent for inpatient hospitalizations (Brown et al., 2010; Brown et al., 2011; Raven et al.,
2017). Very few studies have compared national rates of acute health care services utilization
between older adults experiencing homelessness to those of their housed counterparts. In a
22
study comparing older adults experiencing homelessness in Boston to three nationally
representative samples of older adults, 43 percent of the older homeless adults had been
admitted to the hospital more than once in the prior year compared to 11 percent of the
nationally representative sample. Moreover, whereas 70 percent of the older adults
experiencing homelessness had more than one emergency department visit in the prior year,
only 19 percent of the nationally representative sample of older adults did (Brown et al., 2011).
Further, most older adults experiencing homelessness in the sample had received ambulatory
care (87 percent) within the previous 12 months (Brown et al., 2011). A study using a similar
sample of older adults experiencing homelessness found a small proportion of the sample
accounted for half of all emergency departments and inpatient visits; those who spent the
majority of the past six months homeless, either unsheltered or staying in shelters, had
significantly higher rates of emergency department visits than those who had spent most of
their time housed (Brown et al., 2010).
Older adults experiencing homelessness use the emergency department most frequently for
injuries and exposure to violence; complications resulting from substance use, including alcohol
and tobacco; and treatment of mental health disorders (Raven et al., 2017). Among people
experiencing homelessness, emergency departments remain a low-barrier access point to seek
pain management and medical treatment for chronic medical conditions and pain that could be
managed in outpatient settings. Although over two-thirds of the sample of adults 50 and older
experiencing homelessness in the study reported having a regular non-emergency place for
routine care, it was not associated with reduced use of the emergency department (Raven et
al., 2017).
Older adults and younger adults experiencing homelessness use acute health care services at
similar rates, despite differences in having health insurance and a regular health care place or
provider.
In Brown’s 2010 study of health care utilization by people experiencing homelessness, adults
aged 50 and older were more likely to have health insurance, a regular place for health care,
and a regular health care provider (e.g., medical doctor, nurse practitioner, or registered nurse)
than those under 50. However, both groups had similar rates of acute health care utilization in
the prior year, including emergency department visits (43 percent of older adults vs. 49 percent
of younger adults) and inpatient hospitalizations (32 percent of older adults vs. 40 percent of
younger adults) (Brown et al., 2010). This study showed no significant differences between age
groups in the type of visit; most visits were for physical ailments (85 percent for older adults vs.
88 percent for younger adults) as opposed to emotional problems (19.5 percent for both age
groups) (Brown et al., 2010).
Behavioral Health Needs
Older adults experiencing homelessness, especially women, are more likely to have mental
health conditions than older housed adults.
In studies with samples of older adults experiencing homelessness (Brown et al., 2011; Kaplan
et al., 2019), older adults in permanent supportive housing (Henwood et al., 2018), and
veterans (Schinka et al., 2012), between 40 percent and 58 percent either screened for or

23
reported mental health conditions. For example, 56 percent of older adults in permanent
supportive housing reported at least two chronic mental health conditions (Henwood et al.,
2018). Depression was the most common condition identified; other conditions include
schizophrenia and post-traumatic stress disorder. These rates of mental health conditions are
higher among older adults experiencing homelessness than older housed adults (which range
from 18 percent to 34 percent), measured both by diagnoses and symptomology (Brown et al.,
2011; U.S. CDC, 2008).
Some studies find evidence of gender differences in rates of mental health conditions among
older adults experiencing homelessness. Compared to older homeless men, older homeless
women were two and one-half times more likely to have any chronic mental health condition
and more likely to be diagnosed with more mental health conditions (Winetrobe et al., 2017;
Dickins et al., 2021).
Findings from the Health and Retirement Study indicate race and ethnic differences in the
behavioral health conditions of older adults experiencing homelessness. Compared to their
White counterparts, Black and African American older adults experiencing homelessness are
significantly more likely to report a history of illicit drug use and less likely to report a history of
mental illness or domestic violence than White older adults experiencing homelessness
(Chekuri et al., 2016).
Older adults experiencing homelessness also have more substance use disorders than the
general population.
Although there are no studies that directly compare older homeless adults to their housed
counterparts on substance use, a few studies have compared older homeless adults to
population-based samples and to other samples. Studies generally find that a higher percentage
of older adults experiencing homelessness
report alcohol and/or drug use than population-
based samples (e.g., CDC, 2008). In the HOPE
HOME cohort of older adults experiencing
homelessness, for example, rates of binge
drinking were significantly higher in older
homeless adults than in three large-scale studies
of older adults using population-based samples
(30 percent vs. 1 percent, 7 percent, and 3 percent) and a greater percentage of the older
adults experiencing homelessness reported moderate or greater severity of alcohol use (26
percent) than housed adults of all ages (5 percent) served in a U.S. Department of Veterans
Affairs (VA) primary care clinic (Brown et al., 2019). This sample also had a higher rate of
current illicit substance use (63 percent) than a national community-based sample of adults of
all ages experiencing homelessness (23 percent) (Spinelli et al., 2017).
“I've dealt with a lot of trauma as well. I lost
my best friend that I've known since I was
17 years old due to COVID, so there you go
again now. Setback is you start using again,
just to numb the pain, you know what I
mean?” – Male, 59

24
Studies to date yield inconsistent findings on the differences in mental health conditions and
substance use between older and younger adults experiencing homelessness.
It is unclear whether there are age differences in the prevalence of behavioral health conditions
among individuals experiencing homelessness. Whereas some studies have found a higher
prevalence of mental health conditions such as anxiety, depression, and post-traumatic stress
disorder (Garibaldi et al., 2005; Tompsett et al., 2009) among older adults experiencing
homelessness than among their younger counterparts, other studies have found either no
significant differences in the rates of these conditions (DeMallie et al.,1997; Gelberg et al.,
1990) or the opposite finding (Gordon et al., 2012).
Similarly, the limited studies that contrast rates of substance use between older and younger
adults experiencing homelessness yield mixed findings. Some studies suggest that, among
people experiencing homelessness, younger adults are more likely to use drugs than older
adults while older adults may be more likely to use alcohol (DeMallie et al., 1997; Gordon et al.,
2012). Yet other studies fail to find such differences (Hecht & Coyle, 2001; Gelberg et al., 1990)
or find that there is a lower prevalence of substance use disorders for older versus younger
adults experiencing homelessness (Burt et al., 1999; Dietz et al., 2009).
Preliminary evidence suggests older adults who first experienced homelessness earlier in life
are more likely to have behavioral health conditions than those who first experienced
homelessness after age 50.
In the only study to compare differences between newly and chronically homeless older adults,
Brown and colleagues (2016) found that participant characteristics and life course experiences
differed by age at first homelessness. Compared to
individuals whose first homelessness occurred at
age 50 or older, individuals with first homelessness
before age 50 showed a greater prevalence of
behavioral health disorders at different stages in
life. For example, this group had higher rates of
drug use in childhood and mental health problems
in young and middle adulthood, as well as a higher
prevalence of current mental health issues,
including depressive symptoms and post-traumatic
stress disorder, and drug use, and higher rates of
hospitalizations for mental health problems in
adulthood (Brown et al., 2016).
Individuals who had experienced homelessness as older adults reported high rates of physical
and behavioral health problems, echoing findings from the literature.
All of the older individuals with lived experience of homelessness with whom we spoke
discussed suffering from physical and behavioral health problems, including diabetes, HIV,
traumatic brain injury, glaucoma, arthritis, bipolar disorder, post-traumatic stress disorder, and
substance use disorder. A few people also reported having experienced strokes or cancer in the
past. Many of the interviewees, including all of those who were homeless at the time of our
“I mean, I'm going to be 60 years old. It's
getting cold out and… I'm not settled
carrying a backpack around every
freaking day. It's like my back is starting
to bother me. I got health issues. I only
got one kidney that's functioning 40%
because I had cancer a little over a year
ago. That's the second time I had cancer
in 6 years. So, it's like, you know what? I
need to be settled down in a place.” –
Male, 59
25
interview, reported physical pain and mobility issues, often attributed to being unsheltered. For
example, one individual reported they had lost several toes due to frostbite contracted while
being outside in bad weather.
Basic Needs
Older adults experiencing homelessness have high rates of food insecurity.
Food insecurity coupled with insufficient nourishment complicates chronic disease
management and presents a major challenge for older homeless adults who have a high
prevalence of chronic disease and limited mobility (Brown et al., 2011; Patanwala et al., 2018).
Food insufficiency among older adults is associated with significantly greater odds of
hospitalization for any reason, psychiatric hospitalization, and high emergency department
utilization (Baggett et al., 2011). Individuals who are food insecure -- having limited access to
adequate food due to lack of resources -- have poorer health and are more likely to consume
foods deficient in nutrients (Robaina & Martin, 2013). Also, severely cost-burdened older adults
who are in the bottom income quartile reduce their spending on food by 30 percent more than
those who are not cost-burdened (National Association of Area Agencies on Aging [n4a], n.d. b).
Among participants in the HOPE HOME study, over half reported food insecurity, with one-third
reporting low food security and one-quarter reporting very low food security (Tong et al.,
2018), consistent with food insecurity estimates among other homeless populations (e.g.,
Parpouchi et al., 2016) and nearly two times higher than national estimates among the United
States population living in poverty (Coleman-Jensen et al., 2016).
Lack of transportation poses a significant barrier for older adults experiencing homelessness.
Adults experiencing homelessness commonly indicate their most used modes of transportation
include public transit and walking (Chan et al., 2014; North et al., 2017; Murphy, 2019), which
are more difficult for older individuals with mobility challenges. Lack of transportation has been
cited as a barrier for adults experiencing homelessness, as it reduces access to shelter and
housing, medical and behavioral health care, social engagement, food, and other supportive
services (Greysen et al., 2012; Hui & Habib, 2014, 2017; Niño, Loya, & Cuevas, 2009; Murphy,
2019; Turnbull, Muckle, & Masters, 2007). Among studies of older adults experiencing
homelessness, mobility challenges (i.e., difficulty walking without help) and challenges with
instrumental ADLs such as using public transportation are common (Henwood et al., 2018).
Thus, it is reasonable to conclude that older adults experiencing homelessness face
transportation barriers even beyond those of younger adults experiencing homelessness.
However, there is little available research focused on transportation issues specifically among
older adults experiencing homelessness.
Older adults experiencing homelessness, including those who are newly placed into housing,
experience loss of community.
Many of the experts and providers with whom we spoke noted that mobility limitations,
frequent address changes, receipt of housing assistance in a new neighborhood, and the death
of family and friends contribute to formerly homeless older adults having limited social
networks. Multiple interviewees noted that social and physical isolation among this population
can contribute to further cognitive and physical declines. One housing provider noted that
26
formerly homeless older residents in her organization’s properties often struggle to identify
someone who can serve as their medical power of attorney following years of social isolation.
27
Section 3. Systems and Services Available to Serve Older Adults at Risk
of or Experiencing Homelessness
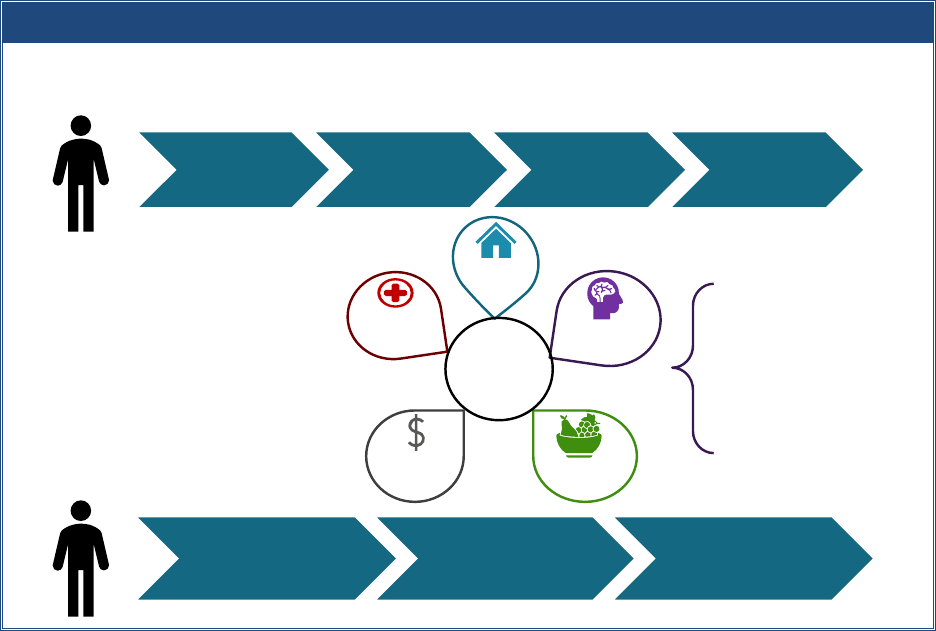
Exhibit 3 presents a conceptual systems framework for understanding the different services
needed by older adults experiencing homelessness and the service delivery systems that may
offer these services. The framework highlights the two subgroups of older adults experiencing
homelessness identified through recent studies and the pathways of services, housing, and
support likely needed to become stably housed. These two subgroups provide a rubric for
understanding the types of assistance older adults experiencing homelessness need, but within
the broader acknowledgement that each person has their own unique history and needs.
Exhibit 3. Systems Framework for Addressing Homelessness Among Older Adults
Older individuals who repeatedly experience homelessness often require extensive outreach
and emergency shelter before obtaining housing and supports. To achieve long-term stability,
many require ongoing case management to help link them to needed health and behavioral
health care, income supports, and other services. In contrast, older adults who have not
previously experienced homelessness, but have experienced adverse events that threaten their
housing stability, tend to need lighter touch or prevention-focused services to regain housing
stability. Critical services for this population are those that help identify them before they
become homeless so that they may be prevented or diverted from homelessness through
various systems’ efforts to connect them to income supports, medical insurance, rental and
utility assistance, nutrition assistance, and transportation assistance. For those who need
Provide crisis
supports
Connect to
housing
Provide
supportive
services
Maintain
supports for
long-term
stability
Prevent/divert
homelessness
Provide housing
assistance, as needed
Connect to needed
long-term supports
First
Homelessness
Earlier in Life
First
Homelessness in
Older Adulthood
Care
coordination
Housing
Behavioral
health
Basic
needs
Income and
Benefits
Systems involved:
- Homeless
- Housing
- Aging
- Veterans
- Health Care & LTC
- Behavioral Health
- Social Services
Health and
Long-Term
Care
28
additional housing assistance, shallow subsidies (limited rental assistance for a longer period of
time) or temporary subsidies and connections to needed supports may be sufficient to help
them get back on their feet (Goldberg et al., 2016; Sermons & Henry, 2010).
We reviewed available information across the systems and sectors shown above for each of the
areas of needs older adults at risk of or experiencing homelessness have (e.g., housing, health
and long-term care, behavioral health, income and benefits, basic needs). We identified the
services, housing, and supports available to low-income older adults and those experiencing
homelessness specifically. We paid particular attention to innovations implemented during the
COVID-19 pandemic that might be continued or expanded to better serve vulnerable older
adults, especially those who experience homelessness. Where documented in the literature, we
discuss the challenges service providers and recipients encounter in providing or receiving
assistance. Finally, we identify the gaps in services and supports in serving older adults
experiencing homelessness.
In this section, we describe the full range of services, housing, and supports available for adults
at risk of or experiencing homelessness available across communities. Not all communities have
all these types of assistance and those that do may have insufficient capacity to meet the need.
In addition, not all are tailored to older adults. We indicate those services that are specifically
targeted to older adults or other activities in place to help older adults access or use the
service.
HOMELESSNESS ASSISTANCE
Homelessness assistance programs are available for older adults who are at risk of or
experiencing homelessness in communities across the country. HUD is the primary funder of
homelessness assistance, which is administered locally through Continuums of Care (CoCs).
Many communities also receive state, local, and private funding for homelessness programs.
This assistance includes:
• Homelessness prevention.
• Identification, engagement, and assessment of people experiencing homelessness such
as outreach programs, drop-in centers, and coordinated entry systems.
• Crisis or interim housing assistance.
Homelessness Prevention
Services available for older adults at risk of becoming homeless that stabilize their housing
situation include energy assistance, home repair programs, and eviction prevention resources.
Local government agencies or non-profit organizations typically administer these programs and
make them available to all low-income households, not specifically elderly households.
Energy assistance programs help with home energy bills, energy crises, weatherization, and
energy-related minor home repairs. These assistance programs are provided through a range of
federal, state, and local funding sources including the U.S. Department of Health and Human
29
Services (HHS) Low-Income Home Energy Assistance Program (LIHEAP) and the Low Income
Household Water Assistance Program, and the U.S. Department of Energy’s Weatherization
Assistance Program.
Home modification and repair assistance programs help older adults address health and safety
hazards in and improve accessibility of their homes to reduce the risk of falls and accidents. The
USDA’s Section 504 Home Repair program and local Area Agencies on Aging offer such
programs. Each program has its own eligibility criteria and application process.
Eviction prevention resources are available for older adults at risk of homelessness. Prior to the
COVID-19 pandemic, this assistance typically included financial assistance for 1-2 months’ rent
and was available through a range of federal, state, and local public and private sources,
including faith-based and non-profit organizations. In response to the financial crisis caused by
the COVID-19 pandemic, the U.S. Department of the Treasury’s (USDT’s) Emergency Rental
Assistance (ERA) Program provided up to 18 months of rental and utility assistance both for
arrears and prospective payments (USDT, n.d.).
3
Eligibility for eviction prevention through this
program was limited to renters with household incomes below 80 percent of the area median
income who experienced COVID-related financial hardship and could demonstrate a risk of
homelessness or housing instability.
Profile of Prevention Services for Older Adults
In New Mexico and Arizona, the Native American Disability Law Center, a non-
profit organization that advocates for the legal rights of Native Americans with
disabilities, creates accounts for their clients in an online benefits application
portal, including setting up email addresses for those who do not have them. This
process helps individuals apply for and track LIHEAP funds, as well as other public
benefits.
The Home Safe Program in California was established in 2018 to support the
safety and housing stability of individuals involved with Adult Protective Services
by providing housing-related assistance using evidence-based practices for
homeless assistance and prevention. Home Safe offers a range of strategies to
prevent homelessness, including housing-related intensive case management,
short-term housing-related financial assistance, deep cleaning to maintain safe
housing, eviction prevention, and landlord mediation (Benioff Homelessness &
Housing Initiative, 2021).
3
Two separate ERA programs were established: ERA1 provides up to $25 billion under the Consolidated
Appropriations Act, 2021, which was enacted on December 27, 2020, and ERA2 provides up to $21.55 billion
under the American Rescue Plan Act of 2021, which was enacted on March 11, 2021. ERA1 ended in September
2022. ERA2 is set to expire in September 2025.

30
Identification, Engagement, and Assessment Programs
Homelessness assistance programs focused on identifying people experiencing homelessness
and engaging them in services include street outreach teams, mobile vans, and drop-in centers,
among others. Most outreach and engagement programs are not limited to older adults;
however, some programs across the country specifically target older adults.
Profile of Outreach Services for Older Adults
Hearth, Inc. in Boston, Massachusetts, funded through both public and private
sources, provides outreach to individuals aged 50 years and older who are at risk
of or experiencing homelessness. A team of six case managers, supervised by a
licensed social worker, visits homeless shelters weekly to identify older adults
needing permanent housing. Outreach workers help these older adults apply for,
locate, and move into subsidized housing and connect to other necessary
services and assistance. The program also employs an “at risk” case manager who
works with older adults who are at risk of homelessness, referred through day
shelters, medical providers, elder services, and visiting nurse association
agencies, among other sources. When at risk elders are identified and enrolled in
the program, the case manager helps to stabilize housing by accessing services
including tenant counseling, landlord mediation, money management, and
eviction prevention (Brown et al., 2013).
Crisis/Interim Housing Programs
Crisis or interim housing
4
is short-term assistance designed to address an immediate housing
crisis. Assistance includes emergency shelter, motel vouchers, and transitional housing.
According to the 2018 Annual Report to the Annual Homeless Assessment Report,
approximately, more than 16 percent of people living in sheltered homeless situations were
over the age of 55 (HUD, 2020), and the rate is increasing. Limited crisis or interim housing
programs are in place specifically for older adults experiencing homelessness.
Profile of Crisis or Interim Housing for Older Adults
One noteworthy program is the Serving Seniors’ Transitional Housing Program in
San Diego, California, which provides transitional housing and supportive services
for 90-120 days to adults aged 62 and older experiencing homelessness. The
program tailors its shelter facilities and services to the specific needs of older
adults, including having facilities accessible to people with mobility challenges
and case management focused on the unique needs of older adults.
4
The terms crisis and interim housing are typically used interchangeably to denote temporary housing situations
people experiencing homelessness may live while looking for permanent housing. In contrast to emergency shelter
and motel vouchers, transitional housing often includes more supportive services and allows longer stays, often up
to 24 months.

31
Challenges with Homelessness Assistance for Older Adults Experiencing Homelessness
Older adults experiencing homelessness may face unique challenges in accessing available
homelessness assistance. In discussions, both experts and providers noted that many older
adults at risk of homelessness do not reach out for assistance until it is too late because they do
not know where to go for help or they are too proud to ask for it. This is particularly true for
those experiencing homelessness for the first time who may lack knowledge about the services
available in their communities or about their eligibility for assistance. For example, many older
renters, particularly those not working prior to the pandemic, may not know they are eligible
for eviction prevention through the ERA Program (Prunhuber, 2021). Providers also report that
older adults who experience homelessness are sometimes difficult to engage in services due to
their belief that participation might result in being “put in a home,” losing their independence
or having their money taken from them (Corporation for Supportive Housing [CSH], 2011).
Finally, age-related hearing and vision loss may contribute to heightened anxiety and lack of
trust.
Those who do know about homelessness assistance may have a hard time accessing it because
of poor health or limited mobility (CSH, 2011; SeniorNavigator, n.d.), or they may lack access to
technology to complete online applications (NCOA, 2022). Accessibility challenges and difficulty
performing ADLs also may make using some assistance, such as emergency shelters, more
difficult (Goldberg et al., 2016).
Equipment such as hearing aids and glasses are
at risk of being broken or lost in both
unsheltered environments and shelters (Kushel,
2012). Shelters closed during the day pose
challenges for older adults who need a safe
location to rest (SeniorNavigator, n.d.). Features
of some shelter environments, such as bunk
beds and shared bathing facilities, may be
difficult for older adults who have medical
conditions and may increase their risk of falls
and injury (Goldberg et al., 2016). Walking long distances or waiting in long lines for food and
other services can limit access for people with mobility issues (National Coalition for the
Homeless, 2009). Finally, limited assistance, such as one-time prevention resources or time-
limited rental assistance, may be insufficient to meet the needs of older adults on limited, fixed
incomes who also have declining health.
Expanded Services During the COVID-19 Pandemic
During the COVID-19 pandemic, numerous federal, state, and local agencies provided additional
assistance to people experiencing homelessness to access shelter, housing, and needed
services. The Coronavirus Aid, Relief, and Economic Security (CARES) Act provided additional
funding for states through existing federal programs, including $45 billion for the Federal
Emergency Management Agency Disaster Relief Fund, $4 billion for Emergency Solutions
“I broke my glasses, because I kept
taking them off and sleeping with them
on the street. I had them cobbled
together with tape, which never quite
fixed them. Eventually, I was given a pair
of hand-me-down glasses [by a case
manager] that were not my prescription,
but it was better than nothing.” –
Female, 51
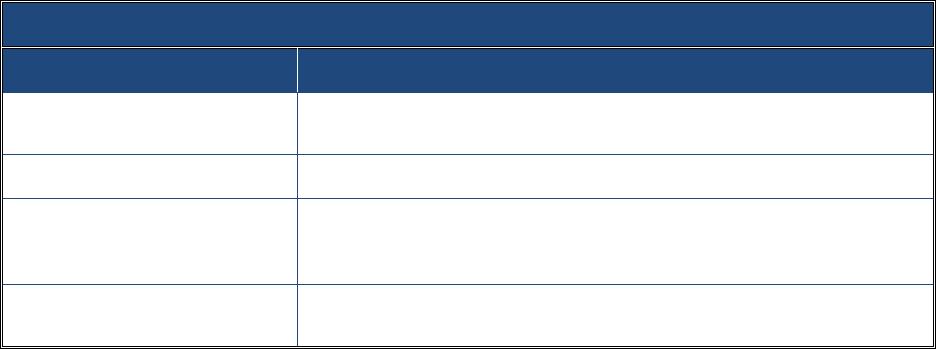
32
Grants, and $5 billion for 11 Community Development Block Grants. Communities could use
these funds to secure, rehabilitate, and maintain sites for non-congregate shelters such as
dorms, motels, and hotels. In discussions, experts and providers noted that efforts such as
California’s Project Roomkey to move older adults experiencing homelessness out of
congregate shelters and off of the streets into motel rooms were practical and compassionate
approaches. These approaches not only provided people with a safe, stable place to stay but
also made it easier for case managers to locate and regularly connect with them.
HOUSING PROGRAMS AND RESIDENTIAL LONG-TERM CARE OPTIONS
Housing assistance programs range from those that provide time-limited assistance to
permanent subsidized options with and without supportive services. Exhibit 4 outlines the
types of housing options available. As noted, however, not all options are available in all
communities or in the quantity needed. Each housing option is described in more detail below.
Based on their examination of the shelter, hospital, and nursing home use by older adults
experiencing homelessness, Culhane and colleagues (2019) argue that the majority of older
adults experiencing homelessness have moderate needs that could be met by rapid re-housing,
shallow rental subsidies, and rental vouchers with light case management. Older adults who
enter homelessness at a later age and have fewer service needs may require more of a “light
touch” approach. Service-intensive assistance, such as permanent supportive housing and
additional supports like palliative care and long-term care (such as personal care to assist with
ADLs), should be reserved for those homeless older adults with the greatest needs (Culhane et
al., 2019). Older adults who have experienced chronic or repeated homelessness are more
likely to fit within this category of higher need.
Exhibit 4. Types of Housing Assistance Available for Older Adults Experiencing Homelessness
Type of Assistance
Description
Rapid re-housing
Time-limited rental assistance, coupled with housing navigation and case
management
Permanent supportive housing
Non-time-limited rental assistance with voluntary supportive services
Subsidized permanent housing
Non-time-limited rental assistance for use in a range of settings, from
scattered single-family houses and apartments to high-rise apartments for
elderly households
Low-income tax credit properties
Properties with certain percentages of units set aside for low-income
households at reduced rents

33
Rapid Re-housing Programs
Rapid re-housing, a Housing First
5
approach, provides access to permanent housing through
time-limited rental assistance along with housing navigation to locate and secure an available
unit, relocation services, and case management (HUD Exchange, n.d.). First developed on a
federal level in 2009 through HUD’s Homelessness Prevention and Rapid Re-housing Program
funded under the American Recovery and Revitalization Act, rapid re-housing has continued to
expand through federal investments, including investments from HUD, VA, HHS, and the U.S.
Department of Labor (DoL). A variety of non-federal investments, including general revenue
funds, and state funding (e.g., federal block grant funds, state housing trust funds) have
increasingly been provided for rapid re-housing programs (Dunton & Brown, 2019).
Most rapid re-housing programs target families or individuals meeting specific eligibility criteria,
such as the Veterans Affairs Supportive Housing program that serves veterans. Although
households served through these programs may include older adults, none are specifically
targeted to older adults (Gubits et al., 2018). According to HUD guidelines, rapid re-housing is
an effective intervention for different types of households experiencing homelessness,
including those with no income, those with disabilities, and those with poor rental history (HUD
Exchange, n.d.). Poor candidates for the intervention, per HUD guidelines, include those
experiencing chronic homelessness and in need of permanent supportive housing, and those
who are seeking a therapeutic residential environment, including those recovering from
substance use disorders (HUD Exchange, n.d.). Additionally, individuals who are on fixed
incomes and unlikely to increase their income over time (including older adults) may be poor
candidates for the intervention as the housing assistance is time-limited.
Permanent Supportive Housing
Permanent supportive housing is a non-time-limited intervention that combines rental
assistance with voluntary supportive services for people experiencing chronic homelessness
(National Alliance to End Homelessness [NAEH], 2021). Eligibility requirements for HUD-funded
permanent supportive housing include one year or more of documented chronic
homelessness,
6
a documented disabling condition (e.g., chronic mental health conditions,
chronic health conditions, and substance use disorders), limited income earning potential, and
a need for intensive case management. Permanent supportive housing programs can be “site-
based” (in an apartment building with multiple units) or “scattered-site” (with units spread
throughout a community).
Permanent supportive housing is an effective solution to homelessness for older adults (Chung
et al., 2018; Henwood et al., 2014; Lipton et al., 2000; Tsemberis et al., 2004), including those
with mental health and substance use disorders (Kushel, 2020; Perl & Bagalman, 2015).
5
Housing First indicates individuals move into permanent housing directly from homelessness rather than
spending a period of time in temporary, service-rich interventions, such as transitional housing, before entering
housing.
6
Chronic homelessness includes one year of consecutive homelessness or four or more episodes of homelessness
within the last three years that accumulate to at least one year.
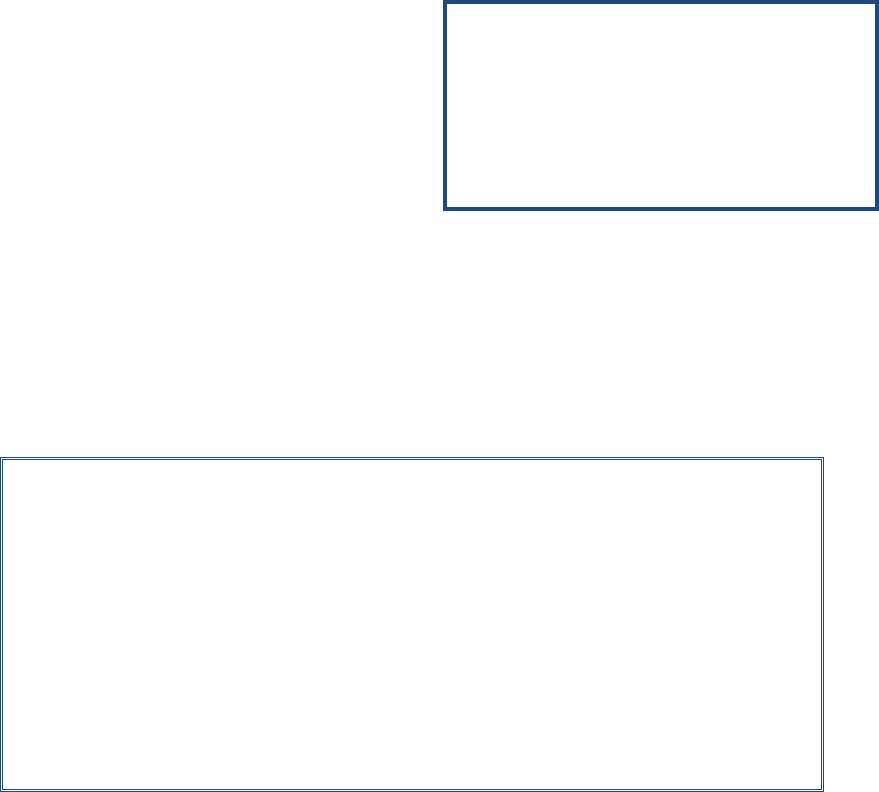
34
Investments in permanent supportive housing have helped decrease the number of chronically
homeless individuals of all ages by 8 percent since 2007 (NAEH, 2021). In addition, through the
use of permanent supportive housing the VA has seen reductions in chronically homeless
veterans, the majority of whom are over the age of 51 (U.S. Interagency Council on
Homelessness, 2018).
Permanent supportive housing is also cost-effective for people with complex health and social
needs (Culhane et al., 2002; Metraux et al., 2003). For example, a study by Bamberger and
Dobbins (2015) found that many formerly homeless older adults who were placed in nursing
homes could be housed successfully in permanent supportive housing at lower cost and with
more independence. Studies of permanent supportive housing serving all populations of adults
document decreases in emergency room visits (Martinez & Burt, 2006), use of emergency
detoxification services (Larimer et al., 2009), and incarcerations (Larimer et al., 2009), as well as
increases in housing stability (Barrow et al., 2004).
Few studies examine outcomes of permanent
supportive housing specifically for older adults.
The few that are available compare older and
younger adults experiencing homelessness. One
study found that older adults in permanent
supportive housing spent fewer days homeless,
had less involvement with the justice system,
and spent more time in independent/single-
room occupancy and congregate/residential settings compared to younger adults in permanent
supportive housing (Henwood et al., 2014). Evidence on other outcomes of permanent
supportive housing for people experiencing homelessness, including severity of mental health
conditions, quality-of-life, substance use, and hospital admissions, is mixed (Aubry et al., 2020).
A number of permanent supportive housing programs across the country are tailored for older
adults who have experienced homelessness.
Profile of Permanent Supportive Housing for Older Adults
In Los Angeles, the Southern California Clinical and Translational Science Institute
is pilot testing the integration of the Community Aging in Place--Advancing Better
Living for Elders (CAPABLE) program with permanent supportive housing for older
adults who have experienced homelessness. CAPABLE is a short-term program
that provides home-based services, such as visiting occupational therapists,
nurses, and handypersons to older adults so that they can age in place. The Los
Angeles pilot program provides CAPABLE services to formerly homeless older
adults who are 50 years or older, live in permanent supportive housing, and
experience difficulties with ADLs.
“I think now the best thing that ever
happened to me, for me to have my own
house, to have a key. I can lay my head
down and I don't have to fear no one
coming in, or being hurt, or anything like
that.” – Male, 59

35
Other Community-Based Housing Options for Older Adults
Housing for older adults is available through local housing providers and public housing
agencies in the form of permanent subsidies (e.g., Section 8 Housing Choice Vouchers and
Section 202 Supportive Housing for the Elderly vouchers), and low-income tax credit properties.
Although these housing options are available to individuals who are at risk of or experiencing
homelessness, eligibility for these options is open to a broader population of low-income older
adults.
Subsidized Permanent Housing involves rental assistance programs that help low-income
individuals afford housing in the private market. Low-income older adults may qualify for long-
term housing assistance through public housing agencies that administer housing assistance
programs and often develop and maintain affordable housing properties. The Housing Act of
1937 first established publicly supported housing to provide decent and safe rental housing for
eligible low-income families, elderly persons, and persons with disabilities (HUD, n.d. a).
Publicly supported housing includes a range of types, from scattered single-family houses and
apartments to high-rise apartments for elderly households.
Two of the largest subsidized housing programs for older adults are the Supportive Housing for
the Elderly (Section 202) and the Housing Choice Voucher (Section 8) programs. Section 202
provides rental assistance and supportive services to low-income households with net incomes
of less than 50 percent of the area median income (or less than 30 percent in some properties)
that include at least one member who is 62 years or older (HUD, n.d. b). Section 202 properties,
operated by private and non-profit housing providers, are designed to accommodate
individuals who need some assistance with ADLs by including grab bars and ramps in the
apartments. Care and supportive services, such as meals, housecleaning, and transportation,
are also typically available at these residences (HUD, n.d. b). The Section 202 program serves
approximately 400,000 households annually (Couch, 2021); residents are, on average, 79 years
old with an average income of less than $10,000. Ninety percent of residents are single women
(Novak, 2018).
Housing Choice Vouchers, formerly referred to as Section 8, can be used in privately owned and
managed properties (i.e., project-based vouchers) or in private units that residents select
themselves (HUD, n.d.). These vouchers are available to households whose total annual income
does not exceed 50 percent of the area median income.
7
Eligibility for Housing Choice
Vouchers is limited to U.S. citizens and non-citizens with eligible immigration status. Housing
Choice Vouchers are not limited to seniors; however, as of 2016, half (51 percent) were elderly
or disabled (Sard, 2018).
Low Income Tax Credit Properties provide another opportunity for affordable housing for older
adults. The Low-Income Housing Tax Credit (LIHTC) program, created by the Tax Reform Act of
1986, provides tax credits for the acquisition, rehabilitation, or new construction of rental
7
A public housing agency is required to provide 75 percent of its vouchers to applicants whose incomes do not
exceed 30 percent of the area median income.
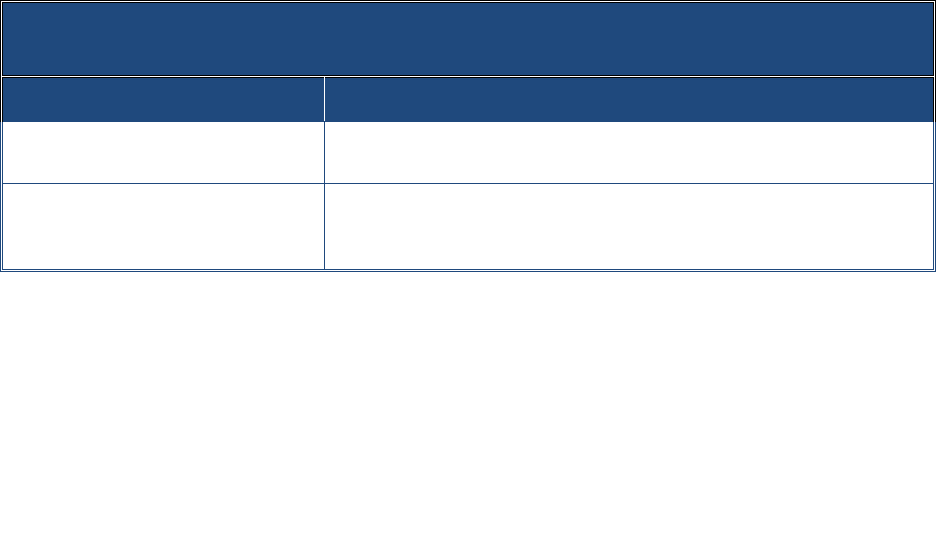
36
housing. LIHTC units are not limited to low-income households; however, 20 percent of units in
LIHTC properties must be rented to households with incomes less than 50 percent of the area
median income or 40 percent of units must be rented to households with incomes less than 60
percent of the area median income. According to HUD data on LIHTC tenant data, more than a
third of households (33.8 percent) in LIHTC properties include at least one resident aged 62 or
older (HUD User, 2019).
Long-Term Care Options for Individuals with High Needs
Exhibit 5 outlines the types of residential long-term care available for individuals needing a high
level of care. These options are primarily for individuals with debilitating health issues or
serious conditions that require frequent medical supervision and round-the-clock care.
Exhibit 5. Types of Residential Long-Term Care Available
for Older Adults Experiencing Homelessness
Type of Assistance
Description
Residential care
A range of congregate care settings that typically include housing,
medical management, supportive services, and social activities
Institutional long-term care
Institutions such as nursing homes for individuals who can no longer live
independently and need a significant amount of supervised care with
meals, assistance with ADLs, and health management
Residential Care settings provide both housing and on-site supportive services for individuals
who need some assistance with ADLs or some amount of supervision because of cognitive
impairments. These residential care settings may provide housing, medical management,
support services, social activities, and, in some cases, assistance with ADLs. Residential care
settings are licensed at the state level. States and localities use over 30 terms to refer to group
housing for older adults, and licensure requirements vary. Depending on the state terminology,
size, and services offered these residential care settings can go by a number of names including
Board and Care Homes, Adult Care Facilities, Residential Care Facilities, and Assisted Living
Facilities (Lewin Group, 2011; n4a, n.d. a).
In some places, residential care homes provide room, board, and services but are not licensed
by the state. Some operate legally, whereas others are operating illegally, raising concerns
about the quality of such places. These homes often serve vulnerable individuals with limited
financial resources.
In addition to residential care facilities, Adult Foster Care Homes provide room, board, and in-
home supports offered in a home-like environment with shared living and dining areas. Most
states limit the size of adult foster care homes to no more than five residents. The majority of
costs associated with adult foster care are private pay, though some states offer limited
support through their Medicaid State Plans.
37
The monthly costs of these residential care settings are far lower than nursing homes, but most
of these residential care facilities are private pay. Financial assistance from Medicaid for
supportive services within residential care settings can be covered through several different
Medicaid authorities. The most common services are Medicaid Home and Community-Based
Services (HCBS) 1915(c) Waivers and through the Medicaid State Plan Personal Care or Personal
Assistance Services. In recent years, states have also started using Medicaid managed care to
provide long-term services and supports.
However, Medicaid does not cover the housing portion of the cost of such residential care, and
therefore cannot cover “room and board”. Some states have enacted policies to make such
settings more available to lower-income residents. For example, some states limit the
maximum amount that can be charged for housing or provide non-Medicaid assistance to
Medicaid-eligible persons (e.g., a resident may spend their SSI income on the room and board
and Medicaid covers the services or the state may provide a state-funded housing supplement).
Finally, many states provide non-Medicaid state assistance to help older adults with low
incomes afford assisted living. Veterans may qualify for assistance paying for congregate living
through the VA’s Aid and Attendance or Housebound programs. In addition, Section 202
subsidies and other funding for housing can cover some of the housing costs for residents in
certain facilities.
Institutional Long-Term Care is available for individuals who can no longer live independently
and need a significant amount of assistance with ADLs. Nursing homes provide the most
comprehensive package of services and are available to individuals who need 24-hour
supervised care with meals, activities, and health management. A physician supervises each
resident’s care, and a medical professional is almost always present. Like assisted living, costs
vary depending on the level of care provided. Costs are extremely high, reaching an average of
$8,000 per month. Medicaid will pay 100 percent of the cost of nursing home care for
beneficiaries.
Challenges with Housing Assistance for Older Adults Experiencing Homelessness
Perhaps the most significant challenge with housing assistance for older adults experiencing
homelessness is that there is not enough housing available to meet the growing need among
low-income older adults. The lack of affordable housing coupled with increases in the numbers
of older adults eligible for housing assistance creates challenges in finding and maintaining
housing for those experiencing homelessness. Only 37 affordable and available homes exist for
every 100 extremely low-income renters in the United States (those with incomes less than 30
percent of the area median income), nearly a third of whom (30 percent) are seniors (Aurand et
al., 2021). The number of low-income older adults who are eligible for rental assistance but do
not receive it also has increased more than 5 percent between 2017 and 2018 (PAHRC, 2020).
Although over time more older adults are living in publicly supported housing (increasing 2.9
percent between 2018 and 2019), the amount of affordable housing available is not keeping
pace with demand. Adults living in the housing are aging, more older adults are entering public
housing for the first time, and seniors living in publicly supported housing are staying longer,
averaging 12.3 years in 2017, an increase of 5 percent since 2013. Yet the share of eligible
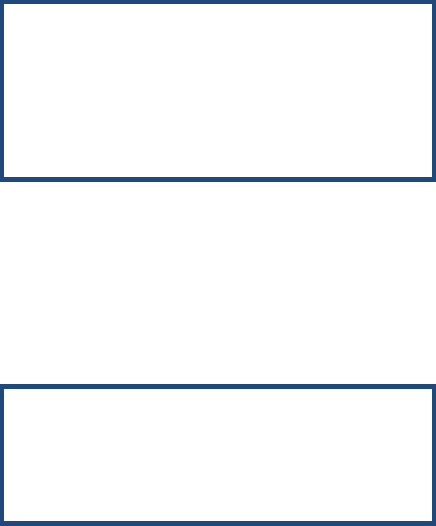
38
seniors who receive housing assistance declined from 41 percent to 40 percent from 2017 to
2018 (PAHRC, 2020).
New funding for the Housing Choice Voucher
program has been largely unchanged since 1983,
and most appropriations maintain existing
operations (Couch, 2020). With respect to
Section 202 units, the supply is not sufficient to
meet the growing number of adults who qualify,
a challenge further exacerbated by low vacancy
rates (Kochera, 2006) and having many facilities in need of repair (Libson, 2005). Long wait
times for eligible older adults often result from these challenges. As an example, the length of
time senior households spent on waitlist for public housing and Housing Choice Voucher
increased by 18 percent between 2016 and 2017, from 22.9 months to 27 months (PAHRC,
2020).
As housing providers noted, lacking necessary
vital documents such as a birth certificate or
Social Security card, which can be lost through
encampment sweeps or while staying on the
street, can be a common barrier for older adults
to receiving housing assistance. In addition,
people experiencing homelessness are often unaware of their eligibility for housing assistance.
The people with lived experience with whom we spoke were unaware of whether they qualified
for housing assistance or reported long waitlists to get it. Others mentioned discrimination by
landlords who did not want to rent to them because they experienced homelessness.
Expanded Services During the COVID-19 Pandemic
The CARES Act included a moratorium on tenant evictions from rental properties that receive
federal funding or have Federal Government-backed mortgages from March 2020 until July
2020. The Centers for Disease Control and Prevention (CDC) announced an additional eviction
moratorium on September 1, 2020, that was extended multiple times and ended in August
2021. In addition, some states, localities, territories, and Tribal areas, continue to implement
statewide and/or local and county eviction moratoriums.
CARES Act funding also allowed communities to provide supportive housing services and more
medium and long-term housing assistance, such as rental assistance and housing navigation
services. Moreover, HUD granted waivers to all communities to help prevent the spread of
COVID-19 and mitigate the pandemic’s economic impacts; these waivers included a suspension
of time limits on temporary assistance programs, such as rapid re-housing, and a series that
facilitate access to public housing. Waivers pertained to income verifications, review of
citizenship and Social Security numbers, and proof of family composition for public
housing tenants and inspections that were not possible or, in some instances, safe during the
pandemic.
“A lot of [landlords] don't want to house
homeless people because of the
baggage that comes with homeless
people.” – Male, 62
“As far as getting housing and stuff, I
really don't have communication with
the housing people. They just tell me I'm
still pending or waiting for a place.” –
Female, 60
39
HEALTH CARE, LONG-TERM CARE, AND BEHAVIORAL HEALTH SERVICES
Physical and behavioral health services play a critical role in the lives of many older adults
experiencing homelessness due to the elevated incidence of health problems they experience
relative to their housed counterparts (Cohen, 1999; Gelberg et al., 1990; HPRI, 2019; Brown et
al., 2016). For many older adults at risk of homelessness, health expenses contribute to their
becoming homeless (Bielenberg et al., 2020; Center for Housing Policy, 2015). The high cost of
health care and long-term services and supports lead to extended periods of poverty for more
than two-thirds of older adults aged 65 and older (Johnson & Favreault, 2021).
Medicare and Medicaid
Health care, long-term care, and behavioral health services, including prescription medications,
are available for older adults at risk of or experiencing homelessness through a variety of
federal and state-funded mechanisms including Medicare, Medicaid, and VA benefits (for
eligible veterans) among others. Benefits provided by each of these programs as well as the
eligibility requirements vary within programs and across states. Medicare and Medicaid serve
as the primary source of health insurance for older adults experiencing homelessness.
Medicare is a federally-funded health insurance program that helps with the cost of health
care, but it does not cover all medical expenses or the cost of most long-term care.
Beneficiaries can receive Medicare benefits through Medicare fee-for-service (FFS)
(“traditional” Medicare) or Medicare Advantage plans. Medicare Advantage Plans are offered
by private companies approved by Medicare. A key limitation of Medicare for older adults
experiencing homelessness is its eligibility criteria. Medicare is limited to individuals aged 65
and older who have a work history or as an entitlement benefit to younger people receiving
Social Security disability benefits for at least two years or with end stage renal disease.
Medicare-eligible individuals with low-incomes (i.e., in 2022, less than $1,153 per month for an
individual and resources limited to $8,400, which would likely apply to a large majority of older
adults experiencing homelessness) can receive additional coverage through the Qualified
Medicare Beneficiary program (i.e., Medicare Savings Programs) (Medicare.gov, n.d.). The
program provides financial assistance with part A premiums (hospital insurance), Part B
(medical insurance) premiums, as well as with deductibles, coinsurance, and copayments for all
individuals who meet the eligibility criteria.
Medicare typically provides full or partial coverage for services from doctors and other health
care providers; outpatient care; preventive services such as screenings, vaccinations, and
wellness visits; inpatient care in hospitals, skilled nursing facilities, and hospice care; and home
health care, as well as for prescription drugs and some medical equipment such as wheelchairs
and walkers. Medicare provides limited vision, hearing, and dental coverage for older adults.
In addition to physical health services, Medicare provides coverage for behavioral health
services including depression screenings, diagnostic tests, individual and group psychotherapy,
40
psychiatric evaluation, medication management, hospitalizations, and treatment of substance
use disorders in both inpatient and outpatient settings.
Medicare is available to a wide range of older adults, but some Medicare Advantage special
needs plans (SNPs), which are designed to provide targeted care and limit enrollment to
defined groups of Medicare beneficiaries, are beginning to focus specifically on people
experiencing homelessness. For instance, LA Care, a health plan based in Los Angeles, has
partnered with SNP Alliance, Massachusetts General Hospital, and other academic,
professional, and non-profit health care organizations to come up with a homelessness-focused
Medicare Advantage SNP (Jain et al., 2020).
Medicaid provides health insurance for low-income Americans, including families with children,
elderly people, and people with medically certified disabilities. Older adults ages 50-64 who are
not yet eligible for Medicare but do meet income eligibility (133 percent of the federal poverty
line) are also eligible for Medicaid in the 38 states and the District of Columbia that broadened
their eligibility under the Affordable Care Act. However, in the 12 states that as of January 2021
have not expanded coverage under the Affordable Care Act, receipt of Medicaid by adults
without children is rare (Garfield & Orgera, 2021). As of 2019, 10.5 percent of all adults ages 50-
64 nationally were uninsured, for which the primary reason reported was that insurance was
not affordable (Cha & Cohen, 2020).
Like Medicare, Medicaid typically provides full or partial coverage for a wide range of health
services, including medical appointments, hospitalizations, preventive services, outpatient care,
medications, and medical equipment as well as limited vision, hearing, and dental coverage.
Medicaid coverage of behavioral health services, in contrast to Medicare coverage, varies
greatly across states. All states provide some mandatory services for all Medicaid clients such as
medically necessary inpatient hospital services, outpatient services, and institutional long-term
care; however, Medicaid coverage for adults 65 and older varies by state for services such as
detoxification, prescribed medications, targeted case management, rehabilitation services,
therapies, medication management, clinic services, licensed clinical social work services, peer
supports, and hospital stays.
State Medicaid programs can cover HCBS for individuals with disabilities and older adults with
functional impairments (Costello, 2021) These services can include assistance with personal
care, care coordination, and non-medical transportation. In addition, states can elect to cover
housing-related services and supports, such as pre-tenancy services, home accessibility
modifications, and transition services (Costello, 2021).
For individuals who are eligible for both programs, referred to as “duals”, Medicaid provides
assistance for Medicare premiums as well as other services not typically covered by Medicare.
As duals are a diverse population with extensive and complex needs, the Centers for Medicare
& Medicaid Services (CMS) has developed the Financial Alignment Initiative in an effort to work
with states to improve the coordination of all Medicare and Medicaid covered benefits and
enhance the care provided to dually eligible beneficiaries. As of January 2020, 11 states are
participating in this initiative (CMS, 2022).

41
Increasingly, to meet the needs of individuals with complex medical needs such as older adults
experiencing homelessness, providers and funders are offering coordinated care models that
integrate primary care, behavioral health services, and social services through a single program.
For example, PACE is a Medicare program, available as a state Medicaid option, that provides
comprehensive medical and social services to certain frail, community-dwelling elderly
individuals, most of whom are dually eligible for Medicare and Medicaid (Medicaid.gov, n.d.). In
several communities, this model is being implemented in partnership with housing providers
and targeted specifically to older adults experiencing homelessness.
Profile of Coordinated Care Models for Older Adults
St. Paul’s PACE program in San Diego, California, provides a coordinated model of
care to formerly homeless older adults aged 55 years or older who are dually
eligible for Medicare and Medicaid. In partnership with local housing developers,
older adults are provided subsidized housing with wrap-around supportive services,
including primary and specialty health services, medication assistance, mental
health services, occupational therapy, dentistry, as well as meals and nutrition
counseling, social activities, social services, and transportation assistance. This
program reports reduced hospital use among older adults and lower rates of
hospital readmissions and potentially avoidable hospitalizations, such as for
congestive heart failure and asthma (Meret-Hanke, 2011; Segelman et al., 2014).
Veterans Affairs Health Care
Some older adults at risk of or experiencing homelessness may also be eligible for health care
through the Veterans Health Administration (VHA). Eligibility includes having served prior to
September 7, 1980; having served after September 7, 1980, and served for 24 months or the
full period of active duty; having been discharged for a disability that was caused or made
worse by active-duty service; and having been discharged for a hardship.
8
Of the 8.7 million
veterans enrolled in health care through the VHA in 2021, 30 percent (2.6 million) were
between ages 45 and 64, and 49 percent (4.2 million) were over age 65 (Wang et al., 2021;
Vespa, 2020). According to HUD, 55 percent of the veterans experiencing sheltered
homelessness in 2021 were aged 55 or older (HUD, 2023).
VHA benefits typically offer coverage for services and medications comparable to Medicare and
Medicaid; however, VHA health care benefits are not the same for all participants and are
subject to change based on funding availability. Participants are assigned to different priority
levels according to various factors, such as income and whether they have any medical
condition that derives from their military service. If federal funding for VHA health care drops or
does not keep pace with costs, individuals in the lower priority groups may lose VHA coverage.
8
A hardship discharge is a mechanism through which activity members of the military can be released from duty
due to hardship such as the death or permanent disability to the member's immediate family, such as the spouse
who is the primary guardian to the children of the family when the military personnel would be deployed.
42
VHA benefits also provide coverage for behavioral health treatment, including a broad range of
mental health conditions, substance use disorders, post-traumatic stress disorder, and serious
mental illness through both inpatient and outpatient settings. Moreover, general and
psychogeriatric mental health services are provided as an integral part of primary care within
the Patient Aligned Care Teams as well as VHA nursing homes and residential care facilities
where many veterans receive care. The VHA also has a set of programs that fall under the
heading Geriatrics and Extended Care, which are designed to help veterans diagnosed with
chronic health issues or life-limiting illnesses. Among other things, these programs can provide
respite care, adult day care, outpatient and inpatient hospital services, nursing homes,
palliative care, and hospice.
Older Americans Act Funded Programs
Older adults experiencing homelessness may also benefit from health and support programs
available through Older Americans Act (OAA) funded programs. The OAA coordinates the
distribution of funds for many programs for older adults, both health-related and otherwise
(ACL, 2022). These funds originate with the federal Administration of Aging, which oversees 56
State Units on Aging, which in turn oversee over 600 Area Agencies on Aging and almost 300
Tribal organizations, totaling around 20,000 service providers (ACL, n.d.; Siegler et al., 2015).
The OAA funds a number of programs and services directly, such as Aging and Disability
Resource Centers, Elder Rights Support programs, and the Alzheimer’s Disease Initiative
(Congressional Research Service, 2022). However, the majority of OAA funds (72.8 percent in
FY2022) go directly to State Units on Aging and Area Agencies on Aging, which allocate funds
locally to address the health and social needs of their constituents (Congressional Research
Service, 2022). One such source is the Title III-D Disease Prevention and Health Promotion
grant, which Area Agencies on Aging use to fund evidence-based disease prevention and health
promotion services in settings such as senior centers, community centers, and various
congregate settings (California Department of Aging, n.d.).
One important development in recent years is the No Wrong Door System initiative, a
collaborative effort by the Administration for Community Living (ACL), CMS, and VHA. The
initiative strives to create a more consumer-driven, efficient system for accessing long-term
services and supports for older adults and individuals with disabilities services. Since 2003, the
No Wrong Door initiative has supported 33 states with funding to help transform their systems
to make it easier for consumers and their families to learn about the services available and how
to access them (ACL, 2022).
Substance Abuse and Mental Health Service Administration Funded Programs
Older adults experiencing homelessness with mental health and/or substance use disorders can
access services through programs of the Substance Abuse and Mental Health Services
Administration (SAMHSA), a federal agency within HHS (SAMHSA, n.d.). Individuals can receive
comprehensive care, including 24/7 crisis services, referrals to clinics and services, and care
coordination, through Certified Community Behavioral Health Clinics (CCBHCs), or through
SAMHSA’s National Helpline (SAMHSA, n.d.). CCBHC services are available to individuals of all
43
ages and are free for those unable to pay (SAMHSA, n.d.). SAMHSA also provides a variety of
grants to states and local organizations specifically assisting those experiencing co-occurring
homelessness and behavioral health disorders with a variety of services, including case
management, peer support, and treatment for mental health and substance use disorders
(SAMHSA, n.d.).
Other Sources of Health Care
Older adults, including those who may be uninsured, can also access health care through
community-based outpatient clinics including Federally Qualified Health Centers (FQHCs),
Health Care for the Homeless clinics, Community Health Centers, Migrant Health Centers, and
Primary Care in Public Housing (Health Resources and Services Administration [HRSA], 2018).
Each of these organizations is grant-funded to provide specific services to underserved
populations.
In particular, the Health Care for the Homeless Program supports FQHCs that provide health
care to people experiencing homelessness. Anyone experiencing homelessness is eligible to
receive assistance from a Health Care for the Homeless clinic, though clinics are primarily
located in urban locations. Eligibility includes people living in unsheltered locations, shelters or
transitional housing, “doubled-up” situations with family or friends, people exiting institutions
without a stable housing situation, and people in any other unstable or non-permanent living
situation. Nearly 300 Health Care for the Homeless clinics across the country provide primary
health, mental health, substance use disorders, and social services with intensive outreach and
case management to link clients with additional services. In 2020, Health Care for the Homeless
clinics served nearly 1 million patients, with 7.43 percent over the age of 65, a proportion that
has been steadily increasing in recent years (HRSA, 2020).
Challenges with Health Services for Older Adults Experiencing Homelessness
Older adults experiencing homelessness face a number of challenges accessing the health care
they need, including lack of health insurance; a need for immediate focus on basic needs, such
as food and housing, instead of health needs; limited appointments and providers; a lack of
transportation to access assistance (Canham et al., 2020; Kushel et al., 2012; Watson et al.,
2008) among others.
Lack of insurance: There are no nationally representative data on rates of health insurance
coverage for older adults experiencing homelessness; however, two studies have been
conducted in single cities. These studies found that the majority of older adults experiencing
homelessness have some type of health insurance, with Medicare and Medicaid being the
primary sources (Lee et al., 2020; Ye et al., 2019). Using Homeless Management Information
Systems data on 1,204 older adults aged 55-90 living in Tampa, Florida who received
homelessness assistance in the last year, Lee and colleagues (2020) found that 88 percent had
insurance. Similarly, in a study of 17 older adults experiencing homelessness in Wilmington,
Delaware, Ye and colleagues (2019) found that all but two participants reported having health
insurance.

44
Older homeless adults who lack health coverage tend to be aged 50-65 and fall between the
cracks of governmental safety nets -- not old enough to qualify for Medicare and ineligible for
Medicaid assistance in many states (Dipietro et al., 2014). In an examination of the Health Care
for the Homeless User Survey, Baggett and colleagues (2011) found that, among people
experiencing homelessness, those aged 45 and older were more likely than younger adults to
have an unmet need for prescription medications (2010).
Primary focus on basic needs: Many older adults experiencing homelessness, including those
with health insurance, do not receive the health care they need because they first focus on
addressing their basic and immediate needs, such as securing shelter and food (Baggett et al.,
2011; Van Dongen et al., 2019). This delay of attention to medical needs often results in older
adults experiencing homelessness relying on emergency departments and street outreach
programs for health care (Chung et al., 2018; McDonald et al., 2006).
Limited appointments or providers: Some research has found that over half of adults aged 50
and older who are experiencing homelessness report having access to a regular place of care
(Chung et al., 2018; Kaplan et al., 2019). Access to health care, including routine exams or
wellness checks, for older adults who are experiencing homelessness is still lower than their
housed counterparts, due in part to individuals not knowing where to go or inability to get and
keep appointments (McDonald et al., 2006; Ye, 2019). Moreover, older adults with memory
problems may struggle to attend scheduled appointments (Grenier et al., 2013).
Lack of transportation: In the limited research available documenting older homeless adults’
barriers to receiving needed health care, research found that a lack of transportation to
appointments or difficulty navigating public transportation was cited as among the most
common reasons for lack of health care receipt among older adults experiencing homelessness
(Canham et al., 2020; Ye et al., 2019).
In discussions, people with lived experience
noted barriers to service receipt including
unreliable telephones, inability to get walk-in
appointments, appointments that were too far
out to remember, and, for two individuals, lost Medicaid cards which prevented them from
getting the health services that they needed.
Additionally, in discussions, experts and housing providers noted that behavioral health care
services are rarely tailored to geriatric populations. Conditions related to aging, such as
memory problems, may be interpreted as behavioral health problems. Moreover, if behavioral
health providers are not attentive to feelings common to older adults, such as shame and
distrust of assistance, they will be less effective in providing them the assistance they need.
Expanded Services During the COVID-19 Pandemic
Various new policies and practices were put into place to facilitate access to health care during
the COVID-19 pandemic. HRSA’s COVID-19 Coverage Assistance Fund and COVID-19 Uninsured
“I have trouble keeping [appointments]
because I forget a lot.” – Female, 60
45
Program covered the costs of administering COVID-19 vaccines to uninsured and underinsured
patients. CMS expanded Medicare coverage of telehealth and provided payment policy and
regulatory flexibility for Medicare-covered services. In addition, the Families First Coronavirus
Response Act required that Medicaid programs keep people continuously enrolled through the
end of the month in which the COVID-19 public health emergency ends.
INCOME SUPPORTS AND OTHER NEEDS
Income Supports
SSI, SSDI, and state-funded general assistance programs provide income supplements to aged,
blind, and disabled people (and some family members) to help meet basic needs such as food,
clothing, and housing. As of 2022, an eligible individual’s monthly maximum federal SSI
payment was $841. All but four states supplement this amount with additional assistance
ranging from $10 to $400 a month. SSDI payment amounts are based on an individual’s lifetime
average earnings before becoming disabled, with average monthly amounts ranging from $800
and $1,800. Because many older adults live on fixed incomes, another strategy some
communities are exploring to assist older adults is to provide shallow rental subsidies (typically
several hundred dollars a month of limited, needs-based payments), such as Santa Monica’s
Preserving Our Diversity program, which provides rental assistance to low-income seniors to
maintain their housing (Sharma, 2019).
For people who were employed and lost their jobs, unemployment insurance benefits can
provide some temporary income supports. The basic unemployment insurance program is
operated by individual states and overseen by the DoL. Most states provide up to 26 weeks of
benefits, replacing about half of a recipient’s wages, on average (Stone & Chen, 2014). Eligibility
and benefit levels differ by state. Some recipients may also be eligible for the Extended Benefit
program, which provides an additional 13-20 weeks of compensation to workers if the state’s
unemployment situation has worsened. Studies estimate unemployment rates among people
experiencing homelessness range from 57 percent to over 90 percent compared to less than 5
percent for the general population (HPRI, 2020); however, it is not clear how many older adults
experiencing homelessness are eligible for or receive unemployment insurance benefits.
Providers and organizations can assist older adults experiencing homelessness with the
application process to apply for these benefits (Perret, 2021; Brown et al., 2013). The SOAR
program, an evidence-based model, also helps older adults with mental illnesses, co-occurring
substance use disorders, or other impairments to apply for SSI and SSDI (Kushel, 2020). One
study found that SOAR applicants were twice as likely to have their initial application approved
than all other homeless applicants (Kauff et al., 2016). On a national level, SOAR applicants who
were of older age and living in an institutional setting, such as a hospital or a residential
treatment center, were associated with a higher rate of application approval among homeless
adults at risk of or experiencing homelessness (Lowder et al., 2017).
46
Food and Nutrition Assistance
Administered by the USDA, SNAP provides monthly benefits to low-income households to
purchase food. It is the largest USDA food assistance program, serving more than 5 million older
adults annually (U.S. Government Accountability Office, 2019). SNAP is funded through
“mandatory” federal funding, meaning that funding for the program is automatically expanded
or contracted to meet demand (Blancato & Whitmere, 2021). State Units on Aging and Area
Agencies on Aging also provide nutrition services to adults aged 60 and older. For example,
Meals on Wheels is a program that delivers meals to home-bound individuals who are unable to
purchase or prepare their own meals.
Transportation Assistance
Transportation assistance for older adults experiencing homelessness is available through a
range of services. At the state level, the Aging Services Division provides a range of services to
eligible older adults, including transportation to shopping and medical appointments (Eldercare
Directory, n.d.). Eligible older adults may contact their local offices to arrange for transportation
to medical appointments and shopping centers, among other locations. Older adults who need
special accommodations, such as those who use a wheelchair or have other mobility
impairments, can use the accessible transportation.
Although service availability and eligibility differ from state to state, older adults receiving
Medicaid coverage may use travel services to reach medical facilities. The transportation
voucher program involves assistance with fares or rides without charge to eligible low-income
older adults and people with disabilities (Haarstad, 2008). In addition, Medicaid Advantage
plans have flexibility to offer expanded benefits that go beyond Medicare FFS and can address
barriers to health, including non-emergency transportation to and from doctor’s appointments,
lab tests, pharmacies, massage therapy, fitness centers, and other health care-related
destinations.
Social Engagement Services
Many communities offer services to combat social isolation that many older adults experience,
including senior centers, adult day centers, and in-home social engagement programs, though
few of these programs are specifically for older adults experiencing homelessness. These
programs are often funded through Area Agencies on Aging but can be supported through
other federal, state, and municipal sources as well as through faith-based and private sources.
Such services typically provide wellness and exercise classes, arts programs, and community
building opportunities (ACL, n.d.; Berg-Weger et al., 2020; Siegler et al., 2015). The availability
of such programs, the services they provide, and eligibility for participation vary nationally.
Adult Protective Services
Adult protective services (APS) programs respond to allegations of abuse, neglect, or
exploitation of vulnerable adults, such as older adults and those with disabilities (National Adult
Protective Services Resource Center [NAPSRC], n.d.). They investigate allegations and, as
needed, address the health and safety needs of the victims through providing a range of

47
services and case management (NAPSRC, n.d.). APS programs collaborate with a number of
professionals in the health, safety, and social services fields to address allegations as well as
other needs victims may require (National Adult Protective Services Association, n.d.). States
receive the majority of their funding for APS programs from the Federal Government through
the Social Services Block Grant, which they can supplement through general revenue funds or
other funding intended for older adults, such as funding through the OAA (Ramsey-Klawsnik,
2018). Program administration varies by state and can occur at the state level, the county level,
through local agencies such as Area Agencies on Aging, or some combination of all three
(Ramsey-Klawsnik, 2018). Each APS program can determine its own eligibility and reporting
requirements in addition to definitions of abuse, neglect, and exploitation; some programs
offer services only to adults over age 60, while others use varying combinations of age and
disability to determine eligibility (Ramsey-Klawsnik, 2018).
Challenges with Income Supports and Other Needs
Older adults experiencing homelessness face a range of challenges in accessing assistance and
services for meeting basic needs, such as income, food, and transportation. People
experiencing homelessness may have difficulty accessing financial benefits for which they are
eligible. Individuals with serious mental illnesses, medical impairments, or substance use
disorders and who are at risk of or experiencing homelessness face challenges when applying
for SSDI benefits (Donaldson et al., 2020). Some applicants find it difficult to produce the
documents needed to establish or maintain their eligibility.
Studies have also identified several barriers in accessing food assistance programs among older
adults experiencing homelessness, such as difficulty applying for or renewing their benefits due
to limited access to technology and no fixed addresses, low health literacy, and cognitive
impairment, that may complicate the ability to understand eligibility criteria and complete
necessary documentation (Tong et al., 2018). USDA researchers suggest that older adults,
especially those who have been self-sufficient for the majority of their life, may feel stigma
around receiving welfare, especially in a public setting such as a grocery store (SNAP, n.d.). Data
on the rate of SNAP participation for older adults experiencing homelessness are not available,
yet data for all eligible elderly households indicate that only about a third participates in SNAP
(e.g., Ziliak & Gundersen, 2020). In response to the low participation levels and unique
economic circumstances of elderly households, the USDA Food and Nutrition Service has
implemented waivers and demonstration projects that aim to reduce barriers to participation,
reduce administrative burden, and improve access to SNAP for elderly people (Levin et al.,
2020).
In discussions, experts and providers echoed this
sentiment, noting that many older adults
experiencing homelessness or recently placed in
housing need assistance applying for and
maintaining benefits, including SSDI, SNAP, and
others, especially those older adults who are not internet savvy, do not have access to the
necessary technology, or struggle to understand the steps required to apply for and maintain
“For me, I don't know how the computer
works… Everything now you have to do it
on the computer.” – Male, 66

48
their benefits. Among people with lived experience of homelessness, two reported needing
help navigating the recertifications for their benefits and, in particular, being confused by all of
the mail they received from different agencies. Others reported not knowing how computers
worked and feeling frustrated that they needed to use computers to apply for benefits and
other assistance.
Yet an additional challenge for older adults experiencing homelessness is that SNAP does not
allow recipients to purchase prepared food, thus requiring access to cooking facilities and an
ability to safely store uncooked food (Tong et al., 2018). However, several states (five as of April
2022) have implemented a SNAP Restaurant Meals Program that allows select SNAP recipients
to use their SNAP benefits to pay for restaurant meals. Eligibility differs across states but is
typically limited to SNAP recipients who are 60 years or older, are experiencing homelessness,
or have a disability (USDA, 2021).
Transportation assistance is available for many
older adults experiencing homelessness;
however, barriers can limit access to some
services, particularly for those in rural areas and
with mobility limitations (Ravensbergen et al.,
2022). Limited research is available on the
accessibility of public transportation for older
adults, though the literature suggests significant variation by city (Ravensbergen et al., 2022).
Individuals with lived experience with homelessness reported transportation difficulties,
including not knowing how to navigate bus systems and feeling vulnerable with using public
transportation due to poor eyesight and the lack of proper eyewear, physical limitations, or
memory problems.
Expanded Services During the COVID-19 Pandemic
Assistance to meet a range of older adults’ basic needs were expanded during the COVID-19
pandemic. The pandemic exacerbated food insecurity for older adults at risk of or experiencing
homelessness due to a loss of, or disruption in, food from nutrition programs (Goger, 2020). To
address this challenge, numerous providers implemented innovative strategies, such as
converting in-person nutrition programs for older adults into “grab and go” programs or home-
delivered meals. Additionally, when some traditional senior nutrition food distribution channels
were overwhelmed, providers found new local and corporate partners. For example, members
of National Association of Nutrition and Aging Services Programs (NANASP) and n4a partnered
with Tivity Health to provide Nutrisystem and South Beach Diet frozen home-delivered meals to
older adults in areas with food shortages. A January 2021 survey of the NANASP members
found that around 90 percent of respondents reported that they were still serving more meals
now than prior to the pandemic, with many providers stating that their demand had doubled or
more (NANASP, 2021).
During the pandemic, states began more widespread adoption of the USDA’s SNAP Online
Purchasing Pilot to allow SNAP participants the option of grocery shopping online, which prior
“[My case manager is] going to give me
bus passes, but the problem is that my
eyesight and it's just not good and I just
don't feel, I feel vulnerable out there.” –
Female, 59
49
to March 2020 was in place in only New York and Washington State. The program has
continued to expand following the pandemic. As of April 2023, the District of Columbia and
every state except Alaska were participating in the program (USDA, 2021).
In addition, during the pandemic, federally-funded unemployment insurance was expanded to
include workers not traditionally covered by unemployment insurance benefits, provide a flat
benefit level to all recipients (at a higher rate than was typically provided by states), and extend
the period of time for which recipients could receive benefits.
In 2021, the Federal Government drastically increased its direct contribution to APS programs
through the CARES ACT and the American Rescue Plan Act (ACL, 2021). No formal APS
administration changes happened at the federal level in response to the pandemic, though
some APS programs took on larger roles in service referrals and direct provision as community-
based organizations and nursing homes struggled to stay open and provide care for older adults
(Liu & Delagrammatikas, 2021).
Providers with whom we spoke noted that several changes implemented during the pandemic
had both positive and negative impacts for the older adults they served. For example, multiple
housing providers were able to provide iPads or other devices to their residents, expanding the
ways to connect with family and friends; however, older adults with limited technological
proficiency were less able to use these new methods of connection. For these older adults, the
pandemic was thought to accelerate physical and cognitive decline. Similarly, many meal
services such as soup kitchens transitioned to meal delivery assistance. This shift was an
advantage for those who struggled to access services, yet also removed an opportunity for
socialization for many older adults.
50
Section 4. Gaps and Potential Strategies
ADDRESSING GAPS IN SERVICE DELIVERY AND COORDINATION
The environmental scan and discussions identified a number of critical gaps in housing and
service availability, accessibility, delivery, and coordination. The following interventions and
policy considerations may help providers and policymakers better meet the housing and
support needs of older adults experiencing housing instability and homelessness.
Identification, Outreach, and Navigation Services
Various interviewees recommended better screening and identification of housing instability
among non-homelessness providers with whom older adults are connected, such as health
clinics and benefits offices, would help prevent many at risk older adults from becoming
homeless. Older adults experiencing homelessness need outreach and navigation that is
targeted sensitive to their specific barriers to receiving assistance. Experts and providers noted,
in particular, that services are needed to help older adults learn about the available supports
that match their eligibility and to navigate the process of applying for and accessing that
assistance.
Individuals with lived experience of
homelessness echoed this sentiment. Two
people who experienced homelessness for the
first time as older adults reported that they did
not know who to turn to for assistance or what
assistance was available. Although most
individuals reported being connected to a case
manager who helped them figure out where to
go, they reported primarily learning about the assistance available through other people on the
street.
Increased Access to Benefits and Services
Experts and providers noted that restrictive eligibility criteria also prevent or complicate access
to key services for this population. Some criteria, such as for Medicaid long-term care (including
HCBS), have strict income and/or asset requirements that require recipients to exhaust nearly
all savings before receiving coverage. The asset limits for Medicaid eligibility for these services
are typically no more than $2,000 for an individual or $3,000 for couple.
9
Other programs, such
as SSI, have strict age and/or disability criteria, limiting services to people over age 60 or 62.
Veterans who have been dishonorably discharged are ineligible for VA assistance. Permanent
supportive housing programs are often limited to those who have experienced chronic
homelessness and are thus unavailable to older adults who are at risk but do not have histories
of homelessness. Undocumented individuals are ineligible for most types of federally-funded
9
California is implementing a new policy that is phasing out this asset limit beginning in July 2022 (Justice in Aging,
2022).
“They should have more people that will
go down there to try to help them to get
off the damn street because once you're
on the street, it is so hard to keep it
together and get off the street.” –
Male, 57
51
assistance.
10
Experts noted that overall, older adults experiencing homelessness are at
increased risk of morbidity and mortality compared to the housed population and need access
to these benefits and services.
Crisis and Interim Housing Tailored for Older Adults
Experts and providers reported a need for homelessness assistance that was tailored to older
adults’ unique challenges. For example, emergency shelter accommodations should include
beds that are on the first floor or bottom bunk, 24-hour access to bedrooms and bathrooms,
and refrigeration or locked storage for medications and medical supplies. Additionally, they
noted, providers who serve older adults at risk of or experiencing homelessness must be
sensitive to the emotional needs of older adults, who may be struggling with shame and
sadness due to needing assistance or being disconnected from their families.
Permanent Supportive Housing Tailored to Older Adults with Histories of Homelessness
Older adults with histories of homelessness often have additional challenges moving into
permanent supportive housing than older adults without such histories. These include greater
functional impairments and behavioral health challenges, as well as limited connection to their
communities. There is a need for additional permanent supportive housing specifically tailored
to these older adults with physical accommodations (e.g., wheelchair accessible buildings, grab
bars in units) to address these needs as well as access to the types of case management and
nursing assistance (e.g., medication management, wound care) that will allow them to age in
place.
Consistent Case Management Assistance
The majority of older adults with lived
experience with whom we spoke indicated that
case management help was critical to getting
the assistance they needed. When asked how
they knew where to go for assistance, ten of the
14 individuals said they learned about help
through their case managers. For those in permanent supportive housing, this case
management was, most often, associated with the housing program. People not in housing
mentioned that case managers at emergency shelters were also helpful in providing guidance
about where to go for help. Four individuals spoke of the difficulties navigating the system
when they did not have case managers or when there was case manager turnover, which
prevented them from getting the help they needed. Research shows that low wages and a
demanding work environment are associated with high rates of case manager and supervisor
turnover in many organizations, both of which can disrupt clients’ access to appropriate and
10
Beginning in May 2022, California expanded Medi-CAL access to all individuals who are 50 years or older
regardless of immigration status. Under this expansion, all individuals who meet Medi-CAL full-scope eligibility
are eligible for primary, specialty, behavioral health, and long-term care as well as in-home supportive services,
HCBS, transportation, vision, and hearing aid coverage (Office of Governor Gavin Newsom, 2022).
“I talked with [my case manager] 1 time
and now he's gone for 2 or 3 weeks
doing something, I don't know what, and
won't be back.” – Female, 59

52
timely services (Gabrielian et al., 2022). A current shortage of direct care workers and case
managers exacerbates the challenges of system navigation for many older adults.
Inadequate Capacity of Affordable Housing
Echoing findings from the research, experts and providers spoke of the need for more
affordable housing for older adults at risk or experiencing homelessness. In particular, they
identified a need for more permanent supportive housing as well as other subsidized housing
for older adults, including Supportive Housing for the Elderly (Section 202) and Housing Choice
Voucher (Section 8) units. For most housing assistance programs, such as Section 8 vouchers,
waitlists can be years long, and once an individual receives a voucher, low housing vacancy
rates and landlord bias can effectively prevent people from securing affordable housing.
Lack of Coordination Across Systems
Across discussions, the most-widely identified issue with serving older adults experiencing
homelessness was a lack of coordination across the various systems that serve older adults at
risk of or experiencing homelessness. This lack of
coordination happens on multiple levels. At a
systems level, cross-systems coordination has
not been a federal priority, funding streams are
often siloed, and eligibility criteria vary. Multiple
experts indicated that many programs, for
example, may make sense fiscally but run into
barriers due to the “wrong pocket problem”
such that the money that needs to be spent
comes from a different coffer than money that
will be saved. For example, greater investments
in prevention services or housing stabilization services will likely result in improved health
outcomes. Yet, the savings that result from those improvements are unlikely to benefit
agencies that provide prevention or housing assistance.
Experts and providers noted that it is no one person’s or agency’s job to coordinate across
systems and social service agencies are often too understaffed to take this on. Others indicated
that most systems are quite complex and use different language and data systems, making it
difficult to communicate. Coordination may be further challenged by program requirements
that are hard for people experiencing homelessness to meet. For example, some PACE
programs serve older adults living in subsidized housing with wrap-around supportive services,
including primary and specialty health services, medication assistance, mental health services,
occupational therapy, dentistry, as well as meals and nutrition counseling, social activities,
social services, and transportation assistance. Although this model has successfully coordinated
care for homeless people in a few select locations, such as San Diego, as a Medicare benefit
option, it was not originally designed to serve this high-need population. Individuals with long
histories of homelessness may have more functional impairments and behavioral health needs
than is covered by PACE payment rates.
“All the different agencies, they don't
communicate with each other like they
should. And, well, a couple of times I've
got responses from the agencies that I
need to recertify and I have sat down
and went through all that paperwork
and sent it off and I still get the
threatening letters.” – Male, 74
53
Finally, many aging, health, and long-term care service systems do not routinely screen for
housing instability among their clients and thus service providers are unaware that they need to
coordinate with housing and homelessness providers. When they are aware of the coordination
that is needed, HIPAA regulations can make it difficult for care providers to communicate about
their shared clients. Moreover, distinct data systems across systems make it difficult for
providers to track individuals’ service receipt to ensure they are getting the assistance they
need.
GAPS IN KNOWLEDGE
The experts and providers interviewed largely concurred that insufficient research has focused
specifically on older adults experiencing homelessness, a small but growing population of
people. Those interviewed provided insight into areas they would like to see additional
research to inform policy and services moving forward.
Research on Equity in Services and Outcomes
One key area raised by many individuals with whom we spoke was the need for more research
focused on equity in services and outcomes for older adults experiencing homelessness. Racism
and language barriers can prevent individuals from accessing the assistance they need, though
providers may not understand the extent to which this occurs. Experts pushed for additional
research unpacking whether there are differences by race and ethnicity in the types and
amount of assistance received by people experiencing homelessness as well as the causes of
those differences. One expert also called for research exploring the extent to which older adults
who are LGBTQ+ receive the assistance they need.
Research on the Connection between Health and Homelessness among Older Adults
Another area in which older adults are understudied is the intersection of health and
homelessness. Experts noted cognitive impairment in older age may contribute to individuals’
risk of homelessness as they struggle to manage their finances. Yet, interviewees called for
more research exploring cognitive decline once individuals become homeless. One expert
noted that individuals experiencing sleep deprivation or severe depression, common conditions
among those who are homeless, may be misdiagnosed with dementia on health assessments.
Another cited preliminary research indicating that cognitive tests for people experiencing
homelessness are far more unstable over time than among their housed counterparts and that
moving into housing results in improved cognition. Yet more research is needed in this field,
including to understand racial-ethnic differences in cognitive decline for people experiencing
homelessness (Nye et al., 2022).
Documentation of Available Assistance
Experts also cited a need for additional documentation of the types of assistance available to
older adults at risk of or experiencing homelessness as well as the eligibility criteria and
enrollment requirements across systems. This work can guide federal and state policymakers
about what help is available, where gaps in assistance exist, and when individuals are most
54
likely to need interventions to help them access and maintain the services they need. This
report serves as a starting point to meet this need, yet additional work is needed to document
the complex eligibility and enrollment requirements for programs, particularly those that vary
by state or municipality. One expert suggested they would like to see a map of all of the
moments that a Medicaid-eligible individual could lose or be denied coverage for failing to
provide necessary documentation. This exercise, they argued, could inform policy
recommendations to simplify the process as well as provide case managers with guidance
about the types of assistance needed.
Additional Data on Older Adults Experiencing Homelessness
Finally, interviewees identified a need for additional data focused on older adults experiencing
homelessness. Some experts pointed to state and local municipalities, such as Washington
State, Rhode Island, Allegheny County, and Los Angeles County, that have integrated databases
that could provide insight into the service needs and experiences of older adults experiencing
homelessness across multiple systems. However, federal homelessness data include limited
information about older adults, making it hard to identify the size and composition of the
population or their service needs.
POTENTIAL STRATEGIES
Through the information identified in this study, we offer a number of potential strategies for
policymakers and service providers to better identify and serve older adults at risk of or
experiencing homelessness. Strategies for policymakers to consider include:
• Additional prevention resources. Experts and providers with whom we spoke identified
prevention services as both cost-effective and compassionate approaches to serving
older adults at risk of homelessness. These services include short-term rental assistance
until affordable housing can be located, permanent shallow rental subsidies, resources
to help with property taxes, and assistance with home maintenance costs.
• Assistance with other costs of living. With increasing costs of food, transportation, and
other expenses, rent-burdened older adults will increasingly struggle to pay for housing.
Providing assistance with these other expenses, through established programs such as
Meals on Wheels and new programs developed during the pandemic, will allow for
additional resources to be allocated towards housing without sacrificing other needs.
• Additional types of affordable housing assistance. Shallow subsidies that provide a
small, ongoing amount of rental assistance to older adults on fixed incomes could
prevent or end their homelessness. In discussions, many experts and providers spoke of
the need for a broader range of affordable housing situations, such as affordable
assisted living for older adults who need limited assistance but do not require nursing
home-level care.
• Expanded state coverage for HCBS for at risk individuals. HCBS can help support older
adults and individuals with disabilities live in the community. Such services include
assistance with medication management and wound care; assistance with ADLs; home
55
management services, such as housekeeping and home repairs; transportation to
medical appointments as well as other locations such as grocery and clothing stores;
opportunities for social engagement; and case management assistance. Strategies might
include ensuring that eligible individuals in transitional housing and permanent
supportive housing have access to needed personal care to help with ADLs. States can
also consider covering housing-related services and supports under their HCBS systems,
such as pre-tenancy services for individuals transitioning from homelessness or
institutions or assistance with home modifications (Costello, 2021).
• Identification of older adults by HUD as a key population. One limitation to
understanding the size and characteristics of the population of older adults experiencing
homelessness is the limited data available. Despite older adults comprising a growing
share of the population of adults experiencing homelessness, HUD does not designate
older adults as a population of focus in its Annual Homelessness Assessment Reports.
Thus, no national data are available on the characteristics (e.g., gender, race, ethnicity)
or geographic distribution of older adults experiencing homelessness and no data exist
on the number of older adults experiencing unsheltered homelessness.
• Better cross-systems coordination. Many interviewees noted that most systems that
serve older adults experiencing homelessness do not coordinate with one other. They
suggested addressing homelessness among this population through cross-systems
coordination needs to be a federal priority and can be fostered through shared goals,
flexible or blended funding streams, and better integrated data systems. On a local
level, CoCs could work with ACL to ensure that No Wrong Door providers and providers
of coordinated entry are well-connected and can easily make referrals between their
programs to best meet the needs of older adults experiencing homelessness.
• Continuation of programs started during the pandemic. A number of programs
adopted or expanded during the pandemic, such as telemedicine and the USDA’s SNAP
Online Purchasing Pilot, provided older adults access to the assistance they needed
when they could not leave their homes. A continuation of these programs would
increase access to assistance for older adults with mobility limitations due to health
impairments, including poor eyesight and poor memory.
Potential strategies for service providers include:
• More proactive identification of older adults at risk of homelessness. Experts and
providers both noted that many older adults at risk of homelessness do not reach out
for assistance until it is too late to maintain their housing because they do not know
where to go for help or they are unwilling to ask for it. While Area Agencies on Aging are
increasingly fielding calls on assistance to address housing instability and homelessness,
there could be more proactive identification of older adults at risk of losing their
housing. Service providers, such as health clinics and those participating in the No
Wrong Door Initiative, may be in a good position to implement strategies (such as
routine screenings) to identify older adults who are severely rent-burdened or
otherwise at risk of homelessness and then work to connect those adults to available
services.
56
• Better documentation of services and supports available in local communities. This
documentation of assistance, as well as the eligibility criteria for receipt of assistance,
will enable more older adults at risk of or experiencing homelessness to know what
assistance is available and how they can access it. This resource must be regularly
maintained and easy for people to access, such as through city or county websites, local
service providers, and locations older adults frequently visit (e.g., public libraries).
• Additional assistance accessing medical equipment for people experiencing
homelessness. Older adults experiencing homelessness face challenges accessing
assistive technology, such as eyeglasses and hearing aids, that may be lost or damaged
while they are living in places not suitable for human habitation or are moving
frequently from shelter to shelter. Homelessness providers could connect with services
in their communities to assist older adults with providing or replacing this equipment. In
addition, shelter and transitional housing providers should provide accommodations for
people with limited mobility such as grab bars and shower safety seats.
• Training for case management staff on issues specific to older adults. With the rate of
older adults experiencing homelessness increasing, CoCs should provide training for
front-line staff on issues specific to older adults experiencing homelessness. Such
training could provide staff with sensitivity to and strategies for addressing feelings of
distrust of assistance, concerns about losing their independence, and difficulty using
public transportation and remembering scheduled appointments. Training could also
address the range of service needs that are more common among older adults
experiencing homelessness and list the providers in the community that can help
address such needs.
• Improved access to sufficient income assistance for eligible individuals. Programs such as
SSI are designed to prevent destitution, premature illness, and death among people who
are 65 and older, blind, or disabled. Yet few older adults experiencing homelessness under
age 65 receive the benefit, despite having significant health and mental health challenges.
More aggressive outreach and enrollment through programs such as SOAR would provide
a sustainable source of income for a significant share of older adults experiencing
homelessness. In addition, SSI payments are insufficient to support individuals with their
living expenses. In 19 states and the District of Columbia, statewide average one-bedroom
rents are higher than monthly SSI payments and in the remaining states, monthly rents are
equal to 75 percent or more of monthly SSI payments (Schaak et al., 2017).
CONCLUSION
Older adults at risk of and experiencing homelessness are an especially vulnerable population
with a higher prevalence and severity of a number of health and behavioral health challenges
than both their housed counterparts and younger adults experiencing homelessness. As the
number of older adults experiencing homelessness continues to grow, it is critical to
understand their unique set of needs as well as the services and supports that are available and
accessible to address them. This environmental scan provides a roadmap for better
understanding this population, including older adults’ pathways into homelessness, their
57
characteristics, and service needs. It outlines the range of services and supports available to
address those needs across service delivery systems. Finally, it documents the unique
challenges older adults experiencing homelessness face in accessing the assistance available
and offers a number of potential strategies for better serving this population.
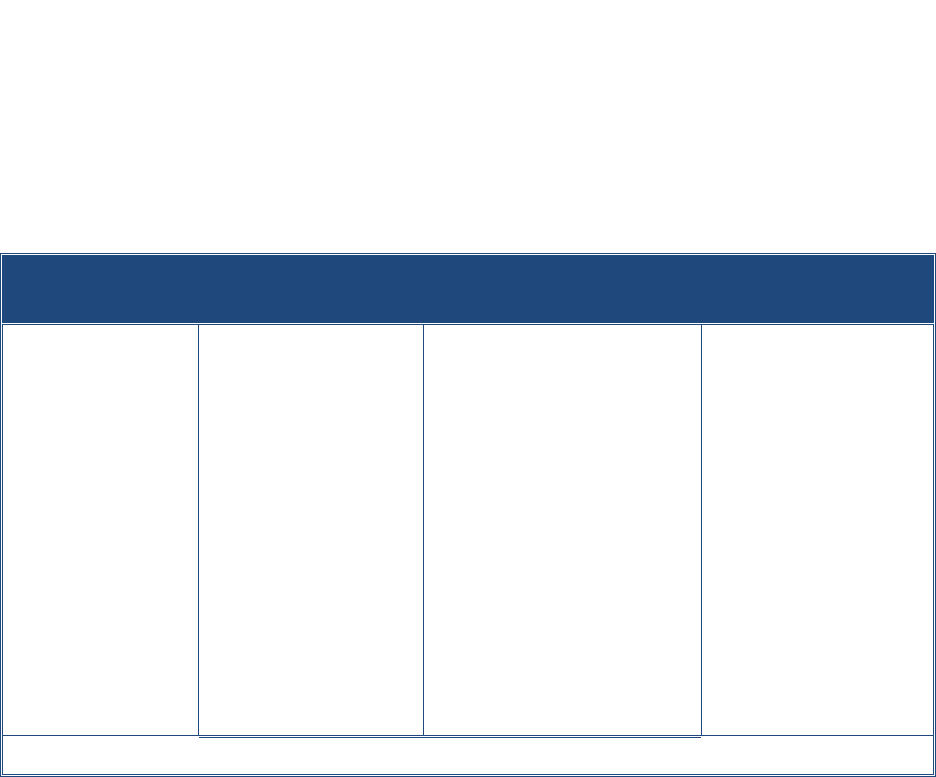
58
Appendix: Overview of Methodology
This report incorporates findings from an environmental scan, including a review and synthesis
of published research, evaluations, and white papers; discussions with subject matter experts
and housing and service providers; and conversations with people with lived experience of
homelessness in older adulthood. Each of these methods is described in further detail below.
ENVIRONMENTAL SCAN
We used a systems approach for identifying key resources, including focused searches on
literature and other resources within the fields of homelessness and housing, health and
behavioral health, and aging. We began the literature review with identification and review of
the seminal articles on older adult homelessness (e.g., Brown et al., 2011, 2016; Brown et al.,
2016; Culhane et al., 2013; Culhane et al., 2019; Kushel, 2020; Shinn et al., 2007) and the
bibliographies of the leading scholars in the field to identify both published and unpublished
relevant resources, including reports, evaluations, and datasets along with research articles.
From this initial review, we developed a list of key words to use in a broader search, augmented
with terms based on our knowledge of services and supports available across systems to serve
older adults at risk of or experiencing homelessness.
Exhibit A-1 outlines the key words and search terms used.
Exhibit A-1. Key Words and Search Terms Used to Identify Relevant
Published and Unpublished Literature
Population:
• Older adults
• Aging adults
• Seniors
• Elderly people
• Veterans
Conditions:
• Low-income
• Equity/
discrimination
• Rent-burdened
• Unsheltered
• Food insecurity
• Uninsured/
underinsured
Services:
• Homelessness prevention
• Outreach/engagement
• Crisis/interim housing
• Rapid re-housing
• Permanent supportive
housing
• Affordable housing/low-
income housing
• Medicare/Medicaid
• Medical respite care
• Income supports (SSI/SSDI)
• Food and nutrition
assistance
• Transportation assistance
Systems:
• Homelessness
• Housing
• Health care
• Behavioral health
• Social services
• Aging services
• VA
The sources searched for relevant literature are detailed in Exhibit A-2.
We conducted a series of systematic searches using the key words to identify the population of
interest in combination with conditions, services, and systems. For example, searches included
“older adults” combined with “low-income”, “homelessness prevention”, “homelessness
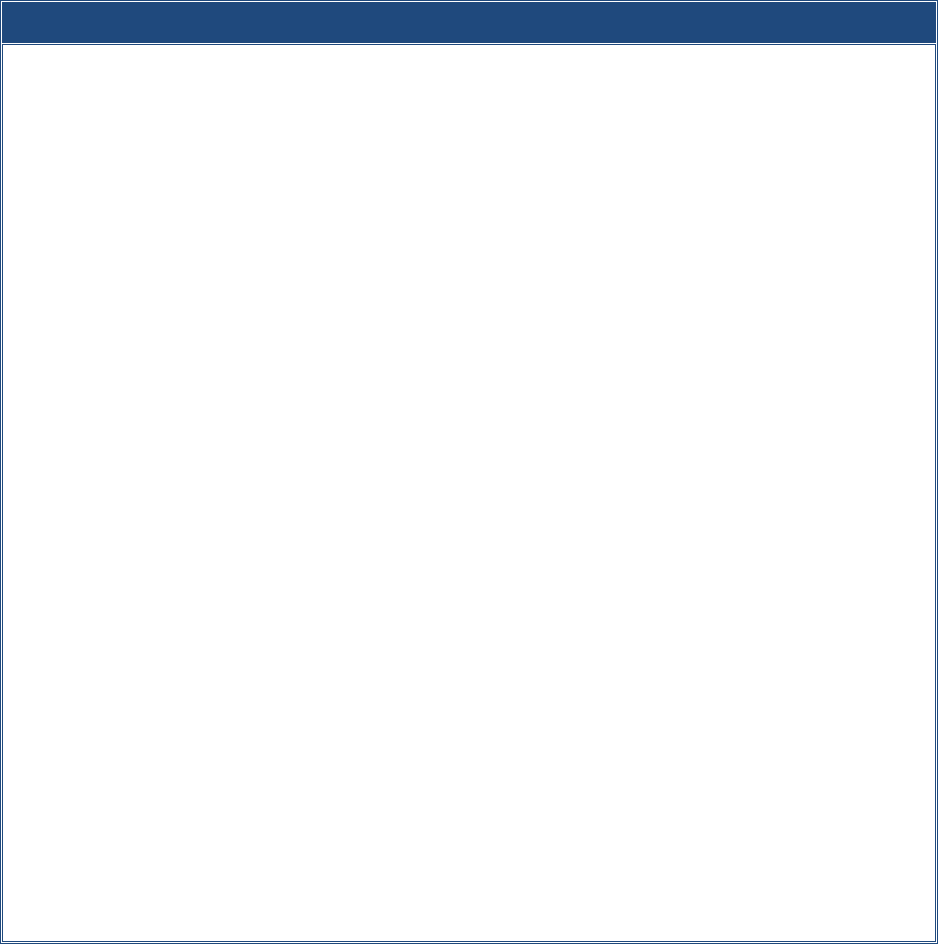
59
services”, and so on. Using these combinations of terms, we searched a variety of databases of
published literature to identify research on characteristics, service needs, and interventions for
older adults experiencing homelessness. We also searched government agency websites for
information about eligibility and coverage of services and supports across a range of systems.
Next, we searched the websites of research organizations, service providers, and advocacy
organizations for additional information about the needs of older adults at risk of or
experiencing homelessness, the challenges they face in accessing assistance, and specific
programs that are working to address these challenges. Finally, we identified additional studies
and reports recommended by experts and providers during the interview phase of the project.
This process identified 364 potential sources.
Exhibit A-2. Sources Searched to Identify Relevant Published and Unpublished Literature
• Seminal articles in field
• Bibliographies of leading scholars
• Databases of published literature (PsycINFO, ProQuest, SAGE Research Methods, FirstSearch, PubMed,
LitCovid)
• Government agencies
– Administration for Community Living/Administration on Aging
– Centers for Disease Control and Prevention
– Centers for Medicare & Medicaid Services
– Substance Abuse and Mental Health Services Administration
– U.S. Department of Health and Human Services
– U.S. Department of Housing and Urban Development
– U.S. Department of Veterans Affairs
– U.S. Interagency Council on Homelessness
– U.S. Social Security Administration
• Research, service, and advocacy organizations
– AmeriCorps
– Assisted Living Org
– Association of Mature American Citizens Foundation
– Benioff Homelessness and Housing Initiative
– Center for Housing Policy
– Center on Budget and Policy Priorities
– Corporation for Supportive Housing
– Council of Large Public Housing Authorities
– Homelessness Policy Research Institute
– Joint Center for Housing Studies, Harvard University
– Abdul Latif Jameel Poverty Action Lab Justice in Aging
– LeadingAge
– National Adult Protective Services Association
– National Adult Protective Services Resource Center
– National Alliance to End Homelessness
– National Association of Area Agencies on Aging
– National Coalition for the Homeless
– National Council on Aging
– National Health Care for the Homeless Council
– National Low Income Housing Coalition
– USAging
60
Once materials were collected, we applied a protocol to appraise the resources for factors that
may influence their interpretation and prioritization. For example, for studies on the
characteristics of the population, we considered the study location, the population included,
and the year of completion. Studies that occurred fully outside of the United States or Canada
were excluded from consideration. For studies on samples that were small or not
representative of all older adults experiencing homelessness (e.g., individuals living in a
particular city or individuals recruited from drop-in centers), we integrated details of the
studies that may influence their generalizability (such as sampling strategy or geographic
location) into the summary of findings to provide appropriate context for the reader. For
literature on program resources and interventions, we prioritized the most current information
available. In the final scan, we incorporated 164 of the materials identified.
Compared to the larger literature on homelessness among all populations, only a few studies
have focused specifically on older homeless adults, and most of these studies have been
conducted within the last decade. Several of the studies reviewed in this report are based on
small samples concentrated in urban areas. These limited samples pose challenges in drawing
generalizations about older adults’ experiences with homelessness and the supports available
for them. Thus, the picture presented here, though illustrative, may not include the experiences
of all older adults, such as those from rural areas. The examination of demographic composition
of the population of older adults experiencing homelessness is especially new; only a few
studies exist examining differences in the needs and trajectories between subgroups of older
adults or the influence of characteristics such as race and ethnicity and immigration status.
Several articles reviewed in this report originate from a single cohort of older adults who
participated in the landmark HOPE HOME study (Brown et al., 2011, 2016; Hurstak et al., 2017;
Kaplan et al., 2019; Kushel, 2020; Lee et al., 2016; Raven et al., 2017). This study followed a
cohort of 350 older adults experiencing homelessness in Oakland, California over three years.
The study used clinical assessments and structured interviews to assess geriatric conditions
(functional, cognitive, and sensory impairment), housing history, behavioral health (mental
health and alcohol and substance use disorders), physical health (chronic diseases), and acute
health care utilization (emergency department visits, inpatient hospitalizations, and skilled
nursing facility placement). As the first study of its kind to focus on this population, it provides
much-needed data on the experiences, trajectories, and consequences of geriatric conditions in
homeless adults aged 50 and older, providing important insights into the type of housing and
services that may be effective for serving this population. Yet there remains a need for
additional research to replicate this study to build on these learnings and assess the
generalizability of the findings for all older adults experiencing homelessness.
DISCUSSIONS
Discussions with Subject Matter Experts and Providers
Between June and October 2022, we conducted a series of discussions with a diverse set of
subject matter experts and housing and service providers on homelessness among older adults.
61
Nine subject matter experts representing different disciplines of research, policy, practice, and
systems with expertise in aging and homelessness were selected, including those with expertise
in population changes, behavioral health, housing, prevention, health care/long-term care,
veteran populations, aging services, and racial equity. We also selected representatives from
eight housing and service provider agencies located throughout the country, including
providers of homelessness prevention, outreach, and drop-in assistance; health care and
respite care; permanent supportive housing, and aging support services. Throughout the
report, we refer to these individuals as experts and providers, respectively.
These expert and provider discussions supplemented information learned through the
literature review. The discussions followed a semi-structured format and focused on providing a
deeper understanding of:
• The characteristics and needs of older adults at risk of or experiencing homelessness.
• Challenges to and potential strategies for identifying older adults in need and engaging
them in assistance.
• The range of services and supports across service sectors that are available to meet their
needs, including innovative interventions to explore.
• Gaps in services and supports that remain.
• Barriers and facilitators of cross-system coordination.
• Areas for which additional research is needed.
Discussions with People Experiencing Homelessness
We collected data through tailored conversations from individuals between the ages of 56 and
74 who were experiencing or had experienced homelessness as older adults. All but one of the
individuals were recruited for participation through three provider agencies -- two permanent
supportive housing programs for older adults located in the northeast and one drop-in center
for older adults located in the southwest. The final individual was identified through her work
as a national mental health consumer advocate and policy consultant who has written a
personal account of the challenges of experiencing homelessness as an older adult. Six people
were currently experiencing homelessness at the time of the discussion, staying in shelter, in
tents, or on the street. Eight people were housed, with seven in permanent supportive housing
and one in low-income housing. The goals of these conversations were to learn more about
their experiences accessing the housing and supports they needed and the challenges they
faced Westat staff conducted six of these conversations, while the remaining eight
conversations were led by case managers from the participating agencies using protocols
developed by Westat.
62
REFERENCES
Administration for Community Living (ACL). (2021) ACL Awards Over $85 Million to Support Adult
Protective Services Programs. https://acl.gov/news-and-events/announcements/acl-awards-over-
85-million-support-adult-protective-services-programs.
Administration for Community Living (ACL). (n.d.). Adult Day Care. Eldercare Locator. Retrieved April 4,
2023, from https://eldercare.acl.gov/public/resources/factsheets/adult_day_care.aspx.
Administration for Community Living (ACL). (2022). Older Americans Act. Retrieved April 4, 2023, from
https://acl.gov/about-acl/authorizing-statutes/older-americans-act.
Airgood-Obrycki, W. (2019). The Growing Problem of Older Adult Homelessness. Joint Center for Housing
Studies of Harvard University. Retrieved March 10, 2022, from
https://www.jchs.harvard.edu/blog/the-growing-problem-of-older-adult-
homelessness#:~:text=While%20the%20number%20of%20people,Housing%20America's%20Older
%20Adults%202019.
Aubry, T., Bloch, G., Brcic, V., Saad, A., Magwood, O., Abdalla, T., Alkhateeb, Q., Xie, E., Mathew, C.,
Hannigan, T., Costello, C., Thavorn, K., Stergiopoulos, V., Tugwell, P., & Pottie, K. (2020).
Effectiveness of permanent supportive housing and income assistance interventions for homeless
individuals in high-income countries: A systematic review. Lancet Public Health, 5(6), e342-e360.
https://doi.org/10.1016/S2468-2667(20)30055-4.
Aurand, A., Emmanuel, D., Threet, D., Rafi, I., & Yentel, D. (2021). The gap: A shortage of affordable
homes. National Low Income Housing Coalition. Retrieved January 31, 2022, from
https://reports.nlihc.org/sites/default/files/gap/Gap-Report_2021.pdf.
Baggett, T.P., Hwang, S.W., O’Connell, J.J., Porneala, B.C., Stringfellow, E.J., Orav, E.J., Singer, D.E., &
Rigotti, N.A. (2013). Mortality among homeless adults in Boston: Shifts in causes of death over a
15-year period. JAMA Internal Medicine, 173(3), 189-195.
https://doi.org/10.1001/jamainternmed.2013.1604.
Baggett, T.P., Singer, D.E., Rao, S.R., O’Connell, J.J., Bharel, M., & Rigotti, N.A. (2011). Food insufficiency
and health services utilization in a national sample of homeless adults. Journal of General Internal
Medicine, 26(6), 627-634. https://doi.org/10.1007/s11606-011-1638-4.
Bamberger, J.D., & Dobbins, S.K. (2015). A research note: Long-term cost effectiveness of placing
homeless seniors in permanent supportive housing. Cityscape, 17(2), 269-278.
http://www.jstor.org/stable/26326949.
Barrow, S., Rodríguez, G.S., & Córdova, P. (2004). Final Report on the Evaluation of the Closer to Home
Initiative. Corporation for Supportive Housing. Retrieved January 31, 2022, from
https://www.hudexchange.info/resource/891/closer-to-home-evaluation-of-the-closer-to-home-
initiative/.
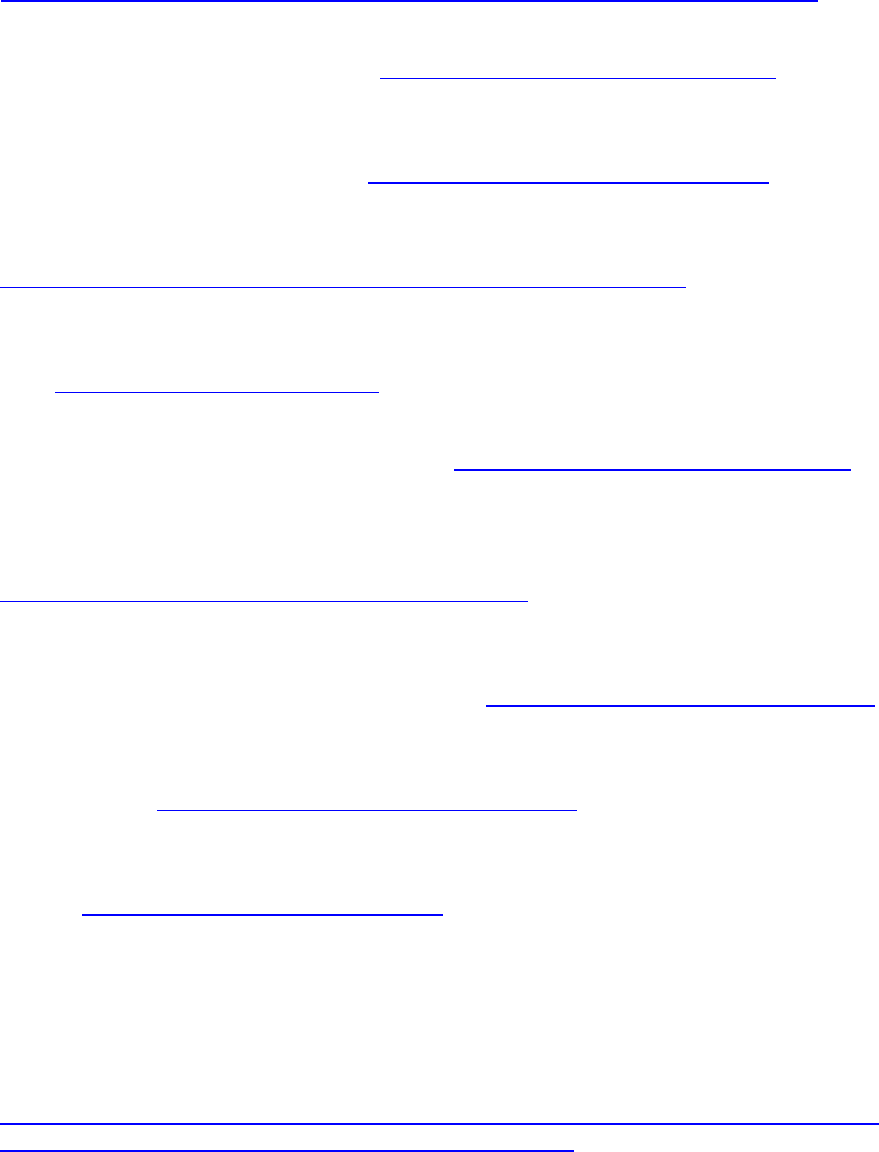
63
Benioff Homelessness and Housing Initiative. (2021). Home Safe Interim Evaluation: Key Findings.
Retrieved March 31, 2022, from
https://homelessness.ucsf.edu/sites/g/files/tkssra5216/f/resources/home_safe_memo.pdf.
Berg-Weger, M., & Morley, J.E. (2020). Loneliness in old age: An unaddressed health problem. Journal of
Nutrition, Health & Aging, 24(3), 243-245. https://doi.org/10.1007/s12603-020-1323-6.
Bielenberg, J.E., Futrell, M., Stover, B., & Hagopian, A. (2020). Presence of any medical debt associated
with two additional years of homelessness in a Seattle sample. INQUIRY: Journal of Health Care
Organization, Provision, & Financing, 57. https://doi.org/10.1177/0046958020923535.
Blancato, R., & Whitmire, M. (2021). The Crucial Role of Federal Nutrition Programs in Promoting Health
among Low-Income Older Adults. American Society on Aging. Retrieved January 31, 2022, from
https://generations.asaging.org/federal-nutrition-programs-key-older-adults.
Brown, R.T., Kimes, R.V., Guzman, D., & Kushel, M. (2010). Health care access and utilization in older
versus younger homeless adults. Journal of Health Care for the Poor and Underserved, 21(3), 1060-
1070. https://doi.org/10.1353/hpu.0.0344.
Brown, R.T., Kiely, D.K., Bharel, M., & Mitchell, S.L. (2011). Geriatric syndromes in older homeless adults.
Journal of General Internal Medicine, 27(1), 16-22. https://doi.org/10.1007/s11606-011-1848-9.
Brown, R.T., Thomas, M.L., Cutler, D.F., & Hinderlie, M. (2013). Meeting the housing and care needs of
older homeless adults: A permanent supportive housing program targeting homeless elders.
Seniors Housing & Care Journal, 21(1), 126-135. Retrieved January 31, 2022, from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3980491/.
Brown, R.T., Miao, Y., Mitchell, S.L., Bharel, M., Patel, M., Ard, K.L., Grande, L.J., Blazey-Martin, D., Floru,
D., & Steinman, M.A. (2015). Health outcomes of obtaining housing among older homeless adults.
American Journal of Public Health, 105(7), 1482-1488. https://doi.org/10.2105/AJPH.2014.302539.
Brown, R.T., Goodman, L., Guzman, D., Tieu, L., Ponath, C., & Kushel, M.B. (2016). Pathways to
homelessness among older homeless adults: Results from the HOPE HOME study. PLOS ONE,
11(5), e0155065. https://doi.org/10.1371/journal.pone.0155065.
Brown, R.T., Hemati, K., Riley, E.D., Lee, C.T., Ponath, C., Tieu, L., Guzman, D., & Kushel, M.B. (2017).
Geriatric conditions in a population-based sample of older homeless adults. Gerontologist,
gnw011. https://doi.org/10.1093/geront/gnw011.
Burt, M., Aran, L., Douglas, T., Valente, J., Lee, E., & Iwen, B. (1999). Homelessness: Programs and the
People They Serve: Findings from the National Survey of Homeless Assistance Providers and Clients.
Technical Report. Washington, DC: Urban Institute.
California Department of Aging. (n.d.). Program Narrative & Fact Sheets--Disease Prevention and Health
Promotion. California Department of Aging. Retrieved April 4, 2023, from
https://www.aging.ca.gov/Providers_and_Partners/Area_Agencies_on_Aging/Disease_Prevention
_and_Health_Promotion/Program_Narrative_and_Fact_Sheets/.
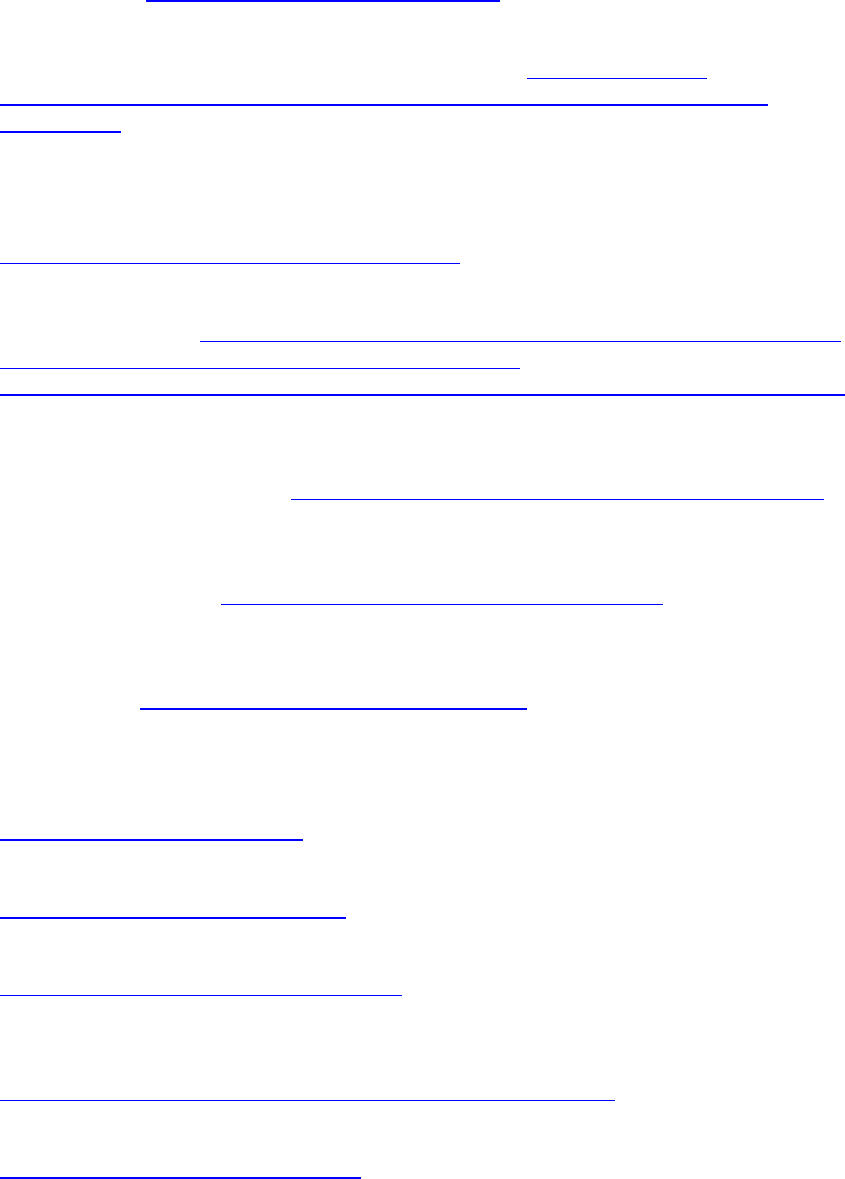
64
Canham, S.L., Custodio, K., Mauboules, C., Good, C., & Bosma, H. (2020). Health and psychosocial needs
of older adults who are experiencing homelessness following hospital discharge. Gerontologist,
60(4), 715–724. https://doi.org/10.1093/geront/gnz078.
Center for Housing Policy. (2015). The Impacts of Affordable Housing on Health: A Research Summary.
Center for Housing Policy. Retrieved March 10, 2022, from https://nhc.org/wp-
content/uploads/2017/03/The-Impacts-of-Affordable-Housing-on-Health-A-Research-
Summary.pdf.
Centers for Disease Control and Prevention (CDC), & National Association of Chronic Disease Directors.
(2008). The State of Mental Health and Aging in America Issue Brief 1: What Do the Data Tell Us?
Atlanta, GA: National Association of Chronic Disease Directors. Retrieved March 10, 2022, from
https://www.cdc.gov/aging/pdf/mental_health.pdf.
Centers for Medicare & Medicaid Services (CMS). (2022). Financial Alignment Initiative (FAI). Retrieved
March 31, 2022, from https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-
Medicaid-Coordination/Medicare-Medicaid-Coordination-
Office/FinancialAlignmentInitiative/FinancialModelstoSupportStatesEffortsinCareCoordination.
Cha, A.E., & Cohen, R.A. (2020). Reasons for Being Uninsured among Adults Aged 18-64 in the United
States, 2019. NCHS Data Brief, No. 382. Hyattsville, MD: National Center for Health Statistics.
Retrieved March 31, 2022, from https://www.cdc.gov/nchs/products/databriefs/db382.htm.
Chan, D.V., Gopal, S., & Helfrich, C.A. (2014). Accessibility patterns and community integration among
previously homeless adults: A geographic information systems (GIS) approach. Social Science &
Medicine, 120, 142-152. https://doi.org/10.1016/j.socscimed.2014.09.005.
Chekuri, L., Turturro, C.L., Nekkalapudi, M., & Mittal, D. (2016). Racial differences in older homeless
adults: Findings in a homeless sample from Little Rock. American Journal of Geriatric Psychiatry,
24(3), S67-S68. https://doi.org/10.1016/j.jagp.2016.01.066.
Chung, T.E., Gozdzik, A., Palma Lazgare, L.I., To, M.J., Aubry, T., Frankish, J., Hwang, S.W., &
Stergiopoulos, V. (2018). Housing First for older homeless adults with mental illness: A subgroup
analysis of the At Home. International Journal of Geriatric Psychiatry, 33(1), 85-95.
https://doi.org/10.1002/gps.4682.
Cohen C.I. (1999). Aging and homelessness. Gerontologist, 39(1), 5-14.
https://doi.org/10.1093/geront/39.1.5.
Cohen S. (2004). Social relationships and health. American Psychologist, 59(8), 676-684.
https://doi.org/10.1037/0003-066X.59.8.676.
Coleman-Jensen, A., Rabbitt, M.P., Gregory, C.A., & Singh, A. (2016). Household Food Security in the
United States in 2016. U.S. Department of Agriculture. Retrieved January 31, 2022, from
https://www.ers.usda.gov/webdocs/publications/84973/err-237.pdf.
Congressional Research Service. (2022). Older Americans Act: Overview and Funding. Retrieved from
https://sgp.fas.org/crs/misc/R43414.pdf.
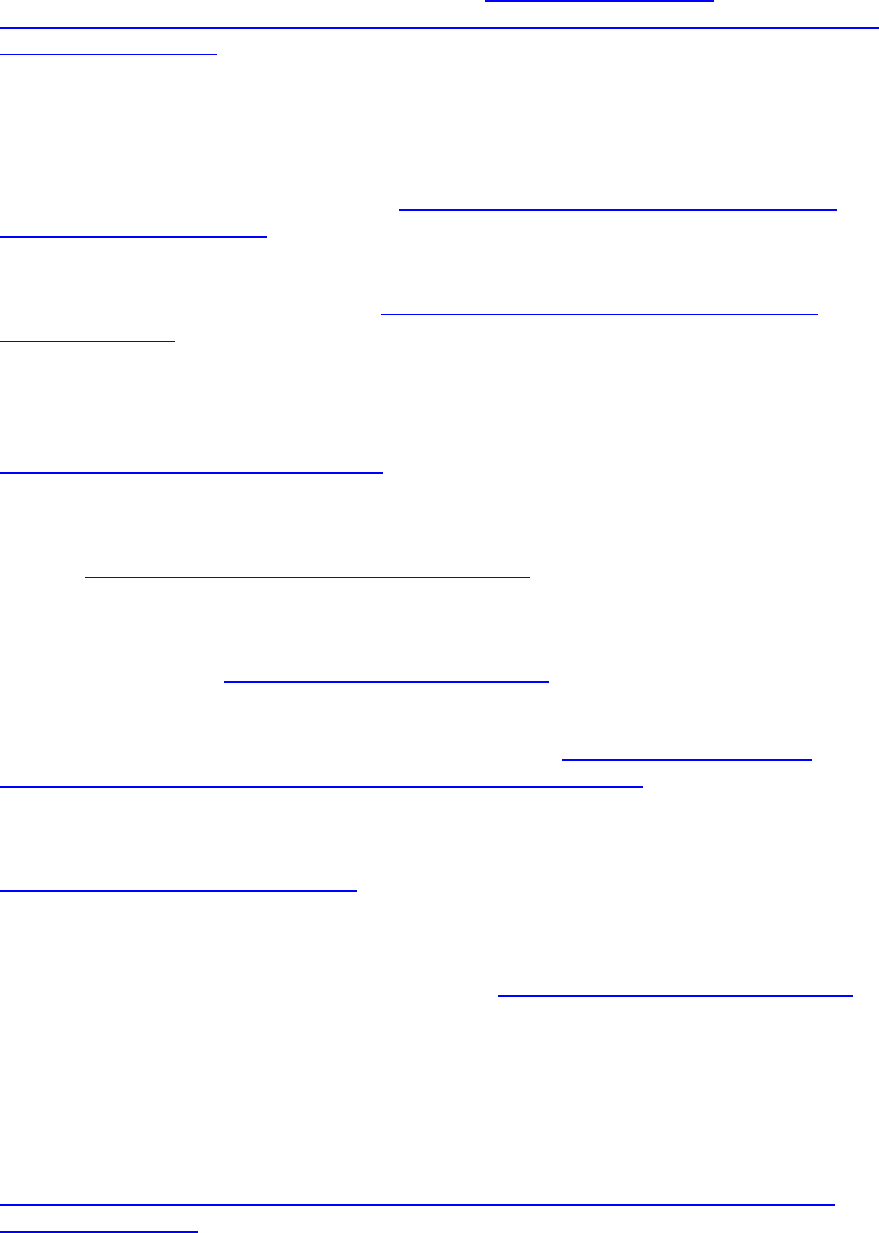
65
Corporation for Supportive Housing (CSH). (2011). Ending Homelessness among Older Adults through
Supportive Housing. Retrieved January 31, 2022, from https://www.csh.org/wp-
content/uploads/2012/01/Report_EndingHomelessnessAmongOlderAdultsandSeniorsThroughSup
portiveHousing_112.pdf.
Costello, A.M. (2021). RE: Opportunities in Medicaid and CHIP to Address Social Determinants of Health
(SDOH). Baltimore, MD.
Couch, L.M. (2020). Falling short: Federal housing assistance is failing older adults. Generations Journal,
44(2), 1-8. Retrieved January 31, 2022, from https://generations.asaging.org/federal-housing-
assistance-older-adults-failing.
Couch, L.M. (2021). Section 202: Supportive Housing for the Elderly. National Low Income Housing
Coalition. Retrieved March 31, 2022, from https://nlihc.org/sites/default/files/AG-2021/04-
13_Section-202.pdf.
Crane, M., Byrne, K., Fu, R., Lipmann, B., Mirabelli, F., Rota-Bartelink, A., Ryan, M., Shea, R., Watt, H.,
Warnes, A.M. (2005). The causes of homelessness in later life: Findings from a 3-nation study.
Journals of Gerontology Series B: Psychological Sciences & Social Sciences, 60(3), S152-S159.
https://doi.org/10.1093/geronb/60.3.S152.
Culhane, D.P., Metraux, S., & Hadley, T. (2002). Public service reductions associated with placement of
homeless persons with severe mental illness in supportive housing. Housing Policy Debate, 13(1),
107-163. https://doi.org/10.1080/10511482.2002.9521437.
Culhane, D.P., Metraux, S., Byrne, T., Stino, M., & Bainbridge, J. (2013). The age structure of
contemporary homelessness: Evidence and implications for public policy. Analyses of Social Issues
& Public Policy, 13, 1-17. https://doi.org/10.1111/asap.12004.
Culhane, D.P., Byrne, T., Metraux, S., Kuhn, R., Doran, K., Johns, E., & Schretzman, M. (2019). Emerging
Crisis of Aged Homelessness. Retrieved January 31, 2022, from https://aisp.upenn.edu/wp-
content/uploads/2019/01/Emerging-Crisis-of-Aged-Homelessness-1.pdf.
DeMallie, D.A., North, C.S., & Smith, E.M. (1997). Psychiatric disorders among the homeless: A
comparison of older and younger groups. Gerontologist, 37(1), 61-66.
https://doi.org/10.1093/geront/37.1.61.
Dickins, K.A., Philpotts, L.L., Flanagan, J., Bartels, S.J., Baggett, T.P., & Looby, S.E. (2021). Physical and
behavioral health characteristics of aging homeless women in the United States: An integrative
review. Journal of Women’s Health, 30(10), 1493-1507. https://doi.org/10.1089/jwh.2020.8557.
Dietz, T.L. (2009). Drug and alcohol use among homeless older adults: Predictors of reported current and
lifetime substance misuse problems in a national sample. Journal of Applied Gerontology, 28(2),
235-255.
DiPietro, B., Artiga, S., & Gates, A. (2014). Early Impacts of the Medicaid Expansion for the Homeless
Population. Kaiser Family Foundation. Retrieved May 1, 2023, from
https://www.kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-
homeless-population/.
66
Donaldson, L.P., Streeter, C.L., Larkin, H., Briar-Lawson, K., Meyer-Adams, N., Lupfer, K., Elder, J., &
Grimshaw, A. (2020). The SOAR Model as an effective mechanism for university--Community
partnerships to end homelessness. Journal of Social Work Education, 56(sup1), S99-S110.
https://doi.org/10.1080/10437797.2020.1741481.
Dunton, L., & Brown, S. (2019). Rapid Re-housing in 2018: Program Features and Assistance Models. U.S.
Department of Housing and Urban Development. Retrieved March 31, 2022, from
https://www.huduser.gov/portal/sites/default/files/pdf/RRH-CommunityScanReport.pdf.
Eldercare Directory. (n.d.). Essential Resources for Senior Citizens and Their Caregivers. Retrieved
January 31, 2022, from https://www.eldercaredirectory.org/state-resources.htm.
Gabrielian, S., Cordasco, K.M., Finley, E.P., Hoffmann, L.C., Harris, T., Calderon, R.A., Barnard, J.M., Ganz,
D.A., & Olmos-Ochoa, T.T. (2022). Engaging stakeholders to inform national implementation of
critical time intervention in a program serving homeless-experienced veterans. Frontiers in
Psychology, 13, 1009467. https://doi.org/10.3389/fpsyg.2022.1009467.
Garfield, R., & Orgera, K. (2021). The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand
Medicaid. Kaiser Family Foundation. Retrieved March 31, 2022, from
https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-
do-not-expand-medicaid/.
Garibaldi, B., Conde-Martel, A., & O’Toole, T.P. (2005). Self-reported comorbidities, perceived needs,
and sources for usual care for older and younger homeless adults. Journal of General Internal
Medicine, 20(8), 726-730. https://doi.org/10.1111/j.1525-1497.2005.0142.x.
Gelberg, L., Linn, L.S., & Mayer-Oakes, S.A. (1990). Differences in health status between older and
younger homeless adults. Journal of the American Geriatrics Society, 38(11), 1220-1229.
https://doi.org/10.1111/j.1532-5415.1990.tb01503.x.
Goger, A. (2020). For Millions of Low-Income Seniors, Coronavirus is a Food-Security Issue. Brookings.
Retrieved March 31, 2022 from https://www.brookings.edu/blog/the-avenue/2020/03/16/for-
millions-of-low-income-seniors-coronavirus-is-a-food-security-issue/.
Goldberg, J., Lang, K., & Barrington, V. (2016). How to Prevent and End Homelessness among Older
Adults. Justice in Aging. Retrieved January 31, 2022, from https://www.justiceinaging.org/wp-
content/uploads/2016/04/Homelessness-Older-Adults.pdf.
Gonyea, J.G., Mills-Dick, K., & Bachman, S.S. (2010). The complexities of elder homelessness, a shifting
political landscape and emerging community responses. Journal of Gerontological Social Work,
53(7), 575-590. https://doi.org/10.1080/01634372.2010.510169.
Gordon, R.J., Rosenheck, R.A., Zweig, R.A., & Harpaz-Rotem, I. (2012). Health and social adjustment of
homeless older adults with a mental illness. Psychiatric Services, 63(6), 561-568.
https://doi.org/10.1176/appi.ps.201100175.
Grenier, A., Barken, R., Sussman, T., Rothwell, D., & Lavoie, J. (2013). Literature Review: Aging and
Homelessness. Retrieved March 31, 2022, from https://aginghomelessness.com/wp-
content/uploads/2012/10/Literature-Review-Aging-and-Homelessness.pdf.
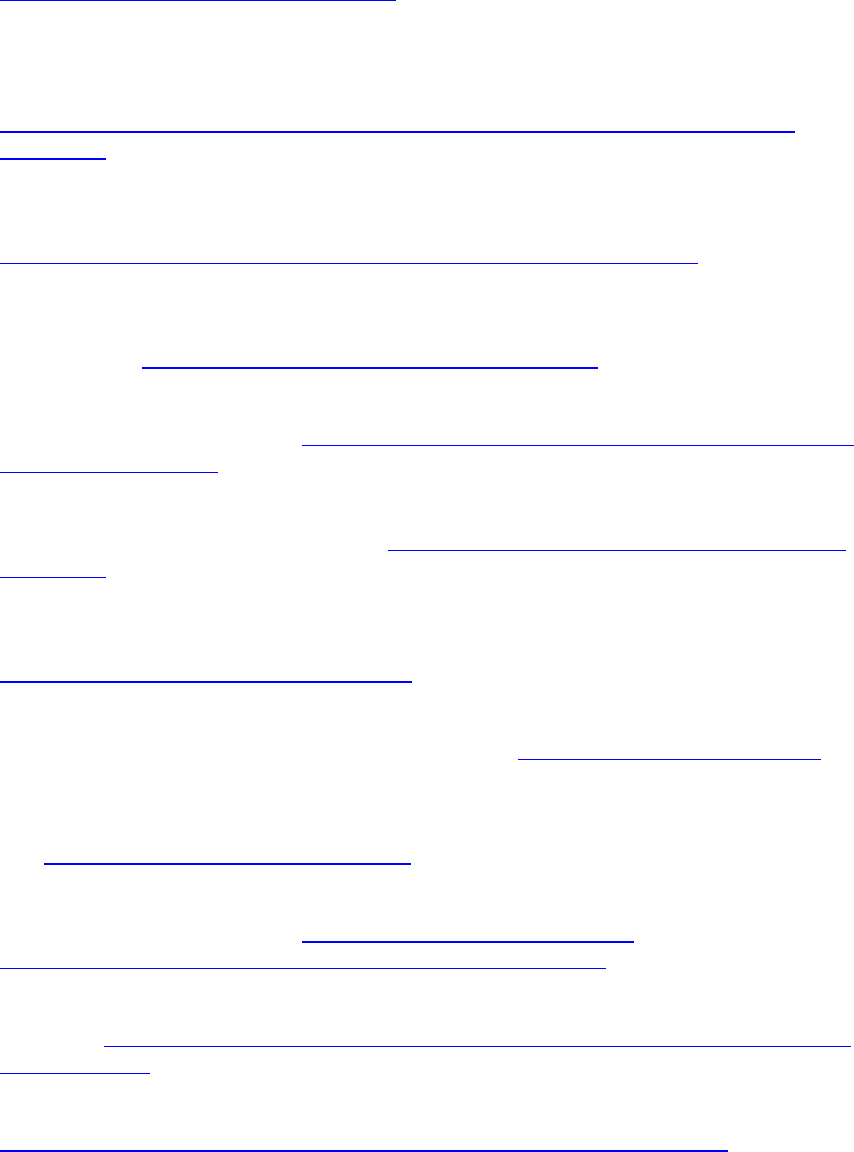
67
Greysen, S.R., Allen, R., Lucas, G.I., Wang, E.A., & Rosenthal, M.S. (2012). Understanding transitions in
care from hospital to homeless shelter: A mixed-methods, community-based participatory
approach. Journal of General Internal Medicine, 27(11), 1484-1491.
https://doi.org/10.1007/s11606-012-2117-2.
Gubits, D., Bishop, K., Dunton, L., Wood, M., Albanese, T., Spellman, B., & Khadduri, J. (2018).
Understanding Rapid Re-housing: Systematic Review of Rapid Re-housing Outcomes Literature.
U.S. Department of Housing and Urban Development. Retrieved March 31, 2022, from
https://www.huduser.gov/portal/sites/default/files/pdf/Systematic-Review-of-Rapid-Re-
housing.pdf.
Haarstad, C. (2008). Transportation Voucher Programs: Facilitating Mobility in Rural Areas. Employment
Transportation Resources. Retrieved January 31, 2022, from
http://www.worksupport.com/documents/transportvouchprogmobilrural.pdf.
Hahn, J.A., Kushel, M.B., Bangsberg, D.R., Riley, E., & Moss, A.R. (2006). Brief report: The aging of the
homeless population: Fourteen-year trends in San Francisco. Journal of General Internal Medicine,
21(7), 775-778. https://doi.org/10.1111/j.1525-1497.2006.00493.x.
Health Resources and Services Administration (HRSA). (2018). Federally Qualified Health Centers.
Retrieved January 31, 2022, from https://www.hrsa.gov/opa/eligibility-and-registration/health-
centers/fqhc/index.html.
Health Resources and Services Administration (HRSA). (2020). 2020 Special Populations Funded
Programs. Retrieved March 31, 2022, from https://data.hrsa.gov/tools/data-reporting/special-
populations.
Hecht, L., & Coyle, B. (2001). Elderly homeless: A comparison of older and younger adult emergency
shelter seekers in Bakersfield, California. American Behavioral Scientist, 45(1), 66-79.
https://doi.org/10.1177/00027640121957024.
Henwood, B.F., Katz, M.L., & Gilmer, T.P. (2014). Aging in place within permanent supportive housing.
International Journal of Geriatric Psychiatry, 30(1), 80-87. https://doi.org/10.1002/gps.4120.
Henwood, B.F., Lahey, J., Rhoades, H., Winetrobe, H., & Wenzel, S.L. (2018). Examining the health status
of homeless adults entering permanent supportive housing. Journal of Public Health, 40(2), 415-
418. https://doi.org/10.1093/pubmed/fdx069.
Homelessness Policy Research Institute (HPRI). (2019). Older Adults Experiencing Homelessness.
Retrieved January 31, 2022, from https://socialinnovation.usc.edu/wp-
content/uploads/2019/08/Older-Adults-Literature-Review-Final.pdf.
Homelessness Policy Research Institute (HPRI). (2020). Homelessness and Employment. Retrieved May 1,
2023, from https://socialinnovation.usc.edu/wp-content/uploads/2020/08/Homelessness-and-
Employment.pdf.
HUD Exchange. (n.d.). Rapid Re-housing. Retrieved March 31, 2022, from
https://files.hudexchange.info/resources/documents/Rapid-Re-Housing-Brief.pdf.
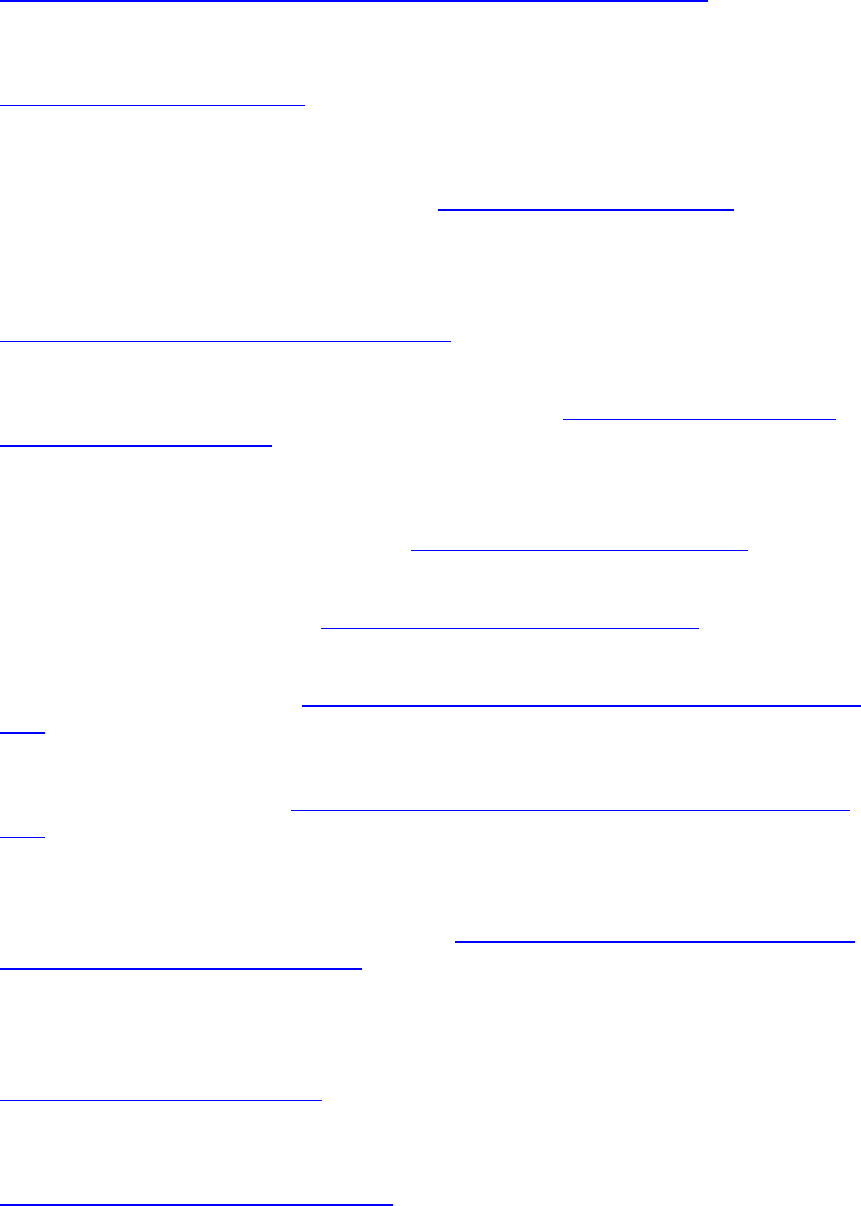
68
HUD User. (2019). Tenants in LIHTC Units as of December 31, 2019. Retrieved March 31, 2022, from
https://www.huduser.gov/portal/Datasets/lihtc/2019-LIHTC-Tenant-Tables.pdf.
Hui, V., & Habib, K.M. (2014). An Investigation of Transport-Related Social Exclusion of the At-Risk
Community (Homeless People) in Toronto, Canada. Retrieved March 31, 2022, from
https://trid.trb.org/view/1287880.
Hui, V., & Habib, K.N. (2017). Homelessness vis-à-vis Transportation-Induced Social Exclusion: An
Econometric Investigation of Travel Behavior of Homeless Individuals in Toronto, Canada.
Transportation Research Record, 2665(1), 60-68. https://doi.org/10.3141/2665-07.
Hurstak, E., Johnson, J.K., Tieu, L., Guzman, D., Ponath, C., Lee, C.T., Jamora, C.W., & Kushel, M. (2017).
Factors associated with cognitive impairment in a cohort of older homeless adults: Results from
the HOPE HOME study. Drug and Alcohol Dependence, 178, 562-570.
https://doi.org/10.1016/j.drugalcdep.2017.06.002.
Hwang, S.W., Orav, E.J., O'Connell, J.J., Lebow, J.M., & Brennan, T.A. (1997). Causes of death in homeless
adults in Boston. Annals of Internal Medicine, 126(8), 625-628. https://doi.org/10.7326/0003-
4819-126-8-199704150-00007.
Hwang, S.W., Colantonio, A., Chiu, S., Tolomiczenko, G., Kiss, A., Cowan, L., Redelmeier, D.A., & Levinson,
W. (2008). The effect of traumatic brain injury on the health of homeless people. Canadian
Medical Association Journal, 179(8), 779-784. https://doi.org/10.1503/cmaj.080341.
Jain, S.H., Baackes, J., & O’Connell, J.J. (2020). Homeless special needs plans for people experiencing
homelessness. JAMA, 323(10), 927. https://doi.org/10.1001/jama.2019.22376.
Joint Center for Housing Studies of Harvard University. (2018). Housing America’s Older Adults.
Retrieved January 31, 2022, from https://www.jchs.harvard.edu/housing-americas-older-adults-
2018.
Joint Center for Housing Studies of Harvard University. (2019). Housing America’s Older Adults.
Retrieved January 4, 2023, from https://www.jchs.harvard.edu/housing-americas-older-adults-
2019.
Johnson, R.W., & Favreault, M.M. (2021). Risk of Economic Hardship Among Older Adults. Washington,
DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and
Human Services. Retrieved January 13, 2023, from https://aspe.hhs.gov/reports/risk-economic-
hardship-among-older-adults-issue-brief.
Kaplan, L.M., Vella, L., Cabral, E., Tieu, L., Ponath, C., Guzman, D., & Kushel, M.B. (2019). Unmet mental
health and substance use treatment needs among older homeless adults: Results from the HOPE
HOME Study. Journal of Community Psychology, 47(8), 1893-1908.
https://doi.org/10.1002/jcop.22233.
Kauff, J.F., Clary, E., Lupfer, K.S., & Fischer, P.J. (2016). An evaluation of SOAR: Implementation and
outcomes of an effort to improve access to SSI and SSDI. Psychiatric Services, 67(10), 1098-1102.
https://doi.org/10.1176/appi.ps.201500247.
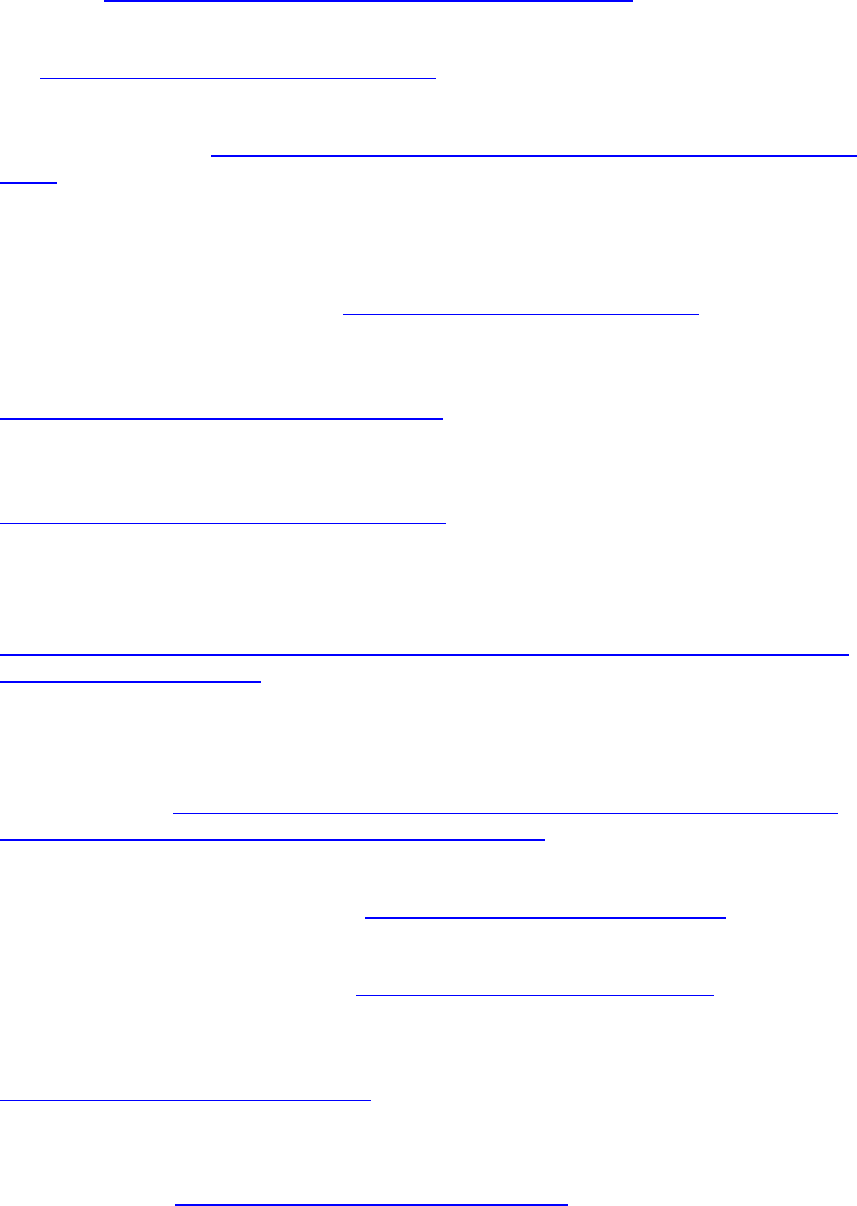
69
Kochera, A. (2006). Developing Appropriate Rental Housing for Low-Income Older Persons: A Survey of
Section 202 and LIHTC Property Managers. AARP Public Policy Institute. Retrieved January 31,
2022, from https://assets.aarp.org/rgcenter/consume/dd149_lihtc.pdf.
Kushel, M. (2012). Older homeless adults: Can we do more? Journal of General Internal Medicine, 27(1),
5-6. https://doi.org/10.1007/s11606-011-1925-0.
Kushel, M. (2020). Homelessness among older adults: An emerging crisis. Generations, 44(2). Retrieved
January 31, 2022, from https://stg-generations.asaging.org/homelessness-older-adults-poverty-
health.
Larimer, M.E., Malone, D.K., Garner, M.D., Atkins, D.C., Burlingham, B., Lonczak, H.S., Tanzer, K., Ginzler,
J., Clifasefi, S.L., Hobson, W.G., & Marlatt, G.A. (2009). Health care and public service use and costs
before and after provision of housing for chronically homeless persons with severe alcohol
problems. JAMA, 301(13), 1349-1357. https://doi.org/10.1001/jama.2009.414.
Lee, C.T., Guzman, D., Ponath, C., Tieu, L., Riley, E., & Kushel, M. (2016). Residential patterns in older
homeless adults: Results of a cluster analysis. Social Science & Medicine, 153, 131-140.
https://doi.org/10.1016/j.socscimed.2016.02.004.
Lee, K., Murphy, E.R., Cassidy, J., Chen, Z., and Rhee, T.G. (2020). Impacts of health insurance on older
adults with histories of homelessness. Journal of Social Distress & Homelessness.
https://doi.org/10.1080/10530789.2020.1819051.
Levin, M., Kauff, J., Negoita, M., Dragoset, L., Goger, A., Baxter, C., Paprocki, A., Makowsky, L., Gutierrez,
I., Brown, E., & Sarver, M. (2020). Evaluation of Alternatives to Improve Elderly Access to SNAP.
USDA Food and Nutrition Service. Retrieved January 31, 2022, from
https://www.fns.usda.gov/snap/evaluation-alternatives-improve-elderly-access-supplemental-
nutrition-assistance-program.
Lewin Group. (2011). Design of a Demonstration of Coordinated Housing, Health and Long-Term Care
Services and Supports for Low-Income Older Adults. Washington, DC: Office of the Assistant
Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Retrieved
April 1, 2022, from https://aspe.hhs.gov/reports/design-demonstration-coordinated-housing-
health-long-term-care-services-supports-low-income-older-0.
Li, Z., & Dalaker, J. (2021). Poverty Among the Population Aged 65 and Older. Congressional Research
Service. Retrieved March 31, 2022, from https://sgp.fas.org/crs/misc/R45791.pdf.
Libson, N. (2005). The sad state of affordable housing for older people. Generations: Journal of the
American Society on Aging, 29(4), 9-15. https://www.jstor.org/stable/26555401.
Lipton, F.R., Siegel, C., Hannigan, A., Samuels, J., & Baker, S. (2000). Tenure in supportive housing for
homeless persons with severe mental illness. Psychiatric Services, 51(4), 479-486.
https://doi.org/10.1176/appi.ps.51.4.479.
Lowder, E.M., Desmarais, S.L., Neupert, S.D., & Truelove, M.A. (2017). SSI/SSDI Outreach, Access, and
Recovery (SOAR): Disability application outcomes among homeless adults. Psychiatric Services,
68(11), 1189-1192. https://doi.org/10.1176/appi.ps.201600568.
70
Liu, P.-J., & Delagrammatikas, L. (2021). Adult protective service’s role in addressing older and
dependent adult abuse in the age of COVID. Frontiers in Public Health, 9.
https://doi.org/10.3389/fpubh.2021.659640.
Martinez, T.E., & Burt, M.R. (2006). Impact of permanent supportive housing on the use of acute care
health services by homeless adults. Psychiatric Services, 57(7), 992-999.
https://doi.org/10.1176/ps.2006.57.7.992.
McDonald, L., Donahue, P., Janes, J., & Cleghorn, L. (2006). In from the Streets: The Health and Well-
being of Formerly Homeless Older Adults. National Research Program of the National
Homelessness Initiative. https://doi.org/10.13140/RG.2.1.4680.2647.
Medicaid.gov. (n.d.). Program of All-Inclusive Care for the Elderly. Retrieved March 31, 2022, from
https://www.medicaid.gov/medicaid/long-term-services-supports/program-all-inclusive-care-
elderly/index.html.
Medicare.gov. (n.d.). Medicare Savings Programs. Retrieved August 29, 2022, from
https://www.medicare.gov/basics/costs/help/medicare-savings-programs#collapse-2624.
Meret-Hanke, L.A. (2011). Effects of the program of all-inclusive care for the elderly on hospital use.
Gerontologist, 51(6), 774-785. https://doi.org/10.1093/geront/gnr040.
Metraux, S., Marcus, S.C., & Culhane, D.P. (2003). The New York-New York Housing Initiative and use of
public shelters by persons with severe mental illness. Psychiatric Services, 54(1), 67-71.
https://doi.org/10.1176/appi.ps.54.1.67.
Metraux, S., Eng, N., Bainbridge, J., & Culhane, D.P. (2011). The impact of shelter use and housing
placement on mortality hazard for unaccompanied adults and adults in family households entering
New York City Shelters: 1990-2002. Journal of Urban Health, 88(6), 1091-1104.
https://doi.org/10.1007/s11524-011-9602-5.
Moses, J. (2019). Building a Conversation: Aged Homelessness on the Rise. National Alliance to End
Homelessness. Retrieved January 31, 2022, from https://endhomelessness.org/blog/building-a-
conversation-aged-homelessness-on-the-rise/.
Murphy, E.R. (2019). Transportation and homelessness: A systematic review. Journal of Social Distress &
the Homeless, 28(2), 96-105. https://doi.org/10.1080/10530789.2019.1582202.
National Adult Protective Services Association. (n.d.). Getting to Know Adult Protective Services.
Retrieved March 6, 2023, from https://www.napsa-now.org/.
National Adult Protective Services Resource Center (NAPSRC). (n.d.). Adult Protective Services, What You
Must Know. National Center on Elder Abuse. Retrieved March 6, 2023, from
https://ncea.acl.gov/NCEA/media/publications/APS-Fact-Sheet.pdf.
National Alliance to End Homelessness (NAEH). (2021). Permanent Supportive Housing. Retrieved
January 31, 2022, from https://endhomelessness.org/ending-homelessness/solutions/permanent-
supportive-housing/.
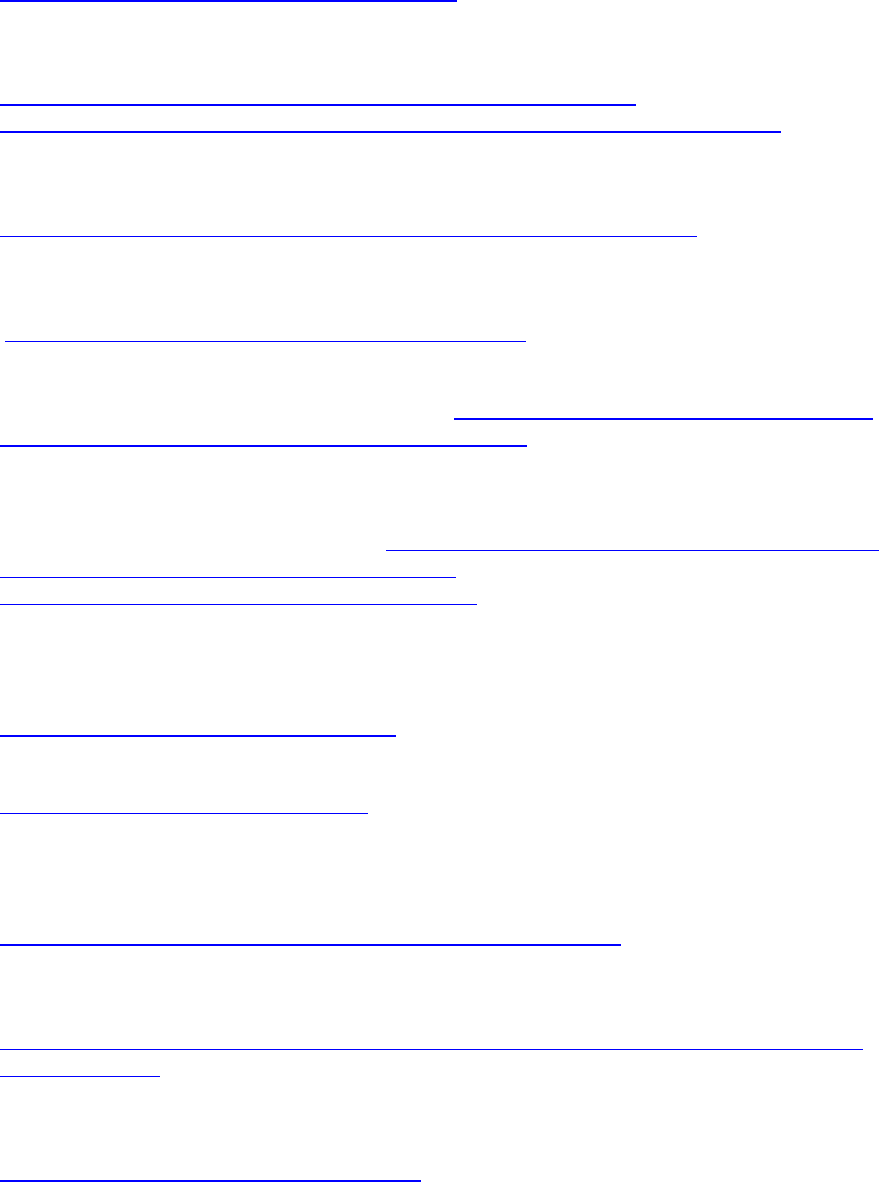
71
National Association of Area Agencies on Aging (n4a). (n.d. a). Housing Options for Older Adults: A Guide
for Making Housing Decisions. Retrieved January 31, 2022, from
https://www.usaging.org/files/HousingOptions.pdf.
National Association of Area Agencies on Aging (n4a). (n.d. b). Housing and Homelessness: Services and
Partnerships to Address a Growing Issue. Retrieved December 22, 2022, from
https://www.usaging.org/Files/Housing%20and%20Homelessness%20-
%20Services%20and%20Partnerships%20to%20Address%20a%20Growing%20Issue.pdf.
National Association of Nutrition and Aging Services Programs (NANASP). (2021). NANASP COVID-19
Relief and Vaccine Survey--January 2021. Retrieved January 31, 2022, from
https://www.nanasp.org/sites/default/files/documents/Data_Q3_210222.pdf.
National Coalition for the Homeless. (2009). Homelessness among Elderly Persons. Retrieved March 10,
2022, from
https://www.nationalhomeless.org/factsheets/Elderly.pdf.
National Council on Aging (NCOA). (2022). How to Make It Easier for Older Adults to Get Energy and
Utility Assistance. Retrieved March 31, 2022, from https://www.ncoa.org/article/how-to-make-it-
easier-for-older-adults-to-get-energy-and-utility-assistance.
Niño, M.D., Loya, M.A., & Cuevas, M. (2009). Who are the chronically homeless? Social characteristics
and risk factors associated with chronic homelessness. Journal of Social Distress & the Homeless,
19, 41-65. Retrieved March 31, 2022, from https://www.semanticscholar.org/paper/Who-are-the-
Chronically-Homeless-Social-and-Risk-Ni%C3%B1o-
Loya/9be479666f4e9c87cd1ea6609fca01a8aca81984.
North, C.S., Wohlford, S.E., Dean, D.J., Black, M., Balfour, M.E., Petrovich, J.C., Downs, D.L., & Pollio, D.E.
(2017). A pilot study using mixed GPS/narrative interview methods to understand geospatial
behavior in homeless populations. Community Mental Health Journal, 53(6), 661-671.
https://doi.org/10.1007/s10597-016-0057-8.
Novak, M. (2018). Issues on Aging. New York, NY: Taylor & Francis Group.
https://doi.org/10.4324/9781315445366.
Nye, E., Lamont, H., & Anderson, L. (2022) Federal Efforts to Address Racial and Ethnic Disparities in
Alzheimer’s Disease and Related Dementias (Issue Brief). Washington, DC: Office of the Assistant
Secretary for Planning and Evaluation, U.S. Department of Health and Human Services.
https://aspe.hhs.gov/reports/federal-efforts-address-adrd-disparities.
Office of Governor Gavin Newsom. (2022). California Expands Medi-Cal to All Eligible Adults 50 Years of
Age and Older. CA.gov. Retrieved March 21, 2023, from
https://www.gov.ca.gov/2022/04/29/california-expands-medi-cal-to-all-eligible-adults-50-years-
of-age-and-older/.
Parpouchi, M., Moniruzzaman, A., Russolillo, A., & Somers, J.M. (2016). Food insecurity among homeless
adults with mental illness. PLOS ONE, 11(7), e0159334.
https://doi.org/10.1371/journal.pone.0159334.
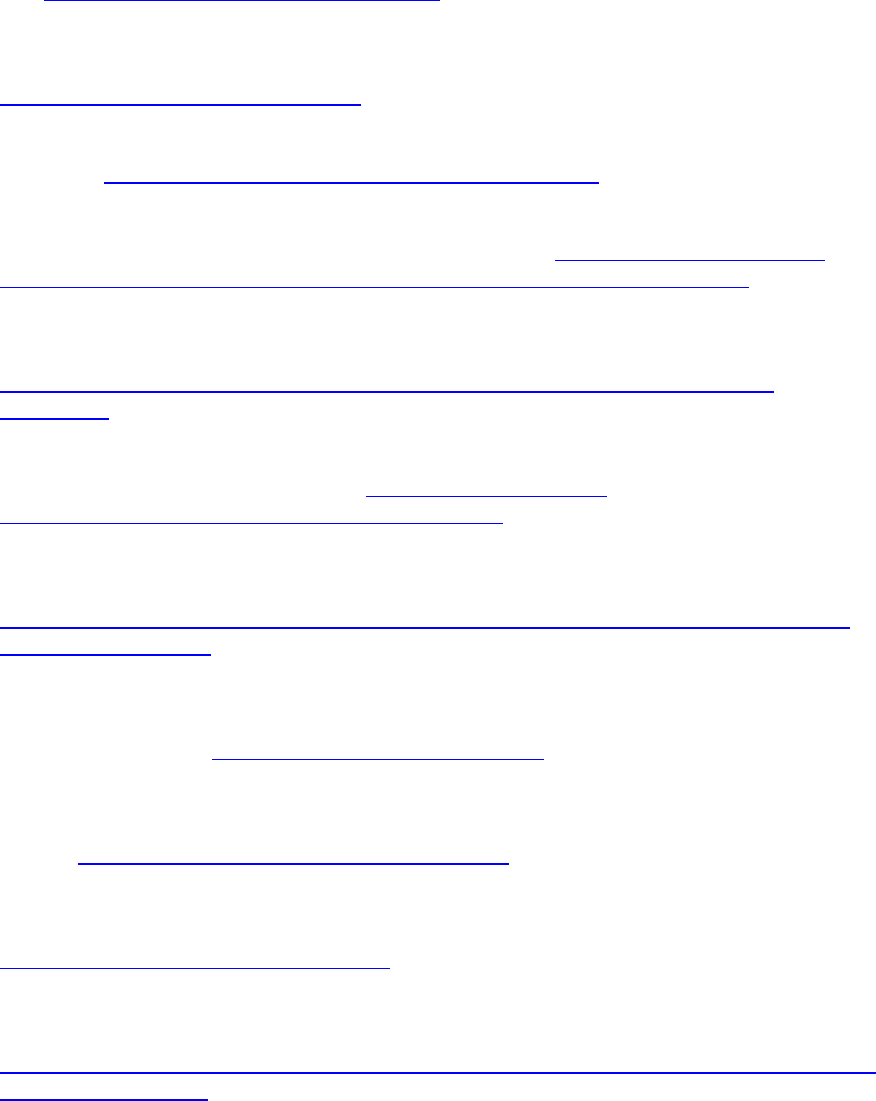
72
Patanwala, M., Tieu, L., Ponath, C., Guzman, D., Ritchie, C.S., & Kushel, M. (2018). Physical,
psychological, social, and existential symptoms in older homeless-experienced adults: An
observational study of the HOPE HOME cohort. Journal of General Internal Medicine, 33(5), 635-
643. https://doi.org/10.1007/s11606-017-4229-1.
Perl, L., & Bagalman, E. (2015). Chronic Homelessness: Background, Research, and Outcomes.
Congressional Research Service. Retrieved January 31, 2022, from
https://sgp.fas.org/crs/misc/R44302.pdf.
Perret, Y.M. (2021). Homelessness and Social Security. Social Security Matters. Retrieved March 31,
2022, from https://blog.ssa.gov/homelessness-and-social-security/.
Prunhuber, P. (2021). Do You Think Older Renters on a Fixed Income Can’t Get Help with Back Rent?
Think Again! Justice in Aging. Retrieved March 31, 2022, from https://justiceinaging.org/wp-
content/uploads/2021/09/Older-Renters-Can-Get-Help-with-Back-Rent-Utilities.pdf.
Prunhuber, P. & Kwok, V., (2021). Low-Income Older Adults Face Unaffordable Rents, Driving Housing
Instability and Homelessness. Justice in Aging. Retrieved March 10, 2022, from
https://justiceinaging.org/wp-content/uploads/2021/02/Older-Adults-Rental-Housing-
Burdens.pdf.
Public and Affordable Housing Research Corporation (PAHRC). (2020). 2020 Housing Impact Report:
Seniors. Retrieved March 31, 2022, from http://www.pahrc.org/wp-
content/uploads/2020/04/Spring2020HIR_Seniors-1.pdf.
Ramsey-Klawsnik, H. (2018). Understanding and Working with Adult Protective Services (APS). National
Adult Protective Services Association & National Center on Elder Abuse.
http://eldermistreatment.usc.edu/wp-content/uploads/2018/05/Understanding-and-Working-
with-APS_May2018.pdf.
Raven, M.C., Tieu, L., Lee, C.T., Ponath, C., Guzman, D., & Kushel, M. (2017). Emergency department use
in a cohort of older homeless adults: Results from the HOPE HOME Study. Academic Emergency
Medicine, 24(1), 63-74. https://doi.org/10.1111/acem.13070.
Ravensbergen, L., Van Liefferinge, M., Isabella, J., Merrina, Z., & El-Geneidy, A. (2022). Accessibility by
public transport for older adults: A systematic review. Journal of Transport Geography, 103,
103408. https://doi.org/10.1016/j.jtrangeo.2022.103408.
Robaina, K.A., & Martin, K.S. (2013). Food insecurity, poor diet quality, and obesity among food pantry
participants in Hartford, CT. Journal of Nutrition Education & Behavior, 45(2), 159-164.
https://doi.org/10.1016/j.jneb.2012.07.001.
Sard, B. (2018). Housing Choice Voucher Program: Oversight and Review of Legislative Proposals. Center
on Budget and Policy Priorities. Retrieved January 31, 2022, from
https://www.cbpp.org/research/housing/housing-choice-voucher-program-oversight-and-review-
of-legislative-proposals.
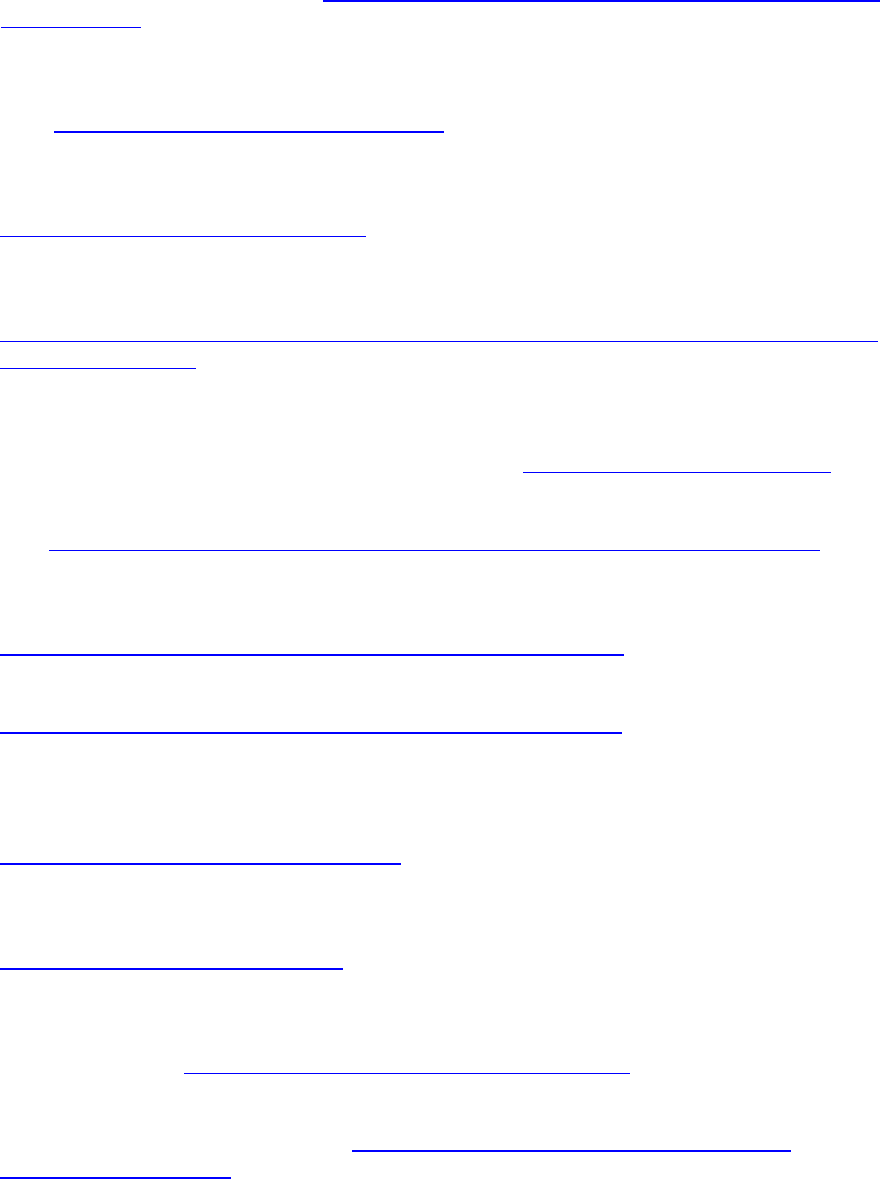
73
Schaak, G., Sloane, L., Arienti, F., & Zovistoski, A. (2017). Priced Out: The Housing Crisis for People with
Disabilities. Technical Assistance Collaborative, Inc., Consortium for Citizens with Disabilities
Housing Task Force. Retrieved from https://www.tacinc.org/wp-content/uploads/2020/04/priced-
out-in-2016.pdf.
Schinka, J.A., Schinka, K.C., Casey, R.J., Kasprow, W., & Bossarte, R.M. (2012). Suicidal behavior in a
national sample of older homeless veterans. American Journal of Public Health, 102(S1), S147-
S153. https://doi.org/10.2105/AJPH.2011.300436.
Schinka, J.A., Curtiss, G., Leventhal, K., Bossarte, R.M., Lapcevic, W., & Casey, R. (2017). Predictors of
mortality in older homeless veterans. Journals of Gerontology: Series B, 72(6), 1103-1109.
https://doi.org/10.1093/geronb/gbw042.
Schinka, J.A., & Byrne, T. (2018). Aging and Mortality in Homeless Veterans: Nine Questions. Retrieved
from
https://www.va.gov/HOMELESS/nchav/docs/Schinka_Byrne_AgingLifeExpectancyHomelessVetera
ns_Sept2018_508.pdf.
Segelman, M., Szydlowski, J., Kinosian, B., McNabney, M., Raziano, D.B., Eng, C., van Reenen, C., &
Temkin-Greener, H. (2014). Hospitalizations in the Program of All-Inclusive Care for the Elderly.
Journal of the American Geriatrics Society, 62(2), 320-324. https://doi.org/10.1111/jgs.12637.
SeniorNavigator. (n.d.). Special Concerns for the Elderly Who are Homeless. Retrieved March 31, 2022,
from https://seniornavigator.org/article/12426/special-concerns-elderly-who-are-homeless.
Sermons, M.W., & Henry, M. (2010). Demographics of homelessness series: The rising elderly
population. Homelessness Research Institute. Retrieved January 31, 2022, from
https://endhomelessness.org/resource/the-rising-elderly-population/.
Sharma, A. (2019). Santa Monica to subsidize rent for hundreds of seniors. LAist.
https://laist.com/news/santa-monica-senior-rental-housing-subsidies.
Shinn, M., Gottlieb, J., Wett, J.L., Bahl, A., Cohen, A., & Baron Ellis, D. (2007). Predictors of homelessness
among older adults in New York City: Disability, economic, human and social capital and stressful
events. Journal of Health Psychology, 12(5), 696-708.
https://doi.org/10.1177/1359105307080581.
Siegler, E.L., Lama, S.D., Knight, M.G., Laureano, E., & Reid, M.C. (2015). Community-based supports and
services for older adults: A primer for clinicians. Journal of Geriatrics, 2015(678625).
https://doi.org/10.1155/2015/678625.
Spinelli, M.A., Ponath, C., Tieu, L., Hurstak, E.E., Guzman, D., & Kushel, M. (2017). Factors associated
with substance use in older homeless adults: Results from the HOPE HOME study. Substance
Abuse, 38(1), 88-94. https://doi.org/10.1080/08897077.2016.1264534.
Stone, C., & Chen, W. (2014). Introduction to Unemployment Insurance. Center on Budget and Policy
Priorities. Retrieved May 1, 2023, from https://www.cbpp.org/research/introduction-to-
unemployment-insurance.
74
Substance Abuse and Mental Health Services Administration (SAMHSA). (n.d.). Programs. Retrieved April
4, 2023, from https://www.samhsa.gov/programs.
Supplemental Nutrition Assistance Program (SNAP). (n.d.). Addressing Barriers & Challenges--Seniors.
Retrieved from
https://www.budget.senate.gov/imo/media/doc/Addressing%20Barriers%20and%20Challenges%
20-%20Seniors.pdf.
Tolbert, J., & Ammula, M. (2022). 10 Things to Know About the Unwinding of the Medicaid Continuous
Enrollment Requirement. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/10-
things-to-know-about-the-unwinding-of-the-medicaid-continuous-enrollment-requirement/.
Tompsett, C.J., Fowler, P.J., & Toro, P.A. (2009). Age differences among homeless individuals:
Adolescence through adulthood. Journal of Prevention & Intervention in the Community, 37(2), 86-
99. https://doi.org/10.1080/10852350902735551.
Tong, M., Tieu, L., Lee, C.T., Ponath, C., Guzman, D., & Kushel, M. (2018). Factors associated with food
insecurity among older homeless adults: Results from the HOPE HOME study. Journal of Public
Health, 41(2), 240-249. https://doi.org/10.1093/pubmed/fdy063.
Tsemberis, S., Gulcur, L., & Nakae, M. (2004). Housing First, consumer choice, and harm reduction for
homeless individuals with a dual diagnosis. American Journal of Public Health, 94(4), 651-656.
https://doi.org/10.2105/AJPH.94.4.651.
Turnbull, J., Muckle, W., & Masters, C. (2007). Homelessness and health. Canadian Medical Association
Journal, 177(9), 1065-1066. https://doi.org/10.1503/cmaj.071294.
U.S. Census Bureau. (2021). U.S. Census Bureau QuickFacts: United States. U.S. Census Bureau. Retrieved
March 3, 2023, from https://www.census.gov/quickfacts/US.
U.S. Department of Agriculture (USDA). (2021). FNS Launches the Online Purchasing Pilot. Retrieved
January 31, 2022, from https://www.fns.usda.gov/snap/online-purchasing-pilot.
U.S. Department of Housing and Urban Development (HUD). (2018). The 2017 Annual Homeless
Assessment Report (AHAR) to Congress: PART 2: Estimates of Homelessness in the United States.
Retrieved March 31, 2022, from https://www.huduser.gov/portal/sites/default/files/pdf/2017-
AHAR-Part-2.pdf.
U.S. Department of Housing and Urban Development (HUD). (2023). 2021 Annual Homeless Assessment
Report (AHAR) to Congress, Part 2: Estimates of Homelessness in the United States. Retrieved
August 21, 2023, from https://www.huduser.gov/portal/sites/default/files/pdf/2021-AHAR-Part-
2.pdf.
U.S. Department of Housing and Urban Development (HUD) (n.d. a). Housing Choice Vouchers Fact
Sheet. Retrieved March 31, 2022, from
https://www.hud.gov/topics/housing_choice_voucher_program_section_8#hcv01.
75
U.S. Department of Housing and Urban Development (HUD) (n.d. b). Section 202 Supportive Housing for
the Elderly Program. Retrieved March 31, 2022, from
https://www.hud.gov/program_offices/housing/mfh/progdesc/eld202.
U.S. Department of the Treasury (USDT). (n.d.). Emergency Rental Assistance Program. Retrieved March
31, 2022, from https://home.treasury.gov/policy-issues/coronavirus/assistance-for-state-local-
and-tribal-governments/emergency-rental-assistance-program.
U.S. Interagency Council on Homelessness. (2018). Homelessness in America: Focus on Veterans.
Retrieved January 31, 2022, from
https://www.usich.gov/resources/uploads/asset_library/Homelessness_in_America._Focus_on_V
eterans.pdf.
U.S. Government Accountability Office. (2019). Food Insecurity: Better Information could help Eligible
College Students Access Federal Food Assistance Benefits. Retrieved January 31, 2022, from
https://www.gao.gov/products/gao-19-95.
Van Dongen, S., Klop, J., Onwuteaka-Philipsen, B., De Veer, A., Francke, A., Slockers, M., Van Laere, I.,
van der Heide, A., & Rietjens, J. (2019). Advance care planning and palliative care for homeless
people in medical respite shelters: A retrospective record review. BMJ Supportive and Palliative
Care, 9(Suppl 2). https://doi.org/10.1136/spcare-2019-acpicongressabs.41.
Vespa, J. (2020). Those Who Served: America’s Veterans from World War II to the War on Terror.
American Community Survey Report. U.S. Census Bureau.
https://www.census.gov/content/dam/Census/library/publications/2020/demo/acs-43.pdf.
Wang, Z.J., Dhanireddy, P., Prince, C., Larsen, M., Schimpf, M., & Pearman, G. (2021). 2021 Survey of
Veteran Enrollees’ Health and Use of Health Care: Data Findings Report. Advanced Survey Design,
LLC. https://www.va.gov/VHASTRATEGY/SOE2021/2021_Enrollee_Data_Findings_Report-
508_Compliant.pdf.
Watson, D.P., George, C., & Walker, C. (2008). “Falling through the cracks”: Health care needs of the
older homeless population and their implications. Jacobs Kronenfeld, J. (Ed.) In Care for Major
Health Problems and Population Health Concerns: Impacts on Patients, Providers and Policy
(Research in the Sociology of Health Care, 26), Emerald Group Publishing Limited, Bingley, pp. 187-
204. https://doi.org/10.1016/S0275-4959(08)26009-6.
Winetrobe, H., Wenzel, S., Rhoades, H., Henwood, B., Rice, E., & Harris, T. (2017). Differences in health
and social support between homeless men and women entering permanent supportive housing.
Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health, 27(3), 286-
293. https://doi.org/10.1016/j.whi.2016.12.011.
Xu, J., Murphy, S.L., Kochanek, K.D., & Arias, E. (2020). Mortality in the United States, 2018. National
Center for Health Statistics. Retrieved January 31, 2022, from
https://www.cdc.gov/nchs/data/databriefs/db355-h.pdf.
Ye, V.M., Caplan, R.J., Consiglio-Ward, L., & Ellison, J.M. (2019). Health care needs of homeless older
adults: Examining the needs of a senior center cohort. Delaware Journal of Public Health, 5(5), 74-
80. https://pubmed.ncbi.nlm.nih.gov/34467082/.
77
ACRONYMS
The following acronyms are mentioned in this report.
ACL
HHS Administration for Community Living
ADL
Activity of Daily Living
APS
Adult Protective Services
CAPABLE
Community Aging in Place--Advancing Better Living for Elders
CARES Act
Coronavirus Aid, Relief, and Economic Security Act
CCBHC
Certified Community Behavioral Health Clinic
CDC
HHS Centers for Disease Control and Prevention
CMS
HHS Centers for Medicare & Medicaid Services
CoC
Continuum of Care
COVID-19
Novel Coronavirus
CSH
Corporation for Supportive Housing
DoL
U.S. Department of Labor
ERA
USDT Emergency Rental Assistance
FFS
Fee-For-Service
FQHC
Federally Qualified Health Center
HCBS
Home and Community-Based Services
HHS
U.S. Department of Health and Human Services
HIPAA
Health Insurance Portability and Accountability Act
HOPE HOME
Health Outcomes in People Experiencing Homelessness in Older
Middle Age
HPRI
Homelessness Policy Research Institute
HRSA
HHS Health Resources and Services Administration
HUD
U.S. Department of Housing and Urban Development
LGBTQ+
Lesbian, Gay, Bisexual, Transgender, Queer or Questioning, Intersex,
Asexual, and More
LIHEAP
HHS Low-Income Home Energy Assistance Program
LIHTC
Low-Income Housing Tax Credit
78
n.d.
not dated
n4a
National Association of Area Agencies on Aging
NAEH
National Alliance to End Homelessness
NANASP
National Association of Nutrition and Aging Services Programs
NAPSRC
National Adult Protective Services Resource Center
NCOA
National Council on Aging
OAA
Older Americans Act
PACE
Program of All-inclusive Care for the Elderly
PAHRC
Public and Affordable Housing Research Corporation
SAMHSA
HHS Substance Abuse and Mental Health Services Administration
SNAP
Supplemental Nutrition Assistance Program
SNP
Special Needs Plan
SOAR
SSI/SSDI Outreach, Access, and Recovery
SSDI
Social Security Disability Insurance
SSI
Supplemental Security Income
USDA
U.S. Department of Agriculture
USDT
U.S. Department of the Treasury
VA
U.S Department of Veterans Affairs
VHA
Veterans Health Administration
October 2023
FINAL REPORT
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Office of the Assistant Secretary for Planning and Evaluation
200 Independence Avenue SW, Mailstop 447D
Washington, D.C. 20201
For more ASPE briefs and other publications, visit:
aspe.hhs.gov/reports
ABOUT THE AUTHORS
Kathryn A. Henderson, Ph.D., Nanmathi Manian, Ph.D., Debra J.
Rog, Ph.D., Evan Robison, M.P.H., Ethan Jorge, Monirah Al-
Abdulmunem, M.S., work in Westat.
SUGGESTED CITATION
Henderson, K.A., Manian, N., Rog, D.J., Robison, E., Jorge, E., Al-
Abdulmunem, M. Addressing Homelessness Among Older Adults
(Final Report). Washington, DC: Office of the Assistant Secretary
for Planning and Evaluation, U.S. Department of Health and
Human Services. October 26, 2023.
COPYRIGHT INFORMATION
All material appearing in this report is in the public domain and
may be reproduced or copied without permission; citation as to
source, however, is appreciated.
___________________________________
Subscribe to ASPE mailing list to receive
email updates on new publications:
aspe.hhs.gov/join-mailing-list
For general questions or general
information about ASPE:
aspe.hhs.gov/about
H

