
SEAFARER MEDICAL
EXAMINATIONS
A PHYSICIAN GUIDE
TC-1002354
*TC-1002354*
Responsible Authority
The Director, Marine Personnel Standards
and Pilotage is responsible for this
document, including any changes,
corrections, or updates.
Approval
______________________________________
Director, Marine Personnel Standards and Pilotage
Marine Safety
Original Date Issued: March 25, 2013 Date Revised:
©
Her Majesty the Queen in Right of Canada, as represented by the Minister of Transport, 2013.
All rights reserved. Unless otherwise stated, information in this publication may be reproduced freely,
provided that Transport Canada, Marine Safety is credited as the source. Important: This publication is
subject to periodical reviews and it is updated accordingly.
ISBN: 978-1-100-19045-7
Catalog No. T29-96/2011E-PDF
TP 11343E
(05/2012)
i
INFORMATION DOCUMENT
Title
Medical Examination of Seafarers - Physician’s Guide
TP No. Revision 01
11343 E
Originator
Marine Personnel Standards and Pilotage
(AMSP)
330 Sparks St., 8
th
floor
Telephone
Fax
(866) 577-7702
(613) 993-4935
MarineSafety@tc.gc.ca
Tower C, Place de Ville
E-mail
MarineSafety@tc.gc.ca
http://www.tc.gc.ca/MarineSafety
Ottawa, Ontario K1A 0N8
URL
http://www.tc.gc.ca/MarineSafety
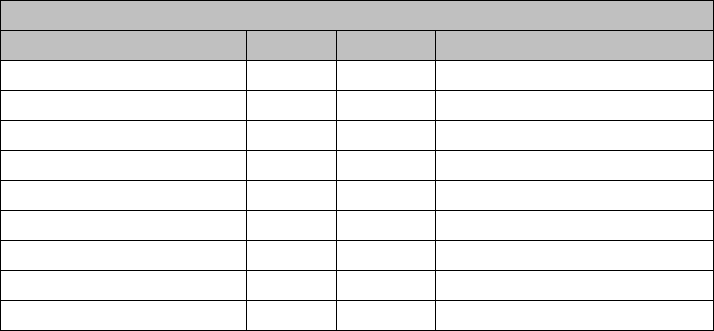
REVISIONS
Last Review
Next Review
Revision
No.
Date of Issue
Affected
Pages
Author(s)
Brief Description of Change

ii
TABLE OF CONTENTS
TABLE OF CONTENTS .......................................................................................... II
1. INTRODUCTION .................................................................................................. 1
1.1 SEAFARER ASSESSMENT ................................................................................................. 1
1.2 SEAFARING LIFE AND WORK ......................................................................................... 2
2. CERTIFICATION PROCEDURES .................................................................... 4
2.1 MARINE MEDICAL EXAMINERS ..................................................................................... 4
2.2 THE APPLICANT (SEAFARER) ......................................................................................... 6
2.3 THE ASSESSMENT FORM ................................................................................................. 7
2.4 THE ASSESSMENT .............................................................................................................. 7
2.5 THE OUTCOME AND PROVISIONAL MEDICAL CERTIFICATE ................................. 8
2.6 VALIDITY PERIODS ........................................................................................................... 9
2.7 CONFIDENTIALITY AND DISCLOSURE ......................................................................... 9
2.8 DUTIES AND RESPONSIBILITIES ...................................................................................10
2.9 CONTACT INFORMATION ...............................................................................................10
2.10 THE CERTIFICATE AND LIMITATIONS.........................................................................10
2.11 DIRECTIVES FOR LIMITATIONS OR DYSQUALIFICATION ......................................15
2.12 APPEALS..............................................................................................................................15
3. REQUIREMENTS ............................................................................................... 17
3.1 FUNCTIONAL ABILITIES .................................................................................................17
3.2 VISUAL REQUIREMENTS.................................................................................................17
3.3 COLOUR VISION REQUIREMENTS ................................................................................19
3.4 HEARING REQUIREMENTS .............................................................................................21
4. MEDICAL CONDITIONS.................................................................................. 22
4.1 CONDITIONS OF ALTERED AWARENESS ....................................................................22
4.2 SEIZURE DISORDER ..........................................................................................................23
4.3 SLEEP DISORDERS ............................................................................................................24
4.3.1 Insomnia ................................................................................................................. 24
4.3.2 Obstructive Sleep Apnea ........................................................................................ 25
4.3.2 Narcolepsy .............................................................................................................. 27
4.3.4 Restless Leg Syndrome ........................................................................................... 27
4.4 DIABETES............................................................................................................................28
4.5 OBESITY ..............................................................................................................................30
4.6 CARDIAC .............................................................................................................................34
4.7 HYPERTENSION .................................................................................................................36
4.8 ANTICOAGULANTS ..........................................................................................................36
4.9 PRESCRIPTION OPIATES ..................................................................................................37
4.10 PSYCHIATRY ......................................................................................................................38
4.10.1 Schizophrenia and Schizoaffective disorder ........................................................... 39
4.10.2 Delusional Disorder ................................................................................................ 40
4.10.3 Brief Psychotic Disorder.......................................................................................... 41
4.10.4 Bipolar I Disorder .................................................................................................... 41
iii
4.10.5 Bipolar II Disorder ................................................................................................... 41
4.10.6 Depression, Dysthymia, Anxiety Disorders ............................................................. 42
4.10.7 Attention Deficit Disorder ...................................................................................... 42
4.10.8 Delirium, Dementia, and Amnestic and Other Cognitive Disorders ....................... 42
4.10.9 Medications ............................................................................................................ 42
4.10.10 Alcohol and Substance Abuse ................................................................................ 43
4.11 ALCOHOL AND DRUGS ....................................................................................................43
4.12 ASTHMA ..............................................................................................................................50
4.13 CHRONIC OBSTRUCTIVE PULMONARY DISEASE .....................................................51
4.14 ANAPHYLAXIS AND ALLERGIES ..................................................................................52
4.15 HIV / AIDS ...........................................................................................................................52
4.16 HEPATITIS ...........................................................................................................................54
4.17 THYROID .............................................................................................................................55
4.18 NEPHROLITHIASIS AND URINALYSIS ..........................................................................55
4.19 SOLITARY KIDNEY ...........................................................................................................55
4.20 STROKE ...............................................................................................................................55
4.21 CEREBRAL ANEURYSM ...................................................................................................58
4.22 MEDICATIONS ...................................................................................................................58
4.23 HERNIA ................................................................................................................................59
4.24 PNEUMOTHORAX .............................................................................................................59
4.25 PREGNANCY ......................................................................................................................60
4.26 INFLAMMATORY BOWEL DISEASE ..............................................................................61
4.27 AORTIC ANEURYSM .........................................................................................................62
4.28 PERIPHERAL VASCULAR DISEASE ...............................................................................62
4.29 HEMOPHILIA AND OTHER CLOTTING DISORDERS ..................................................62
4.30 NEOPLASIA .........................................................................................................................62
5. CONCLUSION..................................................................................................... 63
ANNEX 1: SAMPLE LETTER TO SEAFARER ................................................. 64
ANNEX 2: PHYSICIAN’S REPORT FOR A DIABETIC SEAFARER ............ 65
ANNEX 3: TABLE OF COMMONLY USED LIMITATIONS FOR MARINE
MEDICAL CERTIFICATES .................................................................................. 67
ANNEX 4: REQUIRED LIMITATIONS APPLIED TO MARINE MEDICAL
CERTIFICATES BY CONDITION ....................................................................... 69
ANNEX 5: USEFUL LINKS FOR MARINE MEDICAL EXAMINERS ...... 76
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 1 of 76
1. INTRODUCTION
This Guide is intended to standardize the medical examinations of seafarers. It provides
the tools and guidelines that Marine Medical Examiners can use while assessing the
candidate. It:
• sets out the factors designated Marine Medical Examiners should take into
account when conducting medical examinations;
• highlights the physical requirements seafarers need to meet in order to receive a
medical certificate;
• includes tests to consider for establishing whether a seafarer meets these
requirements; and
• briefly reviews the administrative procedures for the issuance of medical
certificates.
Much of this information takes into consideration the International Labour Organization
and the International Maritime Organization publication entitled Guidelines on the
Medical Examinations of Seafarers.
Part 2, Division 8 of the Marine Personnel Regulations, 2007(MPR) directs a Marine
Medical Examiner to perform medical examinations and advise the Minister of Transport
of the seafarers’ fitness.
These regulations were made by the Governor in Council under section 100 of the
Canada Shipping Act, 2001 in order to specify the crewing and certification requirements
on board vessels. Section 16 of the Act provides for the Minister to specify the manner
Medical Certificates are issued and as such, a Marine Medical Examiner may then issue a
Provisional Certificate that is valid for 6 months. This gives Transport Canada time to:
• oversee the process and ensure standards are met consistently across the country
• prepare and issue the Ministerial Certificate of fitness, also known as a
Canadian Maritime Document, as set out in the Canada Shipping Act, 2001.
1.1 SEAFARER ASSESSMENT
Assessing a Seafarer’s fitness is not without challenges. So too is the job of a seafarer.
Working at sea presents many hazards. Concerns are magnified by the inaccessibility of
medical care if the need arises. This is why seafarer’s must meet such a high standard of
health and fitness.
As an examiner, your assessment will determine if a seafarer can meet the unique safety-
critical demands on board ship. You must also determine and/or try to predict if a
seafarer’s underlying condition could pose an unacceptable risk.
To assist in the seafarer assessment, international organizations cooperated in publishing
Guidelines on the Medical Examinations of Seafarers. These guidelines were developed
to align medical requirements and medical examinations around the world. They are not
intended to replace your professional skill and judgment, but to aid in the determination
of a seafarers’ fitness.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 2 of 76
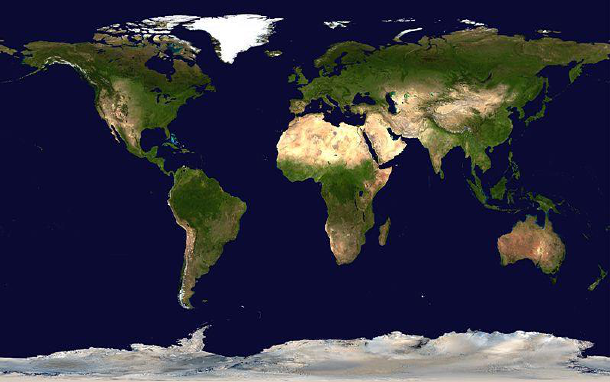
1.2 SEAFARING LIFE AND WORK
The marine environment is unique. This is why you should always consider the
following factors during any assessment and before making any final decision about a
seafarer’s fitness.
The Seafarer
Seafarers must be able to live and work closely with others for weeks and perhaps
months. They must be able to cope effectively with isolation from family, friends, culture,
and supportive medical care.
As a medical examiner, you should:
• Clearly identify the Seafarer’s present role and any intended career plans. This
will help you to identify the standard you measure them by and determine any
specific limitations.
• Consider the type of vessel, duration of the voyages and destinations of the
vessel.
• Identify candidates seeking to start a seafaring career and provide advice about
the implications of a medical condition.
Availability and Quality of Medical Care
Ships, especially when on unlimited voyages, operate in areas that are difficult to access.
An ill seafarer is difficult to replace. The remaining crewmembers may become
overburdened when filling in to perform required tasks. Caring for the ill seafarer puts
further strain on crew.
Crewmembers have limited medical background and most vessels carry only
basic medical supplies.
There may be limits in transporting the ill to receive definitive medical care.
Since seafarers live in close contact with each other and often, for long periods of time,
contagious diseases are a major concern.
It is often impossible to provide or replace required medications.
Work Environment
With the trend to have smaller crews, people have to multitask, especially in
emergency situations.
Hours of work may be burdensome and there may be little to no opportunity to take
time off.
Workplace ergonomics, hazards and living conditions on vessels are often overlooked,
but should be carefully considered. Examples include:
• violent vessel motions
• living and working in cramped spaces
• narrow hatches to pass through
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 3 of 76
• having to stand for long periods of time
• ladders to climb
• heavy weights to lift
• harsh weather conditions
• excessive heat in machinery spaces
• excessive noise levels
• having to travel by air to access their vessel.
Seafarers must be able to respond to emergency situations and stressful situations that
may arise. As in any workplace, violence and harassment may occur on a vessel; however
traditional solutions may not apply.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 4 of 76
2. CERTIFICATION PROCEDURES
2.1 MARINE MEDICAL EXAMINERS
Transport Canada’s Marine Medical Branch issues and revokes appointments.
Appointments cannot be transferred to other clinicians. To become a Marine Medical
Examiner, a medical practitioner must reside and practice in Canada, and apply for the
designation by the Minister of Transport. They should:
• be experienced in occupational medicine.
• have knowledge of living and working conditions on board ships.
• enjoy absolute professional independence from employers, workers and their
representatives in exercising their medical judgment.
• be licensed to practice in the province where examinations are conducted.
• provide proof of Registration and a Certificate of Professional Conduct from
their provincial College of Physicians and Surgeons.
• attend a Transport Canada Marine Medical Seminar before designation.
• attend the Seminar no less than every four years.
Appointments can be terminated in rare circumstances for the following reasons:
• loss or suspension of medical license.
• low quality of Marine Medical Examination Reports and/or evaluations.
• non-attendance of Marine Medical Seminars at prescribed frequency.
The Marine Medical Branch will maintain a list of all designated examiners and make it
available to the public. Examiners should notify the Branch with any:
• change in address,
• prolonged absence, and/or
• inability to provide Marine Medical Exams.
If there is no Marine Medical Examiner within 200 km of where the vessel operates in
Canadian waters or the seafarer’s place of residence, a non-designated physician or
registered nurse may conduct a medical examination if it is within their scope of practice
and issue a provisional medical certificate to the seafarer. In such situations, prior to their
assessment, the seafarer must notify the Marine Medical Branch, who will then send the
appropriate forms and instructions to the examining health professional.
Transport Canada expects a Marine Medical Examiner to be familiar with the certification
process, comply with its standards and requirements and conduct a thorough medical
examination that properly assesses a seafarer’s medical condition and protects public
safety. Such an examination will:
• determine not only fitness to safely perform one’s duties, but to also deal with
emergencies at sea.
• identify conditions or health-related impairments.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 5 of 76
• determine the level of risk and danger caused by that medical problem to the
candidate, the crew and passengers, the vessel, its cargo and the environment.
• identify conditions that may require emergency treatment.
• determine the critical time needed for treatment/access to appropriate land-
based care.
A Marine Medical Examiner shall observe a duty to care and inform the seafarer to
pursue any positive finding. However, this does not translate into an obligation to treat
except in emergency situations. The seafarer should be referred back to their primary
caregiver or specialist for definitive management.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 6 of 76
2.2 THE APPLICANT (SEAFARER)
The Marine Personnel Regulations Part 2, Crewing outlines those seafarers who must
hold a Marine Medical Certificate. Any seafarer who is uncertain should contact their
Transport Canada Marine Safety Examination Centre for assistance. Please refer to links
in Annex 5.
Any seafarer who is required to hold a Marine Medical Certificate must:
• ensure their Marine Medical Certificate is valid; and
• arrange for a medical assessment with a Marine Medical Examiner when
needed.
A Marine Medical Certificate is required for any crewmember of a Canadian Vessel
holding a Certificate of Competency except:
• Master Limited for a Vessel of Less Than 60 Gross Tonnage, Non-
passenger
• Chief Mate, Limited for a Vessel of Less Than 60 Gross Tonnage
• Certificate of Service as Master of a Fishing Vessel of Less Than 60 GT
• Certificate of Service as Watchkeeping Mate of a Fishing Vessel Less
Than 100 GT
• Small Vessel Machinery Operator
• Small Vessel Machinery Operator, Restricted
• Compass Adjuster
• Restricted Proficiency in Survival Craft and Rescue Boats Other Than
Fast Rescue Boat
• Passenger Safety Management
• Specialized Passenger Safety Management (Ro-Ro Vessels)
• Supervisor of an Oil Transfer Operation
• Supervisor of an Oil Transfer Operation in Arctic Waters (North of
60
o
N)
• Supervisor of a Chemical Transfer Operation
• Supervisor of a Liquefied Gas Transfer Operation
• Fishing Master, Fourth Class
• Watchkeeping Mate of a fishing vessel of less than 24 m in length
overall
A Marine Medical Certificate is not required for most members of a crew who are not
required to hold a certificate on board a fishing vessel, a vessel on a Sheltered Waters
Voyage or Near Coastal Voyage , Class 2 or a vessel less than 200 gross tonnage, unless
the vessel is on an international voyage.

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 7 of 76
2.3 THE ASSESSMENT FORM
Marine Medical Examiners must use the most current edition of the Marine Medical
Assessment form. You can order copies by calling 1-888-830-4911 or emailing
[email protected]. You must complete every field in the assessment form and submit the
document to Ottawa in a timely fashion.
The form includes a tear-off to give to the seafarer. The tombstone information and
Marine Medical Examiner fitness determination are critical as it serves as the Provisional
Marine Medical Certificate. While the form is self-explanatory, one field requires
clarification.
The Candidate Document Number (CDN) is a unique number that confirms and
harmonizes a seafarer’s identity information in the Transport Canada Marine Safety
(TCMS) database system. You can learn more about the CDN at:
http://www.tc.gc.ca/eng/marinesafety/bulletins-2010-05-eng.htm
The CDN is required by everyone needing a TCMS issued document. Reports submitted
to Marine Medicine without a CDN are incomplete and cannot be processed. Seafarers
requiring a TCMS Medical Certificate must obtain a CDN before their assessment. They
can do this by visiting the nearest Transport Canada Marine Safety Examination Centre.
The lower portion of the tear off provides the seafarer information and includes the
seafarer’s obligations and their appeal rights.
2.4 THE ASSESSMENT
Check the photo identification of any person requesting a marine medical examination
before you begin an assessment. Existing Seafarers should provide their existing Marine
Medical Certificate so you become aware of any previously determined limitations. It is
important that you identify which Certificates of Competency are presently held or intend
to be obtained.
Collect as much medical information as possible to substantiate the outcome of the fitness
evaluation, especially if you do not know the applicant. Circumstance may require further
testing or a supportive letter from the primary caregiver or specialist. In such cases, gather
and incorporate this information into the assessment. This is also an opportunity to
educate the candidate of the information that will be required for future assessments.
Remember to advise the candidate that they must pay any costs related to proving their
fitness.
Once you have received all the required information and completed the assessment, there
are essentially three courses that you can follow. The candidate may:
1) satisfy all the requirements and can be deemed Fit.
2) require some limitations that allow balancing a health concern with the possible
risk it poses.
3) pose too great a risk and will be determined as Unfit.
You can contact the Marine Medical Branch directly at any time to discuss a case and
receive advice. But, as a Marine Medical Examiner, you must decide whether or not to
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 8 of 76
issue a Provisional Medical Certificate declaring the seafarer fit for sea services with or
without limitations.
The Marine Medical Branch may subsequently review your assessments. A Marine
Medical Certificate, which is a Canadian Maritime Document, will be issued based on the
assessment form and the Provisional Certificate. Assessments older than six months from
the day of the examination will be considered stale and will not be considered for the
purpose of the issuance of a Canadian Maritime Document.
2.5 THE OUTCOME AND PROVISIONAL MEDICAL CERTIFICATE
A Provisional Medical Certificate is valuable because it is equal to a Canadian Maritime
Document in meeting regulatory requirements that allow a seafarer to perform a safety-
critical role. Seafarers may also use their Provisional Medical Certificates to upgrade their
Certificate of Competency.
If a Marine Medical Examiner finds a Seafarer fit, he/she will:
• give the Seafarer a duly completed Provisional Medical Certificate; and
• forward the original Marine Medical Assessment form, any other relevant
medical reports and a copy of the Provisional Medical Certificate to the Marine
Medical Branch.
If a Marine Medical Examiner finds a Seafarer fit with limitations, he/she will:
• give the Seafarer a duly completed Provisional Medical Certificate that outlines
the limitations;
• give the Seafarer a letter addressed to the Seafarer that gives the reasons for the
limitation; and
• forward a copy of this letter, along with the original Marine Medical
Assessment form, any other relevant medical reports and a copy of the
Provisional Medical Certificate to the Marine Medical Branch.
If a Marine Medical Examiner finds a Seafarer unfit, he/she will:
• give the Seafarer a letter addressed to the Seafarer that gives the reasons for not
issuing a Provisional Medical Certificate
• forward a copy of this letter, the actual Provisional Medical Certificate that was
not issued, along with the original Marine Medical Assessment form and any
other relevant medical reports to the Marine Medical Branch.
In all cases, Marine Medical Examiners should keep copies of the Marine Medical
Assessment form and any relevant medical reports as outlined by their respective
Provincial Medical College.
Note: You will find a sample letter that outlines a Seafarer’s limitations or reasons for
being Unfit in Annex 1 of this guide.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 9 of 76
2.6 VALIDITY PERIODS
Provisional Medical Certificate
A Provisional Medical Certificate is valid for up to 6 months after being issued by the
Marine Medical Examiner. The examiner may reduce this time period if circumstances
call for it.
A Provisional Medical Certificate becomes invalid when Transport Canada issues a:
• medical certificate by the Minister (Canadian Maritime Document)
• a letter from the Minister declaring his or her refusal to issue a medical
certificate.
Marine Medical Certificate
The Marine Medical Certificate is a Canadian Maritime Document issued by the Minister
of Transport. This document is valid for a maximum of two years from the date the
medical examination is performed except for candidates under 18 years of age, in which
case the maximum period of validity is one year.
Marine Medical Certificates that expire during a voyage shall remain in force until the
end of the voyage.
A seafarer should be reviewed or assessed by a marine examiner if he or she has:
• been unable to work for 30 or more days because of sickness or injury;
• been evacuated/discharged from ships for health reasons; or
• a significant change in their condition.
Certain circumstances may necessitate more than just a review but a complete Marine
Medical Assessment.
The Marine Personnel Standards and Pilotage Directorate of Marine Safety issues
Medical Certificates on behalf of the Minister of Transport.
2.7 CONFIDENTIALITY AND DISCLOSURE
The information Transport Canada requires to establish medical fitness to issue a Marine
Medical Certificate is collected under Section 16 of the Canada Shipping Act, 2001. It is
considered to be confidential nature and should be protected.
Section 90 of the Canada Shipping Act, 2001 outlines the care-givers responsibility to
disclose information. If a physician or an optometrist has reasonable grounds to believe
that the holder of a certificate has a condition that is likely to constitute a hazard to
maritime safety, they should inform the Minister without delay. Sharing such information
is not restricted to the time of the Marine Medical Assessment.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 10 of 76
Further, the seafarer must inform their caregivers that they are certificate holders and that
holding a certificate means they have consented to the Minister being informed of such
information.
Note: No legal, disciplinary or other proceedings lie against a physician or optometrist for
anything they do in good faith in compliance with this section.
2.8 DUTIES AND RESPONSIBILITIES
The Canada Shipping Act, 2001 also outlines the responsibilities of others. No master of a
Canadian vessel shall operate it unless it is staffed with a crew that is sufficient and
competent for the safe operation of the vessel on its intended voyage, and is kept so
staffed during the voyage.
Crew members also share responsibility for their safe functioning and shall carry out their
duties and functions in a manner that does not jeopardize the safety of the vessel or of any
person on board. They are also responsible to report to the master any safety hazards of
which they become aware and any change in their circumstances that could affect their
ability to carry out their duties and functions safely.
2.9 CONTACT INFORMATION
All calls are welcomed at our Toll Free number: 1-866-577-7702
The Marine Medical Branch’s direct Fax number is: 1-613-993-4935
Address:
Transport Canada
Marine Medicine
8
th
Floor-AMSPM
Place de Ville, Tower C
Ottawa, Ontario
K1A 0N8
2.10 THE CERTIFICATE AND LIMITATIONS
The Marine Medical Certificate is a valuable tool and is recognized internationally. The
information it contains is standardized around the world as outlined by the International
Convention of Standards, Training, Certification and Watchkeeping for Seafarers.
It provides details and limitations that ensure safety of the seafarer, crewmembers,
passengers, the vessel and its cargo and of the environment. These limitations allow for a
balance between a health concern and the possible risk it poses. They are broadly
classified as: Duty, Geographical, Medical and Time Limitations.
Notes:
• It is very important to include any limitations you assign on the certificate, but
do not include medical information.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 11 of 76
• When a seafarer is convalescing from a condition, you should deem them Unfit.
Deeming them fit pending recovery or treatment plan as a limitation is
inappropriate.
Watchkeeping
Watchkeeping is a term that refers to the different safety critical roles on a vessel that
require unconditional cognitive and perceptual function. Thus, anyone with compromised
function may require such a limitation.
Specifically, in Canada’s Marine Personnel Regulations, “Watch” means
a) In respect of a vessel, crewmembers attending to the navigation,
communications, machinery and security of the vessel, and including the
master; and
b) In respect of a crewmember, the period during which he or she is required to be
on call or physically present.
Duty Limitations:
This category is most relevant to those with any cognitive or perceptual functional deficit.
1) No Watchkeeping:
Applies to anyone with a risk of sudden incapacitation. It also reduces the risk
for anyone with risk of impaired cognition as a result of a medical condition or
medication use.
2) No Bridge Watchkeeping:
Applies to those who fulfill the requirements for another department but not
necessarily for the bridge.
3) No Lone Watchkeeping:
Less restrictive for those with possibly full perceptual functioning, with an
ongoing risk of transient cognitive deficiencies such as Hypoglycemia.
4) Present Occupation Only:
Some seafarers fulfill the requirements for only their present job. A career
change would require a reassessment.
Note: ‘Not fit for Emergency Duties’ or ‘As per Transport Canada’ are not valid
limitations.
Geographical Limitations:
Registered Canadian Vessels possess an inspection certificate of their own that prescribes
it geographical limits. Seafarers must possess a Medical Certificate that allows them to
navigate in the regions noted on the vessel’s inspection certificate.
Setting geographical limitations are useful for those individuals who are at risk of needing
urgent medical attention or who do not necessarily meet International Standards, but can
fulfill domestic requirements.

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 12 of 76
One Nautical Mile represents 1.852 KM and is a unit of length used in sea and
air navigation.
These standard limitations are outlined in The Marine Personnel Regulations and The
Vessel Certificate Regulations:
1) Sheltered Waters Voyage:
A voyage that is in Canada, on a lake or a river above tidal waters, where
a vessel can never be further than one nautical mile from the closest shore.
2) Inland Waters Voyage:
A voyage on the Inland Waters of Canada together with any part of any lake
or river forming part of the inland waters of Canada that lies within the
United States or a voyage on Lake Michigan.
3) Canadian Waters Voyage:
A voyage that extends to Canadian Territorial waters to 12 Nautical Miles
from shore.
4) Near Coastal Voyage, Class 2:
A voyage within 25 nautical miles from shore in waters contiguous to Canada,
the United States (except Hawaii) or Saint Pierre and Miquelon, and within 100
nautical miles from a place of refuge.

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 13 of 76
5) Near Coastal Voyage, Class 1:
A voyage that is between places in Canada, the United States (except Hawaii),
Saint Pierre and Miquelon, the West Indies, Mexico, Central America or the
northeast coast of South America.
A voyage during which the vessel is always north of latitude 6 degrees north and
within 200 nautical miles from shore or above the continental shelf.
This class of voyage extends southward to permit the transit of the Panama
Canal and has no limits regarding distances from places of refuge.
6) Limited Contiguous Waters Voyage:
A variation of Near Coastal Class 1 limited to the waters contiguous to Canada,
the United States (excluding Hawaii) and Saint-Pierre-et-Miquelon.
This limitation applies to those individuals that do not necessarily meet
international standards, but can fulfill domestic requirements. Canada and the
United States have a Memorandum of Understanding recognizing the other’s
certificates and thus allow voyages through United States’ waters.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 14 of 76
7) Unlimited Voyages:
No geographical implication
8) Other Geographical Limitation:
Nothing prevents a very specific limitation if it is required such as:
Within ___ nautical miles from a shore or port,
Voyage between Point A and Point B only.
Medical Limitations:
Medical limitations reflect the Seafarer’s medical needs to ensure they can function safely
and address any emergency medical needs.
• Corrective lenses required
• Hearing aids required
• Specialized electrical equipment required while sleeping
• Must carry self-administered medications
• Must avoid specific allergen
Time Limitations:
A provisional medical certificate may have a shorter validity that the six months outlined
by the regulations to ensure the seafarer complies with a specific request for information
or management by their caregivers.
You may choose to set other time limitations as a way of quantifying the urgency to
receive medical attention. It could also be related to a specific medical condition and its
functional limitation. These limitations could include:
• The maximal duration of a voyage
• Not to be away from Home Port overnight
• The maximal time away from a specified medical facility
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 15 of 76
2.11 DIRECTIVES FOR LIMITATIONS OR DYSQUALIFICATION
Listed are some of the possible factors you should consider when making a final decision.
They are derived in part from the challenges of seafaring life and work conditions.
The role of most personal physicians is to advocate for the patient. However, the role of a
Marine Medical Examiner is very specific and that is to determine the fitness of the
seafarer and inform the Minister of any risk to safety.
• Is the known or suspected condition presently stable and what is the probability
of an exacerbation or recurrence?
• Could the condition obstruct in the safe performance of regular duties as well
as emergency duties?
• Could the disorder prevent the person from speaking in a clear and prompt
manner?
• Could there be any personal safety concerns or life-threatening situations?
• Could there be any risk to passengers, crew, vessel, cargo or the environment?
• How quickly could the condition evolve and how quickly would the seafarer
require management?
• Could there be an exacerbation of the underlying condition as a result the
demands of the job or a work related exposure?
• Are there any medical services on board?
• What would be the impact of lost or damaged medications?
• Does the seafarer have sufficient insight and what is the likelihood they will
follow medical advice?
2.12 APPEALS
The Marine Personnel Regulation provides 30 days for a seafarer to appeal the outcome
of a Medical Examination as indicated on the Provisional Medical Certificate.
A seafarer’s employer or prospective employer may also submit a memorandum to the
Minister requesting a review of the Provisional Medical Certificate.
Such submissions should be addressed to:
Director, Personnel Standards and Pilotage
Transport Canada (AMSPM)
Marine Medicine Division
330 Sparks Street - Tower C. 8
th
Floor
Ottawa, ON K1A 0N8

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 16 of 76
The Canadian Shipping Act, 2001 provides a review process for:
• a Canadian Maritime Document declaring a Seafarer fit for sea service with
limitations
• the Minister’s decision to refuse to issue a Canadian Maritime Document.
Such submissions should be addressed to:
Transportation Appeal Tribunal of Canada
333, Laurier Avenue West, Room 1201
Ottawa, ON K1A 0N5
Tel: 613-990-6906
Fax: 613-990-9153
Email: info@tatc.gc.ca
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 17 of 76
3. REQUIREMENTS
3.1 FUNCTIONAL ABILITIES
Physical and mental abilities have to be assessed. Strenuous working conditions and the
potential for rough weather require normal mobility, agility and strength. A seafarer must
be able to climb steep stairs, rope ladders and vertical steel rung ladders. They must be
capable of working in confined spaces and pass through narrow hatches.
Many of these tasks are more difficult while wearing personal life-saving equipment and
breathing apparatus. It is further complicated in emergency situations. Limb amputations,
joint instabilities, dysfunction and pain as well as any balance problems or poor spatial
awareness, require special assessment.
There are some basic requirements that all seafarers must meet to be fit:
a) adequate muscle strength to lift and carry a weight of 22 kg;
b) the physical capacity to wear breathing apparatus and the seafarer’s personal
life-saving equipment while climbing ladders;
c) the agility and strength to carry out the duties that may be assigned to them
regarding fire fighting and vessel abandonment in an emergency;
d) the ability to work in constricted spaces and move through restricted openings
of a maximum dimension of 600 mm by 600 mm; and
e) the physical and mental fitness to meet the occupational and operational
requirements of the position that they occupy or seek to occupy.
As an examiner, you may use alternative methods to assess the applicant’s ability to
perform such tasks and document your approach on the Marine Medical report. More
specific physical abilities are located in a table in Section 4.5 Obesity. The applicant may
use any normally used prosthesis for the evaluation, and have it identified as a
requirement on their Certificate. If these universal standards cannot be met, the applicant
is Unfit.
3.2 VISUAL REQUIREMENTS
Good vision cannot be overstated in any safety-critical role. There are three main
categories of visual requirements for seafarers. They are deck, engine, and catering and
others, each with different requirements.
However, all seafarers must have at least an unaided vision of 6/60 or 20/200 with both or
either eye alone so they can function in emergency situations or at least, be able to
evacuate a ship in the absence of one’s corrective lenses. Any seafarer unable to meet this
standard will be deemed Unfit. This is why unaided vision testing needs to be recorded.
All seafarers who meet their specific visual acuity requirement with the use of corrective
lenses must have a limitation documented on their Certificate of:
Corrective Lenses required
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 18 of 76
Deck:
• require 6/12 or 20/40 in each eye
• normal visual fields*
• near vision of N8
• no diplopia, no night blindness, no progressive eye disease
The inability to meet any specific standard will result in a limitation of:
No Watchkeeping
A unique population exists with Marine Pilots. Depth perception has been identified as a
requirement to transfer vessels and the Marine Medical Examiner or other practitioner has
to ensure the applicant or holder of a Pilotage license or Pilotage certificate, has the depth
perception required to perform Pilotage duties.
Engine:
• require 6/15 or 20/50 in each eye
• sufficient visual fields*
• near vision of N8
• no diplopia, no night blindness, no progressive eye disease
The inability to meet any specific standard will result in a limitation of:
No Watchkeeping
The medical standards for vision do not apply to an engineer who held an Engineer
Certificate of Competency issued before July 30, 2002.
Engineers meeting this exception will result in a limitation of:
No Bridge Watchkeeping
Catering and Others:
• require 6/60 or 20/200 with both or either eye
• sufficient visual fields*
• near vision sufficient for duties
Monocular Vision
Monocular vision is not a total barrier to safely performing one’s duties. Those with
newly acquired monocular vision are Unfit for 6 months to adjust to the condition.
International requirements of Normal Visual Fields for deck personnel will result in a
geographical limitation if the aided better eye can fulfill the acuity standard below. Such a
limitation will not be necessary for Engine Personnel who only require sufficient visual
fields, but will be restricted to the Engine Department.
• Deck Personnel 6/12 or 20/40 in the better eye
• Engine Personnel 6/15 or 20/50 in the better eye
• Deck Personnel: Limited Contiguous Waters Voyage
• Engine Personnel: No Bridge Watchkeeping
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 19 of 76
• All other Personnel: No Watchkeeping
*Visual Fields – Any significant visual field defect could compromise safety. Medical
Examiners who suspect any defect should refer the candidate for further testing.
Notes:
• Typically visual fields in one eye should be no less than 150 contiguous degrees
along the horizontal meridian.
• Central or peripheral scotomas must be taken into account when assessing
visual fields.
• Scotomas and quadrantanopias will require an ophthalmologic assessment
at each evaluation.
• Complete homonymous, bitemporal or binasal hemianopsias would disqualify
the applicant.
3.3 COLOUR VISION REQUIREMENTS
All Deck and all Engine personnel need full colour vision. The International Convention
for Standards, Training, Certification and Watchkeeping for Seafarers has recently
strengthened this requirement. You must carry out colour vision testing at every Marine
Medical Assessment.
Pseudoisochromatic plate tests differentiate people with normal colour vision and those
with defective colour vision that might interfere with safety. The applicant should not
be allowed to wear sunglasses or ‘colour corrective’ lenses.
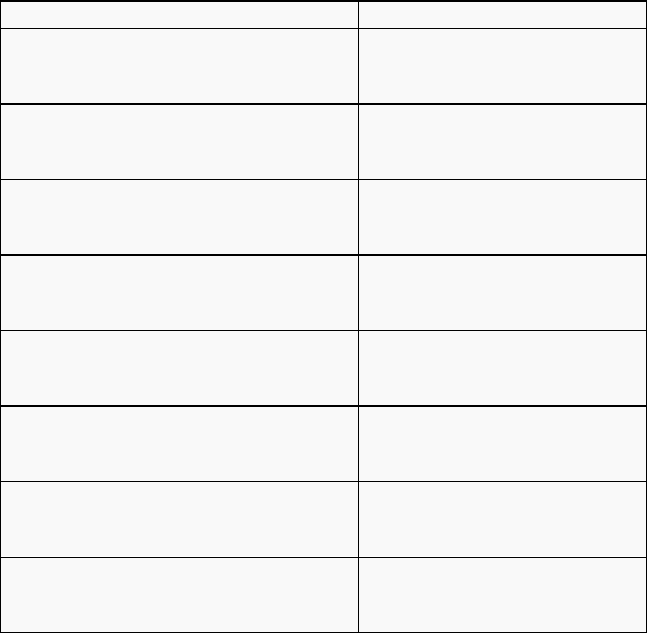
The number of acceptable incorrect responses to each type of plate is shown in the table
below. Record the particular set of Pseudoisochromatic Plates and the number of plates
you use, as well as the number of errors on the Marine Medical Examination Form.
Types of Pseudoisochromatic Plates
Type
Edition
Tested
Errors Allowed
American Optical (1965 Ed.)
18
1-18
3
American Optical HRR
20
1-6
0
Ishihara
16
1-8
1
Ishihara
24
1-15
2
Ishihara
38
1-21
3
Ishihara (concise)
14
1-14
Special explanation with plates
Keystone Orthoscope ®
All
0
Keystone Telebinocular ®
All
0
Titmus
All
0
Any candidate who fails a pseudoisochromatic plate test must be further tested with a
Farnsworth D-15 Hue Test. Not all Marine Medical Examiners will have the Farnsworth
D-15 Hue Test but many optometrists or ophthalmologists can provide such a service.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 20 of 76
Make sure to submit the raw data with any report. Since the outcome of this test is valid
for 6 Years, specialised colour vision testing is not required at every Marine Medical
Assessment. The seafarer should receive a copy of their report to provide at future
Marine Assessments.
Failure of colour vision testing will result in a limitation of:
No Watchkeeping
There are some exceptions:
The medical standards for vision do not apply to an engineer who held an Engineer
Certificate of Competency before July 30, 2002.
Also, Division 8, subsection 270. (3) of the Marine Personnel Regulations, sets out that
the medical standards for colour vision do not apply to a seafarer who:
a) is not required to hold a certificate of competency to perform their duties on
board a vessel; or
b) is required to hold one of the following certificates to perform their duties on
board a vessel:
(i) Engine-room Rating (ERR),
(ii) Ship’s Cook,
(iii) Proficiency in Fast Rescue Boats,
(iv) Proficiency in Survival Craft and Rescue Boats Other Than Fast
Rescue Boats,
(v) Restricted Proficiency in Survival Craft and Rescue Boats Other
Than Fast Rescue Boats,
(vi) Oil and Chemical Tanker Familiarization,
(vii) Liquefied Gas Tanker Familiarization,
(viii) Passenger Safety Management,
(ix) Specialized Passenger Safety Management or
(x) Compass Adjuster.
Limitations to impose: No Bridge Watchkeeping for Engineers and ERR group (i)
No Watchkeeping for all other groups (ii – x)

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 21 of 76
3.4 HEARING REQUIREMENTS
Seafarers must demonstrate the ability to recognize all the occupationally related sounds
in their specific working environment and effectively communicate. Subjective testing
will be continued to be used to screen for hearing and the seafarer must demonstrate the
ability to adequately hear conversation. Failing that, an audiogram must be provided. A
Marine Medical Examiner with appropriately calibrated equipment or a Registered
Audiologist may perform such testing prior to the Marine Medical Exam being finalized.
The audiogram should ensure an average hearing loss of no more than 30dB in the better
ear of all seafarers for the frequencies of 500, 1000, 2000 and 3000 Hz.
Those requiring Hearing Aids must undergo a formal Audiology assessment before each
Marine Medical Exam. A recent Sound Field Test with Hearing Aids performed with six
months or a written report from an Audiologist or Ears, Nose and Throat Specialist will
be required to confirm that hearing acuity falls within the required objective standards.
Not meeting the auditory standard with or without Hearing Aids will result in a limitation
of:
No Watchkeeping
Seafarers who meet the standards with the use of Hearing Aids will require a limitation
of:
Hearing Aids required
The medical standards for hearing do not apply to an engineer who held an Engineer
Certificate of Competency before July 30, 2002.
Engineers meeting this exception will result in a limitation of:
No Bridge Watchkeeping
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 22 of 76
4. MEDICAL CONDITIONS
The role of the Marine Medical Examiner is clearly defined to determine the fitness and
functional abilities of the individual to perform their duties and deal with emergency
situations at sea. It is impossible to provide an all-inclusive list of conditions and
certificate outcomes and limitations.
There has to be a common approach and some consensus taking into account the diversity
of marine occupations, vessels and voyages, and seafarers. The common thread that binds
this all together is safety.
The Minister of Transport requires your opinion of whether a seafarer poses a safety risk
to themselves, the crew, the passengers, the vessel and cargo and the environment.
An added benefit to your assessment is that it will contribute to the overall health of the
seafaring population.
4.1 CONDITIONS OF ALTERED AWARENESS
Many conditions can cause sudden incapacitation that obviously affect one’s ability to
function at their post and could put safety at risk.
These conditions can be broken into seven groups:
1) Neurological, e.g., epilepsy or tumours
2) Metabolic, e.g., hypoglycemia
3) Cardiac, e.g., acute coronary syndrome or pathological rhythms
4) Fatigue, e.g., OSA or narcolepsy
5) Respiratory, e.g., chronic lung disease
6) Medication, e.g., opiates, benzodiazepines, mood-altering
7) Other, e.g., vasovagal, traumatic
Examiners must identify the cause of the condition; and the seafarer will most likely have
to provide more information or undergo further investigations with their family doctor or
specialists.
If the symptom is new with no obvious cause, a seafarer will be Unfit for a
3 month period for health professionals to evaluate the probability of recurrence.
If the episodes are recurrent (they have two or more episodes in a 12 month period) the
seafarer will be Unfit until a diagnosis is made and the condition managed.
If a typical vasovagal syncopal episode is suspected, ask about any provocative features,
prodromal symptoms and postural influences. Obviously, no restriction or limitation is
required if it has typical features and there is a sufficient prodrome to allow them to
manage. However, if it is a recurrent or an atypical vasovagal presentation, a limitation of
No Lone Watchkeeping should be considered.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 23 of 76
4.2 SEIZURE DISORDER
This is a complicated condition with many etiologies that have a common end-effect and
impact on function. It may be associated with a variety of cerebral or systemic disorders;
however, it is idiopathic in up to 75% of young adults. Approximately 2% of the
population will have a seizure during their lifetime. There is a 30% chance of having
a recurrence and likely to occur soon after the initial event and then subsequently decline.
Seizures that begin after the age of 25 are usually secondary to some form of organic
brain disease. Epilepsy has to be distinguished from Syncope or any other cause of loss
of consciousness or awareness.
The best predictor of a recurrence is the duration of time since the last seizure. Also, any
change or cessation of anti-epileptic medication could affect the chance of recurrence.
You may need to ask the seafarer to provide supportive documents that explains their
condition. Determining one to be fit will depend on:
• Whether you believe the seafarer is being truthful about their history,
• If you believe the seafarer is conscientious and will take their medication,
• Whether the seafarer is under regular medical supervision,
• Whether the treatment is working, and
• The treatment doesn’t have any significant side effect that would impair
their function.
Different limitations are applied to stratify seafarers to avoid placing everyone into the
same category and unnecessarily restricting people.
Childhood Febrile Seizure: Fit
New or ongoing seizure,
Ongoing investigation,
Within six months of seizure control: Unfit
Temporary disqualification is not unreasonable as it provides time to determine the cause
of the condition, the impact on function and provide a period of stability.
After six months of being seizure-free with or without medications, the Seafarer may
return to work with limitations to mitigate risks.
Seizure-free with or without Rx
for six months: No Watchkeeping and Near Coastal Class I
After one year of being seizure free, the geographical limitation can be lifted.
Seizure-free with or without Rx
for 12 months: No Watchkeeping
If an individual has been seizure free on or off medications for a five years, they are
deemed fit with no limitations.
Seizure-free with or without Rx
for five years: Fit
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 24 of 76
Special circumstances:
Seafarers who have had fully controlled seizures with medications beyond the 5 year
period and change or stop medication must be limited to No Watchkeeping for six
months and must provide a favourable neurological assessment including a normal EEG.
Once confirmed, they may be deemed fit with no limitations.
Those who are seizure free on medications for at least one year and relapse as a result of a
physician directed change in treatment may be reinstated with their previous limitation
once the treatment has been corrected.
If one suffers a solitary seizure, they are managed as a new onset condition and will
be deemed Temporarily Unfit. They may be reinstated with a No Watchkeeping
limitation for one year after a favourable neurological assessment including a normal
EEG. After the one year, they will be fit with no limitation.
Alcohol related seizures require a thorough neurological assessment to rule out any other
underlying cause and input from an addiction specialist. Case by case decisions are to be
based on the severity of the alcohol abuse/dependence. Despite a provocative factor being
identified you must impose a 12 month observation period during which they would be
Unfit. They may be reinstated after their Substance Abuse Professional provides
supportive documentation. To return to work, they must observe the two year monitoring
program outlined in the Alcohol and Drugs section of this guide.
4.3 SLEEP DISORDERS
Sleep disorders can have a significant impact on normal mental and physical functioning
and are often underestimated. There is a broad classification of sleep disorders. The
Dyssomnias impact a person’s functions and are characterized by either hypersomnulence
or insomnia.
Within the Dyssomnias are:
1) Insomnia
2) Obstructive Sleep Apnea
3) Narcolepsy
4) Restless Leg Syndrome
5) Others such as Circadian Rhythm Sleep Disorders.
The other groups that don’t have such a serious impact on your assessments are the
Parasomnias. There is also a group of secondary conditions that result primarily from
psychiatric conditions.
Common to all these is the impact on one’s function.
4.3.1 INSOMNIA
This is a very common problem with much aetiology. A recent study revealed up
to 58% of adults experienced symptoms of insomnia a few nights a week.
This condition is a double-edged sword. On one side, if untreated, it will affect
performance and slow reaction time. On the other side, the pharmacological
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 25 of 76
treatment includes medications with possible side effects that can impact on
function. Their use is typically recommended for short term, but patients are
often on these medications over the long term.
Ensure the seafarer doesn’t have any functional limitations resulting from the
condition or its treatment. If there is ongoing use of these medications, issue a
No Watchkeeping limitation.
If medication use is only periodic, you may deem a seafarer fit without
limitations but you must make it clear they must not to use the medication
within 48 hours of manning their shift. Document your discussion about the
prohibition period and side effects.
4.3.2 OBSTRUCTIVE SLEEP APNEA
This condition is becoming much more recognized. One study revealed it may
affect nearly 1 in 15 individuals. There are a variety of symptoms that could
affect a fitness determination.
There are several ways to screen for Sleep Apnea. The Adjusted Neck
Circumference (ANC) is a prediction rule that uses four clinical factors. The
ANC is calculated as the sum of the neck circumference and the values for the
presence of hypertension (+4), history of frequent snoring (+3), and reported
chocking, gasping or witnessed apneas (+2). The calculated value predicts the
probability of sleep apnea as follows:
<43 Low Probability
43-48 Intermediate Probability (4-8x as probable)
>48 High Probability (20x as probable)
New England Journal of Medicine, 2002, 347:498-504.
Another easy method of screening would be The Epworth Sleepiness Scale. It
has been validated primarily in obstructive sleep apnea as a measure of excessive
daytime sleepiness and is repeated after treatment (e.g. CPAP or surgery) to
document improvement of symptoms.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 26 of 76
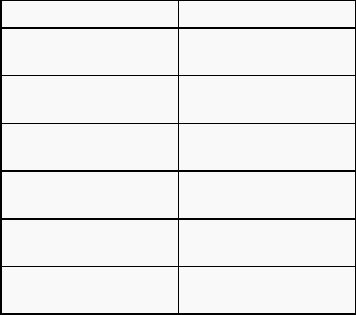
The Epworth Sleepiness Scale
How likely are you to doze off or fall asleep in the following situations, in
contrast to simply feeling tired? This refers to your usual way of life in recent
times. Even if you have not done some of these things recently try to work out
how they would have affected you.
Use the following scale to choose the most appropriate number for each
situation:
• 0 = no chance of dozing
• 1 = slight chance of dozing
• 2 = moderate chance of dozing
• 3 = high chance of dozing
Situation
Chance Of Dozing
Sitting and reading
Watching TV
Sitting inactive in a public place
(e.g. a theatre or a meeting)
As a passenger in a car for an hour without
a break
Lying down to rest in the afternoon when
circumstances permit
Sitting and talking to someone
Sitting quietly after a lunch without
alcohol
In a car, while stopped for a few minutes
in traffic
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 27 of 76
Epworth Sleepiness Scale Interpretation
The score obtained by adding the numbers leads to a total:
0 - 9 average score, normal population
10 - 24 sleep specialist advice recommended
Further testing For Sleep Apnea:
If there is a significant physical finding or a positive screening test, send the
seafarer back to their Family Doctor for referral to a sleep specialist or to the
Sleep Lab for diagnosis or to titrate their existing CPAP machine as needed if
the diagnosis is already apparent. Apply a No Watchkeeping limitation until an
expert is satisfied there is no longer daytime somnolence.
Once a seafarer is using CPAP and there is evidence of ongoing need, apply a
limitation of Specialized electrical equipment required while sleeping.
Since Polysomnograms are not readily available in parts of the country, you may
screen using overnight oximetry.
A desaturation of greater that 3% is significant but you may have to weigh it
against the symptoms and will possibly require a Specialist assessment.
4.3.2 NARCOLEPSY
This is not a common condition, occurring in only 1 person in 2,000 but it has
significant impact on function. It manifests as excessive daytime sleepiness and
can cause a person to fall asleep at inappropriate times. There are a variety of
treatments available. You will need to request specialist documentation, but you
must place a No Watchkeeping limit on all seafarers with this condition.
4.3.4 RESTLESS LEG SYNDROME
This relatively rare condition will likely require some specialist input. This
condition will impact on sleep quality and secondarily on daytime function.
A variety of treatments exist and decisions will be based on severity, impact on
function, medications used and potential medication side effects. It will require a
No Watchkeeping limitation.

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 28 of 76
4.4 DIABETES
This condition is one of our society’s biggest health concerns. It may be so widespread in
your day-to-day practice that we are desensitized to the potential problems it poses for
seafarers with safety critical roles and the inaccessibility to urgent medical care.
Complications can be simplified if viewed as Acute versus Chronic. Acute conditions
include:
• Hypoglycaemia. Precipitating factors that make this important to consider in
seafarers are many and include irregular hours, missed meals, and the physical
requirements of the job. Contributing to this is the care-givers insistence for
tighter glycemic control. The unpredictability and severity of hypoglycaemia
could be a major marine safety hazard.
There is an obligation to look into this potential problem further. You may want
to use the sample questionnaire provided at the end of this guide. (Annex 2)
• Diabetic Ketoacidosis and Nonketotic Hyperglycemic-Hyperosmolar State
or Coma. These have different etiologies, but similar symptoms. DKA often
signals Type 1 DM. However, the Hyperosmolar state results with excessively
high blood glucose levels and should be considered with those with poor
control. Among many symptoms, one can have impaired consciousness and
seizures. If this is the case, you should consider placing limitations on persons
with poor control.
The chronic complications of Diabetes are well known and must not be ignored as they
could have a significant impact on one’s function and longevity. The major system to
consider is cardiovascular.
Diabetes Association’s Clinical Practice Guidelines provides assistance. You can find it
online at:
http://www.diabetes.ca/files/cpg2008/cpg-2008.pdf
It helps identify those at high risk of coronary events. It also gives guidance with
screening requirements of these individuals. It is important to consider that most people
with the condition will be managed by their Primary Caregivers with evidence-based
principles and likely have undergone many of the investigations that would help
determine their risk.
Typical Requirements:
• FBS
• AIC
• Lipid Profile
• ACR or Microalbuminuria
• Determination of Hypoglycemic Risk (statement from Family Physician or
Glucometer Log)
• Annual Optometrist or Ophthalmologist Report
• Baseline ECG if
• Greater that 40 yrs old
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 29 of 76
• Diabetic for more than 15 years
• Diabetic with Hypertension, Peripheral vascular disease or Proteinuria
• Repeat ECG every two years
• Exercise Stress Test (EST) for men greater that 45 and women greater than 50
• EST for anyone younger who is at high risk
• Micro or Macrovascular disease
• Multiple additional risk factors as evaluated by UKPDS or Framingham
• One extreme risk factor
• Duration of greater than 15 years if older than 30 yrs old
• Anyone with typical or atypical cardiac symptoms
• Anomalies on resting ECG
This information will be required at the time of each assessment except the EST, which
should be based on risk and any changes in the condition. Once you receive the
information, you can determine the fitness of the individual and apply any required
limitations to reduce the perceived risk.
Newly diagnosed diabetics beginning any form of treatment or any unstable seafarers will
be deemed Temporarily Unfit until they provide evidence that they are on a stable
regimen with no major complications resulting from their diabetes or its treatment.
Individuals with good glycemic control, who have limited cardiovascular risk, are at low
risk of having a hypoglycemic event and are undergoing regular monitoring may be Fit
without any limitations.
If the assessment reveals the potential for significant hypoglycemic event, then the
seafarer must address the risk and you must apply limitations. Red Flags would include
patients with poor insight of their condition, hypoglycemic unawareness, frequent
episodes and those requiring the aid of another individual to correct the condition. In such
cases, the following limitations may be required:
• No Lone Watchkeeping
• Requires Regular Meals
Using Insulin disqualifies the seafarer for any unlimited voyages based on International
Standards. As a result, Insulin use requires a limitation of:
• Limited Contiguous Waters Voyage
If the assessment uncovers, any significant risk, specifically cardiac, you should direct the
person to their treating physician to address the issue.
If the risk remains, depending on that risk, they may be Unfit or require more stringent
duty or geographical limitations.
You may also choose to impose a time limitation to ensure an appropriate follow-up to
reassess the status for any situation.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 30 of 76
4.5 OBESITY
Obesity is growing in our society. There are several ways to classify it, with the most
familiar being the Body Mass Index (BMI). It has been shown to closely represent one’s
body fat percentage, but has its obvious limitations.
It is calculated as: BMI = Weight (Kg) / Height (m)
2
The most frequently used definition is the one provided by the WHO.
BMI
Classification
< 18.5
Underweight
18.5–24.9
Normal weight
25.0–29.9
Overweight
30.0–34.9
Class I obesity
35.0–39.9
Class II obesity
> 40.0
Class III obesity
However, you can see that Class III may no longer serve in North America and it has
been further stratified to:
• Any BMI > 40 is severe obesity
• A BMI of 40.0–49.9 is morbid obesity
• A BMI of >50 is super obese
Waist Circumference is now the focus of interest and is a marker in Metabolic Syndrome
(Waist, TG, HDL, BP, FBS). It has a strong correlation with cardiovascular disease. It has
a history that dates back to the late 1950’s. However, its relationship to insulin resistance
wasn’t recognized until 1988. There are several definitions of metabolic syndrome but
central to all the current ones is the waist circumference. One of the problems with this is
the standardization of measurements:
Men: greater than 102 cm
Women: greater than 88 cm
The Workplace Health and Public Safety Program of Health Canada have reviewed the
subject and concluded that
“There is no evidence that an obese person cannot medically
perform the tasks of most jobs without increased risk to self, colleagues,
and the public”.
OHAG Advisory/Interpretation 2000-07 Obesity and Occupational
Health Medical Assessment
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 31 of 76
They acknowledge that obesity presents a risk of developing other health problems and
there may be performance issues. It is these performance issues that are the focus of your
evaluation.
To address this issue and we must rely on functional abilities previously reviewed in
Section 3.1. Seafarers are required to meet the following standards:
a) adequate muscle strength to lift and carry a weight of 22 kg;
b) the physical capacity to wear breathing apparatus and the seafarer’s personal
life-saving equipment while climbing ladders;
c) the agility and strength to carry out the duties that may be assigned to them
regarding fire fighting and vessel abandonment in an emergency;
d) the ability to work in constricted spaces and move through restricted openings
of a maximum dimension of 600 mm by 600 mm; and
e) the physical and mental fitness to meet the occupational and operational
requirements of the position that they occupy or seek to occupy.
If you have ongoing concern with the seafarer’s function, if there has been significant
interval weight gain, or if the BMI exceeds 35, you could further assess the effects of
obesity on the individual’s performance by using the following table extracted from
The International Convention on Standards of Training, Certification and Watchkeeping
for Seafarers. It outlines the minimum physical abilities for seafarers. If the seafarer is
unable to pass key components of normal and emergency duties on a vessel, they should
be deemed Unfit.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 32 of 76
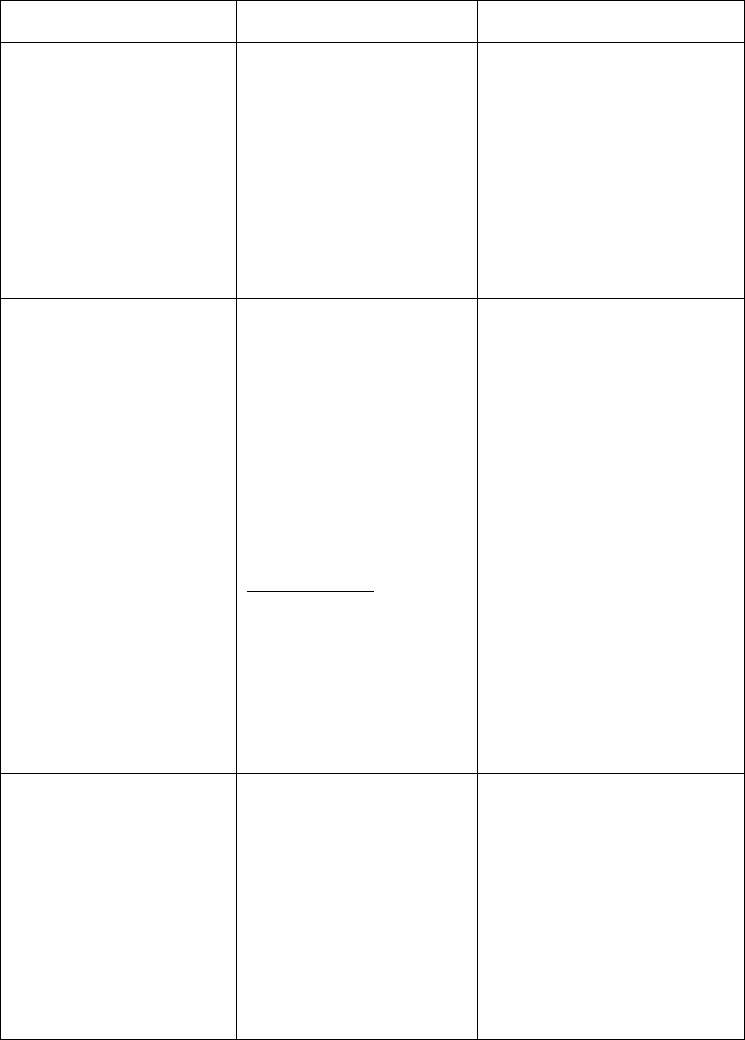
Assessment of minimum entry level and in-service physical abilities for seafarers
3
STCW Table B-I/9
Shipboard task, function,
event or condition
3
Related physical ability
A medical examiner should be
satisfied that the candidate
4
Routine movement around ves-
sel:
• on moving deck
• between levels
• between compartments
Note 1 applies to this row
Maintain balance and move
with agility
Climb up and down vertical lad-
ders and stairways
Step over coamings (e.g., Load
Line Convention requires coam-
ings to be 600 mm high)
Open and close watertight doors
Has no disturbance in sense of bal-
ance
Does not have any impairment or
disease that prevents relevant move-
ments and physical activities
Is, without assistance
5
, able to:
• climb vertical ladders and stair-
ways
• step over high sills
• manipulate door closing systems
Routine tasks on board:
• Use of hand tools
• Movement of ship’s stores
• Overhead work
• Valve operation
• Standing a four-hour watch
• Working in confined spaces
• Responding to alarms,
• warnings and instructions
• Verbal communication
Note 1 applies to this row
Strength, dexterity and stamina to
manipulate mechanical devices
Lift, pull and carry a load
(e.g., 18 kg)
Reach upwards, stand, walk and
remain alert for an extended
period
Work in constricted spaces and
move through restricted openings
(e.g., SOLAS requires minimum
openings in cargo spaces and
emergency escapes to have the
minimum dimensions of
600 mm × 600 mm)
Visually distinguish objects,
shapes and signals
Hear warnings and instructions
Give a clear spoken description
Does not have a defined impairment
or diagnosed medical condition that
reduces ability to perform routine
duties essential to the safe operation
of the vessel
Has ability to:
• work with arms raised
• stand and walk for an extended
period
• enter confined space
• fulfil eyesight standards
• fulfil hearing standards set by
competent authority or take ac-
count of international guidelines
• hold normal conversation
Emergency duties
6
on board:
• Escape
• Fire-fighting
• Evacuation
Note 2 applies to this row
Don a lifejacket or immersion suit
Escape from smoke-filled spaces
Take part in fire-fighting
duties, including use of
breathing apparatus
Take part in vessel
evacuation procedures
Does not have a defined impairment
or diagnosed medical condition that
reduces ability to perform emergency
duties essential to the safe operation
of the vessel
Has ability to:
• don lifejacket or immersion suit
• crawl
• feel for differences in temperature
• handle fire-fighting equipment
• wear breathing apparatus (where
required as part of duties)
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 33 of 76
NOTES FOR TABLE B-I/9:
1) Rows 1 and 2 of the above table describe (a) ordinary shipboard tasks, functions,
events and conditions, (b) the corresponding physical abilities which may be
considered necessary for the safety of a seafarer, other crew members and the
ship, and (c) high-level criteria for use by medical practitioners assessing
medical fitness, bearing in mind the different duties of seafarers and the nature
of shipboard work for which they will be employed.
2) Row 3 of the above table describes (a) ordinary shipboard tasks, functions,
events and conditions, (b) the corresponding physical abilities which should be
considered necessary for the safety of a seafarer, other crew members and the
ship, and (c) high-level criteria for use by medical practitioners assessing
medical fitness, bearing in mind the different duties of seafarers and the nature
of shipboard work for which they will be employed.
3) This table is not intended to address all possible shipboard conditions or
potentially disqualifying medical conditions. Parties should specify physical
abilities applicable to the category of seafarers (such as “Deck officer” and
“Engine rating”). The special circumstances of individuals and for those who
have specialized or limited duties should receive due consideration.
4) If in doubt, the medical practitioner should quantify the degree or severity of any
relevant impairment by means of objective tests, whenever appropriate tests are
available, or by referring the candidate for further assessment.
5) The term “assistance” means the use of another person to accomplish the task.
6) The term “emergency duties” is used to cover all standard emergency response
situations such as abandon ship or fire fighting as well as the procedures to be
followed by each seafarer to secure personal survival.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 34 of 76
4.6 CARDIAC
Cardiac conditions can have a significant impact on one’s function and exercise tolerance.
That is why you should consider conditions that could require immediate attention when
determining fitness. It is impossible to cover every possible cardiac condition and apply
standards to each, especially since each person will suffer different degrees of morbidity
from their condition. A straightforward approach may be taken so you can offer an
opinion on the probability of sudden incapacitation or dysfunction.
Key to a cardiac functional assessment is The New York Heart Classification’s four
functional categories listed below.
The New York Heart Classification
I No symptoms and no limitation in ordinary physical activity.
II Mild symptoms and slight limitation during ordinary activity.
Comfortable at rest.
III Marked limitation in activity due to symptoms, even during less-than-ordinary
activity. Comfortable only at rest.
IV Severe limitations. Experiences symptoms even while at rest.
In the past, a stress test was almost always required. The Canadian Cardiovascular
Society feels that an assessment and report of the relevant functional class above
definitions may sometimes be enough unless one feels it necessary to further determine
function or if it was otherwise clinically indicated.
While this may be a reasonable approach for the average patient, a seafaring population is
unique with safety critical roles and inaccessibility to medical services. Most cardiac
patients already have caregivers and specialists that are using evidence-based
investigations and treatment. In such cases, get their opinions.
You can simplify your decision-making process to individual aspects:
Symptoms
Function
Recent Cardiac Events
Risk
Specialist’s Opinion
Disqualifiers
Symptoms
Any new symptoms (chest pain, palpitations, presyncope, and shortness of breath) must
be investigated. These persons would be deemed Temporarily Unfit until evidence is
provided. Consider this fitness outcome whenever there is a high index of suspicion.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 35 of 76
Function
Regardless of the condition, you must consider function. This is where the NYHC is such
a useful tool. Remember, you have to consider not just their baseline function but also
their abilities in cases of emergency situations. Anyone in Class III or IV would be Unfit.
Recent Cardiac Events
If, for example, a seafarer suffers from an acute coronary syndrome, develops a newly
recognized LBBB or undergo a significant cardiac procedure, deem them as Temporarily
Unfit. Have seafarers get their condition and function assessed by their specialist after a 3
month period. If they get a favourable report from their specialist, you may lift the
restriction. You may shorten the waiting period if a specialist supports it.
Risk
Risk is a major consideration. If there is a significant risk for a first time event or the risk
of recurrence in people with a cardiac condition, be sure to reflect it the fitness outcome.
It may be outside your scope to make such a risk determination and you will often need a
specialist’s opinion. However, one evidence-based method of determining risk is the
Framingham Risk Score. If the risk is considered to be high, there may be little choice but
to apply limitations or even deem the seafarer as Unfit. Such individuals will require
further investigations and management by their treating physicians. If the work-up reveals
significant findings, they will need ongoing specialist management and the following
limitation should be applied:
• No Watchkeeping
• Sheltered Waters.
For persons determined to be low risk on that scale, you now have an evidence-based
assessment that could substantiate your decision to make them Fit.
Specialist Opinion
Seafarers deemed fit with or without limitations may have a specialist recommendation of
a specific management plan or frequency for reassessments that you can incorporate into
the limitations such as ‘Voyages not to exceed 30 days’.
Disqualifiers
Some conditions bring an unacceptable risk. Seafarers with the conditions below will be
deemed Unfit.
• NYHC Class III or IV
• Implanted Cardioverting Defibrillators (ICD) unless used for prophylactic
reasons based on positive genetic screening in a low risk patient and the
cardiologist feels there is <1% risk of sudden incapacity. In this unique
population, No Lone Watchkeeping and LCWV restrictions are required.
• Cardiac Transplant
• Acute Pericarditis, Myocarditis, or Bacterial Endocarditis (risk of embolism)
until fully recovered
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 36 of 76
• Angiographic demonstration of >50% reduction in diameter of LCA
• Mobitz II Second and Third Degree heart blocks
• VT of either hemodynamically unstable or LVEF < 35%
• Symptomatic Sick Sinus Syndrome until successfully treated
• Symptomatic SVT, Atrial Fibrillation, Atrial Flutter until after 3 month period
of stability after treatment
• Within One Month of implantation of Permanent Pacemaker and cardiology
review of function
• Congested Heart Failure with Ejection Fraction < 35%
4.7 HYPERTENSION
Hypertension is primarily considered as a long-term risk factor however; there are some
acute situations that you must consider. It can impact multiple systems, primarily, the
CNS and CVS. While there are different cut-off values and management approaches,
anyone with a blood pressure of >170/100 is Unfit.
4.8 ANTICOAGULANTS
An aging population brings more people with Atrial Fibrillation, valvular disease and
other thrombotic disorders. When we consider the typical patient, we usually realize the
risks involved in the use of an anticoagulant, but it is almost always outweighed by the
benefits (60% reduction of Non-valvular Atrial Fibrillation Strokes for example).
This is not true, however, with Seafarers, where the typical risk/benefit analysis is
skewed. Theirs is physical work which poses an increased risk to injury. The potential
movements on board a vessel and the risks of falling compound this risk of injury.
There is also the inaccessibility of care while at sea that leads to obvious difficulties of
dealing with poorly controlled bleeding as well as the impact of interfering with
monitoring protocols.
The risk of major bleeding while on an anticoagulant has recently been revised and
surpasses 3% annually. New England Journal of Medicine, 2010, 363:1875-76. However,
this doesn’t necessarily apply to seafarers. And even if such a risk would be acceptable,
practical issues of bleeding have to be considered.
Health Canada recently provided a guideline for Warfarin use and Safety Sensitive Work.
They conclude that for the use of Warfarin may not be an automatic disqualification.
OHAG Bulletin 2008-01 – Warfarin use and Safety Sensitive Work
In the past, the focus was dedicated to Warfarin, but there are other agents available,
Clopidogrel and Dabigatran to name some. They may have different monitoring needs,
but the basic issues of trauma and bleeds are the same.
With this in mind, there are some specific issues that are specific to seafarers:
1) Consider the underlying condition for which they are being treated and ensure no
functional limitations as well as no risk of incapacitating recurrence, essentially
that reviewed with the Cardiac Conditions. For example, Atrial Fibrillation that
is not well rate-controlled and other arrhythmias, a Cardiology consult may
be needed.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 37 of 76
2) No ongoing DVT or PE. Once DVT resolved for 1 month and PE resolved for
3 months, reconsideration.
3) For all seafarers using Warfarin, reassurance of INR stability for 3-month period
and planned regular monitoring (monthly).
4) Further determination will depend on the perceived risk of injury. Factors that
will play into this would include:
• Seafarer age
• Size of vessel. A larger vessel will have relatively less movement and risks
of falls.
• Availability of portable INR instruments.
Any seafarer using anticoagulants may not go beyond Near Coastal Class II.
4.9 PRESCRIPTION OPIATES
Significant advances have been made in the management of Acute and Chronic Pain with
the introduction of new and different agents. Side effect profiles have also improved.
However, you must consider a variety of factors. Many seafarers are in safety critical
roles which vary dramatically in emergency situations. It is nearly impossible to
extrapolate the potential influences of any of these agents on the function of these
individuals. Even if one has been on a particular product for any length of time, they may
be called upon to function in an emergency and there may be no room for error. This is
why a firm and strict policy is in place:
• Opiates are prohibited in a Marine Environment
• Any periodic use is not permitted within 48 hours of sailing.
This applies to every member of the crew. People who cannot function without the
regular use of these medications may have to reconsider their career options.
There will be some who use opiates occasionally. They must understand that use is not
permitted within 48 hours of sailing. If there are any concerns regarding their use of
opiates, ask them to provide supporting information from their treating physician or
specialist to confirm:
• the underlying condition and any functional limitation it imposes
• the different treatments and outcomes
• the use of relatively low doses of opiates
• the stability of the dose
• no adverse side effects of the medications
• any impact on the patient’s behaviour and function
• evidence of no signs of abuse of opiates, and
• no aberrant behaviour or other substance abuse

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 38 of 76
While you don’t have to apply a limitation to such a person’s certificate, you must make
sure they understand use is not permitted within 48 hours of sailing. Document this
warning, and the fact you explained it to the seafarer, on his or her medical report.
There will be requests for the use of Tramadol. It is a useful agent and has a different side
effect profile compared to other analgesics. It has the potential of causing seizures,
especially with concomitant use of other medication. There is also the potential to cause
psychological and physical dependence. For these reasons, it will be restricted in the same
way as other opiates.
Methadone use is becoming more prevalent and its purpose is clear in treatment
programs, but it, like other opiates, is also prohibited. However, upon receiving a
supportive letter from their caregiver outlining the cessation of this medication and the
status of the underlying condition, the seafarer will be allowed to resume duties but
possibly with limitation. Similar reports may be requested periodically at an interval of
every 3 months for up to two years based on the circumstances at the prerogative of
Transport Canada’s Marine Medical Branch.
4.10 PSYCHIATRY
There are many challenges in assessing seafarers’ mental fitness, which include the:
• variety of psychiatric conditions that exist,
• diversity of presentations,
• potentially rapid fluctuations in severity and,
• lack of firm statistical data about the effects of these disorders on one’s function
The prevalence of these conditions is rising and is more often reported due to our
society’s more open approach to them.
Within our seagoing population, factors contributing to a greater concern and
susceptibility of such conditions include but not limited to the:
• potential duration away from home,
• lack of support,
• working with authoritive people,
• cramped living quarters,
• different racial, social, religious groups of coworkers,
• irregular hours and sleep,
• dangerous working conditions,
• expectations to function in emergency situations,
• difficulty for ongoing psychological treatment and support,
• unavailability of replacing medication.
A balanced approach is necessary to allow competent individuals work without
compromising safety.
Mental fitness is crucial as it can have a significant impact on cognition, thought
processes, judgement, reaction time, motor function, and perceptual changes. Individuals
may become aggressive, erratic, reckless, and feel invulnerable; to name a few.
Always consider medication use, side effects and the consequences of a missed dose that
could hamper a seafarer with their safety-critical jobs.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 39 of 76
With most medical conditions, supporting documents are essential. This is especially true
for mental health, since it is unrealistic to be able to assess any significant mental health
issue at only one brief visit, which also includes the individual’s entire health review and
physical exam. The seafarer’s Family Physician, Psychiatrist, or Substance Abuse
Professional is a valuable partner that can provide critical information on the seafarer’s
condition and status.
However, keep in mind that many of these providers are frequently advocating for the
patient and may not recognize their patient’s safety-critical role, the inaccessibility
of medical support and services, and the challenges of the job.
This is why, despite supporting documents being a critical part of the assessment, you
must carefully consider:
• Function
• Risk of recurrence
• Risk of a mild condition worsening
• Co-morbidities
• Ability to function in an Emergency Situation
• Side effect of medications
• The patient’s insight, responsibility and compliance with management
• Overall risk to safety.
For most patients, the history they provide may reveal significant information, especially
if they have good insight into their condition. After careful consideration, if it is only a
mild depression or an anxiety disorder, you may determine there is no significant
impairment and deem the seafarer Fit.
For more significant conditions or if an issue arises from your questioning, the obligation
would be to seek more information. Once you receive an outside opinion, the seafarer will
have to be reassessed and the fitness assessment concluded.
If you determine that the psychiatric condition has a low risk you should be comfortable
to assess them as Fit with No Limitations especially if they have good insight, comply
with treatment, are free from any side effects of medications and have good medical
follow-up. This decision must be substantiated.
If, there is evidence of a significant risk of recurrence or a severe impairment, or possibly
significant side effects, then the seafarer would have to be deemed Unfit. You may invite
them to undertake management and request them to provide supportive documentation
and return for a reassessment.
Alternatively, if there is a focal dysfunction, perhaps in cognition resulting from
medications, returning to work with a limitation of No Watchkeeping would be
appropriate. Consider issuing a time limitation to monitor any changes in the condition.
Specific Conditions:
4.10.1 SCHIZOPHRENIA AND SCHIZOAFFECTIVE DISORDER
Common to both are changes in perception, thinking, emotion, and interpretation
of events leading to erratic, bizarre and unpredictable behaviour and
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 40 of 76
relationships. The environment on board ship with the cramped quarters, intense
relationships with a limited number of people, inability to have time alone,
constant noise, separation from family and so on is very difficult for such
individuals.
Even a stable patient on medication may be destabilized in such an environment.
One may have longstanding mild symptoms but may have unpredictable changes
in behaviour and as such, even brief voyages would be dangerous.
This is why any seafarer suffering one of these conditions is Unfit.
4.10.2 DELUSIONAL DISORDER
While similar to the above, the delusions lack the bizarre quality seen with
Schizophrenia. Also, symptoms of a major mood disorder are absent and there is
a variable, but typically no severe impact on psychosocial functioning. However,
a risk still remains as one can develop unpredictable and bizarre behaviour based
on the delusions or changes in delusions.
There is a spectrum here and it depends on the nature of the delusion. Delusions
about specific events distant in time or space such as the knowledge of the true
murderer of a celebrity or having been abducted by a flying saucer 10 years ago,
and that have not been acted upon for several years would be categorized
differently from delusions involving jealousy, persecution, grandiosity or
somatic symptoms as well as delusions being acted upon.
As a result of this spectrum, there will be some stratification of outcomes. The
majority will be Unfit. However, you may decide to deem Fit with Limitations
of No Watchkeeping Duties, seafarers with supportive documentation from
their psychiatrist and evidence of:
• No previous effect on function
• No previous aggression
• Delusions stable
• Delusions not being acted upon
• Delusions irrelevant to life at sea; or
• Good insight, compliance and ongoing follow-up
While unusual, you may decide to issue a certificate that deems a seafarer Fit
with no limitations if he or she is deemed in complete remission is and/or has:
• Lack of delusions for 2 years
• Complete insight
• Delusion seen as unimportant by the patient i.e. ‘true, but I don’t
care now’
• AND no previous effects on function
• AND no previous aggression may be considered.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 41 of 76
4.10.3 BRIEF PSYCHOTIC DISORDER
The key feature is a sudden onset of psychosis, typically florid, that lasts no
longer than one month and the individual has a full return to their premorbid
functioning. It may be with or without a precipitating psychosocial stressor.
During the disorder, the seafarer is Unfit.
In the setting of a precipitating stressor and after three months have passed since
a complete resolution of the disorder, the seafarer can return to work as Fit with
no limitations.
In the absence of a precipitating stressor and after six months have passed since
a complete resolution of the disorder, the seafarer can return to work as Fit with
Limitations of No Watchkeeping. After 2 years have passed, the seafarer may
be considered Fit with no limitations.
Any recurrence of psychotic symptoms necessitates that the seafarer is Unfit.
4.10.4 BIPOLAR I DISORDER
The essential feature of this condition is the occurrence of one or more
Manic Episodes. Further, this disorder (as opposed to Type 2) must have:
• produced “marked impairment” in occupational functioning,
social activities or relationships; or
• required hospitalization; or
• presented with psychotic features.
The same risks posed by schizophrenia exist with this disorder. Individuals
suffering a Manic episode exhibit poor judgement and frequently do not
recognize that they are ill. Some, especially those with psychotic features, may
become violent or suicidal (completed suicide in 10-15% of bipolar type 1).
Many will also have associated Alcohol and other Substance Use Disorders.
Ninety per cent of persons who have a single manic episode have a recurrence.
Some (20-30%) continue to exhibit residual symptoms and many (60%)
experience interpersonal and occupational difficulties between episodes. The
interval between acute episodes tends to decrease with age.
As a result, a seafarer diagnosed with Bipolar Disorder Type 1, is Unfit.
4.10.5 BIPOLAR II DISORDER
This disorder is distinguished from Type 1 by the fact that it has not been severe
enough to:
• cause “marked impairment” in occupational functioning or social
activities
• require hospitalization
• include psychotic features.
A seafarer is Unfit during any stage that this condition is being investigated
and/or treated. By definition, this condition is typically not severe (only
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 42 of 76
Hypomanic), but if it is frequent or if the episodes, which while not psychotic,
cause significant problems at sea or on land, you must deem the seafarer Unfit.
Otherwise, once in remission and the seafarer is complying with treatment, has
good insight and has good function, you may consider them Fit with Limitations
of No Watchkeeping.
After two years have passed without recurrence and off medications, you may
consider the seafarer Fit with no limitations.
4.10.6 DEPRESSION, DYSTHYMIA, ANXIETY DISORDERS
These conditions present a wide range of severity of symptoms. The risks to
safety include reduced performance, slow response, indecisiveness, difficultly in
dealing with emergencies, interpersonal turmoil, and suicidality. The
determination of fitness will depend on the degree of the symptoms and their
influence on function.
Severe symptoms, significant impairment, poor compliance, poor insight, or a
risk of exacerbation at sea will require the Seafarer to be deemed Unfit.
People with less severe symptoms may be considered Fit with Limitations of No
Watchkeeping Duties. Once the condition has resolved, the seafarer may be
considered Fit with no limitations.
4.10.7 ATTENTION DEFICIT DISORDER
Many people with adult ADD can function without medication, but function
better with it. Psychostimulants are the first line medication for this condition so
when making an assessment takes into account the fact that these medications
can be abused or sold.
If there is a way to secure the medication and the seafarer is reliable and
has good insight and good function, you may consider him or her Fit with
no limitations.
4.10.8 DELIRIUM, DEMENTIA, AND AMNESTIC AND OTHER
COGNITIVE DISORDERS
Previously known as Organic Mental Syndromes and Disorders, the key feature
for this group of conditions is a clinically significant change in cognitive
function. You must deem seafarers with these conditions Unfit.
With the exception of Delirium, once the acute condition is resolved and it is
unlikely to recur and there are no sequellae, you may consider the seafarer Fit
with no limitations.
4.10.9 MEDICATIONS
Taking medications is not in itself enough to cause unfitness, but obviously, it is
an important factor you MUST CONSIDER IN ALL CASES. There are too
many variations to make absolute rules. In mild conditions, most medications are

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 43 of 76
helpful, but not necessary. In the absence of any side effects, no limitation will
be required.
However, other conditions require medications and you should advise the
seafarer to continue their treatment. This is also true of medications that have the
potential of a discontinuation syndrome.
Regardless of the condition or the specific medication used or whether used
intermittently, you should question the seafarer about side effects and document
the response. Any evidence or concern about side effects that will affect the
seafarer’s function will require a No Watchkeeping limitation.
The seafarer should be informed that using Benzodiazepines and any sedatives is
prohibited within 48 hours of sailing.
4.10.10 ALCOHOL AND SUBSTANCE ABUSE
Consider this during all assessments. It is addressed in the next section, but it is
often a component of mental disorders and requires special attention when you
assess one’s mental health.
4.11 ALCOHOL AND DRUGS
The Canadian Counsel of Motor Vehicle Administrators state that “Despite alcohol’s
social acceptance, it is simply another sedating drug that interferes with judgement, reflex
control and behaviour.”
Alcohol consumption is accepted and so prevalent in our society that it easy to become
desensitized to it. Since seafarers hold safety sensitive positions in which there is a lot at
stake, you must give this issue special attention.
The problem starts with what constitutes too much alcohol and what is acceptable?
Further, can you the examiner, turn a blind’s eye to any excessive quantity being declared
as consumed only off duties? These are challenging questions but help is available with
Canada’s Low-Risk Alcohol Drinking Guidelines developed by the National Alcohol
Strategy Advisory Committee. These guidelines were developed to reduce immediate
and long-term alcohol consequences. You will need to use your clinical judgment when
assessing acceptable limits of consumption. However a consumption of > 15 standard
alcohol units per week for men and > 10 for women would grounds for further evaluation.
More information can be found at the Canadian Center on Substance Abuse at:
http://www.ccsa.ca/Eng/Priorities/Alcohol/Canada-Low-Risk-Alcohol-Drinking-
Guidelines/Pages/default.aspx
Many question how effective objective markers are to screen and what these markers
really tell about a person’s function and risks. Following are some references pointing to
the advantages of questionnaires.
A 2005 study confirmed that an elevated GGT, MCV and carbohydrate-deficient
transferrin (%CDT) could be a predictive screen up 90% of the time. However, the
authors suggested it was too early to use any biochemical markers for screening.
Addiction. 2005; 100(10): 1477–1486

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 44 of 76
Another study from Helsinki provided a predictive value of only 54% and deemed
objective testing as not being a useful screening tool. They further determined GGT alone
detected only a third of patients having more than 16 "drinks" per day. In contrast, the
brief questionnaires and interviews identified nine out of ten alcoholics.
Lancet 1982 Feb 6;1(8267):325-8.
There are a variety of screening questionnaires. There is the Michigan Alcohol Screening
Test (MAST) and it is a screening tool for alcoholism widely used by courts.
The CAGE questionnaire has a sensitivity of 93% and a specificity of 76% for the
identification of problem drinking. Lancet 1982 Feb 6;1(8267):325-8
The CAGE questionnaire involves 4 questions:
1) Have you ever felt you should cut down on your drinking?
2) Have people annoyed you by criticizing your drinking?
3) Have you ever felt bad or guilty about your drinking?
4) Have you ever had a drink first thing in the morning to steady your nerves
or get rid of a hangover (eye-opener)?
Total scores of 2 or above are thought to be clinically significant and may
indicate alcohol dependence. JAMA 1984, 252: 1905-1907.
An example of its use is a Canadian study trying to identify how big of a problem alcohol
use is in Canada. It identified almost 6% of Canadians with positive results. They were
able to correlate a 7 times greater risk of alcohol related problems with this positive
group. Unfortunately, the majority (85%) were not indentified or seeking help for the
issue. Can Med Assoc J. Dec 1, 1997; 157 (11) 1529
A recent systematic review of the literature has concluded that the AUDIT is the best
screening instrument for the whole range of alcohol problems. The World Health
Organization developed it and it has been validated in six countries. It helps to identify
persons with hazardous and harmful patterns of alcohol consumption. It has been found to
provide an accurate measure of risk across gender, age, and cultures.
There are a couple of definitions that are implemented in this screening test.
Hazardous drinking is a pattern of alcohol consumption that increases the risk of harmful
consequences for the user or others. Hazardous drinking patterns are of public health
significance despite the absence of any current disorder in the individual user.
Harmful use refers to alcohol consumption that results in consequences to physical and
mental health.
Alcohol dependence is a cluster of behavioral, cognitive, and physiological phenomena
that may develop after repeated alcohol usage which includes a strong desire to consume
alcohol, impaired control over its use, persistent drinking despite harmful consequences,
increased alcohol tolerance, and a physical withdrawal reaction when alcohol use is
discontinued.
You will find the entire document at:
http://whqlibdoc.who.int/hq/2001/who_msd_msb_01.6a.pdf
AUDIT consists of 10 questions about recent alcohol use, alcohol dependence symptoms,
and alcohol-related problems.
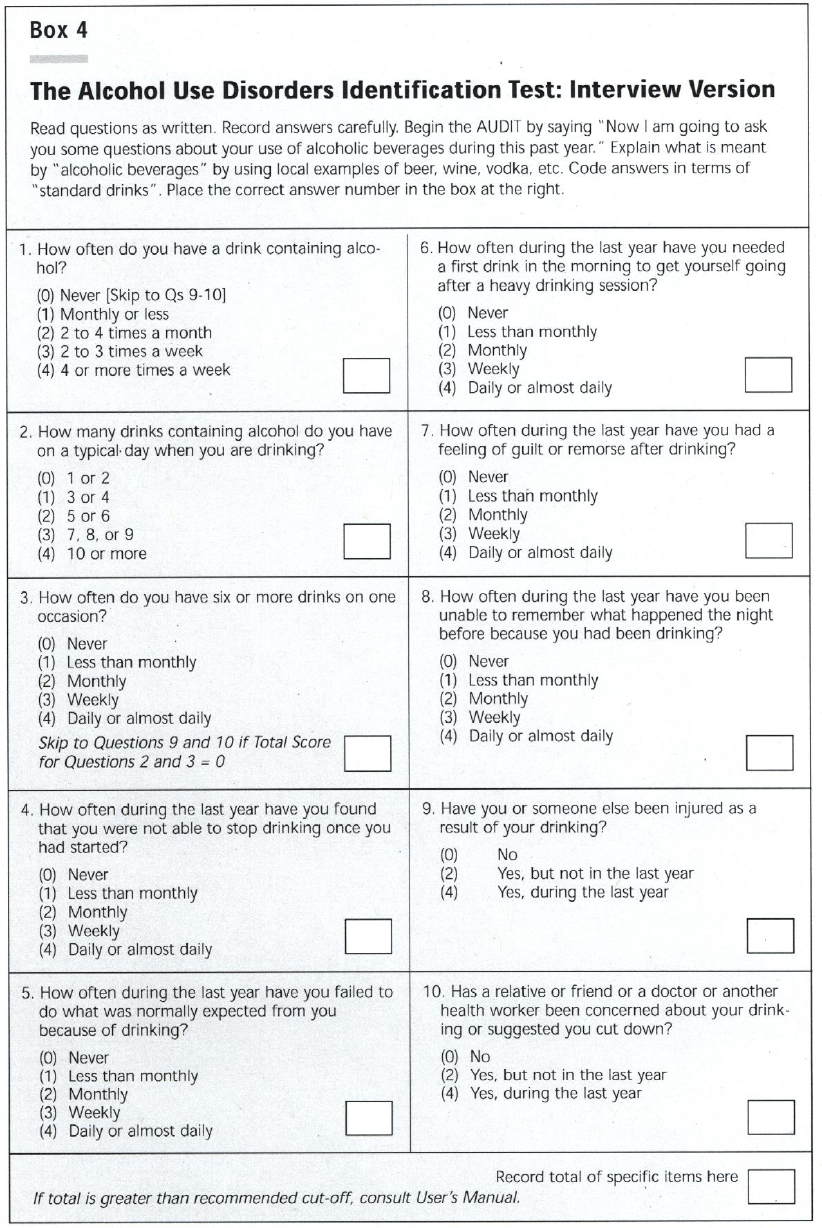
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 45 of 76
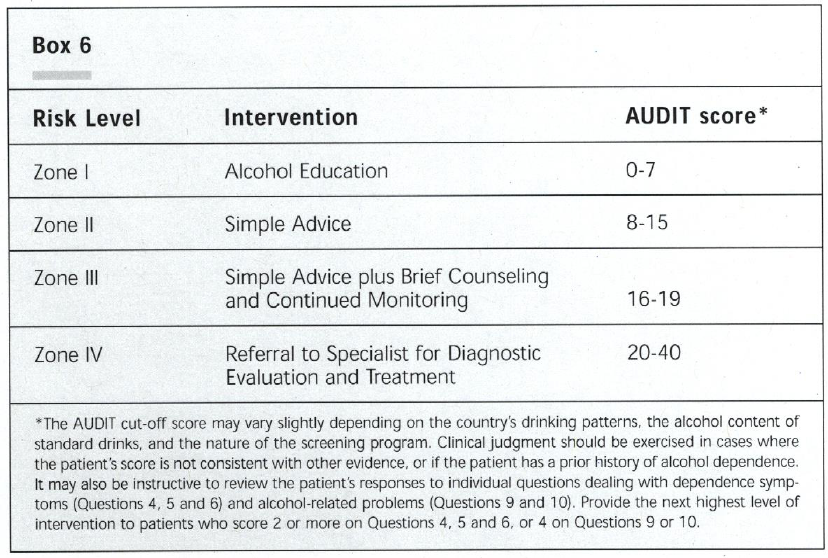
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 46 of 76
There are two ways to interpret the results:
1. the total score reflects the patient’s level of risk related to alcohol; and
2. individual responses differentiate different zones or risk levels and prescribes
different actions.
Scores of 8 or more indicates hazardous and harmful use. If you use a cut off of 10, it
will provide you with greater specificity and give you fewer false positives. For
individuals older than 65 years old, you may consider a cut off of 7.
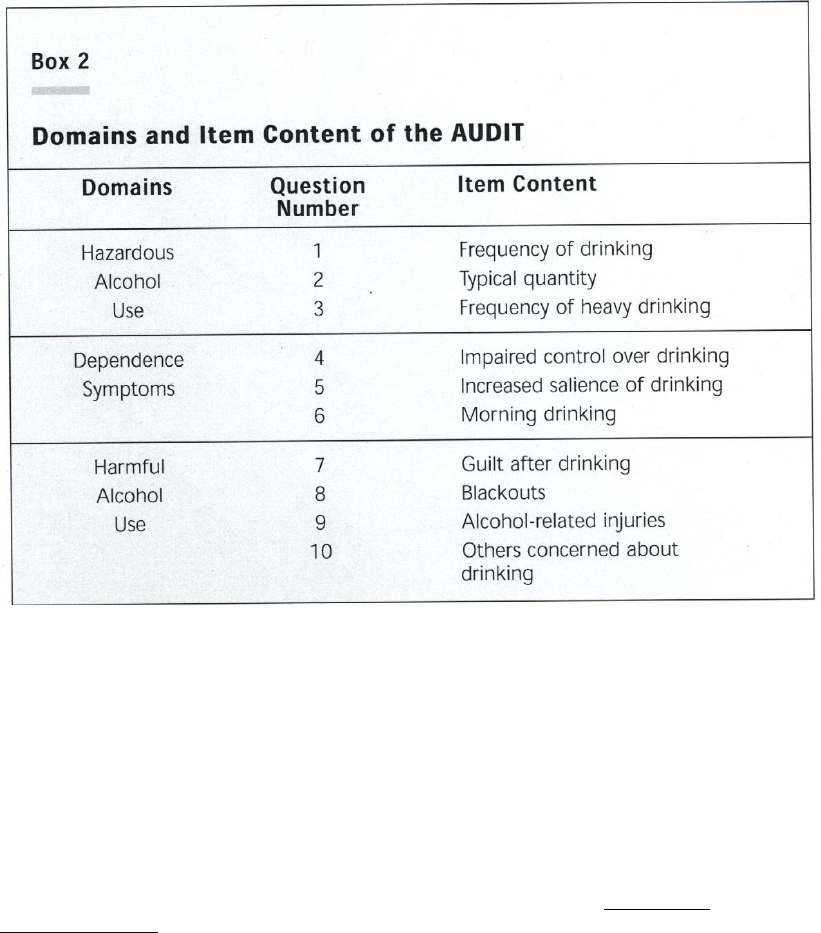
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 47 of 76
Further, the questions are clustered into domains and could differentiate different issues.
Significant scores
• Points in Q#2 or Q#3 Consumption at Hazardous levels
• Points in Q#4 to 6 Presence or incipience of dependence
• Points in remainder Indicate harm is already being experienced
Also, the last two questions 9 and 10, gives insight as to whether there is evidence of a
past problem and may suggest vigilance of the patient.
WHAT ABOUT DRUGS?
Once again, rely on Screening Questionnaires. One useful tool is called the Drug Abuse
Screening Test or DAST-20 that originated from the Addiction Research Foundation
in Toronto.
It is a 20-item instrument that may be given in either a self-report or in a structured
interview format with a "yes" or "no". It is a brief, simple, practical, and valid method for
identifying individuals who are abusing psychoactive drugs. It yields a quantitative index
score of the degree of problems related to drug use and misuse. DAST scores are highly
diagnostic with respect to a DSM diagnosis of psychoactive drug dependence.
The questions concern information about potential involvement with drugs not including
alcoholic beverages during the past 12 months.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 48 of 76
It screens for the use of prescribed or over the counter drugs in excess of the directions
and any non-medical use of drugs. The various classes of drugs may include: cannabis,
solvents, tranquilizers, barbiturates, cocaine, stimulants, hallucinogens or narcotics.
A DAST score of six is typically significant. It is also suggested that a score of 16 or
greater be considered to indicate a very severe abuse or a dependency condition. The
DAST also provides a score that should be sensitive to changes in substance using
experiences over a 6 and 12-months follow-up period, as suggested by the author.
DAST-20
Have you used drugs other than those required for medical reasons?
Have you abused prescription drugs?
Do you abuse more than one drug at a time?
Can you get through the week without using drugs?
(Inverse response scored)
Are you always able to stop using drugs when you want to?
(Inverse response scored)
Have you had "blackouts" or "flashbacks" as a result of drug use?
Do you ever feel bad or guilty about your drug use?
Does your spouse (or parents) ever complain about your involvement
with drugs?
Has drug abuse created problems between you and your spouse or your parents?
Have you lost friends because of your use of drugs?
Have you neglected your family because of your use of drugs?
Have you been in trouble at work because of drug abuse?
Have you lost a job because of drug abuse?
Have you gotten into fights when under the influence of drugs?
Have you engaged in illegal activities in order to obtain drugs?
Have you been arrested for possession of illegal drugs?
Have you ever experienced withdrawal symptoms (felt sick) when you stopped
taking drugs?
Have you had medical problems as a result of your drug use (e.g. memory loss,
hepatitis, convulsions, bleeding, etc.)?
Have you gone to anyone for help for a drug problem?
Have you been involved in a treatment program specifically related to drug use?
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 49 of 76
DAST INTERPRETATION GUIDE
RISK
DAST-20
ACTION
None
0
Monitor
Low
1-5
Brief Counselling
Intermediate (meets DSM Criteria)
6-10
Outpatient (intensive)
Substantial
11-15
Intensive
Severe
16-20
Intensive
Regardless of whether it is alcohol or drugs, there is NO tolerance to allow anyone at risk
to be allowed to hold a safety critical post. It is important to constantly remain vigilant as
individuals are not likely to provide such information readily.
Administer a screening test to, or send to their treating physician, any seafarer that;
• declares excessive use,
• presents behavioral cues,
• has received a Driving Under the Influence charge, and/or
• presents any alcohol or drug-related physical stigmata.
If the screen suggests problems, you should advise the seafarer of your concern and have
them see their family doctor or a Substance Abuse Professional (SAP) to address the issue
further and look at their treatment options.
If there is any evidence of a significant issue, you must deem the seafarer Unfit.
There are many opportunities for a rehabilitation program and ongoing monitoring
of the alcohol or drug use behavior. Remember, Methadone Programs are not permissible.
Those diagnosed with a substance abuse disorder may be reinstated if they produce a
supportive letter from a SAP when at least 3 months has passed since completing a
Rehabilitation Program. You may choose to apply limitations.
You would you base your decision on answers to the questions below.
1) Are there any cognitive deficits?
2) Have there been any withdrawal seizures?
3) Are there any motor deficits?
4) Any maladaptive behaviors?
5) Any co-morbidity such as mental health or liver disease?
It would also depend on documentation from the SAP or family doctor.
1) Are they supportive of a return to duties?
2) Are objective markers such as LFTs responding?
3) Is monitoring ongoing and reflecting abstinence?
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 50 of 76
4) Was the treatment program completed and participation in post-treatment
activities?
If a seafarer meets these criteria, grant him or her a time limited Certificate of 3 months
during which time, their caregiver provides supportive documentation and objective blood
or urine screens. This frequency of evaluation every 3 months will continue for a period
of TWO years and monitoring of such will occur at the Marine Medical Unit.
If there are any doubts, impose a limitation of No Watchkeeping.
Those that are recently diagnosed and elect to not undergo rehab will remain Unfit. Upon
re-applying, they must see a SAP and probably undergo the same 3month-monitoring
program for 2 years dependent on the SAP assessment.
Those with a past history of Substance Abuse and dependent on the Marine Medical
Examiner assessment may require documentation from their SAP or Family Doctor
reflecting abstinence for at least 2 years.
4.12 ASTHMA
Asthma is a chronic respiratory condition that affects 7% of the population. It is more
common in childhood, with a prevalence of up to 15%. Many ‘outgrow’ their symptoms,
but may have some residual hyper-reactivity and symptoms may resurface with the right
conditions. Occupational asthma is the most commonly reported occupational respiratory
disease. The American Thoracic Society identifies up to 23% of new-onset adult asthma
as work related. Asthma requires attention as this condition could be life threatening.
Classifying asthma is straightforward.
1) Intermittent - mild symptoms less than once weekly and easily responds to beta
agonist. FEV1 > 80% predicted
2) Mild Persistent - mild symptoms more often that once weekly. Periodic use of
inhaled steroids and still responds to beta agonist. FEV1 > 80% predicted
3) Moderate Persistent - symptomatic, daily and nightly. Regular use of inhaled
steroids and occasional use of oral steroids. FEV1 60-80% predicted
4) Severe Persistent - symptomatic day and night. Frequent use of Oral steroids.
Frequent hospitalizations. FEV1 < 60% predicted.
5) Exercise Induced - episodes provoked by exertion especially in the cold.
Responds to beta agonist.
Your focus is on the condition’s relationship to fitness to work at sea. Regardless of their
severity, make sure they can wear their emergency breathing apparatus.
You must consider the possibility of an acute exacerbation that could lead to a severe or
life-threatening situation. You can do this by assessing:
• any specific triggers and how to avoid them;
• the severity of their condition and possible previous oral steroid use
and hospitalizations; and
• how successfully they respond to their treatment?
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 51 of 76
The approach to assessing a seafarer’s fitness to join the ship’s complement is as follows:
Anyone who is Intermittent or Mild Persistent and your assessment is
supportive, you may well deem Fit.
Those who are Moderate Persistent will require input from a specialist, but they
will likely be Fit with Limitations. It will likely be Geographical, limiting them
to Inland or Sheltered Waters. Near Coastal Class I or Near Coastal Class II
could only be considered if supported by the specialist.
Seafarers with Exercise Induced may require input from a specialist and their
severity would determine whether they are Fit or alternatively, Unfit keeping in
mind there is no limitation preventing one from emergency duties and exertion.
You must deem those with Severe Persistent asthma Unfit.
You should consider placing Medical limitations such as: Must carry self
administered medications on all seafarers with asthma.
4.13 CHRONIC OBSTRUCTIVE PULMONARY DISEASE
This condition, if severe enough, can be disabling. There are many facets to this group
of respiratory conditions that you can evaluate, but your focus is function. There are
several ways to do this, but one way to do so would be to quantify breathlessness.
A validated tool to assess this is the MRC Breathlessness Scale. It assigns one of five
grades that relate breathlessness that could apply for any respiratory condition to activities
and function.
Grade
Degree of breathlessness related to activities
1
Not troubled by breathlessness except on strenuous exercise
2
Short of breath when hurrying or walking up a
slight hill
3
Walks slower than contemporaries on level ground because of
breathlessness, or has to stop for breath when walking at own
pace
4
Stops for breath after walking about 100m or after a few
minutes on level ground
5
Too breathless to leave the house, or breathless when dressing
or undressing
Occupational Medicine; 2008; 58; 226-227
Any supplementary oxygen use and MRC Grades 4 and 5 would Disqualify the seafarer.
Those with Grade 3 may require more frequent assessments and may have a Time
Limited Certificate to monitor disease progression and be restricted to Sheltered
Waters.
Alternatively, if there are any doubts, a clinical decision can be made with input from
specialists and spirometry.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 52 of 76
In all cases, ensure seafarers can effectively meet four pertinent requirements:
(a) adequate muscle strength to lift and carry a weight of 22 kg;
(b) the physical capacity to wear breathing apparatus and the seafarer’s personal
life-saving equipment while climbing ladders;
(c) the agility and strength to carry out the duties that may be assigned to them
regarding fire fighting and vessel abandonment in an emergency; and
(d) the physical and mental fitness to meet the occupational and operational
requirements of the position that they occupy or seek to occupy.
4.14 ANAPHYLAXIS AND ALLERGIES
Allergies are very complex and can present with a wide range of symptoms. There is a
classification system and the focus is primarily with Type 1 Hypersensitivities. It includes
atopic dermatitis, allergic Urticaria, Hay fever, Allergic asthma, Anaphylaxis from any
source and IgE-mediated food allergies such as peanuts, eggs and seafood. These
conditions may be either local or systemic with their symptoms ranging from a mild
irritation to a full-blown Anaphylactic Reaction.
The key is to determine the severity of the reaction and the possibility of an exposure to
an agent that could cause a life-threatening reaction. If there is a clear history
of what the exact allergen is and precisely how the individual reacts, carry on and make
a fitness determination. However, many times, the condition is never truly defined and
if there is any question, send the seafarer back to his or her family doctor for
a referral to an allergist to determine the facts. The allergist may have to provide
an opinion.
If it is simply a Vespid reaction, it will likely not be an issue to your typical seafarer, but
they may be stung while at a port. However, in this setting, you would have some
expectation that medical services will be available in a near-by land-based facility.
Depending on the specific allergen and their reaction, you may have to declare the
individual Unfit. However, if the condition allows, you can consider a limitation of:
‘Must carry self-administered medications at all times’
‘Avoid Specific Allergen _________’
Seafarers and Medical Certificates are portable. Make sure you indicate any limitations if
they are deemed Fit as the Seafarer’s workplace and exposures are prone to change.
Celiac Disease is not Type 1 hypersensitivity, but rather a Type 4 Cell Mediated
Hypersensitivity mediated by T-cells. It may not be an urgent/life threatening condition,
but it can lead to significant symptoms and dysfunction. For critical crew members you
should consider placing a limitation of:
‘Should avoid eating certain foods’
4.15 HIV / AIDS
Seafarers are not disqualified solely on the basis of this diagnosis. Many infected
individuals will be quite well and may be so for many years. However, your focus should
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 53 of 76
be on function and the risk of the condition significantly deteriorating and requiring
medical attention.
One issue is viral transmission. Exposure and acquisition is concerning, but it is
questionable whether that alone is enough to bar them from a vessel crew. The main
transmission routes of HIV are well established. It is possible to find HIV in the saliva,
tears and urine of infected individuals, but there are no recorded cases of infection by
these secretions, so the risk of infection via these routes is negligible.
There are a variety of ways to view and quantify this condition:
• Clinical stage
• Complications
• CD4 count
The World Health Organization Disease Staging System for HIV Infection and Disease
was first produced in 1990 and updated in September 2005.
Stage I: HIV disease is asymptomatic and not categorized as AIDS
Stage II: include minor mucocutaneous manifestations and recurrent upper respiratory
tract infections.
Stage III: includes unexplained chronic diarrhea for longer than a month, severe bacterial
infections and pulmonary tuberculosis.
Stage IV: includes toxoplasmosis of the brain, candidiasis of the esophagus, trachea,
bronchi or lungs and Kaposi's sarcoma; these diseases are used as indicators
of AIDS.
The CDC Classification System for HIV now factors in the CD4 count (CD4 T-cell count
below 200 cells/µl or a CD4 T-cell percentage of total lymphocytes of less than 14%) and
AIDS defining illnesses that include:
• Candidiasis of bronchi, trachea, or lungs
• Candidiasis esophageal
• Cervical cancer (invasive)
• Coccidioidomycosis, disseminated or extrapulmonary
• Cryptococcosis, extrapulmonary
• Cryptosporidiosis, chronic intestinal for longer than 1 month
• Cytomegalovirus disease (other than liver, spleen or lymph nodes)
• Encephalopathy (HIV-related)
• Herpes simplex: chronic ulcer(s) (for more than 1 month); or bronchitis,
pneumonitis, or esophagitis
• Histoplasmosis, disseminated or extrapulmonary
• Isosporiasis, chronic intestinal (for more than 1 month)
• Kaposi's sarcoma
• Lymphoma Burkitt's, immunoblastic or primary brain
• Mycobacterium avium complex
• Mycobacterium, other species, disseminated or extrapulmonary
• Pneumocystis carinii pneumonia
• Pneumonia (recurrent)
• Progressive multifocal leukoencephalopathy
• Salmonella septicemia (recurrent)
• Toxoplasmosis of the brain
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 54 of 76
• Tuberculosis
• Wasting syndrome due to HIV
CD 4 counts can help predict risk. The major discriminating points are:
• CD 4 < 200 High risk
• CD 4 > 350 Lower risk
A specialist will have to weigh in and help you assess the seafarer’s status. However, as
a framework:
Stage 1(asymptomatic) and CD 4 > 350 Fit.
If one becomes symptomatic up to Stage 2 and the CD 4 remains greater than 350,
Fit with Limitations specific to their circumstances. You may also want to issue a
Time limitation.
A Seafarer beyond Stage 2 or with a CD 4 count below 350 is Unfit.
4.16 HEPATITIS
Regardless of its cause, consider those with any Acute Hepatitis Temporary Unfit.
Subsequently, it all depends on the underlying condition that influences the liver and
any sequellae.
Most viral causes of Hepatitis resolve and leave no significant functional impairment, so
you may deem the Seafarer Fit. However, others are left with ongoing impairment of
liver function or complications such as cirrhosis or portal hypertension. You must request
information from the patient’s family doctor and Hepatologist and may place time
limits to allow for follow-up. Depending on the outcome, you may consider some
individuals Unfit.
Hepatitis C is unique. Between 60-70% of people infected develop no symptoms during
the acute phase. In the minority of patients who experience acute phase symptoms, they
are generally mild and nonspecific, and rarely lead to a specific diagnosis of Hepatitis C.
The patient becomes unwell and symptomatic only when the disease impairs liver
functions. It may be as little as some jaundice and fatigue, but may proceed to fulminant
hepatic failure and require transplant.
Spontaneous viral clearance rates are highly variable and between 10–60%
of persons
infected with HCV clear the virus from their bodies during the acute phase as shown by
normalization in liver enzymes in contrast to 95% of Hep B cases that resolve within
6 months. In the remainder, the immune system cannot manage the virus and they
become chronic.
Those with chronic hepatitis frequently have no symptoms and the only differentiating
factor would be elevated liver function tests. However, about a third remain ill, some
develop cirrhosis and some develop hepatocellular carcinoma. Some individuals will
undergo treatment with Interferon. Treatment can last up to a year.
The treatment with Interferon may be physically demanding, particularly for those with a
prior history of drug or alcohol abuse. Many patients will experience side effects ranging
from a 'flu-like' syndrome (the most common, experienced for a few days after the weekly
injection of interferon) to severe adverse events including anemia, cardiovascular
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 55 of 76
events, and psychiatric problems. Deem individuals undergoing Interferon treatment
temporarily Unfit.
Does the Hep C Viral Load have a role to play in your situation? It is an important factor
in determining the probability of response to interferon-based therapy but it does not
necessarily indicate disease severity nor the likelihood of disease progression.
4.17 THYROID
The fitness of a person with a thyroid condition depends entirely on function. If function
is impaired, redirect the Seafarer back to their Family Doctor to correct the situation.
Attention is required for any possible complications such as cardiac or emotional.
4.18 NEPHROLITHIASIS AND URINALYSIS
This condition may cause incapacitating pain and dysfunction. There is also the risk of
obstruction. Someone with one remote stone form should simply remain vigilant.
However, if such individuals have blood in the urine, or if they have recurrent stones, you
must send them to their family doctor or urologist for an assessment. If at any time there
is a risk of passing a stone, then placing a restriction of Near Coastal Class II would
be appropriate.
There is some controversy regarding the benefits of a screening urinalysis. Recent
reviews have failed to demonstrate any relevance as a screening test except in pregnant
women. Not uncommonly, one spills some blood or protein in their urine, but does that
really impact on one’s fitness to be a seafarer?
For Seafarers, the purpose of this test is to screen for a condition that may develop or be
exacerbated that will influence their function and safety of the ship. The burden of the
Marine Medical Assessment is greater to pre-empt some conditions that may occur at sea.
For a young (less than 40), non-smoking, asymptomatic seafarer, a urinalysis revealing
trace or 1+ blood will not affect their qualification. However, if it is a greater quantity,
you must send the seafarer back to their family doctor for further investigation.
Glucosuria is not consequential in one who we know to be a diabetic as they will not
uncommonly spill sugar. However, in the absence of a previous diagnosis of diabetes, you
should send the seafarer back to their family doctor for further investigation and
management before completing the Marine Medical Assessment.
4.19 SOLITARY KIDNEY
The Canadian Urological Association has no specific Occupational Guidelines for adults
with Solitary Kidneys. Aside from reviewing the cause for having only one kidney, there
are no limitations.
4.20 STROKE
This discussion primarily revolves around function. However, sudden incapacitation
applies to stroke as well. This is especially the case when the outcome of the first
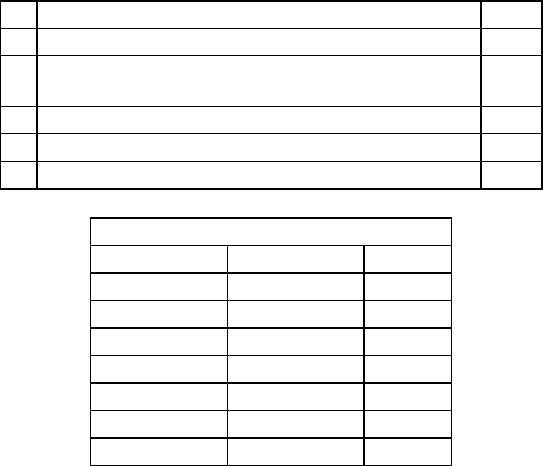
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 56 of 76
ischemic event in an individual with atrial fibrillation could be disabling in 60% of suffers
and fatal in approximately 20% of them.
Strokes can be broadly classified as ischemic or hemorrhagic. The former is much more
common, accounting for 88% of events. There are many causes of ischemic strokes, but
the majority are the result of atrial fibrillation.
Regardless of the cause, if evidence suggests the patient will have a dramatic
deterioration in their condition or have a significant risk of recurrence, deem them
Temporarily Unfit. Send these seafarers back to the family doctor for appropriate
investigation and management.
The CHADS
2
score is one of several clinical prediction tools for estimating the risk of one
with atrial fibrillation developing a stroke. It is used primarily to determine the need for
anticoagulation by stratifying risk.
You can use this tool for seafarers with atrial fibrillation not already anticoagulated. It is
not a proven predictor for those already on anticoagulants, but one can extrapolate and
use it to determine some degree of risk; knowing that there is an approximately 2/3
reduction in stroke prevalence while on therapeutic doses.
Condition
Points
C
Congestive heart failure
1
H
Hypertension: blood pressure consistently above
140/90 mmHg (or treated hypertension on medication)
1
A
Age >75 years
1
D
Diabetes Mellitus
1
S
2
Prior Stroke or TIA
2
Annual Stroke Risk
CHADS
2
Score
Stroke Risk %
95% CI
0
1.9
1.2–3.0
1
2.8
2.0–3.8
2
4.0
3.1–5.1
3
5.9
4.6–7.3
4
8.5
6.3–11.1
5
12.5
8.2–17.5
6
18.2
10.5–27.4
Gage BF, van Walraven C, Pearce L, et al. (2004). "Selecting patients with atrial
fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin”,
Circulation 110 (16): 2287–92.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001).
"Validation of clinical classification schemes for predicting stroke: results from the
National Registry of Atrial Fibrillation", JAMA 285 (22): 2864–70.
If you determine that risk is minimal, assess if any neurological deficit is significant.
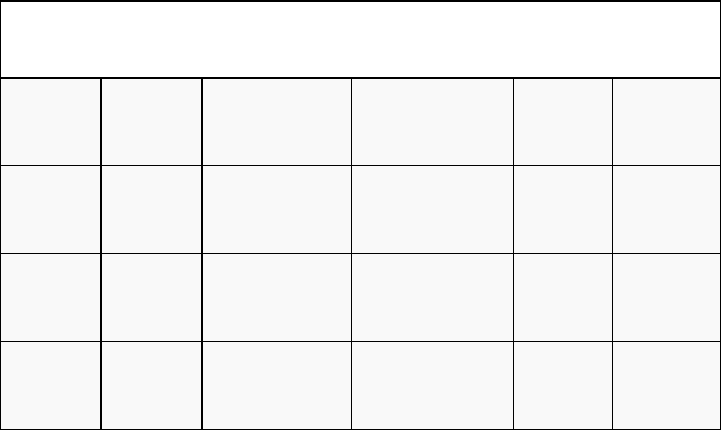
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 57 of 76
Deem any seafarer who recently suffered a stroke as Temporarily Unfit.
Once stabilized and 3 months have passed with no evidence of impending recurrence, you
may reassess the Seafarer for duties.
Pursuant to the MPR a Seafarer is to meet the following standards:
a) adequate muscle strength to lift and carry a weight of 22 kg;
b) the physical capacity to wear breathing apparatus and the seafarer’s personal
life-saving equipment while climbing ladders;
c) the agility and strength to carry out the duties that may be assigned to them
regarding fire fighting and vessel abandonment in an emergency;
d) the ability to work in constricted spaces and move through restricted openings
of a maximum dimension of 600 mm by 600 mm; and
e) the physical and mental fitness to meet the occupational and operational
requirements of the position that they occupy or seek to occupy.
For seafarers who have suffered a Transient Ischemic Attack, investigations are required
to ensure it is not a signal of a more significant condition. By definition, it is a vascular
compromise resulting in brief neurological dysfunction persisting for less than 24 hours.
Symptoms vary widely. One third of people with a TIA later have recurrent TIAs and
another third go on to develop a stroke.
The ABCD
2
determines very short-term risk for stroke after TIA. It may have limited use
for a marine medical examiner, but it may give some guidance.
In general, deem anyone with recurrent TIA Unfit until they have undergone a complete
Neurological assessment to determine the cause, have it rectified and determine any
residual dysfunction.
ABCD
2
score
age
blood pressure
clinical features
duration
diabetes
0 points
<60 years
normal
other than those
specified
less than 10
minutes
no diabetes
1 points
≥60 years
raised (blood
pressure ≥140/90)
speech disturbance
without weakness
10 to 59
minutes
diabetes
present
2 points
unilateral (one-
sided) weakness
≥60
minutes
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 58 of 76
The risk for stroke can be estimated from the ABCD2 score as follows:
• Score 1-3 (low)
• 2 day risk = 1.0%
• 7 day risk = 1.2%
• Score 4-5 (moderate)
• 2 day risk = 4.1%
• 7 day risk = 5.9%
• Score 6–7 (high)
• 2 day risk = 8.1%
• 7 day risk = 11.7%
Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. (January 2007).
"Validation and refinement of scores to predict very early stroke risk after transient
ischaemic attack", Lancet 369 (9558): 283–92.
4.21 CEREBRAL ANEURYSM
If a seafarer has a symptomatic cerebral aneurysm that has not been surgically corrected,
they are Unfit. Once repaired, upon receipt of a favourable opinion for a neurosurgeon at
the 6-month mark, they may be deemed Fit.
If an aneurysm is discovered incidentally and the patient is asymptomatic, they may be
deemed Fit upon a favourable opinion from a neurologist or neurosurgeon.
4.22 MEDICATIONS
In general, unfitness for sea duties for medical reasons is dictated by the nature of an
illness. Conditions of short duration such as pneumonia or a fracture, may dictate a
temporary period away from work. Problems can arise when medications started during
the illness are continued or new drugs are used to suppress or control resulting problems.
Medications that are prescribed by physicians for a specific condition may affect a
seafarer’s ability to perform safety sensitive duties. In these circumstances, the decision
on fitness to work is often difficult.
Side effects of particular concern include; altered vision, impaired judgment, reduced
attention span, diminished motor function, or altered response to an adverse environment
during emergencies.
Many organizations have a lengthy list of medications that would be disqualifying, but
one can realistically argue that ANY medication has the potential to impact on one’s
function and would require further assessment.
An exhaustive list of medications is impossible to produce, but some examples could
include: Anti-depressants, Anti-emetics, Anti-motion sickness agents, Anti-psychotics,
Anti-convulsants, Anti-histamines, Hypnotics and Sedatives, Medical use of
Hallucinogens (medicinal marijuana), Muscle relaxants, and Opiates.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 59 of 76
Specific examples that illustrate the difficulty of providing a finite list of medication
include:
• The makers of Champix recently issued a safety bulletin regarding the side
effects of the product that has resulted in seafarers being temporarily Unfit
while using this product.
• The ILO/WHO Guidelines clearly address this issue. “Consumption of …
psychotropic drugs which adversely affect the health of the seafarer or the
safety of the ship” are grounds to justify restrictions or render the examinee
temporarily or permanently unfit.
However, opiates and sedatives are never acceptable. Anyone on a regular dose of either
of these products is not allowed to be responsible for any safety critical role, regardless of
their history of stability. For those using these classes periodically, the use is forbidden
within 48 hours of sailing.
When assessing Seafarers taking any medications, you must:
• Undertake a thorough review to ascertain any side effects
• Take appropriate action if their medications could interfere with function.
Note: Remind Seafarers that Section 113 of the Canada Shipping Act, 2001 states, “every
crew member on board a vessel shall carry out their duties and functions in a manner that
does not jeopardize the safety of the vessel or of any person on board.” This means that
each seafarer is responsible for any possible side effects.
4.23 HERNIA
A hernia is not typically a barrier to work. It is the grey zone where you must exercise
your judgement. If:
• there are incarcerated or strangulated contents involved; they require urgent
surgical assessment and intervention before being deemed fit to work.
• it is small hernia defect, advise the candidate to follow up with their family
doctor to have the issue addressed and to seek attention if there are any changes.
• you are concerned that the hernia ring is large and there is an increased potential
for problems, consider issuing a 3 month Geographical Limitation such as Near
Coastal Class 2 on the certificate. A seafarer may return to duties after surgical
correction and with support of a General Surgeon.
4.24 PNEUMOTHORAX
This is typically an acute condition in which a patient will not necessarily present for
a Marine Medical Exam.
It most commonly arises:
• Spontaneously (most commonly in tall slim young males and in
Marfan syndrome)
• Following a penetrating chest wound
• Following barotrauma to the lungs
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 60 of 76
• Iatrogenic causes such as pleural biopsies, bronchoscopies, line placements,
positive-pressure ventilation
It may also be due to:
• Chronic lung pathologies including emphysema, asthma
• Acute infections
• Chronic infections, such as tuberculosis
• Lung damage caused by cystic fibrosis
• Cancer
• Rare diseases that are unique to women such as Catamenial pneumothorax (due
to endometriosis in the chest cavity) and lymphangioleiomyomatosis
This condition commonly comes to light in the history. A single episode of a
Pneumothorax with no other underlying condition or sequellae should not be a barrier.
This is of course assuming the treating doctor at the time followed the condition and
performed studies to illustrate resolution and no findings such as residual blebs existed
that could be a reason for recurrence. An average of 30% of patients with a spontaneous
Pneumothorax could experience a recurrence. This risk increases to 50% if they are
a smoker.
If the history is within 3 months, the seafarer must provide x-ray evidence of resolution.
If there is a history of recurrence, more information will be required including a specialist
note to consider any further management to correct a potential underlying problem.
4.25 PREGNANCY
Like other conditions, your role is to consider function and access to medical care.
However, keep in mind that even a normal pregnancy that can be easily managed on
shore can pose increased health risks at sea.
Pregnancy is perhaps a bigger issue for the employer to accommodate the seafarer’s needs
by making changes to the working conditions, hours on duty, shift work, and mitigating
risks such as exposures and injuries.
Life on board ship has specific aggravating factors such as:
• Shocks, vibrations, movements
• Manual handling of loads
• Shift work
• Postures and travelling
• Electromagnetic fields?
• Temperature extremes
• Chemical exposures
• Carbon Monoxide
Pregnancy itself has its own particular health issues:
• Morning Sickness
• Backache
• Varicose Veins
• Hemorrhoids
• Frequency
• Fatigue
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 61 of 76
• Balance with an altered centre of gravity
• Increasing size and discomfort
• Preterm labour
Miscarriage is the most common complication of early pregnancy and often occurs before
a woman knows she is pregnant. The demise of a pregnancy at any stage is not your sole
concern. You must also consider the life threatening risks to the mother with hemorrhage
and infection that could occur.
Assess each pregnant seafarer based on her condition and gestational age against her role,
the vessel purpose (i.e., a chemical carrier), the duration of travel, the distance of
proposed voyages; and make a reasonable decision. The seafarer’s Obstetrician will have
to weigh in, as well.
The seafarer must acknowledge the uniqueness of the work environment and be willing to
take some personal responsibility and recognize the risks working at sea.
Postpartum usually spans 6 weeks, but again, make decisions on a case-by-case basis.
Factors include a significant Post-partum bleed, potential retained products of conception,
post-partum emotional changes.
General Guidelines:
Any complicated pregnancy requires a supportive report from an Obstetrician.
Pregnancies less than 24 weeks will be limited to Near Coastal Class I.
Pregnancies beyond 24 weeks will be limited to Sheltered Waters.
Seafarers must meet the Universal Requirements will still have to be met at any stage
of pregnancy.
You must inform the seafarer of the risks so they can decide if they are willing to work
at sea.
4.26 INFLAMMATORY BOWEL DISEASE
Seafarers with this condition may develop severe symptoms on short notice. They will
frequently require specialist assessment and follow up. Not uncommonly, they will
require supportive care.
If there is evidence of ongoing active disease, you should apply a geographical limitation
such as Near Costal 1. However if the condition has been stable for a period of time,
there has never been any hospitalization and there is a supportive report from their
clinician, they may well be Fit.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 62 of 76
4.27 AORTIC ANEURYSM
The rupture of an aortic aneurysm is catastrophic and requires urgent care. Seafarers
detected to have an aortic aneurysm will require a vascular surgical assessment. Thus a
medical certificate will have to set appropriate time limits to ensure follow-up every 6 to
12 months depending on the rate of growth of the aneurysm or as recommended by the
surgeon.
Assess anyone with an Abdominal Aortic Aneurysm that is equal or greater that 5.5cm as
Unfit. Other aneurismal sites will require vascular surgical opinion.
4.28 PERIPHERAL VASCULAR DISEASE
Intermittent claudication can certainly be symptomatic and affect one’s function.
A specialist report may be required to determine the need for intervention. A functional
assessment will also be required to ensure the seafarer can meet the minimal universal
requirements.
4.29 HEMOPHILIA AND OTHER CLOTTING DISORDERS
This group of conditions has a very broad expression and for obvious reasons, a specialist
report will be required. As can be easily appreciated, these conditions can be challenging
in a marine setting for the same reasons described in the section on anticoagulants.
Seafarers with a severe case will be deemed Unfit. For those with a milder case, upon
receipt of supportive reports from their specialist, a geographic limitation of up to
Limited Contiguous Waters Voyage will be required.
4.30 NEOPLASIA
The diversity of conditions and the variations of expression of this problem will require
specialist input.
Restrictions may include time limitations for required follow up. Also, Geographical
limitations are not unrealistic. If there were any significant impairment in function, then
employment limitations such as No Watchkeeping would be necessary. Here are some
very broad guidelines:
Unfit: If undergoing active investigation and treatment.
Fit with Limitations: If treated and apparent cure and low risk if within 5 years.
Fit: If treated and no evidence of risk of recurrence or any
impairment resulting from condition or treatment after
5 years.
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 63 of 76
5. CONCLUSION
The role as a Marine Medical Examiner has evolved and is not only to report medical
facts but to make a fitness decision and provide that opinion to the Minister of Transport.
The ultimate goal is to MINIMIZE RISK. That is why Transport Canada has the
expectation that Marine Medical Examiners will:
• be familiar with its certification process and comply with its standards and
requirements
• conduct a thorough medical examination and
• obtain any relevant documentation so that a proper assessment may be made
with due regard to the examinees’ medical condition and public safety.
The Marine Medical Exam is also a unique opportunity for you to promote health and
educate your patients. You should:
• encourage all seafarers to maintain healthy lifestyles
• promote the role of primary health care providers and encourage regular
checkups and
• inform the Seafarer of any medical documentation needed at their next
assessment to prevent unnecessary delays at future assessments.
Transport Canada will conduct periodic reviews to keep this Guide current. We encourage
Marine Medical Examiners to provide any feedback and opinions.
Marine Medicine hopes you find this guide useful and looks forward to continue working
with you in the future.
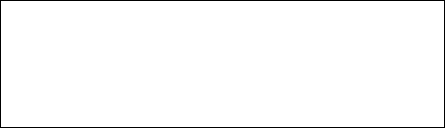
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 64 of 76
ANNEX 1: SAMPLE LETTER TO SEAFARER
Marine Medical Examiner:
Date: ______________________________________
Dear Mr./Ms _____________________________________________ CDN # __________________
Based on the marine medical examination performed on ___________, and conforming to the Marine
Personnel Regulations (MPR), you have been assessed as:
□ Unfit
□ Fit with the following Limitations:
______________________________________________________________________
______________________________________________________________________
______________________________________________________________________
______________________________________________________________________
This decision is based on the following information:
______________________________________________________________________
______________________________________________________________________
______________________________________________________________________
______________________________________________________________________
______________________________________________________________________
As per the MPR, sub-section 278 (1), you have the right to request a reconsideration of this
assessment within 30 days of receipt of this notice. Please address your request to Transport Canada:
Marine Medicine (AMSPM)
Transport Canada
330 Sparks Street
Ottawa, Ontario
K1A 0N8
Sincerely,
Dr. __________________________________________________ MME # ___________________
c.c.: Transport Canada, Marine Medicine

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 65 of 76
ANNEX 2: PHYSICIAN’S REPORT FOR
A DIABETIC SEAFARER
Patients Name______________________________CDN__________________Date_____________
Please provide further information regarding your patient’s condition as part of a Marine
Medical Assessment. There is limited access to medical services at sea that requires a
Diabetic to understand and control their condition.
Note: Any expenses incurred to prove their medical fitness is the seafarer’s responsibility.
1) How long have you treated this patient for Diabetes?
2) When was the initial diagnosis of Diabetes established?
3) Treatment required:
Diet □ Oral medications □ Insulin □
Please list all mediations and doses:
4) Does the patient carry out self ‘blood’ glucose testing?
YES □ NO □
5) Does the patient’s glycemic log suggest good control of their Diabetes?
YES □ NO □
6) Does your patient understand the relationship between their condition, diet,
__exercise and medications?
YES □ NO □
7) Does your patient take appropriate action based on the ‘blood’ glucose levels?
YES □ NO □
8) Can your patient recognize a hypoglycaemic reaction if and when it occurs?
YES □ NO □
9) Please list the symptoms experience during a hypoglycaemic reaction:

MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 66 of 76
10) Has your patent ever had any significant Hypoglycaemic events of which you are
-----aware?
YES □ NO □
If “YES”, please indicate the date and treatment (self-treated, hospitalized, etc):
11) Please provide current results of:
FBS AIC ACR Total Chol
TG HDL LDL Ratio
Exercise Stress Testing:
□ Unnecessary based on risk evaluation defined by Canadian Diabetic
______.Association’s Clinical Practice Guidelines
□ Date and outcome (or attach report):
12) Does your patient suffer any end-organ conditions?
Peripheral Neuropathy? □ Retinopathy? □
Cardiovascular? □ Nephropathy? □
13) Do you have any concerns regarding your patient’s ability to perform their
___safety-critical-job in a Marine Environment where they are inaccessible to
___Medical Services?
YES □ NO □
If “YES”, Please indicate the reason,
THANK YOU,
Physicians Signature Date
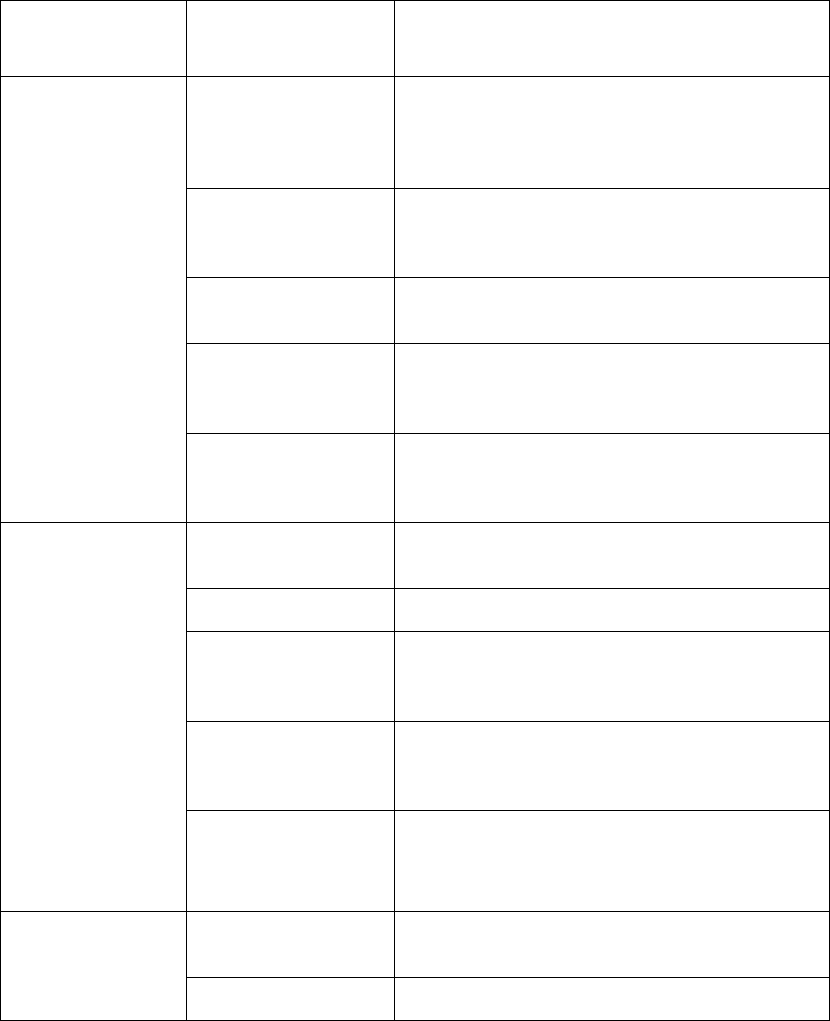
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 67 of 76
ANNEX 3: TABLE OF COMMONLY USED
LIMITATIONS FOR MARINE MEDICAL
CERTIFICATES
TYPE OF
LIMITATION
NAME
APPLICATION/DEFINITION
DUTY
Definition of
Watchkeeping (WK)
Refers to safety critical roles on a vessel that require
unconditional cognitive and perceptual function.
Anyone with a potential for the compromise of
function may require a limitation
No Watchkeeping
For anyone with risk of Sudden Incapacitation or
risk of impaired cognition due to a medical
condition or medications
No Bridge
Watchkeeping
For those who fulfill the requirements for another
department but not for the bridge
No Lone Watchkeeping
For those with possibly full perceptual functioning,
but with an ongoing risk of temporary cognitive
deficiencies
Present Occupation
Only
For those fulfilling the requirements for their
present job only. A reassessment will be required to
make a career change
MEDICAL
Corrective lenses
required
When aid is required to meet the standard
Hearing Aids required
When aid is required to meet the standard
Specialized Electrical
Equipment Required
While Sleeping
Needs accommodations with an appropriate
electrical outlet
Must Carry Self-
administered
Medications
When needs life saving medication like Epipen,
asthma medication
To Avoid Specific
Allergen
When Seafarers have significant allergies to certain
agents
TIME
The maximal duration
of a voyage___
May need regular treatment or medical follow up
Not to be away from
Same as above
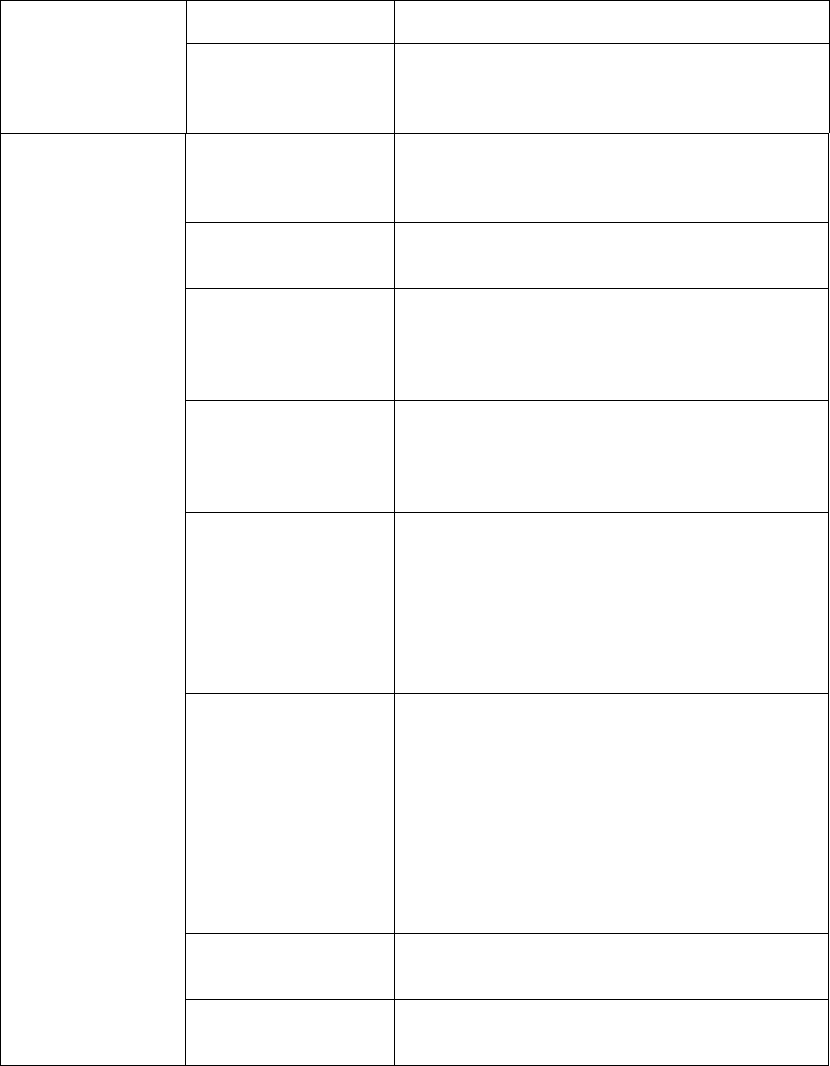
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 68 of 76
Home Port Overnight
The maximal time
away from a specified
medical facility
Same as above
GEOGRAPHICAL
1Nautical Mile(NM)
equals 1.852 KM
Sheltered Waters
Voyage
A voyage that is in Canada, on a lake or a river
above tidal waters, where a vessel can never be
further than one nautical mile from the closest shore
Canadian Waters
Voyage
A voyage that extends to Canadian Territorial
waters to 12 Nautical Miles
Inland Waters voyage
A voyage on the Inland Waters of Canada together
with any part of any lake or river forming part of
the inland waters of Canada that lies within the
United States or a voyage on Lake Michigan
Near Coastal Voyage,
Class 2 (NC2)
A voyage within 25 nautical miles from shore in
waters contiguous to Canada, the United States
(except Hawaii) or Saint Pierre and Miquelon, and
within 100 nautical miles from a place of refuge
Near Coastal Voyage,
Class 1 (NC1)
A voyage that is between places in Canada, the
United States (except Hawaii), Saint Pierre and
Miquelon, the West Indies, Mexico, Central
America or the northeast coast of South America. A
voyage during which the vessel is always north of
latitude 6 degrees north and within 200 nautical
miles from shore or above the continental shelf
Limited Contiguous
Waters Voyage
(LCWV)
A variation of Near Coastal Class 1 limited to the
waters contiguous to Canada, the United States
(excluding Hawaii) and Saint-Pierre-et-Miquelon.
Applicable for those individuals that do not meet
International Standards, but can fulfill domestic
requirements. Canada and the United States have a
Memorandum of Understanding recognizing the
other’s certificates and thus voyages through United
States’ waters are permissible.
Within ___ nautical
miles from port
May need urgent medical care
Voyage between Point
A and Point B
Another way allowing those fulfilling the
requirements for their present voyage only
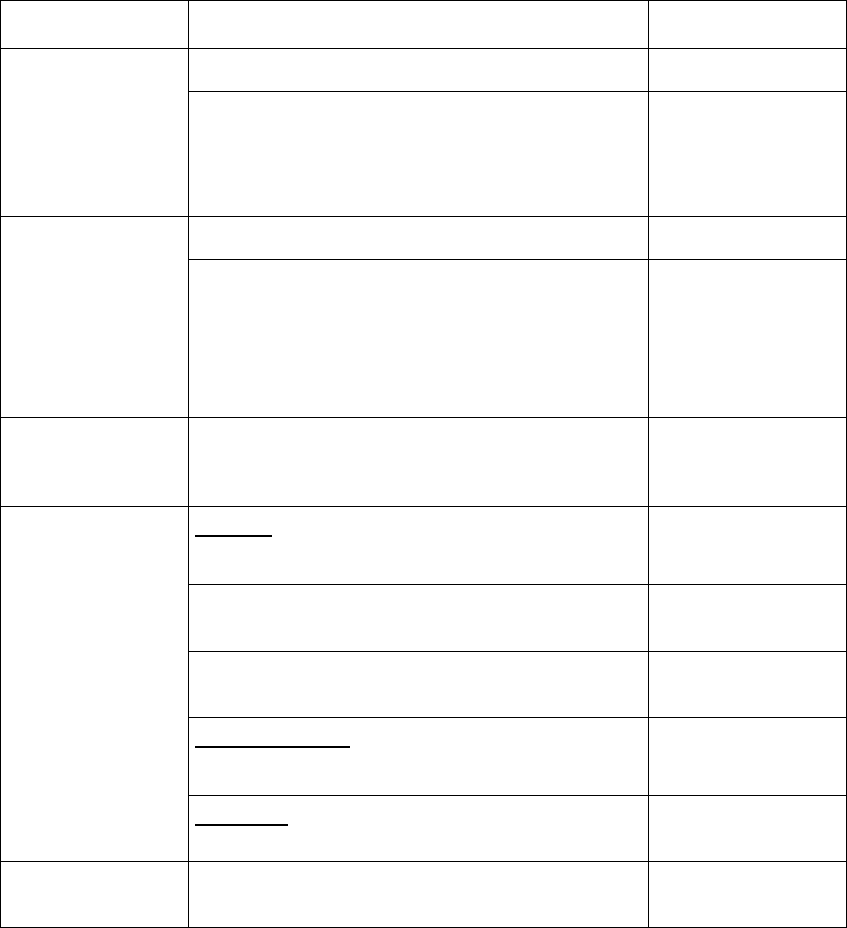
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 69 of 76
ANNEX 4: REQUIRED LIMITATIONS APPLIED TO
MARINE MEDICAL CERTIFICATES BY
CONDITION
CONDITION
ASSESSMENT
LIMITATION
Altered awareness
Not yet diagnosed, ongoing investigation
UNFIT
If there is a potential chance of:
-Hypoglycemia with DM treatment
-Vasovagals
-Medication side effects
No Solo WK
Alcohol and Illicit
Drugs
Evidence of significant issue
UNFIT
After completion of a Rehabilitation Program:
- a minimum of 3 months has passed
- a supportive letter from a Primary
Caregiver or Substance Abuse Specialist confirming
abstinence every 3montns
TIME LIMITATION
(3 months for a period
of TWO years)
+/- No WK
Anaphylaxis/
Allergies
Must carry self
administered
medication
Aneurysm
Cerebral
Symptomatic
UNFIT
- After surgery
- At the 6-month mark
FIT
- Incidentally finding asymptomatic supporting letter
from specialist
FIT
Abdominal Aortic
> 5.5cm
UNFIT
Other sites
Require vascular surgical opinion
Asthma
Intermittent, Mild Persistent, or Mild Exercise Induced
and your assessment is supportive
FIT
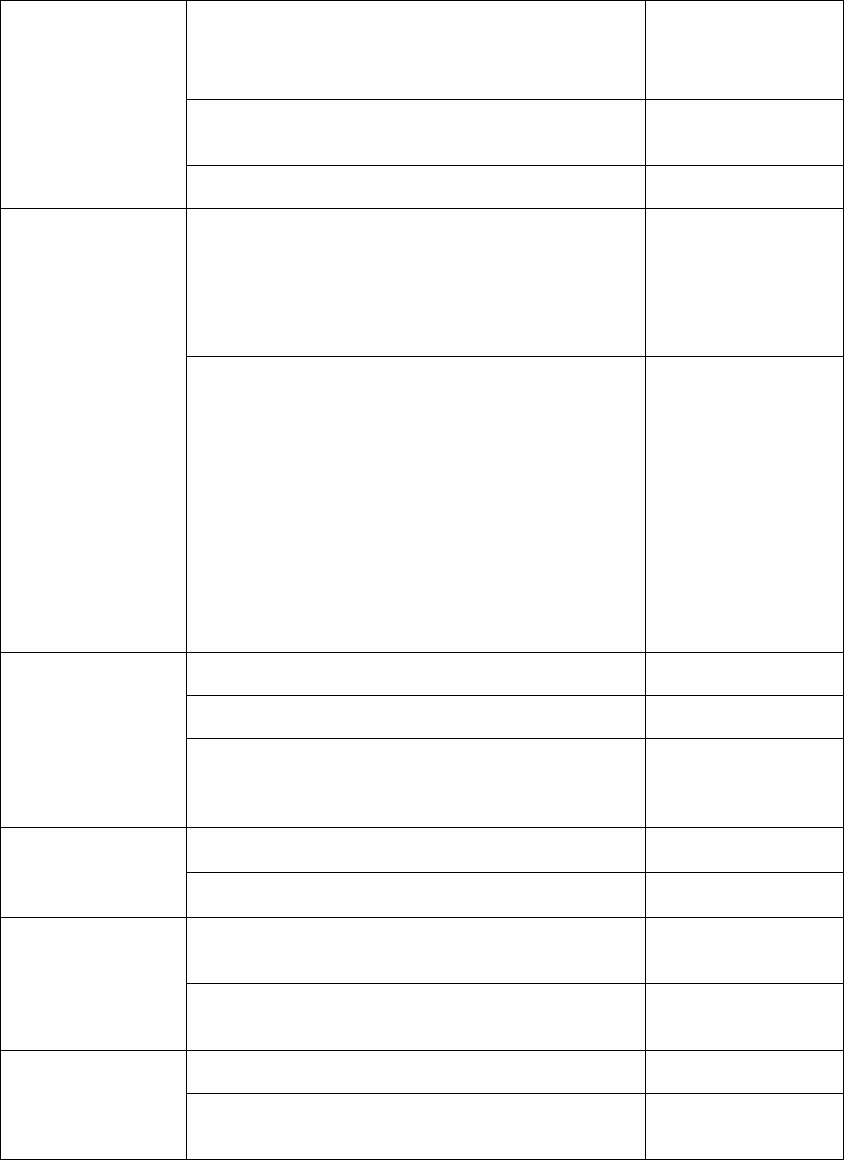
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 70 of 76
For all asthmatics that have ongoing
use of medications.
Must carry self
administered
medications
Moderate Persistent will likely
require input from a specialist
FIT with Limitations
likely Geographical
Severe Persistent and Significant Exercise Induced
UNFIT
Cardiac
- B/P > 170/100
-New symptoms have to be investigated
-< 3 month after an event or a cardiac procedure
-Within One Month of implantation of Permanent
_Pacemaker
Temporally UNFIT
-NYHC Class III or IV
-Implanted Cardioverting Defibrillators (ICD) unless
used prophylacticly based on positive genetic
screening in low risk individuals (then No Lone
Watchkeeping and LCWV)
-Cardiac Transplant
-Angiographic demonstration of >50% reduction in
_diameter of LC
-Mobitz II Second and Third Degree heart blocks
-VT of either hemodynamically unstable or
-LVEF < 35%
-CHF with EF < 35%
UNFIT
Diabetes
Newly Diagnosed or Unstable
Temporarily UNFITt
Hypoglycemia with treatment
No lone WK
Insulin use
- LCWV
- No WK first month
--of use
Hemophilia and
other Clotting
Disorders
Mild case
LCWV
Severe case
UNFIT
Hepatitis
Acutely sick and that would include those undergoing
treatment with Interferon
Temporarily UNFIT
After Acute phase passes/no significant impairments to
liver function and end-stage complications
FIT
Hernia
Small hernia defect
FIT
Large hernia ring
Geographical
Limitation
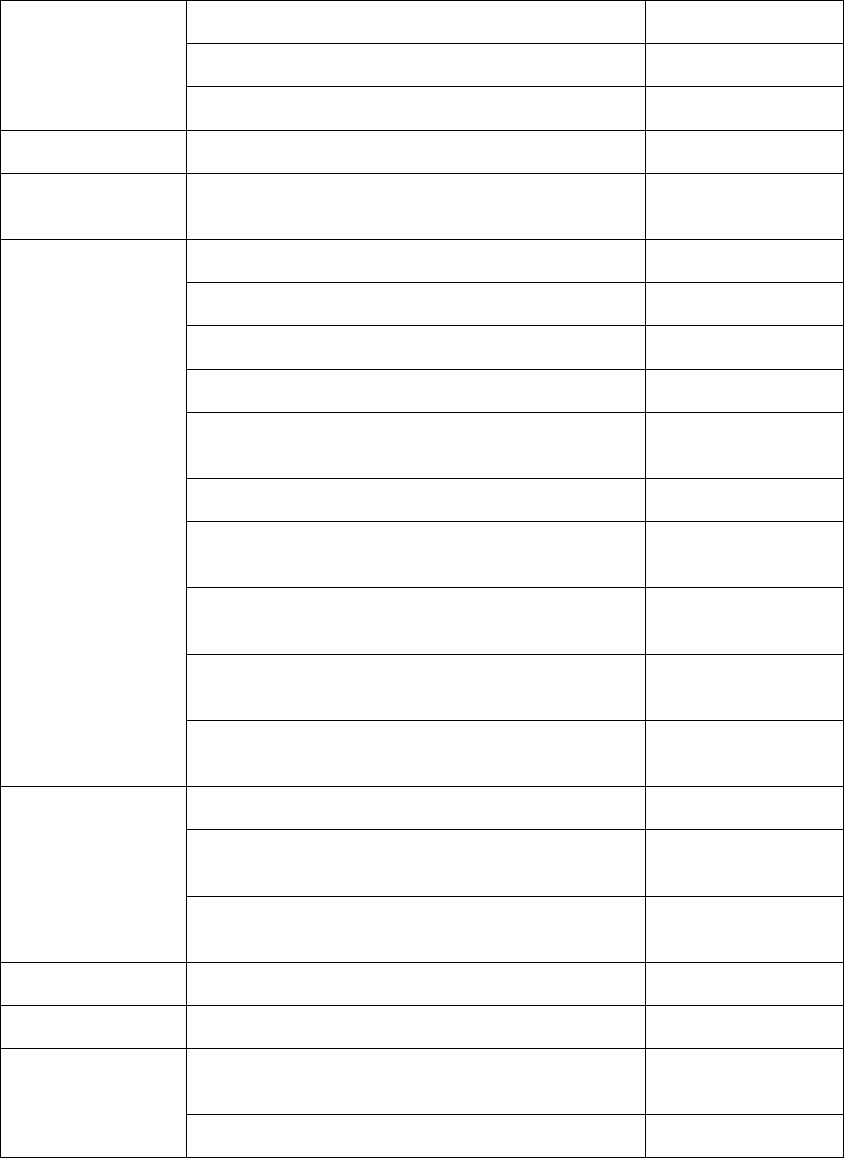
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 71 of 76
HIV
Stage 1 (asymptomatic) and CD 4 > 350
FIT
Stage 2 and the CD 4 > 350
FIT With Limitations
Beyond Stage 2 or a CD 4 < 350
UNFIT
IBD
Evidence of ongoing active disease
NC I
Job specific
For those fulfilling the requirements for their present
job only.
Present Occupation
Only
Medication
Anticoagulant
NC2
Antimetabolites and Biologicals
LCWV
Champix
Temporarily UNFIT
Immunosuppressant
LCWV
Insulin
-LCWV and No WK
first month of use
Interferon
Temporarily UNFIT
Opiates
ongoing use
UNFIT
Opiates
PRN but not within 48 hours of sailing
FIT
Sedatives
ongoing use
No WK
Sedatives
PRN but not within 48 hours of sailing
Fit
Neoplasia
If undergoing Active investigation and treatment
UNFIT
If treated and apparent cure and low risk if within 5
years.
FIT +/- limitations
if treated/ no evidence of recurrence/ no impairment
from condition or treatment after 5 years
FIT
Nephrolithiasis
If there is any risk of passing a stone
NC II
Obesity
If unable to meet Universal Requirements
UNFIT
Pneumothorax
Single episode of a Pneumothorax and confirmatory X
ray
FIT
Recurring episodes with supportive documentation
FIT
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 72 of 76
Pregnancy
Universal
Requirements must
met at any stage of
pregnancy
less than 24 weeks
NC I
beyond 24 weeks
Sheltered Waters
Psychiatry
- Significant risk of recurrence
- Severe impairment
- Significant side effects
- 2 psychotic episodes
UNFIT
Schizophrenia/ schizoaffective disorder/Bipolar I
UNFIT
Seizure
Childhood Febrile Seizure
FIT
New or Ongoing Seizure, Ongoing Investigation
UNFIT
Seizure-free with or without Rx for 6 months
NC I
No WK
Seizure-free with or without Rx for 12 months
No WK
Seizure-free with or without Rx for 5 Years
FIT
Special circumstances
See Text
Sleep disorders
Narcolepsy and Restless Leg Syndrome
No WK
Obstructive sleep apnea
Stable CPAP
Specialized Electrical
Equipment Required
While Sleeping
Symptomatic not treated
No WK
Surgery and asymptomatic
FIT
Solitary kidneys
FIT
Stroke
Minimum three months after event
Temporarily UNFIT
Once stabilized and meet Universal Requirements
FIT
Urinalysis
Hematuria: Trace or 1+ blood
Young (less than 40)/ non-smoking/asymptomatic no
stone history
FIT
Glucosuria
In non diabetic will require diabetic assessment
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 73 of 76
Universal
requirements
a) adequate muscle strength to lift and carry a weight
of 22 kg
b)the physical capacity to wear breathing apparatus
and the seafarer’s personal life-saving equipment while
climbing ladders;
c)the agility and strength to carry out the duties that
may be assigned to them regarding fire fighting and
vessel abandonment in an emergency;
d)the ability to work in constricted spaces and move
through restricted openings of a maximum dimension
of 600mm by 600mm;
e)the physical and mental fitness to meet the
occupational and operational requirements of the
position that they occupy or seek to occupy.
FIT
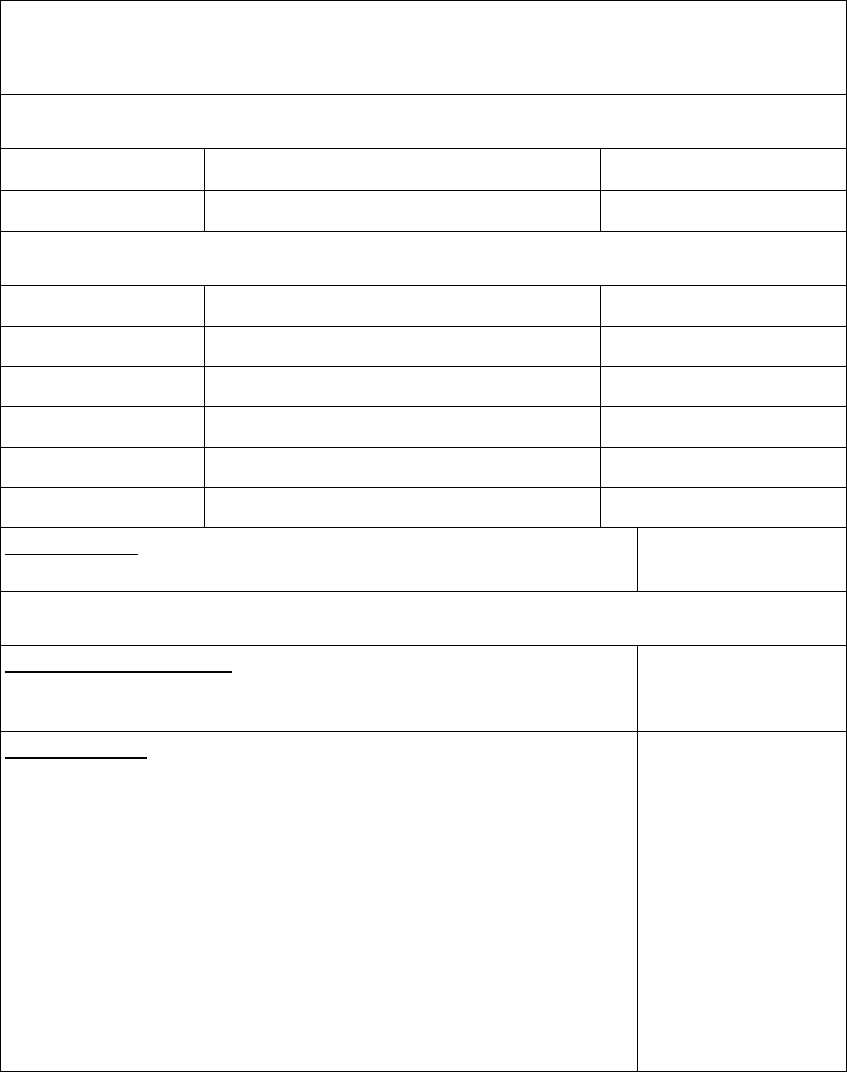
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 74 of 76
Objective standard :VISION* and HEARING
*When there is no diplopia, no night blindness, no progressive eye disease
UNCORRECTED ACUITY
FOR ALL SEAFARERS
< 20200 using one or both eyes
UNFIT
> 20200 and requires correction
Corrective lenses required
CORRECTED ACUITY
DECK
< 20/40 both eyes
No WK
< 20/40 one eye only
LCWV
ENGINE
< 20/50 both eyes
No WK
< 20/50 one eye only
No Bridge WK
CATERING AND OTHER
≥ 20/200 in both or either eye alone
Present Occupation Only
Exception group engine who held an Engineer Certificate of Competency
issued before July 30, 2002
No Bridge WK
COLOUR VISION
Standard for All Seafarers
Ishihara Passed
Ishihara Failed but Farnsworth D 15 Passed
No WK if not met
Exception group
- engineer who held an Engineer Certificate of Competency before July 30, 2002.
- seafarer who:
A)is not required to hold a certificate of competency to perform their duties on board a vessel; or
B)is required to hold one of the following certificates to perform their duties on board a vessel:
(i) Engine-room Rating (ERR)
(ii) Ship’s Cook
(iii) Proficiency in Fast Rescue Boats
(iv) Proficiency in Survival Craft and Rescue Boats Other Than Fast Rescue Boats
(v) Restricted Proficiency Survival Craft and Rescue Boats Other Than Fast Rescue Boats
(vi) Oil and Chemical Tanker Familiarization
(vii) Liquefied Gas Tanker Familiarization
(viii) Passenger Safety Management
(ix) Specialized Passenger Safety Management
(x) Compass Adjuster.
No Bridge WK for
Engineers and Group
B(i)
No WK for group A and
group B (ii – x)
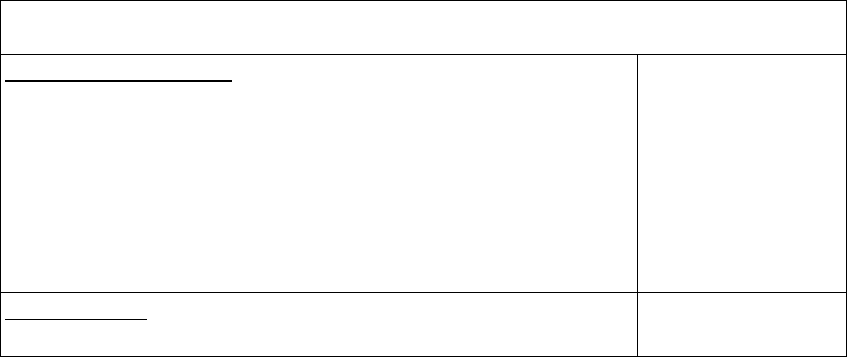
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 75 of 76
HEARING
Standard for All Seafarers
-ability to adequately hear conversation
-Hearing aids and Monaural hearing are permitted
-If fail screening audiogram must be provided
-average of no more that 30 dB loss in the better ear for the frequencies of
500, 1000,2000, and 3000 Hz
-Hearing aid users q2years assessment confirm standard is met
No WK if not met
Exception group engine who held an Engineer Certificate of Competency
issued before July 30, 2002
No Bridge WK
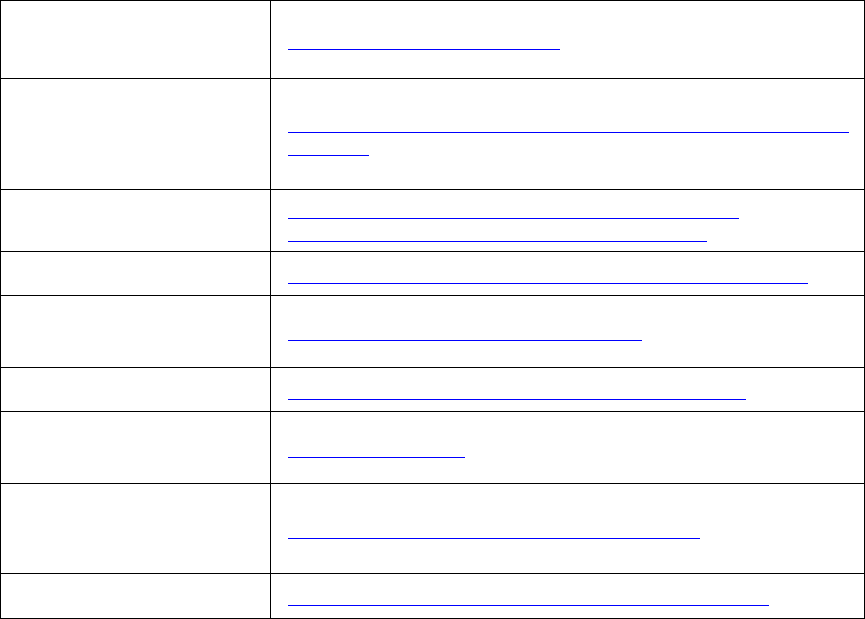
MEDICAL EXAMINATION OF SEAFARERS TP 11343E
PHYSICIAN’S GUIDE 76 of 76
ANNEX 5: USEFUL LINKS FOR MARINE MEDICAL
EXAMINERS
Marine Personnel
Standards and Pilotage
(AMSP)
http://www.tc.gc.ca/MarineSafety
The Guidelines for
Conducting Pre-sea and
Periodic Medical Fitness
Examinations for Seafarers
http://www.ilo.org/public/english/dialogue/sector/techmeet/ilowho97/
index.htm
Marine Personnel
Regulations, 2007(MPR)
http://laws-lois.justice.gc.ca/eng/regulations/SOR-2007-
115/?showtoc=&instrumentnumber=SOR-2007-115
CDN Information
http://www.tc.gc.ca/eng/marinesafety/bulletins-2010-05-eng.htm
Marine Safety Transport
Canada Centers
http://tcinfo/marinesafety/regions/menu.htm
Canada Shipping Act 2001
http://laws-lois.justice.gc.ca/eng/acts/C-10.15/index.html
Transportation Appeal
Tribunal of Canada
http://www.tatc.gc.ca/
The Canadian Diabetes
Association’s Clinical
Practice Guidelines
http://www.diabetes.ca/files/cpg2008/cpg-2008.pdf
AUDIT (Alcohol Screen)
http://whqlibdoc.who.int/hq/2001/who_msd_msb_01.6a.pdf
