
© 2021 Thrivent | For financial professional use only.
1
Thrivent Traditional
Long-Term Care Insurance
Product Guide
Introduction 2
General Overview 3
Target Market and Suitability 4
Basic Product Overview 5
Contract Provisions
• Issue Ages
• Risk Classes
• Premium Payment Types
• Premium Modes
• Rate Guarantee
• Dividends
6
Couples Discount 8
Features and Benefits Overview 9
Base Contract Features and Benefits
• Waiver of Premium
• Contingent Nonforfeiture Benefit–
Lifetime Pay Contracts
• Contingent Nonforfeiture Benefit–
Limited Pay Contracts
• Alternate Care Benefit
• Bed Reservation
• Care Coordinator Services
10
Ancillary Benefits
• Respite Care Benefit
• Equipment/Home Modification Benefit
• Caregiver Training
• International Care Benefit
13
Basic Building Blocks
• Elimination Period
• Benefit Multiplier
• Maximum Monthly Benefit
• Available Benefit
15
Benefit Increase Options
• Flexible Increase Benefit
• Annual Increase Benefit
• Comparing the Benefit
Increase Options
17
Optional Riders
• Waiver of Elimination Period for Home
Care and Adult Day Care
• Cash Benefit
• Return of Premium Upon Death
• Shared Care Benefit
• Survivorship Benefit
• Nonforfeiture Benefit
22
Optional Riders Compatibility Chart 28
Qualifying for Benefits 29
Payment of Benefits 31
Other Important Information 32
Underwriting 33
Suitability 33
Administrative Questions 34
Long-Term Care Insurance
Partnership Information
35
Long-Term Care Insurance Taxation 36
Conversions and Replacements 37
1035 Exchange Overview 38
Appendix A: Tables for Substantial
Premium Rate Increases
39
Table of Contents
© 2021 Thrivent | For financial professional use only.
2
Thrivent Traditional Long-Term Care Insurance
Thrivent Traditional Long-Term Care Insurance is a
comprehensive product that can help clients and
prospects pay for qualified long-term care expenses and
protect income and savings from being redirected to pay
for care.
Thrivent Traditional Long-Term Care Insurance covers
services and care in a variety of settings, from home
care to facility care, giving the insured flexibility to
receive the level of care he or she needs in a location
he or she may prefer.
Full Impact of Long-Term Care Needs
On January 1, 2011, the first of 76 million baby boomers
started to turn 65, a transition that is reported to continue
at a rate of more than 10,000 people per day, every day,
for the next 18 years.
1
By 2050, the number of individuals using paid long-term
care services in any setting (e.g., at home, residential
care such as assisted living, or skilled nursing facilities)
will likely double from 13 million in 2000, to 27 million
people. This estimate is influenced by growth in the
population of older people in need of care.
2
Why Thrivent Traditional Long-Term Care Insurance?
We believe long-term care is an event, not a product.
You may never experience the need for it, but if you do,
the people you love will experience consequences—
emotional, physical and financial.
It’s critical to make an extended care plan (whether you
believe you’ll need it or not). With a strategy in place, your
family won’t have to make hasty, emotional decisions that
too often damage family relationships.
Long-term care insurance is a way to fund the choices
you specify in your strategy (where/how you’ll receive
care, your family’s involvement, how you’ll pay for care).
Caregiving can have a devastating emotional effect on a
family. Care coordination services handle the business
details, so you can focus on being a family.
As a financial professional, you can help guide your
clients throughout their long-term care planning
decisions, as part of an ongoing overall financial strategy.
1
“Combination Insurance Products: What Do Consumers Really Want?” Pokorski, Robert M.D. LIMRA’s MarketFacts Quarterly/Number 1, 2011.
2
U.S. Department of Health and Human Services, and U.S. Department of Labor. The future supply of long-term care workers in relation to the aging
baby boom generation: Report to Congress. Washington, D.C.: Office of the Assistant Secretary for Planning and Evaluation, 2003.
http://aspe.hhs.gov/daltcp/reports/ltcwork.pdf (Jan. 20. 2005)
Introduction
© 2021 Thrivent | For financial professional use only.
3
What Is Long-Term Care?
Long-term care is a range of services and support that
may be needed to meet health or personal needs over a
long period of time. Most long-term care is not medical
care, but rather assistance with the basic personal tasks
of everyday life, called “activities of daily living,” such as:
• Bathing
• Dressing
• Using the toilet
• Transferring (to or from bed or chair)
• Caring for incontinence
• Eating
Many different services help people with chronic
conditions overcome limitations that keep them from
being independent. Long-term care is different from
traditional medical care. Long-term care helps a person
live as he or she does now. However, it may not help to
improve or correct medical conditions.
Long-term care services that help with activities of
daily living may include home health care, respite care,
hospice care, adult day care, care in a nursing home and
care in an assisted living facility. Long-term care may also
include care management services, which will evaluate
needs and coordinate and monitor the delivery of long-
term care services.
Who May Need Long-Term Care?
The need for long-term care may begin gradually
and progress as more and more help is needed with
activities of daily living, such as bathing, dressing,
household chores, meal preparation or managing
money. Or long-term care may be needed suddenly
after a major illness, such as a stroke or heart attack.
It may also be needed due to injuries sustained in an
accident. If care is needed, a stay at a care facility or
home health care services may be necessary—for
months, years or the rest of a person’s life.
What Can Long-Term Care Insurance Do for Clients
and Prospects?
Long-term care insurance can help clients
and prospects:
• Stay at home longer.
• Pay for qualified long-term care expenses
and protect income and savings from
being reallocated to pay for care.
• Receive help with activities of daily living. For example:
– An occupational therapist may be needed to
provide instruction on how to use adaptive
equipment (such as a reacher, sock aid or
long-handled shoe horn) or alternate ways to
perform daily activities.
– A home health aide may help with showers,
general hygiene and setting up daily medications.
– A nurse may be needed to periodically provide
assistance with insulin shots, blood thinners,
routine vital sign checks or wound care.
– A speech therapist might teach techniques to help
a person swallow more effectively if an individual
is experiencing problems eating or drinking.
General Overview
© 2021 Thrivent | For financial professional use only.
4
Target Market
• Preretired
– Ages 45-65.
– Working and saving.
• Goals include:
– Protecting his or her income and savings.
– Paying for long-term care expenses without
depleting savings or redirecting current income.
– Having choices and control over who provides
care and where.
– Making decisions today to preserve/ensure
options and independence in the future.
Secondary Markets
• Women
– The vast majority of those needing care are women.
– Most informal caregivers are women.
• Sandwich generation
– This generation is trying to manage helping their
parents and raising their children.
– They recognize that their parents may not have
planned and may not be able to financially
obtain coverage.
– They may be willing to purchase coverage on
their parents so they can manage their care
instead of provide it.
• Business owners
– Appeal as a key person.
– Potential tax advantages.
Suitability
A person should consider buying long-term care
insurance if he or she:
• Has significant savings and income.
• Wants to protect some of the assets and income.
• Can pay premiums, including possible future
premium increases, without financial difficulty.
• Wants to stay independent of the support of others.
• Wants the flexibility to choose care in the setting
that he or she will be most comfortable in.
A person should not buy long-term care insurance
if he or she:
• Cannot afford the premiums.
• Has limited assets, savings or income.
• Only has a single source of income from a
Social Security benefit or Supplemental
Security Income (SSI).
• Often has trouble paying for utilities, food,
medicine or other important needs.
• Is on Medicaid.
There are several long-term care insurance options
available to clients, including stand-alone long-term
care insurance (like this product), annuities with a
long-term care insurance rider, and life insurance
with a long-term care insurance rider. Each type of
coverage has unique characteristics and features,
and—as a result—it is difficult to make “apples-to-
apples” comparisons.
Stand-alone long-term care insurance may have a
larger benefit over a longer period of time. This type of
insurance is also pure insurance.
You can help clients understand the differences and
develop insights about which type of coverage may
be appropriate for their specific situation. Consider
clients’ overall financial situations and use available
illustrations to highlight the unique product features.
(Additional suitability information on page 33.)
Target Market and Suitability

© 2021 Thrivent | For financial professional use only.
5
Thrivent Traditional Long-Term Care Insurance is intended
to be federally tax-qualified long-term care insurance
pursuant to the Internal Revenue Code 7702B(b).
It is a comprehensive long-term care insurance product,
with coverage that includes home health care, residential
care facilities and adult day care.
Basic Product Overview*
Thrivent Traditional Long-Term Care Insurance Benefits
The benefits below are available after the elimination period has been satisfied and are subject to
the maximum monthly benefit and available benefit. Benefits may vary by state.
Home Health Care
Home health care benefits are qualified long-term care services if they are:
• Necessary to enable the insured to continue to live safely in his or her own residence; and
• Are provided by an employee of a home health agency or other trained personnel in the insured’s
residence. Note: Although family members may be taking care of the insured, family/informal
caregivers cannot bill for services to be reimbursed.
Home care services include:
• Homemaker services.
• Home health aide services.
• Skilled nursing services.
• Nutritional and dietary services.
• Physical, occupational, speech and respiratory therapy.
• Hospice care services.
Homemaker services include the following services when an impairment does not permit a person to
perform them and an informal caregiver is not available:
• Routine housecleaning.
• Preparing meals.
• Laundry.
• Shopping for essentials.
Residential Care
Facility
Residential care facility benefits include nursing homes, assisted living facilities and hospice care.
Residential care facilities do not include any facility that is primarily:
• A clinic, hospital or sanatorium.
• A subacute care or rehabilitation hospital.
• A sheltered living accommodation, a residence home or a similar living arrangement.
• A home or facility that operates primarily for the treatment of alcoholism, drug addiction or
a mental or nervous disorder.
Adult Day Care
Facility
Adult day care benefits provide care and companionship, outside the home, to small groups of adults
(typically six or more) who are chronically ill and need assistance or supervision during the day.
The program offers relief to family members or caregivers and allows them the freedom to go to work,
handle personal business or just relax knowing their loved one is well cared for and safe.
*Refer to individual state contracts for unique contractual definitions/terms.

© 2021 Thrivent | For financial professional use only.
6
Contract Provisions
Feature Details Additional Information
Issue Ages
18 to 79
The age used for the contract is the applicant’s age as of 30 days prior to the
application date.
Example: The applicant’s birthday is on Nov. 10 and she turned 60. She applies
for a long-term care insurance contract on Nov. 28. In this case, her contract age
would be 59 years old, even though her actual age is 60 (30 days prior to Nov. 28
she was 59 years old).
“Saving Age” is not allowed, other than as described above.
Risk Classes
Preferred
Preferred—90% of standard.
Standard
Class 1
Class 2
Class 1—125% of standard.
Class 2—150% of standard.
Gender-distinct pricing (except for Montana).
Premium Payment
Types
Lifetime Pay
10 Pay
This is not a cash accumulation product; no cash value is accumulated with
limited pay or lifetime pay.
Underwriting does not vary based on the premium payment type.
Changes to the premium payment type:
• May change from limited pay to lifetime pay after issue.
– Not subject to underwriting.
– Premium calculated based on the original issue age.
• May NOT change from lifetime pay to limited pay after issue.
• May NOT add/increase any other benefits or riders when a limited pay
premium mode is elected.
– If the insured wants to add or increase benefits or riders, he or she
must go through underwriting and buy a new contract.
Premium Modes
Monthly EFT
Quarterly
Semiannually
Annually
Paying the premium more often than annually will result in higher premiums.

© 2021 Thrivent | For financial professional use only.
7
Contract Provisions (continued)
Feature Details Additional Information
Rate Guarantee
Five year rate
guarantee
The rate guarantee is for five years from the issue date, and applies to the
entire contract, including any flexible increase benefit increases that occur
during that time. The new premium associated with the flexible increase
benefit would be guaranteed for the remaining years of the original five-year
rate guarantee.
Example of the rate guarantee with the flexible increase benefit:
A contract has an issue date of 1/1/13 and an original maximum monthly
benefit of $2,000 and a $550 annual premium. The rate guarantee is in effect
until 1/1/18.
On 1/1/14, the insured accepts a flexible increase offer. The new maximum
monthly benefit is $2,100 and the premium is $585. The new premium of
$585 is guaranteed until 1/1/18 (five years from the original issue date of
the contract).
On 1/1/15, the insured declines the flexible increase offer. The premium
remains $585, guaranteed to 1/1/18.
On 1/1/16, the insured accepts another flexible increase offer. The new
maximum monthly benefit is $2,205 and the premium is $630. The new
premium of $630 is guaranteed until 1/1/18.
Dividends
Eligible for
dividends
Dividends are not guaranteed.
Dividends, if payable, will be applied on an annual basis.
The only available dividend option is to reduce the premium.
• If the dividend exceeds the premium, the amount in excess will be
accumulated and applied toward future premiums.
• Accumulated dividends will earn 3.5% interest until used to pay any
future premiums.
• If the dividend is less than the premium, the balance will be billed.
• Upon termination of the contract, any remaining accumulated dividends
will be paid to the insured or insured’s estate, but only to the extent
that they do not exceed the sum of premiums paid by the insured and
applied to the contract.
– The sum of premiums paid does not include premiums waived or
reduced by dividends.
All distributions of dividends will be taxable and require a 1099.
© 2021 Thrivent | For financial professional use only.
8
Who Qualifies for the Couples Discount?
The couples discount is available to:
• Married couples.
• State partners/civil unions/domestic partners that are
named in a valid certificate or license by the state.
• Two individuals living together for at least
three years in a committed relationship as
partners or family members AND:
– Are committed to sharing expenses.
– Are not married.
– If related, must belong to the same generation
(such as siblings).
Why Do ‘Couples’ Receive a Discount?
In general, research has shown that individuals in a
committed relationship (such as spouses, partners or
family members who live together) provide each other
with informal care when it is needed. They tend to use
fewer paid care services, and if paid care services
are used, they tend to be used later in the process
compared to single people who are in a similar situation.
Having a spouse or partner to assist with care can
make a significant difference in the type of care needed
and where it is received. Care provided in the insured’s
home is typically less expensive than residential care,
thus potentially resulting in lower claim amounts being
paid over time.
Couples Discount
Two Available Discounts
1
Discount Details Additional Information
20% Couples
Discount
2
• Both individuals apply and
are approved for coverage,
or
• One individual has existing
coverage issued by Thrivent,
AAL or LB, and the other
is applying for Thrivent
Traditional Long-Term Care
Insurance coverage.
• When one insured dies or if the couple divorces
or separates:
– Discount remains for life.
– No changes to coverage.
• Marriage/remarriage (or meets the eligibility rules for the
couples discount outlined above):
– Discount may be applied after issue if insured marries
or remarries and the new spouse buys a contract.
5% Couples
Discount
3
• Both individuals apply but only
one is approved for coverage; or
• Only one individual applies.
• Discount may be applied after issue if the insured
marries or remarries (or meets the eligibility rules
for the couples discount outlined above).
• Do not need to submit two applications to qualify
for 5% discount.
3
1
All discounts are subject to eligibility rules as explained in this Product Guide.
2
For MT: 25% Couples Discount.
3
For MT: 10% Couples Discount.
© 2021 Thrivent | For financial professional use only.
9
Features and Benefits Overview
*CA Rider: Waiver of Elimination Period for Home and Community-Based Care.
Thrivent Traditional Long-Term Care Insurance is a
comprehensive product with many built-in features, as
well as optional riders to customize the plan according
to the client’s or prospect’s personal needs.
It may be helpful to think about the coverage in four
buckets: base contract benefits and features, basic
building blocks, inflation protection and optional riders.
• Base contract benefits and features are
built into the base contract. A few examples
include ancillary benefits, bed reservation,
care coordination and waiver of premium.
• The basic building blocks are the required
choices an individual must make when
designing his or her personal long-term
care insurance contract. They include:
– Maximum monthly benefit amount.
– Benefit multiplier.
– Available benefit.
– Elimination period.
• We offer two benefit increase options to help keep
pace with inflation and the rising costs of care:
– Flexible Increase Benefit.
› 5% compound
– Annual Increase Benefit.
› 1% compound
› 2% compound
› 3% compound
› 5% compound
• Optional riders are typically the last choices to
be made. They are available for an additional
cost and customize the long-term care insurance
contract to meet an individual’s specific wants
and needs. The optional riders are:
– Waiver of Elimination Period for Home Care
and Adult Day Care.*
– Cash Benefit.
– Return of Premium Upon Death.
– Shared Care Benefit.
– Survivorship Benefit.
– Nonforfeiture Benefit.
© 2021 Thrivent | For financial professional use only.
10
Base Contract Features and Benefits
Waiver of Premium
This benefit states that premiums will be waived once the elimination period is satisfied as long as
the insured continues to be benefit-eligible. Once the insured is no longer benefit-eligible and no
longer receiving services, the waiver of premium benefit will end and premium payments will resume.
If the insured becomes eligible for benefits again, the waiver of premium benefit will apply again.
Additional Information:
• Ancillary benefits do not trigger waiver of premium.
• Double waiver of premium is included if the insured has the shared care benefit rider.
– This will waive the premium for both individuals even if only one insured is receiving benefits.
• Limited Pay Contracts:
– If the contract goes on waiver for a limited pay contract, it does not change the number of
years the premium will be paid.
Example: The payment type selected on a contract is 10 years. If the individual pays the premium
for five years and then goes on premium waiver for two years and then recovers, he or she would
need to pay the remaining three years of premium payments.
Contingent
Nonforfeiture
Benefit—
Lifetime Pay
Contracts
This benefit states that if the contingent nonforfeiture benefit is triggered, the coverage will continue as
paid-up coverage. If the benefit is triggered by premium default, the paid-up coverage will be effective
on the date the grace period ends. Otherwise, paid-up coverage will be effective the date of the
insured’s notice to cancel the contract.
• Benefits will be paid subject to all of the conditions and limitations of this contract.
• Maximum monthly benefit and elimination period will be the same as were in effect
at the time of lapse.
• No increases will be provided under any increase benefit rider on or after the date paid-up
coverage becomes effective.
• All riders on this contract will terminate on the date paid-up coverage becomes effective.
• The available benefit under the paid-up coverage may be used for all care and services
covered under the terms of the contract.
• The available benefit will be reduced by the amounts that are paid under the paid-up coverage.
• Paid-up coverage will terminate on the date the available benefit reaches zero.
The paid-up coverage will have an available benefit equal to the lesser of:
1. The nonforfeiture credit.
2. The available benefit in effect immediately before the date paid-up coverage becomes effective.
The nonforfeiture credit is equal to the greater of:
1. The total of all premiums paid for the contract.
2. The maximum monthly benefit in effect on the date paid-up coverage becomes effective.
Premiums paid by the insured do not include premiums waived by Thrivent or reduced by dividends.
The Contingent Nonforfeiture Benefit will be triggered if:
1. Thrivent increases the premium rates;
2. The new premium represents a substantial increase in premium;* and
3. Within 120 days after the due date of the new premium if either:
a. The contract terminates due to premium default; or
b. The insured gives notice to cancel the contract. The date of notice is the date Thrivent
receives it or, if later, the date the insured specifies.
*A substantial premium increase is an increase that results in a cumulative percentage increase in premiums
since the contract’s date of issue that equals or exceeds the percentages shown in Appendix A.
Base Contract Features and Benefits

© 2021 Thrivent | For financial professional use only.
11
Base Contract Features and Benefits Continued
Contingent
Nonforfeiture
Benefit—
Limited Pay
Contracts
This benefit states that if the contract has a limited premium payment period, and the contingent
nonforfeiture benefit is triggered, the coverage will continue as paid-up coverage with reduced benefit
maximums. If the benefit is triggered by premium default, the paid-up coverage will be effective on the
date the grace period ends. Otherwise paid-up coverage will be effective the date of the insured’s
notice to cancel the contract.
• Benefits will be paid subject to all of the conditions and limitations of the contract.
• No increases will be provided under any increase benefit rider on or after the date paid-up
coverage becomes effective.
• All riders on the contract will terminate on the date paid-up coverage becomes effective.
• The available benefit under the paid-up coverage may be used for all care and services
covered under the terms of the contract.
• The available benefit will be reduced by the amounts that are paid under the paid-up coverage.
• Paid-up coverage will terminate on the date the available benefit reaches zero.
The contract’s remaining available benefit, maximum monthly benefit and ancillary benefit limits will be
reduced to amounts equal to:
90% of the amounts in eect prior to termination
x
# of months premiums were paid/# of months in the premium paying period
=
Paid-up benefit amount
Premiums paid by the insured do not include premiums waived by Thrivent or reduced by dividends.
The Limited Premium Payment Period Contingent Nonforfeiture Benefit will be triggered if:
1. Thrivent increases the premium rates,
2. The new premium represents a substantial premium,*
3. Prior to the due date of the increased premium, premiums have been paid for
at least 40% of the number of months in the premium payment period, and
4. Within 120 days after the due date of the new premium if either:
a. The contract terminates due to premium default, or
b. The insured gives notice to cancel the contract. The date of notice is the
date Thrivent receives it or, if later, the date the insured specifies.
*A substantial premium increase is an increase that results in a cumulative percentage increase in premiums
since the contract’s date of issue that equals or exceeds the percentages shown in Appendix A.

© 2021 Thrivent | For financial professional use only.
12
Base Contract Features and Benefits Continued
Alternate Care
Benefit
Allowing for an alternate care benefit helps ensure that individuals have access to emerging services
that may develop over time, but are not currently identified or available.
This allows the insured to qualify for benefits not specifically listed elsewhere in the contract.
Alternate care that is not normally covered by the contract may be covered if:
• Thrivent and the insured have a written agreement that describes how the services will be covered.
• The alternate care is prescribed in a plan of care document.
– The care is a cost-effective alternative.
– The plan pays expenses up to the maximum monthly benefit.
– Care is subject to the elimination period and available benefit.
Benefits will be paid according to the terms of the contract (e.g., maximum monthly benefit, available
benefit). No benefits will be paid for alternate services provided prior to the date of the agreement.
Bed Reservation
This feature provides a benefit for bed reservation for temporary absences of up to 60 days per
calendar year.
This means that if the insured is in a residential care facility and temporarily leaves (e.g., to go to
the hospital or attend a family event), the charges incurred to hold a space to enable the insured
to return to that facility will be covered.
If the elimination period has not yet ended, the crediting of days toward the elimination period
will not be interrupted by a temporary absence as described above.
Care Coordinator
Services
If the insured would like to use the services of a care coordinator, Thrivent will identify someone in the
area. The insured is not required to use care coordinator services in order to use his or her insurance
benefits. Expenses for care coordinator services will not be reimbursed from the contract coverage but
rather are covered separately by Thrivent. A care coordinator can help develop the insured’s required
plan of care, which will be used to administer benefits.
A care coordinator is a health care professional with training and expertise in case management.
Services provided by a care coordinator include:
• Performing a comprehensive care needs assessment.
• Developing, implementing and coordinating a plan of care.
• Identifying the services needed.
• Locating local caregivers and care facilities.
• Monitoring ongoing care.

© 2021 Thrivent | For financial professional use only.
13
Ancillary Benefits
Ancillary Benefits*
Ancillary benefits include:
• Respite care.
• Equipment/home modification.
• Caregiver training.
• International care benefit.
These benefits are not subject to the elimination period or the maximum monthly benefit.
In addition, the benefits do not satisfy the elimination period. Ancillary benefits that are paid
will reduce the total available benefit amount.
Each ancillary benefit has its own separate benefit limit. The benefit limits are tied directly to
the maximum monthly benefit. If the maximum monthly benefit increases or decreases, so do
the ancillary benefit limits.
Ancillary benefits = 2x maximum monthly benefit.
Example: The insured has a $5,000 maximum monthly benefit amount, a 60-month benefit
multiplier and the 5% compound annual increase benefit. The available benefit is $300,000
($5,000 x 60 = $300,000).
The ancillary benefit limits would be $10,000 when the contract is issued (2 x $5,000 = $10,000).
After the first contract anniversary when the 5% compound annual increase benefit is applied, the
maximum monthly benefit would be $5,250 and the available benefit would be $315,000. Thus, the
ancillary benefit limits would be $10,500.
If $2,000 is paid for respite care in the second contract year, the available benefit amount would be
reduced to $313,000 ($315,000 - $2,000 = $313,000). The remaining respite care benefit for that
contract year would be $8,500 ($10,500 - $2,000 = $8,500).
*For CA: Referred to as Supplemental Benefits. Respite care is the only ancillary benefit that is available each
calendar year. Equipment/home modification, caregiver training and the international care benefit are lifetime limits.
Respite Care Benefit
Respite care is designed to provide an opportunity for an informal caregiver to have some
needed time off by providing alternative care for the insured.
Respite care means qualified long-term care services are designed to:
• Relieve an informal caregiver.
• Provide on a short-term basis, in a residential care facility, an adult day care facility,
or in a person’s home as home care services.
• Are received in a week where no days are credited toward the elimination period.
– The insured must decide if the days go toward the elimination period or toward
respite care benefits (cannot do both in the same week).
Benefit = 2x current maximum monthly benefit amount each calendar year.

© 2021 Thrivent | For financial professional use only.
14
Ancillary Benefits Continued
Equipment/Home
Modification Benefit
Equipment/home modifications are safety-related alterations to the home. Equipment or home
modifications must be specified in the plan of care and be necessary according to the insured’s
condition to be covered.
Special equipment means:
• Therapeutic equipment such as a hospital bed, wheelchair, crutches or walker.
• Safety-related equipment such as a medical alert system.
• Any other medical equipment that is specified in the insured’s plan of care.
Home modifications are:
• Home safety checks to evaluate the insured’s home to determine if it is a physically
safe environment for the insured and provide recommendations for home modifications.
• Accessibility changes to an insured’s home such as a ramp, chairlift or alterations to
accommodate a wheelchair.
• Safety-related changes to an insured’s home such as installation of grab bars or railings.
• Any other changes to an insured’s home that are specified in his or her plan of care.
Benefit = 2x current maximum monthly benefit amount (lifetime limit).
Caregiver Training
Benefit
The caregiver training benefit allows a qualified health care professional to provide training
that is specific to the needs of the insured so that an informal caregiver can care for that person.
An informal caregiver does not receive compensation for providing care.
Benefit = 2x current maximum monthly benefit amount (lifetime limit).
International Care
Benefit
The international care benefit provides a nominal benefit if covered services are received outside of the
United States, its territories and possessions.
The international care benefit can be used for:
• Nursing home care.
• Assisted living care.
• Home health care.
• Hospice care.
The insured must provide appropriate documentation in English to receive payment.
This documentation includes:
• Certification from a U.S.-licensed health care practitioner that the insured is chronically ill and
received care for the covered expense for which the insured is submitting notice of claim.
• Properly completed claim forms and proof that the insured is receiving covered care
(in the form of fully itemized bills).
• Copy of an airline ticket or other proof acceptable that the insured is outside of the country.
• Copies of medical records which Thrivent deems necessary to support the insured’s claim.
The benefit is paid in U.S. dollars to the insured.
The benefit will not cover expenses incurred in countries where payment would violate economic,
financial or trade sanctions imposed by the U.S. or United Nations.
Benefit = 2x current maximum monthly benefit amount (lifetime limit).
Cash Benefit Rider does not pay when receiving international care.

© 2021 Thrivent | For financial professional use only.
15
Basic Building Blocks
The basic building blocks are the required choices
individuals must make when you are helping design
his or her long-term care insurance and include:
• Elimination period.
• Benefit multiplier.
• Maximum monthly benefit.
• Available benefit.
Basic
Building Block
Details Additional Information
Elimination Period
30, 90 or 180 days*
The elimination period is the time when the insured must pay for
covered services before the insurance begins paying benefits.
Calendar days:
• One day of service in a week receives credit for full week
(seven days).
• Calendar week begins on Sunday and ends Saturday.
The elimination period needs to be satisfied only once while
the contract is in force.
Changes to the elimination period:
• Decreases—Changing to a longer elimination period after issue.
– Subject to the current issue minimums.
– Future premium will be recalculated based on the
decreased coverage and the original issue age.
– Cannot decrease coverage during or after a claim period
has occurred.
• Increases—Changing to a shorter elimination period after issue.
– Subject to underwriting at attained age.
Note: Zero-day elimination is an option for the home care and
adult day care benefit only if the optional waiver of elimination
period for home care and adult day care rider is selected.
Benefit Multiplier
24, 36, 48, 60 or 96 months
The benefit multiplier is a factor based on time (expressed in
months) that is used to determine the insured’s available benefit
or pool of money.
Changes to the benefit multiplier:
• Decreases—Can be decreased after issue.
• Increases—Can be increased after issue.
– Subject to evidence of insurability.
Example: If the insured selects a $5,000 maximum monthly
benefit and a 60-month benefit multiplier, the total available
benefit is $300,000 for long-term care expenses, regardless of
how long it takes to use the benefits.
• $5,000 x 60 = $300,000
If the insured uses the maximum every month, benefits will last
approximately five years. Benefit increase options, which are
discussed later in the guide, would extend the time frame that
the benefit would be paid. If less than the maximum is used, the
available benefit will last longer than five years.
*CT: 180 days Elimination Period is not available.

© 2021 Thrivent | For financial professional use only.
16
Basic Building Blocks Continued
Basic
Building Block
Details Additional Information
Maximum Monthly
Benefit
$1,500–$15,000
(Increments of $100)
The maximum monthly benefit amount is the limit on the amount the
contract would pay, each month, during a claim period for qualified
expenses. The elimination period must be met and there must be a
remaining available benefit.
Changes to the maximum monthly benefit:
• Decreases—Can be decreased after issue.
• Increases—Can be increased after issue.
– Subject to evidence of insurability.
Examples:
• If expenses in a given month during a claim period exceed the
contract’s benefit amount, the expenses would be reimbursed
up to the maximum monthly benefit amount and reduce the total
available benefit.
• If expenses in a given month during a claim period are less than the
contract’s maximum monthly benefit amount, the expenses would be
reimbursed, and the unused portion of the maximum monthly benefit
amount would remain in the total available benefit. The total available
benefit would be reduced only by the amount reimbursed.
– The unused maximum monthly benefit does not increase the
following month’s maximum monthly benefit amount. It does help
the pool of money last longer.
• The chart below shows how a hypothetical claim may be paid
based on a $5,000 maximum monthly benefit and total available
benefit of $300,000.
Long-term
care expense
incurred
Actual amount paid
from long-term care
insurance contract
Available
Benefit
January $2,500 $2,500 $2 97, 50 0
February $3,000 $3,000 $294,500
March $5,000 $5,000 $289,500
April $5,200 $5,000 $284,500
May $4,800 $4,800 $279,700
Available Benefit
The available benefit is the total pool of money available during the
insured’s lifetime to pay for qualified long-term care expenses.
Example:
The maximum monthly benefit amount selected is $5,000. The benefit
multiplier selected is 60 months. So, the available benefit is $300,000.
$5,000 x 60 = $300,000
This amount will increase if the contract has an annual increase
benefit or the flexible increase benefit (and does not decline an
increase offer).
The available benefit is decreased when covered expenses
are reimbursed.
Monthly
Benefit
Benefit
Multiplier
Available
Benefit

© 2021 Thrivent | For financial professional use only.
17
Benefit Increase Options
If you’ve seen recent cost-of-care projections, you know
long-term care expenses are likely to be higher in the
future than they are today. Benefit increase options help
protect against the rising costs of long-term care by
helping the insureds to customize their plans to meet
their current and potential future needs for increased
coverage. Choosing a benefit increase option can be one
of the most important additions a prospective insured
includes in long-term care insurance planning.
Thrivent offers two types of benefit increase options:
• Flexible Increase Benefit (FIB).
• Annual Increase Benefit (AIB).
Benefit increase options:
• Can be added to individual and shared care contracts.
• Cannot be selected together on a contract—
can only have one or the other.
• Both options are available on preferred,
standard, class 1 and class 2 contracts.
Let’s take a closer look at how these options work.
Flexible Increase Benefit (FIB)
Details
Issue ages: 18 to 70
The flexible increase benefit includes an automatic claim increase benefit.
How It Works
Provides an opportunity to increase the maximum monthly benefit and current remaining
available benefit on the contract anniversary by 5% compounded annually. Ancillary benefits
will also increase accordingly.
• Without evidence of insurability.
• All-or-nothing offer each year (5% increase or 0% increase).
The increase will be automatic unless the insured opts out when he or she receives the
annual notification letter.
• Premiums will increase with each offer accepted and premiums will be based on the insured’s
age at the time of the increase.
• Premiums will remain unchanged if the insured does not accept the increase.
Automatic increases will occur if the insured is on claim.
• The insured can decline automatic increases while on claim, but it may not be in
his or her best interest.
• If the insured recovers, he or she will have to pay the increased premium amount
associated with the new coverage.
• If the new premium associated with the automatic increases is not affordable to the insured,
the insured can decrease coverage.
If three consecutive offers are declined, no future increase offers will be extended. However, the rider
will remain on the contract since the insured is still eligible for the automatic claim increases.
Additional
Information
This benefit is not available with:
• 10-pay contracts.
• Survivorship Benefit Rider.
Flexible increase benefit increases occur automatically on the contract anniversary.
A notification letter will be sent prior to the contract anniversary.
Changes
Changes:
• If the flexible increase benefit is dropped after issue, the previous increases will be maintained,
and the future premium will be recalculated without the flexible increase benefit rider load/premium.
• Flexible increase benefit can be added after issue.
– Evidence of insurability will be required.
© 2021 Thrivent | For financial professional use only.
18
$30,000
$25,000
$20,000
$15,000
$10,000
$5,000
$0
50
55
60
65
70
75 80 85 90
Age
Increase Accepted
Increase Declined
Increase Not Oered
Maximum Monthly Benefit
No increases
oered
Increases resume
when receiving
benefits
Three consecutive
declines
Most increases
accepted
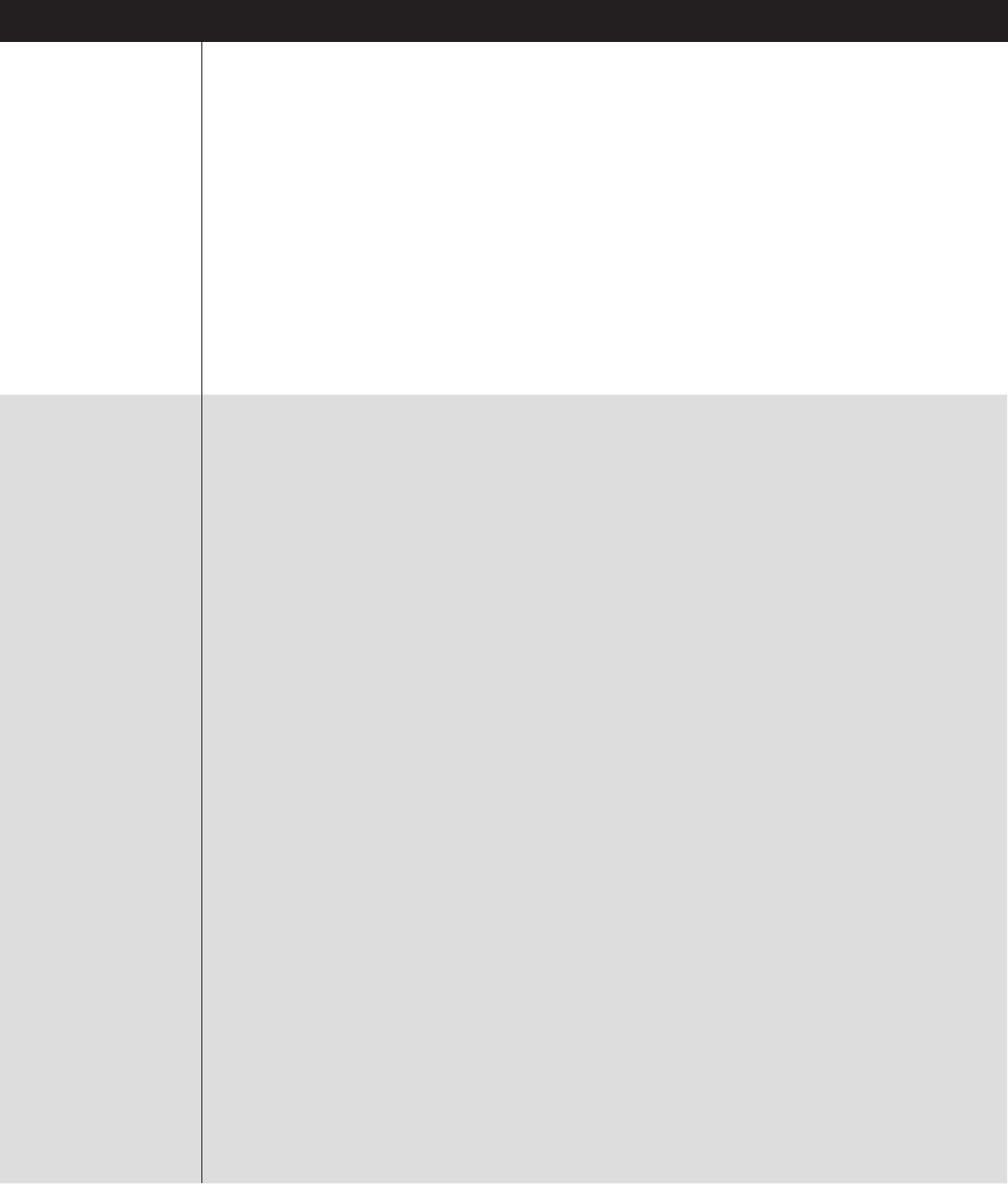
Let’s look at a hypothetical example using the flexible
increase benefit:
Mary, at age 50, purchased Thrivent Long-Term Care
Insurance, choosing the optional flexible increase
benefit rider to help manage her budget. Having the
option to accept or decline the premium increases
was important to her, especially during the years when
her children needed help paying for college. Mary
also knew that in preparing for the future, she wanted
the maximum monthly benefit amount to increase over
time; with a goal to accept increases until her maximum
monthly benefit amount reached at least $15,000.
Over the next 20 years, Mary accepted 13 annual
increase offers, and declined seven. However, she didn’t
decline the offer in three consecutive years, which meant
her flexible increase benefit was offered each year.
When she reached age 70, Mary decided her maximum
monthly benefit of $15,000 was adequate to meet her
needs and declined all future increases. After Mary
declined the increase offer three years in a row, she
was not offered any future increases.
At age 80, Mary’s health declined, and she needed
assistance with daily activities. She began to receive
qualified long-term care services at home according
to her Plan of Care. After meeting her elimination
period, her long-term care insurance benefits started.
Now that Mary is on claim, the flexible increase
benefit rider automatically increases her maximum
monthly benefit and available benefit by 5%,
compounded annually, and will continue to do
so each year while she is receiving care.
Mary doesn’t have to worry about paying premiums
during this time since the premium waiver benefit is
a standard benefit included with her insurance.
Flexible Increase Benefit
Hypothetical Example
Flexible Increase Benefit

© 2021 Thrivent | For financial professional use only.
19
Annual Increase Benefit (AIB)
Details
Issue ages: 18 to 79
How It Works
If the insured chooses this benefit rider, the maximum monthly benefit, available benefit (pool of money)
and ancillary benefits will automatically increase annually on the rider anniversary, depending on the
level selected.
Premiums, however, will remain level over time. That’s because the cost of future increases is
automatically built into the premium. As a result, this benefit may be appropriate for people who want
the convenience of making one decision and not having to decide each year or prefer a level premium
for budgeting purposes.
Four choices are available (compounded annually):
• 1% • 2% • 3% • 5%
Changes
• If the annual increase benefit is dropped after issue, the previous annual increases will be
maintained and the future premium will be recalculated based on the current amount of
maximum monthly benefit coverage (including increases) at the original issue age without the
annual increase benefit rider.
• The compound annual increase benefit can be decreased after issue.
– Allowed decreases include:
› Changing from a higher percent AIB to a lower percent AIB (for example: 5% to 3%, 2%,
or 1% AIB; 3% to 2% or 1% AIB, or 2% to 1% AIB).
– No evidence of insurability required.
› Changing from either AIB (5%, 3%, 2% or 1%) to FIB.
– No evidence of insurability required.
• The compound annual increase benefit can be added or increased after issue.
– Evidence of insurability will be required.
– Allowed additions and increases include:
› Changing from no annual increase benefit to 1%, 2%, 3% or 5%.
› Changing from a lower percent AIB to a higher percent AIB (1% to 2%, 3% or 5% AIB; 2% to
3% or 5% AIB; 3% to 5% AIB).
› Changing from FIB to AIB.

© 2021 Thrivent | For financial professional use only.
20
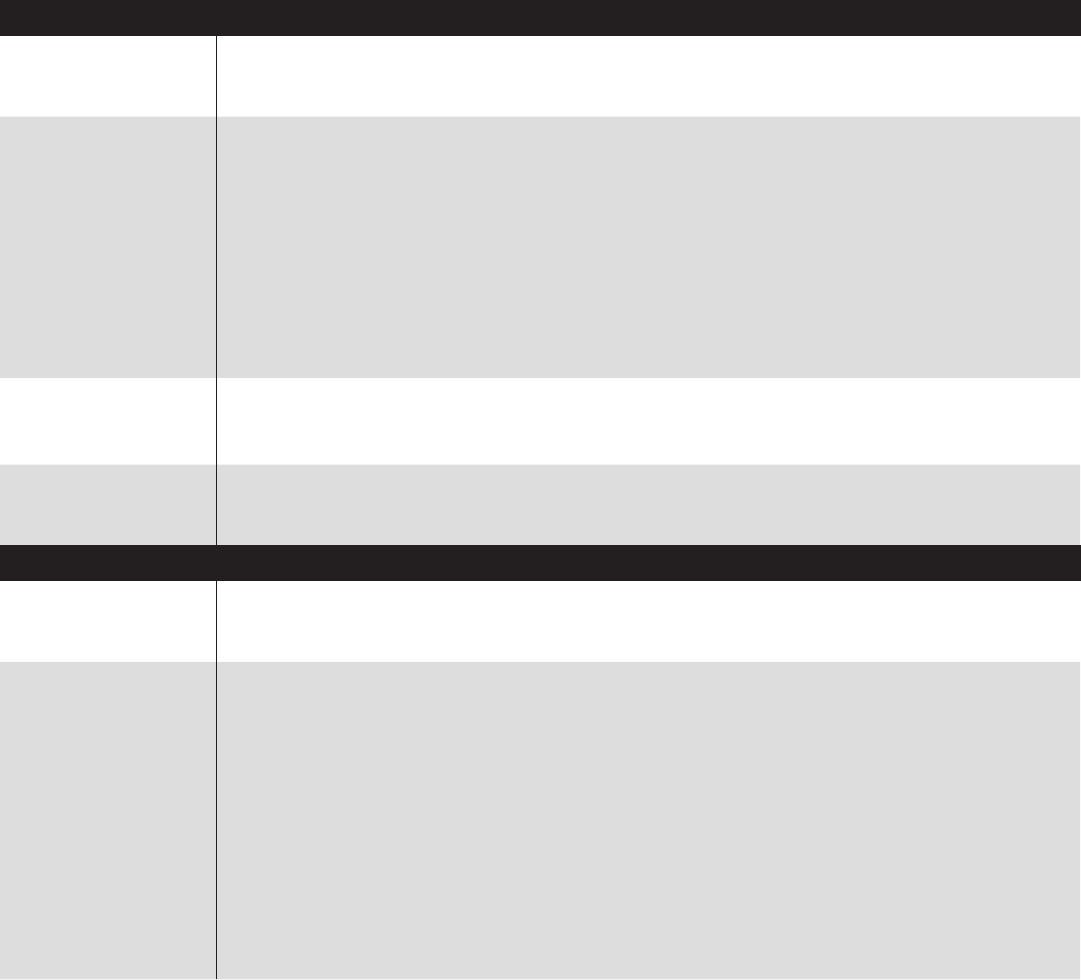
Let’s look at a hypothetical example using the 5%
annual increase benefit.
At age 50, Sue purchases Thrivent Long-Term
Care Insurance with a maximum monthly benefit
amount of $5,700 and a 5% annual increase benefit,
compounded annually. Her desired goal is to have
a maximum monthly benefit of $15,000 when she
reaches age 70.
As you can see from the chart below, Sue’s annual
premiums of $9,638 remain level over time, although
her monthly benefit increases 5% annually.
At age 70, Sue’s maximum monthly benefit has
reached $15,124, and at age 80—when she needs
residential care—her maximum monthly benefit has
grown to $24,635.
Annual Increase Benefit
Hypothetical Example*
*Based on a 5% Annual Increase Benefit (compounded annually), $9,638 annual premium, goal to reach a maximum monthly
benefit of $15,000 by age 70, issue age 50, standard risk class, ignores any other riders and premium discounts that may be
applicable. No changes are made to the contract throughout the years illustrated and no claims are paid. Premiums may increase
after the initial five year rate guarantee.
$30,000
$25,000
$20,000
$15,000
$10,000
$5,000
$0
$12,000
$10,000
$8,000
$6,000
$4,000
$2,000
$0
50 55 60 65 70 75 80
Age
Maximum Monthly Benefit
Annual Premium
AIB Monthly Benefit AIB Premium
Annual Increase Benefit

© 2021 Thrivent | For financial professional use only.
21
• 50-year-old female insured with standard risk
class, no couples discount or additional riders.
• 90-day elimination period with
60-month benefit multiplier.
• Goal is to have approximately $15,000
maximum monthly benefit by age 70.
• Annual increase benefit contract (5%).
– Maximum monthly benefit amount begins at $5,700.
– Annual premium is $9,638.
• Flexible increase benefit contract.
– Maximum monthly benefit amount begins at $8,000.
– Annual premium is $3,256.
– 7 of 20 increases are declined between the
ages of 50 and 70.
– No increases accepted after age 70.
Comparing the Benefit Increase Options
Flexible Increase Benefit Annual Increase Benefit
• Flexible.
• Benefits and premium increase automatically
each year unless declined.
• For people who prefer a lower initial premium.
• For people who prefer a level premium.
• Convenience of making the decision once
instead of each year.
The graph below shows a comparison of the maximum
monthly benefit and premium between the flexible
increase benefit and the annual increase benefit.
This hypothetical comparison is based on the previous
examples used for the flexible increase benefit and the
annual increase benefit:
$30,000
$25,000
$20,000
$15,000
$10,000
$5,000
$0
$12,000
$10,000
$8,000
$6,000
$4,000
$2,000
$0
50 55 60 65 70 75 80
Age
Maximum Monthly Benefit
Annual Premium
AIB Monthly Benefit FIB Monthly Benefit AIB Premium FIB Premium

© 2021 Thrivent | For financial professional use only.
22
Optional riders are typically the final choices to be made. They are available for an
additional cost and help customize the long-term care insurance contract to meet
the individual’s specific wants and needs.
The available riders are:
• Waiver of Elimination Period for Home Care and Adult Day Care.*
• Cash Benefit.
• Return of Premium Upon Death.
• Shared Care Benefit.
• Survivorship Benefit.
• Nonforfeiture Benefit.
Optional Riders
*CA Rider: Waiver of Elimination Period for Home and Community-Based Care.
Waiver of Elimination Period for Home Care and Adult Day Care*
Description
The rider allows the insured to receive home health care and adult day care services on day one—
effectively a zero-day elimination period—specifically for at-home care.
How It Works
The coverage days received under this benefit will be applied toward meeting the elimination period
(so when facility care is needed, the elimination period doesn’t “start over”).
Even though the elimination period is waived, the premium will not be waived until the
elimination period is met.
Additional Details
Available on individual and shared care contracts.
Restriction: This rider is NOT available with the 180-day elimination period.
Changes
• Can be dropped after issue.
• Can be added after issue.
• Subject to evidence of insurability.
Cash Benefit
Description
The cash benefit is a rider that provides additional cash payments above the maximum monthly benefit,
regardless of whether the insured is receiving home care or facility care. It provides the insured with
added flexibility to pay for services that are not typically covered.
How It Works
If the insured is receiving home care services:
• An additional amount equal to 15% of the maximum monthly benefit would be paid
as a cash payment.
If the insured is receiving facility care:
• The cash benefit is equal to 10% of the maximum monthly benefit.
The insured must meet the elimination period and receive at least five days of care per calendar month
to receive the benefit.
The cash benefit is not payable for international care.
Additional Details
Available on individual and shared care contracts.
This benefit is a separate benefit and does not reduce the available benefit.
Elimination period must be met before this benefit will be paid.
If home care and facility care services are paid in the same month, the higher percentage will be paid.
Benefits received may be taxable.
Changes
• Can be dropped after issue.
• Can be added after issue.
– Subject to evidence of insurability.
© 2021 Thrivent | For financial professional use only.
23
Optional Riders Continued
Return of Premium Upon Death
Description
This rider returns the premiums paid to the insured’s estate at the time of death.
How It Works
The rider must be in force for 10 years before a death occurs to be eligible for payment.
Payment = Premiums paid for the base contract and riders less
Any accumulated dividends paid upon death and the sum of any benefit payments that
were paid on the contract, including ancillary benefits.
If the benefits paid exceed premiums paid, then no return of premium is paid.
To pay the benefit under this rider, Thrivent requires:
• Rider must be active; and
• Proof of death; and
• Written notice from a representative of the insured’s estate that no expenses eligible for
payment are outstanding.
Additional Details
Restriction: Only available on individual contracts; not available with shared care contracts.
The sum of premiums paid does not include premiums waived or reduced by dividends.
May have tax implications for the estate.
Changes
• Can be dropped after issue.
• Can NOT be added after issue.
Shared Care Benefit
Description
This rider is for couples who purchase identical Thrivent Long-Term Care Insurance. It’s designed to
provide couples with extra flexibility in their long-term care planning.
How It Works
“Benefit partner” is the term used to identify the two people in a shared care benefit agreement.
The shared care benefit links two individual contracts together. If an insured uses his or her entire
available benefit, then he or she can start drawing from the benefit partner’s remaining available benefit.
• An insured does not need to satisfy a new elimination period to use his or her benefit partner’s
benefits since he or she already met the elimination period under his or her own contract.
• If one insured qualifies for the waiver of premium, neither benefit partner will have to pay premiums.
The joint waiver of premium benefit automatically kicks in.
• If an insured uses all of his or her benefit partner’s benefits, the benefit partner not on claim
can elect to purchase an additional 24-month benefit for his or her use only (without additional
underwriting). This is called the residual benefit.
1
• Other than reducing the contract’s available benefit, payment of benefits to the benefit partner will
not affect the other insured’s eligibility for benefits under his or her contract.
• Both insureds may be on claim at the same time.
1
In Arizona and Connecticut, each person must retain 24 months of benefits in the pool for the contract owner’s sole purpose.
The additional 24-month benefit is not available for purchase.

© 2021 Thrivent | For financial professional use only.
24
Optional Riders Continued
Shared Care Benefit—Continued
Additional Details
Both contracts MUST have identical coverage, issue dates and benefits, including:
• Elimination period
• Benefit multiplier
• Maximum monthly benefit
• Benefit increase options
• Riders
• Premium payment type
(lifetime pay or limited pay)
For contracts with the flexible increase benefit rider:
• Benefit partners must either accept or decline the increase offers together—the maximum
monthly benefit amounts must be identical at all times.
• If one insured is on claim and the other insured is not, both individuals will get the automatic
increase associated with the flexible increase benefit.
– If the insured that is on claim recovers, both individuals will need to pay for
the increases that occurred while on claim.
– If the premium associated with the increase in coverage is not manageable, the benefit
partners are allowed to drop their coverage amounts (benefits must remain identical).
Restrictions: The shared care benefit is not available with the return of premium upon death rider.
Residual Benefit
As mentioned above the residual benefit is available to a contract owner when his or her benefit
partner has used all the benefits from both contracts. The benefit partner not on claim can elect
to purchase an additional 24-month benefit for his or her use only.
The new available benefit will be the current maximum monthly benefit on the date of termination
with a benefit multiplier of 24 months.
• No evidence of insurability is required.
• The new premium will be based on the insured’s attained age.
• Available through age 85.
Eligibility for the residual benefit:
• Insured that is applying for the benefit has not had any days credited to
his or her elimination period.
• Insured that is applying has not been eligible to be certified as chronically ill in the
two years before the application date for the residual benefit.
Who can elect the
shared care benefit?
The shared care benefit rider is available to:
• Married couples.
• State partners/civil unions/domestic partners that are named in a valid certificate or
license by the state.
• Two individuals living together for three consecutive years in a committed relationship
as partners or family members AND:
– Are committed to sharing expenses.
– Are not married.
– If related, must belong to the same generation (such as siblings).

© 2021 Thrivent | For financial professional use only.
25
Optional Riders Continued
Shared Care Benefit—Continued
Death, Divorce
or Separation
Death
• Surviving benefit partner’s contract will be automatically increased by the remainder of the
deceased’s available benefit.
• Shared care rider will terminate.
• The new premium calculation will be the surviving contract holder’s original premium
(with the couples discount still in place) less the premium for the shared care rider.
There is no charge for the increased available benefit.
Example:
Divorce or Separation
Upon divorce or separation, this rider is only terminated if one of the benefit partners cancels the rider.
Otherwise, the rider will continue.
Remarriage/New Partner/New Committed Relationship
(See page 24 for who is eligible to elect the shared care benefit.)
The insured cannot add a new spouse, partner or family member to this coverage (the rider cannot
be added after issue).
Changes
• Can be dropped after issue.
• Can NOT be added after issue.
• Contract changes cannot be made that create unequal benefits while maintaining the shared
care benefit rider.
– Example: If benefit partner A wants to drop his or her maximum monthly benefit from
$5,000 to $3,000, then benefit partner B must do the same.
• If a contract change is made that creates an unequal benefit, the shared care benefit rider
will be terminated.
$500,000 total shared
pool of money at time
of initial purchase
Death occurs:
Person A dies without using
any long-term care benefits
Person B now has the sum
of both pools for covered
long-term care expenses
A B
$250,000 $250,000
A B
$250,000 $250,000
B
$500,000
Let’s take a look at how the shared care benefit rider
would work:
In the example below, Paul and Mary have identical
Thrivent Traditional Long-Term Care Insurance plans
without the shared care benefit rider.
Now, let’s take a look at the options Paul and Mary have
available to them when they purchase identical Thrivent
Traditional Long-Term Care Insurance with the shared
care benefit rider:
Paul Mary
Maximum Monthly Benefit
$6,000
Maximum Monthly Benefit
$6,000
Benefit Multiplier
60 months
Benefit Multiplier
60 months
Total Available Benefit is $360,000 each
Paul Mary
Maximum Monthly Benefit
$6,000
Maximum Monthly Benefit
$6,000
Benefit Multiplier
60 months
Benefit Multiplier
60 months
Total Available Benefit
$360,000
Total Available Benefit
$360,000
Total Available Benefit is $720,000,
which is available to Paul and/or Mary
© 2021 Thrivent | For financial professional use only.
26
Optional Riders Continued
Survivorship Benefit
Description
This rider states if two individuals (benefit partners) have in-force contracts and riders for 10 years
and one individual dies, the surviving benefit partner’s contract will become paid up.
How It Works
If two individuals have in-force contracts with the survivorship rider on both of their contracts
(naming each other as the benefit partner), then upon the death of one insured, the surviving
benefit partner’s contract will become paid up.
• If either benefit partner dies before 10 years, then no benefit will be paid.
• No benefits can have been paid during the first 10 years in force.
Additional
Information
The survivorship benefit is available to individuals who qualify for the couples discount
(see below for eligibility).
The insured’s contracts do not need to be identical, but they both have to have the rider and be
named as the benefit partner on the other insured’s contract.
Restriction: This rider is not available with:
• 10-pay contracts.
• FIB Rider.
Who is eligible for
this rider?
The survivorship benefit rider is available to:
• Married couples.
• State partners/civil unions/domestic partners that are named in a valid certificate or
license by the state.
• Two individuals living together for three consecutive years in a committed relationship as
partners or family members AND:
– Are committed to sharing expenses.
– Are not married.
– If related, must belong to the same generation (such as siblings).
Divorce
Upon divorce/separation, the rider is terminated if one of the insureds cancels the rider;
otherwise the rider will continue.
Changes
• Can be dropped after issue.
• Can NOT be added after issue.

© 2021 Thrivent | For financial professional use only.
27
Optional Riders Continued
Nonforfeiture Benefit
Description
This rider provides an option for the long-term care benefits to continue as reduced paid-up
insurance if the insured chooses to terminate his or her contract for any reason. The contract
must be in force for a minimum of three years before this benefit can be triggered.
How It Works
The amount of paid-up coverage will be equal to the lesser of:
• The nonforfeiture credit (see below); and
• The available benefit in effect immediately before the date paid-up coverage becomes effective.*
The nonforfeiture credit is equal to the greater of:
• The total premiums paid for the contract; and
• The maximum monthly benefit in effect on the date the paid-up coverage becomes effective.
Premiums paid by the insured do not include premiums waived by Thrivent or reduced by dividends.
The shortened benefit period is NOT reduced by any benefit payments paid prior to the date of lapse
but is subject to the remaining available benefit.
The same maximum monthly benefit amount, elimination period and other limits
(except available benefit) remain that were in effect at the time of lapse.
All optional riders will terminate on the date paid-up insurance becomes effective.
*For CA: Three times the maximum monthly benefit in effect on the date the paid-up coverage becomes effective.
Additional
Information
Available on individual and shared care contracts.
If this rider is selected, the insured may also have a contingent nonforfeiture option available BUT
the insured can only be paid under one of the nonforfeiture options. The insured may choose which
nonforfeiture benefit he or she would like to receive if more than one is triggered.
Changes
• Can be dropped after issue.
• Can NOT be added after issue.

© 2021 Thrivent | For financial professional use only.
28
Optional Riders Compatibility Chart
This chart shows the allowable combinations of the optional riders and
limited pay period options.
Annual Increase
Benefit
— No Yes Yes Yes Yes Yes Yes Yes
Flexible Increase
Benefit
No — Yes Yes Yes Yes No Yes No
Nonforfeiture
Benefit
Yes Yes — Yes Yes Yes Yes Yes Yes
Return of
Premium Upon
Death
Yes Yes Yes — Yes Yes Yes No Yes
Cash Benefit
Yes Yes Yes Yes — Yes Yes Yes Yes
Waiver of
Elimination
Period for Home
Care and Adult
Day Care*
Yes Yes Yes Yes Yes — Yes Yes Yes
Survivorship
Benefit
Yes No Yes Yes Yes Yes — Yes No
Shared Care
Benefit
Yes Yes Yes No Yes Yes Yes — Yes
Limited Pay
Period—10 Pay
Yes No Yes Yes Yes Yes No Yes —
Annual Increase
Benefit
Nonforfeiture Benefit
Cash Benefit
Survivorship Benefit
Flexible Increase
Benefit
Return of Premium
Upon Death
Waiver of Elimination
Period for Home Care
and Adult Day Care*
Shared Care Benefit
Limited Pay Period—
10 Pay
*The Waiver of Elimination Period for Home Care and Adult Day Care is not available with the 180-day elimination period.
CA Rider: Waiver of Elimination Period for Home and Community-Based Care.
Note: The Flexible Increase Benefit is available with the Shared Care Benefit. However, both contract owners must accept or decline
their offers at the same time. The coverage must be identical, otherwise, the Shared Care Benefit rider will terminate.
© 2021 Thrivent | For financial professional use only.
29
Qualifying for Benefits
Eligibility for the Payment of Benefits
To be eligible for benefits under the long-term care
insurance contract, all of the following conditions must
be met:
1. Insured is chronically ill and receives qualified
long-term care services;
2. For benefits subject to the elimination period, the
services are received after that period has ended; and
3. Coverage is not listed under the exclusions
(see page 32 for exclusions list).
What does it mean to be chronically ill?
On any given day, an insured is chronically ill if a licensed
health care practitioner has, within the 12-month period
preceding that day, certified in writing that he or she has:
1. A physical impairment that is expected to last at least
90 days, or
2. A cognitive impairment.
A physical impairment is an impairment that prevents a
person from performing two or more activities of daily
living without the substantial assistance of another person.
Substantial assistance means hands-on assistance or
standby assistance.
Activities of daily living include:
1. Bathing. Washing oneself in a tub or shower,
including getting in or out of the tub or shower, or
by sponge bath.
2. Continence. Maintaining control of bowel and bladder
functions or, if unable to do so, taking care of the
personal hygiene associated with incontinence,
including caring for a catheter or colostomy bag.
3. Dressing. Putting on and taking off all items
of clothing and any necessary braces, fasteners
or prostheses.
4. Eating. Feeding oneself by getting food into the
body from a receptacle (such as a plate, cup or table)
or, if necessary, by feeding tube or intravenously.
Eating does not include preparing meals.
5. Transferring. Moving into or out of a bed, chair
or wheelchair.
6. Using the Toilet. Getting to and from the toilet,
transferring on and off the toilet and performing
the associated personal hygiene.
A cognitive impairment is an impairment of the mind that:
1. Is comparable to (and includes) Alzheimer’s disease
and similar forms of irreversible dementia;
2. Is measured by clinical evidence and standardized
tests; and
3. Results in the need for continual supervision.
© 2021 Thrivent | For financial professional use only.
30
Qualifying for Benefits Continued
What are Qualified Long-Term Care Services?
Qualified long-term care services are:
• Required because the insured is chronically ill; and
• Provided pursuant to a plan of care.
What is a plan of care? Why is it required?
A plan of care is a written document that:
1. Is prepared and signed by a licensed health
care practitioner in accordance with accepted
standards of practice;
2. Prescribes qualified long-term care services
that are consistent with an assessment of the
insured’s impairment; and
3. Includes services or treatment that could not
be omitted without adversely affecting the
insured’s health.
Thrivent retains the right to discuss the plan of care
with the licensed health care practitioner who prepared
it. Thrivent may also verify that the plan of care is
appropriate and consistent with generally accepted
standards of care for a person who is chronically ill. The
plan of care must be updated as the insured’s needs
change. Thrivent must receive a copy of the plan of
care upon its completion and each time it is updated.
Thrivent retains the right to request periodic updates not
more often than once every 30 days. Thrivent will make a
copy of the current plan of care available to the insured’s
doctor, when requested. The insured may only have one
plan of care in effect at any time.
Is there a benefit or service available to help the
insured with this process?
Yes. Care Coordination Services are available to the
insured if he or she would like assistance.
The Care Coordination Benefit, if the insured chooses to
use it, pays for a care coordinator to help the insured and
his or her family:
• Perform a comprehensive care needs assessment.
• Identify the services needed.
• Locate local caregivers and facilities.
• Assist in developing, implementing and
coordinating the insured’s plan of care.
• Monitor the insured’s ongoing care.
There is no cost to the insured for the services provided
by a care coordinator referred by Thrivent. In addition,
these services are not subject to the elimination period.
© 2021 Thrivent | For financial professional use only.
31
Payment of Benefits
Payment of Benefits/Claims Process
This is a brief outline of the claims process:
1. Contact Thrivent’s Claims department.
• A notice of claim must be submitted to
Thrivent at our Service Center within 30
days after a covered loss starts or as soon
after this as reasonably possible.
• An acknowledgement letter will be sent to
the insured and the financial professional
upon receipt of the request for benefits.
• A claims representative will review the health
status, physician’s assessment of care needs,
the contract and its available benefits and
services, and the credentials of the health
care provider or facility providing the care.
• When all the information has been received and
reviewed, a letter explaining the claim decision
and next steps will be sent to the insured.
• If a decision cannot be made, a letter explaining
the reason for the delay will be sent to the insured.
2. Contact care coordinator services.
3. Ongoing claim review.
4. Reimbursement for services.
Benefits will be paid to the insured or to the health care
provider to whom the insured has assigned benefits.
Any benefits payable to the insured that are unpaid at his
or her time of death will be paid to his or her estate.
The insured is eligible for reimbursement up to the
maximum monthly benefit, subject to the available benefit.
The insured can receive payment for multiple benefit
services in one day.
Coordination With Other Coverage
If an expense covered under this contract is also covered
by other contracts or a rider issued by Thrivent (or a
predecessor organization), the amount payable for that
expense under this contract will be reduced by the sum
of the amounts that are paid for that expense under the
other coverage.
Coordination of benefits will be determined on multiple
contracts based on the issue date, beginning with the
earliest issued contract paying benefits first.
Coordination of benefits provision applies to: Arizona,
California, District of Columbia, Delaware, Hawaii, Indiana,
Montana and South Dakota.
Medicare Non-Duplication
Medicare non-duplication applies. This means that the
long-term care contract will not pay benefits for expenses
which are reimbursable under Medicare or would be
reimbursable under Medicare but for the application of a
deductible or coinsurance amount.

© 2021 Thrivent | For financial professional use only.
32
Other Important Information
Right to Cancel
The insured is provided a 30-day period upon receipt of the contract to review and/or rescind the
contract. If the insured cancels during this initial 30 days, all premiums paid will be refunded.
Unintentional Lapse
A feature that allows the insured to name someone to be notified if coverage is about to lapse
because the premium has not been paid. This could be a relative, friend or professional such
as a lawyer or accountant.
Grace Period
A window of time (60 days) to pay each premium that is in default.
Reinstatement
If the contract terminates at the end of the grace period for nonpayment of premiums, the insured
may reinstate the contract:
• Within six months after the end of the grace period.
• Must pay any premiums that are in default.
If the insured is NOT chronically ill on the date the unpaid premium was due, the insured must
submit an application for reinstatement.
If the insured is chronically ill on the date the unpaid premium was due, the insured is not required
to submit an application for reinstatement but must provide proof of chronic illness.
Time Limit on
Certain Defenses
A contract may be voided due to misstatements in the application as follows:
1. For the first six months the contract is in force, the contract may be voided if it is shown that a
misstatement is material to the decision to issue the contract.
2. For losses incurred after the first six months but before the contract has been in force for two years,
the contract may be voided if it is shown that a misstatement is both material to the decision to
issue the contract and related to the loss for which benefits are sought.
3. For losses incurred after the contract has been in force for two years, the contract may be
voided only if it is shown that the insured knowingly and intentionally misstated relevant facts
related to his or her health.
This provision applies to any additional coverage that is added from its effective date with regard to
statements made in the application for the additional coverage.
Exclusions
The long-term care insurance contract does not pay benefits for charges billed by a doctor or charges
for prescription drugs.
In addition, the long-term care insurance contract does not cover services:
• Outside the U.S., its territories and possessions, except as provided under the
International Care Benefit.
• Necessary due to an attempt at suicide or an intentionally self-inflicted injury.
• Provided for the treatment of alcoholism or drug addiction.
• Provided by an immediate family member unless:
– He or she is a regular employee of a facility or agency that is providing the treatment,
services or care;
– The facility or agency receives the payment for the treatment, service or care and he or
she receives no compensation other than the normal compensation for employees in his
or her job category; and
– He or she has no ownership or financial interest in the facility or agency providing the
treatment, services or care.
• For which benefits are payable under any state or federal Workers’ Compensation, Occupational
Disease or Employer’s Liability Laws.
An immediate family member means a spouse or partner and anyone who is related to the insured,
spouse or partner by blood, adoption or marriage (including step-relatives) as a parent, grandparent,
child, grandchild, brother, sister, aunt, uncle, nephew or niece.
© 2021 Thrivent | For financial professional use only.
33
Underwriting
For Thrivent Traditional Long-Term Care Insurance
underwriting guidelines, refer to the Underwriting
Guidelines on FieldNet Underwriting page, including
details on:
• Underwriting Requirements by Age
• Preferred Underwriting Checklist
• Uninsurable Conditions
Suitability
National Association of Insurance Commissioners
(NAIC) Suitability:
The sale of a long-term care insurance contract must be
determined to be suitable. You must determine whether
the purchase is appropriate for the needs of the applicant.
Factors that go into determining suitability:
• The prospective insured must have the ability to pay
for the proposed coverage and other pertinent financial
information related to the purchase of the coverage.
• The applicant’s goals or needs with respect to long-
term care and the advantages and disadvantages
of insurance to meet those goals or needs.
• The values, benefits and cost of the applicant’s
existing insurance, if any, when compared
to the values, benefits and cost of the
recommended purchase or replacement.
• The values, benefits and cost of Thrivent’s
Long-Term Care Insurance when assessed
against the applicant’s goals or needs.
What are the guidelines for determining suitability?
• In general, a sale of long-term care
insurance is NOT suitable if:
– The applicant has less than $20,000 in annual
income, or less than $30,000 in assets to protect
(savings and investments), unless premium is being
paid by a family member or other outside source.
– The applicant is eligible or about to become
eligible for Medicaid.
– The applicant’s only source of income is Social
Security or supplemental security income.
– The applicant otherwise has limited assets and
can’t afford to pay the premium over the life of
the contract.
In order to ensure that a particular long-term care
insurance product is suitable, the following elements
must also be taken into consideration:
• Who will pay the premium (applicant, child, etc.).
• Where the premium will come from
(income, savings, investments, etc.).
• The applicant’s living arrangements (e.g., are family
and friends available to assist in care, if needed).
• The actual cost of care in the area where
the applicant lives.
• How the individual will fund his or her care
costs during the elimination period.
• The applicant’s needs and how a particular long-term
care insurance product can satisfy those needs.
• Which benefits have been selected, including benefit
levels, inflation choices, optional benefits, etc.
• What could happen if the individual experiences
a change in financial circumstances.
• Does he or she understand that rates
could possibly change in the future.
© 2021 Thrivent | For financial professional use only.
34
Administrative Questions
Application Processing for Couples
Couples that apply together will be processed together.
Thrivent will hold each applicant’s file until there is a final
underwriting decision on BOTH files. Then they will be
processed and issued together with the same issue date;
one issued and the other declined; or both declined.
Advance Premium Payment for
Conditional Insurance*
The advance premium payment must be at least one
month’s premium for conditional insurance.
Other pertinent information:
• By making an advance premium payment with the
application, underwriting will not be affected by any
change in health status that occurs after the latest of:
– The date the insured makes the advance premium
payment, or
– The date the insured signs the application, or
– The date the insured completes all tests or physical
exams required by Thrivent, if applicable.
• No coverage is effective until the application
is approved and a contract is issued.
• Completing an application or making an
advance premium payment does not guarantee
that the application will be approved.
• If a contract is issued, the insured must pay all
premiums when due to keep his or her contract
in force.
• If a contract is not issued, any advance premium
payment submitted with the application
will be refunded without interest.
Is Premium Required With an Application?
No. Premium is not required with an application.
If at least one month’s premium is submitted or EFT
is selected with the application, Thrivent will consider
health history as of the time of application regardless
of any subsequent changes in health.
NOTE: For CA, premium is not allowed with the application.
Preliminary Declaration of Insurability for Long-Term
Care Insurance
Complete the Preliminary DOI for Long-Term Care
Insurance, form 27253. The state-specific form can be
found on the Thrinven Online Forms Utility page (TOFU).
*This is not available for CA.

© 2021 Thrivent | For financial professional use only.
35
Long-Term Care Insurance
Partnership Information
Some states have long-term care insurance partnership
programs designed to encourage people to plan
ahead for potential long-term care needs by acquiring
long-term care insurance. Under these partnership
programs, when a partnership-eligible long-term care
insurance contract is purchased, the contract owner
will receive protection known as “asset disregard” if
he or she needs to apply for Medicaid. Neither the
state nor federal government issues contracts; private
insurance companies issue long-term care insurance.
The government-provided asset disregard programs
vary by state. The long-term care partnership program
is a creation of federal law allowing states to alter their
Medicaid programs to allow assets to be disregarded
based upon claims paid by eligible qualified long-term
care insurance contracts. Most states allow a dollar-
for-dollar asset disregard for claims paid on qualified
partnership contracts and will not require an insured
to exhaust the benefits offered under the partnership
contract in order to qualify for Medicaid.
Benefits of the Partnership Program
• Partnership long-term care insurance contracts
are tax-qualified plans under federal law and must
contain certain consumer protections and provide
inflation protection benefits for purchasers so that
benefits keep up with the cost of inflation over time.
• The long-term care partnership program provides
an alternative to spending down or transferring
assets by forming a partnership between
Medicaid and private long-term care insurers.
• Once private insurance benefits are used,
special Medicaid eligibility rules are applied
if additional long-term care is needed.
Key Features of Long-Term Care Partnership Plans
• The contracts must be tax-qualified plans.
• Contracts must provide the following inflation protection:
– Insureds under age 61 at date of purchase must
have compound annual inflation protection.
– Insureds at least 61 years of age but under the age
of 76 must have some level of inflation protection.
– Insureds older than age 76 may have, but are not
required to have, inflation protection.
How Will an Insured Know if He or She
Purchased a Partnership Plan?
• If the contract he or she purchased is a partnership
eligible plan, he or she will receive written notice from
the insurance company. Depending upon the state, the
notice will be provided in one of the following ways:
– His or her contract or certificate will be identified
as a partnership plan in the contract itself—
either on the front page or on the schedule page
of the contract.
– He or she will receive a letter from his or her
insurance company advising him or her that he
or she has purchased a partnership contract. If
this is the only notification he or she receives, it
is extremely important to keep this letter.
Please keep in mind that these programs have
specific requirements in each state in which they are
offered. Check with your state insurance department
or counseling program to see if these contracts are
available in your state. Many states with long-term
care partnership programs have information on their
websites. To locate your state’s insurance department
website, visit www. naic.org/state_web_map.htm.
The U.S. Department of Health and Human Services
maintains a website with information on long-term care
insurance and the partnership program at
www.longtermcare.gov.
© 2021 Thrivent | For financial professional use only.
36
Long-Term Care Insurance Taxation
Thrivent’s Traditional Long-Term Care Insurance is
intended to be federally tax-qualified. This means:
• Premiums can be included with other annual
uncompensated medical expenses for deductions
from income in excess of 7.5% of adjusted gross
income up to a maximum amount
adjusted for inflation.
• Benefits received and used to pay for long-term
care services generally will not be counted as
income. For contracts that pay benefits using
the expense-incurred method (like Thrivent’s
contracts), benefits received in excess of the
costs of long-term care services may be taxable.
• To trigger the benefits under the contract,
federal law requires insureds to be
unable to do two activities of daily living
without substantial assistance.
• “Medical necessity” cannot be
used as a trigger for benefits.
• Chronic illness or disability must be
expected to last for at least 90 days.
• For cognitive impairment to be covered, a
person must require substantial supervision.
Please advise your clients to consult his or her
tax consultant or legal advisor regarding the tax
consequences in his or her situation.

© 2021 Thrivent | For financial professional use only.
37
Conversions and Replacements
For Previously Sold, Existing Contracts:
Prior AAL or LB
contracts, Genworth or
John Hancock contracts,
Thrivent Long-Term Care
Insurance or Thrivent
Security One Annuity
With a Long-Term Care
Insurance Rider
No conversion is allowed.
If the insured would like new coverage, he or she would need to buy a new contract and be
underwritten at his or her attained age.
Prior AAL or LB LTCi
contracts, or Thrivent
LTCI contracts for
California residents
For CA, if a client replaces a LTCi contract that we previously issued, they will receive a
credit on their new contract, equal to 5% of the premium on the old contract for each year
the contract was in force, up to 50%.
If the insured would like new coverage, he or she would need to buy a new contract and
be underwritten at his or her attained age.
Disability Insurance
Contracts with GIO
Purchase Option
• Earning Power
(AAL D-Series)*
These contracts offered a long-term care insurance purchase option:
• Only available if the long-term care insurance product is offered in the resident state.
• Premiums are based on attained age.
• Not subject to underwriting.
• Only available at ages 55, 60 and 65—must request within 90 days after the
insured’s birthday.
• Cannot be receiving DI benefits or waiver of premium benefits under the DI contract.
• Must have minimum DI benefit of two years to be eligible.
• Thrivent will require that $1,500 per month be purchased as the minimum since this
is the minimum monthly benefit allowed on the long-term care insurance contract.
State variations apply for states with higher minimum issue limits.
• The coverage offered will be comprehensive coverage.
• Additional coverage can be purchased with underwriting.
Disability Insurance
Contracts with GIO
Purchase Option
• LB 96 Series*
These contracts offered a long-term care insurance purchase option:
• Only available if the long-term care insurance product is offered in the resident state.
• Premiums are based on attained age.
• Not subject to underwriting.
• Only available at ages 50, 55, 60 and 65—must request within 90 days after the
insured’s birthday.
• Have not received DI benefits or waiver of premium benefits for any of the six months
prior to the insured’s birthday.
• Must have minimum DI benefit of two years to be eligible.
• Maximum benefit of:
1. $2,100 per month x 24 months = $50,400 or
2. Minimum allowed by the state.
– Additional coverage can be purchased with underwriting.
All conversions and replacements must meet suitability guidelines.
*For more information on the Disability Insurance Contracts with GIO Purchase Option for Earning Power (AAL D-Series) and LB 96 Series, please see
the Health Insurance page on FieldNet and refer to the Previously Sold Products section.

© 2021 Thrivent | For financial professional use only.
1035 Exchange Overview
Eligible 1035 Exchanges for Long-Term
Care Insurance
• Assignment and surrender requested as part of
a 1035 exchange transaction cannot be reversed
once the transfer process is complete.
• There is no right to a return of the exchanged
contract(s) as a part of the “Right to Cancel” the
new contract. Consequently, any taxable gain
incurred from exchanging a contract(s) cannot be
reversed once the distribution is processed.
• Thrivent cannot request a 1035 exchange
from a foreign company.
For more information on 1035 exchanges, and procedures
for requesting an Internal or External 1035 Exchange,
please see FieldNet.
Transactions eligible for 1035 exchange treatment for long-term care insurance
From To Type of Exchange
Life Insurance
NEW Life Insurance Full exchange only
NEW nonqualified annuity Full exchange only
NEW qualified long-term care (LTC) insurance Full exchange only
EXISTING nonqualified annuity Full exchange only
EXISTING qualified LTC Insurance Full exchange only
Nonqualified Annuity
NEW nonqualified annuity Partial or full exchange
NEW qualified LTC Insurance Partial or full exchange
EXISTING nonqualified annuity Full exchange only
EXISTING qualified LTC Insurance Partial or full exchange
Qualified LTC Insurance
NEW qualified LTC Insurance Partial or full exchange
EXISTING qualified LTC Insurance Partial or full exchange
29023 R1-21
Internal Revenue Code (IRC) Section 1035 is a tax law
provision that enables a contract owner to exchange
an existing contract without incurring a tax on the
transferred value(s) and carries over the cost basis of
the terminated contract to the destination contract.

© 2021 Thrivent | For financial professional use only.
39
Appendix A: Tables for Substantial
Premium Rate Increases
Table 1: Triggering substantial premium
rate increase for lifetime premium
Table 2: Triggering substantial premium
rate increase for limited pay premium
A substantial premium increase is an increase that results
in a cumulative percentage increase in premiums since
the date of issue that equals or exceeds the percentage
shown below:
Issue Ages Percent Increase
29 or under 200%
30 to 34 190%
35 to 39 170%
40 to 44 150%
45 to 49 130%
50 to 54 110%
55 to 59 90%
60 70%
61 66%
62 62%
63 58%
64 54%
65 50%
Issue Ages Percent Increase
Under 65 50%
65-80 30%
Over 80 10%
Issue Ages Percent Increase
66 48%
67 46%
68 44%
69 42%
70 40%
71 38%
72 36%
73 34%
74 32%
75 30%
76 28%
77 26%
78 24%
Issue Ages Percent Increase
79 22%
80 20%
81 19%
82 18%
83 17%
84 16%
85 15%
86 14%
87 13%
88 12%
89 11%
90 or over 10%
