
EXECUTIVE BOARD
EB148/7
148th session
13 January 2021
Provisional agenda item 6
Political declaration of the third high-level meeting
of the General Assembly on the prevention and
control of non-communicable diseases
Report by the Director-General
1. The report is submitted in response to decision WHA72(11) (2019), in which the Health Assembly
requests the Director-General “to consolidate reporting on the progress achieved in the prevention and
control of noncommunicable diseases and the promotion of mental health with an annual report to be
submitted to the Health Assembly through the Executive Board, from 2021 to 2031, annexing reports
on implementation of relevant resolutions, action plans and strategies, in line with existing reporting
mandates and timelines.” Table 1 sets out the corresponding elements of this report.
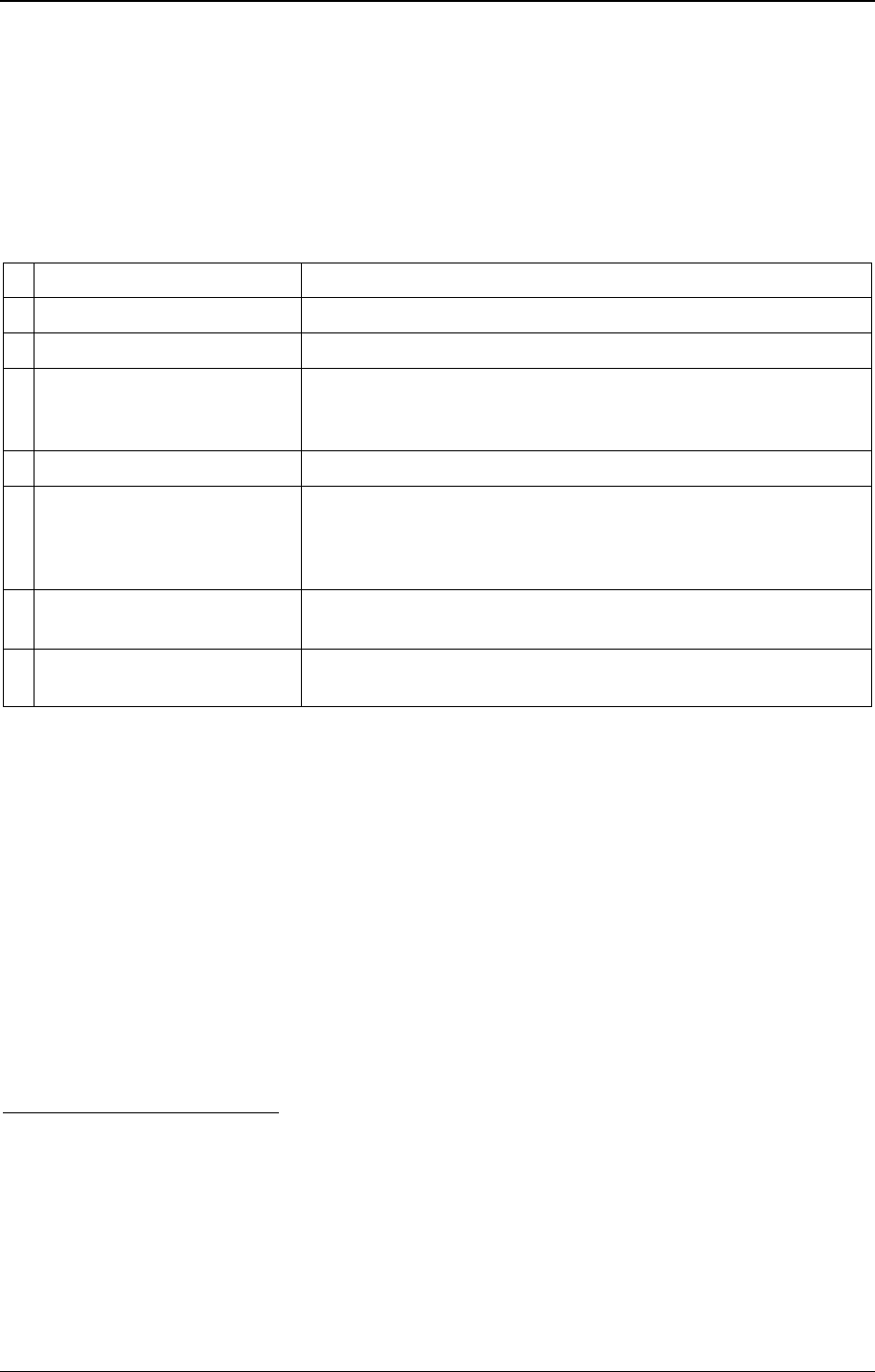
Table 1. Mandates from paragraph 3(e) in decision WHA72(11) for progress reports in this
document.
Progress achieved in the prevention and control of noncommunicable diseases and
the promotion of mental health, including the following topics and the mandating
resolution or decision:
Location in this
document
• resolution WHA53.17 (2000) on prevention and control of noncommunicable
diseases
• resolution WHA66.10 (2013) on follow-up to the Political Declaration of the High-
level Meeting of the General Assembly on the Prevention and Control of Non-
communicable Diseases
• decision WHA72(11) on the follow-up to the political declaration of the third high-
level meeting of the General Assembly on the prevention and control of non-
communicable diseases
Paragraphs
2 to 43
• resolution WHA70.12 (2017) on cancer prevention and control in the context of an
integrated approach
Annex 1
• resolution WHA57.17 (2004) on the global strategy on diet, physical activity and
health
• resolution WHA71.6 (2018) on WHO’s global action plan on physical activity
2018–2030
Annex 2
• resolution WHA65.6 (2012) on comprehensive implementation plan on maternal,
infant and young child nutrition
Annex 3
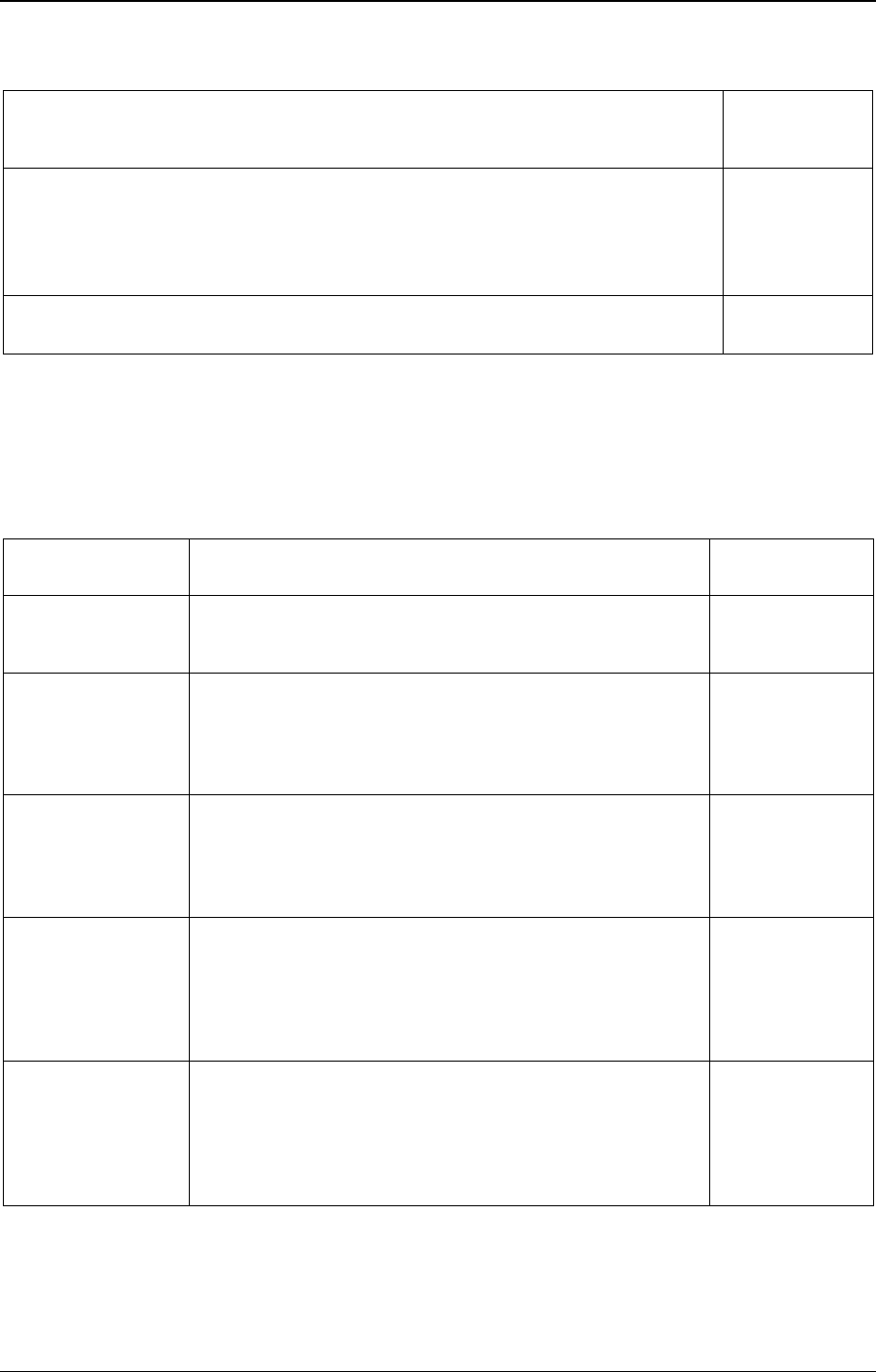
EB148/7
2
Progress achieved in the prevention and control of noncommunicable diseases and
the promotion of mental health, including the following topics and the mandating
resolution or decision:
Location in this
document
• resolution WHA68.19 (2015) on outcome of the Second International Conference
on Nutrition
• decision WHA70(19) (2017) on report of the Commission on Ending Childhood
Obesity: implementation plan
• resolution WHA71.9 (2018) on infant and young child feeding
• resolution WHA68.8 (2015) on health and environment: addressing the impact of air
pollution and decision WHA69(11) (2016) on the related road map
Annex 4
2. In addition, in decision WHA72(11) (2019) the Health Assembly requests the Director-General
to submit information about the following requested actions to the Seventy-fourth World Health
Assembly, through the Executive Board. See Table 2.
Table 2. Further actions requested of the Director-General in decision WHA72(11) (2019)
Relevant
paragraph
Action
Location in this
document
3(a)
to propose updates to the appendices of WHO’s comprehensive
mental health action plan 2013–2030
Annex 5
Appendix 1
Appendix 2
3(f)
to provide further concrete guidance to Member States in order
to strengthen health literacy through education programmes and
population-wide targeted and mass- and social-media campaigns
to reduce the impact of all risk factors and determinants of
noncommunicable diseases
Annex 6
3(g)
to present, based on a review of international experiences, an
analysis of successful approaches to multisectoral action for the
prevention and control of noncommunicable diseases, including
those that address the social, economic and environmental
determinants of such diseases
Annex 7
3(h)
to collect and share best practices for the prevention of
overweight and obesity, and in particular to analyse how food
procurement in schools and other relevant institutions can be
made supportive of healthy diets and lifestyles in order to
address the epidemic of childhood overweight and obesity and
reduce malnutrition in all its forms
Annex 8
1 and paragraph 40
of United Nations
General Assembly
resolution 73/2
(2018)
to provide support for implementation of the following action:
strengthen the design and implementation of policies, including
for resilient health systems and health services and infrastructure
to treat people living with noncommunicable diseases and
prevent and control their risk factors in humanitarian
emergencies
Annex 9
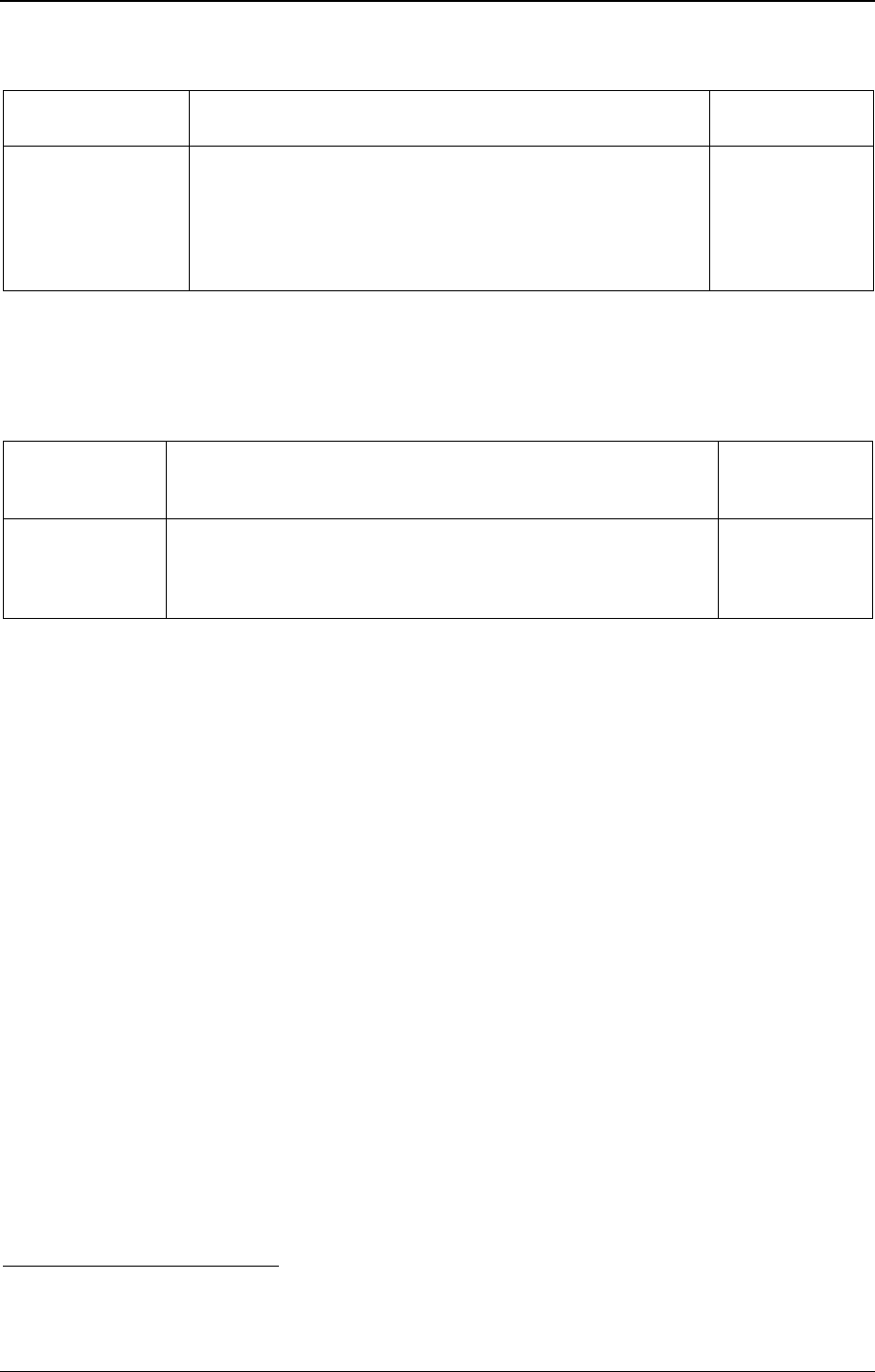
EB148/7
3
Relevant
paragraph
Action
Location in this
document
United Nations
Economic and Social
Council resolution
2014/10
to inform the World Health Assembly on a regular basis about
progress made by the United Nations Inter-Agency Task Force
for the Prevention and Control of Non-communicable Diseases
in the implementation of the WHO’s global action plan for the
prevention and control of noncommunicable diseases
2013–2030.
Annex 10
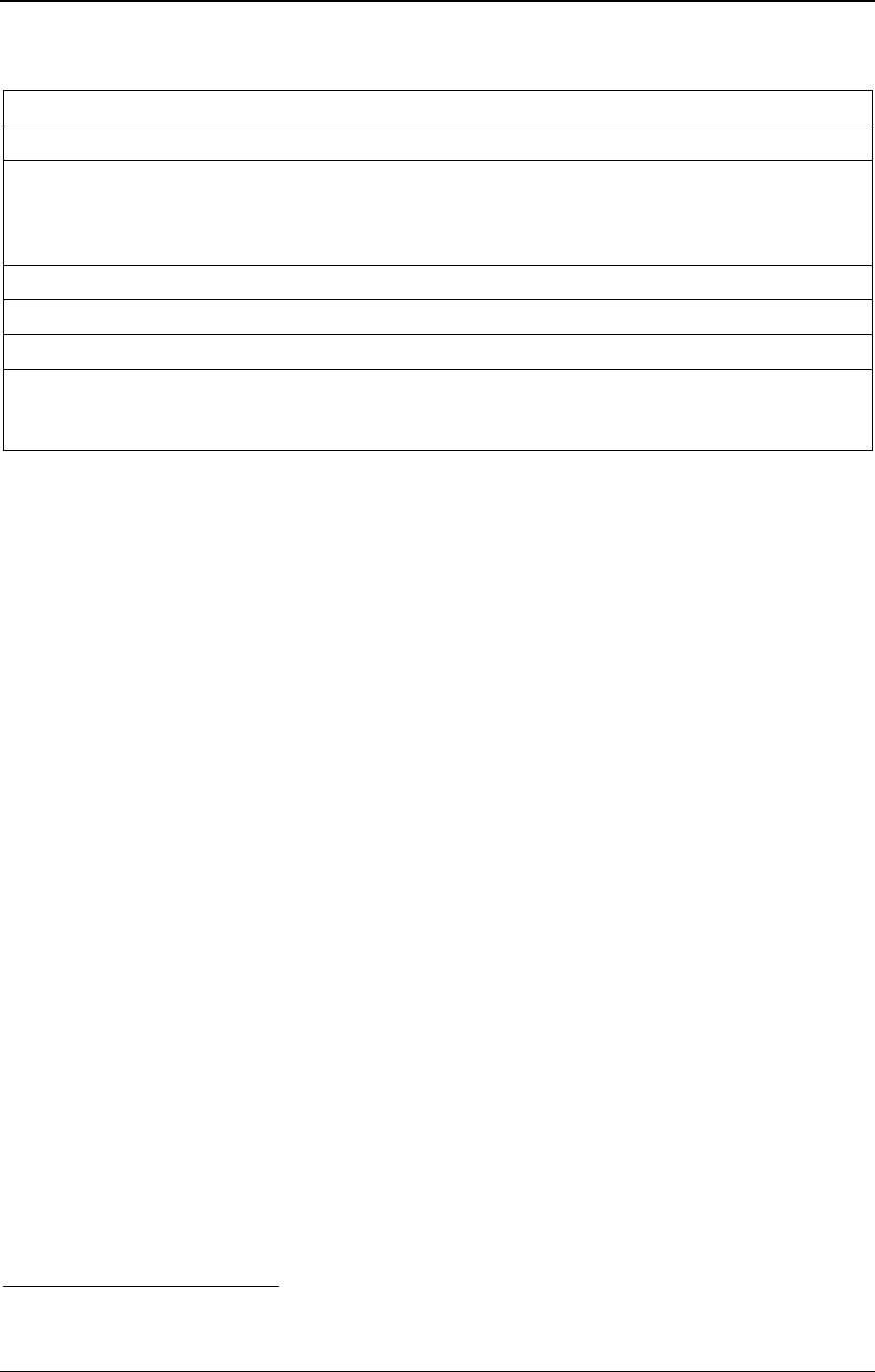
3. Table 3 lists two other mandated evaluations, which are discussed briefly below (see paragraphs
45–47) and will be published separately.
Table 3. Two further mandated evaluations, with source of mandate and document number
Resolution
WHA66.10
(2013)
Mid-point evaluation of the WHO’s global action plan for the
prevention and control of noncommunicable diseases
Document
EB148/7 Add.1
Document
A67/14 Add.1,
Appendix 1,
paragraph 19
Final evaluation of the Global coordination mechanism on the
prevention and control of noncommunicable disease
Document
EB148/7 Add.2
THE BURDEN OF NONCOMMUNICABLE DISEASES (NCDS): WHERE WE STAND
TODAY
1
4. WHO’s World health statistics 2020 reveal that, compared with the advances against
communicable diseases, progress in preventing and controlling premature death from NCDs has been
inadequate.
5. An estimated 41 million people worldwide died of NCDs in 2016, equivalent to 71% of all deaths.
Four NCDs caused most of those deaths: cardiovascular diseases (17.9 million), cancer (9.0 million),
chronic respiratory diseases (3.8 million), and diabetes (1.6 million).
6. An estimated 15 million people worldwide died of NCDs between the ages of 30 and 70 years,
defined as premature death. The probability (risk) of premature death from any one of the four main
NCDs decreased by 18% globally between 2000 and 2016. The most rapid decline was seen for chronic
respiratory diseases (40% lower), followed by cardiovascular diseases and cancer (both 19% lower).
Diabetes, however, showed a 5% increase in premature mortality during the same period.
7. Despite the rapid progress made between 2000 and 2010 in reducing the risk of premature death
from any one of the four main NCDs, the momentum of change has dwindled during 2010–2016, with
annual reductions in premature mortality rates slowing for the main NCDs. In high-income countries,
even though the premature mortality rate due to diabetes decreased from 2000 to 2010, it increased in
2010–2016. In low- and middle-income countries, the premature mortality rate due to diabetes increased
across both periods.
1
WHO. World health statistics 2020: monitoring health for the SDGs. Geneva: World Health Organization; 2020
(https://apps.who.int/iris/handle/10665/332070).

EB148/7
4
8. The rising mortality rates from diabetes are associated with – among other factors – the increasing
prevalence of obesity. Since 2000, the prevalence of obesity among adults (18 years and older) globally
has increased 1.5 times and the prevalence in children (5–18 years) more than doubled (from 2.9% to
6.8%) in 2016.
9. In 2016, the prevalence of physical inactivity for adults aged 18 years or more was 27.5%. Levels
of inactivity are twice as high in high-income countries as in low-income countries, and insufficient
activity increased by 5% in high-income countries between 2001 and 2016.
10. Global prevalence of hypertension decreased by 11% from 2000 to 2015. The prevalence of
hypertension was highest in low-income countries (28.4%) and lowest in high-income countries (17.7%)
in 2015.
11. Tobacco use has decreased steadily globally. A little under one quarter (23.6%) of adults (15 years
and older) globally used tobacco in some form in 2018, down from one third (33.3%) in 2000. The total
number of adult tobacco users remains very high, however: about 1.3 billion in 2018.
12. The burden of mental health conditions remains high. According to the latest global burden of
disease estimates (for 2017), mental, neurological and substance use disorders make up 11.1% of
disability-adjusted life years lost worldwide and 26.7% of years lived with disability (compared to
10.2% and 26.8% respectively in 2012), and an estimated 971 million people have a mental disorder
(compared to 916 million people in 2012). Almost 800 000 people die by suicide each year; it is the
second leading cause of death in 15–29-year-olds.
13. Worldwide, alcohol consumption, measured in litres of pure alcohol per person of 15 years or
older, has been relatively stable since 2010 and was estimated at 6.2 litres in 2018. However, trends
observed and projections made before the pandemic of coronavirus disease (COVID-19) forecast an
increase in global alcohol consumption per capita by 2025. The impact of the COVID-19 pandemic on
the levels of alcohol consumption worldwide and predicted trends still needs to be assessed.
14. In 2016, nine out of 10 people breathed air that did not meet the WHO air quality guidelines and
more than half the world’s population was exposed to air pollution levels at least 2.5 times above the
safety standard set by WHO. Although the proportion of the global population with access to clean
cooking fuels and technologies has increased steadily since 2000 and reached 63% in 2018, the actual
number of people without clean cooking has remained relatively constant over the past three decades.
PROGRESS TOWARDS TARGET 3.4 OF SUSTAINABLE DEVELOPMENT GOAL
AND RELATED TARGETS: WHERE WE STAND TODAY
15. Target 3.4 of Sustainable Development Goal 3 is to reduce premature mortality from NCDs by a
third by 2030 relative to 2015 levels, and to promote mental health and well-being. Only 17 countries
are on track to meet that target for women and 15 for men.
1
There is some reduction in the global
1
NCD Countdown 2030 Collaborators. NCD Countdown 2030: pathways to achieving Sustainable Development
Goal target 3.4. The Lancet, 2020; 396(10255):918-934 (https://www.thelancet.com/journals/lancet/article/PIIS0140-
6736(20)31761-X/fulltext, accessed 29 October 2020).
EB148/7
5
age-standardized suicide rate
1
(8% reduction from 2010 to 2016)
2
but the indicator (3.4.2) shows that
the suicide rate is still far from achieving the target.
16. Target 3.8 is to achieve universal health coverage. All income categories of countries have
demonstrated almost no progress since 2000 in expanding the “universal health coverage service
capacity and access coverage” for the prevention, screening, early diagnosis and appropriate treatment
of NCDs.
3
In particular, between 2010 and 2019, many countries showed lagging performance on
effective coverage indicators for NCDs compared with those for communicable diseases and maternal
and child health, suggesting that many health systems are not keeping pace with the rising NCD burden.
There is a growing awareness that global ambitions to accelerate progress towards universal health
coverage are increasingly unlikely to be realized without concerted action on NCDs.
4
17. Overweight among children has shown a concerning upward trend. Worldwide, an estimated
5.6% – or 38.3 million children under five years of age – were overweight in 2019, compared with about
30.3 million in 2000.
18. Target 3.5 is to strengthen the prevention and treatment of substance abuse, including the harmful
use of alcohol, which is a risk factor for NCDs and other health conditions. Since 2010 little progress
has been made in reducing the harmful use of alcohol, and development and implementation of effective
alcohol control measures have been uneven between countries and WHO regions.
19. Target 3.a is to strengthen the implementation of the WHO Framework Convention on Tobacco
Control in all countries, where progress is measured by the age-standardized prevalence of current
tobacco use among persons aged 15 years and older. WHO estimates that the prevalence of current
tobacco use among persons aged 15 years and older has declined globally since 2015, from 24.9% in
2015 to 23.6% in 2018.
5
However, the implementation progress has been uneven for different articles
of the Convention. Only 32 Member States are currently on track to achieve WHO’s voluntary target of
a relative reduction in tobacco use prevalence of 30% between 2010 and 2025.
20. Over the past decade, the number of countries monitoring and reporting on air quality (indicator
11.6.2 on annual mean levels of fine particulate matter) has improved. Globally, the population exposed
1
WHO. Mental health atlas 2017. Geneva: World Health Organization; 2018
(https://apps.who.int/iris/handle/10665/272735).
2
WHO (https://www.who.int/gho/publications/world_health_statistics/2020/EN_WHS_2020_Main.pdf?ua=1,
accessed 29 October 2020).
3
WHO. Primary health care on the road to Universal Health Coverage: 2019 Monitoring report. Geneva: World
Health Organization; 2019 (https://www.who.int/healthinfo/universal_health_coverage/report/uhc_report_2019.pdf?ua=1,
accessed 29 October 2020).
4
GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of
effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden
of Disease Study 2019. The Lancet, 2020; 396(10258):1250-1284
(https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30750-9/fulltext, accessed 29 October 2020).
5
WHO. The Global Health Observatory. Geneva: World Health Organization
(https://www.who.int/data/gho/data/indicators/indicator-details/GHO/age-standardized-prevalence-of-current-tobacco-
smoking-among-persons-aged-15-years-and-older, accessed 7 December 2020).

EB148/7
6
to PM2.5 levels above the current WHO air quality guidelines (annual average of 10 μg/m
3
) has fallen
by 4%, from 94% in 2010 to 90% in 2016.
1
21. In 2018, 63% (range 56–68%) of the global population had access to clean cooking fuels and
technologies, leaving the global population without such access at 2.8 billion people,
2
a figure
unchanged for around two decades now (indicator 7.1.2 on proportion of population with primary
reliance on clean fuels and technology). Without prompt action, universal access will fall short of the
relevant Goals by almost 30%.
22. In a growing recognition of air pollution as a public health threat, countries are scaling up
commitments to implement air quality policies and to align climate and air quality. At the 2019 Climate
Action Summit, 50 countries with in total more than one billion people committed themselves to reach
WHO air quality guideline values and align climate and air quality policies by 2030.
23. For the poorest one billion people of the world, NCDs account for more than a third of their
burden of disease. That includes almost 800 000 deaths annually among those aged younger than
40 years, more than HIV, tuberculosis and maternal deaths combined.
THE COVID-19 PANDEMIC: A DEADLY INTERPLAY WITH THE NCD EPIDEMIC
24. In May 2020, WHO conducted a rapid assessment survey of the impact of the COVID-19
pandemic on NCD resources and services,
3
to which 163 Member States (84%) responded. In
122 countries, governments are collecting or collating data on comorbidities between persons infected
with SARS-CoV-2 and persons living with NCDs. The Secretariat is analysing the data in order to derive
global estimates on these comorbidities. Initial results seem to indicate that persons living with
hypertension and/or diabetes appear to be two-to-four times more vulnerable to becoming severely ill
with or die from the virus. People living with obesity or using tobacco may be suffering from
undiagnosed or untreated hypertension or diabetes, which may be one of the reasons for a differential
social impact of COVID-19 within countries.
25. More than 80 countries reported complete or partial disruptions to management services for
people with hypertension or diabetes and diabetic complications. Countries most commonly reported
that they used triaging in response to the disruptions to NCD-related services; telemedicine was also
very widely used. However, the disruption of health services is particularly problematic for those living
with NCDs who need regular care.
26. Several examples from countries show how the disruption of NCD services has directly affected
people. Screening, case identification and referral systems for cancer have all been affected by the
COVID-19 pandemic, resulting in a substantial decrease in cancer diagnoses. The fact that fewer patients
with acute coronary syndrome are admitted to hospital often means increases in out-of-hospital deaths
and long-term complications of myocardial infarction. The Secretariat is conducting a modelling
1
Shaddick G, Thomas ML, Mudu P, Ruggeri G, Gumy S. Half the world’s population are exposed to increasing air
pollution. npj Climate and Atmospheric Science 2020; 3:23 (https://doi.org/10.1038/s41612-020-0124-2, accessed
7 December 2020).
2
United Nations, Department of Economic and Social Affairs, Statistics Division. Ensure access to affordable,
reliable, sustainable and modern energy for all (https://unstats.un.org/sdgs/report/2020/goal-07/, accessed 7 December 2020).
3
WHO. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a
rapid assessment. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/334136).
EB148/7
7
exercise to forecast the long-term upsurge in premature deaths from NCDs resulting from the disruption
of health services.
27. WHO’s interim operational guidance on maintaining health services in the COVID-19 context
includes considerations for NCDs, mental health and nutrition.
1
The joint policy brief on responding to
NCDs during and beyond the COVID-19 pandemic provides examples of NCD-specific actions that
could be considered in the development of national COVID-19 response and recovery plans.
2
28. In September 2020, the United Nations General Assembly in its resolution 74/306 on a
comprehensive and coordinated response to the COVID-19 pandemic called upon Member States “to
further strengthen efforts to address non-communicable diseases as part of universal health coverage,
recognizing that people living with non-communicable diseases are at a higher risk of developing severe
COVID-19 symptoms and are among the most impacted by the pandemic”.
3
THE COVID-19 PANDEMIC: RESPONDING TO THE MENTAL HEALTH,
NEUROLOGICAL AND SUBSTANCE USE CONSEQUENCES
29. The COVID‐19 pandemic is profoundly affecting mental health and well-being. Mental and
neurological manifestations, such as depression, anxiety and delirium/encephalopathy, are reported in
COVID-19 patients. Many people with pre-existing mental, neurological and substance use disorders
are facing exacerbation of symptoms due to stressors, while the limited available services are disrupted.
Some people cope with stressors in harmful ways such as turning to alcohol, drugs or risky patterns of
potentially addictive behaviours, including video gaming and gambling. Adversity is a potent risk factor
for mental and behavioural disorders, such as depression and alcohol use disorders.
30. The Secretariat has assessed the impact of COVID-19 on services for mental, neurological and
substance use disorders through a rapid survey between June and August 2020.
4
Out of 130 countries,
121 (93%) countries reported disruptions in one or more of their services for these disorders and
116 (89%) reported that mental health and psychosocial support was part of their national COVID-19
response plans. Countries are responding to the disruptions through teletherapy interventions (70%),
crisis hotlines (68%) and training for health-care providers (60%). The General Assembly
resolution 74/306 encouraged Member States “to address mental health in their response to and recovery
from the pandemic by ensuring widespread availability of emergency mental health and psychosocial
support”.
31. The Secretariat is coordinating different pillars of its COVID‐19 response to integrate mental
health and psychosocial support into the COVID‐19 response effort.
5
WHO co‐chairs the Inter‐Agency
Standing Committee Reference Group on Mental Health and Psychosocial Support in Emergency
1
WHO. Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance,
1 June 2020. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/332240).
2
WHO, United Nations Development Programme. Responding to non-communicable diseases during and beyond the
COVID-19 pandemic. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/334145).
3
United Nations General Assembly, resolution 74/306 (2020), Comprehensive and coordinated response to the
coronavirus disease (COVID-19) pandemic: operative paragraph 9.
4
WHO. The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment.
Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/335838).
5
Tedros AG. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry 2020;
19(2):129-130 (https://onlinelibrary.wiley.com/doi/full/10.1002/wps.20768, accessed 30 October 2020).
EB148/7
8
Settings. A wide range of resources, available in numerous languages and formats, has been developed
by WHO and its partners.
1
WHO established the Global Forum on Neurology and COVID-19 in order
to exchange knowledge and enhance clinical practices.
BUILDING BACK BETTER
32. Over the past 20 years, NCDs have changed the world. They have become the leading cause of
death in most countries, resulting in 200 million premature deaths among people aged between 30 and
70 years, most living in low- and middle-income countries. During the next 10 years, another 150 million
people will die from NCDs between the ages of 30 and 70 years. Most deaths can be avoided or delayed.
33. In adopting resolution WHA53.17 in 2000, the Health Assembly recognized for the first time that
the long-term needs of people living with NCDs are rarely dealt with. Accordingly, the Political
Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of
Non-communicable Diseases in 2011 included a commitment from governments to explore the
provision of adequate resources through, inter alia, domestic and bilateral channels. In 2016, NCDs
represented 27% of domestic public spending and 9% of external funds for health across a dataset
including 16 low-income countries and 24 middle-income countries.
2
Today, NCDs remain the largest,
most internationally-underfunded public health issue globally, where most lives could be saved or
improved.
34. Bilateral donors have not shown increased appetite for funding activities specifically earmarked
as addressing NCDs to establish even the minimal critical capacity, mechanisms and mandates needed
in low- and middle-income countries to pursue change. In the absence of such funding, groups with
economic, market and commercial interests stepped up their efforts to lobby against implementation of
interventions by WHO, discrediting WHO’s scientific knowledge, available evidence and reviews of
international experience, and bringing legal challenges against countries to oppose progress.
3
35. The response to the COVID-19 pandemic must address precisely these failures that are being
exposed and exploited by the pandemic. Investment in the prevention and control of NCDs as part of
COVID-19 recovery is attractive, as cost-effective, high-impact interventions already exist but are not
sufficiently implemented and scaled up in low- and middle-income countries. Tackling NCDs in general
must be an integral part of the immediate response to COVID-19 and of the recovery at global, regional
and national levels, as well as part of the strategies to build back better.
36. Pathway analyses show that every country still has options today for achieving target 3.4 of
Sustainable Development Goal 3. No country could achieve the target by addressing only prevention or
only counselling, screening, early diagnosis and appropriate treatment of NCDs.
1
WHO. Mental health & COVID-19 (https://www.who.int/teams/mental-health-and-substance-use/covid-19,
accessed 30 October 2020).
2
WHO. Public spending on health: a closer look at global trends. Geneva: World Health Organization;
2018 (https://apps.who.int/iris/handle/10665/276728), p. 29.
3
Seventy-first World Health Assembly. Preparation for the third High-level Meeting of the General Assembly on the
Prevention and Control of Non-communicable Diseases, to be held in 2018: report by the Director-General. Geneva: World
Health Organization; 2018. Document A71/14, Table 5, row (v) (https://apps.who.int/iris/handle/10665/276368).
EB148/7
9
37. The final report of WHO’s Independent High-level Commission on Non-communicable Diseases
1
recommended a specific set of the most effective and feasible interventions that should be considered
as a priority to accelerate progress towards target 3.4, reducing premature mortality from NCDs by one
third (Table 4).
Table 4. Interventions against specific risk factors and diseases
Risk factor or disease
2
Interventions
1
Tobacco use
• WHO mPOWER policy package
3
2
Excess sodium consumption
• WHO SHAKE technical package
3
Cervical, liver, colon and other
cancers
• Hepatitis B and human papillomavirus vaccination
• Detection, screening and treatment of cervical and preventable or
treatable cancers
4
Hypertension
• WHO HEARTS technical package for cardiovascular disease
5
Household air pollution
• World Bank: Household Energy for Cooking: Project Design
Principles
• WHO Guidelines for indoor air quality: household fuel
consumption
6
Consumption of industrially-
produced trans-fatty acids
• WHO REPLACE action package
• WHO protocol for measuring trans-fatty acids in foods
7
Harmful use of alcohol
• Taxation; limitation of places and hours of sale; restrictions on
marketing, promotion, and sponsorships
38. The report of the WHO/The Lancet’s NCD Countdown 2030 in 2020 showed that essential
components of any strategy to achieve target 3.4 of Goal 3 must include control of tobacco use and of
the harmful use of alcohol, detection and treatment of hypertension and diabetes, primary and secondary
prevention of cardiovascular diseases in high-risk individuals through multidrug treatment, and
bronchodilators and low-dose inhaled corticosteroids for asthma and selected patients with chronic
obstructive pulmonary disease.
4
39. Progress in noncommunicable diseases towards relevant targets needs a major boost. The
Secretariat is scaling up its programme on NCDs. The immediate aim is to catalyse tangible progress
towards target 3.4 within the next three years, especially through new and bold innovative solutions that
have a multiplier effect across the Sustainable Development Goals.
1
WHO. WHO Independent high-level commission on noncommunicable diseases: final report: it’s time to walk the
talk. Geneva: World Health Organization; 2019 (https://apps.who.int/iris/handle/10665/330023).
2
Physical inactivity is not included, owing to lack of adequate data.
3
Derived from key demand reduction measures in the WHO Framework Convention on Tobacco Control, thus
supporting the achievement of SDG target 3.a.
4
NCD Countdown 2030 collaborators. NCD Countdown 2030: pathways to achieving Sustainable Development
Goal target 3.4. The Lancet, 2020; 396(10255):918-934 (https://www.thelancet.com/action/showPdf?pii=S0140-
6736%2820%2931761-X, accessed 7 December 2020).

EB148/7
10
40. A major contribution to attaining target 3.4 will come from WHO’s new initiative to eliminate
cervical cancer in the next 100 years and reaching the 90-70-90 triple-intervention target by 2030:
• 90% of girls fully vaccinated against human papillomavirus by the age of 15 years;
• 70% of women screened using a high-performance test by the age of 35 years and again by the
age of 45 years;
• 90% of women identified with cervical disease receive treatment (90% of women with
pre-cancer treated and 90% of women with invasive cancer managed).
41. The Secretariat will develop similar strategic cross-cutting initiatives for diabetes, childhood
cancer and breast cancer.
42. The current capacities for NCD surveillance remain inadequate in many countries and urgently
require strengthening. Currently, many countries have few usable mortality data and weak information
on risk factor exposure and morbidity. Data on NCDs are often not well integrated into national health
information systems. Improving country-level surveillance and monitoring remains a top priority in the
fight against NCDs. The Secretariat will continue to support the scaling up of national efforts to
strengthen NCD surveillance and data systems, and expand the provision of strategic information for
policy-making, service provision and accountability.
43. Other organizations in the United Nations system are also committed to aligning their relevant
activities with the comprehensive United Nations response to COVID-19, for example through:
(i) raising national awareness on the return on investment in NCD prevention and treatment so as to
secure domestic budgetary allocations and international finance; (ii) supporting countries in including
NCDs into their socioeconomic plans for the COVID-19 response; and (iii) participating in the WHO
Working Group on COVID-19 and NCDs. The United Nations Inter-Agency Task Force on the
Prevention and Control of NCDs and the Global Action Plan for Healthy Lives and Well-being for All
continue to provide important platforms for many United Nations organizations to work through.
PREPARATORY PROCESS LEADING TO THE FOURTH HIGH-LEVEL MEETING
OF THE UNITED NATIONS GENERAL ASSEMBLY ON THE PREVENTION AND
CONTROL OF NCDs IN 2025
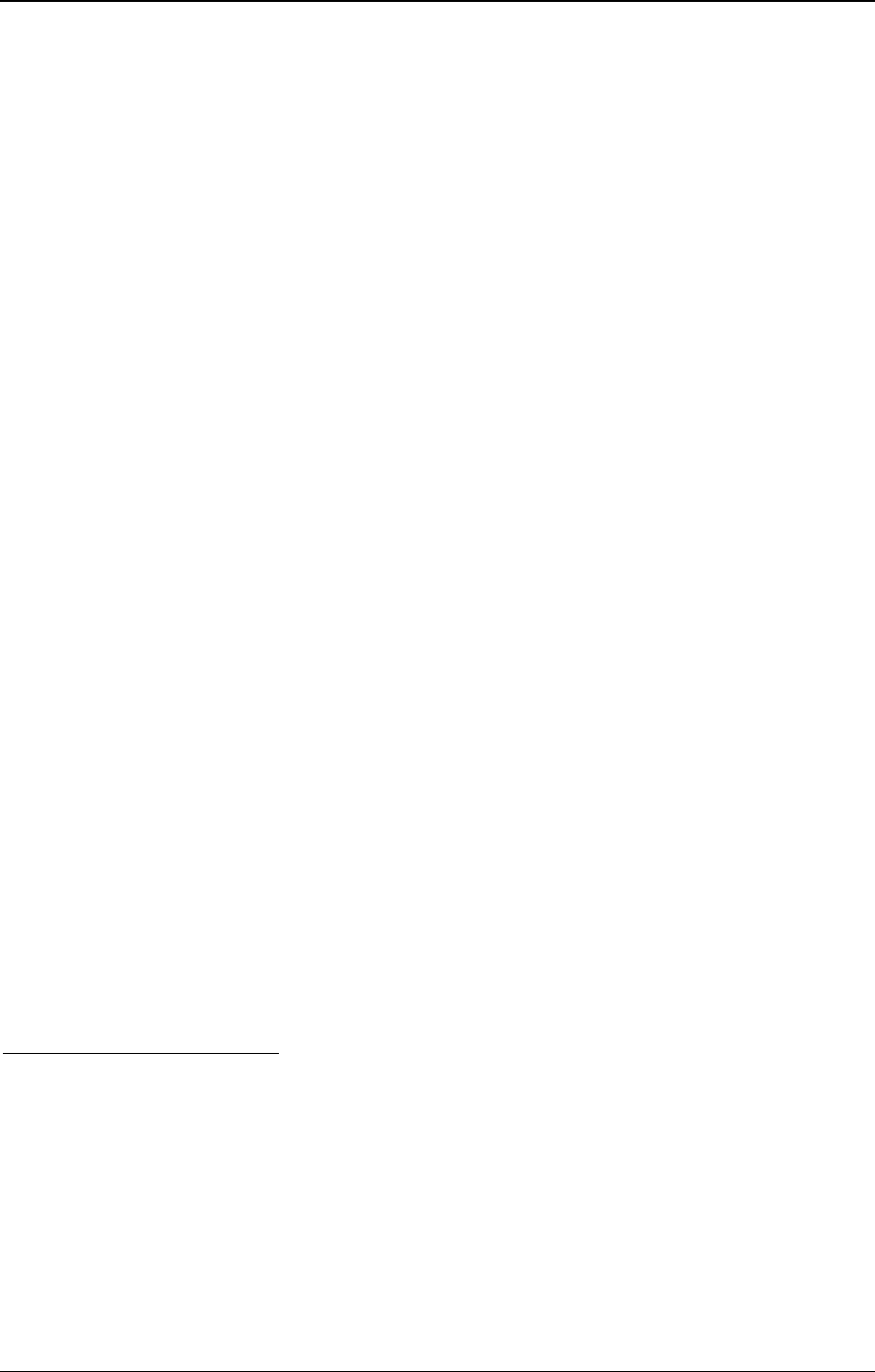
44. Table 5 sets out the process and scheduled meetings in preparation for the fourth high-level
meeting of the General Assembly on the prevention and control of non-communicable diseases.
Outcomes will serve as an input into the process.
Table 5. Meetings planned to prepare for the fourth high-level meeting of the General Assembly
on the prevention and control of non-communicable diseases
2021
• Second WHO global dialogue on financing national NCD responses
• Ninth session of the Conference of the Parties to the WHO Framework Convention on Tobacco Control
• Second Session of the Meeting of the Parties to the Protocol to Eliminate Illicit Trade in Tobacco
Products
2022
EB148/7
11
• Third WHO global meeting of national NCD Programme Directors and Managers
2023
• First WHO global ministerial conference for Small Island Development States on the prevention and
control of NCDs
• Tenth session of the Conference of the Parties to the WHO Framework Convention on Tobacco Control
• Third Session of the Meeting of the Parties to the Protocol to Eliminate Illicit Trade in Tobacco Products
2024
• Third WHO global ministerial conference on the prevention and control of NCDs
2025
• United Nations dialogue with civil society and the private sector
• Fourth high-level meeting of the General Assembly on the Prevention and Control of Non-communicable
Diseases
EVALUATIONS
45. In accordance with paragraph 60 of the Global action plan for the prevention and control of
noncommunicable diseases 2013–2020, in 2019 the Secretariat convened a representative group of
stakeholders, including Member States and international partners, to conduct a mid-point evaluation of
implementation of the global action plan. Its purpose was to assess progress towards the six objectives
of the global action plan and identify the lessons learned throughout its implementation by Member
States, by international partners and by the three levels of the Organization. The evaluation aimed to
document successes and identify challenges and gaps in the implementation of the global action plan
since 2013; to make strategic recommendations for improving implementation up until 2030; and to
provide inputs into WHO’s next global status report on noncommunicable diseases and other relevant
reports. The Secretariat’s Evaluation Office will submit an executive summary of the mid-point
evaluation to the Seventy-fourth World Health Assembly, through the Executive Board (see document
EB148/7 Add.1).
46. As specified in the terms of reference for the Global coordination mechanism on the prevention
and control of noncommunicable diseases,
1
a final evaluation of the mechanism took place in 2020 in
order to assess its effectiveness, its added value and its continued relevance to the achievement of the
2025 voluntary global targets, including its possible extension. The Evaluation Office will submit an
executive summary of the final evaluation to the Seventy-fourth World Health Assembly, through the
Executive Board (see document EB148/7 Add.2).
47. In line with the terms of reference of the United Nations Inter-Agency Task Force on the
Prevention and Control of NCDs, the evaluation of its contribution to the implementation of WHO’s
Global Action plan was described in the mid-point evaluation of that plan.
1
Document A67/14 Add.1, Appendix 1.

EB148/7
12
ACTION BY THE EXECUTIVE BOARD
48. The Board is invited:
• to note the report and its annexes;
• to provide guidance on the continued relevance of WHO’s Global action plan for the prevention
and control of noncommunicable diseases and on any corrective measures which may be taken
where actions have not been effective, and to reorient parts of the plan, as appropriate, in
response to the 2030 Agenda on Sustainable Development and/or the United Nations
Comprehensive Response to COVID-19, as appropriate;
• to provide guidance on the continued relevance of WHO’s Global coordination mechanism for
the prevention and control of noncommunicable diseases and the possible extension of its
lifespan, taking into account the evaluation mentioned in paragraph 46, and decision
WHA72(11) (2019), which extended the lifespan of WHO’s Global action plan for the
prevention and control of non-communicable diseases 2013–2020 to 2030.
49. The Board is further invited to consider the following draft decision:
The Executive Board, having considered the report of the Director-General on the political
declaration of the third high-level meeting of the General Assembly on the prevention and control
of non-communicable diseases,
1
decided to recommend to the Seventy-fourth World Health
Assembly the adoption of the following decision:
The Seventy-fourth World Health Assembly, having considered the report of the
Director-General, decided to adopt the proposed updates to the appendices of WHO’s
comprehensive mental health action plan 2013–2030 (contained in document EB148/7,
Annex 5, appendices 1 and 2).
1
Document EB148/7.
EB148/7
13
ANNEX 1
CANCER PREVENTION AND CONTROL IN THE CONTEXT OF AN
INTEGRATED APPROACH
1. In 2017, the Seventieth World Health Assembly adopted resolution WHA70.12 (2017) on cancer
prevention and control in the context of an integrated approach and requested the Director-General: to
develop, before the end of 2019, the first periodic public health- and policy-oriented world report on
cancer; to prepare a comprehensive technical report on pricing approaches and their impact on the
availability and affordability of cancer medicines; to develop tool kits to establish and implement
comprehensive cancer prevention and control programmes; to strengthen the capacity of the Secretariat
both to support the implementation of cost-effective interventions and country-adapted models of care
and to work with international partners; and to provide technical assistance, including support for the
establishment of centres of excellence. This annex describes progress made in implementing the
resolution.
2. The Secretariat has undertaken the following activities.
3. WHO report on cancer.
1
The report and accompanying cancer country profiles
2
were launched
on World Cancer Day (4 February 2020), in coordination with the launch by the International Agency
for Research on Cancer of its World Cancer Report on cancer research for cancer prevention. The
content of both documents was harmonized.
4. The WHO report included an investment case for cancer, in line with the mandate from resolution
WHA70.12, that demonstrated every US$ 1 invested in cancer control yields a full social return based
on both direct productivity and societal gains of US$ 9.50. By investing US$ 2.70 per person in
low-income countries, US$ 3.95 per person in lower-middle-income countries and US$ 8.15 per person
in upper-middle-income countries, an additional 7.3 million lives could be saved by 2030.
5. Technical report on cancer medicine pricing approaches. The requested comprehensive
technical report on pricing of cancer medicines and its impacts was submitted to and noted by the
Executive Board at its 144th session.
3
In 2020 WHO updated the WHO guideline on country
pharmaceutical pricing policies to support national policy development and implementation.
4
6. Toolkit for cancer prevention and control. Among its multiple toolkits to support Member
States with cancer policy formulation and guidance, WHO, working with the International Agency for
1
WHO. WHO report on cancer: setting priorities, investing wisely and providing care for all. Geneva: World Health
Organization; 2020 (https://apps.who.int/iris/handle/10665/330745).
2
WHO cancer country profiles. Geneva: World Health Organization; 2020 (https://www.who.int/cancer/country-
profiles/en/, accessed 30 October 2020).
3
Technical report: pricing of cancer medicines and its impacts: a comprehensive technical report for the World
Health Assembly Resolution WHA70.12 (2017): operative paragraph 2.9 on pricing approaches and their impacts on
availability and affordability of medicines for the prevention and treatment of cancer. Geneva: World Health Organization;
2020 (https://apps.who.int/iris/handle/10665/277190) and document EB144/2019/REC/2, summary records of the tenth
meeting.
4
WHO. WHO guideline on country pharmaceutical pricing policies, 2nd ed. Geneva: World Health Organization;
2020 (https://apps.who.int/iris/handle/10665/335692).

EB148/7 Annex 1
14
Research on Cancer, has developed one that is linked to the OneHealth tool.
1
It allows for stepwise and
resource-stratified scale-up in cancer prevention and control for adult and childhood cancers. It provides
evidence on the most cost-effective interventions for all age groups and has been used to support five
Member States in implementing cancer interventions.
7. WHO, working with the International Atomic Energy Agency, issues guidance, providing a
framework for Member States to establish comprehensive cancer centres.
8. Technical support to countries. The Secretariat has provided broad technical support to Member
States in the development and formulation of comprehensive programmes and policies on cancer
prevention and control.
9. WHO collaborated with the International Atomic Energy Agency to support countries in enabling
radiotherapy procurement by prioritizing radiotherapy technology aligned with health system capacity.
Technical specifications for radiotherapy were jointly developed as part of inter-agency guidance on
technical specifications for radiotherapy equipment in cancer treatment.
10. WHO has also worked with the International Atomic Energy Agency to increase coordination and
support provided to Member States participating in an “imPACT review”. The imPACT methodology
has been revised to improve the service and to provide more effective and coordinated support to
Member States, including broad partner collaboration.
11. Elimination of cervical cancer. In resolution WHA73.2 (2020), the Seventy-third World Health
Assembly adopted the global strategy to accelerate the elimination of cervical cancer as a public health
problem. The global strategy outlines the 90-70-90 targets to be reached by 2030, on the basis of human
papillomavirus vaccination, screening, and treatment of pre-invasive and invasive cancers, including
palliative care. For the third target of the global strategy (the appropriate management of 90% of women
identified with invasive cervical cancer), the Secretariat is preparing a framework for strengthening and
scaling-up services for the management of invasive cervical cancer.
12. WHO global initiative for childhood cancer. In September 2018, this global initiative was
launched. It aims to double the probabilities of survival from childhood cancer, which would save one
million more lives by 2030, by improving access to and quality of services including treatment and
palliative care. A technical package, CureAll, will be launched in 2021. Support to Member States has
started in 12 countries.
2
13. Collaboration with stakeholders. The Secretariat has strengthened engagement with broad
multisectoral stakeholders within and beyond existing WHO initiatives. This has included enhanced
coordination between the International Agency on Cancer Research and WHO at the management and
working levels, as reflected in the development of standard operating procedures and routine
communication on IARC Handbooks of Cancer Prevention.
3
1
OneHealth Tool. Geneva: World Health Organization; 2020 (https://www.who.int/choice/onehealthtool/en/,
accessed 30 October 2020).
2
Ghana, Mali, Morocco, Myanmar, Pakistan, Peru, Philippines, Senegal, Timor-Leste, Ukraine, Uzbekistan and
Zambia.
3
Coordination and Communication Mechanisms between IARC and WHO – at management and working levels.
Governing Council, Sixtieth Session (document GC/60/13). Lyon: International Agency for Research on Cancer; 2018
(https://governance.iarc.fr/GC/GC60/En/Docs/GC60_13_CoordinationWHO.pdf, accessed 30 October 2020).

Annex 1 EB148/7
15
14. The Secretariat has strengthened capacity, as requested, by increasing the number of staff working
on cancer prevention and control, with more than 20 new staff positions and consultancy posts, equally
distributed among all levels of the Organization. The result has been increased intensity and frequency
of support to Member States.
15. The Secretariat will continue to support Member States in their efforts to prevent, identify and
address cancer prevention and control through integrating cancer care within noncommunicable diseases
policies and programmes and broader work to strengthen national health systems as part of universal
health coverage.

EB148/7
16
ANNEX 2
GLOBAL STRATEGY ON DIET, PHYSICAL ACTIVITY AND HEALTH AND
GLOBAL ACTION PLAN ON PHYSICAL ACTIVITY 2018–2030
1. This annex sets out the progress made in implementing resolutions WHA57.17 (2004) on global
strategy on diet, physical activity and health and WHA71.6 (2018) on global action plan on physical
activity 2018–2030.
GLOBAL STRATEGY ON DIET, PHYSICAL ACTIVITY AND HEALTH:
PROGRESS TO DATE
2. To support Member States in implementing the set of recommendations on physical activity, the
Secretariat produced a series of supporting global technical resources. In addition, regional technical
tools and resources supported policy action across key settings and populations.
3. In 2010, WHO launched the first global recommendations on physical activity for health
1
outlining the substantial range of health benefits of regular physical activity for different age groups.
These guidelines affirmed the substantial health benefits of regular physical activity for healthy growth
and development, prevention of leading noncommunicable diseases and injuries, and improvement of
mental health and well-being.
4. In 2013, the Health Assembly agreed the first global target to reduce physical inactivity by 10%
by 2025 as part of the set of nine voluntary targets to reduce noncommunicable disease by 2025.
2
The
global action plan for the prevention and control of noncommunicable diseases 2013–2020 had
identified public awareness campaigns as a cost-effective intervention (“best buy”), and in 2017 an
updated set of best buys identified an extended set of effective interventions
3
to increase population
levels of physical activity across the life course.
5. In all regions, technical support and multi-country training were developed and capacity-building
workshops conducted, resulting in an increasing number of countries developing national policies or
plans and surveillance. In addition, countries across all regions commenced, or updated, their
surveillance of physical activity in adults and, to a lesser extent, adolescents.
6. Although in all WHO regional offices limited human and financial capacity dedicated to physical
activity constrained the pace and scale of technical assistance to countries, the Regional Office for
1
WHO. Global recommendations on physical activity for health. Geneva: World Health Organization; 2010
(https://apps.who.int/iris/handle/10665/44399).
2
Resolution WHA66.10 (2013).
3
WHO. Tackling NCDs: “best buys” and other recommended interventions for the prevention and control of
noncommunicable diseases. Geneva: World Health Organization; 2017 (https://apps.who.int/iris/handle/10665/259232).
Annex 2 EB148/7
17
Europe developed a regional strategy on physical activity for the period 2016–2025
1
and the Regional
Office for the Eastern Mediterranean issued a regional call for action.
2
7. In 2016, the Commission on Ending Childhood Obesity reaffirmed the importance of addressing
physical inactivity in children, especially young children.
3
Its subsequent implementation plan
4
called
for countries to prioritize and strengthen the promotion of physical activity to children through schools
and child care, to parents and families, and through supportive urban design and transport systems.
8. Throughout the period 2004–2016, the global strategy contributed to increased recognition
globally of the importance of regular physical activity. Overall, however, the impact on the development
and implementation of national policy and approaches was slow and uneven, and mostly limited to
high-income countries. Rising concerns about the lack of progress in reducing levels of physical
inactivity and the apparent widening of disparities prompted the request for a global action plan on
physical activity, drawing on the latest scientific evidence on effective approaches and aligned with the
goals of the 2030 Agenda for Sustainable Development.
GLOBAL ACTION PLAN ON PHYSICAL ACTIVITY 2018–2030: PROGRESS TO DATE
9. In resolution WHA71.6 (2018), the Seventy-first World Health Assembly endorsed the global
action plan on physical activity 2018–2030, which provided an updated set of 20 evidence-based policy
recommendations for accelerating progress towards the interim 2025 target, namely a 10% improvement
in physical activity.
10. The Health Assembly requested five specific actions: (1) implementation of the actions for the
Secretariat in the global action plan, including providing necessary support to Member States for
implementation of the plan, in collaboration with other relevant partners; (2) finalization of a monitoring
and evaluation framework on the implementation of the global action plan; (3) production of a global
status report on physical activity, building on the latest evidence including that on sedentary behaviours;
(4) updating the global recommendations on physical activity for health 2010; and (5) reporting on
progress made in implementing the global action plan to the Health Assembly in 2021, 2026 and 2030.
The following paragraphs respond to that request and outline key priorities for the remainder of the
biennium 2020–2021 and challenges and opportunities for promoting physical activity.
1
WHO Regional Office for Europe. Physical activity strategy for the WHO European Region 2016–2025. World
Health Organization. Regional Office for Europe; 2016 (https://apps.who.int/iris/handle/10665/329407).
2
WHO Regional Office for the Eastern Mediterranean. Promoting physical activity in the Eastern Mediterranean
Region through a life-course approach. Cairo: World Health Organization Regional Office for the Eastern Mediterranean;
2014 (https://apps.who.int/iris/handle/10665/116901).
3
See decision WHA69(12) (2016).
4
Welcomed by the Health Assembly in decision WHA70(19) (2017). Geneva: World Health Organization; 2018
(https://apps.who.int/iris/handle/10665/275415).
EB148/7 Annex 2
18
Responding to requests from Member States to support national efforts for implementing
the recommendations of the global action plan
11. In 2018, WHO launched ACTIVE: a technical package on effective interventions to promote
physical activity.
1
It provides guidance for Member States on how to plan, start and scale up the
implementation of the policy recommendations across the four strategic areas of the global action plan,
including strengthening governance and national policy frameworks and multisectoral collaboration.
12. Technical support on how to reduce disparities in physical activity between subpopulations will
be described in modules on promoting physical activity to older adults, people living with disabilities or
chronic disease, and strengthening community sport-health initiatives and partnerships.
13. At the regional level, tools and resources to support Member States’ actions on physical activity
and for sharing regional best practices have also been developed in priority areas including:
communication campaigns, health-promoting schools, counselling in primary health care, workplaces,
healthy ageing, and healthy cities.
14. Training courses have been held to strengthen skills and knowledge on physical activity within
context of health promotion and/or NCD prevention programmes at the global, regional and national
levels. Often these have been conducted in collaboration with WHO collaborating centres and supported
by stakeholders; during 2018–2019 more than 100 countries have participated.
15. New global comparative analyses of levels and trends in physical activity estimated that in 2016
one quarter of adults and three quarters of adolescents did not meet global recommendations, with
negligible improvements since 2001.
2
Furthermore, gender disparities between men and women, and
boys and girls, appeared to be widening.
Updating the global recommendations on physical activity for health 2010
16. In 2019–2020, the Secretariat completed the requested updating of the global recommendations
from 2010. The work was supported by a 27-member Guideline Development Group and included a
web-based public consultation.
17. WHO’s new guidelines on physical activity and sedentary behaviour
3
have been finalized for
children and adolescents (aged 5–17 years), adults (18–64 years), older adults (65 years and above) and
include, for the first time, specific recommendations on physical activity in subpopulations such as
pregnant women and those living with chronic conditions or disability. The guidelines are thus aligned
with the goals of the global action plan. The global launch took place on 25 November 2020.
4
1
WHO. ACTIVE: a technical package for increasing physical activity. Geneva: World Health Organization; 2018
(https://apps.who.int/iris/handle/10665/275415).
2
WHO. The Global Health Observatory: noncommunicable diseases: risk factors
(https://www.who.int/gho/ncd/risk_factors/physical_activity/en/, accessed 2 November 2020).
3
WHO. WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020
(https://apps.who.int/iris/handle/10665/336656).
4
WHO. Every move counts towards better health – says WHO (https://www.who.int/news/item/25-11-2020-every-
move-counts-towards-better-health-says-who, accessed 7 December 2020).

Annex 2 EB148/7
19
18. To support preparation and accelerate country adoption of the new global guidelines, virtual
workshops were held in each of WHO’s six regions (June–July 2020), bringing together more than
67 Member States responsible for national guideline development across multiple ministries. The
workshops and piloting of the adoption framework will support Member States to develop or update
their national physical activity guidelines.
Developing a global monitoring and evaluation framework to track progress on
implementation of a global action plan
19. In developing a monitoring and evaluation framework the Secretariat has included identification,
where possible, of existing indicators and data sources suitable for tracking progress on implementation
of the 20 policy recommendations (see paragraph 9 of this annex). Consultation with Member States
and relevant stakeholders began with an expert meeting in November 2018 and continues, for instance
with organizations in the United Nations development system, particularly United Nations Development
Programme, United Nations Educational, Scientific and Cultural Organization and United Nations
Human Settlements Programme (UN-Habitat), to ensure alignment with other relevant monitoring
frameworks and Sustainable Development Goals.
20. The framework, comprising a set of process, outcome and impact indicators, is scheduled for
publication as a technical report on the WHO website by the end of 2020.
Global status report on physical activity
21. Preparation of the requested first global status report on physical activity began in parallel with
work on the monitoring and evaluation framework. During 2019–2020 relevant data, including those
from WHO’s global survey in 2019 of national capacity for NCD prevention and control
1
and WHO’s
road safety survey 2018,
2
were analysed.
22. Workplans for 2020, including proposed global and regional consultations, collection and launch
(scheduled for December 2020) of country best practice case studies, have been heavily disrupted by
COVID-19. Consequently, the publication of this report has been postponed to 2021 to allow for full
engagement of all relevant stakeholders.
23. The emerging findings reaffirm that progress on physical activity remains modest and uneven in
reach and scale between and within regions. Further, the rate of country implementation suggests that
continuing a “business as usual” approach is unlikely to achieve the global target of a 15% reduction in
the global prevalence of physical inactivity by 2030. Impediments to implementing recommended,
cost-effective actions at national and subnational levels must be identified and mitigated in order to
accelerate global progress and impact.
Major obstacles to increasing physical activity
24. Impediments identified across all regions include: (1) a lack of prioritization of policy on physical
activity within and beyond the health sector; (2) lack of human and financial resources within the
1
WHO. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2019
global survey. Geneva: World Health Organization 2020 (https://apps.who.int/iris/handle/10665/331452).
2
WHO. Global status report on road safety 2018. Geneva: World Health Organization; 2018
(https://apps.who.int/iris/handle/10665/276462).

EB148/7 Annex 2
20
Secretariat and countries to develop, disseminate and implement policy actions on physical activity;
(3) weak capacity to integrate approaches across multiple sectors and implement whole-of-system
approaches; and (4) insufficient capacity to engage and sustain civil society, research communities and
other key partners at national and subnational levels, particularly between health and relevant authorities
for sport, transport, urban planning, design and environment.
Accelerating increases in physical activity
25. In most Member States multiple opportunities exist to strengthen and accelerate actions aimed at
retaining or increasing physical activity, particularly through walking and cycling, with the achievement
of multiple other policy priorities. Areas of strong policy alignment include: healthy ageing; road safety;
climate change mitigation; air quality; environmental sustainability; liveable cities and communities;
and reduction of inequalities.
26. To support the scaling up of country efforts, WHO has strengthened partnership with
stakeholders, including the sport and technology sectors, and established dialogues with the relevant
private sector operators
1
to engage and align their efforts towards achieving common goals of the global
action plan.
27. Progress in implementation of the global action plan can also be accelerated by increased
investment in the promotion of physical activity to youth and adolescents; expansion of workforce
capacity and skills in the promotion of physical activity; strengthening national multisectoral
coordination; investment in research and knowledge transfer, particularly in low- and middle-income
countries; and removing social, environmental and economic barriers to participation.
Impact of COVID-19 on physical activity and responses
28. COVID-19 has had an unprecedented impact on how, where and for how long people can be
physically active. Ensuring that the importance and protective benefits of physical activity on mental
and physical health are recognized in countries’ responses to COVID-19 is vital, as is securing the
inclusion of policies that embed equitable opportunities for physical activity in strategies to “build back
better”.
1
WHO. Engagement with the private sector for SDG target 3.4 on NCDs and mental health
(https://www.who.int/ncds/governance/private-sector/en/, accessed 9 November 2020).

EB148/7
21
ANNEX 3
ENDING ALL FORMS OF MALNUTRITION
1. Sustainable Development Goal 2 (End hunger, achieve food security and improved nutrition and
promote sustainable agriculture) has set the ambitious targets to eliminate all forms of malnutrition by
the year 2030. The Health Assembly has been concerned about nutrition since its early years. In the past
two decades it has dealt with unhealthy diets through the global strategy on diet, physical activity and
health, endorsed in 2004 (resolution WHA57.17); all forms of malnutrition through the comprehensive
implementation plan on maternal, infant and young child nutrition, endorsed in 2012
(resolution WHA65.6 and later resolution WHA71.9 (2018) on infant and young child feeding); and the
implementation plan of the Commission on Ending Childhood Obesity, welcomed in 2017 (decision
WHA70(19)). The Health Assembly also endorsed the Rome Declaration, the outcome of the Second
International Conference on Nutrition in 2014 (resolution WHA68.19 (2015)), and progress on its
implementation has subsequently been reported biennially, together with the progress on the United
Nations Decade of Action on Nutrition, 2016–2025.
2. This annex provides an overview of the progress in the global nutrition situation and the policy
response and reports more specifically on the outcomes of the Second International Conference on
Nutrition. Progress in implementing resolutions WHA65.6 (2012) and WHA71.9 (2018) and decision
WHA70.19 (2017) are reported in greater detail in the biennial reports delivered in even years.
PROGRESS IN ACHIEVING GLOBAL TARGETS ON DIET AND NUTRITION
3. The concept of “all forms of malnutrition” is reflected in the global nutrition targets established
by the Health Assembly in 2012 (resolution WHA65.6),
1
which cover child wasting, stunting and
overweight; anaemia in women of reproductive age; low birth weight; and exclusive breastfeeding. The
first four targets are included in the formal monitoring system for the Sustainable Development Goals.
In addition, in 2013 the Health Assembly endorsed the global action plan for the prevention and control
of noncommunicable diseases 2013–2020 and adopted its nine voluntary global targets for 2025 in
resolution WHA66.10 (2013), including the targets of halting the rise in diabetes and obesity and
reducing the intake of salt/sodium.
4. The prevalence of adult obesity continues to rise in all WHO regions, from 11.8% in 2012 to
13.1% in 2016, so that the global target to halt the rise in obesity by 2025 is unlikely to be achieved.
Excessive salt consumption is still responsible for an estimated three million deaths from heart disease,
stroke and related causes.
5. In addition, in 2019, before the COVID-19 pandemic, almost 690 million people (8.9% of the
global population) were undernourished and two billion people (25.9% of the global population)
experienced hunger or did not have regular access to nutritious and sufficient food.
1
Document WHA65/2012/REC/1, Annex 2 (Comprehensive implementation plan on maternal, infant and young
child nutrition) (https://apps.who.int/gb/ebwha/pdf_files/WHA65-REC1/A65_REC1-en.pdf).

EB148/7 Annex 3
22
6. Unhealthy diets account for an additional 11 million deaths. Sub-optimal diets are now
responsible for 20% of premature (disease-mediated) mortality worldwide, as well as for 20% of all
disability-adjusted life years lost to ill-health.
PROGRESS IN THE IMPLEMENTATION OF FOOD AND NUTRITION POLICIES
7. WHO’s Global database on the Implementation of Nutrition Action
1
contains information on
national policies and strategies with nutrition goals, strategies or indicators in 194 Member States, of
which 180 have comprehensive or topic-specific nutrition policies (on, for example, healthy diet,
anaemia and breastfeeding). A third
Global Nutrition Policy Review is in process.
8. National strategies that include specific goals, objectives, and actions to promote healthy
diets. Most countries have adopted the global nutrition targets for 2025, covering for example stunting
(117 Member States), anaemia in women (104), low birth weight (119), child overweight (137),
exclusive breastfeeding (130) and wasting (111). The vast majority (186 Member States) include actions
to promote healthy diets in their national policies and strategies, aiming to reduce consumption of fats
(100 Member States), salt/sodium (142) or sugars (86). Population information policies through
counselling or media campaigns are more common (181 Member States) than those that seek to change
the food environment through nutrition labelling, marketing restrictions, fiscal policies or
reformulation (156).
9. Labelling and health claim. Nutrition labelling was the intervention that saw the largest increase
between WHO’s first and second global nutrition policy reviews in 2009–2010 and 2016–2017,
respectively. National nutrition-labelling legislation defines the details on the information that should
be available to consumers on pre-packaged food, including list of ingredients, nutrient declaration and
the health or nutrient claims producers make on labels. As reported to the second review, 73 countries
provided detailed information on their implementation of nutrient declaration and 69 countries on their
regulation of nutrition and health claims.
10. Promotion of food products consistent with a healthy diet. Reformulation of food and
beverage products is being implemented to reduce the content of saturated fatty acids, trans-fatty acids,
sugars and salt/sodium. The recent WHO report on global trans-fatty acid elimination 2020
2
found that
58 countries so far have introduced laws to eliminate trans-fatty acids from the food supply; if
successful, elimination will protect 3.2 billion people from those harmful substances by the end of 2021.
11. Fiscal policies. Currently 73 Member States impose taxes on sugar-sweetened beverages,
although the definitions, type and level of tax and range of products covered vary greatly. Twenty-nine
Member States identify subsidies on healthy foods and beverages (for instance, fruits and vegetables)
as suitable approaches to support healthy diets in their national strategies.
1
WHO. Global database on the Implementation of Nutrition Action (GINA)
(https://extranet.who.int/nutrition/gina/en).
2
WHO. News release: more than 3 billion people protected from harmful trans fat in their food. Geneva: World
Health Organization; 2020 (https://www.who.int/news/item/09-09-2020-more-than-3-billion-people-protected-from-harmful-
trans-fat-in-their-food, accessed 7 December 2020).

Annex 3 EB148/7
23
12. Food programmes. Among the respondents to the Global Nutrition Policy Review 2016–2017,
1
85 countries reported food distribution programmes as part of their social safety nets employed to
address underlying causes of malnutrition, typically either emergency food aid programmes or special
foods for infants and young children (or both).
13. School policies and programmes. The Global Nutrition Policy Review 2016–2017
recommended the strengthening of school health and nutrition programmes to ensure nutrition-friendly
schools where policies, curriculum, environments and services are designed to promote healthy diets
and support good nutrition. Most countries (89% of 160) reported having school health and nutrition
programmes, but individual components of school programmes had largely deteriorated since the first
Global Nutrition Policy Review in 2009–2010.
14. Health and other services. Among respondents to the Global Nutrition Policy Review
2016–2017, 153 countries reported employing nutrition professionals (that is, trained nutritionists or
dieticians). However, the density was low (particularly in the African Region) – six countries had no
nutrition professionals, and the global median among 126 countries providing details was only
2.3 trained nutrition professionals per 100 000 population. Pre-service and in-service training of health
professionals in maternal, infant and young child nutrition was reported to be offered in 140 countries,
although the number of hours in the pre-service curriculum dedicated to this topic was generally less
than the number of hours dedicated to this subject area in WHO’s breastfeeding training course curricula.
SECOND INTERNATIONAL CONFERENCE ON NUTRITION AND THE UNITED
NATIONS DECADE OF ACTION ON NUTRITION
15. Following up on the outcomes of the Second International Conference on Nutrition, governments,
organizations in the United Nations system, civil society and the private sector have been active in
improving awareness and stimulating action to respond to a new nutritional reality characterized by all
forms of malnutrition. A second report of the United Nations Secretary-General on the implementation
of the United Nations Decade of Action on Nutrition was published on 13 April 2020.
2
Mid-term review
16. In keeping with the United Nations Economic and Social Council’s resolution E/RES/1989/84 on
international decades, commitments made in the Rome Declaration on Nutrition should be reviewed at
mid-term and at the end of the Decade of Action on Nutrition, in an open and participatory process.
17. The mid-term review foresight paper
3
summarizes the progress in the six action areas of the
Decade:
(a) Sustainable, resilient food systems for healthy diets. In growing numbers, high-level
reports and resolutions have underlined the crucial role of sustainable, resilient food systems for
1
WHO. Global Nutrition Policy Review 2016–2017: country progress in creating enabling policy environments for
promoting healthy diets and nutrition. Geneva: World Health Organization. 2018
(https://apps.who.int/iris/handle/10665/275990).
2
UN General Assembly. Implementation of the United Nations Decade of Action on Nutrition (2016–2025).
New York: United Nations; 2020 (https://undocs.org/en/A/74/794).
3
United Nations Decade of Action on Nutrition (2016-2025). Mid-term review foresight paper
(https://www.who.int/docs/default-source/nutritionlibrary/departmental-news/mid-term-review---un-decade-of-action-on-
nutrition/nutrition-decade-mtr-foresight-paper-en.pdf?sfvrsn=c3c14085_8, accessed 7 December 2020).

EB148/7 Annex 3
24
healthy diets and improved nutrition. Numerous alliances have been established to bring together
different actors, beyond the traditional nutrition actors, for sustainable food systems. Recognition
of agroecology and biodiversity, increased consideration of sustainability issues in national
food-based dietary guidelines, growing implementation of measures to reduce food loss and
waste, and action to enhance resilience of the food supply in crisis-prone areas have been noticed.
Measures to reduce or eliminate industrially-produced trans-fatty acids have been accelerated,
and voluntary or mandatory reformulation of processed food products has been carried out to
reduce their salt/sodium content.
(b) Aligned health systems providing universal coverage of essential nutrition actions. A
clear understanding of the effective interventions to be delivered by health systems has emerged
during the first half of the Decade, but there has been significant under-investment in both
ensuring adequate coverage of high-impact nutrition interventions and improving their quality.
To accelerate progress on wasting in children under five years of age, a United Nations global
action plan on child wasting: a framework for action to accelerate progress in preventing and
managing child wasting and the achievement of the Sustainable Development Goals
1
was
published on 9 March 2020. This plan will enable organizations of the United Nations
development system to develop a more targeted road map for action in 2021. Strong health
systems are needed to deliver nutrition actions, and the increasing political momentum for
achieving universal health coverage presents new opportunities for expanding coverage and for
mainstreaming WHO’s essential nutrition actions
2
through the life-course.
(c) Social protection and nutrition education. The contributions of social protection to food
security and nutrition will depend on its integration at policy level. To ensure that social protection
policies holistically combat all forms of malnutrition, a nutrition-sensitive approach needs to be
applied in their design and implementation. Policy measures for improving food access, social
protection and food assistance are prevalent in some WHO regions, while in other WHO regions
this continues to be an area of under-investment. Nutrition education is widely implemented in
schools, but policies to ensure that education is supported by healthy school environments are
lacking and implementation of school health and nutrition programmes has deteriorated in recent
years. Although most countries train health workers on nutrition, the level of training is often
inadequate and, more generally, nutrition action continues to be hampered by a lack of trained
nutrition professionals. The potential of multi-component school-based programmes to educate
about food and nutrition has been increasingly recognized as an important programmatic area for
sustainable development.
(d) Trade and investment for improved nutrition. Trade can be a key element in enhancing
food security and nutrition, but there has been increasing recognition of the need for coherence
between trade policy and nutrition action and the importance of governance and cross-sectoral
cooperation. A finance gap persists, despite the need for responsible and sustainable investments
in agriculture and food systems. Certain global value chains and agri-food industries currently
produce environmentally unsustainable food products which commonly are rich in unhealthy fats,
sugars and/or salt/sodium. Increased globalization of the food supply means populations are more
1
WHO. Global action plan on child wasting: a framework for action to accelerate progress in preventing and
managing child wasting and the achievement of the Sustainable Development Goals. Geneva: World Health Organization;
2020 (https://www.who.int/publications/m/item/global-action-plan-on-child-wasting-a-framework-for-action, accessed
7 December 2020).
2
WHO. Essential nutrition actions: mainstreaming nutrition through the life-course. Geneva: World Health
Organization; 2019 (https://apps.who.int/iris/handle/10665/326261).

Annex 3 EB148/7
25
exposed to different food hazards. Rather than driving healthy diets, trade and investment policies
are exacerbating malnutrition in all its forms. Increased foreign direct investment, for example,
has been linked to higher consumption of sugar-sweetened beverages. Prioritizing health over
short-term economic gain has been shown to lead to greater economic gains in the long term.
(e) Safe and supportive environments for nutrition at all ages. Creation of healthy food
environments – encompassing availability, affordability, promotion and quality of food
supporting healthy diets – has become a central consideration in nutrition policy-making. There
is increasing momentum for the creation of healthy urban environments, with food environments
an important element. Policies to create healthy food environments in schools, to protect and
support breastfeeding or to fortify staple foods with micronutrients are widespread, although their
implementation is often inadequate. Implementation of fiscal policies to promote healthy diets
(particularly taxes on sugar-sweetened beverages) has accelerated over the first half of the
Decade. There remains much scope to scale up and improve regulation of the marketing of foods
and non-alcoholic beverages to children, strengthen the focus on adolescent nutrition and
effectively integrate nutrition and water, sanitation and hygiene programmes.
(f) Strengthened governance and accountability for nutrition. Generating commitments
and new financing for nutrition has progressed significantly. Despite considerable advances,
however, the inadequate and highly variable progress towards the global nutrition and diet-related
NCD targets reflects insufficient action to strengthen nutrition governance, policy and
accountability systems. It also points to a persistent gap in global nutrition financing and the
implementation of policy, legislative and regulatory measures, including fiscal measures as
appropriate, aimed at ending all forms of malnutrition. Donor funding for nutrition increased
during the first half of the Decade, but it is estimated that an additional US$ 7 billion is needed to
achieve the global nutrition targets. Improved global data now identify those regions and countries
that are progressing or falling behind, but weak or non-existent nutrition information systems and
insufficient data – particularly on nutritional status in specific groups and over a long enough
period to track trends – remain a substantial challenge.
Contributions by different actors
18. Member States. Action by Member States is described above (paragraphs 7–17). No additional
formal commitments have been made to the Decade besides those already published.
19. The Decade encourages United Nations Member States to strengthen collaboration on nutrition
action by establishing action networks, which are informal coalitions of countries, with global or
regional scope, aimed at accelerating and aligning efforts around specific topics linked to the Decade’s
Work Programme. Led and coordinated by one or more countries, the action networks allow countries
to exchange knowledge and good practices, successes and challenges, and provide mutual support to
accelerate progress with the objective of improving food systems, diets and nutrition for all through
policies and legislation.
1
To date, the following global action networks have been convened under the
Decade:
(a) Global Action Network on Sustainable Food from the Oceans and Inland Waters for Food
Security and Nutrition – lead country: Norway.
1
United Nations Decade of Action on Nutrition 2016-2025. Action networks. New York: United Nations
(www.un.org/nutrition/action-networks, accessed 2 November 2020).

EB148/7 Annex 3
26
(b) Global Action Network on Nutrition Labelling – lead countries: Australia, Chile and
France.
(c) Global Action Network on Traditional, Healthy and Sustainable Diets – lead country: Italy.
20. In October 2019, Germany announced plans to form a world coalition on healthy school meals.
Brazil and Sri Lanka are jointly developing a work programme.
21. Additionally, several regional networks have been convened for the Americas and the Pacific,
namely:
(a) Regional Action Network on Strategies for Reducing Salt Consumption for the Prevention
and Control of Cardiovascular Disease in the Americas – lead countries: Brazil, Colombia and
Costa Rica.
(b) Regional Action Network on Food Guidelines for the Region of the Americas – lead
countries: Brazil and Uruguay.
(c) Regional Action Network for the Americas on Food and Nutrition Security Governance –
lead country: Brazil.
(d) Regional Action Network for the Americas on Public Purchasing of Family-produced
Food – lead country: Brazil.
(e) Regional Action Network for the Americas on Sustainable School Feeding – lead country:
Brazil.
(f) Regional Action Network for the Americas on Healthy Food Environments – lead country:
Chile.
(g) Regional Action Network for Ending Childhood Obesity in the Pacific – lead country: Fiji
22. In order to support the implementation of the Decade, the Food and Agriculture Organization and
WHO published in 2018 a guide
1
for countries to translate the policies and actions recommended in the
Framework for Action of the Second International Conference on Nutrition into country-specific
commitments and a policy brief
2
on driving commitment for nutrition within the Decade.
23. Organizations in the United Nations system have contributed to the Decade in accordance with
their respective mandates. The Food and Agriculture Organization focuses on the role of agriculture
1
FAO, WHO. Strengthening nutrition action: a resource guide for countries based on the policy recommendations of
the Second International Conference on Nutrition (ICN2). Rome and Geneva: Food and Agriculture Organization of the
United Nations and World Health Organization; 2018 (www.fao.org/3/ca1505en/CA1505EN.pdf, accessed
3 November 2020).
2
WHO, FAO. Driving commitment for nutrition within the UN Decade of Action on Nutrition: policy brief. Geneva:
World Health Organization; 2018 (https://www.who.int/publications/i/item/WHO-NMH-NHD-17.11, 12 January 2021).
Annex 3 EB148/7
27
and food systems in reducing malnutrition. Its strategy and vision for its work in nutrition
1
were
informed by the main challenges in nutrition and the Organization’s comparative strengths.
24. WHO published various normative products to support countries in the implementation of the
commitments made at the Second International Conference on Nutrition, including essential nutrition
actions, assessing and managing children at primary health care facilities to prevent overweight and
obesity, fortification of rice with vitamins and minerals,
2
effective actions for improving adolescent
nutrition,
3
and implementation guidance for the revised baby-friendly hospital initiative.
4
25. The International Atomic Energy Agency has focused on strengthening collective actions
across organizations, countries and communities to accelerate work on tackling the double burden of
malnutrition, in particular in assessing the impact of programmes and initiatives targeting that double
burden. Furthermore, attention needs to be paid to the role of stable isotope techniques in understanding
biological pathways.
26. The International Fund for Agricultural Development issued in 2019 its nutrition action plan
2019–2025,
5
with the overall objective to accelerate mainstreaming of nutrition in its investments and
to realize its commitment to increasing the target of mainstreaming nutrition into 50% of projects in
their design stage and improve the nutrition of 12 million people by 2021.
27. The vision of UNICEF’s strategic plan for 2018–2021
6
is to consolidate and expand the
programmatic gains of addressing child malnutrition in all its forms around the world, in order to meet
by 2021 three annual targets of reaching at least: (i) 250 million children under five years of age with
services to prevent stunting and other forms of malnutrition; (ii) 100 million adolescents with services
to prevent anaemia and other forms of malnutrition; and (iii) 6 million children with services to treat
severe wasting and other forms of acute malnutrition in development and humanitarian contexts.
28. The World Food Programme continued delivering optimal nutrition programming on treatment
and prevention as an emergency response, while integrating nutrition-sensitive approaches across the
humanitarian-development nexus.
29. The United Nations Standing Committee on Nutrition continued working towards maximizing
coherence of United Nations policies and accountability, with advocacy for nutrition, building bridges,
exploring new and emerging nutrition-related issues in collaboration with its members and through
various knowledge products.
1
FAO. Strategy and vision for FAO’s work in nutrition. Rome: Food and Agriculture Organization of the United
Nations; 2014 (http://www.fao.org/3/a-i4185e.pdf).
2
WHO. Guideline: fortification of rice with vitamins and minerals as a public health strategy. Geneva: World Health
Organization; 2018 (https://apps.who.int/iris/handle/10665/272535).
3
WHO. Guideline: implementing effective actions for improving adolescent nutrition. Geneva: World Health
Organization; 2018 (https://apps.who.int/iris/handle/10665/260297).
4
WHO, UNICEF. Implementation guidance: protecting, promoting and supporting breastfeeding in facilities
providing maternity and newborn services: the revised baby-friendly hospital initiative. Geneva: World Health Organization;
2018 (https://apps.who.int/iris/handle/10665/272943).
5
IFAD. Mainstreaming nutrition in IFAD: Nutrition action plan 2019-2025. Rome: International Fund for
Agricultural Development; 2019 (www.ifad.org/en/document-detail/asset/41237860, accessed 3 November 2020).
6
UNICEF strategic plan, 2018-2021 (https://www.unicef.org/reports/unicef-strategic-plan-20182021, 12 January
2021).

EB148/7 Annex 3
28
30. The United Nations Inter-Agency Task Force on Non-communicable Diseases, through its
thematic working group on nutrition convened by the Standing Committee on Nutrition, continued to
work on all forms of malnutrition.
31. The 2019 report of the Special Rapporteur on the Right to Food to the General Assembly
focused on the Sustainable Development Goals
1
through a human rights-based approach to nutrition
policies, emphasizing in particular the inequitable distribution of food and productive resources as a
significant barrier to the realization of the right to food and nutrition.
Non-State actors
32. Global initiatives. The Tokyo Nutrition for Growth Summit, postponed to December 2021,
2
will
provide an opportunity for taking stock and making new financial and policy commitments at the
mid-term of the Decade. It will bring together countries, donors and partners to present clear
commitments and demonstrate progress towards the targets endorsed by the Health Assembly and those
of the Sustainable Development Goals. It aims to obtain commitments in five priority areas: (1) health:
making nutrition integral to universal health coverage for sustainable development; (2) food: building
food systems that promote healthy diets and nutrition, ensure livelihoods of producers and are
climate-smart; (3) resilience: tackling malnutrition effectively in fragile and conflict-affected contexts;
(4) promoting data-driven accountability; and (5) securing new investment and driving innovation in
nutrition financing. In 2019, WHO led the development of the universal health coverage component of
the Nutrition for Growth’s commitment framework and published the Nutrition in UHC policy brief.
3
33. In 2021, United Nations will convene a Food Systems Summit as part of the Decade of Action.
The Summit will cover five action tracks: (1) ensuring access to safe and nutritious food for all (enabling
all people to be nourished and healthy, progressive realization of the right to food); (2) shifting to
sustainable consumption patterns (promoting and creating demand for healthy and sustainable diets,
reducing waste); (3) boosting nature-positive production at sufficient scale (acting on climate change,
reducing emissions and increasing carbon capture, regenerating and protecting critical ecosystems and
reducing food loss and energy usage, without undermining health or nutritious diets); (4) advancing
equitable livelihoods and value distribution (raising incomes, distributing risk, expanding inclusion,
promote full and productive employment and decent work for all); and (5) building resilience to
vulnerabilities, shocks and stress (ensuring the continued functionality of healthy and sustainable food
systems). WHO has been asked to be the anchor United Nations body for track (2).
1
UN Special Rapporteur on the right to food. Report on Sustainable development Goal 2 and the right to food.
Geneva: Office of the High Commissioner on Human Right; 2019
(https://www.ohchr.org/EN/Issues/Food/Pages/SDG2.aspx, accessed 7 December 2020).
2
Tokyo Nutrition for Growth Summit 2021 (https://nutritionforgrowth.org/events/, accessed 7 December 2020).
3
WHO. Nutrition in universal health coverage. Geneva: World Health Organization; 2019
(https://apps.who.int/iris/handle/10665/329493).

EB148/7
29
ANNEX 4
HEALTH AND THE ENVIRONMENT:
ADDRESSING THE HEALTH IMPACT OF AIR POLLUTION
1. This annex summarizes progress in the implementation of resolution WHA68.8 (2015) on
addressing the health impact of air pollution and the related road map for an enhanced global response
to the adverse health effects.
1
(For further information see the progress report submitted to the
Seventy-third World Health Assembly.)
2
2. Work has substantially advanced the development of knowledge products and tools to measure
the health effects and health-care cost of air pollution. These include the means to assess health impact
and health economic and sector-specific tools, at both national and subnational levels. The update of the
WHO air quality guidelines is at an advanced stage.
3. WHO has reported and will continue to report regularly on three air pollution-related Sustainable
Development Goal indicators: 3.9.1 (mortality rate attributed to household and ambient air pollution),
7.1.2 (proportion of population with primary reliance on clean fuels and technology) and 11.6.2 (annual
mean levels of fine particulate matter (for example, PM2.5 and PM10) in cities (population weighted)).
To further support countries in monitoring these indicators, the Secretariat has developed more robust
statistical methods and enhanced survey tools to better assess the health impacts of ambient air pollution
and household energy use.
4. WHO’s databases on ambient air pollution and household energy have been updated regularly
and expanded to include more locations, pollutants and sources of exposure.
5. Advances have been made to raise the priority accorded to air pollution on regional agendas
through the development of regional plans of action and the creation of country air pollution and health
profiles in selected Member States at their request.
6. WHO, in collaboration with other organizations in the United Nations development system, has
developed the global BreatheLife Network to raise awareness about the scale and importance of air
pollution as a health risk and to share solutions and mobilize action. Since its launch in October 2016,
76 city, regional or country governments level have officially joined the BreatheLife Network; global
awareness was raised in 2018 through WHO’s First Global Conference on Air Pollution and Health.
With growing recognition of air pollution as a public health threat, countries are scaling up commitments
to implement air quality policies and to align climate and air quality. In 2018, at the first WHO
international conference on air pollution and health, 26 countries, 12 cities, 11 organizations of the
United Nations development system, 39 nongovernmental organizations and the European Union
committed themselves to a range of interventions to address air pollution. At the United Nations Climate
Action Summit in 2019, 50 countries with more than one billion people committed themselves to
reaching WHO air quality guideline values and aligning climate and air quality policies by 2030.
1
Welcomed by the Health Assembly in decision WHA69(11) (2016)
(https://apps.who.int/gb/ebwha/pdf_files/WHA69-REC1/A69_2016_REC1-en.pdf#page=27, accessed 5 November 2020).
2
WHO. Progress reports. Seventy-third World Health Assembly, document A73/32, section I. Geneva: World Health
Organization; 2020 (https://apps.who.int/gb/ebwha/pdf_files/WHA73/A73_32-en.pdf, accessed 5 November 2020).

EB148/7 Annex 4
30
7. WHO, with other organizations of the United Nations development system, launched the Health
and Energy Platform for Action
1
at a side-event at the Seventy-second World Health Assembly in 2019.
The Platform aims to strengthen the political and technical cooperation between the health and energy
sectors at global, regional and country levels to accelerate the transition to clean energy, with an initial
focus on clean cooking and electrification of health care facilities.
8. One highly significant achievement is the recognition of air pollution as a fifth major risk factor
for NCDs at the third High-level Meeting of the General Assembly on prevention and control of
non-communicable diseases in 2018 and the inclusion of air pollution into multisectoral regional and
national NCD action plans. In this context the Secretariat has advanced its work on developing policy
options on ambient and household air pollution that will contribute to the achievement of the objectives
and voluntary global targets of the global action plan for the prevention and control of noncommunicable
diseases 2013–2020. The first phase of this work consists in compiling a compendium of WHO’s and
other United Nations’ guidance on health and environment, including air pollution. Subsequent in-depth
analyses of the effectiveness of existing interventions will draw on the compendium and other existing
WHO guidelines and recommendations.
9. Over the past years, WHO has been developing and enhancing a set of analytical tools to build
the evidence of the health and economic effects of air pollution, for instance the AirQ+ software tool
and sector-specific tools such as the health and economic assessment tool for walking and cycling. The
Secretariat has undertaken rapid situational assessments and stakeholder mappings for the Clean
Household Energy Solutions Toolkit in countries where reliance on the use of biomass for cooking
purposes is heavy. It is currently developing training materials for health-care professionals, aimed at
strengthening capacity to understand the risks of air pollution to health and to communicate them to
patients and communities.
10. The Secretariat has been working continuously to provide direct country support, with targeted
technical training workshops intended to enhance institutional capacities to address air pollution and
health. In addition, WHO has undertaken several joint missions with other United Nations bodies in
order to plan and enhance country support.
1
WHO, UNDP. Accelerating SGD 7 achievement: Action brief 2 – Global energy and health platform of action.
New York: United Nations, Department of Economic and Social Affairs, Division for Sustainable Development Goals; 2019
(https://sustainabledevelopment.un.org/content/documents/24066ab2_cover.pdf, accessed 8 December 2020).

EB148/7
31
ANNEX 5
UPDATES TO THE APPENDICES OF WHO’S COMPREHENSIVE
MENTAL HEALTH ACTION PLAN 2013–2030
1. In response to paragraph 3(a) of decision WHA72(11) (2019), in which the Health Assembly
requests the Director-General, inter alia, to propose updates to the appendices of WHO’s comprehensive
mental health action plan, in consultation with Member States and taking into account the view of other
stakeholders, the Secretariat has taken the following steps to update Appendix 1 (Indicators for
measuring progress towards defined targets) and Appendix 2 (Options for the implementation of the
comprehensive mental health action plan 2013–2020) of that action plan:
• March 2020. A virtual consultation with Member States was organized by the regional offices
for Africa, the Americas, South-East Asia, Europe and the Eastern Mediterranean in order to
seek views on the “zero draft” of updated Appendix 1 and the pre-existing (2013) version of
Appendix 2. Additionally, Member States of the Western Pacific Region were consulted by
email to seek views on the “zero draft” of updated Appendix 1. A web-based consultation for
Member States, organizations in the United Nations system and non-State actors on the “zero
draft” of updated Appendix 1 and the pre-existing (2013) version of Appendix 2 was conducted
• July 2020. Virtual consultations were organized by the Regional Office for the Western Pacific
to seek the views of the Region’s Member States on the pre-existing (2013) version of
Appendix 2.
• August–September 2020. A virtual consultation with Member States was organized by the
regional offices for Africa, the Americas, South-East Asia, Europe and the Eastern
Mediterranean to seek views on the “zero draft” of updated Appendix 2. That text was also the
subject of a web-based consultation for Member States, organizations in the United Nations
system and non-State actors.
2. The resulting updated Appendix 1 (see below) includes the updated indicators and targets to
monitor the comprehensive mental health action plan up to 2030.
3. The resulting updated Appendix 2 (see below) has been modified through strengthened text on
suicide prevention, workplace mental health, universal health coverage, mental health of children,
mental health across the life course, multisectoral work, human rights, and involvement of people with
lived experience of mental health conditions.
EB148/7 Annex 5
32
Appendix 1
PROPOSED UPDATED APPENDIX 1 OF THE COMPREHENSIVE MENTAL
HEALTH ACTION PLAN 2013–2030: INDICATORS FOR MEASURING
PROGRESS TOWARDS DEFINED TARGETS
1. The updated indicators for assessing progress towards meeting the global targets of
Comprehensive mental health action plan 2013–2030 represent a subset of the information and the
reporting needs that Member States require to be able to monitor adequately their mental health policies
and programmes. Given that targets are voluntary and global, each Member State is not necessarily
expected to achieve all the specific targets but can contribute to a varying extent towards reaching them
jointly.
2. The global targets established for each objective provide the basis for measurable collective action
and progress by Member States towards global goals and should not negate the setting of more ambitious
national targets, particularly for those countries that have already reached global ones.
3. As indicated under Objective 4 of the plan, the Secretariat will continue providing guidance,
training and technical assistance to Member States, upon request, on the development of national
information systems for capturing data on indicators of mental health system inputs, activities and
outcomes. The aim is to keep building on existing information systems rather than creating new or
parallel systems.
Objective 1: To strengthen effective leadership and governance for mental health
Global target 1.1: 80% of countries will have developed or updated their policy or plan for mental health in
line with international and regional human rights instruments, by 2030.
Indicator 1.1: Existence of a national policy or plan for mental health that is being implemented and in line
with international human rights instruments.
Means of verification:
Physically available policy or plan; confirmation that it accords with international and regional human rights
standards; and assessment of implementation status.
Comments, assumptions and/or rationale:
For countries with a federated system, the indicator will refer to policies or plans of most states or provinces
within the country. Policies or plans for mental health may be stand-alone or integrated into other general
health or disability policies or plans.
Human rights standards include provisions for (i) transition to mental health services based in the community;
(ii) respect of human rights; (iii) comprehensive support and services; (iv) promotion of a recovery approach;
and (v) participation in decision making processes.
Implementation status includes (i) estimation and allocation of human resources; (ii) estimation and allocation
of financial resources; (iii) monitoring and evaluation of specified indicators or targets.
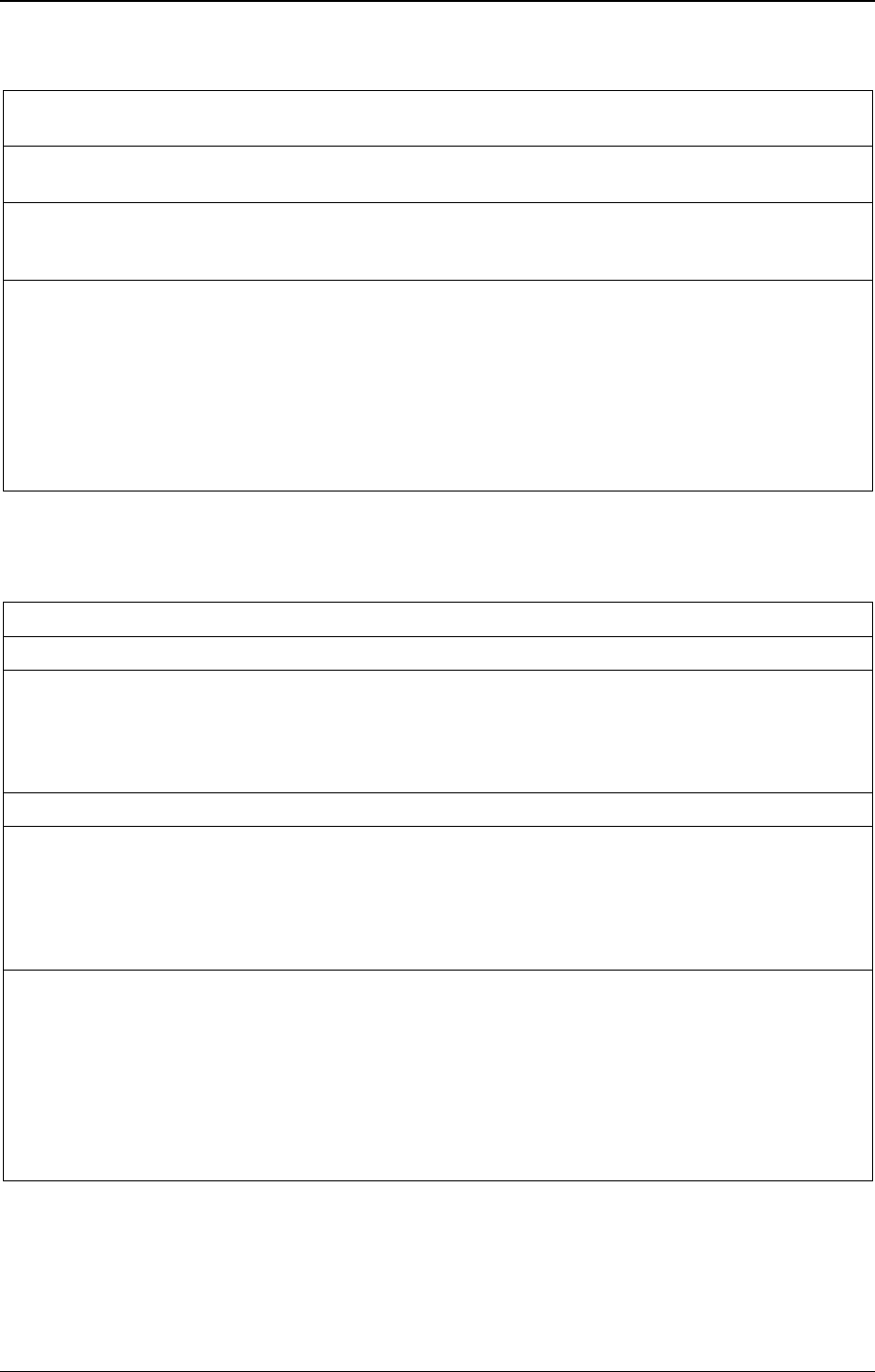
Annex 5 EB148/7
33
Global target 1.2: 80% of countries will have developed or updated their law for mental health in line with
international and regional human rights instruments, by 2030.
Indicator 1.2: Existence of a national law covering mental health that is being implemented and in line with
international and regional human rights instruments.
Means of verification:
Physically available law, confirmation that it accords with international and regional human rights standards,
and assessment of implementation status.
Comments, assumptions and/or rationale:
For countries with a federated system, the indicator will refer to the laws of most states/provinces within the
country. Laws for mental health may be stand-alone or integrated into other general health or disability laws.
Human rights standards include provisions for (i) transition to mental health services based in the community;
(ii) promotion to exercise legal capacity; (iii) prevention of coercive practices; (iv) procedures to file appeals
and complaints; (v) regular inspections of mental health services.
Implementation status refers to (i) existence of a dedicated authority or independent body to assess
compliance with human rights standards; (ii) regular inspection of mental health services by the dedicated
authority or body; and (iii) systematic response to complaints and reporting of its findings.
Objective 2: To provide comprehensive, integrated and responsive mental health and social care
services in community-based settings
Global target 2.1: Service coverage for mental health conditions will have increased at least by half, by 2030.
Indicator 2.1.1: Proportion of persons with psychosis who are using services over the past 12 months [%].
Means of verification:
Numerator: number of people with psychosis in receipt of services, derived from routine information systems
or a baseline and follow-up survey of health facilities in one or more defined geographical areas of a country.
Denominator: total number of people with psychosis in the sample population, derived from national surveys
or, if unavailable, based on subregional prevalence estimates.
Indicator 2.1.2: Proportion of people with depression who are using services over the past 12 months [%].
Means of verification:
Numerator: number of people with depression in receipt of services, derived from household surveys or
epidemiological studies or routine information systems, or a baseline and follow-up survey of health facilities
in one or more defined geographical areas of a country.
Denominator: Total number of people with depression in the sample population, derived from national
surveys or, if unavailable, based on subregional prevalence estimates.
Comments, assumptions and/or rationale:
Estimates of service coverage are needed for all mental disorders, but are restricted here to psychosis and
depression as tracer indicators for severe and common mental disorders respectively to limit measurement
effort.
Health facilities range from primary care centres to general and specialized hospitals; they may offer social
care and support as well as psychosocial and/or pharmacological treatment on an outpatient or inpatient basis.
To limit measurement effort, and where needed, countries may restrict the survey to hospital-based and
overnight facilities only (with some loss of accuracy due to omission of primary care and other service
providers).

EB148/7 Annex 5
34
Global target 2.2: 80% of countries will have doubled number of community-based mental health facilities,
by 2030.
Indicator 2.2: Number of community-based mental health facilities.
Means of verification:
Availability and number of community-based facilities that manage mental health conditions and related
clinical and social problems.
Comments, assumptions and/or rationale:
In the context of improving access to care and service quality, development of comprehensive community-
based mental health and social care services is recommended. Community-based services can be outpatient or
inpatient services as well as home help and support services.
Global target 2.3: 80% of countries will have integrated mental health into primary health care, by 2030.
Indicator 2.3: Existence of a system in place for integration of mental health into primary health care.
Means of verification:
Description from countries using the following criteria: guidelines for integration of mental health into
primary health care available and adopted; pharmacological and psychosocial interventions provided at
primary health care level; and training and supervision for non-specialized health workers at primary care
level.
Comments, assumptions and/or rationale:
Integration of mental health into primary health care is essential to ensure universal health coverage. A range
of mental health services including promotive, preventive, treatment and care services can be provided when
integrated into primary health care.
Objective 3: To implement strategies for promotion and prevention in mental health
Global target 3.1: 80% of countries will have at least two functioning national, multisectoral mental health
promotion and prevention programmes, by 2030.
Indicator 3.1: Functioning programmes of multisectoral mental health promotion and prevention in
existence.
Means of verification:
Inventory or project-by-project description of currently implemented programmes.
Comments, assumptions and/or rationale:
Programmes may – and preferably should – cover both universal, population-level promotion or prevention
strategies or locally-identified vulnerable groups. Examples include programmes on: suicide prevention;
mental health awareness/anti-stigmatization; mental health promotion at the workplace; school-based mental
health; and maternal mental health prevention and promotion.
Criteria to identify functioning include dedicated financial and human resources, defined plan of
implementation, and documented evidence of progress and/or impact.
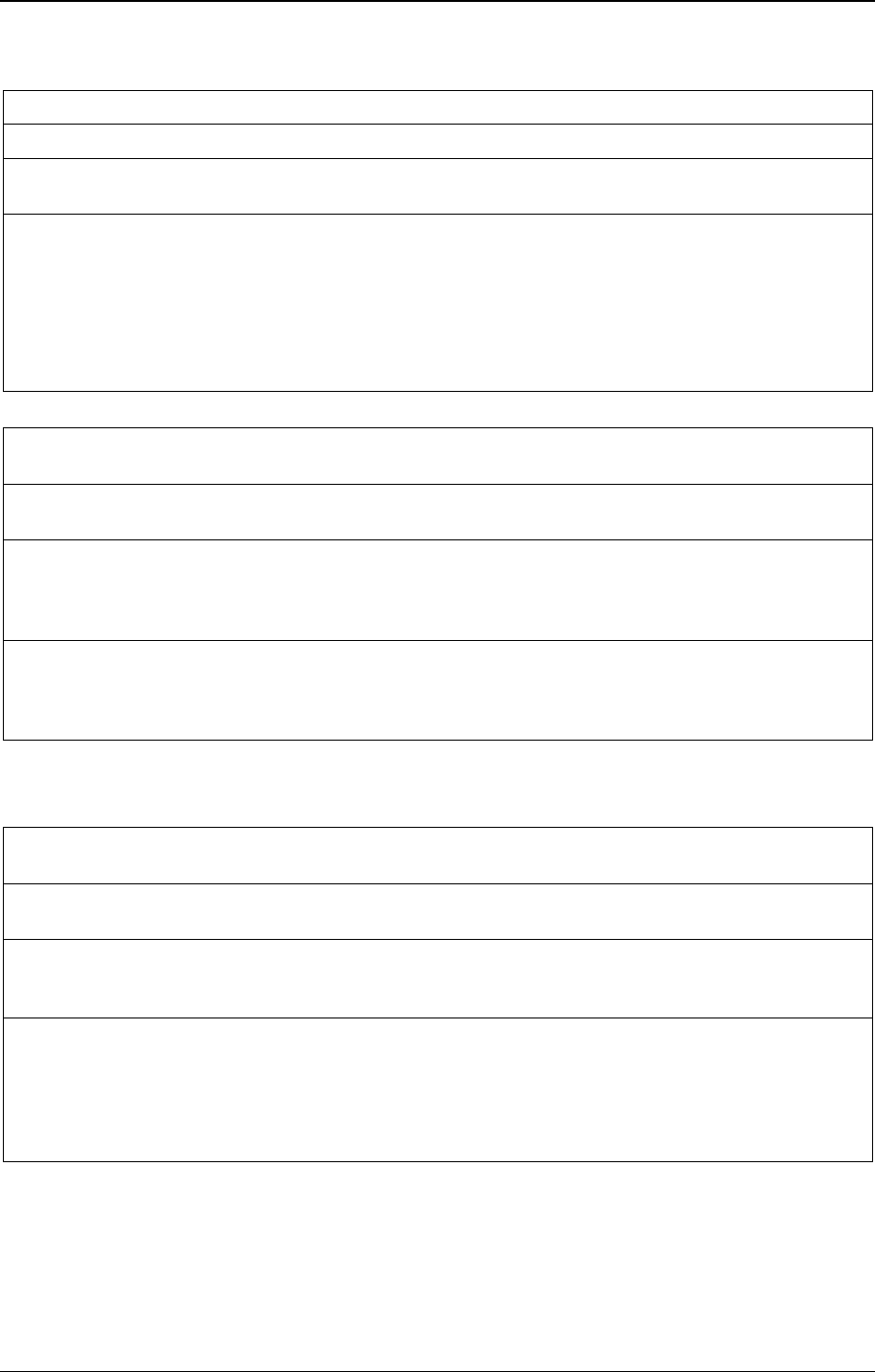
Annex 5 EB148/7
35
Global target 3.2: The rate of suicide will be reduced by one-third, by 2030.
Indicator 3.2: Suicide mortality rate (per 100 000 population).
Means of verification:
Routine annual registration of deaths due to suicide.
Comments, assumptions and/or rationale:
Effective action towards this target requires joint action from multiple sectors outside health/mental health
sector. Obtaining accurate surveillance data is difficult and, because of more accurate reporting of suicides,
population ageing and other possible factors, total recorded suicides may not decrease in some countries;
however, the rate of suicide (as opposed to total suicides) best reflects improved prevention efforts.
The target (and indicator) is aligned with those for Sustainable Development Goal 3 (target 3.4 and
indicator 3.4.2).
Global target 3.3: 80% of countries will have a system in place for mental health and psychosocial
preparedness for emergencies and/or disasters, by 2030.
Indicator 3.3: Existence of a system in place for mental health and psychosocial preparedness for
emergencies/disasters.
Means of verification:
Description from countries for a system in place for mental health and psychosocial preparedness using the
following criteria: defined plan of implementation, dedicated financial and human resources, and documented
evidence of progress and/or impact.
Comments, assumptions and/or rationale:
Planning for disaster and/or emergency response is a priority as expressed in the Sendai Framework for
Disaster Risk Reduction (2015–2030) and in the Inter-agency Standing Committee Guidelines for Mental
Health and Psychosocial Support in Emergency Settings.
Objective 4: To strengthen information systems, evidence and research for mental health
Global target 4.1: 80% of countries will be routinely collecting and reporting at least a core set of mental
health indicators every two years through their national health and social information systems, by 2030.
Indicator 4.1: Core set of identified and agreed mental health indicators routinely collected and reported
every two years.
Means of verification:
Reporting and submission of measurements against the core mental health indicator sent to WHO every two
years.
Comments, assumptions and/or rationale:
Core mental health indicators include those relating to specified targets of this action plan, together with other
essential indicators of health and social system actions (for example, training and human resource levels, and
service availability and utilization). The data need to be disaggregated by sex and age groups. Where needed,
surveys can also be used to complement data from routine information systems. Data will be collected,
analysed and reported by WHO as part of its Mental Health Atlas.
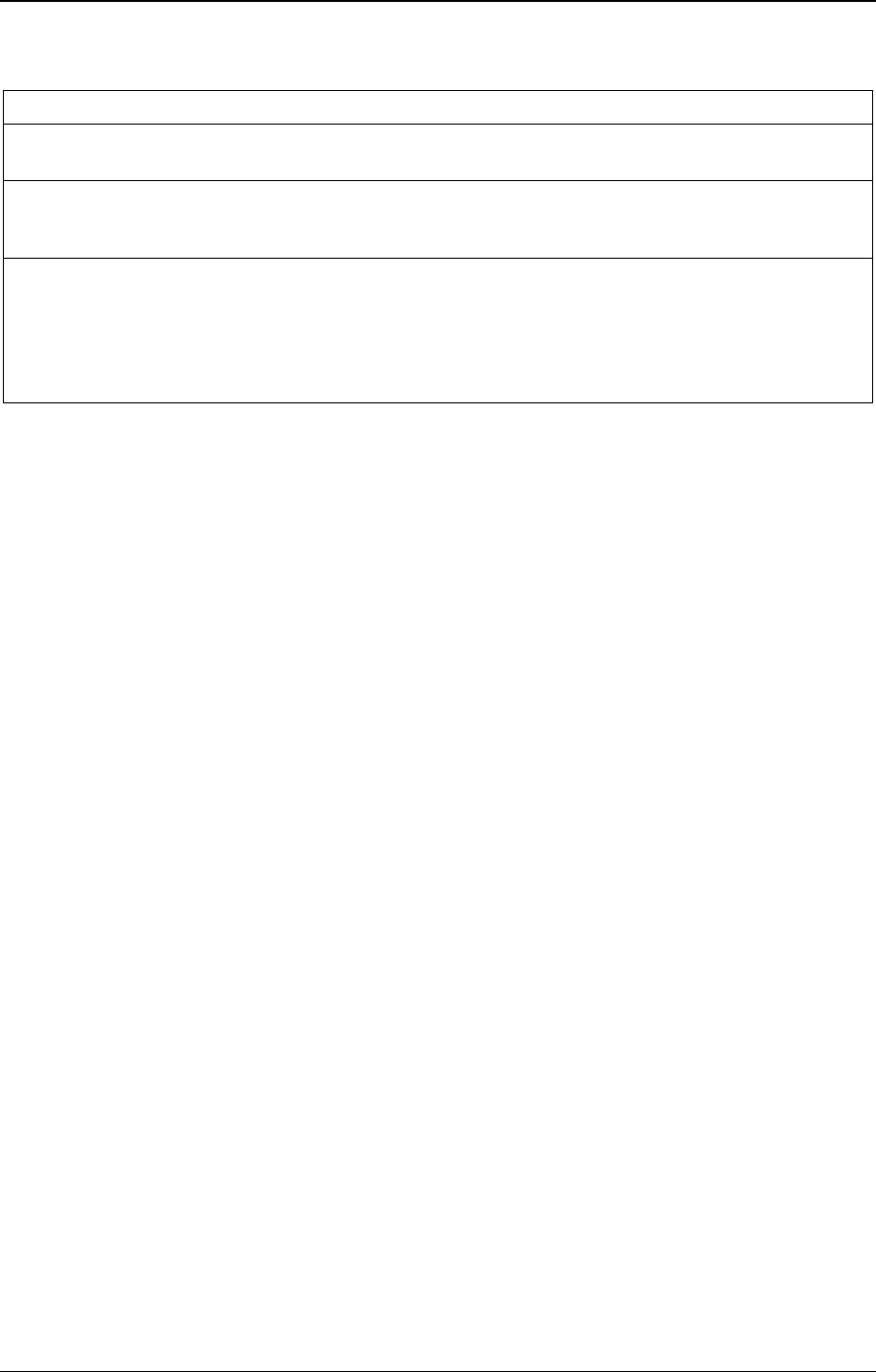
EB148/7 Annex 5
36
Global target 4.2: The output of global research on mental health doubles, by 2030.
Indicator 4.2: Number of published articles on mental health research (defined as research articles published
in the databases).
Means of verification:
Literature searches centrally-conducted every two years, stratified by country of origin, topics and types of
research, using bibliometric data sourced for the most recent calendar year.
Comments, assumptions and/or rationale:
The indicator measures the output of mental health research as defined by national published research studies.
The annual published research output in peer-reviewed and indexed journals is a proxy for the amount (and
quality) of mental health research being conducted in a country. It indirectly assesses a country’s commitment
to mental health research, which will ultimately have an impact on outcomes for people with mental health
conditions.
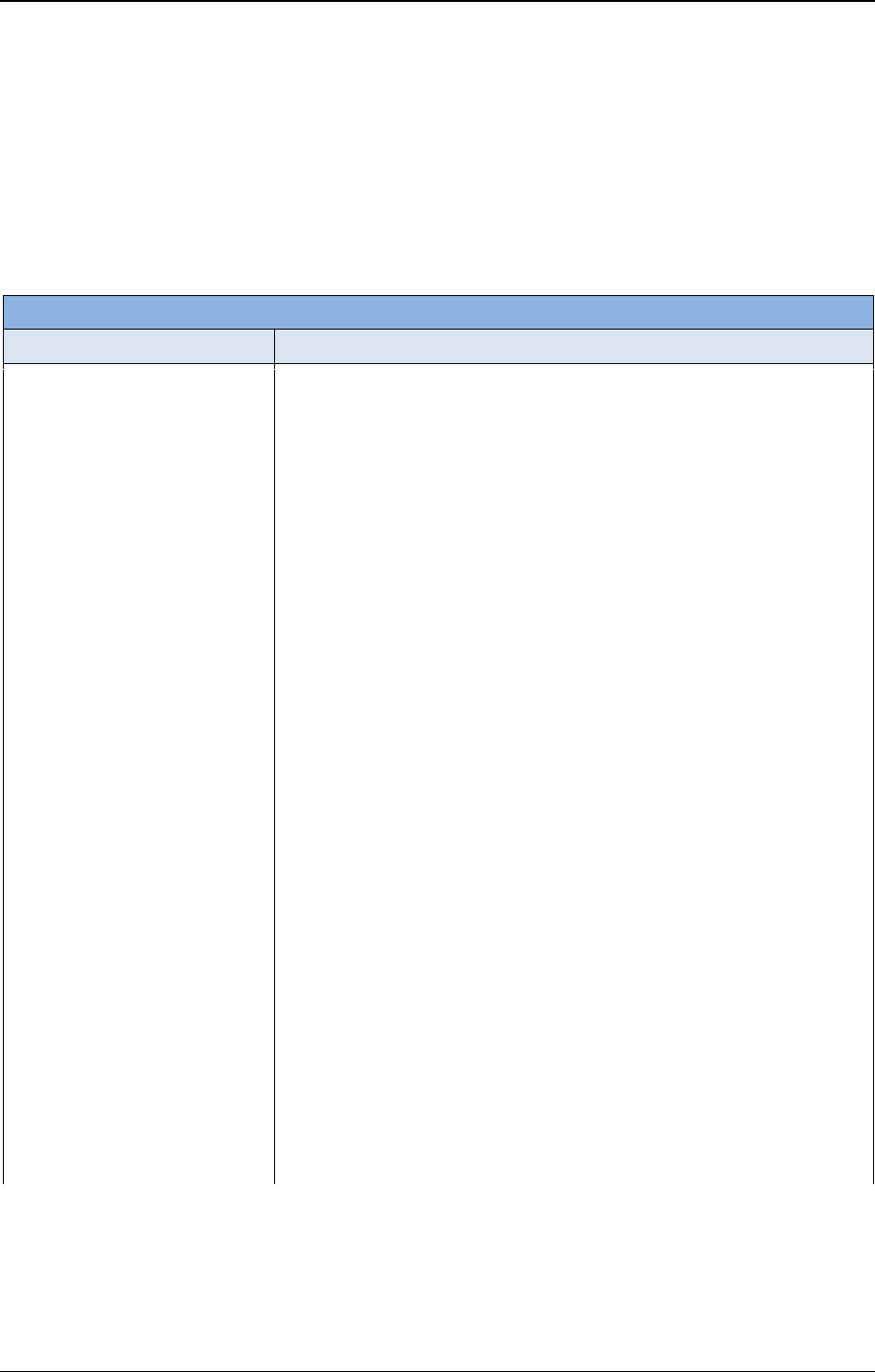
Annex 5 EB148/7
37
Appendix 2
PROPOSED UPDATED APPENDIX 2 OF THE COMPREHENSIVE MENTAL
HEALTH ACTION PLAN 2013-2030
Options for the implementation of the comprehensive mental health
action plan 2013-2020
Objective 1: To strengthen effective leadership and governance for mental health
Actions
Options for implementation
Policy and law: Develop,
strengthen, keep up-to-date and
implement national policies,
strategies, programmes, laws and
regulations relating to mental
health within all relevant sectors,
including protective monitoring
mechanisms and codes of
practice, in line with evidence,
best practice, the Convention on
the Rights of Persons with
Disabilities and other
international and regional human
rights instruments.
• Develop and implement a comprehensive mental health policy and plan
that complies with international human rights instruments, includes
allocated human and financial resources and undergoes regular
monitoring against indicators or targets for implementation.
• Decriminalize suicide, suicide attempts and other acts of self-harm.
• Set up a functional mental health unit or coordination mechanism(s) in
the health ministry, with an allocated budget and responsibility for
strategic planning, coordination, needs assessment, interministerial and
multisectoral collaboration and service evaluation for mental health
across the life-course.
• Ensure coordination of mental health and social care activities at all
relevant subnational levels (for example, district, municipality and
community levels).
• Sensitize policy-makers to mental health and human rights issues
through the preparation of policy briefs and scientific publications and
the provision of leadership courses and other learning and knowledge
exchange opportunities in mental health.
• Undertake capacity-building among stakeholders including
policy-makers regarding strategies to promote respect for people’s will
and preference in mental health and related services.
• Mainstream mental health and the rights of persons with mental
disorders and psychosocial disabilities into all sectoral policies, laws
and strategies (for example, health, social affairs, education, justice and
labour/employment) including emergency preparedness and response,
poverty reduction and development.
• Improve accountability by setting up mechanisms, using independent
bodies, to monitor, prevent and respond to torture or cruel, inhuman
and degrading treatment and other forms of ill-treatment and abuse;
collect data on restrain and seclusion and involuntary treatments; and
involve appropriate stakeholder groups in these mechanisms, for
example, lawyers and people with mental disorders and psychosocial
disabilities, in a manner consistent with international human rights
instruments.
• Amend or repeal legislation that perpetuates stigmatization,
discrimination and human rights violations against people with mental
disorders and psychosocial disabilities.
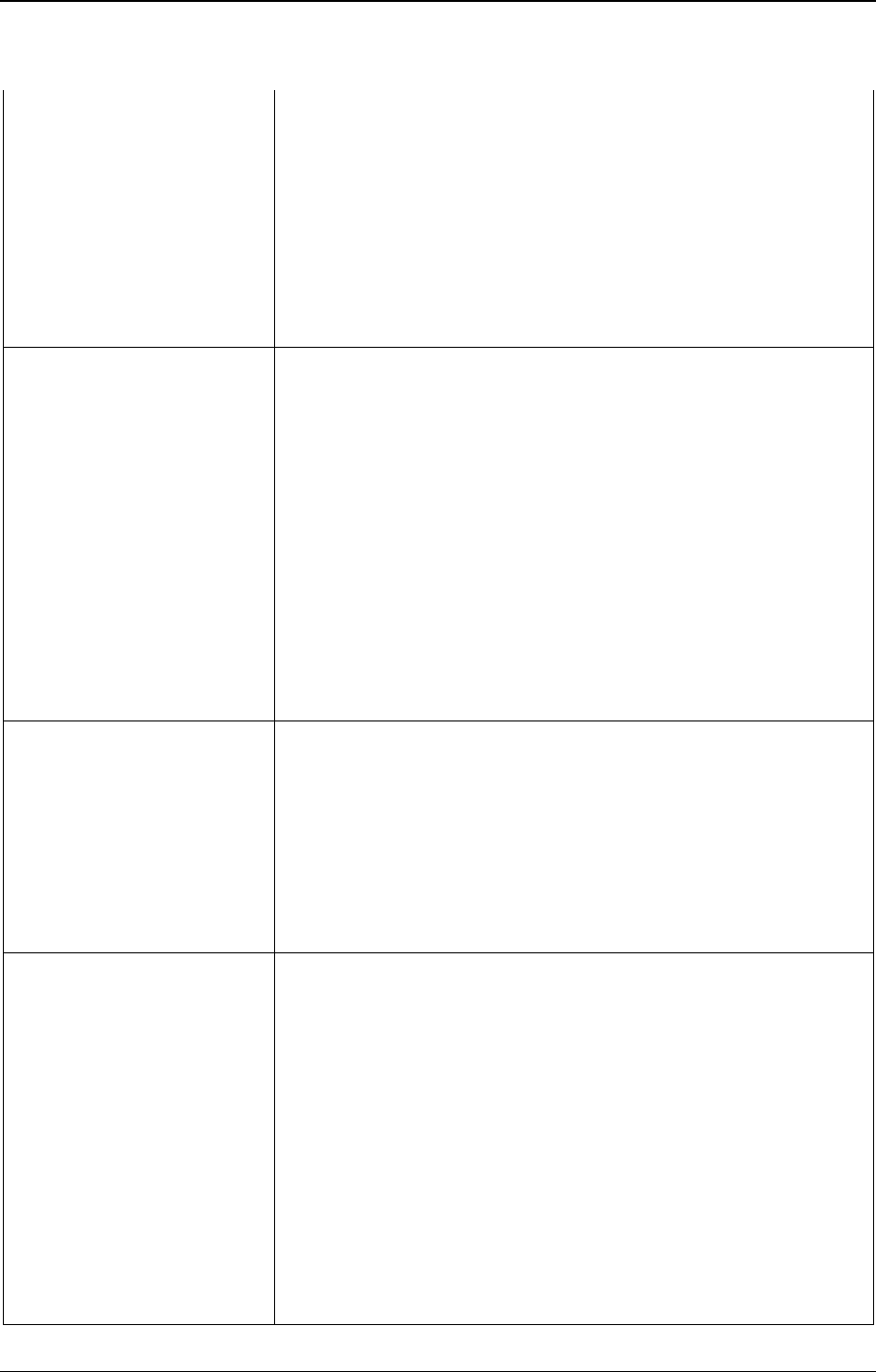
EB148/7 Annex 5
38
• Monitor and evaluate the implementation of policies and legislation to
ensure compliance with international human rights conventions
including the Convention on the Rights of Persons with Disabilities and
the Convention on the Right of the Child, as appropriate, and feed this
information into the reporting mechanism of these conventions.
• Establish supported decision-making mechanisms; help people to
develop advance plans that state their will and preference should they
experience a crisis in the future; and ensure that people have all the
supports they require in order to make a decision, including access to
trusted persons and advocates and provision of valid information about
all matters relevant to their decision.
Resource planning: Plan
according to measured or
systematically estimated need
and allocate a budget, across all
relevant sectors, that is
commensurate with identified
human and other resources
required to implement
agreed-upon, evidence-based
mental health plans and actions.
• Include mental health services, such as psychosocial and psychological
interventions and basic medicines for mental disorders, in universal
health coverage and financial protection schemes and offer financial
protection for socioeconomically disadvantaged groups.
• Use – and if indicated, collect – data on epidemiology and resource
needs in order to inform the development and implementation of
mental health plans, budgets and programmes.
• Set up mechanisms for tracking expenditures for different types of
mental health services in health and other relevant sectors such as
education, employment, criminal justice and social services.
• Identify available funds at the planning stage for specific
community-based, culturally-appropriate, cost-effective activities so
that implementation can be assured.
• Join with other stakeholders to effectively advocate increased resource
allocation for mental health including through investment cases for
mental health.
Stakeholder collaboration:
Engage stakeholders from all
relevant sectors, including
persons with mental disorders,
carers and family members, in
the development and
implementation of policies, laws
and services relating to mental
health, through a formalized
structure and/or mechanism.
• Convene, engage with, and solicit consensus from all relevant sectors
and stakeholders when planning, developing and implementing
policies, laws and services relating to health, including sharing
knowledge about effective mechanisms to improve coordinated policy
and care across formal and informal sectors.
• Build local capacity and raise awareness among relevant stakeholder
groups about mental health, law and human rights, including their
responsibilities in relation to the implementation of policy, laws and
regulations.
Strengthening and
empowerment of people with
mental disorders and
psychosocial disabilities and
their organizations: Ensure that
people with mental disorders and
psychosocial disabilities are
given a formal role and authority
to influence the process of
designing, planning and
implementing policy, law and
services.
• Provide logistic, technical and financial support to build the capacity of
people with mental disorders and psychosocial disabilities and their
organizations, including youth and carers, in understanding and
advocating the realization of human rights conventions, policy, law and
services, based on their needs and preferences.
• Encourage and support the formation of independent national and local
organizations of people with mental disorders and psychosocial disabilities
and establish formal mechanisms to ensure their full and effective
participation in the development and implementation of mental health
policies, laws and services as well as their monitoring and evaluation.
• Involve people with mental disorders and psychosocial disabilities in
the assessment and monitoring of all public and private mental health
services including psychiatric hospitals and social care homes.
• Include people with mental disorders and psychosocial disabilities and
their organizations in capacity-building of stakeholders, including
policy-makers and health workers delivering mental health care.
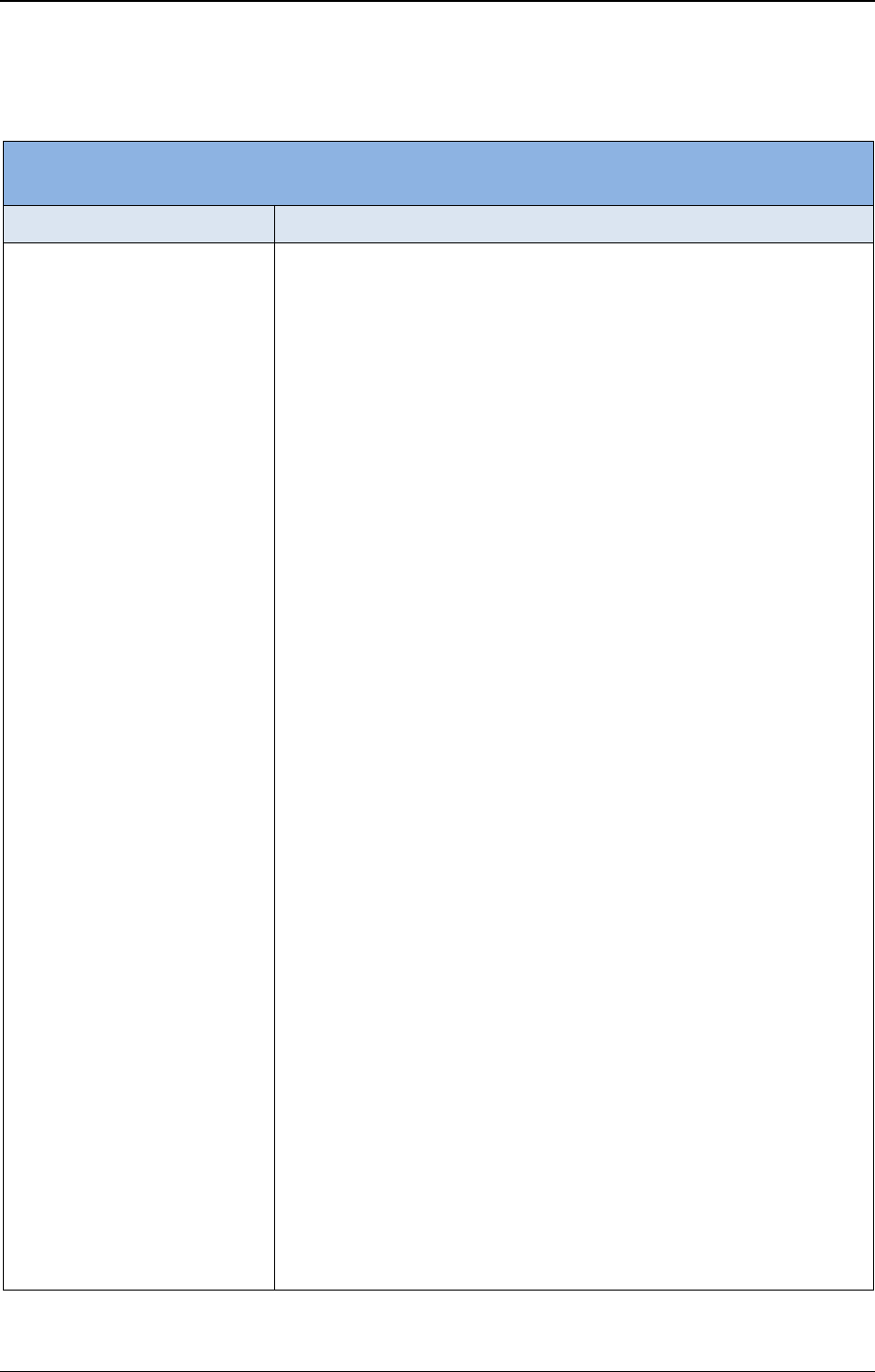
Annex 5 EB148/7
39
Objective 2: To provide comprehensive, integrated and responsive mental health and social care services
in community-based settings
Actions
Options for implementation
Service reorganization and
expanded coverage:
Systematically shift the locus of
care away from long-stay mental
hospitals towards non-specialized
health settings with increasing
coverage of evidence-based
interventions (including the use
of stepped-care principles, as
appropriate) for priority
conditions and using a network
of linked community-based
mental health services, including
short-stay inpatient and
outpatient care in general
hospitals, primary care,
comprehensive mental health
centres, day care centres, support
of people with mental disorders
living with their families, and
supported housing.
• Develop a phased and budgeted plan for scaling down and closing
long-stay psychiatric institutions and replacing them with support for
discharged residents to live in the community.
• Work towards a gradual shift of financial resources and staff towards
community-based care, closing long-stay institutions once there are
adequate community alternatives.
• Accompany the process of scaling down long-stay psychiatric
institutions with (a) human rights protection and improvements in
quality of life in institutions and (b) ensuring continuity of care and
welfare provision for discharged long-stay residents (for example,
livelihoods and housing support, including places in small group
homes).
• Provide outpatient mental health services and an inpatient mental health
unit in general hospitals.
• Build up interdisciplinary community-based mental health services for
people across the life course, through for instance outreach services,
home care and support, primary health care, emergency care,
community-based rehabilitation and supported housing.
• Integrate mental health and social care into disease-specific
programmes and services, such as those for HIV/AIDS, tuberculosis,
noncommunicable diseases and neglected tropical diseases, and into
population-specific programmes and services, such as maternal, sexual
and reproductive health, child and adolescent health, gender-based
violence and family health and well-being programmes and services.
• Engage service users and family members and/or carers with practical
experience as peer support workers.
• Support the establishment and implementation of community mental
health services run by nongovernmental organizations, faith-based
organizations and other community groups, including self-help and
family support groups, which protect, respect and promote human
rights and are subject to monitoring by government agencies.
• Consider the use of evidence-based innovative approaches to provide
psychological support at scale (for example, guided self-help, digital
self-help, collaborative and stepped-care approaches).
• Develop and implement tools or strategies for self-help and care for
persons with mental disorders, including strengthening the use of
electronic and mobile technologies, potentially as part of a stepped-care
system.
• Develop capacity, policies and operational procedures for remote
delivery of services (for example, telehealth) and use digital health
solutions to support practitioners in providing care where feasible.
• Provide in-home and other community-support services for carers of
children and of adults with psychosocial disabilities including carer
skills training and other multidisciplinary services (for example,
physical and occupational therapy, nutritional support, housing,
education support, and early childhood development).
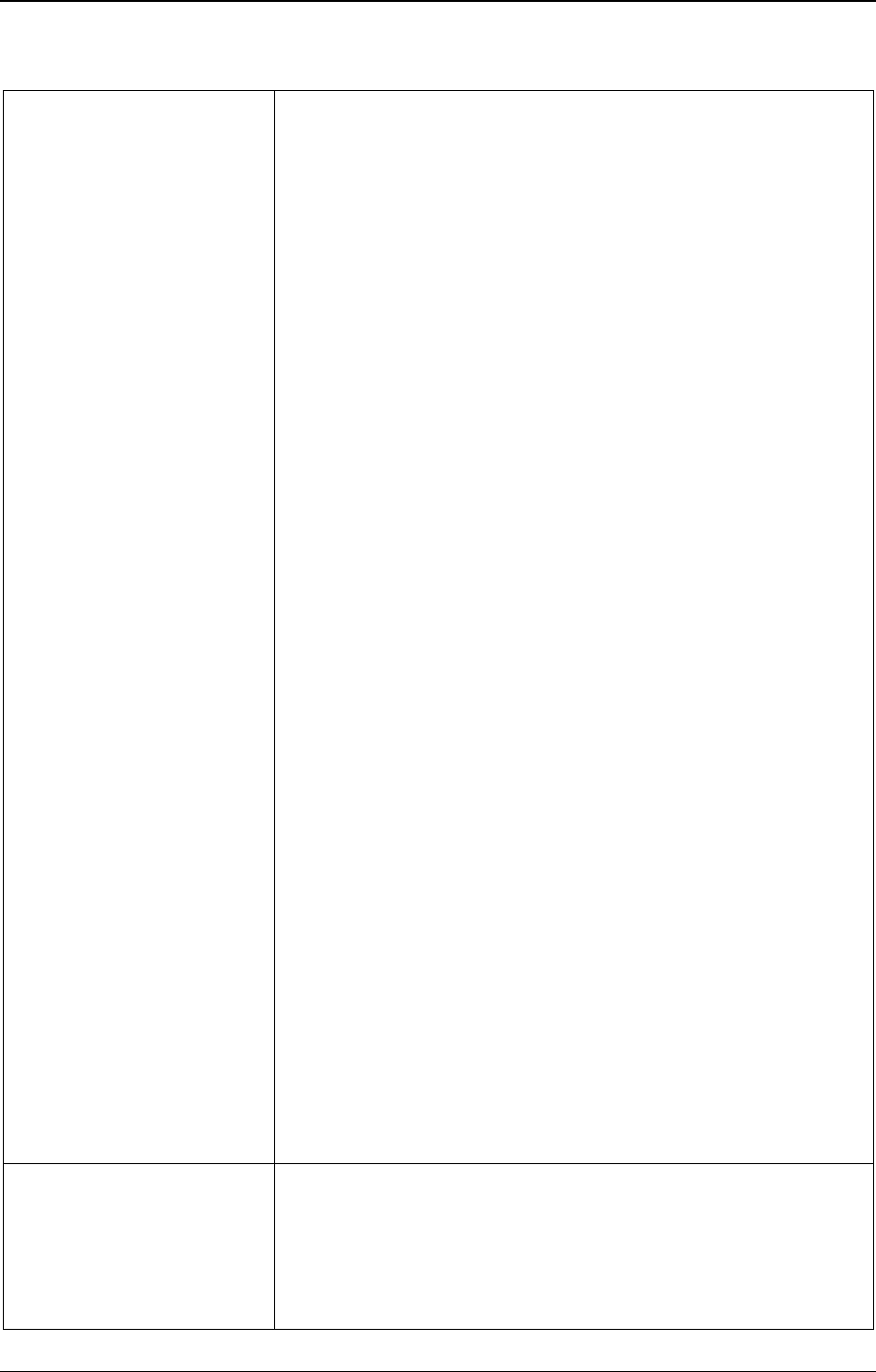
EB148/7 Annex 5
40
Integrated and responsive care:
Integrate and coordinate holistic
prevention, promotion,
rehabilitation, care and support
that aims at meeting both mental
and physical health care needs
and facilitates the recovery of
persons of all ages with mental
disorders within and across
general health and social services
(including the promotion of the
right to employment, housing and
education) through service user-
driven treatment and recovery
plans and, where appropriate,
with the inputs of families and
carers.
• Encourage health workers to initiate and support recovery plans and
link people with services and resources based on their needs and
preferences including education, work, health care, and livelihood
opportunities.
• Develop the planning and delivery of services jointly with people with
mental health conditions and psychosocial disabilities.
• Implement guidelines for the management of physical health in persons
with severe mental health conditions.
• Advocate with other sectors (for example, livelihoods support, housing,
education, vocational training, employment, social welfare and legal
support) the inclusion and support of people with mental disorders and
psychosocial disabilities in their services and programmes.
• Cultivate recovery-oriented and culturally-appropriate care and support
through awareness-building opportunities and training for health and
social service providers.
• Provide information to people with mental disorders, their families and
carers on causes and potential impacts of disorders, treatment and
recovery options, as well as on healthy lifestyle behaviours in order to
improve overall health and well-being.
• Foster the empowerment and involvement of persons with mental
disorders, their families and caregivers in mental health care.
• Procure and ensure the availability of basic medicines for mental
disorders included in the WHO Model List of Essential Medicines at all
health system levels, ensure their rational use, and enable non-specialist
health workers with adequate training to prescribe such medicines.
• Build competencies of health professionals to provide accurate
information about a range of feasible evidence-based psychosocial and
pharmacological interventions and to discuss benefits and risks,
including possible side and withdrawal effects of interventions.
• Address the mental well-being of children and carers when a family
member with severe illnesses (including those with mental disorders)
presents for treatment at health services.
• Provide services and programmes to children and adults who have
experienced adverse life events, including ongoing domestic violence,
civil unrest, conflict or disaster, that meet people’s mental health needs,
promote recovery and resilience, and prevent further distress for those
who seek support.
• Implement interventions to manage family crises and provide care and
support to families and carers in primary care and other service levels.
• Provide early interventions for children and adolescents with mental
health conditions through family-centred and child and adolescent-
responsive health care, at primary health care, school and community
levels.
• Implement the use of WHO QualityRights standards to assess and
improve quality and human rights conditions in inpatient and outpatient
mental health and social care facilities including policies and
procedures to stop the use of coercive practices in services.
Mental health in humanitarian
emergencies (including
isolated, repeated or continuing
conflict, violence, and
disasters): Work with national
emergency committees to include
mental health and psychosocial
• Work across sectors with national and subnational actors on integrating
mental health and psychosocial support in all national and local
emergency preparedness and response policies, plans, procedures and
actions as outlined in the Sphere Handbook’s minimum standards and
the Inter-Agency Standing Committee Guidelines on Mental Health
and Psychosocial Support in Emergency Settings.
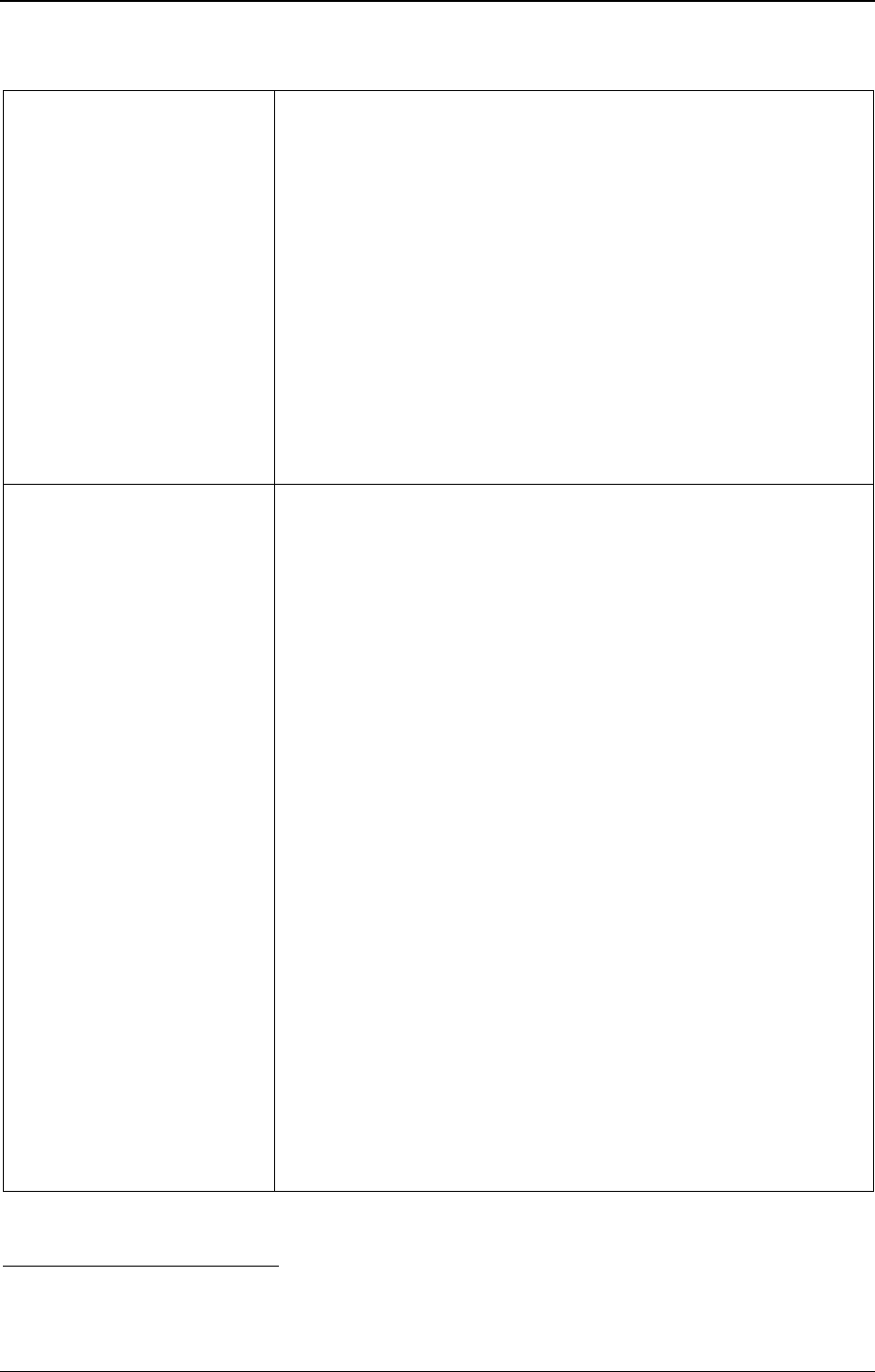
Annex 5 EB148/7
41
support needs in emergency
preparedness, and enable access
to safe and supportive services,
including services that address
psychological trauma and
promote recovery and resilience,
for persons with (pre-existing as
well as emergency-induced)
mental disorders or psychosocial
problems, including for health
and humanitarian workers, during
and following emergencies, with
due attention to the longer-term
funding required to build or
rebuild a community-based
mental health system after the
emergency.
• Prepare for emergencies by training health and community workers in
basic psychosocial support, such as psychological first aid.
• During emergencies, ensure coordination with partners across health,
protection, nutrition and education sectors on the application of the
Sphere Handbook’s relevant minimum standards and the Inter-Agency
Standing Committee guidelines mentioned above.
• Include mental health and psychosocial support as an integral, cross-
cutting component in public health emergency responses (for example,
to COVID-19 and Ebola virus disease) as part of a range of pillars or
domains, such as case management, risk communication and
community engagement, continuation of services, response
coordination, and operations (for instance, staff support).
• Use emergencies as an opportunity to build or rebuild sustainable
community-based mental health and social care systems, and to
demonstrate the feasibility and effectiveness of community models of
care that address the long-term increase in mental disorders in
emergency-affected populations.
Resource planning: Build the
knowledge and skills of general
and specialized health workers to
deliver evidence-based,
culturally-appropriate and human
rights-oriented mental health and
social care services, for children
and adolescents, inter alia, by
introducing mental health into
undergraduate and graduate
curricula and through training
and mentoring health workers in
the field, particularly in non-
specialized settings, to identify
and offer treatment and support
to people with mental disorders
as well as to refer people, as
appropriate, to other levels of
care.
• Develop and implement a strategy for building and retaining human
resource capacity to deliver mental health and social care services
across the life course in health, social and educational settings, such as
primary health care, general hospitals and schools.
• Support pre-service and in-service training of health workers in WHO’s
Mental Health Gap Action Programme’s intervention guide for the
identification and management of mental, neurological and substance
use disorders in non-specialized settings, evidence-based psychological
interventions and associated training and supervision materials for
prioritized expanded care.
1
• Ensure that health and social care workers have access to a cadre of
supervisors with experience in evidence-based interventions who can
provide continued mentoring and support.
• Collaborate with universities, colleges, other relevant educational
entities and professional associations to define and incorporate a mental
health component in undergraduate and postgraduate curricula, to offer
continued education and knowledge exchange on mental health and to
ensure accreditation and oversight of mental health professionals.
• Ensure an enabling service context for training health, education and
social care workers that focuses on the ongoing development,
monitoring and evaluation of competencies and that includes clear task
definitions, referral structures, supervision and mentoring.
• Improve the capacity of health, education and social care workers in all
areas of their work (for example, covering clinical, human rights and
public health domains), including eLearning methods where
appropriate.
• Ensure inclusion of human rights and person-centred recovery-oriented
approaches in the curricula of undergraduate and graduate courses,
continuing professional development opportunities and professional
accreditation mechanisms, and offer internships and learning
placements in services that promote such approaches.
1
See document EB146/7 (2019), Annex 1: Menu of policy options cost-effective interventions to promote mental
health and well-being (https://apps.who.int/gb//ebwha/pdf_files/EB146/B146_7-en.pdf).
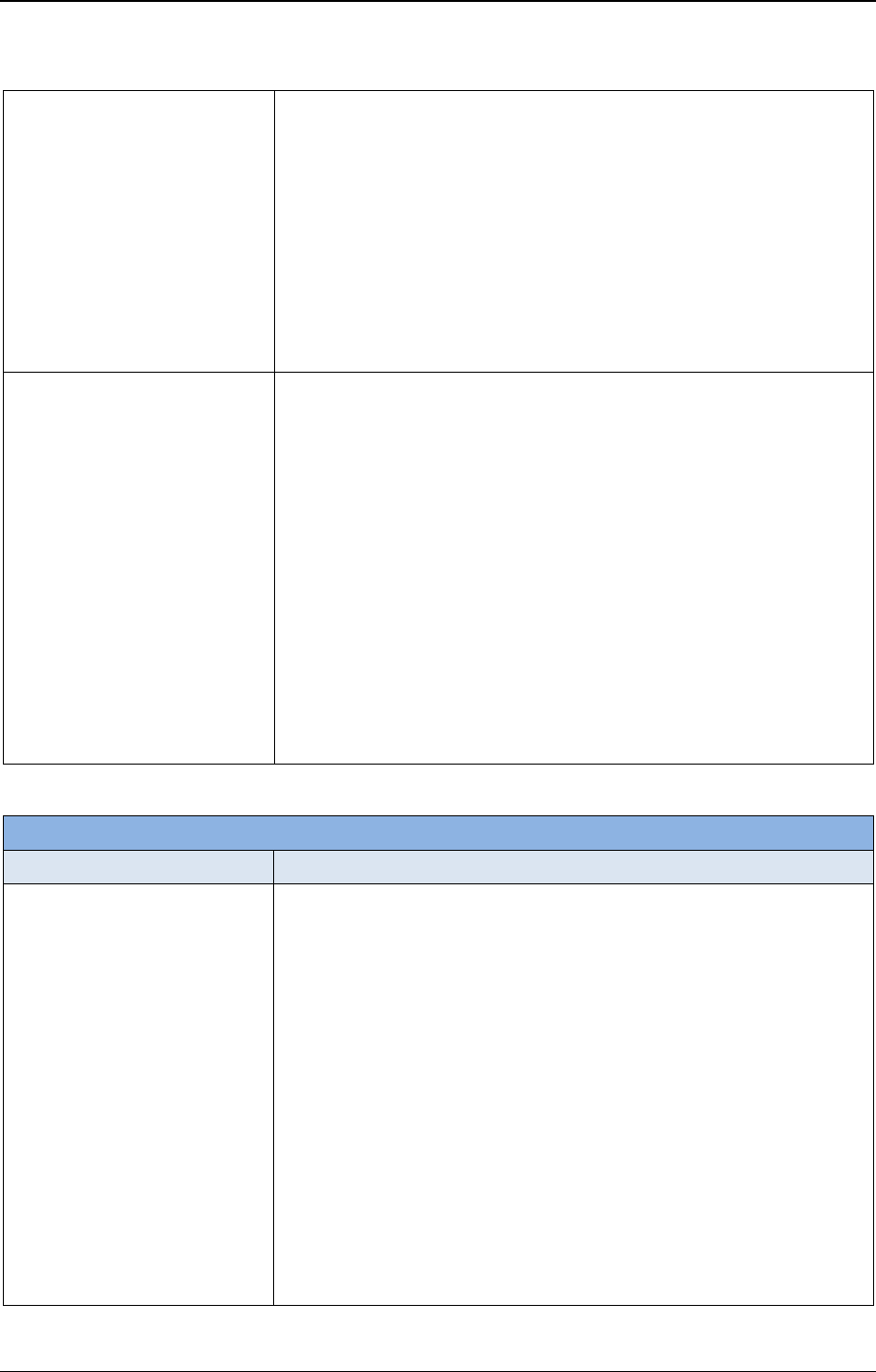
EB148/7 Annex 5
42
• Establish or strengthen supervised clinical training for prospective
mental health professionals, including psychologists, social workers,
psychiatric nurses and psychiatrists.
• Improve working conditions, financial remuneration and career
progression opportunities for mental health professionals and others,
including lay workers, in order to attract and retain the mental health
workforce.
• Collaborate with educational institutions and places of employment to
improve recruitment and retention of persons from various
backgrounds (including persons with lived experience of mental health
conditions and psychosocial disabilities) to amplify their voices and
diversify the mental health workforce and leadership.
Address disparities: Proactively
identify and provide appropriate
support for groups at particular
risk of mental illness who have
poor access to services.
• Identify and assess the mental health needs and determinants of
different sociodemographic groups in the community and also of
vulnerable people who may not be using services (such as people living
with homelessness, children, older people, persons in the criminal
justice system, persons in detention, internally displaced persons,
asylum seekers, refugees, migrants, minority ethnic groups, persons
who identify as LGBTIQ+, indigenous populations, people with
physical and intellectual disabilities, and people affected by emergency
situations) and address the barriers that they face in accessing
treatment, care and support.
• Develop a proactive strategy for targeting these people and groups and
provide services that meet their needs.
• Build competencies of health and social care workers to better
understand the needs of vulnerable people and the social determinants
of mental health, including poverty, inequality, discrimination and
violence, and to respond adequately to these factors when providing
care and support.
Objective 3: To implement strategies for promotion and prevention in mental health
Actions
Options for implementation
Mental health promotion and
prevention: Lead and coordinate
a multisectoral strategy that
combines universal and targeted
interventions for promoting
mental health and preventing
mental disorders and for
reducing stigmatization,
discrimination and human rights
violations, and which is
responsive to specific vulnerable
groups across the lifespan and
integrated within the national
mental health and health
promotion strategies.
• Develop and implement national, multisectoral mental health
promotion and prevention programmes.
• Increase public knowledge and understanding about mental health, how
to stop discrimination and how to access services, through media
awareness campaigns and initiatives that involve persons with lived
experience of mental disorders and psychosocial disabilities.
• Include mental health care and support as part of home- and health
facility-based antenatal and postnatal care for new parents and/or carers
including skills training for carers.
• Provide early childhood programmes that address the cognitive,
sensory-motor and psychosocial development of children as well as
promote healthy child–caregiver relationships.
• Reduce the harmful use of alcohol by implementation of measures
included in WHO’s global strategy to reduce the harmful use of
alcohol.
• Introduce brief interventions for hazardous and harmful substance use.
• Implement programmes to prevent and address domestic violence,
including attention to violence related to alcohol use.
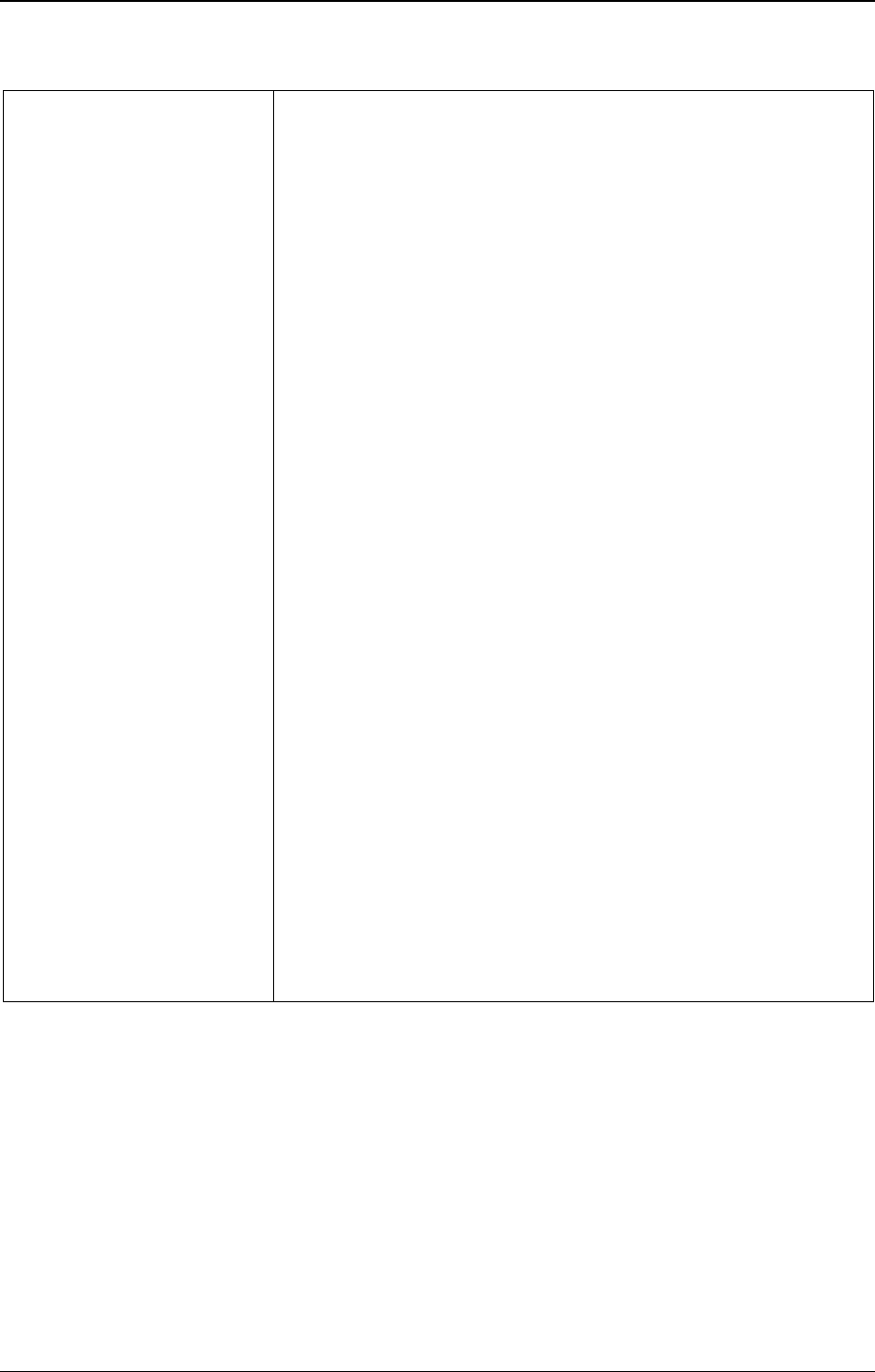
Annex 5 EB148/7
43
• Protect children and adults from abuse by introducing or strengthening
community protection networks and systems.
• Address the needs of children with parents with chronic mental
disorders within promotion and prevention programmes.
• Develop universal and indicated (targeted) school-based promotion and
prevention, including for instance socioemotional life and skills
programmes; programmes to counter bullying and violence;
programmes to counter stigmatization and discrimination of persons
with mental disorders and psychosocial disabilities; raising awareness
of the benefits of a healthy lifestyle and the risks of substance use; and
early detection and intervention for children and adolescents with
emotional or behavioural problems (including disordered eating) or
neurodevelopmental disorders.
• Address discrimination in educational institutions and the workplace
and promote full access to educational opportunities, work participation
and return-to-work programmes for people with mental disorders and
psychosocial disabilities.
• Promote safe, supportive and decent working conditions for all
(including informal workers), with attention to organizational
improvements in the workplace; implement evidence-based
programmes to promote mental well-being and prevent mental health
conditions, including training managers in order to benefit employees’
mental well-being; introduce interventions for stress management and
workplace well-being programmes; and address stigmatization and
discrimination.
• Enhance self-help groups, social support, community networks and
community participation opportunities for people with mental disorders
and psychosocial disabilities and other vulnerable people, using digital
interventions where possible.
• Encourage the use of evidence-based traditional and cultural practices
for promotion and prevention in mental health (such as yoga and
meditation).
• Enhance the use of social media in promotion and prevention strategies.
• Implement preventive and control strategies for neglected tropical
diseases (for instance, taeniasis and cysticercosis) in order to prevent
neurological and associated mental health consequences.
• Develop policies and measures to be implemented by relevant
ministries (for example, finance, labour and social welfare) for the
protection of vulnerable populations during financial and economic
crises.
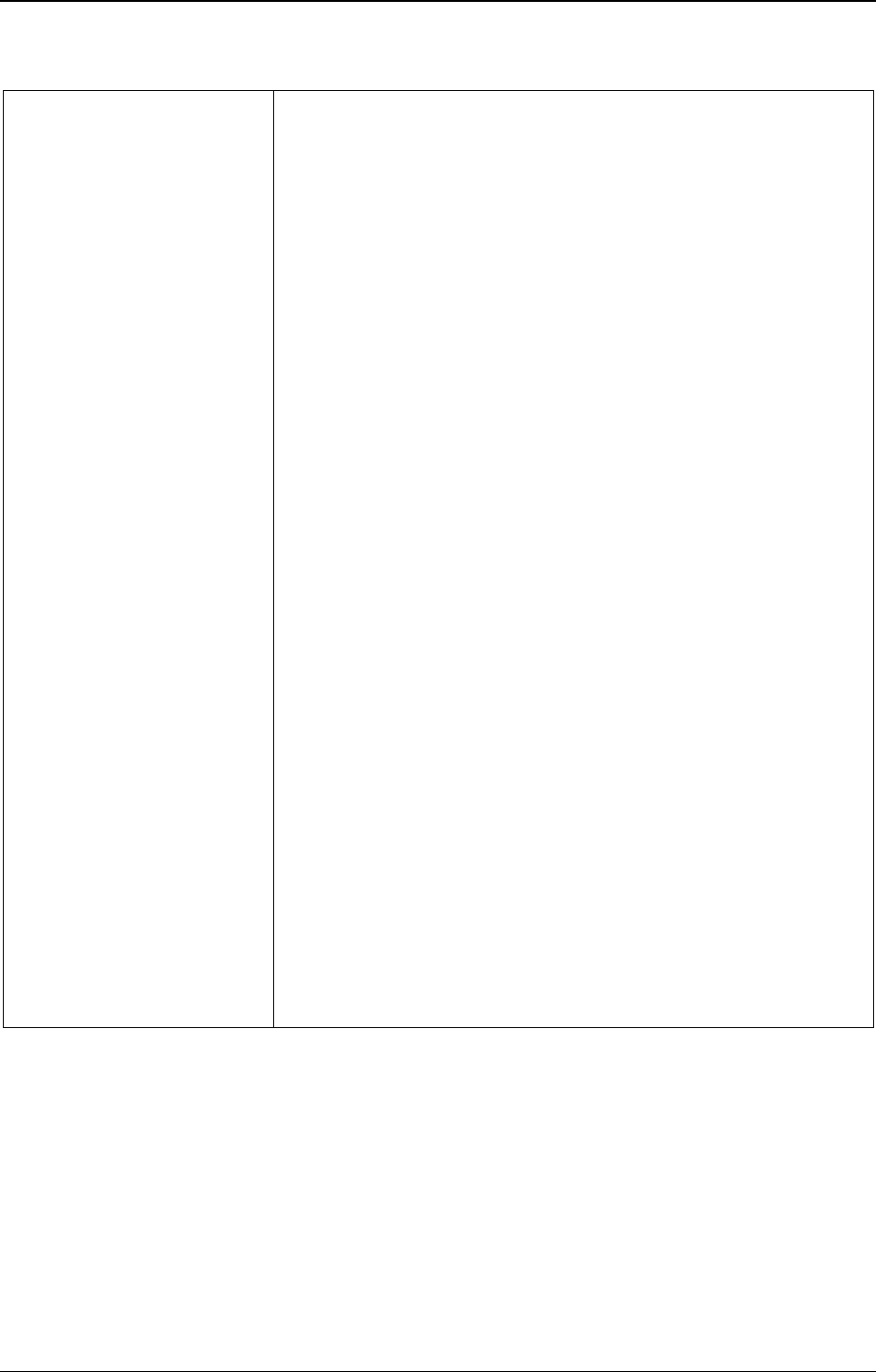
EB148/7 Annex 5
44
Suicide prevention: Develop
and implement comprehensive
national strategies for the
prevention of suicide, with
special attention to groups
identified as at increased risk of
suicide, including lesbian, gay,
bisexual and transgender
persons, youth and other
vulnerable groups of all ages
based on local context.
• Develop, keep up-to-date, implement and evaluate national suicide
prevention strategies that guide governments and stakeholders to
implement effective preventive interventions, raise public awareness,
increase help-seeking and reduce stigmatization of suicidal thoughts
and behaviours.
• Increase public, political and media awareness of the magnitude of the
problem and the availability of evidence-based effective suicide-
prevention strategies.
• Ban highly hazardous pesticides and restrict access to other means of
self-harm and suicide (for instance, high places, medicines and
firearms).
• Promote responsible media reporting in relation to cases of suicide by
training media professionals and others producing content for screen or
stage on how to cover suicide.
• Implement universal and indicated school-based socioemotional
learning programmes and other interventions to support adolescents in
their problem-solving and coping skills.
• Promote workplace, school-based and other community-based
initiatives for suicide prevention that are tailored to groups at risk
including adolescents and older persons.
• Improve responses in the health system and other sectors to self-harm
and suicide, including training of staff (for example, non-specialized
health workers, social workers, teachers, police, persons working in the
criminal justice system, firefighters, other first responders and faith
leaders) in the assessment, management and follow-up of self-harm and
suicide.
• Engage communities in suicide prevention and optimize psychosocial
support from available community resources for both those who self-
harmed or who attempted suicide and families of people who died by
suicide.
• Develop community-level strategies for suicide prevention including
access to formal and informal services, volunteer social support groups
and other culturally-appropriate programmes.
• Ensure financing of suicide prevention by allocating adequate
resources.
• Ensure all relevant groups at risk of suicide, including indigenous
people, are involved in developing suicide-prevention strategies.
• Conduct a situation analysis (for instance, rates of suicide and self-
harm, specific populations at risk, common methods of suicide, existing
suicide prevention activities and gaps) to inform the planning of suicide
prevention activities.
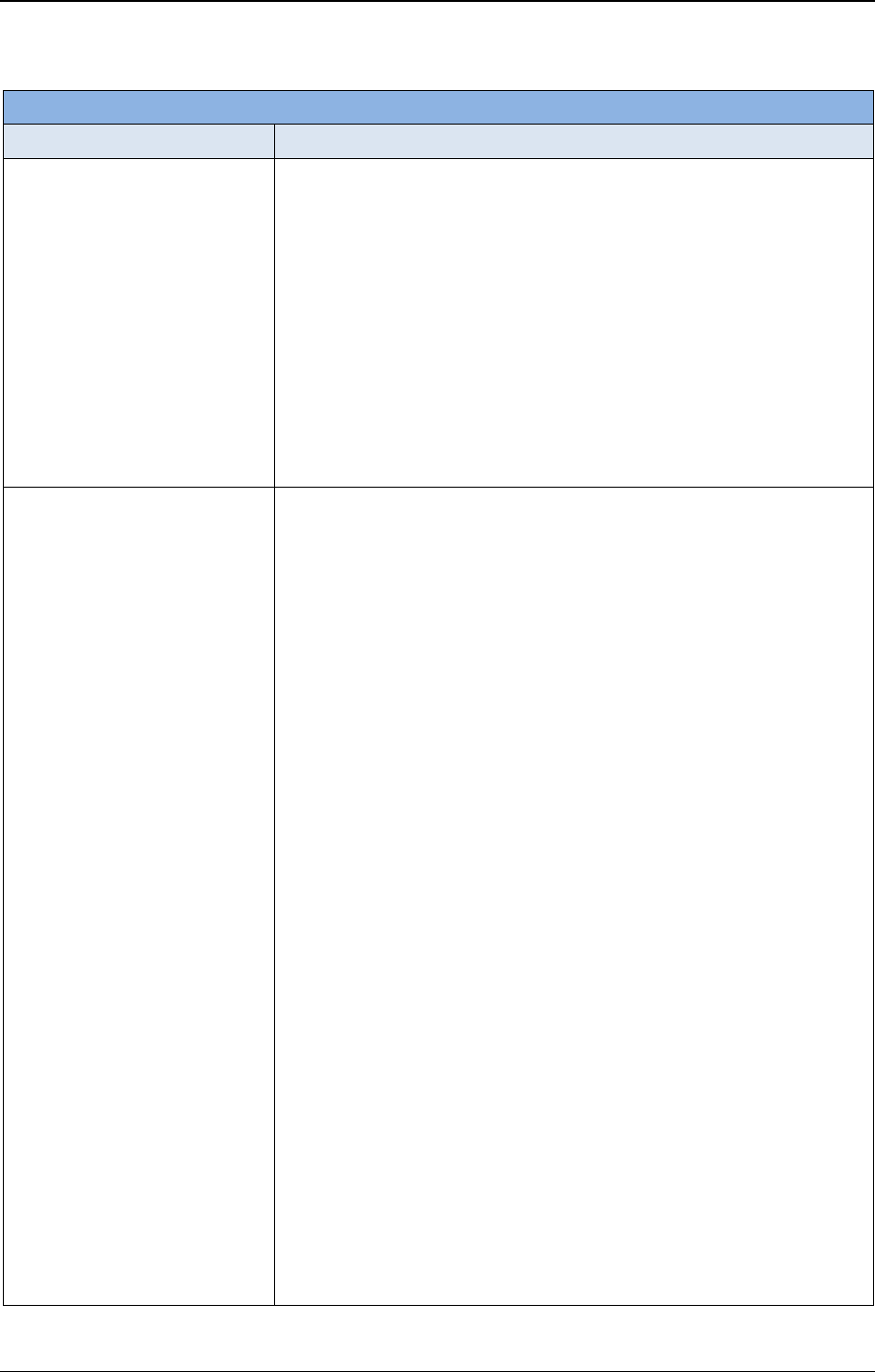
Annex 5 EB148/7
45
Objective 4: To strengthen information systems, evidence and research for mental health
Actions
Options for implementation
Information systems: Integrate
mental health into the routine
health information system and
identify, collate, routinely report
and use core mental health data
disaggregated by sex and age
(including on completed and
attempted suicides) to improve
mental health service delivery,
promotion and prevention
strategies and to feed into the
Global Mental Health
Observatory (as a part of WHO’s
Global Health Observatory).
• Establish a surveillance system for monitoring mental health and self-
harm and/or suicide and suicide attempts, ensuring that records are
disaggregated by facility, gender, age, disability, method and other
relevant variables.
• Embed mental health and self-harm and/or suicide information needs
and indicators, including risk factors and disabilities, within national
population-based surveys and health information systems.
• Collect detailed data from secondary and tertiary services in addition to
routine data collected through the national health information system.
• Include mental health indicators within information systems of other
sectors.
• Analyse and publish data collected on the availability, financing and
evaluation of mental health and social care services and programmes to
improve services and population-based interventions.
Evidence and research:
Improve research capacity and
academic collaboration on
national priorities for research in
mental health, particularly
operational research with direct
relevance to service development
and implementation and the
exercise of human rights by
persons with mental disorders,
including the establishment of
centres of excellence with clear
standards, with the inputs of all
relevant stakeholders including
persons with mental disorders
and psychosocial disabilities.
• Develop and promote a prioritized and funded national research agenda
in the area of mental health, based on consultation with all
stakeholders.
• Improve research capacity to assess needs and to evaluate the
effectiveness, implementation and scale up of services and
programmes, including human rights and recovery-oriented
approaches.
• Enable strengthened cooperation between universities, institutes, and
health and social services and other relevant settings (such as
educational) in the field of mental health research.
• Conduct research, in different cultural contexts, on local
understandings and expressions of mental distress, practices that are
harmful (for instance, human rights violations and discrimination) or
protective (for instance, social supports and traditional customs) and
ways of help-seeking (for instance, traditional healers), as well as the
efficacy, acceptability and feasibility of interventions for treatment and
recovery, prevention and promotion.
• Develop methods for characterizing mental health disparities that occur
among diverse subpopulations in countries, including factors such as
race and/or ethnicity, sex, socioeconomic status and geography (urban
versus rural), and evaluate interventions that are responsive to the needs
of specific groups and address social determinants.
• Strengthen collaboration between national, subnational and
international research centres for mutual interdisciplinary exchange of
research and resources between countries.
• Promote high ethical standards in mental health research, ensuring that:
research is conducted only with the free and informed consent of the
person concerned; researchers do not receive any privileges,
compensation or remuneration in exchange for encouraging or
recruiting people to participate in the research; research is not
undertaken if it is potentially harmful or dangerous; all research is
approved by an independent ethics committee functioning according to
national and international norms and standards; and research is carried
out with meaningful involvement of local collaborators and
stakeholders in the design, implementation and dissemination of
research findings.
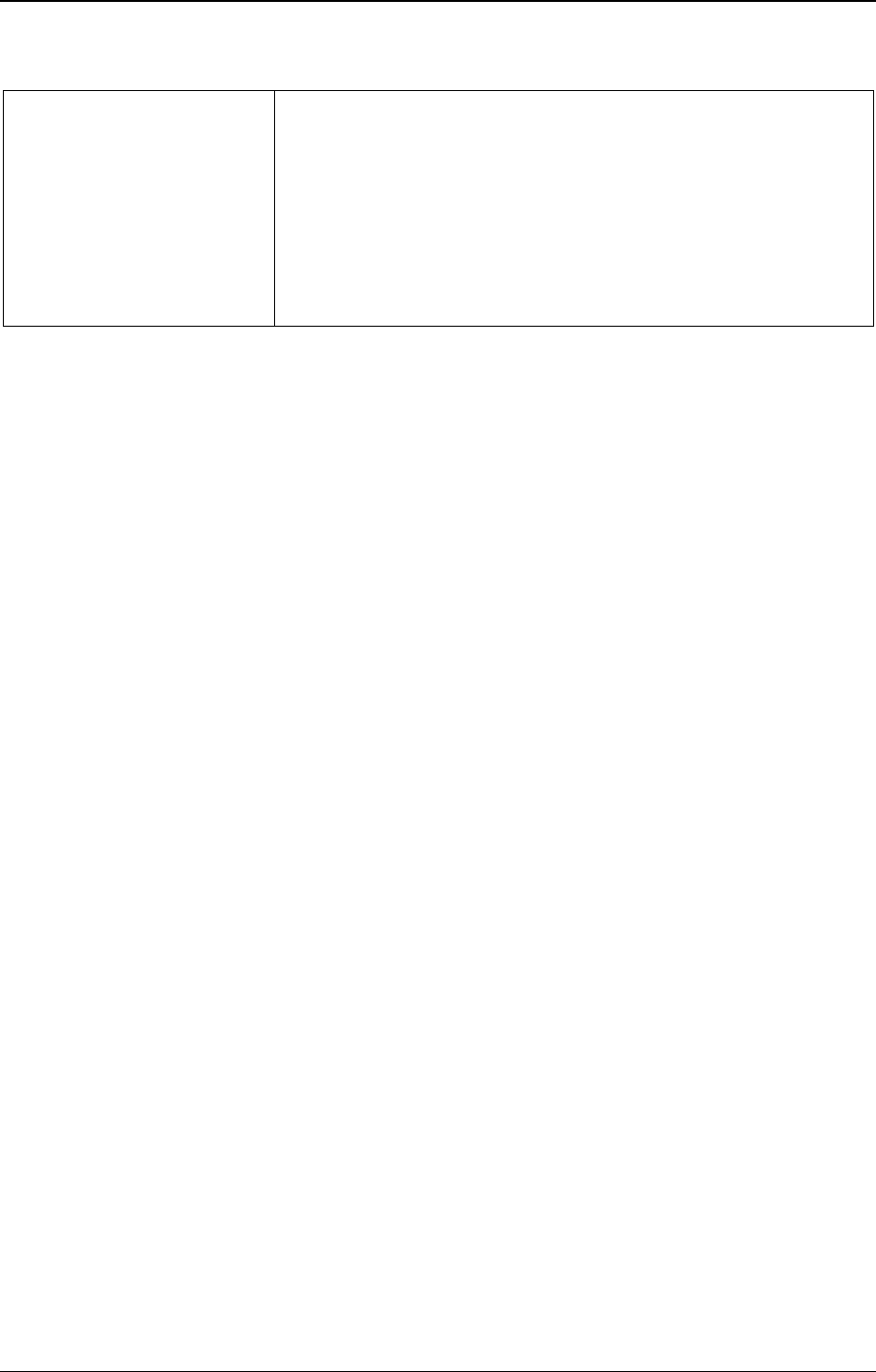
EB148/7 Annex 5
46
• Ensure that people with mental health conditions and psychosocial
disabilities and their organizations contribute to mental health research,
for instance through setting the research agenda, advising on the
research methods and design, and in informing about their lived
experience.
• Ensure the translation of results from research to practice and the
transfer of knowledge from academic to service settings by training
stakeholders, including policy-makers and mental health professionals,
in critical appraisal of evidence and providing open access to unbiased
and easy-to-understand information.

EB148/7
47
ANNEX 6
CONCRETE GUIDANCE TO STRENGTHEN HEALTH LITERACY
1. This annex describes progress in providing Member States with concrete guidance to strengthen
health literacy through education programmes and population-wide targeted and mass- and social-media
campaigns to reduce the impact of all risk factors and determinants of noncommunicable diseases.
Context
2. In 2014, at the second High-level Meeting of the General Assembly on Non-communicable
Diseases, ministers and representatives of States and Governments committed themselves to “continue
to develop, strengthen and implement appropriate multisectoral public policies and action plans to
promote health education and health literacy, with a particular focus on populations with low health
awareness and/or literacy.”
1
3. The Shanghai Declaration on promoting health in the 2030 Agenda for Sustainable Development,
adopted at the 9th Global Conference on Health Promotion, held in China from 21 to
24 November 2016,
2
highlighted health literacy as one of the main pillars of health promotion for
achieving the 2030 Agenda for Sustainable Development.
4. At the third High-level Meeting of the General Assembly on Non-communicable Diseases in
2018, Heads of State and Government committed themselves to “empower the individual to make
informed choices by providing an enabling environment, strengthening health literacy through
education, and implementing population-wide and targeted mass and social media campaigns that
educate the public about NCD risk factors.”
3
5. These commitments remain largely unmet.
6. During the current COVID-19 pandemic, health literacy has been shown to be one of the key
drivers of a successful response, as people’s knowledge and abilities to obtain, understand, judge and
take decisions based on evidenced-based information are essential.
Providing Member States with concrete guidance to strengthen health literacy
approaches for the prevention and control of NCDs and mental health conditions
7. The Director-General convened a working group on health education and health literacy for
NCDs
4
of global experts nominated by Member States from 2017 to 2019 and supported by WHO’s
Global coordination mechanism for the prevention and control of noncommunicable diseases to
recommend ways and means of encouraging Member States and non-State actors to promote health
education and health literacy for the prevention and control of NCDs. The group focused in particular
1
In accordance with paragraph 30(a)(iii) of United Nations General Assembly resolution 68/300.
2
In accordance with preambular paragraph 6 of resolution WHA71.2.
3
In accordance with paragraph 334 of United Nations General Assembly resolution 73/2.
4
WHO. The WHO GCM/NCD Working Group on health education and health literacy for NCDs (Working
Group 3.3, 2016–2017) (https://www.who.int/global-coordination-mechanism/working-groups/working-group-3-3/en/,
accessed 7 December 2020).

EB148/7 Annex 6
48
on populations with low health awareness and/or literacy and took into account WHO’s best buys and
other recommended interventions for the prevention and control of NCDs.
8. The final report from the working group has been designated a WHO Global Public Health Good
for the period 2020–2021 and is being finalized. Its guidance will support the implementation of
practical health literacy approaches to accelerate the prevention and control of NCDs at national level,
including use of an implementation toolkit. The draft final report will be presented for broad
consultation, including Member States, all three levels of WHO, and selected and relevant external
stakeholders, during the first quarter of 2021, before its recommendations are piloted across WHO
regions.
9. Under the auspices of the WHO Working Group on health education and health literacy, the
Secretariat, developed ways to support the implementation of national health literacy demonstration
projects across WHO’s regions.
10. The Secretariat created a community of practice whose members met to build expertise and
resources to improve health literacy approaches for the prevention and control of NCDs and mental
health conditions.
11. The WHO European Action Network on Health Literacy for Prevention and Control of
Noncommunicable Diseases
1
was launched in 2019 to support Member States in the European Region
to attain target 3.4 of Sustainable Development Goal 3 (by 2030 reduce by one third pre-mature mortality
from noncommunicable diseases (NCDs) through prevention and treatment, and promote mental health
and well-being) through interventions based on health literacy.
12. In 2019 the Regional Committee for Europe at its sixty-ninth session, in resolution EUR/RC69/R9
“Towards the implementation of health literacy initiatives through the life course”, took note of the
WHO European road map for implementation of health literacy initiatives through the life course and
urged Member States to strengthen implementation of health literacy initiatives in various areas of
action, environments and settings, including by using innovations.
Providing Member States with concrete guidance to strengthen health literacy through
education programmes and population-wide targeted and mass- and social-media
campaigns to reduce the impact of all risk factors and determinants of NCDs
13. Recommendation 2 of the final report of the WHO Independent High-level Commission on
Noncommunicable Diseases
2
requests the Secretariat to “support countries in their national efforts to
empower individuals to make healthy choices and make the healthiest choice the easiest choice,
including through the creation of enabling environments and the promotion of health literacy”.
14. The Secretariat is developing a toolkit for behavioural change communication campaigns on NCD
risk factors and mental health conditions, targeted at children and adolescents. This toolkit will build on
1
Drapkina O, de Graca Freitas M, Mikkelsen B, Breda J, Salakhov E, Lopatina M, Silva da Costa A, Koylyu A,
Williams J, Wickramasinghe K, Telo de Arriaga M. The WHO European Action Network on Health Literacy for Prevention
and Control of Noncommunicable Diseases. Public Health Panorama 2019; 5(2–3):123–129
(https://apps.who.int/iris/handle/10665/327056, accessed 12 January 2021).
2
WHO. It’s time to walk the talk: WHO Independent High-level Commission on Noncommunicable Diseases –
summary. Geneva: World Health Organization; 2019 (https://www.who.int/ncds/governance/high-level-commission/en/,
accessed 12 January 2021).

Annex 6 EB148/7
49
the WHO Strategic Communications Framework
1
and will prioritize a catalogue of communications
knowledge, skills, contextual best practices, innovative approaches and resources for effective
communication to particular target audiences and the use of emerging technologies in communicating
messages about NCD risk factors and the promotion of healthy behaviours.
15. In 2020, WHO published a handbook on life skills education about prevention of
noncommunicable diseases.
2
Its purpose is to support schools in implementing interventions aimed at
reducing the main modifiable risk behaviours for noncommunicable diseases.
16. The Secretariat will update this annex in its report to the Seventy-fourth World Health Assembly
in May 2021.
1
WHO. WHO Strategic Communications Framework. Geneva: World Health Organization; 2020
(https://www.who.int/mediacentre/framework-at-a-glance-slides.pdf, accessed 7 December 2020).
2
WHO. Life skills education school handbook: prevention of noncommunicable diseases: introduction. Geneva:
World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/331948).

EB148/7
50
ANNEX 7
ANALYSIS OF SUCCESSFUL APPROACHES TO MULTISECTORAL ACTION
FOR THE PREVENTION AND CONTROL OF NONCOMMUNICABLE DISEASES
1. This annex describes the process that the Secretariat will follow to analyse, on the basis of a
review of international experiences, successful approaches to multisectoral action for the prevention and
control of noncommunicable diseases, including those that address their social, economic and
environmental determinants.
2. WHO’s 2008–2013 action plan for the global strategy for the prevention and control of
noncommunicable diseases included an action for the Secretariat to “conduct a review of international
experience in the prevention and control of noncommunicable diseases, including community-based
programmes, and identify and disseminate lessons learned”. Owing to lack of resources, this first global
stocktaking report on multisectoral action for NCDs was not prepared at the time. Taking into account
this gap, decision WHA72(11) (2019) reiterated this request to the Director-General: to submit “in the
consolidated report to the Seventy-fourth World Health Assembly in 2021, based on a review of
international experiences, an analysis of successful approaches to multisectoral action for the prevention
and control of noncommunicable diseases, including those that address the social, economic and
environmental determinants of such diseases”.
3. The Secretariat will take the following actions:
• In 2022, it will launch a publicly-accessible NCD multisectoral action repository to serve as a
tool for governments to:
• draw attention to national or local multisectoral projects in support of target 3.4 of
Sustainable Development Goal 3 (by 2030 reduce by one third pre-mature mortality from
NCDs through prevention and treatment, and promote mental health and well-being) at
the global level;
• submit descriptions of national projects serving as best practices for others, and update
on a continuous basis;
• extend networks by contacting directly project owners in other countries.
• In 2022, it plans to launch the first stocktaking report on multisectoral action for NCDs with
the aim of updating governments and partners on multisectoral activities undertaken to
accelerate progress towards target 3.4. The report will be updated annually, building on calls
for new entries into the database.
• In 2023, the Secretariat will submit an analysis of successful approaches to the Executive Board
at its 150th session.

EB148/7
51
ANNEX 8
ANALYSIS OF HOW FOOD PROCUREMENT IN SCHOOLS AND OTHER
RELEVANT INSTITUTIONS CAN BE MADE SUPPORTIVE OF HEALTHY DIETS
1. This annex reports the progress on the implementation of decision WHA72(11) (2019) that
requested the Director-General “to collect and share best practices for the prevention of overweight and
obesity, and in particular to analyse how food procurement in schools and other relevant institutions can
be made supportive of healthy diets and lifestyles in order to address the epidemic of childhood
overweight and obesity and reduce malnutrition in all its forms”.
Context
2. Every day, foods, beverages, meals and snacks are served and sold in public institutions. In
addition, many governments also purchase foods for government-funded programmes, such as school
meal programmes and social protection programmes. Collectively, these public settings and
programmes have a large population reach, including vulnerable groups such as children and older
people.
3. Governments worldwide therefore have a unique opportunity – as well as responsibility – to lead
by example through the implementation of healthy public food procurement policies that ensure that the
food served or sold in public settings or purchased (or subsidized) by government contributes to
promoting healthy diets and preventing all forms of malnutrition, including obesity and diet-related
NCDs. In addition to these public health benefits, healthy public food-procurement policies can have
economic benefits, improve productivity and educational attainment, help to increase the availability of
healthy, affordable foods and may also contribute to boosting local agriculture.
School food policies
4. In the Global Nutrition Policy Review 2016–2017, most countries (89% of 160) reported having
school health and nutrition programmes, but schools remain an underused delivery platform for
promoting good nutrition and healthy diets, especially as they can address issues related to both
undernutrition and overweight and obesity.
5. The Secretariat has analysed measures applied to foods and beverages served or sold in and
around schools, drawing on 128 documents from 83 Member States included in WHO’s Global database
on the implementation of nutrition action.
1
About half (42 Member States) had legislative measures
(such as laws, decrees and ordinances) published in official gazettes, often including an enforcement
mechanism. These were issued as stand-alone school food and nutrition legislation or incorporated into
broader school-related laws (on, for instance, feeding programmes, health or hygiene) or into other
legislative measures (for example, marketing restrictions, public catering laws, public health codes, and
child health and nutrition laws). Another 10 countries had compulsory standards for foods and beverages
in schools, while 25 countries had government-issued guides for school foods and beverages that were
typically promoted through ministry websites or reports. Nine countries had stated the requirements for
school food and beverages in national school nutrition policies. Among the 77 countries with legislation,
1
This includes 8 countries in the African Region, 17 in the Region of the Americas, 4 in the South-East Asia Region,
37 in the European Region, 6 in the Eastern Mediterranean Region, and 11 in the Western Pacific Region.

EB148/7 Annex 8
52
standards or guides on school foods and beverages, 73 countries covered foods and beverages offered
during school lunches and often also other meals or snacks provided. Furthermore, 52 countries had
measures that covered foods and beverages sold at school, in cafeterias, food stores, snack bars or
vending machines. Less frequently, measures covered foods and beverages available at school activities
or events (10 countries) or extended to sales around schools (for example, in radius of 200 meters around
the school premises – three countries). Several countries (22) extended the measures to foods and
beverages marketed in schools, including sponsorships. Only three countries extended the measures to
foods brought from home.
6. The measures typically involved food-based criteria that promoted healthier foods and beverages
(74 countries) especially fruits and vegetables (69 countries), water for drinking (57 countries) and
whole-grain varieties of cereals and cereal products (43 countries). For proteins, the measures
recommended leaner cuts of meat, fish or eggs (38 countries) or the use of pulses and legumes
(43 countries), often as replacement of animal-sourced products on a number of days of the week. The
measures often recommended the use of unsaturated oils for cooking (26 countries). Fewer measures
promoted fortified foods, including iodized salt (12 countries) or fortified staple foods (six countries).
7. Most countries also listed foods and beverages that were prohibited, to be avoided or to be limited
in schools (67 countries). This most commonly applied to various kinds of confectionary, savoury
snacks, cakes and pastries (49 countries), fried foods (36 countries) and salt and condiments with a high
sodium content (35 countries). For beverages, 48 countries prohibited or limited carbonated and
non-carbonated soft drinks, and 26 countries prohibited energy and sport drinks. Specific prohibitions
or limitations were less common for other sugar-sweetened beverages, such as juice drinks
(22 countries), sweetened flavoured milks (19 countries), beverages prepared from liquid and powder
concentrates (16 countries) or 100% fruit or vegetable juices (12 countries). In fact, many countries
promoted juices (both diluted and 100%) to be served or sold in schools.
8. In 46 countries the measures included nutrient-based criteria for foods and beverages offered in
schools, based on total fat (36 countries), sugars (34 countries), salt/sodium (33 countries), energy
(28 countries), saturated fatty acids (23 countries) or trans-fatty acids (18 countries). Many countries
provided indications on the portions to be served in school, and 28 countries used this policy measure
as a way to limit items that do not form part of healthy diets.
Annex 8 EB148/7
53
Action Framework for Developing and Implementing Public Food Procurement Policies
for a Healthy Diet
1
9. To support Member States in implementing a healthy public food procurement policy, the
Secretariat has collected several country examples and developed an action framework for developing
and implementing public food procurement policies for a healthy diet. The action framework was
peer-reviewed by experts, policy-makers and practitioners from Member States from all WHO regions
and contains various country case studies and best practices.
2
10. The framework illustrates key steps to take in developing or revising a healthy public
food-procurement policy, and ways to prepare an implementation plan and to monitor and enforce the
policy. It proposes how to conduct a landscape analysis and engage with a lead government authority to
review existing policies in consultation with stakeholders. A step-wise approach is also suggested.
Nutrient or food-based criteria, as well as other criteria such as portion size, will have to complement
such policies, and food safety considerations will have to be included. The framework contains the links
to the specific case studies and available tools.
1
WHO. Action Framework for Developing and Implementing Public Food Procurement Policies for a Healthy Diet.
Geneva: World Health Organization; 2020 (https://www.who.int/publications/i/item/9789240018341, accessed 12 January
2021).
2
Settings and facilities considered are: day-care centres or child-care facilities, schools, after-school/summer
programmes, post-secondary institutions, universities, hospitals, long-term and residential aged care facilities, government
workplaces, farmers’ markets, public parks, community centres, sport and recreation facilities, railway stations, public bus
stands, airports, military bases, prisons and juvenile detention facilities, cafeterias/cafes, canteens, restaurants, snack shops,
food kiosks, tuck shops, and vending machines. The analysis also considered school meal programmes, social services, social
support programmes, homeless shelters, food pantries, supplemental feeding programmes, sport events held in public
settings, government-sponsored meetings and conferences.
EB148/7
54
ANNEX 9
GUIDANCE ON HOW TO STRENGTHEN THE DESIGN AND IMPLEMENTATION
OF POLICIES, INCLUDING FOR RESILIENT HEALTH SYSTEMS AND
HEALTH SERVICES AND INFRASTRUCTURE TO TREAT PEOPLE LIVING
WITH NONCOMMUNICABLE DISEASES AND PREVENT AND CONTROL THEIR
RISK FACTORS IN HUMANITARIAN EMERGENCIES
1. This annex describes the process that the Secretariat is following to draw up guidance to Member
States, in response to paragraph 40 of the Political Declaration of the third High-level Meeting of the
General Assembly on the Prevention and Control of Non-communicable Diseases,
1
on how to strengthen
the design and implementation of policies, including those for resilient health systems and health
services and infrastructure to treat people living with NCDs and to prevent and control their risk factors
in humanitarian emergencies.
2. It also provides an update on the Secretariat’s work in response to paragraphs 31, 46 and 48 of
WHO’s global action plan for the prevention and control of noncommunicable diseases 2013–2030
2
to
ensure continuity of essential NCD services, including availability of life-saving technologies and
essential medicines, in humanitarian emergencies.
Context
3. The number of people currently affected by humanitarian emergencies worldwide is
unprecedented. The United Nations Office for the Coordination of Humanitarian Affairs estimated that
168 million people would need humanitarian aid and protection in 2020.
3
The ongoing COVID-19
pandemic is aggravating this situation, placing an additional burden on already fragile health systems
and disrupting essential health services around the world.
4. NCDs such as cancer, cardiovascular disease, chronic respiratory disease and diabetes are the
leading causes of death and disability worldwide, disproportionally affecting low- and middle-income
countries, which are especially vulnerable to the effects of conflict, epidemics, natural disasters, and
forced displacement. In 2017, NCDs accounted for between 24% and 68% of mortality in the top five
source countries for refugees.
5. Interruption of care, sudden shifts in priorities of the health care system, the inability of health
facilities to function safely and provide quality care for all patients, changes in diet and physical activity
habits, increase in stress levels, decrease in medication adherence and precipitation of an acute
1
United Nations General Assembly. Political Declaration of the third High-level Meeting of the General Assembly
on the Prevention and Control of Non-communicable Diseases. Resolution A/RES/73/2
(https://digitallibrary.un.org/record/1648984, accessed 4 November 2020), paragraph 40.
2
Resolution WHA66.10 (2013), Annex.
3
OCHA. Global humanitarian overview 2020. Geneva: United Nations Office for the Coordination of Humanitarian
Affairs; 2019 (https://www.unocha.org/global-humanitarian-overview-2020, accessed 4 November 2020).
Annex 9 EB148/7
55
exacerbation in a chronic condition – all result in excess morbidity and mortality related to NCDs during
emergencies and disasters.
1
6. The health component of humanitarian responses to emergencies has traditionally focused on
communicable diseases and injury management, with NCDs being poorly addressed. Capacity and
resources for NCD service provision are often already inadequate in low- and lower middle-income
settings. A humanitarian emergency makes this more evident, causing NCD-related premature mortality,
morbidity and economic difficulty on top of the damage caused by other aspects of the emergency.
7. The COVID-19 pandemic has brought a new level of urgency to the need for improving NCD
management as part of emergency preparedness and response. NCDs and their risk factors increase both
susceptibility to infection and the likelihood of severe outcomes from COVID-19. At the same time,
NCD services have been severely disrupted,
2
leaving many people with NCDs without the health
services and medicines they need.
Ensuring continuity of NCD services in humanitarian emergencies: work to date
8. Some progress has been made in raising awareness and producing guidance to support Member
States and humanitarian agencies in ensuring continuity of NCD care in emergencies:
• NCDs in emergencies: a WHO/UNHCR policy brief
3
describes global minimum standards and
priority actions for NCD care in preparation for, response to and recovery from humanitarian
emergencies.
• Integration of NCD care in emergency response and preparedness: a technical guidance
document from the Regional Office for South-East Asia
4
outlines relevant priority actions to
integrate NCD interventions into national health emergency preparedness and responses.
• Prevention and control of noncommunicable diseases in refugees and migrants: technical
guidance from the Regional Office for Europe
5
outlines key priority areas for interventions
within refugee and migrant groups.
• In June 2015 an informal working group on NCDs in humanitarian settings was set up as
an informal platform to share lessons learned and to harmonize and draft technical guidance for
1
WHO Regional Office for South-East Asia. Integration of NCD care in emergency response and preparedness.
Manila: World Health Organization Regional Office for South-East Asia; 2018
(https://apps.who.int/iris/bitstream/handle/10665/272964/9789290226352-eng.pdf?sequence=1&isAllowed=y).
2
WHO. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a
rapid assessment. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/334136).
3
WHO. Noncommunicable diseases in emergencies. Geneva: World Health Organization;
2016 (https://apps.who.int/iris/handle/10665/204627).
4
WHO Regional Office for South-East Asia. Integration of NCD care in emergency response and
preparedness. Manila: World Health Organization Regional Office for South-East Asia; 2018
(https://apps.who.int/iris/handle/10665/272964).
5
WHO Regional Office for Europe. Prevention and control of noncommunicable diseases in refugees and migrants:
Technical guidance. Copenhagen: World Health Organization Regional Office for Europe; 2019
(https://apps.who.int/iris/handle/10665/311461).

EB148/7 Annex 9
56
dealing with NCDs in humanitarian settings. It is chaired by the United Nations High
Commissioner for Refugees and WHO participates.
• WHO’s operational guidance for maintaining essential health services in the COVID-19
context
1
provides an entry point for prioritizing essential NCD services in emergencies. The
Secretariat is adapting guidance for the humanitarian context the Global Health Cluster
COVID-19 Task Team.
9. The Inter-Agency Emergency Health Kit
2
has been revised to include essential NCD medicines.
The Regional Office for the Eastern Mediterranean developed an additional NCD kit
3
to provide
essential medicines and medical devices for the management of most common NCDs encountered at
primary health care level. Since 2017, the kit has been used in, Afghanistan, Bangladesh, Central African
Republic, Democratic Republic of the Congo, Ethiopia, Iraq, Libya, Syrian Arab Republic and Yemen,
and is pre-positioned in the occupied Palestinian territory, including east Jerusalem and the WHO
Operations Supply and Logistics Hub in Dubai.
10. NCDs remain a neglected aspect of humanitarian responses, however, with significant gaps in
technical and operational guidance, lack of capacity and resources in the Secretariat at headquarters and
in regions and countries, and insufficient integration of NCDs into emergency preparedness and
response plans, humanitarian data collection systems, and dashboards.
Process to develop guidance to Member States on ensuring continuity of essential NCD
services in humanitarian emergencies
11. In order to support Member States in their commitment to strengthen policies to treat people living
with NCDs and prevent and control their risk factors in humanitarian emergencies, the Secretariat is
undertaking work in the following areas:
• governance: to establish an integrated approach to addressing NCDs in humanitarian
emergencies across the Organization, including the Global Health Cluster.
• normative work: to comprehensively map existing policies, guidelines and tools to address
NCDs in humanitarian settings in order to fill gaps in guidance for governments and
humanitarian agencies.
• technical assistance: to propose ways to improve support to countries across preparedness,
response and recovery, leveraging crises as an entry-point to build health systems back better
through development of sustainable NCD services.
• research: to continue existing work with academic partners to shape the research agenda so as
to inform policies to strengthen emergency preparedness and responses.
1
WHO. Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance,
1 June 2020. Geneva: World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/332240).
2
WHO. The interagency health kit 2017: medicines and medical devices for 10 000 people for approximately three
months. Geneva: World Health Organization; 2019 (https://apps.who.int/iris/handle/10665/279428).
3
Slamam S, Lee J, Aragno M, Laroche S, Hogerzeil H. The development of the noncommunicable diseases
emergency health kit. Eastern Mediterranean Health Journal (special issue on scaling up health workforce in the Eastern
Mediterranean Region), 2018; 24(1):92-98 (https://doi.org/10.26719/2018.24.1.92, accessed 7 December 2020).

Annex 9 EB148/7
57
• financing: to advocate with donors the prioritization of building bridges with a view to
prioritizing NCDs in humanitarian emergencies across the health, development and
peace-building sectors.
12. The Secretariat will update this annex in its report to the Seventy-fourth World Health Assembly
in May 2021.
EB148/7
58
ANNEX 10
UPDATE ON THE WORK OF THE UNITED NATIONS INTER-AGENCY TASK
FORCE ON THE PREVENTION AND CONTROL OF
NON-COMMUNICABLE DISEASES
1. This annex provides an update on the work of the United Nations Inter-Agency Task Force on the
Prevention and Control of Non-communicable Diseases in the implementation of WHO’s global action
plan for the prevention and control of non-communicable diseases 2013–2020, the Political Declaration
on the third High-level Meeting of the General Assembly on the Prevention and Control of
Non-communicable Diseases (General Assembly resolution 73/2 (2018)), Health Assembly decision
WHA72(11) (2019) on follow up to that political declaration, and resolution E/RES/2019/9 of the United
Nations Economic and Social Council on the Task Force.
1
2. The Task Force ensures coordinated action across the United Nations system to support Member
States achieve the Sustainable Development Goals related to NCDs. It delivers high-quality technical
support to advance multisectoral action in countries. Over the past year, three members of the Task
Force – the United Nations High Commissioner for Refugees, International Labour Organization and
Organisation for Economic Co-operation and Development - have published briefs on NCDs; altogether
now 12 members have published briefs under the Task Force.
2
3. The report of the Director-General on the Task Force, submitted to the Economic and Social
Council in March 2020,
3
described progress and achievements over the past year in line with the Task
Force’s strategic priorities,
4
including joint programming missions, joint programmes and initiatives,
the Global Action Plan for Healthy Lives and Well-being for All
5
and progress on establishing a United
Nations NCD and mental health multi-partner trust fund to support countries in scaling up action on
NCDs and mental health. The report also highlighted the linkages between NCDs and COVID-19.
4. The Economic and Social Council, in resolution 2020/22 on the work of the Task Force,
6
called
upon the members of the Task Force to continue to work together to identify additional technical
resources to enhance their support to Member States in line with the Task Force strategy for 2019–2021,
paying particular attention to the needs of Member States during their COVID-19 response and recovery.
1
United Nations Economic and Social Council. United Nations Inter-Agency Task Force on the Prevention and
Control of Non-communicable Diseases: draft resolution. Document E/2019/L.16 (https://undocs.org/E/2019/L.16).
2
WHO. United Nations agency briefs: responding to the challenge of NCDs. Geneva: World Health Organization;
2019 (https://apps.who.int/iris/bitstream/handle/10665/327396/WHO-UNIATF-19.98-eng.pdf?ua=1).
3
United Nations Economic and Social Council. United Nations Inter-Agency Task Force on the Prevention and
Control of Non-communicable Diseases. New York: United Nations; 2020, document E/2020/51
( https://undocs.org/en/E/2020/51).
4
WHO. United Nations Inter-Agency Task Force on the Prevention and Control of Non-communicable Diseases.
2019–2021 strategy. Geneva: World Health Organization; 2019 (https://www.who.int/groups/un-inter-agency-task-force-on-
NCDs, accessed 12 January 2021).
5
WHO. About the Global Action Plan for Healthy Lives and Well-being for All. Geneva: World Health Organization
(https://www.who.int/initiatives/sdg3-global-action-plan/about, accessed 7 December 2020).
6
United Nations Economic and Social Council. Resolution E/RES/2020/22: United Nations Inter-Agency Task Force
on the Prevention and Control of Non-communicable Diseases (https://digitallibrary.un.org/record/3874500?ln=en).

Annex 10 EB148/7
59
5. In September 2020, the publication of WHO, United Nations Development Programme and the
Task Force on responding to NCDs during and beyond the COVID-19 pandemic, to which more than
30 Task Force members contributed, was launched.
1
It builds on WHO’s operational guidance on how
to maintain essential health services for NCDs and mental health during the pandemic. It is aimed at
governments, policy-makers, organizations in the United Nations system and development partners and
explains why strong action on NCDs must be an integral part of the COVID-19 response and recovery.
6. The Economic and Social Council’s resolution E/RES/2019/9 on the work of the Task Force in
2019 encouraged the mobilization of resources through innovative funding mechanisms, including a
dedicated multi-partner trust fund. As a result, the Task Force Secretariat has drafted terms of reference
with the United Nations Multi-Partner Trust Fund Office as the administrative agent. In the first instance,
the trust fund will support low- and middle-income countries accessing catalytic resources to tackle
NCDs, as part of their national COVID-19 response and recovery plans.
7. In February 2020, the Task Force and WHO’s Global Tuberculosis Programme undertook a joint
mission to Nigeria with 15 agencies and bilateral development partners.
8. Members of the Task Force continue to deliver joint programmes to support countries in
advancing action on NCDs. One example is the WHO/United Nations Development Programme joint
project to catalyse multisectoral action on NCDs, which to date has worked with Member States to
deliver 26 cases for investment in NCD prevention and control and mental health. The investment cases
provide countries with evidence and arguments to strengthen legislative, fiscal and regulatory measures
at the country level.
9. An example of a new programme established in reaction to the COVID-19 pandemic is the Access
Initiative for Quitting Tobacco
2
which works with governments, the United Nations and the private
sector to accelerate tobacco cessation in low- and middle-income countries.
10. Task Force members are committed to align their NCD and mental health activities with the
United Nations’ comprehensive response to COVID-19, for example through: (i) raising national
awareness on return on investment in NCD prevention and treatment to secure domestic budgetary
allocations and financing for development discussions: (ii) by helping countries to include NCDs into
their socioeconomic response plans; and (iii) participating in the WHO Working Group on COVID-19
and NCDs. WHO’s global action plan for healthy lives and well-being continues to provide an important
platform for many members of the Task Force to work through.
1
WHO/UNDP. Responding to non-communicable diseases during and beyond the COVID-19 pandemic. Geneva:
World Health Organization; 2020 (https://apps.who.int/iris/handle/10665/334145).
2
WHO. WHO and partners to help more than 1 billion people quit tobacco to reduce risk of COVID-19
(https://www.who.int/news-room/detail/09-07-2020-who-and-partners-to-help-more-than-1-billion-people-quit-tobacco-to-
reduce-risk-of-covid-19, accessed 5 November 2020).

EB148/7 Annex 10
60
11. A “Friends of the Task Force” event was held in the margins of the United Nations General
Assembly on 24 September 2020 that allowed Member States and development partners to provide
updates on their work on NCDs and mental health and for the Task Force to provide an update on its
activities. WHO’s Director-General announced the winners of the 2020 Task Force award.
1
= = =
1
WHO. UNIATF Awards 2020 (https://www.who.int/news-room/detail/25-09-2020-uniatf-awards-2020, accessed
5 November 2020).
