
© 2022 College of American Pathologists (CAP). All rights reserved. For Terms of Use please visit www.cap.org/cancerprotocols . 1
Template for Reporting Results of Biomarker Testing of
Specimens From Patients With Carcinoma of Gynecologic Origin
Version: 1.0.0.0
Protocol Posting Date: December 2022
The use of this protocol is recommended for clinical care purposes but is not required for accreditation
purposes.
Authors
Barbara A. Crothers, DO*; Lara R. Harik, MD, FCAP*; Angela N. Bartley, MD, PhD, FCAP; Russell R.
Broaddus, MD, PhD, FCAP; Linus T. Chuang, MD; Michael B. Cohen, MD; Patricia Salter Jamieson,
CTR; Elke A . Jarboe, MD; Teri A. Longacre, MD; George L. Mutter, MD; Christopher N. Otis, MD; Patrick
L. Fitzgibbons, MD, FCAP; Richard Zaino, MD; Gulisa Turashvili, MD, PhD; Krisztina Hanley, MD.
With guidance from the CAP Cancer and CAP Pathology Electronic Reporting Committees.
* Denotes primary author.
Accreditation Requirements
Completion of the template is the responsibility of the laboratory performing the biomarker testing and/or
providing the interpretation. When both testing and interpretation are performed elsewhere (eg, a
reference laboratory), synoptic reporting of the results by the laboratory submitting the tissue for testing is
also encouraged to ensure that all information is included in the patient’s medical record and thus readily
available to the treating clinical team. This template is not required for accreditation purposes.
Summary of Changes
v 1.0.0.0
• New Protocol

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
2
Reporting Template
Protocol Posting Date: December 2022
Select a single response unless otherwise indicated.
CASE SUMMARY: (Gynecologic Biomarker Reporting Template)
TEST(S) PERFORMED
Completion of the template is the responsibility of the laboratory performing the biomarker testing and / or providing the
interpretation. When both testing and interpretation are performed elsewhere (e.g., a reference laboratory), synoptic reporting of the
results by the laboratory submitting the tissue for testing is also encouraged to ensure that all information is included in the patient’s
medical record and thus readily available to the treating clinical team.
Gene names should follow recommendations of The Human Genome Organisation (HUGO) Nomenclature Committee
(www.genenames.org; accessed October 12, 2022).
All reported gene sequence variations should be identified following the recommendations of the Human Genome Variation Society
(http://varnomen.hgvs.org/; accessed October 12, 2022).
+Testing Performed on Block Number(s) (specify): _________________
+Specimen Type
___ Biopsy / curettage
___ Resection
___ Other (specify): _________________
+Appropriate Controls Verified
___ Yes
___ No
___ Other (specify): _________________
Immunohistochemical Tests Performed (Note A
) (select all that apply)
___ Estrogen Receptor (ER) Status (Note B)
Estrogen Receptor (ER) Status
___ Positive
Percentage of Cells with Nuclear Positivity: _________________ %
Average Intensity of Staining
___ Weak
___ Moderate
___ Strong
___ Negative (less than 1%)
___ Progesterone Receptor (PgR) Status (Note B
)
Progesterone Receptor (PgR) Status
___ Positive
Percentage of Cells with Nuclear Positivity: _________________ %
Average Intensity of Staining
___ Weak
___ Moderate
___ Strong
___ Negative (less than 1%)
___ HER2 Status (for uterine serous carcinoma only) (Note C
)

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
3
HER2 Status
# No staining in tumor cells
___ Negative (score 0)#
## Faint / Barely perceptible, incomplete membrane staining in any proportion, or weak complete staining in less
than 10% of tumor cells
___ Negative (score 1+)##
### Strong complete or basolateral / lateral membrane staining in less than or equal to 30%, or weak to moderate
staining in greater than or equal to 10% of tumor cells
___ Equivocal (score 2+)###
#### Strong complete or basolateral / lateral membrane staining in greater than 30% of tumor cells
___ Positive (3+)####
___ Cannot be determined (indeterminate) (explain): _________________
___ Mismatch Repair (MMR) Protein Status (Note D
)
Mismatch Repair (MMR) Protein Status (select all that apply)
___ MLH1
Nuclear MLH1 Expression
___ Intact
___ Loss
___ Other (specify): _________________
___ PMS2
Nuclear PMS2 Expression
___ Intact
___ Loss
___ Other (specify): _________________
___ MSH2
Nuclear MSH2 Expression
___ Intact
___ Loss
___ Other (specify): _________________
___ MSH6
Nuclear MSH6 Expression
___ Intact
___ Loss
___ Other (specify): _________________
___ Background non-neoplastic tissue / internal control shows intact nuclear expression
+Additional Comment (specify percentage loss or other): _________________
Immunohistochemistry (IHC) Interpretation for Mismatch Repair (MMR) Proteins# (Note D
)
# There are exceptions to these IHC interpretations. These results should not be considered in isolation, and
clinical correlation with genetic counseling is recommended to assess the need for germline testing.
___ No loss of nuclear expression of MMR proteins: low probability of microsatellite instability-high
(MSI-H) phenotype#
___ Loss of nuclear expression of MLH1 and PMS2: testing for methylation of the MLH1 promoter is
indicated (the presence of MLH1 methylation suggests that the tumor is sporadic and germline
evaluation is probably not indicated; absence of MLH1 promoter methylation suggests the possibility of
Lynch syndrome, and sequencing and / or large deletion / duplication testing of germline MLH1 is
indicated)#
___ Loss of nuclear expression of MSH2 and MSH6: high probability of Lynch syndrome, genetic
counseling is recommended#
___ Loss of nuclear expression of MSH6 only: high probability of Lynch syndrome, genetic counseling

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
4
is recommended#
___ Loss of nuclear expression of PMS2 only: high probability of Lynch syndrome, genetic counseling
is recommended#
___ Other (specify): _________________
___ p53 Status (Note E
)
p53 Status
___ Normal expression (wild type)
___ Abnormal expression (mutated)
___ Overexpression (strong, diffuse basilar nuclear expression in greater than 90% of cells)
___ Null (lack of nuclear or cytoplasmic expression)
___ Cytoplasmic staining, diffuse (with or without nuclear expression)
ADDITIONAL TESTS PERFORMED
+HER2 by in situ Hybridization (Note C
)
"Number of Observers" and "Number of Invasive Tumor Cells Counted" are required only when Negative or Positive is selected.
___ Negative (not amplified)
___ Positive (amplified)
___ Cannot be determined (indeterminate) (explain): _________________
___ Not performed
___ Pending
Number of Observers: _________________
Number of Invasive Tumor Cells Counted: _________________ cells
Method (select all that apply)
___ Not applicable (not performed)
___ Dual probe assay
+Average Number of HER2 Signals per Cell: _________________
+Average Number of CEP17 Signals per Cell: _________________
+HER2 / CEP17 Ratio: _________________
___ Single probe assay
+Average Number of HER2 Signals per Cell: _________________
+Aneusomy (as defined by vendor kit used)
___ Not identified
___ Present (explain): _________________
+Heterogeneous Signals
___ Not identified
___ Present
+Percentage of Cells with Amplified HER2 Signals
___ Specify percentage: _________________ %
___ Other (specify): _________________
___ Cannot be determined

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
5
+Microsatellite Instability (MSI) Interpretation (Note F)
The presence of MSI-H / deficient mismatch repair may also be an indication for additional testing for Lynch syndrome and genetic
counselling.
___ MSI-Stable (MSS)
___ MSI-Low (MSI-L)
+___ 1-29% of the markers exhibit instability
+___ 1 of the 5 NCI or mononucleotide markers exhibits instability
+___ Other (specify): _________________
___ MSI-High (MSI-H)
+___ Greater than or equal to 30% of the markers exhibit instability
+___ 2 or more of the 5 NCI or mononucleotide markers exhibit instability
+___ Other (specify): _________________
___ MSI-Cannot be determined (explain): _________________
___ Pending
+MLH1 Promoter Methylation Analysis (Note G
)
___ MLH1 promoter methylation present
___ MLH1 promoter methylation absent
___ Cannot be determined (explain): _________________
___ Pending
+Image Analysis
___ Not performed
___ Performed
+Specify Method: _________________
+Biomarkers Scored by Image Analysis (select all that apply)
___ ER
___ PgR
___ HER2 by IHC
___ HER2 by ISH
___ Other (specify): _________________

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
6
Explanatory Notes
A. Biomarker Testing in Gynecologic Carcinoma
Biomarker testing in gynecologic malignancies is an evolving practice with numerous candidates under
investigation for targeted therapies.
1,2,3,4
Only a few of these tests have status in clinical guidelines or
recommendations. Many of these markers have a major role in the diagnostic assessment of tumor type.
American Society of Clinical Oncology (ASCO) and the College of American Pathologists (CAP)
guidelines for breast cancer tissue ischemia and fixation for testing ER, PgR, and HER2 have been
proposed for gynecologic tumors and may be adopted but are not currently required.
5,6
References
1. Jiang P, Jia M, Hu J, Huang Z, Deng Y, Hu Z. A nomogram model involving
immunohistochemical markers for predicting the recurrence of stage I-II endometrial cancer.
Front Oncol. 2021; 10:586081.
2. Gülseren V, Kocaer M, Özdemir IA, Çakır I, Sanci M, Güngördük K. Do estrogen, progesterone,
p53, and Ki67 receptor ratios determined from curettage materials in endometrioid-type
endometrial carcinoma predict lymph node metastasis? Curr Probl Cancer. 2020; 44(10);100498.
3. Vrede SW, van Weelden WJ, Visser NCM, et al. Immunohistochemical biomarkers are prognostic
relevant in addition to the ESMO-ESGO-ESTRO risk classification in endometrial cancer. Gynec
Oncol. 2021; 161;787-794.
4. Ramon-Patino JL, Ruz-Caracuel I, Heredia-Soto V, et al. Prognosis stratification tools in early-
stage endometrial cancer: could we improve their accuracy? Cancers. 2022; 14(4):912.
5. Allison KH, Hammond MEH, Dowsett M, et al. Estrogen and progesterone receptor testing in
breast cancer: American Society of Clinical Oncology/College of American Pathologists guideline
update. Arch Pathol Lab Med. 2020;144(5):545-563.
6. Wolff AC, Hammond MEH, Allision KH, et al. HER2 testing in breast cancer: American Society of
Clinical Oncology/College of American Pathologists clinical practice guideline focused update.
Arch Pathol Lab Med. 2018; 142:1364–1382.
B. ER and PgR Immunohistochemistry
Hormone receptor expression is occasionally assessed on primary invasive endometrial carcinomas at
the request of the treating clinician in order to predict response to endocrine therapy.
1,2
Guidelines for
reporting results of hormone receptor testing in breast carcinomas published by the American Society of
Clinical Oncology (ASCO) and the College of American Pathologists (CAP) require recording specific
preanalytic and analytic variables that can affect test results.
3
This information has not been required for
endometrial carcinomas and is optional. However, appropriate positive and negative controls should be
used and evaluated.
Hormone receptor status is typically performed in formalin-fixed, paraffin-embedded tissue sections by
immunohistochemistry (IHC). Only nuclear staining is considered positive. There are many tissue and
technical variables that can affect test results, and the assays must be validated to ensure their accuracy.
In the endometrium, benign endometrial glands, endometrial stroma, or myometrium may serve as
internal control tissue. If internal controls are not present, consider repeating the test on another
specimen with internal controls (if available). Reasons for false-negative results include the following:
• Exposure of tumor cells to heat (e.g., carcinomas transected by using cautery during surgery)
• Prolonged cold ischemic time, which may result in antigenic degradation
CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
7
• Under- or over-fixation; fixation for at least 6 hours in buffered formalin is recommended;
prolonged fixation can also diminish immunoreactivity
• Type of fixative: ER is degraded in acidic fixatives such as Bouin’s and B-5; formalin should be
buffered to ensure pH range between 7.0 and 7.4
• Decalcification, which may result in loss of immunoreactivity
• Non-optimized antigen retrieval or use of (weeks) old tissue sections
• Type of antibody
• Dark hematoxylin counterstain obscuring faintly positive diaminobenzidine (DAB) staining
False-positive results occur less frequently. Rare reasons would be the use of an impure antibody that
cross-reacts with another antigen or misinterpretation of entrapped normal or hyperplastic cells as
invasive carcinoma. False-positive tests can also be generated by image analysis devices that mistakenly
count overstained nuclei.
Reporting Guidelines
There are currently no outcome-driven consensus opinions that have been developed for the reporting of
the results of immunohistochemical assays for ER and PgR for endometrial cancer. In absence of robust
data, the CAP recommends using a modified reporting format similar to that used for reporting the results
of immunohistochemical assays for ER and PgR for breast cancer (Table 1).
4
As there is a wide range of receptor levels in individual cancers, a uniform reporting scheme using the
proportion of positive cells as well as the intensity of immunoreactivity is recommended:
• Number of positive cells: The number of positive cells can be reported as a percentage or within
discrete categories (e.g., 10-20%).
• Intensity: Refers to degree of nuclear positivity (i.e., pale to dark). The intensity can be affected
by the amount of protein present, as well as the antibody used and the antigen retrieval system.
In most cancers, there is heterogeneous immunoreactivity with pale to darkly positive cells
present.
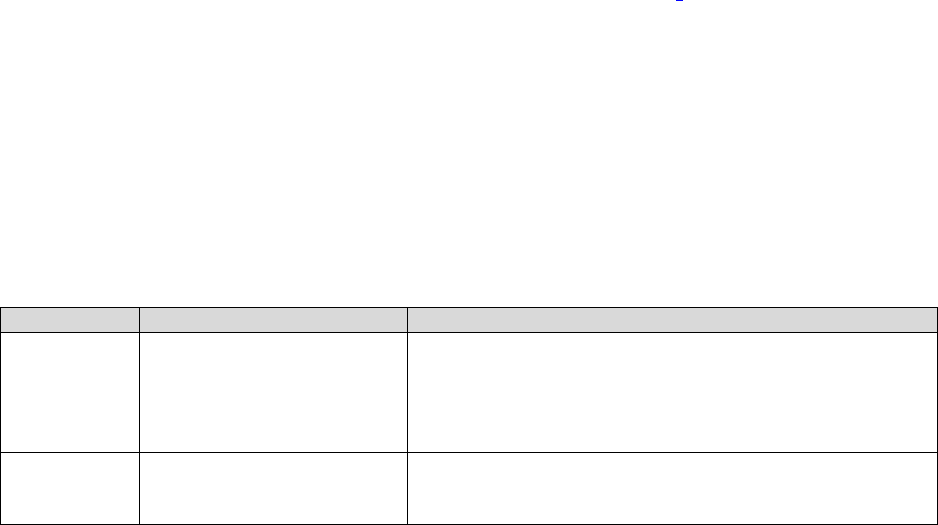
Table 1. Reporting Results of Estrogen Receptor (ER) and Progesterone Receptor (PgR) Testing
Result
Criteria
Comments
Positive
Immunoreactive tumor
cells present
(greater
than or equal to 1%
)
The percentage of immunoreactive cells may
b
e
determined by visual estimation or
quant
itation.
Quant
itation should be provided by reporting the
percentag
e
of positive cells in the entire section. If there is significant
regional variation, that should also be reported.
Negative
Less than
1% immunoreactive
tumor cells
presen
t
References
1. Guan J, Xie L, Luo X, et al. The prognostic significance of estrogen and progesterone receptors
in grade I and II endometrioid endometrial adenocarcinoma: hormone receptors in risk
stratification. J Gynecol Oncol. 2019; 30(1):e13.
2. Jrezak KJ, Duska L, MacKay HJ. Endocrine therapy in endometrial cancer: an old dog with new
tricks. Gynecol Oncol. 2019; 153(1):175-183.

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
8
3. Allison KH, Hammond MEH, Dowsett M, et al. Estrogen and progesterone receptor testing in
breast cancer: American Society of Clinical Oncology/College of American Pathologists guideline
update. Arch Pathol Lab Med. 2020;144(5):545-563.
4. Fitzgibbons PL, Dillon DA, Alsabeh R, et al. Template for reporting results of biomarker testing of
specimens from patients with carcinoma of the breast. Arch Pathol Lab Med. 2014;138(5):595-
601.
C. HER2 (ERBB2) Testing
The HER2 (ERBB2) gene is located on chromosome 17 and codes for a tyrosine kinase receptor from the
epidermal growth factor receptor (EGFR) family. This protein is critical in signaling pathways that regulate
cell division, proliferation, differentiation, and apoptosis. There are currently no consensus guidelines that
have been developed for reporting of the results of HER2 testing in endometrioid carcinoma, but HER2
has been proposed as a biomarker, and testing is recommended by the National Comprehensive Cancer
Network (NCCN) guidelines for advanced or recurrent uterine serous carcinoma.
1,2,3
Heterogeneity of
expression within a tumor is a common problem. Unlike the patterns seen in breast carcinoma, staining is
usually lateral or basolateral and spares the apical portion of cells (U-shaped membranous
pattern).
3
Approximately 25-30% of uterine serous carcinoma will show HER2 overexpression and/or
gene amplification, but divergent results between the two testing methods are common and concordance
may be less than 50%.
4,5,6
Although there is an increased progression-free survival in patients with
homozygous HER2 protein expression treated with targeted chemotherapy, the overall response rate is
low, and most uterine serous carcinomas tend to show heterogeneous HER2 expression. This has
implications for treatment and negative HER2 results on small samples might erroneously exclude
patients from HER2 targeted therapy.
7
In the absence of conclusive data, CAP suggests using a similar reporting format as that used for
reporting the results of HER2 testing for breast cancer, with modifications below.
4,5,8,9
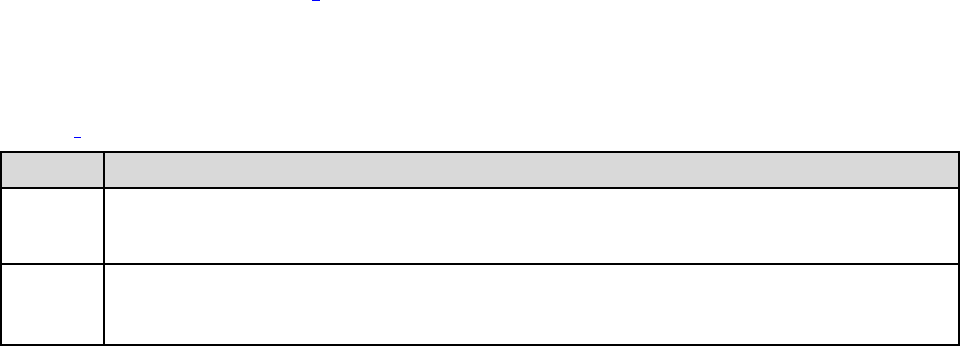
Table 2. Reporting Results of HER2 Testing by Immunohistochemistry for Endometrial Serous
Carcinoma
Result
Criteria
Negative (Score 0)
No staining observed
Negative (Score 1+)
Incomplete membrane staining that is faint/barely perceptible in any proportion of cells or
Weak complete staining in less than 10% of tumor cells*
Equivocal (Score 2+)
†
Intense complete or basolateral/lateral membrane staining in 30% or less tumor cells*or
Weak to moderate staining in greater than or equal to 10% of tumor cells*
Positive (Score 3+)
Intense complete or basolateral/lateral membrane staining in over 30% of tumor cells*
* Readily appreciated using a low-power objective and observed within a homogeneous and contiguous population of
invasive tumor cells.
† Must order reflex test (same specimen using ISH) or order a new test (new specimen if available, using IHC or
ISH).
HER2 Testing by In Situ Hybridization
The propensity for HER2 heterogeneity in uterine serous carcinoma is mirrored by intratumoral HER2
heterogeneity in fluorescent in situ hybridization (FISH) studies. FISH is performed on tumors with a 2+
IHC score, using the largest tumor area with HER2 immunoreactivity for testing.
5
Currently, there are no
recommendations to perform FISH in lieu of IHC testing. Based on a large clinical trial, only HER2/CEP17
ratios of greater than or equal to 2.0 are considered amplified and serve as baseline guidance for
CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
9
reporting pending further studies.
4
Several unanswered questions remain, such as whether endometrial
biopsy or hysterectomy is the optimal specimen, whether multiple specimens should be tested, whether
metastases should be tested, and if so, how to clinically manage discordant results.
Table 3. Reporting Results of HER2 Testing by Fluorescent In Situ Hybridization (single-probe
assay)
5
Result
Criteria (single-probe assay)
Negative
· FISH HER2/CEP17 ratio less than 2.0 and
· Average HER2 copy number less than 6 per nucleus
Positive
· FISH HER2/CEP17 ratio greater than or equal to 2.0 or
· FISH HER2/CEP17 ratio less than 2.0, copy number equal to or greater than 6 per nucleus
References
1. Saito A, Yoshida H, Nishikawa T, Yonemon K. Human epidermal growth factor receptor 2
targeted therapy in endometrial cancer: clinical and pathological perspectives. World J Clin
Oncol. 2021; 12(10):868-881.
2. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology
Uterine Neoplasms. Version 1. 2021 [cited 14 December 2021] Available from:
https://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf
3. Buza N, English DP, Santin AD, Hui P. Toward standard HER2 testing of endometrial serous
carcinoma: 4-year experience at a large academic center and recommendations for clinical
practice. Mod Pathol. 2012; 26(12):1605-12.
4. Buza N. HER2 testing in endometrial serous carcinoma: time for standardized pathology practice
to meet the clinical demand. Arch Pathol Lab Med. 2021; 145:687-691.
5. Buza N. HER2 testing and reporting in endometrial serous carcinoma: practical recommendations
for HER2 immunohistochemistry and fluorescent in situ hybridization: proceedings of the ISGyP
companion society session at the 2020 USCAP annual meeting. Int J Gynecol Pathol. 2020;
40(1):17-23.
6. Rottmann D, Assem H, Matsumoto N, Wong S, Hui P, Buza N. Does specimen type have an
impact on HER2 status in endometrial serous carcinoma? Discordant HER2 status of paired
endometrial biopsy and hysterectomy specimens in the presence of frequent intratumoral
heterogeneity. Int J Gynecol Pathol. 2020; 40:263-271.
7. Banet N, Shahi M, Batista D, et al. HER-2 amplification in uterine serous carcinoma and serous
endometrial intraepithelial carcinoma. Am J Surg Pathol. 2021; 45(5):708-715.
8. Wolff AC, Hammond MEH, Allision KH, et al. HER2 testing in breast cancer: American Society of
Clinical Oncology/College of American Pathologists clinical practice guideline focused update.
Arch Pathol Lab Med. 2018; 142:1364–1382.
9. Buza N. Immunohistochemistry in gynecologic carcinomas: practical update with diagnostic and
clinical considerations based on the 2020 WHO classification. Semin Diagn Pathol. 2022;
39(1):58-77.
D. Mismatch Repair (MMR) Immunohistochemistry Testing
Screening for the autosomal dominant Lynch syndrome can be performed by universal MMR testing of
endometrioid carcinoma, one of the most common presentations. Immunohistochemical (IHC) testing for

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
10
DNA MMR protein expression (i.e., MLH1, MSH2, MSH6, and PMS2 expression) is performed on
formalin-fixed, paraffin-embedded tissue.
MMR testing in endometrioid carcinoma has been included in the molecular classification system for
endometrioid carcinoma proposed by the World Health Organization.
1
MMR-deficient patients are eligible
for immune checkpoint inhibitors, although in many cases, treatment is currently restricted to clinically
challenging cases.
2
If the results of DNA MMR IHC and MSI (microsatellite instability) testing are discordant (e.g., MSI-H
phenotype with normal IHC or abnormal IHC with MSS phenotype), then the laboratory should make sure
that the same sample was used for MSI and IHC testing and that there was no sample mix-up.
1
Another
possible source of discordance is low tumor volume in the MSI sample. Note that loss of MSH6 protein
expression may occur in absence of MSI-H phenotype.
3,4
Microsatellite instability is a primary pathway of
endometrial carcinogenesis and should be considered when all MMR protein expression is intact.
Any positive reaction in the nuclei of tumor cells is considered as intact expression (normal), and it is
common for intact staining to be somewhat patchy. An interpretation of expression loss in tumor cells
should be made only if a positive reaction is seen in internal control cells, such as the nuclei of stromal,
inflammatory, or non-neoplastic epithelial cells.
4,5
Loss of expression of MLH1 may be due to Lynch
syndrome or methylation of the MLH1 promoter region (as occurs in sporadic MSI carcinoma).
Patients with patterns reflecting a high likelihood of Lynch syndrome should be referred for consultation
with a geneticist. No loss of nuclear expression of MMR proteins indicates a low probability of
microsatellite instability-high (MSI-H). Loss of DNA MMR protein expression is likely to be due to mutation
(either genetic or somatic) in one of the mismatch repair genes.
6,7,8
This information will help identify the
gene that is most likely to have a mutation (e.g., a patient whose tumor shows loss of MSH2 and MSH6
expression, but retention of MLH1 and PMS2 expression, may have an MSH2 germline mutation). Loss of
nuclear expression of MHL1 and PMS2 should be triaged for MLH1 methylation studies. The presence of
MLH1 methylation suggests a sporadic tumor rather than a germline mutation, and further germline
testing is likely not indicated. Absence of MLH1 methylation suggests Lynch syndrome and sequencing
and/or large deletion/duplication testing of germline MLH1 is indicated. Loss of nuclear expression of
MSH2 and MSH6, loss of MSH6 only, or loss of PMS2 only all have a high probability of Lynch syndrome
and genetic counseling should be considered.
References
1. Matias-Guiu X, Oliva E, McCluggage WG, et al. Tumours of the uterine corpus. In: WHO
Classification of Tumours Editorial Board. Female genital tumours [Internet]. Lyon (France):
International Agency for Research on Cancer; 2020 [cited 2020 Nov 20]. (WHO classification of
tumours series, 5th ed.; vol. 4).
Available from: https://tumourclassification.iarc.who.int/chapters/34
2. Casey L, Singh N. POLE, MMR, and MSI testing in endometrial cancer: proceedings of the
ISGyP Companion Society session at the USCAP 2020 annual meeting. Int J Gynecol Pathol.
2020; 40(1):5-16.
3. McConechy MK, Talhouk A, Li-Chang HH, et al. Detection of DNA mismatch repair (MMR)
deficiencies by immunohistochemistry can effectively diagnose the microsatellite instability (MSI)
henotype in endometrial carcinomas. Gynecol Oncol. 2015; 137(2):306-310.

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
11
4. Stelloo E, Jansen AML, Osse EM, et al. Practical guidance for mismatch repair-deficiency testing
in endometrial cancer. Ann Oncol. 2017; 28:96-102.
5. Watkins JC, Nucci MR, Ritterhouse LL, Howitt BE, Sholl LM. Unusual mismatch repair
immunohistochemical patterns in endometrial carcinoma. Am J Surg Pathol. 2016; 40(7):909-916.
6. Haraldsdottir S, Hampel H, Tomsic J, et al. Colon and endometrial cancers with mismatch repair
deficiency can arise from somatic, rather than germline, mutations. Gastroenterology. 2014;
147(6):1308-1316.
7. Ligtenberg MJ, Kuiper RP, Chan TL, et al. Heritable somatic methylation and inactivation of
MSH2 in families with Lynch syndrome due to deletion of the 3’ exons of TACSTD1. Nat Genet.
2009; 41(1):112-117.
8. Geurts-Giele WR, Leenen CH, Dubbink HJ, et al. Somatic aberrations of mismatch repair genes
as a cause of microsatellite-unstable cancers. J Pathol. 2014; 234(4):548-559.
E. p53 Expression
p53 is a tumor suppressor protein that induces expression of p21, a cyclin-dependent kinase inhibitor that
is involved in the arrest of cellular proliferation at the G1 phase. Essentially, p53 regulates cell
proliferation, DNA repair, apoptosis, and genetic stability. Inactivation of p53 occurs through mutations of
TP53 or inactivation of p53 through binding proteins, resulting in dysregulated growth. Mutations result in
abnormal cellular expression of the protein (overexpression or lack of expression) that can be detected by
immunohistochemical methods. In gynecologic malignancies, p53 expression is frequently used as a
diagnostic tool but can be employed as a marker for targeted chemotherapy. Mutations of TP53 occur
more commonly (~90%) in serous carcinoma than in endometrioid carcinoma (~10-40%) and are
associated with significantly poorer outcomes.
1,2
Recently the WHO has included TP53 evaluation into its molecular classification of endometrial
carcinoma.
3
The vast majority of serous-type endometrial carcinomas exhibit mutations in TP53. While
most low-grade endometrioid endometrial tumors are not associated with TP53 mutations, a significant
subset of high-grade endometrioid tumors are; thus, any ancillary testing for the presence of a TP53
mutation should be performed with an awareness of the limitations of the IHC result with respect to
providing a conclusive answer as to classification.
4,5
On occasion, p53 testing may be requested for
treatment purposes, but sequencing of the TP53 gene may be more appropriate to select patients for
targeted therapy.
6
Extent of p53 specific nuclear immunostaining can be used to assess TP53 gene integrity in endometrial
carcinoma. Normal endometrial glands with an intact TP53 gene express the protein at low levels,
reaching a threshold of immunohistochemical detection (positive staining) in only a small percentage of
cells. Generally, this is 1% to 5% of nuclei but may increase under conditions of cellular damage or repair.
Two different staining patterns are each considered diagnostic of abnormalities of the TP53 gene itself.
Most common are mutations resulting in a qualitatively abnormal p53 protein that stabilizes the p53
complex, resulting in intense nuclear staining in >90% of affected cells. In most cases that harbor
mutations in TP53 that are associated with overexpression, intense nuclear staining is present in over
90% of affected cells. Second is genomic damage causing loss of expression, with a complete absence
of protein in all affected cells. The latter “null” phenotype must be distinguished from a failed stain. Low
levels of expression within internal control tissues (stroma, or nonmalignant epithelium) can be used for
this purpose. It should be noted that p53 expression is significantly affected by non-optimized antigen
retrieval or use of archival (weeks old) tissue sections.

CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
12
References
1. Nakamura M, Obata T, Daikoku T, Fujiwara H. The association and significance of p53 in
gynecologic cancers: the potential of targeted therapy. Int J Mol Sci. 2019; 20:5482.
2. Zheng W, Xiang L, Fadare O, Kong B. A proposed model for endometrial serous carcinogenesis.
Am J Surg Pathol. 2011; 35:1-14.
3. Matias-Guiu X, Oliva E, McCluggage WG, et al. Tumours of the uterine corpus. In: WHO
Classification of Tumours Editorial Board. Female genital tumours [Internet]. Lyon (France):
International Agency for Research on Cancer; 2020 [cited 2020 Nov 20]. (WHO classification of
tumours series, 5th ed.; vol. 4).
Available from: https://tumourclassification.iarc.who.int/chapters/34
4. Cancer Genome Atlas Research Network. Integrated genomic characterization of endometrial
carcinoma. Nature. 2013;497(7447):67-73.
5. Hoang LN, McConechy MK, Kobel M, et al. Histotype-genotype correlation in 36 high-grade
endometrial carcinomas. Am J Surg Pathol. 2013;37(9):1421-1432.
6. Beinse G, Rance B, Just PA, et al. Identification of TP53 mutated group using a molecular and
immunohistochemical classification of endometrial carcinoma to improve prognostic evaluation for
adjuvant treatments. Int J Gynecol Cancer. 2020; 30(5):640-647.
F. Microsatellite Instability Testing
Detection of hereditary defective mismatch repair has clinical implications for treatment of the affected
patient and family members. Patients with a microsatellite instability-high (MSI-H) phenotype in their
cancer tissues may have a germline mutation in one of several DNA mismatch repair (MMR) genes (e.g.,
MLH1, MSH2, MSH6, or PMS2) or an altered EPCAM (TACSTD1) gene.
1,2,3
After appropriate genetic
counseling, patients may want to consider testing to identify the causative heritable abnormality. An MSI-
H phenotype is more frequently observed in sporadic endometrioid carcinoma (about 15% of cases) due
to somatic abnormalities, usually hypermethylation of the MLH1 gene promoter.
MSI testing protocols are similar to those developed for colon cancer. These are briefly summarized
here, but more complete details are available in the separately issued “Template for Reporting Results of
Biomarker Testing of Specimens From Patients With Carcinoma of the Colon and Rectum”.
4
Testing is
generally performed with at least 5 microsatellite markers, generally mononucleotide or dinucleotide
repeat markers. In 1998, a National Institutes of Health consensus panel proposed that laboratories use a
5-marker panel consisting of 3 dinucleotide and 2 mononucleotide repeats for MSI testing. Recent data
suggest that dinucleotide repeats may have lower sensitivity and specificity for identifying tumors with an
MSI-H phenotype. As a consequence, there has been a move towards including more mononucleotides
and fewer dinucleotides in MSI testing panels. Many laboratories now use a commercially available kit for
MSI testing that utilizes 5 mononucleotide markers.
If DNA MMR IHC has not been performed, this testing should be recommended for any case that shows
an MSI-H phenotype, because this information will help identify the gene that is most likely to have a
germline (or somatic) mutation.
5
References
1. Haraldsdottir S, Hampel H, Tomsic J, et al. Colon and endometrial cancers with mismatch repair
deficiency can arise from somatic, rather than germline, mutations. Gastroenterology.
2014;147(6):1308-1316.
CAP Approved
Gynecologic.Bmk_1.0.0.0.REL_CAPCP
13
2. Ligtenberg MJ, Kuiper RP, Chan TL, et al. Heritable somatic methylation and inactivation of
MSH2 in families with Lynch syndrome due to deletion of the 3’ exons of TACSTD1. Nat Genet.
2009;41(1):112-117.
3. Geurts-Giele WR, Leenen CH, Dubbink HJ, et al. Somatic aberrations of mismatch repair genes
as a cause of microsatellite-unstable cancers. J Pathol. 2014;234(4):548-559.
4. Burgart LJ, Chopp WV, Jain D, Bellizzi AM, Fitzgibbons PL. Template for Reporting Results of
Biomarker Testing of Specimens From Patients With Carcinoma of the Colon and Rectum.
https://documents.cap.org/protocols/ColoRectal.Bmk_1.3.0.0.REL_CAPCP.pdf Published June
2021. Accessed October 12, 2022.
5. Casey L, Singh N. POLE, MMR, and MSI testing in endometrial cancer: proceedings of the
ISGyP Companion Society session at the USCAP 2020 annual meeting. Int J Gynecol Pathol.
2020; 40(1):5-16.
G. MLH1 Promoter Methylation Analysis
Defective mismatch repair in sporadic endometrial cancer is most often due to inactivation of the MLH1
gene promoter by methylation (epigenetic silencing). Most laboratories utilize a methylation-specific real-
time polymerase chain reaction (PCR) assay to determine the presence of methylation.
