
Guidelines on surveillance among
populations most at risk for HIV
UNAIDS/WHO Working Group
on Global HIV/AIDS and STI Surveillance
WHO Library Cataloguing-in-Publication Data
Procurement process resource guide.
(WHO Medical device technical series)
1.Appropriate technology. 2.Equipment and supplies - supply and distribution. 3.Technology
assessment, Biomedical I.World Health Organization.
ISBN 978 92 4 150137 8 (NLM classification: WX 147)
© World Health Organization 2011
All rights reserved. Publications of the World Health Organization can be obtained from WHO
Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41
22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to
reproduce or translate WHO publications – whether for sale or for noncommercial distribution
– should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail:
The designations employed and the presentation of the material in this publication do not
imply the expression of any opinion whatsoever on the part of the World Health Organization
concerning the legal status of any country, territory, city or area or of its authorities, or
concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent
approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that
they are endorsed or recommended by the World Health Organization in preference to others
of a similar nature that are not mentioned. Errors and omissions excepted, the names of
proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by the World Health Organization to verify
the information contained in this publication. However, the published material is being
distributed without warranty of any kind, either expressed or implied. The responsibility for
the interpretation and use of the material lies with the reader. In no event shall the World
Health Organization be liable for damages arising from its use.
Design & layout: L’IV Com Sàrl, Le Mont-sur-Lausanne, Switzerland.

Guidelines on surveillance among
populations most at risk for HIV
UNAIDS/WHO Working Group
on Global HIV/AIDS and STI Surveillance
ii
Acknowledgements
Global surveillance of HIV and sexually transmitted infections is a joint effort of the World Health Organization
(WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS). The UNAIDS/WHO Working Group
on Global HIV/AIDS and STI Surveillance, initiated in November 1996, provides technical guidance on
conducting HIV and STI surveillance. Its mandate is to improve the quality of data available for informed
decision-making and planning at the national, regional and global levels.
This document is based on experience in countries and expert reviews from WHO/UNAIDS and the Centers
for Disease Control and Prevention (CDC), USA, which have contributed to the writing and revision of the
final document. All the persons involved declared no conflicts of interest.
WHO and UNAIDS would like to thank the individuals who contributed to this document including: Donna
Stroup, Carolyn Smith, members of the UNAIDS/WHO Working Group on HIV and STI Surveillance, and
members of the US Government’s Surveillance and Surveys Technical Working Group.
Guidelines on surveillance among populations most at risk for HIV
1
Contents
Acknowledgements ii
1 Introduction 3
1.1. Purpose 3
1.2. Background 4
1.3. Classification of HIV epidemics 4
1.4. Ethical issues with populations most at risk for HIV 5
Protect participants’ privacy and rights 5
Provide benefits to the community 5
Handle incentives for participation ethically 5
Protect young people 5
Provide protection to participants with illegal behaviours 6
1.5. Process 6
2 Plan surveillance of populations most at risk for HIV 7
2.1. Step 1: Prepare to set up the surveillance system 7
2.1.1 Collaborate with stakeholders 7
2.1.2 Conduct a pre-surveillance assessment 8
2.1.3 Identify populations at increased HIV risk from high-risk behaviour 9
2.1.4 Estimate the size of populations at increased risk for HIV 10
2.1.5 Decide on the geographical areas 10
2.1.6 Consider special issues related to each population of interest 10
2.1.7 Integrate with existing surveillance and monitoring plans 13
2.2 Step 2: Decide on the surveillance design 13
2.2.1 HIV case reporting 13
2.2.2 Programme data used for surveillance 14
2.2.3 Sentinel surveillance 14
2.3. Step 3: Decide on a surveillance sampling strategy 15
2.3.1 Simple random sampling 15
2.3.2 Stratified sampling 16
2.3.3 Cluster or targeted sampling 17
2.3.4 Snowball sampling 17
2.3.5 Respondent-driven sampling 18
2.3.6 Convenience sampling 20
2.3.7 Time–location sampling 20
2.3.8 Sample size 21
2.3.9 Sampling strategies for populations most at risk for HIV 22
3 Conduct surveillance of populations most at risk for HIV 25
3.1 Step 4: Address operational issues 25
3.1.1 Plan staffing and training 25
3.1.2 Develop data collection instruments 26
3.1.3 Plan handling of specimens and HIV testing 27
3.2. Step 5: Data management 27
3.2.1 Plan the data management system 27
3.2.2 Use data management best practices 28
3.2.3 Create a dataset for analysis 28
3.2.4 Document the steps used to create the database 28
3.2.5 Maintain confidentiality and security 29
2
3.3. Step 6: Data analysis 29
3.3.1 Handling non-response 29
3.3.2 Using weighting 29
3.3.3 Determining HIV prevalence 30
3.3.4 Determining HIV prevalence trends 30
3.3.5 Determining HIV incidence 30
3.3.6 Dealing with uncertainty 31
3.3.7. Ensuring validity 31
4 Use the results/Evaluate the surveillance plan 32
4.1.1 Share the results 32
4.1.2 Develop a dissemination plan 32
4.1.3 Protect the population from stigma or legal action 32
4.1.4 Use the results to improve programmes 33
4.2. Step 8: Evaluate the system 34
Appendix A: List of additional surveillance resources 35
Appendix B: Glossary and acronyms 36
Appendix C: Links 39
References 40

Guidelines on surveillance among populations most at risk for HIV
3
The overall goal of this document is to provide guidance on how to develop and maintain HIV surveillance
among populations most at risk for HIV. Ultimately, these surveillance activities should improve the overall
understanding of HIV in countries and improve the response to HIV.
This guide complements the second generation surveillance guidelines on how to conduct HIV surveillance
activities in low- and middle-income countries. Those guidelines recommend that all countries conduct HIV
surveillance among populations with behaviours that increase their risk for HIV, or populations most at risk
for HIV infection.
1.1. Purpose
This document provides guidance on methods for conducting surveillance among populations most at risk
for HIV.
Public health surveillance for HIV is the systematic, ongoing collection of data on the occurrence, distribution
and trends in HIV infection. In general, the objectives of surveillance include:
n to estimate the magnitude of a health problem in a population at risk
n to understand the natural history of a disease
n to evaluate prevention and control activities
n to monitor changes in trends in the epidemic
n to detect changes in health practices or risk factors
n to identify research needs and facilitate research
n to contribute to the planning process (1).
Additional reasons to conduct HIV surveillance among populations most at risk for HIV are:
n to guide HIV prevention programming at the local level
n to inform priority-setting and resource allocation at the national level
n to contribute to the scientific understanding of HIV transmission in populations most at risk for HIV
infection as a result of high-risk behaviour
n to inform disease burden and treatment needs among most-at-risk populations.
When monitoring the HIV epidemic, it is important to identify populations that are most at risk for infection.
The sexual and drug-use behaviours of populations contribute to the overall burden of HIV in the country.
People with these behaviours are often the first to become infected and are at risk of being infected at a
higher rate than those in the general population.
The primary target audience of this guide includes surveillance specialists. In addition, this guide will be
useful for programme managers at national and subnational levels to better understand the strengths
and weaknesses of the data they are using to make decisions. Finally, this guide will also be useful for
donor agencies that support HIV surveillance activities and measure the success of their activities through
surveillance data.
Most countries and their development partners already have some form of HIV surveillance among most-
at-risk populations. This guide is intended to help refine and standardize their HIV strategies and activities
for HIV surveillance among these populations. It presents different approaches along with their advantages
and disadvantages. It is hoped that this guide will empower managers and decision-makers to consider
additional options for strengthening their HIV surveillance systems so that they are able to compare trends
over time.
1. Introduction

4
This guide does not cover all the issues related to HIV surveillance; rather, it serves as a general hands-
on reference specifically for surveillance among most-at-risk populations. It cites additional materials and
resources for further information on surveillance and includes country examples.
1.2. Background
This document complements a number of other guidelines that provide further information on specific
surveillance activities. A complete list of reference materials is provided in Appendix A. These guidelines
are available on the UNAIDS and WHO web sites.
Some of the core sources include the following:
n Guidelines for estimating the size of populations most at risk to HIV presents a process for creating local
and national size estimates.
n An update to Guidelines on second generation surveillance explores new tools and techniques from a
field perspective to enhance the first guideline published in 2000.
There are a number of documents that describe monitoring and evaluation activities among populations
most at risk for HIV, including the Framework for monitoring and evaluating HIV prevention programmes
among most-at-risk populations (2007). (http://data.unaids.org/pub/Manual/2008/jc1519_framework_for_
me_en.pdf). Operational guidelines for the monitoring and evaluation of HIV-related programmes targeting
persons who inject drugs and men who have sex with men are anticipated in 2011.
For more in-depth information on the topics covered here as well as a self-teaching manual on surveillance
among most-at-risk populations, see Surveillance of most-at-risk populations (http://globalhealthsciences.
ucsf.edu/PPHG/surveillance/surv_modules.html).
1.3. Classification of HIV epidemics
UNAIDS/WHO and partners have identified three epidemic categories to help countries focus surveillance
activities. These categories are suggestions. Countries should know best where new infections are coming
from and what type of epidemic exists in their country.
Each country has a unique epidemic and usually has multiple subepidemics within different parts of the
country. Because of the diversity among HIV epidemics, it is critical to “know your epidemic”. That means
understanding how the epidemic differs within subpopulations and in geographical areas. Surveillance
data will provide the information to allow programme managers to better know their epidemics. Moreover,
they will allow programme managers to respond more effectively to the epidemic. As more surveillance
data become available, surveillance officers should evaluate their surveillance system to ensure that it is
appropriate for the type of epidemic. Table 1.1 will help determine where to focus the surveillance system
and whether the focus needs to shift over time.
Table 1.1. Base surveillance activities on the type of epidemic
Epidemic state, situation Surveillance focus
Low-level
n HIV has not reached significant levels in populations most at
risk for HIV infection as a result of high-risk behaviour.
n HIV is largely confined to people within populations most at risk
for HIV infection as a result of high-risk behaviour.
n Focus surveillance activities in populations most at risk for HIV.
Concentrated
n HIV has spread rapidly in one or more populations most at risk
for HIV infection as a result of high-risk behaviour.
n The epidemic is not yet well established in the general
population.
n Continue surveillance among most-at-risk populations.
n Begin surveillance activities in the general population,
especially in urban areas.
Guidelines on surveillance among populations most at risk for HIV
5
Generalized
n The epidemic has matured to a level where transmission occurs
in the general population, independent of populations most at
risk for HIV.
n Without effective prevention, HIV transmission continues at
high rates in populations most at risk.
n With effective prevention, prevalence will drop in populations
most at risk before they drop in general population.
n Focus routine surveillance on the general population.
n Conduct surveillance among populations most at risk for HIV.
As described in Table 1.1, each type of epidemic should maintain some surveillance of populations most at
risk for HIV. Use these guidelines to facilitate surveillance in all settings.
1.4. Ethical issues with populations most at risk for HIV
Collection of any data requires attention to human subjects’ concerns. Before considering surveillance of
populations most at risk for HIV, the following principles should be considered.
Protect participants’ privacy and rights
In many cases, populations that are the target of HIV surveillance are vulnerable and might be accorded
special protection under ethical regulations. Handling of data on risk behaviours and HIV status may increase
the risk of harm to these populations due to stigma, economic loss or legal liability (2).
Participating in surveillance activities should either be voluntary or, in specific circumstances, should be
based on unlinked anonymous testing of blood samples. Unlinked anonymous testing should be used as
a surveillance strategy only when data from clinical settings and other studies cannot provide an accurate
measure of the prevalence or trends of HIV infection (3). Respect each person’s right to privacy. It is critical
to offer privacy and assurances of confidentiality during data collection. Keep data confidential. In turn, the
perception of confidentiality will influence the completeness of reporting and disclosure of risk.
Provide benefits to the community
Public health research should always provide a benefit to society. Extend the ethical principle of do no harm
to providing benefits to surveillance subjects. Whenever possible, provide individuals participating in the
survey with:
n test results
n information about HIV and AIDS
n counselling (on preventing HIV or on other health or social needs)
n treatment and care to the extent possible with local resources
n referrals to other services.
Consider how the results will be used before starting a surveillance activity among most-at-risk populations.
The results should be used for the good of public health while minimizing any harm to the participants.
Handle incentives for participation ethically
Providing benefits in the form of cash payment or vouchers for goods and services is often a useful
recruitment and retention technique (4). However, the use of incentives should be considered carefully
during the ethical review. Any incentive must consider the customs of the community but should not be so
large that it is considered coercive or exploitative (5). The ethical concern here is that the offer of financial
compensation, medical services or some goods might cause participants to consider only their short-term
benefits and they might underestimate the long-term costs. This might entice some participants to provide
data and could create a bias to the results (6).
Protect young people
When surveillance of most-at-risk populations includes collecting data from adolescents, additional ethical
issue arise. Young people may be particularly vulnerable to exploitation, abuse and other harmful outcomes
(legal, physical and social). Follow the guidelines for collecting data on adolescents (4,7).
6
Provide protection to participants with illegal behaviours
Safeguard participants from situations in which they might face legal persecution. This is critical for HIV
surveillance in any context. Some of the behaviours that cause increased risk for HIV are illegal in some
settings. Legal protection of confidentiality are constantly in flux (8). This can be avoided by including
members of the population who can provide information on the local context in surveillance pre-planning.
For additional information, see Ethical issues to be considered in second generation surveillance (http://www.
who.int/hiv/pub/epidemiology/en/sgs_ethical.pdf). Additional guidelines on ethics and HIV surveillance will
be available on the WHO web site shortly.
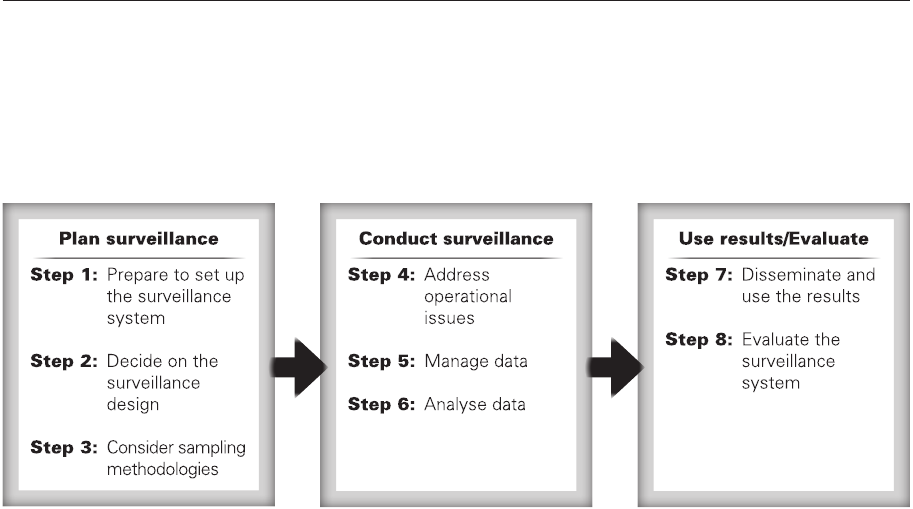
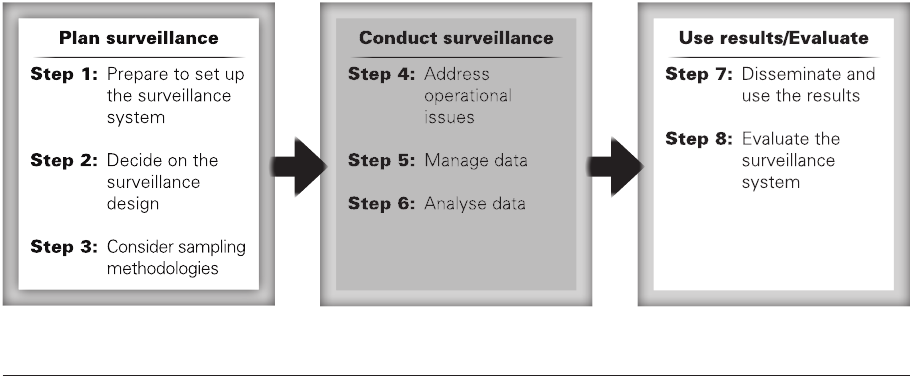
1.5. Process
Planning and conducting surveillance among populations most at risk for HIV can be summarized by the
eight steps shown below.
Figure 1.1. Planning and conducting surveillance among populations most at risk for HIV
The remainder of this document discusses the processes shown in Figure 1.1. Guidance and examples are
provided on methods:
n to plan surveillance activities, steps 1–3, Section 2
n to conduct surveillance, steps 4–6, Section 3
n to disseminate results and evaluate the surveillance system, steps 7–8, Section 4.
Guidelines on surveillance among populations most at risk for HIV
7
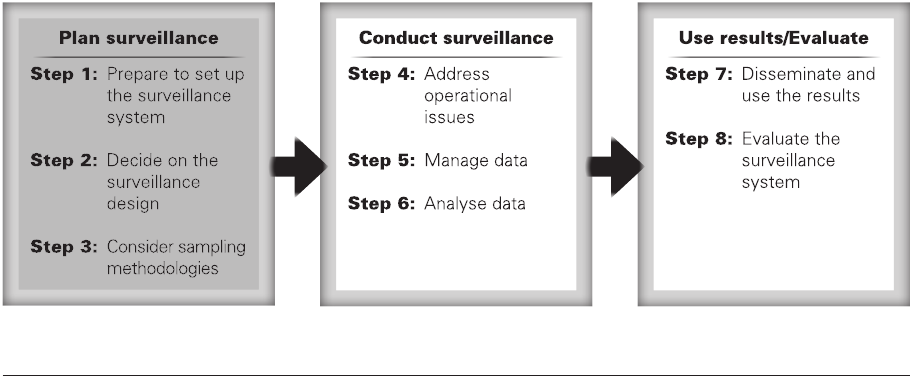
The first three steps of the process are general preparations for conducting surveillance among populations
most at risk for HIV. Some countries might have an existing surveillance system. It might still be useful to
review the first steps to ensure that the system is well designed.
Figure 2.1. Plan HIV surveillance among populations most at risk for HIV
2.1. Step 1: Prepare to set up the surveillance system
While preparing the surveillance system, it is important to develop a protocol to ensure the success of the
surveillance system. This will help ensure that accurate, appropriate and useful data will be captured by the
surveillance system. Be sure the protocol covers the following areas:
n how surveillance stakeholders will be involved in activities
n planned pre-surveillance assessment
n populations of interest, with explicit definitions of these populations, based on the behaviours that put
them at increased risk for HIV
n the size of the population or populations
n geographical boundaries, sites or location of surveillance
n coverage and descriptions of the representativeness of the population
n frequency of surveillance
n how surveillance activities will be merged with other monitoring and evaluation plans.
2.1.1 Collaborate with stakeholders
HIV surveillance cannot be done in isolation. Use a team approach to improve the quality and credibility
of the results. Table 2.1 provides a list of possible stakeholders and what they can bring to the surveillance
activities. Plan to involve members of HIV prevention programmes, monitoring and evaluation programmes,
and resource planning structures. Identify a team of stakeholders to help in designing and implementing
HIV surveillance activities.
2. Plan surveillance of populations most
at risk for HIV
8
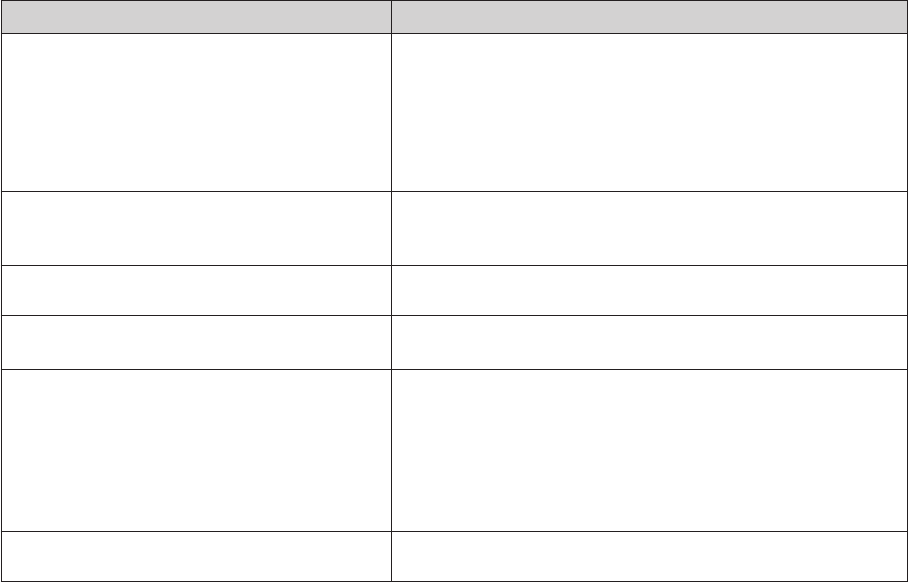
Table 2.1. Potential stakeholders to include in planning surveillance activities among populations most at
risk for HIV
Stakeholder What they bring
Members of the populations most at risk for HIV n Provide insight into:
• thetimingofsurveillance
• theappropriatenessofthesamplingstrategy
• thewordingforthequestionnaire,and
• instrumentdesign
n Provide study legitimacy in the community
n Provide the legal and social context
Nongovernmental organizations or civil society
organizations working with most-at-risk populations
n Provide information on the needs of most-at-risk populations
n Have experience in reaching the population to inform the sampling
strategy and instrument design
HIV prevention experts Ensure that the surveillance results provide information on a timely basis for
programme planning or advocacy
Survey and census implementers n Advice on sampling strategies
n Additional data for size estimation activities
Monitoring and evaluation staff n Ensure that surveillance activities are part of the national monitoring and
evaluation plan
n Reduce the chances that efforts will be duplicated by different
organizations
n Combine data/analysis of results with other monitoring and evaluation
activities
n Disseminate combined results
Staff engaged in surveillance for sexually transmitted
infections
Improve efficiency by combining HIV surveillance activities with surveillance
for sexually transmitted infections
2.1.2 Conduct a pre-surveillance assessment
Conduct a pre-surveillance assessment before starting surveillance activities. The purpose of this assessment
is to understand the epidemic in the country. Review existing HIV and STI surveillance results as well as
findings from behavioural surveys. Consider which populations are at increased risk for HIV and how their
behaviours put them at increased risk. Guidelines on how to conduct a pre-surveillance assessment are
available at: http://data.unaids.org/pub/Manual/2005/20050101_gs_guidepresurveillanceassmnt_en.pdf.
In brief, pre-surveillance activities should gather information on the subpopulations and geographical areas
to be included in the surveillance. The assessment should include qualitative fieldwork
• toidentifyandverifyhotspots,
• toverifythedenitionofthepopulation,and
• toguidetheplanningandlogisticsofsurveillanceeldwork.
The pre-surveillance assessment will ensure that the right subpopulations are being considered and are
defined correctly. If the population is defined incorrectly, the surveillance team might fail to detect emerging
epidemics and miss the opportunity to target interventions where they will make the most difference.
Qualitative research is necessary to describe the patterns of behaviour, points of access and barriers to
surveillance for the populations (9). Surveillance methods will differ depending on whether the person is
self-identified and, if so, whether the person is part of a subculture (10).
It is worth taking the extra time and effort to go through the pre-surveillance process to plan appropriately
and refine the surveillance protocol. Conducting the assessment could help avoid mistakes that might
ultimately cost lives, time and money.
Guidelines on surveillance among populations most at risk for HIV
9
2.1.3 Identify populations at increased HIV risk from high-risk behaviour
Specific behaviours put individuals at increased risk for HIV. During the pre-surveillance assessment, the
available resources are compiled to help identify populations with these behaviours. Very high transmission
rates are found in groups that engage in the following behaviours:
n inject drugs with used needles
n have anal sex
n have sex with many partners without protection.
Specific populations with behaviours that put individuals at increased risk for HIV have been identified as
being important for HIV surveillance (11):
n Sex workers
n Clients of sex workers
n People who inject drugs
n Men who have sex with men.
Identify the actual behaviour that puts people at increased risk for HIV when selecting subpopulations for
surveillance activities. For example:
n Sex workers have large numbers of partners, often within a very short time, increasing their exposure to
HIV and sexually transmitted infections. Sex workers are often at a disadvantage in negotiating condom
use because their partners pay for their services.
n Clients of sex workers are also at increased risk for infection because of the sex workers’ high turnover
of sex partners. Clients of sex workers often act as a bridge to low-risk populations, which means that
they are often the link between the populations with behaviours that put them at increased risk for HIV
and low-risk populations. For example, a client of a sex worker may transmit HIV to his regular partner.
n Persons who inject drugs are at increased risk because of the high transmissibility of HIV when injecting
equipment is shared. When a needle, syringe or other injecting equipment is shared, the blood from the
first injector is often still in the equipment. It is injected into the next user’s body. This is a very efficient
method for transmitting HIV or hepatitis B and C.
n Men who have sex with men are often identified as another population at increased risk for HIV. This is
because unprotected anal sex has much higher transmissibility than vaginal sex.
n Women who receive anal sex are also at increased risk for HIV.
Carefully consider the difference between vulnerable populations (such as persons with disabilities) and
populations with behaviours that put them at increased risk. Conducting surveillance among vulnerable
populations whose risk-taking behaviours are not well understood is not useful (although it might be useful
for programming for those populations).
Transgender persons often have unique networks of sexual partners or clients. The risk behaviours are
often the same as described above – anal sex or selling sex – but they take place in select venues or with
select populations. Given the high levels of HIV prevalence among this population, it is important to carry
out special surveys to estimate the size of this population and estimate the HIV prevalence in this population.
Transgender populations can vary from an individual who dresses as the other sex (transvestite) to persons
who have had surgery to modify body parts (trans-sexual). The population is difficult to categorize and
often identifies with different terminology. Formative research is critical among this population to ensure
that the correct terms and questions are included in any survey. Participation from the community is also
essential. For guidance on how to conduct surveys among transgender populations, see http://transpulse.
ca/documents/OHTN-%20Best%20Practices%20for%20Trans%20Participants-%20GBauer%202009%20
vFINAL.pdf
10
Decide on a clear and specific definition of the populations that will be covered with surveillance activities.
Here are some examples:
n Sex workers – “Women who have received money for sex at a brothel in the past six months”
n Persons who inject drugs – “Persons who have injected any non-medical drug in the past three weeks”.
Definitions will depend on the surveillance strategy and design so no global guidance can be provided
on these definitions. Keep in mind that definitions should be precise, time-bound, measurable, valid and
reliable.
Proxy populations
It is often necessary to use proxy definitions for at-risk populations that are not a distinct social group. A
proxy definition uses a sociodemographic characteristic of a group, such as occupation, or places where
persons engaging in risk behaviours are likely to be found (such as men at bars, male migrants living in
dormitories, etc.).
The proxy definition is not the cause of the increased risk for HIV. For example, truck drivers are often used
as a proxy definition for clients of sex workers because some studies show that a higher proportion of
truckers are reported to be clients of sex workers than men in the general population. However, on its own,
driving a truck is not a risk for acquiring HIV. Similarly, prisoners are often a proxy definition for most-at-risk
populations. In some settings, prisoners have been found to inject drugs or have anal sex.
A proxy definition is almost always imperfect:
n Some people who meet the proxy definition may not engage in the risk behaviour.
n Some people who have the risk behaviour may not meet the proxy definition.
A proxy definition is useful only if there is evidence that a large proportion of individuals in the group
practise the high-risk behaviour of interest. When using data from proxy groups to describe the epidemic,
be clear why a proxy group has been adopted. Document any local data which demonstrate that the proxy
group does define a population with higher risk behaviours.
2.1.4 Estimate the size of populations at increased risk for HIV
Estimates of the size of at-risk populations are critical for interpreting surveillance results and can be used to
justify surveillance activities to stakeholders and funders. Estimates can be a strong force in policy change
and resource allocation by describing the potential population at risk. In addition, estimates of population
size inform the development, implementation, and monitoring and evaluation of interventions.
Population sizes can often be estimated at the same time as surveillance activities. Information on how to
conduct size estimation studies is available in the Guidelines on estimating the size of populations most at
risk to HIV (12).
2.1.5 Decide on the geographical areas
Population members in different regions of the country may have different behaviours and thus different
risks. These differences are important for planning surveillance efforts.
Differences by region may make it difficult to generalize surveillance results from one city to the rest of the
country. Surveillance activities will be needed in multiple locations within the country to ensure that these
differences are captured.
Again, the information gathered during the pre-surveillance assessment should assist in deciding on the
geographical regions where surveillance will be conducted.
2.1.6 Consider special issues related to each population of interest
Sex workers
Sex workers – people who exchange sex for money or goods – are an important group in the HIV epidemics
of many countries, especially in countries where condom use by sex workers and their clients is low. Sex
workers may have a higher prevalence of HIV than other populations because of their high turnover of
sexual partners and financial incentives by clients to not use condoms.
Guidelines on surveillance among populations most at risk for HIV
11
Sex workers differ markedly from one place to another and by the level of the HIV epidemic (13). In addition,
there may be many different categories of sex work. In pre-surveillance activities, it is especially important
to get the community to support the research so that they can provide input on the surveillance design.
In addition, researchers should forge alliances with individuals and organizations in a position to deliver
specific intervention programmes. These include:
n sex workers’ groups
n local authorities
n gatekeepers, such as brothel owners
n women’s groups.
Data that should be collected in addition to HIV status include: frequency of sex work, time since initiation
in sex work, frequency of condom use, non-client partners, questions on the reach of prevention and care
programmes available in the area, other high-risk behaviours and other relevant variables.
Clients of sex workers
Clients of sex workers are at increased risk of infection because they have sex with sex workers who have
large numbers of sex partners. As described earlier, clients of sex workers act as a bridging population to
the general population. Surveillance among clients of sex workers is increasingly being conducted among
clients recruited at sex work venues (14,15, 16).
Surveillance of client populations can also be done using proxy populations that are believed to have sexual
contact with sex workers. These include:
n commercial drivers
n military personnel
n patients at STI clinics who report visiting sex workers.
In addition to HIV status, some additional data which should be collected among clients include: frequency
of visits to sex workers, sexual behaviour with regular partners, condom use frequency, other high-risk
behaviours and other relevant variables.
Persons who inject drugs
In most societies, the illegal nature of injecting drug use and its associated stigma mean that persons who
inject drugs are often a hidden population (17). Implementing surveillance among persons who inject drugs
requires some general principles:
n Combine HIV surveillance activities with a larger surveillance framework, including other health issues
such as hepatitis B and C surveillance.
n Work with organizations that have links to drug users:
• formerusers
• drug-abusetreatmentprogrammes
• lawenforcementsettings
• communityoutreachworkerswhooftenarerecruitedfromamongcurrentusers
• treatmentandrehabilitationcentres(18).
In many countries, the population of those who inject drugs varies from year to year, so plan to conduct size
estimation studies regularly rather than relying on old data. As described earlier, preventive services for
persons who inject drugs should accompany HIV surveillance activities (19).
Collect data on risk and preventive behaviours, including information on screening and vaccination for
hepatitis. Include needle-sharing, sexual activity (such as condom use), access to free sterile injection
equipment, participation in prevention activities and access to antiretroviral treatment (20, 21). See Technical
guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting
drug users. (http://www.who.int/hiv/pub/idu/idu_target_setting_guide.pdf)
Different drug-injecting behaviours may contribute to HIV transmission, for example:
n needle-sharing
n indirect sharing (“backloading” or “frontloading”)
n sharing filters or cookers.
12
In indirect sharing, one syringe is used to prepare the drug solution, which is then divided into one or more
syringes for injection. The solution is transferred between syringes with the needle removed (frontloading)
or plunger removed (backloading). This allows virus transmission if the preparation syringe is not clean.
The importance of each of these methods of sharing may depend on local behaviour. For example, if
direct sharing has been virtually eliminated due to intervention programmes and behaviour change, then
surveillance should monitor indirect sharing.
Surveillance should also monitor sharing that involves many different “sharing partners” within a short
period (“rapid partner-change” behaviour), since this behaviour is associated with rapid transmission of HIV
among persons who inject drugs. Technical guidelines that provide specific guidance on monitoring and
evaluating interventions for injecting drug use are available. (http://www.who.int/hiv/pub/idu/idu_target_
setting_guide.pdf)
Finally, collect information on access to sterile injecting equipment. Easy access to sterile injection equipment
is critical for HIV prevention among persons who inject drugs.
In summary, surveillance among persons who inject drugs should incorporate:
n data on drug injection risk behaviour
n sexual risk behaviour
n size and growth of the population
n patterns of drug use
n access to sterile injecting equipment
n participation in prevention activities, including screening for hepatitis
n access to antiretroviral therapy.
Men who have sex with men
HIV among men who have sex with men is increasing in many countries of the world (22,23,24). Surveillance
in this population has often underestimated the magnitude of infection and risk among this population.
Many countries do not include men who have sex with men in their regular surveillance activities because
homosexuality is illegal and highly stigmatized (25).
The impact of risk among men who have sex with men varies, depending on the level of the epidemic.
Even in some regions with a generalized epidemic, men who have sex with men may have a higher HIV
prevalence than among the general population (26).
Use formative research to enlist the cooperation of the community.
Behavioural questions that should be included in surveys with men who have sex with men include: the
number of partners, sexual behaviour and frequency of sex with female partners, time since initiation of
male-to-male sex, frequency of condom use, participation in HIV prevention or care programmes and other
relevant variables.
Other populations
In some countries, access to populations most at risk for HIV may be limited. As a result, surveillance
activities may be planned among proxy populations. In some cases, regular and consistent HIV testing and
counselling will be available from proxy populations (for example, prisoners), providing an opportunity to
analyse potential trends. It is important to ensure that ethical processes were followed to generate these
data before using them.
Surveillance systems based on proxy populations might not be adequate. Although they can be useful for
supplementing surveillance, they will typically not provide full and representative information on the actual
group of interest. As a result, they suffer from the same problems and weaknesses of such sampling or
selection biases (sampling biases and weaknesses are described later in this document). Additional variables
that should be asked of these populations depend on the behaviour that puts the group at increased risk.

Guidelines on surveillance among populations most at risk for HIV
13
Incarcerated populations
Persons in prison might be more likely to engage in behaviours that increase their risk for acquiring HIV
through injecting drugs, engaging in anal sex with fellow prisoners (27,28) or tattooing (29). While these
behaviours occur in many prison settings, incarcerated populations are not a proxy population for all
injecting drug users or men who have sex with men.
Prison populations are often used as proxy populations. Surveillance among prisoners should include the
reason for each prisoner’s incarceration (this can provide potential information to determine if they were
infected before imprisonment).
Keep in mind that incarcerated persons may have been infected before they were incarcerated.
Military recruits
In some countries, military recruits are more likely to visit sex workers. This makes them a useful proxy
population for clients of sex workers. In addition, this population is often routinely tested for sexually
transmitted infection (including HIV) through existing medical systems.
However, being in the military is not on its own a risk factor for HIV infection so interpret results with caution.
2.1.7 Integrate with existing surveillance and monitoring plans
After conducting all of these preliminary activities, including the formative assessment and size estimation,
revise and review the HIV surveillance protocol. Ensure that the protocol documents the decisions made
and plans future surveillance activities on a timeline. Make sure that the surveillance protocol is incorporated
into the national monitoring and evaluation plan to avoid overburdening staff and duplicating efforts. Use
the surveillance protocol to develop funding requests for surveillance activities.
2.2 Step 2: Decide on the surveillance design
Surveillance results will help determine:
n how many people are infected with HIV among the population most at risk, and
n the factors that might be associated with their HIV status.
Therefore, surveillance activities must collect biological and behavioural data.
There are a few ways to collect biological data. Options include:
n HIV case reporting
n using programme data for surveillance
n sentinel surveillance.
Regardless of the biological surveillance design, behavioural data should also be collected. Tracking HIV
prevalence or incidence may show the progress in implementing prevention programmes. However,
these data alone will not indicate why the programmes succeeded or failed. Behavioural data can show
associations with particular aspects of risk.
Historically, surveillance activities for biomarkers and for behavioural indicators were conducted as separate
activities. When planning surveillance activities that collect information on biomarkers, it is currently
recommended to also collect data on risk and preventive behaviours.
2.2.1 HIV case reporting
Many developed countries rely on HIV case reporting (and the self-reported transmission route) for
surveillance among most-at-risk populations. However, this method has several limitations:
n Many individuals are not diagnosed until long after they have been infected, or not at all, leading to
underreporting.
n The self-reported mode of transmission is potentially biased, as individuals may not want to disclose
high-risk behaviours to health-care providers.
n HIV case reporting generally provides only limited data on the risks of HIV transmission or behaviour.
14
Therefore, if HIV case reporting will be used, it is important to conduct alternative or additional surveillance
activities to supplement the case reporting data.
Because of the time lag of almost a decade between infection and development of AIDS, AIDS case reporting
does not reflect the recent dynamics of the HIV epidemic. In addition, as the number of people receiving
antiretroviral therapy increases, the number of new AIDS cases will decline. AIDS case reporting is therefore
not very useful for surveillance. Instead, building on systems for the delivery of antiretroviral therapy,
surveillance of advanced HIV is recommended (30).
Case reporting often needs to be based on names or national identity numbers to avoid double counting.
If individuals are required to report on behaviours that might be illegal or highly stigmatized, storing
identifying information along with self-reports of those data might be unethical.
2.2.2 Programme data used for surveillance
Many countries collect biological results from their programmes, such as sexually transmitted infection
(STI) clinics or HIV testing and counselling services. Routine programmes often focus on populations at
increased risk for HIV.
STI clinics or voluntary counselling and testing services collect information on risk behaviours. This allows
programme managers to separate the test results of men who have sex with men, women who have anal
sex, sex workers and persons who inject drugs. Annual measures of the HIV prevalence in these separate
populations provide an indication of HIV trends in most-at-risk populations.
However, data from voluntary counselling and testing and other services are often biased, depending on
who decides to participate in these services. For example, when the services charge fees, these services will
be attended by more wealthy members of the population. Moreover, the bias is likely to change over time
as more or less people access these services as programmes expand or undergo budgetary restrictions.
Similar to case reporting, this method relies on self-reported behaviours provided in a setting that might
not be confidential. Data may be biased depending on the stigma attached to the behaviour in the country.
2.2.3 Sentinel surveillance
Sentinel surveillance uses selected sites for collecting measures of HIV prevalence in a population.
Sentinel surveillance can take the form of:
n a community survey or
n a facility-based survey.
Both require the identification of subgroups of the population who are at increased risk. The section on
sampling later in this document describes the methods available for sentinel surveillance.
Similar to case reporting, this method relies on self-reported behaviours to determine the mode of
transmission. In many survey settings, interviewers are unknown to the respondent. This ensures some
level of confidentiality.
Sentinel surveillance at the community level has several challenges. All of these factors influence the validity
of the data and the generalizability of the data to a larger population.
n Sampling of most-at risk-populations is often challenging because no complete sampling frame (list
of members of the population) is available. Because of this, the resulting sample may be biased and
difficult to replicate over time.
n When random selection rules are not used, interviewer and self-selection sampling biases may result.
As a result, the survey may under-sample members of a given population who do not occupy obvious
niches in the community or who do not approach outreach workers. In other words, the survey may not
reach hidden subpopulations.

Guidelines on surveillance among populations most at risk for HIV
15
n Sampling of subgroups of interest may only recruit those who are at higher risk for HIV infection and
only later recruit those at lower risk (31).
n In sampling populations of interest, geographical areas may not be sampled in proportion to numbers
of the population of interest. For example, drug users may not be sampled in proportion to the intensity
of drug use in the region. The probability of selecting drug users may not be known.
All of these issues are discussed further in the section on sampling.
2.3. Step 3: Decide on a surveillance sampling strategy
Surveillance is conducted to allow comparisons of data from the same group over time. Thus, samples
should be:
n representative of the population
n able to be repeated (or replicable) in a later survey.
For most-at-risk populations, it is difficult to replicate surveys. Populations may be difficult to reach (hidden)
or transient; that is, people move into or out of the population. To address these issues, HIV prevalence
studies among most-at-risk populations often use probability, convenience or snowball sampling methods,
which are not always replicable over time.
While selecting a sampling strategy, consider the following:
n It should be feasible to sample from the same population in future surveys.
n The sample should be as representative of the population as possible.
n The sampling strategy should match available resources for this round and future rounds of the survey.
n It should be possible to carry out the survey (reaching all persons in the sample) in a reasonably short
period of time.
n The cost involved should be affordable.
n Legal and ethical issues of implementing the sampling strategy should be taken into account.
2.3.1 Simple random sampling
Description
The way a sample is selected determines the scientific viability of the study. A simple random sample is the
gold standard for sampling considerations. Simple random sampling assumes that everyone in the target
population has the same, known probability of being included in the sample, like drawing numbers or
names from a hat. More commonly, each member of the population is identified by a number and random
number tables or computer algorithms are used to select the required sample size.
Advantages
From a statistical perspective, simple random sampling:
n eliminates bias from a sample of volunteers who might have different characteristics than the complete
population
n provides each member of the population with the same chance of being selected
n provides a sample that contains members with characteristics similar to the population as a whole.
Limitations
As straightforward as this seems, implementing a true simple random sample in fieldwork can be expensive,
inconvenient or impossible:
n Implementing a random sample requires a sampling frame or list of the target population. Clearly, this
requirement is not met for many populations at increased risk for HIV. (See Box 1.)
n Even if a list does exist, the sample population might be dispersed throughout a geographical area,
making it expensive and time-consuming to carry out.
n A random sample may miss people or behaviours that are not common in the population.
16
In cases where a sampling frame and easy access to the population are not available, alternatives are
necessary. Excellent reviews of conventional sampling techniques can be found elsewhere (32,33,34). Several
variants of classical sampling are important for surveillance among populations at increased risk for HIV (35).
These variants are presented below.
Box 1: What is a sampling frame?
A sampling frame is simply a list of all of the individuals eligible to be in the survey. Persons participating
in the survey are selected from the sampling frame and are considered the survey sample. An
incomplete sampling frame can result in a biased sample and inaccurate results if the people excluded
from the frame have different characteristics than those included in the sampling frame.
2.3.2 Stratified sampling
Description
Stratified sampling is modified simple random sampling. Stratified sampling may provide an economic
saving over simple random sampling:
n Divide the target population into groups (strata) that are more similar within the group than the groups
are to each other.
n Now take a simple random sample from each group independently.
Define strata by the nature of the sampling question. For example, if the variable of interest is condom use,
and different types of sex workers used condoms at different frequencies, the strata could be defined as the
various types of sex workers (street-based, brothel-based, home-based) in the population.
Advantages
When data are collected in this way, statistical methods allow weighting schemes to be used to estimate the
variability and potential error of the survey due to the sampling design (36). (See Box 2.)
Limitations
It is important to have a clear understanding of the population and the differences within the population
to be able to stratify it. In the example above, we would need to know the different types of sex workers
and their behaviours. Once the strata are known, a sampling frame is needed for each stratum. Choose the
sample from these lists.
Box 2: How to weigh survey results
When a sample is drawn from a sampling frame, it is common to draw more from one section of the
population than another. This is referred to as stratified or cluster sampling.
When stratified sampling is used, it is possible to correct the bias in the sample by calculating a
variable that truly represents the population of interest. For example:
n If one subgroup of the population is overrepresented in the survey, give this subgroup a weight of
less than one.
n If a subgroup is underrepresented in the survey, give them a weight greater than one.
n The overall weighted frequency is equal to the total number of people in the survey.
All survey variables are then calculated using these weights to correct for the biases introduced from
the sampling strategy. In addition, weights are used to calculate the precision of the estimate and the
potential error as a result of the survey design or the design effect.
Guidelines on surveillance among populations most at risk for HIV
17
2.3.3 Cluster or targeted sampling
Description
Cluster or targeted sampling is also a modified simple random sampling. The target population may
be naturally divided into groups (as with stratified sampling). Within the groups there is diversity in the
variable of interest but, on average, one group is similar to the other. Each cluster should be a fairly good
representation of the entire population on a smaller scale. Often, clusters are geographical areas, such as:
n villages
n regions of a rural area
n sections of a town or city
n physical units such as brothels, bars or streets.
To conduct cluster sampling, randomly select the clusters and then perform simple random sampling within
the clusters (37).
Advantages
As with stratified sampling, weighting allows for calculation of the sampling error (38). Using the sex worker
example, if most of the population of interest is street-based, cluster sampling may be appropriate. Cluster
sampling commonly uses maps to guide the stratification. This allows for a greater generalizability to a
geographical area.
Limitations
It is usually easy to break groups into clusters when using geographical areas. Use mapping of the population
to be sure that a sample of the entire population in the region is included. A sampling frame from which to
draw the sample is needed for each cluster.
As described earlier, stratified and cluster samples can use weighting schemes to create statistical estimates
of variability and errors. This means that they can produce probability samples. Properly conducted, these
adaptations can produce estimates with as much or more accuracy as simple random sampling but with a
substantial saving of resources.
However, these designs could lead to higher estimates of error compared with that from simple random
sampling. When surveys are structured with stratifications or clusters, they are described as having a design
effect. The design effect of the study needs to be considered when planning the sampling strategy and
calculating sample sizes. Involve a statistician on the surveillance team for these types of issues.
The first three options described above are often not feasible when working with most-at-risk populations.
There are usually no sampling frames if the entire most-at-risk population in a geographical area is
considered the sampling universe. Therefore, non-probability sampling is often necessary for surveillance
of most-at-risk populations.
2.3.4 Snowball sampling
Description
Snowball sampling is one type of non-probability sampling. Persons already interviewed or measured are
used to find study subjects. Generally, subjects first contacted are asked to name acquaintances who are
then approached, interviewed and asked for additional names. In this way, a sufficient number of subjects
can be accumulated to give a study adequate power (39).
For example, if the goal is to study persons who inject drugs, sampling from needle exchange programmes,
while accessible, will miss many women, youth and those who have recently started injecting. This would
produce a statistically representative sample of an unrepresentative part of the target population. Snowball
sampling was developed to address this problem by reaching individuals in diverse social networks.
Advantage
The method allows the sampling of populations that are networked when there is no sampling frame.
18
Limitations
Snowball sampling has many limitations.
n If the goal is repeated surveillance on the same group, snowball sampling will not be appropriate. There
can be no way to compare the results over time.
n Bias can result since most people tend to name acquaintances who are similar to themselves
demographically: by race, ethnicity, education, income or religion.
2.3.5 Respondent-driven sampling
Description
Respondent-driven sampling is a modification of snowball sampling which uses a mathematical model to
weight the sample data to compensate for the fact that the sample is not a simple random sample (40,41).
Respondent-driven sampling is an important method for sampling hard-to-reach groups, including when
the groups may be small relative to the general population or when a list (sampling frame) of population
members does not exist.
To conduct respondent-driven sampling:
n Identify and recruit seeds (initial survey respondents). The number of seeds required varies by the total
sample size required and the diversity of the target population.
n Give each seed coupons and ask them to recruit three to five acquaintances.
n Each recruit who visits the study site brings a coupon that identifies (by number) who referred them.
n No names are provided, just study identification numbers combined to develop a list of the numbers of
acquaintances per study participant.
n Give each recruit coupons and ask them to recruit three to five acquaintances.
n Recruiting may go on for several waves.
n A mathematical model based on the Markov chain theory and network theory weights the sample to
address the probability that people will refer their friends, making the sample less random.
Advantages
The resulting statistical theory controls for the biases associated with chain-referral methods, providing
both population estimates and estimates of variability for those estimates (42).
Individuals are accessed through their social networks, making it more likely to reach those who shun large
public venues and avoid the street.
Limitations
As a method, respondent-driven sampling is costly and time-consuming. Sources of significant bias can
exist if the population is not well networked. Entire sections of the population of interest can be missed if
they are not connected to the initial seeds.
Depending on the number of initial seeds, the start-up of a respondent-driven sampling study can be slow.
Respondent-driven sampling requires specific software for analysis (available at: http://www.
respondentdrivensampling.org/main.htm). Recent research has found that there is large variation in the
estimates produced through respondent-driven sampling. Large sample sizes should improve on the
estimates (43).
There have been mixed results using respondent-driven sampling with different most-at-risk populations.
In some contexts, the populations were not well networked, making respondent-driven sampling a difficult
sampling strategy.
A more detailed description of how to conduct respondent-driven sampling is available at: http://www.
respondentdrivensampling.org/.
Guidelines on surveillance among populations most at risk for HIV
19
Respondent-driven sampling in Beijing, China
Respondent-driven sampling was used for three rounds of surveys to recruit men who have sex with
men in Beijing, China in 2004, 2005 and 2006. The surveys included a structured interview to collect
behavioural data and blood specimens to test for HIV, syphilis, hepatitis B virus and hepatitis C virus.
The number of participants in the surveys was 325, 427 and 540 in the 2004, 2005 and 2006 surveys,
respectively. In the 2004 survey, only one seed was recruited; in the 2005 and 2006 surveys, 10 and 8
seeds were recruited, respectively.
Special software (RDSAT) was used to adjust for the chain referral recruitment process used to select
the sample for the survey. The software allowed researchers to make adjustments to reflect the make-
up of the target population based on information from the networks of the respondents.
Once adjusted, the results were representative of the population, allowing the researchers to compare
the results over time. The researchers found a rise in HIV prevalence among men who have sex with
men in Beijing over the three years and recommended urgent services for this population to slow the
spread of HIV. This study was one of the first to use respondent-driven sampling for basic surveillance
– comparing prevalence trends. (41)
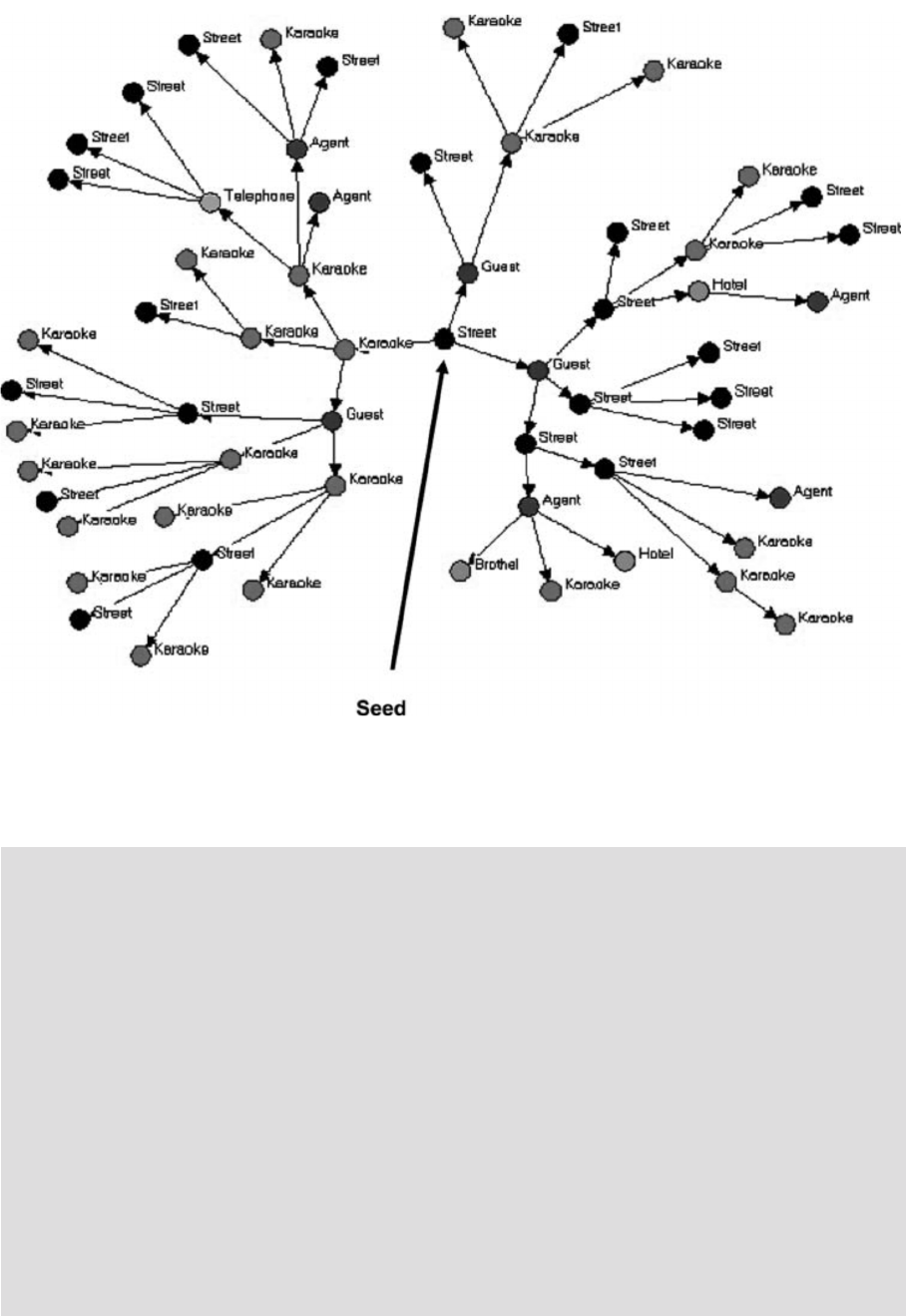
Figure 2.2. Respondent-driven sampling recruitment network for one seed by type of female sex worker
in Viet Nam
Source: Johnston LG et al. Effectiveness of respondent-driven sampling to recruit female sex workers in two cities in Vietnam.
Journal of Urban Health,
2006, 83 (Suppl 7):16–28.
http://www.springerlink.com/content/j31w862u2v65538n
20
2.3.6 Convenience sampling
Description
A convenience sample includes persons in the sample who are easy to reach or convenient to sample. An
example might be testing and interviewing all sex workers attending an STI clinic.
Advantages
Although convenience sampling is not a form of probability sampling, data from convenience samples may
be the only information available on populations most at risk for HIV transmission.
Limitations
In convenience sampling, no rules are used for sample selection. There is no way to estimate error or bias
in this sampling scheme.
2.3.7 Time–location sampling
Description
Many of the sampling methods discussed above rely on non-probability methods or tend to overestimate
people who are more networked. Time–location sampling methods can avoid these limitations.
This is a probability-based surveillance method that relies on a sampling frame derived from the times
when and locations where members of a target population congregate rather than where they live (44).
To conduct time–location sampling:
n List all the venues where the population congregates as the primary sampling unit. For example, the
population may meet in certain clubs.
n Randomly select specific times, days and venues.
n The selected venues are visited during the day and time specified.
n Subjects are systematically approached and asked to participate.
This represents a probability-based sample if:
n Every member of the target population has an equal probability of being at the venue at any given time
or day.
n Every person selected agrees to participate.
n Everyone gives truthful responses.
Time–location sampling requires good-quality formative research to ensure that no bias is entered into
selection of the venue, day and time.
Advantages
A time–location sample can be derived from key informant interviews which describe where members of
the population congregate. Once a full census of these sites has been identified, a random selection of
these sites can be chosen for inclusion in the sample. This information will also be useful for prevention
activities.
Limitations
A number of limitations exist.
n The venues selected might not necessarily be frequented by all of the target population.
n It is difficult to estimate the probability of missing someone who does not attend any of the venues.
n Some venues offer little privacy for disclosure of sensitive information.
n The accuracy of self-reported data given in a public setting is questionable.
n Identifying venues that most-at-risk populations frequent could be exposing them to unwanted attention.
Although it is time- and labour-intensive, time–location sampling does have utility for surveillance among
groups at higher risk for HIV infection as a result of high-risk behaviour (45).
More guidance on how to conduct a time–location survey can be found at: http://globalhealthsciences.ucsf.
edu/PPHG/assets/docs/tls-res-guide.pdf.

Guidelines on surveillance among populations most at risk for HIV
21
Time–location sampling in Harare, Zimbabwe
“Spatial–temporal” sampling, or time–location sampling, was used for a cross-sectional survey in
Harare, Zimbabwe of men who frequent beer halls. These men are a proxy group for men who have
high-risk sexual behaviour or frequent sex workers. To create the sample, the researchers:
n created a list of all beer halls owned by one operator (which accounted for 75% of the beer halls in
Harare),
n created a calendar of 4-hour recruitment events,
n randomly selected the beer halls to fill each calendar event,
n approached every third man who entered the beer hall to assess his eligibility for the survey
(eligibility criteria included that the man was not intoxicated).
Interviews were conducted in the privacy of nearby vans and biological samples were taken to test for
HIV. Prevention efforts were provided at the same time as the survey. Prevalence of HIV was found to
be 30% among men attending beer halls in Harare. Sex while intoxicated, unprotected sex with casual
partners, and paying for sex were highly correlated with recent HIV seroconversion. The results of this
study suggested that prevention efforts should be focused on patrons of beer halls (46).
Comparison of time–location sampling and respondent-driven sampling
Time–location sampling and respondent-driven sampling are the most common sampling techniques
currently used among populations most-at-risk for HIV. They both have limitations. Sometimes one is
preferred over the other (47).
Use respondent-driven sampling when:
n the target population is truly hidden
n it is useful to understand the social connections within the population for programme planning.
Use time–location sampling when:
n the target population is visible
n knowledge of the environment will also assist with programme planning.
2.3.8 Sample size
Sample size is an important aspect of the sample design and requires a number of considerations.
n What are the key variables in the study (usually HIV prevalence or behavioural factors)?
n How precise do the estimated results for those variables need to be?
n Does the survey need to be large enough to detect change over time between surveys or differences
between key subgroups?
In general, larger sample sizes are better than smaller ones:
n Larger samples provide the ability to distinguish true differences among subgroups of the population
or to analyse trends in incidence and risk behaviour. Because most hidden or high-risk populations are
themselves heterogeneous, surveillance requires large sample sizes to analyse subgroups.
n Larger samples are needed to make the sample more likely to accurately represent the population (i.e.
there is less uncertainty around the estimate).
n It is important to note that a large sample does not necessarily guarantee estimates that are unbiased. It
is possible to have a very precise estimate of a biased value.
For more detailed information on calculating sample size, see Surveillance of populations at high risk for
HIV transmission (48).
22
2.3.9 Sampling strategies for populations most at risk for HIV
Sex workers
Sex workers may be working legally or illegally:
n If they are legal and registered, routine screening for sexually transmitted infection may be required. If
so, a list of workers may be available from authorities or clinics. In this case, simple random sampling
or enumeration may be possible from the list. If no such list is available, time–location sampling may be
used. For reasons of comparability, surveillance should be conducted during the same period each year.
n For illegal sex workers who are venue based, time–location sampling at street, brothel, agent or other
venues can be used for HIV surveillance. If sex workers are not venue based but are well networked,
respondent-driven sampling might be appropriate.
Surveillance in institutional settings such as clinics is less subject to refusal bias, but more subject to
participation bias when compared with population-based surveillance. Clinics may overrepresent sex
workers at either end of the economic spectrum, depending on whether services are free or not. Some
populations may avoid clinics due to legal implications or stigma toward their behaviour.
Clients of sex workers
Researchers may use time–location sampling focusing on the locations where persons meet sex workers to
provide estimates of behavioural risk and infection prevalence (49). Researchers may also use convenience
sampling. In this case, an interviewer approaches clients leaving the room of a female sex worker to invite
the client for an interview and to provide an oral fluid sample for rapid testing (15,16). Clients of sex workers
are often not well networked so snowball or respondent-driven sampling is not effective in this population.
Persons who inject drugs
For out-of-treatment drug users, street- or venue-based sampling or network sampling will be necessary. For
in-treatment drug users, convenience samples can be useful. For example, needle exchange programmes
can be useful in assessing the changing characteristics of illicit drug markets, even though the data are
not representative of the broader population of persons who inject drugs (18). Behavioural surveillance is
important to document the effectiveness of prevention programmes in this population (20). Injecting drug
users are often well networked in order to purchase drugs so network sampling methods are appropriate.
Men who have sex with men
Sampling approaches for HIV surveillance among men who have sex with men again depends on the stigma
attached to the behaviour.
Convenience sampling, such as patients at a clinic (50) is often difficult as few countries have clinics devoted
to men who have sex with men. In those that do, such clinics are usually limited to large urban centres.
For men who have sex with men, it may be more appropriate to conduct repeated biological and behavioural
surveys at venues identified through formative research. If the population is hidden and venues are not
available, respondent-driven sampling can be used. Repeating these surveys at consistent sites will be
crucial for tracking trends over time.
Guidelines on surveillance among populations most at risk for HIV
23
Surveillance among men who have sex with men in Bangkok, Thailand
Three cross-sectional surveys were carried out in Bangkok, Thailand between 2003 and 2007. The
surveys focused on men who have sex with men using a time–location sampling methodology.
Venues where the men congregated were identified through a mapping exercise followed by a count
of the men attending each venue. Venues were then selected for participation in the survey.
HIV prevalence was calculated and regression analyses were used to evaluate differences and trends
over time adjusting for time–location cluster sampling. HIV prevalence in 2003, 2005 and 2007 was
17.3%, 28.3% and 30.8%, respectively.
There was a significant increase between 2003 and 2005 but the difference between 2005 and 2007 was
not significant. Additional analysis was done by looking at proxy measures of incidence and changes
in behaviour over time (see section 3.3.5). Based on the prevalence levels and the behavioural data,
the authors identified key prevention strategies that would be useful for reversing the epidemic among
men who have sex with men in Bangkok (51).
Table 2.2 provides a quick overview of sampling strategies for populations at higher risk for HIV because of
high-risk behaviour.
Table 2.2. Sampling strategies for various populations
At higher risk Possible sampling strategies
Sex workers n Time–location sampling: At hotspots where sex workers sell their trade
n Convenience: List of registered sex workers
n Convenience: List of STI clinics attendees
Clients of sex workers n Cluster sampling: survey of proxy populations (truck drivers, fishermen)
n Time–location sampling: hotspots where clients meet sex workers
n Convenience: list of STI clinic attendees reporting sex worker visits
Persons who inject drugs n Respondent-driven sampling: starting seeds from an injecting arcade
n Time–location sampling: at street venues where people inject
n Convenience: List of treatment centre attendees
Men who have sex with men n Respondent-driven sampling: starting seeds from a club
n Time–location sampling: at venues (bars, parks, etc.)
n Cluster sampling: using surveys of proxy populations (prisoners)
24
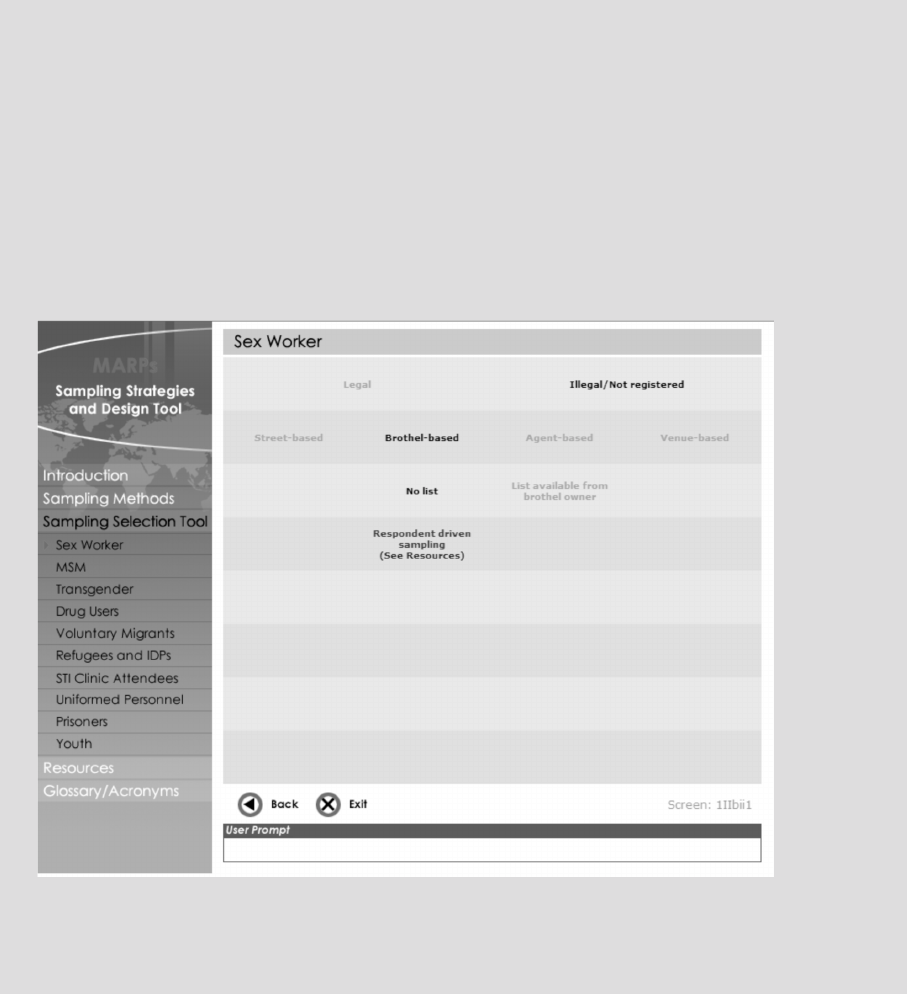
Sampling strategies and design tool
A useful tool for determining the most appropriate sampling tool is hosted at
http://globalhealthsciences.ucsf.edu/PPHG/surveillance/CDC-MARPs/sampling_selection.htm.
This tool provides sampling strategies based on the population that is being surveyed. It includes most-
at-risk populations as well as some populations that are commonly considered proxy populations for
surveillance of those most at risk. Figure 2.3 provides a snapshot of the tool and the results for brothel-
based sex workers.
Figure 2.3. Example from the sampling strategies and design tool
Developed for Centers for Disease Control and Prevention by Design and Learning Interactive, Inc.,
www.designandlearning.com, a Northrop Grumman subcontractor, 2009.
Guidelines on surveillance among populations most at risk for HIV
25
The next part of the process concerns conducting surveys. Populations most at risk for HIV have special
requirements. Focus on their special needs and how to avoid legal repercussions and stigma.
Figure 3.1. Conduct surveillance of most-at-risk populations
3.1 Step 4: Address operational issues
3.1.1 Plan staffing and training
Recruiting and training staff for a surveillance project is a critical and challenging task. The surveillance
programme staff should include:
• managementandtechnicalpersonnel
• supportstaff
• eldworkstaff
• dataentrystaff
• analysisstaff.
3. Conduct surveillance of populations
most at risk for HIV
26
Table 3.1 provides a surveillance staff list and job responsibilities. Regular and ongoing training of staff is
critical to ensure the success of the surveillance programme. All staff should be aware of all aspects of the
programme. Use every opportunity to cross-train staff. For example, give data entry staff field experience in
collecting data. They will be better team members.
Table 3.1 Example responsibilities of surveillance programme staff
Staff categories Example responsibilities
Surveillance management and technical personnel
Surveillance director n Overall surveillance, statistical and financial direction
n Technical lead for the project
Surveillance and statistical specialist n Surveillance methods, statistical survey design, enumeration areas, sampling frames
n Fieldstafftraining,supervision,qualitycontrol
n Data management, statistical analysis, report writing
Financial manager n Surveillance budget accounts
n Spending monitor
n Contractsandacquisitions
Support staff n General administrative support for surveillance staff
(May include drivers and tracking of fuel and mileage)
Fieldwork
Team leader n Team supervisor
n Meetings with community leader and members
Interviewer n Interviewing and obtaining specimens for HIV testing
n Completingquestionnairesandeditstoquestionnaires
Laboratory technician n Obtaining specimens for HIV tests if the survey protocol does not allow interviewers to do
this
n Performing tests in the laboratory
n Quality control of laboratory data
Data entry and processing
Data manager Manager for:
n Data entry, program and database development
n Dataediting,qualitycontrol
Data entry personnel n Questionnaire management
n Final hand-editing
n Dataentryfromquestionnairesintoelectronicdatales
Analyst n Supervisor, construction of documentation
n Data analysis
n Interpretation of results for relevant audiences
n Report writing
Statistician n Review sample design including sample size calculation
n Consult on analysis and interpretation of results
3.1.2 Develop data collection instruments
When designing a questionnaire, be sure to capture all the variables that are needed. Do not include
unnecessary questions in the questionnaire. Consistent questions are important to monitor trends over
time, but continuing to ask old questions about treatments that have changed is not useful.
To decide which questions to include in a survey, create a tabulation plan. A tabulation plan is a set of mock
tables that will be used in the final report. Include exactly which variables will be presented in the analytical
report of a survey.
Developing a tabulation plan helps to focus the questions on the necessary data. It also ensures that all of
the critical questions needed for the analysis are included in the questionnaire.
Guidelines on surveillance among populations most at risk for HIV
27
When constructing a questionnaire, consider other major data collection efforts within the country. Avoid
re-creating questions. Copy word-for-word questions that have been used in previous surveys:
n to allow comparison of results between surveys
n to reduce field-testing of questions.
Make sure the survey questionnaires evolve as the epidemic evolves. Family Health International has
developed questionnaires for use among populations most at risk. Consult those examples for ideas (52).
(http://www.fhi.org/en/hivaids/pub/guide/bssguidelines.htm).
Consider international reporting needs and indicators required for national commitments before
finalizing the questionnaire. Also be sure to translate and back-translate the questionnaire to identify any
misunderstandings, and pretest the questionnaire in a community outside of the sample.
3.1.3 Plan handling of specimens and HIV testing
WHO and UNAIDS have developed guidelines for HIV using testing technologies for surveillance (53). These
guidelines consider a country’s laboratory infrastructure and surveillance needs, and then suggest methods
for selecting, evaluating and implementing HIV testing technologies and strategies. These guidelines
provide recommendations for:
n specimen selection
n collection, storage and testing of specimens
n selection and evaluation of appropriate HIV testing strategies
n technologies that meet surveillance objectives
n quality assurance issues.
HIV testing among most-at-risk populations presents unique challenges as well as opportunities. The
development of rapid testing technologies allows testing to move from the laboratory to the field. Providing
results at the time of the test is very useful when working with populations that are hard to reach, as
opportunities for these populations to learn their HIV status might not occur often. Depending on the
surveillance design, two strategies have been proposed for most-at-risk populations. See Table 3.2.
Table 3.2. Testing strategies for most-at-risk populations
Country/surveillance situation Testing algorithm
Strategy 1:
n For unlinked anonymous surveillance – when
test results and counselling are not provided to
respondents
Use a two-test strategy
n Both tests need high sensitivity and high negative predictive value.
n Specimens reactive to both tests are considered HIV-positive.
Strategy 2:
n For linked surveillance – when test results and
counselling are provided to respondents at the time of
the survey
Use a three-test strategy
n Confirmatory results are needed according to the algorithms used for
diagnosis.
n Specimens reactive to three different assays are considered positive.
3.2. Step 5: Data management
The reward for careful planning and implementation of surveillance comes with the analysis.
3.2.1 Plan the data management system
The structure and content of the database should be specified before data collection begins. Database
development involves five steps.
28
Procedure: Five steps for developing the survey database
Step Do this…
1 Determineasystemforidentication(ID)ofrecords.MaketheIDsystemconsistentandcomprehensivetouniquelyidentify
each record:
n createauniqueIDforeachparticipant
n protect personal identity. It should be possible to verify ID numbers and analyse results but not disclose who the participant
is. All names, registration numbers or addresses should be deleted.
2 Design a master file for information across multiple datasets, such as demographic information, which will be included in both
behavioural interviews and laboratory data. This allows analysts to link datasets for analysis:
n Ensure that the relevant IDs are entered on all forms before data collection.
n Include checks between the different files (for example, birth date).
3 Design the database. The structure of the database will reflect the various types of data and the timing of data collection.
n Include a directory for each dataset collected with separate subdirectories for software programs, datasets and
documentation.
n This will ensure that all data files can be traced accurately from data collection through analysis to published paper.
4 Plan data entry and data analysis.
n If the data are collected on paper, ensure that no errors are made during data entry. Develop a reliable data entry system
using independent double entry.
n If data are collected electronically, select a reliable transfer method from the machine used for data collection into the
project database.
n Regardless of the mode of collection, give data entry staff a list of:
• acceptablevalues(thatis,validranges)foreachvariable(questionitem)
• eldsthataremandatory(forexample,subjectIDordateofdatacollection).
5 Ensure that the protocol is followed and maintained. Be especially aware of ethical issues when designing the database.
3.2.2 Use data management best practices
The purpose of data management is to preserve data integrity between data collection and analysis/reporting
(54). Data management best practices are particularly important for HIV surveillance among most-at-risk
populations due to the sensitive nature of the data (55,56). Sound data management is an ethical obligation
for anyone engaged in data collection.
Family Health International (FHI) has produced guidelines for the management of behavioural data (57).
(http://www.fhi.org/en/HIVAIDS/pub/survreports/firstthingsfirst.htm)
Begin data verification for quality assurance as data are collected and entered during fieldwork. Use the data
entry software program for quality assurance. For example, check all fields to make sure that the values are
acceptable and internally consistent.
3.2.3 Create a dataset for analysis
Most data management experts recommend that permanent datasets for analyses be created only when
data are completely entered, cleaned and frozen; no further changes are allowed.
3.2.4 Document the steps used to create the database
In professional data management, all decisions are apparent at every stage, from data collection through
analysis.
n Document and explain all the decisions made when cleaning the data.
n Document the steps used to create new variables.
n Document how missing variables are handled.
n Label all variables in each dataset in a manner that conveys information even after the datasets are
merged.
n Create codebooks or annotated forms to describe each instrument, map variable names onto the data
collected.

Guidelines on surveillance among populations most at risk for HIV
29
3.2.5 Maintain confidentiality and security
Surveillance staff must ensure and maintain confidentiality during data entry and processing, and should
have been trained in ethical issues important for surveillance.
n All personal identifying information (such as name, identification number, address) should be removed
from forms before data entry.
n Store identifying information in locked files or destroy it.
n Do not store computer data files with personal information on computer networks.
n If personal information is stored on a computer, password protect or encrypt it.
Linking behavioural data with HIV status from laboratory data is important for HIV surveillance. However,
linking data increases the likelihood of inadvertent disclosure of protected health information.
3.3. Step 6: Data analysis
No matter how rigorous the method of analysis, if compromises were made in the surveillance design
or data collection, the analysis will be flawed. General guidelines for surveillance analysis can be found
elsewhere (58,59). Discussed here are analytical methods for specific issues relating to HIV surveillance
among populations most at risk for HIV.
3.3.1 Handling non-response
Despite careful data collection, there will be some missing data. Decide how to handle these missing data.
For example, for some questions, a respondent (the person responding) may not give an answer or items
may not apply. Include an explanation of missing data in the database documentation.
There are two ways to deal with missing data:
n Ignore it. That is, analyse the data as they exist and omit them when they are missing. Do this if the
team believes that people who do not respond to a particular question are, on average, like those who
do respond with respect to other data collected (60). While we might question the wisdom of such an
assumption for HIV surveillance, this is the assumption that most statistical analysis packages make.
n If the team agrees that missing data cannot be ignored, consider imputation methods. Values are filled
in (imputed) for the missing data, based on other data that were supplied by that person (61). Depending
on the extent and nature of the missing values, the unadjusted data may produce biased estimates (62).
3.3.2 Using weighting
Most surveys require sampling weights to be calculated and applied to adjust the results during analysis
and avoid bias. For example, if the sampling strategy has oversampled one subgroup of the population (for
example, younger sex workers or brothel-based sex workers), the analyst would need to adjust the general
results for the whole population to reflect the true probability of being selected.
Similarly, weighting can adjust for cluster or stratified sampling designs.
Weights can also correct for different response rates. For example, if one subpopulation was more likely to
refuse to participate in the survey than other subpopulations, the statistician might adjust the weighting to
account for the non-response of this group.
In many surveillance designs and sampling strategies described in this document, it will not be possible to
create sampling weights.
n If cluster sampling was used with different probabilities of selection by cluster, it will be not be possible
to develop weights. Consult a sampling statistician in this case.
n For time–location sampling and respondent-driven sampling methods, sampling weights are used.
• For respondent-driven sampling, see the tools for respondent-driven sampling analysis at www.
respondentdrivensampling.org.
• Fortime–locationsampling,seehttp://globalhealthsciences.ucsf.edu/PPHG/assets/docs/tls-res-guide.
pdf.
30
3.3.3 Determining HIV prevalence
To calculate HIV prevalence, divide the total number of people testing HIV-positive by the total number who
were tested (33).
Programme managers often require the number of individuals in the population of interest who are infected,
even though everyone in the population is not tested during the survey. To make this extrapolation, it
is necessary to estimate the size of the population for the denominator. Size estimation has numerous
challenges, which are described in the size estimates guidelines (10).
Prevalence data combine new and old infections. HIV prevalence is difficult to interpret in regions where
treatment is expanding and thus people who are HIV-positive are living longer. A rising prevalence may be
interpreted, as people are living longer because they are receiving ART. Stable or declining HIV prevalence
may also be interpreted, as the number of new infections is declining or more infected persons are dying.
In populations most-at-risk for infection, prevalence estimates might also reflect:
n the impact of turnover in populations. For example, new sex workers may enter the industry and older
sex workers may leave the industry, or
n sample saturation may occur when the same injecting drug users are tested at a syringe exchange
programme over multiple rounds of a survey.
3.3.4 Determining HIV prevalence trends
Data on trends provide an important indicator of the trajectory of the epidemic. To be able to accurately
compare data and assess trends, the data will need to meet many statistical requirements. These include
the following:
n Achieve a sufficient survey sample size to detect a change over time.
n Conduct consistent sample recruitment between surveys. For example:
• Ifonesurveyusesrespondent-drivensamplingandthenextsurveyusestime–locationsampling,the
populations in the surveys will be different. Therefore, they are not comparable. However, changing
the sampling design to adopt a stronger or more accurate method is encouraged.
• Ifnon-probabilitysamplingisused,itisnotpossibletodeterminewhetherthesampleisrepresentative
of the population.
• Ifthesampleispulledfromavoluntarycounsellingandtestingclinicandtherehasbeenachangein
the fee structure since the last survey, there could be changes in the population attending the clinic.
Use sites consistently included in the surveillance system over time. If additional sites are added or dropped,
it is important to adjust for the fact that prevalence might be systematically different in those sites. Be sure
to describe any systematic changes in the final report.
If the samples are comparable over time, conduct tests to see if the trends are statistically significant. The
conventional approach to trend analysis is to test the significance of the results through different statistical
tests:
n a linear chi-square (63)
n a linear regression (64)
n an exponential regression (65) or
n a categorical (66) model.
Descriptions of these techniques of analyses can be found elsewhere.
3.3.5 Determining HIV incidence
When interpreting cross-sectional HIV prevalence data, some people assume that: trends in HIV prevalence
reflect trends in transmission, or prevalence is a reasonable surrogate for risk of infection. These assumptions
have been shown to be false in some situations (67).
Guidelines on surveillance among populations most at risk for HIV
31
HIV incidence (recent infection) is a better measure for understanding the projection of the epidemic and the
progress of HIV prevention efforts. However, it is more difficult to measure. Methods include:
n statistical or mathematical modelling (68,69,70,71)
n directly measuring incidence through laboratory assays. These methods are still being developed
(72,73,74,75). Since 2006, a series of meetings have been held to discuss progress towards validating a
protocol for the use of existing HIV incidence assays and the development of future incidence assays.
WHO has established a Technical Incidence Assay Working Group (HIVIWG). Detailed information can be
accessed on the WHO web site: (http://www.who.int/diagnostics_laboratory/en/).
n proxy measures of incidence. Measuring HIV prevalence trends in a population of newly exposed
individuals may be a reasonable proxy for incidence (76). For example, assessing HIV prevalence trends
among individuals who have just started injecting drugs or selling sex can be used as a proxy for
incidence (77,78).
n longitudinal cohort studies. These studies require large numbers of persons at risk and frequent testing
to determine ranges for seroconversion (79,80,81).
3.3.6 Dealing with uncertainty
Unless a census is done of the population of interest, the individuals in these surveys will be chosen from
larger populations. The individuals might not have the same characteristics as the larger population. Survey
results will thus have some level of uncertainty, which should be considered when analysing the results.
Describe the uncertainty with the results. Ideally, the statistician on the team would calculate standard
errors or confidence intervals around the estimates to indicate the uncertainty of the estimate.
3.3.7. Ensuring validity
Validity refers to the degree to which the results from the surveillance activity accurately measure the
indicator or related public health problem (82). In the context of surveillance of most-at-risk populations,
validity is determined primarily by the sample design, sample size, questionnaire construction and accuracy
of participants’ responses (83).
n Base the sampling strategy or design on a probability sample if possible. If this is not possible, use a
strategy that best represents the population.
n Choose the correct sample size to ensure that the data collection is adequate to measure the characteristics
of interest. Many populations most at risk for HIV have varied behaviours. Large samples permit analysis
of subgroups of the population.
n Reduce bias by constructing a good questionnaire for collecting accurate information from
respondents (84).
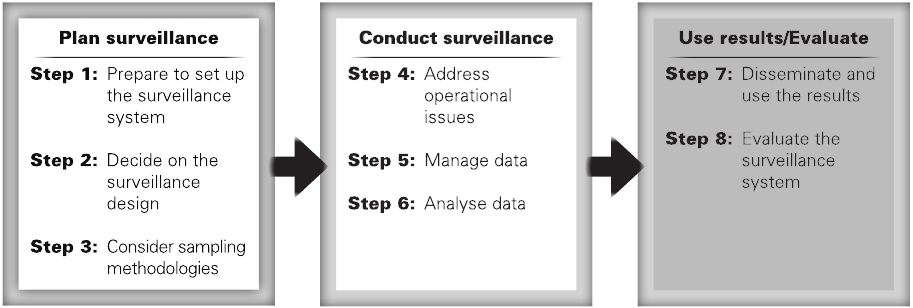
32
4. Use the results/Evaluate the
surveillance plan
The final two steps of the process are using the results and evaluating the surveillance system.
Figure 4.1. Use the results collected and evaluate the surveillance system
4.1.1 Share the results
Sharing the surveillance results is an ethical imperative. The results of these efforts can have an important
impact on the HIV response. Therefore, once the results and recommendations are available, they should
be shared in a responsible manner.
Plan to provide the stakeholders involved in the study with the preliminary results. Use their expertise to
interpret the data collected.
4.1.2 Develop a dissemination plan
Develop a dissemination plan for the stakeholders involved in the planning phase. Consider these questions:
n Who needs to know the results?
n How should the results be presented to each audience?
n When are the results needed by that audience?
n What are the key messages to get across?
Consider sharing the findings in newsletters, which are published faster than peer-reviewed journals. Also
consider that the affected community might not have access to journals.
4.1.3 Protect the population from stigma or legal action
Ethical questions on how to share the results will vary by the populations affected. Shared surveillance
information may cause political pressure in the case of restrictive policies. This may result in harm to the
members of risk groups and make it even harder to contact them in future.
It is important that the results are transformed into messages that are clear and not harmful or further
stigmatizing to the population.
Guidelines on surveillance among populations most at risk for HIV
33
4.1.4 Use the results to improve programmes
Use the results to inform prevention, care and treatment programmes. The information may have been
disseminated widely to a broad group of stakeholders. However, it is critical to take the data to the next step
for use by decision-makers.
Make an effort to ensure that programme managers have access to the results to plan appropriate
interventions based on the surveillance results. Surveillance results should help improve services for most-
at-risk populations and reduce their risk of acquiring HIV infection. Involve the most-at-risk populations not
only in the research but also in the development of intervention programmes based on the results.
Analyse data to generate strategic information. Use the information for decision-making and planning. Only
in this way can resources devoted to surveillance be justified and used to curb the epidemic in populations
most at risk for HIV.
Try to report on a regular basis to communities at risk, partner organizations and national AIDS councils.
Support these stakeholders to determine how the results best inform their services. Make this a part of the
ongoing activities of surveillance. Surveillance staff should have access to and proactively participate in the
HIV response planning process.
Examples of how surveillance data have been used to improve programmes have been highlighted in recent
conferences (85).
n In a number of countries in sub-Saharan Africa, surveillance data have been used in simple models (see
example below) to estimate where new HIV infections are occurring.
n In Kazakhstan, surveillance data from prison populations have been used to develop an appropriate
prevention response for the prison population.
n In Bangladesh, sophisticated subtyping of HIV strains has provided evidence of how HIV has spread
between populations and neighbourhoods.
Example of use of surveillance data
Surveillance data on most-at-risk populations can be used to improve HIV programmes with “Modes
of Transmission” models. Modes of Transmission is a simple spreadsheet model that allows countries
to predict where new infections will occur in their country. Using data on HIV prevalence among
different subpopulations and most-at-risk populations, a team of epidemiologists from Kenya was
able to identify populations where estimates of new infections can be expected. These data were
used to help plan interventions in the national strategic plan. This exercise led to a recommendation
to increase service provision for men who have sex with men, persons who inject drugs, other drug
users and sex workers.
Figure 4.2: Distribution of new infections in Kenya
Heterosexual sex within union/regular partnership
Casual heterosexual sex
Female sex workers and clients
MSM and prison
Injecting Drug Use (IDU)
Health Facility Related
More information on the Modes of Transmission software can be found at www.unaids.org.
Source: Kenya National AIDS Control Council. HIV prevention response and modes of transmission analysis. 2009. (http://www.unaidsrstesa.org/files/u1/Kenya_MoT_
Country_Synthesis_Report_22Mar09.pdf).

34
4.2. Step 8: Evaluate the system
Any surveillance activity that is implemented must be evaluated regularly to ensure that it is meeting its
objectives (86).
More informal routine monitoring is also useful. Reflect on these aspects of the surveillance system:
n Frequency and timeliness of data collection
n Appropriateness of populations under surveillance
n Consistency of sites and groups measured over time
n Coverage/representativeness of the groups for the target populations.
When evaluating the HIV surveillance system, include the following:
n Can the system describe where new infections are occurring?
n Can the system describe how the epidemic is changing?
n Are the data being used to inform programming?
n Are the right data elements being collected?
n Is the choice of methodology appropriate for the situation?
n Does the data collection process adhere to the protocol?
n Has the analysis been conducted with appropriate tools/methods, including weighting, adjustment for
design effects, etc.?
n Is data collection restricted to essential data?
n Is there appropriate process documentation?
n Does the activity conducted meet ethical standards?
Look for additional information on surveillance evaluation guidelines on the WHO and UNAIDS web sites
in 2011.
Guidelines on surveillance among populations most at risk for HIV
35
Appendix A: List of additional
surveillance resources
Title Year Topic
Guidelines on estimating the size of populations most
at risk to HIV
2010 Update on methodologies for estimating the size of
most-at-risk populations http://data.unaids.org/pub/
Manual/2010/guidelines_popnestimationsize_en.pdf
Evaluation guidelines for HIV second generation
surveillance system
Forth-coming 2011 How to assess and evaluate HIV surveillance systems
and adapt them to the needs of countries
Ethical issues in HIV surveillance: guidelines Forth-coming 2011 Ethical principles for conducting HIV surveillance
activities
Guidelines for using HIV testing technologies in
surveillance:
selection, evaluation and implementation: 2009
update
2009 An update in guidance on selecting and utilizing
appropriate HIV tests for surveillance purposes
http://www.who.int/hiv/pub/surveillance/hiv_
testing_technologies_surveillance_.pdf
HIV triangulation resource guide: synthesis of results
from multiple data sources
for evaluation and decision-making
2009 Guidelines on conducting triangulation, users’ manual
developed with examples based on experiences in
Africa. http://www.who.int/hiv/pub/surveillance/
hiv_triangulation_guide.pdf
The pre-surveillance assessment: guidelines for
planning serosurveillance of HIV, prevalence of
sexually transmitted infections and the behavioural
components of second generation surveillance of HIV
2005 Tools for preparing to implement second generation
surveillance including defining and selecting risk
groups, sites and feasibility of methods
http://www.who.int/hiv/pub/surveillance/sti/en/
index.html
Guidelines for measuring HIV prevalence in
population-based surveys
2005 Guidelines for national population-based surveys with
HIV testing
http://data.unaids.org/pub/Manual/2005/20050101_
GS_GuideMeasuringPopulation_en.pdf
Guidelines for HIV surveillance among tuberculosis
patients
2004 How to conduct HIV surveillance among TB patients
http://www.searo.who.int/LinkFiles/Facts_and_
Figures_05_GuidelinesHIV_surveillancTBpatients_
final_version.pdf
Guidelines for effective use of data from HIV
surveillance systems
2004 Guidance on how to analyse, interpret and present
surveillance data
http://data.unaids.org/Publications/IRC-pub06/
JC1010-UsingData_en.pdf
36
Appendix B: Glossary and acronyms
AIDS
Late stage of HIV infection, including the development of one or more opportunistic illnesses (illnesses
that occur because of low levels of CD4 lymphocytes or immunodeficiency)
Active surveillance
A system in which health authority personnel take the lead in identifying and reporting cases, as opposed
to “passive surveillance”
AIDS case
surveillance
The identification and reporting of persons meeting the definition of an AIDS case to permit public health
authorities to track the disease over time. Also known as ”AIDS case reporting”
Anonymous
Having no known name or identity. For example, removing all personal identifying information from a
sample that will be tested for HIV, in order to protect the patient’s identity
Antiretroviral drugs
Drugs used to fight infections caused by retroviruses such as HIV
Antiretroviral therapy
(ART)
Treatment with drugs that inhibit the ability of HIV to multiply in the body
Behavioural
surveillance
SurveysofbehaviourthatmayresultinacquiringHIV.Thismayinvolveaskingasampleofpeopleabout
risk behaviours such as sexual practices and drug use.
Bias
A systematic error in the collection or interpretation of data
Bridging populations
Persons belonging to high-risk subpopulations who interact with people at lower risk in the general
population, making it more likely for the HIV epidemic to shift from high-risk (“concentrated”) populations
to the general population
Case reporting
A surveillance system in which persons who are identified as meeting the case definition are reported to
public health authorities
Concentrated HIV
epidemic
The epidemic state in which HIV has spread to a high level in a defined subpopulation but is not well
established in the general population. This epidemic state is characterized by an HIV prevalence that is
consistently >5% in at least one defined subpopulation, but <1% in pregnant women in urban areas.
Confidentiality
Protecting information that concerns a study participant or patient from release to those who do not need
to have the information
Convenience
sampling
The selection of subjects from a population based on accessibility and availability
Demographic
information
The “person” characteristics of epidemiology (usually collected with “place” and “time”) – age, sex, race
and occupation – used to characterize the populations at risk
Denominator
The population (or population experience, as in person-years, etc.) at risk in the calculation of a proportion
or rate. The denominator is the lower portion of a fraction used to calculate a rate or ratio.
Epidemic
The occurrence of a disease (or other health-related event) at a substantially increased level and at a given
period of time in relation to a baseline
Epidemiology
The study of the distribution and determinants of health-related states or events in specified populations,
and the application of this study to the control of health problems
Generalized HIV
epidemic
The epidemic state in which HIV is firmly established in the general population. This epidemic state is
characterized by an HIV prevalence that is consistently >1% in pregnant women.
High-risk behaviours
Behaviours that increase the risk of a person contracting a disease
Highly active
antiretroviral therapy
(HAART)
The use of at least three antiretroviral drugs in combination to suppress viral replication and progression of
HIV disease by reducing the viral load to undetectable levels
HIV
Acronym for human immunodeficiency virus

Guidelines on surveillance among populations most at risk for HIV
37
Human
immunodeficiency
virus (HIV)
A retrovirus that causes AIDS by infecting T-cells of the immune system
HIV counselling and
testing (HCT)
A programme that provides both counselling and testing services to communities, allowing persons who
are tested to obtain emotional and medical support before and after their HIV tests
Incidence
Ameasureofthefrequencywithwhichanevent,suchasanewcaseofillness,occursinapopulation
over a period of time. The denominator is the population at risk; the numerator is the number of new cases
occurring during a given time period.
Informed consent
Informedconsentistheprovisionofadequateinformationtoactivelydecidetoconsenttoaprocedure.
It protects the person’s freedom of choice and respects their autonomy with regard to decisions affecting
their body and health.
Laboratory-based
reporting
A surveillance system in which the reports of cases come from clinical laboratories
Linked anonymous
HIV testing
A person is tested for HIV, and the specimen is labelled with a code without a name or identifiers that
couldrevealtheperson’sidentity.Thismethodisvoluntaryandrequiresobtaininginformedconsentand
making the test results available (with appropriate counselling) to the person tested.
Linked confidential
HIV testing
A person agrees to have an HIV test with the assurance that the test result will be kept confidential and
onlyselectedhealth-careprovidersmaybeinformed.Thismethodisvoluntaryandrequiresobtaining
informed consent and discussing the test results with the person. Linked confidential testing also allows
for the collection of more detailed demographic and risk-behaviour information.
Linking
Refers to whether a tested individual’s name or identifying information is associated with their HIV test
results
Low-level HIV
epidemic
The epidemic state in which HIV has not reached significant levels in any subpopulation, although HIV
infection may have existed for many years. This epidemic state is characterized by an HIV prevalence that
has not consistently exceeded 5% in any defined subpopulation. This state suggests that networks of risk
are rather diffuse or that the virus has only recently been introduced.
MSM
Acronym for men who have sex with men
Natural history of
disease
Acronym for men who have sex with men
Odds ratio
A measure of the strength of an association between exposure and disease, calculated by taking the ratio
of the odds of disease with the exposure to those odds without exposure. For a rare disease, the odds ratio
is a reasonable approximation of the relative risk. Odds ratios are commonly used for case–control studies
and result easily from logistic regression analysis.
Passive surveillance
A system in which a health-care provider or worker notifies the health authority of any cases of diseases,
as opposed to “active surveillance”
Random sample
A sample derived by selecting individuals such that each individual has the same probability of selection
Proxy population
A population in which a large proportion of the members have a behaviour that puts individuals at
increased risk for HIV. Proxy populations are used when it is not possible to specifically sample the most-
at-risk population.
Relative risk
A measure of the association between a disease or condition and a factor under study, calculated by
dividing the incidence rate among those exposed to the factor by the incidence rate among those not
exposed to the factor
Representative
sample
A sample whose characteristics correspond to those of the original or reference population
Representativeness
The extent to which the sample resembles the true population
Selection bias
A systematic error in the process of respondent selection for a study or survey
Sensitivity
The proportion of persons with disease who are correctly identified by a screening test or case definition
as having the disease
Sentinel case
reporting
Reporting cases of a disease from sentinel sites
Sentinel populations
Populations that are subject to sentinel surveillance activities. They may not necessarily be representative
of the general population, but they might be the first to be affected by HIV. Examples include persons with
sexually transmitted infection or truck drivers.
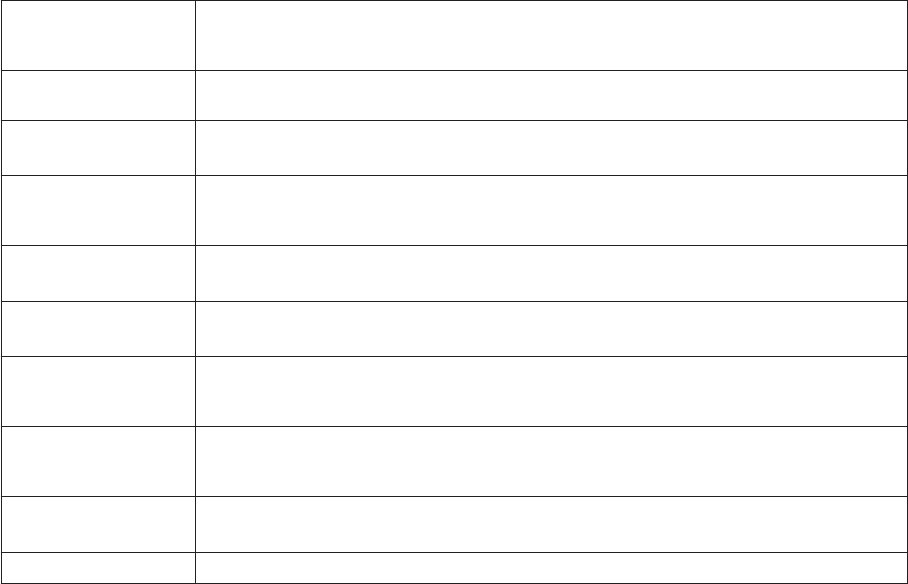
38
Sentinel sites
Sites at which sentinel surveillance activities take place, including clinics attended by individuals who may
not be representative of the general population but represent groups initially infected or at higher risk for
infection than the general population
Sentinel surveillance
A surveillance system that samples populations from facilities or communities for a short period of time on
a regular basis
Seroprevalence
surveys
Surveys that estimate the HIV prevalence by testing blood for HIV antibody
Serosurveillance
Collecting blood samples for surveillance. Latent, subclinical infections and carrier states can be detected,
in addition to clinical cases. This is especially important in the case of HIV and other sexually transmitted
infections, which often have a long latent period before symptoms become apparent.
Sexually transmitted
infection (STI)
Diseases that are spread by the transfer of organisms from person to person during sexual contact
Simple random
sampling
Asamplingmethodthatrequirestheuseofarandomnumbertableorothermethod(forinstance,
computer-based) to generate random numbers that identify the persons to be included in the sample
Surveillance
The systematic collection, analysis, interpretation and dissemination of health data on an ongoing basis, to
gain knowledge of the pattern of disease occurrence and potential in a community, in order to control and
prevent disease in the community
Systematic sampling
A sampling method that consists of randomly selecting the initial patient who meets the inclusion
criteria and then selecting every “nth” (for example, third or fifth) eligible patient thereafter until the
predetermined sample size is reached or the survey period is over
Unlinked anonymous
testing
In unlinked anonymous testing, a sample of blood originally collected for other purposes is tested for HIV
after all information that could identify the source of the blood is eliminated from the sample.
Validity
The degree to which a measurement actually measures or detects what it is supposed to measure
Guidelines on surveillance among populations most at risk for HIV
39
Appendix C: Links
UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance
Global surveillance of HIV/AIDS and sexually transmitted infections is a joint effort of WHO and UNAIDS.
The UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance, initiated in November 1996, is
the coordination and implementation mechanism for UNAIDS and WHO to compile and improve the quality
of data needed for informed decision-making and planning at national, regional and global levels. http://
www.unaids.org/en/HIV_data/Epidemiology/epiworkinggrp.asp
A good selection of key HIV/AIDS surveillance reports and documents include the following:
n New strategies for HIV/AIDS surveillance in resource-constrained countries (http://data.unaids.org/
Topics/Epidemiology/Reports/hivsurveillanceconference-addis_en.pdf)
n Ethical issues to be considered in second generation surveillance (http://www.who.int/hiv/pub/
epidemiology/en/sgs_ethical.pdf)
n Guidelines for conducting HIV sentinel serosurveys among pregnant women and other groups
(http://data.unaids.org/publications/irc-pub06/jc954-anc-serosurveys_guidelines_en.pdf)
n HIV/AIDS epidemiological surveillance update for the WHO African Region 2002 (http://www.who.int/hiv/
pub/epidemiology/pubafro2003/en/)
n Guidelines for second generation HIV surveillance
(www.who.int/hiv/pub/surveillance)
Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections
These fact sheets provide country-specific information on numerous key indicators relevant to HIV.
Journal supplements specifically on HIV surveillance
AIDS 2001 Supplement 3
AIDS 2005 Supplement 2 on the first global HIV surveillance conference in Addis Ababa, Ethiopia
Journal of HIV/AIDS Surveillance and Epidemiology 2010 issue 2 on the second global HIV surveillance
conference in Bangkok, Thailand
40
1 Teutsch SM. Considerations in planning a surveillance system. Chapter 2. In: Teutsch SM, Churchill
RE, eds. Principles and practice of public health surveillance. 2nd edition. New York, Oxford University
Press, 2000.
2 Fairchild AL et al. Public goods, private data: HIV and the history, ethics, and uses of identifiable
public health information. Public Health Reports, 2007, 122:7–15.
3 WHO/UNAIDS. Ethical issues in HIV surveillance: guidelines. (In press).
4 Rhodes SD et al. Exploring Latino men’s HIV risk using community-based participatory research.
American Journal of Health Behavior, 2007, 31:146–158.
5 Council for International Organizations of Medical Sciences. The international ethical guidelines for
biomedical research involving human subjects: guideline 7. Geneva, WHO, 2002.
6 Emanuel EJ et al. Undue inducement in clinical research in developing countries: is it a worry?
Lancet, 2005, 366:336–340.
7 Schenk K, Williamson J. Ethical approaches to gathering information from children and adolescents
in international settings: guidelines and resources. Washington, DC, Population Council, 2005.
8 Baker MG, Fidler DP. Global public health surveillance under new international health regulations.
Emerging Infectious Diseases, 2006, 12:1058–1065.
9 Baral S et al. Elevated risk for HIV infection among men who have sex with men in low- and middle-
income countries 2000–2006: a systematic review. PLoS Medicine, 2007, 4:e339. doi:10.1371/journal.
pmed.0040339.
10 Introduction to sampling most-at-risk populations: sampling strategies and design tool. Available at:
http://www.theagencyfordesign.com/clients/cdc/marps (accessed 12 March 2011).
11 UNAIDS. A framework for monitoring and evaluating HIV prevention programmes for most-at-risk
populations. Geneva, UNAIDS, 2008. Available at: http://data.unaids.org/pub/Manual/2008/jc1519_
framework_for_me_en.pdf (accessed 28 October 2010).
12 UNAIDS/WHO. Guidelines on estimating the size of populations most at risk to HIV. Geneva, UNAIDS/
WHO, 2010. Available at: http://data.unaids.org/pub/Manual/2010/guidelines_popnestimationsize_
en.pdf (accessed 28 October 2010).
13 Ghys PD, Jenkins C, Pisani E. HIV surveillance among female sex workers. AIDS, 2001, 15 (suppl
3):S33–S40.
14 Subramanian T et al. HIV, sexually transmitted infections and sexual behaviour of male clients of
female sex workers in Andhra Pradesh, Tamil Nadu and Maharashtra, India. AIDS, 2008, 22:S69.
15 Vuylsteke BL et al. HIV prevalence and risk behavior among clients of female sex workers in Abidjan,
Côte d’Ivoire. AIDS, 2003, 17:1691–1694.
16 Lowndes CM et al. Management of sexually transmitted diseases and HIV prevention in men at high
risk: targeting clients and non-paying sexual partners of female sex workers in Benin. AIDS, 2000,
14:2523–2534.
17 Des Jarlais DC, Dehne K, Casabona J. HIV surveillance among injecting drug users. AIDS, 2001, 15
(suppl 3):s13–s22.
References
Guidelines on surveillance among populations most at risk for HIV
41
18 Topp L et al. Representativeness of injecting drug users who participate in HIV surveillance. Journal
of Acquired Immune Deficiency Syndromes, 2008, 47:632638.
19 Lau JTF et al. Changes in the prevalence of HIV-related behaviors and perceptions among 1832
injecting drug users in Sichuan, China. Sexually Transmitted Diseases, 2008, 35:325–335.
20 Lansky A et al. Developing an HIV behavioral surveillance system for injecting drug users: the
national HIV behavioral surveillance system. Public Health Reports, 2007, 122(S1):48–55.
21 Hammett TM et al. Patterns of HIV prevalence and HIV risk behaviors among injection drug users
prior to and 24 months following implementation of cross-border HIV prevention interventions in
northern Vietnam and southern China. AIDS Education and Prevention, 2006, 18:97–115.
22 CDC. Trends in HIV/AIDS diagnoses among men who have sex with men—33 states, 2001–2006.
MMWR Morbidity and Mortality Weekly Reports, 2008, 57:681–686.
23 McFarland W, Caceres CF. HIV surveillance among men who have sex with men. AIDS, 2001, 15 (suppl
3):S23–S32.
24 Family Health International. Surveillance and assessment reports. Available at: http://www.fhi.org/en/
HIVAIDS/pub/survreports/index.htm (accessed 12 March 2011).
25 Cloete A et al. Stigma and discrimination experiences of HIV-positive men who have sex with men in
Cape Town, South Africa. AIDS Care, 2008, 20:1105–1110.
26 Smith A et al. Men who have sex with men and HIV/AIDS in sub-Saharan Africa. Lancet, 2009,
374:416–422. DOI:10.1016/S0140-6736(09)61118-1.
27 Teplin LA et al. HIV and AIDS risk behaviors in juvenile detainees: implications for public health policy.
American Journal of Public Health, 2003, 93:906–911.
28 Dolan K, Kite B, Black E, et al. HIV in prison in low-income and middle-income countries. Lancet, 2007,
7:32–41.
29 Rotily M et al. Surveillance of HIV infection and related risk behavior in European prisons: a
multicentre pilot study. European Journal of Public Health, 2001, 11:243–250.
30 WHO. WHO case definitions of HIV for surveillance and revised clinical staging and immunological
classification of HIV-related disease in adults and children. Geneva, WHO, 2007. Available at: http://
www.who.int/hiv/pub/guidelines/hivstaging/en/index.html (accessed on 12 March 2011).
31 Iguchi M et al. Interpreting HIV seroprevalence data from a street-based outreach program. Journal of
Acquired Immune Deficiency Syndromes, 1994, 7:491–499.
32 American Statistical Association. Survey research methods section. Available at: http://www.amstat.
org/sections/srms/Proceedings/ accessed on 28 March 2011.
33 WHO. Guidelines for measuring national HIV prevalence in population-based surveys. Geneva, WHO,
2006. Available at: http://www.who.int/hiv/pub/surveillance/guidelinesmeasuringpopulation.pdf
(accessed 12 March 2011).
34 WHO. Guidelines for conducting behavioural surveillance. New Delhi, WHO SEARO, 2001. Available
at: http://www.searo.who.int/LinkFiles/Publications_aids-123.pdf (accessed on 12 March 2011).
35 Ostrow DG, Kessler RC. Methodological issues in AIDS behavioral research. New York, Plenum Press,
1993.
36 Foreman EK. Survey sampling principles. New York, Marcel Dekker, 1991.
37 Munro HL et al. Prevalence and determinants of HIV and sexually transmitted infections in a general
population-based sample in Mysore district, Karnataka state, southern India. AIDS, 2008, 22 (suppl
5):s117–s125.
38 Som RK. Practical sampling techniques. Boca Raton, FL, CRC Press, 1996.
39 Faugier J, Sargeant BA. Sampling hard to reach populations. Journal of Advanced Nursing, 2008,
26:790–797.
42
40 Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations.
Social Problems, 1997, 44:174–199.
41 Heckathorn DD. Extensions of respondent-driven sampling: analyzing continuous variables and
controlling for differential recruitment. Sociological Methodology, 2007, 37:151–207.
42 Ma X et al. Trends in prevalence of HIV, syphilis, hepatitis C, hepatitis B, and sexual risk behavior
among men who have sex with men: results of 3 consecutive respondent-driven sampling surveys in
Beijing, 2004 through 2006. Journal of Acquired Immune Deficiency Syndromes, 2007, 45:581–587.
43 Goel S, Salganik MJ. Assessing respondent-driven sampling. Proceedings of the National Academy of
Sciences, 2010, 107:6743–6747.
44 Robbins CL et al. Multicity HIV seroprevalence in street youth, Ukraine. International Journal of STD &
AIDS, 2010, 21:489–496.
45 Stueve A et al. Time–space sampling in minority communities: results with young Latino men who
have sex with men. American Journal of Public Health, 2001, 91:922–926.
46 Fritz KE et al. The association between alcohol use, sexual risk behavior, and HIV infection among
men attending beerhalls in Harare, Zimbabwe. AIDS and Behavior, 2002, 6:221–228.
47 Johnson L, Sabin K, Prybylski D. Update for sampling most-at-risk and hidden populations for HIV
biological and behavioral surveillance. Journal of HIV/AIDS Surveillance & Epidemiology, 2010, 2:2.
48 WHO. Surveillance of populations at high risk for HIV transmission. Module 6. New Delhi, WHO
Regional Office for South-East Asia, 2007. Available at: http://www.searo.who.int/LinkFiles/
Publications_Module-6.pdf (accessed on 12 March 2011).
49 Subramanian T et al. HIV, sexually transmitted infections, and sexual behavior of male clients of
female sex workers in Andhra Pradesh, Tamil Nadu and Maharashtra, India: results of a cross-
sectional survey. AIDS, 2008, 22 (suppl 5):s69–s79.
50 Soto RJ et al. Sentinel surveillance of sexually transmitted infections/HIV and risk behaviors in
vulnerable populations in 5 Central American countries. Journal of Acquired Immune Deficiency
Syndromes, 2007, 46:101–111.
51 van Griensven F et al. Trends in HIV prevalence, estimated HIV incidence, and risk behavior among
men who have sex with men in Bangkok, Thailand, 2003–2007. Journal of Acquired Immune
Deficiency Syndromes, 2010, 53:234–239. 210.1097/ QAI.1090b1013e3181c1092fc1086.
52 Family Health International. Behavioral surveillance surveys: guidelines for repeated behavioral
surveys in populations at risk of HIV. Arlington, FHI, 2000. Available at: http://www.fhi.org/en/hivaids/
pub/guide/bssguidelines.htm (accessed on 6 December 2010).
53 UNAIDS/WHO Working Group on Global HIV/AIDS and STD Surveillance. Guidelines for using HIV
testing technologies in surveillance: selection, evaluation and implementation: 2009 update. Geneva,
UNAIDS/WHO, 2009. Available at: http://www.who.int/hiv/pub/surveillance/hiv_testing_technologies_
surveillance_.pdf (accessed 6 December 2010).
54 Dean AG. Computerizing public health surveillance systems. In: Teutsch SM, Stroup DF, eds.
Principles and practice of public health surveillance. 2nd edition. New York, Oxford University Press,
2000.
55 Payne L. Information sharing and assessment (ISA): can data management reduce risk? Children &
Society, 2004, 18:383–386.
56 Mohania M, Ananthanarayanan R, Gupta A. Some issues in privacy data management. Data &
Knowledge Engineering, 2007, 63:591–596.
57 Family Health International. First things first: guidelines on management and coding of
behavioural surveillance data. Arlington, FHI, 2006. Available at: http://www.fhi.org/NR/rdonlyres/
em3sbmf74plnwbkg3y64zrajqbktch66cijjvijog3xiyit44muehtnaayszwyq7u6acvbdkrmaxkj/
datamanagementguideline1.pdf (accessed on 6 December 2010).
58 Janes GR et al. Descriptive epidemiology: analyzing and interpreting surveillance data. In: Teutsch
SM, Stroup DF, eds. Principles and practice of public health surveillance. 2nd edition. New York,
Oxford University Press, 2000.
Guidelines on surveillance among populations most at risk for HIV
43
59 Brookmeyer R, Stroup DF (eds). Monitoring the health of populations: statistical principles and
methods for public health surveillance. New York, Oxford University Press, 2004.
60 Groves RM et al. Survey nonresponse. New York, Wiley and Sons, 2002.
61 Harrison KM et al. Risk factor redistribution of the national HIV/AIDS surveillance data: an alternative
approach. Public Health Reports, 2008, 123:618–627.
62 Marston M, Jarris K, Slaymaker E. Non-response bias in estimates of HIV prevalence due to the
mobility of absentees in national population-based surveys: a study of nine national surveys. Sexually
Transmitted Infections, 2008, 84:i71–i77.
63 Gouws E et al. The epidemiology of HIV infection among young people aged 15–24 years in southern
Africa. AIDS, 2008, 22 (suppl 4):s5–s16.
64 Van der Loeff MFS et al. Sixteen years of HIV surveillance in a West African research clinic reveals
divergent epidemic trends of HIV-1 and HIV-2. International Journal of Epidemiology, 2006, 35:1322–
1328.
65 Gouws E, and the International Group on Analysis of Trends in HIV Prevalence and Behaviours in
Young People in Countries most Affected by HIV. Trends in HIV prevalence and sexual behaviour
among young people aged 15–24 years in countries most affected by HIV. Sexually Transmitted
Infections, 2010, 86 (Suppl 2):72–83.
66 Fleiss JL. The comparison of proportions for many samples. In: Statistical methods for rates and
proportions. New York, John Wiley; 1973:99–102.
67 McFarland W et al. Detection of early HIV infection and estimation of HIV incidence using a sensitive/
less sensitive testing strategy at anonymous counseling and testing sites in San Francisco. Journal of
Acquired Immune Deficiency Syndromes, 1999, 22:484–489.
68 Hallett TB et al. Estimating incidence from prevalence in generalised HIV epidemic: methods and
validation. PLoS Medicine, 2008, 5:e80. doi:10.1371/journal.pmed.0050080.
69 Gregson S et al. Demographic approaches to the estimation of incidence of HIV-1 infection among
adults from age-specific prevalence data in stable endemic conditions. AIDS, 1996, 10:1689–1697.
70 Williams B et al. Estimating HIV incidence rates from age prevalence data in epidemic situations.
Statistics in Medicine, 2001, 20:2003–2016.
71 Stover J et al. Estimated HIV trends and program effects in Botswana. PloS ONE, 2008, 3:e3729.
72 Parekh BS, McDougal JS. Application of laboratory methods for estimation of HIV-1 incidence. Indian
Journal of Medical Research, 2005, 121:510–518.
73 Janssen RS et al. New testing strategy to detect early HIV-1 infection for use in incidence estimates
and for clinical and prevention purposes. Journal of the American Medical Association, 1998, 280:42–
48.
74 Busch MP et al. Beyond detuning: ten years of progress and new challenges in the development and
application of assays for cross-sectional HIV incidence estimation, AIDS, 2010, 24:2763–2771.
75 Guy R et al. Accuracy of serological assays for detection of recent infection with HIV and estimation of
population incidence: a systematic review. Lancet Infectious Diseases, 2009, 9:747–759.
76 Zaba B, Boerma T, White R. Monitoring the AIDS epidemic using HIV prevalence data among young
women attending antenatal clinics: prospects and problems. AIDS, 2000, 14:1633–1645.
77 Garfein RS et al. Prevalence and incidence of hepatitis C virus infection among young adult injection
drug users. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology, 1998,
18(suppl 1):s11–s19.
78 Mahy M et al. A proxy measure for HIV incidence among populations at increased risk to HIV. Journal
of HIV/AIDS Surveillance and Epidemiology, 2010, 2:8.
79 Kingsley LA et al. Temporal trends in human immunodeficiency virus type 1 seroconversion 1984–
1989. A report from the Multicenter AIDS Cohort Study (MACS). American Journal of Epidemiology,
1991, 134:331–339.
44
80 Des Jarlais DC et al. Continuity and change within an HIV epidemic: injecting drug users in New York
City, 1984 through 1992. Journal of the American Medical Association, 1994, 271:121–127.
81 Wambura M et al. HIV prevalence and incidence in rural Tanzania: results from 10 years of follow-up
in an open-cohort study. Journal of Acquired Immune Deficiency Syndromes, 2007, 46:616–623.
82 United States Population Council. AIDSQuest: The HIV/AIDS Survey Library
Appendix E: selected bibliography of research on validity and reliability of HIV/AIDS-related survey
instruments. Available at: http://www.popcouncil.org/Horizons/ORToolkit/AIDSQuest/index.html
(accessed on 28 March 2011).
83 Boerma JT Sommerfelt AE. Demographic and health surveys (DHS): contributions and limitations.
World Health Statistics Quarterly, 1993, 46:222–226.
84 Seha AM, Klepp KI, Ndeki SS. Scale reliability and construct validity: a pilot study among primary
school children in Northern Tanzania. AIDS Education and Prevention, 1994, 6:524–534.
85 Mahy M, et al. Maximizing the use of surveillance data: innovative examples from around the world.
Journal of HIV/AIDS Surveillance & Epidemiology, 2010, 2:11.
86 UNAIDS. National AIDS programmes: a guide to monitoring and evaluation. Geneva, UNAIDS, 2000.
Available at: http://data.unaids.org/publications/IRC-pub05/jc427-mon_ev-full_en.pdf (accessed on 12
March 2011).

48
For more information, contact:
World Health Organization
Department of HIV/AIDS
Avenue Appia 20
1211 Geneva 27
Switzerland
E-mail: [email protected]
www.who.int/hiv
