
Building the City of Solutions
Evaluating the Addiction
Crisis Response
in Huntington/Cabell County WV
Principle Investigator
-Todd Davies, PhD
Quantitative Team Lead
-Hannah Redman, MSHI, MHA
Team
-Tim Babine, MS, MSHI
-Jonathan Willis, MS
-Jing Tian, MS
Qualitative Team Lead
-Taylor Maddox-Rooper, MS
Team
-Ryan Crouse, MA
-Fortune Ezemobi, MPH
-Kassandra Flores, MS
-Paris Johnson, MPH
-Benjamin Thompson, MS
-Sarah Matson, MPH
Tool Development
-Debra Koester, PhD, DNP,
MSN, RN
MARSHALL TEAM
Evaluation Lead
-Debra Dekker, PhD
Directoral Support
-Chris Aldridge, PhD, MSW
-Aaron Alford, PhD, MPH, PMP
Fidelity Team
-Shawna Newton
-Kellie Hall
-Caden Gabriel
NACCHO TEAM
Project Lead
-Michael Meit, MPH, MA
ACEs Team
-Lucianna Rocha, MPH
-Michelle Dougherty, MPH
-Victoria Hallman
-Megan Heffernan, MPH
-Margaret Cherney
Partner Analytics
-Brandon Sepulvado, PhD
-Keshav Vemuri, MS
NORC TEAM
Project Director
-Christopher Jones,
PharmD, DrPH, MPH
Project Coordination
-Brian Corry, MS
-Akadia Kacha-Ochana,
MPH
Technical Assistance
-Steven Sumner, MD
-Gaya Myers, MPH, CHES
-Manisha Patel, MD, MS
-Vikram Krishnasamy, MD
CDC TEAM

© MUSOM 2021| www.jcesom.edu
Addiction Response | September 2021
Understanding Declining Rates of Drug Overdose Mortality in Eastern Kentucky NORC at the University of Chicago
jcesom.marshall.edu September 2021
Introduction
By 2014, Huntington/Cabell County found itself in
the midst of an addiction epidemic that put the
entire community into crisis mode. The community
came together to create a response to the
epidemic, which was built on an unprecedented
level of collaboration. This report evaluates the
development of that response and outlines the
critical timing and resources that made it
successful.
Prior to the community response, Huntington, WV
and surrounding Cabell County was much like
many communities in regards to addiction. The
focus of services were primarily on the clinical
aspects of treatment and recovery. Agencies
operated separately and often functioned as
competitors. Medication assisted treatment (MAT)
providers and peer-based or 12-step programs
spoke of each other with distain. The local
governmental approach to addiction was
channeled through the police department. As the
number of people struggling with addiction
increased across the community, it became clear to
many that those approaches were not sufficient to
address the growing problem. Frontline workers
often felt that with control over the resources (Key
Stakeholders) did not understand the full
consequences of addiction and were not
empowered to address many critical issues.
“I think we spend a lot of time with
people with initials after their names
thinking they have the answer and the
only thing they've been in is a book.”
- Frontline Worker
Those attitudes changed when the political, health,
and university leadership publically admitted that
the community was in trouble and worked together
to create an
environment
of
collaboration
across the
community.
Frontline
workers and
patients were
sought out for their expertise and encouraged to
build natural connections between agencies. The
overall result was a large increase in referrals to
treatment and a decrease in overdose deaths.
Project Description
With funding from the Centers for Disease Control and Prevention (CDC) and the National Association of County and
City Health Officials (NACCHO), the Division of Addiction Sciences within the Joan C. Edwards School of Medicine at
Marshall University (Marshall) conducted this study to Identify and describe the impact of critical elements of a
community-wide response in Huntington/Cabell County, WV to the addiction epidemic. The community response resulted
in an increase in the number of individuals with substance use disorder identified and referred to treatment that correlated
with a two-year drop in overdose deaths just prior to the COVID-19 pandemic. This study describes the severity of the
epidemic including the significant barriers. Key actionable components for other communities are reported with the
approach and timing required to deploy them.
Building the City of Solutions
Evaluating the Addiction Crisis Response in Huntington/Cabell County WV
Executive Summary
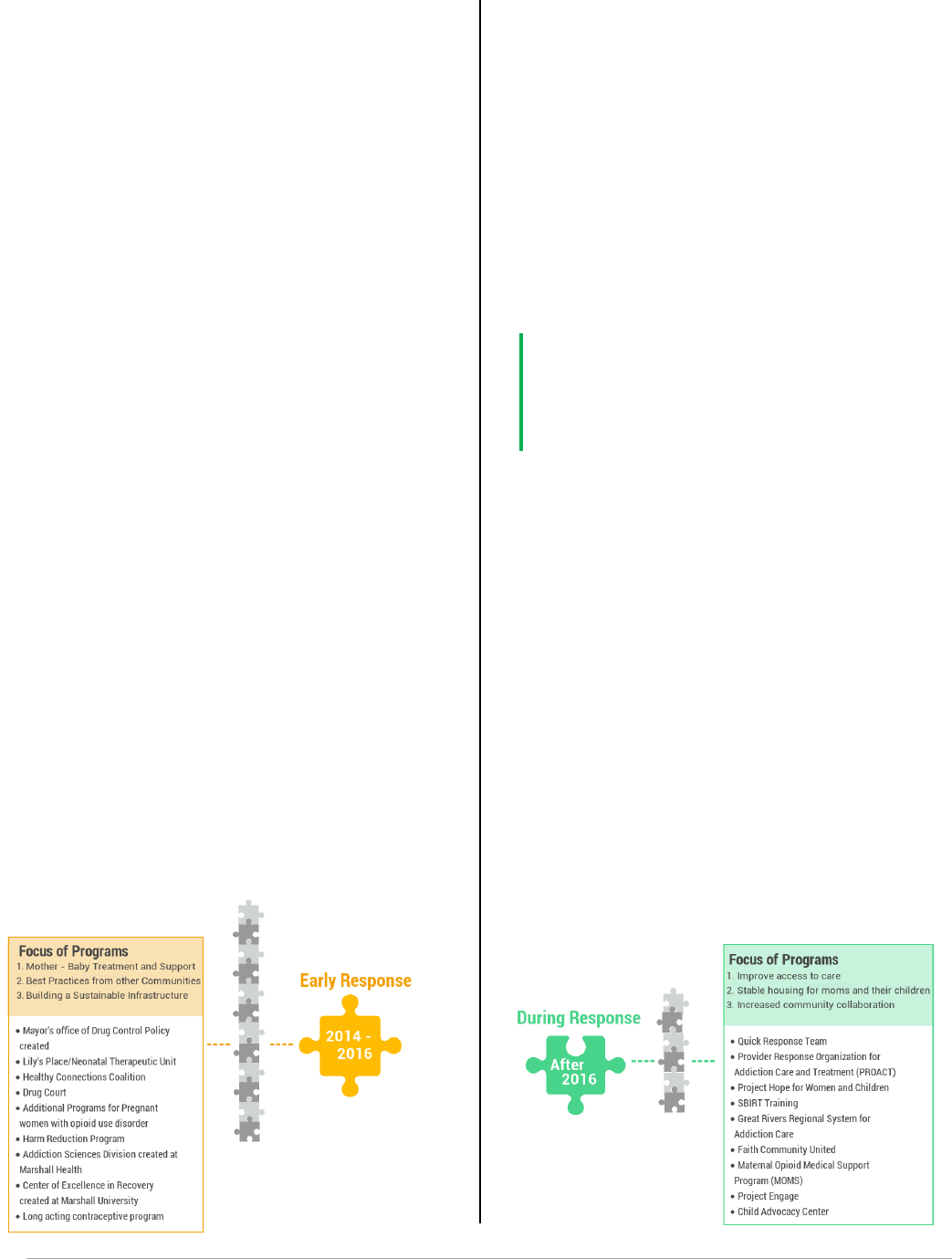
Figure 1: Programs prior to response
Figure 2: Critical leadership entities.
© MUSOM 2021| www.jcesom.edu
Addiction Response | September 2021
Figure 3: Programs early in the response
Methods
A multi-layered mixed methods approach was
used by evaluators. Data was collected and
analyzed use a variety of complementary
methodologies.
• Qualitative data from those involved
with the Huntington/Cabell County
addiction epidemic response was
collected by semi-structured
interviews with 44 Key Stakeholders
(administrative level) and 56 Frontline
Workers (those who with work directly
with those affected by substance use).
• A non-affiliated “client survey” was
conducted of individuals with
substance use disorder (SUD) to
collect the patient perspective of the
response.
• A partnership survey and network
analysis was used to determine the
level of agency collaboration.
• Evaluators also conducted a review of
SUD and Cabell County-related media
activity.
• A community shared data system was
developed to aggregate clinical data to
determine success of the evaluation
through existing data.
Findings
Building the Response
The response to the addiction epidemic in
Huntington/Cabell County, WV was a process with
the community searching for answers. The key
attribute that made the response successful was
the attitude and approach of leadership that the
community should search for answers
together. Community buy-in was still a challenge early
on, so efforts were focused on adopting best practices
from other communities (such as establishing a drug
court) while building a sustainable infrastructure that
would allow the community to react quickly as the
consequences of widespread addiction.
As part of creating infrastructure, local government,
county health officials, and university members
emphasized the collection and analysis of more real-
time data for the community to convince State and
Federal agencies of the critical nature of the situation.
Data available to these agencies was not timely or
representative of the size of the problem, making it
difficult to secure grant funding for the area.
“I think having access to data, just
information is so crucial because people
don't understand what's happening.”
- Key Stakeholder
Community agencies began immediately building
collaborations, but with an emphasis on mother –
baby resources. As part of the epidemic, Cabell
County was experiencing an alarming number of
births in which the neonate was prenatally exposed
to drugs. Most of the community viewed these babies
as innocent, and community support for these
resources met with minimum stigma.
Buy-in from the larger community for patients with
substance use disorder outside of exposed neonates
did not happen until August 2016 when the area
experienced 26 overdoses in a single day. After this
day, the response became focused on improving
access to care and building community collaboration.
These later efforts were directly responsible for the
success of the response, but would not have been
possible without the earlier infrastructure and
collaboration already in place.
Figure 4: Programs during the full response

Evaluating the Addiction Crisis Response in Huntington/Cabell County WV
Division of Addiction Sciences Research
© MUSOM 2021| www.jcesom.edu
Addiction Response | September 2021
What Worked?
Key Stakeholders and Frontline Workers agreed that collaboration, community buy-in, and a client-centered
approach are what made the response effective. The collaboration structure in Huntington/ Cabell County, WV
is unstructured, denoting an environment of collaboration and not a controlled process. There was a strong
sense from the community members that participated in data collection that, while the new programs are an
important part of the response, the collaborative approach was the key to identifying and deploying the
programs that were best suited to this community specifically. Culture, or cultural specificity, was an important
part of the overall process. All of the programs developed after 2016 also have a peer component in order to
extend that cultural sensitivity directly to the clients in need of support or care.
Key Stakeholders also discussed that data collection and the willingness to try new methods and approaches
were key factors, while Frontline Workers and surveyed clients focused on more practical aspects of recovery
(access to care, transportation, fulfilling personal commitments, etc.).
Recommendations for other
communities:
•
Admit there is a problem:
This will likely
require strong political leadership
•
Empower existing resources:
Many
answers were found existing within the
community already
•
Create an environment of
Collaboration:
Natural collaborations are
the most effective, but can require
encouragement.
•
Focus attention on whole life recovery
and families:
Every patient represents a
larger group that needs support.
•
Treat patients as human beings:
Services will not be utilized to the fullest
extent if the clients don’t feel welcome.
•
Control the message with shared data:
Tell others about your community; don’t
wait for them to decide who you are.
•
Watch out for compassion fatigue:
Those in the thick of the fight need to
know that their efforts are worthwhile.
ABOUT NAACHO
National Association of County and City Health Officials
(NACCHO) was established in 1965 to improve the
health of communities by strengthening and advocating
for local health departments. NACCHO currently serves
over 3000 local health departments and is the leader in
providing cutting-edge, skill-building, professional
resources and programs, seeking health equity, and
supporting effective local public health practice and
systems. NACCHO is dedicated to supporting local
health departments, optimizing strategic partnerships
and alliances, and advocating for local health
departments.
ABOUT MU Joan C. Edwards School of Medicine
The Joan C. Edwards School of Medicine at Marshall
University is a community-based, Veterans Affairs
affiliated medical school established in 1977 to address
health disparities in rural tri-state region of southern
West Virginia, southeastern Ohio, and eastern Kentucky
and dedicated to providing high quality medical
education and post graduate training programs to foster
a skilled physician workforce to meet the unique
healthcare needs of the population we serve. The
mission was and still is today to provide healthcare and
education to Appalachia.

Table of Contents
Introduction ........................................................................................................................... 1
Background .................................................................................................................. 1
A Community in Trouble ............................................................................................... 2
Methodology ......................................................................................................................... 5
Interviews ..................................................................................................................... 5
Surveys ........................................................................................................................ 6
Quantitative Methodology ............................................................................................ 6
Media Analysis ............................................................................................................. 7
Findings ............................................................................................................................... 8
Addressing the Barriers ................................................................................................ 8
Building Collaboration is a multi-Step Process ........................................................... 10
Evaluation of Community Collaborative Structure ...................................................... 10
Process of Developing a Community-Wide Collaborative Environment ...................... 12
Finding Common Ground ................................................................................... 12
Leadership ......................................................................................................... 13
Community Response Approach ....................................................................... 16
Collaboration Creates Opportunity for Sustainable Programs ................................... 20
Stigma, Misunderstanding, and Educating the Community ........................................ 21
Financing the Response-Data is the Key ................................................................... 24
Indicators of Success ................................................................................................. 25
Future Directions .................................................................................................................. 30
Limitations ............................................................................................................................ 32
Conclusion ............................................................................................................................ 33
Lessons for Other Communities ........................................................................................... 34
Index of Response Participants Mentioned in Evaluation: .................................................... 35
Resources ............................................................................................................................ 36
Funding from the CDC was made possible through the Center for State, Tribal, Local, and
Territorial Support (CSTLTS) Cooperative Agreement OT18-1802 "Strengthening Public Health
Systems and Services through National Partnerships to Improve and Protect the Nation's
Health.”

1 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Introduction: For the last few decades, a major epidemic grew and the United States saw an
increase in the incidence and complication rates of drug addiction.
1
This epidemic would result
in deaths by drug poisoning surpassing death by suicide, homicide, firearms and motor vehicles
accidents by 2017.
2
A culmination of events placed the small Appalachian city of Huntington,
West Virginia at the epicenter. Huntington and surrounding Cabell County, developed a
community response that included an unprecedented level of collaboration and a number of
novel solutions. In Dec 2019, the Centers for Disease Control and Prevention (CDC) through
the National Association of County and City Health Officials (NACCHO) funded an evaluation of
the community response to the addiction epidemic to:
1. Identify and describe the impact of critical elements defined as part of the response in
Huntington/Cabell County, WV
2. Understand the role of public health system partners on the effectiveness of system
delivery and utilization in the response in Huntington/Cabell County
3. Identify the actionable factors for translating the Huntington/Cabell County response to
other communities.
Utilizing a mixed methods approach, evaluators conducted 100 interviews with Key
Stakeholders (administrative level) and Frontline workers (those who work directly with those
affected by substance use). By conducting a partnership survey to determine the level of
agency collaboration; a client survey of individuals with substance use disorder (SUD); a review
of SUD-related media activity and a quantitative clinical data system, evaluators were able to
report on the response to the addiction epidemic in Huntington/Cabell County. This report will
describe the severity of the epidemic, the response, and report indicators of effectiveness. The
ultimate goal is to identify the key components of the response that may be adapted and used in
other communities to respond to public health crises.
Background: Cicero et al demonstrated that the pattern of first opioid use changed significantly
in the last 40 to 50 years. Eighty percent of individuals who had their first opioid use in the
1960’s reported that first exposure to be heroin. Contrast this with the 2000’s, where 75% of
users reported prescription opioids as their first exposure.
3
Despite an increased likelihood of
abuse, only 4.2% of those using opioids non-medically turned to heroin
4
. Some researchers
speculate OxyContin abuse may have increased the rates of heroin abuse,
5
6
but as OxyContin
prescribing decreases heroin use continues to rise.
5
As efforts continue to reduce the over-prescribing of opioids, availability of opioids made
significant inroads. Data from the Centers for Disease Control and Prevention (CDC) WONDER
Database found increases in overdose deaths associated with heroin and synthetic opioids like
fentanyl.
7
8
In fact, heroin related overdose deaths jumped from 1,842 in 2000 to 10,574 in
2014
9
with heroin use increasing significantly in most demographic groups.
4
The influence of
overprescribing on the addiction epidemic may have waned with prescribing restrictions, but the
substance abuse continued to grow as an increasing number of patients reported heroin as their
first opioid
8
, reversing the trend of the previous few decades.
By 2015, claims were being made of Middle America being specifically targeted by opioid
producers and “Mexican drug lords.”
11
Heroin became more readily available in areas not
traditionally considered centers for drug distribution
12
and the cost per gram dropped from
$2,690 in 1982 to less than $600.
13
2 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
This increased availability and lower cost of heroin, coupled with the poor economic conditions
and isolating terrain throughout Central Appalachia, created a fertile soil for this targeted drug
activity to grow. West Virginia (WV), the only state located entirely in Central Appalachia, ranks
consistently as one of the worst states for health and economic status. WV had the highest age-
adjusted death rate from drug poisoning in the country.
14
The state reported a rapid growth in
the rates of opiate overdoses,
15,16
Hepatitis C and other communicable diseases related to
sharing needles, and Neonatal Abstinence Syndrome (NAS)
17
throughout WV with the most
severe effect on Southern WV.
18
This culmination of evidence indicates that West Virginia was,
likely, the most impacted state in the union and Huntington/Cabell County was the most affected
part of the state.
Numerous anecdotal accounts report the
majority living in the Huntington or Cabell
County, WV either struggled with SUD or
had a loved one who did. Because of the
widespread personal impact, the
community was quick to set aside biases
and individual agendas to work toward a
comprehensive solution.
A Community in Trouble: Prior to 2013,
during the building stages of the epidemic, there were a few already aware of the continued
increase in substance use in Huntington/Cabell County. The number and variety of available
SUD resources suited a community its size, but would prove inadequate in the face of the high
volume of individuals with SUD within the community. There were faith-based programs, like
Celebrate Recovery and Loved One’s, as well as both Alcoholics Anonymous and Narcotics
Anonymous. Huntington’s numerous sober living houses demonstrated some success helping
those who
sought
recovery. A
peer-based
recovery
facility that
would
eventually
become
Recovery Point
of West
Virginia
opened in
2011. In 2012,
First Steps
Wellness &
Recovery
Center opened
to serve people
experiencing homelessness and the opioid using population. During this time, the Huntington
Comprehensive Treatment Center and Valley Heath Systems provided medication-assisted
treatment options to the community. All of this was in addition to the county’s behavioral health
I always kind of have to smile to myself when I hear
people talk about how the opioid crisis became a
big thing in the 2000s, because, I was here in
ninety-seven and it was already a fairly big thing
then. It was, of course, more pain pills at that time.
– Key Stakeholder
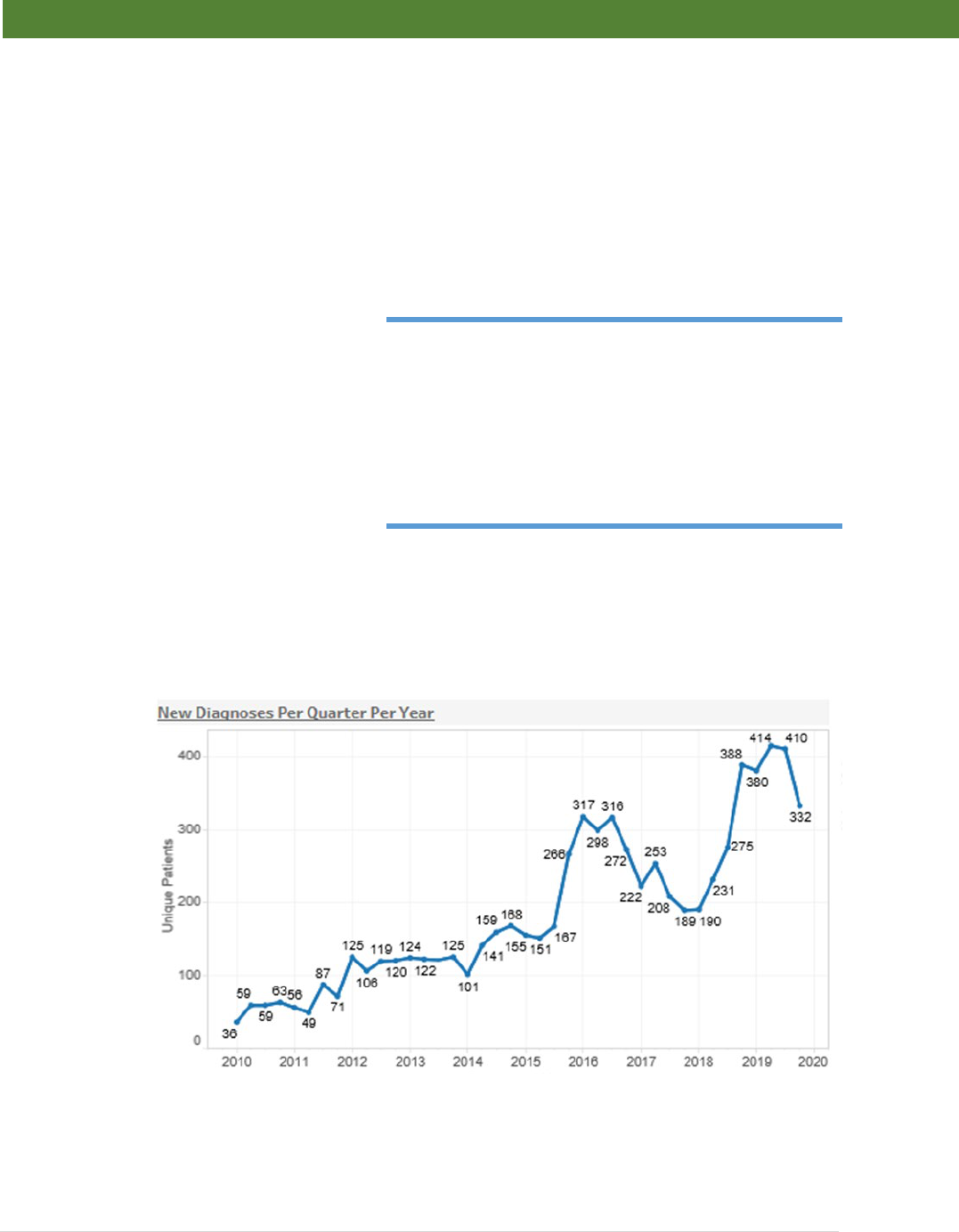
Figure 1: Incidence of new diagnosis of opioid use disorder within WV CAD partner agencies.

3 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
facility, Prestera Center, which ran a variety of programs across the community for decades by
this time.
While many resources existed in the
community, they were largely working
in isolation. Independently, those
involved in these organizations were
noticing a sharp rise in patient volume.
Data would later confirm these observations, but official reports of both incidence and
prevalence are often years behind. A retrospective report using data assembled from the CDC’s
Wonder Database shows that, in 2014, West Virginia led the U.S. in Overdose Death Rate with
35.5 deaths per 1000, almost 2.5 times the national average and 35% more than the next
closest state (New Mexico and New Hampshire are tied with 26.2 deaths per 1000 each).
19
Overdose deaths were not the only data to demonstrate the severity of the substance use
problem at the time. The number of individuals diagnosed with opioid use disorder (OUD)
continued to rise during this period. (Figure 1) Hepatitis C (HCV) infection present in infants at
the time of delivery in West
Virginia was the highest in the
nation at 22.6 per 1000 live in
2014
20
, suggesting that the
number of substance abusers
was quite high the area. Anil
and Simmons published a
comprehensive report on
Hepatitis B (HBV) and HCV
incidence in WV.
21
The
incidence of acute HBV
infection in 2015 was 14.7 per
every 100,000 West Virginia
residents, nearly 14 times the
national average. By 2015,
West Virginia had almost 5
times the HCV infection rate as
the rest of the country
combined (3.4 per 100,000
compared to 0.7 per 100,000)
21
. In developed countries,
about 90% of people infected
It doesn't seem like the community became aware
at the same time, but we felt little changes
happening – Frontline Worker
The initial reaction was, frankly, one of being overwhelmed with the sheer number of
patients we were caring for… but also overwhelming resources and not being able to care
for babies that truly needed an intensive care unit and having to turn those patients away. –
Sean Loudin: Former Medical Director of Lily’s Place and Cabell-Huntington Hospital
Neonatal Therapeutic Unit
Figure 2: Verified number of babies born prenatally-exposed to opioids in
Cabell County, WV per 1000 births Between 2010 and 2019.

4 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
with HCV are former or current injection drug users
22
. Although increased infectious disease
transmission rates are a significant part of the overall societal cost, infection rates are
dependent on several factors (harm reduction, sexual activity, transmission rates, etc.) and does
not include non-injection misuse of opioids exclusively.
Perhaps the most impactful and alarming aspect of the addiction epidemic was the surge of
babies born with in utero exposure to opioids and other substances and those that developed
Neonatal Abstinence Syndrome (NAS). Among 28 states with publicly available data in the
Healthcare Cost and Utilization Project during 1999-2013, the overall NAS incidence increased
300% from 1.5 per 1000 hospital births in 1999, to 6 per 1000 hospital births in 2013. Using
state-based data, the CDC reports that WV has the highest rate of babies born with NAS in
2013 at 33.4 per 1000
17
. It has also been reported using the WV Health Care Authority (HCA)
database and the Uniform Billing Database that southeastern region of WV has the highest
incidence of NAS in the state at 48.76 per 1000 births.
18
Based on a comprehensive review of
cases from Cabell County’s primary birthing hospital, Cabell Huntington Hospital (CHH), it is
possible that the numbers from these databases vastly under-reported the true severity of the
situation. The 33.4 per 1000 NAS patients for West Virginia in 2013 is much lower than the 76.4
per 1000 patient treated for severe withdrawal due to prenatal exposure in the same year and
163.9 neonates per 1000 live births with known in utero exposure to drugs, also in 2013. Those
numbers continued to increase and were reported as 94.3 neonates with severe withdrawal per
1000 live births and 185.8 per 1000 with known in utero exposure in 2015.
23
That number rose
to 236 per 1000 by its peak with 123 per 1000 of those neonates exhibiting severe enough
symptoms to be diagnosed with NAS. (Figure 2)
Of course, in 2011 and 2012, none of these statistics were available. Tolia et al reported in 2015
that NAS was increasing in frequency and represented a large percentage of admissions to
some NICUs across the country.
24
This was certainly true in Huntington/Cabell County. The
NICU at Cabell-Huntington Hospital was so inundated with withdrawing neonates that newborns
with more severe medical needs were often sent to regional hospitals hours away.
Huntington and the surrounding community were desperate for solutions. Those who treated
SUD felt isolated, community sentiment to those suffering was unkind, and there was a distinct
lack of leadership. While the members of this small community suffered across the board, the
data lagged behind the reality of the devastation. State and Federal agencies, who only had
access to data that was years old, were largely dismissive of the gravity of the problem. Without
numbers to reinforce the claims, the outside world could not see the signs of the epidemic
ravaging on the inside. Discussions of SUD and Cabell County, WV were rarely held outside the
region. The community felt invisible. As the epidemic increased in intensity, the community went
from relative obscurity to intense scrutiny. By 2017, four percent (4%) of all media and social
media coverage related to addiction worldwide mentioned Huntington or Cabell County. That
number had dropped to less than 2% by 2019.
In the face of doubt, feelings of isolation, and general hopelessness the Huntington/Cabell
County community developed a collaborative response perceived by the individuals connected
to the local SUD population as being highly successful. This response has been credited for a
decrease in overdose deaths and building the infrastructure necessary for long-term community-
wide recovery. Many communities face, or will face, similar public health crises and could
potentially benefit by developing a similar response. An evaluation of the community response
to the addiction epidemic was conducted to fully understand the key components, aggregate the
community-wide measures of success, and create a roadmap for other communities.

5 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Methodology: A mixed methods approach was applied to explore the perceived effectiveness
of the addiction epidemic response in Huntington/Cabell County by key stakeholders, frontline
workers, and individuals in treatment. Participants were asked to identify the effective
components of the response, barriers, and remaining gaps. To support this data, a partnering
survey was conducted to determine the level of interagency collaboration across the community
and a media analysis was completed for 2014 through 2019. One or all of the above
instruments were used to collect data representing 67 separate agencies or major divisions
including representation for treatment, recovery, public health, education, recovery and family
services, criminal justice, economic/workforce development, and advocacy. The Marshall
Institutional Review Board (IRB) reviewed and approved all study mechanics and participant
interactions. Before each interview, the interviewer conducted informed consent with the
participant to assure voluntary participation.
Interviews:
1. Definitions:
a. Key stakeholders (KS) – defined as individuals that were directly involved
with the response and had decision-making authority (or significant influence
over decision making authority) for an agency with regular interaction with
the SUD population
i. Data was collected from 44 KS by in-person individually interviews.
b. Frontline workers (FL) – defined as individuals who had substantial direct
client contact with individuals with SUD or their family members during the
response.
i. The original intent was to conduct focus groups of FL based on sector
representation. COVID-19 restrictions required a shift to individual
telephone interviews. Fifty-six (56) FL were interviewed.
2. Interview Design: An interview guide was developed for each population type (KS
and FL) to maintain consistency between interviews. Conduct of the interviews
were semi-structured to allow participants to express themselves freely thus
allowing for more accurate data capture. As Marshall University is imbedded in the
Huntington/Cabell County community; evaluators had internal knowledge and
experience of the response. This knowledge was augmented by additional local
stakeholders not related to the study team, including individuals with lived
experience, to formulate value-based questions aimed at identifying the critical
elements of the response in Huntington/Cabell County, WV. Interview guides were
then independently reviewed by members of NACCHO and the CDC for
appropriateness and project relevance. In addition to an accounting of the history
of the development of the community response, questions identifying critical areas
are best surmised with the following questions:
1. At a community level what is working and how has the community gaged that
progress or success? How do you know it is ‘working’?
2. What barriers must be overcome?
3. What gaps remain currently in the community response? Has the community
tried to address them to date – why or why not?
4. What changes occurred at the community level as a result of the community
response in Huntington/Cabell County?
5. What are the most important ways in which the community responded from
2015 to 2019 that other communities should understand?

6 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Participants were initially identified based on their association with agencies known
to participate in the response or interact with a significant portion of the SUD
population in Huntington/Cabell County. Further participants were identified using
snowball sampling. Interviews were recorded and transcribed. Partners at NACCHO
independently screened interviews to assure fidelity and identify bias prior to
analysis. The research team conducted an analysis of qualitative data using NVivo
qualitative analysis software (QSR International Pty Ltd., Melbourne, Australia). We
developed a codebook to identify themes and topics of interest based on the
research hypotheses.
Surveys:
1. Partnering Survey – Individuals participating in the KS and FL interviews were provided
a partnering survey at the conclusion of the interview. The survey received 75.7%
participation with all agencies represented. Participants were provided a comprehensive
list of agencies involved with the SUD population and asked to rate the relationship
based on the level of collaboration with their own agency. The strength of the tie
between agencies was rated on a scale from 0 to 5.
a. No Interaction (0): No interaction with your organization at all.
b. Networking (1): Aware of organization - Loosely defined roles - little
communication - All decisions are made independent from this organization.
c. Cooperation (2): Provide information to each other - Somewhat defined roles -
Formal communication - All decisions are made independently
Figure 3: Distribution of community interviews by organization type.

7 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
d. Coordination (3): Share information and resources - Defined roles - Frequent
communication - Some shared decision making
e. Coalition (4): Share ideas - Share resources - Frequent and prioritized
communication - All members have a vote in decision making
f. Collaboration (5): Members participate in programs that function as one system -
Frequent communication is characterized by mutual trust - Consensus is reached
on many or all decisions.
2. Anonymous Client Survey: Individuals in SUD treatment or served by recovery
supportive programs were surveyed to determine client perceptions of the response.
Questions were designed to determine, in the last five years, which programs were most
helpful in their recovery journey, key factors in recovery, barriers to recovery, and
changes in access to care. Surveys were distributed to individuals in all aspects of
addiction, treatment, or recovery throughout the community including Medication
Assisted Treatment (MAT) programs, peer-based programs, sober living facilities, those
with SUD that are experiencing homelessness, and individuals served by Lily’s Place
NAS treatment facility. Surveys were provided online and email using Qualtrics
(Qualtrics, Provo, UT) or via paper. Paper surveys were later entered into the system by
research staff.
Quantitative Methodology: In addition to the primary qualitative and survey data collection
mechanisms, the West Virginia Community Data System (WV CAD) was developed to
aggregate substance use disorder data from multiple agencies. WV CAD brings the data from
different agencies using different data collection systems into a single-dimensional database
that can identify unique individuals across the community system in a way that protects patient
privacy utilizing a “Safe Harbor” concept. Our methodology allows us to aggregate private
health information (PHI) while complying with regulations promulgated under HIPAA, HITECH,
42 C.F.R. Part 2 (in regards to PHI, and other substance use disorder information as
contemplated by the confidentiality regulations of 42 CFR Part 2), as well as W. Va. Code § 27-
3C-1 and W. Va. Code § 16-3C-1 et seq., as amended.
WV CAD currently houses data from ten separate programs and agencies representing 70-80%
of the substance use treatment and related programs (by patient volume - approximately
440,000 unique patients that receive care in Cabell County, WV) in Huntington, WV. Data
elements include treatment, program utilization, success measures, substance use data, and a
variety of social determinants of health. Initial quantitative data representing referrals to
treatment, increases in those receiving treatment, and 90-day success rates related directly to
the response, as well as SUD population demographics, were extracted from this system.
Media Analysis: Data was collected Cision Communications Cloud (Cision, Chicago, Il) for
media monitoring of the keywords: substance use disorder, addiction, opioids, opioid use
disorder, drug epidemic, opioid epidemic co-mentioned with Huntington or Cabell County, West
Virginia between 2014 and 2019. Cision combs a collection of global online news, blogs, social,
print and broadcast channels for relevant mentions. Then, we analyzed those mentions by key
topics, audience reach, ad value equivalency, and sentiment.

8 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Findings: Addressing the Barriers: Interviewees reported that attitudes across the
community varied from compassionate to outright hostile towards individuals with SUD in
the early 2010’s. The broader community was not aware of the severity of the situation and
a great deal of stigma permeated the community. When asked about the barriers that
needed to be overcome both KS (40.9% of interviews) and FL (28.8% of interviews)
answered “stigma” more often than any other answer. (Figure 4) The two groups similarly
agreed for the need of funding as the second most significant barrier. Finances were a
common theme across the interviews as many referred to a data gap between what was
available to federal agencies and the local reality as a major struggling in attracting funding
in the early days of the response. Both groups also mentioned lack of education along with
poor understanding of addiction and mental health. Beyond those main issues, there was
some variance between the groups. KS, whose responsibilities are primarily
administrative, discussed agency level barriers, such as silos between agencies, employee
burnout, access to care, and the politicizing of SUD. Frontline workers focused more on
patient levels barriers like access, long-term facilities, housing, and transportation.
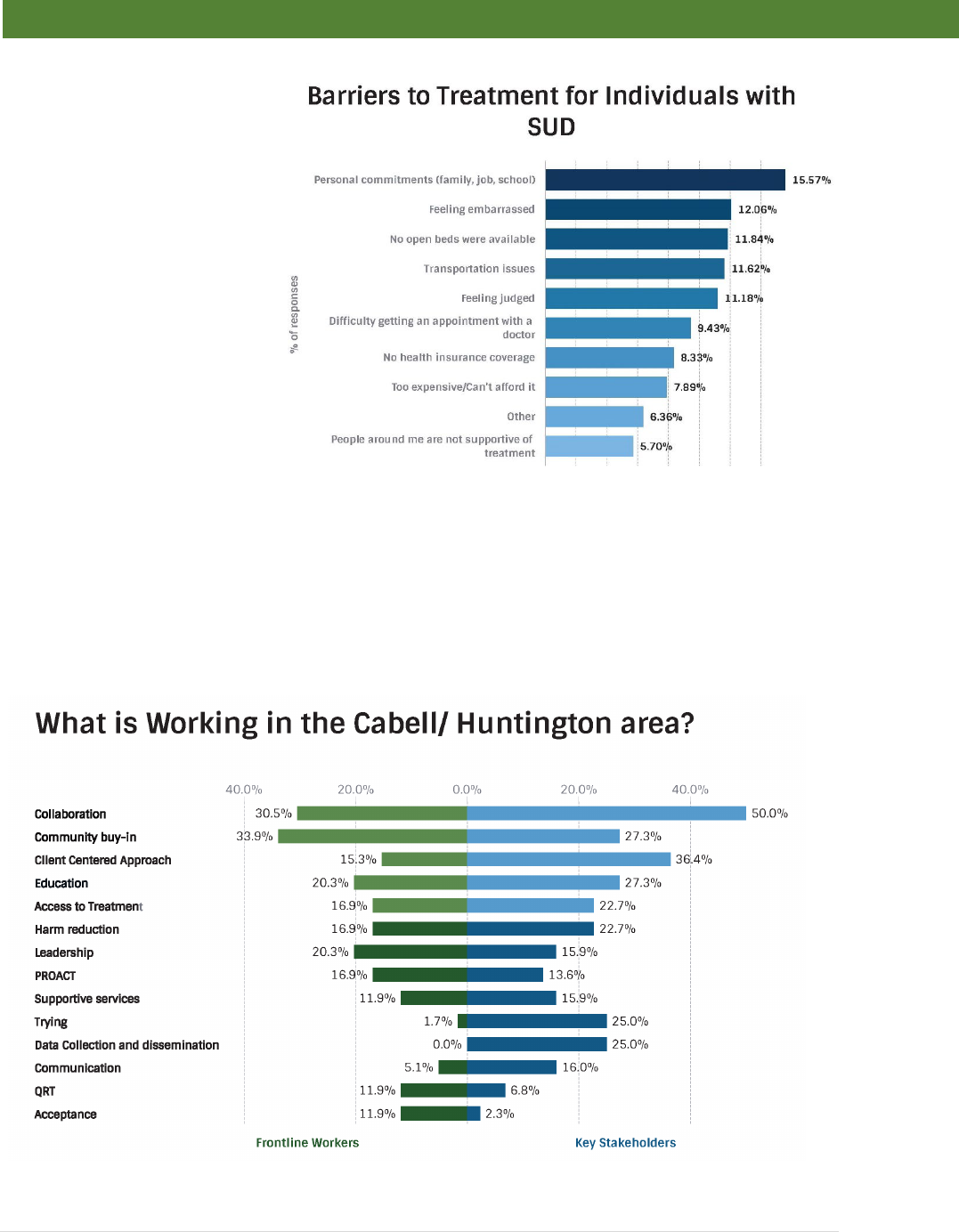
The perception of the most impactful barriers by KS and FL were slightly different from those
identified by those with SUD. An anonymous survey of clients receiving services in the
community showed that “personal commitments” was the biggest barrier. A second tier of
barriers were reported by clients that suggest issues with access to care (“transportation and
“no open beds available”) and stigma (“feeling embarrassed” and “feeling judged”). (Figure 5)
While stigma is important to all of the groups, it seems to be viewed as a more significant
barrier by KS and FL than the clients; who see their personal commitments and basic access
as larger barriers.
Figure 4: Answers given to the question, "What were the barriers?" answered by more than 10% of interviewees.
9 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Despite these barriers, the
overwhelming tone from the
interviews was in regards to
a remarkable level of
collaboration. Both KS
(50.0%) and FL (30.5%)
reported “collaboration”
more than any other
response when asked,
“What is working?” (Figure
6) Many KS and FL
interviews also mentioned
community buy-in,
education, and a client-
centered approach as
functional aspects of the
community response. Similar
to the barriers question, the
consensus answers from FL
interviewees focused on
their impression of what
helped the clients directly, naming a number of specific programs (PROACT and QRT). While
KS interviewees mentioned access to care and approach issues, many discussed how efforts
to collect and disseminate data was critical to attracting funding and changing policies. Another
theme by KS was coded as “trying,” or the willingness of a variety of individuals and agencies to
step outside of their standard procedures to attempt new methods and approaches.
Figure 5: Patients with SUD were asked to identify the barriers to treatment with the
question: "
Whenever you’ve thought about getting treatment (either residential or
outpatient), which of the following would you say are the biggest barriers for you
to get
into a treatment program?” N=456
Figure 6: Answers given to the question, "What is working?" answered by more than 10% of interviewees.

10 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
While KS listed siloes between agencies and competition between agencies as barriers, those
barriers were often considered less critical than others. Several FL interviewees did discuss
problems in the continuity of care while others associated access to care issues with poor
communication between agencies. These barriers may have been more impactful than
suggested by discussing specific issues. There was agreement across the interviews that the
mechanism for overcoming many of the identified and potentially unidentified barriers was an
unprecedented level of collaboration. Unity of purpose and a collaborative spirit was
overwhelmingly credited as the primary reason for the success of the community response to
the addiction epidemic.
Building Collaboration is a multi-Step Process: Collaboration was identified as the key factor
in the Huntington/Cabell County Response to the Addiction Epidemic. While the participants in
the response were, by their own admission, learning as they went, the process that developed
was deliberate and should be replicable. The tangible elements of the response came into effect
because of the community-wide sense of collaboration. This allowed Huntington/Cabell County
to identify and address gaps quickly by optimizing existing programs and creating a few new
programs strategically to take advantage of limited resources. Creating this collaborative
environment required a number of key elements and followed a precarious timing of events. The
steps of the process and the timing of those steps were equally important.
Evaluation of Community Collaborative Structure: An analysis of the collaborative structure
in the Huntington/Cabell County community showed a lot of collaboration that was unstructured.
The absence of central point, or even cluster of collaboration suggests that the community
developed an environment of collaboration that encouraged natural connections to occur
instead of an institutionally driven collaborative structure.
In order to understand the nature of this community-wide collaboration, we conducted a
partnering survey in which we asked agencies from across the community to rate the strength of
the tie between their agency and a list of 80 different organizations across the community on a
scale from 0 to 5. With a 75.7% response rate to the survey, there were 52 organizations
represented in the survey response data (39 of which were among the 80 partners included as
questionnaire items). Of these 52 organizations, 35 were represented by at least one FL
respondent, 27 were represented by at least one KS respondent, and 10 were represented by at
least one of each type of respondent. Participants were requested to indicate the level of
interaction between their agencies and 79 other agencies based from 0 to 5. No Interaction (0):
No interaction with your organization at all. Networking (1): Aware of organization - Loosely
defined roles - Little communication - All decisions are made independent from this
organization. Cooperation (2): Provide information to each other - Somewhat defined roles -
Formal communication - All decisions are made independently. Coordination (3): Share
information and resources - Defined roles - Frequent communication - Some shared decision
making. Coalition (4): Share ideas - Share resources - Frequent and prioritized communication -
All members have a vote in decision making. Collaboration (5): Members participate in
programs that function as one system - Frequent communication is characterized by mutual
trust - Consensus is reached on many or all decisions. There was no clear community structure
indicated by either group. A- Key stakeholders were evenly distributed while B- Frontline
workers were either weak (<3) or strong (5). Lighter lines represents weaker collaboration
strength while darker lines represent stronger collaboration strength. There were 4 instances
where 2 FL respondents from the same organization participated in the survey and 4 more
instances where 2 KS respondents from the same organization participated in the survey; we

11 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
obtained a single response vector in each of these cases by taking the entry-wise maximum of
the dual responses present.
Organizations tend to be listed as
collaborators by roughly 20 other
organizations normally distributed
between Key Stakeholders and
Frontline workers (in-degree), while
the collaborations an organization
claims to have are uniformly
distributed (out-degree) (Figure 7).
This is an indication that many
organizations are less collaborative
than they report, particularly when
reported by Key Stakeholders. The
differential distribution pattern is
likely an indication of a collaborative
environment in which there was
social pressure to appear
collaborative. Even with the variance
of in-degree vs (no comma) out-
degree distribution patterns, the large
amount of interagency collaboration
mentioned in the interviews appears
to be functional.
Key Stakeholders, most having administrative authority, reported a strong sense of collaboration
and the expectation of collaboration from the community. The partner survey responses indicate
this phenomenon. Undirected network maps show an even distribution of the strength of
interagency collaborations, but no clear community structure is indicated. (Figure 8A) This
suggests an effective environment of collaboration instead of a specifically directed structure.
FL had a slightly different distribution by reporting primarily either weak (<3) or very strong
collaboration (=5). FL partnering analysis still failed to show a clear community structure.
(Figure 8B)
Weak ties in social networks are associated with distant clusters within a social system. As this
study is measuring across a community, it is likely that weak ties (<3) are more representative of
Figure 8: The partnership study results for A- Key stakeholders and B- Frontline workers.
A
B
Figure 7: Distribution of partner survey collaborators. Organizations tend
to be listed as collaborators by roughly 20 other organizations. (in-
degree) This number tends to be normally distributed. The number of
collaborations that an organization says it has tends to vary uniformly.
(out-degree) “Count” indicates the strength of collaboration (0-5).
“Degree” is the number of agencies indicated as having some a level of
collaboration >0.

12 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
individual relationships interacting across agencies. Strong ties (=5) are official or public
collaborations recognized by every level of the organization. Intermediate ties (3,4) in this study
would represent the interagency collaboration that go beyond individual relationships, but are
not yet official or public agency connections. Under the suggested model of a widespread
environment of collaboration, this data would then suggest that KS, as the administrative
officials, have a wider view of agency collaboration. FL on the other hand see the most
collaboration at a personal level or when the collaboration reaches widely across the
organization, but not necessarily collaboration in the intermediate stages.
Process of Developing a Community-Wide Collaborative Environment: Several
interviewees credited the togetherness of the Appalachian culture for the collective nature of the
response to the addiction epidemic. It is unclear how much of the cooperation was cultural, or if
the desire to work together for the common good is necessarily unique to Appalachia. The data
suggests however, in addition to the general building of infrastructure, that major components
were necessary to allow the community to come together in such a way. Based on interview
responses and the timeline and focus of the efforts; three key approaches were determined to
be a necessary part of overcoming
the barriers and building an
environment of collaborative healthy
recovery in the face of the epidemic.
• Finding Common Ground
• Leadership
• Community Response Approach
1. Finding Common Ground:
Despite community-wide stigma,
there was one population who
shared ubiquitous support, the
prenatally-exposed neonate. One
Key Stakeholder summed up the
consensus that prenatally-exposed
children were not subject to the
same stigma presented to others in
the SUD population by stating, “…it
is easy to get people to support
babies, even if they won’t support
their mothers.” The large number of
babies who had become victims of
the addiction epidemic became a
rallying point for the community.
Interview respondents, regardless of
position, discussed a need for support for children, particularly those exposed to substances in
utero. Supporting this perception, the first programs developed that enjoyed broad community
support were related to these youngest victims of the epidemic.
While Prestera Center had women and children’s program for years, a number of new
programs changed the landscape of treatment for pregnant women with SUD. Marshall Health
developed the Maternal Addiction Recovery Center, a medication assisted treatment program
You know, the building for Lily's place donated by a
prominent family, each nursery room within Lily's
place was donated, every bit of that facility; the
flooring, the cribs, the paint, the furniture within each
nursery was donated by a family or a church or
something. That Lily's place has never bought or
purchased a diaper in its existence in 2014 because
the community has always donated diapers and
wipes and baby clothing and bubble bath and
everything else. So that, you know, that is how this
community has rallied around that you will see.
We've seen children forgoing their birthday parties or
presence at their birthday parties so that they could
throw a baby shower for a little place…
…because it’s babies.
– Sean Loudin: Former Medical Director of Lily’s Place
and Cabell-Huntington Hospital Neonatal Therapeutic
Unit

13 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
for pregnant women up to six weeks postpartum. Valley Health System, a local Federally
Qualified Health Center, developed their own pregnancy program, co-currently. Cabell-
Huntington Hospital created a specialized unit just for withdrawing neonates. These programs
helped provide the necessary infrastructure to handle the rapidly growing need, but one effort
captured the community psyche more than any other— Lily’s Place. Despite the fact that this
outside facility had a lower capacity than the hospital’s Neonatal Therapeutic Unit, interviewees
from both groups, who mentioned babies or NAS, also mentioned Lily’s Place.
Lily’s Place is a private not-for-profit facility where prenatally exposed babies with no other
medical problems can recover in a more homebound setting. Lily’s Place uses therapeutic
handling methods and weaning techniques to treat patients. Developing this unique facility was
truly a community effort with donations from around the community and shared resources with
other medical facilities. Lily’s Place
changed the discussion. It was a
positive story of helping the helpless
that allowed many within the
community to begin to see the
severity of the epidemic. Once the
community rallied around saving the
neonates, it was a short step to
getting support to get more
resources to their mothers, leading
eventually to the coalition Healthy
Connections, Project Hope for
Women and Children, Hope House,
and numerous programs and
resources targeted at helping new
mothers with SUD.
2. Leadership
When it comes to identifying those
primarily for the response, a few
names rose to the top. However, it
was very clear that Key Stakeholders and Frontline workers all felt that the
Huntington/Cabell County response to the addiction epidemic was a broad effort with too
many champions to mention. At the end of the day, everyone was expected to do their
part and most delivered above and beyond expectation. This community collaboration
did not happen in a vacuum.
Although early on it was important to give the community a single program on which to focus
support there were other more difficult programs critical to an effective response that required
taking political risks. The individuals who took those risks were identified by key stakeholders in
the community as the primary champions of the response. It likely is no accident that the
named champions represent the most influential organizations in Cabell County, i.e, the City of
Huntington, the Cabell-Huntington Health Department, and Marshall University. It is clear that
the leadership had to come from these three entities (Figure 9) while being supported strongly
by the two major hospitals in town (St. Mary’s Hospital and Cabell-Huntington Hospital), the
County’s Behavioral Health Center - Prestera Center, and the area’s largest Federally Qualified
Health Center – Valley Health System. These agencies developed their own response while
Political Leader
(Mayor)
Top Public Health
Official (County
Health
Department)
Most Trusted non-
Political Agency
(Marshall
University)
Figure 9: Three major leadership components in Huntington/Cabell
County

14 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
working together to create an environment that allowed a single unified community response
that started with treating those patients already on the front lines of the epidemic and
approaching patients as the content experts. Thus, it was not just that the recognized
community leaders came together, but the approach they used empowered those most able to
make the critical changes. Many Frontline personnel interviewed indicated that prior to the
founding of the Mayor’s Office of Drug Control Policy and the Division of Addiction Sciences at
Marshall University, they and their counterparts were often underappreciated.
Of the six individuals named by more than ten percent of interviewees as “Champions” of the
community response (Figure 10) to the addiction epidemic, four (Mayor Steve Williams, Dr.
Michael Kilkenny, Dr. Stephen Petrany,
and Former Police Chief Jim Johnson)
admitted to having a steep learning
curve. Some of the critical individuals
involved with making the response a
success knew very little about addiction
or recovery at the beginning. However,
each was able to put their reservations
and biases aside to bring the
community together and focus on
developing a response based on best
practice and improving the community
as a whole.
a. Mayor Steve Williams – City of Huntington
In 2014, shortly after being elected Mayor, Steve Williams responded to citizen complaints
about the growing epidemic by supporting the “River to Jail” program, which took a at law
enforcement approach to addressing the addiction problem. Like many before him, Mayor
Williams thought that increased arrests and drug seizures would stem the tide of drugs entering
Huntington. The Mayor quickly realized that he did not understand the epidemic that was now
plaguing the City in which he was
responsible. So, leaving politics aside
(as many might not do), he changed
his approach.
In 2015, the Mayor’s Office of Drug
Control Policy (MODCP) was
established. Former Police Chief Jim
Johnson, and Fire Chief Jan Rader
were tasked with developing a
comprehensive plan for the community. Chief Johnson and Chief Rader used the influence of
their office to bring together anybody and everybody who were spending resources to address
SUD or were strongly affected by the epidemic. Stakeholders in the community responded well
to the formation of the new office. Everyone involved with the Mayor’s Office of Drug Control
Policy used each meeting to learn from those who had been working with the substance using
population. In addition to the specific question of “Champions,” Jan Rader was mentioned
specifically throughout the interview transcripts. Her association with the MODCP was noted as
Figure 10: Top responses of both KS and FL In response to the
ques
tion, "Who are the Champions?" in discussion of the response.
I didn't go to city council and ask for an action on it.
This is just something that we needed to do. I called it
the Mayor's Office of Drug Control Policy. We just got
moving, started meeting with people. Now, I was a
bit naive at the time in January of 2015. – Steve
Williams: Mayor Huntington, WV

15 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
important for changing the perception of the SUD population. Experts in addiction from across
the area started to feel more empowered than isolated, and the siloes started to break.
While actively working to establish a community resolve to respond to the addiction epidemic,
the City of Huntington began a campaign to address the critical data gap. Police data analyst
Scott Lemley was assigned to create a database of addiction related information. Through this
effort, the Mayor’s Office of Drug Control Policy was able to demonstrate that a large portion of
crime in the City of Huntington was drug related and that the number of overdoses in the City
were rising rapidly well ahead of the State Medical Officer’s report on overdose deaths.
b. Michael Kilkenny, MD – Cabell-Huntington Health Department
As the Mayor’s office was establishing its response, the Cabell-Huntington Harm Reduction
Program (CHHRP) began at the Cabell-Huntington Health Department (CHHD). This program
began providing an array of harm
reduction services including
infectious disease care, wide-
spread naloxone distribution, as
well as providing syringes to 1,155
Cabell County residents that were
persons who inject drugs (PWID),
primarily heroin and drugs sold as
heroin
25
in the first year. Harm
reduction has been a critical part of
controlling infectious disease outbreaks during the epidemic while providing a path to
treatment for PWIDs. By keeping his message focused on best practice and scientific
methodology while engaging and addressing concerns, Dr Kilkenny and his staff were able to
gain tentative acceptance in a resistant community to establish this program. Thus, despite
public resistance, Cabell County has widely distributed naloxone and maintained a functional
syringe exchange program.
As in the efforts of the Mayor’s Office, CHHD focused on utilizing the data collected to obtain
more accurate estimates of the epidemic. The City and Dr. Kilkenny alike were confronted with
sorting the differences between available data and the reality on the ground.
c. Marshall University
Marshall University has always had a special relationship with the City of Huntington. While this
is true of many universities, a full community response would not have been possible in
Huntington/Cabell County without the full participation of Marshall. This is why the University
was one of the earliest visits made by the Mayor’s office.
The University reacted immediately along two major efforts paths. 1) The Marshall University
President created a task force to coordinate University resources directed at addressing the
epidemic. This effort coordinated a variety of activities from a number of different colleges and
departments. 2) Developed the Division of Addiction Science within the Joan C. Edwards
School of Medicine to provide infrastructure for research and expanded SUD treatment. The
physician’s group of the medical school (Marshall Health) would also provide clinical
infrastructure for the creation of sustainable programs. In 100 of 100 interviews, Marshall was
mentioned as a partner, champion, or key to a long-term successful response in addressing
SUD in the community. Throughout the response, various Marshall University Colleges and
departments were collaborating in dozens of different community efforts. Per the interviews,
The champions, can I say the Health Department as
one of the champions? They would be one of the
champions because it's a group effort, it’s not just
harm reduction, it’s nurses, it’s environmental.-
Frontline Worker

16 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
many Key Stakeholders and Frontline workers did not specifically name an individual,
department, or project at the University. More than a dozen individuals from Marshall University
were identified as “Champions,” but only two were indicated by at least 10% of interviewees.
• Dr. Stephen Petrany, Chair of the Department of Family and Community Health in
Marshall’s medical school, created the Division of Addiction Sciences which would
provide the infrastructure for sustaining new programs (described below) designed to fill
critical gaps in the continuum of care across the community.
• Bob Hansen, former CEO of Prestera Center was hired as the first Director of the
Division of Addiction Science, becoming the primary architect for major components of
the full community response. After serving as Director, Bob moved on to lead the Office
of Drug Control Policy for the State of West Virginia.
Results from the frontline worker interviews clearly show a strong emphasis on the overall
sense of collaboration across the community and that the groundwork laid for the NAS focused
response and the leadership framework were critical to the response being effective and timely.
Without the coordination of resources and the support from those who managed such
resources, a collaborative effort of community members would have proven ineffective. As
evidence, on May 22, 2005 four teens were found dead in Huntington after prom in a violent
crime that was a direct result of illegal drug activity. Police reported that one of the teens was
targeted while the rest were killed to eliminate witnesses.
27,28
The community rallied and there
were many “calls to action,” community coalitions started to form, and the event even garnered
national attention.
27
The incident was severe enough to capture the attention of the community
as was the 28 person in one day overdose event of 2016, which caused the community to
respond. However, without a concerted effort from the community leaders, who largely
disregarded events of a growing addiction problem in the community and considered the
circumstances a police matter, there was little in the way of effective response.
Huntington still celebrates a “Day of
Hope” on the anniversary of these
murders. Two projects developed
from the efforts of private citizens,
Hope House and what would become
Recovery Point of WV, but both
programs struggled for 5+ years
before becoming an effective part of
the Huntington/Cabell County
recovery community.
Community Response Approach: Having little knowledge of the collective opinion of the KS,
FL, and clients across the community, local leaders set out to understand how to address the
growing issues. The first step in this process was for the community leaders to admit there was
a problem and face the epidemic. KS and FL interviews often (53 of 100) mentioned that a key
component in beginning a response was the willingness of social and political leadership to
admit that the community was in trouble. How they approached the next phase was equally
important. Several interviewees commented that having a number of KS in certain positions
with extensive experience as Frontline workers made a big difference in the response
approach.
I think that the mayor really was being honest and
open about what the problem were, that the city was
having problems and he was willing to talk about it.
You know, there are other mayors and other political
officials around the country and certainly in West
Virginia that wouldn’t face issues. –Key Stakeholder

17 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
While the leadership in
Huntington/Cabell County pulled
together in both purpose and
approach, agencies across the
community came together quickly in
response. Clinical agencies and
those that deal with substance using
populations joined the effort very
quickly. This was particularly true of efforts or resources directed specifically at helping
newborn babies who were prenatally exposed to opioids and other neuroactive substances.
Many of the existing agencies began collaborating despite long-held differences based on
philosophical differences in recovery approach. Agencies that had programs in place noted
by both Key Stakeholders and Frontline workers as early contributors and collaborators in
the response are as follows (alphabetical order):
• Cabell County Drug Court
• Cabell County Prosecutor’s Office
• Cabell County Child Protective Services
• Harmony House (including First Steps) - a day shelter for people experiencing
homelessness and families
• Lifehouse – Sober living facility
• Lily’s Place – Independent treatment facility for neonates experiencing withdrawal
• Marshall’s Maternal Addiction Recovery Center – MAT program for pregnant women
• Mountain Health Network - owns the Cabell Huntington Hospital and St. Mary’s Medical
Center in Huntington
• Prestera Center – County Behavioral Health Center
• Recovery Point of West Virginia – Residential peer recovery facility
According to many interviewees,
the community at large came
along more slowly, despite the fact
that a growing number of families
were directly affected by the
epidemic. Individuals outside the
agencies that routinely deal with
an SUD population, particularly
those in the faith community,
reported a growing sense of
urgency and often felt isolated
dealing with the increases in
crime, used syringe litter, and
trying to find help for loved ones. A
response to the epidemic was
underway, but it was not yet a full
community response.
On 15 August, 2016 everything
changed. That was the day that
Not a normalization of an opioid epidemic. But
making it no longer something that has to be hidden,
I think is one of the first steps of a much stronger
response. -Frontline Worker
Twenty six overdose calls are called within a four hour
period. Twenty eight people overdosed that day.
However, two of the individuals were never called in.
They used drugs by themselves. They both,
unfortunately did pass. But however, all 26 people
who were called in on that single day, all were saved
from an overdose. And that was the first time that we
knew that we had a band from heroin to fentanyl and
car fentanyl mixed into the drugs being far more
potent. And that's all public knowledge because of
some court papers. Certainly went after the individual
who distributed those drugs in the community. So on
that day, it became national and international news.
So if you had had your head buried in the sand, it was
no longer possible. –Key Stakeholder

18 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
fentanyl and fentanyl analogs arrived and were responsible for 28 overdoses in Cabell
County. Twenty six of these overdoses were responded to by emergency medical services
within 4 hours.
26
This single event galvanized the majority of the community into a single
response, because the leadership had been preparing a response and could offer
immediate, well-vetted answers. Cries of “What can we do?” and “Who is going to stop this?”
were quickly marginalized with people asking, “What can I do?” More than half (23 of 44) of
the Key Stakeholders mentioned this day as a seminal event in the response. After August
2016, whatever remained of the interagency siloes were (temporarily) torn down.
Agencies and services for SUD prior to the addiction epidemic and subsequent response in
Huntington/Cabell County were primarily focused on recovery and treatment. As the increasing
number of individuals with SUD were
recognized by frontline agencies across the
community, programs were developed that
either focused on the agreed sub-population
(prenatally-exposed babies) and adopted as
best practice from other communities (Drug
Court, Harm Reduction), or were attempts by
leadership organizations to develop a
functional plan (Mayor’s Office, Marshall)
(Figure 12). These programs were largely
developed in isolation or with a limited group of
interested parties that simply did what they
could. After the events of August 15, 2016, the
establishment of programs became more
directed.
In meetings joint hosted by Marshall University’s Division of Addiction Science and the Mayor’s
Office of Drug Control Policy, community members that work with SUD populations were asked
for their opinion of what should be the focus of the community response. For the many
individuals and agencies that had felt underappreciated from traditional approaches, this was a
significant change in approach. In that meeting several needs were identified:
• Lack of Detox Beds
• Poor access to care across the population, i.e., need to “meet population where they
are.”
• Not enough housing for new mothers with SUD
• Programs do not work well together
New programs developed after this meeting largely addressed one of these defined needs.
Prestera Center immediately doubled the number of Detox beds. Project Hope for Women and
Children was developed to address
the need for more housing for new
mothers with SUD. Collaborative
efforts designed programs that either
Improved access to care or
developed a community
collaboration to continuously improve
Figure 11: One example of the national reports about the
overdoses on 15 August, 2016 in Huntington/Cabell
County.
I think we spend a lot of time with people with initials
after their names thinking they have the answer and
the only thing they've been in is a book. –Frontline
Worker

19 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
system optimization (Figure 12). These new programs developed quickly because agencies in
the community were willing to share infrastructure. All of the post-Aug 2016 programs went from
concept to implementation in less than two years, with early results realized by early in 2018.
Timing seems to have been critical. Many interviewees reported a lack of public support prior to
Aug 2016. However, had the leadership structures not been in place when the events of that
day occurred, there is a strong possibility that the overall response would have been too slow to
effectively change the course of the epidemic.
Prior to the response (before 2014)
programs largely focused on
treatment or recovery exclusively.
Without widespread support,
Figure 12: Programs for individuals and Families with SUD in Huntington/ Cabell County established before the response,
early in the response, or during the full community effort.
We had people hiding in plain sight. –Key Stakeholder

20 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
agencies created the programs that were sustainable through medical reimbursement claims.
As these agencies were at the forefront of addiction in the community, they often understood
the need for additional services and recovery support, but did not have the resources to fund
such efforts with grants that are time consuming and unreliable long-term. Thus, many
programs developed by community agencies throughout the years prior to the epidemic were
ultimately short-lived.
In the early days of the response, public support for those struggling with addiction was largely
restricted to prenatally-exposed babies. Thus, the steps taken to establish the Mayor’s Office of
Drug Control Policy, the Cabell-Huntington Harm Reduction Program, and the Marshall
University Division of Addiction Sciences and Center of Excellence for Addiction Care required
leaders to shoulder a fair amount of political risk.
The Client Survey (n=219) identified PROACT and Harmony House (a drop in center for
individuals experiencing homelessness) as the most impactful organizations by being used by
>30% of respondents with >90% of those that used the agencies labeling them as ‘helpful.’ All
of the agencies labeled in Figure 13, with the exception of PROACT, existed prior to the
response, but have made significant changes to their services during the response.
Figure 13: Indication of usefulness of agencies in the response to the addiction epidemic in Huntington/ Cabell County, WV.
Participants in the client survey (n=219) identified which community services they utilized which agency or services they uti
lized
and indicated which (yes/no) if that agency or service was helpful to their recovery. Labeled organizat
ions represent those
agencies who were identified as used by >30% of participants and 80% of those who used the agency in their recovery indicated
that agency as ‘helpful.’
Harmony House and PROACT very closely overlap in the figure.

21 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Collaboration Creates Opportunity for Sustainable Programs: All 44 Key Stakeholders
reported that expanded services either improved utilization or created new programs during the
response. Many attributed open dialogue across the community or better communication with
partner agencies for these expansions. This is a strong example of how collaboration helped to
overcome critical barriers and optimize existing agencies. While the community-wide
collaboration helped to improve utilization of existing programs, new programs were developed
through partnerships to fill critical gaps.
Quick Response Team (QRT) – QRT is a response team that visits victims of overdose
within 24-72 hours after the event. The concept is to engage those with severe SUD at their
most vulnerable time in order to get these most at risk individuals into treatment. Operated by
Cabell County Emergency Medical Services (CCEMS), the QRT was originally developed as a
collaboration between CCEMS, the City of Huntington, Marshall University’s Joan C. Edwards
School of Medicine, Prestera Center, Recovery Point of WV, Huntington Police Department,
and the faith community. The QRT is responsible for an increase in referrals to treatment. This
program was funded by grants awarded to the City of Huntington.
Project Engage – Project Engage is a program adapted from a similar program
developed at Christiana Health in Delaware. This program uses specially trained clinical staff
and peer recovery coaches to identify and engage individuals with SUD in the hospitals so they
can be referred to treatment. Project Engage was established through a collaborative effort of
Mountain Health, which operates both Cabell-Huntington and St. Mary’s hospitals in
Huntington, Recovery Point of WV, and Marshall University. Project Engage was established
with grants from the State Targeted Response Program and funding from both hospitals and is
sustained through medical reimbursements.
Provider Response Organization for Addiction Treatment (PROACT) – PROACT is a
standalone facility designed to improve time to treatment for individuals referred. The goal of
PROACT is to get patients treatment with 72h of interaction with the healthcare system.
PROACT provides appropriate therapy, including Medication Assisted Treatment while
connecting patients to recovery support programs. PROACT is the centerpiece of the
community response. Initial funding for PROACT was provided by grants and donations from
across the community with additional support from Mountain Health Network, Valley Health
Systems (a local Federally Qualified Health Center) providing clinical support, Recovery Point
of WV providing peer support. The physician’s group of the Joan C. Edwards School of
Medicine at Marshall University (Marshall Health) operates the facility while providing additional
recovery support. Valley Health Systems would eventually leave the collaboration once
PROACT was able to operate independently through medical reimbursement.
Project Hope for Women and Children (Project Hope) – Project Hope, and later the
transitional living facility Hope House, filled a critical need by significantly expanding the
residential space for new mothers with SUD and their prenatally-exposed children. Operated by
Marshall Health, Project Hope is a facility owned by and located at the Huntington City Mission
that provides treatment and extensive support to mothers with SUD in conjunction with
PROACT. Renovations of an existing building was made possible through grants from the Ryan
Brown Foundation and SAMHSA with substantial private donations from the Huntington/Cabell
County community.
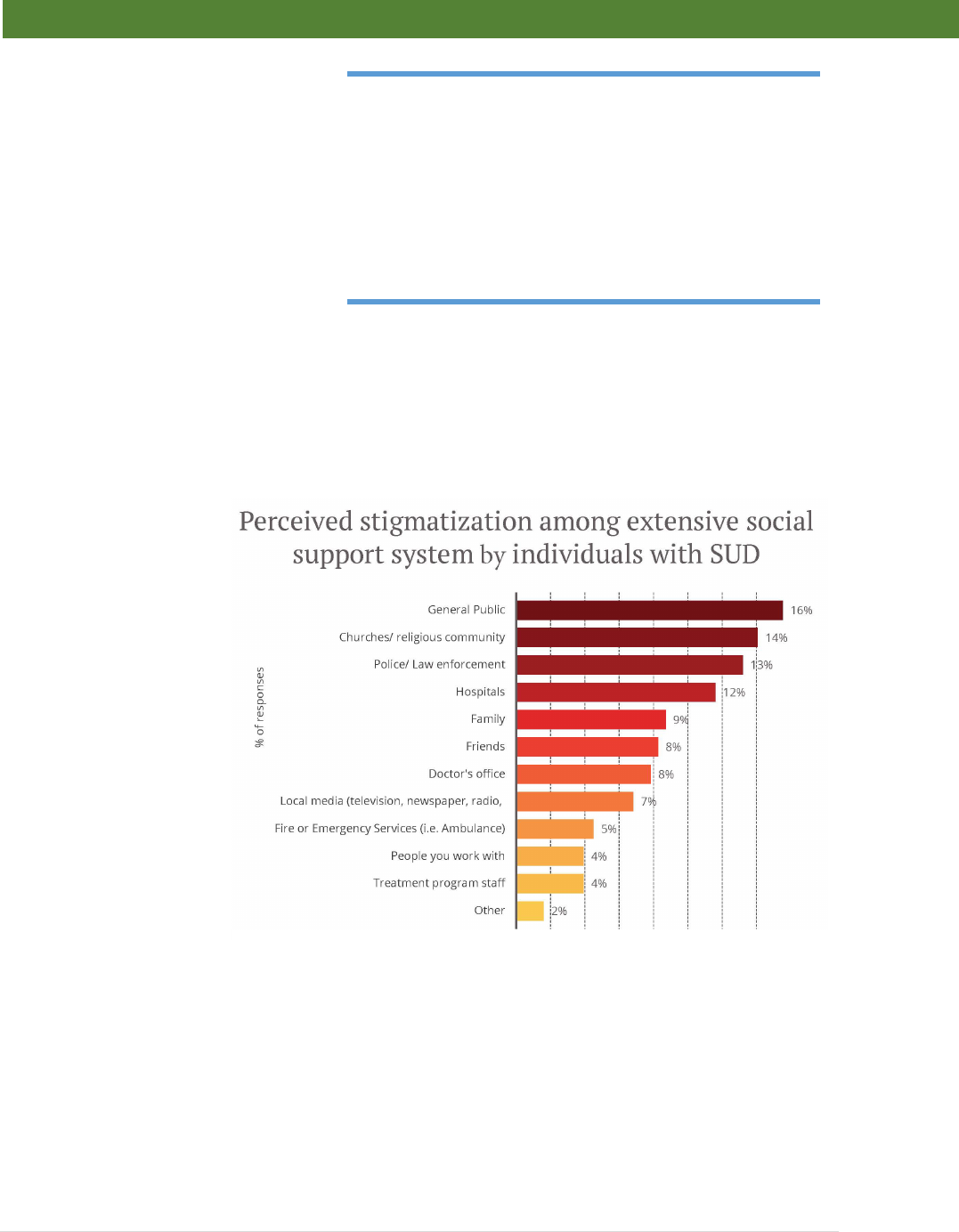
22 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Stigma, Misunderstanding, and
Educating the Community: The top
barrier mentioned by both KS and FL
was stigma. For this evaluation,
based on the interviews, stigma is
defined as “a negative attitude and/or
treatment toward persons with
substance use disorder.” Stigma is
often mentioned as a major issue in
individuals struggling with SUD. In the
same vein, “lack of education” and
“lack of understanding of addiction” were also mentioned as significant barriers; these were
both considered contributors to stigma and poor treatment of individuals with SUD. Several FL
recounted stories of individuals not seeking care due to feeling stigmatized by the general
public and healthcare workers. Clients reported the “General Public” as the social group in
which they received the highest level of stigma. (Figure 14) It is not clear if this perception is
derived from individual interactions across the community or from media depictions of those
with SUD. “Churches/ religious community,” “Police/ Law enforcement,” and “Hospitals” had the
next highest selections
in the survey. Each of
these areas were
addressed in different
ways.
While a campaign that
was specifically
designed to reduce
stigma across the
community was
deployed in
Huntington/Cabell
County, implementation
of the plan did not occur
until late in 2019. Thus,
the outcomes of the
anti-stigma campaign
are part of the ongoing
plans and not the
response as evaluated
in this report. Anti-
stigma efforts during the
response were far more grassroots. Both KS and FL mentioned both community buy-in and
education as key areas of success when asked, “What is working?”(Figure 6) Many
interviewees specifically discussed in open dialogs about how the mechanisms and
consequences of addiction helped many start to see the SUD population as individuals
suffering instead of people with intent to harm the community. There were three areas broadly
mentioned throughout the interviews credited with reductions in stigma:
Figure 14: Patients with SUD were asked to indicate where they experienced stigma with
the question: "Where in Huntington / Cabell County would you identify as having
high levels
of stigma?” N=219
I don’t know of the right words, understanding that
they have a little more sympathy towards the
problem, and I think it was brutal there for a while. I
mean, I would go out to eat…[and]…they would come
up and they'd really get on my case. Why are you
wasting money? Let these people die. We don't need
them. –Key Stakeholder

23 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
1. Community leaders and medical professionals having a better understanding of
addiction and insisting that
their respective staff followed
suit.
2. Education of people across
the community, particularly
those in positions of power.
3. Engagement of the faith
community.
The educational programs mentioned throughout the interviews were, in reality, a mix of
clinicians, researchers, and public health officials from Marshall University and the Cabell-
Huntington Health Department providing educational sessions. Individuals from these
organizations volunteered their time to provide addiction education and training sessions to any
organization willing to support such a session. Despite the lack of a comprehensive curriculum
or program, almost all of these educational sessions included some level of anti-stigma
education.
While our client survey
indicated a slight overall
improvement in stigma as
reported by individuals with
SUD (Mean of 5.91 on a 1
to 10 Likert scale) (Figure
15), it is not clear how much
these educational sessions
affected the improvement
of stigma outside of the
organizations that
specifically received the
training. Client survey
respondents indicated an
improvement in stigma
57.21% of the time, with
23.88% reporting stigma
worsening, and 18.91% of
responding that stigma did
not change.
KS and FL interviewees mentioned “Community by in” and “Education” as two of the strongest
factors working within the response. (Figure 6) One factor discussed through both KS and FL
interviews was the individual impact of Fire Chief Jan Rader. Chief Rader, by her own volition,
engaged in a public campaign in which she openly discussed the importance of the appropriate
treating for people dealing with addiction. Both KS and FL widely mentioned Jan Rader as a
key contributor to changing the public conversation.
Figure 15: Patients with SUD were asked to rate on a scale of 0 (Much Worse) to 10
(Much Improved) – with 5 indicating “ No Change” on the change in access to
treatment with the question: " In the past five years have you seen a change in how
those with substance use disorder are viewed by others in the community?" N=218
“I've-, seen a lot I've seen a lot more acceptance. And
yes, there are some people out there who have
certain beliefs, but I’ve seen more willingness to
explore and to challenge those beliefs within
themselves.”– Key Stakeholder

24 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
One group of religious leaders formed a
coalition, Faith Community United, to
utilize the above-mentioned voluntary
resources and bring education and
understanding to the larger faith
community. Faith Community United held
special sessions in churches across the
community in 2017 and 2018. A
significant portion of these sessions
included the importance of person-first
approaches and the power of stigma.
While the vast majority of anti-stigma
activity was a matter of time and sweat
equity, there was one grant-funded
program that served to provide a structure
to educate people on the use of non-stigmatizing language. Marshall University began training
individuals in 2016 thanks to a grant from the Substance Abuse and Mental Health Services’
(SAMHSA) SBIRT (Screening, Brief Intervention, and Referral to Treatment) Program (Amy
Saunders, PI). Through 2016 and 2018, the Marshall team trained over 5000 individuals from
across clinical and behavioral health services. SBIRT is designed to enhance the continuum of
care for substance use disorder by improving the recognition of individuals with SUD and
referring them to the appropriate care. A large part of the training, conducted primarily by a
single individual – Program Director Lyn O’Connell, included the best way to make SUD
patients more comfortable and responsive to treatment options. The SBIRT program was the
only widespread education program that included dedicated anti-stigma education during the
community
response.
Battling Stigma
can be difficult,
particularly when
the general public
(who SUD clients
indicated as
expressing the
highest levels of
negative attitudes)
are subject to
negative media
attention. There
was a reduction in
the ad
equivalency
required to
counter negative
media and social
media reports about SUD in Cabell County from 2017 to 2018, (Figure 16) but we cannot
definitively determine if the community effort was causative. There was a slight rise from 2018
The faith community was having to reconsider as in
addiction as a moral failing. We had to get additional
training. Interestingly, when we created the quick
response team pastors became part of the quick
response team. They started undergoing training
instruction. Early on when we were seeking to get the
faith community involved this one pastor was very
honest, he said, “honestly I don't know what to say.
I'll pray for you? What do we do?” As a result, we
helped put together some instruction for the pastors,
That was quite helpful. – Key Stakeholder
Figure 16: Ad Equivalency in media and social media articles about SUD and Huntington/Cabell
County with negative sentiments
. Ad Equivalency shows how much it would potentially cost to buy
the total press coverage. It is calculated by multiplying the readership, potential viewership, and
average ad cost. Sentiment analysis is performed by measuring the tonality of the keywords seen
in the headlines and bodies of each article.

25 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
to 2019 in negatively worded media, although this rise is primarily due to reports about the
opioid lawsuits with the negative sentiment directed towards pharmaceutical companies and
distributors and not SUD patients. A concerted effort was initiated to reduce negative publicity
about Huntington/ Cabell County, (comma) after several community leaders became frustrated
with a growing amount of negative media attention in 2017. The Huntington-Cabell County
Chamber of Commerce, the Cabell-Huntington Health Department, Marshall University, and the
City of Huntington worked together to 1-educate local media on addiction and non-stigmatizing
language and 2- limit access to key community leaders by media members that were not
dedicated to developing a balance story without unnecessary negativity.
Financing the Response – Data is the Key: Key Stakeholders, particularly those in leadership
positions, discussed a great deal of discontent with the response from funding agencies at the
State and Federal level in the early
days of the response. Both KS and
FL indicated “finances/funding” as
the second most significant barrier. It
was difficult to attract funding and
other resources when the reality of
the large scope of the problem in
Huntington was not yet clear in the
data reported to State and Federal
agencies. Community agencies were
not able to attract the funding for
programs until the community was
able to present more real-time data.
Grants that funded the later stages of the response were all developed through this model. KS
and FL discussed throughout the interviews about how there was an emphasis on data
collection. This was particularly the case from the three leadership agencies discussed
previously. One Key Stakeholder summarized the data problem as, “We had to stop waiting for
Charleston [State Capital of WV] and
Washington to tell us who we are;
we had to provide the data that
explained who we are, on our
terms.”
When KS and FL interviewees were
asked how to measure success the
majority of responses required
quantitative measures. These
measures varied from system monitoring and longitudinal tracking (15 KS and 37 FL) to “more
accurate numbers” (18 KS and 8 FL) and continuity of care tracking (4 KS and 19 FL). Social
and lifestyle measures were also mentioned by a number of interviewees (11 KS and 24 FL)
emphasizing a greater need for longer-term measures of success.
I think having access to researchers is really
important to collect the data and understand. I think
having access to data, just information is so crucial
because people don't understand what's happening.
They don't have access to that. You know data can be
like a year old sometimes even, or older. And so most
people in the communities don't have access to data.
– Key Stakeholder
Everything from in law enforcement with the fire
department, in finance just but making it all
evidence-based. You don't want any of this stuff that
is just a political thing. If the numbers support it, let
the data speak. – Key Stakeholder

26 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
In addition to the approach of taking their lead from information about addiction in
Huntington/Cabell County from the patients and frontline workers, the three leadership entities,
along with Mountain Health Network and many of the SUD treatment and recovery providers,
put a strong focus on accurate data collection. Most agencies, even in the face of limited funds,
assigned resources (FTEs, new data systems, contractual data assistance) to improving the
availability and timeliness of data related to SUD in the community. This focus on data collection
culminated in the development of the West Virginia Community Addiction Data System
(WVCAD). The WVCAD brings the data from all of these services, from different agencies,
using different data collection systems
into a single-dimensional database that
can identify unique individuals across the
community system in a way that protects
patient privacy by utilizing the “Safe
Harbor” concept.
Indicators of Success:
Huntington/Cabell County response
efforts resulted in an increase in referrals
to care for those with SUD from 20 to 30
per month to over two hundred per
month directly associated with programs initiated as part of the response. (Figure 17). Peer
recovery coaches were utilized in all the programs initiated as part of the response that resulted
in an increase in referrals to treatment. The area saw a corresponding decrease in overdose
deaths. Charleston WV (Kanawha County), a city of similar size with more resources and
infrastructure that sits approximately 50 miles east of Huntington, did not have a coordinated
community response and saw no decrease in overdose deaths during the same period. (Figure
18)
The collaborative efforts are working, since overdose
rates are going down. You know, when we, and I can
only kind of look at a mom angle. Look at the number
of moms and some of the drug free moms and babies
data, I look at that data and I see improvements.
Fewer moms being addicted three months after, so
we see that it’s working. – Key Stakeholder
Figure 17: Monthly referrals from response programs.
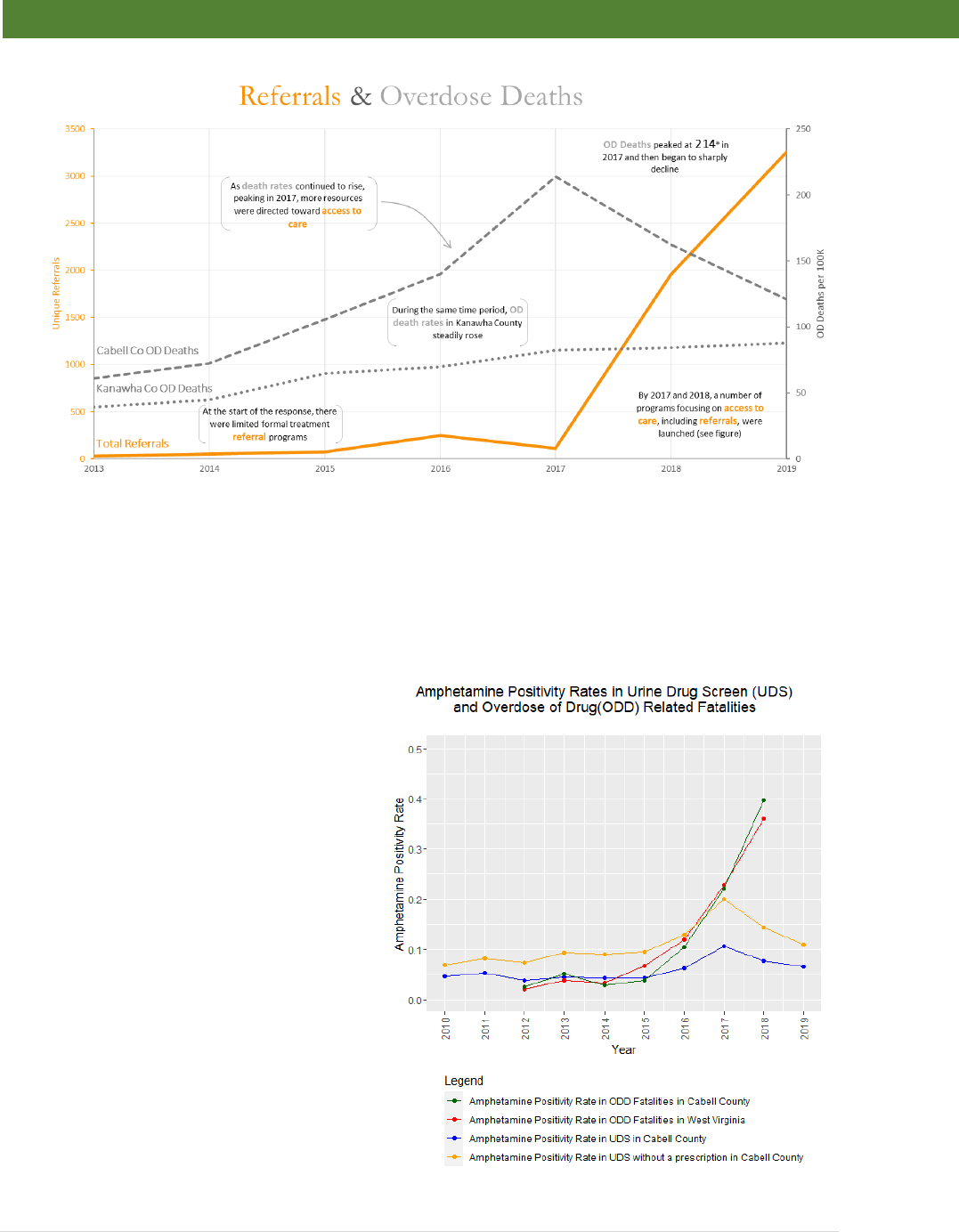
27 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Several explanations have been suggested for the decrease in overdose deaths in
Huntington/Cabell County:
1. Increase in the availability of naloxone. The Cabell-Huntington Health Department began
public distribution of Narcan (naloxone) as part of the harm reduction program in 2015.
Due to this effort, many citizens,
especially those who live and/or
associate with individuals at risk
for overdose had Narcan
available. While it seems likely
that the wide availability of
naloxone had a positive effect on
controlling overdose deaths, the
overall decrease in the Cabell
County was not observed until
2018 (based on annual reports)
and Narcan has been available
on emergency response units
since the late 1990’s. Additionally,
as a comparator, Charleston
replicated the Cabell County
distribution of naloxone with no
decrease in overdose deaths.
2. Transition to methamphetamine:
An increase in methamphetamine
use is another potential reason
for the decrease in overdose
Figure 18: Monthly referrals from response programs cross-referenced with annual overdose deaths from Cabell County
(Huntington) and Kanawha County (Charleston).
Figure 19: Percentage of drug toxicology results testing positive
for amphetamines.

28 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
deaths as amphetamines do not create the respiratory depression caused by opioids.
There was also an increase in methamphetamine in overdose death toxicology, although
those individuals also tested positive for opioids, with few exceptions. A similar
phenomenon of co-use of amphetamines and opioids was observed in new MAT
patients. This suggests that the increase methamphetamine use did not substantively
reduce opioid use across the population. Charleston saw a similar transition of some of
the SUD population from opioids to methamphetamine with no decrease in overdose
deaths. Urine Drug screen (UDS) toxicology indicated that the percentage of hospital
tests showing positive for amphetamine decreased in 2018 and 2019 suggesting that a
switch in use across the population to methamphetamine from opioids may not have
been a strong factor in reducing overdose deaths. (Figure 20)
3. Increase in Individuals in Treatment: The increase in referrals was recorded with
a corresponding increase in treatment initiation over existing programs. Initial increases
in treatment initiation were first observed in abstinence-based recovery programs,
followed by
MAT-based
treatment as
the necessary
medical
infrastructure
was
established at
both the State
and local
levels. (Figure
20) West
Virginia
passed the
1115 Waiver
exemption in 2017 resulting in a 10-fold increase in MAT prescribers by 2019. Existing
programs in Huntington/Cabell County reported that they remained at capacity for the
entirety of the reported time
period. Increases in
treatment initiation is the
only available data that
corresponds with the
decrease in overdose
deaths.
As the number of treatment
initiations increased, patients
maintaining program compliance
increased in a similar fashion. New
programs initiated experienced a
high percentage of patient
continuity beyond 90 days initially
when the provider to patient ratios
Figure 21: Total number of individuals from new or expanded programs
staying in treatment longer than 90 days.
Figure 20: Treatment initiation above existing patient capacity.

29 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
were high and the patient population was self-selected for those willing to utilize new programs.
Program effectiveness, as determined by individuals maintaining program compliance for
greater than 90 days, leveled off to approximately 40% as programs reached capacity. (Figure
21) The majority of individuals referred and initiated in treatment are in active.
The decrease in overdose deaths,
increase in referrals, and treatment
initiation correspond with a
decrease in opioid used detected
by UDS. There was a State-wide
change in opioid prescribing
practices. It is unclear how much
impact the decrease in overall
opioid prescribing had on overdose
deaths, but the percentage of
overdose deaths that included
opioids did not change.
Referrals to treatment and the
increased availability of services
improved access to care as
experienced by the patient
population (Mean of 7.77 on a 1 to
10 Likert scale). Respondents
reported improvements in access
to care 85.91% of the time, 4.70%
indicated a decrease in access, and
7.65% responded no change. A
survey of individuals with SUD evenly
distributed between MAT patients,
individuals in peer (abstinence)-based
recovery, and those with SUD who are
also experiencing homelessness indicated a large improvement in their perception of access to
treatment (Figure 22).
Despite a clear impression of the response as being successful, many interviewees expressed
concern at the lack of programs for children and
families. The focus on programs reducing overdose
deaths, increasing access to care, and individuals in
treatment were considered good and necessary, but
short term. Similarly, the efforts towards treating
prenatally-exposed babies were considered a small
piece of a larger problem. FL Interviewees strongly
support a more integrated approach to SUD care that
focus’ on prevention and comprehensive family issue.
(Figure 23)
As the focus of the response was initially on reducing overdose deaths, increasing access to
care, and individuals in treatment, prevention efforts were initiated slower than other programs.
Figure 23: Single word broad concepts for next
steps derived from FL interviews.
So I do believe when I'm saying that person needs
support after their treatment, it's really the whole
family that needs support. – Frontline Worker
Figure 22: Patients with SUD were asked to rate on a scale of 0 (Much Worse) to
10 (Much Improved)
– with 5 indicating “ No Change” on
the change in access to
treatment with the question: "
How has access to treatment and recovery for
substance use disorder changed within the past 5 years? Please
rate on the
sliding scale below." N=218
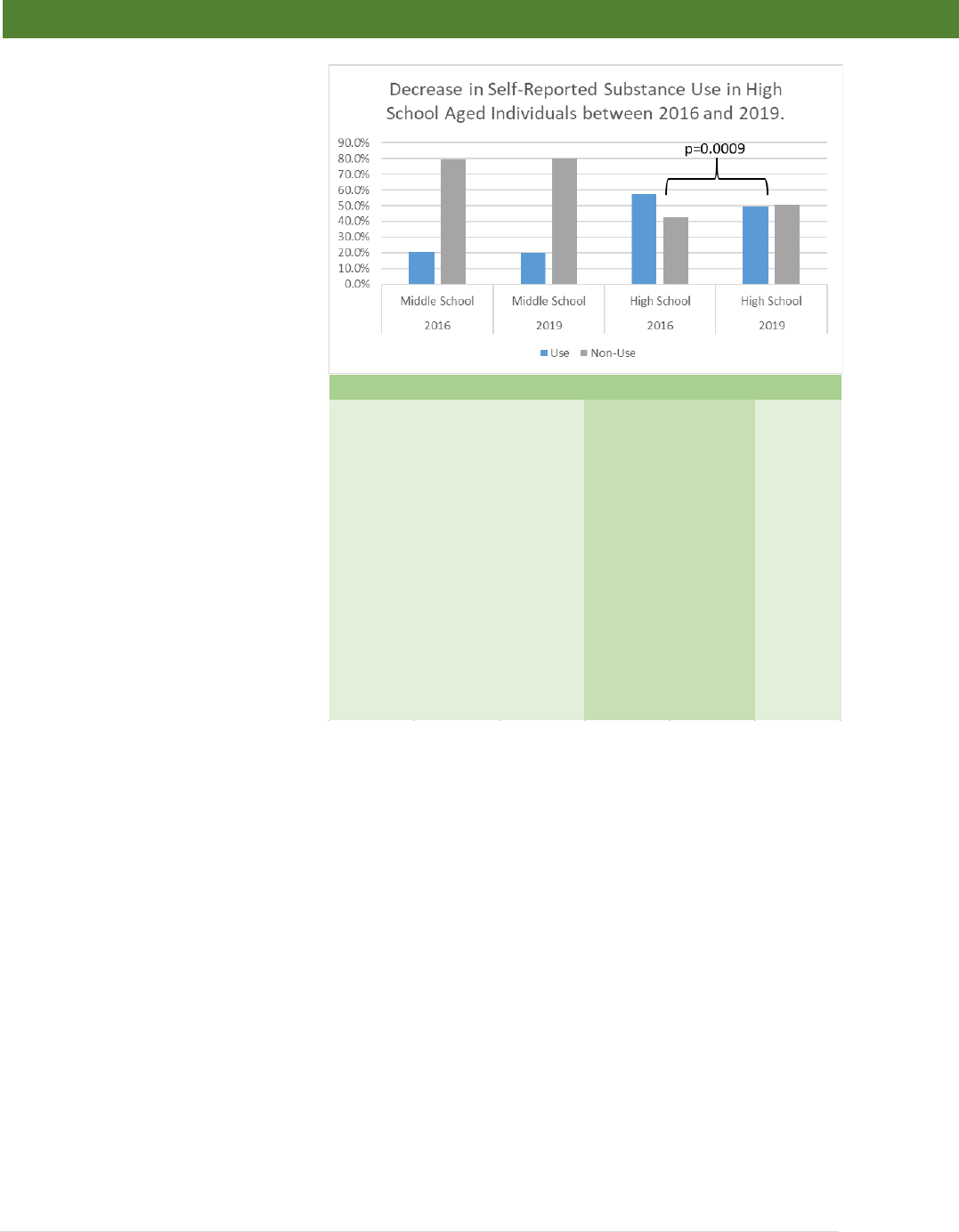
30 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Some evidence-based practices
prevention practices and improved
social emotional learning were
initiated several years prior to the
response (2012-2014), but were
not ubiquitously utilized. Response
related programs were not initiated
until the 2018-2019 school year.
Despite this lag, the number of
High School age children self-
reporting substance use decreased
from 57.5% to 49.7%. (Figure 24) It
is not clear whether this decrease
is due to the earlier or later
prevention efforts, or if it is a
positive consequence of the active
efforts of the larger response. This
reduction could be a result of
secondary prevention due to their
family members receiving
treatment, increase awareness and
attention from teachers or coaches,
or awareness on the part of the
students themselves based on the
publicity created by the epidemic
and subsequent community
response. FL interviews, whose
participants work directly with the
SUD population, including children,
revealed strong themes related to
the consequences of addiction on
children.
2016
2019
Tobacco 18.5% 16.6% p=0.0575
Alcohol 31.7% 29.0% p=0.0575
Marijuana 16.3% 17.3% p=0.7733
Cocaine 2.4% 1.1% p=0.0016
Inhalants 3.1% 1.8% p=0.0076
Hallucinogens 3.0% 1.7% p=0.0047
Heroin 1.8% 0.7% p=0.0013
Steroids 3.1% 2.1% p=0.0596
Ecstasy 2.6% 0.8% p<0.0001
Methamphetamine 1.7% 0.6% p=0.0019
Prescription Drugs 5.2% 3.6% p=0.0132
Over the Counter Medication 3.7% 1.9% p=0.0004
Figure 24: Self-report data collected by the Prevention Empowerment
Partnership from the Pride Survey indic
ates a decrease in substance use in High
School age students between 2016 and 2019. n=4179
A
B

31 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Gaps and Future Directions: The response to the addiction epidemic was focused on
improving access to treatment and reducing overdose deaths. This evaluation has provided
evidence that the efforts put forth by the community were successful. Preventing overdose
deaths and getting more individuals into treatment is the first critical step. The effects of
addiction in the Huntington/Cabell County are more pervasive than these early stages. KS and
FL were
largely in
agreement
about the
gaps in the
current
system. It is
clear that both
groups believe
that better
access to
“mental and
behavioral
healthcare”
and
“resources for
children” were
the two most important gaps in the community’s ability to assist individuals and families
struggling with addiction. While several of the programs are now sustained through
reimbursement models, sustainability is still a struggle as KS, and to a lesser extent FL, listed
“funding” as the third most critical gap. KS continued to be focused on “timely treatment
referrals” more than FL. Both groups strongly supported patient lifestyle issues like “integration
in the workforce” and “affordable housing.” Issues addressed during the response “timely
treatment referrals” and “stigma” were mentioned by both, but more strongly by KS. FL, on the
other hand, were more concerned with “long-term treatment, “Adverse childhood experiences,”
(ACEs) and “resources for grandparents” (specifically referring to grandparents who are raising
grandchildren because of issues in the family related to SUD). (Figure 25)
Based on the identified gaps, a few key programs developed during the later stages of the
evaluated response or after (late 2019+) may be important to the long-term recovery of the
community. Recent programs are directed at improvements in behavioral health capacity,
resources for children and childhood trauma, and special programs for long-term self-care.
Mental Health and Behavioral Healthcare: Despite improvements in capacity and access to
care, the Huntington/Cabell County community still has a deficit of behavioral health
professionals. Many KS and FL expressed a great deal of concern about the ability to attract
qualified therapists to the area. Having enough therapists that have the appropriate training and
experience to treat children with several behavioral health issues, including SUD, was reported
as being particularly difficult. These sentiments are reflected in the gap analysis. Marshall
University’s Departments of Social Work and Psychology have been attempting to address the
problem directly through the training of more therapists and counselors. The Joan c. Edwards
Figure 25: Answers given to the question, "What are the remaining gaps?" answered by more than 10% of
interviewees.

32 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
School of Medicine at Marshall University has also started an Addiction Science Fellowship to
expand the number of addiction specialists in the area.
Resources for Children: The Prevention Empowerment Partnership (PEP) is a coalition of
concerned citizens that work with the schools and other agencies to engage in primary
prevention activities. PEP has deployed a litany of structured and evidence-based interventions
in education, outreach, and engagement of school age children specifically designed to reduce
substance initiation and use.
Funding: Attracting extramural funding and reimbursable models remains a challenge. While
most agencies remain collaborative, attracting funding for programs remains a competitive
process. The community has been able to optimize funding by sharing responsibilities with
agencies that already have the necessary expertise. For example, the Child Advocacy Center in
Cabell County basic operations is subsidized by Cabell-Hunting Hospital (part of the Mountain
Health Network), but relies on reimbursable therapists from Prestera Center and Valley Health
System. Similarly, Project Hope for Women and Children clients receive services through
PROACT. Collaboration allows agencies to optimize their expertise whereby improving
sustainability and reducing resource requirements for some projects. Despite this, funding
remains a challenge considering the scope of the problem.
Integration into the workforce: Frontline workers and clients have expressed the need for
employment assistance through this evaluation process. Creating Opportunities for Recovery
Employment (CORE) was established at Marshall Health to address this gap. Initially funded by
Appalachian Regional Commission and established late in 2018, CORE was not in full operation
in time to contribute to the response evaluation, but all sectors agree that it is critical for long-
term community health. Through CORE, patients of the majority of SUD treatment providers or
recovery programs can receive workforce readiness training and job placement services that
coincide with their care. CORE has also worked with the WV State Chamber of Commerce and
WV Jobs and Hope to establish an employer’s tool kit to provide advice and human resource
recommendations to establish a drug-free and recovery friendly work environment.
Timely Treatment Referrals: The timeline from referral to treatment initiation can be critical to
establishing some individuals in treatment. Despite the development success of PROACT and
Project Engage to ease the transition from initial interaction with the healthcare system to
initiation of treatment, there remain barriers to a fully functional process. PROACT has
increased hours of availability regularly since it opened, but is limited by the number of patients
treated in those expanded hours due to issues related to sustainability. Project Engage, on the
other hand, is dependent on finding the right staff to run the program and has struggled with
culture shifts within the hospitals. Both programs have dramatically improved access to care,
but still have some growing pains to overcome before they are optimal.
Affordable Housing: Affordable, recovery-friendly, housing that accepts clients that struggle with
the challenges often experienced by those in recovery remains a problem. Two major efforts are
addressing this gap. The first is the opening of Hope House in 2020, an extension of Project
Hope for Women and Children that provides longer-term housing for families that graduated
from the transitional program at Project Hope. A new effort Local provider OVB Health has

33 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
partnered with Fannie Mae, the Fletcher Group, and Marshall University to create a recovery
housing strategy for the area.
Stigma: Marshall University and Quality Insights have developed a number of anti-stigma
initiatives. The first is a highly targeted and measurable digital advertising campaign specific for
and only promoted to hospital staff via their mobile devices. In addition an e-learn curriculum
was developed as an interactive training session created and tested by a combination of
physicians and nurses who have extensive experience with SUD and non-clinical individuals.
This curriculum has clinical and non-clinical tracks designed to reach, educate, and impact
individuals with the most effective stigma-reduction training for their work environment.
Lack of Communication: Communication in any community across agencies can be difficult, and
Cabell County, WV is no different. Despite an unprecedented level of collaboration, the area still
has challenges in communication. The WV Community Addiction Dashboard (describe in
Methods) was designed to not only share data across SUD providers, but also to create a
platform for continued cross-community collaboration. Governance of the data in the WVCAD is
overseen by a committee of individuals from around the community to assure that the public
health efforts of the data system was representative of the needs and will of the community as a
whole.
Adverse Childhood Experiences (ACEs): In the process of the evaluation, an ACEs Advisory
Group comprised primarily of frontline workers developed a plan for addressing ACEs with
NORC and the research team. That Advisory Group is now in the process of developing an
implementation strategy for that plan (attached as Appendix B to this report).
Resources for Grandparents: Cabell County Schools have developed a program targeted at
helping grandparents who are now raising their grandchildren due to problems related to SUD.
This program was developed late in the response and was not able to be fully implemented due
to the COVID-19 pandemic response requirements.
Limitations: The evaluators recognize that there are several limitations associated with this
study. Researchers consciously worked to gather a broad spectrum of thoughts and opinions
from both stakeholders of various levels of interaction with the SUD population across Cabell
County, WV. However, study findings are limited to those stakeholders willing to participate in
the research. The Client Survey, despite representing a sampling of individuals with SUD taken
evenly from the population, had a small number of respondents (219). As a qualitative study that
identified correlations suggesting an effective community response, it is impossible to
definitively determine which components of the response had the greatest impact. Consistent
themes were identified across respondents; however, the findings may not be generalizable to
other settings. Additionally, the COVID-19 social distancing requirements delayed data
collection and could potentially have influenced data collection.

34 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Conclusion: The City of Huntington and surrounding Cabell County, WV has been called,
“Ground Zero of the Opioid Epidemic.” While the validity of that statement can be debated, there
is little doubt that this modest city with just over 100,000 people in the metro area became
synonymous with the addiction crisis now facing many communities. A number of novel
programs were developed as part of the response to this epidemic, some worked, others did
not. A lot of the ideas behind these programs came from other communities, the QRT, Project
Engage, Drug Court. Even the Mayor’s Office of Drug Control Policy contained concepts
borrowed from other communities. Since the response, several communities have developed
programs similar to those used in Huntington/Cabell County without the positive results.
However, many of these programs work and are necessary to fill the critical gaps that many
communities are experiencing.
For years, frontline workers asked for help or complained about poor access to care for their
clients. First responders wearied of seeing the same individuals committing drug-related crimes
or overdosing. Those families struggling with the consequences of addiction were often pushed
aside because of lack of resources or programmatic bureaucracy. The three people who would
eventually be named as the champions of the response by their peers were a mayor that initially
thought it was a police problem, a health department director that did not fully believe in harm
reduction, and a family physician who wanted nothing to do with addiction. All of this amongst a
community that largely just didn’t want to deal with the people suffering from addiction lent to a
weak or no response. This may sound familiar if you are in a community that is losing hope
against this epidemic. These champions, along with countless individuals across the
community, would put their preconceived notions aside to learn the realities of the situation and
move forward without hesitation. Thus, Huntington/ Cabell County found its hope in ownership,
collaboration, and knowledge.
From the top down the Huntington/ Cabell County community took ownership of the problem.
Ignoring addiction was no longer an option and everyone was expected to do their part.
Ownership quickly turned into a remarkable environment of collaboration as the problem was
simply too big for any one group or agency. With this came the recognition that the data
collection and analytics had to far exceed the methods of the past.
Extraordinary things came out of this new environment beyond just what was outlined through
this report. Some brief examples include: Marshall Heath and Valley Health Systems –
traditional competitors – worked together to operate PROACT. The Greater Huntington
Chamber of Commerce helped teach businesses how to be “recovery friendly.” MAT programs
engaged in peer-support to improve outcomes of their patients while peer-based programs that
traditionally shunned medication worked collaboratively with MAT. Perhaps most importantly,
individuals suffering from addiction are now looked at as families in trouble.
The fundamental lesson from this evaluation of the Huntington/Cabell County response to the
addiction epidemic is that selecting and adapting the appropriate programs for your community
is important, but far less important than the implementation process.

35 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Lessons for Other Communities: When a community responds to a crisis and other
communities face similar challenges, there is often talk about the services and programs that
helped the community recover. While there were certainly innovative approaches like Lily’s
Place, PROACT, the Quick Response Team, and Faith Community United, the true story of the
Addiction Epidemic Response in Huntington/ Cabell County, WV lies in how these programs
developed through collaboration and willingness to change. Here are the recommendations for
any community facing an addiction crisis that wishes to develop a full community response
based on lessons learned from Huntington/ Cabell County, WV:
1. Admit there is a problem: The community leadership is Huntington/ Cabell County, WV did
not shrink from the problem. An open and public admission of crisis was the first critical step
to an effective response.
2. Empower existing resources: While there were new programs developed during the
response, increased capacity and response came from existing agencies or collaborations
between existing agencies. Every individual and agency in the community should be
encouraged to do what they can and empowered to be creative with solutions. It is likely that
the knowledge of the critical gaps in any given community exists within the frontline workers
and patient population, but the key
stakeholders hold the resources
and authority to make that
knowledge actionable.
3. Create Collaboration: The
overarching theme of the evaluation
of the Huntington/ Cabell County response was collaboration. Everybody in the community
has a role to play. Ego, status quo, and siloed organizations will inhibit any response.
4. Focus attention on whole life recovery and families: Substance use disorder has a
collateral effect on all those connected to it. Community recovery includes all members of
the community.
5. Treat patients as human beings: Stigma is an important part of creating an environment
that encourages recovery. Individuals with SUD, like most people, respond better when they
are treated with respect and kindness. When clients do not feel like a program or service will
treat them well, they will not use it.
6. Control the message: Communities can control the message foremost through data
collection. Federal and state agencies do not have access to the same real-time data as the
local community, nor can they understand how that data relates to the reality of any crisis.
To conduct a timely response, the local community has to inform federal and state agencies
of the reality of a crisis through shared real-time data.
7. Watch out for compassion fatigue: Frontline workers and first responders often deal with
difficult and frustrating situations related to SUD. Supervisors of these critical members must
actively address compassion fatigue. Frontline workers, in the evaluation of the Huntington/
Cabell County response, reported lack of feedback as one of the most frustrating issues.
First responders especially feel the need to know if those they arrest or treat with SUD find
recovery; as the positive outcomes of their work may not be measured or shared.
…just do the best you can. Focus on trying to do 150
percent every day at all times and just be supportive
and positive... – Frontline Worker

36 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
Index of Community Members Mentioned in Evaluation:
In order of appearance:
• Sean Loudin
o Former Medical Director of Lily’s Place and Cabell-
Huntington Hospital Neonatal Therapeutic Unit
• Steve Williams
o Mayor, City of Huntington
• Jim Johnson
o Former Director, Mayor’s Office of Drug Control
Policy
• Jan Rader
o Huntington Fire Chief
• Scott Lemley
o Former Police Data Analyst
• Michael Kilkenny
o Medical Director, Cabell-Huntington Health
Department
• Stephen Petrany
o Chair, Joan C. Edwards School of Medicine,
Department of Family Medicine
• Bob Hansen
o Director, Division of Addiction Sciences
• Amy Saunders
o Principle Investigator, Marshall SBIRT Program
• Lyn O’Connell
o Former Program Director, Marshall SBIRT Program

37 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
References:
1. Manchikanti L, Helm S, 2nd, Fellows B, et al. Opioid epidemic in the United States. Pain
Physician 2012;15:ES9-38.
2. National Drug Threat Assessment Summary 2016. Washington, DC: Department of
Justice, Drug Enforcement Administration; 2017.
3. Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United
States: a retrospective analysis of the past 50 years. JAMA Psychiatry 2014;71:821-6.
4. Jones CM, Logan J, Gladden RM, Bohm MK. Vital Signs: Demographic and Substance
Use Trends Among Heroin Users - United States, 2002-2013. MMWR Morb Mortal Wkly Rep
2015;64:719-25.
5. Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in
the United States. N Engl J Med 2015;372:241-8.
6. Cicero TJ, Ellis MS, Surratt HL. Effect of abuse-deterrent formulation of OxyContin. N
Engl J Med 2012;367:187-9.
7. Wide-ranging online data for epidemiologic research (WONDER). In: Statistics NCfH, ed.
Atlanta, GA: Centers for Disease Control and Prevention; 2016.
8. Cicero TJ, Ellis MS, Kasper ZA. Increased use of heroin as an initiating opioid of abuse.
Addict Behav 2017;74:63-6.
9. Prevention. CfDCa. Wide-ranging Online Data for Epidemiologic Research (WONDER),
Multiple-Cause-of-Death file, 2000–2014. 2015.
10. Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-
Opioid Use and Heroin Use. N Engl J Med 2016;374:154-63.
11. Quinones S. Dreamland : the true tale of America's opiate epidemic. New York:
Bloomsbury Press; 2015.
12. National Drug Threat Assessment Summary 2014. Washington, DC: Department of
Justice, Drug Enforcement Administration; 2015.
13. National Drug control strategy: Data Supplement 2014. Washington, DC: Office of
National Drug Control Policy, Office of the President of the United States; 2014.
14. Paulozzi LJ, Mack KA, Hockenberry JM, Division of Unintentional Injury Prevention
NCfIP, Control CDC. Vital signs: variation among States in prescribing of opioid pain relievers
and benzodiazepines - United States, 2012. MMWR Morb Mortal Wkly Rep 2014;63:563-8.
15. Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose
Deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep 2016;65:1445-52.
16. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in Drug and Opioid Overdose
Deaths--United States, 2000-2014. MMWR Morb Mortal Wkly Rep 2016;64:1378-82.
17. Ko JY, Patrick SW, Tong VT, Patel R, Lind JN, Barfield WD. Incidence of Neonatal
Abstinence Syndrome - 28 States, 1999-2013. Morbidity and Mortality Weekly Report
2016;65:799-802.
18. Stabler ME, Long DL, Chertok IR, Giacobbi PR, Jr., Pilkerton C, Lander LR. Neonatal
Abstinence Syndrome in West Virginia Substate Regions, 2007-2013. J Rural Health 2016.
19. Rossen L, Bastian B, Warner B, Khan D, Chong Y. Drug Poisoning Mortality: United
States, 2002–2014. National Center for Health Statistics: Centers for Disease Control and
Prevention; 2016.
20. Patrick JL, Elliott GD, Comizzoli P. Structural integrity and developmental potential of
spermatozoa following microwave-assisted drying in the domestic cat model. Theriogenology
2017;103:36-43.
21. Anil LS, A. West Virginia Viral Hepatitis B and C Surveillance. Charleston, WV: WV
DHHR; 2016.
22. WHO Fact Sheet. 2000. at http://www.who.int/inf-fs/en/fact164.html
.)

38 | Evaluating the Addiction Crisis Response in
Huntington/Cabell County WV
23. Loudin S, Werthammer J, Prunty L, Murray S, Shapiro JI, Davies TH. A management
strategy that reduces NICU admissions and decreases charges from the front line of the
neonatal abstinence syndrome epidemic. Journal of Perinatology 2017.
24. Tolia VN, Patrick SW, Bennett MM, et al. Increasing incidence of the neonatal
abstinence syndrome in U.S. neonatal ICUs. N Engl J Med 2015;372:2118-26.
25. Kilkenny M. Cabell-Huntington Harm Reduction Program Client Intake Survey Report
2016: Cabell-Huntington Board of Health; 2016.
26. Massey J, Kilkenny M, Batdorf S, et al. Opioid Overdose Outbreak - West Virginia,
August 2016. MMWR Morb Mortal Wkly Rep 2017;66:975-80.
27. The quadruple homicide: A timeline. Herald Dispatch 2008 May 21, 2008.
28. Hedrick C. Teens Remembered Ahead of Homicide Anniversary. Herald Dispatch 2017
May 20, 2017.
