
Supplement / Vol. 69 / No. 1 August 21, 2020
U.S. Department of Health and Human Services
Centers for Disease Control and Prevention
Morbidity and Mortality Weekly Report
Youth Risk Behavior Surveillance —
United States, 2019

Supplement
The MMWR series of publications is published by the Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention (CDC),
U.S. Department of Health and Human Services, Atlanta, GA 30329-4027.
Suggested citation: [Author names; first three, then et al., if more than six.] [Title]. MMWR Suppl 2020;69(Suppl-#):[inclusive page numbers].
Centers for Disease Control and Prevention
Robert R. Redfield, MD, Director
Anne Schuchat, MD, Principal Deputy Director
Chesley L. Richards, MD, MPH, Deputy Director for Public Health Science and Surveillance
Rebecca Bunnell, PhD, MEd, Director, Office of Science
Arlene Greenspan, PhD, Acting Director, Office of Science Quality, Office of Science
Michael F. Iademarco, MD, MPH, Director, Center for Surveillance, Epidemiology, and Laboratory Services
MMWR Editorial and Production Staff (Serials)
Charlotte K. Kent, PhD, MPH, Editor in Chief
Christine G. Casey, MD, Editor
Mary Dott, MD, MPH, Online Editor
Terisa F. Rutledge, Managing Editor
David C. Johnson, Lead Technical Writer-Editor
Catherine B. Lansdowne, MS, Project Editor
Marella Meadows, Project Editor
Guest Editors: Zewditu Demissie, PhD; J. Michael Underwood, PhD
Martha F. Boyd, Lead Visual Information Specialist
Maureen A. Leahy, Julia C. Martinroe,
Stephen R. Spriggs, Tong Yang,
Visual Information Specialists
Quang M. Doan, MBA, Phyllis H. King,
Terraye M. Starr, Moua Yang,
Information Technology Specialists
MMWR Editorial Board
Timothy F. Jones, MD, Chairman
Michelle E. Bonds, MBA
Matthew L. Boulton, MD, MPH
Carolyn Brooks, ScD, MA
Jay C. Butler, MD
Virginia A. Caine, MD
Katherine Lyon Daniel, PhD
Jonathan E. Fielding, MD, MPH, MBA
David W. Fleming, MD
William E. Halperin, MD, DrPH, MPH
Jewel Mullen, MD, MPH, MPA
Jeff Niederdeppe, PhD
Patricia Quinlisk, MD, MPH
Patrick L. Remington, MD, MPH
Carlos Roig, MS, MA
William Schaffner, MD
Morgan Bobb Swanson, BS
CONTENTS
Overview and Methods for the Youth Risk Behavior
Surveillance System — United States, 2019..............................................1
Condom and Contraceptive Use Among Sexually Active High School
Students — Youth Risk Behavior Survey, United States, 2019
......... 11
Trends in Violence Victimization and Suicide Risk by Sexual Identity
Among High School Students — Youth Risk Behavior Survey,
United States, 2015–2019
............................................................................. 19
Interpersonal Violence Victimization Among High School Students —
Youth Risk Behavior Survey, United States, 2019
...................................... 28
Prescription Opioid Misuse and Use of Alcohol and Other Substances
Among High School Students — Youth Risk Behavior Survey,
United States, 2019
......................................................................................... 38
Suicidal Ideation and Behaviors Among High School Students —
Youth Risk Behavior Survey, United States, 2019
................................. 47
Tobacco Product Use Among High School Students — Youth Risk
Behavior Survey, United States, 2019
....................................................... 56
Dietary and Physical Activity Behaviors Among High School
Students — Youth Risk Behavior Survey, United States, 2019
......... 64
Transportation Risk Behaviors Among High School Students —
Youth Risk Behavior Survey, United States, 2019
................................. 77

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Overview and Methods for the Youth Risk Behavior
Surveillance System — United States, 2019
J. Michael Underwood, PhD
1
; Nancy Brener, PhD
1
; Jemekia Thornton, MPA
1
; William A. Harris, MM
1
; Leah N. Bryan, MPH
1
;
Shari L. Shanklin, MPH
1
; Nicholas Deputy, PhD
1,2
; Alice M. Roberts, MS
3
; Barbara Queen, MS
4
, David Chyen, MS
1
; Lisa Whittle, MPH
1
;
Connie Lim, MPA
1
; Yoshimi Yamakawa, MPH
1
; Michelle Leon-Nguyen, MPH
1
; Greta Kilmer, MS
1
; Jennifer Smith-Grant, MSPH
1
;
Zewditu Demissie, PhD
1
; Sherry Everett Jones, PhD, JD
1
; Heather Clayton, PhD
1
; Patricia Dittus, PhD
1
1
Division of Adolescent and School Health, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC;
2
Epidemic Intelligence Service;
3
ICF International, Rockville, Maryland;
4
Westat, Rockville, Maryland
Abstract
Health risk behaviors practiced during adolescence often persist into adulthood and contribute to the leading causes of morbidity
and mortality in the United States. Youth health behavior data at the national, state, territorial, tribal, and local levels help monitor
the effectiveness of public health interventions designed to promote adolescent health. The Youth Risk Behavior Surveillance
System (YRBSS) is the largest public health surveillance system in the United States, monitoring a broad range of health-related
behaviors among high school students. YRBSS includes a nationally representative Youth Risk Behavior Survey (YRBS) and separate
state, local school district, territorial, and tribal school–based YRBSs. This overview report describes the surveillance system and
the 2019 survey methodology, including sampling, data collection procedures, response rates, data processing, weighting, and
analyses presented in this MMWR Supplement. A 2019 YRBS participation map, survey response rates, and student demographic
characteristics are included. In 2019, a total of 78 YRBSs were administered to high school student populations across the United
States (national and 44 states, 28 local school districts, three territories, and two tribal governments), the greatest number of
participating sites with representative data since the surveillance system was established in 1991. The nine reports in this MMWR
Supplement are based on national YRBS data collected during August 2018–June 2019. A full description of 2019 YRBS results
and downloadable data are available (https://www.cdc.gov/healthyyouth/data/yrbs/index.htm).
Efforts to improve YRBSS and related data are ongoing and include updating reliability testing for the national questionnaire,
transitioning to electronic survey administration (e.g., pilot testing for a tablet platform), and exploring innovative analytic methods
to stratify data by school-level socioeconomic status and geographic location. Stakeholders and public health practitioners can
use YRBS data (comparable across national, state, tribal, territorial, and local jurisdictions) to estimate the prevalence of health-
related behaviors among different student groups, identify student risk behaviors, monitor health behavior trends, guide public
health interventions, and track progress toward national health objectives.
Introduction
Adolescence is typically a healthy period of life, and CDC
reports that youths continue to make better decisions for
their health (1). However, some high school–aged youths
experience disparate health risks that increase the possibility
of acquiring a sexually transmitted disease (STD), including
human immunodeficiency virus (HIV) infection, and increase
opportunities for substance use, mental health problems, and
interpersonal violence or self-harm. Risky health behaviors
practiced during adolescence often persist into adulthood
(2). In 2018, CDC reported that the leading causes of death
Corresponding author: J. Michael Underwood, PhD, Division of
Adolescent and School Health, National Center for HIV/AIDS, Viral
Hepatitis, STD, and TB Prevention, CDC. Telephone: 404-718-1471;
E-mail: [email protected].
among U.S. adolescents were attributable to motor-vehicle
crashes, followed by suicide and homicide (3). In contrast,
that same year, a separate study reported the leading causes of
death among persons of all ages were heart disease, followed
by cancer and unintentional injuries (e.g., burns, drowning,
falls, poisoning, and motor-vehicle crashes) (4).
The Youth Risk Behavior Surveillance System (YRBSS)
monitors health behaviors, conditions, and experiences among
high school students throughout the United States. The system
includes a national Youth Risk Behavior Survey (YRBS),
conducted by CDC, and separate state, local school district,
territorial, and tribal school–based YRBSs, which are referred
to as site-level surveys. YRBSS is designed to monitor priority
health risk behaviors that contribute to the leading causes of
mortality, morbidity, and social problems among youths and
adults. The following categories of behaviors are included
in the system: 1) behaviors that contribute to unintentional

Supplement
2 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
injury and violence; 2) tobacco use; 3) alcohol and other
drug use; 4) sexual behaviors that contribute to unintended
pregnancy and STD/HIV infection; 5) dietary behaviors; and
6) physical inactivity.
This report describes the 2019 YRBS methodology,
including sampling, data collection, processing, weighting,
and analyses. Results include a 2019 YRBS participation
map, survey response rates (1991–2019), and student
demographic characteristics from the national survey.
Furthermore, this overview report is one of nine featured
in this MMWR Supplement. Each report uses YRBS data to
assess a priority public health topic among adolescents. In
addition to this overview report, this supplement includes
national YRBS updates regarding condom and contraceptive
use; violence victimization and suicide ideation by sexual
identity; interpersonal violence victimization; opioid, alcohol,
and other substance use behaviors; suicide ideation and
behaviors; tobacco use, including vaping; dietary behaviors
and physical activity; and transportation risk behaviors. Each
report might not include all national YRBS data related to the
topics that were collected in 2019, and this supplement does
not include any data from site-level surveys; however, all the
data are publicly available. (YRBS data and documentation
are available at https://www.cdc.gov/healthyyouth/data/yrbs/
data.htm.) Stakeholders and public health practitioners can
use YRBS data (comparable across national, state, tribal, and
local jurisdictions) to estimate the prevalence of health-related
behaviors among different student groups, identify student
risk behaviors, monitor health behavior trends, guide public
health interventions, and track progress toward national
health objectives.
National YRBS Methodology
Overview
The national YRBS is conducted biennially during the
spring of odd-numbered years and allows CDC to assess how
risk behaviors change temporally among the U.S. high school
population. The national YRBS provides comparable data
across years and allows state and local entities conducting their
own YRBS to demonstrate how the behaviors of their youths
compare with those at the national level. YRBS is conducted
among students in grades 9–12 who attend U.S. public and
private schools. A nationally representative sample of schools
and a random sample of classes within those schools are selected
to participate. The survey is self-administered anonymously by
using a computer-scannable questionnaire booklet and takes
one class period (approximately 45 minutes) to complete.
Questionnaire
In 2019, the YRBS questionnaire consisted of 99 questions.
Eighty-nine of those questions were included in the standard
questionnaire* used by sites. Ten additional questions were
added to the standard questionnaire that reflect areas of interest
for CDC and other stakeholders, forming the 99-question
national YRBS questionnaire. As in all cycles, both the standard
questionnaire and additional national-only questions were
revised to ensure that emerging and prevailing risk behaviors
among high school students were measured. Subject matter
experts from CDC and elsewhere proposed changes, additions,
and deletions to the questionnaire. New and revised questions
were reviewed for format, readability, and clarity and were
subjected to cognitive testing. CDC made further refinements
to the questions on the basis of those testing results.
All questions, except those assessing height, weight, and
race, were multiple choice, with a maximum of eight mutually
exclusive response options and only one possible answer per
question. The survey questions have undergone test-retest
analysis and demonstrated good reliability (5,6). The wording
of each question, including recall periods and response options,
and operational definitions for each variable, are available by
reviewing the 2019 YRBS questionnaire and data user’s guide.
(YRBSS data and documentation are available at https://www.
cdc.gov/healthyyouth/data/yrbs/data.htm.)
Sampling
The 2019 YRBS sampling frame consisted of all regular
public (including charter schools), parochial, and other
nonpublic schools with students in at least one of grades 9–12
in the 50 U.S. states and the District of Columbia. Alternative
schools, special education schools, schools operated by the U.S.
Department of Defense, the Bureau of Indian Education, and
vocational schools serving only students who also attended
another school were excluded. Schools with an enrollment
of ≤40 students across grades 9–12 also were excluded. The
sampling frame was based on data sets obtained from Market
Data Retrieval, Inc., and the National Center for Education
Statistics (NCES). NCES data sets were based on the Common
Core of Data (https://nces.ed.gov/ccd) for public schools
and the Private School Universe Survey (https://nces.ed.gov/
surveys/pss) for nonpublic schools.
A three-stage cluster sampling design was used to produce
a nationally representative sample of students in grades 9–12
* The standard YRBSS questionnaire includes 89 questions. YRBS coordinators
(located in CDC-funded states, local school districts, territories, and tribes)
voted for or against each proposed change, addition, and deletion. Final content
of the standard YRBS questionnaire was decided on the basis of the results of
this voting process.
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
who attend public and private schools. The first-stage sampling
frame comprised 1,257 primary sampling units (PSUs),
consisting of entire counties, groups of smaller adjacent
counties, or parts of larger counties. The 1,257 PSUs were
categorized into 16 strata according to their metropolitan
statistical area status (e.g., urban or rural) and the percentages
of non-Hispanic black (black) and Hispanic students in each
PSU. From the 1,257 PSUs, 54 were sampled with probability
proportional to overall school enrollment size for that PSU. For
the second-stage sampling, secondary sampling units (SSUs)
were defined as a physical school with grades 9–12 or a school
created by combining nearby schools to provide all four grades.
From the 54 PSUs, 162 SSUs were sampled with probability
proportional to school enrollment size. To provide adequate
coverage of students in small schools, an additional 15 small
SSUs were selected from a subsample of 15 PSUs from the 54
PSU sample. These 177 SSUs corresponded to 184 physical
schools. The third stage of sampling comprised random
sampling of one or two classrooms in each of grades 9–12
from either a required subject (e.g., English or social studies)
or a required period (e.g., homeroom or second period).
All students in sampled classes were eligible to participate.
Schools, classes, and students who refused to participate were
not replaced in the sampling design.
Data Collection Procedures
CDC’s Institutional Review Board approved the protocol
for the YRBS. Survey procedures were designed to protect
students’ privacy by allowing for anonymous and voluntary
participation. Before survey administration, local parental
permission procedures were followed. During survey
administration, students completed the self-administered
questionnaire during one class period and recorded their
responses directly on a computer-scannable booklet.
Response Rates and Data Processing
For the 2019 YRBS, 13,872 questionnaires were completed
in 136 schools. The national data set was cleaned and edited
for inconsistencies. Missing data were not statistically imputed.
A questionnaire failed quality control when <20 responses
remained after editing or when it contained the same answer
to ≥15 consecutive questions. Among the 13,872 completed
questionnaires, 195 failed quality control and were excluded
from analysis, resulting in 13,677 usable questionnaires. The
school response rate was 75.1%; the student response rate was
80.3%; and the overall response rate (i.e., [student response
rate] × [school response rate]) was 60.3%.
Race/ethnicity was ascertained from two questions:
1) “Are you Hispanic or Latino?” (with response options of
“yes” or “no”) and 2) “What is your race?” (with response
options of “American Indian or Alaska Native,” “Asian,” “black
or African American,” “Native Hawaiian or other Pacific
Islander,” or “white”). For the second question, students
could select more than one response option. For this report,
students were classified as Hispanic/Latino and are referred
to as Hispanic if they answered “yes” to the first question,
regardless of how they answered the second question. Students
who answered “no” to the first question and selected only black
or African American to the second question were classified as
black or African American and are referred to as black. Students
who answered “no” to the first question and selected only white
to the second question were classified and are referred to as
white. Race/ethnicity was classified as missing for students
who did not answer the first question and for students who
answered “no” to the first question but did not answer the
second question.
To obtain a sufficient sample size for analyses of health-
related behaviors by sexual identity and sex of sexual contacts,
students were divided into groups (Table 1). Students who had
no sexual contact were excluded from analyses related to sexual
behaviors, female students who had sexual contact with only
females were excluded from analyses on condom use and birth
control use, and male students who had sexual contact with
only males were excluded from analyses on birth control use.
Weighting
A weight based on student sex, race/ethnicity, and grade
was applied to each record to adjust for school and student
nonresponse and oversampling of black and Hispanic students.
The overall weights were scaled so that the weighted count
of students equals the total sample size, and the weighted
proportions of students in each grade match the national
population proportions. Therefore, weighted estimates
are nationally representative of all students in grades 9–12
attending U.S. public and private schools.
Analytic Methods
Findings presented in this MMWR Supplement and Youth
Online (https://nccd.cdc.gov/Youthonline/App/Default.aspx),
an interactive data analysis tool that allows access to all YRBSS
data, follow analytic methods similar to what is described in
this overview report. For more information regarding the
analyses presented in this supplement (e.g., variables analyzed,
custom measures, and data years), see the Methods section in
each individual report.
All statistical analyses were conducted on weighted data by
using SAS (version 9.4; SAS Institute) and SUDAAN (version
11.0.1; RTI International) software to account for the complex
Supplement
4 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Processing of sexual identity and sex of sexual contacts questions — Youth Risk Behavior Survey, United States, 2019
Question Student response Analytic description
Sexual identity
Which of the following best describes you?
1) Heterosexual (straight), 2) gay or lesbian, 3) bisexual, or
4) not sure
Heterosexual (straight)
Gay or lesbian or bisexual
Not sure
Heterosexual students
Lesbian, gay, or bisexual students
Not-sure students
Sex of sexual contacts
During your life, with whom have you had sexual contact?
1) I have never had sexual contact, 2) females, 3) males, or
4) females and males
What is your sex?
1) Male or 2) female
I have never had sexual contact* Students who had no sexual contact
Contact:
Female
Male
Student:
Male
Female
Students who had sexual contact with only the
opposite sex
Contact:
Male
Females and males
Female
Females and males
Student:
Male
†
Male
Female
†
Female
Students who had sexual contact with only the
same sex or with both sexes
* Excluded from analyses on sexual behaviors.
†
Excluded from analyses on birth control use and condom use.
sampling designs. In all reports, prevalence estimates and
confidence intervals were computed for variables in the YRBS
data set. Pairwise differences between populations (e.g., sex, race/
ethnicity, grade, sexual identity, and sex of sexual contacts) were
determined using t-tests. Prevalence estimates were considered
statistically significant if the t-test p value was <0.05.
In reports that analyzed data related to temporal trends,
prevalence estimates for variables assessed with identically
worded questions were examined. Logistic regression analyses
were used to account for all available estimates; control for
sex, grade, and racial/ethnic changes over time; and assess
long-term linear and quadratic trends. A p value associated
with the regression coefficient that was <0.05 was considered
statistically significant. Linear and quadratic time variables
were treated as continuous and were coded by using orthogonal
coefficients calculated with PROC IML in SAS. A minimum
of 3 survey years was required for calculating linear trends,
and a minimum of 6 survey years was required to calculate
quadratic trends. Separate regression models were used to
assess linear and quadratic trends for every variable. When a
significant quadratic trend was identified, Joinpoint software
was used to automate identification of the year when the
nonlinear (i.e., quadratic) trend changed. Regression models
were used to identify linear trends occurring in each segment.
Cubic and higher-order trends were not assessed. A quadratic
trend indicates a statistically significant but nonlinear trend
in prevalence over time. A long-term temporal change that
includes a significant linear and quadratic trend demonstrates
nonlinear variation (e.g., leveling off or change in direction) in
addition to an overall increase or decrease over time.
In reports that analyzed 2-year changes in health-related
behaviors, prevalence estimates from 2017 and 2019 were
compared by using t-tests for variables assessed with identically
worded questions in both survey years. Prevalence estimates were
considered statistically different if the t-test p value was <0.05.
Data Availability and Dissemination
YRBS data (1991–2019) are available from the YRBSS
data and documentation website (https://www.cdc.gov/
healthyyouth/data/yrbs/data.htm), as are additional resources,
including data documentation and analysis guides. Data are
available in both Access and ASCII formats. SAS and SPSS
programs are provided for converting the ASCII data into
SAS and SPSS data sets. Variables are standardized to facilitate
trend analyses and for combining data. YRBSS data are also
available online by using Youth Online (https://nccd.cdc.gov/
Youthonline/App/Default.aspx), a tool that allows point-and-
click data analysis and creation of customized tables, graphs,
maps, and fact sheets. Youth Online also performs statistical
tests by health topic and filters and sorts data by race/ethnicity,
sex, grade, and sexual orientation (sexual identity and sex of
sexual contacts). Finally, YRBS Explorer is a new application
featuring user-friendly options to view and compare national,
state, and local data via tables and graphs (https://yrbs-explorer.
services.cdc.gov). Data requests and other YRBSS-related
questions can be sent to CDC by using the data request form
(https://www.cdc.gov/healthyyouth/data/yrbs/contact.htm).
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 5
US Department of Health and Human Services/Centers for Disease Control and Prevention
State, Local School District,
Territorial, and Tribal YRBS
Methodology
Overview
Biennial administration of site-level YRBSs allows state
and local education and health agencies to assess how risk
behaviors change temporally among the high school population
in their respective jurisdiction. Site-level YRBS data provide
comparable data across years and allow comparisons of student
behaviors across jurisdictions (e.g., national or state). Site-
level surveys are conducted among students in grades 9–12
attending public schools by using samples representative of
the state, local, territorial, or tribal jurisdiction where they are
administered. The survey is self-administered anonymously
and takes one class period (approximately 45 minutes) to
complete. State and local institutional review boards approved
the protocol for their respective YRBSs. Survey methodology
for data collection, processing, and analytic methods were the
same as those described for the national YRBS.
Questionnaires
The 2019 YRBS standard questionnaire contained
89 questions and was used as the starting point for site-level
YRBS questionnaires. Sites could add or delete questions but
were required to use at least 60 of the questions on the standard
questionnaire. This flexibility allows YRBS coordinators and
other local stakeholders the opportunity to pursue topics of
interest by customizing their survey.
Sampling
Sites used a two-stage cluster sampling design to produce
a representative sample of students in grades 9–12 in their
jurisdiction. In 41 states, three local school districts, and one
territory, in the first sampling stage, public schools with any
of grades 9–12 were sampled with probability proportional
to school enrollment size. In two states, 25 local school
districts, and two territories, all schools in the jurisdiction
were selected to participate (i.e., a census of schools). In the
second sampling stage, intact classes from either a required
subject (e.g., English or social studies) or a required period
(e.g., homeroom or second period) were sampled randomly.
In three sites (Vermont, the District of Columbia, and Palau),
a census of students was eligible to participate.
Response Rates and Nonresponse
Bias Analyses
Before the 2019 YRBS cycle, CDC required a minimum
60% overall response rate for data from a jurisdiction to be
weighted. As response rates in federal surveys continue to
decline (7), a better understanding of the complex association
between nonresponse and nonresponse bias is needed. In 2019,
CDC chose three YRBS sites with overall response rates of
50%–60% (Nebraska; Texas; and Spartanburg County, South
Carolina) to pilot nonresponse bias analyses to evaluate data
representativeness. Because of data limitations, comparisons
were limited to responding and nonresponding schools by
school size and responding and nonresponding students by
grade. Weighted sample and population percentages by grade,
sex, and race/ethnicity were also compared. Overall, few
statistically significant differences between comparison groups
were found, which suggested that the data were generally
representative of their respective populations. For the 2019
cycle, CDC used nonresponse bias analysis results to help
determine whether data were weighted for sites with overall
response rates <60%.
Weighting
YRBS data were weighted if sites collected data from a
representative sample of students (determined either by an
overall response rate of ≥60% or nonresponse bias analysis
indicating no significant bias). A weight based on student sex,
race/ethnicity, and grade was applied to each record to adjust
for school and student nonresponse in each jurisdiction. The
weighted count of students equals the student population in
each jurisdiction. Data from 44 states and 28 local school
districts were weighted. In 26 states and 13 local school
districts, weighted estimates are representative of all students
in grades 9–12 attending regular public schools, and in
13 states and eight local school districts, weighted estimates are
representative of regular public school students plus students in
grades 9–12 in other types of public schools (e.g., alternative
or vocational schools).
Data Availability and Dissemination
A combined data set including national, state, local school
district, territorial, and tribal YRBS data (1991–2019) is available
from the YRBSS data and documentation website (https://nccd.
cdc.gov/Youthonline/App/Default.aspx). Availability of site
data depends on survey participation, data quality, and data-
sharing policies. Information about YRBSS data is available at
the participation maps and history website (https://www.cdc.
gov/healthyyouth/data/yrbs/participation.htm). Data requests
Supplement
6 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
and other YRBS-related questions can be sent to CDC by
using the data request form. (The YRBSS question, comment,
and data request form is available at https://www.cdc.gov/
healthyyouth/data/yrbs/contact.htm.) Site-level YRBS data
(from high school and middle school surveys) collected during
1991–2019 are available through Youth Online (https://nccd.
cdc.gov/Youthonline/App/Default.aspx) and YRBS Explorer
(https://yrbs-explorer.services.cdc.gov).
YRBS Response Rates and 2019
Demographic Characteristics
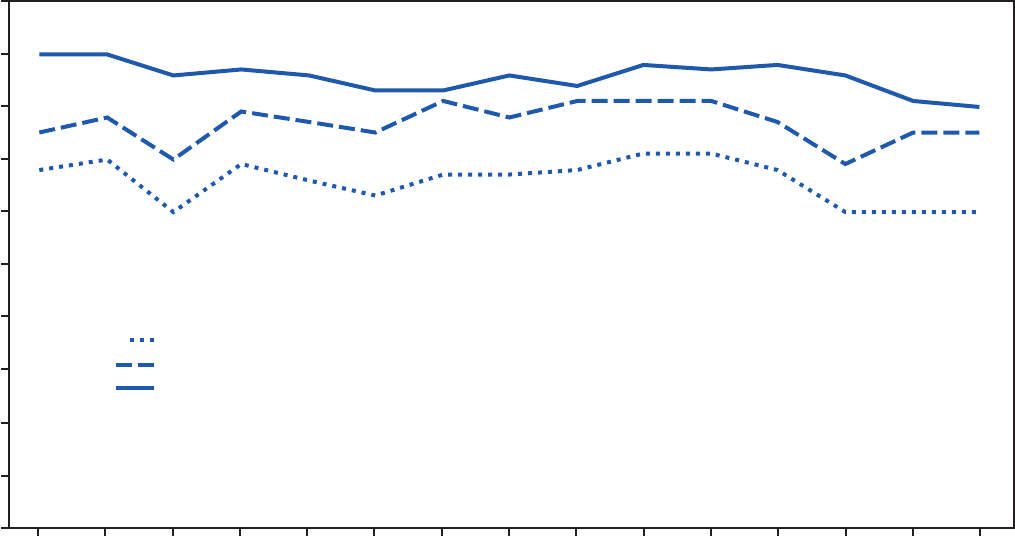
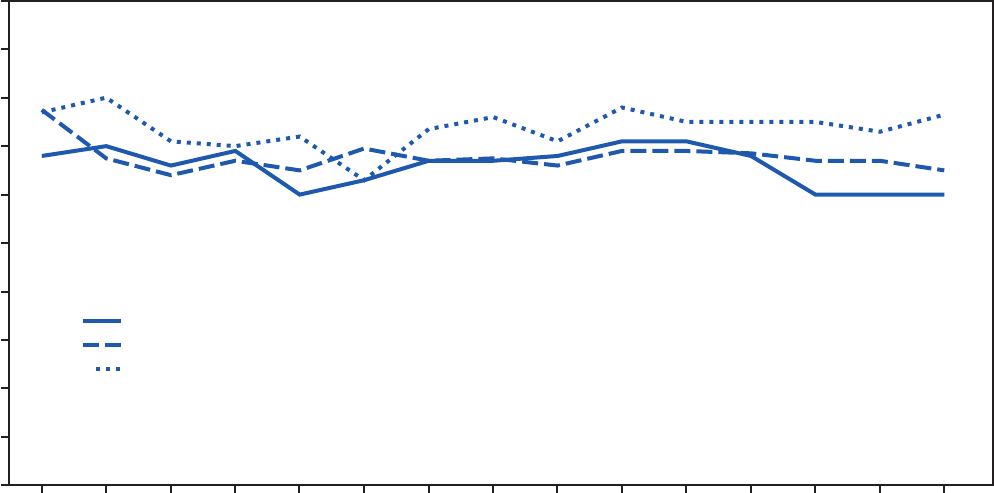
During 1991–2019, national YRBS overall response rates
remained at >60% (Figure 1). They reached a high of 71%
during the 2009 and 2011 YRBS cycles, followed by steady
decreases; response rates have remained in the low 60% range
during the 2015–2019 cycles. Since 1991, school response
rates have varied from 70% to the low 80% range, whereas
student participation rates have been consistent at 80%–90%.
Data were weighted to match national population
proportions. Thus, 50.6% of students were male, and 26.6%
were in 9th grade; 25.5% were in 10th grade; 24.2% were in
11th grade; and 23.5% were in 12th grade (Table 2). In regard
to race/ethnicity, the majority of students were no-Hispanic
FIGURE 1. Overall, school, and student response rates for the national Youth Risk Behavior Surveys — United States, 1991–2019
0
10
20
30
40
50
60
70
80
90
100
1991 1993 1995 1997 1999 2001 2003 2005 2007 2009 2011 2013 2015 2017 2019
Percentage
Year
School response rate
Student response rate
Overall response rate
white (white) (51.2%), followed by Hispanic (26.1%), black
(12.2%), and other (10.6%), which is defined as American
Indian or Alaska Native, Asian, Native Hawaiian or other
Pacific Islander, or multiracial but non-Hispanic.
Nationwide, 84.4% of students self-identified as heterosexual,
2.5% as gay or lesbian, and 8.7% as bisexual; 4.5% were not
sure of their sexual identity (Table 3). In 2019, 45.4% of
students had sexual contact with only the opposite sex, 2.2%
with only the same sex, and 4.8% with both sexes; 47.6% had
had no sexual contact.
2019 Site-Level YRBS Participation and
Student Response Rates
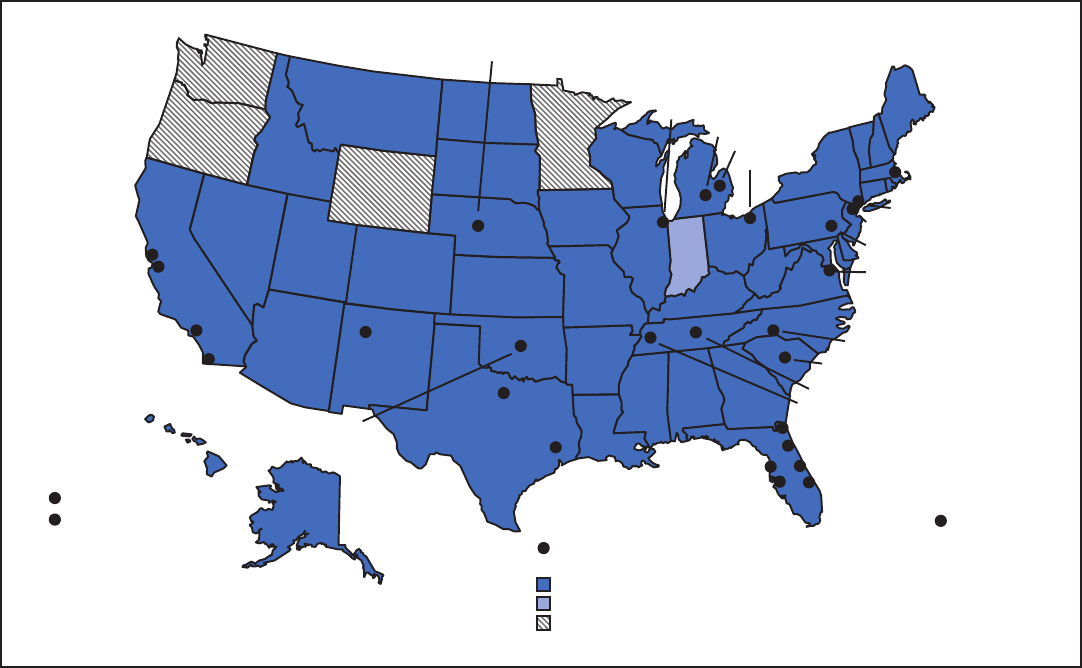
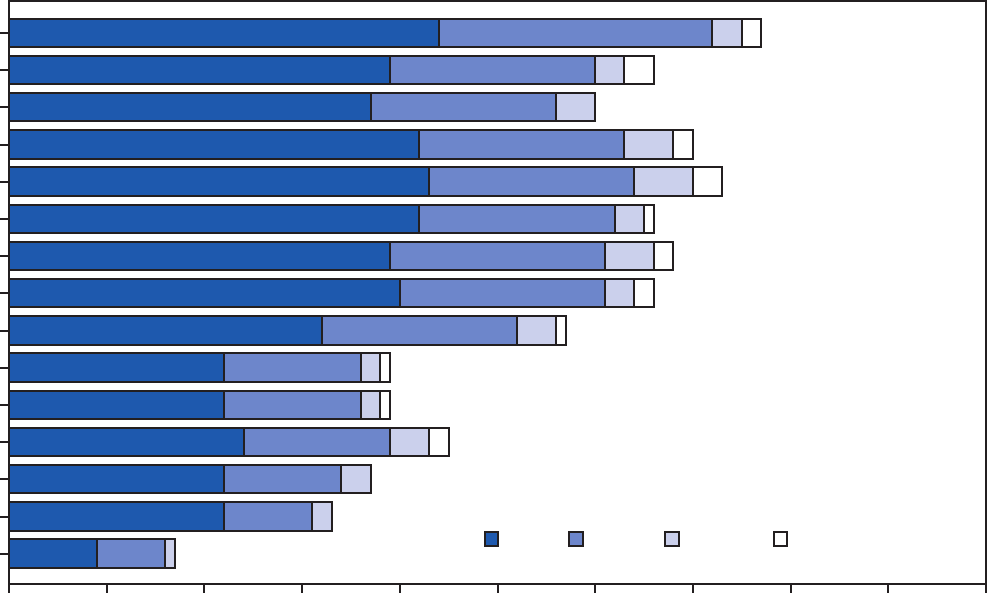
In 2019, a total of 44 states, 28 local school districts, three
territories, and two tribal governments had representative
data (Figure 2). In 2019, the median response rate for state
YRBSs with representative data was 65.0% (Figure 3), which
has typically remained at 60%–70% since 1991. The median
response rate for local school district YRBSs with representative
data was 76.5% (Figure 3) and has typically remained at
70%–80% since 1991. Since the inception of YRBSS in 1991,
the number of sites with representative data has increased,
reaching a high of 77 in 2019 (Figure 4).
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 7
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Youth Risk Behavior Survey student demographic
characteristics — United States, 2019
Characteristic No. (%)
Participating schools 136 (100)
Student sample size 13,677* (100)
Response rates
Schools (75.1)
Students (80.3)
Total (60.3)
Sex
†
Male 6,641 (50.6)
Female 6,885 (49.4)
Race/Ethnicity
†,§
White, non-Hispanic 6,668 (51.2)
Black, non-Hispanic 2,040 (12.2)
Hispanic 3,038 (26.1)
Other 1,493 (10.6)
Grade
†,§
9 3,637 (26.6)
10 3,717 (25.5)
11 3,322 (24.2)
12 2,850 (23.5)
* Among the 13,872 completed questionnaires, 195 failed quality control and
were excluded from analysis, resulting in 13,677 usable questionnaires.
†
Does not included students who responded “ungraded” or “other grade.”
§
Percentages might not total 100% because of rounding.
Discussion
YRBSS is the largest public health surveillance system in the
United States, monitoring multiple health-related behaviors
among high school students. Since 1991, YRBSS has collected
data from approximately 4.9 million high school students in
approximately 2,100 separate surveys. Survey response rates
have remained slightly above 60%, since YRBSS inception.
Consistent and relatively high response rates allow for
long-term trend analyses of student health behaviors and
experiences. During the 2019 cycle, 78 separate jurisdictions
successfully collected YRBS data from a broad diversity of
high school students. Nationally representative data from
adolescents of various demographic profiles (e.g., sex, race
and ethnicity, sexual identity) provide information regarding
TABLE 3. Number and percentage of students, by sexual identity and sex of sexual contacts — Youth Risk Behavior Survey, United States, 2019
Characteristic
Total Male Female
No. (%) 95% CI No. (%) 95% CI No. (%) 95% CI
Sexual identity
Heterosexual 10,853 (84.4) 83.4–85.3 5,728 (91.2) 90.1–92.3 5,048 (77.6) 75.9–79.3
Gay or lesbian 380 (2.5) 2.1–3.0 157 (2.1) 1.6–2.7 211 (2.9) 2.3–3.6
Bisexual 1,151 (8.7) 8.0–9.4 201 (3.4) 2.8–4.1 929 (13.9) 12.7–15.2
Not sure 591 (4.5) 3.9–5.0 223 (3.2) 2.7–3.9 350 (5.6) 4.7–6.6
Sex of sexual contacts
Opposite sex only 4,856 (45.4) 42.8–48.1 2,642 (49.5) 46.2–52.8 2,214 (41.3) 38.7–44.0
Same sex only 292 (2.2) 1.8–2.7 99 (1.6) 1.2–2.0 193 (2.8) 2.2–3.6
Both sexes 526 (4.8) 4.2–5.5 90 (1.8) 1.4–2.3 436 (7.8) 6.7–9.1
No sexual contact 4,953 (47.6) 44.8–50.4 2,346 (47.1) 43.9–50.4 2,607 (48.0) 45.1–50.9
Abbreviation: CI=confidence interval.
disparities in health-related behaviors and highlight long-term
trends in the prevalence of these behaviors.
In 2019, CDC launched the Public Health Data
Modernization Initiative to enhance the potential of using
data for disease detection and elimination. The initiative
envisions a future in which data drives action efficiently,
flexibly, rapidly, and with impact. CDC leverages technology,
knowledge, leadership, access, and collaboration to harness
the life-saving power of data. YRBSS has both longstanding
and newly implemented features that align with the
modernization initiative. CDC scientists provide technical
support to help state and local education and health agencies
administer their YRBS. Flexibility in the questionnaire
design process allows stakeholders to collect data of interest
across student populations. Detailed YRBS site reports are
rapidly returned to state and local departments of health and
education, often within 16 weeks of survey administration.
In 2019, YRBSS reach (measured by the number of sites with
representative data) has increased to 78 sites including the
national survey, the most in YRBSS history. These data will
help identify student risk behaviors, affect decision-making,
and guide public health interventions.
The public release of YRBS data coincides with the
publication of this nine-part MMWR Supplement and is an
agencywide collaboration. Subject matter experts from selected
CDC programs contributed to this supplement to highlight
public health concerns among U.S. high school students.
YRBS data dissemination is managed through online requests,
Youth Online, and YRBS Explorer. This year, CDC updated
Youth Online to strengthen data presentation, improve user
experience, and ultimately expand reach for YRBS data. These
improvements to data dissemination will improve YRBS access,
expand usage, and maximize impact.
CDC continually works to strengthen YRBSS, and new
developments are under way. In 2019, CDC launched a
project to update reliability testing for the national YRBS
questionnaire. As other school-based surveys move toward
Supplement
8 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 2. State, local school district, territorial, and tribal government Youth Risk Behavior Surveys — selected U.S. sites, 2019
State: representative data
State: no representative data
Local school district, territory,
or tribal government: representative data
Did not participate
New York City
Newark
Philadelphia
District of Columbia
Boston
Cleveland
Genesee
Eaton
Chicago
Duval County
Orange County
Palm Beach County
Broward County
Gaston County
Spartanburg County
Nashville
Shelby County
Northern Mariana Islands
Guam
Puerto Rico
San Francisco
Oakland
San Diego
Los Angeles
Pasco County
Hillsborough County
Houston
Fort Worth
Albuquerque
Cherokee Nation
Winnebago Tribe of Nebraska
electronic platforms (e.g., computer, smart phone, or tablet),
some site-level YRBSs have also transitioned to electronic
survey administration. CDC recently completed pilot
testing for a tablet-based survey administration of the YRBS
questionnaire and is considering using tablets for future
YRBSs. Finally, CDC is exploring innovative analytic methods
to stratify YRBS data by school-level socioeconomic status
and geographic location. A recent study using this approach
reported students attending schools in low socioeconomic
areas were more likely to experience violence, poor emotional
well-being, and suicidality (8).
Limitations
Reports in this supplement include a limitations section
describing the analyses pertaining to that particular report. In
general, YRBSS findings are subject to at least six limitations.
First, these data apply only to youths who attend school and
therefore are not representative of all persons in this age group.
In 2019, approximately 5% of high school–aged youths (ages
14–17 years) were not enrolled in school (9). Those youths
might engage in riskier health behaviors than their peers, and
those behaviors are not captured in the school-administered
YRBS. Second, the extent of underreporting or overreporting
of health-related behaviors cannot be determined, although
the survey questions demonstrate good test–retest reliability
(5,6). Third, not all states and local school districts administer
YRBS, and those that did administer it might not include all
the standard questions on their YRBS questionnaire; therefore,
data for certain variables are not available for some sites. Fourth,
YRBS data analyses are based on cross-sectional surveys and
can only provide an indication of association, not causality.
Moreover, the survey is descriptive and not designed to explain
the reasons behind any observed trends. Fifth, limitations exist
related to assessment of sexual and gender identity. Students
might not be fully aware of their sexual identity at the time of
assessment or might not have understood the sexual identity
question. The category of students who are not sure of their
sexual identity might encompass students who are unsure of
their sexuality, students who were uncomfortable answering
the question, or students who did not understand the question.
In addition, although some sites asked questions about
transgender students, the national YRBS does not include a
question about gender identity; therefore, national prevalence
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 9
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 3. National, state, and local school district Youth Risk Behavior Survey response rates — United States and selected U.S. sites,
1991–2019*
0
10
20
30
40
50
60
70
80
90
100
1991 1993 1995 1997 1999 2001 2003 2005 2007 2009 2011 2013 2015 2017 2019
National response rate
State median response rate
Local school district median response rate
Year
Percentage
* Does not include Youth Risk Behavior Survey data from U.S. territories and tribal governments.
estimates for this population of students cannot be assessed.
Finally, a limitation exists regarding the aggregation of race
and ethnicity data. The national YRBS aggregates these data
into broad categories of white, black, and Hispanic. All other
students are classified as “other.” More detailed racial/ethnic
information, as published elsewhere, provides valuable data
regarding health disparities among high school students (10).
Conclusion
YRBSS is the best source for quality data at the national,
state, territorial, tribal, and local school district levels for
monitoring health-related behaviors that contribute to the
leading causes of mortality and morbidity among U.S. high
school students and that can lead to health problems as adults.
A recent report from the National Academies of Sciences,
Engineering, and Medicine used YRBS as its data source
on the basis of the strengths of the system (11). In 2019, in
addition to the national data, 44 states, 28 local school districts,
three territories, and two tribal governments received data
representative of their high school student populations.
This overview report describes YRBSS methods for guiding
the analyses presented in this MMWR Supplement. A full
description of 2019 YRBS results and downloadable data
are available (https://www.cdc.gov/healthyyouth/data/yrbs/
index.htm).
Conicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. CDC. Youth Risk Behavior Survey: data summary and trends report,
2007–2017. Atlanta, GA: US Department of Health and Human
Services, CDC; 2018. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/
trendsreport.pdf
2. Wiium N, Breivik K, Wold B. Growth trajectories of health behaviors
from adolescence through young adulthood. Int J Environ Res Public
Health 2015;12:13711–29. https://doi.org/10.3390/ijerph121113711
3. Murphy SL, Xu J, Kochanek KD, Arias E. Mortality in the United States,
2017. NCHS Data Brief 2018; (328):1–8.
4. Curtin SC, Heron M, Miniño AM, Warner M. Recent increases in injury
mortality among children and adolescents aged 10–19 years in the United
States: 1999–2016. Natl Vital Stat Rep 2018;67:1–16.
5. Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG.
Reliability of the 1999 youth risk behavior survey questionnaire.
J Adolesc Health 2002;31:336–42. https://doi.org/10.1016/
S1054-139X(02)00339-7
Supplement
10 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 4. Number of states, local school districts, territories, and tribal governments with representative Youth Risk Behavior Survey data, by
year of survey — selected U.S. sites, 1991–2019
0 10 20 30 40 50 60 70 80 90 100
1991
1993
1995
1997
1999
2001
2003
2005
2007
2009
2011
2013
2015
2017
2019
Number of representative sites
Year
States Districts Territories Tribal governments
6. Brener ND, Mcmanus T, Galuska DA, Lowry R, Wechsler H. Reliability
and validity of self-reported height and weight among high school
students. J Adolesc Health 2003;32:281–7. https://doi.org/10.1016/
S1054-139X(02)00708-5
7. Czajka JL, Beyler A. Declining response rates in federal surveys: trends
and implications. Final report. Vol. I. Washington, DC: Mathematica
Policy Research; 2016. https://aspe.hhs.gov/system/files/pdf/255531/
Decliningresponserates.pdf
8. Everett Jones S, Underwood JM, Pampati S, et al. School-level poverty
and persistent feelings of sadness or hopelessness, suicidality, and
experiences with violence victimization among public high school
students. J Health Care Poor Underserved 2020;30 [In press].
9. US Department of Education, National Center for Education Statistics.
Fast facts: enrollment trends. Washington, DC: US Department of
Education; 2019. https://nces.ed.gov/fastfacts/display.asp?id=65
10. Lowry R, Eaton DK, Brener ND, Kann L. Prevalence of health-risk
behaviors among Asian American and Pacific Islander high school
students in the U.S., 2001–2007. Public Health Rep 2011;126:39–49.
https://doi.org/10.1177/003335491112600108
11. National Academies of Sciences, Engineering, and Medicine. Promoting
positive adolescent health behaviors and outcomes: thriving in the 21st
century. Washington, DC: The National Academies Press; 2019. http://
www.nap.edu/catalog/25552/promoting-positive-adolescent-health-
behaviors-and-outcomes-thriving-in-the

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 11
US Department of Health and Human Services/Centers for Disease Control and Prevention
Condom and Contraceptive Use Among Sexually Active High School
Students — Youth Risk Behavior Survey, United States, 2019
Leigh E. Szucs, PhD
1
; Richard Lowry, MD
2
; Amy M. Fasula, PhD
3
; Sanjana Pampati, MPH
4
; Casey E. Copen, PhD
5
; Khaleel S. Hussaini, PhD
3
;
Rachel E. Kachur, MPH
5
; Emilia H. Koumans, MD
3
; Riley J. Steiner, PhD
3
1
Division of Adolescent and School Health, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention,
CDC;
2
Office of the Director, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC;
3
Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC;
4
Oak Ridge Institute for Science and Education;
5
Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention CDC
Abstract
Preventing unintended pregnancy and sexually transmitted diseases (STDs), including human immunodeficiency virus (HIV)
infection, among adolescents is a public health priority. This report presents prevalence estimates for condom and contraceptive
use among sexually active U.S. high school students from the 2019 Youth Risk Behavior Survey. Behaviors examined included
any condom use, primary contraceptive method use, and condom use with a more effective contraceptive method, all reported at
last sexual intercourse. Analyses were limited to sexually active students (i.e., those who had sexual intercourse with one or more
persons during the 3 months before the survey). Except for any condom use, students reporting only same-sex sexual contact were
excluded from analyses. Weighted prevalence estimates were calculated, and bivariate differences in prevalence were examined
by demographic characteristics (sex, race/ethnicity, and grade) and other sexual risk behaviors (age of sexual initiation, previous
3-month and lifetime number of sex partners, and substance use before last sexual intercourse). Nationwide, 27.4% of high school
students reported being sexually active (n = 3,226). Among sexually active students who reported having had sexual contact with
someone of the opposite sex (n = 2,698), most students (89.7%) had used a condom or a primary contraceptive method at last
sexual intercourse. Prevalence of any condom use at last sexual intercourse was 54.3%, and condoms were the most prevalent
primary contraceptive method (43.9% versus 23.3% for birth control pills; 4.8% for intrauterine device [IUD] or implant; and
3.3% for shot, patch, or ring). Approximately 9% had used condoms with an IUD, implant, shot, patch, ring, or birth control pills.
Using no pregnancy prevention method was more common among non-Hispanic black (23.2%) and Hispanic (12.8%) students
compared with non-Hispanic white students (6.8%); compared with Hispanic students, using no pregnancy prevention method
was more common among non-Hispanic black students. Prevalence of condom use was consistently lower among students with
other sexual risk behaviors. Results underscore the need for public health professionals to provide quality sexual and reproductive
health education and clinical services for preventing unintended pregnancy and STDs/HIV and decreasing disparities among
sexually active youths.
Introduction
Preventing unintended pregnancy and sexually transmitted
diseases (STDs), including human immunodeficiency virus
(HIV) infection, is a U.S. public health priority, particularly
among adolescents (1). U.S. birth rates among youths aged
15–19 years have decreased to record lows; evidence suggests
that increasing use of a range of contraceptive options,
including intrauterine devices (IUDs) and implants, also
known as long-acting reversible contraception, is a contributing
factor (2). However, U.S. birth rates among adolescents
remain higher than rates in comparable Western industrialized
nations (3). In 2018, U.S. birth rates for persons aged 15–17
Corresponding author: Leigh E. Szucs, PhD, Division of Adolescent
and School Health, National Center for HIV/AIDS, Viral Hepatitis,
STD, and TB Prevention, CDC. Telephone: 404-718-6785; E-mail:
and 18–19 years were 7.2 and 32.3 births per 1,000 females,
respectively (4). Moreover, racial/ethnic, geographic, and
socioeconomic disparities persist (4). For example, in 2018,
birth rates among non-Hispanic black (black) (26.3) and
Hispanic (26.7) persons aged 15–19 years were almost two
times the rate for non-Hispanic white (white) (12.1) persons (4).
Contraceptive methods vary in effectiveness and highly and
moderately effective methods do not prevent STDs, which
disproportionately affect adolescents (5). Highly effective
reversible contraceptive methods (IUDs and implants) are
associated with a <1% failure rate during the first year of typical
use; moderately effective contraceptive methods (injectables,
patches, rings, and birth control pills) are associated with a
4%–7% failure rate during the first year of typical use; and
less effective methods (condoms, diaphragm, and spermicides)
are associated with a >10% failure rate during the first year
of typical use (6). Condoms, although categorized as a less
Supplement
12 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
effective method of pregnancy prevention (6), remain vital
for STD/HIV prevention and promoting condom use is
particularly important given increasing STD rates in the
United States (5). Professional medical organizations (7,8) and
federal agencies, including CDC, recommend using condoms
for STD/HIV prevention with a more effective method of
contraception for optimal protection against unintended
pregnancy (9). However, recent decreases in condom use
have been documented, and the proportion of adolescents
using condoms with more effective methods of contraception
has been consistently low, with recent national estimates of
approximately 9% of sexually active high school students (10).
Because of these challenges to pregnancy- and STD/HIV-
prevention goals, monitoring condom and contraceptive use
behaviors among sexually active youths is essential. This study
reports prevalence estimates from the 2019 Youth Risk Behavior
Survey (YRBS) for any condom use at last sexual intercourse
among sexually active U.S. high school students. In addition,
prevalence estimates of primary contraceptive method use and
condom use with more effective methods of contraception
at last sexual intercourse among sexually active students who
had sexual contact with the opposite sex during their lifetime
are reported. Variations in these behaviors by demographic
characteristics and sexual risk behaviors were examined to
support public health professionals in implementing quality
sexual and reproductive health education and clinical services
that prevent STDs/HIV and unintended pregnancy.
Methods
Data Source
This report includes data from the 2019 YRBS, a cross-
sectional, school-based survey conducted biennially since
1991. Each survey year, CDC collects data from a nationally
representative sample of public and private school students in
grades 9–12 in the 50 U.S. states and the District of Columbia.
Additional information about YRBS sampling, data collection,
response rates, and processing is available in the overview report
of this supplement (11). The prevalence estimates for all sexual
behavior questions for the overall study population and by
sex, race/ethnicity, grade, and sexual orientation are available
at https://nccd.cdc.gov/youthonline/App/Default.aspx. The
full YRBS questionnaire is available at https://www.cdc.gov/
healthyyouth/data/yrbs/pdf/2019/2019_YRBS-National-HS-
Questionnaire.pdf.
Measures
Behaviors analyzed included any condom use, primary
contraceptive method, and condom use with more effective
methods of contraception, all reported at last sexual intercourse.
Any condom use was assessed by the question, “The last time
you had sexual intercourse, did you or your partner use a
condom?” Response options included the following: I have
never had sexual intercourse, yes, or no. Primary contraceptive
method was assessed through a separate question, “The last
time you had sexual intercourse, what one method did you or
your partner use to prevent pregnancy?” Respondents could
select only one response from the following list of options:
I have never had sexual intercourse; no method was used to
prevent pregnancy; birth control pills; condoms; an IUD
(such as Mirena or ParaGard) or implant (such as Implanon
or Nexplanon); a shot (such as Depo-Provera), patch (such
as Ortho Evra), or birth control ring (such as NuvaRing);
withdrawal or some other method; or not sure. Dichotomous
(yes versus no) variables for each response option were created,
except for “not sure”; although participants selecting this
response (n = 93; 3.9%) were included in the analytic sample,
prevalence estimates for this category are not reported.
A dichotomous (yes versus no) variable for any condom
use with an IUD, implant, shot, patch, ring, or birth control
pills was constructed by using the separate items for any
condom use and primary contraceptive method at last sexual
intercourse. These two items were also used to create the
following dichotomous (yes versus no) indicators: condom
use only (yes to any condom use and condoms or no method
for pregnancy prevention); highly or moderately effective
contraceptive use only (no to any condom use and an IUD,
implant, shot, patch, ring, or birth control pills for pregnancy
prevention); withdrawal or some other contraceptive method
use only (no to any condom use and withdrawal or some other
method for pregnancy prevention); and use of no condom and
no primary contraceptive method (no to any condom use and
no method for pregnancy prevention).
Condom and contraceptive use were examined by
demographic characteristics and sexual risk behaviors.
Demographic characteristics included sex (female or male),
race/ethnicity (non-Hispanic white [white], non-Hispanic
black [black], or Hispanic; other/multiple responses are not
reported), and grade (9, 10, 11, or 12). Four dichotomous
sexual risk behaviors were created: age of sexual initiation
(<13 years versus ≥13 years); lifetime number of sex partners
(1–3 versus ≥4); number of sex partners during the previous
3 months (1 versus ≥2); and alcohol or drug use before last
sexual intercourse (yes versus no).
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 13
US Department of Health and Human Services/Centers for Disease Control and Prevention
Analysis
The analytic sample was restricted to sexually active students
(i.e., those who reported having had sexual intercourse with
one or more persons during the 3 months before the survey).
Analyses involving pregnancy prevention methods excluded
students who only had same-sex sexual contacts during their
lifetime, on the basis of an item about respondents’ sex (“What
is your sex?” with response options including female or male)
and another item assessing the sex of sexual contacts (“During
your life, with whom have you had sexual contact?” with
response options including I have never had sexual contact,
females, males, and females and males).
All analyses were conducted using SUDAAN (version 11.0.0;
RTI International) to account for the complex sampling design.
Weighted prevalence estimates and 95% confidence intervals
were calculated for each outcome. Chi-square statistics
were used to examine bivariate differences by demographic
characteristics and sexual risk behaviors. For significant overall
differences by race/ethnicity and grade, t-tests were used to
identify pairwise differences. Differences were considered
significant if p<0.05.
Results
Among the 27.4% of sexually active students (n = 3,226),
approximately half were female (52.2%) and white (52.3%);
approximately one third were in grade 12 (36.9%) (Table 1).
Regarding sexual risk behaviors among those sexually active
students, 7.0% had sexual intercourse for the first time before
age 13 years (3.0% of all YRBS respondents reported having
had sexual intercourse for the first time before age 13 years);
26.9% had sexual intercourse with ≥4 persons during their
lifetime (8.6% of all YRBS respondents reported having had
sexual intercourse with ≥4 persons during their lifetime);
20.5% had sexual intercourse with ≥2 persons during the
previous 3 months; and 21.2% had drunk alcohol or used
drugs before last sexual intercourse.
Among sexually active students, prevalence of any condom
use at last sexual intercourse was 54.3% (Table 2). Among
sexually active students who reported having had sexual
contact with someone of the opposite sex (i.e., excluding
those who reported only same-sex sexual contact) (n = 2,698),
condoms (43.9%) were the most prevalent primary pregnancy
prevention method, based on responses to the distinct item
assessing pregnancy prevention method, followed by birth
control pills (23.3%); withdrawal or other method (10.1%);
IUD or implant (4.8%); and shot, patch, or ring (3.3%). (Of
participants excluded from the analytic sample for primary
method of pregnancy prevention, 95 students reported having
had only same-sex sexual contact and 433 students did not
answer the questions, “What is your sex?” or “During your life,
with whom have you had sexual contact?”) Approximately one
tenth (10.7%) had not used a pregnancy prevention method
at last sexual intercourse; 9.1% had used a condom with an
IUD, implant, shot, patch, ring, or birth control pills at last
sexual intercourse. Prevalence of condom and IUD or implant
use (<1.0%) and condom and shot, patch, or ring use (<1.0%)
was lower than condom and birth control pills use (7.5%).
Prevalence estimates for mutually exclusive categories that
reflect both pregnancy and STD/HIV prevention effectiveness
and account for any condom use in addition to a primary
pregnancy prevention method indicate that condom use
only was most common (44.3%), followed by highly or
moderately effective contraceptive method use only (22.2%)
(Figure). Prevalence of condom use with an IUD, implant,
shot, patch, ring, or birth control pills (9.1%) was similar to
prevalence of using withdrawal or other method only (9.5%)
and using no condom and no primary pregnancy prevention
method (10.3%).
Analyses revealed significant differences in any condom
use and primary pregnancy prevention method at last sexual
intercourse by demographic characteristics (Table 2). By
sex, no differences occurred in not using any method of
pregnancy prevention (i.e., no method); however, differences
were identified in type of method used. Compared with male
students’ report of contraceptive use by their female partner,
prevalence as reported by female students was higher for shot,
patch, or ring (4.5% versus 2.1%) and birth control pills
(26.1% versus 20.2%). In contrast, prevalence of condom use
as the primary method for pregnancy prevention reported by
male students (49.4%) was higher than female students’ report
of condom use by their male partner (38.8%), as was any
condom use at last sexual intercourse (60.0% versus 49.6%).
A similar pattern emerged when examining prevalence of
any condom and primary contraceptive method use by grade.
The prevalence of using no method was the same across grades;
however, differences occurred in method type. Any condom
use and condom use as the primary pregnancy prevention
method was more prevalent in lower versus higher grades. In
contrast, use of an IUD or implant; birth control pills; and
condom with an IUD or implant, shot, patch, ring, or birth
control pills was typically more prevalent in higher versus lower
grades. For example, condom use as the primary pregnancy
prevention method was more common among students in
grades 9 (55.3%), 10 (47.7%), and 11 (45.3%) versus students
in grade 12 (37.4%) (and grade 9 versus grade 11), whereas
IUD or implant use was less common among 9th-grade
Supplement
14 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Prevalence of demographic characteristics and sexual risk behaviors among sexually active* high school students — Youth Risk
Behavior Survey, United States, 2019
Characteristic No.
†
(%
§
) 95% CI
Sex
Female 1,679 (52.2) 49.4–55.0
Male 1,510 (47.8) 45.0–50.6
Race/Ethnicity
¶
Black, non-Hispanic 474 (11.2) 8.9–14.0
Hispanic 771 (28.4) 22.3–35.5
White, non-Hispanic 1,602 (52.3) 46.4–58.1
Grade
9 389 (11.3) 9.8–13.0
10 741 (21.4) 19.3–23.6
11 967 (30.4) 27.8–33.2
12 1,089 (36.9) 33.4–40.4
Sexual risk behavior
Had sexual intercourse before age 13 years 242 (7.0) 5.7–8.5
Had sexual intercourse with ≥4 persons during their lifetime 854 (26.9) 24.3–29.7
Had sexual intercourse with ≥2 persons during the previous 3 months 658 (20.5) 18.5–22.7
Had drunk alcohol or used drugs before last sexual intercourse 652 (21.2) 18.8–23.9
Abbreviation: CI = confidence interval.
* Defined as having had sexual intercourse with at least one person during the 3 months before the survey (n = 3,226).
†
Unweighted.
§
Weighted estimates.
.
¶
Race/ethnicity values do not total 100% because “other/multiple” responses are not reported (i.e., American Indian/Alaska Native, Asian, Native Hawaiian/Other
Pacific Islander, and multiple race).
students (<1.0%), compared with students in grades 10 (3.3%),
11 (3.2%), and 12 (8.2%). Prevalence of IUD or implant use
among 10th- and 11th-grade students was also lower than
among 12th-grade students.
In contrast with sex and grade, not using a pregnancy
prevention method differed by race/ethnicity, with higher
prevalence of no method among black (23.2%) and Hispanic
(12.8%) students, compared with white students (6.8%);
compared with Hispanic students, using no pregnancy
prevention method was more common among black students.
Additional racial/ethnic differences in type of method were
identified, with the general pattern that prevalence of using
a more effective method of contraception was lower among
black and Hispanic students compared with white students.
Specifically, prevalence among black and Hispanic students
was lower than among white students for use of an IUD or
implant (2.0% and 1.6% versus 6.7%, respectively); birth
control pills (12.1% and 15.5% versus 29.7%, respectively);
and condom use with an IUD, implant, shot, patch, ring, or
birth control pills (7.5% and 4.8% versus 12.4%, respectively).
In contrast, prevalence of withdrawal or other method use was
higher among black (13.9%) and Hispanic (13.1%) students
than among white students (7.7%). Condom use as the
primary method for pregnancy prevention was higher among
Hispanic students (49.6%), compared with black (37.2%) and
white (42.3%) students, and any condom use at last sexual
intercourse was higher among Hispanic (56.2%) and white
(55.8%) students compared with black students (48.2%).
Differences by sexual risk behaviors in the prevalence of using no
contraceptive method and in the type of method used, including
any condom use, also were observed (Table 3). Comparing
students who had initiated sex before age 13 years with students
who had not, differences in no method use were not significant;
however, prevalence was lower for any condom use at last sexual
intercourse (40.9% versus 55.4%), condom use as the primary
method of pregnancy prevention (30.4% versus 44.8%), and
withdrawal or other method use (5.5% versus 10.4%). Students
who had ≥4 lifetime partners had higher prevalence of no method
use (14.7% versus 9.2%) and lower prevalence of any condom
use (46.6% versus 57.1%); condom use as the primary pregnancy
prevention method (36.2% versus 46.6%); and condom use with
an IUD, implant, shot, patch, ring, or birth control pills (6.5%
versus 10.1%) compared with students who had <4 lifetime sex
partners. A similar pattern was observed for students who reported
having had ≥2 recent partners, although no significant differences
in no method use were observed. Comparing students who had
drunk alcohol or used drugs before last sexual intercourse with
students who had not, use of no method was higher (14.7%
versus 9.6%), whereas any condom use (47.4% versus 56.0%)
and condom use as the primary pregnancy prevention method
(39.3% versus 45.1%) were lower.
Discussion
This report provides the most recent nationally representative
estimates of condom and contraceptive use among sexually
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 15
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Prevalence of condom and primary contraceptive use at last sexual intercourse among sexually active* high school students, by
demographic characteristics — Youth Risk Behavior Survey, United States, 2019
Demographic
characteristic
Any
condom use
†
Primary contraceptive method Condoms and IUD,
implant, shot,
patch, ring, or
birth control pills
IUD or
implant
Shot, patch,
or ring
Birth control
pills
Condom
Withdrawal or
other method
No
method
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
Total 54.3
(52.0–56.6)
NA 4.8
(3.3–7.0)
NA 3.3
(2.3–4.7)
NA 23.3
(19.8–27.2)
NA 43.9
(40.6–47.3)
NA 10.1
(8.5–12.0)
NA 10.7
(8.8–12.8)
NA 9.1
(7.4–11.2)
NA
Sex NA <0.01 NA 0.20 NA <0.05 NA <0.01 NA <0.01 NA 0.34 NA 0.21 NA 0.10
Female 49.6
(45.6–53.6)
NA 5.6
(4.0–7.6)
NA 4.5
(2.9–6.8)
NA 26.1
(22.1–30.5)
NA 38.8
(34.0–44.0)
NA 10.8
(8.9–13.0)
NA 11.9
(9.1–15.3)
NA 10.3
(8.3–12.7)
NA
Male 60.0
(57.0–63.0)
NA 4.0
(2.1–7.4)
NA 2.1
(1.2–3.6)
NA 20.2
(16.4–24.7)
NA 49.4
(45.8–53.1)
NA 9.3
(7.1–12.2)
NA 9.3
(7.1–12.1)
NA 7.9
(5.8–10.7)
NA
Grade NA <0.05 NA <0.01 NA 0.29 NA <0.01 NA <0.01 NA 0.20 NA 0.63 NA <0.01
9 61.3**
(54.6–67.5)
NA 0.1**
,††,§§
(0.0–0.7)
NA 2.4
(0.9–6.2)
NA 10.9**
,††
(6.0–19.1)
NA 55.3**
,††
(47.4–62.9)
NA 10.6
(6.9–15.9)
NA 14.1
(9.1–21.2)
NA 4.7**
(2.7–8.2)
NA
10 55.4
(50.2–60.4)
NA 3.3**
(2.0–5.6)
NA 2.1
(1.0–4.4)
NA 18.2**
,††
(13.4–24.3)
NA 47.7**
(41.2–54.3)
NA 12.5
(9.5–16.4)
NA 10.5
(7.2–15.1)
NA 7.0**
(4.7–10.3)
NA
11 56.3
(51.9–60.6)
NA 3.2
**
(1.8–5.8)
NA 4.2
(2.6–6.7)
NA 25.8
(21.0–31.3)
NA 45.3**
(39.4–51.4)
NA 7.9
(5.9–10.5)
NA 10.1
(7.9–12.8)
NA 8.9
(6.1–12.9)
NA
12 50.3
(46.9–53.8)
NA 8.2
(5.5–12.2)
NA 3.6
(2.0–6.3)
NA 27.7
(23.3–32.5)
NA 37.4
(33.4–41.6)
NA 10.3
(7.9–13.3)
NA 10.2
(6.9–14.9)
NA 11.6
(8.9–15.0)
NA
Race/Ethnicity NA <0.05 NA <0.01 NA 0.07 NA <0.01 NA <0.01 NA <0.01 NA <0.01 NA <0.01
Black, non-Hispanic 48.2
¶¶,
***
(43.2–53.3)
NA 2.0
¶¶
(1.0–4.0)
NA 5.4
(2.9–9.9)
NA 12.1
¶¶
(8.7–16.5)
NA 37.2***
(31.2–43.6)
NA 13.9
¶¶
(8.4–22.2)
NA 23.2
¶¶,
***
(19.2–27.7)
NA 7.5
¶¶
(5.1–10.8)
NA
Hispanic 56.2
(52.0–60.3)
NA 1.6
¶¶
(0.7–3.4)
NA 1.4
(0.6–3.2)
NA 15.5
¶¶
(11.5–20.5)
NA 49.6
¶¶
(44.7–54.4)
NA 13.1
¶¶
(10.0–17.0)
NA 12.8
¶¶
(9.1–17.8)
NA 4.8
¶¶
(3.1–7.4)
NA
White, non-Hispanic 55.8
(52.9–58.6)
NA 6.7
(5.0–9.0)
NA 4.0
(2.5–6.4)
NA 29.7
(25.7–34.0)
NA 42.3
(38.2–46.5)
NA 7.7
(6.1–9.8)
NA 6.8
(5.3–8.6)
NA 12.4
(10.1–15.2)
NA
Abbreviations: CI = confidence interval; IUD = intrauterine device; NA = not applicable.
* Defined as having had sexual intercourse with at least one person during the 3 months before the survey (n = 3,226). Except for any condom use at last sexual intercourse, students
reporting only same-sex sexual contact use were excluded; therefore, the analytic sample was restricted to sexually active students who reported having had sexual contact with someone
of the opposite sex (n = 2,698). Among sexually active students, excluding those who only had same-sex sexual contact, a total of 93 (3.9%) students answered the pregnancy prevention
question “not sure”; findings are not presented for this group.
†
Any condom use at last sexual intercourse was measured by a separate item from condoms as the primary method used for preventing pregnancy.
§
Weighted estimates.
¶
Significance is defined as p<0.05, by chi-square test.
** Significantly different than grade 12, by linear contrast t-test
††
Significantly different than grade 11, by linear contrast t-test.
§§
Significantly different than grade 10, by linear contrast t-test.
¶¶
Significantly different than white, non-Hispanic race/ethnicity, by linear contrast t-test.
*** Significantly different than Hispanic race/ethnicity, by linear contrast t-test.
active U.S. high school students. In addition, notable differences
in these behaviors by demographic characteristics and sexual
risk behaviors are identified that can support implementation
of interventions to improve condom and contraceptive use
among adolescents most in need. Doing so will help to achieve
unintended pregnancy and STD/HIV prevention goals,
including reducing disparities by race/ethnicity.
Overall, most (89.7%) sexually active students (excluding
those who only reported same-sex sexual contact) used a
condom or a primary contraceptive method at last sexual
intercourse, yet approximately one fifth (19.8%) reported
using withdrawal or some other method only or no condom
and no primary contraceptive method. Moreover, prevalence
estimates by method type, as well as differences by demographic
characteristics and sexual risk behaviors, underscore the
importance of meeting the unintended pregnancy and STD/
HIV prevention needs of all sexually active high school students.
Only 9.1% of sexually active students (excluding those who
only reported same-sex sexual contact) reported having used a
condom with a more effective contraceptive method, which is
the recommended approach for preventing both unintended
pregnancy and STDs/HIV because the most effective forms of
contraception confer no STD/HIV protection (7–9). Although
use of condoms alone can prevent both adverse outcomes and
was the most prevalent method used, only approximately half
of sexually active students reported any condom use at last
sexual intercourse, which is concerning given the high risk
for STDs among this population (5). Moreover, condoms are
categorized as a less effective pregnancy prevention method,
given that they are associated with a 13.0% pregnancy risk
during the first year of typical use (6), and prevalence of
any highly or moderately effective method use at last sexual
intercourse was only 31.4%.
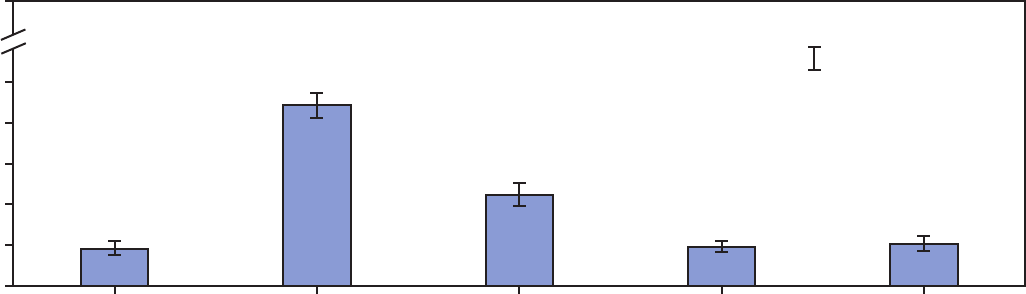
Supplement
16 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. Prevalence of condom and primary contraceptive use* at last sexual intercourse among sexually active
†
high school students —
Youth Risk Behavior Survey, United States, 2019
0
10
20
30
40
50
100
Condom with highly or
moderately eective
contraceptive
method
Condom
only
Highly or
moderately eective
contraceptive
method only
Method used
Withdrawal or other
contraceptive
method only
No condom and
no primary
contraceptive
method
Prevalence (%)
95% Condence interval
* Condom with highly or moderately effective contraceptive method = students who responded “yes” to any condom use at last sexual intercourse and intrauterine
device or implant; shot, patch, or ring; or birth control pills (i.e., highly or moderately effective methods) as primary pregnancy prevention method. Condom only =
students who responded “yes” to any condom use at last sexual intercourse and condom or no method as primary pregnancy prevention method. Highly or
moderately effective contraceptive method only = students who responded “no” to any condom use at last sexual intercourse and intrauterine device or implant;
shot, patch, or ring; or birth control pills (i.e., highly or moderately effective methods) as primary pregnancy prevention method. Withdrawal or other contraceptive
method only = students who responded “no” to any condom use at last sexual intercourse and withdrawal or some other method as primary pregnancy prevention
method. No condom and no primary contraceptive method = students who responded “no” to any condom use at last sexual intercourse and no method of
pregnancy prevention.
†
Defined as having had sexual intercourse with at least one person during the 3 months before the survey (n = 2,698). Students reporting only same-sex sexual
contact were excluded from the analytic sample.
Notable demographic differences in condom and contraceptive
use warrant particular attention. Compared with white students,
black and Hispanic students had higher prevalence of no
pregnancy prevention method use and lower prevalence of
highly and moderately effective contraceptive method use. Black
students also had lower prevalence of any condom use at last sexual
intercourse than white and Hispanic students. On the basis of
these findings and the documented racial/ethnic disparities in birth
and STD rates among adolescents (4,5), meeting the unintended
pregnancy and STD/HIV prevention needs of black and Hispanic
youths is vital. Understanding and addressing structural barriers
that might contribute to the observed differences are important
next steps. As for grade, differences indicate that younger students
are more likely to use condoms, whereas older students are more
likely to use an IUD or implant, birth control pills, and condoms
with a more effective contraceptive method. Therefore, improving
younger adolescents’ knowledge of, comfort with, and access to the
most effective methods of pregnancy and STD/HIV prevention is
needed. Whereas findings related to race/ethnicity and grade have
clear practice implications, patterns by sex might largely reflect
reporting differences on the basis of who uses a given method. As
compared with female students, the proportion of male students
reporting condom use was higher, and the proportion reporting
their partners’ use of shot, patch, or ring, and birth control pill use
was lower. For the latter female-controlled methods, self-report
by females is considered more accurate (12).
Finally, differences in condom and contraceptive use by
sexual risk behaviors reveal that use of preventive strategies
is suboptimal among high school students who engage in
those behaviors. The general pattern was that students with a
given risk indicator, compared with those without, had lower
prevalence of condom use and higher prevalence of using
no method of contraception, although not all differences
were significant. Such findings might reflect potential
disempowerment in sexual interactions (13) and the challenge
of using condoms correctly and consistently while under the
influence of alcohol or drugs (14). Because number of partners
is an indicator of STD/HIV risk, findings that students
with ≥2 recent or ≥4 lifetime partners had lower prevalence
of condom use, alone or with a highly or moderately effective
contraceptive method, are particularly concerning.
Collectively, these findings from the 2019 YRBS highlight the
importance of programmatic efforts that can improve condom
and contraceptive use among adolescents. The effectiveness of
sexual risk reduction education is well documented (15); because
of given decreasing attention to condom-related topics in school-
based instruction (16), efforts to strengthen implementation
are warranted. Such education should ensure that highly and
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 17
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 3. Prevalence of condom and primary contraceptive use at last sexual intercourse among sexually active* high school students, by
sexual risk behaviors — Youth Risk Behavior Survey, United States, 2019
Sexual risk behavior
Any
condom use
†
Primary contraceptive method Condom and IUD,
implant, shot,
patch, ring, or
birth control pills
IUD or
implant
Shot, patch,
or ring
Birth control
pills
Condom
Withdrawal or
other method
No
method
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
%
§
(95%
CI)
p
value
¶
Had sexual
intercourse before
age 13 years
NA <0.05 NA 0.05 NA 0.83 NA 0.81 NA <0.05 NA <0.05 NA 0.05 NA 0.12
Yes 40.9
(30.4–52.4)
NA 2.6
(1.1–6.0)
NA 3.0
(1.0–8.2)
NA 22.1
(13.4–34.1)
NA 30.4
(19.3–44.2)
NA 5.5
(2.9–10.3)
NA 22.8
(12.6–37.7)
NA 4.8
(1.7–13.3)
NA
No 55.4
(52.9–57.9)
NA 5.0
(3.4–7.2)
NA 3.4
(2.3–4.9)
NA 23.4
(19.7–27.5)
NA 44.8
(41.4–48.3)
NA 10.4
(8.6–12.5)
NA 9.8
(8.0–12.0)
NA 9.4
(7.6–11.6)
NA
Had sexual
intercourse with
≥4 persons during
their lifetime
NA <0.01 NA <0.01 NA 0.60 NA 0.43 NA <0.01 NA 0.32 NA <0.05 NA <0.05
Yes 46.6
(42.9–50.2)
NA 7.4
(5.0–10.8)
NA 2.9
(1.6–5.2)
NA 21.5
(17.0–26.9)
NA 36.2
(31.0–41.7)
NA 11.5
(8.7–15.0)
NA 14.7
(10.9–19.6)
NA 6.5
(4.3–9.8)
NA
No 57.1
(54.3–59.8)
NA 3.9
(2.6–5.8)
NA 3.5
(2.3–5.4)
NA 23.9
(19.7–28.6)
NA 46.6
(43.1–50.1)
NA 9.6
(7.7–11.9)
NA 9.2
(7.3–11.7)
NA 10.1
(8.1–12.4)
NA
Had sexual
intercourse with
≥2 persons during
the previous
3 months
NA <0.01 NA 0.69 NA <0.05 NA 0.13 NA <0.05 NA 0.14 NA 0.20 NA <0.01
Yes 47.1
(43.1–51.1)
NA 5.0
(3.1–8.0)
NA 1.7
(0.6–4.5)
NA 19.9
(15.1–25.8)
NA 39.3
(35.1–43.7)
NA 12.7
(9.2–17.3)
NA 14.0
(9.5–20.0)
NA 5.2
(3.2–8.4)
NA
No 56.2
(53.4–58.9)
NA 4.7
(3.3–6.8)
NA 3.7
(2.6–5.3)
NA 24.1
(20.4–28.3)
NA 45.1
(41.3–48.9)
NA 9.4
(7.7–11.4)
NA 9.8
(8.2–11.7)
NA 10.1
(8.3–12.4)
NA
Had drunk alcohol or
used drugs before
last sexual
intercourse
NA <0.05 NA 0.35 NA 0.35 NA 0.10 NA <0.05 NA 0.68 NA <0.05 NA 0.10
Yes 47.4
(42.0–52.9)
NA 5.7
(3.6–8.9)
NA 2.3
(1.1–5.1)
NA 20.5
(16.2–25.7)
NA 39.3
(33.4–45.5)
NA 10.6
(7.4–15.0)
NA 14.7
(11.0–19.3)
NA 6.4
(3.9–10.5)
NA
No 56.0
(53.1–58.8)
NA 4.7
(3.1–6.9)
NA 3.5
(2.3–5.4)
NA 24.0
(20.4–28.1)
NA 45.1
(41.7–48.6)
NA 9.7
(7.9–11.9)
NA 9.6
(7.6–12.2)
NA 9.6
(7.6–12.1)
NA
Abbreviations: CI = confidence interval; IUD = intrauterine device; NA = not applicable.
* Defined as having had sexual intercourse with at least one person during the 3 months before the survey (n = 3,226). Except for any condom use at last sexual intercourse, students reporting
only same-sex sexual contact use were excluded; therefore, the analytic sample was restricted to sexually active students who reported having had sexual contact with someone of the
opposite sex (n = 2,698). Among sexually active students, excluding those who only had same-sex sexual contact, a total of 93 (3.9%) students answered the pregnancy prevention question
“not sure”; findings are not presented for this group.
†
Any condom use at last sexual intercourse was measured by a separate item from condoms as the primary method used for preventing pregnancy.
§
Weighted estimates.
¶
Statistical significance is defined as p<0.05, by chi-square test.
moderately effective contraceptive methods are clearly addressed,
including in earlier grades (e.g., middle school). Doing so in the
context of broader education about health services might be a
developmentally appropriate approach.
Engaging directly with communities most affected by
unintended pregnancy and STD/HIV can be one strategy to help
identify and address social determinants of health that contribute
to disparities in condom and contraceptive use. Furthermore,
education and clinical services can be delivered through
community- and school-based programs tailored to serve young
persons most in need. Fostering community–clinic partnerships
through youth-serving organizations is one strategy for reaching
the most vulnerable adolescents. Such partnerships can help
address barriers and improve access to sexual and reproductive
health care, either through referral or service integration (17).
In addition to access, delivery of comprehensive, client-
centered, and adolescent-friendly care by well-trained
providers is essential. For example, same-day initiation of
long-acting reversible contraception methods (i.e., providing
the method during the initial appointment) is a best practice
that can facilitate adolescents’ access to these methods (17).
Another example is provider counseling about condom use
with more effective contraceptive methods, which has been
associated with adolescents’ use of this prevention strategy (18).
Integrating unintended pregnancy and STD/HIV prevention
in school-, clinic-, and community-based health promotion
likely requires explicit attention to individual prevention goals as
well as preferences related to the various prevention strategies (19).
Supplement
18 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Limitations
General limitations for the YRBS are available in the overview
report of this supplement (11). The findings in this report are
subject to at least five additional limitations. First, male students’
report of their female partners’ contraceptive use might not be
accurate (11). Second, distinguishing the intended purpose of
condom use in relation to pregnancy and STD/HIV prevention
is not feasible. Although YRBS assesses condom use as a primary
method for pregnancy prevention, condom use for STD/HIV
prevention is not explicitly measured. Third, condom use with
a more effective contraceptive method might be underestimated
because respondents could only select one method of pregnancy
prevention at last sexual intercourse. Fourth, the estimates
for highly and moderately effective contraception could be
underestimated if respondents viewed a less effective option (i.e.,
condoms or withdrawal or some other method) as their primary
contraceptive method used at last sexual intercourse. Finally,
because the sex of last sex partner is not measured, the analytic
sample might include students with same-sex partners at last
sexual intercourse for whom pregnancy prevention is not needed.
Conclusion
Ongoing national surveillance will remain important to
understanding the population-level effects of public health and
clinical approaches to preventing unintended pregnancy and
STDs/HIV among young persons. To complement these efforts,
implementation science and observational research should
address unresolved questions (e.g., young men’s role in condom
and contraceptive use, barriers and facilitators to integration of
pregnancy and STD/HIV prevention, and effective strategies
for addressing disparities, including racial/ethnic differences).
Taken together, these data can be used to improve condom and
contraceptive use for all sexually active adolescents.
Conflicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. US Department of Health and Human Services. Healthy people 2020:
sexually transmitted diseases. Washington, DC: US Department of
Health and Human Services; 2020. https://www.healthypeople.
gov/2020/topics-objectives/topic/sexually-transmitted-diseases
2. Lindberg LD, Santelli JS, Desai S. Changing patterns of contraceptive
use and the decline in rates of pregnancy and birth among US
adolescents, 2007–2014. J Adolesc Health 2018;63:253–6. https://doi.
org/10.1016/j.jadohealth.2018.05.017
3. Sedgh G, Finer LB, Bankole A, Eilers MA, Singh S. Adolescent
pregnancy, birth, and abortion rates across countries: levels and recent
trends. J Adolesc Health 2015;56:223–30. https://doi.org/10.1016/j.
jadohealth.2014.09.007
4. Martin J, Hamilton B, Osterman M, Driscoll A. Births: final data for
2018. Hyattsville, MD: National Center for Health Statistics; 2019.
https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_13-508.pdf
5. CDC. Sexually transmitted disease surveillance 2018. Atlanta, GA: US
Department of Health and Human Services, CDC; 2019. https://www.
cdc.gov/std/stats18/default.htm
6. Trussell J, Aiken ARA, Micks E, Guthrie KA. Efficacy, safety, and personal
considerations. In: Contraceptive technology. 21st ed. Atlanta, GA:
Managing Contraception; 2018.
7. Committee on Adolescent Health Care Long-Acting Reversible
Contraception Working Group, American College of Obstetricians and
Gynecologists. Committee opinion no. 539: adolescents and long-acting
reversible contraception: implants and intrauterine devices. Obstet
Gynecol 2012;120:983–8. https://doi.org/10.1097/
AOG.0b013e3182723b7d
8. Committee on Adolescence. Contraception for adolescents. Pediatrics
2014;134:e1244-56. https://doi.org/10.1542/peds.2014-2299
9. Gavin L, Moskosky S, Carter M, et al. Providing quality family planning
services: recommendations of CDC and the U.S. Office of Population
Affairs. MMWR Recomm Rep 2014;63(No. RR-04).
10. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—
United States, 2017. MMWR Surveill Summ 2018;67(No. SS-8).
https://doi.org/10.15585/mmwr.ss6708a1
11. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
12. Brauner-Otto S, Yarger J, Abma J. Does it matter how you ask? Question
wording and males’ reporting of contraceptive use at last sex. Soc Sci
Res 2012;41:1028–36. https://doi.org/10.1016/j.ssresearch.2012.04.004
13. Seth P, DiClemente RJ, Loworn AE. State of the evidence: intimate
partner violence and HIV/STI risk among adolescents. Curr HIV Res
2013;11:528–35.
14. Parkes A, Wight D, Henderson M, Hart G. Explaining associations
between adolescent substance use and condom use. J Adolesc Health
2007;40:180.e1-18.
15. Chin HB, Sipe TA, Elder R, et al; Community Preventive Services Task
Force. The effectiveness of group-based comprehensive risk-reduction
and abstinence education interventions to prevent or reduce the risk of
adolescent pregnancy, human immunodeficiency virus, and sexually
transmitted infections: two systematic reviews for the Guide to
Community Preventive Services. Am J Prev Med 2012;42:272–94.
https://doi.org/10.1016/j.amepre.2011.11.006
16. Lindberg LD, Maddow-Zimet I, Boonstra H. Changes in adolescents’
receipt of sex education, 2006–2013. J Adolesc Health 2016;58:621–7.
https://doi.org/10.1016/j.jadohealth.2016.02.004
17. Brittain AW, Tevendale HD, Mueller T, et al. The teen access and quality
initiative: improving adolescent reproductive health best practices in
publicly funded health centers. J Community Health 2020;45:615–25.
https://doi.org/10.1007/s10900-019-00781-z
18. Morroni C, Heartwell S, Edwards S, Zieman M, Westhoff C. The impact
of oral contraceptive initiation on young women’s condom use in 3
American cities: missed opportunities for intervention. PLoS One
2014;9:e101804. https://doi.org/10.1371/journal.pone.0101804
19. Steiner RJ, Liddon N, Swartzendruber AL, Pazol K, Sales JM. Moving
the message beyond the methods: toward integration of unintended
pregnancy and sexually transmitted infection/HIV prevention. Am J
Prev Med 2018;54:440–3. https://doi.org/10.1016/j.amepre.2017.10.022

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 19
US Department of Health and Human Services/Centers for Disease Control and Prevention
Trends in Violence Victimization and Suicide Risk by Sexual Identity
Among High School Students — Youth Risk Behavior Survey,
United States, 2015–2019
Michelle M. Johns, PhD
1
; Richard Lowry, MD
2
; Laura T. Haderxhanaj, PhD
3
; Catherine N. Rasberry, PhD
1
; Leah Robin, PhD
1
; Lamont Scales, MA
4
;
Deborah Stone, ScD
5
; Nicolas A. Suarez, MPH
1
1
Division of Adolescent and School Health, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC;
2
Office of the Director, National
Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC;
3
Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD,
and TB Prevention, CDC;
4
Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC;
5
Division of Injury Prevention, National Center for Injury Prevention and Control, CDC
Abstract
Lesbian, gay, and bisexual (LGB) youths continue to experience more violence victimization and suicide risk than heterosexual
youths; however, few studies have examined whether the proportion of LGB youths affected by these outcomes has varied over
time, and no studies have assessed such trends in a nationally representative sample. This report analyzes national trends in violence
victimization and suicide risk among high school students by self-reported sexual identity (LGB or heterosexual) and evaluates
differences in these trends among LGB students by sex (male or female) and race/ethnicity (non-Hispanic black, non-Hispanic
white, or Hispanic). Data for this analysis were derived from the 2015, 2017, and 2019 cycles of CDC’s Youth Risk Behavior Survey
(YRBS), a cross-sectional, school-based survey conducted biennially since 1991. Logistic regression models assessed linear trends
in prevalence of violence victimization and indicators of suicide risk among LGB and heterosexual students during 2015–2019;
in subsequent models, sex-stratified (controlling for race/ethnicity and grade) and race/ethnicity-stratified (controlling for sex
and grade) linear trends were examined for students self-identifying as LGB during 2015–2019. Results demonstrated that LGB
students experienced more violence victimization and reported more suicide risk behaviors than heterosexual youths. Among LGB
youths, differences in the proportion reporting violence victimization and suicide risk by sex and race/ethnicity were found. Across
analyses, very few linear trends in these outcomes were observed among LGB students. Results highlight the continued need for
comprehensive intervention strategies within schools and communities with the express goal of reducing violence victimization
and preventing suicide risk behaviors among LGB students.
Introduction
Lesbian, gay, and bisexual (LGB) youths experience more
violence victimization and suicide risk than heterosexual youths
(1–3). In 2015, CDC’s Youth Risk Behavior Surveillance
System (YRBSS) added two new questions to the national
questionnaire regarding sexual identity and sexual behavior.
These questions facilitated the first nationally representative
estimates of the health behaviors and experiences of sexual
minority youths (students who identify as LGB or those who
have sexual contact with persons of the same or both sexes)
and affirmed the presence of substantial health disparities (i.e.,
differences in health outcomes between social groups driven
by unequal social or environmental circumstances) in violence
victimization and suicide risk between LGB and heterosexual
youths . Findings from the 2017 Youth Risk Behavior Survey
Corresponding author: Michelle M. Johns, PhD, National Center
for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC.
Telephone: 404-718-8858. E-mail: [email protected].
(YRBS) revealed that LGB high school students experienced
more bullying at school (33% among LGB students and 17%
among heterosexual students), more sexual dating violence
by dating partners (LGB, 16%; heterosexual, 6%), and more
suicide attempts (LGB, 23%; heterosexual, 5%) (3) than their
heterosexual peers.
Notably, the 2019 YRBS data collection cycle presented
the first opportunity for examining linear trends in violence
victimization and suicide risk trends for LGB students across
time in a nationally representative sample. Few studies have
examined whether prevalence of violence victimization and
suicide risk varies among LGB youths over time (4). School
environments in the United States might be improving in their
ability to meet the needs of LGB youths (5); for example, recent
surveillance data from CDC’s 2018 School Health Profiles,
which include representative data from 43 states, provide
evidence that many schools are implementing supportive
practices. In the 2018 School Health Profiles, an average of
78.5% of schools across U.S. states included in the sample
reported identifying safe spaces for LGB and transgender
Supplement
20 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
and questioning youths, and an average of 96.1% of schools
across these states prohibited harassment based on a student’s
perceived or actual sexual orientation or gender identity
(6). A recent study (4) that pooled local YRBS data during
2009–2017 to examine trends in suicide risk found that reports
among LGB youths of suicide risk might be decreasing but
that LGB students still are as much as three times more likely
to have attempted suicide than heterosexual students. National
U.S. trends have not been estimated.
LGB youths are a heterogenous population with intersecting
social identities (e.g., sex, race/ethnicity, or gender identity), and
important differences might exist among LGB youths regarding
risk for violence and suicide. For example, LGB females appear
to be at higher risk for dating and sexual violence than LGB
males (7,8). In examinations of racial/ethnic differences among
LGB youths, clear patterns of differences in experiences of
violence victimization and suicide risk are less consistent (9,10).
For example, one study of interpersonal violence among sexual
minorities reported that physical victimization from an intimate
partner was 1–4 times higher among non-white youths than
among white youths (9). Another study reported that non-
Hispanic white and Hispanic LGB youths were more likely to
be bullied than non-Hispanic white heterosexual youths but
that non-Hispanic black LGB youths were not more likely to
be bullied than non-Hispanic white heterosexual youths (10).
This same study reported that all LGB youths, regardless of
race/ethnicity, were at increased risk for suicidal ideation (10).
More systematic evaluations of the within-group differences in
violence victimization and suicide risk behaviors among sexual
minority youths are warranted.
This analysis contributes to the evidence base regarding LGB
students, violence victimization, and suicide risk. YRBS data
were used to examine national trends in violence victimization
and suicide risk among high school students by self-reported
sexual identity and evaluated differences among LGB students
by sex and race/ethnicity. The analysis was guided by the
following four questions:
1. How did the prevalence of violence victimization
and suicide risk among LGB students vary during
2015–2019?
2. To what extent did violence victimization and suicide
risk trends differ from these trends among heterosexual
students during the same period?
3. Among LGB students, to what extent did violence
victimization and suicide risk trends vary by sex (male
or female)?
4. Among LGB students, to what extent did violence
victimization and suicide risk trends vary by race/ethnicity
(non-Hispanic black, non-Hispanic white, or Hispanic)?
Methods
Data Source
This report includes data from the 2015 (n = 15,624), 2017
(n = 14,765), and 2019 (n = 13,677) cycles of the national
YRBS (pooled n = 44,066), a cross-sectional, school-based
survey conducted biennially since 1991. Each survey year,
CDC collects data from a nationally representative sample
of public and private school students in grades 9–12 in the
50 U.S. states and the District of Columbia. Additional
information about YRBS sampling, data collection, response
rates, and processing is available in the overview report of this
supplement (11). The prevalence estimates for all questions
on violence victimization and suicide risk for the overall
study population and by sex, race/ethnicity, grade, and sexual
orientation are available at https://nccd.cdc.gov/youthonline/
App/Default.aspx. The full YRBS questionnaire is available at
https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2019/2019_
YRBS-National-HS-Questionnaire.pdf.
Measures
All measures analyzed for this report are provided
(Table 1). Students responded to seven questions about
violence victimization, including ever experiencing forced
sexual intercourse; experiencing sexual dating violence, physical
dating violence, bullying at school, electronic bullying, and
being threatened or injured with a weapon at school during
the previous 12 months; and missing school because of feeling
unsafe at or on the way to or from school during the previous
30 days. Students responded to five questions about suicide
risk during the previous 12 months, including having felt
persistently sad or hopeless; having seriously considered suicide;
and having made a suicide plan, having attempted suicide,
or having made a suicide attempt that had to be treated by
a doctor or nurse. Students responded to five demographic
questions relating to sex, sexual identity, grade, race, and
ethnicity, which were used as covariates and to create relevant
strata in all trend analyses.
Analysis
Data from the 2015, 2017, and 2019 national YRBS were
examined for trends in the prevalence among LGB students in
experiences of violence victimization and indicators of suicide
risk. Data were analyzed by using SAS (version 9.4; SAS
Institute) and SUDAAN (version 11.0.0; RTI International) to
account for the complex sampling designs. Data were assessed
using complete case analysis; missing data were not imputed.
All outcomes were dichotomized as either yes or no, ≥1 time
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 21
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Measures for demographic characteristics, violence victimization, and suicide risk behaviors among high school students — Youth
Risk Behavior Survey, United States, 2019
Construct Measure
Demographic characteristics
Sexual identity Which of the following best describes you?
A. Heterosexual (straight)
B. Gay or lesbian
C. Bisexual
D. Not sure
Sex at birth What is your sex?
A. Female
B. Male
Race What is your race? (Select one or more responses.)
A. American Indian or Alaska Native
B. Asian
C. Black or African American
D. Native Hawaiian or Other Pacific Islander
E. White
Ethnicity Are you Hispanic or Latino?
A. Yes
B. No
Grade In what grade are you?
A. 9th grade
B. 10th grade
C. 11th grade
D. 12th grade
E. Ungraded or other grade
Violence victimization*
Forced sex Have you ever been physically forced to have sexual intercourse when you did not want to?
Sexual dating violence During the past 12 months, how many times did someone you were dating or going out with force you to do sexual things
that you did not want to do? (Count such things as kissing, touching, or being physically forced to have sexual intercourse.)
Physical dating violence During the past 12 months, how many times did someone you were dating or going out with physically hurt you on
purpose? (Count such things as being hit, slammed into something, or injured with an object or weapon.)
Bullying at school During the past 12 months, have you ever been bullied on school property?
Electronic bullying During the past 12 months, have you ever been electronically bullied? (Count being bullied through texting,
Instagram, Facebook, or other social media.)
Felt unsafe at, to, or from school During the past 30 days, on how many days did you not go to school because you felt you would be unsafe at school
or on your way to or from school?
Threatened or injured with a weapon
at school
During the past 12 months, how many times has someone threatened or injured you with a weapon, such as a gun,
knife, or club, on school property?
Suicide risk behaviors*
Persistent feelings of
sadness/hopelessness
During the past 12 months, did you ever feel so sad or hopeless almost every day for 2 weeks or more in a row that you
stopped doing some usual activities?
Seriously considered suicide During the past 12 months, did you ever seriously consider attempting suicide?
Made a suicide plan During the past 12 months, did you make a plan about how you would attempt suicide?
Attempted suicide During the past 12 months, how many times did you actually attempt suicide?
Suicide attempt requiring
medical treatment
If you attempted suicide during the past 12 months, did any attempt result in an injury, poisoning, or overdose that
had to be treated by a doctor or nurse?
* All violence victimization and suicide risk measures were dichotomized as either “yes” (i.e., ≥1 time, ≥1 day) or “no” (i.e., 0 days, 0 times).
or 0 times, or ≥1 day or 0 days. Weighted prevalence estimates
with 95% confidence intervals (CIs) were calculated by using
Taylor series linearization to produce nationally representative
prevalence estimates for each survey year.
Logistic regression models were used to assess linear trends
in the prevalence of violence victimization and indicators
of suicide risk among LGB and heterosexual students for
2015–2019, controlling for sex, race/ethnicity, and grade.
Main effects odds ratios (ORs) comparing LGB students with
heterosexual students also were calculated for the 2015–2019
period. In subsequent models, sex-stratified (controlling
for race/ethnicity and grade) and race/ethnicity-stratified
(controlling for sex and grade) linear trends, were examined
for students self-identifying as LGB on the survey. Main
effects ORs comparing sex and race/ethnicity groups also were
calculated for these subsequent regression models. Linear trends
were considered statistically significant if p<0.05. Main effects
ORs were considered statistically significant if 95% CIs did
not include 1.0.
Supplement
22 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Results
Violence Victimization
Among all students (Table 2), LGB students had greater
odds of violence victimization than heterosexual students
across all seven indicators, as evidenced by statistically
significant main effects of sexual identity on each indicator
(Table 2). Among LGB students, the percentage who reported
experiencing physical dating violence during 2015–2019
significantly decreased from 17.5% to 13.1%. No other
violence victimization outcomes varied significantly among
LGB students in this period.
Among LGB students stratified by sex (Table 3), male
students reported greater odds of feeling unsafe at or on the way
to or from school (aOR: 1.61) and being threatened or injured
with a weapon (aOR: 1.54) than female students. Conversely,
male LGB students reported reduced odds of electronic
bullying (aOR: 0.71), sexual dating violence (aOR: 0.66), and
forced sex (aOR: 0.51) than female LGB students. Among male
LGB students, the percentage reporting being threatened or
injured with a weapon at school significantly increased from
2015 (11.6%) to 2019 (15.9%), as did the percentage reporting
forced sex (2015: 8.0%; 2019: 15.6%). Among female LGB
students, the percentage reporting physical dating violence
significantly decreased from 2015 (16.9%) to 2019 (12.1%).
Among LGB students stratified by race (Table 4), non-
Hispanic black (black) and Hispanic students reported higher
odds of feeling unsafe at or on the way to or from school
than non-Hispanic white (white) students (aOR: 1.63 and
aOR: 1.46, respectively), and black students also reported
greater odds of being threatened or injured with a weapon than
white students (aOR: 1.60). With regard to bullying, black
and Hispanic LGB students reported reduced odds of both
bullying at school (black, aOR: 0.31; Hispanic, aOR: 0.56) and
electronic bullying (black, aOR: 0.41; Hispanic, aOR: 0.55),
compared with white LGB students. Black LGB students also
reported reduced odds of sexual dating violence, compared
with white LGB students (aOR: 0.44). The only significant
trend among violence models stratified by race/ethnicity was
among Hispanic LGB students, who had reduced percentage
of reporting experiencing physical dating violence in 2019
(9.8%), compared with 2015 (22.6%).
Suicide Risk
Among all students (Table 2), LGB students had greater
odds of suicide risk than heterosexual students across all five
indicators, as evidenced by significant main effects for each
variable. The percentage of LGB students reporting these
outcomes did not vary significantly during 2015–2019.
Among LGB students stratified by sex (Table 3), male
students had lower odds of all five suicide risk indicators than
female students. Among female LGB students, the percentage
reporting suicide attempts decreased significantly from 2015
(32.8%) to 2019 (23.6%). All other trends in suicide risk in
these sex-stratified models remained stable.
Among LGB students stratified by race (Table 4), black
and Hispanic students had lower odds than white students
of reporting persistent feelings of sadness or hopelessness
(black, aOR: 0.42; Hispanic, aOR: 0.69) and seriously
considering attempting suicide (black, aOR: 0.43; Hispanic,
aOR: 0.65). Black LGB students also had lower odds than
white LGB students of making a suicide plan (aOR: 0.61).
The percentage of LGB students reporting these outcomes in
the race/ethnicity-stratified models did not vary significantly
during 2015–2019.
Discussion
Overall, these results underscore that LGB students continue
to have a greater prevalence of violence victimization and
suicidal behavior than their heterosexual peers. The higher
prevalence of violence and suicide among LGB students is
consistent with results from other studies regarding sexual
minorities and minority stress (12,13). Minority stress is the
preeminent framework for understanding disparities among
sexual minorities and refers to the process by which social
stigma directed toward LGB and other nonheterosexual
persons is enacted through external stressors (e.g., violence,
discrimination, or harassment) and internal stressors (e.g.,
identity concealment or expectations of rejection) (12). Both
types of stress shape mental and physical health (12,14), and
the impact of violence victimization on LGB youths (15) and
its connection to elevated suicide risk is well-documented
(16). LGB students’ disproportionate experience of violence
victimization and suicide risk, compared with their heterosexual
peers in this study, underscores the continued relevance of
minority stress among LGB youths and the continued public
health need for action that addresses these sizeable disparities.
Notably, the proportion of LGB students experiencing
violence victimization or suicide risk remained fairly stable
during 2015–2019. One exception is reports of physical dating
violence; fewer LGB students reported experiencing physical
dating violence in 2019 than in 2015. This downward trajectory
of physical dating violence appears to be a continuation of
an already documented population trend of a decrease in
experiences of dating violence among adolescents (17), and its
detection among LGB youths is promising. Regarding suicide
risk, a recent study examined local trends since 2009 and

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 23
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Trends in the prevalence of violence victimization and suicide risk behaviors among high school students, by self-identied sexual
identity — Youth Risk Behavior Survey, United States, 2015–2019*
Health risk behavior
Main effect 2015 2017 2019 Linear trend
aOR (95% CI) % (95% CI) % (95% CI) % (95% CI) Beta p value
†
Violence victimization
Feeling unsafe at school (past 30 days)
Lesbian, gay, or bisexual 1.98 (1.70–2.30) 12.5 (10.2–15.3) 10.0 (8.1–12.3) 13.5 (11.0–16.5) 0.0619 0.65
Heterosexual 1.0 (Ref.) 4.6 (3.9–5.4) 6.1 (5.1–7.3) 7.5 (6.3–8.9) 0.3749 0.00
Threatened or injured with a weapon at school (past 12 months)
Lesbian, gay, or bisexual 2.09 (1.80–2.43) 10.0 (7.9–12.7) 9.4 (7.4–11.8) 11.9 (9.3–15.2) 0.2463 0.12
Heterosexual 1.0 (Ref.) 5.1 (4.5–5.9) 5.4 (4.8–6.0) 6.3 (5.5–7.3) 0.1629 0.02
Bullied at school (past 12 months)
Lesbian, gay, or bisexual 2.10 (1.87–2.37) 34.2 (29.6–39.0) 33.0 (27.4–39.0) 32.0 (29.5–34.6) –0.0847 0.28
Heterosexual 1.0 (Ref.) 18.8 (17.3–20.3) 17.1 (16.1–18.2) 17.1 (15.7–18.7) –0.0800 0.10
Electronically bullied (past 12 months)
Lesbian, gay, or bisexual 1.94 (1.72–2.20) 28.0 (24.0–32.3) 27.1 (23.1–31.4) 26.6 (23.3–30.2) –0.0775 0.43
Heterosexual 1.0 (Ref.) 14.2 (13.1–15.3) 13.3 (12.4–14.4) 14.1 (12.9–15.4) –0.0047 0.92
Physical dating violence (past 12 months)
Lesbian, gay, or bisexual 2.06 (1.77–2.40) 17.5 (14.4–21.2) 17.2 (14.3–20.5) 13.1 (10.5–16.1) –0.2264 0.04
Heterosexual 1.0 (Ref.) 8.3 (7.5–9.3) 6.4 (5.8–7.1) 7.2 (6.2–8.3) –0.1448 0.047
Sexual dating violence (past 12 months)
Lesbian, gay, or bisexual 2.08 (1.69–2.57) 22.7 (18.0–28.2) 15.8 (12.3–20.1) 16.4 (12.7–20.9) –0.2420 0.15
Heterosexual 1.0 (Ref.) 9.1 (8.2–10.0) 5.5 (4.8–6.3) 6.7 (5.9–7.5) –0.2785 <0.001
Forced sexual intercourse (lifetime)
Lesbian, gay, or bisexual 3.31 (2.90–3.77) 17.8 (14.4–21.8) 21.9 (19.0–25.0) 19.4 (16.2–23.1) 0.0650 0.59
Heterosexual 1.0 (Ref.) 5.4 (4.6–6.4) 5.4 (4.7–6.2) 5.5 (4.9–6.2) 0.0200 0.82
Suicide risk behaviors
Persistent feelings of sadness or hopelessness (past 12 months)
Lesbian, gay, or bisexual 3.60 (3.22–4.03) 60.4 (55.1–65.4) 63.0 (59.5–66.5) 66.3 (62.2–70.2) 0.1566 0.13
Heterosexual 1.0 (Ref.) 26.4 (24.6–28.4) 27.5 (25.9–29.2) 32.2 (30.8–33.7) 0.1949 0.00
Seriously considered attempting suicide (past 12 months)
Lesbian, gay, or bisexual 4.51 (4.07–4.99) 42.8 (38.4–47.3) 47.7 (43.7–51.8) 46.8 (43.1–50.6) 0.0936 0.26
Heterosexual 1.0 (Ref.) 14.8 (13.7–15.9) 13.3 (12.5–14.3) 14.5 (13.4–15.7) –0.0242 0.62
Made a suicide plan (past 12 months)
Lesbian, gay, or bisexual 4.28 (3.84–4.77) 38.2 (34.0–42.6) 38.0 (34.5–41.7) 40.2 (36.6–44.0) 0.0646 0.45
Heterosexual 1.0 (Ref.) 11.9 (10.8–13.1) 10.4 (9.3–11.7) 12.1 (11.1–13.1) 0.0031 0.96
Attempted suicide (past 12 months)
Lesbian, gay, or bisexual 4.54 (3.89–5.28) 29.4 (25.7–33.3) 23.0 (18.6–28.0) 23.4 (20.0–27.1) –0.1901 0.06
Heterosexual 1.0 (Ref.) 6.4 (5.6–7.3) 5.4 (4.6–6.4) 6.4 (5.6–7.4) –0.0148 0.85
Suicide attempt requiring medical treatment (past 12 months)
Lesbian, gay, or bisexual 3.78 (3.02–4.73) 9.4 (7.3–12.1) 7.5 (5.7–9.8) 6.3 (4.8–8.3) –0.2852 0.07
Heterosexual 1.0 (Ref.) 2.0 (1.5–2.7) 1.7 (1.4–2.1) 1.7 (1.4–2.2) –0.1197 0.40
Abbreviations: aOR = adjusted odds ratio; CI = confidence interval; Ref. = referent group.
* Logistic regression models were used to assess linear trends in the prevalence of violence victimization, and indicators of suicide risk among lesbian, gay, or bisexual
students and heterosexual students for 2015–2019, controlling for sex, race/ethnicity, and grade.
†
Statistical significance is defined as p<0.05 or a 95% CI that does not include 1.0.
reported a decrease in reported suicide risk behaviors among
LGB students (4). The national trends reported in this analysis
warrant continued monitoring over time to assess whether the
downward trajectory in local contexts (4) reflects the general
trajectory of suicide risk and LGB youths nationally.
Results from sex-stratified models highlight important
differences between male and female experiences of violence
victimization among LGB students. In this sample, male LGB
students were more likely to report feeling unsafe at school
and being threatened with a weapon; conversely, female LGB
students were more likely to report bullying both at school
and electronically. This finding is consistent with observational
studies of bullying during adolescence; males tend to report
more physical forms of bullying and harassment, whereas
females tend to report experiencing more verbal and social
bullying (18). In addition, female LGB students had a greater
prevalence of sexual dating violence and forced sex than male
LGB students. This sex difference is also consistent with what
is known about dating and sexual violence among LGB youths
(7) and mirrors national trends in dating and sexual violence,
in which females are consistently disproportionately affected
by these types of victimization (19).
Of concern, the percentage of male LGB students who
reported being threatened or injured with a weapon at school
and who reported forced sexual intercourse significantly
increased over time. Although both male and female LGB
students are negatively affected by violence, these percentages
highlight an increasing trend in violence among male LGB
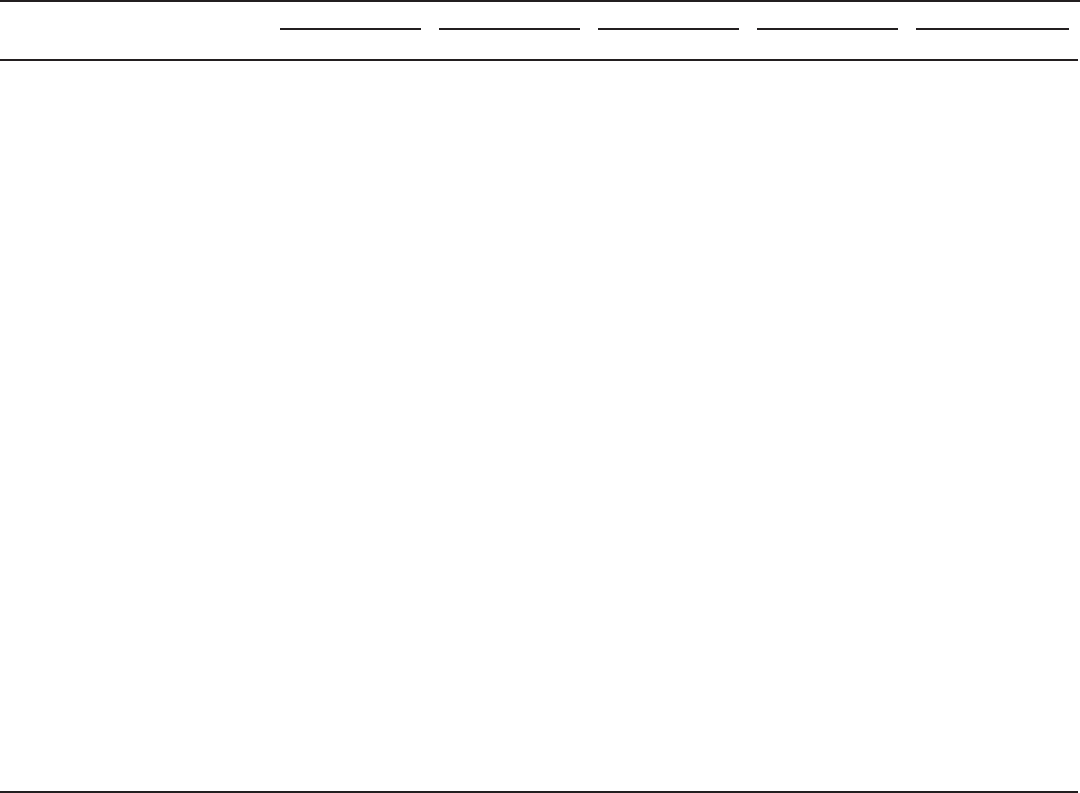
Supplement
24 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 3. Trends in violence victimization and suicide risk behaviors among lesbian, gay, and bisexual high school students, by sex and sexual
identity — Youth Risk Behavior Survey, United States, 2015–2019*
Health risk behavior
Main effect 2015 2017 2019 Linear trend
aOR (95% CI) % (95% CI) % (95% CI) % (95% CI) Beta p value
†
Violence victimization
Feeling unsafe at school (past 30 days)
Gay or bisexual male 1.61 (1.14–2.28) 15.5 (9.5–24.4) 12.3 (7.4–19.6) 18.3 (12.4–26.1) 0.1623 0.55
Lesbian or bisexual female 1.0 (Ref.) 10.8 (8.6–13.5) 9.1 (6.9–11.9) 11.5 (9.5–14.0) 0.0435 0.72
Threatened or injured with a weapon at school (past 12 months)
Gay or bisexual male 1.54 (1.14–2.08) 11.6 (7.5–17.5) 14.6 (9.8–21.2) 15.9 (11.4–21.8) 0.3973 0.04
Lesbian or bisexual female 1.0 (Ref.) 9.1 (6.6–12.4) 7.4 (5.6–9.7) 10.6 (8.1–13.9) 0.1944 0.29
Bullied at school (past 12 months)
Gay or bisexual male 0.86 (0.69–1.08) 26.3 (19.4–34.7) 35.0 (25.4–45.9) 31.7 (25.7–38.4) 0.0942 0.58
Lesbian or bisexual female 1.0 (Ref.) 37.2 (32.7–42.0) 32.2 (26.9–38.1) 32.0 (28.6–35.7) –0.1550 0.09
Electronically bullied (past 12 months)
Gay or bisexual male 0.71 (0.57–0.89) 22.4 (16.3–30.1) 22.3 (16.5–29.4) 25.5 (18.7–33.8) 0.0786 0.71
Lesbian or bisexual female 1.0 (Ref.) 30.5 (26.0–35.4) 28.5 (24.4–33.1) 27.1 (23.7–30.7) –0.1076 0.28
Physical dating violence (past 12 months)
Gay or bisexual male 1.06 (0.72–1.58) 19.9 (12.9–29.4) 16.8 (10.0–27.0) 15.9 (9.4–25.6) –0.0798 0.78
Lesbian or bisexual female 1.0 (Ref.) 16.9 (13.9–20.4) 16.9 (13.5–21.0) 12.1 (9.3–15.6) –0.2638 0.04
Sexual dating violence (past 12 months)
Gay or bisexual male 0.66 (0.44–0.98) 20.9 (12.7–32.6) 13.5 (7.5–23.0) 10.3 (5.6–18.3) –0.4638 0.20
Lesbian or bisexual female 1.0 (Ref.) 22.6 (18.0–27.9) 16.3 (12.8–20.6) 18.2 (13.6–23.8) –0.2166 0.18
Forced sexual intercourse (lifetime)
Gay or bisexual male 0.51 (0.38–0.68) 8.0 (4.8–13.1) 15.6 (10.3–22.9) 15.6 (10.7–22.0) 0.4388 0.047
Lesbian or bisexual female 1.0 (Ref.) 21.1 (17.0–25.9) 23.7 (20.6–27.2) 21.0 (17.3–25.4) –0.0203 0.87
Suicide risk behaviors
Persistent feelings of sadness or hopelessness (past 12 months)
Gay or bisexual male 0.39 (0.33–0.47) 43.9 (35.9–52.3) 45.5 (38.9–52.2) 53.5 (46.3–60.4) 0.2667 0.12
Lesbian or bisexual female 1.0 (Ref.) 66.5 (61.4–71.2) 68.8 (65.1–72.2) 70.5 (66.6–74.2) 0.1167 0.25
Seriously considered attempting suicide (past 12 months)
Gay or bisexual male 0.59 (0.47–0.73) 32.7 (23.6–43.3) 37.0 (31.5–42.8) 40.4 (33.9–47.2) 0.1960 0.30
Lesbian or bisexual female 1.0 (Ref.) 46.6 (42.1–51.1) 51.0 (46.1–55.9) 49.0 (44.8–53.3) 0.0553 0.55
Made a suicide plan (past 12 months)
Gay or bisexual male 0.57 (0.46–0.71) 27.0 (20.3–34.9) 28.7 (22.8–35.5) 33.0 (26.4–40.3) 0.2350 0.21
Lesbian or bisexual female 1.0 (Ref.) 42.0 (37.1–47.2) 40.8 (36.8–45.0) 42.4 (38.4–46.4) 0.0130 0.89
Attempted suicide (past 12 months)
Gay or bisexual male 0.73 (0.55–0.96) 19.4 (13.6–27.0) 18.3 (11.5–27.9) 23.8 (17.8–31.1) 0.1626 0.45
Lesbian or bisexual female 1.0 (Ref.) 32.8 (28.1–37.9) 23.7 (19.4–28.5) 23.6 (20.0–27.6) –0.2929 0.01
Suicide attempt requiring medical treatment (past 12 months)
Gay or bisexual male 0.63 (0.42–0.97) 7.0 (3.6–13.1) 3.8 (1.9–7.3) 5.9 (3.2–10.6) –0.2535 0.53
Lesbian or bisexual female 1.0 (Ref.) 10.3 (7.8–13.4) 8.2 (6.2–10.7) 6.6 (5.0–8.7) –0.2977 0.05
Abbreviations: aOR = adjusted odds ratio; CI = confidence interval; Ref. = referent group.
*
Logistic regression models were used to assess linear trends in the prevalence of violence victimization and indicators of suicide risk among lesbian, gay, and bisexual
high school students, by sex and self-identified sexual identity for 2015–2019, controlling for race/ethnicity and grade.
†
Statistical significance is defined as p<0.05 or a 95% CI that does not include 1.0.
students. Among adults, gay men are at greater risk for physical
violence than lesbians (20), and the increasing prevalence
in these types of violence among male LGB students might
suggest an increasing disparity between sexual minority men
and women in violence victimization. Continued monitoring of
this trend is needed, in both adolescent and adult populations.
Female LGB students reported fewer experiences of physical
dating violence over time, whereas male LGB students’ reports
of experiencing physical dating violence remained stable. This
pattern might indicate that the overall reduction in physical
dating violence in the population is not occurring among
sexual minority males, which might be supported by the data
regarding being threatened or injured with a weapon and
experiencing forced sex. An assessment of the ways that violence
in schools and in dating relationships affects sexual minority
males is warranted, both through research to understand
underlying mechanisms and in practice to ensure violence
prevention programming is directly addressing the needs of
sexual minority males.
Despite a trend of decreasing suicide attempts among
LGB females during 2015–2019, LGB females consistently
reported more suicide risk behaviors than LGB males. This
pattern echoes larger population trends in which both adult
and youth females report more suicidal ideation than adult and
youth males (21). Notably, this same literature finds that males
experience more deaths by suicide (i.e., completed suicide
attempts) than females (21); thus, an important remaining
question for LGB youths is whether these sex-specific patterns
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 25
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 4. Trends in violence victimization and suicide risk behaviors among lesbian, gay, and bisexual high school students, by
race/ethnicity — Youth Risk Behavior Survey, United States, 2015–2019*
Health risk behavior
Main effect 2015 2017 2019 Linear trend
aOR (95% CI) % (95% CI) % (95% CI) % (95% CI) Beta p value
†
Violence victimization
Feeling unsafe at school (past 30 days)
Black, non-Hispanic 1.63 (1.13–2.35) 17.8 (11.4–26.6) 12.5 (7.4–20.4) 15.2 (8.3–26.2) –0.0269 0.93
Hispanic 1.46 (1.07–1.99) 15.6 (11.5–21.0) 12.4 (8.4–18.0) 13.7 (9.5–19.5) –0.0688 0.75
White, non-Hispanic 1.0 (Ref.) 9.0 (6.7–12.0) 8.6 (6.4–11.6) 11.1 (8.0–15.1) 0.1309 0.41
Threatened or injured with a weapon at school (past 12 months)
Black, non-Hispanic 1.60 (1.07–2.41) 15.6 (8.0–28.1) 15.7 (11.7–20.7) 12.9 (7.2–22.0) –0.0494 0.89
Hispanic 0.89 (0.63–1.27) 9.0 (5.5–14.3) 9.4 (6.7–13.0) 7.7 (4.9–11.8) –0.1270 0.61
White, non-Hispanic 1.0 (Ref.) 8.2 (5.5–12.0) 7.1 (4.9–10.1) 12.9 (8.6–18.9) 0.4292 0.09
Bullied at school (past 12 months)
Black, non-Hispanic 0.31 (0.22–0.44) 21.4 (12.2–34.7) 17.2 (10.6–26.9) 18.2 (12.2–26.2) –0.0651 0.82
Hispanic 0.56 (0.45–0.70) 31.2 (25.1–38.0) 26.6 (21.0–33.1) 27.6 (23.2–32.5) –0.1077 0.44
White, non-Hispanic 1.0 (Ref.) 42.2 (34.8–50.0) 40.8 (32.8–49.3) 37.6 (33.6–41.7) –0.1265 0.31
Electronically bullied (past 12 months)
Black, non-Hispanic 0.41 (0.31–0.54) 17.0 (12.6–22.6) 16.3 (12.1–21.5) 20.5 (12.5–31.6) 0.1336 0.61
Hispanic 0.55 (0.42–0.71) 24.8 (17.8–33.4) 17.7 (13.3–23.2) 25.4 (20.1–31.5) 0.0619 0.75
White, non-Hispanic 1.0 (Ref.) 36.0 (29.1–43.5) 36.0 (30.1–42.4) 28.2 (22.8–34.1) –0.2484 0.09
Physical dating violence (past 12 months)
Black, non-Hispanic 1.19 (0.81–1.75) 14.2 (8.8–22.2) 23.8 (15.5–34.7) 11.6 (7.0–18.6) –0.1425 0.53
Hispanic 1.13 (0.83–1.54) 22.6 (16.3–30.4) 19.1 (14.2–25.2) 9.8 (5.8–16.2) –0.7080 0.003
White, non-Hispanic 1.0 (Ref.) 15.3 (11.9–19.5) 14.1 (10.4–18.7) 13.8 (10.6–17.6) –0.0883 0.55
Sexual dating violence (past 12 months)
Black, non-Hispanic 0.44 (0.27–0.72) 20.4 (11.5–33.7) 6.4 (3.3–12.0) 10.3 (5.5–18.7) –0.7987 0.11
Hispanic 0.97 (0.68–1.39) 23.0 (14.8–34.1) 18.6 (11.4–29.0) 18.3 (11.3–28.2) –0.2334 0.41
White, non-Hispanic 1.0 (Ref.) 22.3 (16.8–29.1) 18.2 (13.7–23.8) 16.7 (11.8–23.1) –0.2426 0.21
Forced sexual intercourse (lifetime)
Black, non-Hispanic 0.92 (0.66–1.29) 16.0 (8.3–28.7) 23.9 (17.7–31.6) 15.4 (9.8–23.4) 0.0759 0.77
Hispanic 1.10 (0.85–1.43) 24.0 (18.7–30.3) 21.8 (17.6–26.8) 19.1 (13.3–26.7) –0.2740 0.17
White, non-Hispanic 1.0 (Ref.) 15.5 (11.5–20.6) 21.0 (16.8–26.1) 21.3 (16.6–26.9) 0.2531 0.12
Suicide risk behaviors
Persistent feelings of sadness or hopelessness (past 12 months)
Black, non-Hispanic 0.42 (0.33–0.55) 44.8 (35.2–54.7) 52.1 (42.6–61.4) 51.1 (44.6–57.5) 0.1107 0.56
Hispanic 0.69 (0.54–0.89) 58.2 (50.6–65.5) 61.2 (52.9–69.0) 64.1 (56.0–71.4) 0.1766 0.30
White, non-Hispanic 1.0 (Ref.) 67.4 (60.3–73.8) 66.3 (60.9–71.3) 71.6 (65.7–76.8) 0.1679 0.24
Seriously considered attempting suicide (past 12 months)
Black, non-Hispanic 0.43 (0.34–0.55) 34.4 (25.7–44.3) 28.4 (21.3–36.7) 35.1 (29.2–41.4) –0.0389 0.85
Hispanic 0.65 (0.54–0.79) 40.7 (34.7–46.9) 45.3 (38.7–52.0) 39.2 (33.2–45.6) –0.0625 0.63
White, non-Hispanic 1.0 (Ref.) 48.9 (42.2–55.7) 54.1 (50.4–57.6) 52.4 (47.1–57.7) 0.0959 0.44
Made a suicide plan (past 12 months)
Black, non-Hispanic 0.61 (0.46–0.82) 32.9 (23.6–43.7) 24.1 (16.8–33.2) 36.0 (28.8–43.9) 0.0564 0.81
Hispanic 0.86 (0.69–1.06) 37.9 (31.3–45.0) 35.5 (29.5–42.0) 40.0 (32.8–47.7) 0.0765 0.62
White, non-Hispanic 1.0 (Ref.) 40.1 (34.5–46.0) 42.8 (37.7–48.0) 40.3 (35.8–45.0) 0.0044 0.97
Attempted suicide (past 12 months)
Black, non-Hispanic 0.97 (0.70–1.34) 29.2 (23.1–36.1) 20.7 (12.5–32.3) 27.2 (18.0–38.8) 0.0293 0.91
Hispanic 1.06 (0.83–1.37) 31.4 (26.4–36.9) 24.6 (18.3–32.2) 23.2 (17.3–30.4) –0.2610 0.12
White, non-Hispanic 1.0 (Ref.) 28.6 (23.1–34.7) 21.8 (16.4–28.4) 22.3 (18.1–27.3) –0.2078 0.13
Suicide attempt requiring medical treatment (past 12 months)
Black, non-Hispanic 0.83 (0.50–1.40) 5.9 (3.2–10.7) 6.4 (3.1–12.9) 7.3 (3.0–16.6) 0.2889 0.50
Hispanic 1.20 (0.83–1.75) 13.3 (9.2–19.0) 8.7 (5.2–14.3) 6.8 (4.3–10.5) –0.4683 0.05
White, non-Hispanic 1.0 (Ref.) 9.3 (6.4–13.2) 7.5 (5.2–10.8) 5.6 (3.5–8.7) –0.3545 0.11
Abbreviations: aOR = adjusted odds ratio; CI = confidence interval; Ref. = referent group.
* Logistic regression models were used to assess linear trends in the prevalence of violence victimization and indicators of suicide risk among lesbian, gay, and bisexual
high school students, by race/ethnicity for 2015–2019, controlling for sex and grade.
†
Statistical significance is defined as p<0.05 or a 95% CI that does not include 1. 0.
in deaths by suicide hold in this group; however, reliable data
regarding sexual orientation and rates of death by suicide are
unavailable. Such data could aid in further illuminating how
LGB youths are affected by suicide risk behaviors and guide
interventions for addressing this public health concern.
In models stratified by race/ethnicity, black and Hispanic
LGB students were more likely to feel unsafe and were more
likely to be threatened or injured with a weapon than white
LGB students. This finding might highlight black and Hispanic
LGB students being at greater risk for the forms of victimization
Supplement
26 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
that directly compromise physical safety (18). Conversely,
white LGB students were more likely to report school and
electronic bullying, indicating they might be at greater risk
for verbal and social victimization. Although the types of
racial/ethnic disparities in violence victimization presented in
this report do not mirror those reported in previous studies
(9,10), these findings underscore that differences by race/
ethnicity among sexual minority youths exist. Schools seeking
to address victimization through policies and practices designed
to address safety concerns for LGB students can benefit from
acknowledging differences in the experiences of LGB youths
across races/ethnicities and ensuring all youths are served
through these intervention strategies.
Regarding suicide risk, although a significantly lower
percentage of black and Hispanic LGB youths reported feeling
sad and hopeless or considering suicide than white LGB
youths, no differences existed among races/ethnicities in suicide
attempts or medically serious suicide attempts. These findings
are similar to those from other studies highlighting that all
LGB youths are at increased risk for suicide, regardless of race/
ethnicity (10) and might again highlight the mental health
impact of minority stress among all racial/ethnic groups (12).
Limitations
General limitations for the YRBS are available in the
overview report of this supplement (11). The findings in this
report are subject to at least five additional limitations. First,
although three cycles of national data to examine trends among
LGB youths are available, the brief 2015–2019 period might
be inadequate to assess trends. Continued monitoring of these
indicators over time to detect progress regarding disparities
experienced by LGB high school students is needed. Second,
the overall proportion of students identifying as LGB was
small: 2015, 8.3% (n = 1,246); 2017, 10.9% (n = 1,494);
and 2019, 11.7% (n = 1,531). Therefore, these analyses
might be underpowered for detecting statistical differences
in trends in models stratified by sex and race/ethnicity. As
more data are collected from LGB youths in future cycles
of the national YRBS, pooling data across cycles to improve
statistical power will be essential for increasing the likelihood
of detecting trends in stratified models. Third, this report does
not include differences in violence victimization and suicide
risk for students who identified their sexual identity as “not
sure” or across sexual behavior categories; future studies might
benefit from assessing these youths to further understand the
experiences of sexual minority students, violence victimization,
and suicide risk. Fourth, by pooling 2015–2019 data, the aOR
for the difference between groups on all outcomes might mask
heterogeneity over time within each subpopulation (e.g., the
size of the difference between LGB and heterosexual students
might vary between years); however, a disparity between LGB
and heterosexual students on these outcomes has been observed
since sexual identity data began to be collected on the national
YRBS in 2015. Finally, three survey measures had relatively large
amounts of missing data in 2019: forced sex (approximately
2,400 observations), sexual dating violence (approximately 3,400
observations), and attempted suicide with injury (approximately
4,900 observations). Most of these missing data can be attributed
to some selected schools administering YRBS questionnaire
versions that did not include these questions. Consequently, not
all students in the national sample were given the opportunity
to answer these questions and were counted as missing.
Conclusion
These findings highlight the continued need for policies and
practices within school environments that reduce victimization
and bolster the mental health of LGB students. Substantial
evidence exists for the role of antiharassment policies, gay-
straight alliances (or other student-led clubs designed to
support sexual minority students), and programs aimed at
improving staff support of LGB students in improving school
environments for these students (22). In addition to in-school
programs and policies, schools might consider engagement
with community organizations and stakeholders to collaborate
on implementation of comprehensive violence and suicide
prevention strategies that address a range of risk and protective
factors at the individual, relationship, community, and societal
levels. Comprehensive packages designed to inform these
prevention efforts are available from CDC (https://www.
cdc.gov/violenceprevention/pub/technical-packages.html).
For example, comprehensive approaches to suicide reduction
help to prevent suicide risk, support persons at increased risk,
prevent reattempts, and help survivors of suicide loss. When
refining such practices to meet the needs of LGB students,
special consideration of the impact of physical violence on LGB
males, suicide risk among LGB females, and the interactions
between race/ethnicity and these outcomes is warranted.
Furthermore, continued monitoring of these disparities
between LGB and heterosexual students over time is needed
until these disparities can be eradicated.
Conflicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 27
US Department of Health and Human Services/Centers for Disease Control and Prevention
References
1. Johns MM, Lowry R, Rasberry CN, et al. Violence victimization,
substance use, and suicide risk among sexual minority high school
students—United States, 2015–2017. MMWR Morb Mortal Wkly Rep
2018;67:1211–5. https://doi.org/10.15585/mmwr.mm6743a4
2. Kann L, Olsen EOM, McManus T, et al. Sexual identity, sex of sexual
contacts, and health-related behaviors among students in grades 9–12—
United States and selected sites, 2015. MMWR Surveill Summ 2016;65.
https://doi.org/10.15585/mmwr.ss6509a1
3. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—
United States, 2017. MMWR Surveill Summ 2018;67(No. SS-8).
https://doi.org/10.15585/mmwr.ss6708a1
4. Raifman J, Charlton BM, Arrington-Sanders R, et al. Sexual
orientation and suicide attempt disparities among US adolescents:
2009–2017. Pediatrics 2020;145:e20191658. https://doi.org/10.1542/
peds.2019-1658
5. Demissie Z, Rasberry CN, Steiner RJ, Brener N, McManus T. Trends
in secondary schools’ practices to support lesbian, gay, bisexual,
transgender, and questioning students, 2008–2014. Am J Public Health
2018;108:557–64. https://doi.org/10.2105/AJPH.2017.304296
6. CDC. School Health Profiles 2018: characteristics of health programs
among secondary schools. Atlanta, GA: US Department of Health and
Human Services, CDC; 2019. https://www.cdc.gov/healthyyouth/data/
profiles/pdf/2018/CDC-Profiles-2018.pdf
7. Dank M, Lachman P, Zweig JM, Yahner J. Dating violence experiences
of lesbian, gay, bisexual, and transgender youth. J Youth Adolesc
2014;43:846–57. https://doi.org/10.1007/s10964-013-9975-8
8. Walters ML, Chen J, Breiding MJ. The National Intimate Partner
and Sexual Violence Survey (NISVS): 2010 findings on victimization
by sexual orientation. Atlanta, GA: US Department of Health and
Human Services, CDC, National Center for Injury Prevention and
Control; 2013. https://www.cdc.gov/violenceprevention/pdf/NISVS_
Report2010-a.pdf
9. Whitton SW, Newcomb ME, Messinger AM, Byck G, Mustanski B. A
longitudinal study of IPV victimization among sexual minority youth. J Interpers
Violence 2016;34:912–45. https://doi.org/10.1177/0886260516646093
10. Mueller AS, James W, Abrutyn S, Levin ML. Suicide ideation and
bullying among US adolescents: examining the intersections of
sexual orientation, gender, and race/ethnicity. Am J Public Health
2015;105:980–5. https://doi.org/10.2105/AJPH.2014.302391
11. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
12. Meyer IH, Frost DM. Minority stress and the health of sexual minorities.
In: Patterson CJ, D’Augelli AR, eds. Handbook of psychology and sexual
orientation. New York, NY: Oxford University Press; 2013: 252–66.
13. Bouris A, Everett BG, Heath RD, Elsaesser CE, Neilands TB. Effects
of victimization and violence on suicidal ideation and behaviors
among sexual minority and heterosexual adolescents. LGBT Health
2016;3:153–61. https://doi.org/10.1089/lgbt.2015.0037
14. Frost DM, Lehavot K, Meyer IH. Minority stress and physical health
among sexual minority individuals. J Behav Med 2015;38:1–8. https://
doi.org/10.1007/s10865-013-9523-8
15. Zaza S, Kann L, Barrios LC. Lesbian, gay, and bisexual adolescents:
population estimate and prevalence of health behaviors. JAMA
2016;316:2355–6. https://doi.org/10.1001/jama.2016.11683
16. Burton CM, Marshal MP, Chisolm DJ, Sucato GS, Friedman MS.
Sexual minority-related victimization as a mediator of mental health
disparities in sexual minority youth: a longitudinal analysis. J Youth
Adolesc 2013;42:394–402. https://doi.org/10.1007/s10964-012-9901-5
17. CDC. Youth Risk Behavior Survey: data summary & trends report
2007–2017. Atlanta, GA: US Department of Health and Human
Services, CDC, Division of Adolescent and School Health; 2018. https://
www.cdc.gov/healthyyouth/data/yrbs/pdf/trendsreport.pdf
18. Carbone-Lopez K, Esbensen F-A, Brick BT. Correlates and consequences
of peer victimization: gender differences in direct and indirect forms
of bullying. Youth Violence Juv Justice 2010;8:332–50. https://doi.
org/10.1177/1541204010362954
19. Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner and
Sexual Violence Survey (NISVS): 2015 data brief—updated release. Atlanta,
GA: National Center for Injury Prevention and Control, CDC; 2018.
https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf
20. Stotzer RL. Comparison of hate crime rates across protected and
unprotected groups—an update. Los Angeles, CA: University of
California at Los Angeles, The Williams Institute; 2012. https://
escholarship.org/uc/item/43z1q49r
21. Beautrais AL. Gender issues in youth suicidal behaviour. Emerg Med (Fremantle)
2002;14:35–42. https://doi.org/10.1046/j.1442-2026.2002.00283.x
22. Johns MM, Poteat VP, Horn SS, Kosciw J. Strengthening our schools to
promote resilience and health among LGBTQ youth: emerging evidence
and research priorities from The State of LGBTQ Youth Health and
Wellbeing Symposium. LGBT Health 2019;6:146–55. https://doi.
org/10.1089/lgbt.2018.0109

Supplement
28 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Interpersonal Violence Victimization Among High School Students —
Youth Risk Behavior Survey, United States, 2019
Kathleen C. Basile, PhD
1
; Heather B. Clayton, PhD
2
; Sarah DeGue, PhD
1
; John W. Gilford, PhD
1
; Kevin J. Vagi, PhD
1
;
Nicolas A. Suarez, MPH
2
; Marissa L. Zwald, PhD
1
; Richard Lowry, MD
3
1
Division of Violence Prevention, National Center for Injury Prevention and Control, CDC;
2
Division of Adolescent and School Health, National Center for HIV/AIDS,
Viral Hepatitis, STD, and TB Prevention, CDC;
3
Office of the Director, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC
Abstract
Adolescent interpersonal violence victimization is an adverse childhood experience and a serious public health problem for
youths, their families, and communities. Violence victimization includes dating violence, sexual violence, and bullying. Youth
Risk Behavior Survey data for 2019 were used to examine physical and sexual dating violence; sexual violence by anyone; and
bullying victimization, whether on school property or electronic, of U.S. high school students by sex, race/ethnicity, and sexual
identity. In addition, this report explores frequency of dating violence and frequency of sexual violence among students who
reported these forms of victimization and presents composites of dating violence and bullying. Findings reveal that 8.2% of
students reported physical dating violence; 8.2% reported sexual dating violence; 10.8% reported sexual violence by anyone, of
which 50% of cases were by a perpetrator other than a dating partner; 19.5% reported bullying on school property; and 15.7%
reported electronic bullying victimization during the previous 12 months. Approximately one in eight students reported any
dating violence, and one in four reported any bullying victimization. Female students; lesbian, gay, and bisexual students; and
students not sure of their sexual identity reported the highest prevalence estimates across all five violence victimization types, any
and both forms of dating violence, and any bullying victimization. Non-Hispanic white students reported the highest prevalence
of bullying victimization. Among students experiencing physical or sexual dating violence or sexual violence by anyone, the most
common frequency reported was one time during the previous year; higher frequency was more prevalent among male students
compared with female students. These findings provide a contextual understanding of the prevalence of interpersonal violence
of U.S. high school students, highlighting those with highest prevalence. Findings can be used by public health professionals to
guide prevention efforts with youths in schools and communities.
Introduction
Interpersonal violence, or aggression perpetrated by another
person, including dating violence, sexual violence, and bullying,
is a serious problem for students, schools, and communities.
Violence can reoccur across the lifespan and is associated with
multiple health effects and negative health behaviors (e.g.,
risky sexual behaviors, substance misuse, and physical health
symptoms) (1). Victimization often begins during adolescence
and can be viewed as an adverse childhood experience (ACE). For
example, nationally representative data from adults during 2015
indicate that 43.2% of females and 51.3% of males who had
been raped were first raped before age 18 years (2). Prevalence
studies of adolescents confirm this finding. For example, a survey
Corresponding author: Kathleen C. Basile, PhD, Division of Violence
Prevention, National Center for Injury Prevention and Control, CDC.
Telephone: 404-398-8317; E-mail: [email protected].
of students in grades 7–12 found that 56% of females and 48%
of males reported some form of sexual violence victimization by
a peer (e.g., unwelcome comments, touching, or being forced
to do something sexual) during the 2010–11 school year (3).
Approximately 20% of adolescents reported physical dating
violence and 9% reported sexual dating violence (4). These
studies indicate that sexual violence during adolescence occurs
inside and outside of the dating context. In addition, 20% of
students in grades 6–12 reported bullying victimization during
the 2017 school year (5).
Scientific literature indicates that certain groups (e.g., females,
racial/ethnic minorities, and sexual minority youths)
disproportionately experience interpersonal violence during
adolescence (1). For instance, in a sample of northeastern
10th-grade students, sexual minority youths reported more
bullying, sexual violence, and dating violence victimization
than heterosexual youths, with sexual minority females
reporting particularly high levels (91% of sexual minority
females and 79% of sexual minority males reported at least
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 29
US Department of Health and Human Services/Centers for Disease Control and Prevention
one form of victimization) (6). Furthermore, in a study of
sexual violence victimization of college students, females had
higher odds of victimization than did males, and non-Hispanic
black (black) students and students of other races/ethnicities
had higher odds of victimization than did non-Hispanic
white (white) students; moreover, these racial differences were
greater for males. For females, Hispanics had lower odds of
sexual violence victimization than whites, and for males, no
substantial differences existed between Hispanics and whites
(7). Understanding these disparities in the experience of
violence victimization is crucial for identifying those at highest
risk and for guiding prevention efforts. Contextual factors also
are valuable in describing victimization (e.g., frequency of
victimization or co-occurrences of violence subtypes). These
factors increase understanding of these violence types and
further contextualize prevalence estimates. For example, in
a report using 2013 data, approximately 21% of female and
10% of male high school students who reported dating in the
previous year experienced sexual or physical dating violence,
and 6% of females and 3% of males experienced both physical
and sexual dating violence (8).
This report presents 2019 prevalence estimates for dating
violence, sexual violence, and bullying victimization of U.S.
high school students by sex, race/ethnicity, and sexual identity,
and includes frequency of dating violence and sexual violence
victimization by demographic characteristics. Combined
prevalence of different forms of dating violence and bullying
also is presented to provide the most current estimates of each
violence type. These findings can guide prevention efforts
in addressing adolescent interpersonal violence at different
levels of the social ecology (i.e., individual, relationship, and
community or societal levels).
TABLE 1. Violence victimization measures — Youth Risk Behavior Survey, United States, 2019
Violence victimization Questionnaire item Coding for analysis
Physical dating violence
victimization
“During the past 12 months, how many times did someone you were dating or going out
with physically hurt you on purpose? (Count such things as being hit, slammed into
something, or injured with an object or weapon.)” [Question excludes students who did
not date or go out with anyone during the previous 12 months.]
≥1 time versus 0 times;
1 time, 2 or 3 times, ≥4 times
Sexual dating violence
victimization*
“During the past 12 months, how many times did someone you were dating or going out
with force you to do sexual things that you did not want to do? (Count such things as
kissing, touching, or being physically forced to have sexual intercourse.)” [Question
excludes students who did not date or go out with anyone during the previous
12 months.]
≥1 time versus 0 times;
1 time, 2 or 3 times, ≥4 times
Sexual violence victimization
by anyone
†
“During the past 12 months, how many times did anyone force you to do sexual things
that you did not want to do? (Count such things as kissing, touching, or being physically
forced to have sexual intercourse.)”
≥1 time versus 0 times;
1 time, 2 or 3 times, ≥4 times
Bullied on school property “During the past 12 months, have you ever been bullied on school property?” Yes versus no
Electronically bullied “During the past 12 months, have you ever been electronically bullied?” Yes versus no
Abbreviation: YRBS = Youth Risk Behavior Survey.
* A total of 3,324 students had missing data for this variable, mostly attributed to the use of different versions of the YRBS questionnaire that did not include the
sexual violence questions in certain selected schools.
†
A total of 3,439 students had data missing for this variable, mostly attributed to the use of different versions of the YRBS questionnaire that did not include the sexual
violence questions in certain selected schools.
Methods
Data Source
This report includes data from CDC’s 2019 Youth Risk
Behavior Survey (YRBS), a cross-sectional, school-based
survey conducted biennially since 1991. Each survey year,
CDC collects data from a nationally representative sample
of public and private school students in grades 9–12 in the
50 U.S. states and the District of Columbia (N = 13,677).
Additional information about YRBS sampling, data collection,
response rates, and processing is available in the overview
report of this supplement (9). The prevalence estimates for
all violence questions for the overall study population and by
sex, race/ethnicity, grade, and sexual orientation are available
at https://nccd.cdc.gov/youthonline/App/Default.aspx. The
full YRBS questionnaire is available at https://www.cdc.gov/
healthyyouth/data/yrbs/pdf/2019/2019_YRBS-National-HS-
Questionnaire.pdf.
Measures
This analysis included five standard measures of violence
victimization and three composite variables created from those
standard measures. The standard measures included 1) having
experienced physical dating violence, 2) having experienced
sexual dating violence, 3) having experienced sexual violence
by anyone, 4) having been bullied on school property, and
5) having been bullied electronically (Table 1). For each of
these five standard measures, dichotomous categories were
created: ≥1 time versus 0 times for all sexual violence and dating
violence measures and “yes” versus “no” for both bullying
Supplement
30 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
victimization measures. The manner in which the data were
collected (see Limitations) means that approximately 25% of
respondents were missing data for sexual violence victimization
by anyone (3,439) out of a sample of 13,677 students. The
denominators for dating violence victimization measures are
students who reported dating during the 12 months before
the survey (66.1% [n = 8,703 students] for physical dating
violence victimization and 66.2% [n = 6,847 students] for
sexual dating violence victimization), whereas the denominator
for the sexual violence by anyone and bullying victimization
measures are the full sample of students for which data were
available. Three of these standard measures included levels
of victimization frequency. For each of three measures (i.e.,
physical dating violence, sexual dating violence, and sexual
violence by anyone), frequencies were collapsed into three
levels: 1 time, 2 or 3 times, or ≥4 times.
The two dating violence victimization measures were
combined into composite measures: experienced any dating
violence victimization and experienced both physical and
sexual dating violence victimization. Because of the manner
in which the data were collected, approximately 25% of
respondents were missing data for sexual dating violence
victimization (3,324 observations out of a sample of 13,677
students). When calculating the “any dating violence
victimization” measure, responses missing data for either the
sexual or the physical dating violence measure were removed
from the analysis. Any “yes” responses to either the physical
dating violence measure or the sexual dating violence measure
were combined for the numerator, with all responses without
missing data as the denominator. Similarly, to create the
“both physical and sexual dating violence” measure, “yes”
responses to both physical dating violence and sexual dating
violence were required for the numerator, with all nonmissing
responses in the denominator. A similar strategy was also used
for creating a bullying victimization “any” measure. “Any
bullying victimization” included any “yes” response to either
experiencing bullying at school or experiencing electronic
bullying, with all nonmissing responses in the denominator.
The option of exploring “both bullying at school and electronic
bullying” was not pursued. Use of personal electronic devices
in the school setting is increasing; therefore, the amount of
overlap between electronic bullying and bullying at school
might be considerable and combining these items could result
in an overestimate of their prevalence. Additional analysis
examined overlap between the sexual dating violence measure
and the sexual violence by anyone measure.
Three demographic characteristics were included in the
analyses: student sex (male or female), race/ethnicity (white,
black, Hispanic, or other), and sexual identity (heterosexual;
lesbian, gay, or bisexual [LGB]; or not sure). Although students
of multiple or other race/ethnicity are included in these
analyses, data are not presented for this group because small
sample sizes and unknown heterogeneity within this group
resulted in limited interpretability.
Analysis
Weighted prevalence estimates and corresponding 95%
confidence intervals were determined for all violence victimization
measures. Comparisons by demographic characteristics were
conducted with the chi-square test (p<0.05). When differences
among groups were demonstrated, additional t-tests were
performed to determine pairwise differences between groups.
Differences between prevalence estimates were considered
statistically significant if the t-test p value was <0.05 for main
effects (sex, race/ethnicity, or sexual identity).
Results
Among the approximately two thirds of U.S. high school
students who reported dating during the 12 months before the
survey, 8.2% reported experiencing physical dating violence,
and 8.2% experienced sexual dating violence (Table 2).
Sexual violence victimization perpetrated by anyone during
the 12 months before the survey was reported by 10.8% of
students. When comparing the sexual dating violence measure
with the sexual violence by anyone measure, half (50%) of the
10.8% of students who reported sexual violence by anyone
were victimized only by someone other than a dating partner.
Experiences of bullying victimization during the 12 months
before the survey varied, with 15.7% of students reporting
experiencing electronic bullying and 19.5% reporting bullying
on school property. For all violence victimization measures,
the prevalence varied by both sex and sexual identity, and
variation by race/ethnicity was only observed for bullying
victimization. Specifically, female students, LGB students,
and students not sure of their sexual identity consistently
had the highest prevalence across all five of the violence
victimization indicators. In addition, compared with Hispanic
or black students, white students had the highest prevalence
of experiencing bullying victimization at school and electronic
bullying. The prevalence of electronic bullying among Hispanic
students was also significantly greater than the prevalence
among black students.
Among students who experienced physical dating violence,
sexual dating violence, or sexual violence by anyone during the
previous year, the most common frequency reported was 1 time for
each (Figure). The pattern of frequency for violence victimization
differed by type of victimization. The distribution of frequency
for physical dating violence victimization was U-shaped, with
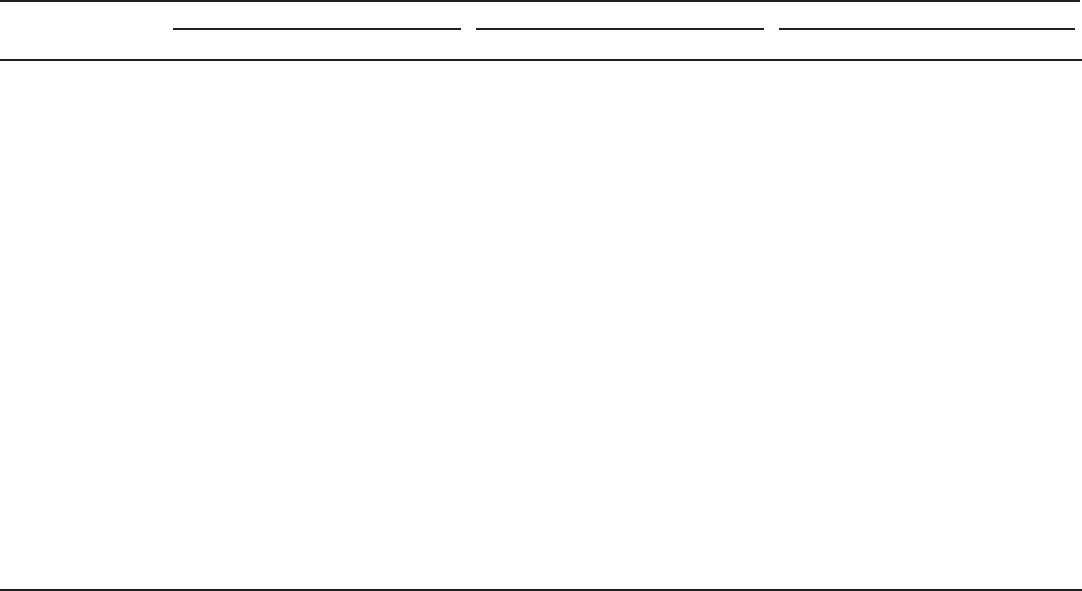
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 31
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Percentage of high school students who experienced violence victimization,* by demographic characteristics and type of violence —
Youth Risk Behavior Survey, United States, 2019
Characteristic
Experienced physical dating violence
†
Experienced sexual dating violence
§
Experienced sexual violence by anyone
¶
% (95% CI) p value** % (95% CI) p value** % (95% CI) p value**
Total 8.2 (7.2–9.4) NA 8.2 (7.4–9.1) NA 10.8 (9.9–11.7) NA
Sex
Female 9.3 (8.0–10.8) 0.01 12.6 (11.2–14.2) <0.01 16.6 (15.1–18.2) <0.01
Male 7.0
††
(5.8–8.4) NA 3.8
††
(3.1–4.7) NA 5.2
††
(4.4–6.1) NA
Race/Ethnicity
White, non-Hispanic 7.5 (6.4–8.7) 0.43 8.1 (6.9–9.6) 0.11 10.2 (9.1–11.4) 0.23
Black, non-Hispanic 8.2 (6.1–10.8) NA 6.2 (4.5–8.6) NA 10.3 (8.0–13.1) NA
Hispanic 8.9 (7.4–10.8) NA 8.7 (6.9–10.8) NA 12.2 (10.6–14.0) NA
Sexual identity
Heterosexual 7.2 (6.2–8.3) 0.01 6.7 (5.9–7.5) <0.01 9.0 (8.2–9.9) <0.01
Lesbian, gay, or bisexual 13.1
§§
(10.5–16.1) NA 16.4
§§
(12.7–20.9) NA 21.5
§§
(18.2–25.2) NA
Not sure 16.9
§§
(11.1–24.9) NA 15.0
§§
(9.5–23.0) NA 16.2
§§
(11.7–22.0) NA
Characteristic Bullied on school property Electronically bullied — —
Total 19.5 (18.2–20.9) NA 15.7 (14.6–16.9) NA — —
Sex
Female 23.6 (21.8–25.5) <0.01 20.4 (18.9–22.0) <0.01 — —
Male 15.4
§§
(14.0–16.9) NA 10.9
††
(9.6–12.4) NA — —
Race/Ethnicity
White, non-Hispanic 23.1 (21.4–24.8) <0.01 18.6 (17.1–20.2) <0.01 — —
Black, non-Hispanic 15.1
¶¶
(13.1–17.4) NA 8.6
¶¶
(7.4–10.0) NA — —
Hispanic 14.8
¶¶
(12.8–17.1) NA 12.7
¶¶,
*** (11.1–14.5) NA — —
Sexual identity
Heterosexual 17.1 (15.7–18.7) <0.01 14.1 (12.9–15.4) <0.01 — —
Lesbian, gay, or bisexual 32.0
§§
(29.5–34.6) NA 26.6
§§
(23.3–30.2) NA — —
Not sure 26.9
§§
(22.2–32.2) NA 19.4
§§,†††
(15.5–24.0) NA — —
Abbreviations: CI=confidence interval; NA = not applicable; YRBS = Youth Risk Behavior Survey.
* During the 12 months before the survey.
†
Being physically hurt on purpose (counting such things as being hit, slammed into something, or injured with an object or weapon) by someone they were dating
or going out with, ≥1 time, among the 66.1% (n = 8,703) of students nationwide who dated or went out with someone during the 12 months before the survey.
§
Being forced to do “sexual things” (counting such things as kissing, touching, or being physically forced to have sexual intercourse) they did not want to do by
someone they were dating or going out with, ≥1 time, among the 66.2% (n = 6,847) of students nationwide who dated or went out with someone during the
12 months before the survey. Of 13,677 students, this variable was missing for 3,324, mostly attributed to the use of different versions of the YRBS questionnaire
that did not include the sexual violence questions in certain selected schools. This resulted in complete data for 10,353 students, of which 66.2% (6,847) reported
dating in the 12 months before the survey.
¶
Being forced to do “sexual things” (counting such things as kissing, touching, or being physically forced to have sexual intercourse) they did not want to do by
anyone, ≥1 time, during the 12 months before the survey. Data were missing for 3,439 students for this variable, mostly attributed to the use of different versions
of the YRBS questionnaire that did not include the sexual violence questions in certain selected schools.
** Chi-square test (p<0.05).
††
Significantly different from female students, based on t-test (p<0.05).
§§
Significantly different from heterosexual students, based on t-test (p<0.05).
¶¶
Significantly different from white students, based on t-test (p<0.05).
*** Significantly different from black students, based on t-test (p<0.05).
†††
Significantly different from lesbian, gay, or bisexual students, based on t-test (p<0.05).
the highest levels of frequency at 1 time and ≥4 times, whereas
for both sexual dating violence victimization and sexual violence
victimization by anyone, the most common frequency was 1 time,
with a decreasing prevalence as the frequency increased.
The frequency of physical and sexual dating violence varied
significantly by sex (Table 3). Specifically, the prevalence of
physical dating violence was significantly greater at higher
frequency levels (≥4 times) among male students compared
with female students (41.6% versus 21.6%, respectively).
This frequency distribution pattern was similar for sexual
dating violence. The prevalence at the higher end of frequency
for sexual dating violence was significantly greater for male
students compared with female students (41.0% versus 20.8%,
respectively). Higher frequency (≥4 times) was also reported
for sexual violence by anyone for male students compared
with female students (33.9% versus 18.6%, respectively). No
significant differences existed by race/ethnicity in frequency
of physical and sexual dating violence or sexual violence by
anyone. These analyses could not include sexual identity
because of limited data (i.e., group counts <30).
Overall, 12.2% of students experienced any type of dating
violence victimization, and 3.0% experienced both types
(Table 4). Both dating violence composite measures varied
substantially by sex and sexual identity but not by race/ethnicity.
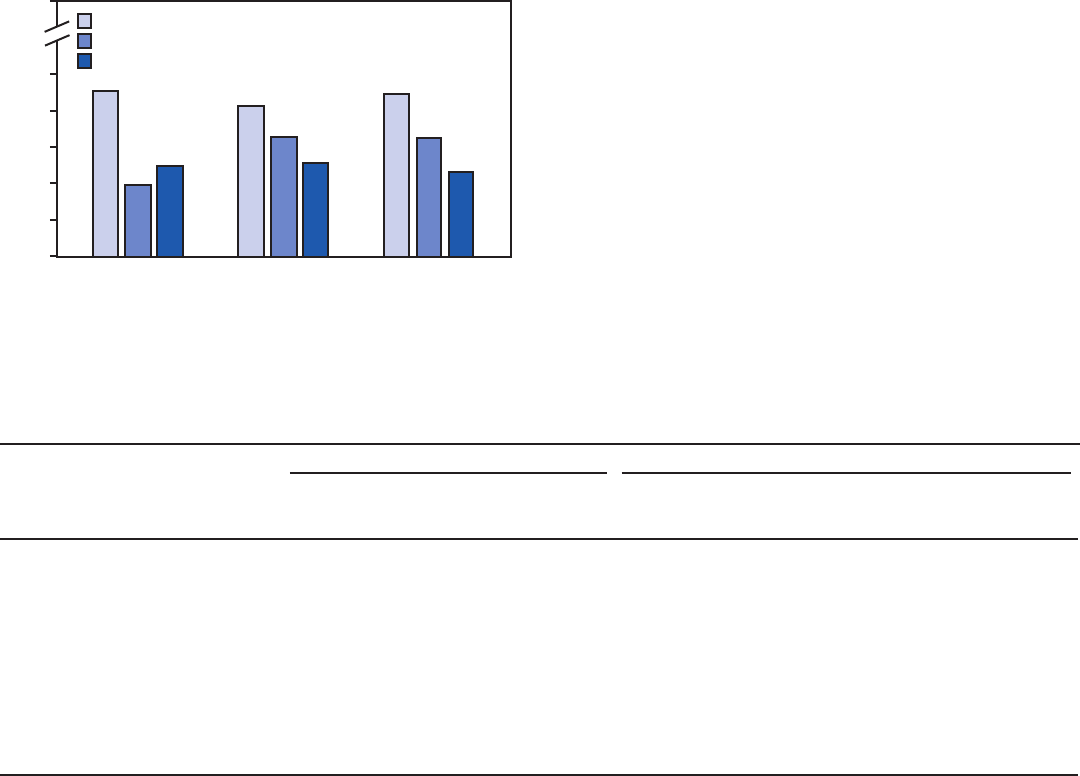
Supplement
32 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
The prevalence of the dating violence composite variables was
significantly greater for female students compared with male
students (16.4% versus 8.2% for any dating violence type;
3.8% versus 2.1% for both dating violence types). Students
who did not identify as heterosexual had substantially greater
prevalence of both dating violence composites. For any type of
FIGURE. Percentage of high school students who experienced violence,
by type of victimization (physical dating violence, sexual dating
violence, or sexual violence by anyone) and by number of times during
the previous year — Youth Risk Behavior Survey, United States, 2019
1 time
2–3 times
≥4 times
0
10
20
30
40
50
Physical dating
violence
(n = 799)
Sexual dating
violence
(n = 558)
Sexual violence
by anyone
(n = 1,159)
Percentage
Type of victimization
100
dating violence, the prevalence was 22.3% for LGB students
and 18.7% for students who were not sure of their sexual
identity versus 10.5% for heterosexual students. For both types
of dating violence, the prevalence was 5.8% for LGB students
and 9.4% for students not sure of their sexual identity versus
2.4% for heterosexual students.
The prevalence of experiencing any type of bullying
victimization was 24.8% (Table 4), and prevalence varied
significantly by sex, race/ethnicity, and sexual identity. The
prevalence of experiencing any bullying victimization was
significantly greater for female students compared with male
students (30.2% versus 19.2%, respectively) and significantly
greater for white (28.8%) compared with black (18.0%) or
Hispanic (19.2%) students. Both LGB students (39.5%)
and students not sure of their sexual identity (32.7%) had
significantly higher prevalence of any bullying compared with
heterosexual students (22.2%), with LGB students reporting
greater prevalence than students not sure of their sexual identity.
Discussion
This report describes the 2019 prevalence and frequency
of different forms of interpersonal violence victimization
experienced by U.S. high school students. Similar to
TABLE 3. Frequency of types of violence victimization,* by demographic characteristics among high school students reporting experiencing
specific types of violence — Youth Risk Behavior Survey, United States, 2019
Type of violence victimization
Sex Race/Ethnicity
Male
% (95% CI)
Female
% (95% CI) p value
†
White, non-
Hispanic
% (95% CI)
Black, non-Hispanic
% (95% CI)
Hispanic
% (95% CI) p value
†
Experienced physical dating violence
§
NA NA <0.01 NA NA NA 0.21
1 time 38.0 (32.2–44.2) 51.7 (44.2–59.2) NA 47.9 (39.7–56.2) 47.5 (37.6–57.7) 40.9 (31.3–51.3) NA
2 or 3 times 20.4 (14.2–28.4) 26.7 (21.6–32.5) NA 25.5 (18.7–33.8) 16.7 (10.3–25.9) 27.0 (19.5–36.0) NA
≥4 times 41.6 (34.6–48.9) 21.6 (16.9–27.1) NA 26.6 (20.1–34.3) 35.8 (25.0–48.2) 32.1 (24.9–40.3) NA
Experienced sexual dating violence
¶
NA NA 0.05 NA NA NA 0.39
1 time 33.3 (23.8–44.4) 44.0 (36.5–51.8) NA 42.2 (33.7–51.2) 29.0 (15.5–47.6) 45.0 (33.3–57.3) NA
2 or 3 times 25.7 (16.8–37.2) 35.2 (28.4–42.6) NA 32.3 (25.8–39.4) 38.6 (23.8–56.0) 33.3 (22.3–46.5) NA
≥4 times 41.0 (28.0–55.3) 20.8 (15.3–27.6) NA 25.5 (18.8–33.7) 32.4 (15.4–55.7) 21.6 (14.4–31.2) NA
Experienced sexual violence by anyone** NA NA 0.006 NA NA NA 0.36
1 time 36.6 (28.7–45.4) 47.3 (42.8–52.0) NA 47.6 (41.2–54.1) 39.7 (30.0–50.2) 44.0 (36.6–51.6) NA
2 or 3 times 29.5 (21.8–38.6) 34.1 (29.9–38.5) NA 31.2 (26.3–36.6) 34.9 (27.1–43.7) 34.5 (28.1–41.6) NA
≥4 times 33.9 (25.3–43.8) 18.6 (15.2–22.5) NA 21.2 (16.1–27.4) 25.4 (17.1–36.0) 21.5 (15.7–28.7) NA
Abbreviations: CI=confidence interval; NA =not applicable; YRBS = Youth Risk Behavior Survey.
* During the 12 months before the survey.
†
Chi-square test (p<0.05).
§
Being physically hurt on purpose (counting such things as being hit, slammed into something, or injured with an object or weapon) by someone they were dating
or going out with, ≥1 time, among the 66.1% (n = 8,703) of students nationwide who dated or went out with someone during the 12 months before the survey.
¶
Being forced to do “sexual things” (counting such things as kissing, touching, or being physically forced to have sexual intercourse) they did not want to do by
someone they were dating or going out with, ≥1time, among the 66.2% (n = 6,847) of students nationwide who dated or went out with someone during the
12 months before the survey. Of 13,677 students, this variable was missing for 3,324, mostly attributed to the use of different versions of the YRBS questionnaire
that did not include the sexual violence questions in certain selected schools. This resulted in complete data for 10,353 students, of which 66.2% (6,847) reported
dating in the 12 months before the survey.
** Being forced to do “sexual things” (counting such things as kissing, touching, or being physically forced to have sexual intercourse) they did not want to do by
anyone during the 12 months before the survey. These data were missing for 3,439 students for this variable, mostly attributed to the use of different versions of
the YRBS questionnaire that did not include the sexual violence questions in certain selected schools.
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 33
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 4. Percentage of high school students who experienced any dating violence or both physical and sexual dating violence* and any form
of bullying victimization,
†
by demographic characteristics — Youth Risk Behavior Survey, United States, 2019
Characteristic
Dating violence composite variables Bullying victimization composite
Experienced any dating violence
§
Experienced both physical and sexual
dating violence
¶
Experienced any bullying**
% (95% CI) p value
††
% (95% CI) p value
††
% (95% CI) p value
††
Total 12.2 (11.3–13.3) NA 3.0 (2.5–3.7) NA 24.8 (23.4–26.3) NA
Sex
Female 16.4 (14.7–18.2) <0.01 3.8 (3.0–5.0) 0.006 30.2 (28.4–32.1) <0.01
Male 8.2
§§
(7.1–9.4) NA 2.1
§§
(1.6–2.9) NA 19.2
§§
(17.6–20.9) NA
Race/Ethnicity
White, non-Hispanic 12.1 (10.8–13.5) 0.42 2.8 (2.2–3.5) 0.51 28.8 (26.9–30.7) <0.01
Black, non-Hispanic 10.6 (7.9–14.1) NA 3.0 (1.7–5.2) NA 18.0
¶¶
(15.7–20.6) NA
Hispanic 12.7 (11.1–14.6) NA 3.3 (2.1–5.1) NA 19.2
¶¶
(17.4–21.1) NA
Sexual identity
Heterosexual 10.5 (9.5–11.6) <0.01 2.4 (2.0–2.9) 0.007 22.2 (20.6–23.8) <0.01
Lesbian, gay, or bisexual 22.3***
(17.9–27.5) NA 5.8***
(3.9–8.4) NA 39.5*** (36.6–42.5) NA
Not sure 18.7*** (13.2–26.0) NA 9.4*** (5.0–16.9) NA 32.7***
,†††
(27.6–38.3) NA
Abbreviations: CI=confidence interval; NA = not applicable.
* During the 12 months before the survey, among students who dated or went out with someone during the 12 months before the survey.
†
During the 12 months before the survey.
§
Combined any “yes” responses to physical dating violence and sexual dating violence. Because of the manner in which this variable was calculated, missing values
in both the physical dating violence and sexual dating violence measures resulted in 3,355 missing values in the “experienced any dating violence” composite measure.
¶
Combined where responses to both physical dating violence and sexual dating violence were “yes.” Because of the manner in which this variable was calculated,
the missing values in both the physical dating violence and sexual dating violence measures resulted in 3,355 missing observations in the “experienced both
physical and sexual dating violence” composite measure.
** Combined any “yes” responses to bullied at school and electronic bullying.
††
Chi-square test (p<0.05).
§§
Significantly different from female students, based on t-test (p<0.05).
¶¶
Significantly different from white, non-Hispanic students, based on t-test (p<0.05).
*** Significantly different from heterosexual students, based on t-test (p<0.05).
†††
Significantly different from lesbian, gay, or bisexual students, based on t-test (p<0.05).
findings from previous YRBSs (https://www.cdc.gov/
violenceprevention/pdf/2012FindingsonSVinYouth-508.pdf),
physical dating violence, sexual dating violence, sexual violence
by anyone, bullying on school property, and electronic bullying
victimization are adverse childhood experiences (ACEs) that are
occurring at high rates. Examining their prevalence individually
and in combination by key demographic characteristics
provides an overall observation and contextual understanding
of interpersonal violence experienced by U.S. high school
students and helps identify disparities in health and safety
among U.S. youths, which can guide prevention efforts.
All five types of victimization, including any or both forms of
dating violence and any form of bullying, were more common
among female and sexual minority students, highlighting their
more frequent victimization. These findings are consistent
with previous studies that reported disparities in interpersonal
violence victimization, particularly dating violence and sexual
violence, by sex and sexual identity (6,7). Although findings
did not reveal substantially greater prevalence for racial/ethnic
minority youths for the forms of violence examined, research
has consistently shown that racial/ethnic minority youths are
at greater risk for homicides and other community violence
victimization (https://www.cdc.gov/violenceprevention/
pub/technical-packages.html). Disparities in health and risk
for violence have been linked to sexism, homophobia, and
structural disadvantage (10).
Half of students who reported sexual violence victimization
by anyone did not report sexual violence by a dating partner,
indicating that students who experience sexual violence are often
victimized by someone other than a dating partner. This finding
is consistent with previous research (3) documenting that sexual
violence happening in school during adolescence is frequently
perpetrated by peers and not necessarily by dating partners.
Indeed, perpetrators of sexual violence during youth can be
acquaintances, family members, persons in a position of authority,
and strangers, in addition to dating partners (https://www.cdc.
gov/violenceprevention/pdf/2012FindingsonSVinYouth-508.
pdf). This indicates that efforts might need to be focused on
preventing sexual violence both inside and outside the context
of dating relationships to be most helpful.
Males who experienced dating violence or sexual violence
reported high frequencies of victimization (≥4 times during
Supplement
34 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
the previous year) substantially more often than did females.
That is, although male students do not report higher prevalence
of victimization than do female students, when they do
report it, they report experiencing it at a higher frequency.
Previous research has documented that, among youths at
high risk (i.e., previously exposed to violence in the home or
community), adolescent males reported higher frequency of
victimization than did females for sexual dating violence (11).
However, male adolescents might also be more likely to disclose
dating violence and sexual violence when the victimization has
happened more than once.
In this study, bullying victimization was the only type
of violence victimization examined for which racial/ethnic
differences existed, with substantially higher prevalence
occurring among white students compared with black or
Hispanic students. This result for bullying is supported in
part by previous research (12). In addition, Hispanic students
reported substantially higher prevalence of electronic bullying
victimization compared with black students. Other research
has indicated that black students might underreport bullying
victimization when presented with a definition-based measure
of bullying that includes a form of the word “bully,” as is used
in YRBS, as opposed to behaviorally specific measures that
describe the victimization behaviors but do not use the word
“bully” (13). The measurement of bullying in this study might
have differentially affected reporting across racial/ethnic groups.
Overall, these findings highlight the importance of early
engagement in effective, evidence-based efforts for preventing
violence victimization and perpetration before they begin or
stopping them from continuing. Findings from this study
also demonstrate substantial differences in exposure to these
types of violence by sex, race/ethnicity, and sexual identity,
highlighting the need for prevention efforts that address the
unique needs of these groups. To help communities focus
their prevention efforts on what works and to address risk
and protective factors for violence and other ACEs across the
social ecology, CDC developed a series of technical packages
that identify key violence prevention strategies and approaches
on the basis of the best available research evidence. (CDC’s
technical packages for violence prevention are available at
https://www.cdc.gov/violenceprevention/pub/technical-
packages.html.) This series includes packages focused on sexual
violence, intimate partner violence (including dating violence),
and youth violence (including bullying). Preventing Adverse
Childhood Experiences (ACEs): Leveraging the Best Available
Evidence compiles evidence focused on ACEs from across the
technical packages (https://www.cdc.gov/violenceprevention/
pdf/preventingACES.pdf ).
Multiple evidence-based interpersonal violence prevention
approaches are directly related to the findings in this study.
For example, social-emotional learning programs that
support development of skills for communication, emotion
regulation, empathy, and respect and that target risk factors for
interpersonal violence (e.g., impulsivity or drug use) have been
reported to decrease adolescent sexual violence perpetration
and homophobic name-calling, with indirect effects on peer
bullying, cyberbullying, and sexual harassment perpetration
when mediated by delinquency (14,15). By addressing shared
risk and protective factors across types of violence, social-
emotional learning programs can build the skills youths
need for engaging in healthy relationships with family, peers,
dating partners, and others, thus preventing multiple forms of
adolescent interpersonal violence and long-term consequences
into adulthood. In addition, bystander programs teach youths
how to safely act when they see behaviors that increase risk
for violence and change social norms within their peer groups.
Although originally conceptualized as a means of challenging
heterosexist attitudes to prevent sexual and dating violence
(16), such programs might also prevent other forms of
adolescent violence, including bullying and violence targeting
sexual, gender, and racial minorities by focusing the training
on recognizing and challenging these specific harmful attitudes
and behaviors (17,18).
Modifying the social and physical environment in schools
and neighborhoods might improve safety and reduce risk
for violence for more of the population than individual- or
relationship-level approaches alone. For example, one school-
based prevention approach that includes a building-level
intervention (e.g., addressing physical areas in the school
identified by students as less safe) has been reported to reduce
sexual violence victimization and perpetration by peers
and dating partners (19). In addition, the development of
safe and supportive environments in schools that promote
protective factors (e.g., school connectedness and professional
development regarding lesbian, gay, bisexual, and transgender
[LGBT] youths) can help create accepting school environments
for LGBT youths and reduce the risk for bullying and other
violence (20). Results from this report indicate that LGB
youths, specifically, are at a disproportionately higher risk
for interpersonal violence victimization compared with
heterosexual youths. As of 2019, gender identity has not been
assessed by the YRBS nationwide. However, during 2017,
gender identity was assessed in YRBSs conducted in 10 states
and nine large urban school districts; these data show that
transgender students consistently report greater prevalence
of violence victimization than their cisgender peers (21).
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 35
US Department of Health and Human Services/Centers for Disease Control and Prevention
Promotion of gay-straight alliances and support of LGBT
students can help provide these youths with an accepting school
environment, which might also reduce the risk for school-based
violence against these youths (22). (Information about CDC’s
current school health programs is available at https://www.
cdc.gov/healthyyouth/fundedprograms/1807/resources.htm.)
CDC is engaged in ongoing research and programmatic
activities for expanding the research evidence and adding to
the knowledge base of effective primary prevention programs,
policies, and practices available to communities for preventing
interpersonal violence among youths. For example, CDC’s
Dating Matters: Strategies to Promote Healthy Teen Relationships
is a comprehensive adolescent dating violence prevention
model. Dating Matters includes multiple integrated prevention
strategies that address risk factors for youths and their families,
schools, and neighborhoods with demonstrated effects on
adolescent dating violence, bullying, and peer violence in
middle school. (Additional information about Dating Matters
is available at https://www.cdc.gov/violenceprevention/
intimatepartnerviolence/datingmatters/index.html.)
In addition, since 2001, CDC has provided funding for
primary prevention of sexual violence through the Rape
Prevention and Education Program to state health departments
in all 50 states, the District of Columbia, and four U.S.
territories. Funded organizations implement initiatives that
address youths in their communities, including community-
and societal-level approaches (e.g., improving education and
leadership opportunities for girls). (Additional information
about the Rape Prevention and Education Program is available
at https://www.cdc.gov/violenceprevention/sexualviolence/rpe/
index.html.) CDC also sponsors youth violence prevention
research through its National Centers of Excellence in Youth
Violence Prevention. Their goal is to build the scientific
infrastructure and community partnerships necessary for
stimulating new youth violence prevention research and
practice across the country, including a focus on the impact
of structural factors (e.g., housing, education, or systemic
discrimination) that limit access to positive social determinants
of health.
Prevention of interpersonal violence among adolescents
might be most successful when a comprehensive strategy is
used that addresses these ACEs at multiple levels of the social
ecology simultaneously and recognizes that these different
forms of victimization can be co-occurring (1). The findings
reported here also highlight the importance of acknowledging
the disproportionate prevalence of these forms of victimization
on certain youths (i.e., females and sexual minorities) and
addressing these disparities in prevention efforts.
Limitations
General limitations for the YRBS are available in the overview
report of this supplement (9).The findings in this report are
subject to at least five additional limitations. First, substantial
overlap likely existed in the measures that examined experiences
of sexual violence victimization (i.e., sexual dating violence
victimization and sexual violence victimization by anyone),
and among the bullying victimization measures (i.e., electronic
bullying and bullied at school). For these reasons, composites
for the sexual violence measures and a “both” composite for
bullying (i.e., experienced both electronic bullying and bullying
at school) were not created. Second, because of the breadth of
topics included in the YRBS, violence victimization subtype
measures included in the YRBS tend to be broad in nature and,
in this study, were assessed by single items. More specific and
detailed measures of violence victimization would allow for a
comprehensive analysis of the prevalence and overlap between
different forms of interpersonal violence victimization. Third,
the YRBS bullying items include the word “bullied,” which
might have decreased disclosure (13). Fourth, the interpersonal
violence victimization types that could be included in this
study (i.e., dating violence, sexual violence, and bullying), as
a whole, do not reflect the breadth of interpersonal violence
victimization experienced by youths (i.e., other forms of youth
violence experienced in the community) and might partially
explain why few racial/ethnic differences were found. Finally,
the sexual violence measures (and composite measures that
were created with the sexual violence measures) in this report
had a relatively large amount of missing data (approximately
3,400 observations) in 2019. Most of this missing data can
be attributed to the use of different versions of the YRBS
questionnaire that did not include the sexual violence questions
in certain selected schools. Consequently, not all students in
the national sample were given the opportunity to answer the
sexual violence questions and were counted as missing. When
constructing the composite measures for any dating violence,
and both physical and sexual dating violence victimization, the
analytic sample was restricted to students who had complete
data for both physical and sexual dating violence victimization,
which reduced the potential for biased estimates.
Future Directions
To increase understanding of the differential experiences
of adolescent interpersonal violence victimization, future
research that focuses in more detail on the demographic
groups highlighted in this study can be beneficial. For
example, on the basis of these findings, additional research
Supplement
36 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
to better understand the characteristics and consequences
of these forms of interpersonal violence on sexual minority
youths is warranted. Research exploring sex differences in the
frequency of victimization across additional types of violence
can add to the findings reported here. Future studies that
include more detailed measures of dating violence, sexual
violence, and bullying for capturing and isolating understudied
subtypes of these forms of violence (e.g., psychological dating
violence, nonconsensual sexting, or relational bullying) would
increase knowledge of the full prevalence of these forms of
violence among youths. Finally, studies that examine the
co-occurrence and cumulative impact of different forms of
violence victimization during adolescence and into adulthood
can guide more comprehensive prevention efforts.
Conclusion
Interpersonal violence victimization experiences of high
school students are a form of ACEs and represent a substantial
public health problem in the United States. Multiple forms
of interpersonal violence, including dating violence, sexual
violence, and bullying, negatively affect youths and can
continue to have damaging effects throughout a person’s
life. The findings in this report are consistent with those in
previous studies about disparities in interpersonal violence
victimization by demographic characteristics; the report also
provides additional insight about the specific groups of students
who are at highest risk for particular types of interpersonal
violence and who might benefit most from prevention
efforts. In addition, the findings increase understanding of
the contextual factors associated with interpersonal violence
victimization (e.g., frequency, location, and co-occurrence of
subtypes) and can guide how violence prevention professionals
select and implement prevention approaches for addressing
dating violence, sexual violence, and bullying. Prevention
approaches at the individual, relationship, and school or
community levels (e.g., those that seek to increase youths’ skills
in preventing violence, change social norms related to violence,
and modify the physical and social environment in schools and
communities to increase protection against violence) are crucial
for building a comprehensive strategy to reduce interpersonal
violence victimization among youths.
Conicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. CDC. Preventing multiple forms of violence: a strategic vision for
connecting the dots. Atlanta, GA: US Department of Health and Human
Services, CDC, National Center for Injury Preventon and Control,
Division of Violence Prevention; 2016.
2. Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner
and Sexual Violence Survey (NISVS): 2015 data brief. Atlanta, GA: US
Department of Health and Human Services, CDC, National Center for
Injury Prevention and Control; 2018. https://www.cdc.gov/
violenceprevention/datasources/nisvs/2015NISVSdatabrief.html
3. Hill C, Kearl H. Crossing the line: sexual harassment at school. Washington,
DC: American Association of University Women; 2011. https://www.aauw.
org/resources/research/crossing-the-line-sexual-harassment-at-school
4. Wincentak K, Connolly J, Card N. Teen dating violence: a meta-analytic
review of prevalence rates. Psychol Violence 2017;7:224–41. https://
doi.org/10.1037/a0040194
5. Seldin M, Yaez C. Student reports of bullying: results from the 2017
School Crime Supplement to the National Crime Victimization Survey.
Report no.: NCES 2019–054. Washington, DC: US Department of
Education, National Center for Education Statistics; 2019. https://nces.
ed.gov/pubsearch/pubsinfo.asp?pubid=2019054
6. Norris AL, Orchowski LM. Peer victimization of sexual minority and
transgender youth: a cross-sectional study of high school students.
Psychol Violence 2020;10:201–11. https://doi.org/10.1037/vio0000260
7. Coulter RWS, Mair C, Miller E, Blosnich JR, Matthews DD,
McCauley HL. Prevalence of past-year sexual assault victimization among
undergraduate students: exploring differences by and intersections of
gender identity, sexual identity, and race/ethnicity. Prev Sci
2017;18:726–36. https://doi.org/10.1007/s11121-017-0762-8
8. Vagi KJ, O’Malley Olsen E, Basile KC, Vivolo-Kantor AM. Teen dating
violence (physical and sexual) among US high school students: findings
from the 2013 National Youth Risk Behavior Survey. JAMA Pediatr
2015;169:474–82. https://doi.org/10.1001/jamapediatrics.2014.3577
9. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
10. Popkin SJ, Bogle M, Zweig JM, Saxena PD, Breslav L, Michie M. Let
girls be girls: how coercive sexual environments affect girls who live in
disadvantaged communities and what we can do about it. Washington,
DC: Urban Institute; 2015. https://www.urban.org/sites/default/files/
publication/72466/2000490-Let-Girls-Be-Girls.pdf
11
. Reidy DE, Kearns MC, Houry D, Valle LA, Holland KM, Marshall KJ.
Dating violence and injury among youth exposed to violence. Pediatrics
2016;137:e20152627. https://doi.org/10.1542/peds.2015-2627
12
. Spriggs AL, Iannotti RJ, Nansel TR, Haynie DL. Adolescent bullying
involvement and perceived family, peer and school relations:
commonalities and differences across race/ethnicity. J Adolesc Health
2007;41:283–93. https://doi.org/10.1016/j.jadohealth.2007.04.009
13
. Sawyer AL, Bradshaw CP, O’Brennan LM. Examining ethnic, gender,
and developmental differences in the way children report being a victim
of “bullying” on self-report measures. J Adolesc Health 2008;43:106–14.
https://doi.org/10.1016/j.jadohealth.2007.12.011
14
. Espelage DL, Low S, Ryzin MJV, Polanin JR. Clinical trial of Second
Step Middle School Program: impact on bullying, cyberbullying,
homophobic teasing, and sexual harassment perpetration. School Psych
Rev 2015;44:464–79. https://doi.org/10.17105/spr-15-0052.1
15
. Espelage DL, Low S, Polanin JR, Brown EC. The impact of a middle
school program to reduce aggression, victimization, and sexual violence.
J Adolesc Health 2013;53:180–6. https://doi.org/10.1016/j.
jadohealth.2013.02.021
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 37
US Department of Health and Human Services/Centers for Disease Control and Prevention
16. Storer HL, Casey E, Herrenkohl T. Efficacy of bystander programs to
prevent dating abuse among youth and young adults: a review of the
literature. Trauma Violence Abuse 2016;17:256–69. https://doi.
org/10.1177/1524838015584361
17
. Nelson JK, Dunn KM, Paradies Y. Bystander anti‐racism: a review of
the literature. Anal Soc Issues Public Policy 2011;11:263–84. https://
doi.org/10.1111/j.1530-2415.2011.01274.x
18
. National Academies of Sciences. Preventing bullying through science,
policy, and practice. Rivara F, Le Menestrel S, eds. Washington, DC:
The National Academies Press; 2016. https://www.nap.edu/read/23482/
chapter/1
19
. Taylor BG, Stein ND, Mumford EA, Woods D. Shifting boundaries:
an experimental evaluation of a dating violence prevention program in
middle schools. Prev Sci 2013;14:64–76. https://doi.org/10.1007/
s11121-012-0293-2
20
. Bonell C, Hinds K, Dickson K, et al. What is positive youth development
and how might it reduce substance use and violence? A systematic review
and synthesis of theoretical literature. BMC Public Health 2016;16:135.
https://doi.org/10.1186/s12889-016-2817-3
21
. Johns MM, Lowry R, Andrzejewski J, et al. Transgender identity and
experiences of violence victimization, substance use, suicide risk, and
sexual risk behaviors among high school students—19 states and large
urban school districts, 2017. MMWR Morb Mortal Wkly Rep
2019;68:67–71.
22. Marx RA, Kettrey HH. Gay-straight alliances are associated with lower
levels of school-based victimization of LGBTQ+ youth: a systematic
review and meta-analysis. J Youth Adolesc 2016;45:1269–82. https://
doi.org/10.1007/s10964-016-0501-7

Supplement
38 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Prescription Opioid Misuse and Use of Alcohol and Other Substances
Among High School Students — Youth Risk Behavior Survey,
United States, 2019
Christopher M. Jones, PharmD, DrPH
1
; Heather B. Clayton, PhD
2
; Nicholas P. Deputy, PhD
2,3
; Douglas R. Roehler, PhD
4
; Jean Y. Ko, PhD
5
;
Marissa B. Esser, PhD
6
; Kathryn A. Brookmeyer, PhD
7
, Marci Feldman Hertz, MS
2
1
Office of the Director, National Center for Injury Prevention and Control, CDC;
2
Division of Adolescent and School Health, National Center for HIV/AIDS,
Viral Hepatitis, STD, and TB Prevention, CDC;
3
Epidemic Intelligence Service, CDC;
4
Division of Overdose Prevention, National Center for Injury Prevention
and Control, CDC;
5
Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC;
6
Division of Population
Health, National Center for Chronic Disease Prevention and Health Promotion, CDC;
7
Division of STD Prevention, National Center for HIV/AIDS, Viral
Hepatitis, STD, and TB Prevention, CDC
Abstract
Adolescence is an important period of risk for substance use initiation and substance use–related adverse outcomes. To examine
youth substance use trends and patterns, CDC analyzed data from the 2009–2019 Youth Risk Behavior Survey. This report
presents estimated prevalence of current (i.e., previous 30-days) marijuana use, prescription opioid misuse, alcohol use, and binge
drinking and lifetime prevalence of marijuana, synthetic marijuana, cocaine, methamphetamine, heroin, injection drug use, and
prescription opioid misuse among U.S. high school students. Logistic regression and Joinpoint analyses were used to assess 2009–
2019 trends. Prevalence of current and lifetime substance use by demographics, frequency of use, and prevalence of co-occurrence
of selected substances among students reporting current prescription opioid misuse are estimated using 2019 data. Multivariable
logistic regression analysis was used to determine demographic and substance use correlates of current prescription opioid misuse.
Current alcohol, lifetime cocaine, methamphetamine, heroin, and injection drug use decreased during 2009–2019. Lifetime use
of synthetic marijuana (also called synthetic cannabinoids) decreased during 2015–2019. Lifetime marijuana use increased during
2009–2013 and then decreased during 2013–2019. In 2019, 29.2% reported current alcohol use, 21.7% current marijuana use,
13.7% current binge drinking, and 7.2% current prescription opioid misuse. Substance use varied by sex, race/ethnicity, grade,
and sexual minority status (lesbian, gay, or bisexual). Use of other substances, particularly current use of alcohol (59.4%) and
marijuana (43.5%), was common among students currently misusing prescription opioids. Findings highlight opportunities for
expanding evidence-based prevention policies, programs, and practices that aim to reduce risk factors and strengthen protective
factors related to youth substance use, in conjunction with ongoing initiatives for combating the opioid crisis.
Introduction
Substance use and associated adverse outcomes contribute
to substantial morbidity, mortality, and economic costs to
society each year in the United States (1). Data from national
surveys indicate the majority of adolescents will engage in
some form of substance use before they graduate from high
school (https://www.samhsa.gov/data/report/2018-nsduh-
detailed-tables). During adolescence, areas of the brain
associated with emotional responses and reward systems
develop before those associated with executive functioning,
judgement, and decision making (2). This uneven maturation
results in increased susceptibility for engaging in risky and
impulsive behaviors, including substance use, and increases
Corresponding author: Christopher M. Jones, PharmD, DrPH, Office
of the Director, National Center for Injury Prevention and Control,
CDC. Telephone: 404-498-0756; E-mail: [email protected].
vulnerability to reinforcing and rewarding effects of substances
(2,3). Preventing or delaying substance use initiation among
youths can reduce later risk for substance use and substance
use disorders (1,3,4). Beyond the individual negative effects
of substance use during youth and into adulthood, substance
use among youths also increases the likelihood for negative
consequences that affect peers, families, and communities
(5). Youth substance use is associated with increased risk for
delinquency, academic underachievement, teenage pregnancy,
sexually transmitted diseases, perpetrating or experiencing
violence, injuries, and mental health problems (1,3–6).
As the United States confronts its decades-long opioid
overdose epidemic (1,2), preventing opioid misuse among
youth is a public health imperative. Previous research has
documented that misuse of prescription opioids among
youths is associated with multiple adverse health outcomes
and risk behaviors, including use of alcohol and other illicit
drugs, injection drug use, suicidal ideation, youth violence,
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 39
US Department of Health and Human Services/Centers for Disease Control and Prevention
delinquency, having four or more lifetime sexual partners, not
using a condom at last sexual intercourse, increased risk for
acquisition of human immunodeficiency virus infection and
sexually transmitted diseases (6), and increasing overdoses (7).
Studies also have demonstrated that prescription opioid misuse
among youths is strongly linked with subsequent initiation
and use of heroin and increased risk for injecting prescription
opioids and developing an opioid use disorder (8–10).
Preventing substance use among youths is necessary because
of the health and social effects of youth substance use. To
inform substance use prevention initiatives and to improve
understanding of youth substance use patterns, including
misuse of prescription opioids and other substances, this
analysis 1) examines trends and patterns in substance use
among high school students overall and by demographic
characteristics, 2) characterizes the frequency of use of
specific substances among high school students, 3) explores
co-occurring substance use among high school students who
misuse prescription opioids, and 4) examines the demographic
and substance use correlates of prescription opioid misuse
among high school students. Findings from this analysis can
help inform efforts by public health practitioners, clinicians,
and the substance use prevention community to expand
the implementation of evidence-based prevention policies,
programs, and practices that aim to reduce risk factors and
strengthen protective factors related to youth substance use.
Methods
Data Source
This report includes data from CDC’s 2009–2019 Youth
Risk Behavior Survey (YRBS), a cross-sectional, school-based
survey conducted biennially since 1991. Each survey year,
CDC collects data from a nationally representative sample
of public- and private-school students in grades 9–12 in
the 50 U.S. states and the District of Columbia. Additional
information about YRBS sampling, data collection, response
rates, and processing is available in the overview report of this
supplement (11). The prevalence estimates for all substance
use questions for the overall study population and by sex,
race/ethnicity, grade, and sexual orientation are available at
https://nccd.cdc.gov/youthonline/App/Default.aspx. The
full YRBS questionnaire is available at https://www.cdc.gov/
healthyyouth/data/yrbs/pdf/2019/2019_YRBS-National-HS-
Questionnaire.pdf.
Measures
This report addresses four current (i.e., previous 30 days
before the survey) and seven lifetime substance use behaviors.
The four current substance use behaviors include 1) marijuana
use (ascertained by the question, “During the past 30 days,
how many times did you use marijuana?”), 2) alcohol use
(“During the past 30 days, on how many days did you have
at least one drink of alcohol?”), 3) binge drinking (“During
the past 30 days, on how many days did you have 4 or more
drinks of alcohol in a row, that is, within a couple of hours
[if you are a female] or 5 or more drinks of alcohol in a row,
that is, within a couple of hours [if you are a male]?”), and
4) prescription opioid misuse (“During the past 30 days, how
many times have you taken prescription pain medicine without
a doctor’s prescription or differently than how a doctor told you
to use it?”). The current prescription opioid misuse question
is new for the 2019 YRBS, providing opportunities to explore
substance use patterns and individual characteristics associated
with this variable for the first time.
The seven lifetime substance use behaviors include
1) marijuana use (“During your life, how many times have you
used marijuana?”), 2) synthetic marijuana (also called synthetic
cannabinoids) use (“During your life, how many times have you
used synthetic marijuana?”), 3) cocaine use (“During your life,
how many times have you used any form of cocaine, including
powder, crack, or freebase?”), 4) methamphetamine use (“During
your life, how many times have you used methamphetamines
[also called speed, crystal meth, crank, ice, or meth]?”), 5) heroin
use (“During your life, how many times have you used heroin
[also called smack, junk, or China White]?”), 6) prescription
opioid misuse (“During your life, how many times have you
taken prescription pain medicine without a doctor’s prescription
or differently than how a doctor told you to use it?”), and
7) injection drug use (“During your life, how many times have
you used a needle to inject any illegal drug into your body?”).
Substance use behaviors were dichotomized to indicate
current or lifetime use versus no use. With three exceptions,
frequency of use for each substance was categorized as
1–2 times, 3–9 times, 10–39 times, or ≥40 times. Frequency of
current alcohol use and current binge drinking were categorized
as 1–2 days, 3–9 days, 10–19 days, or ≥20 days. For injection
drug use, frequency of use was categorized as 1 time or ≥2 times.
Four demographic characteristics were included in the analysis:
sex (male or female), race/ethnicity (non-Hispanic white [white],
non-Hispanic black [black], Hispanic, or other), grade (9/10
or 11/12), and sexual identity (heterosexual; lesbian, gay, or
bisexual; or not sure). Students reporting “other” race/ethnicity
are included in all analyses; however, data are not presented for
that group because of limited interpretability.
Supplement
40 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Analysis
First, annual prevalence of each substance use behavior was
estimated for all years with available data. Second, to identify
temporal trends, logistic regression analyses were used to
model linear and quadratic time effects while controlling for
sex, grade, and racial/ethnic group changes over time; for
significant quadratic time effects, Joinpoint software was used
to identify the year the trend changed direction (11). Trends
were assessed during 2009–2019 for current alcohol, current
marijuana, lifetime marijuana, lifetime cocaine, lifetime
methamphetamine, lifetime heroin, and lifetime injection
drug use. Synthetic marijuana use was first assessed by YRBS in
2015; therefore, trend analysis for this variable was conducted
for 2015–2019. Third, to identify 2-year changes in substance
use behaviors, prevalence estimates from 2017 and 2019 were
compared by using t-tests; changes were considered statistically
different if the p value was <0.05.
Four additional analyses were conducted by using 2019
YRBS data only. First, prevalence estimates and associated
95% confidence intervals (CIs) for each substance use behavior
were calculated by demographic characteristics. Statistically
significant pairwise differences between demographic groups
for each of the substance use behaviors were determined by
t-tests; differences were considered statistically significant if the
p value was <0.05. Second, to examine frequency of use among
students who reported engaging in each substance use behavior,
prevalence estimates and 95% CIs of students reporting each
frequency of use category were calculated. Third, prevalence
estimates of co-occurring use of selected substances among
students reporting current prescription opioid misuse were
estimated. Finally, multivariable logistic regression analysis
was used to determine demographic and substance use
correlates of current prescription opioid misuse. Because the
use of one substance is generally strongly associated with use
of one or more other substances, it is important to account
for multiple substance use behaviors during the modeling
process. Therefore, all demographic and substance use variables
were included in a single model to examine the independent
effect of each variable on current prescription opioid misuse.
This modeling strategy is consistent with previous research
examining substance use behaviors among youths (6).
To improve model stability during multivariable analyses,
three composite substance use variables were created. A
composite variable regarding alcohol consumption was created
with three levels: 1) no previous 30-day use, 2) previous
30-day use (current drinking but no binge drinking), and
3) previous 30-day binge alcohol use. A marijuana composite
variable also was created with three levels: 1) no lifetime use,
2) lifetime use but no previous 30-day use, and 3) previous
30-day use. A composite lifetime use of cocaine, heroin,
or methamphetamine variable was created by combining
answers of “1 or more times” for each of the three constituent
variables. Because substance use variables are known to be
highly correlated with each other, the Variance Inflation Factor
was used to assess multicollinearity. None was observed (i.e.,
no values >10).
Adjusted prevalence ratios (aPRs) and corresponding
95% CIs were calculated; estimates were considered
statistically significant if the 95% CI did not include 1.0. All
analyses were conducted by using SAS-callable SUDAAN
(version 11.0.1; RTI International) to account for survey
weights and the complex sample design of the YRBS. No
imputation methods were used for data that were missing.
Results
Substance use was common among U.S. high school
students during 2019 and varied by substance, year, and
demographic groups (Table 1). Among current substance
use measures, the highest prevalence estimates were for
alcohol (29.2%) and marijuana use (21.7%). Current binge
drinking was reported by 13.7% of high school students,
and 7.2% reported current prescription opioid misuse.
Among lifetime use measures, marijuana use was reported
by 36.8% of high school students, followed by misuse of
prescription opioids (14.3%) and use of synthetic marijuana
(7.3%), cocaine (3.9%), methamphetamine (2.1%), or heroin
(1.8%). Lifetime injection drug use was reported by 1.6% of
high school students.
Trend data were available for eight of the 11 substance
use measures included in the analyses. Among these
measures, current alcohol use, lifetime cocaine, lifetime
methamphetamine, lifetime heroin, and lifetime injection drug
use decreased during 2009–2019. Lifetime use of synthetic
marijuana decreased during 2015–2019. The prevalence
of lifetime marijuana use increased during 2009–2013
(36.8%–40.7%) and then decreased during 2013–2019
(40.7%–36.8%). No statistically significant changes from 2017
to 2019 were observed for any of the substance use behaviors.
Compared with females, males had a significantly higher
prevalence of lifetime use of cocaine (4.9% versus 2.7%),
methamphetamine (2.7% versus 1.5%), heroin (2.3% versus
1.0%), and injection drug use (2.1% versus 1.1%) (Table 2).
Compared with males, females had a significantly higher
prevalence of current alcohol use (31.9% versus 26.4%), binge
drinking (14.6% versus 12.7%), current prescription opioid
misuse (8.3% versus 6.1%), and lifetime prescription opioid
misuse (16.1% versus 12.4%). Among racial/ethnic groups,
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 41
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Prevalence of and trends in prevalence of lifetime and current use of specific substances and use behaviors among high school
students — Youth Risk Behavior Survey, United States, 2009–2019
Behavior
Prevalence
Linear change* Quadratic change*
Change
from
2017 to 2019
†
2009 2011 2013 2015 2017 2019
Current use
§
Marijuana 20.8 23.1 23.4 21.7 19.8 21.7 No change No change No change
Alcohol 41.8 38.7 34.9 32.8 29.8 29.2 Decreased 2009–2019 No change No change
Binge drinking — — — — 13.5 13.7 NA
¶
NA
¶
No change
Prescription opioid misuse — — — — — 7.2 NA
¶
NA
¶
NA
¶
Lifetime use
Marijuana 36.8 39.9 40.7 38.6 35.6 36.8 No change Increased 2009–2013
Decreased 2013–2019
No change
Cocaine 6.4 6.8 5.5 5.2 4.8 3.9 Decreased 2009–2019 No change No change
Methamphetamine 4.1 3.8 3.2 3.0 2.5 2.1 Decreased 2009–2019 No change No change
Heroin 2.5 2.9 2.2 2.1 1.7 1.8 Decreased 2009–2019 No change No change
Injection drug use 2.1 2.3 1.7 1.8 1.5 1.6 Decreased 2009–2019 No change No change
Synthetic marijuana — — — 9.2 6.9 7.3 Decreased 2015-2019 NA
¶
No change
Prescription opioid misuse — — — — 14.0 14.3 NA
¶
NA
¶
No change
Abbreviation: NA = not available.
* Based on trend analyses by using a logistic regression model controlling for sex, race/ethnicity, and grade (p<0.05).
†
Based on t-test analysis (p<0.05).
§
Previous 30 days before the survey.
¶
Insufficient years of data to assess trends.
TABLE 2. Prevalence of lifetime and current use of specific substances and use behaviors among high school students, by demographic
characteristics — Youth Risk Behavior Survey, United States, 2019
Behavior
Sex Race/Ethnicity Grade Sexual identity
Male
(n = 6,641)
%
(95% CI)
Female
(n = 6,885)
%
(95% CI)
White,
non-Hispanic
(n = 6,668)
%
(95% CI)
Black,
non-Hispanic
(n = 2,040)
%
(95% CI)
Hispanic
(n = 3,038)
%
(95% CI)
9/10
(n = 7,354)
%
(95% CI)
11/12
(n = 6,172)
%
(95% CI)
Heterosexual
(n = 10,853)
%
(95% CI)
LGB
(n = 1,531)
%
(95% CI)
Not sure
(n = 591)
%
(95% CI)
Current use*
Marijuana 22.5
(20.6–24.5)
20.8
(18.7–23.1)
22.1
(19.9–24.6)
21.7
(19.1–24.5)
22.4
(20.4–24.6)
17.1
(15.5–18.8)
26.6
†
(23.6–29.7)
20.9
(19.0–23.0)
31.1
§
(27.4–35.1)
19.5
¶
(14.8–25.3)
Alcohol 26.4
(24.4–28.6)
31.9
**
(29.6–34.3)
34.2
(31.7–36.8)
16.8
††
(13.5–20.7)
28.4
††,§§
(26.1–30.8)
22.8
(20.6–25.2)
36.0
†
(33.8–38.3)
28.8
(26.8–30.8)
33.9
§
(29.8–38.2)
25.3
¶
(20.0–31.4)
Binge drinking 12.7
(11.0–14.6)
14.6
**
(13.2–16.2)
17.3
(15.1–19.7)
6.2
††
(4.2–9.2)
12.4
††,§§
(11.0–14.0)
8.9
(7.4–10.7)
18.8
†
(17.0–20.8)
13.4
(12.0–15.0)
15.6
(12.8–18.8)
13.1
(9.0–18.8)
Prescription
opioid misuse
6.1
(5.3–7.1)
8.3
**
(7.0–9.9)
5.5
(4.4–6.9)
8.7
††
(6.5–11.6)
9.8
††
(8.2–11.6)
7.0
(5.8–8.4)
7.3
(6.1–8.8)
6.4
(5.4–7.5)
12.0
§
(9.6–14.9)
11.5
§
(8.2–15.9)
Lifetime use
Marijuana 37.0
(34.2–40.0)
36.5
(34.1–38.9)
36.8
(33.9–39.8)
37.5
(34.0–41.1)
39.2
(36.5–41.9)
29.2
(26.7–31.8)
44.8
†
(41.5–48.2)
36.0
(33.3–38.7)
49.6
§
(45.1–54.1)
27.5
§,¶
(22.4–33.3)
Cocaine 4.9
(4.2–5.8)
2.7
**
(2.0–3.7)
2.9
(2.2–3.7)
4.0
(2.7–5.9)
5.6
††
(4.5–6.9)
2.8
(2.0–3.7)
5.0
†
(4.1–6.1)
3.3
(2.7–4.0)
7.0
§
(4.8–10.1)
7.6
§
(4.3–12.9)
Methamphetamine 2.7
(2.1–3.4)
1.5
**
(1.0–2.2)
1.2
(0.9–1.6)
3.8
††
(2.4–6.0)
2.7
††
(1.8–4.0)
1.5
(1.0–2.3)
2.6
†
(1.9–3.3)
1.5
(1.2–1.9)
5.0
§
(3.1–7.9)
6.1
§
(3.4–10.8)
Heroin 2.3
(1.8–3.1)
1.0
**
(0.6–1.8)
0.9
(0.6–1.2)
3.4
††
(2.2–5.3)
2.4
††
(1.5–3.9)
1.6
(1.0–2.5)
1.8
(1.3–2.5)
1.2
(0.9–1.6)
3.8
§
(2.1–7.0)
6.2
§
(3.4–11.0)
Injection drug use 2.1
(1.5–2.9)
1.1
**
(0.6–1.9)
0.8
(0.6–1.2)
2.9
††
(1.5–5.5)
2.5
††
(1.8–3.5)
1.6
(1.1–2.3)
1.5
(1.0–2.4)
1.1
(0.8–1.6)
3.5
§
(2.1–5.7)
5.1
§
(2.5–10.2)
Synthetic marijuana 7.2
(6.2–8.4)
7.4
(6.2–8.7)
6.7
(5.6–8.0)
5.7
(4.4–7.4)
9.8
††,§§
(8.6–11.3)
6.2
(5.3–7.3)
8.3
†
(7.2–9.7)
6.7
(5.8–7.7)
11.6
§
(9.0–14.7)
10.4
(6.9–15.5)
Prescription
opioid misuse
12.4
(11.0–14.1)
16.1
**
(14.1–18.4)
12.7
(10.9–14.7)
15.3
(12.9–18.1)
16.0
(13.5–18.8)
13.6
(11.9–15.5)
14.9
(13.2–16.7)
12.7
(11.2–14.4)
23.9
§
(19.9–28.3)
19.1
§
(14.6–24.5)
Abbreviations: CI = confidence interval; LGB = lesbian, gay, or bisexual.
* Previous 30 days before the survey.
†
Significantly different from 9/10 grade students, based on t-test analysis (p<0.05).
§
Significantly different from heterosexual students, based on t-test analysis (p<0.05).
¶
Significantly different from lesbian, gay, or bisexual students, based on t-test analysis (p<0.05).
**
Significantly different from male students, based on t-test analysis (p<0.05).
††
Significantly different from white students, based on t-test analysis (p<0.05).
§§
Significantly different from black students, based on t-test analysis (p<0.05).
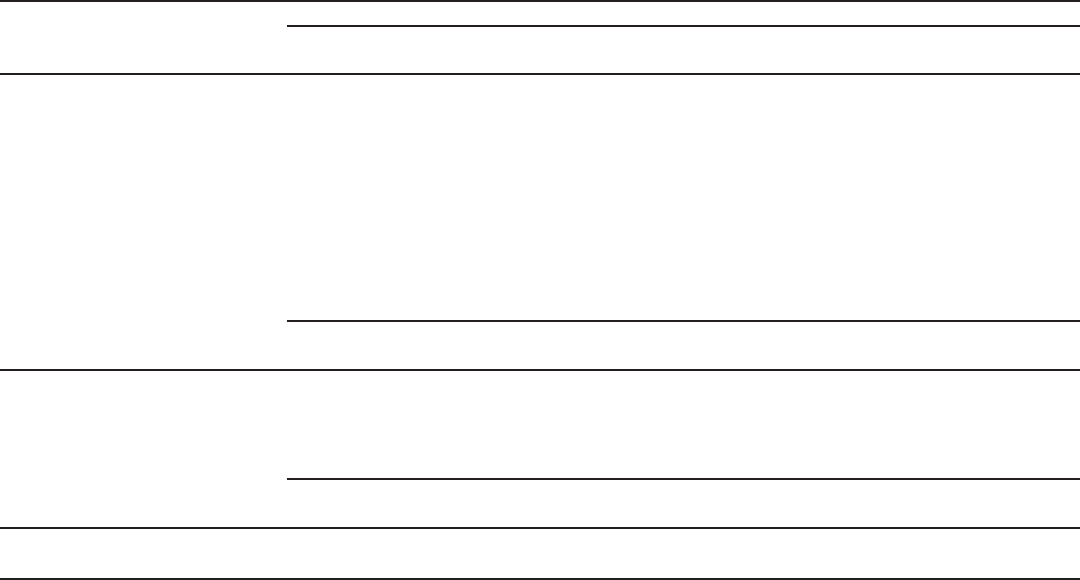
Supplement
42 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
notable differences in prevalence estimates were identified for
current use of alcohol, binge drinking, current prescription
opioid misuse, and lifetime use of cocaine, methamphetamine,
heroin, injection drug use, and synthetic marijuana. However,
no clear pattern emerged. For example, the prevalence of
current prescription opioid misuse was significantly lower
among white students (5.5%) compared with black (8.7%)
or Hispanic students (9.8%). Conversely, the prevalence of
current alcohol use was lower among black students (16.8%)
compared with white (34.2%) or Hispanic students (28.4%).
Approximately half of the substance use behaviors varied
substantially by grade, with consistently higher prevalence
among 11th-
and 12th-grade students compared with 9th- and
10th-grade students for current marijuana use, current alcohol
use and binge drinking, lifetime marijuana use, lifetime cocaine
use, lifetime methamphetamine use, and lifetime synthetic
marijuana. Prevalence of all but one of the substance use
behaviors (i.e., binge drinking) varied considerably by sexual
identity. Students who identified as lesbian, gay, or bisexual
had a higher prevalence of all substance use behaviors, except
binge drinking, compared with students who identified as
heterosexual. Similarly, students who identified as not sure of
their sexual identity also had higher prevalence of approximately
TABLE 3. Frequency of lifetime and current use among high school students reporting use of specific substances — Youth Risk Behavior Survey,
United States, 2019
Behavior
Frequency
1–2 times
% (95% CI)
3–9 times
% (95% CI)
10–39 times
% (95% CI)
≥40 times
% (95% CI)
Current use*
Marijuana (n = 2,946) 36.7 (33.7–39.8) 21.8 (19.7–24.1) 23.5 (21.4–25.8) 18.0 (15.1–21.3)
Prescription opioid misuse (n = 661) 53.2 (47.9–58.5) 23.3 (18.9–28.3) 13.7 (11.0–16.9) 9.8 (6.3–14.8)
Lifetime use
Marijuana (n = 4,219) 24.6 (22.4–27.1) 20.9 (19.3–22.6) 20.8 (19.2–22.5) 33.6 (30.5–36.9)
Prescription opioid misuse (n = 2,000) 48.8 (45.7–51.9) 24.7 (22.4–27.2) 15.9 (14.0–18.1) 10.6 (8.8–12.7)
Synthetic marijuana (n = 955) 48.8 (44.9–52.6) 20.8 (17.8–24.3) 18.5 (14.9–22.8) 11.9 (9.2–15.3)
Cocaine (n = 557) 45.0 (38.7–51.5) 20.3 (15.7–25.9) 18.5 (14.4–23.6) 16.1 (11.8–21.7)
Methamphetamine (n = 351) 42.9 (34.7–51.5) 15.5 (10.8–21.7) 13.7 (9.0–20.3) 27.9 (19.1–39.0)
Heroin (n = 316) 31.7 (24.4–40.1) 18.6 (12.8–26.2) 16.9 (11.8–23.6) 32.9 (21.7–46.3)
Behavior
Frequency
1–2 days
% (95% CI)
3–9 days
% (95% CI)
10–19 days
% (95% CI)
≥20 days
% (95% CI)
Current use
Alcohol use (n = 3,669) 54.8 (52.6–57.0) 36.6 (34.4–38.8) 5.1 (4.1–6.4) 3.5 (2.6–4.7)
Binge drinking (n = 1,657) 61.2 (56.5–65.7) 31.1 (27.7–34.7) 4.1 (2.7–6.2) 3.6 (2.4–5.3)
Behavior
Frequency
1 time
% (95% CI)
≥2 times
% (95% CI)
Lifetime use
Injection drug use (n = 200) 47.8 (35.4–60.4) 52.2 (39.6–64.6)
Abbreviation: CI = confidence interval.
* Previous 30 days before the survey.
half of the substance use behaviors compared with heterosexual
students, including current prescription opioid misuse, lifetime
cocaine use, lifetime methamphetamine use, lifetime heroin
use, lifetime injection drug use, and lifetime prescription opioid
misuse. However, students who identified as not sure of their
sexual identity had lower prevalence of certain substance use
behaviors compared with students identifying as lesbian, gay,
or bisexual, including current marijuana use, current alcohol
use, and lifetime marijuana use.
Frequency of use (i.e., number of times used or number
of days used) varied across specific substance use behaviors
(Table 3). Among students reporting marijuana use during the
30 days before the survey (i.e., current use), 18.0% reported
using it ≥40 times; 23.5%, 10–39 times; 21.8%, 3–9 times;
and 36.7%, 1–2 times. For current prescription opioid misuse,
9.8% reported misuse ≥40 times; 13.7%, 10–39 times; 23.3%,
3–9 times, and 53.2%, 1–2 times. Among students reporting
lifetime use of specific substances, marijuana had the highest
percentage of students reporting use ≥40 times (33.6%),
followed by heroin (32.9%), methamphetamine (27.9%),
and cocaine (16.1%). Lifetime prescription opioid misuse and
lifetime synthetic cannabinoid use were the two substances
with the highest percentages reporting use 1–2 times (48.8%
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 43
US Department of Health and Human Services/Centers for Disease Control and Prevention
each), followed by cocaine (45.0%), and methamphetamine
(42.9%). Among students reporting current alcohol use or
current binge drinking, more than half of students (54.8%
and 61.2%, respectively) reported those behaviors on 1–2 days.
Among students who had ever injected drugs (1.2%), 47.8%
reported injecting drugs 1 time, and 52.2% reported injecting
drugs ≥2 times.
Students reporting current prescription opioid misuse
commonly indicated use of other substances (Figure). Overall,
43.5% of students reporting current prescription opioid misuse
also reported current marijuana use, 59.4% reported current
alcohol use, and 30.3% reported current binge drinking.
Lifetime use of other substances among students reporting
current prescription opioid misuse was 62.9% for marijuana,
30.3% for synthetic marijuana, 20.5% for cocaine, 15.0%
for methamphetamine, and 14.0% for heroin. Approximately
12.4% of students reporting current prescription opioid misuse
also reported lifetime injection drug use.
In adjusted analyses, current prescription opioid misuse
varied by sex, race/ethnicity, and sexual identity (Table 4).
Specifically, males were significantly less likely to report
engaging in current prescription opioid misuse (aPR: 0.69;
95% CI: 0.57–0.84) compared with females (referent group);
black and Hispanic students were significantly more likely to
have engaged in prescription opioid misuse (black students,
aPR: 1.49; 95% CI: 1.05–2.10; Hispanic students, aPR: 1.52;
95% CI: 1.12–2.05) compared with white students (referent
group); and students identifying as lesbian, gay, or bisexual
were more likely to report current prescription opioid misuse
(aPR: 1.35; 95% CI: 1.02–1.79) compared with students
identifying as heterosexual (referent group). All substance
use behaviors included in the model, except for marijuana
use, were significantly associated with current prescription
opioid misuse, ranging from aPR= 2.13 (95% CI: 1.59–
2.86) for lifetime synthetic marijuana use and aPR = 2.13
(95% CI: 1.58–2.86) for previous 30-day binge drinking, to
aPR=5.08 (95% CI: 2.72–9.49) for lifetime injection drug use.
Discussion
This report provides key insights into substance use
behaviors of U.S. high school students during 2009–2019.
Encouraging findings include decreasing prevalence of current
alcohol use and decreases in the prevalence of lifetime use of
marijuana, cocaine, methamphetamine, heroin, synthetic
marijuana, and injection drug use. However, the findings in
this report underscore that substance use among high school
students remains common, with approximately one in three
students reporting current alcohol use, one in five reporting
current marijuana use, and one in seven reporting current
binge drinking. Because of the ongoing U.S. opioid crisis, of
particular concern are the high rates of lifetime (one in seven
students) and current prescription opioid misuse (one in 14
students) and high rates of co-occurring substance use among
students currently misusing prescription opioids.
Notable demographic differences and patterns in substance
use among high school students are identified in this report.
Specifically, males had substantially higher rates of cocaine,
methamphetamine, heroin, and injection drug use compared
with females, and females had substantially higher rates of
current alcohol use and current binge drinking. In addition,
females had higher rates of current prescription opioid misuse
compared with males, and this pattern persisted in multivariable
models where males had lower adjusted prevalence ratios for
current prescription opioid misuse compared with females.
Differences also occurred in substance use patterns across
racial/ethnic groups. For example, black and Hispanic students
reported higher rates of current prescription opioid misuse
compared with white students; in contrast, white students
reported the highest rates of current alcohol use and binge
drinking, followed by Hispanic and black students. These
substance use patterns by racial/ethnic groups are similar to
those identified in other U.S. youth substance use surveys
(https://www.samhsa.gov/data/report/2018-nsduh-detailed-
tables). This heterogeneity in substance use patterns among
demographic groups can be used to guide development of
tailored and targeted prevention messages and interventions.
Particularly noteworthy were the universally elevated rates
of substance use among self-identified sexual minority youths
compared with heterosexual youths, which is consistent with
previous research (12). In addition to findings regarding
broader substance use patterns, this report provides actionable
information on prescription opioid misuse among high school
students that can be applied to ongoing efforts for preventing
opioid misuse, use disorders, and overdoses. Specifically, the
high rates of co-occurring substance use, especially alcohol and
marijuana use, among students currently misusing prescription
opioids highlights the importance of prevention efforts that focus
on general substance use risk and protective factors. Notably,
these associations are not limited to high school students because
binge drinking and marijuana use are associated with increased
prescription opioid misuse among both adults and adolescents
(13). Finally, sexual minority youths also had significantly
higher prevalence of current prescription opioid misuse even
after controlling for other demographic and substance use
characteristics, which is consistent with their overall pattern
of higher rates of substance use in this study. It also further
emphasizes the importance of identifying tailored prevention
strategies to address disparities among this vulnerable population.
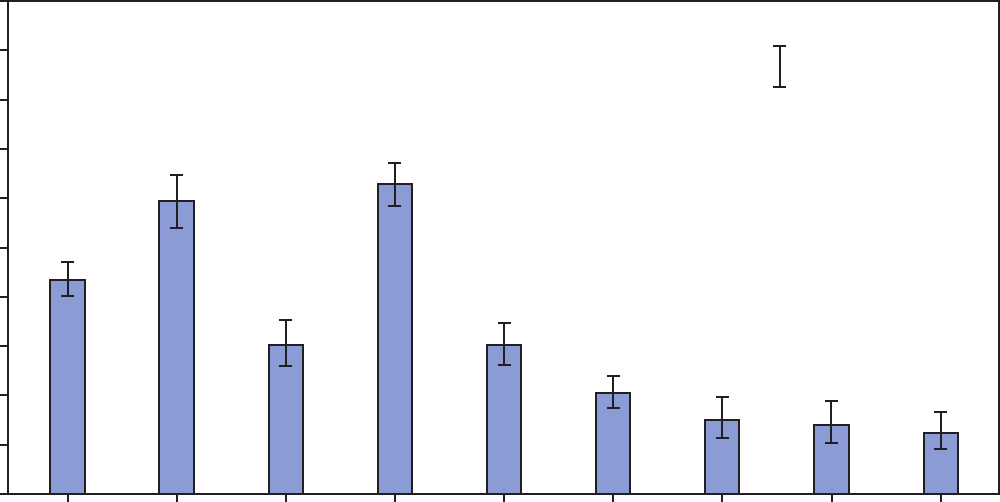
Supplement
44 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. Percentage of co-occurring substance use behaviors among high school students who reported previous 30-day prescription opioid
misuse* — Youth Risk Behavior Survey, United States, 2019
0
10
20
30
40
50
Percentage
60
70
80
90
100
Previous
30-day
marijuana
use
Previous
30-day
alcohol
use
Previous
30-day
binge
alcohol
use
Lifetime
marijuana
use
Lifetime
synthetic
marijuana
use
Lifetime
cocaine
use
Lifetime
meth-
amphetamine
use
Lifetime
heroin
use
Lifetime
injection
drug
use
95% Condence interval
Substance use behaviors
* Unweighted N = 661.
Scientific evidence for the effective prevention of substance
use indicates the importance of interventions that target risk
and protective factors at the individual, family, and community
levels to maximize their public health impact (1–3). Risk
factors include adverse childhood experiences at the individual
level, limited parental monitoring and involvement and
active substance use in the home at the family level, and easy
availability and accessibility to alcohol and other substances
and community norms favorable toward use of alcohol and
other substances at the community level (1,2,5). In addition,
studies have demonstrated that youth alcohol use is associated
with adult alcohol use, and that both community-level and
individual-level alcohol use are affected by population-level
alcohol policies (e.g., those that reduce the availability and
accessibility of alcohol and increase its price) (14).
The ability to reach young persons during early elementary
ages, before they begin using substances, and throughout
adolescence makes the school environment well-suited
for prevention programming. School-based substance use
prevention programs that focus on broad-based skill building
(e.g., psychosocial development, life-skills development, and
social-emotional learning and connectedness) have greater
promise than substance-specific programs (15,16). In addition,
multifaceted programs that incorporate aspects of individual,
school, and family interventions (e.g., the Promoting School-
community-university Partnerships to Enhanced Resilience
[PROSPER] program and Communities That Care [CTC])
have demonstrated effectiveness at reducing or preventing
youth substance use (17,18).
Broader prevention policies for changing the environment
in which youths live (e.g., those that reduce the availability of
substances) can also be used as part of a comprehensive approach
for reducing youth substance use. The U.S. Community
Preventive Services Task Force recommends certain population-
level strategies (e.g., increasing alcohol taxes and regulating
the number and concentration of places that sell alcohol as
interventions for reducing excessive alcohol use, including
alcohol use among youths) (https://www.thecommunityguide.
org/resources/what-works-preventing-excessive-alcohol-
consumption). Enhanced enforcement of existing substance
use policies (e.g., prescription drug monitoring programs
that are used universally with near–real-time data and laws

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 45
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 4. Multivariable logistic regression model examining
individual-level characteristics associated with previous 30-day
prescription opioid misuse among high school students — Youth
Risk Behavior Survey, United States, 2019
Characteristic
Adjusted*
prevalence ratios
(95% CI)
Demographics
Sex
Female Referent
Male 0.69 (0.57–0.84)
Race/Ethnicity
White, non-Hispanic Referent
Black, non-Hispanic 1.49 (1.05–2.10)
Hispanic 1.52 (1.12–2.05)
Grade
9 or 10 Referent
11 or 12 0.85 (0.66–1.10)
Sexual identity
Heterosexual Referent
Lesbian, gay, or bisexual 1.35 (1.02–1.79)
Not sure 1.37 (0.86–2.17)
Substance use and use behaviors
Alcohol use
No previous 30-day use Referent
Previous 30-day nonbinge drinking 2.28 (1.63–3.19)
Previous 30-day binge drinking 2.13 (1.58–2.86)
Marijuana use
No lifetime use Referent
Lifetime use, but no previous 30-day use 1.21 (0.89–1.65)
Previous 30-day use 1.31 (0.95–1.80)
Lifetime synthetic marijuana use
No Referent
Yes 2.13 (1.59–2.86)
Lifetime use of cocaine, heroin, or methamphetamine
No Referent
Yes 2.49 (1.89–3.27)
Lifetime injection drug use
No Referent
Yes 5.08 (2.72–9.49)
Abbreviation: CI = confidence interval.
* Adjusted prevalence ratios were calculated from a single logistic regression
model that included all covariates listed in this table.
prohibiting sales of alcohol to persons aged <21 years) also
can help reduce substance use among youths (19,20). In
addition, strategies for expanding access to evidence-based pain
treatment and improving prescribing of prescription opioids
through safer prescribing practices can help reduce opioid
misuse and overdoses. Improving opioid prescribing can have
dual benefits by reducing the environmental availability of
prescription opioids for diversion and misuse and reducing
the risk for misuse associated with the prescription of opioids
to youths (2).
Limitations
General limitations for the YRBS are available in the overview
report of this supplement (11). The findings in this report are
subject to at least three additional limitations. First, the questions
assessing lifetime and current prescription opioid misuse refer
to prescription pain medicine; however, the questions provide
examples of opioid-containing prescription medications only.
Therefore, if students considered nonopioid prescription pain
medications when answering, an overestimation of prescription
opioid misuse prevalence might have occurred. Second, many
of the substance use questions included common street names
for drugs; however, newly introduced street names or street
names specific to certain geographic areas were not included,
which might have resulted in underreporting of substance
use behaviors. Finally, there was variation in the amount of
missing data for some substance use variables (e.g., the largest
amount missing was for current prescription opioid misuse
[5,000 missing observations]). Missing data might result from
a variety of factors, such as students choosing not to answer
questions or inconsistent responses to similar questions that
are set to missing during the data cleaning process (11). In
addition, schools selected to participate in the national YRBS
and in a state or local YRBS only complete the local version
of the survey; as a result, questions included on the national
survey but not the local survey are set to missing.
Conclusion
The findings in this report indicate that youth substance use
has declined in recent years; however, substance use, including
misuse of prescription opioids, remains common among
U.S. high school students. Opportunities exist for bringing
to scale evidence-based policies, programs, and practices
that aim to reduce risk factors and strengthen protective
factors among youths in conjunction with initiatives already
underway for combating the U.S. opioid overdose epidemic.
Disproportionately affected populations (e.g., sexual minority
youths) might benefit from tailored substance use interventions
combined with more widespread implementation of broader
population-level policy strategies.
Conicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
Supplement
46 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
References
1. Office of the Surgeon General. Facing addiction in America: the Surgeon
General’s report on alcohol, drugs, and health. Rockville, MD: US
Department of Health and Human Services; 2016. https://addiction.
surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf
2. Compton WM, Jones CM, Baldwin GT, Harding FM, Blanco C,
Wargo EM. Targeting youth to prevent later substance use disorder:
an underutilized response to the U.S. opioid crisis. Am J Public
Health 2019;109(Suppl3):S185–9. https://doi.org/10.2105/
AJPH.2019.305020
3. Steinberg L. Risk taking in adolescence: new perspectives from brain
and behavioral science. Curr Dir Psychol Sci 2007;16:55–9. https://doi.
org/10.1111/j.1467-8721.2007.00475.x
4. DuPont RL, Han B, Shea CL, Madras BK. Drug use among youth:
National survey data support a common liability of all drug use. Prev
Med 2018;113:68–73. https://doi.org/10.1016/j.ypmed.2018.05.015
5. Hawkins JD, Jenson JM, Catalano R, et al. Unleashing the power
of prevention. Am J Med Res (N Y) 2016;3:39–74. https://doi.
org/10.22381/AJMR3120162
6. Clayton HB, Bohm MK, Lowry R, Ashley C, Ethier KA. Prescription
opioid misuse associated with risk behaviors among adolescents. Am J Prev
Med 2019;57:533–9. https://doi.org/10.1016/j.amepre.2019.05.017
7. Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in
hospitalizations for opioid poisonings among children and adolescents,
1997 to 2012. JAMA Pediatr 2016;170:1195–201. https://doi.
org/10.1001/jamapediatrics.2016.2154
8. Cerda M, Santaella J, Marshall BD, Kim JH, Martins SS. Nonmedical
prescription opioid use in childhood and early adolescence predicts
transitions to heroin use in young adulthood: a national study. J Pediatr
2015;167:605–12e1–2.
9. Jones CM. Trends and key correlates of prescription opioid injection
misuse in the United States. Addict Behav 2018;78:145–52. https://doi.
org/10.1016/j.addbeh.2017.10.018
10. Jones CM, Christensen A, Gladden RM. Increases in prescription
opioid injection abuse among treatment admissions in the United States,
2004-2013. Drug Alcohol Depend 2017;176:89–95. https://doi.
org/10.1016/j.drugalcdep.2017.03.011
11. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
12. Rostad WL, Clayton HB, Estefan LF, Johns MM. Substance use and
disparities in teen dating violence victimization by sexual identity
among high school students. Prev Sci 2020;21:398–407. https://doi.
org/10.1007/s11121-019-01049-7
13. Esser MB, Guy GP Jr, Zhang K, Brewer RD. Binge drinking and
prescription opioid misuse in the U.S., 2012–2014. Am J Prev Med
2019;57:197–208. https://doi.org/10.1016/j.amepre.2019.02.025
14. Xuan Z, Blanchette JG, Nelson TF, et al. Youth drinking in the
United States: relationships with alcohol policies and adult drinking.
Pediatrics 2015;136:18–27. https://doi.org/10.1542/peds.2015-0537
15. Griffin KW, Botvin GJ. Evidence-based interventions for preventing
substance use disorders in adolescents. Child Adolesc Psychiatr Clin N
Am 2010;19:505–26. https://doi.org/10.1016/j.chc.2010.03.005
16. Faggiano F, Minozzi S, Versino E, Buscemi D. Universal school-
based prevention for illicit drug use. Cochrane Database Syst Rev
2014;12:CD003020. https://doi.org/10.1002/14651858.CD003020.
pub3
17. Spoth R, Redmond C, Shin C, Greenberg MT, Feinberg ME, Trudeau L.
PROSPER delivery of universal preventive interventions with young
adolescents: long-term effects on emerging adult substance misuse and
associated risk behaviors. Psychol Med 2017;47:2246–59. https://doi.
org/10.1017/S0033291717000691
18. Oesterle S, Kuklinski MR, Hawkins JD, Skinner ML, Guttmannova K,
Rhew IC. Long-term effects of the Communities That Care trial on
substance use, antisocial behavior, and violence through age 21 years.
Am J Public Health 2018;108:659–65. https://doi.org/10.2105/
AJPH.2018.304320
19. Elder R, Lawrence B, Janes G, et al. Enhanced enforcement of laws
prohibiting sale of alcohol to minors: systematic review of effectiveness
for reducing sales and underage drinking. Washington, DC:
Transportation Research Board; 2007:181–8. Transportation Research
Circular no. E-C123.
20. Haegerich TM, Jones CM, Cote PO, Robinson A, Ross L. Evidence
for state, community and systems-level prevention strategies to address
the opioid crisis. Drug Alcohol Depend 2019;204:107563. https://doi.
org/10.1016/j.drugalcdep.2019.107563

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 47
US Department of Health and Human Services/Centers for Disease Control and Prevention
Suicidal Ideation and Behaviors Among High School Students —
Youth Risk Behavior Survey, United States, 2019
Asha Z. Ivey-Stephenson, PhD
1
; Zewditu Demissie, PhD
2
; Alexander E. Crosby, MD
1
; Deborah M. Stone, ScD
1
; Elizabeth Gaylor, MPH
1
;
Natalie Wilkins, PhD
2
; Richard Lowry, MD
3
; Margaret Brown, DrPH
1
1
Division of Injury Prevention, National Center for Injury Prevention and Control, CDC;
2
Division of Adolescent and School Health, National Center for HIV/AIDS,
Viral Hepatitis, STD, and TB Prevention, CDC;
3
Office of the Director, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC
Abstract
Suicide is the second leading cause of death among high school-aged youths 14–18 years after unintentional injuries. This
report summarizes data regarding suicidal ideation (i.e., seriously considered suicide) and behaviors (i.e., made a suicide plan,
attempted suicide, and made a suicide attempt requiring medical treatment) from CDC’s 2019 Youth Risk Behavior Survey.
Results are reported overall and by sex, grade, race/ethnicity, sexual identity, and sex of sexual contacts, overall and within sex
groups. Trends in suicide attempts during 2009–2019 are also reported by sex, race/ethnicity, and grade. During 2009–2019,
prevalence of suicide attempts increased overall and among female, non-Hispanic white, non-Hispanic black, and 12th-grade
students. Data from 2019 reflect substantial differences by demographics regarding suicidal ideation and behaviors. For example,
during 2019, a total of 18.8% of students reported having seriously considered suicide, with prevalence estimates highest among
females (24.1%); white non-Hispanic students (19.1%); students who reported having sex with persons of the same sex or with
both sexes (54.2%); and students who identified as lesbian, gay, or bisexual (46.8%). Among all students, 8.9% reported having
attempted suicide, with prevalence estimates highest among females (11.0%); black non-Hispanic students (11.8%); students
who reported having sex with persons of the same sex or with both sexes (30.3%); and students who identified as lesbian, gay, or
bisexual (23.4%). Comprehensive suicide prevention can address these differences and reduce prevalence of suicidal ideation and
behaviors by implementing programs, practices, and policies that prevent suicide (e.g., parenting programs), supporting persons
currently at risk (e.g., psychotherapy), preventing reattempts (e.g., emergency department follow-up), and attending to persons
who have lost a friend or loved one to suicide.
Introduction
Suicidal behavior presents a major challenge to public
health in the United States and globally (1). Although fatal
(i.e., suicide) and nonfatal (e.g., suicide attempts) suicidal
behaviors are a public health concern across the life span,
they are of particular concern for youths and young adults
aged 10–24 years. During 2018, a total of 48,344 persons
(all ages) died from suicide, and suicide was the 10th leading
cause of death overall in the United States, accounting for
approximately 1.7% of all deaths (2). Among high school–
aged youths (14–18 years), 2,039 suicides occurred that year,
making it the second leading cause of death for this age group
after unintentional injuries (n = 2,590). Suicide accounted
for approximately 33.9% or approximately one of every
three injury-related deaths among this age group (2). During
2009–2018, suicide rates among youths aged 14–18 years
Corresponding author: Asha Z. Ivey-Stephenson, PhD, Division of
Injury Prevention, National Center for Injury Prevention and Control,
CDC. Telephone: 770-488-0940; E-mail: [email protected].
increased by 61.7% from 6.0 to 9.7 per 100,000 population
(2). Although suicide is a major public health problem, many
more youths make suicide attempts and struggle with suicidal
ideation. For example, during 2018, according to data from
a nationally representative sample of emergency departments
(EDs), approximately 95,000 youths aged 14–18 years visited
EDs for self-harm injuries (2).
One objective of the Healthy People 2020 Mental Health
and Mental Disorders is to reduce suicide attempts by
adolescents that resulted in an injury, poisoning, or overdose
that had to be treated by a doctor or nurse (3). The Youth Risk
Behavior Survey (YRBS) monitors six categories of priority
health behaviors and experiences among adolescents, with
four questions specifically related to suicide (4). This report
summarizes 2019 YRBS data regarding suicidal ideation and
behaviors among high school students and presents trends in
suicide attempts among this population during 2009–2019.
The report is intended for decision-makers, prevention
program practitioners, and those who work in youth-serving
organizations so that they can identify vulnerable youths and
take appropriate action to direct prevention resources to those
young persons.
Supplement
48 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Methods
Data Source
This report includes data from the 2009–2019 cycles of
the YRBS, a cross-sectional, school-based survey conducted
biennially since 1991. Each survey year, CDC collects data
from a nationally representative sample of public and private
school students in grades 9–12 in the 50 U.S. states and the
District of Columbia. Additional information about YRBS
sampling, data collection, response rates, and processing
is available in the overview report of this supplement (4).
The overview report also includes information about the
classification of sexual identity and sex of sexual contacts and
standard data analysis methods. The prevalence estimates for
all suicidal ideation and behavior questions for the overall
study population and by sex, race/ethnicity, grade, and sexual
orientation are available at https://nccd.cdc.gov/youthonline/
App/Default.aspx. The full YRBS questionnaire is available at
https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2019/2019_
YRBS-National-HS-Questionnaire.pdf.
Measures
Four suicidal ideation and behavior variables are included in
this report. Suicidal ideation was measured with the question,
“During the past 12 months, did you ever seriously consider
attempting suicide?” Making a suicide plan was measured
with the question, “During the past 12 months, did you
make a plan about how you would attempt suicide?” (These
two questions had “yes” or “no” response options.) Suicide
attempts were measured with the question, “During the
past 12 months, how many times did you actually attempt
suicide?” Suicide attempts were assessed by frequency of
attempts, but the variable was dichotomized into yes or no
responses for analytic purposes. Lastly, students were asked,
“If you attempted suicide during the past 12 months, did any
attempt result in an injury, poisoning, or overdose that had to
be treated by a doctor or nurse?” This question is referred to
in this report as, “made a suicide attempt requiring medical
treatment.” The response options for the last question were,
“I did not attempt suicide during the past 12 months,” “yes,”
or “no”; however, this variable was also dichotomized into yes
or no responses for analysis.
Analysis
Analyses of these suicidal ideation and behavior variables
included examining associations between each item and
demographic characteristics, including sex (male/female), race/
ethnicity (non-Hispanic white [white], non-Hispanic black
[black], or Hispanic), grade (9, 10, 11, or 12), sexual identity
(heterosexual; lesbian, gay, or bisexual [LGB]; or not sure), or
sex of sexual contacts (sexual contact with only the opposite
sex, sexual contact with only the same sex or both sexes, and
no sexual contact). Associations by race/ethnicity, grade, sexual
identity, and sex of sexual contacts were calculated for the
overall study population but also separately for male and female
students. Statistical differences were determined by using
chi-square analyses at the p <0.05 level of significance. Linear
trends for 2009–2019 were examined for attempted suicide by
sex, race/ethnicity, and grade. All analyses of suicidal ideation
and behaviors were conducted among the full sample, and
analysis of behavior variables was not limited to students who
reported suicidal ideation (i.e., analysis conducted among the
full sample). Additional information about the methods used
to conduct YRBS trend analyses are provided in the overview
report of this supplement (4).
Results
Suicidal Ideation and Behaviors,
Overall and by Sex
During the 12 months before the survey, 18.8% of students
nationwide reported seriously considered attempting suicide
(prevalence significantly higher among female [24.1%] than
male [13.3%] students), and among students nationwide,
15.7% of students had made a plan about how they would
attempt suicide (prevalence significantly higher among female
[19.9%] than male [11.3%] students), and 8.9% of students
had attempted suicide ≥1 time (prevalence significantly higher
among female [11.0%] than male [6.6%] students) (Table 1).
Nationwide, 2.5% of students had made a suicide attempt
requiring medical treatment, with a prevalence significantly
higher among female (3.3%) than male (1.7%) students.
Suicidal Ideation and Behaviors by Race/
Ethnicity and Grade, Overall and by Sex
Overall, a significant difference occurred in having seriously
considered attempting suicide by race/ethnicity (white: 19.1%;
black: 16.9%; Hispanic: 17.2%) (Table 2), with a significant
difference by race/ethnicity among male students (white:
13.8%; black: 10.7%; Hispanic: 11.4%) but not among female
students. No significant differences (overall or by sex) occurred
in having seriously considered attempting suicide by grade.
Among students reporting having made a suicide plan, a
significant difference occurred by race and ethnicity overall
(white: 15.7%; black: 15.0%; Hispanic: 14.7%) but not among
male or female students. No significant difference occurred in
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 49
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Percentage of high school students who had seriously considered attempting suicide, had made a suicide plan, had attempted
suicide, or had made a suicide attempt requiring medical treatment during the 12 months before the survey, by sex — Youth Risk Behavior
Survey, United States, 2019
Behavior
Female
% (95% CI)
Male
% (95% CI)
Total
% (95% CI)
Chi-square
(p value)
Seriously considered attempting suicide 97.922 (<0.001)
Yes 24.1 (22.3–26.0) 13.3 (12.2–14.5) 18.8 (17.6–20.0) NA
No 75.9 (74.0–77.7) 86.7 (85.5–87.8) 81.2 (80.0–82.4) NA
Made a suicide plan 109.568 (<0.001)
Yes 19.9 (18.4–21.6) 11.3 (10.3–12.4) 15.7 (14.6–16.9) NA
No 80.1 (78.4–81.6) 88.7 (87.6–89.7) 84.3 (83.1–85.4) NA
Attempted suicide 27.037 (<0.001)
Yes 11.0 (9.7–12.5) 6.6 (5.5–8.1) 8.9 (7.9–10.0) NA
No 89.0 (87.5–90.3) 93.4 (91.9–94.5) 91.1 (90.0–92.1) NA
Made a suicide attempt requiring medical treatment* 10.313 (0.003)
Yes 3.3 (2.6–4.2) 1.7 (1.3–2.3) 2.5 (2.1–3.0) NA
No 96.7 (95.8–97.4) 98.3 (97.7–98.7) 97.5 (97.0–97.9) NA
Abbreviations: CI = confidence interval; NA = not applicable.
* Made a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse.
having made a suicide plan by grade overall or among female
students, but a significant difference was identified among male
students (9th grade: 9.5%; 10th grade: 10.4%; 11th grade:
12.1%; 12th grade: 13.6%). Students who had attempted
suicide were significantly different by race/ethnicity overall
(white: 7.9%; black: 11.8%; Hispanic: 8.9%) and among
female students (white: 9.4%; black: 15.2%; Hispanic: 11.9%)
but not among male students. No significant differences
existed in having attempted suicide by grade (overall or by
sex). In addition, no significant difference in having made a
suicide attempt requiring medical treatment was noted by race/
ethnicity or grade, overall or by sex.
Suicidal Ideation and Behaviors by Sexual
Identity and Sex of Sexual Contacts,
Overall and by Sex
A significant difference occurred in having seriously
considered attempting suicide by sexual identity overall
(heterosexual: 14.5%; LGB: 46.8%; not sure: 30.4%) (Table 3)
and among both female (heterosexual: 18.0%; LGB: 49.0%;
not sure: 35.9%) and male (heterosexual: 11.4%; LGB:
40.4%; not sure: 21.7%) students. Similarly, having seriously
considered attempting suicide varied by sex of sexual contacts,
overall (had sexual contact with only the opposite sex: 19.4%;
had sexual contact with only the same sex or both sexes:
54.2%; had no sexual contact: 13.0%), among female (had
sexual contact with only the opposite sex: 25.3%; had sexual
contact with only the same sex or both sexes: 59.2%; had no
sexual contact: 16.2%), and among male (had sexual contact
with only the opposite sex: 14.6%; had sexual contact with
only the same sex or both sexes: 39.1%; had no sexual contact:
9.7%) students.
Overall, a significant difference occurred in having made
a suicide plan by sexual identity (heterosexual: 12.1%; LGB:
40.2%; not sure: 23.9%), with a significant difference among
both female (heterosexual: 14.6%; LGB: 42.4%; not sure:
28.1%) and male (heterosexual: 9.9%; LGB: 33.0%; not sure:
17.4%) students. Similarly, a significant difference was noted
among students having made a suicide plan by sex of sexual
contacts, overall (had sexual contact with only the opposite
sex: 16.5%; had sexual contact with only the same sex or both
sexes: 44.0%; had no sexual contact: 10.9%), with a significant
difference among both female (had sexual contact with only
the opposite sex: 20.7%; had sexual contact with only the same
sex or both sexes: 48.2%; had no sexual contact: 13.8%) and
male (had sexual contact with only the opposite sex: 12.9%;
had sexual contact with only the same sex or both sexes: 31.2%;
had no sexual contact: 7.9%) students.
A significant difference existed in having attempted suicide
by sexual identity, overall (heterosexual: 6.4%; LGB: 23.4%;
not sure: 16.1%) and among both female (heterosexual: 7.9%;
LGB: 23.6%; not sure: 15.2%) and male (heterosexual: 5.1%;
LGB: 23.8%; not sure: 16.4%) students. Similarly, a significant
difference was identified in having attempted suicide by sex
of sexual contacts, overall (had sexual contact with only the
opposite sex: 9.3%; had sexual contact with only the same
sex or both sexes: 30.3%; no sexual contact: 4.8%), with a
significant difference among both female (had sexual contact
with only the opposite sex: 11.4%; had sexual contact with
only the same sex or both sexes: 31.4%; no sexual contact:
6.1%) and male (had sexual contact with only the opposite
sex: 7.5%; had sexual contact with only the same sex or both
sexes: 26.5%; no sexual contact: 3.5%) students.
Finally, a significant difference occurred in having made a
suicide attempt requiring medical treatment by sexual identity,
Supplement
50 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Percentage of high school students who had seriously considered attempting suicide, had made a suicide plan, had attempted
suicide, or had made a suicide attempt requiring medical treatment during the 12 months before the survey, by sex, race/ethnicity, and
grade — Youth Risk Behavior Survey, United States, 2019
Behavior
Female
% (95% CI)
Chi-square
(p value)
Male
% (95% CI)
Chi-square
(p value)
Total
% (95% CI)
Chi-square
(p value)
Seriously considered attempting suicide
Race/Ethnicity —* 1.504 (0.230) — 4.989 (0.005) — 5.870 (0.002)
White, non-Hispanic 24.3 (21.9–26.9) — 13.8 (12.3–15.3) — 19.1(17.6–20.8) —
Black, non-Hispanic 23.7 (20.7–27.1) — 10.7 (8.2–13.7) — 16.9 (15.3–18.7) —
Hispanic 22.7 (19.3–26.5) — 11.4 (9.8–13.3) — 17.2 (15.2–19.4) —
Grade — 0.209 (0.889) — 0.790 (0.507) — 0.820 (0.491)
9 23.7 (20.7–27.0) — 11.9 (9.9–14.2) — 17.7 (15.7–19.8) —
10 23.6 (20.3–27.3) — 13.2 (11.1–15.8) — 18.5 (16.1–21.1) —
11 24.9 (22.5–27.6) — 13.6 (11.5–16.0) — 19.3 (17.7–21.1) —
12 24.0 (20.7–27.6) — 14.9 (12.4–17.7) — 19.6 (17.5–21.9) —
Made a suicide plan
Race/Ethnicity — 1.652 (0.194) — 2.358 (0.087) — 3.043 (0.041)
White, non-Hispanic 19.2 (16.9–21.8) — 12.0 (10.6–13.5) — 15.7 (14.1–17.4) —
Black, non-Hispanic 20.4 (17.6–23.5) — 10.1 (7.3–13.9) — 15.0 (12.9–17.5) —
Hispanic 19.6 (16.9–22.6) — 9.6 (8.0–11.4) — 14.7 (13.0–16.7) —
Grade — 0.461 (0.711) — 3.195 (0.035) — 0.652 (0.587)
9 20.4 (17.9–23.2) — 9.5 (7.9–11.4) — 14.8 (13.1–16.6) —
10 20.3 (17.2–23.7) — 10.4 (8.6–12.4) — 15.4 (13.4–17.7) —
11
20.4 (17.6–23.5) — 12.1 (10.3–14.2) — 16.4 (14.5–18.5) —
12 18.5 (15.7–21.6) — 13.6 (11.4–16.1) — 16.2 (14.3–18.3) —
Attempted suicide
Race/Ethnicity — 2.973 (0.044) — 1.505 (0.229) — 2.866 (0.050)
White, non-Hispanic 9.4 (7.8–11.3) — 6.4 (5.1–7.8) — 7.9 (6.9–9.1) —
Black, non-Hispanic 15.2 (10.8–20.9) — 8.5 (5.6–12.9) — 11.8 (8.7–15.9) —
Hispanic 11.9 (9.0–15.6) — 5.5 (3.9–7.6) — 8.9 (7.1–11.1) —
Grade — 1.878 (0.150) — 0.384 (0.765) — 0.311 (0.817)
9 12.8 (10.7–15.3) — 6.0 (4.5–7.9) — 9.4 (7.9–11.1) —
10 11.0 (9.1–13.3) — 6.5 (4.7–9.0) — 8.8 (7.4–10.5) —
11 10.4 (8.1–13.3) — 6.7 (5.2–8.8) — 8.6 (7.1–10.4) —
12 9.4 (6.9–12.6) — 7.3 (5.2–10.0) — 8.5 (6.8–10.6) —
Made a suicide attempt requiring medical treatment
†
Race/Ethnicity — 0.446 (0.721) — 1.583 (0.210) — 1.387 (0.262)
White, non-Hispanic 2.9 (1.9–4.4) — 1.2 (0.8–1.9) — 2.1 (1.5–2.8) —
Black, non-Hispanic 3.8 (2.3–6.2) — 2.9 (1.5–5.5) — 3.3 (2.2–4.9) —
Hispanic 3.6 (2.6–4.9) — 2.3 (1.4–3.9) — 3.0 (2.3–3.8) —
Grade — 0.406 (0.750) — 0.571 (0.638) — 0.274 (0.844)
9 3.3 (2.3–4.8) — 1.3 (0.7–2.3) — 2.3 (1.7–3.1) —
10 3.6 (2.3–5.5) — 1.7 (0.9–3.3) — 2.7 (1.8–3.9) —
11 2.7 (1.7–4.3) — 2.0 (1.2–3.2) — 2.3 (1.7–3.3) —
12 3.4 (2.2–5.3) — 1.9 (1.0–3.9) — 2.7 (2.0–3.7) —
Abbreviation: CI = Confidence interval.
* Not applicable.
†
Made a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse.
overall (heterosexual: 1.7%; LGB: 6.3%; not sure: 5.2%) and
among both female (heterosexual: 2.3%; LGB: 6.6%; not
sure: 3.8%) and male (heterosexual: 1.3%; LGB: 5.9%; not
sure: 7.6%) students. A significant difference also was noted
in having made a suicide attempt requiring medical treatment
by sex of sexual contacts, overall (had sexual contact with only
the opposite sex: 2.6%; had sexual contact with only the same
sex or both sexes: 10.2%; had no sexual contact: 1.0%) and
among both female (had sexual contact with only the opposite
sex: 3.4%; had sexual contact with only the same sex or both
sexes: 10.4%; had no sexual contact: 1.4%) and male (had
sexual contact with only the opposite sex: 1.9%; had sexual
contact with only the same sex or both sexes: 9.4%; had no
sexual contact: 0.5%) students.
Trends in Suicide Attempts, Overall and by
Sex, Race/Ethnicity, and Grade
Among the total student population, the percentage of
students who had attempted suicide ≥1 time during the
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 51
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 3. Percentage of high school students who had seriously considered attempting suicide, had made a suicide plan, had attempted sui-
cide, or had made a suicide attempt requiring medical treatment during the 12 months before the survey, by sex, sexual identity, and sex of
sexual contacts — Youth Risk Behavior Survey, United States, 2019
Behavior
Female
% (95% CI)
Chi-square
(p value)
Male
% (95% CI)
Chi-square
(p value)
Total
% (95% CI)
Chi-square
(p value)
Seriously considered attempting suicide
Sexual identity — 75.728 (<0.001) — 22.231 (<0.001) — 88.194 (<0.001)
Heterosexual 18.0 (16.3–20.0) —* 11.4 (10.4–12.6) — 14.5 (13.4–15.7) —
LGB 49.0 (44.8–53.3) — 40.4 (33.9–47.1) — 46.8 (43.1–50.6) —
Not sure 35.9 (29.5–42.9) — 21.7 (14.8–30.5) — 30.4 (25.4–35.9) —
Sex of sexual contacts — 64.007 (<0.001) — 13.972 (<0.001) — 66.938 (<0.001)
Opposite sex only 25.3 (22.8–28.0) — 14.6 (12.9–16.5) — 19.4 (17.6–21.4) —
Same sex only or both sexes 59.2 (52.5–65.6) — 39.1 (29.3–49.9) — 54.2 (49.0–59.3) —
No sexual contact 16.2 (14.2–18.3) — 9.7 (8.1–11.7) — 13.0 (11.8–14.3) —
Made a suicide plan
Sexual identity — 66.568 (<0.001) — 19.732 (<0.001) — 90.368 (<0.001)
Heterosexual 14.6 (13.2–16.0) — 9.9 (8.9–11.0) — 12.1 (11.1–13.1) —
LGB 42.4 (38.4–46.4) — 33.0 (26.4–40.3) — 40.2 (36.6–44.0) —
Not sure 28.1 (22.1–35.0) — 17.4 (11.8–24.8) — 23.9 (19.4–29.0) —
Sex of sexual contacts — 56.442 (<0.001) — 18.435 (<0.001) — 62.470 (< 0.001)
Opposite sex only 20.7 (18.4–23.3) — 12.9 (11.5–14.6) — 16.5 (14.9–18.1) —
Same sex only or both sexes 48.2 (42.8–53.6) — 31.2 (23.8–39.7) — 44.0 (39.7–48.4) —
No sexual contact 13.8 (12.3–15.6) — 7.9 (6.7–9.4) — 10.9 (9.8–12.1) —
Attempted suicide
Sexual identity — 26.919 (<0.001) — 15.972 (<0.001) — 40.352 (<0.001)
Heterosexual 7.9 (6.6–9.4) — 5.1 (4.2–6.3) — 6.4 (5.6–7.4) —
LGB 23.6 (20.0–27.6) — 23.8 (17.8–31.1) — 23.4 (20.0–27.1) —
Not sure 15.2 (9.6–23.3) — 16.4 (9.9–26.0) — 16.1 (11.1–22.8) —
Sex of sexual contacts — 58.123 (<0.001) — 12.379 (<0.001) — 66.202 (<0.001)
Opposite sex only 11.4 (9.5–13.5) — 7.5 (5.8–9.6) — 9.3 (7.9–10.8) —
Same sex only or both sexes 31.4 (27.0–36.1) — 26.5 (17.5–38.0) — 30.3 (25.9–35.0) —
No sexual contact 6.1 (4.8–7.8) — 3.5 (2.6–4.8) — 4.8 (4.0–5.8) —
Made a suicide attempt requiring medical treatment
†
Sexual identity — 7.893 (0.001) — 5.592 (0.008) — 13.034 (<0.001)
Heterosexual 2.3 (1.6–3.2) — 1.3 (0.9–1.9) — 1.7 (1.4–2.2) —
LGB 6.6 (5.0–8.7) — 5.9 (3.2–10.6) — 6.3 (4.8–8.3) —
Not sure 3.8 (1.6–8.4) — 7.6 (3.6–15.2) — 5.2 (3.0–9.0) —
Sex of sexual contacts — 14.728 (<0.001) — 10.517 (<0.001) — 23.046 (<0.001)
Opposite sex only 3.4 (2.4–4.8) — 1.9 (1.3–2.9) — 2.6 (2.0–3.3) —
Same sex only or both sexes 10.4 (7.5–14.2) — 9.4 (4.9–17.6) — 10.2 (7.6–13.4) —
No sexual contact 1.4 (0.8–2.4) — 0.5 (0.3–1.1) — 1.0 (0.6–1.5) —
Abbreviations: CI = confidence interval; LGB = lesbian, gay, or bisexual.
* Not applicable.
†
Made a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse.
12 months before the survey experienced a significant linear
increase from 6.3% during 2009 to 8.9% during 2019
(Figure 1–3). Among female students, a significant linear
increase (from 8.1% to 11.0%) occurred in the prevalence of
having attempted suicide. No significant linear change was
observed for the prevalence of having attempted suicide among
male students. By race/ethnicity, significant linear increases in
having attempted suicide were observed for white (from 5.0%
to 7.9%) and black (from 7.9% to 11.8%) but not Hispanic
students. By grade, a significant linear increase in having
attempted suicide was observed only for 12th-grade students
(from 4.2% to 8.5%).
Discussion
During 2019, approximately one in five (18.8%) youths had
seriously considered attempting suicide, one in six (15.7%)
had made a suicide plan, one in 11 (8.9%) had made an
attempt, and one in 40 (2.5%) had made a suicide attempt
requiring medical treatment. Linear trends in suicide attempts
have increased during 2009–2019 overall and among certain
demographic groups.
The 2019 YRBS data highlight considerable differences
in suicidal ideation, plans, attempts, and attempts requiring
medical treatment. Consistent with previous research, during
2019, females had more suicidal ideation, suicide plans,
and suicide attempts, including attempts requiring medical
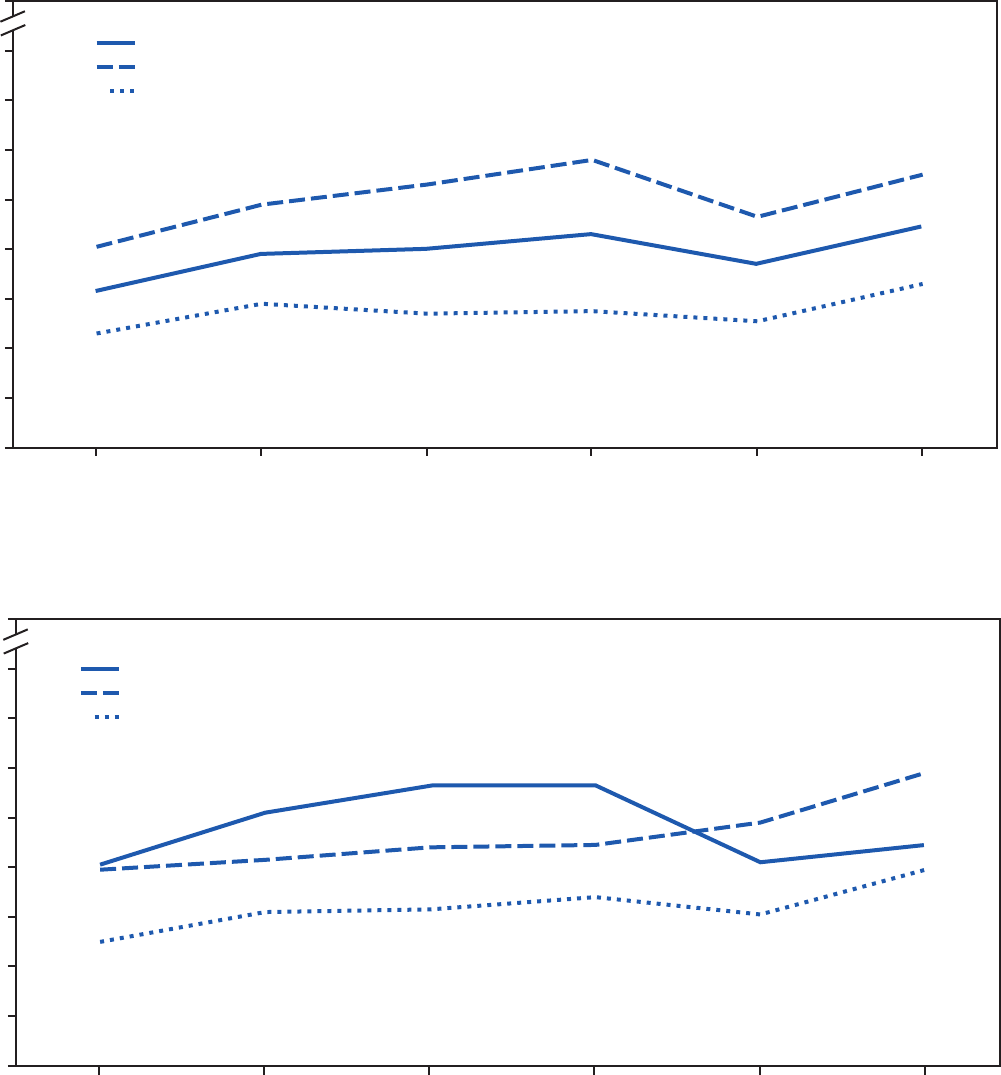
Supplement
52 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 1. Percentage of high school students who attempted suicide during the 12 months before the survey, overall and by sex — Youth Risk
Behavior Survey, United States, 2009–2019
0
2
4
6
8
10
12
14
16
100
2009 2011 2013 2015 2017 2019
Female
Overall
Male
Percentage
Year
FIGURE 2. Percentage of high school students who attempted suicide during the 12 months before the survey, by race/ethnicity — Youth Risk
Behavior Survey, United States, 2009–2019
0
2
4
6
8
10
12
14
16
100
2009 2011 2013 2015 2017 2019
Percentage
Year
White, non-Hispanic
Black, non-Hispanic
Hispanic
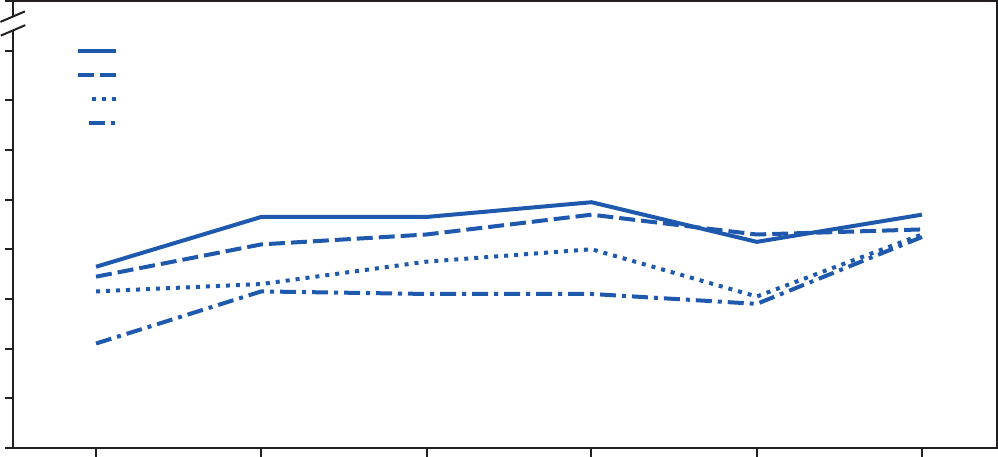
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 53
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 3. Percentage of high school students who attempted suicide during the 12 months before the survey, by grade — Youth Risk Behavior
Survey, United States, 2009–2019
0
2
4
6
8
10
12
14
16
100
2009 2011 2013 2015 2017 2019
Percentage
Year
9th
10th
11th
12th
treatment, than males (5). Certain racial/ethnic differences
also were identified. For example, black male students had
the lowest prevalence estimates of suicidal ideation. Regarding
suicide attempts, black students (male and female) had the
highest prevalence estimates. This finding is consistent with
previous research (6). Also consistent with previous research are
the study findings regarding sexual orientation and sex of sexual
contacts (5). Namely, prevalence estimates of suicidal ideation,
suicide plans, attempts, and attempts requiring medical
treatment were highest among sexual minority youths, those
who identified as LGB, and youths who reported having had
sexual contact with the same or with both sexes during 2019.
Adolescence is a developmental stage often characterized
by rapid and extensive physical and psychosocial changes (7).
It also represents a time for expanded identity development,
with sexual identity development representing a complex,
multidimensional, and often stressful process for youths (8).
The potential dissonance between sexual identity and behavior
and the social rejection sexual minority youths often experience
can contribute to increased suicidal ideation and behaviors
along with an increased risk for suicide (9,10). Because of the
high prevalence of suicidal ideation and behaviors among sexual
minority youths, additional research is needed to determine
how best to support this vulnerable group. Such research
might evaluate strategies designed to reduce sexual minority
stress (e.g., discrimination and victimization resulting from
sharing one’s sexual orientation) (11) and unhealthy behaviors
(e.g., substance use) and the resultant impact on suicidal
ideation and behaviors.
Suicide attempts are a known risk factor for and the greatest
predictor of death by suicide (12), which is the rationale for
investigating trends only on this outcome. The number of
children and adolescents who sought medical treatment at EDs
for suicide attempts increased sharply from 2007 (540,000)
to 2015 (960,000) (13). Either a linear increase or no change
in suicide attempts by variables reported here (i.e., sex, race/
ethnicity, and grade) was identified for 2009–2019. Although
for a different period (1991–2017), other researchers also
have reported that suicide attempts among black students
increased significantly (6). More specifically, previous findings
indicated that suicide attempts increased at an accelerating rate
among black females, and black male youths had a substantial
increase in attempts requiring medical treatment during the
period (6). Future studies are needed to continue monitoring
trends in suicidal ideation and behavior for black students and
other race/ethnicity groups. For example, such studies might
include more detailed analyses among the American Indian/
Alaska Native youth population who have been reported to
be at increased risk for suicidal behaviors (6).
In this analysis, one notable finding emerged by sex and
grade; a substantial increase in making a suicide plan occurred
among males as grade increased. To address this trend, schools
can consider a sex-by-grade–specific approach to implementing
suicide prevention or intervention activities.
Supplement
54 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Limitations
General limitations for the YRBS are available in the
overview report of this supplement (4). The findings in this
report are subject to at least one additional limitation. This
analysis is conducted among all students (i.e., does not separate
ideation from behaviors); suicide patterns might differ between
those who experienced suicidal ideation and those who did not.
Future Directions
To address the health differences in suicidal ideation and
behaviors observed by student demographics and to decrease
these outcomes overall, a comprehensive approach to suicide
prevention, including programs, practices, and policies based
on the best available evidence, is needed. Such an approach
addresses the range of risk and protective factors occurring
across the individual, relationship, community, and societal
levels. A comprehensive approach also seeks to prevent suicide
risk, identify and support youths at increased risk, prevent
attempts and reattempts, and help survivors of suicide loss (i.e.,
those grieving the death of a friend or loved one). States and
communities, including school communities, can use strategies
with such best available evidence as that documented in the
CDC Preventing Suicide Technical Package (14).
Preventing adverse childhood experiences (e.g., child
maltreatment) can help reduce suicide risk among adolescents
through strategies that promote safe, stable, nurturing
relationships and environments in childhood (15). Other
strategies in a comprehensive approach to suicide prevention
include supporting families by strengthening economic
supports and teaching coping and problem-solving skills
among children, adolescents, and their parents; promoting
connectedness between youths and their schools, teachers,
peers, and family; creating protective environments in schools
and at home (e.g., limiting access to such lethal means among
students at risk as medications and firearms); promoting help-
seeking behaviors; reducing stigma; and training teachers and
adults in recognizing signs of suicide and responding effectively
through referrals to evidence-based treatment (e.g., cognitive-
behavioral therapy) (14). Finally, schools and the media should
respond to and report on suicides in ways that are supportive
and responsible (e.g., not sensationalizing deaths), thereby
avoiding additional suicides (i.e., suicide contagion) (14).
Conclusion
Suicide is a leading cause of death among youths; however,
many more youths are at risk for suicide as a result of
experiencing suicidal ideation, making suicide plans, and
attempting suicide, making a focus on nonfatal suicidal
behavior a crucial public health priority. During 2009–2019,
trends in suicide attempts among adolescents increased overall
and among many demographic groups. Prevalence estimates
of suicidal ideation, suicide plans, attempts, and attempts
requiring medical treatment were highest among sexual
minority youths and youths who reported having had sexual
contact with the same or with both sexes. Regarding differences
by race/ethnicity, black students had the highest prevalence
estimates for attempted suicide. Factors at the individual,
relationship, community, and societal levels likely contribute
to the differences in suicide attempts among different racial/
ethnic groups and sexual minority youths and the differences
observed by sex and grade. More research is needed to better
understand the risk and protective factors to determine which
suicide prevention strategies might best serve each group.
The findings in this report underscore the importance of a
comprehensive approach to suicide prevention, which would
provide necessary support to those at risk, decrease suicidal
ideation and behaviors, and ultimately prevent suicide among
youths and save lives.
Conflicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. World Health Organization. Preventing suicide: a global imperative.
Geneva, Switzerland: World Health Organization; 2014. https://apps.
who.int/iris/bitstream/handle/10665/131056/9789241564779_eng.pdf
2. CDC. Web-based Injury Statistics Query and Reporting System
(WISQARS). Atlanta, GA: US Department of Health and Human
Services, CDC, National Center for Injury Prevention and Control;
2020. https://www.cdc.gov/injury/wisqars/index.html
3 US Department of Health and Human Services. Healthy people 2020.
Washington, DC: US Department of Health and Human Services,
Office of Disease Prevention and Health Promotion; 2020. https://www.
healthypeople.gov
4. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 55
US Department of Health and Human Services/Centers for Disease Control and Prevention
5. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—
United States, 2017. MMWR Surveill Summ 2018;67(No. SS-8):1–114.
https://doi.org/10.15585/mmwr.ss6708a1
6. Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of suicidal behaviors
among high school students in the United States: 1991–2017. Pediatrics
2019;144:e20191187. https://doi.org/10.1542/peds.2019-1187
7. Tsang SK, Hui EK, Law BC. Positive identity as a positive youth
development construct: a conceptual review. ScientificWorldJournal
2012;2012:529691. https://doi.org/10.1100/2012/529691
8. Rosario M, Schrimshaw EW, Hunter J, Braun L. Sexual identity
development among lesbian, gay, and bisexual youths: consistency and
change over time. J Sex Res 2006;43:46–58. https://doi.
org/10.1080/00224490609552298
9. Annor FB, Clayton HB, Gilbert LK, et al. Sexual orientation discordance
and nonfatal suicidal behaviors in U.S. high school students. Am J Prev
Med 2018;54:530–8. https://doi.org/10.1016/j.amepre.2018.01.013
10. Hong JS, Espelage DL, Kral MJ. Understanding suicide among sexual
minority youth in America: an ecological systems analysis. J Adolesc
2011;34:885–94. https://doi.org/10.1016/j.adolescence.2011.01.002
11. Meyer IH. Minority stress and mental health in gay men. J Health Soc
Behav 1995;36:38–56. https://doi.org/10.2307/2137286
12. Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts
and behaviors: A meta-analysis of 50 years of research. Psychol Bull
2017;143:187–232. https://doi.org/10.1037/bul0000084
13. Burstein B, Agostino H, Greenfield B. Suicidal attempts and ideation
among children and adolescents in US emergency departments, 2007–
2015. JAMA Pediatr 2019;173:598–600. https://doi.org/10.1001/
jamapediatrics.2019.0464
14. Stone DM, Holland KM, Bartholow B, Crosby AE, Davis S, Wilkins
N. Preventing suicide: a technical package of policies, programs, and
practices. Atlanta, GA: US Department of Health and Human Services,
CDC, National Center for Injury Prevention and Control; 2017. https://
www.cdc.gov/violenceprevention/pdf/suicideTechnicalPackage.pdf
15. CDC. Preventing adverse childhood experiences (ACEs): leveraging the
best available evidence. Atlanta, GA: US Department of Health and
Human Services, CDC, National Center for Injury Prevention and
Control; 2019. https://www.cdc.gov/violenceprevention/pdf/
preventingACES.pdf

Supplement
56 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Tobacco Product Use Among High School Students — Youth Risk
Behavior Survey, United States, 2019
MeLisa R. Creamer, PhD
1
; Sherry Everett Jones, PhD, JD
2
; Andrea S. Gentzke, PhD
1
; Ahmed Jamal, MBBS
1
; Brian A. King, PhD
1
1
Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC;
2
Division of Adolescent and School Health,
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC
Abstract
Tobacco product use is the leading cause of preventable disease, disability, and death in the United States. This report used data
from the 2019 Youth Risk Behavior Survey to assess the following among U.S. high school students: ever use of cigarettes and
electronic vapor products, current use (≥1 day during the 30 days before the survey) of tobacco products, frequent use (≥20 days
during the 30 days before the survey) among current users of tobacco products, trends in use over time, and usual source of
electronic vapor products among current electronic vapor product users. In 2019, a total of 50.1% of U.S. high school students
had ever used electronic vapor products, and 24.1% had ever tried cigarette smoking. Current electronic vapor product use was
32.7%, current cigarette smoking was 6.0%, current cigar smoking was 5.7%, and current smokeless tobacco use was 3.8%.
Approximately 36.5% of students were current users of any tobacco product, and 8.2% were current users of two or more tobacco
products. Frequent use among users of individual products was 32.6% for electronic vapor products, 28.5% for smokeless tobacco,
22.2% for cigarettes, and 18.4% for cigars. Among current electronic vapor product users who were aged ≤17 years, the most
commonly reported source was borrowing them from someone else (42.8%). Significant decreases occurred in current cigarette
smoking (1991: 27.5%; 2019: 6.0%), cigar smoking (1997: 22.0%; 2019: 5.7%), and smokeless tobacco use (2017: 5.5%;
2019: 3.8%). However, significant increases occurred in current electronic vapor product use (2015: 24.1%; 2019: 32.7%)
and any tobacco product use (2017: 19.5%; 2019: 36.5%). Although current cigarette smoking, cigar smoking, and smokeless
tobacco use has decreased among high school students, the increased prevalence of electronic vapor product use among youths
is concerning. Continued surveillance for all tobacco product use is warranted for guiding and evaluating public health policy at
the local, state, tribal, and national levels.
Introduction
Smoking is the leading cause of preventable premature
disease and death in the United States (1). An estimated 88%
of adult daily cigarette smokers report first trying cigarette
smoking before age 18 years (2). Previous reports indicate
decreases in current cigarette smoking (i.e., use during the
30 days before the survey) among U.S. high school students
from a high of 36.4% in 1997 to 8.8% in 2017 (3). However,
there are a variety of tobacco products, including smokeless
tobacco products, cigars, and most recently, electronic vapor
products (e.g., e-cigarettes).
Electronic vapor products have evolved since entering the
U.S. marketplace in 2007. Initial products were disposable,
resembled the size and shape of conventional cigarettes,
and used free-base nicotine; however, newer products are
rechargeable, resemble common objects (e.g., USB flash
drives), and typically deliver nicotine salts (4,5), which
Corresponding author: Andrea S. Gentzke, PhD, Office on Smoking and
Health, National Center for Chronic Disease Prevention and Health
Promotion, CDC. Telephone: 404-498-1795; E-mail: [email protected].
allow higher levels of nicotine to be inhaled more easily by
the user (6). Sales of these newer generation, or “pod-mod,”
products have increased in the United States during recent
years. For example, sales of JUUL, the most commonly sold
e-cigarette in the United States since December 2017, increased
approximately 600% during 2016–2017 from 2.2 million
unit sales to 16.2 million unit sales (7). By December 2018,
JUUL accounted for an estimated 76% of the $322.1 million
total e-cigarettes sales that occurred that month in the United
States (8). The popularity of these electronic vapor products
among youths is likely the result of multiple factors, including
advertising exposure, availability of youth-appealing flavors,
curiosity, and social exposure through friends and others (4–6).
In 2014, prevalence of electronic vapor product use among
high school students surpassed prevalence of cigarette smoking
(9), and according to data from the 2017 Youth Risk Behavior
Survey (YRBS), 13.2% of high school students had used
electronic vapor products during the previous 30 days (3).
These findings align with increases in use observed in other
national surveys of youth in the United States. For example,
according to the National Youth Tobacco Survey (NYTS),
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 57
US Department of Health and Human Services/Centers for Disease Control and Prevention
current electronic vapor product use among high school students
increased 78% (11.7% to 20.8%) during 2017–2018 (9).
Youth use of tobacco products in any form is unsafe (1,4).
Cigarette smoking harms nearly every organ in the body, and
smokeless tobacco product use is associated with multiple health
risks, including cancers of the mouth (1). Moreover, the aerosol
in electronic vapor products can contain harmful ingredients,
including heavy metals, ultrafine particles, and nicotine (4).
Nicotine is highly addictive, can harm the developing adolescent
brain, and can prime the brain for addiction to other drugs
(4,10). In addition, a growing body of scientific literature
suggests that youths who use e-cigarettes are more likely to smoke
conventional cigarettes in the future (4,10).
Surveillance for tobacco product use among youths is crucial
for guiding and evaluating tobacco control strategies at local,
state, tribal, and national levels. This report presents the latest
data from the 2019 YRBS to assess the following among U.S.
high school students: ever use of cigarettes and electronic
vapor products; current use (≥1 day during the 30 days before
the survey) of tobacco products (electronic vapor products,
cigarettes, cigars [cigars/cigarillos/little cigars], smokeless
tobacco [chewing tobacco, snuff, dip, snus, or dissolvable
tobacco products], any tobacco product, and two or more
products); frequent use (≥20 days during the 30 days before
the survey) of tobacco products among current users of those
products; trends in tobacco product use over time; and usual
source of obtaining electronic vapor products among current
electronic vapor product users.
Methods
Data Source
This report includes data from the 1991–2019 cycles of
CDC’s national YRBS, a cross-sectional, school-based survey
conducted biennially since 1991. Each survey year, CDC
collects data from a nationally representative sample of public
and private school students in grades 9–12 in the 50 U.S. states
and the District of Columbia. Additional information about
YRBS sampling, data collection, response rates, and processing
is available in the overview report for this supplement (11). The
prevalence estimates for all tobacco product use questions for
the overall study population and by sex, race/ethnicity, grade,
and sexual orientation are available at https://nccd.cdc.gov/
youthonline/App/Default.aspx. The full YRBS questionnaire
is available at https://www.cdc.gov/healthyyouth/data/yrbs/
pdf/2019/2019_YRBS-National-HS-Questionnaire.pdf.
Measures
Ever use, which was defined as having used the product
at least one time during their lifetime, was assessed for two
distinct tobacco products: cigarettes and electronic vapor
products. Ever cigarette smoking was assessed by the question,
“Have you ever tried cigarette smoking, even one or two
puffs?” Ever electronic vapor product use was assessed by the
question, “Have you ever used an electronic vapor product?”
with a preamble that read, “The next 3 questions ask about
electronic vapor products, such as JUUL, Vuse, MarkTen, and
blu. Electronic vapor products include e-cigarettes, vapes, vape
pens, e-cigars, e-hookahs, hookah pens, and mods.”
Current use (≥1 day during the 30 days before the survey)
was assessed for four tobacco products: 1) current electronic
vapor product use was assessed by the question, “During the
past 30 days, on how many days did you use an electronic
vapor product?” 2) current cigarette smoking was assessed by
the question, “During the past 30 days, on how many days did
you smoke cigarettes?” 3) current cigar smoking was assessed
by the question, “During the past 30 days, on how many days
did you smoke cigars, cigarillos, or little cigars?” and 4) current
smokeless tobacco use was assessed by the question, “During
the past 30 days, on how many days did you use chewing
tobacco, snuff, dip, snus, or dissolvable tobacco products, such
as Copenhagen, Grizzly, Skoal, or Camel Snus? (Do not count
any electronic vapor products.)” Response options for each of
the four questions were 0 days, 1–2 days, 3–5 days, 6–9 days,
10–19 days, 20–29 days, and all 30 days. Among current users
of each individual product, frequent use was also calculated.
Frequent use was defined as having used the respective product
on ≥20 days during the 30 days before the survey.
Two composite measures were also investigated in this
analysis. Any current tobacco product use was defined as any
use of electronic vapor products, cigarettes, cigars, or smokeless
tobacco during the 30 days before the survey. Use of two or
more products was defined as current use of two or more of
the four assessed tobacco products.
Respondents also were asked how they usually obtained
electronic vapor products by the question (referred to as source
hereinafter), “During the past 30 days, how did you usually
get your own electronic vapor products? (Select only one
response.)” Response options were as follows: I did not use any
electronic vapor products during the past 30 days; I bought
them in a store such as a convenience store, supermarket,
discount store, gas station, or vape store; I got them on the
Internet; I gave someone else money to buy them for me; I
borrowed them from someone else; a person who can legally
buy these products gave them to me; I took them from a store
Supplement
58 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
or another person; or I got them some other way. Analysis of this
variable was limited to current electronic vapor product users.
The demographic characteristics of students analyzed for
this report included sex (female or male), grade (9, 10, 11, or
12), age (≤15 years, 16 or 17 years, or ≥18 years), and sexual
identity (heterosexual; lesbian, gay, or bisexual; or not sure).
In addition, students were classified into four racial/ethnic
categories: non-Hispanic white (white); non-Hispanic black
(black); Hispanic or Latino of any race (Hispanic); and other
or multiple races (non-Hispanic). The numbers of students
in the other or multiple racial/ethnic groups were too small
to produce statistically stable estimates; therefore, those data
are not presented as a separate group in this report but were
retained in the overall analytic sample.
Analysis
Prevalence of use for each respective tobacco product was
estimated for all years for which data were available. For 2019,
statistically significant pairwise differences by sex, grade, race/
ethnicity, age, and sexual identity were determined for each of
the assessed tobacco product use behaviors by using t-tests. For
each tobacco product, changes in prevalence were compared for
2017 and 2019 by using t-tests. In addition, t-tests were used
to compare how students who were ≤17 years and ≥18 years
usually obtained their electronic vapor products; these age
groups were used because age 18 years was the federal legal
age of sale for tobacco products at the time of the survey.
Prevalence estimates were considered statistically different if
the p value was <0.05.
To identify temporal trends, logistic regression analyses
were used to model linear and quadratic time effects while
controlling for sex, grade, and race/ethnicity. Linear time
effects were analyzed for current electronic vapor products
use (2015–2019), and both linear and quadratic time effects
were analyzed for current cigarette smoking (1991–2019) and
current cigar smoking (1997–2019). Because of substantial
changes in the question wording for smokeless tobacco
products in 2017, trends were not assessed for smokeless
tobacco. Additional information about the methods used to
conduct YRBS trend analyses are provided in the overview
report of this supplement (11).
Results
Among U.S. high school students in 2019, a total of 50.1%
(95% confidence interval [CI]: 48.1–52.2) had ever used
electronic vapor products, and 24.1% (CI: 21.3–27.0) had
ever tried cigarette smoking (data not shown). Prevalence of
current use was 32.7% for electronic vapor products, 6.0% for
cigarettes, 5.7% for cigars, and 3.8% for smokeless tobacco. In
addition, 36.5% of students had currently used any tobacco
products, and 8.2% had currently used two or more tobacco
products (Table 1).
Prevalence of tobacco product use varied by demographic
groups, with current use of cigarettes, cigars, smokeless tobacco,
and two or more tobacco products being higher among male
students than female students. Although differences in tobacco
product use varied by grade, prevalence of current use of each
individual product, any tobacco product, and two or more
tobacco products was higher among 12th-grade students than
9th-grade students. Prevalence of current use of electronic
vapor products, cigarettes, any tobacco product, and two or
more tobacco products was higher among white and Hispanic
students than black students, and the prevalence of electronic
vapor products and any tobacco product use was higher among
white than Hispanic students. Prevalence of current cigar use
was higher among students aged ≥18 years than those aged 16
or 17 years and those aged ≤15 years. For all other individual
products, any tobacco product, and two or more tobacco
products, prevalence increased in each age category. Among
sexual identity groups, prevalence of electronic vapor product
use was higher among heterosexual students and lesbian, gay, or
bisexual students than not-sure students. Prevalence of current
use of cigarettes, cigars, any tobacco product, and two or more
tobacco products was higher among lesbian, gay, or bisexual
students than heterosexual students. Finally, the prevalence
of any tobacco product use was higher among lesbian, gay, or
bisexual students than not-sure students.
In 2019, among the 32.7% of current electronic vapor
product users, 32.6% were frequent users; among the 5.7%
current cigarette smokers, 22.2% were frequent users; among
the 3.8% current cigar smokers, 18.4% were frequent users;
and among the 6.0% current smokeless tobacco product users,
28.5% were frequent users. From 2017 to 2019, among current
electronic vapor product users, a significant increase occurred
in frequent use (from 25.1% to 32.6%), and among current
cigarette smokers, a significant decrease occurred in frequent
use (from 30.0% in 2017 to 22.2% in 2019) (Figure 1). No
significant changes in frequent use of smokeless tobacco or
cigars were observed among users of these products from
2017 to 2019.
The usual source of electronic vapor products among current
users varied by age (Table 2). Among current electronic vapor
product users who were aged ≤17 years, the most commonly
reported usual source of electronic vapor products was
borrowing them from someone else (42.8%). Among those
aged ≥18 years, the most commonly reported source was
buying them in a store (56.4%). Compared with students
aged ≤17 years, a higher prevalence of students aged ≥18 years
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 59
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Percentage of high school students who were current tobacco users, by selected characteristics and type of tobacco product — Youth
Risk Behavior Survey, United States, 2019
Characteristic
Electronic vapor products* Cigarettes
†
Cigars
§
Smokeless tobacco
¶
Any tobacco product** ≥2 products
††
% (95% CI) % (95% CI) % (95% CI) % (95% CI) % (95% CI) % (95% CI)
Total 32.7 (30.7–34.8) 6.0 (5.0–7.2) 5.7 (4.8–6.7) 3.8 (3.2–4.6) 36.5 (33.6–39.5) 8.2 (7.0–9.5)
Sex
§§
Male 32.0 (29.7–34.3) 6.9 (5.7–8.4) 7.4 (6.4–8.6) 5.8 (4.7–7.1) 36.3 (33.3–39.3) 10.4 (9.0–11.9)
Female 33.5 (30.9–36.1) 4.9 (3.8–6.4) 3.8 (2.8–5.1) 1.6 (1.2–2.1) 36.6 (33.1–40.2) 5.8 (4.5–7.5)
Grade
¶¶
9 25.0 (22.8–27.4) 3.8 (2.8–5.1) 3.8 (2.7–5.2) 2.0 (1.4–3.0) 27.7 (24.8–30.9) 5.3 (4.2–6.6)
10 30.5 (27.3–33.8) 5.2 (3.9–6.9) 4.7 (3.5–6.2) 3.6 (2.6–5.0) 34.3 (30.3–38.6) 7.3 (5.6–9.6)
11 35.9 (32.3–39.8) 5.9 (4.5–7.7) 6.0 (4.6–7.8) 3.9 (3.0–5.1) 39.8 (35.7–44.1) 8.4 (6.7–10.4)
12 40.4 (37.5–43.4) 9.0 (7.6–10.7) 8.5 (6.9–10.4) 5.5 (4.3–7.1) 45.0 (41.3–48.7) 11.9 (10.3–13.7)
Race/Ethnicity***
Black, non-Hispanic 19.7 (16.9–22.8) 3.3 (2.3–4.6) 5.3 (4.1–6.8) 2.8 (1.8–4.4) 24.7 (21.3–28.4) 4.8 (3.7–6.2)
Hispanic 31.2 (28.6–33.8) 6.0 (4.3–8.4) 6.1 (4.7–8.0) 3.1 (2.3–4.3) 33.8 (31.1–36.7) 7.9 (6.2–10.0)
White, non-Hispanic 38.3 (36.0–40.7) 6.7 (5.3–8.4) 5.9 (4.7–7.4) 4.4 (3.3–5.7) 42.0 (38.3–45.9) 9.5 (7.8–11.5)
Age group (yrs)
†††
≤15 25.9 (24.1–27.9) 4.2 (3.2–5.4) 4.2 (3.1–5.6) 2.7 (2.0–3.8) 29.1 (26.2–32.1) 5.8 (4.6–7.2)
16 or 17 35.2 (32.3–38.3) 6.0 (4.8–7.4) 5.7 (4.5–7.0) 3.7 (3.0–4.6) 38.8 (35.2–42.4) 8.4 (6.8–10.1)
≥18 42.8 (39.0–46.7) 10.9 (8.6–13.6) 10.2 (8.1–12.7) 7.2 (5.5–9.2) 49.1 (44.9–53.4) 14.2 (12.0–16.7)
Sexual identity
§§§
Heterosexual 32.8 (30.5–35.2) 5.2 (4.3–6.3) 5.2 (4.4–6.1) 3.7 (3.1–4.4) 36.1 (33.1–39.2) 7.8 (6.7–9.0)
Lesbian, gay, or bisexual 34.1 (30.8–37.6) 10.4 (7.8–13.7) 8.1 (5.9–11.1) 3.2 (2.0–5.2) 40.3 (36.2–44.4) 10.4 (8.0–13.5)
Not sure 24.9 (19.8–30.7) 7.4 (4.8–11.3) 7.2 (4.3–12.0) 5.5 (3.1–9.5) 30.0 (23.3–37.6) 8.1 (5.4–11.9)
Abbreviation: CI = confidence interval.
* Percentage of students who used an electronic vapor product, including e-cigarettes, e-cigars, e-pipes, vape pipes, vaping pens, e-hookahs, and hookah pens
(e.g., blu, NJOY, Vuse, MarkTen, Logic, Vapin Plus, eGo, and Halo), on ≥1 day during the 30 days before the survey.
†
Percentage of students who smoked cigarettes on ≥1 day during the 30 days before the survey.
§
Percentage of students who smoked cigars, cigarillos, or little cigars on ≥1 day during the 30 days before the survey.
¶
Percentage of students who used smokeless tobacco, including chewing tobacco, snuff, dip, snus, or dissolvable tobacco products (e.g., Red Man, Levi Garrett,
Beechnut, Skoal, Skoal Bandits, Copenhagen, Camel Snus, Marlboro Snus, General Snus, Ariva, Stonewall, or Camel Orbs), but not including any electronic vapor
products, on ≥1 day during the 30 days before the survey.
** Percentage of students who smoked cigarettes or cigars or used smokeless tobacco or an electronic vapor product, on ≥1 day during the 30 days before the survey.
††
Percentage of students who used ≥2 of the following tobacco products: cigarettes, cigars (cigars, cigarillos, or little cigars), an electronic vapor product, or smokeless
tobacco, on ≥1 day during the 30 days before the survey.
§§
Sex pairwise comparisons assessed by t-test (p<0.05): for cigarettes, cigars, smokeless tobacco, and ≥2 products, male students were significantly different (p<0.05)
from female students.
¶¶
Grade pairwise comparisons assessed by t-test (p<0.05): for electronic vapor products and any tobacco product: all pairwise comparisons were significantly
different (p<0.05); for cigarettes, cigars, and ≥2 products: 12th grade was significantly different (p<0.05) than 9th, 10th, and 11th grades; 11th grade was significantly
different (p<0.05) than 9th grade; for smokeless tobacco: 12th grade was significantly different (p<0.05) than 9th, 10th, and 11th grades; 10th and 11th grades
were significantly different (p<0.05) than 9th grade.
*** Race/ethnicity pairwise comparisons assessed by t-test (p<0.05): for electronic vapor products and any tobacco product: all pairwise comparisons were significantly
different (p<0.05); for cigarettes and ≥2 products: white and Hispanic were significantly different (p<0.05) than black.
†††
Age pairwise comparisons assessed by t-test (p<0.05): for electronic vapor products, cigarettes, smokeless tobacco, any tobacco product, and ≥2 products: all
pairwise comparisons were significantly different (p<0.05); for cigars: ≥18 years was significantly different (p<0.05) than 16–17 years and ≤15 years.
§§§
Sexual identity pairwise comparisons assessed by t-test (p<0.05): for electronic vapor products: heterosexual and lesbian, gay, or bisexual were significantly
different (p<0.05) than not-sure students; for cigarettes, cigars, and ≥2 products: lesbian, gay, or bisexual was significantly different (p<0.05) than heterosexual;
for any tobacco product: lesbian, gay, or bisexual was significantly different (p<0.05) than heterosexual and not-sure students.
usually bought electronic vapor products in a store. In contrast,
compared with older students, a higher prevalence of students
aged ≤17 years got them on the Internet, gave someone else
money to buy them, borrowed them from someone else, got
them from a person who could legally buy them, or got them
some other way.
Trend analyses indicated that during 2015–2019, a significant
linear increase occurred in prevalence of current electronic
vapor products use (from 24.1% to 32.7%) (Figure 2). Trend
analyses also indicated that during 1991–2019, a significant
linear decrease in current cigarette smoking was observed (from
27.5% to 6.0%). A significant quadratic trend in cigarette
smoking also was identified: a 6-year increase in prevalence
(from 27.5% in 1991 to 36.4% in 1997) was followed by
a 22-year decrease (from 36.4% in 1997 to 6.0% in 2019).
Additionally, during 1997–2019, a significant linear decrease
(from 22.0% to 5.7%) occurred in the overall prevalence
of current cigar smoking. A significant quadratic trend also
was identified: a 16-year decrease in prevalence (from 22.0%
in 1997 to 12.6% in 2013) was followed by another 6-year
decrease, but at a different rate of decrease (from 12.6% in
2013 to 5.7% in 2019).
During 2017–2019, a significant increase occurred in current
electronic vapor products use (from 13.2% to 32.7%) and
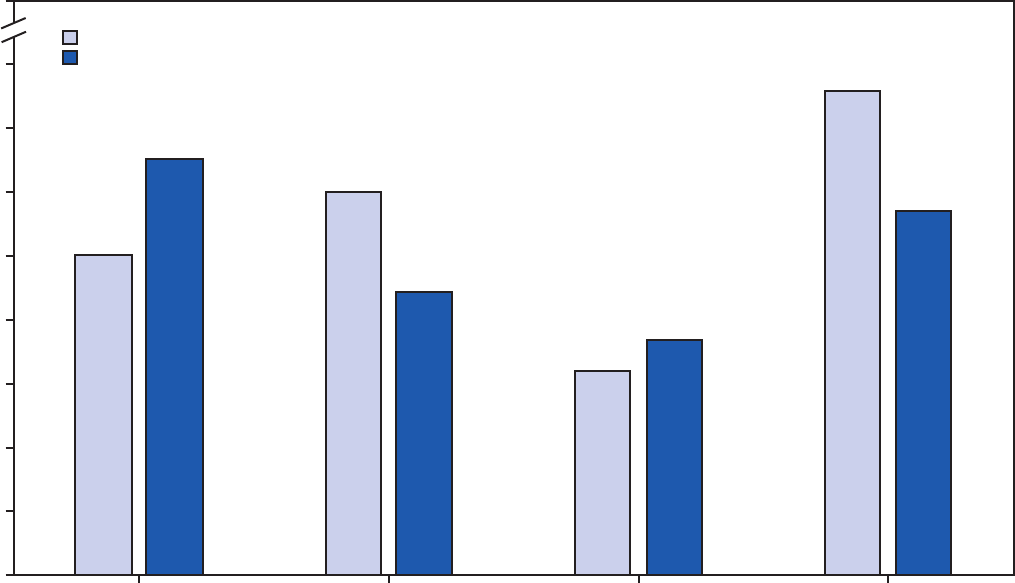
Supplement
60 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 1. Prevalence of frequent tobacco use* among current users, by type of tobacco product
†
— Youth Risk Behavior Survey, United States,
2017 and 2019
§
0
5
10
15
20
25
30
35
40
100
Electronic vapor products Cigarettes Cigars Smokeless tobacco
Prevalence (%)
Tobacco product
2019
2017
* Frequent use was defined as use on ≥20 days during the 30 days before the survey.
†
Frequent use was assessed among respondents who reported current use (on ≥1 day during the 30 days before the survey) of each tobacco product. In 2017, among
the 13.2% of students nationwide who used electronic vapor products on ≥1 day during the 30 days before the survey; among the 8.8% of students nationwide
who smoked cigarettes on ≥1 day during the 30 days before the survey; among the 8.0% of students nationwide who smoked cigars on ≥1 day during the 30 days
before the survey; among the 5.5% of students nationwide who used smokeless tobacco on ≥1 day during the 30 days before the survey. In 2019, among the 32.7%
of students nationwide who used electronic vapor products on ≥1 day during the 30 days before the survey; among the 6.0% of students nationwide who smoked
cigarettes on ≥1 day during the 30 days before the survey; among the 5.7% of students nationwide who smoked cigars on ≥1 day during the 30 days before the
survey; among the 3.8% of students nationwide who used smokeless tobacco on ≥1 day during the 30 days before the survey.
§
Differences from 2017 to 2019 were assessed by t-test (p<0.05): A significant increase occurred in frequent use of electronic vapor products; a significant decrease
occurred in frequent use of cigarettes; and no change occurred in frequent use of cigars/cigarillos/little cigars and smokeless tobacco.
any tobacco product use (from 19.5% to 36.5%). During
2017–2019, significant decreases were observed in current
cigarette smoking (from 8.8% to 6.0%), current cigar smoking
(from 8.0% to 5.7%), and current smokeless tobacco use (from
5.5% to 3.8%). No change occurred in use of two or more
tobacco products during 2017–2019.
Discussion
In 2019, a total of 36.5% of high school students currently
used any tobacco product, with electronic vapor products being
the most commonly used product. This reflects an increase in
use of electronic vapor products from 2017 to 2019, findings
that are consistent with those from other national surveillance
systems, including NYTS (9,12) and Monitoring the Future
(13). For example, NYTS results demonstrated that, among
high school students, e-cigarette use increased from 11.7%
in 2017 to 27.5% in 2019 (9,12). These increases align
with the increasing popularity of newer electronic vapor
product devices, including JUUL (7). The dramatic increase
in electronic vapor product use among high school students
has led to increases in overall tobacco product use among
U.S. youths, erasing gains made in previous years and leading
the U.S. Surgeon General to declare youth e-cigarette use an
epidemic in the United States (10).
Use of any tobacco product among youth is unsafe, regardless
of frequency of use or number of products used. Although the
2019 national YRBS results indicate that most current youth
tobacco product users are infrequent users, variations exist by
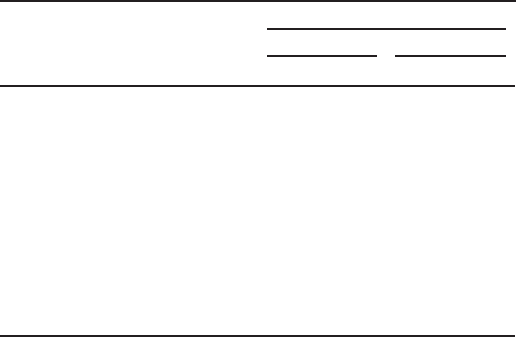
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 61
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Usual source* of obtaining electronic vapor products among
current electronic vapor product users,
†
by age — Youth Risk
Behavior Survey, United States, 2019
Usual source
Age group
§
≥18 yrs ≤17 yrs
% (95% CI) % (95% CI)
Bought them in a store (e.g., a
convenience store, supermarket,
discount store, gas station, or
vape store)
56.4 (51.0–1.6) 8.1 (6.8–9.6)
Got them on the Internet 1.8 (0.9–3.4) 3.6 (2.8–4.6)
Gave someone else money to buy
them for me
3.1 (1.5–6.1) 21.3 (19.5–23.2)
Borrowed them from someone else 27.5 (23.4–32.0) 42.8 (40.2–45.4)
A person who can legally buy these
products gave them to me
3.9 (2.4–6.3) 11.1 (9.9–12.3)
Took them from a store or
another person
2.0 (0.8–5.0) 1.6 (1.1–2.4)
Got them some other way 5.4 (3.3–8.8) 11.6 (10.1–13.4)
Abbreviation: CI = confidence interval.
* Students were limited to selecting only one response.
†
Including e-cigarettes, e-cigars, e-pipes, vape pipes, vaping pens, e-hookahs,
or hookah pens (e.g., blu, NJOY, Vuse, MarkTen, Logic, Vapin Plus, eGo, and
Halo) among students who used electronic vapor products during the 30 days
before the survey.
§
Comparisons between age groups were assessed by t-test (p<0.05). All
comparisons were statistically different with the exception of “took them from
a store or another person.”
product; for example, frequent use ranged from 18.4% for
cigars to 32.6% for electronic vapor products. In addition, these
results indicate that frequent use of electronic vapor products
increased during 2017–2019; whereas frequent use of other
products decreased or did not change. Even infrequent tobacco
product use, particularly cigarette smoking, is predictive of
progression to daily smoking (14). Nearly all tobacco products
include nicotine, and even infrequent use of tobacco products
has been linked to symptoms of nicotine dependence (15).
Further, 8.2% of high school students currently used two or
more tobacco products in 2019. Multiple tobacco product use is
associated with substance use disorders (16) and might increase
nicotine exposure and risk for nicotine dependence (15).
In 2019, electronic vapor product users aged ≤17 years
usually obtained their products from social sources (e.g.,
by borrowing them from someone). This is consistent with
results from both the Population Assessment of Tobacco and
Health Study and NYTS, which also determined that social
sources were the most common way for adolescents to obtain
electronic vapor products (17,18). These social sources might
include older students who are of legal age for purchasing
the products in their state or community. In 2016, electronic
vapor products were deemed to be tobacco products under
the Family Smoking Prevention Tobacco Control Act (https://
www.federalregister.gov/documents/2016/05/10/2016-10685/
deeming-tobacco-products-to-be-subject-to-the-federal-food-
drug-and-cosmetic-act-as-amended-by-the), thus setting the
federal minimum purchase age for electronic vapor products
at 18 years. However, on December 20, 2019, federal
legislation increased the minimum age of sales of tobacco
products from 18 to 21 years nationwide; the law does not
preempt more stringent state or local age of sale laws (https://
www.fda.gov/tobacco-products/retail-sales-tobacco-products/
selling-tobacco-products-retail-stores). Before this federal
law, 19 states, the District of Columbia, Guam, and Palau
had enacted laws that increased the age of sale for tobacco
products to 21 years, including 13 laws enacted during 2019
(19). Such laws might limit the ability for high school students
to obtain tobacco products from their peers, including those
older students who were of legal age to purchase these products
in their state or community before the law’s implementation.
Multiple factors continue to promote and influence tobacco
product use among youths, including exposure to tobacco
product advertising and imagery through media, as well as the
availability of flavored tobacco products. The sustained and
comprehensive implementation of population-based strategies,
in coordination with the regulation of tobacco products by
the U.S. Food and Drug Administration (FDA), can reduce
all forms of tobacco product use and initiation among U.S.
youths. Such strategies include increasing the price of tobacco
products, implementing comprehensive smoke-free policies,
implementing advertising and promotion restrictions and
national antitobacco public education media campaigns,
restricting youth access to flavored tobacco products, and
implementing policies that increase the minimum age of
purchase for tobacco products to 21 years (1,2,4,10). In
addition to population-level policies for preventing and
reducing initiation of tobacco product use among youths,
tools from the National Cancer Institute (e.g., https://
teen.smokefree.gov) and the Truth Initiative (e.g., https://
truthinitiative.org/thisisquitting) provide resources to help
youth quit tobacco product use.
Limitations
Limitations for YRBS overall are available in the overview
report of this supplement (11). This report is subject to at least
three additional limitations. First, changes in question wording
for smokeless tobacco use in 2017 prohibit comparability with
previous years’ data and long-term trend analyses for prevalence
of smokeless tobacco use, any tobacco product use, and use of
two or more tobacco products. Second, the question addressing
how students usually obtained electronic vapor products requires
that respondents select only one response, although they might
have obtained these products through multiple sources; therefore,
the full scope of the sources students use to access these products
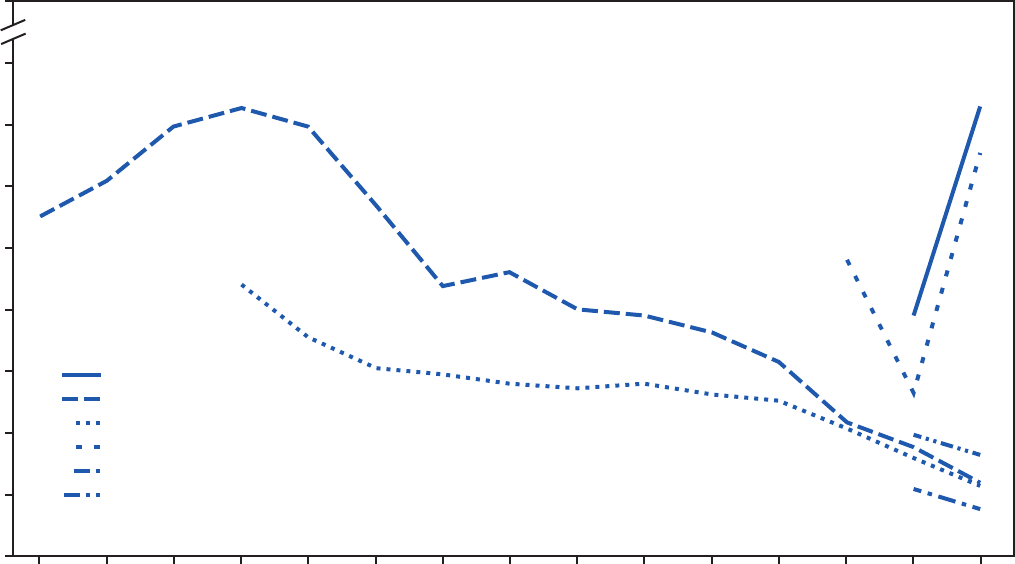
Supplement
62 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 2. Prevalence of current tobacco product use, by year — Youth Risk Behavior Survey, United States, 1991–2019*
* Logistic regression analyses were used to model linear and quadratic time effects while controlling for sex, grade, and race/ethnicity. Electronic vapor products:
significant linear increase (2015–2019); cigarettes: significant linear decrease (1991–2019); significant quadratic trend: increase during 1991–1997, decrease during
1997–2019; cigars/cigarillos/little cigars: significant linear decrease (1997–2019); significant quadratic trend: decrease 1997–2013; decrease 2013–2019 (different
rate of decrease). Differences from 2017 to 2019 were assessed by t-test (p<0.05): A significant increase occurred in use of electronic vapor products and any tobacco
product; a significant decrease occurred in use of cigarettes, cigars/cigarillos/little cigars and smokeless tobacco; and no change occurred in use of ≥2 products.
0
5
10
15
20
25
30
35
40
100
1991 1993 1995 1997 1999 2001 2003 2005 2007 2009 2011 2013 2015 2017 2019
Prevalence (%)
Year
Any tobacco product
Cigarettes
Cigars/cigarillos/little cigars
Electronic vapor products
Smokeless tobacco
≥2 products
might not have been addressed. Finally, the questions related to
electronic vapor products and cigars do not specifically exclude
the possibility of marijuana use in either product (e.g., blunt use).
Conclusion
Although current use of cigarettes, cigars, and smokeless
tobacco among U.S. high school students has decreased,
tobacco product usage has evolved, and the increasing
prevalence of electronic vapor product use among youths
during recent years is concerning. Implementing evidence-
based tobacco control strategies, combined with FDA’s
regulatory efforts, is important for preventing and reducing
all forms of tobacco product use among youths. In addition,
continued surveillance of all tobacco products is warranted for
guiding and evaluating public health policy at the local, state,
tribal, and national levels.
Conflicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. US Department of Health and Human Services. The health consequences of
smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA:
US Department of Health and Human Services, CDC; 2014. https://www.
ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf
2. US Department of Health and Human Services. Preventing tobacco use
among youth and young adults. Atlanta, GA: US Department of Health
and Human Services, CDC; 2012. https://www.cdc.gov/tobacco/data_
statistics/sgr/2012/index.htm
3. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—
United States, 2017. MMWR Surveill Summ 2018;67(No. SS-8). https://
doi.org/10.15585/mmwr.ss6708a1
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 63
US Department of Health and Human Services/Centers for Disease Control and Prevention
4. US Department of Health and Human Services. E-cigarette use among
youth and young adults: a report of the Surgeon General. Atlanta, GA:
US Department of Health and Human Services, CDC; 2016. https://
www.cdc.gov/tobacco/data_statistics/sgr/e-cigarettes/pdfs/2016_sgr_
entire_report_508.pdf
5. Spindle TR, Eissenberg T. Pod mod electronic cigarettes—an emerging
threat to public health. JAMA Netw Open 2018;1:e183518. https://
doi.org/10.1001/jamanetworkopen.2018.3518
6. Jackler RK, Ramamurthi D. Nicotine arms race: JUUL and the high-
nicotine product market. Tob Control 2019;28:623–8. https://doi.
org/10.1136/tobaccocontrol-2018-054796
7. King BA, Gammon DG, Marynak KL, Rogers T. Electronic cigarette
sales in the United States, 2013–2017. JAMA 2018;320:1379–80.
https://doi.org/10.1001/jama.2018.10488
8. King BA, Gammon DG, Coats EM, Marynak K, Loomis BR, Rogers
T. The rise of the pod mod: trends in e-cigarette sales in the United
States, 2013–2017. Society for Research on Nicotine and Tobacco annual
meeting. San Francisco, CA; February 20–23, 2019.
9. Gentzke AS, Creamer M, Cullen KA, et al. Vital signs: tobacco product
use among middle and high school students—United States, 2011–2018.
MMWR Morb Mortal Wkly Rep 2019;68:157–64. https://doi.
org/10.15585/mmwr.mm6806e1
10. US Department of Health and Human Services. Surgeon General’s
advisory on e-cigarette use among youth. Washington, DC: US
Department of Health and Human Services, Office of the Surgeon
General; 2018. https://e-cigarettes.surgeongeneral.gov/documents/
surgeon-generals-advisory-on-e-cigarette-use-among-youth-2018.pdf
11. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
12. Wang TW, Gentzke AS, Creamer MR, et al. Tobacco product use and
associated factors among middle and high school students—United
States, 2019. MMWR Surveill Summ 2019;68(No. SS-12). https://doi.
org/10.15585/mmwr.ss6812a1
13. Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Trends
in adolescent vaping, 2017–2019. N Engl J Med 2019;381:1490–1.
https://doi.org/10.1056/NEJMc1910739
14. Saddleson ML, Kozlowski LT, Giovino GA, Homish GG, Mahoney
MC, Goniewicz ML. Assessing 30-day quantity-frequency of U.S.
adolescent cigarette smoking as a predictor of adult smoking 14 years
later. Drug Alcohol Depend 2016;162:92–8. https://doi.org/10.1016/j.
drugalcdep.2016.02.043
15. Apelberg BJ, Corey CG, Hoffman AC, et al. Symptoms of tobacco
dependence among middle and high school tobacco users: results from
the 2012 National Youth Tobacco Survey. Am J Prev Med
2014;47(Suppl 1):S4–14. https://doi.org/10.1016/j.amepre.2014.04.013
16. Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Grucza RA, Bierut LJ.
Youth tobacco use type and associations with substance use disorders.
Addiction 2014;109:1371–80. https://doi.org/10.1111/add.12567
17. Tanski S, Emond J, Stanton C, et al. Youth access to tobacco products
in the United States: findings from wave 1 (2013–2014) of the
population assessment of tobacco and health study. Nicotine Tob Res
2019;21:1695–9. https://doi.org/10.1093/ntr/nty238
18. Liu ST, Snyder K, Tynan MA, Wang TW. Youth access to tobacco
products in the United States, 2016–2018. Tob Regul Sci 2019;5:491–501.
https://doi.org/10.18001/TRS.5.6.2
19. Marynak K, Mahoney M, Williams KS, Tynan MA, Reimels E, King
BA. State and territorial laws prohibiting sales of tobacco products to
persons aged <21 years, United States, December 31, 2019. MMWR
Morb Mortal Wkly Rep 2020;69:189–92. https://doi.org/10.15585/
mmwr.mm6907a3

Supplement
64 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Dietary and Physical Activity Behaviors Among High School
Students — Youth Risk Behavior Survey, United States, 2019
Caitlin L. Merlo, MPH
1
; Sherry Everett Jones, PhD, JD
2
; Shannon L. Michael, PhD
1
; Tiffany J. Chen, MSPH
3
;
Sarah A. Sliwa, PhD
1
; Seung Hee Lee, PhD
3
; Nancy D. Brener, PhD
2
; Sarah M. Lee, PhD
1
; Sohyun Park, PhD
3
1
Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion, CDC;
2
Division of Adolescent and School Health,
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC;
3
Division of Nutrition, Physical Activity, and Obesity, National Center for
Chronic Disease Prevention and Health Promotion, CDC
Abstract
Establishing healthy dietary and physical activity patterns among youths is an important public health strategy for improving
health and preventing chronic diseases; however, few adolescents meet U.S. government recommendations for dietary or physical
activity behaviors, and disparities by sex and race/ethnicity exist. CDC analyzed data from the 2019 Youth Risk Behavior Survey to
update estimates of dietary and physical activity behaviors among U.S. high school students overall and by sex and race/ethnicity.
In addition, 2-year comparisons (2017 and 2019) and trends in prevalence of these behaviors during 2009–2019 were examined.
In 2019, overall, during the 7 days before the survey, 41.8% of students had eaten fruit or drunk 100% fruit juices <1 time/day;
40.7% had eaten vegetables <1 time/day; and 16.7% had not eaten breakfast on all 7 days. Moreover, although 57.4% of students
had played on ≥1 sports team during the 12 months before the survey, less than half of students had been physically active for
≥60 minutes/day on all 7 days (23.2%), had exercised to strengthen or tone their muscles on ≥3 days/week (49.5%), had met both
aerobic and muscle-strengthening physical activity guidelines (16.5%), or had attended physical education classes on all 5 days in
an average school week (25.9%). Trend data indicate limited progress in shifting dietary and physical activity behaviors. That is,
with the exception of decreases in the percentage of students who had consumed soda ≥1 time/day (2009: 29.2%; 2019: 15.1%),
sports drinks ≥1 time/day (2015: 13.8%; 2019: 10.6%), and <3 glasses/day of plain water (2015: 50.5%; 2019: 44.6%), high
school students’ dietary and physical activity behaviors have not improved and, in certain cases, have worsened. These findings
support the need for multicomponent approaches, including policy and environmental changes, and opportunities for adolescents
to learn about and practice making healthy choices.
Introduction
Nutrition and physical activity are important for optimal
growth and development and chronic disease prevention.
Approximately half of U.S. adults have a chronic disease that
is related to inadequate diet quality and physical activity,
including type 2 diabetes, cardiovascular diseases, or obesity
(1). Such diseases can affect productivity and quality of life and
contribute to high health-care costs. Dietary and physical activity
behaviors develop during childhood and can create a trajectory
that continues into adulthood (1,2). Establishing healthy dietary
and physical activity behaviors early in life is a vital public health
strategy for promoting lifelong physical health.
The U.S. government establishes recommendations for
healthy dietary and physical activity patterns for persons of
different ages, including adolescents. The Dietary Guidelines
Corresponding author: Caitlin L. Merlo, MPH, Division of Population
Health, National Center for Chronic Disease Prevention and Health
Promotion, CDC. Telephone: 770-488-6171; E-mail: [email protected].
for Americans 2015–2020 outlines key recommendations for
following a healthy eating pattern within calorie levels that are
appropriate for a person’s age, sex, height, weight, and physical
activity level (1). Recommendations include eating a variety
of vegetables, fruits, and whole grains, and limiting sodium,
added sugars, and saturated and trans fats.
The Physical Activity Guidelines for Americans, 2nd Edition,
recommends that children and adolescents ages 6–17 years
engage in ≥60 minutes of moderate-to-vigorous physical
activity daily (2). Most of this daily physical activity should
be aerobic activity, whereas muscle- and bone-strengthening
physical activity should each be done ≥3 days each week (2).
Previous data indicate that most adolescents are not meeting
recommendations for healthy eating (1) or physical activity
(3), which increases the risk for chronic diseases later in life.
In addition, disparities by sex and race/ethnicity exist (4).
To update national estimates of dietary and physical activity
behaviors among U.S. high school students overall and by
sex and race/ethnicity and to determine how these behaviors
have changed over time, CDC analyzed data from the 2019
Youth Risk Behavior Survey (YRBS) and examined trends in
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 65
US Department of Health and Human Services/Centers for Disease Control and Prevention
prevalence of these behaviors during the previous 10 years.
Public health and school health researchers and practitioners
can use these findings to inform policies and practices that
support healthy eating and physical activity among adolescents.
Methods
Data Source
This report includes data from the 2009–2019 cycles of
the YRBS, a cross-sectional, school-based survey conducted
biennially since 1991. Each survey year, CDC collects data
from a nationally representative sample of public and private
school students in grades 9–12 in the 50 U.S. states and the
District of Columbia. Additional information about YRBS
sampling, data collection, response rates, and processing is
available in the overview report of this supplement (5). The
prevalence estimates for all physical activity, nutrition, and
body weight questions for the overall study population and by
sex, race/ethnicity, grade, and sexual orientation are available
at https://nccd.cdc.gov/youthonline/App/Default.aspx. The
full YRBS questionnaire is available at https://www.cdc.gov/
healthyyouth/data/yrbs/pdf/2019/2019_YRBS-National-HS-
Questionnaire.pdf.
Measures
The student demographic characteristics analyzed included
sex (female or male) and race/ethnicity. Students were classified
into four racial/ethnic categories: non-Hispanic white (white);
non-Hispanic black (black); Hispanic or Latino of any race
(Hispanic); and other or multiple races. The numbers of
students in the other or multiple racial/ethnic groups were
too small for meaningful analysis; therefore, findings for
those groups are not presented; however, the corresponding
data remain in the analytic sample. This analysis included six
dietary variables and five physical activity variables (Table 1).
The dietary variables included the following: during the 7 days
before the survey, had eaten fruit or drunk 100% fruit juices
<1 time/day, had eaten vegetables <1 time/day, had not eaten
breakfast on all 7 days, had drunk soda or pop ≥1 time/day
(not counting diet soda or diet pop), had drunk a sports drink
≥1 time/day, and had drunk <3 glasses/day of plain water. The
physical activity variables included the following: during the
7 days before the survey, had been physically active for a total
of ≥60 minutes/day on all 7 days, had exercised to strengthen
or tone muscles on ≥3 days, had met both aerobic and muscle-
strengthening physical activity guidelines (defined as being
physically active for a total of ≥60 minutes/day on all 7 days
and doing exercises to strengthen or tone muscles on ≥3 days),
had attended physical education classes on all 5 days in an
average school week, and had played on ≥1 sports team during
the 12 months before the survey.
Analysis
Prevalence estimates and 95% confidence intervals for each
2019 dietary and physical activity behavior were calculated
overall and for each sex and racial/ethnic group. Statistically
significant pairwise differences by sex and race/ethnicity were
determined by t-tests. In addition, prevalence of each dietary
and physical activity behavior was compared for 2017 with
2019 by using t-tests. Differences between prevalence estimates
were considered statistically significant if the t-test p value
was <0.05.
To identify 10-year temporal trends, logistic regression analyses
were used to model linear and quadratic time effects while
controlling for sex, grade (9, 10, 11, and 12), and racial/ethnic
changes over time (6). All variables had data available for
2009–2019, except for did not eat breakfast on all 7 days; were
physically active for a total of ≥60 minutes/day on all 7 days; did
exercises to strengthen or tone muscles on ≥3 days and met both
aerobic and muscle-strengthening physical activity guidelines,
which had data for 2011–2019 only; and drank a sports drink
≥1 time/day and drank <3 glasses/day of plain water, which had
data for 2015–2019 only. Additional information about the
methods used to conduct YRBS trend analyses are provided in
the overview report of this supplement (5).
Results
Dietary Behaviors
Overall
In 2019, nationwide, 41.8% of students had eaten fruit
or drunk 100% fruit juices <1 time/day; 40.7% had eaten
vegetables <1 time/day; 16.7% had not eaten breakfast on
all 7 days; 15.1% had drunk sugar-sweetened soda or pop
≥1 time/day (not counting diet soda or diet pop); 10.6%
had drunk a sports drink ≥1 time/day; and 44.6% had drunk
<3 glasses/day of plain water (Table 2). A higher percentage of
male students than female students had drunk sugar-sweetened
soda or pop ≥1 time/day (18.2% versus 11.7%) and had drunk
a sports drink ≥1 time/day (14.0% versus 7.1%). A higher
percentage of black students than white and Hispanic students
had eaten fruit or drunk 100% fruit juices <1 time/day (47.8%
versus 42.1% and 39.5%, respectively), had eaten vegetables
<1 time/day (54.8% versus 35.5% and 46.8%, respectively),
had drunk a sports drink ≥1 time/day (15.6% versus 9.3%

Supplement
66 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Question wording and details for included dietary and physical activity behavior variables — Youth Risk Behavior Survey, United
States, 2019
Variable Question Response options
Years of data
available for 10-year
trend analysis Coding for analysis
Dietary behaviors
Ate fruit or drank
100% fruit juices
<1 time/day
During the past 7 days, how many times did you . . .
• drink 100% fruit juices such as orange juice,
apple juice, or grape juice? (Do not count
punch, Kool-Aid, sports drinks, or other
fruit-flavored drinks.)
• eat fruit? (Do not count fruit juice.)
I did not [drink 100% fruit juice]/[eat
fruit] during the past 7 days, 1–3 times
during the past 7 days, 4–6 times
during the past 7 days,1 time/day,
2 times/day, 3 times/day, or
≥4 times/day
2009–2019 <1 time/day versus
≥1 time/day
Ate vegetables
<1 time/day
During the past 7 days, how many times
did you eat . . .
• green salad?
• potatoes? (Do not count French fries, fried
potatoes, or potato chips.)
• carrots?
• other vegetables? (Do not count green salad,
potatoes, or carrots.)
I did not eat [green salad]/[potatoes]/
[carrots]/[other vegetables] during
the past 7 days, 1–3 times during the
past 7 days, 4–6 times during the past
7 days, 1 time/day, 2 times/day,
3 times/day, or ≥4 times/day
2009–2019 <1 time/day versus
≥1 time/day
Did not eat breakfast
on all 7 days
During the past 7 days, on how many days did
you eat breakfast?
0 days, 1 day, 2 days, 3 days, 4 days,
5 days, 6 days, or 7 days
2011–2019 <7 days versus 7 days
Drank soda or pop
≥1 time/day
During the past 7 days, how many times did you
drink a can, bottle, or glass of soda or pop, such
as Coke, Pepsi, or Sprite? (Do not count diet
soda or diet pop.)
I did not drink soda or pop during the
past 7 days, 1–3 times during the past
7 days, 4–6 times during the past
7 days, 1 time/day, 2 times/day,
3 times/day, or ≥4 times/day
2009–2019 ≥1 time/day versus
<1 time/day
Drank a sports drink
≥1 time/day
During the past 7 days, how many times did you
drink a can, bottle, or glass of a sports drink,
such as Gatorade or Powerade? (Do not count
low-calorie sports drinks such as Propel or G2.)
I did not drink sports drinks during the
past 7 days, 1–3 times during the past
7 days, 4–6 times during the past
7 days, 1 time/day, 2 times/day,
3 times/day, or ≥4 times/day
2015–2019 ≥1 time/day versus
<1 time/day
Drank <3 glasses/day
of plain water
During the past 7 days, how many times did you
drink a bottle or glass of plain water? (Count
tap, bottled, and unflavored sparkling water.)
I did not drink water during the past
7 days, 1–3 times during the past
7 days, 4–6 times during the past
7 days, 1 time per day, 2 times per day,
3 times/day, or ≥4 times/day
2015–2019 ≥3 times/day versus
<3 times/day
Physical activity behaviors
Were physically
active for a total of
≥60 minutes/day
on all 7 days
During the past 7 days, on how many days were
you physically active for a total of at least
60 minutes per day? (Add up all the time you
spent in any kind of physical activity that
increased your heart rate and made you
breathe hard some of the time.)
0 days, 1 day, 2 days, 3 days, 4 days,
5 days, 6 days, or 7 days
2011–2019 7 days versus <7 days
Did exercises to
strengthen or tone
muscles on ≥3 days
During the past 7 days, on how many days did you
do exercises to strengthen or tone your muscles,
such as push-ups, sit-ups, or weightlifting?
0 days, 1 day, 2 days, 3 days, 4 days,
5 days, 6 days, or 7 days
2011–2019 ≥3 days versus <3 days
Met both aerobic
and muscle-
strengthening
physical activity
guidelines
[See “were physically active for a total of
≥60 minutes/day on all 7 days” and “did
exercises to strengthen or tone muscles on
≥3 days.”]
Not applicable 2011–2019 Physically active for
≥60 minutes/day on all
7 days
and did exercises
to strengthen or tone
muscles on ≥3 days
versus physically active
for <60 minutes/day on
all 7 days or did exercises
to strengthen or tone
muscles on <3 days
Attended physical
education classes
on all 5 days
In an average week when you are in school, on
how many days do you go to physical
education (PE) classes?
0 days, 1 day, 2 days, 3 days, 4 days, or
5 days
2009–2019 ≥5 days versus <5 days
Played on ≥1 sports
team
During the past 12 months, on how many sports
teams did you play? (Count any teams run by
your school or community groups.)
0 teams, 1 team, 2 teams, or ≥3 teams 2009–2019 ≥1 team versus <1 team
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 67
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Percentage of high school students who engaged in selected dietary and physical activity behaviors, by sex and race/ethnicity —
Youth Risk Behavior Survey, United States, 2019
Variable
Total
% (95% CI)
Sex Race/Ethnicity
Female
% (95% CI)
Male
% (95% CI)
White,
non-Hispanic
% (95% CI)
Black,
non-Hispanic
% (95% CI)
Hispanic
% (95% CI)
Dietary behaviors
Ate fruit or drank 100% fruit juices
<1 time/day*
41.8 (39.8–43.8) 43.0 (40.7–45.4) 40.6 (38.2–43.1) 42.1 (39.2–45.1) 47.8
†,§
(43.6–51.9) 39.5 (36.7–42.3)
Ate vegetables <1 time/day
¶
40.7 (38.0–43.4) 40.4 (37.2–43.6) 41.1 (38.1–44.3) 35.5 (33.2–37.8) 54.8
†,§
(50.1–59.4) 46.8
†
(41.8–52.0)
Did not eat breakfast on all 7 days during the
7 days before the survey
16.7 (15.3–18.1) 16.7 (15.2–18.3) 16.6 (14.9–18.4) 15.3 (13.9–16.8) 21.1
†
(17.3–25.6) 16.9 (14.1–20.0)
Drank sugar-sweetened soda or pop ≥1
time/day**
15.1 (13.1–17.2) 11.7 (9.9–13.8) 18.2
††
(15.9–20.8) 15.2 (12.7–18.0) 16.9 (13.5–21.0) 16.1 (13.1–19.6)
Drank a sports drink ≥1 time/day
§§
10.6 (9.2–12.3) 7.1 (5.7–8.8) 14.0
††
(11.9–16.4) 9.3 (7.7–11.2) 15.6
†,§
(12.9–18.8) 11.9
†
(10.2–13.8)
Drank <3 glasses/day of plain water
¶¶
44.6 (42.7–46.5) 44.1 (42.0–46.1) 45.0 (42.3–47.6) 44.2 (41.7–46.7) 54.8
†,§
(49.0–60.4) 44.2 (41.8–46.7)
Physical activity behaviors
Were physically active for a total of
≥60 minutes/day on all 7 days***
23.2 (21.9–24.6) 15.4 (14.2–16.6) 30.9
††
(28.9–33.1) 25.6 (24.1–27.2) 21.1
†
(17.6–25.2) 20.9
†
(18.6–23.5)
Did exercises to strengthen or tone muscles
on ≥3 days
†††
49.5 (47.6–51.3) 39.7 (37.2–42.4) 59.0
††
(56.8–61.0) 50.8 (48.2–53.4) 47.0 (42.7–51.2) 48.1 (44.5–51.9)
Met both aerobic and muscle-strengthening
physical activity guidelines
§§§
16.5 (14.6–18.6) 10.1 (8.7–11.6) 23.1
††
(20.4–26.0) 18.4 (15.8–21.4) 13.4
†
(9.5–18.4) 16.0 (13.7–18.6)
Went to physical education classes on
all 5 days
¶¶¶
25.9 (21.5–31.0) 22.8 (17.9–28.5) 28.9
††
(24.6–33.7) 24.3 (18.8–30.7) 23.8 (17.4–31.7) 29.9 (24.5–36.0)
Played on ≥1 sports team**** 57.4 (54.3–60.4) 54.6 (51.1–58.0) 60.2
††
(56.9–63.4) 62.0 (58.1–65.7) 56.1
†
(51.4–60.7) 51.6
†
(46.5–56.6)
Abbreviation: CI = confidence interval.
* Such as orange juice, apple juice, or grape juice, not counting punch, Kool-Aid, sports drinks, or other fruit-flavored drinks during the 7 days before the survey.
†
Significantly different than white students based on t-test analysis (p<0.05).
§
Significantly different than Hispanic students based on t-test analysis (p<0.05).
¶
Green salad, potatoes (not counting French fries, fried potatoes, or potato chips), carrots, or other vegetables during the 7 days before the survey.
** Such as Coke, Pepsi, or Sprite, not counting diet soda or diet pop, during the 7 days before the survey.
††
Significantly different than female students based on t-test analysis (p<0.05).
§§
Such as Gatorade or PowerAde, not counting low-calorie sports drinks such as Propel water or G2, during the 7 days before the survey.
¶¶
Counting tap, bottled, and unflavored sparkling water during the 7 days before the survey.
*** Adding up time spent in any kind of physical activity that increased their heart rate and made them breathe hard some of the time during the 7 days before the survey.
†††
Such as push-ups, sit-ups, or weightlifting during the 7 days before the survey.
§§§
Were physically active for ≥60 minutes/day on all 7 days and did exercises to strengthen or tone muscles on ≥3 of the 7 days before the survey.
¶¶¶
In an average week when the student was in school.
**** Counting any teams run by their school or community groups during the 12 months before the survey.
and 11.9%, respectively), and had drunk <3 glasses/day of
plain water (54.8% versus 44.2% and 44.2%, respectively).
In addition, a higher percentage of Hispanic students than
white students had eaten vegetables <1 time/day (46.8% versus
35.3%) and had drunk a sports drink ≥1 time/day (11.9%
versus 9.3%), and a higher percentage of black students than
white students had not eaten breakfast on all 7 days (21.1%
versus 15.3%).
Trends
Trend analyses indicated that, during 2009–2019, a
significant linear increase occurred in the percentage of students
who had eaten fruit or drunk 100% fruit juices <1 time/day
overall and among female, male, white, black, and Hispanic
students (Table 3). Significant quadratic trends were not
identified except among black students. The percentage of
black students who had eaten fruit or drunk 100% fruit
juices <1 time/day did not change during 2009–2015 and
then increased during 2015–2019. During 2017–2019, the
percentage of students who had eaten fruit or drunk 100%
fruit juices <1 time/day increased among male students and
black students.
During 2009–2019, a significant linear increase occurred
in the percentage of students who had eaten vegetables
<1 time/day overall and among male, white, and black students.
Significant quadratic trends were not identified, except among
black students. The percentage of black students who had eaten
vegetables <1 time/day did not change during 2009–2015 and
then increased during 2015–2019.
During 2011–2019, a significant linear increase occurred in
the percentage of students who had not eaten breakfast on all
7 days overall and among female, male, and white students.
During 2017–2019, the percentage of students who had not
eaten breakfast on all 7 days increased among students overall
and among female, male, white, and black students.
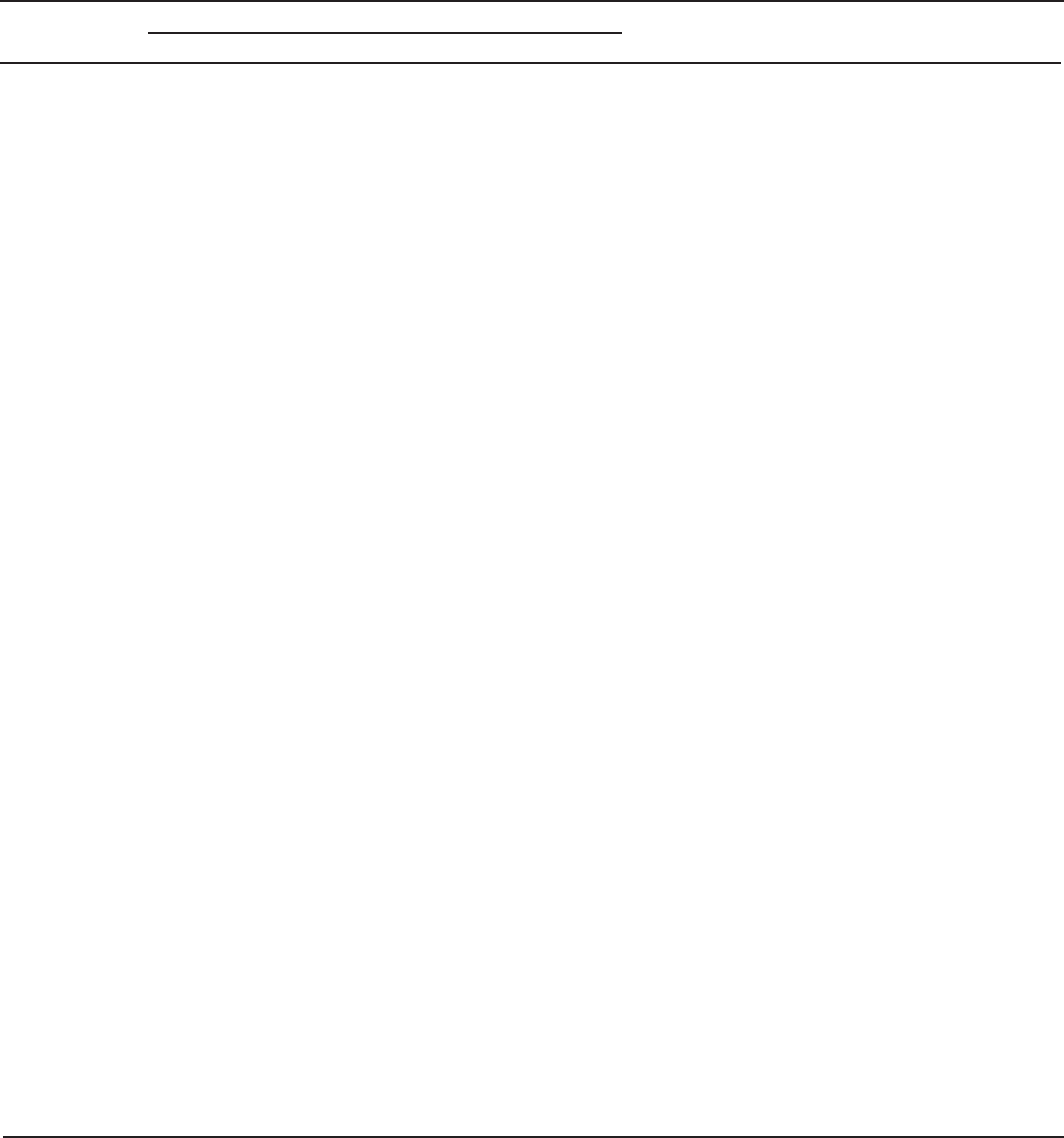
Supplement
68 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 3. Percentage of high school students who engaged in selected dietary behaviors, by sex, race/ethnicity, and survey year — Youth Risk
Behavior Survey, United States, 2009–2019
Behavior
Prevalence (%)
Linear change* Quadratic change*
Change during
2017–2019
†
2009 2011 2013 2015 2017 2019
Ate fruit or drank 100% fruit juices <1 time/day
§
Total 35.2 36.0 37.4 36.7 39.2 41.8 Increased during
2009–2019
None None
Female 37.6 38.4 40.0 37.9 41.8 43.0 Increased during
2009–2019
None None
Male 33.0 33.9 34.7 35.4 36.7 40.6 Increased during
2009–2019
None Increased
White, non-Hispanic 34.4 35.8 39.3 37.0 40.4 42.1 Increased during
2009–2019
None None
Black, non-Hispanic 39.2 36.4 36.5 37.8 39.3 47.8 Increased during
2009–2019
None during
2009–2015
Increased during
2015–2019
Increased
Hispanic 35.6 35.3 35.0 35.9 37.6 39.5 Increased during
2009–2019
None None
Ate vegetables <1 time/day
¶
Total 37.3 37.7 38.5 39.0 40.6 40.7 Increased during
2009–2019
None None
Female 38.4 38.4 38.7 40.0 40.7 40.4 None None None
Male 36.3 37.2 38.5 38.0 40.6 41.1 Increased during
2009–2019
None None
White, non-Hispanic 32.7 34.3 35.2 35.8 37.2 35.5 Increased during
2009–2019
None None
Black, non-Hispanic 48.8
45.7 48.1 47.5 50.6 54.8 Increased during
2009–2019
None during
2009–2015
Increased during
2015–2019
None
Hispanic 45.9 43.6 43.1 43.5 43.9 46.8 None None None
Did not eat breakfast on all 7 days during the 7 days before the survey
Total —** 13.1 13.7 13.8 14.1 16.7 Increased during
2011–2019
—
††
Increased
Female —** 13.9 13.8 14.2 14.5 16.7 Increased during
2011–2019
—
††
Increased
Male —** 12.3 13.5 13.3 13.6 16.6 Increased during
2011–2019
—
††
Increased
White, non-Hispanic —** 12.0 11.5 12.0 12.8 15.3 Increased during
2011–2019
—
††
Increased
Black, non-Hispanic —** 16.1 16.0 18.0 15.2 21.1 None —
††
Increased
Hispanic —** 14.4 17.4 14.7 16.0 16.9 None —
††
None
Drank sugar-sweetened soda or pop ≥1 time/day
§§
Total 29.2 27.8 27.0 20.4 18.7 15.1 Decreased during
2009–2019
None during
2009–2013
Decreased during
2013–2019
Decreased
Female 23.3 24.0 24.1 16.4 15.4 11.7 Decreased during
2009–2019
None during
2009–2013
Decreased during
2013–2019
Decreased
Male 34.6 31.4 29.9 24.3 22.3 18.2 Decreased during
2009–2019
None Decreased
White, non-Hispanic 29.0 28.8 29.0 19.7 19.6 15.2 Decreased during
2009–2019
None Decreased
Black, non-Hispanic 33.7 28.0 30.2 22.7 21.5 16.9 Decreased during
2009–2019
None None
Hispanic 28.1 27.0 22.6 21.7 17.0 16.1 Decreased during
2009–2019
None None
See table footnotes on the next page.
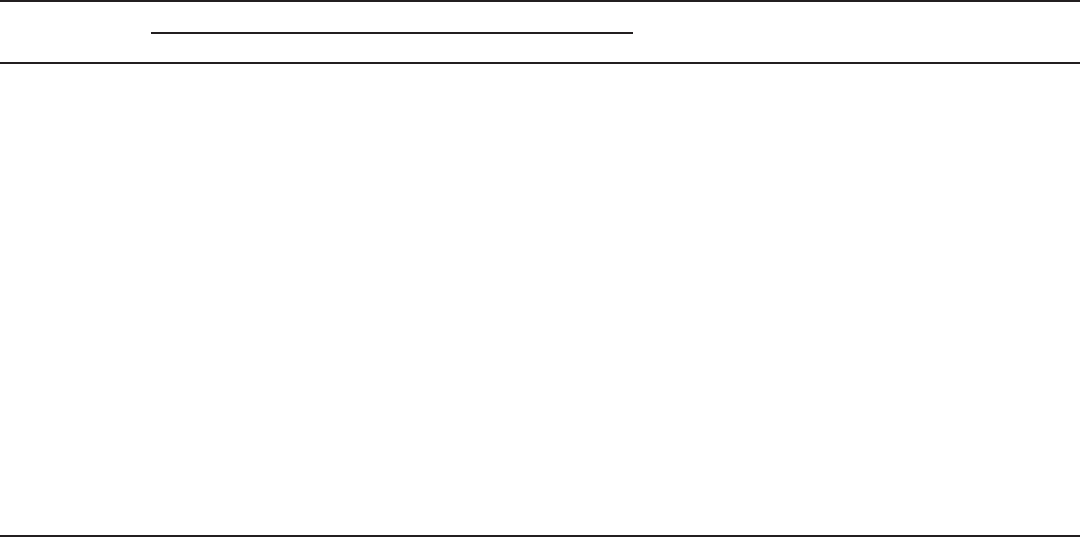
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 69
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 3. (Continued) Percentage of high school students who engaged in selected dietary behaviors, by sex, race/ethnicity, and survey year —
Youth Risk Behavior Survey, United States, 2009–2019
Behavior
Prevalence (%)
Linear change* Quadratic change*
Change during
2017–2019
†
2009 2011 2013 2015 2017 2019
Drank a sports drink ≥1 time/day
¶¶
Total —** —** —** 13.8 12.4 10.6 Decreased during
2015–2019
—
††
None
Female —** —** —** 8.8 8.2 7.1 None —
††
None
Male —** —** —** 18.7 16.9 14.0 Decreased during
2015–2019
—
††
Decreased
White, non-Hispanic —** —** —** 12.4 10.7 9.3 Decreased during
2015–2019
—
††
None
Black, non-Hispanic —** —** —** 19.7 21.1 15.6 None —
††
Decreased
Hispanic —** —** —** 15.7 13.5 11.9 Decreased during
2015–2019
—
††
None
Drank <3 glasses/day of plain water***
Total —** —** —** 50.5 48.7 44.6 Decreased during
2015–2019
—
††
Decreased
Female —** —** —** 51.9 48.8 44.1 Decreased during
2015–2019
—
††
Decreased
Male —** —** —** 49.0 48.6 45.0 Decreased during
2015–2019
—
††
Decreased
White, non-Hispanic —** —** —** 50.1 48.8 44.2 Decreased during
2015–2019
—
††
Decreased
Black, non-Hispanic —** —** —** 60.9 52.7 54.8 None —
††
None
Hispanic —** —** —** 49.7 47.5 44.2 Decreased during
2015–2019
—
††
Decreased
* Based on trend analyses by using a logistic regression model controlling for sex, race/ethnicity, and grade (p<0.05).
†
Based on t-test analysis (p<0.05).
§
Such as orange juice, apple juice, or grape juice, not counting punch, Kool-Aid, sports drinks, or other fruit-flavored drinks, during the 7 days before the survey.
¶
Green salad, potatoes (not counting French fries, fried potatoes, or potato chips), carrots, or other vegetables during the 7 days before the survey.
** Data not available. Question not asked in that year.
††
Insufficient years of data to assess quadratic trends.
§§
Such as Coke, Pepsi, or Sprite, not counting diet soda or diet pop, during the 7 days before the survey.
¶¶
Such as Gatorade or PowerAde, not counting low-calorie sports drinks such as Propel water or G2, during the 7 days before the survey.
*** Counting tap, bottled, and unflavored sparkling water during the 7 days before the survey.
During 2009–2019, a significant linear decrease occurred
in the percentage of students who had drunk sugar-sweetened
soda or pop ≥1 time/day overall and among female, male, white,
black, and Hispanic students (Figure 1). Significant quadratic
trends were identified overall and among female students.
Overall and among female students, the percentage of students
who had drunk sugar-sweetened soda or pop ≥1 time/day did
not change during 2009–2013 and then decreased during
2013–2019. During 2017–2019, the percentage of students who
had drunk sugar-sweetened soda or pop ≥1 time/day decreased
overall and among female, male, and white students.
During 2015–2019, a significant linear decrease occurred
in the percentage of students who had drunk a sports drink
≥1 time/day overall and among male, white, and Hispanic
students (Figure 2). During 2017–2019, the percentage of
students who had drunk a sports drink ≥1 time/day decreased
among male students and black students.
During 2015–2019, a significant linear decrease occurred
in the percentage of students who had drunk <3 glasses/day
of plain water overall and among female, male, white, and
Hispanic students. During 2017–2019, the percentage of
students who had drunk <3 glasses/day of plain water decreased
overall and among female, male, white, and Hispanic students.
Physical Activity Behaviors
Overall
In 2019, nationwide, 23.2% of students had been physically
active for ≥60 minutes/day on all 7 days; 49.5% had exercised
to strengthen or tone their muscles on ≥3 days/week; 16.5%
had met both aerobic and muscle-strengthening physical
activity guidelines; 25.9% had attended physical education
classes on all 5 days in an average school week; and 57.4% had
played on ≥1 sports team (Table 2). A higher percentage of
male students than female students had been physically active
for ≥60 minutes/day on all 7 days (30.9% versus 15.4%), had
exercised to strengthen or tone muscles on ≥3 days (59.0%
versus 39.7%), had met both aerobic and muscle-strengthening
physical activity guidelines (23.1% versus 10.1%), had
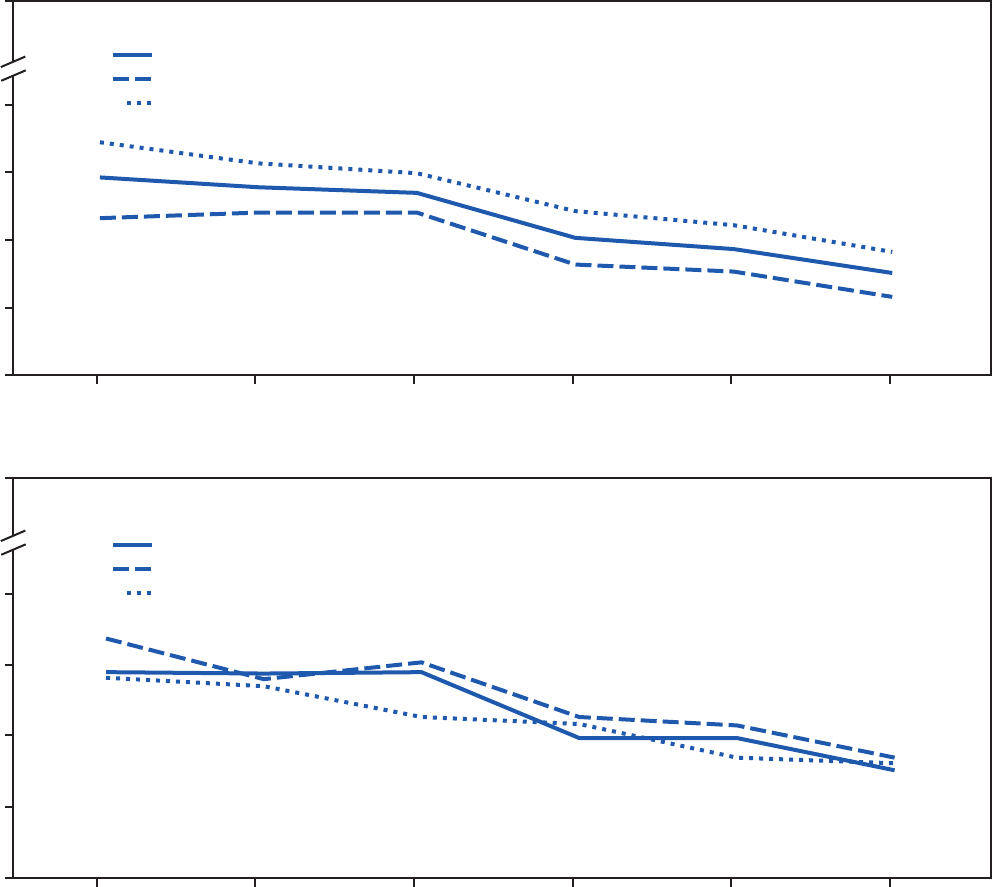
Supplement
70 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 1. Percentage of high school students who had drunk sugar-sweetened soda or pop ≥1 time per day during the 7 days before the
survey, overall and by sex and race/ethnicity* — Youth Risk Behavior Survey, United States, 2009–2019
Overall
Female
Male
0
10
20
30
40
2009 2011 2013 2015 2017 2019
Percentage
0
10
20
30
40
Percentage
2009 2011 2013 2015 2017 2019
White, non-Hispanic
Black, non-Hispanic
Hispanic
100
100
Year
Year
* During 2009–2019, a significant linear decrease was observed in the percentage of students who had drunk sugar-sweetened soda or pop ≥1 time/day overall and among
female, male, white, black, and Hispanic students. Based on trend analyses by using a logistic regression model controlling for sex, race/ethnicity, and grade (p<0.05).
attended physical education classes on all 5 days in an average
school week (28.9% versus 22.8%), and had played on
≥1 sports team (60.2% versus 54.6%) (Figure 3). A higher
percentage of white students than black students had been
physically active for ≥60 minutes/day on all 7 days (25.6%
versus 21.1%), had met both aerobic and muscle-strengthening
physical activity guidelines (18.4% versus 13.4%), and had
played on ≥1 sports team (62.0% versus 56.1%). In addition,
a higher percentage of white students than Hispanic students
had been physically active for ≥60 minutes/day on all 7 days
(25.6% versus 20.9%) and had played on ≥1 sports team
(62.0% versus 51.6%) (Table 2).
Trends
During 2011–2019, a significant linear decrease occurred
in the percentage of students who had been physically active
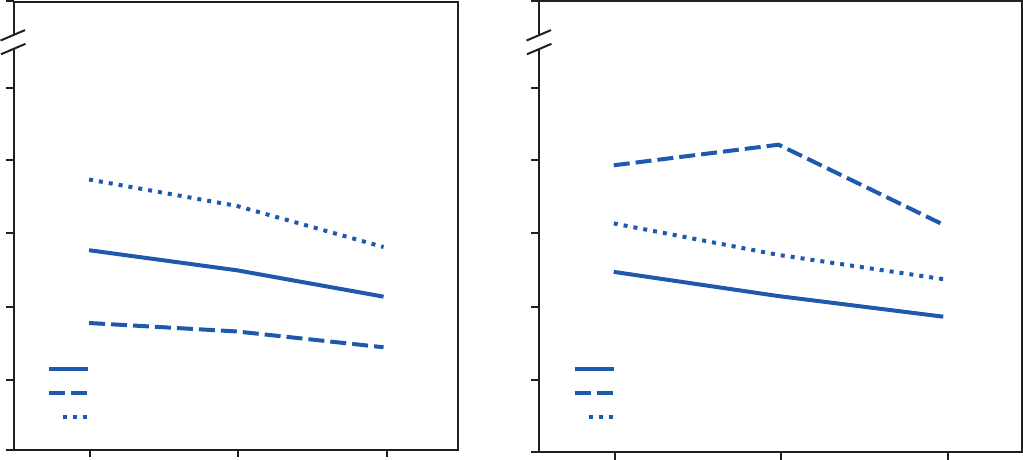
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 71
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 2. Percentage of high school students who had drunk a sports drink ≥1 time per day during the 7 days before the survey, overall and
by sex and race/ethnicity* — Youth Risk Behavior Survey, United States, 2015–2019
Overall
Female
Male
0
2015 2017 2019
0
5
10
15
20
25
2015 2017 2019
Percentage
Percentage
100
100
White, non-Hispanic
Black, non-Hispanic
Hispanic
Year Year
5
10
15
20
25
* During 2015–2019, a significant linear decrease was observed in the percentage of students who had drunk a sports drink ≥1 time/day overall and among male,
white, and Hispanic students. Based on trend analysis by using a logistic regression model controlling for sex, race/ethnicity, and grade (p<0.05).
for ≥60 minutes/day on all 7 days overall and among female,
male, white, black, and Hispanic students (Table 4). During
2017–2019, the percentage of students who had been
physically active for ≥60 minutes/day on all 7 days decreased
overall and among male students and Hispanic students.
During 2011–2019, a significant linear decrease occurred in
the percentage of students who had exercised to strengthen or
tone their muscles on ≥3 days/week overall and among male,
white, black, and Hispanic students. During 2017–2019, no
significant changes occurred in the percentage of students
who had exercised to strengthen or tone their muscles on
≥3 days/week overall or among the sex or racial/ethnic groups.
During 2011–2019, a significant linear decrease occurred
in the percentage of students who had met both aerobic and
muscle-strengthening physical activity guidelines overall
and among female, male, white, and black students. During
2017–2019, the percentage of students who had met both
aerobic and muscle-strengthening physical activity guidelines
did not significantly change overall but decreased among male
students and Hispanic students.
During 2009–2019 and during 2017–2019, no significant
linear changes occurred in the percentage of students who had
attended physical education classes on all 5 days in an average
school week or had played on ≥1 sports team overall or among
the sex and racial/ethnic groups, except among female students.
Among female students, a significant linear decrease occurred
in the percentage who had attended physical education classes
on all 5 days in an average school week.
Discussion
With the exception of decreases in the percentages of
students who had consumed soda ≥1 time/day, sports drinks
≥1 time/day, and <3 glasses/day of plain water, high school
students’ dietary and physical activity behaviors have not
improved during the previous 10 years and, in certain cases,
have worsened. This is cause for concern because healthy
dietary and physical activity behaviors are important for
growth and development, academic outcomes, and prevention
of chronic diseases, including type 2 diabetes, heart disease,
hypertension, and obesity (1,7). Recent data demonstrate
that approximately one in five adolescents have prediabetes,
which increases the risk for type 2 diabetes and cardiovascular
diseases (8). In addition, data from the National Health and
Nutrition Examination Survey reveal that, in the United States
during 2007–2008, approximately 18.1% of youths aged
12–19 years had obesity and this increased to 20.6% during
2015–2016 (9). In this analysis, in which differences by race/
ethnicity exist, black and Hispanic high school students have
poorer dietary and physical activity behaviors, compared
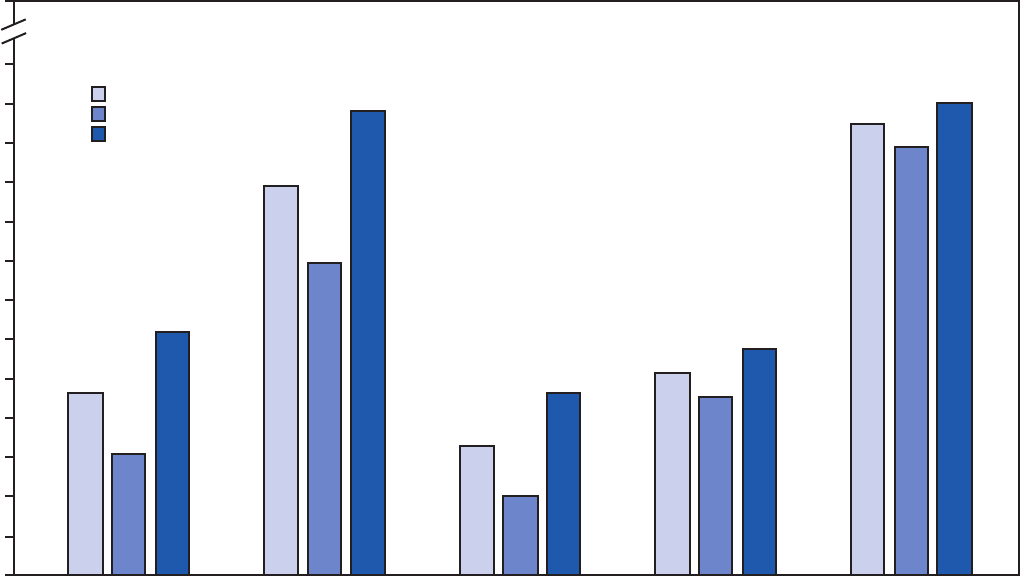
Supplement
72 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 3. Percentage* of high school students who had engaged in physical activity
†
and physical education during the 7 days before the
survey, overall and by sex
§
— Youth Risk Behavior Survey, United States, 2019
Overall
Female
Male
0
5
10
15
20
25
30
35
40
45
50
55
60
65
Were physically active
for a total of
≥60 minutes/day
on all 7 days
Did exercises to
strengthen or tone
muscles on ≥3 days
Met both aerobic
and muscle-strengthening
physical activity guidelines
Attended physical
education classes
on all 5 days
Played on ≥1
sports team
during the past
12 months
100
Percentage
Activity
* Bars represent the percentage of respondents with a “yes” response, overall and by sex.
†
The “met both aerobic and muscle-strengthening physical activity guidelines” variable is defined as being physically active for a total of ≥60 minutes/day on all
7 days and doing exercises to strengthen or tone muscles on ≥3 days during the 7 days before the survey (Source: U.S. Department of Health and Human Services.
Physical activity guidelines for Americans. 2nd ed. Washington, DC: US Department of Health and Human Services; 2018. https://www.hhs.gov/fitness/be-active/
physical-activity-guidelines-for-americans/index.html).
§
In 2019, a significantly higher percentage of male than female students had been physically active for ≥60 minutes/day on all 7 days during the 7 days before the
survey, had exercised to strengthen or tone muscles on ≥3 days during the 7 days before the survey, had met the aerobic and muscle-strengthening physical activity
guidelines during the 7 days before the survey, had attended physical education classes on all 5 days in an average school week when the student was in school,
and had played on ≥1 sports team during the past 12 months. Based on t-test analysis (p<0.05).
with white high school students. These findings also indicate
that male students have poorer dietary behaviors but better
physical activity behaviors than do female students. Addressing
dietary and physical activity behaviors can benefit all students
and is especially important for those with increased risk for
chronic diseases (e.g., students from low-income families and
racial/ethnic minorities).
Dietary Behaviors
No improvements occurred in fruit or vegetable consumption
during 2009–2019 and, in many cases, have worsened. Overall,
consumption of fruits and vegetables remained low in 2019.
For example, four of 10 high school students had eaten fruit
or drunk 100% fruit juices <1 time/day. Similarly, four of 10
had eaten vegetables <1 time/day. Although the prevalence of
having eaten fruit or drunk 100% fruit juice <1 time/day and
having eaten vegetables <1 time/day is similar for male students
and female students, recommended daily intakes differ by age
and sex. Females and males aged 14–18 years need 1.5 cups
and 2 cups, respectively, of fruits, and 2.5 cups and 3 cups,
respectively, of vegetables (https://www.choosemyplate.gov/
resources/MyPlatePlan). Although YRBS measures frequency
of intake and not the amount consumed, children and
adolescents who meet the recommended amounts typically
consume fruits and vegetables multiple times throughout the
day (10); therefore, consuming fruits or vegetables <1 time/day
is likely insufficient. Strategies that encourage adolescents to
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 73
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 4. Percentage of high school students who engaged in selected physical activity behaviors, by sex, race/ethnicity, and survey year —
Youth Risk Behavior Survey, United States, 2009–2019
Behavior
Prevalence (%)
Linear change* Quadratic change*
Change during
2017–2019
†
2009 2011 2013 2015 2017 2019
Were physically active for a total of ≥60 minutes/day on all 7 days
§
Total —
¶
28.7 27.1 27.1 26.1 23.2 Decreased during
2011–2019
—** Decreased during
2017–2019
Female —
¶
18.5 17.7 17.7 17.5 15.4 Decreased during
2011–2019
—** None
Male —
¶
38.3 36.6 36.0 35.3 30.9 Decreased during
2011–2019
—** Decreased during
2017–2019
White, non-Hispanic —
¶
30.4 28.2 29.0 27.1 25.6 Decreased during
2011–2019
—** None
Black, non-Hispanic —
¶
26.0 26.3 24.2 24.5 21.1 Decreased during
2011–2019
—** None
Hispanic —
¶
26.5 25.5 24.6 25.8 20.9 Decreased during
2011–2019
—** Decreased during
2017–2019
Did exercises to strengthen or tone muscles on ≥3 days
††
Total —
¶
55.6 51.7 53.4 51.1 49.5 Decreased during
2011–2019
—** None
Female —
¶
43.8 41.6 42.7 40.8 39.7 None —** None
Male —
¶
66.7 61.8 63.7 62.1 59.0 Decreased during
2011–2019
—** None
White, non-Hispanic —
¶
55.7 52.4 54.5 50.6 50.8 Decreased during
2011–2019
—** None
Black, non-Hispanic —
¶
54.0 48.8 52.3 51.0 47.0 Decreased during
2011–2019
—** None
Hispanic —
¶
56.6 53.3 52.4 52.3 48.1 Decreased during
2011–2019
—** None
Met guidelines for aerobic and muscle-strengthening physical activity
§§
Total —
¶
21.9 21.6 20.5 20.0 16.5 Decreased during
2011–2019
—** None
Female —
¶
12.7 13.0 12.2 12.1 10.1 Decreased during
2011–2019
—** None
Male —
¶
30.7 30.3 28.6 28.5 23.1 Decreased during
2011–2019
—** Decreased during
2017–2019
White, non-Hispanic —
¶
23.9 22.6 22.7 20.8 18.4 Decreased during
2011–2019
—** None
Black, non-Hispanic —
¶
18.4 20.6 15.7 17.7 13.4 Decreased during
2011–2019
—** None
Hispanic —
¶
18.9 20.5 18.7 20.0 16.0 None —** Decreased during
2017–2019
See table footnotes on the next page.
increase the quantity of fruits and vegetables each time they
consume them are likely needed to help them meet the daily
recommendations (10). For example, schools can offer students
multiple fruit and vegetable choices each day through school
meal programs, including through grab-and-go salads (11).
Sugar-sweetened beverages (SSBs) are the primary source
of added sugars in U.S. youths’ diets (1). Frequently
drinking SSBs is associated with health conditions, including
obesity, type 2 diabetes, heart disease, and tooth decay (12).
Alternatively, drinking enough water every day is good for
overall health and is associated with higher Healthy Eating
Index scores among adolescents (13). (More information about
the Healthy Eating Index is available at https://www.fns.usda.
gov/resource/healthy-eating-index-hei.) YRBS asks about two
specific types of SSBs, soda or pop and sports drinks. This study
identified substantial decreases in the percentage of students
who had drunk soda or pop ≥1 time/day overall and among all
sex and racial/ethnic groups. In addition, decreases occurred
in the percentage of students who had drunk a sports drink
≥1 time/day overall and among female, white, and Hispanic
students. Despite these improvements in soda and sports drink
consumption, consumption of these beverages is common.
Differences also existed by sex and race/ethnicity. Similar to
this study, previous studies reported that SSB intake was higher
among males than among females (14) and among black and
Hispanic adolescents than among white adolescents (15). One
possible explanation for the differences between racial/ethnic
groups is that beverage companies disproportionately market
SSBs to black and Hispanic youths (16).
Supplement
74 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 4. (Continued) Percentage of high school students who engaged in selected physical activity behaviors, by sex, race/ethnicity, and survey
year — Youth Risk Behavior Survey, United States, 2009–2019
Behavior
Prevalence (%)
Linear change* Quadratic change*
Change during
2017–2019
†
2009 2011 2013 2015 2017 2019
Went to physical education classes on all 5 days
¶¶
Total 33.3 31.5 29.4 29.8 29.9 25.9 None None None
Female 31.9 27.2 24.0 25.5 25.3 22.8 Decreased during
2009–2019
None None
Male 34.6 35.5 34.9 33.8 34.7 28.9 None None None
White, non-Hispanic 30.6 33.0 27.1 25.4 27.2 24.3 None None None
Black, non-Hispanic 37.0 27.6 26.6 35.8 28.5 23.8 None None None
Hispanic 40.5 30.0 37.7 37.7 37.4 29.9 None None None
Played on ≥1 sports team***
Total 58.3 58.4 54.0 57.6 54.3 57.4 None None None
Female 52.3 52.6 48.5 53.0 49.3 54.6 None None None
Male 63.8 64.0 59.6 62.2 59.7 60.2 None None None
White, non-Hispanic 61.1 60.9 55.2 62.4 54.5 62.0 None None None
Black, non-Hispanic 57.3 57.0 55.2 57.6 59.1 56.1 None None None
Hispanic 53.2 54.1 51.2 48.5
52.2 51.6 None None None
* Based on trend analyses by using a logistic regression model controlling for sex, race/ethnicity, and grade (p<0.05).
†
Based on t-test analysis (p<0.05).
§
Adding up time spent in any kind of physical activity that increased their heart rate and made them breathe hard some of the time during the 7 days before the survey.
¶
Data not available. Question not asked in that year.
** Insufficient years of data to assess quadratic trends.
††
Such as push-ups, sit-ups, or weightlifting during the 7 days before the survey.
§§
Were physically active for ≥60 minutes/day on all 7 days and did exercises to strengthen or tone muscles on ≥3 of the 7 days before the survey.
¶¶
In an average week when the student was in school.
*** Counting any teams run by their school or community groups during the 12 months before the survey.
During the 2014–15 school year, the Smart Snacks in School
nutrition standards were implemented, which decreased
students’ access to SSBs at school. (More information about
the Smart Snacks in School nutrition standards is available at
https://www.gpo.gov/fdsys/pkg/FR-2013-06-28/pdf/2013-
15249.pdf.) Additional policy and educational approaches
(e.g., health education classes or communitywide campaigns)
might help further reduce SSB access in schools and other
settings and help adolescents choose healthier beverage options,
including plain water.
Physical Activity Behaviors
Overall, prevalence of health-promoting physical activity
behaviors was low in 2019 and either decreased or did not
change during the previous 10 years. Healthy People 2020
monitors four of the five physical activity behaviors included
in this study (https://www.healthypeople.gov/), and these
behaviors will continue to be monitored with Healthy People
2030. Healthy People 2020 objective PA-3 aims to increase the
proportion of adolescents who meet federal physical activity
guidelines for aerobic physical activity to ≥31.6% (PA-3.1),
muscle-strengthening activity to ≥61.2% (PA-3.2), and both
aerobic physical activity and muscle-strengthening activity to
≥24.1% (PA-3.3). The proportions of students meeting the
aerobic, muscle-strengthening, or both guidelines decreased
during 2011–2019, and 2019 data indicate that adolescents
continue to fall short of achieving these targets.
One of the Healthy People 2020 objectives (PA-5) is to increase
the proportion of adolescents who participate in daily school
physical education to ≥36.6%. Given no increase in this behavior
during 2009–2019 and that only 25.9% of high school students
attended daily physical education class during 2019, the target
for this objective is unlikely to be met in 2020. Students can
accumulate approximately 40% of their daily physical activity
through participation in physical education (17), demonstrating
that physical education at school is an effective strategy for helping
high school students meet the federal physical activity guidelines.
During 2015–2016, although the majority of U.S. states required
public high schools to provide physical education, few states
mandated a time requirement for high school students, and many
states permitted students to substitute other activities for their
physical education requirement. (More information about the
status of physical education in the United States is available at
https://www.shapeamerica.org/MemberPortal/SHAPE_Sign_I.
aspx?WebsiteKey=c03f2b51-3ee7-46fa-b587-de18213dcae5&Lo
ginRedirect=true&returnurl=%2fadvocacy%2fson%2f.)
The 2019 release of the National Youth Sports Strategy
highlighted youth sports participation for its physical activity,
psychosocial, and academic achievement benefits. (More
information about the National Youth Sports Strategy is
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 75
US Department of Health and Human Services/Centers for Disease Control and Prevention
available at https://health.gov/our-work/physical-activity/
national-youth-sports-strategy.) Despite these benefits, only
57.4% of high school students reported participating in
sports. The National Survey of Children’s Health also assesses
participation in youth sports, with similar estimates to YRBS
for youths aged 14–17 years (3).
Across all the physical activity behaviors, a higher percentage
of males than females met aerobic, muscle-strengthening, or
both guidelines, participated in daily physical education, and
played on ≥1 sports team. These differences might be caused
by gender stereotypes, self-efficacy, self-consciousness, or
social influences (18). When overcoming barriers to physical
activity, particularly for adolescent females, strategies that
span the Social-Ecological Model by addressing individual,
interpersonal, organizational, community, and societal
components might need to be considered.
Addressing Dietary and
Physical Activity Behaviors
Improving dietary and physical activity behaviors among
adolescents requires efforts across multiple settings. For
example, schools can implement policies and practices (e.g.,
local school wellness policies) (https://www.fns.usda.gov/tn/
local-school-wellness-policy) that support healthy eating and
physical activity, including ensuring the following: 1) that
foods and beverages sold during the school day meet Smart
Snacks in School nutrition standards, 2) that school meals are
appealing and include menu items that students enjoy, and
3) that students have access to free drinking water during the
school day (11). Schools can also help students meet the federal
physical activity guidelines by providing physical activity
opportunities before, during, and after the school day. This
can be achieved by developing, implementing, and evaluating
a comprehensive school physical activity program, which serves
as a national framework for physical education and physical
activity in schools. (More guidance on comprehensive school
physical activity programs is available at https://www.cdc.gov/
healthyschools/physicalactivity/pdf/13_242620-A_CSPAP_
SchoolPhysActivityPrograms_Final_508_12192013.pdf.)
Health education is another way that schools can help students
develop the knowledge and skills needed for making health-
enhancing decisions. These school efforts can be addressed and
coordinated through the Whole School, Whole Community,
Whole Child Model, which highlights the interconnectedness
of multiple health behaviors and outcomes and promotes
collaboration among diverse partners, including mental health
professionals, school leaders, school nurses, physical and health
educators, and parents for promoting health and well-being for
all students. (More information about the Whole School, Whole
Community, Whole Child approach is available at https://www.
cdc.gov/healthyschools/wscc/index.htm.)
Community members and parents can reinforce the
messages promoted within the school and can participate on
the school wellness or school health teams that are addressing
healthy eating, physical education, and physical activity. (More
information about parent engagement in school health is
available at https://www.cdc.gov/healthyyouth/protective/
pdf/parent_engagement_strategies.pdf.) In addition, parents
and community members can engage in physical activity
with adolescents, provide social supports for adolescents that
increase physical activity while decreasing sedentary behaviors,
and make choices that support healthy eating.
Community-based interventions that address healthy eating
and physical activity through policy and environmental
changes can improve dietary and physical activity behaviors
and weight-status outcomes among youths (19–21). These
kinds of community-based approaches often adopt multiple
strategies, including providing information (e.g., messaging
campaigns and healthy recipe demonstrations), providing
incentives, and improving access to opportunities for practicing
healthy behaviors through policy and systems changes. Having
multiple activities that target specific behaviors and using a
mix of behavioral change strategies appear to be important
for making health behavior changes (19). Community-
based interventions that also include the school setting are
more effective in influencing outcomes among youths than
interventions that occur only in the community (20).
Limitations
General limitations for the YRBS are available in the
overview report of this supplement (5). The findings in this
report are subject to at least one additional limitation. Certain
questions about dietary behaviors (e.g., fruit consumption)
ask about frequency rather than portion size; therefore, these
data cannot directly determine whether students are meeting
specific recommendations for age and sex (22).
Conclusion
Because of the limited progress in increasing the prevalence
of healthy dietary and physical activity behaviors among U.S.
high school students, multicomponent approaches, including
policy and environmental changes and opportunities for
adolescents to learn about and practice making healthy choices,
are needed to facilitate healthy dietary and physical activity
patterns. Schools, communities, and families can work together
in creating healthy environments where adolescents thrive.
Supplement
76 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Conicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. US Department of Health and Human Services; US Department of
Agriculture. 2015–2020 dietary guidelines for Americans. 8th ed.
Washington, DC: US Department of Health and Human Services; US
Department of Agriculture; 2015. http://health.gov/
dietaryguidelines/2015/guidelines
2. US Department of Health and Human Services. Physical activity
guidelines for Americans, 2nd ed. Washington, DC: US Department of
Health and Human Services; 2018. https://health.gov/sites/default/
files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
3. The Child and Adolescent Health Measurement Initiative. National
Survey of Children’s Health. Baltimore, MD: Johns Hopkins University,
Bloomberg School of Public Health; 2016. https://www.childhealthdata.
org/learn-about-the-nsch/NSCH
4. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—
United States, 2015. MMWR Surveill Summ 2016;65(No. SS-6).
5. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
6. Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral
sciences. 5th ed. Boston, MA: Houghton Mifflin; 2003.
7. Rasberry CN, Tiu GF, Kann L, et al. Health-related behaviors and
academic achievement among high school students—United States,
2015. MMWR Morb Mortal Wkly Rep 2017;66:921–27. http://dx.doi.
org/10.15585/mmwr.mm6635a1
8. Andes LJ, Cheng YJ, Rolka DB, Gregg EW, Imperatore G. Prevalence
of prediabetes among adolescents and young adults in the United States,
2005–2016. JAMA Pediatr 2019;174:e194498. https://doi.org/10.1001/
jamapediatrics.2019.4498
9. Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity,
and severe obesity among children and adolescents aged 2–19 years:
United States, 1963–1965 through 2015–2016. Hyattsville, MD: US
Department of Health and Human Services, CDC, National Center for
Health Statistics; 2018. https://www.cdc.gov/nchs/data/hestat/obesity_
child_15_16/obesity_child_15_16.htm
10. Moore LV, Hamner HC, Kim SA, Dalenius K. Common ways Americans
are incorporating fruits and vegetables into their diet: intake patterns
by meal, source and form, National Health and Nutrition Examination
Survey 2007–2010. Public Health Nutr 2016;19:2535–9. https://doi.
org/10.1017/S1368980016000586
11. CDC. School health guidelines to promote healthy eating and physical
activity. MMWR Recomm Rep 2011;60(No. RR-5).
12. Dietary Guidelines Advisory Committee. Scientific report of the 2015
Dietary Guidelines Advisory Committee: advisory report to the Secretary
of Health and Human Services and the Secretary of Agriculture.
Washington, DC: US Department of Agriculture, Agricultural Research
Service; 2015. https://health.gov/our-work/food-nutrition/2015-2020-
dietary-guidelines/advisory-report
13. Leung CW, DiMatteo SG, Gosliner WA, Ritchie LD. Sugar sweetened
beverage and water intake in relation to diet quality in U.S. children. Am J
Prev Med 2018;54:394–402. https://doi.org/10.1016/j.amepre.2017.11.005
14. Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage
consumption among U.S. youth, 2011–2014. NCHS Data Brief
2017;(271):1–8.
15. Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage
consumption among children and adults, 2003–2014. Obesity (Silver
Spring) 2018;26:432–41. https://doi.org/10.1002/oby.22056
16. Harris JL, Schwartz MB, LoDolce M, et al; Sugary Drink FACTS 2014.
Some progress but much room for improvement in marketing to youth.
Hartford, CT: University of Connecticut Rudd Center for Food Policy
and Obesity; 2014. http://sugarydrinkfacts.org/resources/
SugaryDrinkFACTS_Report.pdf
17. Bassett DR, Fitzhugh EC, Heath GW, et al. Estimated energy
expenditures for school-based policies and active living. Am J Prev Med
2013;44:108–13. https://doi.org/10.1016/j.amepre.2012.10.017
18. Spencer RA, Rehman L, Kirk SF. Understanding gender norms, nutrition,
and physical activity in adolescent girls: a scoping review. Int J Behav
Nutr Phys Act 2015;12:6. https://doi.org/10.1186/s12966-015-0166-8
19. Ritchie LD, Woodward-Lopez G, Au LE, et al; Healthy Communities
Study Team. Associations of community programs and policies with
children’s dietary intakes: the Healthy Communities Study. Pediatr Obes
2018;13(Suppl 1):14–26. https://doi.org/10.1111/ijpo.12440
20. Wang Y, Cai L, Wu Y, et al. What childhood obesity prevention
programmes work? A systematic review and meta-analysis. Obes Rev
2015;16:547–65. https://doi.org/10.1111/obr.12277
21. Pate RR, Frongillo EA, McIver KL, et al; Healthy Communities Study
Team. Associations between community programmes and policies and
children’s physical activity: the Healthy Communities Study. Pediatr
Obes 2018;13(Suppl 1):72–81. https://doi.org/10.1111/ijpo.12426
22. Eaton DK, Olsen EO, Brener ND, et al. A comparison of fruit and
vegetable intake estimates from three survey question sets to estimates
from 24-hour dietary recall interviews. J Acad Nutr Diet
2013;113:1165–74. https://doi.org/10.1016/j.jand.2013.05.013

Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 77
US Department of Health and Human Services/Centers for Disease Control and Prevention
Transportation Risk Behaviors Among High School Students —
Youth Risk Behavior Survey, United States, 2019
Merissa A. Yellman, MPH
1
; Leah Bryan, MPH
2
; Erin K. Sauber-Schatz, PhD
1
; Nancy Brener, PhD
2
1
Division of Injury Prevention, National Center for Injury Prevention and Control, CDC;
2
Division of Adolescent and School Health, National Center for
HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC
Abstract
Motor-vehicle crashes are a leading cause of death and nonfatal injury among U.S. adolescents, resulting in approximately 2,500
deaths and 300,000 nonfatal injuries each year. Risk for motor-vehicle crashes and resulting injuries and deaths varies, depending
on such behaviors as seat belt use or impaired or distracted driving. Improved understanding of adolescents’ transportation risk
behaviors can guide prevention efforts.
Therefore, data from the 2019 Youth Risk Behavior Survey were analyzed to determine
prevalence of transportation risk behaviors, including not always wearing a seat belt, riding with a driver who had been drinking
alcohol (riding with a drinking driver), driving after drinking alcohol, and texting or e-mailing while driving. Differences by
student characteristics (age, sex, race/ethnicity, academic grades in school, and sexual identity) were calculated. Multivariable
analyses controlling for student characteristics examined associations between risk behaviors. Approximately 43.1% of U.S. high
school students did not always wear a seat belt and 16.7% rode with a drinking driver during the 30 days before the survey.
Approximately 59.9% of students had driven a car during the 30 days before the survey. Among students who drove, 5.4% had
driven after drinking alcohol and 39.0% had texted or e-mailed while driving. Prevalence of not always wearing a seat belt was
higher among students who were younger, black, or had lower grades. Riding with a drinking driver was higher among Hispanic
students or students with lower grades. Driving after drinking alcohol was higher among students who were older, male, Hispanic,
or had lower grades. Texting while driving was higher among older students or white students. Few differences existed by sexual
identity. Multivariable analyses revealed that students engaging in one transportation risk behavior were more likely to engage in
other transportation risk behaviors. Traffic safety and public health professionals can use these findings to reduce transportation
risk behaviors by selecting, implementing, and contextualizing the most appropriate and effective strategies for specific populations
and for the environment.
Introduction
Motor-vehicle crashes are predictable and preventable.
However, in the United States, they remain the second leading
cause of death among adolescents and the fourth leading
cause of nonfatal injury. During 2018, approximately 2,500
adolescents (persons aged 12–19 years) died in motor-vehicle
crashes; of those deaths, >75% were occupants of passenger
vehicles (i.e., cars, pickup trucks, vans, or sport utility vehicles)
(1). Motor-vehicle crashes also resulted in approximately
297,000 nonfatal injuries among adolescents during 2018.
Moreover, fatal and nonfatal motor-vehicle–crash injuries
among adolescents resulted in approximately $12 billion in
medical and work-loss costs during 2018 (https://www.cdc.
gov/injury/wisqars).
Passenger-related transportation risk behaviors (e.g., nonuse
of seat belts or riding with a driver who had been drinking
Corresponding author: Merissa A. Yellman, MPH, Division of Injury
Prevention, National Center for Injury Prevention and Control.
Telephone: 404-498-5299; E-mail: [email protected].
alcohol) increase the risk for injury or death in a crash or
risk for a crash itself. Seat belt use among adolescents and
young adults is typically lower than among adults of other
age groups (1) (https://crashstats.nhtsa.dot.gov/Api/Public/
ViewPublication/812781). For instance, the National
Occupant Protection Use Survey Controlled Intersection
Study uses a probability-based sample of observational surveys
conducted on an annual basis to produce estimates of seat belt
use nationwide at a typical daylight moment. Results during
2016–2018 indicate that seat belt use among adolescents and
young adults aged 16–24 years was approximately 87% each
year, whereas seat belt use among adults aged ≥25 years was
90% or higher (https://crashstats.nhtsa.dot.gov/Api/Public/
ViewPublication/812781). Previous research also demonstrates
that high school students put themselves at risk by riding with
drivers who have been drinking alcohol (2).
Per mile driven, drivers aged 16–19 years have crash rates
approximately four times greater than those of drivers aged
≥20 years (1); a leading contributor is driver inexperience
(1,3). Because of this elevated crash risk, engagement in
driver-related transportation risk behaviors (e.g., driving after
Supplement
78 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
drinking alcohol or texting or e-mailing while driving) puts
adolescents at even higher risk. For example, drinking alcohol
negatively affects a person’s ability to drive safely regardless of
age. However, even at the same blood alcohol concentration
(BAC), drivers aged 16–20 years have a much higher risk for
being involved in a crash than older drivers (1,4). Similarly, the
negative effects of driver inexperience on driving performance
are worsened by cell phone–related driver distraction (5).
For this report, 2019 data from the Youth Risk Behavior
Survey (YRBS) were analyzed by student characteristics to
determine the prevalence of four transportation risk behaviors
among U.S. high school students. Associations between
engagement in multiple transportation risk behaviors also were
calculated. This study provides an update on which adolescent
groups have an elevated prevalence of engaging in transportation
risk behaviors and reveals the extent to which adolescents engage
in multiple transportation risk behaviors. The findings can help
traffic safety and public health professionals appropriately select,
tailor, and implement effective strategies to have a greater impact
on reducing risk behaviors, thereby preventing crashes, injuries,
and deaths among adolescents.
Methods
Data Source
This report includes data from CDC’s 2019 YRBS, a cross-
sectional, school-based survey conducted biennially since
1991. Each survey year, CDC collects data from a nationally
representative sample of public and private school students in
grades 9–12 in the 50 U.S. states and the District of Columbia.
Additional information about YRBS sampling, data collection,
response rates, and processing is available in the overview
report of this supplement (6). The prevalence estimates for all
unintentional injury questions for the overall study population
and by sex, race/ethnicity, grade, and sexual orientation are
available at https://nccd.cdc.gov/youthonline/App/Default.
aspx. The full YRBS questionnaire is available at https://
www.cdc.gov/healthyyouth/data/yrbs/pdf/2019/2019_YRBS-
National-HS-Questionnaire.pdf.
Measures
This study examined two passenger- and two driver-related
transportation risk behaviors among U.S. high school students.
The overall analytic sample was used for the passenger-related
risk behaviors, which included not always wearing a seat belt
when riding in a car driven by someone else and riding with a
driver who had been drinking alcohol (riding with a drinking
driver). Not always wearing a seat belt was assessed with the
question, “How often do you wear a seat belt when riding in
a car driven by someone else?” Response options included
“always,” “most of the time,” “sometimes,” “rarely,” or “never,”
with any response other than “always” being defined as not
always wearing a seat belt. Riding with a drinking driver was
assessed with the question, “During the past 30 days, how many
times did you ride in a car or other vehicle driven by someone
who had been drinking alcohol?” Responses were dichotomized
(0 times versus ≥1 time). Students who reported riding with a
drinking driver at least once during the previous 30 days were
classified as having engaged in the behavior.
Driver-related transportation risk behaviors included driving
when they had been drinking alcohol (driving after drinking
alcohol) and texting or e-mailing while driving (texting while
driving). Driving after drinking alcohol was assessed with
the question, “During the past 30 days, how many times did
you drive a car or other vehicle when you had been drinking
alcohol?” Texting while driving was assessed with the question,
“During the past 30 days, on how many days did you text or
e-mail while driving a car or other vehicle?” Students who
indicated they had not driven a car or other vehicle during the
past 30 days on each respective question were excluded from
the analysis for these questions. Responses among drivers were
categorized as 0 times or days versus ≥1 time or day.
An approximation of driving prevalence among students is
presented to provide context for the driver-related behaviors.
However, driving prevalence is not directly captured in the 2019
YRBS. For this approximation, students who chose a response
other than “I did not drive a car or other vehicle during the past
30 days” for both driver-related questions (driving after drinking
alcohol and texting while driving) were classified as drivers, and
students who indicated that they did not drive a car or other
vehicle during the past 30 days were classified as nondrivers.
Driver classification was independent of students’ responses to
the two questions about passenger-related transportation risk
behaviors because students who drove during the past 30 days
could also be passengers when they were not driving during the
same 30-day period.
All transportation risk behaviors were analyzed by self-
reported student characteristics, including age (14, 15,
16, 17, or ≥18 years), sex (male or female), race/ethnicity
(non-Hispanic white [white]; non-Hispanic black [black]; or
Hispanic or Latino of any race [Hispanic]), academic grades in
school (mostly As or Bs versus mostly Cs, Ds, or Fs), and sexual
identity (heterosexual; lesbian, gay, or bisexual; or not sure).
Although data from students in other or multiple racial/ethnic
groups were collected, the numbers were too small to produce
statistically stable estimates specific to other or multiple racial/
ethnic groups; therefore, these data are not presented as a
separate group in this report but were retained in the analytic
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 79
US Department of Health and Human Services/Centers for Disease Control and Prevention
sample. In addition, students aged <14 years (n = 87) were not
included in the analysis by age because the sample of students
in this age category was too small for meaningful analysis and
because these students cannot legally drive anywhere in the
United States (1).
Analysis
For this report, unadjusted weighted prevalence estimates and
corresponding 95% confidence intervals were calculated, and
posthoc t-tests were used to assess between-group differences.
Differences between prevalence estimates were considered
statistically significant if the t-test p value was <0.05. In the
results, only statistically significant differences in prevalence
estimates are reported.
Logistic regression models that controlled for age, sex,
race/ethnicity, academic grades in school, and sexual
identity produced adjusted prevalence ratios and examined
the associations between transportation risk behaviors. For
passenger-related transportation risk behaviors, students who
did not engage in the risk behaviors were designated as the
referent group. For driver-related transportation risk behaviors,
students who drove but did not engage in the risk behaviors
were designated as the referent group. Adjusted prevalence
ratios were considered statistically significant if their pairwise
comparison between groups (risk versus referent) was p <0.05.
Results
In 2019, a total of 43.1% of U.S. high school students had
not always worn a seat belt and 16.7% had ridden with a
drinking driver during the 30 days before the survey (Table 1).
Among the 59.9% of respondents who had driven a car or other
vehicle during the 30 days before the survey, 5.4% had driven
after drinking alcohol and 39.0% had texted while driving.
Both driving after drinking alcohol and texting while driving
usually increased with age. Specifically, prevalence of driving
after drinking alcohol was higher among students aged ≥18
years (8.9%) than among students aged 16 (4.0%), 15 (2.6%),
or 14 (2.7%) years (Table 1). In addition, prevalence was higher
among students aged 17 (5.9%) years than among those aged
15 (2.6%) years. For texting while driving, prevalence was
higher among students aged ≥18 (59.5%) years than among
students aged 17 (50.9%), 16 (30.5%), 15 (15.5%), or
14 (15.5%) years. Prevalence also was higher among students
aged 17 years than among those aged 16, 15, or 14 years and
higher among students aged 16 years than among those aged
15 or 14 years.
Conversely, not always wearing a seat belt usually decreased
with age. Prevalence of not always wearing a seat belt was lower
among students aged ≥18 years (39.4%) than among students
aged 16 (43.5%), 15 (46.9%), or 14 (45.7%) years. Similarly,
prevalence was lower among students aged 17 (38.9%) years
than among all younger students. For riding with a drinking
driver, no differences occurred by age.
Differences by race/ethnicity were detected for all four
transportation risk behaviors but did not demonstrate a
consistent pattern. Prevalence of not always wearing a seat
belt was higher among black students (61.7%) than among
Hispanic students (48.2%) or white students (36.6%). In
addition, prevalence among Hispanic students was higher than
among white students. For the alcohol-related transportation
risk behaviors, Hispanic students (20.8%) had a higher
prevalence of riding with a drinking driver than black students
(15.9%) or white students (15.1%), and Hispanic students
(6.6%) had a higher prevalence of driving after drinking alcohol
than black students (4.1%). In contrast, prevalence of texting
while driving was higher among white students (43.9%) than
among black students (29.5%) or Hispanic students (35.2%).
Students whose academic grades in school were mostly Cs, Ds,
or Fs had a higher prevalence of not always wearing a seat belt
(57.0%), riding with a drinking driver (20.1%), and driving
after drinking alcohol (7.4%) than students whose academic
grades in school were mostly As or Bs (38.8%, 15.3%, and
4.7%, respectively); however, prevalence of texting while
driving did not differ by this characteristic.
Few differences were identified when examining behaviors by
sex and by sexual identity. Only alcohol-related transportation
risk behaviors demonstrated differences. Among students who
had driven during the 30 days before the survey, male students
(7.0%) had a higher prevalence of driving after drinking alcohol
than female students (3.6%). By sexual identity, students who
were not sure of their sexual identity (21.9%) had a higher
prevalence of riding with a drinking driver than heterosexual
students (15.7%); however, the prevalence was not different
from lesbian, gay, or bisexual students (19.2%).
Multivariable analyses indicated that, for each transportation
risk behavior, students engaging in that behavior were more likely
to engage in each of the other transportation risk behaviors,
after controlling for age, sex, race/ethnicity, academic grades
in school, and sexual identity (Table 2). For passenger-related
transportation risk behaviors, students who did not always
wear a seat belt were 1.80 times as likely to have ridden with a
drinking driver, 2.73 times as likely to have driven after drinking
alcohol, and 1.29 times as likely to have texted while driving than
students who always wore a seat belt. Students who had ridden
with a drinking driver during the 30 days before the survey were
1.42 times as likely to not always wear a seat belt, 9.87 times as
likely to have driven after drinking alcohol, and 1.50 times as
likely to have texted while driving than students who had not
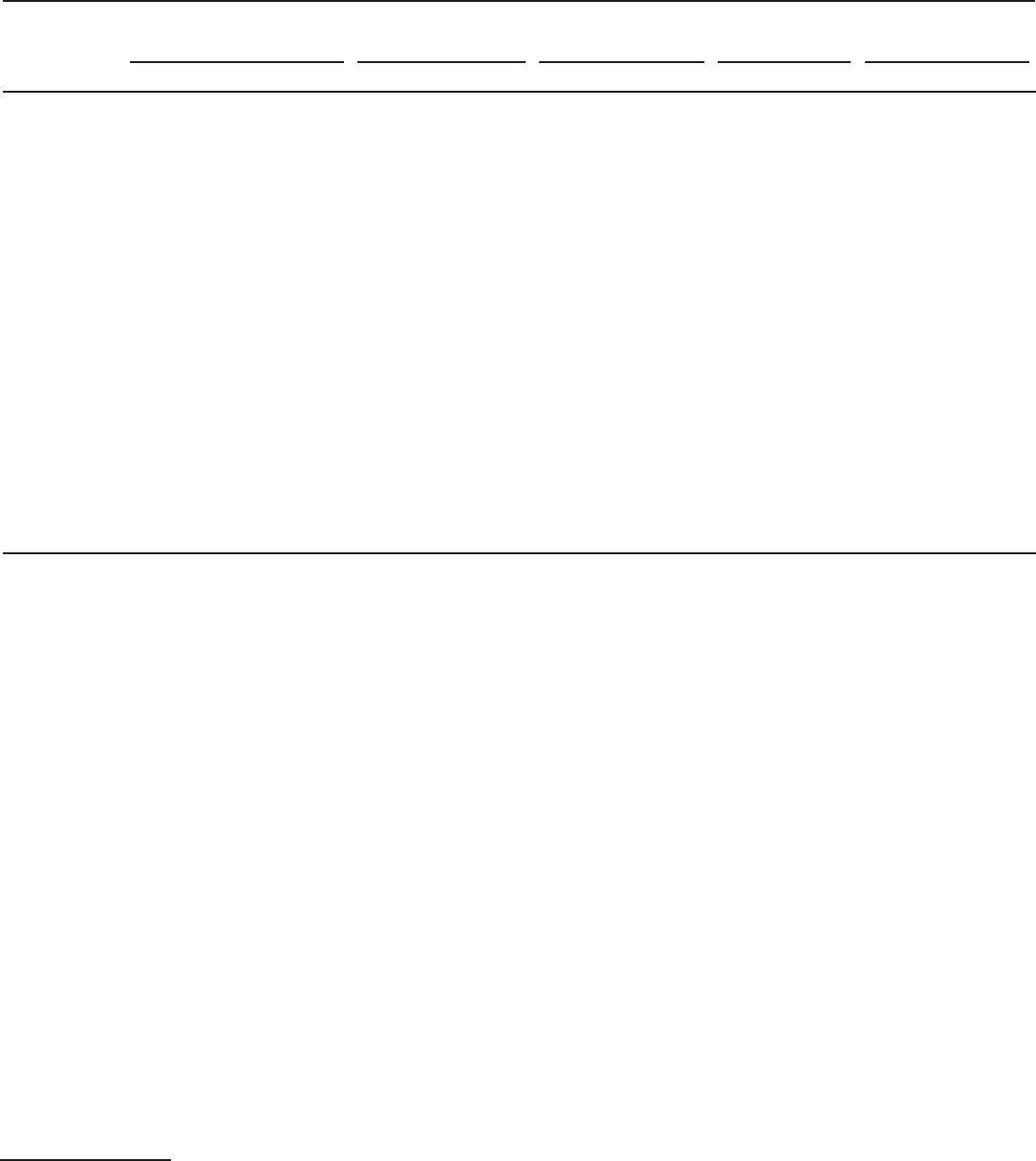
Supplement
80 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Unweighted number and unadjusted weighted prevalence estimates of high school students* who engaged in transportation risk
behaviors, by selected characteristics — Youth Risk Behavior Survey, United States, 2019
Characteristic
Total
Did not always wear a
seat belt
¶
Rode with a driver who
had been drinking
alcohol**
Drove when they had
been drinking
alcohol**
,††
Texted or e-mailed while
driving
††,§§
No.
†
% (95% CI) No.
§
% (95% CI) No.
§
% (95% CI) No.
§
% (95% CI) No.
§
% (95% CI)
Total 13,677 NA 4,852 43.1 (40.2–45.9) 2,214 16.7 (15.2–18.2) 423 5.4 (4.5–6.5) 2,784 39.0 (36.4–41.7)
Age (yrs)
¶¶
14 1,699 11.9 (10.9–13.0) 573 45.7 (40.9–50.5) 276 16.4 (13.9–19.1) 14 2.7 (0.9–7.5) 51 15.5 (11.2–21.0)
15 3,473 24.8 (23.5–26.0) 1,283 46.9 (42.7–51.1) 557 16.7 (14.6–19.1) 49 2.6 (1.7–3.9) 211 15.5 (11.8–20.2)
16 3,628 25.6 (24.5–26.7) 1,318 43.5 (39.5–47.6) 564 16.0 (13.8–18.5) 112 4.0 (2.8–5.6) 730 30.5 (25.8–35.5)
17 3,102 23.7 (22.5–24.8) 1,045 38.9 (35.6–42.4) 481 16.0 (13.8–18.5) 138 5.9 (4.3–7.9) 1,072 50.9 (46.5–55.3)
≥18 1,616 13.7 (12.6–14.9) 574 39.4 (36.6–42.4) 279 18.4 (15.4–21.7) 91 8.9 (6.4–12.4) 672 59.5 (54.9–63.9)
Sex
Male 6,641 50.6 (49.1–52.1) 2,369 43.3 (40.0–46.7) 1,015 15.6 (14.1–17.2) 257 7.0 (5.6–8.8) 1,434 39.6 (36.6–42.6)
Female 6,885 49.4 (47.9–50.9) 2,440 42.7 (39.7–45.7) 1,141 17.5 (15.6–19.5) 149 3.6 (2.8–4.6) 1,311 38.4 (35.5–41.4)
Race/Ethnicity***
White,
non-Hispanic
6,668 51.2 (46.4–56.0) 2,079 36.6 (33.8–39.6) 986 15.1 (13.5–16.8) 207 5.1 (3.9–6.5) 1,608 43.9 (40.4–47.5)
Black,
non-Hispanic
2,040 12.2 (10.2–14.6) 901 61.7 (56.3–66.8) 325 15.9 (13.3–18.7) 47 4.1 (2.6–6.4) 312 29.5 (24.3–35.2)
Hispanic 3,038 26.1 (21.8–30.9) 1,237 48.2 (45.0–51.4) 605 20.8 (18.7–23.1) 107 6.6 (5.2–8.5) 562 35.2 (30.8–39.8)
Academic grades
†††
Mostly As or Bs 9,785 75.1 (72.2–77.8) 3,152 38.8 (36.0–41.6) 1,449 15.3 (13.8–17.0) 248 4.7 (3.8–5.9) 2,070 40.4 (37.8–43.1)
Mostly Cs, Ds, or Fs 2,677 20.6 (18.3–23.2) 1,226 57.0 (53.4–60.5) 547 20.1 (17.7–22.8) 133 7.4 (5.7–9.6) 548 37.1 (32.2–42.4)
Sexual identity
Heterosexual 10,853 84.4 (83.4–85.3) 3,741 42.1 (39.1–45.2) 1,656 15.7 (14.1–17.4) 322 5.2 (4.2–6.4) 2,268 39.6 (36.6–42.6)
Lesbian, gay, or
bisexual
1,531 11.2 (10.4–12.0) 564 44.7 (39.4–50.1) 283 19.2 (16.0–22.9) 39 4.7 (2.4–9.0) 257 34.7 (28.4–41.7)
Not sure 591 4.5 (3.9–5.0) 208 43.3 (37.6–49.2) 125 21.9 (16.8–28.1) 24 9.5 (4.8–17.7) 93 31.7 (22.0–43.4)
Abbreviations: CI = confidence interval; NA = not applicable.
* Unadjusted weighted prevalence estimates and corresponding 95% CIs were calculated and are presented in the table. Posthoc t-tests were used to assess
between-group differences. Differences were considered statistically significant if the t-test p value was <0.05. Statistical significance is not indicated in the table
due to the large number of different pairwise comparisons; however, all significant differences are described in the results.
†
The unweighted number of students for each characteristic only includes students who selected a response on the survey question pertaining to that characteristic.
Students who did not select a response were not included in the analysis for that characteristic but were retained in the analytic sample for every question on
which they provided a response.
§
Students who selected any response on the survey question pertaining to a risk behavior were included in the analysis for that behavior; however, only the
unweighted numbers of students who engaged in that behavior are presented in the table. Students who did not select a response were not included in the
analysis for that behavior but were retained in the analytic sample for every question on which they provided a response.
¶
Most of the time, sometimes, rarely, or never wore a seat belt when riding in a car driven by someone else.
** ≥1 time during the 30 days before the survey.
††
Among students who had driven a car or other vehicle during the 30 days before the survey.
§§
On ≥1 day during the 30 days before the survey.
¶¶
The total column percentages for age do not add up to 100% because students aged <14 years are not presented because they cannot drive legally in any U.S. state.
*** The total column percentages for race/ethnicity do not add up to 100% because other non-Hispanic race categories are not presented.
†††
The total column percentages for academic grades do not add up to 100% because students who were not sure about their grades or who responded “none of
these grades” are not presented.
ridden with a drinking driver. For driver-related transportation
risk behaviors, students who had driven after drinking alcohol
at least once during the 30 days before the survey were 1.65
times as likely to not always wear a seat belt, 4.91 times as likely
to have ridden with a drinking driver, and 2.38 times as likely
to have texted while driving than students who had not driven
after drinking alcohol. Students who had texted while driving
on at least one day during the 30 days before the survey were
1.32 times as likely to not always wear a seat belt, 1.96 times as
likely to have ridden with a drinking driver, and 12.64* times
* Estimate should be interpreted with caution because the 95% confidence
interval is wide.
as likely to have driven after drinking alcohol than students who
had not texted while driving.
Discussion
Transportation risk behaviors varied by student characteristics,
with age, race/ethnicity, and academic grades demonstrating
the most differences. Increased engagement in driver-related
transportation risk behaviors as students become older has been
reported in other studies (7–9). This finding is not surprising
because adolescents engage in certain risky driver–related
behaviors less often when an adult supervisor is present in the
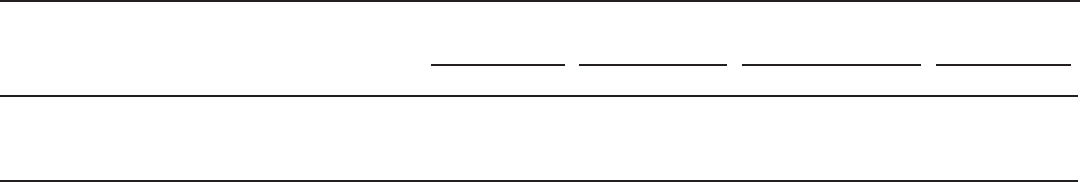
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 81
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Adjusted prevalence ratios* for high school students who engaged in multiple transportation risk behaviors — Youth Risk Behavior
Survey, United States, 2019
Transportation risk behavior
†
Did not always wear
a seat belt
§
Rode with a driver who
had been drinking
alcohol
¶
Drove when they had been
drinking alcohol
¶,
**
Texted or
e-mailed while
driving**
,††
aPR (95% CI) aPR (95% CI) aPR (95% CI) aPR (95% CI)
Did not always wear a seat belt
§
NA 1.80 (1.59–2.04) 2.73 (1.81–4.11) 1.29 (1.19–1.41)
Rode with a driver who had been drinking alcohol
¶
1.42 (1.32–1.53) NA 9.87 (7.14–13.64) 1.50 (1.37–1.65)
Drove when they had been drinking alcohol
¶,
** 1.65 (1.40–1.95) 4.91 (4.17–5.77) NA 2.38 (2.15–2.63)
Texted or e-mailed while driving**
,††
1.32 (1.20–1.44) 1.96 (1.69–2.27) 12.64 (8.45–18.91)
§§
NA
Abbreviations: aPR = adjusted prevalence ratio; CI = confidence interval; NA = not applicable.
* Multivariable logistic regression models that controlled for age, sex, race/ethnicity, academic grades, and sexual identity were used to produce the aPRs and
corresponding 95% CIs presented in the table. The aPRs were considered statistically significant if the p value of their pairwise comparison between groups (risk
versus referent) was <0.05. All aPRs in the table are significant.
†
Students who engaged in protective behaviors (i.e., always wearing a seat belt) or did not engage in risk behaviors (i.e., riding with a driver who had been drinking
alcohol, driving when they had been drinking alcohol among students who had driven, or texting or e-mailing while driving among students who had driven)
were the referent group.
§
Most of the time, sometimes, rarely, or never wore a seat belt when riding in a car driven by someone else.
¶
≥1 time during the 30 days before the survey.
** Among students who had driven a car or other vehicle during the 30 days before the survey.
††
On ≥1 day during the 30 days before the survey.
§§
Estimate should be interpreted with caution because the 95% CI is wide.
vehicle, as is required when adolescents possess a driver’s permit
(https://aaafoundation.org/distracted-driving-among-newly-
licensed-teen-drivers). As adolescents age, begin to drive without
adult supervision, and gain driving experience, driver-related
risk behaviors can be more common (9) (https://aaafoundation.
org/distracted-driving-among-newly-licensed-teen-drivers).
The positive association between age and texting while driving
illustrates the need to sustain attention to preventing the behavior
throughout adolescence (9). On the other hand, the prevalence
of not always wearing a seat belt decreased by age, possibly
indicating that although adolescents are typically more willing
to engage in risky transportation behaviors as they become older,
they still maintain a sense of self-preservation and risk perception
and therefore take precautions by wearing seat belts.
This study demonstrated that Hispanic students had a higher
prevalence of riding with a drinking driver and driving after
drinking alcohol than white students or black students. One
study described similar findings about drinking and driving
among Hispanics in the literature (10). Additional research
to explore which Hispanic populations might be at higher
risk found that U.S.-born Hispanic youths were more likely
to initiate drinking and driving behavior compared with first-
generation immigrant Hispanic youths, even after adjusting
for demographic variables (10). Additional research is needed
to determine whether different strategies to reduce alcohol-
impaired driving should be selected for or tailored to specific
Hispanic populations based on nativity status.
Other studies have reported that students with lower
academic grades were more likely to engage in other health-
related risk behaviors (e.g., risky sexual behaviors or substance
use) (11). The 2019 YRBS illustrates that this association
extends to engagement in transportation risk behaviors. Lower
academic achievement might be indicative of an underlying
tendency to make riskier decisions, or risky behaviors
themselves might lead to lower academic achievement. More
research into a potential causal association and the temporality
of that association is warranted. Of note, texting while driving
was the one transportation risk behavior that did not differ
by academic achievement. One potential explanation is that
although adolescents understand that texting while driving
is unsafe, the perceived benefits of texting while driving and
the motivations for engaging in the behavior often differ
from other transportation risk behaviors and can outweigh
the perceived risks for adolescents at the moment when they
choose to do it (8,9).
In this study, students engaging in any given transportation
risk behavior were more likely to engage in each of the other
measured transportation risk behaviors, even after controlling
for student characteristics. Associations with alcohol-
related behaviors were highest, particularly for driving after
drinking alcohol. Students who engaged in any of the other
transportation risk behaviors were approximately 3–13 times
as likely to have also engaged in driving after drinking alcohol
at least once during the 30 days before the survey. This might
signify a general willingness to engage in risky behaviors among
students who choose to drink and drive. This finding is also
concerning because of the potential additive effects of these
transportation risk behaviors. For example, adolescents who
drive after drinking alcohol, thus increasing their risk for a
crash, are also more likely to not always wear a seat belt, which
increases their risk for injury or death during a crash.
Because students engaged in multiple transportation
risk behaviors, interventions designed to address multiple
transportation risk behaviors might concurrently help reduce
Supplement
82 MMWR / August 21, 2020 / Vol. 69 / No. 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
those behaviors. Existing infrastructure and resources for
comprehensive school and community programs designed
to address different health behaviors could be leveraged to
expand the benefits of these programs to transportation risk
behaviors. For example, programs that already rely on family
engagement could incorporate safe driving, because parental
involvement is crucial for teaching adolescents how to drive
by providing varied practice opportunities, promulgating
safe driver behaviors, and instilling the importance of
avoiding transportation risk behaviors (https://www.cdc.
gov/parentsarethekey/parents/index.html). Programs that
provide counseling and social services for adolescents could
incorporate brief alcohol interventions, which are promising
for reducing drinking and driving among adolescents at high
risk for engaging in the behavior (12,13).
Engagement in all of these transportation risk behaviors
across the United States remains high. Considering that
adolescent drivers (16–19 years of age) have the highest crash
rates (1), the fact that only six of 10 adolescents in this study
always wore seat belts is concerning. Measures that are effective
for increasing seat belt use, such as primary enforcement seat
belt laws that allow police to ticket drivers or passengers for
being unrestrained even in the absence of other violations (13),
also can be beneficial for preventing crashes or crash injuries
involving other contributing factors. For example, evidence
indicates that primary enforcement seat belt laws are effective
for reducing fatal alcohol-related crashes among underage
drivers aged 15–20 years (14).
Although this study did not find many differences in riding
with a drinking driver by student characteristics, approximately
one of every five students engaged in the behavior
. Riding with
a drinking driver is intrinsically unsafe and also is associated
with adolescent drinking and driving
(15). Longitudinal
research has revealed that adolescent passengers who are
exposed to drinking and driving at a young age are more likely
to engage in drinking and driving themselves as they become
older and begin to drive (16). Additional research about
the drinking drivers with whom adolescents ride and their
relationships with the drinking drivers (e.g., parents, other
family members, or peers) might be useful for designing and
implementing targeted interventions.
In every U.S. state, minimum legal drinking age (MLDA)
laws stipulate that drinking alcohol is illegal for anyone aged
<21 years, as is driving after drinking any amount of alcohol
(zero tolerance laws) (1,13). Despite these laws, approximately
one fifth of drivers aged 16–20 years killed in crashes during
2018 had BACs of ≥0.08% (1). This study found that in 2019,
a total of 5.4% of students who drove did so after drinking
alcohol at least once in the previous 30 days. Driving after
drinking alcohol is risky and unacceptable at any age; however,
the risk is even higher among adolescent drivers aged 16–20
years, even at BACs below the legal limit for adults (4). Zero
tolerance laws (7,13,14), graduated driver licensing systems
(7), and MLDA laws (7,13,14) are effective in helping reduce
drinking and driving and alcohol-related crashes and injuries
among adolescents, and they should continue to remain
universally implemented. Other general population deterrent
approaches that are effective for preventing alcohol-impaired
driving overall also can be beneficial for specifically preventing
adolescent drinking and driving. For example, publicized
sobriety checkpoints are highly effective for reducing drinking
and driving overall (13), and evidence indicates that they can
reduce alcohol-impaired driving (17) and alcohol-related
crashes among underage drivers (14).
Consistent with two recent studies, this analysis determined
that texting while driving among adolescents remains high,
increases with age, and is more common among white students
than students of other races/ethnicities (8,9). Similar to the
other studies, this analysis also determined that adolescents
who engage in texting while driving are more likely to engage
in other transportation risk behaviors (8,9). Awareness
campaigns, education, and changes in policy related to texting
while driving have had mixed effectiveness (9,13). Because of
this, such technologic interventions as in-vehicle cell phone
blocking technologies can serve as potential solutions; however,
the effectiveness and acceptability of such solutions require
more research (9,13).
Lack of parental monitoring and supervision is a common
underlying contributor to many health risk behaviors, and
parental involvement can be especially important for reducing
transportation risk behaviors. For example, one study found
that adolescents with supportive parents who monitor their
behavior were less likely to engage in multiple passenger- and
driver-related transportation risk behaviors, including seat belt
nonuse, cell phone use while driving, and drinking and driving,
than adolescents with uninvolved parents (18). Parents/guardians
also can play a vital role in teaching adolescents to drive by
helping ensure they gain valuable driving experience and by
setting rules and expectations for adolescent drivers, including
rules and expectations for not engaging in transportation
risk behaviors. Parent-teen driving agreements (https://www.
cdc.gov/parentsarethekey/parents/index.html) can formalize
those expectations and demonstrate a commitment between
parents and adolescents to adhere to safe driving practices while
adolescents gain new driving privileges over time.
Supplement
MMWR / August 21, 2020 / Vol. 69 / No. 1 83
US Department of Health and Human Services/Centers for Disease Control and Prevention
Limitations
General limitations for the YRBS are available in the overview
report of this supplement (6). The findings in this report are
subject to at least two additional limitations. First, YRBS does
not quantify driving or riding exposure in general or during the
30 days before the survey. How many trips each student takes as
a driver or as a passenger and the amount of time each student
spends on the road are unknown. High school students who
take more frequent trips or drive for longer times or distances
might have more opportunity to engage in transportation risk
behaviors because of a higher exposure that is not captured by the
survey. Second, for riding with a driver who had been drinking
alcohol, the relationship between the student and the drinking
driver (e.g., parent/guardian, other family member, a peer, or
someone else) is unknown. The nature of this relationship
might have implications for designing potential strategies and
prevention messages for empowering adolescents so that they
can intervene (15).
Conclusion
Motor-vehicle–crash injuries remain a leading cause of
death among adolescents. Despite this, passenger- and driver-
related transportation risk behaviors that increase the risk for
crashes, injuries, and deaths remain too common. Reducing
transportation risk behaviors among adolescents by using proven
strategies, especially those that can target multiple transportation
risk behaviors, can help prevent crashes, reduce injuries, and
save lives. Because driver-related transportation risk behaviors
increased with age, continued emphasis on implementation
of effective strategies for preventing these behaviors with high
school juniors and seniors should be considered.
Conicts of Interest
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. No potential conflicts of interest
were disclosed.
References
1. Insurance Institute for Highway Safety. Teenagers. Arlington, VA:
Insurance Institute for Highway Safety, Highway Loss Data Institute;
2019. https://www.iihs.org/topics/teenagers
2. O’Malley PM, Johnston LD. Driving after drug or alcohol use by US
high school seniors, 2001-2011. Am J Public Health 2013;103:2027–34.
https://doi.org/10.2105/AJPH.2013.301246
3. McCartt AT, Shabanova VI, Leaf WA. Driving experience, crashes and
traffic citations of teenage beginning drivers. Accid Anal Prev
2003;35:311–20. https://doi.org/10.1016/S0001-4575(02)00006-4
4. Voas RB, Torres P, Romano E, Lacey JH. Alcohol-related risk of driver
fatalities: an update using 2007 data. J Stud Alcohol Drugs
2012;73:341–50. https://doi.org/10.15288/jsad.2012.73.341
5. Llerena LE, Aronow KV, Macleod J, et al. An evidence-based review:
distracted driver. J Trauma Acute Care Surg 2015;78:147–52. https://
doi.org/10.1097/TA.0000000000000487
6. Underwood JM, Brener N, Thornton J, et al. Overview and methods
for the Youth Risk Behavior Surveillance System—United States, 2019.
In: Youth Risk Behavior Surveillance—United States, 2019. MMWR
Suppl 2020;69(No. Suppl 1).
7. CDC. Vital signs: drinking and driving among high school students
aged ≥16 years—United States, 1991-2011. MMWR Morb Mortal
Wkly Rep 2012;61:796–800.
8. Olsen EO, Shults RA, Eaton DK. Texting while driving and other risky
motor vehicle behaviors among US high school students. Pediatrics
2013;131:e1708–15. https://doi.org/10.1542/peds.2012-3462
9. Li L, Shults RA, Andridge RR, Yellman MA, Xiang H, Zhu M. Texting/
emailing while driving among high school students in 35 states, United
States, 2015. J Adolesc Health 2018;63:701–8. https://doi.org/10.1016/j.
jadohealth.2018.06.010
10. Maldonado-Molina MM, Reingle JM, Jennings WG, Prado G. Drinking
and driving among immigrant and US-born Hispanic young adults:
results from a longitudinal and nationally representative study. Addict
Behav 2011;36:381–8. https://doi.org/10.1016/j.addbeh.2010.12.017
11. Rasberry CN, Tiu GF, Kann L, et al. Health-related behaviors and
academic achievement among high school students—United States,
2015. MMWR Morb Mortal Wkly Rep 2017;66:921–7. https://doi.
org/10.15585/mmwr.mm6635a1
12. Steinka-Fry KT, Tanner-Smith EE, Hennessy EA. Effects of brief alcohol
interventions on drinking and driving among youth: a systematic review
and meta-analysis. J Addict Prev 2015;3:1–22.
13. Richard CM, Magee K, Bacon-Abdelmoteleb P, Brown JL. Countermeasures
that work: a highway safety countermeasure guide for state highway safety
offices. 9th ed. Washington, DC: National Highway Traffic Safety
Administration (NHTSA); 2018. Report no. DOT HS 812 478. https://
www.nhtsa.gov/sites/nhtsa.dot.gov/files/documents/812478_
countermeasures-that-work-a-highway-safety-countermeasures-guide-.pdf
14. Romano E, Scherer M, Fell J, Taylor E. A comprehensive examination of
U.S. laws enacted to reduce alcohol-related crashes among underage drivers.
J Safety Res 2015;55:213–21. https://doi.org/10.1016/j.jsr.2015.08.001
15. Leadbeater BJ, Foran K, Grove-White A. How much can you drink before
driving? The influence of riding with impaired adults and peers on the
driving behaviors of urban and rural youth. Addiction 2008;103:629–37.
https://doi.org/10.1111/j.1360-0443.2008.02139.x
16. Li K, Simons-Morton BG, Vaca FE, Hingson R. Association between
riding with an impaired driver and driving while impaired. Pediatrics
2014;133:620–6. https://doi.org/10.1542/peds.2013-2786
17. Nelson TF, Xuan Z, Babor TF, et al. Efficacy and the strength of evidence
of U.S. alcohol control policies. Am J Prev Med 2013;45:19–28. https://
doi.org/10.1016/j.amepre.2013.03.008
18. Ginsburg KR, Durbin DR, García-España JF, Kalicka EA, Winston FK.
Associations between parenting styles and teen driving, safety-related
behaviors and attitudes. Pediatrics 2009;124:1040–51. https://doi.
org/10.1542/peds.2008-3037

ISSN: 2380-8950 (Print)
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free
of charge in electronic format. To receive an electronic copy each week, visit MMWR at https://www.cdc.gov/mmwr/index.html.
Readers who have difficulty accessing this PDF file may access the HTML file at https://www.cdc.gov/mmwr/ind2020_su.html. Address all inquiries about
the MMWR Series, including material to be considered for publication, to Executive Editor, MMWR Series, Mailstop E-90, CDC, 1600 Clifton Rd., N.E.,
Atlanta, GA 30329-4027 or to [email protected]v.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations
or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of these sites. URL addresses
listed in MMWR were current as of the date of publication.
