®
AOTA
THE AMERICAN OCCUPATIONAL THERAPY ASSOCIATION
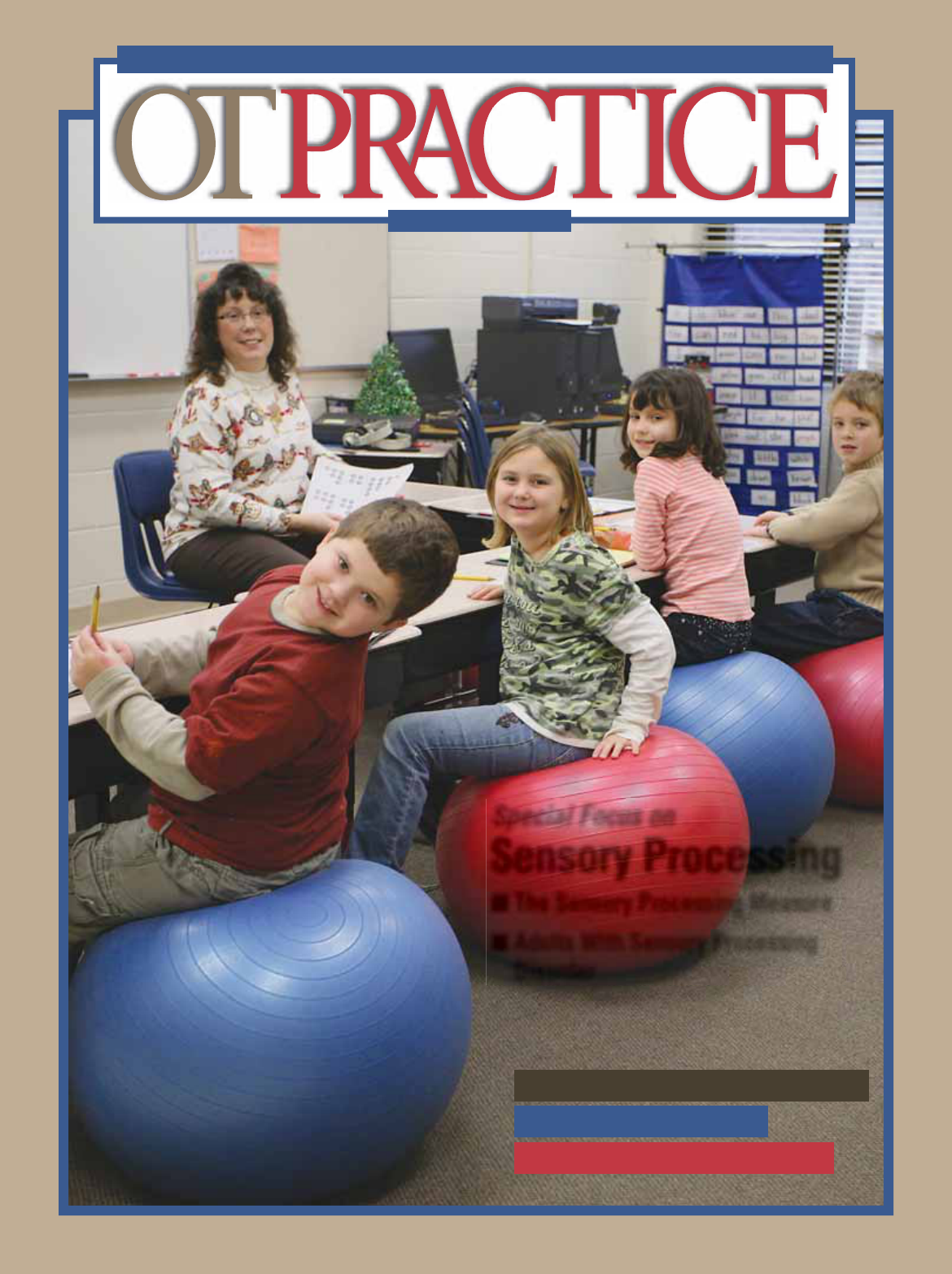
Special Focus on
Sensory Processing
■ The Sensory Processing Measure
■ Adults With Sensory Processing
Disorder
JUNE 15, 2009
PLUS
Proposed Medicare Regulations
Handwriting Training
The Dance of Independence
1
DEPARTMENTS
News 3
Capital Briefi ng 6
Medicare Proposed Regulations
In the Clinic 8
Handwriting Training
for the Nondominant Hand
Continuing Competence 20
Volunteer Service as
Professional Development
Occupation in Action 21
A Strong Foundation
for Independent Living
Calendar 23
Continuing Education Opportunities
Employment Opportunities 27
Living Life To Its Fullest 32
OT Refl ections From the Heart
The Dance of Independence
AOTA • THE AMERICAN OCCUPATIONAL THERAPY ASSOCIATION
VOLUME 14 • ISSUE 10 • JUNE 15, 2009
Discuss OT Practice articles at www.OTConnections.org in the OT Practice Discussions Forum.
Send e-mails regarding editorial content to [email protected].
Visit our Web site at www.aota.org for OT Practice online,
contributor guidelines, and additional news and information.
OT PRACTICE • JUNE 15, 2009
OT Practice serves as a comprehensive source for practical information to help occupational therapists and occupational therapy
assistants to succeed professionally. OT Practice encourages a dialogue among members on professional concerns and views.
The opinions and positions expressed by contributors are their own and not necessarily those of OT Practice’s editors or AOTA.
Advertising is accepted on the basis of conformity with AOTA standards. AOTA is not responsible for statements made by advertisers,
nor does acceptance of advertising imply endorsement, offi cial attitude, or position of OT Practice’s editors, Advisory Board, or
The American Occupational Therapy Association, Inc. For inquiries, contact the advertising department at 800-877-1383, ext. 2715.
Changes of address need to be reported to AOTA at least 6 weeks in advance. Members and subscribers should notify the Membership
department. Copies not delivered because of address changes will not be replaced. Replacements for copies that were damaged in
the mail must be requested within 2 months of the date of issue for domestic subscribers and within 4 months of the date of issue for
foreign subscribers. Send notice of address change to AOTA, PO Box 31220, Bethesda, MD 20824-1220, e-mail to [email protected],
or make the change at our Web site at www.aota.org.
Back issues are available prepaid from AOTA’s Membership department for $16 each for AOTA members and $24.75 each for
nonmembers (U.S. and Canada) while supplies last.
Members who prefer to access this publication electronically may view it as a PDF at www.aota.org. To request each issue in Word
format (without graphics or other design elements), send an e-mail to [email protected].
FEATURES
Using the 9
Sensory Processing
Measure (SPM) in
Multiple Practice Areas
Diana A. Henry, Cheryl E. Ecker, Tara
J. Glennon, & David Herzberg show how
the SPM is used in children’s school and
home environments to help identify the
most appropriate interventions.
Occupational Therapy 15
Intervention for
Adults
With Sensory Processing
Disorder
Teresa A. May-Benson describes a
personalized, intensive protocol
that is tailored to adults and
designed for quick results.
COVER PHOTOGRAPH COURTESY OF DIANA HENRY
Chief Operating Offi cer: Christopher Bluhm
Director of Marketing & Member Communications:
Beth Ledford
Editor: Laura Collins
Senior Editor: Molly Strzelecki
CE Articles Editor: Sarah D. Hertfelder
Art Director: Carol Strauch
Production Manager: Sarah Ely
Director of Sales & Corporate Relations: Jeffrey A. Casper
Account Executive: Tracy Hammond
Advertising Assistant: Clark Collins
Ad inquiries: 800-877-1383, ext. 2715,
or e-mail [email protected]
OT Practice External Advisory Board
Asha Asher, Chairperson, Developmental
Disabilities Special Interest Section
Salvador Bondoc, Chairperson, Physical
Disabilities Special Interest Section
Barbara E. Chandler, Chairperson, Early
Intervention & School Special Interest Section
Sharon J. Elliott, Chairperson, Gerontology
Special Interest Section
Jyothi Gupta, Chairperson, Education Special
Interest Section
Kimberly Hartmann, Chairperson, Technology
Special Interest Section
Christine Kroll, Chairperson, Administration
& Management Special Interest Section
Lisa Mahaffey, Chairperson, Mental Health
Special Interest Section
Kathy Maltchev, Chairperson, Work and
Industry Special Interest Section
Pamela Toto, Chairperson, Special Interest
Sections Council
Karen Vance, Chairperson, Home &
Community Health Special Interest Section
Renee Watling, Chairperson,
Sensory Integration Special Interest Section
AOTA President: Penelope Moyers Cleveland
Executive Director: Frederick P. Somers
Chief Public Affairs Offi cer: Christina Metzler
Chief Financial Offi cer: Chuck Partridge
Chief Professional Affairs Offi cer: Maureen Peterson
© 2009 by The American Occupational Therapy Association, Inc.
OT Practice (ISSN 1084-4902) is published 22 times a year,
semimonthly except only once in January and December by
the American Occupational Therapy Association, Inc., 4720
Montgomery Lane, Bethesda, MD 20814-3425; 301-652-2682.
Periodical postage is paid at Bethesda, MD, and at additional
mailing offi ces.
U.S. Postmaster: Send address changes to OT Practice, AOTA,
PO Box 31220, Bethesda, MD 20824-1220.
Canadian Publications Mail Agreement No. 41071009. Return
Undeliverable Canadian Addresses to PO Box 503, RPO West
Beaver Creek, Richmond Hill ON L4B 4R6.
Mission statement: The American Occupational Therapy Asso-
ciation advances the quality, availability, use, and support of
occupational therapy through standard-setting, advocacy, edu-
cation, and research on behalf of its members and the public.
Annual membership dues are $225 for OTs, $131 for OTAs, and
$75 for Student-Plus members, of which $14 is allocated to the
subscription to this publication. Standard Student membership
dues are $53 and do not include OT Practice. Subscriptions in
the U.S. are $142.50 for individuals and $216.50 for institutions.
Subscriptions in Canada are $205.25 for individuals and $262.50
for institutions. Subscriptions outside the U.S. and Canada
are $310 for individuals and $365 for institutions. Allow 4 to 6
weeks for delivery of the fi rst issue.
Copyright of OT Practice is held by The American Occupational
Therapy Association, Inc. Written permission must be obtained
from AOTA to reproduce or photocopy material appearing in
OT Practice. A fee of $15 per page, or per table or illustration,
including photographs, will be charged and must be paid before
written permission is granted. Direct requests to Permissions,
Publications Department, AOTA, or through the Publications
area of our Web site. Allow 2 weeks for a response.

9
OT PRACTICE • JUNE 15, 2009
PHOTOS COURTESY OF THE AUTHORS
S
ince its publication in
2007, the Sensory Pro-
cessing Measure (SPM)
1
has received positive
reviews for applicabil-
ity in both clinical and
school-based practice, in
part because it can be scored quickly
and easily. This article illustrates
usage through case examples, as well
as discusses important psychometric
properties of the tool.
FOCUS ON COLLABORATION
The SPM is unique in that it was stan-
dardized on the same group of children
in their home and school environ-
ments. Rating forms for both parents
and school staff affords everyone a
chance to document their perspectives
of the child within their respective
environments. As one teacher stated,
“The SPM provides a ‘bird’s eye view’
of the student’s sensory processing
performance in various environments,
including those where I do not see the
student.” This format helps clinicians
realize that the adults in each of the
child’s environments have important
perspectives that must be considered.
In addition to the home and main
classroom, the perspectives of staff
members in that student’s art, music,
and physical education (PE) classes;
during recess; on the bus; and in the
cafeteria can be quickly taken into
consideration via six SPM environment
(reproducible) forms. Each contains
only 15 questions, except the Bus form,
which contains 10. The following case
examples illustrate the importance of
obtaining information from others in
order to gain insight into the student’s
daily sensory processing challenges,
as well as to collaborate for developing
strategies.
SCHOOL-BASED SERVICES
Case Example: Cafeteria Intervention
Before the fi ndings of the SPM had
been implemented, 8-year-old Bob, a
DIANA A. HENRY
CHERYL E. ECKER
TARA J. GLENNON
DAVID HERZBERG
Sensory Processing
Measure
(
SPM
)
The SPM is a quick, easy-to-use, reliable measure of
children’s sensory processing and praxis at home and
in school environments.
Using the
in Multiple
Practice Areas
Figure 2. Chair balls are used for students
with vestibular-seeking behaviors and
postural control issues.

10
JUNE 15, 2009 • WWW.AOTA.ORG
student with attention defi cit hyperac-
tivity disorder, was being reprimanded
daily in the cafeteria, unbeknownst to
other school personnel or his parents.
Bob was self-initiating activities he had
learned in occupational therapy and
speech therapy (e.g., sucking apple-
sauce through a tiny straw), but the
cafeteria worker had not been privy to
Bob’s oral-motor and sensory-seeking
needs. Taking seriously her responsi-
bilities to keep the cafeteria clean and
orderly, she was concerned that Bob’s
oral motor activities often caused a
mess and did not “appear” to be appro-
priate behavior in the cafeteria.
Although the team discussed Bob’s
activities as appropriate sensory seek-
ing/proprioceptive input, the cafete-
ria worker who completed the SPM
Cafeteria form
2
helped the team realize
that Bob was not demonstrating appro-
priate behavior based on what she
expected in the cafeteria. At the same
time, completing the SPM afforded the
worker the opportunity to understand
why Bob was demonstrating what she
considered inappropriate behavior.
She became aware of Bob’s sensory
processing challenges and their impact
on his occupational performance
throughout the school day. This mutual
understanding opened the door for
implementing a successful intervention
plan within all environments, includ-
ing the cafeteria. Progress measured
via the SPM posttest 5 months later
revealed that the strategies, listed
below, were working.
■ Bob learned to appropriately
explain his sensory needs.
■ A sport bottle for sucking was made
available to Bob throughout the day.
■ Bob used an oral motor transition
tool on the way to lunch.
■ Bob drank thick yogurt through
a straw, using a cup with a lid to
obtain oral motor input while keep-
ing the contents from spilling over.
■ Bob took responsibility for cleaning
up after himself.
Case Example:
Response to Intervention (RtI)
Student Study Teams (SST), often com-
posed of classroom and special educa-
tion teachers, a school administrator,
and hopefully an OT, meet to develop
early intervention services when there
is a problem behavior in a classroom.
Under RtI, an SST used the SPM to
identify potential sensory barriers to a
class of children maintaining attention,
resulting in the team suggesting more
movement opportunities throughout
day. In fact, many teachers report
that breaks in general are essential for
alertness and that increased move-
ment experiences positively infl uence
cognition. The staff in this school
implemented movement breaks (e.g.,
shakes and wiggles) (see Figure 1) as a
Tier 1 intervention (general education
strategies for all students) and provided
chair balls for desk work to students
who demonstrated vestibular seeking
behaviors and postural control issues
(a Tier II intervention) (see Figure 2 on
p. 9). This strategy was supported by
research on chair ball use in the class-
room, which reported improved in-seat
behavior and legible word productivity.
3
Case Example: Gym Class
The SPM (including the PE form)
was used for Lucas, a student with
autism, and revealed proprioceptive
concerns, vestibular challenges, poor
bilateral integration, diffi culty with
praxis, and decreased social participa-
tion. Although Lucas was successfully
included in his 4th grade classroom, he
was unable to participate in many PE
activities, including volleyball. He was
unable to maintain focus on the ball, or
to motor plan the timing and sequenc-
ing of his movements to volley back
and forth. Lucas’s school occupational
therapist, PE teacher, and clinic-based
occupational therapist (at his mother’s
suggestion, as Lucas had received
Ayres sensory integration intervention
during the summer) collaborated and
created a plan to have Lucas be a PE
helper as part of his special education
support plan (Tier III intervention).
The ability of the SPM to promote
collaboration between school- and
clinic-based therapists yielded positive
results for Lucas. For example, during
volleyball, he indicated which team
was serving by pushing a milk crate
with weighted materials from one side
of the net to the other (see Figure 3
on p. 11). Several sensory and praxis
goals were addressed in this way, and
his self-esteem increased as he assisted
his teacher in this functional task. This
strategy served as a mechanism for
Lucas to stay engaged in the game,
interact with the other students, and
obtain the sensory input he needed.
CLINIC-BASED SERVICES
Regardless of setting, the SPM can
facilitate a team approach, help guide
discussion, and provide a quantifi able
picture of the child’s sensory process-
ing, with statistical assurance that the
SPM is measuring sensory process-
ing. The SPM has been instrumental
in helping many families and medical
teams to reframe children’s behaviors.
Many parents have described a sense
Figure 1. Students engage in shakes and wiggles as part of a movement break.

11
OT PRACTICE • JUNE 15, 2009
of relief and empowerment when their
descriptions of their children were
quantifi ed to demonstrate sensory pro-
cessing problems. The following section
highlights some of SPM’s clinical uses.
Case Example: Quantifying Dysfunction
for Professionals
Jared, a 6 year old, avoided using any
public bathrooms because of the sound
of the toilet, had bitter fi ghts over teeth
brushing, and had a prolonged morning
routine because of discomfort with his
clothing. His pediatrician responded
to these concerns by prescribing
anti-anxiety medication and providing
instructions to Jared’s parents on set-
ting limits. When Jared’s parents later
found an occupational therapist trained
in sensory integration and completed
the SPM Home form, they fi nally had
quantifi able information that Jared
had “some problems” for hearing and
“defi nite dysfunction” for touch. In
communications with the pediatrician,
the occupational therapist was able to
reframe Jared’s functional problems
by identifying the underlying sensory
processing problems, thus demonstrat-
ing that the behavior issues were not
caused by “poor parenting.” With the
support of the pediatrician Jared began
participating in occupational therapy,
with positive functional outcomes in
the initially identifi ed areas of concern.
Case Example: Reframing Symptoms of
Sensory Processing Disorder
At school, 8-year-old Thomas was
having trouble with social relationships,
following directions, and sitting still.
Because he performed academically at
grade level and his school psychologist
Figure 3. Lucas pushes a milk crate with weighted materials to indicate which team is serving,
which allowed him to participate while addressing his sensory needs.
THE MOST THOROUGH AND PRACTICAL SENSORY INTEGRATION TRAINING IN THE WORLD
USC/WPS Comprehensive Program
in Sensory Integration
This four-course series covers sensory integration theory,
assessment, interpretation, and intervention.
• Learn how sensory systems affect everyday functioning
• Learn how to administer and interpret the
Sensory Integration and Praxis Tests (SIPT)
• Learn how to design and implement effective intervention
• Attain your USC/WPS Certificate in Sensory Integration
For a complete schedule or to register:
Visit wpspublish.com
Call 800-648-8857
Upcoming Courses in:
Cincinnati, OH
Santa Rosa, CA
Miami, FL
Dallas, TX
Western Psychological Services
P-4146

12
JUNE 15, 2009 • WWW.AOTA.ORG
and teacher felt he just had behavior
problems, he did not qualify for occu-
pational therapy services in school. At
the suggestion of a friend, Thomas’s
mother contacted an occupational
therapist in a clinic setting. As part
of the assessment, both the Home
and Main Classroom SPM forms were
completed. The results confi rmed that
Thomas’s challenges at school were
related to sensory processing. When
Thomas’s mother completed the SPM,
she realized that Thomas had extreme
responses to sensory input in his home
and community that she had never
noticed before, because she had been
unknowingly accommodating him. For
example, Thomas was bothered by the
feel of his sheets and clothing; seemed
to not get dizzy; leaned on other peo-
ple; and tended to do everything with
too much force, including petting his
neighbor’s dog and hugging his mother
and sister. The SPM results enabled the
clinic-based therapist to identify goals
that would be medically relevant and
reimbursed by the insurance carrier
(i.e., in 6 months, Thomas will dem-
onstrate increased body awareness
when hugging his mother and sibling
as demonstrated by appropriate force,
lack of injury, and no expression of pain
or discomfort from either recipient,
90% of the time). In addition, the SPM
enabled the clinic-based occupational
therapist to provide suggestions for
sensory-based activities that could be
infused into Thomas’s school day (i.e.,
more movement opportunities between
deskwork activities because his SPM
scores refl ected dysfunction in his
vestibular and proprioception systems.
These suggestions resulted in Thomas
being able to listen more attentively
and sit still more often.
Case Example: Food Sensitivity
Seven-year-old Sera was referred to
occupational therapy because of her
narrow, unhealthy repertoire of foods.
Her scores on the SPM fell in the
typical range, potentially indicating
that there were other reasons for her
disordered eating. However, as the SPM
manual indicates, the therapist should
examine individual items if there is any
reason for concern.
1
A review of the
SPM questions with Sera’s parents, and
clinical observations, indicated sensory
integration problems. For example,
Sera’s parents commented that she
“never” had certain responses to sen-
sory input because she had “overcome”
her sensitivities. When answering
the SPM item, “Does your child show
distress at smells that other children
do not notice?” they reported that she
was not distressed, but she noticed the
slightest fragrances or odors. The SPM
item analysis indicated slight varia-
tions in scores, thus clinical reasoning
yielded additional information, allowing
for a more specifi c intervention plan
and leading Sera to tolerate and accept
a greater range of different nutritious
foods, with less tension during meals.
PSYCHOMETRIC STRENGTH
OF THE SPM
For an assessment tool to be reliable
for clinical practice, it must provide
accurate and consistent information.
This section summarizes evidence dem-
onstrating that the SPM is a valid and
reliable measure of sensory processing,
praxis, and social participation.
The SPM was developed with a
large, demographically representative
normative sample, consisting of 1,051
typically developing children, ranging
in age from 5 to 12 years. The norma-
tive sample was roughly divided among
males and females, ethnically diverse,
and representative of various levels of
socioeconomic status.
A normative sample provides clini-
cians with the expected SPM scores for
typically developing children. There-
fore, when determining whether a child
has a sensory processing disorder, the
clinician simply compares the SPM
scores to the average scores of the
normative sample. This comparison
classifi es the child into one of three
SPM interpretive ranges: (1) typical,
(2) some problems, or (3) defi nite
dysfunction.
Some measurement error is possible
in all tests. When developing the SPM,
a premium was placed on establishing
high reliability, or reducing the amount
of measurement error as much as
possible. One important aspect of reli-
ability is internal consistency, which
expresses how well the items of the
SPM “hang together” to measure clear,
well-defi ned aspects of sensory pro-
cessing. For example, the SPM Hearing
scale is intended to measure problems
with auditory processing. If some of
the items on the Hearing scale had
measured some other construct (e.g.,
attention span, aggressiveness, etc.),
the Hearing scale’s internal consistency
would have been lower. Internal con-
sistency is expressed as a correlation
coeffi cient that ranges in value from
0 to 1, with higher values indicating
greater reliability. In the SPM norma-
tive sample, all of the scales on the
Home and School forms have internal
consistency greater than .70 (and most
are greater than .80), indicating that
they are reliable enough to support
clinical assessment.
Another important aspect of reliabil-
ity is test-retest reliability, or temporal
stability. The SPM and other behavioral
rating scales are presumed to measure
characteristics of children that are
stable over short periods. For example,
one would not expect a child’s level of
dysfunction in auditory processing to
change appreciably over 2 weeks, all
else being equal. The 2-week test-
retest correlations for the SPM scales
are almost all .95 or above, indicating
excellent temporal stability.
The validity of an assessment has
various facets, some theoretical and
some practical. Discriminant validity
refers to the SPM’s ability to differenti-
ate between typically developing chil-
dren and those with sensory processing
dysfunction. As part of the SPM devel-
opment research, a clinical sample was
collected, consisting of 345 children
FOR MORE INFORMATION
AOTA CEonCD™: Response to Intervention:
A Role for Occupational Therapy Practitioners
By G. Frolek Clark, 2008. (Earn .2 AOTA CEUs
[2 NBCOT PDUs/2 contact hours.] $68 for
members, $97 for nonmembers. To order, call
toll free 877-404-AOTA or shop online at http://
store.aota.org. Order #4826-MI.)
FAQ on Response to Intervention
American Occupational Therapy Association,
2008. Bethesda, MD: Author.
http://www.aota.org/Practitioners/PracticeAreas/
Pediatrics/Browse/School/FAQ-Response-to-
Intervention.aspx
Online chat between school and clinic based
therapists hosted on www.otexchange.com
by Deanna Iris Sava and Diana A. Henry.
Go to www.ateachabout.com home page and
click on Discussion chat about the SPM.
Sensory Processing Measure Web site
www.sensoryprocessingmeasure.com
13
OT PRACTICE • JUNE 15, 2009
who were currently receiving occupa-
tional therapy intervention for sensory
and motor problems. These children
had a wide range of conditions, from
sensory processing disorder, to atten-
tion defi cit disorder, to autism.
The SPM scores of the children in the
clinical sample were signifi cantly higher
(worse) on all eight scales than the
scores of typically developing children
from the normative sample. A measure
of effect size was used to determine
whether these SPM score differences
were clinically meaningful, in addition
to being statistically signifi cant. In every
instance, the effect size of these differ-
ences exceeded .8, which is the thresh-
old for a large, clinically signifi cant
effect.
4
These results allow clinicians to
use the SPM with the confi dence that it
identifi es children who need treatment
for sensory processing disorder.
CONCLUSION
The applicability of the SPM in both
school- and clinic-based practice is
clear. In addition to providing fi rst-hand
information from those who are part
of the child’s life and facilitating team
communication, this statistically sound
assessment tool gives therapists the
ability to document the need for occu-
pational therapy services and design
appropriate interventions. (Case
studies under development with the
Sensory Processing Measure—
Preschool [SPM-P, for 2- to 5-year-olds]
are indicating that it too will aid clini-
cians who support children in various
environments.)
■
Acknowledgments
The authors offer grateful thanks to staff, parents,
and students at Horseshoe Trails and Desert Sun
Elementary schools in Arizona; Monroe Road
Elementary in Michigan; and therapists at Rehab
Dynamics in Ohio.
References
1. Parham, L. D., Ecker, C., Miller-Kuhaneck, H.,
Henry, D. A., & Glennon, T. J. (2007). Sensory
Processing Measure (SPM): Manual. Los Ange-
les: Western Psychological Services.
2. Miller-Kuhaneck, H., Henry, D. A., & Glennon, T.
J. (2007). Sensory Processing Measure (SPM)
School Environments Form. Los Angeles: West-
ern Psychological Services.
3. Schilling, O. L., Washington, K., Billingsley, F.
F., & Deitz, J. (2003). Classroom seating for
children with attention defi cit hyperactivity
disorder: Therapy balls versus chairs. American
Journal of Occupational Therapy, 57, 534–541.
4. Cohen, J. (1992). A power primer. Psychological
Bulletin, 112, 155–159.
Diana A. Henry, MS, OTR/L, FAOTA, president of
Henry Occupational Therapy Services, presents
workshops on the SPM as well as on Sensory Tools
for Tots, Teens, Teachers, and Parents. Traveling
full-time in her RV, she can be reached at www.
ateachabout.com.
Cheryl L. Ecker, MA, OTR/L, BCP, SWC, is the
clinical director at Therapy in Action in Tarzana,
California.
Tara J. Glennon, EdD, OTR/L, FAOTA, is a profes-
sor of Occupational Therapy at Quinnipiac Univer-
sity in Hamden, Connecticut. She is also the owner
of the Center for Pediatric Therapy in Fairfi eld and
Wallingford, Connecticut.
David Herzberg, PhD, is vice president of
Research and Development at Western Psychologi-
cal Services, the publisher of the SPM. He can be
reached at [email protected].
To discuss this article,
go to
www.otconnections.org. Click on
Forums, Public Forums, then
OT Practice Magazine discussion.
Western Psychological Services
wpspublish.com • 800-648-8857
Order your copy of the SPM today!
Easy to Score and Interpret
Other tests make this claim, but the SPM actually lives up
to it. AutoScore™ forms with built-in Profile Sheets give
you rapid scoring and a quick visual summary of results.
Clear Results
SPM scales are described in
simple, nontechnical language:
• Social Participation
• Vision
• Hearing
• Touch
• Body Awareness
• Balance and Motion
• Planning and Ideas
• Total Sensory Systems
Because it’s easy to explain what
you’re measuring, it’s also easy to explain results.
You get a comprehensive, clinically rich picture of
the child that parents intuitively understand.
Direct Comparison of Sensory
Functioning at Home and at School
With Home and School Forms standardized on
the same group of children, the SPM is the only
assessment that allows you to directly compare
the child’s functioning across environments.
Home Form
L. Diane Parham, Ph.D., OTR/L, FAOTA, and Cheryl Ecker, M.A., OTR/L
Main Classroom and School Environments Forms
Heather Miller Kuhaneck, M.S., OTR/L, Diana A. Henry, M.S., OTR/L,
and Tara J. Glennon, Ed.D., OTR/L, FAOTA
The best in every sense
Sensory Processing Measure
KITS
COMPREHENSIVE KIT (W-466) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . $149.00
Includes 25 Home AutoScore™ Forms; 25 Main Classroom AutoScore™ Forms;
School Environments Form CD; Manual
SCHOOL KIT (W-466S) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . $120.00
Includes 25 Main Classroom AutoScore™ Forms; School Environments Form CD; Manual
HOME KIT (W-466H) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . $95.00
Includes 25 Home AutoScore
™
Forms; Manual
At a Glance…
benefit: Provides a complete
picture of children’s sensory processing difficulties
at school, at home, and in the community
ages: 5 to 12 years
administration time: 15 to 20 minutes
format: Parent and/or teacher rating scale; additional
rating sheets completed by other school personnel
norms: Based on a nationally representative sample
of 1,051 children. Additional data were collected on
a clinical sample of 345 children.
P-4147
