i
Medicare Communications and Marketing Guidelines (MCMG)
Date: 02/09/2022
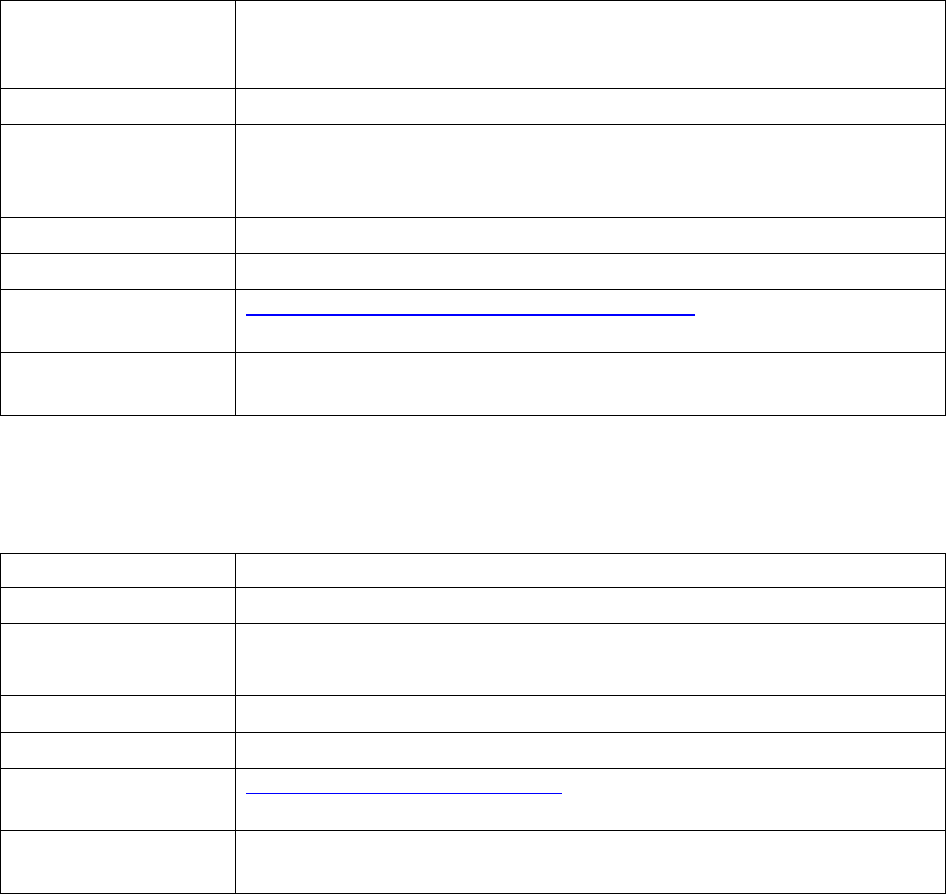
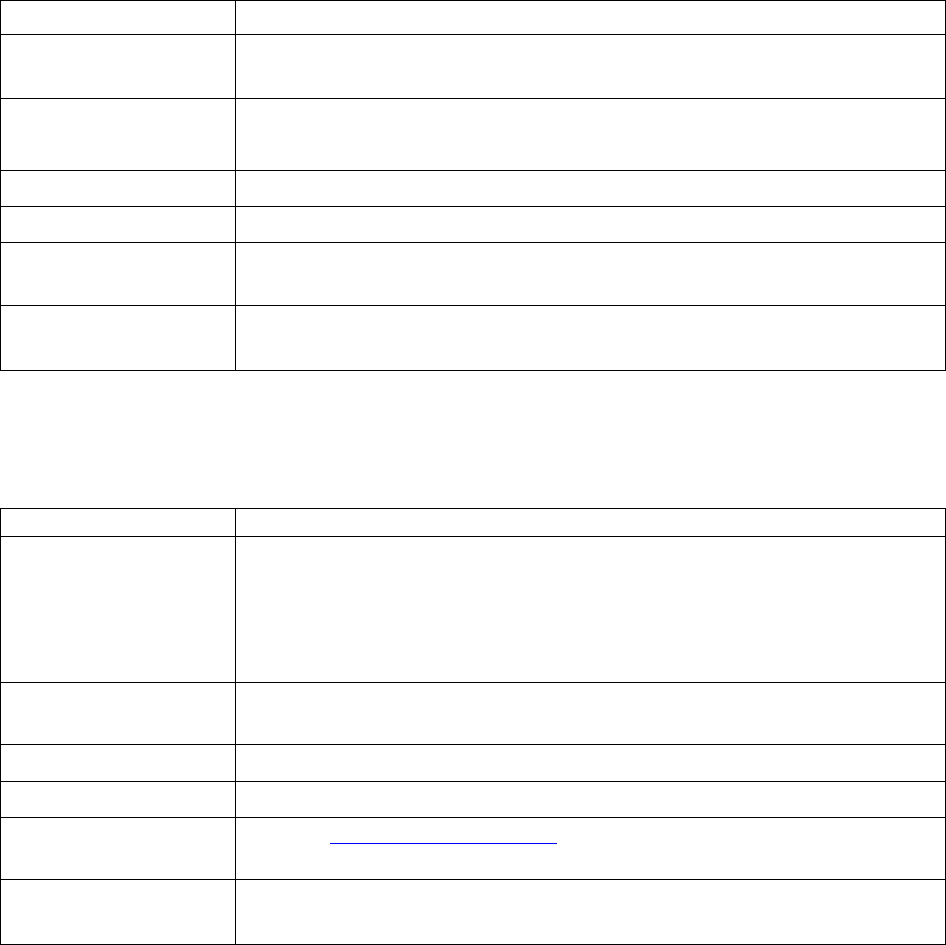
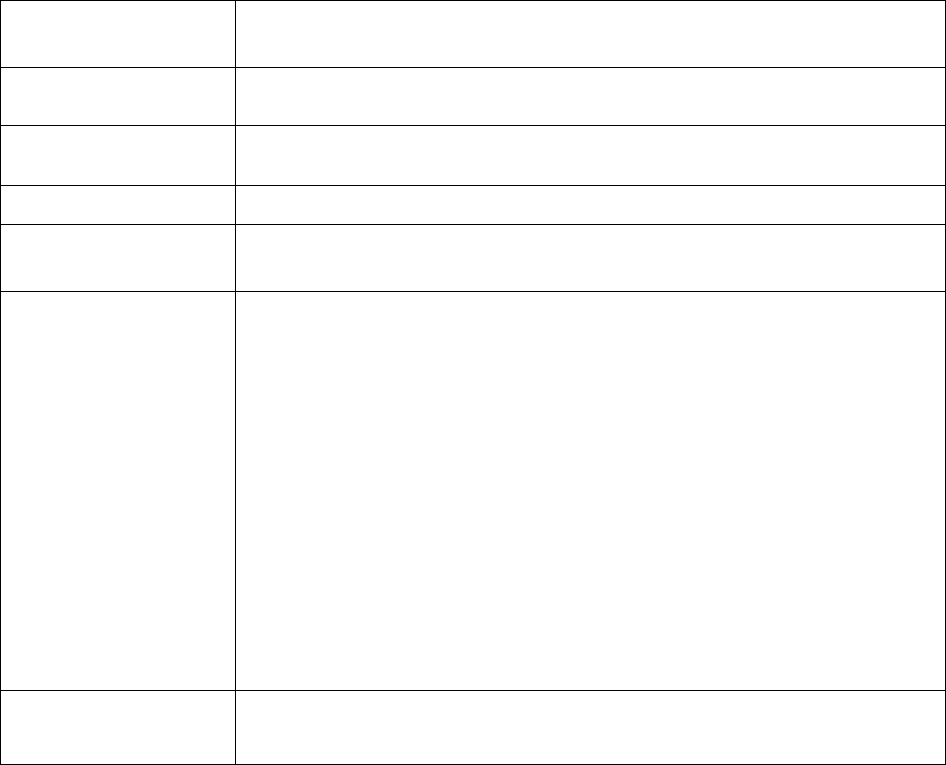
Table of Contents
Introduction .................................................................................................................................................. 3
Definitions (42 CFR §§ 422.2260, 423.2260) ............................................................................................... 3
CMS Required Materials – Materials that are required under 42 CFR §§ 422.2267(e) and
423.2267(e) .................................................................................................................................................... 5
Submission, Review, and Distribution of Materials (42 CFR §§ 422.2261, 423.2261) ...........................
6
§§ 422.226
1(a), 423.2261(a) - General requirements .................................................................................. 6
§§ 422.2261(a)(1), 423.2261(a)(1) – The HPMS Marketing Module ......................................................... 6
§§ 422.2261(a)(3), 423.2261(a)(3) – Third-party submissions .................................................................... 7
§§ 422.2261(b)(3), 423.2261(b)(3) – File and Use (F&U) .......................................................................... 9
§§ 422.2261(d), 423.2261(d) – Standards for CMS Review ....................................................................... 9
General Communications Materials and Activities Requirements (42 CFR §§ 422.2262,
423.2262) . 11
§§ 422.226
2(a) 423.2262(a) - General rules .............................................................................................. 11
§§ 422.2262(a)(1)(x), 423.2262(a)(1)(x) – Plan type in plan name ........................................................... 11
General Marketing Requirements (42 CFR §§ 422.2263, 423.2263) .....................................................
11
§§ 422.226
3(b)(2), 423.2263(b)(2) – Nominal gifts .................................................................................. 11
§§ 422.2263(b)(3), 423.2263(b)(3) – Exclusion of meals as a nominal gift .............................................. 12
§§ 422.2263(b)(7), 423.2263(b)(7) – Prohibition of marketing during the Open Enrollment Period (OEP)
.......................................................................................................................................................... 12
Beneficiary Contact (42 CFR §§ 422.2264, 423.2264) .............................................................................
13
§§ 422.226
4(a)(2)(i), 423.2264(a)(2)(i) – Prohibition on the use of door to door solicitation .................. 13
§§ 422.2264(a)(2)(iv), 423.2264(a)(2)(iv) - Telephone solicitation .......................................................... 13
§§ 422.2264(b), 423.2264(b) - Contact for plan business .......................................................................... 13
§§ 422.2264(c), 423.2264(c) - Events with beneficiaries .......................................................................... 13
Websites (§§ 422.2265, 423.2265) ..............................................................................................................
13
§§ 422.226
5(a), 423.2265(a) - General website requirements ................................................................... 13
§§ 422.2265(b), 423.2265(b) – Required content ...................................................................................... 14
§§ 422.2265(c), 423.2265(c) - Required posted materials ......................................................................... 14
Activities with Healthcare Providers or in the Healthcare Setting
(42 CFR §§ 422.2266, 423.2266) . 14
§§ 422.2266(c)(7), 423.2266(c)(7) – Announcing new or continuing affiliations ..................................... 14
ii
Required materials and content (42 CFR §§ 422.2267, 423.2267) ......................................................... 15
§§ 422.226
7(a)(2), 423.2267(a)(2) - For markets with a significant non-English speaking population .... 15
§§ 422.2267(d)(1), 423.2267(d)(1) - When multiple enrollees are living in the same household ............. 15
§§ 422.2267(d)(2), 423.2267(d)(2) – When materials are delivered electronically ................................... 15
§§ 422.2267(d)(2)(i), 423.2267(d)(2)(i) – When materials are delivered electronically without prior
authorization from the enrollee ........................................................................................................ 15
§§ 422.2267(e), 423.2267(e) - CMS Required Materials and content ....................................................... 15
Disclaimers .................................................................................................................................................. 31
Agent/Broker Requirements (42 CFR §§ 422.2274, 423.2274) ............................................................... 36
§§ 422.2274(b), 423.2274(b) - Agent/broker requirements ....................................................................... 36
§§ 422.2274(c), 423.2274(c) - MA organization oversight ....................................................................... 36
§§ 422.2274(a), 423.2274(a) - Definitions ................................................................................................. 36
§§ 422.2274(d)(3), 423.2274(d)(3) - Renewal compensation .................................................................... 36
§§ 422.2274(d)(5)(iii)(B) - Rapid Disenrollment Compensation ............................................................. .36
Appendix 1 – St
andardized Pre-Enrollment Checklist (422.2267(e)(4), 423.2267(e)(4)) ..................... 37
Appendix 2 – Model Summary of Benefits Instructions (422.2267(e)(5), 423.2267(e)(5)) ...................
39
Appendix 3 – Employer/Union Group Health Plans ............................................................................... 42
Appendix 4 – Use o
f Medicare Mark for Part D Sponsors ..................................................................... 43
Appendix 5 – Ext
ernal Links ..................................................................................................................... 48
Introduction
The Medicare Advantage (MA) and Part D Marketing and Communications (MCMG) provides
the marketing and communications requirements for Medicare Advantage (MA) plans, section
1876 cost plans, and Medicare Prescription Drug Plans (collectively referred to as “plans”)
governed under Title 42 of the Code of Federal Regulations (CFR), Parts 417, 422, and 423.
These requirements also apply to Medicare-Medicaid Plans (MMPs), except as modified in
state-specific marketing guidance for each state’s demonstration. State-specific guidance for
MMPs is considered an addendum to the regulations and MCMG, and is generally posted at the
Medicare-Medicaid Plan (MMP) Marketing Information & Resource
page on CMS.gov. The
MCCG has been structured to align with the regulatory requirements in 42 CFR Part 422
Subpart V and 42 CFR Part 423 Subpart V. The MCMG should be used in conjunction with the
regulatory requirements to aid plans in understanding and complying with the regulations.
Compliance
Plans are responsible for ensuring compliance with applicable Federal laws and regulations,
including CMS’ marketing and communications regulations. This includes monitoring and
overseeing the activities of their subcontractors, downstream entities, and/or delegated entities.
Failure to comply with applicable rules may result in compliance and/or enforcement actions,
including, but not limited to, intermediate sanctions and/or civil money penalties.
Note: Plans may impose additional restrictions on their subcontractors, downstream entities,
and/or delegated entities, provided they do not conflict with the requirements outlined in
regulations or the MCMG.
Definitions (42 CFR §§ 422.2260, 423.2260)
Communications means activities and use of materials created or administered by the plans or
any downstream entity to provide information to current and prospective enrollees. All activities
and materials aimed at prospective and current enrollees, including their caregivers, are
“communications” within the scope of the regulations at 42 CFR Parts 417, 422, and 423.
Note: Where the term enrollee is used, whether a current or prospective enrollee, the term
encompasses representatives of the enrollee who are authorized to act on the enrollee’s behalf.
Marketing is a subset of communications and must, unless otherwise noted, adhere to all
communication requirements. To be considered marketing, communications materials must meet
both intent and content standards. In evaluating the intent of an activity or material, CMS will
consider objective information including, but not limited to, the audience, timing, and other
context of the activity or material, as well as other information communicated by the activity or
material. The organization's stated intent will be reviewed but not solely relied upon.
1
Intent
Material or activities that CMS determines, as described above, are intended to:
• Draw a beneficiary's attention to a plan or plans,
• Influence a beneficiary's decision-making process when making a plan selection, or
• Influence a beneficiary's decision to stay enrolled in a plan (retention-based marketing).
Content
Materials or activities that include or address content regarding:
• The plan's benefits, benefits structure, premiums, or cost sharing,
• Measuring or ranking standards (for example, Star Ratings or plan comparisons), or
• Rewards and incentives as defined under 42 CFR § 422.134(a) (for MA and section 1876
cost plans only).
Below are examples to assist in identifying marketing versus communication.
1.
A flyer reads “Swell Health is now offering Medicare Advantage coverage in Nowhere
County. Call us at 1-800-BE-SWELL for more information.”
Marketing or Communication? Communication. While the intent is to draw a
beneficiary’s attention to Swell Health, there is no marketing content.
2.
A billboard reads “Swell Health Offers $0 Premium Plans in Nowhere County”
Marketing or Communication? Marketing. The advertisement includes both the
intent to draw the viewer’s attention to the plan and has content that mentions
zero-dollar premiums being available.
3.
A letter is sent to enrollees to remind them to get their flu shot. The body of the letter
says, “Swell Health enrollees can get their flu shot for $0 copay at a network
pharmacy…”
Marketing or Communication? Communication. While the letter mentions cost
sharing, the intent is not to steer the reader into selecting a plan or to stay with
their current plan, but to encourage current enrollees to get a flu shot. The letter
contains factual information and was provided only to current enrollees in the
plan.
4.
A third-party television commercial where an actor says: “Call us to hear about plans
that can provide hearing and dental benefits, zero-dollar monthly premiums, and can
even lower your Medicare Part B costs.”
Marketing or Communications? Marketing. While a specific plan is not
mentioned by name, the commercial’s intent is to draw the beneficiary to a MA
plan or plans and the content addresses plan premium, cost-sharing, and benefit
information for plans being represented and sold by the third party.
2
CMS’s regulations at 42 CFR §§ 422.2267(e) and 423.2267(e) designate all required materials
and content as either communications or marketing. Plans will need to review regulations at 42
CFR §§ 422.2260 and 423.2260 and these guidelines to determine if a “Plan-Created Material”
(i.e., something not listed as a required material in 42 CFR §§ 422.2267(e) and 423.2267(e)) is
considered a communication or marketing material. Plans are also encouraged to consult with
their Regional Office Account Manager or Marketing Reviewer about any marketing or
communications questions.
Materials are static in nature, whereas activities are more dynamic. Interactions with a
beneficiary could begin as a communication activity but become a marketing activity. For
example, an enrollee calls the plan’s customer service number for questions related to coverage
under the plan in which in the caller is currently enrolled; during the call, the enrollee asks about
other health plan options, moving the call from communications to marketing. The plan must
comply with all applicable requirements during communications and marketing activities. In
cases where an interaction transitions from a communication activity to a marketing activity, the
plan must comply with all applicable requirements for each type of activity during the relevant
portion of the interaction.
Other Definitions
Age-ins - An individual who is aging into Medicare eligibility. Such individuals typically elect
to enroll in a plan during the seven-month period consisting of three months before they turn age
65, the month they turn 65, and the three months after they turn 65.
Co-Branding - A relationship between two or more separate legal entities, where at least one
party is a plan. Co-branding is when a plan displays the name(s) or brand(s) of the co-branding
entity or entities on its materials to signify a business arrangement. Co-branding relationships
are independent of the contract that the plan has with CMS. Plans are responsible for ensuring
that co-branded materials include appropriate disclaimers and other model content as specified
by CMS regulations at 42 CFR §§ 422.2267(e)(36) and 423.2267(e)(37) where applicable.
CMS Required Materials
– Materials that are required under 42 CFR §§ 422.2267(e) and
423.2267(e)
Plan Created Materials – Materials created by plans, typically advertisements, that are not
required under 42 CFR §§ 422.2267(e) and 423.2267(e).
3
Submission, Review, and Distribution of Materials (42 CFR §§ 422.2261,
423.2261)
§§ 422.2261(a), 423.2261(a) - General requirements
• All marketing materials, election forms, and certain designated communications
materials used by a plan, including those used by third-party and downstream entities,
must be submitted to CMS for review.
§§ 422.2261(a)(1), 423.2261(a)(1) – The HPMS Marketing Module is the primary system
of record for the collection, review, and storage of materials that must be submitted for
CMS review
•
In limited situations and with prior approval from CMS, plans may submit materials
outside of HPMS.
•
Non-English/Alternate Format Materials
• Plans are not required to submit non-English language materials that are
translations of a previously submitted English version. The English Version
of the Standardized material identification (SMID) may be used on non-
English translations.
• If a plan creates a material to be used only in a non-English language, the
plan must submit an English translation to HPMS via a zip file containing
both the material and the translations.
• Plans are not required to submit alternate format versions of a previously
submitted standard material.
•
Submission of Required Websites –Websites that plans are required to maintain
pursuant to 42 CFR §§ 422.2265 and 423.2265 do not require submission if they are
limited to only providing the content and materials required under 42 CFR §§
422.2265(b), 423.2265(b), 422.2265(c), and 423.2265(c). Required websites that
contain additional marketing content must be submitted to CMS on an annual basis
(contract year). Submission is done by selecting “Plan Required Website” under the
“CMS Required” section of the HPMS Marketing Module. Regardless of submission,
websites must include the current Material ID on all web pages. The following outlines
how applicable websites must be submitted.
• Each Contract Year’s initial website submission must use a Microsoft Word
document (or similar) listing the items on the website and must contain the
website’s URL. Screenshots, test sites, etc. are not needed. The Standardized
Material Identification (SMID) used for the submission must correspond to
the material ID on the website, except it will end with an underscore
followed by the contract year (e.g., H1234_abcwebsite_M_2022). The
contract year is not required on the actual webpages.
• Updates made to the website for the same contract year, must be submitted
using a Microsoft Word document (or similar) containing the URL and a list
of all changes. The same material ID on the site’s pages are permitted (e.g.
H1234_abcwebsite_M). However, updated submissions must use the
website’s material ID followed by an underscore and contract year, followed
by an underscore and a letter (“A”, “B”, “C”, etc.) corresponding to each
4
resubmission (e.g., H1234_abcwebsite_M_2020_A). The contract year and
the letter do not have to be shown on the actual website.
• Plans are not required to submit web page updates when only
communication content or content required in 42 CFR §§ 422.2265,
423.2265 has been updated.
• As outlined under §§ 422.2261(b)(3) and 423.2261(b)(3), plans must wait
five (5) days following the submission of a website or website change(s)
before going live with the website. However, plans are not required to take
down their website while they are making updates.
§§ 422.2261(a)(3), 423.2261(a)(3) – Third-party submissions
Consultant Submitted Multi-Plan Marketing Materials - CMS permits third parties to submit
marketing materials directly to CMS, on behalf of contracted plans, when the marketing
materials created by a third party include marketing content of and used by multiple (two or
more) plans. For example, if the third party operates a website that lists all contracted plans and
their cost sharing, and is used by beneficiaries to select and enroll into a plan, the third party
may submit the website on behalf of the contracted plans.
Note: The multi-plan submission process is intended for third parties that submit for multiple
organizations. If the third party’s marketing materials only mention one organization, then the
plan should submit the material directly to CMS using the standard submission process.
Providing Consultant Access – The following steps are for third-party access to the HPMS
marketing module for multi-plan submissions.
• Prepare an official letter that states the user’s name, CMS user ID, consultant company
name, the type of consultant access being requested, and the contract/multi-contract
entity (MCE) number(s) for which consultant access is needed. The letter must be
provided on the organization’s official letterhead and signed by a senior official of the
organization. Organizations can submit one letter and include multiple consultants on that
letter if they are all obtaining the same consulting access type. CMS recommends the use
of the following sample language:
(Name of organization) hereby requests that (name of consultant user, the CMS
user ID, and consultant company name) be granted Marketing Consultant Access
for Multi-Plan Submissions for the following contract number(s): (list specific
contract numbers or provide the MCE number).
• Submit the official letter via e-mail in scanned PDF format to
HPMSConsultantAccess@cms.hhs.gov. To facilitate timely processing, please indicate
the type of consultant access in the subject line of the e-mail. It is a best practice for the
plan to cc the third-party for which they are requesting access.
• An email confirmation will be provided to all included in the original e-mail (sender and
all cc’d) when access has been granted. Unless the third-party was cc’d on the original e-
mail request, plans are responsible for informing the third-party that the access has been
approved.
• It is important to note that consultant user access is limited in HPMS to only the multi-
plan portion of the marketing module. Third parties cannot see or access other plan
5
related marketing information outside of multi-plan submissions.
• For more information, please refer to the May 26, 2021 HPMS memo,
“Updated -
Instructions for Requesting Consultant Access to the Health Plan Management System (HPMS).”
Note: Ultimately, it is the responsibility of the plan to manage and maintain the set of users for
whom they have authorized access to HPMS. User access can be viewed under the “User
Resources > User Access Administration” link in HPMS. If a user within an organization does
not currently have access to the “plan user access” reports, organizations must submit a request
to hpms_access@cms.hhs.gov.
Multi-Plan Submission Process – Third-party Perspective – Once consultant access has been
granted to the third party by at least one contract/MCE, the third party may begin submitting
multi-plan marketing materials. The following applies to multi-plan submitted materials:
• The submissions process is the same as the plan submissions process (i.e. collection of
marketing content, audience, life cycle, media types, etc.), however, multi-plan
submissions can only be made for Plan Created Materials
• During the initial submission process, the third party is able to select from any
contracts/MCEs who have authorized access
• The third-party will select a reviewer from a list of multi-plan dedicated CMS reviewers
• Review timeframes are the same as they would be for plan submitted materials (e.g., 45-
day or file and use (“F&U”))
• After the material has been approved (or accepted for F&U submissions), all plans whose
contract/MCE was selected as a part of the submission will be notified (no plan
notification is provided up until this point)
• Upon receipt of the email, plans whose contract/MCE was selected must “Opt-In” or
“Opt-Out” of the material
• The third-party may not use the material for an associated contract/MCE unless the plan
has opted-in
• HPMS sends an e-mail to the third-party for all submission updates, including when each
plan provides an “Opt-In” or “Opt-Out”
• A plan opting in or out of a material does not impact the material’s review status (i.e.
approved or accepted)
• The third-party can add additional contracts/MCEs after the material has been approved
• The third-party will see a “tab” for each contract/MCE that is associated with the
material (plans are only able to see their own “tab”)
Note: Please refer to §§ 422.2262(d) and 423.2262(d) for SMID requirements for multi-plan
materials.
Multi-Plan Submission Process – Plan Perspective – After the plan grants access to the
marketing module for multi-plan submissions, the following happens after a material has been
submitted for the plan’s contract/MCE and approved (or accepted for F&U) <OR> when a
plan’s contract/MCE number has been added to an already approved material:
• The plan will receive an email from HPMS notifying the plan that a multi-plan material
has been submitted that includes their contract/MCE number.
6
• Upon receipt of the email, the plan should review the material and “opt-in” or “opt-out”.
o “Opting-In” – indicates that the plan is aware of the material and is providing
their concurrence that they will be associated with the submission (i.e. that the
material will be used by the third-party for the contract/MCE noted)
o “Opting-Out” – indicates that the plan does not want to be associated with the
submission (i.e. that the material will not be used by the third-party for the
contract/MCE noted)
o Opting-in/out does not impact the status of the material in HPMS (e.g., it will
remain approved/accepted)
• Plans are responsible for the content of multi-plan materials they have opted into and
responsible for ensuring the materials remain compliant with the most current
requirements. See 42 CFR §§ 422.503(b)(4)(vi), 422.504(i), 423.504(b)(4)(vi),
423.505(i).
Note: The expectation is that all conversations and external reviews of the material have
already occurred prior to the material being submitted into HPMS. The multi-plan submission
process is not the vehicle for plan review of third-party submitted materials.
§§ 422.2261(b)(3), 423.2261(b)(3) – File and Use (F&U)
CMS designates certain marketing materials as F&U eligible based on the material's content,
audience, and intended use, as they apply to potential risk to the beneficiary. A material
submitted under F&U may be used five days following its submission, provided the plan
certifies the material complies with all applicable standards.
•
The “Marketing Lookups” function in the HPMS Marketing Module identifies what
materials (for CMS Required Materials) and what media types (for Plan Created
Materials) qualify for F&U submissions. Plans without an executed contract may
submit F&U materials. However, once the contract is executed, CMS presumes that the
plan has, by submission of the materials, attested that the material complies with all
requirements regardless if the materials were submitted before or after contract
execution.
•
Plans may be subject to compliance actions if:
• Materials are used before they are “accepted” (i.e. five days following the
submission of the material), or
• Materials are found during a CMS review to be out of compliance with the
applicable requirements under §§422.2260 through 422.2267 and §§ 423.2260
through 423.2267.
§§ 422.2261(d), 423.2261(d) – Standards for CMS Review
•
Placeholders (formerly “template materials”) –CMS permits the use of placeholders
to represent certain variable data in required or Plan Created Materials (except for SBs,
as provided in Appendix 2). Variable data fields for premiums, cost sharing, benefits
should only be used when the document is applicable for more than one plan. The type
of data that will populate the placeholder dictates how the material is submitted.
• Plans have the choice on whether to use placeholders. If a plan does not want to
7
use placeholders the data in the submitted materials must be bracketed (e.g., [$10
Copay/$15 Copay/$20 Copay]). If the plans are using placeholders, the plan
must include the data type in brackets along with a reference to where the data
can be found in the spreadsheet or table (e.g. [Copay, see column “A”]). The
submission for materials with placeholders consists of a zipped file which
contains the material and a spreadsheet or table identifying the actual data for
each variable field. Spreadsheets or tables must only include the variable data
found in the submitted material for the contracts/plans associated with the
submitted material.
• When using placeholders that include non-marketing content, the content can be
represented in the material by the data type in brackets (e.g. [date], [hours of
operation], [agent name]). In this instance, a table containing the actual data is not
required with the submission, however, such data must be made available upon
request.
•
Remedying a previously disapproved material - Plans should clearly indicate all
changes/updates when resubmitting materials that were previously disapproved, such as
highlighting text changes or inserting notes or identifying changes in the comments
section.
•
Material Replacement - For the specified materials below, HPMS now has a “material
replacement” functionality to allow updated materials to be resubmitted as a
replacement file attachment using the same SMID. Material replacement is available
for:
• Annual Notice of Change (ANOC)
• Summary of Benefits (SB)
• Evidence of Coverage (EOC)
• Star Ratings Document
• Sales scripts and presentations
• Enrollment scripts
• Enrollment forms (online and paper)
If the material replacement function is used, do not mark the original material as “no
longer in use.”
The material replacement function is not available for previously submitted materials
other than those listed above; any other materials that require changes/updates must be
marked as “no longer in use” and resubmitted with a new SMID.
•
Updates to CMS Required Materials - Plans must review all required documents for
accuracy and resubmit if changes or corrections to previously submitted CMS Required
Materials are identified (e.g., the benefit or cost-sharing information differs from that in
the approved bid). In addition, the following requirements apply:
• ANOC, EOC, and formulary errata must be sent in hard copy within a
reasonable timeframe or electronically if the enrollee has opted into
receiving electronic versions, and
• SB addenda or reprints must be sent only to existing enrollees if the plan
mass mailed the SB.
8
General Communications Materials and Activities Requirements (42 CFR §§
422.2262, 423.2262)
§§ 422.2262(a) 423.2262(a) - General rules
• To avoid misleading or confusing beneficiaries, plans must make it clear when an
encounter with a beneficiary is moving from a communications activity to a marketing
activity, such as when a beneficiary is being transferred to a sales or enrollment
representative. Before transferring, the beneficiary must clearly consent to being
transferred.
§§ 422.2262(a)(1)(x), 423.2262(a)(1)(x) – Plan type in plan name
• When a plan’s communications activities or materials include the plan name, the plan
type must also be included. The plan is not required to repeat the plan type when the plan
name is used multiple times in the material, but should include the plan type, at the end
of the plan name, when the plan name is first mentioned or in a way that prominently
conveys the plan type to the recipient.
General Marketing Requirements (42 CFR §§ 422.2263, 423.2263)
§§ 422.2263(b)(2), 423.2263(b)(2) – Nominal gifts
CMS’s regulations governing marketing prohibit plans from offering gifts to beneficiaries unless
the gifts are of nominal value. The regulations refer to guidance published by the HHS Office of
Inspector General (HHS OIG) for the meaning of “nominal value.” HHS OIG’s current
interpretation of “nominal value” is set forth in “Office of Inspector General’s (OIG’s) Policy
Statement Regarding Gifts of Nominal Value To Medicare and Medicaid Beneficiaries,” and is
no more than $15 per item or $75 in the aggregate, per person, per year. CMS’ interpretation of
the terms “nominal gifts” and “cash equivalents,” as described below, is intended to align with
HHS OIG’s interpretations of the same (or in the case of “nominal gifts,” similar) terms.
The following rules apply to nominal gifts:
• Nominal gifts must be offered to similarly situated beneficiaries without discrimination
and without regard to whether the beneficiary enrolls in a plan.
• Nominal gifts may not be in the form of cash, including cash-equivalents, or other
monetary rebates.
• CMS is adopting OIG’s interpretation of cash equivalents. OIG has interpreted the term
“cash equivalents” to encompass items convertible to cash (such as a check) or items that
can be used like cash (such as a general-purpose debit card, but not a gift card that can be
redeemed only for certain categories of items or services, like a fuel-only gift card
redeemable at gas stations). See 85 Fed. Reg. 77,684, 77,789-90 (Dec. 2, 2020),
81 Fed.
Reg. 88,368, 88,393 n. 19 (Dec. 7, 2016). CMS’s interpretation of “cash equivalents” for
the purposes of this regulation mirrors OIG’s interpretation subject to the following,
additional guidance.
o A general gift card that is not restricted to specific retail chains or to specific
items and categories would fall under those types that would be considered a
cash equivalent (e.g. Visa gift card).
o Gift cards for retailers or online vendors that sell a wide variety of consumer
9
products would also fall under this prohibition (e.g., Walmart and Amazon).
o A gift card that can be used for a more limited selection of items or food,
would not be considered a cash equivalent (e.g. Starbucks or a Shell Gas gift
card).
§§ 422.2263(b)(3), 423.2263(b)(3) – Exclusion of meals as a nominal gift
• Refreshments and light snacks are not considered “meals.” Plans should ensure that
items provided could not be reasonably considered a meal and/or that multiple items are
not being “bundled” and provided as if a meal.
• Meals may be provided at educational events that meet CMS’s regulations and other
events that would fall under the definition of communications.
§§ 422.2263(b)(7), 423.2263(b)(7) – Prohibition of marketing during the Open Enrollment
Period (OEP)
• The term “knowingly”, as used in the regulation, considers the recipient and content of
the message. For example, if messaging specifically calling out the OEP is sent, it would
be knowingly targeting. Likewise, if a plan was aware that an individual had already
made an AEP enrollment decision, sending unsolicited marketing materials to that
individual, even if the OEP was not mentioned, would be considered “knowingly
targeting.”
• The requirement does not restrict a plan from:
o Providing educational materials or marketing materials if and when the
beneficiary proactively reaches out looking for OEP help. Providing marketing
materials and other information in response to a request from a beneficiary is at
the beneficiary’s request and hence not unsolicited.
o Marketing to dual-eligible and LIS beneficiaries who, in general, may make
changes at least once per calendar quarter during the first nine (9) months of the
year.
o Marketing from 5-Star plans, as individuals can enroll into the 5-Star plan at any
time using the 5 Star SEP.
o Using mailings or other marketing aimed at individuals aging into the Medicare
program unless the plan knows the individual has already made an enrollment
decision. For example, a plan buys a list of age-ins and sends marketing mailers
to all addressing their newly eligible Medicare status. Since the plan has no way
to know if any of these age-ins already selected a plan it is not considered
knowingly targeting during the OEP, provided the content of the message is
about their Initial Coverage Election Period and does not address or include any
references to the OEP.
o Including educational information, excluding marketing, on the plan’s website
about the existence of OEP.
• Marketing messages aimed at generating interest or leads during the OEP are generally
prohibited, unless as noted above. For example, a generic marketing line of “not happy
with your plan, change now” would be considered inappropriate marketing.
10
Beneficiary Contact (42 CFR §§ 422.2264, 423.2264)
§§ 422.2264(a)(2)(i), 423.2264(a)(2)(i) – Prohibition on the use of door to door solicitation
• Agents/brokers who have a pre-scheduled appointment with a potential enrollee who is a
“no-show” may leave information at that enrollee’s residence.
§§ 422.2264(a)(2)(iv), 423.2264(a)(2)(iv) - Telephone solicitation
• Other types of electronic direct messaging, such as through social media analogous to
text messaging are not permitted.
• Text messages regarding care and care coordination are permissible with prior current
enrollee consent. An opt-out process must be included on each communication.
§§ 422.2264(b), 423.2264(b) - Contact for plan business
• Plans may not market prior to October 1 (§§ 422.2263(a) and 423.2263(a)) under the
pretext of plan business.
• CMS provides Medicare beneficiary data to plans for the purpose of enrolling,
disenrolling, and providing care to members in their plan. The permitted uses of data
provided by CMS are outlined in the data use agreement signed by plans.
§§ 422.2264(c), 423.2264(c) - Events with beneficiaries
• As established under §§ 422.62(a)(2)(iii) and 423.38(b)(3), the annual coordinated
election period for the following calendar year is October 15 through December 7. As
such, enrollment applications may not be solicited or accepted for a January 1 effective
date until October 15 of the preceding calendar year, unless the beneficiary has an SEP.
Note: Plans are reminded that other laws – such as the HIPAA privacy rules - may limit the use
of information gathered from other sources or in connection with other products offered by the
plan. Nothing in this guidance creates an exemption or exception to other applicable laws.
Websites (§§ 422.2265, 423.2265)
As required under §§ 422.111(h)(2), 422.2265, 423.128(d)(2), and 423.2265, all plans must have
a website that includes specific documents and content. The following operational guidance
should be used in conjunction with the regulatory requirements, with an emphasis on those
requirements found under §§ 422.2265 and 423.2265.
Note: This guidance only pertains to plan required websites.
§§ 422.2265(a), 423.2265(a) - General website requirements
•
Notification must be provided when beneficiary leaves the plan’s Medicare information
website, noting that the individual will go to non-Medicare information website or to a
different website.
•
Websites must comply with anti-discrimination provisions, such as Section 508 of the
Rehabilitation Act, with regard to providing access to websites and other materials. See
also 45 CFR § 92.104.
11

§§ 422.2265(b), 423.2265(b) – Required content
•
CMS considers it a best practice to provide instructions on how to appoint a
representative and a link to the downloadable version of the CMS Appointment of
Representative Form (CMS Form-1696)
•
To ensure that eligible beneficiaries are able to enroll without restriction, CMS also
considers it a best practice for plans to provide enrollment instructions and forms
•
When providing required content regarding how to file a grievance (§§ 422.562(a)(2)
and 423.562(a)(2)), request an organization determination, and an appeal, plans should
include the following:
o
Written procedures for filing;
o
A direct link on the grievance/coverage determination webpage to the
Medicare.gov complaint, where an enrollee can enter a complaint in lieu of
calling 1-800-MEDICARE;
o
Phone number(s) for receiving oral requests;
o
Mailing address for written requests;
o
Fax number (optional);
o
Links, if applicable, to any forms created by the plan for appeals and grievances;
o
Information on how to obtain an aggregate number of grievances, appeals, and
exceptions filed with the plan; and
o
Contact numbers for enrollees and/or physicians to use for process or status
questions.
§§ 422.2265(c), 423.2265(c) - Required posted materials
•
All required materials must be clearly labeled and easily found.
•
Plans must include the last update date of the material, in close proximity to the
material link (e.g. in file name, next to link, etc.) For example, a link that reads “Super
MA Plan EOC, updated 11/23/2021.”
•
Updates (e.g., to correct an error) to materials must be posted as soon as possible.
Activities with Healthcare Providers or in the Healthcare Setting (42 CFR §§
422.2266, 423.2266)
§§ 422.2266(c)(7), 423.2266(c)(7) – Announcing new or continuing affiliations
•
Provider affiliation announcements made by plans that do not include marketing are
considered communications. If the announcement contains marketing, the
announcement must be submitted into HPMS.
•
Provider affiliation announcements made by providers may not include marketing
content. For example, an announcement that says Dr. Smith is now accepting Medicare
Advantage X, and then provides cost sharing or other marketing content/intent (e.g.
Plan X is the greatest Medicare Advantage Plan) would be prohibited.
12
Required materials and content (42 CFR §§ 422.2267, 423.2267)
Unless otherwise noted, the materials below designated as communications materials do not
require HPMS submission.
§§ 422.2267(a)(2), 423.2267(a)(2) - For markets with a significant non-English speaking
population
•
ID cards are exempt from the translation requirements for markets with a significant
non-English speaking population described at §§ 422.2267(a)(2) and 423.2267(a)(2).
§§ 422.2267(d)(1), 423.2267(d)(1) - When multiple enrollees are living in the same
household
•
When mailing materials to more than one individual living in the same household, the
materials (e.g., envelope, cover letter) must clearly notate each individual name.
•
Members in community residences (e.g., nursing facilities, group homes) must receive
their own copy of non-beneficiary-specific materials, regardless of whether they have
the same address.
§§ 422.2267(d)(2), 423.2267(d)(2) – When materials are delivered electronically
•
Documents delivered electronically will be considered to be received by the enrollee as
of the date the plan sends it; not when the enrollee opens/accesses it.
§§ 422.2267(d)(2)(i), 423.2267(d)(2)(i) – When materials are delivered electronically
without prior authorization from the enrollee
•
It is acceptable to state “currently available” if the documents have been posted prior to
the notice.
§§ 422.2267(e), 423.2267(e) - CMS Required Materials and content
Unless otherwise noted, any CMS Required Material not listed below (or required under §§
422.2267(b)(e) and 423.2267(b)(e)) are considered communications.
Plans may enclose additional benefit/plan operation materials with CMS Required Materials
unless prohibited below or in instructions (e.g., ANOC instructions). These materials should be
made distinct from the required material(s) and be related to the beneficiary’s plan.
13

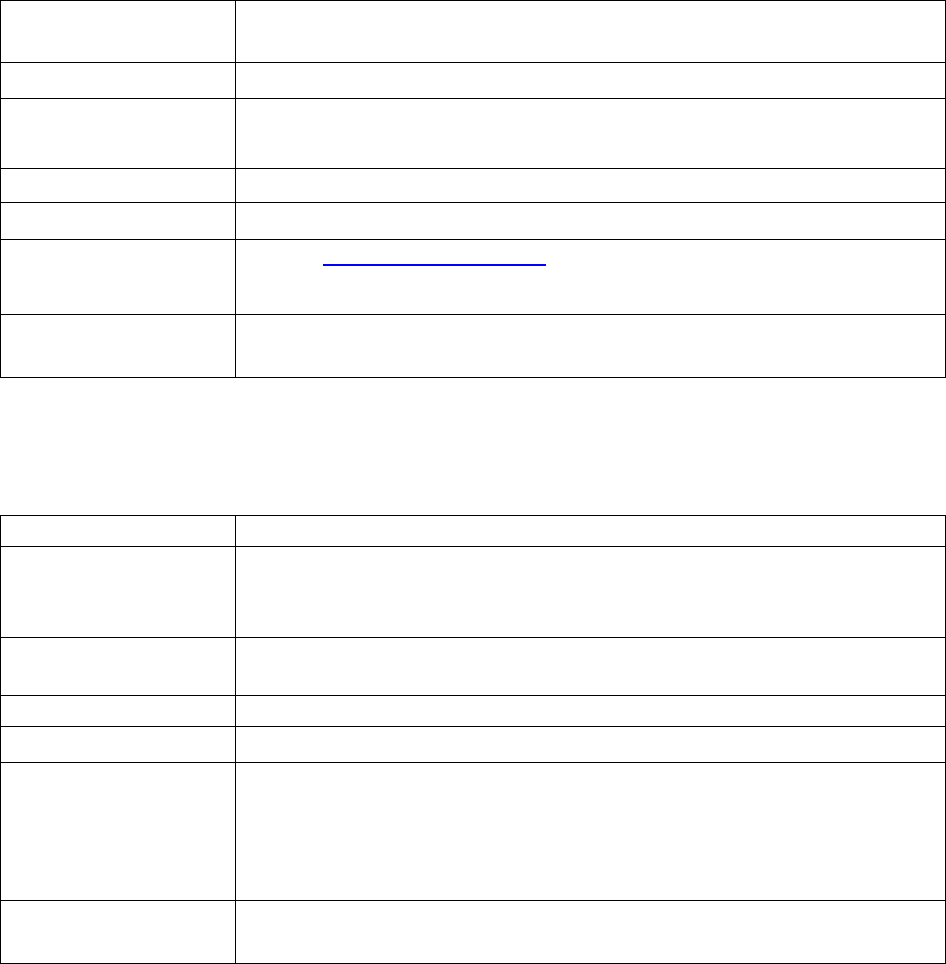
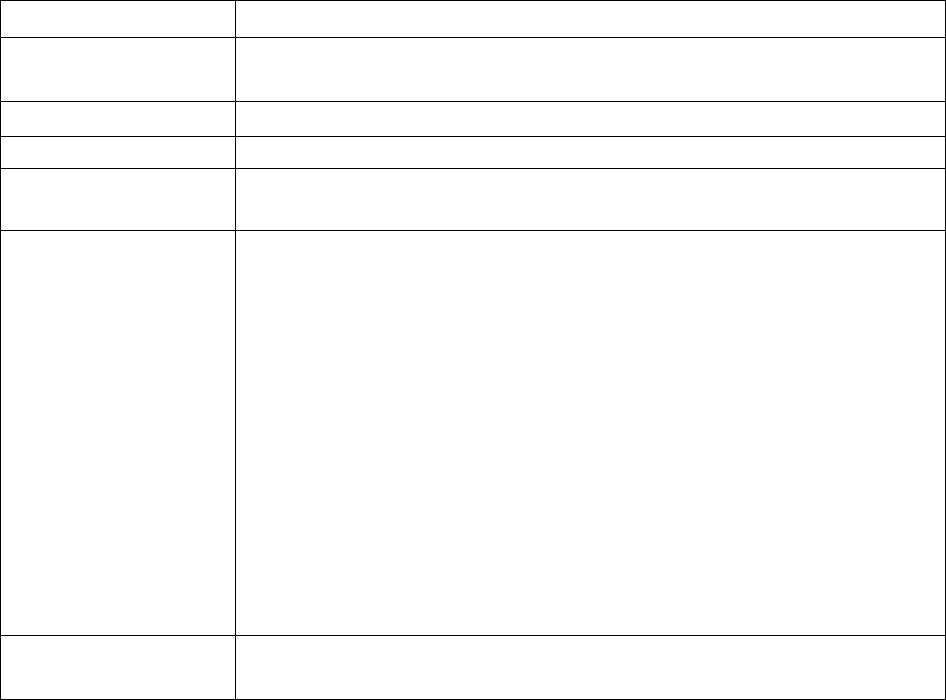
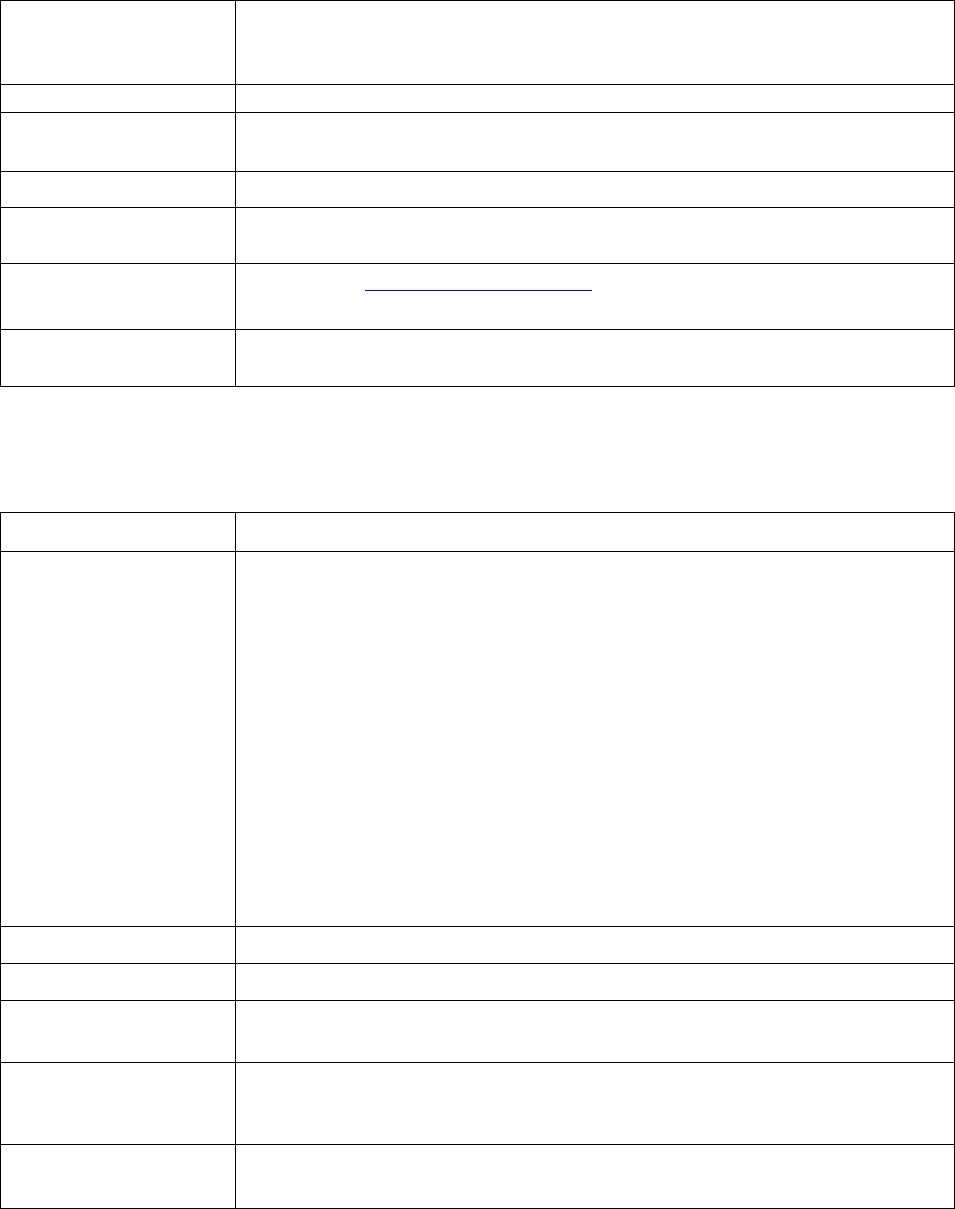
Annual Notice of Change (Marketing)
(42 CFR §§ 422.111(d)(2), 422.2267(e)(3), 422.2265(c)(1)(ii), 423.128(g)(2), 423.2267(e)(3),
423.2265(c)(1)(ii))
To Whom
Required:
Provided to current enrollees of plan, including those with October 1,
November 1, and December 1 effective dates.
Timing:
• Must send for enrollee receipt no later than September 30 of each year.
Note: ANOC must be posted on Plan/Part D website by October 15.
• October 1, November 1, and December 1 enrollees must receive within
10 calendar days from receipt of CMS confirmation of enrollment or
by last day of month prior to effective date, whichever is later.
Method of
Delivery:
Hard copy, or electronically, if enrollee has opted into receiving electronic
version as permitted in 42 CFR §§ 422.2267(d) and 423.2267(d).
HPMS:
File and Use. Must be submitted at least five days prior to mailing.
Format
Specification:
Standardized Material.
Guidance and
Other Relevant
Information:
Marketing Models, Standard Documents, and Educational Material | CMS
Translation
Required (5%
Threshold):
Yes.
ANOC (Marketing) and EOC (Communications) Errata
(42 CFR §§ 422.2261, 422.2262, 423.2261, 423.2262)
To Whom
Required:
Provided to current enrollees when errors are found in the ANOC or EOC.
Timing:
Must send to enrollees immediately following CMS approval.
Method of
Delivery:
Hard copy, or electronically if enrollee has opted into receiving electronic
version as permitted in 42 CFR §§ 422.2267(d) and 423.2267(d).
HPMS:
Where required, ANOC errata must be submitted by October 15, and EOC
errata must be submitted by November 15.
Format
Specification:
Standardized material.
Guidance and
Other Relevant
Information:
Refer to the annual Health Plan Management System memo “Issuance of
Contract Year Model Materials” and “Contract Year Annual Notice of
Change and Evidence of Coverage Submission Requirements and Yearly
Assessment” memos.
Translation
Required (5%
Threshold):
Yes.
14
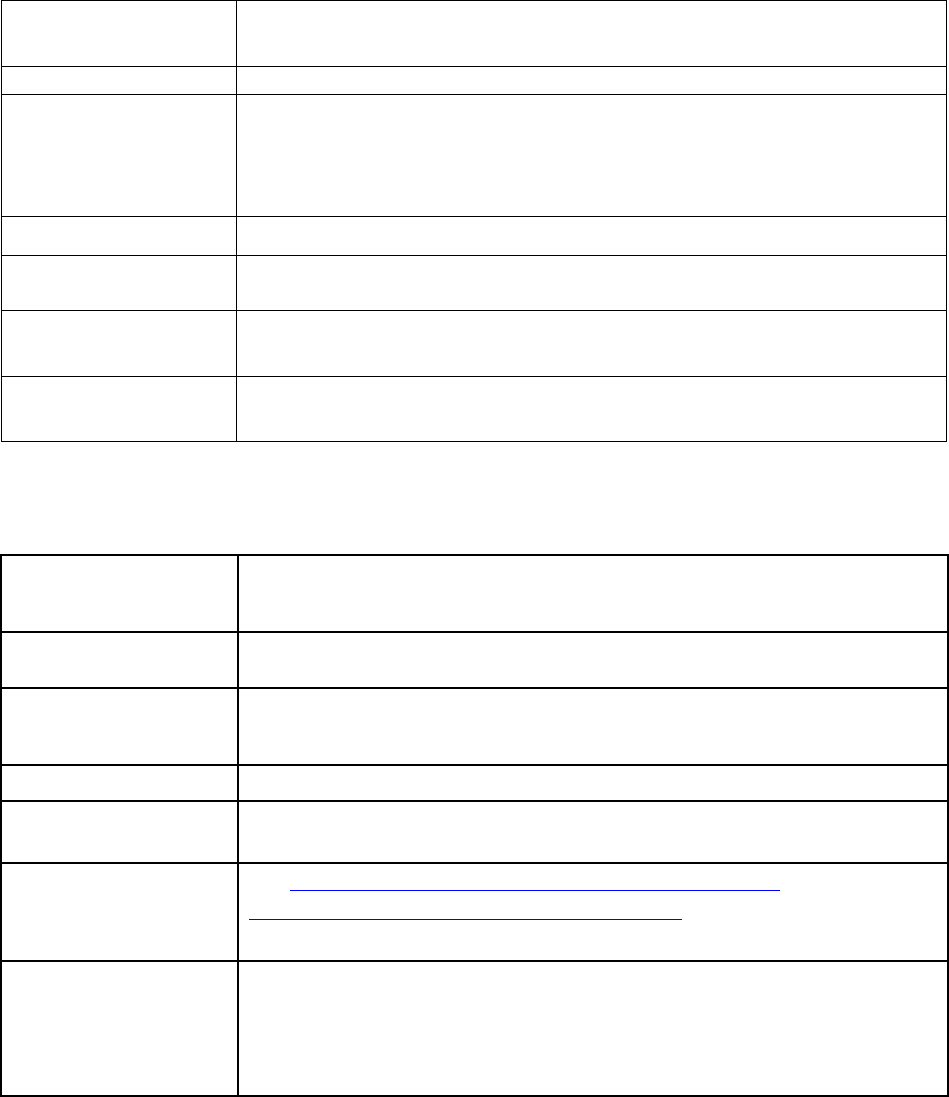
Comprehensive Medication Review Summary (Communication)
(42 CFR §§ 423.153(d)(1)(vii)(B) and (D))
To Whom
Required:
Provided to enrollees in a plan’s Medication Therapy Management
(MTM) program after receiving a comprehensive medication review
(CMR).
Timing:
May be provided to enrollee immediately following a CMR, or if
distributed separately, materials should be sent out within 14 calendar days.
Method of
Delivery:
Hard copy, or electronically if enrollee has opted into receiving electronic
version as permitted in § 423.2267(d).
HPMS:
Not applicable.
Format
Specification:
Standardized OMB-approved Format (Form CMS-10396, OMB Control
Number 0938-1154).
The Format cannot be modified, but the specific content to populate the
Format must be tailored to address issues unique to the individual enrollee
and may be customized for the Part D plan and MTM program.
Guidance and
Other Needed
Information:
See https://www.cms.gov/Medicare/Prescription-Drug-
Coverage/PrescriptionDrugCovContra/MTM for
• CMR Standardized Format and detailed implementation
instructions, and
• Annual MTM Program Submission Instructions memo.
Note
: MTM program materials should not include any marketing or
promotional messages.
Translation
Required (5%
Threshold):
Yes.
15
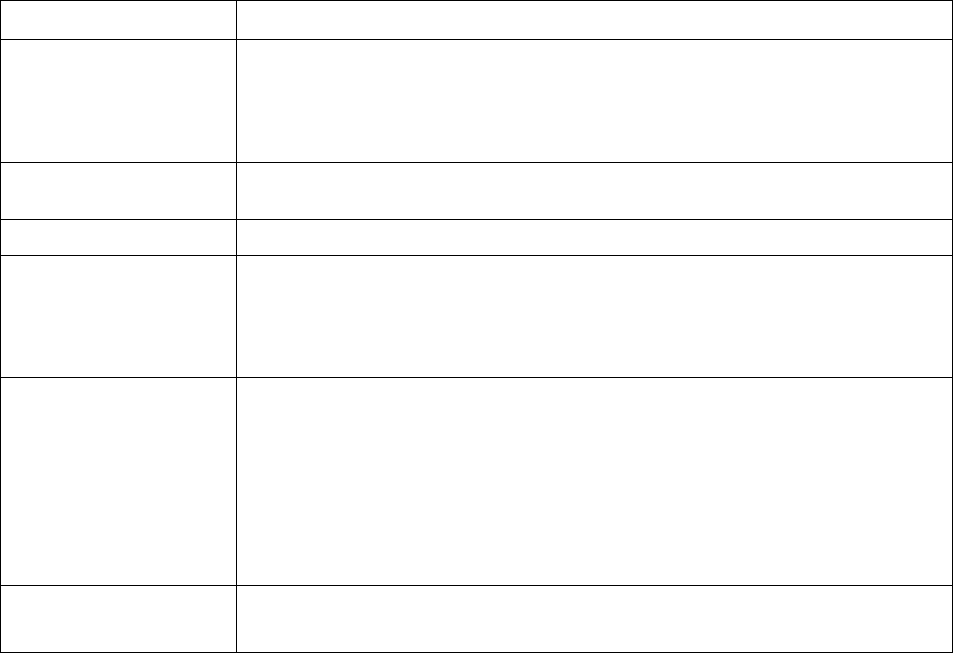
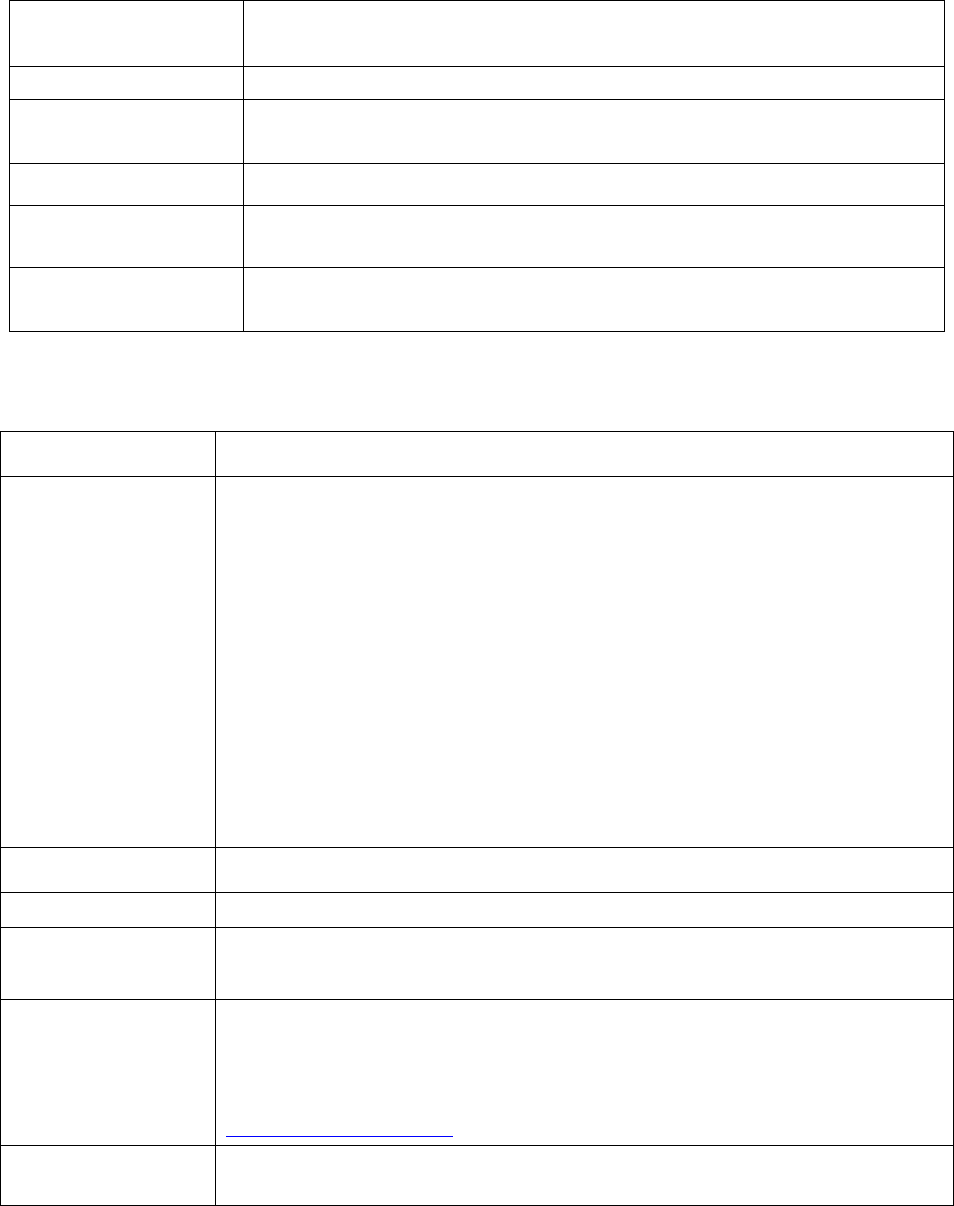
Coverage/Organization Determination, Discharge, Appeals and Grievance Notices
(Communications)
(42 CFR §§ 422.2267(e)(14) and (16)-(29), 423.2267(e)(18) and (20)-(31))
To Whom
Required:
Provided to enrollees who have requested an appeal or have had an
appeal requested on their behalf.
Timing:
Provided to enrollees on an ad hoc basis, based on required timeframes
in 42 CFR Parts 422 and 423, subpart M.
Method of
Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR §§ 422.2267(d) and
423.2267(d).
HPMS:
Not applicable.
Format
Specification:
Standardized OMB-approved denial notices for initial coverage denials
(e.g. NDMCP); model notices for plan level appeals (Notice of Right to
an Expedited Grievance).
Guidance and
Other Relevant
Information:
Parts C & D Enrollee Grievances, Organization/Coverage
Determinations, and Appeals Guidance
Medicare Managed Care Appeals & Grievances | CMS
Translation
Required (5%
h h ld)
Yes.
Enrollment/Election Form/Request (Communications)
(Sections 1851(h)(1) and 1860D-01(b)(1)(vi) of the Social Security Act; 42 CFR §§ 422.60(c),
422.2267(e)(6); 423.32(b), 423.2267(e)(6))
To Whom Required:
Provided upon request.
Timing:
Not applicable.
Method of Delivery:
Paper enrollment forms may be in hard copy or electronic format (e.g.,
PDF file). Plans are permitted to send via email (when the beneficiary
has authorized), online (e.g. portal) for current members (when the
enrollee has authorized), and upon request (e.g., if beneficiary does not
want to enroll telephonically or electronically).
HPMS:
Submission required by statute.
Format
Specification:
Model Material. Must follow requirements for enrollment mechanisms
and required data elements outlined in enrollment guidance.
Guidance and Other
Relevant
Information:
Eligibility, Enrollment, and Disenrollment – Medicare Managed Care
Manual - Chapters 2 and 17d (collectively “Enrollment Guidance), and
Parts C & D Enrollee Grievances, Organization/Coverage
Determinations, and Appeals Guidance
Translation Required
(5% Threshold):
Yes.
16
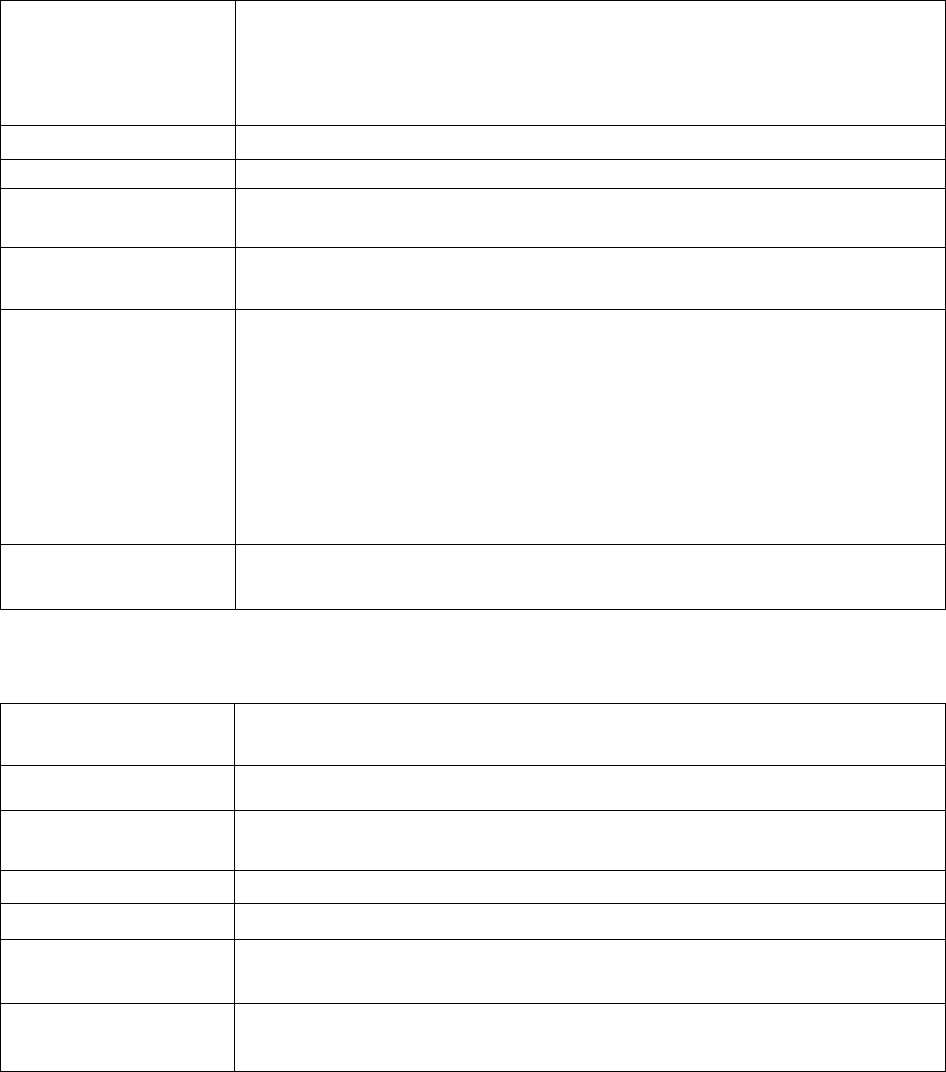
Enrollment and Disenrollment Notices (Communications)
(42 CFR §§ 422.60(e)(3), 422.74(b), 422.2267(e)(7), 422.2267(e)(8), 423.32(d), 423.36(b)(2),
423.2267(e)(7), 423.2267(e)(8))
To Whom Required:
Provided as outlined in enrollment guidance.
Timing:
Must follow required timeframes as outlined in enrollment guidance.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR §§ 422.2267(d) and
423.2267(d).
HPMS:
Not applicable.
Format
Specification:
Model material. Include elements as outlined in enrollment guidance.
Guidance and Other
Relevant
Information:
Eligibility, Enrollment, and Disenrollment – Medicare Managed Care
Manuals:
• Chapter 2 - Medicare Advantage Enrollment and Disenrollment
• Chapter 17d - Subchapter D – Medicare Cost Plan Enrollment and
Disenrollment Instructions
Parts C & D Enrollee Grievances, Organization/Coverage
Determinations, and Appeals Guidance
Translation
Required (5%
Threshold):
Yes.
Evidence of Coverage (Communications)
(42 CFR §§ 422.111(b), 422.2267(e)(1), 423.128(b,) 423.2267(e)(1))
To Whom Required:
Provided to all plan enrollees. October 1, November 1, and December 1
enrollees must receive the current EOC and the next calendar year EOC.
Timing:
• Provided to current plan enrollees by October 15 of each year.
• Pr
ovided to new plan enrollees within 10 calendars days from receipt
of CMS confirmation of enrollment
or by last day of month prior to
effective date, whichever is later.
Method of Delivery:
Hard copy, or electronically, as permitted in 42 CFR §§ 422.2267(d) and
423.2267(d).
HPMS:
File and Use.
Format Specification:
Standardized Material
Guidance and Other
Relevant Information:
No additional information.
Translation Required
(5% Threshold):
Yes.
17
Excluded Provider Notice (Communications)
(42 CFR §§ 422.2267(e)(15), 423.2267(e)(19))
To Whom Required:
Provided to members who have used a provider who has been excluded
from participating in the Medicare Program based on an OIG exclusion
or the CMS preclusion list.
Timing:
Provided on an ad hoc basis.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR §§ 422.2267(d) and
423.2267(d)
.
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Relevant Information:
Office of the Inspector General Exclusion Program
Translation Required
(5% Threshold):
Yes.
Explanation of Benefits – Part C (Communications)
(42 CFR §§ 422.111(k), 422.2267(e)(2))
To Whom Required:
Provided to enrollees anytime a Part C benefit is utilized.
Timing:
Plan may send monthly or per claim with a quarterly summary.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR § 422.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Relevant Information:
Medicare Managed Care Manual, Chapter 4, Section 190.
Translation Required
(5% Threshold):
Yes.
18
Explanation of Benefits – Part D (Communications)
(42 CFR §§ 423.2267(e)(2), 423.128(e))
To Whom Required:
Provided to enrollees anytime their prescription drug benefit is utilized.
Timing:
Must be provided by the end of month following the month when
benefit was utilized.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR § 423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Relevant Information:
Medicare Prescription Drug Manual Chapters 5 and 6.
Translation Required
(5% Threshold):
Yes.
Formulary (Communications)
(42 CFR §§ 423.2267(e)(9), 423.128(b)(
4))
To Whom Required:
Provided to all enrollees of plan.
Timing:
• Must be provided to current enrollees of plan by October 15 of each
year.
• Provide to new enrollees within 10 calendars days from receipt of
CMS confirmation of enrollment or by last day of month prior to
effective date, whichever is later.
Method of Delivery:
Hard copy, or electronically, as permitted in 42 CFR § 423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Relevant Information:
Refer to Part D Model Materials and Medicare Prescription Drug
Benefit Manual, Chapter 6.
Translation Required
(5% Threshold):
Yes.
19
Low Income Subsidy (LIS) Notice (Communications)
(42 CFR § 423.2267(c)(10))
To Whom Required:
Provided to potential enrollees once they are eligible for Extra Help and
receive the low-income subsidy.
Timing:
Provided prior to effective date of enrollment.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Relevant Information:
Refer to Part D Model Materials
Translation Required
(5% Threshold):
Yes.
Low Income Subsidy (LIS) Rider (Communications)
(42 CFR § 423.2267(e)(11))
To Whom Required:
Provided to all current enrollees who qualify for Extra Help.
Timing:
• Provided at least once per year by September 30.
• Sent to enrollees who qualify for Extra Help or have a change in
LIS levels within 30 days of receiving notification from CMS.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR § 423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Relevant Information:
D-SNP enrollees who have $0 cost-sharing for all Part D drugs are
exempt from sending a separate LIS Rider since the EOC’s cost-sharing
Information for drug copays is the same for everyone
Medicare Prescription Drug Benefit Manual, Chapter 13, Section 70.2.
Translation Required
(5% Threshold):
Yes.
20
Membership ID Cards (Communications)
(42 CFR §§ 417.427, 422.111(i), 423.120(c))
To Whom Required:
Provided to all plan enrollees.
Timing:
Provided to new enrollees within 10 calendars days from receipt of CMS
confirmation of enrollment or by last day of month prior to effective
date, whichever is later. Must also be provided to all enrollees if
information on existing card changes.
Method of Delivery:
Provided in hard copy. In addition to the hard copy, plans may also
provide a digital version (e.g., app).
HPMS:
Not applicable.
Format Specification:
Model material. Combination health and drug cards must follow the
Workgroup for Electronic Data Interchange (WEDI) standards.
Standalone Part D cards must follow the National Council for
Prescription Drug Program (NCPDP) standards.
Guidance and Other
Relevant Information:
• Cards must include Plan’s/Part D sponsor’s website address,
customer service number, and contract/PBP number.
• The front of the Part D sponsor card must include the Medicare
Prescription Drug Benefit Program Mark.
• PPO and PFFS ID cards must include the phrase “Medicare limiting
charges apply.”
• May not use social security number (SSN).
Translation Required
(5% Threshold):
No.
21
Mid-Year Change Notification to Enrollees (Communications)
(42 CFR §§ 422.2267(e)(9), 423.2267(e)(12), 423.120(b)(5))
To Whom Required:
Provided to all applicable enrollees when there is a mid-year change in
benefits, plan rules, formulary.
Timing:
Ad hoc, based on specific requirements for each issue.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR §§ 422.2267(d) and
423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model Material.
Guidance and Other
• Notices of changes in plan rules unless otherwise addressed in
Relevant Information:
regulation must be provided 30 days in advance.
• National Coverage Determination (NCD) changes announced or
finalized less than 30 days before effective date, notification
required as soon as possible.
• Mid-year NCD or legislative changes must be provided no later than
30 days after the NCD is announced or the legislative change is
effective.
• Plans may include change in next plan mass mailing (e.g.,
newsletter), provided it is within 30 days and must be reflected on
Plan/Part D website.
• Medicare Prescription Drug Benefit Manual - Chapter 6 for
guidance related to midyear formulary changes and required notice.
Updates to the chapter related to immediate generic substitutions
consistent with 42 CFR 423.120(b)(5)(iv) are forthcoming.
Sponsors should refer to the relevant regulation at 42 CFR
423.120(b)(5).
• National Coverage Determination website.
Translation Required
(5% Threshold):
Yes.
22
Non-Renewal Notices (Communication)
(42 CFR §§ 417.492(a)(ii) and (b)(ii), 422.74(d)(7), 422.506, 422.2267(e)(10), 423.44(d)(6),
423.507, 423.2267(e)(13))
To Whom Required:
Provided to enrollees affected by a non-renewal or service area
reduction.
Timing:
At least 90 days before the end of the current contract year. Cost Plans,
without Part D, at least 60 days before the end of the current contract year.
Method of Delivery:
Notices must be hard copy and sent via U.S. mail. First class postage is
recommended.
HPMS:
Not applicable.
Format Specification:
Model material. - current contract year. Modifications permitted per
instructions.
Guidance and Other
Needed Information:
• Information about non-renewals or service area reductions may not be
released to the public, including current enrollees, until notice is
received from CMS.
• Plans may elect to share Non-Renewal and Service Area Reduction
(NR/SAR) information only with first tier, downstream, and related
entities (FDRs) or anyone that the plan does business with (i.e.,
contracted providers).
• Plans must provide a NR/SAR notice to beneficiaries who enroll in a
non-renewing plan on October 1, November 1, or December 1 of the
current contract year (e.g., less than 90 days before the effective date
of the non-renewal).
• Additional NR/SAR notice information can be found in the annual
“Non-Renewal and Service Area Reduction Guidance and Enrollee
Notification Models” HPMS memo.
Translation Required
(5% Threshold):
Yes.
23
Outbound Enrollment Verification (Communications)
(42 CFR §§ 422.2272(b), 423.2272(b))
To Whom Required:
Provided for all agent/broker assisted enrollments.
Timing:
Must be conducted within 15 calendar days following the receipt of the
enrollment request.
Method of Delivery:
Hard copy, telephonic, email.
HPMS:
Not applicable.
Format Specification:
Model material. Must include required content.
Guidance and Other
Needed Information:
•
Communication must address enrollment into plan and provide
customer service number for beneficiary questions regarding costs,
benefits, rules, or any other question about plan.
•
May be completed via phone call (including during welcome call) or
via email, if email is requested by an enrollee.
•
Must send a written communication if the plan
fails to speak with the
individual within 15 calendar days of enrollment requests.
•
Agent/brokers are not permitted to be part of the enrollment
verification call.
•
Enrollment verification processes must stop if plan is notified that
beneficiary is ineligible to enroll in plan or if beneficiary has
canceled the enrollment.
•
Method and timing of the enrollment verification must be
documented (date, time, and method of contact).
Translation Required
(5% Threshold):
Yes.
24
Part D Transition Letter (Communications)
(42 CFR § 423.2267(e)(14))
To Whom Required:
Provided when a beneficiary receives a transition fill for a non-
formulary drug.
Timing:
Sent within three (3) days of adjudication of temporary transition fill.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR § 423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material. Modifications permitted.
Guidance and Other
Needed Information:
Medicare Prescription Drug Benefit Manual Chapter 6, Section
30.4.10.
Pharmacy Directory (Communications)
(42 CFR §§ 423.128, 423.2267(e)(15))
To Whom Required:
Provided to all plan enrollees.
Timing:
• Provided to current plan enrollees by October 15 of the year prior to the
applicable year.
• Provided to new plan enrollees within 10 calendars days from receipt
of CMS confirmation of enrollment or by last day of month prior to
effective date, whichever is later.
• Must be provided to current enrollees upon request, within three (3)
business days of the request.
• Part D plans must update pharmacy directory information any time
they become aware of changes. All updates to the online provider
directories must be completed within 30 days of receiving information
requiring update. Updates to hardcopy provider directories must be
completed within 30 days, however, hardcopy directories that include
separate updates via addenda are considered up-to-date.
Method of Delivery:
Hard copy, or electronically, as permitted in 42 CFR § 423.2267(d).
HPMS:
Not applicable.
Format
Specification:
Model material. Current Contract Year Pharmacy Directory. Modifications
permitted per instructions.
Guidance and Other
Needed
Information:
See the HPMS memo dated August 16, 2016 (Pharmacy Directories and
Disclaimers) for information regarding electronic and hard copy directory
requirements.
Part D Model Materials
Translation
Required (5%
Yes.
25
Plan Termination Notices (Communication)
(42 CFR §§ 422.508(a), 422.510(b), 422.512(b), 422.2267(e)(10), 423.508(b), 423.509(b), 423.510(b),
423.2267(e)(13))
To Whom Required:
Provided to affected enrollees before the plan termination effective date.
Timing:
CMS and Plan/Part D provider-initiated terminations require enrollee
notices be sent as specified in CFR Title 42.
Method of Delivery:
• Notices must be hard copy and sent via U.S. mail. First class
postage is recommended.
• Notice to the general public requires publishing in one or more
newspapers of general circulation.
HPMS:
Not applicable.
Format Specification:
Model required - Current contract year.
Guidance and Other
Needed Information:
Relevant plan termination notice requirements are provided at §§
422.111, 422.508, 422.510, 422.512, 422.2267, 423.508, 423.509,
423.510 and 423.2267.
Translation Required
(5% Threshold):
Yes.
Pre-Enrollment Checklist (Communications)
(42 CFR §§ 422.2267(e)(4), 423.2267(e)(4))
To Whom Required:
Provided to potential enrollees with the Summary of Benefits (SB) when
the SB is accompanying an enrollment form.
Timing:
Prior to enrollment.
Method of Delivery:
In the same format the SB was provided.
HPMS:
Not applicable.
Format Specification:
Standardized material. Modifications to disclaimer language not
permitted, however, plans may delete bullets that do not apply to a
specific plan type. If the pre-enrollment checklist is used for multiple
products, additional language may be added before or after the
disclaimer to clarify or distinguish how a disclaimer applies to products.
Guidance and Other
Needed Information:
Must accompany the SB. Refer to Appendix 1.
Translation Required
(5% Threshold):
Yes.
26
Prescription Transfer Letter (Communications)
(42 CFR § 423.2267(e)(16))
To Whom Required:
Provided to enrollees if a Part D sponsor is requesting permission to fill
a prescription at a different network pharmacy than the one currently
being used by enrollee.
Timing:
Ad hoc.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in 42 CFR § 423.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Needed Information:
Refer to the Part D Model Materials
Translation Required
(5% Threshold):
Yes.
Provider Directory (Communications)
(42 CFR §§ 422.111(b)(3), 422.2267(e)(11))
To Whom Required:
Provided to all plan enrollees.
Timing:
• Provided to current plan enrollees by October 15 of the year prior to
the applicable year.
• Provided to new plan enrollees within 10 calendars days from
receipt
of CMS confirmation of enrollment or by last day
of month prior to
effective date, whichever is later.
• Must be provided to current enrollees upon request, within three (3)
business days of the request.
• Plans must update directory information any
time they become aware
of changes. All updates to the online provider directories must be
completed within 30 days of receiving information requiring update.
Updates to hardcopy provider directories must be completed within 30
days, however, hardcopy direc
tories that include separate updates via
addenda are considered up-to-date
Method of Delivery:
Hard copy, or electronically, as permitted in 42 CFR § 422.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material. Current Contract Year Provider Directory. Modifications
permitted per instructions.
Guidance and Other
Needed Information:
Chapter 4 of the Medicare Managed Care Manual, and Medicare
Advantage and Section 1876 Cost Plan Provider Directory Model.
Translation Required
(5% Threshold):
Yes.
27
Provider Termination Letter to Beneficiaries (Communications)
(42 CFR §§ 422.111(e), 422.2267(e)(12))
To Whom Required:
Provided to all applicable enrollees, per 42 CFR §422.111(e), when their
provider will no longer be part of the plan network.
Timing:
At least 30 days prior to the termination effective date.
Method of Delivery:
Notices must be hard copy and sent via U.S. mail (first class postage
recommended). Plans may also send notices electronically if enrollee
has opted into receiving electronic version as permitted in 42 CFR §
422.2267(d).
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Needed Information:
Chapter 4 of the Medicare Managed Care Manual.
Translation Required
(5% Threshold):
Yes.
Safe Disposal Information (Communication)
(42 CFR §§ 422.111(j), 423.153(d)(1)(vii)(E) and (F))
To Whom Required:
Provided to enrollees in a plan’s MTM program as part of the CMR,
targeted medication review, or other MTM correspondence or service.
Timing:
At least once annually beginning on January 1, 2022.
Method of Delivery:
Hard copy, or electronically if enrollee has opted into receiving
electronic version as permitted in §§ 422,2267(d) and 423.2267(d).
HPMS:
Not applicable.
Format Specification:
No model required. This information must comply with all
requirements of § 422.111(j).
Guidance and Other
Needed Information:
See https://www.cms.gov/Medicare/Prescription-Drug-
Coverage/PrescriptionDrugCovContra/MTM for Annual MTM
Program Submission Instructions memo.
Translation Required
(5% Threshold):
Yes.
28

Scope of Appointment (Communications)
(
Sections 1851(j)(2)(A) and 1860D-04(l) of the Social Security Act;
42 CFR §§422.2264(c), 422.2266(d)-(f), 422.2274(b)-(c), 423.2264(c), 423.2266(d) and (e),
422.2274(b)-(c))
To Whom Required:
Documented for all marketing activities, in-person, telephonically,
including walk-ins to plan or agent offices.
Timing:
Prior to the appointment.
Method of Delivery:
Signed hard copy, telephonic recording (telephonic appointments only),
or electronically signed.
HPMS:
Not applicable.
Format Specification:
Model material.
Guidance and Other
Needed Information:
The following requirements must be on the scope of appointment form
or on the recorded call:
•
Product types to be discussed.
•
Date of appointment.
•
Beneficiary and agent contact information.
•
Statement stating, no obligation to enroll, current or future
Medicare enrollment status will not be impacted, and
automatic enrollment will not occur.
A new SOA is required if the beneficiary requests information regarding
a different plan type than previously agreed upon.
Translation Required
(5% Threshold):
Yes.
29
Star Ratings Document (Marketing)
(42 CFR §§ 422.2267(e)(13), (423.2267(e)(17))
To Whom Required:
Provided to all prospective enrollees when an enrollment form is
provided. For online enrollment, Star Ratings document must be made
available electronically (e.g., via link) prior to the completion and
submission of enrollment request.
Timing:
Provided prior to enrollment.
Method of Delivery:
Hard copy or via electronic mechanism.
HPMS:
Must be uploaded within 21 calendar days of the release of the updated
information.
Format Specification:
Standardized. Star Ratings document is generated from HPMS.
Guidance and Other
Needed Information:
• New plans that have no Star Ratings are not required to provide until
the following contract year.
• Updated Star Ratings must be used within 21 calendar days of
release of updated information on Medicare Plan Finder.
• Updated Star Ratings must not be used until CMS releases Star
Ratings on Medicare Plan Finder.
• Only the plan logo may be added to the document (no other changes
or alterations are permitted).
Translation Required
(5% Threshold):
Yes.
Summary of Benefits (Marketing)
(42 CFR §§ 422.2267(e)(5), 423.2267(e)(5))
To Whom Required:
Provided to all prospective enrollees when an enrollment form is
provided.
Timing:
Available by October 15 of each year.
Method of Delivery:
Hardcopy or electronic, depending on the format of the enrollment
mechanism.
HPMS:
Submitted prior to October 15 of each year.
Format Specification:
Model material.
Guidance and Other
Needed Information:
Refer to Appendix 2
Translation Required
(5% Threshold):
Yes.
30
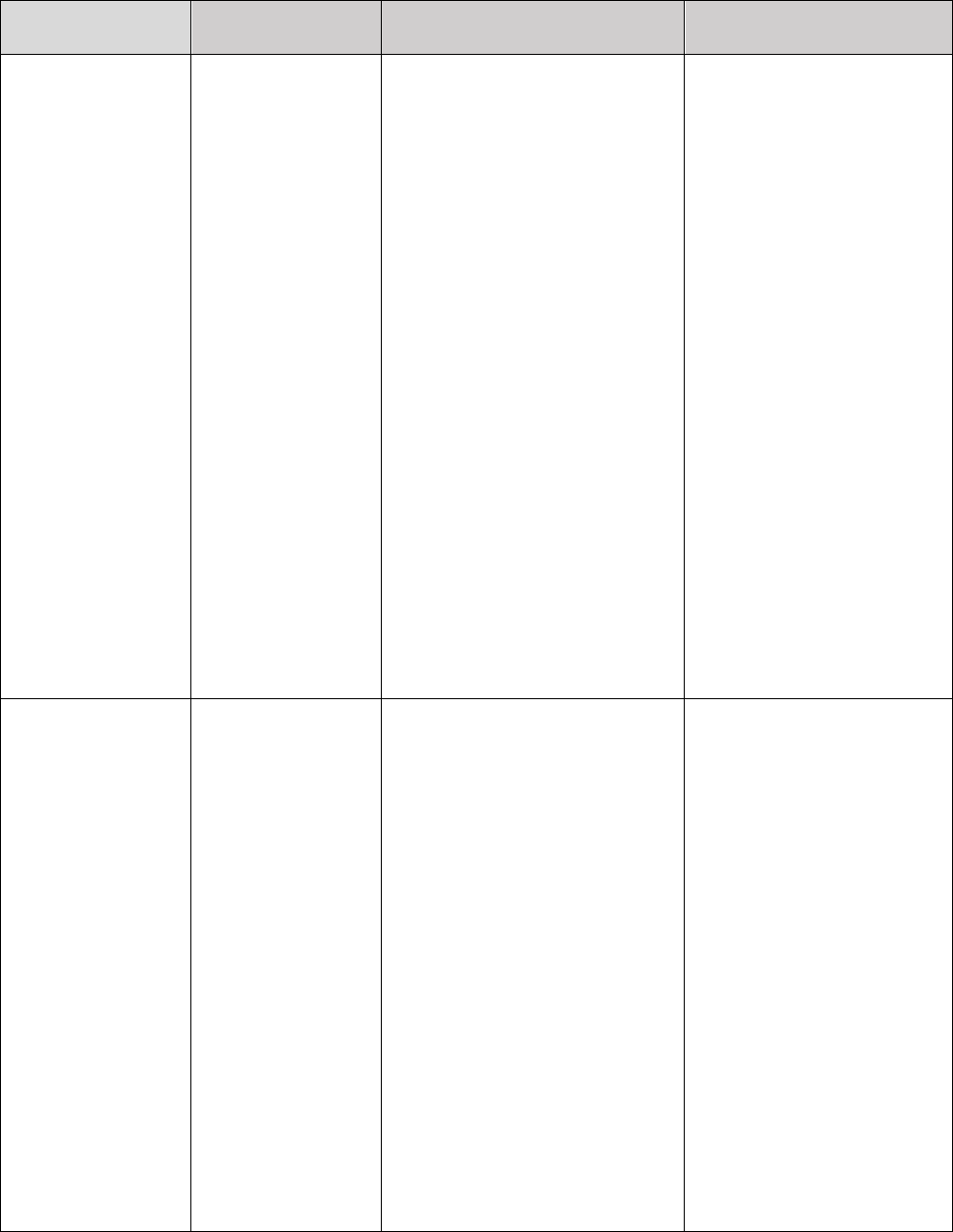
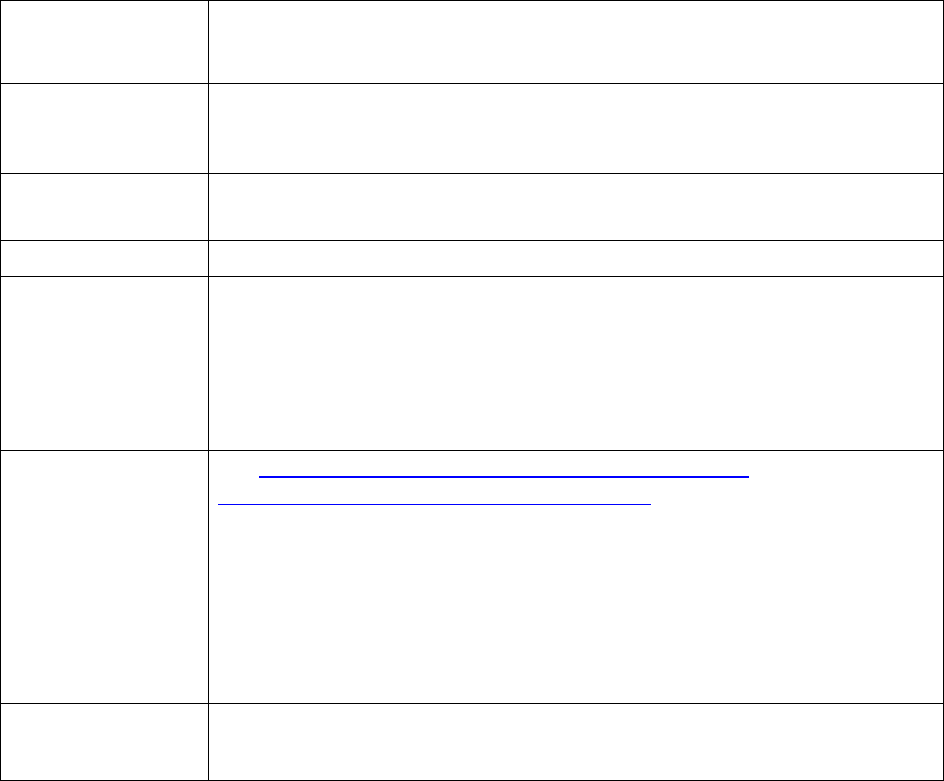
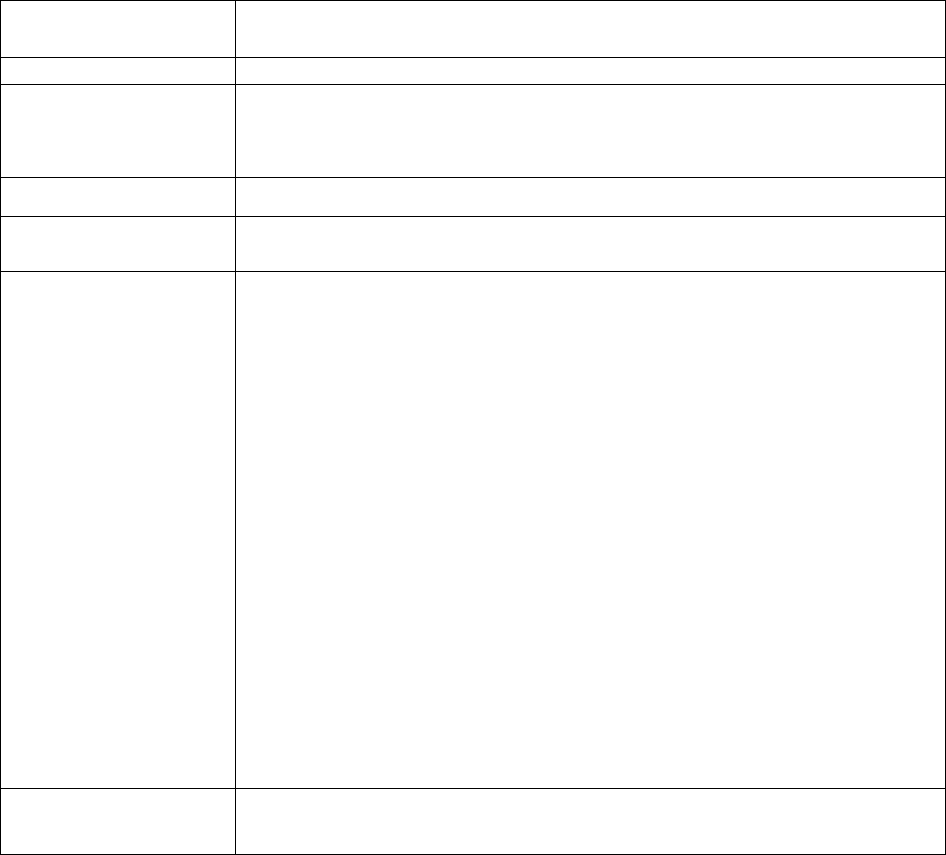
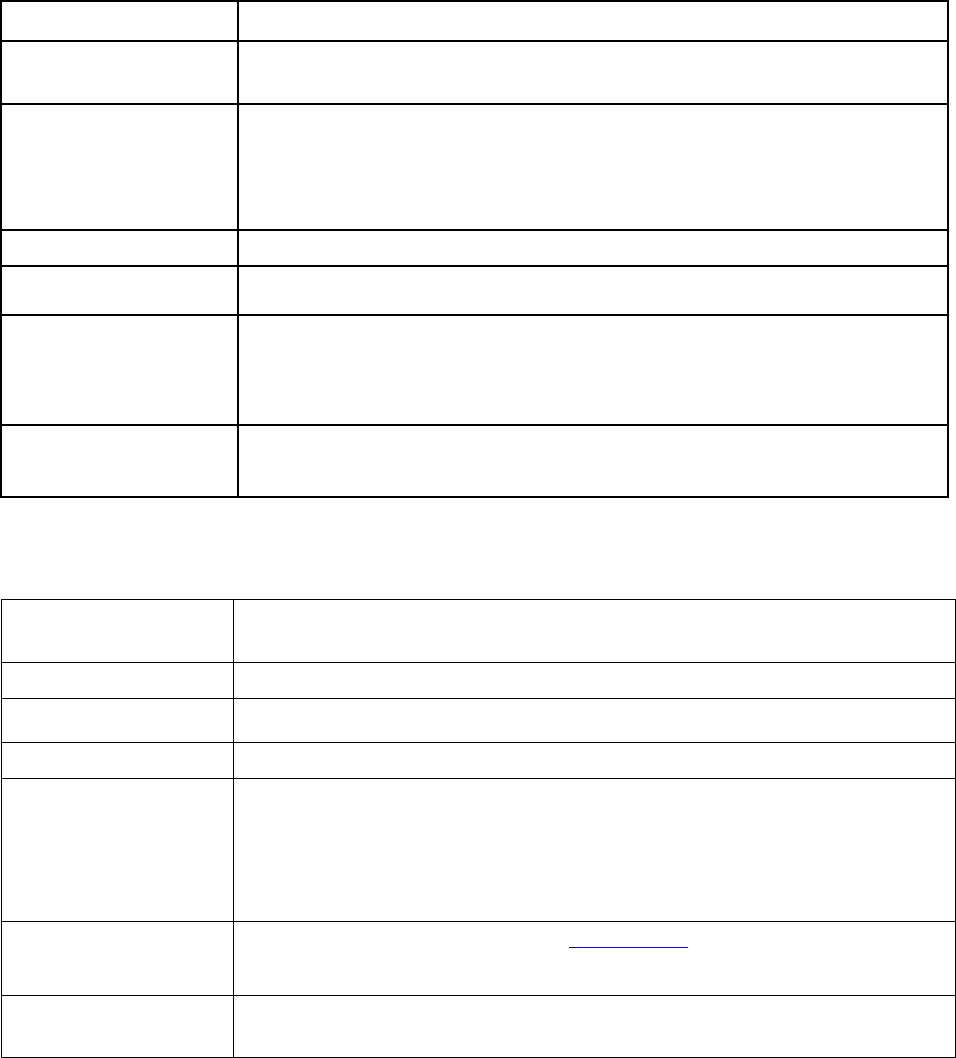
Disclaimers
Disclaimer
42 CFR
Section(s)
Model or Standardized
Content
Applicable Documents
and Notes
Federal
422.2267(e)(30)
Model Content:
Required on all marketing
Contracting 423.2267(e)(32) Disclaimer must include: materials except: Banners
Statement
• Legal or marketing name
of the organization.
• Type of plan (e.g., HMO,
HMO SNP, PFFS, PDP).
• A statement that the
organization has a
contract with Medicare
(when applicable, plans
may also state that the
organization has a
contract with the
state/Medicaid program).
• A statement that
enrollment depends on
contract renewal.
Example:
“[Plan’s legal or marketing
name] is a [plan type] with a
Medicare contract.
Enrollment in [Plan’s legal or
marketing name] depends on
contract renewal.”
and banner-like
advertisements, outdoor
advertisements, text
messages, social media,
and envelopes.
Plans should incorporate
contract with
state/Medicaid Program
when appropriate.
Star Ratings
422.2267(e)(31)
423.2267(e)(33)
Model Content:
• Convey that plans are
evaluated yearly by
Medicare
• Convey that the ratings are
based on a 5-star rating
system
Example:
“Every year, Medicare
evaluates plans based on a 5-
star rating system.”
Must be used whenever
Star Ratings are
mentioned in marketing
materials, with the
exception of when Star
Ratings are published on
small objects (e.g., that
pens or rulers).
Model content may be
provided in disclaimer
form or within the
material.
Because of the space
limitations associated with
electronic media such as
search ads and social
media, it is acceptable to
provide the Star Ratings
31
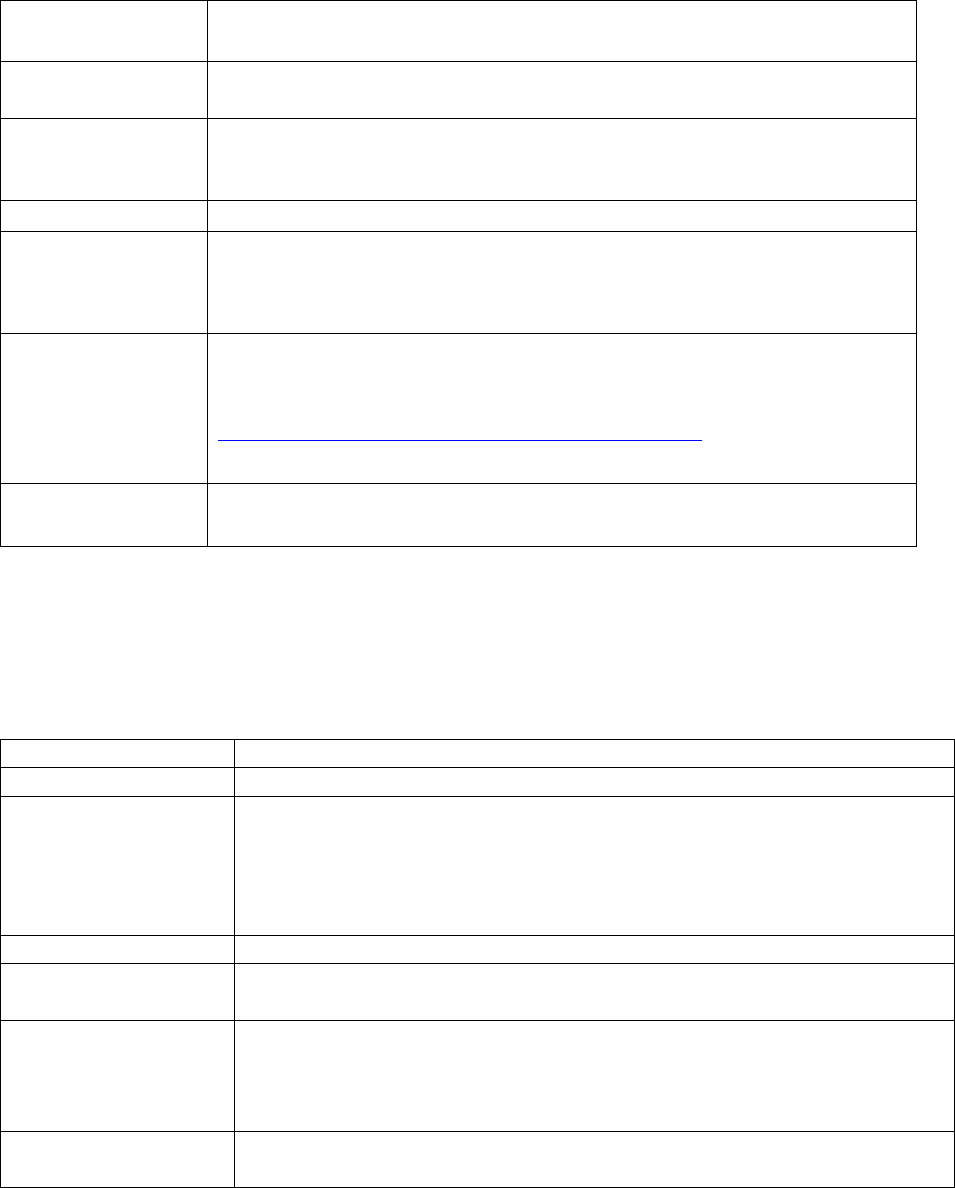
Disclaimers
Disclaimer
42 CFR
Section(s)
Model or Standardized
Content
Applicable Documents
and Notes
disclaimer to the viewer
when they click on the ad.
Accommodations
422.2267(e)(33)
423.2267(e)(34)
Model Content:
• Convey that
accommodations for
persons with special needs
is available.
• Provide a telephone
number and TTY number.
Example:
“For accommodations of
persons with special needs at
meetings call <insert phone
and TTY number>.”
Must be in any
advertisement of
invitations to all events as
described under §§
422.2264(c) and
423.2264(c).
Model content may be
provided in disclaimer
form or within the
material.
Special
422.2267(e)(32)
Model Content:
Must be used whenever
Supplemental
• Convey the benefits
SSBCI benefits are
Benefits for the
mentioned are special
mentioned.
Chronically Ill
supplemental benefits.
(SSBCI)
• Convey that not all
members will qualify.
Example:
“The benefits mentioned are a
part of special supplemental
program for the chronically
ill. Not all members qualify.”
Model content may be
provided in disclaimer
form or within the
material.
32
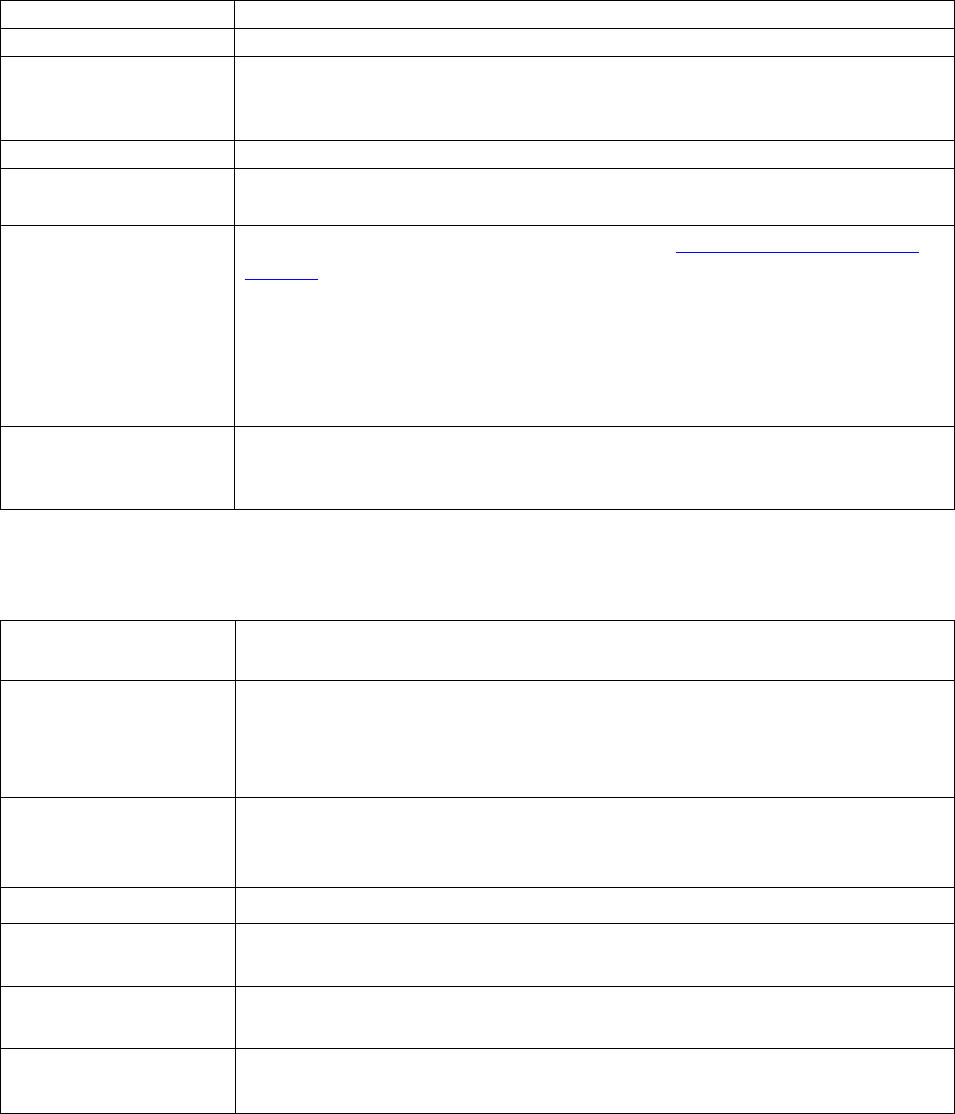
Disclaimers
Disclaimer
42 CFR
Section(s)
Model or Standardized
Content
Applicable Documents
and Notes
Mailing
Statements
422.2267(e)(34)
423.2267(e)(35)
Standardized Content:
• Include the following
statement when mailing
information about the
enrollee's current plan:
“Important [Insert Plan
Name] information.”
• Include the following
statement when mailing
health and wellness
information: “Health and
wellness or prevention
information.”
Must be included when
mailing applicable
information to current
members.
Must include the plan
name. If the plan name is
elsewhere on the
envelope, it does not need
to be repeated in the
disclaimer.
Delegated or sub
-
contracted entities and
downstream entities that
conduct mailings on
behalf of a multiple plans
must also comply with
this requirement;
however, they do not have
to include a plan name.
Promotional
Give-Away
422.2267(e)(35)
423.2267(e)(36)
Model Content:
• Convey that there is no
obligation to enroll in a
plan.
Examples:
“Eligible for a free drawing,
gift, or prizes with no
obligation to enroll.”
“Free gift without obligation
to enroll.”
Required when offering
promotional giveaways
such as drawings, prizes,
or free gifts.
Model content may be
provided in disclaimer
form or within the
material.
33
Disclaimers
Disclaimer
42 CFR
Section(s)
Model or Standardized
Content
Applicable Documents
and Notes
Provider Co-
422.2267(e)(36)
Model Content:
Must be used whenever
branded Material 423.2267(e)(37)
• Convey, as applicable, that
other pharmacies,
physicians or providers are
available in the plan's
network.
Example:
“Other
<Pharmacies/Physicians/Provi
ders> are available in our
network.”
co-branding relationships
with network provider are
mentioned, unless (for
MA and cost plans
(including MA-PD plans)
only) the co-branding is
with a provider network or
health system that
represents 90 percent or
more of the network as a
whole.
Out of Network
422.2267(e)(37)
Standardized Content:
Must be included
Non-Contracted “Out-of-network/non- whenever materials
Provider contracted providers are under
no obligation to treat Plan
members, except in
emergency situations. Please
call our customer service
number or see your Evidence
of Coverage for more
information, including the
cost-sharing that applies to
out-of-network services.”
reference out-of-
network/non-contracted
providers.
Does not apply to
standalone PDP plans.
NCQA SNP
422.2267(e)(38)
Model Content:
Required on all
Approval
• Convey that the MA
documents that reference
Statement
organization has been
approved by the National
Committee for Quality
Assurance (NCQA) to
operate as a Special Needs
Plan (SNP).
• Include the last contract
year of NCQA approval.
• Convey that the approval is
based on a review of [insert
Plan Name's] Model of
Care.
• May not include numeric
SNP approval scores.
Example:
“Based on a Model of Care
review, [Insert Plan Name]
NCQA SNP approval.
Must be used by SNPs
who have received NCQA
approval.
34
Disclaimers
Disclaimer
42 CFR
Section(s)
Model or Standardized
Content
Applicable Documents
and Notes
has been approved by the
National Committee for
Quality Assurance (NCQA) to
operate a Special Needs Plan
(SNP) through [insert last
contract year of NCQA
approval].”
35
Agent/Broker Requirements (42 CFR §§ 422.2274, 423.2274)
§§ 422.2274(b), 423.2274(b) - Agent/broker requirements
State law determines activities that require a licensed agent/broker. Unless required by
state law, the following do not require the use of state-licensed marketing representatives:
o Providing factual information;
o Fulfilling a request for materials; or,
o Taking demographic information in order to complete an enrollment application.
•
To ensure beneficiaries are not mislead or confused, licensed agents/brokers who are
customer service representatives cannot act simultaneously as both a customer service
representative and a sales/marketing agent/broker. The agent/broker must clearly state
to the beneficiary when their role changes to a marketing/sales role, subject to
beneficiary request and concurrence.
§§ 422.2274(c), 423.2274(c) - MA organization oversight
•
Plans must report, to their CMS Account Manager, all enrollments made by unlicensed
agent(s) and for-cause terminations of agents/brokers.
•
Plans must provide annual training and testing that meets CMS’ requirements as found
in the Agent and Broker Training and Testing Guidelines, posted yearly on the
CMS.gov website.
§§ 422.2274(a), 423.2274(a) - Definitions
A “like plan type” enrollment includes:
• PDP replaced by another PDP
• An MA, MA-PD, or MMP to another MA, MA-PD, or MMP, or
• A Section 1876 Cost Plan to another Section 1876 Cost Plan.
§§ 422.2274(d)(3), 423.2274(d)(3) - Renewal compensation
•
Renewal compensation may only be paid for enrollments into an MMP plan if
permitted per state MMP policy.
§§ 422.2274(d)(5)(iii)(B), - Rapid Disenrollment Compensation
• Rapid disenrollment compensation recovery does not apply when dual eligible
beneficiaries move from an MAPD to an MMP.
36

□
□
□
□
□
Appendix 1 – Standardized Pre-Enrollment Checklist (422.2267(e)(4),
423.2267(e)(4))
Instructions:
Plans must include the Standardized Pre-Enrollment Checklist with the enrollment form and the
SB.
Plans may remove parts or portions of the checklist that are not applicable to a particular plan
type or product. When the pre-enrollment checklist is used for multiple products, they may add
additional language before or after the disclaimer to clarify or distinguish how a disclaimer
applies to different products.
Pre-Enrollment Checklist
Before making an enrollment decision, it is important that you fully understand our benefits and
rules. If you have any questions, you can call and speak to a customer service representative at
[insert customer service phone number].
Understanding the Benefits
The Evidence of Coverage (EOC) provides a complete list of all coverage and services.
It is important to review plan coverage, costs, and benefits before you enroll. Visit
[insert Plan website] or call [insert plan phone number] to view a copy of the EOC.
Review the provider directory (or ask your doctor) to make sure the doctors you see now
are in the network. If they are not listed, it means you will likely have to select a new
doctor.
Review the pharmacy directory to make sure the pharmacy you use for any prescription
medicine is in the network. If the pharmacy is not listed, you will likely have to select a
new pharmacy for your prescriptions.
Review the formulary to make sure your drugs are covered.
Understanding Important Rules
In addition to your monthly plan premium [plans may delete the monthly plan premium
portion for $0 premium plans], you must continue to pay your Medicare Part B
premium. This premium is normally taken out of your Social Security check each month.
[Note: Fully integrated dual SNPs may elect to remove this section or modify it to
convey that the Part B premium is already paid. Plans that have a Part B buy-down
may alter the language to convey the amount the plan pays and the beneficiary
owes.]
37
□
□
□
□
□
□
□
Benefits, premiums and/or copayments/co-insurance may change on January 1, [insert
year].
[For plans that do not offer out of network coverage] Except in emergency or urgent
situations, we do not cover services by out-of-network providers (doctors who are not
listed in the provider directory).
[For PPO, PFFS, and other plans that offer out of network coverage] Our plan allows
you to see providers outside of our network (non-contracted providers). However, while
we will pay for covered services [HMO-POS may insert “certain covered services”], the
provider must agree to treat you. Except in an emergency or urgent situation, non-
contracted providers may deny care. [If applicable, plans must add the following
language] In addition, you will pay a higher co-pay for services received by non-
contracted providers.
[For C-SNP plans] This plan is a chronic condition special needs plan (C-SNP). Your
ability to enroll will be based on verification that you have a qualifying specific severe
or disabling chronic condition.
[For D-SNP plans] This plan is a dual eligible special needs plan (D-SNP). Your ability
to enroll will be based on verification that you are entitled to both Medicare and medical
assistance from a state plan under Medicaid. [D-SNPs may provide additional
information if they impose restrictions to specific Medicaid eligibility category(ies)]
[For I-SNP plans] This plan is an institutional special needs plan (I-SNP). Your ability to
enroll will be based on verification that you, for 90 days or longer, have had or are
expected to need the level of services provided in a skilled nursing facility, a nursing
facility, an intermediate care facility for individuals with intellectual and developmental
disabilities, a psychiatric hospital or unit, a rehabilitation hospital or unit, a long-term
care hospital, a swing-bed hospital, or a facility approved by CMS that furnishes similar
services.
[For MSAs] MSA Plans combine a high deductible Medicare Advantage Plan and a trust
or custodial savings account (as defined and/or approved by the IRS). The plan deposits
money from Medicare into the account. You can use this money to pay for your health
care costs, but only Medicare-covered expenses count toward your deductible. The
amount deposited is usually less than your deductible amount, so you generally have to
pay money out of pocket before your coverage begins.
Medicare MSA Plans do not cover prescription drugs. If you join a Medicare MSA Plan,
you can also join any separate Medicare Prescription Drug Plan.
There are additional restrictions to join an MSA plan, and enrollment is for a full
calendar year unless you meet certain exceptions. Those who disenroll during the
calendar year will owe a portion of the account deposit back to the plan. Contact the plan
at [insert customer service and TTY] for additional information.
38
Appendix 2 – Model Summary of Benefits Instructions (422.2267(e)(5),
423.2267(e)(5))
Plans must reflect Part C and Part D benefits and cost sharing in the SB. If there is no cost
sharing, plans must notate no costs (e.g., $0 cost for day six (6) and beyond). If the benefit is not
offered, then notate that it is not offered. Part C benefits and cost sharing must be in the
following order:
•
Monthly plan premium (Part C and D premium combined);
•
Part B premium buy-down, if applicable;
•
Deductibles, including plan level and category level deductible;
•
Maximum Out-of-Pocket Responsibility (does not include prescription drugs);
•
Inpatient Hospital coverage;
•
Outpatient Hospital coverage;
•
Ambulatory Surgical Center (ASC) Services;
•
Doctor Visits (Primary Care Providers and Specialists);
•
Preventive Care;
•
Emergency Care;
•
Urgently Needed Services;
•
Diagnostic Services/Labs/Imaging (include diagnostic tests and procedures, labs,
diagnostic radiology, and X-rays);
•
Hearing Services (Include mandatory and optional supplemental benefits);
•
Dental Services (Include mandatory and optional supplemental benefits);
•
Vision Services (Include mandatory and optional supplemental benefits); and,
•
Mental Health Services.
In addition to the benefits in §§ 422.2267(e)(5)(ii), plans should include the following five
(5) benefits in the SB under Part C:
•
Skilled Nursing Facility;
•
Physical Therapy;
•
Ambulance;
•
Transportation; and
•
Medicare Part B Drugs.
Part D benefits must include:
•
Cost sharing for deductible, the initial coverage phase, coverage gap, and catastrophic
coverage. Cost sharing must be broken down by the tier number/name (e.g., tier 1
generic).
When applicable, a notation that costs may differ based on pharmacy type or status (e.g.,
preferred/non-preferred, mail order, long-term care (LTC), and 30- or 90-day supply).
To avoid beneficiary confusion when comparing plans, plans must maintain the above order of
the data elements. The monthly premium, deductible and the maximum out-of-pocket cost must
always be displayed first. Plans may then decide whether to display drug or health benefits next.
39

If any of the benefits are not offered (e.g., transportation), indicate them as “not covered.” Plans
may remove certain benefits if they are not applicable to a particular plan type (e.g., Part D only
plan removes Part C benefits).
Additional benefits may be listed after all the required elements are provided in the SB. They
may be listed after Part C or after Part C and D benefits.
Plans may list supplemental benefits for the chronically ill (SSBCI) in addition to Part C benefits
and Part D.
When adding Value Added Items and Services (VAIS) in the SB:
• They should be placed in a separate section, distinguishable from the benefits;
• Services/items should not be called benefits as they are not part of the Medicare plan
benefit package; and,
• Plans should provide language in the SB to make it clear that these additional
services/items are not part of the plan benefit package or the Medicare benefit.
Please refer to Medicare Managed Care Manual
, Chapter 4, Section 80 for additional
information on VAIS.
Other required information in the SB:
•
The document must be labeled as “Summary of Benefits” noting the plan year;
•
The plan name and type must be clearly labeled for all Plans in the SB. For example,
<Plan name, HMO or PPO, SNP, MSA, etc.>;
•
Service area and eligibility requirements, including the Medicaid eligibility criteria
applicable to Dual Eligible Special Needs Plans (D-SNPs);
•
Phone number, including TTY/TDD;
•
Days and hours of operation;
•
Website address;
•
In-network and out-of-network cost-sharing information for applicable plan types;
•
Applicable disclaimers;
•
Language stating that the complete list of services is found in the Evidence of Coverage
(EOC), as well as language directing readers how to access or order the EOC;
•
Language that directs readers how to access or order the "Medicare & You" handbook;
•
If the SB includes plans with and without Part D prescription drug coverage, the
distinction between plans must be clear;
•
Notate services that require a physician referral or prior authorization; and
•
If offering optional supplemental benefits, plans must include the additional premium
amount.
D-SNPs
We encourage FIDE SNPs to work with their contracted State Medicaid agencies in developing
an SB that displays integrated benefits.
40
Medicare Premium and Deductible:
Plans that use Medicare premium, deductible, or cost sharing amounts (e.g., inpatient hospital)
must insert the current year’s Medicare amounts. In addition, the category must also note that
these amounts may change for the following year and the plan will provide updated rates at
[insert website] as soon as Medicare releases them.
Overall design and layout:
Plans may present multiple plan benefit packages (PBPs) in the same document by displaying
the benefits in separate columns. Plans using this option may include similar or different plan
types (e.g., HMO to HMO, or HMO to PFFS, or HMO to PPO). Plans may also:
•
Make use of colors to enhance the ability to navigate the document, or
•
Incorporate various icons/graphics to help locate important information, such as how to
complete an application online or contact customer service (e.g., phone number).
Note: SNPs must remain separate from non-SNP plans to avoid confusion for beneficiaries.
Recommendations:
The following recommendations are based on consumer testing:
•
Avoid the use of multiple folds and large charts as it may make it cumbersome and
difficult to use;
•
Include definitions and purpose of the document;
•
Avoid using dimensions that are too large as it could diminish the usefulness of the SB;
and,
•
Avoid the use of footnotes. If necessary to include footnoted information, visually
emphasize (e.g., larger or bold font) the inclusion of superscripts in coverage charts.
HPMS Submission Process:
The SB is a File & Use document, and therefore must be submitted in HPMS under “CMS
Required” as one document.
41
Appendix 3 – Employer/Union Group Health Plans
Sections 1857(i) and 1860D-22(b) of the Social Security Act; 42 CFR §§ 422.2276, 423.458,
423.2276
Plans offering employer group health plans including Employer Group Waiver Plans (EGWPs)
are not required to submit communication and marketing materials specific only to those
employer plans. However, as a condition of CMS providing particular waivers or modifications
to employer group plans, CMS may request and review any materials in the event of beneficiary
complaints or for any other reason it determines to ensure the information accurately and
adequately informs Medicare beneficiaries about their rights and obligations under the plan.
CMS waivers to employer group plans are limited in scope to their stated parameters, and
employer group plans (including EGWPs) must follow all rules in these guidelines unless CMS
explicitly waives them. For specific guidance regarding these waivers, please refer to Chapter 9
of the Medicare Managed Care Manual and Chapter 12 of the
Medicare Prescription Drug
Benefit Manual.
Marketing Provisions Table – Employer/Union Group Plans
These requirements are applicable to the transaction between the agent/broker selling the plan to
the employer/union. All activities conducted by the employer/union or its designees to sign up
individual employees to the plan(s) selected by the employer/union are excluded from these
provisions.
Note: This table contains a partial list of exclusions.
Applicable Provisions (Not Waived)
Not Applicable Provisions
(Waived)
Nominal Gifts
Unsolicited Contacts
Sales/Marketing in Health Care Settings
Cross-selling
Sales/Marketing at Educational Events
Scope of Appointments
Co-branding
Provision of Meals
Appointment of Agents/Brokers
Agent/Broker Compensation
State Licensure Requirements
Agent/Broker Testing
Reporting of Terminated Agents/Brokers
CMS Prior Review of
Marketing Materials
Agent/Broker Training
Agents must be thoroughly familiar with the products
they are selling, including the plan specific details and
the Medicare rules that apply to the specific products.
The organization/sponsor is responsible for ensuring
that the agents selling for them have sufficient
knowledge.
Pre-Enrollment Checklist
42

Appendix 4 – Use of Medicare Mark for Part D Sponsors
Section 1140 of the Social Security Act
All plans may use the Medicare Prescription Drug Benefit Program Mark only after
electronically executing the Medicare Mark License Agreement in HPMS. Only a CEO, CFO, or
COO who is designated as an authorized signer in HPMS is eligible to execute the Medicare
Mark License Agreement. In certain circumstances, the Medicare Mark License Agreement may
be signed in hard copy. The license agreement is effective for a single contract year and plans
must renew annually to continue using the mark. Unless otherwise approved, no individuals,
organizations, and/or commercial firms may distribute materials bearing the Medicare
Prescription Drug Benefit Program Mark. Plans may use the mark on communications and
marketing materials consistent with this chapter.
Use of Medicare Prescription Drug Benefit Program Mark on Items for Sale or
Distribution
Section 1140 of the Social Security Act
All plans may use the Medicare Prescription Drug Benefit Program Mark on items they
distribute, provided the item(s) follow(s) guidelines for nominal gifts, as provided in 42 CFR §
423.2263(b)(2). Plans cannot sell items with the Medicare Prescription Drug Benefit Program
Mark for profit.
Approval to Use the Medicare Prescription Drug Benefit Program Mark
Plans must submit requests to distribute other items (materials that are not included in this
chapter) bearing the Medicare Prescription Drug Benefit Program Mark to CMS at least 30 days
prior to the anticipated date of distribution. Plans should send requests sent to:
Office of the Administrator
Office of Communications
Visual & Multimedia Communications Group
7500 Security Blvd.
Baltimore, MD 21244-1850
Once CMS has approved a request, the following will apply: 1) approval will be effective for a
period not to exceed one year; and 2) approval will be granted only for those items for which use
of the mark was requested in the request letter and for which CMS granted written approval.
Prohibition on Misuse of the Medicare Prescription Drug Benefit Program Mark Section
1140 of the Social Security Act
42 U.S.C. section 1320b-10 prohibits the misuse of the Medicare name and marks. In general, it
authorizes the Inspector General of DHHS to impose penalties on any person who misuses the
term Medicare or other names associated with DHHS in a manner which the person knows or
should know gives the false impression that DHHS has approved, endorsed, or authorized it.
Offenders are subject to fines of up to $5,000 per violation or in the case of a broadcast or
telecast violation, $25,000.
43

Mark Guidelines
Section 1140 of the Social Security Act
The Medicare Prescription Drug Benefit Program Mark is a logotype comprised of the words
Medicare Rx with the words Prescription Drug Coverage directly beneath.
Always use reproducible art available electronically. Do not attempt to recreate the Program
Mark or combine it with other elements to make a new graphic. Artwork will be supplied in
.EPS, .TIFF or .JPG format after notification of approval into the program.
Mark Guidelines - Negative Program Mark
Section 1140 of the Social Security Act
The Medicare Prescription Drug Benefit Program Mark may be reversed out in white. The entire
mark must be legible.
Mark Guidelines - Approved Colors
Section 1140 of the Social Security Act
The two (2)-color mark is the preferred version. It uses PMS 704 (burgundy) and sixty-five (65)
percent process black. It is recommended that if the CMS mark is used in conjunction with the
brand mark, that the black versions of those logos be used.
44
"
I
l
The 1-color version in one-hundred (100) percent black also is acceptable.
Mark Guidelines on Languages
Section 1140 of the Social Security Act
The Spanish version of the Medicare Prescription Drug Benefit Program Mark may be used in
place of the English language version on materials produced entirely in Spanish. The two (2)-
color version is preferred, but the grayscale, black and negative versions may be used.
Mark Guidelines on Size
Section 1140 of the Social Security Act
To maintain clear legibility of the Program Mark, never reproduce it at a size less than one (1)
inch wide. The entire mark must be legible.
Mark Guidelines on Clear Space Allocation
Section 1140 of the Social Security Act
The clear space around the Medicare Prescription Drug Benefit Program Mark prevents any
nearby text, image or illustration from interfering with the legibility and impact of the mark. The
measurement “x” can be defined as the height of the letter “x” in “Rx” in the Program Mark.
Any type or graphic elements must be at least “x” distance from the mark as shown by the
illustration.
45

•1
"x"
I
I I
~p,
~t~
o
~i.~{t~~
~&. j I
·~
I ]
"x"
x I
I I
------------------------
~
-------
I
Mark Guidelines on Bleed Edge Indicator
Section 1140 of the Social Security Act
The Program Mark may not bleed off any edge of the item. The mark should sit at least one--
eighth (1/8) inch inside any edges of the item.
Mark Guidelines on Incorrect Use
Section 1140 of the Social Security Act
Following are rules for preventing incorrect use of the Medicare Prescription Drug Benefit
Program Mark:
•
Do not alter the position of the mark elements;
•
Do not alter the aspect ratio of the certification mark;
•
Do not stretch or distort the mark;
•
Always use the mark only as provided in the CMS approval/license agreement;
•
Do not rotate the mark or any of its elements;
•
Do not alter or change the typeface of the mark;
•
Do not alter the color of any of the mark elements;
•
Do not position the mark near other items or images. Maintain the clear space
allocation;
•
Do not position the mark to bleed off any edge. Maintain one-eighth (1/8) inch safety
from any edge;
•
Do not use any of the mark elements to create a new mark or graphic; and
•
Do not use the mark on background colors, images or other artwork that interfere with
the legibility of the mark.
Mark Guidelines for Part D Standard Pharmacy ID Card Design
Section 1140 of the Social Security Act
Use of the Medicare Prescription Drug Benefit Program Mark on an ID card must be consistent
with guidance mentioned in this section.
46
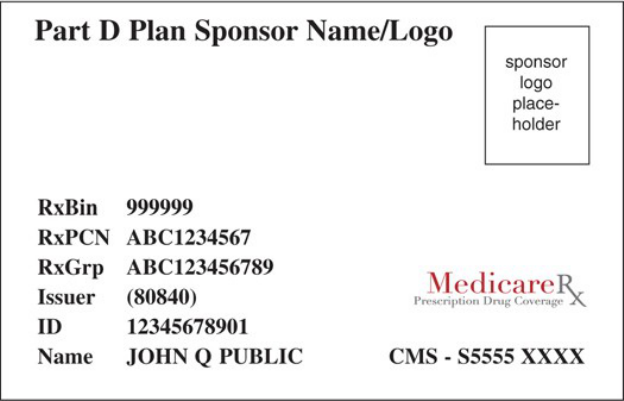
D
Plan
Sponsor Name/Logo
RxBin
RxPCN
RxGrp
Iss
uer
ID
Name
999999
ABC1234567
ABC123456789
(80840)
12345678901
JOHN
Q PUBLIC
sponsor
logo
place-
holder
Pn
~
~
l£~}
n
~~
>
~~
~
~
CMS - S5555
XXXX
47
Appendix 5 – External Links
CMS Eligibility and Enrollment Guidance
https://www.cms.gov/Medicare/Eligibility-and-Enrollment/MedicareMangCareEligEnrol
CMS Medicare Online Enrollment Center:
https://www.medicare.gov/plan-compare/
CMS Plan Finder
https://www.medicare.gov or 1-877-486-2048)
https://www.medicare.gov/plan-compare/
CMS Star Ratings
https://www.cms.gov/Medicare/Prescription-Drug-
Coverage/PrescriptionDrugCovGenIn/PerformanceData
HIPAA Privacy Rule and Disclosure Requirements
https://www.hhs.gov/hipaa/index.html
HIPAA Privacy Rule and Security Requirements
https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/significant-aspects/index.html
Internal Revenue Service (IRS) Tax publications
https://www.irs.gov or 1-800-TAX-FORM (1-800-829-3676)
Medicare.gov Complaint Website
https://www.medicare.gov/MedicareComplaintForm/home.aspx
Medicare Managed Care Manual
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Internet-Only-Manuals-
IOMs-Items/CMS019326
Medicare Part D Model Materials
https:www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Part-
D-Model-Materials
Medicare Prescription Drug Benefit Manual
https://www.cms.gov/Medicare/Prescription-Drug-
Coverage/PrescriptionDrugCovContra/PartDManuals
Medicare Coverage Database
https://www.cms.gov/medicare-coverage-database/indexes/ncd-alphabetical-index.aspx
Medicare Coverage Determinations (MCD)
https://www.cms.gov/medicare-coverage-database/reports/reports.aspx
Section 508 of the Rehabilitation Act
https://www.hhs.gov/web/section-508/index.html
State-specific marketing guidance for MMPs
48