MEDICAL RECORDS
Fees and Challenges
Associated with
Patients’ Access
Report to Congressional Committees
May 2018
GAO-18-386
United States Government Accountability Office

United States Government Accountability Office
Highlights of GAO-18-386, a report to
c
ongressional committees
May 2018
MEDICAL RECORDS
Fees and Challenges Associated with
Patients’
Access
What GAO Found
Available information suggests that the fees charged for accessing medical
records can vary depending on the type of request and the state in which the
request is made. Under the Health Insurance Portability and Accountability Act of
1996 (HIPAA) and its implementing regulations, providers are authorized to
charge a reasonable, cost-based fee when patients request copies of their
medical records or request that their records be forwarded to another provider or
entity. In the case of third-party requests, when a patient gives permission for
another entity—for example, an attorney—to request copies of the patient’s
medical records, the fees are not subject to the reasonable cost-based standard
and are generally governed by state law. According to stakeholders GAO
interviewed, the fees for third-party requests are generally higher than the fees
charged to patients and can vary significantly across states.
The four states GAO reviewed have state laws that vary in terms of the fees
allowed for patient and third-party requests for medical records. For example,
three of the states have per-page fee amounts for patient and third-party records
requests. The amounts charged are based on the number of pages requested
and vary across the three states.
• One of the three states has established a different per-page fee amount for
third-party requests. The other two do not authorize a different fee for patient
and third-party requests.
• One of the three states also specifies a maximum allowable fee if the
provider uses an electronic health records system. The other two do not
differentiate costs for electronic or paper records.
In the fourth state, state law entitles individuals to one free copy of their medical
record. The statute allows a charge of up to $1 per page for additional copies.
Patient advocates, provider associations, and other stakeholders GAO
interviewed identified challenges that patients and providers face when patients
request access to their medical records.
• Patients’ challenges include incurring what they believe to be high fees when
requesting medical records—for example, when facing severe medical
issues that have generated a high number of medical records. Additionally,
not all patients are aware that they have a right to challenge providers who
deny them access to their medical records.
• Providers’ challenges include the costs of responding to patient requests for
records due to the allocation of staff time and other resources. In addition,
according to provider associations and others GAO interviewed, fulfilling
requests for medical records has become more complex and challenging for
providers, in part because providers may store this information in multiple
electronic record systems or in a mix of paper and electronic records.
View GAO-18-386. For more information,
contact
Carolyn L. Yocom at (202) 512-7114
or
Why GAO Did This Study
HIPAA and its implementing
regulations, as amended by the Health
Information Technology for Economic
and Clinical Health Act, require health
care providers to give patients, upon
request, access to their medical
records, which contain protected health
information (i.e., diagnoses, billing
information, medications, and test
results). This right of access allows
patients to obtain their records or have
them forwarded to a person or entity of
their choice—such as another
provider—in a timely manner while
being charged a reasonable, cost-
based fee. Third parties, such as a
lawyer or someone processing
disability claims, may also request
copies of a patient’s medical records
with permission from the patient.
The 21st Century Cures Act included a
provision for GAO to study patient
access to medical records. Among
other things, this report describes (1)
what is known about the fees for
accessing patients’ medical records
and (2) challenges identified by
patients and providers when patients
request access to their medical
records. GAO reviewed selected
HIPAA requirements and implementing
regulations and guidance, and relevant
laws in four states selected in part
because they established a range of
fees associated with obtaining copies
of medical records. GAO also
interviewed four provider associations,
seven vendors that work for providers,
six patient advocates, state officials,
and Department of Health and Human
Services’ (HHS) officials. The
information GAO obtained and its
analysis of laws in the selected states
are not generalizable. HHS provided
technical comments on this report.
Page i GAO-18-386 Patient Access to Medical Records
Letter 1
Background 4
Available Information Suggests That Fees for Accessing Patient
Medical Records Vary by Type of Request and State 8
Stakeholders Identified Fees and Other Challenges for Patients
Accessing Medical Records and Challenges for Providers in
Allocating Resources to Respond to Requests 13
OCR Investigates Complaints, Audits Providers, and Educates
Patients and Providers about Patient Access 18
Agency Comments 23
Appendix I GAO Contact and Staff Acknowledgments 24
Tables
Table 1: Health Insurance Portability and Accountability Act
Access Guidance Options for Calculating Reasonable,
Cost-Based Fees for Patient and Patient-Directed
Requests 9
Table 2: Allowable Fees for Requests for Medical Records in
Selected States 11
Figures
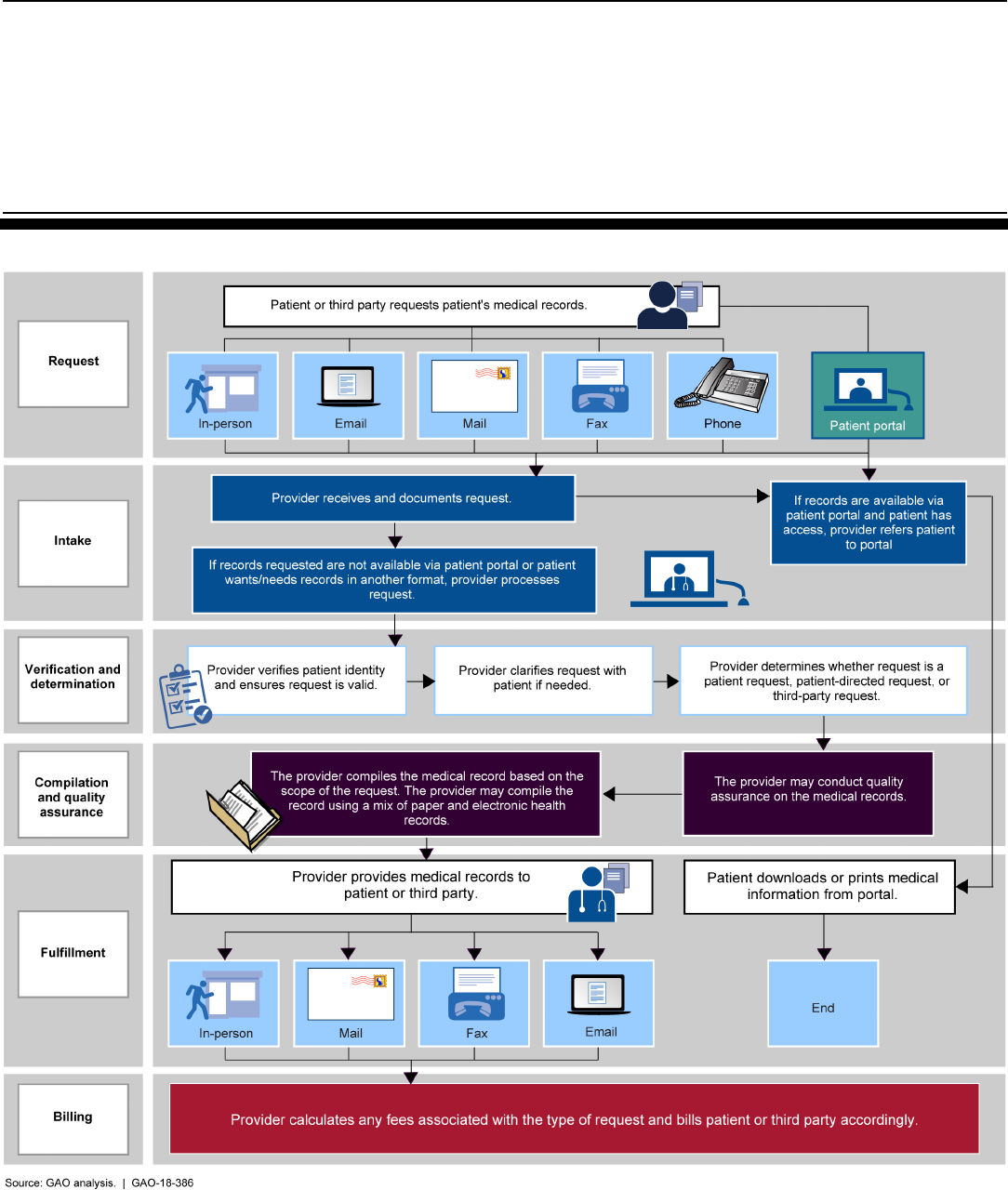
Figure 1: Provider and Vendor Process for Fulfilling Medical
Record Requests 7
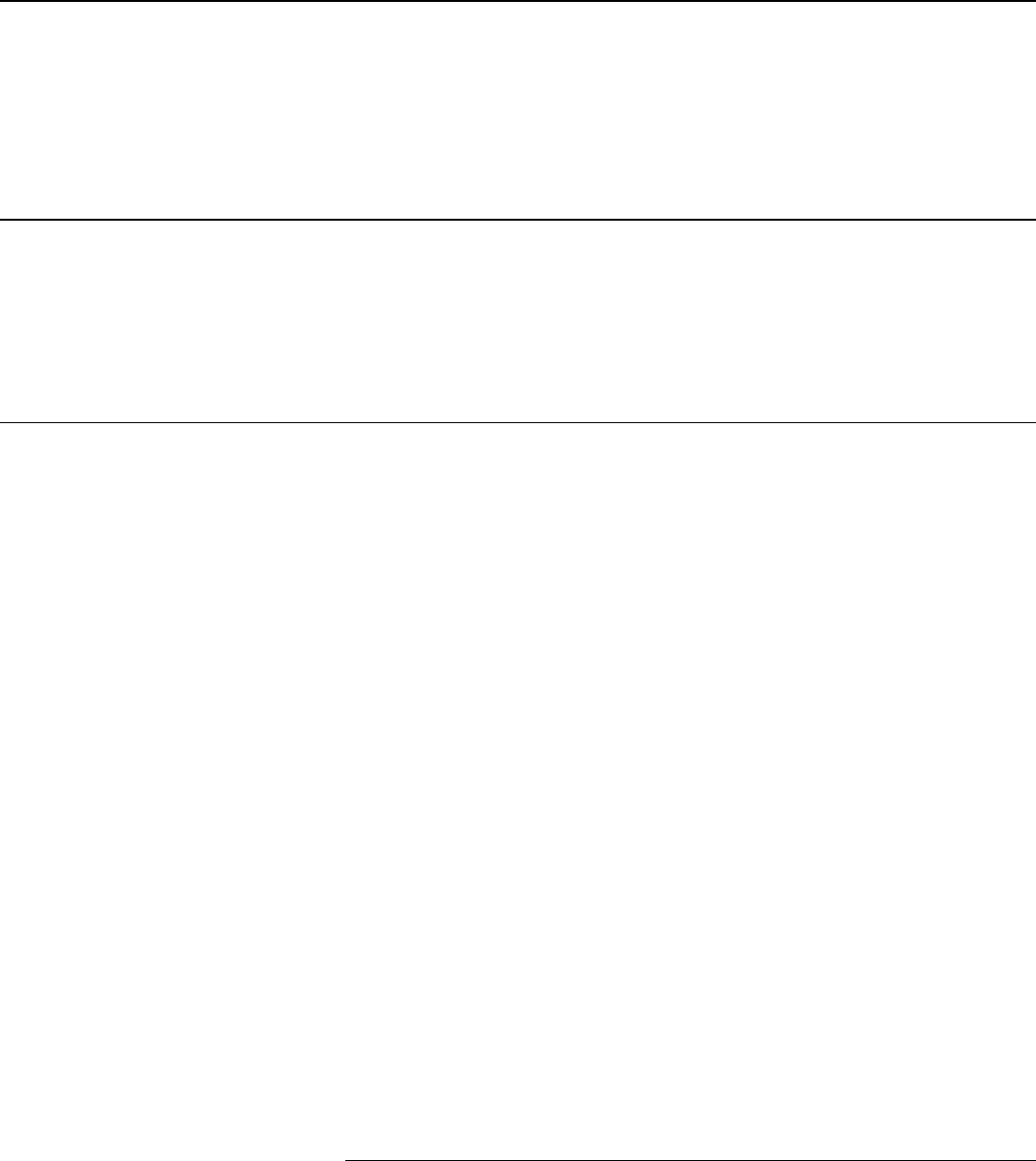
Figure 2: HHS Office for Civil Rights Time to Close Complaints
Received between February 2016 and June 2017 20
Contents
Page ii GAO-18-386 Patient Access to Medical Records
Abbreviations
EHR electronic health record
HHS Department of Health and Human Services
HIPAA Health Insurance Portability and Accountability Act
of 1996
HITECH Act Health Information Technology for Economic and
Clinical Health Act
OCR Office for Civil Rights
OIG Office of Inspector General
ONC Office of the National Coordinator for Health
Information Technology
ROI release-of-information
This is a work of the U.S. government and is not subject to copyright protection in the
United States. The published product may be reproduced and distributed in its entirety
without further permission from GAO. However, because this work may contain
copyrighted images or other material, permission from the copyright holder may be
necessary if you wish to reproduce this material separately.
Page 1 GAO-18-386 Patient Access to Medical Records
441 G St. N.W.
Washington, DC 20548
May 14, 2018
The Honorable Lamar Alexander
Chairman
The Honorable Patty Murray
Ranking Member
Committee on Health, Education, Labor, and Pensions
United States Senate
The Honorable Greg Walden
Chairman
The Honorable Frank Pallone Jr.
Ranking Member
Committee on Energy and Commerce
House of Representatives
In the course of seeking or obtaining health care, patients may request
and obtain their medical records. They may, for example, want to take
their medical records to another health care provider, or use the records
to apply for disability coverage or resolve a dispute over insurance
coverage.
1
Patients may obtain their records directly in an electronic or
paper form or direct one provider to send these records to another
provider or entity, such as an insurer or lawyer. In other cases, a third
party, such as a lawyer or someone processing disability claims, may
directly contact a provider to request access to a patient’s medical
records with permission from the patient.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA),
as amended, and its implementing regulations, require HIPAA-covered
entities (e.g., providers and insurers) to provide individuals, upon request,
with access to their medical records, which contain protected health
information (e.g., information on diagnoses, billing, medications, and test
results).
2
This right of access allows patients to obtain their medical
records in a timely manner while being charged a reasonable, cost-based
1
For the purposes of this report, we use the term “provider” to refer to physicians,
hospitals, and other health care practitioners.
2
The Health Information Technology for Economic and Clinical Health (HITECH) Act
amended HIPAA and its implementing regulations. As relevant here, the HITECH Act
specified requirements in the application of the patient access regulation. Pub. L. No. 111-
5, § 13405(e), 123 Stat. 115, 268 (2009).
Letter
Page 2 GAO-18-386 Patient Access to Medical Records
fee. Federal law also states that an individual can direct a provider to
send the records to a person of the individual’s choice.
3
In 2016, the
Department of Health and Human Services’ (HHS) Office for Civil Rights
(OCR), which is responsible for enforcing the rights established under
HIPAA, issued guidance about the right of access. Among other things,
the guidance states that when a patient requests that his or her medical
records be forwarded to a person or entity, a reasonable, cost-based fee
can be charged.
The 21st Century Cures Act included a provision for us to study patient
access to medical records and issue a report by June 13, 2018.
4
In this
report we describe
1. what is known about the fees charged for accessing patients’ medical
records,
2. challenges identified by patients and providers when patients request
access to their medical records, and
3. efforts by OCR to ensure patients’ access to their medical records.
To describe what is known about the fees charged for accessing patients’
medical records, we reviewed selected HIPAA requirements and
implementing regulations and guidance. We conducted interviews with
relevant stakeholders, including representatives from seven release-of-
information (ROI) vendors and nine individuals or entities with expertise in
HIPAA, including HIPAA lawyers in both private practice and who work in
health policy.
5
We selected these stakeholders based on our initial
background research, prior work, and input from other stakeholders.
During our interviews, we asked about examples of state laws that govern
the fees for obtaining copies of medical records. Using this information,
we judgmentally selected four states for closer review—Kentucky, Ohio,
Rhode Island, and Wisconsin. We selected these states based on input
3
Given that this report is about patient access to medical records, in some instances we
use the term “patient” to refer to an individual with regard to his or her HIPAA access
rights and “provider” to refer to providers who are the relevant HIPAA-covered entities.
The Privacy Rule defines “covered entity” as a health plan, a health care clearinghouse,
and a health care provider who transmits any health information in electronic form in
connection with a transaction covered by the regulations. 45 C.F.R. § 160.103 (2017).
4
Pub. L. No. 114-255, § 4008, 130 Stat. 1033, 1184-1185 (2016).
5
ROI vendors gather and release medical records on behalf of providers.

Page 3 GAO-18-386 Patient Access to Medical Records
from stakeholders, a review of state laws, and because these states have
a range of different types of fees. In Ohio, Rhode Island, and Wisconsin,
we interviewed officials in the state agencies responsible for oversight of
patients’ access to medical records. Officials from Kentucky declined an
interview but provided written responses to our questions. The
information we obtained from stakeholders and our analysis of laws in the
selected states are not generalizable.
To describe challenges identified by patients and providers when patients
request access to their medical records, we interviewed relevant
stakeholders. Specifically, we interviewed individuals or entities with
expertise in the topic of patients’ access to health information (referred to
hereafter as experts), six patient advocates, representatives from four
organizations that represent providers (provider representatives), and
representatives from seven ROI vendor companies. We judgmentally
selected these stakeholders based on our previous studies, presentations
at conferences, relevant testimony at Congressional hearings, and
recommendations by other interviewees. We also interviewed officials
from HHS’s OCR, Office of the National Coordinator for Health
Information Technology (ONC), and Office of Inspector General (OIG).
We obtained specific examples of situations when patients have faced
challenges accessing their medical records; these examples were
provided to us by OCR and an organization that collects anecdotes from
patients about their experiences. The information we obtained from
stakeholders is not generalizable.
To describe efforts by OCR to ensure patients’ access to their medical
records, we reviewed data from OCR on all patient access complaints
received between February 2016 and June 2017. We assessed the
reliability of these data by (1) performing electronic testing of required
data elements, (2) reviewing existing information about the data and the
system that produced them, and (3) consulting agency officials who are
knowledgeable about the data. We determined that these data were
sufficiently reliable for the purposes of our reporting objectives. We also
reviewed relevant OCR documentation, including policies and
procedures, audit guidelines, and reports on HIPAA violations, as well as
10 examples of patient access complaints provided to us by OCR. Finally,
we interviewed officials from OCR and ONC.
We conducted this performance audit from March 2017 to May 2018 in
accordance with generally accepted government auditing standards.
Those standards require that we plan and perform the audit to obtain
sufficient, appropriate evidence to provide a reasonable basis for our
Page 4 GAO-18-386 Patient Access to Medical Records
findings and conclusions based on our audit objectives. We believe that
the evidence obtained provides a reasonable basis for our findings and
conclusions based on our audit objectives.
Patients may request copies of their medical records, or request that
copies of their records be sent to a designated person or entity of their
choice.
• In a patient request, a patient or former patient requests access to or
copies of some or all of her medical records, in either paper or
electronic format. For example, a patient might want to keep copies
for her own personal use or to bring with her when moving or
changing providers.
• In a patient-directed request, a patient or former patient requests
that a provider or other covered entity send a copy of the patient’s
medical records directly to another person or entity, such as another
provider. For example, a patient might request that her medical
records be forwarded to another provider because the patient is
moving or wants to seek a second opinion.
• In a third-party request, a third party, such as an attorney, obtains
permission from a patient (via a HIPAA authorization form that is
signed by the patient) to access the patient’s medical records. For
example, with permission from the patient, a lawyer might request
copies of a patient’s medical records to pursue a malpractice case.
6
HIPAA’s Privacy Rule—the regulations that implement HIPAA’s privacy
protections—requires that upon request, HIPAA-covered entities, such as
health care providers and health plans, provide individuals with access to
6
A patient’s records may be released by means of a patient-directed request or a third-
party request. A key difference between patient, patient-directed, and third-party requests
is that in the case of the two types of patient requests, a provider is required to disclose
the record, except when an exception applies. In contrast, in a third-party request with a
valid HIPAA authorization, the provider is permitted (but not required) to disclose the
record.
Background
Medical Record Requests
HIPAA
Page 5 GAO-18-386 Patient Access to Medical Records
their medical records.
7
Under HIPAA’s implementing regulations,
providers and other covered entities must respond to a patient or patient-
directed request for medical records within 30 days. The Privacy Rule
also establishes an individual’s right to inspect or obtain a copy of his or
her medical records which, as amended in 2013, includes the right to
direct a covered entity to transmit a copy of the medical records to a
designated person or entity of the individual’s choice.
8
Individuals have
the right to access their medical records for as long as the information is
maintained by a covered entity or by a business associate on behalf of a
covered entity, regardless of when the information was created; whether
the information is maintained in paper or electronic systems onsite,
remotely, or is archived; or where the information originated. Finally, the
HIPAA Privacy Rule also describes the circumstances under which
protected health information in medical records may be released to
patients and third parties.
9
In February 2016, OCR issued guidance to explain its 2013 regulations.
10
Among other things, this guidance states that as part of a patient’s right of
access, patients have the right to obtain copies of their medical records
and the right to have their records forwarded to a person or entity of their
7
See 45 C.F.R. pt. 164 (2017). Medical records contain protected health information that
is kept in designated record sets maintained by the covered entity. The designated record
set is defined at 45 CFR §164.501 as a group of records maintained by or for a covered
entity that comprises the medical records and billing records about individuals maintained
by or for a covered health care provider; enrollment, payment, claims adjudication, and
case or medical management record systems maintained by or for a health plan; or other
records that are used, in whole or in part, by or for the covered entity to make decisions
about individuals.
8
45 C.F.R. §§ 164.502(a)(1), 164.524(c)(3)(ii) (2017). In 2013, HHS issued a final rule to
implement statutory amendments to HIPAA made under the HITECH Act. See 78 Fed.
Reg. 5566 (Jan. 25, 2013).
9
In addition to HIPAA’s Privacy Rule, there are several other HIPAA rules related to
protected health information and patient medical records. For example, the HIPAA
Security Rule establishes national standards to protect electronic health information and
requires certain safeguards to ensure the confidentiality, integrity, and availability of such
information (see 45 CFR Part 160 and Subparts A and C of Part 164). The HIPAA Breach
Notification Rule requires covered entities to notify affected individuals and HHS following
a breach of unsecured protected health information (see 45 CFR Part 160 and Subparts A
and D of Part 164).
10
OCR’s guidance on individuals’ rights under HIPAA to access their health information
can be found online. See Department of Health and Human Services, Individuals’ Right
under HIPAA to Access Their Health Information 45 CFR § 164.524, accessed December
21, 2017,
https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html.
Page 6 GAO-18-386 Patient Access to Medical Records
choice; in these circumstances, patients are only to be charged a
“reasonable, cost-based fee.”
11
The guidance further notes that state laws
that provide individuals with greater rights of access to their medical
records are not preempted by HIPAA and still apply. With respect to fees,
patients may not be charged more than allowed under the Privacy Rule,
even if state law provides for higher or different fees.
12
To respond to medical record requests, providers either use staff within
their organization or may contract with ROI vendors to conduct this work.
In general, both providers’ staff and ROI vendors follow the same process
when fulfilling requests for medical records for both individual patients
and third parties. (See fig. 1.)
11
45 C.F.R. § 164.524(c)(4) (2017).
12
In general, state laws that are contrary to the HIPAA Privacy Rule are preempted by
HIPAA unless a specific exception applies. One exception is if the state law provides
greater privacy rights (including patient access rights) with respect to such information.
Fulfilling Medical Record
Requests
Page 7 GAO-18-386 Patient Access to Medical Records
Figure 1: Provider and Vendor Process for Fulfilling Medical Record Requests
Page 8 GAO-18-386 Patient Access to Medical Records
Available information suggests that the allowable fees for accessing
medical records vary by type of request—that is, whether a patient or
third party is making the request—and by state. Federal laws establish
limits on the fees that may be charged for two of the three types of
requests for medical records: (1) patient requests, when patients request
access to their medical records, and (2) patient-directed requests, when
patients request that their records be sent to another person or entity,
such as another provider. HIPAA does not establish limits on fees for
third-party requests.
For patient and patient-directed requests, providers may charge a
“reasonable, cost-based fee” under HIPAA’s implementing regulations.
OCR’s 2016 guidance gives examples of options providers (or a ROI
vendor responding to requests for medical records on behalf of a
provider) may use in determining a “reasonable cost-based fee.”
13
(See
table 1.)
13
On January 8, 2018, Ciox Health, LLC, a ROI vendor, filed suit against HHS regarding
the “reasonable, cost-based fee” applicable to patient-directed requests. Ciox Health, LLC
v. Azar, No. 1:18-cv-0040 (D.D.C. filed Jan. 8, 2018). As of April 2018, no decision had
been rendered in this case.
Available Information
Suggests That Fees
for Accessing Patient
Medical Records Vary
by Type of Request
and State
Page 9 GAO-18-386 Patient Access to Medical Records
Table 1: Health Insurance Portability and Accountability Act Access Guidance Options for Calculating Reasonable, Cost-
Based Fees for Patient and Patient-Directed Requests
Option 1
Actual costs
Option 2
Average costs
Option 3
Flat fee
Method for calculating
portion of fee for labor
costs
Provider calculates actual labor
costs to fulfill the request.
Provider develops a schedule
of costs for labor based on
average labor costs to fulfill
standard types of requests.
A provider may charge individuals a
flat fee for all requests for electronic
copies of protected health
information that is maintained
electronically, provided the fee does
not exceed $6.50.
Types of labor/materials for
which fee applies
Labor for copying (and creating a
summary or explanation if the
individual requests or agrees),
applicable supplies (CD or USB
drive), and postage.
Providers may add to the
average labor cost amount any
applicable supply (e.g., paper,
or CD or USB drive) or postage
costs.
Charge may not exceed $6.50 and
is inclusive of all labor, supplies,
and postage.
Types of labor/materials
that must be provided free
of charge
Review of access request; searching for, retrieving, and otherwise preparing the responsive information
for copying; ensuring information relates to the correct individual; segregating, collecting, compiling, and
otherwise preparing the response information for copying.
Per page fees are not permitted for paper or electronic copies of protected health information maintained
electronically.
Source: Department of Health and Human Services’ Office for Civil Rights 2016 guidance. | GAO-18-386
In addition to the HIPAA requirements, some states have established
their own fee schedules, formulas, or limits on the allowable fees for
patient and patient-directed requests. State laws that allow for higher fees
than permitted under HIPAA are preempted by the federal law, but those
providing for lower fees are not preempted.
14
Representatives from ROI
vendors, provider representatives, and other stakeholders we interviewed
told us that not all states have established their own requirements
governing the fees for medical record requests and, among the states
that have, the laws can vary. For example, states can vary as to whether
they set a maximum fee that may be charged or whether they establish a
fee schedule that is applicable to paper records, electronic records, or
both. While states may establish per-page amounts that can be charged
for a copy of a patient’s medical records, these per-page amounts can
vary.
14
OCR’s 2016 access guidance does not establish a fee schedule and does not specify a
dollar amount that is to be charged for every request for records. Instead, it describes
three permissible methods of calculating the reasonable, cost-based fee permitted by the
regulation.
Page 10 GAO-18-386 Patient Access to Medical Records
In contrast with patient and patient-directed requests, the fees for third-
party requests are not limited by HIPAA’s reasonable, cost-based
standard for access requests and are instead governed by state laws,
regulations, or other requirements. For third-party requests, providers and
vendors working on their behalf may charge whatever is allowed under
these state requirements. According to ROI vendors and other
stakeholders we interviewed, such fees are typically higher than the
reasonable, cost-based fees permitted under HIPAA for patient and
patient-directed requests and may be established by formulas that vary
by state. For example, states can vary as to whether they establish per-
page copy fees, allow providers to charge a flat fee, or charge different
fees based on the type of media requested (e.g., electronic copies, X-
rays, microfilm, paper, etc.). Additionally, state laws of general
applicability (for example, the commercial code) may govern the
permissible fees applicable to ROI release of records. Representatives of
ROI vendors we interviewed stated that there is significant variation in the
state laws that govern the fees for third-party requests, and companies
employ staff to track the different frameworks.
Across the four selected states, we found examples of the kinds of
variation stakeholders have described in the allowable fees for patient
and third-party requests for medical records. (See table 2.)
• Three of the states— Ohio, Rhode Island, and Wisconsin—have
established per-page fee amounts. The amounts charged are based
on the number of pages requested and vary across the three states.
These three states have also established specific fee rates for
requesting media such as X-ray or magnetic resonance imaging scan
images.
• One state—Ohio—has established a different per-page fee amount
for third-party requests. The other three states have not established
different fees for different types of requests (i.e., between patient and
third-party requests).
• One state—Rhode Island—specifies a maximum allowable fee if the
provider uses an electronic health records (EHR) system for patient
and patient-directed requests.
• One state—Kentucky—entitles individuals to one free copy of their
medical record under state law. The statute allows a charge of up to
$1 per page for additional copies of a patient’s medical records.
Page 11 GAO-18-386 Patient Access to Medical Records
Table 2: Allowable Fees for Requests for Medical Records in Selected States
State and statute
Methods of
charging fees for
patient and
patient-directed
requests
a
Methods of charging
fees for third- parties
Does the statute
distinguish between
paper and electronic
records?
Special fees for
other types of
media
Other allowed
fees
Kentucky
KY. REV. STAT.
§ 422.317
Copy of medical
record provided
without charge.
Copying fee not to
exceed $1 per page for
second copy upon
request by patient,
patient’s attorney or
authorized
representative.
Statute does not
distinguish between
paper and electronic
records.
Fees for other
media not
specified.
Other allowed
fees are not
explicitly
mentioned.
Ohio
OHIO REV. CODE
§ 3701.741
For paper or
electronic data, per
page fees of $2.74
for pages 1-10,
$0.57 for pages 11-
50, $0.23 for pages
51 and higher.
Initial fee of $16.84,
$1.11 per page for
pages 1-10, $0.57 per
page for pages 11-50,
and $0.23 per page for
pages 51 and higher.
Statute refers explicitly
to paper or electronic
data but does not
specify different rates.
$1.87 per page
for CAT, MRI, or
X-ray images on
paper or film (all
requests).
Actual cost of
postage.
Rhode Island
b
R.I.Gen. Laws § 23-
1-48
For electronic
records, fee of
$0.50 for pages 1-
100, $0.25 for
pages 101 and
higher, with $100
cap.
For paper records,
$0.50 for pages 1-
100 and $0.25 for
pages 101 and
higher, with no cap.
Same as for patient
requests.
Yes, cap of $100 for
electronically stored
medical records.
Copies of X-rays
or films not
producible by
photocopy shall
be provided at
actual costs for
materials and
supplies.
Up to $25 for
clerical services
(including
research handling
and data retrieval)
for both paper and
electronic.
c
Wisconsin
WIS. STAT. §146.83
For paper copies:
$1 per page for
pages 1-25; $0.75
cents per page for
pages 26-50; $0.50
cents per page for
pages 51-100; and
$0.30 cents per
page for pages 101
and higher.
Statute does not
explicitly refer to third
parties.
Statute does not
explicitly refer to the
charges for electronic
records.
For microfiche or
microfilm copies,
$1.50 per page.
For a print of an
X-ray, $10 per
image.
Actual shipping
costs and
applicable taxes.
Source: GAO analysis of state laws. | GAO-18-386
a
The state statutes do not explicitly refer to patient-directed requests.
b
Rhode Island enacted a new statutory fee schedule in July 2017 and does not specify a different rate
for patient and third-party requests. Prior to enactment of the new statute, the state’s fee schedule
specified a maximum allowable fee of $127.49 for patient requests but did not establish a maximum
allowable fee for third-party requests. Under the new statute, Rhode Island also allows providers or
ROI vendors to charge a $25 clerical and retrieval fee for patient requests (including patient-directed
requests) for medical records. However, the Department of Health and Human Services’ Office for
Page 12 GAO-18-386 Patient Access to Medical Records
Civil Rights’ 2013 Final Rule and 2016 guidance states that retrieval costs are not permitted under the
Privacy Rule and may not be charged to individuals even if authorized by state law.
c
Other allowable fees in Rhode Island are a special handling fee of $10 if records must be delivered
within 48 hours.
In some cases, questions have been raised about the fee structure that
should be applied to certain types of requests. Representatives from ROI
vendors we interviewed told us that they have seen an increase in third
parties (primarily law firms) submitting requests for medical records and
indicating that the requests are patient-directed and therefore subject to
HIPAA’s reasonable, cost-based fee standard.
15
According to these
representatives, it is sometimes difficult for them to determine whether it
is an attorney making a third-party request or an attorney submitting a
patient-directed request because, for example, patient-directed requests
are submitted by a patient’s attorney and appear similar to traditional
third-party requests (e.g., they appear on legal letterhead).
16
As a result,
the representatives said that they are often unsure about which fee
structure to apply to the request: a reasonable, cost-based fee or a fee for
a third-party request, which ROI vendors told us is typically higher.
17
When asked about the reported distinction between fees for patient-
directed and third-party requests, OCR officials told us that they are in the
process of considering whether any clarification is needed to their 2016
guidance. This guidance describes the requirements of HIPAA and the
Health Information Technology for Economic and Clinical Health
(HITECH) Act, as well as their implementing regulations. HIPAA provides
patients with a legally enforceable right of access to their medical records.
OCR officials explained that the HITECH Act amended HIPAA and
15
As noted earlier, in 2013, HHS amended its regulations to state that the patient right of
access includes patient-directed requests. In 2016, OCR issued guidance stating that the
fee limitations applicable to individual patient requests are also applicable to patient-
directed requests.
16
OCR’s guidance states that a covered entity (i.e., a health care provider) may not
require an individual to provide a reason for requesting access and that the individual’s
rationale for requesting access, if voluntarily offered or known by the provider, cannot be
used to deny access to the medical records.
17
Third-party requests must contain a valid HIPAA authorization, the requirements for
which are set forth in regulation. 45 C.F.R. § 164.508(c) (2017). Patient directed requests
that direct that records to be sent to a third party have fewer requirements than are
required in a HIPAA authorization. To direct a copy to a third party, the patient’s request
must be in writing, signed, and must clearly identify the designated person or entity and
the location to which the protected health information should be sent. 45 C.F.R. §
164.524(c)(3)(ii) (2017).
Page 13 GAO-18-386 Patient Access to Medical Records
specifies that a patient’s right of access includes the right to direct a
provider to transmit the records directly to an entity or individual
designated by the individual.
18
According to OCR officials, the same
requirements for providing a medical record to an individual, such as the
limits on allowable fees and the format and timeliness requirements,
apply to patient-directed requests. OCR officials told us that they are
considering whether—and if so, how—they could clarify the 2016
guidance within the constraints of HIPAA and the HITECH Act.
Patient advocates and others we interviewed described challenges
patients face accessing medical records, such as high fees. Provider
representatives described challenges providers face, including allocating
staff time and other resources to respond to requests for medical records.
18
Pub. L. No. 111-5, § 13405(e)(1), 123 Stat. 115, 264 (Feb. 7, 2009). The HITECH Act
also states that any fee a covered entity may impose shall not be greater than the entity’s
labor costs.
Stakeholders
Identified Fees and
Other Challenges for
Patients Accessing
Medical Records and
Challenges for
Providers in
Allocating Resources
to Respond to
Requests

Page 14 GAO-18-386 Patient Access to Medical Records
Multiple stakeholders we interviewed—patient advocates, a provider
representative, experts, and a representative from an ROI vendor—told
us that some patients have incurred high fees when requesting access to
their medical records. Stakeholders noted that in some cases the fees
reported by patients appear to exceed the reasonable, cost-based
standard established under HIPAA.
19
One patient advocacy organization,
which collects information on patients’ access to their medical records,
described the following examples reported to them by patients:
• Two patients described being charged fees exceeding $500 for a
single medical record request.
• One patient was charged $148 for a PDF version of her medical
record.
• Two patients were directed to pay an annual subscription fee in order
to access their medical records.
• One patient was charged a retrieval fee by a hospital’s ROI vendor for
a copy of her medical records. Retrieval fees are prohibited under
HIPAA.
20
In addition, according to patient advocates we interviewed, high fees can
adversely affect patients’ access to their medical records. For example,
one patient advocate told us that some patients simply cancel their
requests after learning about the potential costs associated with their
request. Another patient advocate told us that patients are often unable to
afford the fees charged for accessing their medical records, even in cases
when the fees are allowed under HIPAA or applicable state law. This
advocate explained that per-page fees, even if legally authorized, can
pose challenges for patients; in particular, patients who have been
seriously ill can accumulate medical records that number in the
19
According to an April 2017 article, fees that appear to exceed HIPAA’s reasonable, cost-
based standard may be driven in part by the existence of state laws that are inconsistent
with—and are preempted by—HIPAA’s fee limitations. See A.W. Jaspers, J.L. Cox, H.A.
Krumholz, “Copy Fees and Limitation of Patients’ Access to Their Own Medical Records,”
JAMA Internal Medicine, vol. 177, no. 4 (2017). State laws that provide individuals with
greater rights of access to their protected health information than the Privacy Rule, such
as those states that require records to be provided free of charge once per year or that are
not contrary to the Privacy Rule, are not preempted by HIPAA and thus still apply.
20
According to one patient advocate with whom we spoke, some ROI vendors do not
itemize the fees they charge for access to medical records, which makes it difficult to
determine whether the fees are “reasonable.”
Patient Advocates and
Other Stakeholders
Described High Fees for
Obtaining Medical
Records, While Providers
and Patients May Be
Unaware of Patients’
Access Rights
Page 15 GAO-18-386 Patient Access to Medical Records
thousands of pages and can, as a result, face fees in excess of $1,000 for
a single copy of their records.
Stakeholders we interviewed told us that in many cases, providers may
also be unaware of patients’ right to access their medical records and the
laws governing the fees for doing so.
• Two patient advocates and an expert said that patients are sometimes
denied access to their medical records.
21
• Patient advocates and experts told us that some providers are not
aware of the 2016 OCR guidance, which describes patients’ rights to
access their medical records, as well as the permitted fees for such
access.
• One patient advocate and a provider representative also noted that
providers may be confused about caregivers’ and family members’
access to medical records. For example, providers sometimes
incorrectly deny family members’ access to a patient’s health
information, which HIPAA allows under certain circumstances.
22
• Provider representatives, patient advocates, and an expert agreed
that providers could benefit from more training on medical record
access issues, including training on the options patients have for
accessing their medical records.
Stakeholders we interviewed also noted that patients themselves are not
always aware of their right to access their medical records, do not always
know that they can submit a formal complaint to HHS’s OCR when denied
access, and could benefit from specific educational efforts that raise
awareness of these issues. For example, patient advocates said that the
“notice of privacy practices” form that patients receive and are asked to
sign when they first seek care from a provider could be improved to raise
awareness of the rights associated with accessing medical records. This
form is used to explain a provider’s privacy policies and obligations, and
what patients have to do to obtain access to their medical records.
However, a provider association and an expert told us that these forms
21
One stakeholder noted that one reason for denying patients access to their medical
records was fear that patients will use the information to sue the provider.
22
For example, when a family member is involved in the patient’s care, the Privacy Rule
does not require written consent for a provider to share health information with family
members as long as the patient does not object (and other conditions are met). 45 C.F.R.
§ 164.510 (2017).
Page 16 GAO-18-386 Patient Access to Medical Records
are not always easy for patients to understand, and patients might not
always read them. OCR has developed a standard privacy notice that
providers may adopt if they choose. However, a patient advocate told us
that most providers are still using their own versions of the notice.
Multiple stakeholders we interviewed told us that responding to patient
requests for medical records can be challenging because it requires the
allocation of staff and other resources and as a result, responding to such
requests can be costly. Furthermore, a provider representative, three
representatives from ROI vendors, and a patient advocate confirmed that
providers and their staff may lack the expertise needed for responding to
requests for medical records in a manner that complies with HIPAA and
applicable state laws. Providers can receive training on HIPAA related
issues; however, a patient advocate told us that this training, which may
be provided by private companies, often focuses on security issues (i.e.,
maintaining secure medical record systems) and not on the rights of
patients.
In addition, stakeholders we interviewed commonly stated that the
increased use of electronically stored health information in EHRs has
resulted in a more complex and challenging environment when
responding to requests for patients’ medical records. For example, these
stakeholders noted the following:
• Extracting medical records from EHRs is not a simple “push of a
button” and often requires providers or their ROI vendors to go
through multiple systems to compile the requested information.
Stakeholders noted that printing a complete record from an EHR
system can result in a document that is hundreds of pages long due to
the amount of data stored in EHR systems.
• Representatives from three ROI vendors told us that as providers
have transitioned from using paper records to using EHR systems,
information has been scanned into electronic medical records. This
has, in some cases, resulted in records being incorrectly merged
(e.g., the records of two patients merged into a single record). As a
result, when responding to a medical record request, providers or their
vendors must carefully go through each page of the record to ensure
only the correct patient’s medical records are being released.
• A provider representative, representatives from four ROI vendors, and
two experts noted that providers often have multiple active EHR
systems, or have legacy EHR systems in which some medical records
Provider Representatives
and Other Stakeholders
Described Challenges of
Allocating Staff Time and
Other Resources, While
Technology Has Improved
Patients’ Ability to Access
Records
Page 17 GAO-18-386 Patient Access to Medical Records
are stored. This requires providers and their vendors to go through
multiple EHR systems to extract information in response to a medical
record request.
• Some providers still have a mix of paper and electronic records, which
ROI vendors and provider representatives told us makes responding
to medical record requests more difficult and time consuming.
• A provider representative and other stakeholders said that while
patients can request copies of their records in an electronic format,
providers may have security concerns about sending information via
unsecured email or providing electronic information via a patient’s
USB stick, which increases the risk of a provider’s system becoming
infected with malware.
While health information technology has created some challenges for
providers, numerous stakeholders we interviewed told us that the
technologies have made accessing medical records and other information
easier and less costly for patients. For example, multiple stakeholders we
interviewed told us that an increase in the use of patient portals has
reduced the number of patient requests for access to their medical
records because patients are able to directly access some health
information through the portals.
23
As we have previously reported, patient
portals have facilitated patient access to medical records and patients
have noted the benefits from having such electronic access, even though
portals do not always contain all the information patients need.
24
The use
of patient portals has not eliminated patient requests for access to their
medical records; a provider representative we interviewed said that many
patients still prefer to obtain paper copies of their records.
23
A patient portal is a secure online website that gives patients 24-hour access to their
personal health information and medical records anywhere with an Internet connection.
Portals are purchased by providers and generally only include health information
generated and made available by that individual provider. We have reported on the
information providers generally make available via patient portals. See GAO, Health
Information Technology: HHS Should Assess the Effectiveness of Its Efforts to Enhance
Patient Access to and Use of Electronic Health Information, GAO-17-305 (Washington,
D.C.: Mar. 15, 2017).
24
See GAO-17-305.
Page 18 GAO-18-386 Patient Access to Medical Records
To enforce patients’ right of access under HIPAA’s Privacy Rule, the HHS
OCR undertakes four types of efforts. OCR (1) investigates complaints it
receives from patients and others regarding access to patient medical
records, (2) audits a sample of providers to determine the extent to which
their policies and procedures are compliant with HIPAA, (3) reports to
Congress on compliance with HIPAA, and (4) educates patients and
providers about patients’ rights to access their medical records.
OCR has established a process for investigating patients’ complaints over
access to their medical records. Via an online portal on its website, OCR
receives complaints submitted by patients.
25
Staff in OCR’s headquarters
office conduct an initial review of the information provided by the
complainant.
26
According to OCR officials, complaints that cannot be
immediately resolved are generally assigned to a regional office
investigator, who is responsible for reviewing the complaint and obtaining
additional information from the complainant and provider, if needed.
27
After the investigator completes the investigation, OCR issues a letter to
both the provider and patient explaining what OCR has found. Depending
on the nature of the findings, OCR may, for example, issue technical
assistance to the provider; close the complaint without identifying a
violation; require the provider to implement a corrective action plan;
conduct a more detailed investigation; and, if warranted, levy a civil
monetary penalty.
28
According to OCR officials, the use of civil monetary
penalties is rare and reserved for situations where providers’ behavior is
particularly egregious.
25
OCR’s online portal is available online. See Department of Health and Human Services
Office for Civil Rights, Complaint Portal, accessed April 2, 2018,
https://ocrportal.hhs.gov/ocr/cp/wizard_cp.jsf
26
OCR officials noted that if a complainant refuses to sign a release form allowing OCR to
speak with the provider in question and obtain the patient’s information, OCR does not
conduct any investigation. OCR staff stated that patients sometimes refuse to sign such a
release form.
27
OCR comprises nine regional offices.
28
Under HIPAA, OCR has the authority to take enforcement action and impose civil
monetary penalties on providers and other covered entities that violate HIPAA. 42 U.S.C.
§ 1320d-5. As of October 2017, OCR officials confirmed that the agency has levied a civil
monetary penalty on one provider for violating the patient right of access under HIPAA.
OCR Investigates
Complaints, Audits
Providers, and
Educates Patients
and Providers about
Patient Access
Investigation of Patient
Complaints
Page 19 GAO-18-386 Patient Access to Medical Records
Examples of patient access complaints provided to us by OCR included
complaints about the following:
• providers not responding even after the patient made multiple
requests, or providers taking longer than 30 days to respond to a
request for medical records or other information ;
29
• providers charging excessive fees for copies of patients’ medical
records;
• providers not responding to requests from personal representatives or
caregivers; and
• providers denying medical records requests from a parent or parents
of children.
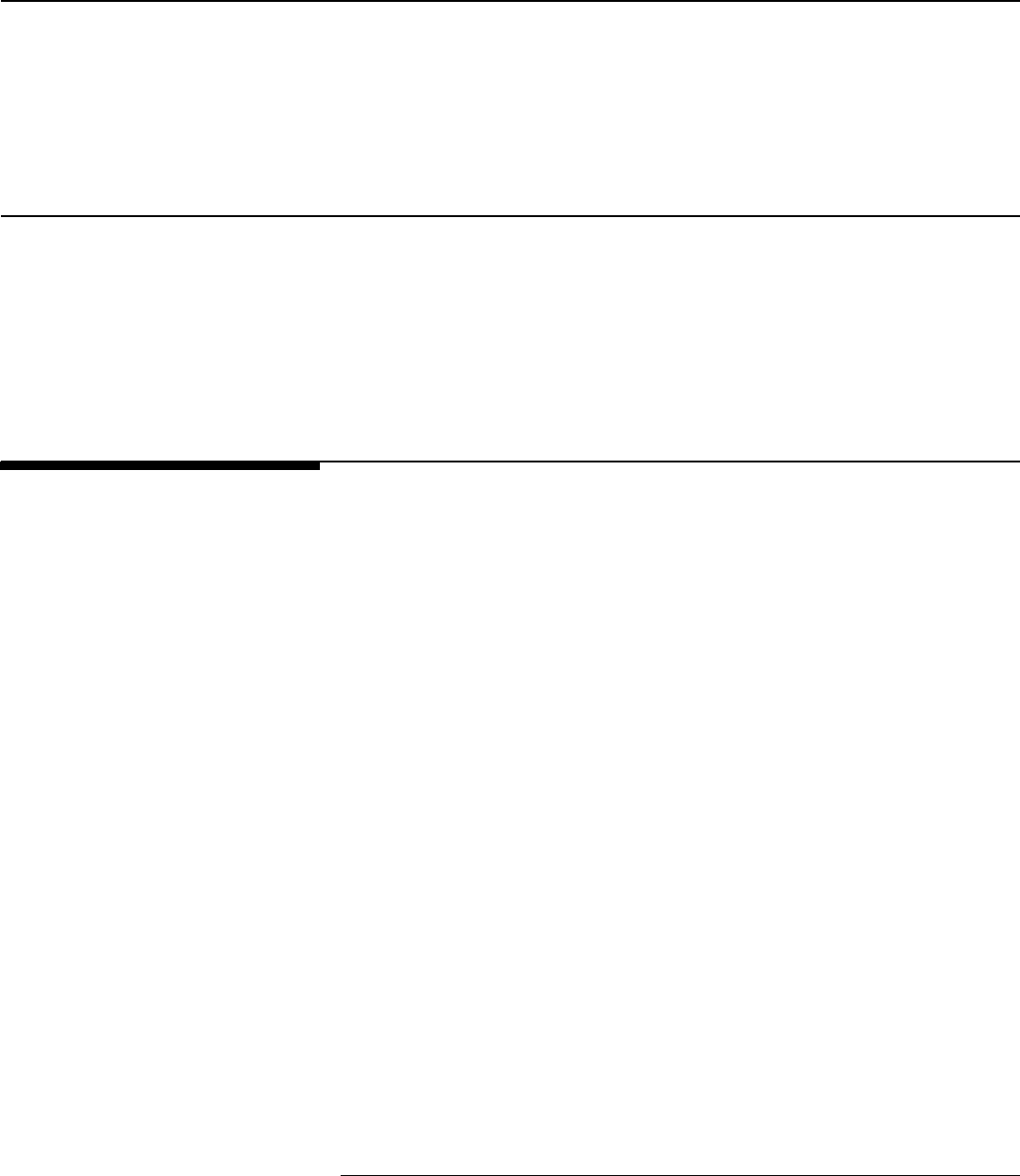
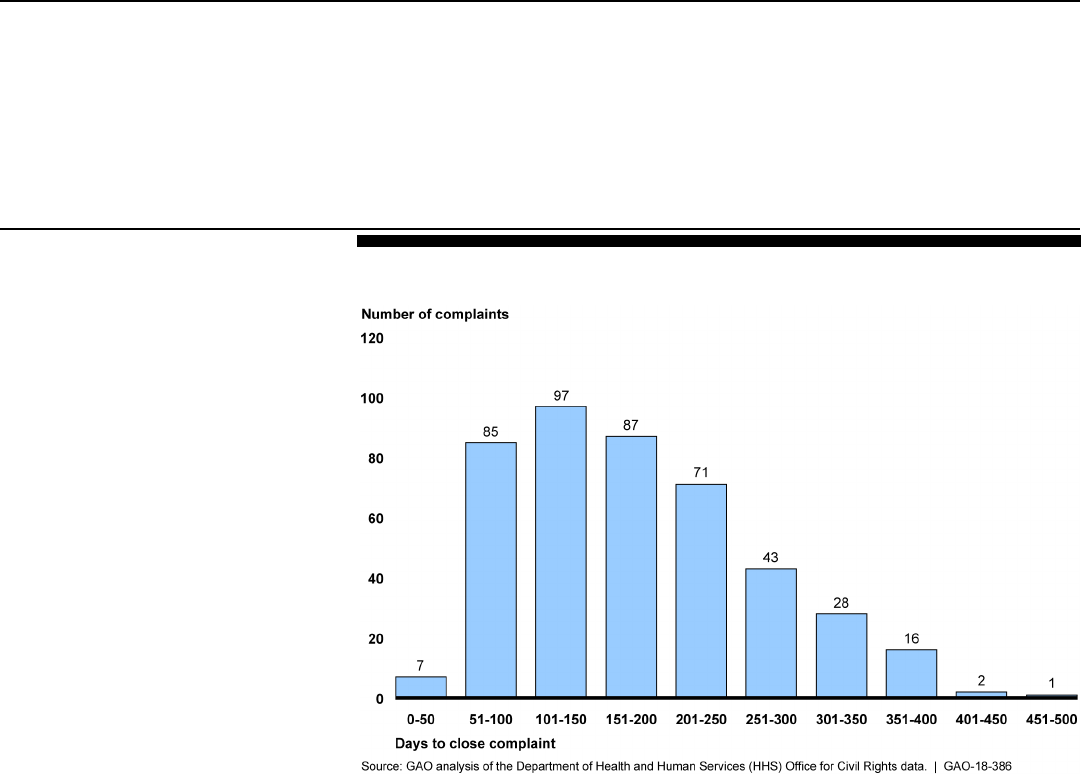
Our analysis of OCR data also shows that the amount of time OCR takes
to investigate and close a patient access complaint varies. OCR received
a total of 583 patient access complaints between February 2016 and
June 2017, closing 437 of these complaints during that same time period.
These 437 complaints took anywhere from 11 to 497 days to close. (See
fig. 2.) The majority of these 437 complaints (63 percent) were closed in
200 or fewer days. OCR officials stated that while there is no required
time frame for closing a complaint involving patients’ access to their
medical records, they aim to close cases in fewer than 365 days.
29
Under HIPAA’s implementing regulations, providers and other covered entities must
respond to a patient or patient-directed request for medical records within 30 days. 45
C.F.R. § 164.524(b) (2017).
Page 20 GAO-18-386 Patient Access to Medical Records
Figure 2: HHS Office for Civil Rights Time to Close Complaints Received between
February 2016 and June 2017
According to OCR officials, while there is no required time frame for
closing a patient access case, investigators aim to get patients access to
their medical records as soon as possible, which typically occurs before
the case is formally closed (i.e., a formal letter is issued to provider and
patient). OCR officials noted a number of reasons why complaints can
take a significant amount of time to close. In some cases, the patient
receives her records early in the investigation, but the complaint is kept
open by OCR to ensure that agreed-upon or recommended corrective
actions are taken by the provider—for example, training staff on patient
access rights or demonstrating that the provider’s policies pertaining to
patient access have been changed. In other complaints, time is needed
for OCR to obtain consent from the patient who filed the complaint. OCR
officials noted that in some instances, patients ultimately decide they do
not want to give OCR consent to investigate their complaint, due to
concerns that the provider will learn their identity. OCR officials also noted
that complaints that are moving towards more serious enforcement
actions, such as civil monetary penalties, may also take a long time to
close. Finally, OCR officials noted that their own staffing limitations in
regional offices can sometimes result in complaints taking additional time
to close.
Page 21 GAO-18-386 Patient Access to Medical Records
The HITECH Act requires OCR to conduct periodic audits of selected
covered entities in order to review the policies and procedures the
covered entities have established to meet HIPAA requirements and
standards.
30
The right of patients to access their medical records is
included in these requirements. As part of its most recent audit, OCR
officials stated that they reviewed 103 covered entities regarding their
policies related to patient access to health information, including the
entities’ notice of privacy practices.
31
In addition, OCR reviewed any
access requests the covered entities received from patients, including
both requests that were granted and requests that were denied. OCR
examined these access requests to determine whether access was
provided in a manner that was consistent with the covered entities’
policies and procedures and whether the entities fulfilled the requests
they received within the 30-day time frame established under the Privacy
Rule. OCR also examined any fees that were charged for access and
whether those fees met HIPAA’s reasonable, cost-based standard. OCR
officials said that after completing each audit, OCR submitted a draft
report for the audited entity for review. The entity had 10 days to review
and submit any feedback to OCR, which OCR reviewed and incorporated
into the entity’s final audit report. According to OCR officials, OCR has
completed this phase of the audit program and will release a final report
in 2018.
30
42 U.S.C. § 17940.
The HITECH Act requires OCR to conduct periodic audits of covered entity and business
associate compliance with the HIPAA Privacy, Security, and Breach Notification Rules. In
2011 and 2012, OCR implemented a pilot audit program to assess the controls and
processes implemented by 115 covered entities to comply with HIPAA’s requirements.
Additionally, in 2013, OCR conducted an evaluation of the effectiveness of the pilot
program. OCR completed the second phase of the audit program in which it audited
covered entities and business associates for compliance with HIPAA rules.
31
Every covered entity and business associate in the country was eligible to be selected
for an audit; however, business associates were not audited on the patient access
standard since they are not subject to this provision. To select its 103 covered entities,
OCR identified pools of covered entities that represented a range of health care providers
and other organizations that are considered covered entities under HIPAA. Sampling
criteria for selecting entities to audit included size of entity, type of entity, geographic
location, and current enforcement activity with OCR. OCR did not select entities for audit
that had an open complaint investigation with OCR or were currently undergoing a
compliance review by OCR.
OCR Audits
Page 22 GAO-18-386 Patient Access to Medical Records
The HITECH Act directs HHS to submit an annual report to Congress on
compliance with HIPAA that includes details about complaints of alleged
violations of the Privacy Rule and the resolution of these complaints.
32
The patient right of access is part of the HIPAA and Privacy Rule
requirements. The report, which is issued by OCR, includes information
on the patient access complaints OCR has received, the number of
investigations it has conducted, and the fines OCR has levied. OCR
issued its most recent report in 2016. The report summarized complaints
and enforcement actions for the 2013 through 2014 calendar years. OCR
officials stated that they are in the process of reviewing a draft report that
will be released in mid-2018 and contain information and data from
calendar years 2015 and 2016.
As part of its responsibilities to enforce HIPAA’s Privacy Rule, OCR also
provides a variety of educational materials that aim to educate both
patients and providers about patients’ right to access their medical
records. These materials include the following:
• In September 2017, OCR published a pamphlet that aims to educate
consumers, particularly caregivers, about patients’ rights to access
their medical records, including how to file a complaint if denied
access.
33
• OCR has worked with ONC to produce three videos (“Your Health
Information, Your Rights!”) and an infographic aimed at educating
32
Section 13424(a) of the HITECH Act requires the Secretary of the Department of Health
and Human Services to prepare and submit an annual report to Congress regarding
compliance with the Privacy and Security Rules promulgated under HIPAA. In addition,
Section 13424(a)(2) of the HITECH Act requires that each report be made available to the
public on the web site of the Department. OCR submits the reports to Congress every 2
years and posts the reports, as well as submission letters to the applicable Congressional
committee. See Department of Health and Human Services, Report to Congress on
Privacy Rule and Security Rule Compliance, accessed April 4, 2018,
https://www.hhs.gov/hipaa/for-professionals/compliance-enforcement/reports-
congress/index.html; and Reports to Congress on Breach Notification Program, accessed
April 4, 2018, https://www.hhs.gov/hipaa/for-professionals/breach-notification/reports-
congress/index.html
33
This pamphlet and other consumer information can be found online. See Department of
Health and Human Services, Get It. Check It. Use It., accessed April 4 2018,
https://www.hhs.gov/hipaa/for-individuals/right-to-access/index.html.
Annual Report to
Congress
Provider and Patient
Education Efforts
Page 23 GAO-18-386 Patient Access to Medical Records
patients and others about patients’ rights to access their medical
records.
34
• OCR has developed provider education videos that aim to educate
providers on the rights of patients to access their medical records and
how such access can enable patients to be more involved in their own
care. Providers can receive continuing education credits for watching
these videos.
To assist providers, OCR has worked with ONC to develop a model
notice of privacy practices to help providers adequately communicate
access rights to patients in a standardized, easy-to-understand way.
35
We provided a draft of this report to HHS for review. HHS provided us
with technical comments, which we incorporated as appropriate.
We are sending copies of this report to the appropriate congressional
committees, the Secretary of Health and Human Services, and other
interested parties. In addition, the report is available at no charge on the
GAO website at http://www.gao.gov.
If you or your staffs have any questions about this report, please contact
me at (202) 512-7114 or at [email protected]. Contact points for our
Office of Congressional Relations and Office of Public Affairs can be
found on the last page of this report. Other major contributors to this
report are listed in appendix I.
Carolyn L. Yocom
Director, Health Care
34
These resources are available online. See Department of Health and Human Services,
Your Rights under HIPAA, accessed April 4, 2018, https://www.hhs.gov/hipaa/for-
individuals/guidance-materials-for-consumers/index.html.
35
The model notice can be found online. See Department of Health and Human Services,
Model Notices of Privacy Practices, accessed January 12, 2018,
https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/model-notices-privacy-
practices/index.html.
Agency Comments
Appendix I: GAO Contact and Staff
Acknowledgments
Page 24 GAO-18-386 Patient Access to Medical Records
Carolyn L. Yocom, (202) 512-7114 or yocomc@gao.gov
In addition to the contact named above, Tom Conahan, Assistant
Director; Andrea E. Richardson, Analyst-in-Charge; Krister Friday; and
Monica Perez-Nelson made key contributions to this report.
Appendix I: GAO Contact and Staff
Acknowledgments
GAO Contact
Staff
Acknowledgments
(101949)
The Government Accountability Office, the audit, evaluation, and investigative
arm of Congress, exists to support Congress in meeting its constitutional
responsibilities and to help improve the performance and accountability of the
federal government for the American people. GAO examines the use of public
funds; evaluates federal programs and policies; and provides analyses,
recommendations, and other assistance to help Congress make informed
oversight, policy, and funding decisions. GAO’s commitment to good government
is reflected in its core values of accountability, integrity, and reliability.
The fastest and easiest way to obtain copies of GAO documents at no cost is
through GAO’s website (https://www.gao.gov). Each weekday afternoon, GAO
posts on its website newly released reports, testimony, and correspondence. To
have GAO e-mail you a list of newly posted products, go to https://www.gao.gov
and select “E-mail Updates.”
The price of each GAO publication reflects GAO’s actual cost of production and
distribution and depends on the number of pages in the publication and whether
the publication is printed in color or black and white. Pricing and ordering
information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077, or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard,
Visa, check, or money order. Call for additional information.
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or E-mail Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
Contact:
Website: https://www.gao.gov/fraudnet/fraudnet.htm
Automated answering system: (800) 424-5454 or (202) 512-7470
Orice Williams Brown, Managing Director, WilliamsO@gao.gov, (202) 512-4400,
U.S. Government Accountability Office, 441 G Street NW, Room 7125,
Washington, DC 20548
Chuck Young, Managing Director, youngc1@gao.gov, (202) 512-4800
U.S. Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
James-Christian Blockwood, Managing Director, s[email protected]ov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814,
Washington, DC 20548
GAO’s Mission
Obtaining Copies of
GAO Reports and
Testimony
Order by Phone
Connect with GAO
To Report Fraud,
Waste, and Abuse in
Federal Programs
Congressional
Relations
Public Affairs
Strategic Planning and
External Liaison
Please Print on Recycled Paper.
