
DRAFT FOR CONSULTATION
JUNE 2022
10 proposals to build
a safer world together
Strengthening the Global Architecture for Health
Emergency Preparedness, Response and Resilience

DRAFT FOR CONSULTATION
JUNE 2022
10 proposals to build
a safer world together
Strengthening the Global Architecture for Health
Emergency Preparedness, Response and Resilience

DRAFT FOR CONSULTATION
JUNE 2022
ii
10 proposals to build a safer world together – Strengthening the Global Architecture for Health Emergency Preparedness, Response and
Resilience
WHO/2022
© World Health Organization 2022
Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence
(CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo).
Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work
is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specic
organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license
your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add
the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization
(WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding
and authentic edition”.
Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the
World Intellectual Property Organization
(http://www.wipo.int/amc/en/mediation/rules/).
Suggested citation. 10 proposals to build a safer world together – Strengthening the Global Architecture for Health Emergency
Preparedness, Response and Resilience Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris .
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders . To submit requests for commercial
use and queries on rights and licensing, see
http://www.who.int/about/licensing .
Third-party materials. If you wish to reuse material from this work that is attributed to a third party, such as tables, gures or
images, it is your responsibility to determine whether permission is needed for that reuse and to obtain permission from the
copyright holder. The risk of claims resulting from infringement of any third-party-owned component in the work rests solely
with the user.
General disclaimers. The designations employed and the presentation of the material in this publication do not imply the
expression of any opinion whatsoever on the part of WHO concerning the legal status of any country, territory, city or area or
of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent
approximate border lines for which there may not yet be full agreement.
The mention of specic companies or of certain manufacturers’ products does not imply that they are endorsed or
recommended by WHO in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the
names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by WHO to verify the information contained in this publication. However, the published
material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and
use of the material lies with the reader. In no event shall WHO be liable for damages arising from its use.
Cover photo: WHO is reaching the most vulnerable people in 15 African countries, including South Sudan, who are facing humanitarian situations such as drought,
natural disasters and displacement. © WHO

DRAFT FOR CONSULTATION
JUNE 2022
iii
Contents iii
Foreword from the Director-General iv
Executive summary v
Introduction 1
Purpose of the white paper 2
Proposals for strengthening global health emergency
preparedness, response and resilience 3
Governance 4
Systems 6
Financing 11
Equity, inclusivity and coherence 14
Next Steps 17
Annex 1: Strengthening HEPR systems capacities 18
Annex 2: Application of principles of equity,
inclusivity, and coherence 32
Contents

DRAFT FOR CONSULTATION
JUNE 2022
iv
Foreword from the Director-General
The COVID-19 pandemic has revealed deep aws in the world’s defences
against health emergencies, exposed and exacerbated profound inequities
within and between countries, and eroded trust in governments and
institutions.
The world was, and remains, unprepared for large-scale health
emergencies. But this lesson is not a new one. For decades the emergence
of new epidemic-prone diseases, conicts, and other humanitarian
emergencies has caused global panic and alarm, followed by neglect and
underinvestment in health emergency preparedness, prevention and
response as public and political attention wanes.
Three interlinked priorities are key to the renewal and recovery of national
and global health systems that we need to break the cycle of panic and
neglect, improve population health, and make countries better prepared for
and more resilient against future health emergencies.
We must tackle the root causes of disease and ill-health; we must reorient
health systems towards primary health care and universal health coverage; and we must rapidly strengthen the global
architecture for health emergency preparedness and response. This white paper presents WHO’s proposals for how we can
achieve this third priority together.
In response to a request at our Executive Board, and in consultation with Member States and other stakeholders, we set
out ten proposals for a stronger global health security architecture, based on the principles of equity, inclusivity, and
coherence. The proposals build on the more than 300 recommendations from the various independent reviews of the
global response to COVID-19, and reports into previous outbreaks.
We call for stronger governance that is coherent, inclusive and accountable; stronger systems and tools to prevent,
detect and respond rapidly to health emergencies; stronger nancing, domestically and internationally; and a stronger,
empowered and sustainably nanced WHO at the centre of the global health security architecture.
Finally, to be able to implement these proposals eectively, we need a new international accord, which WHO’s Member
States are now negotiating. Since the Second World War, countries have entered into treaties on tobacco, nuclear, chemical
and biological weapons, climate change and many other threats to our shared security and well-being. It is common sense
now for countries to agree on a common approach to common threats, with common rules for a common response to
health emergencies.
The COVID-19 pandemic has taught us all many painful lessons. The greatest tragedy would be not to learn them. Now is the
time to make the bold changes that must be made to keep future generations safer.
Dr Tedros Adhanom Ghebreyesus
WHO Director-General

DRAFT FOR CONSULTATION
JUNE 2022
v
The coronavirus disease (COVID-19) pandemic continues to
highlight the need for a stronger, inclusive, equitable and
coherent health emergency preparedness, response, and
resilience (HEPR) architecture.
Building on the work of numerous reviews, panels, and
consultations, this White Paper outlines the Director-
General’s 10 proposals to strengthen HEPR under the aegis
of a new overarching Pandemic Accord that is currently
under negotiation. The recommendations are grouped
by the three main constituents of the global pandemic
architecture.
Governance
1 Establish a Global Health Emergency Council and
Committee on Health Emergencies for the World Health
Assembly
2 Make targeted amendments to the International Health
Regulations (2005)
3 Scale-up Universal Health and Preparedness Reviews
and strengthen independent monitoring
Systems
4 Strengthen global health emergency alert and
response teams that are trained to common standards,
interoperable, rapidly deployable, scalable and
equipped
5 Strengthen health emergency coordination through
standardized approaches to strategic planning,
nancing, operations and monitoring of health
emergency preparedness and response
6 Expand partnerships and strengthen networks for a
whole-of-society approach to collaborative surveillance,
community protection, clinical care, and access to
countermeasures
Financing
7 Establish a coordinating platform for nancing to
promote domestic investment and direct existing and
gap-lling international nancing to where it is needed
most
8 Establish a nancial intermediary fund for pandemic
preparedness and response to provide catalytic and gap-
lling funding
9 Expand the WHO Contingency Fund for Emergencies to
ensure rapidly scalable nancing for response
10 Strengthen WHO at the centre of the global HEPR
architecture
The Director-General’s proposals are designed to support
and contribute to decision-making in the various fora
within and beyond WHO that will determine the future
global architecture of HEPR.
The Secretariat welcomes comments from Member
States and partners on these proposals through informal
consultations and feedback in writing.
Executive summary
DRAFT FOR CONSULTATION
JUNE 2022
1
This is the description of the plague of Athens in 430 BCE,
as told by the ancient Greek historian Thucydides in his
History of the Peloponnesian War. Almost two-and-a-
half millennia later, the coronavirus disease (COVID-19)
pandemic has demonstrated that although much has
changed, much has not.
At the time of writing, almost 6.3 million deaths have been
reported to WHO, but the true toll is much higher. Health
systems have been overwhelmed, and many health workers
have lost their lives or le their jobs because of burnout,
stress and anxiety. The global economy was plunged into its
deepest recession since the Second World War, forcing 135
million people into poverty. Widespread misinformation
and disinformation have caused confusion and distrust,
dividing families, communities and societies.
The pandemic has exposed divisions and inequities within
and between countries, and gaps in the world’s ability
to prepare for, prevent, detect and respond rapidly to
epidemics, pandemics and other health emergencies.
COVID-19 hit the poor and vulnerable hardest, while
reminding even the most privileged that infectious diseases
still have the power to upend not only health systems, but
also societies and economies.
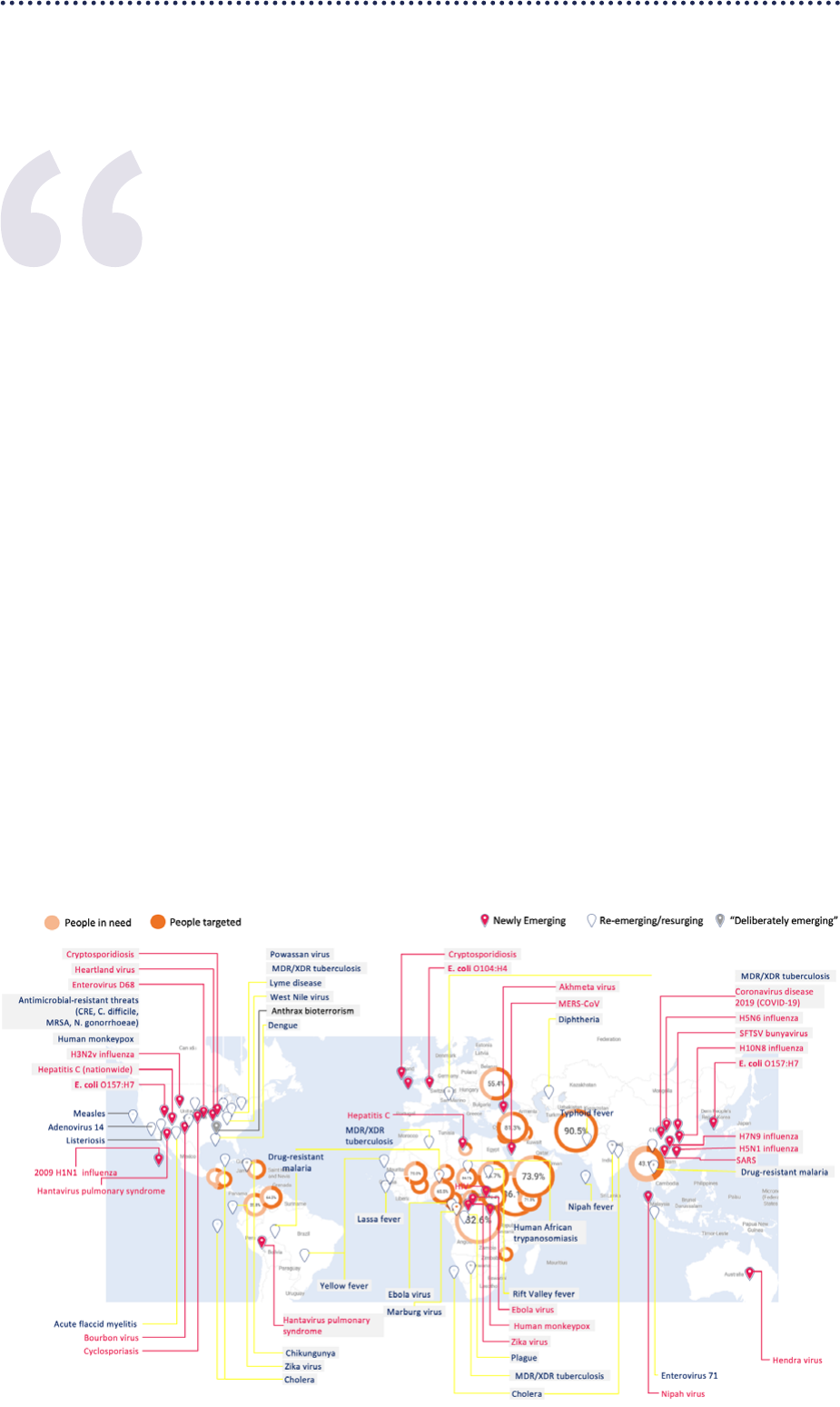
The risk of new health emergencies continues to increase,
driven by the escalating climate crisis, environmental
degradation, and increasing geo-political instability,
disproportionately impacting the poor and most vulnerable
(Figure 1). Humanitarian crises aected 300 million people
in 2022, putting them at an increased risk of the health
emergencies that inevitably follow.
The overall lesson is clear: the world is not prepared. This
lesson is not a new one. Just this century, epidemics of
SARS, H5N1, H1N1, MERS, Ebola and Zika have emerged,
only to be followed by a pattern of panic and neglect, in
which concern during emergencies gives way to apathy and
underinvestment in their aermath.
Thucydides wrote his account of the Plague of Athens
so that future generations might avoid the suering he
experienced. While COVID-19 has taken so much, it has
also given us the opportunity to learn the painful lessons
it has taught us, and use them to build a healthier, safer,
fairer world for the generations to come. We must seize that
opportunity before the world moves on to other priorities.
Introduction
The doctors were unable to cope, since they were treating the disease for the rst time and in ignorance:
indeed, the more they came into contact with suerers, the more liable they were to lose their own lives.
No other device of men was any help. Moreover, supplication at sanctuaries, resort to divination, and
the like were all unavailing. In the end, people were overwhelmed by the disaster and abandoned eorts
against it. … I shall give a statement of what it was like, which people can study in case it should ever
attack again, to equip themselves with foreknowledge so that they shall not fail to recognize it. I can give
this account because I both suered the disease myself and saw other victims of it.
Figure 1: Scale of health emergencies from all hazards (2021/2022)

DRAFT FOR CONSULTATION
JUNE 2022
2
There have been many expert reviews of the HEPR
architecture and the global response to the COVID-19
pandemic, yielding more than 300 recommendations
that have been analysed and discussed through
multiple international processes (Figure 2). The quality
of contributions to these reviews reects the depth of
thought, expertise and engagement of a broad spectrum
of stakeholders. Maintaining this engagement and
strengthening the links between stakeholders will be a
crucial determinant of the success of an agile, responsive
and exible HEPR architecture in the future.
Building on the work done to date, this white paper outlines
the Director-General’s 10 proposals to strengthen HEPR
under the aegis of a new overarching pandemic accord,
which is currently being developed by the Intergovernmental
Negotiating Body to dra and negotiate a WHO convention,
agreement or other international instrument on pandemic
prevention, preparedness and response.
The proposals focus on the architecture that will be needed
to ensure a signicantly more prepared world, and may need
to be adapted for specic threats and contexts. The proposals
do not attempt to assign roles and responsibilities within that
architecture. The capabilities and partnerships developed
during the response to COVID-19 will contribute to achieving
this ambitious agenda, and WHO will continue to engage with
others in determining wider roles and responsibilities.
Many of the proposals below are designed to build on,
complement and strengthen existing frameworks and
capacities established aer previous crises, strengthening
the bonds between global health partners. Other proposals
build on new and innovative mechanisms put in place
during the COVID-19 pandemic to ll critical gaps. In many
cases, these initiatives now need to be adapted and rened
according to the lessons of the pandemic in consultation
with Member States and partners. A small number of
proposals call for the establishment of new mechanisms
or structures that are currently being discussed in ongoing
Member State processes.
The proposals are grouped by the three main pillars of
the global HEPR architecture: governance, systems and
nancing, and are based on three key principles.
• They must promote equity, with no one le behind –
equity is both a principle and a goal, to protect the most
vulnerable.
• They should promote an HEPR architecture that is
inclusive, with the engagement and ownership of all
countries, communities and stakeholders from across
the One Health spectrum. Commitment to diversity,
equity and inclusivity is key to eective HEPR at all
levels, including equal participation in leadership and
decision-making, regardless of gender.
• They must promote coherence, reducing fragmentation,
competition and duplication; be aligned with existing
international instruments such as the International
Health Regulations (2005) and the Pandemic Inuenza
Preparedness Framework for the sharing of inuenza
viruses and access to vaccines and other benets; ensure
synergy between institutional capabilities for systems
strengthening and nancing; and promote the integration
of HEPR capacities into national health and social systems
based on universal health coverage and primary health care.
Purpose of the white paper
Figure 2. Reviews, reports and processes that have
informed this white paper
P
a
n
d
e
m
i
c
A
c
c
o
r
d
G
o
v
e
r
n
a
n
c
e
S
y
s
t
e
m
s
F
i
n
a
n
c
i
n
g
Equity
Inclusivity
Coherence
Independent Panel for Pandemic
Preparedness and Response report
GPMB and IOAC reports
Other reports
IHR Review Committee on the
Functioning of the International
Health Regulations (2005) during
the COVID-19 Response
Pan-European Commission on
Health and Sustainable Development
High Level Independent Panel on
Financing the Global Commons
for Pandemic Preparedness and
Response report
INB and WGPR processes
G20 and G7 processes
Other processes
GPMB: Global Preparedness Monitoring Board; Intergovernmental Negotiating Body to dra and negotiate a WHO convention, agreement or other international instrument on
pandemic prevention, preparedness and response; IOAC: Independent Oversight and Advisory Committee for the WHO Health Emergencies Programme; WGPR: Member States
Working Group on Strengthening WHO Preparedness and Response to Health Emergencies.
More than 300
recommendations
DRAFT FOR CONSULTATION
JUNE 2022
3
Health emergency preparedness, response and
resilience is multi-sectoral by nature
Dealing eectively with the multiplying complex and
multi-dimensional threats of the 21st century requires a
strengthened and agile approach to the way we prepare for
and respond to health emergencies. Where previously there
has been chronic neglect and underinvestment in national
capacities, we need to make smart, evidence-based
investments that deliver the best possible return in terms
of lives saved, sustainable development, global economic
stability and long-term growth. That means recognizing
that strengthening the global HEPR architecture must be
part of the broader eort towards the 2030 Sustainable
Development Goals.
Countries were already o track to meet their commitments
under the health-related Sustainable Development Goals
before COVID-19, and the pandemic has set back progress
even further. Achieving the health-related Goals will
therefore require a plan for recovery and renewal based
on rapidly accelerating progress in three interdependent
priority areas:
• Health promotion: preventing disease by addressing its
root causes;
• Primary health care: supporting a radical reorientation
of health systems towards primary health care, as the
foundation of universal health coverage; and
• Health security: urgently strengthening the global
architecture for HEPR at all levels.
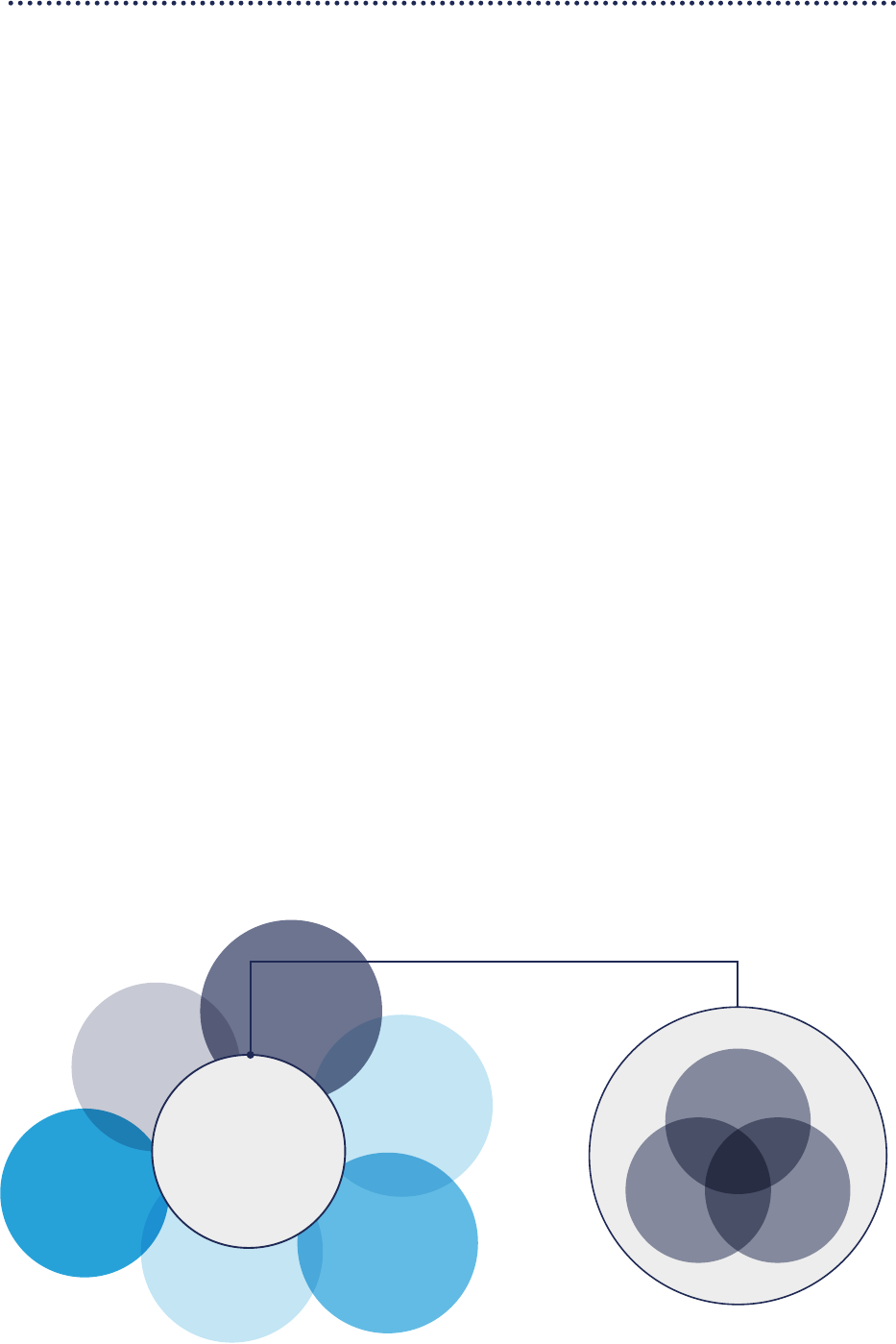
These priorities stem from the simple principle that there
is one health system, encompassing the common functions
and structures that are crucial for health security, for
primary health care, and for health promotion (Figure 3).
Targeting these common capacities for investment will
accelerate progress towards the health-related Sustainable
Development Goals at the same time as boosting national
and global health security. A renewed global architecture
for HEPR must be built on a foundation of strong national
health systems that are deeply connected with and
accountable to the communities they serve, and which
advance gender equity and human rights.
Many HEPR capacities straddle the boundary of the health
system and other governmental and societal sectors and
systems, such as education, nance, animal health and
agriculture, and the environment. Investments are also
needed to strengthen these links, and ensure greater
coherence in multi-sectoral planning, readiness and
response.
The need for greater coherence and coordination of
eort and investment extends to the global level. The
international community needs ways of working together
that deliver collaboration and coordinated, collective
action, and that address the fragmentation that impairs
the current global architecture for HEPR. That means
considering carefully the creation of new mechanisms, and
the addition of new organizations or institutes to what is
already a crowded landscape.
Figure 3. Investing in health security strengthens primary healthcare and health promotion, and vice versa,
within the broader health system
Animal health
and agriculture
Environment
Humanitarian and
disaster management
Economics and finance
Social welfare
and protection
Health system
Security
H
e
a
l
t
h
s
y
s
t
e
m
Primary
health care
Health
promotion
Health
security

DRAFT FOR CONSULTATION
JUNE 2022
4
Figure 4. Summary of proposed solutions for the
strengthening of the global architecture for health
emergency preparedness, response and resilience
Within the broader context of recovery and renewal for
achieving the health-related Sustainable Development
Goals, and the need for greater coherence of the global
HEPR architecture under the aegis of a new Pandemic
Accord, 10 proposals for strengthening HEPR are outlined
below (Figure 4).
Governance
Eective governance is essential to bring greater equity,
inclusivity and coherence to the global architecture of
HEPR, enabling Member States and partners to work
collectively around a shared plan, galvanized by political
will, and with the resources to sustain positive changes.
Proposal 1. Establish a Global Health Emergency
Council and a Committee on Health Emergencies
of the World Health Assembly
HEPR must be elevated to the level of heads of state and
government to ensure sustained political commitment, and
break the cycle of panic and neglect that has characterized
the response to previous global health emergencies.
Several panels have proposed the establishment of a
high-level body on global health emergencies, comprising
heads of state and other international leaders. The
Director-General supports this concept, and proposes the
establishment of a Global Health Emergency Council, linked
to and aligned with the constitution and governance of
WHO, rather than creating a parallel structure, which could
lead to further fragmentation of the global architecture
of HEPR. Head of State participation, especially during
health emergencies, would further strengthen WHO’s
primary constitutional function to act as the directing
and coordinating authority on international health work
(WHO Constitution, Article 2(a)).
The Council would address health emergencies as well as
their broader context and social and economic impact. It
would have three primary responsibilities:
• Address obstacles to equitable and eective HEPR,
ensuring collective, whole-of-government and whole-
of-society action, aligned with global health emergency
goals, priorities and policies;
• Foster compliance with and adherence to global health
agreements, norms and policies; and
• Identify needs and gaps, swily mobilize resources, and
ensure eective deployment and stewardship of these
resources for HEPR.
The Council would be composed of heads of state and
government, attended by the United Nations Secretary
General and WHO Director-General, with heads of relevant
international organizations and other bodies as observers.
The Council would meet annually to review progress in
pandemic preparedness and response, and as required
in the event of a public health emergency of international
concern.
P
a
n
d
e
m
i
c
A
c
c
o
r
d
G
o
v
e
r
n
a
n
c
e
S
y
s
t
e
m
s
F
i
n
a
n
c
i
n
g
Equity
Inclusivity
Coherence
Systems
Capacity – strengthened health emergency alert
andresponse teams that are interoperable and
rapidly deployable
Coordination: standardized approaches for
coordinating strategy, nancing, operations
and monitoring of preparedness and response
Collaboration: expanded partnerships and
strengthened networks for collaborative surveillance,
community protection, clinical care and access to
countermeasures
Financing
Predictable nancing for preparedness –
coordinating platform for nancing with increased
domestic investment and more eective/innovative
international nancing
Rapidly scalable nancing for response – expanded
contingency fund for emergencies
Catalytic, gap-lling funding – expanded nancing
through a new nancial intermediary fund
Governance
Leadership – Global Health Emergency Council,
WHO Committee for Emergencies
Regulation – targeted amendments to the
International Health Regulations (2005)
Accountability – universal health and preparedness
review, independent monitoring mechanisms
Proposals for strengthening global health
emergency preparedness, response and resilience

DRAFT FOR CONSULTATION
JUNE 2022
5
The work of the Council would complement and be
linked with the work of a Standing Committee on Health
Emergencies, which the Executive Board established at its
151st session in May 2022.
To strengthen integrated governance, the Health
Assembly could also establish a new main committee on
emergencies, a Committee E. Such a new main committee
could be linked with both the Council and the Standing
Committee on Health Emergencies, and as an open-ended
committee of all WHO Member States, Committee E would
help to ensure global inclusivity. The Oicers of Committee
E and of the Standing Committee could be invited to attend
meetings of the Council to further promote coordination
among the three bodies.
Further, a Committee E could:
• Review the work of WHO in health emergency
preparedness, response and resilience;
• Act as a conference of State Parties to the International
Health Regulations (2005);
• Act as the peer review mechanism for the Universal
Health and Preparedness Review; and
• Consider any recommendation by the Executive Board
based on advice from the Standing Committee on Health
Emergencies.
Such an interlinked arrangement could strengthen WHO’s
constitutional role as the directing and coordinating
authority on international health work.
Proposal 2. Make targeted amendments
to the International Health Regulations (2005)
The International Health Regulations (2005) (IHR) are the
international legally binding framework that denes the
rights and obligations of its 196 States Parties and of the
WHO Secretariat for handling public health emergencies
with potential to cross borders. The IHR remains an
essential legal instrument for public health emergencies
preparedness and response.
The COVID-19 pandemic has revealed some weaknesses in
the interpretation of, application of and compliance with
the IHR. The inherent tension between the aim to protect
health and the need to protect economies by avoiding
travel and trade restrictions has been noted by the IHR
Review Committee on the Functioning of the International
Health Regulations (2005) during the COVID-19 Response as
the most important factor limiting compliance with the IHR.
In addition, too many countries still do not have suicient
public health capacities to protect their own populations,
and to give timely warnings to WHO. The current reporting
mechanism on the implementation of plans of action to
ensure that the core capacities required by the IHR are
present and functioning lacks incentives for compliance.
The absence of a conference of the States Parties to the IHR
is an overarching limitation in their eective application
and compliance.
Further strengthening of IHR implementation compliance
will require some targeted amendments. Areas of focus
may include: improved accountability by establishing
the national responsible authority for the overall
implementation of the IHR, and a conference of State
Parties (see proposal 1 above); more specicity in relation
to notication, verication and information sharing;
capacity-building and technical support for surveillance,
laboratory capacity and public health rapid response; and
streamlining the process to bring IHR amendments into
force.
Ensuring that the IHR can be eiciently and eectively
strengthened to accommodate evolving global health
requirements is key to their continued relevance and
eectiveness as a global health legal instrument.

DRAFT FOR CONSULTATION
JUNE 2022
6
Proposal 3. Scale up Universal Health and
Preparedness Reviews and strengthen
independent monitoring
In response to a proposal from several Member States, the
introduction of the Universal Health and Preparedness
Review (UHPR) was announced by the WHO Director-
General in November 2020, with the goal of building
solidarity, mutual trust and accountability for health,
through an innovative intergovernmental review process.
The UHPR is a Member State-led mechanism in which
countries agree to a voluntary, regular and transparent peer
review of their comprehensive national health emergency
preparedness capacities, incorporating lessons learned
from the COVID-19 pandemic on preparedness assessment.
It aims to:
• Enhance transparency and understanding of a country’s
comprehensive preparedness capacities among relevant
national stakeholders;
• Promote whole-of-government and whole-of-society
dialogue on preparedness in countries, including close
cooperation with governments, regional organizations
and civil society;
• Encourage compliance with commitments made under
the IHR and related Health Assembly resolutions in the
eld of emergency preparedness;
• Elevate considerations for preparedness beyond
the health sector and ensure the comprehensive
implementation of recommendations; and
• Promote national, regional and global solidarity,
dialogue and cooperation.
A pilot phase of the UHPR mechanism was completed in
2021. Based on lessons learned from the pilot phase, the
UHPR should now be scaled up to complement existing
assessment tools and processes, and a peer review
mechanism should be included as part of the UHPR
process.
Self-assessment and peer review of national capacities,
including through the UHPR, should be complemented
by independent monitoring at the international level. The
independent monitoring mechanism should be modelled
on best practice in independent monitoring of international
instruments, and should build on and strengthen existing
monitoring mechanisms, such as the Global Preparedness
Monitoring Board and the Independent Oversight and
Advisory Committee for the WHO Health Emergencies
Programme. The mechanism would be composed of an
independent body of leaders and experts, supported by a
transparent, evidence-based, expert-led data collection and
review process, to ensure objectivity and credibility. It would
have a broad scope, encompassing the global architecture
of HEPR systems, nancing and governance. It would report
its ndings and recommendations to the World Health
Assembly, the Global Health Emergency Council, and the
proposed coordination platform for nancing.
Together, these accountability tools for governments,
international organizations and other stakeholders across
all sectors will: identify the risks and determinants of health
emergencies; reveal gaps and weaknesses in the capacity
and performance of health emergency systems and
their nancing and governance; develop and implement
solutions to ensure equity, eectiveness and eiciency; and
promote compliance with obligations under international
law, including the IHR and the pandemic accord currently
under negotiation.
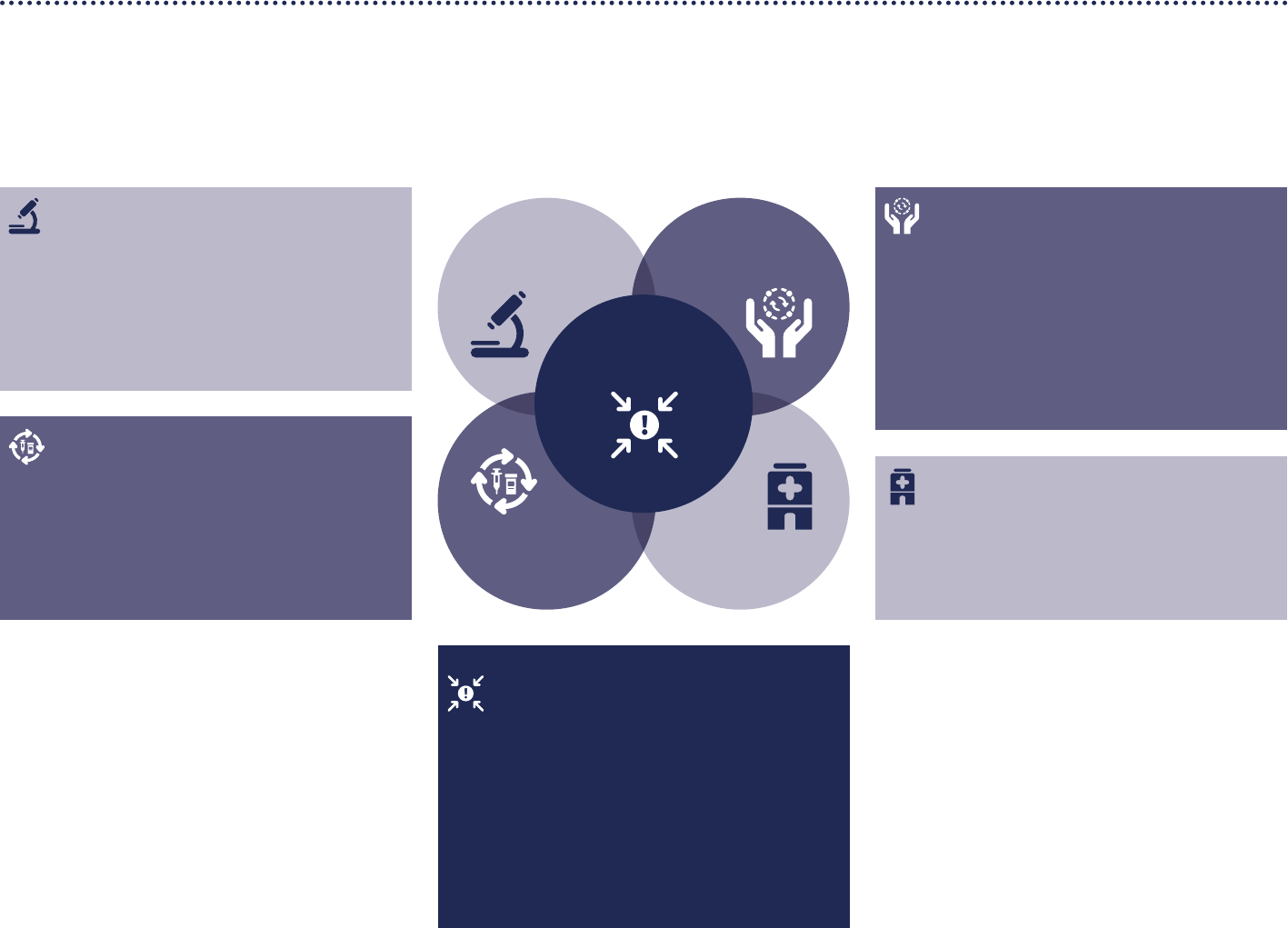
Systems
The ability to prepare for, prevent, detect and respond
eectively to health emergencies at national, regional and
global levels depends on the operational readiness and
capacities in ve core subsystems (Figure 5; expanded
on in Annex 1).
• Collaborative surveillance and public health intelligence
through strengthened multisectoral disease, threat
and vulnerability surveillance; increased laboratory
capacity for pathogen and genomic surveillance; and
collaborative approaches for risk assessment, event
detection and response monitoring.
• Community protection through two-way information
sharing to inform, educate and build trust; community
engagement to create public health and social measures
based on local contexts and customs; a multisectoral
approach to social welfare and livelihood protection to
support communities during health emergencies, and
mechanisms to ensure the protection of individuals from
sexual exploitation, abuse and harassment.
• Clinical care that is safe and scalable, with eective
infection prevention and control that protects, patients,
health workers and communities; and resilient health
systems that can maintain essential health services
during emergencies.
• Access to countermeasures through fast-track research
and development, with pre-negotiated benet sharing
agreements and appropriate nancing instruments; a
seamless link between research and development and
scalable manufacturing platforms and agreements for
technology transfer; coordinated procurement and
emergency supply chains; and strengthened population-
based services for immunization and other public health
measures.
• Emergency coordination with a trained health
emergency workforce that is interoperable, scalable
and ready to rapidly deploy; coherent national action
plans for health security to drive preparedness and
prevention; operational readiness through risk
assessment and reduction and prioritization of critical
functions; and rapid detection of and scalable response
to threats through the application of a standardized
emergency response framework.
DRAFT FOR CONSULTATION
JUNE 2022
7
Access to
countermeasures
Emergency
coordination
Community
protection
Clinical care
Collaborative
surveillance
Emergency coordination
Strengthened health emergency alert and
response teams that are interoperable and
rapidly deployable
Coherent national action plans for
preparedness, prevention, risk reduction and
operational readiness
Scalable health emergency response
coordination through standardized and
commonly applied Emergency Response
Framework
Community protection
Proactive risk communication and infodemic
management to inform communities and build trust
Community engagement to co-create mass
population and environmental interventions
based on local contexts and customs
Multi-sectoral action to address community
concerns such as social welfare and livelihood
protection
Clinical care
Safe and scalable emergency care
Protecting health workers and patients
Health systems that can maintain essential
health services during emergencies
Collaborative surveillance
Strengthened national integrated disease, threat
and vulnerability surveillance
Increased laboratory capacity for pathogen and
genomic surveillance
Collaborative approaches for risk assessment,
event detection and response monitoring
Access to countermeasures
Fast track R&D with pre-negotiated benet
sharing agreements
Scalable manufacturing platforms and
agreements for technology transfer
Coordinated procurement and emergency
supply chains to ensure equitable access
Figure 5. Interconnected core subsystems for health emergency preparedness, response and resilience
DRAFT FOR CONSULTATION
JUNE 2022
8
These capacities must be embedded in strengthened
national health systems, and will require investment in
essential public health functions, primary health care and
health promotion. Strengthening integrated surveillance,
community engagement, health promotion, routine
immunization and other essential health services will reduce
the risk of health emergencies, and enable communities
to be ready for and more resilient to emergencies.
Strong primary health and public health systems enable
communities to better assess context-specic threats
and vulnerabilities to reduce risk through prevention and
readiness. The link between communities and national
health emergency systems is critical to rapidly communicate
risk and scale up support once an event has been detected.
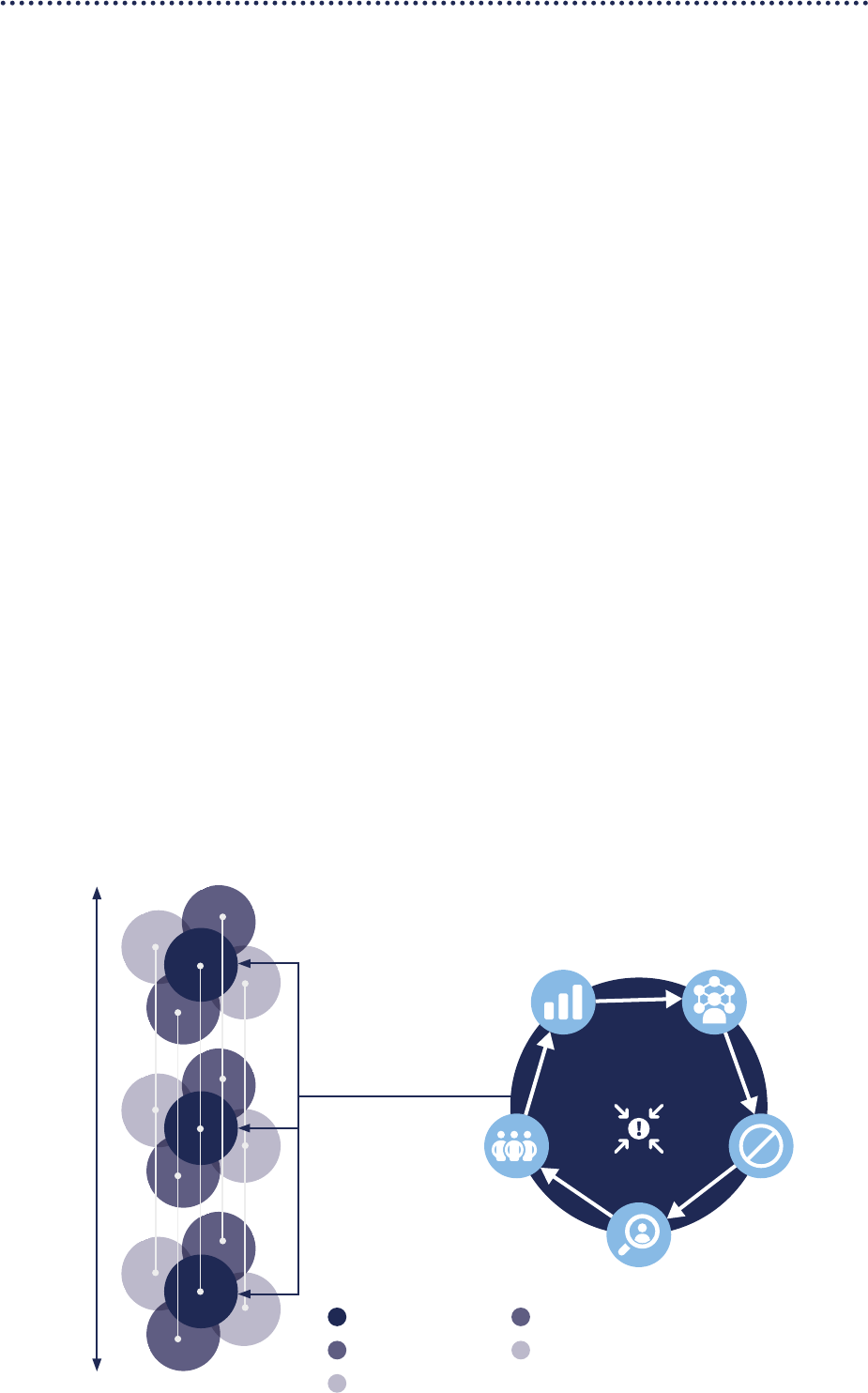
Given these interdependencies and the breadth of actors
involved, it is critical that the ve core subsystems are
well integrated within countries, and have strong links to
structures for support, coordination and collaboration at
regional and global levels across all phases of the health
emergency cycle of prepare, prevent, detect, respond and
recover (Figure 6).
Proposals for strengthening both the subsystems and the
linkages between them are outlined below.
Proposal 4. Strengthen global health emergency
alert and response teams that are trained to
common standards, interoperable, rapidly
deployable, scalable and equipped
The COVID-19 pandemic continues to expose national-level
decits in the core capacities required for eective HEPR.
National capacities are the fundamental building blocks
of global health security; therefore, these decits confer
profound systemic risks.
Mitigating these risks will require substantial investments
in many countries to build and strengthen professionalized
multidisciplinary health emergency teams, fully integrated
into national resilient health systems and other relevant
sectors under the One Health approach. The scale and
nature of workforce needs depend on national context, but
the most substantial and widespread gaps highlighted by
COVID-19 are in the areas of epidemiology and surveillance,
including laboratories; the health system workforce required
to rapidly scale up safe emergency clinical care and maintain
essential services during an emergency; the non-clinical
aspects of protection, such as working conditions and
fair remuneration; and the community engagement and
infodemic management resources needed to strengthen
trust in health authorities and build community resilience to
health emergencies.
Figure 6. Interlinkages between ve core subsystems for health emergency preparedness, response and resilience across
the emergency cycle
National
Regional
Global
Recover Prepare
Respond
Detect
Prevent
Emergency
coordination
Emergency coordination Community protection
Clinical care
Access to countermeasures Collaborative surveillance
Global
National
Regional
DRAFT FOR CONSULTATION
JUNE 2022
9
Smart investments in strengthening national capacities
will enable the development of globally deployable health
emergency alert and response teams to strengthen regional
and global preparedness, detection and response. Combined
with mechanisms for emergency coordination (see Proposal
5) to support training, accreditation and deployment,
strengthened national alert and response teams can give rise
to a country-owned yet internationally deployable global
health emergency workforce.
Proposal 5. Strengthen health emergency
coordination through standardized approaches
to strategic planning, nancing, operations and
monitoring of health emergency preparedness
and response
Health emergency subsystems are dependent on each other
for operational eectiveness. At national level, COVID-19
demonstrated that overall health emergency preparedness
and response management systems were oen fragmented.
At regional and global levels, the pandemic highlighted
a lack of consistency in national approaches, a lack of
eective mechanisms to coordinate and communicate
action between countries, and challenges in eiciently
channelling international support to where it was most
needed.
Remedying this fragmentation will require further
investment in ensuring greater consistency and
standardization in emergency coordination at national
level, including through a commonly applied emergency
response framework. Application of this framework must
be enabled by strengthened infrastructure, workforce and
leadership that is resourced and empowered to: strengthen
operational readiness through assessment of risks and
vulnerabilities, and prioritization of critical functions across
all core subsystems; develop context-specic strategies
and plans for preparedness, prevention, readiness and
response; mobilize the necessary resources; and monitor
and evaluate actions. Health emergency management
should be embedded in broader whole-of-government
national disaster management systems.
A strengthened and redesigned network of public health
emergency operations centres can connect international
and regional technical, nancial and operational support to
national emergency management systems, and at the same
time can improve coordination between countries and
international partners across the health emergency cycle.
Box 1.
Detecting and preventing
spillovers: a planetary perspective
to health emergency preparedness,
response and resilience
What do the past four public health emergencies of
international concern (PHEIC) have in common? Ebola
virus disease in Western Africa in 2014; the 2015–16
Zika virus epidemic; the 2018–20 Kivu Ebola epidemic;
and the COVID-19 pandemic: all were the result of
zoonotic “spillover” events, in which a pathogen jumps
the species barrier from another animal into a human
population. In each of the above cases, viral pathogens
were able to spread in human populations before
being detected.
Foreshortening the time between a spillover event and
its initial detection is a major focus of the One Health
movement, and a crucial component of strengthening
the global HEPR architecture. The intrinsic links
between health and disease in humans, domestic
animals and wildlife means that an early warning
system linked to surveillance and risk analysis at and
beyond the three-way interface of humans, animals, and
the environment is essential if we are to detect spillover
events while containment is still a feasible option.
The rapid introduction of new technologies for
surveillance, such as genomic sequencing, that has
followed in the wake of COVID-19 in many countries
has brought us an increment closer to realising the
vision set out by the tripartite of WHO, FAO and OIE in
their landmark 2004 report that relaunched the One
Health concept. Fully implementing the tripartite’s
2004 recommendations will be a key consideration as
consultations on reforms to the governance, nancing,
and systems of global HEPR continue.
Ultimately, our collective approach to spillovers
must move beyond detection to embrace prevention.
Global deforestation, the trade in wildlife and wildlife
products, and over-intensive animal rearing are
not only disastrous for ecosystems and the global
environment, they also drastically amplify the risk
of spillover events. And as the rate of environmental
degradation and ecosystem loss increases, so to does
the risk of spillovers with epidemic and pandemic
potential. Investments in HEPR only make sense in
the context of a broader concerted and coordinated
international eort to protect the health of the planet
itself. Detecting and containing spillovers as close to
when and where they rst occur is the key to stopping
outbreaks from becoming epidemics and pandemics,
but addressing the root causes of spillovers is the key
to preventing those outbreaks in the rst place.
DRAFT FOR CONSULTATION
JUNE 2022
10
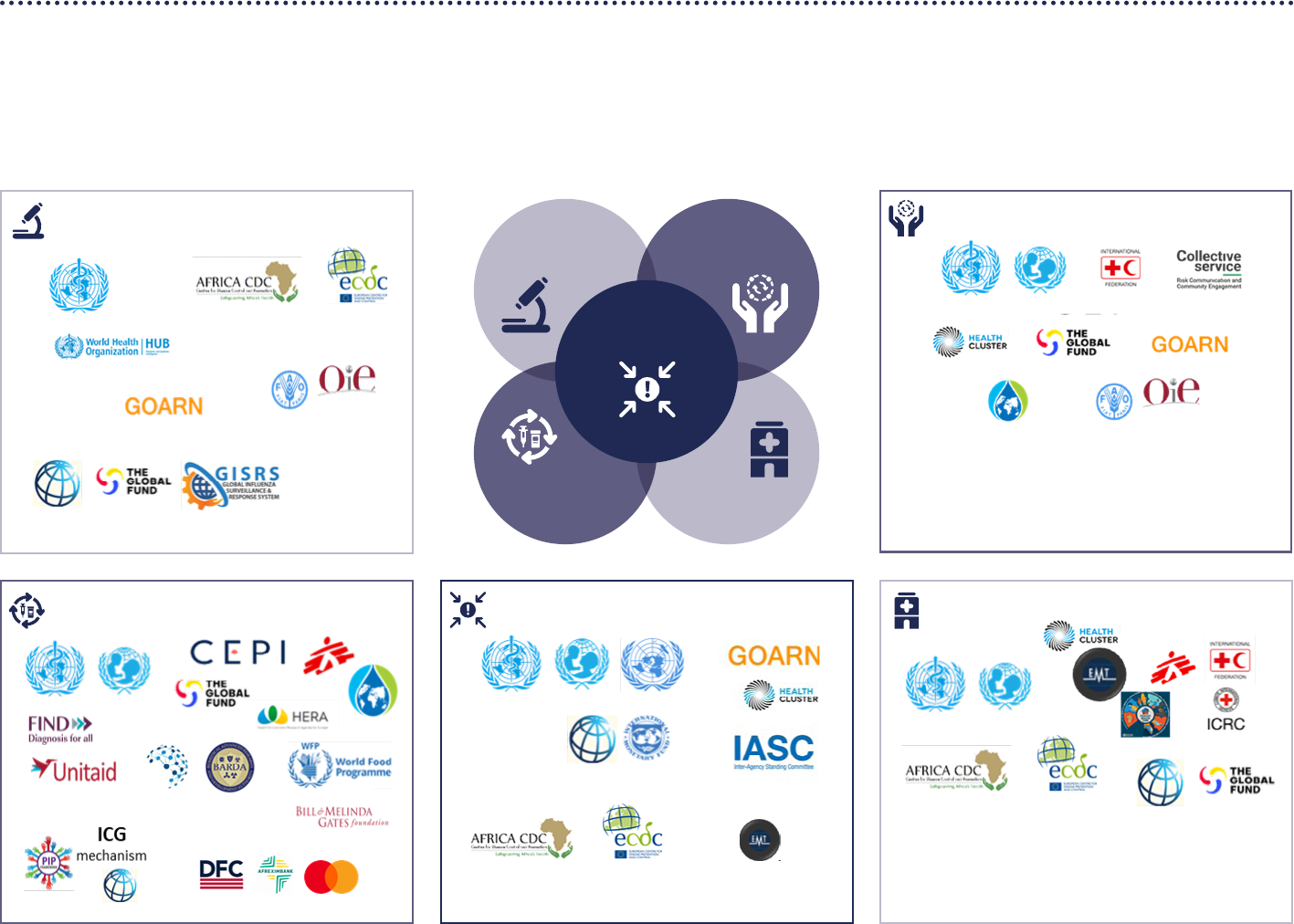
Proposal 6. Expand partnerships and strengthen
networks for a whole-of-society approach to
collaborative surveillance, community protection,
clinical care, and access to countermeasures
COVID-19 has shown that resilience to health emergencies
can be strengthened in key areas by broader and closer
collaboration between organizations and institutions at
national, regional and global levels before health emergencies
hit. This will require the strengthening and, where required,
the establishment of whole-of-society, interdisciplinary,
multi-partner networks for collaborative surveillance, clinical
care, community protection and access to countermeasures.
This will enable the extensive ecosystem of HEPR partners
at the global, regional and national levels to fully participate
according to their strengths and capabilities to co-create
innovative and timely solutions in an agile and collaborative
way (see Figure 7 for a non-exhaustive illustration of the
ecosystem of international partners for COVID-19).
Ad hoc and time-limited regional and global collaborations
between national authorities, multilateral institutes and
the private sector, such as the Access to COVID-19 Tools
Accelerator (including COVAX) and the African Union Vaccine
Acquisition Trust, played a crucial role in accelerating
the development of COVID-19 medical countermeasures.
Consolidating and building on these COVID-19 successes,
while ensuring that collaborative arrangements are in place
and build on existing networks between various global
health agencies, industry and the scientic community to
ensure fair access and scalable manufacturing, will help
to protect the world from both known and theoretical
pandemic threats.
At the same time, forecasting pandemic risks and
detecting infectious threats can be transformed by closer
interdisciplinary collaboration nationally, regionally
and globally. The WHO Hub for Pandemic and Epidemic
Intelligence is a new initiative that will play a leading role in
strengthening collaborative surveillance. The WHO Hub will
also drive further development of initiatives such as Epidemic
Intelligence from Open Sources and the International
Pathogen Surveillance Network. Established global
surveillance systems for specic pathogens, such as the Global
Inuenza Surveillance and Response System, also provide a
strong foundation upon which to build.
COVID-19 has also highlighted the role that collaborative
eorts play in building the resilience of communities to health
emergencies. The need to invest in collaborative arrangements
that bring communities of practice and communities of
circumstance together to design response and resilience
measures has been highlighted aer every major health
emergency of the past two decades: COVID-19 makes these
calls impossible to ignore.
The ecosystem of international partners for COVID-19 can
be used as the basis for expanding the network of relevant
partners, strengthening the links between them, and
developing collaboration hubs for each of the ve core
subsystems to further strengthen the global architecture for
HEPR.
Box 2.
Strengthening every link
in the countermeasure chain
The unprecedented global eort to develop vaccines
and diagnostics for COVID-19 is oen portrayed as an
overnight success. But, as with many such successes,
it was built on many years of diligent work before the
pandemic.
In 2016, in the wake of the world’s deadliest recorded
outbreak of Ebola virus disease, the WHO R&D
Blueprint was launched to bring together a broad cast
of researchers from academia and industry, regulators,
governmental and non-governmental organizations,
and multilateral institutes to prioritize action against
a list of potential pandemic threats. Stemming from
these eorts the Coalition for Emerging disease
Preparedness Innovations, which was also launched
in 2016, funded several of the ambitious vaccine-
development programmes that ultimately yielded
three of the vaccines that have received WHO
Emergency Use Listing for use against COVID-19.
Getting these vaccines to where they are needed has
proven more challenging. Despite the eorts and some
notable successes of COVAX – the vaccines pillar of the
Access to COVID-19 Tools Accelerator (ACT-A) – vaccine
access remains highly inequitable more than two
years into the pandemic. Many of the world’s most
vulnerable populations remain unprotected, which has
prolonged the acute phase of the pandemic.
Learning the lessons of COVID-19 will mean building
on the strengths and successes of the organizations
and initiatives that existed before the pandemic,
consolidating and institutionalizing what worked
during time-limited collaborations such as ACT-A, and
addressing the shortfalls that have resulted not only
in inequitable access to countermeasures, but also
in disparities in the speed, quantity and eiciency
with which dierent categories of countermeasures –
vaccine, therapeutics, and diagnostics – have been
developed, tested, approved, and distributed to where
they are needed most.
Much of this work will need to be done at the global
and regional level to bring together partners from
the length and breadth of the value chain through
formal and informal mechanisms that span dierent
pathogens and categories of countermeasures. These
mechanisms, or mechanism, will need to provide the
necessary incentives – with appropriate tolerances
for risk – and benet-sharing agreements to ensure
that future countermeasures are delivered equitably,
rapidly, and at scale.
Continued on next page …
DRAFT FOR CONSULTATION
JUNE 2022
11
Box 2. (continued)
The Pandemic Inuenza Preparedness Framework,
which celebrated its 10th anniversary last year,
provides a case study in how to guarantee the access of
developing countries to vaccines and other pandemic-
related supplies. However, as COVID-19 has shown,
the nal step in the value chain can oen be the most
diicult step to take. The vaccine and immunization
programmes of countries, along with the capacity of
countries to rapidly adopt and adapt to new vaccines,
diagnostics and therapeutics, have been implicated
in every public health emergency of international
concern to date. Building these capacities, which lie at
the heart of resilient national health systems, will be
crucial to prevent and respond to future epidemics and
pandemics.
Key features of an agile, equitable, and risk-
tolerant global system to ensure the development,
manufacture, and distribution of medical
countermeasures for pandemic threats
• End-to-end partnerships, built on the pre-existing
trust that exists between core partners such as CEPI,
Gavi, Global Fund, UNICEF and WHO, and which
provides a forum for new stakeholders
• Inclusive governance, with a strong voice for low-
income countries, lower middle-income countries,
and civil society organizations
• Rapid decision making, based on the “no regrets”
principle of emergency response
• Streamlined and coordinated regulatory processes
across high-income, middle-income and low-
income countries, balancing the need for speed and
safety
• A multi-country platform for clinical trials to obtain
statistically signicant results more quickly from
broad and representative populations
• Links to resilient emergency supply chains
• Pre-agreed, rapidly accessible funding for
global procurement, and appropriate, risk-
tolerant mechanisms to fund development and
manufacturing
• Seamless linkage of the development process to
distributed manufacturing capacity, with rapid
transfer of knowhow from innovator companies
• Support to strengthen the science–policy interface
and decision making in countries, and to strengthen
the readiness of health systems to rapidly access
and deploy countermeasures
Financing
Financing an eective health emergency preparedness
and response architecture will require approximately an
additional US$ 10 billion per year, according to WHO–World
Bank analyses presented in 2022 to the G20. However,
eective nancing depends not only on more funds, but
also on strengthened and innovative mechanisms to ensure
that funds are accessed and delivered in ways that are agile
and risk tolerant, to ensure the best possible return on
investment and the most eective and timely allocation of
resources to ll critical gaps.
Proposal 7. Establish a coordinating platform
for nancing to promote domestic investment
and direct existing and gap-lling international
nancing to where it is needed most
Every country should step up domestic investments to
prepare for health emergencies, but low-income countries
and some lower middle-income countries need urgent
international support to strengthen HEPR.
International nancial support can come from many
dierent actors, both public and private, with oen
overlapping and competing priorities. Greater coordination
and simplication is needed across this funding landscape
to ensure that existing funding ows are coordinated
and targeted to the most critical gaps in the global HEPR
architecture, such as national-level preparedness gaps,
funding for regional and global institutions that support
HEPR, investments in upstream and emergency research
and development and downstream manufacturing and
procurement, and rapidly accessible funding to initiate
and scale emergency response operations. Where existing
funding ows are insuicient to ll critical gaps in core
national and global HEPR capacities, these ows should be
augmented by additional catalytic and gap-lling funding
through a nancial intermediary fund (see below).
To bring coherence and eiciency across domestic
and international investments, including additional
investments through a proposed nancial intermediary
fund, a new coordination platform is required that unites
the technical work of WHO and other HEPR partners
as needed, with the nancial investments of the World
Bank and other international nancial institutions. This
coordinating platform for nance and health would monitor
the performance of HEPR funding ows, improve eective
allocation to critical priorities, and help to mobilize and
direct catalytic and gap-lling nancial support. This new
mechanism should strive for worldwide representation,
building on the work of the G20’s Joint Finance and Health
Task Force.
DRAFT FOR CONSULTATION
JUNE 2022
12
Community protection
Access to
countermeasures
Emergency
coordination
Community
protection
Clinical care
Collaborative
surveillance
and other One Health
stakeholders
Other major contributors include nongovernmental
organizations, civil society organizations and the
private sector
Collaborative surveillance
and other One Health
stakeholders
and other donors
and other regional centres
for disease control
Emergency coordination
and other regional centres
for disease control
and other donors
Access to countermeasures
and other donors
Clinical care
and other donors
and other regional centres
for disease control
Other major contributors include nongovernmental
organizations, civil society organizations and the
private sector
Figure 7. Illustrative ecosystem of international partners for COVID-19 (non-exhaustive)

DRAFT FOR CONSULTATION
JUNE 2022
13
Proposal 8. Establish a nancial intermediary
fund for pandemic preparedness and response to
provide catalytic and gap-lling funding
Existing funding ows do not cover gaps in the HEPR
architecture. A new pooled fund has been proposed by
several reviews and organizations as a potential solution
for international nancing to better support national
preparedness and response, and global public goods.
Most recently, WHO and the World Bank recommended
to the G20’s Joint Finance and Health Task Force the
establishment of a Financial Intermediary Fund (FIF),
to be hosted by the World Bank.
The FIF should avoid duplication and ensure
complementarity with existing HEPR nancing eorts
and institutions. Critical design elements for a FIF should
include:
• A central role for WHO to enable direct linkage between
national and global HEPR assessment and planning
processes and the investments proposed by the FIF;
• Governance mechanisms that include a coalition of
participating donors, and that are informed by objective
assessments of HEPR needs and the perspectives of
beneciary country governments;
• Work with existing multilateral development banks
and implementing partners, who should be eligible for
nancing; and
• Funding proposals would be based on national action
plans for health security and related nancing plans,
lling gaps identied through the IHR monitoring
framework and UHPR (see above).
Proposal 9. Expand the WHO contingency fund for
emergencies to ensure rapidly scalable nancing
for response
At present, funding mechanisms for emergency response
are fragmented and unpredictable. The WHO contingency
fund for emergencies (CFE) is able to disburse relatively
modest amounts rapidly for early response, but it is not
designed to directly nance elements of national response,
nor the eorts of key partners, oen leading to operational
gaps when implementing multi-disciplinary and multi-
sectoral response plans. In addition, in the event that
initial containment eorts fail, WHO’s CFE is not designed
to support the scale-up and adaptation of response, nor
sustain a response over durations longer than the initial
few months. In the absence of pre-negotiated draw-down
mechanisms to enable access to larger tranches of exible
funding triggered by the escalation of health emergencies,
critical windows for scale-up are oen missed due to a
reliance on unpredictable, oen inexible, and frequently
insuicient funding from ad hoc appeals.
Addressing the problems above will require two
innovations. First, the CFE should be expanded in size
and scope to enable the direct nancing of national and
international partners in the rst stages of the response,
including deployments through the health emergency
workforce and emergency supply chain. This will ensure
that multisectoral health emergency response plans can be
fully and rapidly implemented. Second, in the event that
initial response eorts are unable to contain an infectious
threat or suiciently mitigate the eects of a non-infectious
hazard, an additional substantial draw-down facility should
be triggered to ensure that the multisectoral response
can be scaled up to cover additional geographical areas
and populations for an extended duration. The triggers
for activation of this draw-down facility should be pre-
negotiated, transparent and based on the “no regrets”
precautionary principle.
An expanded CFE could satisfy both needs, with
contingency funds accessed via two transparent
mechanisms: a rapid response facility and a sustained
scale-up facility, both of which would be linked to a
standardized and commonly applied emergency response
framework for alert, verication, risk assessment and jointly
developed strategic plans and resource requirements for
rapid and scalable response.

DRAFT FOR CONSULTATION
JUNE 2022
14
Equity, inclusivity and coherence
IEquity, inclusivity, and coherence are key principles
reected in the WHO Constitution, and central to the
“happiness, harmonious relations and security of all
people”.
In all countries, the burden of risks of and vulnerabilities
to health emergencies inevitably fall disproportionately
on the most socially and economically disadvantaged
and marginalized. As the ongoing experience of COVID-19
shows, the failure of the HEPR architecture to adequately
address equity, particularly equitable access to medical
countermeasures, has magnied and prolonged the
acute phase of the pandemic. As Member States have
emphasized, equity is not limited to access to medical
countermeasures, but includes universal health coverage
and national health systems strengthening.
An eective, equitable, inclusive, trusted and accountable
HEPR architecture must meet the needs of all countries
and communities, including the most marginalized and
those in fragile, vulnerable and conict-aected contexts.
It is therefore essential that all countries be involved, and
all communities be represented, in the translation of the
proposals set out here into context-specic solutions, and
in the allocation of investments for HEPR, with an equal
role for low-income and middle-income countries in the
leadership and accountability mechanisms of a new HEPR
architecture.
Member States have also highlighted the importance of
coherence, acknowledging ‘the central role of WHO in the
global health architecture, with its normative and standard-
setting functions, and provision of technical assistance
and support, as well as its convening power at the global,
regional and national levels.’ Broadening inclusion in global
HEPR must go hand in hand with strengthening the links
between current stakeholders to: empower coordination;
reduce fragmentation, competition and duplication; and
accelerate investment in HEPR within the broader context
of the drive towards the Sustainable Development Goals.
Only in applying these principles of equity, inclusivity
and coherence consistently and rigorously in the design
and operations of the HEPR architecture at all levels, and
monitoring their application, can we achieve the outcomes
we seek. They apply across the three pillars of Governance,
Systems and Financing, and are, in eect, a pillar in their
own right, as they are at the heart of strengthening WHO
in fullling its constitutional functions at the heart of the
global architecture of HEPR.
This requires a shared understanding of how equity,
inclusivity and coherence will be applied in practice,
and how they will be monitored, based on measurable,
objective metrics, to ensure action and accountability.
Annex 2 provides details of how these principles will be
applied and monitored in each of the 10 proposals.
.
Figure 8. Equity, inclusivity and coherence at the heart of
the global architecture for health emergency preparedness,
response and resilience
E
q
u
i
t
y
I
n
c
l
u
s
i
v
i
t
y
C
o
h
e
r
e
n
c
e
Trust
P
a
n
d
e
m
i
c
A
c
c
o
r
d
Inclusivity
• All 194 Member States with an equal voice
• Whole of government & whole of society approach
• Collaborative networks of multi-sectoral & multi-
disciplinary partners
Coherence
• Science, evidence and expertise to set the norms,
standards and regulations
• Trusted, impartial and authoritative information to
communicate risk
• Coordinated assessment, strategy, nancing,
operations & monitoring
Equity
• Highest level of health for all
• Equitable access to countermeasures and other
essential resources
• First responder and last resort to protect the most
vulnerable
DRAFT FOR CONSULTATION
JUNE 2022
15
Proposal 10. Strengthen WHO at the centre of the
global HEPR architecture
Sustained commitment to equity, inclusivity and coherence
(Annex 2) will be best served by the strengthening of and
sustained investment in the only multilateral organization
with a mandate that encompasses the systems, nance
and governance of HEPR: WHO. To achieve this, the world
needs a strengthened WHO, with the authority, nancing
and accountability to eectively full its unique mandate
as the directing and coordinating authority on international
health work.
The Organization has essential responsibilities: for setting
international norms and standards; for promoting and
conducting research in the eld of health; for providing
data and information; for developing evidence-based
policy and guidance; for investigating and responding to
health emergencies as a rst responder and as a provider
of last resort, including in the most vulnerable and
fragile contexts; and for maintaining strong relationships
within the global health ecosystem. Discharging these
responsibilities requires adequate and sustainable
nancing. A pandemic accord, adopted by WHO Member
States, would reinforce the legitimacy and authority of WHO
and complement steps that Member States are already
taking to ensure sustainable nancing of the Organization.
The accord would also ensure that the technical expertise
of WHO, its oices and its various scientic, normative,
operational and monitoring bodies and networks, are
utilized most eectively and eiciently within an equitable,
inclusive and coherent architecture for health emergency
preparedness and response.
Strengthening WHO at the core of the global HEPR
architecture will continue to build and sustain trust in
its mission, contributing to a safer world built on equity,
inclusivity and coherence. A world with fewer health
emergencies, with rapid detection and response when
they do occur, with equitable access, with reduced health,
social and economic impacts, and with rapid and equitable
recovery (Figure 8).
Box 3.
Context is key to eective health
emergency preparedness, response
and resilience in fragile, conict-
aected and vulnerable settings
As COVID-19 has shown, health emergencies can have
markedly dierent impacts even among countries and
communities with seemingly similar capacities, risks,
and vulnerabilities. One size of response does not
t all, and nowhere is this more true than in fragile,
conict-aected and vulnerable settings (FCVs). In
these settings, the causes of and responses to health
emergencies can interact with and oen amplify
pre-existing risks and vulnerabilities in unpredictable
ways. In these contexts, operational readiness for
preparedness and response must account for a
number of key challenges, including:
• Shis in resources required for critical measures
for prevention, control and mitigation of infectious
outbreaks may further compromise the already
limited capacity to deliver essential health services
• Limitations on testing capacity may impact
surveillance capabilities, requiring additional
approaches to obtain a correct picture of the situation
• Capacity to scale up treatment and readiness to
utilize new diagnostics, therapeutics and vaccines is
oen limited locally due to existing health systems
challenges
• Social and public health measures, as applied
in higher resource settings, may be harmful and
threaten the livelihoods and social cohesion of
communities in the absence of adequate measures
to support communities
• In areas with armed conict, violence and
insecurity, preparedness, prevention and response
measures must be carefully negotiated and
designed with communities to avoid amplifying
conict and any existing mistrust in authorities
• Communities in fragile, conict-aected and
vulnerable settings may oen be in geographically
and socio-economically isolated areas, and pose
unique logistical and security challenges
Strong community engagement is needed to build
trust and protection, as well as ensure eective
implementation of HEPR measures. Eective disease
control in FCVs must be based on a pragmatic and
contextualised adaptation of global guidance and
goals that accounts for other public health threats
and social economic realities. Done in this way, HEPR
measures can reinforce the key role of health as a
driver of peace and sustainable development.
DRAFT FOR CONSULTATION
JUNE 2022
16
Box 4.
Understanding the disproportionate eects of the COVID-19 response on
women and children can strengthen health emergency preparedness,
response and resilience in the future
The past two years have seen increasing evidence of the
unique impact that COVID-19 and the public health and
social measures of the response have had on women,
children, and men.
Although men generally have higher mortality rates
from COVID-19 than women, women and girls are
disproportionately aected by the social and economic
consequences of the pandemic. For example, women
comprise around 70% of health and social care workers
globally and 90% of the nursing and midwifery workforce
and yet they hold only 25% of leadership roles in health.
Women are typically clustered into lower-status, lower
paid jobs in health and social care. Investing in equal pay
– which includes recognizing unpaid health care work – is
fair and urgent.
As in other health emergencies, the COVID-19 pandemic
has intensied pre-existing gender inequalities, as
reected by:
• Increased burden of unpaid care work, which falls
mainly on women and girls, due to the impacts of
COVID-19 on the caregiving infrastructure
• Increased burden of paid health and social work
during the pandemic falls disproportionately on
women, who represent the largest share of health and
social care workers globally
• Increased risk of domestic and gender-based violence
due to the combined eect of enforced home-
based connement, restrictions on movement, and
disruptions to health and social services
• Increased risk of unintended pregnancies and
maternal deaths from disruptions to sexual and
reproductive health services
• Higher probability of loss of job and/or income
for women
• Exacerbation of existing barriers to services, driving
inequitable coverage, such as inability to leave
children unattended
Children of all ages and in all countries have been
aected various ways by the socio-economic impacts
of the COVID-19 pandemic and response measures,
including through:
• Disruptions in essential nutrition and health services
and increased food insecurity, mainly due to
decreased purchasing power of families
• Disruptions in education and learning caused by
school closures, which has also aected access to
school meals and signicantly increased rates of
stress, anxiety and other mental health issues. It is
estimated that 24 million children may never return to
school, due to the economic impact of the pandemic
• An increased likelihood that children experience and
observe physical, psychological and sexual abuse at
home
• Increased threat of child labour, child marriage and
child traicking as a result of increased economic
vulnerability
As with other health emergencies, COVID-19 has hit the
most vulnerable hardest at the same time as increasing
the number of vulnerable people. It is crucial to learn
from and recognize how and why COVID-19 has had a
disproportionate impact on women and children, and
ensure that our collective priorities for strengthening the
health emergency preparedness, response and resilience
architecture are anchored in the principles of equity,
inclusivity and coherence.

DRAFT FOR CONSULTATION
JUNE 2022
17
Next Steps
The HEPR systems, nance and governance proposals
described in this white paper represent a coherent
approach to developing a t-for-purpose HEPR
architecture. Operationalizing that architecture will require
an additional level of detail, followed by implementation
by both WHO and our partners. Change will not be easy, but
time is of the essence – health emergencies can strike at any
time and the COVID-19 pandemic is not over. WHO stands
ready to build from the work done during the pandemic to
develop the new capabilities required of it and to engage
closely in ongoing processes, including the development of
a Pandemic Accord.
The Director-General’s proposals are designed to support
and contribute to decision-making in the various fora within
and beyond WHO that will determine the future global
architecture of HEPR. History tells us that the world has a
small window of opportunity to endorse and implement the
proposals in this white paper before global attention shis
and we begin another cycle of panic and neglect.
The Secretariat welcomes comments and feedback on
the proposals contained in the white paper. Consultations
will continue to take place over the coming months with
Member States, UN partners, other international and
regional organizations, civil society, and other major
stakeholders to discuss and further develop these
proposals to build a safer world together.
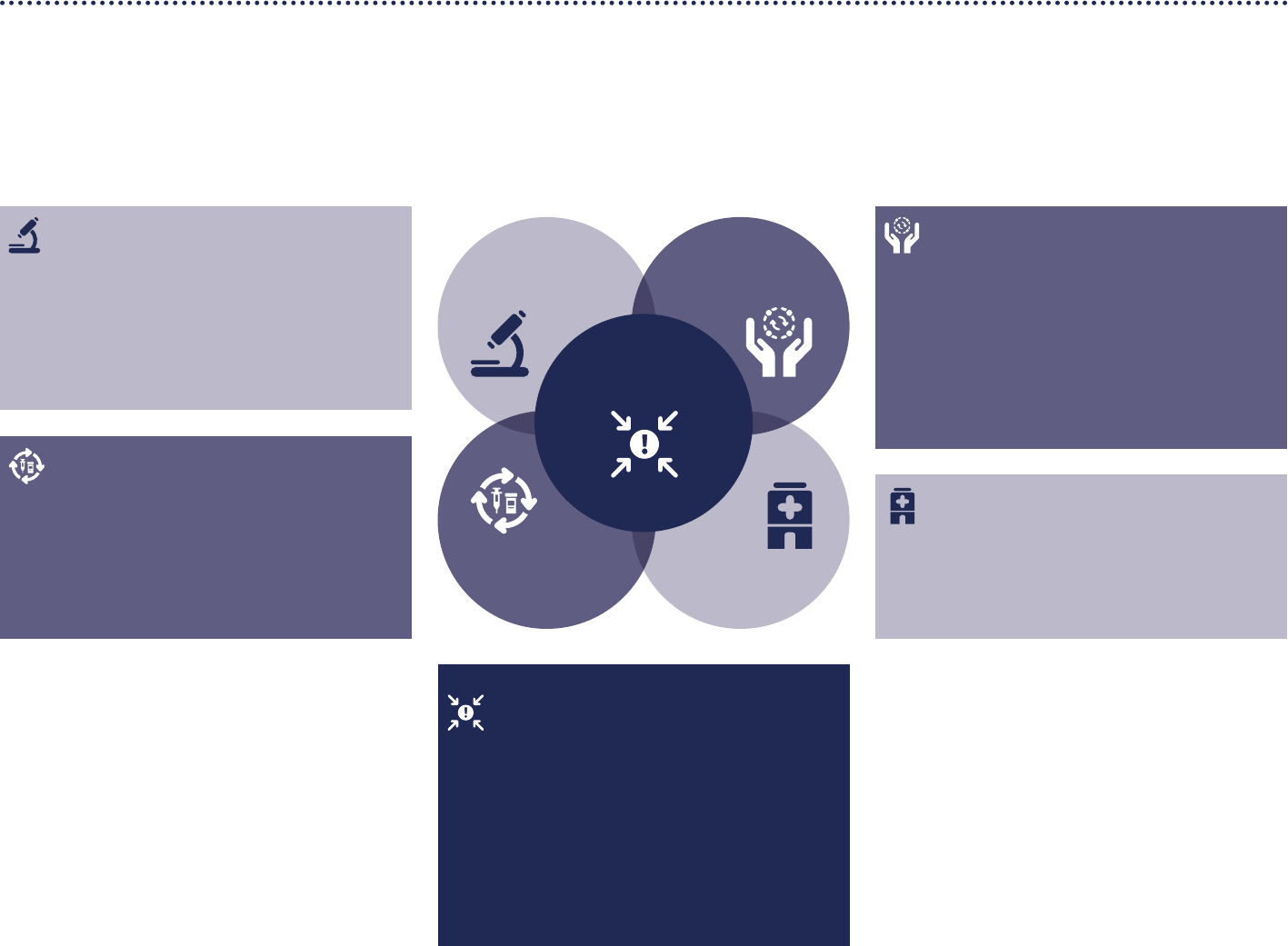
DRAFT FOR CONSULTATION
JUNE 2022
18
Clinical care
Safe and scalable emergency care
Protecting health workers and patients
Health systems that can maintain essential
health services during emergencies
Figure 1: Interconnected core capacities and solutions for HEPR systems
Access to
countermeasures
Emergency
coordination
Community
protection
Clinical care
Collaborative
surveillance
Emergency coordination
Strengthened health emergency alert and
response teams that are interoperable and
rapidly deployable
Coherent national action plans for
preparedness, prevention, risk reduction and
operational readiness
Scalable health emergency response
coordination through standardized and
commonly applied Emergency Response
Framework
Community protection
Proactive risk communication and infodemic
management to inform communities and build trust
Community engagement to co-create mass
population and environmental interventions
based on local contexts and customs
Multi-sectoral action to address community
concerns such as social welfare and livelihood
protection
Collaborative surveillance
Strengthened national integrated disease, threat
and vulnerability surveillance
Increased laboratory capacity for pathogen and
genomic surveillance
Collaborative approaches for risk assessment,
event detection and response monitoring
Access to countermeasures
Fast track R&D with pre-negotiated benet
sharing agreements
Scalable manufacturing platforms and
agreements for technology transfer
Coordinated procurement and emergency
supply chains to ensure equitable access
Annex 1: Strengthening HEPR systems capacities
This Annex complements the White Paper by providing a rst dra of additional details about HEPR systems key capacities (Figure 1). Each section describes a system, followed by
subsystem key capacities and/or relevant considerations. This work is ongoing and will continue to be rened through consultations and expert technical input.

DRAFT FOR CONSULTATION
JUNE 2022
19
Collaborative surveillance
A truly interconnected global system for public health intelligence can revolutionise our ability to detect an emerging
outbreak, communicate information fast, and rapidly initiate an appropriate response. Accurate, timely information
about emergence, transmission, susceptibility, morbidity, and mortality, along with in-depth contextual insights
on risk and vulnerability, are crucial for initiating and adjusting appropriate response measures, including targeting
countermeasures towards the most vulnerable populations. Enhancing and expanding lab capacity, networks,
mechanisms and incentives for sharing pathogens, biological samples and genomic data are vital to global pandemic
preparedness.
Collaborative surveillance includes strengthened national integrated disease, threat and vulnerability surveillance,
increased laboratory capacity for pathogen and genomic surveillance and collaborative approaches for risk assessment, event
detection and response monitoring.
1.1 Strengthened national integrated disease,
threat and vulnerability surveillance
National disease surveillance, starting at the lowest
administrative level in a health system, is the foundation
upon which a global HEPR must be built. There is therefore
a pressing need to strengthen, expand, consolidate,
modernise, automate and improve the coordination,
sustainability, resilience and scalability of surveillance
systems.
It is also crucial that links between national, regional and
global surveillance systems are strengthened. Established
global surveillance systems for specic pathogens or
domains of surveillance, such as the Global Inuenza
Surveillance and Response System Plus (GISRS+) and the
Global Early Warning System Plus (GLEWS+), represent
a strong foundation upon which to build. GISRS+ and
its sentinel systems have integrated SARS-CoV-2 since
March 2020 and respiratory syncytial virus since 2015. The
development of GISRS for inuenza, SARS-CoV-2 and other
novel respiratory viruses of pandemic potential should be
an essential component of surveillance capacity building,
and was supported by Member States at the 150th meeting
of the Executive Board in January 2022, and recommended
by the IHR Emergency Committee for COVID-19 in its 11th
statement of April 2022.
The integration of polio and other vertical surveillance
programs into national capacities could provide a key
route to accelerate the strengthening of national integrated
disease surveillance. Completing the transition of vertical
pogram assets into broader national health systems can
ensure that their unique strengths, including community
based surveillance, translate into improved national
capabilities.
To be eective, all the surveillance capabilities have to feed
into a dened body in every government for synthesis and
decision-making. These bodies could be ministries of health
or national public health institutions.
Key capacities include:
• Integrated surveillance, including indicator-based
and syndromic surveillance, grounded in eective
healthcare delivery services
Integrated surveillance, including traditional indicator-
based and syndromic surveillance, is anchored in
health systems with a national disease surveillance
strategy based on IHR core capacities, focused on a list
of priority and epidemic-prone diseases and syndromes
informed by local risks. It also includes non-traditional
approaches such as community-based, participatory,
and event-based surveillance (including rumour
surveillance, public information monitoring and social
media listening).
• Expanded One Health surveillance
One Health surveillance is the systematic collection,
validation, analysis, interpretation of data and
dissemination of information collected on humans,
animals and the environment. It expands surveillance to
encompass the broader ecosystem and associated risks,
such as zoonoses, and food borne illnesses.
• Strengthened active surveillance and event
monitoring
Rapid verication, risk assessment and eective
response to new public health events depends on strong
eld epidemiology, including: timely case investigation;
contact tracing; and monitoring of key operational
performance indicators such as vaccination coverage
and health service delivery. Field epidemiology and
information management training programs and agile
eld data collection systems are core to this capability.
• Interconnected multisectoral threat and vulnerability
surveillance
Multisectoral surveillance provides a contextualized view
of threats and vulnerabilities to understand and manage
the drivers of health risk as they emerge and evolve. It
integrates demographic, social and economic drivers of
health risk, based on local contexts.

DRAFT FOR CONSULTATION
JUNE 2022
20
1.2 Increased laboratory capacity for pathogen and
genomic surveillance
Increased laboratory capacity benets both public
health surveillance systems and health care delivery. A
comprehensive laboratory network incorporating clinical,
sentinel, and reference laboratories performing appropriate
public health functions will serve both, ongoing disease
programs and emerging infectious disease detection.
Access to surge capacity during emergencies, including
through agreements to access regional and/or global
auxiliary capacity, should be established, maintained, and
regularly tested to ensure system readiness.
The Director-General launched the pilot testing phase
of the WHO BioHub System in 2021. Its goal is to oer a
reliable, safe and transparent mechanism for Member
States to voluntarily share novel biological materials,
without replacing or competing with existing systems, and
contribute to the acceleration of research and innovation
before and during epidemics and potential pandemics.
Key capacities include:
• Expanded laboratory and testing capacity
National laboratory and testing capabilities, compliant
with internationally and nationally recognized quality
standards, should be closely linked to national public
health systems. Strategies to ensure accurate and
timely pathogen detection should be adapted to the
local context and incorporate tools such as multiplex
platforms, point-of-care diagnostics, and mobile
laboratory infrastructure as appropriate. This should be
with appropriate mechanisms to ensure functional and
integrated specimen collection, transport, and result
reporting.
• Established and scaled genomic surveillance
capabilities
Advanced capabilities, such as genomic sequencing
capacity, must be established, scaled, and linked to
regional and global initiatives to guide the public
health response. Such capacities should cover emerging
pathogen and outbreak detection, epidemiological
investigation, monitoring, and research and
development of countermeasures during outbreaks.
• Laboratory data systems integrated into broader
health and surveillance systems
Laboratory data for pathogen diagnostics should be
shared in a timely manner for public health action, and
data systems should be integrated into the broader
health system. Data systems should be based on
interoperable laboratory management information
systems and networks, according to agreed standards
and principles, and ensuring data security and patient
anonymity where necessary.
• Strengthened international platforms to enable
sharing of biological samples and genetic data
Rapid sharing of biological and genetic data is critical for
eective pandemic and epidemic intelligence globally.
Eective sharing is essential not only for outbreak
identication and control eorts, but also for expediting
research and development process for medical
countermeasures.
• Enhanced biosafety and biosecurity to limit biorisk
Strengthening laboratory and diagnostic capacity
should include enhanced capacities to carry out risk
assessment, informing biosafety and biosecurity policies
and practice. This can only be achieved if relevant
standards are routinely maintained in laboratories at all
times.

DRAFT FOR CONSULTATION
JUNE 2022
21
1.3 Collaborative approaches for risk assessment,
event detection and response monitoring
The collaboration between various surveillance actors at the
local, national, regional and global level, as well as between
diverse sectors, is essential for a full understanding of risks,
vulnerabilities, event detection and response monitoring.
Mechanisms that integrate and harness information from
divergent sources combined with advanced data and
analytical tools that can provide valuable insights for
eective detection and response.
At the global level, the WHO Hub for Pandemic and
Epidemic Intelligence fosters such a collaborative
approach to surveillance by connecting data, solutions,
and communities of practice globally; by innovating
solutions and processes; and strengthening capabilities
for forecasting, detection and assessment of risks
to provide of actionable intelligence for prevention,
preparedness, response and recovery from health threats
and emergencies. The WHO Hub for Panemic and Epidemic
Intelligence aims to build a collaborative, trust-based
community involving a diverse set of multi-disciplinary
entities, including National Public Health Institutes (NPHIs).
For example, the initiative Epidemic Intelligence from
Open Sources (EIOS) brings together initiatives, networks
and systems to create a unied all-hazards, One Health
approach to early detection, verication, assessment and
communication of public health threats using publicly
available information.
Key capacities include:
• Expanded networks for collaborative intelligence and
decision making
Data and information sharing among local and
national health authorities (such as National Public
Health Institutes), regional bodies and WHO can guide
responses to emerging and established threats, and
improve decision making. Collaborative networks
should convene a broad range of expertise at local,
national, regional, and global levels.
• Strengthened data-sharing platforms to connect and
integrate multi-sectoral sources of information
Innovative data-sharing platforms are required to
connect, integrate and harness information from
diverse sources, and can be strengthened through the
promotion of best practices in data governance and
management.
• Interconnected multidisciplinary communities to co-
create advanced analytical and modelling tools
Easily accessible and adaptable advanced analytical
and modelling tools can enhance advanced cross-
sectoral surveillance, improve outbreak detection, and
guide response decision making. A multidisciplinary
community is best placed to co-create models based
on relevant health emergency use cases, and should be
fostered and enabled.
• Open access to tools and analysis to inform tactical
and strategic operations and decision-making
Integrated data, tools, and apps to improve data-
driven decision making should be made available and
openly accessible through a community-owned virtual
marketplace to promote innovation and co-creation
of open source solutions. Tools should enable risk and
vulnerability characterisation, and impact monitoring
and assessment. An eective marketplace would require
modern data systems and infrastructure, and agreed
standards for data quality, privacy and security. Such
a marketplace would give decision makers access
to analytical insights and tools for data visualisation
(including dashboards) to inform and enable rapid,
evidence-based decision making.
DRAFT FOR CONSULTATION
JUNE 2022
22
Community protection
Building trust with communities fosters engagement and enables the adaptation of public health and social measures.
Trust can also be strengthened, and the eectiveness of public health and social measures improved, through multisectoral
collaboration to protect social welfare and livelihoods during health emergency response. Reinforcing ties between local
networks and communities of practice at a global scale can enhance protection of the most vulnerable and marginalised
populations.
Two-way communication can build trust and inform the co-creation and co-ownership of preparedness and response
measures. WHO’s EPI-WIN initiative enables work with international and local partners to establish priority actions with
faith and religious leaders, youth networks, the labour force, fact-checking organizations and infodemic managers to
foster trust and understanding about how health emergencies are aecting lives, and what can be done to support each
community in their own unique contexts to respond eectively.
The RCCE Collective Service is intended to develop and sustain structures and mechanisms that promote coordinated
community-centred, evidence-based and participatory approaches to risk communication and community engagement.
It aims to embed risk communication and community engagement across public health, humanitarian and development
response eorts. The Service brings together key assets of partnering organizations into a holistic and consistent approach.
Community protection includes risk communication and infodemic management, community engagement to help design and
implement public health and social measures, and multisectoral action to address community concerns.
2.1 Proactive risk communication and infodemic
management to inform communities and build
trust
Enduring trust and resilience can only be built through
consistent and eective engagement with, participation
and ownership of communities before, during and aer
health emergencies. Infodemic management, combined
with adequate risk communication and consistent
community engagement can improve uptake of and
participation in public health and social measures (PHSM),
and increase trust in and demand for countermeasures
such as vaccines.
Key capacities include:
• Social listening and sentiment analysis
Understanding individual and community behaviours
enables the detection of information decits. Platforms
to monitor dynamic changes in perceptions and
attitudes should be used routinely and leveraged
during health emergencies to adapt risk messaging.
Fostering a dynamic understanding of public attitudes
and perceptions, concerns and feedback, as well as
conversations about infectious pathogens and public
health and response measures is essential to inform
the design and implementation of plans for risk
communication and community engagement. Novel
approaches, such as social listening and sentiment
analysis, oer new ways to understand community
perceptions and concerns.
• Health messages adapted to community context
Risk communications can be co-created and
tailored to local contexts on the basis of social and
behavioural data and community feedback. Testing
risk communications through participatory processes
enables communications to be tailored to target
sub-populations. Monitoring of the eectiveness of
communications can enable messages to be adapted in
step with evolving contexts and community concerns.
• Empowering communities to strengthen resilience
against mis/disinformation
Communities should be empowered to co-create
interventions to mitigate potential impacts of PHSM
and build resilience against mis/disinformation.
Understanding community concerns and characteristics
of target populations can inform the design of
interventions. It should be done in partnerships with a
range of stakeholders. Design and implementation of
interventions should be tied with eectiveness tracking.
2.2 Community engagement to co-create
population and environmental interventions
based on local contexts and customs
Dynamic adaptation and co-creation of PHSM with
communities means that those measures are more likely
to be inclusive, equitable, and adapted to local context,
practices, risks and threats. Co-creation requires thoughtful
community engagement, through established consultation
processes, engagement and feedback mechanisms
and platforms to capture community views, needs and
experiences, including those of the most vulnerable. PHSM
should be adjusted to local contexts based on social and
behavioural data and community feedback.

DRAFT FOR CONSULTATION
JUNE 2022
23
PHSM, dynamically co-created with communities, should
be systematically integrated in national, subnational and
community health preparedness and response plans,
nancing and monitoring and evaluation frameworks,
agreed on at the highest level of government and supported
by legislation. PHSM should be implemented and adjusted
based on continuous analysis of epidemiological data,
health system capacity and contextual factors that
inuence the eectiveness and burden of interventions, so
that benets are maximized while the health, social and
economic burden is kept to a justiable minimum.
Global collaborations are needed to build evidence and
further understanding of how PSHM work in dierent
contexts, combinations and durations, to balance risks and
benets. Ethical considerations for the implemention of
interventions should be carefully considered. Monitoring
of the operational performance of PSHM and community
attitudes and perceptions can inform further adaptation.
Specic strategies can include:
• Building community resilience
Communities need to be ready for and resilient to
health emergencies and shocks, such as climate-related
hazards, natural disasters, conicts, and pandemics.
Readiness and resilience measures should be adapted
to local contexts, taking into consideration specic risks
and threats. Adaptations should factor in the specic
requirements of at-risk groups.
• Emergency vaccination
Community-centred development of emergency
vaccination plans, based on evidence and consultations,
can increase condence, trust and demand for vaccines.
Community-centred approaches can foster a better
understanding of at-risk groups, inform adaptations
to service delivery (including mobile vaccination
sites) to better reach specic sub-populations, and
understanding and addressing perceptions of vaccine
safety and benets.
• Vector control and other environmental measures to
contain spillover
To mitigate risks at the animal–human interface, specic,
localized risk-reducing interventions and direct vector-
control interventions may be needed. Interventions
should target drivers of emergence and spillover, and
be adapted to local contexts. Where measures impinge
on livelihoods due to their impact on agriculture and/
or livestock, appropriate incentives and compensatory
mechanisms may be required to oset lost earnings and
maximise community consent and participation.
• Travel and trade measures
Travel-related measures, including those mplemented
at points of entry should be risk-based, evidence-
based, context-specic. They should be discussed and
appropriately communicated with all key stakeholders
involved, including local communities and cross-border
authorities. Essential travel and transport operations
should be prioritized for emergency and humanitarian
actions, with priority given to essential personnel,
repatriations and cargo transport of essential supplies
such as food, medicines, vaccines and fuel, with the aim
of ensuring supply chain continuity.
• Other public health and social measures to interrupt
human-to-human chains of transmission
Measures to interrupt chains of transmission include
locally tailored isolation and quarantine, improved
sanitation and hygiene, safe and dignied funerary
rites, and a risk-based approach to mass gatherings
and population movements. Careful assessment of the
impact of any restrictions on movement is required to
minimize exacerbation of existing inequities.

DRAFT FOR CONSULTATION
JUNE 2022
24
2.3 Multisectoral action, including social welfare
and livelihood protection, to address community
concerns
Communities should be early partners across all stages of
health emergency preparedness, response and recovery,
and should be closely consulted on the design of all PHSM
that have a direct impact on the lives and livelihoods of
local communities. Community support for PHSM relies
on fostering a clear understanding of the public health
rationale underpinning those PHSM. This understanding
should be based on condence that interventions will
come at the lowest possible cost to livelihoods, education,
and social and mental wellbeing. Whole-of-society and
whole-of-government approaches require multisectoral
engagement and feedback mechanisms to address
community needs through contextual adaptation,
community participation and ownership. Adaptation based
on close consultation is particularly important to drive
participation and minimize harm to vulnerable groups,
including women and children.
Key considerations include:
• Social welfare and protection
The health, social and economic burdens experienced by
individuals and societies should be carefully measured,
considered in decision-making and implementation,
and minimized. This should include strengthening
protection of vulnerable groups, such as women and
children. Decision makers should pay careful attention
to addressing risks of physical, psychological and sexual
abuse.
• Livelihood and economic safety nets
Understanding of the impact of measures may further
guide the design and implementation of socio-economic
support systems and safety nets to alleviate unintended
harms. Additionally, the design and calibration of
population and environmental measures should be
inuenced by socioeconomic considerations, including
impact on businesses and the broader economy.
• Continuity of education and learning
Learning and continuation of education is an essential
right to children worldwide. In addition, schools can
provide protection, but also school-meals and social
support. Careful consideration to ensure access
isneeded, especially among vulnerable groups. Enabling
platforms need to be adapted to local contexts and
resources.
• Food security
Food supply chains should be maintained, limiting
impacts on food supply and demand. International
and border measures should be assessed for potential
disruptions, with mitigation measures co-created with
the most aected communities, such as food delivery or
equitable economic allocations.
DRAFT FOR CONSULTATION
JUNE 2022
25
Clinical care
A strong HEPR architecture is anchored in strong national health systems and primary health care. High-quality health
services and capacity are necessary to detect, prevent and respond to health emergencies. Existing gaps in health systems
were generally understood before COVID-19, and are already targeted for strengthening through the Universal Healthcare
Agenda. However, a resilient health system goes beyond the availability of resources, and ultimately depends on its
capacity to re-organize and re-deploy existing resources in response to shocks such as health emergencies. The most
safe and resilient health systems have the agility and exibility to surge to meet increased demands imposed by health
emergencies whilst maintaining essential services, and protecting and supporting health workers and patients. Resilient
health systems ensure equitable access to care, mitigating nancial, contextual, and cultural barriers.
Clinical care includes lifesaving and scalable clinical care, protection of healthcare workers and patients, and health systems
that can maintained essential health services.
3.1 Safe and scalable emergency care
All countries should invest in capacities to ensure that
adequately trained sta, resources and infrastructure are
available for the management, referral and transportation
of all patients aected by health emergencies, based on risk
and vulnerability assessments. The ability to provide safe
and scalable emergency care in health emergencies can be
reinforced by strengthening essential capacities in strong,
resilient health systems. Capacities should be anchored
within rapidly deployable clinical care protocols at facility
level to prioritize patient ows during a health emergency,
including through patient screening, isolation, acuity-based
triage and targeted referral pathways. Ensuring access
and adapting services for at-risk populations should be
a priority. Non-essential services should be reintroduced
as the emergency abates. Global collaboration should
reinforce capacities through the establishment of a global
network of experts than can rapidly inform and disseminate
novel clinical care information, guiding the development of
best practices.
Key capacities include:
• Resilient infrastructure and safe health facilities
Health infrastructure should be resilient to disruptions
caused by health emergencies. Safe health facilities
should remain accessible and fully functional following
an emergency, ensuring continuous clinical care.
Infrastructure considerations include the use of
renewable energy sources to increase resilience and
lessen environmental impact.
• Emergency clinical care pathways
Emergency clinical care pathways should prioritize
access to high quality care, especially among at-
risk populations. Eective pathways require the
establishment of mechanisms for pre-hospital and
emergency patient ows, such as patient triage and
isolation, and adapted referral pathways triggered
by specic emergencies. Strategies should focus on
promoting exibility safety, and equitable access
including through the use of modular infrastructure and
alternative facilities. Evaluations of case management
procedures and protocols should inform the design of
care pathways.
• Surge capacity for clinical care
Clinical capacity, including workforce, should be able
to surge in anticipation of and in response to health
emergencies. Training and long-term planning for
health workforce development is a crucial aspect of
preparation for scenarios in which health workers
must be redeployed to meet a surge in demand.
Phased reallocation of workforce from routine services
towards emergency services should be determined by
established triggers and thresholds. In situ capacity
may be augmented by rapidly deployable national
and international Emergency Medical Teams (EMTs) to
support emergency clinical needs.
• Stockpiles of emergency supplies and medicines
Supplies and equipment should be pre-dened based
on priority listing, adapted to local contexts, risks, and
vulnerability. Equitable access should be planned pre-
emergency, using strategies such as stockpiles and pre-
negotiated contracts, based on transparent allocation
frameworks.
3.2 Protecting health workers and patients
Protecting health workers and patients is essential in
health systems and communities before, during, and
aer health emergencies. Protection includes protecting
health facilities and health workers from attacks. Investing
in infection prevention and control (IPC) is one of the
most cost-eective interventions available to reduce
infection and anti-microbial resistance (AMR) in health
care facilities. Immediate access to suicient personal
protective equipment (PPE) and rapid IPC training early in
an emergency can reduce morbidity and mortality, while
generating substantial net nancial savings. IPC should be
anchored in strong water, sanitation and hygiene (WASH)
capacities.
IPC should be embedded and monitored within broader
health systems, in synergy with other programmes such as
those dedicated to AMR, quality of care, patient safety and
occupational health. IPC strategy should address a range of
threats, pathogens and emergency contexts.

DRAFT FOR CONSULTATION
JUNE 2022
26
Key capacities include:
• Mechanisms to monitor and mitigate attacks on
health
Attacks on health facilities and health workers deprive
people of care and endanger health care providers. The
nature of attacks vary across contexts, and can range
from physical attacks with heavy weapons to threats
and intimidation. The systematic collection of evidence
of attacks, advocacy and political intervention to end
such attacks, and the promotion of good practices for
protecting health facilities and workers from attacks
are necessary to save lives and maintain strong health
systems.
• Access to IPC materials and training
IPC should improve health worker and patient safety
at the point of care, with optimal practices supported
by IPC materials embedded within the patient pathway
and clinical care. Materials and training are essential
tools for the prevention and containment of outbreaks.
Interventions to change practices and the continuous
training, supportive supervision and mentorship of
health workers and essential sta on IPC measures and
the rational use of PPE are necessary to ensure that
patients, health workers, caregivers and visitors are
protected.
• Adequate WASH services in health facilities
WASH infrastructure should be a permanent and
accessible element throughout health facilities,
extending beyond isolation wards to other wards.
Access to WASH services should also be provided in
public places and community spaces based on risk
analyses, with special consideration given to sites used
by vulnerable communities and community isolation
centres.
3.3 Health systems that can maintain essential
health services
Resilient health systems are core to achieving universal health
access and the maintenance of essential services during
emergencies. Solutions to strengthen resilient health systems
must address foundational health system gaps and essential
public health functions, which provide a cost-eective, holistic
approach to strengthening public health capacities.
Maintaining access to essential health services hinges on a
strong primary healthcare foundation that can be adapted in
the context of an emergency, and should also seek to detect
and address changes in patient behaviour, including fear of
healthcare settings and its impact on care seeking.
Key capacities include:
• Protection of essential health services
Essential services should be pre-dened and scaled on
the basis of recommendations adapted to local contexts
based on needs and threats, and should encompass a
wide range of services along the life course, including
maternal and child care, and routine immunizations.
A primary healthcare approach can help to ensure
the continuation of essential health services during
health emergencies, because a primary health care
system provides a exible and adaptable care-deliver
platform with strong links to local communities. Health
emergencies should trigger dedicated protocols,
including nancial processes, for scaling and protecting
essential services, with careful consideration given to
user fees and co pays.
• Monitoring disruptions to essential health services
Mechanisms to monitor the delivery of and access to
essential services should be embedded in prioritization
processes that incorporate specic thresholds to trigger
support and ameliorative action. Monitoring should
enable detection and characterisation of disruptions,
and is crucial from the onset of emergencies and
throughout an evolving response.
• Resilient and adaptable health workforce
The deployment of the health care workforce across
the health system should be managed during health
emergencies based on pre-dened trigger thresholds
adapted to a wide range of potential scenarios.
Resilience of the health workforce includes non-clinical
aspects of protection, such as working conditions, fair
remuneration, the availability of hazard pay, professional
education and development and mental health support.
Gender dynamics should also be considered, given that
women make up the majority of the health workforce in
most countries.
• Recovery of health systems aer emergencies
Health systems should return to a pre-emergency
operational posture based on dened thresholds as
health emergencies subside. The post-emergency
recovery phase should include mechanisms to capture
lessons from aer-action reviews and other review
processes to further strengthen resilience through
a process of continuous learning, adaptation and
improvement.
DRAFT FOR CONSULTATION
JUNE 2022
27
Access to countermeasures
Seamless, concerted and coordinated eorts across every step of the countermeasures value chain is necessary to continue
accelerating development and equitable deployment of countermeasures. This should be enabled by innovative nancing
mechanisms that are appropriately tolerant of the risk inherent in countermeasure research and development, in which
most candidates will fail. Few countries will have the capacity to complete this end-to-end process within their own borders,
therefore regional approaches should be considered as the most eicient way to ensure equitable global access to new
countermeasures.
Several existing partnerships and legal agreements have increased access to countermeasures, primarily against specic
pathogens such as inuenza, smallpox, yellow fever, cholera, and meningitis. These have paved the way for stronger, global
multisectoral collaboration. The International Coordinating Group (ICG) on Vaccine Provision provides a framework to
manage and coordinate the provision of emergency vaccine supplies and antibiotics to countries during major outbreaks.
The Pandemic Inuenza Preparedness (PIP) Framework enables developing country access to vaccines and other pandemic-
related supplies, acting as the only mechanism securing real time access. The R&D blueprint allows for rapid activation of R&D
activities during epidemics, using R&D roadmaps and target product proles for priority diseases. In response to COVID-19, the
ACT-Accelerator was launched in 2020 to accelerate the development of COVID-19 tests, treatments and vaccines and to ensure
their equitable distribution.
Equitable access to countermeasures should be based fast-tracked and prioritized R&D with pre-negotiated benet-sharing
agreements, scalable manufacturing platforms and agreements for technology transfer, and coordinated procurement and
emergency supply chains.
4.1 Fast-tracked R&D with pre-negotiated benet-
sharing agreements
A well-resourced, globally shared R&D roadmap should
build on the lessons and strengths of the WHO R&D
Blueprint, COVID-19 Solidarity Trials, PIP Framework and
other initiatives. Such a roadmap should encompass
multiple priority pathogens and prioritize and incentivize
the development, manufacturing and rapid deployment
of countermeasures in response to both the emergence of
known pathogens and a hypothetical ‘disease X’ scenario.
Key capacities include:
• Shared global R&D agenda to strengthen coordination
A shared global R&D agenda would set clear priorities,
establish roadmaps and ensure global coordination
of R&D activities. It should include platforms for the
coordination of research, with representation from all
major stakeholder groups, including LICs and LMICs.
Aligned and coordinated scale-up plans in case of the
emergence of new pathogens are needed. Essential R&D
activities should be well dened, to enable mitigation
strategies to minimize disruptions in the context
of emergencies. High-quality operational research
should feed back into the shared global R&D agenda
and continuously inform the prioritization of research
activities.
• Enabling environment for research and discovery
Pre-negotiated benet-sharing agreements and
frameworks for accelerated emergency research and
development of countermeasures can ensure global
coordination and collaboration and avoid duplication.
Agile nancing with adequate risk tolerance, such
as forgivable loans, can align incentives between
stakeholders. Frameworks to enhance collaboration
should include means to facilitate information and
sample sharing. Safety and ethics are central prerequisites
for eective enabling environments.
• Standardized platforms to scale clinical trials equitably
Global collaboration on clinical trials through
standardized protocols, processes and programs
enable rapid scaling and improve the diversity of trial
participants. Pre-established protocols for participation in
international clinical trials during emergencies should be
created and/or adopted at the national level.
• Adapted regulatory and legal frameworks to accelerate
clinical trials
Agile yet thorough and comprehensive emergency use
listing and pre-qualication processes are required for
emergency situations to expedite clinical testing and
approval of novel countermeasures at the same time as
ensuring compliance with appropriate safety standards.
National emergency regulatory approval procedures
should be developed, and may be expedited by
harmonization with global authorization processes.
4.2 Scalable manufacturing platforms and
agreements for technology transfer
There is a clear need for additional global, geographically
diversied manufacturing capacity that can be rapidly
pivoted to emergency needs during crises. Globally
distributed manufacturing capacity can ensure that
more people will have early and equitable access to
countermeasures in the future. Manufacturing platforms
and agreements for technology transfer can enhance equity
among countries.
Key capacities include:
• Adapted manufacturing platforms that can scale
rapidly
Manufacturing platforms should be built with the goal of
scaling rapidly, leveraging multiproduct technology to be
rapidly adaptable to new needs. These platforms should
be aligned with prioritized needs and coordinated at a

DRAFT FOR CONSULTATION
JUNE 2022
28
national, regional, and global level as needed, based on
local contexts and capabilities.
• Distributed manufacturing capacity with pre-
negotiated agreements to ensure equitable access
Pre-negotiated and equitable access to production
capacity, markets, and appropriate risk-tolerant capital
agreements should be established. Reaching collective
agreements on equitable access to countermeasures
requires among others the relevant clauses in
manufacturing contracts and standardized and
collaborative procurement processes.
Equitable manufacturing capacity implies an even
distribution across global regions to balance aggregation
of demand with proximity to end users. Enabling access
to technologies, including global technology transfer,
licensing agreements and facilitated access to knowhow,
equipment and raw materials is necessary to operate and
appropriately scale-up manufacturing capacities.
• Expanded ever-ready capability for rapid mobilization
Manufacturing for all major categories of emergency
medical countermeasures (including vaccines,
therapeutics and diagnostics) should be dual use
wherever possible to maintain a constant state of
readiness. Dual use in this context may mean the
integration of emergency capacity into the manufacturing
of non-emergency products, such as vaccines for routine
immunization programmes. Installing and strengthening
global coordination and access to manufacturing capacity
(including equipment and raw materials) can ensure
equitable access to meet the needs of LICs and LMICs.
• Strengthened regulatory, legal, and enabling
frameworks to scale manufacturing platforms
Capacity should be complemented by pre-dened
mechanisms for licensing and intellectual property
sharing. Strengthening national regulatory capacities
is needed for eective and eicient oversight of the
quality, safety and eicacy of medical products, and
marketing authorization/registration of medical products.
This should include the adoption and/or adaption of
regulatory, quality assurance, indemnication / liability,
and labelling standards. Regulatory exibility enables
rapid access to existing and novel products. Policy and
regulatory hurdles that limit equitable access should be
addressed.
4.3 Coordinated procurement and emergency
supply chains to ensure equitable access
Supply scarcity in the context of an outbreak can paralyse
response mechanisms and increase inequity. Emergency
supply chains are needed to ensure that supplies are
available when and where they are most needed, and that
the logistics to access them are robust enough to hold up
in times of crisis. Capacities established during COVID-19
can be further strengthened and sustained on the basis of
lessons learned.
Key capacities include:
• Pre-dened list of essential supplies and medicines
An essential supplies and medicines list should be
developed based on national treatment guidelines and
prioritized threats. Primary, secondary, and tertiary
suppliers should be identied to ensure continuous
access, even in the event of supply chain disruptions.
• Pre-negotiated coordinated procurement to ensure
access
Agile, transparent, pre-negotiated and coordinated
procurement processes should be developed and
include bridge and/or innovative nancing, such as
demand pooling mechanisms, advance purchase
commitments and/or early use agreements. Processes
should be agile and address any potential barrier to
product delivery, such as payment delays. Global and/or
regional procurement processes can facilitate large-scale
procurement eorts.
• Coordinated global demand aggregation to optimize
risk sharing
National response authorities should coordinate demand
aggregation, using consolidated approaches to demand
forecasting and t-for-purpose technology platforms.
National-level partners should work closely with a
network of global partners to coordinate global demand
aggregation.
• Ensured equitable and transparent access
Equitable and transparent allocation frameworks can
ensure equitable national access to a necessary minimum
quantity of supplies. Strengthening equitable and
transparent allocation frameworks should include the
establishment of coordinated governance mechanisms,
collective agreements, and political commitment to
ensure equitable access to goods, especially for supply-
constrained countermeasures.
• Strengthened global, regional and national logistics
and distribution that rely on pre-negotiated and
coordinated contracts
Strong, resilient, tested, diversied and coordinated
national and local supply chains have clear plans for the
delivery and implementation of countermeasures that are
t for purpose for inter-pandemic years as well as during
emergencies. Comprehensive review of trade practices,
frameworks and incentives, and existing agreements can
identify potential hurdles and enable a free ow of raw
materials and goods during emergencies to maximize
the supply of products. National supply chains rely on
pre-negotiated and coordinated distribution contracts,
drawing on stockpiling and logistics hubs, with clear
protocols for allocation and replenishment.
DRAFT FOR CONSULTATION
JUNE 2022
29
Emergency coordination
Coordination of HEPR systems is critical to systematically marshal and deploy the appropriate resources (knowledge
and data, nancial, materiel, technical and operational) to prepare for, prevent, detect, alert, and respond rapidly to any
health emergency. Eective coordination enables all the other sub-systems to deliver on their potential. At all levels of
organization, accountable leadership must be underpinned by eective multisectoral and multidisciplinary coordination,
particularly in incident management of acute response and broader health emergency workforce development.
Emergency coordination should draw on health emergency alert and response teams that are interoperable and rapidly
deployable; coherent national action plans for preparedness, prevention, risk reduction and operational readiness; and
scalable health emergency response coordination through a standardized and commonly applied emergency response
framework.
5. 1 Health emergency alert and response teams
that are interoperable and rapidly deployable
Health emergency alert and response teams should
constitute a global, professional and interoperable
network that is ready to respond to health emergencies
worldwide. The concept of such a global health emergency
workforce builds on existing global, regional, and national
organisations and networks. Alert and response teams
would strengthen national capacities for readiness and
response, be locally embedded and locally responsive,
while being globally coordinated and able to deploy
regionally and internationally. The broader public health
emergency workforce requires training and equipping to
ensure a strong pipeline of team members. Teams would
be well-trained and ready to investigate and respond
eectively to public health emergencies wherever they
arise, at the same time as supporting local public health
capacity outside of emergencies. National teams would
be representative of and trusted by the communities they
serve.
Key capacities include:
• Common standards for interoperable health
emergency alert and response teams
Ensuring interoperability of alert and response teams
relies on common global standards and certication.
Operating procedures and multidisciplinary team
composition should be adapted for various emergency
scenarios.
• Trained, equipped, and expanded global, regional,
and national networks
Ensuring a well-trained, professional, multi-sectoral and
equipped alert and response teams that strengthens
existing networks (such as GOARN, EMTs, GHC) requires
an understanding of existing networks and what they
can deliver, along with adequate support and nancing.
Additional training and equipment will expand existing
national, regional, and global alert and response
networks.
• Scaled coordination and support for team
deployment
Rapid international and national deployments of
teams would be facilitated by standardized protocols,
operating guidelines and activation procedures and
mechanisms. Deployment should be based on alert
denitions at global, regional, national and local levels;
specify team congurations adapted to respond to
specic alerts; call on up-to-date registries of experts;
coordinated processes for employment. Support for
deployment should draw on contingency planning,
including rapidly available nancing. Post-deployment
debrieng and support should be mandatory.
• Evidence-based learning and development
Measuring impact and eectiveness of teams requires
ongoing monitoring of progress and fostering a
community of practice, codifying learnings, and sharing
best practices, tools and resources. Action plans should
be rened and adapted rapidly on the basis of insights
from the eld. Infrastructure to enable information
management, including databases and platforms for
eective networking and knowledge sharing, will need
to be developed and maintained.
5.2 Coherent, resourced national action plans for
health security
Coherent national action plans for health security (NAPHS)
are critical for maintaining and strengthening IHR (2005)
capacities and progressing towards the eective prevention,
detection and mitigation of health emergency threats, as
well as the immediate response to and recovery from them.
Comprehensive multisectoral planning should be integrated
within national health systems planning. Prevention and
readiness, including the routine integration of One Health
approaches and scaled-up vaccine coverage of high-priority
groups for epidemic or pandemic prone diseases, must be
a cornerstone of HEPR. At the national level, authorities
should align their NAPHS or equivalent with broader
cross-government One Health and whole-of-government
strategies, engaging with key stakeholders such as national
parliaments. Planning and activities to ensure operational
readiness should be driven by regular assessment of risks
and vulnerabilities at national and subnational levels.
Operational capacities should be prioritized and tested on a
dynamic basis as risks and vulnerabilities evolve over time.
Key capacities include:
• Standardized assessment of preparedness capacities
Transparent peer-reviewed processes are needed to
assess national capacity as part of dynamic monitoring.
Assessments can include IHR monitoring and evaluation
processes, including the Universal Health and

DRAFT FOR CONSULTATION
JUNE 2022
30
Preparedness Reviews, which augment voluntary Joint
External Evaluations, and State Party Self-Assessment
Annual Reports. National capacity assessments are
essential to inform NAPHS.
• Updated threat and vulnerability mapping and risk
identication
National planning eorts should be based on context-
specic, up-to-date threat and vulnerability mapping,
including tools such as the Strategic Tool for Assessing
Risks (STAR) methodology to conduct strategic risk
assessments and forecasting, which in turn serve as a
basis for NAPHS and their equivalents. These should link
to broader national frameworks of risk reduction (e.g.,
Sendai Framework for Disaster Risk Reduction including
climate and economic risks).
• Development of prioritized, costed national plans for
risk reduction, prevention, and readiness
NAPHS and their equivalents play an important role
in setting country-wide priorities and facilitating
and supporting multisector engagement, including
civil society, the private sector, military, academia,
the media and communities. NAPHS integrate One
Health approaches, and establish costed plans and
cross-government strategies to guide investments in
national systems. Costing should account for required
one-o investments and recurring costs, including core
capacity building for risk reduction. NAPHS should be
integrated within broader national health and disaster
management strategies.
• Mapping gaps and mobilizing technical and nancial
resources
The development and implementation of NAPHS
and their equivalents can unite a broad range of
technical, operational and nancial support behind a
single coherent national vision on health security. It
supports the planning and strengthening of sustainable
preparedness capacities, identifying resources within
and beyond the health security agenda. It needs to be
aligned with national health policies and strategies
including annual planning and budgeting cycles. It
can increase and/or improve better use of domestic
budget, while oering a unied vision for gap lling
catalytic funding. Strengthened resource mobilization
and dynamic monitoring of implementation can
support greater national leadership, governance, and
international solidarity for preparedness, while ensuring
alignment with broader health system priorities.
• Simulation exercises to strengthen readiness and
mobilization of resources
Simulation exercises, coupled with aer-action reviews,
and dynamic preparedness and risk assessments, can
strengthen resource mobilization and implementation.
Continuous pressure testing and simulation training can
support greater national leadership, governance, and
international solidarity for preparedness, readiness and
response, while ensuring alignment with broader health
system priorities. Translating learnings from exercises
and reviews into NAPHS and their equivalents can
increase accountability and transparency.
5.3 Scalable health emergency response
coordination through standardized and commonly
applied emergency response framework
Pre-existing coordination mechanisms should facilitate
whole-of-government and whole-of-society responses
to emergencies, including multifaceted crises such as
COVID-19. Integration and coordination between dierent
capacity-strengthening initiatives across the health
emergency cycle can enhance coherence at national level.
Particularly in acute response incident management,
accountable leadership must be underpinned by eective
multisectoral and multidisciplinary coordination and
bringing together core partners for health emergency
response under government leadership.
WHO’s Emergency Response Framework (ERF) provides
guidelines, operational criteria and standards from
early detection, verication, risk assessment (of acute
events), situational analysis (for protracted emergencies),
grading and response coordination (through the incident
management system). Applying a similarly standardized
and commonly applied framework globally could enhance
alignment and strengthen preparedness and response.
Specic roles and responsibilities should be dened for
each HEPR partner, strengthening and building on existing
networks.
Key capacities include:
• Timely verication, investigation, and risk
assessment of alerts
Early warning and surveillance should be anchored on
the systematic collection, analysis and communication
of any information used to detect, verify, and investigate
events and health risks. Data should be rapidly
disseminated and based on alert triggers, establish,
strengthen and operationalize rapid response teams that
are responsible for the rapid investigation of alerts, eld
risk assessment and, when required, early operational
response.
• Rapidly scalable, adaptable, and interconnected
emergency coordination structures
Standardized and commonly applied emergency
response framework agreements can enhance
scalability and coordination of the health emergency
response. Grading is an internal activation procedure
that triggers emergency procedures and activities for
the management of the response, indicating the level
of operational response and nancing required. This
includes pre-dened incident management support
team (IMST) and emergency coordination structure
scale-up. Coordination and leadership capacities at
national level can be further reinforced through Public
Health Emergency Operation Centers (PHEOCs).
• Prompt synthesis and dissemination of key evidence
to inform action
Building and sustaining knowledge management
can uphold standards of quality before, during, and
aer health emergencies. Knowledge management
depends on maintinaing access to a network of experts,

DRAFT FOR CONSULTATION
JUNE 2022
31
the timely synthesis of evidence into key insights to
drive action and policy, and broad dissemination.
Development of rapid feedback loops to adjust plans,
build specic capacities, and support a culture of
continuous improvement can strengthen preparedness
and response for a given event.
• Strengthened development mobilization and
monitoring of strategies, plans and nancing for
emergency operations
IMST and EOCs are responsible for emergency planning,
and rapidly developing and mobilizing necessary
strategies and nancing. Ongoing collaboration with
international, national and community actors can ensure
eective, scalable coordination of response. Lessons
from operational reviews, intra-action reviews and
debriefs at global/regional/national levels should inform
course correction of emergency operations. Progress
against pre-agreed and regularly reviewed indicators
should systematically track implementation towards the
objectives of the operational response plan.
• Operations, support and logistics
Management of operations and logistics includes human
resources, nances, infrastructure, logistics and supplies
which helps ensure standardized emergency response.
Rapid and scalable responses require rapid supply,
rapid deployment of teams, and safety and security
including protection from sexual exploitation and
abuse a. Best practices and standards can strengthen
interoperability through unied tools and systems.
DRAFT FOR CONSULTATION
JUNE 2022
32
Annex 2: Application of principles of equity,
inclusivity, and coherence
Equity, inclusivity, and coherence are goals as well as principles. Only in applying them consistently and rigorously in the
design and operations of the HEPR architecture at all levels, and monitoring their application, will we achieve the outcomes
we seek.
The following table demonstrates how these principles can be applied and monitored across the ten proposals for
strengthening the global architecture of HEPR.
Pillars Proposal Application of principles
Governance
Proposal 1. Establish a Global Health
Emergency Council and committee for
emergencies of the World Health Assembly
• Alignment with the Constitution and governance of WHO
• Broad multi-sectoral and multistakeholder engagement to inform
agendas
• Gender equity and diversity in membership and leadership
Proposal 2. Make targeted amendments to
the International Health Regulations (2005)
• Alignment of regulatory frameworks relevant to HEPR, including
IHR, proposed pandemic accord, Nagoya protocol, TRIPS and BWC
Proposal 3. Scale-up Universal Health
and Preparedness Reviews and strengthen
independent monitoring
• Whole of government and whole of society engagement in dialogue
and assessments
• Peer assessment to build solidarity, mutual trust, and accountability
for health
• National assessments linked to national action plans for health
security (NAPHS), with nancing, implementation and monitoring
• Harmonization and alignment of multisectoral monitoring
frameworks for HEPR across the spectrum of prevention,
preparedness, response, and recovery
Systems
Proposal 4. Strengthen global health alert
and response teams that are trained to
common standards, interoperable, rapidly
deployable, scalable and equipped
• Multidisciplinary health emergency workforce reecting the
cultural, ethnic, and racial diversity of the communities it serves
• Workforce drawn from and fully integrated into national health
systems and other relevant One Health sectors
• Application of a gender lens to strategic priorities and policies
Proposal 5. Strengthen health emergency
coordination through standardized
approaches to strategic planning, nancing,
operations and monitoring of health
emergency preparedness and response
• Interdependence and interoperability of health emergency
coordination hubs with common standards and operating
framework
• Health emergency management embedded in broader whole-of-
government national disaster management systems
Proposal 6. Expand partnerships and
strengthen networls for a whole-of-society
approach to collaborative surveillance,
community protection, clinical care, and
access to countermeasures
• Equitable sharing of benets, including allocation and access to
countermeasures for HEPR within and among Member States
• Meaningful engagement of communities and civil society in HEPR
at all levels
• Eective collaboration between national authorities, multilateral
organizations and non-State Actors at all levels
Finance
Proposal 7. Establish a coordinating
platform for nancing to promote domestic
investment and direct existing and gap-lling
international nancing to where it is needed
most
• Financing priorities aligned with global, regional and national plans
and priorities
• Inclusive and representative membership of coordinating platform
Proposal 8. Establish a nancial
intermediary fund for pandemic
preparedness and response to provide
catalytic and gap-lling funding
• Contributions based on burden sharing among all Member States,
with additional contributions from non-State Actors
• Allocations aligned with global and national priorities and plans
• Financing gaps lled for low-income and lower middle-income
countries
• Non-competitive with and supportive of existing nancing
instruments for HEPR
• Governance inclusive of contributors and beneciaries
Proposal 9. Expand the WHO Contingency
Fund for Emergencies to ensure rapidly
scalable nancing for response
• Financing for national and international partners aligned with
responsibilities within common emergency response framework
• Implementing mechanisms link nancing to impact, especially
among the most vulnerable
Equity,
inclusivity,
and
coherence
Proposal 10. Strengthen WHO at the centre
of the global HEPR architecture
• Adoption of a pandemic accord as an overarching framework for an
equitable, inclusive and coherent architecture of HEPR
• Sustainable nancing to better align the mandate of WHO with
planning and implementation

