
Medicare General Information, Eligibility,
and Entitlement
Chapter 2 - Hospital Insurance and Supplementary
Medical Insurance
Table of Contents
(Rev. 12046, 05-18-23)
Transmittals for Chapter 2
10 - Hospital Insurance Entitlement
10.1 - Insured Status
10.2 - Hospital Insurance for the Aged
10.3 - Hospital Insurance for Disability Beneficiaries
10.4 - Hospital Insurance for Persons Needing Kidney Transplant or Dialysis
10.4.1 - Effective Date of Entitlement for Persons on Dialysis
10.4.2 - Entitlement Based on Transplant
10.4.3 - Effect on Self-dialysis Training on Entitlement
10.4.4 - End of Coverage Based on ESRD
10.4.5 - Reentitlement for Beneficiaries with ESRD
20 - Hospital Insurance Obtained by Premium Payment
20.1 - Eligibility Requirements
20.2 - Premiums for Hospital Insurance
20.2.1 - Premiums Paid by Other Than Enrollee
20.2.1.1 - Part A Buy-in States
20.2.1.2 - Part A Group Payer States
20.3 - Beginning of Coverage
20.3.1 - Initial Enrollment Period (IEP)
20.3.2 - General Enrollment Period (GEP)
30 - End of Coverage for Hospital Insurance
40 - Supplementary Medical Insurance (SMI)
40.1 - Eligibility for Enrollment
40.2 - Automatic Enrollment in SMI
40.3 - Enrollment Periods
40.3.1 - Enrollment During the Individual's Initial Enrollment Period
40.3.2 - Enrollment During General Enrollment Period
40.3.3 - Enrollment During the Individual's Special Enrollment Period
(SEP) Related to Coverage Under Group Health Plans
40.3.4 SEP for International Volunteers
40.3.5 SEP for Certain TRICARE Beneficiaries
40.3.6 SEP for Beneficiaries for Whom Medicare is Now the
Primary Payer (D-SEP)
40.3.7 –Special Enrollment Period for Exceptional Conditions
40.3.7.1 SEP for Individuals Impacted by an Emergency or
Disaster
40.3.7.2 SEP for Individuals Affected by Employer
Misrepresentation
40.3.7.3 SEP for Formerly Incarcerated Individuals
40.3.7.4 SEP for Termination of Medicaid Coverage
40.3.7.5 SEP for Other Exceptional Conditions
40.4 - Nature and Purpose of State Buy-in
40.5 - End of Coverage
40.6 - Termination and Reenrollment
40.7 - Premiums
40.7.1 - Amount of Premiums
40.7.2 - Increase in Base Premium Amount
40.7.3 - Collection of Premiums
40.7.4 - Grace Period for Payment
40.7.5 - Payment After Grace Period Applies
40.7.6 - Premiums Paid by Other Than the Enrollee
40.7.6.1 - Informal Arrangement
40.7.6.2 - Premium Payer
40.7.6.3 - Formal Group Arrangement
40.7.6.4 - Premium Surcharge Payment
40.7.6.5 – Premiums Under Buy-In
40.7.7 - Late Enrollment Penalty for Premium Part A
40.7.8 – Late Enrollment Penalty for Premium Part B
40.8 - Waiver of Enrollment Period Requirements Due to Administrative Error
40.9 - Extended Coverage for Part B Immunosuppressive Drugs (PB-ID)
40.9.1 - Part B-ID Eligibility Requirements
40.9.2 - Other Health Coverage Making an Individual Ineligible for Part
B-ID
40.9.3 - Effective Date of Entitlement to Part B-ID
40.9.4 - Initial Enrollment & Reenrollment in Part B-ID
40.9.5 - Procedure for Enrolling in Part B-ID
40.9.6 - Termination of Part B-ID
40.9.7 - Part B-ID Premiums
40.9.8 - Procedure for Termination of Part B-ID
40.9.9 - Medicare Savings Programs for Part B-ID Premiums
50 - Identifying the Patient's Health Insurance Record Using the Medicare Card
50.1 - Medicare Beneficiary Identifier (MBI)
60 - Medicare Part C, Medicare+Choice
10 - Hospital Insurance Entitlement
(Rev. 1, 09-11-02)
Hospital insurance (HI), as well as supplementary medical insurance (SMI), is available
to three basic groups of "insured individuals"- the aged, the disabled, and those with end
stage renal disease. Following is an explanation of how an individual becomes "insured"
as well as an explanation of the eligibility requirements for each group.
10.1 - Insured Status
(Rev. 1, 09-11-02)
To be eligible for premium-free HI, an individual must be "insured" based on his or her
own earnings or those of a spouse, parent, or child. To be insured, the worker must have
a specific number of quarters of coverage (QCs); the exact number required is dependent
upon whether the person is filing for HI on the basis of age, disability, or end stage renal
disease. QCs are earned through payment of payroll taxes under the Federal Insurance
Contributions Act (FICA) during the person's working years. QCs earned by an
individual who pays the full FICA tax are usable to insure the person for both monthly
social security benefits and HI.
Federal employees were exempt from payment of FICA taxes prior to January 1983.
However, beginning in January 1983, Federal employees became subject to the HI
portion of the FICA tax (those actually employed in January 1983 were also deemed to
have earned HI quarters of coverage for their Federal service prior to January 1983).
Also, Government employees who pay only the HI portion of the FICA tax are only
insured for HI; they are not insured for monthly social security benefits.
State and local Government employees hired after March 31, 1986, are eligible for
Medicare coverage and must pay the HI portion of the FICA tax. A State may elect to
cover employees hired prior to April 1986 for the Medicare portion of the FICA tax by
requesting an agreement or modification of its existing agreement under section 218 of
the Social Security Act.
10.2 - Hospital Insurance for the Aged
(Rev. 1, 09-11-02)
To be eligible for HI on the basis of age, a person must be age 65 or older and either
eligible for monthly social security or railroad retirement cash benefits, or would be
eligible for such benefits if the worker's Government QCs were regular social security
QCs. An individual who is insured for monthly benefits need not actually file for
benefits to receive HI benefits. If such a person continues to work beyond age 65, he or
she may instead elect to file an application for HI only.
Premium-free HI for the aged begins with the month in which the individual attains age
65, provided he or she files an application for HI or for cash benefits and HI within 6
months of the month in which he or she attains age 65. If the application is filed later
than that, HI entitlement can be retroactive for only 6 months. An individual attains age
65 on the day before his or her 65th birthday. For example, if an individual is born on
August 1, the attainment date is July 31, and HI begins with July 1. Entitlement
generally does not end until death.
10.3 - Hospital Insurance for Disability Beneficiaries
(Rev. 1, 09-11-02)
A disabled person who is entitled to social security or railroad retirement benefits on the
basis of disability is automatically entitled to HI after 24 months of entitlement to such
benefits. Since there is a 5-month disability benefits waiting period, the person actually
becomes entitled to HI after being disabled for 29 months.
In addition, disabled persons who are not insured for monthly Social Security disability
benefits but would be insured for such benefits if Government QCs were treated as social
security QCs, are deemed to be entitled to disability benefits and automatically entitled to
HI after being disabled for 29 months.
The months in the Medicare qualifying period need not be consecutive so that months
from a previous period of disability benefit entitlement generally may be counted in
determining when the qualifying period requirement is met. HI entitlement on the basis
of disability is available not only to the worker, but to the widow, widower, or child of a
deceased, disabled, or retired worker if any of them become disabled within the meaning
of the Social Security or Railroad Retirement Acts.
If an individual recovers from a disability, HI entitlement ends with the month after the
month he or she is notified of the disability termination. For example, if notification is
November 15, entitlement ends December 31. However, if the individual's disability
benefit entitlement ends only because he or she was working, HI entitlement may
continue for up to 78 additional months.
10.4 - Hospital Insurance for Persons Needing Kidney Transplant or
Dialysis
(Rev. 1, 09-11-02)
Individuals of any age with end stage renal disease (ESRD) who receive dialysis on a
regular basis or a kidney transplant are eligible for HI (and are deemed enrolled for
Supplementary Medical Insurance (SMI) unless such coverage is refused) if they file an
application. They must also meet certain work requirements for insured status under the
social security or railroad retirement programs, or be entitled to monthly social security
benefits or an annuity under the Railroad Retirement Act, or be the spouse or dependent
child of an insured or entitled person.
10.4.1 - Effective Date of Entitlement for Persons on Dialysis
(Rev. 1, 09-11-02)
Entitlement usually begins after a 3-month waiting period has been served, i.e., with the
first day of the third month after the month in which a course of regular dialysis begins.
Entitlement begins before the waiting period has expired if the individual receives a
transplant or participates in a self-dialysis training program during the waiting period.
10.4.2 - Entitlement Based on Transplant
(Rev. 1, 09-11-02)
Entitlement begins with the month the individual is admitted as an inpatient to a hospital
for procedures in preparation for or in anticipation of a kidney transplant, provided the
transplant surgery takes place within the following 2 months. If the transplant is delayed
more than 2 months after the preparatory hospitalization, entitlement begins with the
second month prior to the month of transplant. Under the Medicare, Medicaid, and State
Children's Health Insurance Program (SCHIP) Benefits Improvement and Protection Act
of 2000, Congress extended immunosuppressive drug benefits to lifetime, as long as the
beneficiary is entitled to Medicare and was entitled to Medicare when his/her transplant
took place.
10.4.3 - Effect on Self-dialysis Training on Entitlement
(Rev. 1, 09-11-02)
Entitlement begins with the first month of the course of dialysis if the individual is
expected to complete the self-dialysis training program and self-dialyze thereafter.
10.4.4 - End of Coverage Based on ESRD
(Rev. 1, 09-11-02)
HI coverage based on ESRD ends with the earliest of the following dates:
• The day an individual dies,
• The last day of the 12th month after the month the course of dialysis is
discontinued, unless the individual receives a kidney transplant during that period
or begins another course of dialysis, or
• The last day of the 36th month after the month the person receives a kidney
transplant.
10.4.5 - Reentitlement for Beneficiaries with ESRD
(Rev. 1, 09-11-02)
If a person whose entitlement based on ESRD has ended begins a new course of regular
dialysis or has a kidney transplant, reentitlement begins without a waiting period.
20 - Hospital Insurance Obtained by Premium Payment
(Rev. 1, 09-11-02)

20.1 - Eligibility Requirements
(Rev. 1, 09-11-02)
Individuals who want hospital insurance coverage but who are not otherwise eligible (i.e.,
do not qualify under either the regular or deemed insured provisions, in §§10.1, 10.2,
10.3, 10.4 in this chapter) may obtain such coverage by enrolling timely, paying a
monthly premium, and upon meeting the following three requirements:
• Attaining age 65,
• Enrolling or already having enrolled in the SMI program,
• Being a resident of the U.S., and either:
o A citizen, or
o An alien lawfully admitted for permanent residence who has resided
continuously in the U.S. for the 5 years prior to the month of enrollment.
20.2 - Premiums for Hospital Insurance
(Rev. 1, 09-11-02)
Each year, the Secretary of the Department of Health and Human Services announces the
amount of the hospital insurance premium payable for each month in the following
calendar year. The applicable premium amount is 33/76 (about 43.4 percent) of the
hospital insurance deductible for that calendar year. The premium is rounded to the
nearest $1. An individual who is not entitled to free Part A and wishes this type of
coverage must enroll him/herself during the appropriate enrollment period. A premium is
due for each month of entitlement under Premium HI.
20.2.1 - Premiums Paid by Other Than the Enrollee
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
The following subsections describe Medicare Part A premiums paid by other than the
enrollee.
20.2.1.1 - Part A Buy-in States
(Rev .11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
States that include the payment of Medicare Part A premiums for Qualifying Medicare
Beneficiaries (QMBs) in their state buy-in agreements are known as Part A buy-in states.
Individuals in Part A buy-in states can file for Premium Part A at any time, without
regard to enrollment periods. Late enrollment penalties do not apply. Please see the
Manual for State Payment of Medicare Premiums, chapter 1, sections 1.7 and 1.11 for
additional information about Part A buy-in states.

20.2.1.2 - Part A Group Payer States
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
States that do not include the payment of Medicare Part A premiums for QMBs in their
state buy-in agreements are known as group payer states. To become entitled to Part A,
individuals in group payer states can file for premium Part A during their Initial
Enrollment Period (IEP) or the General Enrollment Period (GEP). Part A premiums and
any applicable late enrollment penalties are paid under a group payer arrangement. Please
see the Manual for State Payment of Medicare Premiums, chapter 1, section 1.7 and 1.11
for additional information about Part A group payer states.
20.3 - Beginning of Coverage
(Rev. 1, 09-11-02)
20.3.1 - Initial Enrollment Period (IEP)
(Rev. 1, 09-11-02)
Persons may enroll for premium hospital insurance by filing a request during the IEP
which begins the third month before the month of first eligibility and lasts for 7 months.
The individual's IEP for premium hospital insurance is in most cases the same 7-month
period as the IEP for SMI.
The individual may enroll for hospital insurance when he or she enrolls for SMI, or later
during his or her IEP. The beginning date of an individual's premium hospital insurance
coverage period is determined by the rules applicable to SMI coverage based on an SMI
enrollment during an IEP. (See chapter 2 §40 in this chapter.)
20.3.2 - General Enrollment Period (GEP)
(Rev. 1, 09-11-02)
Eligible persons who have not enrolled for premium hospital insurance during their IEP,
or whose premium hospital insurance has been terminated, may enroll during a GEP
(January 1 - March 31 of each year) if they are enrolling or have enrolled for SMI. As
with SMI, an eligible person who enrolls for hospital insurance during a GEP will have
hospital insurance coverage beginning the following July.
The same restrictions on enrollment and reenrollment apply as in the SMI program.
Individuals who enroll late may pay a 10 percent premium penalty.
30 - End of Coverage for Hospital Insurance
(Rev. 1, 09-11-02)
A beneficiary's entitlement under the provision terminates:

• With the month of the individual's death,
• With the last day of the third month following the premium billing month (for
nonpayment of premiums),
• With the end of the month following the month in which he or she files a
voluntary request for termination,
• With the month SMI coverage is terminated, or
• With the month before the month in which he or she becomes entitled to hospital
insurance under the regular or ESRD provisions. (See §2, §10.4 of this chapter.)
40 - Supplementary Medical Insurance (SMI)
(Rev. 1, 09-11-02)
Unlike the HI benefits program, which is largely financed by compulsory taxes on
employers, employees, and the self-employed, the SMI benefits program is a voluntary
program financed from premium payments by enrollees, together with contributions from
funds appropriated by the Federal Government, and certain deductible and cost-sharing
provisions.
40.1 - Eligibility for Enrollment
(Rev. 1, 09-11-02)
To obtain SMI coverage, eligible individuals must enroll in the plan during an enrollment
period open to them and pay the required premiums. They are eligible to enroll if they
are entitled to premium-free HI, or are age 65 and resident citizens or resident aliens. To
qualify as a resident alien, an individual must have been lawfully admitted for permanent
residence and have resided continuously in the United States during the 5 years
immediately preceding the month of enrollment.
40.2 - Automatic Enrollment in SMI
(Rev. 1, 09-11-02)
Beneficiaries (except those residing in foreign countries or Puerto Rico) are deemed to
have enrolled in SMI in the month before the month for which they are entitled to HI so
that HI and SMI coverage start in the same month. Thus, monthly beneficiaries other
than disability beneficiaries are deemed to enroll in the month before attainment of age
65. Disability beneficiaries are deemed to enroll in the 24th consecutive month of
entitlement to disability benefits.
Every potential "deemed" enrollee is given a reasonable opportunity (at least 2 months) to
decline SMI enrollment by filing notice to this effect. He or she is deemed not to have
enrolled and does not incur any premium liability. A refusal of SMI not timely filed is
treated as a request for voluntary termination under existing disenrollment rules once it
has been established that the individual does not wish to have SMI.
40.3 - Enrollment Periods
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Enrollment is possible only during specified enrollment periods:
• An individual's initial enrollment period (IEP) is of 7 months duration. It begins 3
full calendar months before and ends 3 full calendar months after the month in
which the individual first meets all the requirements for enrollment.
• A general enrollment period (GEP) occurs each year from January 1 through
March 31. Coverage is effective the month following the month of enrollment.
• Special enrollment periods (SEP) are available to enable certain individuals to
enroll in Medicare outside of the IEP and the GEP.
40.3.1 - Enrollment During the Individual's Initial Enrollment Period
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Coverage begins on the first day of:
• The month in which the individual first becomes eligible for SMI if enrollment
takes place during the first 3 months of the initial enrollment period,
• The month following the month of enrollment if enrollment occurs during the
fourth through seventh month of the initial enrollment period.
40.3.2 - Enrollment During General Enrollment Period
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Coverage begins the first day of the month following the month of enrollment.
40.3.3 - Enrollment During the Special Enrollment Period (SEP)
Related to Coverage Under Group Health Plans
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
If an individual enrolls in SMI or premium HI while still covered under a GHP or LGHP
or during the first full month when not enrolled in a GHP/LGHP based on current
employment status, coverage begins either with:
• The first day of the month of SMI or premium HI enrollment, or
• At the individual's option, with the first day of any of the following 3 months.
If the individual enrolls during any of the 7 remaining months of the special enrollment
period, coverage begins with the first day of the month following the month of
enrollment.
40.3.4 - SEP for International Volunteers
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals who do not enroll in Part B or Premium Part A when first eligible because
they were performing volunteer service outside of the United States may enroll during
this SEP.
Eligible Individuals may enroll if:
• They volunteered outside of the United States through a program that covers at
least a 12-month period; and
• Is sponsored by a tax exempt organization; and
• The individual has (or had) health insurance that provided coverage to the
individual while he or she was outside of the U.S. for the duration of the volunteer
service.
The SEP for volunteers is the 6-month period that begins the earlier of the first day of the
month following the month for which the:
• Individual was no longer serving as a volunteer outside of the United States;
• Organization no longer has tax-exempt status; or
• Individual no longer has health insurance that provides coverage outside of the
United States.
Coverage begins the first day of the month following enrollment.
40.3.5 - SEP for Certain TRICARE Beneficiaries
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals who enroll in Part A based on disability or ESRD, but do not enroll in Part B
because they were eligible for TRICARE standard or TRICARE prime, may enroll during
this SEP. Eligible individuals are those who are:
• Under age 65, and
• Eligible for TRICARE Standard at the time of HI entitlement and:
• A military retiree or military retiree family member, or
• On active duty or a family member of an active duty service member with
Medicare based on ESRD.
Eligible individuals may enroll:
• If notified of Medicare entitlement during the IEP -The month after the end of the
IEP, or
• If notified of Medicare entitlement after the IEP -The month of notification of
Medicare entitlement.
Coverage begins:
If notified of Medicare entitlement during the IEP:
• The month of enrollment, or
• The first month after the end of the IEP
If notified of Medicare entitlement after the IEP:
• The month of enrollment, or
• The month SMI terminated based on the refusal.
If entitlement is based on ESRD, coverage begins:
• The month of HI entitlement, or
• The month of enrollment, or
• The month after the end of the IEP.
40.3.6 - SEP for Beneficiaries for Whom Medicare is Now the Primary
Payer (D-SEP)
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals entitled to Medicare Part A based on disability, but who did not enroll in Part
B because Medicare was the secondary payer for covered services, may enroll using this
7-month SEP.
Eligible individuals may enroll with the later of:
• The month in which the employer notifies the beneficiary that Medicare is the
primary payer, or
• The month Medicare becomes the primary payer.
Coverage begins either:
• The first day of the month of filing for Part B, or
• During any month of the 7-month D-SEP, or
• Retroactive to the month Medicare becomes the primary payer provided the
beneficiary makes arrangements to pay the past due premiums; either by a lump
sum payment or by monthly installments.
40.3.7 – SEP for Exceptional Conditions
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Effective January 1, 2023, the following SEPs for exceptional conditions are available
for Premium Part A and Part B, respectively.
40.3.7.1 - SEP for Individuals Impacted by an Emergency or Disaster
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals who do not enroll in Part B or Premium Part A when first eligible due to
having an emergency or disaster as declared by a federal, state, or local government
entity may enroll during this SEP.
Eligible Individuals may enroll as early as:
• The month of the emergency or disaster, or
• Up to six months after the emergency or disaster has ended.
NOTE: they may also be able to use this SEP if the disaster or emergency takes place
where their authorized representative, legal guardian, or person who makes health care
decisions on their behalf resides.
The SEP begins the date an emergency or disaster is declared, or the start date identified
in the emergency declaration, whichever is earlier. The SEP ends six months after the
end of the date which is the later of:
• The end date identified in the disaster or emergency declaration, or
• The end date of any extensions or the date when the declaration has been
determined to have ended or has been revoked, or
• The date of the declaration, if such date is after the end of the disaster.
Coverage begins the first day of the month following enrollment.
40.3.7.2 – SEP for Individuals Affected by a Health Plan or Employer
Misrepresentation
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals who do not enroll in Part B or Premium Part A when first eligible due to
misrepresentation or reliance on incorrect information provided by their employer or
GHP, agents or brokers of health plans, or any person authorized to act on behalf of such
entity may enroll during this SEP.
An eligible person must demonstrate (by documentation or written attestation) both of the
following:
• They did not enroll in Part B or Premium Part A during another enrollment
period in which they were eligible based on information received from an
employer or GHP, agents or brokers of health plans, or any person authorized to
act on such organization’s behalf.
• An employer, GHP, agent or broker of a health plan, or their representative
materially misrepresented information or provided incorrect information relating
to enrollment in Part B or Premium Part A.
The SEP begins the day an individual notifies the Social Security Administration and
ends six months later.
Coverage begins the first day of the month following enrollment.
40.3.7.3 - SEP for Formerly Incarcerated Individuals
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals who do not enroll in Part B or Premium Part A when first eligible because
they were incarcerated may enroll during the SEP.
An eligible person can sign up anytime within the 12 months after their release from
incarceration.
The SEP begins the day an individual is released from the custody of penal authorities.
However, individuals have the option to select a retroactive effective date (not to begin
prior to their release date and not to exceed 6 months). If individuals choose this
retroactive option, they will be responsible for paying Medicare premiums back to the
date of coverage.
Coverage begins the first day of the month following enrollment or up to six months
retroactive.
40.3.7.4 - SEP for Termination of Medicaid Coverage
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals whose Medicaid eligibility terminated may enroll during this SEP.
A person may be eligible based on this condition if they have:
• Lost Medicaid entirely,
• Missed a Medicare enrollment period, and
• Their Medicaid coverage was terminated on or after January 1, 2023.
The SEP begins when an individual is notified of an upcoming termination of Medicaid
eligibility and ends six months after the Medicaid termination. Medicare benefits start the
month after Medicare enrollment unless the individual elects a start date back to the first

day of the month the individual lost Medicaid and agrees to pay all prior premiums.
Note: Individuals who are still eligible for Medicaid, including a Medicare Savings
Program, and have not received notice of an upcoming Medicaid termination are not
eligible for this SEP.
40.3.7.5 - SEP for Other Exceptional Conditions
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
Individuals who do not enroll in Part B or Premium Part A when first eligible because
conditions beyond their control caused them to miss an enrollment period may enroll
during the SEP. This SEP is available for individuals whose unique conditions do not
qualify for other SEPs.
An eligible person must demonstrate (by documentation or written attestation) that
conditions outside of their control that occurred on or after January 1, 2023, caused
them to miss an enrollment period.
An individual’s request for this SEP will only be granted in conditions that are truly
exceptional in nature, and will not be used to grant individual’s enrollment due to
forgetfulness, lack of knowledge, or failure to make premium payments.
SSA will determine when this SEP begins on a case-by-case basis, but the SEP will end
no less than 6 months after it begins.
Coverage begins the first day of the month following enrollment.
40.4 - Nature and Purpose of State Buy-in
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
Under the State Buy-in program, states, the District of Columbia, and the U.S. territories
may enter into buy-in agreements with CMS to enroll certain individuals who are dually
eligible for Medicare and Medicaid into Medicare Part B and pay the premiums on their
behalf.
Most states have expanded their buy-in agreements to also include payments of Part A
premiums for individuals who must pay a premium to enroll in Medicare Part A and who
are eligible for the Qualified Medicare Beneficiary (QMB) eligibility group. State buy-in
agreements maximize the number of full-benefit Medicaid recipients enrolled in
Medicare, which ensures that Medicare pays primary to Medicaid. State buy-in
agreements also facilitate enrollment in Medicare for low income individuals who are not
eligible for full-benefit Medicaid coverage by paying Medicare premiums and cost
sharing. Please see the Manual for State Payment of Medicare Premiums, chapter 1,
section 1.2 for additional state buy-in information.

40.5 - End of Coverage
(Rev. 1, 09-11-02)
An individual may notify CMS in writing, at any time, that he or she no longer wishes to
participate in the supplementary medical insurance plan. Termination of coverage takes
effect at the close of the calendar month following the calendar month in which the
request for termination was filed.
Enrollment under medical insurance is terminated because of nonpayment of premiums.
Termination is effective with the end of the grace period provided for payment of
premiums. (See chapter 2, §40.7.4 of this manual.)
For individuals under age 65, enrollment is terminated because HI entitlement ended.
SMI terminates at the same time as HI.
If not terminated sooner, coverage ends with the beneficiary's death.
40.6 - Termination and Reenrollment
(Rev. 1, 09-11-02)
An individual whose enrollment has terminated may reenroll only in a general enrollment
period or a special enrollment period if the requirements are met.
40.7 – Premiums
(Rev. 1, 09-11-02)
A premium is due for each month of entitlement under SMI. The SMI premium covers
about one-fourth of the cost of the Part B program.
40.7.1 - Amount of Premiums
(Rev. 1, 09-11-02)
In the third quarter of each calendar year, the Secretary of the Department of Health and
Human Services announces the base premium for SMI coverage that is payable as of the
following January 1. The SMI premium is the same for all enrollees even though the cost
to the program is greater for ESRD enrollees and the disabled than it is for the aged. The
SMI premium is refigured each year and is based on the lower of one-half of SMI
program costs per aged enrollee or the general percentage by which social security
benefits were increased during the calendar year in which the announcement occurs.
(During the 5-year period, January 1984 through December 1988, the formula for
computing the SMI premium has been modified to provide that the Part B premium
reflects exactly one-fourth of the cost of the Part B program. Beginning with the
premium announced for the period beginning January 1989, however, the method of
computing the SMI premium reverts back to the pre-January 1984 rules.)
40.7.2 - Increase in Base Premium Amount
(Rev. 1, 09-11-02)
The base premium that is announced by the Secretary is paid by most enrollees.
However, it is increased for those who enroll late or reenroll after a prior termination of
entitlement. The amount of the increase is 10 percent of the base rate for each full 12-
month period during which the individual could have been but was not enrolled in the
program. However, months in which an individual has GHP coverage based on current
employment status are not counted as months in which the individual "could have been,
but was not enrolled." This exception does not apply to individuals who are entitled to
Medicare on the basis of ESRD.
40.7.3 - Collection of Premiums
(Rev. 1, 09-11-02)
SMI premiums are collected from benefits payable (in order of priority) by the Railroad
Retirement Board, SSA, or Office of Personnel Management (Civil Service) unless the
individual is covered under a State buy-in agreement. If the individual is entitled to such
benefits but the payments are in suspense, e.g., due to work deductions, he or she is billed
for the amounts due. Uninsured beneficiaries are also billed directly for the premiums
due.
Premium bills are sent every 3 months unless the individual specifically requests a
monthly bill or is also entitled to Premium - HI (in which case a monthly combined SMI-
Premium-HI bill is sent).
40.7.4 - Grace Period for Payment
(Rev. 1, 09-11-02)
A grace period has been provided for payment of premiums by those who are billed
directly. The period extends for 90 days after the month in which the bill is mailed. If
the premiums are not received in that prescribed time, entitlement terminates at the end of
the grace period. This 90-day grace period for paying overdue SMI premiums and
continuing SMI coverage may be extended by CMS for good cause for up to an
additional 90 days. Good cause, for example, is found if the enrollee was mentally or
physically incapable of paying his or her premiums timely, or had some reasonable basis
to believe that payment had been made, or the failure to pay was due to administrative
error.
40.7.5 - Payment After Grace Period Applies
(Rev. 1, 09-11-02)
If an extension to the grace period (additional 90 days; a total not to exceed 180 days) has
been granted, an enrollee may retain SMI entitlement by paying all past due premiums if
there was a good cause for his/her failure to pay premiums within the initial grace period.
40.7.6 - Premiums Paid by Other Than the Enrollee
(Rev. 1, 09-11-02)
The following subsections describe premiums paid by other than the enrollee.
40.7.6.1 - Informal Arrangement
(Rev. 1, 09-11-02)
Enrollees who are being billed directly for Medicare premiums may turn over their
premium bills to a friend, relative, employer lodge, union or other organization to pay
premiums on their behalf. The third party payer forwards the proper amount of payment
for each enrollee to CMS's Premium Collection Center. Enrollees participating in this
type of informal arrangement continue to receive their premium notice (Form CMS-500),
and remain responsible for assuring that premiums paid on their behalf are paid timely in
order to avoid termination of Medicare coverage.
40.7.6.2 - Premium Payer
(Rev. 1, 09-11-02)
Individuals may be designated as the premium payer for an enrollee and receive the
enrollee's premium bills, if it is judged to be in the enrollee's best interest (e.g., the
enrollee is competent, but too physically ill or infirm to be able to handle such matters).
The individual receiving the premium bill must be a relative or friend showing personal
interest in the welfare of the enrollee.
40.7.6.3 - Formal Group Arrangement
(Rev. 1, 09-11-02)
Employers, religious orders, lodges, unions or other organizations may enter into a
formal agreement with CMS in order to receive a single bill and pay a lump sum for the
premiums due from a group of individuals. Group payments under a formal group
agreement may be made only on behalf of individuals who are already enrolled and are
being billed for direct remittance. This type of arrangement is referred to as a "Formal
Group Payer" arrangement. While included in a formal group payer arrangement,
enrollees will no longer receive a premium notice (Form CMS-500). This arrangement is
available only where the number of enrollees in the group is large enough to make it
practicable to send one bill to the group payer and where the following conditions are
also met:
• Enrollees included under the formal group arrangement are directly billed for
their premium, and are not having his/her premiums deducted from a Social
Security, Railroad Retirement, or Civil Service benefit, or, are not having
premiums paid by a State Medicaid agency under a State buy-in agreement;
• The enrollee authorizes the formal group payer to pay premiums on his/her
behalf;

• The formal group payer has a minimum of 20 enrollees; and
• The formal group payer agrees to submit premium payments via electronic funds
transfer.
If the formal group payer agreement is terminated, or if the group payer alerts CMS to
remove an individual from the group payer arrangement, CMS will resume collection of
premiums from the individual through the direct billing process.
40.7.6.4 - Premium Surcharge Payment
(Rev. 1, 09-11-02)
States or local Governments may pay a lump sum for the total amount of the SMI late
enrollment premium surcharge for a group of individuals. In order to pay the premium
surcharge, States or local Governmental entities are required to enter into a formal
agreement with CMS. An individual is not billed for the premium surcharge portion of
his/her SMI premium while under a premium surcharge agreement, however, he/she is
billed for the base premium amount. If the enrollee is receiving a Social Security,
Railroad Retirement, or Civil Service annuity, the agencies responsible for these
programs will continue to withhold the base premium amount from the annuity.
Enrollees who are billed directly for premiums will continue to receive a premium bill for
the base premium amount.
The ultimate responsibility for paying premiums rests with the enrollees.
40.7.6.5 - Premiums Under Buy-In
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
States pay the Part B premiums for any eligible individual specified in the state’s buy-in
agreement. Under buy-in agreements, states can enroll individuals in Part B at any time
without regard to Medicare enrollment periods or late enrollment penalties. Please see the
Manual for State Payment of Medicare Premiums, chapter 1, section 1.4 for additional
information about state payment of premiums under a buy-in agreement.
40.7.7 – Late Enrollment Penalty (LEP) for Premium Part A
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
If an individual did not enroll in premium Part A when first eligible, they may have to pay
a higher monthly premium if they decide to enroll later. The monthly premium for Part A
may increase up to 10%. The individual will have to pay the higher premium for twice the
number of years the individual could have had Part A, but did not sign up.
For individuals enrolling using the SEP Related to Coverage Under Group Health
Plans, the premium Part A LEP is calculated by adding the months that have elapsed
between the close of the individual’s IEP and the end of the month in which the individual
enrolls. For enrollments after your IEP has ended, months where you had group health
plan coverage are excluded from the LEP calculation.
For individuals enrolling using an Exceptional Conditions SEP, the International
Volunteers SEP, or the SEP for Certain TRICARE Beneficiaries, no LEP will be applied.
40.7.8 – Late Enrollment Penalty (LEP) for Premium Part B
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
If an individual did not sign up for Part B when first eligible, the individual may have to
pay a late enrollment penalty for as long as the individual has Medicare. The individual’s
monthly premium for Part B may go up 10% for each full 12-month period that the
individual could have had Part B, but did not sign up for it.
For individuals enrolling using the SEP Related to Coverage Under Group Health Plans,
the Part B LEP is calculated by adding the months that have elapsed between the close of
the individual’s IEP and the end of the month in which the individual enrolls. For
enrollments after your IEP has ended, months where you had group health plan coverage
are excluded from the LEP calculation.
For individuals enrolling using an Exceptional Conditions SEP, the International
Volunteers SEP, or the SEP for Certain TRICARE Beneficiaries, no LEP will be applied.
For individuals enrolling using the D-SEP, the Part B LEP is calculated by adding all
months during which the large group health plan (LGHP) was secondary payer
beginning with the end of the IEP, or the date LGHP coverage began.
40.8 - Waiver of Enrollment Period Requirements Due to
Administrative Error
(Rev. 1, 09-11-02)
CMS and SSA are authorized to take necessary action to correct an erroneous SMI or
premium hospital insurance enrollment or nonenrollment which was based upon the
action, inaction, or error of a Government officer, employee, or agent. The action may
include designating special individual enrollment periods and premium adjustments.
For the purpose of this provision, an individual's enrollment or nonenrollment in SMI is
considered to have been prejudiced and due to the "action, inaction, or error" of an
officer, employee, or agent of the Government, if there is an official record or other
evidence showing that:
• The individual took reasonable appropriate and timely measures to assert his or
her rights, and
• Due to administrative fault or other action, which may or may not have been
erroneous at the time taken, his or her rights have been or are likely to be
impaired unless relief is given.
This authority applies to all Part B cases which have arisen since the Medicare program
began on July 1, 1966. It is applied to cases that come to CMS's or SSA's attention;
however, MACs should not search their files.
40.9 - Extended Coverage for Part B Immunosuppressive Drugs (PB-
ID)
(Rev. 11646; Issued:10-19-22; Effective:01-01-23; Implementation:01-03-23)
The Consolidated Appropriations Act of 2021 amended section 1836(b) of the Social
Security Act to add a new form of coverage that provides solely for coverage of
immunosuppressive drugs beginning January 1, 2023, for eligible individuals whose
entitlement to Medicare based on End-Stage Renal Disease (ESRD) ends the 36th month
after the month in which the individuals receive a successful kidney transplant.
This new benefit is referred to as the Part B immunosuppressive drug benefit or “Part B-
ID.”
Beneficiaries enrolled in Part B-ID will not be covered for any other Medicare benefit or
for any items or services other than Part B Immunosuppressive Drugs.
40.9.1 - Part B-ID Eligibility Requirements
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
An individual is eligible for Part B-ID if he or she:
1. Is or was entitled to Medicare Part A based on ESRD that ends 36 months after a
successful kidney transplant; and
2. Attests that he or she is not enrolled in other health coverage that would make
them ineligible for Part B-ID, as outlined in section 40.9.2. Every individual
enrolling in Part B-ID must:
i. Attest that they are not enrolled in other health coverage and do not
expect to enroll in other coverage which would make them
ineligible for Part B-ID; and
ii. Agree to notify SSA within 60 days of enrolling in other health
coverage.
NOTE: An individual can inform SSA of other health coverage up
to 6 months in advance
40.9.2 - Other Health Coverage Making an Individual Ineligible for Part
B-ID
(Rev . 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
An individual who has other certain health coverage is not eligible for Part B-ID. Other
health coverage includes:
• Group Health Plans or Individual Health Plans;
• Enrolled in the patient enrollment system of the Department of Veterans Affairs
(VA) or otherwise eligible to receive immunosuppressive drugs from the VA;
• TRICARE for Life;
• Health Insurance Marketplace qualified health plans; and
• Medicaid or State Children’s Health Insurance Program (CHIP) coverage that
includes immunosuppressive drugs.
40.9.3 - Effective Date of Entitlement to Part B-ID
(Rev. 11646; Issued:10-19-22; Effective:01-01-23; Implementation:01-03-23)
The effective date of an individual’s eligibility for the Part B-ID benefit depends on
when their entitlement to Medicare Part A based on ESRD ends and when they
submit the attestation described in section 40.9.1 of this chapter.
When an individual’s Medicare Part A entitlement based on ESRD ends on or after
January 1, 2023:
• If they submit the attestation before the end of the 36
th
month after the
month of the kidney transplant (i.e. before their Medicare Part A
entitlement based on ESRD ends), Part B-ID begins effective at the start
of the month after their Medicare Part A on the basis of ESRD ends.
• If they submit the attestation after their Medicare Part A entitlement ends,
Part B-ID begins at the start of the month following the month in which
the attestation is submitted.
When an individual’s Medicare Part A entitlement based on ESRD ends prior to
January 1, 2023:
• If they submit the attestation to enroll from October 1, 2022 through
December 31, 2022, Part B-ID begins effective January 1, 2023.
• If they submit the attestation to enroll after December 31, 2022, Part B-ID
begins the following month.
40.9.4 - Initial Enrollment & Reenrollment in Part B-ID
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
There are no enrollment periods associated with Part B-ID. Therefore, eligible
individuals can enroll at any time without regard to Medicare enrollment periods. The
earliest date on which they may initially enroll depends on when their Medicare Part A
entitlement based on ESRD ends, under the following two scenarios:
1. When an individual’s Medicare Part A entitlement based on ESRD ends on or
after January 1, 2023, they may enroll in Part B-ID any time after their Medicare
Part A on the basis of ESRD entitlement ends.
2. When an individual’s Medicare Part A entitlement based on ESRD ends prior to
January 1, 2023, they may enroll in Part B-ID beginning October 1, 2022 and
their coverage will start the later of January 2023 or the month after they enroll.
Individuals who had previously enrolled in Part B-ID can reenroll at any time if they
meet the eligibility requirements in section 40.9.1.
NOTE: Late enrollment penalties are not applicable to Part B-ID enrollment. Additional
information is outlined under subsection 40.9.7 (Part B-ID Premiums).
40.9.5 - Procedure for Enrolling in Part B-ID
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
Eligible individuals may enroll by:
1. calling SSA at 1-877-465-0355 and providing an oral attestation, or
2. completing and filing the Application for Enrollment in Part B-ID.
Immunosuppressive Drug Coverage Form CMS-10798 and mailing it to the
following address:
SOCIAL SECURITY ADMINISTRATION
OFFICE OF CENTRAL OPERATIONS
PO Box 32914
BALTIMORE, MARYLAND 21298
Note: The Office of Central Operations Office of Disability Operations teleservice
center (ODO TSC) will only be handling the telephonic enrollments and PC 7 will
process the enrollment for Part B-ID.
40.9.6 - Termination of Part B-ID
(Rev. 11646; Issued:10-19-22; Effective:01-01-23; Implementation:01-03-23)
1. Individuals enrolled in other health coverage are required to notify
SSA and terminate Part B-ID
a. When a Part B-ID covered individual notifies SSA that they have
enrolled in other coverage, and if not otherwise specified, Part B-
ID terminates effective with the first day of the month following
the month SSA receives the notification.

b. If the individual states that their other health insurance begins in
the future, the individual may request a termination date up to 6
months in the future.
Example: If an individual enrolls in employer health coverage
during an employer’s open enrollment period in October, for a
January 1
st
effective date, the individual can submit their request
for termination of the Part B-ID benefit in October or November,
and not lose their Part B-ID benefit prior to the January 1
st
effective date.
c. When a state ends buy-in for Part B-ID because an individual
gained full Medicaid eligibility that includes immunosuppressive
drug coverage, the individual must report this new eligibility to
SSA and terminate Part B-ID coverage.
If a Part B-ID covered individual fails to notify SSA of their enrollment in
other health coverage, including employer and Medicaid, Part B-ID will
terminate effective the first day of the month after the month in which
SSA discovers the individual has other health coverage.
2. Voluntary termination request – In general, Part B-ID terminates
effective with the first day of the month following the month in which we
receive the request.
There is an exception to this general rule for individuals who had state
payment of their Part B-ID premium under a Medicare Savings Program
(as described in section 40.9.9) and who are notified by SSA that their
state will no longer pay their Medicare Part B-ID premiums. For these
individuals the following entitlement end dates apply:
a. If the individual files a voluntary termination request within 30
days after the date of the notice that state payment of premiums
will end or has ended, the individual's Part B-ID entitlement ends
on the last day of the last month for which the state paid the
premium.
b. If the individual files the voluntary termination request more than
30 days but not more than 6 months after state payment of
Medicare Part B-ID premiums ends, Part B-ID entitlement ends on
the last day of the month in which the request is filed.
c. If the individual files the voluntary termination request later than
the 6th month after state payment of Medicare Part B-ID premiums
ends, entitlement ends at the end of the month after the month in
which request is filed.
We note that individuals who lose eligibility for state payment of Medicare Part B-ID
premiums through a Medicare Savings Program will continue to be eligible for the Part
B-ID benefit without interruption with the individual assuming responsibility for paying
the Part B-ID premiums, unless they voluntarily terminate. The options for financial
relief from Part B billing in SSA’s Program Operations Manual System (POMS), section
HI.00815.042, also apply for the Part B-ID coverage here.
3. Death - Entitlement to Part B-ID continues into the month of death, up to
and including the date of death.
4. Non-payment of premiums – Part B-ID coverage will terminate for non-
payment of premiums following the same rules, including grace periods,
used for Medicare Part B for monthly billing in sections 40.5 and 40.7.4 of
this manual. Note that section 40.5 provides end of coverage information,
and section 40.7.4 provides grace period payment information.
5. Individual becomes entitled to Medicare on another basis – In cases
where a Part B-ID enrollee becomes eligible for Medicare based on age,
disability, or ESRD, Part B-ID will terminate effective with the last day of
the month prior to the month in which they become entitled on the other
basis. Equitable relief for retroactivity may apply.
40.9.7 - Part B-ID Premiums
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
Part B-ID premiums may be adjusted based on rounding, the income-related monthly
adjusted amounts (IRMAA), and the hold harmless provision, but will not be increased
based on late enrollment.
If the individual is directly billed for premiums, billing will be on a monthly basis.
40.9.8 - Procedure for Termination of Part B-ID
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
Individuals enrolled in the Part B-ID benefit can report other coverage and request to
terminate their enrollment by either:
1. calling SSA at 1-877-465-0355 to disenroll over the phone to verbally request
termination, or
2. completing and submitting Form CMS-1763, Request for Termination of
Premium Hospital and/or Supplementary Medical Insurance, and mailing it to:
SOCIAL SECURITY ADMINISTRATION
OFFICE OF CENTRAL OPERATIONS
PO Box 32914
BALTIMORE, MARYLAND 21298
3. any other request to SSA that shows the unequivocal desire to end coverage.
Note: The Office of Central Operations Office of Disability Operations teleservice
center (ODO TSC) only will handle the telephonic disenrollment and PC 7 will
process the disenrollment for Part B-ID.
When the individual is reporting other coverage and choosing a future termination date, a
termination effective date that is more than 6 months in the future cannot be processed
40.9.9 - Medicare Savings Programs for Part B-ID Premiums
(Rev. 11764; Issued 12-22-22; Implementation: 01-01-2023; Effective 01-03-23)
Individuals enrolled in Part B-ID with limited income and resources may be eligible for
assistance through the Medicare Savings Programs (MSPs). The MSPs include three
eligibility groups that cover Part B-ID premiums and sometimes cost sharing, including:
• Qualified Medicare Beneficiary (QMB)
• Specified Low-Income Medicare Beneficiary (SLMB)
• Qualifying Individuals (QI)
There are two ways to enroll in the MSPs for the payment of the Part B-ID premiums.
First, once enrolled in Part B-ID, individuals may apply for the MSPs and be determined
eligible by their state for an MSP eligibility group based on Part B-ID.
Second, individuals who are enrolled in an MSP group and lose Medicare entitlement
based on ESRD 36 months after the month in which they receive a kidney transplant can
transition to an MSP based on Part B-ID enrollment without a break in coverage if:
(1)they attest that they do not have other health coverage as described in 40.9.1 by the
end of the 36th month after the month in which they receive a kidney transplant; and (2)
the state redetermines the individual’s Medicaid eligibility on all bases and does not
otherwise find the individual ineligible for the MSP group.
50 - Identifying the Patient's Health Insurance Record Using the
Medicare Card
(Rev. 124, Issued: 05-17-19, Effective: 06-18-19, Implementation: 06-18-19
As part of health insurance electronic data processing, Medicare cards are issued by CMS
to individuals who have established entitlement to health insurance.
Below is an example of the Medicare card.
New Medicare Card
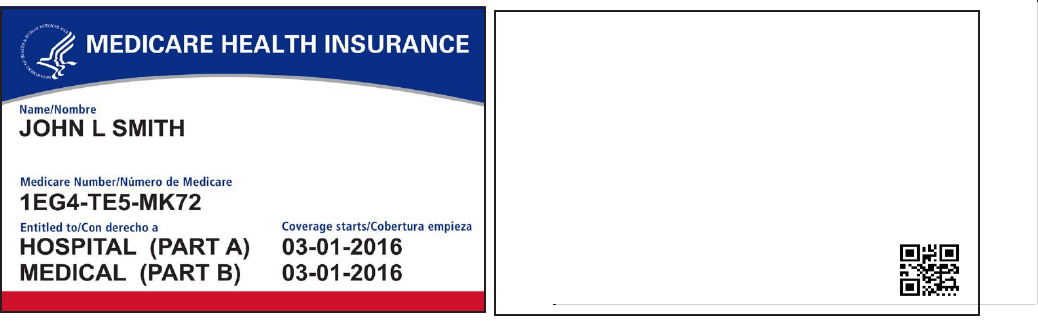
New Medicare Card Front New Medicare Card
Back
The Medicare card is used to identify the individual as being entitled and also serves as a
source of information required to process Medicare claims or bills. It displays the
beneficiary's name, Medicare number, and effective date of entitlement to hospital
insurance and/or medical insurance. The Social Security Administration's Social Security
Office assists in replacing a lost or destroyed Medicare cards.
50.1 - Medicare Beneficiary Identifier (MBI)
(Rev. 12046, Issued:05-18-23, Effective:01-01-23, Implementation:06-21-23)
The term Medicare beneficiary identifier (MBI) is a general term describing a
beneficiary’s Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
60 - Medicare Part C, Medicare+Choice
(Rev. 1, 09-11-02)
Medicare Part C, which is also known as Medicare+Choice, is a Medicare program that
gives beneficiaries more choices among health plans. Everyone who has Medicare Parts
A and B is eligible, except those who have end stage renal disease, and were not in a
Medicare+Choice plan at the onset of this condition.
Public Law 105-33, the Balanced Budget Act of 1997, establishes a new authority
permitting contracts between CMS and a variety of different managed care and fee-for-
service entities. The types of entities that may be granted contracts under this new
authority include:
• Coordinated care plans, including Health Maintenance Organizations (HMOs),
Preferred Provider Organizations (PPOs), and Provider-Sponsored Organizations
You may be asked to show this card when you get health care services.
Only give your personal Medicare information to health care providers,
your insurers, or people you trust who work with Medicare on your behalf.
WARNING: Intentionally misusing this card may be considered fraud
and/or other violation of federal law and is punishable by law.
Es posible que le pidan que muestre esta tarjeta cuando reciba servicios de
cuidado médico. Solamente dé su información personal de Medicare a los
proveedores de salud, sus aseguradores o personas de su confianza que
trabajan con Medicare en su nombre.
¡ADVERTENCIA! El mal uso intencional de esta tarjeta puede ser
considerado como fraude y/u otra violación de la ley federal y es sancionada
por la ley.
1-800-MEDICARE (1-800-633-4227 /
TTY: 1-877-486-2048); Medicare.gov
(PSOs). A PSO is defined as a public or private entity established by health care
providers, which provide a substantial proportion of health care items and services
directly through affiliated providers who share, directly or indirectly, substantial
financial risk.
• Religious fraternal benefit society plans which may restrict enrollment to
members of the church, convention or group with which the society is affiliated.
Payments to such plans may be adjusted, as appropriate to take into account the
actuarial characteristics and experience of plan enrollees.
• Private fee-for-service plans which reimburse providers on a fee-for-service basis,
and are authorized to charge enrolled beneficiaries up to 115 percent of the plan's
payment schedule (which may be different from the Medicare fee schedule).
In addition to the Medicare+Choice contractors, beginning in January, 1999, up to
390,000 beneficiaries will have the choice (on a demonstration basis ending January 1,
2003) of enrolling in a Medical Savings Account (MSA) option. Under this option,
beneficiaries would obtain high deductible health policies that pay for at least all
Medicare-covered items and services after an enrollee meets the annual deductible of up
to $6,000. The difference between the premiums for such high deductible policies and
the applicable Medicare+Choice premium amount would be placed into an account for
the beneficiary to use in meeting his or her deductible expenses.
Past 1876 Contracts - HMO/CMP risk plans that remain in compliance with current
contracting standards and comply with new requirements established under this statutory
authority automatically transitioned into the Part C Medicare+Choice program. Section
1876 risk-based contractors were paid under a new Medicare+Choice payment
methodology rather than the prior method in section 1876(a), and were subject to certain
other Medicare+Choice provisions. The Secretary no longer accepts new 1876 risk
applications. As of January 1, 1999, existing 1876 risk-based contracts were terminated,
and plans in good standing transitioned to the Medicare+Choice program.
Repeal of Cost Option - As of August 5, 1997, the Secretary is prohibited from entering
into any new 1876 cost-based contracts, unless the plan is a Health Care Prepayment Plan
with an agreement under section 1833 of the Social Security Act. The 1876 cost-based
payment authority is repealed and all cost contracts are terminated as of December 31,
2002.
Limited HCPP Option - Beginning January 1, 1999, the Secretary may only contract
with those HCPPs that are sponsored by Union or Employer groups, or HCPPs that do
not "provide, or arrange for the provision of, any inpatient hospital services ...." This
amendment will result in the termination of section 1833 agreements with any
organization that does not meet the new definition. CMS will establish transition rules
for 1876 risk-based contractors that currently receive reimbursement on a cost basis for
enrollees remaining under a previous HCPP agreement.
For more information, see the Managed Care Manual.
Transmittals Issued for this Chapter
Rev #
Issue Date
Subject
Impl Date
CR#
R12046GI
05/18/2023
Update to the Internet Only Manual (IOM)
Publication (Pub.) 100-01, IOM Chapter 2
Hospital Insurance and Supplementary
Medical Insurance
06/21/2023
13189
R11764BP
12/22/2022
New Medicare Part B Immunosuppressant
Drug Benefit (PBID) - Implementation
01/03/2023
12804
R11646GI
10/19/2022
New Medicare Part B Immunosuppressant
Drug Benefit (PBID) – Implementation –
Rescinded and Replaced by Transmittal
11764
01/03/2023
12804
07/28/2022
New Medicare Part B Immunosuppressant
Drug Benefit (PBID) – Implementation
SENSITIVE/CONTOVERSIAL DO NOT
POST- Rescinded and Replaced by
Transmittal 11646
01/03/2023
12804
R124GI
05/17/2019
Update to Publication (Pub.) 100-01 to
Provide Language-Only Changes for the
New Medicare Card Project
06/18/2019
11240
R01MGI
09/11/2002
Initial Publication of Manual
NA
NA
Back to top of Chapter
