
2010
Illinois
Emergency Medical Services
for Children
Guidelines for the
Nurse in the
School Setting

Illinois Emergency Medical Services for Children
isacollaborativeprogrambetweenthe
Illinois Department of Public Health
and
Loyola University Medical Center
www.luhs.org/emsc

Table of Contents
Acknowledgements
1
Introduction
3
Pediatric Educational Recommendations for Professional
Health Care Providers
5
Assessment and Triage
9
Tables and Figures
Figure 1 Pediatric Assessment Triangle
12
Table 1 Initial (ABCDE) Assessment
14
Figure 2 Pulse Points
16
Table 2 AVPU Scale
17
Table 3 SAMPLE History
19
Table 4 PQRST History for Pain Assessment
20
Figure 3 Wong–Baker FACES Pain Rating Scale
20
Table 5 Focused (FHGI) Physical Examination
21
Table 6 Pediatric Vital Signs by Age
21
Table 7 Temperature Equivalents
22
Table 8 Triage Categories and Disposition
24
School Nurse Protocols
Systematic Assessment/Immediate Care
31
Triage
33
Abdominal Pain
35
Anaphylaxis/Allergic Reaction
37
Asthma Attack (Acute)/Reactive Airway Disease
39
Bites and Stings
41
Burns
43
Burn Assessment
44
Chest Pain
45
Chest Trauma
47
Child Maltreatment, Suspected
49
Indications of Child Maltreatment
50
Cold-related Injuries (Hypothermia/Frostbite)
51
Dental, Oral, and Maxillofacial Emergencies
53
Diabetic Emergencies
55
Disaster/Emergency Response: Mass-casualty Incidents
57
START/JumpSTART Algorithms for MCI Triage
58
Ear Emergencies
59
Eating Disorders
61
Eye Emergencies
63
Foreign Body Airway Obstruction
65
AHA Airway Clearing Maneuvers
66
Headache
67
Head/Spinal Cord Trauma
69
Heat-related Injuries
71
Hemophilia
73
Increased Intracranial Pressure in a Student With a VP Shunt
75
Lacerations/Abrasions
77
Musculoskeletal Injury
79
Interventions for Musculoskeletal Injuries
80
Near-drowning/Submersion
81
Nose Emergencies
83
Obstetric Emergencies
85
Emergency Neonatal Care
86
Respiratory Distress
87
Seizures
89
Sexual Abuse/Assault, Teen Dating Violence
91
Sickle Cell Anemia
93
Substance Abuse
95
Suicide Prevention
97
Syncope/Unconsciousness
99
Throat Emergencies
101
Toxic Exposure (Ingestion/Environmental)
103
Toxidromes
104
Trauma
105
Interventions for Musculoskeletal Trauma
106
Violent Behavior
107
Violent Behavior: Safety Tips
108
DevelopmentoftheseguidelineswassupportedinpartbyafederalgrantfromtheAssistantSecretaryfor
PreparednessandResponse(ASPR)andfundingthroughanEMSCPartnershipgrant,HealthResourcesand
ServicesAdministration,U.S.DepartmentofHealthandHumanServices.

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
1
Acknowledgements
Guidelines for the Nurse in the School Setting contains excerpts from the Illinois EMSC School
Nurse Emergency Care (SNEC) Course manual, 4
th
Edition (2010), which was developed under
the direction of the Illinois EMSC School Nurse Emergency Care Course Review Committee.
The Illinois Emergency Medical Services for Children Advisory Board gratefully acknowledges
the commitment and dedication of the committee members, who contributed countless hours of
collaboration as well as perspectives that reflect the diverse conditions and environments in
which school emergency nursing is delivered in Illinois. Their collective efforts have aided the
Illinois EMSC program tremendously in striving toward the goal of improving pediatric
emergency care within our state.
Special thanks are extended to the Illinois Association of School Nurses, the Illinois State Board
of Education, and the School Health Program within the Illinois Department of Human
Services, for their ongoing guidance and support.
Review Committee
Laveda Albright, RN, TNS, CEN
Emergency Services Nurse
Consultant
Lori Miller Cataldo, RN, BSN
School Nurse Arlington Heights
School District 25
Julie D’Agostino, RN, MS, APN-CS,
CEN, TNS Clinical Instructor,
School of Nursing William Rainey
Harper College
Mary Fisher, RN, BSN, MA,
NBCSN, TNS Health Services
Supervisor Rockford School
District
Mary Fecht Gramley, RN, PhD,
CEN, TNS Clinical Instructor
Waubonsee Community College
School of Nursing
Susan Fuchs, MD, FAAP, FACEP
Assistant Director, Pediatric
Emergency Medicine Children’s
Memorial Hospital
Margaret Gbur, RN, MSN, IL CSN
School Nurse Richards High
School
Sandy Hancock, RN, MS, TNS
EmergiKids St Alexius Medical
Center
Victoria Jackson, RN, MS, NCSN
Coordinator, School Health
Program Illinois Department of
Human Services
Evelyn Lyons, RN, MPH EMSC
Manager Illinois Department of
Public Health
Patricia McGleam, RN, BSN
EMSC Educator Loyola University
Medical Center
Miriam Miller, MPH EMSC
Preparedness Coordinator Loyola
University Medical Center
Jody Moncado, RN, MS, IL CSN
School Nurse Rockford School
District
Pat O’Connor, RN, BA, MEd,
IL CSN School Nurse
Community Unit School District
200
Phyllis Pelt, RN, MS, IL CSN
Health and Safety Chair, Illinois
PTA Adjunct Instructor and
Consultant University of Illinois–
Chicago, College of Nursing
Linda Reimel, RN, BSN, MS
Regional EMS Coordinator Illinois
Department of Public Health
Deborah Rice, RN, MSN, IL CSN
School Nurse Aptakisic-Tripp
Community Consolidated School
District 102
Debra Sansone, RN, MSN, IL CSN
School Nurse Hinsdale South
High School
Debra Tauber, RN, BSN, TNS, CEN
Director of Nursing SunRise at
Fountain Square–Lombard

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
2

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
3
Introduction
Illinois Emergency Medical Services for Children (EMSC) recognizes the unique field of school
nursing and the multiple roles that the nurse in the school environment is called upon to
perform. The intent of the Guidelines for the Nurse in the School Setting is to provide nurses
working in the school setting with a set of emergency care guidelines that can be utilized during
the delivery of care to the ill or injured student.
It is important to note that there exist variations in school settings, services and access to
resources and personnel. These differences can impact upon delivery of care. Illinois EMSC has
made every effort to ensure that the information presented in this document is accurate and
represents current accepted practice in the United States. However, the recommendations in
this document are not intended to indicate an exclusive course of treatment or to be applicable
in all circumstances or to serve as a substitute for the professional advice of a physician. It is
recommended that care must always be based upon the student’s clinical presentation and on
authorized policies. We also recommend that you use the information in this document as a
guide for developing local school policies and protocols. It is hoped that this document becomes
a valuable addition to the nursing practice resources already available to school nurses.
Because schools provide services to students throughout the childhood and adolescent years,
school nurses must be cognizant of pediatric developmental stages and able to provide age
appropriate services and information. A baseline understanding of pediatric developmental
characteristics and a general knowledge of appropriate approaches in the assessment and
management of the varied age groups will be beneficial. The assessment and treatment
approach when dealing with an injured or ill kindergartner is quite different from that of a high-
school student, particularly when considering student participation in the decision making
process, provision of educational information, and level of parental involvement. In addition,
children with special needs or chronic conditions may require more frequent emergency care
interventions due to their physical or mental disability and/or chronic illness.
The school nurse has a key role not only in providing emergency care to students, but also in
developing prevention strategies. Many emergencies are avoided in the schools each day
because school nurses have assisted in the education of teachers/school staff, parents/guardians
and students in prevention and early intervention techniques. Proactive development of
individualized health care plans and emergency care plans can also play a key role in prevention.
By working collaboratively with school administrators/staff, medical advisors, local EMS
agencies, local health care practitioners, and parents/guardians, the school nurse can be
instrumental in establishing a comprehensive program of emergency care aimed at reducing
student morbidity and mortality.
Keeping abreast of practice changes and trends within the field of school nursing is critical.
Resources that can assist in this effort are available through a variety of sources, particularly the
Illinois Association of School Nurses (www.iasn.org) and the National Association
of School Nurses (www.nasn.org).

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
4
Lastly, educational programs leading to certification in the specialty of school nursing can
enhance the practice of school nursing and the management of a comprehensive school health
program. Certification represents a national standard of preparation, knowledge, and practice.
The National Board for Certification of School Nurses (NBCSN) endorses the concept of
voluntary certification by examination for all school nurses. Professional certification in school
nursing provides an ongoing, quality credentialing process for eligible school nurses. The
NBCSN provides the opportunity for school nurses to set the standards for their specialty area
through voluntary professional certification.
In addition, Type 73 certification is available for school nurses in Illinois. There are currently
four approved programs in our state through which the school nurse internship for the Type 73
School Nurse Certification may be obtained. These are listed below, along with contact
information.
Milikin University, 1184 W. Main St., Decatur, IL 62522; 217-424-6374
National Louis University, 1000 Capitol Dr., Wheeling, IL 60090; 847-465-0575, x5373
Southern Illinois University at Edwardsville, School of Nursing, Edwardsville, IL 62026;
618-650-2000 or 1-800-234-4844
University of Illinois-Chicago, 1200 West Harrison, Chicago, IL 60607; 312-996-4350 or
312-413-0544
We hope that you find the Guidelines for the Nurse in the School Setting useful. Please feel free
to contact the Illinois EMSC program at (708) 327-EMSC for any questions you may have or
access our website at www.luhs.org/emsc for other pediatric emergency care resources.
Illinois EMSC has made every effort to ensure that the information presented in this document is accurate and represents
current accepted practice in the United States. However, the recommendations in this document are not intended to indicate an
exclusive course of treatment or to be applicable in all circumstances. We recommend that you use this document as a guide for
developing local school policies and protocols.

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
5
Pediatric Educational
Recommendations for Professional
Health Care Providers
Because many aspects of emergency care are different for children than for adults, health care
professionals with responsibility for children must have the specific knowledge, understanding
and skills necessary to provide appropriate care. In addition, many health care practitioners
have limited opportunities to apply their pediatric knowledge and skills. This emphasizes the
need for ongoing education in order to refresh one's knowledge and skill base as well as to
ensure clinical consistency with current practice guidelines. A statewide needs assessment
conducted by Illinois Emergency Medical Services for Children (EMSC) identified that many
prehospital and hospital health care practitioners feel the need for greater preparedness when
caring for the critically ill or injured pediatric patient. Integration of pediatric focused
educational curricula into healthcare provider primary and continuing education will assist in
addressing this need. The educational needs of healthcare practitioners should be addressed
through curricula that can focus on recognizing characteristic signs of serious illness or injury in
children of all ages, timely pediatric assessment, stabilization and treatment modalities that
favor improved outcomes. Pediatric focused education is emphasized for all practitioners whose
duties bring them into contact with the pediatric population including first responders, EMT’s at
basic, intermediate and paramedic levels, emergency physicians, emergency nurses, pediatric
nurses, pediatricians, family practitioners, clinic or office based personnel, school nurses and
mid-level practitioners among others. In addition, the development of instructors with a strong
pediatric knowledge base will provide the most effective means of ensuring the longevity of
pediatric emergency care education. The Illinois Emergency Medical Services for Children
(EMSC) Advisory Board supports the inclusion of the following pediatric focused educational
initiatives into healthcare practitioner primary and continuing education. Pediatric emergency
care course information can be viewed in the Education section of the Illinois EMSC web site at
www.luhs.org/emsc.
School Nurse Emergency Care Course (SNEC)
The Illinois EMSC program sponsors this 3 day course within our state. The targeted audience is
specifically school nurses. The course is designed to enhance the assessment and appropriate
triaging skills of the school nurse when confronted with the acutely ill or injured child. With the
increasing number of urgent health related conditions seen within the changing school
environment and the need to assure emergency and disaster preparedness, this course supports
the school nurse's core knowledge base in responding to these situations. The School Nurse
Emergency Care course recognizes school nurses as skilled professionals, while remaining
cognizant of the limited support and resources for emergency care interventions afforded by the
school health environment. The course is team taught by both school nurses and emergency
department nurses since both perspectives are essential in delivering the emergency training.
Course content contains lectures, case presentations and skill stations. Contact hours are

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
6
obtained through the American Nurses Credentialing Center’s Commission on Accreditation.
CPDU hours are available through the Illinois Association of School Nurses. Course renewal is
recommended every four years.
The SNEC curriculum emphasizes an appropriate assessment and triage approach and
addresses the following topics:
Your Role in Emergency Planning
Legal Issues in Nursing
Assessment and Triage
Trauma
Respiratory Emergencies
Shock
Neurologic Emergencies
Eye, Ear, Nose, Throat, and Dental
Emergencies
Environmental Emergencies
Abdominal and Genitourinary
Emergencies
Musculoskeletal Emergencies
Emergencies Involving Mental or
Behavioral Health
Medical Emergencies
Planning for Students With Special
Health Care Needs
School Emergency Response and Crisis
Management
Advanced Pediatric Life Support (APLS)
This two day course focuses on the initial management of illnesses and injuries that, if left
untreated, could lead to life threatening pediatric conditions requiring resuscitation. The course
content is primarily oriented toward emergency diagnosis and response. The course format
combines lectures with small group sessions that allow for case presentations and hands-on
experience. Sponsored by the American College of Emergency Physicians (ACEP) and American
Academy of Pediatrics (AAP), this course is recommended for all physicians and other
healthcare professionals who are responsible for the management of acutely ill or injured
children. For more information, go to www.acep.org.
Emergency Nursing Pediatric Course (ENPC)
This 16 hour comprehensive pediatric course is sponsored by the Emergency Nurses Association
(ENA) and is tailored specifically to meet the educational needs of the nurse in an emergency
setting. The focus of this course is to teach nurses the various aspects of pediatric emergency
nursing care. Lectures and skill stations emphasize the appropriate triage, assessment and
management of the ill or injured pediatric patient. The course is designed to provide core-level
pediatric knowledge and psychomotor skills associated with the delivery of professional nursing
care to the pediatric patient. For more information, go to www.ena.org.
ITLS Pediatric – International Trauma Life Support Pediatric Provider Course
This course builds upon a core knowledge base of trauma care. The course emphasizes the
practical training needed to assure that the prehospital provider is confident and competent
when faced with caring for the critically injured child. The course focuses specifically on
prehospital care of the pediatric trauma patient. The Illinois College of Emergency Physicians
(ICEP) sponsors the ITLS Pediatric Provider course which is approved by International Trauma
Support. For more information, go to www.itrauma.org/education.

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
7
NRP – Neonatal Resuscitation Program
This joint American Heart Association (AHA) and American Academy of Pediatrics (AAP)
sponsored course was designed to teach an evidence-based approach to resuscitation of the
newborn. The causes, prevention, and management of mild to severe neonatal asphyxia are
carefully explained so that health professionals may develop optimal knowledge and skill in
resuscitation. For more information, go to www.aap.org.
Pediatric Advanced Life Support (PALS)
This American Heart Association (AHA) and American Academy of Pediatrics (AAP) sponsored
course focuses primarily on pediatric resuscitation. It provides the information needed for
recognizing the child at risk for cardiopulmonary arrest, strategies for preventing
cardiopulmonary arrest in the pediatric population and reinforcement of the cognitive and
psychomotor skills necessary for resuscitating and stabilizing the infant and child in respiratory
failure, shock or cardiopulmonary arrest. This two day course is geared toward all advanced
healthcare professionals who provide care to children. For more information, go to
www.americanheart.org.
Pediatric Education for Prehospital Professionals (PEPP)
The American Academy of Pediatrics (AAP) sponsors this course which aims to prepare
prehospital professionals in the management of the pediatric patient. This highly interactive
course combines lectures, videos, hands-on skill stations and small group scenarios. The course
has a one day BLS format or a two day ALS format. For more information, go to
www.peppsite.com.
PEARS – Pediatric Emergency Assessment, Recognition and Stabilization Course
This American Heart Association (AHA) sponsored one-day course is designed for healthcare
professionals who infrequently see critically ill children. It supports those who are not
credentialed in advanced pediatric skills and who do not routinely provide pediatric advanced
life support. PEARS prepares students to assess, categorize, decide, and act early to stabilize the
child. The main focus of PEARS is prevention, and specifically the assessment, recognition and
stabilization of pediatric victims at risk of severe cardiopulmonary distress. PEARS is a video-
based course with instructor-led discussion. For more information, go to www.heart.org.
JumpSTART - Pediatric Multicasualty Incident Triage
Illinois JumpSTART Workshop
JumpSTART is a pediatric triage algorithm/process that was developed to help meet the needs
of children and responders at disaster/mass casualty incidents. It was developed by Lou Romig,
MD, FAAP, FACEP, Miami Children’s Hospital, Miami, FL. In conjunction with Children’s
Memorial Hospital (Chicago), the Illinois EMSC program sponsors a training workshop that
reviews the unique needs of children in a disaster, mass casualty triage principles, the START
(Simple Triage and Rapid Treatment) system for adults and the JumpSTART MCI Triage
System for Children. The workshop also includes interactive scenarios/exercises. This
education targets first responders, prehospital personnel, nurses, physicians and other
healthcare professionals. For more information on JumpSTART, go to
www.jumpstarttriage.com.

G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
8

G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
9
3 | Assessment and Triage
This section reviews key steps in the assessment and triage process, as well as
various tools that may be useful in your practice.
Assessment as a Lifesaving Tool
To the students in your school, your importance as a health care provider cannot
be overstated. Each day, you may treat 5% to 10% of the total student population
for problems ranging from mild stomach aches or minor lacerations to life-
threatening asthma or traumatic brain injury. Over the course of a typical career
as a school nurse, you will alleviate pain and prevent suffering on a daily basis;
and in all likelihood, you will save lives.
When a student experiences emergent illness or injury, your actions can, in some
cases, make the difference between permanent disability and full recovery. With
so much in the balance, it is essential to assess the student’s condition swiftly and
accurately, without overlooking important physical and historical findings. These
findings provide the basis for selecting and prioritizing interventions, evaluating
the student’s response, and determining disposition.
A systematic, consistent approach is key to this process.
Five Components of a Systematic Assessment
A systematic assessment can be broken down into 5 major components, each of
which has a specific role in emergency nursing care:
Scene safety assessment
Ensure that it’s safe to approach, or call for backup assistance as necessary.
Across-the-room assessment
Immediately activate EMS if the situation is obviously emergent.
Initial assessment (ABCDE)
Identify and treat problems that threaten life, limb, or vision.
History
Gather background information essential to your triage decision.
Focused physical examination (FGHI)
Measure and record vital signs; inspect, auscultate, and palpate to identify or
investigate additional problems.
These components can be adapted to virtually any situation you may face in the
course of a day, giving you a safe, consistent basis for clinical decision-making
and nursing interventions. The culmination of the systematic assessment is an
accurate triage determination, appropriate interventions, and final disposition.
NOTE
During an actual emergency, you’ll go through these 5 components
almost simultaneously, in far less time than it takes to describe them.

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
10
Additional actions
Once the emergency is over, it’s also important to attend to
Documentation, including data collection
Evaluation and follow-up
Planning and prevention
This chapter provides an overview of the steps needed to complete each of these
components, from assessment to triage to postincident activities. Additional
details and examples of how you’ll use these tools in specific situations are the
focus of the chapters that follow. Your own experience and common sense are
what bring the steps together into a congruent whole.
Three key points
Three of the techniques that foster a successful approach to assessment are
briefly noted below. You may find it helpful to keep them in mind as you visualize
applying these steps in your own practice.
Use developmentally appropriate language
KEY POINT
Remember to use developmentally appropriate language when addressing students,
especially younger children.
It’s important to talk to the student throughout the assessment process,
explaining your actions and providing reassurance. Be sure to use
developmentally appropriate language and techniques as you interact and
communicate. You must also try to attune yourself to the various ways a child
could interpret your meaning. For example, the phrase take your blood pressure
could be interpreted to mean that you are literally about to take away something
having to do with blood. To prevent misunderstandings, say instead, I’m going to
measure your blood pressure, or for younger students, I’m going to give your
arm a hug.
NOTE
Language, culture, technology, and environment may affect the
assessment process. Enlist special resources as needed to help you
communicate effectively with the student.
Gather history information throughout the process
KEY POINT
If possible, gather focused history information as you perform each step of the
assessment.
As you talk to the student and explain what you’re doing, it’s natural to ask
questions about the injury or illness you’re assessing. Use this technique to gather
as much of the focused history information as possible while you perform the
initial assessment and provide interventions, as this will help you to evaluate
your findings more accurately. If the student is unable to respond to your
questions, query others who were present when the incident arose.
| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
11
Treat significant problems as you go
KEY POINT
It is essential to take any necessary actions before moving on to the next step of the
assessment.
As you progress through the assessment components, it is essential to take any
necessary actions before moving on to the next step. Immediately treating such
life-threatening problems as airway obstruction or inadequate ventilation will
help to ensure optimal outcome.
Similarly, although triage is presented as the end result of a complete assessment,
in practice you will activate EMS at the earliest sign of an emergent situation.
Scene Safety Assessment
Hazards
Before rendering aid, you must ensure your own safety as well as that of the
student and others present. Even within the health office, maintain a constant
awareness of circumstances that could affect your own safety or that of others
present. To determine whether you can safely approach the student, look for the
following hazards:
Substances
Blood or other body fluids, noxious fumes, toxic chemicals.
Situational dangers
An armed perpetrator, hostages, weapons.
Environmental dangers
An unstable structure, fire, electrical hazards, or other potential mechanisms of
injury.
KEY POINT
Never place yourself in danger. If you cannot control a hazard, do not approach the
student.
Never place yourself in danger. If you cannot control hazards, do not approach
the student—call 911 or your local emergency number to activate backup
assistance.
Resources
If the situation does not appear hazardous, you may find it useful to consider
briefly whether you have the equipment and resources you need to manage the
incident at this time. For example, you might send for
Additional personnel to help you with interventions or to manage bystanders
Personal protective gear or specialized equipment (such as an automated external
defibrillator, backboard, cold packs, or splints) that isn’t in your portable
emergency kit

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
12
Breathing
Visible movement
Work of breathing
(normal/increased)
Circulation
Color
Pediatric Assessment Triangle
General Assessment
Appearance
Mental status
Muscle tone
Body position
NOTE
Always be prepared for unexpected emergencies. Carry disposable
gloves and a resuscitation mask at all times, and make sure these
items are available in key locations for anyone who might need them.
Across-the-room Assessment
KEY POINT
The across-the-room assessment is a quick overall appraisal of the student’s
condition based on appearance, breathing, and circulation.
FIGURE 1. PEDIATRIC ASSESSMENT TRIANGLE
The across-the-room
assessment is a natural
continuation of the scene
safety assessment as you
focus your attention on the
student. Briefly evaluate
the student’s appearance,
breathing, and circulation
as illustrated in the
Pediatric Assessment
Triangle (Figure 1). This
allows you to decide in a
few moments how quickly
you must proceed with
further assessments and
interventions.
Reprinted with permission from the
Teaching Resource
for Instructors in Prehospital Pediatrics
–BLS, ed 2 (2006).
During the initial assessment that follows, you will revisit these areas to perform
a hands-on evaluation with interventions. At this point, you simply want to form
an overall impression of vital functions.
Appearance
Appearance refers to mental status, muscle tone, and body position.
Mental status, in turn, is based on both level of consciousness and the
student’s interactions with others. Ask yourself the following questions:
Does the student appear to be awake and aware of surroundings? Is the student
aware of the injury or illness?
If awake, what is the student’s emotional response to the current situation?
(calm, confused, anxious, agitated, angry, depressed)
Does the student seem appropriately responsive to others present (looking
around, responding to questions) or dull and apathetic?
Is there evidence of normal muscle tone (sitting or standing upright, able to
walk), or does the student appear limp?
How is the student positioned? (sitting normally, maintaining a tripod position,
lying supine)

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
13
Breathing
Breathing refers to the presence or absence of visible movement at the chest or
abdomen and work of breathing:
Can you confirm at a glance that the student is breathing?
Is there evidence that the student is working hard to maintain adequate
ventilation? (flaring nostrils, retractions, difficulty speaking)
Circulation
Circulation refers to visible skin color, an indication of perfusion to vital
organs.
Does the student’s color appear normal?
If not, does it appear pallid, dusky, mottled, cyanotic, or flushed?
Conclusions
Combine the evidence of your observations with your intuition and experience to
form a first impression of the student’s level of distress: Compared with baseline,
does this student look well, ill, or seriously ill? Take into account any clearly
visible signs and symptoms of illness or injury, such as emesis, bleeding,
deformities, or expressions of pain.
Next steps
If the student’s condition is clearly emergent—for example, the student is
struggling to breathe, turning dusky or cyanotic, exhibiting seizure activity,
bleeding profusely—activate EMS immediately, then approach the student and
proceed with the initial assessment and interventions.
Initial Assessment
The initial (ABCDE) assessment focuses on Airway, Breathing, Circulation,
Disability (neurologic status), and a brief physical Exposure to examine parts of
the body directly related to the chief complaint. Table 1 provides an overview of
the process.

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
14
T
ABLE 1. INITIAL (ABCDE) ASSESSMENT
Assessment Interventions
A Airway
Position, sounds, obstruction
Stabilize cervical spine if trauma is possible or
mechanism of injury is unknown. Open airway if
necessary, using jaw thrust or chin lift as
appropriate. Position student to maintain airway
patency. Look and listen for signs of obstruction.
Perform airway-clearing maneuvers as indicated.
B Breathing
Rate, depth/pattern, symmetry, sounds,
work of breathing, odors, injuries
Position student for maximum ventilatory ability.
Give oxygen as tolerated if available. Provide
mouth-to-mask ventilation if needed.
C Circulation
Heart rate and quality of pulses, capillary
refill time, skin color, temperature, and
moisture, bleeding
Initiate CPR if needed; control bleeding with
pressure dressings and elevation of the affected
limb.
D Disability (neurologic status)
Level of consciousness via AVPU;
pupillary response
Provide reassurance; position to maintain
comfort; give oxygen if available.
E Exposure with Environmental control
to prevent heat loss
Observe and inspect for additional
emergent problems
Treat wounds or other findings as appropriate.
Treat as necessary to maintain normothermia.
As you interpret your assessment findings, keep in mind that many factors
besides illness or injury can contribute to deviations from the norm. It is
important to be aware of these factors so that you can take them into account. For
example:
Certain medications can cause the breathing rate and heart rate to be fast or slow
A cold ambient temperature can delay capillary refill and affect other skin
findings
Fear, fever, and pain typically increase the respiratory rate and heart rate
Students with certain chronic conditions may have baseline vital signs that fall
outside the normal range for age
Also note that, since children’s vital signs vary by age, subtle abnormalities are
easily overlooked. During the initial assessment, however, you are looking
primarily for overt discrepancies compatible with severe conditions. If none are
present, you’ll have time to assess for less obvious signs during the focused
physical examination.
KEY POINT
The goal of the initial assessment is to identify and treat life-threatening
emergencies. Activate EMS as soon as the need becomes evident.
The goal of the initial assessment is to identify and treat life- or limb-threatening
emergencies. As you progress through the assessment, provide interventions as
necessary to maintain the airway, breathing, and circulation before continuing
on to the next step. If at any time the student cannot maintain airway patency,

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
15
adequate ventilation, or adequate perfusion, immediately activate EMS. Notify
the parent/guardian as soon as you are able to do so.
NOTE
When performing a physical assessment, always observe
standard precautions to prevent exposure to body fluids.
Spinal stabilization
If there is any possibility of injury to the head or spine, provide manual
stabilization of the cervical spine before you begin the airway assessment. Note
that you will need to maintain spinal stabilization until EMS personnel arrive.
Airway
Look, listen, and feel for signs of patency:
Can you see movement of the chest or abdomen?
Can you hear airway sounds, such as stridor, wheezing, or coughing?
Can you feel air exchange at the mouth or nose?
Open the student’s mouth and inspect for sources of airway obstruction.
Interpreting your findings
Drooling or inability to talk may indicate upper airway edema from infection or
anaphylaxis
Stridor (a crowing sound) indicates upper airway obstruction
Facial injuries can compromise the airway
Breathing
Note the respiratory rate (normal, fast or slow, apnea), the depth and pattern of
breathing (shallow, gasping, irregular), and bilateral symmetry of chest
movement
Listen for adventitious breath sounds, such as wheezing or grunting
Watch for signs indicating increased work of breathing (retractions, nasal flaring,
difficulty speaking)
Note any unusual breath odors (fruity; reminiscent of petroleum products,
tobacco, or alcohol)
Evaluate chest wall integrity, noting any obvious injuries
Interpreting your findings
Increased work of breathing and audible breath sounds indicate respiratory
compromise
Fast breathing is an early compensatory mechanism for hypoxia; breathing slows
as hypoxia worsens
Decreased, absent, or unequal breath sounds may indicate airway obstruction, a
pneumothorax, hemothorax, or atelectasis

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
16
Grunting is a late sign of severe respiratory distress that is worsening into
respiratory failure
Circulation
During the Circulation assessment, you will
Assess heart rate and quality of pulses
Evaluate perfusion by assessing
à Capillary refill time (normally less than 2 seconds)
à Skin color (normal, pallid, dusky, mottled, cyanotic, flushed)
à Skin temperature and moisture (warm, dry, cool, clammy)
Look for active bleeding (none, minor, moderate, profuse; controlled or
uncontrolled)
Heart rate and quality of pulses
Measure the heart rate by palpating the pulses. Evaluate the quality of the pulses
and note discrepancies between the central and peripheral pulses at the same
time. Pulse points are shown in Figure 2.
FIGURE 2. PULSE POINTS
Although you won’t actually measure the
student’s blood pressure until after the
history and pain assessment, the pulses
can be roughly correlated with blood
pressure as follows:
If you can palpate the carotid pulse, the
systolic blood pressure is at least
60 mm Hg.
If you can palpate the femoral pulse, the
pressure is at least 70 mm Hg.
If you can palpate the radial pulse, the
pressure is at least 80 mm Hg.
Perfusion
Capillary refill time
Assess capillary refill at the distal
extremities with the limb positioned
so that it is level with the heart. Firmly
press and release the skin to blanch
the underlying capillary bed. Color
should return in less than 2 seconds.
Color
Inspect skin color at the lips and tongue. Note whether skin color seems normal,
pale or flushed, mottled or cyanotic.

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
17
NOTE
To assess skin color in students with dark skin pigmentation, check
the nail beds, palms, or mucous membranes
Temperature
Feel skin temperature at the extremities and compare with temperature at the
more central body regions. It may be significant if skin is either unusually hot or
cold.
Moisture and quality
Note dryness or clamminess. Pinch gently to check for normal elasticity.
Bleeding
Look for profuse external bleeding.
Interpreting your findings
Tachycardia is usually the earliest sign of developing shock in children;
tachycardia combined with a fast respiratory rate is a strong indicator of
compensated shock (see Chapter 6: Shock)
Thready or weak pulses, cool, clammy extremities, and delayed capillary refill
time are also associated with shock
A discrepancy between the central and peripheral pulses may be an early sign of
decreasing stroke volume
Hypotension with bradycardia is a late, ominous sign of decompensated shock
Skin that is inelastic and prone to tenting usually signifies dehydration
Disability
The Disability assessment is a brief evaluation of neurologic function. Assess level
of consciousness using the AVPU Scale (Table 2), then evaluate pupil size and
reactivity.
TABLE 2. AVPU SCALE
Mnemonic Associated Findings
A
Aler
t
The student is awake and able to speak or
interact spontaneously
V
Verbal
(responds to verbal stimulus)
A verbal stimulus elicits some response; for
example, the student’s eyes may open when
you call loudly, or agitation may lessen in
response to a command
P
Painful
(responds to painful stimulus)
The student responds to a painful stimulus by
moaning, crying, or withdrawing from pain
U
Unresponsive
The student shows no response to verbal or
painful stimuli

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
18
Interpreting your findings
Level of consciousness is an important indicator of adequate perfusion. A
significant reduction in responsiveness is an ominous sign in a student who has a
mechanism that may cause respiratory compromise or shock.
Exposure
Remove clothing as needed to briefly assess specific factors related to the
presenting problem, such as injuries, rashes, bites, or stings. Watch for signs of
internal hemorrhage. Control ambient temperature if possible or drape the
student with coverings as necessary to prevent heat loss. Replace clothing as soon
as you are able to do so.
History
Information gathered from the health history helps you form a plan of care. You
may already be familiar with the student’s history from information supplied by
the parent/guardian, primary health care provider, and school staff or from
previous interactions with the student. Make sure your understanding of current
health issues is up-to-date, and get specific details relevant to the incident at
hand.
NOTE
In younger students, obtain the history from the parent/guardian, if
available, or from the student’s health record as time permits.
Some of the useful mnemonics for the health history include SAMPLE (Table 3),
PQRST (Table 4), a pain assessment tool, and CIAMPEDS (pronounced see I am
peds), which is outlined below.
Chief complaint
Immunizations, Isolation
Allergies
Medications
Past health history
Events preceding the problem
Diet/elimination
Symptoms associated with the problem

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
19
TABLE 3. SAMPLE HISTORY
Topic Questions
S
Symptoms
Ask the student to describe
current symptoms, particularly
pain.
What problem brings the student to the health office?
How long has the problem persisted?
If an injury, how and when did it occur?
Is the student having pain, apprehension, or guarding?
What is the location, quality, and duration of the pain?
Does positioning make the pain better or worse?
What strategies make other symptoms better or worse?
What is the student’s impression of his or her condition?
A
Allergies
Does the student have any known allergies to food,
medications, latex or other materials, or environmental
elements, such as bee stings?
M
Medications
List medications the student
takes regularly, including
dosage regimen and time of the
last dose.
Is the student using any prescription, over-the-counter,
home, herbal, or cultural remedies? For what reasons?
When was the last dose taken?
Did the student take any medications before coming to
the health office? What was the result?
Has the student used any illicit drugs?
P
Past health histor
y
Note preexisting physical or
psychological disabilities,
previous trauma, and chronic
conditions. Check immunization
status, including tetanus
prophylaxis.
Does the student have a chronic illness? (asthma,
diabetes, hemophilia, seizure disorder)
Does the student have special health care needs?
a
Does the student rely on a medical device? (oxygen,
tracheostomy, nebulizer, central venous line,
gastrostomy tube)
Are immunizations up to date?
Is isolation necessary? (pediculosis, varicella exposure,
immunosuppression)
L
Last meal
Document when and what the
student last ate or drank.
Is the student able to eat?
When was the last meal?
Has there been any nausea, vomiting, diarrhea?
Are bowel and bladder function normal?
E
Events
Ask the student to describe
events that led up to the illness
or injury.
When did the problem begin?
Were there precipitating factors?
If an injury occurred, were there witnesses? What did
they report?
a
You may need to modify your evaluation of assessment findings for students with special needs,
as their baseline findings may vary from accepted averages.
Pain Assessment
Pain has been referred to as the fifth vital sign because of its significance in
assessing pathophysiology. The PQRST assessment tool (Table 4) outlines a
detailed, systematic interview that covers many clinically significant aspects of
pain.

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
20
T
ABLE 4. PQRST HISTORY FOR PAIN ASSESSMENT
Assessment Points
P
Problem: How does the student describe the chief complaint?
Provoke: What makes the pain worse?
Palliate: What makes the pain better?
Q
Quality: What is the quality or character of the pain?
R
Radiate: Does the pain or discomfort seem to travel or move?
S
Severity: Using a developmentally appropriate assessment tool (eg,
numeric or FACES
a
scale), how does the student rate the severity of pain
or discomfort?
Signs: What clinical signs accompany the problem?
Symptoms: What subjective problems does the student report?
T
Timing: When did the pain start? Was the onset sudden or gradual?
a
FACES indicates Wong-Baker FACES Pain Rating Scale
Severity may be the most challenging aspect of pain to assess, since it is largely a
subjective determination. Various assessment tools can help students quantify
the severity of their pain; it’s important to select one that is suitable to the
student’s age, cognitive development, and cultural background. For example,
school-aged children with average developmental abilities can often rate their
pain using a simple numeric scale (On a scale of 0 to 10, if 0 is no pain at all and
10 is the worst pain you’ve ever felt, tell me how bad the pain is right now).
For younger students (aged about 3 years and older), those who are less
comfortable with numbers, and those who lack the cognitive skills to think about
pain in relative terms, the Wong-Baker FACES Scale may be useful (Figure 3).
The scale allows a student to point to a cartoon face with an expression that
reflects the student’s pain experience.
FIGURE 3. WONG-BAKER FACES PAIN RATING SCALE
From Hockenberry MJ, Wilson D:
Wong’s Essentials of Pediatric Nursing
. Ed 8. St. Louis, MO:
Mosby; 2009. Used with permission. Copyright Mosby.
Pain may be assessed in infants and those with developmental impairment or
other impediments to verbal communication by observing behavioral cues, such
as facial grimace, and physiologic parameters, such as heart rate.
Interventions
Comfort measures for pain may include applying a cold pack, stabilizing
suspected fractures, or dressing wounds.

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
21
Focused Physical Examination
The focused physical examination may be limited or complete (head-to-toe)
depending on the circumstances, the student’s health status, and applicable
protocols. At minimum, you will measure and document a full set of vital signs.
Table 5 provides a mnemonic to help you remember steps you may perform.
TABLE 5. FOCUSED (FGHI) PHYSICAL EXAMINATION
Assessment Comments
F Full set of vital signs
Measure and document baseline vital signs, including
blood pressure, heart rate, respiratory rate, and
temperature. If possible, note weight and blood glucose
level as well.
G Give comfort measures
Perform interventions to alleviate pain, such as applying a
cold pack, immobilizing a suspected fracture, or dressing
a wound.
H Head-to-toe assessment
Inspect, palpate, auscultate—
limited or complete
Perform specialized assessment procedures as indicated,
such as cranial nerve assessments, abdominal palpation,
or range of motion assessments.
I Isolate; Injuries; additional
Interventions
Assess the potential for communicable disease and
isolate as indicated. If you find injuries in varying stages of
healing, consider the possibility of child maltreatment.
Provide additional interventions according to your findings.
Baseline vital signs
During the initial assessment, your goal was simply to identify clearly abnormal
vital signs suggestive of an emergent condition. At this point, establishing
baseline vital signs is essential to both the triage determination (discussed in the
following section) and ongoing reassessment. It is also an important element in
continuity of care if the student is referred for further medical evaluation.
Normal vital signs vary with the student’s age (Table 6). As noted earlier, other
factors that can affect normal vital signs include certain chronic medical
conditions or physical disabilities, medications, environmental conditions, and
the student’s emotional state.
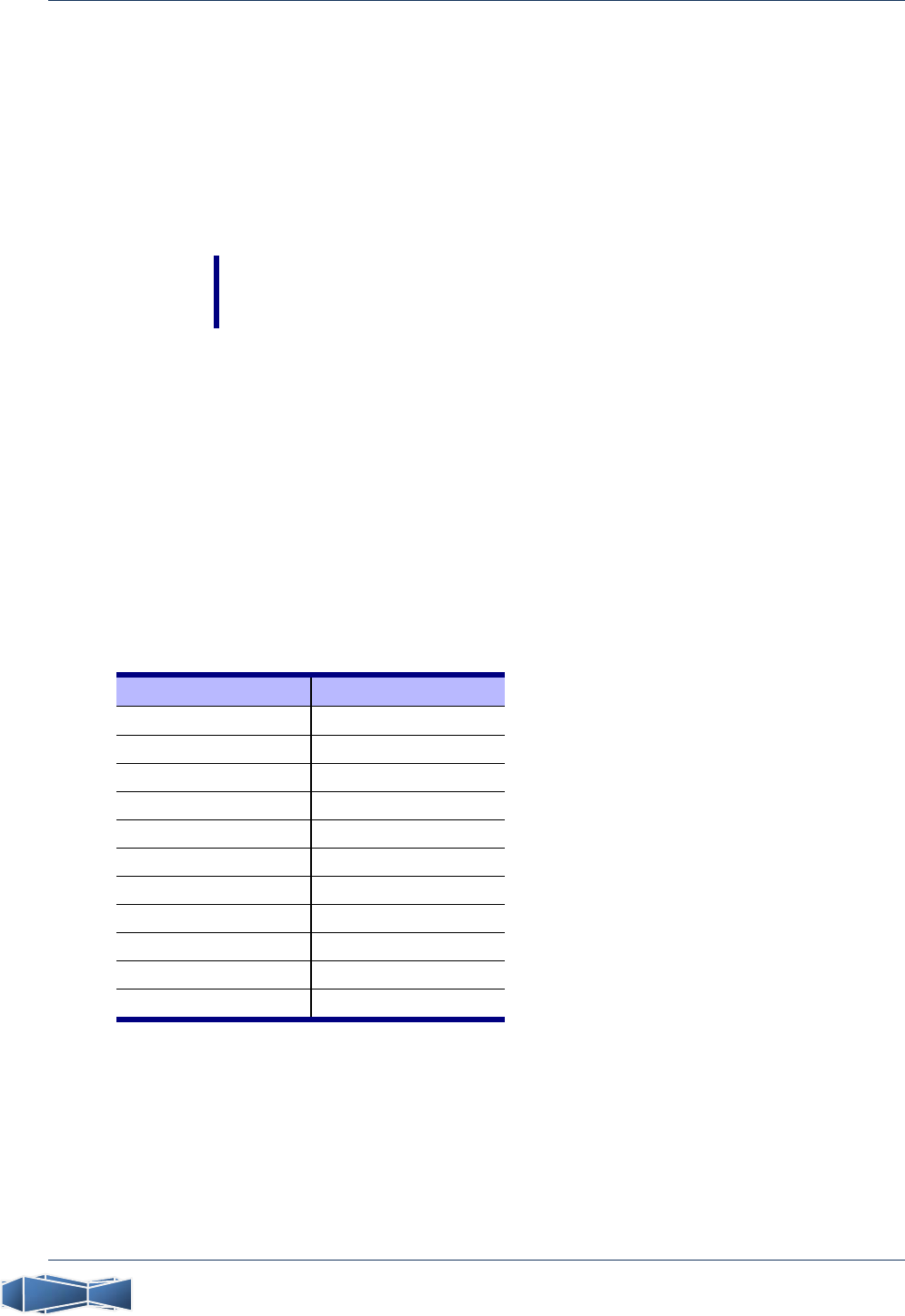
TABLE 6. PEDIATRIC VITAL SIGNS BY AGE
Age RR HR BP
Neonate (birth-30 days) 30-60 100-180 50-90
Infant (1-12 months) 24-50 100-160 60-100
Toddler (1-3 years) 24-40 90-150 80-105
Preschooler (3-5 years) 20-30 80-140 95-105
School-aged (5-12 years) 18-30 65-120 95-120
Adolescent (12 years and older) 12-20 60-100 100-128
BP indicates systolic blood pressure (mm Hg); HR, heart rate; RR, respiratory rate
A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
22
Measuring blood pressure
To measure blood pressure accurately, use a cuff that is two-thirds as wide as the
student’s upper arm from the elbow to the axilla. If you do not have a table of
normal blood pressure rates, you can use the following formula to approximate
the lowest acceptable limit for systolic blood pressure:
BP=70+(2×age in years)
This formula is appropriate for children older than 2 years.
NOTE
Do not rely solely on blood pressure to indicate the severity of the
student’s condition. Children can maintain normal blood pressure until
decompensated shock is imminent.
Temperature and other measurements
Note the student’s temperature; if possible, include weight and blood glucose
levels as well.
Temperature conversion
Use the following formulas to perform temperature conversions between
Fahrenheit and centigrade:
To convert centigrade to Fahrenheit: (1.8¯°C)¨32=°F
To convert Fahrenheit to centigrade: (°F–32)¯0.556=°C
Alternatively, use the information in Table 7.
TABLE 7. TEMPERATURE EQUIVALENTS
°C °F °C °F
34.2 93.6 38.6 101.5
34.6 94.3 39.0 102.2
35.0 95.0 39.4 102.9
35.4 95.7 39.8 103.6
35.8 96.4 40.2 104.4
36.2 97.2 40.6 105.1
36.6 97.9 41.0 105.8
37.0 98.6 41.4 106.5
37.4 99.3 41.8 107.2
37.8 100.0 42.2 108.0
38.2 100.8 42.6 108.7
C indicates centigrade; F, Fahrenheit
Orthostatic vital signs
Orthostatic vital signs can help you assess for dehydration or volume depletion.
Record the student’s blood pressure and heart rate while the student is supine
and again 1 minute after the student sits up or stands. If the blood pressure falls

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
23
by more than 20 mm Hg, or if the heart rate increases by 20 bpm, orthostasis is
present.
Additional assessments
Inspect, palpate, and auscultate for additional problems as time permits. Look for
bleeding, abrasions, wounds, hematomas, or ecchymoses, as well as rashes,
petechiae, edema, or pupura.
Reassess the student’s activity level (talking or silent; walking or immobile;
sitting or supine) and emotional state; compare with your observations from
earlier assessments to detect possible trends. Assess orientation to time, place,
and person as indicated.
Triage
Principles of Triage
School nursing practice is unpredictable. There may be times when you
have several students as well as staff or visitors waiting in the health office, some
reporting for scheduled interventions, others presenting with unexpected
problems. You must also respond to episodes of acute illness or injury arising
elsewhere around the facility. Consequently, you must be able to determine
quickly who needs immediate interventions and who can wait. You will not
always treat your students in order of arrival—rather, you must treat them
according to the seriousness of the presenting illness or injury, placing those
whose condition is most critical ahead of others. Triage—derived from the
French word meaning to sort—provides an objective way to do this.
Through your initial assessment findings, you can “sort” 1 or more students into
emergent, urgent, or nonurgent categories according to whether a condition
exists that has the potential to threaten life, limb, or vision. Treatment priorities
and disposition are associated with each triage category.
If the student’s condition changes during ongoing monitoring and reassessment,
the triage category may be changed as appropriate.
Remember that it’s better to overtriage than to undertriage, particularly if your
intuition tells you that there is a significant underlying problem. Experience can
also help you decide to upgrade your triage determination. For example, if a
student who has a history of severe asthma presents with mild dyspnea, you
might immediately consider this student’s condition emergent and activate EMS
transport, knowing that in the past, the student has developed respiratory
distress very quickly.
KEY POINT
Do not delegate tasks related to the initial assessment and triage. Only an
experienced registered nurse has the expertise to categorize ill and injured students.
While you may delegate tasks associated with ongoing health care, do not
delegate tasks related to the initial assessment and triage. Only an experienced

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
24
registered nurse has the requisite knowledge and expertise to quickly recognize
and categorize ill and injured students.
Performing Triage
Table 8 describes the 3 commonly recognized triage categories (emergent,
urgent, nonurgent) with examples of problems that fall within each category.
TABLE 8. TRIAGE CATEGORIES AND DISPOSITION
Category Examples Disposition
Emergent
Student
requires
immediate
medical
attention.
Condition is
acute and has
the potential to
threaten life,
limb, or vision.
Cardiopulmonary arrest
Altered LOC
Burns, severe/major
Caustic chemical exposure
Childbirth, imminent
Head injury, history of loss of consciousness
Pain, severe or significant location (eg, chest)
Poisoning/drug overdose
Respiratory distress, severe, or respiratory failure
Shock, any type
Spinal cord injury, suspected
Status epilepticus or first-time seizure
Threatens harm to self or others
Trauma, severe or trauma to limb, no distal pulse
Monitor
a
in health
office
Transport to
emergency care
facility via ground
or air EMS
Urgent
Student
requires
additional
medical
intervention
within 2 hours.
Condition is
acute but not
severe or life-
threatening.
Burns, minor
Deformity/suspected closed fracture without
circulatory compromise
Febrile illness (T exceeds 100°F/37.8°C)
GI symptoms (nausea, vomiting, diarrhea)
Lacerations requiring sutures without excessive
blood loss
Pain, moderate, after abdominal trauma
Seizure, atypical, in student with history of seizures
Wheezing
Monitor in health
office
Transport to
emergency care
facility via EMS,
parent/guardian, or
other adult as
appropriate
Nonurgent
Student may
require referral
for routine
medical care.
Minor or
nonacute
condition.
Essentially well; S/S of mild noncommunicable
illness or URI
Headache without fever/abnormal findings
Injury, minor (abrasions/ecchymoses, muscle
sprains/strains)
Pain, mild (eg, abdominal or menstrual pain,
headache or toothache)
Monitor in health
office
Contact
parent/guardian
Return student to
class or send
home as indicated
a
Monitoring should be performed by school nurse. EMS indicates emergency medical services; F,
Fahrenheit; GI, gastrointestinal; LOC, level of consciousness; S/S, signs/symptoms; T,
temperature; URI, upper respiratory infection
Ongoing Monitoring and Reassessment
Ongoing monitoring and reassessment are an essential part of nursing care. Your
initial triage decision allows you to formulate a nursing diagnosis and develop the
plan of care; you may need to adjust the triage category as well as disposition,

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
25
however, after you have evaluated the student’s response to interventions and
determined whether health status has improved or worsened. A student whose
condition initially appeared nonurgent may abruptly deteriorate, requiring
immediate attention. This means that you must conduct frequent reevaluations
and arrange for ongoing monitoring and observation while you are busy
elsewhere.
Follow applicable protocols regarding appropriate monitoring.
Completing the Process
Documentation and Data Collection
Document your assessment findings and triage category in the student’s health
record. List interventions and the student’s response. Record the final disposition
as well. Be sure relevant information, such as permission to treat the student,
allergies, medications, immunizations, and contact information, is passed on to
prehospital care providers so that they can include it in their report to emergency
department personnel.
Collect and analyze data to identify injury and illness patterns so that you can
monitor and prevent recurrences.
Follow-Up
If possible, follow up any student health care incident with the student’s primary
health care provider, the emergency department physician, the prehospital care
professionals, or the parent/guardian. Document the outcome in the student’s
health record and incident report, as appropriate.
Prevention
Prevention should be considered the final component in any health care visit. You
have an instrumental role in initiating and maintaining measures to minimize the
effects of injury or illness and reduce the risk of inaccurate triage decisions, such
as
Establishing written triage guidelines or protocols
Designating experienced registered nurses to perform triage
Maintaining knowledge and practice requirements related to triage and decision-
making skills
Knowing which students have emergency care plans on file and reviewing the
necessary interventions with others who may have a responsibility for carrying
them out.
Developing and maintaining individualized health care plans and emergency care
plans for students with special needs.
Ensuring that critical information from these care plans is shared with teachers,
aides, coaches, and lunchroom or playground monitors as appropriate.

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
26
NOTE
Under the Family Educational Rights and Privacy Act, parent/guardian
consent is not required in order to share student health records with
school personnel provided they have a legitimate educational interest
in the student or a need to know the information to protect their
welfare before releasing the information.
Students With Special Needs
Although the pediatric assessment techniques outlined in this chapter are equally
applicable to students who have special health care needs, you must adjust these
techniques to accommodate the student’s developmental age, rather than basing
them on chronologic age. Note also that baseline vital signs for a student with a
chronic condition may be outside the range of same-age peers who do not have
special needs.
As a school nurse, you see the day-to-day variations among your school’s
students and are often the first to notice changes in a student’s condition. With
special needs students, it’s particularly important to become familiar with the
student’s baseline status so that you can tell when the student’s condition has
changed.
Use developmentally appropriate language, gestures, and techniques when
communicating with a student who has cognitive impairment or developmental
delay. When assessing students who depend on technologic assistive devices,
don’t allow yourself to be distracted by the specialized equipment they use. Your
focus should always be directed toward the student.
Summary
One of your primary responsibilities as school nurse is to recognize severe illness
or injury among the students in your school. It is best to do this using a
systematic, consistent assessment schema. Your initial assessment findings give
you a basis for determining the urgency of each student’s condition through
triage. Triage categories allow you to treat students according to acuity of need.
Written triage protocols and policies are important in facilitating this process.
References and Information Sources
Emergency Nurses Association. Core Curriculum for Pediatric Emergency
Nursing. 2nd ed. Sudbury, MA: Jones and Bartlett Publishers; 2002.
Emergency Nurses Association. Emergency Nursing Core Curriculum. 6th ed.
Philadelphia, PA: WB Saunders Co; 2007.
Emergency Nurses Association. Emergency Nursing Pediatric Course Provider
Manual. 3rd ed. Des Plaines, IL: Emergency Nurses Association; 2004.
Emergency Nurses Association. Trauma Nursing Core Course Provider Manual.
6th ed. Philadelphia, PA: WB Saunders; 2007.

| A SSESSMENT AND T RIAGE
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
27
Emergency preparedness for children with special health care needs. American
Academy of Pediatrics Web site. http://www.aap.org/advocacy/epquesansw.htm.
Accessed December 30, 2009.
Health, mental health and safety guidelines for schools.
http://www.nationalguidelines.org/. Accessed December 30, 2009.
Hockenberry MJ, Wilson D. Wong’s Essentials of Pediatric Nursing. 8th ed. St
Louis, MO: Mosby; 2009.
Illinois Emergency Medical Services for Children. Pediatric Pain Management in
the Emergency Department [educational module].
http://www.luhs.org/depts/emsc/ped_pain_manag_report.pdf. Published
August 2002. Accessed December 30, 2009.
National Association of Emergency Medical Technicians. PHTLS: Basic and
Advanced Prehospital Trauma Life Support. 6th ed. St Louis, MO: Mosby; 2007.
Romig LE. PREP for peds—patient physiology, rescuer responses, equipment,
protocols. Size-up & approach tips for pediatric calls. JEMS. 2001;26(5):24-33.
Tunik M, Treiber M, Kim J, Cooper A, Foltin G, eds. Teaching Resource for
Instructors in Prehospital Pediatrics–Basic Life Support. 2nd ed. New York, NY:
Center for Pediatric Emergency Medicine; 2006.

A SSESSMENT AND T RIAGE |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
28

G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
29
A | Protocols
Systematic Assessment/Immediate Care
................................................
31
Triage .................................................................................................. 33
Abdominal Pain ................................................................................... 35
Anaphylaxis/Allergic Reaction ............................................................... 37
Asthma Attack (Acute)/Reactive Airway Disease .................................... 39
Bites and Stings .................................................................................... 41
Burns ................................................................................................... 43
Burn Assessment ................................................................................ 44
Chest Pain ........................................................................................... 45
Chest Trauma ...................................................................................... 47
Child Maltreatment, Suspected ............................................................ 49
Indications of Child Maltreatment ...................................................... 50
Cold-related Injuries (Hypothermia/Frostbite) ....................................... 51
Dental, Oral, and Maxillofacial Emergencies ........................................ 53
Diabetic Emergencies........................................................................... 55
Disaster/Emergency Response: Mass-casualty Incidents ........................ 57
START/JumpSTART Algorithms for MCI Triage ...................................... 58
Ear Emergencies ................................................................................... 59
Eating Disorders ................................................................................... 61
Eye Emergencies .................................................................................. 63
Foreign Body Airway Obstruction ......................................................... 65
AHA Airway Clearing Maneuvers ........................................................ 66
Headache ............................................................................................ 67
Head/Spinal Cord Trauma ................................................................... 69
Heat-related Injuries ............................................................................ 71
Hemophilia ......................................................................................... 73
Increased Intracranial Pressure in a Student With a VP Shunt ............... 75
Lacerations/Abrasions ........................................................................... 77
This section contains protocols that have been developed by Illinois EMSC to guide school
nurses as they assess and manage students with emergency health issues in the school setting.
Please note that Illinois EMSC has made every effort to ensure that the information presented
in this document is accurate and represents current accepted practice in the United States.
However, the recommendations in this document are not intended to indicate an exclusive
course of treatment or to be applicable in all circumstances. We recommend that you use this
document as a guide for developing local school policies and protocols.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
30
Musculoskeletal Injury
.........................................................................
79
Interventions for Musculoskeletal Injuries ............................................ 80
Near-drowning/Submersion ................................................................. 81
Nose Emergencies ................................................................................ 83
Obstetric Emergencies ......................................................................... 85
Emergency Neonatal Care .................................................................. 86
Respiratory Distress .............................................................................. 87
Seizures ............................................................................................... 89
Sexual Abuse/Assault, Teen Dating Violence ........................................ 91
Sickle Cell Anemia ............................................................................... 93
Substance Abuse .................................................................................. 95
Suicide Prevention ............................................................................... 97
Syncope/Unconsciousness ................................................................... 99
Throat Emergencies ........................................................................... 101
Toxic Exposure (Ingestion/Environmental) ........................................... 103
Toxidromes ...................................................................................... 104
Trauma .............................................................................................. 105
Interventions for Musculoskeletal Trauma ......................................... 106
Violent Behavior ................................................................................ 107
Violent Behavior: Safety Tips ............................................................ 108

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
31
Systematic Assessment/Immediate Care
Every nursing encounter begins with a systematic assessment. The 5 components of a comprehensive
assessment are listed below. Suggested actions should be performed if indicated and in accordance with
applicable protocols and available resources. Take any necessary actions before progressing to the next
step of the assessment.
NOTE
Triage determination and EMS activation should occur as soon as the need becomes apparent.
SCENE SAFETY ASSESSMENT
Call for assistance as indicated before proceeding.
ACROSS-THE-ROOM ASSESSMENT
Use Pediatric Assessment Triangle (PAT)
Appearance (mental status muscle tone/body position interaction)
Breathing (work of breathing, including nasal flaring, retractions; abnormal airway
sounds)
Circulation (visible skin color)
INITIAL (ABCDE) ASSESSMENT/IMMEDIATE INTERVENTIONS
Standard precautions
C-spine stabilization
Airway (positioning)
Breathing (O
2,
mouth-to-mask)
Circulation (control bleeding CPR/AED)
Disability (AVPU, pupil check)
Exposure (brief inspection)
HISTORY/PAIN ASSESSMENT
SAMPLE (Symptoms Allergies Medications Past health history Last food/drink Events)
Pain—PQRST, numeric or FACES scale (comfort measures)
FOCUSED PHYSICAL EXAMINATION
Full vital signs, temperature, weight, blood glucose
Limited or complete examination (inspect auscultate palpate)
TRIAGE (E–U–N)
Emergent (activate EMS)
Urgent (determine need for EMS)
Nonurgent (return to class or send home)
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
32
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
33
Triage
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO.
DETERMINE TRIAGE CATEGORY
The assessment findings allow you to determine a triage category, which dictates subsequent
actions. Key findings associated with each triage category are listed below, together with general
interventions. Specific actions will vary according to the situation.
EMERGENT
Findings that suggest a potential threat to
life or function requiring immediate
medical attention include
Cardiopulmonary arrest
Altered LOC
Burns, severe/major
Caustic chemical exposure
Childbirth, imminent
Head injury with any history of loss
of consciousness
Pain, severe, or significant location
(eg, chest)
Poisoning/drug overdose
Respiratory distress, severe, or
respiratory failure
Shock (hypovolemic, anaphylactic,
cardiogenic)
Spinal cord injury, suspected
Status epilepticus or first-time
seizure
Suicidal behavior
Trauma, severe, or trauma to limb,
distal pulse absent
Violent/homicidal behavior
INTERVENTIONS
Support ABCs
Activate EMS
Initiate appropriate interventions as
per specific protocol or IHP/ECP
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Findings that suggest an acute,
severe, but non–life-threatening
condition requiring additional medical
intervention within 2 hours include
Burns, minor
Deformity/suspected closed
fracture without circulatory
compromise
Fever exceeding 100°F/37.8°C
GI symptoms, persistent
(nausea, vomiting, diarrhea)
Lacerations requiring sutures
without excessive blood loss
Pain, moderate, following
abdominal trauma
Seizure, atypical, in a student
with a history of seizures
Wheezing
INTERVENTIONS
Support ABCs as indicated
Determine need for EMS
Observe student closely
Initiate appropriate
interventions as per specific
protocol or IHP/ECP
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Findings that suggest a
nonacute condition that is not
severe (but may require
referral for routine medical
care) include
Essentially well with S/S
of mild noncommunicable
illness or URI
Headache without fever
or other abnormal findings
Injury, minor (abrasions,
ecchymoses,
sprains/strains)
Pain, mild (eg, abdominal
or menstrual pain,
headache or toothache),
without fever or other
abnormal findings
INTERVENTIONS
Initiate appropriate
interventions or
administer medications as
per specific protocol or
IHP/ECP
Observe student
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
34
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
35
Abdominal Pain
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR ABDOMINAL PAIN
Focused abdominal assessment
Time of last bowel movement
Urinary symptoms
Events preceding episode, including trauma
Menstrual history and possibility of pregnancy
History/pattern of previous occurrences
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Capillary refill time exceeds 2 sec
Orthostatic vital signs
a
Change in mental status, LOC
Decreased or absent bowel sounds
Abdominal/GU trauma (see Trauma
protocol)
Abdominal distention, rigidity, or
guarding
Bluish discoloration of flank or
periumbilical area (Grey Turner
sign)
Severe abdominal pain
Imminent childbirth (see Obstetric
Emergencies protocol)
Pregnant with vaginal bleeding
INTERVENTIONS
Support ABCs
Activate EMS
Place student supine
Give nothing by mouth
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Stable vital signs with
Moderate abdominal pain or
dysuria
Nausea/vomiting or
significant diarrhea
Significant pain with fever
Mucus or frank blood in
stool; tarry stools
Abnormal vaginal bleeding or
discharge without pregnancy
INTERVENTIONS
Determine need for EMS
Observe student closely
Give nothing by mouth
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Stable vital signs with
Mild or intermittent
abdominal pain/cramps
Onset related to menses
INTERVENTIONS
If recurrent abdominal pain
(RAP) has been diagnosed,
allow student to rest in
health office
Observe student
Contact parent/guardian
Return student to class or
send home as indicated
Refer to medical care or
school support services as
indicated for frequent
complaints
Follow up
a
Orthostatic vital signs
Assess BP and HR while student is supine. Have student sit up or stand and reassess 1 min later. If BP decreases
by more than 20 mm Hg or HR increases by 20 bpm, orthostasis is present.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
36
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
37
Anaphylaxis/Allergic Reaction
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR ANAPHYLAXIS
Respiratory assessment
Focused assessment of skin findings
History of systemic allergic reaction
History of food allergy
Events preceding reaction, such as a bite/sting
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of cardiopulmonary compromise
(see reverse)
Airway compromise
Change in mental status, LOC
Cyanosis at mouth and lips
S/S of severe respiratory distress
(wheezing, dyspnea)
Signs of shock/hypotension
History of anaphylaxis
Edema of face, lips, eyes, tongue
Generalized hives involving large area
Diaphoresis
C/o tightness in throat or chest
C/o apprehension, weakness
INTERVENTIONS
Support ABCs
Activate EMS
Administer prescribed Epi-Pen/Epi-Pen Jr
if available
Repeat Epi-Pen/Epi-Pen Jr in 10 min if no
response
Initiate CPR if necessary
For severe respiratory distress, administer
prescribed bronchodilator
Consult IHP/ECP
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
S/S of mild systemic
reaction; eg, localized
hives, abdominal
cramps, nausea,
vomiting
Edema of extremities
Persistent coughing
Tingling, itching of
face, ears, nose
History of allergy
INTERVENTIONS
Determine need for
EMS
Consult IHP/ECP
Observe student
closely
Administer prescribed
Epi-Pen/Epi-Pen Jr if
available and activate
EMS
Contact
parent/guardian to
transport student to
medical care or home
Follow up
NONURGENT
Local reaction only
Responsive to medications
Nasal congestion
Persistent sneezing
INTERVENTIONS
Consult IHP/ECP
Apply cold pack to site
Observe student
Contact parent/guardian
Return student to class or send
home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
38
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
39
Asthma Attack (Acute)/Reactive Airway Disease
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR ACUTE ASTHMA ATTACKS
Airway inspection to R/O obstruction due to
infection or foreign body aspiration
Respiratory assessment
Skin assessment
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
Help student into a position of comfort
Perform peak flow assessment if possible
Note: Obtain peak expiratory flow reading
before administering bronchodilator and again
20 min later (or per ECP orders)
Administer prescribed bronchodilator or
other medication as directed
Note: Use spacer or holding chamber with
MDI/nebulizer, if available
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of severe asthma (see
reverse)
INTERVENTIONS
Support ABCs
Prepare to ventilate if necessary
Activate EMS if S/S are not
relieved by medication or if
medication is not available
Administer high-flow O
2
if
available
Repeat prescribed
bronchodilator/ other
medications
Directly/continuously observe
student
Consult IHP/ECP
Contact parent/guardian
Notify school administrator
Follow up
URGENT
S/S of moderate asthma (see
reverse)
Cannot tolerate normal activity
No improvement within 15–30 min
of bronchodilator administration
Bronchodilator unavailable
INTERVENTIONS
Determine need for EMS
Administer high-flow O
2
if
available
Repeat prescribed
bronchodilator/other medications
Consult IHP/ECP
Directly/continuously observe
student
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
S/S of mild asthma (see
reverse)
Symptoms respond to
bronchodilator
Student is able to maintain
normal level of activity
INTERVENTIONS
Repeat prescribed
bronchodilator/other
medications
Consult IHP/ECP
Monitor student
Contact parent/guardian
Return student to class or
send home as indicated
Assess need for
parent/guardian–student
asthma education
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
40
Tools for Assessing Students
ASSESSMENT FINDINGS IN ASTHMA
Assessment Mild Asthma Moderate Asthma Severe Asthma
PEFR
70%–90% of predicted
or personal best
50%–70% of predicted or
personal best
less than 50% of predicted
or personal best
RR
Less than 30% above
mean
30%–50% above mean
More than 50% above
mean
LOC Normal Normal Normal or decreased
Dyspnea
Absent or mild; able to
speak in complete
sentences
Moderate; speaks in
phrases or partial
sentences
Severe; speaks only in
single words or short
phases
Accessory
muscle use
None or mild intercostal
retractions
Moderate intercostal
retractions, suprasternal
retractions
Severe intercostal
retractions, suprasternal
retractions, nasal flaring
during inspiration
Color Normal Pallid Pallid or cyanotic
Auscultation
End-expiratory wheeze
only
Wheeze throughout
expiration and inspiration
Decreasing or absent
breath sounds
O
2
saturation Exceeds 95% 90%–95% Less than 90%
LOC indicates level of consciousness; O
2
, oxygen; PEFR, peak expiratory flow rate; RR, respiratory rate
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
I
NDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
41
Bites and Stings
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR BITES AND STINGS
Time bite/sting occurred
Location of bite/sting on body
Type of bite/sting
Number of bites/stings
Intensity of pain
Previous exposure/allergic reaction to same
type of bite/sting
Wound characteristics (erythema, edema,
ecchymoses, drainage, size/depth)
Inspection for foreign body (stinger, tooth, tick)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of anaphylaxis or
history of anaphylactic
reaction (see Anaphylaxis
protocol)
S/S of respiratory distress
Hypotension
Cardiac arrest
Loss of consciousness
Known exposure to toxin
(see Toxic Exposure
protocol)
Severe pain
INTERVENTIONS
Support ABCs
Activate EMS
Perform CPR as appropriate
Administer IM epinephrine
as per ECP
Directly/continuously
observe student
Report animal bites to
appropriate local official
Contact PCC as appropriate
(800-222-1222)
Contact parent/guardian
Notify school administrator
Follow up
URGENT
S/S of mild systemic reaction
with wheezing, progressive
pain/edema but normal vital
signs (see Anaphylaxis protocol)
Deep puncture wounds
Moderate pain
Lacerations requiring sutures
(see Lacerations/Abrasions
protocol)
Nausea/vomiting
Human bite with broken skin
INTERVENTIONS
Determine need for EMS
Wash lacerations with soap and
water; irrigate as indicated
Observe student closely
Report animal bites to
appropriate local official
Refer all incidents involving
human bites to ED
Contact PCC as appropriate
(800-222-1222)
Contact parent/guardian to
transport to medical care or
home
Follow up
NONURGENT
Mild localized allergic reaction
without systemic/respiratory S/S
Mild pain
Mild pruritus
Stinger/tick present
INTERVENTIONS
Stinger
Remove stinger by scraping with
stiff cardboard/credit card; do
not squeeze
Apply cold pack
Observe student for 20 min
before returning to class
Tick
Grasp tick with fine-point
tweezers as close to skin as
possible
Pull firmly
Wash bite area and hands with
soap and water
In All Cases
Observe student
Contact parent/guardian
Return student to class or send
home as indicated
Follow up
First Aid Don’ts
Do not apply a tourniquet, as it can lead to ischemia
Do not incise wound or apply suction, as these measures are ineffective and potentially dangerous
NOTE
Refer student for tetanus booster if it has been 5 years or more since the
last vaccination. Tetanus booster is recommended every 10 years.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
42
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
43
Burns
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR BURN INJURIES
Scene safety (eg, live electrical wire)
Burn characteristics (see reverse)
Duration of contact with burn source
Student’s age, weight, and general health status
Associated injuries
Pediatric GCS score
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
Remove student from burn source (eg, heat/electricity)
Remove jewelry, rings, constricting clothing
(Do not remove clothing that has adhered to skin!)
Begin irrigation of chemical burns with cool water
Cool thermal burns if less than 20% BSA is involved
NOTE: Protect student from hypothermia
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Apnea or pulselessness
Full-thickness burn (tough, brownish surface)
Deep partial-thickness burn (charred/white)
Burns involving face, hands or feet, eyes or ears,
genitalia (see Eye or Ear Emergencies protocols)
Electrical burns
S/S of inhalation injury (singed nasal hair,
carbonaceous sputum) or other complicating injuries
Altered LOC
Respiratory distress (see Respiratory Distress protocol)
Suspected child maltreatment (see Child Maltreatment
protocol after providing burn care)
Severe pain
INTERVENTIONS
Support ABCs
Activate EMS
Electrical burns
Safely remove student from burn source
Initiate CPR as needed/have AED ready
Inspect for entrance and exit wounds
Chemical burns
Continue copious irrigation of chemical burns with cool
running water for at least 20 min
Consider contacting PCC (800-222-1222)
Send burn agent and MSDS to ED with student
Do not apply cold packs
Thermal burns
Cover with dry, sterile dressings or clean sheet
In all cases
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Superficial partial-thickness burn
without complicating factors
Moderate pain
Erythema/edema, wet/oozing
blisters
Too large to cover with adhesive
bandage
Signs of associated infection
INTERVENTIONS
Determine need for EMS
Flush copiously with cool running
water
If unable to immerse, apply clean,
wet, cool cloth
Do not apply cold packs
Do not break blisters
Bandage loosely
Observe student closely
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
Superficial burn (eg,
sunburn)
Minor erythema
Local, mild pain
Student is alert
INTERVENTIONS
Immerse area in cool
water 2–5 min
Apply tepid cloths
Bandage loosely
Observe student
Contact
parent/guardian
Return student to
class or send home
as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
44
Burn Assessment
The depth, extent, and location of a burn provide a consistent basis for conveying
information about a burn injury to EMS and other health care providers. The following
parameters are used to describe depth:
A superficial burn involves only the epidermis. It is characterized by erythema
and local pain.
A superficial partial-thickness burn involves both the epidermis and the
corium. This type of burn generally produces erythema and blisters.
A deep partial-thickness burn may appear white and dry, with locally reduced
sensitivity to touch and pain.
A full-thickness burn has a tough brownish surface and a hard eschar. The area
will be locally insensitive to touch or pain. This type of burn will not heal without
intervention.
Extent is described as a percentage of the body surface area (%BSA). A quick way to
determine %BSA for small or irregular burns is to use the student’s hand (including the
palm and fingers) as a reference, since this is roughly equal to 1% of the student’s total
body surface area. The figures below illustrate %BSA by anatomic area for an infant,
child, and adult.

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
45
Chest Pain
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR CHEST PAIN
Consider etiology
Cardiac
Respiratory
Musculoskeletal
Trauma
Psychosocial stress
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Severe chest pain
Bradycardia/tachycardia
Cyanosis of lips and nail beds
Decreased LOC
Palpitations
Dyspnea
Peripheral pulses weak/thready/absent
Diaphoresis; clammy, cool skin
Restlessness
Hypotension
Nausea
Weakness
Capillary refill exceeds 2 sec
INTERVENTIONS
Support ABCs
Activate EMS
Have AED readily available
Maintain position of comfort
Directly/continuously observe student
Reassess vital signs every 5 min
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Moderate, persistent chest
pain
Anxiety
Stable vital signs
No history of
recent chest trauma
recent asthma attack
loss of consciousness
INTERVENTIONS
Support ABCs
Determine need for EMS
Maintain position of
comfort
Observe student closely
Reassess vital signs
Contact parent/guardian
to transport student to
medical care or home
Follow up
NONURGENT
Mild chest pain
Normal vital signs
No history of
recent chest trauma
recent asthma attack
loss of consciousness
INTERVENTIONS
Support ABCs
Maintain position of
comfort
Monitor closely
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
46
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
47
Chest Trauma
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
KEY ASSESSMENT POINTS FOR CHEST TRAUMA
Respiratory assessment
Chest wall inspection for symmetry, wounds,
ecchymoses
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
If student is apneic, perform rescue breathing
using mouth-to-mask
If pulseless, initiate CPR; consider AED
Apply clean dressing to open chest wounds
(occlude on 3 sides only)
Apply direct pressure for profuse hemorrhage
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of respiratory distress
Open chest wound
Crush injury
Uncontrollable hemorrhage
Muffled heart sounds
S/S of pneumothorax or cardiac tamponade:
Apprehension
Rapid/shallow respiration
Painful respiration
Jugular vein distension
Cyanosis
Muffled heart sounds
Hypotension (late/ominous sign)
INTERVENTIONS
Support ABCs
Activate EMS
Maintain spinal stabilization
Cover open chest wounds (occlude on 3 sides
only)
Elevate head and shoulders 30° unless neck
injury is suspected
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Closed chest injury
without respiratory
distress
S/S of closed rib fracture
(shallow/painful but
unimpaired respiration)
INTERVENTIONS
Support ABCs
Determine need for EMS
Monitor
respiratory/cardiac
status
Observe student closely
Contact parent/guardian
to transport student to
medical care or home
Follow up
NONURGENT
Stable vital signs
Ecchymoses
No S/S of rib fracture
INTERVENTIONS
Apply cold packs as
appropriate
Observe student
Contact
parent/guardian
Return student to
class or send home
as indicated
Follow up
NOTE
Pneumothorax/cardiac tamponade may develop slowly during a 24- to 48-hour
period following chest trauma, making reassessment crucial.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.
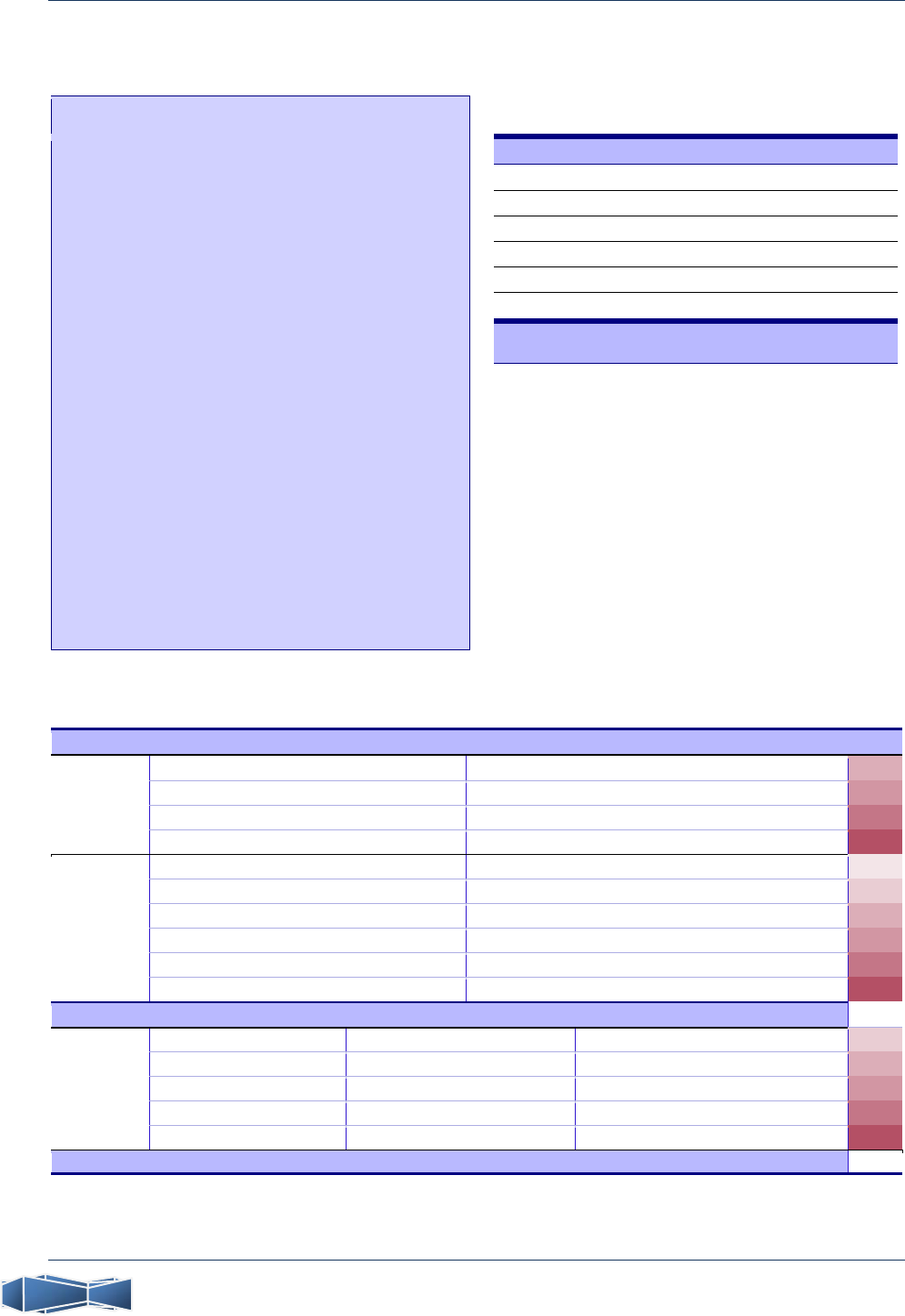
P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
48
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
49
Child Maltreatment, Suspected
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol),
performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR SUSPECTED CHILD MALTREATMENT
Indications of neglect Indications of abuse (See reverse)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Multiple new suspicious injuries
(see Trauma protocol)
History of chronic life-threatening
illness without appropriate medical
treatment
INTERVENTIONS
Support ABCs
Activate EMS
Treat injuries
Provide emotional support
Directly/continuously observe
student
Report suspicions to DCFS:
800-25-ABUSE (22873)
Notify crisis response team
Notify school administrator
Document all findings
Follow up
URGENT
New injuries and history of
suspicious injuries (see
Trauma protocol)
Appears inadequately fed,
clothed, or sheltered
Inadequate medical care
INTERVENTIONS
Treat injuries
Provide emotional support
Observe student closely
Report suspicions to
DCFS: 800-25-ABUSE
(22873)
Notify crisis response team
as appropriate
Document all findings
Follow up
NONURGENT
Student reports
abandonment by
parent/guardian
Student reports
maltreatment
INTERVENTIONS
Provide emotional
support
Report suspicions to
DCFS: 800-25-ABUSE
(22873)
Notify crisis response
team as appropriate
Observe student
Document all findings
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
50
Indications of Child Maltreatment
You are required by law to report any suspicion of child maltreatment (abuse or neglect)
to the appropriate agency in your state. In Illinois, you can reach the Child Abuse Hotline
maintained by the Department of Children and Family Services by calling
800-25-ABUSE (22873). The law provides immunity for mandated reporting.
INDICATORS OF ABUSE INDICATORS OF NEGLECT
The following findings should increase
your suspicion of child abuse:
The reported history of injury is inconsistent
with the physical examination findings.
Details of the reported history change from
one telling to the next.
There was a prolonged delay between the
time of injury and the time medical
assistance was sought.
The child has a history of repeated trauma.
The parent/guardian responds to questions
inappropriately or does not comply with
medical advice.
Suspicious injuries include
Injuries involving soft tissue of the face,
neck, abdomen, or similar areas
Injuries involving areas that are normally
shielded, including the back and chest
Fractures of long bones in children younger
than 3 years
Old scars or injuries in different stages of
healing
Injuries with an appearance suggesting
deliberate infliction, such as human bite
marks, cigarette burns, rope marks, or the
imprint of a belt or other object
Trauma affecting the genital or perianal
area
Sharply demarcated burns in unusual areas
Scald patterns that appear to involve
dipping the area in hot water, such as burns
to the hands, feet, or buttocks
The following findings should increase
your suspicion of child neglect:
Unsafe conditions are evident in the home
environment (eg, weapons within reach,
open windows without screens or window
guards, perilously unsanitary conditions).
The parent/guardian has not provided for
medical treatment, refuses to permit
medical treatment, or fails to seek
necessary and timely medical care for a
child who has an acute or chronic life-
threatening illness.
A child younger than 10 years has been left
unattended or unsupervised. (Although
some situations permit a parent/guardian to
leave a young child alone without
endangerment, you cannot make this
determination.)
The child appears to be abandoned.
The parent/guardian appears to be
incapacitated due to intoxication, disabling
psychiatric problems, debilitating illness, or
similar impairment, and cannot adequately
care for the child.
The child appears to be malnourished
(seriously underweight, emaciated, or
dehydrated), inadequately clothed, or
inadequately sheltered.
The child is found to be intoxicated or under
the influence of an illicit substance.
All instances of suspected child maltreatment must be reported to the DCFS for investigation.
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
51
Cold-related Injuries (Hypothermia/Frostbite)
GENERAL GUIDELINES
Hypothermia: rewarm slowly
Frostbite: rewarm quickly
Do not rub affected area
When rewarming, use warm
water, never hot
Educate students regarding
susceptibility to hypothermic injury,
need for precautions
FROSTBITE CATEGORIES
a
Frostnip
Blanched, white skin, cold to touch
Superficial frostbite
Firm, waxy skin, softer tissue underneath
Blisters develop in 24 to 48 hours
Deep frostbite
Mottled or gray-blue skin, firm to touch
Severity not apparent until frostbitten area is rewarmed
Sensory: cold; pruritus or paresthesia
Necrosis develops over time
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR COLD-RELATED INJURIES
Skin assessment
Events preceding episode
Duration of exposure
Focused physical examination of extremities
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Altered LOC
Cyanosis
Slow/shallow respiration
Weak, thready pulses, no pulses, or
bradycardia
Hypotension
Extremities edematous and discolored
No shivering (severe hypothermia)
Slurred speech
Abnormally low body temperature
S/S of deep frostbite
a
INTERVENTIONS
Activate EMS
Remove student’s wet clothing
Keep student warm and completely
covered
Assess vital signs for 1 full minute
If pulseless, initiate CPR
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Normal LOC or drowsy
Shivering (mild
hypothermia)
S/S of superficial frostbite
or frostnip
a
INTERVENTIONS
Remove wet clothing and
keep student warm
Determine need for EMS
Observe student closely
If alert, give sips of warm
liquid
Warm area with warm
water
Reinforce need for
precautions when exposed
to cold
Contact parent/guardian to
transport student to
medical care or home
Follow up
NONURGENT
Alert
Slight shivering
Exposed skin feels cold
No signs of frostbite or
frostnip
a
INTERVENTIONS
Remove wet clothing and
replace with dry coverings
If student is alert, give sips
of warm liquid
Warm cold skin with warm
water
Observe student
Reinforce need for
precautions when exposed
to cold
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
52
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
53
Dental, Oral, and Maxillofacial Emergencies
NOTE
Refer student for tetanus booster if it has been 5 years or more since the
last vaccination. Tetanus booster is recommended every 10 years.
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
KEY ASSESSMENT POINTS FOR DENTAL, ORAL, AND MAXILLOFACIAL EMERGENCIES
Inspect teeth
Assess facial bones, including mandible
Assess ability to open and close mouth
IMMEDIATE INTERVENTIONS
Even before you determine triage category, ensure the adequacy of the student’s airway
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Airway compromise
Change in mental status, LOC
Excessive bleeding
Suspected fracture of mandible or other
facial bones (see Trauma protocol as
indicated)
INTERVENTIONS
Maintain c-spine stabilization
Support ABCs
Activate EMS
Treat hemorrhage with direct pressure
Apply cold packs to reduce pain/edema
For suspected mandible fracture only,
stabilize jaw by wrapping cravat around
the point of the chin, securing it on top
of the head, avoiding pressure on neck
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Displacement of multiple
teeth
Avulsion of permanent tooth
a
Major chip/fracture of
permanent tooth
Broken orthodontic appliance
Severe toothache
INTERVENTIONS
If possible, save large tooth
chips; cover jagged edge of
tooth with gauze
For wire protruding from
appliance, gently attempt to
bend away from oral tissue;
if unsuccessful, cover end
with gauze or dental wax (do
not remove embedded wire)
Observe student closely
Contact parent/guardian to
transport student to dental
care or home
Follow up
NONURGENT
Caries
Exfoliation of primary
tooth
Eruption of permanent
tooth
Bleeding gums
Minor chip/fracture of
tooth
INTERVENTIONS
For minor tooth chip,
have student rinse
mouth with warm salt
water
Apply cold compress to
edematous areas
Observe student
Contact parent/guardian
Return student to class
or send home as
indicated
Follow up
a
Avulsion of permanent tooth
Note: Replantation is most likely to succeed if attempted within 60 minutes.
Activate EMS or transport immediately to dentist
Handle the tooth by the crown, not the root
If the tooth is dirty, gently rinse in milk or water
Gently replace tooth in socket (do not use force)
only if student is alert and able to cooperate
Instruct student to keep pressure on tooth by
biting gently on clean gauze; if unable to do so,
place tooth in milk for transport
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
54
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
55
Diabetic Emergencies
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR DIABETIC EMERGENCIES
Respiratory assessment
Skin assessment
Last insulin dose/type of insulin used and route
Last meal/carbohydrate intake
Precipitating factors (exercise, change in eating
habits/diet, stress, missed insulin dose, illness)
Current blood glucose level
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Severe hypoglycemia
Glucose less than 60 mg/dL with loss of
consciousness or seizures (see Seizures
protocol)
Severe hyperglycemia/DKA
Glucose exceeds 250 mg/dL with at least
1 of the following:
Moderate to severe dehydration
Abdominal pain/tenderness
Kussmaul respiration, fruity breath
odor
Tachycardia
Cool extremities
Altered LOC (lethargic to comatose)
INTERVENTIONS
Support ABCs
Activate EMS
Directly/continuously observe student
Place in left lateral recovery position to
prevent aspiration
Consult IHP/ECP
Hypoglycemia
Administer 1 mg glucagon IM/SQ if
available per ECP
Severe hyperglycemia
Administer insulin per ECP
Diabetic ketoacidosis
Prepare for immediate transport
Give nothing by mouth
In all cases
Contact parent/guardian
Notify school administrator
Determine need for diabetes education
(parent/guardian, student, school
personnel)
Follow up
URGENT
S/S of moderate hypoglycemia
(glucose less than 60; student
awake and responsive)
S/S of moderate hyperglycemia
(glucose 120–250 mg/dL; student
awake and responsive with mild
abdominal pain/tenderness,
nausea, headache, tachycardia,
fruity breath odor)
INTERVENTIONS
Support ABCs
Determine need for EMS
Monitor student closely
Consult IHP/ECP
Hypoglycemia
Give glucose tablets/instant glucose
equivalent to 15 grams carbs or 4
oz regular soda or juice
(orange/apple) followed by
snack/next meal
As indicated, give extra snack (eg,
2 peanut butter crackers or half
sandwich and 8 oz milk)
Hyperglycemia
Administer insulin per ECP
Increase intake of water
Test for ketonuria
In all cases
Contact parent/guardian to
transport student to medical care
or home
Determine need for diabetes
education (parent/guardian,
student, school personnel)
Follow up
NONURGENT
S/S of mild hypoglycemia (glucose
60–80 mg/dL; student awake,
alert)
S/S of mild hyperglycemia (glucose
120–250; student awake, alert)
INTERVENTIONS
Consult IHP/ECP
Mild hypoglycemia
Give glucose tablets/instant
glucose equivalent to 15 grams
carbs or 4 oz regular soda or juice
(orange/apple) followed by
snack/next meal
As indicated, give extra snack (eg,
2 peanut butter crackers or half
sandwich and 8 oz milk)
Recheck glucose in 15 min; if no
improvement, repeat treatment
If improvement is noted, return
student to class or send home as
indicated
Instruct student to refrain from
tasks requiring intense
concentration or exertion for 1 hr
Mild hyperglycemia
Administer insulin per ECP
Increase intake of water
Return student to class or send
home as indicated
In all cases
Contact parent/guardian
Determine need for diabetes
education (parent/guardian,
student, school personnel)
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
56
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
57
Disaster/Emergency Response: Mass-casualty Incidents
DEFINITION
A mass-casualty incident is a situation in which
medical care requirements overwhelm local emergency response resources
IMMEDIATE ACTIONS
Assess scene safety
Determine approximate number of casualties
Activate EMS
Activate incident command
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Perform triage assessment using START/JumpSTART (see reverse)
Assign appropriate triage categories
Dispatch casualties to designated field treatment area
EMERGENT (RED)
Life-threatening
Shock
Respiratory
distress/failure
Major burns
Fracture of long bone
with circulatory
compromise
INTERVENTIONS
Assign team members
to multiple casualties
Maintain ABCs
Ensure direct,
continuous observation
until transfer of care
Notify parent/guardian
as specified in
emergency response
plan
Assist EMS as
appropriate
Follow up
URGENT (YELLOW)
Care required within 2 hr
Fracture of long bone
without circulatory
compromise
Laceration without
significant blood loss
Head injury without
loss of consciousness
INTERVENTIONS
Maintain ABCs
Initiate appropriate
care
Notify
parent/guardian as
specified in
emergency response
plan
Assist EMS as
appropriate
Provide for counseling
Follow up
NONURGENT (GREEN)
Nonacute/minor condition
Major abrasions/
ecchymoses
Muscle
sprains/strains
Emotional distress
INTERVENTIONS
Initiate appropriate
care
Monitor for changes
Notify
parent/guardian as
specified in
emergency response
plan
Provide for
counseling
Follow up
DELAY CARE (BLACK)
Survival unlikely
Massive open head
trauma
Cardiac arrest
INTERVENTIONS
Do not render care
until adequate
resources and
personnel permit
Follow up
EMS TRIAGE CATEGORIZATION FOR MASS-CASUALTY INCIDENTS
Category Condition
Red
Potential threat to life or function requiring immediate intervention
Yellow
Acute condition that is not life- or limb-threatening, requiring care within 1–2 hours
Green
Nonacute or minor condition
Black
Catastrophic injury or condition such that survival is unlikely (in a disaster situation, resources do
not allow for resuscitation of such patients)
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
58
START/JumpSTART Algorithms for MCI Triage
MCI denotes mass-casualty incident

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
59
Ear Emergencies
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
KEY ASSESSMENT POINTS FOR EAR EMERGENCIES
Skin assessment for wounds, blisters,
erythema, edema, hematomas, bleeding
Hearing evaluation
Focused physical assessment
(external/otoscopic)
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
Control bleeding
Apply appropriate dressing
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Change in mental status, LOC
Laceration/avulsion/hematoma of
external ear with uncontrollable
bleeding (see Head/Spinal Cord
protocol as indicated)
Burn or direct thermal injury
Acute hearing loss
INTERVENTIONS
Maintain spinal stabilization if
applicable
Support ABCs
Activate EMS
Directly/continuously observe
student
Maintain position of comfort
Keep student calm
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Foreign body in ear
Mild hematoma
Abrasions/minor lacerations of external
ear (see Lacerations/Abrasions protocol)
INTERVENTIONS
Determine need for EMS
Foreign body
Do not attempt to remove unless object
is visible and can be gripped with forceps
or fingers
If object is a live insect, instill 1–2 drops
of mineral oil
In All Cases
Closely monitor student
Contact parent/guardian to transport
student to medical care or home
Maintain position of comfort
Observe student
Follow up
NONURGENT
Mild earache
without drainage
Associated low-
grade fever
INTERVENTIONS
Send student home
if pain is persistent
or accompanied by
fever
Contact
parent/guardian
Return student to
class or send home
as indicated
Follow up
NOTE
Refer student for tetanus booster if it has been 5 years or more since the
last vaccination. Tetanus booster is recommended every 10 years.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
60
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
61
Eating Disorders
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR EATING DISORDERS
Skin assessment
History of food intake and level of exercise
Menstrual history
Mental status examination or other brief
psychosocial profile
Focused physical assessment of weight (have
student remove shoes/bulky outer wear)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Cardiac arrest
Seizure activity (see
Seizures protocol)
Hypotension
Bradycardia
Lethargy
INTERVENTIONS
Support ABCs
Activate EMS
Directly/continuously
observe student
Contact parent/guardian
Notify school
administrator
Follow up
URGENT
Orthostatic vital signs
a
Significant weight loss
Tooth enamel erosion
Weakness
Poor skin turgor
INTERVENTIONS
Support ABCs
Determine need for EMS
Encourage fluid intake in small quantities
Provide nonthreatening environment
Observe student closely
Discuss the need for medical
evaluation/counseling with
parent/guardian
Contact parent/guardian to transport
student to medical care or home
Follow up
NONURGENT
Normal vital signs
Suspicion or early signs of
eating disorder
b
INTERVENTIONS
Provide nonthreatening
environment
Observe student
Discuss health
consequences of behavior
Contact parent/guardian
Refer to school counselor
Return student to class or
send home as indicated
Follow up
a
Orthostatic vital signs
Assess BP and HR while student is supine. Have student sit up or stand and reassess 1 min later. If BP decreases
by more than 20 mm Hg or HR increases by 20 bpm, orthostasis is present.
b
Early signs/psychosocial attributes associated with eating disorders
High achiever/perfectionist
Low self-esteem/depression
History of substance abuse
Intense fear of weight gain
Evidence of body dysmorphia
Rigid self-control
Decreased food intake, self-induced vomiting,
use of laxatives/diuretics/emetics
Vigorous exercising to achieve weight loss
rather than fitness
Recent history of weight loss/weight fluctuations
Preference for oversized clothing
Amenorrhea
Hypothermia
Lanugo (downy hair)
Weakness
Poor skin turgor
Esophagitis, oral lesions
Dental caries, tooth enamel erosion
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
62
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
63
Eye Emergencies
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if spinal injury is suspected!
KEY ASSESSMENT POINTS FOR EYE EMERGENCIES
Events leading up to injury (eg, chemical exposure, other burn)
AS TOLERATED, focused physical examination of the eye/vision assessment for
visible wounds, drainage, foreign body
extraocular movement
PERRLA
visual acuity
IMMEDIATE INTERVENTIONS
For chemical burns involving the eye, IMMEDIATELY activate EMS, then ensure scene safety and begin flushing eye
copiously with saline, eyewash solution, or water
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Change in mental status, LOC
Penetrating injury
Chemical/thermal burn
Unequal/irregular pupils
Blunt injury (see Head/Spinal Cord protocol)
Embedded foreign body
Hyphema (haze or blood in iris)
Decreased visual acuity/loss of vision
INTERVENTIONS
Maintain c-spine stabilization as applicable
Support ABCs
Activate EMS
Protect eye from further injury
Chemical burns
Continue irrigation while awaiting EMS
Send copy of MSDS to ED
Penetrating injuries
Stabilize object with gauze pads
Tape disposable drinking cup over dressing (do not
allow it to contact object)
Thermal burns
Do not inspect eyes
Apply loose, moist dressing
Radiation burns
(eg, from arc welder, sunlight, sun lamp)
Cover with eye patch
In all cases
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Blunt trauma without vision
changes
S/S extraocular muscle
entrapment
Suspected corneal abrasion
Laceration of lid
Blurry/impaired vision
Diplopia
Eye pain/guarding
Sensation of foreign body
persisting more than 1 hr
Bilateral periorbital ecchymoses
(raccoon eyes)
INTERVENTIONS
Determine need for EMS
If no evidence of injury, apply
cool compress for 20 min
Instruct student not to move
rapidly, bend over, or cough
Observe student closely
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Superficial foreign body
Subconjunctival
hemorrhage (may follow
violent coughing or
vomiting)
Minor periorbital
lacerations
Minor periorbital
ecchymoses
INTERVENTIONS
Foreign body
If foreign body is visible
in sac of lower lid,
remove with cotton-
tipped applicator
If unsuccessful after 2
attempts, or if foreign
body is located
elsewhere, flush with
saline, eyewash solution,
or water
In all cases
Observe student
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
64
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
65
Foreign Body Airway Obstruction
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol),
performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR FOREIGN BODY AIRWAY OBSTRUCTION
Evaluation of airway/respiratory status
Suddenness of onset
Events leading up to incident (eg, witnessed
ingestion/aspiration of small object, toy, or food
Note: Fever or S/S of respiratory illness decreases the likelihood of foreign body etiology
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Severe airway obstruction
Choking, silent cough or
Unable to cough, speak, or make any
sound
Apnea
Pallor or cyanosis
Loss of consciousness
INTERVENTIONS
Severe Obstruction
Begin AHA airway clearing maneuvers.
See reverse for detailed procedure.
In infants younger than 1 yr, apply 5
back slaps and 5 chest thrusts
In children older than 1 yr, perform
abdominal thrusts (Heimlich
maneuver)
Continue until either the object is
expelled or the infant or child
becomes unresponsive
Begin CPR, checking inside the mouth
before each series of rescue breaths
to see whether the object is visible
and can be removed
Note: Do not attempt blind finger
sweeps! Foreign body may be pushed
further into the airway, exacerbating
obstruction.
Activate EMS if efforts are
unsuccessful after 1 minute
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Mild airway obstruction
History of aspiration
Fast breathing
Intermittent wheezing or
stridor
Gagging, choking, coughing
Pink skin color
Mild to moderate dyspnea
INTERVENTIONS
Encourage forceful cough
Do not interfere in any
other way
Monitor for worsening distress,
ineffective cough, inspiratory
wheezing, labored breathing,
tachycardia
If signs of severe obstruction
develop, triage as Emergent
and begin AHA airway clearing
maneuvers (see reverse)
If student’s efforts clear the
obstruction, contact
parent/guardian to transport
student to medical care or
home
Notify school administrator
Provide psychological support
Follow up
NONURGENT
Witnessed
ingestion/aspiration
Student clears obstruction
by coughing
No S/S of continued
obstruction
INTERVENTIONS
Observe student at
frequent intervals
throughout day
Contact parent/guardian
Provide psychological
support
Return student to class or
send home as indicated
Follow up
NOTE: If student
continues to cough the
next day, suspect retained
bronchial foreign body,
bronchitis, or pneumonia.
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
66
AHA Airway Clearing Maneuvers
Responsive Infant
Sit or kneel, holding the infant prone. Rest your forearm on your thigh
and support the infant’s head by firmly holding the infant’s face and jaw.
Place your other hand on the infant’s back, supporting the occiput. The
infant should be sandwiched between your forearms, with the head
lower than the trunk.
Using the heel of your hand, deliver 5 forceful back slaps (Figure 1).
Turn the infant supine while continuing to support the head and neck.
Position the infant on your thigh, keeping the head lower than the trunk.
Continue to support the occiput with one hand. Place your other hand
just below the intermammary line, as you would to deliver chest
compressions. Deliver 5 quick downward chest thrusts (Figure 2).
Continue to alternate back slaps and chest thrusts until either the object
is expelled or the infant becomes unresponsive.
Figure 1
Figure 2
Figure 3
Unresponsive Infant
Look in the infant’s mouth. Attempt to remove the object if it is visible.
Open the airway using a jaw-thrust maneuver. Attempt rescue breaths.
If the breaths are not effective, reposition the infant’s head and try
again.
Begin CPR, compressing the sternum with 2 fingers just below the
intermammary line.
Look inside the mouth before each series of rescue breaths and attempt
to remove the object if it is visible. Repeat these steps up to 1 minute
until either the object is dislodged or rescue breathing is successful.
If attempts are not successful after 1 minute, activate EMS.
Return to CPR until efforts are successful or EMS responders arrive.
Responsive Child
Stand or kneel behind the child. Place your arms directly under the
child’s axillae, encircling the chest.
Place the radial side of your fist against the child’s abdomen at the
midline, slightly above the navel and well below the tip of the xiphoid
process.
Grasp your fist with your other hand. Deliver a series of quick abdominal
thrusts, directed inward and upward (Figure 3). Make each thrust
separate and distinct. Use sufficient force to dislodge the obstruction,
but do not compress the xiphoid process or the lower margins of the rib
cage, as this could damage internal organs.
Repeat the series of abdominal thrusts until the object is expelled or the
child becomes unresponsive.
Unresponsive Child
Look in the child’s mouth. Attempt to remove the object if it is visible.
Open the airway using a jaw-thrust maneuver. Attempt rescue breaths.
If the breaths are not effective, reposition the child’s head and try again.
Position yourself either kneeling beside or straddling the child’s hips.
Begin CPR (Figure 4).
Look inside the mouth before each series of rescue breaths and attempt
to remove the object if it is visible. Continue CPR up to 1 minute, until
either the object is dislodged or rescue breathing is successful.
If attempts are not successful after 1 minute, activate EMS.
Return to CPR until efforts are successful or EMS responders arrive.
Figure 4
Figs: American Heart
Association, Pediatric
Advanced Life Support
Provider Manual, 2000
AHA indicates American Heart Association

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
67
Headache
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR HEADACHES
Mental status/neurologic assessment
Past health history of headaches or recent
head injury
Events leading up to onset, such as stress,
exposure to a known trigger, aura
Focused physical assessment for neck stiffness
Assessment for visual disturbances (see Eye
Emergencies protocol)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Change in mental status, LOC
Acute neurologic deficit
Seizure activity (see Seizures
protocol)
Severe headache (eg, c/o “worst
headache of my life”)
Stiff neck with fever
Recent head injury
Hypertension
INTERVENTIONS
Support ABCs
Activate EMS
Consult IHP/ECP
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Moderate headache with vomiting
History of aura
Exposure to known trigger
Blurred vision, dizziness,
photophobia
No neurologic deficit
History of migraines
INTERVENTIONS
Determine need for EMS
Provide rest in quiet, darkened
room
Consult IHP/ECP
Administer medication per
IHP/ECP
Observe student closely
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
Generalized mild headache
S/S of URI
S/S of sinus infection
INTERVENTIONS
Allow student to rest
supine for 30 min
Consult IHP/ECP
Administer medication per
IHP/ECP
Observe student
Reassess
Educate about avoiding
triggers
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.
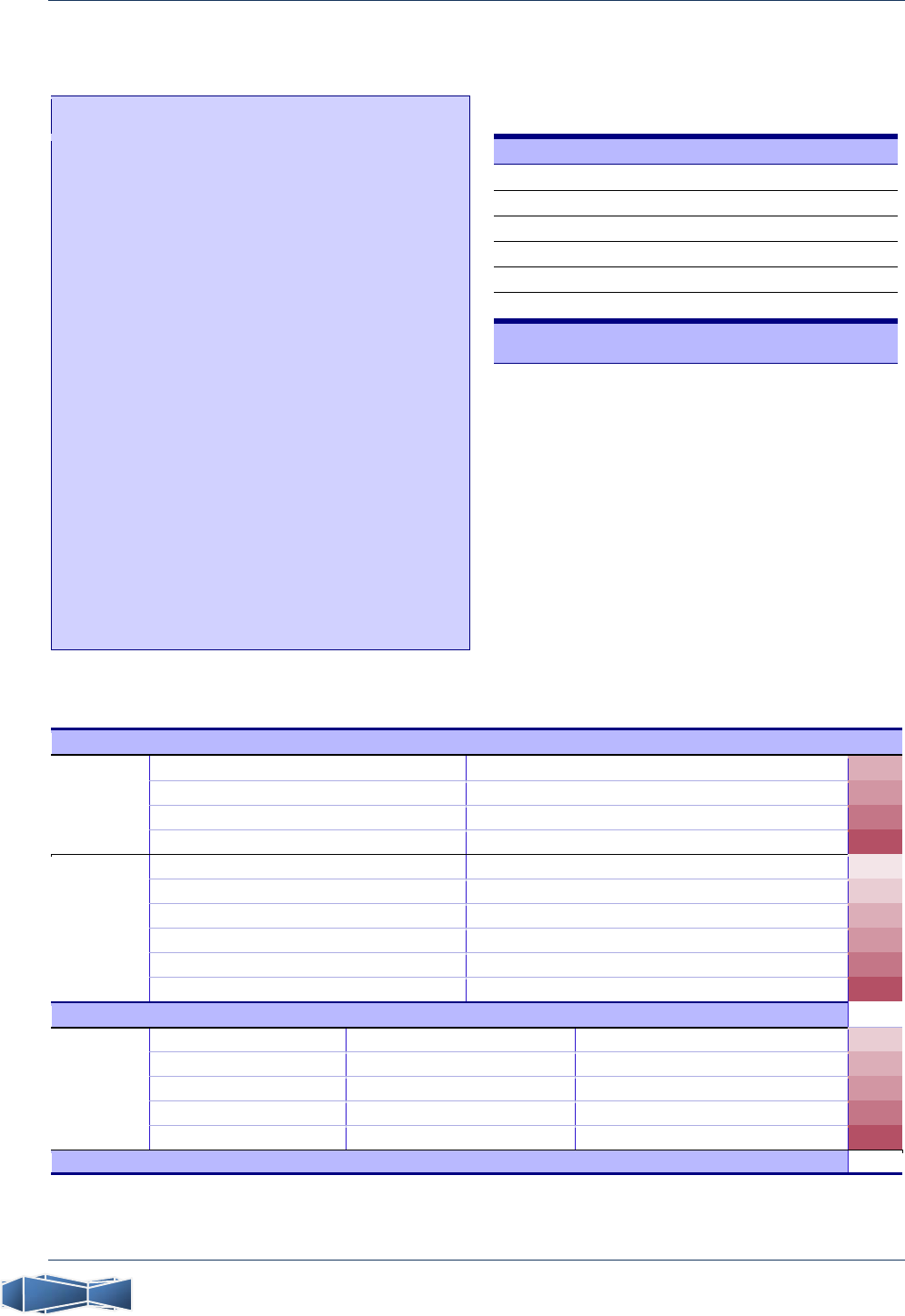
P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
68
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
69
Head/Spinal Cord Trauma
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO.
Stabilize c-spine—DO NOT move student!
KEY ASSESSMENT POINTS FOR HEAD/SPINAL CORD TRAUMA
Mental status/neurologic assessment
Events leading up to injury
Mechanism of injury
Assessment for visual disturbances (see Eye
Emergencies protocol)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Change in mental status, LOC
(including drowsiness, lethargy)
Abnormal behavior/loss of
normal abilities
Seizure activity (see Seizures
protocol)
Loss of/decreased movement or
sensation in extremities
Blood/CSF discharge from
nose/ears
Significant trauma to head/neck
or high-risk mechanism of
injury
Evidence of depressed skull
fracture
Paresthesia
INTERVENTIONS
Support ABCs
Activate EMS
Maintain c-spine stabilization
Apply direct pressure to
bleeding except over depressed
skull injury
Keep student warm
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Brief period of
confusion/amnesia
Neck pain
Dizziness
Blurred vision/diplopia
Headache
Nausea/vomiting
Laceration requiring sutures
(see Lacerations/Abrasions
protocol)
INTERVENTIONS
Support ABCs
Determine need for EMS
Maintain c-spine stabilization
Control bleeding with direct
pressure
Apply cold packs to swollen
areas
Keep student warm
Observe student closely
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Alert
Minor abrasions, lacerations, or
edema
INTERVENTIONS
Apply cold packs as indicated
Observe student closely
Reassess after 15–30 min
Contact parent/guardian
Return student to class or send
home as indicated
Advise parent/guardian, teachers,
coaches of injury and emphasize
need for observation over next
24–48 hours, seeking medical
care if the student exhibits any of
the following:
dizziness
headache
nausea
photophobia
diplopia
irritability
poor concentration
decline in academic ability
personality changes
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
70
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
71
Heat-related Injuries
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR HEAT-RELATED INJURIES
Skin assessment (eg, color, other skin findings)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of heat stroke
Hyperthermia (T exceeding
104°F/40°C)
Confusion/diminished LOC
Hot/dry/red skin
Tachycardia/weak peripheral
pulses
Syncope
Ataxia
Seizure activity (see Seizures
protocol)
INTERVENTIONS
Heat stroke is a life-
threatening emergency!
Support ABCs
Activate EMS
Immediately remove from heat
to a cool environment
Immediately initiate cooling
measures:
Loosen clothing
Apply cool, wet towels to
neck, groin, axillae
Sponge with cool compresses
Fan student
Place in left lateral recovery
position in case of vomiting
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Oriented
Mild tachycardia
S/S of heat exhaustion
Cool, moist, pale skin
Dilated pupils
Mild to moderate headache
Nausea/vomiting
Muscle cramps
Weakness, dizziness
Normothermic to mildly
hyperthermic (T less than
101°F/38.3°C)
Diaphoresis
Orthostatic vital signs
a
INTERVENTIONS
Determine need for EMS
Observe continuously
Allow to rest in cool environment
Loosen clothing
Apply cool, wet towels
Fan student
In the absence of vomiting,
encourage fluid replacement with
water or a diluted electrolyte-
replacement drink as permitted
by applicable protocols
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
Mild cramping of calves,
thighs, shoulders
Normothermic
Awake and alert
INTERVENTIONS
Allow to rest in cool
environment
Loosen clothing
Observe student
Encourage fluid replacement
with water or a diluted
electrolyte-replacement
drink as permitted by
applicable protocols
Educate student about
maintaining adequate
hydration during higher-risk
activities
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
a
Orthostatic vital signs
Assess BP and HR while student is supine. Have student sit up or stand and reassess 1 min later. If BP decreases
by more than 20 mm Hg or HR increases by 20 bpm, orthostasis is present.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
72
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
73
Hemophilia
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR HEMOPHILIA
History relating to recent surgery, medical
procedures, dental extractions, or injuries
Focused physical examination for external
bleeding, lacerations, ecchymoses, abrasions,
hematomas
IMMEDIATE INTERVENTIONS
Even before you determine triage category, attempt to control external bleeding by applying
firm pressure for 10 min
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of internal bleeding:
Headache
Dizziness
Visual disturbances
Neurologic deficit
Altered LOC/pupillary
changes
Signs of shock
Profuse, uncontrollable
hemorrhage
Severe abdominal pain
INTERVENTIONS
Support ABCs
Activate EMS
For shock, place in
Trendelenburg position
Consult IHP/ECP
Directly/continuously
observe student
Frequently reassess vital
signs and AVPU
Contact parent/guardian
Notify school
administrator
Follow up
URGENT
Acute joint swelling/pain
Abdominal discomfort, tenderness on
palpation, nausea
External bleeding not responsive to
prolonged pressure
Indications of intramuscular hematoma
(most commonly felt in knees, ankles,
elbows): tingling, pain, limited ROM,
edema, increased warmth/tenderness
INTERVENTIONS
Support ABCs
Determine need for EMS
Consult IHP/ECP
Reassess vital signs
Apply cold pack to swollen joint
Observe student closely
Contact parent/guardian to transport
student to medical care or home
Follow up
NONURGENT
Minor lacerations,
ecchymoses, abrasions
Bleeding responds to
pressure
INTERVENTIONS
Apply firm, direct pressure
Apply cold pack as
indicated
Consult IHP/ECP
Observe student
Contact parent/guardian
Return to class when
bleeding stops or send
home as indicated
Educate student
parent/guardian and school
personnel about
playground/sport safety
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
74
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
75
Increased Intracranial Pressure in a Student With a
Ventriculoperitoneal Shunt
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR STUDENTS WITH VP SHUNTS
Facial symmetry
Gag reflex
Pupil size/reactivity
Extraocular eye movements
Neurologic function
Pediatric GCS score
Symmetry of function/strength, posture, gait,
balance, spontaneous movement
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Change in mental status, LOC
Lethargy
Acute neurologic deficit
Inability to look up/roll eyes
upward
New onset eye deviation
Seizure (see Seizures protocol)
INTERVENTIONS
Support ABCs
Activate EMS
Consult IHP/ECP
Directly/continuously observe
student
Contact physician for
instructions
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Early S/S of shunt dysfunction:
Headache
Irritability
Vomiting
Decreased appetite
Change in personality
Loss of existing skills or abilities
Swelling/erythema along shunt
path
Seizures
Loss of balance
S/S of shunt tract infection
INTERVENTIONS
Support ABCs
Determine need for EMS
Place student supine
Elevate head
Allow student to rest
Reduce environmental stimuli
Consult IHP/ECP
Observe student closely
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
Headache
Normal neurologic
assessment and PGCS
score
INTERVENTIONS
Consult IHP/ECP
Allow student to rest 30
min, then reassess
Contact parent/guardian
Return student to class or
send home as indicated
Reassess every 2 hours if
student remains at school
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
76
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
77
Lacerations/Abrasions
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR LACERATIONS AND ABRASIONS
Inspection of wound
Neurovascular assessment distal to injury:
Pain, pulse, pallor, paresthesia, paralysis (5 Ps mnemonic)
Capillary refill
Edema
Skin temperature
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Absent distal pulses
Significant blood loss
Crush injury
Amputation (see Trauma protocol)
Penetrating wound
Capillary refill exceeds 2 sec
Altered LOC
S/S of respiratory distress
INTERVENTIONS
Support ABCs
Activate EMS
Control hemorrhage
Elevate/immobilize extremity
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Stable vital signs
Pulses present distal to injury
Significantly contaminated
lacerations
Facial lacerations
Puncture wounds of foot
Wounds requiring sutures
Controllable bleeding
INTERVENTIONS
Support ABCs
Determine need for EMS
Control bleeding with direct
pressure
Observe student closely
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Stable vital signs
Superficial abrasion,
scrape, or wound
Small splinter or foreign
body
INTERVENTIONS
Remove splinter
Cleanse wounds using
aseptic technique
a
Bandage wounds
Observe student
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
a
General wound care/aseptic cleansing
Clean wounds thoroughly with soap.
Rub abrasions gently with 4x4 gauze to remove debris and crusts.
Rinse copiously with water.
Bandage abrasions loosely, using nonadherent gauze to allow air circulation.
Apply butterfly bandage to lacerations after bleeding has been controlled.
Due to high risk of infection, all deep puncture wounds of the foot must be
referred to a physician.
NOTE
Refer student for tetanus booster if it has been 5 years or more since the
last vaccination. Tetanus booster is recommended every 10 years.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
78
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
79
Musculoskeletal Injury
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
KEY ASSESSMENT POINTS FOR MUSCULOSKELETAL INJURIES
Focused physical examination of affected area:
Bilateral symmetry
ROM/strength
Visual inspection for abnormalities
Neurovascular status distal to injury:
Pain, pulse, pallor, paresthesia, paralysis (5 Ps)
Edema
Capillary refill
Skin temperature
IMMEDIATE INTERVENTIONS
Even before you determine triage category,
immobilize and support affected area proximal and distal to injury
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Open fracture
Amputation (see Trauma protocol)
Degloving injury
Neurovascular compromise
Severe edema/deformity at joint or
extremity
Joint deviation
Suspected femoral fracture
INTERVENTIONS
Support ABCs
Activate EMS
Instruct student to avoid weight-
bearing/movement of injured area
Immobilize and position suspected
fractures/dislocations (see reverse)
Reassess neurovascular status distal
to injury every 5–10 min
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Stable vital signs
Moderate deformity/discoloration
without open wound
Moderate edema at joint or
extremity
Moderate pain/guarding
Normal neurovascular findings
INTERVENTIONS
Support ABCs
Determine need for EMS
Immobilize and position suspected
fracture/dislocation (see reverse)
Elevate extremity
Apply cold packs
Observe student closely
Reassess neurovascular status
distal to injury every 5–10 min
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
Normal vital signs
No deformity
Mild soft tissue
edema
Mild pain/point
tenderness
Able to bear weight
Normal neurovascular
findings
INTERVENTIONS
Apply cold pack
Elevate area
Observe student
Contact
parent/guardian
Return student to
class or send home
as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.
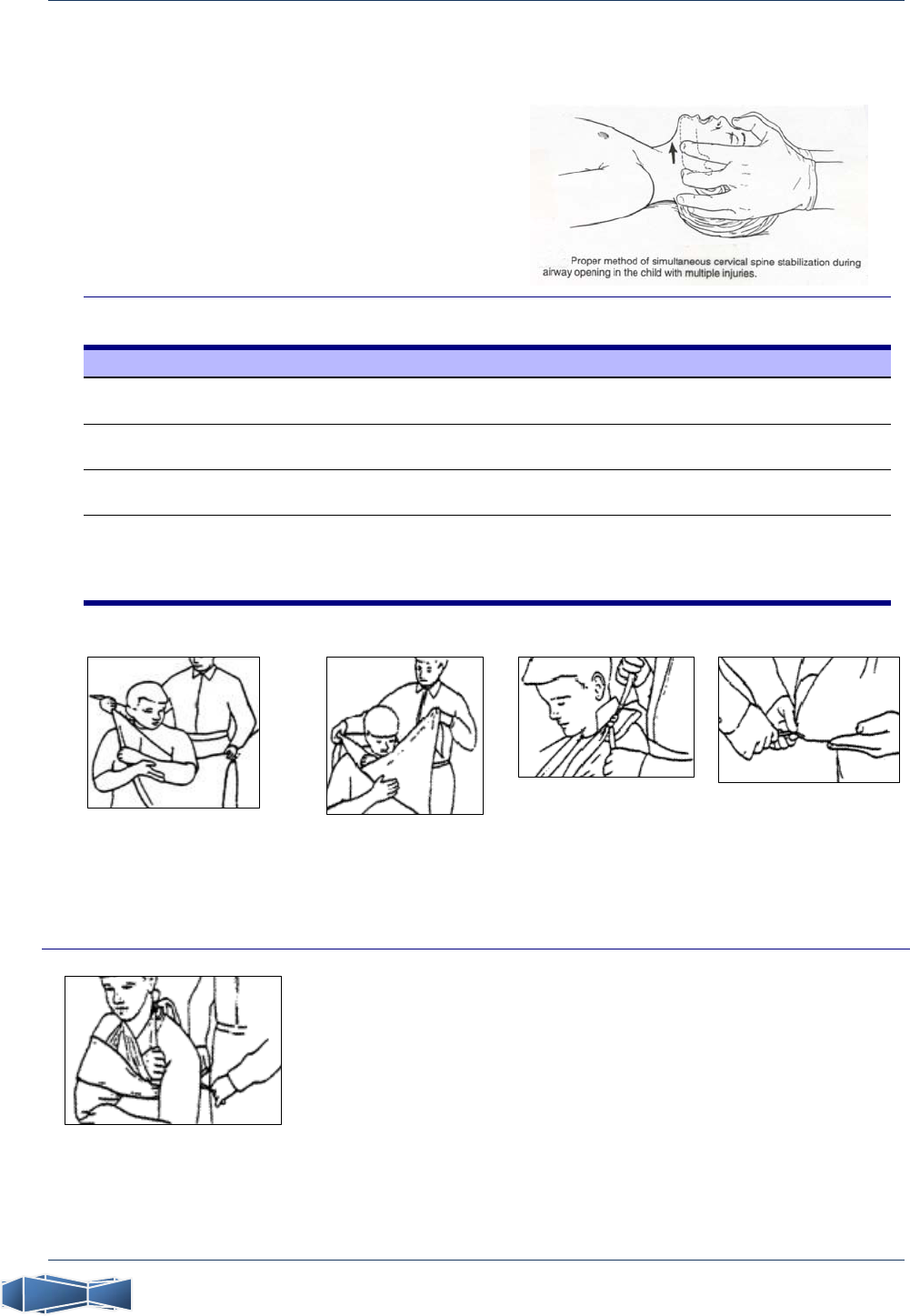
P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
80
Interventions for Musculoskeletal Injuries
MANUAL CERVICAL SPINE STABILIZATION
Position student supine
Place both hands along lateral aspect of student’s
head
Position the head so that the neck is in neutral
alignment with the spine
Continue to support the head to maintain neutral
cervical alignment
IMMOBILIZATION/POSITIONING OF FRACTURES AND DISLOCATIONS
Area/Injury Treatment
Upper extremity Apply sling/triangular bandage
Swathe if additional immobilization is indicated
Clavicular injury/dislocation Apply sling/triangular bandage
Swathe if additional immobilization is indicated
Angulation with unimpaired
circulation
Immobilize as presented
Do not move extremity
Angulation with absent distal
pulse, cyanosis
Return extremity to proper physiologic position
Apply gentle traction until pulse is restored
Splint or immobilize area, including joints proximal and distal to injury
Reassess pulses every 5–10 minutes
SLING AND SWATHE IMMOBILIZATION
Place the arm across the chest
and position as shown. Bring the
bandage over the arm and
behind the neck.
Adjust the length as
necessary and tie the
ends. The arm should
be well supported,
relieving pressure on
the shoulder.
Place the knot so that it
lies over the shoulder
rather than against the
cervical spine. Placing a
pad under the knot will
enhance comfort.
Secure the sling at the
elbow with a safety pin
or knot, creating a
pocket in which the
elbow rests securely.
Reassess neurovascular
integrity.
If further immobilization is needed to secure the
extremity and a second bandage is available,
swathe the arm as permitted by applicable
protocols. Lay the second bandage flat, then fold it
several times lengthwise. Use the folded bandage
to swathe the injured arm against the chest wall,
immobilizing it.

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
81
Near-drowning/Submersion
CAUTION
Ensure scene safety! Never attempt a water rescue unless you are trained to do so.
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR SUBMERSION INJURIES
Skin assessment
Duration of exposure
Inspection for associated injuries
KEY FINDINGS
Dyspnea, rales, rhonchi, wheezing, or apnea
Bradycardia or asystole
Cyanosis/pallor
Altered LOC
Fixed, dilated pupils
Hypothermia, cool skin
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
The triage category for ALL instances of near-drowning is EMERGENT!
INTERVENTIONS
Activate EMS
EMS transport to ED for evaluation is REQUIRED in
all cases of near-drowning!
If still in water
Do not remove student without assistance
Keep student afloat face-up
Support head and neck in neutral alignment with spine
Open airway using jaw thrust and support ventilation
When adequate assistance is available, place student
supine on backboard or other rigid support for removal
from water
If out of water
Support ABCs (use jaw thrust technique if spinal injury is
suspected)
Assess Pediatric Glasgow Coma Scale score
Cover student and maintain warmth to prevent
hypothermia
In all cases
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
82
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
83
Nose Emergencies
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
KEY ASSESSMENT POINTS FOR EMERGENCIES INVOLVING THE NOSE
Airway status
Mechanism of injury/events preceding episode
Physical assessment/inspection for
abnormalities, bleeding, drainage
IMMEDIATE INTERVENTIONS
Even before you determine triage category, begin to control bleeding with pressure
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Suspected nasal fracture
with potential head/neck
injury (see Head/Spinal
Cord protocol)
Change in mental status,
LOC
Airway compromise
CSF drainage
INTERVENTIONS
Maintain spinal
stabilization as applicable
Support ABCs
Activate EMS
Directly/continuously
observe student
Keep student calm
Contact parent/guardian
Notify school
administrator
Follow up
URGENT
Suspected nasal fracture, no
possibility of head/neck
injury
Tenderness on palpation
Epistaxis not controlled after
10 min
Moderate periorbital edema
INTERVENTIONS
Determine need for EMS
Prolonged epistaxis
Pinch nostrils closed and
apply pressure for 10 min
If epistaxis continues,
consider activating EMS
Suspected nasal fracture
Apply cold packs
See Lacerations/Abrasions
protocol for treatment of
associated wounds
In all cases
Observe student closely
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Foreign body
Controllable epistaxis
S/S of acute sinusitis:
Pain/pressure over sinus areas
Throbbing
Headache, malaise, fever
Mucopurulent secretions
Mild periorbital edema
INTERVENTIONS
Epistaxis
Pinch nostrils closed and apply pressure
for 10 min
Foreign body
Have student blow nose while occluding
unobstructed nostril
Attempt removal only if object is
visible and can be grasped with forceps
or fingers
During extraction, occlude nostril
superior to object so that it cannot be
pushed further in
If object cannot be removed, reclassify
as urgent
In all cases
Observe student
Contact parent/guardian for referral to
primary care physician
Return student to class or send home
as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
84
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
85
Obstetric Emergencies
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol),
performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR OBSTETRIC EMERGENCIES
Obstetric history:
Anticipated due date
Recent drug use
Possibility of multiple births
Prenatal care (name/phone # of obstetrician)
Delivery hospital
Color of amniotic fluid (clear, red, green, yellow-
tinged)
Progression of labor
Bloody show/expulsion of mucous plug
Timing/strength of contractions
Inspection for crowning
Reported urge to move bowels
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of shock
Seizure activity (see Seizures protocol)
S/S of preeclampsia:
BP equals or exceeds 140/90 or
BP elevated by 30 mm Hg (systolic) or
15 mm Hg (diastolic) above known
baseline
Crowning
Breech presentation
Prolapsed umbilical cord
Abruptio placentae
Placenta previa/vaginal bleeding
Multigravida
Premature labor
Contractions less than 10 min apart
INTERVENTIONS
Support ABCs
Activate EMS
For signs of shock, if delivery is not
imminent, place in left lateral recovery
position
If delivery is imminent, prepare for
emergency delivery (see reverse for
neonatal care)
Directly/continuously observe student
Notify school administrator
Follow up
URGENT
Pregnancy-induced
hypertension
History of trauma
Active labor, amniotic sac
intact
Contractions more than 10 min
apart
INTERVENTIONS
Determine need for EMS
Observe student closely
Contact parent/guardian to
transport student for medical
care
Monitor closely
Follow up
NONURGENT
Variable
contractions
Amniotic sac intact
Vomiting with stable
vital signs
INTERVENTIONS
Observe student
Contact
parent/guardian to
transport student
for medical care
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
86
Emergency Neonatal Care
IMMEDIATE INTERVENTIONS
Suction the infant’s mouth first, then the nose
Dry the infant with a towel
Rewrap the infant in a warmed, clean, dry towel or blanket; cover head
Stimulate breathing by rubbing infant’s back or flicking feet
Resuscitate if necessary according to current AHA guidelines
Calculate Apgar score (below)
NOTE
Do not interrupt resuscitation procedures to calculate Apgar score.
Directly/continuously observe student and infant
Contact significant others per student’s request
APGAR SCORING CRITERIA
Unless resuscitation measures are needed, assess the baby’s Apgar score 1 minute
after birth and again 5 minutes after birth. The Table summarizes categories and scoring.
APGAR EVALUATION OF THE NEONATE
Sign 0 1 2
A
Appearance (color)
Cyanotic or pallid
Centrally pink,
extremities cyanotic
Completely pink
P
Pulse rate
Absent
Slower than 100
bpm
Faster than 100
bpm
G
Grimace (reflex
irritability)
a
No response Grimace Cough/cry/sneeze
A
Activity (muscle
tone)
Limp
Some flexion
(extremities)
Active movement
R
Respiratory effort
Absent Slow/irregular Good; cries
a
In response to nasal or oral stimulation. bpm indicates beats per minute
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
87
Respiratory Distress
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR RESPIRATORY DISTRESS
Breathing assessment
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
Loosen restrictive clothing Help student into position of comfort Maintain airway patency
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
S/S of severe respiratory distress or failure
Apnea or dyspnea
Grunting, drooling
S/S of impending respiratory failure
Cyanosis
Tachycardia
Shallow respiration
Decreasing LOC/restlessness
Hypotension
S/S of airway obstruction (see Foreign Body
protocol)
Severe asthma attack (see Asthma protocol)
S/S of epiglottitis (dysphagia, drooling, high
fever, stridor, tripod positioning)
INTERVENTIONS
Support ABCs
Activate EMS
Maintain position of comfort
Administer high-flow O
2
as tolerated if
available
Epiglottitis
Do not inspect hypopharynx
Keep student calm
Respiratory failure
Assist ventilation via mouth-to-mask
Anticipate need for CPR
In all cases
Directly/continuously observe student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
S/S of moderate
respiratory distress
Fever, chills
Persistent or barky
cough
Stridor, wheezing
Nasal flaring
Retractions
Pleural pain
Mild to moderate
asthma (see Asthma
Attack protocol
INTERVENTIONS
Support ABCs
Determine need for EMS
Maintain position of
comfort
Observe student closely
Contact parent/guardian
to transport student to
medical care or home
Follow up
NONURGENT
Hyperventilation
S/S of mild URI
Cough
Nasal congestion
Sore throat
Hoarseness
Low-grade fever
INTERVENTIONS
For hyperventilation
Encourage student to
relax
In all cases
Observe student
Contact
parent/guardian
Return student to
class or send home as
indicated (send home
for fever in which T
exceeds
100°F/37.8°C)
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
88
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
89
Seizures
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
Open airway as necessary, using jaw-thrust maneuver
KEY ASSESSMENT POINTS FOR SEIZURES
Past health history, particularly of
Epilepsy
Syncope
Diabetes
Events preceding episode, particularly head injury
Indicators of drug overdose, meningitis,
hypoglycemia (see Diabetic Emergencies and
Substance Abuse protocols)
IMMEDIATE INTERVENTIONS
During an active seizure, perform the following actions before you proceed with triage:
Do not put anything in student’s mouth—do not restrict movement in any way
Provide privacy
Protect student from injury
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
First-time seizure/no known history
of seizures
History of seizures and medication
noncompliance with no recent
seizures
Seizure/series of seizures
persisting more than 5 min
Associated respiratory compromise
Associated head injury or trauma
INTERVENTIONS
Support ABCs
Activate EMS
Consult IHP/ECP
Directly/continuously observe
student
Provide psychological support
Document time, characteristics,
duration of seizure
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Atypical seizure in student
with history of seizures
INTERVENTIONS
Support ABCs
Determine need for EMS
Consult IHP/ECP
Check glucose if possible
Allow to rest in left lateral
recovery position
Provide psychological
support
Observe student closely
Document characteristics/
duration of seizure
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Typical seizure in student with
baseline history of frequent
seizures
INTERVENTIONS
Consult IHP/ECP
Check glucose if possible
Allow to rest in left lateral
recovery position during
postictal phase
Provide psychological support
Observe student
Document characteristics/
duration of seizure
Contact parent/guardian
Return student to class or
send home as indicated
For persistent drowsiness,
notify parent/guardian to
transport student home
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
90
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
91
Sexual Abuse/Assault, Teen Dating Violence
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR SEXUAL ABUSE OR ASSAULT
Psychosocial history
Menstrual status/possibility of pregnancy
Focused physical examination for injuries
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
Provide a safe, nonthreatening environment
Ask questions that will help student recognize
what has happened
Reinforce student’s courage in seeking help
Try to ascertain whether sexual assault took
place
(NOTE: Any instance of suspected sexual
assault requires ED treatment and local
law enforcement notification)
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Thoughts of death or suicide
Severe/life-threatening injuries
(see Trauma protocol)
Suspected sexual assault
INTERVENTIONS
Support ABCs
Activate EMS
Directly/continuously monitor
student
Refer to school counselor as
appropriate
Report suspicions to DCFS at
800-25-ABUSE (22873)
and/or local law
enforcement as appropriate
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Ecchymoses/injuries, not
life-threatening
Alcohol/drug use
Current, previous, or
potential pregnancy
INTERVENTIONS
Support ABCs
Determine need for EMS
Observe student closely
Provide support
Refer to school counselor
Report suspicions to
DCFS at 800-25-ABUSE
(22873) and/or local law
enforcement
Contact parent/guardian to
transport student to
medical care or home
Follow up
NONURGENT
History of truancy
Sudden change in dress or makeup
Difficulty making decisions
Abrupt changes in
mood/personality
Combative, possessive, or jealous
behavior
Withdrawal/self-isolation
INTERVENTIONS
Refer to school counselor
Observe student’s behavior with
others
Document findings
Provide support
Contact parent/guardian
Return student to class or send
home as indicated
Report suspicions to DCFS at
800-25-ABUSE (22873) and/or
local law enforcement
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
92
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
93
Sickle Cell Anemia
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR SICKLE CELL ANEMIA
Past health history, including recent illness
Last food/drink (likelihood of dehydration)
Events leading up to episode, including
exposure to temperature extremes
Focused physical examination/palpation for
localized pain, edema, other abnormalities
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Fever (T exceeds 100°F/37.8°C)
S/S of infection, sepsis
Severe, continuous pain in extremities, back,
chest, or abdomen
Seizure activity (see Seizures protocol)
Change in mental status, LOC
Dyspnea
Chest pain
Priapism/penile pain
Severe splenomegaly and S/S of shock
Pallor, lethargy with other abnormal findings
S/S of impending respiratory collapse:
Cyanosis
Tachycardia
Shallow respiration
Decreasing LOC/restlessness
Hypotension
Decreased breath sounds
Respiratory distress (acute chest syndrome)
INTERVENTIONS
Support ABCs
Activate EMS
Refer to IHP/ECP
Respiratory distress/shock
Administer high-flow O
2
if available
Help to maintain position of comfort (shock
position as indicated)
In all cases
Directly/continuously observe student
Reassess vital signs every 5 min
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Fever (T exceeds
100°F/37.8°C)
Mild to moderate pain
Severe
edema/tenderness of
affected areas
INTERVENTIONS
Support ABCs
Determine need for EMS
Refer to IHP/ECP
Provide oral hydration
(4–8 oz/hour)
Allow to rest
Elevate affected
extremity
Observe student closely
Contact parent/guardian
to transport student to
medical care or home
Educate student about
need for good oral
hydration, protection
from temperature
extremes
Follow up
NONURGENT
Minor localized pain
INTERVENTIONS
Refer to IHP/ECP
Provide oral hydration
(4–8 oz/hour)
Allow to rest
Reassess pain
Contact parent/guardian
Observe student
Return student to class
or send home as
indicated
Reassess every 2 hr if
student remains at
school
Educate student about
need for good
hydration, protection
from temperature
extremes
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
94
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
95
Substance Abuse
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR SUBSTANCE ABUSE
Respiratory assessment
Orientation to person/place/time
Ability to recall event/injuries incurred
Type/amount of substance involved (request
medication/drug container if available)
Time/route of exposure (dermal, ocular,
inhalation, ingestion)
Underlying health problems (SAMPLE history)
Other students involved
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Respiratory/cardiac arrest
Unconscious/can’t be roused
Change in LOC
Labored/shallow breathing
Hallucinations, violent
behavior, extreme agitation
S/S of trauma or injury
Seizure activity (see Seizures
protocol)
INTERVENTIONS
Support ABCs
Initiate CPR as appropriate
Activate EMS
Place student in left lateral
recovery position
Directly/continuously observe
student
Monitor airway/respiratory
status
See Trauma protocol as
appropriate
Contact PCC as indicated
a
Contact parent/guardian
Notify school administrator
Initiate counseling/support
measures per school policy
Follow up
URGENT
Somnolence, emesis, unusual
behavior
Unsteady gait
Memory problems
Mild agitation/restlessness
Suspicious odors
Needle marks/drug residue on
skin, nose, clothes
Previous loss of consciousness
Complicating health problems
INTERVENTIONS
Determine need for EMS
Observe student continuously
Give nothing by mouth
Remain with student
See Trauma protocol as
appropriate
Contact PCC as indicated
a
Contact parent/guardian to
transport student to medical care
or home
Notify school administrator
Initiate counseling/support
measures per school policy
Follow up
NONURGENT
Coherent and oriented
Stable vital signs
No loss of consciousness
INTERVENTIONS
Support ABCs
Observe student
Remain with student
Contact PCC as indicated
a
Notify school administrator
Contact parent/guardian
Return student to class or
send home as indicated
Initiate counseling/support
measures per school policy
Follow up
a
When calling the Poison Control Center (800-222-1222), identify yourself as a health care professional
and provide the following information: your name and phone number; student’s name, age, weight, and
vital signs; substance involved (if known); amount, time, route, and duration of exposure; abnormal
S/S; first aid and immediate interventions rendered.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
96
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
97
Suicide Prevention
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR POTENTIAL SUICIDE
Focused Psychosocial Examination/Risk Factor Assessment
Precipitating events
Parents recently divorced
Multiple life stressors
Recent breakup with girlfriend or boyfriend
Unplanned pregnancy
Preparatory actions
Acquiring the means
Putting affairs in order
Suicide talk
Giving away prized possessions
Precautions against discovery
Current Symptoms
Hopelessness/powerlessness
Depressed mood
Suicidal ideation
Abrupt change in personality
History
Previous suicide attempts
Affective disorders or conduct disorder
Family history of mental illness, suicidal
behavior, or affective disorders
Alcoholism or substance abuse
Chronic health condition
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Thoughts of death
Suicide plan, preparations
Suicide attempt
Previous suicide attempt
INTERVENTIONS
Support ABCs as indicated
Activate EMS
Remove personal effects
Do not leave student alone
under any circumstances!
Listen to student carefully
Take conversation seriously
Notify crisis response team
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Suicidal ideation
Depression
Withdrawal
Self-blame
Self-reproach
INTERVENTIONS
Determine need for EMS
Remain with student at all
times
Listen to student
Notify crisis response team
Contact parent/guardian to
transport student to medical care
or home
Follow up
NONURGENT
Frequent physical complaints
Sad affect
INTERVENTIONS
Observe student regularly
Refer to school counselor
Notify crisis response team of
your concerns and findings
Contact parent/guardian
Return student to class or
send home as indicated
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
98
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
99
Syncope/Unconsciousness
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
Stabilize c-spine if head/spinal injury is suspected!
KEY ASSESSMENT POINTS FOR SYNCOPE
Mental status/neurologic assessment
Psychosocial history
Past health history/current menstrual status
Medications taken
Events leading up to episode, including
activities, weather conditions
Last food/drink taken
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Acute change from baseline
mental status/LOC
Irregular pulse
Acute neurologic deficit
Head injury/headache with
altered LOC or vomiting
Severe headache with altered
LOC
Head injury/history of anemia,
hemophilia, other coagulopathy
Associated seizure activity (see
Seizures protocol)
INTERVENTIONS
Maintain c-spine stabilization as
applicable
Support ABCs
Activate EMS
Directly/continuously observe
student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Possible VP shunt dysfunction
Orthostatic vital signs
a
S/S of moderate
hypoglycemia
Signs of dehydration
Severe headache without
altered LOC
Persistent or severe dizziness
Exercise-induced syncope
(possible cardiac etiology)
Possible medication reaction
without emergent findings
History of substance abuse or
eating disorder
INTERVENTIONS
Support ABCs as indicated
Determine need for EMS
Contact parent/guardian to
transport student to medical
care or home
Closely observe student
Follow up
NONURGENT
Hyperventilation
Vasovagal reaction to
anxiety/pain or other known
trigger
Exposure to ambient heat
Evidence of carotid sinus reaction
(eg, subsequent to neck hold by
classmate)
No associated injuries
INTERVENTIONS
Place student supine
Allow student to wake
spontaneously
For hyperventilation, encourage
student to relax
Observe student
Contact parent/guardian
Return student to class or send
home as indicated
Follow up
a
Orthostatic vital signs
Assess BP and HR while student is supine. Have student sit up or stand and reassess 1 min later. If BP decreases
by more than 20 mm Hg or HR increases by 20 bpm, orthostasis is present. Note: Syncopal episodes that are
not associated with rising or standing require further evaluation.
See the following protocols as appropriate:
Diabetic Emergencies Increased ICP in a Student With a VP Shunt
Head/Spinal Cord Trauma Seizures
Heat-related Injuries Trauma
Hemophilia
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
100
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
101
Throat Emergencies
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see reverse), performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR THROAT EMERGENCIES
Across-the-room assessment (note tripod
positioning)
Respiratory assessment
Events preceding illness/suddenness of onset
Focused physical examination with inspection of
pharynx, palpation of lymph nodes
IMMEDIATE INTERVENTIONS
Even before you determine triage category, perform the following actions as indicated
Loosen restrictive clothing
Maintain airway patency
Help student into position of comfort
TRIAGE CATEGORY/ADDITIONAL INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Airway compromise
Change in mental status, LOC
S/S of epiglottitis:
Sudden onset
Stridor, drooling, dysphagia
High fever
Anaphylactic reaction (see Anaphylaxis
protocol)
S/S of retropharyngeal abscess:
Fever
Stiff, painful neck
Asymmetric edema of posterior pharyngeal
wall
Dyspnea
INTERVENTIONS
Activate EMS
Support ABCs
Keep student calm
Administer high-flow O
2
as tolerated if
available
Epiglottitis
Do not inspect hypopharynx
Maintain position of comfort
In all cases
Directly/continuously observe student
Reassess vital signs every 5 min
Contact parent/guardian
Notify school administrator
Follow up
URGENT
S/S of peritonsillar
abscess:
Severe pain
Fever
INTERVENTIONS
Support ABCs
Determine need for EMS
Maintain position of
comfort
Contact parent/guardian
to transport student to
medical care or home
Observe student closely
Follow up
NONURGENT
Swollen, tender lymph
nodes
S/S of
tonsillitis/pharyngitis:
Tonsillar exudate
Erythema
Deviation of tonsils
toward midline
INTERVENTIONS
Observe student
Contact
parent/guardian
Return student to class
or send home as
indicated (send home
for fever exceeding
100°F/37.8°C)
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
102
Tools for Assessing Students
SYSTEMATIC ASSESSMENT
PEDIATRIC VITAL SIGNS BY AGE
NOTE: Perform interventions AS YOU GO. Determine
triage/activate EMS at EARLIEST INDICATION of need.
Scene safety assessment
Call for assistance as indicated
Across-the-room assessment
Use Pediatric Assessment Triangle (PAT)
Appearance Breathing Circulation
Initial assessment
Standard precautions C-spine stabilization
Airway Breathing Circulation D isability
a
Exposure
History/pain assessment
SAMPLE history PQRST/other pain assessment
Focused physical examination
Vital signs, temperature, weight, blood glucose
Inspect auscultate palpate
Triage
Emergent Urgent Nonurgent
a
Disability Assessment
Assess responsiveness (AVPU):
A Alert
V Responds to Verbal stimulus
P Responds to Painful stimulus
U Unresponsive
Assess pupils
Assess for transient paresthesia
Age RR HR BP
Neonate (0-30 days)
30-60 100-180 50-90
Infant (1-12 mo)
24-50 100-160 60-100
Toddler (1-3 yr)
24-40 90-150 80-105
Preschooler (3-5 yr)
20-30 80-140 95-105
School-aged (5-12 yr)
18-30 65-120 95-120
Adolescent (12 yr /up)
12-20 60-100 100-128
RR indicates respiratory rate; HR, heart rate; BP,
systolic blood pressure (mm Hg)
INDICATORS OF CARDIOPULMONARY
COMPROMISE IN CHILDREN
Tachycardia
Weak, thready, or absent peripheral pulses
Decreasing consciousness
Tachypnea/respiratory difficulty
Central cyanosis and coolness
Hypotension (late sign)
Bradycardia (ominous sign)
No palpable BP (ominous sign)
PEDIATRIC GLASGOW COMA SCALE
1 Yr or Older Younger than 1 Yr Score
Eye opening
Spontaneous Spontaneous 4
To verbal command To shout 3
To pain To pain 2
No response No response 1
Best motor
response
Obeys commands Spontaneous 6
Localizes pain Localizes pain 5
Flexion–withdrawal Flexion–withdrawal 4
Flexion–abnormal (decorticate rigidity) Flexion–abnormal (decorticate rigidity) 3
Extension (decerebrate rigidity) Extension (decerebrate rigidity) 2
No response No response 1
Older Than 5 Yr 2–5 Yr Younger than 2 Yr
Best verbal
response
Oriented Appropriate words/phrases Smiles/coos appropriately
5
Disoriented/confused Inappropriate words Cries, inconsolable 4
Inappropriate words Persistent cries/screams Persistent inappropriate cries/screams 3
Incomprehensible sounds Grunts Grunts, agitated, restless 2
No response No response No response 1
Total Score

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
103
Toxic Exposure (Ingestion/Environmental)
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol),
performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR TOXIC EXPOSURES
Assess/ensure scene safety (notify school administrator as indicated to activate hazmat protocols)
Respiratory assessment
Skin assessment
LOC/neurologic assessment, including PERRLA
Type/amount of substance (get container if
available)
Time/route of exposure (dermal, ocular,
inhalation, ingestion)
Location where exposure occurred
Subsequent S/S, especially respiratory status,
LOC, emesis
Ability to recall event, including injuries incurred
Underlying health problems (SAMPLE history)
Focused physical assessment, including injury,
odors
Other students involved
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
Refer to Toxidrome table (see reverse)
EMERGENT
Respiratory arrest
Seizures (see Seizures protocol)
Loss of consciousness
Dyspnea, severe respiratory
distress
Signs of shock/hypotension
INTERVENTIONS
Support ABCs
Activate EMS
Initiate CPR as necessary
Contact PCC
a
Refer for medical care as
recommended by PCC
Send MSDS and substance (if
possible) to ED with student
Contact parent/guardian
Notify school administrator
Follow up
URGENT
Unusual behavior
History of emesis
Minor abnormal findings
INTERVENTIONS
Determine need for EMS
Contact PCC
a
Refer for medical care as
recommended by PCC
Consult MSDS
Contact parent/guardian to
transport student to medical care
or home
Notify school administrator
Follow up
NONURGENT
Asymptomatic
Stable vital signs
INTERVENTIONS
Observe student
Consult MSDS
Contact PCC
a
Refer for medical care as
recommended by PCC
Provide supportive care as
indicated
Contact parent/guardian
Return student to class or
send home as indicated
Notify school administrator
Follow up
NOTE
a
When calling the Poison Control Center (800-222-1222), identify yourself as a health care
professional and provide the following information: your name and phone number; student’s
name, age, weight, and vital signs; substance involved (if known); amount, time, route, and
duration of exposure; abnormal S/S; first aid and immediate interventions rendered.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that
caremust be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
104
Toxidromes
If assessment findings suggest a toxic ingestion and you do not know what substance is
involved, it may be helpful to look for signs of identifiable toxic syndromes (toxidromes).
Toxidromes involve a recognizable group of signs and symptoms that tend to occur
consistently with particular toxins. The Table describes the 4 major toxidromes and
provides mnemonics that can help you remember the associated findings. Examples of
substances that can cause each toxidrome are also included.
TOXIDROMES
Toxidrome Clinical Findings Causative Substances
Opioid
Constricted pupils
CNS depression
Respiratory depression
Heroin
Codeine
Fentanyl
Methadone
Sympathomimetic
Hypertension
Tachycardia
Hyperthermia
Diaphoresis
Dilated pupils
Epinephrine
OTC diet aids
Amphetamines
Oral decongestants (eg,
pseudoephedrine)
Bronchodilators
Anticholinergic
Listed phrases
may help you
recall clinical
findings
Hyperthermia (Hot as a hare)
Flushed skin (Red as a beet)
Hypertension, dry skin (Dry as a
bone)
Delirium (Mad as a hatter)
Dilated pupils (Blind as a bat)
Urinary retention (Full as a flask)
Tachycardia
Absent bowel sounds
Antihistamines
GI antispasmodics
Certain toxic plants (eg, jimson
weed, deadly nightshade,
amanita muscaria)
Certain toxic mushrooms
Atropine
Tricyclic antidepressants
Cholinergic
Diarrhea
Urination
Miosis, Muscle fasciculations
Bradycardia, Bronchorrhea
Emesis
Lacrimation
Salivation, Sweating
Weakness
Organophosphate and
carbamate insecticides
Mushrooms containing
muscarine (imocybe species,
amanita species, ibotenic
muscimol)
Physostigmine
CNS indicates central nervous system; OTC, over-the-counter; GI, gastrointestinal

| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
105
Trauma
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol), performing interventions AS YOU GO
Ensure scene safety before approaching
Stabilize c-spine if head/spinal injury is suspected
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Slow or fast RR, other S/S of respiratory distress/failure
Capillary refill exceeds 2 seconds, other S/S of shock
Currently/previously unconscious
Profuse hemorrhage
Penetrating wound or significant blunt trauma to head,
chest, or abdomen
Open chest wound
Suspected pelvic/femoral fracture
Suspected spinal injury with paresthesia
Amputation/crush injury
S/S of intra-abdominal injury:
Hematuria
Grey Turner sign (bluish discoloration of
flank/periumbilical area)
Abdominal asymmetry/distention
Tenderness/guarding/pain on gentle palpation
INTERVENTIONS
Support ABCs
Activate EMS
Maintain spinal stabilization
Place supine or in shock position
Keep student warm
Give nothing by mouth
Stabilize impaled object with dressings—do not remove
Splint/elevate suspected fracture
Control hemorrhage
Directly/continuously observe
Frequently reassess vital signs/AVPU
Contact parent/guardian
Notify school administrator
Follow up
Amputation management
Wrap part in gauze slightly moistened with sterile saline
Place in plastic bag, seal securely, and label
Place bag on cold packs for transport
Follow up
URGENT
Stable vital signs
No loss of consciousness
Deformity/suspected closed
fracture without
neurovascular compromise
Controllable bleeding
Significant mechanism of
injury without other
significant abnormalities
INTERVENTIONS
Support ABCs
Reassess vital signs
Determine need for EMS
Control bleeding
Proceed with detailed physical
examination
Splint/immobilize suspected
fractures, elevate extremity,
and apply cold packs
Blunt abdominal injury
Observe closely 15 min for
S/S of intra-abdominal injury
(listed under Emergent)
Reassess in 1 hour or if S/S
recur
In all cases
Contact parent/guardian to
transport student to medical
care or home
Follow up
NONURGENT
Stable vital signs
No deformity or
suspicion of fracture
Minor abrasions or
lacerations
Mild muscle strain or
sprain
INTERVENTIONS
Proceed with detailed
physical examination
Refer to appropriate
protocol
a
Blunt abdominal injury
Observe closely 15
min for S/S of intra-
abdominal injury (see
Emergent)
Reassess in 1 hour or
if S/S recur
In all cases
Contact
parent/guardian
Return student to
class or send home as
indicated
Follow up
a
See protocols as appropriate: Abdominal Burns Chest Trauma Head/Spinal Cord Lacerations/Abrasions Musculoskeletal
NOTE
Refer student for tetanus booster if it has been 5 years or more since the last
vaccination. Tetanus booster is recommended every 10 years.
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
106
Interventions for Musculoskeletal Trauma
MANUAL CERVICAL SPINE STABILIZATION
Position student supine
Place both hands along lateral aspect of
student’s head
Position the head so that the neck is in
neutral alignment with the spine
Continue to support the head to maintain
neutral cervical alignment
IMMOBILIZATION/POSITIONING OF FRACTURES AND DISLOCATIONS
Area/Injury Treatment
Upper extremity Apply sling/triangular bandage
Swathe if additional immobilization is indicated
Clavicular
injury/dislocation
Apply sling/triangular bandage
Swathe if additional immobilization is indicated
Angulation with
unimpaired circulation
Immobilize as presented
Do not move extremity
Angulation with absent
distal pulse, cyanosis
Return extremity to proper physiologic position
Apply gentle traction until pulse is restored
Splint or immobilize area, including joints proximal and distal to injury
Reassess pulses every 5–10 minutes
SLING AND SWATHE IMMOBILIZATION
Place the arm across the chest
and position as shown. Bring the
bandage over the arm and
behind the neck.
Adjust the length as
necessary and tie the
ends. The arm should
be well supported,
relieving pressure on
the shoulder.
Place the knot so that it
lies over the shoulder
rather than against the
cervical spine. Placing a
pad under the knot will
enhance comfort.
Secure the sling at the
elbow with a safety pin
or knot, creating a
pocket in which the
elbow rests securely.
Reassess neurovascular
integrity.
If further immobilization is needed to secure the
extremity and a second bandage is available,
swathe the arm as permitted by applicable
protocols. Lay the second bandage flat, then fold it
several times lengthwise. Use the folded bandage
to swathe the injured arm against the chest wall,
immobilizing it.
| P ROTOCOLS
G
UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
107
Violent Behavior
SYSTEMATIC ASSESSMENT
Begin the 5 components of assessment (see Assessment protocol),
performing interventions AS YOU GO
KEY ASSESSMENT POINTS FOR VIOLENT INCIDENTS
Assess/ensure scene safety before approaching (notify police liaison/security)
Perform across-the-room assessment followed by mental status examination (below)
Appearance: general; grooming; posture
Mood: cooperative, frightened, irritable
Speech: soft/loud, fast, slurred
Behavior: fidgeting, pacing, eye contact
Memory: recent memory/immediate recall
Orientation: realistically oriented to
person/place/time
Thought process: mental activity; evidence
of delusions/hallucinations
Thought content: what the student says;
suicidal ideation, hopelessness
Insight: recognizes responsibilities or blames
others for problems
Judgment: decision-making ability (superficial,
impulsive)
Perception: awareness of self and thoughts
(guilt, indecisiveness)
TRIAGE CATEGORY/APPROPRIATE INTERVENTIONS
Determine triage category and activate EMS AS SOON AS the need becomes apparent!
EMERGENT
Danger to self/others
Brandishing weapon
Physical cues indicate
escalation
Drug or alcohol
intoxication
Physical restraint
necessary
History of violence
INTERVENTIONS
Initiate lockdown
procedures
Activate EMS/security
Never intervene alone
See reverse for safety
tips
Contact parent/guardian
Notify school
administrator
Monitor behavioral
progress
Follow up
URGENT
Moderately agitated but not violent
Expressing verbal anger without physical
aggression
INTERVENTIONS
Determine need for EMS/security
Speak in low, measured tones
Explain that you know something is bothering
student and you will help student control
behavior
Walk with student to diffuse agitation
Repeat/restate what student says:
“You’re feeling angry.”
“I’m concerned for you. I’m going to help
you control yourself.”
“What do you need? What do you need to
do?”
“When you felt like this before, what helped
you?”
Notify crisis response team
Contact parent/guardian to transport student
to medical care or home
Monitor behavioral progress
Follow up
NONURGENT
Mildly anxious or
frightened
Previously angry but
now calm
INTERVENTIONS
Take student to a quiet
area with backup
support available
Provide reassurance as
needed
Speak in low,
measured tones
Contact
parent/guardian
Allow student to return
to class if student is
calm, ready, and able
to identify ways to deal
with feelings; or send
home as indicated
Monitor behavioral
progress
Follow up
The Illinois Emergency Medical Services for Children School Nurse Committee has exercised extreme caution that all information
presented is accurate and in accordance with professional standards in effect at the time of publication. The information does
not serve as a substitute for the professional advice of a physician/advanced practice nurse; does not dictate an exclusive course
of treatment; and should not be construed as excluding other acceptable methods of treatment. It is recommended that care
must be based on the student’s clinical presentation and on authorized policies.

P ROTOCOLS |
G UIDELINES FOR THE N URSE IN THE S CHOOL S ETTING | 2010
108
Violent Behavior: Safety Tips
Emergent situation
Do not invade student’s personal space (stand back at least 5 ft)
Stand at 45° angle to student, not directly in front
Maintain open posture
Maintain a clear exit route
Be prepared to move quickly
Do not make any abrupt moves unless necessary
Be sure student has no weapons before approaching
Give student brief, clear, assertive directions before any action
Establish yourself as a concerned professional
Proceed without hesitation
Enlist adequate, trained assistance (at least 6 people, if possible) before
attempting physical restraint
Urgent situation
Speak in low, measured tones
Explain that you know something is bothering student and you will help student
control behavior
Walk with student to diffuse agitation
Repeat/restate what student says:
à “You’re feeling angry.”
à “I’m concerned for you. I’m going to help you control yourself.”
à “What do you need? What do you need to do?”
à “When you felt like this before, what helped you?”
