
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 2
Table of Contents
Part I: Introduction to the IHI Open School and Curriculum Integration 3
About this Guide 3
A Brief History and Overview 3
A Closer Look at the IHI Open School Courses 4
Introduction to Curriculum Integration 6
Part II: Planning for Success 9
Curricular Structure 9
Curricular Design 10
Part III: Securing Buy-in and Sustaining Your Efforts 15
Engaging Key Stakeholders 15
Sustaining Local Integration 18
Part IV: Appendix and Additional Resources 20
IHI Open School Course List 20
How to Appropriately Credit the IHI Open School 21
Resources to Support Curriculum Integration and Curriculum Design Efforts 22
Authors:
Wendy Madigosky, MD, MSPH, Director, Foundations of Doctoring Curriculum and
Interprofessional Education and Development, University of Colorado Anschutz Medical Center;
Faculty Network Advisor, IHI Open School
Gina Deitz, Community Manager, IHI Open School
Laura Fink, Senior Managing Editor, IHI
Acknowledgements: Special thanks to the members of our faculty network for their contributions
and feedback through individual survey responses and interviews with our team.
Access this guide online at any time at:
http://www.ihi.org/education/IHIOpenSchool/Courses/Pages/OSInTheCurriculum.aspx
.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 3
Part I: Introduction to the IHI Open School
and Curriculum Integration
About this Guide
Before we begin, here’s a quick overview of how we hope this guide will help you:
Who is this guide for?
This guide is for educators in health care who would like to take advantage of content from the IHI
Open School to help teach quality improvement and patient safety. We created the guide with the
hope that anyone interested in using the Open School as a teaching tool would find it valuable.
University faculty, leaders of residency programs and other graduate or post-licensure programs,
and trainers in hospitals and health care organizations should find plenty of relevant and
actionable advice.
Why have a guide to curriculum integration?
More than 1,000 universities and hospitals have used Open School courses in some capacity. Over
the years, the Open School has heard from many educators who are interested in teaching quality
and safety or are inspired by the Open School, but who aren’t always sure how to integrate the
courses into their teaching. In other cases, educators who are already teaching with the Open
School have asked how to improve or sustain their teaching of this material.
What does this guide cover?
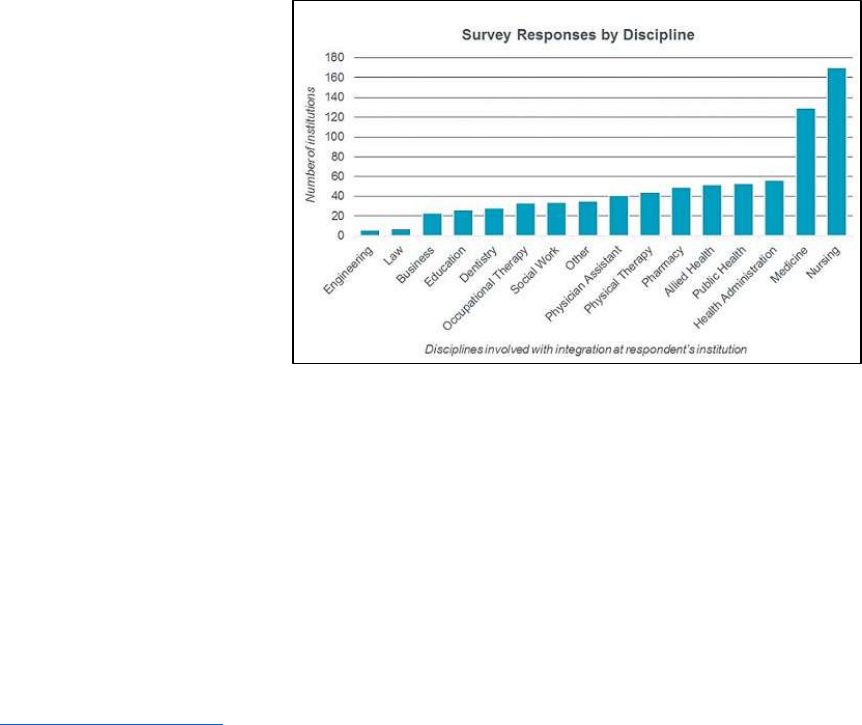
In 2016, the Open School
surveyed hundreds of faculty
who use the Open School
courses in their teaching.
These educators represented a
diverse set of health
professional programs from 16
countries, and this guide
brings together their collective
expertise and experiences.
This guide touches upon the
following aspects of teaching
with the Open School: typical
approaches to integration,
strategies for supplementing the courses with other learning tools, tips for securing approval from
critical stakeholders, and advice on sustaining changes over time once an effective program is in
place. Whether you are associated with a university, post-licensure or graduate training program,
or a professional organization, this guide will help you use the Open School to pursue your unique
educational goals.
A Brief History and Overview
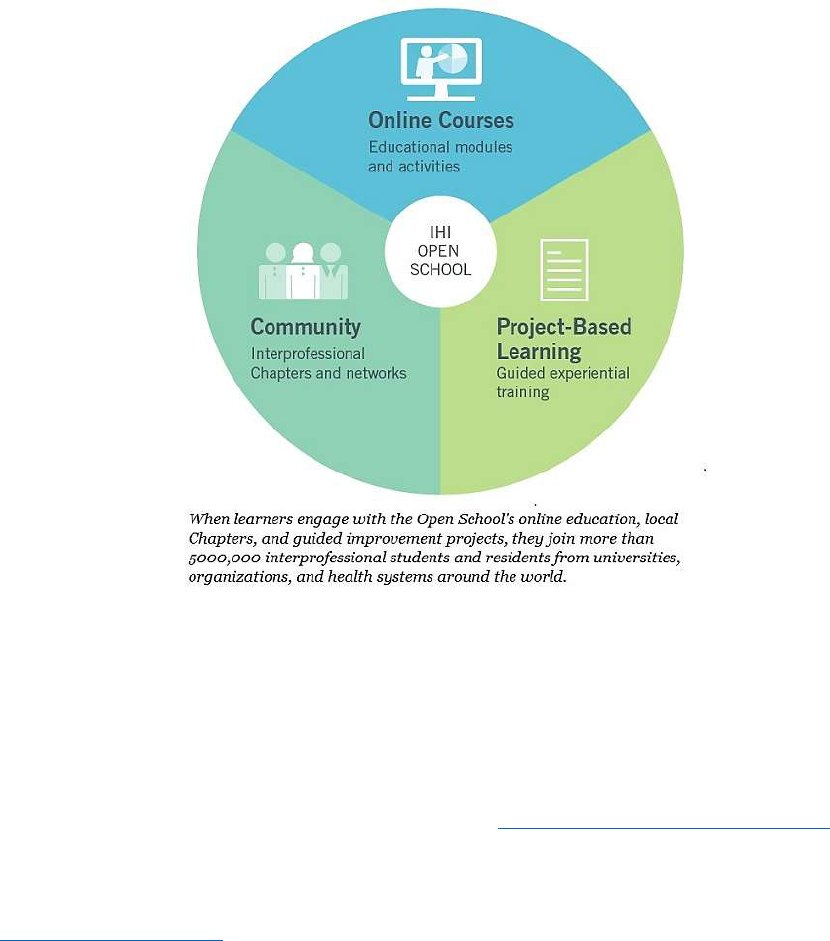
The IHI Open School began as a handful of online courses, first published in September 2008,
designed to provide a basic education in quality and safety for all health professions students.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 4
Since then, the online course catalog has grown to include more than 30 courses, including
courses designed for Graduate Medical Education (GME) faculty and professionals.
Meanwhile, the scope of the Open School has also evolved to include a large and vibrant
interprofessional Chapter Network, which is comprised of more than 830 local Chapter groups
that meet face-to-face at university campuses and organizations around the world. Chapter
activities include learning together about the principles of quality improvement, teaching others
on campus or at a health system about quality improvement, and working on quality
improvement projects.
Today, there is also a third arm of the Open School, which helps learners gain practical experience
with improvement in their local settings. Through project-based learning opportunities, the Open
School provides expert guidance and coaching to help learners achieve real results in improving
health and health care.
The tireless efforts of university faculty and other educators around the world have been
instrumental to the Open School’s success in each of these three areas. These individuals have
been vital in bringing the skills of improvement, safety, system design, and leadership to the next
generation of health care professionals.
A Closer Look at the IHI Open School Courses
For educators who are unfamiliar with the Open School courses, here is a brief overview of what
they include and how you might use them.
The Open School offers more than 30 online courses in quality, safety, leadership, the Triple Aim,
and patient-centered care. Thirteen of the introductory level courses (QI 101–Q105, PS 101–105,
TA 101, PFC 101, and L 101) comprise the Open School’s Basic Certificate in Quality and Safety.
(When you enter the catalog, look for the courses indicated with an asterisk.)
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 5
Beyond the Basic Certificate, there are other 100-level courses that teach introductory concepts
for all health professions. There are also 200-level courses, which teach intermediate concepts
and specialized topic areas, and there is a 300-level course — a project-based learning module,
which we will discuss later.
The courses incorporate mixed media, including video and interactive discussion, to engage
learners and cater to different learning styles. Courses are grouped into catalogs and broken down
into lessons, which take 15–45 minutes to complete. As you are thinking through what to assign to
learners in your program, keep these different options for “chunking” material in mind.
Educators are often surprised to learn the Open School courses are free for students, residents,
and faculty to access. We provide open access to these audiences because we are committed to
making quality and safety education available to future health professionals. Please note that
when learners or faculty make use of Open School materials, we ask that they credit us
appropriately, including throughout course materials such as assessments or syllabi. (For
guidance on the preferred language to acknowledge the Open School, see page 21 in the
Appendix.)
To provide free access to health professionals in training, IHI offers individual and group
subscriptions to professionals, who can earn continuing education credits. Academic and
professional groups can purchase subscriptions that provide access to the Team Tracking Tool.
These tools help educators teach the content and monitor learners’ progress.
Open School courses can help faculty and organizations achieve several goals:
Introducing learners to the fundamental concepts and importance of quality improvement
and patient safety worldwide.
Meeting structural or accreditation standards.
Creating a shared understanding of improvement and a common language within an
organization or a class.
Helping prepare students or staff members to be leaders in their careers.
We’ll share many strategies to help accomplish these goals throughout this guide.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 6
Introduction to Curriculum Integration
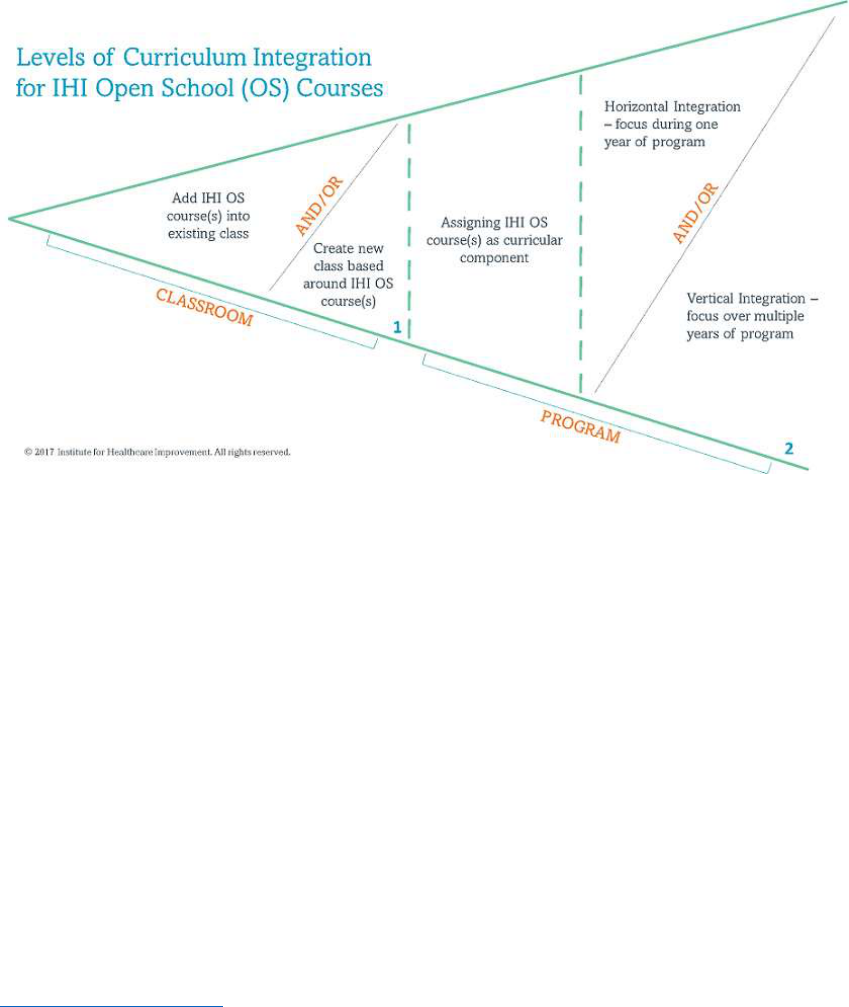
When we talk about “curriculum integration,” we are referring to the intentional inclusion of one
or more Open School courses within a broader educational experience. As far as what a
“curriculum” entails, that is up to you, the educator, to define. The Open School courses may be
included by one professor in the curriculum for a single class; or, they may be a central curricular
component of a multi-year clinical program. For example, an institutional committee may assert
that Open School courses should be covered incrementally, at multiple points throughout a
student’s training.
For simplicity, we will describe two levels of integration, which we will call “classroom
integration” and “program integration.” Although this depiction should not limit you (on the
contrary, we welcome you to go outside the lines), we hope that understanding common
approaches, and some of their benefits and challenges, will give you a place to start as you think
about integrating the courses in your own way.
As you begin to envision how you will integrate the Open School courses into your curriculum,
consider two key questions:
How deep will the learning experience be?
Experts have defined five levels of competency in quality improvement: novice, advanced
beginner, competent, proficient, and expert (see the article “Designing Education to Improve
Care” on page 22 in the Appendix). On the simpler side, the goal may be basic exposure to a few
key concepts — perhaps the Model for Improvement or the fundamentals of patient safety. On the
more ambitious side, some educators choose to weave the Open School courses with other forms
of content and applied learning opportunities. Consider: What level of proficiency do you want
learners to achieve?
How broad will the integration be?
Integrating the Open School courses may begin and end with one faculty member and a single
course. Or, the integration may span a year of training or more, as an integral component of
For this guide,
“curriculum
integration” is the
intentional
inclusion of one or
more Open School
courses within a
broader
educational
experience.

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 7
program-level requirements. Consider: To what extent will the education be a coordinated effort,
taking place across different classes, semesters, or years of training?
As previously mentioned, there are two main levels of integrating the Open School courses into
the curriculum: the classroom level and the program level. This section of the Guide will provide
some description of each of these levels — including where they will naturally overlap — and
successful models within them.
Level 1: Classroom integration
Adding Open School courses to the curriculum of an individual class can be a simple way to bring
quality and safety training to a select group of learners, especially in situations that require little
or no involvement from administration or more than one faculty member. Depending upon the
existing infrastructure, here are two common forms of classroom-level integration.
A. Embed IHI Open School courses into existing teaching material.
Understanding quality and safety can enhance health professionals’ effectiveness in virtually
every area of work, so opportunities to weave the courses into existing teaching material
should be easy to find. At the classroom level, “integration” in its simplest form is the step of
adding a few Open School courses (or even part of one course, perhaps a lesson) to the
syllabus, teaching material, or homework for an existing class.
With this approach, look for ways to anchor the content to existing material. As part of a class
on maternal health, for example, you might include one or more Open School courses on
person- and family-centered care, and relate the learning back to the clinical topic area. If you
already teach quality improvement concepts, classroom integration can be as intuitive as
adding Open School courses to the relevant discussion.
B. Create a new class inspired by the IHI Open School courses.
With more than 30 online courses (comprising more than 80 more narrowly focused lessons),
the Open School can easily serve as the foundation for learning about quality and safety; the
courses provide excellent building blocks for educators who want to design from the ground
up. The courses could be the primary source of learning about quality and safety concepts or
could play a key supportive role.
Although tied to a specific classroom, this form of curriculum integration requires
coordination at the program level. For example, programmatic leadership will likely want to
establish how a new class will factor into overall learning goals and requirements. This model
of classroom integration therefore overlaps with our next discussion, which focuses on
program-level integration. (Note: For advice on making the case for inclusion of a new class
in a competitive curricular environment, see pages 15–18.)
Level 2: Program integration
Integration at the program level means the Open School courses are a central component of
program-wide curricular goals. The education may still be tied to the classroom setting or may be
entirely independent of classroom learning. For example, Graduate Medical Education programs
often rely on the courses to introduce quality and safety concepts to residents, which faculty then
reinforce in the clinical setting. Compared to classroom-level integration, the educational design
may be more or less complicated; however, more people will likely need to be involved in
approving, coordinating, and perhaps teaching the material. This need for coordination can create
a challenge at the outset, but the collaborative effort helps ensure the Open School integration will

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 8
last. As with classroom-level integration, there are different ways to approach integration at the
program level.
A. Assign IHI Open School courses as a stand-alone requirement.
The Open School online courses can offer a stand-alone introduction to key topic areas, and
many organizations rely on them as a way to provide this training independent of classroom
learning or everyday work responsibilities. For example, many programs ask trainees or staff
to complete the Basic Certificate in Quality and Safety (the Open School’s pre-packaged
curriculum of 13 foundational courses) outside of their clinical duties, and learners submit
their certificates of completion as proof of their work. Other programs assign a hand-picked
selection of courses and subscribe to the Open School’s Team Tracking Tool to monitor
learners’ progress.
Although this option does not provide the depth of learning of the approaches we’ll describe
next, assigning Open School courses as independent learning is effective for programs that
wish to introduce some fundamental concepts without significant changes to the existing
structures. It’s a good place to start for hospitals who want to create a common language in
patient safety and quality improvement across the organization. It’s also a good place to start
for academic programs that aren’t yet able to invest significant time or resources into teaching
quality and safety.
B. Assign IHI Open School courses as part of a broader effort to teach quality and
safety.
Including the Open School courses as part of a centralized curriculum to teach quality and
safety requires significant coordination among educators and program leadership, but the
result can be worth the effort. Teaching Open School content in multiple encounters across
classes or program years can help learners understand its ongoing connection to their
primary studies. Two ways institutions can structure a coordinated, multi-faceted Open
School integration effort include:
○ Horizontal program integration:
Horizontal integration refers to teaching Open School content over multiple time frames
within a program year. It is a coordinated effort among faculty so that learners are taking
courses each semester or across planned didactic sessions that build upon each other over
the training year.
As with individual classroom integration, if the institution already has quality and safety
programming in place, integrating the Open School courses can be as simple as making
appropriate connections to existing subject matter.
○ Vertical program integration:
Vertical integration takes the use of the Open School courses a step further, spanning
across multiple program years. In this approach, quality and safety may become a focus
throughout the full health professional program or associated training. It is a highly
coordinated effort, in which faculty and learners understand the education to be a core
competency.
Achieving this extensive level of integration requires bringing together a group of
educators that represent each stage of training. This group, which may be
interprofessional, must design a synchronized plan for presenting different aspects of
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 9
safety and quality over time. The potential payoff is a cooperative group of faculty and
learners who share a common commitment to patient safety and quality improvement.
For more examples and models of curriculum integration, including the Six-Step Approach for
Curriculum Development in Medical Education, see page 22 in the Appendix.
Part II: Planning for Success
Curricular Structure
The most common question educators have when they begin to think about teaching with the
Open School is: “Where do I start?”
Faculty around the world who have already integrated the courses respond with the same advice:
Don’t wait for a state of readiness — just dive in. And as you do, follow the same general advice
you would give to others at the outset of an improvement project: Set an aim, establishing what
you are trying to accomplish, for whom, and by when; create a list of the key measures you’ll
track; and start with a small test of change. Starting small — with one course, topic area, or small
group of students (e.g., learners in one discipline) — can help secure buy-in across the institution
and keep things manageable for individual faculty.
As with any improvement effort, you’ll want to stay focused on outcomes, with the needs of your
learners at the center. Planning will be a critical step that can make all the difference in your
success. Be sure to answer the following questions at the outset of your integration effort.
How will I choose what to teach?
There is no need to assign all the Open School courses right away or at once. Instead, start small,
and start with yourself. If you are a university faculty member, the courses are all free. Personally
reviewing as many Open School courses as you can will allow you to note the most relevant topics
or the ones you feel are most important to teach first. We also recommend two resources to help
you and your colleagues identify the material you’d like to teach:
The course catalog offers a high-level view of the entire curriculum.
For greater detail, course summaries include lesson-by-lesson outlines of key learning
content.
Taking time to get acquainted with the breadth of content available should help you envision your
ideal curriculum. In your vision, be sure to keep overall program-level objectives in mind.
When you feel comfortable with the content, you may want to start by assigning the courses in
one topic area (e.g., patient safety, quality improvement, or population health). Or start with just
one introductory course, such as PFC 101: Introduction to Patient-Centered Care. After some
early success (defined by positive feedback from students, for example), you can gradually expand
to other content areas or more advanced coursework.
Will the content be required or optional?
There are many programs that require Open School courses for class credit, graduation, or
certification. There are also many programs that offer the courses as a voluntary opportunity for
Visit the “How to
improve” section
on IHI.org for
resources and
general advice on
leading
improvement
projects using the
Model for
Improvement as
your guide.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 10
intrinsically motivated students or staff. Both of these are great options, but one may work better
for your context.
If you are planning to require the courses, consider using the Open School’s Team Tracking Tool
to understand your learners’ progress. Available by subscription, this tool captures overall course
completions, names of participants, post-lesson assessment scores, and other useful data for
faculty.
How will I ensure learners have time to complete the content?
As you envision your assignments, keep the time requirements in mind. Every course and course
lesson include an estimated completion time, usually between 15–45 minutes per lesson, on the
first page. If you are adding courses to an already packed curriculum or syllabus, try to think of
what you can shorten or remove. In the professional setting, think of how you can help create
time for staff to participate.
How will the Open School fit into the broader quality and safety curriculum, if
applicable?
The Open School courses provide strong foundational knowledge in the areas of quality
improvement, patient safety, and several other health care improvement topics. However,
supporting the course learning with additional resources, group discussion, activities, and
projects can raise learners’ confidence and proficiency. Think of how you can connect the courses
to classwork and these other types of learning opportunities — starting with some of the ideas
below.
Curricular Design
Weaving different content types and teaching formats together can reinforce concepts and bring
them to life. When it comes to selecting additional subject matter to pair with the Open School
courses — whether for assignments, lectures, or group activities — consider supplemental content
from within the Open School and beyond. The Open School offers many free educational activities
on its website, outside of the courses.
You should also look beyond the Open School to find compelling content that’s relevant to your
group — perhaps in relation to the discipline of study, local current events, or a particular topic of
interest. Here are a few formats you may want to include in your teaching and some ideas to get
you started:
Reading materials
Many faculty assign academic papers and books, such as specific sections of The Improvement
Guide, to dive more deeply into specific topics of interest. Check the “Additional Resources” pages
within the Open School courses, usually included at the end of each lesson (prior to the post-
lesson assessment). These resource pages list helpful books, articles, and other opportunities to
further explore the topic area. We’ve listed a few reading recommendations in the Appendix as
well.
To keep the content fresh and relevant to your particular setting, consider adding news articles
into the mix. Current events can contextualize concepts and add urgency to the learning —
especially if learners see a chance to make a difference.
Access this guide
online at any time
at
http://www.ihi.or
g/education/IHIOp
enSchool/Courses/
Pages/OSInTheCur
riculum.aspx.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 11
Classroom activities or didactic sessions
Group activities — especially with instructor support — are important for learners’ long-term
retention of concepts. Just like with clinical skills, improvement methodology takes practice and
requires mentorship. To give learners the opportunity to discuss new ideas and to practice new
skills right away, consider these examples for classroom or group learning sessions:
Flipped classroom
Instead of waiting for learners to come together to introduce them to a new concept, ask them to
do independent learning first. If you assign a course as pre-work, the group will have a head start
when they meet. This can allow more time for richer discussion.
Example: At the University of Colorado School of Medicine, students review PS 105:
Responding to Adverse Events in preparation for a panel discussion about error
disclosure. The panel presentation, which includes patients, providers, and hospital
representatives who have been involved in adverse events, is followed by small group
discussion and a role-play activity. Faculty lead Dr. Wendy Madigosky says using the
Open School course as pre-work elevates the students’ level of reflection and engagement
during the discussion.
Learner-led presentations
As educators know, one of the best ways to master a topic is to teach it. With this in mind, some
faculty use the teach-back method with the Open School courses. It’s an effective way to both
assess the presenter’s learning and re-engage the audience in the topic (or introduce them to it,
depending how the content is divvied up).
Examples: At Universiti Tunku Abdul Rahman in Malaysia, faculty Nem-Yun Boo
requires learners to take courses independently and then create their own presentations
based on the material, in which they explain what they’ve learned. The presentations
provide faculty with a face-to-face opportunity to identify and clarify important points
learners may have missed.
All residents at Boston Medical Center complete a selection of Open School courses as
part of the core curriculum of their intern year. In their second year, internal medicine
residents participate in a quality or safety initiative. Residents looking for additional
learning complete the Open School’s Basic Certificate and spend three weeks on rotation
at the VA Boston Healthcare System. The VA provides opportunities for residents to join
institutional improvement initiatives and present their work, learnings, and experience to
their peers and the leadership team.
Games
Games are a fun way to break up didactic content and expand upon that learning. Look for games
and exercises on the Open School website, including the following games that reinforce important
improvement concepts and include instructional videos, learning objectives, and discussion
questions for facilitators:
○ Measurement — How Do You Measure the Banana?
○ Systems Design — The Paper Airplane Game
○ Plan-Do-Study-Act (PDSA) Cycles — The Coin Spinning Game
○ Variation — Candy Counting Activity
○ Leadership and Management — The Red Bead Experiment

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 12
Case studies
Also available through the Open School, case studies help learners understand how concepts
relate to real-life situations. Case studies can put a human face on ideas in the abstract, engaging
learners on a more personal level — and perhaps inspiring them to take action. The Open School’s
case studies include facilitator guides with learning objectives and discussion questions. (See page
23 in the Appendix for a list of the Open School’s most popular case studies.) Faculty also use and
discuss real-life examples and cases, which may be drawn from learners’ own experiences, to
create meaningful teaching moments.
Examples: At Texas Woman’s University School of Nursing, Master’s students in the
Nursing Health Systems Management track have to find a completed improvement project
at their place of work (clinical or not) and describe how they’d sustain or continue to
improve the results of that project.
As part of the patient safety curriculum at Vanderbilt University’s School of Medicine in
Tennessee, students complete a reflection exercise about adverse events and near misses.
They reflect on personal experiences as well as those of team members who are not
physicians.
Simulated project work
Project-based work is necessary to master the skills and understand the idiosyncrasies of quality
improvement. Learners with busy schedules may feel intimidated by the idea of finding time for
larger projects, especially those that require teamwork. It can help to provide class time or
protected time from clinical training for learners to create and work on team-based projects,
whether real or simulated, especially when faculty and mentors make themselves available for
coaching.
Examples: At the University of Texas at Austin School of Nursing, students work in teams
to plan a quality improvement project to tackle a theoretical problem, including writing a
project charter, creating aims, and developing measurement plans. Assistant Professor
Terry Jones, RN, PhD, says it’s valuable to provide class time to practice this critical
planning phase.
During their rotation at the VA Boston Healthcare System, Boston Medical Center
residents are expected to lead an interdisciplinary one-hour lunch session on a specific
case, facilitating small groups to run rapid root cause analyses and propose potential
interventions. Drs. Lakshman Swamy and Christopher Worsham, Chief Residents who
supervise these sessions, bring the proposals to decision makers who often use them to
effect real change.
Observation
Observing how quality and safety principles relate to the real world of health care (or even other
high-risk industries) can contextualize and enhance learners’ understanding.
Examples: At the University of Colorado School of Medicine, students review PS 104:
Teamwork and Communication in a Culture of Safety and attend a lecture reinforcing
the importance of teamwork. Then, they shadow local hospital teams to see best practices
in action.
At East Carolina University in North Carolina, PFC 201: A Guide to Shadowing: Seeing
Care through the Eyes of Patients and Families is pre-work before a half-day patient
shadowing event. Students follow patients and families through their health care journey
to better understand the care experience from patients’ points of view.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 13
Learning assessments
Generally, you will want to include some type of learning evaluation in your curriculum. Almost
every Open School course includes a short assessment, usually consisting of five or six multiple
choice questions, at the end of each lesson. (Learners must score 75 percent or higher to complete
a course.) However, you may want to create additional assessments to track collective learning
over time or evaluate specific outcomes that are important to you. Many GME faculty use the
Accreditation Council for Graduate Medical Education (ACGME)’s Clinical Learning Environment
Review (CLER) program to measure learning outcomes, for example. Other faculty create their
own written assessments, and others opt for a face-to-face format, which allows instructors to
identify and clarify misunderstandings in real-time. Improvement projects, which we’ll discuss
next, provide a more rigorous (and potentially even more valuable) opportunity to assess learners’
ability to apply concepts and improve patient care. (For tools to assess training program
outcomes, see page 22 in the Appendix).
Example: At the University of Texas at Austin, educator Terry Jones, RN, PhD,
administers a self-assessment at the beginning of her class to check students’ knowledge of
quality and safety (e.g., conducting root cause analysis, writing project charters, etc.).
When the class is concluding, she asks them the same questions again, to see how far
they’ve come.
Project-based learning
Reading, case studies, group activities, and observation can go a long way toward bringing
concepts to life, but there is no replacement for the actual experience of setting up and leading a
quality improvement project in the real world. Quality and safety experts and experienced faculty
strongly recommend pairing didactic content with applied learning, such as project work or
practical experience. These types of opportunities can take some work to set up, but the learning
will be meaningful. Here are a few tips to get started:
Find projects that are institutionally supported
Your institution may already have improvement projects in progress that learners can join. Try
starting there. If you are looking to design a new project, make sure it aligns with leadership-level
goals. Keep in mind that Open School Chapters around the world are working on local
improvement projects every day, so check for a Chapter in your area; they may be able to help you
find a project or involve your learners in their efforts.
Examples: The Duke University Chapter in North Carolina has developed a strong
partnership with the Duke Health System. Alongside faculty, the Chapter helped build the
Quality and Innovation Scholars Program (QISP). Now moving into its third year, QISP
matches students from multiple professions with physicians and health system leaders,
who immerse them in interdisciplinary, systems-level quality improvement and
innovation. Learn more, including how students and faculty got the program off the
ground, from the Open School Blog.
The internal medicine residency program at Boston Medical Center follows a case-based
model to teach quality improvement. During rotation at the VA Boston Healthcare
System, residents have protected time to focus on quality improvement and patient
safety. They review patient safety incidents and screen them for improvement
opportunities, with the chance to begin a project or join an existing project during the
rotation.

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 14
Build partnerships with service organizations or local hospitals
Look for local hospitals and organizations that are willing to accept help from students. Some
potential partners may meet you with skepticism, but ask faculty and administrative colleagues for
contacts who might be willing to build a relationship. Some schools have established student-run
free health clinics, which create a perfect avenue for incorporating quality improvement in the
clinic’s standard work and processes. Forming a long-term relationship with a partner organization
can create enduring opportunities for many learners to come.
Examples: The University of Dundee in Scotland invites small groups of medical students
to work with clinical teams and learn how to gather information about patient
experiences and feed it back to the clinical teams. These encounters begin in year one of
the curriculum, and the students have the option for more in-depth work related to
improvement and human factors science. Dr. Peter Davey, a lead faculty for the program,
says it’s a chance for the participants to establish meaningful relationships with patients
and other providers. They learn about the people — instead of just the tasks — of
medicine, and they can begin to incorporate a person-centered mindset into their
improvement work.
The University of Cincinnati Open School Chapter in Ohio established an interprofessional
student-run clinic that operates in partnership with St. Vincent de Paul, a local charitable
organization. This collaboration helped establish numerous health services for patients
and clients, as well as opportunities for students to meaningfully practice quality
improvement.
Use the IHI Open School’s project-based learning opportunities
Through two project-based learning opportunities, the Open School provides expert guidance and
coaching to help learners achieve real results in improving health and health care. Refer to QI
301: Guide to the IHI Open School Quality Improvement Practicum (for learners) and GME 207:
Faculty Advisor Guide to the IHI Open School Quality Improvement Practicum (for faculty
advisors) in the main Open School course catalog. Also look for offerings of the semi-synchronous
course Leadership and Organizing for Change.
Examples: At Pennsylvania State University School of Nursing, students who had
completed Open School courses on leadership, quality, and patient safety in their
leadership class suggested incorporating Leadership and Organizing for Change into the
program’s leadership practicum the following semester. Associate Professor Karen Wolf,
PhD, was pleasantly surprised that her students were so enthusiastic to continue to
advance their learning and leadership.
After learning the basics of quality and safety through other Open School courses,
students of Frontier Nursing University take the Open School’s Practicum to support
them through their first improvement projects at local hospitals and rural health clinics.
Lead faculty Diana Jolles, MSN, PhD, has seen her students develop greater mastery of
the content, and many partner organizations have praised the level of skills her students
bring to the work with their local teams.
Similarly, faculty at the University of Stirling in Scotland have integrated the Basic
Certificate in Quality and Safety and the Open School Practicum into the nursing
curriculum, and more than 600 students have completed improvement projects as a
result. Teaching fellow Brian James reiterated how important it was for students to
participate in projects outside the comfort of the classroom, to gain first-hand experience
Opportunities for
students to learn
about people –
instead of just the
tasks – of
medicine help
them incorporate
a person-centered
mindset into their
improvement
work.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 15
with the challenges of leading improvement. He said although some students were
deterred by initial setbacks, they often shared overwhelmingly positive feedback at the
conclusion of projects — having observed the meaningful changes they helped create.
For three specific models for facilitating experiential learning at the point of care, see pages 23–
28 in the Appendix or review GME 205: A Roadmap for Facilitating Experiential Learning in
Quality Improvement.
Part III: Securing Buy-in and Sustaining Your
Efforts
Engaging Key Stakeholders
In addition to the tasks described in Section II, focused on structuring and designing your
curriculum, you’ll need to think about building support for your efforts. Adding Open School
materials into educational programming may require approval from fellow faculty and leadership,
depending upon what you are planning. In some cases, securing buy-in can be the biggest
challenge you’ll face, especially when you’re starting a new class or planning program integration.
However, the same advice for any improvement effort continues to apply: Start small and expand
your efforts with each incremental success.
As you progress further into integrating Open School courses into the curriculum, it’s unlikely all
your learners and colleagues will readily agree on exactly how the courses should be incorporated.
(Frankly, some will feel they should not be added to a jam-packed curriculum in any form.)
Faculty, students, administrators, and/or professional colleagues may not understand the
importance of quality and safety training. And, very likely, they may feel overcommitted in their
current responsibilities. All this can inhibit those around you from appreciating and supporting
your vision.
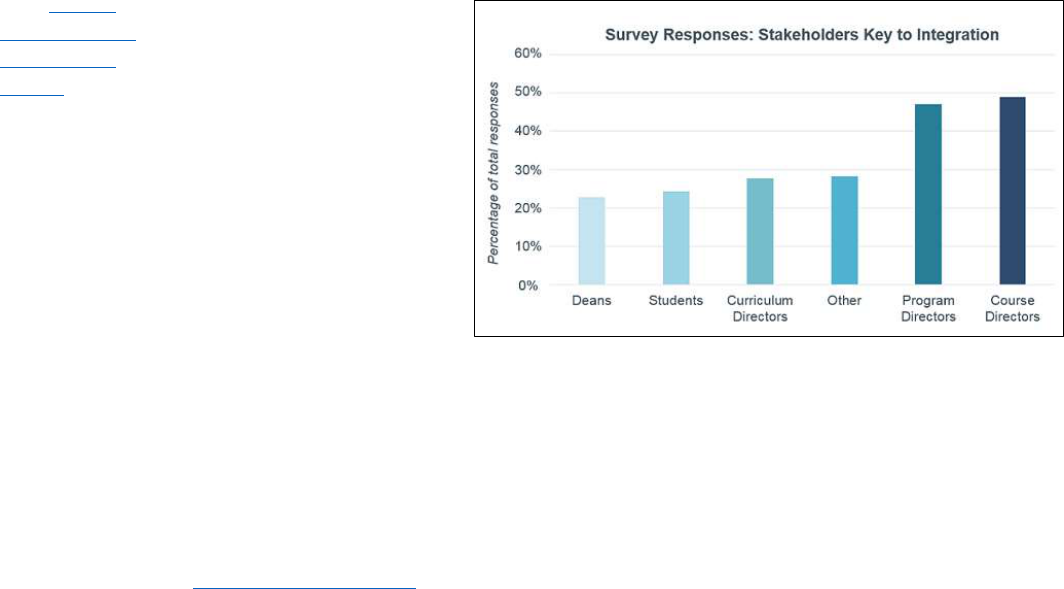
How do you overcome these
hurdles? Time and again,
faculty and other leaders of
Open School integration
efforts have underscored the
importance of gathering
support from across their
institutions: students,
curriculum and program
directors, faculty, and deans
are all groups you can and
should engage. You never
know who will become your
biggest champions, and,
ideally, you should strive to develop a multi-tiered network of ongoing support.
Students and Learners
Learners who have taken an Open School course or two can speak to the importance of quality
improvement and patient safety as part of their learning experience. Ideally, find learners within
Familiarize
yourself with our
goals, mission,
and work to
inform your
conversations
with
stakeholders.
Take OS 101:
Introduction to
the IHI Open
School.

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 16
your organization who can provide testimonials to help bring other faculty, administration, or
students on board. Student champions can describe the relevance of the courses to their
education, increasing peers’ willingness to accept the courses as meaningful work. Here are a few
tips to begin building your cohort of student champions:
Connect with the IHI Open School Chapter at your institution
Look for the Open School Chapter nearest to you. With luck, there may be one at your institution
— in which case, be sure to involve them in your efforts to integrate the courses into the
curriculum. You can also start your own Chapter.
Examples: At the University of British Columbia, Chapter Leaders were instrumental in
leading multiple efforts to integrate quality improvement into programming. With the
support of Chapter Faculty Advisors, they led efforts to design a Quality Improvement
Practicum Program that connects students with local improvement projects. They also
spurred a successful initiative to add the Basic Certificate in Quality and Safety as an
elective credit.
At University of South Carolina School of Medicine, students are required to go to at least
one Open School Chapter meeting as part of their training.
Be clear about how the courses will grow students’ skills and provide long-term
benefits
At all costs, avoid suggesting the courses are one more hurdle to jump or box to check for busy
students and staff. Instead, explain that the science of improvement will help learners be better
health care professionals and that it will contribute to greater success and satisfaction in their
careers. For example, remind students they can add the Basic Certificate to their resumes and that
the Open School offers chances to both learn about and practice health care leadership.
Understanding patient safety concepts will help them prevent adverse events, and improvement
methodology will help them be more efficient in their work.
Provide clear instructions to make taking the courses as easy as possible
Before you assign Open School courses to students, provide clear instructions to ensure they will
have no trouble finding the online content. For example, institutional subscribers should
distribute the log-in information they receive with their subscription. Making things as easy as
possible for your learners will help reduce fears that assignments will be confusing or time
consuming.
Align the course work with project work
As previously mentioned, there is nothing as motivating as seeing real results, especially those
that benefit patients or colleagues. Working on local improvement projects can elicit buy-in as
you help learners gain a deeper appreciation of quality improvement as a method to lead
meaningful change.
Show that you value feedback
Don’t be shy about asking for feedback. Soliciting feedback from learners helps them feel valued
and personally invested, and improving your own curriculum shows that you practice what you
preach.
Faculty
Oftentimes, a lack of trained faculty makes it difficult for programs to teach quality and safety and
becomes a limiting factor for integrating the topics within a curriculum. If possible, help create
opportunities for faculty to study quality and safety. The more they know, the better luck you will
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 17
have in building a network of educators who can promote and spread the Open School. Here are a
few tips to grow a network of devoted faculty:
Develop your own background in quality improvement
Others will gain trust in you if you can point to your own quality and safety expertise or successful
improvement efforts. Beyond that, you may find you can apply quality improvement to your
course integration initiative. If you don’t have the necessary experience to inspire others, join
forces with someone who does. Adding an expert’s voice will add legitimacy and can be
persuasive.
Develop faculty awareness of the principles of quality and safety
If possible, bring together a group of educators, perhaps representing different disciplines or
learning stages, to work together to develop capacity for teaching quality and safety across your
institution. As a place to begin, the Open School offers seven courses for Graduate Medical
Education faculty, listed in the Appendix of this guide, to support efforts to train residents in
quality and safety and develop didactic curriculum on these topics.
Examples: East Carolina University has not only integrated Open School courses into
training for students and medical residents, but it has made the Open School’s Basic
Certificate a requirement for a year-long interprofessional fellowship program for faculty,
called “Teachers of Quality Academy.” As part of that program, faculty complete a quality
improvement project, which they present at an annual quality symposium. According to
Dr. Elizabeth Baxley, faculty development became a clear goal for her institution when
they recognized a significant return on investment.
Introduce faculty to the IHI Open School and the benefits of using the courses
In addition to this guide, there are many Open School resources that explain its mission and value
to educators. Refer colleagues to the Open School Overview, or, better yet, direct them to specific
materials from the Overview that you think will be persuasive. For example, you can share an
introductory course, OS 101: Introduction to the IHI Open School: Join the Movement to
Improve Health & Health Care. We’ve mentioned the value of local testimonials. As you get
started with your campaign, you can also point to user ratings on the course overview pages.
Examples: During a faculty meeting, Connie Boerst, President and CEO of Bellin College
in Wisconsin, proved to colleagues that the Open School was more than “busy work”: She
took the room through an Open School course, page by page. The demonstration opened
their eyes to the high-quality, interactive learning experience the courses provide.
Administration and Organizational Leaders
Integrating the Open School courses, especially at the program level, requires program,
curriculum, and administrative directors to carve out time for students, trainees, or other learners
to complete the work. The support of leadership over time is crucial for long-term success of Open
School course integration. Here are some ideas to get leaders interested in your work:
Show how the IHI Open School can fill an educational gap
Identify and highlight ways in which the Open School courses can help fill gaps in the curriculum,
especially in meeting outside requirements from overseeing bodies, such as accreditation
committees. Look to standard nursing requirements and to the ACGME’s Clinical Learning
Environment Review program, for example. Compare requirements to the course summaries,
which you can also print and distribute.
Example: Many organizations and schools identify interprofessional learning as a
priority, but struggle to find ways to bring health care disciplines together. The Open

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 18
School courses and Chapter Network can help fill this gap. Advocates of the Open School
have often emphasized the potential for quality and safety learning events and activities
to build common ground and establish shared goals across health professions.
Partner early in the curriculum development process
Want to make sure administrators feel invested? Involve key partners in the development of the
curriculum early on. Consider including deans, course and program directors, and other experts
in quality and safety (at hospitals, this may include your quality improvement team staff or other
clinical leaders).
Highlight your support network of student and faculty champions
Although support from leadership is critical, the reality is that it may come only after a critical
mass of other stakeholders are onboard. As you identify and develop “early adopters,” raise those
people up, and help increase the volume of their voices.
These tips should help you begin using Open School courses in the curriculum. In addition to the
integration examples throughout this guide, you can find other resources in the Appendix,
including John Kotter’s 8-Step Change Model on page 22.
Sustaining Local Integration
Once you’ve successfully integrated the courses into your curriculum — whatever that means to
you, based on the definitions and aims you’ve set forth — be sure to celebrate! However, keep in
mind that a crucial step remains: Developing a sustainability plan. Planning for how you will
sustain the work in the future will help ensure many cycles of learners will continue to benefit
from the Open School.
The sooner you can start thinking about long-term plans, the better. Here are few
recommendations:
○ Continue to look for opportunities to link Open School content to institutional priorities
and/or program requirements and competencies.
○ Keep reminding administrators of the value of the Open School for students, staff, and
customers, and point to positive results (the more concrete, the better, so look for
opportunities for long-term assessment and evaluation).
○ Continue to grow dedication to improvement science from faculty and educators — if you
leave your role, there should be others who will pick up where you left off.
○ Join forces with your local Open School Chapter or start one. A local Chapter provides a
ready-made cohort of learners eager to support the use of the Open School.
○ Lastly, always practice what you preach! Use improvement science in the integration
process every step of the way: Even after you have a successful curriculum, continue to
gather feedback from students and other faculty, and run PDSA (plan-do-study-act)
cycles to improve.
Ongoing Inspiration and Support
Remember, you are not alone in this work. Please look to the Open School for support, as well as
to hundreds of faculty, students, and other leaders who are driving efforts to integrate the Open
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 19
School into institutions and organizations around the world. Here are a few key ways to stay
connected:
Join improvement communities online
Online support networks give you access to a wide group of educators who are doing similar work
all over the world. The Open School’s Faculty Network, for example, is a place to connect and
share ideas, experiences, and learning. You can also join the Open School Faculty Advisor listserv
by emailing openschool@ihi.org.
Connect with the improvement community at conferences or events throughout
the year
Nothing proves you’re not alone like a large-scale event of like-minded people. IHI’s annual
world-class conferences, including the National Forum on Quality Improvement in Health Care,
offer opportunities to learn the latest improvement ideas and best practices for generating change
in your organization. Be sure to inquire about faculty scholarships, which are often available for
conferences.
Keep in touch with the IHI Open School
The Open School regularly updates its courses and other content and is constantly adding new
material. For example, changes in 2016 included redesigning the Basic Certificate, releasing a new
suite of improvement games, and developing this guide. Provide a valid email address when you
register on ihi.org to ensure you’re aware of changes that can affect you and your learners.
Consider, also, subscribing to the Open School newsletter for updates, coming events, and new
content.
Join or start an IHI Open School Chapter at your institution
We cannot emphasize enough: Having an organized group of learners who are interested in
quality improvement and patient safety — and are passionate about spreading the learning —
offers a terrific advantage for sustaining and expanding course integration efforts. Learn more
about the Chapter Network, including how to get a new Chapter started or become a Faculty
Advisor.
And as always, please feel free to reach out to our team at openschool@ihi.org any time. We hope
to hear from you, and we wish you the best of luck!

IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 20
Part IV: Appendix and Additional Resources
IHI Open School Course List
Improvement Capability
○ QI 101*: Introduction to Health Care Improvement
○ QI 102*: How to Improve with the Model for Improvement
○ QI 103*: Testing and Measuring Changes with PDSA Cycles
○ QI 104*: Interpreting Data: Run Charts, Control Charts, and other Measurement Tools
○ QI 105*: Leading Quality Improvement
○ QI 201: Planning for Spread: From Local Improvement to System-Wide Change
○ QI 301: Guide to the IHI Open School Quality Improvement Practicum
Patient Safety
○ PS 101*: Introduction to Patient Safety
○ PS 102*: From Error to Harm
○ PS 103*: Human Factors and Safety
○ PS 104*: Teamwork and Communication in a Culture of Safety
○ PS 105*: Responding to Adverse Events
○ PS 201: Root Cause and Systems Analysis
○ PS 202: Building a Culture of Safety
○ PS 203: Partnering to Heal: Teaming Up Against Healthcare-Associated Infections
○ PS 204: Preventing Pressure Ulcers
Person- and Family-Centered Care
○ PFC 101*: Introduction to PFCC
○ PFC 102: Dignity and Respect
○ PFC 201: Seeing Care Through the Eyes of Patients and Families
○ PFC 202: Basic Skills for Conversations about End-of-Life Care
Triple Aim for Populations
○ TA 101*: Introduction to the Triple Aim for Populations
○ TA 102: Improving Health Equity
Leadership
○ L 101*: Introduction to Health Care Leadership
*To complete the Basic Certificate in Quality & Safety, one must complete this course.
Project-Based Learning
○ QI 301: Guide to the IHI Open School Quality Improvement Practicum
○ Leadership and Organizing for Change
Take one of our
sample courses to
familiarize
yourself with our
design and
approach.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 21
Graduate Medical Education
○ GME 201: Why Engage Trainees in Quality and Safety?
○ GME 202: A Guide to the Clinical Learning Environment Review (CLER) Program
○ GME 203: The Faculty Role: Understanding & Modeling Fundamentals of Quality &
Safety
○ GME 204: The Role of Didactic Learning in Quality Improvement
○ GME 205: A Roadmap for Facilitating Experiential Learning in Quality Improvement
○ GME 206: Aligning Graduate Medical Education with Organizational Quality & Safety
Goals
○ GME 207: Faculty Advisor Guide to the IHI Open School Quality Improvement Practicum
How to Appropriately Credit the IHI Open School
When Open School courses, lessons, videos, figures, text, assessment questions, or other
materials are used for classroom or program integration, they must be appropriately referenced
by learners and educators. Here is the format IHI requests:
For an IHI Open School Online Course:
Author(s). Lesson Title. In: Course Title [IHI Open School online course]. Boston,
Massachusetts: Institute for Healthcare Improvement; year published:page number.
www.ihi.org/onlinecourses. Updated date of last update. Accessed date.
Example: Lloyd R, Murray S, Provost L. Lesson 1: An overview of the Model for
Improvement. In: QI 102: The Model for Improvement: Your Engine for Change [IHI
Open School online course]. Boston, Massachusetts: Institute for Healthcare
Improvement; 2009:3. www.ihi.org/onlinecourses. Updated August 19, 2015. Accessed
October 15, 2015.
For an IHI Open School Activity:
Author(s). Activity title. Institute for Healthcare Improvement Open School website. url. date
accessed.
Example: Hilliard R. An extended stay. Institute for Healthcare Improvement Open
School website.
http://www.ihi.org/education/ihiopenschool/resources/Pages/Activities/CaseStudyAnE
xtendedStay.aspx. Accessed November 6, 2015
If referring to content that is referenced within Open School resources, please include both Open
School information as well as the original reference. If you’re unsure how to reference content,
please don’t hesitate to email openschool@ihi.org.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 22
Resources to Support Curriculum Integration and Curriculum
Design Efforts
The following is just a sampling of the resources that faculty are using to supplement the courses
and design quality and safety training programs. The Open School is beginning to develop a more
comprehensive list of resources to assist educators, which will be available later this year.
Models to Support Program Development
○ Armstrong G, Headrick L, Madigosky W, Ogrinc G. Designing education to improve
care. The Joint Commission Journal on Quality and Patient Safety. 2012;38(1):5-
14. https://ipecollaborative.org/uploads/S2-JQPS-0212_Armstrong.pdf. Accessed
January, 24 2017.
○ Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical
Education: A Six-Step Approach. 2nd ed. Baltimore, Maryland: Johns Hopkins
University Press; 2009.
○ Kotter, JP. Leading Change. 2nd ed. Boston, Massachusetts: Harvard Business School
Press; 2012.
Assessment Tools
There are a number of ways in which faculty measure program or class outcomes in addition to the
Open School assessment questions at the end of each lesson. Here are a few assessment tools
faculty shared with us:
All disciplines
Quality improvement curricular assessments used across disciplines include the Quality
Improvement Knowledge Application Tool (QIKAT) and the Systems Quality
Improvement Training and Assessment Tool (SQITAT).
Graduate Medical Education
Most GME faculty consider ACGME CLER guidelines in their program design. You can revisit the
CLER goals and approach for strengthening clinical training for medical residents in GME 202: A
Guide to the Clinical Learning Environment Review (CLER) Program.
Commonly Required Readings
○ Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement
Guide: A Practical Approach to Enhancing Organizational Performance. Hoboken, New
Jersey: John Wiley & Sons. 2009.
○ Kohn LT, Corrigan JM, Donaldson MS, eds. (Committee on Quality of Health Care in
America, Institute of Medicine). To Err Is Human: Building a Safer Health System.
Washington, DC: National Academies Press; 2000.
○ Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st
Century. Washington DC: National Academies Press; 2001.
○ Galt KA, Paschal KA. Foundations in Patient Safety for Health Professionals. Sudbury,
Massachusetts: Jones and Bartlett Publishers, LLC; 2011.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 23
IHI Open School Content
Top Case Studies:
○ Code Blue — Where To (AHRQ)
○ The Unfortunate Admission
○ A Downward Spiral: A Case Study in Homelessness
Most Watched Videos:
○ What Happened to Josie?
○ How Do You Use a Driver Diagram?
○ How Can We Define ‘Quality’ in Health Care?
Learning from Other Curriculum Integration Efforts
Through conversations with faculty in compiling this guide, the Open School gathered a multitude
of examples of how organizations, faculty, and students are using our courses. Of course, we
couldn’t fit all of these stories here. For additional case studies and examples, we encourage you
to visit our website, where you can find continued inspiration and ideas.
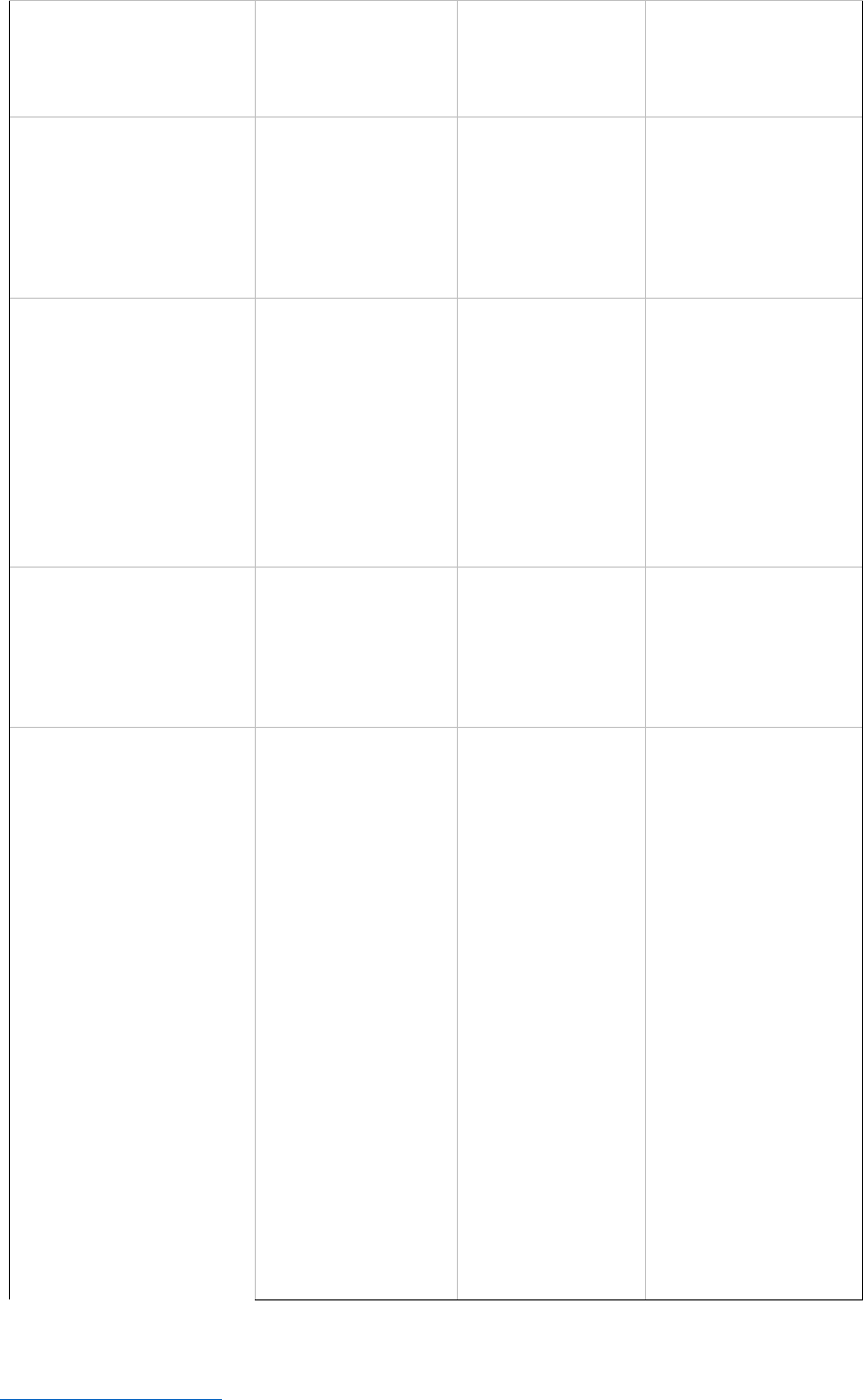
Facilitating Experiential Learning in Quality Improvement
The table below introduces IHI’s adaptable three-model framework for supporting project-based
learning. The guide for implementing this three-model framework with trainees at the point of
care is available in GME 205: A Roadmap for Facilitating Experiential Learning in Quality
Improvement.
Team-Based
Model
Unit-Based
Model
Systems-Based
Model
Definition
Focused on behavior
change and limited
process change to
improve a workflow that
is within the control of
the interdisciplinary
medical team
Focused on a
workflow in a
particular unit or
clinic with aims that
are tied to
institutional priorities
Focused on a workflow
that crosses multiple
units/clinics with an aim
to improve systems at the
departmental or
institutional level
Scenario
An inpatient team
composed of an
attending physician, two
residents, medical
students, nurses a
pharmacist, and a social
worker will spend the
next two weeks together
on service, integrating
quality and safety into
their daily routine of
bedside
interdisciplinary rounds
(if in an ambulatory
A group of four to six
trainees will be
rotating at one-month
intervals through an
inpatient unit,
working clinically with
various attending
physicians but
assigned to a QI
project with a single
advisor
A group of six to eight
trainees will be rotating
through many units within
a hospital during the
period but conducting a
QI project in a selected
unit with a single advisor
and a small team of
involved attending
physicians
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 24
setting, the
interdisciplinary team
may have a slightly
different composition)
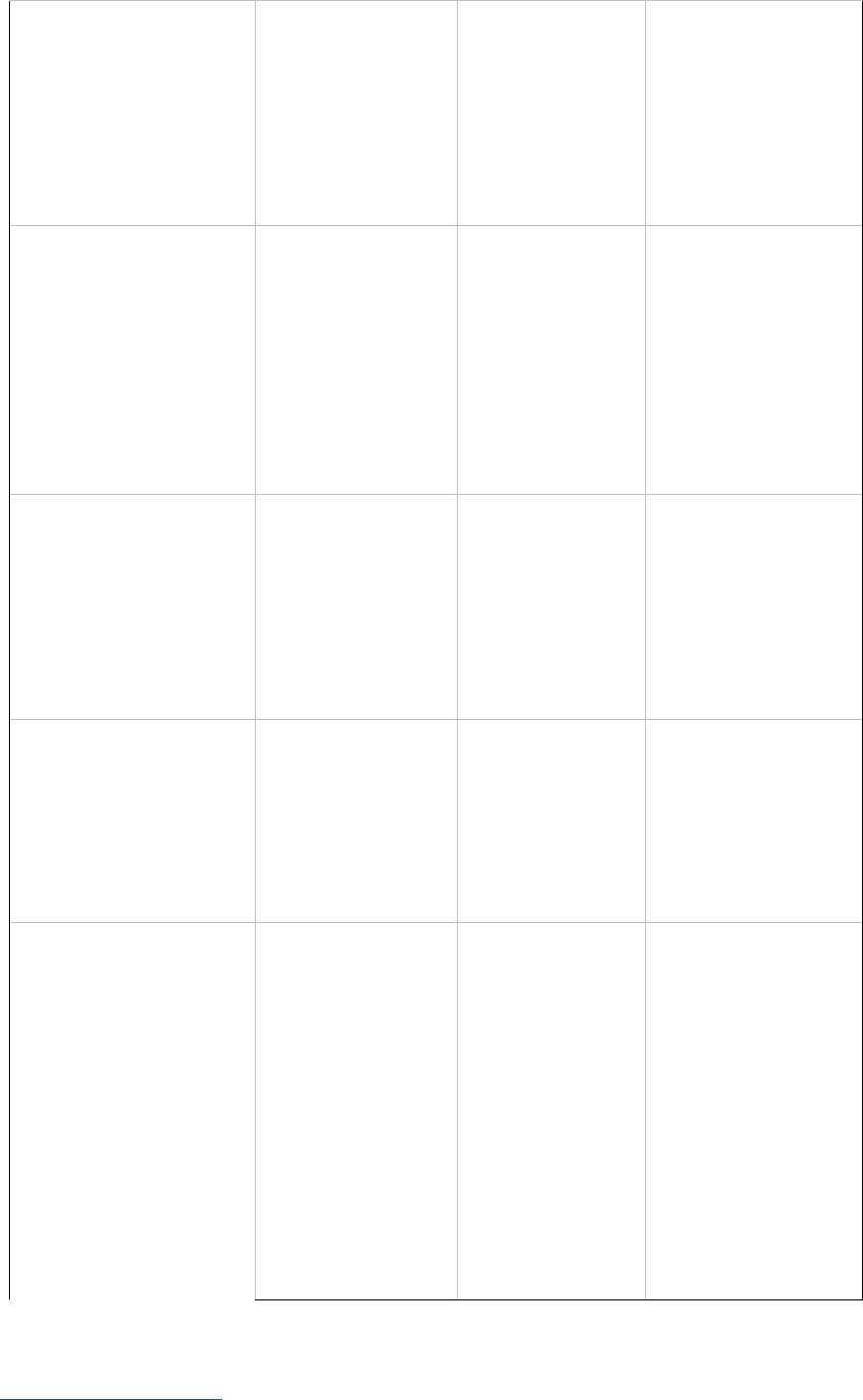
Improvement
objective
Discover a new practice
or innovation relating to
team
behavior/workflow, or
solve a problem that
pertains to routine
patient care
To develop a new
practice or innovation
that serves the unit or
clinic as a whole
To make system-level
change that helps achieve
institutional objectives
around quality and safety
Educational
objective
To motivate trainees to
incorporate
improvement principles
and systems-based
thinking into their daily
clinical routines, and to
move toward
integrating QI/PS into
clinical care rather than
thinking of it as a
separate activity
To demonstrate to the
trainee that even with
a limited amount of
time in a unit, she or
he can and should
play a vital role in
accelerating the
progress of that unit’s
improvement
initiatives
To integrate trainees into
the larger institutional
objectives for quality and
safety; to make robust
direct connections
between clinical care
trainees are providing at
the bedside and the larger
quality and safety aims of
the institution in which
they train
“Owned” by
The rounding team in
an inpatient unit, or a
clinical team in an
ambulatory setting
The nursing leader
and clinical director of
the unit/clinic
The quality
director/leader and a
nursing director who
oversee one or more
units/clinics or the
department as a whole
Required faculty
leadership
Led by faculty members
while they are working
to clinically supervise
trainees (for example, as
attending physicians on
an inpatient service or
as preceptors in a clinic
or emergency
department); faculty
should consider
themselves “competent
to proficient” in QI/PS,
with basic knowledge in
QI/PS and a clear
understanding of the
workflow and behaviors
of the team/unit/clinic/
department
Led by faculty
members who are
“unit owners” (have
QI/PS as a key aspect
of their job
description and are
responsible for the
quality output of their
area); may be a
clinical director of a
unit, or the unit-
specific quality leader;
are proficient in
QI/PS knowledge and
skills; have a deep
understanding of the
unit’s workflow and
priorities; are in a
position to influence
changes in workflows
and systems beyond
the behaviors of a
particular team of
physicians; have the
ability to influence the
Led by faculty members
who are directors of
quality or quality officers
for a department, or
clinical leaders such as
Vice Chair for Clinical
Services, with quality
playing a central role in
their job description; are
in a position of leadership
that allows them to
influence multiple clinical
leaders across units of
their department; have a
deep understanding of
departmental priorities
and functioning; are
“proficient to expert” in
their understanding of
QI/PS
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 25
culture of the
attending physicians
they oversee, and have
strong links to
interprofessional
clinical leaders
(nursing, pharmacy,
social work, and case
management)
Scope of
improvement(s)
Scope should be
appropriate to the team
structure/workflow and
the available timeframe
based on trainees’
rotation schedule; the
problem that becomes
the focus for the
improvement effort
must be a “felt need” of
the team
Scope of
improvements or
changes is appropriate
for the unit/clinic
setting; efforts focus
on systems
improvements that
are mainly contained
within the unit/clinic
Can involve systems and
processes that cut across
multiple units or clinics;
larger systems are
restructured
Duration
Can be as short as two
weeks, or as long as a
month or two
Flexible, but typically
will last two to six
months (or even up to
a year, depending on
local capability and
whether the clinical
experience is
rotational or
longitudinal)
Can last anywhere from
several months to a year
or more, depending on the
time required for buy-in
and the duration of each
PDSA cycle
Interprofessionalism
Does not require
significant
modifications to the
workflow of providers
who are not on the
improvement team
Interprofessional
collaboration required
among a group of care
providers and staff in
one particular unit or
clinic (nurses,
pharmacists, medical
assistants, etc.)
Interprofessional
collaboration is critical to
success; requires buy-in
from multiple
stakeholders
Defining the
problem to be
addressed
The problem should be
limited to something
that the team can
address; the problem
should be a “felt need”
of the team (not
necessarily a unit or
institutional priority);
finally, the
improvement efforts
should target a problem
of inconsistency in
team’s operations or
processes or in its care
delivery.
The problem should
be a unit priority that
is relatively focused
and very achievable
within the constraints
of two to six months.
You will likely
determine your
problem of focus
based on your unit’s
particular weaknesses
with respect to the
overall organization’s
quality and safety
strategy.
Due to the longitudinal
nature of this project, the
problem could be a sub-
project of one of the stated
hospital-wide aims. (For
example, it could be
related to reducing length
of stay, hospital-acquired
infections, mortality,
readmissions, etc.) The
aim is tied to a specific
outcome measure.
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 26
Encouraging buy-in
Since the projects will
have such rapid
turnover, it is important
to ensure that the
clinical staff who are
involved in each “new”
project be supportive of
the structure of rapid
turnover of
improvement teams and
projects, which is why
the team must
determine the focus of
the project and why the
project must be based
on an actual “felt need”
of the team.
The team could use
multidisciplinary
rounds with nursing,
social work,
respiratory therapy,
etc., as a venue to
discuss quality and
safety issues and
suggest areas for
improvement that
could become a
medium-term QI
project.
Buy-in from the unit
leadership will help
facilitate buy-in from the
clinicians and caretakers
on the front lines.
Designing metrics
Metrics will be specific
to the project and the
timeframe. In such a
short-term project, you
should record
measurements daily.
Metrics will be
specific to the project
and the timeframe. In
unit-based projects,
you should record
measurements on a
weekly basis.
Metrics will be specific to
the project and the
timeframe. In medium- to
longer-term projects like
these, the measurement
system is likely to be more
complex. You can review
process measures every
couple of weeks and
outcome measures on a
monthly basis.
Institutional resources
might be available to
capture these
measurements and report
them.
Baseline data
collection
You should collect
baseline data (i.e.,
assess the current state
of the problem) within
the first 48 hours of the
clinical team’s
assembling, selecting a
topic, and starting their
on-service time
together.
You can collect
baseline data over a
week or two,
depending on the
scope of the project
and the sample size of
patients that will serve
as the baseline
population.
You can collect baseline
data over whatever time
frame you deem optimal
to collect sufficient data.
Institutional resources
may be mobilized to help
with data collection,
analysis, and reporting.
Improvement cycles
Conduct tests of change
on a daily basis over a
span of two or three
weeks, and evaluate the
results of each test the
following day or shortly
thereafter.
PDSA cycles will vary
from a few days to a
few weeks each.
PDSA cycles require more
planning to move forward
than in the other models,
and will vary from a few
weeks to a month each.
Tracking changes
As part of the daily
routine, perhaps at the
beginning or end of
Track weekly
summary statistics
This model lends itself to
summary statistics every
two to four weeks with a
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 27
bedside rounds, the
team can huddle to
discuss progress since
the prior day on their
improvement initiative.
with a continuously
updated run chart.
continuously updated run
chart, with monthly to
quarterly aggregated
statistics and bigger-
picture run charts to
demonstrate perturbation
of the system. (Updates
may occur more often
toward the beginning of
the initiative, and less
frequently over time.)
Pros
The rapid cycling
inherent in this
approach requires that
the improvement work
be completely
integrated into clinical
care rather than
separate/superimposed.
The ability to work on a
problem that the team
feels is important will
achieve more buy-in.
The goal here is not
necessarily to transform
the system, but to allow
trainees to participate
meaningfully in an
improvement effort that
matters to them.
The change that
happens provides
instant feedback to the
team on whether or not
their interventions were
successful.
Opportunities for
improvement are
addressed in real time
and immediately, as
opposed to over a six to
12-month period.
This timeframe is
quite flexible and may
fit well with the
rhythm of clinical
schedules of trainees
and their attending
physicians. The team
can collaborate and
take turns moving the
project forward as
different trainees
rotate through the
same unit and address
the same aim.
The truly
interdisciplinary
nature of these unit-
based projects is
valuable for
understanding
teamwork and
interprofessionalism.
The greater alignment
of these projects with
institutional priorities
may make resources
available that are not
available to smaller-
scope projects.
Learners truly understand
the iterative process of QI
by monitoring key metrics
over time with run charts.
There is sufficient time to
make significant changes
to the system, which may
lead to more profound
improvements and more
sustainability.
The longer timeframe
gives learners the chance
to formally work through
the steps of a mentored QI
experience including a
charter, a driver diagram,
and a continuously
updated run chart.
Participants learn about
institutional priorities in
quality and safety, and
they also learn how to
work in interprofessional
teams.
Cons
In such a short period of
time, system
transformation is
neither likely nor
possible. Altering
workflows is the more
likely outcome.
There is real risk of
“improvement fatigue”
and substantial
The medium-term
timeframe may be too
short to accomplish
significant system-
level change or too
long to accomplish
rapid, real-time
change.
The trainees typically
do not select the topic
This model requires
commitment to a single
aim over a relatively long
period of time, so it may
be difficult to sustain
momentum.
Team members will not
receive as much “instant”
feedback on whether their
interventions were
IHI Open School Faculty Guide: Best Practices for Curriculum Integration
Return to the Table of Contents Institute for Healthcare Improvement • ihi.org 28
improvement burden
among staff, as a new
team with a new aim
comes along every
month or so. Those who
work continuously in
the unit or clinic may be
less invested because of
the rapid cycling
involved.
Tracking true change
may be difficult if
patient volume (i.e., the
number of patients with
the condition you are
focusing on) is not
sufficiently large in a
two to four week period
to conducts tests of
change and draw
conclusions.
or problem to work
on. These are
determined by
institutional
priorities, which may
or may not be “felt
needs” of the trainee.
This may have the
effect of decreasing
trainee buy-in for the
projects.
successful, because the
tests of change are
conducted over longer
periods of time.
It may take longer to
change a system.
The trainees typically do
not select the topic or
problem to work on. These
are determined by hospital
priorities, which may or
may not be “felt needs” of
the trainee. This may have
the effect of decreasing
trainee buy-in to the
projects.
Examples of
opportunities for
experiential learning
Improving
documentation of DVT
prophylaxis for patients;
improving medication
reconciliation upon
transfer out of the
intensive care unit;
removing urinary
catheters as soon as
clinically indicated;
decreasing time to
discharge after rounds
for patients who are
clinically ready for
discharge; improving
verbal communication
of STAT orders to
nurses once ordered in
the electronic medical
record
Consistent provision
of Asthma Home
Management Care
Plans (AHMCP) to
pediatric patients
upon discharge;
improving
communication
around direct
admissions from
outside the hospital;
improving
empanelment of
patients with a
primary care provider;
reducing wait times to
be seen with a new
diagnosis of breast
cancer; reducing the
number of patients
who have undergone a
procedure who are
transferred to a unit
without verbal pass-
off from the physician
who performed the
procedure
In both the pediatric and
adult emergency
departments, decreasing
the time it takes for
patients with sickle cell to
receive their first dose of
pain medication upon
presentation for care;
increasing the monthly
rate of patients admitted
for asthma who are
discharged after a
pharmacist delivers their
medications to their
hospital room and
educates the family on
their use; optimizing
communication when a
patient is transferred to a
long-term care facility;
implementation of the
surgical checklist or
central venous catheter
bundle in the ICU

