Walden University Walden University
ScholarWorks ScholarWorks
Walden Dissertations and Doctoral Studies
Walden Dissertations and Doctoral Studies
Collection
2019
Nursing Knowledge on Pressure Injury Prevention in the Intensive Nursing Knowledge on Pressure Injury Prevention in the Intensive
Care Unit Care Unit
Yanick Jacob
Walden University
Follow this and additional works at: https://scholarworks.waldenu.edu/dissertations
Part of the Nursing Commons
This Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies
Collection at ScholarWorks. It has been accepted for inclusion in Walden Dissertations and Doctoral Studies by an
authorized administrator of ScholarWorks. For more information, please contact [email protected].

Walden University
College of Health Sciences
This is to certify that the doctoral study by
Yanick Jacob
has been found to be complete and satisfactory in all respects,
and that any and all revisions required by
the review committee have been made.
Review Committee
Dr. Carolyn Sipes, Committee Chairperson, Nursing Faculty
Dr. Patricia Senk, Committee Member, Nursing Faculty
Dr. Joanne Minnick, University Reviewer, Nursing Faculty
Chief Academic Officer and Provost
Sue Subocz, Ph.D.
Walden University
2019
Abstract
Nursing Knowledge of Pressure Injury Prevention in the Intensive Care Unit
by
Yanick Jacob
MS, Walden University, 2019
BS, Long Island University College, 1985
Project Submitted in Partial Fulfillment
of the Requirements for the Degree of
Doctor of Nursing Practice
Walden University
November 2019
Abstract
Over 60,000 hospital patients die each year from complications associated with hospital-
acquired pressure injuries (HAPIs). Pressure-injury rates have increased by 2% within the
past decade as life expectancy has also increased due to high cost in Medicare. Evidence
shows that the incidence of pressure injuries (PIs) in healthcare facilities is increasing,
with high rates of occurrence in intensive care units (ICUs). At the clinical site for which
this project was developed, multiple in-services had been provided to staff regarding PIs,
but uncertainty persisted about how knowledgeable the nurses were. This project, using
the Academic Center for Evidence Star Model of Knowledge Transformation improved
the nurses’ knowledge and their practice related to PI prevention in the ICU, as well as to
translate evidence into nursing practice. A literature review was conducted on PI
prevention to inform the project. The project provided an educational program for
intensive care nurses on PI prevention and determined, based on participants’ pre- and
posttest responses, that nurses’ knowledge improved as a result of participation. This
project, involving 55 nurses, includes information on the Pieper-Zulkowski Pressure
Ulcer Knowledge Test (PZ-PUKT) measuring pressure knowledge which resulted in an
85% improvement on injury prevention, 76% in wound description, as well as, 62% in
the Braden Scale. Improvements in knowledge and practice resulting from nurses’
participation in an evidence-based education session on PI prevention may bring positive
social change to the organization at which this project was conducted.
Nursing Knowledge of Pressure Injury Prevention in the Intensive Care Unit
by
Yanick Jacob
MS, Walden University, 2019
BS, Long Island University, 1985
Project Submitted in Partial Fulfillment
of the Requirements for the Degree of
Doctor of Nursing Practice
Walden University
November 2019
Dedication
I would like to dedicate my Doctor of Nursing Practice (DNP) final project to
God, who gave me the strength to pursue my dreams. To my family, especially Claudel,
my husband, who was always there for me, staying up me while I was working on my
project. Without his help, this dream could not have been a success. I wanted to thank my
kids, Vanessa and Tamara, for understanding and cooperating with me. Many times, I
wanted to quit, but they kept me going and said they believed in me. To all family
members (with special thanks to my sister Gladys), friends, and coworkers, who have
helped and supported me along this process, this is for you.
Acknowledgments
I would like to acknowledge the team of faculty—Dr. Carolyn Sipes, Dr. Patricia
Senk, Dr. Joanne Minnick, and Dr. Nancy Moss—who helped me achieve this journey;
their mentorship enabled me to get to this point. I would like to thank all my family and
friends who have supported me reach this goal.

i
Table of Contents
List of Tables ..................................................................................................................... iv
Section 1: Nature of the Project ...........................................................................................1
Introduction ....................................................................................................................1
Problem Statement .........................................................................................................2
Purpose ...........................................................................................................................3
Addressing the Gap in Practice ......................................................................................4
Practice-Focused Question.............................................................................................5
Nature of the Doctoral Project .......................................................................................6
Approach Used...............................................................................................................6
Significance of the DNP Doctoral Project .....................................................................7
Stakeholder Analysis .....................................................................................................8
Contributions to Nursing Practice ..................................................................................8
Transferability of Knowledge ........................................................................................8
Implications for Positive Social Change ........................................................................9
Summary ........................................................................................................................9
Section 2: Background and Context ..................................................................................11
Introduction ..................................................................................................................11
Concepts, Models, and Theories ..................................................................................11
Literature Review.........................................................................................................13
Search Strategy ............................................................................................................15
Local Background and Context ...................................................................................16
ii
Relevance to Nursing Practice .....................................................................................17
Role of the DNP Student..............................................................................................18
Professional Role in the Project ............................................................................ 19
Motivation for Completing the Project ................................................................. 19
Potential Biases ..................................................................................................... 20
Expert Panel .......................................................................................................... 20
Summary ......................................................................................................................21
Section 3: Collection and Analysis of Evidence ................................................................23
Introduction ..................................................................................................................23
Practice-Focused Question...........................................................................................23
Sources of Evidence .....................................................................................................23
Setting and Sample Population ....................................................................................24
Participants ...................................................................................................................24
Procedures ....................................................................................................................25
Instrumentation and Materials .....................................................................................26
Protection of Participants .............................................................................................27
Project Ethics and Institutional Review Board (IRB) ..................................................27
Data Analysis and Synthesis ........................................................................................27
Summary ......................................................................................................................28
Section 4: Findings and Recommendations .......................................................................29
Findings and Implications ............................................................................................30
Recommendations ........................................................................................................36
iii
Strengths and Limitations ..................................................................................... 37
Future Directions .................................................................................................. 39
Section 5: Dissemination Plan ...........................................................................................40
Plan for Dissemination .................................................................................................40
Analysis of Self ............................................................................................................42
As Scholar ............................................................................................................. 42
Project Manager .................................................................................................... 43
Summary ......................................................................................................................44
References ..........................................................................................................................45
Appendix A: Power Point Presentation for Expert Panel ..................................................54
Appendix B: Pieper Pressure Ulcer Knowledge Pretest ....................................................59
Appendix C: Pieper Pressure Ulcer Knowledge Posttest ..................................................61
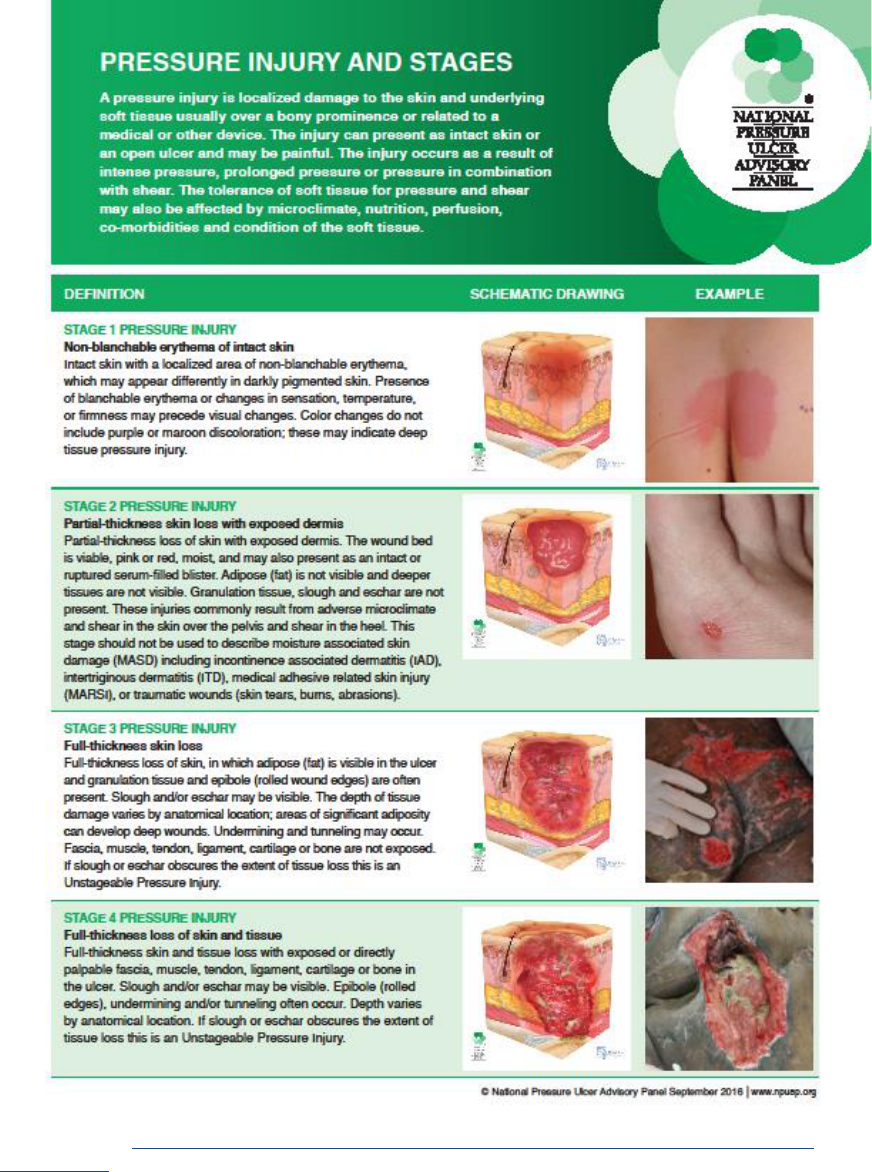
Appendix D: Education Packet ..........................................................................................63
Appendix E: Best Practice Checklist/Pressure Injury Prevention Bundle .........................65
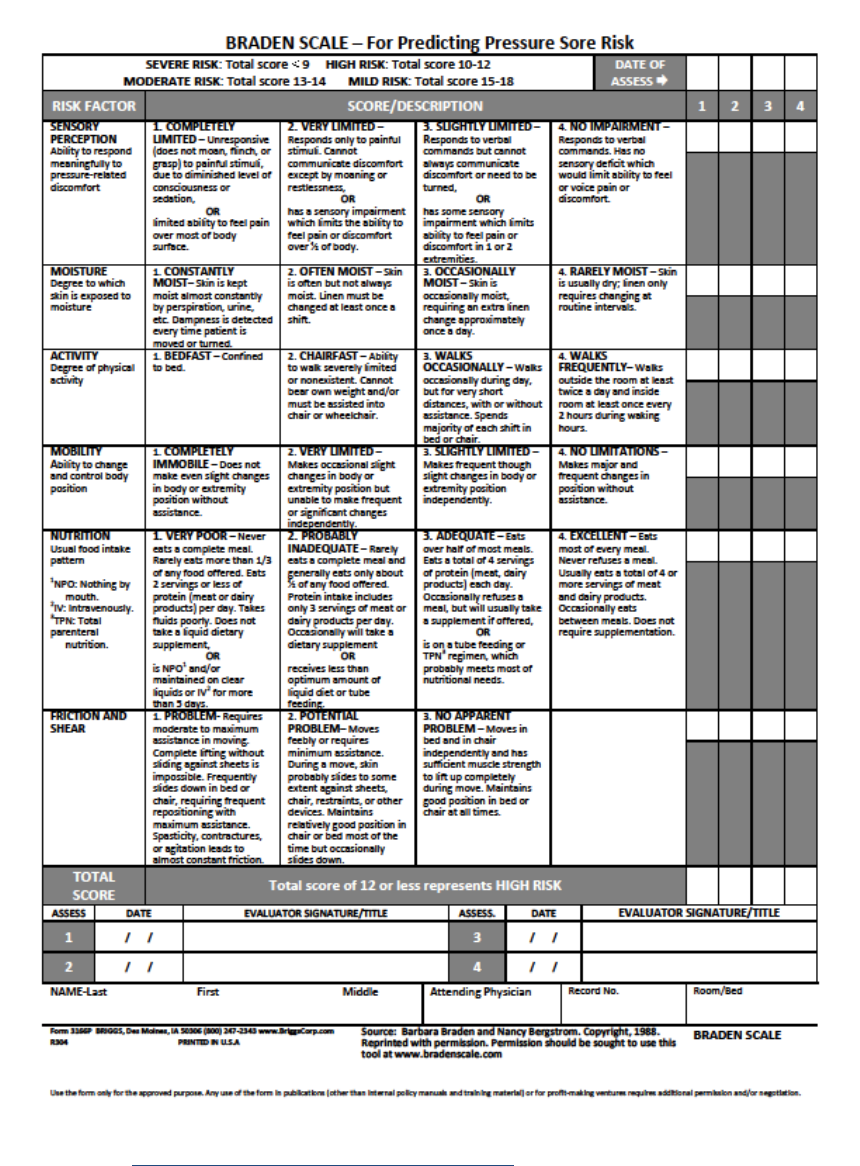
Appendix F: Braden Scale Risk Assessment Tool ............................................................66
Appendix G: Permission for NPUAP Product ...................................................................67
Appendix H: Permission for Pieper-Zulkowski Pressure Ulcer Knowledge Test .............68
iv
List of Tables
Table 1. Comparison of Nurses’ Knowledge on Pressure Injury Prevention ..................326
Table 2. Comparison of Nurses' Knowledge on Staging ...................................................37
Table 3. Comparison of Nurses’ Knowledge on Braden Scale .........................................38
Table 4. Comparison of Nurses’ Knowledge on Education Program ................................39

1
Section 1: Nature of the Project
Introduction
The quality of care provided by acute-care facilities is being scrutinized by many
government agencies, such as the Centers for Medicare and Medicaid Services (CMS).
The Institute of Medicine and the Institute of Healthcare Improvement have voluntarily
joined organizations such as the Leapfrog Group and Hospital Quality Initiative (HQI) to
ensure healthcare quality for the public by identifying when nursing may influence
negative outcomes in hospitals (Leapfrog Group, 2011). Quality indicators include
hospital-related conditions such as catheter-associated urinary tract infections (CAUTIs)
and hospital-acquired pressure injuries (HAPIs). Pressure injuries (PIs), formerly known
as pressure ulcers, continue to be a problem in the hospital setting. As defined by the
National Pressure Ulcer Advisory Panel (NPUAP, 2016), a PI is “a localized injury to the
skin and/or underlying tissue over a bony prominence, as a result of pressure, or pressure
in combination of shear.”
In the United States, it is estimated that 2.5 million patients per year are affected
with PIs (Agency for Healthcare Research and Quality [AHRQ], 2014). In the intensive
care unit (ICU), pressure injuries are associated with an increased risk of death, longer
length of stay, and discomfort (Apostolopoulou et al., 2014). In addition, the
development of PIs has been used as a measure of the quality of care that is provided to
patients (Meddings et al., 2015).
The goal of this project was to provide education to critical-care nurses on PI
prevention and to assess participants’ knowledge and practice improvement after
2
completion of the education. A staff education project was developed to meet the need
for an evidence-based educational program to support nursing knowledge about PI
prevention and assessment. The target population consisted of critical-care registered
nurses in a medical ICU. In this 30-bed ICU in a tertiary-care facility in the southeastern
United States, PIs remain at 0.3% to 1% per month, as compared to the national incidence
rate of 2.5% (Padula, 2017).
Problem Statement
The practice problem for this DNP project was the high occurrence of PIs
developing in the ICU. Patients in the ICU are critically ill, with many experiencing
multiorgan failure, so prevention of PI is essential. PI affects the comfort of the patient
and extends the patient’s duration of stay in the hospital. On average, the organization
admits several patients with life-threatening disease, infection, and PIs. The facility
provides numerous opportunities for nurses to learn about PIs, including skills fair and a
routine in-service on PI prevention, but PI has always seemed to be an issue. The facility
also has new staff members whose knowledge base on prevention is unknown. The
problem is significant because nurses frequently do not use the preventive measures
available to them. To help nurses gain a better understanding of how best to prevent PIs,
this project was developed to provide evidence-based information to the nurses in the
ICU. I sought to assess nurses’ knowledge and practice related to PI prevention in order
to identify any supports that might be needed for an improvement or change in practice.
Currently, HAPIs represent a national concern due to increased patient morbidity, the
high cost of treatment, and medical expenses (Zaratkiewicz et al., 2011). The

3
development of pressure injuries is linked to poor patient outcomes, but most HAPIs can
be prevented if hospitals improve the quality of their care. However, since July 2015, due
to higher incidents of HAPIs, PI has increased by 2% as life expectancy has also
increased (Cano, Anglade, Stamp, & Young, 2015).
Currently, there is evidence that the incidence of PIs in healthcare facilities is
increasing. Over 60,000 hospital patients die each year from complications associated
with HAPIs. HAPI rates vary depending on the clinical setting, ranging from 2.2% to
23.9% in long-term care to 0% to 17% in home care (Health Research & Educational
Trust, 2017). According to NPUAP (2015), PI care in the United States costs around $11
billion annually. Costs for an individual PI can vary from $500 to $70,000. According to
the Wound, Ostomy, and Continence Nurses Society (WOCN, 2017), PI is a complex
problem due to multiorgan failure and comorbidities. Recognizing that PIs cannot be
completely eliminated, the WOCN (2017) issued a position statement on avoidable
versus unavoidable PIs. Policies and campaigns have been implemented to encourage
hospitals to improve the quality of care in an effort to reduce unnecessary and
preventable costs. Medical devices related to PI have come to be more than 30% of the
overall hospital-acquired pressure ulcer injury (HAPU/I) rate therefore to treat PIs
quickly, to reduce the cost and improve quality interventions must be implemented
(Health Research & Educational Trust, 2017).
Purpose
The purpose of this staff education project was to provide an educational program
to intensive care nurses on PI prevention and to determine whether nursing knowledge
4
improved when measured by pre- and posttest responses. Nurses perform and inspect all
pressure points on admission, on transfers, at the beginning of each shift, for each end-of-
shift report, and at discharge, but PI remains a concern in the project agency.
Addressing the Gap in Practice
A better understanding of the gap between theory and practice may encourage
healthcare providers to pay more attention to evidence-based practice (EBP)
recommendations in order to reduce PI incidence in healthcare settings. In this case, there
is a gap in nursing education and application of knowledge regarding PI prevention.
The staff education project was developed to address the gap in practice regarding
EBP for PI prevention by improving nurses’ knowledge of PIs. In order to ensure
superior prevention of PIs, it is necessary to assess nurses’ knowledge and practice (Joint
Commission Resources, 2012). The Pieper-Zulkowski Pressure Ulcer Knowledge Test
(PZ-PUKT) was used to measure PI knowledge in addition to factors attributed to
development of pressure injuries (Pieper & Zulkowski, 2014). It has been reported that
many nurses have inadequate knowledge concerning PIs and the staging of wounds
(Delmore et al., 2018) and need to be educated on PI prevention.
Waugh (2014) conducted a systematic review using seven studies to examine
nursing knowledge and PI prevention and found that there was no relation to the
application of adequate PI prevention. Furthermore, nurses with higher levels of
education have scored higher in knowledge in some studies, whereas other studies have
shown no difference in knowledge associated with nurses’ education (Waugh, 2014).

5
The WOCN (2017) recommended further research to identify the development of
risk factors for PI and interventions for clinical practice. The WOCN has noted the need
for a fuller understanding of the conditions and risk factors associated with avoidable and
unavoidable PIs.
Practice-Focused Question
The practice-focused question for this project helped to identify the clinical
problem relating to PI prevention (Fineout-Overholt, Melynk, Stillwell, & Williamson,
2010). The question was as follows: To what extent will the nurses’ knowledge on
pressure injuries improve after attending a structural education program?
Due to a lack of documentation on PI prevention, it appeared that the nursing staff
did not understand the importance of adequate preventative measures for PIs. For
example, the Braden Scale is highly predictive of PI development, although it is utilized
inefficiently. In 2014, wound experts with NPUAP affirmed that not all PIs can be
prevented in the ICU, suggesting that the development of PI may be unavoidable in
critically ill patients (Cox, Roche, & Murphy, 2018). In the facility, the Braden Scale is
used as an assessment tool for patients at risk of PI. Understanding the scale and its
scoring assist in determining the level of risk. A score of 15-18 identifies a patient at risk,
a score of 13-14 identifies moderate risk, a score of 10-12 indicates high risk, and a score
below 9 identifies greater risk (Cox et al., 2018). However, Bergstrom and Braden (2002)
recommended that low subscale scores are to be used for prevention protocols, as these
are now required by CMS (Cox et al., 2018). In addition, there may be a lack of research
6
evidence on the effectiveness of some interventions that are available (Gray, Grove &
Sutherland, 2017).
Nature of the Doctoral Project
The evidence that was used to meet the purpose of this doctoral project included
information obtained from various literatures. In identifying the research problem, I used
research from Cumulative Index of Nursing and Allied Health (CINAHL), Medline,
Joanna Briggs Institute, and Cochrane. The population involved in this project included
wound care nurses, the wound care champion RN of the unit, dieticians, and a physical
therapist. A questionnaire tool was provided to all nurses in the critical care units in the
medical ICU to measure knowledge and practice on PIs. The doctoral project was
conducted to assess nursing knowledge of an EBP for PI prevention in intensive care
nurses after providing an educational program. I used a validated questionnaire tool to
assess nurses’ knowledge of PI prevention and practice. The staff education project
involved pretest-posttest administration of a questionnaire to determine the effect of
education on nursing knowledge on PI. ICU nurses involved in delivering regular care to
any patient at risk of PI were included.
Approach Used
The approach that was used for this doctoral project included a comprehensive
literature review on PI prevention and practice in the ICU. The project was directed by
the Academic Center for Evidence (ACE) Star Model of Knowledge Transformation to
translate evidence into nursing practice, which has been used as a guide to increase
understanding of the use of EBP in nursing practice and its relevance in clinical decision
7
making (Stevens, 2013). The development of nursing knowledge is relevant.
Furthermore, it will be evaluated to appropriately answer the research question. The ACE
model was used to assist in nursing education, PI prevention, practice, skin assessment,
and the Braden Scale.
Significance of the DNP Doctoral Project
The NPUAP has developed many educational materials regarding PI. The
persistence of PIs as a problem in the hospital setting can be attributed to the inadequacy
of efforts to disseminate the knowledge required to prevent these injuries (NPUAP,
European Pressure Ulcer Advisory Panel, & Pan Pacific Pressure Injury Alliance, 2014).
I discussed the need for this project with the nurse manager and how it might be
beneficial to assess nursing knowledge and practice. In 2011, the Center for Medical
Surveillance began reporting HAPI rates for hospitals on its Hospital Compare website,
and in 2014, the Affordable Care Act began reducing reimbursement to hospitals that
were in the highest quartile for incidence of hospital-acquired conditions (HAC) for
Medicare patients (Meddings et al., 2015). PI is considered as a localized injury to the
skin or underlying body tissue that occurs over bony prominences (NPUAP, 2016).
Working in ICU exposes staff to the rigors of PI prevention in immobile patients, and
despite the many protocols that are available to deal with the issue, it keeps occurring.
Efforts to assess nursing knowledge and practice can be useful if problems can be
identified and improvements in the quality of patient care can be achieved. Such efforts
to support PI prevention are important because the incidence of HAPIs has increased
nationally in medical ICUs (Institute for Clinical Systems Improvement, 2012).
8
Stakeholder Analysis
Stakeholders in this project were the hospital administrators, the nurse manager
for the unit, and the wound care specialists. These experts were informed of the project
and were asked to offer guidance. The stakeholders may be impacted by the results of the
pretest/posttest questionnaires, and could further impact the rate of PI incidence in the
facility.
Contributions to Nursing Practice
PIs can contribute to increased length of hospital stay, increased chance of death,
missed employment days, social isolation, pain, suffering, and financial burden
(Strazzieri-Pulido, Gonazalez, Nogueria, Padilha, & Santos, 2019). Hospital mortality
rates have increased to 11.2% with patients who developed HAPIs and the rate of
mortality with readmission within 30 days after discharge was 15.3% (Lyder et al., 2012).
This project assessed nurses’ knowledge of PI prevention and practice with the
implementation of an evidence-based education program. Nursing knowledge of
prevention and assessment of PIs is essential to lowering PI rates.
Transferability of Knowledge
Through this DNP project, critical-care nurses gained knowledge and experience
on PI prevention in nursing practice. An additional goal of this project is to support
positive change by sharing the findings with others in similar practice areas with similar
issues such as PIs. Dealing with PI is a major concern in hospitals because CMS will no
longer reimburse for PIs caused while patients are hospitalized (Cooper, 2013).
9
Implications for Positive Social Change
There have been a number of suggestions to increase nursing knowledge over the
years. Some of the most effective involve providing standard operating protocols in the
practice setting, providing summaries of information at conferences and workshops, and
recognizing continuous educational achievements through certifications and honors.
Assessing critical-care nurses’ knowledge and practice through an evidence-based
educational program on PI prevention may bring positive social change to the
organization at which this project was conducted. Educational program can bring
knowledge closer to nurses, alleviate the strain of nurses’ workload, and give nurses
motivation to receive continuing education. In efforts to transfer knowledge, professional
bodies require that all nurses complete a required continuing education regimen over a
period of time. Several resolutions in assisting continuing education have been proposed,
such as making required reading material available in summary form as well as having
the material available for staff through electronic means. However, these methods have
not been taken up effectively (Clark et al., 2015; Coventry, Maslin-Prothero, & Smith,
2015).
Summary
In the field of acute care, critically ill patients are at a high risk for developing
PIs. Preventing PIs is a healthcare concern in the hospital where I implemented this DNP
project, and this project was an effort to mitigate PIs by determining the level of nurses’
knowledge of PI prevention and practice in the ICU through an educational program. In
Section 2, I present the background and context of project, which are supported by a
10
comprehensive literature review on PI prevention and practice.

11
Section 2: Background and Context
Introduction
In the hospital- and home-care settings, there are an increasing number of
patients who are immobilized by illness. This situation has led to an increase in the
incidence of PIs. PIs represent a significant concern in the hospital-care setting. The
focus question for this project was the following: To what extent will the nurses’
knowledge on pressure injuries improve after attending a structural education program?
This project assessed the impact of an evidence-based education program on nurses’
knowledge of PI prevention and assessment.
The DNP project focused on assessing the information that was possessed by
nurses and disseminating information in regard to PI prevention. It encompassed a
literature review on the prevention of PIs. Using a pre- and posttest questionnaire as the
chief study design, I obtained information from nurses on their knowledge of current
practice guidelines. In this section, I present the theoretical models for the project, a
literature review, and the project’s relevance to nursing practice.
Concepts, Models, and Theories
Theoretical frameworks create a reference for interpretation or generalization of
the literature. The theoretical framework suggested that evidence-based practice (EBP) is
valid; therefore, confirming the need to understand research findings. Furthermore,
evidence-based nursing practice is the identification of theories on human health and
human experiences to direct modalities of care. Using EBP to make changes in current
practices have proven effective and demonstrate positive outcomes. Failure to apply EBP

12
to guide nursing care increases the risk of poor effects (Chrisman, Jordan, Davis, &
Williams, 2014). With this in mind, I used the evaluation criteria proposed Chrisman, et,
al, 2014) to guide the direction of this project.
Nurses have developed numerous EBP models to help in understanding evidence
in the context of nursing practice. The ACE model assists in examining and applying
EBP in a manner that is useful for nursing. (Academic Center for Evidence-Based
Practices [ACEBP], 2012).
Using the ACE Star Model of Knowledge Transformation, one can discover
barriers when moving evidence into practice and implementing solutions grounded in
EBP. The ACE model includes competencies for essential skills of knowledge
management, accountability for the scientific basis of nursing practice, organizational and
policy changes, and the development of scientific foundations for EBP. This model was
developed for clinical and educational use to assess nurses’ willingness to practice
evidence-based care and to measure the impact of related professional development. The
model, represented by a five-pointed star, defines knowledge and integrates best research
evidence with clinical expertise to achieve EBP. Point 1 of the star represents primary
research studies; Point 2 represents evidence summary; Point 3 refers to evidence-based
clinical practice guidelines; Point 4 represents evidence in action; and Point 5 represents
evaluation of the impact of the EBP on satisfaction, efficacy, patient health outcomes,
and health policy (Correa-de-Araujo, 2015).
Another model that can be considered is the health benefit model (HBM), which
was developed as a way to understand the perceived benefits and consequences of
13
decision-making behaviors (Roden, 2004). Garrett-Wright (2011) applied the HBM to
perceived behavioral control and behavioral intention from the theory of planned
behavior.
Literature Review
Bradshaw (2010) acknowledged that an important feature that distinguishes the
nursing profession is taking accountability for practice and examining the best way to
deliver care; this statement fully reflects the essence of EBP related to PI treatment.
However, the main problem in PI treatment lies in the fact that there is a gap between
theory and practice. To prove the validity of this assumption, PI treatment should be
considered in terms of risk assessment strategies. Consistency in nursing assessment,
documentation, and relevance to the interventions planned will improve PI prevention
and decrease the risk of PI development. Identification of extrinsic and intrinsic risk
factors for PI development is necessary.
However, a retrospective observational study conducted using the U.S. Premier
Healthcare Database (PHD) showed the importance of identifying risk factors for HAPIs
and improving best practice for PI prevention (Dreyfus, Gayle, Trueman, Delhougne, &
Siddiqui, 2018). Patients who may receive a mixture of treatments for other pathologies
may not be receiving proper nutrition as income constraints may dictate diet. In addition,
literature indicates that unmodifiable factors associated with patients with disease
processes and comorbidities have a great effect on PI development and patients’ ability to
adhere to preventive measures (NPUAP, 2017; WOCN Society, 2017).
14
PIs are responsible for over 60,000 annual cases of hospital death in the United
States due to complications (ICSI, 2012). Meanwhile, difficulty in obtaining
reimbursement for ulcer treatment raises operating costs in healthcare institutions. The
cost of treatment has been set at a figure of around $11 billion every year, which
underscores the need to reduce the incidence of PI at a local and national scale (Bauer,
Rock, Nazzal, Jones, & Qu, 2016).
Several comprehensive reviews addressing PI prevention and nursing knowledge
were identified. The NPUAP provides information on identifying and staging PI along
with current treatment and served as a resource for project. Waugh (2014) discovered that
there was no significant nursing knowledge with PI prevention when nursing knowledge
was effectively identified. However, the lack of knowledge to nursing practice scored
higher with higher application of PI prevention. Furthermore, although nurses who scored
high were highly educated, there was no major difference in knowledge scores for nurses
with higher levels of education (Waugh, 2014).
Moore and Cowman (2014) compared PI incidence between patients assessed
with the Braden risk assessment tool (n = 74) and patients examined through unstructured
risk evaluation (n = 76), concluding that there was no statistical difference between the
groups. They further compared PI assessment using the Waterlow risk assessment tool (N
= 420), the Ramstadius risk screening tool (N = 420), and no formal risk assessment (N =
420). The findings they obtained gave Moore and Cowman reason to assert that there was
no statistical difference in PI incidence across the three patient groups.
15
In the facility studied, wound care prevention is essential, and the Braden Scale
has been used as the most complete process for validation (Garcia-Fernandez, Pancorbo-
Hildago, & Agreda, 2014). Depending on the score, the nurse assessing the patient may
initiate preventive measures. The Braden score system consists of six subscales—sensory
perception, moisture, activity, mobility, nutrition, and friction/shear—for identifying
patients at risk for pressure injury (AHRQ, 2016).
Search Strategy
A comprehensive literature review was conducted using CINAHL, Medline,
Cochrane, and the Walden library database. Boolean operators were used for key words
such as pressure injury, knowledge, prevention, critical care, skin assessment, education,
staging, and Braden Scale. With high occurrence of PI’s in mind, there have been broad
attempts to develop methods for reducing the incidence of PI in high-risk patients. To this
end, there have been several proposed methods that have taken into account the type of
care setting and the patient group. Some of the methods proposed are inspecting the skin
frequently, relieving pressure on risk areas, reducing moisture by applying creams,
preventing friction and forces of shear when moving the patient, making sure that the
patient receives proper nutrition, and paying special attention to patients at risk during
rounding (Tayyib, Coyer, & Lewis, 2015).
The knowledge and skills required for preventing PIs consist of patient-risk
assessment, practice protocols for prevention of ulceration, assessment of ulcers, and
management of PIs. The accumulation of such knowledge is the essence of this DNP
project. I sought to implement an evidence-based PI prevention program that was
16
dedicated to increasing the knowledge of nurses. The logical premise underlying the
project was that with sufficient knowledge, a nurse should be able to handle and prevent
PIs.
Local Background and Context
The clinical site where this staff education project was piloted was a 30-bed
medical ICU in a tertiary-care facility in a hospital in the southeastern United States.
Patients in a ICU setting such as the project site may be unconscious and
immunocompromised. They may also be receiving medications that increase the risk of
developing PI. Hospitalized patients being treated for a variety of illnesses require
constant monitoring by nurses to ensure that the risk of PI is minimal. Many of these
patients have multiorgan failure. It is essential to note that immobilization is one of the
chief contributors to the PI problem (Cox et al., 2018).
Under new CMS guidelines, Stage 2-4 or unstageable PIs that were not present on
admission were considered injuries. Suspected deep-tissue injury was replaced by deep-
tissue injury (CMS, 2018). Evidence-based guidelines provide essential vision to
clinicians and stakeholders related to patients who received interventions and offered to
support HAPI that was unavoidable due to critically ill patients. With the implementation
of a quality-improvement initiative 67% reduction in HAPIs were reflected avoidable
(Jacobson, Thompson, Halvorson, & Zeitler, 2016).
The implementation of continuing education programs in PI prevention seems to
be eliminating the incidences of the injury. It is a reference point from which the need to
17
develop other novel solutions or to intensify the use of the existing ones can be
supported.
DNP-prepared nurses must take roles of leadership and advocate for changes that
better serve the patient. They are also required to take part in the generation of nursing
wisdom and the dissemination of information to others. This role of dissemination was
integral to this project. The aim was to ensure that the delivery methods were effective.
Being in the ICU makes one realize that despite the bulletin boards and booklets
available in the area and the nurses’ lounge advocating PI prevention, a large part of the
nurses’ day is spent tending to already-developed PIs. With an increasing number of
geriatric ICU patients, there is need to consider all approaches that could prevent this
susceptible group of patients from developing PIs. This calls into question the validity of
the methodologies suggested for prevention. However, scrutiny of these methods yields
evidence that the recommendations are valid in practice (Mallah, Nassar, & Badr, 2015).
The question of how much of the available knowledge is actually disseminated and
internalized successfully therefore arises. This seems to be the logical progression to
finding a solution to the practice problem.
Relevance to Nursing Practice
PI continues to represent a financial problem for the healthcare system and a
challenge to patients’ quality of life (Parnham, 2015). Although the NPUAP has provided
many protocols, guidelines, and educational materials related to PIs to all organizations,
PIs remain a problem in the hospital setting, which can be attributed to the inadequacy of
efforts to disseminate the knowledge required to prevent these injuries (NPUAP et al.,
18
2014). Nuru, Zewdu, Amsalu, and Mehretie (2015) found PI knowledge to be good in
over half of the nurses in an institutional study, but they found practice essentials to be
good in less than half of the nurses. In the study, many reasons were given for the
development of this problem, including inadequate resources and equipment and a staff
shortage, which may have affected work performance and caused fatigue (Nuru et al.,
2015).
In another study by Gunningberg et al. (2015), the thematic description of this PI
knowledge was found to be weak. Using a PI knowledge tool, the researchers were able
to test for the themes of nutrition, classification and observation, risk assessment, and
etiology and causes. From their findings, they recommended an extensive educational
campaign. This is why the knowledge base of nurses was an important factor to consider
in the current project.
Role of the DNP Student
My role as the DNP student in this project was to assess nurses’ knowledge and
practice related to PI prevention in the ICU. To achieve this, I used pre- and posttest
questionnaires.
My primary objectives as a DNP-prepared nurse are to serve as a role model and
to engage in EBP research, identifying gaps that exist and undertaking to structure and
implement projects to fill those gaps. The DNP-prepared nurse should provide incentive
for nurses to undertake interventions and research. My role in this project also involved
evaluating the success of the project in terms of the set of objectives, which involved
19
determining whether nurses’ knowledge of PI prevention and practice improved after an
educational session.
Professional Role in the Project
The professional obligation of registered nurses is to ensure that all of the
knowledge that their colleagues acquire through education and experience is passed on.
In order for information to be raised the levels of knowledge and wisdom, it must be
tested in the crucible of evidence. The interventions have already been tested. Therefore,
I sought in this DNP project to establish whether the dissemination of this knowledge was
complete and the effect it had on the incidence and management of PIs.
Motivation for Completing the Project
I was a key figure in an interprofessional practice team, serving as a conduit for
information, a conflict arbitrator, a leader, and a project director. While working in the
ICU and seeing many protocols for PI prevention, documentation, and skin assessment, I
noted that PIs continued to occur. During past practicum experiences, I had noticed that
there seemed to be a gap concerning PI prevention related to knowledge. My role was to
educate the nursing staff on the importance of skin assessment for patients in the ICU and
to assess nurses’ knowledge on PI prevention before and after education was provided.
My motivation for this doctoral project derived from my interest in determining
what research was currently available that would support and identify the need to
implement a PI prevention program and its impact on nurse knowledge. I had no bias for
this project.

20
Potential Biases
During the project, one potential challenge that I identified was staff cooperation,
which could have affected the accuracy of questionnaire results. Although EBP is used
for guiding advanced nursing practice, there are some barriers involved when
implementing interventions. The educational intervention in this project was based on
quality improvement models that can be applied in the healthcare setting.
Expert Panel
I conducted a staff education project using the staff education plan. A PowerPoint
(PPT) presentation was presented to the participants (Appendix A). I explained the
pretest, which was a 47-item questionnaire administered to the nursing staff prior to staff
education in order to determine participants’ current knowledge and understanding of PI
prevention (Appendix B), as well as the posttest, which was a 47-item questionnaire that
was administered to the nursing staff after the completion of the education program to
determine new knowledge and understanding of PI prevention (Appendix C).
I will present the education packet (Appendix D) which I will have reviewed with
the expert panel of: nurse manager, two clinical managers, and RNs on that unit. The
education packet will include current evidence on Pressure Injury Prevention from the
NPAUP including: wound description and staging information and risks factors. I will
also include a Best Practice check list, which will provide information on Pressure Injury
Prevention and what should be applied for each patient (Appendix E), and finally, I
include the Braden Scale, concerning risk assessment on pressure injury and level of
intervention to follow (Appendix F). I will explain the conduction of the pre-
21
test, develop the intervention with feedback from your expert panel, revise the education
packet present the information then conduct the post-test and evaluate it then work with
the expert panel and make recommendations.
The overall goal is to educate staff on Pressure Injury prevention as studies have
shown that educating staff will lead to improvement in clinical outcomes (Kavanagh et
al., 2012). The DNP project is an integral part of developing the skills to research and
develop evidence-based nursing knowledge. The DNP project proposed seeks to mitigate
this by first assessing the degree of knowledge the nurses have on Pressure Injury
prevention and then charting a course for their continuous education.
The DNP prepared nurse must take the role of leadership and advocate for
changes that better serve the patient. They are also required to take part in the generation
of nursing wisdom and in disseminating this knowledge to others. This role of
dissemination is the key part of this project. The aim is to ensure that the delivery
methods are effective.
Summary
The role of the DNP nurse as a leader and advocate is best exemplified by the
DNP project. In the same breath, the DNP nurse is able to sharpen their research skills
while contributing to the body of nursing wisdom. A practicum stint in the ICU revealed
that despite the large amount of information available on PIs, there are still many cases of
ICU-related pressure injuries. In light of this, a new strategy must be adopted.
The project proposes to couple an evaluation of the degree of knowledge with a
subsequent educational initiative for nurses in the ICU. The results of this project are
22
aimed at improving the patient outcome, quality care, and the management of hospital
and patient resources as well as adding to the body of nursing knowledge. Through
evidence-based practice research modalities, we are able to understand the problem and
generate the most viable solutions for the good of the entire healthcare system. Section 3
details the collection and analysis of evidence on nursing knowledge on pressure injury
prevention and practice.

23
Section 3: Collection and Analysis of Evidence
Introduction
HAPIs remain a national concern due to patient morbidity, the high cost of
treatment, and reimbursement cases (Zaratkiewicz et al., 2011). The aim of this staff
education project was to provide education to critical-care nurses on PI prevention and to
assess staff knowledge after completion of the education. In this section, I describe the
collection and analysis of evidence, addressing the following topics: (a) practice-focused
question, (b) setting/population sample, (c) participants, (d) procedures, (e)
instrumentation materials, (f) data analysis, (g) protection of participants, and (h) project
ethics and Institutional Review Board (IRB), concluding with a summary. The project
plan was to obtain data and analyze evidence through the use of a questionnaire on PI
prevention. The questionnaires were distributed, collected, and analyzed to ensure that
the research questions had been answered as predicted.
Practice-Focused Question
According to Stillwell, Fineout-Overholt et al. (2010), a practice-focused question
identifies a clinical problem for staff to recognize and understand. The focus question for
this staff education project was the following: To what extent will the nurses’ knowledge
of PIs improve after attending a structural education program?
Sources of Evidence
The sources of evidence that were used for this doctoral project were obtained
from numerous articles in the literature. All articles were reviewed and organized into
sections related to PIs, prevention, skin bundle, knowledge, staging, wounds, and best
24
practice. Sources of evidence were gathered from CINAHL, Joanna Briggs Institute,
Medline, and Cochrane. Recommendations and further research related to knowledge and
practice of PI prevention were considered in order to address the practice-focused
question. My aim was for the staff education project to address a gap in the knowledge of
critical-care nurses and provide the necessary evidence to improve nurses’ practice and
maintain PI prevention. The staff education project site was an acute-care tertiary Level 1
trauma unit consisting of 763 beds.
Setting and Sample Population
The selected setting was a 30-bed ICU in a medical ICU located in the
southeastern region of the United States Working in the ICU exposes staff to the rigors of
PI due to patient immobility and hemodynamic instability. The sample population
consisted of 20 RNs working in the ICU. As the DNP student directing this project, I had
the stakeholders assist in the selection of the healthcare individuals. The stakeholders
who assisted in the process were the wound care nurse, the wound care RN of the unit,
and the clinical specialist of the unit. In this organization, nurses are expected to
formulate and communicate changes to practice and management in the healthcare
setting.
Participants
All participants for this staff education project were registered nurses working in
intensive care with direct patient care responsibilities. The age range for participants was
23-65 years. Participants were informed of this staff educational project and informed

25
that all data, questionnaires, and surveys would be kept confidential and anonymous in a
locked cabinet in the ICU charge office.
Procedures
The staff education project took 2 weeks. A PPT presentation was shown to the
participants and took approximately 60 minutes (Appendix A). I explained the pretest,
which was a 47-item questionnaire administered to the nursing staff prior to the staff
education in order to determine their current knowledge and understanding of PI
prevention (Appendix B), as well as the posttest, a 47-item questionnaire administered to
the nursing staff after the completion of the education program to determine new
knowledge and understanding of PI prevention (Appendix C). I presented the education
packet (Appendix D), which I had reviewed with an expert panel consisting of the nurse
manager, two clinical managers, and RNs on that unit. The education packet included
current evidence on PI prevention from the NPAUP, including wound description,
staging information, and risk factors. I also included a best practice checklist, which
provided information on PI prevention and what should be applied for each patient
(Appendix E). Finally, I included the Braden Scale concerning risk assessment for PIs
and levels of intervention to follow (Appendix F). The duration of each test was
approximately 20-30 minutes. The posttest questionnaire consisted of 47 questions used
by Pieper and Zulkowski (2014) utilizing a Likert scale. The Likert scale was used to
evaluate the self-reported knowledge before the pre-test and after the posttest. A
nonparametric t -test result was used to identify the trends between ordered groups and to
examine the frequency and knowledge with respect to PI prevention test completion
26
(Terry, 2015). The findings from the pre- and posttest were analyzed to determine change
in practice.
Instrumentation and Materials
Due to its high reliability, the Pressure Ulcer Knowledge Test (the Pieper test)
was used to assess nurses’ knowledge of PI prevention, referring to the research question.
This test has a Cronbach’s alpha of 0.8 and shows good validity for PI prevention and
skin assessment and staging (Pieper & Zulkowski, 2014).
Through this staff educational project, I sought to address the PI concern by
getting an overall perspective on information dynamics as they related to PI prevention.
The quantity and quality of information that is available to the nursing staff were
assessed. The data collection method consisted of performing a skin assessment on all
patients who met the inclusion criteria, at the beginning of the shift and at the end-of-shift
report. Skin assessment was the driver for a nursing intervention to identify early skin
damage and to prevent skin damage (Tume, Siner, Scott, & Lane, 2014). Other data
collection involved documenting the Braden Scale for each patient. The Braden score
system consists of six subscales: sensory perception, moisture, activity, mobility,
nutrition, and friction/shear (Tayyib et al., 2015). The first subscale uses a scale of 1 to 3,
and the remaining five subscales use a scale of 1 to 4. The lower the score, the higher the
patient’s risk of developing sores or injuries is. Depending on the score, the nurse
assessing the patient then initiates preventive measures.
27
Protection of Participants
All participants for this project were registered nurses working in intensive care
with direct patient care. Upon conducting a project, it is crucial to ensure the protection
of human subjects in terms of autonomy, confidentiality, nonmaleficence, and
beneficence (Gray et al., 2017). All participants were protected, as all data,
questionnaires, and surveys were kept confidential in a locked cabinet in the ICU charge
office.
Project Ethics and Institutional Review Board (IRB)
As per protocol regarding rules and ethical and federal regulations, I submitted
the DNP project to the Walden University IRB for approval.
Data Analysis and Synthesis
The need to evaluate the incidence of PIs in critically ill patients in the ICU was
closely related to the clinical question. The pre- and posttest questionnaire helped to
closely represent the clinical question when exploring the outcomes of nurse-driven
behaviors to decrease PIs. After the education session, posttest questionnaires were given
to the participating nurses in anonymously labeled packets. Responses from these
questionnaires were evaluated and analyzed. DNP projects are crucial in evaluating
practice guidelines and settings to ensure that the quality of care continuously increases.
This particular staff education project was conducted to ensure that the body of
knowledge that was available to the nurses reached its target audience efficiently and
therefore enabled them to meet the needs of their immobilized and sometimes
unconscious patients.
28
Summary
In summary, the need to assess nurses’ knowledge and practice related to PI
prevention in the ICU continues to be a concern. Although PIs may remain an issue,
having ongoing education, training, assessment, and a guidelines tool on PI prevention to
improve nurses’ knowledge and practice related to PI is essential to preventing further
injuries. In order to raise information to the levels of knowledge and wisdom, it must be
tested in the crucible of evidence. In Section 4, I present the findings and
recommendations.

29
Section 4: Findings and Recommendations
The local problem serving as inspiration for this DNP project was the high
occurrence of PIs developing in the ICU. In Section 3, I addressed the gap in practice
concerning PI and explored how to mitigate risks by assessing nurses’ knowledge. In the
following section, I evaluate current practice pertaining to PIs and conduct pre- and
posttest evaluations. The findings from this PI study may support the need for
improvement or change in practice. Better understanding of the gap between theory and
practice may encourage healthcare providers to pay more attention to EBP
recommendations in order to reduce PI incidence in healthcare settings. As a reminder,
the guiding practice-focused question for this project was the following: To what extent
will the nurses’ knowledge on pressure injuries improve after attending a structural
education program? The purpose of this educational project was to provide further
education on PI prevention and to identify whether nurses’ knowledge improved based on
the training. The focus of the training was assessment and understanding of better
methods of PI prevention.
The aim of this educational project was to identify whether nurses’ knowledge
improved after an educational session. PIs in the ICU are inevitable; however, assessing
and analyzing new evidence and strategies for PI prevention could reduce the incidence
of PIs in the hospital. This study was based on multiple sources of evidence to support the
conclusion. The sources of evidence used for the staff education included literature
obtained from CINAHL Plus with Full-Text, Joanna Briggs Institute, Medline, Cochrane,
and ProQuest. Development of the process included a pretest and posttest on nursing

30
knowledge of PI prevention that were administered to the nursing staff. Results of the
pretest and posttest were compared to identify outcomes. The comparison between the
pretest and posttest responses determined that nurses’ understanding had increased after
the intervention. Section 4 contains a discussion of the findings, implications, strengths,
and limitations of the study, as well as my analysis of myself.
Findings and Implications
The project objective was to assess nurses’ knowledge of PI prevention in the
ICU after attending a structured educational program. The aim of conducting this study of
a staff education project was achieved by using the Pieper Knowledge Test. The Pieper
Knowledge Test was used to measure five categories: (a) PI prevention, (b) staging, (c)
wound description, (d) the Braden Scale and (e) program education. Permission to
conduct the project was pursued, reviewed, and obtained from the project agency’s
Institutional Review Board (IRB), which issued project approval on June 21, 2019,
(Reference # 005544). A PPT was presented to the participants (Appendix A). This
project required the distribution of a pretest questionnaire on current knowledge and
understanding of PI prevention (Appendix B) and was administered to the nurses. In
order to understand the change in nurse’s knowledge to determine the presence of new
knowledge and understanding of PI prevention, a posttest questionnaire was administered
to the nursing staff by the expert panel after the completion of the educational program
(Appendix C). An educational packet on PI prevention was presented to the nurses
(Appendix D). Using the NPAUP guidelines, the education packet included current
evidence on PI prevention, including wound description and staging information and risk
31
factors. The packet included a best practice checklist, which provided information on PI
prevention (Appendix E), and the Braden Scale: risk assessment on PI and interventions
Appendix F). The results from the pre- and posttest assessment of the participants’
practice and knowledge of PI prevention were analyzed. Among the 47 questionnaires
from the Pieper Knowledge Test, I selected 14 of the questions related to prevention,
staging, knowledge, the Braden Scale, and education to determine knowledge deficits and
any needs for improvements in knowledge.
There were 75 nurses in the ICU. Seventy-five (100%) nurses were administered
the pretest and provided with the education packet on PI prevention in the ICU. Seventy-
five participants completed a color-coded pretest. Following the completion of the
pretest, 75 participants were administered the education presentation and packet.
Participants were allowed to ask questions throughout presentation, which lasted 30
minutes. After the education presentation, the participants were given the color-coded
posttests, which they were allowed 2 weeks to complete. Upon return, each participant’s
pretest and posttest were matched. Of the 75 initial participants, only 55 (73%) nurses
completed both the pretest and the posttest. Therefore, 55 total participants were included
in the complete data set to determine any change in knowledge.
The following results reflect responses to two general questions on nurses’
knowledge on PI prevention and show strong improvement in nurses’ knowledge on PI
prevention (see Table 1). Prior to education, only 30 nurses (54%) demonstrated
knowledge concerning patient assessment for PI development on admission to the
hospital, compared to 45 nurses (81%) on the posttest; thus, there was an increase of
32
27%. The second question concerning care given to prevent or to treat PI and to treat PI
documentation demonstrated that 34 (61%) of participants indicated that this idea was
important on the pretest, compared to 43 (78%) of participants on the posttest,
demonstrating 16% improvement in understanding. In both cases, participants’
knowledge increased.
Table 1
Comparison of Nurses’ Knowledge on Pressure Injury Prevention
Question item
Pre-test
Strongly agree
N = 55 (%)
Posttest
Strongly agree
N = 55 (%)
Percent
change
All individuals should be
assessed on admission to a
hospital for risk of pressure
injury development
30 (54%)
45 (81%)
27%
All care given to prevent or
treat pressure injuries must
be documented
34 (61%)
43 (78%)
17%
The next four questions focused on the staging of wounds, differentiating Stage I
and Stage II (see Table 2). The first question asked participants about the definition of
Stage I and the description of a lightly pigmented person. Prior to education, 33 (60%) of
the nurses were able to define Stage I in a lightly pigmented person. Post education, there
was an increase so that 42 (76%) nurses were able to define Stage I in a lightly pigmented
person. The results indicated that after education, there was increased knowledge for
Question 1. The second question asked participants about the description of Stage II and
how to identify full thickness skin loss. On the pretest, 22 (40%) participants indicated
that full thickness of the skin loss is described as Stage II. On the posteducation
33
assessment, 20 (36%) participants demonstrated knowledge on full thickness skin loss in
Stage II. As noted below, there was a decrease by 4% on the posttest for Question 2.
Although there was a decrease of 4% on the Stage II description, results demonstrated
improvement of knowledge on staging. Question 3 asked participants to identify whether
Eschar is healthy. The results for the third question indicated that prior to education, 25
(45%) of the participants described healthy tissue as Eschar. After education, 7 (13%) of
the nurses indicated that Eschar is not considered healthy tissue. The fourth question
asked each participant to describe slough; 32 (58%) participants identified slough as
“yellow cream necrotic tissue” on the pretest, and 40 (73%) did so education. The results
for Question 4 on slough indicate that there was an increase in knowledge.
Table 2
Comparison of Nurses’ Knowledge on Staging
Question item
Pre-test
Strongly agree
N = 55 (%)
Posttest
Strongly agree
N = 55 (%)
Percent
change
Stage I pressure injuries are
defined as intact with non-
blanche erythema in lightly
pigmented persons
Stage II pressure injuries are
full thickness skin loss
33 (60%)
22 (40%)
42 (76%)
20 (36%)
16%
4%
Eschar is healthy tissue
Slough is yellow or cream
necrotic tissue on a wound
bed
25 (45%)
32 (58%)
7 (13%)
40 (73%)
32%
15%
The next two questions related to the nurses’ knowledge on the Braden Scale (see
Table 3). The first question showed that 24 (44%) of the participants indicated an
34
understanding about risk factors for the development of PIs such as immobility,
incontinence, impaired nutrition, and altered level of consciousness. On the posttest, 43
(78%) of the participants were able to identify the risk factors for patients concerning PIs.
This result indicates that the overall knowledge of risk factors improved significantly for
the participants. For the second question, 22 (40%) participants agreed that a low Braden
score is associated with a higher risk of PI. In the posttest results, 28 (50%) of the nurses
agreed that the increase of PI is contributed to a low Braden score. Results for Question 2
showed a 10% change in knowledge after education.
Table 3
Comparison of Nurses’ Knowledge on Braden Scale
Question item
Pre-test
Strongly agree
N = 55 (%)
Posttest
Strongly agree
N = 55 (%)
Percent
change
Risk factors for
development of pressure
injuries are immobility,
incontinence, impaired
nutrition, and altered level
of consciousness
24(44%)
43(78%)
34%
A low Braden score is
associated with increased
pressure injury risk
22(40%)
28 (50%)
10%
In the next two questions, participants were asked about the values of education as
a direct impact on nurses’ knowledge (see Table 4). The first question involved the issue
of whether the incidence of PIs can be decreased after an education session; 34 (62%) of
the participants agreed on the pretest, and 50 (90%) of the participants agreed on the
posttest, indicating 28% improvement. Question 2 asks about participants knowledge of
35
government intervention regarding risk, prevention, and treatment, 32 (58%) of the
nurses agreed. Following education, 42 (76%) of the participants acknowledged that PIs
were increasing tremendously. Results showed 18% improvement. After education, in
responding to both questions, participants showed improved knowledge.
Table 4
Comparison of Nurses’ Knowledge on Education Program
Question item
Pre-test
Strongly agree
N = 55 (%)
Posttest
Strongly agree
N = 55 (%)
Percent
change
Educational programs may
reduce the incidence of
pressure injuries
34 (62%)
50 (90%)
28%
The incidence of pressure
injury is so high that the
government has appointed a
panel to study risk,
prevention, and treatment
32 (58%)
42 (76%)
18%
The implications noted show an improvement in nursing knowledge and a
decrease in nurses’ knowledge on staging. The improvements seen were in nurses’
knowledge on PI prevention, wound description, the Braden Scale, and the education
program. The results indicate that with education, nurses’ scope of knowledge can be
expanded. As a result, from a practical standpoint, patient care can be improved. If nurses
can successfully understand PI, can correctly identify wound description, can understand
the metric of the Braden Scale, and can see the value in an education program, patients
can continue to reap the benefit of more informed nurses. From a reverse viewpoint,
being able to understand where nurses have fallen short in understanding can yield better
36
opportunities for implementing education during follow-up. The need to understand the
implication on decreased staging knowledge could provide an opportunity to develop
better programs that can help nurses understand the implications of full thickness skin
loss. As a result, future nurses may be able to identify staging better and make
adjustments in practice more quickly.
Recommendations
This doctoral project was conducted to assess nurses’ knowledge on PI prevention
and to understand whether nurses’ knowledge decreased or increased following an
educational program in the ICU. There are significant issues facing nurses in relation to
their knowledge on PIs. The findings from the posttest strongly indicate that the
educational program may decrease the incidence of PI, resulting in better patient care.
The overall goal is to educate staff on PI prevention, as studies have shown that educating
staff leads to improvement in clinical outcomes. According to Henry and Foronda (2017),
improving nurses’ knowledge of PI prevention results in preventing HAPI incidents. The
results from this project indicated positive outcomes in two areas:
1. Increased education on PI prevention: When nursing staff are given education
about a topic, they can apply that knowledge for better outcomes. This project
clearly demonstrated that when the nursing staff was educated, their knowledge
about PIs increased. The results may translate into better patient care and
earlier identification of the start of PI. Henry and Foronda (2017) reviewed and
discussed the nurse education programs for the prevention and identification of
HAPI and concluded that education programs increased nurses’ knowledge of
37
HAPIs. In addition, creating a culture of success education can promote high-
quality care and safety for patients (Henry & Foronda, 2017).
a. Development of useable tools pertaining to PI and skin condition and
placement of these tools in accessible areas: This educational program
demonstrated different models of what is considered healthy skin and what is
considered a PI. Hospitals and institutions might consider adding visual
guidelines for nurses to reference (see Appendix E) provided by WOCN
(2017). They also might consider placing guidelines in high-traffic or high-
visibility areas as a reminder for nurses between educational programs. Henry
and Foronda (2017) suggested including a number of PI and wound pictures
for each stage to help solidify nurses’ education. Furthermore, Ebi, Hirko, and
Mijena (2019) did a cross-sectional study design on nurses’ knowledge of
pressure ulcers and certified the use of an educational program on PIs to keep
nurses well-informed regarding current knowledge. In addition, reviewing PI
prevention guidelines on a regular basis is useful in increasing nurses’
knowledge on PI prevention (Ebi et al., 2019).
Strengths and Limitations
The strengths of the doctoral project are the use of a reliable and valid tool to
assess the nurses’ knowledge on pressure injury prevention and documentation. This has
not been previously attempted in this ICU. The results were startling, with far fewer
nurses than expected having a robust knowledge of pressure injury prevention and
documentation. The positive post-test results clearly demonstrate the impact of an
38
educational program on increasing knowledge of pressure injury prevention. In the
future, such programs should be presented regularly to all existing and new staff to
ensure that all staff is competent and knowledgeable regarding pressure injury prevention
and documentation.
Study limitations include the fairly large attrition number in participation. There
are 75 nurses on the Intensive Care Unit but only 55 (73%) nurses participate in the
educational periods. Although participants were informed of the anonymity of their
participation, only 55 (73%) participated in the complete pre-test and post-test. The
significance of this attrition is not known, but it may be concluded that there is a lack of
commitment to pressure injury prevention. Other interpretations of this limitation might
be because of the demanding nature of the profession and other education programs
occurring simultaneously. Lastly, part of the limitation on the study may have been the
design in that completing questionnaires may not be desirable to participants may affect
results (Ebi et al., 2019). Other limitations of this project were the limited participant
pool-specifically one facility, one ICU and to distribute only to nurses. Also, the small
sample size of this group prevents generalizability to a larger audience. Although, new
evidence-based practice suggested that the Pieper Pressure Ulcer knowledge test has
proven to be a safe practice for adult learners to self-identify, self -learn and self-correct
knowledge (Delmore, et al., 2018).
The Pieper Knowledge Test has been tested before to determine the strengths and
limitation in clinical practice to measure the staff knowledge. Negativity on PI prevention
can lead to lack of knowledge on preventive measures and may influence the nurses’
39
performance. Research suggests pressure injury prevention can result from a lack of
knowledge on pressure injury prevention, and may contribute to lack of adequate
validation therefore the results cannot be generalized (Dalvand, Ebadi & Geshiagh,
2018).
Future Directions
The future directions for researchers interested in pressure injury prevention could
include routine educational programs on pressure injury prevention, and assessing nurses’
knowledge on staging, on wound description and Braden Scale. Having accurate, up–to-
date and ongoing knowledge regarding pressure injury, prevention, risk, staging, and
treatment is one way to prevent pressure injuries (Pieper & Zulkowski, 2014). Providing
a structured staff educational project is important to closing the gap and can be effective
in changing the culture in the intensive care unit with the development of guidelines and
protocols.
40
Section 5: Dissemination Plan
The purpose of this project was to determine whether nursing knowledge
improved when comparing intensive-care nurses’ responses to a pre- and posttest
questionnaire after an educational program on PI prevention. My plan is to disseminate
the project’s findings and share the results with clinicians within the organization. Nurses
are the primary audience with which I intend to share the project’s outcomes. The
following paragraphs outline the plan for dissemination and describe the rationale for the
audience of nurses as the primary recipients.
Plan for Dissemination
The dissemination of a project is a crucial procedure to transfer findings to
stakeholders. Presenting the findings to the organization’s leadership provided a valuable
opportunity for the organization leader to stimulate change. The promotion of new
strategies to develop advanced levels of clinical judgment, systems thinking, delivering,
and evaluating evidence-based care practices will be undertaken with the intention of
improving patient outcomes (Association of Critical Care Nurses [AACN], 2015). The
most tremendous impact has been to provide the findings. I plan to disseminate the
findings in three tiers: internally within the organization, externally as a publication, and
in an ongoing fashion at a selection of local and national conferences. The rationale for
choosing these stakeholders stems from the idea that the results generated from the DNP
project can be contributed in multiple outlets. First, from the perspective of internal
dissemination, I plan to share the results in my facility through ongoing education in the
ICU. The project demonstrated the effectiveness of staff response to an educational
41
program. Therefore, an ongoing PI prevention and documentation program will be
developed to be presented at the mandatory quarterly critical care skills fair in the facility
for improving the knowledge of the bedside nurses. This process will translate evidence
into practice by creating a culture change. Keyton (2017) suggested that culture results
from shared patterns of values and artifacts (in this case, knowledge and training) that are
passed through member interactions. Ideally, the internal culture can reflect better
practices.
From an external perspective, I plan to publish this project to serve as a resource
guide at clinical sites such as critical-care nursing seminars or symposia regarding
nursing knowledge on PI prevention. The publications that I may consider submitting to
are the American Journal of Nursing and Nursing 2019 Critical Care. I chose these two
magazines for publication because these magazines are the most informative, reliable
sources for EBP for critical-care nurses.
Lastly, I will submit my project to organizations holding relevant local or national
conferences, specifically, the Broward County Chapter of the American Association of
Critical Care Nurses (BCCAACN) and the National Nurses Teaching Institute of the
American Association of Critical Care Nurses (NTIAACN). BCCAACN is a local
chapter for critical-care nurses whose members meet monthly and that provides lectures,
continuing educational programs on health, school fairs, and other programs on topics
related on current issues pertinent to critical care. NTIAACN is the world’s largest
specialty nursing organization and provides current literature, lectures, and education on
current EBP to critical-care nurses.
42
Analysis of Self
This project has given me the opportunity to expand myself in numerous ways.
The DNP program prepares nurses to be scholars, practitioners, and project developers.
The AACN (2006) defined a DNP-prepared nurse as one who is challenged by rapidly
changing practices and dynamic work environments. My experience in this project
indicates that I am capable of focusing on one area of medical concern, developing a
project accordingly, conducting research accurately and with validity, and producing
interpretable results. As a result, in the future, I will have the skill set needed to develop
new policies and procedures focusing on new clinical practice. As a practitioner, my role
is to be committed as a patient advocate and to promote positive patient outcomes. My
project indicates that I am capable not only of interpreting results by analyzing numerical
outcomes from a pretest and posttest, but also of transferring data into tangible
recommendations for better practice. The DNP program is designed to train nurses to
demonstrate the highest levels of knowledge, leadership, communication skills, and
ability to translate evidence into practice (AACN, 2015). The completion of this project
indicates that I will be able to conduct future projects as a capable and competent project
manager.
As Scholar
As a scholar, I will continue to translate evidence into practice and assist with
health care functions and conferences. This project initiative has improved my nursing
skills, as well as my presentation and writing skills. This DNP project has increased my
nursing knowledge to achieve better outcomes for patients and higher levels of safety.

43
Additionally, as a scholar, my goal is that a publication of this project may contribute to
the greater body of knowledge available to other scholars learning about PI prevention.
Lastly, from the perspective of evaluation evidence, and implementing the evidence into
practice, the results from this study may contribute to better training materials. This
project, which focused on PI prevention, contributes knowledge based on actual nurses
engaging in patient care. These kinds of projects contribute outcomes that can be used in
the development of training materials that can be transferable across many similar
settings and are not unique to the participant pool used (Almaki, 2016). As a bonus,
quantitative data similar to the data gathered during this DNP project can be used to
inform future studies that collect interview data from participants (Murphy, Staffileno, &
Carlson, 2015).
Project Manager
Completing this project has improved my skills and critical thinking. For a DNP-
prepared nurse, understanding project development is important. In the future, I hope to
engage in continued professional collaboration with the organization. This project has
allowed me to develop a start-to-finish opportunity to create knowledge from the findings
of pre- and posttest comparisons. From this work, I have learned that the effort of
coordinating a project can yield a better understanding of how to assess knowledge and
build on that knowledge toward the end goal of successful patient care. The leadership
role of the DNP-prepared nurse involves developing EBP into a plan that improves
outcomes for a target population. This project has allowed me to increase my confidence
in translating theory into EBP.
44
Summary
The practice problem of PI continues to be a challenge in the acute-care setting.
Specifically, the need to assess knowledge and practice of PI prevention in the ICU will
continue to be a concern. Providing ongoing education, training, assessment, guideline
tools, and best practice for PI prevention can have a positive impact on nurses’
knowledge and practice. For a PI to be prevented there must be a well-documented plan
for interventions to be delivered to the patient (Jacobson et al., 2016; Pittman et al.,
2016). Furthermore, the development of this doctoral project has enabled me to apply my
expertise to problem solving within the facility to promote improved patient outcomes.
45
References
Academic Center for Evidence-Based Practice. (2012). The ACE Star model. Retrieved
from http://www.acestar.uthsca.edu/acestar-model.asp
Agency for Healthcare Research and Quality. (2016). Preventing pressure ulcers in
hospitals: Are we ready for this change? Retrieved from http://www.ahrq.gov
/professionals/systems/hospital/pressureulcertoolkit/putool17a.html
Almalki, S. (2016). Integrating quantitative and qualitative data in mixed methods
research: Challenges and benefits. Journal of Education and Learning, 5(3), 288-
296.
Apostolopoulou, E., Tselebis, A., Konstantinos, T., Kamarrnnu, E., Lambnopoulos, I., &
Kallnakmans, A. (2014). Pressure ulcer and risk factors in ventilated intensive
care patients. Health Science Journal, 8(3), 333-342. Retrieved from
http://www.hsj.gr/medicine/pressure-ulcer-incidence-and-risk-factors-in-
ventilated-intensive-care-patients.pdf
Association of Colleges of Nursing. (2015). The essentials of doctoral education for
advanced nursing practice. Retrieved from http://www.aacn.nche.edu/dnp
/Essentials.pdf
Bauer, K., Rock, K., Nazzal, M., Jones, O., & Qu, W. (2016). Pressure ulcers in the
United States inpatient population from 2008 to 2012: Results of a retrospective
nationwide study. Ostomy Wound Management, 62(11), 30-38.
Bergstrom, N., & Braden, B. J. (2002). Predictive validity of the Braden Scale among
Black and White subjects. Nursing Research, 51(6), 398-403.

46
Braden, B. J., Bergstrom, N. B. J., Laguzza, A., & Holman, V. (1987). The Braden scale
for predicting pressure sore risk. Nursing Research, 36(4), 205-210.
https://doi.org/10.1097/00006199-198707000-00002
Bradshaw, W. G. (2010). Importance of nursing leadership in advancing evidence-based
nursing practice. National Network, 1(29), 117-122.
Cano, A., Anglade, D., Stamp. H., & Young. D. L. (2015). Improving outcomes by
implementing a pressure ulcer prevention program (PUPP): Going beyond the
basics. Healthcare, 3(3), 574-585.
Centers for Medicare & Medicaid Services. (2018, September). Changes in skin integrity
post-acute care: pressure ulcer/injury. Retrieved from
https://www.cms.gov/.../September_2018_IRF_LTCH_Section_M_Webinar_with
out_...
Chrisman, J., Jordan, R., Davis, C., & Williams, W. (2014). Exploring evidence-based
practice research. Nursing Made Incredibly Easy, 12(4), 8-12.
https://doi.org/10.1097/01.NME.0000450295.93626.e7
Clark, M., Julmisse, M., Marcelin, N., Merry, L., Tuck, J., & Gagnon, A. J. (2015).
Strengthening healthcare delivery in Haiti through nursing continuing education.
International Nursing Review, 62(1), 54-63.
Cooper, K. L. (2013). Evidence-based prevention of pressure ulcers in the intensive care
unit. Critical Care Nurses, 33(6), 57-66.

47
Correa-de-Araujo, R. (2015). Evidence-based practice in the United States: Challenges,
progress, and future directions. Health Care for Women International, 37(1), 2–
22. https://doi.org/10.1080/07399332.2015.1102269
Coventry, T. H., Maslin‐Prothero, S. E., & Smith, G. (2015). Organizational impact of
nurse supply and workload on nurses continuing professional development
opportunities: An integrative review. Journal of Advanced Nursing, 71(12), 2715-
2727.
Cox, J., Roche, S., & Murphy, V. (2018). Pressure injury risk factors in critical care
patients: A descriptive analysis. Advances in Skin & Wound Care, 31(7), 328-334.
Currey, J., Considine, J., & Khaw, D. (2012). Clinical nurse research consultant: A
clinical and academic role to advance practice and the discipline of nursing.
Journal of Advanced Nursing, 67(10), 2275-2283.
Dalvand, S., Ebadi, A., & Geshiagh, R. G. (2018). Nurses’ knowledge on pressure injury
prevention: A systematic review and meta-analysis based on pressure ulcer
knowledge assessment tool. Retrieved from https://www.ncbi.nlm.nih.gov
Dreyfus, J., Gayle, J., Trueman, P., Delhougne, G., & Siddiqui, A. (2018). Assessment of
risk factors associated with hospital-acquired pressure injuries and impact on
health care utilization and cost outcomes in U.S. hospitals. American Journal of
Medical Quality, 33(4), 348-358. https://doi.org/10.1177/1062860617746741
Ebi, W.E., Hirko, F.F., & Minejena, D.A. (2019). Nurses’ knowledge to pressure ulcer
prevention in public hospitals in Wollega: a cross-sectional study design. BMC
Nursing, 18(20). 2-12. Retrieved from https://doi.org/10.1186/s12912-019-0346y
48
Garcia-Fernadez, F. P., Agreda, J., & Pancorbo-Hildago. (2014). A new theoretical model
for the development of pressure ulcers and other dependence-related lesions.
Journal of Nursing Scholarship, 46(1),28-38.doi:10.1111/jnu.12051.
Garrett-Wright, D. (2011). Parental perception of preschool child body weight. Journal of
Pediatric Nursing, 26(5), 435-455. https.//doi.org/10.1016/j.pedn.2010.07.009
Gillam, S., & Siriwardena, A. N. (2013). Frameworks for improvement: Clinical audit,
the plan- do-study-act cycle and significant event audit. Quality In Primary Care,
21(2), 123-130.
Gray, J. R., Grove, S. K., & Sutherland, S. (2017). The practice of nursing research:
Appraisal, synthesis, and generation of evidence (8
th
ed.). St. Louis, MO:
Saunders Elsevier.
Gunningberg, L., Mårtensson, G., Mamhidir, A. G., Florin, J., Muntlin Athlin, Å., &
Bååth, C. (2015). Pressure ulcer knowledge of registered nurses, assistant nurses
and student nurses: A descriptive, comparative multicenter study in Sweden.
International Wound Journal, 12(4), 462-468.
Health Research & Educational Trust (2017, April). Hospital Acquired Pressure Ulcers/
Injuries (HAPU/I): 2017. Chicago, IL: Health Research & Educational Trust.
Accessed at http://www.hret-hiin.org/ Accessible at: http://www.hret-hiin.org/
Henry, M., & Foronda, C. (2017). Evaluation of evidence-based nursing education of
hospital acquired pressure injury prevention in clinical practice: An integrative
reiew. Journal of Nursing Education and Practice, 8(1), 1-15.
http://doi.org/10.5430/jnep.

49
Institute for Clinical Systems Improvement. (2012). Health care protocol: Pressure ulcer
prevention and treatment protocol. Retrieved from
https://www.dhs.wisconsin.gov/regulations/training/c10-h03.pdf
Jacobson, T. M., Thompson, S. L., Halvorson, A. M., & Zeitler, K. (2016). Enhancing
documentation of pressure ulcer prevention intervention. Journal of Nursing Care
Quality, 31(3), Wolters Kluker. doi:
https://doi.org/201197/NCQ.0000000000000175.
Joint Commission Resources. (2012). Pressure ulcer prevention toolkit. Retrieved from
http://www.jointcommissioninternational.org/assets/1/14/PUT11_Sample_Pages.
pdf
Kavanagh, K. T., Cimiotti, J. P., Abusalem, S., & Coty, M. (2012). Moving healthcare
quality forward with nursing-sensitive value-based purchasing. Journal Of
Nursing Scholarship, 44(4), 385-395.
Keyton, J. (2017). Culture, Organizational. The International Encyclopedia of
Organizational Communication, 1-20.
Leapfrog Group (2011). Leapfrog Hospital Quality and Safety Survey Results.
www.leafrodgroup.org/cp
Lyder C., Wang, Y., Metersky, M., Curry, M., Kliman, R., Verzier, & Hunt D. (2012).
Hospital-acquired pressure ulcers: Results from the National Medicare Patient
Safety Monitoring System Study. Journal of The American Geriatrics Society
60(9),1603-1608.
50
Mallah, Z., Nassar, N., & Badr, L. K. (2015). The effectiveness of a pressure ulcer
intervention program on the prevalence of hospital acquired pressure ulcers:
Controlled before and after study. Applied Nursing Research, 28(2), 106-113.
Meddings, J., Reichert, H., Rogers, M. A., Hofer, T. P., McMahon, L. F., & Grazier, K.
L. (2015). Under pressure: Financial effect of the Hospital‐Acquired Conditions
Initiative–A statewide analysis of pressure ulcer development and payment.
Journal of the American Geriatrics Society, 63(7), 1407-1412.
Merrill, M. D. (2002). First principles of instruction. Education Technology Research and
Development. 50(3), 43-59.
Moore, Z. E., & Cowman, S. (2014). Risk assessment tools for the prevention of pressure
ulcers. Cochrane Database of Systematic Reviews, 2014(2).
doi:10.1002/14651858.CD006471.pub3
Murphy, M. P., Staffileno, B. A., & Carlson, E. (2015). Collaboration among DNP-and
PhD-prepared nurses: Opportunity to drive positive change. Journal of
Professional Nursing, 31(5), 388-394.
National Pressure Ulcer Advisory Panel. (2014). Prevention and treatment of pressure
ulcers: Quick reference guide. Perth, Australia: Cambridge Media.
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and
Pan Pacific Pressure Injury Alliance. (2014). Prevention and treatment of
pressure ulcers: Clinical Practice Guidelines. Haesler, E, Ed. Osborne Park,
Western Australia: Cambridge Media.
National Pressure Ulcer Advisory Panel (NPUAP) NPUAP Mission.Retrieved from:

51
https://www.npuap.org/wp-content/uploads/.../Padula-William-NPUAP-13FEB17.pdf
National Pressure Ulcer Advisory Panel. (2016). NPUAP pressure injury staging.
Retrieved from: http://www.npuap.org/resources/educational-and-clinical-
resources/npuap-pressure-injury-stages/
National Pressure Ulcer Advisory Panel. (2017). NPUAP pressure injury staging.
Retrieved from: http://www.npuap.org/resources/educational-and-clinical-
resources/npuap-pressure-injury-stages/
Nuru, N., Zewdu, F., Amsalu, S., & Mehretie, Y. (2015). Knowledge and practice of
nurses towards prevention of pressure ulcer and associated factors in Gondar
University Hospital, Northwest Ethiopia. BMC Nursing, 14(1), 34. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4450466/
Parnham, A., Pankhurst, S., & Dabell, W. (2015). Reducing avoidable pressure ulcers in
the community. Nursing Standard (Royal College of Nursing (Great
Brtain):1987), 29(26), 62. Doi:10.7748/ns.29.26.62.e9656
Pieper, B., & Zulkowski, H. (2014). The Pieper-Zulkowski pressure ulcer knowledge test.
Advance Skin Wound Care, 27(9), 413-419.
Pittman, J., Beeson,T., Terry, C., Dillon, J., Hampton, C., Kerley, D., Tucker, J. (2016).
Unavoidable pressure ulcers: Development and testing of the Indiana University
Health Pressure Ulcer Prevention Inventory. J Wound Ostomy Continence Nurs,
43(1), 32-38. doi:10.1097/won.0000000000000191.
52
Roden, J. (2004). Validating the revised health belief model for young families;
Implications for nurses’ health promotion practice. Nursing and Health Sciences,
6(4), 247-259. https://doi.org/10.111/j.1442-2018.2004.0198x
Rycroft-Malone, J., & McInnes, E. (2000). Pressure ulcer risk assessment and prevention
(Technical report). London, UK: Royal College of Nursing.
Stillwell, S., Fineout-Overholt, E., Melnyk, B., & Williamson, K. (2010). Evidence-based
practice step by step: Critical appraisal of the evidence: Part 1: An introduction to
gathering, evaluating, and recording the evidence. American Journal of Nursing,
110(7), 47-52. Retrieved from
https://hsl.osu.edu/sites/hsl.osu.edu/files/Critical%20Appraisal%20Part%201.pdf
Strazzieri-Pulido, K.C., Gonzalez, C.V., Nogueira, P. C., Padilha, K., & Santos, V.L.C.
(2019). Pressure injuries in critical patients: Incidence, patient-associated factors,
and nursing workload. J Nurs Manag, 2019; 27;301-
310.https://doi.org/10.1111/jonm.12671.
Tayyib, N., Coyer, F., & Lewis, P. A. (2015). A two-arm cluster randomized control trial
to determine the effectiveness of a pressure ulcer prevention bundle for critically
ill patients. Journal of Nursing Scholarship, 47(3), 237-247.
Titler, M. G. (2008). The evidence for evidence-based practice implementation. In R. G.
Hughes (Ed.), Patient safety and quality: An evidence-based handbook for
nursing (pp. 1113-1161). Rockville, MD: Agency for Healthcare Research and
Quality.

53
Tume, L. N., Siner, S., Scott, E., & Lane, S. (2014). The prognostic ability of early
Braden Q scores in critically ill children. Nursing in Critical Care, 19(2), 98-103.
Doi:10.1111/nicc.12035
Waugh, S. M. (2014). Attitudes of nurses toward pressure ulcer prevention: A Literature
Review. MedSurg Nursing, 23(5), 350-358.
Wound, Ostomy and Continence Nurses Society. (2017). WOCN position statement on
avoidable versus unavoidable pressure. Retrieved from
https://cdn.ymaws.com/www.wocn.on.org/resource/resmgr/publications/Avoidabl
e_vs._Unavoidable_Pr.pdf
Wound, Ostomy and Continence Nurses Society. (2017). WOCN guidelines for
prevention and management of pressure injuries (ulcers). Retrieved from
https://www.jwocnonline.com
Zaratkiewicz, S., Whitney, J. D., Lowe, J. R., Taylor, S., O’Donnell, F., & Minton-Foltz,
M. (2011). Development and implementation of a hospital-acquired pressure ulcer
incidence tracking system and algorithm. Journal of Healthcare Quality, 32(6),
44-51.

54
Appendix A: Power Point Presentation for Expert Panel

55
56
57
58
*Click on the slide to view entire presentation
59
Appendix B: Pieper Pressure Ulcer Knowledge Pretest
Select options to respond: 1) True, 2) False or 3) Do not know using a check mark
1Stage pressure ulcers are defined as intact skin with nonblanche erythema in
lightly pigmented persons
1
2
3
2. Risk factors for development of pressure ulcers are immobility, incontinence,
impaired nutrition, and altered level of consciousness.
3. All hospitalized individuals t risk for pressure ulcers should have a systematic
skin inspection at least daily and those in long term care at a once a week.
4. Hot water and soap may dry the skin and increase the risk for pressure ulcers.
5. It is important to massage bony prominences.
6. A stage III pressure ulcer is a partial thickness skin loss involving the
epidermis and/ or dermis.
7. All individuals should be assessed on admission to a hospital for risk of
pressure ulcer development.
8. Cornstarch, creams, transparent dressings (e.g., tegaderm, opsite), and
hydrocolloid dressings (e.g., Duoderm, Restore) do not protect against the
effects of friction.
9. A stage IV pressure ulcer is a full thickness skin loss with extensive
destruction, tissue necrosis, damage to muscle, bone, or supporting structure.
10. An adequate dietary intake of protein and calories should be maintained
during illness
11. Persons confined to bed should be repositioned every 3 hours.
12. A turning schedule should be written and placed at the bedside.
13. Heel protectors relieve pressure on the heels.
14. Donut devices/ring cushions help to prevent pressure ulcers.
15. In a side lying position, a person should be at a 30-degree angle with the bed
unless inconsistent with the patient’s condition and other care needs that take
priority.
16. The head of the bed should be maintained at the lowest degree of elevation
(hopefully, no higher than a 30-degree angle) consistent with medical
conditions.
17 A person who cannot move him or herself should be repositioned every 2
hours while sitting in a chair.
18. Persons who can be taught should shift their every 30 minutes while sitting
in a chair.
19. Chair –bound persons should be fitted for a chair cushion.
20. Stage II pressure ulcers are full thickness skin loss.
21 The epidermis should remain clean and dry.
22. The incidence of press ulcers is so high that the government has appointed a
panel to study risk, prevention, and treatment.
60
23. A low-humidity environment may predispose a person to pressure ulcers.
24. To minimize the skin’s exposure to moisture on incontinence, underpads
should be used to absorb moisture.
25. Rehabilitation should be instituted if consistent with the patient’s overall
goals of therapy.
26. Slough is yellow or cream necrotic tissue on a wound bed.
27. Eschar is good for wound healing.
28. Bony prominences should not have direct contact with one another.
29. Every person assessed to be at risk for developing pressure ulcers should be
placed on a pressure-redistribution bed surface.
30. Undermining is the destruction that occurs under the skin.
31. Eschar is healthy tissue.
32. Blanching refers to whiteness when pressure is applied to a reddened area.
33. A pressure redistribution surface reduces tissue interface pressure below
capillary closing pressure.
34. Skin macerated from moisture tears more easily.
35. Pressure ulcers are sterile wounds.
36. A pressure ulcer scar will break down faster than unwounded skin.
37. A blister on the heel is nothing to worry about.
38. A good way to decrease pressure on the heels is to elevate them of the bed.
39. All care given to prevent or treat pressure ulcers must be documented.
40. Devices that suspend the heels protect the heels from pressure.
41.Shear is the force that occurs when the skin sticks to a surface and the body
slides.
42. Friction may occur when moving a person up in bed.
43. A low Braden score is associated with increased pressure ulcer risk.
44. The skin is the largest organ of the body.
45. Stage II pressure ulcers may be extremely painful due to exposure of nerve
endings.
46. For persons who have incontinence, skin cleaning should occur at the time
of soiling and at routine intervals.
47 Educational programs may reduce the incidence of pressure ulcers.
Retrieved from http://www.ahrq.gov/professioals/systems/hpsital/preseureulcertoolkit/putool7a.htm

61
Appendix C: Pieper Pressure Ulcer Knowledge Posttest
Select options to respond: 1) True, 2) False or 3) Do not know using a check mark
1Stage pressure ulcers are defined as intact skin with nonblanche erythema in
lightly pigmented persons
1
2
3
2. Risk factors for development of pressure ulcers are immobility, incontinence,
impaired nutrition, and altered level of consciousness.
3. All hospitalized individuals t risk for pressure ulcers should have a systematic
skin inspection at least daily and those in long term care at a once a week.
4. Hot water and soap may dry the skin and increase the risk for pressure ulcers.
5. It is important to massage bony prominences.
6. A stage III pressure ulcer is a partial thickness skin loss involving the
epidermis and/ or dermis.
7. All individuals should be assessed on admission to a hospital for risk of
pressure ulcer development.
8. Cornstarch, creams, transparent dressings (e.g., tegaderm, opsite), and
hydrocolloid dressings (e.g., Duoderm, Restore) do not protect against the
effects of friction.
9. A stage IV pressure ulcer is a full thickness skin loss with extensive
destruction, tissue necrosis, damage to muscle, bone, or supporting structure.
10. An adequate dietary intake of protein and calories should be maintained
during illness
11. Persons confined to bed should be repositioned every 3 hours.
12. A turning schedule should be written and placed at the bedside.
13. Heel protectors relieve pressure on the heels.
14. Donut devices/ring cushions help to prevent pressure ulcers.
15. In a side lying position, a person should be at a 30-degree angle with the bed
unless inconsistent with the patient’s condition and other care needs that take
priority.
16. The head of the bed should be maintained at the lowest degree of elevation
(hopefully, no higher than a 30-degree angle) consistent with medical
conditions.
17 A person who cannot move him or herself should be repositioned every 2
hours while sitting in a chair.
18. Persons who can be taught should shift their every 30 minutes while sitting
in a chair.
19. Chair –bound persons should be fitted for a chair cushion.
20. Stage II pressure ulcers are full thickness skin loss.
21 The epidermis should remain clean and dry.
22. The incidence of press ulcers is so high that the government has appointed a
panel to study risk, prevention, and treatment.
62
23. A low-humidity environment may predispose a person to pressure ulcers.
24. To minimize the skin’s exposure to moisture on incontinence, underpads
should be used to absorb moisture.
25. Rehabilitation should be instituted if consistent with the patient’s overall
goals of therapy.
26. Slough is yellow or cream necrotic tissue on a wound bed.
27. Eschar is good for wound healing.
28. Bony prominences should not have direct contact with one another.
29. Every person assessed to be at risk for developing pressure ulcers should be
placed on a pressure-redistribution bed surface.
30. Undermining is the destruction that occurs under the skin.
31. Eschar is healthy tissue.
32. Blanching refers to whiteness when pressure is applied to a reddened area.
33. A pressure redistribution surface reduces tissue interface pressure below
capillary closing pressure.
34. Skin macerated from moisture tears more easily.
35. Pressure ulcers are sterile wounds.
36. A pressure ulcer scar will break down faster than unwounded skin.
37. A blister on the heel is nothing to worry about.
38. A good way to decrease pressure on the heels is to elevate them of the bed.
39. All care given to prevent or treat pressure ulcers must be documented.
40. Devices that suspend the heels protect the heels from pressure.
41.Shear is the force that occurs when the skin sticks to a surface and the body
slides.
42. Friction may occur when moving a person up in bed.
43. A low Braden score is associated with increased pressure ulcer risk.
44. The skin is the largest organ of the body.
45. Stage II pressure ulcers may be extremely painful due to exposure of nerve
endings.
46. For persons who have incontinence, skin cleaning should occur at the time
of soiling and at routine intervals.
47 Educational programs may reduce the incidence of pressure ulcers.
Retrieved from http://www.ahrq.gov/professioals/systems/hpsital/preseureulcertoolkit/putool7a.htm
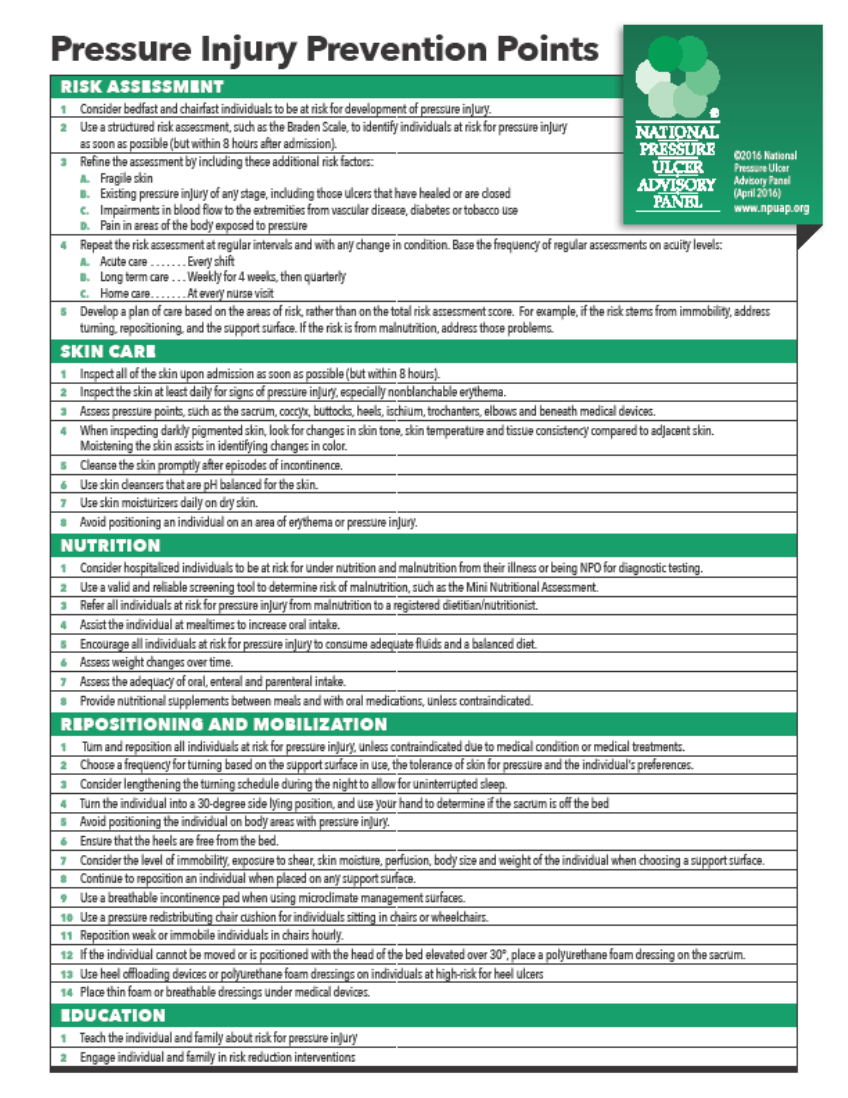
63
Appendix D: Education Packet
65
Appendix E: Best Practice Checklist/Pressure Injury Prevention Bundle
Identify a bundle of best practices
A clinical pathway has been created
Key elements of a comprehensive skin assessment have been identified
Approaches to document and report results of skin assessment have been explored
A tool for assessing risk has been chosen
An appropriate bundle of best practices has been identified for our organization
___
___
___
___
___
Develop pressure ulcer care plan based on identified risk
Approaches to document and communicate care plan have been identified
A system linking care planning to assessment has been developed
All levels of staff are aware of care plan
___
___
___
Customize the bundle for specific work units
Retrieved from: https://www.ahrq.gov/professionals/systems/hospital/pressureulcertoolkit/putool3a.html
67
Appendix G: Permission for NPUAP Product
68
Appendix H: Permission for Pieper-Zulkowski Pressure Ulcer Knowledge Test