
1
Crest
®
+ Oral-B
®
at dentalcare.ca
Course Author(s): Tanya Villalpando Mitchell, RDH, MS
CE Credits: 1 hour
Intended Audience: Dentists, Dental Hygienists, Dental
Assistants, Dental Students, Dental Hygiene Students, Dental
Assistant Students
Date Course Online: 06/04/2020
Last Revision Date: N/A
Course Expiration Date: 06/03/2023
Cost: Free
Method: Self-instructional
AGD Subject Code(s): 490
Online Course: www.dentalcare.ca/en-ca/professional-education/ce-courses/ce617
Disclaimer: Participants must always be aware of the hazards of using limited knowledge in integrating new techniques or procedures into their
practice. Only sound evidence-based dentistry should be used in patient therapy.
Conflict of Interest Disclosure Statement
• The author reports no conflicts of interest associated with this course.
Introduction – Periodontal Screening and Recording
Periodontal Screening and Recording (PSR) is a rapid and inexpensive method of screening patients
to decide if a more comprehensive assessment is necessary. After taking Periodontal Screening and
Recording: Its Use When Detecting Periodontal Disease, the participant will be able to explain the
benefits of the PSR system, use the PSR system in a clinical setting, interpret a patient’s PSR score,
identify who should be assessed with a more comprehensive periodontal exam and discuss the PSR
system with patients.
Periodontal Screening and Recording:
Its Use When Detecting Periodontal Disease
Continuing Education
Brought to you by

2
Crest
®
+ Oral-B
®
at dentalcare.ca
Course Contents
• Overview
• Learning Objectives
• Introduction
• Objectives of Screening
• Interpretation of Codes
• Guidelines for Patient Management
• Advantages and Limitations
• Conclusion
• Course Test
• References
• About the Author
Overview
A complete periodontal assessment includes
a thorough review of the patient’s medical
and dental histories, as well as the recording
of gingival findings including probing depths,
clinical attachment levels, tooth mobility and
position, furcation involvement, bleeding on
probing, occlusal relationships, and bone levels.
6
It is important the dentist or dental hygienist
monitor and evaluate a patient’s periodontal
status on a regular basis. Periodontal diseases
are the leading cause of tooth loss in adults.
1
The Centers for Disease Control and Prevention
reports 47.2% of adults in the United States
have a form of periodontal disease. The rate
increases to 70.1% for those Americans age
65 and older.
9
A 2012 study by Eke et al. found
periodontal disease to be more common
in men than in women and in adults who
had not completed high school.
10
Every oral
examination should include an evaluation
of the periodontium. The ultimate goal of
the periodontal assessment is to identify
and classify periodontal disease.
3
Although
the Periodontal Screening and Recording
®
(PSR) is not intended to replace a full mouth
probing and recording of findings, it is a rapid
method of screening patients to decide if a
more comprehensive assessment is necessary.
The dentist or dental hygienist must decide,
upon completion and documentation of their
patient’s PSR scores, whether the patient should
receive a full periodontal examination. This
would result in the patient’s classification of
periodontal disease characterized by the staging
and grading system as recommended by the
American Academy of Periodontology (AAP).
15
Learning Objectives
Upon completion of this course, the dental
professional should be able to:
• Explain the benefits of the PSR system.
• Use the PSR system in a clinical setting.
• Interpret a patient’s PSR score.
• Identify who should be assessed with a
more comprehensive periodontal exam.
• Discuss the PSR system with patients.
Introduction
Gingivitis and periodontitis fall into the
category of periodontal diseases. Both are
microbial infections of the periodontium, where
the microorganisms operate in conjunction
with a person’s host response.
7
The dental
hygienist is most often the person in the
professional dental setting who screens
patients and assesses periodontal health or
disease. The most commonly used screening
method for the measurement of depth of the
gingival sulcus and the clinical attachment
level is periodontal probing.
6
The clinician,
by measuring probing depths, can make
assumptions of the state of health of the
periodontium. Early detection and diagnosis
are significant components in the prevention
of periodontal disease. The American Academy
of Periodontology (AAP) recommends every
dental patient should receive a comprehensive
periodontology evaluation annually.
11
The
Periodontal Screening and Recording
®
(PSR)
system is one example of a diagnostic aid used
to assess the periodontal health of patients.
The PSR system has been used to study the
relationship in overweight and obese patients
who smoke as well as a way to estimate the
periodontal health statuses of a representative
military population.
2,8
A study by Khocht et al
found the PSR to be an effective tool in the
screening of periodontal diseases.
4
The PSR has
been used to detect the periodontal status of
individuals with immunoglobulin A deficiency.
12
Overall, there are a limited number of studies
involving use of the PSR.
Background
In 1982, the World Health Organization (WHO)
created the Community Periodontal Index
of Treatment Needs (CPITN). This method of
evaluation estimated the periodontal disease
3
Crest
®
+ Oral-B
®
at dentalcare.ca
prevalence and severity based on the probing
depths and condition of the periodontium.
In 1992, the AAP modified the Simplified
Periodontal Examination (SPE), used in New
Zealand, and developed the PSR system for
use in North America (journal article). With the
corporate sponsorship of the Procter & Gamble
Company, the AAP and the American Dental
Association (ADA) adopted the PSR system.
3
The PSR system was designed to initiate the
promotion, prevention, and early treatment of
periodontal diseases by:
• Introducing a simplified screening method
that met legal dental recording requirements.
• Encouraging dentists to incorporate the PSR
system into every oral examination.
• Educating members of the public to
value periodontal health and to request a
periodontal screening from dentists (PSR
Training Program, 1992).
Objectives of Screening
The PSR system does not replace the need for
a comprehensive periodontal examination. It
acts as a time saving screening of periodontal
health to indicate when a partial or full-
mouth examination is required. When the
clinician becomes familiar with the PSR system
examination process, it should only take a few
minutes to conduct a screening.
Similar to a traditional comprehensive
periodontal examination, the PSR system
measures each tooth individually, with implants
examined the same way as natural teeth.
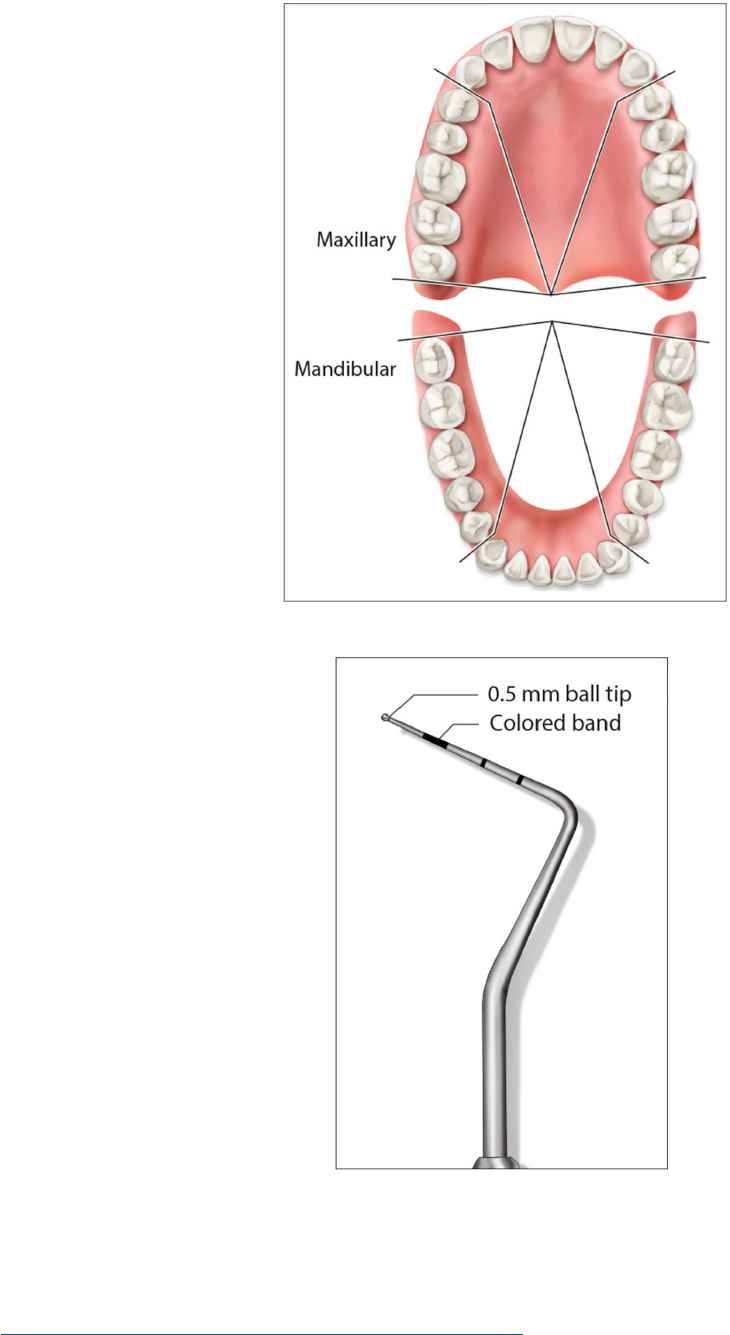
However, the mouth is divided into sextants
instead of quadrants (Figure 1).
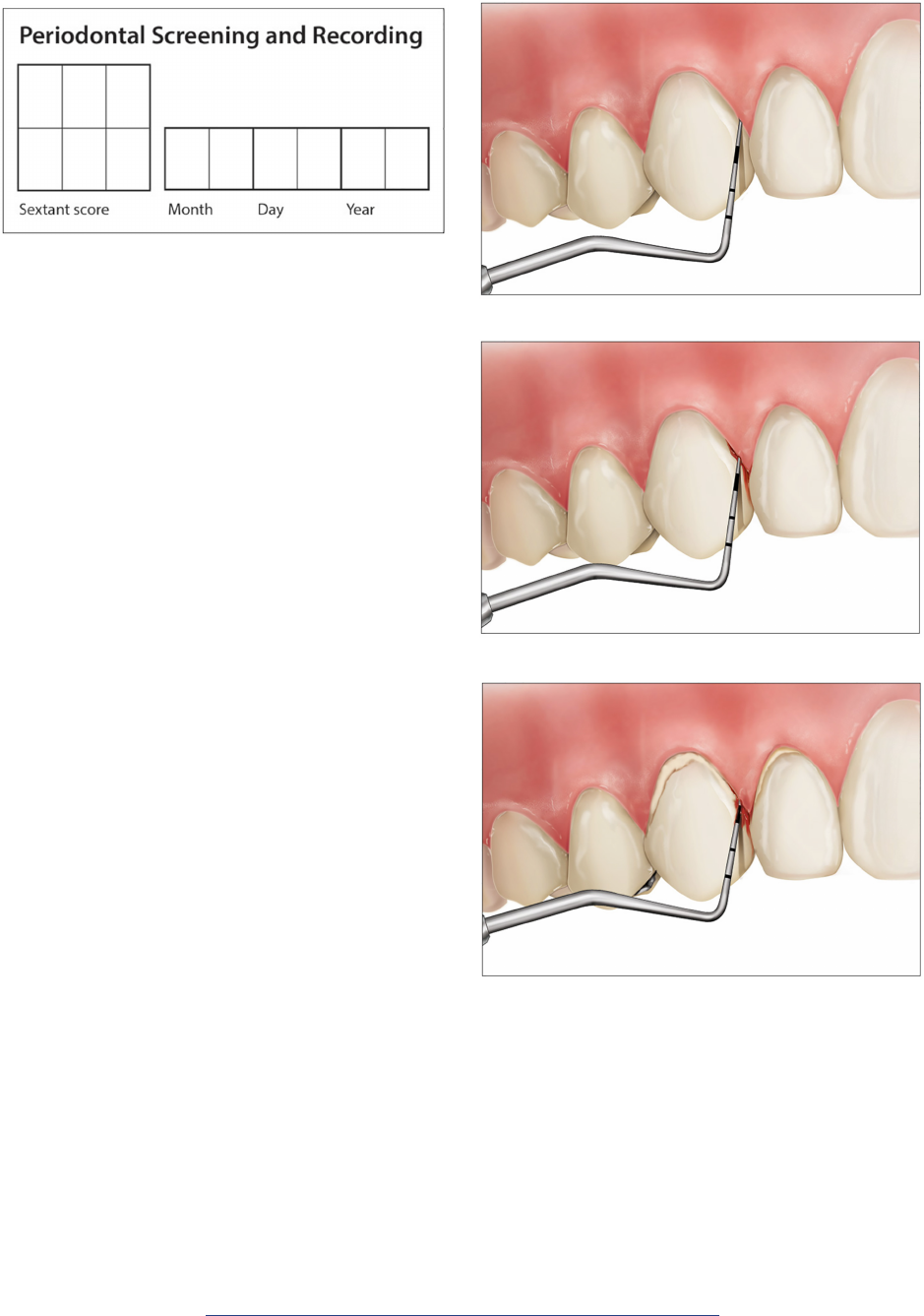
Six measurements for each tooth are obtained,
utilizing a special ball-tipped probe. This probe
has a 0.5 mm ball at the tip and a color-coded
area 3.5 to 5.5 mm from the tip. The probe may
be plastic or metal. The ball at the end of the
probe is intended to enhance patient comfort
and assist in detecting overhanging margins and
subgingival calculus (Figure 2).
The probe is inserted into the sulcus or pocket
and walked around the circumference of each
tooth. This method is the same technique
Figure 1. Sextants of Mouth.
Figure 2. Special Ball-tipped Probe.
4
Crest
®
+ Oral-B
®
at dentalcare.ca
method of more specifically defining individual
cases. This system will be discussed in further
depth under 5(b) Periodontitis.
Code 1:
The colored area of the probe remains
completely visible in the deepest probing
depth in the sextant; this indicates that probing
used as with a comprehensive periodontal
examination. However, the PSR system is
unique in the way the probe is read. The
clinician need only observe the position of the
color-coded band in relation to the gingival
margin. The color-coded band is commonly
known as a reference mark, which spans
between 3.5 mm to 5.5 mm. For each area
probed, the clinician will decide if the colored
band is either totally visible, partly visible, or
not at all visible.
14
The presence of furcation
involvement, mobility, mucogingival problems,
or recession should also be noted with an
asterisk. After each tooth in the sextant has
been examined, only the highest code obtained
is recorded and only one score is recorded
for each sextant. If a sextant is edentulous, an
“X” is placed. Measurements are recorded by
sextants as shown below (Figure 3).
Interpretation of Codes
Code 0:
The colored area of the probe remains
completely visible in the deepest crevice of
the sextant; this indicates that probing depths
in the sextant range between 1 mm to 3 mm.
There is no calculus or defective margins
detected. The gingival tissues are healthy with
no bleeding after gentle probing.
With this model in mind, the concept of
creating more individualized patient case
definitions came to fruition. Using the medical
model of staging and grading, the authors of
the new classification were able to combine
some of the factors typically used in disease
determination such as severity, extent, rate
of progression, risk factors, etc. to create a
Figure 3. Recording Scores.
Code 1
Code 2
Code 0

5
Crest
®
+ Oral-B
®
at dentalcare.ca
The Symbol “*”:
The symbol “*” should be added to a sextant
score whenever the following is found: furcation
involvement, mobility, mucogingival problems,
or recession extending to the colored area of the
probe (indicating 3.5 mm or greater).
Guidelines for Patient Management
Code 0:
Appropriate preventive care should be given as
well as a review of daily plaque control habits.
Code 1:
Individualized oral hygiene instructions should be
reinforced with the patient. Appropriate therapy,
including subgingival plaque removal should be
performed.
Code 2:
Individualized oral hygiene instruction and
appropriate therapy, including subgingival plaque
removal, as well as the removal of calculus and
the correction of plaque-retentive margins and
restorations should be performed.
Code 3:
A comprehensive periodontal examination and
charting of the affected sextant are necessary
to determine an appropriate care plan. This
examination and documentation should include
the following: identification of probing depths,
clinical attachment levels (gingival recession),
bleeding on probing, mobility, mucogingival
problems, furcation involvement, and
radiographs. If one or more sextants score a
Code 3, a comprehensive full mouth examination
and charting are indicated.
Code 4:
A comprehensive full mouth periodontal
examination and charting are necessary to
determine an appropriate care plan. This
examination and documentation should include
the following: identification of probing depths,
clinical attachment levels (gingival recession),
bleeding on probing, mobility, mucogingival
problems, furcation involvement, and
radiographs. It can be assumed that advanced
periodontal treatment will be required.
Symbol (*):
If an abnormality exists in the presence of Codes
0, 1, or 2, the clinician should make a specific
depths range between 1 mm to 3 mm. There
is no calculus or defective margins detected.
However, there is bleeding after probing.
Code 2:
The colored area of the probe remains
completely visible in the deepest probing depth
in the sextant; this indicates probing depths
range between 1 mm to 3 mm. Supragingival or
subgingival calculus and/or defective margins
are detected.
Code 3:
The colored area of the probe remains partly
visible in the deepest probing depth in the
sextant; this indicates that probing depths may
range between 4 mm to 5 mm.
Code 4:
The colored area of the probe completely
disappears indicating a probing depth of greater
than 5.5 mm.
Code 3
Code 4

6
Crest
®
+ Oral-B
®
at dentalcare.ca
notation and/or treatment for that condition
as needed. If an abnormality exists in the
presence of Code 3 or 4, a comprehensive
periodontal examination and charting are
necessary to determine an appropriate care
plan.
Advantages and Limitations
The advantages of using the PSR system
include early detection, speed, simplicity,
cost-effectiveness, ease of recording, and risk
management.
• Early detection: Since all sites are
evaluated, the risk of periodontal disease
can be made early and appropriate
treatment can be performed.
• Speed: Once the technique of the PSR
system is learned, it should take only a
few minutes to perform the screening.
This saves time versus a comprehensive
examination.
• Simplicity: It is easy to do and understand
for patients.
• Cost-effectiveness: It is not necessary to
purchase expensive equipment since all that
is needed is a ball-tipped probe.
• Ease of recording: Only one number is
recorded for an entire sextant.
• Risk management: The dental team
is monitoring and recording a patient’s
periodontal status to stay compliant
with standards of care and for legal
requirements.
There are limitations when using the PSR
system. As stated earlier, it is not intended to
replace a full-mouth periodontal examination.
Those patients who have received treatment
for periodontal diseases and/or are in a
maintenance phase of care should receive
comprehensive periodontal examinations
routinely. There is also limited use of the
PSR system in children. It is necessary to
differentiate pseudo-pockets from true
periodontal pockets with these younger
patients. In any patient exhibiting enlarged
gingiva or recession, the PSR score may give
false results.
14
Landry and Jean reported that
since the PSR does not measure epithelial
attachment, the severity of periodontal
disease may be underestimated with its use.
5
While a study by Rams and Loesche found
a pretreatment PSR score of 4 or greater
in 110 adults to be a good predictor of
periodontal access surgery needs, this same
study concluded after performing non-surgical
periodontal therapy the score overestimated
surgical access needs.
13
Conclusion
The PSR system is a valuable tool in the early
detection of periodontal disease. This system
can indicate when a more comprehensive
periodontal examination should be performed.
The unique way the probe is read and
the limited amount of recordings needed
when performing an examination is easy to
incorporate into every patient’s appointment.

7
Crest
®
+ Oral-B
®
at dentalcare.ca
Course Test Preview
To receive Continuing Education credit for this course, you must complete the online test. Please
go to: www.dentalcare.ca/en-ca/professional-education/ce-courses/ce617/test
1. What makes the PSR system unique?
A. The way the probe is read.
B. The way the probe is inserted into the sulcus.
C. Its adoption by the ADA and AAP.
D. Its intended use on patients.
2. A new patient presented to the dental office for an initial examination. The PSR would be
an appropriate method to comprehensively assess the patient’s periodontal status.
A. True
B. False
3. Which of the following describes a PSR Code 2?
A. Colored area of the probe remains partly visible; no calculus or defective margins detected;
gingival tissues healthy.
B. Colored area of the probe remains visible in deepest probing depth; no calculus or defective
margins detected; there is bleeding on probing.
C. Colored area of the probe completely disappears; probing depth > 5.5 mm.
D. Colored area of the probe is completely visible in deepest probing depth in sextant; supra-
or subgingival calculus detected or defective margins present.
4. Which of the following patients would NOT be a good candidate for the PSR system?
1. Child patient
2. Periodontal maintenance patient
3. Recall patient with no bleeding upon probing
4. Patient screened at a health fair
A. 3
B. 3 and 4
C. 1
D. 1 and 2
5. For each sextant, only the lowest PSR score is recorded.
A. True
B. False
6. The patient management of a PSR Code 4 is _______________.
A. individualized oral hygiene instruction and removal of subgingival calculus; as well as
removal of calculus and correction of plaque-retentive margins and restorations
B. individualized oral hygiene instructions should be reinforced; subgingival plaque removal
C. comprehensive full mouth periodontal examination and charting
7. If one or more sextants score a Code 3, what is the appropriate protocol?
A. Removal of subgingival plaque
B. Full mouth exam and charting
C. Refer to a periodontist
D. Oral hygiene instruction

8
Crest
®
+ Oral-B
®
at dentalcare.ca
8. All of the following are advantages to using the PSR except one. Which one is the
EXCEPTION?
A. Excessive cost
B. Simplicity
C. Risk management
D. Speed
9. The probe used with the PSR system has a 0.5 mm ball tip. Which of the following is
NOT a purpose for this tip?
A. Gives a more accurate reading.
B. Enhances patient comfort.
C. Detects subgingival calculus.
D. Detects overhanging margins.
10. In which of the following conditions could the scores of the PSR give a false reading?
A. Excessive plaque
B. Gingival health
C. Gingival bleeding
D. Gingival recession
9
Crest
®
+ Oral-B
®
at dentalcare.ca
References
1. American Dental Association and The American Academy of Periodontology. June 1992.
2. Covington LL, Breault LG, Hokett SD. The application of Periodontal Screening and Recording
(PSR) in a military population. J Contemp Dent Pract. 2003;4(3):36-51. Published 2003 Aug 15.
3. Hodges KO. Concepts in nonsurgical periodontal therapy. Albany, NY. Delmar Publishers. 1998.
4. Khocht A, Zohn H, Deasy M, Chang KM. Screening for periodontal disease: radiographs vs. PSR.
J Am Dent Assoc. 1996;127(6):749-756. doi:10.14219/jada.archive.1996.0310.
5. Landry RG, Jean M. Periodontal Screening and Recording (PSR) Index: precursors, utility and
limitations in a clinical setting. Int Dent J. 2002;52(1):35-40. doi:10.1111/j.1875-595x.2002.
tb00595.x.
6. Weinberg MA. Comprehensive periodontics for the dental hygienist. Upper Saddle River, NJ.
Prentice Hall. 2001.
7. Weinberg MA, Fine JB. Comprehensive periodontics for the dental hygienist. Upper Saddle River,
NJ. Pearson Education. 2010.
8. Wood N, Johnson RB. The relationship between smoking history, periodontal screening and
recording (PSR) codes and overweight/obesity in a Mississippi dental school population. Oral
Health Prev Dent. 2008;6(1):67-74.
9. CDC. Oral Health Conditions. Periodontal Disease. Accessed June 1, 2020.
10. Eke PI, Dye BA, Wei L, Thornton-Evans GO, et al. Prevalence of periodontitis in
adults in the United States: 2009 and 2010. J Dent Res. 2012 Oct;91(10):914-920.
doi:10.1177/0022034512457373.
11. American Academy of Periodontology. Comprehensive periodontal therapy: a statement by
the American Academy of Periodontology*. J Periodontol. 2011;82(7):943-949. doi:10.1902/
jop.2011.117001.
12. Jorgensen GH, Arnlaugsson S, Theodors A, Ludviksson BR. Immunoglobulin A deficiency and
oral health status: a case-control study. J Clin Periodontol. 2010;37(1):1-8. doi:10.1111/j.1600-
051X.2009.01494.x.
13. Rams TE, Loesche WJ. Relationship Between Periodontal Screening and Recording Index Scores
and Need for Periodontal Access Surgery. J Periodontol. 2017;88(10):1042-1050. doi:10.1902/
jop.2017.170070.
14. Gehrig JS, Shin DE, Willmann DE. Foundations of periodontics for the dental hygienist.
Philadelphia, PA. Wolters Kluwer. 2019.
15. Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-
implant diseases and conditions - Introduction and key changes from the 1999 classification.
J Periodontol. 2018;89 Suppl 1:S1-S8. doi:10.1002/JPER.18-0157.
Additional Resources
• No Additional Resources Available.
About the Author
Tanya Villalpando Mitchell, RDH, MS
Ms. Mitchell is Professor and Director, Graduate Studies at the University of
Missouri Kansas City School of Dentistry, Division of Dental Hygiene. She is a
member of the American Dental Hygienists’ Association and the American Dental
Education Association.
Email: [email protected]
