
NO TIME TO WAIT:
SECURING THE FUTURE
FROM DRUG-RESISTANT
INFECTIONS
REPORT TO THE
SECRETARY-GENERAL
OF THE UNITED NATIONS
APRIL 2019
TABLE OF CONTENTS
Key messages in this report ............................................................................................................................. 1
Summary of IACG recommendations ............................................................................................................. 2
1. Context for this report ................................................................................................................................... 3
2. Process of developing the IACG recommendations ............................................................................... 3
3. Background to the IACG recommendations ............................................................................................. 4
4. IACG recommendations ................................................................................................................................ 9
IACG Members ...................................................................................................................................................... 24
No Time to Wait: Securing the future from drug-resistant infections • 1
Antimicrobial resistance is a global crisis that threatens
a century of progress in health and achievement of the
Sustainable Development Goals.
• Antimicrobial (including antibiotic, antiviral, antifungal
and antiprotozoal) agents are critical tools for ghting
diseases in humans, terrestrial and aquatic animals
and plants, but they are becoming ineffective.
• Alarming levels of resistance have been reported in
countries of all income levels, with the result that
common diseases are becoming untreatable, and
lifesaving medical procedures riskier to perform.
• Antimicrobial resistance poses a formidable
challenge to achieving Universal Health Coverage and
threatens progress against many of the Sustainable
Development Goals, including in health, food security,
clean water and sanitation, responsible consumption
and production, and poverty and inequality.
• Misuse and overuse of existing antimicrobials in
humans, animals and plants are accelerating the
development and spread of antimicrobial resistance.
• Inadequate access to clean water, sanitation and
hygiene in health care facilities, farms, schools,
households and community settings; poor infection
and disease prevention; lack of equitable access
to affordable and quality-assured antimicrobials,
vaccines and diagnostics; and weak health, food and
feed production, food safety and waste management
systems are increasing the burden of infectious
disease in animals and humans and contributing
to the emergence and spread of drug-resistant
pathogens.
There is no time to wait. Unless the world acts urgently,
antimicrobial resistance will have disastrous impact
within a generation.
• Drug-resistant diseases already cause at least 700,000
deaths globally a year, including 230,000 deaths from
multidrug-resistant tuberculosis, a gure that could
increase to 10 million deaths globally per year by
2050 under the most alarming scenario if no action
is taken. Around 2.4 million people could die in high-
income countries between 2015 and 2050 without a
sustained effort to contain antimicrobial resistance.
• The economic damage of uncontrolled antimicrobial
resistance could be comparable to the shocks
experienced during the 2008-2009 global nancial
crisis as a result of dramatically increased health care
expenditures; impact on food and feed production,
trade and livelihoods; and increased poverty and
inequality.
• In higher-income countries, a package of simple
interventions to address antimicrobial resistance
could pay for itself due to costs averted. In lower-
income countries, additional but still relatively
modest investments are urgently needed.
• If investments and action are further delayed, the
world will have to pay far more in the future to
cope with the disastrous impact of uncontrolled
antimicrobial resistance.
Because the drivers of antimicrobial resistance lie in
humans, animals, plants, food and the environment, a
sustained One Health response is essential to engage
and unite all stakeholders around a shared vision and
goals.
• National Antimicrobial Resistance Action Plans are
at the heart of a multisectoral One Health response,
but nancing and capacity constraints in many
countries need to be urgently addressed to accelerate
implementation.
• Strengthening infection prevention and control in
health care facilities and farms using available tools
and ensuring access to clean water, sanitation and
hygiene in health facilities, farms, schools, household
and community settings are central to minimizing
disease transmission and the emergence and
transmission of antimicrobial resistance in humans,
animals, plants, food and the environment.
• Strengthening surveillance, regulatory frameworks,
professional education and oversight of antimicrobial
prescription and use, and increasing awareness
among all stakeholders are also signicant challenges
that need to be urgently addressed to ensure the
responsible use of antimicrobials and to minimize
resistance in humans, animals, plants, food and the
environment.
• Immediately stopping the use of the antimicrobials
on the WHO List of Highest Priority Critically
Important Antimicrobial Agents for Human Medicine
as growth promoters is an essential rst step towards
completely phasing out the use of antimicrobials for
growth promotion.
• Additional effort, investments and incentives
are needed to spur innovation in antimicrobial
medicines, diagnostics, vaccines, waste management
tools, safe and effective alternatives to antimicrobials
and alternative practices, as well as operational and
implementation research, in human, animal and plant
health.
• Many people around the world still do not have
access to antimicrobials. Ensuring equitable and
affordable access to quality antimicrobial agents and
their responsible and sustainable use is an essential
component of the global response to antimicrobial
resistance.
• Stronger political leadership, advocacy, coordination
and accountability are needed at all levels to enable
a sustained One Health response to antimicrobial
resistance. All stakeholder groups – including
governments, civil society and the private sector
– need to be engaged and to collaborate in an
unprecedented effort across the human, animal,
plant, food and feed production and environmental
sectors, based on a shared vision and goals.
• The challenges of antimicrobial resistance are complex
and multifaceted, but they are not insurmountable.
Implementation of the recommendations in this
report will help to save millions of lives, maintain
economic and other development gains, and secure
the future from drug-resistant diseases.
KEY MESSAGES IN THIS REPORT
No Time to Wait: Securing the future from drug-resistant infections • 1
2 • No Time to Wait: Securing the future from drug-resistant infections
SUMMARY OF IACG RECOMMENDATIONS
A. ACCELERATE PROGRESS IN
COUNTRIES
C. COLLABORATE FOR MORE
EFFECTIVE ACTION
D. INVEST FOR A SUSTAINABLE
RESPONSE
E. STRENGTHEN ACCOUNTABILITY
AND GLOBAL GOVERNANCE
B. INNOVATE TO SECURE THE
FUTURE
A1: The IACG calls on all Member States to ensure equitable
and affordable access to existing and new quality-assured
antimicrobials as well as alternatives, vaccines and
diagnostics, and their responsible and prudent use by
competent, licensed professionals across human, animal
and plant health.
C1: The IACG calls for the systematic and meaningful
engagement of civil society groups and organizations
as key stakeholders in the One Health response to
antimicrobial resistance at global, regional, national and
local levels.
D1: The IACG calls on governments; global, regional,
national, bilateral and multilateral nancing and
development institutions and banks; and private
investors to systematically apply standards to assess
risks and impacts related to antimicrobial resistance (an
antimicrobial resistance and One Health “lens”) when
making investments.
E1: The IACG requests the Tripartite agencies (FAO, OIE
and WHO) together with UN Environment, other UN
agencies and the World Bank, in the context of UN reform,
to further strengthen joint One Health action, based on
target-setting, country priorities and needs, by enhancing
their organizational capacity and providing adequate and
sustainable core funding for antimicrobial resistance-
related activities.
B1: The IACG calls on public, private and philanthropic
donors and other funders to increase investment and
innovation in quality-assured, new antimicrobials
(particularly antibiotics), novel compounds, diagnostics,
vaccines, waste management tools, and safe and effective
alternatives to antimicrobials for human, terrestrial and
aquatic animal and plant health, as well as implementation
and operational research.
B2: The IACG recommends that existing and future global
access initiatives should promote and support equitable
and affordable access to existing and new, quality-assured
antimicrobials, diagnostics, vaccines, waste management
tools and safe and effective alternatives to antibiotics for
human, terrestrial and aquatic animal and plant health.
B3: The IACG calls on public, private and philanthropic
research funders and other stakeholders to build upon
current research and development efforts for new
antimicrobials, diagnostics, vaccines, waste management
tools, and safe and effective alternatives to antimicrobials;
and to strengthen implementation and operational
research and research coordination and collaboration in
a One Health context.
A2: The IACG calls on all Member States to accelerate the
development and implementation of One Health National
Antimicrobial Resistance Action Plans within the context
of the SDGs.
C2: The IACG calls for the systematic and meaningful
engagement of and enhanced action by the private
sector as key stakeholders in the One Health response to
antimicrobial resistance at global, regional, national and
local levels.
D2: The IACG emphasizes the need for increased
investments in the response to antimicrobial resistance,
including from domestic nancing in all countries; urges
existing and future nancing mechanisms in human,
animal and plant health, food and feed production and
the environment to give greater priority to antimicrobial
resistance in their resource allocations; calls on public,
private and philanthropic donors to contribute additional
funding, including to support implementation of National
Antimicrobial Resistance Action Plans.
E2: The IACG recommends the urgent establishment of
a One Health Global Leadership Group on Antimicrobial
Resistance, supported by a Joint Secretariat managed by
the Tripartite agencies (FAO, OIE and WHO).
E3: The IACG requests the Secretary-General, in close
collaboration with the Tripartite agencies (FAO, OIE
and WHO), UN Environment and other international
organizations, to convene an Independent Panel on
Evidence for Action against Antimicrobial Resistance in a
One Health context to monitor and provide Member States
with regular reports on the science and evidence related
to antimicrobial resistance, its impacts and future risks,
and recommend options for adaptation and mitigation.
E4: The IACG recognizes the ongoing process led by
Member States to develop the Global Development
and Stewardship Framework to Combat Antimicrobial
Resistance and urges the Tripartite agencies (FAO, OIE and
WHO) and UN Environment to expedite its development
in line with the scope described in the 2015 World Health
Assembly resolution on antimicrobial resistance (WHA68.7).
As Member States nalize this process, they should also
consider the need for new international instruments.
A3: The IACG calls on all Member States to phase out the
use of antimicrobials for growth promotion, consistent
with guidance from the Tripartite agencies (FAO, OIE and
WHO) and Codex Alimentarius, starting with an immediate
end to the use of antibiotics categorised as the Highest
Priority Critically Important Antimicrobial Agents on the
WHO List of Critically Important Antimicrobials for Human
Medicine.
No Time to Wait: Securing the future from drug-resistant infections • 3
1. CONTEXT FOR THIS REPORT
The 2016 Political Declaration of the High-level Meeting of the United Nations General Assembly on
Antimicrobial Resistance (1) represented a landmark in the world’s commitment to tackling antimicrobial
resistance, calling for greater urgency and action in response to its many challenges. In the political
declaration, Member States requested the Secretary-General, in consultation with the Food and Agriculture
Organization of the United Nations (FAO), the World Organisation for Animal Health (OIE) and the World
Health Organization (WHO) to convene an ad hoc interagency coordination group (IACG) co-chaired by the
Executive Ofce of the Secretary-General and the Director-General of WHO to provide practical guidance for
approaches needed to ensure sustained, effective global action to address antimicrobial resistance. It also
requested the Secretary-General to submit a report for consideration by Member States by the seventy-
third session of the General Assembly in 2019 on the implementation of the political declaration and on
further developments and recommendations emanating from the IACG, including on options to improve
coordination, considering the 2015 Global Action Plan on Antimicrobial Resistance (2).
This report presents the IACG’s response to the request from Member States in the 2016 political declaration
and makes recommendations for urgent action for consideration by the Secretary-General, Member States
and other stakeholders in the global response to antimicrobial resistance.
2. PROCESS OF DEVELOPING THE
IACG RECOMMENDATIONS
The IACG was convened in March 2017. Its membership
consisted of representatives of United Nations and
multilateral agencies and individuals with expertise
across human, animal and plant health, as well as
the food, animal feed, trade, development and
environment sectors. The IACG’s mandate was to
provide practical guidance for approaches needed to
ensure sustained effective global action to address
antimicrobial resistance. Its terms of reference
included promoting, planning and facilitating
collaborative action to align activities so that gaps
are closed and resources are optimally utilized;
exploring the feasibility of developing global goals
and targets related to antimicrobial resistance;
and reporting back to the Secretary-General by the
seventy-third UN General Assembly in 2019. The IACG
was supported by a Secretariat hosted by WHO with
staff seconded from FAO, OIE and WHO.
Between March 2017 and December 2018, the IACG
met formally either in-person or by teleconference
eight times, and held many other conference calls,
including meetings of thematic sub-groups. To guide
its activities, the IACG developed a workplan (3)
and an IACG Framework for Action on Antimicrobial
Resistance (4) that describes key content areas and
relevant levers to address them, building on the
2016 political declaration, the Global Action Plan
on Antimicrobial Resistance and the Sustainable
Development Goals (SDGs). Country visits by IACG
members to Argentina, Thailand and Vietnam in
2018 provided valuable insights into successes
and challenges in national and local responses to
antimicrobial resistance.
In the course of its deliberations, the IACG
analysed critical issues in the response to
antimicrobial resistance to inform its report
and recommendations. In 2018, it developed
discussion papers for public consultation in six
thematic areas: 1) Public awareness, behaviour
change, and communication; 2) National Action
Plans on Antimicrobial Resistance; 3) Optimizing
use of antimicrobials; 4) Innovation, research and
development, and access; 5) Surveillance and
monitoring; and 6) Global governance and alignment
with the SDGs (5,6,7,8,9,10). Targeted outreach and
consultations were conducted with key stakeholders
during this analytic phase, particularly with regard
to governance, access, research and development
issues. A web-based public consultation process on
the six discussion papers was held between June
and August 2018 and received 153 submissions from
a wide range of stakeholders.
The IACG conducted a wide range of stakeholder
engagement activities, including discussions with
FAO, OIE, WHO and UN Member States based in
Rome, Paris, Geneva and New York respectively;
discussions with civil society and the private
sector; and inputs from more than 350 participants
attending the Call to Action on Antimicrobial

4 • No Time to Wait: Securing the future from drug-resistant infections
Resistance event in Accra, Ghana, in November
2018. A mapping exercise and critical appraisal of
recommendations made in previous global reports
on antimicrobial resistance were conducted by the
IACG Secretariat to provide guidance to the IACG and
help ensure that its recommendations addressed
key bottlenecks in the response, rather than
duplicating those in previous reports. In January and
February 2019, additional public discussions on the
draft IACG recommendations were held with more
than 400 people representing 68 Member States, 39
civil society organizations, 49 private sector groups
and 11 international organizations. Concurrently, a
web-based forum on the draft recommendations
drew more than 80 additional written submissions
from Member States, civil society organizations, the
private sector and individuals.
Further information on the IACG process and relevant
materials, including the written submissions
received, are available on the IACG website.
3. BACKGROUND TO THE IACG RECOMMENDATIONS
3.1. Antimicrobial resistance is a global crisis that
risks reversing a century of progress in health
Antimicrobial agents are critical tools to ght
diseases in humans, animals, plants and crops.
But growing levels of resistance to these agents
is placing a century of progress in human health
at risk. Common infections are becoming much
more difcult to treat, and lifesaving medical
procedures and treatments riskier to perform. At the
same time, there is a lack of scientic innovation
resulting in part from market failure, with too few
new antimicrobials, vaccines, diagnostics tools and
alternatives to antimicrobials for use in humans,
animals and plants in the research and development
pipeline.
Alarming levels of antimicrobial resistance have been
reported in countries of all income levels. In some
member countries of the Organization for Economic
Cooperation and Development (OECD), about 35
per cent of common human infections are already
resistant to currently available medicines, and in
some low- and middle-income countries (LMICs),
resistance rates are as high as 80 to 90 per cent for
some antibiotic-bacterium combinations (11). More
than a third of countries providing data to WHO in
2017 reported widespread resistance to common
pathogens (12). Resistance to second- and third-line
antibiotics – the last lines of defence against some
common diseases – are projected to almost double
between 2005 and 2030 (11). Concurrently, millions
of lives are lost every year due to lack of access to
existing antimicrobial agents: inadequate access
to antibiotics alone kills nearly 6 million people
annually, including a million children who die of
preventable sepsis and pneumonia (13,14,15).
Although antimicrobial resistance can develop
naturally, misuse and overuse of antimicrobial
agents in humans, terrestrial and aquatic animals,
plants and crops are greatly accelerating its
development and spread. In human health,
poor medical prescribing practices and patient
adherence to therapies, weak regulation and
oversight including over-the-counter sales, and
the proliferation of substandard and falsied
antimicrobials are all contributing to the problem.
The use of antimicrobials to promote growth and
routinely prevent disease in healthy animals and
crops without appropriate indication and in the
absence of good agricultural practices to prevent
infectious diseases on farms are further contributing
to the development and spread of antimicrobial
resistance (16). Drivers of the use of antimicrobials
in animal health – especially in many LMICs – include
the large and growing burden of animal diseases,
the increasing scale of animal production, and
underinvestment in veterinary services and animal
health. These underlying issues require attention
as part of efforts to reduce the unnecessary use of
antimicrobials in animals.
3.2 There is no time to wait. Unless the world
acts urgently, antimicrobial resistance will
have disastrous impact within a generation
Although antimicrobial resistance is not mentioned
in the SDGs, it is recognized in the Global Action
Plan for Healthy Lives and Well-being for All (17) as
a barrier to achievement of SDG 3 on human health
and directly jeopardizes progress against other SDGs
related to food security, clean water and sanitation,
and responsible consumption and production. Due
to cascading impacts on economic development and
inequality, antimicrobial resistance also indirectly
threatens progress against the SDGs that aim to
reduce poverty and inequality.
No Time to Wait: Securing the future from drug-resistant infections • 5
The true magnitude of antimicrobial resistance in
humans is not fully known, but estimates suggest
that resistant infections already cause at least
700,000 deaths every year, including 230,000 deaths
from multidrug-resistant tuberculosis (18,19). A
worst-case scenario developed by the World Bank
has suggested that this gure could rise to 10 million
deaths every year by 2050, if no action is taken (20).
In countries where resistance can be measured
accurately, the OECD predicts that around 2.4 million
people could die in Europe, North America and
Australia between 2015 and 2050 without a sustained
effort to contain antimicrobial resistance (11).
The economic impact of uncontrolled antimicrobial
resistance would also be catastrophic. As drug-
resistant pathogens spread, health care expenditures
would increase dramatically, and sustainable food
and feed production – including global trade in
food, feed and livestock – will increasingly be at risk.
As a result, the World Bank estimates that by 2030
up to 24 million people could be forced into extreme
poverty, mainly in low-income countries, and annual
economic damage as a result of antimicrobial
resistance could be comparable to the shocks
experienced during the 2008-2009 global nancial
crisis – but with no end in sight (20).
Although evidence remains limited, concerns are also
growing about the impact of antimicrobial resistance
on the environment and natural ecosystems due to
overuse and discharge of antimicrobials and resistant
micro-organisms in manure and waste from health
care facilities and pharmaceutical manufacturing,
commercial livestock and plant production, and sh
and seafood farming, a problem that may be fuelled
by changes in the world’s climate (21,22).
3.3. A sustained One Health response
to antimicrobial resistance is essential
to engage and unite all stakeholders
around a shared vision and goals
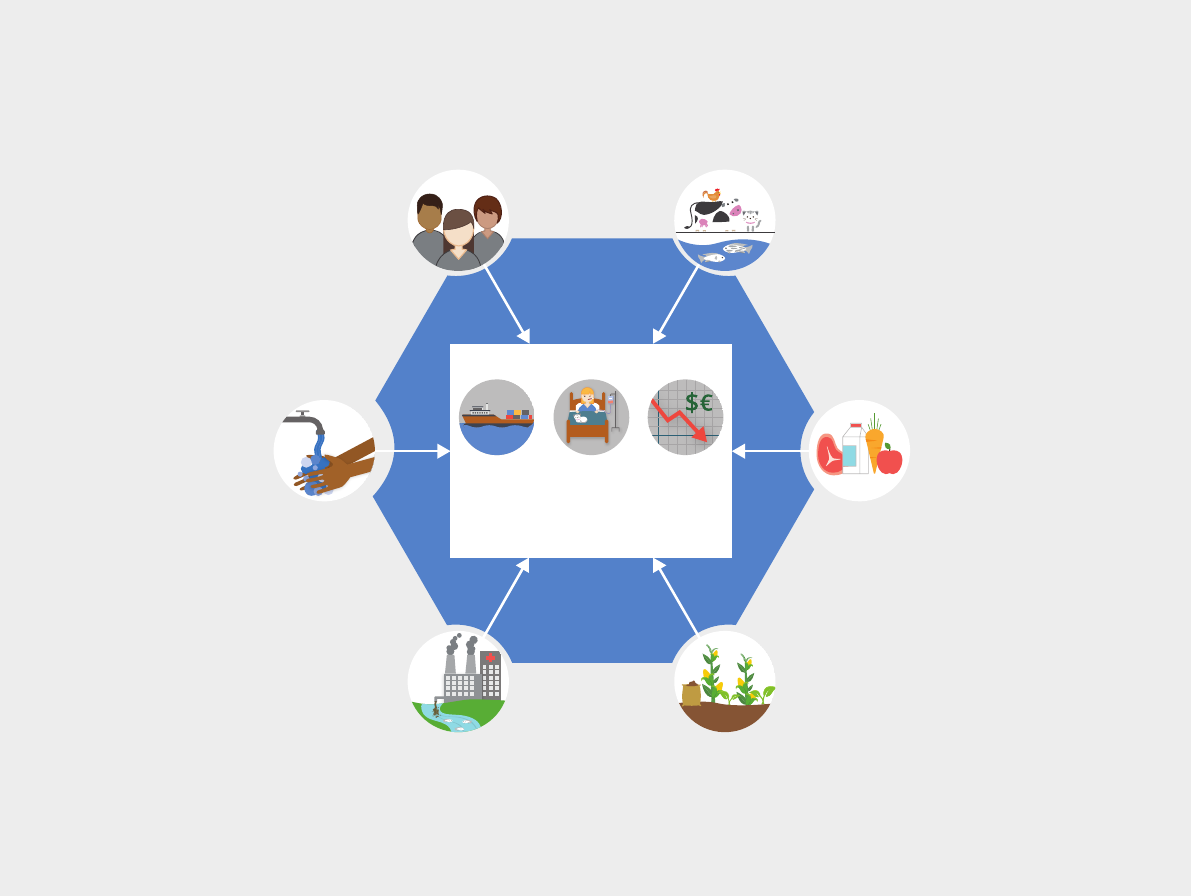
Because the drivers and impact of antimicrobial
resistance lie in humans, terrestrial and aquatic
animals, plants, food, feed and the environment,
and are interconnected, a One Health approach is
essential to addressing it on multiple fronts (Fig.1).
Misuse and overuse of
antimicrobials; poor access to
quality, affordable medicines,
vaccines and diagnostics; lack
of awareness and knowledge;
movement of animals
Misuse and overuse of
antimicrobials; poor access to
quality, affordable medicines,
vaccines and diagnostics; lack
of awareness and knowledge;
population movement
Poor infection and
disease prevention and
control; transmission of
resistant pathogens in
food production, storage,
distribution and preparation
Misuse and overuse of
antimicrobials; poor
infection and disease
prevention and control
Lack of access to clean
water, sanitation and
hygiene; poor infection
and disease prevention
and control in health
care facilities and farms
Discharge of waste from
health care facilities,
pharmaceutical
manufacturing and farms
F
o
o
d
&
F
e
e
d
H
u
m
a
n
s
T
e
r
r
e
s
t
r
i
a
l
&
A
q
u
a
t
i
c
A
n
i
m
a
l
s
W
a
t
e
r
,
S
a
n
i
t
a
t
i
o
n
&
H
y
g
i
e
n
e
P
l
a
n
t
s
&
C
r
o
p
s
E
n
v
i
r
o
n
m
e
n
t
DRIVERS OF ANTIMICROBIAL RESISTANCE
Risks to food
and feed
production,
businesses and
trade;
interaction with
climate change
Economic
damage, loss of
productivity
and increased
health care
expenditures
Increased
morbidity and
mortality in
humans and
animals
IMPACT OF ANTIMICROBIAL RESISTANCE
Fig 1. A One Health response to address the drivers and impact of antimicrobial resistance
“One Health” refers to designing and implementing programmes, policies, legislation and research in a way that enables multiple sectors
and stakeholders engaged in human, terrestrial and aquatic animal and plant health, food and feed production and the environment to
communicate and work together to achieve better public health outcomes.
No Time to Wait: Securing the future from drug-resistant infections • 5
6 • No Time to Wait: Securing the future from drug-resistant infections
3.3.1. Accelerated implementation of One Health
national action plans must be at the heart of the
global response to antimicrobial resistance
Since the launch of the Global Action Plan on
Antimicrobial Resistance in 2015, at least 100
countries have developed National Antimicrobial
Resistance Action Plans, and there is a wealth of
normative guidance from the Tripartite agencies
(FAO, OIE and WHO) and the Codex Alimentarius to
support their implementation (23). But efforts to
implement national action plans are currently too
slow and must be accelerated.
Although antimicrobial resistance affects all
countries at all levels of development, not all
countries are equally equipped to respond
effectively, and national plans need to be tailored
to local needs, context and capacities. Many LMICs
facing a higher burden of disease and risk of
antimicrobial resistance still need to improve basic
water, sanitation and hygiene in health care facilities,
farms, schools, households and community settings;
strengthen infection prevention and control in health
facilities, farms and food and feed production; and
improve waste management and environmental
protection. At the same time, they face signicant
barriers to implementation of National Antimicrobial
Resistance Action Plans, including inadequate
political awareness and commitment, and lack
of informed people to champion a One Health
approach. Many countries also lack a compelling
narrative to engage policy-makers and the general
public in a way that links antimicrobial resistance
to core national health and economic interests. At
the same time, mechanisms and capacity for One
Health collaboration across Ministries and sectors
are frequently inadequate or under-resourced.
Many national action plans focus mainly on the
health of humans and livestock, paying insufcient
attention to plants, food and feed production,
waste management and the environment. Plans
are often not costed or prioritized, largely because
few countries have developed robust, national
antimicrobial resistance investment cases that
identify priorities, estimate returns on investment
and costs of inaction and assess risks to the
attainment of the SDGs.
Many countries require support to implement
national action plans in key areas such as
building and analysing the evidence base; setting
targets; developing regulatory frameworks and
professional capacities to support responsible use
of antimicrobials; mainstreaming antimicrobial
resistance into existing programming across the
SDGs; and mobilizing additional human and nancial
resources. Depending on country context, additional
investments and capacity building are needed to
develop and implement critical components such as
antimicrobial stewardship programs; professional
education, training, certication and development;
behaviour change, awareness and communications
activities; and strengthening supply chain
management and legal and regulatory frameworks
across the One Health spectrum.
Strengthening monitoring and surveillance
is particularly important to track the use of
antimicrobials and the spread of resistance in
humans, animals, plants and food; build the evidence
base for action; support multisectoral collaboration;
and monitor progress. Implementing surveillance
systems requires signicant, long-term investments
in personnel, training, laboratory, data collection
and other infrastructure. All countries, as well as
their donors and development partners, have a vital
interest in building these critical capacities at the
country level, ensuring that data is used to guide
responses, and supporting global-level surveillance
through initiatives such as WHO GLASS and AGISAR
and surveillance work undertaken by OIE and FAO.
3.3.2. More innovation is needed to
tackle antimicrobial resistance across
the One Health spectrum
The research and development pipeline for health
technologies to address priority pathogens has long
been inadequate (24,25,26). A sustained effort is
needed to spur increased innovation in medicines,
diagnostics, vaccines and safe and effective
alternatives to antimicrobials across human,
terrestrial and aquatic animal and plant health, as
well as waste and environmental management.
Previous reports have emphasized that the lack of
incentives for manufacturers of pharmaceuticals
and active pharmaceutical ingredients to invest in
research and development is the major impediment
to innovation to tackle antimicrobial resistance
(18,27). They have also proposed a range of incentives
– including push, pull and delinkage mechanisms –
to address different research and development
bottlenecks, optimize existing funding for research
and development and attract new investments.
The G20 has twice committed to further examine
practical market incentive options for antimicrobial
resistance-related research and development (28,29).
No Time to Wait: Securing the future from drug-resistant infections • 7
But more attention and effort are needed to
determine which of these mechanisms will be the
most effective in stimulating the pipeline for priority
pathogens, while also guaranteeing access to and
stewardship of new and existing antimicrobial
products.
Several international initiatives launched in the
last few years have helped to catalyse the pipeline
of new antibiotics and accelerate products from
early stages to proof of concept, as well as to direct
donor funding towards priority areas. However,
additional resources and incentives are needed to
expand the scope and scale of these efforts and to
move products more rapidly into clinical trials and
through to regulatory approval. There are currently
few research and development initiatives dedicated
to addressing antimicrobial resistance in terrestrial
and aquatic animals, or in plants, food, feed and the
environment.
The benets of scientic innovation in the response
to antimicrobial resistance will be lost if new health
products are not made available to everyone who
needs them, and they are not used in a responsible
and sustainable manner. Access to current
antimicrobials and diagnostics is already inadequate
in many LMICs. Use of available diagnostics and
vaccines is also sub-optimal due to factors such
as cost, lack of trained health care workers and
veterinarians, delays in providing test results, cold
chain requirements and complexity of dosing. In
the animal and plant sectors, the potentially higher
costs of new products may lead farmers to prefer
older, less effective antimicrobials or products of
unknown quality. In addition, fragile production
and supply chains for existing antimicrobials due to
the small number of producers, leading to frequent
shortages of these products around the world and
further contributing to growing rates of disease and
outbreaks and an increased risk of antimicrobial
resistance in both humans and animals (30).
3.3.3. The world must act and invest now
to address antimicrobial resistance,
or pay far more in the future
The World Bank estimates that the current cost of
antimicrobial resistance containment measures
is around USD 9 billion annually, but making
investments now could be cost-saving, depending
on country context and the proportion of costs
averted (20). In human health, the OECD estimates
that in high-income and many middle-income
countries, the costs of implementing measures to
reduce resistance are so low – USD 2 per person per
year for an effective package of measures – and the
benets so great that investments are likely to pay
for themselves (11). In many lower-income countries,
additional but still relatively modest investments
are urgently needed. If investments and action
are delayed, the world will have to pay far more in
the future to cope with the catastrophic impact of
uncontrolled antimicrobial resistance.
The few dedicated funds that currently address
antimicrobial resistance – such as the UK’s
Fleming Fund and Joint Programming Initiative
on Antimicrobial Resistance (JPI-AMR), which is
supported by 27 Member States and the European
Commission, and several research and development
initiatives – have helped to catalyze action in
priority areas, but they are limited in scope,
duration and/or geographic coverage. There is also
little appetite on the part of donors to establish new
global funding instruments specically to address
antimicrobial resistance. Nevertheless, existing
funding mechanisms in human health [including the
Coalition for Epidemic Preparedness Innovations
(CEPI); Gavi, the Vaccine Alliance; the Global Fund
to Fight AIDS, Tuberculosis and Malaria; Medicines
Patent Pool; and Unitaid] can be expanded and
leveraged, and additional investments are needed
to bring the One Health response in countries and at
the global level to a scale that is truly commensurate
with the threats posed by antimicrobial resistance.
3.3.4. The One Health response to antimicrobial
resistance requires stronger leadership, advocacy,
coordination and accountability at all levels
The current global response to antimicrobial
resistance is inadequate.
Although the impact of antimicrobial resistance
on human health and in food production has
received considerable attention, there is still
inadequate political commitment and stakeholder
engagement in these areas globally and at country
level. Antimicrobial resistance in animals and plants
requires increased attention, advocacy, political
commitment, and engagement, while efforts to
address antimicrobial resistance in the environment
lag far behind in attention, advocacy, political
commitment, engagement and the evidence base.
Stronger leadership, coordination and accountability
are needed at all levels to address these challenges.
Enhanced capacity to develop normative guidance
and provide technical support is also urgently
8 • No Time to Wait: Securing the future from drug-resistant infections
needed. The Tripartite collaboration between WHO,
FAO and OIE has provided critical leadership on
antimicrobial resistance in recent years but remains
seriously under-resourced. The engagement of UN
Environment in the work of the Tripartite agencies
is also important to support its Member States
in addressing antimicrobial resistance within
environmental policy-making. At the same time,
many other initiatives on antimicrobial resistance
have emerged outside the Tripartite arrangement.
The result is that no single entity is presently tasked
to take on the essential functions of global One
Health leadership and coordination across sectors,
based on a vision and goals that are shared by all
stakeholders - including governments, civil society
and the private sector – and an agreed approach
to setting targets and ensuring accountability
for action. A more systematic and coordinated
effort is also needed to synthesize the evidence
base and identify knowledge gaps across sectors
and disciplines to guide One Health policy and
implementation.
The challenges of antimicrobial resistance
are complex and multifaceted, but they are
not insurmountable. Implementation of the
recommendations in this report will help to save
millions of lives, preserve antimicrobials for
generations to come and secure the future from
drug-resistant diseases.
But there is no time to wait.
No Time to Wait: Securing the future from drug-resistant infections • 9
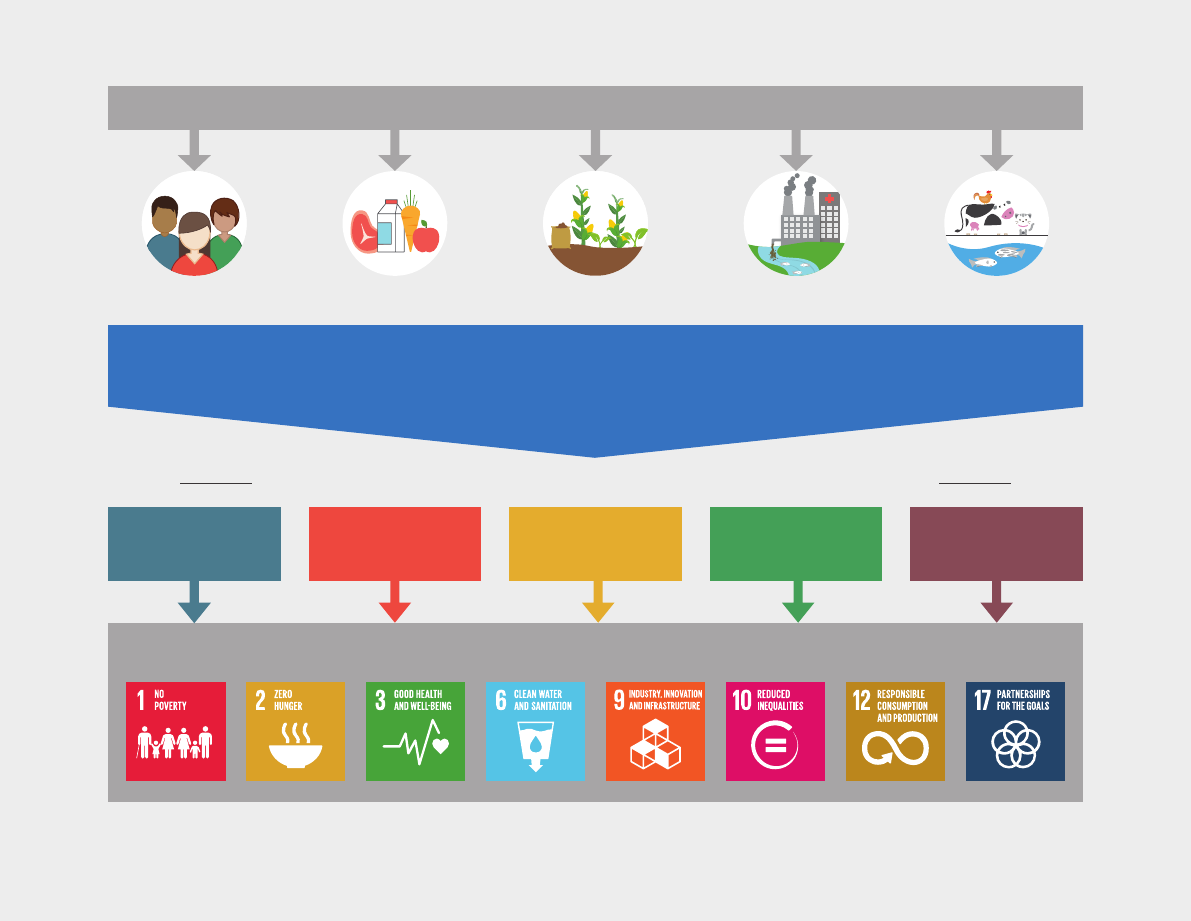
SUSTAINABLE DEVELOPMENT GOALS
ONE HEALTH RESPONSE TO ANTIMICROBIAL RESISTANCE
Humans Food & Feed Plants & Crops Environment Terrestrial &
Aquatic Animals
Antimicrobial resistance is a global crisis. There is no time to wait.
A sustained One Health response with a shared vision and goals is essential to tackle antimicrobial
resistance and achieve the Sustainable Development Goals.
Interagency Coordination Group on Antimicrobial Resistance Recommendations
ACCELERATE
PROGRESS
IN COUNTRIES
INNOVATE TO
SECURE THE
FUTURE
COLLABORATE FOR
MORE EFFECTIVE
ACTION
INVEST FOR A
SUSTAINABLE
RESPONSE
STRENGTHEN
ACCOUNTABILITY AND
GLOBAL GOVERNANCE
Fig. 2: One Health, IACG recommendations and the Sustainable Development Goals
4.1 Guiding principles for recommendations
In the course of developing its recommendations,
the IACG was guided by the following principles:
• The recommendations should promote and
support a One Health approach to antimicrobial
resistance cutting across human, terrestrial and
aquatic animal and plant health, as well as food
and feed production and the environment;
• The recommendations should focus
on strengthening existing systems and
mainstreaming of efforts to combat
antimicrobial resistance so as to leverage gains
across the SDGs;
• The recommendations should address
major challenges identied in addressing
antimicrobial resistance and build upon
best practices across health, development,
nancing, and research and development;
• To the extent possible, the recommendations
should not duplicate those made in previous
reports, but instead focus on catalyzing the
implementation of earlier recommendations
by addressing key gaps and bottlenecks in the
current response to antimicrobial resistance;
• The recommendations should support
mobilization and action by all stakeholders,
including governments, international
organizations, academia, civil society and the
private sector, at global, regional, national and
local levels, with a strong emphasis on enabling
country-level action and with due consideration
to country-specic context, capacity and
infrastructure; and
• The recommendations should be practical
and feasible to implement, support a targeted
response based on country and disease-specic
context, and contribute to achieving signicant
impact against antimicrobial resistance.
4. IACG RECOMMENDATIONS
No Time to Wait: Securing the future from drug-resistant infections • 9

10 • No Time to Wait: Securing the future from drug-resistant infections
4.2 Recommendations
A. ACCELERATE PROGRESS IN COUNTRIES
Aim of the recommendations in this section: These recommendations emphasize the importance of building
and sustaining effective and tailored national responses to address antimicrobial resistance through increased
political commitment and more coordinated multisectoral efforts across the One Health spectrum, while also
leveraging gains across the SDGs. Implementing these recommendations is the primary responsibility of
national governments which should have the central role in developing and implementing national policies
and programmes to address antimicrobial resistance based on guidance from the Tripartite agencies and
other international organizations.
Considerations for this recommendation:
• The IACG recognizes that effective systems for
infection prevention and control, including
vaccination, clean water, sanitation and hygiene,
as well as awareness creation, good management
practices, biosecurity and good animal welfare in
farming, avert infections in health care and farm
settings. These approaches will ensure patient
safety and protect health and farm workers, as
well as animals and plants, thereby reducing
the future need for antimicrobials, protecting
the environment and ensuring sustainable food
and feed production. Furthermore, effective
standards and practices in environmental
protection and the proper management and
handling of soil, water, health facility and
pharmaceutical waste, as well as manure used
as fertilizer, can further reduce the spread of
antimicrobial residues along the food and feed
production chain and in the environment.
• The IACG recognizes that in settings where
trained prescribers are in short supply, non-
physicians (such as nurses, paramedics and
community health workers) and veterinary
paraprofessionals may also be trained
and authorized to prescribe or administer
some antimicrobial agents, including under
professional supervision.
• The IACG emphasizes that ensuring equitable
and affordable access to and stewardship of
existing and new quality-assured antimicrobial
Recommendation A1: The IACG calls on all Member States to ensure equitable and affordable access to
existing and new, quality-assured antimicrobials as well as alternatives, vaccines and diagnostics and their
responsible and prudent use by competent, licensed professionals across human, animal and plant health.
This recommendation must be supported by efforts to reduce the need for antimicrobials, enhance their
responsible and prudent use and improve access through:
a. Lowering the prevalence of infection through clean water, sanitation and hygiene in health care facilities,
farms, schools and in household and community settings;
b. Decreasing the likelihood of diseases and their spread through delivery of existing vaccines and
diagnostics and through strengthening infection prevention and control measures, beginning with
improved hand hygiene and strengthening laboratory and diagnostic services for human, animal and
plant health;
c. Ensuring best practices in terrestrial and aquatic animal and plant health, food and feed production and
waste management;
d. Supporting behaviour change through effective awareness creation, communication and appropriate
incentives targeted at the public and professionals in human, terrestrial and aquatic animal and plant
health, as well as food and feed production and the environment;
e. Developing national processes and instruments based on international guidelines and standards
to support equitable access to and responsible and prudent use of existing and new quality-assured
antimicrobials in humans, animals, plants and food and feed production, as well as access to diagnostics
and vaccines, waste and water management in health care, manufacturing and farming-related activities;
and
f. Strengthening and maintaining national regulatory and accountability mechanisms and integrated
monitoring and surveillance systems.
No Time to Wait: Securing the future from drug-resistant infections • 11
medicines, diagnostics and vaccines is a function
of effective health systems and is essential for
effective national responses to antimicrobial
resistance. This can be achieved in several ways,
including:
o Addressing shortages and stockouts:
Governments should establish national
medicine, vaccine and diagnostics shortage
notication systems to allow them to
take rapid action in relation to shortages
and stockouts of these health products.
WHO and OIE should provide guidance
to countries on developing or improving
existing national medicine and vaccine
shortage notication systems for human
and animal health that are harmonized and
employ the same denitions, approaches
and methodologies, where appropriate.
This should be complemented by efforts
to strengthen supply chain and health
information management systems with the
aim of preventing shortages and stockouts.
A strong supply chain requires sustainable
supplies of active pharmaceutical ingredients
to avoid supply inefciencies.
o Effective national-level antibiotic demand
forecasts: Improved forecasting is needed in
both human and animal health to improve
access to antibiotics and to strengthen
procurement and supply chain management.
This will in turn support efforts by WHO and
OIE to develop a global demand forecast
model for antibiotics that can be shared with
manufacturers and procurement agencies on
a regular basis and made publicly available.
However, the IACG notes the complexity of
and challenges associated with developing
forecasts for bacterial infections, even in
countries with robust public health and
pharmaceutical reporting and surveillance
systems.
o Establishing antimicrobial production
facilities: Some governments or regional
entities may consider establishing
production facilities or contracting
manufacturers to help mitigate shortages
and ensure sustainable production and
supply of antimicrobials, particularly
antibiotics for human and animal health,
paying due consideration to manufacturing
and environmental standards and quality
assurance for health commodities.
o Providing affordable access: Governments
should establish policies, measures and
mechanisms that provide existing and new
antimicrobial medicines, diagnostics and
vaccines at affordable prices, including to
people who are unable to pay for them. This
will ensure that the benets of antimicrobials
are made available to the population at large,
especially those most in need of treatment,
regardless of their capacity to pay.
o Pooled procurement mechanisms: Leveraging
and learning lessons from existing pooled
procurement mechanisms in human health
and potentially establishing them for
animal health could help to secure both the
supply of quality-assured medicines, ensure
predictability of demand for manufacturers
and promote sustainable procurement
practices.
o Tackling substandard and falsied medical
products is an important component of
ensuring access to quality antimicrobials,
including stewardship. Strengthening national
regulatory pathways and implementing
complementary efforts to improve
antimicrobial resistance surveillance and
supply chain mechanisms – including the
implementation of low-cost technologies
and track-and-trace systems – could help to
address this problem in low- and middle-
income countries. Furthermore, efforts to
ensure Universal Health Coverage also promote
access to quality-assured and appropriate use
of antimicrobials and play a role in reducing
the development of antimicrobial resistance.
• The responsible and prudent use of antimicrobials
across the human, animal and plant health
sectors requires appropriate attention to
and investment in professional education,
training, certication and development as
well as regulation of professionals, including
physicians, dentists, pharmacists, veterinarians
and other specialists across human, terrestrial
and aquatic animal and plant health, food and
feed production, and the environment.
• The IACG emphasizes that there is an urgent
need to strengthen national surveillance and
regulatory frameworks and enforcement capacity
in all countries to support effective national
responses to antimicrobial resistance, including
monitoring antimicrobial resistance; access to,
affordability of and the responsible and prudent
use of antimicrobials and their importation
and sale, particularly over-the-counter and
on the internet, and sustainable practices
for waste and environmental management.

12 • No Time to Wait: Securing the future from drug-resistant infections
Surveillance systems should include a set of
specic, dened and standardized indicators
to enable monitoring of access, availability
and affordability of antimicrobials and related
commodities.
• The IACG recognizes that efforts to achieve
Universal Health Coverage and to expand
basic and essential health services are critical
to ensuring equitable and affordable access
to quality-assured health products and the
responsible and prudent use of antimicrobials.
Because achieving Universal Health Coverage
depends to a signicant degree on the continued
effectiveness of antimicrobials, these challenges
must be addressed simultaneously.
Recommendation A2: The IACG calls on all Member States to accelerate the development and implementation
of One Health National Antimicrobial Resistance Action Plans within the context of the SDGs that, at a
minimum, include:
a. Prioritized actions and interventions that are specic to the national context, capacity and infrastructure,
and that are costed and funded, including with adequate domestic resource allocations;
b. Strengthening key national systems for vaccination; infection prevention and hygiene in health care
and farming settings; integrated laboratory systems for human, animal and plant health; monitoring;
integrated surveillance; sustainable procurement of health commodities; and waste management;
c. Technical co-operation, capacity development, research and advocacy components, including support
for champions and civil society at national and local levels to mobilize action on antimicrobial resistance;
and
d. Effective national coordination, accountability and governance mechanisms that ensures collaboration
between government ministries, parliamentarians, civil society organizations, the private sector and
regional and international partners.
Considerations for this recommendation:
• This recommendation is relevant to all countries.
However, the IACG recognizes that approaches
to tackling antimicrobial resistance and the
development and implementation of National
Antimicrobial Resistance Action Plans differ
among countries, particularly between high-
income and low- and middle-income countries.
These differences are based on country-specic
context, capacity and infrastructure, and will
determine the type and level of actions and
interventions required to address antimicrobial
resistance at national and local levels.
• Furthermore, such differences between
countries should inform and help to dene the
mainstreaming of responses to antimicrobial
resistance within existing sustainable
development strategies as well as social and
political agendas across human, terrestrial and
aquatic animal and plant health, food and feed
production and the environment at country
level.
• The IACG notes that national actions on
antimicrobial resistance are relevant to several
SDGs, including those that relate to human health,
food security, clean water and sanitation, as well
as responsible consumption and production,
illustrating the importance of mainstreaming
action on antimicrobial resistance into national
efforts to achieve the SDGs.
• The IACG further recognizes that cooperation
and solidarity are required among all countries
for an effective global response to antimicrobial
resistance, including to tackle cross-border
issues and ensure that adequate nancial and
technical resources are available to support
implementation of national action plans,
including in low- and middle-income countries.
Furthermore, such cooperation should consider
the high burden of disease and increased risk of
antimicrobial resistance in some countries, and
efforts should be directed where the needs are
greatest and action will have the most impact.
Mechanisms to promote the exchange of best
practices and experience through north-south
and south-south collaboration will be useful
to accelerate implementation of National
Antimicrobial Resistance Action Plans in low-
and middle-income countries.
• The IACG emphasizes that One Health
surveillance and monitoring systems need to
be established, coordinated and integrated,
covering human, terrestrial and aquatic animal
and plant health, food and feed production and

No Time to Wait: Securing the future from drug-resistant infections • 13
the environment. To the extent possible, they
should also provide harmonized, veriable or
equivalent data that can be easily aggregated,
compared, exchanged and appropriately used
for decisions locally, nationally and globally.
Building on recent efforts, the Tripartite
agencies – working together with Member States
and other organizations – need to develop and
monitor core indicators that cut across human,
animal, plant, food and environmental health.
• The IACG underlines the importance of
creating and strengthening integrated
laboratory platforms and services for
antimicrobial resistance in collaboration
with other priority human, animal and plant
health programmes of a country, aligned with
existing national laboratory strategic plans.
Recommendation A3: The IACG calls on all Member States to phase out the use of antimicrobials for growth
promotion, consistent with guidance from the Tripartite agencies (FAO, OIE and WHO) and Codex Alimentarius,
starting with an immediate end to the use of antibiotics categorised as the Highest Priority Critically
Important Antimicrobial Agents on the WHO List of Critically Important Antimicrobials for Human Medicine
(i.e. quinolones, third- and higher- generation cephalosporins, macrolides and ketolides, glycopeptides and
polymyxins).
Considerations for this recommendation:
• The IACG recognizes that the use of antimicrobials
in animal production may be as high as or
exceed use in the human health sector. The IACG
emphasizes that this recommendation should
be implemented by Member States as a matter
of urgency and that it should be complemented
by the adoption of global standards and best
practices established by the Tripartite agencies
and other international and national authorities.
• The IACG emphasizes that eliminating the use
of the Highest Priority Critically Important
Antimicrobial Agents for growth promotion is
only a rst step towards reducing the overuse
and misuse of antimicrobials in food and feed
production, including in both animals and crops.
• The IACG underlines the importance of collateral
measures to address challenges that could
arise from the phasing out of antimicrobials in
growth promotion, including using alternatives
to antimicrobials; infection control and
hygiene; education and provision of economic
incentives to farmers as they transition from
using antimicrobials as growth promoters, as
well as promoting research to identify effective
interventions. It also recognizes the need for
enhanced capacity and technical expertise
on animal husbandry to facilitate the phasing
out of antimicrobials for growth promotion,
particularly in LMICs.
• The IACG notes that while some countries
continue to use antimicrobials for animal growth
promotion and in crops, others – particularly
low-income countries – experience difculties
in accessing effective antimicrobials to treat
diseases in animals. Moreover, both situations –
excessive use and poor access – can co-exist in
the same country. Although efforts to implement
this recommendation should recognize
these challenges in different countries, it is
important that countries work together in a
spirit of solidarity to address them. Countries
authorizing antimicrobials for non-veterinary
medical use, such as growth promotion, should
employ appropriate risk analysis – the process
of hazard identication and risk assessment,
management and communication – as described
in the OIE Terrestrial Animal and Aquatic Animal
Health Codes. Such risk analyses should be
unbiased assessments that transparently
present the evidence base for ndings and
recommendations and be subject to peer review.

14 • No Time to Wait: Securing the future from drug-resistant infections
B. INNOVATE TO SECURE THE FUTURE
Aim of the recommendations in this section: These recommendations emphasize that current efforts to support
research into and development of new antimicrobials, diagnostics, vaccines, waste management tools, and
safe and effective alternatives to antimicrobials across the One Health spectrum remain inadequate and need
to be intensied, with sustained investment and increased scientic engagement and collaboration. They also
aim to promote equitable and affordable access to and stewardship of new health products, through both
existing and future global access initiatives.
Considerations for this recommendation:
• The IACG recognizes that the absence of
quality data and the inability to generate such
information in all settings across the One Health
spectrum are a major barrier in the global
response to antimicrobial resistance, including
data to enable a complete understanding of the
burden and demonstrate a strong investment
case.
• The IACG notes that the limited market
potential of antibiotics, diagnostics and
vaccines discourages innovation, primarily due
to scientic barriers, the high cost of research
and development and low success rates for
new compounds, as well as limited revenue
due to low price and volume of new products.
Accordingly, additional, sustained investments
and collaborations are needed on the part of
governments, the private sector and civil society
to accelerate research and development, pull
new products through to market and ensure
effective stewardship.
• The IACG reiterates that all research and
development efforts to address antimicrobial
resistance should be needs-driven, evidence-
based and guided by the principles of
affordability, effectiveness, efciency and equity,
as well as delinking the cost of investments in
research and development on antimicrobial
resistance from the price and volume of sales.
• The IACG recognizes the need to develop and
provide appropriate nancial and non-nancial
market incentives for research and development
to address antimicrobial resistance and
recommends that these incentives should be
aligned with dened research and development
needs and priorities, including the WHO List
of Priority Pathogens and the OIE proposed
priorities for vaccine development for chicken,
swine, sheep, goat, bovine and sh diseases, and
appropriately targeted to address bottlenecks
and market barriers across the product life
cycle, from fundamental research to registration
and equitable and affordable access and
stewardship. This could include incentives such
as grant funding and tax credits to support early
stage research (push mechanisms) and rewards
for new research and development products
including market entry rewards, milestone
prizes, advance market commitments and other
market incentives (pull mechanisms).
• The IACG acknowledges the important and
encouraging role of existing international
mechanisms to support research and
development in human health, including CARB-X,
Global Antibiotic Research and Development
Partnership, Innovative Medicines Initiative,
JPI-AMR, TB Alliance, European and Developing
Countries Clinical Trials Partnership, CEPI and
others. It recommends full and sustained funding
for such initiatives and other approaches to
Recommendation B1: The IACG calls on public, private and philanthropic donors and other funders to
increase investment and innovation in quality-assured, new antimicrobials (particularly antibiotics),
novel compounds, diagnostics, vaccines, waste management tools, and safe and effective alternatives to
antimicrobials for human, terrestrial and aquatic animal and plant health, as well as implementation and
operational research through:
a. Financial and non-nancial incentives strategically targeting the most important research and
development needs, scientic challenges, and market barriers based on the principles of affordability,
effectiveness, efciency and equity, as outlined in the 2016 UN Political Declaration on Antimicrobial
Resistance; and
b. Building upon existing Product Development Partnerships in human health and possibly establishing
more of them, particularly for terrestrial and aquatic animal and plant health.

No Time to Wait: Securing the future from drug-resistant infections • 15
improve innovation and affordable access to
health products through public, private and
philanthropic sources.
• The IACG acknowledges that terrestrial and
aquatic animal health research and development
are under-nanced, limiting the development of
tools that reduce the need for antimicrobials in
animals. It emphasizes the need for increased
funding for animal health research and
development from public and private sources,
drawing upon lessons from successful Product
Development Partnerships in human health,
and replicating them in terrestrial and aquatic
animal and plant health.
• The IACG underlines that additional funding
combined with appropriate nancial and non-
nancial incentives is particularly required to
bring innovative products from fundamental
research to registration and implementation,
including to accelerate clinical trials in
humans and experimental work in animals and
plants, and to create a sustainable innovation
ecosystem that overcomes the challenges faced
in research and development by small and
medium enterprises.
• The IACG recognizes that beyond product
development, funding is also required for
repurposing existing antimicrobials, and
development of suitable drug regimens
and child-friendly formulations. Similarly,
implementation and operational research
require adequate investment, including on
burden and mechanisms of transmission of drug
resistant infections; implementation of existing
tools and effective approaches; innovative
practices; behavior change, awareness creation
and communication; infection prevention;
quality improvement interventions; responsible
and prudent use of antimicrobials; smart
approaches to livestock management and
animal husbandry practices; and effective soil,
water and waste management.
Recommendation B2: The IACG recommends that existing and future global access initiatives should
promote and support equitable and affordable access to existing and new, quality-assured antimicrobials,
diagnostics, vaccines, waste management tools and safe and effective alternatives to antibiotics for human,
terrestrial and aquatic animal and plant health.
Considerations for this recommendation:
• While the IACG recognises that governments
have the central responsibility to ensure
equitable and affordable access to existing
and new antimicrobials, diagnostics, vaccines,
waste management tools and safe and effective
alternatives to antibiotics and alternative
practices for human, terrestrial and aquatic
animal and plant health, it notes that there
are few global access initiatives, particularly
to address the needs of LMICs. The IACG
therefore emphasizes the need to leverage
the use of existing global access and scale-
up initiatives and platforms in human health
wherever possible (e.g. CEPI, Gavi, the Global
Fund to Fight AIDS, Tuberculosis and Malaria,
Medicines Patent Pool, Unitaid) to ensure
access to existing and new, quality-assured
antimicrobials, diagnostics and vaccines to
address antimicrobial resistance. This could be
done by assessing the comparative advantage
and strengths of each of these organizations
and determining the levels of funding required.
• The IACG recognizes the need to develop new
global initiatives to ensure access to and
responsible and prudent use of existing and
new antimicrobials, diagnostics, vaccines,
waste management tools and safe and effective
alternatives to antibiotics in terrestrial and
aquatic animal and plant health, including for
low-income countries.
• The IACG notes that harmonized regulatory
guidance for new antimicrobials, vaccines,
and alternatives to antimicrobials – possibly
including strengthening global and regional
mechanisms - will help to prevent existing
registration and commercialization challenges
resulting from divergent approval requirements
and processes.

16 • No Time to Wait: Securing the future from drug-resistant infections
Recommendation B3: The IACG calls on public, private and philanthropic research funders and other
stakeholders to build upon current research and development efforts for new antimicrobials, diagnostics,
vaccines, waste management tools, and safe and effective alternatives to antimicrobials; and to strengthen
implementation and operational research and research coordination and collaboration in a One Health
context by:
a. Supporting, facilitating and strengthening coordinated global mapping of research and development
activities and funding to address antimicrobial resistance;
b. Establishing and maintaining platforms for sharing information on research and products in development
in both ongoing and completed research and development activities;
c. Promoting synergies and opportunities for collaboration among funders, researchers and research
platforms in human, animal and plant health, and the environment; and
d. Promoting openness and transparency in data from all research, monitoring and surveillance sources,
including overcoming data protection provisions that restrict such data sharing.
Considerations for this recommendation:
• The IACG emphasizes that lack of information,
collaboration and transparency across different
research and development activities, funding
agencies and partners continue to act as signicant
barriers to advancing research and development
related to antimicrobial resistance. It recognizes
past and current efforts to promote and enhance
research collaboration and interdisciplinary
approaches to address antimicrobial resistance
and particularly acknowledges ongoing efforts
to map research activities, including through
JPI-AMR, the Global Antimicrobial Resistance
Research & Development Hub and the STAR-IDAZ
International Research Consortium on Animal
Health, as well as in the private sector.
• The IACG notes that information sharing,
collaboration and coordination of research
and development through ongoing and future
initiatives across all sectors will help in
identifying global research and development
priorities; ensure that funding addresses
those priorities along the full research and
development pipeline; enable gaps to be
identied and monitored; maximize the impact
of research and development; facilitate the work
of small and medium enterprises and contribute
to reducing costs and avoiding duplication of
effort.
• The IACG recommends that, wherever possible,
existing research and development platforms
for animal and human health, and for the
environment, should formalize information-
sharing and collaboration arrangements in line
with relevant international agreements and
ongoing discussions.
C. COLLABORATE FOR MORE EFFECTIVE ACTION
Aim of the recommendations in this section: Multisectoral efforts involving all stakeholders are essential to
tackle the many challenges posed by antimicrobial resistance. These recommendations aim to strengthen the
systematic engagement of civil society and the private sector to optimize their contributions to the response
to antimicrobial resistance, including working with national governments. All stakeholders should make
appropriate declarations of conicts of interest.
Recommendation C1: The IACG calls for the systematic and meaningful engagement of civil society groups
and organizations as key stakeholders in the One Health response to antimicrobial resistance at global,
regional, national and local levels through:
a. Strengthening their roles in accountability, advocacy, planning, monitoring progress and ensuring
responsible and prudent use of antimicrobials;
b. Promoting synergies with consumer and civil society groups active in other sectors, including in climate
change and the environment; responses to sexual and reproductive health and rights; HIV, TB and
malaria; patient safety; water, sanitation and hygiene; Universal Health Coverage; and other aspects of
the SDGs; and
c. Provision of political, nancial and technical support for civil society organizations to enhance their
engagement, including for work with governments while keeping their independence.

No Time to Wait: Securing the future from drug-resistant infections • 17
Considerations for this recommendation:
• The IACG emphasizes that closer engagement
of civil society is essential to advance efforts
against antimicrobial resistance at global,
regional, national and local levels. This includes
professional societies (e.g. medical, veterinary),
organizations (e.g. non-governmental
and community-based), associations (e.g.
consumers, farmers, patients, service providers)
trade unions and federations, academia and
other non-state actors (e.g. foundations,
research networks).
• The IACG notes that civil society groups
have a particularly important role to play in
the development of National Antimicrobial
Resistance Action Plans; ensuring
transparency of governance and monitoring;
undertaking advocacy, awareness creation
and communications; and enabling citizens
to become agents of change. Depending on
country context, civil society actors can be
strong drivers for mobilization and action to
address antimicrobial resistance. For example,
consumer groups have advocated successfully
for responsible and prudent antibiotic use in
food production by some companies, mainly
in high-income countries. In other countries,
farmers’ groups have mobilized to respond to
the challenges that antimicrobial resistance
poses to their livelihoods. The IACG notes that
efforts are particularly needed to strengthen the
engagement of civil society stakeholders from
the environment sector and to encourage and
engage consumer groups in LMICs in efforts to
address antimicrobial resistance.
• Experiences from advanced global health
initiatives that address HIV, TB and malaria, and
from the climate change and environment sectors
that have resulted in demonstrable impact, can
be drawn upon to advance this recommendation.
The IACG particularly emphasizes the need
for stakeholders engaged in antimicrobial
resistance to work with these groups to identify
synergies and opportunities to achieve shared
gains by addressing antimicrobial resistance in
their advocacy and programming efforts.
• The IACG highlights the importance of providing
political, nancial and technical support to
civil society organizations to enhance their
engagement, including to work effectively with
governments and to ensure that their efforts are
aligned with and contribute to evidence-based
national policies and approaches. Innovative
approaches to nancing the engagement
of community-based organizations include
the Collaborative Fund for HIV Treatment
Preparedness, Global Fund Advocates Network,
the Civil Society Challenge Facility of the Stop
TB Partnership, and the Global Environment
Facility’s Small Grants Programme. These and
other initiatives have successfully mobilized
community action and ownership in their
respective elds and have signicant potential
to do the same across sectors in the response to
antimicrobial resistance.
Recommendation C2: The IACG calls for the systematic and meaningful engagement of and enhanced action
by the private sector as key stakeholders in the One Health response to antimicrobial resistance at global,
regional, national and local levels to support:
a. Affordable access, responsible and prudent use and stewardship of antimicrobials;
b. Ethical production, distribution and marketing practices, including through environmentally sustainable
production and waste management and the elimination of inappropriate incentives to sell antimicrobials;
c. Engagement by the private sector in collaborative efforts to collect, analyze and use data and realign
economic incentives to improve production, distribution and marketing practices; and
d. Contributions to addressing antimicrobial resistance through testing of innovative approaches, corporate
social responsibility, and similar initiatives.
Considerations for this recommendation:
• The IACG recognizes the diverse range of private
sector actors that need to be engaged in the ght
against antimicrobial resistance. This includes
industries such as generic and non-generic
manufacturers producing pharmaceuticals,
health technologies and pesticides/biocides for
human, animal and plant health; commercial
food and feed producers and retailers; private
nancial institutions and venture capital
including banking, insurance, investors and
investment fund managers; and private
practitioners in human and animal health.

18 • No Time to Wait: Securing the future from drug-resistant infections
• The IACG also recognizes encouraging efforts by
the private sector to engage in the response to
antimicrobial resistance, including in voluntary,
collaborative approaches to responsible and
prudent distribution and use of antimicrobials,
and through organized industry collaboration
related to both human and animal health.
However, the IACG emphasizes that the urgency
and threat posed by antimicrobial resistance
demand signicantly more action by and
enhanced engagement of the private sector to
advance efforts against antimicrobial resistance
at global, regional and national levels.
• In addition to the activities described in this
recommendation, private sector actors in
human, plant, and animal health, as well as in
the food and feed production and retail sectors,
have important contributions to make in the
areas of nancing and resource mobilization;
information and data sharing; monitoring and
surveillance; behaviour change, awareness
creation and communication; advocacy and work
with government on key policy issues; research
and development; and effective environmental
management.
D. INVEST FOR A SUSTAINABLE RESPONSE
Aim of the recommendations in this section: Financing is a critical bottleneck to advancing the global response
to antimicrobial resistance. These recommendations emphasize the need for innovative approaches to
mainstream antimicrobial resistance-related activities and leverage resources from existing funding streams,
as well as to mobilize new and additional funding. The recommendations further underline that domestic
nancing commitments by national governments are essential to advance priority actions and ensure long-
term, sustainable responses to antimicrobial resistance.
Considerations for this recommendation:
• The IACG notes that experiences of main-
streaming gender and climate change into grants
and loans of bilateral agencies, the World Bank
and regional development banks demonstrate
the feasibility of introducing a similar approach
of applying an antimicrobial resistance and
One Health “lens” to existing funding streams
and approaches. Applying this “lens” entails
the development and application of standards
to assess antimicrobial resistance-related risks
and impacts and accountability measures to
ensure that that these investments do mitigate—
and do not worsen—the emergence, prevalence
and impact of antimicrobial resistance.
• The IACG notes that the direct and indirect
costs to the health sector and food production
systems of treating and managing drug-
resistant infections are already signicant
and are likely to increase in the absence of
concerted action. These costs may be offset
by adequate investments to lower the burden
of infections through water, sanitation and
hygiene; vaccination and infection prevention
and control measures; universal health coverage;
and by promoting sustainable production and
supply. Overall, the IACG emphasizes the need
to further leverage existing funding streams and
investments, and to mobilize new and additional
resources to strengthen existing efforts and
ensure a more effective and sustainable
global response to antimicrobial resistance. It
underlines that such investments not only help
to tackle the challenges currently posed by
Recommendation D1: The IACG calls on governments; global, regional, national, bilateral and multilateral
nancing and development institutions and banks; and private investors to systematically apply standards
to assess risks and impacts related to antimicrobial resistance (an antimicrobial resistance and One Health
“lens”) when making investments through:
a. Ofcial Development Assistance;
b. South-South cooperation;
c. The International Development Association (IDA) replenishment process from IDA19 onwards;
d. Financial support, grants, loans, credits and insurance for terrestrial and aquatic animals and plants;
health, water and sanitation; development; food systems; manufacturing of health products; the
environment; and other relevant areas.

No Time to Wait: Securing the future from drug-resistant infections • 19
antimicrobial resistance but will also avert the
need for even greater investments in the future
and will help to mitigate the economic impact of
antimicrobial resistance.
• The IACG notes that that there is an urgent
need to elevate the challenges of antimicrobial
resistance as crucial elements of the global
social, economic development and nancing
agenda, including the SDGs. The spread of
untreatable drug-resistant diseases poses a
serious threat to the achievement of the SDGs,
including those that relate to human health;
food security; clean water and sanitation; and
responsible consumption and production. The
IACG recognizes the importance and urgency of
developing robust analyses and indicators that
capture both the direct and indirect impact of
antimicrobial resistance on efforts to achieve
the SDGs.
• The IACG recognizes the indirect benets that
broader nancial investments in areas related to
human, terrestrial and aquatic animal and plant
health, as well as food and feed production, can
have in addressing antimicrobial resistance.
Applying an antimicrobial resistance and
One Health “lens” to and monitoring such
investments will help to inform and leverage
further nancing for antimicrobial resistance.
Recommendation D2:
a. The IACG emphasizes the need for additional and increased investment in the global response to
antimicrobial resistance, including from domestic nancing in all countries;
b. The IACG urges existing and future nancing mechanisms in human, animal and plant health, as well as
food and feed production and the environment – including Gavi, the Vaccine Alliance; the World Bank;
the Global Fund to Fight AIDS, Tuberculosis and Malaria; Global Financing Facility; Multilateral Climate
Funds; and Unitaid, as well as future nancing streams for Universal Health Coverage; water, sanitation
and hygiene; and other priority development issues, and their donors, to give antimicrobial resistance
greater priority in their resource allocations, including by assessing the need to expand their scope and
mandate, where appropriate.
c. The IACG further calls on public, private and philanthropic donors in human, animal and plant health, as
well as food and feed production and the environment, to contribute additional funding to addressing
antimicrobial resistance, including to support implementation of National Antimicrobial Resistance
Action Plans.
Considerations for this recommendation:
• The IACG notes that signicant opportunities
exist within existing human health nancing
mechanisms – notably Gavi, the Vaccine Alliance;
the Global Fund to Fight AIDS, Tuberculosis and
Malaria; and Unitaid – to contribute to the
external nancial needs of low-income countries
in implementing National Antimicrobial
Resistance Action Plans.
• The IACG acknowledges both the added value
of and the need to further strengthen nancing
mechanisms dedicated to antimicrobial
resistance, such as JPI-AMR, which is supported
by 27 Member States and the European
Commission, as well as the Fleming Fund of the
UK government, to advance the global response,
particularly through support for implementation
in low-income countries while also ensuring
long-term sustainability through domestic
nancing.
• The IACG highlights the importance of
increased engagement by the private sector
and other stakeholders to advance innovative
nancing concepts for antimicrobial resistance,
including livestock insurance programs and
other incentives to support the transition to
sustainable food and feed production practices,
as well as accredited medicine dispensing
outlets and social impact bonds.
• The IACG emphasizes that efforts to leverage
resources within existing funding mechanisms
must be supported by effective global, regional
and national governance and coordination
mechanisms to help direct limited resources
to agreed priorities and goals across the One
Health spectrum.

20 • No Time to Wait: Securing the future from drug-resistant infections
E. STRENGTHEN ACCOUNTABILITY
AND GLOBAL GOVERNANCE
Aim of the recommendations in this section: Stronger and sustained global leadership and advocacy and a more
powerful global narrative and vision are all needed to advance the global response to antimicrobial resistance.
These recommendations promote the creation of a platform that will be instrumental in raising the prole
and urgency of addressing antimicrobial resistance, building and maintaining political momentum and public
support, enabling more comprehensive monitoring of the science and evidence related to antimicrobial resistance,
ensuring accountability among all stakeholders and recognizing the central role of national governments.
Recommendation E1: The IACG requests the Tripartite agencies (FAO, OIE and WHO) together with UN
Environment, other UN agencies and the World Bank, in the context of UN reform, to further strengthen joint
One Health action, based on target-setting, country priorities and needs, by enhancing their organizational
capacity and providing adequate and sustainable core funding for antimicrobial resistance-related activities
in order to:
a. Integrate antimicrobial resistance into UN country-level activities, including UN Development Assistance
Frameworks and Country Programme Documents;
b. Provide and update effective normative guidance, standards and tools, where necessary;
c. Advise on priority evidence-based interventions and actions;
d. Provide coordinated technical co-operation and capacity building, including One Health regional
platforms for technical co-operation;
e. Guide, support, monitor and evaluate implementation, including on infection prevention and control;
antimicrobial stewardship; integrated surveillance; data quality and harmonization; risk assessment;
procurement and demand forecasting; and supply management;
f. Identify priorities for research and development and facilitate implementation research in a One Health
context; and
g. Dene the nancial needs and gaps for national and global responses to antimicrobial resistance,
including the costs of inaction and anticipated returns on investment.
Considerations for this recommendation:
• The IACG acknowledges the critical and core
mandate of the Tripartite agencies (FAO, OIE
and WHO) and Codex Alimentarius in providing
Member States with normative guidance,
standards and tools to tackle antimicrobial
resistance for human, aquatic and terrestrial
animal and plant health, as well as in food
and feed production and food safety. The
IACG also recognizes the important role of UN
Environment in addressing environment-related
antimicrobial resistance issues. Other UN and
international agencies have key roles to play
in accelerating action against antimicrobial
resistance, including at country level, for
example, through UN Development Assistance
Frameworks and ensuring a whole-UN approach
to antimicrobial resistance.
• The IACG applauds recent positive developments
from the Tripartite agencies (FAO, OIE and
WHO), including the signing of a Memorandum
of Understanding and a joint workplan that
includes UN Environment. However, the IACG
believes that the response of the Tripartite
agencies (FAO, OIE and WHO) needs to be stepped
up and requires further consolidation and
strengthening through enhanced organizational
capacity and commitment of additional human
and nancial resources, including adequate
and sustainable core funding for their activities
related to antimicrobial resistance.
• The IACG emphasizes that formalizing the
antimicrobial resistance-related core and shared
roles and responsibilities of the Tripartite agencies
(FAO, OIE and WHO) and UN Environment based
on their mandate in their respective sectors will
facilitate collaborative and coordinated action.
For example, the Tripartite agencies (FAO, OIE
and WHO) and UN Environment can collectively
dene key antimicrobial resistance-related
activities which they will undertake separately,
jointly or in collaboration with other UN and
international agencies.
• The IACG recognizes that lessons can be drawn
from experience and best practice models and
platforms of the Tripartite agencies (FAO, OIE

No Time to Wait: Securing the future from drug-resistant infections • 21
and WHO) within the One Health context that
were demonstrated in responses to zoonoses
and emerging infections. These experiences can
be used to guide and further strengthen the
Tripartite agencies’ response to antimicrobial
resistance through building national capacity,
creating a platform and repository to share best
practices and materials (e.g. in awareness creation,
communications, integrated surveillance,
antimicrobial stewardship promoting responsible
and prudent use) and developing tools to support
the implementation of National Antimicrobial
Resistance Action Plans.
• The IACG recommends that lessons should also
be drawn from other areas with advanced global
responses, such as TB, HIV, malaria and the
Joint External Evaluations of the International
Health Regulations. For example, the Tripartite
agencies and UN Environment in collaboration
with other stakeholders including civil society
and the private sector could conduct Joint
Periodic Review missions on antimicrobial
resistance every three to ve years within a
One Health context that are complemented
by regular monitoring in priority countries.
Such Joint Reviews provide national advocacy
opportunities and a useful model for advancing
action and impact at country level, including
to enhance accountability. Regional models
for technical cooperation and coordination can
also inform efforts to address antimicrobial
resistance. For example, the UNAIDS regional
technical support facilities and the TBTEAM
mechanism of WHO provide technical support
to countries on HIV and TB, respectively.
Recommendation E2: The IACG recommends the urgent establishment of a One Health Global Leadership
Group on Antimicrobial Resistance, supported by a Joint Secretariat managed by the Tripartite agencies
(FAO, OIE and WHO), to:
a. Maintain urgency, public support, political momentum and visibility of the antimicrobial resistance
challenge on the global agenda;
b. Advocate for action, including support for the expanding work of the Tripartite agencies (FAO, OIE and
WHO), UN Environment and other international and regional entities;
c. Monitor and report on progress, gaps and accountability in the global response to antimicrobial resistance;
d. Advocate for multi-stakeholder engagement by facilitating a partnership platform with the participation
of Member States, UN agencies, international and intergovernmental organisations and regional entities,
civil society, the private sector, researchers and other key stakeholders to develop and work towards a
shared global vision, goals and coordinated action on antimicrobial resistance;
e. Provide advice and guidance on reports of the Independent Panel on Evidence for Action against
Antimicrobial Resistance (recommendation E3);
f. Monitor and advocate for the inclusion of antimicrobial resistance and a One Health “lens” in investments
and programmes of major nancing instruments for agriculture, health, development, food and feed
production and other relevant areas (recommendation D1).
Considerations for this recommendation:
• The SDGs cannot be achieved if antimicrobial
resistance is not addressed with greater urgency.
The IACG stresses the importance of increasing
and maintaining the urgency and visibility of
the need to address antimicrobial resistance on
the global agenda through political and public
support, and target setting. The One Health
Global Leadership Group on Antimicrobial
Resistance will play a pivotal role in addressing
these challenges.
• The IACG recognizes that its work has played an
important role in ensuring that antimicrobial
resistance is prominent on the global health
and development agenda, including in the work
of the Tripartite agencies (FAO, OIE and WHO).
However, the IACG mandate is time-limited and
the scale of its efforts are insufcient considering
the global threat posed by antimicrobial
resistance. Therefore, the complex responses
that are required need to be addressed over the
long-term through the establishment of a One
Health Global Leadership Group. Furthermore,
the IACG notes that other models in health
and development illustrate the practicality and
feasibility of establishing a Global Leadership
Group on Antimicrobial Resistance. Examples
include:
o The Global Preparedness Monitoring Board
for Health Emergencies is co-convened

22 • No Time to Wait: Securing the future from drug-resistant infections
by WHO and the World Bank to monitor
progress, identify gaps and advocate for
sustained, effective action to ensure global
preparedness for disease outbreaks and
other health emergencies. The Board
succeeded the UN Secretary-General’s Global
Health Crises Task Force, created in 2016 in
response to the West Africa Ebola outbreak.
o Scaling Up Nutrition (SUN) Movement Lead
Group, which has overall responsibility for
the Movement’s progress towards addressing
global under-nutrition. The SUN Lead Group
succeeded the High-Level Task Force on Food
and Nutrition Security, established by the
UN Secretary-General in 2008. A high-level
Lead Group was established in 2012 with
membership nominated by the Secretary-
General and is supported by a Coordinator
and Secretariat based in Geneva. The SUN
Movement Executive Committee acts on
behalf of the SUN Movement Lead Group to
oversee development and implementation
of the Movement’s strategy.
o The Committee on World Food Security
(CFS) reporting to the UN General Assembly
through the Economic and Social Council
and the FAO Conference brings together
stakeholders working on food security
and nutrition globally. Created in 1974 as
an intergovernmental UN body, the CFS
currently involves 130 Member States and
includes both a Civil Society Mechanism
and a Private Sector Mechanism. It is
supported by a multi-agency Secretariat
comprised of FAO, the International Fund
for Agricultural Development and the World
Food Programme, and includes a High-Level
Panel of Experts.
• The IACG proposes that the One Health Global
Leadership Group on Antimicrobial Resistance
be composed of a small group of current and
former Heads of State; Ministers of Agriculture,
Environment, Finance, Health, and Water and
Sanitation; Heads of the Tripartite agencies; other
UN and international agencies; Heads of Regional
Banks and other prominent global leaders and
eminent persons representing human, animal
and plant health, as well as food and feed
production and the environment, including
members from the private sector and civil society,
and with appropriate gender and geographic
representation. Proper declarations of conict of
interest should be made. The One Health Global
Leadership Group should be supported by a small
Secretariat managed by the Tripartite agencies.
This Secretariat can also develop and facilitate a
partnership platform for global coordination and
action. The One Health Global Leadership Group
should oversee the preparation of a plan of action
with key performance indicators, particularly to
ensure that its activities are supporting country-
level action.
• The IACG reiterates the urgent need to develop
a shared global vision, narrative and targets to
tackle antimicrobial resistance and mobilize all
relevant stakeholders, including Member States;
UN agencies; international and intergovernmental
organisations and regional entities; civil society;
the private sector; and researchers, and to support
country-level action. The IACG recommends
the establishment of a constituency-based
partnership platform facilitated and managed by
the Tripartite agencies with diverse representation
(e.g. governments, private sector and civil
society representing human, animal, plant and
environment health, as well as agriculture and food
and feed production) to develop and implement
a shared global vision, narrative and targets.
• The IACG notes that such a partnership platform,
with support from the Secretariat, would create
opportunities to collectively address diverse
areas of importance by all stakeholders,
serve as a venue for information sharing and
collaboration, and promote leadership by key
partners around the shared global vision and
narrative. This is consistent with existing models
such as the End Malaria Partnership and the
Partnership for Maternal, Newborn & Child
Health. The Secretariat of the Global Leadership
Group and partnership platform could also
provide support to the Independent Panel
on Evidence for Action against Antimicrobial
Resistance [Recommendation E3].
Recommendation E3: The IACG requests the Secretary-General, in close collaboration with the Tripartite
agencies (FAO, OIE and WHO), UN Environment and other international organizations, to convene an
Independent Panel on Evidence for Action against Antimicrobial Resistance in a One Health context to
monitor and provide Member States with regular reports on the science and evidence related to antimicrobial
resistance, its impacts and future risks, and to recommend options for adaptation and mitigation.

No Time to Wait: Securing the future from drug-resistant infections • 23
Considerations for this recommendation:
• The IACG notes that limited data and the lack
of targets, as well as inadequate expertise and
in some cases limited consensus on approaches
to addressing antimicrobial resistance and
its associated threats across the One Health
spectrum, present key challenges that hamper
global progress. There is an urgent need to
shape the global antimicrobial resistance
agenda to stimulate the generation of evidence
and its translation and dissemination into policy
change and effective interventions.
• The IACG recognizes the need for an Independent
Panel on Evidence for Action against
Antimicrobial Resistance to provide robust and
authoritative assessments of the science, data
and evidence related to antimicrobial resistance
across all sectors, asses its impacts and future
risks and recommend options for adaptation and
mitigation to governments and all stakeholders
in the form of periodic reports.
• The IACG notes that the composition of
the Independent Panel should include
representation across the One Health spectrum,
including experts from human, terrestrial and
aquatic animal and plant health, as well as the
environment, food and feed production and
food safety sectors.
• The IACG notes that the Independent Panel
on Evidence for Action against Antimicrobial
Resistance should draw on the experiences and
lessons of similar, existing entities, including
the Intergovernmental Panel on Climate Change,
the Joint FAO/WHO Expert Committee on Food
Additives, the Joint FAO/WHO Expert Meetings
on Microbiological Risk Assessment, and
the International Assessment of Agricultural
Knowledge, Science and Technology for
Development. The costs of convening experts,
commissioning expert analysis, and maintaining
Secretariat functions are anticipated to be
modest.
Recommendation E4: The IACG recognizes the ongoing process led by Member States to develop the Global
Development and Stewardship Framework to Combat Antimicrobial Resistance and urges the Tripartite
agencies (FAO, OIE and WHO) and UN Environment to expedite its development in line with the scope
described in the 2015 World Health Assembly resolution on antimicrobial resistance (WHA68.7). As Member
States nalize this process, they should also consider the need for new international instruments.
Considerations for this recommendation:
• The IACG acknowledges the current debates
and discussions about binding or non-
binding international instruments to combat
antimicrobial resistance and recognises
the enormous challenge of developing and
negotiating such international instruments
among Member States. The IACG recommends
that priority be given to adopting and
implementing global standards and best
practices established by the Tripartite agencies
(FAO, OIE and WHO) and other international
and national authorities, and that the current
debates and discussions should not distract
from this priority.
• The IACG recognizes that the ongoing process
of developing the Global Development and
Stewardship Framework to Combat Antimicrobial
Resistance led by Member States with
facilitation by the Tripartite agencies (FAO, OIE
and WHO) and UN Environment has not yet been
nalized. The Framework was rst called for in
the 2015 World Health Assembly resolution on
antimicrobial resistance and later in the 2016
Political Declaration on antimicrobial resistance.
The IACG therefore urges Member States, the
Tripartite agencies (FAO, OIE and WHO) and UN
Environment to bring the development of the
Framework to a conclusion as soon as possible
consistent with the scope described in the 2015
World Health Assembly resolution and with all
due consideration to and inclusion of relevant
recommendations in this report.
• The IACG recognizes that ongoing discussions
and nalization of the process to develop
the Global Development and Stewardship
Framework to Combat Antimicrobial Resistance
can be used as an initial platform by Member
States to advance a stepwise approach
towards potential new, binding or non-binding
international instruments. Such instruments
need to include a stronger focus on supporting
the distribution, responsible and prudent use
of existing and new antimicrobial medicines,
diagnostics, vaccines and other interventions,
while also preserving existing antimicrobial
agents, including using the WHO ACCESS, WATCH
and RESERVE categorization of antibiotics.
24 • No Time to Wait: Securing the future from drug-resistant infections
MEMBERS OF THE AD HOC INTERAGENCY COORDINATION
GROUP (IACG) ON ANTIMICROBIAL RESISTANCE
Co-Chairs
Ms Amina Mohammed
Deputy Secretary-General,
United Nations (UN)
Dr Tedros Adhanom Ghebreyesus
Director-General, World Health
Organization (WHO)
Co-conveners
Professor Junshi Chen
Senior Research Professor,
National Center for Food Safety
Risk Assessment, China
Professor Dame Sally Davies
Chief Medical Ofcer, United Kingdom
of Great Britain and Northern Ireland
Professor Anthony D. So
Director, IDEA (Innovation+Design
Enabling Access) Initiative, Johns
Hopkins Bloomberg School
of Public Health; Director,
Strategic Policy Program, ReAct,
United States of America
Members in individual capacity
Dr Fajer Al Salloom
Ministry of Works, Municipality
Affairs and Urban Planning –
Agriculture Affairs, Bahrain
Dr Hanan H. Balkhy
Executive Director, Infection
Prevention & Control, Ministry of
National Guard Health Affairs,
Saudi Arabia
Professor Otto Cars
Senior Professor, Infectious
Diseases, Senior Adviser - ReAct,
Uppsala University, Sweden
Dr Lyalya Gabbasova
Assistant to the Minister of Health
for AMR issues, TB, HIV/AIDS and
other infectious diseases, Ministry
of Health, Russian Federation
Ms Martha Gyansa-Lutterodt
Director of Pharmaceutical Services,
Ministry of Health, Ghana
Dr Jaana Husu-Kallio
Permanent Secretary, Ministry of
Agriculture and Forestry, Finland
Mr Martin Khor
Malaysia
Dr Marco Marzano de Marinis
Italy
Dr Gérard Moulin
Deputy Director, National Agency
for Veterinary Medicinal Products,
and Research Director, French
Agency for Food, Environmental and
Occupational Health & Safety, France
Ms Sunita Narain
Director General, Centre for
Science and Environment, India
Dr Donald A. Prater
Acting Assistant Commissioner for
Food Safety Integration, Ofce of
Foods and Veterinary Medicine,
Food and Drug Administration,
United States of America
Dr Mesrak Mokonnen Yetneberk
General Secretary of the Ofce
of Parliament, Ethiopia
Member Organization
representatives
Food and Agriculture Organization
of the United Nations (FAO)
Ms Maria Helena Semedo,
Deputy Director-General, Climate
and Natural Resources
The Global Fund to Fight AIDS,
Tuberculosis and Malaria
Dr Marijke Wijnroks, Chief of Staff
Organization for Economic
Cooperation and Development (OECD)
Mr Mark Pearson, Deputy
Director of Employment,
Labour and Social Affairs
World Organisation for
Animal Health (OIE)
Dr Matthew Stone, Deputy
Director-General, International
Standards and Science
Joint United Nations Programme
on HIV/AIDS (UNAIDS)
Mr Simon Bland, Director,
New York Liaison Ofce
UN Environment
Ms Jacquline Alvarez, Science
and Risk Unit Leader, Chemicals
and Waste Branch
Unitaid
Ms Sanne Wendes, Senior Adviser
to the Executive Director
United Nations Children’s
Fund (UNICEF)
Dr Stefan Peterson, Associate
Director and Global Chief of Health
World Bank
Dr Enis Baris, Practice
Manager, Health, Nutrition and
Population Global Practice
World Customs Organization (WCO)
Ms Ana Hinojosa, Director,
Compliance and Facilitation
World Health Organization (WHO)
Dr Ranieri Guerra, Assistant Director-
General, Strategic Initiatives
World Intellectual Property
Organization (WIPO)
Mr Minelik Alemu Getahun, Assistant
Director-General, Global Issues Sector
World Trade Organization (WTO)
Ms Christiane Wolff, Head, Sanitary
and Phytosanitary Measures Section,
Secretary, Committee on Sanitary
and Phytosanitary Measures
The IACG on Antimicrobial Resistance and its Secretariat were nancially supported by the Governments of Canada, France,
Japan, Norway and Sweden, the Wellcome Trust and the World Health Organization. The work of the IACG and its subgroups
was also supported by external experts, partners, organizations, consultants, past IACG Secretariat staff and technical
advisors from IACG member organizations. The IACG Secretariat was supported by staff from WHO, FAO and OIE, directed
by Haileyesus Getahun and included Tim Corrigan, Rosalie Edma, Ziena Elsawi, Ian Grubb, Saija Kalenius, Eva Nathanson
and Alessandro Patriarchi. Taona Kuo provided coordination on behalf of the Executive Ofce of the UN Secretary-General.
No Time to Wait: Securing the future from drug-resistant infections • 25
REFERENCES
1 United Nations. Political Declaration of the High-level Meeting of the General Assembly on Antimicrobial
Resistance, A/71/L.2. 22 September 2016.
2 World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015.
3 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. IACG Terms of Reference. May 2017.
4 Interagency Coordination Group on Antimicrobial Resistance. AMR Framework for Action Supported by the
IACG. Working document. August 2017.
5 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. Meeting the challenge of antimicrobial
resistance: From communication to collective action. IACG discussion paper. July 2018.
6 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. Antimicrobial resistance: National
Action Plans. IACG discussion paper. June 2018.
7 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. Reduce unintentional exposure and the
need for antimicrobials, and optimize their use. IACG discussion paper. July 2018.
8 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. Antimicrobial resistance: Invest in
innovation and research and boost R&D and access. IACG discussion paper. June 2018.
9 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. Surveillance and monitoring for
antimicrobial use and resistance. IACG discussion paper. June 2018.
10 Ad hoc Interagency Coordination Group on Antimicrobial Resistance. Future global governance for
antimicrobial resistance: IACG discussion paper. July 2018.
11 Organization for Economic Cooperation and Development. Stemming the superbug tide: Just a few dollars
more. November 7, 2018.
12 World Health Organization. Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early
Implementation 2016-17. 29 January 2018.
13 Laxminarayan R. et al. Access to effective antimicrobials: A worldwide challenge. Lancet. 2016; 387:168-75
14 Rochforsd C. et al. Global governance of antimicrobial resistance. Lancet Vol. 391. May 19, 2018.
15 Daulaire N. et al. Universal access to effective antibiotics is essential for tackling antibiotic resistance. J Law
Med Ethics 2015;43;17-21
16 World Organisation for Animal Health. Annual report on antimicrobial agents intended for use in animals.
2018.
17 GAVI, Global Financing Facility, The Global Fund to Fight AIDS, TB and Malaria, UNAIDS, UNDP, UNFPA, UNICEF,
Unitaid, UN Women, World Bank Group and World Health Organization. Towards a global action plan for
healthy lives and well-being for all. Uniting to accelerate progress towards the health-related SDGs. 2018.
18 O’Neill J. Antimicrobial resistance: Tackling a crisis for the health and wealth of nations. The review on
antimicrobial resistance. December 2014.
19 World Health Organization. Global tuberculosis report 2018 (2017 data).
20 World Bank. Drug-resistant infections: A threat to our economic future. March 2017.
21 MacFadden D. et al. Antibiotic resistance increases with local temperatures. Nature Climate Change 8,
510–514 (2018)
22 United Nations Environment Program. Frontiers 2017: Emerging issues of environmental concern. 2017.
23 World Health Organization. Tenth meeting of the Strategic and Technical Advisory Group on Antimicrobial
Resistance. Status update on STAG February 2018 recommendations. 4 December 2018.
24 Ventola CL. The antibiotic resistance crisis. PT. 2015;40(4):277– 83
25 Deak D. et al. Progress in the ght against multidrug-resistant bacteria? A review of U.S. Food and Drug
Administration–approved antibiotics, 2010–2015. Ann Intern Med. 2016;165(5):363–72.
26 World Health Organization. Antibacterial agents in clinical development: Ann analysis of the antibacterial
clinical development pipeline, including tuberculosis. 2017.
27 DRIVE-AB. Revitalizing the antibiotic pipeline: Stimulating innovation while driving sustainable use and
global access. March 2018.
28 G20 Leaders’ Declaration 2017: Shaping an interconnected world. Hamburg, July 8, 2017.
29 G20 Leaders’ Declaration 2018: Building consensus for fair and sustainable development. Buenos Aires,
December 1, 2018.
30 World Health Organization. Addressing the global shortage of, and access to, medicines and vaccines.
Executive Board, 142nd session. EB142/13. 12 January 2018.

26 • No Time to Wait: Securing the future from drug-resistant infections
