
Section 1332 State Relief and
Empowerment Waiver Concepts
Discussion Paper
November 29, 2018
Centers for Medicare & Medicaid Services
Center for Consumer Information & Insurance Oversight
2
Contents
Overview of 1332 Waiver Concepts.................................................................................................... 3
Waiver Concept A: State-Specific Premium Assistance………………………………………………………………….. 8
Waiver Concept B: Adjusted Plan Options………………………………………………………………………………………. 13
Waiver Concept C: Account-Based Subsidies………………………………………………………………………………….. 20
Waiver Concept D: Risk Stabilization Strategies……………………………………………………………………………….25
Appendix A: Types of Waiver Concepts and Policy Options …………………………………………………………….37

3
Overview of 1332 Waiver Concepts
Introduction to Section 1332 Waivers
Under section 1332 of the Patient Protection and Affordable Care Act (PPACA), states can apply for a
State Innovation Waiver (also referred to as a “section 1332 waiver” or “1332 waiver”) from the
Department of Health and Human Services (HHS) and the Department of the Treasury (collectively, the
Departments), which allows states, if approved, to implement innovative programs to provide access to
quality health care. The overarching goal of 1332 waivers is to empower states to develop innovative
health coverage options that best fit the states’ individual needs. This goal aligns with the
Administration’s goal to give all Americans the opportunity to gain quality and affordable health
coverage regardless of income, geography, age, sex, or health status. Through section 1332 waivers, the
Departments aim to assist states with developing health insurance markets that offer more choice,
competition, and affordability to Americans.
These waiver concepts are intended to foster discussion with states by illustrating how states might take
advantage of new flexibilities provided in recently released guidance
1
related to section 1332 on
October 24, 2018, which replaced the previous guidance released on December 16, 2015. The new
guidance aims to lower barriers to innovation for states seeking to reform their health insurance
markets, increases flexibility with respect to the manner in which a section 1332 state plan may meet
section 1332 standards in order to be eligible to be approved by the Departments, clarifies the
adjustments the Secretaries may make to maintain federal deficit neutrality, and allows for states to use
existing state legislative authority to authorize section 1332 waivers in certain scenarios. These waivers
are now called State Relief and Empowerment Waivers to reflect this new direction and opportunity.
The Departments are committed to empowering states to innovate in ways that will strengthen their
health insurance markets, expand choices of coverage, target public resources to those most in need,
and meet the unique circumstances of their state.
Under a section 1332 waiver, a state may receive pass-through funding associated with the resulting
reductions in federal spending on Exchange financial assistance (that is, premium tax credits under
section 36B of the Internal Revenue Code (PTC), small business health insurance tax credits under
section 45R of the Code (SBTC), or cost-sharing reductions (CSR)) consistent with the statute and the
state’s waiver plan. Pass-through funding may only be used to implement the state waiver plan.
To receive approval for a section 1332 waiver, states must demonstrate that the waiver will provide
access to health insurance coverage that is at least as comprehensive and affordable as would be
provided under the PPACA without the waiver, will provide coverage to at least a comparable number of
residents of the state as would be provided coverage without a waiver, and will not increase the federal
deficit. These statutory criteria are referred to as the “guardrails.” Before submitting its section 1332
waiver application, a state must have enacted a law providing for implementation of the waiver,
provided a public notice and period for public comment, and held public hearings sufficient to ensure a
meaningful level of public input.
1
https://www.federalregister.gov/documents/2018/10/24/2018-23182/state-relief-and-empowerment-waivers

4
Support of Section 1332 Waivers and Release of 1332 Waiver Concepts
Since 2015, the Departments have approved a number of state waivers,
2
and continue to work with
states on future waivers. The Departments have developed this series of 1332 Waiver Concepts
(“waiver concepts”) in an effort to spur conversation and innovation with states. The Departments look
forward to engaging with states on these waiver concepts, which are intended to show states concepts
that the Administration supports and that fit within the 1332 framework. States are not required to use
these concepts in their waiver applications; states may use these waiver concepts alone or in
combination with other waiver concepts, state proposals, or policy changes. We encourage states to
couple waiver concepts with other innovative ideas. See Appendix A: Types of Waiver Concepts and
Policy Options for an overview of all waiver concepts included in this document. The four waiver
concepts discussed in this document are:
• Waiver Concept A: State-Specific Premium Assistance;
• Waiver Concept B: Adjusted Plan Options;
• Waiver Concept C: Account-Based Subsidies; and
• Waiver Concept D: Risk Stabilization Strategies.
These waiver concepts are offered to serve as a springboard for innovative ideas that may improve the
health care markets in individual states, and the concepts discuss policy and implementation ideas that
we look forward to discussing with states. However, in order to gain approval, states’ section 1332
waiver applications must meet section 1332 statutory requirements, including satisfaction of the four
guardrails under section 1332(b)(1) (comprehensiveness, affordability, coverage, and federal deficit
neutrality). The Departments cannot assess whether or not a proposal meets the guardrails until we
receive a specific proposal from a state. A state’s incorporation of any waiver concept into a section
1332 waiver application is not a guarantee that the Departments will ultimately approve the waiver.
The Departments retain the discretion to decide whether to grant a 1332 waiver based on the particular
circumstances of each state’s application, and the Departments must in all cases evaluate each
application for compliance with section 1332 statutory requirements. The Departments’ waiver
authority is limited to requirements described in section 1332(a)(2) of the PPACA. Thus, for example, the
Departments have no authority to waive any provision of the Employee Retirement Income Security Act
(ERISA).
The Departments continue to encourage states to propose other innovative approaches to meet the
unique needs of their population, and recommend that states interested in applying for a section 1332
waiver reach out to the Departments promptly for assistance in formulating an approach that meets the
requirements of section 1332. These waiver concepts do not represent the full range of provisions of the
PPACA that can be waived under section 1332; states can and might want to consider developing
applications to use section 1332 waivers to waive other provisions as outlined in the statute, such as the
employer mandate, or the metal tiers. Further questions and comments, including comments on these
waiver concepts, should be directed to StateInnovat[email protected]hs.gov
.
2
For a list of all received waiver applications (including approved waivers) please see:
https://www.cms.gov/CCIIO/Programs-and-Initiatives/State-Innovation-
Waivers/Section_1332_State_Innovation_Waivers-.html#Section 1332 State Waiver Applications
5
Expectations Regarding 1332 Waivers, Guardrails, and Application Timing
As with all 1332 waiver applications, states leveraging waiver concepts designed by the Departments will
need to ensure their proposed plans meet all of the statutory requirements, including satisfying the four
guardrails (comprehensiveness, affordability, coverage, and federal deficit neutrality).
To provide flexibility under the statute to states to explore different options for coverage, the new
guidance issued in October 2018 explains how the Departments’ new interpretation of the
comprehensiveness and affordability guardrails now focuses on access to comprehensive and affordable
coverage. This shift in focus to access ensures that state residents who wish to retain coverage similar
to that provided under the PPACA can continue to do so, while permitting a state 1332 waiver plan to
also provide access to other options that may be better suited to consumer needs and more attractive
or affordable to many individuals. The updated guidance interprets the comprehensiveness and
affordability guardrails to mean that the waiver must provide access to coverage that is at least as
comprehensive and affordable as coverage absent the waiver. The coverage guardrail will be met so
long as a comparable number of residents are covered under the waiver as would have been covered
absent the waiver. The new guidance expands the definition of coverage for purposes of this guardrail
to include more forms of coverage. The guidance also focuses on the aggregate effects of the waiver for
the guardrails.
In light of the requirement to have continued access to comprehensive and affordable coverage, the
new guidance maintains the same strong-protections for people with pre-existing conditions as the law
currently provides absent a 1332 waiver. To be clear, the waiver concepts presented here do not open
any flexibility for states to undermine these protections. This Administration remains firmly committed
to maintaining protections for all Americans with pre-existing conditions, and believes that states can
develop programs that improve upon the status quo and provide necessary support for people with pre-
existing and/or chronic conditions.
States will also need to establish evaluation requirements for the program as outlined in the waiver
specific terms and conditions. Programs will be evaluated periodically for how well they achieve
program goals. Evaluation criteria may include: the number of uninsured, the number of persons
covered, the change in premiums, coverage options, the accessibility of providers and the change in
cost-sharing, the extent of expected choice available to consumers, the extent of expected competition
between insurers, the efficiency of the health care system, and best use of public dollars.
Consistent with the statute, states must have legal authority to pursue a waiver by enacting state laws
or enacting revisions to existing state laws to apply for and implement a state plan for a section 1332
waiver. Per the 2018 guidance, the Departments clarified that in certain circumstances, a state may
satisfy the requirement that the state enact a law under section 1332(b)(2) by using existing legislation
that provides statutory authority to implement or enforce PPACA provisions and/or the state plan,
combined with a duly-enacted state regulation or executive order.
Consistent with the regulations at 31 CFR 33.108(b) and 45 CFR 155.1308(b), states are required to
submit initial waiver applications sufficiently in advance of the requested waiver effective date,
including an appropriate implementation timeline, to allow for enough time to review and to maintain
smooth operations of the Exchange in the state, and for affected stakeholders or issuers of health
insurance plans that are (or may be) affected by the waiver plan to take necessary action based on the
6
approval of the waiver plan, particularly when the waiver impacts premium rates. States should
generally plan to submit their initial waiver applications no later than the end of the first quarter of the
year prior to the year the waiver would take effect in order to allow for sufficient time for review. The
Departments may be able to review waiver concepts discussed in this paper more quickly than novel
waiver applications. However, the Departments cannot guarantee a state’s request for review or
approval by a certain date earlier than the 180-day statutory deadline.
States may propose to leverage the federal platform, HealthCare.gov, to perform eligibility, plan display,
plan selection, and enrollment functions. If a state wishes to rely on the federal platform to implement
its waiver plan and such reliance requires technical changes to the federal platform’s information
technology system or to the operating procedures of the federal platform, additional time may be
needed. States should engage with HHS early in the section 1332 waiver application process to
determine whether the federal platform can accommodate the technical changes that support their
state needs and requested flexibilities. Similarly, states considering a waiver of any federal tax provision
should engage with the Departments early in the process to assess whether the waiver proposal is
feasible for the Internal Revenue Service (IRS) to implement, and to assess the administrative costs to
the IRS of implementing the waiver proposal.
Under state innovation waivers, including waivers that incorporate these waiver concepts, states are
responsible for ensuring that consumers whose coverage choices are impacted by a waiver are aware of
changes that will result from the implementation of a state’s waiver plan. Consumers need to
understand these changes in order to be empowered to make decisions about their health care. States
that are requesting a waiver should consider and describe in their applications how consumers will be
educated about their new coverage options and how they will purchase this coverage.
Financing and Pass-Through Funding
Under a section 1332 waiver, if the waiver proposal is approved, a state may receive funding equal to
the amount of forgone federal financial assistance that would have been provided to its residents
pursuant to programs under title I of the PPACA. A state may only use this funding, known as pass-
through funding, to implement the state’s plan as described in the 1332 waiver application and/or the
state’s specific terms and conditions. In order for a state to receive pass-through funding, a state must
demonstrate that federal spending on financial assistance if the waiver is approved is equal to or less
than the amount the federal government would pay if the waiver were not approved and implemented.
Under the statute, the state will be entitled to funding based on the amount of PTC, SBTC, and CSR that
would have been provided to individuals in the state absent the waiver. Pass-through funding levels will
be reduced by any other increase in spending or decrease in revenue as necessary to ensure the deficit
neutrality guardrail is met.
As part of a state’s waiver application, if the state is seeking pass-through funding, it should include an
explanation of how, due to the structure of the state plan and the waiver of a provision listed under
section 1332(a)(2), the state anticipates that individuals would not qualify for, or would qualify for less
PTC, SBTC, or CSR for which they would otherwise be eligible. The state should also explain how the
state plans to use that funding to implement the state waiver plan.
The Departments will evaluate the estimated pass-through funding amount requested by a state for the
period of the waiver. The actual pass-through amount for the period of the waiver will be calculated by
the Departments annually. If a state receives pass-through funding, the state must use pass-through
7
funding solely for purposes of implementing the state's 1332 waiver plan as approved by the
Departments. Any unused pass-through funds must be returned to the federal government by the end
of the waiver, as specified in the specific terms and conditions. The state is responsible for ensuring any
necessary state funding is available to implement its state plan, as described in its application.
The PPACA includes a provision that applies abortion coverage limitations to plans that are sold through
the Exchange for all individuals who receive federal income-based subsidies to purchase private health
insurance. Furthermore, the Hyde Amendment prohibits federal funds, including section 1332 pass-
through funds, from being used to pay for abortion outside of the exceptions for rape, incest, or if the
pregnancy is determined to endanger the woman’s life. States must ensure that any pass-through
funding complies with these requirements as well.
Administrative Expenses
Under the deficit neutrality requirement, the projected federal spending net of federal revenues under
the waiver must be equal to or lower than projected federal spending net of federal revenues in the
absence of the waiver. The effect on federal spending includes all changes in financial assistance
provided to eligible Exchange enrollees and other direct spending that result from implementation of
the waiver. Projected federal spending under the waiver proposal also includes all administrative costs
to the federal government, including any changes in IRS administrative costs, federal Exchange
administrative costs, or other administrative costs associated with the waiver. Subject to the
requirements of the Intergovernmental Cooperation Act (ICA) and OMB Circular A-97, if a waiver
requires the Centers for Medicare & Medicaid Services (CMS) to make technical changes to the federal
eligibility and enrollment platform, the state will be responsible for reimbursing CMS for any costs
incurred for certain technical and specialized services covered under the ICA (either with 1332 pass-
through funds and/or funds provided by the state to fully reimburse CMS).
Additional Information
In developing a 1332 waiver proposal, states will need to establish program requirements to help
guarantee the integrity and success of their new program. All programs are at risk of waste, fraud, and
abuse; states are responsible for ensuring appropriate measures are in effect to minimize these risks. In
addition, under all 1332 waivers, states must have a plan in place to guarantee that pass-through
funding is only used for the approved waiver plan.
States with an approved waiver must comply with all Federal laws including the applicable civil rights
authorities that prohibit discrimination in healthcare programs and activities on the basis of race, color,
national origin, disability, age, and sex.

8
Waiver Concept A: State-Specific Premium Assistance
With Waiver Concept A: State-Specific Premium Assistance, states could consider options to create and
implement a new state subsidy structure that changes the distribution of subsidy funds compared to the
current PTC structure. A state may design a subsidy structure that meets the unique needs of its
population in order to provide more affordable healthcare options to individuals in their state broadly to
a wider range of individuals or to address structural issues that create perverse incentives, such as the
subsidy cliff
3
. If the waiver is expected to reduce federal spending on PTC, the state will receive federal
pass-through funding that may be used to implement the section 1332 state waiver plan and help fund
the state subsidy program.
Policy
In the State-Specific Premium Assistance waiver concept, states have the flexibility to design a new
subsidy structure implemented by the state in lieu of the federal PTC structure.
States need to ensure that any new subsidy structure meets the 1332 guardrails, including the
affordability guardrail, which is generally measured by comparing each individual’s expected out-of-
pocket spending for health coverage and services to their incomes. Out-of-pocket spending for health
care includes premiums (or equivalent costs for enrolling in coverage) and spending such as deductibles,
co-pays, and co-insurance associated with the coverage, or direct payments for healthcare.
This new state subsidy structure can redefine the amount of financial assistance provided as a state
subsidy, such as a state tax credit, or redefine the populations eligible for such financial assistance, or
both. For example, a state might:
• Replace the federal PTC structure with a new per-member per-month, state premium credit
based on age.
• Determine eligibility using an affordability percentage and award financial assistance when the
costs of health coverage exceed a set percentage of household income.
• Leverage a similar state subsidy or state tax credit structure already in place that could be easily
modified for this purpose.
Implementation Approaches (Concept A: State-Specific Premium Assistance)
In the State-Specific Premium Assistance waiver, states would receive waiver of the PTC for plans offered
through the Exchange in the state (section 36B of the Code and section 1401of the PPACA, both waived
in entirety), in addition to provisions around QHPs, such as 1301(a) and the Exchange’s operations,
1311(d)(2)(B)(i). Under this approach, in place of the PTC, states could develop a state premium subsidy
program. This would likely be easier for existing State-based Exchanges (SBE) to operationalize using
existing SBE infrastructure as outlined in the options below since there are already connections to
federal data sources.
States can also consider how to implement the new subsidy structure. An advanceable subsidy structure
based on consumers’ projecting their income requires much more complexity than an age-adjusted tax
3
The subsidy cliff refers to the point at which a consumer’s income changes and they are ineligible for PTC.

9
credit. Income-based subsidies could also provide perverse incentives that discourage upward mobility
and work, and states may wish to avoid these problems. States considering a subsidy structure based on
income should also consider how consumers can report changes in income or if the state will perform an
income reconciliation. States are encouraged to also consider additional innovations within the subsidy
program. Subsidy design will also have an impact on participation.
Under the State-Specific Premium Assistance waiver, there would not be a FFE operating in the state.
Rather, applications for state financial assistance would be made available to consumers as part of the
state’s plan and administered by the state, and the state would assume all responsibilities associated
with providing financial assistance. These responsibilities specifically include development of the new
subsidy structure, creation and processing of applications, eligibility determinations, payment of
subsidies to issuers, providing consumer support and education to applicants and enrollees, and
adjudicating appeals of eligibility determinations. States would be required to reimburse CMS for
waivers that require CMS to make technical changes to the federal eligibility and enrollment platform.
• Implementation Approach 1: One implementation option for states would be to perform the
eligibility determination using existing Medicaid or CHIP system connections to federal data
sources (e.g., Department of Homeland Security and the Social Security Administration). States
would be required to cost allocate expenses with Medicaid
4
in these circumstances, and
perform data matching issue processing for individuals who are not able to be electronically
verified. This may require new data use agreements or updates to existing data use agreements
with federal agencies, but would have the benefit of streamlining health coverage assistance
programs and consumer support channels within the state. States would be required to have
the authority to access these federal data sources.
o Note: Due to technical limitations and build constraints on the FFE system, this waiver
option may be feasible for implementation as early as Open Enrollment (OE) 7 (plan
year 2020), but the state’s plan and needed technical changes would need to be
confirmed by CMS by the August prior to the start of the same plan year (i.e., August
2019 for implementation in plan year 2020).
• Implementation Approach 2: A second implementation option for states would be to perform
the eligibility determination using authorities and technologies currently in place through the
FFE connections to federal data sources (e.g., Department of Homeland Security and the Social
Security Administration). Under this approach, the state would request that the FFE perform
verification of certain eligibility factors, such as citizenship and immigration status, on behalf of
the state. Related to the verification requests, the FFE would perform downstream data
matching issue processing, and support the state in related appeals adjudication. States would
use this federally-verified data (for example citizenship/immigration status) in combination with
application responses and other state-verified data (for example state income) to make an
eligibility determination.
o A table outlining state and federal responsibilities for FFE-platform states considering
this approach is included below.
o Note: Due to technical limitations and build constraints on the FFE system, this waiver
option is feasible for implementation as early as OE8 (plan year 2021) and the state’s
plan and needed technical changes would need to be confirmed by CMS by January of
4
Per 2 CFR 200 (previously OMB-A-87), cost allocation principles would apply unless otherwise waived.
10
the prior plan year (i.e., January 2020 for implementation in plan year 2021). CMS will
need detailed design elements to evaluate feasibility and provide estimates on costs.
For either implementation approach, states would communicate the eligibility result to the individual
and provide the individual with information on how to use the subsidy when enrolling in health
coverage. Current FFE states should consider the option described below in Implementation Approach
2. Where necessary, the state would provide follow up information to the individual regarding the
successful resolution of data matching issues (DMIs), or regarding the failure to resolve a DMI and the
associated loss of subsidy eligibility.
Once an eligibility determination is made, consumers could take advantage of the market’s existing sales
channels to purchase coverage. States are encouraged to consider waiving additional Exchange
requirements (section 1311 of the PPACA) in order to maximize flexibility in implementing their tailored
financial assistance program. Examples of policy options and implementation approaches related to
plan option flexibility and provided in the adjusting plan options waiver concept section.
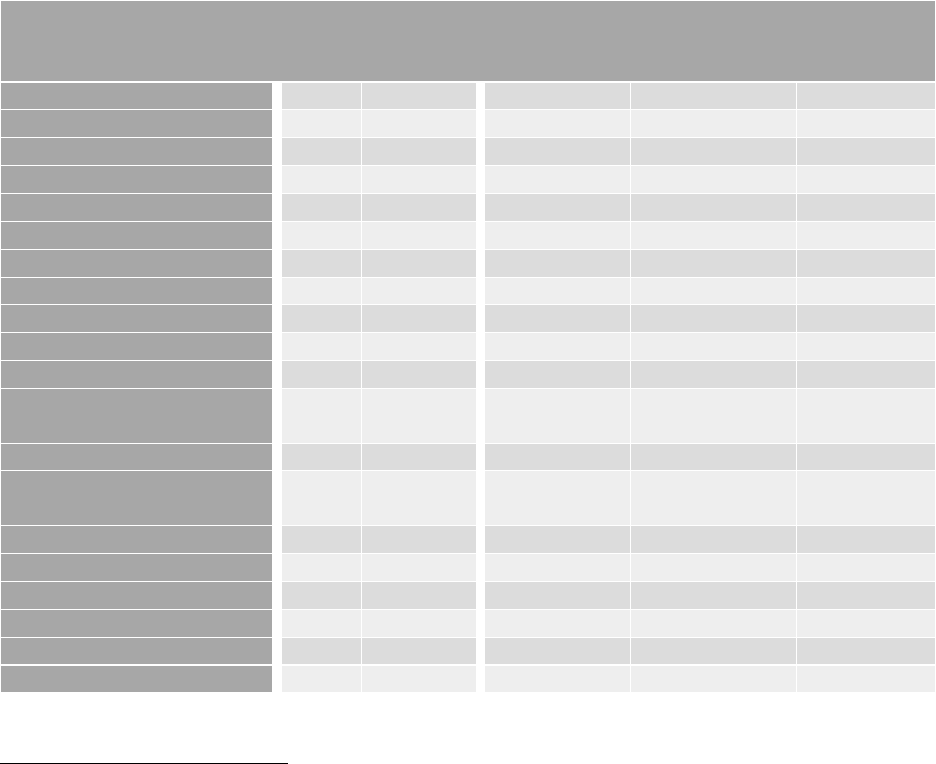
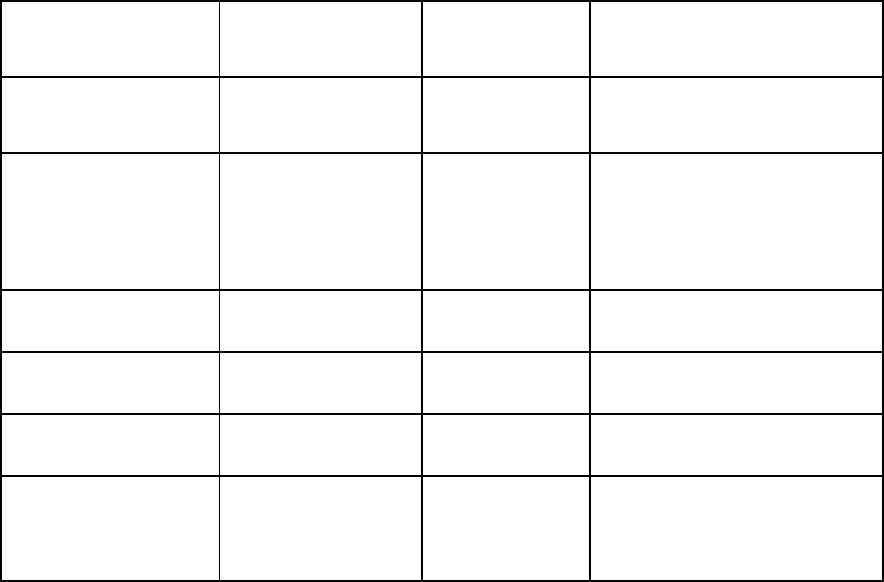
State and federal responsibilities for implementing a new subsidy structure under a new State-Specific
Premium Assistance Waiver (Concept A)
Without Waiver
(FFE platform state
status quo)
Option for FFE support of State-specific
Premium Assistance Waiver
State
Federal
State
State or Vendor
Federal
Consumer call center
X
X
Consumer website
X
X
Consumer marketing
X
X
Consumer noticing
X
X
DMI only
Agent/broker support
X
X
X
X
Assister support
X
Optional
5
Plan certification
X
X
Optional
Anonymous shopping
X
Optional
ID proofing
X
X
Application
X
X
Verifications:
citizenship/immigration
X
X
Verifications: income
X
Optional
Optional
Verifications: non-ESI
coverage check
X
Optional
Verifications: SEP
X
Optional
DMI follow up
X
X
Eligibility determination
X
X
Benefit calculation
X
X
Appeals
X
X
Casework
X
X
X
5
Items listed as optional are listed as optional since they are waivable provisions under section 1332 of the PPACA.
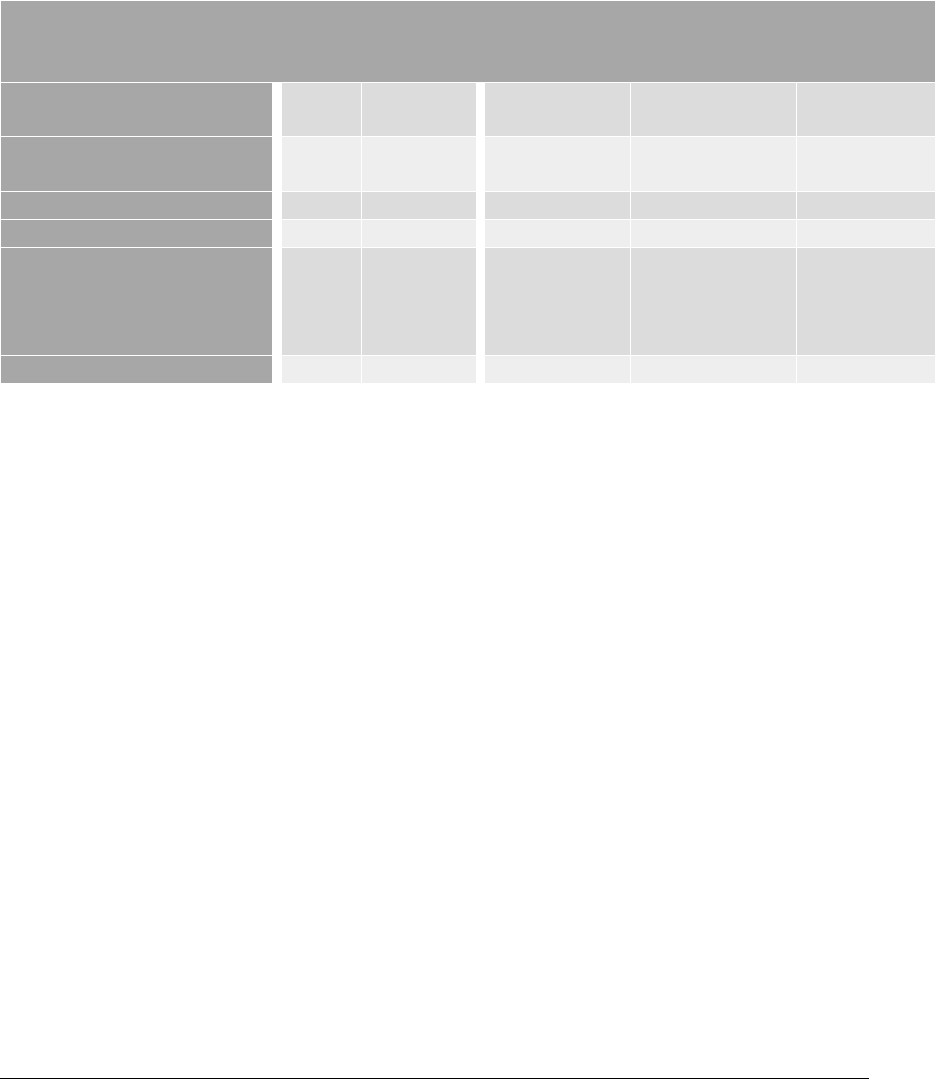
11
Without Waiver
(FFE platform state
status quo)
Option for FFE support of State-specific
Premium Assistance Waiver
Account transfer –
Medicaid/CHIP
X
X
Optional
Plan shopping and
selection
X
Optional
Enrollment transactions
X
Optional
Enrollment reconciliation
X
Optional
1095A generation
X
Not a part of
Implementation
for this waiver
option
Issuer payment
X
X
Administrative Expenses
States may use pass-through funding associated with waived PTC to implement the state plan and help
fund the alternative state subsidy program. Any additional costs to fund the state subsidy program
would be the state’s responsibility. For example, if additional state premium subsidy costs are incurred
through additional enrollment under these policy changes, the state would be responsible for covering
that additional cost (either with 1332 pass-through funds or funds provided by the state). Please refer
to the Overview of 1332 Waiver Concepts for information on when states can receive pass-through
funding, and administrative costs to the federal government associated with the waiver.
• Implementation Approach 1: States would perform the eligibility determination using existing
Medicaid or CHIP system connections to federal data sources
o Administrative Expenses: In this option, very few costs would be incurred by CMS, and
the state would be treated by CMS in a similar manner as a state operating its own
Exchange with a redirect to the independent state website.
• Implementation Approach 2: States would perform the eligibility determination using
authorities and technologies currently in place through the FFE’s connections to federal data
sources
o Administrative Expenses: In this option, costs would be incurred by the state to support
up-front technical changes and ongoing processing of citizenship or immigration-related
DMIs. The state will be responsible for reimbursing CMS for both types of costs incurred
as part of the section 1332 state waiver program.
Things to consider and/or additional information on implementation approaches under Concept A
Below are some questions to consider as the state develops these programs, and to include in the 1332
waiver application.
Questions for Concept A:
1) How will the state implement a new subsidy structure?
12
a. Which entity will administer the program? Is it a new or existing entity? To what extent
will the entity be subject to state insurance laws? To what extent will the entity
coordinate activities with other public programs (e.g., Medicaid and CHIP)?
b. How much funding is necessary for the subsidy structure?
c. What populations or eligibility requirements will the state have for this program (e.g.,
age, income, etc.?
d. What plan options will be available?
e. If state funding is required, how much funding does the state anticipate will be
necessary to implement the state plan and how will the state generate the required
state funding?
2) When and how will consumers be notified of their subsidy amount?
3) Will there be a process for consumers to report changes to eligibility criteria (i.e. income, age,
address etc.)?
4) What process will be used for consumers to appeal their eligibility determination and subsidy
amount?
5) What sources is the state using to verify eligibility for coverage and/or the subsidy (if
applicable)? Will the state be using their Medicaid/CHIP Agency or the FFE to do eligibility
verifications and determinations? Is the state using any state sources for verification?
6) How will issuers receive payments for the subsidy? What is the timing and mechanism for pay-
out?
7) Will the state reconcile state subsidy amounts based on current or prior year household income
or some other income definition If so, how will that be operationalized?
8) Will the new subsidy program include incentives for providers, enrollees, and plan issuers to
continue managing health care costs and utilization and lower overall health care spending (if
any)?
9) Does the state have the authority/ability to adjust the program requirements on a yearly or
other basis to account for market changes? If so what is the schedule and process for this?
10) Will the state require issuers to include the impact of the program in initial and/or final rates?
11) Is there any existing legislation and/or regulations related to the state program, or is new state
legislation and/or regulation needed?
12) If the state is leveraging the FFE’s system, does the state anticipate requesting any changes to
the FFE? If the state is leveraging the SBE, does the state anticipate requesting any changes to
the SBE? Related to question #2 above, does the state envision that applicants will be able to
see their subsidy amount during the plan selection process?
13) If implementing a state subsidy program what (if any) federal tax consequences will there be for
the individuals enrolled and/or reporting requirements for the state as a result?
14) How does the state plan to ensure access to health coverage that is at least as comprehensive
and affordable as would be provided under the PPACA as compared to without the waiver?

13
Waiver Concept B: Adjusted Plan Options
In the Adjusted Plan Options waiver concept, states would have the flexibility to provide state financial
assistance for non-QHPs, potentially increasing consumer choice and making coverage more affordable
for individuals. States also could choose to expand the availability of catastrophic plans beyond the
current eligibility limitations by waiving section 1302(e)(2) of the PPACA, for example, to make them
available to a broader group of individuals. With the Adjusted Plan Options waiver, states may be able
to increase consumer choice and affordability by allowing consumers to use a state subsidy towards
catastrophic plans, individual market plans that are not QHPs, or plans that do not fully meet PPACA
requirements. Under the PPACA, consumers can use PTC only towards non-catastrophic QHPs offered
through the Exchanges. Under this waiver concept, states may be able to waive the QHP requirement
under section 36B of the Code and allow PTC for a non-QHP if the non-QHP is offered through the
Exchanges and if certain other conditions are met.
As with all 1332 waiver requests, a state must ensure that the waiver plan meets the four statutory
guardrails including affordability, comprehensiveness, coverage, and federal deficit neutrality. In
particular, to the extent the proposal impacts the individual market risk pool in any adverse way, a state
will need to clearly identify how the waiver plan will continue to provide access to coverage that is at
least as affordable and comprehensive as without the waiver. Under each of the options for
implementing this concept, the state would need to take on responsibilities for certification of plans.
Option 1: Allow state financial assistance for non-QHPs
Policy
States should consider what, if any, state requirements there will be for the state subsidy to apply to
non-QHPs and what types of plans would be eligible for the state subsidy. For example, a state may
wish to prevent subsidies for people purchasing products that do not meet some minimum standard.
States may allow state-specific financial assistance to be applied to QHPs and/or non-QHPs such as: all
plans approved for sale in the individual market (including non-QHP off-exchange individual market
plans); plans that do not meet (or that exceed) a specific AV/metal level; short-term, limited-duration
plans; catastrophic plans, employer -based plans, association health plans; plans that do not meet all
EHB requirements, but are at least as comprehensive as those that do; value-based insurance design
(VBID) plans; or condition-specific benefit plans that might exceed EHB requirements. In designating
plans eligible for subsidies, states would need to ensure that any changes result in a plan that will meet
the 1332 guardrails and other requirements of the Departments. This option could allow for more plan
options for consumers. States should consider if the subsidies may have federal tax consequences for
consumers and whether the subsidies may lead to IRS reporting requirements for the state.
Implementation Approaches
In Option 1: Allow state financial assistance for non-QHPs, states would request to waive provisions
relating to the PTC under section 36B of the Code and section 1402 of the PPACA. In addition states
would receive a waiver of provisions related to QHPs, such as section 1311(d)(2)(B)(i) of PPACA, which
14
prohibits Exchanges from making available any health plan that is not a QHP. Due to the way the federal
Exchange platform operates, a state interested in this option would have to administer a state-specific
premium assistance program as described in Waiver Concept A: State-Specific Premium Assistance
waiver component if it wants to offer a subsidy to non-QHPs. Besides looking at the type of plans
offered, one other area for innovation is in cost sharing, which would likely require waiving the PPACA’s
metal level requirements in section 1301(a)(C)(ii).
Below is a discussion of how the state could implement the policy options, with a focus on plan design,
enrollment processing, and payment to issuers. All implementation approaches under Option 1 assume
that a state is also administering its own state-specific premium assistance program.
Plan design implementation approaches:
1) While meeting state innovation waiver guardrails, a state could choose how broadly or narrowly
to define eligibility for the subsidies that would apply to plans that do not meet the cost-sharing
or actuarial value (AV) level requirements. All or a select group of people or employers such as
small employers or consumers eligible for a different existing state tax credit (for example, state
EITC programs) could be offered subsidy eligibility. These changes could apply across the state’s
insurance market or to a select group via a new coverage level. States may refer to Waiver
Concept A: State-Specific Premium Assistance.
2) A state may also wish to support innovation in the benefits provided by plans. The 2019
Payment Notice provided substantially more options in what states can select as an EHB-
benchmark plan, starting for plan year 2020.
6
Enrollment implementation approaches:
1) One implementation option for states is to allow enrollment to occur directly with participating
issuers or web broker websites; similar to how small businesses enroll in FF-SHOP plans, how
individuals are currently enrolled when they purchase coverage off-Exchange, and the direct
enrollment process for consumers signing up for individual market coverage through Exchanges
that use HealthCare.gov. To activate subsidies, consumers would provide a voucher or other
proof of subsidy eligibility when enrolling. This may be more appropriate for states wishing to
keep the set of subsidy-eligible plans as broad as possible.
a. Note: Due to technical limitations and build constraints on the FFE system, this waiver
option may be feasible for implementation as early as OE8 (plan year 2021) and the
state’s plan and needed technical changes would need to be confirmed by CMS by
January of the prior plan year (i.e., January 2020 for implementation in plan year
2021). CMS will need detailed design elements to evaluate feasibility and provide
estimates on costs.
2) A second implementation option for states is to design a system where enrollment would occur
through a specific website separate from the HealthCare.gov website and back-end platform
used by the FFE. For example, states may consider developing their own portal. This could be
paired with the subsidy determination process and host the subsidy eligibility application to save
6
https://www.federalregister.gov/public-inspection/current
15
on administrative costs, and may be more appropriate for states wishing to restrict plan options
to a specific plan or set of plans.
a. Note: Due to technical limitations and build constraints on the FFE system, this waiver
option may be feasible for implementation as early as Open Enrollment (OE) 7 (plan
year 2020), but the state’s plan and needed technical changes would need to be
confirmed by CMS by the August prior to the start of the same plan year (i.e., August
2019 for implementation in plan year 2020).
In either implementation approach above, states would be responsible for communicating to issuers
and to individuals in the states information on what types of plans are eligible for the state subsidy. Part
of a state’s implementation plan should include how it will inform the public of the upcoming changes
for plan options. In this option, the Exchange call center would no longer be available for consumers to
enroll in or select a plan, so the state will want to consider whether or not to offer a similar type of
service.
The state would receive pass-through funding from the federal government to the extent that it waives
PTC under section 36B of the Code or waives another provision under section 1332(a)(2) that results in
savings of PTC. The state would determine a method for applying such funding to the state subsidy. The
state also would remain responsible for any costs in excess of the pass-through amount that are
necessary to implement its plan as described in the state’s approved application. Costs could exceed
expectations if the state lacks adequate controls on eligibility determinations, if the selection of plans
was wide enough to attract many new subsidy-eligible enrollees, or for other reasons.
Payment implementation approaches:
1) One implementation option for states is to aggregate payment to issuers to cover appropriate
levels of premium subsidy payment per enrollment.
2) A second implementation option for states is to make payment to individuals at the time of
subsidy eligibility determination, and direct the individuals to make payment to their
participating issuer (similar to an Electronic Benefit Transfer (EBT) card)
Administrative Expenses (Option 1: Allow state financial assistance for non-QHPs)
Because this change in plan options would require a state to concurrently waive the PTC and implement
a state-run eligibility program as outlined in the Waiver Concept A: State-Specific Premium Assistance,
states should review the waiver options for additional information on administrative expenses. Please
refer to the Overview of 1332 Waiver Concept for information on when states can receive pass-through
spending, and on administrative costs to the federal government associated with the waiver.
Option 2: Allow non-QHPs to be sold on the existing Exchange and/or expand the availability of
catastrophic plans (additional option to apply PTC to catastrophic plans and non-QHPs sold on the
existing Exchange)
Policy
States with FFEs or with State-based Exchanges that rely on the federal platform (SBE-FPs) that maintain
the basic tenets of PPACA QHPs may elect to make plan oversight changes that can provide additional
flexibility while maintaining the technical requirements to continue use of the HealthCare.gov platform.
16
Note that some flexibility in performing QHP certification reviews already exists for states that perform
plan management functions in FFEs, and additional flexibility is available for SBEs, so a waiver may not
be necessary for some changes. This option focuses on changes that may require a state innovation
waiver. Under this option, the state could waive the requirement in section 36B(c)(2)(A)(i) of the Code
that to be eligible for PTC, the taxpayer or a member of the taxpayer’s family must be enrolled in a QHP
through the Exchange for one or more months during the year. States should consider whether plans
offered under a waiver can conform to the data elements required for QHP templates when this option
would use HealthCare.gov. If a state waiver allows PTC for a non-QHP offered through the Exchange,
the state must ensure that the non-QHP provides Form 1095-A to individuals with all the same
information that QHPs provide now, and also provides Form 1095-A information to the IRS in the
manner that QHPs provide now. In addition, the non-QHP must perform certain eligibility activities to
ensure that consumers enrolling in the non-QHP coverage generally are eligible for PTC. This option
could potentially allow for multiple plan options for consumers.
Implementation Approaches (Option 2)
The second policy option would have a smaller impact on plan design, such that a state could maintain
the option to continue using HealthCare.gov and to continue to have the PTC available to their
population.
• In order to determine eligibility for PTC and calculate the amount of premium tax credit
available to consumers on the FFE, issuers must continue to submit traditional silver-level QHPs
for sale on the Exchange in order to calculate the state’s benchmark plan.
• A state may want to allow issuers to sell a plan without the plan having to meet all QHP
certification standards by waiving some or all of section 1311(c) of the PPACA, while still making
it available through HealthCare.gov. In these cases, technical feasibility may limit variation from
existing federal Exchange data structures. The state would need to collaborate with CMS early
in the process to assure that new plans conform to the data elements required for the QHP plan
templates. This option could be helpful for states that do not want to implement their own
subsidy structure.
• Regarding catastrophic plans, states could expand the availability of catastrophic plans beyond
the current eligibility limitations by waiving section 1302(e)(2) of the PPACA, for example, to
make them available to a broader group of individuals. Currently, catastrophic plans are
available only to individuals under the age of thirty, or to individuals who have qualified for an
Exchange affordability or hardship exemption. Catastrophic plans’ risk is adjusted separately
from other metal level plans. Waiving these limitations would expand plan options to more
individuals. However, wider enrollment in catastrophic plans is likely to lead to issuers
increasing their cost because it would change the risk profile of their enrollees.
• In addition to making non-QHP and expanded catastrophic plans available through the
Exchange, states should determine whether or not PTC (and APTC) could be applied to such
plans. Currently, individuals enrolling in catastrophic plans are not eligible for PTC. A state may
choose to waive this limitation and thereby make the plans more affordable, in addition to
allowing PTC to be applied to new non-QHP plans. Note that such an option may have an
impact on PTC spending and premiums which would be evaluated as part of the overall waiver
analysis.

17
The state would receive pass-through funding from the federal government to the extent that it waives
eligibility for PTC under section 36B of the Code or waives another provision under section 1332(a)(2)
that results in savings of PTC, for example if the waiver lowers premiums as a result of improving the risk
pool. The state would remain responsible for any costs in excess of the pass-through amount that are
necessary to implement its plan as described in the state’s application. Costs could exceed expectations
if the selection of plans was wide enough to attract many new subsidy-eligible enrollees, or for other
reasons.
Catastrophic or non-QHP plans offered on the Exchange for which PTC is allowable will need to provide
certain information to IRS and taxpayers about these plans on Form 1095-A. There would need to be
technical changes to allow APTC or PTC to apply to catastrophic or non-QHP plans on HealthCare.gov.
Note: Due to technical limitations and build constraints on the FFE system, this waiver option may be
feasible for implementation as early as Open Enrollment (OE) 7 (plan year 2020) for catastrophic plans
on the FFE, but the state’s plan and needed technical changes would need to be confirmed by CMS by
the January prior to the start of the same plan year (i.e., January 2019 for implementation in plan year
2020). We expect this would involve a moderate cost to the FFE for catastrophic plans, and may be a
higher cost depending on the type of non-QHPs offered on the Exchange. The state would be
responsible for funding the technical build to adjust the HealthCare.gov system for this purpose.
Administrative Expenses (Option 2)
Technical changes to the federal Exchange would be necessary in order to support changes to
catastrophic plan eligibility or the application of APTC to non-QHPs. States are encouraged to reach out
to the Departments with proposals early in the process, in order for cost estimates and feasible
technical timelines to be determined. Please refer to the Overview of 1332 Waiver Options for
information on when states can receive pass-through spending, and administrative costs to the federal
government associated with the waiver.
Things to consider and/or additional information on implementation approaches under Concept B
Options 1 and 2
Below are some questions to consider as the state develops these programs, and to include in the 1332
waiver application.
Questions for Concept B Option 1:
1) How will the state implement a new subsidy structure?
a. Which entity will administer the program? Is it a new or existing entity? To what extent
will the entity be subject to state insurance laws? To what extent will the entity
coordinate activities with other public programs (e.g., Medicaid and CHIP)?
b. How much funding is necessary for the subsidy structure?
c. What populations or eligibility requirements will the state have for this program (e.g.,
age, income, etc.?
d. What plan options will be available?
e. If state funding is required, how much funding does the state anticipate will be
necessary to implement the state plan and how will the state generate the required
state funding?
2) When and how will consumers be notified of their subsidy amount?
18
3) Will there be a process for consumers to report changes to eligibility criteria (i.e. income, age,
address etc.)?
4) What process will be used for consumers to appeal their eligibility determination and subsidy
amount?
5) What sources is the state using to verify eligibility for coverage and/or the subsidy (if
applicable)? Will the state be using their Medicaid/CHIP Agency or the FFE to do eligibility
verifications and determinations? Is the state using any state sources for verification?
6) How will issuers receive payments for the subsidy? What is the timing and mechanism for pay-
out?
7) Will the state reconcile state subsidy amounts based on actual or earned income? If so, how will
that be operationalized?
8) Will the new subsidy program includes incentives for providers, enrollees, and plan issuers to
continue managing health care costs and utilization and lower overall health care spending (if
any)?
9) Does the state have the authority/ability to adjust the program requirements on a yearly or
other basis to account for market changes? If so what is the schedule and process for this
adjustment?
10) Will the state require issuers to include the impact of the program in initial and/or final rates?
11) Is there any existing legislation and/or regulations related to the state program, or is new state
legislation and/or regulation needed?
12) If the state is leveraging the FFE’s system, does the state anticipate requesting any changes to
the FFE? If the state is leveraging the SBE, does the state anticipate requesting any changes to
the SBE? Related to question #2 above, does the state envision that applicants will be able to
see their subsidy amount during the plan selection process?
13) If implementing a state subsidy program what (if any) federal tax consequences will there be for
the individuals enrolled and/or reporting requirements for the state as a result?
14) How does the state plan to ensure access to health insurance that is at least as comprehensive
and affordable as would be provided under the PPACA as compared to without the waiver?
15) How will a state monitor affordability and coverage for new plans offered that may have
different cost sharing, annual and lifetime limits, and may not have reporting requirements
equal to comprehensive coverage?
19
Questions for Concept B Option 2:
1) Which non-QHPs will be newly available on or off-Exchange?
a. What is the eligibility criteria for these plans and how does it differ from QHPs? Are they
eligible for PTC and if so, are they also eligible for APTC?
b. What is the duration of these plans and how does it differ from QHPs?
c. Will the plans be available only during an open enrollment period, or will they also offer
special enrollment periods?
d. What additional information will need to be collected from consumers in order to
determine their eligibility for these plans?
e. Are there enrollment caps under these plans?
f. Do these new plans meet state licensing requirements?
2) How will consumers be able to identify the non-QHP plans?
a. Will they need to be displayed differently?
b. Is there new or additional information about these plans that will need to be available?
How will consumers learn how these plans differ from QHPs?
3) Will the state provide supplemental information about these plans?
4) If expanding eligibility for catastrophic plans, what new population will be newly eligible for
these plans?
5) Is the state leveraging the federal system? In what ways does this program require changes to
the FFE?
a. Changes to application questions? (not possible at this time)
b. Changes to plan display? (not possible at this time)
c. Changes to information elsewhere on HealthCare.gov (outside of the application)?
d. Changes to APTC eligibility or calculation?
e. Changes to plan enrollment, i.e. enrollment caps?
6) If PTC is made available for non-QHPs on the Exchange, how will the state ensure that the non-
QHP or the Exchange (1) provides Form 1095-A to consumers and the IRS, and (2) screens
consumers for PTC eligibility during the enrollment process (for example, verifying lawful
presence; determining eligibility for other minimum essential coverage, including Medicaid; and
determining affordability of any employer coverage, etc. for all family members enrolling in the
plan)?

20
Waiver Concept C: Account-Based Subsidies
In the Waiver Concept C: Account-Based Subsidies waiver option, states would have the flexibility to
direct public subsidies into a defined-contribution, consumer-directed account that an individual uses to
pay health insurance premiums or other health care expenses. The account could be primarily funded
with pass-through funding made available by waiving the PTC (section 36B of the Code and section 1401
of the PPACA) or the SBTC (section 45R of the Code), along with any additional state funds to implement
the 1332 waiver plan. The account could also allow individuals to aggregate funding from additional
sources, including individual and employer contributions. An account-based approach, depending on
how the state designs the program, could give beneficiaries more choices, improve incentives to make
cost-conscious health care spending decisions through the responsibility for managing a health care
budget, and better enable them to maintain health coverage regardless of changes in income or other
life circumstances. This approach could also allow a consumer greater ability to select a plan based on
the individual’s or their family’s needs, including a higher deductible plan with lower premiums.
States will need to create their own subsidy structure, consider which plan options will be offered, and
how to aggregate funding from various sources. More specifically, in the Waiver Concept A: State-
Specific Premium Assistance waiver option, states could have the flexibility to design a new subsidy
structure to target public assistance to better help the vulnerable and to expand the risk pool. In the
Waiver Concept B: Adjusted Plan Options waiver concept, states could change the types of plans that are
eligible for premium subsidies to make coverage more affordable for individuals and to increase
consumer choice. The type of subsidy and types of plans would depend on the state plan. Depending
on how the health expense account is structured it may have tax implications for the individual or
states.
As a reminder, a state must ensure that the waiver meets the four statutory guardrails of affordability,
comprehensiveness, coverage, and federal deficit neutrality and any other requirements of the
Departments. As discussed in the 2018 guidance and principles, the state should also address in the
application for the section 1332 waiver how the section 1332 state plan addresses the Administration’s
priority to support and empower those people with low incomes as well as those people with high
expected health care costs. In particular, this model could be structured in a variety of ways that may
have diverging impacts on individual market coverage and affordability. For example, there may be
scenarios where even though a state provides subsidies to an account on behalf of a consumer, the
consumer’s overall cost for premiums and out of pocket health care spending would increase. The
state’s waiver plan should take into account how the plan will meet the affordability guardrail.
Health Expense Account
Policy
Similar to Waiver Concept A: State-Specific Premium Assistance, in the Account-Based Subsidies waiver
concept, states would have the flexibility to design a new subsidy structure to, for instance, make
coverage more affordable for a wider range of individuals and to attract more young and healthy
consumers into their market. One option is to use subsidies as a contribution towards funding a
defined-contribution, consumer-directed Health Expense Account (HEA). This would be a new type of
account a state could create where consumers could use an HEA to pay health insurance premiums and
other health care expenses. An HEA promotes a number of important policy goals. Giving the
21
beneficiary ownership and control over a health care budget creates better incentives for them to
obtain higher value from their spending decisions. An HEA could potentially also help people maintain
continuous coverage and reduce churn in and out of health programs because under the plan a
consumer could maintain private coverage.
An HEA establishes a personal health care budget for beneficiaries to manage. A state could consider
whether the HEA would need to first be used to pay premiums to guarantee the beneficiary maintained
health coverage. States would need to consider if and how any money left over in the account could be
used on a yearly basis. For example, such funds could:
• Stay with the individual to be used to pay other health care expenses incurred during the year or
saved to pay for future health care expenses for that plan year or future plan years.
• Be split between who contributed to the account (for example the state and the individual) for
eligible health care expenses.
• Be directed to wellness programs.
• Be directed to programs that support personal health (i.e. smoking cessation programs)
The structure of the subsidy could also be tailored to accomplish the same policy goals as Waiver
Concept A: State-Specific Premium Assistance, including making coverage more affordable for a wider
range of individuals. Like state-specific premium assistance, a state can adjust contributions to redefine
eligibility parameters to accomplish specific goals and reach specific populations. For example:
• A state may provide a flat, per-member per-month contribution to the account based on age.
• A state may provide a sliding scale per-member per-month credit based on income and other
eligibility factors.
• A state can structure the contribution on a sliding scale to those over 400% of the federal
poverty level (FPL) or under 100% FPL to reduce or eliminate the current subsidy cliffs.
(See Waiver Concept A: State-Specific Premium Assistance for additional subsidy structure ideas.)
A state may choose to provide an additional state contribution towards the state subsidy program than
what is provided by waiving section 36B of the Code to increase the generosity of the subsidy. A state
might also allow employers to contribute to the account.
Implementation Approaches
In the HEA option, states could request to waive federal laws relating to PTC (section 36B of the Code
and section 1402 of the PPACA) to establish a new subsidy program and also fund HEAs.
States could continue using the current Exchange enrollment platform and plan certification, create a
new platform, or waive the PPACA’s Exchange and QHP provisions and rely entirely on the private
market. If a state chooses to waive the PPACA’s provisions related to Exchanges (section 1311) and
QHPs (section 1301), the implementation could be similar to the implementation approach for Waiver
Concept B: Adjusted Plan Options, Option 1, which allows state-specific financial assistance to be applied
to non-QHPs. This has the potential for consumers to use the account to purchase a wider variety of
plans.

22
Another approach is for a state to leverage the existing FFE in the state. States would need to work with
the FFE and effectively “turn off” the financial assistance component of the FFE for the state. In this
option, states would cover costs incurred for the technical build to adjust the HealthCare.gov website
and backend system and changes to consumer support channels (including the call center, messaging,
etc.). This option would be similar to the Waiver Concept A: State-Specific Premium Assistance as
outlined above.
In establishing HEAs, states will need to consider a number of design elements and issues, including:
• Contribution Amount: A state will need to establish a framework for setting the contribution
amount. For instance, the contribution amount could be a flat amount by age and family size or
scaled for income or a percentage of the premium for a benchmark plan.
o A state could set up a matching program where the HEA contribution would match a
portion of contributions from an individual and/or employer.
o A state could couple the account with a wellness program. Consumers could earn
contributions towards their account by participating or meeting certain requirements
outlined in the wellness program.
• Restrictions on the Use of Funds: While a state generally could allow the funds to pay for health
plans and health expenses, a state may want to restrict what the HEA can reimburse. For
instance, a state may want to limit an HEA to paying for plans with an actuarial value that
minimizes out-of-pocket exposure or health expenses that go toward reaching out-of-pocket
spending limits; or a state may choose to limit the HEA to premium payments, a new standard,
or another existing standard like section 213(d) of the Internal Revenue Code.
• Family Account Structure: Having multiple family members under a single account generally
makes it easier to administer for both the state and the family. However, a single account
approach requires procedures for removing family members from the account under certain
circumstances, such as a divorce or a child aging out of the plan. To avoid issues with removing
family members from the account, a state may opt for an approach that provides an individual
account for each family member. Or a state may consider an approach where all dollars remain
with the family in one account.
• Account Administrator: States would be responsible for setting up and administering these
accounts. A state could establish each HEA as a trust administered by a private financial
institution on behalf of the beneficiary or the state itself could hold and administer the HEA.
• HEA Savings: States would need to consider if and how an enrollee can use savings built up
within the HEA, including what will happen with any money left over after the plan year. For
example any money left over in the account (or a portion) could be used as a funding source to
implement part of the state’s waiver plan for healthcare coverage or services as defined in the
Specific Terms and Conditions (STCs) for the period of the waiver
7
:
o Go back to the state to use towards the state waiver plan (this option would have less of
an impact on consumer behavior).
o Stay with the individual irrespective of whether they were still in the individual market
to be used to pay other health care expenses incurred during the month or saved to pay
for future health care expenses for that plan year or future plan years.
7
Note funds remaining at the end of a waiver will be returned to Treasury consistent with the STCs.
23
o Be split between the state and the individual for health related expenses and/or the
state waiver plan.
o Be directed to wellness programs.
o Be directed to programs that support personal health (i.e. smoking cessation programs)
• Tax Implications: States should consider what (if any) federal tax consequences there will be for
the individual and/or reporting requirements for the state as a result of establishing an HEA.
Administrative Expenses
States may use pass-through funding associated with waiving section 36B of the Code for the Account-
Based Subsidies waiver option to implement the state plan and help partially fund the state account-
based subsidy program. In place of the PTC, states could receive federal pass-through funding in the
amount individuals would have otherwise received in PTC. States would use this federal funding to
contribute to the HEAs based on rules established by the state and consistent with Federal law.
As a reminder, a state must ensure that the waiver meets the four statutory guardrails of affordability,
comprehensiveness, coverage, and federal deficit neutrality. Any additional costs to fund the account-
based subsidy program would be the state’s responsibility.
Please refer to the Overview of 1332 Waiver Concept for information on when states can receive pass-
through spending, and administrative costs to the federal government associated with the waiver.
Things to Consider and/or additional information on implementation approaches under Option 1
Below are some questions to consider as the state develops these programs, and to include in the 1332
waiver application.
Questions for Concept A Option 1 that are applicable for Concept C:
1) How will the state implement a new subsidy structure?
a. Which entity will administer the program? Is it a new or existing entity? To what extent
will the entity be subject to state insurance laws? To what extent will the entity
coordinate activities with other public programs (e.g., Medicaid and CHIP)?
b. How much funding is necessary for the subsidy structure?
c. What populations or eligibility requirements will the state have for this program (e.g.,
age, income, etc.?
d. What plan options will be available?
e. If state funding is required, how much funding does the state anticipate will be
necessary to implement the state plan and how will the state generate the required
state funding?
2) When and how will consumers be notified of their subsidy amount?
3) Will there be a process for consumers to report changes to eligibility criteria (i.e. income, age,
address etc.)?
4) What process will be used for consumers to appeal their eligibility determination and subsidy
amount?
5) What sources is the state using to verify eligibility for coverage and/or the subsidy (if
applicable)? Will the state be using its Medicaid/CHIP Agency or the FFE to do eligibility
verifications and determinations? Is the state using any state sources for verification?
24
6) How will issuers receive payments for the subsidy (i.e. is the individual responsible for paying
the issuer directly with savings from their HEA?)? What is the timing and mechanism for pay-
out?
7) Will the state reconcile state subsidy amounts based on actual or earned income? If so, how will
that be operationalized?
8) Will the new subsidy program includes incentives for providers, enrollees, and plan issuers to
continue managing health care costs and utilization and lower overall health care spending (if
any)?
9) Does the state have the authority/ability to adjust the program requirements on a yearly or
other basis to account for market changes? If so what is the schedule and process for this?
10) Will the state require issuers to include the impact of the program in initial and/or final rates?
11) Is there any existing legislation and/or regulations related to the state program, or is new state
legislation and/or regulation needed?
12) If the state is leveraging the FFE’s system, does the state anticipate requesting any changes to
the FFE? If the state is leveraging the SBE, what operational changes does it intend to make?
Related to question #2 above, does the state envision that applicants will be able to see their
subsidy amount during the plan selection process?
13) If implementing an HEA what (if any) federal tax consequences will there be for the individuals
enrolled and/or reporting requirements for the state as a result?
14) How does the state plan to ensure access to health insurance that is at least as comprehensive
and affordable as would be provided under the PPACA as compared to without the waiver?
Questions for Concept C Option 1 specific to the Account-Based Subsidies Option:
1) Would an individual be allowed to withdraw any portion of his or her contributions at the end of
the year?
2) What entity owns the account and/or administers the account as part of the state’s plan?
3) What expenses can the account be used for?
4) What protections will be in place to protect program integrity and reduce improper payments?
5) What entities can contribute to the account?
6) How will the state treat any savings remaining in the account at the end of the year? Will the
savings be rolled over to the next year and how can the consumer use them?
7) What are the eligibility requirements for an individual to access the account?
a. Are they for certain types of plans?
b. Would a person be required to enroll in coverage in order to receive the contribution? If
so, what would be the requirements on the coverage?
c. What happens if the individual or a family member becomes eligible for Medicaid or
CHIP during the year? Could he or she use the savings in the account to pay for any cost
sharing that Medicaid/CHIP require?
8) Does the state plan to have a single account for a family or individual account for each family
member?
9) What is the structure for the contribution amount? Is there a match and/or other requirements?
10) Can employers contribute to the account?

25
Waiver Concept D: Risk Stabilization Strategies
In the risk stabilization strategies waiver component, states can consider ways to address the costs of
individuals with expensive medical conditions to mitigate the impact of those expenses on people who
purchase coverage in the individual market. For example, states can implement a state-operated
reinsurance program or high-risk pool by waiving the single risk pool under 1312(c)(1) of the PPACA and
can be coupled with the other waiver idea options discussed. Reinsurance programs have lowered
premiums for consumers, improved market stability, and increased consumer choice. Some states have
chosen to use a claims cost-based model (OR, MN, WI), a conditions-based model (AK), or a hybrid
conditions and claims cost-based model (ME) for their reinsurance program. This paper includes
examples of state approaches to date, but states are encouraged to think creatively about what model
makes the most sense for their state. If the state shows an expected reduction in federal spending on
PTC, the state will receive federal pass-through funding to help partially fund the state’s high-risk
pool/reinsurance program.
Policy Options to Design a Risk Stabilization Program
Option 1: Implement a Reinsurance Program
Policy
Reinsurance programs compensate insurers for people with significant medical expenditures during a
year, lowering premiums in the individual market (both in and outside the Exchange). Reinsurance
payments are based on actual costs, so along with high-risk individuals it also helps mitigate insurer
losses for low-risk individuals who may have unexpectedly high costs (such as costs incurred due to an
accident or sudden onset of an illness). Under reinsurance, some plans may receive payments for high-
cost enrollees and below we discuss three choices for states to design reinsurance programs. As a
reminder to states, the risk adjustment high-cost risk pool has been effective since plan year 2018 and
will reimburse 60% of claims above $1 million, with no cap. This risk adjustment high-cost risk pool
program will work in conjunction with state reinsurance programs to provide relief from catastrophic
claims costs so states should take this into consideration as they establish parameters for their
reinsurance program so the state-operated reinsurance program does not duplicate claims covered
under the risk adjustment high-cost risk pool.
Choice 1 - Claims cost-based reinsurance program: One option for states is a claims cost-based
reinsurance program where issuers are reimbursed for a portion of the costs of enrollees whose
claims exceed a certain threshold (i.e. the attachment point). Typically, issuers are reimbursed
for only a portion of costs (i.e., the coinsurance rate) above the attachment point, and in some
cases, up to a set cap. High-cost individuals remain in the same risk pool as other enrollees (for
both claims cost-based reinsurance programs and conditions-based reinsurance programs) and
enroll in the same commercial plans available to the general public. Claims are eligible for
payment through a reinsurance program using funds separately raised for that purpose when
certain criteria are met. A few state examples of this option are outlined below in Table 1.
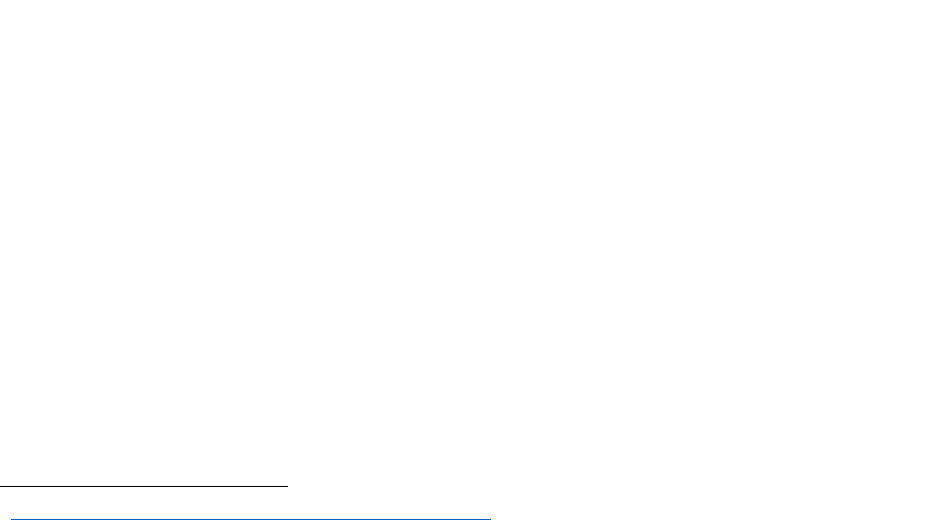
Table 1: Examples of reinsurance programs using the claims-cost based option:
26
Program Attachment Point
Coinsurance
Rate Cap
Minnesota
$50,000
(2018/2019)
80%
(2018/2019)
$250,000 (2018/2019)
Oregon
$95,000 (2018)
$90,000 (2019)
50%
(2018/2019)
$1,000,000 (2018/2019)
Wisconsin $50,000 (2019) 50% (2019) $250,000 (2019)
New Jersey $40,000 (2019) 60% (2019) $215,000 (2019)
Maryland $20,000 (2019) 80% (2019) $250,000 (2019)
Federal Reinsurance
Program
$45,000
(2014/2015)
$90,000 (2016)
80% (2014)
50%
(2015/2016)
$250,000 (2014-2016)
Choice 2 –––– Condition-based reinsurance program: Instead of identifying people based on
their claims costs, another option is a conditions-based reinsurance program where insurers are
reimbursed for costs of individuals with one or more of a list of pre-determined high cost
conditions. This program would operate in a very similar fashion as a claims-based reinsurance
program as enrollees remain in the individual market risk pool and the funding and structure is
invisible to them. However, because claims are only reimbursed for people with a specific set of
conditions (determined either in a prior year or current year), insurers must still pay claims for
people who run up high claims due to an accident or other health event. The reinsurance
program would pay the entire claims of all individuals meeting any of the conditions. Alaska
provides an example of a conditions-based reinsurance program:
Alaska: The Alaska Reinsurance Program began in 2017 and uses a retrospective
reinsurance model. The program covers all costs for enrollees with one or more of 33
high-cost conditions based on the state’s analysis of 2015 claims data. If an enrollee was
treated for one of the designated conditions, that enrollee will be ceded to the
reinsurance program retrospectively for the year. Beginning in 2018, the program is
operating under a 1332 waiver. Premiums were reduced by an estimated 20% due to
the reinsurance program. The program was estimated to pay claims totaling $60 million
in 2018 with federal pass-through funding covering about 97% of this amount. For 2019,
the state’s analysis expects the reinsurance program will pay approximately $71 million
in claims.
Choice 3 - Hybrid Reinsurance Program: Another option is a hybrid where the state could
implement a reinsurance program that is both conditions-based and claims based, where issuers
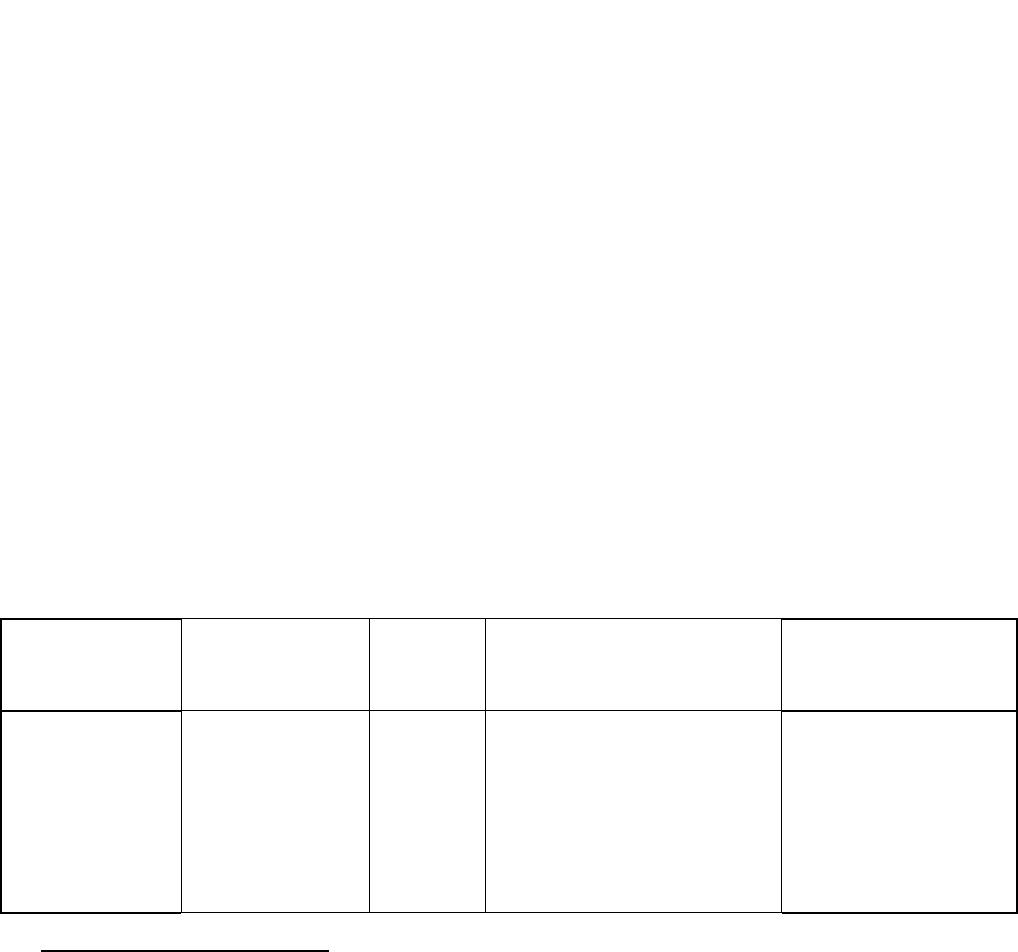
27
are reimbursed for the costs (or a fraction of costs) of individuals within a specified range with
one or more of a list of pre-determined high-cost conditions. For the purposes of a 1332 waiver,
the state would need to define the list of conditions as well as the parameters for
reimbursement. Example of a hybrid reinsurance program is below:
Maine: Maine reinstated the Maine Guaranteed Access Reinsurance Association
(MGARA) that was initially operated in 2012 to 2013.
8
Under Maine’s reinsurance
model, insurers are reimbursed for costs of individuals with one of eight medical
conditions
9
as identified in ICD-10 codes, and any other individuals identified within 60
days of enrollment by the insurer as posing high enough risk to be worth paying the
reinsurance premium, which is 90% of the underlying policy premium. Maine’s
reinsurance is subject to an attachment point and coinsurance as outlined below. The
enrollee remains free to choose any health plan and the funding and structure is
invisible to him or her. Maine’s original program was often called an invisible high-risk
pool because high risks were identified prospectively through the underwriting process,
much like a traditional high-risk pool and the operation of the program was invisible to
the high risk individuals who had access to all of the insurance products available to any
consumer. Reinsurance is applied on a policy year basis, and individuals with one or
more of the eight designated conditions are reinsured retroactively to the beginning of
the policy year. Maine’s program also continues to allow discretionary ceding, but
discretionary ceding will remain subject to the tight window in MGARA’s original Plan of
Operation – 60 days following effective date of the underlying primary coverage. In this
way the Maine program carries forward an element of identifying high risks
prospectively, similar to a more traditional high risk pool. Only a small amount of
discretionary ceding is expected due to the high attachment points and issuer loss of the
ceded premium.
Program
Eligibility
Attachme
nt Point Coinsurance Rate Cap
Maine
(Hybrid model-
attachment point/
conditions based)
All policies covering
individuals with
one of
eight listed conditions
or other high-risk
individuals as
identified by the
issuer.
$47,000
90% (for $47,000-$77,000)
100% (for > $77,000) net the
difference of any claims above $1
million, which are partially
covered by the federal high cost
risk adjustment program
None, but for claims
above $1,000,000, the
program pays net of
amounts covered by the
federal high cost risk
adjustment program
8
Maine’s previous reinsurance program that operated from 2012-2013 before the PPACA reinsurance program,
similarly enrolled individuals with the same eight conditions but had different parameters The plans ceded 90
percent of the premiums paid for these enrollees to the reinsurance pool. For those enrolled, the reinsurance
covered 90 percent of claims between $7,500 and $32,500, and covered 100 percent of claims over $32,500 with
no cap.
9
Ceded conditions include: Uterine Cancer, Metastatic Cancer, Prostate Cancer, Chronic Obstructive Pulmonary
Disease (COPD), Congestive heart Failure, HIV Infection, Renal Failure, and Rheumatoid Arthritis.
28
Implementation approaches (Option 1 Reinsurance program - Choice 1, 2, and 3):
As part of the “risk stabilization waiver concept,” the 1312(c)(1) individual market single risk pool
requirement would be waived in connection with the implementation of a state-operated reinsurance
or individual risk pool program (to the extent it would otherwise require excluding total expected state
reinsurance payments when establishing the market wide index rate).
10
• Setting up a reinsurance program: A new reinsurance program, whether a claims-based or
conditions-based model, will require new activities both for the state and for carriers. Initially,
there will be one-time start-up costs. Once a program is under way, there will be operating and
oversight expenses of several kinds. Set-up activities include: creating a governance structure
and mechanisms (e.g., board, plan of operations); contracting for administrative services and
systems; acquiring claims and accounting software; entering into contracts for professional
services such as law and accounting; hiring or arranging for actuarial support; and establishing
budgetary and financial systems, including holding of fiscal reserves, and arranging for banking
services.
For a conditions-based model, there may need to be more analysis to look at claims and identify
which conditions are the greatest cost-drivers and could be ceded to the reinsurance program,
making it slightly harder to administer than a claims based model. A hybrid model also might
add an additional level of analysis.
In the context of a section 1332 waiver, states have used their existing high-risk pools to
administer the state-operated reinsurance program by leveraging some of the existing
infrastructure and/or legal authority. Other states have the Department of Insurance administer
the program. For example the Alaska Reinsurance Program (ARP) is administered by Alaska
Comprehensive Health Insurance Association (ACHIA). The Minnesota Premium Security
Program (MPSP) is run by the Minnesota Comprehensive Health Association (MCHA). The
Oregon Reinsurance Program (ORP) is administered by the State of Oregon and the Department
of Consumer and Business Services (DCBS).
• Prospective vs Retrospective model for reinsurance programs: As part of implementation of a
reinsurance program, states should consider whether they want to do a prospective or
retrospective reinsurance model. Generally speaking, a prospective model is significantly more
complex to design and operate, both for the state and for carriers, than a retrospective model.
This is often because a prospective model requires development of a way to identify which
consumers have certain conditions and/or expect to have certain claim costs and auto-cede
them into the reinsurance program.
A prospective model generally pays nothing for people who incur unpredictable claims and,
therefore, follows a more traditional insurance model. Insurers may therefore still be subject to
large claims. By contrast, a retrospective reinsurance model cedes claims that meet the
10
https://www.cms.gov/CCIIO/Programs-and-Initiatives/State-Innovation-Waivers/Downloads/Checklist-for-
Section-1332-State-Innovation-Waiver-Applications-5517-c.pdf
29
reinsurance parameters after looking at claims data for the year. By paying all large claims that
exceed a certain amount, a retrospective model may reduce incentives to manage costs for
large claims. As a result, states could consider ways to incorporate managing costs into their
reinsurance programs.
• While the prospective model requires both advance selection of auto-ceded conditions and
significant activity by carriers to identify those consumers, the retrospective model requires
neither. In a prospective model the state would need to establish how to prospectively identify
high risks for the program.
Administrative expenses (Option 1 Reinsurance program - Choice 1, 2, and 3):
Overall, administrative costs should not be as large as a percentage of claims payouts for a reinsurance
program compared to a high risk pool. From prior experience, we estimate that state administrative
costs would amount to at most an additional 1 to 3 percent of claims costs, depending upon how active
administrators are. States can use pass-through funding towards operation of a reinsurance program
under its waiver plan. As an example, the Alaska Reinsurance program (ARP) cost was $717,000 for 2017
and included some one-time only start-up costs. The state budgeted $590,800 for administrative costs
for the ARP in 2018.
To help new states in the start-up years of implementing their reinsurance program, CMS is offering the
following flexibilities for states to administer their reinsurance program as outlined in Option 1.
• Transitional assistance for administering a reinsurance (RI) program: States can request that
the federal government calculate issuers’ state RI payments based on the state RI
parameters as part of the state’s waiver plan. States would still be responsible for making
reinsurance claims payments to issuers. States that are interested in this transitional
program should notify CMS early in the process about the state’s parameters for CMS to
assess the feasibility of the proposal. This option is only available for the first two years of a
waiver, at which point the state is expected to fully operate their RI program to include the
program calculations, collections, and payments. The state would be responsible for the
Federal cost of this service, including development, implementation, maintenance,
operations, and customer support. States will be responsible for reimbursing CMS for these
services.
• Assistance with a state database for reinsurance program: CMS has made the EDGE server
software that issuers use in relation to CMS’s risk adjustment program available for states to
use for developing their own database for the state’s reinsurance program. The software
available is for the enrollment and claims data processing, and program calculation.
o State Database: Any IT security applications will need to be developed and
maintained by the state. There is no additional cost to the state for this software,
and no additional administrative cost to the federal government for states using this
option. Under this approach, the state would incur the full burden of running its
state reinsurance program. If the state were to ask for assistance there would be
costs that the state would incur and be responsible for.
o State Database (i.e. EDGE Server): Some IT security applications will need to be
developed and maintained by the state, will other applications would have to be

30
created and maintained by CMS. Although the state must maintain hardware and
software updates, there is an administrative cost to the federal government. Under
this approach, the state would require support from CMS for creating/updating the
state-specific calculations, providing customer service and tracking.
Please refer to the Overview of 1332 Waiver Options for information on when states can receive pass-
through spending, and administrative costs to the federal government associated with the waiver.
Option 2: High-Risk Pool
Policy
Another option is a High-Risk pool (HRP), which is a mechanism that states can consider to lower
premiums and risk in the individual market by removing high-risk enrollees from the commercial market.
In a traditional high-risk pool, individuals who failed to maintain continuous coverage at risk of high-cost
conditions are covered through a separate pool outside of the individual market, and funded by high-
risk pool premiums and external funding, which is most often necessary. In a risk pool that is invisible to
the individual as described above, individuals who qualify for the high-risk pool enroll in an individual
plan offered by a commercial, state-licensed health insurance issuer, but their claims (either total claims
or claims at certain specific attachment points) are subject to payment using the additional funding
available through the risk pool arrangement. Insuring the high losses incurred by such individuals
through a separate pool prevents the need to raise average premiums for commercial consumers to
offset those losses.
Traditional HRP Pre-PPACA: Prior to the PPACA implementation, 35 states operated high-risk
pool programs. Eligibility categories varied by state and generally covered individuals with pre-
existing conditions that made them uninsurable in the commercially underwritten market, or
insurable only at premium rates significantly higher than standard, and who were not eligible for
group coverage or Medicare or Medicaid. State high-risk pools were also often employed as an
alternative mechanism for HIPAA continuation purposes for those who lost group coverage.
PCIP: The Pre-existing Condition Insurance Plan (PCIP) program, authorized by the PPACA,
provided $5 billion to create high-risk pools in each state from 2010 until the end of 2013. The
PCIP program provided coverage to those individuals uninsured for at least 6 months prior to
enrollment with a pre-existing condition or who had been denied coverage. States had the
option to create a new program or build on an existing program. Otherwise the federal
government operated the PCIP program directly. The Office of the Actuary within the Centers
for Medicare & Medicaid Services (CMS) projected enrollment of 375,000 by the end of 2010,
but as of April 10, 2011 enrollment was only about 15,800 in the state-run PCIPs and 5,700 in
the federally run PCIPs. Enrollment in state-run PCIPs was higher on average than enrollment in
federally run PCIPs primarily due to these states having an aggregate population that was about
55 million more than the aggregate population of states in the federally run PCIP (based on 2010
US Census Data).
11
Some risk pools developed conditions-based lists that often required an
attestation from the individual. PCIP premiums were set at the standard market rate for
comparable coverage, as opposed to traditional state high-risk pool programs that generally set
premiums at 110-200% of standard market rates. As of January 1, 2014, PPACA prohibits issuers
11
https://www.gao.gov/new.items/d11662.pdf

31
from denying coverage or charging differential premium rates based on pre-existing conditions,
which has changed the landscape of the individual market. States are allowed to set up their
own, self-funded high-risk pool where the product is not designated as health insurance, which
are usually administered by a third-party administrator (TPA) which is sometimes a health
insurance issuer. Plans sold must comply with any applicable state regulations and rules.
Products that are not considered health insurance products are not subject to the Public Health
Service Act.
HRP Today under PPACA: Currently, under guaranteed availability rules that apply to licensed
health insurance issuers, consumers cannot be required to purchase coverage only from a high-
risk pool. As such, if a state pursues a high-risk pool, consumers will likely choose the plan that
best meets their needs in terms of costs and benefits, so states should consider whether the
plan in the high-risk pool would be enticing to consumers as they design their high-risk pools.
For example, if the high-risk pool offers an attractive plan with robust provider networks or
benefits for a certain condition, this may entice consumers with that condition to enroll in the
high-risk pool. States can establish eligibility standards for the high-risk pool (e.g., based on
certain conditions or other parameters).
States could also consider implementing a state subsidy program as described in the State-
Specific Premium Assistance waiver component option if the state wanted to make the high-risk
pool enrollees eligible for financial assistance. Another way to approach high-risk pools is to
make them self-funded where they do not count as insurance products and as such do not have
to comply with certain protections under the ACA.
Examples of State-Administered Traditional High-Risk Pools (some of which are still operational)
Note: these are not section 1332 waiver proposals:
• North Dakota: The Comprehensive Health Association of North Dakota became operational
in 1982 and is still operational. The pool is financed by assessments on accident and health
insurers that write more than $100,000 in premium volume within the state. The premium
cap is set at 135 percent of the individual premium rate charged for similar coverage
throughout the state. There is a lifetime limit of $1,000,000 in benefits. At the end of 2005,
just over 1,730 persons receive coverage from the pool. There were 647 enrollees in the
pool as of 2015.
• New Mexico: New Mexico’s Medical Insurance Pool (NMMIP) is still in operation and
included 2,700 enrollees in 2016. The program is actively trying to shift enrollees into a QHP
to comply with the program limit of 1,000 participants.
States also might want to consider high-risk pools more as options for certain populations to market
them in a different way to consumers, while similar to the high-risk pools described above. For example,
a state may have a high-risk pool designed for certain high cost conditions with certain benefits that are
enticing to individuals such as provider networks or other benefits.
Implementation approaches (Option 2 high-risk pool):
To implement a traditional high-risk pool program as part of the “risk stabilization model,” states would
waive section 1312(c)(1) (the individual single risk pool requirement) in connection with implementation
32
of a state-operated high-risk pool program (to the extent it would otherwise require excluding total
expected impact of the high risk pool when establishing the market wide index rate).
12
A traditional high-risk pool would require new activities both for the state and for health insurance
issuers. For a traditional high-risk pool the state would also need to make sure there’s an
eligibility/enrollment system, adequate provider networks, claims processing and operations, and
customer service and communications system in place. The high-risk pool would receive all premium
dollars and pay all claims for its members. Assuming the high-risk pool uses a health insurance issuer to
process claims and perform other functions, the issuer would receive a TPA fee as sole compensation,
and would assume no risk. States would also need to determine a governance structure, requirements
for contracting with carriers, etc.
In the context of a section 1332 waiver, states may be able to leverage existing high-risk pool authority,
particularly if a high-risk pool is still operating. States may need to establish authority to set standards
for products that are not health insurance and/or amend their current standards depending on the
types of products the state wants the high-risk pool to sell to consumers.
States may also want to consider if the coverage in the state high-risk pool would meet the definition of
coverage in the 1332 guidance released in October 2018.
13
States can consider if the coverage offered
would meet the definition of minimum essential coverage (MEC) and apply for this designation if so.
Administrative expenses (Option 2 high-risk pool):
The administrative cost for high risk pools established by the state in lieu of the federal PCIP program
over the life of the program was about 5% of total spend (vs. 7% for the federal PCIP), but the range was
between 2% - 15%. Administrative costs do typically go down over the life of the program.
States should evaluate if additional state funding is required to fully fund the state plan.
Please refer to the Overview of 1332 Waiver Options for information on when states can receive pass-
through spending, and administrative costs to the federal government associated with the waiver. We
do not anticipate any additional administrative costs to the federal government with this option, but
would need to evaluate the specific proposal by the state.
Additional information on implementation approaches under Option 1 and 2
Things to Consider in Designing a High-Risk Pool/Reinsurance Program:
As mentioned above, states have flexibility in how they design and administer their reinsurance program
to work best in their state. Below are some things to consider as the state develops a high-risk pool/
state-operated reinsurance program, and to include in the 1332 waiver application.
1. How will the state implement a high-risk pool/reinsurance program?
12
https://www.cms.gov/CCIIO/Programs-and-Initiatives/State-Innovation-Waivers/Downloads/Checklist-for-
Section-1332-State-Innovation-Waiver-Applications-5517-c.pdf
13
Coverage for section 1332 waivers refers to minimum essential coverage as defined in 26 USC 5000A(f) and 26
CFR 1.5000A-2, and health insurance coverage as defined in 45 CFR 144.103.
33
a. What is the entity that will administer the program? Is it a new or existing entity? To
what extent will the entity be subject to state insurance laws?
b. How much is the necessary funding for the high-risk pool/reinsurance program and
what premium reduction is the state trying to achieve?
c. If state funding is required, how much funding does the state anticipate will be
necessary to implement the state plan and how will the state generate the required
state funding?
d. If implementing a traditional high-risk pool, what are the eligibility requirements and
plan metal tiers available (if applicable)?
2. What will be the data collection timing and mechanism for collecting claims information and
generally for pay-out?
a. How will the state identify and pay claims?
3. Will the state be using a conditions-based list for reinsurance and/or an attachment point
model?
4. Will the reinsurance program include incentives for providers, enrollees, and plan issuers to
continue managing health care cost and utilization for individuals eligible for the described
reinsurance program (if any)?
5. Will the state specify a co-insurance amount, or a cap, based on available funds, similar to the
federal program?
a. When will the parameters be finalized?
b. Further, does the state have the ability to adjust the parameters to account for market
changes? If so, what is the schedule and process for finalizing the parameters on a year
by year basis?
6. Will the state require issuers to include the impact of the reinsurance program and/or high-risk
pool in initial and/or final rates?
7. Are there any legislation and/or regulations related to the state reinsurance program?
a. Are any additional regulations needed? If so what is the timing of those regulations?
Information on the federal reinsurance program, which may provide helpful lessons for states
considering creating state-run programs, information on reinsurance contributions, as well as materials
and timelines by benefit year, can be found here
14
. If you are interested in learning more about federal
reinsurance payments, please refer to this overview
15
and this document
16
on how CMS calculates
reinsurance payments and reports. These documents and others are also available through CCIIO’s
technical assistance
portal
17
(once registered, search under Library, filter by ‘reinsurance’, ‘Reinsurance-
contributions’, and ‘distributed data…’).
Cost-containment strategies
14
https://www.cms.gov/CCIIO/Programs-and-Initiatives/Premium-Stabilization-Programs/The-Transitional-
Reinsurance-Program/Reinsurance-Contributions.html
15
https://www.regtap.info/uploads/library/RP_OverviewPresentation_111314_v4_5CR_111314.pdf
16
https://www.regtap.info/uploads/library/RP_Slides_063016_v1_5CR_070116.pdf
17
https://www.regtap.info/index.php
34
In general, the most expensive 5% of insured individuals account for over half of the costs (55%) of the
total market.
18
It’s important that along with the reinsurance program, the state also help mitigate the
costs associated with this population to lower overall health care spending.
19
In May 2017, the Departments released a checklist
20
for states on information to include in their 1332
waiver application. We also asked whether the reinsurance program includes incentives for providers,
enrollees, and plan issuers to continue managing health care cost and utilization for individuals eligible
for the described high-cost risk pool/reinsurance (if any). For example, while lower attachment points
and higher coinsurance percentages offer the greatest opportunity to lower premiums, without issuer
incentives to control costs, policy objectives for issuers to be fully engaged in cost control would not be
met. In addition, without incentives to control costs, there is no long-term impact on lowering costs
associated with premium increases outside the period of the waiver.
In an effort to encourage states to design high-risk pool/reinsurance programs that lower costs and
encourage cost containment below are some ideas for states to strongly consider:
o Mandating significant and effective care management protocols.
o Requiring case management for individuals that have either a certain condition or reach a certain
claim threshold
o Using value-based designs specific to the state-operated reinsurance program members.
21
o Modifying reimbursement rates to issuers/providers – establish a coinsurance rate under 100%
o Making per-capita payments to insurers instead of reinsurance; essentially the state would give
insurers a flat PMPM for each enrollee which would cause issuers to lower premiums by that
amount.
o Including options that cede risk should include parameters that put downward pressure on costs, for
example, by reimbursing based on a cap or coinsurance rate to a certain claims dollar amount for
outlier costs, particularly in geographic areas where there are few issuers and dominant providers.
This could create an opportunity to lower overall costs.
Funding for High-Risk Pool/Reinsurance Programs:
As part of a section 1332 waiver to implement a high-risk pool/state-operated reinsurance program,
states must evaluate their goals for their individual market. Perhaps the state is looking at this option to
help reduce premiums for consumers in the individual market, attract or retain issuers in their market,
or help address high costs.
Under a section 1332 waiver, a state may receive pass-through funding associated with the resulting
reductions in federal spending on Exchange financial assistance consistent with the statute. For states
submitting a section 1332 waiver application implementing a high-risk pool/state-operated reinsurance
program and seeking a pass-through of funding, their state legislation must provide that the high-risk
18
http://us.milliman.com/insight/2017/Reinsurance-and-high-risk-pools-Past--present--and-future-role-in-the-
individual-health-insurance-market/?lng=1048578
20
https://www.cms.gov/CCIIO/Programs-and-Initiatives/State-Innovation-Waivers/Downloads/Checklist-for-
Section-1332-State-Innovation-Waiver-Applications-5517-c.pdf
21
https://www.urban.org/sites/default/files/alfresco/publication-pdfs/1000983-Implementing-Government-
Funded-Reinsurance-in-the-Context-of-Universal-Coverage.pdf
35
pool/state-operated reinsurance program (either the funding or authorization for the program) is
contingent upon federal approval of the waiver (or will become effective only if the section 1332 waiver
is approved). By applying for a section 1332 waiver, a state can apply federal pass-through funding to
fund a portion of a state reinsurance program and achieve premium reductions. The amount of funding
for a reinsurance program will depend on the type of premium reduction the state wants to achieve, the
geographic makeup of the state’s population, and what percentage of the market is subsidized.
As part of a section 1332 waiver, states must submit an actuarial analysis to show the impact the
reinsurance program will have on premiums in the state, among other analysis described above. A state
may look at its claims data and Marketscan data to predict how much financing it will take to reduce
premiums by the desired amount.
Some examples of how states have considered funding the state share of their reinsurance programs are
outlined in Table 2 (note similar funding mechanisms could also be used to fund a HRP):
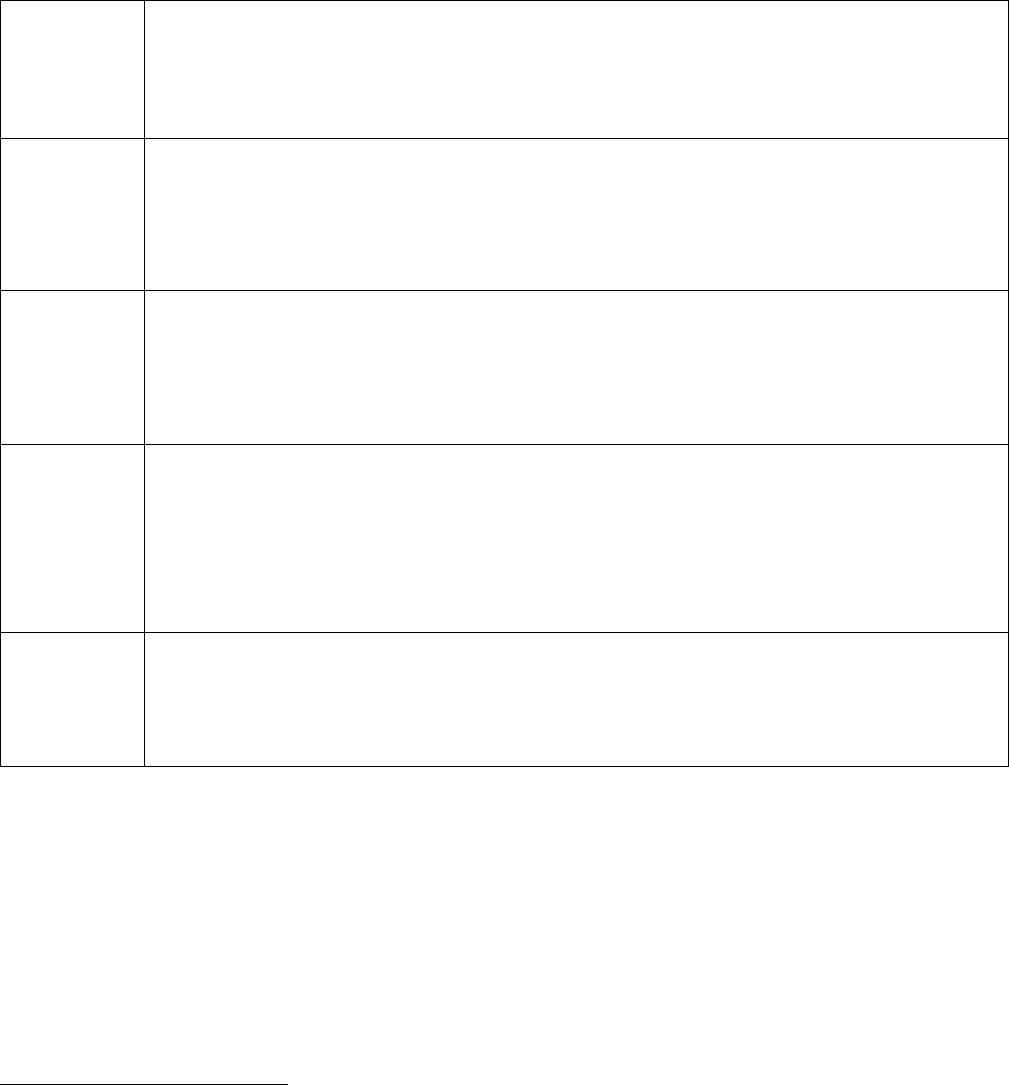
36
Table 2: Examples of State Funding Approaches for Reinsurance Programs
Minnesota
$271 million dollar reinsurance program for 2018 which reduced premiums by an estimated
20%; Minnesota funded the state portion of the reinsurance program through their general
fund and a portion of the state’s 2% provider tax which applied to hospitals and other
providers.
Oregon
$90 million dollar reinsurance program for 2018 which reduced premiums by an estimated
7.5%; 95.4 million dollar reinsurance program for 2019 which reduced premiums by an
estimated 7.8%; Oregon funded the state portion of the reinsurance program through a
premium assessment levied on major medical premiums for policies issued in this state and
through excess fund balances currently held in two state programs.
22
Wisconsin
$200 million reinsurance program for 2019 which will reduce premiums by an estimated 11%;
Wisconsin funded the state portion of the reinsurance program through state general
purpose revenue (GPR), which
consists of general taxes, miscellaneous receipts and revenues
collected by the state,
and federal pass-through dollars. Act 138 creates a sum sufficient
appropriation for WIHSP, which allows the state to appropriate GPR.
Alaska
$60 million dollar reinsurance program for 2018 which reduced premiums by an estimated
20%; Alaska funded the state portion of the reinsurance program in a separate fund set up
within their general fund which is financed by the state’s premium tax that applies to all lines
of insurance. Specifically: Reinsurance program funding for 2017- 2018 is appropriated by the
Legislature from premium tax assessed on all insurers (not just health insurers) in Alaska.
Note: taxes rates vary from .75% to 6% depending on insurer type.
Maine
$93 million dollar reinsurance program for 2019 which will reduce premiums by an estimated
9%; Maine funded the state portion of the reinsurance program through a market-wide
assessment ($4 per member/per month) and ceding 90% of premiums received from
consumers with at least one of eight high-risk health conditions to MGARA.
22
The ORP will be funded by a portion of the 1.5% assessment described in Section 5 of HB 2391. HB 2391 creates
a 1.5% assessment on fully insured commercial major medical premiums, including premium equivalents for self-
insured public plans, for eight calendar quarters beginning at plan renewal on or after Jan. 1, 2018. In 2018, the
balance of two existing funds – the Oregon Health Insurance Marketplace (OHIM) fund in excess of six-months
operating budget and the Oregon Medical Insurance Pool (OMIP) account balance – will also be used to fund the
ORP.
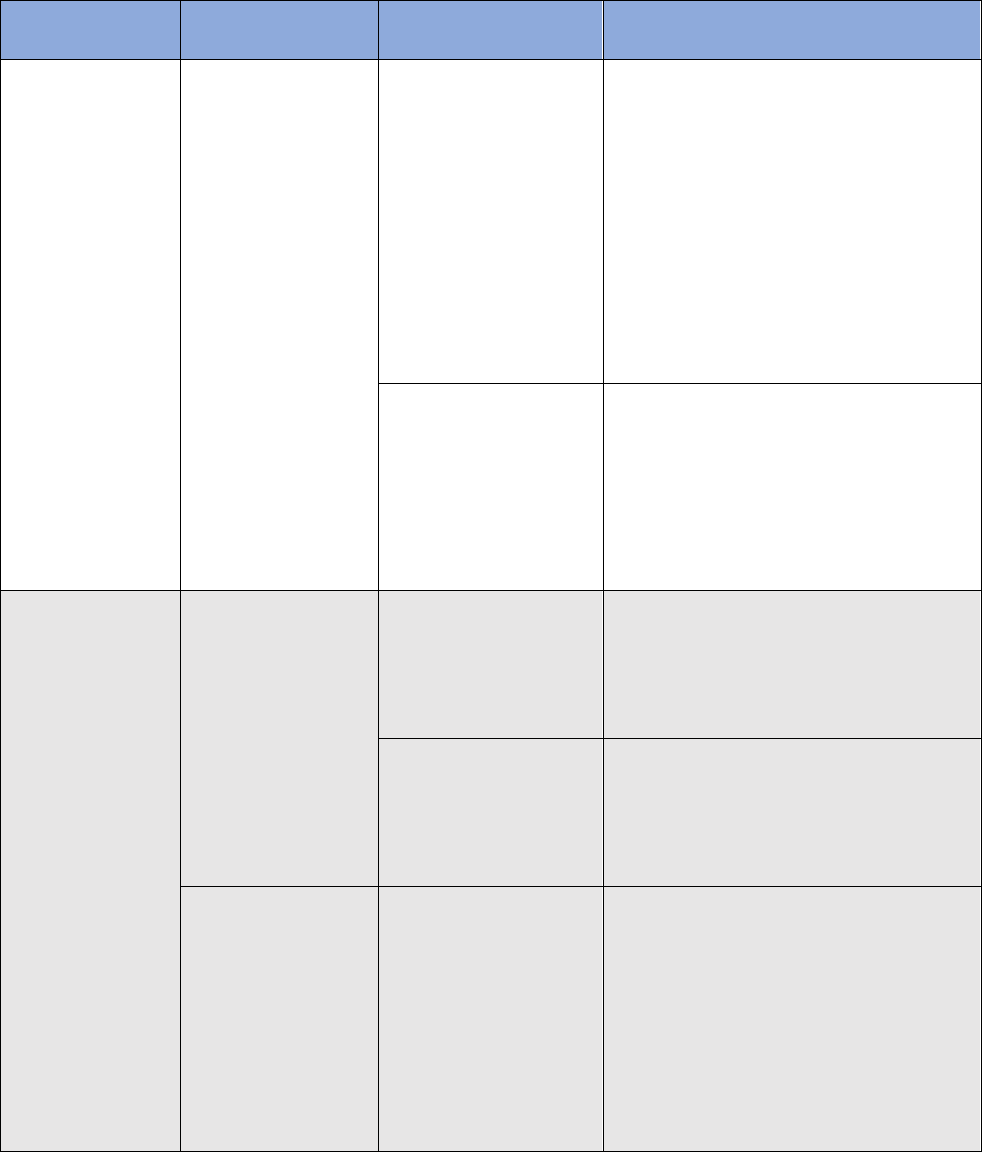
37
Appendix A: Types of Waiver Concepts and Policy Options
Waiver Concept
Policy options
Implementation
approaches/Decisions
Considerations
Waiver Concept
A: State-Specific
Premium
Assistance
Policy goal:
target specific
populations
and/or increase
affordability
Create a State-
Specific Premium
Assistance Program
to target certain
age, federal
poverty levels
(FPL), or
demographic
groups (for
example, based on
conditions,
vulnerable
populations, etc.)
Use state’s Medicaid
system for eligibility
determinations for
new structure
• Requires concurrence of relevant
federal partners
• Must identify authority (or existing
state authority) for relevant federal
partners to provide data to support
1332 program eligibility
requirements
• Must draft/update data use
agreements with federal agencies
• No HealthCare.gov Exchange
possible
Build new eligibility
system and leverage
HealthCare.gov
backend for
citizenship and
immigration
verification checks
• State must reimburse CMS for
significant federally-facilitated
Exchange (FFE) technical build, in
support of tailored system use
• No HealthCare.gov Exchange
possible, but federal platform could
be leveraged
Waiver Concept
B: Adjusted Plan
Options
Policy goal:
increase
affordability
and/or increase
consumer choice
Option 1: Allow
state-specific
financial assistance
to be applied to
non-QHPs
Enrollment to occur
directly with
participating issuers or
web broker websites
• Requires concurrent waiver of PTC
and state implementation of
eligibility
• No HealthCare.gov Exchange
possible
Enrollment to occur
through a specific
website, which hosts
program eligibility
application as well
• Requires concurrent waiving of PTC
and state implementation of
eligibility
• No HealthCare.gov Exchange
possible
Option 2: Allow
sale and/or
application of
federal PTC and
Advance Payments
of the PTC (APTC)
to additional on-
Exchange plans
(catastrophic plans)
Implement on
Exchange
• HealthCare.gov Exchange platform
used (some level of customization)
• States do not have to create their
own subsidy structure
• If allowing APTC/PTC, requires
Exchange screening of consumers
for APTC/PTC eligibility and Form
1095-A provided to consumers and
the IRS
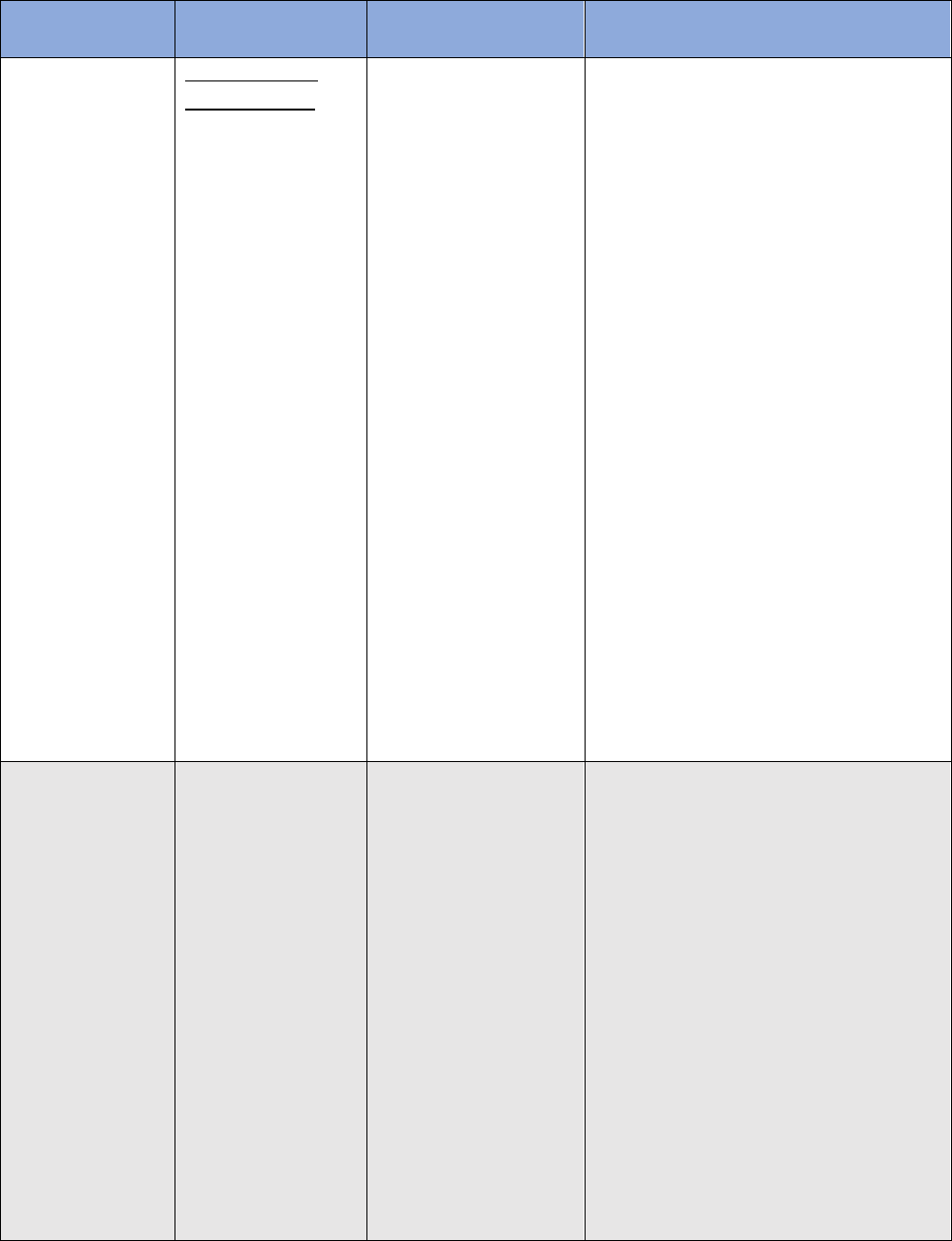
38
Waiver Concept
Policy options
Implementation
approaches/Decisions
Considerations
Waiver Concept
C: Account-Based
Subsidies
Policy goals:
• Target specific
populations;
• Increase
consumer
choice and
control;
• Minimize
market
distortions;
and/or
• Increase
affordability
Health Expense
Account (HEA):
Provide consumer
directed HEA to
targeted
populations to use
to pay premiums
and/or other
health expenses
Combine with
Concept A (where the
State implements a
state specific premium
assistance program.)
or B (where states
change the types of
plans eligible for
subsidies).
State restricts the use
of the funds to pay
only certain health
expenses
• Coverage must be verified before
account can be used to pay health
expenses other than premiums
• Administrative tools depending on
state plan to restrict funds to
certain health care expenses
• No HealthCare.gov Exchange
possible
Waiver Concept
D: Risk
Stabilization
Strategies
Policy goal:
Account for
regional
premium
variation in a
way that lowers
premiums
Option 1:
Implement a State-
Operated
Reinsurance
Program
Choice 1: Claims cost-
based (attachment
point model): Issuers
are reimbursed for a
portion of the costs of
enrollees whose
claims exceed a
certain threshold (i.e.,
the attachment point)
Choice 2 Conditions-
based: Issuers are
reimbursed for a
portion of the costs
above a certain
threshold for
individuals with one
• State-administered reinsurance
program
• Option for federal help with
administering the program; for
example use of the EDGE server for
reinsurance calculations
• HealthCare.gov Exchange platform
used (no customization)
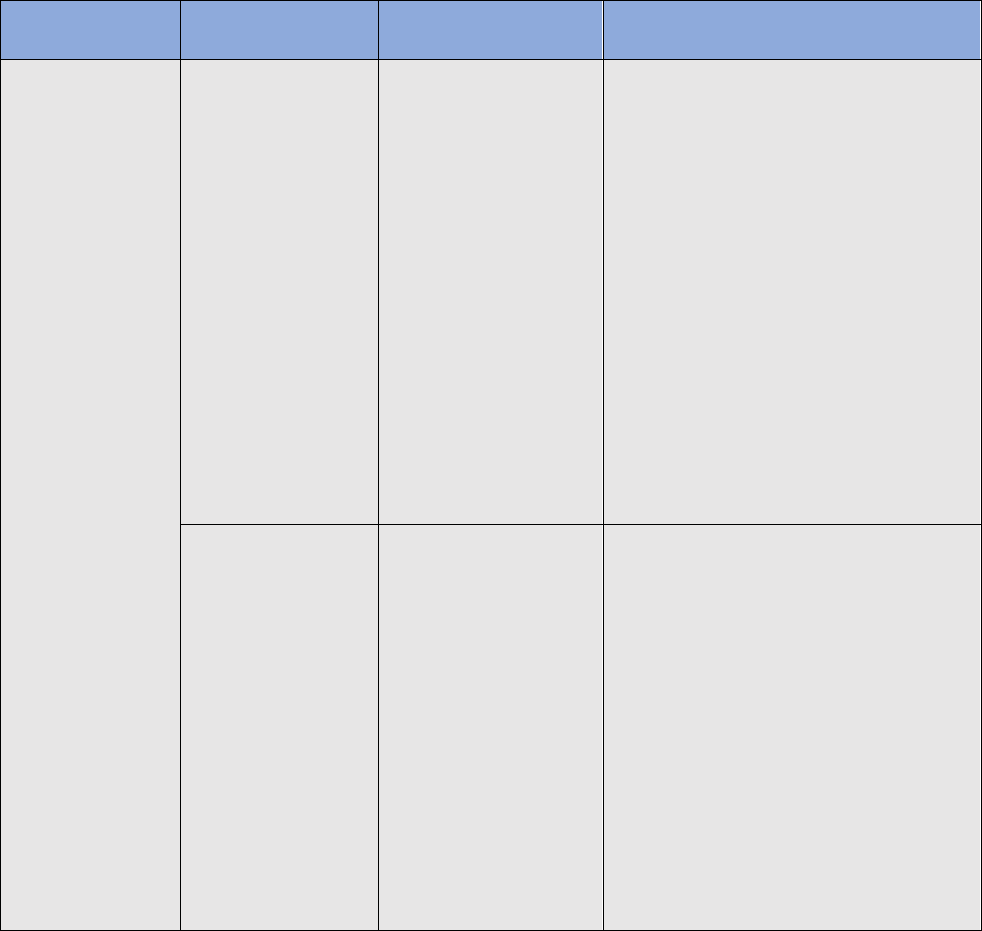
39
Waiver Concept
Policy options
Implementation
approaches/Decisions
Considerations
or more of a list of
pre-determined high-
cost conditions
Choice 3: Hybrid:
Combination of a
claims cost-based and
conditions based
model
In each approach
individuals remain in
the same risk pool as
other enrollees so it is
“invisible” to the
consumer
Option 2:
Implement a
traditional high-risk
pool (HRP)
In a traditional high
risk pool individuals at
risk of high-cost
conditions are
covered through a
separate pool outside
of the individual
market risk pool;
funded by high-risk
pool premiums and
external funding,
which is often
necessary
• State-administered program
• HealthCare.gov Exchange platform
may or may not be used (no to
moderate customization)
