
Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
1
Department of Rehabilitation Services
Physical Therapy
Standard of Care: Total Hip Replacement
Inpatient Physical Therapy management of the patient following total hip arthroplasty,
hemiarthroplasty, hip resurfacing, or revision total hip arthroplasty.
ICD 9 Codes:
Choose the primary diagnosis for the first ICD9 when entering charges. Use secondary
supporting ICD9 codes depending upon impairments per individual patient.
Table 1: ICD 10 Codes: may include, but are not limited to:
M16.9 Hip Osteoarthritis
M08.059 Juvenile Rheumatoid Arthritis
affecting the hip
M08.059 Rheumatoid Arthritis with
Rheumatoid factor affecting the hip
M08.859 Rheumatoid Arthritis without
Rheumatoid Factor affecting the hip
M87.059 Osteonecrosis affecting the hip
M16.300A Hip Osteoarthritis secondary to hip
dysplasia
S72.009A Femoral Neck Fracture
M84.453A Pathological femoral neck fracture
M93.259 Osteochondritis Dissecans affecting
the hip
S73.006A Hip Dislocation
Case Type / Diagnosis:
This standard of care applies to patients following hip hemiarthroplasty, total hip arthroplasty
(THA), and hip resurfacing as a result of disorders that include, but are not limited to:
• Osteoarthritis (OA)
• Rheumatoid arthritis (RA)
• Avascular necrosis (AVN)
• Congenital hip dysplasia
• Tumors/Osteosarcoma
• Traumatic joint injuries
• Rotrusio Acetabuli
• Arthritis associated with Paget's
Disease
• Ankylosing Spondylitis
• Juvenile Rheumatoid Arthritis
This standard of care serves as a guide for clinical decision-making for physical therapy (PT)
management of this patient population at Brigham and Women’s Hospital (BWH) acute care PT
services.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
2
The purpose of hip hemiarthroplasty, THA, and hip resurfacing is to reduce pain, restore
function and correct deformity by improving the biomechanics of the hip joint. This is done by
replacing the damaged joint with a prosthetic implant, realigning the soft tissues, and eliminating
structural and functional deficits. The Center of Disease Control and Prevention (CDC) reports
that each year in the United States 332,000 total hip replacements are performed
1
. In 2013
approximately 500 total hip replacements were performed at BWH
2
. The demand for primary
total hip arthroplasties is estimated to grow by 174% by the year 2030, with the demand for
revision procedures to grow by 137% within the same time frame
3
.
Surgical Techniques:
Total Hip Arthroplasty
If both the acetabulum and the femoral head are damaged then a THA may be indicated. A THA
consists of a femoral and acetabular component. During a THA the hip is dislocated exposing the
joint cavity and femoral head. The deteriorated femoral head is removed. The acetabulum is
prepared by cleaning and enlarging it with circular reamers of gradually increasing size
1
. The
new acetabular shell is implanted securely within the prepared hemispherical socket. The
acetabular socket can be made of metal, ultra-high molecular-weight polyethylene, or a
combination of polyethylene backed by metal. The plastic inner portion of the implant is placed
within the metal shell and fixed into place. Next, the femur is prepared to receive the stem. The
stem portions of most hip implants are made of titanium- or cobalt/chromium-based alloys. They
come in different shapes and some have porous surfaces to allow for bone in growth. A femoral
neck osteotomy is performed, and the hollow center portion of the bone is cleaned and enlarged,
creating a cavity that matches the shape of the implant stem. The top end of the femur is
smoothed allowing the stem to be inserted flush with the bone surface. If the ball is a separate
piece, the proper size is selected and attached. Cobalt/chromium-based alloys or ceramic
materials (aluminum oxide or zirconium oxide) are used in making the ball portions, which are
polished smooth to allow easy rotation within the prosthetic socket. The ball is seated within the
cup allowing proper alignment of the joint.
Hip replacements may be cemented, cementless, or hybrid (a combination of cemented and
cementless components), depending on the type of fixation used to hold the implant in place.
Cemented THA are more commonly recommended for older patients, for patients with
conditions such as RA, and for younger patients with compromised health or poor bone quality
and density. These patients are less likely to put stresses on the cement that could lead to fatigue
fractures
4
.
Figure 1: Total Hip Arthroplasty
http://orthoinfo.aaos.org/topic.cfm?topic=a00377

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
3
Hip Hemiarthroplasty
If only one part of the joint is damaged or diseased, a partial hip replacement, or hip
hemiarthroplasty, may be recommended. In most instances, the acetabulum is left intact and the
head of the femur is replaced, using components similar to those used in a total hip replacement.
A hip hemiarthroplasty can be either a unipolar or bipolar prosthesis. The most common form of
partial hip replacement is unipolar
1
. In a unipolar prosthesis the head is fixed to the stem. In a
bipolar prosthesis there is an additional polyethylene bearing between the stem and the
endoprosthetic head component
5
.
Hip Resurfacing
Hip resurfacing is a technique for hip arthroplasty that has recently emerged. BWH is one of the
few New England Hospitals that offers hip resurfacing. The acetabular component is replaced
similar to a total hip replacement, however the head of the femur is covered or "resurfaced" with
a hemispherical component. This fits over the head of the femur and spares the bone of the
femoral head and the femoral neck. It is fixed to the femur with cement around the femoral head
and has a short stem that passes into the femoral neck
1
. Hip resurfacing conserves bone, restores
the proximal femoral anatomy, and has lower wear rates. A meta-analysis found that patients
following hip resurfacing have better functional outcomes on the Western Ontario and the
McMaster Universities Osteoarthritis Index (WOMAC) and Harris hip score (HHS) than those
following THA
6
. Indications for hip resurfacing can include osteoarthritis, developmental
dysplasia of the hip and avascular necrosis
7
. Hip resurfacing is an option for younger patients
with more demanding lifestyles that would put them at higher risk for earlier failure of a THA.
Certain patients, however, are at greater risk for requiring revision of resurfacing, including those
with smaller femoral head size, older patients, and patients with developmental dysplasia
7
.
Figure 2: THA vs. Hip Resurfacing
http://www.methodistorthopedics.com/hip-resurfacing-arthroplasty
Revision Total Hip Arthroplasty:
Primary total hip arthroplasties have a 95% survivorship at 10 years or greater. With life
expectancy growing and younger patients with higher activity levels undergoing THA, revision
total hip arthroplasties are an unfortunate necessity
8
. The incidence of revision THA in a
fourteen month span of October 2005 to December 2006 was 51,345 patients in the United
States
9
. The reasoning for revision varies and can be due to complications following THA along
with other causes. These reasons for hip revision can be separated into three main categories:
implant-related factors, patient related factors, and failures related to surgical technique. The
most common indications may include the following:

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
4
Table 3: Reasons for Hip Revisions
Implant-related factors:
Surgical technique factors:
Periprosthetic fracture
Recurrent dislocation/instability*
Delamination of the porous coating
Infection*
Osteolysis
Malpositioning of components
Aseptic loosening*
*= leading factors requiring revision
Certain risk factors put patients at jeopardy for adverse events requiring revision THA. Patients
with RA have a higher baseline risk for infectious disease compared to the general population.
Patients with RA were found to have higher risk of prosthetic joint infections compared to
patients with OA, resulting in a need for revision
10
. Sickle cell anemia, poor bone density,
obesity, the male gender, and younger age are also risk factors that result in complications
requiring revision total hip replacement
8
.
Surgical Approach:
There are different approaches that can be used in order to perform a THA. The approach that is
chosen is based on the surgeon’s experience and patient factors. Knowing which approach was
used in addition to the specifics of the patient’s operating room report will help guide the
therapist in postoperative rehabilitation management. Each approach has a specific location for
the incision that is defined by its relation to the gluteus medius.
Posterior Approach:
The posterior (Moore) approach accesses the hip by splitting the gluteus maximus posterior to
the gluteus medius. The posterior capsule and external rotators are divided. The femur is then
flexed and internally rotated to complete exposure of the hip joint
11
.This approach gives
excellent access to the acetabulum and preserves the hip abductors. The external rotators and the
posterior capsule are repaired at the end of the procedure.
Figure 3: Posterior Approach
http://www.jaaos.org/content/15/12/707/F1.expansion
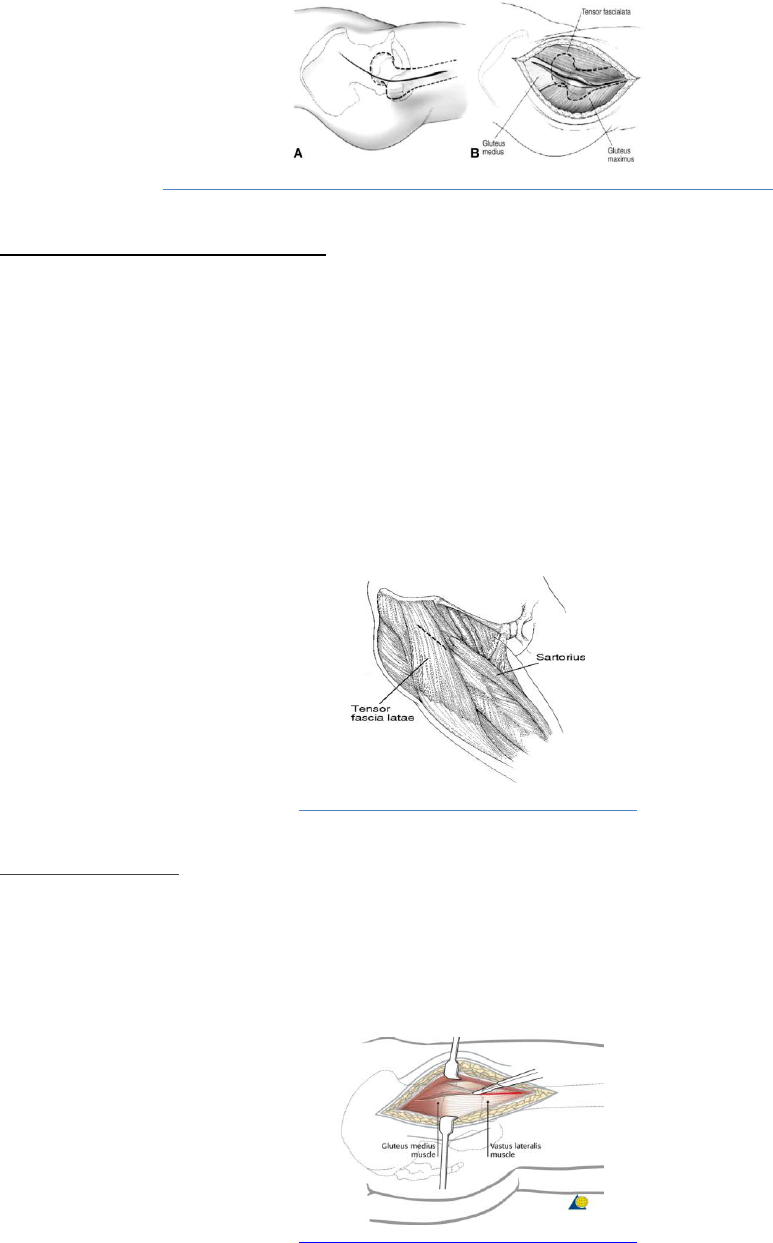
Anterior Lateral Approach:
The anterolateral (Watson-Jones) approach accesses the hip joint through the interval between
the tensor fasciae latae and the gluteus medius. The hip is dislocated anteriorly and a femoral
neck osteotomy is performed or the neck osteotomy is made in situ. The anterior fibers of
gluteus medius are often reflected from the greater trochanter and repaired at the conclusion of
the surgery
12
.
Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
5
Figure 4: Anterior Lateral Approach
http://synapse.koreamed.org/DOIx.php?id=10.5371/jkhs.2011.23.2.95&vmode=PUBREADER
Direct Anterior Approach (DAA):
The direct anterior (Heuter) approach is a modification of the Smith-Peterson (Anterior)
approach. The incision is made lateral to the anterior superior iliac spine and is carried down
through the skin and subcutaneous tissues to the fascia. The fascia over the tensor fascia lata
muscle is then split. An interval is made between the tensor fascia lata and rectus femoris
muscles. The leg is then externally rotated and the rectus femoris muscle is detached from the
anterior capsule and the femoral neck is divided. The capsule is then released. Traction is applied
to the femur to expose the acetabulum, the femoral head is removed, and the acetabular
component is placed. The femur is exposed by external rotation, extension and abduction in
order for the femoral stem to be placed. The subcutaneous tissue and fascia are sutured and the
skin is closed at the end of the procedure
13
.
Figure 5: Direct Anterior Approach
http://www.jaaos.org/content/15/12/707/F4.large.jpg
Lateral Approach:
The lateral (Bauer’s) approach requires elevation of the hip abductors (gluteus medius and
gluteus minimus) in order to access the joint. The abductors may be lifted up by osteotomy of the
greater trochanter and reapplied afterwards using wires. The hip abductors could also be divided
at their tendinous portion or through the functional tendon and repaired using sutures.
Figure 6: Lateral Approach
http://www.jaaos.org/content/15/12/707/F4.large.jpg

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
6
Trochanteric Osteotomy:
This may be an additional aspect of the surgery for any of the above procedures. This allows for
additional exposure of the hip joint by lifting the hip abductors off the greater trochanter with an
osteotomy.
Peri-Operative Medical Management:
Anticoagulation Therapy
Patients undergoing THA are often started on anticoagulants such as warfarin, heparin, low
molecular weight heparin (Lovenox), or aspirin the night before surgery to decrease risk for
blood clots. This dose is adjusted after surgery depending on the patient’s international ratio
(INR) hematology values. At the time of discharge, patients who are at a high risk for deep vein
thrombosis (DVT) will remain on anticoagulation therapy for approximately 3weeks. High-risk
patients include those who have undergone bilateral THA, have a history of prior DVT, are on
estrogen therapy, have a recent history of cancer, or have undergone THA secondary to hip
fracture
14
.
Pain Management
There are different modes of analgesia used during and after a THA. Either general or spinal
anesthesia is used during surgery. A local anesthetic pericapsular injection is also commonly
used, however not all the time, for additional pain control. General anesthesia is a combination of
intravenous (IV) drugs and inhaled gasses to produce unconsciousness and an inability to feel
pain during surgery. Spinal anesthesia is a spinal block that forms regional anesthesia. An
injection of local anesthetic is placed into the subarachnoid space typically at the level of T8.
Patients that receive spinal anesthesia are under conscious sedation during their surgery. The
pericapsular injection most commonly consists of Clonidine®, Toradol®, Epinephrine®, and
Ropivacaine® used for pain control. Clonidine® is an antihypertensive that decreases blood
pressure. Toradol® is a nonsteroidal anti-inflammatory drug (NSAID) that treats pain and
inflammation. Epinephrine® is sympathomimetic agent that relaxes muscles and tightens blood
vessels. Ropivacaine® is a local anesthetic that blocks pain by causing decreased sensation and
numbness. A study of 325 patients found that a pericapsular injection is effective in decreasing
post-operative pain and allows for early mobilization with resulting earlier discharge
15,16
. After
surgery, the patient is brought to the post anesthesia care unit (PACU) where anesthesiologists
and nurses assist with pain control. Patient’s pain is treated with IV narcotics, most often
Dilaudid® and/or Morphine®. IV pain management is often discontinued on post-operative day
1 (POD#1) and the patient is then transitioned to oral (PO) pain medication consisting of short
and long acting narcotics. Short-acting narcotics such as Oxycodone® or oral Dilaudid® are
used as needed for breakthrough pain control. If necessary, IV infusions of Morphine® or
Dilaudid® are also provided to the patient for additional breakthrough pain relief. Long-acting
narcotics such as Oxycontin® are slow release and are used to treat pain around-the-clock.
Pain management is necessary to allow patient comfort and to facilitate mobility following THA.
At BWH PT is coordinated with the nursing staff to allow for patients to receive pain medication
approximately 30-45 minutes prior to mobility. This allows for the medication to be effective
during treatment sessions. While pain management plays an important role in assisting with
mobility, there are negative side effects that narcotics can have limiting PT treatment. Nausea,
vomiting, dizziness, and drowsiness as a result of narcotics can restrict PT intervention in the

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
7
acute care setting
15
. These side effects should be assessed by the physical therapists during their
examination of the patient and should be communicated with the nurse and responding clinician.
Indications for Treatment:
The typical length of stay at BWH for patients following THA is two to three days excluding the
day of surgery. Due to the short length of stay following THA, the focus of PT management
begins on POD#1 with initial evaluation and an afternoon treatment session. Patients are then
seen by PT once a day for a treatment session on POD#2 and POD#3. The PT evaluation
includes patient education, mobility, and functional training as well as increasing ROM and
motor control of the articular and peri-articular structures of the hip joint. It is important to keep
in mind that ROM, along with proper soft tissue balance, is required to ensure proper
biomechanics in the hip joint. Therefore, PT must address both impairments in order to ensure
good outcomes.
The World Health Organization developed the International Classification of Functioning
Disability and Health (ICF) as a framework to define the spectrum of problems that patients face
with different diagnoses, including OA. Osteoarthritis causes musculoskeletal pain and is one of
the primary reasons why patients elect for THA. One study found that the ICF core set for OA
allows there to be focus on aspects of patient’s everyday life that may not have been taken into
account otherwise in their treatment when following up at three weeks, three months and six
months post THA
17
. A study of 64 patients looked at their desired functional improvements
before and after THA. The study found that a majority of the patients were concerned with
activities and partition such as walking, moving around, and recreation/leisure activities.
However at three months post THA majority of their concern was regarding dressing
18
.
Therefore PT treatment should focus on the full picture of the patient’s health, using the ICF
model as guide when tailoring treatments for patients following THA. The following are lists of
potential body structures, body functions, activities and participation limitations that may
indicate treatment in patients following THA.
Table 4: ICF: Total Hip Arthroplasty
19
Body Structure/Function(s):
Activity Limitations:
Participation Restrictions:
• Range of motion (ROM)
• Muscle performance
(including strength, power,
and endurance)
• Motor control
• Balance
• Gait
• Tissue integrity
• Pain
• Sensation
• Knowledge deficit
• Aerobic capacity/endurance
• Ventilation/gas exchange
• Bed mobility
• Transfers
• Ambulation
• Stair climbing
• Functional activities
• Basic/instrumental
activities of daily
living (B/IADLs)
• Quality of life
• Community
Mobility
• Driving
• Working

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
8
Contraindications / Precautions for Treatment:
The following post-operative activity recommendations are often included in the PT consults for
patients following THA in the acute care setting. Specific orders regarding precautions and the
approach used, however is not always included in the PT consult. It is important to review the
operative note along with the patients chart to ensure the proper activity restrictions and
precautions are followed. It may be necessary to contact the responding clinician to clarify orders
if the operative note or chart are not clear. Orders and precautions can include but are not limited
to the following:
• Weight bearing Status:
o Weight bearing as tolerated (WBAT) to full weight bearing (FWB)
o WBAT with bilateral upper extremity support
o Partial weight bearing (PWB)
• Hip Dislocation Precautions: based on the surgical approach used:
o Posterior Precautions: No hip flexion greater than ninety degrees, no hip adduction or
internal rotation beyond neutral, and none of the above motions combined.
o Limited Posterior Precautions: No combination of hip flexion greater than ninety
degrees, no hip adduction or internal rotation beyond neutral.
o Anterior Precautions: No lying flat, no prone lying, no bridging and no hip external
rotation.
o Modified Anterior Precautions: No prone lying, no bridging and no hip external
rotation.
o Direct Anterior Precautions: no bridging
o Lateral Precautions: The patient will likely have hip abduction restrictions.
o Global Precautions: most often ordered for a patient following a hip resurfacing
surgery or a revision hip surgery following multiple dislocations. This set of
precautions are a combination of both posterior and anterior dislocation precautions.
This is due to the large incision into both the posterior and anterior hip capsule to
expose the femoral head.
• Trochanteric osteotomy: If a trochanteric osteotomy is performed the orders may include
restrictions for hip abduction. It may be stated as, “passive abduction only” or “functional
abduction only.” This is to allow for bone healing and to prevent a non-union
20
.
• Positioning of the operative extremity: Positioning recommendations may include:
o Positioning the operative extremity in neutral rotation with a towel roll proximal to
the knee to prevent external rotation
o Locking the foot control of the bed in extension to prevent the operative knee from
resting in a flexed position
o Use of a hip abduction pillow or folded pillow between the patient’s lower
extremities to prevent the operative extremity from adducting

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
9
Early Post-Operative Complications:
It is important to recognize signs and symptoms of early post-operative complications and
consult with other health care providers as appropriate. The common acute care complications
following THA are:
• Blood loss requiring transfusion
15
o Decreased blood pressure, pallor appearance, fatigue, shortness of breath,
dizziness
21
• Deep vein thrombosis (DVT)
22
o calf pain or tenderness, swelling with pitting edema, increased skin temperature,
cyanosis
21
• Pulmonary embolism
22
o Chest pain, chest wall tenderness, back pain, upper abdominal pain, syncope,
shoulder pain, shortness of breathing, hemoptysis, new onset of wheezing, painful
respiration, new cardiac arrhythmia
21
• Excessive joint bleeding
o Excessive swelling, discoloration, pain
21
• Hematoma
23
o Excessive swelling, discoloration, pain
21
• Joint infection
8
o Swelling, warmth, fatigue, temperature, wound drainage, erythema
21, 24
• Joint dislocation
23, 25
o Pain, limb shortening and internal rotation, decreased hip ROM
21
• Sciatic nerve injury
24, 26
If a patient presents during the first few days post-operatively with increased pain not consistent
with surgical pain, excessive swelling, decreased muscle strength or sensation along a motor
and/or sensory nerve distribution, sudden shortness of breath and decreased oxygen saturation
along with increased resting heart rate, PT interventions must be stopped, and the medical team
consulted.
Late-Onset Post-Operative Complications:
• Skin necrosis:
o Devitalized tissue that consists of necrotic cells called eschar. Eschar is dry,
leathery and rigid. This requires drainage and potentially surgery to correct the
defect
24
.
• Persistent joint drainage in the weeks following THA:
o This complication is often treated with joint aspiration, antibiotics, and at times
debridement and joint lavage. A wound vacuum may be placed.
• Large hematoma formation:
o Patients are often advised by the surgeon to rest the hip joint, use ice to help
decrease the size of the hematoma, and stop taking anticoagulants. If the
hematoma does not resolve, patients may need surgical evacuation
21
.
• Wound healing complications in the first few weeks after surgery:
o This typically occurs in patients who are on chronic steroids or chemotherapy,
have RA, obesity, diabetes, or are active smokers. The signs and symptoms

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
10
include increased joint swelling, pain, and redness in the joint or at the site of the
incision
21
.
• Dislocation:
o A systematic literature review found that rates of hip dislocation vary depending
on the surgical approach: anterior lateral 0.70%, lateral 0.43%, and posterior
lateral with soft tissue repair 1.01%
27
. Reported dislocation rates following the
direct anterior approach were found to be 0.96% in 1037 procedures, 0.61% in
437 procedures, 1.3% in 2132 procedures and 1.5% in 1374 procedures
23
.
• Heterotrophic ossification:
o Abnormal bone growth in the muscle or other connective tissue that causes
swelling, warmth near the hip joint, and erythema along with elevated serum
alkaline phosphatase levels. Heterotrophic ossification can lead to decreased
ROM and stiffness
24
.
Evaluation:
Medical History: A patient’s past medical history should be reviewed detailing both pre-
existing medical conditions and past surgical interventions. It should be noted if
additional consults were requested prior to surgery for medical clearance. Some co-
morbid conditions that can affect outcomes are:
o Diabetes
22
o asthma
o medication-controlled hypertension
o coronary artery disease or prior myocardial infarction
o stroke with residual neurological deficits
o cancer
o renal disease requiring dialysis
o peripheral vascular disease with claudication
o Parkinson’s disease
o Rheumatoid arthritis
22
o systemic disorders
o obesity
28
History of Present Illness: Attention to pre-operative ROM, hip muscle strength, and
functional mobility are among the most important data for the physical therapist during
the medical history review. It is also imperative to review relevant diagnostic imaging
and other tests that lead to the current diagnosis and decision to pursue surgical
management. Inquire about presenting signs and symptoms, including: duration/severity,
impact on function, and any prior management of symptoms via PT, medication, or other
conservative means.
Hospital Course: Read the operative report and note positioning, approach used, if the
surgeon needed to perform a trochanteric osteotomy, or additional fixation was required.
Record the surgeon, date of surgery, type of anesthesia used and note any complications
or additional procedures intra-operatively in the initial evaluation.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
11
When reviewing the chart and orders, note any consults that were placed, post-operative
complications, and the trend of lab values, along with post-operative precautions based
on approach. Post-operative laboratory workup, especially hematocrit and INR level,
need to be monitored when evaluating a patient following THA in the acute care setting.
INR levels should not exceed 3.0 or higher and appropriateness of treatment must be
discussed with the medical team. Please refer to the General Surgery Standard of care for
further details on hematocrit and INR parameters.
Social History: Include general demographics of age, sex, and primary language. This
also consists of a review of the patient’s home environment, family/caregiver support,
occupation, patient’s goals, use of assistive devices, possession of durable medical
equipment (DME) and prior level of function considering self-care and home
management activities. For patients following THA this may also include previous
exercise routines or programs, activity levels, history of falls and participation in PT.
Medications: Review current pharmacological management of existing medical
conditions. Common pain medications used in the acute management of patients
following THA are:
o Dilaudid
o Hydromorphone
o Oxycodone
o Oxycontin
Take note of the route of administration for medications (i.e. via IV, PO, etc), as this will
help guide the examination. Record the type of pain medication the patient is receiving
and when it was last administered in the initial evaluation. Patients are also often on the
anticoagulant medication, such as Warfarin, to prevent DVT.
Examination:
Observation: Upon observation note the patient position, appearance, and
lines/drains/tubes. Foley catheters are typically discharged by 6am on POD#1 prior to the
patient being seen by PT. The following is a list of common lines/drains/tubes and
positioning devices that may be seen with patients following THA:
• Nasal Cannula for oxygen therapy
• Pneumatic (compression) boots for DVT prophylaxis
• Telemetry/cardiac depending on if there is specific co-morbid conditions
• Continuous oxygen saturation monitors
• Towel roll next to the distal thigh to prevent lower extremity external rotation
• Hemovac or Jackson Pratt (JP) drain to extract excess fluid from the operated hip
joint
• Hip abduction pillow placed between the patient’s lower extremities
o This may be removed POD #1. See posture under Musculoskeletal
examination for more details.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
12
Communication, Affect, Mental Status/Cognition, Language, and Learning Style:
The patient’s level of arousal/alertness, orientation, ability to follow commands,
communicate/make needs known, primary language and learning preferences is taken
into account and documented in the examination.
Pain:
Intensity of pain is documented at every inpatient encounter using the visual analogue
scale (VAS) or verbal report scale (VRS) if possible. Plan of action such as pre-
medication or cryotherapy is also included in the systems review. Other qualitative
details of pain that are important to obtain include the frequency, alleviating/aggravating
factors, and descriptors of pain. Pain assessment should be made pre, during and post
PT.
Musculoskeletal:
• Anthropometrics: Body Mass Index (BMI) and/or height and weight of the patient
should be included in the systems review to assist with guiding your examination and
proper fit of necessary assistive devices.
• Range of Motion: Observation or goniometric measurement of ROM of all lower
extremity (LE) joints and gross assessment of ROM of the upper extremity (UE)
joints are to be documented in the systems review. Active and passive ROM of the
operative hip is measured in supine, seated and standing. Hip flexion, extension and
abduction are measured in the supine position, flexion in the seated position, and
extension in the standing position. Limitations in ROM are also documented to
further describe the end-feel of the joint (i.e. firm, bony, empty/painful).
• Strength: Manual muscle test (MMT) or gross measurement of the LE and UE
muscles is assessed and documented. Special attention is given to assess quadriceps,
hip abductor and hip flexor strength, and the quality of an isometric quad contraction
of the quadriceps, and gluteals (i.e. trace, poor, fair, and good) via palpation and
observation. Even though joint surgery is successful at eliminating many joint related
factors, reduced muscle mass, muscle length, and weakness are not addressed by
surgical interventions. Therefore, attention to these impairments is important in
developing an appropriate treatment plan and achieving good outcomes.
• Posture: Assessment and documentation of posture and positioning in supine, sitting,
or standing are included in a systems review. Special attention should be paid to the
degree of hip rotation of the lower extremities to maintain hip precautions according
the patients specific surgical approach. If the patient has posterior precautions they
may have a hip abduction pillow between their legs that can be removed on POD #1
and a folded pillow can be placed between the patient’s lower extremities while in
supine to assist in preventing the patient from adducting their operative leg.
• Leg length: Patients will often have a shortened extremity pre-operatively secondary
to degenerative changes. Equal leg length is difficult to achieve after THA and the
surgeon will perform systematic and reproducible perioperative steps to minimize
major leg length discrepancy. Post-operatively, if the operative extremity was
lengthened, the patient may experience hip flexor tightness and pain. If a leg length
discrepancy is found after THA it can result in limping, neurological damage, patient

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
13
dissatisfaction, lumbar pain and the need for contralateral shoe lifts. A study of
twenty patients found that a leg length inequality from 1-20 mm at follow up of 16
months post-operatively does not impair the symmetry of hip kinematics and kinetics
during gait and stair climbing
29
. The patient may perceive a leg length discrepancy in
the early post-operative phase secondary to soft tissue tightness. This may take time
to resolve.
• Gait: Qualitative gait assessment is detailed with comments on the type, pattern, and
biomechanics of gait, as well as the type of assistive device used and amount of
assistance provided. Changes in stride and step length, as well as cadence should be
documented in patients with hip OA both before and after THA.
Neuromuscular:
• Sensation: Sensation testing along peripheral nerve distributions in bilateral LE for
light touch is assessed on POD#1-2 to ensure that there is no nerve damage.
Peripheral nerve palsy after primary THA ranges from 0.09% to 3.7% and in revision
THA from 0% to 7.6%. In addition to sensation changes patients may present with
other symptoms if nerve damage did occur during surgery. The following is a list of
possible nerves that may be damaged and associated symptoms
26
:
o Sciatic Nerve: the incidence of sciatic nerve palsy related to THA ranges from
0.05% to 1.9%. Patients may present with foot drop if the sciatic nerve is
injured during surgery and further neurological evaluation may be warranted
to asses both divisions of the sciatic nerve
26
. The sciatic nerve is most often
injured with use of a posterior approach for THA
30
.
▪ Peroneal Nerve: the incidence of peroneal nerve injury is 0.3% to
2.1%
26
.
o Femoral Nerve: the incidence of femoral neuropathy related to THA is 0.01%
to 2.3%. Patients will present with thigh pain, quadriceps weakness, and
anteromedial and medial paresthesias of the leg
26
. The femoral nerve can be
damaged when the direct anterior approach or anterolateral approach is used
for THA
23, 30
.
o Obturator Nerve: the incidence of obturator nerve injury is 0.01%. Injury to
the obturator nerve can present as hip adductor weakness, and groin or thigh
pain
26
. Injury to the obturator nerve with use of the lateral approach for
THA
30
.
o Superior Gluteal Nerve: There is no reported cases of injury to the superior
gluteal nerve following THA, however it is important to note that
postoperative pain and weakness of the abductors of the hip may mask injury
to this nerve
26
. Use of the lateral approach for THA puts the superior gluteal
nerve at risk for injury
30
.
• Proprioception: Hip joint proprioceptive testing may be indicated depending on where
the patient is in their post-operative course, as this may impact balance, gait, strength
and functional mobility.
• Balance: Following THA qualitative observations should be documented:
o Static and dynamic sitting balance. This may include with and without UE
support.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
14
o Static and dynamic standing balance. This may include use of an assistive
device, wide and narrow base of support, and level and uneven surfaces as
appropriate.
Particularly in the acute post-operative phase, sitting and standing balance may be
impaired, thereby impacting the overall plan of care. In the sub-acute period, patients
after THA should be examined in their ability to perform static and dynamic standing
without assistive devices, as well as unilateral standing as appropriate.
Cardiovascular/Pulmonary:
• Vital Signs: Blood pressure, heart rate, respiratory rate, and peripheral oxygen
saturation should be assessed and documented as appropriate during PT
evaluation/treatments based on the patient’s symptomatology, particularly in the early
post-operative days. As previously referenced, anemia and concomitant orthostatic
hypotension are common complications immediately after THA. They can cause
clinical symptoms such as shortness of breath, lightheadedness or dizziness, blurred
vision, and nausea. The clinical signs include drop in blood pressure with positional
changes, tachycardia, diaphoresis, and vomiting. Attention to these signs and
symptoms including appropriate documentation is important during the patient
examination following THA, in addition to communication with the clinical team
21, 24
.
• Pulmonary Status: Assess and document auscultation of breath sounds, breathing
pattern, cough quality and cough production
24
• Endurance: Examination of activity tolerance by utilizing the rate of perceived
exertion (RPE) scale or a gross subjective and objective assessment of fatigue level
should be documented in patients following THA. This should detail the amount of
functional activities the patient was able to tolerate during the exam
24
.
Integumentary:
• Dressing/Incision: The surgical incision is closed with either staples or dermabond
and covered with a clean sterile dressing of gauze held in place with tegaderm while
the patient is in the operating room. This dressings remains in place for 3-5 days to
decrease risk of infection. After 3-5 days the dressing is removed, if the incision is
draining then the gauze is replaced until it becomes clean and dry. Once the incision
is clean and dry then it will be left open to air. If the sterile dressing that placed in
operating room becomes saturated, then the dressing will be changed by the medical
team while the patient is admitted to BWH.
• Skin: Skin assessment is noted, including observation of presence/absence of
dressing, surgical incision location, discoloration/erythema, drainage, or ecchymosis.
Any pressure points due to immobility or bracing should also be assessed.
• Edema: Soft tissue edema commonly occurs immediately after THA, as well as in the
sub-acute phase. Therefore, the amount of LE edema is documented by gross
qualitative assessment, or via circumferential measurements as appropriate.
Functional Tests and Outcome Measures:
The following functional tests and measures may be used in the acute care setting and

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
15
during the home or outpatient phase of rehabilitation to assess locomotor and functional
capacity of patients status post THA:
• Timed Get Up and Go (TUG)
31
o To assess balance, fall risk, and walking ability
• Six Minute Walk Test (6MWT)
31, 32
o To assess aerobic capacity/endurance
• Hip and Knee Satisfaction Scale
33
o To assess patient satisfaction following hip/knee replacement
• Harris Hip Score (HHS)
6, 18, 32
o To assess patient satisfaction following hip/knee replacement
• Oxford Hip Score
31
o To assess patient satisfaction following hip/knee replacement
• The Hip Dysfunction and Osteoarthritis Outcome Score (HOOS)
18, 34
o To assess patient satisfaction following hip/knee replacement
• Western Ontario and the McMaster Universities Osteoarthritis Index (WOMAC)
6,
17, 31, 32, 34, 35
o To assess pain, physical function and stiffness in patients with hip/knee
OA
• Lower Extremity Functional Scale (LEFS)
36
o To assess impairment and set functional goals
• Short-Form-36 (SF-36)
17, 31
o To assess quality of life
Assessment:
PT Diagnosis:
Based on the Guide to Physical Therapist Practice
19
, patients following THA are classified
into the following practice pattern:
• 4H: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of
Motion Associated with Joint Athroplasty
19
.
Problem List:
In the first days following THA patients impairments will result in decreased independence
with bed mobility, transfers, ambulation, functional activities, basic/instrumental activities of
daily living and quality of life. Please refer to Rehabilitation Management under Indications
for Treatment for further details.
Figure 7: ICF Model
http://www.canchild.ca/en/canchildresources/internationalclassificationoffunctioning.asp

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
16
Table 4: ICF: Total Hip Arthroplasty
19
Body Structure/Function(s):
Potential impairments in body
structure may include but are
not limited to:
Activity Limitations:
Potential functional
limitations may include but
are not limited to:
Participation Restrictions:
Potential participation
restrictions may include but
are not limited to:
• Range of motion
(ROM)
• Muscle performance
(including strength,
power, and endurance)
• Motor control
• Balance
• Gait
• Tissue integrity
• Pain
• Sensation
• Knowledge deficit
• Aerobic
capacity/endurance
• Ventilation/gas
exchange
• Bed mobility
• Transfers
• Ambulation
• Stair climbing
• Functional activities
• Basic/instrumental
activities of daily
living (B/IADLs)
• Quality of life
• Community Mobility
• Driving
• Working
Prognosis:
Most patients are expected to ambulate without assistive devices within three to six weeks
after their surgery. Patients should exhibit operative hip strength >/=4+/5 MMT within 3
months following THA. The overall long-term goal for the patient is to at least return to their
pre-operative level of function with less pain; however most tend to see an overall
improvement when compared to their pre-operative function.
The degree to which patients reach these projected goals depends in part on the reason for the
THA, prior functional level, co-morbidities and post-op complications. Patients with lower
pre-operative
function may require more intensive PT intervention. This may extend recovery
times
because the patient is less likely to achieve functional outcomes
similar to those of
patients who have less pre-operative dysfunction
37
. A review of publications on the recovery
of physical functioning after THA showed improvements in: perceived physical functioning,
functional capacity such as walking and rising from a chair, and actual daily activity as
measured by WOMAC-PF, SF-36-PF and walking speed with gait analysis, 6-8 months post-
surgery
31
. A study of 437 patients found that the largest improvements for physical
impairment, activity limitations, and social participation restrictions occurs within 3 months
post-surgery. There is a rapid improvement in physical impairment seen within the first two
weeks post-surgery. Participation restrictions worsen early after THA and then quickly
improve over the next 3 months post THA. Patients that are male, non-obese, that do not

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
17
have low back pain, and that are of younger age were found to have statistically significant
better outcomes over time post THA. This study also found that although the greatest
improvements occurs by 3 months post-operatively, a 28% of total improvements in ICF
constructs occurs between 3 and 12 months post THA
34
.
Goals: Typical goals following THA are as follows and should be tailored/individualized
based on the unique characteristics of each individual patient:
Short Term Goals: The short term goals for this patient population during their hospital
course are:
Within 2-3 days:
1. The patient will be independent and able to demonstrate knowledge of safety and
compliance with hip precautions and positioning with all mobility.
2. The patient will perform all bed mobility and transfers with least amount of assistance
and devices.
3. The patient will ambulate household distances (50-100 feet) and negotiate stairs with
a step-to or step-through pattern, with least amount of assistance and devices.
4. The patient will demonstrate a fair to good isometric quad contraction and MMT of
>/= 3-/5 to increase independence with bed mobility, transfers, and ambulation.
5. The patient will be independent with home exercise program and activity precautions.
*These short term goals will vary depending on the patient’s prior level of function, as
well as the patient’s own personal goals.
Long Term Goals: The long term goals for this patient population are:
Within 2-4 weeks:
1. Independent gait with unilateral upper extremity support of a crutch/cane for
greater than or equal to three hundred feet.
2. Initiation of standing and balance therapeutic exercise program.
3. Initiation of use of stationary bicycle within precautions if one is available.
Within 4-6 weeks:
1. Ambulate greater than or equal to five hundred feet with least restrictive device.
2. Progression to use of no assistive device by home/outpatient PT.
3. Initiation of outpatient PT program.
Within 8-10 weeks:
1. Return to work as applicable.
2. Ambulate community distances with no assistive device.
Treatment Planning / Interventions
Established Pathway ___ Yes, see attached. _X_ No
Established Protocol _X__ Yes, see attached. __ No

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
18
Interventions most commonly used for this case type/diagnosis:
A study of 57 patients following primary THA randomly assigned twice daily PT and
showed earlier achievement of functional milestones than those of the control group who
received PT only once-daily
38
. At BWH patients receive PT twice on POD#1 and are
educated on independent therapeutic exercise program and encouraged to complete the
program 3-5 times a day. Their independent therapeutic exercise program typically
consists of exercise that target muscles of the hip, knee and ankle and are focused on
increasing strength and ROM. Treatments that may be initiated in a patient following
THA as deemed appropriate by the evaluating PT are as follows:
• Flexion, extension, abduction (if indicated), and adduction Active/Active
Assisted/Passive ROM of operative hip
32, 39
.
• Therapeutic exercise/strength training with focus on isometric and functional hip
flexor and quadriceps control, hamstrings, as well as hip abductors, adductors,
and gluteal muscles
32, 39
.
• Respiratory and circulatory exercises starting POD#1, to include deep breathing,
coughing, and ankle pumps. A systematic review that looked at a study of 14
patients found that a progressive arm-interval exercise program with an arm
ergometer improved patient’s distances with the 6-minute-walk test following
THA
32
.
• Seated closed chain exercises progressing to standing closed chain exercises when
the patient demonstrates good pain control, muscle strength, and balance
32, 40
.
• Resistive Exercises for the quadriceps and hamstrings are generally not used in
the acute phase of rehabilitation. However a study of 36 patients found that a
progressive resistive training program for the first 12 weeks post operatively
improved maximal dynamic muscle strength by 30% and improved stair climbing
power by 35% when compared to use of electrical stimulation and standard
rehabilitation
32, 41
.
• Gait training on even surfaces, stair training and uneven terrain as indicated
• Balance and coordination activities
• Body mechanics and postural exercises
Functional Training in Self-Care and Home Management:
Starting on POD#1 bed mobility and transfer and basic/instrumental activities of daily
living training is started in order to promote the patient’s independence. Patients are
educated on the use of proper assistive devices and equipment as indicated. This can
include use of a bedrail, or transfer devices. The goal is to gradually progress patient’s
mobility without assistive equipment by POD#2-3 to allow them to function safety and
independently in their home environment. Vehicle transfers are also introduced and
reviewed with the patient prior to discharge home.
Prescription and Application of Appropriate Assistive Devices/Durable Medical
Equipment:
Patients are measured, fit, and trained with the most appropriate assistive device to
increase safety and independence during ambulation and transfers. The most common
ambulatory devices used in patients immediately following THA are walkers (standard or

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
19
rolling), axillary crutches, and in some cases, only a straight cane or a single crutch. As
patients mobility improves and as safety allows they will be progressed to the least
restrictive assistive devices. Other durable medical equipment (DME) generally used or
recommended to facilitate safe and independent transfers include commodes, raised toilet
seats, ADL equipment, and tub/shower seats.
Frequency & Duration:
Patients are generally in the hospital for 2-3 days post-operatively. Patients are followed
at a frequency of five to seven times per week and are reassessed every 7-10 days if they
remain in BWH. Most patients do not stay in the acute care hospital greater than 3 days
unless there are post-operative complications. The expected number of visits per episode
of care ranges from 12 to 60. The various episodes of care following THA consist of
inpatient acute care PT, short-term rehabilitation or home PT, and outpatient PT (when
indicated). Based on the Guide to Physical Therapist Practice, it is anticipated that 80%
of patients will achieve their anticipated goals and expected outcomes during this time
frame of visits
19
.
During the acute care stay, THA patients are typically seen once daily,
except on POD#1 when they are seen for their initial evaluation and an afternoon
treatment session. The focus of treatment during this time is on improving hip joint
ROM, muscle control and balance, and functional independence. If outpatient care is
required, ROM, strength, proprioception, gait, balance, and swelling impairments should
be assessed and treatment should be progressed as appropriate in order to maximize
functional outcomes.
Patient / family education:
Education for patients undergoing a THA is an integral component of the clinical
pathway for these patients. Pre-operative joint class is available for patients to prepare
them for their surgery and recovery. Most orthopedic surgeons at BWH refer and highly
recommend that their patients attend joint class to obtain knowledge in preoperative
preparation, hospital stay, surgical procedure, expectations following surgery and
rehabilitation. Interdisciplinary handouts and educational videos are offered as part of
BHW’s pre-operative education and are available on the orthopedic website. Pre-
operative education can reduce a patient’s hospital stay by twenty four hours by
promoting early functional recovery and improving functional outcomes
15
. Pre-operative
exercise programs are also beneficial for patient outcomes after surgery. A systematic
review of randomized control studies found that exercise-based intervention prior to a
total hip replacement reduces pain and improves physical function
35
.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
20
Education for patients and their families/caregivers is continued throughout their stay at
the hospital. On POD #1 they are educated on:
• Correct positioning of the operative LE
• Hip dislocation precautions
• Importance of initiating early mobility
• Safety with mobility and use of appropriate assistive devices
• Weight bearing precautions (if indicated)
• PT plan of care: including independent exercises, and the expected discharge
goals and outcomes.
Patients are provided with education handouts that outlines the above information for
future reference and for use at home after discharge. The white boards located in each
patient room can also be utilized to write down goals and recommendations for nursing
staff.
Recommendations and referrals to other providers:
• Occupational Therapy (OT): Patients who are in need of assistance for B/IADL
are referred to occupational therapy for training with appropriate adaptive
equipment. OT is generally consulted immediately post-operatively in
conjunction with PT. Occupational therapy will assess a patient if the patient’s
plan is to discharge home, or if a patient may potentially have specific OT needs
secondary to pre-existing co-morbidities. Occupational therapy is consulted to
assess a patient’s ability to comply with dislocation precautions during activities
such as toileting, dressing, and ADL’s. OT generally evaluates a patient on
POD#2 to maximize participation and independence with B/IADL’s. OT can
provide a patient with special equipment to optimize a patient’s independence
with ADL’s. Equipment could include: sock donner, long handled sponge, shoe
horn, grabber, elastic shoe laces, leg lifter etc. If the patient’s plan is to discharge
to a rehab facility generally OT is deferred while in the inpatient setting to the
rehab setting to optimize ability to participate.
• Ortho Tech: Ortho techs are consulted on a case by case basis to place a bed
frame and trapeze on the beds of patients following a THR to allow the patient to
perform bed mobility and weight shifting as appropriate. Ortho techs will also be
consulted if a hip abduction brace is indicated. A hip abduction brace is used if a
patient has had pervious hip surgery with multiple dislocations, or during the
surgery the surgeon assessed that the patient was going to require external support
to prevent dislocation. Fitting a hip abduction brace can be performed the day
that the order is placed and the physical therapist should accompany the ortho
tech for the initial fitting. It is the physical therapists role to clarify ROM orders
for the brace and a wearing schedule, as well as progress the patient’s bed and
transfer mobility. Please see the hip abduction procedure guide on the T drive for
additional information.
• Social Work: Social workers may be consulted in complicated situations where
patients may have difficulty coping with recovery and have limited social
supports.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
21
• Care Coordination: An appointment is made for most patients prior to their THA
with a Care Coordinator at the Preoperative Clinic. A Care Coordinator is a
registered nurse that specializes in discharge planning. Since the length of stay
following a THA is short it is important to initiate discharge planning prior to
surgery. A Care Coordinator will screen patients based on their living situation,
social supports, prior level of function, and home environment to help create safe
discharge plans based on each patient’s individual needs. They will meet with
patients following THA on POD#1 and facilitate all discharges both to home and
rehabilitation facilities, provide clinical updates to insurance companies, and
arrange transportation to another facilities as needed.
Re-evaluation
The average inpatient length of stay following THA is 3 days. Patients are re-evaluated on a
daily basis with respect to their ROM, quality of movement, muscle contraction, pain intensity,
gait quality, and functional independence. If the patient’s hospital course is prolonged due to
complications, a formal re-evaluation will be performed every 7-10 days to re-assess progression
towards the previously outlined goals and outcomes. In the outpatient setting, the patient is to be
formally re-evaluated every 30 days; however impairments such as ROM should be monitored
each visit. A re-evaluation is also indicated if there has been a significant change in signs and
symptoms.
Discharge Planning
Commonly expected outcomes at discharge:
It is expected that most patients following THA will be discharged home after the
inpatient acute care phase. Several factors including age, co-morbidities, living situation
and support at home all may contribute to a patients discharge to short term rehabilitation
versus home. Commonly expected outcomes for discharge home are the ability to
comply with hip dislocation precautions with all mobility, the ability to perform bed
mobility and functional transfers independently, safely ambulate household distances of
50-100ft on even and uneven surfaces with an assistive device, and improve hip ROM
and strength as identified in the goals.
Transfer of Care:
Discharge planning is often started at the patient’s pre-operative visit with Care
Coordination. During the initial PT evaluation discharge recommendations are
established from a PT perspective. Communication with care coordination and patient’s
multidisciplinary team will help to ensure successful transition of care and should be
docummented in the patient’s medical record. Discharge recommendations should be
documented in the initial physical therapy evaluation and any other encounter notes as
appropriate. The selection of a discharge destination takes planning and careful
consideration of multiple factors such as patient’s social supports, living environment,
and their functional mobility progress with skilled PT while at BWH. Proper
documentation and communication of discharge recommendations will facilitate in the
patients transfer of care to either home with services or to an extended care facility.

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
22
Patient’s discharge instructions:
• Review with the patient and family/caregivers dislocation precautions, safety,
assist needed at home, use of proper assistive devices and equipment, proper gait
and stair climbing techniques, positioning and home therapeutic exercise.
• Provide patients and their family/caregivers with education handouts that outline
importance information that has been reviewed throughout PT sessions while at
BWH.
Authors: Reviewed by:
Jessica Lesage, PT Brendan Connor, PT
December, 2015 Carolyn Beagan, PT
PUT ON ELLUCID AWAITING LINDA”S FINAL APPROVAL

Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
23
REFERENCES:
1. American Academy of Orthopedic Surgeons. Orthopedic Hip Replacement. Available
at:http://www.niams.nih.gov/Health_Info/Hip_Replacement/default.asp Retrieved
October 24, 20014.
2. Brigham and Women’s Hospital. Hip Replacement. Available at:
http://www.brighamandwomens.org/Departments_and_Services/orthopedics/resources/hi
p-replacement.aspx Retrieved October 24,2014
3. Kurtz, S., Ong, K., Lau, E., Mowat, F., & Halpern, M. (2007). Projections of primary and
revision hip and knee arthroplasty in the united states from 2005 to 2030. The Journal of
Bone and Joint Surgery.American Volume, 89(4), 780-785.
4. Joint Replacement Institute. Types of Hip Replacement and Methods of Fixation.
Available at: http://www.jri-docs.com/hip-resurfacing-replacement/hip-
replacement/resources/types-of-hip-replacement-and-methods-of-fixation Retrieved
February 23, 2015.
5. Bhattacharyya, T., & Koval, K. J. (2009). Unipolar versus bipolar hemiarthroplasty for
femoral neck fractures: Is there a difference? Journal of Orthopaedic Trauma, 23(6),
426-427.
6. Smith, T. O., Nichols, R., Donell, S. T., & Hing, C. B. (2010). The clinical and
radiological outcomes of hip resurfacing versus total hip arthroplasty: A meta-analysis
and systematic review. Acta Orthopaedica, 81(6), 684-695.
7. Prosser, G. H., Yates, P. J., Wood, D. J., Graves, S. E., de Steiger, R. N., & Miller, L. N.
(2010). Outcome of primary resurfacing hip replacement: Evaluation of risk factors for
early revision. Acta Orthopaedica, 81(1), 66-71.
8. Ulrich, S. D., Seyler, T. M., Bennett, D., Delanois, R. E., Saleh, K. J., Thongtrangan, I.,
et al. (2008). Total hip arthroplasties: What are the reasons for revision? International
Orthopaedics, 32(5), 597-604.
9. Bozic, K. J., Kurtz, S. M., Lau, E., Ong, K., Vail, T. P., & Berry, D. J. (2009). The
epidemiology of revision total hip arthroplasty in the united states. The Journal of Bone
and Joint Surgery.American Volume, 91(1), 128-133.
10. Bongartz, T., Halligan, C. S., Osmon, D. R., Reinalda, M. S., Bamlet, W. R., Crowson, C.
S., et al. (2008). Incidence and risk factors of prosthetic joint infection after total hip or
knee replacement in patients with rheumatoid arthritis. Arthritis and Rheumatism, 59(12),
1713-1720.
Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
24
11. Suh, K. T., Park, B. G., & Choi, Y. J. (2004). A posterior approach to primary total hip
arthroplasty with soft tissue repair. Clinical Orthopaedics and Related Research,
(418)(418), 162-167.
12. Masonis, J. L., & Bourne, R. B. (2002). Surgical approach, abductor function, and total
hip arthroplasty dislocation. Clinical Orthopaedics and Related Research, (405)(405),
46-53.
13. Lovell, T. P. (2008). Single-incision direct anterior approach for total hip arthroplasty
using a standard operating table. The Journal of Arthroplasty, 23(7 Suppl), 64-68.
14. Beksac, B., Gonzalez Della Valle, A., & Salvati, E. A. (2006). Thromboembolic disease
after total hip arthroplasty: Who is at risk? Clinical Orthopaedics and Related Research,
453, 211-224.
15. Ibrahim, M. S., Khan, M. A., Nizam, I., & Haddad, F. S. (2013). Peri-operative
interventions producing better functional outcomes and enhanced recovery following
total hip and knee arthroplasty: An evidence-based review. BMC Medicine, 11, 37-7015-
11-37.
16. Kerr, D. R., & Kohan, L. (2008). Local infiltration analgesia: A technique for the control
of acute postoperative pain following knee and hip surgery: A case study of 325 patients.
Acta Orthopaedica, 79(2), 174-183.
17. Pisoni, C., Giardini, A., Majani, G., & Maini, M. (2008). International classification of
functioning, disability and health (ICF) core sets for osteoarthritis. A useful tool in the
follow-up of patients after joint arthroplasty. European Journal of Physical and
Rehabilitation Medicine, 44(4), 377-385.
18. Heiberg, K. E., Ekeland, A., & Mengshoel, A. M. (2013). Functional improvements
desired by patients before and in the first year after total hip arthroplasty. BMC
Musculoskeletal Disorders, 14, 243-2474-14-243.
19. Guide to Physical Therapist Practice; 2nd Edition, APTA. Phys Ther 2001; 81: 9-744.
20. Lakstein, D., Backstein, D. J., Safir, O., Kosashvili, Y., & Gross, A. E. (2010). Modified
trochanteric slide for complex hip arthroplasty: Clinical outcomes and complication rates.
The Journal of Arthroplasty, 25(3), 363-368.
21. Dutton, M. (2008). Orthopaedic examination, evaluation, and intervention (2nd ed.). New
York: McGraw-Hill Medical.
22. Soohoo, N. F., Farng, E., Lieberman, J. R., Chambers, L., & Zingmond, D. S. (2010).
Factors that predict short-term complication rates after total hip arthroplasty. Clinical
Orthopaedics and Related Research, 468(9), 2363-2371.
Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
25
23. Barton, C., & Kim, P. R. (2009). Complications of the direct anterior approach for total
hip arthroplasty. The Orthopedic Clinics of North America, 40(3), 371-375.
24. Sullivan, S. (2007). Physical rehabilitation (5th ed.). Philadelphia: F.A. Davis.
25. Kotwal, R. S., Ganapathi, M., John, A., Maheson, M., & Jones, S. A. (2009). Outcome of
treatment for dislocation after primary total hip replacement. The Journal of Bone and
Joint Surgery.British Volume, 91(3), 321-326.
26. Brown, G. D., Swanson, E. A., & Nercessian, O. A. (2008). Neurologic injuries after total
hip arthroplasty. American Journal of Orthopedics (Belle Mead, N.J.), 37(4), 191-197.
27. Kwon, M. S., Kuskowski, M., Mulhall, K. J., Macaulay, W., Brown, T. E., & Saleh, K. J.
(2006). Does surgical approach affect total hip arthroplasty dislocation rates? Clinical
Orthopaedics and Related Research, 447, 34-38.
28. Huddleston, J. I., Wang, Y., Uquillas, C., Herndon, J. H., & Maloney, W. J. (2012). Age
and obesity are risk factors for adverse events after total hip arthroplasty. Clinical
Orthopaedics and Related Research, 470(2), 490-496.
29. Benedetti, M. G., Catani, F., Benedetti, E., Berti, L., Di Gioia, A., & Giannini, S. (2010).
To what extent does leg length discrepancy impair motor activity in patients after total
hip arthroplasty? International Orthopaedics, 34(8), 1115-1121.
30. Uskova, A. A., Plakseychuk, A., & Chelly, J. E. (2010). The role of surgery in
postoperative nerve injuries following total hip replacement. Journal of Clinical
Anesthesia, 22(4), 285-293.
31. Vissers, M. M., Bussmann, J. B., Verhaar, J. A., Arends, L. R., Furlan, A. D., & Reijman,
M. (2011). Recovery of physical functioning after total hip arthroplasty: Systematic
review and meta-analysis of the literature. Physical Therapy, 91(5), 615-629.
32. Di Monaco, M., Vallero, F., Tappero, R., & Cavanna, A. (2009). Rehabilitation after total
hip arthroplasty: A systematic review of controlled trials on physical exercise programs.
European Journal of Physical and Rehabilitation Medicine, 45(3), 303-317.
33. Mahomed, N., Gandhi, R., Daltroy, L., & Katz, J. N. (2011). The self-administered
patient satisfaction scale for primary hip and knee arthroplasty. Arthritis, 2011, 591253.
34. Davis, A. M., Perruccio, A. V., Ibrahim, S., Hogg-Johnson, S., Wong, R., Streiner, D. L.,
et al. (2011). The trajectory of recovery and the inter-relationships of symptoms, activity
and participation in the first year following total hip and knee replacement. Osteoarthritis
and Cartilage / OARS, Osteoarthritis Research Society, 19(12), 1413-1421.
35. Gill, S. D., & McBurney, H. (2013). Does exercise reduce pain and improve physical
function before hip or knee replacement surgery? A systematic review and meta-analysis
Standard of Care: Total Hip Replacement
Copyright © 2015 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved
26
of randomized controlled trials. Archives of Physical Medicine and Rehabilitation, 94(1),
164-176.
36. Yeung, T. S., Wessel, J., Stratford, P., & Macdermid, J. (2009). Reliability, validity, and
responsiveness of the lower extremity functional scale for inpatients of an orthopaedic
rehabilitation ward. The Journal of Orthopaedic and Sports Physical Therapy, 39(6), 468-
477.
37. Petersen, M. K., Andersen, N. T., & Soballe, K. (2008). Self-reported functional outcome
after primary total hip replacement treated with two different periopera-tive regimes: A
follow-up study involving 61 patients. Acta Orthopaedica, 79(2), 160-167.
38. Stockton, K. A., & Mengersen, K. A. (2009). Effect of multiple physiotherapy sessions
on functional outcomes in the initial postoperative period after primary total hip
replacement: A randomized controlled trial. Archives of Physical Medicine and
Rehabilitation, 90(10), 1652-1657.
39. Jesudason, C., & Stiller, K. (2002). Are bed exercises necessary following hip
arthroplasty? The Australian Journal of Physiotherapy, 48(2), 73-81.
40. Trudelle-Jackson, E., & Smith, S. S. (2004). Effects of a late-phase exercise program
after total hip arthroplasty: A randomized controlled trial. Archives of Physical Medicine
and Rehabilitation, 85(7), 1056-1062.
41. Suetta, C., Andersen, J. L., Dalgas, U., Berget, J., Koskinen, S., Aagaard, P., et al. (2008).
Resistance training induces qualitative changes in muscle morphology, muscle
architecture, and muscle function in elderly postoperative patients. Journal of Applied
Physiology (Bethesda, Md.: 1985), 105(1), 180-186.
