1
REPORT
Evaluation of Postdoctoral NRSA T32 Institutional Training Grant Program
National Institute of General Medical
S
c
i
ence
Panel Roster
Chair
Schwinn, Debra A., M.D.
Professor of Anesthesiology, Pharmacology, Biochemistry
Associate Vice President for Medical Affairs
Carver College of Medicine
University of Iowa
Members
Beaudet, Arthur L., M.D.
Professor
Department of Molecular and Human Genetics
Baylor College 0f Medicine
Coopersmith, Craig M., M.D.
Professor of Surgery
Emory University School of Medicine
Gutierrez-Hartmann, Arthur, M.D.,
Professor Departments of Medicine and of Biochemistry & Molecular Genetics
University of Colorado Anschutz Medical Campus
Mayeux, Philip R., Ph.D.
Department of Pharmacology and Toxicology
University of Arkansas For Medical Sciences
Nakamoto, Robert K., Ph.D.
Professor, Department of Mol. Physiology & Biophysics
University of Virginia
Whittington, Robert A, M.D.
Professor, Dept of Anesthesiology
Columbia University-
John G Younger, M.D.
Chief Technology Officer and Director
Akadeum Life Sciences, Inc
2
Executive Summary
NIGMS’s postdoctoral National Research Service Award (NRSA) T32 Institutional Training Grants
seek to increase physician involvement in research in 4 areas of biomedicine that fall within
NIGMS’s purview due to broad, systemic mechanisms of disease/treatment. These areas include
Medical Genetics; Clinical Pharmacology; Burn, Trauma, and Perioperative Injury; and
Anesthesiology. In May 2018, the NIGMS convened an external panel of experts as a working group
of the NIGMS Advisory Council to examine whether these institutional clinical postdoctoral research
training (CPRT) T32 programs are achieving their goal.
Overall, the panel noted that postdoctoral institutional T32 grants are a common NIH-wide pathway
for developing physician scientists through mentored research during later years of training (e.g.,
residency, fellowship, transition to faculty). This makes them distinct from predoctoral programs
such as the NIGMS Medical Scientist Training Program (MSTP leading to the MD-PhD degree).
U.S. MD-PhDs practice in surgical disciplines, anesthesiology, emergency medicine, or critical care
medicine only 13% of the time, whereas 21% of all U.S. physicians are in these fields. This means
fewer medical scientists trained at the predoctoral stage are active in these focus areas. Given this,
the panel found that the NIGMS CPRT T32 program supports physician scientist research training
opportunities in these research areas that are not supported by other categorical NIH Institutes.
While the panel was able to make a meaningful assessment of NIGMS postdoctoral T32 program
outcomes with the considerable amount of data provided by the NIGMS Office of Program Planning,
Analysis and Evaluation (OPAE), it should be noted that outcome parameters may have been
underestimated as some data were not accessible (e.g., research funding by industry or other
national federal/non-federal entities, details of faculty appointment, etc.). Overall, NIGMS
postdoctoral T32 programs demonstrate similar outcomes in terms of grant applications/awards,
publications, and faculty status, compared with other postdoctoral T32s across the NIH.
Achievement of senior faculty status (%) also compares favorably with MSTP graduates. Of note,
in terms of diversity (higher % under-represented minorities and women), NIGMS CPRT T32s
compare favorably with other postdoctoral T32 and MSTP programs, and significantly better than
K08/K23 programs. Approximately 34% of all NIGMS postdoctoral T32 trainees ultimately apply for
investigator-initiated NIH research grants, with 54% of those applicants receiving subsequent NIH
funding (≈20% overall). Those with at least one funded grant averaged 3.1 to 4.4 grants per funded
trainee depending upon their CPRT focus area. This proportion of trainees receiving NIH grant
funding is approximately half that achieved by individual K08 awardees. However, panel members
cited the need for trainees to generate data (often within the context of a postdoctoral T32 training
program) to compete successfully for K08/K23 or R01 funding. Panel members also noted that the
impact of institutional T32 training grants goes beyond supporting individuals, to positively
influencing programs and institutions in developing physician scientists.
Given these findings, the panel recommends that NIGMS maintain its support for the CPRT
postdoctoral NRSA programs and that the focus be assessed with regards to changes in clinical
research and practice, as well as changes in financial obstacles to training of clinician scientists
that have occurred since the inception of the programs. The issues for each research focus are
unique and need to be considered individually. Finally, the panel notes that NIGMS (and ideally,
3
the NIH more broadly) should delineate clear goals for all training programs and develop metrics
that will allow continuous assessment of program success individually and nationally.
Introduction
Institutional Postdoctoral T32s are part of the Ruth L. Kirschstein National Research Service Award
(NRSA)s established in 1974 by the National Research Service Award Act; this award mechanism
has been in continuous operation since that time. Within NIGMS, postdoctoral institutional T32s
support researchers in 4 specified shortage areas: 1) Medical Genetics; 2) Clinical Pharmacology;
3) Burn, Trauma, and Perioperative Injury; and 4) Anesthesiology. These clinical research programs
are located in NIGMS because they address broad, systemic mechanisms of disease/treatment
and therefore do not fit into the missions of the disease- or organ systems-based categorical NIH
Institutes. NIGMS’s NRSA program has been a primary means of supporting clinical postdoctoral
research training programs relevant to the NIH mission for the last 40 years. Physicians interested
in research often do not have the protected time necessary to begin or continue scientific
training/work through their residency, fellowship, and early career years. Programs developed with
these institutional training grants provide protected and mentored research time for physicians to
develop skills and identities as scientists, and to train in basic or clinical/translational areas. These
institutional grants aim to prepare trainees for careers that have a significant impact on the health-
related research needs of the Nation.
Institutions receiving these awards are expected to include training opportunities in the fundamental
concepts of multidisciplinary research, as well as research techniques critical to trainee areas of
focus. Additional program activities have included attendance at local and national scientific
meetings and workshops, training in specific methods or analytic techniques (sometimes including
working toward a MS or MPH degree), and training designed to enhance research independence
and scientific capability. This clinical postdoctoral research training (CPRT) program aims to
enhance and develop research training for physicians interested in research careers relevant to the
NIH mission. Specific program goals focus on increasing the number of clinicians trained in
research methodology and the number of physicians involved in research throughout the course of
their careers.
Overview of NIGMS Postdoctoral T32 Program (1990-2016)
History: Program began in 1974; data examined by the evaluation panel covered years 1990-
2016.
Goal: Develop physician scientists through mentored research during later years of clinical training.
Why Train Physician/Clinician Scientists? Clinician scientists are uniquely trained to bridge the
gap between scientific discoveries and clinical medicine. This small cadre of physicians, trained in
both clinical medicine and science (basic, translational, clinical) identify challenging clinical
problems and bring them to the laboratory, as well as translate new laboratory discoveries to the
clinic. As reported in the NIH Physician-Scientist Workforce Working Group Report in 2014,
1
physician scientists are considered an endangered species in the medical workforce, making
dedicated training pathways imperative.
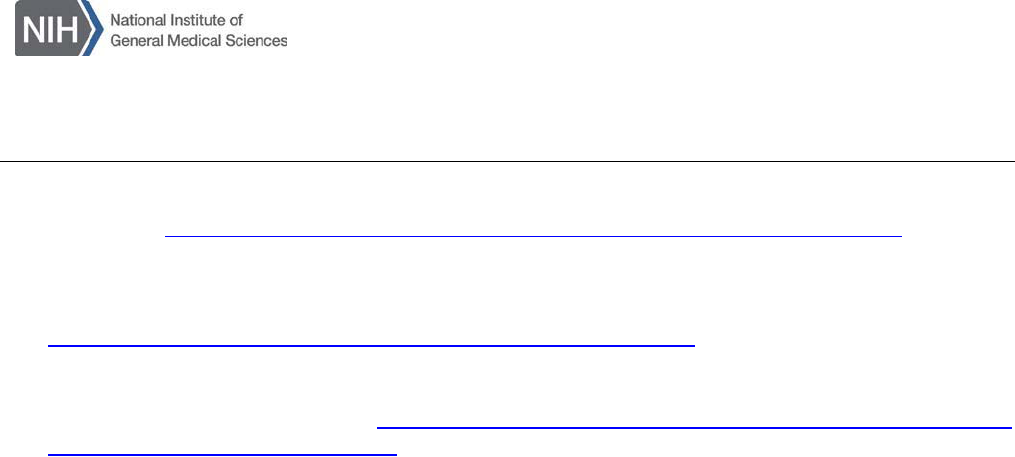
Postdoctoral T32 Intervention Timing: Postdoctoral research training occurs during post-
medical school residency, fellowship, or transition to faculty years (Figure 1).
4
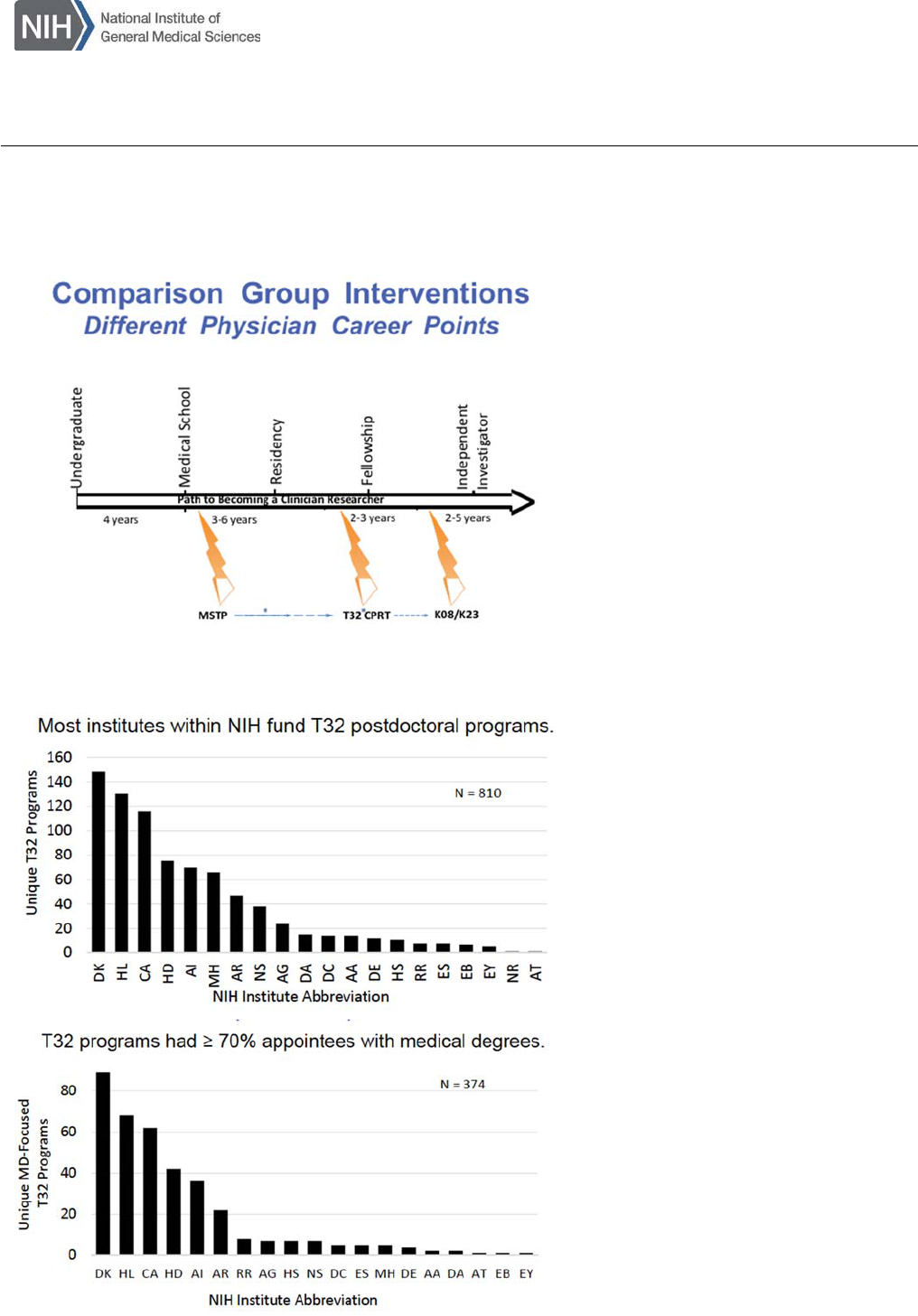
NIH Institutes Participating in Postdoctoral T32 Research Training: Virtually all NIH Institutes
participate in postdoctoral T32 training programs. Specifically, 20 NIH Institutes besides NIGMS
sponsor primarily clinical postdoctoral T32 programs. Between 1999 and 2003 there were 810
unique postdoctoral programs funded by these 20 institutes (defined as programs with >90%
postdoctoral trainees) and of these, 374 have ≥70% trainees with medical degrees (Figure 2).
Years of CPRT T32 Training: At least 2 years of training are expected (80% overall research
effort).
Location of Current NIGMS CPRT T32 Awardees: In 2016, NIGMS supported 45 T32 programs
at 35 institutions in 21 states across the U.S.
Total number of NIGMS CPRT program participants (1990-2016): 2119
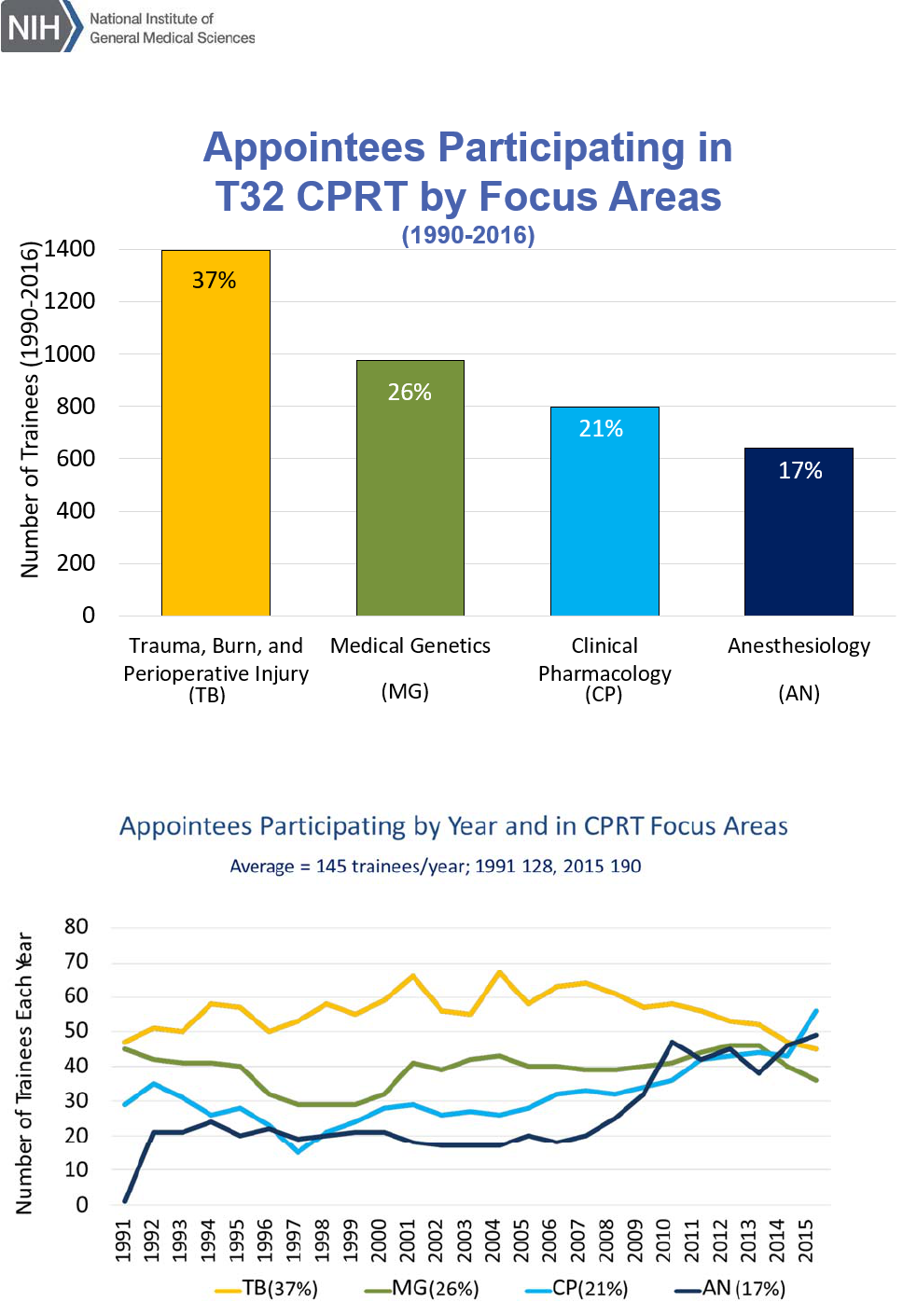
Four Current NIGMS CPRT (T32) Programs / Focus Areas (Figures 3 and 4):
Medical Genetics (26%)
Clinical Pharmacology (21%)
Burn, Trauma, and Perioperative Injury (37%)
Anesthesiology (17%)
Number of CPRT T32 Awards Per Year: From 1992-2015, the number of CPRT T32 trainees
grew from 120 to 190/year, averaging 145/year over that time period. Given 190 trainees in 45 T32
programs in the U.S. in 2015/2016, this averages 4.2 trainees per program (including all training
years).
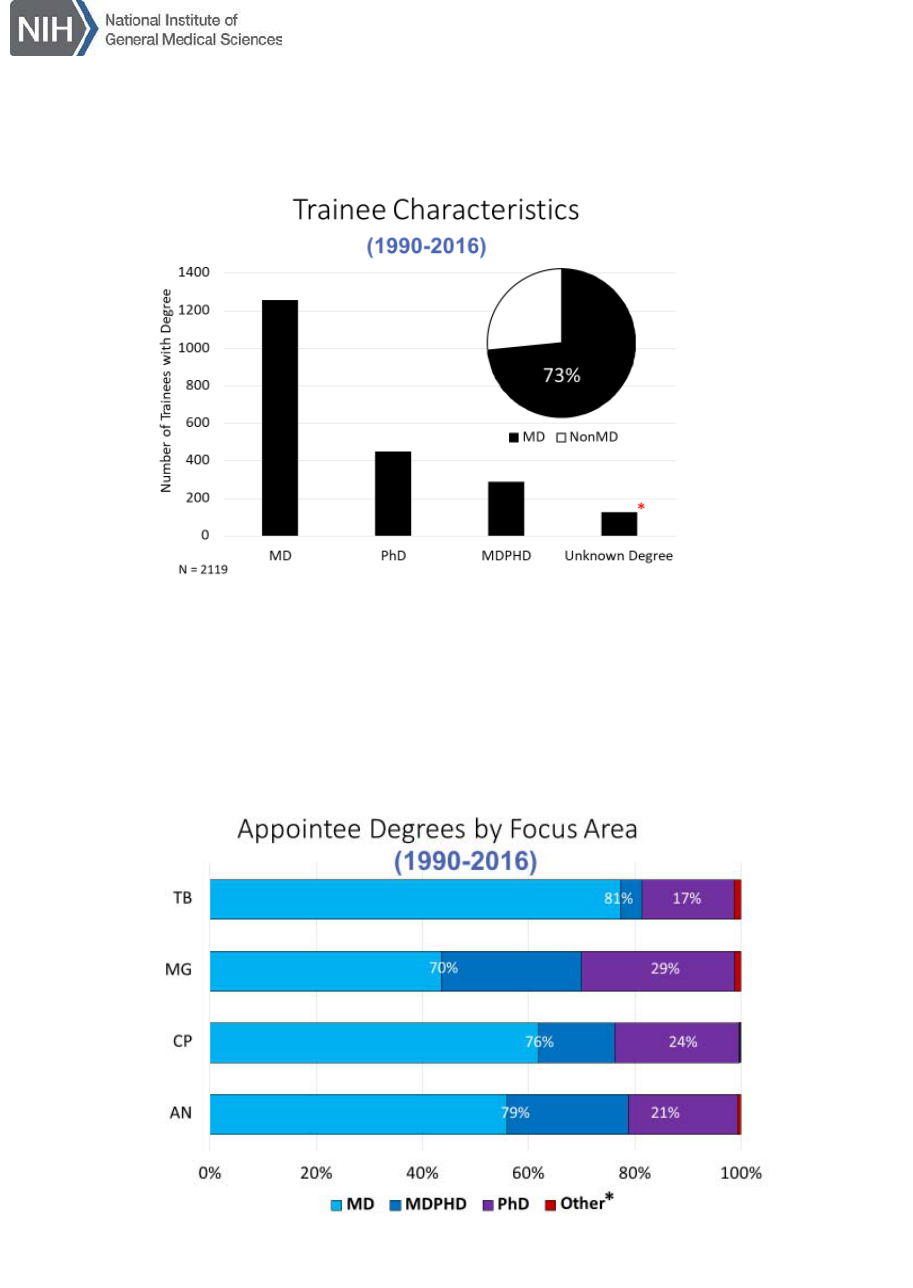
Trainee Characteristics: On average 73% of the 2119 program trainees are physicians (MD 60%,
MD-PhD 13%) (Figure 5). The percentage of MD versus PhD trainees for each T32 program is
shown in Figure 6.
Percent NIGMS CPRT T32 Trainees Who Completed the MSTP Program: 4% of NIGMS T32
trainees were former NIGMS MSTP trainees.
Comparison Groups
The panel determined that the best comparator group for NIGMS postdoctoral CPRT T32 programs
is similar postdoctoral T32 programs supported by other NIH Institutes. However, data available for
this comparison was limited to application and success data for NIH awards. Since MSTP programs
train MD-PhD students and the training is longer, occurs during medical school in generally a much
wider array of research areas, the committee felt MSTP programs were not a good comparison for
the CPRT programs. Similarly, the K mechanisms support trainees at later career stages and differ
in the type of mentorship and in their selection criteria. Thus, although not good comparators for
this assessment, the latter groups proved useful in providing some insights into the broader issues
and nature of training and support of physician scientists.
Caveats
NIGMS Postdoctoral CPRT T32 Programs in Context: In assessing the CRPT programs it is
critical to recognize broader issues in the overall national effort to train and develop a highly skilled
workforce of physician scientists.
1
Since these programs are targeted to a specific stage in the
training path (Figure 1) and highly focused on 4 specific areas relevant to NIGMS, assessment of

5
the data must be made in this context.
Data Limitations: The panel recognized that data collection for these programs over time is
challenging and the efforts of OPAE staff were commendable and extensive (in several cases this
required integrating several internal/external databases, which required individual validation before
being presented to the review group). In spite of these efforts, some data were not available (e.g.,
research career outcomes in government and industrial settings, grants obtained by trainees from
non-NIH government sources [NSF, DOD, PCORI] or national foundations, details of faculty status,
additional degrees obtained [MS, MPH], co-investigator status on grants, some publications not
associated with a NIH grant, or even data complicated by name changes). As a result, there is
likely under-reporting in all groups, but particularly with this group of physician scientists who are
commonly funded via a combination of NIH and non-NIH sources over their careers. Despite these
limitations, the panel was able to make a reasonable assessment of the program.
Evolution of Scientific Fields: A final key factor is that these 4 programs have been in existence
for many years and the nature of medical research and research training in each specialty have
evolved over time. These factors are not captured in the data collected, and are therefore outside
the scope of this evaluation, but they are critical to future planning by NIGMS. Some of these issues
include the establishment of the National Human Genome Research Institute (NHGRI), which funds
basic science aspects of human genome science and which might be able to partner in some clinical
genetics/genomics training; introduction of pharmacogenetics as an important discipline within
clinical pharmacology; integration of pain medicine more closely with anesthesiology; and blurring
of boundaries between burn, trauma, and perioperative injury and resuscitation science and surgical
critical care outcomes.
Evaluation of Program Effectiveness
Evaluation of the NIGMS CPRT T32 programs by the review committee started with answering the
4 questions listed below.
QUESTION 1: Has the T32 Clinical Postdoctoral Research program been successful in
increasing clinician’s participation in the research community?
Overall the panel consensus was YES, NIGMS CPRT T32 programs have had a positive impact in
increasing clinician participation in research. This is because rigorous research training can occur
at various points throughout a physician’s education (pre-medical school, medical school,
residency, fellowship, beginning faculty years; Figure 1). Acceptance into most MD-PhD and MSTP
programs occurs during application to medical school or in year 1, yet some medical students
discover an interest in science later. Reviewers noted that the concept of “multiple on-ramps” to a
scientific career better reflects optimal physician scientist training opportunities than the classic
“pipeline” description. Thus, the ability to train physician scientists in the 4 NIGMS CPRT programs
later in their careers is important. Each specialty has some unique variations in training needs and
field-specific challenges (e.g., financial issues and/or clinical time commitments) that influence the
path and length of time to a successful research career, yet all share key similarities that aid in
increasing clinician participation in research.
NIGMS CPRT programs target MD and MD-PhD degree holders; the pool for this training are MDs
who develop a strong interest in these areas of research most often during residency. Overall 73%
6
of all NIGMS T32 trainees have MD degrees and the most of the rest have PhD degrees (Figure
5). In the very clinically-focused programs, 80% of the trainees had MD degrees and in Medical
Genetics programs 70% of the trainees had MD degrees (Figure 6).
T32 programs provide trainees with financial support for protected research time coupled with
programmatic activities and mentored research instruction aimed at preparing them for pursuit of
research careers. While the 2014 NIH Physician-Scientist Workforce Working Group suggested
shifting somewhat from T32 toward individual investigator-initiated training awards (e.g., NIH K or
F series),
1
the panel noted that for this group of investigators, 18-24 months of T32 research is often
needed to obtain preliminary data facilitating successful individual K08/K23 applications. As has
been reviewed elsewhere, such investigator-initiated training awards are an important step toward
successful K99 and R01 awards, and ultimately long-term research careers as physician scientists.
The panel noted that within an institution CPRT T32 programs facilitate development of a research-
oriented environment and a more discipline-diverse research training community of mentors,
collaborators, and non-T32-supported fellows. One panel member described this as providing more
research “oxygen” within departments. Another member pointed out that MSTP program directors
generally advise medical students interested in surgical/trauma/anesthesiology specialties to apply
specifically to residency programs that have T32 grants since this is viewed as a marker of serious
scientific commitment by a division, department, or program.
The review panel noted that NIGMS CPRT T32 programs have contributed significantly to
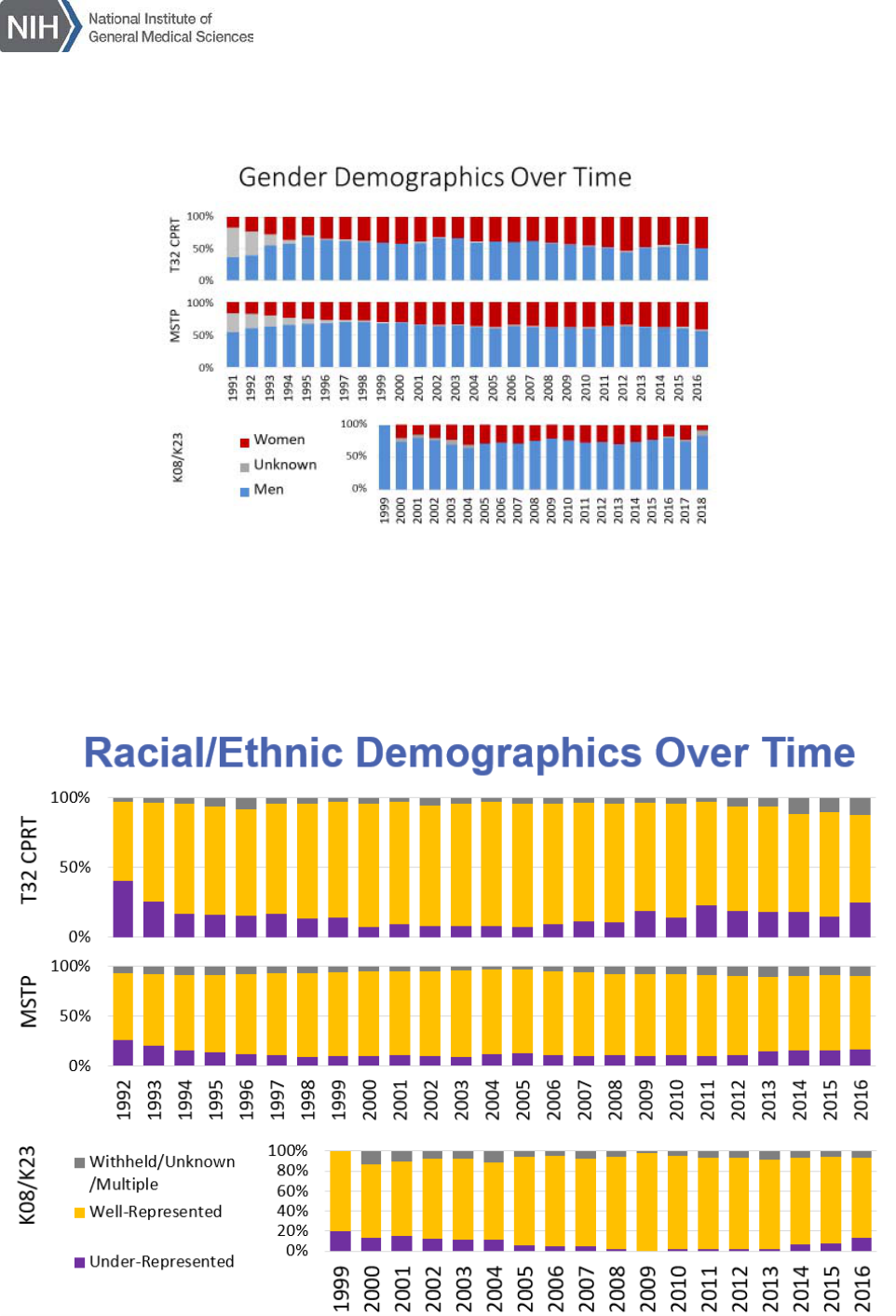
development of a more diverse clinical research workforce. Figure 7 shows gender demographics
for NIGMS programs over time. In terms of training women physician scientists, the CPRT T32
program compares favorably with MSTP and K08/K23 programs. Figure 8 shows racial/ethnic
demographics over the same period. Again, institutional T32s racial/ethnic inclusion compare
favorably with both MSTP and K08/K23 programs.
In terms of program outcomes, the proportion of CPRT T32 graduates who seek and garner
research support, and ultimately have independent research programs, is comparable to trainees
from other postdoctoral training programs across the NIH that seeking to involve MDs in research.
These outcomes are considered in detail in answering the next three questions.
QUESTION 2: Do T32 appointee career trajectories continue towards research and scientific
enterprise?
It is important to note that surgery, anesthesiology, and clinical genetics have long clinical residency
and fellowship training periods. Depending on when research training occurs, many years may
pass before faculty status is possible. Therefore, the review panel focused on intermediate and
long-term outcomes following completion of the CPRT T32 program, since grants and publications
may be shifted several years later compared to other programs. Ultimately, attainment of a senior
level academic career position is a marker for overall long-term research/academic success.
For question 2, the review panel examined whether CPRT T32 program graduates stay in academic
medicine. Physician scientists have many pathways beyond academic medicine by which they may
stay involved in science. These include working for government agencies, pharmaceutical or
biotechnology companies, non-profit organizations, and in science policy leadership positions.
Unfortunately, the panel could not evaluate these career pathways since currently such data are
7
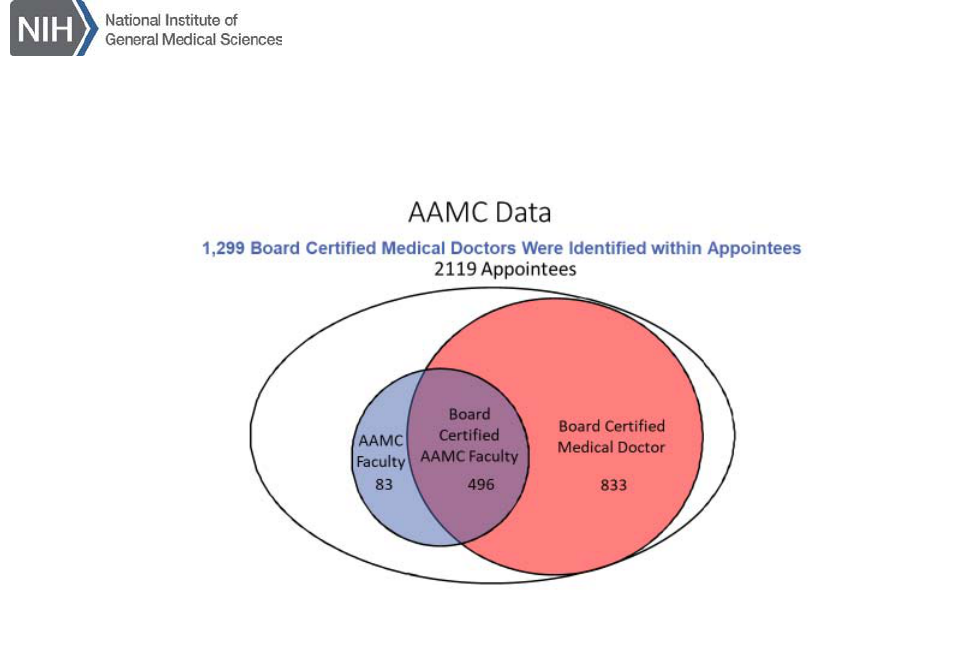
not captured in a consistent manner. In terms of faculty status, Figure 9 shows a merging of AAMC
faculty data with national data on board certification. These data suggest that of the 2119 CPRT
T32 trainees from 1990-2016, 1299 (61%) have clinical board certification and 579 (27%) are
current members of the faculty at an academic medical center (AMC). The panel noted that board
certification numbers appear internally consistent. Given that ≈70% of T32 trainees are MDs, recent
MD T32 trainees (e.g., surgery disciplines) may not have completed their residency, and for many
specialties board certification can take up to 1-5 years post-residency to accomplish, trainees from
the last 5 years might not yet be board certified or been able to join the faculty.
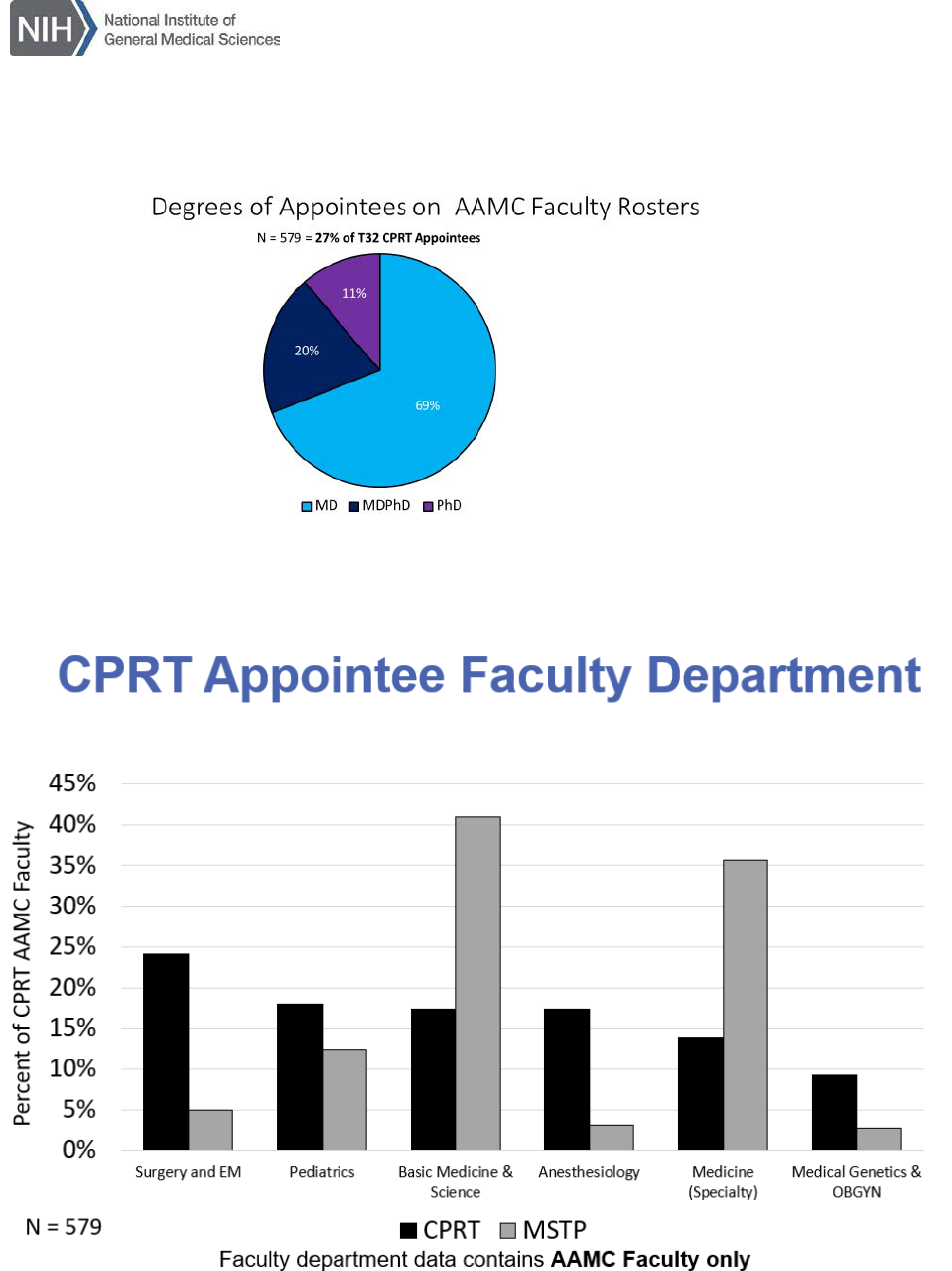
For those CPRT T32 trainees with faculty appointments, 89% have an MD degree. Figure 11 shows
which department CPRT T32 and MSTP graduates join. Overall, T32 graduates join surgery,
anesthesia, basic science, medicine and pediatrics departments, all areas relevant to the 4 NIGMS
focus areas, at higher rates relative to MSTP trainees. Figure 12 compares CPRT T32 and MSTP
faculty at their highest AAMC rank; in this comparison, CPRT T32 graduates compare favorably in
terms of the percent of graduates who ultimately reach Associate Professor and Full Professor rank.
Taken together, CPRT T32 trainees appear to join the faculty and to be promoted to more senior
levels at approximately similar rates to other relevant NIH-funded physician scientist trainees.
However, more nuanced analysis is not possible. The review panel noted that data for comparison
of faculty promotion track were not available, and even if available might be complicated by
inconsistent definitions across universities. In general, tenure track and clinician scientist promotion
tracks at academic medical centers reflect more research-intensive careers compared with more
clinically-oriented clinical educator or clinician promotion tracks. As such, capturing promotion track
information might provide a marker for guiding evaluation of effectiveness of individual physician
scientist training pathways going forward. However, it is important to remember that mentoring is
an important aspect of being a faculty member. Research training provides a unique vantage point
from which to mentor the next generation of physician scientists, no matter what the faculty
member’s career track.
Question 3: What outcomes are correlated with completion of T32 training programs?
Key indicators of a successful research career are research funding and publications. The review
panel therefore examined research grant applications, grant awards, and scientific publications for
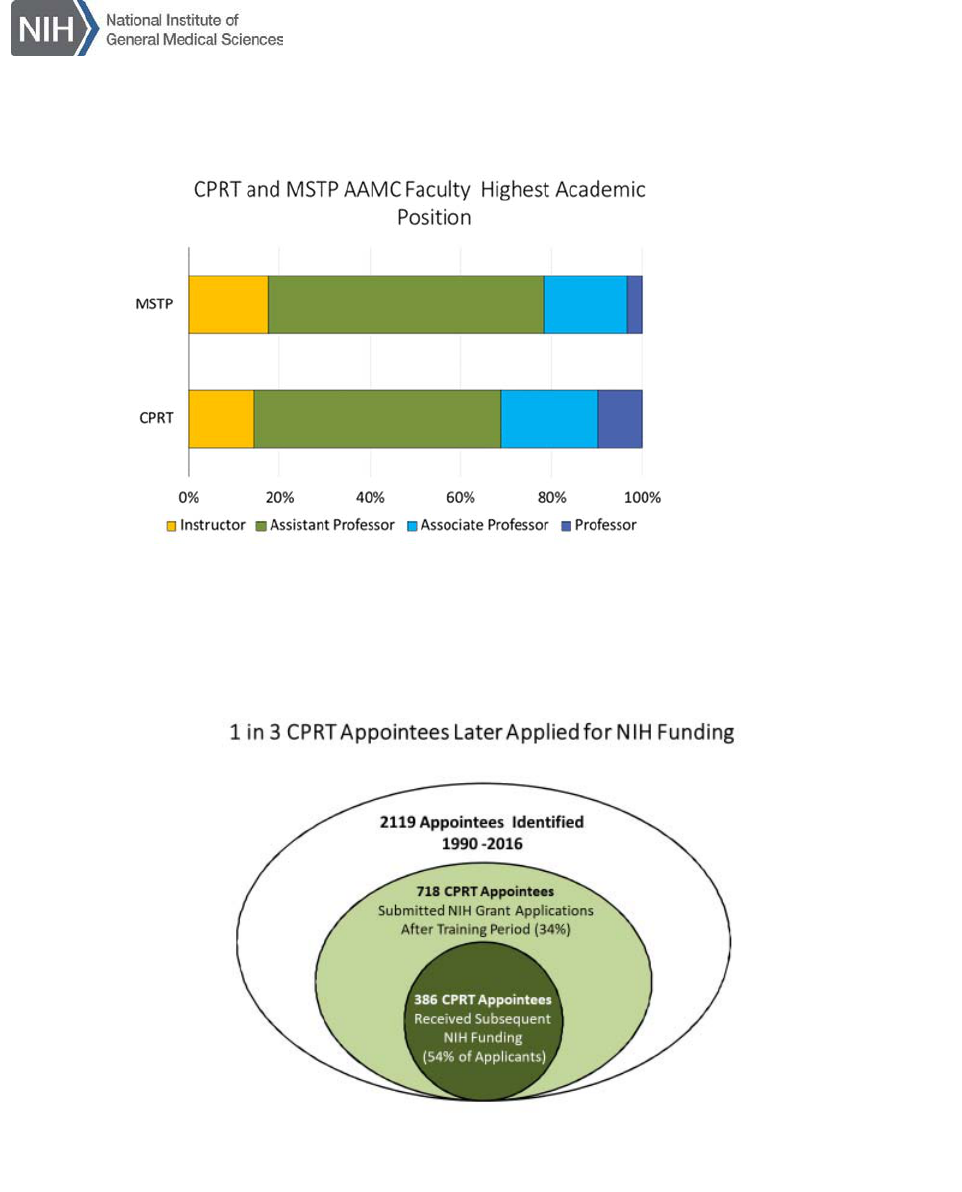
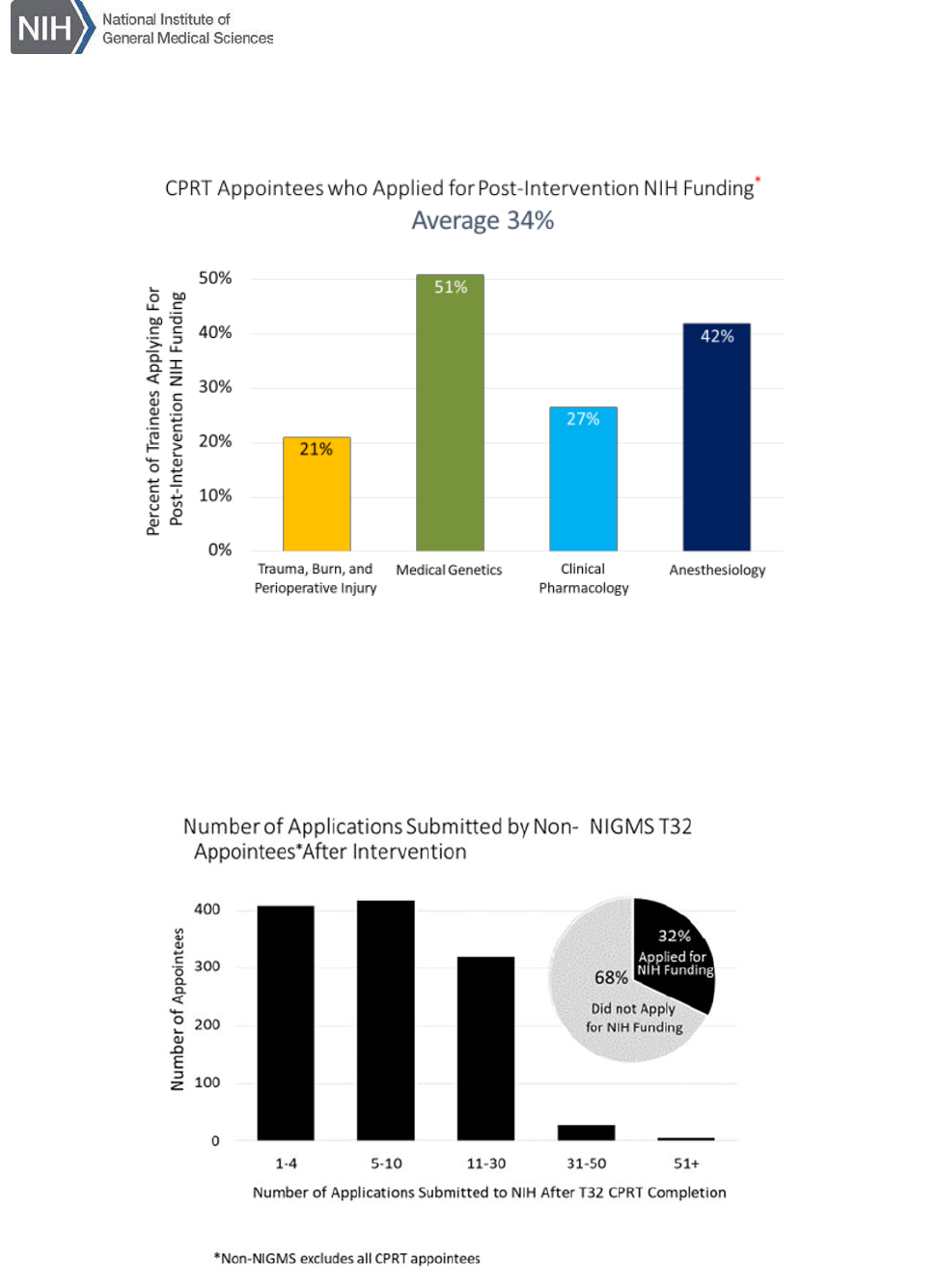
CPRT T32 trainees. Of the 2119 CPRT trainees identified from 1990-2016, 718 (34%) submitted
NIH grant applications after the training period (Figure 13). Figure 14 shows distribution of these
application by individual focus program, with alumni of the medical genetics and anesthesiology
programs having the highest percentage of NIH applications (51% and 42%, respectively). The
overall 34% NIGMS T32 NIH grant submission rate is comparable with 32% seen with non-NIGMS
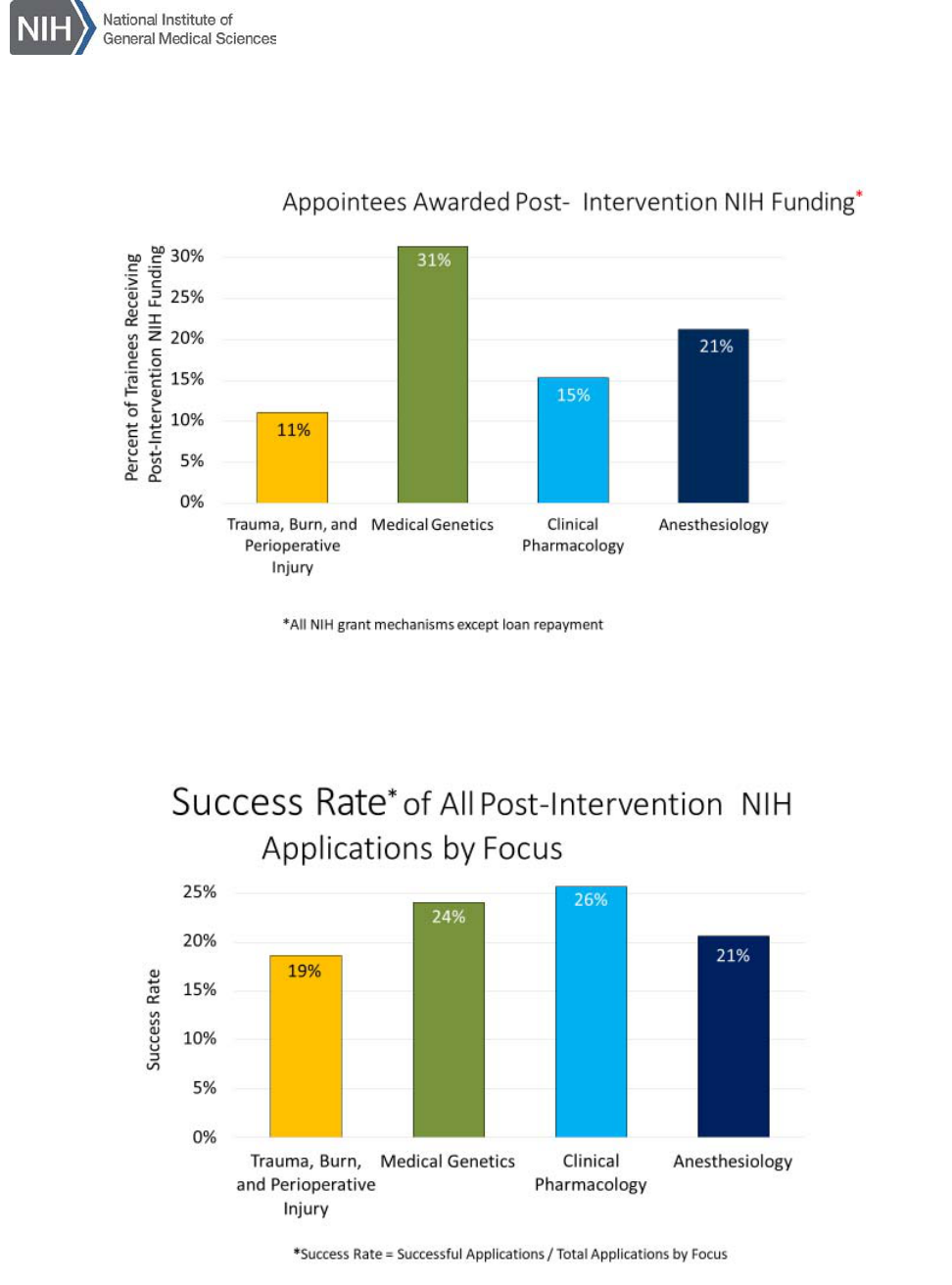
T32 programs across the NIH (Figure 15). Figure 13 shows that 386 (54% of the NIH grant
applicants) received NIH funding (≈20% of all CPRT trainees), with the highest percent securing
NIH grants from medical genetics and anesthesiology focus areas (Figure 16). However, taking
into account the success rate (success rate = number of applications submitted / total applications
by focus), the overall success rate is similar in all 4 focus areas at ≈23% (burn/trauma 19%, medical
genetics 24%, clinical pharmacology 26%, anesthesiology 21%; Figure 17).
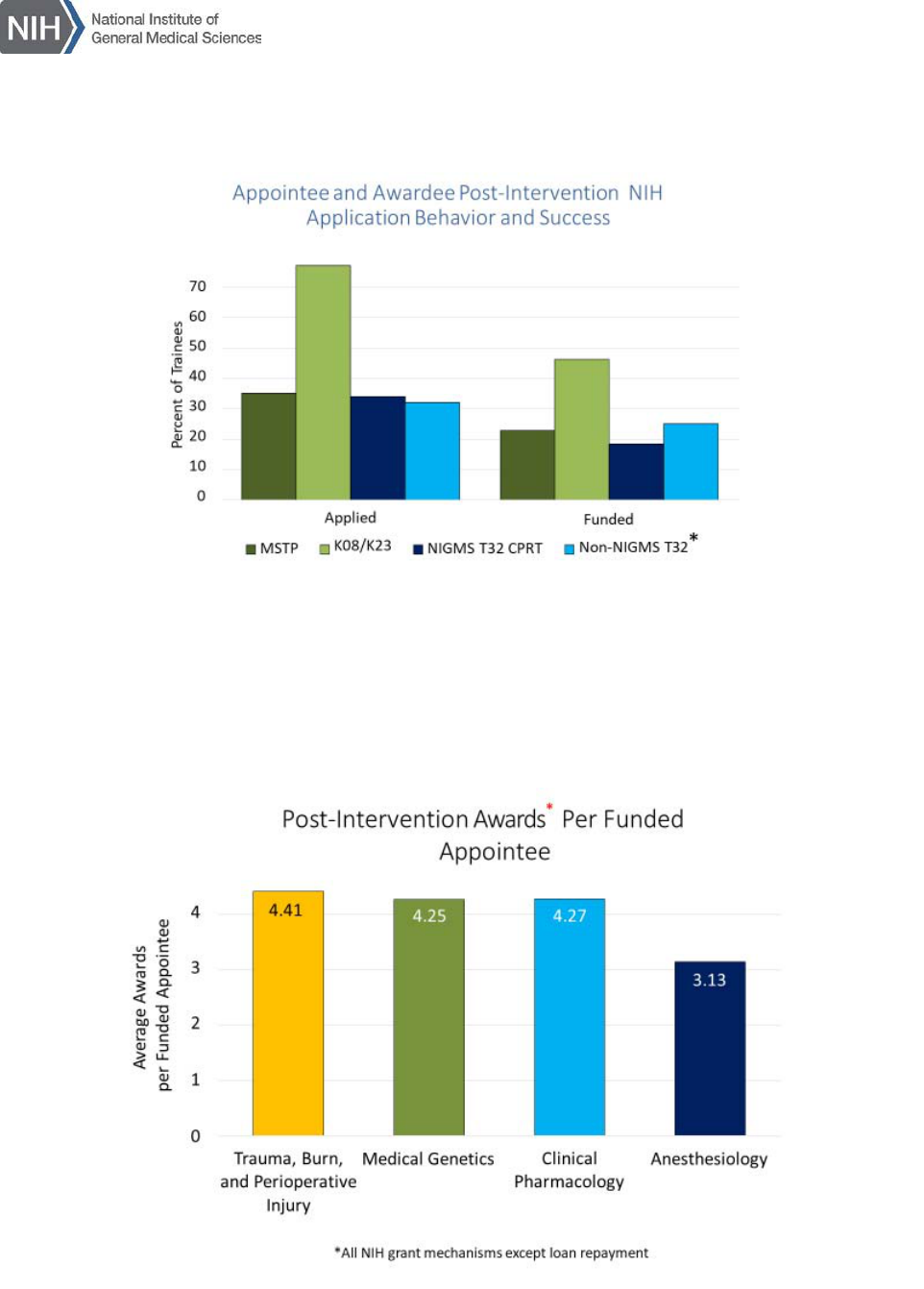
Figure 18 compares NIGMS T32 CPRT trainees with other training pathways within the NIH.
NIGMS CPRT T32 graduates apply for NIH funding at similar rates as non-NIGMS T32 and MSTP
8
graduates, although CPRT trainees have slightly fewer funded NIH grants. Both MSTP and all T32
trainees apply for, and receive, NIH grants at approximately half the rate of K08/K23 awardees.
K08/K23 graduates most often have had prior research experience (e.g., T32 or MSTP training)
since successful applications for these awards tend to require preliminary data. The CPRT T32 or
MSTP graduates who are successful in receiving a K08/K23 awards are captured in the K-series
outcomes, as well as in their original training mechanism.
Another potentially strong indicator of continued research career success is receipt of multiple NIH
grants, which was seen for 5-6% for CPRT T32 graduates. Figure 19 shows that for this subset of
CPRT T32 graduates, the total number of NIH grants ranges from 3.1 to 4.4 per funded appointee,
depending on focus area.
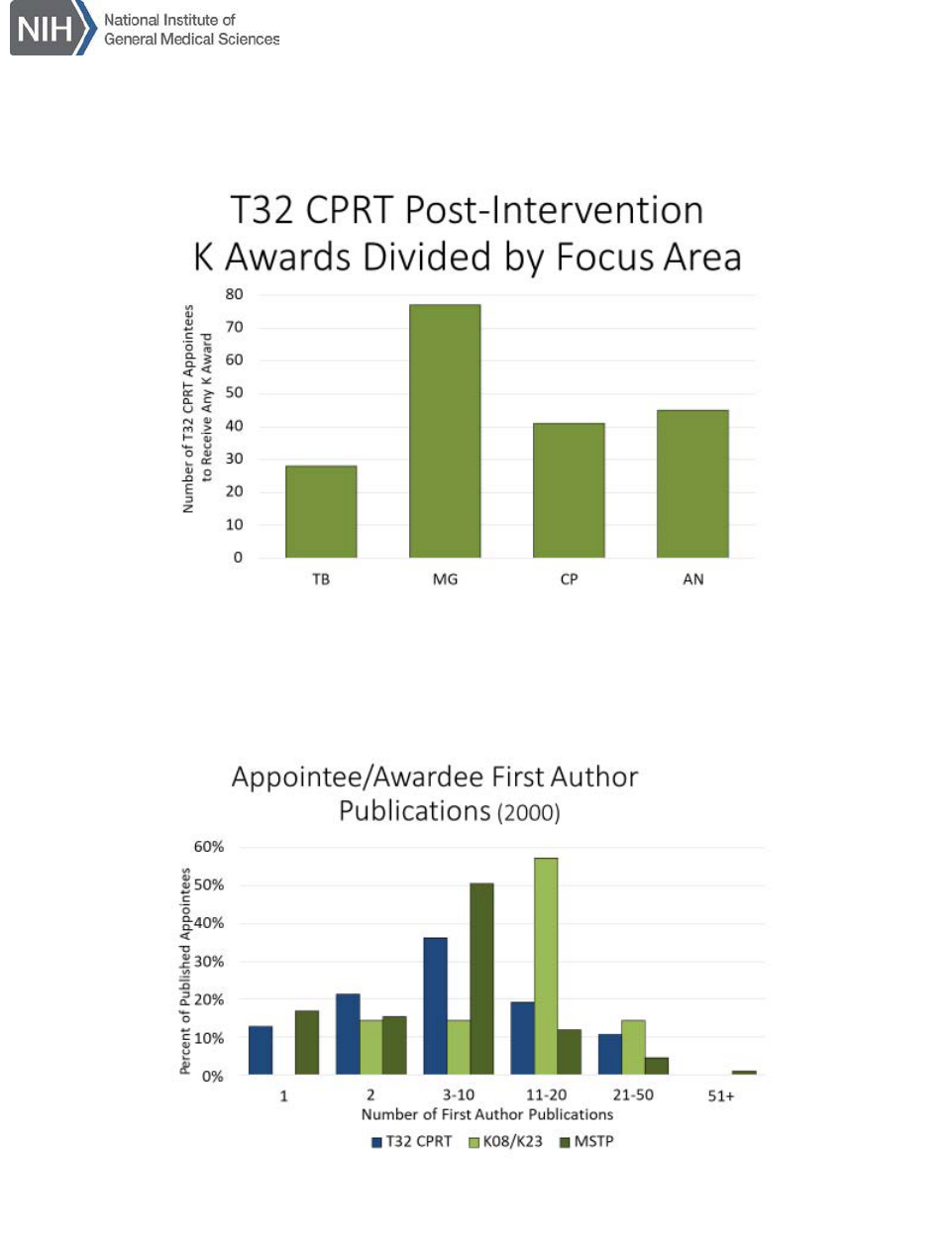
Since it is known that K awardees are twice as likely to apply for, and receive, NIH research support
than other trainees, application for K awards provides a good indicator of movement toward a
research career. For the period examined, 185 K awards were obtained by CPRT graduates from
any NIH institute (roughly 9% of the graduates): 28 burn/trauma, 75 medical genetics, 40
pharmacology, 42 anesthesia (Figure 20). It should be noted that NIGMS K awards are made only
in the areas of anesthesiology, clinical pharmacology and trauma/burn injury, and not in medical
genetics. Indeed, it is not uncommon for CPRT T32 trainees to apply for K awards from other NIH
institutes, since once a research project is defined, it may ultimately fit better within specific mission
of other NIH institutes. The panel viewed any NIH K award, no matter the institute of origin, a
success metric for NIGMS CPRT T32 graduates.
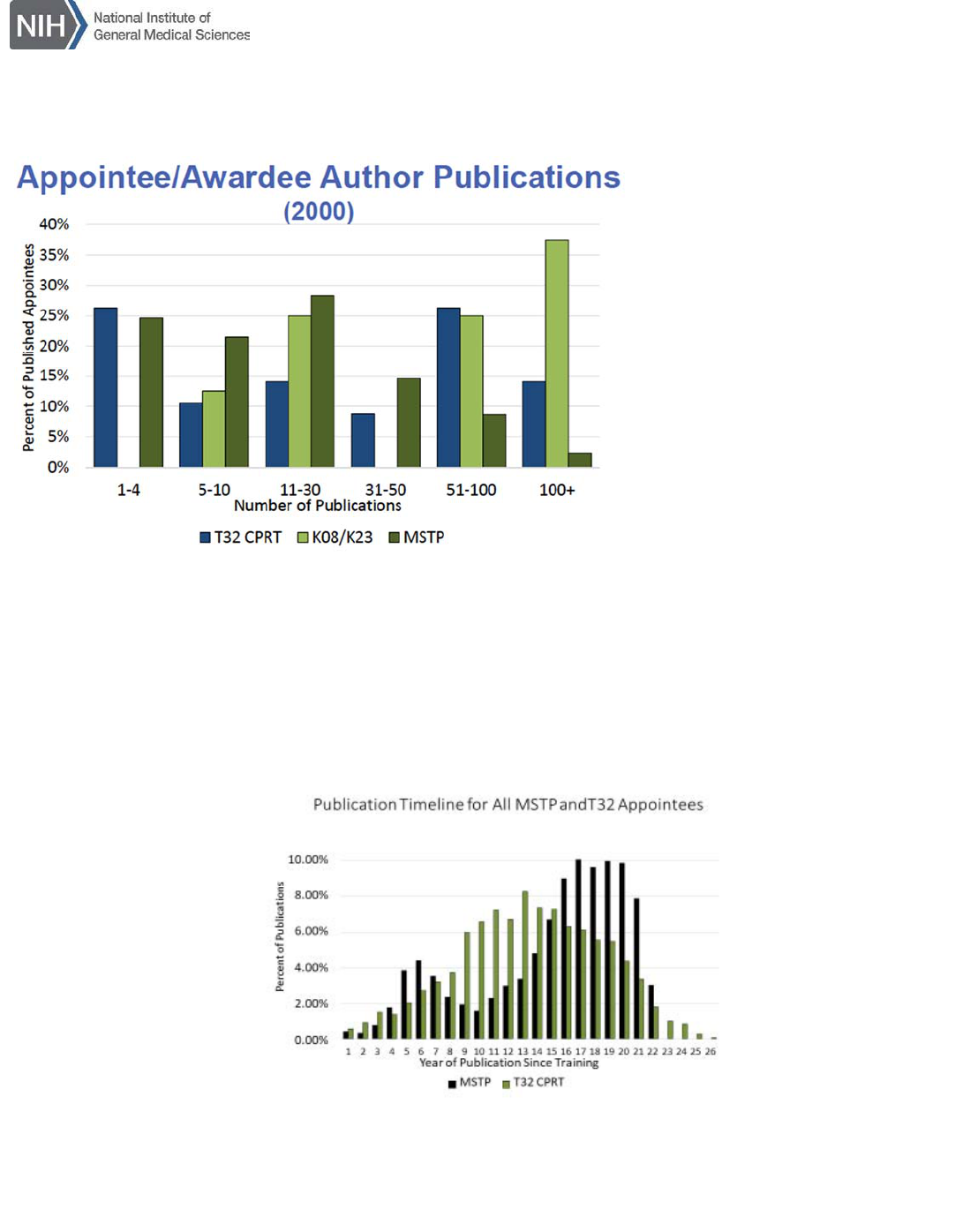
Scientific publications offer another measure of a successful research trajectory. About 11-14% of
the CPRT trainees cited an NIH grant in their publications after completion of the program. First
author publications for the subset of CPRT T32 trainees appointed in 2000 are shown in Figure 21
and total publications in Figure 22. Compared with K08/K23 and MSTP graduates, CPRT T32
trainees who publish have remarkably similar publication rates; this is surprising given their
significantly shorter training time (2 versus 4-5 years). These data also suggest K08/K23 grantees
have a somewhat higher number of publications compared with CPRT T32 and MSTP trainees.
Figure 23 shows publication time lines for both CPRT T32 and MSTP trainees. It should be
remembered that MSTP (MD-PhD) training occurs for 3-4 years during medical school and followed
by a hiatus where MSTP graduates complete clinical portions of medical school, residency and
sometimes fellowship; the bi-modal distribution of publications for MSTP graduates in Figure 23
shows this clearly. In contrast, T32 training usually comes at the end of residency or fellowship and
is most often 2 years in duration.
Question 4: Do trainees remain clinically in their area of research focus after research
training is completed?
YES. AAMC Faculty department membership in surgical disciplines, anesthesiology, emergency
medicine, medical genetics, and critical care medicine, indicate that CPRT T32 trainees are
overrepresented in the focus areas of this training program compared with MSTP trainees. Since
CPRT T32 research occurs during either residency, fellowship, or transition to faculty, clinical
aspects of trainee careers are generally set by the time they begin their T32 research experience.
What can change is the precise focus of research within those disciplines as a subset of trainees
move from mentored to independent investigators. The panel viewed this as healthy since science
9
changes continually and cutting-edge scientific approaches are then integrated into these clinical
disciplines.
Summary
Overall, NIGMS CPRT T32 programs demonstrate similar outcomes, in terms of grant
applications/awards, publications, and faculty status, as other postdoctoral T32s across the NIH.
Achievement of senior faculty status (%) also compares favorably with that of MSTP graduates.
Approximately 34% of all NIGMS postdoctoral T32 trainees ultimately apply for investigator-initiated
NIH research grants, with 54% of those applicants receiving subsequent NIH funding (≈20%
overall); those with at least one grant averaged 3.1 to 4.4 per trainee. This is approximately half
that achieved by individual K08 awardees. However, panel members cited the need for trainees to
generate data (often within the context of a postdoctoral T32 training program) to compete
successfully for K08/K23 or R01 funding. Panel members also noted that the impact of institutional
T32 training grants goes beyond supporting individuals, to positively influencing programs and
institutions in developing physician scientists. Given these data, the panel felt NIGMS T32
programs fulfill a critical niche in physician scientist research training not supported by other
categorical NIH Institutes.
Panel Recommendations
1. The panel recommends that NIGMS continue its support of the postdoctoral NRSA CPRT T32
programs and re-assess the emphasis of the programs in regard to changes in clinical research
and practice, as well as changes in financial obstacles to training of clinician scientists that have
occurred since the inception of the programs (e.g., income differential compared to clinical
pursuits). The issues for each research area have unique characteristics that need to be
considered individually.
2. NIGMS should define clear goals for its clinically focused research training programs (CPRT
T32, MSTP, K08/K23) and develop metrics than can be routinely collected by each CPRT
program and collectively by NIGMS for all CPRT programs. Such data could provide a basis for
measuring success and continuing enhancement for each program and for CPRT programs
overall. The committee felt that, if required, support for such data collection would be beneficial
for all institutional and individual training grant mechanisms.
3. Medicine and clinical research have evolved over the last 30 years; research technology, clinical
pressures and research areas have changed, and NIGMS should reexamine the focus areas of
these programs to ensure they are best serving the clinical research workforce needs.
Some suggestions:
Medical Genetics training has undergone significant changes including the establishment of
NHGRI, success of human genome study, introduction of genomic technology into the clinic,
and board certification. The Institute should explore with NHGRI areas of commonality with
the possibility of co-funding or the transfer of medical genetics training to NHGRI.
Broaden Trauma, Burn, and Injury to include emergency and critical care medicine (e.g.,
Trauma, Burn, Injury and Critical Care research)

10
Examine clinical pharmacology to see what it encompasses today (for example,
pharmacogenetics, systems biology, mathematical models, big data), current workforce
needs, and how this fits within the NIH. It is recommended that input be sought from
experts credentialed in this field.
Consider incorporating pain medicine more clearly within the Anesthesiology focus area.
4. Examine the feasibility of expanding loan repayment eligibility for this group of clinical
investigators in the 4 NIGMS focus areas, once updated. This is important since these trainees
fulfill critical niche in medical research not supported by other categorical NIH Institutes.
11
References
1. Physician-Scientist Workforce Working Group Report. National Institutes of Health, Bethesda, MD,
June 2014 (https://acd.od.nih.gov/documents/reports/PSW_Report_ACD_06042014.pdf).
2. 2016 Physician Specialty Data Report. Association of American Medical Colleges (AAMC),
Washington, D.C., 2016 (see Table 1.1. Active Physicians in the Largest Specialties, 2015,
http://www.aamc.org/data/workforce/reports/458480/1-1-chart.html)
3. National MD-PhD Program Outcomes Study. Association of American Medical Colleges (AAMC),
Washington, D.C., April 2018 (https://members.aamc.org/eweb/upload/AAMC-National-MDPhD-
Program-Outcomes-Study-2018.pdf). See Figure 12 and Table 4 for data cited.
12
APPENDIX: Supporting Material
Figure 1: Timing of Postdoctoral T32 (CPRT) Programs Compared with Other Physician Research
Training Grants
Figure 2: Non-NIGMS T32 Postdoctoral Programs (1999-2003)
13
Figure 3: Trainees Participating in NIGMS T32 CPRT by Focus Area
Figure 4: Trainees Participating in NIGMS T32 CPRT by Year and Focus Area Over Time
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 5: Majority of NIGMS CPRT Postdoctoral T32 Trainees Are Physicians (73%)
Figure 6: Percent MD or MD-PhD versus PhD Trainees for Each Focus Area
[73% of T32 CPRT Trainees held a medical degree (MD)]
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 7: NIGMS CPRT T32 Programs Recruitment of Women to Science Training
Figure 8: NIGMS CPRT T32 Programs Recruitment of Under Represented Minorities to Science
Training
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 9: Board Certification and Faculty Status of CPRT T32 Trainees (1990-2016)
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 10: Degrees Of CPRT T32 Trainees Who Joined Academic Medical Faculty
Figure 11: Departments Joined As Faculty By CPRT T32 versus MSTP Trainees
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 12: Highest Academic Position for CPRT T32 versus MSTP
Figure 13: Schematic of NIGMS CPRT T32 Trainees Who Later Applied for NIH Funding
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 14: Distribution of NIGMS CPRT T32 Trainees Who Applied For NIH Funding By Focus
Area
Figure 15: Non-NIGMS T32 Program Trainees Who Submitted NIH Grants
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 16: Distribution of NIGMS CPRT T32 Trainees Who Received NIH Funding By Focus Area
Figure 17: Success Rate (Successful Applications / Total Applications by Focus) For NIGMS
CPRT T32 Trainees Who Received NIH Funding
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 18: Comparison of NIGMS CPRT T32 Trainees With Other NIH Training Pathways In
Terms of NIH Grant Applications and Funded Grants
Figure 19: Average NIH Awards For 5-6% of CPRT T32 Trainees Who Received Multiple NIH
Grants Over Their Career, By Focus Area
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 20: Number of T32 CPRT Trainees Who Received Any K Award, By Focus Area
Figure 21: First Author Publications Per Appointee By Training Mechanism (Year 2000)
T32ClinicalPostdoctoralResearchTraining(CPRT)Progra
m
EvaluationRepor
t
Figure 22: Total Publications Per Appointee By Training Mechanism (Year 2000)
Figure 23: Publication Timeline For All MSTP and T32 Trainees
