DO NOT WRITE IN THIS BINDING MARGIN
Page 1 of 6
(Afx identication label here)
URN:
Family name:
Given name(s):
Address:
Date of birth: Sex: M F I
© The State of Queensland (Queensland Health) 2021
Except as permitted under the Copyright Act 1968, no part of this work may be
reproduced communicated or adapted without permission from Queensland Health
To request permission email: ip_of[email protected].au
Facility: .........................................................................................................
Iron Infusion Consent
Adult (18 years and over) OR
Child/Young Person (under 18 years)
IRON INFUSION CONSENT
v1.00
Clinical content review: 2021
Clinical check: 08/2021
Published: 09/2021
SW9511
C. Patient OR substitute decision-maker OR parent/
legal guardian/other person* requests the following
procedure(s)
Iron infusion
Ferric Carboxymaltose (Ferinject
®
)
Ferric Derisomaltose (Monofer
®
)
Iron Polymaltose (Ferrosig
®
)
Iron Sucrose (Venofer
®
)
Is this off-label use? Yes No
D. Risks specic to the patient in having an iron
infusion
(Doctor/clinician to document additional risks not included in
the patient information sheet):
E. Risks specic to the patient in not having an iron
infusion
(Doctor/clinician to document specic risks in not having an
iron infusion):
F. Alternative treatment options
(Doctor/clinician to document alternative treatment not
included in the patient information sheet):
G. Information for the doctor/clinician
The information in this consent form is not intended to be
a substitute for direct communication between the doctor/
clinician and the patient OR substitute decision-maker OR
parent/legal guardian/other person*.
I have explained to the patient OR substitute decision-maker
OR parent/legal guardian/other person* the contents of this
form and am of the opinion that the information has been
understood.
Name of doctor/clinician:
Designation:
Signature: Date:
A. Does the patient have capacity?
Complete for ADULT patient only
Yes è GO TO section B
No è COMPLETE section A
You must adhere to the Advance Health Directive (AHD),
or if there is no AHD, the consent obtained from a substitute
decision-maker in the following order: Category 1. Tribunal-
appointed guardian; 2. Enduring Power of Attorney; or
3. Statutory Health Attorney.
Name of substitute decision-maker:
Category of substitute decision-maker:
Complete for CHILD/YOUNG PERSON patient only
Yes
Although the patient is a child/young person, the patient may
be capable of giving informed consent and having sufcient
maturity, understanding and intelligence to enable them to
fully understand the nature, consequences and risks of the
proposed procedure/treatment/investigation/examination and
the consequences of non-treatment – ‘Gillick competence’
(Gillick v West Norfolk and Wisbech Area Health Authority
[1986] AC 112)
è GO TO section B
No
Parent/legal guardian/other person* with parental rights and
responsibilities to provide consent and complete this form
è COMPLETE section A
* Formal arrangements, such as parenting/custody orders, adoption, or
other formally recognised carer/guardianship arrangements. Refer to the
Queensland Health ‘Guide to Informed Decision-making in Health Care’
and local policy and procedures. Complete the source of decision-making
authority as applicable below.
If applicable, source of decision-making authority (tick one):
Court order è Court order veried
Legal guardian è Documentation veried
Other person* è Documentation veried
Name of parent/legal guardian/other person*:
Relationship to child/young person:
B. Is an interpreter required?
If yes, the interpreter has:
provided a sight translation of the informed consent form
in person
translated the informed consent form over the telephone
Name of interpreter:
Interpreter code: Language:
Page 2 of 6
(Afx identication label here)
URN:
Family name:
Given name(s):
Address:
Date of birth: Sex: M F I
DO NOT WRITE IN THIS BINDING MARGIN
© The State of Queensland (Queensland Health) 2021
Except as permitted under the Copyright Act 1968, no part of this work may be
reproduced communicated or adapted without permission from Queensland Health
To request permission email: ip_of[email protected].au
Iron Infusion Consent
Adult (18 years and over) OR
Child/Young Person (under 18 years)
H. Patient OR substitute decision-maker OR parent/
legal guardian/other person* consent
I acknowledge that the doctor/clinician has explained:
• the “Iron infusion” patient information sheet
• the medical condition and proposed treatment, including the
possibility of additional treatment
• the general and specic risks and benets of the procedure
• the prognosis, and risks of not having the procedure
• alternative treatment options
• that there is no guarantee the procedure will improve the
medical condition
• that if a life-threatening event occurs during the procedure:
- an adult/young person will be treated based on
documented discussions (e.g. AHD or ARP [Acute
Resuscitation Plan])
- a child’s health care will be provided in accordance with
good clinical practice and in the best interests of the patient
• that a doctor/clinician other than the consultant/specialist
may assist with/conduct the clinically appropriate treatment;
this may include a doctor/clinician undergoing further training
under supervision
• that if the doctor/clinician wishes to record video, audio or
images during the procedure where the recording is not
required as part of the treatment (e.g. for training or research
purposes), I will be asked to sign a separate consent form.
If I choose not to consent, it will not adversely affect my
access, outcome or rights to medical treatment in any way.
I was able to ask questions and raise concerns with the
doctor/clinician.
I understand I have the right to change my mind regarding
consent at any time, including after signing this form (this
should be in consultation with the doctor/clinician).
I/substitute decision-maker/parent/legal guardian/other
person* have received the following consent and patient
information sheet(s):
“Iron infusion”
On the basis of the above statements,
I/substitute decision-maker/parent/legal guardian/other
person* consent to having an iron infusion.
Name of patient/substitute decision-maker/parent/legal
guardian/other person*:
Signature: Date:
If the patient is a young person:
I am not aware of any legal or other reason that prevents
me from providing unrestricted consent for this young
person for this treatment (not applicable if the young
person is Gillick competent and signs this form).
DO NOT WRITE IN THIS BINDING MARGIN
© The State of Queensland (Queensland Health) 2021
Except as permitted under the Copyright Act 1968, no part of this work may be
reproduced communicated or adapted without permission from Queensland Health
To request permission email: ip_of[email protected].au
Adult and Child/Young Person | Informed consent: patient information
A copy of this form should be given to the
patient/substitute decision-maker/parent/legal guardian/
other person*
to read carefully and allow time to ask any questions about the procedure. The
consent form and patient information sheet should be included in the patient’s medical record.
Iron infusion patient information
SW9511 v1.00 Clinical content review: 2021 Clinical check: 08/2021 Published: 09/2021 Page 3 of 6
Iron use in children
The product information for each of the following products state they are not indicated for use in
children; however, iron infusions are commonly used in children. This is called off-label use and
is common in paediatric medical practice. If you have any questions about off-label use, please
discuss these with your doctor/nurse/midwife. For further information on off-label use in children
go to section 6 “Where can I nd support or more information?”. The information in these guides
refers to the best available evidence and best practice protocols that support the safety and
benet of these products for paediatric use.
1. What is an iron infusion and how will it help me/the patient?
Our bodies need iron. Iron is used to make haemoglobin, this is the part of the red blood cell
that transports oxygen around the body. Iron is also important for muscle strength, energy
and mental function. If your iron levels are low you may feel tired and not be able to perform
your normal daily activities. As the iron levels drop lower, the haemoglobin levels drop below
normal. This is known as iron deciency anaemia.
The most common way to treat iron deciency is
to take iron by mouth as a tablet or liquid. This
works for most people and is usually tried rst.
You might need an iron infusion if you:
• are not able to take iron tablets/liquids
• are not responding to iron tablets/liquids
• need to increase your iron levels quickly
(e.g. before major surgery, late in pregnancy
or to avoid a blood transfusion)
• if you have chronic kidney disease, chronic
heart failure, or inammatory bowel disease.
Sometimes more than one iron infusion is
required to fully elevate your iron levels.
An intravenous (IV) iron infusion is an infusion made up of iron, not blood, that is infused
directly into your bloodstream. A plastic cannula is placed into one of your veins and is
attached to a pump that infuses the iron into your body. Iron infusions work faster to replace
iron than tablets or liquids taken by mouth.
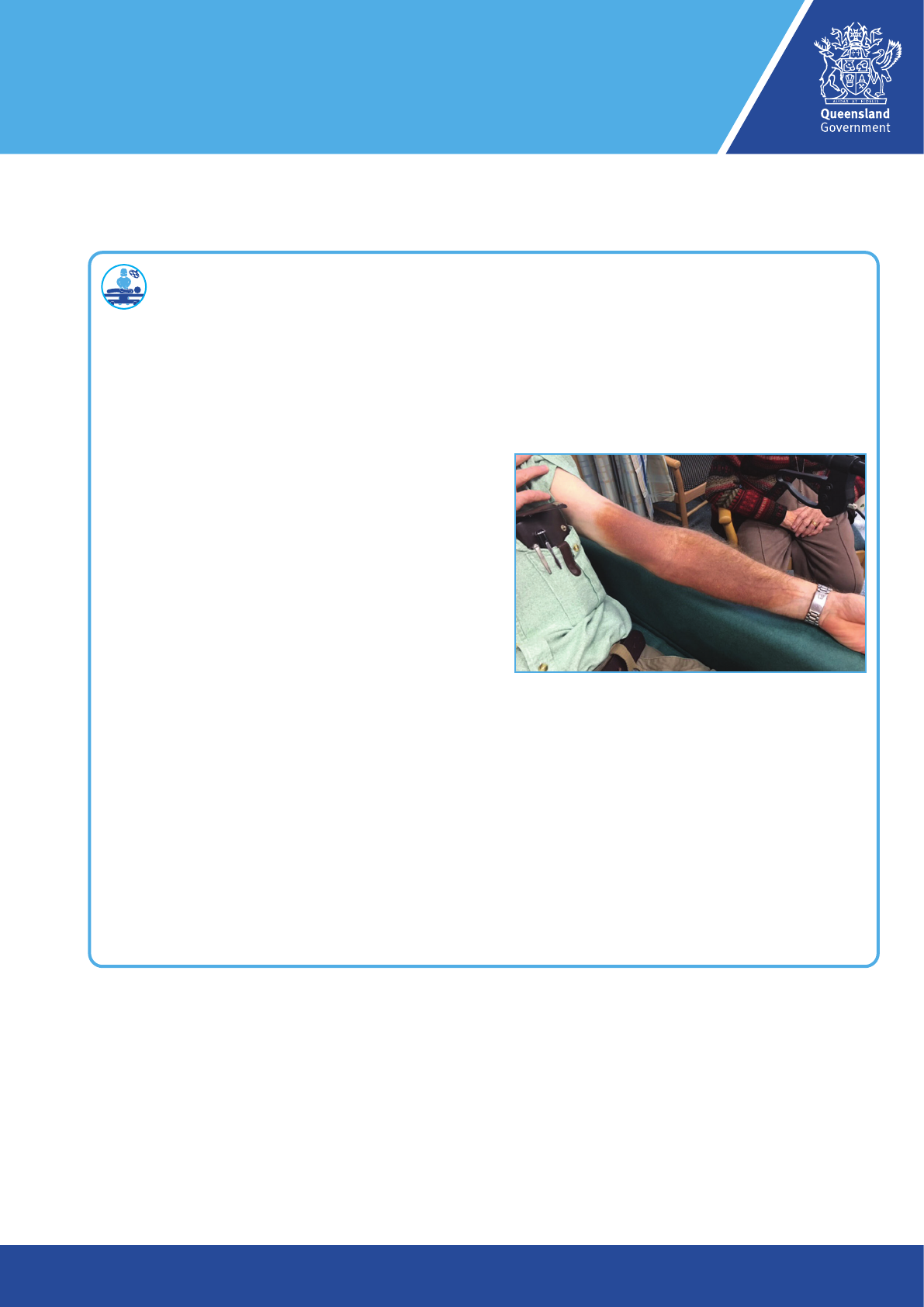
Staining of the skin from intravenous iron is uncommon, but when it occurs the stain can be
long lasting or permanent (see image above). The leakage occurs in the area around the
cannula (drip site) into the surrounding tissues.
Iron infusion
Image: Iron staining.
Source: Canning, M & Grannell, L. 2020, ‘A Stain on iron
therapy,’ Australian Prescriber, vol. 43, no. 5, pp.160-3,
retrieved 29/08/2021 (www.nps.org.au/assets/p160-Canning-
Grannell.pdf). Image used under CC BY-NC-ND 4.0 licence.
Iron infusion patient information
SW9511 v1.00 Clinical content review: 2021 Clinical check: 08/2021 Published: 09/2021 Page 4 of 6
Preparing for the treatment
Before you have an iron infusion, you must
tell your doctor/nurse/midwife and the nurses
performing the infusion if you:
• are pregnant/trying to get pregnant, as an
IV iron infusion should be avoided in the
rst trimester
• have a history of asthma, eczema or other
allergies
• have had a reaction to any type of iron
injection or infusion in the past
• have a history of high iron levels
(haemochromatosis) or liver problems
• have (or may have) an infection at the
moment.
You may want to ask your doctor/nurse/
midwife about the following:
• Why do I need an IV iron infusion?
• What are the other options?
• How many infusions will I need to get
enough iron?
• (If you are currently taking iron tablets/
liquids) When do I stop taking the iron
tablets/liquids and will I need to use them
again?
• How long will it take for my iron levels to
improve?
• Any questions about side effects that may
worry you.
The day of the treatment
There is preparation needed for an iron
infusion. Here are some useful tips:
• It is helpful if you are well hydrated prior
to your iron infusion so that putting in a
cannula may be easier.
• Have your regular breakfast/lunch – you do
not need to fast.
• Take all your regular medications.
• Tell your nurse/midwife administering the
iron infusion if you are pregnant or not.
• If you experience any side effects, inform
your nurse/midwife immediately.
• Adults can drive home after the iron
infusion and all patients can resume
usual activities (unless you experienced
an unexpected reaction and medical staff
inform you otherwise).
• Very little iron crosses into breast milk
so breast feeding mothers may safely
breastfeed.
All the iron products listed on this consent
form have Australian marketing approval
from the Therapeutic Goods Administration
(TGA). The Australian approved product
information lists the approved indications
(uses) and any age restrictions. Off-label use
occurs when an iron infusion is prescribed
outside the approved product information
(either the indication or the age restriction)
and is common in paediatric medical practice.
A doctor/nurse/midwife will discuss the
suitable treatment options for your child.
The indications and age restrictions for iron
infusion are as follows:
• Ferric Carboxymaltose (Ferinject
®
)
– Treatment of iron deciency when
oral iron preparations are ineffective or
cannot be used. The diagnosis must be
based on laboratory tests. Precaution:
The product information states that Ferric
Carboxymaltose is not recommended in
children under 14 years.
• Ferric Derisomaltose (Monofer
®
) –
Product information states that Ferric
Derisomaltose Iron Supplement is for
Adults 18 years and older, for use in iron
deciency when oral preparations are
ineffective, inappropriate or when rapid iron
delivery is necessary.
• Iron Polymaltose (Ferrosig
®
) –
Product information states that there
is no age restriction. Treatment of iron
deciency anaemia when oral therapy
is contraindicated, gastrointestinal
absorption of iron is defective or when
patient noncompliance or persistent
gastrointestinal intolerance makes oral
therapy impractical. Iron supplement
for Iron deciency anaemia where oral
treatment not appropriate or gastrointestinal
absorption is defective.
• Iron Sucrose (Venofer
®
) – Treatment
of iron deciency anaemia in patients
undergoing long-term haemodialysis
and who are receiving supplemental
erythropoietin therapy (a drug used to
stimulate red blood cell production in bone
marrow for anaemia). The diagnosis of iron
deciency must be based on appropriate
laboratory tests. Precaution: The product
information states that the safety and
efcacy of Iron Sucrose in children has not
been established.
Iron infusion patient information
SW9511 v1.00 Clinical content review: 2021 Clinical check: 08/2021 Published: 09/2021 Page 5 of 6
Rare risks and complications
• anaphylaxis – rare and usually occurs in
the rst few minutes of the iron infusion and
is characterised by breathing difculties,
which may be life threatening. You will be
closely monitored whilst the iron infusion is
given and for at least 30 minutes
• rapid heart beat (tachycardia) and low
blood pressure
• skin staining (brown discoloration) may
occur due to leakage of iron into the tissue
around the cannula (drip) site. This is not
common, but the stain can be long lasting
or permanent (see image)
• inform the nurse straight away of any pain,
discomfort, burning, prickling, redness,
staining or swelling at the cannula (drip) site
• death as a result of this procedure is
possible. You will be closely monitored
whilst the iron infusion is given and for at
least 30 minutes following completion.
This treatment does not require an
anaesthetic.
What are the risks of not having an
iron infusion?
There may be health consequences if you
choose not to have the proposed treatment.
Please discuss these with the doctor/nurse/
midwife.
If you choose not to have the treatment, you
will not be required to sign a consent form.
If you have signed a consent form, you have
the right to change your mind at any time
prior to the treatment. Please contact the
doctor/nurse/midwife to discuss.
3. Are there alternatives?
Making the decision to have a procedure
requires the patient/substitute decision-
maker/parent/legal guardian/other person*
to understand the options available. Please
discuss any alternative treatment options
with your doctor/nurse/midwife before signing
the consent form.
During the treatment
The duration of the iron infusion varies
depending on the product used. Your
iron infusion may take 15 to 30 minutes,
1 to 2 hours or 4 to 6 hours.
You will also need to allow time for the IV
cannula to be inserted and removed, and for
clinical observation before and after the iron
infusion (30 to 60 minutes).
2. What are the risks?
There are risks and complications with this
procedure. There may also be risks specic
to each person’s individual condition and
circumstances. Please discuss these with
the doctor/nurse/midwife and ensure they
are written on the consent form before you
sign it. Risks include but are not limited to the
following:
Common risks and complications
• low blood pressure
• palpitations
• facial ushing
• dizziness
• vomiting and nausea
• headache
• injection site reactions (see also below skin
staining in rare risks)
• joint and/or muscle pain
• changes in taste (e.g. metallic)
• (Ferric carboxymaltose [Ferinject
®
] only)
hypophosphataemia (low blood phosphate
level). This can cause muscle weakness,
respiratory failure, heart failure and in
rare circumstances osteomalacia (bone
softening), fractures, seizures and/or coma.
You may require oral medication to raise
your blood phosphate level.
Uncommon risks and complications
• dizziness and feeling faint
• chest and/or back pain
• chills and fever
• skin irritation and rash
• swelling of the face, mouth and limbs
• generalised lymphadenopathy (swollen
lymph nodes)
• difcult breathing.
© The State of Queensland (Queensland Health) 2021. Except as permitted under the Copyright Act 1968, no part of this work may be reproduced communicated or adapted without permission
from Queensland Health. To request permission email: ip_of[email protected]
Iron infusion patient information
SW9511 v1.00 Clinical content review: 2021 Clinical check: 08/2021 Published: 09/2021 Page 6 of 6
More information on off-label use can be
found at:
www.blood.gov.au/system/les/Corrected-
Paed-and-Neonatal-IDA-Guide-dosing-for-
iron-polymaltose.pdf
www.mja.com.au/journal/2006/185/10/
label-use-medicines-consensus-
recommendations-evaluating-
appropriateness
Staff are available to support patients’
cultural and spiritual needs. If you would like
cultural or spiritual support, please discuss
with your doctor/nurse/midwife.
Queensland Health recognises that
Aboriginal and Torres Strait Islander patients
will experience the best clinical care when
their culture is included during shared
decision-making.
7. Questions
Please ask the doctor/nurse/midwife if
you do not understand any aspect of this
patient information sheet or if you have any
questions about your/the patient’s medical
condition, treatment options and proposed
treatment.
If you require additional information about
the intravenous iron preparation prescribed
for you, please speak to the clinician/doctor/
nurse/pharmacist who can arrange to provide
you with a Consumer Medicines Information
(CMI) leaet.
8. Contact us
In an emergency, call Triple Zero (000).
If it is not an emergency, but you have
concerns, contact 13 HEALTH (13 43 25 84),
24 hours a day, 7 days a week.
4. What should I expect
after the treatment?
In some cases, iron tablets/liquids are
recommended after the infusion. If oral iron
therapy is recommended it should not start
until at least one week after your IV iron
infusion as the iron within the tablets/liquids
will not be absorbed.
Tell your doctor/nurse/midwife or
seek urgent medical attention/call an
ambulance (000) if you have:
• chest pain
• trouble breathing
• dizziness
• neck/mouth swelling.
5. Who will be performing
the treatment?
A doctor/nurse/midwife other than the
consultant/specialist may assist with/conduct
the clinically appropriate treatment. This
could be a doctor/nurse/midwife undergoing
further training, all trainees are supervised
according to relevant professional guidelines.
If you have any concerns about which
doctor/nurse/midwife will be performing the
treatment, please discuss with the doctor/
nurse/midwife.
6. Where can I nd support
or more information?
Hospital care: before, during and after is
available on the Queensland Health website
www.qld.gov.au/health/services/hospital-
care/before-after where you can read about
your healthcare rights.
More information on iron infusions can be
found on the TGA website:
www.tga.gov.au/sites/default/les/auspar-
ferric-carboxymaltose-191001.pdf
www.tga.gov.au/sites/default/les/auspar-
ferric_derisomaltose-181105.pdf
