

Carpenters Benefit Funds
350 Fordham Road, Wilmington, MA 01887
HEALTH FUND
NEW ENGLAND CARPENTERS
SUMMARY PLAN
DESCRIPTION
BENEFITS
GREAT BENEFITS
The New England Carpenters
Health Benefits Fund
FOR LIFE

HEALTH
BENEFITS
FUND
GREAT BENEFITS
As a member of the New
England Carpenters Health
Benefits Fund, you and your
family are eligible for a
generous benefits package
that offers you well-being,
security and protection.
FOR LIFE
The New England Carpenters Health Benefits Fund
350 Fordham Road
Wilmington, MA 01887
Phone: (800) 344-1515
Fax: (978) 657-8724
August 2005
Dear Participant:
The Board of Trustees of the New England Carpenters Health Benefits Fund is pleased to
issue this revised Summary Plan Description. This handbook has been written to reflect
the changes in the Health Benefits Fund since the last version was printed.
As your Board of Trustees, we continually evaluate the benefits for opportunities for
enhancement while maintaining a financially sound Health Benefits Fund. When we
design our benefit programs and make improvements, we try to do what’s best for the
participants. This revised Summary Plan Description is a reflection of our efforts.
Note that medical benefits and weekly accident and sickness benefits are provided
directly by the Fund. Life insurance and accidental death and dismemberment benefits
are underwritten by Hartford Life Insurance Company.
A New Approach
This book has been designed to be easy to read and understand. “Fast Facts” appear at
the beginning of each section to give you a quick overview of what is contained within
that section. Also, useful information—such as phone numbers and definitions—appear
in the margin as a quick reference.
In addition, this book provides the required information about your rights and protection
under the law in order to comply with the Employee Retirement Income Security Act of
1974 (ERISA). This information is on page 67.
We encourage you and your family to read this Summary Plan Description carefully to
make the best use of the benefits the New England Carpenters Health Benefits Fund offers.
If you have any questions concerning the benefits or your eligibility, please feel free to
contact the Fund Office at (800) 344-1515.
Sincerely,
Board of Trustees
1
Health Benefits Fund

Employer Trustees
William J. Sullivan
Secretary/Treasurer
Stephan A. Adamic
Co-Secretary/Treasurer
George M. Bidgood
Theodore H. Brodie
Donald L. Colavecchio
Thomas J. Gunning
Michael Shaughnessy
William Shea
Thomas Steeves
Union Trustees
Thomas J. Harrington
Chairman
Mark L. Erlich
Co-Chairman
Thomas J. Flynn
Simon R. James
Bruce King
John Murphy
Michael Nelson
David Wallace
Jack Winfield
David A. Woodman
2
Executive Director
Harry R. Dow
Director and Field Representative
James W. Buckley, Jr.
Legal Counsel
O’Reilly, Grosso & Gross
Krakow & Souris, LLC.
Consultants and Actuaries
The Segal Company
The Board of Trustees reserves the right to terminate or amend the
Plan at any time. This includes the right to amend or terminate
benefits or eligibility for any class of participant, including retirees,
when in their sole discretion the Board determines such action is in
the best interest of the Fund and its participants.
Changes to your plan of benefits can happen at any time, so if you
have a question about a particular service or program, contact the
Fund Office for the most up-to-date information.
BOARD OF TRUSTEES

TABLE OF CONTENTS
Key Contact Phone Numbers and Addresses . . . . . . .4
Your Health Benefits Fund . . . . . . . . . . . . . . . . . . . . .5
Eligibility . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6
Maintaining Your Eligibility . . . . . . . . . . . . . . . . . . .7
If You’re Short of Hours . . . . . . . . . . . . . . . . . . . . . .7
Eligible Dependents . . . . . . . . . . . . . . . . . . . . . . . . .8
If Your Child’s Eligibility for Benefits Changes . . . . .9
Extension of Benefits for Totally
Disabled Members . . . . . . . . . . . . . . . . . . . . . . . . .9
When Coverage Ends . . . . . . . . . . . . . . . . . . . . . . . .9
Retiree Health Benefits Plan . . . . . . . . . . . . . . . . . .10
Continuing Your Coverage . . . . . . . . . . . . . . . . . . . . .11
COBRA Continuation Coverage . . . . . . . . . . . . . . .11
Life Events . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .19
If You Move . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .19
If You Get Married . . . . . . . . . . . . . . . . . . . . . . . . .19
If You Have a Baby . . . . . . . . . . . . . . . . . . . . . . . . .20
If You Adopt a Child . . . . . . . . . . . . . . . . . . . . . . . .21
If You Divorce . . . . . . . . . . . . . . . . . . . . . . . . . . . . .21
If You Enter Active Military Service . . . . . . . . . . . .22
If You Become Disabled . . . . . . . . . . . . . . . . . . . . .23
If You Become Eligible for Medicare . . . . . . . . . . . .23
Upon Your Death . . . . . . . . . . . . . . . . . . . . . . . . . .24
Your Medical Plan . . . . . . . . . . . . . . . . . . . . . . . . . . .25
Lifetime Maximum Plan Benefit . . . . . . . . . . . . . . .25
Managed Health Care Program —
Preauthorization . . . . . . . . . . . . . . . . . . . . . . . . .27
Wellness Benefits . . . . . . . . . . . . . . . . . . . . . . . . . . .30
Annual Physical Exams . . . . . . . . . . . . . . . . . . . . .30
Annual Pap Tests and Mammograms . . . . . . . . . . .30
Well-Child Exams . . . . . . . . . . . . . . . . . . . . . . . . .30
Hospitalization and Surgery . . . . . . . . . . . . . . . . . . .31
Hospitalization . . . . . . . . . . . . . . . . . . . . . . . . . . . .31
Surgeon’s Charges . . . . . . . . . . . . . . . . . . . . . . . . . .33
Mental Health and Substance Abuse . . . . . . . . . . . . .35
Preauthorization . . . . . . . . . . . . . . . . . . . . . . . . . . .36
3
Home Health Care . . . . . . . . . . . . . . . . . . . . . . . . . . .37
Hospice Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . .38
Carpenters Assistance Program . . . . . . . . . . . . . . . . .39
Prescription Drugs . . . . . . . . . . . . . . . . . . . . . . . . . . .40
Dental Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .43
Vision Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .45
Life Insurance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .47
Coverage for Your Spouse . . . . . . . . . . . . . . . . . . . .47
If Your Coverage Ends . . . . . . . . . . . . . . . . . . . . . .48
Accidental Death and Dismemberment . . . . . . . . . . .49
Seatbelt Benefit . . . . . . . . . . . . . . . . . . . . . . . . . . . .50
Weekly Accident and Sickness . . . . . . . . . . . . . . . . .51
General Exclusions . . . . . . . . . . . . . . . . . . . . . . . . . .52
Coordination of Benefits . . . . . . . . . . . . . . . . . . . . . .54
Reimbursement and Subrogation . . . . . . . . . . . . . .56
Filing Your Claims . . . . . . . . . . . . . . . . . . . . . . . . . . .58
When Claims Must Be Filed . . . . . . . . . . . . . . . . . .59
When A Claim Is Considered Received By
The Health Benefits Fund . . . . . . . . . . . . . . . . . .59
Urgent, Pre-Service and Concurrent Claims . . . . . .60
Prescription Drug Claims . . . . . . . . . . . . . . . . . . . .60
Claims Communications . . . . . . . . . . . . . . . . . . . .60
Comprehensive Medical Benefits Claims . . . . . . . . .60
Disability Claims (Weekly Accident and
Sickness Benefit) . . . . . . . . . . . . . . . . . . . . . . . . .63
Appeal Process . . . . . . . . . . . . . . . . . . . . . . . . . . . .64
Your ERISA Rights . . . . . . . . . . . . . . . . . . . . . . . . . . .67
Plan Facts . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .69
Schedule of Benefits for Plan I . . . . . . . . . . . . . . . . .71
Schedule of Dental Benefits for Plan I . . . . . . . . . . . .74
Schedule of Benefits for Plan II . . . . . . . . . . . . . . . . .75
Schedule of Benefits for the Retiree Plan . . . . . . . . .78
Glossary of Terms . . . . . . . . . . . . . . . . . . . . . . . . . . .80
New England Carpenters Health Benefits
Fund Privacy Notice . . . . . . . . . . . . . . . . . . . . . . . .83

4
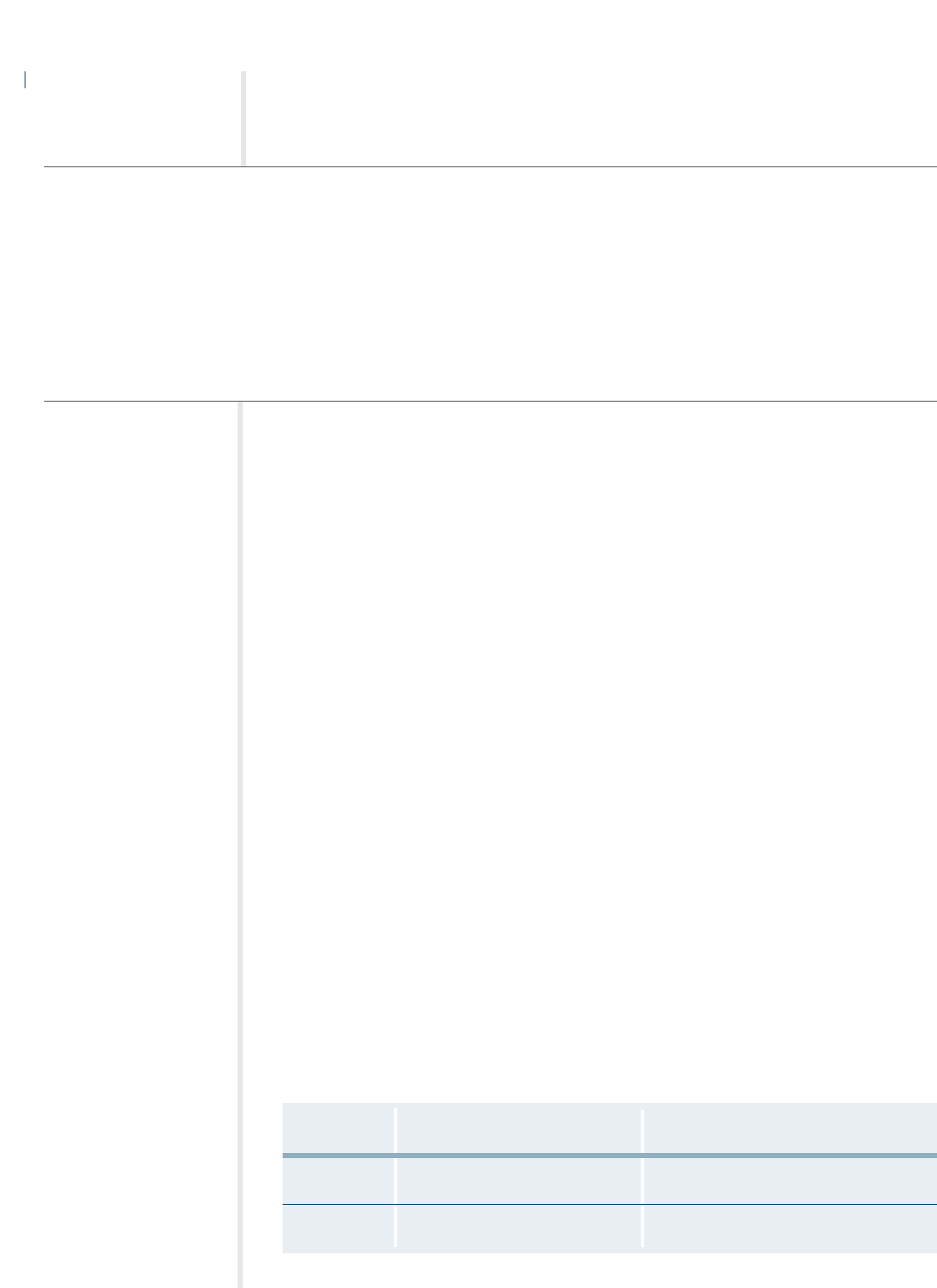
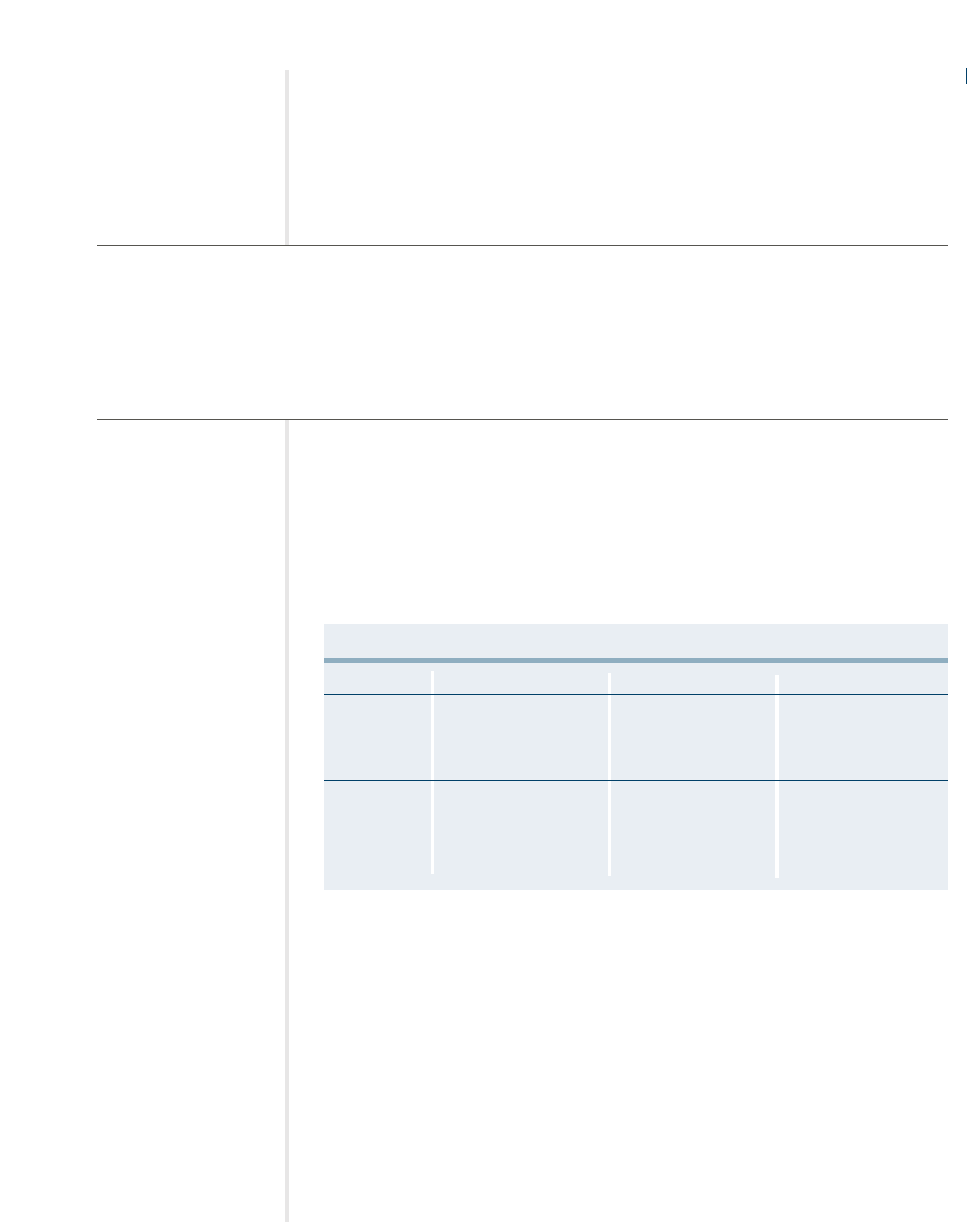
Benefit Address Phone Number Website
Medical Care The Fund Office 978-694-1000 www.carpentersfund.org
350 Fordham Road 800-344-1515
Wilmington, MA 01887
Dental Care Delta Dental 800-872-0500 www.deltadental.com
465 Medford Street
Boston, MA 02129
Vision Care Carpenters Vision Center 617-782-0100
250 Everett Street
Allston, MA 02134
Davis Vision 800-999-5431 www.davisvision.com
159 Express St. TTY: 800-523-2847
Plainview, NY 11803
Prescription Drugs Ullicare Rx/Medco 800-818-6602 www.medcohealth.com
100 Parsons Pond Drive
Franklin Lakes, NJ 07417
Carpenters 350 Fordham Road 978-694-1000
Assistance Program Wilmington, MA 01887 800-344-1515
Health Management Hines & Associates 800-944-9401 www.hinesassoc.com
Program
(Preauthorization)
KEY CONTACT PHONE NUMBERS
AND ADDRESSES

YOUR HEALTH BENEFITS FUND
The New England Carpenters Health Benefits Fund offers eligible
members and their families comprehensive health care coverage.
Benefits include office visits, hospitalization and surgery, home
health care, coverage for prescription drugs, mental health and
substance abuse treatment, dental and vision care.
You want the comfort of knowing that your family will be
protected if something happens to you. Eligible members qualify
for a life insurance benefit, accidental death and
dismemberment insurance benefits and weekly accident and
sickness benefits. The Fund also offers an extension of medical
benefits for you and your family if you become disabled, or for
your family—at no charge—in the event of your death.
HOW THE HEALTH BENEFITS FUND WORKS
The Health Benefits Fund contains three comprehensive health
care plans, which offer coverage depending on your eligibility:
•
PLAN I, for active members and their dependents;
•
PLAN II, for active members and their dependents; and
•
THE RETIREE PLAN, for eligible retirees and their dependents.
5
Your eligibility to participate in Plan I or Plan II is based on the number of hours you
work in covered employment and the contribution rate your employer is required to
make to the Fund on your behalf. Plan I offers coverage for members that work 600
hours or more in a six-month period. Plan II offers a lower level of coverage for members
that work at least 350 hours (but fewer than 600) in a six-month period. These rates are
outlined in a Collective Bargaining Agreement between your employer and the New
England Carpenters Health Benefits Fund.
Hours Requirements
Your eligibility for benefits—which is different from your eligibility to participate—
depends on the number of hours you work in covered employment during a six-month
“work period.” If you work the required number of hours—and your employer
contributes to the Fund for those hours—you and your eligible dependents will be eligible
for coverage for six months. The hours requirements for a six-month work period are:
• Plan I—600 hours in one work period or 1,250 hours in
two consecutive work periods.
• Plan II—350 hours in one work period
• Local 1996
– Plan I— 750 hours in one work period or 1,550 hours in
two consecutive work periods.
– Plan II— 425 hours in one work period.
Work Periods and Coverage Periods
There are two work periods per year. The hours you work during the work period are
used to determine whether you’re eligible for coverage during the six-month coverage
period. Coverage periods begin on April 1 or October 1.
6
What is Covered
Employment?
Covered employment is
work you do for which
contributions are made by
a contributing employer
under the terms of a col-
lective bargaining agree-
ment or signed participa-
tion agreement.
What is a Collective
Bargaining Agreement?
A Collective Bargaining
Agreement is a written
agreement between a
union and an employer
that requires the employer
to make contributions to
the Fund on behalf of its
employees.
•
You must work a specified number of hours in a six-month work
period to be able to initially participate in the Plan.
•
You must also work a specified number of hours to be eligible to receive benefits
for you and /or your eligible dependents.
•
When you don’t work enough hours to qualify for benefits, you may be able to purchase
Continuation Coverage under the Federal program known as COBRA.
•
When you retire, you may be able to purchase coverage under the Retiree Plan if
you meet all the requirements.
ELIGIBILITY
FAST FACTS:
Review Date If you work the required hours You’ll be eligible for coverage
during the work period... during the coverage period...
April 1 August, September, October, April, May, June, July, August
November, December and January and September
October 1 February, March, April, May, October, November, December,
June and July January, February and March

7
MAINTAINING YOUR ELIGIBILITY
Once you gain eligibility, that will continue as long as you work at least 600 hours
(Plan I) or 350 hours (Plan II) in the six-month work period prior to the coverage period.
If you do not work the required number of hours, you may be able to maintain your
coverage, as explained below, by:
•“Buying-In” to the Fund; or
• Using the banked hours you’ve accumulated in your Hours Bank for hours
worked before 1989. Banked hours are removed once you retire.
Plan I — Active Members
Plan I members may continue coverage provided they work at least 1,250 hours in the
previous two consecutive six-month work periods preceding the period they were
covered.
Local 51 and Shops in Plan I Only
Shop employers contribute a set dollar amount for hours worked in the current month to
be covered for the following month. Members must work one hour and the employer
must make the monthly contribution to be covered. For example, a member who works
one hour in May is entitled to full Plan I coverage for the month of June.
IF YOU’RE SHORT OF HOURS
If you do not qualify for continued coverage based on your hours worked, coverage may
be continued in two other ways—through the use of a Buy-In or Banked Hours.
Short Hours Buy-In
If you do not work enough hours during a work period to maintain your eligibility, you
may purchase Buy-In coverage if you were short by 30 hours or less. In order to take
advantage of the buy-in provision, you must have been eligible during the preceding
coverage period under that plan with worked hours only.
You may buy into the plan of coverage you were eligible for in the prior coverage period at
the special buy-in rate per hour. For example, if you are in Plan I and you had worked at
least 570 hours, you could buy the 30 hours you were short (600 required – 570 worked)
for the buy-in rate times 30. To buy into Plan II coverage, you must work at least 320
hours in a work period. For the most up-to-date buy-in rate, contact the Fund Office.
Payment must be made in one lump sum. You have only until the end of April or
October to choose this buy-in option. Otherwise, continuation coverage would be
available under COBRA at COBRA rates. (See page 11 for information on COBRA
Continuation Coverage.) If late hours are received and would bring you into 30 hours
short, you would have 30 days from the date of notification to choose this buy-in option.
Special Rule for New Members
New members may buy into Plan II after working eight hours in the current
work period.

An eligibility statement with the monthly cost will be mailed to you in March or
September (the end of the insured period) indicating the cost for coverage starting the
following month, the next coverage period. Be sure to keep your address current with the
Fund Office so you can receive this statement.
Banked Hours
Hours that were banked prior to August 1, 1989, may be drawn upon to maintain your
coverage when you do not work the required number of hours in a work period for
active members. You will be permitted to use hours from your bank to continue
eligibility, provided you worked some hours in covered employment during the previous
or current work period. You must be eligible to buy into COBRA to exercise this option.
Banked hours are credited at $1.90, which was the actual dollar value of the contribution
rate in effect at the time the hours were banked. Therefore, the total banked hours used
to maintain eligibility will reduce the actual cost of the insurance coverage.
✍
To use your banked hours, you must indicate your wishes on a COBRA form
(continuation coverage) or send a letter of request to the Fund Office.
ELIGIBLE DEPENDENTS
When you become eligible for coverage in the New England Carpenters Health Benefits
Fund, your eligible dependents are also eligible for coverage.
Plan’s Definition of Dependent
The term “dependent” means (1) your lawful spouse; (2) your unmarried children
(including a legally adopted child) who are under 19 years of age; and your unmarried
children who are at least 19 but less than 24 years of age who are enrolled as full-time
students in an accredited school, college or university, not employed on a full-time basis
and dependent upon you for financial support.
If Your Child is Disabled
If an unmarried dependent child is incapable of self-sustaining employment because of
physical handicap or mental retardation and he or she is dependent upon you for
support and maintenance, his/her coverage will be continued provided his/her incapability
commenced prior to attaining age 19 or age 24 if a full-time student. You must submit
proof of your dependent child’s incapability to the Fund Office on the later of 31 days
after the date he/she attains 19 years of age or age 24 if a full-time student or 31 days
after you are notified of his/her eligibility. Benefits will continue to be provided for your
child as long as you remain covered under the Fund.
No person may be eligible for benefits both as a member and as a dependent.
Proof of the continued existence of such incapability shall be furnished to the Fund
Office yearly.
The term “child” also includes a stepchild or foster child, provided the child depends
upon you for support and maintenance and has been reported to the Fund Office.
8
Proving Eligibility for
Dependents
You are required to furnish
the following documenta-
tion for dependent cover-
age if you have not already
done so:
• Marriage certificate from
City Hall or Town Hall;
• Birth certificate document
showing both parents’
names, court document or
written statement on let-
terhead from appropriate
governmental agency
showing legal guardian-
ship and date of birth of
each child;
• Divorce decree if
applicable;
• Proof of a dependent
child’s attendance at an
accredited school or col-
lege as a full-time student
upon attainment of age 19
must be submitted to the
Fund Office twice each
year, as directed by the
Fund Office, on an original
form which contains the
accredited institution’s
seal. He or she must
provide a letter from the
registrar.
The letter should include:
–Verification of his or her
enrollment;
– The number of course
hours for which he or she
is enrolled; and
– The beginning and ending
dates of the term.

9
When Coverage Ends
Your dependents’ eligibility for coverage will end on:
• The date your child or spouse no longer meets the definition
of an eligible dependent under the Fund; or
• The date your eligibility ends.
IF YOUR CHILD’S ELIGIBILITY FOR BENEFITS CHANGES
If your child’s eligibility status changes, you must notify the Fund Office as soon as possible.
Your child may be eligible for COBRA Continuation Coverage for up to 36 months. See
page 11 for more information.
EXTENSION OF BENEFITS FOR TOTALLY DISABLED MEMBERS
If you become totally disabled while covered for benefits under this Fund, you may be
eligible for an extension of benefits for up to two consecutive coverage periods. Your
coverage will be under the same Plan you had at the time of your disability, subject to
proper documentation. This option is available only once per lifetime. If only one free
coverage period is required, the option for a second coverage period is voided. Contact
the Fund Office for an Extension of Benefits form.
If you are eligible for a Social Security Disability Pension, you may be eligible for
coverage under the Retiree Health Benefits Plan for up to 24 months or until you are
covered by Medicare, whichever comes first.
Widow(er) Extension
If a member is covered by this Fund under worked hours or buying into Plan I at the
time of his or her death, the surviving spouse and eligible dependents will be covered
by the Fund for a maximum of three additional years under Plan I. Coverage is provided
at no premium cost, provided that the spouse and dependents have no other health
insurance, including Medicare. However, if the member was buying into Plan II at the
time of his or her death, the surviving spouse and eligible dependents are only eligible
for coverage under Plan II.
WHEN COVERAGE ENDS
Generally, your coverage under the New England Carpenters Health Benefits Fund will end:
• For Shop Employees, the first day of the following month in
which you stop working in covered employment;
• The date you do not meet the requirements for eligibility; or
• The date the Plan terminates.
What You Need to Do
If you are adopting a child,
the following is needed:
•A copy of the birth certifi-
cate once it is available;
•A copy of the paperwork
from the adoption agency
showing the date the child
was placed in the home.
(Coverage for an adopted
child will begin on the date
the child was placed in the
home.)
If you are the legal
guardian, the following is
needed:
•A copy of the birth
certificate;
•A copy of the court
document stating that
the member is the legal
guardian of the child.
(Coverage will begin on
the date of the legal
document.)
If you have not adopted
the child or do not have
legal guardianship and
are only the stepparent
by marriage, then the fol-
lowing is needed:
•A copy of the birth
certificate;
•A copy of the natural par-
ent’s divorce decree, the
medical insurance section,
along with the front page
that has the name of the
defendant and plaintiff’s
names.
•A copy of the tax return.
See page 20 for more
information.

RETIREE HEALTH BENEFITS PLAN
If you retire on or after April 1, 1995, with a Service, Normal, Early or Disability Pension
and meet the Plan’s other eligibility requirements, you and your eligible dependents are
eligible for the New England Carpenters Retiree Health Benefits Plan. There are five
requirements:
•You must be eligible for five out of the past ten coverage periods, have 3,000 hours
during the five-year period immediately prior to retirement and be covered by
the Plan in the period immediately preceding your application for retiree coverage.
•You must have no other group health insurance, including Medicare.
•You must share the cost of coverage with the Fund. Your monthly premiums will
increase from time to time.
•You must obtain medical services from providers in the Carpenters Preferred Provider
Network unless you do not live within a 20-mile radius of the nearest network
provider.
•You must obtain pre-certification for all inpatient hospital stays.
Continued Eligibility for Retirees
Eligibility to participate ends on the earlier of:
• The last day of the month when you do not pay the premium when required;
• The date your pension benefit is suspended for any reason;
• The date you become eligible under another group health plan;
• The date you or your eligible dependent become entitled to Medicare; or
• The date the Plan terminates.
Local 108 cannot participate in the Retiree Plan.
Eligibility for Widow(ers) and Dependent Children
If you were eligible for a Service, Normal, Early or Disability Pension from the New
England Carpenters Pension Fund at the time of your death, your widow(er) and eligible
dependent children may continue coverage under the Retiree Health Plan on a self-
payment basis. If a dependent child is covered under a member who is purchasing the
Retiree Health Plan and the child reaches the age limit, the dependent is eligible to buy
into Plan II under COBRA.
10
What You Need To Do
If your child is no longer
eligible for coverage under
the Fund, he or she may
elect to continue coverage
under COBRA. You or your
child must:
• Contact the Fund Office
within 60 days of losing
eligibility; and
• Enroll in COBRA
Continuation Coverage.
Failure to contact the Fund
Office and provide notice
of the “Qualifying Event”
(discussed in more detail
on page 11) will result in a
loss of rights to COBRA.
These same rules apply
to a Spouse who loses
coverage due to a separa-
tion or divorce.
Continuing Your
Coverage Under COBRA
When your coverage
under this Fund ends,
you may be eligible to
continue some of the
same coverage you had
under the Health Benefits
Fund for a limited time
under COBRA. For infor-
mation about COBRA
Continuation Coverage,
see page 11.
11
COBRA CONTINUATION COVERAGE
If your coverage under the New England Carpenters Health Benefits Fund ends due to a
“Qualifying Event” (see below), you and/or your covered dependents may be eligible to
continue your health care coverage under the Consolidated Omnibus Budget
Reconciliation Act of 1985 (COBRA).
By making monthly payments, you and/or your dependents may continue the same
medical, dental, vision and prescription drug coverage that you had before your coverage
ended. Your coverage can last for up to 18, 29 or 36 months, depending on the
Qualifying Event that resulted in your loss of coverage.
Qualifying Events
To be eligible to elect COBRA Continuation Coverage, you (as the member) and/or your
dependent(s) must lose coverage due to any one of the Qualifying Events, which are
listed in the first column in the table below. The last column indicates how individuals
find out that they’re eligible for continuation coverage, which are explained below.
•You and your dependents may continue certain medical benefits if your coverage ends due to a
“Qualifying Event.”
•Your children are eligible to continue coverage under COBRA when they no longer satisfy the
Fund’s definition of eligible dependent because of age, marriage or student status.
•To keep your coverage under COBRA, you must make monthly payments to the Fund Office on
time. You are fully responsible for the payment of your benefits through COBRA.
CONTINUING YOUR COVERAGE
FAST FACTS:
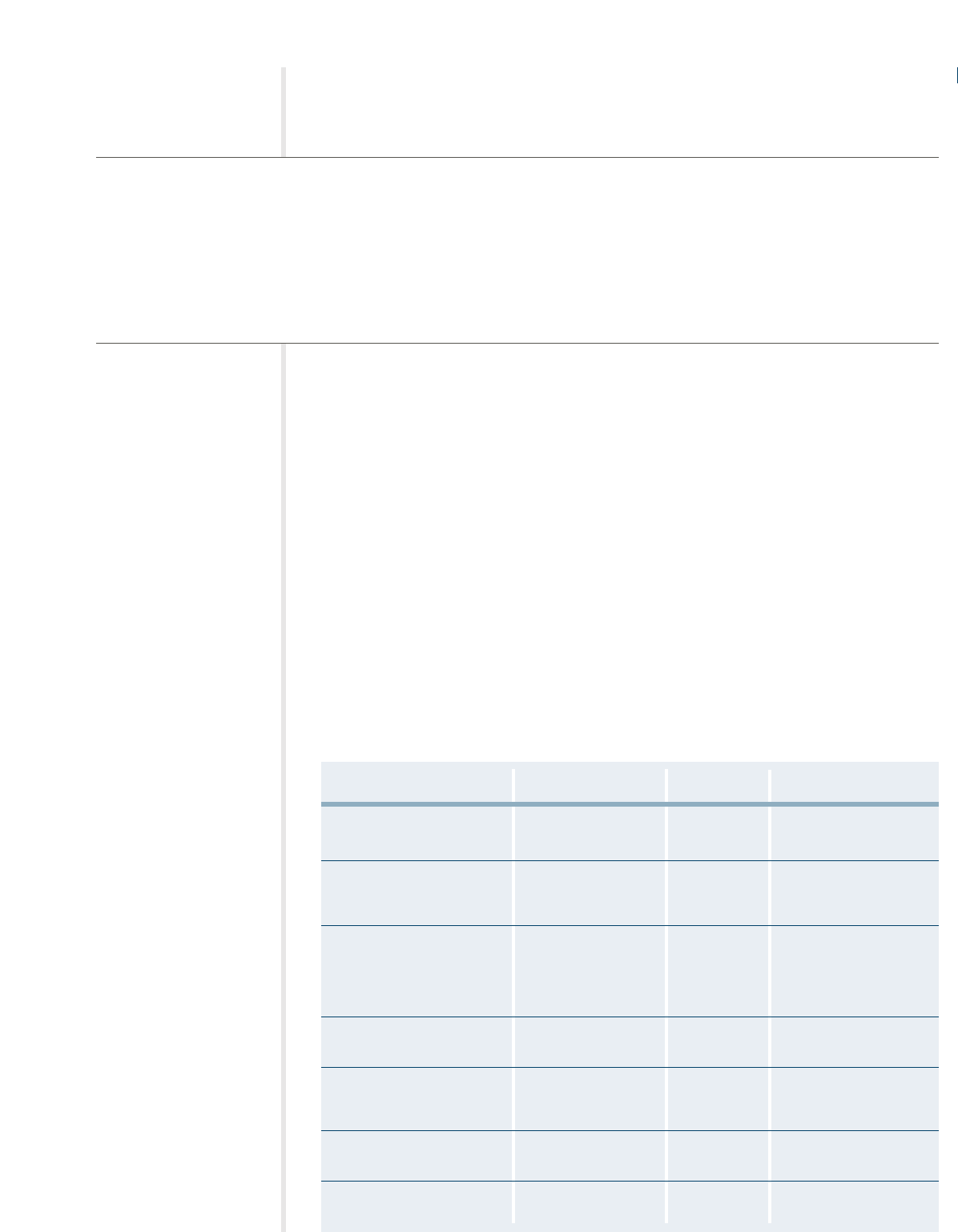
Qualifying Event Who May Purchase Eligibility Notification Requirements
(Qualified Beneficiary)
Member terminated for Member, spouse and/or 18 months Fund Office will
other than gross misconduct dependent children advise eligible participants
(including retirement)
Member reduction in hours Member, spouse and/or 18 months Fund Office
worked (making Member inel- dependent children
igible for coverage or the same
coverage under the Plan)
Member becomes Spouse and/or 36 months Fund Office will advise
entitled to Medicare dependent children eligible participants when
member reaches 65. If
member becomes eligible
before 65, he or she must
advise Fund Office
Member becomes Member, spouse 11 months in Member must advise
eligible for disability through and/or children addition to the Fund Office
Social Security 18 months
Death of Member Spouse and/or 36 months minus Family member must
dependent children the number of notify Fund Office
months covered
since the divorce
Member is divorced or legally Spouse and/or 36 months Member or Spouse must
separated from spouse dependent children advise Fund Office so
notification can occur
Child ceases to be a Dependent child 36 months Member must advise
dependent child under Fund Office so
Plan definition notification can occur

Who May Elect COBRA?
Under the law, only “Qualified Beneficiaries” are entitled to elect COBRA Continuation
Coverage. A Qualified Beneficiary is any member, his or her spouse or dependent who
was covered by the New England Carpenters Health Benefits Fund when a Qualifying
Event occurs. A child who becomes a dependent child by birth, adoption or placement
for adoption with the Member during a period of COBRA Continuation Coverage is also
a qualified beneficiary. However, a dependent purchasing COBRA who acquires a spouse
during COBRA Continuation Coverage is not a qualified beneficiary.
!! One or more of your family members may elect COBRA even if you do not.
Additionally, one member may elect COBRA for all Qualified Beneficiaries. However,
in order to elect COBRA Continuation Coverage, the members of the family must
have been covered by the Plan on the date of the Qualifying Event. A parent may
elect or reject COBRA Continuation Coverage on behalf of dependent children living
with him or her.
How to Elect COBRA Continuation Coverage
✍
In order to elect COBRA Continuation Coverage, the Fund Office must be notified
when you experience a Qualifying Event. You must notify the Fund Office within 60
days from the date that the Qualifying Event occurs, or the date that you would lose
coverage under the Fund because of the Qualifying Event, whichever is later. See the
following Notification Procedures.
✍
When the Fund Administrator receives notice of the Qualifying Event, he or she will
mail you an election form, information about COBRA and the date on which your
coverage will end.
Under the law, you and/or your covered dependents have 60 days from the later of the date:
•You would have lost coverage because of the Qualifying Event; or
•You and/or your covered dependents received the election form and COBRA information.
If you and/or any of your covered dependents do not elect COBRA within 60 days of the
Qualifying Event (or, if later, within 63 days from the mailing date), you and/or your
covered dependents will not have any group health coverage from this Fund after your
coverage ends.
COBRA Notification Procedures
As a covered Member or Qualified Beneficiary you are responsible for providing the Fund
Administrator with timely notice of certain qualifying events. You must provide the Fund
Administrator notice of the following qualifying events:
• The divorce or legal separation of a covered Member from his or her spouse.
•A beneficiary ceasing to be covered under the Plan as a dependent child of a member.
• The occurrence of a second qualifying event after a Qualified Beneficiary has become
entitled to COBRA with a maximum of 18 (or 29) months. This second qualifying
event could include a Member’s death, entitlement to Medicare, divorce or legal
separation or child losing dependent status.
12

13
In addition to these qualifying events, there are two other situations when a covered
Member or Qualified Beneficiary is responsible for providing the Fund Administrator
with notice within the timeframe noted in this section:
• When a Qualified Beneficiary entitled to receive COBRA coverage with a maximum
of 18 months has been determined by the Social Security Administration to be
disabled. If this determination is made at any time during the first 60 days of COBRA
coverage, the Qualified Beneficiary may be eligible for an 11-month extension of the
18 months maximum coverage period, for a total of 29 months of COBRA coverage.
• When the Social Security Administration determines that a Qualified Beneficiary is
no longer disabled.
You must make sure that the Fund Administrator is notified of any of these five
occurrences listed above. Failure to provide this notice within the form and
timeframes described below may prevent you and/or your dependents from obtaining
or extending COBRA coverage.
How Should a Notice Be Provided?
In order to provide the Fund notice of any of these five situations you must complete and
sign the Fund’s “COBRA Notice Form for Covered Employees and Qualified Beneficiaries.”
You can obtain a copy of the form by calling the Fund Office at (800) 344-1515.
Alternatively, you may send a letter to the Fund containing the following information:
your name, for which of the five events listed above you are providing notice, the date of
the event, the date in which the participant and/or beneficiary will lose coverage.
To Whom Should the Notice Be Sent?
Notice should be sent to the Fund at the following address:
Director and Field Representative
The New England Carpenters Health Benefits Fund
P.O Box 7075
Wilmington, MA 01887
Phone: (800) 344-1515
Fax: (978) 657-8724
When Should the Notice Be Sent?
If you are providing notice due to a divorce or legal separation, a dependent losing
eligibility for coverage or a second qualifying event, you must send the notice no later
than 60 days after the later of (1) the date upon which coverage would be lost under the
Plan as a result of the qualifying event (2) the date of the qualifying event or (3) the date
on which the Qualified Beneficiary is informed through the furnishing of a summary
plan description or initial COBRA notice of the responsibility to provide the notice and
the procedures for providing this notice to the Fund Administrator.
If you are providing notice of a Social Security Administration determination of disability,
notice must be sent no later than the end of the first 18 months of continuation coverage.

If you are providing notice of a Social Security Administration determination that you are
no longer disabled, notice must be sent no later than 30 days after the later of (1) the
date of the determination by the Social Security Administration that you are no longer
disabled or (2) the date on which the Qualified Beneficiary is informed through the
furnishing of a summary plan description or initial COBRA notice of the responsibility to
provide the notice and the procedures for providing this notice to the Fund
Administrator.
Who Can Provide a Notice?
Notice may be provided by the covered Member, Qualified Beneficiary with respect to
the qualifying event, or any representative acting on behalf of the covered Member or
Qualified Beneficiary. Notice from one individual will satisfy the notice requirement for
all related qualified beneficiaries affected by the same qualifying event. For example, if a
member and his or her spouse and child are all covered by the Plan, and the child ceases
to become a dependent under the Plan, a single notice sent by the spouse would satisfy
this requirement.
Where you or your dependents have provided notice to the Fund Administrator of
a divorce or legal separation, beneficiary ceasing to be covered under the Plan as a
dependent or a second qualifying event, but are not entitled to COBRA, the Fund
Administrator will send you a written notice stating the reason why you are not eligible
for COBRA.
Paying for COBRA Continuation Coverage
You are responsible for the entire cost of COBRA Continuation Coverage. When you
and/or your dependents become eligible for this coverage, the Fund Administrator will
notify you of the COBRA premium amounts that you must pay.
Your COBRA premiums may be as high as 102% of the Plan’s cost, except in the case of
Social Security disability. (See the section below entitled “COBRA Continuation Coverage
for Disabled Participants.”)
You must send the first COBRA payment to the Fund Office within 45 days from the date
on which the Fund Office receives your COBRA election form, as determined by postage
cancellation. You must make payments so that coverage is continuous—there can be no
lapse in coverage. If you choose COBRA within the election period but after the date on
which your eligibility ended, you must pay the required COBRA premiums retroactively
to cover the elapsed period.
Late COBRA Payments
Your monthly payments are due on the 1st day of each month. You will have 30 days
in which to pay. Payments should be mailed to the Fund Office. If you do not make
payment by the end of the 30 days, your coverage will be cancelled retroactively to the
last day of the previous month and you will lose your right to continuation coverage.
14
Notify The Fund Office
You or a family member
should notify the Fund
Office when any
Qualifying Event occurs
to avoid confusion over
the status of your health
care in the event that
your Employer does not
provide prompt or correct
information.
What You Need To Do:
If you lose coverage due
to a Qualifying Event:
• Inform the Fund Office
of the Qualifying Event
and request a COBRA
election form.
• Complete and mail back
the election form within
63 days of the date of
the mailing, or 60 days of
the date the Qualifying
Event occurred, which-
ever is later.
• Make your first payment
to the Fund Office within
45 days from the date the
Fund Office receives your
COBRA election form.

15
COBRA Continuation Coverage for Disabled Participants
If you are covered under COBRA for 18 months, and within the first 60 days of coverage
you (or your covered dependent) become disabled, you (and your Qualified Beneficiaries
who elected COBRA) may be eligible to continue your COBRA coverage for an additional
11 months for a total of 29 months.
To be eligible, the Social Security Administration must make a formal determination that
you (or your dependent) were disabled effective within the initial 60-day period of the
start of your COBRA coverage and therefore entitled to Social Security Disability income
benefits. You (or your dependent) must notify the Fund Office of the Social Security
determination of disability by the end of the 18-month initial COBRA period if you wish
to continue with the 11-month extension.
If you are eligible for the 11-month extension, your COBRA premiums may be as high as
150% of the regular premiums for the additional 11 months of coverage.
This extended period of COBRA coverage will end on the earlier of:
• The last day of the month that occurs 30 days after Social Security has
determined that you and/or your dependent(s) are no longer disabled;
• The end of the 29 months’ COBRA Continuation Coverage;
• The date the disabled person becomes entitled to Medicare.
If you recover from your disability before the end of the initial 18 months of COBRA
Continuation Coverage, you will not have the right to purchase extended coverage. You
must notify the Fund Office within 30 days of:
• The date that you receive a final Social Security determination that you
and/or your dependent(s) are no longer disabled; or
• The date that the disabled person becomes entitled to Medicare.
Multiple Qualifying Events While Covered Under COBRA
The maximum period of coverage under COBRA is 36 months, even if you experience
another Qualifying Event while you’re already covered under COBRA. If you’re covered
under COBRA for 18 months because of your termination of employment or reduction in
hours, your affected spouse or dependent may extend coverage for another 18 months in
the event of your death or if:
•You get divorced or legally separated;
•You become entitled to Medicare; or
•Your child is no longer a dependent under the Fund’s definition.
For example, you stop working (the first COBRA-Qualifying Event), and you enroll yourself
and your dependents for COBRA Continuation Coverage for 18 months. Three months after
your COBRA Continuation Coverage begins, your child turns 19 and no longer qualifies as a
dependent child under the Fund’s definition. Your child then can continue COBRA coverage
separately for an additional 33 months, for a total of 36 months’ COBRA Continuation Coverage.

You, as the member, are not entitled to COBRA Continuation Coverage for more than a
total of 18 months if your employment is terminated or you have a reduction in hours
(unless you are entitled to additional COBRA Continuation Coverage on account of
disability). Therefore, if you experience a reduction in hours followed by a termination
of employment, the termination of employment is not treated as a second Qualifying
Event and you may not extend your coverage.
Coverage for Your Dependents if You’re Enrolled in Medicare
If you are entitled to or enrolled in Medicare and you have a termination of employment
or reduction in hours, your eligible dependents would be entitled to COBRA for a period
of 18 months (29 months if the 11-month Social Security Disability extension applies)
from the date of your termination of employment or reduction in hours or 36 months
from the date you became entitled to Medicare, whichever is longer.
Special COBRA Enrollment Rights
If you marry, have a newborn child, adopt a child or have a child placed with you for
adoption while you are enrolled in COBRA, you may enroll that spouse or child for
coverage for the balance of the period of COBRA Continuation Coverage. You must
enroll your new dependent within 31 days of the marriage, birth, adoption or placement
for adoption, with proper documentation.
In addition, if you are enrolled for COBRA Continuation Coverage and your spouse or
dependent child loses coverage under another group health plan, you may enroll that
spouse or child for coverage for the balance of the period of COBRA within 31 days after
the termination of the other coverage.
To be eligible for this special enrollment right, your spouse or dependent child must have
been eligible for coverage under the terms of the Plan but declined when enrollment was
previously offered because they had coverage under another group health plan or had
other health insurance coverage, with proper documentation.
Confirmation of Coverage to Health Care Providers
Under certain circumstances, federal rules require the Fund to inform your physician and
health care providers as to whether you have elected and/or paid for COBRA
Continuation Coverage. This rule only applies in certain situations where the physician
or provider is requesting confirmation of coverage and you are eligible for, but have not
yet elected, COBRA coverage, or you have elected COBRA coverage but have not yet paid
for it.
Termination of COBRA Continuation Coverage
COBRA Continuation Coverage will terminate on the last day of the maximum period of
coverage unless it is cut short for any of the following reasons:
•You do not make all required payments on time;
• The person receiving the coverage becomes covered by another group health plan
that does not contain any legally applicable exclusion or limitation with respect to
pre-existing conditions that the covered person may have;
16

17
• The person receiving the coverage becomes entitled to Medicare;
•The Plan terminates its group health plan and no longer provides group health
insurance coverage to its members; or
• The Employer that employed you prior to the Qualifying Event has stopped
contributing to the Plan; and
• The Employer establishes one or more group health plans covering a significant
number of the employer’s employees formerly covered under this Plan; or
• The Employer starts contributing to another multiemployer plan that is a group
health plan.
If continuation coverage is terminated before the end of the maximum coverage period,
the Fund Administrator will send you a written notice as soon as practicable following
the Fund Administrator’s determination that continuation coverage will terminate. The
Notice will set out why continuation coverage will be terminated early, the date of
termination, and your rights, if any, to alternative individual or group coverage.
☎
If you have questions about COBRA Continuation Coverage, contact the Fund Office
at (800) 334-1515.
Additional COBRA Election Period and Tax Credit in Cases of
Eligibility for Benefits Under the Trade Act of 1974
If you are certified by the U.S. Department of Labor (DOL) as eligible for benefits under
the Trade Act of 1974, you may be eligible for both a new opportunity to elect COBRA
and an individual Health Insurance Act Credit. If you and/or your dependents did not
elect COBRA during your election period, but are later certified by the DOL for Trade
Act benefits or receive pensions managed by the Pension Benefit Guaranty Corporation
(PBGC), you may be entitled to an additional 60-day COBRA election period beginning
on the first day of the month in which you were certified. However, in no event would
this benefit allow you to elect COBRA later than six months after your coverage ended
under the Plan.
Also under the Trade Act, eligible individuals can either take a tax credit or get advance
payment of 65% of premiums paid for qualified health insurance, including continuation
coverage. If you have questions about these tax provisions, you may call the Health Care
Tax Credit Customer Contact Center toll-free at 1-866-628-4282. TTD/TTY callers may
call toll-free at 1-866-626-4282. More information about the Trade Act is also available at
www.doleta.gov/tradeact/2002act_index.asp. The Fund Administrator may also be able to
assist you with your questions.
Keep the Fund Informed of Address Changes
In order to protect your family’s rights, you should keep the Fund Administrator
informed of any changes in the addresses of your family members. You should also keep
a copy, for your records, of any notices that you send to the Fund Administrator.

18
Consequences of Failing to Elect COBRA
In considering whether to elect continuation coverage, you should take into account that
a failure to continue your group health coverage will affect your future rights under
federal law. First, you can lose the right to avoid having pre-existing exclusions applied
to you by other group plans if you have more than a 63-day gap in health coverage, and
election of continuation coverage may help you prevent such a gap. Second, you will lose
the guaranteed right to purchase individual health insurance policies that do not impose
these pre-existing condition exclusions if you do not get continuation coverage for the
maximum time available to you. Finally, you should take into account that you have
special enrollment rights under federal law. You have the right to request special
enrollment in another group health plan for which you are otherwise eligible (such as a
plan sponsored by your spouse’s employer) within 30 days after your group health
coverage ends because of the qualifying events listed above. You will also have the same
special enrollment right at the end of continuation coverage if you get continuation
coverage for the maximum time available to you.
Certificate of Creditable Coverage
When your coverage ends, the Fund Office will mail you and/or your dependents a
Certificate of Creditable Coverage that indicates the period of time that you were covered
under the New England Carpenters Health Benefits Fund.
If you become eligible for coverage under another group health plan within 62 days of
the date you lose coverage under the New England Carpenters Health Benefits Fund, this
certificate may be necessary if your new group health plan has pre-existing condition
limitations that apply to you.
The Fund Office will mail this certificate to you shortly after they learn that your
coverage has ended. You may request a certificate from the Fund Office within two years
from the date your coverage ended. To request a Certificate of Creditable Coverage,
contact:
Director and Field Representative
New England Carpenters Health Benefits Fund
P.O. Box 7075
Wilmington, MA 01887
Phone: (800) 344-1515
Fax: (978) 657-8724

LIFE EVENTS
Your benefits are designed to adapt to your needs at different stages of your life. This
section describes how your coverage is affected when you experience certain “life events”
and what you must do to make sure you get the most from your coverage.
19
•You should notify the Fund Office as soon as possible if you experience a life event that may affect
your coverage.
•You and/or your dependents may qualify to continue coverage under COBRA in the event of a loss of
eligibility, divorce, or your termination or reduction of your work hours.
• If you become disabled, you may be entitled to receive an extension of coverage for up to 12 months.
The following life events may affect your coverage:
Moving to a new address Entering active military service
Getting married Becoming disabled
Having a baby Retiring
Taking family medical leave Becoming eligible for Medicare
Adopting a child Death
Getting divorced
If you have a change of address, contact the Fund Office for a change of address form
as soon as possible to make sure your records are up to date and to avoid a delay in
payment of claims.
If you legally marry, your spouse is eligible to receive dependent benefits under the New
England Carpenters Health Benefits Fund.
What You Need To Do
If you get married, you should provide the Fund Office with the following information:
•A copy of your marriage certificate, available from the town or city hall where you were married;
•Your spouse’s date of birth and Social Security number; and
•A copy of your spouse’s medical insurance information, if he or she is covered under another
group insurance plan.
✍
Once you provide the required information, your spouse is eligible for coverage
under the Fund as of the date of your marriage. If you wish to name your spouse as
your beneficiary for your life insurance benefit or accidental death and dismember-
ment benefit, contact the Fund Office for “Change of Beneficiary” form.
If your spouse is covered under another group medical plan, you must report this other
coverage to the Fund Office. The amount of benefits payable under this Fund will be
coordinated with your spouse’s other coverage. Benefits for your spouse under this Fund
will be paid after any benefits are payable from your spouse’s plan. For more information,
see “Coordination of Benefits” on page 54.
FAST FACTS:
IF YOU MOVE
IF YOU GET MARRIED
If You Acquire a Child Through Marriage
Notify the Fund Office if you are planning to cover a stepchild under this Fund. You
must provide certain information in order to cover your stepchild:
1. If the natural parents were married, the following is needed:
• The child’s birth certificate;
• The child’s Social Security card;
• The divorce decree; and
•A joint tax return showing that the Member claims the child as a dependent.
2. If the natural parents were never married, the following is needed:
• The child’s birth certificate;
• The child’s Social Security card;
•A joint tax return showing that the Member claims the child as a dependent; and
• The court order. If no court order exists, you must provide a written statement
indicating whether the natural mother has insurance for the child(ren) and
whether the natural father has insurance for the child(ren).
3. If one of the natural parents has passed away, the following is needed:
• The child’s birth certificate;
• The child’s Social Security card;
•A joint tax return showing that the Member claims the child as a dependent; and
•A copy of the death certificate of the natural parent.
Once your child is born, notify the Fund Office as soon as possible. You will need to
provide certain information in order to have your child covered by this Fund.
What You Need To Do
If you have a baby, you should provide the Fund Office with the following information:
•A copy of the baby’s birth certificate listing both parents;
•A copy of the child’s Social Security card; and
•A copy of your baby’s other medical insurance information if he or she is covered under
another group insurance plan.
The Health Benefits Fund covers expenses related to maternity, prenatal care and child
wellness exams. For information, see pages 30-34.
20
IF YOU HAVE A BABY
If you adopt a child, contact the Fund Office. Your child will be covered as of the
effective date of the adoption placement as long as you are responsible for health care
coverage and your child meets the Fund’s definition of a dependent child (see page 8).
What You Need To Do
If you need to add a child to your coverage, you must provide the Fund Office with the
following information:
•A copy of the child’s birth certificate, when it becomes available;
•A copy of the child’s Social Security card, when it becomes available;
•A copy of the Adoption Agency paperwork indicating the specific date the child
was placed in your home; and
•A copy of the initial adoption paperwork, when it becomes available.
Legal Guardianship
If you become a child’s Legal Guardian, coverage for the child will be effective as of the
date specified on court documents. You must provide the Fund Office with:
•A copy of the child’s birth certificate;
•A copy of the child’s Social Security card, when available;
•A copy of the court document indicating that you as the
Member are the legal guardian of the child.
Family Medical Leave Act
If you take leave in certain circumstances such as serious illness, birth of a child, or
caring for a seriously ill parent or spouse, your employer may be obligated to continue
contributions on your behalf under the Family Medical Leave Act (FMLA). Talk to your
employer for details.
If you divorce from your spouse, notify the Fund Office as soon as possible. The Plan
will cover your ex-spouse as required by the divorce, but under no circumstances will the
Plan cover both the ex-spouse and a current spouse.
What You Need To Do
If you get legally divorced, you must provide the Fund Office with the following information:
•A copy of your divorce decree; and
• If you have children and you do not have custody, a copy of any
Qualified Medical Child Support Order (QMCSO), if applicable.
If your spouse wants to continue coverage, he or she must:
• Contact the Fund Office; and
• Enroll in COBRA Continuation Coverage.
Your former spouse may continue coverage under COBRA for up to 36 months. He or
she must notify the Fund Office within 60 days of the day that the divorce becomes final.
The Fund Office will then send the COBRA Notice and enrollment information to your
former spouse. For more information, see page 11.
21
IF YOU ADOPT A CHILD
IF YOU DIVORCE
Under certain situations, the Fund is required to continue to provide coverage to a
divorced spouse of a Member who continues to maintain eligibility and coverage under
the Plan. The Fund will only maintain coverage for a former spouse if presented with a
court separation or alimony agreement stipulating that the Member is required to provide
health coverage for the former spouse. A continuation of benefits under this Plan to a
former spouse shall only be maintained until the termination date set forth in the Order
or the date the Member or spouse remarries, whichever occurs first. Coverage for the
former spouse will terminate when coverage for the Member terminates.
Qualified Medical Child Support Order (QMCSO)
A Qualified Medical Child Support Order (QMCSO) is a court order, judgment or decree
that recognizes that an alternative recipient may be entitled to benefits under this Fund in
the event of a divorce or other family law action. Orders must be submitted to the Fund
Office to determine whether the order is a QMCSO under federal law. As required under the
Employee Retirement Income Security Act (ERISA), this Fund will recognize a QMCSO that:
•Provides for health coverage to the child(ren) under state
domestic relations law (including a community property law); and
• Relates to benefits under this Fund.
Please notify the Fund Office if your situation involves a QMCSO for information about
how these orders are handled. Or, you and/or your beneficiary(ies) can obtain, without
charge, a copy of the Plan’s QMCSO procedures from the Fund Administrator.
If you are on active duty for 31 days or less, you will continue to receive health care
coverage for up to 31 days, according to the Uniformed Services Employment and
Reemployment Rights Act of 1994 (USERRA).
If you are on duty for more than 31 days, USERRA permits you to continue medical and
dental coverage under COBRA (see page 11) for you and your dependents at your own
expense for up to 18 months. COBRA will be offered after your active eligibility and
coverage runs out. Your dependent(s) may be eligible for health care coverage under
TRICARE. The New England Carpenters Health Benefits Fund will coordinate coverage
with TRICARE, as explained on page 56.
Coverage under this Fund will not be offered for any illness or injury determined by the
Secretary of Veterans Affairs to have incurred in, or been aggravated during, performance
of service in the uniformed services. The uniformed services and the Department of
Veterans Affairs will provide care for service-connected disabilities.
When you are discharged (not less than honorably) from “service in the uniformed
services,” your full eligibility will be reinstated on the day you return to the Union Office
for work with a Contributing Employer, provided that you return within:
• Ninety (90) days from the date of discharge if the period of service was more than
one hundred eighty days; or
• Fourteen (14) days from the date of discharge if the period of service was 31 days or
more but less than one hundred eighty days; or
22
IF YOU ENTER ACTIVE
MILITARY SERVICE

• At the beginning of the first full regularly scheduled working period on the first
calendar day following discharge (plus travel time and an additional eight hours) if
the period of service was less than thirty-one (31) days.
•You will be granted the same plan of coverage you had when you began active duty.
If you are hospitalized or convalescing from an injury caused by active duty, these time
limits are extended up to two years.
What You Need To Do:
If you are called to military leave, you should:
• Notify your employer and the Fund Office; and
• Make any required self-payments to the Fund Office to continue your coverage.
If you become disabled and cannot work, you may be eligible for a Weekly Accident and
Sickness Benefit for up to 26 weeks. See page 51 for more information.
Extension of Coverage for Totally Disabled Members
If you are totally disabled due to an injury or illness and your coverage under the Health
Benefits Fund ends, you will be eligible to extend coverage for up to 12 consecutive
months (two coverage periods) from the date your coverage ends. This is a once-per-
lifetime benefit. For more information, see page 9.
If you or your covered spouse become eligible for Social Security Retirement Benefits at
age 65, you are also eligible for Medicare. Medicare is the federally sponsored health care
program consisting of hospital insurance (Part A) and supplementary medical insurance
(Part B).
You should enroll in Medicare Parts A and B as soon as you are eligible—three months
before your 65th birthday or in certain cases when you become disabled—in order to
avoid a gap in coverage.
To Enroll in Medicare:
•Visit your local Social Security Office;
• Call 1-800-MEDICARE (1-800-633-4227); or
• Go to the Medicare website at www.medicare.gov.
If you remain actively employed beyond age 65, you will continue to receive coverage
provided you work the required number of hours. You (and your spouse) may elect to
participate on a self-pay basis in the group Medicare supplemental plan, provided
through the Fund. This supplemental plan is Blue Cross Blue Shield Medex Gold, which
includes prescription drug coverage.
For information about how your benefits are paid through the New England Carpenters
Health Benefits Fund when you are enrolled in Medicare, see page 55.
23
IF YOU BECOME DISABLED
IF YOU BECOME ELIGIBLE
FOR MEDICARE
In the event of your death from any cause while you’re covered under Plan I or Plan II,
the Fund may provide an extension of health benefits at no cost to your surviving spouse
and children for a period of up to three years. This extended coverage will be available if
these family members have no other health coverage. Coverage for survivors is provided
under the same Plan that you were covered under at the time of your death. See page 10
for more information.
✍
Your designated beneficiary must provide a certified copy of the death certificate in
order to receive a benefit.
What Your Beneficiary Needs To Do:
In the event of your death, your spouse or beneficiary must:
• Notify the Fund Office;
• Provide the Fund Office with an original copy of your death certificate; and
• Apply for your life insurance benefit (and AD&D benefit, if applicable).
24
UPON YOUR DEATH
YOUR MEDICAL PLAN
The New England Carpenters Health Benefits Fund provides a comprehensive medical
plan with coverage for office visits, hospitalization and surgery, home health care, mental
health and substance abuse treatment.
25
• If you are covered under Plan I or Plan II, as an active member or dependent, you may visit any
physician you’d like, including a physician in or out of the PPO.
• If you are in the Retiree Plan, you must use a physician in the PPO to receive benefits,
unless you live outside of a 20-mile radius of a PPO provider.
• Before any hospital admission, you must notify the Fund’s managed health care
program, for pre-approval.
•Your hours worked determine which Plan you’re eligible for. (Refer to page 6 for more information.)
Plans I and II offer a broad range of medical services. You have the freedom to visit any
provider you wish, either one that participates in the Plan’s Preferred Provider
Organization (PPO) network, or an out-of-network provider. Plans I and II offer coverage
both in and out-of-network; however, you’ll save money for you, your family and for the
Fund if you use a provider in the PPO. For a summary of the benefits offered, refer to
the Schedule of Benefits on pages 71-77.
The Retiree Plan is a self-pay plan for retirees and their dependents. Coverage is
provided when services are obtained only from a network (PPO) provider. For a
summary of the benefits offered, refer to the Schedule of Benefits on pages 78-79.
LIFETIME MAXIMUM PLAN BENEFIT
The Lifetime Maximum amount that the Fund will pay toward eligible expenses per
covered individual per lifetime is $1,000,000 if the Member or eligible dependent is
covered under Plan I or the Retiree Plan, or $500,000 if covered under Plan II.
Automatic Reinstatement of Lifetime Maximum Plan Benefit
Each year, the amount of expenses that you or your dependents incur during the
previous year is added back to the Lifetime Maximum Plan benefit—up to $50,000 for
Plan I and up to $10,000 for Plan II. Note that the total maximum can never exceed
$1,000,000 for Plan I or $500,000 for Plan II. Automatic reinstatement can apply if there
is a minimum of one benefit cent remaining at the end of the calendar year.
The Lifetime Maximum Plan Benefit is separate among all three plan options per covered
individual. For example, if a covered individual switches between Plan II and Plan I and
then to the Retiree Plan, each Plan has a separate maximum benefit.
Preferred Provider Organization
The Fund contracts with CCN, and pays a monthly fee for access to its network of
doctors, hospitals and other health care providers that contract with the CCN PPO.
FAST FACTS:
Using the PPO provides savings and convenience to you, your family and the Fund.
When you use a PPO:
• The provider bills the Fund directly; and
• Just one claim form is required each calendar year for each family member.
Your Share of the Cost
To help cover health care expenses, you are responsible for sharing some of the cost for
services. You are responsible for:
• Copayments;
•The calendar year deductible;
•Your coinsurance; and
• Charges (if any) above the Reasonable and Customary amount
if you obtain services outside of the PPO network.
The Calendar Year Deductible
The deductible is the amount you (and/or your family) must pay in medical expenses
before the Fund will begin to pay benefits. The amount of your calendar year deductible
depends on the Plan of Benefits you’re covered under, as shown below.
Calendar Year Deductible
Plan I Plan II Retiree Plan
$150 individual $300 individual $250 per person
$300 family $600 family N/A
!! Any amount you pay toward the deductible under Plan I or Plan II for services
rendered in October, November or December of that year is applied to the deductible
for the following calendar year. That way, you are saved from having to meet the
deductible twice in a short period of time.
Office Visit Copayment
If you visit an in-network provider, there is a $10 copayment due the provider at the
time of the visit. Copayments do not count toward meeting your deductible, coinsurance
or out-of-pocket maximums.
Emergency Room Penalty
If you visit a hospital emergency room for non-urgent care, there is a $50 penalty.
Coinsurance
Once you satisfy the calendar year deductible for all eligible expenses, the Fund may pay
a portion of the benefit. The remainder is your share, or coinsurance amount. Refer to
the Schedule of Benefits, beginning on page 71, for specific coinsurance information.
26
Need to Find a PPO
provider?
Visit the CCN website
at www.ccnusa.com
to locate a PPO provider
near you.
Reasonable and Customary Charges
A Reasonable and Customary (R&C) charge is the “going rate,” as determined by the
Plan based on published guidelines, for a particular medical service or supply in a
specific geographic area. If your health care provider charges more than the R&C rate for
a particular service, you will be responsible for paying that additional amount. For
example, if your doctor charges $500 for a service, but the R&C charge is $475, you will
be responsible for paying $25 in addition to your coinsurance.
Out-of-Pocket Maximums
The Fund has limits on the amount that you must pay out of your own pocket for
eligible medical expenses (your coinsurance and deductibles) each year. After you’ve
reached that limit, the Fund will pay 100% of your eligible medical expenses for the
remainder of the calendar year, up to the Lifetime Maximum.
Out-of-Pocket Maximum
Plan I Plan II Retiree Plan
$1,500 per person $3,000 per person $3,000 per person
Coinsurance for mental health or alcohol/substance abuse inpatient and outpatient
services does not apply toward the out-of-pocket maximum per calendar year.
MANAGED HEALTH CARE PROGRAM — PREAUTHORIZATION
You or your medical provider must contact Hines & Associates in advance if you are
going to be admitted to the hospital for any reason or will receive home health care
services or hospice care upon discharge from an inpatient stay. The Hines & Associates
provider will contact your doctor and evaluate your proposed treatment needs and
medical care standards in your community.
What Services Require Preauthorization?
Contact Hines & Associates at 1-800-944-9401 for authorization before you receive
any of the following treatments or services:
• Inpatient hospitalization;
• Certain out-patient surgeries;
• Home health care services; or
• Hospice care.
27

Preauthorization for Hospitalization
The managed health care program helps the Health Benefits Fund keep down the cost of
a hospital admission and helps you to make better decisions when you need care. This
program is mandatory for all eligible Members and dependents under all Plans of
Benefits. It is your responsibility to contact Hines & Associates before any inpatient
hospitalization. If you do not receive prior authorization for any hospital admission, your
hospitalization benefit will be reduced by $500.
Precertification Requirement for Outpatient Surgical Procedures
Hines & Associates must be contacted to Pre-certify the Outpatient Surgical Procedures
listed below:
• EVLT (Endovenous Laser Therapy) for Varicose Veins
• Septoplasty
• Blepharoplasty
•Breast Reduction
• Abdominoplasty (Panniculectomy)
• Biopsy
• LeForte Osteotomy
• UPPP (Uvulopalatopharyngoplasty)
The following is an example of the medical information Hines & Associates may request:
• Clinical History
•Office Notes
• Photos
This is only a partial list of procedures that need precertification and medical information
Hines & Associates may require. Please contact the Fund office for more information.
What You Need To Do:
Contact Hines & Associates by calling 1-800-944-9401 for authorization prior to your
inpatient Hospitalization.
Make sure you have the following information available:
• Name and Social Security number of the patient;
• Name and Social Security number of the covered Member if different
from the patient;
• Date of proposed admission;
•Name, address and telephone number of the attending physician; and
•Name, address and telephone number of the hospital.
You will be notified in writing of the authorization. If you have not received a written
authorization by the day of your admission, call Hines & Associates.
28

29
Emergency Admission Review Procedure
If you have a medical emergency, you (or a family member) must notify Hines &
Associates within 24 hours of your admission. Show your insurance identification card to
your doctor and the admissions office of the hospital. For your convenience, Hines &
Associates phone number is printed on your card. Failure to notify Hines & Associates
will result in a $500 penalty.
What’s Covered
The New England Carpenters Health Benefits Fund provides eligible Members and
their dependents with a comprehensive plan of benefits. Coverage includes office visits,
hospitalization and surgery, wellness benefits, substance abuse and mental health
treatment, coverage for prescription drugs, dental care (Plan I only) and vision care.
The benefits are described in more detail on the following pages of this book.
For more information about what’s covered under your Plan of Benefits, refer to the
Schedule of Benefits on pages 71-79.
What’s Not Covered
A comprehensive listing of the Fund’s general exclusions are listed on page 52 and 53.
30
WELLNESS BENEFITS
ANNUAL PHYSICAL EXAMS
You and your spouse are entitled to one physical exam per calendar year, up to a
maximum of $150 for Plan I, $75 for Plan II and $100 for the Retiree Plan.
Flu shots can be considered under this benefit if the available dollars are not exhausted.
Any additional charges such as laboratory and/or x-ray charges that exceed the maximum
amount the Plan will pay will be your financial responsibility.
ANNUAL PAP TESTS AND MAMMOGRAMS
Annual Pap tests and mammograms are covered as a sickness benefit and are not subject
to the maximum for the routine physical exam.
WELL-CHILD EXAMS
Plan I
Your children are covered for routine well-child exams at 100% of charges after a $10
copayment from birth up through age five. Your children age six and older are covered at
100% for annual physical exams to a maximum of $70 per calendar year until they turn
19 (or through age 23 if a full-time student).
Plan II
Your children through age five only are covered at 100% with a $10 copayment for
annual physical exams when network providers are used. Well-child exams for children
aged six or older are not covered under Plan II.
Retiree Plan
Your children in the Retiree Plan are not covered for well-child exams.
Refer to the Schedule of Benefits on pages 71-79 for more information.
31
HOSPITALIZATION AND SURGERY
The New England Carpenters Health Benefits Fund provides hospitalization and surgery
coverage for you and your eligible family members. Your specific coverage depends on
your Plan of Benefits and whether you use a hospital and/or a surgeon in the PPO network.
HOSPITALIZATION
Inpatient and outpatient hospital expenses will be billed to the Fund Office. Covered
eligible expenses will be reimbursed according to the chart below, after you’ve met your
deductible. If you are in Plan I or Plan II, you may use any hospital you’d like; however, if
you use a hospital in the PPO, your costs may be less. Retiree Plan participants must use
a PPO hospital to receive benefits, unless you live more than 20 miles from a PPO hospital.
• All inpatient hospitalization must be precertified prior to any hospital stay. If you do not pre-certify
your hospital stay you will have to pay a penalty, and your hospitalization may not be covered.
• Emergency treatment is covered at 100% when you use a PPO Urgent Care Center instead of an
emergency room.
• Doctor’s charges for maternity care, including pre-natal care and delivery, are covered at 100% of
R&C through a PPO provider.
FAST FACTS:
Inpatient Hospitalization
Plan I Plan II Retiree Plan
PPO Network 100% of network charges 80% of network charges 80% of network charges
up to the first $10,000. after you’ve met your after you’ve met your
Then, 90% after you’ve deductible. deductible.
met your deductible.
Out-of-Network 85% of charges 75% of charges 80% of charges after
after you’ve met your after you’ve met your you’ve met the deductible,
deductible. deductible. provided you live outside
a 20-mile radius from a
PPO provider.
☎
Precertify your hospitalization by calling 1-800-944-9401.
Mandatory Pre-Hospitalization Review
If you are going to be hospitalized, you or your doctor must call Hines & Associates,
the Fund’s Health Management provider, within 24 hours to have your hospitalization
authorized in advance. If you do not contact Hines & Associates and receive prior
authorization for your hospital stay, your benefits will be reduced by $500 for that
claim. See page 27 for more information.
Emergency Care
Emergency care is limited to treatment of major illness or injuries requiring urgent
attention. Surgery (including but not limited to sutures, casting, cast removal, strapping,
removal of foreign bodies) and/or supplies that you may require are subject to the
calendar year deductible and provisions of regular plan benefits.
What You Need To Do:
When you call Hines &
Associates, make sure
you have the following
information available:
• Name or Social Security
number of the patient;
• Name or Social Security
number of the covered
Member, if different from
the patient;
• Date of proposed
admission.
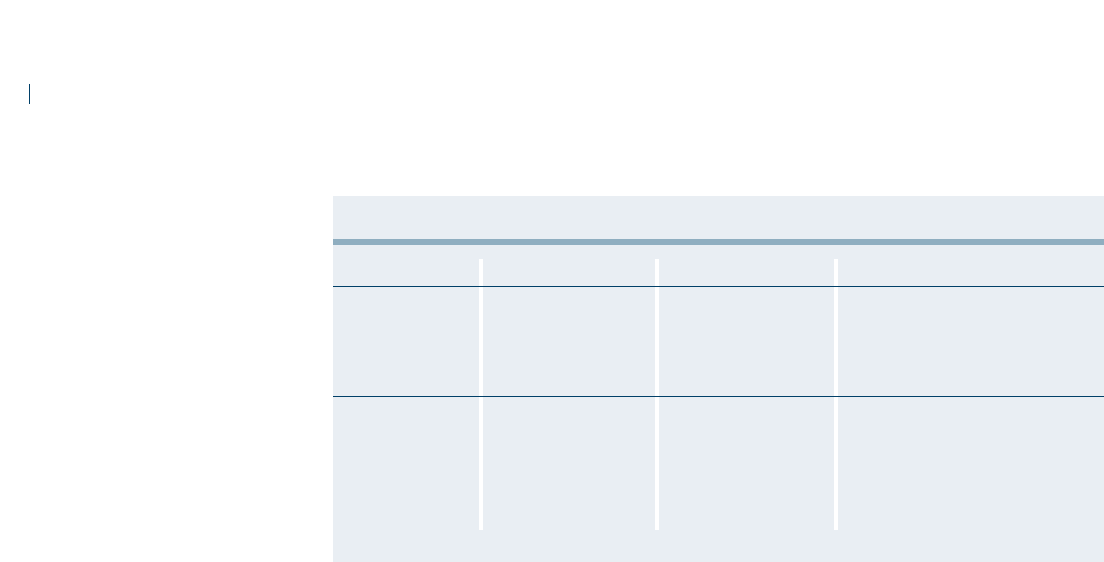
!! You are strongly encouraged not to use a hospital emergency room for urgent care
unless there is a life-threatening condition. You will incur a $50 penalty for any visit
to a hospital emergency room for routine urgent care that is not life-threatening.
Life-Threatening Conditions Include:
32
Emergency Room
Plan I Plan II Retiree Plan
PPO Network 90% of network 80% of network 80% of network charges after
charges after you’ve charges after you’ve your deductible. 50% of network
met your deductible. met your deductible. charges for non life-threatening
emergencies.
Out-of-Network 85% of charges 75% of charges 80% of charges after you’ve
after you’ve met after you’ve met met your deductible. 50% of
your deductible. your deductible. the out-of-network charges for
non life-threatening emergencies
provided you live outside a 20-
mile radius from a PPO provider.
• Abdominal pain
• Accidental injuries
• Acute allergic reactions
• Acute asthma
• Acute gallbladder attack
• Appendicitis
• Cerebral or cardiac spasms
• Coma
• Diabetic coma
• Hypothermia
• Insertion of catheter for
acute retention
•Insulin shock and overdose
• Kidney stone
• Maternity complications
• Pneumonitis
•Respiratory distress
• Severe chest pain
• Severe effects of exposure (frostbite,
sun or heat stroke)
• Shock
• Spontaneous pneumothorax
• Strangulated hernia
• Stroke
• Sudden loss of vision
• Suspected heart attack
• Thrombosis and/or phlebitis
• Unconsciousness

33
SURGEON’S CHARGES
The chart below shows the amount payable for eligible surgical expenses based on your
Plan of Benefits.
!! Please note that certain charges that are related to surgery, such as facility charges,
anesthesia or laboratory charges are not included in the physician’s charges for your
surgery. For more information, see the Schedule of Benefits on pages 71-79.
Maternity
Doctor’s charges for maternity care, including pre-natal care and delivery, are covered at
100% of the PPO fee schedule, otherwise subject to R&C charges. Expectant mothers
covered under Plan I or II are covered for alpha-fetoprotein and other related pre-natal
testing at 100% of the charges when a PPO provider performs the tests. Any laboratory
work sent outside the PPO network for processing or analysis will be covered, subject to
the deductible, according to your Plan’s Schedule of Benefits.
Voluntary Maternity Early Discharge Benefit
The early Maternity discharge program is offered to mothers who choose to be discharged
within one day after normal vaginal delivery, or three days after a Caesarean section.
Those mothers may receive ONE Registered Nurse Home Health Care visit.
The hospital must notify Hines & Associates to obtain prior approval for this benefit.
Hines & Associates will recommend an in-network provider, if available. If an in-
network provider is used, the benefit for the Home Health visit will be paid at 100% of
contract, after your plan deductible is satisfied.
If an out-of-network provider is used, the Home Health visit will be paid at the out-of-
network level of your plan benefits.
Newborns’ and Mothers’ Health Protection Act of 1996
Group health plans and health insurance issuers generally may not, under federal (or state)
law, restrict benefits for any hospital length of stay in connection with childbirth for the
Surgery
Plan I Plan II Retiree Plan
Surgeon’s Charges 100% of fee schedule. 100% of fee schedule. 100% of fee schedule.
(PPO Network) Otherwise subject to Otherwise subject to Otherwise subject to
R&C charges. R&C charges. R&C charges.
Surgeon’s Charges 85% of R&C charges 75% of R&C charges 80% of R&C charges
(Out-of-Network) for eligible expenses for eligible expenses for eligible expenses
after you’ve met your after you’ve met your after you’ve met your
deductible. deductible. deductible, provided you
live outside a 20-mile
radius from a PPO
provider.

Plan I Plan II Retiree Plan
Calendar Year Deductible $150 per person $300 per person $250 per individual
$300 per family $600 per family
Surgeon’s Expenses 100% of PPO fee 100% of PPO fee 100% of PPO fee
(PPO) schedule. schedule. schedule.
Otherwise subject to Otherwise subject to Otherwise subject to
R&C charges. R&C charges. R&C charges.
Surgeon’s Expenses 85% of R&C charges 75% of R&C charges 80% of R&C charges
(Out-of-Network) after deductible after deductible after deductible
Hospital Room and 100% of the first 80% after deductible 80% after deductible
Board (PPO) $10,000, then payable
at 90% after deductible
Hospital Room and 85% after deductible 75% after deductible 80% after deductible
Board (Out-of-Network)
Hospital Physician Expense 90% of charges after 80% of charges after 80% after deductible
Benefit (PPO) deductible deductible
Hospital Physician Expense 85% of R&C charges 75% of R&C charges 80% of R&C charges
Benefit (Out-of-Network) after deductible after deductible after deductible
mother or newborn child to less than 48 hours following a vaginal delivery, or less than 96
hours following a Cesarean section. However, federal law generally does not prohibit the
mother’s or newborn’s attending provider, after consulting with the mother, from discharging
the mother or her newborn earlier than 48 hours (or 96 hours as applicable). In any case,
plans and issuers may not, under federal law, require that a provider obtain authorization
from the plan or issuer for prescribing a length of stay not in excess of 48 hours (or 96 hours).
Women’s Health and Cancer Rights Act of 1998 (WHCRA)
If you have or are going to have a mastectomy, you may be entitled to certain benefits
under the Women’s Health and Cancer Rights Act of 1998 (WHCRA). For individuals
receiving mastectomy-related benefits, coverage will be provided in a manner determined
in consultation with the attending physician and the patient, for:
• All stages of reconstruction of the breast on which the mastectomy was performed;
• Surgery and reconstruction of the other breast to produce a symmetrical appearance;
•Prostheses; and
•Treatment of physical complications of the mastectomy, including lymphedema.
Your physician must contact Hines & Associates at 1-800-944-9401 in advance for
pre-approval of these services.
These benefits will be provided subject to the same deductibles and coinsurance
applicable to medical and surgical benefits provided under yout Plan’s Schedule of
Benefits. Therefore, the following deductibles and coinsurance apply:
34
If you would like more information on WHCRA benefits, call the Fund Office at
(800) 344-1515.

35
MENTAL HEALTH AND SUBSTANCE ABUSE
The Fund provides certain coverage under Plan I, Plan II and the Retiree Plan for
treatment of Mental Health and Substance Abuse for you and your eligible dependents.
Mental Health and Substance Abuse Treatment
Plan I Plan II Retiree Plan
Outpatient
100% of network charges 100% of network charges 100% of network charges
Mental Health to a calendar year to a calendar year to a calendar year
PPO Network; maximum of 25 visits per maximum of 10 visits per maximum of 25 visits per
requires a $10 person per calendar year. person per calendar year. person per calendar year.
copay
Outpatient 50% of R&C charges to 50% of R&C charges to 50% of R&C charges up to
Mental Health a calendar year maximum a calendar year maximum a calendar year maximum
Out-of-Network of 25 visits per person per of 10 visits per person per of 25 visits per person,
calendar year, after you’ve calendar year, after you’ve after you’ve met your
met your deductible. met your deductible. deductible, if you live
outside a 20-mile radius
from a PPO provider.
Inpatient 90% of network charges 80% of network charges 80% of network charges
Mental Health to a calendar year to a calendar year to a calendar year
PPO Network maximum of 30 days maximum of 30 days maximum of 15 days
per person, after you’ve per person, after you’ve per person, after you’ve
met your deductible. met your deductible. met your deductible.
Inpatient 85% of charges to a 75% of charges to a 80% of charges to a
Mental Health calendar year maximum calendar year maximum calendar year maximum
Out-of-Network of 30 days per person, of 30 days per person, of 15 days per person,
after you’ve met your after you’ve met your after you’ve met your
deductible. deductible. deductible.
Outpatient 100% of network charges 100% of network charges 100% of network charges
Substance Abuse to a calendar year to a calendar year to a calendar year
PPO Network; maximum benefit of maximum benefit of maximum benefit of
requires a $10 $500 per calendar year $500 per calendar year $500 per calendar year
copay per person. per person. per person.
Outpatient 85% of R&C charges to a 75% of R&C charges to a 80% of R&C charges to a
Substance Abuse calendar year maximum calendar year maximum calendar year maximum
Out-of-Network benefit of $500 per benefit of $500 per benefit of $500 per
calendar year per person, calendar year per person, calendar year per person,
after you’ve met your after you’ve met your after you’ve met your
deductible. deductible. deductible.
Inpatient 90% of network charges, 80% of network charges, 80% of network charges,
Substance Abuse after you’ve met your after you’ve met your after you’ve met your
(Drug & Alcohol) deductible deductible deductible
PPO Network Maximum of 30 Inpatient Maximum of 30 Inpatient Maximum of 15 Inpatient
Days Per Calendar Year Days Per Calendar Year Days Per Calendar Year
Per Person Per Person Per Person
Maximum of Two (2) Maximum of Two (2) Maximum of Two (2)
LIFETIME Occurrences LIFETIME Occurrences LIFETIME Occurrences
Per Person Per Person Per Person
Inpatient 85% of charges after 75% of charges after 80% of charges after
Substance Abuse you’ve met your deductible you’ve met your deductible you’ve met your deductible
(Drug & Alcohol) Maximum of 30 Inpatient Maximum of 30 Inpatient Maximum of 15 Inpatient
Out-Of-Network Days Per Calendar Year Days Per Calendar Year Days Per Calendar Year
Per Person Per Person Per Person
Maximum of Two (2) Maximum of Two (2) Maximum of Two (2)
LIFETIME Occurrences LIFETIME Occurrences LIFETIME Occurrences
Per Person Per Person Per Person

36
PREAUTHORIZATION
If your doctor recommends inpatient care for the treatment of Mental Health or
Substance Abuse, you must obtain pre-approval through the Fund’s Health Management
provider, Hines & Associates, by calling 1-800-944-9401 for authorization before your
admission. You will be notified in writing of the authorization. If you have not received a
written authorization by the day of your admission, call Hines & Associates.
A person who does not complete the prescribed treatment plan that is established at
the beginning of his/her treatment will be responsible for paying the full cost of the
treatment.
Payment for the treatment of inpatient substance abuse, whether alcohol or drugs, will
be limited to two occurrences in a lifetime.
The Health Fund’s utilization review firm, Hines & Associates, along with the Carpenters
Assistance Program, will assist the Fund in assuring that our Members receive the
highest level of care in the appropriate facilities.

HOME HEALTH CARE
Home Health Care helps the Fund to keep down hospital expenses by providing an
alternative to inpatient hospital care. Home Health Care can not only decrease the length
of a hospital admission but can also, in some cases, eliminate a hospital admission
altogether. This service can save the Fund 50% or more on the cost of inpatient care. In
addition, Home Health Care provides a sense of security during a time of illness. You or a
family member can receive many services at home in familiar surroundings and close to
family and friends.
37
•A Home Health Care Agency is a licensed organization that provides skilled nursing and other therapeutic
services for participants that are recovering from an injury or illness in the comfort of their own home.
• Home Health Care through a PPO provider is covered at 100% after you meet the deductible.
• Help with daily living (custodial care) is covered if provided in your home at the direction of a
hospice organization.
The Fund’s Managed Health Care provider will arrange for medically necessary home
health care through the PPO. To be covered, your doctor must submit a letter of medical
necessity to the Fund Office. Benefits for Home Health Care are shown in the chart below.
FAST FACTS:
Home Health Care
Plan I Plan II Retiree Plan
PPO Network 100% of network charges, 90% of network charges, 100% of network charges,
after you’ve met your after you’ve met your after you’ve met your
calendar year deductible calendar year deductible calendar year deductible
if care begins within if care begins within if care begins within
7 days of discharge from 7 days of discharge from 7 days of discharge from
an inpatient stay; an inpatient stay; an inpatient stay;
otherwise, 90% after otherwise, 80% after otherwise, 80% after
deductible. deductible. deductible.
Out-of-Network 90% of R&C charges, 80% of R&C charges, 80% of R&C charges
after you’ve met your after you’ve met your if you’ve met your
calendar year deductible calendar year deductible deductible and you live
if care begins within if care begins within outside a 20-mile radius
7 days of discharge from 7 days of discharge from from a PPO provider
an inpatient stay; an inpatient stay; if care begins within
otherwise, 85% after otherwise, 75% after 7 days of discharge from
deductible. deductible. an inpatient stay.
To be covered, charges by a Home Health Care Agency for care at home must start within
seven days of a prior hospital confinement for the same or for a related condition OR in
order to prevent a proposed hospital confinement.

What’s Covered
Note that only medically necessary services that are prescribed by the attending physician
and under the supervision of the attending physician are covered. The following is a
partial list of health services available through a Home Health Care Agency:
• Part-time or intermittent nursing care by a registered nurse or by a licensed practical
nurse under the supervision of a registered nurse, if services of a registered nurse are
unavailable;
• Part-time or intermittent home health aide services, consisting primarily of patient
care of a medical or therapeutic nature by other than a registered or licensed practical
nurse;
• Physical therapy, speech therapy, medical social work and nutritional consultations
provided by the Home Health Care Agency; and
• Medical supplies, medications prescribed by a physician and laboratory services by or
on behalf of the Home Health Care Agency to the extent such items would have been
covered if the insured had remained in the hospital. Visits must be medically necessary.
HOSPICE CARE
Hospice Care is covered at 100% through the PPO for Plans I and II only. A hospice is a
facility that provides care and services for the terminally ill and that:
•Provides 24-hour a day nursing care for the terminally ill person with necessary
physical, psychological and spiritual needs, with acute inpatient and outpatient care,
home care, bereavement counseling directly or indirectly;
• Has a medical director who is a physician;
• Has an interdisciplinary team that coordinates the care and services it provides
and that includes at least one physician, one registered professional nurse and one
social worker;
•Maintains central clinical records on all patients; and
• Is licensed or accredited as a hospice if required.
38
What is a Home
Health Aide?
A home health aide is
a person who provides
care of a medical or
therapeutic nature and
reports to and is under
the direct supervision
of a Home Health Care
Agency.
! NOTE: Custodial care
is covered as part of your
hospice care benefits
if provided in your home
at the direction of a
hospice organization.
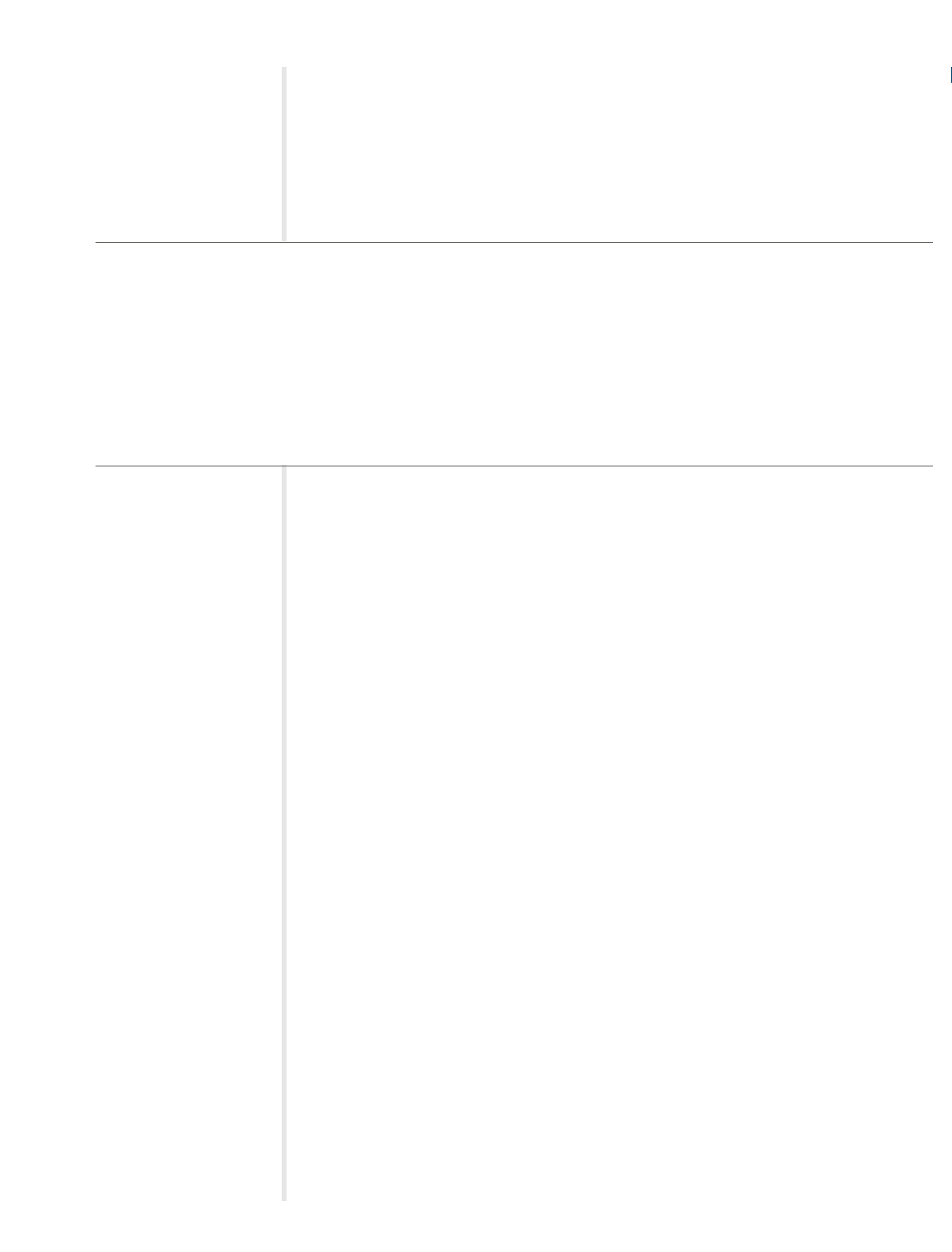
CARPENTERS ASSISTANCE PROGRAM
The Carpenters Assistance Program (CAP) provides free, confidential assistance for you
and your family members when confronting stress, depression, alcoholism, drug abuse,
and job or family problems.
39
How to Contact the CAP
Call 1-800-344-1515
extension 1160 to speak
confidentially with a
counselor or to make an
appointment.
☎
CAP, in association with the Employee Assistance Program (EAP) service of the
Mount Auburn Hospital, provides assistance through a network of facilities
throughout the area. Professionals determine an appropriate treatment plan for
you and/or your covered dependents. To contact Mount Auburn (EAP),
call 617-661-0090 or 1-800-888-5105.
You and your family are eligible for the following benefits:
• Assessment for drug, alcohol, marital, emotional or legal difficulties and/or career
problems;
• Referral to the appropriate facility for the treatment of drug or alcohol dependency
(see Mental Health and Substance Abuse on page 35);
• Diagnostic evaluation and referral to inpatient and/or residential treatment facilities;
• Full coverage for short-term counseling provided by the EAP services of Mount
Auburn Hospital for up to eight one-hour visits per incident;
• Case management and follow-up services for one year; and
• Educational seminars, outreach activities and consultation.
☎
If you are admitted to a hospital or other facility for emergency care for a mental
disorder or for substance abuse treatment, you, a member of your family, your doctor,
or the hospital must call Hines & Associates at 1-800-944-9401 within 24 hours of
your admission.
!! Note: Court-ordered or random drug testing is not covered under the
Carpenters Assistance Program.
• The Carpenters Assistance Program is available to participants and eligible dependents in Plan I, Plan II
and the Retiree Plan.
• When you call, a CAP counselor will assess your situation and set up an appointment for short-term
counseling or refer you to the appropriate provider for treatment.
•Treatment you receive through the Carpenters Assistance Program is strictly confidential.
• If you receive a referral for inpatient treatment of mental health or substance abuse, you must contact
Hines & Associates, the Fund’s Health Management provider, at 1-800-944-9401 for pre-admission
certification within 24 hours of your admission.
FAST FACTS:

PRESCRIPTION DRUGS
The prescription drug benefit offers you and your family a convenient and cost-effective
way to receive your prescription medication. You may have your prescriptions filled by
mail or at a pharmacy. If you use generic drugs, you will save money for yourself and for
the Health Benefits Fund.
40
•Present your Ullicare Rx/Medco card at a participating pharmacy and make the applicable copayment to
receive your prescription drugs.
•You can save time and money by using the mail order program. You can order a 90-day supply of generic
prescription drugs for just $20.
• For retirees, a $15,000 per individual per calendar year maximum applies.
The chart below shows your copayments for prescription drugs based on whether you
receive your prescription medication from a retail pharmacy or through the mail.
FAST FACTS:
Prescription Drugs*
Generic Brand Preferred Brand Non-Preferred
Retail (34-day supply) $10.00 $20.00 $30.00
Mail (90-day supply) $20.00 $40.00 $60.00
Generic Drugs
The Health Benefits Fund encourages the use of generic drugs. Generic drugs are a less
expensive alternative to brand name drugs. The generic version of any drug contains
identical active chemical ingredients and must meet the same manufacturing standards
and federal requirements for safety and effectiveness as a brand name drug. Your
copayments for generic drugs are lower whether you use a retail pharmacy or order your
prescription drugs by mail.
Brand Preferred
This category of medications consists of brand name and generic medications that are the
most commonly used, the most cost efficient and the most therapeutically beneficial in
the treatment of common health conditions.
Brand Non-Preferred
All brand name and generic medications not falling into the above categories.
How to Get Your Prescription Drugs
When you fill a prescription at a pharmacy, you simply present your Ullicare Rx/Medco
card when you request your medication and pay the applicable copayment.
Mail Order Program
The mail order program is a convenient way for you to receive any medication—
especially “maintenance drugs” that you need to take on a regular basis. Because you
* The calendar year maximum is $15,000 per individual in the Retiree Plan.
know in advance that you will need this medication, it’s easy to establish a routine of
filling such prescriptions by mail. Through the mail order program, you are eligible to
receive medication for up to a 90-day supply. Contact the Fund Office for a mail order
form.
What’s Covered
Coverage for prescription drugs is provided for the following non-hospital items:
• Legend drugs;
• Injectable insulin and supplies, including hypodermic needles, syringes and test
material;
• Compounded medication of which at least one ingredient is a prescription legend
drug; or any other drug which, under state law, may only be dispensed upon the
written prescription of a physician;
• Oral contraceptives;
•Viagra (6 tablets every 30 days).
What’s Not Covered
No benefits are payable for:
• The difference in charges between a generic drug and brand name drug unless
“Dispensed as Written” appears on the prescription;
•Drugs or medicines lawfully obtainable without a prescription order of a physician or
dentist except insulin;
• Birth control devices (other than oral contraceptives);
• Levonorgestrel (Norplant);
• Therapeutic devices or appliances and support garments;
• Immunization agents, biological sera, blood or blood plasma;
•Drugs labeled “Caution—limited by federal law to investigational use” or with
similar language or experiment drugs even though a charge is made to the person;
• Any charge for the administration of prescription legend drugs or insulin;
• Any medication, legend or not, which is consumed or administered at the place
where it is dispensed;
• Medication which is to be taken by or administered to the person in whole or in part
while he or she is a patient in a licensed hospital, rest home, sanitarium, extended
care facility, convalescent hospital, nursing home or similar institution which
operates on its premises, a facility for dispensing pharmaceuticals;
• Refilling of a prescription in excess of the number specified by the physician or
dentist or any other refill dispensed after one year from the order of a physician or
dentist;
•Prescription drugs that may be properly received without charge under local, state or
federal programs, including Workers’ Compensation or similar law;
41
How to Fill a
Mail Order Prescription
Obtain a written prescrip-
tion from your doctor for a
90-day supply of medica-
tion. The prescription must
include:
• The patient’s full name
• The doctor’s name, phone
number and address
• Exact strength, quantity
and dosage; and
• Diagnosis, if required for
that drug.
• Call the Fund Office to
request a mail order form.
What are
Maintenance Drugs?
Maintenance drugs are
those that you require on
an ongoing basis such as
medication for high blood
pressure, heart conditions
or diabetes.

• The following drugs:
– Aero Chamber (covered under the Medical Plan with a letter of medical
necessity);
– Hepatitis A or B (covered under the Medical Plan with a letter of medical
necessity);
– Rogaine (Minoxidil or Loniten) when prescribed for hair restoration;
– Retin-A (Tretinoin Cream, Gel, Liquid) except when prescribed by a physician for
acne or a skin disorder for an eligible dependent child before age 24 (covered
under the medical plan for adults with letter of medical necessity);
– Smoking deterrent medications;
– Fertility drugs* such as, but not limited to:
– Pergonal (menotropins);
–Profasi HP (HCG-Human Chorionic Gonadotropin);
–Pro-Ception;
– Serophene (Clomiphene Citrate);
–Clomid (Dienestrol);
–Lupron;
– Ephinephrine – primatine mist;
– Ephedrine sulfate – absolute decongestant;
– Ferrous sulfate – iron supplement;
– Elixir terpin hydrate – expectorant;
– Over the counter vitamins with or without fluoride; and
–Growth hormones.
*Certain fertility drugs are covered under the Medical Plan.
42

DENTAL CARE
Healthy teeth and gums are an important part of your overall health. That’s why the Health
Benefits Fund offers comprehensive dental benefits through Delta Dental, the nation’s
largest dental network. Dental benefits are provided for participants in Plan I only.
43
•You do not have to meet a deductible to receive dental care.
•You may visit any dentist you’d like, but you’ll save money if you use a provider in the Delta Dental
network— “Delta Preferred Option USA Plus.”
• There are no claim forms to file if you use a Delta Dental Network provider.
• Dental benefits are available to Plan I participants and their eligible dependents.
• The Plan covers orthodontia, even for adults.
FAST FACTS:
If you are covered for benefits under Plan I, you and your dependents are eligible for
dental benefits through Delta Dental. Dentists that participate in the Delta Dental network
have agreed to provide services at a pre-negotiated discounted rate. When you visit a
Delta Dental provider, show your Delta Dental ID card to receive the discounted rates.
The chart below shows the amount the Plan pays for Dental Care through the Delta
Dental network.
Dental Benefits (Plan I only) Plan Pays
Diagnostic and Preventive (includes cleanings and x-rays) 100% of network charges
Restorative, Oral Surgery, Periodontics, Endodontics, Prosthetic 80% of network charges
Maintenance and Emergency Dental Care
Prosthodontics (dentures) and Major Restorative 50% of network charges
Orthodontics 100% of network, up to $2,000
per person per lifetime
Out-of-Network Benefits
If you do not use a Delta Dental provider, you will be billed for any amount that your
out-of-network dentist charges that is more than the pre-negotiated Delta Dental network
charge.
Maximum Benefits
A $1,500 calendar year maximum dental benefit applies to each covered person for
dental services per calendar year. The lifetime maximum benefit for orthodontia is
$2,000 per covered person. There’s no age limit for orthodontia.

Covered Dental Surgical Services
The following surgical procedures are covered under the New England Carpenters Health
Benefits Fund:
• Surgical removal of unerupted teeth or impacted teeth when imbedded
in the bone or soft tissue
– Soft tissue impaction
– Partial bony impaction
– Complete bony impaction
• Extraction of seven or more permanent teeth
• The excision of a benign or cancerous growth other than a radicular cyst
• Radicular cysts involving the roots of three or more teeth
• Gingivectomies involving two or more gum quadrants
• Gingival flap
• Mucogingival surgery
• Osseous surgery
• Osseous graft
• Soft tissue graft
• Apicoectomy
44
Questions about
What’s Covered?
Contact Delta Dental
Customer Service at
1-800-872-0500 for
information about
limitations or exclusions
that may apply to a
particular procedure.

Routine vision examinations are essential for maintaining healthy eyes and good vision.
Vision benefits are provided under Plans I, II and the Retiree Plan and for Members and
their spouses who are retired and are collecting a pension from the Carpenters Union
and are current in their monthly dues. Also eligible are spouses of deceased pensioned
Members who continue to collect the Member’s pension after their death provided the
Member was current with dues at the time of his or her death.
The Plan provides:
• For adults – routine eye exam and glasses once every two years; and
• For children – (up to age 19 or 24 if full-time students) routine eye exam and glasses
once every year.
“Glasses” means one pair of bifocals or two pairs of single-vision glasses, one for distance
and one for close-up. Special lens materials and coatings that are not covered under the
vision benefit are available for a reasonable copayment through the Vision Center and
Davis Network.
!! Note: When using the Davis Network, you must obtain your examination and glasses at the same time
and from one provider.
*You also have the option of choosing contact lenses instead of eyeglasses at the Vision
Center or through a Davis Vision Network Provider, with a copayment. The contact lens
benefit guidelines are as follows:
• New wearers, either new to the doctor or first-time obtaining contacts — routine eye
examination, a comprehensive fitting and two standard lenses or two boxes of either
disposable lenses or planned replacement lenses; and
• Existing wearers — routine eye examination, a reassessment fitting and two standard
lenses or two boxes of planned replacement lenses or four boxes of disposable lenses.
45
FAST FACTS:
VISION CARE
•You and your spouse may receive an eye exam and a pair of glasses or contacts* once every 24 months
from the Carpenters Vision Center or from a Davis Vision provider. Your dependent children are
eligible for an eye exam and a pair of glasses or contacts once every 12 months.
• The Optional Vision Benefit may also be available to you, allowing you to visit a vision care specialist
of your choice and receive partial reimbursement for examinations and glasses.

The contact lens benefit is not available through the Optional Vision Benefit
explained below.
You have three alternatives for receiving vision benefits:
• Carpenter Vision Center — owned and operated under the New England Carpenters
Health Benefits Fund. It offers complete eye examinations and the largest selection of
frames available under the Plan. Optical services that aren’t provided under the Plan
are available at a discounted rate through the Vision Center. The Vision Center is at
250 Everett St., Allston, MA, and offers afternoon, evening and Saturday
appointments. Call (617) 782-0100 for an appointment.
• Davis Vision Program—a network of private doctors under contract to provide
routine eye exams and eyeglasses or contact lenses. There is a select group of frames
available under the Davis Vision Plan. Network doctors are located throughout New
England. To find a convenient doctor, call 1-800-999-5431or visit their website at
www.davisvision.com.
Be sure to choose a full-service doctor who can provide both the exam and eyeglasses
or contact lenses. When you make your appointment and at the time of your visit,
tell the staff you are in the Davis Vision program. If you are retired, you must contact
the Carpenter Vision Center (617-782-0100) before contacting Davis Vision.
• Optional Vision Benefit — allows you to see any eye doctor you choose and receive a
partial reimbursement. This option is available only to members of Plan I or Plan II
or members of Local 1996 who live in Maine, Vermont or Northern New Hampshire.
Reimbursement is as follows, regardless of the fee the provider charges:
– Eye exam (routine) — $50
– Frames (one pair only) — $40
– Eyeglass lenses (one pair only) — $60
– Contact lenses — no reimbursement
The following Plan participants must use either the Carpenters Vision Center or a Davis
Vision Network Provider:
• Retirees covered under the Retiree Plan.
• Retired members (and their spouses) who are collecting a pension from
the Carpenters Pension Plan and are current in their dues.*
•A surviving spouse who is receiving the Pension of a retired Member who
was current in his or her dues at the time of his or her death.*
*Members in these categories must contact the Vision Center at 617-782-0100 before
utilizing their vision benefit.
!! The PPO Network ophthalmologists are not part of the vision care benefit.
46
Questions about
Vision Coverage
Call the Carpenter Vision
Center (617) 782-0100
or the Carpenters
Health Benefits Fund
Office if you have ques-
tions (1-800-344-1515).
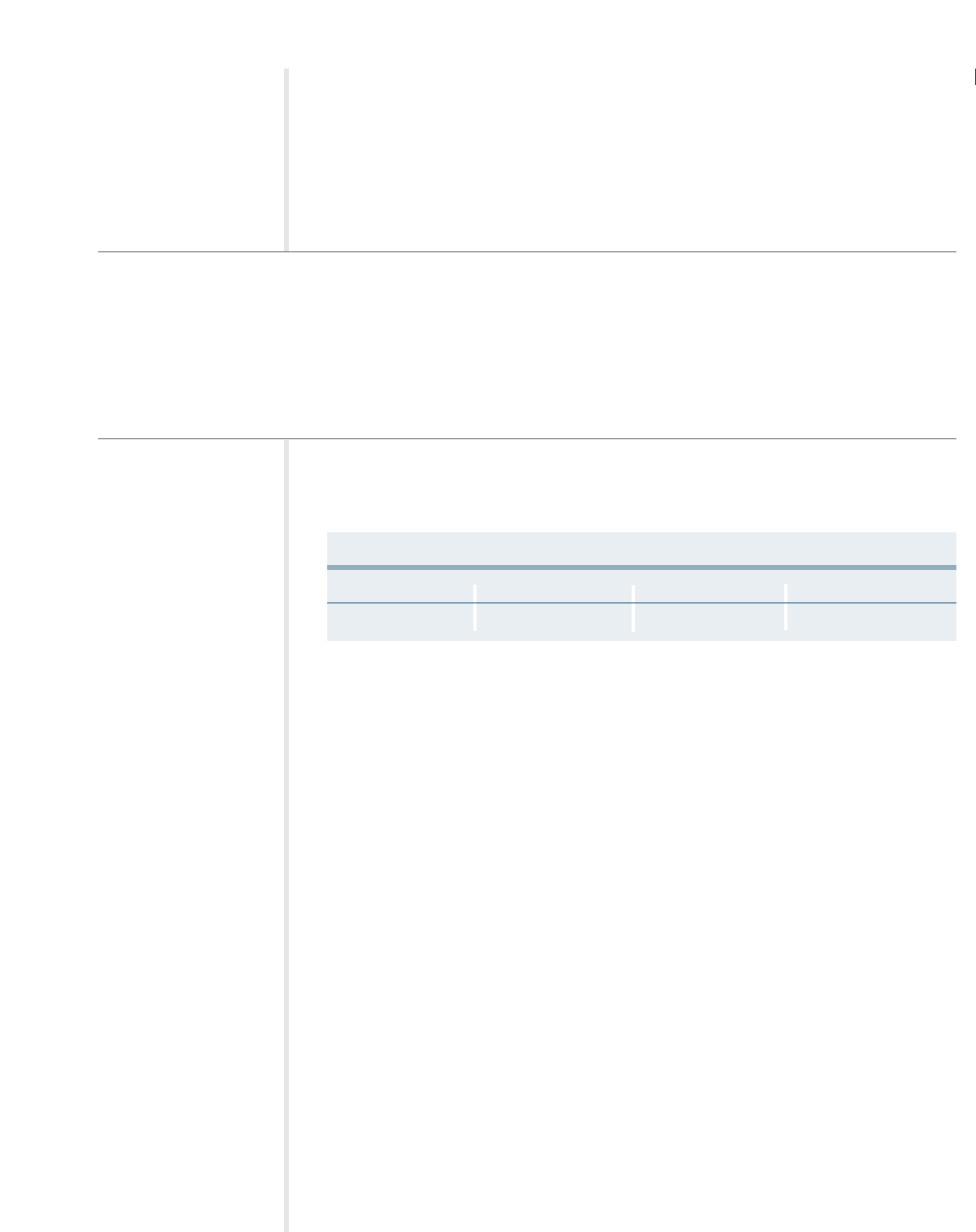
LIFE INSURANCE
Your designated beneficiary will be eligible for a life insurance benefit from this Fund if
you die from any cause while you’re an active member and you’re covered by the New
England Carpenters Health Benefits Fund.
47
•Your designated beneficiary will receive a lump sum benefit if you die while you are an active
member covered by this Fund.
•Your beneficiary must provide the Fund Office with a certified copy of your death certificate in order
to receive a benefit.
• If your current legal spouse dies while you are an active member covered by this Fund, you will be
eligible for a lump sum benefit of $2,000.
The chart below shows the lump sum that is payable to your designated beneficiary upon
your death.
Life Insurance
Plan I Plan II Retiree Plan
Benefit $20,000 $10,000 No Benefit
Naming a Beneficiary
✍
You may name anyone you wish to be your beneficiary and you may change this
designation at any time. To change your beneficiary, call the Fund Office for the
appropriate form. You do not need to get your beneficiary’s consent to make this
change. Your change will be effective when the Fund Office receives your completed
form.
!! Your beneficiary designation must be on file at the Fund Office at the time of your
death to be valid.
If you do not have a designated beneficiary form on file at the Fund Office at the time of
your death, or if your designated beneficiary does not survive you, your life insurance
benefit will be paid to your estate.
COVERAGE FOR YOUR SPOUSE
The Fund also provides a life insurance benefit for your spouse. If your current legal
spouse dies from any cause while covered under the New England Carpenters Health
Benefits Fund, you, as the Member, will be eligible for a lump sum benefit of $2,000.
Note that ex-spouses are not eligible for this benefit.
Keep Your Beneficiary
Information Up-To-Date
Contact the Fund Office
if you’d like to change
your beneficiary if you get
married, have a child or
get divorced.
FAST FACTS:

Continuing Coverage If You Become Disabled
✍
If you become totally and permanently disabled while you're covered under the
Health Benefits Fund, your life insurance benefit will be continued at no cost to you
unless you recover from your disability or attain age 65. You must complete and file
an application for total and permanent disability with the Fund Office within one
year of the date you become disabled and prior to your 60th birthday. The Fund
Office will require proof of your continued disability to keep your life insurance in
force. Contact the Fund Office to request an application.
IF YOUR COVERAGE ENDS
Extended Benefits
If you die within 31 days from the date your coverage under the New England
Carpenters Health Benefits Fund ends, the full amount of life insurance will be payable
to your beneficiary.
Converting Your Coverage
✍
You may convert your life insurance to an individual policy if your coverage under
the Health Benefits Fund ends. To apply, contact the Fund Office for an application
for conversion through the Hartford Life Insurance Company within 31 days of the
date your coverage ends.
48
What is Total and
Permanent Disability?
The Health Benefits Fund
considers you totally and
permanently disabled if
you are not working at any
job for wage or profit, and
you are unable to work in
any job that is reasonably
suited to you by your edu-
cation, training or experi-
ence due to an illness or
injury.
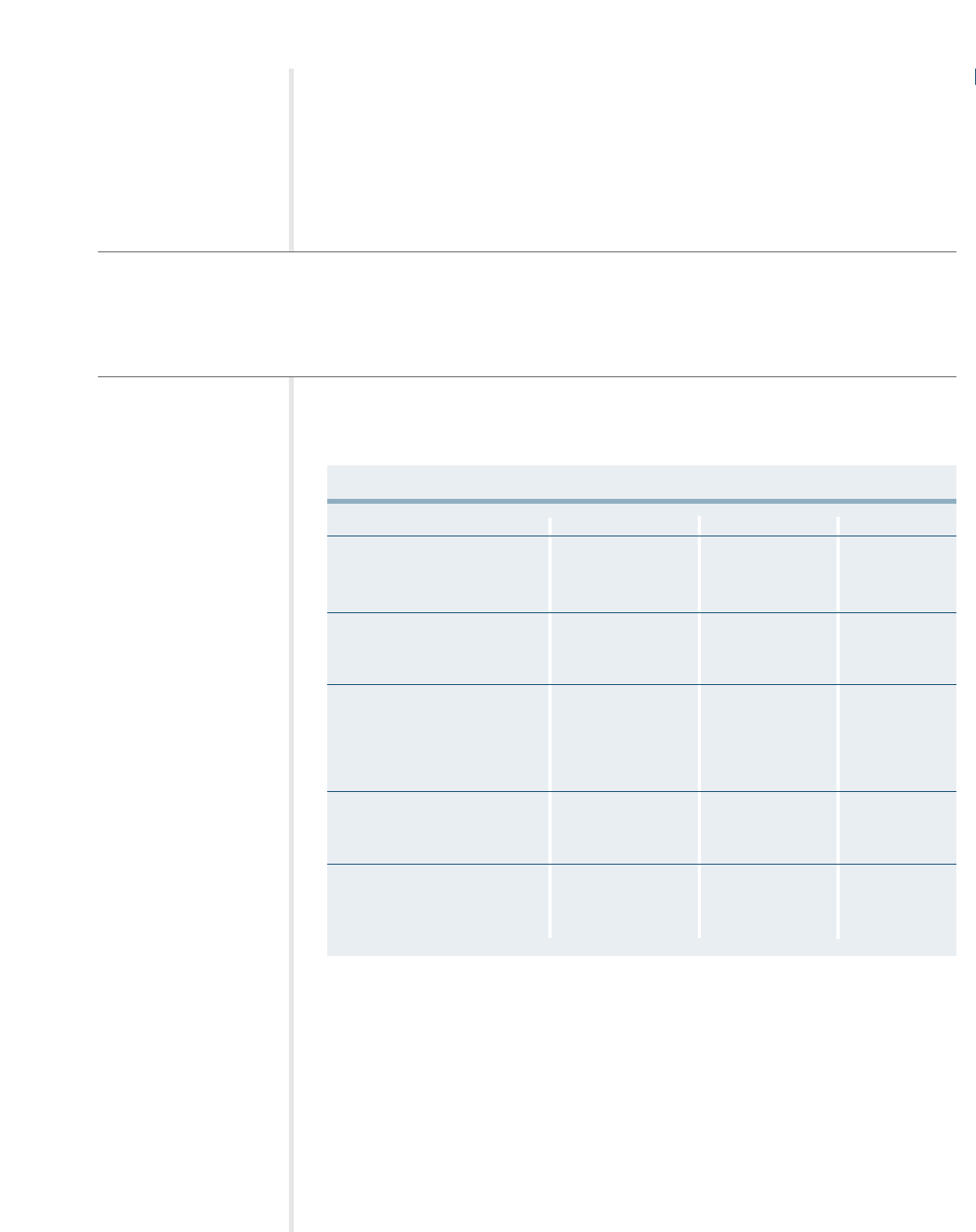
ACCIDENTAL DEATH AND DISMEMBERMENT
Accidental Death and Dismemberment (AD&D) Insurance provides a benefit for Plan I
and II Participants for accidental loss of life, limbs or eyesight while you are covered by
the New England Carpenters Health Benefits Fund.
49
• This benefit is available for the Member only; dependents are not covered under the AD&D benefit.
• The AD&D benefit is payable in addition to and separate from the life insurance benefit.
• Benefits are payable if the loss is a direct result of any injury caused by an accident.
FAST FACTS:
The chart below shows the amount that is payable to you in the case of accidental dismem-
berment. In the event of your death, the benefit is payable to your designated beneficiary.
Accidental Death and Dismemberment
Plan I Plan II Retiree Plan
Loss of Life or loss of $20,000 $10,000 No benefit.
movement of both upper and
lower limbs (quadriplegia)
Loss of movement of three limbs $15,000 $7,500 No benefit.
(triplegia) or loss of movement of
both lower limbs (paraplegia)
Loss of a hand, a foot, an eye, $10,000 $5,000 No benefit.
speech or hearing. Loss of
movement of both upper and
lower limbs on one side of the
body (hemiplegia)
Loss of thumb and index finger $5,000 $2,500 No benefit.
on either hand or loss of
movement of one limb (uniplegia)
More than one of the above $20,000 or the sum $10,000 or the sum No benefit.
resulting from one accident of the benefits of the benefits
payable for each loss, payable for each loss,
whichever is less. whichever is less.
Loss means the following:
• Loss of a hand or foot means that it is completely cut off at or above the wrist or ankle joint.
• Loss of an eye means that sight in the eye is completely lost and cannot be recovered
or restored.
• Loss of speech or hearing means that speech or hearing is lost entirely and the loss
cannot be recovered or restored. Hearing must be lost in both ears.
• Loss of movement of limbs means that the movement is completely lost and irreversible.
• Loss of thumb and index finger means actual severance through or above the
metacarpophalangeal joints.

50
SEATBELT BENEFIT
If you are properly wearing a seatbelt (as verified on the police report) at the time of an
automobile accident and you suffer a loss that is payable under the AD&D benefit, you
may be eligible for a “seatbelt benefit.” To be eligible, you must be a passenger riding in
an automobile or the licensed operator of the automobile that is involved in the accident.
For Plan I, the seatbelt benefit is $2,000. For Plan II, the seatbelt benefit is $1,000. There
is no seatbelt benefit for members in the Retiree Plan.
What’s Not Covered
The Fund will not pay an AD&D benefit for death or any loss resulting from or caused
directly, wholly or partly by:
• Sickness;
• Disease;
• Medical treatment for sickness or disease;
• Any infection, except a pus-forming infection of an accidental cut or wound;
•War or any act of war, whether war is declared or not;
• Any injury received while in any armed service of a country that is at war or engaged
in armed conflict;
• Any intentionally self-inflected injury, suicide, or suicide attempts, whether sane or insane;
• The injured person’s intoxication. Intoxication means that blood alcohol content or the
results of other means of testing blood alcohol level meet or exceed the legal
presumption of intoxication under the law of the state where the accident took place;
• Participation in the commission of a felony; or
•Taking drugs, sedatives, narcotics, barbituates, amphetamines, or hallucinogens
unless prescribed for or administered by a licensed physician.
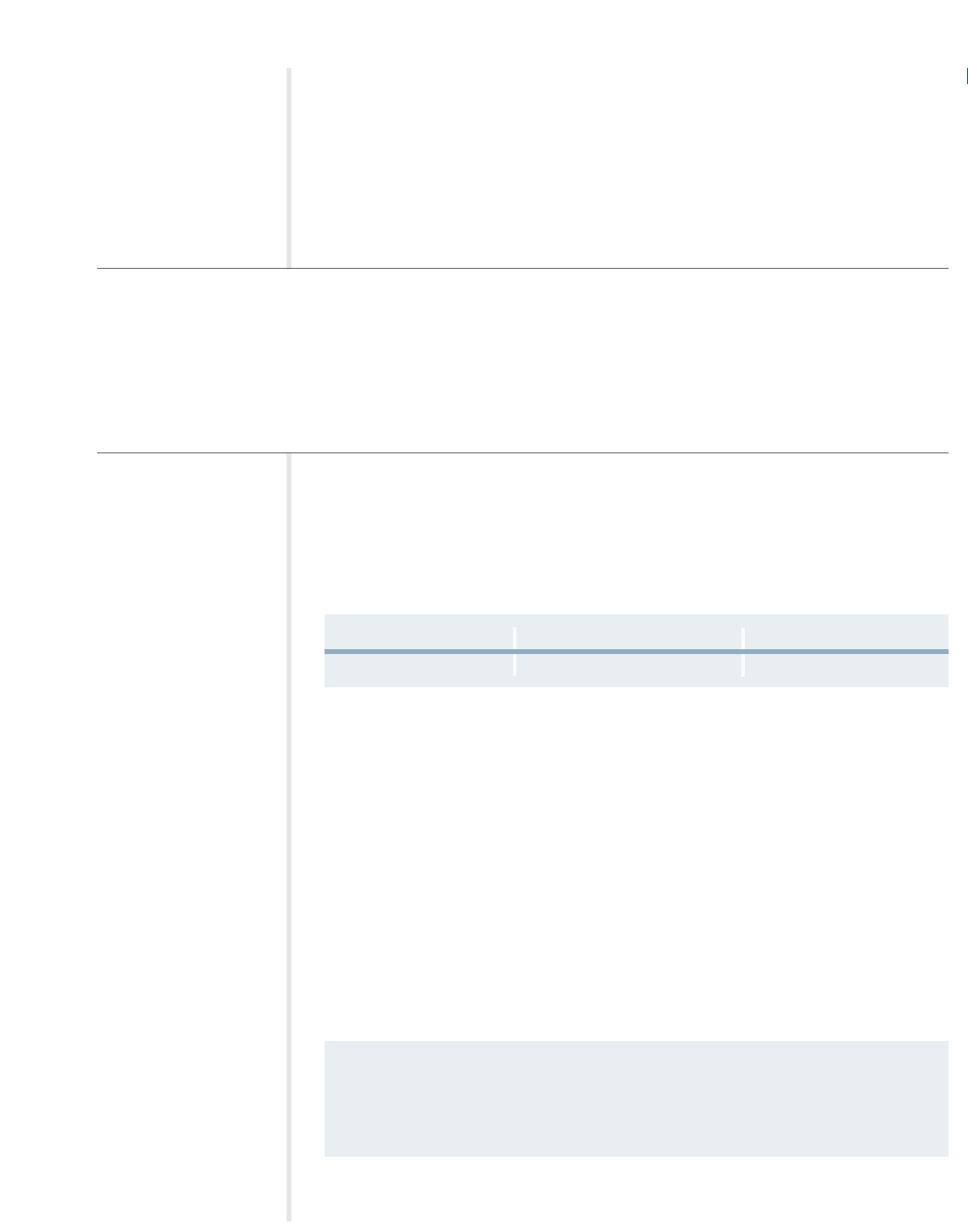
FAST FACTS:
WEEKLY ACCIDENT AND SICKNESS
If you become totally disabled and cannot work due to a non-work related injury or
illness, you are eligible for a weekly accident and sickness benefit through the New
England Carpenters Health Benefits Fund. This benefit is only available to Members in
Plan I with worked hours.
51
• If you are an eligible Plan I Member and you become disabled while covered under Plan I, you may
receive a weekly benefit of $250 from the Health Benefits Fund for up to 26 weeks.
• The Weekly Accident and Sickness benefit is only available to you while you are under the care of a
physician.
• If you are receiving a benefit under Workers’ Compensation or unemployment benefit, Occupational
Disease Law or similar legislation, you are not eligible for the Weekly Accident and Sickness benefit.
Payment of Benefits
Your benefit of $250 per week will begin on the first day of the disability if it is due to an
accident or the eighth day of the disability if it is due to an illness. Payment will
continue during your disability for a maximum of 26 weeks for any one continuous
period of disability due to the same or related cause or causes.
When Benefits Begin Day 1 (Accident) Day 8 (Illness)
Maximum Benefit 26 Weeks 26 weeks
Successive periods of disability that are separated by less than two weeks of continuous
active covered employment are considered one period of disability. If you suffer another
disability due to a different and unrelated cause, you must return to active work for a
period of more than two weeks to receive a benefit for another period of disability.
!! It is not necessary for you to be confined to your home in order to collect a weekly
accident and sickness benefit, but you must be under the care of a legally qualified
physician licensed to practice medicine.
Pregnancy-Related Disability
If you are totally disabled and medically unable to work because of pregnancy, childbirth
or miscarriage, your weekly accident and sickness benefit is payable from the eighth day
of disability on the same basis as any other illness.
Please Note
• Payments you receive
from the weekly accident
and sickness benefit are
considered taxable income
and must be reported on
your federal income tax
return. The Fund Office
will withhold state and
federal income taxes.
• No Social Security (FICA)
tax is deducted from your
payment. The Fund pays
this tax for you.
•You are not eligible for this
benefit if you are using
Banked Hours to maintain
your eligibility.
• For information about filing
weekly accident and sick-
ness claims, see page 63.
• If your disability is related
to a motor vehicle acci-
dent, the Fund does not
pay until the benefit from
the automobile insurance
has been exhausted.
• If your disability is due to
an injury but you do not
stop working at the time
of the injury, the disability
is considered an illness
and the waiting period
applies.
• It is your responsibility to
provide updates of your
condition to the Fund
Office.
If You’re Injured on the Job
If you become disabled due to a work-related illness or injury, you may be eligible for a
Workers’ Compensation benefit. Contact your employer or Local for information on how to
apply for benefits.

52
GENERAL EXCLUSIONS
The following is a partial list of plan exclusions for Plan I, II and the Retiree Plan. You
may call the Fund Office to request specific information as to whether or not a service or
supply is a covered expense. The Plan excludes expenses or charges:
• For services or supplies not recommended by a physician or surgeon or not
medically necessary in treating the injury or illness;
• That are in excess of Reasonable and Customary (R&C) charges;
• For medical care or treatment and services or supplies for charges that are made by a
nursing home, rest home, convalescent home or similar establishment;
• For services or supplies that are:
–Not provided in accordance with generally accepted professional medical
standards; or
– For experimental or investigational treatment;
• Custodial care, when not provided in your home at the direction of a hospice
care organization;
• That result from cosmetic or reconstructive surgery except:
– When surgery is performed on an eligible dependent child because of a
congenital disease or anomaly that has resulted in a functional defect as
determined by his or her attending physician or surgeon; or
– In the case of an accidental bodily injury;
•In connection with dental work, x-rays or surgery (unless part of the dental benefits
for Plan I participants), except expenses for services that are required for correction
of damage caused by an accidental injury to a sound and natural tooth sustained by
an eligible person, or for tumors or cysts of an eligible person;
• Under Plan I and Plan II Temporomandibular Joint Disorders (TMJ) are excluded for
appliances and services, supplies or procedures to increase the height of teeth
(increase vertical dimension or restore occlusion) except for (1) disorders caused by
or result in a specific medical condition, such as degenerative arthritis and jaw
fractures or dislocations. The medical condition must be proven to exist by means of
diagnostic x-ray tests or other generally accepted diagnostic procedures; and a
mandibular orthopedic repositioning appliance (MORA);
•Temporomandibular Joint Disorders (TMJ) for Retirees;
• Early Intervention Services;
• Made by a Veterans’ Administration Hospital or by a physician employed by a
Veterans’ Administration Hospital if the disability is service related, except as
mandated by law;
• That the member is not legally required to pay or that is for medical care furnished
without charge, paid for or reimbursable by or through a government agency or
county, except where specifically prohibited by applicable statute;
• For special home construction to accommodate a disabled person;
• For medical or surgical treatment of obesity, including but not limited to, gastric
restrictive procedures, intestinal bypass and reversal procedures, weight loss
programs, dietary instructions, and any complications thereof;

•For medical or surgical treatment of severe underweight, including, but not limited
to high calorie and/or high protein food supplements, other food or nutritional
supplements, or nutritional counseling, except in conjunction with medically
necessary treatment of anorexia, bulimia or acute starvation. Severe underweight
means a weight more than 25 percent under normal body weight for the patient’s age,
sex, height and body frame based on weight tables generally used by physicians to
determine normal body weight;
• For memberships in or visits to health clubs, exercise programs, gymnasiums, and/or
any other facility for physical fitness programs;
• For sterilization reversals;
•For failure to appear for an appointment as scheduled, for completion of claim forms,
attorneys’ reports or late stay charges;
•For injury, illness or dental treatment for which an eligible person has received or is
entitled to receive benefits under a Workers’ Compensation or Occupational Disease
Law or that arises out of or in the course of any occupation or employment;
•For any loss, expense or charge resulting from an eligible person’s participation in the
commission of a felony;
•For any loss, expense or charge resulting from an act of declared or undeclared war,
armed aggression or act of terrorism;
•For any loss, expense or charge incurred while an eligible person is on active duty or
in training in the Armed Forces, National Guard or Reserves of any state or country;
• For supplies or equipment for personal hygiene, comfort or convenience such as air
conditioning, humidifier, physical fitness and exercise equipment, tanning bed or
water bed;
• For court-ordered or random drug testing;
• For Infertility Treatment under the Retiree Plan;
• For acupuncture unless rendered by an M.D. (Medical Doctor);
• For services rendered when not an eligible participant; and
• Claims not received in the Fund Office within 12 months from date of service.
☎
Contact the Fund Office at (800) 344-1515 for specific information about whether or
not a service or supply is a covered expense.
53
54
COORDINATION OF BENEFITS
Members of a family are often covered under more than one group health plan, which
could result in duplication of health coverage. To avoid this, the health care benefits
provided by this Fund are coordinated with similar benefits payable under other plans.
•You must report any duplicate group health coverage for yourself and/or your dependents
on any claim you submit to the Fund Office.
• Benefits under this Fund are coordinated with HMO, PPO, Medicare or other group health care coverage.
FAST FACTS:
Under the Coordination of Benefits provision, if you are covered under any other group
health plan, the total payment you receive from all programs may not be more than 100%
of the “allowable expenses.” Allowable expenses are the necessary and reasonable expenses
for treatment or supplies covered by the primary plan that you are covered under.
Methods of Coordination
The plan under which benefits are payable first is the primary plan. All other plans are
called secondary plans. The following rules determine which plan’s benefits are payable
first and follow the National Association of Insurance Commissioner’s Model Rules:
•A plan that does not contain a Coordination of Benefits provision is always primary.
•A plan that covers you as a Member is primary.
• If you are covered as a Member under two plans, the plan that has covered you for
a longer period is primary.
•A plan that covers you as an active Member pays before a plan which covers you as
a laid-off Member or retiree.
Rule 2: Dependent Child Covered Under More Than One Plan
A. If the parents of a child are married or are living together, then the plan that covers
the parent whose Birthday falls earlier in the calendar year pays first; and the plan
that covers the parent whose Birthday falls later in the calendar year pays second. If
the parents are not living together but a court decree awards joint custody to both
parents without specifying that one parent has the responsibility to provide health
care coverage for the child, this rule also applies.
B. If both parents have the same Birthday, the plan that has covered one of the parents
for a longer period of time pays first; and the plan that has covered the other parent
for the shorter period of time pays second.
C. The word “Birthday” refers only to the month and day in a calendar year; not the
year in which the person was born.
D. If the specific terms of a court decree state that one parent is responsible for the
child’s health care expenses or health care coverage, and the plan of that parent has
actual knowledge of the terms of that court decree, that plan pays first. If the parent
with financial responsibility has no coverage for the child’s health care services or
expenses, but that parent’s current spouse does, the plan of the spouse of the parent
with financial responsibility pays first. However, this provision does not apply during
any Plan Year during which any benefits were actually paid or provided before the
plan had actual knowledge of the specific terms of that court decree.
E. If the parents are divorced, separated or not living together (regardless of whether
they were ever married), and there is no court decree allocating responsibility for the
child’s health care services or expenses, the order of benefit determination among the
plans of the parents and their spouses (if any) is:
1. The plan of the custodial parent pays first; and
2. The plan of the spouse of the custodial parent pays second; and
3. The plan of the non-custodial parent pays third; and
4. The plan of the spouse of the non-custodial parent pays last.
Coordination of Benefits with Health Maintenance Organizations (HMOs),
Preferred Provider Organizations (PPOs) and Similar Organizations
If you or your dependents are covered by an HMO, a PPO, or a similar health care organ-
ization and that group health plan is primary, you must utilize all health care alternatives
available to you through the other provider(s) before this Fund will honor any claim
for benefits. Also, if a member or his/her dependents violates the provisions of the HMO,
such as neglecting to use that plan’s facilities or following managed care or precertifica-
tion provisions, no benefits will be payable under this Plan.
Coordination of Benefits with Medicare
When you reach age 65 or if you become disabled, you are eligible for hospital insurance
benefits (“Part A”) and supplementary medical insurance (“Part B”) under Medicare. The
chart below illustrates how your benefits are paid at that time.
55
Type of Plan Participant Primary Plan Secondary Plan
Retiree or dependent who is Medicare eligible Medicare This Fund
(and unemployed) unless you are covered under
work hours, then it is reversed
Retiree who is not Medicare eligible This Fund N/A
Active Member and/or dependent who is This Fund Medicare
Medicare eligible
Disabled Active Member This Fund Medicare
Coverage for Disabled Members or Members’ Disabled Dependents with
End-Stage Renal Disease (ESRD)
If you are actively employed and you or any of your covered dependents become entitled
to Medicare because of end-stage renal disease (ESRD), this Plan pays first and Medicare
pays second for 30 months starting the earlier of:
• The month in which Medicare ESRD coverage begins; or
• The first month in which the individual receives a kidney transplant.
Then, starting with the 31st month, Medicare pays first and this Plan pays second.
Any covered charges incurred by such disabled individual should be submitted to this
Plan for payment. Afterward, any unpaid balance should be submitted to Medicare, for
their consideration.
To Enroll in Medicare...
•Visit your local Social
Security Office,
• Call 1-800-MEDICARE
(1-800-633-4227), or
• Log on to
www.medicare.gov.
56
Enrolling in Medicare
You must enroll in Medicare Parts A and B as soon as you are eligible—three months
before your 65th birthday or in certain cases when you become disabled—in order to
avoid a gap in coverage.
TRICARE Military Coverage
If you and/or your family are covered by both this Fund and TRICARE, the coordination
of benefits depends on whether you are called up to active duty for more than 30 days
and whether your family continues coverage under this Plan. If you are on active duty
for more than 30 days, TRICARE will be primary and this Plan will be secondary.
However, if your eligible dependents elect COBRA and continue benefits under this Plan,
this Plan would be primary and TRICARE would be secondary for them.
Motor Vehicle No-Fault Coverage Required by Law
If you are covered by both this Fund and any motor vehicle no-fault coverage that is
required by law, the motor vehicle no-fault coverage pays first, and this Fund pays second.
Workers’ Compensation
This Fund does NOT provide benefits if the medical expenses are covered by Workers’
Compensation or Occupational Disease Law.
REIMBURSEMENT AND SUBROGATION
You or one of your eligible dependents may incur medical expenses in a situation where
a third party—for example, Workers’ Compensation or an auto insurance carrier— may
be held responsible for their payment. In this case, the Fund has all rights of recovery
that you or your dependents would have, including the right to bring suit in your name.
You must cooperate with the Fund to secure the recovery of the payment, and you must
do nothing before or after payment by the Fund to prejudice its rights. If you recover from
the third party or its insurer, you must reimburse the Fund for expenses that it has paid.
When you and/or your eligible dependents incur medical expenses where a third party
may be held responsible for payment you must:
• Notify the Fund Office
• Execute a Subrogation and reimbursement agreement
The subrogation and reimbursement agreement must be executed by you and/or your
covered dependent, and received by the Fund Office within 90 days from the date of the
incident and in no event later than 12 months from the date of the incident.
The amount of reimbursement due to the Fund is based on the following schedule:
Total Recovery Fund’s Share of Recovery
1. Equal or less than benefits 50% of the benefits
2. Greater than one, but less than twice benefits 65% of the benefits
3. Greater than two, but less than three times benefits 75% of the benefits
4. Greater than three, but less than four times benefits 85% of the benefits
5. Greater than four times 100% of the benefits

In no event shall the Fund’s share of recovery be greater than 50% of the total recovery
following the deduction of the participant’s reasonable attorney’s fees (not to exceed 33% of
the total recovery).
Before paying benefits for expenses that may be the responsibility of a third party, you and/or your
dependents will be required to sign an agreement affirming the obligation of you and your depend-
ents to reimburse the Fund from the proceeds of any recovery. The Fund may withhold payments on
any claim until a reimbursement agreement is executed. Your obligation to reimburse the Fund, how-
ever, is not dependent on whether you sign a reimbursement agreement. By accepting the payment of
benefits, you and your dependents agree to the Fund’s subrogation and reimbursement policies.
You and/or your eligible dependent must execute the reimbursement agreement and submit it
for receipt by the Fund Office within 90 days of the date of the accident or injury. If it is not
reasonably possible to submit the executed reimbursement agreement within 90 days, it must
be received by the Fund Office as soon as reasonably possible but in no event later than one
year from the date of the accident or injury. If you fail to comply with this obligation to sign
and submit the reimbursement agreement within the deadline, the Fund will deny claims relat-
ing to the accident or injury.
If you receive payment from a third party under any circumstances, you must reimburse the
Fund in accordance with the schedule above from the proceeds. Reimbursement is mandatory
regardless of whether:
•a claim was ever asserted for the amount received.
• the proceeds were paid by way of settlement, judgment, arbitration award or otherwise.
• you feel that you were “made whole” for your losses by recovery.
• the amount received is characterized as attributable to medical expenses, lost income, pain
and suffering, loss of consortium or otherwise.
• part of the recovery is received by family members other than the primary injured party
such as on a loss of consortium.
The Fund has an equitable interest and lien in the amount that you receive, and you, your
dependents, and those acting on your behalf are under obligation to keep the amount received
in a separate segregated account until your obligations to the Fund are satisfied and all dis-
putes concerning those obligations are settled. The Fund may enforce this obligation by seek-
ing equitable relief in court.
In the event that the participant or dependent submits additional claims for benefits following
settlement of a liability claim and reimbursement to the Fund, the Fund will withhold future
benefits, but only to the extent that the additional benefits would have been reimbursable
under the formula had the settlement occurred later.
If you or your dependents do not reimburse the Fund after receiving payment from a third
party, the Fund may institute legal and/or equitable action in court. In such event, you will be
responsible for all the costs and attorney’s fees associated with that court proceeding, and will
be obligated to pay all interest on all amounts owed from the date they were due. If you or a
dependent fails to reimburse the Fund, the Fund may withhold payment of future benefits
from you as well as all of your dependents up to the amount due plus interest.
57
58
FILING YOUR CLAIMS
A claim for benefits is a request for Plan benefits made in accordance with the Plan’s
reasonable claims procedures. In order to file a claim for benefits offered under this Plan,
you must submit a completed claim form unless your hospital, doctor or other health
care provider uses a standard billing form, such as a UB 92 or HCFA 1500, and files it
directly with the Fund on your behalf.
General inquiries about the Plan’s provisions that are unrelated to any specific benefit
claim or requests to add or improve the Plan’s benefits will not be treated as a claim for
benefits. In addition, a request for pre-approval of a benefit that does not require prior
approval by the Plan is not a claim for benefits.
All of the following information must be completed on the claim form that you get from
your provider(s) in order for your request for benefits to be a claim, and for the Fund
Office to be able to decide your claim.
• Member’s name and Social Security
number
• Member’s address
• Member’s date of birth
• Member’s marital status
• Coordination of benefits information
• Spouse’s name and Social Security
number (if applicable)
• Spouse’s date of birth and
employment status (if applicable)
•Name, address and telephone number
for spouse’s employer
• Patient name and address (if different
from Member)
• Patient’s relationship to insured
•Patient date of birth
• Patient’s sex
• Patient’s student status
•Was condition related to patient’s
employment, or accident
• Date(s) of service
• Date patient able to return to work
•Date of total/partial disability
• Name of referring physician
•Hospitalization dates, if applicable
• CPT-4 (the code for physician
services and other health care services
found in the Current Procedural
Te rminology, Fourth Edition or
later, as maintained and distributed
by the American Medical
Association)
•ICD-9 (the diagnosis code found in
the International Classification of
Diseases, 9th Edition or later, Clinical
Modification as maintained and
distributed by the U.S. Department
of Health and Human Services)
• Billed charge, amount paid and
balance due
• Signature of service provider
• Federal taxpayer identification
number (TIN) of the provider
•Provider billing name and address
Most accepted standard claim forms contain an assignment of benefits agreement, in the
event you wish to assign your hospital or surgical benefits directly to the hospital or
doctor. Upon receipt of the assignment agreement, the Fund Office will directly pay these
benefits to your health care provider. Please remember that any CCN provider will be
paid directly by the Fund. You are only responsible for the copayment amount at the
time of the service and any coinsurance and deductible, depending on the benefit.

WHEN CLAIMS MUST BE FILED
Claims should be filed within 90 days from the date the charges were incurred.
Failure to file claims within the time required shall not invalidate or reduce any claim if
it was not reasonably possible to file the claim within such time. However, in that case,
the claim must be submitted as soon as reasonably possible and in no event later than
one year from the date the charges were incurred.
When you and/or your eligible dependents incur charges in circumstances where a third
party may be liable, you and/or your eligible dependent must:
• Notify the Fund Office.
• Execute and return a reimbursement agreement within 90 days of the accident or
injury. (See section of this book on Reimbursement and Subrogation).
WHEN A CLAIM IS CONSIDERED RECEIVED BY THE HEALTH BENEFITS FUND
Post-Service Claims
A post-service claim for benefits (as defined on page 62) is considered received by the
Fund as follows:
For Medical, Hospital, and Accident and Sickness (Disability) Claims
• On the first business day when the claim is received by U.S. mail or hand- delivered
to the Fund Office at the following address:
New England Carpenters Health Benefits Fund
350 Fordham Road
Wilmington, MA 01887
Phone: (800) 344-1515
Fax: (978) 657-8724
• It is submitted electronically by your provider and received by the Health and Welfare
Fund.
For Dental Claims
• On the first business day when the claim is received by U.S. mail by Delta Dental at
the following address:
Delta Dental Plan of Massachusetts
P.O. Box 9695
Boston, MA 02114
• The claim is submitted electronically by your provider and received by Delta Dental.
For Vision Claims
• On the first business day when the claim is received by U.S. mail by Davis Vision at
the following address:
Davis Vision
159 Express St.
Plainview, NY 11803
• The claim is submitted electronically by your provider and received by Davis Vision.
59

60
URGENT, PRE-SERVICE AND CONCURRENT CLAIMS
Urgent, pre-service and concurrent claims (as defined on pages 60-62) are generally
requests for preauthorization or precertification of a treatment or hospital stay. An
urgent, pre-service or concurrent claim is considered received when a telephone call is
made by you or your provider to Hines & Associates at 1-800-944-9401, or your
provider electronically contacts the Hines & Associates requesting precertification.
PRESCRIPTION DRUG CLAIMS
Ullicare Rx/Medco provides drug preauthorizations for specified drugs. For a complete
listing of these drugs, call (800) 818-6602.
When you present a prescription to a pharmacy to be filled under the terms of this Plan,
that request is not a “claim” under these procedures. However, if your request for a
prescription is denied, in whole or in part, you may file a claim and appeal regarding the
denial by using these procedures.
CLAIMS COMMUNICATIONS
All claims communications will be addressed to and sent to the Member unless the patient
makes a written request to the Health Benefits Fund Office specifically requesting that any
claims communications be sent under the patient’s name and/or to a different address.
Authorized Representatives
An authorized representative, such as your spouse, may complete the claim form for you
if you are unable to complete the form yourself and have designated an individual to act
on your behalf. A form can be obtained from the Fund Office to designate an authorized
representative. The Plan may request additional information to verify that this person is
authorized to act on your behalf. A health care professional with knowledge of your medical
condition may act as an authorized representative in connection with an Urgent Care
Claim (defined below) without you having to complete the special authorization form.
COMPREHENSIVE MEDICAL BENEFITS CLAIMS
The claims procedures for comprehensive medical benefits will vary depending on
whether your claim is for a Pre-Service Claim, an Urgent Care Claim, a Concurrent
Care Claim, a Post-Service Claim, or a Disability Claim. Read each section carefully to
determine which procedure is applicable to your request for benefits:
Pre-Service and Urgent Care Claims
A Pre-Service Claim is a claim for a benefit for which the Plan requires approval of the
benefit (in whole or in part) before medical care is obtained. Under this Plan, prior
approval of services is required for all hospital admissions, complementary medicine,
home health care, hospice care, certain prescription drugs, inpatient and partial day
mental/nervous disorders and alcohol/substance abuse disorders.

Important: Failure To Comply Could Result In A Minimum Penalty Of $500 To
Complete Denial Of The Claim.
The Fund has a contract with Hines & Associates to administer Pre-Service, Urgent and
Concurrent Care Claims.
For properly filed Pre-Service Claims, you and/or your doctor will be notified of a deci-
sion within 15 days from receipt of the claim unless additional time is needed. The time
for response may be extended up to an additional 15 days if necessary due to matters
beyond the control of Hines & Associates. You will be notified of the circumstances requir-
ing the extension of time and the date by which a decision is expected to be rendered.
If an extension is needed because Hines & Associates needs additional information from
you, the extension notice will specify the information needed. In that case you and/or
your doctor will have 45 days from receipt of the notification to supply the additional
information. If the information is not provided within that time, your claim will be
denied. During the period in which you are allowed to supply additional information,
the normal period for making a decision on the claim will be suspended. The deadline is
suspended from the date of the extension notice until either 45 days or the date you
respond to the request (whichever is earlier). Hines & Associates then has 15 days to
make a decision on the Pre-Service Claim and notify you of the determination.
If you or your doctor improperly file a Pre-Service Claim, Hines & Associates will notify
you as soon as possible but not later than 5 days after receipt of the claim, of the proper
procedures to be followed in filing a claim. You will only receive notice of an improperly
filed Pre-Service Claim if the claim includes (i) your name, (ii) your specific medical
condition or symptom, and (iii) a specific treatment, service or product for which
approval is requested. Unless the claim is re-filed properly, it will not constitute a claim.
An Urgent Care Claim is any claim for medical care or treatment with respect to which
the application of the time periods for making Pre-Service claim determinations:
1. could seriously jeopardize the life or health of the claimant or the ability of the
claimant to regain maximum function, or
2. in the opinion of a physician with knowledge of the claimant’s medical condition,
would subject the claimant to severe pain that cannot be adequately managed
without the care or treatment that is the subject of the claim.
Any claim that a physician with knowledge of your medical condition determines is an
Urgent Care Claim within the meaning described above, will be treated as an Urgent
Care Claim. Absent a determination by that physician, whether your claim is an Urgent
Care Claim will be determined by Hines & Associates applying the judgment of a
prudent layperson who possesses an average knowledge of health and medicine.
If you are requesting precertification of an Urgent Care Claim, the time deadlines are
different than those that apply to Pre-Service Claims. Hines & Associates will respond to
you and/or your doctor with a determination by telephone as soon as possible taking
into account the medical condition, but not later than 72 hours after receipt of the claim
by Hines & Associates. The determination will also be confirmed in writing.
61

62
If an Urgent Care Claim is received without sufficient information to determine whether
or to what extent benefits are covered or payable, Hines & Associates will notify you
and/or your doctor as soon as possible, but not later than 24 hours after receipt of the
claim, of the specific information necessary to complete the claim. You and/or your
doctor must provide the specified information within 48 hours of receiving notice. If the
information is not provided within that time, your claim will be denied. Unless the claim
is re-filed properly, it will not constitute a claim.
Notice of the decision will be provided no later than 48 hours after Hines & Associates
receives the specified information or the end of the period given for you to provide this
information, whichever is earlier.
Concurrent Claims
A concurrent claim is a claim for additional treatment or hospital days or a claim that is
reconsidered after an initial approval was made and results in a reduction, termination or
extension of a benefit. (An example of this type of claim would be an inpatient hospital
stay originally approved for five days that is reviewed at three days to determine if the
full five days is appropriate.) In this situation a decision to reduce, terminate or extend
treatment is made at the same time or “concurrently” with the provision of treatment.
A reconsideration of a benefit with respect to a concurrent claim that involves the termina-
tion or reduction of a previously approved benefit (other than by plan amendment or termi-
nation) will be made by Hines & Associates as soon as possible, but in any event early
enough to allow you to have an appeal decided before the benefit is reduced or terminated.
Any request by a claimant to extend approved urgent care treatment will be acted upon
by Hines & Associates within 24 hours of receipt of the claim, provided the claim is
received at least 24 hours prior to the expiration of the approved treatment. A request to
extend approved treatment that does not involve urgent care will be decided according to
pre-service or post-service timeframes, whichever applies.
Post-Service Claim
The following procedure applies to Post-Service Claims. A Post-Service Claim is a claim
that is not a Pre-Service, Urgent Care, or Concurrent Claim (for example, a claim
submitted for payment after health services and treatment have been obtained).
Your provider should submit all claims on your behalf to the Fund Office or to CCN.
If you experience a problem submitting a claim, call the Fund Office.
You do not have to submit an additional claim form with your bills or statements, if you
have filed the annual health claim during the calendar year. Mail any further bills or
statements for any medical or hospital services covered by the Plan to the address shown
on your I.D. Card as soon as you receive them. Your provider may also submit bills on
your behalf.
Ordinarily, you will be notified of the decision on your Post-Service Claim within 30
days from the Plan’s receipt of the claim. This period may be extended once by the Plan
for up to 15 days if the extension is necessary due to matters beyond the control of the

Plan. If an extension is necessary, you will be notified before the end of the initial 30-day
period of the circumstances requiring the extension of time and the date by which the
Plan expects to render a decision.
If an extension is needed because the Plan needs additional information from you, the
extension notice will specify the information needed. In that case you will have 45 days
from receipt of the notification to supply the additional information. If the information is
not provided within that time, your claim is deemed denied. During the period in which
you are allowed to supply additional information, the normal period for making a
decision on the claim will be suspended. The deadline is suspended from the date of the
extension notice until either 45 days or until the date you respond to the request
(whichever is earlier). The Plan then has 15 days to make a decision on a Post-Service
Claim and notify you of the determination.
DISABILITY CLAIMS (WEEKLY ACCIDENT AND SICKNESS BENEFIT)
You must file a claim for Weekly Accident and Sickness Benefits with the Fund Office no
later than 90 days after the date your disability began.
For Disability Claims, the Plan will make a decision on the claim and notify you of the
decision within 45 days. If the Plan requires an extension of time due to matters beyond
the control of the Plan, the Plan will notify you of the reason for the delay and when the
decision will be made. This notification will occur before the expiration of the 45-day
period. A decision will be made within 30 days of the time the Plan notifies you of the
delay. The period for making a decision may be delayed an additional 30 days, provided
the Plan administrator notifies you, prior to the expiration of the first 30-day extension
period, of the circumstances requiring the extension and the date as of which the Plan
expects to render a decision.
If an extension is needed because the Plan needs additional information from you, the
extension notice will specify the information needed. In that case you will have 45 days
from receipt of the notification to supply the additional information. If the information is
not provided within that time, your claim will be denied. During the period in which you
are allowed to supply additional information, the normal period for making a decision on
the claim will be suspended. The deadline is suspended from the date of the extension
notice until either 45 days or until the date you respond to the request (whichever is
earlier). Once you respond to the Plan’s request for the information, you will be notified
of the Plan’s decision on the claim, or the need for an extension, within 30 days.
Notice Of A Denied Claim
You will be provided with written notice of a denial of a claim (whether denied in whole
or in part). This notice will state:
• The specific reason(s) for the determination.
• Reference to the specific Plan provision(s) on which the determination is based.
•A description of any additional material or information necessary to perfect the
claim, and an explanation of why the material or information is necessary.
63

64
•A description of the appeal procedures (including voluntary appeals, if any) and
applicable time limits.
•A statement of your right to bring a civil action under ERISA Section 502(a) following
an adverse benefit determination on review.
• If an internal rule, guideline or protocol was relied upon in deciding your claim, you will
receive either a copy of the rule or a statement that it is available upon request at no charge.
• If the determination was based on the absence of medical necessity, or because the treat-
ment was experimental or investigational, or other similar exclusion, you will receive an
explanation of the scientific or clinical judgment for the determination applying the terms
of the Plan to your claim, or a statement that it is available upon request at no charge.
Appeal Process for Denied Claims
If your claim is denied in whole or in part, or if you disagree with the decision made on a claim,
you may ask for a review. Your request for review must be made in writing to the Fund Office
and must be received within 180 days after you receive a notice of denial. Appeals involving
Urgent Care Claims may be made orally by calling the Fund Administrator at (800) 344-1515
for urgent and concurrent claim appeals only. There is a second level of appeal for Post-
Service and Disability claims, and appeals to the second level concerning those claims must be
received by the Fund Office within 60 days of the date of the decision at the first level of appeal.
APPEAL PROCESS
The appeal process works as follows:
Urgent, Pre-Service and Concurrent Claim Appeals
For Urgent, Pre-Service and Concurrent Claim Appeals, there is one level of appeal.
Appeals should be made in writing to the Fund Office. A subcommittee of the Board of
Trustees will review Urgent, Pre-Service and Concurrent Claim appeals. In certain
circumstances such as Urgent Claim appeals where medical conditions exist that require an
expedited review process, appeals may be made orally via telephone.
Post-Service and Disability Claim Appeals
For Post-Service and Disability claims appeals, there is a two-level appeal process. Appeals at
both levels must be in writing and must be submitted to the Fund Office. The first level of
appeal will consist of a review by the Fund Administrator. First level appeals must be
received by the Fund Office within 180 days after you receive the Fund’s notice of its denial
of your claim. If the Fund Administrator denies your first level appeal, you have the right to a
second level appeal to the full Board of Trustees. Second level appeals must be received by the
Fund Office within 60 days of the date of the Fund Administrator’s decision at the first level.
Information To Which You Are Entitled
You have the right to review documents relevant to your claim. A document, record or
other information is relevant if it was relied upon by the Plan in making the decision; it was
submitted, considered or generated (regardless of whether it was relied upon in making the
decision); it demonstrates compliance with the Plan’s administrative processes for ensuring
consistent decision making; or it constitutes a statement of Plan policy regarding the denied
treatment or service.

Upon request, you will be provided with the identification of medical or vocational
experts, if any, who gave advice to the Plan on your claim, without regard to whether
their advice was relied upon in deciding your claim.
A different person will review your claim than the one who originally denied the claim or
the previous appeal. The reviewer will not give deference to the previous adverse benefit
determinations. The decision will be made on the basis of the record, including such
additional documents and comments that may be submitted by you.
If your claim was denied on the basis of a medical judgment (such as a determination
that the treatment or service was not medically necessary, or was investigational or
experimental), a health care professional who has appropriate training and experience in
a relevant field of medicine will be consulted.
Timing of Notice of Decision on Appeal
• Pre-Service Claims: You will be sent a notice of decision on review within 30 days of
receipt of the appeal by the Fund Office.
• Urgent Care Claims: You will be notified of a decision on your appeal, either orally
or in writing (or both) within 72 hours of receipt of the appeal by the Fund Office.
• Post-Service Claims: For first level appeals, a decision will be made on the appeal
within 30 days of receipt of the appeal by the Fund Administrator. For second level
appeals, decisions will be made at the next regularly scheduled meeting of the Board
of Trustees following receipt of your request for review. However, if your request for
review is received within 30 days of the next regularly scheduled meeting, your
request for review will be considered at the second regularly scheduled meeting
following receipt of your request. In special circumstances, a delay until the third
regularly scheduled meeting following receipt of your request for review may be
necessary. You will be advised in writing in advance if this extension will be
necessary. Once a decision on review of your claim has been reached, the Fund Office
will give you written notice of the decision as soon as possible, but no later than 5
days after the decision has been reached.
• Disability Claims: For first level disability claim appeals a decision will be made by
the Fund Administrator within 45 days of receipt of the appeal at the Fund Office. If
the Fund Administrator determines that special circumstances require an extension
of time, then you will receive a written notice of the extension before the end of the
45-day period. The notice will include the reasons required for the extension and the
approximate date the Plan expects to make a decision.
For second level appeals, decisions will be made at the next regularly scheduled
meeting of the Board of Trustees following receipt of your request for review.
However, if your request for review is received within 30 days of the next regularly
scheduled meeting, your request for review will be considered at the second regularly
scheduled meeting following receipt of your request. In special circumstances, a delay
until the third regularly scheduled meeting following receipt of your request for
review may be necessary. You will be advised in writing in advance if this extension
65

66
will be necessary. Once a decision on review of your claim has been reached, the Fund
Office will give you written notice of the decision as soon as possible, but no later than 5
days after the decision has been reached.
• Concurrent Claims: Appeals of concurrent claims involving a termination or reduction
of benefits of previously approved care shall be completed before the termination or
reduction. The claimant shall be given notice sufficiently in advance of the termination
or reduction to allow the claimant to appeal before the benefit is terminated or reduced.
Appeals of concurrent claims involving an extension of care shall be conducted within
the timeframe for urgent, pre-service or post-service appeals described above, depending
on which category applies to the appeal.
Notice of Decision on Review
The decision on any review of your claim will be given to you in writing. The notice of a
denial of a claim on review will state:
• The specific reason(s) for the determination.
• Reference to the specific Plan provision(s) on which the determination is based.
•A statement that you are entitled to receive reasonable access to and copies of all
documents relevant to your claim, upon request and free of charge.
•A statement of your right to bring a civil action under ERISA Section 502(a) following
an adverse benefit determination on review.
• If an internal rule, guideline or protocol was relied upon by the Plan, you will receive
either a copy of the rule or a statement that it is available upon request at no charge.
• If the determination was based on medical necessity, or because the treatment was experi-
mental or investigational, or other similar exclusion, you will receive an explanation of
the scientific or clinical judgment for the determination applying the terms of the Plan
to your claim, or a statement that it is available upon request at no charge.
Limitation on When a Lawsuit May Be Started
You may not start a lawsuit to obtain benefits until after you have exhausted all levels of
appeal and final decisions have been reached on those appeals, or until the appropriate time
frame described above has elapsed since you filed a request for review and you have received
a final decision or notice that an extension will be necessary to reach a final decision. The
law also permits you to pursue your remedies under section 502(a) of the Employee
Retirement Income Security Act without exhausting these appeal procedures if the Plan has
failed to follow them. No lawsuit to recover Plan benefits may be started more than 15
months after the date of loss (that is, the date you incurred the expense you are seeking to
have the Plan pay) upon which the lawsuit is based. Because the Plan grants its fiduciaries
discretionary authority to determine eligibility for benefits and to construe the terms of the
Plan, the issue in a lawsuit will be limited to whether or not the Board of Trustees (or its
delegates, including the subcommittee for Urgent Care, Pre-service and Concurrent Claims)
acted arbitrarily or capriciously in making its determination. No lawsuit to recover Plan
benefits may be started more than 12 months after the date the Board of Trustees makes its
final decision on an appeal, or after the date the Fund was required but failed to act in
accordance with its appeal procedures.

YOUR ERISA RIGHTS
As a participant in the New England Carpenters Health Benefits Fund, you are entitled to
certain rights and protections under the Employee Retirement Income Security Act of
1974 (ERISA). ERISA provides that all Plan participants are entitled to:
Receive Information About Your Plan and Benefits
• Examine, without charge, at the Fund Administrator’s office and at other specified
locations, such as worksites and union halls, all documents governing the Plan,
including insurance contracts and Collective Bargaining Agreements, and a copy of
the latest annual report (Form 5500 Series) filed by the Fund with the U.S.
Department of Labor and available at the Public Disclosure Room of the Employee
Benefits Security Administration.
• Obtain, upon written request to the Fund Administrator, copies of documents
governing the operation of the Plan, including insurance contracts and Collective
Bargaining Agreements, and copies of the latest annual report (Form 5500 Series)
and updated Summary Plan Description. The Administrator may make a reasonable
charge for the copies.
• Receive a summary of the Fund’s annual financial report. The Fund Administrator is
required by law to furnish each participant with a copy of this summary annual report.
• Continue health care coverage for yourself, spouse or dependents if there is a loss of
coverage under the Plan as a result of a qualifying event. You or your dependents
may have to pay for such coverage. Review this Summary Plan Description and the
documents governing the Plan on the rules governing your COBRA Continuation
Coverage rights.
•Reduce or eliminate exclusionary periods of coverage for pre-existing conditions
under your group health plan, if you have creditable coverage from another plan.
When you lose coverage under the New England Carpenters Health Benefits Fund,
your group health plan or health insurance issuer should provide you with a
certificate of creditable coverage, free of charge when:
–You become entitled to elect COBRA Continuation Coverage,
–Your COBRA coverage ceases, if you request it before losing coverage, or if you
request it up to 24 months after losing coverage.
Prudent Actions By Plan Fiduciaries
In addition to creating rights for Fund participants, ERISA imposes duties upon the
people who are responsible for the operation of the employee benefit plan. The people
who operate your Fund, called “fiduciaries” of the Fund, have a duty to do so prudently
and in the interest of you and other Fund participants and beneficiaries. No one,
including your employer, your union, or any other person, may fire you or otherwise
discriminate against you in any way to prevent you from obtaining a welfare benefit or
exercising your rights under ERISA.
Enforce Your Rights
If your claim is denied or ignored, in whole or in part, you have a right to know why this
was done, to obtain copies of documents relating to the decision without charge, and to
appeal any denial, all within certain time schedules.
67

Under ERISA, there are steps you can take to enforce the above rights. For instance, if
you request a copy of the Plan documents or the latest annual report from the Fund and
do not receive them within 30 days, you may file suit in a federal court. In such a case,
the court may require the Fund Administrator to provide the materials and pay you up to
$110 a day until you receive the materials, unless the materials were not sent because of
reasons beyond the control of the Administrator.
If you have a claim for benefits that is denied or ignored, in whole or in part, you may
file suit in a state or federal court. In addition, if you disagree with the Fund’s decision or
lack thereof concerning the qualified status of a domestic relations order or a medical
child support order, you may file suit in federal court. If it should happen that Fund
fiduciaries misuse the Fund’s money, or if you are discriminated against for asserting
your rights, you may seek assistance from the U.S. Department of Labor, or you may file
suit in a federal court. The court will decide who should pay court costs and legal fees. If
you are successful the court may order the person you have sued to pay these costs and
fees. If you lose, the court may order you to pay these costs and fees, for example if it
finds your claim is frivolous.
Assistance with Your Questions
If you have any questions about your Plan, you should contact the Fund Administrator.
If you have any questions about this statement or about your rights under ERISA, or if
you need assistance in obtaining documents from the Fund Administrator, you should
contact the nearest office of the Employee Benefits Security Administration, U.S.
Department of Labor, listed in your telephone directory or the Division of Technical
Assistance and Inquiries, Pension and Welfare Benefits Administration, U.S. Department
of Labor, 200 Constitution Avenue, N.W., Washington D.C. 20210. You may also obtain
certain publications about your rights and responsibilities under ERISA by calling the
publications hotline at the Employee Benefits Security Administration.
68
69
Name of Plan The New England Carpenters Health Benefits Fund
Type of Plan A self-funded Employee Health and Welfare Benefit Plan that
provides coverage for medical care, prescription drugs, dental care,
vision care, weekly accident and sickness benefits, life insurance and
accidental death and dismemberment benefits to eligible members
and their qualified dependents.
Name of Plan Sponsor Board of Trustees
New England Carpenters Health Benefits Fund
Fund Office Address 350 Fordham Road, Wilmington, MA 01887
Agent for Service of Service of legal process may be made upon any Fund Trustee.
Legal Process
Plan Administrator Board of Trustees
New England Carpenters Health Benefits Fund
Type of Administration Collectively Bargained, jointly trusteed labor management trust
of the Plan
Plan Number 501
IRS Employer 04-2191579
Identification Number
Plan Fiscal Year January 1—December 31
Sources of Financing Payments made to the trust by individual employers under the
provisions of the Collective Bargaining or Participation Agreements,
employee contributions, and any income earned from investment of
employer and employee contributions.
The Fund Office will provide you, upon written request, with
information as to whether a particular employer is contributing to this
Plan on behalf of Participants working under the Collective Bargaining
Agreement and, if so, with that employer’s address.
All monies are used exclusively for providing benefits to eligible
employees, early retirees, and their dependents, and the paying of all
expenses incurred with respect to the operation of the Plan. The
Trustees shall review annually the funding status of the Plan.
Organizations Through Which Plan Benefits
are Provided or Administered
PPO Network Access Only Medical Care
CCN
PPO Network Access Only Substance Abuse and Mental Health
CCN
Utilization Review Vendor Hines & Associates
Self-funded Prescription Drugs
Ullicare Rx/Medco
Self-funded, Network Dental Care
access and dental claims Delta Dental
administration
Self-funded benefit, Vision Care
Network access and vision Davis Vision
claims administration
Insurance Policies Life Insurance and Accidental Death and Dismemberment Insurance–
Hartford Life Insurance Company
PLAN FACTS

The Board of Trustees
The Board of Trustees is made up of an equal number of Representatives and Union
Representatives who serve without compensation. Under a Trust Agreement, the Board
has full authority and discretion to operate and administer this Plan.
Discretionary Authority of the Board of Trustees and its Designees
In carrying out their respective responsibilities under the Plan, the Board of Trustees, the
Fund Administrator and other individuals with delegated responsibility for the
administration of the Plan will have discretionary authority to interpret the terms of the
Plan and to determine eligibility and entitlement to Plan benefits in accordance with the
terms of the Plan. Any interpretation or determination will be given full force and effect,
unless it can be shown that the interpretation or determination was arbitrary and
capricious.
Collective Bargaining Agreement
A collective bargaining agreement is a written agreement between a union and an
employer that requires the employer to make contributions to the Fund on behalf of its
employees. To inquire about whether a particular employer contributes to this Fund, or
to request a copy of the collective bargaining agreement, contact the Fund Office.
Plan Amendment and Termination
The Board of Trustees reserves the right to terminate or amend the Plan including the
right to amend or terminate benefits or eligibility for any class of participant, including
retirees, when in their sole discretion they determine such action is in the best interest of
the Fund and its participants. Eligibility requirements are reviewed regularly by the
Trustees.
In addition, the Plan may be terminated by the Trustees if there is no longer an
agreement in effect between the Employers and the Union requiring contributions to the
Health Benefits Fund.
Should the Plan terminate, the Trustees will apply remaining assets of the Fund to
continue benefits beyond the date of termination. The Trustees reserve the right to
amend the eligibility rules at the time of termination. Retiree benefits are funded from
current contributions and are not guaranteed or vested. In any case, the Trustees will use
any remaining assets of the Fund to provide benefits and pay administration expenses or
otherwise to carry out the purpose of the Plan in accordance with the Plan Document
and Trustee Agreement until the entire remainder of the Fund has been disbursed.
70
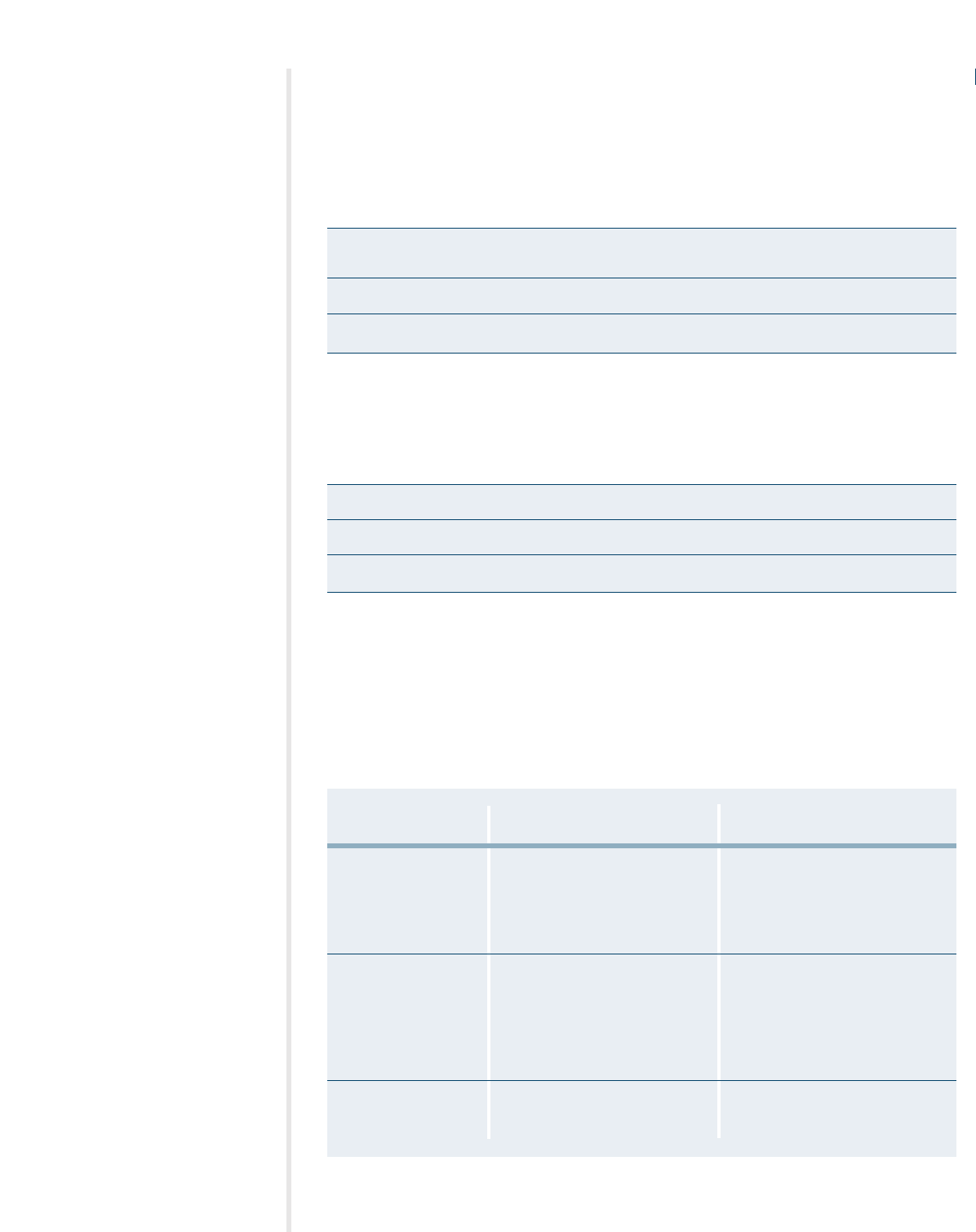
SCHEDULE OF BENEFITS FOR PLAN I
The chart that follows highlights the benefits of the New England Carpenters Health
Benefits Fund. For more detailed information, contact the Fund Office.
Your Calendar Year Deductible $150 per person
$300 per family
Your Calendar Year Out-of-Pocket Maximum $1,500 per person
Maximum Benefit the Plan Will Pay Per Person Per Lifetime $1,000,000
The Life Insurance benefit is available to members and spouses. Accidental Death
and Dismemberment and Weekly Accident and Sickness benefits are available to
Members only.
Life Insurance $20,000 for Member; $2,000 for spouse
Accidental Death and Dismemberment Refer to page 49
Weekly Accident and Sickness $250 per week for up to 26 weeks per period of disability
The following schedule shows the percentage of charges that the Fund pays under Plan I,
whether medical services are obtained in the PPO network or out-of-network. Note:
Charges for benefits provided by PPO network providers are based on a negotiated
contract. Charges for benefits provided by out-of-network providers are based on
reasonable and customary rates as described on page 27. You are responsible for any
provider charges in excess of reasonable and customary rates.
Plan Pays Plan Pays
PPO Network Out-of-Network
Ambulance Service 90% after deductible. 85% after deductible.
Air Ambulance service payable Air Ambulance service payable
at 90% after deductible to a at 85% after deductible to a
maximum of $2,000 per maximum of $2,000 per
life-threatening emergency life-threatening emergency
Cardiac Rehabilitation 90% after deductible when 85% after deductible when
medically necessary following medically necessary following
heart attack or stroke, upon heart attack or stroke, upon
recommendation of and with recommendation of and with
supervision of attending physician, supervision of attending physician,
to a lifetime maximum of $3,000 to a lifetime maximum of $3,000
Chiropractic Care 100% after $10 copay per visit 85% after deductible to a
to a calendar year maximum of calendar year maximum of
20 visits per person 20 visits per person
71
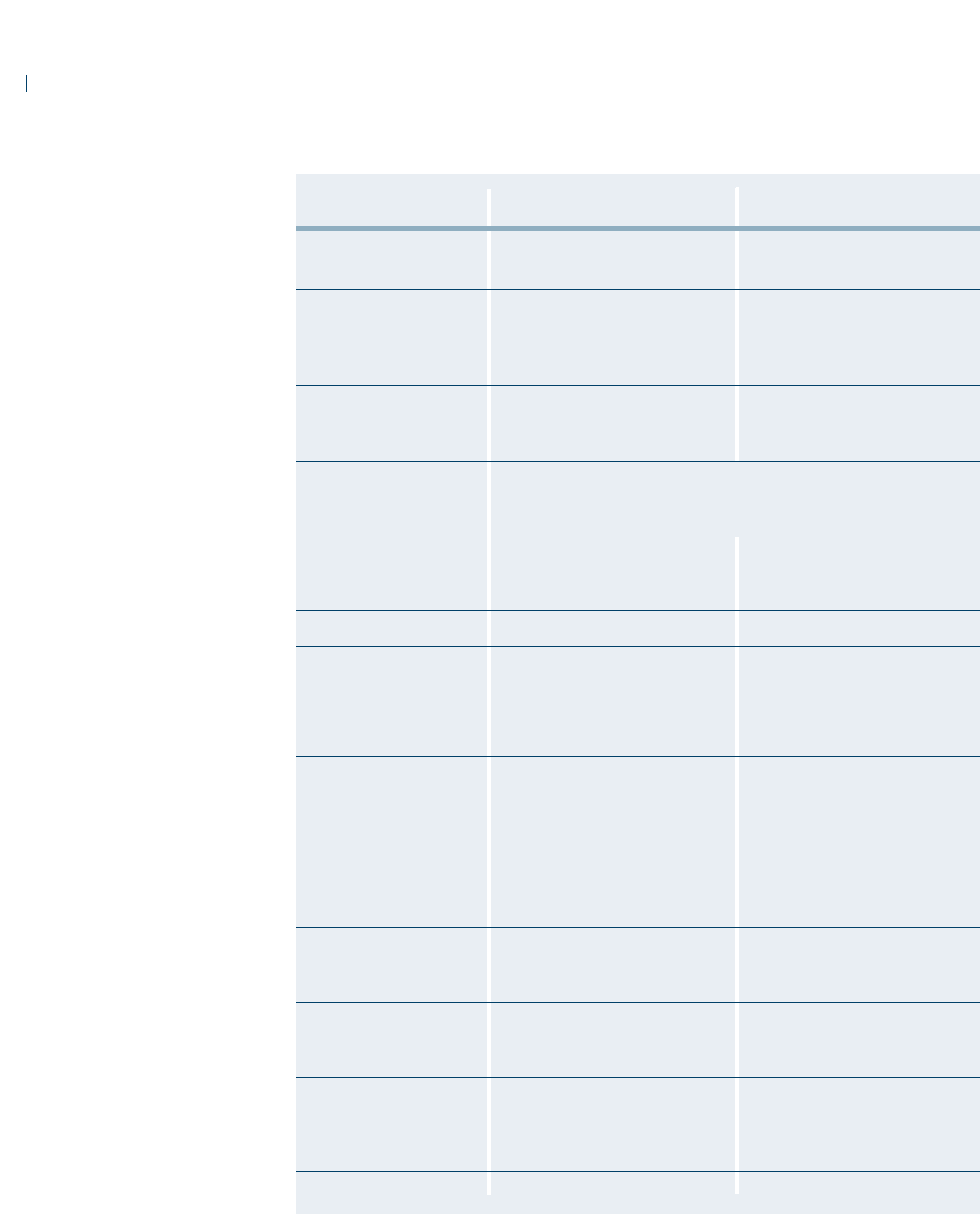
72
Plan Pays Plan Pays
PPO Network Out-of-Network
Diagnostic Laboratory 100% 85% after deductible
and X-Ray
Durable Medical 90% after deductible. 85% after deductible.
Equipment Payments will not exceed the Payments will not exceed the
(requires physician letter actual purchase price actual purchase price
of medical necessity)
Emergency Room 90% after deductible. 85% after deductible.
(refer to page 31) $50 penalty for $50 penalty for
non-life-threatening care non-life-threatening care
Hearing Aids Up to $1,500 per hearing aid to a maximum of $3,000 once every
five-year period. Covered through selected providers only.
Contact the Fund Office for a listing and to set up an appointment
Home Health Care See page 37 for specific coverage See page 37 for specific coverage
(requires physician letter information information
of medical necessity)
Hospice Care 100% after deductible 85% after deductible
Hospital Room and Board 100% of the first $10,000, then 85% after deductible
payable at 90% after deductible
Hospital Physician 90% after deductible 85% after deductible
Expense Benefit
Infertility Treatment Lifetime maximum $5,000. Lifetime maximum $5,000.
Lab and x-ray: 100% of PPO fee; After deductible, 85% of R&C
Surgeon’s fee: 100% of PPO fee charges to the lifetime
schedule, otherwise subject to maximum of $5,000.
R&C charges;
Anesthesia: 100% of PPO fee.
All other services subject to
deductible, then payable at 90%.
Mental Health Treatment 90% after deductible to a 85% after deductible to a
(Inpatient) calendar year maximum of calendar year maximum of
30 days per person 30 days per person
Mental Health Treatment 100% after $10 copay per visit, 50% after deductible to a
(Outpatient) to a maximum of 25 visits per maximum of 25 visits per
person per calendar year person per calendar year
Occupational Therapy 100% after $10 copay per visit 100% up to combined lifetime
(requires physician letter up to combined lifetime maximum maximum of $40,000 for physical,
of medical necessity) of $40,000 for physical, speech speech and occupational therapy
and occupational therapy
Office Visits (Illness) 100% after $10 copay per visit 85% after deductible
SCHEDULE OF BENEFITS FOR PLAN I
CONTINUED
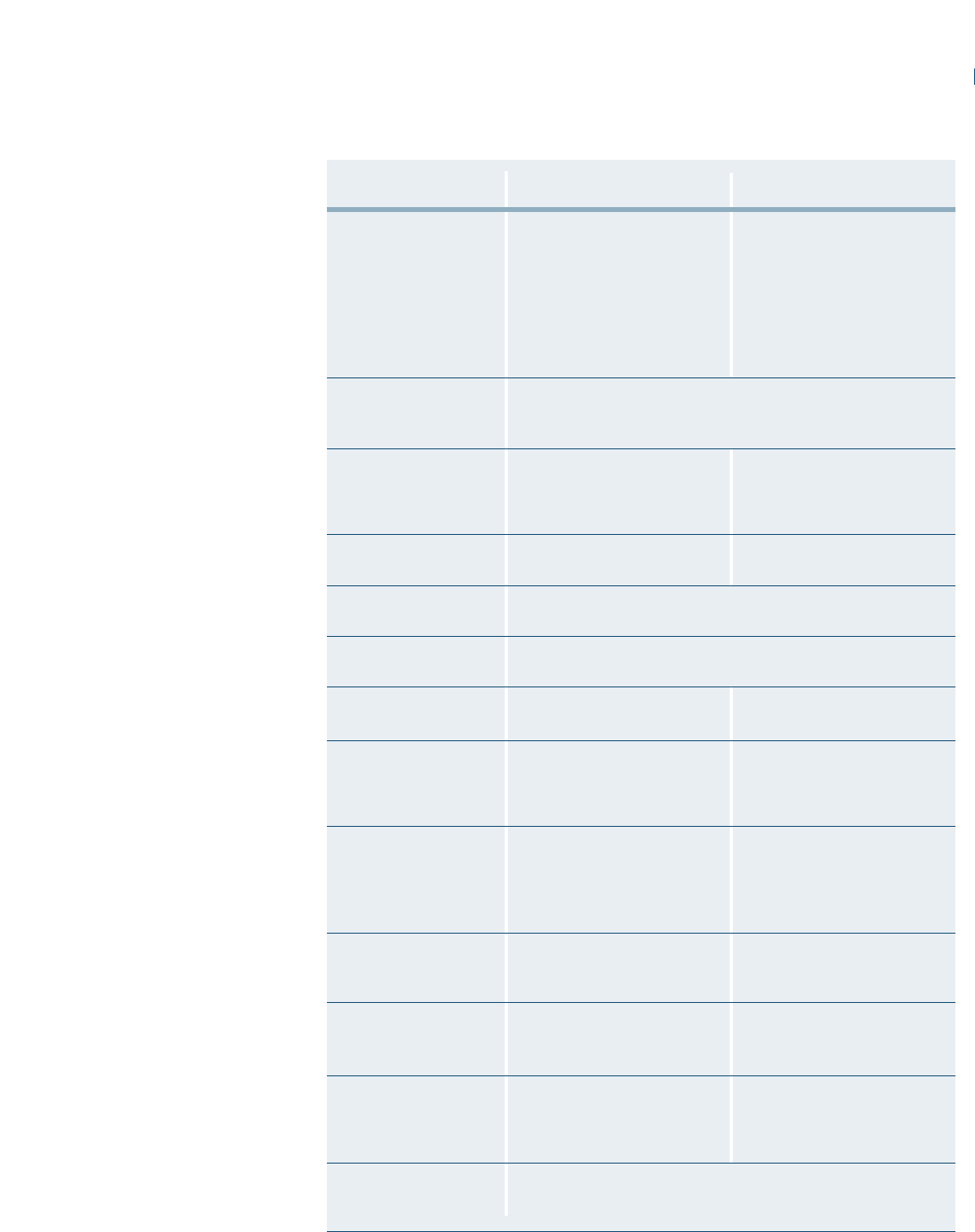
73
Plan Pays Plan Pays
PPO Network Out-of-Network
Organ Transplants $250,000 per transplant maximum. $250,000 per transplant maximum.
Hospital: 100% of the first $10,000 Hospital: 85% after deductible
then 90% after deductible Surgeon’s fee: 85% of R&C
Surgeon’s fee: 100% of PPO fee charges after deductible
schedule otherwise subject to Anesthesia: 85% of charges
R&C charges. after deductible
Anesthesia: 100% of PPO fee
schedule
Physical Exams Covered for Member and spouse only
(includes all lab, x-ray Paid at 100% up to calendar year maximum of $150
and immunizations)
Physical Therapy 100% after $10 copay per visit, up 85% after deductible, up to
(requires physician letter to a combined lifetime maximum a combined lifetime maximum
of medical necessity) of $40,000 for physical, speech of $40,000 for physical, speech
and occupational therapy and occupational therapy
Podiatrist Services 100% after $10 copay to a calendar 85% after deductible to a calendar
year maximum of $500 per person year maximum of $500 per person
Prescription Drugs $20 copay for generics, $40 for Brand Preferred and $60 for
(Mail Order, 90-day supply) Brand Non-Preferred
Prescription Drugs $10 copay for generics, $20 for Brand Preferred and $30 for Brand
(Retail, 34-day supply) Non-Preferred
Skilled Nursing Facility 100% of the first $10,000 then 85% after deductible
payable at 90% after deductible
Speech Therapy 90% after deductible up to a 85% after deductible up to a
(requires physician letter combined lifetime maximum of combined lifetime maximum of
of medical necessity) $40,000 for physical, speech and $40,000 for physical, speech
occupational therapy and occupational therapy
Substance Abuse 90% after deductible to a 85% after deductible to a
Treatment (Inpatient) maximum of 30 days per person maximum of 30 inpatient days
per calendar year. per calendar year per person.
Maximum of two lifetime Maximum of two lifetime
occurrences per person occurrences per person
Substance Abuse 100%, after a $10 copay, to a 85% after deductible to a
Treatment (Outpatient) maximum of $500 per person maximum of $500 per person
per calendar year per calendar year
Surgeon’s Expenses 100% of PPO fee schedule 85% of R&C charges after
otherwise subject to R&C deductible
schedule
Temporomandibular 100% after a $10 copay to a 85% after deductible to a
Joint Disorders (TMJ) lifetime maximum of $1,500, lifetime maximum of $1,500,
within limitations covered under within limitations covered under
Plan exclusions (page 52) Plan exclusions (page 52)
Well-Child Care 100% after a $10 copayment for children from birth through age 5;
(includes all lab, x-ray For children 6 and older, 100% to a calendar year maximum of $70
and immunizations) until they turn 19 (or through 23 if a full-time student)
SCHEDULE OF BENEFITS FOR PLAN I
CONTINUED
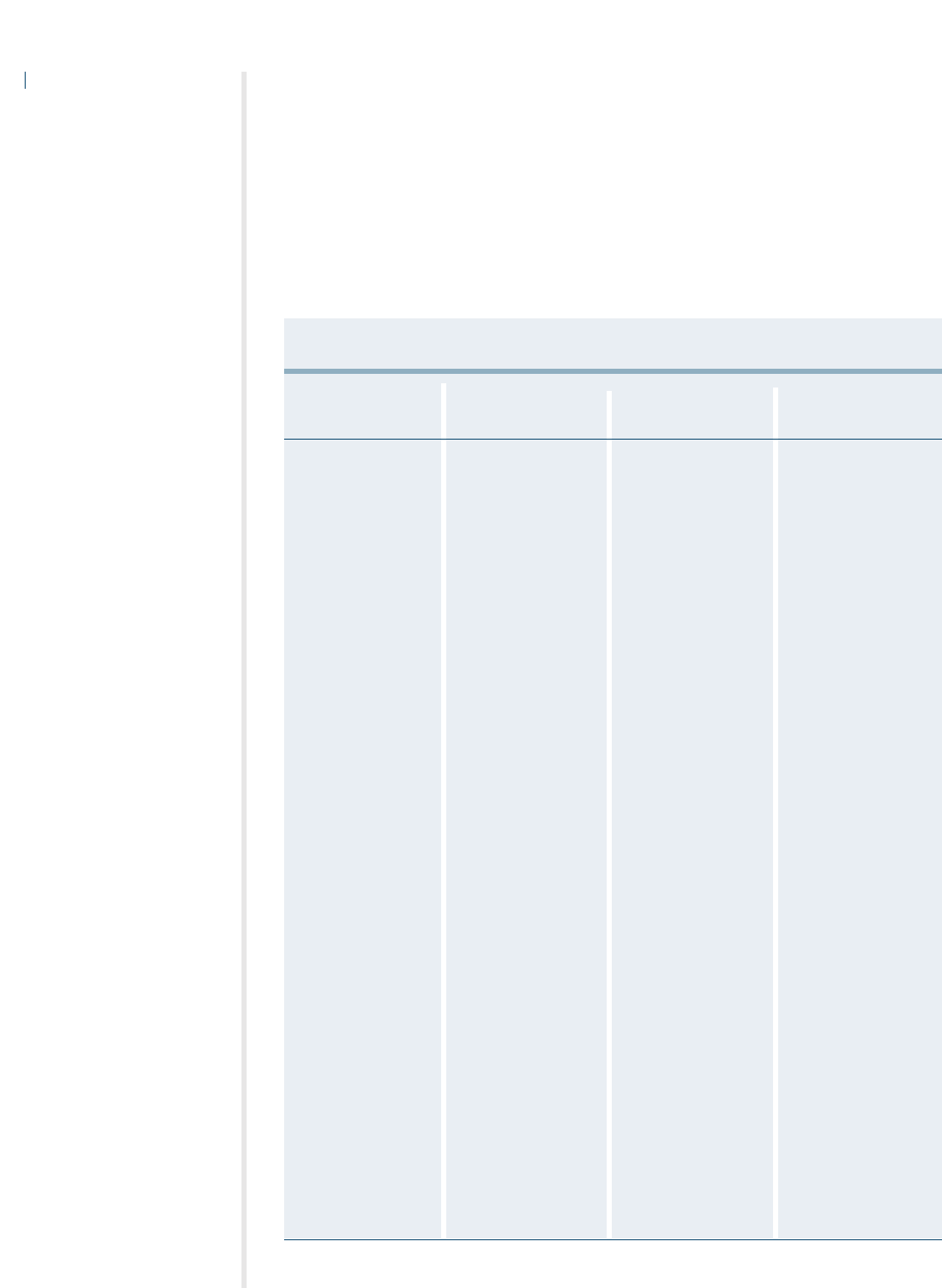
SCHEDULE OF DENTAL BENEFITS FOR PLAN I
The following chart shows the benefits payable when you use a participating Delta
Dental provider. For out-of-network benefits, you will be billed for any amount that
your out-of-network dentist charges that is more than the pre-negotiated Delta Dental
network charge. Please refer to your Delta Dental benefits guide for more specific
coverage information.
74
Dental Care Benefits
Type I
Plan Pays 100%
Diagnostic
One complete initial
oral exam and charting
Periodic oral exams
Full mouth x-rays
Bitewing x-rays
Single tooth x-rays
Sturdy models and
casts
Preventive
Cleaning
Fluoride treatments
Space maintainers
Sealants
Type II
Plan Pays 80%
Restorative
Amalgam fillings
Composite fillings
Treatment fillings
Stainless steel crowns
Oral Surgery
Simple extractions
Surgical extractions
Periodontics
Periodontal surgery
(including
gingivectomy)
Scaling and root planing
Gingival curettage
Endodontics
Root canal therapy
Pulpal therapy
Pulp Capping
Prosthetic
Maintenance
Bridge or Denture
Repair
Rebase or Reline of
Dentures
Recement Crowns,
Inlays and Onlays
Emergency
Dental Care
Type III
Plan Pays 50%
Prosthodontic
Complete or partial
dentures, fixed bridges
and crowns when part
of a bridge; once every
60 months per tooth
Major Restorative
Crowns, inlays and
onlays when teeth
cannot be restored with
regular fillings due to
severe decay or fracture;
once every 60 months
per tooth
Orthodontics
Plan Pays 100%
Orthodontics
Complete Orthodontic
Examination
Active Orthodontic
Treatment
(Comprehensive or
limited including
appliances)

SCHEDULE OF BENEFITS FOR PLAN II
The chart that follows highlights the benefits of the New England Carpenters Health
Benefits Fund. For more detailed information, contact the Fund Office.
Your Calendar Year Deductible $300 per person
$600 per family
Your Calendar Year Out-of-Pocket Maximum $3,000 per person
Maximum Benefit the Plan Will Pay Per Person Per Lifetime $500,000
The Life Insurance benefits are available to Members and spouses. Accidental Death and
Dismemberment Insurance benefits are available to Members only.
Life Insurance $10,000 for Member; $2,000 for spouse
Accidental Death and Dismemberment Refer to page 49
The following schedule shows the percentage of charges that the Fund pays under
Plan II, whether medical services are obtained in the PPO network or out-of-network.
Note: Charges for benefits provided by PPO network providers are based on a negotiated
contract. Charges for benefits provided by out-of-network providers are based on
reasonable and customary rates as described on page 27. You are responsible for any
provider charges in excess of reasonable and customary rates.
75
Plan Pays Plan Pays
PPO Network Out-of-Network
Ambulance Service 80% after deductible. 75% after deductible.
Air Ambulance service payable Air Ambulance service payable
at 80% after deductible to a at 75% after deductible to a
maximum of $2,000 per maximum of $2,000 per
life-threatening emergency life-threatening emergency
Cardiac Rehabilitation 80% after deductible when 75% after deductible when
medically necessary following medically necessary following
heart attack or stroke, upon heart attack or stroke, upon
recommendation of and with recommendation of and with
supervision of attending physician supervision of attending physician,
to a lifetime maximum of $1,500 to a lifetime maximum of $1,500
Chiropractic Care 100% after $10 copay per visit to 75% after deductible to a
a calendar year maximum of 20 calendar year maximum of 20
visits per person visits per person
Diagnostic Laboratory 100% 75% after deductible
and X-Ray
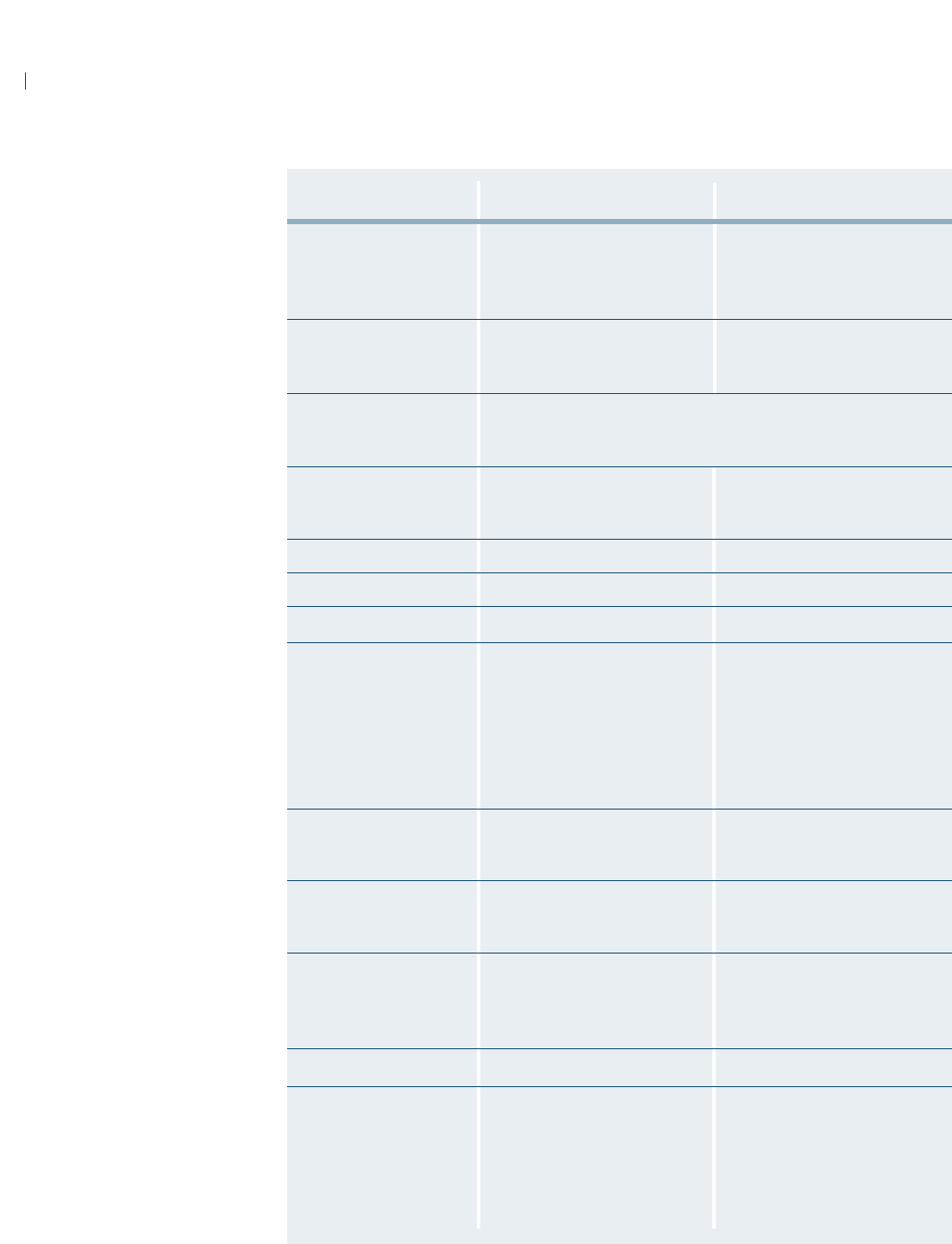
76
Plan Pays Plan Pays
PPO Network Out-of-Network
Durable Medical 80% after deductible. 75% after deductible.
Equipment Payments will not exceed the Payments will not exceed
(requires physician letter actual purchase price actual purchase price
of medical necessity)
Emergency Room 80% after deductible 75% after deductible
(refer to page 31) $50 penalty for non-life-threatening $50 penalty for non-life-threatening
care care
Hearing Aids Up to $1,500 per hearing aid to a maximum of $3,000 once every five-
year period. Covered through selected providers only. Contact the Fund
Office for a listing and to set up an appointment.
Home Health Care See page 37 for specific coverage See page 37 for specific coverage
(requires physician letter information information
of medical necessity)
Hospice Care 100% after deductible 75% after deductible
Hospital Room and Board 80% after deductible 75% after deductible
Hospital Physician Expense 80% after deductible 75% after deductible
Infertility Treatment Lifetime maximum $5,000. Lifetime maximum $5,000. After
Lab and x-ray: 100% of PPO fee; deductible, 75% of R&C charges
Surgeon’s fee: 100% of PPO fee to the lifetime maximum of
schedule, otherwise subject to $5,000.
R&C charges
Anesthesia: 100% of PPO fee.
All other services subject to
deductible, then payable at 80%.
Mental Health Treatment 80% after deductible to a 75% after deductible to a
(Inpatient) calendar year maximum of calendar year maximum of
30 days per person 30 days per person
Mental Health Treatment 100% after $10 copay per visit, 50% after deductible to a
(Outpatient) to a maximum of 10 visits per maximum of 10 visits per
person per calendar year person per calendar year
Occupational Therapy 100% after $10 copay per visit up 100% up to a combined lifetime
(requires physician letter to a combined lifetime maximum maximum of $30,000 for physical,
of medical necessity) of $30,000 for physical, speech speech and occupational therapy
and occupational therapy
Office Visits (Illness) 100% after $10 copay per visit 75% after deductible
Organ Transplants $250,000 per transplant maximum $250,000 per transplant maximum
Hospital: 80% after deductible Hospital: 75% after deductible
Surgeon’s fee: 100% of PPO fee Surgeon’s fee: 75% of R&C
schedule otherwise subject to charges after deductible
R&C charges Anesthesia: 75% of charges
Anesthesia: 100% of PPO fee after deductible
schedule
SCHEDULE OF BENEFITS FOR PLAN II
CONTINUED
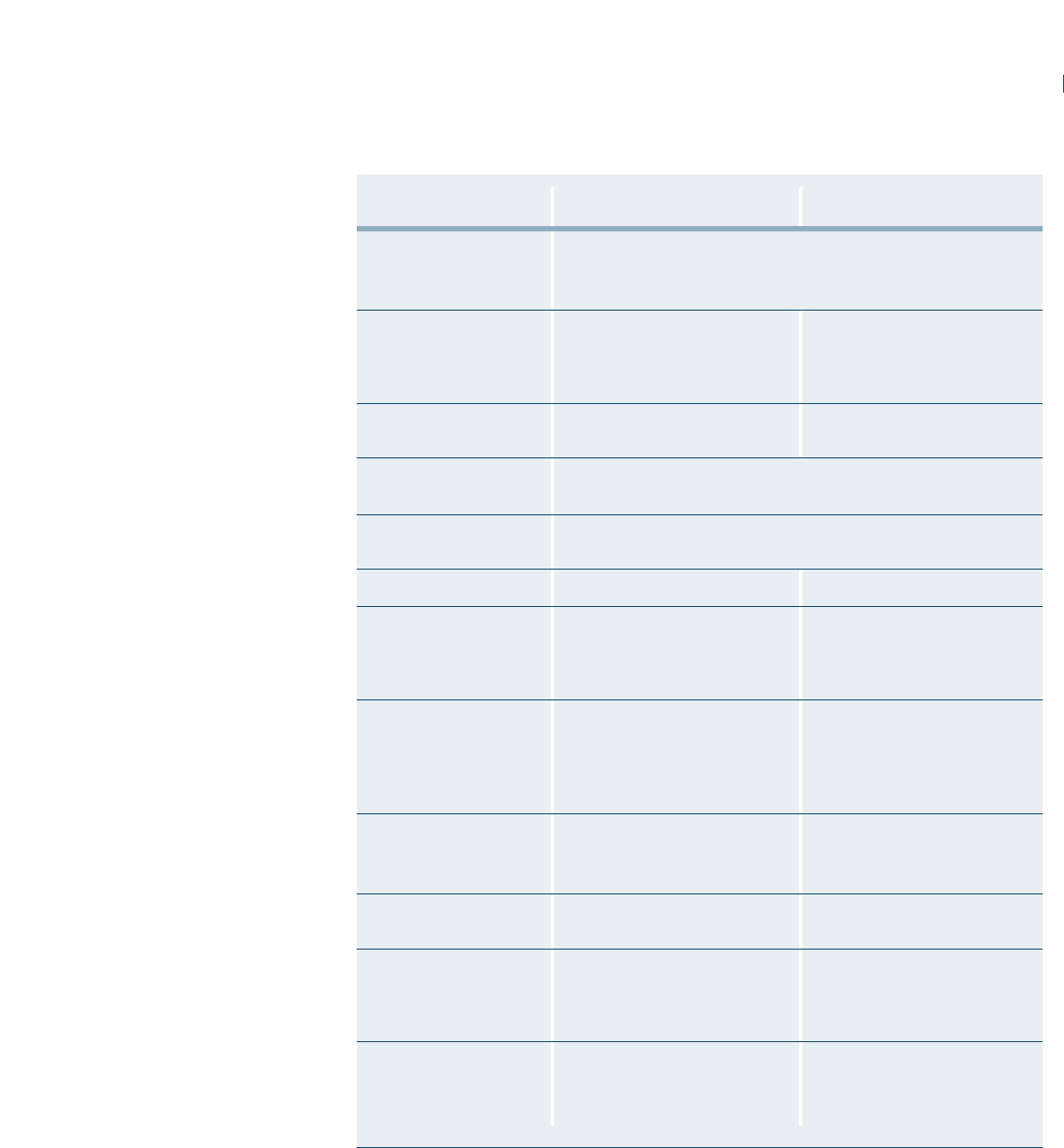
77
Plan Pays Plan Pays
PPO Network Out-of-Network
Physical Exams Covered for Member and spouse only
(includes all lab, x-ray Paid at 100% to a calendar year maximum of $75
and immunizations)
Physical Therapy 100% after $10 copay per visit, up 75% after deductible, up
(requires physician letter to a combined lifetime maximum to a combined lifetime maximum
of medical necessity) of $30,000 for physical, speech of $30,000 for physical, speech
and occupational therapy and occupational therapy
Podiatrist Services 100% after $10 copay to a calendar 75% after deductible to a calendar
year maximum of $500 per person year maximum of $500 per person
Prescription Drugs $20 copay for generics, $40 for Brand Preferred and $60 for Brand
(Mail Order, 90-day supply) Non-Preferred
Prescription Drugs $10 copay for generics, $20 for Brand Preferred and $30 for Brand
(Retail, 34-day supply) Non-Preferred
Skilled Nursing Facility 80% after deductible 75% after deductible
Speech Therapy 80% after deductible up to a 75% after deductible up to a
(requires physician letter combined lifetime maximum of combined lifetime maximum of
of medical necessity) $30,000 for physical, speech and $30,000 for physical, speech and
occupational therapy occupational therapy
Substance Abuse 80% after deductible to a 75% after deductible to a
Treatment (Inpatient) maximum of 30 days per person maximum of 30 days per person
per calendar year. per calendar year.
Maximum of two lifetime Maximum of two lifetime
ocurrences per person ocurrences per person
Substance Abuse 100% after $10 copay to a 75% after deductible to a
Treatment (Outpatient) maximum of $500 per person per maximum of $500 per person
calendar year per calendar year
Surgeon’s Expenses 100% of PPO fee schedule 75% of R&C charges after
otherwise subject to R&C charges deductible
Temporomandibular 100% after $10 copay to a lifetime 75% after deductible to a lifetime
Joint Disorders (TMJ) maximum of $1,000 within maximum of $1,000 within
limitations covered under limitations covered under
Plan Exclusions (page 52) Plan Exclusions (page 52)
Well-Child Care 100% after $10 copayment Not covered
(includes all lab, x-ray for children from birth
and immunizations) through age 5; not covered for
children age 6 and older
SCHEDULE OF BENEFITS FOR PLAN II
CONTINUED
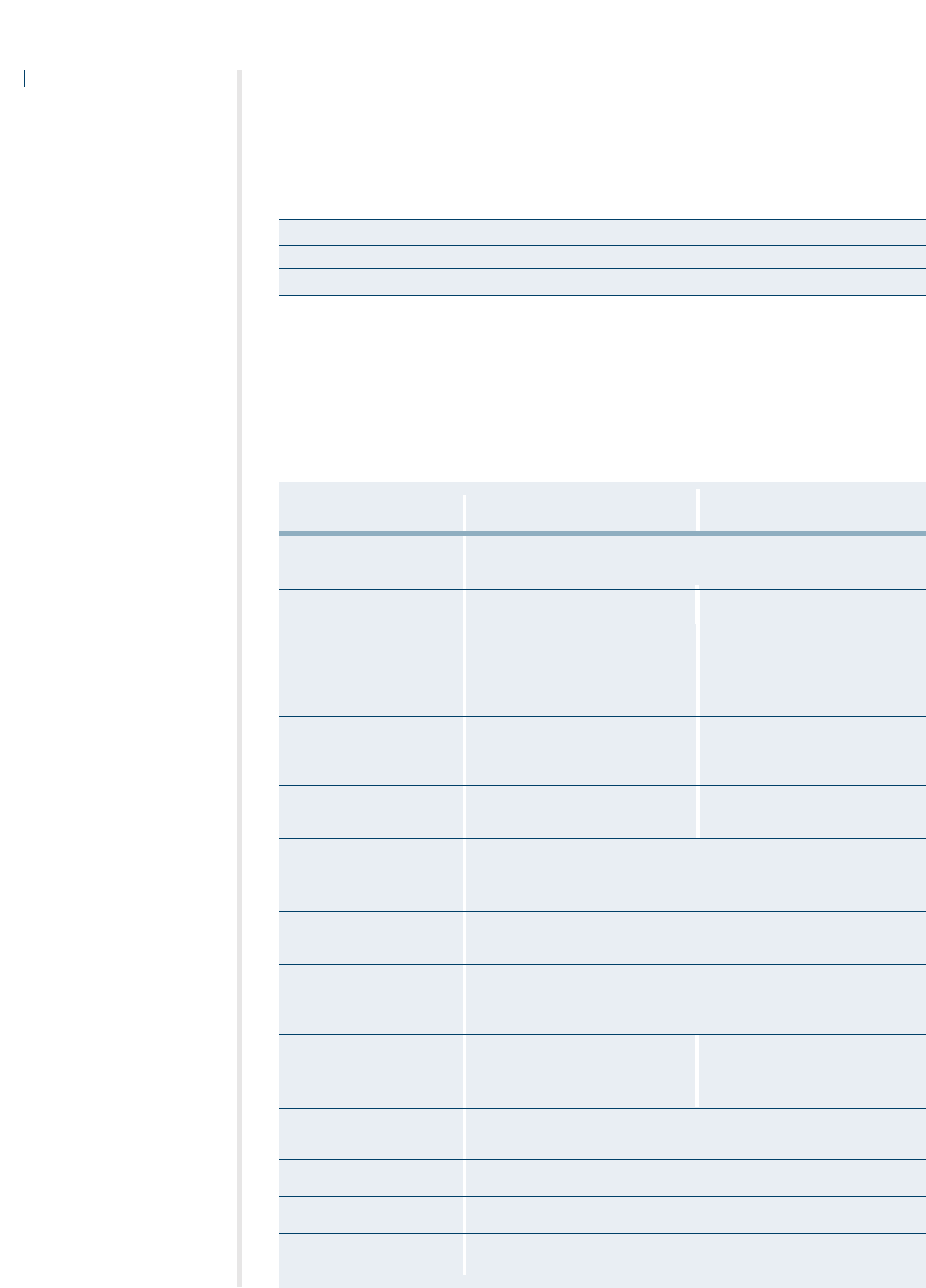
SCHEDULE OF BENEFITS FOR THE RETIREE PLAN
The chart that follows highlights the benefits of the New England Carpenters Health Benefits
Fund. For more detailed information, contact the Fund Office.
Your Calendar Year Deductible $250 per individual
Your Calendar Year Out-of-Pocket Maximum $3,000 per individual
Maximum Benefit the Plan Will Pay Per Person Per Lifetime $1,000,000
!! YOU MUST USE THE PPO NETWORK TO RECEIVE BENEFITS FROM THE RETIREE PLAN
UNLESS YOU LIVE OUTSIDE A 20-MILE RADIUS FROM A PREFERRED PROVIDER.
78
Plan Pays Out-of-Area
PPO Network Benefits
Ambulance Service 80% after deductible. Air Ambulance service payable at 80% after
deductible to a maximum of $2,000 per life-threatening emergency
Cardiac Rehabilitation 80% after deductible, when 80% after deductible when
medically necessary following medically necessary following
heart attack or stroke, upon heart attack or stroke, upon
recommendation of and with recommendation of and with
supervision of attending physician supervision of attending physician,
to a lifetime maximum of $1,500 to a lifetime maximum of $1,500
Chiropractic Care 100% after $10 copay per visit 80% after deductible to a calendar
to a calendar year maximum year maximum of 20 visits per
of 20 visits per person person
Diagnostic Laboratory 100% 80% after deductible
and X-Ray
Durable Medical Equipment 80% after deductible.
(requires physician letter Payments will not exceed the actual purchase price
of medical necessity)
Emergency Room 80% after deductible.
50% after deductible for non-life-threatening care
Hearing Aids Up to $1,500 per hearing aid to a maximum of $3,000 once every five-
year period. Covered through selected providers only. Call the Fund
Office for a listing and to set up an appointment.
Home Health Care See page 37 for specific See page 37 for specific
(requires physician letter information information
of medical necessity)
Hospice Care/Extended Not covered
Care Facility
Hospital Physician Expenses 80% after deductible
Hospital Room and Board 80% after deductible
Infertility Treatment Not covered
The following schedule shows the percentage of charges that the Fund pays under the Retiree Plan
whether medical services are obtained in the PPO Network or Out-of-Area. Note: Charges for
benefits provided by PPO network providers are based on a negotiated contract. Charges for benefits
provided by out-of-area providers are based on reasonable and customary rates described on page
27. You are responsible for any provider charges in excess of the reasonable and customary rates.

79
Plan Pays Out-of-Area
PPO Network Benefits
Mental Health Treatment 80% after deductible to a maximum of 15 days per calendar year
(Inpatient) per person
Mental Health Treatment 100% after $10 copay to a calendar 50% after deductible to a calendar
(
Outpatient) year maximum of 25 visits per person year maximum of 25 visits per person
Occupational Therapy 100% after $10 copay up to a 100% up to a combined lifetime
(requires physician letter combined lifetime maximum of maximum of $30,000 for physical,
of medical necessity) $30,000 for physical, speech and speech and occupational therapy
occupational therapy
Office Visits (Illness) 100% after $10 copay 80% after deductible
Organ Transplants $250,000 per transplant maximum $250,000 per transplant maximum
Hospital: 80% after deductible Hospital: 70% after deductible
Surgeon’s fee: 100% of PPO fee Surgeon’s fee: 70% of R&C
schedule otherwise subject to charges after deductible
R&C charges Anesthesia: 70% of charges
Anesthesia: 100% of PPO fee after deductible
schedule
Physical Exams Covered for Members and spouses only
(includes all lab, x-ray Paid at 100% to a calendar year maximum of $100
and immunizations)
Physical Therapy 100% after $10 copay up to 80% after deductible up to
(requires physician letter combined lifetime maximum of combined lifetime maximum of
of medical necessity) $30,000 for physical, speech and $30,000 for physical, speech and
occupational therapy occupational therapy
Podiatrist Services 100% after $10 copay up to a 80% after deductible up to a
calendar year maximum of $500 calendar year maximum of $500
per person per person
Prescription Drugs $20 copay for generics, $40 for Brand Preferred and $60 for Brand
(Mail Order, 90-day supply) Non-Preferred. Calendar year maximum of $15,000 per person
Prescription Drugs $10 copay for generics, $20 for Brand Preferred and $30 for Brand
(Retail, 34-day supply) Non-Preferred. Calendar year maximum of $15,000 per person
Speech Therapy 80% after deductible up to a 80% after deductible up to a
(requires physician letter combined lifetime maximum of combined lifetime maximum of
of medical necessity) $30,000 for physical, speech and $30,000 for physical, speech and
occupational therapy occupational therapy
Substance Abuse 80% after deductible to a 80% after deductible to a
Treatment (Inpatient) maximum of 15 days per person maximum of 15 days per person
per calendar year per calendar year
Substance Abuse 100% after $10 copay to a 80% after deductible to a
Treatment (Outpatient) maximum of $500 per person maximum of $500 per person
per calendar year. per calendar year.
Maximum of two lifetime Maximum of two lifetime
occurrences per person occurrences per person
Surgeon’s Expenses 100% of PPO fee schedule 80% of R&C charges after deductible
otherwise subject to R&C charges
Temporomandibular Not covered
Joint Disorders (TMJ)
SCHEDULE OF BENEFITS FOR THE RETIREE PLAN
CONTINUED
80
GLOSSARY OF TERMS
This section defines some of the terms used in this document. Please take the time to read these terms
carefully. They will help you to better understand your benefits. Also, in order for benefits to be payable,
the expenses must meet the requirements of these terms.
Ambulatory Surgical Facility means an establishment
licensed as such by the state with an organized med-
ical staff of physicians with permanent facilities that
are equipped and operated primarily for the purpose
of performing surgical procedures and continuous
physician services and registered professional nursing
services whenever a patient is in the facility.
Coinsurance – Once you satisfy the calendar year
deductible, depending on the type of service you
receive, the Fund may pay a portion of the benefit.
The remainder is your share, or coinsurance amount.
Refer to the Schedule of Benefits, beginning on page
71, for specific coinsurance information.
Copayment – A copayment is a fixed dollar amount
that you pay for certain services that are covered
under the Plan. For example, doctor’s office visits in
the PPO network for Plan I require a $10 copayment.
Covered Medical Expenses means expenses for
medical (including prescription drug, vision, hearing
and mental health/substance abuse) and/or dental
services or supplies, but only to the extent that:
• they are Medically Necessary, as defined in this
Definitions chapter of the document; and
• the charges for them are the negotiated fees for in-
network services or the Reasonable and Customary
Charges for out-of-network services; and
• coverage for the services or supplies is not
excluded, as provided in the General Exclusions
Section; and
•the charges do not exceed the calendar year
maximum, lifetime maximum or the Plan’s
individual lifetime maximum benefit.
Custodial Services means any services that are not
intended primarily to treat a specific injury or sickness
(including mental illness, alcohol or drug abuse).
Custodial Services include, but are not limited to:
• Services related to watching or protecting a person;
• Services related to performing or assisting a
person in performing any activities of daily living,
such as walking, grooming, bathing, dressing,
getting in or out of bed, toileting, eating,
preparing foods or taking medications that can be
self-administered; and
• Services not required to be performed by trained
or skilled medical or paramedical personnel.
Deductible – The deductible is the amount you
(and/or your family) must pay in medical expenses
before the Fund will begin to pay benefits. The
amount of your calendar year deductible depends on
the Plan of Benefits you’re covered under.
Eligible Dependent – The term “dependent” means (1)
your lawful spouse; (2) your unmarried children
(including a legally adopted child) who are under 19
years of age; (3) your unmarried children who are 19
through 23 years of age and who are enrolled as full-
time students in an accredited school, college or
university, not employed on a full-time basis and
dependent upon you for financial support.
IMPORTANT: You are required to furnish the
following documentation for dependent coverage if
you have not already done so:
1. Marriage certificate;
2. Birth certificate document showing both parents’
names, court document or written statement on
letterhead from appropriate governmental agency
showing legal guardianship and date of birth of
each child;
3. Divorce decree if applicable;
4. Proof of a dependent child’s attendance at an
accredited school or college as a full-time student
upon attainment of age 19 must be submitted to
the Fund Office twice each year as directed by the
Fund Office on an original form which contains
the accredited institution’s seal.
The term “child” also includes a stepchild or foster
child provided the child depends upon you for
support and maintenance and has been reported to
the Fund Office. See page 8 for details.
If an unmarried dependent child is incapable of self-
sustaining employment because of physical handicap
or mental retardation and he is dependent upon you
for support and maintenance, his coverage will be
continued provided his incapability commenced prior
to attaining age 19 or age 24 if a full-time student.
You must submit proof of your dependent child’s
incapability to the Fund Office on the later of 31 days
after the date he attains 19 years of age or age 24 if a
full-time student or 31 days after you are notified of
his eligibility. Contact the Fund Office for an
application.
Proof of the continued existence of such incapability
shall be furnished to the Fund Office from time to
time at its request.
Emergency Treatment means treatment for an injury
or sudden serious illness that poses an urgent or
pressing need and is treated within hours of the
commencement of the illness or injury.
Experimental Treatment/Procedure means a treatment
or procedure performed to demonstrate a known
truth, examine the validity of a hypothesis, to
determine the efficacy of something previously
untried or which has not been proven.
Extended Care Facility means an institution or a
distinct part of an institution which
• is operated pursuant to law and is primarily
engaged in providing, for compensation from its
patients, skilled nursing care for patients who
require medical care because of injury or sickness;
•provides 24-hour-a-day nursing service under the
supervision of a full-time employee who is either
a doctor or a registered nurse;
• maintains clinical records on all patients;
•provides for having a doctor available to furnish
necessary medical care in case of emergency; and
•provides appropriate methods and procedures for
the dispensing and administering of drugs and
biologicals.
In no event shall “Extended Care Facility” include
any institution or part of an institution which is a
hospital or which is primarily for the care of mental
illness, drug addiction, alcoholism or tuberculosis or
which is primarily engaged in providing domiciliary,
custodial or educational care or care for the aged.
Home Health Aide means a person who provides care
of a medical or therapeutic nature and reports to and
is under the direct supervision of a Home Health Care
Agency.
Home Health Care Agency means an agency or
organization (or a distinct part of) which:
• is primarily engaged in providing skilled nursing
and other therapeutic services for and in the
private residence of participants recovering from
an injury or sickness;
• is properly licensed or approved according to any
applicable state or local standards and is federally
certified as a Home Health Care Agency;
• is operated according to policies established by a
professional staff including at least one physician
and at least one registered nurse;
•provides for supervision of its services by a
physician or a registered nurse;
• maintains medical records for all patients.
Hospital – The term “hospital” means an institution
operated pursuant to law which is primarily engaged
in providing for compensation from its patients
medical, surgical and diagnostic facilities for the care
and treatment of sick and injured persons on an in-
patient basis and which provides such facilities under
the supervision of a staff of physicians and with 24-
hour-a-day nursing services by registered graduate
nurses. Unless it meets this definition, the term
“hospital” shall not include any institution or part
thereof which is used principally as a rest facility,
nursing facility, convalescent facility or facility for the
aged. A licensed institution used principally for the
care and treatment of alcoholics will be included
under the definition of “hospital” with the applicable
coverage in accordance with the schedule of benefits
for which you or a family member are eligible for
confinement in such institution. A licensed
institution used principally for the care and treatment
of mental illness will be included under the definition
of “hospital” with the applicable coverage for
81
confinement in such institution in accordance with
the schedule of benefits for which you or a family
member are eligible.
Hospital Charges, Surgical Charges and Medical
Charges –
The term “hospital charges” means the
charges for covered medical expenses, which are:
• made by a legally constituted hospital for board
and room and for other hospital services and
supplies (but not including charges for special
nursing services or for services for physicians or
surgeons) furnished by the hospital during
confinement;
• The term “surgical charges” means the charges for
covered medical expenses for surgery and for
necessary post-operative treatment in connection
with the surgery.
• The term “medical charges” means those charges
for covered medical expenses that are other than
hospital charges or surgical charges as defined
above.
Hospital Confinement – The term “period of hospital
confinement” includes successive periods of hospital
confinement for the same or a related disease or
bodily injury unless separated by complete recovery
from the disease or bodily injury which caused the
previous period of hospital confinement or, in the
case of the Member, a return to active work for at
least one day.
Hospice Care Facility means an institution that
provides care and service for terminally ill persons
and which:
a. provides 24-hour-a-day nursing care for the
terminally ill person with the necessary physical,
psychological and spiritual needs, with acute
inpatient and outpatient care, home care,
bereavement counseling directly or indirectly;
b. has a medical director who is a physician;
c. has an interdisciplinary team that coordinates the
care and services it provides and which includes
at least one physician, one registered professional
nurse and one social worker;
d. maintains central clinical records on all patients; and
e. is licensed or accredited as a Hospice if required.
Medically Necessary means any service, supply,
treatment or hospital confinement (or part of a
hospital confinement) which is essential to the
treatment of the injury or illness for which it is
prescribed or performed, meets generally accepted
standards of medical practice and is ordered by a
physician. The fact that a Physician or other
provider may prescribe, order, recommend, or
approve a service or supply does not, of itself, make
it Medically Necessary or make the expense a
Covered Charge.
Physician means a licensed medical practitioner who
is practicing within the scope of his license and who
is licensed to diagnose, prescribe and administer
drugs or to perform surgery. It will also include any
other licensed medical practitioner whose services are
required to be covered by law in the locality where
the policy is issued if he is:
• operating within the scope of his license, and
• performing a service for which benefits are
provided under this plan when performed by
a physician.
Reasonable and Customary Charges – The term
“reasonable and customary” means the amount
normally charged for similar services and supplies
which does not exceed the amount ordinarily charged
for comparable services and supplies in the locality
where the services or supplies are received.
82

SECTION 1: PURPOSE OF THIS NOTICE AND
EFFECTIVE DATE
THIS NOTICE DESCRIBES HOW MEDICAL
INFORMATION ABOUT YOU MAY BE USED AND
DISCLOSED AND HOW YOU CAN GET ACCESS
TO THIS INFORMATION. PLEASE REVIEW IT
CAREFULLY.
This Privacy Notice applies to the Fund Office of the
New England Carpenters Health Benefits Fund (“the
Fund”) and the services that the Fund provides through
Hines & Associates, CCN, Delta Dental, Ullicare
Rx/Medco., Davis Vision and other business associates of
the Fund. The Fund’s insurers will send you a notice of
their privacy practices separately.
Effective date.
The effective date of this Notice is April 14, 2003.
This Notice is required by law.
The Fund is required by law to take reasonable steps
to ensure the privacy of your personally identifiable
health information and to inform you about:
1. The Fund’s uses and disclosures of Protected
Health Information (PHI),
2. Your rights to privacy with respect to your PHI,
3. The Fund’s duties with respect to your PHI,
4. Your right to file a complaint with the Fund and
with the Secretary of the United States
Department of Health and Human Services
(HHS), and
5. The person or office you should contact for
further information about the Fund’s privacy
practices.
SECTION 2: YOUR PROTECTED HEALTH
INFORMATION
Protected Health Information (PHI) Defined
The term “Protected Health Information” (PHI)
includes all individually identifiable health
information related to your past, present or future
physical or mental health condition or to payment for
health care. PHI includes information maintained by
the Fund in oral, written, or electronic form.
When the Fund May Disclose Your PHI
Under the law, the Fund may disclose your PHI
without your consent or authorization, or the
opportunity to agree or object, in the following cases:
• For treatment, payment or health care
operations. The Fund and its business associates
will use PHI in order to carry out:
1. Treatment,
2. Payment, or
3. Health care operations.
Tr e atment is the provision, coordination or
management of health care and related services. It
also includes but is not limited to consultations
and referrals between one or more of your
providers.
For example, the Fund may disclose to a treating
orthodontist the name of your treating dentist so
that the orthodontist may ask for your dental x-
rays from the treating dentist.
Payment includes but is not limited to actions to
make coverage determinations and payment
(including billing, claims management,
subrogation, Fund reimbursement, reviews for
medical necessity and appropriateness of care and
utilization review and preauthorizations).
For example, the Fund may tell a doctor whether
you are eligible for coverage or what percentage
of the bill will be paid by the Fund. If we contract
with third parties to help us with payment
operations, such as a physician that reviews
medical claims, we will also disclose information
83
NEW ENGLAND CARPENTERS HEALTH BENEFITS FUND
PRIVACY NOTICE

to them. These third parties are known as
“business associates.”
Health care operations includes but is not limited
to quality assessment and improvement,
reviewing competence or qualifications of health
care professionals, underwriting, premium rating
and other insurance activities relating to creating
or renewing insurance contracts. It also includes
disease management, case management,
conducting or arranging for medical review, legal
services, and auditing functions including fraud
and abuse compliance programs, business
planning and development, business management
and general administrative activities.
For example, the Fund may use information
about your claims to refer into a disease
management program, a well-pregnancy program,
project future benefit costs or audit the accuracy
of its claims processing functions.
• Disclosure to the Fund’s Trustees
The Fund will also disclose PHI to the Fund
Sponsor, which is the Board of Trustees of the
New England Carpenters Health Benefits Fund,
for purposes related to treatment, payment, and
health care operations, and has amended the Plan
Document to permit this use and disclosure as
required by federal law. For example, we may
disclose information to the Board of Trustees to
allow them to decide an appeal or review a
subrogation claim.
• In addition, the Fund may disclose “summary
health information” to the Board of Trustees for
obtaining premium bids or modifying, amending
or terminating the Fund’s group health plan.
Summary information summarizes the claims
history, claims expenses or type of claims
experience by individuals for whom a Plan
Sponsor such as the Board of Trustees has
provided health benefits under a group health
plan. Identifying information will be deleted
from summary health information, in accordance
with federal privacy rules.
• At your request. If you request it, the Fund is
required to give you access to certain PHI in order
to allow you to inspect and/or copy it.
• When required by applicable law.
• As required by HHS. The Secretary of the United
States Department of Health and Human Services
may require the disclosure of your PHI to
investigate or determine the Fund’s compliance
with the privacy regulations.
• Public health purposes. To an authorized public
health authority if required by law or for public
health and safety purposes. PHI may also be used
or disclosed if you have been exposed to a
communicable disease or are at risk of spreading a
disease or condition, if authorized by law.
• Domestic violence or abuse situations. When
authorized by law to report information about
abuse, neglect or domestic violence to public
authorities if a reasonable belief exists that you
may be a victim of abuse, neglect or domestic
violence. In such case, the Fund will promptly
inform you that such a disclosure has been or will
be made unless that notice would cause a risk of
serious harm.
• Health oversight activities. To a health oversight
agency for oversight activities authorized by law.
These activities include civil, administrative or
criminal investigations, inspections, licensure or
disciplinary actions (for example, to investigate
complaints against health care providers) and
other activities necessary for appropriate oversight
of government benefit programs (for example, to
the Department of Labor).
• Legal proceedings. When required for judicial or
administrative proceedings. For example, your
PHI may be disclosed in response to a subpoena
or discovery request that is accompanied by a
court order.
• Law enforcement health purposes. When
required for law enforcement purposes (for
example, to report certain types of wounds).
84

• Law enforcement emergency purposes. For
certain law enforcement purposes, including:
1. identifying or locating a suspect, fugitive,
material witness or missing person, and
2. disclosing information about an individual
who is or is suspected to be a victim of a
crime.
• Determining cause of death and organ donation.
When required to be given to a coroner or
medical examiner to identify a deceased person,
determine a cause of death or other authorized
duties. We may also disclose PHI for cadaveric
organ, eye or tissue donation purposes.
• Funeral purposes. When required to be given to
funeral directors to carry out their duties with
respect to the decedent.
• Research. For research, subject to certain
conditions.
• Health or safety threats. When, consistent with
applicable law and standards of ethical conduct,
the Fund in good faith believes the use or
disclosure is necessary to prevent or lessen a
serious and imminent threat to the health or
safety of a person or the public and the disclosure
is to a person reasonably able to prevent or lessen
the threat, including the target of the threat.
• Workers’ compensation programs. When
authorized by and to the extent necessary to
comply with workers’ compensation or other
similar programs established by law.
• Specialized Government Functions. When
required, to military authorities under certain
circumstances, or to authorized federal officials
for lawful intelligence, counter intelligence and
other national security activities.
Except as otherwise indicated in this notice, uses and
disclosures will be made only with your written
authorization subject to your right to revoke your
authorization.
When the Disclosure of Your PHI Requires Your
Written Authorization
Although the Fund does not routinely obtain
psychotherapy notes, it must generally obtain your
written authorization before the Fund will use or
disclose psychotherapy notes about you. However,
the Fund may use and disclose such notes when
needed by the Fund to defend itself against litigation
filed by you.
Psychotherapy notes are separately filed notes about
your conversations with your mental health
professional during a counseling session. They do not
include summary information about your mental
health treatment.
The Fund may provide health information for the
purpose of evaluating and processing a claim for
disability benefits or to process a hardship loan from
the Annuity Fund; however, the Fund will obtain
your written authorization before it will use or
disclose any health information for this purpose.
When You Can Object and Prevent the Fund from
Using or Disclosing PHI
Disclosure of your PHI to family members, other
relatives, your close personal friends and any other
person you choose is allowed under federal law if:
• The information is directly relevant to the family
or friend’s involvement with your care or payment
for that care, and
•You have either agreed to the disclosure or have
been given an opportunity to object and have not
objected.
Other Uses or Disclosures
The Fund may contact you to provide you with
information about treatment alternatives or other
health-related benefits and services that may be of
interest to you.
85

SECTION 3: YOUR INDIVIDUAL PRIVACY RIGHTS
You May Request Restrictions on PHI Uses and
Disclosures
You may request the Fund to:
1. Restrict the uses and disclosures of your PHI to
carry out treatment, payment or health care
operations, or
2. Restrict uses and disclosures to family members,
relatives, friends or other persons identified by
you who are involved in your care.
The Fund, however, is not required to agree to your
request.
You or your personal representative will be required
to complete a form to request restrictions on uses and
disclosures of your PHI. Make such requests to the
Privacy Official at:
The New England Carpenters Health Benefits
Fund
350 Fordham Road
Wilmington, MA 01887
Phone: (800) 344-1515
You May Request Confidential Communications
The Fund will accommodate an individual’s
reasonable request to receive communications of PHI
by alternative means or at alternative locations
where the request includes a statement that
disclosure could endanger the individual.
You or your personal representative will be required
to complete a form to request restrictions on uses and
disclosures of your PHI. Make such requests to the
Privacy Official (at the address listed above).
You May Inspect and Copy PHI
You have a right to inspect and obtain a copy of your
PHI contained in a “designated record set,” for as
long as the Fund maintains the PHI.
The Fund must provide the requested information
within 30 days if the information is maintained on
site or within 60 days if the information is
maintained offsite. A single 30-day extension is
allowed if the Fund is unable to comply with the
deadline.
You or your personal representative will be required
to complete a form to request access to the PHI. A
reasonable fee may be charged. Requests for access to
PHI should be made to the Privacy Official (at the
address listed at left).
If access is denied, you or your personal
representative will be provided with a written denial
setting forth the basis for the denial, a description of
how you may exercise your review rights and a
description of how you may complain to the Fund
and HHS.
Designated Record Set: includes your medical
records and billing records that are maintained by or
for a covered health care provider. Records include
enrollment, payment, billing, claims adjudication and
case or medical management record systems
maintained by or for a health plan or other
information used in whole or in part by or for the
covered entity to make decisions about you.
Information used for quality control or peer review
analyses and not used to make decisions about you is
not included.
You Have the Right to Amend Your PHI
You have the right to request that the Fund amend
your PHI or a record about you in a designated
record set for as long as the PHI is maintained in the
designated record set subject to certain expectations.
See the Fund’s Right to Amend Policy (available on
request from the Fund’s Privacy Official) for a list of
exceptions.
The Fund has 60 days after receiving your request to
act on it. The Fund is allowed a single 30-day
extension if the Fund is unable to comply with the
60-day deadline. If the Fund denied your request in
whole or part, the Fund must provide you with a
written denial that explains the basis for the decision.
You or your personal representative may then submit
a written statement disagreeing with the denial and
have that statement included with any future
disclosures of that PHI.
86

You should make your request to amend PHI to the
Privacy Official (at the address listed above). You or
your personal representative will be required to
complete a form to request amendment of the PHI.
You Have the Right to Receive an Accounting of the
Fund’s PHI Disclosures
At your request, the Fund will also provide you with
an accounting of certain disclosures by the Fund of
your PHI. We do not have to provide you with an
accounting of disclosures related to treatment,
payment, or health care operations, or disclosures
made to you or authorized by you in writing. See the
Fund’s Accounting for Disclosure Policy (available on
request from the Fund’s Privacy Official) for the
complete list of disclosures for which an accounting
is not required.
The Fund has 60 days to provide the accounting. The
Fund is allowed an additional 30 days if the Fund
gives you a written statement of the reasons for the
delay and the date by which the accounting will be
provided.
If you request more than one accounting within a 12-
month period, the Fund may charge a reasonable,
cost-based fee for each subsequent accounting.
You Have the Right to Receive a Paper Copy of This
Notice Upon Request
To obtain a paper copy of this Notice, contact the
Privacy Official (at the address listed above).
Your Personal Representative
You may exercise your rights through a personal
representative who will be required to produce
evidence of authority to act on your behalf before the
personal representative will be given access to your
PHI or be allowed to take any action for you. Proof of
such authority will be a completed, signed and
approved Appointment of Personal Representative
form. You may obtain this form by calling the Fund
Office.
The Fund retains discretion to deny access to your
PHI to a personal representative to provide protection
to those vulnerable people who depend on others to
exercise their rights under these rules and who may
be subject to abuse or neglect.
The Fund will recognize certain individuals as
personal representatives without you having to
complete an Appointment of Personal Representative
form. For example, the Fund will automatically
consider a spouse, parent of a Member, or an adult
child (age 18 or over) of a Member to be the personal
representative of an individual covered by the Fund.
In addition, the Fund will consider a parent or
guardian as the personal representative of an
unemancipated minor except in a few types of
situations. A spouse, a parent, or child may act on an
individual’s behalf, including requesting access to
their PHI. Spouses and unemancipated minors may,
however, request that the Fund restrict information
that goes to family members as described above at the
beginning of Section 3 of this Notice.
You should also review the Fund’s Policy and
Procedure for the Recognition of Personal
Representatives (available upon request from the
Fund’s Privacy Official) for a more complete
description of the circumstances where the Fund will
automatically consider an individual to be a personal
representative for purposes of exercising your rights
under this Privacy Notice.
87

SECTION 4: THE FUND’S DUTIES
Maintaining Your Privacy
The Fund is required by law to maintain the privacy
of your PHI and to provide you with notice of its
legal duties and privacy practices.
This notice is effective beginning on April 14, 2003
and the Fund is required to comply with the terms of
this notice. However, the Fund reserves the right to
change its privacy practices and to apply the changes
to any PHI received or maintained by the Fund prior
to that date. If a privacy practice is changed, a revised
version of this notice will be provided to you and to
all past and present participants and beneficiaries for
whom the Fund still maintains PHI.
The Privacy Notice will be provided by first class mail
to all named participants. Any other person,
including dependents of named participants, may
receive a copy upon request.
Any revised version of this notice will be distributed
within 60 days of the effective date of any material
change to:
1. The uses or disclosures of PHI,
2. Your individual rights,
3. The duties of the Fund, or
4. Other privacy practices stated in this notice.
Disclosing Only the Minimum Necessary Protected
Health Information
When using or disclosing PHI or when requesting
PHI from another covered entity, the Fund will make
reasonable efforts not to use, disclose or request more
than the minimum amount of PHI necessary to
accomplish the intended purpose of the use,
disclosure or request, taking into consideration
practical and technological limitations.
However, the minimum necessary standard will not
apply in the following situations:
1. Disclosures to or requests made by a health care
provider for treatment,
2. Uses or disclosures made to you,
3. Uses or disclosures made pursuant to your
written authorization,
4. Disclosures made to the Secretary of the United
States Department of Health and Human Services
pursuant to its enforcement activities under
HIPAA,
5. Uses or disclosures required by law, and
6. Uses or disclosures required for the Fund’s
compliance with the HIPAA privacy regulations.
This notice does not apply to information that has
been de-identified. De-identified information is
information that:
1. Does not identify you, and
2. With respect to which there is not reasonable
basis to believe that the information can be used
to identify you.
SECTION 5: YOUR RIGHT TO FILE A COMPLAINT
WITH THE FUND OR THE HHS SECRETARY
If you believe that your privacy rights have been
violated, you may file a complaint with the Fund in
care of the Privacy Official (at the address listed
above).
You may also file a complaint with the Secretary of
the U.S. Department of Health and Human Services
(“HHS”). Please contact the nearest office of the
Department of Health and Human Services, listed in
your telephone directory, visit the HHS website at
www.hhs.gov, or call the Privacy Official for more
information about how to file a complaint.
The Fund will not retaliate against you for filing a
complaint.
SECTION 6: IF YOU NEED MORE INFORMATION
If you have any questions regarding this notice or the
subjects addressed in it, you may contact the Privacy
Official at the Fund Office.
88

SECTION 7: CONCLUSION
PHI use and disclosure by the Fund is regulated by
the federal Health Insurance Portability and
Accountability Act, known as HIPAA. You may find
these rules at 45 Code of Federal Regulations Parts
160 and 164. This notice attempts to summarize the
regulations. The regulations will supersede this notice
if there is any discrepancy between the information in
this notice and the regulations.
89

Employer Trustees
William J. Sullivan, Secretary/Treasurer
Daniel O’Connell’s Sons, Inc.
480 Hampden Street
P.O. Box 267
Holyoke, MA 01041
Stephan A. Adamic
Co-Secretary/Treasurer
P.O. Box 302
Grantham, NH 03753
George M. Bidgood
Bidgood Associates, Inc.
99 Essex Street
Melrose, MA 02176
Theodore H. Brodie
A.F. Underhill, Inc.
P.O. Box 376
Canton, MA 02021-0376
Donald L. Colavecchio
105 Reflection Drive
Sandwich, MA 02563
Thomas J. Gunning
The Building Trades Employers Assoc.
1400 Hancock Street, 7th Floor
Quincy, MA 02169
Michael Shaughnessy
Shaughnessy Crane Service, Inc.
P.O. Box 366
South Boston, MA 02127-0992
William Shea
J.F. White Contracting Company
10 Burr Street
Framingham, MA 017001-4617
Thomas Steeves
T.J. McCartney, Inc.
3 Capitol Street, Suite 1
Nashua, NH 03063
Union Trustees
Thomas J. Harrington, Chairman
New England Regional Council of
Carpenters
803 Summer Street, 4th Floor
South Boston, MA 02127
Mark L. Erlich
Carpenters Local Union 40
10 Holworthy Street
Cambridge, MA 02138
Thomas J. Flynn
Carpenters Local Union 67
760 Adams Street, 2nd Floor
Dorchester, MA 02122
Simon R. James
Local Union No. 108
29 Oakland Street
Springfield, MA 01108
Bruce King
Local Union 1996
60 Industrial Drive
August, ME 04330-9302
John Murphy
New England Regional Council
of Carpenters
803 Summer Street
Boston, MA 02127
Michael Nelson
Local Union 424
21 Mazzeo Drive, Suite 201
Randolph, MA 02368
David R. Wallace
CLMP
803 Summer Street
Boston, MA 02127
Jack Winfield
Local Union 1121
90 Braintree Street
Allston, MA 02134
David A. Woodman
Local Union 56
Marine Industrial Park/EDIC
22 Drydock Avenue, 3rd Floor
Boston, MA 02210-2386
90
BOARD OF TRUSTEES
NOTES
91
92
NOTES

