
1
Medical Orders for Scope of Treatment:
Implementation in North Carolina
North Carolina Institute of Medicine
2013
The Medical Orders for Scope of Treatment (MOST) document is a standardized form that
patients can use to designate treatment preferences which can be used as medical orders across
healthcare facilities. The form must be completed by both the patient (or his or her authorized
representative) and the physician, nurse practitioner or physician assistant. The MOST form
includes care preferences in regards to cardio-pulmonary resuscitation, antibiotics, intravenous
fluids, and feeding tubes, including scope of care (full care, limited care, comfort measures
only). These types of care preferences may be of particular use in nursing home settings. Studies
have shown that the patients’ preferences are more likely to be honored with use of similar
forms.
1,2
Despite generally high support of the MOST form by health professionals, there has
been some concern regarding time, complexity, literacy level, and need for annual update.
Nursing homes in NC are thought to have excellent compliance with documenting advanced care
directives, but the type of process used by most nursing homes in NC is widely varied. In
addition, we have no knowledge of the use of the MOST form in North Carolina, how it is
perceived by staff in health care settings, and whether there are barriers to its use. Also, while we
have some understanding of the use of advance care directives in nursing homes, less is known
about the role of the MOST form and other types of advanced directives in adult care homes and
assisted living facilities. Planning for advance care preferences often starts after a change in
health status concurrent with an acute care hospitalization, therefore understanding the role of
hospitals in advanced care planning and documentation is an important part of understanding the
use of the MOST form in NC.
In 2007, the NC General Assembly passed a bill regarding advanced directives, which, among
other things, authorized the creation of the MOST form for use across settings of care in North
Carolina. This legislation codified the requirements that must be followed in using the MOST
form, including when it will be used, what parties must sign the form, and how often it must be
updated. In addition, the legislation set forth that the North Carolina Institute of Medicine
(NCIOM) would study the process of end-of-life care in 2013.
3
Specifically, the NCIOM was
directed to:
“study issues related to the provision of end-of-life medical care in North
Carolina. As part of the study, the Division of Health Service Regulation,
Department of Health and Human Services, and the North Carolina Board of
Medicine shall provide to the Institute non-identifying information regarding
claims and complaints related to end-of-life medical treatment by health care
providers that was contrary to the express wishes of either the patient or a person
authorized by law to make treatment decisions on behalf of the patient. The
Institute may review any other data related to end-of-life medical care and
treatment the Institute determines is relevant.
2
The purpose of this study is to determine whether statutory changes related to
advance directives and health care powers of attorney impact the type and
quantity of end-of-life medical care provided to patients, whether the patient's or
patient representative's express wishes regarding the provision of treatment at the
end of life are being honored, and whether there is any change in the number of
persons who request continued treatment at the end of their lives, but do not
receive that treatment.”
The North Carolina Institute of Medicine took two approaches to study the use of the MOST
form in North Carolina. First, we conducted a series of interviews with key informants to better
understand how the MOST form was perceived and whether or not there were any formal
complaints about the use of the MOST form. The second part of the study was a web-based
survey of professionals involved in hospital discharge planning and ongoing care in a long-term
care facility (e.g. nursing home, assisted living, or adult care home to better understand their
advanced care planning process generally and their use of the MOST form more specifically.
Methods:
Key informant interviews
The key informant survey included discussions (face to face or by telephone) or email dialogues
with 20 stakeholders knowledgeable in end-of-life care and the delivery in NC. This included
directors or representatives of the NC Medical Board, the NC Medical Society, the Office of
Emergency Medical Services, the NC Bar Association, the NC Division on Aging, the NC
Health Care Facilities Association, hospice agencies, physicians (geriatric/palliative care),
attorneys, and ethicists. The interviews were framed around three issues: 1) perceptions around
the use of MOST forms, DNR forms, and health care power of attorney, 2) claims or complaints
that the MOST form was used contrary to the express wish of the patient regarding end-of-life
care, and 3) changes in end-of-life care related to the 2007 statute.
Web-based survey
To gather more broad-based input on the use of the MOST form in clinical settings, we
conducted a web-based survey of health professionals that are often involved in or supervising
advanced care planning. This was done using Qualtrics, a commercial platform for administering
web-based surveys.
Subjects
Representatives of four organizations agreed to send a link to a web-based survey: the NC Health
Care Facilities Association (representing nursing facilities in North Carolina), the NC
Association of Long Term Care Facilities (representing assisted living and adult care homes), the
NC Assisted Living Association (representing assisted living facilities), and the NC Chapter of
the American Case Management Association (representing hospital discharge planners). The lists
were not provided directly to the NCIOM. We included professionals from all four of these
organizations to gain a better understanding of the advance care planning across the spectrum of
long-term care facilities and from the perspective of the hospital-based discharge planning
professional.

3
Survey instrument
Staff from the NCIOM wrote the first draft of the survey instrument. The items were based on
the findings of a qualitative study of experience with the MOST form by nursing home
professionals.
4
Additional items were added to assure that we addressed the questions raised by
the North Carolina General Assembly in the authorizing statute. A draft survey was reviewed by
representatives of the participating organizations and by several members of the North Carolina
Partnership for Compassionate Care (a group of healthcare and community leaders dedicated to
improving communication and education about end-of-life care through local and statewide
initiatives). The survey was revised based on their feedback.
The survey included questions on the respondents’ familiarity with the MOST form, the types of
advanced care planning forms used by the institution, whether the MOST form is honored in the
institution, and any barriers or concerns about use of the MOST form. The survey specifically
asked respondents whether they had received complaints that treatment was provided in excess
of the wishes expressed by the patient on the MOST form, and if so, whether care was less
aggressive or more aggressive than wishes expressed on the MOST form. The study sent to
administrators of various ongoing care organizations was nearly identical. The survey of the
hospital-based care managers differed somewhat to capture the perspective of a patient upon
being discharged from the hospital, but included most of the same concepts regarding use of the
MOST form, barriers and complaints with the MOST form, and tools used for advance care
planning more generally.
Procedures:
A link to an online survey was sent to the four previously mentioned groups of professionals. If
they followed the link and agreed to the study conditions on the consent, they were directed to a
brief (<5 minutes) online survey. The survey was anonymous. After one week, the surveys were
re-sent to encourage participation. The study was approved by the UNC Committee on Human
Subject Research.
Results:
In the key informant interviews, stakeholder expressed varied perspectives on the uptake of
MOST forms. Generally, stakeholders felt that other forms were more common, including Don
Not Resuscitate (DNR) and 5 Wishes (a combined living will and healthcare power of attorney
that address comfort care and spirituality). Several informants mentioned that use of the forms
was dependent on the local physicians, most of whom were unfamiliar with the form or felt that
it was too cumbersome. When the form was being used, it was often due to local champions who
spread the use of the form in their communities. Several informants mentioned that the biggest
problem with the MOST, DNR, and other forms is when a family wants to override the wishes of
a critically ill loved one, creating conflict at the time of crisis. One respondent noted that at
his/her facility they did not accept the most form as an ‘order’ but stated that admitting
physicians generally reviewed the form and translated it into similar parameters available in the
institution’s computerized order entry system. Several informants commented that the law posed
challenges because it requires the use of original signed forms (e.g., copies are not valid). This
necessitated the patient to keep multiple originals at different locations. No stakeholder could
provide data on how often the forms were being used in their organization or facility.

4
The authorizing legislation required that the Division of Health Service Regulations, Department
of Health and Human Services, and the NC Medical Board provide the NCIOM with non-
identifying information regarding claims and complaints related to end-of-life medical treatment
by health care providers that was contrary to the express wishes of either the patient or a person
authorized by law to make treatment decisions on behalf of the patient. The NCIOM staff
interviewed the executive director of the NC Medical Board and the Director of Complaints for
the NC Medical Board. The Board receives approximately 1300 complaints per year, but the
complaints are not searchable in a way to conclusively examine the issues raised in the
authorizing legislation. However, the Director of Complaints has worked for the medical board
for 15 years, and reviews all complaints. She reported no increase in complaints regarding end-
of-life care since the authorizing legislation. She had vague recollection of one complaint in
which care exceeded that which was desired by the patient. She recalled that no action was taken
on this complaint, and could not recall whether or not this was related to any type of advanced
directive. The Executive Director and Director of Complaints reported that the Board gets
infrequent complaints about end-of-life care in which family members report that their wishes
are not met for end-of-life care when all family members are not in agreement or when there is a
disagreement between physician and family members. The Director of the Division of Health
Services Regulation and the Director of the Office of Emergency Medical Services reported that
they had not received specific complaints about the MOST form. They did report that they
maintained a record of the number of forms ordered and by which institutions, but they have no
way of knowing how many are completed. In a personal communication with the director of the
Office of Emergency Medical Services, she reported that 110,846 MOST forms were distributed
in 2012-2013 (compared to 185,829 DNR forms). The number of forms given to patients/clients
and the number of completed forms remain unknown. Though there is an option for keeping
DNR forms, living wills, and healthcare power of attorney forms online in a registry for a small
fee, there is no such registry option for MOST forms in NC.
The web-based survey yielded 242 responses. It is important to note that the number of potential
respondents is unknown and no response rate is reported. The respondents were well distributed
across the four organizations, representing responses from a spectrum of levels of care.
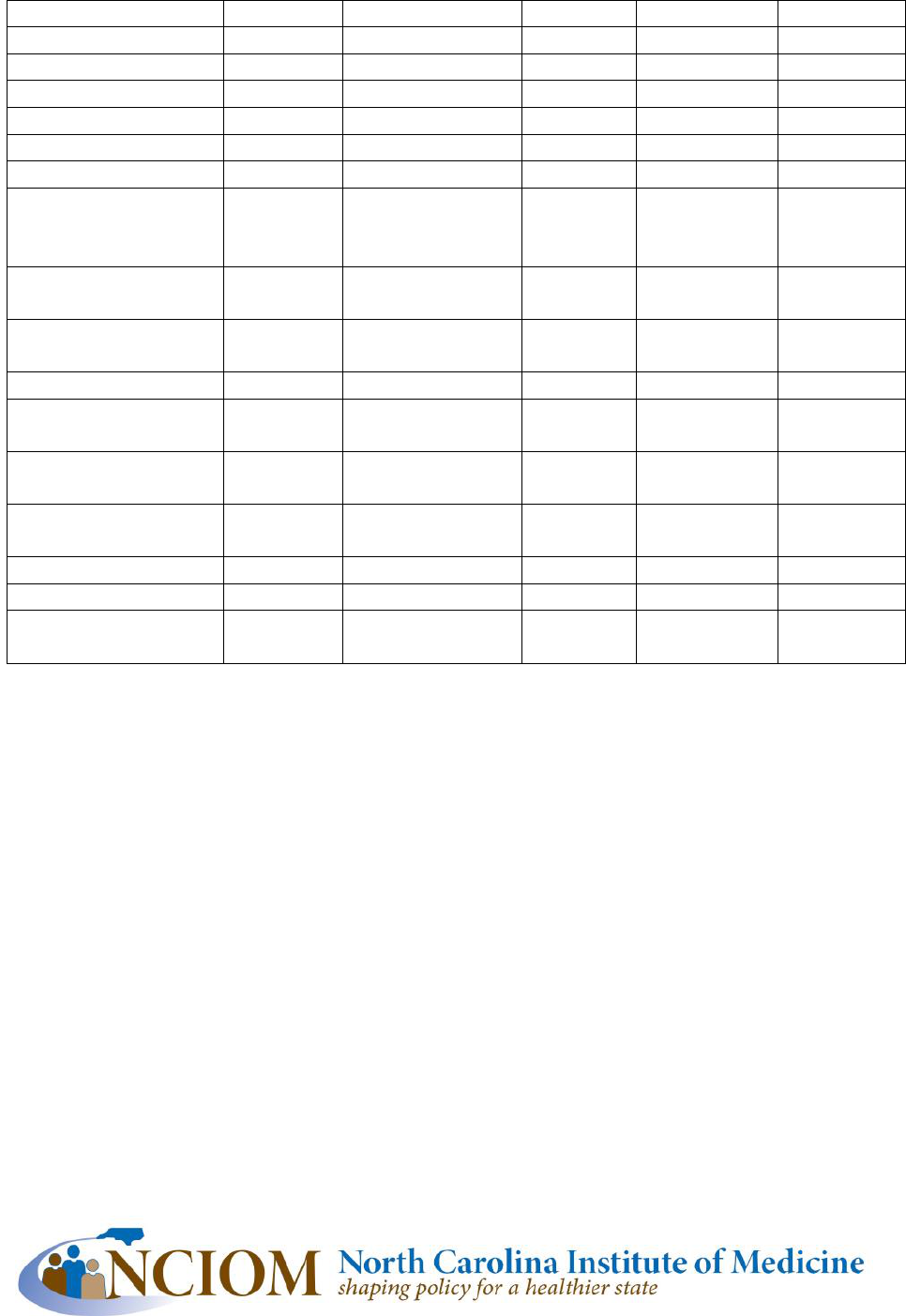
The general approach to advanced care planning and use of the MOST form is summarized in
Table 1. Advanced care planning is required or strongly recommended by the majority of
ongoing care organizations. DNR forms, living wills, and health care power of attorney forms
are more common than the MOST form. The majority of respondents have heard of the MOST
form, but the majority report that few residents or patients at their organization have a MOST
form. The overwhelming majority of organizations honor a MOST form completed elsewhere.
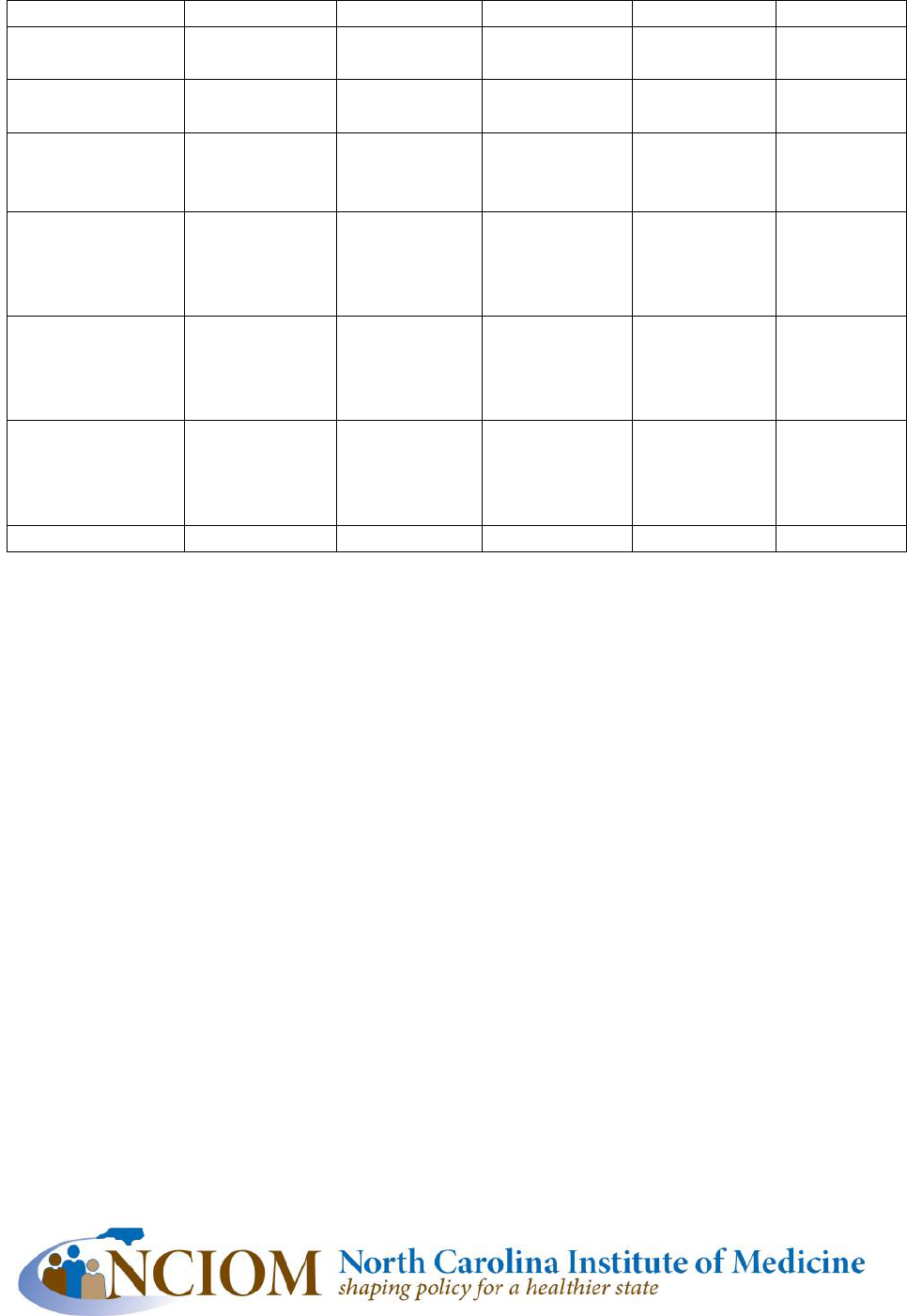
Respondents reported that they had heard few complaints with the MOST form, and the majority
of complaints were in regard to difficulty in understanding the form. Three respondents reported
that they had received complaints that more aggressive care was delivered in excess of care
wishes expressed on the MOST form. No respondents reported care that was less aggressive than
care wishes expressed on the MOST form, a finding consistent with previous research on the
POLST form.
2
(Reported complaints are summarized in Table 2.)
5
Table 1: Advanced Care Planning and Use of MOST Form
NCHCFA
1
NCALA
2
NCLTCF
3
NCCM
4
Total
Respondents (N)
76
41
61
64
242
Use MOST (%)
64
28
30
47
45
Use 5 Wishes (%)
5
3
3
6
5
Use DNR (%)
99
100
90
100
97
Use HCPOA (%)
66
95
77
94
81
Use Living Will (%)
65
87
60
87
74
Advanced Care
Planning required
(%)
33
23
15
NA
24
Strongly
recommended (%)
46
41
37
NA
42
Report >50% have
plan (%)
73
55
34
23
47
Heard of MOST (%)
97
76
63
94
84
Report >50% have
MOST (%)
17
6
6
4
9
26-50% Have MOST
(%)
9
3
0
12
7
1-25% Have MOST
(%)
54
76
51
48
55
None MOST (%)
13
14
43
36
27
Honors MOST (%)
80
100
91
86
88
Received complaints
about MOST (N)
1
6
2
5
14
1
NC Health Care Facilities Association
2
NC Assisted Living Association
3
NC Association of Long-Term Care Facilities
4
NC Chapter of the American Case Management Association
6
Table 2: Problems with MOST FORM (reported providers in an organization)
NCHCFA
1
NCALA
2
NCLTCF
3
NCCM
4
Total
Form difficult to
understand (N)
1
4
2
5
12
Scary to discuss
end of life(N)
-
1
-
2
3
Form too
comprehensive
(N)
1
2
1
1
5
Form too
specific/not
comprehensive
enough (N)
-
1
-
1
2
Care provided in
excess of wishes
on MOST form
(N)
-
2
-
1
3
Care less
aggressive than
wishes on
MOST form (N)
-
-
-
-
0
Other (N)
-
4
-
2
6
1
NC Health Care Facilities Association
2
NC Assisted Living Association
3
NC Association of Long-Term Care Facilities
4
NC Chapter of the American Case Management Association
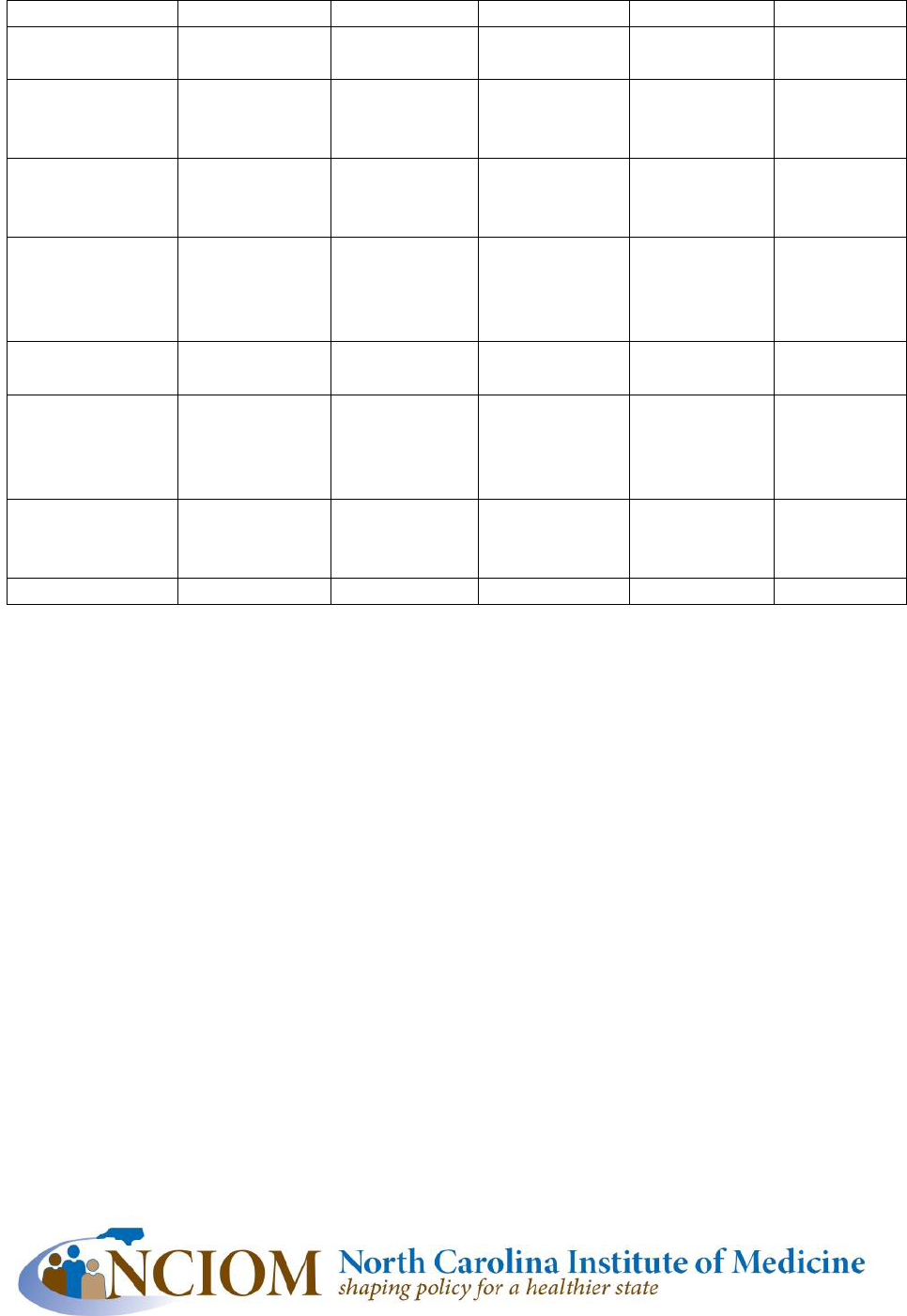
The perceived barriers to the use of the MOST form are summarized in Table 3. The common
concerns included: the form takes too much time, it is hard to match treatment goals to the form,
the review requirements are cumbersome, the form is difficult to understand, the form is
redundant of other paperwork, the form might be lost in transfer, and the form might not be
accepted upon transfer to other agencies. Closer look at the response by organization type reveal
some possible additional information. For example, time requirement is a much bigger problem
for hospital-based care managers than at ongoing care organizations. This may reflect the short
duration of relationship with patients and families in an acute care facility, the high acuity of
medical need, and the short duration of stays. Administrators at ongoing care facilities may feel
like admission to a long-term care facility is too late to start the discussion of advanced care
planning, but the feedback from care-managers may reflect the unique challenge of that
environment, indicating the need to start advanced care planning before acute illness or
decompensation of chronic disease. Concern that a form might be lost or not honored seems to
be a bigger problem for ongoing care organizations than for hospitals.
7
Table 3: Identified Barriers (reported by providers in an organization)
NCHCFA
1
NCALA
2
NCLTCF
3
NCCM
4
Total
Takes too much
time (%)
34
22
34
68
41
Hard to match
goals to
treatment (%)
13
30
29
42
28
Review
requirements
(%)
26
22
17
26
23
Difficult for
patients and
families to
understand (%)
33
48
40
32
37
Redundant
paperwork (%)
20
37
20
14
21
Concern form
would be lost
during transfer
(%)
38
37
20
8
25
Concern form
would not be
honored (%)
16
33
29
14
22
Other (%)
18
4
9
26
16
1
NC Health Care Facilities Association
2
NC Assisted Living Association
3
NC Association of Long-Term Care Facilities
4
NC Chapter of the American Case Management Association
Discussion:
This study of MOST implementation should serve two purposes. First, it provides assurance that
the authorizing statute requiring this study did not lead to large numbers of complaints about
ongoing care. There are no complaints that we could identify that the MOST form or its
authorizing legislation resulted in treatment being withheld at the end of life or treatment being
given in excess of that which was desired by the patient or his/her family. Likewise, concerns
about matching end-of-life treatment with wishes, and navigating family discord at the end of
life were not problems created by the MOST form nor will they be entirely solved by the MOST
form. Unfortunately, there was no baseline by which to examine a change in these problems over
time.

8
The second purpose of this study is to help providers of medical and long-term care in NC to
better understand the role, application, and limitations of the MOST form. The study points to a
number of possible program and policy changes that may improve the use and utility of the
MOST form. Similar barriers and challenges were identified after implementation of the POLST
form in California.
5
Universal acceptance of a MOST form upon transfer would be an important
solution to one perceived barrier. Also, efforts to simplify the form and processes may be
important solutions to improving utilization of the form. For example, if a copy of the form could
be honored, this would safeguard against losing the form. Another option would be the creation
of an electronic MOST form with accessibility between electronic health systems. In Oregon,
completed POLST (Physician Orders for Life Sustaining Treatment) health care providers who
complete a POLST form are required by law to enter the POLST form elements into a registry
which represents a valid order and is available 24 hours a day to emergency personnel and
hospitals unless a patient opts out.
6
This is quite different from the system in North Carolina,
where a MOST form can be sent to the Secretary of State by a patient, but the documents housed
in this registry do not represent valid orders as only the original documents can be used as valid
orders.
Perhaps the most important finding from this study is that advanced care planning is incorporated
at high rates at hospital discharge and admission to ongoing care facilities, at least those
represented by respondents to this study. Patients and providers at these facilities use a variety of
forms, incorporate advanced care planning into discharge and admission processes at high rates,
and report that high proportions of their clients have advanced care plans. Forms, processes and
regulations that facilitate discussion between family members, clients, and care providers will
help to maximize the chance that care preferences are honored at the end-of-life. The forms and
processes that encourage clients to consider a broader range of issues and options are likely to
lead to care that is more closely aligned with their wishes.

9
References
1. Hickman S, Tolle S, Brummel-Smith K, Carley M. Use of the physician orders for life-
sustaining treatment program in Oregon nursing facilities: Beyond resuscitation status. J Am
Geriatr Soc. 2004;52(9):1424-1429.
2. Hickman S, Nelson C, Perrin N, Moss A, Hammes B, Tolle S. A comparison of methods to
communicate treatment preferences in nursing facilities: Traditional practices versus the
physician orders for life-sustaining treatment program. J Am Geriatr Soc. 2010;58(7):1241-1248.
3. General Assembly of North Carolina. Session law 2007-502 house bill 634 an act to clarify the
right to make advance directives and to designate health care agents; and to improve and
simplify the means of making these directives and designations. 502(2007).
4. Caprio A, Rollins V, Roberts E. Health care professionals’ perceptions and use of the medical
orders for scope of treatment (MOST) form in North Carolina nursing homes. Journal of the
American Medical Directors Association. 2012;13(2):162-168.
5. Wenger N, Citko J, O'Malley K, et al. Implementation of physician orders for life sustaining
treatment in nursing homes in California: Evaluation of a novel statewide dissemination
mechanism. Journal of General Internal Medicine. 2013;28(1):51-57.
6. Fromme E, Zive D, Schmidt T, Olszewski E, Tolle S. POLST registry do-not-resuscitate
orders and other patient treatment preferences. JAMA. 2012;307(1):34-35.
