
Population
Pharmacokinetics
Guidance for Industry
U.S. Department of Health and Human Services
Food and Drug Administration
Center for Drug Evaluation and Research (CDER)
Center for Biologics Evaluation and Research (CBER)
February 2022
Clinical Pharmacology
Population
Pharmacokinetics
Guidance for Industry
Additional copies are available from:
Office of Communications,
Division of Drug Information
Center for Drug Evaluation and Research
Food and Drug Administration
10001 New Hampshire Ave., Hillandale Bldg., 4
th
Floor
Silver Spring, MD 20993-0002
Phone: 855-543-3784 or 301-796-3400; Fax: 301-431-6353
Email: druginfo@fda.hhs.gov
https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs
and/or
Office of Communication, Outreach and Development
Center for Biologics Evaluation and Research
Food and Drug Administration
10903 New Hampshire Ave., Bldg. 71, Room 3128
Silver Spring, MD 20993-0002
Phone: 800-835-4709 or 240-402-8010
Email: ocod@fda.hhs.gov
https://www.fda.gov/vaccines-blood-biologics/guidance-compliance-regulatory-information-biologics/biologics-guidances
U.S. Department of Health and Human Services
Food and Drug Administration
Center for Drug Evaluation and Research (CDER)
Center for Biologics Evaluation and Research (CBER)
February 2022
Clinical Pharmacology
Contains Nonbinding Recommendations
i
TABLE OF CONTENTS
I.
INTRODUCTION ...................................................................................................... 1
II. BACKGROUND ........................................................................................................ 2
III. APPLICATION OF POPULATION PK ANALYSIS ............................................... 2
A. Application of Population PK Analysis in Drug Development ........................................... 3
B. Application of Population PK Analysis to Inform Drug Use in Labeling ............................ 5
IV. DATA USED FOR POPULATION PK ANALYSIS ................................................. 7
A. Study Subjects and Covariates ....................................................................................... 7
B. PK Sampling Schedule .................................................................................................. 7
V. DATA ANALYSIS ..................................................................................................... 8
A. Preliminary Examination of the Data ............................................................................. 9
B. Model Development ...................................................................................................... 9
C. Model Validation .........................................................................................................10
D. Simulations Based on Population PK Models .................................................................12
VI. LABELING BASED ON THE RESULTS OF POPULATION PK ANALYSIS ..... 14
VII. POPULATION PK STUDY REPORTING ............................................................. 14
A. Format and Content of the Population PK Study Report ................................................14
B. Submitting Electronic Files to the Agency ......................................................................17
VIII. GLOSSARY OF SELECTED TERMS .................................................................... 19
IX. REFERENCES......................................................................................................... 20
Contains Nonbinding Recommendations
1
Population Pharmacokinetics
Guidance for Industry
1
This guidance represents the current thinking of the Food and Drug Administration (FDA or Agency) on
this topic. It does not establish any rights for any person and is not binding on FDA or the public. You
can use an alternative approach if it satisfies the requirements of the applicable statutes and regulations.
To discuss an alternative approach, contact the FDA office responsible for this guidance as listed on the
title page.
I. INTRODUCTION
This guidance is intended to assist sponsors and applicants
2
of new drug applications (NDAs),
biologics license applications (BLAs), abbreviated new drug applications (ANDAs), and
investigational new drugs (IND) applications in the application of population pharmacokinetic
(PK) analysis. Population PK analysis is frequently used to guide drug
3
development and inform
recommendations on therapeutic individualization (e.g., through tailored dosing) (Marshall et al.
2015; Lee et al. 2011; Bhattaram et al. 2005). Adequate population PK data collection and
analyses submitted in marketing applications have in some cases alleviated the need for
postmarketing requirements or postmarketing commitments.
This guidance includes common applications of population PK analysis to inform drug
development and drug use. This list of applications is not meant to be comprehensive, but rather
provides illustrative examples. This guidance also includes the FDA’s current thinking on the
data and model submissions to support regulatory decisions, recommendations on how to
incorporate information from population PK analyses in labeling, and the general expectations
regarding the format and content for population PK reports submitted to the Agency.
The contents of this document do not have the force and effect of law and are not meant to bind
the public in any way, unless specifically incorporated into a contract. This document is
intended only to provide clarity to the public regarding existing requirements under the law.
FDA guidance documents, including this guidance, should be viewed only as recommendations,
1
This guidance has been prepared by Office of Clinical Pharmacology in the Center for Drug Evaluation and
Research (CDER) and the Center for Biologics Evaluation and Research (CBER) at the Food a nd Drug
Administration.
2
Herea fter, the term sponsor will be used to refer to both sponsors and applicants.
3
For purposes of this guidance, references to drugs and drug and biological products includes drugs approved
under section 505 of the Federal Food, Drug, and Cosmetic Act (the FD&C Act) (21 U.S.C. 355) and biological
products licensed under 351 of the Public Health Service Act (PHSA) (42 U.S.C. 262) that are drugs.

Contains Nonbinding Recommendations
2
unless specific regulatory or statutory requirements are cited. The use of the word should in
Agency guidances means that something is suggested or recommended, but not required.
II. BACKGROUND
Population PK analysis is a well-established, quantitative method that can explain some of the
variability in drug concentrations among individuals (Sheiner, Rosenberg, and Marathe 1977;
Grasela Jr and Sheiner 1991). The focus of this guidance is on the use of this approach in
explaining the variability in drug concentrations observed among human trial subjects from
intrinsic factors, extrinsic factors, differences in dosing, and routes of administration. Drug
concentrations can vary significantly among individuals who are following the same dosing
regimen. This variability can be attributed to intrinsic factors, such as differences in body weight,
presence and extent of liver or renal impairment, or the presence of genetic polymorphisms, or to
extrinsic factors, such as effects of food on drug absorption or concomitant medications that can
interact with the administered drug’s absorption and/or metabolism. In some cases, intrinsic or
extrinsic factors lead to clinically relevant changes in drug concentrations that require clinical
management strategies, such as a change in the dose or dosing regimen.
Intrinsic and extrinsic factors that commonly influence drug exposure are often investigated in stand-
alone clinical pharmacology studies.
4
Stand-alone studies are well controlled and can provide a
robust assessment of these interactions. However, stand-alone studies are usually designed to
focus on intrinsic and extrinsic factors with the highest potential to affect drug exposure, leaving
many possible interactions unstudied. Such stand-alone studies also typically have a limited
number of subjects, are designed as single-dose studies, and might not be conducted in the target
patient population. Population PK analysis typically includes data directly collected from both
patients and healthy volunteers, allowing for an assessment of multiple intrinsic and extrinsic
factors that are not otherwise evaluated in a single trial or population. In addition, the relatively
large numbers of patients included in population PK analysis can improve the precision of the
estimated effect of the factors that affect drug exposures and confirm which factors do not
change drug exposures.
Population PK analysis has the potential to integrate all relevant PK information across a range
of doses and populations to identify factors that can affect a drug’s exposure. Such information
can come from studies with rich or sparse PK sampling, after a single dose or multiple doses,
and/or at steady state, and from healthy individuals, subjects with organ impairment, or the
patient population. These analyses, in turn, can inform strategies to select initial dosage
regimens, manage dosing and administration for a given subpopulation, plan subsequent studies,
or support labeling.
III. APPLICATION OF POPULATION PK ANALYSIS
4
See section IX for references for specific FDA guidances for industry that address stand-alone clinica l
pha rmacology studies.
Contains Nonbinding Recommendations
3
Sponsors seeking advice on the use of population PK analysis for drug development decisions
are encouraged to do so at appropriate milestone meetings with the Agency. While this guidance
focuses on typical applications of population PK analysis, it is recognized there are many novel
applications of population PK analyses beyond those described in this guidance. For example,
application of population PK, model-based approaches can be an alternative for evaluating the
bioequivalence of long-acting injectables, products with sparse PK sampling, or other scenarios
when non-compartmental analysis (NCA) becomes challenging (Zhao et al. 2019). For such
applications, the model’s intended use and its regulatory impact determine the level of robustness
needed for model evaluation. As an example, the model-integrated approach used should be
expected to reliably control the error rate for confirmatory bioequivalence applications.
Sponsors are encouraged to contact the Agency to discuss such novel applications of population
PK analyses to inform drug development and use.
Confidence in a given population PK analysis to support an intended objective is increased by
the following:
• Understanding of the drug’s PK properties
• Prespecified questions in the population PK data analysis plan that will be addressed by a
population PK analysis
• PK data of sufficient quantity and quality (Bonate et al. 2012) from subjects who
represent the indicated population and subpopulations of interest
• Good model performance (i.e., the model should describe the data with acceptable
accuracy and precision and should be evaluated for model misspecification) and validity
for the intended objective
A. Application of Population PK Analysis in Drug Development
1. Selecting Dosing Regimens To Be Tested in Clinical Trials
Population PK analyses are capable of identifying intrinsic and extrinsic factors that can
significantly impact the pharmacokinetics of the drug and inform dosing regimens for testing in
clinical trials to help minimize the variability of treatment response in patients. For example, an
observed strong relationship between body weight and drug exposure can provide support for
body weight-based dosing schemes (e.g., mg/kg dosing or categorical dosing based on body
weight cut points). Such analyses should be combined with a robust understanding of the
relationship between drug exposure and drug effect (e.g., by using pharmacodynamic biomarkers
or clinical endpoints), target engagement (e.g., receptor occupancy), or drug toxicity to inform
the clinical relevance and further refine dosing.
Population PK models can also be used to simulate drug exposures that are expected to occur
following doses or dosing regimens that have not been directly investigated in prior clinical
studies (see section V.D for a discussion on simulation strategies). For example, a population
PK analysis can be used to predict PK changes resulting from the inclusion of a loading dose,

Contains Nonbinding Recommendations
4
changing the dose, or altering the dosing frequency of a dosing regimen for later trials in the drug
development program. When appropriately justified, such analyses, in conjunction with
exposure-response data, have been used to approve dosing regimens that have not been directly
evaluated in the clinical trials (Kimko and Peck 2010). In such cases, sponsors are encouraged
to seek Agency input in advance of performing the analyses.
2. Deriving Sample Size and Sampling Scheme Requirements
Simulations and optimal design methods can maximize the utility of population PK data
collection and analyses. For example, the trial sample size and PK sampling schedule can be
optimized so that the PK parameters and the estimates for major covariate (bolded terms are
defined in section VIII upon first use) effects of interest can be estimated with a defined degree
of precision (see section IV.B for a discussion on various sampling schedules). Simulations with
population PK models can help determine the number of patients in a subpopulation that
achieves sufficient power to detect a significant covariate given a defined covariate effect size
(e.g., the number of patients receiving a concomitant medication that should be included in an
analysis to detect a significant drug-drug interaction (DDI); see section III.B.2).
3. Deriving Exposure Metrics for Conducting Exposure-Response Analysis
The importance and application of exposure-response (E-R) relationships for new drugs are
outlined in the FDA guidance entitled Exposure-Response Relationships — Study Design, Data
Analysis, and Regulatory Applications (May 2003).
5
Population PK analysis can be used to
derive patient PK exposure metrics that are appropriate for sequential E-R analyses. When
relevant, the derivation of exposure metrics should account for: (1) dose interruptions or
modifications; and (2) variations in the pharmacokinetics of a drug over time due to intrinsic or
extrinsic subject factors (e.g., time-varying exposure due to disease state or anti-drug antibodies
for some monoclonal antibodies).
Population PK models can predict individual patient exposures at specific time points regardless
of the spread in sampling times (e.g., trough concentrations can be predicted for all subjects).
When PK data are missing in a small number of subjects, population PK models can predict the
most likely concentration-time profile based on individual covariates including both time-
varying and subject-level covariates (e.g., body weight, genetic polymorphism, sex) (Wählby U
2004). Such predictions are useful, assuming that the residual error and the between-subject
variability are low, and the effect of observed covariates on the PK characteristics of the drug is
considerably larger (see section V.D).
Individual patient exposure metrics are generated based on Empirical Bayes Estimates (EBEs).
When parameter shrinkage is high (i.e., the standard deviation-based shrinkage is usually
greater than 20 to 30 percent), EBEs might be considered less reliable (Savic and Karlsson
2009). The informativeness of individual data (e.g., in cases with sparse data) should be
assessed using individual shrinkage estimates. In addition to parameter shrinkage, the reliability
5
We update guidances periodically. For the most recent version of a guidance, check the FDA guidance web page
at https://www.fda.gov/regulatory-information/search-fda-guidance-documents.

Contains Nonbinding Recommendations
5
of individual PK patient exposure metrics is dependent on the nature of the collected PK data and
the validity of model assumptions. See section V.C for discussions on model validation and
section IV for discussions regarding the adequacy of the data used for population PK analysis.
4. Pediatric Trial Designs
The use of modeling and simulation can help evaluate potential trial designs and optimize dose
selection for pediatric patients.
6
Additional sample size considerations for pediatric studies have
been presented in the literature (Wang et al. 2012). Population PK analysis is especially
appropriate in children because it allows the use of infrequent (i.e., sparse) sampling compared to
the rich sampling associated with traditional PK analyses, thus minimizing the total volume of
blood sampled.
Selecting a dosing regimen for pediatric studies can be based on simulations using a population
PK model developed with adult PK data and incorporating the following when scientifically
justified: (1) principles of allometry; (2) knowledge of developmental changes that can influence
the pharmacokinetics of a drug (ontogeny); and (3) data on the bioavailability of the pediatric
formulation (Holford, Heo, and Anderson 2013; Barbour, Fossler, and Barrett 2014; Zhang et al.
2015; Mahmood I 2014). Incorporating the latest understanding in the population PK model on
the effect of maturation of physiology in pediatric patients across various ages, especially in
those less than 2 years old, can further improve the ability to identify appropriate pediatric
dosing. Dose selection should also consider information on disease similarity and dose- and
exposure-response relationships in adults and pediatrics.
B. Application of Population PK Analysis to Describe Drug Use in Labeling
Population PK analysis using data from early- and late-stage clinical trials, together with results
from stand-alone clinical pharmacology studies, can be used to support the absorption,
distribution, and elimination (metabolism and excretion) (ADME) information in the labeling of
the drug.
In addition, population PK analysis, together with relevant information from stand-alone studies,
nested studies, or other sources, is routinely used to evaluate the effects of covariates on the PK
parameters of a drug and its relevant metabolites to support dosing recommendations. The need
for dose adjustments due to the effect of a covariate on the exposure of the drug should be
evaluated in the context of all available data, including the known E-R relationships for efficacy
and safety. The E-R relationships should be used to establish concentration boundaries within
which dose adjustments are not clinically relevant (i.e., covariate effects within these boundaries
might not warrant a dose alteration; however, covariate effects outside these boundaries could
require a dose modification to optimize the benefit-risk profile of the drug).
6
For more information, see the FDA guida nce entitled General Clinical Pharmacology Considerations for
Pediatric Studies for Drugs and Biological Products (December 2014). When final, this guida nce will represent the
FDA’s current thinking on this topic.
Contains Nonbinding Recommendations
6
1. Specific Populations
Results from population PK analyses can be incorporated into drug product labeling to describe
the PK properties in general patient populations or specific populations, as appropriate. Whether
a covariate analysis supports labeling statements depends on multiple factors, such as the number
of subjects with the covariate included in the analysis, the distribution of the covariate (for
continuous covariates), and the amount of available PK data (see section IV.A).
Some examples of these situations are listed below:
• Stand-alone renal or hepatic impairment studies in the general population might not be
ethical with some drugs (e.g., highly toxic agents). In such cases, adequate representation
of patients in clinical trials with the intrinsic factor of interest, as well as adequate PK
sampling to reliably characterize the effects of the intrinsic factor, can allow for the use
of population PK analysis to characterize the exposure of the drug and its relationship to
response and thus support dosing recommendations in that population.
• Some defined specific populations are traditionally not studied in stand-alone, clinical
pharmacology studies because of the lack of an expected clinically meaningful effect on
the drug’s pharmacokinetics due to prior knowledge of the drug’s ADME characteristics.
Instead, factors such as the influence of sex, age, body weight, or race on the
pharmacokinetics of the investigational drug are often studied without stand-alone trials.
Population PK analysis can be used to describe the pharmacokinetics of a drug in these
subgroups.
• Simulations from population PK models established from pediatric and adult data can be
used to compare the exposure of the drug in pediatric patients and adults, and then derive
the recommended pediatric doses.
2. DDIs
Clinical DDIs (e.g., nested studies as part of a phase 3 trial) can be evaluated using population
PK analysis. General design considerations for nested DDI studies are found in the FDA
guidance entitled Clinical Drug Interaction Studies - Cytochrome P450 Enzyme- and
Transporter-Mediated Drug Interactions (January 2020). Using population PK approaches to
characterize the DDI potential of a drug is not without limitations, and methodological
considerations for using population PK analysis to evaluate DDIs have been described elsewhere
(Bonate et al. 2016; Wang et al. 2017). Specific considerations for the use of a population PK
approach to evaluate DDIs include the following:
• DDIs should be characterized for individual drugs and not for therapeutic classes of
drugs, although exceptions are possible (e.g., multiple proton pump inhibitors can be
pooled if the interaction mechanism is pH-dependent).
• Multiple perpetrators can be pooled to form one covariate category provided that the
perpetrators belong to the same class of index inhibitors/inducers (i.e., weak, moderate,
Contains Nonbinding Recommendations
7
or strong) as identified by the Agency. The pooled perpetrators should all have the same
mechanism of interaction with similar specificity for their respective metabolizing
enzymes. In cases where a clear classification is not recognized by the Agency (i.e.,
transporter inhibitors), pooling should be prespecified whenever possible and is
considered on a case-by-case basis.
• An adequate number of subjects with the concomitant medication should be included in
the trial. The PK sampling schedule should allow for appropriate characterization of the
PK parameters of interest. Adequate information on the dose, timing of administration,
and duration of treatment for the interacting drugs should be available. Simulations can
determine the number of subjects needed to detect an interaction of a defined magnitude
within a given trial design.
• Interactions should be investigated on all physiologically plausible structural elements of
the PK model (e.g., apparent clearance (CL/F), relative bioavailability (F
rel
), rate of
absorption) based on the mechanism of the interaction.
IV. DATA USED FOR POPULATION PK ANALYSIS
Sponsors are encouraged to use all relevant data to support the population PK model. The
sponsor should justify the omission of data from certain studies, certain individuals, or certain
time points and prespecify such omissions in the population PK data analysis plan or study
protocol whenever possible. The sponsor should demonstrate that the data are adequate for the
purpose of the analysis in their report. For example, sponsors can conduct model-based power
analyses showing that the given study design has sufficient power to detect clinically meaningful
covariate relationships under the proposed population PK model (see section III.B).
A. Study Subjects and Covariates
Determining if the data are adequate to address the intended study question is a vital step in any
population PK analysis (see section V.C). The dataset should include a sufficient number of
subjects with an adequate number of PK samples at informative time points. Covariates cannot
be claimed to be influential or not influential on the exposure of a drug if the covariate
distribution is narrow (for continuous covariates) or if the number of subjects in the category is
inadequate (for categorical covariates). Many continuous covariates have established cutoff
values that define category levels. If dosing recommendations are proposed for these categories,
the range of the continuous covariates should preferably span the entire category and not just the
upper or lower ends. An increase in the range and frequency of the covariates tends to increase
the likelihood of finding a true clinically significant covariate relationship and decreases the
likelihood of finding false-positive relationships (Wählby et al. 2002; Wählby, Jonsson, and
Karlsson 2001).
B. PK Sampling Schedule
Contains Nonbinding Recommendations
8
The precision and bias of model-derived PK parameters are dependent on multiple factors,
including the complexity of the model, the number of subjects, the number of samples per
subject, and the sampling schedule. As the number of samples per subject decreases, the
importance of the timing of PK samples increases. For example, if the purpose of an analysis is
to match the maximum concentration (C
max
) observations across populations or dosage forms,
then a sufficient number of PK samples should be collected in the absorption phase. Sponsors
are encouraged to prospectively plan the PK sampling schedule so that the population PK model
is maximally informative.
The methodology and available software for the optimal design of the population PK model are
covered in multiple reviews in the literature (Dodds, Hooker, and Vicini 2005; Nyberg et al.
2015; Ogungbenro and Aarons 2007; Ogungbenro and Aarons 2008). The list below shows
some examples of sampling schedules. Depending on the purpose of the analysis, one or a
combination of the listed strategies can be employed:
• Patients are randomly assigned sampling windows that are derived based on optimal
design methods. The number of samples per patient and the number of sampling
windows are also determined based on optimal design methods.
• Patients randomly contribute two or more samples that, when combined, cover the entire
dosing interval.
• Most patients contribute one sample at a specified time point, often immediately before
the next dose when there is sufficient prior PK knowledge about the study drug.
Sponsors are encouraged to use all relevant PK data for the intended use. However, the extent of
sampling per individual patient and the percentage of sampled patients should ultimately depend
on the intended use of the data. For example, if the C
max
will be used in subsequent E-R
analyses, then there should be adequate sampling around the time to the maximum concentration
(T
max
) (see section III.A.3). In any situation, it is important to verify that patients with missing
PK data do not differ from other patients. For example, patients with missing PK data should not
have higher dropout rates because of a lack of effect or adverse events. If between-occasion
variability will be estimated, the design should be sufficient to assess the presence and
magnitude of effect, requiring at least multiple samples per individual at more than one occasion.
Ignoring large between-occasion variability can lead to biased population parameter estimates
(Karlsson and Sheiner 1993). Similarly, multiple samples per individual should be collected if
time-varying covariates, such as the influence of anti-drug antibodies on drug exposure, are
expected.
V. DATA ANALYSIS
This section of the document provides some guiding principles on the methodological aspects of
population PK analysis. Further methodological considerations and good practices, including
topics not covered here, have been described by others (Ette and Williams 2007; Bonate PL
Contains Nonbinding Recommendations
9
2011; Mould and Upton 2013; Byon et al. 2013; Tatarinova et al. 2013; Lunn et al. 2002;
Schmidt and Radivojevic 2014).
A. Preliminary Examination of the Data
Population PK analysis often begins with a visual examination of the observed data. Preliminary
examination of the data reveals patterns and features in the population dataset using graphical
and statistical techniques and can provide powerful diagnostic tools for confirming assumptions
or, when the assumptions are not met, for suggesting corrective actions (Tukey 1977; Ette and
Ludden 1995). For example, strong correlations between covariates can preclude the ability to
make inferences about individual covariate effects and have implications for the choice of
covariate modeling approach. The scientific (i.e., pharmacologic, biologic, pathophysiologic, or
clinical) merits of including highly correlated covariates should be assessed. This scenario is
often the case with, for example, body weight and creatinine clearance as calculated by the
Cockcroft-Gault Equation. Relevant preliminary examination of the data should be concisely
described in the population PK analysis report.
B. Model Development
Model development methods and best practice recommendations are constantly evolving.
Specific advice on how to develop population PK models is beyond the scope of this guidance.
However, to facilitate the regulatory review of population PK models, sponsors should explicitly
describe their model development procedures (see section VII for more discussion on population
PK reporting). Some aspects of model development that are important for regulatory review are
provided below:
• Model development issues can be addressed through several valid approaches, each with
its own benefits and drawbacks. For example, covariate analysis can be performed based
on several approaches or their possible combinations (e.g., stepwise covariate analysis,
full covariate model approach, the Lasso) (Wählby, Jonsson, and Karlsson 2002;
Gastonguay 2004; Ribbing et al. 2007). In such cases, sponsors should justify why a
particular approach was used.
• The choice of the structural model should be informed from exploration of the observed
data, previous modeling results (when applicable), and a common scientific rationale.
Otherwise, an inappropriate structural model (e.g., missing the covariance between
clearance and volume of distribution in the structural model) could result in incorrect
covariate identification.
• Covariate-parameter relationships can be formulated based on the current knowledge of
biology, physiology, or allometric principles,
and should take into account any data-
driven information on the covariate-parameter relationship (e.g., time-dependent
covariates). Correct identification of the true covariate-parameter relationship is essential
when applying a population PK model to describe drug exposure in patients based on
covariates included in the population PK analysis or when applying the population PK
model to untested scenarios.
Contains Nonbinding Recommendations
10
• Issues regarding missing data, including missing covariates and data below the limit of
quantification (LOQ), should be addressed with appropriate analysis methods (Beal 2001;
Bergstrand and Karlsson 2009; Johansson and Karlsson 2013; Keizer et al. 2015). The
sponsor should justify their methodological approach with regard to missing data using
approaches such as sensitivity analysis.
• The sponsor should distinguish between outlying individuals and outlier data points.
Individual data points that are suspected outliers could be omitted during the model
development process. However, the sponsor should investigate the influence of the
outliers on the final parameter estimates by refitting the final model to the complete
dataset. Removal of suspected outlying individuals is generally discouraged unless the
reason for the outlier is a protocol violation or other human error. Sponsors should
specify how outliers are identified and handled in the analysis. The reasons for declaring
a data point to be an outlier should be prespecified in the data analysis plan. For
example, data points with a normalized weighted residual greater than five could be
considered outliers in some cases. The number of excluded outliers should be kept to a
minimum and clearly documented in reports and datasets.
C. Model Validation
Model validation is a critical step for any population PK analysis and should be conducted to
examine whether the developed model can sufficiently characterize the observed data and
generate reliable modeling and simulation results to meet the needs of the analysis. No single
model validation method is generally sufficient to evaluate all components of a model. Several
methods are generally used so that the relative strengths and weaknesses of each method can
complement each other. In general, models should describe the data with an acceptable level of
bias and an acceptable degree of precision.
Model validation depends on the objective of the analysis and should follow a fit-for-purpose
approach. In some cases, a model can be valid for one purpose but not for another. When
parameter shrinkage is high (standard deviation-based shrinkage: usually greater than 20-30
percent), EBEs might be less reliable (Savic and Karlsson 2009). The informativeness of
individual data should be assessed using individual shrinkage estimates, and the reliability of
individual drug exposure levels to be used in a sequential E-R analysis (see section III.A.3)
needs to be carefully evaluated. However, such a model can still be useful for a covariate
analysis provided that the method for covariate modeling is insensitive to shrinkage (Mould and
Upton 2013).
Submissions to the Agency should contain a detailed description of the model validation
methods used, an explanation of why those methods were selected, model diagnostics supporting
use of the model, and sensitivity analyses, as needed, to demonstrate the impact of assumptions
on the conclusions (see section VII.A). Sponsors are encouraged to discuss model validation
approaches with the Agency, particularly if the population PK analyses are critical for
understanding and supporting proposed dosing.

Contains Nonbinding Recommendations
11
1. Common Approaches for Model Validation
Procedures for conducting a thorough model validation are continuously evolving, and the
Agency welcomes innovations in this field. Several common methods of model validation are
reported in the literature (Karlsson and Savic 2007; Byon et al. 2013, Nguyen et al. 2017) and are
discussed in the sections below.
Basic goodness-of-fit (GOF) plots illustrate how well the model describes the observed data.
GOF plots are also used to evaluate model assumptions (e.g., normality of the random effects)
and to guide model development. Although GOF plots can show that the overall fitting is
acceptable, additional evaluation of the model in subgroups of patients is often necessary
depending on the context of use. For example, if the model will be used to predict drug
exposures in pediatric patients, model validation should be conducted for all relevant age groups.
GOF plots that are stratified for important patient characteristics (e.g., stratified by age group or
cytochrome (CYP) polymorphisms), trial design (e.g., dose or formulation), sampling design
(e.g., sparse versus full), or other important variables are often more convincing of the adequate
performance of a model than GOF plots of the full dataset. Because few patients could be
included in some analysis subgroups, the sponsor should include justifications, as needed,
regarding the sufficiency of the available data to support its intended use.
The following is a list of some of the GOF plots that are considered informative:
• The dependent variable (DV) versus the individual predictions (IPRED)
• The DV versus population predictions (xPRED), where ‘x’ could be nothing, C
(conditional), or P (simulation-based)
• The absolute individual weighted residuals (|IWRES|) versus IPRED or time
7
• The appropriate form of weighted residuals (xWRES) versus xPRED or time, where ‘x’
is defined as above
• A representative sample of IPRED, xPRED, and observations versus time (one plot per
subject)
7
• A histogram or Quantile-Quantile (Q-Q) plot of random effects
• The correlations between random effects
• The random effects versus covariates
8
7
Time should be evaluated as continuous time and as time after dose.
8
This plot is most informative when it is compared before and after the inclusion of covariates.
Contains Nonbinding Recommendations
12
The individual parameters, IPRED and IWRES, tend to shrink towards the population estimate in
individuals with few observations. When shrinkage is high (the standard deviation-based
shrinkage is usually greater than 20-30 percent), diagnostic plots that rely on EBEs, IPRED, or
IWRES can become uninformative, and correlations between random effects and covariates can
be obscured (Savic and Karlsson 2009, Xu et al. 2012, Lavielle and Riba 2016). Furthermore,
high shrinkage can limit the value of using individual post hoc estimates for E-R analysis (see
section III.A.3). However, simulation-based, diagnostic plots are not affected by shrinkage in a
similar manner and can be more informative for diagnostic purposes when shrinkage is high.
Model selection based on parameter shrinkage is not necessary. There are several available
simulation-based diagnostics, including but not limited to, Visual Predictive Check (VPC), the
prediction corrected VPC (pcVPC), the Numerical Predictive Check (NPC), and Normalized
Prediction Distribution Errors (NPDE) (Bergstrand et al. 2011, Brendel et al. 2006).
GOF criteria can also be reflected by some numerical metrics, such as the estimate of the
precision of a parameter. Estimates of parameter precision can provide valuable information
regarding the adequacy of the data to support that parameter. Parameter uncertainty can be
estimated through several methods, such as bootstrap procedures, sampling importance
resampling, log-likelihood profiling, or using the asymptotic standard errors of parameter
estimates. In addition to parameter uncertainty, it is important to compare parameter point
estimates with previous analyses and to evaluate the physiological plausibility of the point
estimates. Another useful numerical metric to evaluate models is the condition value. A large
condition number (the ratio of the largest and the smallest eigenvalue), typically interpreted as
values greater than 1000) indicates that the observed data cannot support the estimation of one or
several parameters (Montgomery, Vining, and Peck 2012). Over-parameterized models can be
simplified and updated as additional data from well-designed clinical trials become available.
An appropriate model should be biologically plausible, consistent with current knowledge, and
have mathematically identifiable parameters. Performance of the model can be checked against
a set of test data, either internal or external. A validation approach relying on the data used for
model building is considered as internal validation. External validation, on the other hand, relies
on the data not used for model building. Data collected in a drug development program can be
split into a model building dataset and a testing dataset. The testing dataset is commonly used
for external validation. Data splitting is a powerful method for model checking. However,
before deciding on a data splitting approach, sponsors should consider the potential impact of the
loss of data on the model’s power to detect covariate relationships and estimate parameters with
an acceptable degree of precision.
There is an additional level of uncertainty when the purpose of the model is to simulate PK
profiles for scenarios that are beyond those that have been clinically studied. Such uncertainty
can be addressed by a sensitivity analysis of the parameter estimates and their impact on the
metric used to inform a decision (Kimko and Peck 2010).
D. Simulations Based on Population PK Models
Simulations should be based on protocols that outline the simulation study to be performed. The
level of detail in the protocol should correspond to the complexity and impact of the question the
Contains Nonbinding Recommendations
13
simulation addresses. Models used for simulations should be validated to address the specific
question the simulation study is trying to answer. Although a model could have been previously
used and validated, it needs to be revalidated if the new purpose is different from the original
purpose. Depending on the purpose of the model, various levels of uncertainty and variability
can be added to the simulations. Some examples are discussed below.
1. Simulations Based on Fixed-Effect Estimates
In their simplest form, simulations are used to illustrate the drug-concentration profile for a
typical individual. Such simulations are based on the typical estimates of the fixed-effect
parameters. Note that predictions based on typical parameter estimates do not correspond to
mean predictions. Mean predictions are obtained by calculating the mean concentration-time
profiles based on simulations with between-subject variability in population PK parameters and
residual error.
2. Simulations Based on Uncertainty of Fixed-Effect Estimates
Uncertainty in parameter estimates can be accounted for if the desire is to illustrate the
probability of the typical subject’s drug exposure to reach or stay above a specific cutoff point or
if one wishes to illustrate the effect of covariates. The choice, if uncertainty of fixed effects is
considered, should be objective driven. For example, forest plots that illustrate the effect of
covariates on the area under the concentration time curve (AUC) or other parameters can be
generated based on simulations with uncertainty in fixed-effect parameters, thereby facilitating
the interpretation of the relative importance of covariates on exposure. Alternatively, if the
effect on exposure estimates is the objective, the uncertainty of all fixed effects should be
considered.
These types of simulations are also useful to evaluate the performance of new
dosing regimens for testing in future trials. Additionally, simulations with parameter uncertainty
can be used to graphically illustrate the effect of parameter precision on PK profiles.
3. Simulations Based on Estimates of Between-Subject Variability
Between-subject variability in PK parameters is accounted for in simulations when the purpose is
to show the range of individual predictions of concentrations in the studied population. Residual
error is added to the individual prediction when the range of observed concentrations is the main
interest.
If the purpose is to predict the observed concentration range of a future population, then
uncertainty in the between-subject variability should be accounted for in addition to the fixed-
effect parameters and residual error.
The correlation between random effects should be accounted for to avoid unrealistic parameter
combinations in subjects. Simulations that account for between-subject variability and include
covariate effects should be conducted in a population with realistic demographic variables.
Demographic variables can be obtained from databases or generated by resampling with
replacement of the individuals in the original study or by sampling the covariate distributions and
their correlations in the target population.
Contains Nonbinding Recommendations
14
VI. LABELING BASED ON THE RESULTS OF POPULATION PK ANALYSIS
Results from population PK analysis can be presented in the CLINICAL PHARMACOLGY
section and summarized in other sections of labeling, as appropriate. Other relevant labeling
sections should not repeat this detailed information but rather provide a succinct description or
recommendation based upon these results followed by a cross-reference to the CLINICAL
PHARMACOLGY section, as appropriate. In general, there is no need to explicitly state in
labeling that the information is based on population PK analysis. Recommendations for
developing the CLINICAL PHARMACOLOGY section are discussed in the FDA guidance for
industry entitled Clinical Pharmacology Labeling for Human Prescription Drug and Biological
Products — Content and Format (December 2016).
VII. POPULATION PK STUDY REPORTING
This section outlines the recommended format and content for a sponsor to submit a population
PK analysis in support of its drug’s clinical pharmacology program. Population PK analyses can
be appropriate at multiple points in the drug development process, for example in the IND, NDA,
BLA, ANDA, or postmarketing stages. The depth and breadth of population PK analyses at each
stage can vary because of the availability or quality of clinical data.
Population PK study reports that are important for regulatory decisions should be included in the
electronic common technical document (eCTD) module 5.3.3.5 and the corresponding programs,
datasets, and define files under the datasets folder within eCTD module 5.
A. Format and Content of the Population PK Study Report
To enable the efficient and consistent review of population PK analyses, the FDA recommends
that the results from population PK analyses should be accompanied with a structured population
PK report. The report should contain the following sections: (1) executive summary, (2)
introduction, (3) materials and methods, (4) results, (5) discussion, (6) conclusions, and (7)
appendix (if applicable). Expected information and elements to be included in these sections are
discussed briefly in Table 1. Sections of the annotated labeling that contain information based
on population PK analysis should include hyperlinks to the population PK report. Additional
discussion regarding reporting is available in the scientific literature (Dykstra et al. 2015).
Contains Nonbinding Recommendations
15
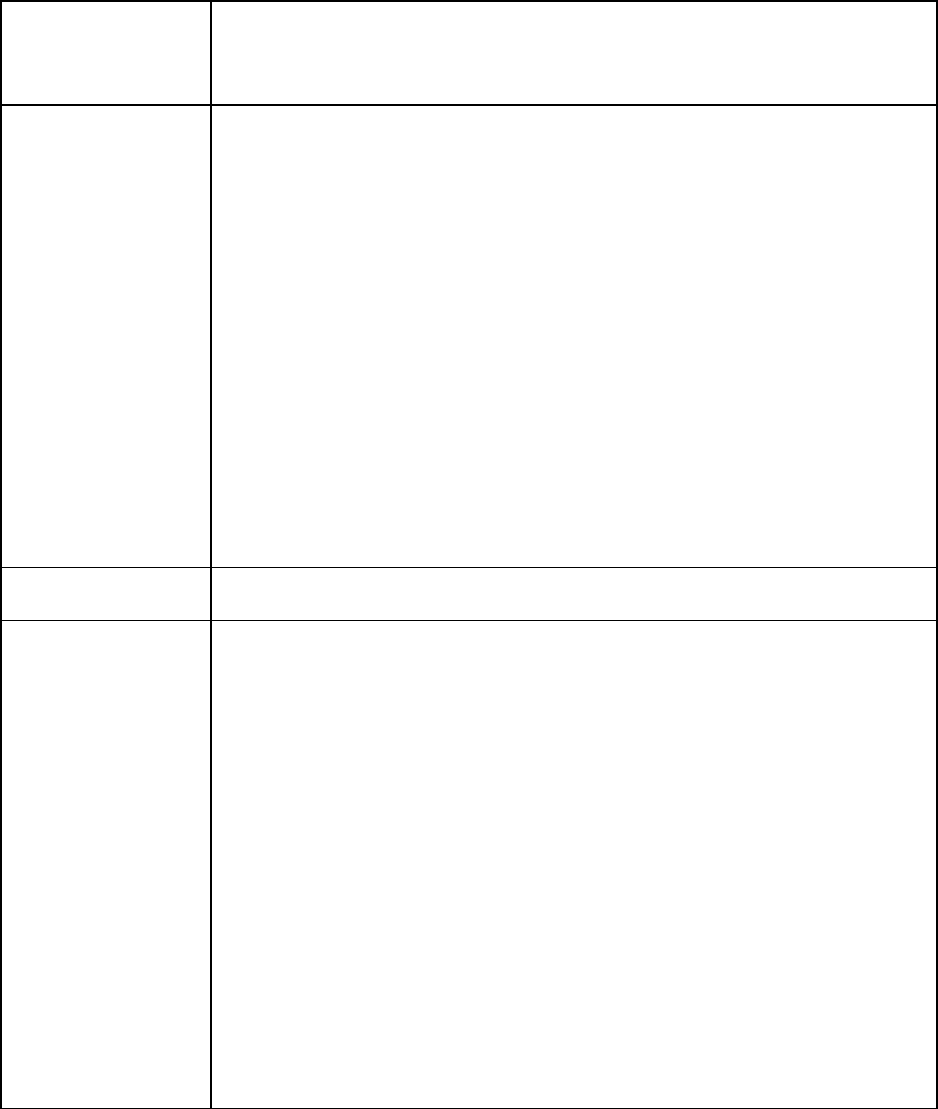
Table 1: Expected Content in Each Section of the Population PK Study Report
Sections
Expected Content
Executive
Summary
• The purpose of the analysis
• The key findings that affect drug use or labeling
• A plain language summary of objectives, data, methodology, and conclusions
• Results presented as their effect on clinically relevant drug exposures, not
model parameters
• Visual presentations of relevant exposure metrics to illustrate how identified
subpopulations differ from the typical population
Introduction
• The background to place the population PK study in the context of the overall
clinical development program
• The objectives for the population PK analysis
• The PK characteristics of the drug
Materials
and Methods
• A description of the trials and the trial data included in the population PK
analysis with information on:
o Dose, including the frequency and duration of dosing, as well as the
number of subjects, number of samples, and number of below the level
of quantification (BLOQ) samples
o Reasons for not including trials with available and potentially
informative data, if applicable
o A distinction between all available relevant data versus final data used
for model building and evaluation
• Hyperlinks to the original trial reports of data used for the analysis and the
bioanalytical evaluation reports for each trial
• Detailed demographic information and other covariate information
• Planned criteria, table of assumptions, and procedures for model building and
evaluation, including:
o Handling of outliers and missing data (e.g., methods of imputation)
o Model-estimation method
o Equations for all model structures and covariate relationships
o Equations for parameter transformations, if parameters are presented in
dimensions other than those in the model output file
Continued
Contains Nonbinding Recommendations
16
Table 1 continued: Expected Content in Each Section of the Population PK Study Report
Sections
Expected Content
Materials
and Methods
o Equations for parameter transformations, if parameters are presented in
dimensions other than those in the model output file
o The method for incorporating variability or parameter uncertainty or
for deriving confidence intervals or prediction intervals
• Detailed descriptions of planned simulations and sensitivity analyses used to
support conclusions and recommendations
• Software and version used for the analysis and simulation*
* Note: The FDA does not recommend or require the use of particular
software for conducting population PK analysis. The sponsor should report
the software used and submit the electronic files supporting the analysis and
simulations (see section VII.B below). If necessary, consult the FDA
regarding the submission of certain file types.
Results
• Summary of the data and data exploration, with adequate graphical and tabular
displays
• A description of the final model, model building steps, validation, final
parameter estimates, and deviations from planned analyses, if applicable
• Application of the model to the objectives, including the relevance of
covariates on PK parameters and simulations of alternative dosing, if
applicable
• Accompanying tables and figures to place findings into context
• Typically, tables and figures should include the following, with other tables
and figures included in the Appendix and cross-referenced in the report body,
as applicable:
o Key modeling building steps, including a description of the structural
and covariate models and objective function changes
o A comparison of parameter estimates from the base to the final model
o Parameter estimates and their associated uncertainty, with variability
reported as the coefficient of variation (CV%) and precision reported
as the percent relative standard error (RSE%) or the 95 percent
confidence interval. Shrinkage should be included in the parameter
estimates table.
o Key diagnostic plots
o GOF plots stratified by the relevant covariates to illustrate model
performance in specific subgroups
Continued
Contains Nonbinding Recommendations
17
Table 1 continued: Expected Content in Each Section of the Population PK Study Report
Results
o Results of model evaluations/validation, such as VPCs,
pcVPCs, NPCs, and NPDEs, etc., should also be included
• A description of simulation results or scenarios, if applicable
Discussion
• An interpretation of the modeling results, including discussions on:
o The adequacy or limitation of the data and model to support
conclusions and recommendations
o The rationale for the modeling approach, assumption
verification, and assessment of uncertainty
o Consistency or inconsistency between the results from
population PK and stand-alone clinical pharmacology studies
and/or previously completed related population analyses
• An assessment of the clinical relevance of the results, including
physiological plausibility and clinical significance of the identified
relationships
• An assessment of any alternative dosing regimens in the context of E-R
analyses for safety and efficacy
Conclusions
• A short summary of major findings from the analysis written in plain
language
Appendix
Additional materials should be included in the Appendix, as needed. The
Appendix does not need to contain full line listings from datasets. Materials
from the Appendix should be cross-referenced in the report body, as
appropriate. Appropriate materials for the Appendix include but are not limited
to:
• Supplemental tables and figures for summaries and analyses included
in the report that support model development or conclusions but are not
critical to the primary purpose of the report
• Methods and codes for generating the key figures and tables
(preferably, codes are submitted as separate files from the study report)
• Listing of samples removed from the analysis and reasons for removal
• A run record describing the steps during model development
• A diagram showing the connection between input datasets,
codes/control streams, and output datasets presented in the E-R report
B. Submitting Electronic Files to the Agency

Contains Nonbinding Recommendations
18
Sponsors should refer to the FDA web page
9
for general advice on submitting data and related
files (e.g., coding scripts). It is critical that datasets and model files submitted for the base, final,
and key intermediate models are the same as those used for generating the model outputs in the
appendices of the report. In addition, FDA staff should be able to identify the source data for
any dataset constructed using output files or postprocessed results from population PK analyses.
For example, if exposure metrics from population PK analyses are included in datasets for E-R
analyses, the sponsor should ensure the traceability between the population PK model output and
any postprocessing steps involved in the construction of the dataset. This can be accomplished
by providing definition files, reviewer guides, and/or codes utilized for dataset assembly.
All conclusions drawn from the population PK analysis should be reproducible by the Agency
with the available codes and data. It is also important to include the unique subject identifier
information for each subject in the population PK dataset and ensure that the identifiers are the
same in the individual clinical trial datasets. This information is vital if data integration is
required between the individual-level outputs (e.g., individual, post hoc estimates for clearance
or volume of distribution generated from the population PK model) and the efficacy or safety
datasets from the individual clinical study reports.
9
The FDA web page on submitting data can be accessed at https://www.fda.gov/about-fda/center-drug-evaluation-
and-research-cder/modeldata-format.
Contains Nonbinding Recommendations
19
VIII. GLOSSARY OF SELECTED TERMS
Covariate
An observed factor that correlates with drug exposure in patients (e.g.,
renal function, body weight, age, sex, genetic polymorphism)
DV
Dependent variable (e.g., drug plasma concentrations)
EBE
Empirical Bayes Estimates, or individual parameter estimates in a
mixed-effects model
GOF
Goodness of fit, a collection of diagnostic criteria used to evaluate
model performance
IPRED
Individual Predicted Data, based on Individual Empirical Bayes
parameter estimates
IWRES
Individual Weighted Residuals, a type of residual
Model validation
The use of various methods to validate model performance for a
specific purpose
NPC
Numerical Predictive Check, a GOF method related to VPC
pcVPC
Prediction corrected VPC, a type of GOF plot related to VPC
Q-Q
Quantile-quantile, a type of GOF plot
Residual
The difference between the predicted and the observed value
Residual error
An estimate of the remaining unexplained variability
Shrinkage
A measure of the extent to which EBE depends on the population
parameters versus the individual observed data
VPC
Visual predictive check, a type of GOF plot
xPRED
Predicted data, based on population parameter estimates, where ‘x’ can
be nothing, C (conditional), or P (simulation-based)
xWRES
Weighted Residuals, a type of diagnostic, where ‘x’ can be nothing, C
(conditional), or P (simulation-based)
Contains Nonbinding Recommendations
20
IX. REFERENCES
Barbour, AM, MJ Fossler, and J Barrett, 2014, Practical Considerations for Dose Selection in
Pediatric Patients to Ensure Target Exposure Requirements, AAPS J, 16(4):749-55.
Beal, SL, 2001, Ways to Fit a PK Model With Some Data Below the Quantification Limit, J
Pharmacokinet Pharmacodyn, 28(5):481-504.
Bergstrand, M, AC Hooker, JE Wallin, and MO Karlsson, 2011, Prediction-Corrected Visual
Predictive Checks for Diagnosing Nonlinear Mixed-Effects Models, AAPS J, 13(2):143-
51.
Bergstrand, M and MO Karlsson, 2009, Handling Data Below the Limit of Quantification in
Mixed Effect Models, AAPS J, 11(2):371-80.
Bhattaram, VA, BP Booth, RP Ramchandani, BN Beasley, Y Wang, V Tandon, JZ Duan, RK
Baweja, PJ Marroum, and RS Uppoor, 2005, Impact of Pharmacometrics on Drug
Approval and Labeling Decisions: A Survey of 42 New Drug Applications, AAPS J,
7(3):E503-E512.
Bonate, PL, A Strougo, A Desai, M Roy, A Yassen, JS van der Walt, A Kaibara, and S
Tannenbaum, 2012, Guidelines for the Quality Control of Population Pharmacokinetic-
Pharmacodynamic Analyses: An Industry Perspective, AAPS J, 14(4):749-58.
Bonate, PL, 2011, Pharmacokinetic-Pharmacodynamic Modeling and Simulation, 2
nd
edition.
New York, Springer.
Bonate, PL, M Ahamadi, N Budha, A de la Pena, JC Earp, Y Hong, MO Karlsson, P Ravva, A
Ruiz-Garcia, H Struemper, JR Wade, 2016, Methods and Strategies for Assessing
Uncontrolled Drug-Drug Interactions in Population Pharmacokinetic Analyses: Results
from the International Society of Pharmacometrics (ISOP) Working Group, J
Pharmacokinet Pharmacodyn, 43(2):123-35.
Brendel K, E Comets, C Laffont, C Laveille, F Mentré, 2006, Metrics for External Model
Evaluation with an Application to the Population Pharmacokinetics of Gliclazide, Pharm
Res, 23(9):2036-49.
Byon, W, MK Smith, P Chan, MA Tortorici, S Riley, H Dai, J Dong, A Ruiz‐Garcia, K
Sweeney, and C Cronenberger, 2013, Establishing Best Practices and Guidance in
Population Modeling: An Experience With an Internal Population Pharmacokinetic
Analysis Guidance, CPT Pharmacometrics Syst Pharmacol, 2(7):1-8.
Dodds, MG, AC Hooker, and P Vicini, 2005, Robust Population Pharmacokinetic Experiment
Design, J Pharmacokinet Pharmacodyn, 32(1):33-64.
Contains Nonbinding Recommendations
21
Dykstra, K, N Mehrotra, CW Tornøe, H Kastrissios, B Patel, N Al‐Huniti, P Jadhav, Y Wang,
and W Byon, 2015, Reporting Guidelines for Population Pharmacokinetic Analyses, J
Pharmacokinet Pharmacodyn, 42(3):301-14.
Ette, EI and TM Ludden,1995, Population Pharmacokinetic Modeling: The Importance of
Informative Graphics, Pharma Res, 12(12):1845-55.
Ette, EI and PJ Williams, 2007, Pharmacometrics: The Science of Quantitative Pharmacology,
John Wiley & Sons.
Gastonguay, MR, 2004, A Full Model Estimation Approach for Covariate Effects: Inference
Based on Clinical Importance and Estimation Precision, J AAPS, 6(S1):W4354.
Grasela Jr, TH and LB Sheiner, 1991, Pharmacostatistical Modeling for Observational Data, J
Pharmacokinet Biopharm, 19(S3):S25-S36.
Holford, N, YA Heo, and B Anderson, 2013, A Pharmacokinetic Standard for Babies and Adults,
J Pharmaceut Sci, 102(9):2941-52.
Johansson, ÅM and MO Karlsson, 2013, Comparison of Methods for Handling Missing
Covariate Data, J AAPS, 15(4):1232-41.
Karlsson, MO and RM Savic, 2007, Diagnosing Model Diagnostics, Clin Pharmacol Ther,
82(1):17-20.
Karlsson, MO and LB Sheiner, 1993, The Importance of Modeling Interoccasion Variability in
Population Pharmacokinetic Analyses, J Pharmacokinet Biopharm, 21(6):735-50.
Keizer, RJ, RS Jansen, H Rosing, B Thijssen, JH Beijnen, JHM Schellens, and ADR Huitema,
2015, Incorporation of Concentration Data Below the Limit of Quantification in
Population Pharmacokinetic Analyses, Pharmacol Res Perspect, 3(2):e00131.
Kimko, HHC and CC Peck, 2010, Clinical Trial Simulation and Quantitative Pharmacology:
Applications and Trends, Springer Science & Business Media.
Lavielle, M and B Ribba, 2016, Enhanced Method for Diagnosing Pharmacometric Models:
Random Sampling from Conditional Distributions, Pharm Res, 33(12):2979-88.
Lee, JY, CE Garnett, JVS Gobburu, VA Bhattaram, S Brar, JC Earp, PR Jadhav, K Krudys, LJ
Lesko, and F Li, 2011, Impact of Pharmacometric Analyses on New Drug Approval and
Labelling Decisions, Clin Pharmacokinet, 50(10):627-35.
Lunn, DJ, N Best, A Thomas, J Wakefield, and D Spiegelhalter, 2002, Bayesian Analysis of
Population PK/PD Models: General Concepts and Software, J Pharmacokinet
Pharmacodyn, 29(3):271-307.
Contains Nonbinding Recommendations
22
Mahmood I. 2014, Dosing in Children: a Critical Review of the Pharmacokinetic Allometric
Scaling and Modelling Approaches in Paediatric Drug Development and Clinical
Settings. Clin Pharmacokinet, 53(4): 327-46.
Marshall, SF, R Burghaus, V Cosson, SYA Cheung, M Chenel, O DellaPasqua, N Frey, B
Hamren, L Harnisch, and F Ivanow, 2016, Good Practices in Model‐Informed Drug
Discovery and Development (MID3): Practice, Application and Documentation, CPT:
Pharmacometrics Syst Pharmacol, 5(3):93-122.
Montgomery, DC, GG Vining, and EA Peck, 2012, Introduction to Linear Regression Analysis,
Wiley.
Mould, DR and RN Upton, 2013, Basic Concepts in Population Modeling, Simulation, and
Model-Based Drug Development—Part 2: Introduction to Pharmacokinetic Modeling
Methods, CPT: Pharmacometrics Syst Pharmacol, 2(4):e38.
Nguyen, THT, M-S Moukassi, N Holford, N Al-Huniti, I Freedman, AC Hooker, J John, MO
Karlsson, DR Mould, JJ Pérez Ruixo, 2017, Model Evaluation of Continuous Data
Pharmacometric Models: Metrics and Graphics, CPT Pharmacometrics Syst Pharmacol,
6(2):87-109.
Nyberg, J, C Bazzoli, K Ogungbenro, A Aliev, S Leonov, S Duffull, AC Hooker, and F Mentré,
2015, Methods and Software Tools for Design Evaluation in Population
Pharmacokinetics–Pharmacodynamics Studies, Br J Clin Pharmacol, 79(1):6-17.
Ogungbenro, K and L Aarons, 2007, Design of Population Pharmacokinetic Experiments Using
Prior Information, Xenobiotica, 37(10-11):1311-30.
Ogungbenro, K and L Aarons, 2008, Optimisation of Sampling Windows Design for Population
Pharmacokinetic Experiments, J Pharmacokinet Pharmacodyn, 35(4):465-82.
Ribbing, J, J Nyberg, O Caster, and EN Jonsson, 2007, The Lasso—A Novel Method for
Predictive Covariate Model Building in Nonlinear Mixed Effects Models, J
Pharmacokinet Pharmacodyn, 34(4):485-517.
Savic, RM and MO Karlsson, 2009, Importance of Shrinkage in Empirical Bayes Estimates for
Diagnostics: Problems and Solutions, J AAPS, 11(3):558-69.
Schmidt, H and A Radivojevic, 2014, Enhancing Population Pharmacokinetic Modeling
Efficiency and Quality Using an Integrated Workflow, J Pharmacokinet Pharmacodyn,
41(4):319-34.
Sheiner, LB, B Rosenberg, and VV Marathe, 1977, Estimation of Population Characteristics of
Pharmacokinetic Parameters From Routine Clinical Data, J Pharmacokinet Biopharm,
5(5):445-79.
Contains Nonbinding Recommendations
23
Tatarinova, T, M Neely, J Bartroff, M van Guilder, W Yamada, D Bayard, R Jelliffe, R Leary, A
Chubatiuk, and A Schumitzky, 2013, Two General Methods for Population
Pharmacokinetic Modeling: Non-Parametric Adaptive Grid and Non-Parametric
Bayesian, J Pharmacokinet Pharmacodyn, 40(2):189-99.
Tukey, JW, 1977, Exploratory Data Analysis, Addison-Wesley.
Wählby, U, MR Bouw, EN Jonsson, and MO Karlsson, 2002, Assessment of Type I Error Rates
for the Statistical Sub-Model in NONMEM, J Pharmacokinet Pharmacodyn, 29(3):251-
69.
Wählby, U, EN Jonsson and MO Karlsson, 2001, Assessment of Actual Significance Levels for
Covariate Effects in NONMEM, J Pharmacokinet Pharmacodyn, 28(3):231-52.
Wählby, U, EN Jonsson and MO Karlsson, 2002, Comparison of Stepwise Covariate Model
Building Strategies in Population Pharmacokinetic-Pharmacodynamic Analysis, AAPS
PharmSci, 4(4):E27.
Wählby U, Thomson AH, Milligan PA, Karlsson MO, 2004. Models for time-varying covariates
in population pharmacokinetic-pharmacodynamic analysis, Br J Clin Pharmacol, 58(4):
367–377.
Wang, Y, PR Jadhav, M Lala, and JV Gobburu, 2012, Clarification on Precision Criteria to
Derive Sample Size When Designing Pediatric Pharmacokinetic Studies, J Clin Pharm,
52(10):1601-06.
Wang, DD, Y Yu, N Kassir, M Zhu, WD Hanley, JC Earp, AT Chow, M Gupta, C Hu, 2017,
The Utility of a Population Approach in Drug-Drug Interaction Assessments: A
Simulation Evaluation, J Clin Pharmacol, 57(10):1268-1278.
Xu, SX, M Yuan, MO Karlsson, A Dunne, P Nandy, A VErmeulen, 2012, Shrinkage in
Nonlinear Mixed-Effects Population Models: Quantification, Influencing Factors, and
Impact, AAPS J, 14(4):927-36.
Zhang, Y, X Wei, G Bajaj, JS Barrett, B Meibohm, A Joshi, and M Gupta, 2015, Challenges and
Considerations for Development of Therapeutic Proteins in Pediatric Patients, J Clin
Pharmacol, 55(S3):S103-15.
Zhao, L, MJ Kim, L Zhang, R Lionberger, 2019, Generating Model Integrated Evidence for
Generic Drug Development and Assessment. Clin Pharmacol Ther, 105(2):338-349.

Contains Nonbinding Recommendations
24
FDA guidances for industry:
10
Clinical Pharmacology Labeling for Human Prescription Drug and Biological Products —
Content and Format (December 2016)
Clinical Drug Interaction Studies—Cytochrome P450 Enzyme- and Transporter-Mediated Drug
Interactions (January 2020)
Exposure-Response Relationships — Study Design, Data Analysis, and Regulatory Applications
(May 2003)
In Vitro Drug Interaction Studies – Cytochrome P450 Enzyme- and Transporter-Mediated Drug
Interactions (January 2020)
Pharmacokinetics in Patients With Impaired Hepatic Function — Study Design, Data Analysis,
and Impact on Dosing and Labeling (May 2003)
10
See also the following FDA guidances: (1) Assessing the Effects of Food on Drugs in INDs and NDAs —
Clinical Pharmacology Considerations (February 2019); (2) General Clinical Pharmacology
Considerations for Pediatric Studies for Drugs and Biological Products (December 2014); and (3)
Pharmacokinetics in Patients With Impaired Renal Function — Study Design, Data Analysis, and Impact
on Dosing and Labeling (September 2020). When final, these guidances will represent the Agency’s
current thinking on these topics.
