1 of 4
Center for Mississippi Health Policy
�
Brief: Birth Centers and Midwifery Care
�
May 2020
As Mississippians cope with a lack of obstetric services in over half of counties
in the state, an increasing number of women desire to have less-medicalized
births outside of a typical hospital setting. e number of planned births that
occurred outside of a hospital in Mississippi grew by 68 percent between 2007
and 2017 as did births attended by midwives. Midwifery care is being explored
across the country as a way to alleviate workforce shortages and oer safe,
community-based care in low-risk pregnancies.
Midwives are trained professionals who help healthy women during pregnancy,
labor and delivery, and after birth. Research indicates that integration of midwifery
care in a health system and better access to midwives are associated with higher
rates of vaginal delivery, vaginal delivery after prior cesarean (c-section), and
breastfeeding as well as lower rates of premature births, low birth-weights, and
neonatal death. While most births that occur in Mississippi are uncomplicated, just
over two percent of pregnancies and births are managed by midwives annually,
and few women have access to safe, non-medicalized birth options.
Midwives have been instrumental in providing uncomplicated pregnancy-
related care in previous times of provider shortages and poor birth outcomes in
Mississippi. (See sidebar.) Mississippi is currently experiencing a shortage of
obstetric providers; women in forty-six Mississippi counties must drive an hour
or more to see an obstetrician (OBGYN) for prenatal, delivery, and post-partum
care. From 2015 to 2017 Mississippi had the highest rates of cesarean deliveries,
pre-term births, and low birth weight in the nation. In response to similar shortages
and poor birth outcomes, several states have broadened access to maternity care
through midwives and birth centers for women with uncomplicated pregnancies.
KEY POINTS
� Midwives and birth centers provide a model of maternity care that research
shows can be appropriate for low-risk pregnancies and deliveries with
similar or better outcomes as typical obstetric care with lower healthcare
costs.
� Certied Nurse Midwives currently practice in Mississippi hospitals, while
Certied Professional Midwives and Direct Entry Midwives legally practice
unregulated in homes and community settings.
� Birth centers provide midwifery care and operate independently from
hospitals. These providers are currently licensable, but none currently
operate in Mississippi.
MIDWIFERY CARE &
BIRTH CENTERS
PUBLISHED MAY 2020
A BRIEF HISTORY OF MIDWIFERY IN
MISSISSIPPI
In 1927, more than 3,000 lay midwives
were documented across Mississippi. The
mostly black midwives served white women
and black communities with no access to
doctors. Many were recruited and trained
as public health nurses by the Department
of Health in response to poor public health
and limited access to physicians. By 1975
only 217 lay midwives were active. Greater
availability of physicians and hospital beds,
improved education about medical care, and
the availability of Medicaid funds for care
contributed to a shift from home births to
hospital-based, medicalized deliveries.
In response to limited capacity at local
hospitals and high infant and maternal
mortality rates, the Mississippi State
Department of Health developed maternal
and child health (MCH) clinics during the
1970s. The clinics employed certied
nurse-midwives to provide prenatal care
and hospital-based deliveries to low-
income expectant mothers in several
counties including Warren, Hinds, Bolivar,
Washington, Holmes, and Jackson counties.
Nurse midwives practicing in the MCH
clinics were trained in partnership with the
University of Mississippi Medical Center.
In 1978 nurse midwives conducted over
5,200 visits and delivered 376 infants in
Jackson County alone.
There is currently no school of nurse-
midwifery in the state, and prenatal care has
not been provided in public health clinics
since 2017.
Source: Beck, T. (2019). ; Mississippi State Board
of Health. (1973-1983). Annual Reports.
DRAFT COPY-NOT FOR DISTRIBUTIONDRAFT COPY-NOT FOR DISTRIBUTION
2 of 4
Center for Mississippi Health Policy
�
Issue Brief: Birth Centers and Midwifery Care
�
May 2020
Three types of midwives are known to practice in Mississippi. Certied Nurse
Midwives (CNMs or nurse-midwives), 29 of whom are currently licensed to
practice and attend over 800 births (or two percent) annually across the state.
Other types of midwives in the state include Certied Professional Midwives
(CPMs) and Direct Entry Midwives (or lay midwives). In Mississippi, CPMs
and lay midwives practice legally but unregulated, and the number of these
practitioners active in the state is unknown. These midwives are available for
women who wish to give birth in home-like settings, but no state-level oversight
exists.
Certied Nurse
Midwife
Certied Professional
Midwife
Direct Entry
Midwife
Currently
Licensable
Licensed by State
Board of Nursing
Not currently, but licensed in 35
states
No
Training
Registered nurse
training with
advanced practice
degree in midwifery
National certication* after 3-5 years
of apprenticeship including at least
2 years of clinical education and
observing 55 or more births
None required
Site of
Practice
Primarily hospitals
and
birth centers
Home and community settings
Home and
Community
Payment
Reimbursable
via Medicaid and
commercial insurers
Mostly self-pay; reimbursable by
some commercial insurance plans;
Medishare
Self-pay; No
known insurance
coverage;
Medishare
Source: The American College of Nurse-Midwives. (2017). * North American Registry of Midwives. (2020).
Nurse midwives practice in all 50 states, and CPMs are licensed to practice
in 37 states including Tennessee, Louisiana, Arkansas, Alabama, and Florida.
Lawmakers in Florida have formally recognized the role of midwives in reducing
a shortage of providers of prenatal and delivery services and have provided for
Medicaid reimbursement for CPMs in addition to nurse midwives.
Birth centers oer another option for uncomplicated deliveries.
Birth centers operate according to the midwife model of care and are an option
for pregnant women at low risk of complications who want a non-medical delivery
but not at home. Medicaid and commercial insurers cover birth center services,
which have signicantly lower costs due to fewer medical interventions and less
expensive sta. Because midwife-managed care limits intervention and allows for
normal progression of labor, data show the risk of some birth-related injuries is less,
although risk of shoulder dystocia may be higher. (See sidebar.) Studies indicate that
fewer than 10 percent of births initiated in birth centers require transfer to medical
care during labor. State law requires that birth centers maintain written agreements
with acute care facilities for transfer of laboring women in case of emergency. Birth
centers currently operate in Tennessee, Arkansas, and Louisiana. There are no
birth centers that meet the state minimum standards currently providing this care in
the state.
DOULAS
Doulas, often confused for midwives, act as
part of a birth support team and provide non-
clinical, emotional support and advocacy for
pregnant and laboring women in any setting.
MINIMUM STANDARDS OF OPERATION FOR
BIRTHING CENTERS
Mississippi Code 41-77-1 thru 25 authorizes
the licensure and regulation of "birthing
centers" by the State Department of Health.
Services are limited to those typical in
uncomplicated childbirth and do not include
cesarean section. Labor in birthing centers
is allowed to progress without medically
unnecessary intervention.
State Minimum Standards require birthing
centers to be operationally independent from
hospital delivery units. They may operate
under the direction of a nurse midwife or a
physician, and are required to maintain a
referral agreement with a hospital that has
an organized obstetrical staff and 24-hour
emergency care and cesarean section
capability within 30 minutes. Patients stays
in birth centers are limited to 24 hours.
Source: MSDH. (2016) Health Facilities
Regulation.
DRAFT COPY-NOT FOR DISTRIBUTIONDRAFT COPY-NOT FOR DISTRIBUTION
TABLE 1. A COMPARISON OF TYPES OF MIDWIVES CURRENTLY PRACTICING IN MISSISSIPPI
Midwives as Providers of Maternity Care
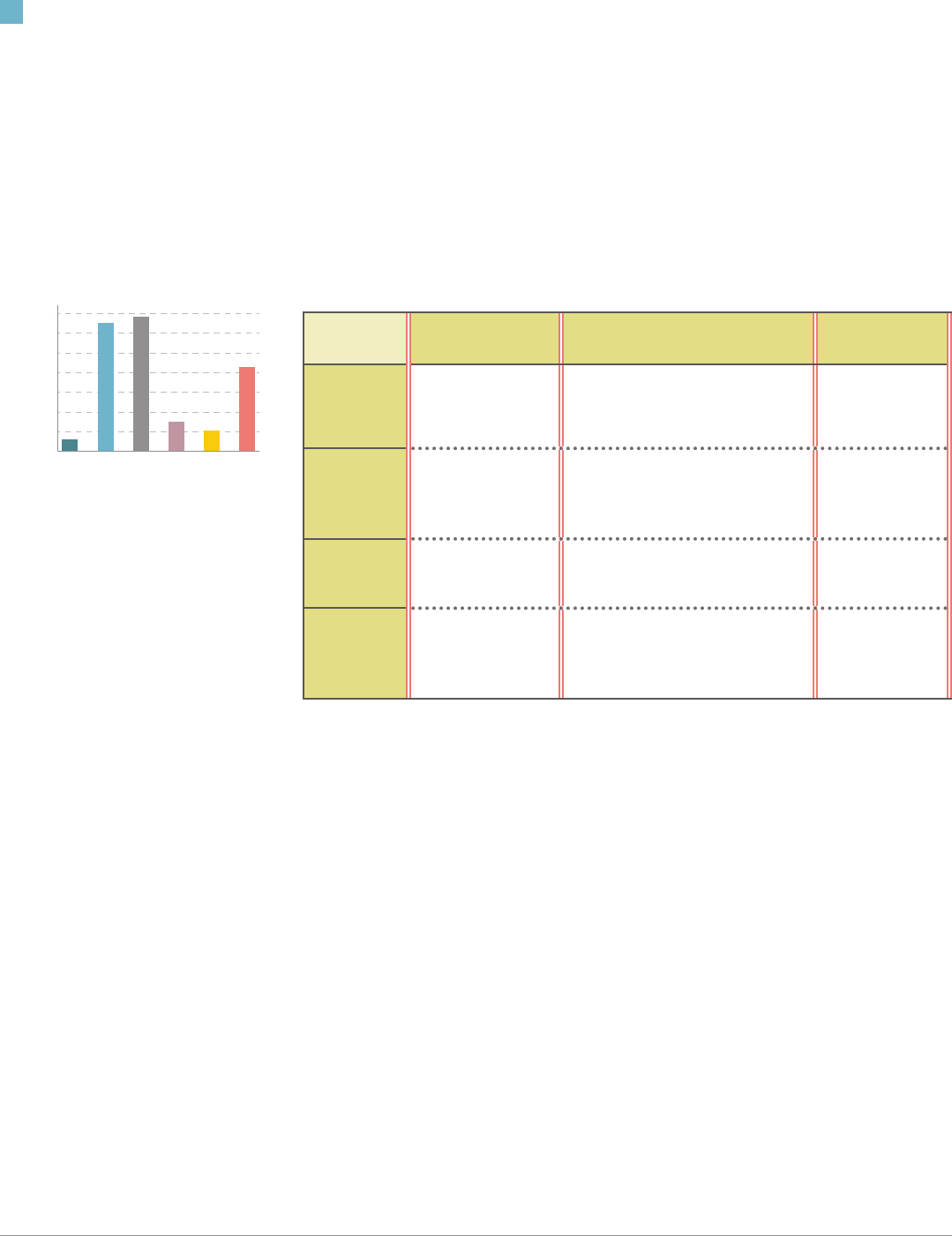
AL FL GA LA MS TN
Percent of all births
PERCENTAGE OF BIRTHS ATTENDED BY MIDWIVES
IN SOUTHEASTERN STATES, 2018
0%
2%
4%
6%
8%
10%
12%
14%
8.6%
2.1%
3.0%
13.7%
13.0%
1.2%
Source: CDC. (2019). National Center for Health
Statistics. Natality Reports (2016-2018).
RISK OF BIRTH INJURY
While research reects decreased risk
of birth injury due to less intervention,
one study has shown an increased risk of
shoulder dystocia associated with midwife-
manged births among women with two or
more previous deliveries.
Source: Souter, V., et al. (2019). Comparison of
Midwifery and Obstetric Care in Low-Risk Hospital
Births
3 of 4
Center for Mississippi Health Policy
�
Issue Brief: Birth Centers and Midwifery Care
�
May 2020
Midwives in any setting practice what is known as the Midwifery Model of Care,
which views pregnancy and birth as normal, healthy physiologic processes.
Midwives support women throughout pregnancy, delivery, and post-partum
periods. Midwife-managed prenatal care includes pregnancy assessment as
well as lifestyle and behavioral interventions, and emotional support. In case of
complications at any point in the pregnancy or delivery, women are referred to
a physician's care. Induction, articially accelerated labor, c-section deliveries,
anesthesia, and intensive electronic monitoring are avoided under midwives’ care
but may be provided by medical clinicians as necessary. Midwives may order lab
tests and medication as credentials allow and medical necessity requires.
Midwifery oers comparable or better outcomes and cost savings.
Research shows that in any setting of care, midwife-managed births result in
signicantly lower rates of induced labor and c-sections which negatively impact
maternal health, and poor outcomes like pre-term births and low birth weight that
endanger infant health. Prenatal and postnatal care are more comprehensive than
typical medical maternity care and supports improved outcomes like breastfeeding
and postpartum contraception use, both of which contribute to long-term health of
mothers and infants.
Research also shows that costs improve under a model of care that promotes
minimal intervention and the natural progression of labor and birth via vaginal
delivery. In 2018, the average total charge to Mississippi Medicaid for an
uncomplicated cesarean delivery was $27,510 while the average total charge for
an uncomplicated vaginal delivery was $15,854 (inclusive of pre-and postnatal
care and infant care). Approximately 70 percent of Medicaid deliveries billed that
year were uncomplicated.
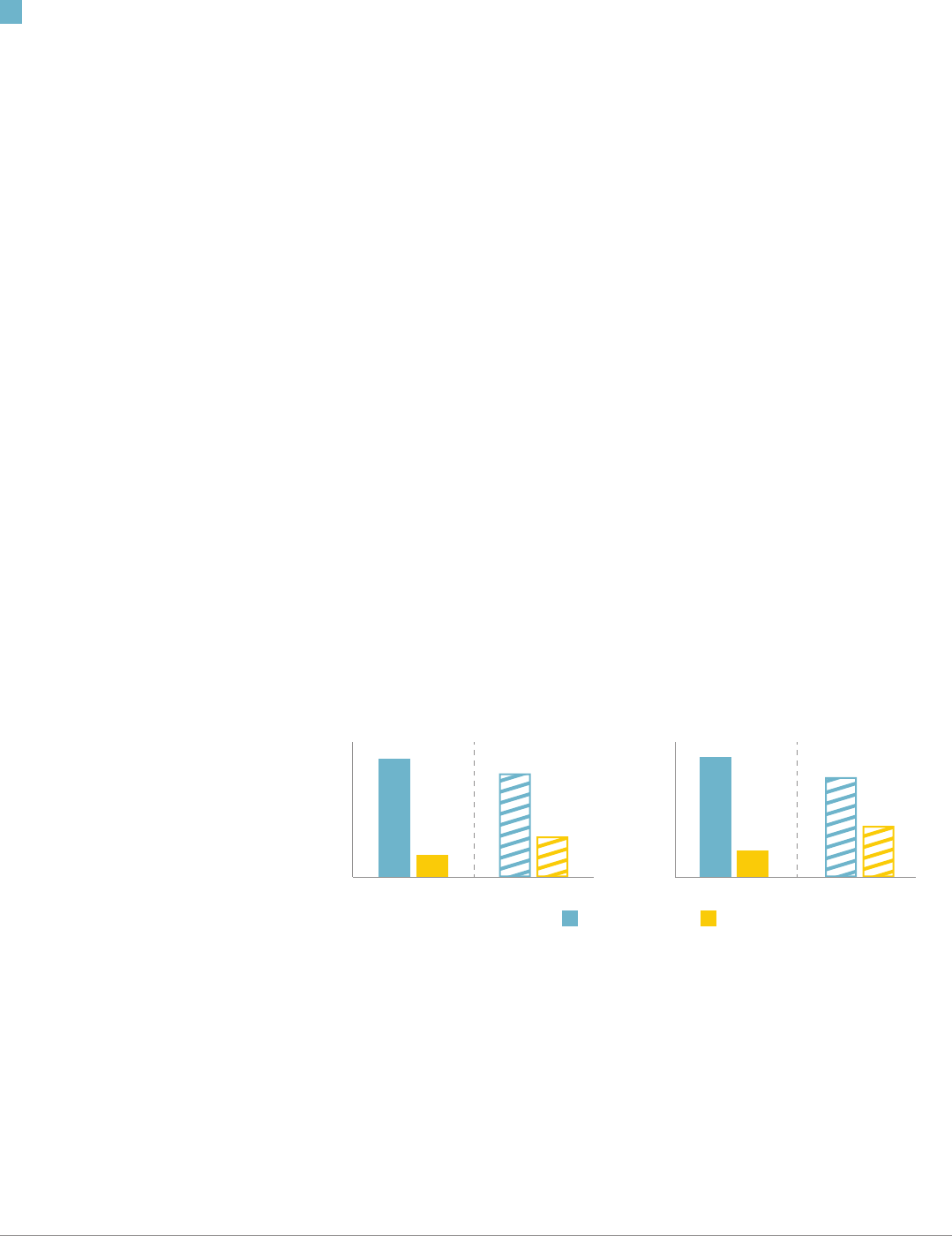
FIGURE 1. LOW RISK CESAREAN AND VBAC BIRTH RATES IN MISSISSIPPI COMPARED WITH THE U.S., 2013
& 2018.
Mississippi may benet from greater integration of midwifery.
Mississippi mothers with low risk for complications deliver via c-section at the
highest rate in the country (Figure 1.). They also attempt vaginal delivery after prior
c-section at half the national rate. Rates of uncomplicated c-sections can vary
widely across hospital systems (from 15 to 37 percent in Mississippi hospitals)
which suggests clinical practice patterns and limitations on time, stang, and labor
rooms may play a role rather than population-level health risks. Births initiated under
midwifery care are very likely to be delivered vaginally (as many as 93 percent of
births in one study). Greater utilization of midwifery would reduce unnecessary
c-sections, as well as risk to maternal and infant health and costs of care.
PRENATAL VISITS
An average prenatal visit with a physician in
a medical setting lasts approximately 15 to
20 minutes while visits with certied nurse
midwives in birth centers last at least 30
minutes.
Source: Urban Institute. (2016). Strong Start for
Mothers and Newborns.
STRONG START FOR MOTHERS AND
NEWBORNS
From 2013-2017 the Centers for Medicare
and Medicaid Innovation studied alternate
models of maternity care including birth
centers. Birth centers demonstrated better
outcomes compared to the national average
for births in all settings including hospitals.
Some results included:
reduced induction of labor
(16.4% v. 24.5%);
reduced primary c-section deliveries
(8.7% v. 21.8%);
increased breastfeeding at discharge
(92.9% v. 83.1%); and
lower rates of NICU admissions
(2.8% v. 8.7%).
Source: Alliman, et al. (2019). Strong Start in Birth
Centers.
UNCOMPLICATED DELIVERY
An uncomplicated delivery involves a single
baby delivered vaginally at full term and
positioned head-down.
COST OF CPM CARE FOR ONE YEAR
One year of care including prenatal,
home-based delivery, and postpartum
care, provided by a Certied Professional
Midwife costs $3000-$4000 on average.
Source: Hillman, R. (2020).
Key Differences in Midwifery Model of Maternity Care
0%
5%
10%
15%
20%
25%
30%
35%
USMS
0%
5%
10%
15%
20%
25%
30%
35%
USMS
Vaginal Birth after Cesarean (VBAC)Primary Cesarean
2013 2018
30.7%
26.9%
31.2%
7.0%
13.3%
25.9%
5.8%
10.6%
CESAREAN SECTIONS AND RISK
C-section is a surgical procedure, and
women who undergo them are at increased
risk of blood clots, post-partum hemorrhage,
infection, internal organ injury, and need for
blood transfusion. Subsequent deliveries
become more risky, too. Risks to newborns
include surgical injury and breathing
problems.
Source: Maternal Safety Foundation. (2018).

4 of 4
Center for Mississippi Health Policy
�
Issue Brief: Birth Centers and Midwifery Care
�
May 2020
Plaza Building, Suite 700
120 N. Congress Street
Jackson, MS 39201
Phone 601.709.2133
Fax 601.709.2134
www.mshealthpolicy.com
@mshealthpolicy
Discussion
The United States is grappling with a host of reversals in decades-long health and
public health gains in maternal and child health. Avoidable pregnancy-related deaths
and illnesses have increased for all mothers and infants, but especially black women
and their children. The burden is heaviest among states in the Southeast, including
Mississippi where obstetric providers are in short supply. It is unlikely that Mississippi
will attract enough OBGYNs to meet recommended coverage levels in the near future.
However, as many states and other highly developed nations have demonstrated in
numerous studies, midwifery care is sucient and benecial for many pregnancies. The
midwifery model of care has been integrated into national and state-level initiatives to
reduce perinatal death and illness as well as racial health disparities in maternal and
child health.
Use of birth centers and midwifery care in Mississippi has lagged behind other states
despite existing enabling policies, such as Medicaid reimbursement for nurse-midwives
and licensure of birth centers. Additional policy options that would foster greater
integration of midwifery into the existing maternity care system in Mississippi include:
� Licensure and regulation of Certied Professional Midwives currently practicing
without regulation in the state
� Promoting collaboration between medical and non-clinical maternity care providers
within medical systems, including both midwives and birth centers
� Creation of in-state training programs for Certied Nurse Midwives to expand the
maternity care workforce for low risk pregnancies
Studies have shown that integration of midwifery in medical settings yields
more favorable outcomes for low-risk pregnancies than medical settings
that do not include midwifery—even in deliveries that are not ultimately
managed by a midwife. Greater inclusion of midwifery would benet the
uncomplicated pregnancies midwives manage as well as relieve strain on
obstetric providers to care for high risk pregnancies
Sources
Stapleton, S., Osborne, C., and Illuzzi, J. (2013). Outcomes of Care in Birth Centers: Demonstration of a Durable Model. Journal of
Midwifery & Women s Health, 58: 3-14. doi:10.1111/jmwh.12003.
Vedam, S., Stoll, K., MacDorman, M., Declercq E., Cramer, R., Cheyne,y M. et al. (2018). Mapping integration of midwives across the
United States: Imp.act on access, equity, and outcomes. PLoS ONE 13(2): e0192523.
Souter, V., Nethery, E., Kopas, M., Wurz, H., Sitcov, K., and Caughey, A. Comparison of Midwifery and Obstetric Care in
Low-Risk Hospital Births, Obstetrics & Gynecology: November 2019 - Volume 134 - Issue 5 - p 1056-1065 doi: 10.1097/
AOG.0000000000003521
Alliman, J, Stapleton, S., Wright, J., Bauer, K., Slider, K., Jolles D. (2019). Strong Start in birth centers: Socio-demographic character-
istics, care processes, and outcomes for mothers and newborns. Birth. 2019;46:234-243.
American College of Nurse-Midwives. Comparison of Certied Nurse-Midwives, Certied Midwives, Certied Professional Midwives
Clarifying the Distinctions Among Professional Midwifery Credentials in the US. (2017). https://www.midwife.org/acnm/les/ccLibrary-
Files/FILENAME/000000006807/FINAL-ComparisonChart-Oct2017.pdf
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary
cesarean delivery. Obstetric care consensus no. 1. Am J Obstet Gynecol, 210 (2014).
Maternal Safety Foundation. (2018). Mississippi State Dashboard. www.cesareanrates.org
Mississippi State Department of Health. (2017). Hospital discharge data cesarean and vaginal deliveries, 2017.
North American Registry of Midwives. (2020). Certifed Professional Midwives (CPM) Candidate Information Booklet. http://narm.org/
pdles/CIB.pdf
Centers for Disease Control and Prevention. (2017). Infant Mortality Rates by State. https://www.cdc.gov/nchs/pressroom/sosmap/
infant_mortality_rates/infant_mortality.htm
Centers for Disease Control and Prevention (CDC). (2019). National Center for Health Statistics (NCHS), Division of Vital Statistics,
Natality public-use data 2016-2018, on CDC WONDER Online Database. http://wonder.cdc.gov/natality-expanded-current.html
The Big Push for Midwives. (2019). Licensure for CPMs: State Chart. http://PushforMidwives.org.
The Birth Place Lab. (2018). Midwifery Integration State Scoring System Report Card. https://www.birthplacelab.org/how-does-your-
state-rank/
Urban Institute. (2016). Strong Start for Mothers and Newborns Evaluation: Year 2 Report. https://downloads.cms.gov/les/cmmi/
strongstart-enhancedprenatalcare_evalrptyr2v1.pdf
Beck, T. (2019, September). Phone interview.
Mississippi State Department of Health. (2016). Minimum Standards of Operation for Birthing Centers. wwww.msdh.state.ms.us.
Mississippi State Board of Health. Annual Reports. (1973-1983). Mississippi Department of Archives.
Hillman, R. (2020, January). Email interview.
MISSISSIPPI MATERNAL AND
CHILD HEALTH OUTCOMES
Mississippi has one of the highest
rates of preterm birth and low
birth weight infants in the country,
particularly among black infants.
ALLIANCE FOR INNOVATION ON
MATERNAL HEALTH (AIM)
AIM is a federally funded, national
collaboration of healthcare
associations working to reduce
severe maternal morbidity and
mortality through maternal and
non-obstetric safety bundles
including a reduction in primary
cesarean sections, a key
contribution of midwifery.
