Ed Kubacki
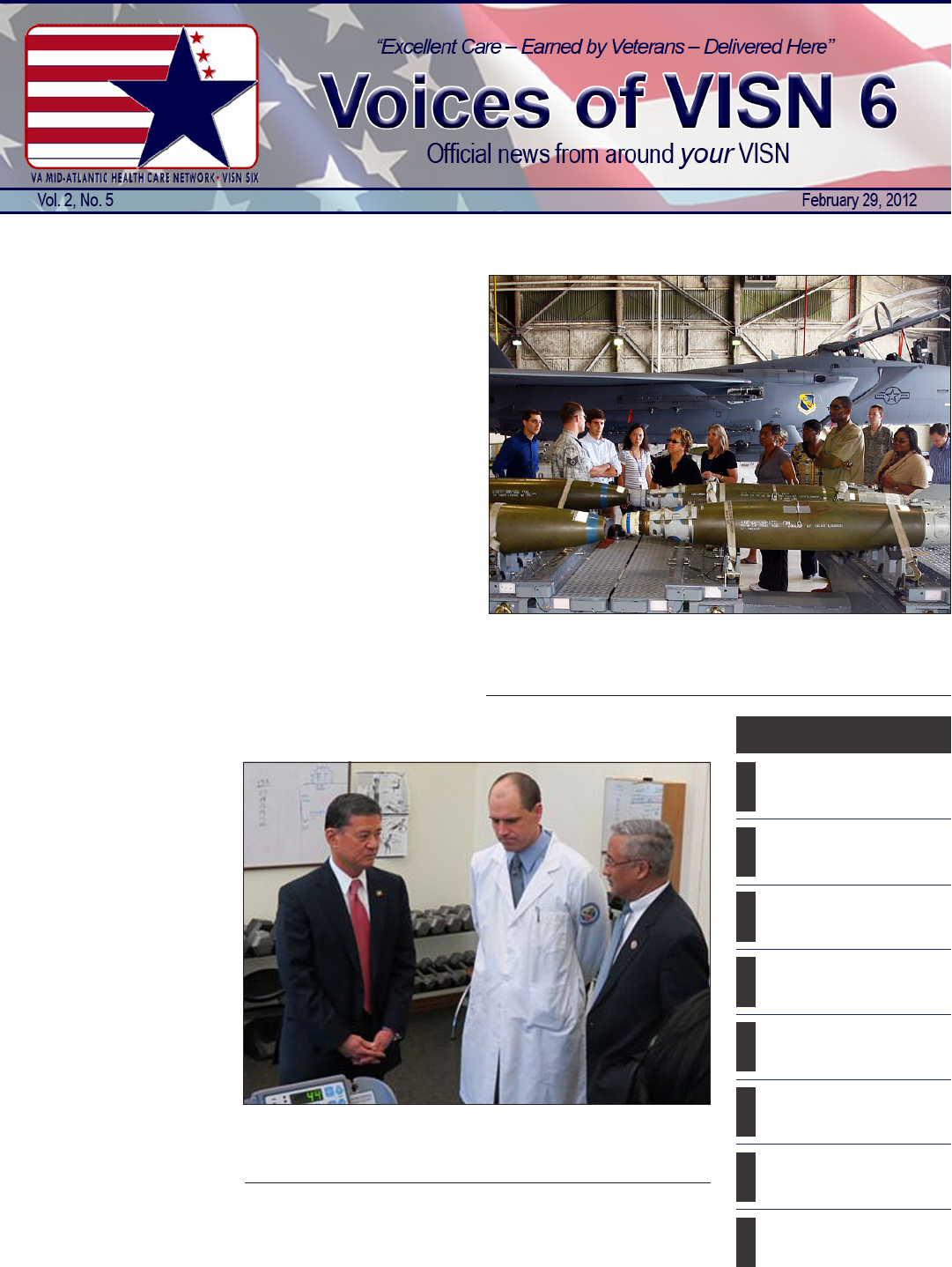
A 4th Fighter Wing munitions maintainer shows Durham VAMC
staff the various munitions which can be delivered by the F-15E
Strike Eagle.
By Hampton & Richmond
VAMC public affairs
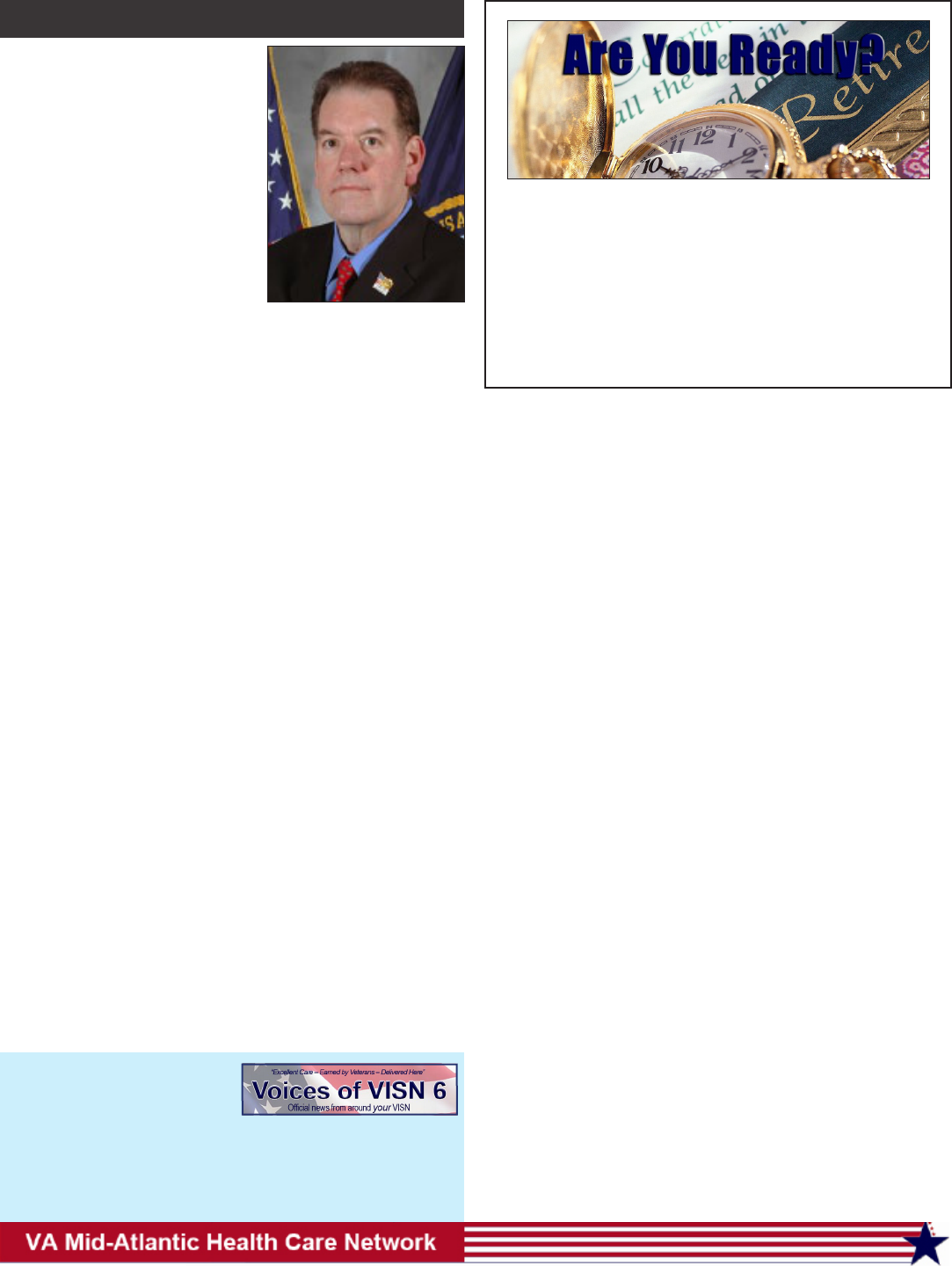
Secretary of Veterans Af-
fairs Eric K. Shinseki paid vis-
its to the Mid-Atlantic Health
Care Network region on two
occasions in February, rst on
Feb. 3 when he toured Rich-
mond VAMC and on Feb. 9
when he made a stop in the
Hampton VAMC area to visit
a trade school with a growing
population of student Veterans.
During his visit to Rich-
mond, the Secretary received
a rsthand look at two of the
medical center’s most highly
touted programs, the McGuire
Polytrauma Rehabilitation
Center and the Servicemember
Transitional Amputee Rehabili-
tation (STAR) program.
Secretary Shinseki also
toured projects the facility has
implemented to become more
energy efcient. Virginia Con-
gressman Bobby Scott accom-
panied the secretary during his
visit.
McGuire’s Polytrauma
Rehabilitation Center is one
of ve facilities in the country
designed to provide intensive
rehabilitative care to Veterans
Inside in Brief
By Jeff Melvin
VISN 6 public affairs
Seeking to gain greater
understanding of the military,
Durham VAMC staff formu-
lated a plan to reach their ob-
jective. The journey began with
online Military Cultural Aware-
ness training, followed by a
continuing series of roundtable
discussions with Veterans, and
culminated with an exchange
of eld trips with the Airmen
of Seymour Johnson Air Force
Base in Goldsboro, N.C.
Durham VAMC Public Af-
fairs Ofcer Pete Tillman, one
of the lead organizers of the
initiative, offered his assess-
ment of the undertaking and the
desired outcome.
According to Tillman the
rst step began when about 30
staff members wanting to learn
more about military culture
took a 90-minute Military Cul-
tural Awareness training course
available in VA’s Talent Man-
agement System. The idea was
simple; Durham VAMC staff
would take the course to bet-
ter understand the military, and
in turn would be able to better
provide health care to those
who served.
“The informative training
explained military culture from
the ground zero,” Tillman said.
“In Jeopardy-style format, staff
learned about military branch-
es, ranks, and conicts. After
completion of the course, they
were primed for an experience
of real life proportions.”
The next step was for the
Durham Staff Enhances Military Awareness
Richmond podiatrist earns
recognition; New arrivals
enhance eld support.
VA Secretary Makes Two Stops In VISN 6
N.C. American Legion
Winter Conference.
Durham receives “gold
heart” from NC preven-
tion partners.
National salute tells Veter-
ans We Care.
Ofcers transition to new
baton; Sun to set on US
Treasury checks.
Marriage vow renewal cer-
emony; Vietnam Veterans
homecoming 2012.
Women can suffer same
deployment ills as men;
Facts about women Vets.
VISN 6 Sites of Care with
addresses and phone num-
bers for each location.
Pg 3Pg 4Pg 5Pg 6Pg 7Pg 8Pg 10Pg 12
Continued on Pg 5
Darlene Edwards
VA Secretary Eric Shinseki discusses Polytrauma with Dr. Shane
McNamee, chief, physical medicine and rehabilitation, Richmond
VAMC, and U.S. Rep. Bobby Scott.
Continued on Pg 4
This month, I’ll shift to a more
clinical focus and shine a light on
some very important work going on
behind the scenes that really speaks
to the heart of being a Veteran-cen-
tered health care organization.
It is well known that service-
members have experiences that
few who have not served can iden-
tify with. These can leave emotional
scars that may be invisible to the
eye, but are just as real as the physi-
cal scars we can see. I’d like to take
this opportunity to tell you about
what VISN 6 is doing to treat the in-
visible wounds of war.
VA is the undisputed leader in mending the physical traumas
of war. Equally as important, VA also leads national and interna-
tional efforts to heal psychological trauma as well.
Within VA, there are 15 specialized mental health centers of
excellence which include 10 Mental Illness Research, Education
and Clinical Centers (MIRECCs), four Mental Health Centers of
Excellence, and the National Center for PTSD.
The MIRECCs were established by Congress with the goal of
researching the causes and treatments of mental disorders and us-
ing education to put new knowledge into routine clinical practice
in VA. Each center addresses a particular mental illness, problem,
or environmental situation.
Post-deployment mental health challenges have been evident
for many years and in 2005, VA addressed this issue by awarding
the VISN 6 MIRECC a multidisciplinary team of clinicians, edu-
cators and researchers charged with the goal of bringing best prac-
tices in mental health care into deployment related mental health.
The overarching goal of Mid-Atlantic MIRECC is the clinical
assessment and treatment of post-deployment mental illness and
readjustment related problems, and the development of new men-
tal health interventions through basic and clinical research.
The MIRECC’s organizational structure includes three major
components: research, clinical, and education.
Locating a MIRECC in this network makes perfect sense be-
cause of the large population of Veterans within our boundaries.
Installations like Fort Bragg, Camp Lejuene, Norfolk Naval Base,
Langley and Seymour Johnson Air Force Bases, along with the
numerous Guard and Reserve bases allows the research registry
access to large numbers of Veterans who are willing to help their
fellow servicemembers by sharing their own stories.
The clinical component seeks to dene, model, champion and
rene the continuum of care for OEF/OIF/OND mental health.
Key to their approach is that there should be “no wrong door” for
Veterans seeking care or for their families in helping them nd and
work with that care. To achieve this, they have created an innova-
tive collaboration with state governments in North Carolina and
Virginia.
Finally, the education component works to bridge the gap be-
tween research and clinical care. The education component trans-
lates best practices and research concepts into educational materi-
als and ensures that the knowledge is shared with all health care
Voices of VISN 6 is published
monthly by VA Mid-Atlantic
Health Care Network.
Questions or comments about
the newsletter, e-mail Bruce.
[email protected] or call 919-
956-5541.
2
From the Director
Daniel F. Hoffmann, Network Director
Augustin Davila, Deputy Network Director
Mark Shelhorse M.D., Chief Medical Ofcer
Bruce Sprecher, Director, Public Affairs
Steve Wilkins, Network Public Affairs
Jeffery Melvin, Network Public Affairs
Patrick W. Schuetz, Newsletter Editor
The VISN 6 Retirement Specialty Center (RSC) is here
to assist you with your CSRS/FERS optional, disability,
military and civilian service deposit, and annuity estimate
retirement needs.
For retirement assistance, please contact us at our toll
free number 1-877-645-6015 or at [email protected]. Our
hours of operation are Monday – Friday, 8 a.m. to 4:30 p.m.
Face-to-face consultations are available by appointment
only.
Retirement Specialty Center Can Help
personnel, patients and families through a variety of accessible
means which include live presentations, print materials, record-
ings, and even the web.
So, why am I focusing on this work at this time?
Unlike past conicts where mental help for Veterans came too
little, too late, VA has made the commitment to address our Veter-
ans needs as soon as humanly possible and to assist our Veterans
with their transition back to their civilian environment.
It’s important to note that an unprecedented number, 53 per-
cent of the 2.2 million returning Veterans, have already sought care
within VA. However, this means that 47 percent have not. Those
who have not will likely seek care from community providers, who
may not have access to the resources necessary to fully address
traumatic brain injury or PTSD or related depression.
This is where MIRECC comes in. MIRECC is in constant
collaboration with North Carolina’s Area Health Education Cen-
ter and Citizen Soldier Support Program. The MIRECC team has
created training for community providers, such as primary care
doctors, caseworkers, and mental health providers to help them
better understand the culture of Veterans and their families. The
team also works to teach community providers how to best iden-
tify, assess, and treat mental health problems that may occur as a
result of war experiences. These workshops are available to all at
www.ahecconnect.com/citizensoldier. Of note, these presentations
are the basis for the rst national AHEC project ever approved! To
date, more than 12,000 community providers have received train-
ing about deployment mental health issues and about how to work
in partnership with VA to ensure the best possible care for Veterans
through this collaboration.
While participation is voluntary, all returning OIF/OEF/OND
Veterans are invited to participate in ongoing research about the
effects of recent deployments on the physical and mental health
of servicemembers, especially as they transition from deployment
back to civilian life. Our goals are to learn more about the readjust-
ment process, to recognize problems earlier, and to improve care.
We are interested in learning about Veterans who have problems as
well as those who have no problems at all.
In this network, we are working to ensure that there is no
wrong door from which a Veteran or his/her family can seek help.
Again, I encourage all Veterans and families to learn more about
what is being done and what is being offered to those who need as-
sistance. For more information, please go to www.mirecc.va.gov/
visn6/index.asp.
Sincerely,
Dan Hoffmann
3
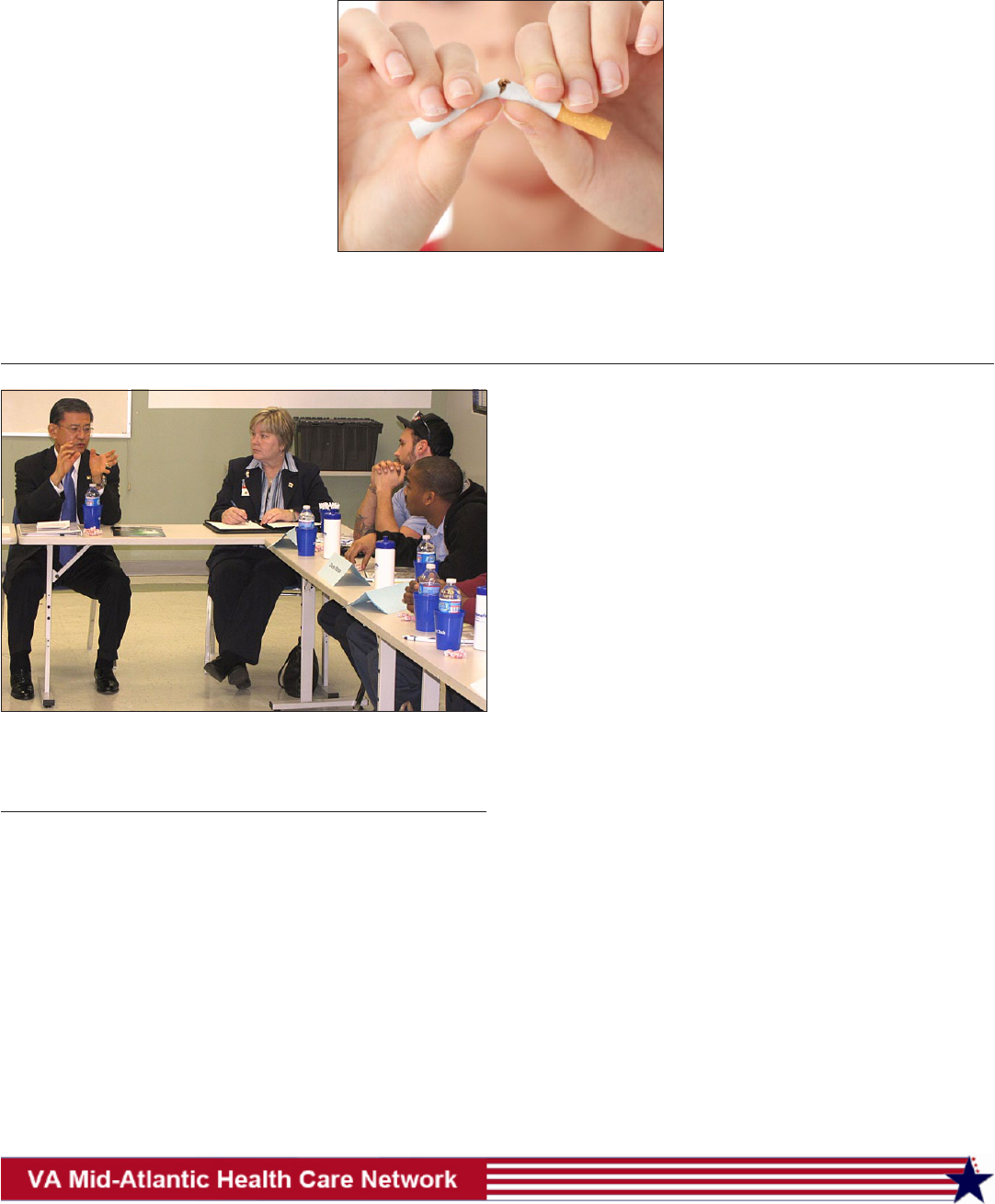
By Darlene Edwards
Richmond VAMC public affairs
Dr. Jonathan Brantley,
chief of podiatry, Richmond
VAMC recently received the
Excellence in Education for the
Profession of Podiatry Award
from the Veterans Health Ad-
ministration for his dedication
and commitment to the educa-
tion of future podiatrists.
Among the many accom-
plishments the doctor of po-
diatric medicine is credited
with is his establishment of
the podiatric medical and sur-
gical residency program at the
medical center. The active resi-
dency program encompasses
a two-year training program.
Dr. Brantley also frequently
lectures to leading colleagues
in the eld most recently at a
national conference, the Desert
Foot Conference, in Phoenix
attended by more than 500 par-
ticipants.
Visitors to the podiatry
clinic will often nd Brantley
providing a detailed overview
of healthy foot care to his pa-
tients and explaining needed
procedures. He will even in-
clude diagrams, photos and
models to support his educa-
tional efforts to ensure the pa-
tient understands the informa-
tion related to their health.
The Richmond VAMC’s
busy podiatry clinic offers com-
prehensive foot and ankle care
to Veterans, ranging from rou-
tine preventative care for some
to surgery for others with com-
plex foot deformities.
Dr. Brantley grew up in
Edgewater Park, N.J., and at-
tended New York College of
Podiatric Medicine.
Richmond Podiatrist
Earns Recognition
Darlene Edwards
Richmond VAMC podiatrist Dr. Joseph Brantley has earned Veter-
ans Health Administration’s Excellence in Education for the Pro-
fession of Podiatry Award.
There are some new fac-
es in unfamiliar spaces and
old faces in new spaces in an
around the VISN 6. The fol-
lowing are some of the new
hires and position changes
since last August.
SaMonia Ford joined
VA and the
VISN in Au-
gust as trans-
portation
assistant.
Before join-
ing VA, Ford
served in the
U.S. Army for eight years and
most recently worked for the
NC National Guard. In her role
for the VISN, Ms. Ford is re-
sponsible for providing assis-
tance preparing transportation
needs.
Cathy
Hendrix
joined VISN
6 in No-
vember as a
management
and program
assistant.
Cathy is a newcomer to VA and
comes to us from the North
Carolina Department of Rev-
enue where she worked as the
administrative assistant for the
special corporate compliance
initiatives division for four
years. Prior to working for the
State of North Carolina, she
worked in logistics and admin-
istration in the private sector
from 1991 to 2003. Cathy was
an active duty Soldier with the
U.S. Army where she worked
in maintenance as a welder and
logistics as a medical supply
specialist. In her key role for
the VISN, Cathy is responsible
for providing administrative
support to the program of-
cials and network executives.
Patrick
March is the
telehealth
data manage-
ment coor-
dinator for
the VISN.
He joined
the VISN staff in January and
comes to us from the Depart-
ment of the Army where he
served as a DoD civilian in-
formation technology data
management specialist. Addi-
tionally, Patrick is a Navy Vet-
eran with 26 years of dedicated
service. In his new role for the
VISN, Patrick is responsible
for providing telehealth pro-
gram analysis.
Katherine McMullin
joined the
organization
last fall as a
health sys-
tems special-
ist for tertiary
care. She
transferred
from the Durham VAMC
where she started as a coordi-
nator in process and systems
improvement working on
process action teams, patient
satisfaction improvement ac-
tivities, and data gathering and
analysis. She also worked as a
program analyst in ambulatory
care, where her duties includ-
ed data analysis and managing
space and equipment. Kathi is
a native of Rockville, MD, and
moved to North Carolina in
2002 to attend graduate school
at UNC. She is responsible for
providing administrative lead-
ership for tertiary care.
Allen
Moye is the
new VISN
6, Health
Administra-
tion Service
Lead. Born
and raised in
Beckley, W. Va., Moye was a
mechanic and airborne-quali-
ed Sergeant in the U.S. Army,
serving for six and a half years.
He joined the VA in 1995 and
has served in various admin-
istrative roles at the Beckley
VAMC where he is currently,
chief, HAS. In his key role
as VISN HAS Lead, Moye is
responsible for serving as the
point of contact for matters
relating to Health Administra-
tion Service.
James
R. Payne III
has served
as a VISN 6,
Area Emer-
gency Man-
ager since
August. He
James is a North Carolina na-
tive and holds a bachelor’s and
master’s degrees from Western
Carolina University. A mili-
tary retiree, James brings 20
years of leadership in various
military and forward deployed
roles including two combat
tours to his new position. His
certications include certied
emergency manager, hospital
emergency coordinator (Level
III), and anti-terrorism special-
New Arrivals, Roles Enhance VISN 6 Field Support
Continued on Pg 4

4
group to participate in several
roundtable discussions to put
the online lessons into action.
Tillman, who served as
facilitator for the discussions,
said compelling stories poured
out of Veteran panelists from
various branches, genders, and
periods of service, respond-
ing to questions like, “Tell
me about the day you enlist-
ed; why did you choose that
branch of service; and how did
your family react when you
told them.”
“The stories were real and
the atmosphere was priceless,”
said Tillman. “By stepping
back from looking at Veterans
as patients, and learning to look
at them as brothers, sisters,
fathers, and friends, the staff
gained valuable insight about
the sacrices of all of the brave
people who served. The inter-
nal connection with VA’s mis-
sion took form in ways both
emotional and authentic.”
Energized by the online
training and the roundtable dis-
cussions, the group was eager
to learn more.
North Carolina is home to
eight military bases. Why not
arrange a trip to one of these in-
stallations to see rsthand how
the military operates? Most of
the participants were not Veter-
ans and had little idea what life
on a military base was like.
A mutually benecial col-
laboration was born. Thirty
staff, and several VA contrac-
tors, embarked on a special tour
of the Seymour Johnson AFB.
“Seeing impressive aircraft
like the F-15E Strike Eagle and
the Boeing KC-135 Stratotank-
er, energized the group,” Till-
man said. “While the aircraft
were intriguing, talking with
the Airmen was truly remark-
able and gave us a new appre-
ciation for Veterans.”
The trip spawned a recip-
rocal visit to further cement
the partnership. About 30 Air-
men from the Seymour John-
son AFB visited the Durham
VAMC for rsthand military
cultural exchange. The Air-
men learned about enrollment,
observed clinicians, and were
briefed on various VA pro-
grams.
Most recently, the Airmen
returned once again and took
part in the National Salute to
Hospitalized Veterans. The Air-
men delivered Valentine’s cards
and spent time enjoying the
company of inpatient Veterans,
including those in the Commu-
nity Living Center.
“The concept was simple
but the experience was complex
as well as profoundly meaning-
ful,” Tillman concluded. “Our
exploration opened the eyes of
staff even further to the life ex-
periences of those that choose
to wear our nation’s uniform.
We took the military cultural
awareness training to a whole
new level and have become a
more understanding workforce
because of it.”
He said medical center
leaders were ooded with posi-
tive comments from training
participants about how the ini-
tiative has given new perspec-
tive to the work they do every
day. Next up, Durham VAMC
is planning to do training and
visit Fort Bragg near Fayette-
ville, one of the Army’s largest
installations.
Steve Wilkins
N.C. American Legion Winter Conference
D. Mack Wood, a retired American Legion district manager,
greets VISN 6 Deputy Network Director Gus Davila following
Davila’s presentation to the North Carolina American Legion
Winter Conference in Raleigh. Davila highlighted VISN con-
cerns including beneciary travel and partnerships with com-
munity organizations to enhance health care opportunities for
Veterans during his talk.
Courtesy Photo
Duke and Durham VAMC Medical Residents Leon Cannizzaro and
Edward Coverstone sit in the cockpit of an Air Force KC-135 Stra-
totanker while learning more about Air Force operations.
Durham continued from Pg 1
ist. He is also a basic and ad-
vanced disaster life support in-
structor and homeland security
exercise evaluation program
instructor.
Barbara A. Rountree
joined the
VISN 6 staff
in December
as telehealth
program as-
sistant. She
transferred
from the Dur-
ham VAMC, where she served
as a program support assistant
in the home telehealth pro-
gram, while participating in
other programs. She graduated
from the Mid-Atlantic Devel-
opment Program in 2009 and
Leadership Development In-
stitute Program in 2010. She is
a certied mentor. In her new
role, Barbara is responsible
for providing administration
and program assistance to the
VISN Telehealth Manager.
Sheila K. Zeto became
VISN rural
coordina-
tor in Au-
gust. She has
served as
rural health
Integrator at
the Beckley
VAMC since January 2010
and as acting VRC since April
2011. She brings an extensive
background in project manage-
ment and data analysis to her
new position, stemming from
her experience as a research
biologist and administrative
ofcer with the U.S. Depart-
ment of Agriculture and as a
VA safety manager and emer-
gency preparedness coordina-
tor prior to her work in rural
health. Zeto is responsible
for providing project manage-
ment, technical expertise and
team leadership in order to co-
ordinate VISN 6 rural health
programs. She will also serve
as liaison between VISN 6 and
the Ofce of Rural Health at
VA Central Ofce.
New Arrivals
Continued from Pg 3
5
By Durham VAMC
public affairs
NC Prevention Partners
(NCPP), a non-prot leader
in reducing preventable ill-
ness and early death, recently
awarded the Gold Heart stan-
dard to the Durham VAMC for
its comprehensive treatment of
tobacco dependence in Veter-
ans.
“This distinction is a
tribute to all of the Durham
VAMC staff members who are
working here and at our afli-
ated community-based outpa-
tient clinics to help Veterans
get healthier by quitting tobac-
co,” says Dr. Clint McSherry,
Durham VAMC’s HBC. “And
it’s also a testament to the val-
ue and effectiveness of VA’s
national tobacco cessation
standards, guidelines, and pro-
grams.”
The Durham VAMC is
one of
the rst
of North
Caro-
lina’s
acute
care hos-
pitals to
achieve
Gold
Heart
status.
It mer-
ited the
award
by meeting NCPP’s key re-
quirements for a successful
quit-tobacco system for pa-
tients. The criteria include
screening patients for tobacco
use as a “vital sign,” providing
team-based cessation counsel-
ing, promoting evidence-based
treat-
ment,
and
evaluat-
ing the
system
on a
con-
tinuous
basis.
NCPP
has
part-
nered
with
several organizations to help
hospitals across the state suc-
cessfully implement effective,
empirically based quit-tobacco
systems similar to the one in
place at each of the Durham
VAMC facilities. As part of its
mission of “prevention rst for
a healthier North Carolina,”
NCPP plans to continue to
collaborate with the Durham
VAMC on additional wellness
initiatives.
“We are especially proud
of this achievement because
Durham VAMC is one of only
four hospitals in the state to
have earned the Gold Heart
award from NCPP,” says Mc-
Sherry, a health psychologist
with 20 years of experience in
tobacco cessation. “We’re go-
ing to continue to help VA lead
the way in its commitment to
promoting health and prevent-
ing disease in our nation’s Vet-
erans.”
Durham Receives “Gold Heart” From NC Prevention Partners
and servicemembers who experienced severe injuries (including
brain injuries) to more than one organ system. During his visit, the
Secretary underscored themes from the State of the Union address,
in which President Obama outlined his strong commitment to Vet-
erans.
He also met with patients and staff at the polytrauma center
and the center’s in-patient unit.
Following the visit to the polytrauma center, Secretary Shin-
seki and Congressman Scott participated in a demonstration of the
simulator now available for patients in the STAR program and to
discuss the simulator’s role in the program.
The STAR program provides comprehensive vocational and
physical rehabilitation to facilitate the transition of servicemem-
bers with amputations into unrestricted military duty or competi-
tive civilian employment.
The simulator, provided by Caterpillar and Simformotion,
provides patients an opportunity to gain an understanding of heavy
equipment machine controls and to learn proper operating proce-
dures well before their training on actual machines.
The simulated environment provides the patient a safe place
to learn about the machinery, while enhancing their performance
skills.
Hydraulic Excavator training is set in a construction environ-
ment and progressively takes the operator from basic controls ori-
entation through more complex training exercises.
The simulator provides hands-on learning in a safe and eco-
nomical way to enhance traditional operator training programs.
The equipment is an excellent addition to the STAR program, pro-
viding another tool that can be used toward achieving the goal of
returning servicemembers to full time employment in their com-
munities.
Less than a week later, the Secretary returned to the Mid-At-
lantic Health Care Network region when he made a short stop in
Hampton Roads/Norfolk, Va., area to bring attention to another VA
priority, helping Veterans nd jobs.
He visited Tidewater Tech, a trade school that recently began
accepting military Veterans using the Post-9/11 GI Bill. The school
offers training in auto repair, welding, building maintenance, and
heating, ventilation and air conditioning. A new provision that
went into effect in October extended the GI Bill’s benets to in-
clude apprenticeships, on-the-job training, vocational schools and
non-degree programs.
According to school ofcials, the number of Veterans enroll-
ing in its programs has increased signicantly since the change
took effect. Approximately 15 percent of Tidewater’s 200 students
are Veterans using the GI Bill. In addition, about half the school’s
instructors are Veterans
Shinseki began his visit by meeting privately with a handful
of student Veterans, followed by a quick tour of the school. Speak-
ing to reporters after the visit the VA Secretary said that, although
unemployment among Iraq and Afghanistan Veterans is slowly
falling, it is still far too high.
He said the original GI Bill helped remake America after
World War II, and that with the benets that include trade schools,
he thinks this GI Bill will do the same.
“I’m very condent,” Shinseki said, “that this generation is
equally capable of rebuilding our nation.”
Jennifer Askey
VA Secretary Eric Shinseki meets with Veterans attending Tide-
water Tech Feb. 9 to discuss Post-9/11 GI Bill changes that allow
student Veterans to enter the labor force with skills gained from
vocational training programs.
Shinseki continued from Pg 1
6
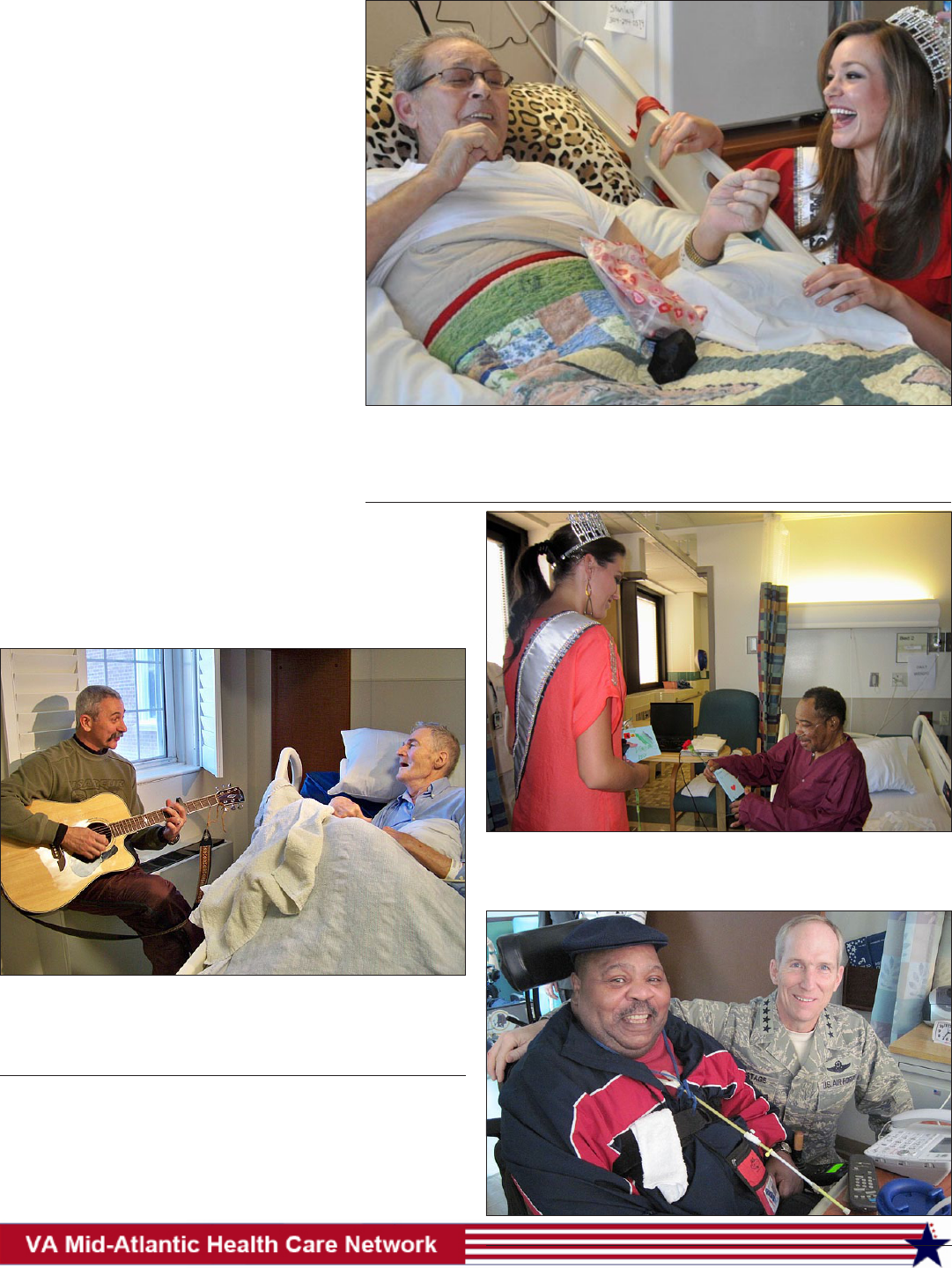
By VISN 6 public affairs
Veterans receive high quality care in VA fa-
cilities every day. The message that they are tru-
ly appreciated for their service and sacrices in
defending our country should never go unspoken
even when the demands of everyday life loom
large.
Because VA and its employees appreciate
the lives and sacrices of each and every Veter-
an, VA health facilities around the nation partici-
pate in a weeklong National Salute to Veterans
to celebrate Veteran patients, and remind them
VA doesn’t take Veterans for granted. The salute
usually takes place throughout a week in Febru-
ary spanning Valentines’ Day.
Executed by VA medical center voluntary
services staff, the annual VA National Salute to
Veteran Patients program began in 1978. Vet-
erans in and around VA facilities are treated to
special meals and activities, visits from distin-
guished guests and special entertainment events
meant to honor the service and lives of Ameri-
ca’s heroes.
More than a million cards and letters are sent to VA patients
each year during the National Salute. VISN 6 activities included
the various festivities held at each facility along with a “Valen-
tines’ For Veterans” concert featuring country music star Aaron
Tippin Feb. 9 in Salem, Va. Although Veterans have the respect
and devotion of VA employees every day, the National Salute to
Veteran Patients pronounces in an obvious way that we care.
National Salute Tells
Veterans We Care
Debbie Voloski
Country music star Aaron Tippin sings a tune for Veteran Mark
Sharp during Tippin’s visit to Salem VAMC Feb. 9. Later that eve-
ning, Tippin gave a “Valentine For Veterans” Concert at the Sa-
lem Civic Center.
Debbie Voloski
Air Force Retired Veteran Larry Snuffer entertains Miss West Virginia USA Andrea
Rogers with a story during her visit to Beckley VAMC in honor of VA’s National
Salute to Veteran Patients. Snuffer told staff that visits such as this “make him feel
lifted, elated, and help to make his last days worthwhile.”
Jennifer Askey
(Right) Air Force Gen. Gilmary M. “Mike” Hostage, commander,
Air Combat Command, delivers a card to Veteran Eugene Hodge
in the Hampton VAMC Spinal Cord Injury Unit during the Na-
tional Salute to Veterans Week.
Pete Tillman
Sydney Perry, Miss North Carolina USA, brought a smile to the
face of inpatient Hudson Huff as she delivered a Valentine’s Day
card and carnation at the Durham VAMC.
7
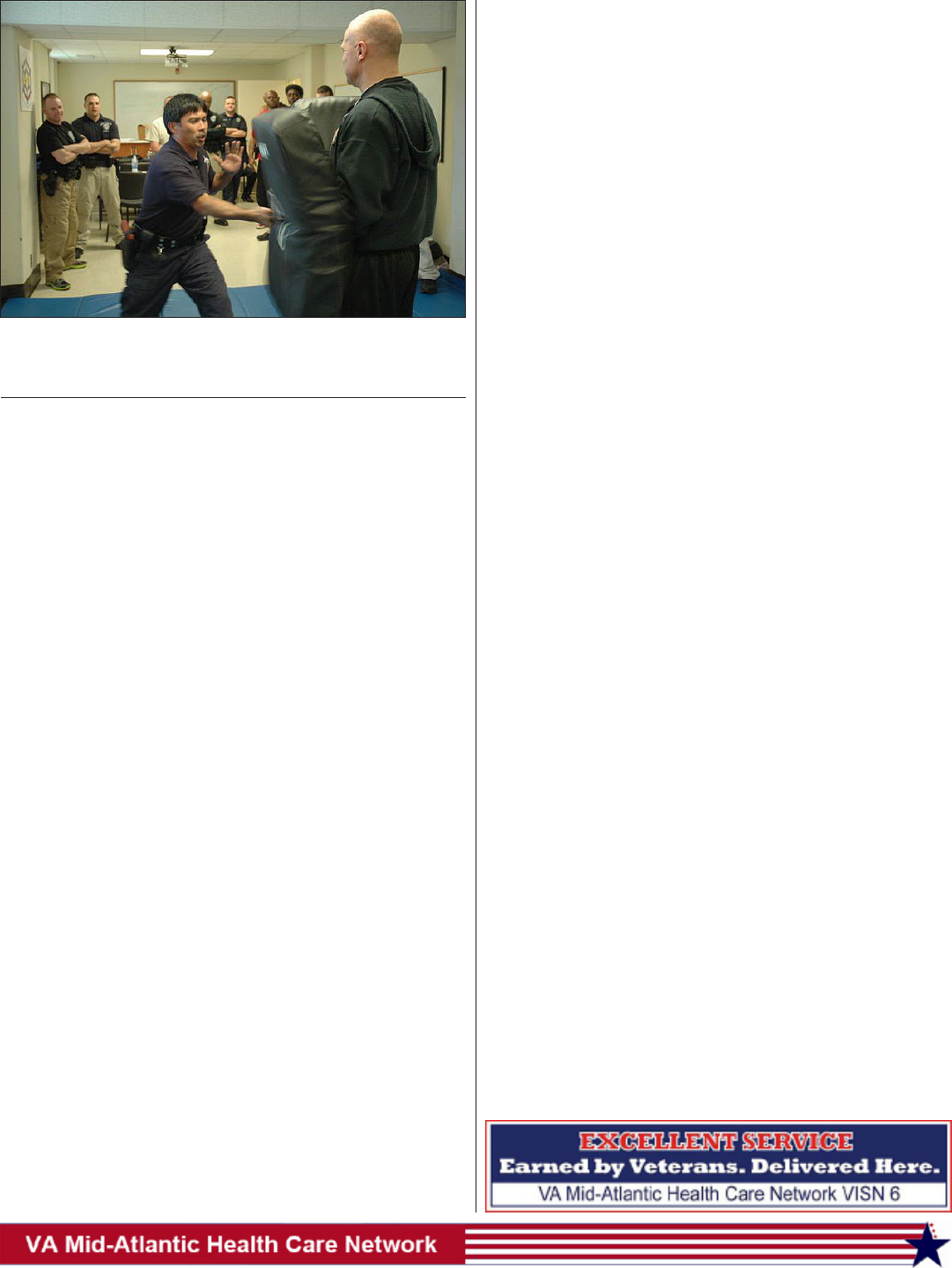
By Robin DeMark
Fayetteville VAMC
Eleven police instructors
from ve states along the East
Coast joined the Fayetteville
VAMC Police Service to com-
plete a new law enforcement
baton training and certication
course conducted by the mobile
training team from the VA Law
Enforcement Training Cen-
ter in North Little Rock, Ark.,
Feb. 3. The training comes as
VA Police Services nationwide
transition from carrying side
handle batons to new expand-
able straight batons.
“The new baton is de-
signed to stun our primary tar-
gets, the large muscle groups
of the body, and is less likely
to break bones or cause per-
manent paralysis,” said Sgt.
Peter McDannell, Fayetteville
VAMC Police Services. “We
are here to serve the Veterans
and seek voluntary compliance
rst.”
According to McDannell,
the primary mission for all VA
police ofcers is to provide
professional law enforcement
service to ensure the safety of
Veterans, patients and employ-
ees. Encounters require differ-
ent defensive techniques and
control measures that require
police ofcers to elevate or de-
escalate the level of force need-
ed.
Special Agent Anthony
Everett, who is the physical
branch lead at the LE Training
Center, served as lead instruc-
tor for the mobile training team.
He said police ofcers are often
placed in situations where they
must use force to control an in-
dividual while at the same time
employing a force option that is
necessary and justied.
“Batons are tools that al-
low a different force option
between empty hand controls
and deadly force,” Everett said.
“The goal is to achieve con-
trol without causing unneces-
sary injury or to use the least
amount of force to achieve that
control. This is how we educate
our trainers to teach our police
ofcers.”
He added the LETC in-
structors were as good as any
at other law enforcement agen-
cies across the country. “Law
enforcement trainers must
have the maturity and passion
to teach, and believe in their
mission always; to get their
students to the highest standard
without fail,” Everett said.
VA law enforcement is re-
sponsible for the protection of
patients, visitors, employees,
property, and maintaining law
and order on property as di-
rected by the Veterans Health
Administration.
For more information
about the VA Law Enforcement
Center or VISN 6 Police Ser-
vices, visit www.osp.va.gov/
Law_Enforcement_Training_
Center_LETC or http://vaww.
visn6.va.gov/police.aspx, re-
spectively.
Ofcers Transition To New Baton
Brad Garner
Fayetteville VAMC Police Ofcer Sgt. Allen Tolentino strikes ‘sus-
pect,’ lead mobile training team instructor Special Agent Anthony
Everett, with the expandable straight baton.
By Bruce Sprecher
VISN 6 public affairs
Like many items of the
past, U.S. Treasury checks are
being replaced by safer, more
efcient electronic means.
People and organizations pre-
viously paid by check will soon
receive payment via electronic
funds transfer to their bank ac-
counts.
During Fiscal Year 2010,
the U.S. government spent
more than $540 million to pro-
cess U.S. Treasury checks. In
December 2010, the Treasury
decided to eliminate, with few
exceptions, checks by May
2013.
In line with the Treasury
directive, VA will stop issuing
checks by Dec. 31, 2012.
The shift to EFT should be
welcome news to Veterans as
there will be no chance of lost
checks and people will spend
less time waiting in line at the
cashier’s window, according to
VA ofcials. Efforts are under-
way nationwide to prepare all
recipients to receive their funds
electronically.
Gus Davila, VA Mid-At-
lantic Health Care Network
deputy director, said the net-
work spent more than $47
million on beneciary travel
during Fiscal Year 2011. “Ac-
complishing these payments
required tens of thousands of
transactions that cost money
that will be better spent on pa-
tient care when the EFT pro-
cess is up and running,” Davila
said.
Davila went on to say that
while the medical centers are
each progressing toward the
EFT process, all efforts are be-
ing made to ensure the transi-
tion does not cause a hardship
for anyone. Because the transi-
tion to the EFT process requires
the inputting of data for mil-
lions of Veterans nationwide,
the implementation is being
staggered throughout the coun-
try and throughout the network.
VHA is working with the
nance service center in Aus-
tin, Texas, to automate the pro-
cess and has also undertaken an
initiative to reduce cash pay-
ments through use of a debit
card program through Treasury
and Comerica Bank. The pilot
debit card will debut later this
year in some locations around
the country. Until then, manu-
ally lling out the EFT Form
will be the way to go.
Although some Veterans
are seen at multiple VA sites,
only one EFT Form is required.
When turning in vouchers, Vet-
erans should inform the clerks
if they have previously turned
in the form. Filling out multiple
EFT forms may actually cause
delays in getting paid. The only
time a new EFT form should
be accomplished, ofcials said,
is when there is a change to a
Veteran’s banking information,
such as changing banks or hav-
ing the money go to a different
account.
While the goal is to reduce
cash on hand and eliminate
check payments, cash reim-
bursement will remain an op-
tion for those without resources
to return home that day or who
are unable to maintain a depos-
itory account.
To ensure no one is caught
off guard or experiences a
hardship, medical centers are
notifying patients through the
mail and with signage located
throughout each facility detail-
ing the dates of the conversion.
“Durham and Hampton
medical centers have begun the
changeover and both facilities
have sent letters to all patients
who received travel payments
in the past year explaining the
need to ll out and turn in an
electronic funds transfer form
SF -3881,” Davila said.
The forms can be picked
up at the medical centers, or
downloaded off the web from
www.fms.treas.gov/pdf/3881.
pdf. Veterans should ll out the
middle and bottom sections.
The medical center will ll out
the top portion.
Sun To Set On Treasury Checks
8
More than 216,000 North
Carolina residents served in
Vietnam, and some 1,600 made
the ultimate sacrice in that
war. The USO of North Caroli-
na and Charlotte Motor Speed-
way, with support from the
North Carolina Association of
Broadcasters, will honor their
service with a Vietnam Veter-
ans Homecoming Celebration.
The Vietnam Veterans
Homecoming Celebration
2012 is set to be an unforget-
table experience featuring live
entertainment, displays and
demonstrations, and military
salutes.
Representatives from VA
medical centers from North
and South Carolina will be on
hand to provide information
and enroll eligible Veterans.
Additionally, counselors from
area Vet Centers, along with
a team from the Winston Sa-
lem VBA regional ofce and
a representative from National
Cemetery Administration will
be on hand. Veterans interest-
ed in enrolling should bring a
copy of their DD-214.
Homecoming For Vietnam Veterans
George C. Duggins,
North Carolina
Vietnam Veterans of America
Region 3 Conference
Date: March 28 to April 1, 2012
Location: Doubletree Biltmore Hotel, 115 Hendersonville
Road, Asheville, NC, 828-771-2277
Contact person: Joe Kristek, Pres. NC VVV State Council,
910-673-4562
Room Reservations: Call 828-274-1800. Make sure you tell
them you are attending the Region 3 conference to receive
the group rate.
Conference and Hotel Registration Information available on
NC VVA State Council website: www.vva-nc.org
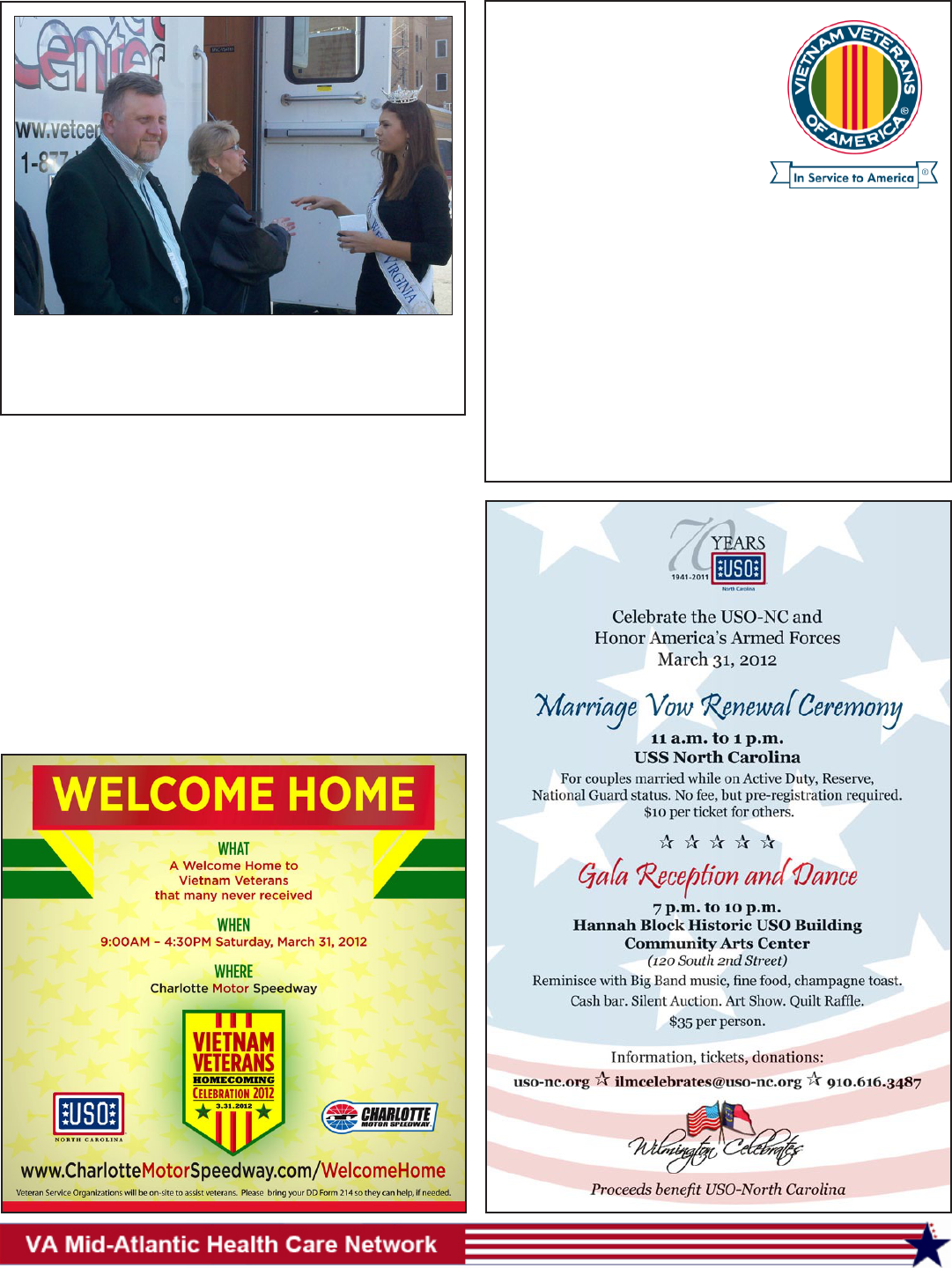
Courtesy Photo
Spenser Wempe, Miss West Virginia, toured Beckley’s new
Mobile Vet Center, a customized vehicle designed to provide
Veterans with vital, on-the-spot counseling and reintegration
services Feb. 17.
9
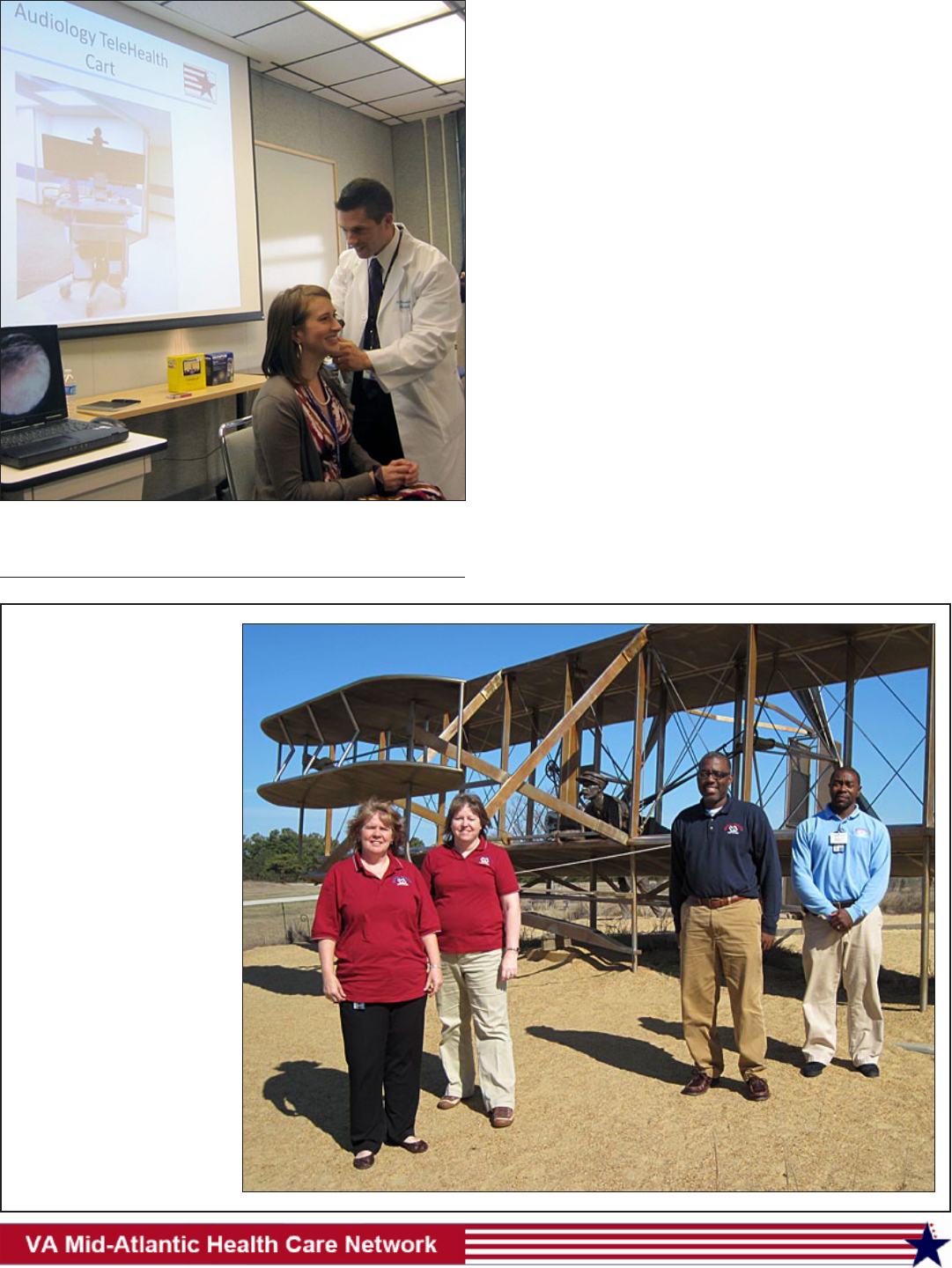
As part of the rural health ini-
tiative, Hampton’s Rural Health
Team reaches out in every di-
rection in their effort to enroll
Veterans for VA health care.
Hampton VAMC’s Rural Health
Initiative team members trav-
eled to the Outer Banks area
of North Carolina, Feb 22, to
conduct a Veteran’s benet out-
reach event in Kill Devil Hills.
The team (from left) Deborah
Frondelli, nurse educator, Eliz-
abeth Halvorsen, program sup-
port assistant, Eddie Hughes,
medical support assistant,
Carvin Harmon, social worker,
take a brief pause in front of the
monument to the Wright Broth-
ers at Kill Devil Hills.
James Coty
Hampton’s Rural
Health Team
Reaches Out
By Tim Devine
Durham VAMC
Last year the Durham VAMC Audiology Clinic was selected
as one of only 10 VA Centers nationally to participate in a pilot
program that allows an audiologist in Durham to program hearing
aids on a patient at a local CBOC.
With the help of an audiology health technician who travels
to the patient site, the doctor at Durham uses a teleconferencing
camera and specialized computer software to control the audiol-
ogy instruments located at the CBOC to verify hearing aid perfor-
mance and make needed adjustments.
An obvious benet of this new service is that patients will no
longer have to travel to Durham for follow-up hearing healthcare.
An equally important benet, said Dr. Nancy Jones, chief of au-
diology and speech pathology at Durham, may be that Veterans
will get better use of their amplication because, by providing this
service at a more convenient location, patients will be more likely
to attend follow-up appointments.
“We hope that instead of giving up on their hearing aids, Vet-
erans will now come back and talk with us about the situations that
still give them problems,” Jones said. “Often all that’s required is
a minor adjustment in the program.”
So far, patient feedback has been overwhelmingly positive.
One Veteran volunteered that the care was “just like being at Dur-
ham, but without the long trip.”
Currently, Veterans must still travel to Durham for their hear-
ing tests, but phase II of this pilot program will allow for many of
these exams to be performed at CBOCs too. This phase is due to
begin in September 2012.
Tele-Audiology Reduces Trips
Pete Tillman
Durham audiology staff demonstrate how the tele-audiology pro-
gram is used to help Veterans reduce travel and get high quality
care.
By Terri Moon Cronk
American Forces Press Service
WASHINGTON – It once was thought that servicewomen neither
were exposed to the same combat situations as men nor developed
the same psychological injuries. Ofcials now recognize other-
wise.
“With the type of combat we’re in now, it’s probably the only
place where men and women really are equal,” therapist Jeanine
Aversa says in “The Long Road Home,” February’s installment of
the Pentagon Channel series “Recon.”
Ofcials estimate that the percentage
of women in the military has doubled in the
past 30 years. But that increase, the “Recon”
segment noted, has come with a rise in prob-
lems such as homelessness, drug addiction
and post-traumatic stress disorder among
female Veterans.
The Defense and Veterans Affairs de-
partments work together to address service
members’ physical, mental and emotional
injuries, including those of women, so of-
cials say it’s now easier for female Veterans
to ask for help.
Kate McGraw, acting deputy direc-
tor for the psychological health, clinical
standards of care at the Defense Centers
for Excellence for Psychological Health
and Traumatic Brain Injury at the Walter
Reed National Military Medical Center in
Bethesda, Md., said a “huge inux” of con-
gressional funding and Defense Department
support on the issues facing female Veterans
have helped address psychological health
and traumatic brain injury.
Focus groups, growing numbers of sup-
port groups and a mental health anti-stigma
campaign are part of the DOD and VA support for female Veterans,
she said.
Battling the stigma of seeking mental health counseling also
has remained a concern among military leaders, McGraw noted.
Some servicemembers don’t seek help, she explained, because
they believe doing so could hurt their careers. So “The Long Road
Home” is an attempt to try to de-stigmatize those fears.
Peculiar to women is an apparent higher rate of “co-occur-
rence” of PTSD and depression when compared with men after
returning from deployment, McGraw said. Other behaviors also
can play a part in women’s lives, she said.
“Women tend to have a higher incidence of binge drinking …
and a higher incidence of eating disorder behavior … as compared
to males,” McGraw said, citing recent literature on studies con-
ducted during the past ve years.
More doors are open to women in the military now than be-
fore. That progress has come with a price.
Veteran Jen Crane knows about that price. She began to have
panic attacks while searching for work after she left the military.
She couldn’t continue her military job as a paralegal in the civilian
sector, so she took a bartending job. There, she was introduced to
cocaine. She said it brought her anxiety down and made her social.
Eventually, her penchant for drugs nearly cost her everything.
Crane turned to prostitution to support her drug habit, and
became homeless and broke. As her situation spiraled downward,
she decided to take her life. But before she could act on her plan,
police arrested her for drug possession.
Crane went to court, and began receiv-
ing counseling from Aversa. With support
from her therapist, the courts and her family,
today she is married, has a child and is the
national spokeswoman for a nonprot orga-
nization, traveling around the country to tell
her story.
Experiences like Crane’s are helping
to change the care female Veterans receive.
“We’re undergoing a culture change within
the Department of Veterans Affairs,” Pa-
tricia Hayes, the VA’s chief consultant on
women’s health, told “Recon.”
VA estimates that 6,500 female Veter-
ans are homeless and live on the nation’s
streets – double the number from 10 years
ago. VA also reported that one in ve wom-
en Veterans reported military sexual trauma
during their military service, and the num-
ber of women with PTSD is increasing.
McGraw outlined signs that someone
is struggling with readjustment issues. She
cited symptoms such as the inability to get
good sleep, nightmares, or the feeling of
reliving events from a deployment when
awake, disturbing dreams about deployment
events, changes in mood, irritability feeling increasingly on edge
or keyed up, or getting startled easily.
Veteran Genevieve Chase, who suffered a traumatic head in-
jury after the vehicle she was riding in exploded, told “Recon” that
in spite of the struggles women try to overcome, their patriotism
remains intact.
“Even the women who are trying to get on their feet or have
been struggling through military sexual trauma, substance abuse,
suicide or any major issue, when they come home, every single
one of them is still proud of their service,” Chase said.
The Pentagon Channel’s “Recon” series is a monthly, 30-min-
ute broadcast that provides an in-depth look at operations, mis-
sions, military events, history and other subjects highlighting the
accomplishments of U.S. military men and women. All “Recon”
programs are posted on the Pentagon Channel’s website at www.
pentagonchannel.mil/recon/.
10
Ofcials: Women Can Suffer Same Deployment Ills As Men
Women Veterans comprise one of the fastest growing populations of Vet-
erans. Today, there are more than 1.8 million living women Veterans of
the nearly 22.7 million Veterans. Mid-Atlantic Health Care Network (VISN 6) totals are as follows: North Carolina - 70,729,
Virginia - 93,637, West Virginia - 12,015. The population of women Veterans has increased from 1.1 million in 1980 to nearly
2 million today, and women are projected to be more than 10 percent of the Veteran population by 2020. The average age of
female Veterans is 48 (male 63). Of the 1.8 million U.S. women Veterans, more than 500,000 have enrolled in the VA health care
system. That number is expected to grow by 30% in the next ve years. Women currently comprise more than 14% of the active
duty military, nearly 18% of Guard and Reserves, and nearly 6% of VA health care users. More than 50% of female OEF/OIF
Veterans have received VA health care.
Facts About Women Veterans
11
WASHINGTON – The Depart-
ment of Veterans Affairs part-
nered with the First Army at
Camp Shelby, Miss., to launch
a streamlined version of its on-
line application for VA health
benets (VA Form 1010EZ)
for service members return-
ing from deployment. VA will
introduce it at demobilization
sites nationwide by early spring
2012.
“This online application
demonstrates VA’s commitment
to work with the Department of
Defense to make it easier for
servicemembers to get the care
they earned by their service,”
said Secretary of Veterans Af-
fairs Eric K. Shinseki. “The
new, online system noticeably
reduces the paperwork and re-
duces a 10-day process to three
days.”
The application is used to
enroll in the VA health care sys-
tem, which has more than 1,000
sites of care across the country.
Enrollment for VA health
care is done as part of a service-
member’s demobilization. The
online form allows the appli-
cation to be completed during
a regularly scheduled brieng
for all service members on VA
benets.
Quick enrollment is im-
portant for returning troops
because recently discharged
combat Veterans are eligible
for ve years of cost-free care
and medications for conditions
potentially related to combat
service.
The new application was
piloted as part of the demobili-
zation process at Camp Shelby.
Based on the results, VA plans
to collaborate with DoD to of-
fer this online application at all
61 demobilization sites nation-
ally.
For more information,
contact VA at 1-877-222 VETS
(8387) or visit www.va.gov/
healthbenets.
Streamlined Online Application To
Launch At Demobilization Sites
WASHINGTON – Building
upon a 66-year partnership
with the states, the Department
of Veterans Affairs has signed
a formal agreement with the
National Association of State
Directors of Veterans Affairs
(NASDVA) to enhance their re-
lationship.
“State agencies are invalu-
able partners in providing ser-
vices to Veterans,” said Sec-
retary of Veterans Affairs Eric
K. Shinseki. “Our historic col-
laboration with NASDVA has
ensured that countless Veterans
receive the benets they have
earned.”
The agreement pledges the
two groups to maintain “effec-
tive communications, an ex-
change of ideas and informa-
tion, identication of emerging
needs, and continuous reevalu-
ation of existing programs.”
NASDVA represents the
state departments of Veterans
affairs in dealings with VA and
with Veterans residing in their
respective states. The states
fund about $5 billion in benets
and services for Veterans.
The involvement of state
governments in Veterans af-
fairs goes back to the Ameri-
can Revolution, with the fed-
eral government becoming
involved after the Civil War. In
1946, NASDVA was created to
coordinate programs between
VA and the states, territories
and the District of Columbia.
Secretary Shinseki signed
the agreement Feb. 13 during
the NASDVA mid-winter con-
ference in Alexandria, Va.
VA, NASDVA Sign Partnership Pact
Yearly u vaccination
should begin in September, or
as soon as the vaccine is avail-
able, and continue throughout
the u season, which can last
as late as May. This is because
the timing and duration of u
seasons vary. While u season
can begin as early as October,
seasonal u activity peaks in
January, February or later.
Inuenza is responsible for
200,000 hospital admissions
and 36,000 deaths nationwide
every year. According to the
federal Centers for Disease
Control and Prevention, vacci-
nation of all health care work-
ers is strongly recommended
to prevent transmission of the
illness to patients, especially
those with long-term medical
conditions who are at high risk
for serious complications from
the u. The CDC recommends
that all health care workers –
even those who are not directly
involved in patient care (e.g.,
clerical, housekeeping and ad-
ministrative staff, volunteers,
etc.) – be vaccinated annually.
If you have questions
about whether you should get a
u vaccine, consult your health
care provider.
When To Get Seasonal Flu Vaccine
WASHINGTON – VA an-
nounced its participation in the
largest state-federal legal settle-
ment in history that deals with
problems within the mortgage
industry.
VA joined with the Depart-
ment of Justice, a coalition of
state attorneys general and oth-
er federal agencies in the settle-
ment.
The nation’s ve largest
mortgage servicers have agreed
to this landmark $25 billion
settlement that addresses past
mortgage loan servicing and
foreclosure abuses, provides
substantial nancial relief to
borrowers, and establishes sig-
nicant new homeowner pro-
tections in the future.
In addition to cash pay-
ments to avoid litigation, the
banks also agree to undertake
other activities, such as prin-
cipal forgiveness, interest-
rate-reduction renancing, and
forbearance during unemploy-
ment.
The settlement also en-
hances protections available
under the Servicemembers
Civil Relief Act and provides
additional assistance when ser-
vicemembers are forced to sell
their home at a loss due to reas-
signment to another location.
VA has always provided
assistance to Veterans and ser-
vicemembers who experience
trouble paying their mortgage,
whether they have a VA loan
or not. Depending on the situ-
ation, VA’s loan specialists can
intervene on a Veteran’s behalf
to help pursue home-retention
options such as repayment
plans, forbearances and loan
modications.
To get help, Veterans and
servicemembers – even those
without a VA guaranteed loan
– may call a national toll-free
number, 877-827-3702 to speak
with VA loan specialists who
will provide information about
the process of obtaining a VA-
guaranteed home loan, or as-
sistance in retaining their home
loan or avoiding foreclosure.
Information about the VA
Home Loan Guaranty program
is also available online at www.
benefits.va.gov/homeloans.
To see videos of Veterans who
reached out to VA and were able
to keep their homes or avoid
foreclosure, please visit www.
benets.va.gov/homeloans/alt-
foreclosure.asp.
VA Joins Mortgage Bank Settlement
Volunteer Opportunities
For info. on opportunities to volunteer in your area, contact:
Asheville Darlene Laughter 828-299-2514
Beckley Cheryl Yost 304-255-2121, ext. 4162 or 4165
Durham Ronni Miller 919-286-0411, ext. 7810
Fayetteville Norma Fraser 910-822-7027
Hampton Judith Curtis 757-722-9961, ext. 3124
Richmond Janet Langhorne 804-675-5000, ext. 4989
Salem Ann Benois 540-224-1919
Salisbury Nancy Perry 704-638-3409

Albemarle POC
1845 W City Drive
Elizabeth City, NC
252-331-2191
Asheville VAMC
1100 Tunnel Road
Asheville, NC 28805
828- 298-7911, 800-932-6408
www.asheville.va.gov/
Beckley VAMC
200 Veterans Avenue
Beckley, WV 25801
304-255-2121, 877-902-5142
www.beckley.va.gov/
Beckley Vet Center
1000 Johnstown Road
Beckley, WV 25801
304-252-8220
Brunswick Outreach Clinic
20 Medical Campus Drive
Supply, NC 28462
910-754-8574
Charlotte Vet Center
2114 Ben Craig Dr.
Charlotte, NC 28262
704-549-8025
Charlotte CBOC
8601 University East Drive
Charlotte, NC 28213
Charlottesville CBOC
650 Peter Jefferson Pkwy
Charlottesville, VA 22911
434-293-3890
Danville CBOC
705 Piney Forest Rd.
Danville, VA 24540
434-710-4210
Durham VAMC
508 Fulton St.
Durham, NC 27705
919-286-0411, 888-878-6890
www.durham.va.gov/
Emporia CBOC
1746 East Atlantic Street
Emporia, VA 23847
434-348-1500
Fayetteville VAMC
2300 Ramsey St.
Fayetteville, NC 28301
910-488-2120, 800-771-6106
www.fayettevillenc.va.gov
Fayetteville Vet Center
4140 Ramsey St.
Fayetteville, NC 28311
910-488-6252
Franklin CBOC
647 Wayah St.
Franklin, NC 28734-3390
828-369-1781
Fredricksburg CBOC
1965 Jefferson Davis Highway
Fredericksburg, VA 22401
540-370-4468
Greensboro Vet Center
2009 S. Elm-Eugene St.
Greensboro, NC 27406
336-333-5366
Greenbrier County CBOC
804 Industrial Park Rd.
Maxwelton, WV 24957
304-497-3900
Greenville CBOC
800 Moye Blvd.
Greenville, NC 27858
252-830-2149
Greenville Vet Center
1021 W.H. Smith Blvd.
Greenville, NC 27834
252-355-7920
Hamlet CBOC
100 Jefferson Street
Hamlet, NC 28345
910-582-3536
Hampton VAMC
100 Emancipation Dr.
Hampton, VA 23667
757-722-9961, 888-869-9060
www.hampton.va.gov/
Hickory CBOC
2440 Century Place, SE
Hickory, NC 28602
828-431-5600
Hillandale Rd. Annex
1824 Hillandale Road
Durham, North Carolina 27705
919-383-6107
Jacksonville CBOC
241 Freedom Way
Midway Park, NC 28544
910-353-6406, 910-353-6406
Jacksonville, N.C. Vet Center
110-A Branchwood Driv
Jacksonville, NC 28546
910-577-1100
Lynchburg CBOC
1600 Lakeside Drive
Lynchburg, VA 24501
434-316-5000
Morehead City CBOC
5420 U.S. 70
Morehead City, NC 28557
252-240-2349
Norfolk Vet Center
1711 Church Street
Norfolk, VA 23504
757-623-7584
Princeton Vet Center
905 Mercer Street
Princeton, WV 24740
304-425-5653
Raleigh CBOC
3305 Sungate Blvd.
Raleigh, NC 27610
919-212-0129
Raleigh II Annex
3040 Hammond Business Place
Raleigh, NC 27603
919-899-6259
Raleigh Vet Center
1649 Old Louisburg Rd.
Raleigh, NC 27604
919-856-4616
Richmond VAMC
1201 Broad Rock Blvd.
Richmond, VA 23249
804-675-5000, 800-784-8381
www.richmond.va.gov/
Roanoke Vet Center
350 Albemarle Ave., SW
Roanoke, VA 24016
540-342-9726
Robeson County CBOC
139 Three Hunts Drive
Pembroke, NC 28372
910-521-8452
Rutherford County CBOC
374 Charlotte Rd.
Rutherfordton, NC 28139
828-288-2780
Salem VAMC
1970 Roanoke Blvd.
Salem, VA 24153
540-982-2463, 888-982-2463
www.salem.va.gov/
Salisbury VAMC
1601 Brenner Ave.
Salisbury, NC 28144
704-638-9000, 800-469-8262
www.salisbury.va.gov/
Staunton CBOC
102 Business Way
Staunton, VA 24401
540-886-5777
Tazewell CBOC
123 Ben Bolt Ave.
Tazewell, VA 24651
276-988-2526
Virginia Beach CBOC
244 Cleareld Avenue
Virginia Beach, VA
757-722-9961, ext. 1900
Virginia Beach Vet Center
324 Southport Circle, Suite 102
Virginia Beach, VA, 23452
757-248-3665
Wilmington CBOC
736 Medical Center Drive
Wilmington, NC 28401
910-763-5979
Winston-Salem CBOC
190 Kimel Park Drive
Winston-Salem, NC 27103
336-768-3296
Winston-Salem Annex
2101 Peters Creek Parkway
Winston-Salem, NC 27127
336-761-5300
Wytheville CBOC
165 Peppers Ferry Rd.
Wytheville, VA 24382-2363
276-223-5400
12
VISN 6 Sites of Care
