Patient Experience Journal Patient Experience Journal
Volume 6 Issue 3 Article 12
2019
Enhancing emergency care environments: Supporting suicidal Enhancing emergency care environments: Supporting suicidal
distress and self-harm presentations through environmental distress and self-harm presentations through environmental
safeguards and the built environment safeguards and the built environment
Stephanie Liddicoat
Swinburne University, Melbourne, Australia
Follow this and additional works at: https://pxjournal.org/journal
Part of the Environmental Design Commons, Health Services Research Commons, Interior
Architecture Commons, Other Architecture Commons, Other Mental and Social Health Commons, and the
Psychiatric and Mental Health Commons
Recommended Citation Recommended Citation
Liddicoat S. Enhancing emergency care environments: Supporting suicidal distress and self-harm
presentations through environmental safeguards and the built environment.
Patient Experience Journal
.
2019; 6(3):91-104. doi: 10.35680/2372-0247.1361.
This Research is brought to you for free and open access by Patient Experience Journal. It has been accepted for
inclusion in Patient Experience Journal by an authorized editor of Patient Experience Journal.

Enhancing emergency care environments: Supporting suicidal distress and self-Enhancing emergency care environments: Supporting suicidal distress and self-
harm presentations through environmental safeguards and the built environment harm presentations through environmental safeguards and the built environment
Cover Page Footnote Cover Page Footnote
This article is associated with the Environment & Hospitality lens of The Beryl Institute Experience
Framework. (http://bit.ly/ExperienceFramework). You can access other resources related to this lens
including additional PXJ articles here: http://bit.ly/PX_EnvtHosp
This research is available in Patient Experience Journal: https://pxjournal.org/journal/vol6/iss3/12
Patient Experience Journal
Volume 6, Issue 3 – 2019, pp. 91-104
Patient Experience Journal, Volume 6, Issue 3 – 2019
© The Author(s), 2019. Published in association with The Beryl Institute
Downloaded from www.pxjournal.org 91
Research
Enhancing emergency care environments: Supporting suicidal distress and
self-harm presentations through environmental safeguards and the built
environment
Stephanie Liddicoat, Swinburne University, sliddicoat@swin.edu.au
Abstract
Self-harming and suicidal distress are prevalent, worldwide healthcare issues. Existing literature explains that both self-
harm and suicidal presentations at Emergency Departments are increasingly occurring, correlating to high costs in
healthcare service delivery. This scoping review aimed to (1) identify the current body of literature which examined the
relationship between design practice and service user experiences within Emergency Departments for self-harm and
suicidal distress presentations, and (2) identify the ways in which the built environment could increase the efficacy of
therapeutic efforts through improving service user outcomes and experiences. This scoping review established that there
was a paucity of research at the time of the review linking the design of the built environment with the provision of care
for self-harm and suicidal distress presentations specifically in Emergency Departments. This is despite the fact that
there is a significant body of literature pronouncing the links between good design practice and support of mental
wellbeing. However, this scoping review established the existence of a limited range of articles related to how design
practice can assist in addressing challenging behaviours, such as service user violence, and issues associated with triage of
clients with a mental illness. Design strategies from the literature are collated and discussed. Limitations of the field and
potential methodologies to address these limitations are also presented.
Keywords
Self-harm, suicidal distress, emergency department design, built environment, evidence-based design, environmental
safeguards
Introduction
In studies worldwide, it is cited that as many as 4% of
adults regularly self-harm, though this is likely not
representative of the full number of self-harming
individuals.
1
In the United States there are 650,000
presentations of self-harm per year,
2
and the strongest risk
factor predictive for suicide is previous self-harm.
3
It is
noted that at least 1% of patients who present to
emergency departments in the United Kingdom after self-
harm complete suicide within a year, and a further 3-5%
do so within the following 5-10 years.
4
Recent Australian
studies demonstrate that there were more than 26,000
hospitalisations for self-harm across Australia in 2010-
2011
5
and that this was a significantly rising trend over a
ten year period
5
. Presentations of self-harm and suicidal
distress are also often recurring; Lilley et al. note that 25%
of individuals presenting at hospital after self-injuring have
a history of self-harm,
6
and Owens and colleagues note
that 15-25% of individuals are likely to repeat within
twelve months.
7
The number of patients who have a mental illness
presenting to emergency departments (EDs) has been
consistently increasing. This has been attributed to the
mainstreaming of mental health services into general
services.
8
There is evidence suggesting that, in addition to
the increases in presentations by patients with a mental
illness, these patients are also presenting with increased
acuity.
9, 10
Morphet and colleagues suggest that 5-10% of
all presentations to Australian EDs are mental health
presentations.
11
Mental health patients present some of
the most challenging clinical situations to ED staff in
regards to their assessment and management
12-15
and are
commonly taxing to the ED due to long stays,
12
high
hospital admission rates
16, 17
and repeat use of the ED.
18
These issues are likely to increase with growth of
population and individuals experiencing mental
disorders.
19
Many service users present to the ED in an
acute crisis. Service users with challenging behaviours,
such as those who are acutely agitated, psychotic, or
aggressive, present ED staff with clinical situations that are
very demanding.
8
Presentation to EDs due to suicidal
distress and/or self-harm are frequent. Service users may
need urgent medical attention due to self-injury, and
community services may not be easily accessible.
8
Given
the interplay between architectural design and quality of
care, several researchers underscore the need for co-
operation among architects/designers and the service

Enhancing emergency care environments, Liddicoat
92 Patient Experience Journal, Volume 6, Issue 3 – 2019
users and staff who will experience the facilities they
create.
20, 21, 50
Built environment/architecture and mental wellbeing
There is a considerable body of literature affirming links
between mental wellbeing and good design practice.
Evaluations of specific design interventions have shown
that good design of a hospital’s environment leads to
better clinical outcomes and less stress for the users; both
patients and staff.
22-26
Research also links environmental
aspects, such as landscaping or natural elements, to the
reduction of stress and the promoting of recovery from
illness.
23, 27
Relative to psychiatric inpatient units, various dimension
of the built environment have shown to elicit supportive
therapeutic benefits for patients.
28
Multiple researchers
address the importance of a ‘deinstitutionalised’ and/or
‘homelike’ environment.
29-32
An orderly or organised
environment is also considered beneficial,
33, 34
as is an
environment that is well maintained.
35
Furnishings that
resist damage and are easily repaired or replaced are
considered a priority.
35, 36
Research has found that design
interventions which reduce incidences of aggression lead
to increased feelings of staff safety and security, and
reduced staff absences.
37
Design which encourages staff-
patient interactions is supported in the literature,
38
which
may include open nurse stations, among other design
features.
31, 35
Further, providing spaces for staff support
and respite is considered best practice.
39, 40
Multiple
researchers emphasise the need to provide spaces for
socialisation for both service users and staff, and the
development of a sense of community,
41-44
as well as
spaces which foster opportunities for autonomy.
45
Following a review of the literature, Karlin and Zeiss
concluded that within psychiatric settings, soft, indirect,
and pervasive or full-spectrum lighting are generally
recommended
46
Studies indicate that increased exposure
to daylight may reduce depressive symptoms
47
and reduce
agitation in patients.
30
Gutkowski and Gutman found that
well-lit spaces supported a therapeutic environment.
48
View to nature, natural landscapes and inclusion of nature
content within psychiatric settings is well discussed within
the literature.
49-51
A series of potential limitations are acknowledged within
the field linking environments with mental health
outcomes. These include:
• Difficulty in measuring of empirical evidence;
• Ill-defined, broad or generic nature of the research
terms and concepts;
• Lack of defined design initiatives.
There are some suggestions to mitigate these possible
limitations, which include the defining of specific user
groups, situations and contexts specific to the research
study, and the undertaking of post occupancy evaluations
which are closely related to defined users and research
terms. These suggestions are discussed below.
Difficulty in measuring empirical evidence and the ill-defined, broad
or generic nature of research terms and concepts
Existing literature acknowledges limitations regarding the
measuring and empirical evidence of the role of the built
environment in increased mental wellbeing.
52
This
limitation is attributed to both the generalised nature of
the research pertaining to mental health,
53
mental health
being a wide sphere
54
containing a multitude of mental
conditions, and also attributed to the definition of mental
health, which is commonly a fluid, ill-defined and
subjective concept and thus difficult to consistently
measure. Limitations are also acknowledged on the
definition of perceived value which design can add, and
the ability to measure such concepts or outcomes. How
the built environment could be broken down into
measurable components is a challenge in research in this
area. Again, this results in difficulty in empirical measuring
through the lack of defined concepts, terms and
interventions within the scope/aims of the research
project. Further, the literature acknowledges that the
analysis of environments and the identification of elements
which relate to various behavioural demands or mental
health symptoms is a neglected issue in psychology.
Importantly, it is acknowledged that the external “built
environment represents a modifiable feature to which
[patients] are exposed and is therefore important for
public health research,”
55
yet a need remains for research
identifying mechanisms by which the built environment
adversely and positively impacts health in order to develop
appropriate interventions.
53
Lack of defined design initiatives
Existing research in design and health seeks to mitigate the
limitations associated with the perceived and measurable
value of design initiatives and concepts through addressing
design for specifically defined user groups. It is made
apparent through existing literature that differing user
groups will respond to their environments in differing
ways, thus it is important to address any design initiatives
to the specific user group’s needs and experiences of space
in order to be effective.
56, 57
It is noted that more research
is needed to provide “more detailed, evidence-based
guidelines for designing optimal restorative environments
for different groups, contexts and activities.”
54
Predominant research methodologies, such as those
employed by Fornara and colleagues, are supportive of
defining specific user groups in order to tailor design
responses and mitigate this limitation of the lack of
empirical evidence. Defining user groups is a
methodology viewed as most reliably influential,
predictable and able to generate the outcomes of
bolstering mental wellbeing or clinical efficacy.
56, 58

Enhancing emergency care environments, Liddicoat
Patient Experience Journal, Volume 6, Issue 3 – 2019 93
As acknowledged by Ke-Tsung and others, there is a gap
in the literature and more research is required in order to
test ways in which theories of restorative environments
and design supportive of mental wellbeing could be
manifest in design practice.
59
It is suggested by these
authors that defined research concepts and post
occupancy evaluation of designs are the means to address
this ambiguity of testing. It is recognised by Ulrich,
Parsons and Kaplan that much further research is required
in the areas relating to specific design outcomes. They
also note that further investigation is needed regarding the
validation of concepts used as guides to assess the
environmental aspects of a space conducive to supporting
mental wellbeing, for example the tangible valuation of the
aesthetic and psychological benefits of ‘attractive visual
landscapes.’
51
This ambiguity leads to difficulty in making
assessments and drawing research conclusions. Difficulty
also lies in defining the environments or modifications in
commensurate terms, which increases difficulty in
quantifying the effects of environments on individuals.
60
By defining research concepts clearly and in relation to a
specific user group and context/situation, the
quantification process and methodologies and design
suggestions can become more clear. Within studies, built
features or elements of the environment are often broadly
defined, examined variables including ‘territoriality’ for
example.
55
More broadly, the fluid definitions found of
‘mental health’ may be related to the paucity of definition
of spatial features or design guidelines. Researchers in this
area note that “the health measures… may have been too
global in content to reflect the influence of the more
specific design factors.”
61
Further, spatial and physical
features are not typically included in surveys examining
patient satisfaction or experience.
59, 62
The literature
reinforces the notions of user specific design and post
occupancy evaluation as potentially a core contributor to
the efficacy of design practice for improving mental
health.
In summary, although a considerable body of literature
exists affirming the links between good design practice and
the promoting of mental wellbeing, there are many
limitations of the research. These limitations include
definition of concepts within the studies, such as the value
of design initiatives, and actual testable design proposals or
suggestions to be employed in the built environment. The
existing body of literature aims to mitigate these
acknowledged limitations through research design
addressing a specific user group, with the purpose of
providing more measurable, defined outcomes. These
findings inform the scoping review focus discussed herein.
This scoping review aimed to (1) identify the current body
of literature which examined the relationship between
design practice and service user experiences within EDs
for self-harm and suicidal distress presentations, and (2)
identify the ways in which the built environment could
increase the efficacy of therapeutic efforts through
improving service user outcomes and experiences.
Methods
This scoping review assessed the existing literature in
relation to the below research question:
Does the design of Emergency Department built environments impact
the service user experience and mental health outcomes, specifically in
the case of self-harm and suicidal distress presentations?
This scoping review was undertaken by the author using
the methodology described by Arksey and O’Malley,
however it does not rule out the possibilities of relevant
existing studies that are subsumed under other conditions,
misnamed, or not correctly indexed by the databases
consulted.
63
Sources
Three reference databases were searched with no limits
applied to year of publication: Medline,
a
PsycINFO
b
and
the Avery Index to Architectural Periodicals.
c
These three
databases ensure that a broad scope is achieved which
encapsulates literature containing primarily architecture-
focused articles and those drawing on medical and
psychological content.
These databases were explored for relevant publications
via a series of set keywords and topic areas.
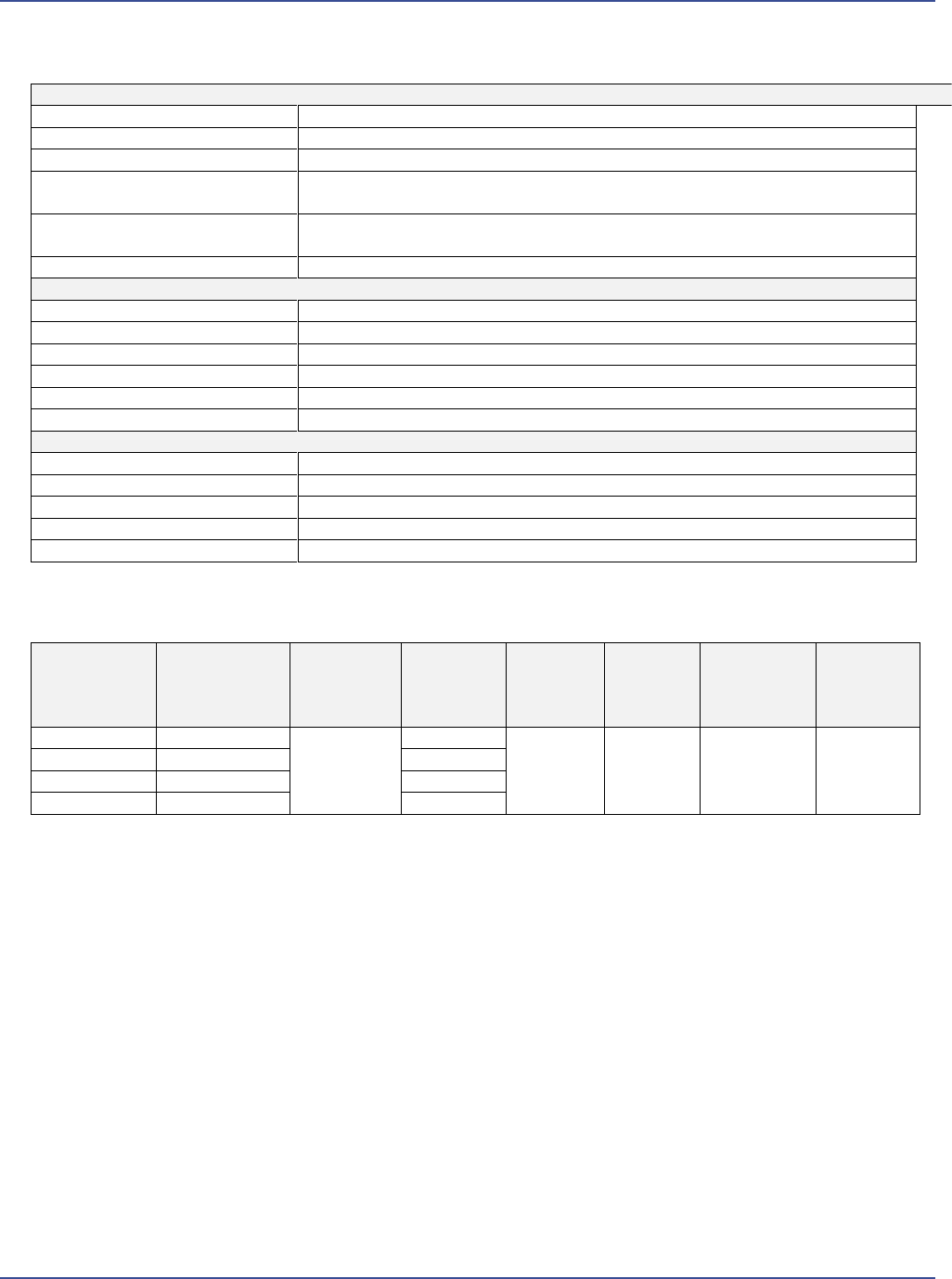
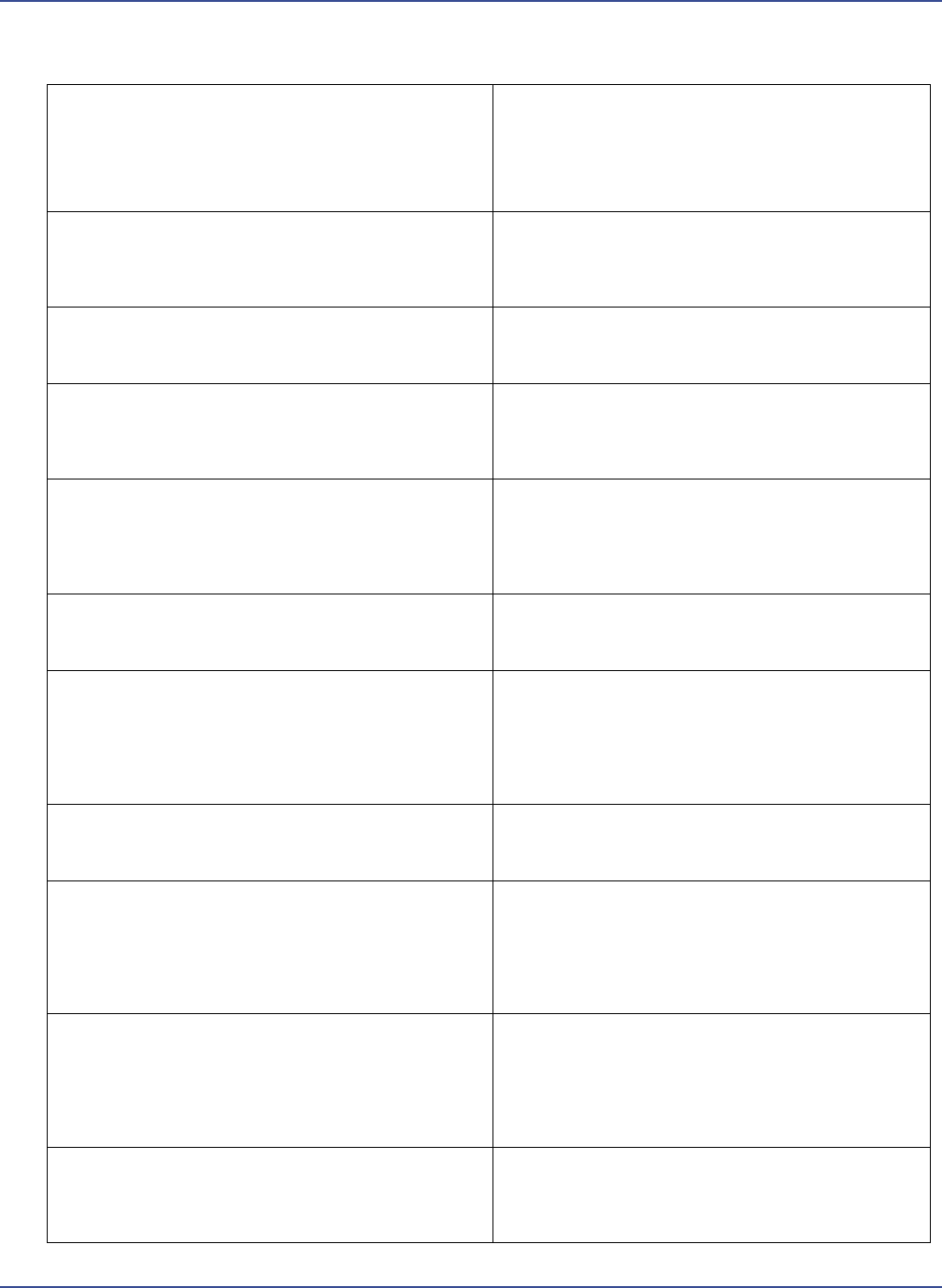
Search terms
Preliminary search terms were defined to reflect a number
of core concepts as defined by this scoping review (see
Table 1). These terms varied relative to the database being
searched and the appropriate subject indexing terms native
to that particular database. The record identification is
detailed in Table 2.
Article screening
Within the three databases searched, a review of all titles
was undertaken first, followed by a review of the abstracts
of publications whose title implied relevance or
titles where the relevance remained ambiguous. Articles
not written in the English language or with obviously
irrelevant titles were removed from the analysis. A
second screening process then took place, whereby the
abstract content was compared against the terms and
concepts of the review. Retrieval of the full text occurred
for the abstracts that suggested relevance as per the
research question and definitions, and also for those
abstracts which left further need for clarification of
relevance. A final selection of 29 articles were the subject
of review in full by the author. Where relevant, references
from articles were scanned to identify other papers that
may not have been identified through the initial database
Enhancing emergency care environments, Liddicoat
94 Patient Experience Journal, Volume 6, Issue 3 – 2019
search. A further 48 articles were identified from the
reference list of these articles for inclusion in the study. A
total of 77 articles were utilised in this scoping
review.
50
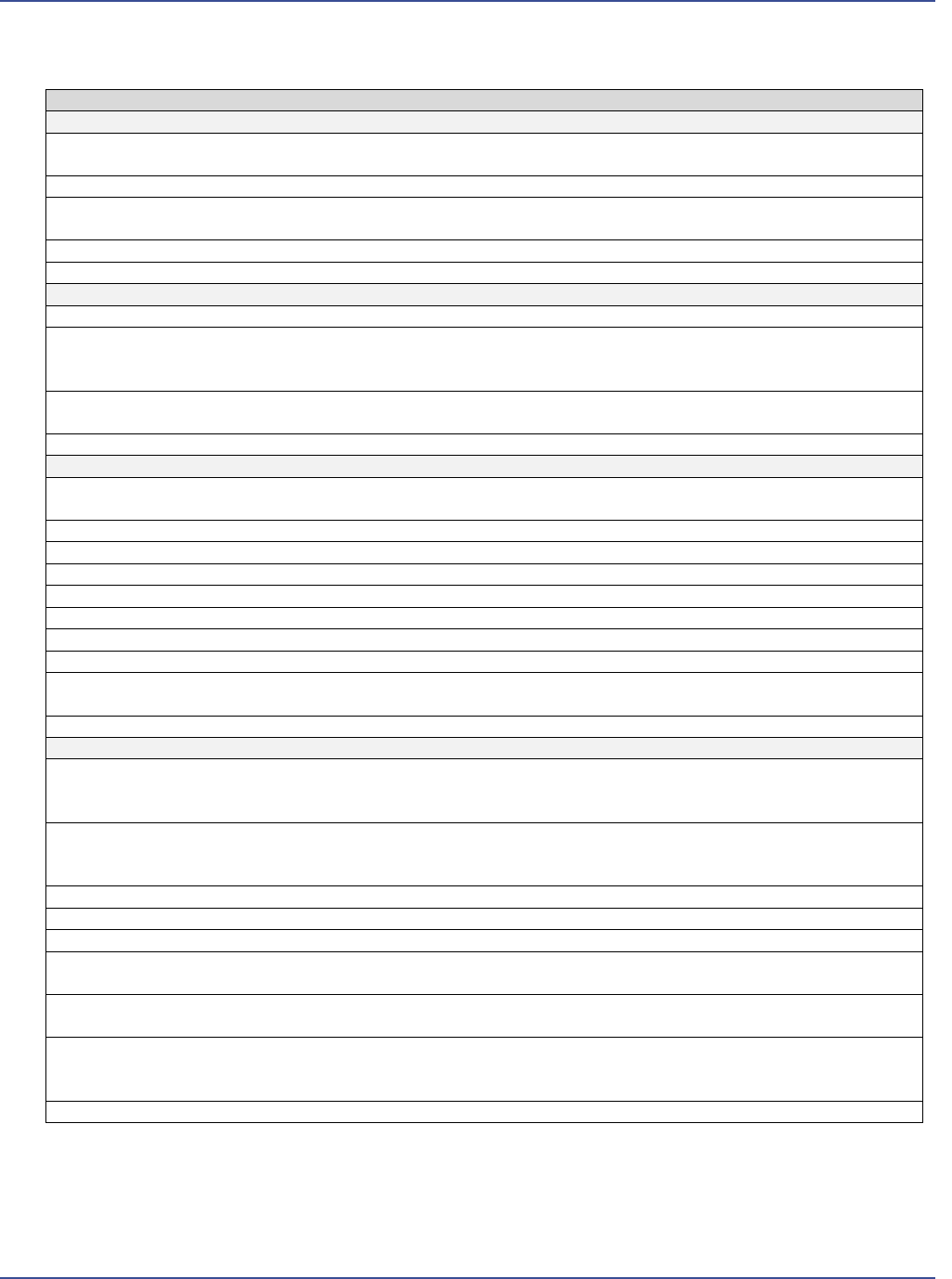
The twenty articles considered particularly
informative are presented in Table 3, alongside their main
contents.
A further step of the study reported herein included the
identification of design strategies contained in the
literature relative to providing environmental safeguards
and improving service user care specifically. This step
involved an identification of supplementary literature,
sourced from the articles’ reference lists, then reviewed in
order to supplement design guidance and compile a more
comprehensive list of design strategies.
Results
Summary findings from this scoping review are reported
across three areas: (1) built environment/architecture
relative to self-harm and suicidal distress; (2) emergency
department design and planning relative to self-harm and
suicidal distress presentations; and (3) design strategies.
Built environment/architecture relative to self-harm
and suicidal distress
After review of articles retained and relevant articles
identified through reference lists, this scoping review
confirmed a scarcity of research linking the treatment of
individuals who self-harm to the design of the built
environment specifically. Warzocha and colleagues
discussed the associations between deliberate self-harm
episodes and selected environmental factors; however, this
Table 1. Databases and Research Terms
Avery Index of Architectural Periodicals
Topic Area
Search Term(s) Used
Built Environment/Architecture
N/A
Self-Harm
“self-harm” OR “self-mutilation” OR “self-injurious behaviour”
Mental Health
“mental health” OR “mental health facilities” OR “psychiatric hospitals” OR
“environmental psychology”
Emergency department
“emergency department” OR “emergency room” OR “accident and emergency”
OR “accident & emergency” OR “a&e” OR “a & e”
Suicidal distress
“suicide” OR “suicidal distress” OR “suicidal ideation”
Medline
Topic Area
Search Term(s) Used
Built Environment/Architecture
“built environment” OR “environment design”
Self-Harm
“self-harm”
Suicidal distress
“suicide” OR “suicidal distress” OR “suicidal ideation”
Mental Health
“mental health”
Emergency department
“emergency department design” OR “emergency department design and planning”
PsycINFO
Topic Area
Search Term(s) Used
Built Environment/Architecture
“built environment” OR “architecture” OR “environmental effects”
Self-Harm
“self-injurious behaviour”
Suicidal distress
“suicide” OR “suicidal distress” OR “suicidal ideation”
Emergency department
“emergency department design” OR “emergency department design and planning”
Table 2. Records Identified
Database
Records
identified
from searches
Duplicates
Abstracts
reviewed
Full text
accessed
Excluded
Full text
accessed
and
included
Additional
records
sourced
Avery
49
11
49
96
67
29
48
Medline
295
78
PsycINFO
1145
87
Total
1489
214
Enhancing emergency care environments, Liddicoat
Patient Experience Journal, Volume 6, Issue 3 – 2019 95
Table 3. Articles Considered Partially Informative
Bost, N., Johnston, A., Broadbent, M., & Crilly, J. (2018).
Clinian perspectives of a mental health consumer flow
strategy in an emergency department. Collegian 25, 415-
420.
Clinicians involved in the provision of care to consumers with a mental
illness who presented to the ED participated in this qualitative study;
themes explored include the built environment (although briefly
presented); findings discuss communication in the ED and strategies to
implement and sustain a new consumer flow in the ED
Broadbent, M., Moxham, L., & Dwyer, T. (2014).
Implications of the emergency department triage
environment on triage practice for clients with a mental
illness at triage in an Australian context. Australasian
Emergency Nursing Journal, 17, 23-29.
This paper details an observational ethnographic approach exploring
the implications of the emergency triage environment on the triage
practice of nurses who triage clients with a mental illness; this paper
confirms that the triage environment has a direct influences on the
nurses’ abilities to conduct an accurate and timely triage, particularly
for a client presenting with a mental illness; various dimensions of the
environment are discussed including security ,noise, visibility, among
others
Broadbent, M., Moxham, L., & Dwyer, T. (2010). Issues
associated with the triage of clients with a mental illness in
Australian emergency departments. Australasian Emergency
Nursing Journal, 13, 117-123.
This paper presents a summary of literature relative to the emergency
triage of clients with a mental illness; various dimensions of triage are
presented and analysed, including content covering waiting times,
models of care, and the values of recovery-oriented practice in this
context
Cardell, R., Bratcher, K. S., & Quinnett, P. (2009).
Revisiting 'suicide proofing' an inpatient unit through
environmental safeguards: A review. Perspectives in
Psychiatric Care, 45(36-44).
This paper identifies strategies in the literature to facilitate
environmental safeguards within psychiatric facilities to protect suicidal
individuals from harming themselves; strategies are presented across
several themes including bathrooms, bedrooms, the psychiatric unit, the
use of cameras, restriction of personal belongings, training of staff,
administrative responsibilities
Clark, D., Dusome, D., & Hughes, L. (2007). Emergency
department from the mental health client's perspective.
International Journal of Mental Health Nursing, 16(2), 126-131.
Focus groups held with mental health patients and their families to
determine their level of satisfaction with care at regional EDs; results
indicate long waiting periods for these patients, impact of attitudes of
care providers, and cover family needs, diagnostic overshadowing, ‘no
where else to go’, and ‘what is missing’; emphasis on design strategies
to address perceived long waiting periods
Fay, L., Carll-White, A., & Harrell, J. (2017). Coming full
cycle: Linking POE findings to design application. Health
Environments Research & Design Journal, 10(3), 83-98.
This paper presents a full-cycle post occupancy evaluation and design
charrette for an emergency department; methods are detailed; findings
include the significance of workflow, communication, privacy and
confidentiality, safety and security; entry sequence redesign is presented
with associated design strategies/recommendations
Gharaveis, A., Hamilton, D. K., Pati, D., & Shepley, M.
M. (2017). Impact of visibility on teamwork, collaborative
communication, and security in emergency departments:
An exploratory study. Health Environments Research & Design
Journal. doi:1937586717735290
This study investigated the impact of visibility on teamwork,
collaborative communication and security issues in the ED; using
interview and on-site observation, this paper presents findings
pertaining to visibility and teamwork, patient assessment, comfort,
communication, security, and related design considerations; layouts,
workstation design, light and acoustics are among the environmental
aspects discussed
Guinther, L., Carll-White, A., & Real, K. (2014). One size
does not fit all: A diagnostic post-occupancy evaluation
model for an emergency department. Health Environments
Research & Design Journal, 7(3), 15-37.
This paper presents the detailed process and methods used in a post-
occupancy evaluation in an urban hospital emergency department; core
areas of evaluation are defined including environment, experience and
operations; connections made between privacy/confidentiality, noise,
occupancy levels and ED layout; a series of design suggestions provided
Huddy, J., & McKay, J. I. (1996). The top 25 problems to
avoid when planning your new emergency department.
Journal of Emergency Nursing, 22(4), 296-301.
Drawing on experience from work in an architectural firm, the
authors present 25 key themes for consideration when planning an
ED; related design dimensions are presented throughout
Enhancing emergency care environments, Liddicoat
96 Patient Experience Journal, Volume 6, Issue 3 – 2019
Table 3. Articles Considered Partially Informative (cont’d.)
Kaar, S. J., Walker, H., Sethi, F., & McIvor, R. (2017). The
function and design of seclusion rooms in clinical settings.
Journal of Psychiatric Intensive Care, 13(81-91).
This paper provides a review of current literature on seclusion room
design; government and other guidance regarding architectural design
specifications is presented; related dimensions from environmental
psychology are discussed including light and nature, safety,
communication, location of seclusion, walls, ceilings and floors,
sanitation; detailed design guidance is provided
Lanza, M. L., Kayne, H. K., Hicks, C., & Milner, J. (1994).
Environmental characteristics related to patient assault. Issues in
Mental Health Nursing, 15(3), 319-335.
This study purpose was to examine the influence of environmental factors
on assault; three survey instruments are used to explore the links between
ward atmosphere and assault frequency; locations of highest assault
frequency are tabled; discussions presented relative to clinical implications,
including ward conditions and ward climate
Lenaghan, P. A., Cirrincione, N. M., & Henrich, S. (2018).
Preventing emergency department violence through design.
Journal of Emergency Nursing, 44(1), 7-12.
This paper provides a review of best design practice pertaining to preventing
ED violence; design strategies are tabled across several themes including
parking zone, entry zone, traffic management, care zones and room
clustering, specialised rooms
Marynowski-Traczyk, D., Moxham, L., & Broadbent, M. (2013).
A critical discussion of the concept of recovery for mental health
consumers in the emergency department. Australian Emergency
Nursing Journal, 16(3), 96-102.
This paper details Australian mental health reforms and their impact on
the ED; unique dimensions of care relative to mental health presentations
at the ED; the concept of recovery in the ED and related care initiatives
for optimal management of these service users, emphasis on best
understanding recovery-oriented approaches in order to inform care provision
Morphet, J., Innes, K., Munro, I., O/Brien, A., Gaskin, C., &
Reed, F. (2012). Managing people with mental health
presentations in emergency departments - A service exploration
of the issues surrounding responsiveness from a mental health
care consumer and carer perspective. Australian Emergency Nursing
Journal, 15(3), 148-155.
This paper presents a literature review, survey and focus group data
collection, analysing the issues associated with access to care in ED settings
for clients presenting with a mental illness; participants’ perspectives of the
ED are presented in key themes, including spatial requirements and how
the ED environment could be improved
Nayeri, N. D., & Aghajani, M. (2010). Patients' privacy and
satisfaction in the emergency department: A descriptive analytical
study. Nursing Ethics, 17(2), 167-177.
Questionnaires were administered in this study to examine the perceptions
of privacy and its relationships with patient satisfaction in three emergency
departments; types and frequency of privacy breaches are detailed;
implications for safety and perceptions of care are discussed
Pati, D., Harvey, T. E., Willis, D. A., & Pati, S. (2015).
Identifying elements of the health care environment that
contribute to wayfinding. Health Environments Research & Design
Journal, 8, 44-67.
This paper details a multi-method study designed to investigate the aspects
of the physical environment that contribute to wayfinding experiences in
hospital settings; physical design elements contributing to wayfinding
experiences include signs, architectural features, structural elements,
furniture, interior elements, among others; how such features contribute to
wayfinding is analysed; design strategies/information as relevant is
presented
Shafiei, T., Gaynor, N., & Farrell, G. (2011). The characteristics,
management and outcomes of people identified with mental
health issues in an emergency department. Journal of Psychiatric and
Mental Health Nursing, 18(1), 9-16.
This paper details a retrospective observational study of adults who attended
and ED and with an ED discharge diagnosis of a mental health disorder;
this study confirms that mental health clients had longer wait times in the
ED and many left before being assessed
Sheehan, B., Burton, E., Wood, S., Stride, C., Henderson, E., &
Wearn, E. (2013). Evaluating the built environment in inpatient
psychiatric wards. Psychiatric Services, 64(8), 789-795.
This study examined the relationships between staff satisfaction and design
features in psychiatric wards; using spatial observation (checklist of design
features) and multi-level modelling, the study confirms that objective
measurement of inpatient psychiatric facilities is feasible and can be used to
identify features which enhance service user satisfaction; non-corridor designs
and personal bathrooms had a strong positive association with staff ratings
of the built environment
Shepley, M. M., Watson, A., Pitts, F., Garrity, A., Spelman, E.,
Kelkar, J., & Fronsman, A. (2016). Mental and behavioural
health environments: Critical considerations for facility design.
General Hospital Psychiatry, 42, 15-21.
An extensive literature review and focus groups/interviews are reported in
this paper, with the aim of identifying the features in the physical
environment that are believed to positively impact staff and patients in
psychiatric environments; a table of design topics and references is provided;
key aspects of the physical environment are analysed in more detail and
with supporting data from the focus groups/interviews; design strategies are
presented
Zamani, Z. (2018). Effects of emergency department physical
design elements on security, wayfinding, visibility, privacy, and
efficiency and its implications on staff satisfaction and
performance. Health Environments Research & Design Journal, 1-17.
doi:10.1177/193758618800482
This paper presents a mixed-method study exploring the connections
between ED physical design, attributes, performance and staff satisfaction;
a table of key descriptive statistics on staff satisfaction levels is provided;
themes include privacy, efficiency, security, visibility, wayfinding, which are
presented alongside design implications

Enhancing emergency care environments, Liddicoat
Patient Experience Journal, Volume 6, Issue 3 – 2019 97
referred to the environment in terms of their exposure to
abuse and their family situation. The authors found that
past suicide attempt(s), alcohol issues within the family,
sustained physical and sexual abuse, and lack of family
support were significantly associated with undertaking self
harm.
64
The research identified linking the built
environment/architecture to suicide and self-harm was
focused predominantly on suicide or self-harm prevention
measures (simply inhibiting access to suicide
opportunities/means), rather than the ways in which the
built environment might provide a psychologically
nurturing or supportive environment for users who may
be in suicidal distress. This research acknowledges the role
of the built environment in mediating attempted and
completed suicides, and that service users are “very
knowledgeable about how to attempt suicide in hospital
settings, possibly more so than hospital staff.”
65
Interestingly however, service users were found to feel
reassured of their safety when hospitals took active
measures to ensure their safety.
65
Environmental safeguards are the structural features in
healthcare facilities which limit the means with which to
commit suicide. Whilst these safeguards cannot guarantee
suicide prevention, they have been shown to reduce the
incidence.
65
The function and design of seclusion rooms in
clinical settings is also discussed, relative to service users
who may be in suicidal distress or at risk of self-harming.
The literature supports the use of natural light and well-lit
environments as contributing to therapeutic settings
generally, however there is no literature relating light and
nature specifically to seclusion rooms.
66
This highlights a
need for research in this area, further supported by the
notion that user specific mental health design is important
to generate relative, effective and supportive design
interventions, as established in broader research.
Emergency department design and planning relative
to self-harm and suicidal distress presentations
The practice environment of the Emergency Department
(ED) refers to the people who inhabit this environment
and the physical space(s)/architecture in which the health
care is provided. As noted by Broadbent and colleagues,
“the triage environment does influence the ED triage and
assessment and the management of clients who present
seeking mental health care.”
67
A common feature in the
literature is that mental health presentations also spend
many hours within the ED.
8, 11, 50, 68
This paper presents
various design strategies/recommendations for ED design
and planning relative to mental health presentations.
Whilst these are not specific to suicidal distress and self-
harm presentations only, these design strategies may
provide a useful platform for future research to develop
design solutions specifically addressing suicidal distress
and self-harm presentations. The collected design aspects
and implications are presented in brief across five
headings: (1) privacy; (2) visibility; (3) entry sequence; (4)
flexibility and spatial layouts; and (5) wayfinding.
d
Privacy
A key goal of health services involves respecting privacy
and service users’ satisfaction. Intrusions of privacy, as
defined by Curtin,
69
may include: the physical presence of
unwanted persons; unwanted observation of or by a
person; dispersal of private, inaccurate, or misleading
information about a person; or encroachment on personal
decisions make in a person’s own sphere.
Installing privacy screens between registration stations is
suggested to ensure privacy and confidentiality, together
with ample circulation space and an area for queuing while
waiting to register.
70
Design attributes evidenced in the
literature which contribute to lowering noise levels and
increasing audial privacy include the use of single patient
rooms (which are also preferred by service users, as
detailed in Morphet and colleagues’ 2012 study), floor to
ceiling solid partitions, acoustical tiles/dividers, solid core
wood doors on most treatment rooms, provision of
private consultation rooms throughout the ED, curtain
partitioning in seated waiting areas which will house
multiple groups of waiting service users (and their
companions), and provision of secluded areas for cell
phone usage in close proximity to the waiting area
70, 71
It is
noted that provision of space for cell phone calls reduces
the overhearing of confidential information being
discussed, and thus minimises privacy and confidentiality
breaches, in addition to being a noise control measure
71
. It
is also important to provide spaces for staff to talk
confidentially to other staff members, which is noted as
lacking in EDs.
70
Further, provision of space for
ambulatory personnel or police to complete reports and
make telephone calls confidentially is necessary to
maintain privacy, and to reduce interference with the work
flow of the unit.
72
Privacy and security are implicated in the particular
challenges unique to management of triage and
management of clients with a mental illness in the ED.
Minimising public scrutiny of a person in mental distress is
considered imperative.
67
Research underscores the role of
environmental characteristics in affecting client behaviour
and outcomes, and emphasise the consideration of the
provision of a private, safe and quiet area to wait that is
visible from the ED triage area.
67
Vulnerable clients, who
are emotionally disturbed, possibly aggressive or agitated,
and “may be exhibiting bizarre behaviours often remain in
the waiting room in the absence of suitable alternative
areas.”
67
ED triage nurses have also identified the need for
a secure, private place for patients in mental distress,
whilst remaining visible by the ED triage nurse.
67
Mental
health clients, too, have reported that a separate space for
people with mental health illnesses would improve the ED
journey.
4,11
Further, consideration of privacy and how it is

Enhancing emergency care environments, Liddicoat
98 Patient Experience Journal, Volume 6, Issue 3 – 2019
afforded through design has implications for
communication between staff and clients regarding plans
of care.
11,50
Indeed, lack of privacy “has a negative
influence on the ability to garner accurate information
critical for ED triage decision-making and to provide
effective ongoing management of the client with a mental
illness.”
67
Visibility
Visibility in EDs linked to safety considerations and to
communication. Research highlights that architectural
design solutions should integrate principles of visibility and
surveillance which are critical to the ED triage process.
73
In Fay and colleagues’ study, nursing staff commented that
it was difficult for patients seated in the waiting area to
hear their name called, which could be attributed to limited
visibility into the waiting areas from the triage doors.
70
Open layouts are suggested as leading to increased face-to-
face communication. Research on nursing unit design
notes that enhanced visibility within centralised pods
promotes increased team interaction, communication, a
greater sense of cohesion and interdisciplinary
collaboration.
73-75
Further, location of the consultation
rooms is implicated in the staff’s ability to communicate
with service users, and the easy location of the registration
desk ensures ease of access to information about their visit
for both service users and visitors.
70
Staff workstations
should also be located to be within view of each other,
which is linked to reduced staff isolation, improved staff
morale, increased service user monitoring and improved
communication among caregivers.
50,76
Providing direct sight lines for security, registration and
nursing staff to treatment doors and waiting areas is
considered essential to maintain safety and security.
70
Clinicians who cannot see each other cannot help each
other if incidences of violence or aggression occur.
76
Eliminating columns or walls at check-in, waiting and pod
areas enhances visibility, as well as safety, communication
and delivery of care.
50,
73, 74
Physical security barriers may impact the provision of
visibility and have the potential to generate negative
feelings about a service user’s access to staff.
76
Appropriate
security features can be implemented discreetly, in a
manner that will not diminish the service user experience.
Further, spatial delineation can assist the facilitation of
safety in the ED. Clear distinction between waiting and
treatment areas can help define acceptable activities and
minimise risks of violence.
76
A safe room may also be
considered for integration into the ED. This room should
have capacity to be locked from the inside for staff, service
users and visitors to retreat, and equipped with a
telephone, duress alarm, reinforced door, a peephole and
external lock and key access.
76
Entry sequence
The entry sequence should be carefully considered in an
ED setting with respect to mental health presentations.
Huddy and colleagues suggest that “‘uncomfortable’ front
doors where ambulatory patients and family members
must enter at the same point with ambulance patients”
72
are problematic and should be avoided. Further, the
exterior of the ED needs to be designed simultaneously
with the interior to achieve appropriate patient flow. EDs
should have separate parking outside a walk-in entrance;
lighting and wayfinding from arriving vehicles is crucial to
facilitate a quick transfer to care.
76
Appropriately designed entries can also assist in the
management of ED violence and challenging behaviours.
It is suggested that all parking and ambulatory areas should
have security surveillance, and additional security support
should manage ED entries.
76
Further, entrances should be
positioned at an angle from driveways in order to prevent
intentional or accidental ramming or vehicular intrusion.
76
Weather cover for the ambulatory docking areas should be
considered as an important design issue.
72
Further, exhaust
fumes from ambulances queued in the ambulatory docking
configuration can infiltrate the ED and impair the ward
comfort and atmosphere. It is suggested that considered
placement of the vehicles, mechanical air pressure in
entrance vestibules, and exhaust openings in canopies can
deter exhaust fumes.
72
Placing security officers at the entrance gives patients and
others the psychological benefit of a visible security
presence, whilst allowing for active intervention when
needed.
77
As Lenaghan and colleagues note, “properly
placed, a security person can step in to restrict access when
necessary, manage high-risk situations, and communicate
and enforce hospital policies and curfews. Their
knowledge of the community can serve as a calming
presence, leading to early detection of threats and a greater
overall sense of control and security”
76
which is a useful
addition to the entry space.
50
Flexibility and spatial layouts
Flexibility of spatial usage is considered important in
maximising the effectiveness of the ED. It is suggested
that the design of the unit should not limit the types of
care that can be delivered in various treatment spaces; for
example, an examination room can be planned with air
change capacities to allow it to be used for an isolation
patient.
72
Further, provision of appropriate storage is
essential, and can also support flexibility of spatial use.
Where fast track components are included in EDs,
separation of the fast track and urgent/emergent care areas
of the ED can be accomplished in order to broaden the
functionality of both areas. If examination rooms are
placed between these functional areas, they may function
as fast track rooms or emergency care rooms, as needed,
accommodating patient overflow in each area.
72
Excessive

Enhancing emergency care environments, Liddicoat
Patient Experience Journal, Volume 6, Issue 3 – 2019 99
distances between fast track and emergency care areas
should be minimised in the ED layout. Excessive distances
require additional support and storage spaces in both
areas, creating duplication of spaces which may be
managed by appropriate design planning.
72
A locked, roll-
down wall, locked cabinetry and gates, and impact resistant
laminate can be used to hide and store equipment and to
prevent patients from harming themselves.
76
Such
measures assist in the flexibility of spatial use and allow
equipment to be exchanged or replaced as required.
50
Wayfinding
Ineffective wayfinding and signage cause inefficiency and
workplace stress among healthcare providers. In the
absence of clear wayfinding strategies, patients may
wander, and may become abusive or aggressive to care
providers.
76
However, there is an acknowledged lack of
empirical research on the impact of navigation and
wayfinding in hospital-based ED facilities.
74
Including
waiting areas which are in direct line of sight from
registration spaces is recommended to promote intuitive
wayfinding and direct movement flows.
74
Meaningful spatial cues and design elements also
contribute to wayfinding. Pati and colleagues
78
identify
several aspects of the physical environment that contribute
to wayfinding, including maps, signs, logical clustering of
functions, furniture, logical pairing of interior architecture
elements, structural elements, architectural features, and
other elements such as artwork, maps and indoor plants.
They provide a series of tangible strategies for integrating
these features into positive wayfinding experiences. Whilst
not focused on ED environments specifically, these
strategies may provide useful in this context. Additionally,
it should be noted that mental health clients have
identified that replacing the term ‘mental health’ with
‘wellbeing’ in ED settings would improve their ED
experiences. This is due to a perception that stigma was
attached to the term ‘mental health.’
11
This should be
integrated into effective signage for the ED.
50
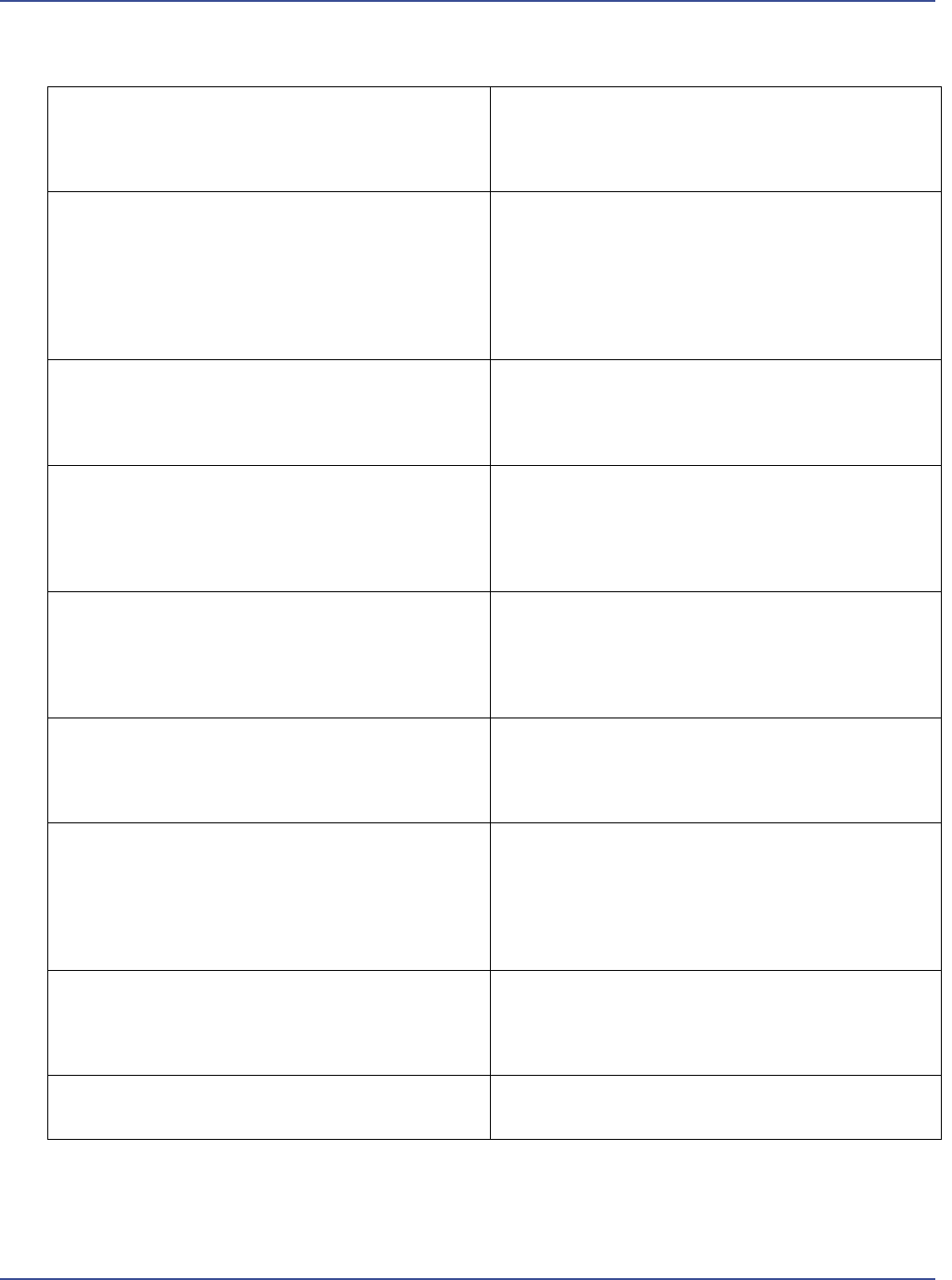
Design strategies
In addition to those strategies discussed in the previous
section, the research identified in this study also provides a
selection of tangible design strategies specifically to
facilitate environmental safeguards and improve service
user care across clinical settings. Supplementary literature,
sourced from the articles’ reference lists, were also
reviewed in order to compile a more comprehensive list of
design strategies (summarised in Table 4).
Discussion and summary
This paper affirms the existence of a body of literature
linking the environment with mental health outcomes,
there are many limitations within the research identified
and within the field as a whole. The limitations of the field
include:
• a difficulty in measuring of empirical evidence;
• the utilising of broad or generic research terms; and
• the lack of defined design initiatives.
Suggested methodologies to mitigate these limitations
include:
• designing for specific user groups; and
• the incorporation of defined research concepts and
terms;
• in conjunction with a specific user group and
context/situation.
Patient safety is acknowledged as an issue linked to the
built environment. The use of environmental psychology
and design theory related to aggression may be
hypothesised to have an effect on patient safety in terms
of reducing patient aggression and stress, and therefore
reducing measures such as restraint and incidences of self-
harm. Aspects of environmental psychology aimed at
reducing stress and aggression
30
may be useful to increase
service user safety within psychiatric settings. Most
existing literature related to safety concerns details aspects
of physical considerations, such as reducing ligature points
and fixtures which might be used as weapons.
79-81
This paper affirms the presence of a body of literature
linking good design practice with improved mental
wellbeing, yet highlights both the lack of design
implications contained in this research and the design
initiatives appropriate to varying mental health user
groups, including self-harm and suicidal distress
presentations specifically, particularly in EDs. This
scoping review confirmed a scarcity of research in the
databases searched linking ED design and planning with
supportive therapeutic effects for self-harm and suicidal
distress presentations specifically. Research identified
provided various design strategies/recommendations for
ED design and planning relative to mental health
presentations. Whilst these are not specific to suicidal
distress and self-harm presentations only, these design
strategies provide a useful platform for development of
possible design solutions for suicidal distress and self-harm
presentations through future research. This scoping review
thus verifies the need for further research studies in this
area.
The limitations of this scoping review are firstly associated
with the fact that findings are not a final output in their
own right, and a process of quality assessment was not
included in the present study. The results are further
constrained by the selection of search keywords and
criteria applied in the process, not least constrained by the
Enhancing emergency care environments, Liddicoat
100 Patient Experience Journal, Volume 6, Issue 3 – 2019
Table 4. Design suggestions for providing environmental safeguards and improving service user care
Providing environmental safeguards and improving service user care
Bathrooms
Shower heads should be flush or slanted so they will not support knotted clothing or sheets or other potential ligatures
that could be used in a hanging attempt.
Minimise breakaway shower heads, shower rods, clothes hooks, curtain rods and railings.
All fixtures should be considered as possible anchors for attempted hangings, including shelves, fire sprinklers, towel
racks and ceiling lights.
The provision of personal bathrooms tends to improve the dignity, privacy and safety of patients.
References:
65, 83-88
Bedrooms
Bedrails should be avoided where possible.
Minimise access to ligatures than patients may use to hang or asphyxiate themselves, such as belts, shoestrings,
bathrobe ties, telephone and receiver cords, ties, sheets that can be torn into strips, stockings, intravenous tubing or
other medical tubing.
Designs of beds that are free from multiple leverage points in order to minimise hangings are ideal, whilst also being
fireproof.
References:
65, 83-87
Within the ward
Non-protruding wing doorknobs are recommended.
Door hinges should be filed to a slant.
There should be no exposed pipes, sprinkler heads, light fixtures, vents, or ducts.
Ventilator grilles should have security screens with holes no more than 3/16 inches wide, or 16-mesh per square inch.
Plumbing should be concealed.
Non-breakable glass in windows and secure windows that do not open are recommended.
Doors should open outward or in both directions to prevent patients from barricading themselves into a room.
Limit access to roofs or high places, open stairwells, screen porches or elevator shafts.
If possible, there should be no electrical outlets in rooms.
Noncorridor designs, such as spoke designs and courtyard arrangements lend themselves to easier observation of
patients and, research shows, are preferred by patients and staff.
References:
65, 83-88
Seclusion Suites
High performance sound-absorbing ceiling and floor tiles are recommended to reduce the noise of the seclusion
environment. This is particularly important when designing seclusion environments providing care for multiple
patients simultaneously.
Features to reduce spatial disorientation are beneficial, and may include signage, environmental cues such as changes in
floor treatments, colour to denote different spaces and assist the patient to identify different functions of different
spaces.
Include views to nature where possible.
In the absence of views to nature, include nature art and prints on the walls.
White or grey should be avoided in seclusion rooms; in general, warm blue tones have a calming effect.
15m² should be considered as the minimum area required for the seclusion room and ensuite bathroom. A further
15m² should be provided for the staff observation area, giving a total of 30m².
Temperature control should be facilitated in order to ensure heating and cooling can be provided in a manner
responsive to patient needs without introducing undue noise.
Include a whiteboard or other display device that provides information to the patient. As suggested by Kaar and
colleagues, this information may include: “(1) orientation to time, place and person; (2) understanding of the treatment
they have been given; (3) knowledge of the team delivering care; and (4) expectations for decision making” (p. 89).
References:
46, 66, 89-93

Enhancing emergency care environments, Liddicoat
Patient Experience Journal, Volume 6, Issue 3 – 2019 101
complexity of this multidisciplinary research and possible
omissions amongst the linked disciplines. Extension of the
searches conducted to grey literatures and other databases
may augment the records identified and may form the
subject of future reviews.
As noted by Broadbent and colleagues, “the triage, and
subsequent care, of clients with a mental illness in the ED
remains one of the biggest unresolved issues in
contemporary emergency care.”
82
By building creative and
innovative partnerships across clinical and design
disciplines, including service users, it is possible to develop
a more comprehensive understanding of the potential
support mechanisms the built environment may facilitate
in ED environments.
End Notes
a. Medline is the United States National Library of
Medicine’s database providing information from the
fields of Medicine, Nursing, Dentistry, Veterinary
Medicine, Allied Health and Pre-clinical Sciences. This
database contains research sourced from over 5,500
biomedical journals published in the United States and
internationally.
b. PsycINFO is the database of the American
Psychological Association and is the largest resource
devoted to peer-reviewed literature in behavioural
science and mental health.
c. The Avery Index to Architectural Periodicals covers
research within the architectural field, indexing over
700 international journals including scholarly literature
as well as publications of professional associations and
major international serials on architecture and design.
d. Further detail on specific design strategies can be
found in Reference 50.
References
1. Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate
self-harm in a nonclinical population: Prevalence and
psychological correlates. Am J Psychiatry.
2003;160:1501-8.
2. Wong N. Book review, sk goldsmith, tc pellmar, am
kleinman, we bunney jr (eds): Reducing suicide: A
national imperative. Am J Psychiatry. 2003;160:1534-5.
3. Hawton K, Zahl D, Weatherall R. Suicide following
deliberate self harm: Long term follow up of patients
who presented to a general hospital. Br J Psychiatry.
2003;182:537-42.
4. Hawton K, Fagg J. Suicide and other causes of death,
following attempted suicide. Br J Psychiatry.
1988;152:359-66.
5. Pointer S. Trends in hospitalised injury, Australia.
Canberra: Australian Institute of Health and Welfare;
2013.
6. Lilley R, Owens D, Horrocks J, A H, Noble R, Bergen
H, et al. Hospital care and repetition following self-
harm: Multicentre comparison of self-poisoning and
self-injury. Br J Psychiatry. 1998;192:440-5.
7. Owens D, Horrocks J, House A. Fatal and non fatal
repetition of self-harm: At repeat episodes: Findings
from a multicentre cohort study. J Affect Disord.
2002;180:44-51.
8. Shafiei T, Gaynor N, Farrell G. The characteristics,
management and outcomes of people identified with
mental health issues in an emergency department. Int J
Ment Health Nurs. 2011;18(1):9-16.
9. Wand T, Schaecken P. Consumer evaluation of a
mental health liason nurse service in the emergency
department. Contemp Nurse. 2006;21(1):14-21.
10. Marynowski-Traczyk D, Moxham L, Broadbent M. A
critical discussion of the concept of recovery for
mental health consumers in the emergency department.
Aust Emerg Nurs J. 2013;16(3):96-102.
11. Morphet J, Innes K, Munro I, O/Brien A, Gaskin C,
Reed F. Managing people with mental health
presentations in emergency departments - a service
exploration of the issues surrounding responsiveness
from a mental health care consumer and carer
perspective. Aust Emerg Nurs J. 2012;15(3):148-55.
12. Heslop L, Elson S, Parker N. Improving continuity of
care across psychiatric and emergency medicine
services: Combining patient data within a participatory
action research framework. J of Adv Nurs. 2000;31:135-
43.
13. Wand T, Happell B. The mental health nurse:
Contributing to improved outcomes for patients in the
emergency department. Accid Emerg Nurs. 2001;9:166-
76.
14. Happell B, Summers M, Pinikahana J. The triage of
psychiatric patients in the hospital emergency
department: A comparison between emergency
department nurses and psychiatric nurse consultants.
Accid Emerg Nurs. 2002;10:65-71.
15. Wynaden D, Chapman R, McGowan S, McDonough S,
Finn M, Hood S. Emergency department mental health
triage consultancy service: A qualitative evaluation.
Accid Emerg Nurs. 2003;11:158-65.
16. Hazlett SB, McCrthy ML, Londoner MS, Onyike CU.
Epidemiology of adult psychiatric visits to us
emergency departments. Acad Emerg Med. 2004;11:193-
5.
17. Kunen S, Prejean C, Gladney B, Harper D, Mandry
CV. Deposition of emergency department patients
with psychiatric comorbidity: Results from the 2004
national hospital ambulatory medical care survey. Emerg
Med J. 2016;23:274-5.
18. Curran GM, Sullivan G, Williams K, Han X, Collins K,
Keys J, et al. Emergency department use of persons
with comorbid psychiatric and substance abuse
disorders. Ann Emerg Med. 2003;41:659-67.

Enhancing emergency care environments, Liddicoat
102 Patient Experience Journal, Volume 6, Issue 3 – 2019
19. Slade T, Johnston a, Teesson M, Whiteford H, Burgess
P, Pirkis J, et al. The mental health of Australians 2. Report
on the 2007 national survey of mental health and wellbeing.
Canberra: Department of Health and Ageing; 2009.
20. Dvoskin JA, Radonski SJ, Bennett C, Olin JA, Hawkins
RL, Dotson LA, et al. Architectural design of a secure
forensic state psychiatic hospital. Behavioural Sciences &
the Law. 2002;20:481-93.
21. Howard T. Physical environment and use of space. In:
Campling P, Davies S, Farquharson G, editors. From
toxic institutions to therapeutic environments. London:
Gaskell; 2004. p. 69-78.
22. Ulrich RS. Essay evidence-based health-care
architecture. Medicine and Creativity.
2006;368(December):538-9.
23. Ulrich RS. Effects of interior design on wellness:
Theory and recent scientific research. J Health Care Inter
Des. 2001;3(1):97-109.
24. Ulrich RS, Zimring C, Zhu X, DuBose J, Seo H, Choi
Y, et al. A review of the research literature on
evidence-based healthcare design (part i). HERD.
2008;1:61-125.
25. Marberry S, editor. Improving healthcare with better building
design. Chicago: Health Administration Press; 2006.
26. Berry LL, Parker D, Coile RC, Hamilton DK, O'Neill
DD, Sadler BL. The business case for better buildings.
Front Health Serv Manag. 2004;21:3-24.
27. Laumann K, Garling T, Morten Stormark K. Rating
scale measures of restorative components of
environments. J Environ Psychol. 2001;21:31-44.
28. Shepley MM, Watson A, Pitts F, Garrity A, Spelman E,
Kelkar J, et al. Mental and behavioural health
environments: Critical considerations for facility
design. Gen Hosp Psychiatry. 2016;42:15-21.
29. Tapak DM. Don't speak about us without us: Design
considerations and recommendations for inpatient
mental health environments for children and
adolescents. Winnipeg, Canada: University of
Manitoba; 2012.
30. Ulrich RS, Bogren I, Lundin S, editors. Towards a
design theory for reducing aggression in psychiatric
facilities. Arch 12; Architecture/Research/Care/Health
Conference; 2014; Gothenburg, Sweden: Chalmers
Institute of Technology.
31. Whitehead CC, Polsky RH, Crookshank L, Fik F.
Objective and subjective evaluation of psychiatric ward
design. Am. J. Psychiatry. 1984;141:639-44.
32. Wilson MR, Soth N, Robak R. Managing disturbed
behavior by architectural changes: Making spaces fit
the program. Residential Treatment for Children & Youth.
1992;10(2):63-74.
33. Eklund M, Harrison L. Ward atmosphere, client
satisfaction and client motivation in a psychiatric work
rehabilitation unit. Community Ment Health J.
2001;37(2):169-77.
34. Middelbow T, Schjodt T, Byrsting K, Gjerris A. Ward
atmosphere in acute psychiatric in-patient care:
Patients' perceptions, ideals and satisfaction. Acta
Psychiatrica Scandinavica. 2001;103(3):212-9.
35. Christenfeld R, Wagner J, Patsva G, Acrish WP. How
physical settings affect chronic mental patients. Psychiatr
Q. 1989;60:253-64.
36. Liddicoat S. Perceptions of spatiality: Supramodal
meanings and metaphors in therapeutic environments.
Interiority. 2018.
37. Martin JH. Improving staff safety through an
aggression management program. Arch Psychiatr Nurs.
1995;9(4):211-5.
38. Tyson G, Lambert G, Beattie L. The impact of ward
design on the behaviour, occupational satisfaction and
well-being of psychiatric nurses. Int J Ment Health Nurs.
2002;11:94-102.
39. Nejati A, Rodiek S, Shepley MM. Using visual
stimulation to evaluate restorative qualities of access to
nature in hospital staff break areas. Landsc Urban Plan.
2016;148:132-8.
40. Nejati A, Shepley MM, Rodiek S. A review of design
and policy interventions to promote nurses' restorative
breaks in healthcare workplaces. J Workplace Health Saf.
2016;64(2):70-7.
41. Davis C, Glick ID, Osow I. The architectural design of
a psychotherapeutic milieu. Hosp Community Psychiatry.
1979;30(7):453-60.
42. Gutkowski S, Ginath Y, Guttmann F. Improving
psychiatric environments through minimal architectural
change. Hosp Community Psychiatry. 1992;43(9):920-3.
43. Sidman J, Moos RH. On the relation between
psychiatric ward atmosphere and helping behavior. J
Clin Psychology. 1973;29(1):74-8.
44. Turlington R. Creating a planetree inpatient psychiatric
unit. Health Facilities Managament Magazine.
2004;17(6):12-3.
45. Sorlie T, Parniakov A, Rezvy G, Ponomarev O.
Psychometric evaluation of the ward atmosphere scale
in a russian psychiatric hospital. Nordic J Psychiatry.
2010;64(6):377-83.
46. Karlin BE, Zeiss RA. Best practices: Environmental
and therapeutic issues in psychiatric hospital design:
Toward best practices. Psychiatr Serv. 2006;57(10):1376-
8.
47. Evans GW. The built environment and mental health. J
Urban Health. 2003;80(4):536-55.
48. Gutkowski S, Guttmann F. Program and process:
Designing the physical space of a day hospital. Isr J
Psychiatry Relat Sci. 1992;29(3):167-73.
49. Frumkin H. Beyond toxicity: Human health and the
natural environment. Am J Prev Med. 2001;20(234-240).
50. Liddicoat S. Designing a supportive emergency
department environment for people with self harm and
suicidal ideation: A scoping review. Australas. Emeg.
Care. 2019. https://doi.org/10.1016/j.auec.2019.04.006
51. Ulrich RS. Human responses to vegetation and
landscapes. Landscape Urban Plan. 1986;13:29-44.

Enhancing emergency care environments, Liddicoat
Patient Experience Journal, Volume 6, Issue 3 – 2019 103
52. Evans G, McCoy J. When buildings don't work: The
role of architecture in human health. J Environ Psychol.
1998;18:85-94.
53. Srinivasan S, O'Falton LR, Dearry A. Creating health
communities, healthy homes, healthy people: Initiating
a research agenda on the built environment and public
health. Am J Public Health. 2003;93(9):1446-50.
54. Joye Y, van den Berg AE. Restorative environments.
2012. In: Environmental Psychology: An introduction
[Internet]. New Jersey: Wiley-Blackwell; [57-66].
55. Messer LC, Maxson P, Miranda ML. The urban built
environment and associations with women's
psychosocial health. J Urban Health. 2012;90(5):857-71.
56. Fornara F, Bonaiuto M, Bonnes M. Percieved hospital
environment quality indicators: A study of orthopaedic
units. J Environ Psychol. 2006;26:321-34.
57. Gifford R. Environmental psychology: Principles and practice.
5 ed. Colville: Optimal Books; 2015.
58. Mourshed M, Zhao Y. Healthcare providers'
perception of design factors related to physical
environments in hospitals. J Environ Psychol.
2012;32:362-70.
59. Ke-Tsung H. A reliable and valid self-rating measure of
the restorative quality of natural environments.
Landscape Urban Plan. 2003;64:209-32.
60. Perkins DV, Perry J, C. Dimensional analysis of
behaviour setting demands in a community residence
for chronically mentally ill women. J Community Psychol.
1985;13:350-9.
61. Duffy M, Willson VL. The role of design factors of the
residential environment in the physical and mental
health of the elderly. J Housing Elderly. 1985;2(3):37-46.
62. Devlin AS, Arneill AB. Healthcare environments and
patient outcomes. Environ Behav. 2003;35:665-94.
63. Arksey H, O'Malley L. Scoping studies: Towards a
methodological framework. Int J Soc Res. 2005;8:19-32.
64. Warzocha D, Pawelczyk T, Gmitrowicz A.
Associations between deliberate self-harm episodes in
psychiatrically hospitalised youth and the type of
mental disorders and selected environmental factors.
Arch Psychiatry Psychother. 2010;2(23-29).
65. Cardell R, Bratcher KS, Quinnett P. Revising 'suicide
proofing' an inpatient unit through environmental
safeguards: A review. Perspect Psychiatr Care. 2009;45(36-
44).
66. Kaar SJ, Walker H, Sethi F, McIvor R. The function
and design of seclusion rooms in clinical settings.
Journal of Psychiatric Intensive Care. 2017;13(81-91).
67. Broadbent M, Moxham L, Dwyer T. Implications of
the emergency department triage environment on
triage practice for clients with a mental illness at triage
in an australian context. Aust Emerg Nurs J. 2014;17:23-
9.
68. Clarke DE, Dusome D, Hughes L. Emergency
department from the mental health client's perspective.
Int J Ment Health Nurs. 2007;16:126-31.
69. Curtin LL. Patient privacy in a public institution. Nurs
Manag. 1993;24(6):26-7.
70. Fay L, Carll-White A, Harrell J. Coming full cycle:
Linkig poe findings to design application. HERD.
2017;10(3):83-98.
71. Guinther L, Carll-White A, Real K. One size does not
fit all; a diagnostic post-occupancy evaluation model
for an emergency department. HERD. 2014;7(3):15-37.
72. Huddy J, McKay JI. The top 25 problems to avoid
when planning your new emergency department. J
Emerg Nurs. 1996;22(4):296-301.
73. Gharaveis A, Hamilton DK, Pati D, Shepley MM.
Impact of visibility on teamwork, collaborative
communication, and security in emergency
departments: An exploratory study. HERD. 2017.
74. Zamani Z. Effects of emergency department physical
design elements on security, wayfinding, visibility,
privacy, and efficiency and its implications on staff
satisfaction and performance. HERD. 2018:1-17.
75. Bost N, Johnston A, Broadbent M, Crilly J. Clinian
perspectives of a mental health consumer flow strategy
in an emergency department. Collegian 25. 2018:415-20.
76. Lenaghan PA, Cirrincione NM, Henrich S. Preventing
emergency department violence through design. J
Emerg Nurs. 2018;44(1):7-12.
77. Lanza ML, Kayne HK, Hicks C, Milner J.
Environmental characteristics related to patient assault.
Iss Ment Health Nurs. 1994;15(3):319-35.
78. Pati D, Harvey TE, Willis DA, Pati S. Identifying
elements of the health care environment that
contribute to wayfinding. HERD. 2015;8:44-67.
79. Watts BV, Young-Xu Y, Mills P, DeRosier P, Kemp J,
Shiner B, et al. Examination of the effectiveness of the
mental health environment of care checklist in
reducing suicide on impatient mental health units. Arch
Gen Psychiatry. 2012;69(6):588-92.
80. Geddes JR. Suicideand homicide in mentally ill
patients. BMJ. 1999;318(1225-1226).
81. Carr R. Psychiatric facility 2011. Available from:
http://www.wbdg.org/design.psychiatric.php.
82. Broadbent M, Moxham L, Dwyer T. Issues associated
with the triage of clients with a mental illness in
australian emergency departments. Aust Emerg Nurs J.
2010;13:117-23.
83. Joint Commission Resources. Suicide prevention: Toolkit
for implementing national patient safety goal 15a. Oakbrook
Terrace: Joint Commission Resources; 2007.
84. National Center on Institutions and Alternatives.
Suicide prevention and 'protrusion-free' design of
correctional facilities. Jail Suicide/Mental Health Update.
2003;12(1-20).
85. Sine DM, Hunt JM. Design guide for the built environment of
behavioural health facilities. 2 ed. Washington, DC:
National Association of Psychiatric Health Systems;
2007.
Enhancing emergency care environments, Liddicoat
104 Patient Experience Journal, Volume 6, Issue 3 – 2019
86. Taiminen TJ, Strandberg J, Kujari H. Inpatient suicide
on general hospital psychiatric ward. Arch Suicide Res.
1996;2(119-124).
87. Shepley MM, Pasha S. Design for mental and behavioural
health. London: Routledge; 2017.
88. Sheehan B, Burton E, Wood S, Stride C, henderson E,
Wearn E. Evaluating the built environment in inpatient
psychiatric wards. Psychiatr Serv. 2013;64(8):789-95.
89. Ulrich RS, Zimring C, Quan X, Joseph A. The role of
the physical environment in the hospital of the 21st
century. Robert Wood Johnson Foundation; Centre for
Health Design; 2004.
90. Carpman J, Grant M, Simmons D. No more mazes.
Research about design for wayfinding in hospitals. Ann Arbor:
University of Michigan Hospitals, Patient and Visitor
Participation Project; 1984.
91. Ulrich RS. Effects of interior design on wellness:
Theory and recent scientific research. J Health Care Inter
Des. 1991;3(1):97-109.
92. Nanda U, Elsen S, Zadeh RS, Owen D. Effect of
visual art on patient anxiety and agitation in a mental
health facility and implications for the business case. J
Psychiatr Ment Health Nurs. 2011;18(5):386-93.
93. Ministry of Health. Secure rooms and seclusion standards and
guidelines: A literature and evidence review. British Columbia:
Government of British Columbia; 2012.
