
NEW MEXICO
HUMAN SERVICES
DEPARTMENT
5
-
YEAR
STRATEGIC
PLAN
NEW MEXICO
PRIMARY CARE
COUNCIL
2023
Version
2
: Updated from
2022

New Mexico Primary Care Council 2023
Page 1 of 48
Contents
Honor Native Land ........................................................................................................................................ 2
Letter from the Primary Care Council Chair .................................................................................................. 3
Executive Summary ....................................................................................................................................... 4
Background and Introduction ....................................................................................................................... 5
New Mexico Overview .................................................................................................................................. 5
Primary Care Council Overview .................................................................................................................... 6
Primary Care Council Timeline of Strategic Activities ................................................................................... 7
Medicaid Primary Care Payment Reforms .................................................................................................. 21
Primary Care Residency Expansion ............................................................................................................. 23
Conclusion ................................................................................................................................................... 25
Acknowledgments ....................................................................................................................................... 26
Appendix ..................................................................................................................................................... 27
Primary Care Return on Investment ....................................................................................................... 27
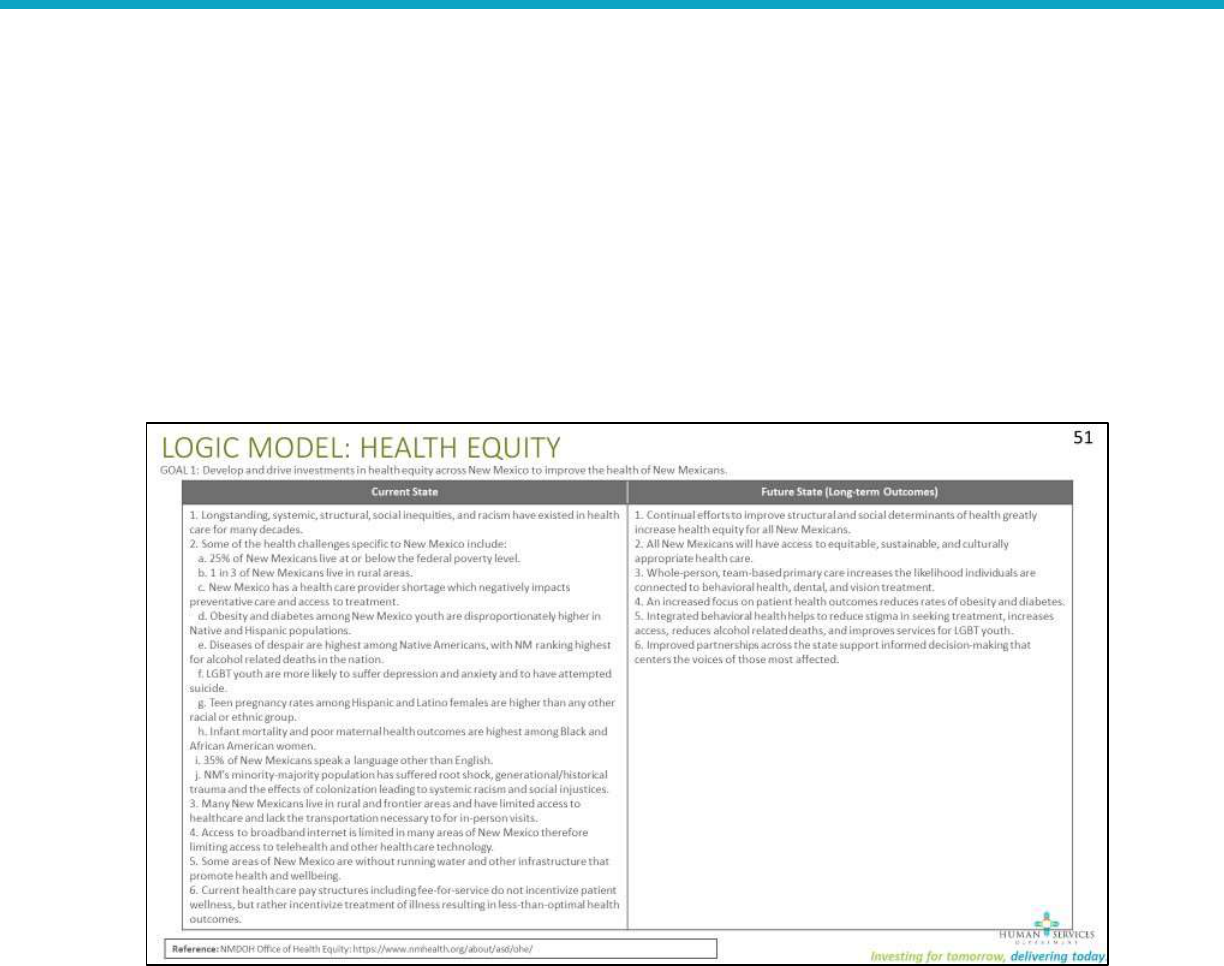
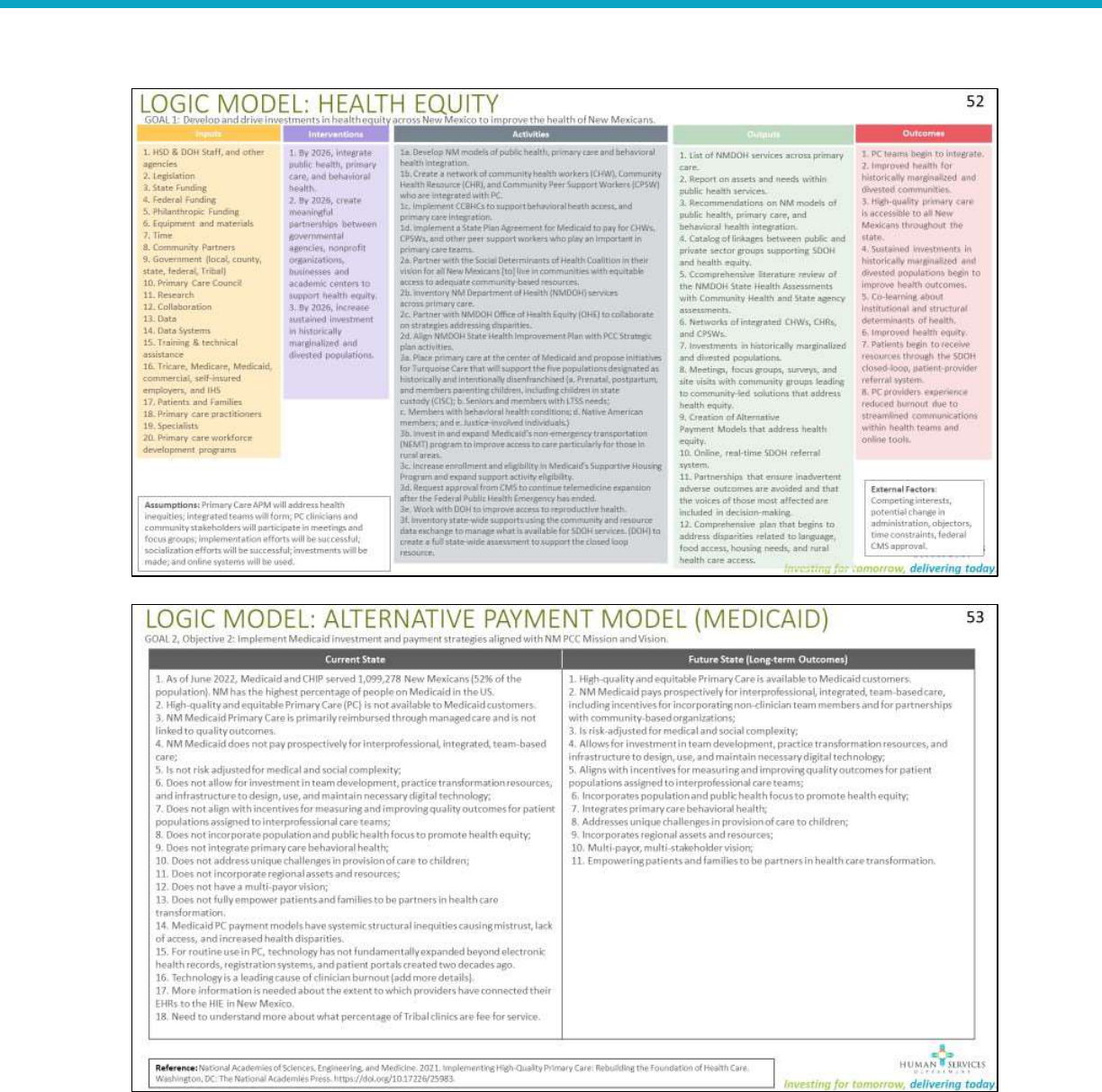
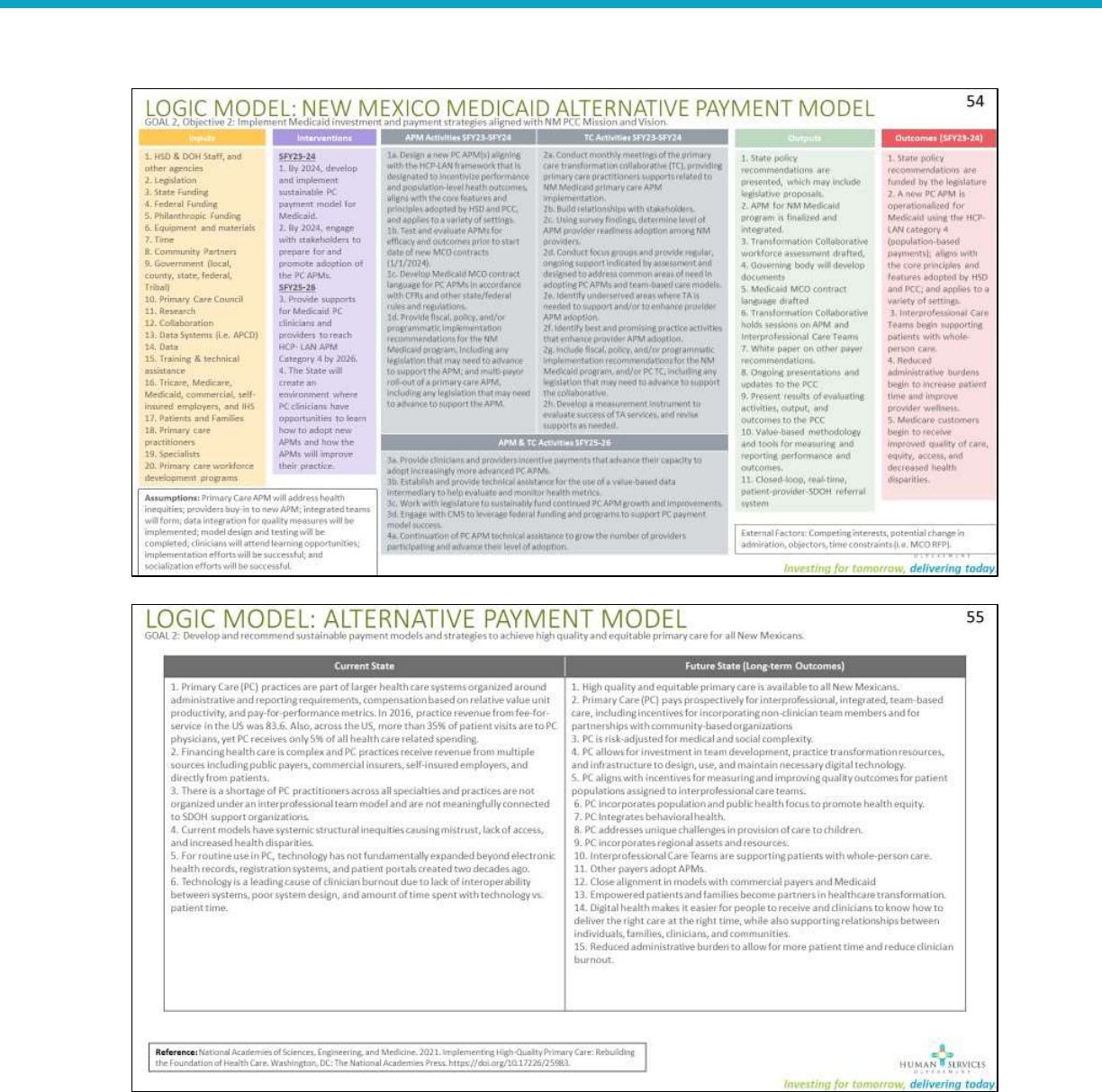
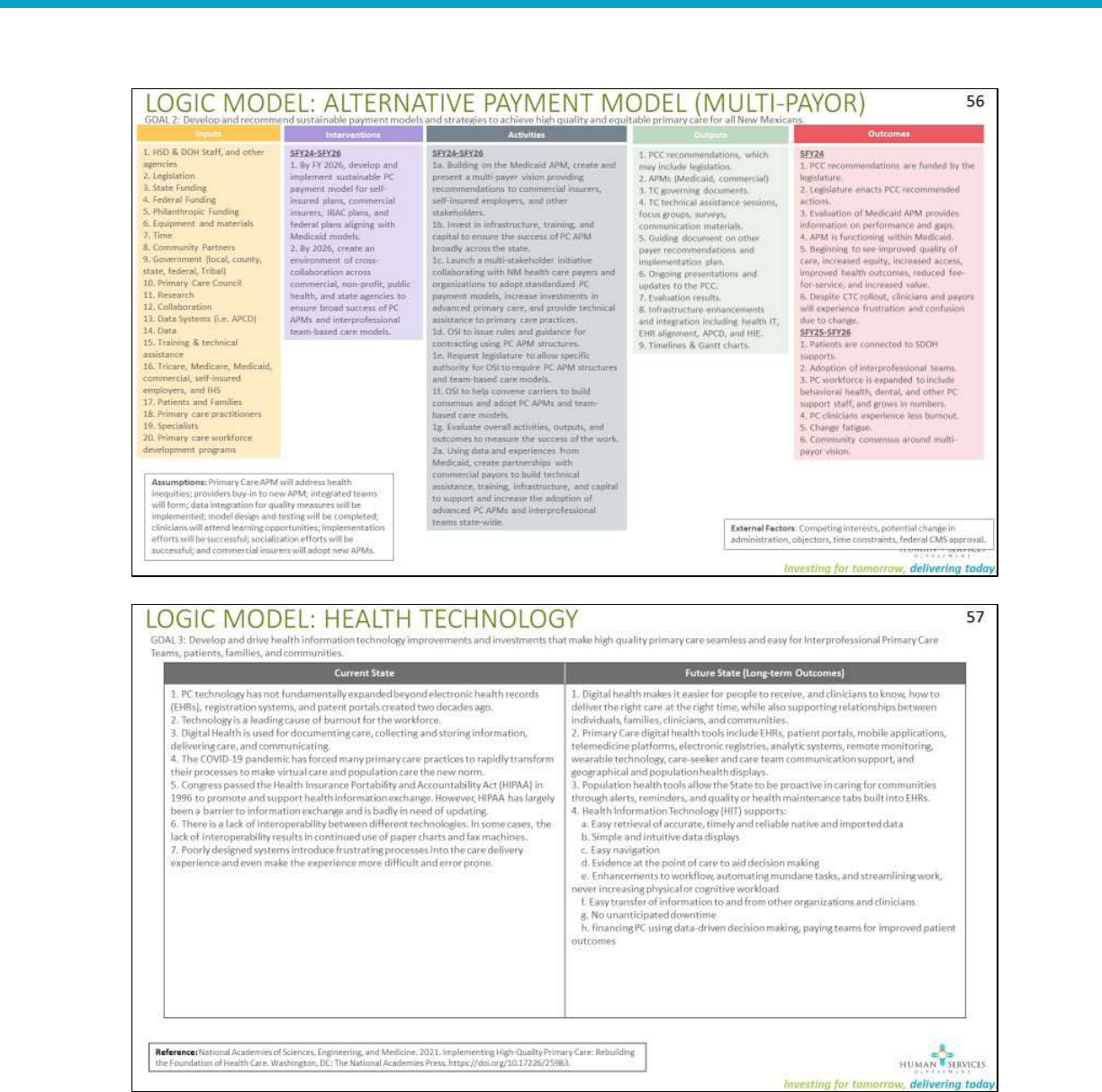
Primary Care Logic Models ..................................................................................................................... 28
Primary Care Best and Promising Practices ............................................................................................ 33
References .................................................................................................................................................. 44
New Mexico Primary Care Council 2023
Page 2 of 48
Honor Native Land
On behalf of all colleagues at the Human Services Department, we
humbly acknowledge we are on the unceded ancestral lands of the
original peoples of the Pueblo, Apache, and Diné past, present, and
future.
With gratitude we pay our respects to the land, the people and the
communities that contribute to what today is known as the State of
New Mexico.
Evening drive through Corrales, NM in October 2021.
By HSD Employee, Marisa Vigil

New Mexico Primary Care Council 2023
Page 3 of 48
Letter from the Primary Care Council Chair
Welcome to New Mexico's Primary Care Council.
In 2019, providers, clinicians, and primary care advocates across New Mexico urged the state legislature
to form the New Mexico State Primary Care Council (PCC). Passed as House Bill 67 in 2021, the PCC is
tasked with addressing the immediate and urgent issues plaguing primary care.
I have the honor of serving as chair of the Primary Care Council since its formation. The PCC understands
the urgent need for a primary care revolution to ensure health equity for patients, families,
communities, and primary care workforce; initiate payment strategies to support high-quality primary
care; make health technology investments and improvements; and build a sustainable workforce. At the
heart of our work, is a desire to:
revolutionize primary care through innovation and creativity;
ensure primary care data is valid, reliable, and specific to understand our system;
develop equitable interprofessional primary care teams who value and honor every member of
the team equally and provide person-centered care;
use an intersectional approach to ensure primary care is fairly and justly provided for all New
Mexicans;
support holistic primary care, factoring in a unique array of ancestral approaches to living and
healing;
ensure healthy communities through partnerships designed with the needs of community at
the center.
Over the past year, the Council has focused on developing primary care payment and care delivery
reforms for Medicaid. In 2023, we will announce the new payment models which were developed in
collaboration with, and to meet the needs of, providers and clinicians across the state. I look forward to
sharing and learning together with you as we provide technical assistance and training for the adoption
of these reforms.
Revolutionizing, reimagining, and investing in primary care in is an enormous, yet essential task, for
ensuring the health of all New Mexicans. As you review the Primary Care Council’s 2023 Strategic Plan, I
hope you see a future where New Mexico exemplifies same-day access to high-quality, equitable,
primary care for all persons, families, and communities.
With sincere gratitude,
Jennifer K. Phillips, M.D.
Family Medicine Physician

New Mexico Primary Care Council 2023
Page 4 of 48
Executive Summary
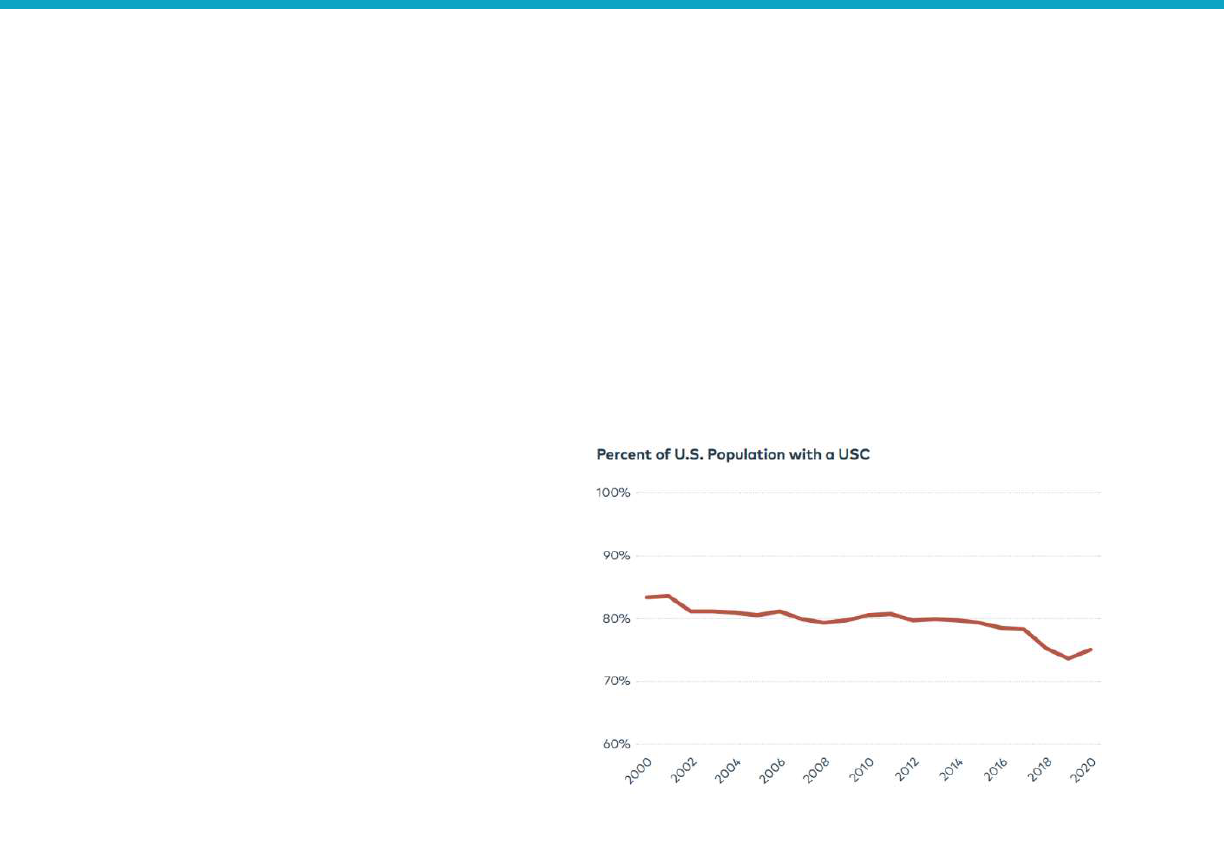
Over the past twenty years, there has been a significant shift in health care resulting in only one in five
Americans having access to a routine or usual source of care. [1] In New Mexico we refer to this usual
source of care as “primary care.” The COVID-19 crisis has brought to the forefront shortcomings in the
current primary care system including a declining workforce experiencing severe burnout; a decline in
patient-physician relationships; profound societal health inequities; and an overall underinvestment in
Primary Care. [2] [3] [4] [5]
A wealth of research shows primary care helps prevent illness and death, and findings in both national
and international studies illustrate primary care results in a more equitable distribution of community
health. [6] Primary care is the only health care component where an increased supply results in
improved population health and more equitable outcomes. Primary care is a common good, which
makes the strength and quality of the country’s primary care services a public concern.
[7]
The primary
care workforce is also key in the promotion of health equity by supporting patients and families in
attaining their full health potential, while ensuring neither social position nor other socially determined
circumstances disadvantages them from achieving their potential.
[8]
In 2022, the Primary Care Council (PCC) and New Mexico Human Services Department (HSD) led a state-
wide collaborative process in to establish new primary care payment models for Medicaid that will
launch on January 1, 2024. Stakeholders across all aspects of primary care were engaged in listening
sessions, surveys, focus groups, and individual conversations. These payment reforms are built to
support the needs of the New Mexico primary care workforce, patients, families, communities, and
payors. Medicaid Turquoise Care Managed Care Organizations (MCO) will be required to adhere to any
payment reform recommendations promulgated by the New Mexico Primary Care Council. The work of
the PCC is also reflected in the State of New Mexico Medicaid federal 1115 waiver demonstration
including:
Expanded Centennial Home Visiting Pilot Programs
Expanded Access to Supportive Housing
Medicaid Services for High-Need Justice-involved Populations 30 Days Before Release
Member-Directed Traditional Healing Benefits for Native Americans
Home-Delivered Meals Pilot Programs
Addition of a Closed-Loop Referral System
Medical Respite for Members Experiencing Homelessness
Primary Care Residency Expansion funding and program technical assistance
In 2023, the PCC will continue their work to revolutionize primary care across the four goals of the
council. Health Equity and wellness for the primary care workforce will continue to be at the center of
the work of the PCC. We will partner with NM Department of Health in the increasing the Community
Health Worker workforce, collaborate on strategies to address health disparities in the state, and begin
to modernize the state’s health IT systems.
HSD, in collaboration with members of the community-based PCC, worked together to develop this
strategic plan. This strategic plan outlines a thoughtful, achievable, and bold plan to improve the many
elements of primary care throughout New Mexico; and the PCC will update it annually over the next
four years.
New Mexico Primary Care Council 2023
Page 5 of 48
Background and Introduction
The 2021 House Bill 67 (Primary Care Council Act)
[9]
charges HSD to establish an unpaid, statewide PCC
to advise the State in finding means to increase New Mexicans’ access to primary healthcare while
improving overall health and lowering total healthcare costs. As enacted, the statute outlines eight
duties for the Council, which are outlined below:
1. Develop a shared description of primary care practitioners and services;
2. Analyze annually the proportion of health care delivery expenditures allocated to primary care
statewide;
3. Review national and state models of primary care investment with the objectives of increasing
access to primary care, improving the quality of primary care services and lowering the cost of
primary care delivery statewide;
4. Review New Mexico state and county
data and information about barriers to
accessing primary care services faced by
New Mexico residents;
5. Recommend policies, regulations and
legislation to increase access to primary
care, improve the quality of primary
care services and reduce overall health
care costs;
6. Coordinate efforts with the graduate
medical education expansion review
board and other primary care workforce
development initiatives to devise a plan
that addresses primary care workforce
shortages within the state;
7. Report annually to the interim legislative health and human services committee and the legislative
finance committee on ways that primary care investment could increase access to primary care,
improve the quality of primary care services, lower the cost of primary care delivery, address the
shortage of primary care providers and reduce overall health care costs; and,
8. Develop and present to the [Human Services Department] secretary a five-year plan to determine
how primary care investment could increase access to primary care, improve the quality of primary
care services, lower the cost of primary care delivery, address the shortage of primary care
providers and reduce overall health care costs.
New Mexico Overview
Prior to their encounter with the Spanish in 1540, the Pueblo, Navajo, Ute, and Apache communities
(including the Fort Sill, Jicarilla and the Mescalero) lived on the land known today as the state of New
Mexico.
In 2021, the New Mexico state population is 2,106,319
[10], with over 68% identifying as racial or ethnic
minorities.
[10] Though the State’s population centers are in urban areas, New Mexico is a rural and
frontier state, with an average population density of 17.5 persons/square mile. [11] Further 18.5% [10]
FIGURE 1: PERCENT OF POPULATION WITH A USUAL SOURCE OF
(PRIMARY) CARE
New Mexico Primary Care Council 2023
Page 6 of 48
of state residents in 2020 were 65 years or older, and is projected to reach 26.5% by 2030, making it the
third oldest state in the U.S. [12] This older population, low population density combined with long
distances make the provision of healthcare particularly challenging. New Mexico has a shortage of
healthcare providers across all specialties, including in primary care. One estimate projects a national
primary care physician shortage of over 20,000 by 2033.
[13] Another estimate lists New Mexico among
three states with the largest shortage of registered nurses by 2030. [14] This healthcare workforce
shortage means healthcare access is challenging, as many New Mexicans cannot access timely primary
care, especially rural and frontier communities.
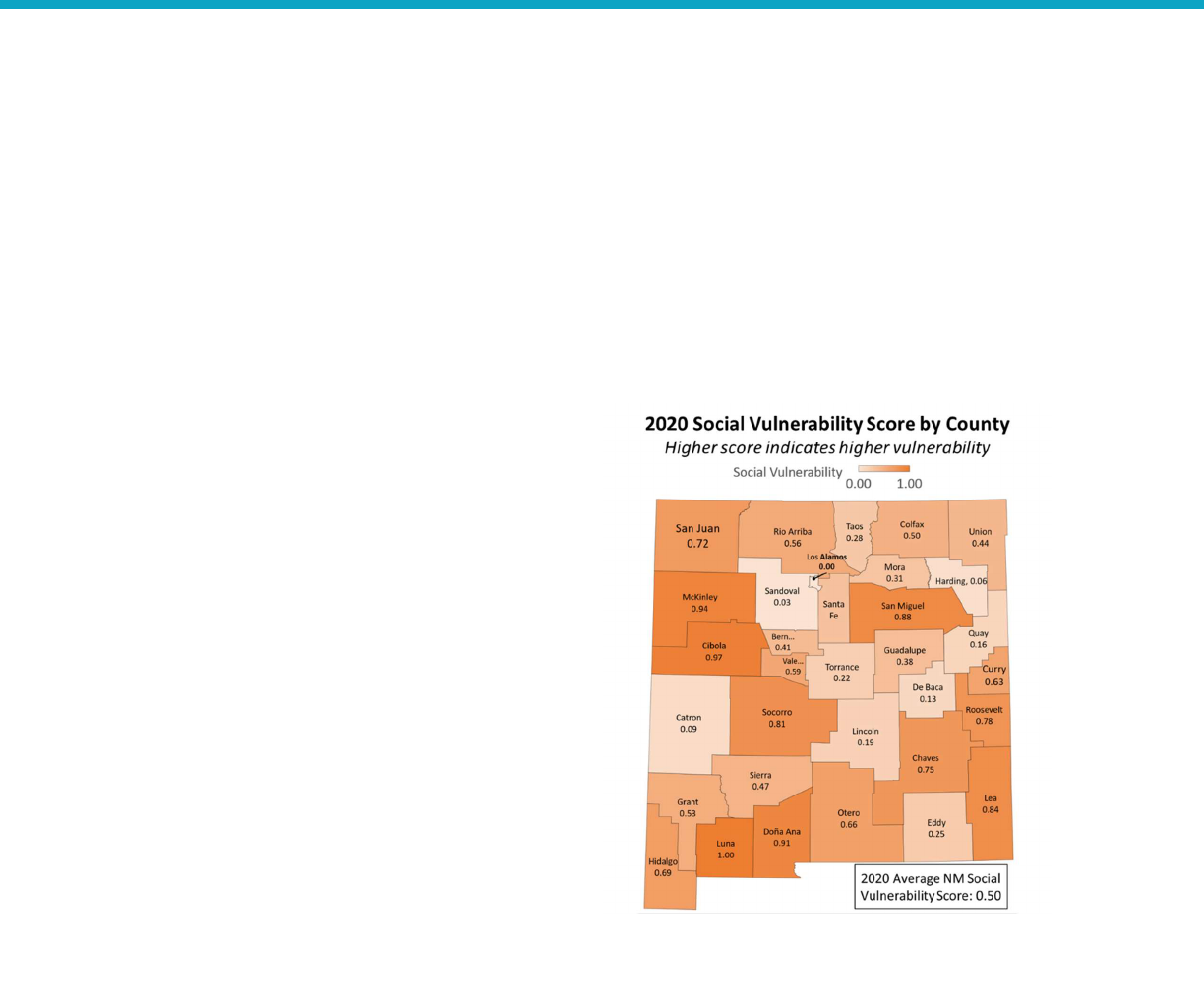
In many health and socioeconomic indicators, New Mexico fares worse when compared to other states
such as per capita personal income ($50,311 4
th
lowest). [15] New Mexico ranks third in U.S. child
poverty (24%), and third in the U.S. in elder
poverty (12.8%). [16] The substantial enrollment
in the Medicaid program reflects the extent of the
state’s poverty: 984,335 New Mexicans enrolled
in the Medicaid public health insurance program
in December 2022, (45% of the State’s
population).
[17]
Although NM has lower death
rates than the national average for heart disease
and cancer, it has much higher death rates for
unintentional injuries, specifically overdose,
motor vehicle injuries, and falls.
The PCC has outlined several activities to support
health equity in New Mexico. Care coordination
and Community Health Workers (CHWs) are
particularly important for achieving access to care
and connection to social supports such as healthy
food, housing, employment, and transportation.
Additionally, HSD is requesting funding for a
closed-loop referral service to connect patents to
social services in their community.
Primary Care Council Overview
The following definition of primary care (adapted from the National Academy of Sciences, Engineering
and Medicine) guides the work of the PCC, setting the stage for the PCC’s mission, vision, and goals:
“High-quality primary care is the provision of whole-person, integrated, accessible, and equitable
healthcare by inter-professional teams and community partners who are accountable for addressing the
majority of individuals’ health and well-being across settings and through sustained relationships with
patients, families, and communities.” [7]
FIGURE 2: NM SOCIAL VULNERABILITY BY COUNTY.
SOURCE, U.S. CENTERS FOR DISEASE CONTROL AND
PREVENTION [66]

New Mexico Primary Care Council 2023
Page 7 of 48
The PCC definition of high-quality primary care is not a description of the current state of primary care in
New Mexico. It is aspirational and defines what the foundation of the health care system can, should,
and must be for all New Mexicans. Thus, the PCC mission is to revolutionize—to change radically and
fundamentally—how we deliver primary care; to transform primary care into a team-based approach
that values and rewards equitable, accessible, comprehensive, coordinated, high-quality, and cost-
efficient care.
As outlined in statute, [9] the PCC is a public-private body that includes nine voting members and
thirteen advisory members, appointed by the Human Services Department (HSD) Secretary. Members
include representatives from HSD, Department of Health, Office of Superintendent of Insurance, and the
NM Primary Care Association. In 2022, the PCC expanded to include community partners who
participate in quarterly meetings and workgroups to provide additional perspectives.
Primary Care Council Timeline of Strategic Activities
In 2022, the PCC developed and adopted the list of strategic activities below designed to be
accomplished in the next several years. These activities align with the eight duties outlined in House Bill
67. The PCC will annually publish updates in subsequent strategic plans.
FIGURE 3: PRIMARY CARE COUNCIL MISSION, VISION, AND GOALS
New Mexico Primary Care Council 2023
Page 8 of 48
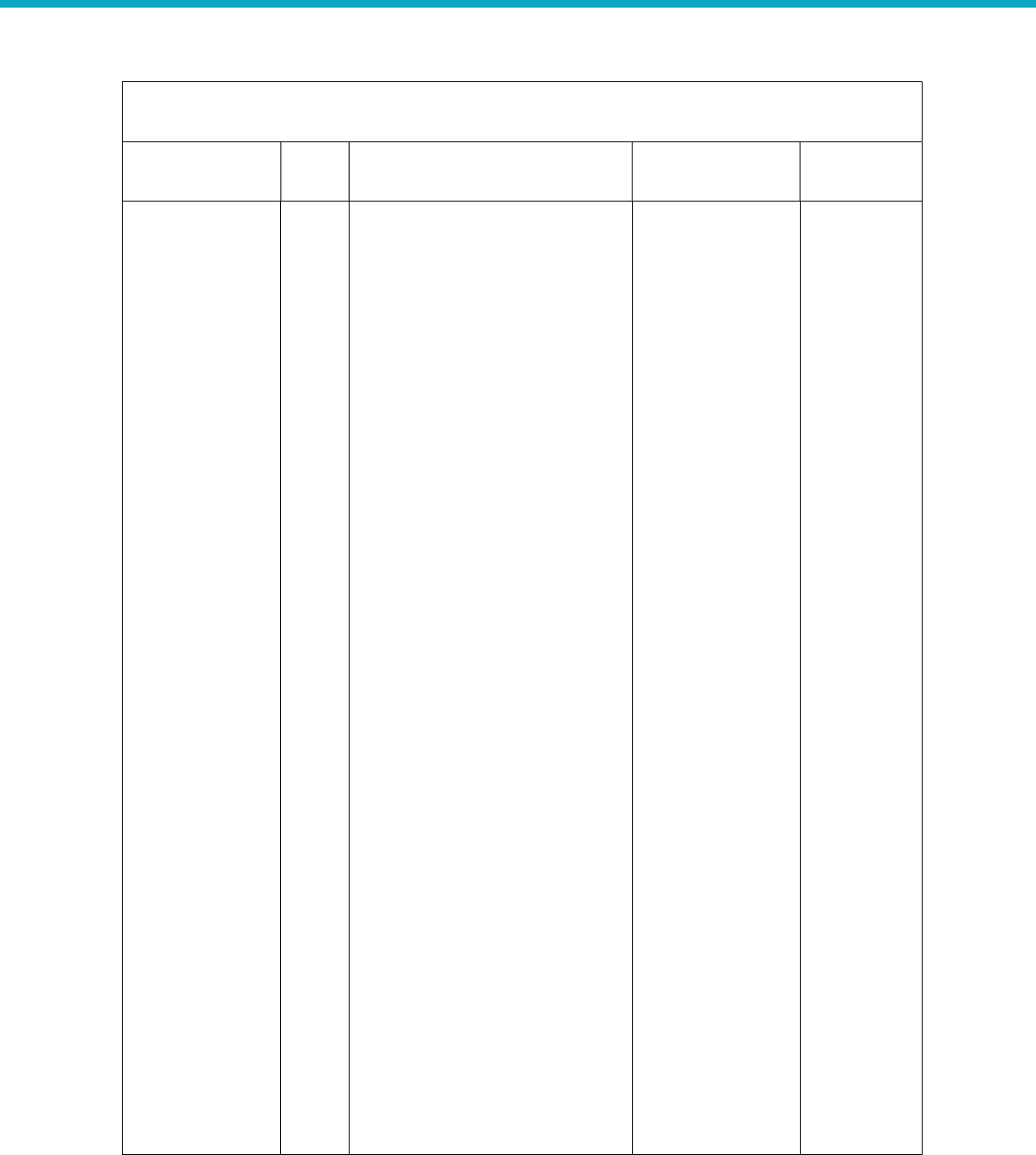
GOAL 1: Develop and drive investments in
health
equity across New Mexico to improve the health of
New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
1.
By 2026,
establish a
standard for
health equity in
New Mexico that
includes the
expectations,
tools, and
resources are
available for
Primary Care.
1,
4,
8
1
a
.
In partnership with
the
Department of Health (DOH),
develop a framework for equity at
the clinic level, community,
patient, and family levels.
1b. DOH in partnership with state
agencies, tribal, and community
stakeholders, will identify and
implement strategies to improve
primary care and health equity in
the State Health Improvement
Plan (SHIP).
1c. Submit a 5-year 1115 waiver
renewal application to CMS that
includes strategies to address
health equity in the state’s
Medicaid program with an
anticipated effective date of
January 1, 2024.
1d. Implement strategies in Goal 3
(Health Equity) of the 1115 waiver
to identify groups that have been
historically and intentionally
disenfranchised and address
health disparities through strategic
program changes to enable an
equitable chance at living healthy
lives.
HSD
(1
c
,e
)
DOH (1b)
HSD & DOH (1a,d)
SFY2
3
(1c)
SFY23 (1a,c)
SFY23-26
(1b)
SFY24-26
(1d)
2. By 2026,
integrate public
health, primary
care, and
behavioral health.
4,5
2a.
In coordination and alignment
with payment reforms, develop
models for interprofessional team-
based care with an emphasis on
behavioral health integration.
2b. In coordination and alignment
with payment reforms, provide
technical assistance and training
for clinics to succeed under
models of interprofessional team-
HSD
(
2a
,b,
c)
DOH (2d,f)
HSD & DOH (2g)
New Mexico
Primary Care
Association
(NMPCA) (2e)
SFY23
(2a,d,e)
SFY23-SFY26
(2b,c,f,g)
New Mexico Primary Care Council 2023
Page 9 of 48
GOAL 1: Develop and drive investments in
health
equity across New Mexico to improve the health of
New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
based
care with an emphasis on
behavioral health.
2c. Implement Certified
Community Behavioral Health
Clinics (CCBHCs) to support
behavioral health access; care
coordination including services
provided to assist and support
individuals in developing their
skills to gain access to needed
medical, behavioral health,
housing, employment, social,
educational, and other services
and help advance primary care
integration. [18]
2d. Inventory DOH services across
New Mexico primary care settings,
including staff presence, grants,
and contracts for services.
2e. Conduct needs and
assets assessment for public
health services in primary
care settings across New Mexico.
2f. Develop and implement
strategies to build out co-located
public health in primary care
settings.
2g. Invest in public health and the
public health workforce to
improve disease surveillance
systems and expand and diversify
the public health workforce so we
can address the impacts of the
social and structural determinants
of health, health inequities,
counter spread of health
misinformation and
disinformation, strengthen
New Mexico Primary Care Council 2023
Page 10 of 48
GOAL 1: Develop and drive investments in
health
equity across New Mexico to improve the health of
New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
partnerships across clinical and
community settings and consider
other societal factors that shape
well-being.
3. By 2026, create
meaningful
partnerships
between
governmental
agencies,
nonprofit
organizations,
businesses, and
academic centers
to support health
equity.
4,5
3a.
A
lign efforts
and
develop
partnerships with social support
organizations who will provide
social services to patients
connected to the closed-loop
referral system.
3b. Align efforts and develop
partnerships with state agencies
and community groups to
establish Accountable
Communities of Health (ACH). [19]
New Mexico
CONNECT
Collaborative (3a,
b)
SFY
23
-
26
(3a,b)
4
. By 2026,
establish
networks of care
coordinators who
support patients
in equitable
access to care,
connection to
social services,
and facilitate
action between
interdisciplinary
care teams.
4,5
4
a.
Improve linkages between
Community Health Workers
(CHW), Community Health
Representatives (CHR), and
Community Peer Support Workers
(CPSW) with primary care clinics to
support integrated team-based
models in primary care.
4b. Standardize training and
certification for CHWs.
4c. Provide training and technical
assistance to CHWs and other care
coordinators on how to use tools,
support equity, connect patients
to social resources, and facilitate
connections and conversations
with interdisciplinary care teams.
4d. Submit a Medicaid state plan
amendment to allow
reimbursement for CHWs and
other care coordinators.
HSD (
4
d
)
DOH (4b,c)
HSD & DOH (4a)
SFY23 (
4
b,
d
)
SFY24-26
(2a,c)
New Mexico Primary Care Council 2023
Page 11 of 48
GOAL 1: Develop and drive investments in
health
equity across New Mexico to improve the health of
New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
5. Analyze
proportion of
health care
delivery
expenditures
allocated to
primary care.
2
5a. In alignment with HB67 duty 2,
annually analyze the proportion of
health care delivery expenditures
allocated to primary care.
5b. Identify and implement policy
changes that can increase the
proportion of health care delivery
expenditures allocated to primary
care.
5c. Once available, utilize the All-
Payer Claims Database to calculate
percentage of primary care spend.
HSD (5a
,b
,c
)
SFY2
4
-
26
(5a,c)
SFY25-26
(5b)
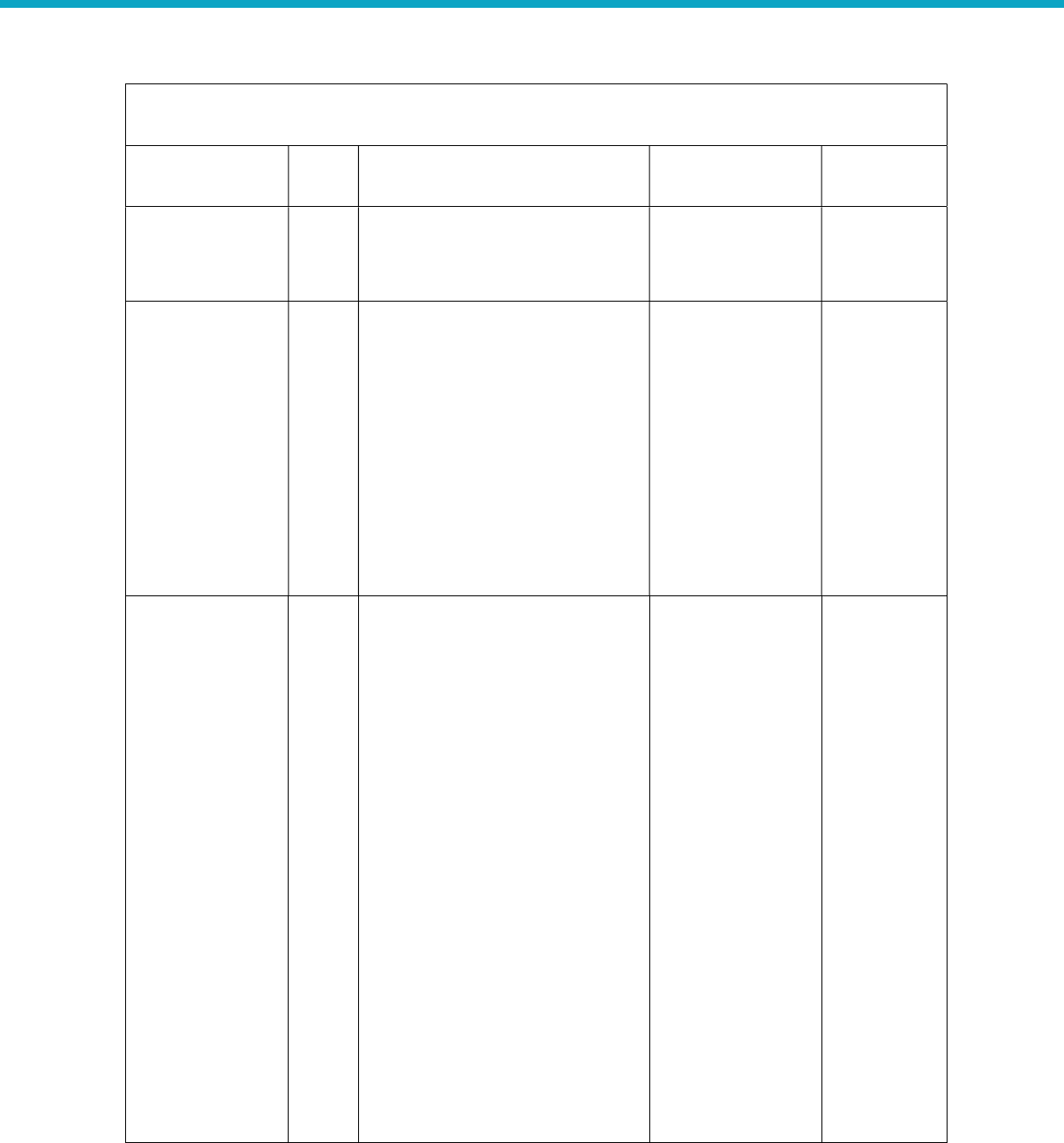
GOAL 2: Develop and recommend sustainable payment models and strategies to achieve high quality
and equitable primary care for all New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
1. By 2024, develop
and implement
sustainable primary
care payment
model(s) for
Medicaid that move
away from fee-for-
service and volume
to payment for
quality, health
outcomes, and
patient wellness.
3,
4,
5
1a. Design a new
primary care
payment model(s) that aligns with
the Health Care Payment Learning
and Action Network (HCP-LAN)
[20] framework to incentivizing
performance and population-level
health outcomes, aligns with the
core features and principles
adopted by HSD and PCC, and
applies to a variety of settings.
1b. Test and evaluate primary care
payment model(s) for efficacy and
outcomes prior to start date of
new Medicaid MCO contracts
(1/1/2024).
1c. Develop Medicaid MCO
contract language for primary care
payment reforms in accordance
with the Code of Federal
Regulations (CFRs) and other
HSD
(1a,b,c,e,h,I,j,k)
HSD & DOH (f)
OSI (1d)
NMFA & DOH
(1g)
SFY2
3
(1a,b,c,e,k)
SFY23-26
(1d,f,g,h,i,j)
New Mexico Primary Care Council 2023
Page 12 of 48
GOAL 2: Develop and recommend sustainable payment models and strategies to achieve high quality
and equitable primary care for all New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
state/federal rules and
regulations.
1d. Provide fiscal, policy, and/or
legislation that may be needed to
advance and support primary care
payment reform; and a multi-
payor roll-out of primary care
payment reform.
1e. Develop and define the quality
metrics (including health equity)
that will be a part of the Medicaid
payment model and harmonized
across the different Medicaid
MCOs.
1f. Create investment
opportunities that support
practices engaged in Medicaid
payment reform implementation
and progression from tier 1 to 4
(e.g., PMPM investments for a
year before moving to additional
tier, up-front investment in
staffing, tech, training, resources).
1g. Through its Primary Care and
Behavioral Health Capital Fund,
the State will provide capital
project financing to community-
based nonprofit clinics located in
rural and underserved areas of
New Mexico.
1h. Work with MCOs to create
consistency across administrative
processes and reduce
administrative burden.
1i. Work with legislature to
sustainably fund continued
primary care payment reform
growth and improvements.
New Mexico Primary Care Council 2023
Page 13 of 48
GOAL 2: Develop and recommend sustainable payment models and strategies to achieve high quality
and equitable primary care for all New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
1
j
.
Engage with CMS to leverage
federal funding and programs to
support primary care payment
model success.
1k. Participate in the Center for
Health Care Strategies “Medicaid
Primary Care Population-Based
Payment Learning Collaborative”
to receive technical assistance
focused on developing,
implementing, and improving
primary care population-based
payment models within Medicaid.
2. Build the
foundation for long-
term engagement
with stakeholders
that began in 2022
to prepare for and
promote adoption of
primary care
payment reforms in
Medicaid.
3,4,5
,8
2a. Conduct meetings of the
Primary Care Transformation
Collaborative (TC), providing
primary care practitioners
supports related to NM Medicaid
primary care payment model
implementation.
2b. Continue to build relationships
with stakeholders through
listening sessions, webinars, and
ongoing support to address
common areas of need to support
the adoption and success for
clinics in adopting primary care
payment reforms.
2c. Publish survey findings and
recommendations for clinician and
provider readiness in adopting
primary care payment reforms.
2d. Identify underserved areas
where additional technical
assistance is needed to support
and/or to enhance provider and
clinician adoption of primary care
payment reforms.
HSD
(2a,b,c,d,e,f)
SFY22 (2c
,e
)
SFY22-23
(2f)
SFY23 (2d)
SFY23-26
(2a,b)
New Mexico Primary Care Council 2023
Page 14 of 48
GOAL 2: Develop and recommend sustainable payment models and strategies to achieve high quality
and equitable primary care for all New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
2e.
Identify and distribute best
and promising practice activities
that enhance provider and
clinician primary care payment
reform adoption.
2f. Develop a measurement
instrument and evaluate success
of technical assistance services,
and revise supports as needed.
3. Provide supports
for Medicaid primary
care clinicians and
providers to reach
HCP-LAN Category 4
by 2026.
3,5,8
3a. Provide clinicians and
providers incentive payments that
advance their capacity to adopt
increasingly more advanced
primary care payment reforms.
3b. Establish a value-based data
intermediary to help evaluate and
monitor population health
metrics.
3c. Provide technical assistance for
the use of a value-based data
intermediary to help evaluate and
monitor population health
metrics.
3d. Provide technical assistance to
providers and clinicians in
supporting adoption of
increasingly more advanced
primary care payment and
interprofessional-team models.
HSD (3a
,b,c,
d
)
SFY
23
-
26
(3d)
SFY24 (3b)
SFY23-26
(3a,c)
4. By
2026
,
create an
environment where
primary care
providers and
clinicians have
opportunities to
learn how to adopt
new payment and
interprofessional
5,
8
4a. Contin
ue
primary care
payment and interprofessional
technical assistance to grow the
number of providers and clinicians
participating in advanced primary
care in the state.
HSD (4a)
SFY2
3
-
26
(4a)
New Mexico Primary Care Council 2023
Page 15 of 48
GOAL 2: Develop and recommend sustainable payment models and strategies to achieve high quality
and equitable primary care for all New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
team
-
based models
and how those
models will improve
their practice.
5. By FY 2026,
develop and
implement
sustainable payment
reforms for self-
insured plans,
commercial insurers,
IBAC plans, and
federal plans
aligning with
Medicaid models.
3,5,8
5
a. Building on Medicaid
payment
reforms, create and present a
multi-payer vision providing
recommendations to commercial
insurers, self-insured employers,
and other stakeholders.
5b. Invest in infrastructure,
training, and capital to ensure the
success of multi-payor primary
care payment reforms broadly
across the state.
5c. Launch a multi-stakeholder
initiative collaborating with NM
health care payers and
organizations to adopt
standardized advanced primary
care payment models, increase
investments in advanced primary
care, and provide technical
assistance to primary care
practices.
5d. Issue rules and guidance for
contracting using PC APM
structures.
5e. Request legislature to allow
specific authority for OSI to
require advanced primary care
payment structures and team-
based care models.
5f. OSI to help convene carriers to
build consensus and adopt PC
APMs and team-based care
models.
HSD
(
5
a
,b,
c,g)
OSI (5d,e,f)
SFY24
(5
a,
c
)
SFY25-26
(5b,d,e,f)
New Mexico Primary Care Council 2023
Page 16 of 48
GOAL 2: Develop and recommend sustainable payment models and strategies to achieve high quality
and equitable primary care for all New Mexicans.
Objectives
HB 67
Duty Activities Lead Timeframe
6
.
Measure the
improvements in
health outcomes
and system-wide
cost savings of
improving an
innovative and
integrated system
that encourages care
coordination,
optimally designed
care management,
and care transition.
3,5,8
6
a. Create state
-
level metrics to
measure population health
outcomes and system-wide health
care savings under primary care
payment reforms.
HSD
, DOH
(
6a
)
SFY2
5
(6a)
GOAL 3: Develop and drive health information technology improvements and investments that make
high quality primary care seamless and easy for Interprofessional Primary Care Teams, patients,
families, and communities.
Objectives
HB 67
Duty Activities Lead Timeframe
1. By 2026, develop,
invest in, and
implement health IT
improvements to
support advanced PC
practice, payment,
and interprofessional
teams.
2,3,4,8
1a. Assess the needs for providers to
connect their EHRs to the HIE to adopt
advanced primary care payment in their
practice.
1b. Contract with business analysts and
project managers to revalidate
requirements for EHRs and modernize
current DOH systems and begin
implementation.
1c. Establish an Office of Informatics to
help manage data and information
exchange between systems.
1d. The All Payor Claims Database
(APCD) will begin collecting data from
various data submitters throughout the
state with an implementation date in 4Q
SFY23.
HSD (1a
,e,i
)
DOH
(1b,c,d,e,f)
Syncronys
(1g,h)
SFY
23
(1a,b,d,f)
SFY24
(1c,e,h)
SFY24-26
(1g)

New Mexico Primary Care Council 2023
Page 17 of 48
GOAL 3: Develop and drive health information technology improvements and investments that make
high quality primary care seamless and easy for Interprofessional Primary Care Teams, patients,
families, and communities.
Objectives
HB 67
Duty Activities Lead Timeframe
1e.
Create a collaborative plan for
implementation of health technologies
across multi-payors to reduce
administrative burdens, enable
successful PC APM implementation, and
team-based care models that include
patient and provider identity
management, attribution, care
management and coordination, financial
benchmarking and management, quality
reporting, and feedback.
1f. Collect data from various data
submitters throughout the state with an
implementation date in 4Q SFY23.
1g. If funding becomes available, partner
with HSD on a Social and Structural
Determinants of Health (SDOH) referral
system which is designed to better
connect patients who need social
services with the resources through
creating HIE data collection and
reporting capabilities.
1h. Expand operability of the Healthcare
Information Exchange (HIE) to support
advanced primary care payment models
including risk stratification and
population management.
1i. Receive Centers for Medicare and
Medicaid Services (CMS) certification to
be a modular system which will allow
the HIE to be a National Committee for
Quality Assurance (NCQA) data
aggregator validator.
New Mexico Primary Care Council 2023
Page 18 of 48
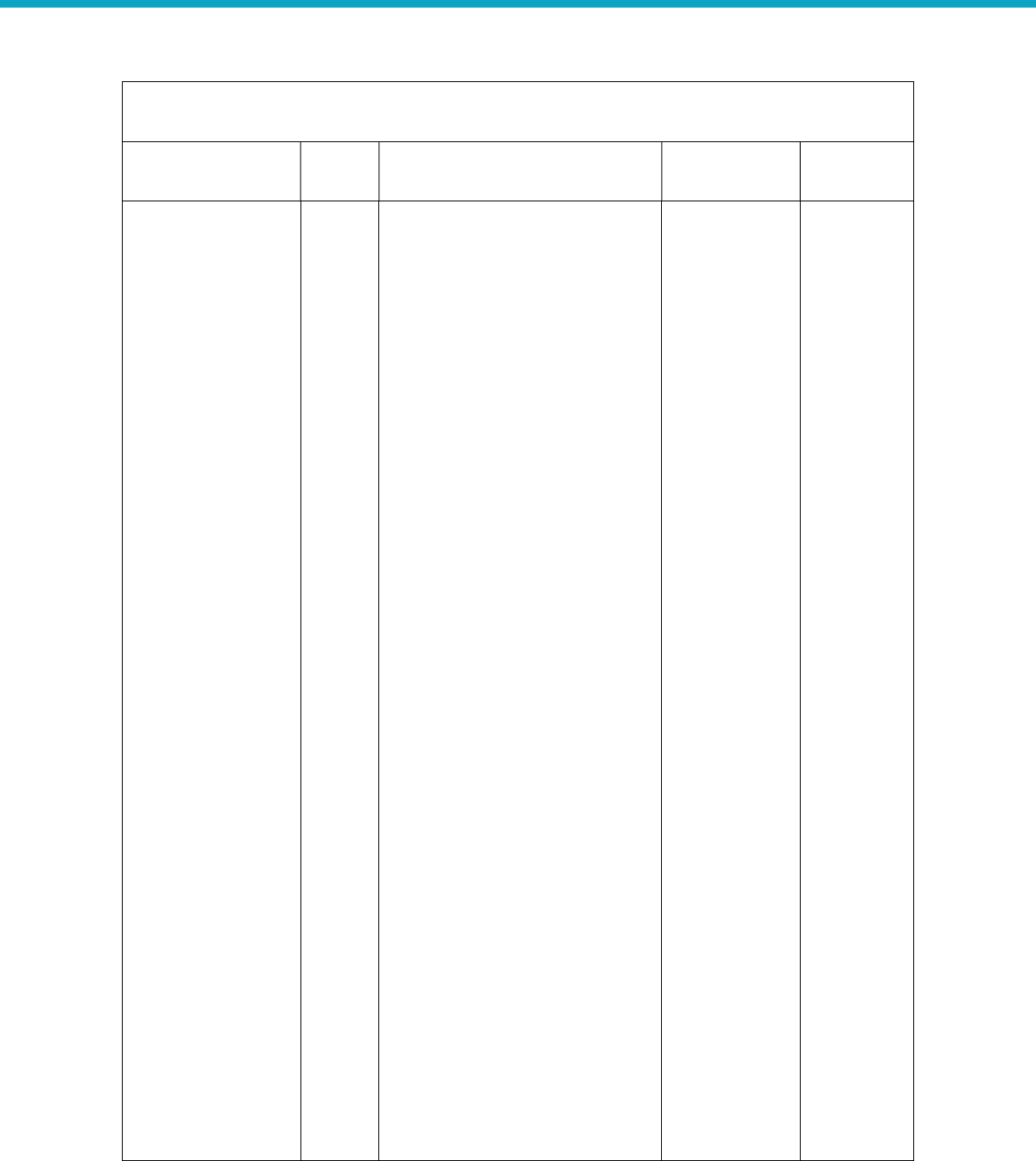
GOAL 4: Create a sustainable workforce, financial model, and budget to support our mission and
secure necessary state and federal funding.
Objectives
HB 67
Duty Activities Lead Timeframe
1. By 2026, develop
a
system for data and
monitoring of the
heath care workforce
across state and
private entities
responsible for
collecting workforce
data.
1,
3,5,6
1a. Conduct a comprehensive,
statewide primary care workforce
analysis to determine the current
provider-to-population ratios,
provider demographics, utilization
of primary care interprofessional
teams.
1b. Understand effectiveness of
loan repayment programs
in recruitment and retention in
rural areas, understand the current
state of provider well-being, and
healthcare career programs that
will inform tactics to address
workforce shortages and
sustainability.
1c. Collaborate with primary care
licensure boards to improve data
collection and analyses.
HSD
(1a
,b,
c
)
SFY2
3
-
26
(1a)
SFY24 (1b)
SFY23-26
(1c)
2. By 2024,
implement
sustainable Medicaid
PC rate adjustments.
2,5
2a.
Develop fair and
equitable
methodology for Medicaid provider
rate reimbursements that support
the healthcare workforce.
2b. Raise Medicaid reimbursement
rates for primary care, behavioral
health, and maternal and child
health to 120% of Medicare.
2c. Raise Medicaid reimbursement
rates for all other services to 100%
of Medicare.
HSD (2a
,b,
c
)
SFY2
3
(2a,b,c)
3. By 2024, develop
plans to expand
existing workforce
capacity and future
workforce
development.
3,5,6
3a. Expand the capacity of
C
ertified
Peer Support Workers (CPSWs)
through training and certification of
existing and future workforces.
3b. Expand the capacity of and
community health workers (CHWs)
HSD (3a
,c
-
g
)
DOH (3b)
SFY24 (
3
c
)
SFY24-26
(3a,b,d)
SFY26 (3e-
g)
New Mexico Primary Care Council 2023
Page 19 of 48
GOAL 4: Create a sustainable workforce, financial model, and budget to support our mission and
secure necessary state and federal funding.
Objectives
HB 67
Duty Activities Lead Timeframe
through training and certification of
existing and future workforces.
3c. Identify strategies the State can
take to promote healthcare
providers and clinicians practice at
the top of their license.
3d. Promote the New Mexico
Health Service Corps (NMHSC) to
recruit, place, and offer financial
assistance to designated health
professionals in rural and medically
underserved areas of the state.
3e. Expand the number of
accredited primary care residency
programs from 8 to 16.
3f. Increase the number of
community primary care residency
positions (from 142 to 264) in NM
by 2025 through expansion of
existing residency programs and
development of new programs,
especially in rural areas.
3g. A minimum of 60% of primary
care residents who complete an
HSD-affiliated residency program
remain in NM and practice primary
care by 2025, reaching 70% by
2030.
4.
By 2024,
expand
and make
improvements to
current recruitment
and retention
efforts.
4a. Make financial incentives and
assistance opportunities for the
health care workforce clear,
transparent, and easy to find.
4b. Identify financial and
nonfinancial barriers to the
recruitment and retention of the
non-licensed primary care
workforce.
DOH (4
a,d)
HSD (4b)
HSD & DOH
(4c)
SFY24
(4a,b,c)
SFY23-26
(4d)
New Mexico Primary Care Council 2023
Page 20 of 48
GOAL 4: Create a sustainable workforce, financial model, and budget to support our mission and
secure necessary state and federal funding.
Objectives
HB 67
Duty Activities Lead Timeframe
4c.
Examine NM state policies that
may be punitive for health care
workers seeking mental health
care, advancing legislation to
protect health workers seeking
help if appropriate.
4d. Provide financial assistance to
rural primary care clinics to sustain
a minimum level of delivery of
primary care services pursuant to
the provisions of the Rural Primary
Health Care Act (RPHCA). [21]
5.
B
y
2026,
implement
recommendations
provided by the US
Surgeon General on
addressing health
worker burnout and
implement programs
relevant needs in
NM. [2]
5
a
.
Examine state health
professional licensing board
questions in applications and
renewal forms for licensure so that
health workers are only asked
about “conditions that currently
impair the clinicians’ ability to
perform the job,” as recommended
by The Joint Commission in 2020,
Federation of State Medical
Boards, and aligned with the
American with Disabilities Act.
5b. Determine extent of workplace
violence against health workers,
and pass legislation to address it if
needed.
5c. Ensure that state boards and
legislatures approach burnout from
a nonpunitive lens by considering
offering options for “safe haven”
non-reporting for clinicians and
providers receiving appropriate
treatment for mental health or
substance use.
5d. Increase access to quality,
confidential mental health, and
HSD
(5a,b,c,d,e,
f,g,h,i)
SFY23
(5,d,e,f)
SFY24
(5a,b,c,g,h)
New Mexico Primary Care Council 2023
Page 21 of 48
GOAL 4: Create a sustainable workforce, financial model, and budget to support our mission and
secure necessary state and federal funding.
Objectives
HB 67
Duty Activities Lead Timeframe
substance use care for all health
workers.
5e. Track timeframes for Medicaid
provider enrollment, simplify
enrollment process and develop a
manual on how to enroll.
5f. Propose updates to the current
MCO credentialling process to
make the process more
streamlined.
5g. Engage with NM Health
Professional Wellness Program
(NMHPWP) to re-design Physician
Health Programs and wellness
programs to provide early
intervention and destigmatize
seeking help.
5h. Analyze licensure questions
about diagnoses and treatment and
determine how to limit questions
to only those necessary for safety,
lowering barriers to seeking
treatment, and easing physician
concerns about their medical
license being suspended or
revoked.
Medicaid Primary Care Payment Reforms
The PCC is beginning its payment reform efforts with the Medicaid program, shifting primary care
financing from a fee-for-service to payments that drive population and patient wellness. This new
payment model will begin January 2024 aligning with the launch of New Mexico Medicaid Turquoise
Care.
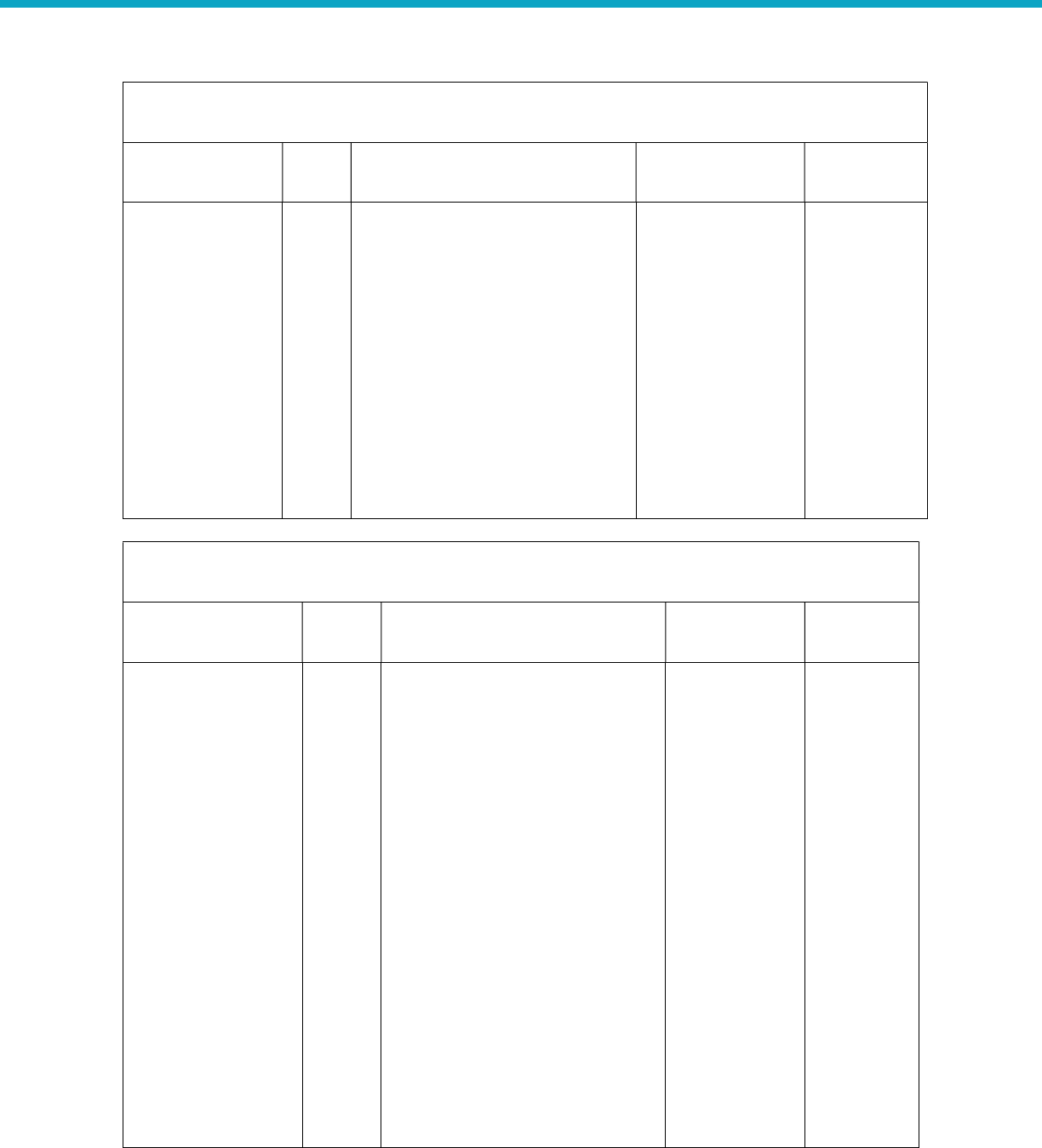
Designing the parameters of the new payment model
HSD has begun the preliminary work to develop the framework for the payment model, and the
approach is strongly influenced by the Health Care Payment Learning and Action Network’s alternative
payment model framework. The framework will enable primary care providers and clinicians to engage
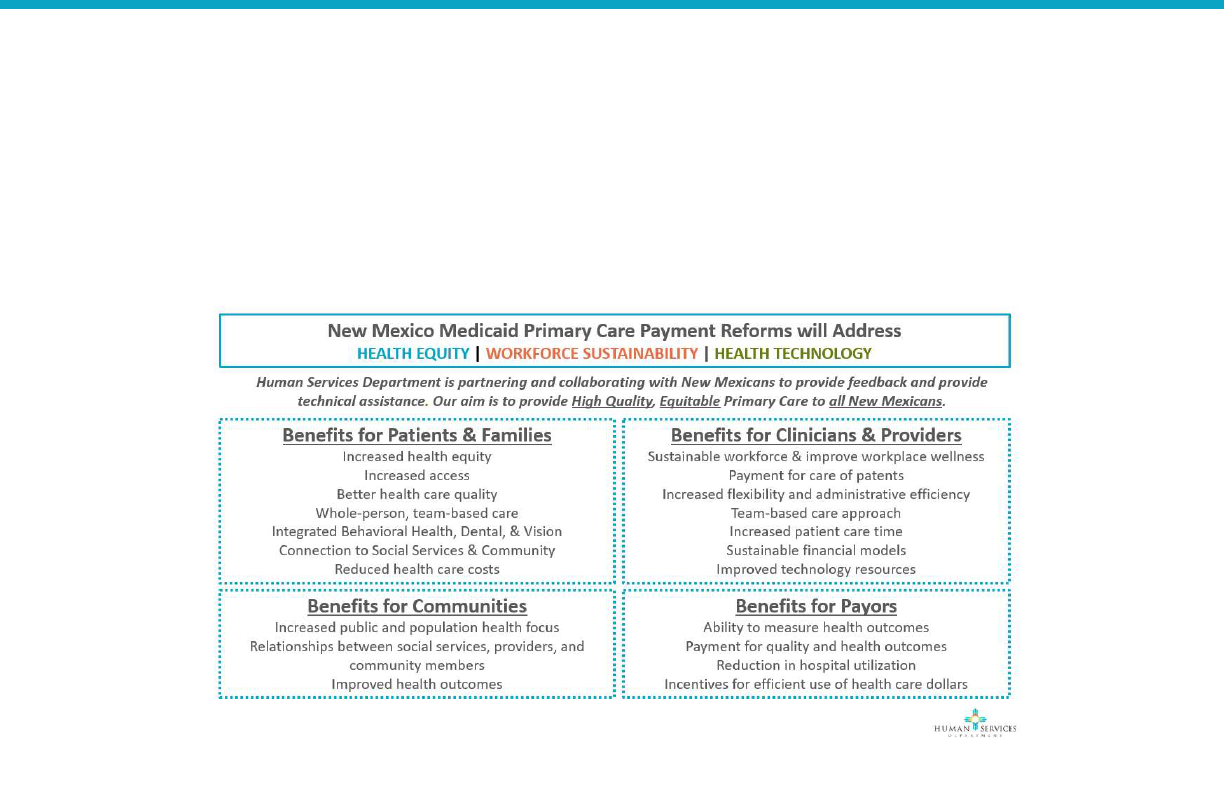
New Mexico Primary Care Council 2023
Page 22 of 48
in value-based payment at a level of risk that is appropriate for their organizations and to move to more
advanced levels of payment over time, in phases. As part of the analysis, HSD and the PCC identified the
benefits of the payment model to patients and providers, including designing a preliminary tiered
measurement framework to create appropriate incentives to improve patient health outcomes and
minimize provider burden. The PCC team will continue to refine the payment model and determine
appropriate incentives and quality measures, and other performance metrics.
Building a new payment model built on community wisdom
Throughout 2022 HSD has met with providers, clinicians, professional societies and associations, and
community-based organizations to obtain input on considerations for payment reform design and
implementation, including provider associations such as:
New Mexico Medical Society
Native American Technical Advisory Committee
New Mexico Pediatrics Association
New Mexico Primary Care Association
New Mexico Medical Society
New Mexico Behavioral Health Providers Association
This engagement was a precursor to conducting a primary care payment reform provider and clinician
readiness survey, where we received 70 responses across the state. The purpose of this survey was to
better understand clinical organizations’ capacity to accept risk, barriers and facilitators to payment
reform implementation, actionable information on primary care providers’ readiness to succeed in
payment reforms, and to identify critical gaps that need to be addressed. The survey was coupled with
four focus groups with representatives of federally qualified health centers, small and medium-sized
physician practices, hospitals, and interprofessional teams (i.e., behavioral health providers, oral health
FIGURE 4: NEW MEXICO MEDICAID PRIMARY CARE PAYMENT REFORM BENEFITS
New Mexico Primary Care Council 2023
Page 23 of 48
providers, and pharmacies). The findings from the survey and focus groups are presented in the
readiness assessment report included in this strategic plan.
Finally, in 2022 the PCC established the Primary Care Clinician and Provider Transformation
Collaborative and its Governing Council and Collaborative Cohort as a mechanism to provide input to
payment reform development and implementation and to bidirectionally communicate with
communities and constituencies.
During 2023, the PCC will continue to refine the new, primary care payment model, meet with
community members and stakeholders, and offer training and technical assistance to primary care
clinical organizations to help them succeed in preparation for the launch of the new payment model in
2024.
Primary Care Residency Expansion
A key strategy to PCC Goal 4 is the expansion of primary care physician residency programs. Pursuant to
2019 House Bill 480 (Graduate Medical Education Expansion Program Act), HSD provides funding to
new and expanded primary care residency programs (Family Medicine, General Pediatrics, General
Internal Medicine, and General Psychiatry). The statute also creates a governing body to oversee the
program and make funding recommendations to the HSD Secretary.
Since 2019, HSD, in collaboration with members of the community-based Primary Care Residency
Expansion Board & Advisory Group, have worked together to develop a strategic plan for residency
expansion throughout the state by:
Financially supporting new residency development and expansion of existing residencies,
particularly in rural and frontier communities. (Since FY 2019, 6 programs have received
development funding, totaling $1,554,811).
Increasing in-state retention post-residency.
Developing a statewide technical assistance resource center that supports programs with
resident recruitment and retention, staff and faculty development, curriculum development etc.
Amending state Medicaid policies, rules, and regulations to incentivize primary care residency
development.
As a result of these activities and the dedicated work of residency program leaders, over a 5-year period,
starting in 2019, primary care residencies are expected to grow from 8 to 16 (a 100% increase) in New
Mexico. At program maturity, this is expected to result in an increase in the number of primary care
residents in training from 142 to 264 (86% increase), and an increase in the number of graduates each
year will grow from 48 to 82, a 71% increase.
5-Year Timeline of Primary Care Residency Expansion in NM
Number of New First-Year Residents
Program 2020 2021 2022 2023 2024 2025 Total new
Residents
New
Graduates per
Year
Family Medicine 3 9 11 12 14 12 61 14
General Psychiatry 0 0 0 5 10 10 25 10
General Pediatrics 0 5 5 5 5 0 20 5
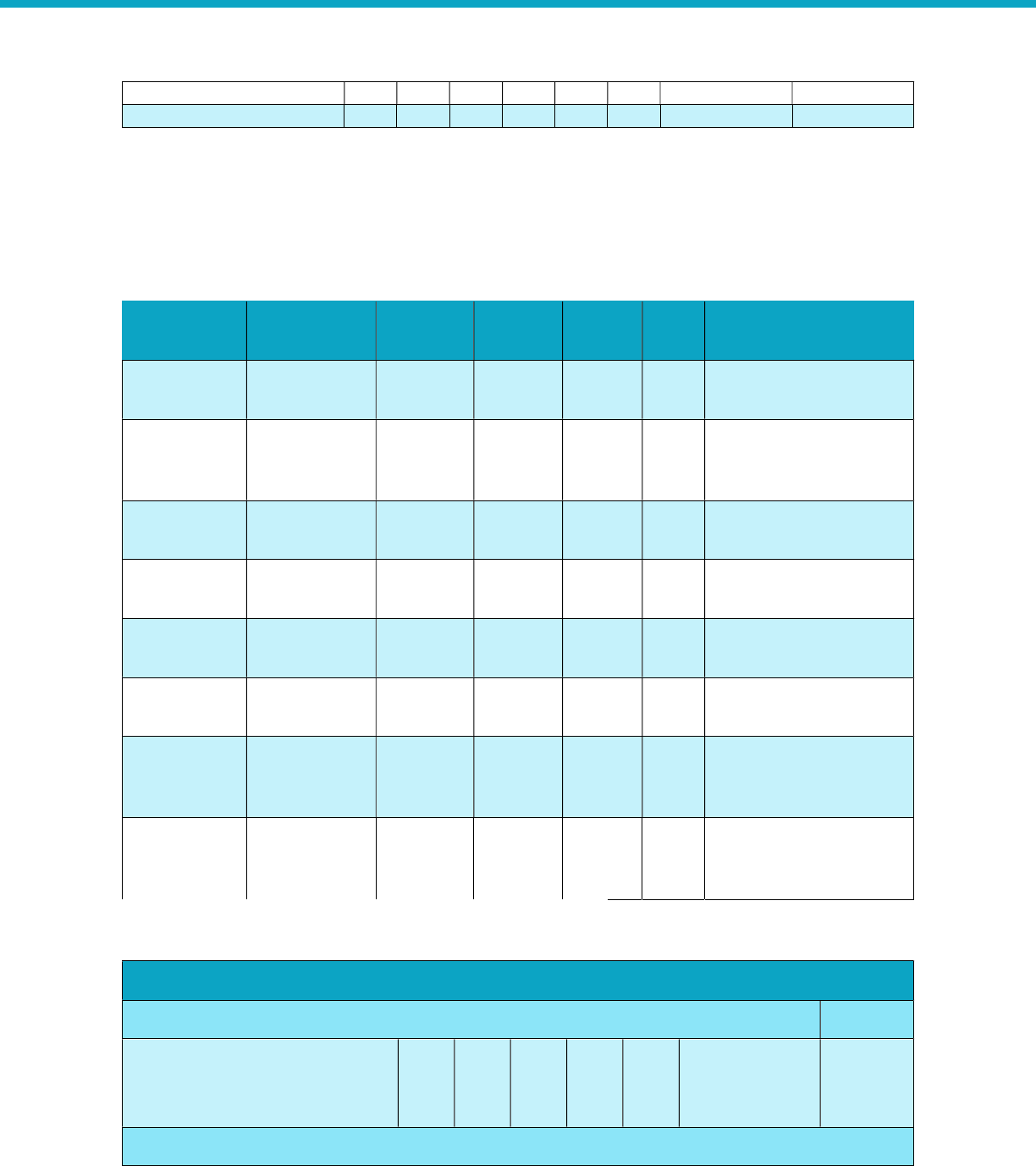
New Mexico Primary Care Council 2023
Page 24 of 48
General Internal Medicine 2 2 2 0 5 5 16 5
Total Residents per Year 5 16 18 22 34 27 122 34
The organizations outlined below have consulted with the New Mexico Primary Care Training
Consortium (NMPCTC) and HSD to begin developing or expanding their programs. Access to necessary
resources may impact projected start dates. Table 1 provides a high-level overview of residency
expansion and Tables 2 and 3 describes expansion in more detail (by program and specialty).
Sponsoring
Institution
Type Location Specialty
Resident
Capacity
Status Notes
NMPCTC New Las Cruces
Gen.
Psychiatry
3 2024
ACGME application under
development
NMPCTC New Española
Family
Medicine
(FM)
4 2023
ACGME application
submitted, awaiting site
visit
Covenant
Health Hospital
New Hobbs FM 6 2024 Early Development
Covenant
Health Hospital
New Hobbs
Gen.
Psychiatry
2 2024 Early Development
Covenant
Health Hospital
New Hobbs
Internal
Medicine
TBD TBD Early Development
San Juan
Regional
New Farmington FM TBD TBD Early Stages
Three Crosses
Regional
Hospital
New Las Cruces IM 5 2024 Early Development
Hidalgo
Medical
Services
Reaccreditation Silver City FM 2 2024
Actively recruiting to re-
establish program
5
-
Year Timeline of New or Expanded Primary Care Residency Programs in NM (detailed)
Number of New First
-
Year Residents
Program 2020
2021
2022
2023
2024
2025
Total
new
Residents
Family Medicine (3 Year Program)
TABLE 1: 5-YEAR TIMELINE OF PRIMARY CARE RESIDENCY EXPANSION IN NM
TABLE 2: 5-YEAR TIMELINE OF PRIMARY CARE RESIDENCY EXPANSION IN NM
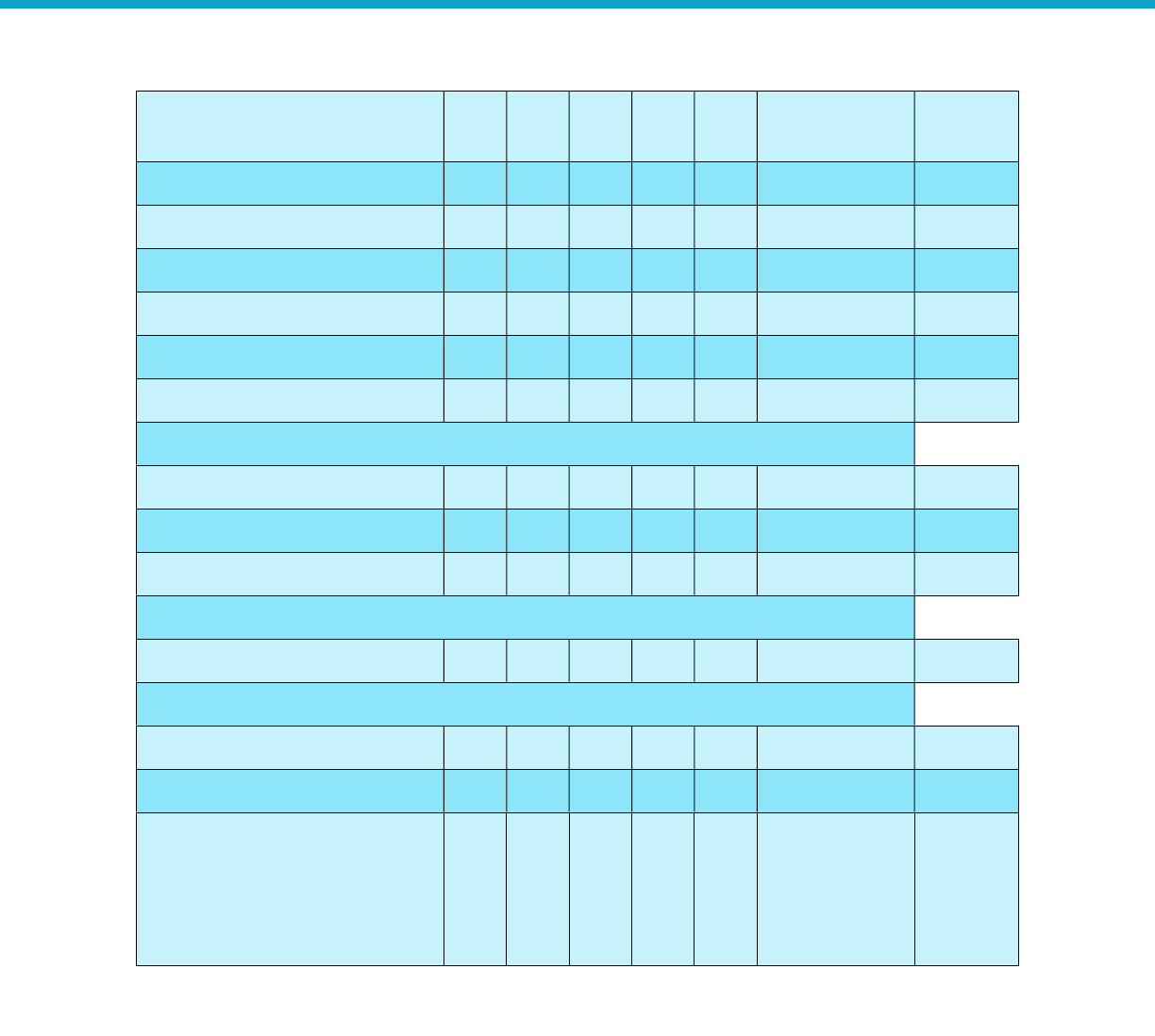
New Mexico Primary Care Council 2023
Page 25 of 48
Memorial Medical
Center (MMC)
& Gerald Champion
3
3
3
-
-
-
9
MMC & La Clínica de Familia
-
4
4
4
-
-
12
UNM & Shiprock
-
-
2
2
2
-
6
CHRISTUS St. Vincent
-
2
2
2
-
-
6
El Centro Family Health
-
-
-
4
4
4
12
Covenant Health Hospital
-
-
-
-
6
6
12
Hidalgo
Medical Services
-
-
-
-
2
2
4
General Psychiatry (4 Year Program)
UNM (expansion)
-
-
-
5
5
5
15
DAC Psychiatry
-
-
-
-
3
3
6
Covenant Health Hospital
-
-
-
-
2
2
4
General Pediatrics (3 Year Program)
UNM (expansion)
-
5
5
5
5
-
20
General
Internal Medicine (3 Year Program)
UNM (expansion)
2
2
2
-
-
-
6
Three Crosses Regional Hospital
-
-
-
-
5
5
10
Total Residents
Per Year
5
16
18
22
34
27
Total
new
residents
trained
=122
Conclusion
The NM Primary Care Council was established because the legislature listened to providers and clinicians
who demanded an urgent response to the crises in primary care. The current work of the council is in
response to that need. Payment reforms for Medicaid that will go live on January 1, 2024, have been
created in collaboration with providers and clinicians, and was built for the specific needs of New
Mexicans. As we prepare for these payment reforms, HSD and the PCC will offer technical assistance
and training. Establishing payment reforms will lay a foundation for future initiatives of the PCC in
supporting workforce sustainability, health equity, and health technology.
TABLE 3: 5-YEAR TIMELINE OF NEW OR EXPANDED PRIMARY CARE RESIDENCY PROGRAMS IN NM (DETAILED)

New Mexico Primary Care Council 2023
Page 26 of 48
Acknowledgments
The contributions, wisdom, and talents of our esteemed colleagues make this five-year strategic plan
designed to improve primary care in New Mexico possible:
Primary Care Council Board and Advisory Members
1. Eileen Goode, RN: CEO, NM Primary Care Association
2. Jennifer K. Phillips, MD: CMO UNM Medical Group, Professor, Family Medicine, UNM School of
Medicine
3. Kathy R. Fresquez-Chavez, NP: CEO, Bella Vida Healthcare
4. Aaron Jacobs, MD: Physician, Associate Professor, Pediatrics Critical Care, UNM Health Sciences
5. Matthew Probst, PA: Chief Quality Officer, El Centro Family Health
6. Valory Wangler, MD: Founding Executive Director, Gallop Community Health
7. Deputy Secretary Laura Parajon, M.D.: NM Department of Health
8. Julie Weinberg: Director, Life and Health Division, NM Office of Superintendent of Insurance
9. Alisha Parada, MD: Chief Division of General Internal Medicine, Geriatrics and Integrative Medicine,
UNM Health Sciences Center
10. Anjali Taneja, MD: Executive Director, Casa de Salud
11. Keenan Ryan, PhC: Pharmacist, UNM Health
12. Jason Mitchell, MD: Senior Vice President, Chief Medical and Clinical Transformation Officer,
Presbyterian Healthcare Services
13. Jon Helm, RN: Nurse Flow Manager, First Choice Community Healthcare
14. Maggie McCowen, LISW: Executive Director, NM Behavioral Health Provider Association
15. Rohini McKee, MD: Chief Quality & Safety Officer, UNM Hospital
16. Ruby Ann Esquibel: Health Policy Coordinator, NM Legislative Finance Committee
17. Mercy Jones: Patient Advocate, Senior, College of Population Health UNM Health Sciences Center
18. Susan Wilson: Executive Director, NM Coalition for Healthcare Value
19. Pamela Blackwell: Director, Government Relations & Communications, NM Hospital Association
20. Wei-Ann Bay, MD: Retired
21. Carolyn Thomas Morris, PhD: Psychiatrist
22. Alanna Dancis, MSN, CNP, Medicaid Medical Director, New Mexico Human Services Department
Community Partners
1. Pamela Stanley, LPCC, Consultant, Caraway Solutions
2. Dan Otero, DBA: Chief Executive Officer, Hidalgo Medical Services
3. Jessica Osenbrügge, Community Initiatives Manager – Health & Nutrition, Road Runner Food Bank
4. Nancy Rodriguez, Executive Director, NM Alliance for School-Based Health Care
Primary Care Council Staff
1. Secretary David R. Scrase, M.D.: Secretary, Human Services Department
2. Nicole Comeaux: State Medicaid Director, Human Services Department
3. Alex Castillo Smith: Acting Deputy Cabinet Secretary, Human Services Department
4. Tim Lopez: Director, Office of Primary Care and Rural Health, New Mexico Department of Health
5. Roberto Martinez, M.D., MPH: Interim Health Equity Director, New Mexico Department of Health,
Public Health Division
6. Elisa Wrede: Project Manager, Food Security & Primary Care, New Mexico Human Services
Department

New Mexico Primary Care Council 2023
Page 27 of 48
Appendix
Primary Care Return on Investment
Healthcare System Savings
A 2019 analysis from The Commonwealth Fund [22]
found several rigorous studies that incorporate a
variety of care management models — which link high-risk patients to needed medical and nonmedical
community supports — reduce utilization of costly health care services, lower costs of care, and produce
a return on investment (ROI). A few programs provided care management through multidisciplinary
teams made up of social workers, case managers, nurses, or physicians and connected patients with
community-based resources as needed. These demonstrated reduced ED visits, hospitalizations, home
health episodes, and skilled nursing home admissions. Several studies also evaluated the impact of
community health workers (CHWs) that connected at-risk patients with social services. A subset of these
studies showed CHWs contributed to a higher follow-up visit show rate, lower ED visits, reduced
Medicaid spending, and an ROI as high as $2.92 for every $1 spent.
Return on Investment: Local Economies
We can consider the economic value of increasing the primary care workforce in several ways. For
example, we can estimate the direct and indirect economic impact of physicians across medical
revenues generated during patient care (output), jobs, wages and benefits, and state and local tax
revenue. We calculate the direct impact from physician activity, and the indirect economic impact from
the industries supported by physicians. On average, each physician supports $3,166,901 in output, an
average of 17.07 jobs, approximately $1.4 million in total wages and benefits, and $126,000 in state and
local tax revenues.
[23]
Primary care dividends are not limited to physicians. Research shows other members of the primary care
interprofessional team produce economic savings. For example, a systematic review of 37 studies found
consistent evidence that cost-related outcomes such as length of stay, emergency visits and
hospitalizations for nurse practitioner care are equivalent to those of physicians.
[24]
Primary care generates additional revenue into the healthcare economy. A study of the economic
impact of a family practice clinic illustrated that for every $1 billed for ambulatory primary care, there
was $6.40 billed elsewhere in the healthcare system. Each full-time equivalent family physician
generated a calculated sum of $784,752 in direct, billed charges for local hospitals and $241,276 in
professional fees for other specialists. [25]
Return on Investment: Population Health
Research has shown the availability of a primary care physician in a rural area to lead to better health
outcomes, such as those relating to all-cause mortality (including cancer) and heart disease. An increase
in one primary care physician per 10,000 individuals results in: 1) an 11% decrease in emergency room
visits; 2) 6% decrease in hospital inpatient admissions; and, 3) 7% decrease in surgery utilization. [6] [26]
These improvements persist after controlling for sociodemographic characteristics. Ultimately, people
who identify a primary care physician as their primary source of care are healthier, regardless of health
status or demographics.
New Mexico had the 12
th
highest drug overdose death rate in 2019 (30.4 per 100,000 population), and
the highest alcohol-related death rate in the U.S. (73.8 deaths per 100,000 population). [27]
Addressing
New Mexico Primary Care Council 2023
Page 28 of 48
the many and complex behavioral health needs of New Mexicans through a fully integrated behavioral
health primary care model is paramount. It is possible to deliver behavioral health services that are
integrated with primary care at relatively low cost, of high quality, and result in improved access.
[28]
Integrating behavioral healthcare in primary care settings provides opportunities to address concerns
before they escalate to crises: screenings to diagnosis an illness; warm handoffs to reduce barriers to
transitioning into behavioral healthcare; guidance from behavioral health specialists acting as
consultants rather than direct service providers; and assessment and triage to short-term therapy or
coaching.
[28] [29]
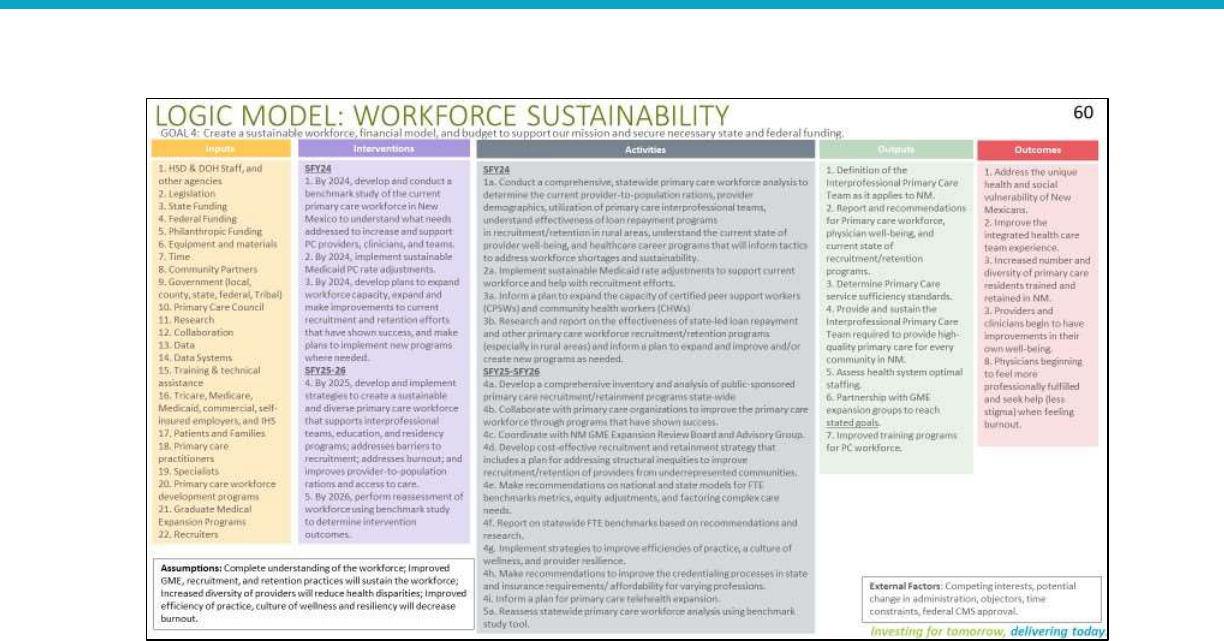
Primary Care Logic Models
New Mexico Primary Care Council 2023
Page 29 of 48
New Mexico Primary Care Council 2023
Page 30 of 48
New Mexico Primary Care Council 2023
Page 31 of 48

New Mexico Primary Care Council 2023
Page 32 of 48
New Mexico Primary Care Council 2023
Page 33 of 48
Primary Care Best and Promising Practices
Topic: Dental Medicaid Managed Care
State: Oklahoma
Description: The Oklahoma Health Care Authority (OHCA) released on September 1, 2022, a request for
proposals (RFP) seeking at least two Medicaid dental managed care plans to serve 919,000 members.
[30] [31] Contracts will run from the award date, which is expected to be between January and June
2023, with six one-year renewal options. Enrollment will begin on October 1, 2023, and proposals are
due by October 31, 2022. Current dental benefit plans are DentaQuest, Liberty Dental Plan of Oklahoma,
and MCNA Dental.
Performance measures and outcome measures are on pp. 289-291 of the RFP. The quality measures are:
Percentage of children receiving an oral evaluation
Percentage of children receiving fluoride treatments
Percentage of children who receive sealants on their first molars
Percentage of all members who receive an annual dental visit
Percentage of periodontal evaluations for adults with periodontitis
Each of the measures includes specifications for data source, improvement targets, and the payment
incentive (withholds from the capitation rate).
State: New Hampshire
Description: The New Hampshire Department of Health and Human Services released on August 25,
2022, an RFP for a Medicaid dental managed care organization to serve approximately 88,000 adults.
[32]The program will be implemented on April 1, 2023, and run through March 31, 2026, with an
additional two-year option. Proposals are due September 30, 2022. The contract does not specify quality

New Mexico Primary Care Council 2023
Page 34 of 48
measures but rather asks the bidders to propose their quality management plan metrics, APM strategy,
and quality expectations for the bidders’ provider network.
Relevance/applicability to New Mexico:
These three states’ RFPs for managed Medicaid dental care could help inform New Mexico’s alternative
payment model and how oral health is integrated into primary care. The Oklahoma performance metrics
seem to be particularly useful as a starting point for New Mexico’s performance measures for oral
health services.
Topic: Behavioral Health
State: Colorado
Description: Since 2019, CMS has worked with six states – Colorado, Illinois, Michigan, New Mexico,
Oregon, and South Dakota – to add additional behavioral health services to their state “benchmark”
plan. [33] Colorado recently created a Behavioral Health Administration (BHA) led by a cabinet-level
commissioner. [34] The BHA will lead a statewide behavioral health strategy, coordinating policy,
payment, and system design through the networked government with other state agencies. This
includes leading policy for children and youth behavioral health strategy with a senior child and youth
advisor working with the commissioner to ensure a coherent child and youth system of care. The BHA’s
governance structure includes an advisory council that will raise individual and community voice in the
state and a commitment to ensuring community-centered practices. The BHA intends to establish a
system for addressing complaints and grievances with behavioral health care; a system for monitoring
the performance of behavioral health providers; a comprehensive behavioral health safety-net system,
including emergency care, outpatient services, and case management; and a new system for licensing
behavioral health organizations and providers.
State: Minnesota
Description: The Minnesota Department of Human Services released on August 15, 2022, an RFP seeking
a current Minnesota Health Care Programs provider agency to provide school-linked substance use
disorder (SUD) services to students and families. [35] The contract is anticipated to begin on January 1,
2023 and run through June 30, 2026. Proposals are due on October 17, 2022. The detailed obligations
and additional measures of performance will be defined in the final negotiated contract.
Relevance/applicability to New Mexico:
The Colorado beneficiary advisory council may be a worthwhile model to emulate for engaging
members with lived experience and obtaining their input on quality measures and benchmarks.
The Minnesota school-based SUD model may help inform primary care SUD performance measures,
particularly once the contracts are awarded, and the performance measures are established.
Topic: Benchmarks for Health Equity
States: (multiple; Massachusetts)
A Kaiser Family Foundation survey conducted in 2021 found that 12 states are measuring health
disparities as a focus for financial incentives: California, Colorado, Connecticut, Hawaii, Illinois, Iowa,
Massachusetts, Michigan, Oregon, Pennsylvania, Tennessee, and Wisconsin. This is an increase from
only two states doing so just two years previously. [36]

New Mexico Primary Care Council 2023
Page 35 of 48
Massachusetts is requesting a new Section 1115 waiver amendment to provide incentive payments to
provider networks and hospitals that collect accurate social risk factor data, identify and monitor
inequities through stratified data reporting, and achieve measurable reductions in health disparities.
[37]
Relevance/applicability to New Mexico:
Focusing on these 12 states’ – and in particular, Massachusetts’s – health equity benchmarks and
performance measures could help inform the development of health equity measures in New Mexico.
Topic: Behavioral Health Integration with Primary Care
The Substance Abuse and Mental Health Services Administration (SAMHSA) and the Health Resources
and Services Administration (HRSA) created a framework for progressive levels of integration between
behavioral health (BH) and primary care providers (PCPs). The three levels are:
1. Coordinated Care: Screen & Consultation | Minimal Collaboration
Care is provided in geographically disparate facilities. Providers communicate about shared patients.
BH providers work to meet care goals established by PCPs.
Examples of this approach include:
PCPs refer BH patients to services: Screening, Brief Intervention, and Referral to Treatment
(SBIRT) [38]
BH providers work with patients to meet goals identified by PCPs: Vermont’s Hub and Spoke
Model
2. Co-Located Care: Co-Located | Better Collaboration
BH providers and PCPs share the same facility, aiding in better coordination.
Examples of this approach include:
BH providers are embedded with primary care practices, provide treatment, and monitor
progress: Collaborative Care Model and Comprehensive Primary Care Plus Model
PCPs and BH providers are embedded in the same facility: Common in FQHCs, [39] like the
Cherokee Heath Systems [40] and Golden Valley Health Centers. [41]
3. Integrated Care: Fully Transformed Care (also see: National Center of Excellence for Integrated
Health Solutions) [42]
Close collaboration in partly integrated practices or comprehensive partnerships in fully merged
practices. Integrated, patient-centered care plans, coordination, complex care management, SDoH
considerations, shared information systems, measurement of patient outcomes, and shared
decision-making.
Examples of this approach include:
Ongoing complex care management, treatment, and referrals: Medicaid Health Homes [43]
PCPs and BH providers operate under one management system: Intermountain Healthcare [44]
State: Colorado
Sustaining Healthcare Across Integrated Primary Care Efforts (SHAPE) aimed to examine the integration
of behavioral health and primary care through a global payment system. Practices that received global
payments showed a 4.8% lower total cost of care for attributed patients. [45]

New Mexico Primary Care Council 2023
Page 36 of 48
State: Texas
The Harris County Hospital District Community Behavioral Health Program (CBHP) program integrates
behavioral health services into 12 Harris County (Houston suburbs) community primary care centers,
two school-based clinics, and a homeless services program. Services include evaluation and treatment of
scheduled patients and walk-in services for patients in crisis, including “curbside” consultations with
PCPs to support psychiatric care. CBHP expanded its capacity to address acute psychiatric service
shortages, reducing average wait times for new appointments from seven months to three weeks, and
admissions to hospital psychiatric emergency centers by 18%. [46]
State: Massachusetts
The Massachusetts Child Psychiatry Access Program (MCPAP) is an interdisciplinary healthcare initiative
that assists PCPs who treat children and adolescents for psychiatric conditions. [47] MCPAP’s goal is to
expand access to BH treatment across the Commonwealth by making child psychiatry services available
to all PCPs. The model staffs each program team with two full-time child and adolescent psychiatrists,
licensed behavioral health clinicians, resource and referral specialists, and program coordinators. The
team aligns with and assists PCPs with the following integrated BH services:
Screening, identification, and assessment.
Treating mild to moderate cases of behavioral health disorders.
Making effective referrals and coordinating care for patients who need community-based specialty
behavioral health services.
State: Utah
Intermountain Healthcare, a non-profit healthcare system serving metropolitan Salt Lake City, launched
a project to integrate mental healthcare services into primary care practices. [48] Early results showed
that patients with depression treated in integrated clinics were 54% less likely to visit the emergency
department. In addition, patients treated in the integrated clinics had a 27% lower growth in the total
cost of care.
Relevance/Applicability to New Mexico:
Integrated care is crucial for expanding access to and improving the quality of behavioral health services
in New Mexico. Given the widespread barriers to accessing behavioral healthcare, especially with an
acute shortage of behavioral health providers, primary care practitioners may be seen as the default for
seeking behavioral health services. Integrated care becomes necessary to enable comprehensively
managed and optimally coordinated care, in addition to giving New Mexico primary care practitioners
practical tools for diagnosis and treatment. It also expands a culturally and linguistically tailored
workforce, including community health workers or peer support specialists who offer counseling, care
management, and social support. This approach has empirical support in improved behavioral health
access and outcomes across age groups and diagnoses. The approaches of other states may be useful
models for HSD payment systems and/or provider operations.
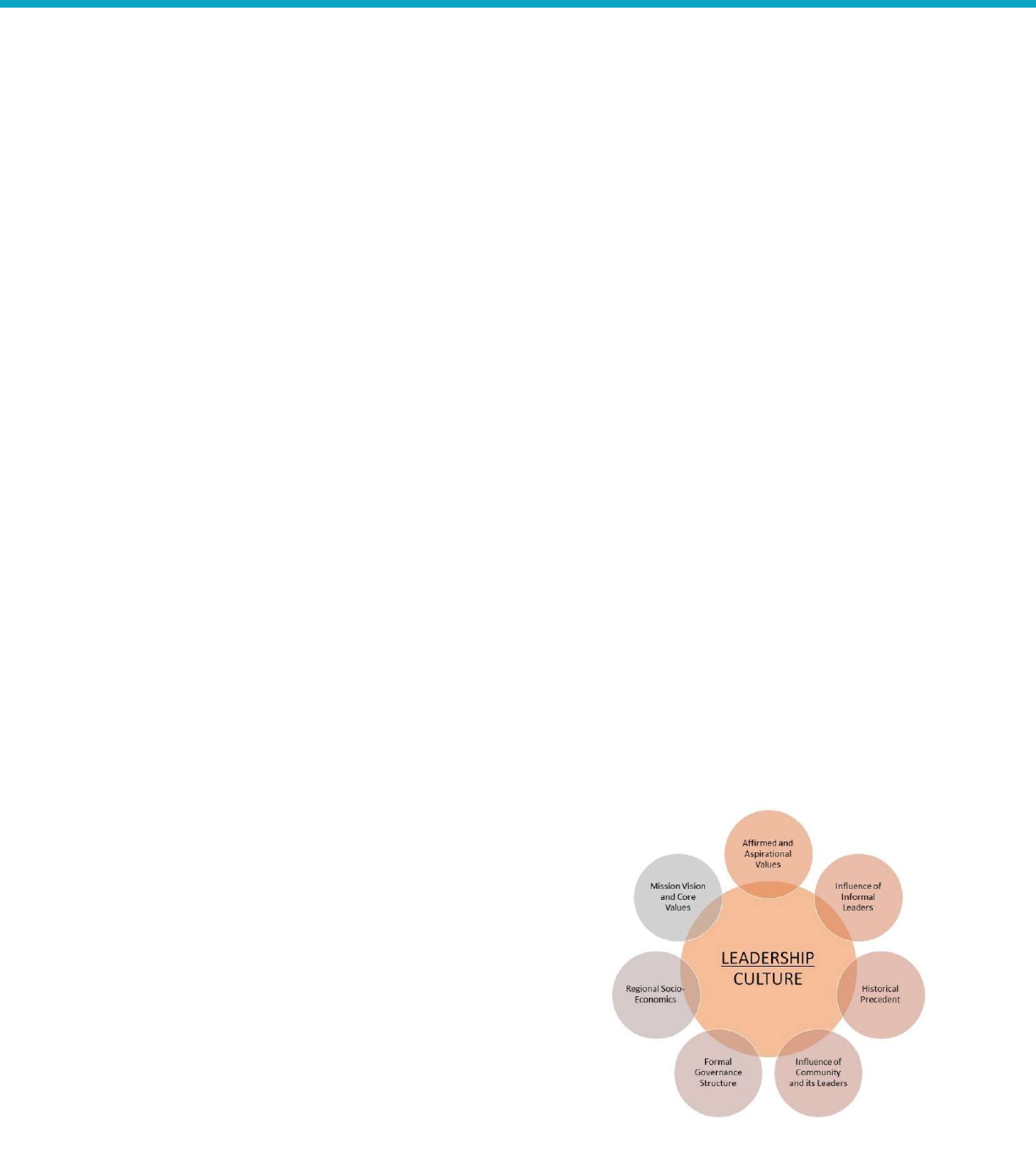
Topic: Leadership and Governance Considerations for Movement Toward Value-Based Care
Leadership must be committed to pursuing value-based care (VBC) and payment (VBP). There needs to
be a clear VBP strategy that includes the “why” and the “how” and it must be communicated
throughout the organization. A multidisciplinary committee structure charged with in-depth analysis and
making recommendations to the leadership governance board is often pivotal, where healthy discussion
and debate can occur to inform critical strategic decisions.
New Mexico Primary Care Council 2023
Page 37 of 48
The framework for these recommendations is primarily based on the Accountable Care Learning
Collaborative Atlas framework, [49] evidence-based practices from large clinically integrated networks
that operate in risk contracts across lines of business, [50]
and models of leadership principles.
Success factors for operating a high-performing value-based organization:
1. Experienced and respected leadership governance board with an established track record of growth
and success.
2. Broad representation on the leadership board, including physicians.
3. Mix of young emerging leaders with more senior leadership.
4. Shared leadership and organizational vision for pursuing advanced alternative payment models.
5. Leaders engaged in rigorous analysis and debate of recommendations; these conversations should
be viewed as a constructive exercise.
6. The decision to pursue risk should be based on rigorous analysis of historical claims data,
identification of opportunities for improvement, a strategic and operational plan to address these
opportunities, and a financial pro forma that estimates cost and probability for profitability.
7. Leaders should be guided by performance metrics, timelines, and targets to monitor the successful
management of risk.
8. Leadership incentive structure should be aligned with key performance indicators to succeed in
global risk.
9. The leadership group should focus on success in value-based care and payment, including global risk
and a committee structure (clinical, operational, information technology, and finance) to feed
recommendations to this group.
10. Achieve consensus among leadership and staff in pursuing global risk.
Applicability to New Mexico
The New Mexico HSD and New Mexico Medicaid provider organizations are now at an inflection point
where they must pivot from the fee-for-service environment into a value-based environment with
delegation, capitation, upside, and downside risk. Organizations must accept that the healthcare
landscape is an environment of continual change, so the leadership of primary care provider
organizations must guide their staff and teams to embrace and benefit from a changing environment
rather than resist change. Marginal improvements, multiplied by time and teamwork, can magnify
actions, and these modest successes can catalyze the momentum for organizational change. Harnessing
the power of small incremental changes will gradually transform the organization and position it to
succeed under APMs.
Governance Structure
The following leadership governance structure designed for larger clinical organizations can serve as a
broad recommendation for more tailored governance within individual healthcare entities. Smaller
organizations will not need as elaborate a structure, but the critical processes and measures to track are
similar.
1. Establish an Executive Leadership Team (ELT) responsible for the vision and setting of the strategic
priorities and a multidisciplinary Operations Leadership Team (OLT) comprised of clinical and non-
clinical staff to execute the strategic priorities.
2. The ELT should comprise the senior executive leadership. The ELT will identify the organization's
strategic priorities and allocate resources. The ELT must align in the pursuit of value-based care and
payment timelines. Once the strategy is identified, they need to articulate the rationale and
methodology to the entire organization and review performance across the organization. This could
New Mexico Primary Care Council 2023
Page 38 of 48
include dashboards with membership trends, quality, and utilization trends for the practice and
individual providers. Any “adverse trends” or outliers should be identified and prioritized for
intervention by the OLT.
3. The OLT should be comprised of multidisciplinary leadership (physician and nursing leadership,
operations, and finance) and tasked with analyzing the data and dashboards to identify the root
cause of adverse trends. Once identified, they will share findings with the ELT and recommend
potential strategic interventions to mitigate or reverse the negative trends. This team will ideally
utilize LEAN and Six Sigma methods to plan, implement, evaluate, and modify initiatives to improve
population health and care coordination and the performance of strategic utilization management
and quality initiatives. This group will ideally have subcommittees focusing on VBC/VBP, population
health, HEDIS, Stars, and CAHPs results. They will track month-over-month and year-over-year
trends. These meetings should be a safe space where diverse perspectives are welcomed with
constructive dialogue leading to collaborative decision-making. Agreed-upon performance metrics,
timelines, and goals should guide resource allocation and prioritization. Organizational priorities,
interventions, and outcomes should be communicated with all staff to understand their unique role
in optimizing individual patient outcomes, clinical performance, and organizational/enterprise
performance. Dissemination of best practices with recognition of individual and team contributions
should also be shared and successes recognized and celebrated.
4. OLT priorities may include (modified from NEJM Catalyst):
a. Improve Quality of Care. Multiple measures of quality can be utilized and may include but
are not limited to Stars, HEDIS, Never Events, readmissions, and ambulatory sensitive
(inappropriate) ER utilization. As New Mexico Medicaid moves toward APMs that reward
outcomes, organizations can leverage LEAN principles to incentivize every employee to
identify opportunities to improve quality, care coordination, and population health to
impact clinical outcomes and cost-effectiveness positively.
b. Improve Operational Efficiencies. According to LEAN principles, idle time for patients or
employees is an opportunity for improvement. Patients sitting in waiting areas, a late start
for team meetings, appointment waiting lists, and unused equipment are all areas that
represent opportunities for healthcare organizations to become more efficient.
c. Optimize Capital Allocation and Cost Control. Surplus real estate, medical supplies,
medications, and outdated equipment may contribute to suboptimal performance.
Leadership | Culture and Trust
Organizational culture offers a mechanism for leaders to
influence and propel extensive change management efforts,
such as the move toward value-based care. Leaders need to
understand and incorporate the values of internal
stakeholders and approach change with empathy. Leaders are
more successful when they operate within the framework of
transparency, fairness, and objectivity. A. Bhardwaj
3
explains
that recruiting and retaining the right leaders is critical, and
the cultural fit between the organization and leadership is a
crucial determinant of success.
Figure 5: Factors that Influence Organizational Culture
[51] represents common factors that act as influencers on
FIGURE 5: FACTORS THAT INFLUENCE ORGANIZATIONAL
CULTURE
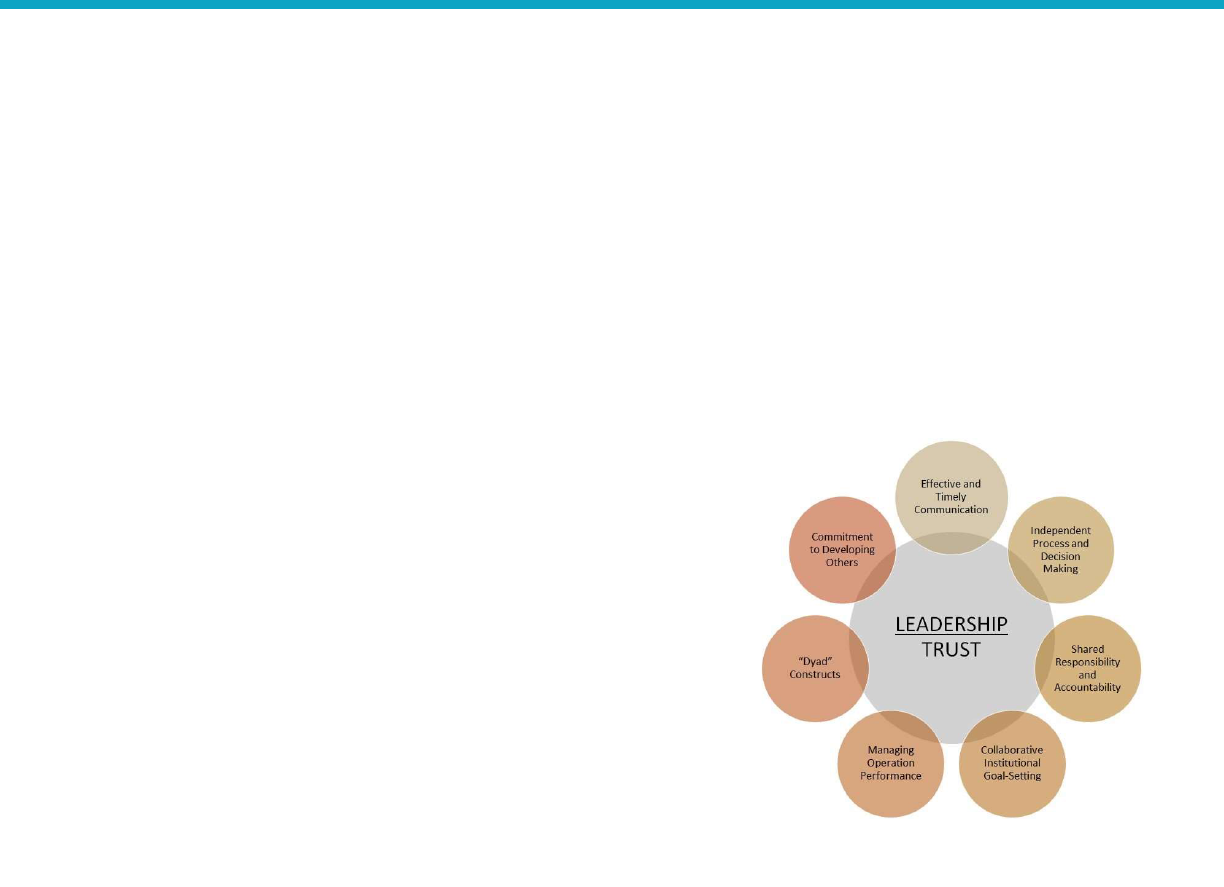
New Mexico Primary Care Council 2023
Page 39 of 48
organizational culture. Each element offers consideration for leadership to understand, accommodate,
and influence. These considerations include:
Sharing a compelling vision
Inspiring a shared purpose
Team engagement and accountability
Nurturing proficiency
Promoting collectivism and group thinking
Promoting collaborative teamwork among groups and departments
Hierarchical governance
Distributive model of leadership with shared responsibility and accountability propels the
growth and development of future leaders
Figure 6: Importance of Trust for Effective Leadership
[51] illustrates leadership that lends itself to promoting a culture
of trust with disparate constituents is crucial for alignment and
directly affects consistency in teamwork and organizational
cohesiveness. Key considerations include (adapted from Bhardwaj
A., Organizational Culture and Effective Leadership):
Leaders should consider operating as a meritocracy
Display transparency, fairness, and objectivity toward
programmatic development and growth
This transparency framework extends to realizing staffing
needs, including recruitment, and retention of personnel,
operating and capital budgets, analyzing clinical outcomes
and operational performance, cost-containment,
compensation, and incentive plans.
As New Mexico’s primary care environment negotiates the
movement toward value-based care, leaders must negotiate the
revenue model, identify, and help mitigate gaps in systems,
processes, and services, serve as trusted advisors to team members across the organization, and
collaborate and build trust across the practice.
Topic: Existing Value-Based Payment Programs & Messaging Strategies
Introduction
Value-based payment program implementation requires stakeholder buy-in, including from clinical
organizations. Achieving provider buy-in may be easier when models focus on increasing provider
compensation or financial stability than on cost savings and the extent to which value-based payment is
seen as a threat or an opportunity. [52] In addition, aligning with federal policy helps garner support
from providers and health systems.
According to the Center for Health Care Strategies report cited above, a fundamental goal of a value-
based payment program is quality improvement. Using or adapting existing quality programs can
minimize administrative burden and align quality incentives across Medicaid programs and statewide
through a multi-payer approach. Several states are also increasing the focus on health equity.
FIGURE 6: IMPORTANCE OF TRUST FOR EFFECTIVE
LEADERSHIP

New Mexico Primary Care Council 2023
Page 40 of 48
This report summarizes the value-based payment programs in seven states, highlights the state’s quality
measurement and tracking approach, and presents how the state is messaging the payment model’s
quality improvement components to stakeholders.
State: Colorado
Value-based payment program: Known as APM2, Colorado’s payment model is a partially capitated
primary care model influenced by the Center for Medicare and Medicaid Innovation (CMMI)
Comprehensive Primary Care Plus Model. The state pays a portion of primary care reimbursement as a
capitated payment and the remainder through fee-for-service (FFS). The focus is on chronic conditions:
primary care providers (PCPs) can earn shared savings by decreasing the total cost of care (TCOC) for
patients with one or more chronic conditions.
Quality measurement and tracking: The state has appropriated funds to build a data dashboard to help
PCPs track and address utilization in real time. PCPs are accountable for ten quality measures from a
menu of 30 (3 are mandatory, and the PCPs choose 7). PCPs must meet a quality threshold to be eligible
for gainsharing payments and can earn an enhanced capitation rate based on quality performance. [53]
Messaging quality improvement: The Primary Care Alternative Payment Model (APM) Guidebook cited
above includes a section on support and resources available to PCPs. Regional Accountable Entities are
responsible for helping PCPs in the following ways: assist PCPs in implementing practice transformation
and process improvement efforts; designate and communicate a single point of contact for questions
and support with the APM; help PCPs select appropriate measures for participating in the APM
(accounting for the PCP’s client panel and/or community); provide ongoing education and support to
help ensure successful participation in the APM; and attest to the PCP’s achievement of structural
measures and patient-centered medical home (PCMH) recognition. The Guidebook includes links to the
APM Measure Set, measure specifications, and workbooks to help PCPs model performance; PCMH
recognition resources; and information specific to federally qualified health centers (FQHCs).
State: Maryland
Value-based payment program: Maryland’s Total Cost of Care (TCOC) Model is a multi-payer partnership
with CMMI and an all-payer hospital population-based payment – hospitals are paid with consistent
rates across Medicare, Medicaid, and commercial payers. The model also includes a care redesign
program in which hospitals can spend savings on incentives to clinical partners to help achieve the
hospitals’ care delivery goals and a partially capitated primary care provider program.
Quality measurement and tracking: Medicare, commercial payers, and Medicaid select quality metrics
and incentives for their respective primary care models.
Messaging quality improvement: The Maryland Health Services Cost Review Commission developed the
Episode Quality Improvement Program as an episodic incentive payment model for specialist physicians
that will help increase participation in advanced APMs and allow for physician alignment with hospitals
under the TCOC Model. [54] [55]
State: Massachusetts
Value-based payment program: In Massachusetts’ Accountable Care Partnership Plan (ACPP), providers
and managed care organizations jointly form an accountable care organization (ACO). ACOs are paid a

New Mexico Primary Care Council 2023
Page 41 of 48
capitated per member per month (PMPM) rate and may receive shared savings if quality benchmarks
are met, including for health equity.
Quality measurement and tracking: MassHealth defined 22 quality measures that started as pay-for-
reporting and evolved to pay-for-performance. Capitated payments are medical and socially risk-
adjusted (for disability, behavioral health, housing stability, rural status, and for a Neighborhood Stress
Score).
Messaging quality improvement: Goals for the program extension approved earlier this year include (1)
continue the path of restructuring and re-affirm accountable, value-based care – increasing expectations
for how ACOs improve care; (2) reform and invest in primary care, health, and pediatric care that
expands access and moves the delivery system away from FFS health care; (3) and to advance health
equity, addressing health-related social needs and disparities. [56] [57]
State: New York
Value-based payment program: New York’s Value-Based Payment Innovator Program is for providers
willing to take on full risk. Managed Care Organizations (MCOs) must pass 90-95% of premiums to the
innovator (the exact amount is determined during contract negotiations). The state sets administrative
requirements for utilization review, utilization management, and disease management, plus five
additional tasks to be determined during negotiations.
Quality measurement and reporting: The innovators and the MCOs select their own quality metrics but
must use at least one that the Delivery System Reform Incentive Program (DSRIP) Clinical Advisory
Group recommends for each subpopulation.
Messaging quality improvement: Through its Medicaid Analytics Performance Portal, the state enables
providers to use state-of-the-art data and analytics tools to explore their performance on key quality
measures, identify members, providers, or ZIP codes responsible for high or low scores, monitor trends,
and explore some of the common drivers of better or poorer performance. New York publishes the total
risk-adjusted cost of care available per provider and MCO for the total population and per integrated
care service (e.g., maternity care, integrated primary care, HIV/AIDS). This tool combines 3M™ Clinical
Risk Grouping (CRG) groupers for population-based analyses and the Health Care Incentive
Improvement Institute (HCI
3
)/ Prometheus episode grouper, including the appropriate risk-adjustment
methodologies. The state believes having these costs and the outcomes of these services available and
transparent is crucial for any transformation towards payments based on value rather than volume. [58]
State: Oregon
Value-based payment program: The Coordinated Care Organization (CCO) program provides financial
rewards to CCOs for improving the quality of care provided to Oregon Health Plan members.
Quality measurement and reporting: The Oregon Health Authority’s (OHA) Quality Incentive Program
published a new CCO performance metric dashboard in December 2022. The dashboard is OHA’s first
presentation of quality measures broken out by race, ethnicity, language, and disability (REALD)
data. The state uses 14 incentivized performance measures.
Messaging quality improvement: To explain its dashboard that presents REALD data, the state says the
purpose is to foster conditions needed for communities to engage in data justice, provide data back to
the communities that advocated for and led to the creation of the REALD legislation and standards,
New Mexico Primary Care Council 2023
Page 42 of 48
identify strengths and inequities in communities that experience structural racism and other forms of
discrimination, and inform how OHA allocates resources to increase health equity effectively. In their
words, “people are not numbers.” [59]
State: Pennsylvania
Value-based payment program: Pennsylvania’s Rural Health Model collaborates with CMMI – this
all-payer program pays rural hospitals a global budget. The global budget covers all inpatient and
outpatient services, and Medicare, Medicaid, and commercial plans contribute.
Quality measurement and reporting: There are eight statewide quality measures, and each participating
hospital must develop its transformation plan to improve quality and population health outcomes.
Messaging quality improvement: Pennsylvania does not include statements about quality on its website;
rather, it defers to the Rural Health Redesign Center and CMMI.
State: Washington
Value-based payment program: Washington’s Multi-Payer Primary Care Transformation Model will be
designed to support quality improvement and payment alignment across Medicaid managed care, public
employee, and commercial plans (this model is still in the design phase). There are three certification
levels: Level 1 providers will receive additional PMPM transformation payments for up to 3 years; Level
2 participants will receive transformation payments and possibly a hybrid fee-for-service
(FFS)/population-based payment to help graduate to Level 3 and may receive quality incentive
payments; and Level 3 providers will be paid prospective comprehensive care payments and quality
incentive payments. Participating providers will have to demonstrate competencies across ten domains.
Quality measurement and reporting: The Washington Health Care Authority (HCA) Primary Care
Measure Set Workgroup has defined a core set of 12 measures to be included in payer and provider
contracts. The core set of measures to gauge the clinical quality delivered by an integrated, whole-
person care model, using HEDIS measurement standards where feasible:
1. Child and Adolescent Well-Care Visit (WCV)
2. Childhood Immunization Status (CIS) (Combo 10)
3. Breast Cancer Screening (BCS)
4. Cervical Cancer Screening (CCS)
5. Colorectal Cancer Screening (COL)
6. Depression Screening and Follow up for Adolescents and Adults (DSF-E)
7. Controlling High Blood Pressure (CBP)
8. Asthma Medication Ratio (AMR)
9. Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%)
10. Antidepressant Medication Management (AMM)
11. 11. Follow-up after ED visit for Alcohol and Other Drug Abuse of Dependence (FUA)
12. Ambulatory Care - Emergency Department (ED) Visits per 1,000 (AMB) [60]
Messaging quality improvement: According to the state, aligning quality measurement has the potential
to reduce the administrative burden for both providers and payers. It also increases the likelihood of
success on the most important measures by reducing focus fragmentation.
New Mexico Primary Care Council 2023
Page 43 of 48
Topic: Tribal stakeholder engagement
State: Oregon
The Oregon Health Authority (OHA) developed the SHARE (Supporting Health for All through
REinvestment) Initiative to implement the legislative requirements in Oregon House Bill 4018 (2018)
regarding social determinants of health. [61] The SHARE Initiative began in 2020, and its primary goals
are to safeguard public dollars by requiring that a portion of coordinated care organizations’ (CCOs’)
profits be reinvested in their communities and to improve member and community health by requiring
reinvestments go toward upstream factors that impact health (e.g., housing, food, and transportation).
One of the requirements (Requirement 4) for CCOs established by the Oregon Health Policy Board’s CCO
2.0 policies is that CCOs must designate a role for their community advisory councils (CACs) related to
SHARE Initiative spending decisions regarding Social Determinants of Health and Equity (SDOH-E)
organizations. The CACs must have a majority representation by consumers, and tribal representatives
must be invited to participate. An SDOH-E partner is defined by Oregon as an organization, local
government, federally recognized Oregon tribal governments, the Urban Indian Health Program, or a
collaborative that delivers SDOH-E-related services. The CCO must invite the tribe to participate in the
shared community health assessment and community health improvement plans. [62]
Relevance/applicability to New Mexico:
The Oregon SHARE Initiative is a potential model for requiring managed care organizations and/or
accountable care organizations to engage tribal communities in planning and spending decisions for
their communities.
Model suggests a framework for developing coordinated community health assessments and
community health improvement plans driving population health improvement.
Topic: Behavioral Health
State: Florida
Description: On August 3, 2022, Florida announced a new pilot program in seven counties to address
the opioid epidemic (a subsequent phase will expand the program to five additional counties; this
program was initially piloted in Palm Beach County). [63] According to state officials, the Coordinated
Opioid Recovery (CORE) initiative is the first of its kind in the nation, coordinated through the
Department of Health, the Department of Children and Families, and the Agency for Health Care
Administration. [64] Governor DeSantis also announced the appointment of Dr. Courtney Phillips as the
first Statewide Director of Opioid Recovery. Florida asserts that standard treatment programs have had
limited success in creating long-term recoveries for opioid addiction and other substance use disorders.
This model of care will establish the following patient flows: (1) overdose occurs; (2) emergency
response and care navigation; (3) bypass other hospitals; (4) transport to a specialty subject matter
hospital (similar to a trauma center); (5) stabilize the patient; (6) initiate medication for opioid use
disorder (MOUD); (7) transfer the patient to a sustained multi-specialty medical group; and (8) focus on
a sustainable clinical pathway and system of care.
Relevance/applicability to New Mexico:
Opioid use disorder is a challenge for New Mexico and the Florida model may be worth considering.
The three-phase pilot structure (single county, then seven counties, then five more counties) may
also be of interest, as well as creating a Statewide Director of Opioid Recovery position.
Model of care suggests pragmatic coordination and continuity of care framework which addresses
the epidemiology, pharmacology, screening, assessment, and treatment of OUD.

New Mexico Primary Care Council 2023
Page 44 of 48
References
[1]
G. A. A. J. M. e. a. Yalda Jabbarpour A, "Relationships Matter: How Usual is Usual Source of
(Primary) Care? PCC EVIDENCE REPORT," 2022. [Online]. Available:
https://www.pcpcc.org/sites/default/files/resources/pcc-evidence-report-2022_1.pdf.
[2]
"Addressing Health Worker Burnout The U.S. Surgeon General’s Advisory on Building a
Thriving Health Workforce," 2022.
[3]
M. Ollove, "Health Worker Shortage Forces States to Scramble,"
The PEW Charitable Trusts
Stateline, 25 March 2022.
[4]
Y. C. e. a. Diana
-Lyn Baptiste, "COVID-19: Shedding light on racial and health inequities in the
USA," Journal of Clinical Nursing, 2020.
[5]
"Primary Care Collaborative State Primary Care Investment Hub," [Online]. Available:
https://www.pcpcc.org/primary-care-
investment#:~:text=Underinvestment%20in%20primary%20care%20gives,of%20specialty%2
0undermines%20primary%20care.. [Accessed 11 January 2023].
[6]
B. Starfield, L. Shi and J. Macinko, "Contribution of Primary Care to Healt
h Systems and
Health," The Milbank Quarterly, vol. 83, no. 3, pp. 457-502, 2005.
[7]
E. a. M. National Academies of Sciences, "Implementing High
-
Quality Primary Care," 2021.
[8]
CDC, "Advancing Health Equity in Chronic Disease Prevention and Managemen
t," [Online].
Available: https://www.hsd.state.nm.us/wp-content/uploads/FINAL-2022-NM-PCC-
Strategic-Plan.pdf. [Accessed 11 01 2023].
[9]
N. M. Legislature, "Primary Care Council Act," 2021. [Online]. Available:
https://www.nmlegis.gov/Sessions/21%20Regular/final/HB0067.pdf. [Accessed 11 1 2023].
[10]
U. C. Bureau, "Population Estimates Program (PEP), Vintage 2020," Published 2021. [Online].
[Accessed 11 1 2023].
[11]
U. C. Bureau, "Historical Population Density Data (1910
-
2020)," Published 2021.
[Online].
Available: https://www.census.gov/data/tables/time-series/dec/density-data-text.html.
[Accessed 11 January 2023].
[12]
S. D. C. o. Iowa, "Census Demographics
-
Population, Housing, Economy, Government,"
[Online]. Available: https://www.iowadatacenter.org/browse/projections.html. [Accessed
11 January 2023].
[13]
I. M. Ltd., "The Complexities of Physician Supply and Demand: Projections From 2019 to
2034," 2021.

New Mexico Primary Care Council 2023
Page 45 of 48
[14]
S. Juraschek, X. Zhang and e. al., "United States Registered Nurse Workforce Report Card
and Shortage Forecast," American Journal of Medical Quality, 2019.
[15]
F. E. D. |. S. L. FED, "Per Capita Personal Income by State, Annual," Economic Research.
[1
6]
K. F. Foundaiton, "State Health Facts | Poverty by Age Range," 2021.
[17]
N. M. H. S. Department, "Social Impact: Data Over Time," 2022.
[18]
S. A. a. M. H. S. A. (SAMHSA), "Criteria for the Demonstration Program to Improve
Community Mental Health Centers and to Establish Certified Community Behavioral Health
Clinics".
[19]
W. S. H. C. Authority, "Accountable Communities of Health (ACHs)," [Online]. Available:
https://www.hca.wa.gov/about-hca/programs-and-initiatives/medicaid-transformation-
project-mtp/accountable-communities-health-achs. [Accessed 12 January 2023].
[20]
H. C. P. L. a. A. N. (HCP
-
LAN), "APM Framework," [Online]. Available: https://hcp
-
lan.org/apm-framework/. [Accessed 23 January 2023].
[21]
N. M. D. o. Health, "RHPCA," [
Online]. Available: https://nmrphca.nmhealth.org/. [Accessed
12 January 2023].
[22]
T. C. Fund, "Review of Evidence on the Health Care Impacts of Interventions to Address the
Social Determinants of Health," [Online]. Available:
https://www.commonwealthfund.org/publications/2019/jun/roi-calculator-evidence-guide.
[Accessed 12 January 2023].
[23]
IQVIA, "The National Economic Impact of Physicians," 2018.
[24]
S.
-
H. J. W. K. J. M. B. E. Z. G. W. R. F. L. S. D. H. L. W. J. Newhouse RP, "Advanced practice
nurse outcomes 1990-2008: a systematic review," Nurs Econ, 2011.
[25]
M. Ronald Schneeweiss, M. M. Kathleen Ellsbury, P. L. Gary Hart and e. al, "The Economic
Impact and Multiplier Effect of a Family Practice Clinic on an Academic Medical Center,"
JAMA, 1989.
[26]
M. M. Sara Martin, M. M. Robert L. Phillips Jr, P. Stephen
Petterson and e. al, "Primary Care
Spending in the United States, 2002-2016," JAMA Internal Medicine, 2020.
[27]
N. M. D. o. Health, "Drug Overdose in New Mexico," 2022.
[28]
F. T. Chang TE, "A blueprint for integrated mental health care: Commentary
for "Costs of
using evidence-based implementation strategies for behavioral health integration in a large
primary care system"," Health Services Research, 2020.

New Mexico Primary Care Council 2023
Page 46 of 48
[29]
N. D. T. P. J. e. a. Melek S P, "Potential Economic impact of integrated medical
-
behavi
oral
healthcare," 2017.
[30]
T. O. H. C. Authority, "SoonerSelect Dental RFP 8070001412," [Online]. Available:
https://oklahoma.gov/ohca/about/procurement/soonerselect-dental-rfp-8070001412.html.
[Accessed 12 January 2021].
[31]
T. O. H. C. Authority, "SoonerSelect Dental Program Request for Proposals," 2022.
[32]
N. H. D. o. H. &. H. Services, "RFP
-
2023
-
DMS
-
06
-
MEDIC: Medicaid Care Management Dental
Services," 2022.
[33]
A. U. S. D. W. D. Thomas
-
Henkel C, "Bolstering the Youth".
[34]
C. D. o. H. Services, "Bill to establish Behavioral Health Administration sign
ed into law,"
2022.
[35]
M. D. o. H. Services, "Open grants, RFPs and RFIs," 2022.
[36]
A. S. Guth M, "Medicaid and Racial Health Equity,"
Kaiser Family Foundation,
2022.
[37]
MassHealth, "Section 1115 Demonstrations State Waivers List".
[38]
S.
A. a. M. H. S. A. (SAMHSA), "Screening, Brief Intervention, and Referral to Treatment
(SBIRT)," 2022.
[39]
S. S. P. J. Nardone M, "Integrating Physical and Behavioral Health Care: Promising Medicaid
Models," Kaiser Family Foundation, 2014. [Online]. [Accessed 12 January 2023].
[40]
S. Klein, "Behavioral Health Integration: Approaches from the Field,"
The Commonwealth
Fund, 2014.
[41]
"Golden Valley Health Centers | Behavioral Health," [Online]. Available:
https://www.gvhc.org/services/behavioral-health/. [Accessed 12 January 2023].
[42]
"National Council for Mental Wellbeing | Center of Excellence," 2022. [Online]. Available:
https://www.thenationalcouncil.org/program/center-of-excellence/. [Accessed 12 January
2023].
[43]
C. f. M. a
. M. Services, "Medicaid Health Homes: An Overview," 2022.
[44]
I. Healthcare, "A Team
-
Based Approach to Mental Health Integration in Primary Care," 2014.
[45]
P. C. Collaborative, "Sustaining Healthcare Across Integrated Primary Care Efforts (SHAPE),
"
[Online]. Available: https://www.pcpcc.org/initiative/sustaining-healthcare-across-
integrated-primary-care-efforts-shape. [Accessed 12 January 2023].

New Mexico Primary Care Council 2023
Page 47 of 48
[46]
A. H. Association, "Harris County Hospital District
-
Community Behavioral Health
Program,"
[Online]. Available: https://www.aha.org/case-studies/2012-04-13-harris-county-hospital-
district-community-behavioral-health-program. [Accessed 12 January 2023].
[47]
M. C. P. A. P. (MCPAP), "Connecting Primary Care with Child Psychiatry," [Onl
ine]. Available:
https://www.mcpap.com/. [Accessed 12 January 2023].
[48]
I. H. Care, "Behavioral Health," [Online]. Available:
https://intermountainhealthcare.org/medical-specialties/behavioral-health/. [Accessed 12
January 2023].
[49]
I. f. A. H. V. a. W. G. University, "Health Value Atlas," [Online]. Available:
https://atlas.advancinghealthvalue.org/. [Accessed 12 January 2023].
[50]
"Evidence
-
based practices from large clinically integrated networks that operate in risk
contracts across lines of business.," NEJM Catalyst, 2018.
[51]
B. A., "Organizational Culture and Effective Leadership in Academic Medical Institutions,"
in
J
Healthc Leadersh, 2022.
[52]
A. S. a. K. B. C. f. H. C. S. Rob Houston, "Medicaid Population
-
Based Payment: The Current
Landscape, Early Insights, and Considerations for Policymakers," Center for Health Care
Strategies, 2022.
[53]
C. D. o. H. C. P. &. Financing, Primary Care Alternative Payment Model Guidebook, 2021.
[54]
M. H. S. C. R. Commission, "Maryland’s Total Cost of Care Model," [Online]. [Accessed 12
January 2023].
[55]
M. H. S. C. R. Commission, "Episode Quality Impro
vement Program (EQIP) Specifications,"
2021.
[56]
M. E. O. o. H. a. H. Services, "MassHealth Partners with 17 Health Care Organizations to
Improve Health Care Outcomes for Members," 2017.
[57]
MassHealth, "1115 MassHealth Demonstration ("Waiver")," 20
22
-
2027.
[58]
N. Y. S. D. o. H. M. R. Team, "A Path toward Value Based Payment: Annual Update New York
State Roadmap for Medicaid Payment Reform," 2019.
[59]
O. H. Authority, "Oregon's Coordinated Care Organizations (CCO) Performance Metrics
Dashboard," 2021.
[60]
W. S. H. C. Authority, "WA Multi
-
payer Primary Care Transformation Model (PCTM)," 2022.
[61]
O. H. Authority, "Supporting Health for All through REinvestment: the SHARE Initiative,"
2023.

New Mexico Primary Care Council 2023
Page 48 of 48
[62]
O. H. Authority, "CCO Guidance:
Community Health Assessments and Community Health
Improvement Plans," 2019.
[63]
R. Dailey, "State leaders roll out a 'massive' public
-
private program to stem the opioid
epidemic," Health News Florida, 2022.
[64]
Staff, "Governor Ron DeSantis Announces New Opioid Recovery Program in Florida,"
Florida
Governor Ron DeSantis, 2022.
[65]
"AACN Fact Sheet
-
Nursing Shortage," 2022.
[66]
CDC, "The Social Vulnerability Index (SVI): Interactive Map".
