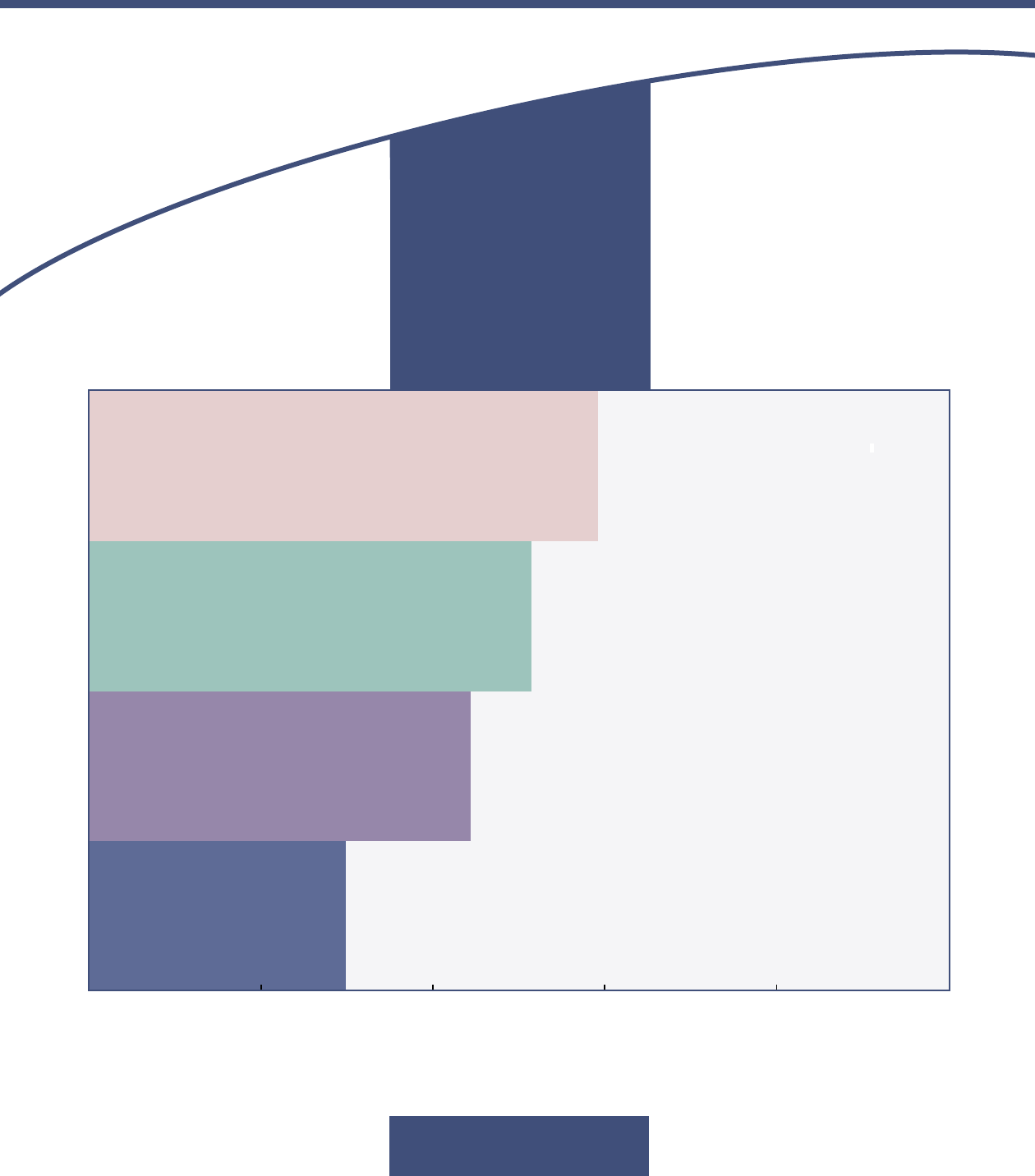
Percentage of People Eligible for Full Benefits from
Medicare and Medicaid Who Have Various Characteristics
Elderly
Originally Qualified for
Medicare Because of
Disability or Kidney Disease
Rather Than Age
Diagnosed With a Mental Illness
Receiving Long-Term
Services and Supports
0 20 40 60 80 100
CONGRESS OF THE UNITED STATES
CONGRESSIONAL BUDGET OFFICE
CBO
Dual-Eligible
Beneficiaries of
Medicare and
Medicaid:
Characteristics, Health
Care Spending, and
Evolv
ing Policies
JUNE 2013

CBO
Notes
Unless otherwise indicated, all of the calculations in this report are based on analysis by the
Congressional Budget Office (CBO) and reflect spending by Medicare (by the federal
government) and Medicaid (by the federal and state governments). CBO does not have access
to data on spending by other payers. Out-of-pocket payments by Medicare and Medicaid
enrollees are excluded from the analysis. Most cost sharing incurred under Medicare for
dual-eligible beneficiaries is paid by Medicaid, and those payments are counted as Medicaid
spending. However, payments by Medicaid to cover the Medicare premiums of dual-eligible
beneficiaries are not included in estimates of Medicaid spending in this report because of data
constraints. Information about the data used in the analysis appears in the appendix.
Numbers in the text, tables, and figures may not add up to totals because of rounding.
Definitions of various terms used in this report appear in the glossary at the end of the report.
Correction:
On March 27, 2014, CBO reposted this document with various small corrections.
Misclassifying some people as eligible beneficiaries of Medicaid and misclassifying the reason
for some others’ eligibility affected the results of various calculations, which are reported
mostly in Tables 1 and 2 and Figure 3 and in the passages in the text that discuss those results.
Corrections are noted on the pages where they occurred.
Pub. No. 4374

Contents
CBO
Summary 1
Why Are Policymakers Concerned About Dual-Eligible Beneficiaries? 1
What Characteristics and Spending Patterns Distinguish the Dual-Eligible Population? 2
What Strategies Are States and the Federal Government Pursuing to Reduce Costs and
Improve the Quality of Care for Dual-Eligible Beneficiaries? 2
What Actions Might Federal Lawmakers Take and How Might They Affect the Budget? 2
Characteristics of Dual-Eligible Beneficiaries That Affect Health Care Needs and Spending 4
Prevalence of Disabilities and Health Risks 4
BOX: PARTIAL DUAL-ELIGIBLE BENEFICIARIES 6
Use of Long-Term Care and Related Services 6
Diversity of Services Needed 8
Spending by Medicare and Medicaid for Dual-Eligible Beneficiaries 8
Medicare’s and Medicaid’s Current Payment Systems for Dual-Eligible Beneficiaries 11
Managed Care Plans in Medicare and Medicaid 11
BOX: ADJUSTING MEDICARE’S PAYMENTS FOR THE HEALTH RISKS OF BENEFICIARIES 12
Dual-Eligible Beneficiaries’ Enrollment in Different Service-Delivery Systems 12
Efforts to Integrate Medicare’s and Medicaid’s Financing and Coordinate Care for
Dual-Eligible Beneficiaries 15
Multipayer Medical-Home Programs 17
Fully Integrated Dual-Eligible Special-Needs Plans 17
Initiatives to Integrate Behavioral and Physical Health Care 17
Managed Long-Term Services and Supports 19
Financial Alignment Demonstration Projects 20
Challenges Facing Efforts to Integrate Financing and Coordinate Care 25
Potential Legislative Actions Targeting Dual-Eligible Beneficiaries and Their
Impact on the Federal Budget 28
Potential Legislative Changes 28
Possible Budgetary Effects of Legislative Changes 29
Appendix: Data Used in This Analysis 31
List of Tables and Figures 38
About This Document 39
Glossary 41

CBO
Dual-Eligible Beneficiaries of
Medicare and Medicaid:
Characteristics, Health Care Spending, and
Evolving Policies
Summary
In 2009, the federal and state governments spent a total
of more than $250 billion on health care benefits for the
9 million low-income elderly or disabled people who
are jointly enrolled in Medicare and Medicaid. Medicare
is a federal program that provides health insurance cover-
age to people who have disabilities, are diagnosed with
certain medical conditions, or are age 65 or older (50 mil-
lion people in 2009). Medicaid, which is funded jointly
by the federal government and the states, provides health
care coverage to low-income people who meet specific
requirements for income and assets and other eligibility
criteria (65 million in 2009).
1
People who are eligible to
receive benefits from both programs at the same time are
known as “dual-eligible beneficiaries.” All of those benefi-
ciaries qualify for full Medicare benefits, but they differ in
the amount of Medicaid benefits for which they are eligi-
ble. Seven million are “full duals,” who qualify for full
benefits from both programs. The other 2 million are
“partial duals,” who do not meet the eligibility require-
ments for full Medicaid benefits but qualify to have
Medicaid pay some of the costs they incur under
Medicare.
This report examines the characteristics and costs of dual-
eligible beneficiaries, focusing on 2009, the most recent
year for which comprehensive data were available when
the Congressional Budget Office (CBO) began this
analysis. The report also examines the different payment
systems that Medicare and Medicaid use to fund care for
dual-eligible beneficiaries and recent efforts at the federal
and state levels to integrate those payment systems and to
coordinate the care that such beneficiaries receive from
the two programs.
Why Are Policymakers Concerned About
Dual-Eligible Beneficiaries?
Federal and state policymakers have growing concerns
about the high costs of dual-eligible beneficiaries—par-
ticularly full duals—as well as about the appropriateness
of the care they receive and the ways in which the sepa-
rate structures of Medicare and Medicaid may affect their
costs and care. Medicare generally pays for acute care
(hospitalization and other short-term care) and postacute
care (services provided in skilled nursing facilities or
elsewhere to help people recover from an acute illness
or surgery). Medicaid pays for long-term services and
supports (LTSS)—which includes long-term care as well
as social support services designed to help people stay in
their homes rather than move to institutions—and other
benefits that Medicare does not cover, such as dental and
vision services.
Those separate funding streams, and the different
payment rates and coverage rules within them, create
conflicting financial incentives for the federal and state
governments and for health care providers, potentially
increasing the costs of care. In addition, receiving care
through separate programs with different payment
and approval procedures increases the likelihood that
full duals—especially those who have many chronic
1. Those enrollment figures are based on total annual enrollment
rather than on average monthly enrollment or enrollment at a
particular point in time.

2 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
conditions and functional limitations—will be treated by
a variety of health care providers who are not coordinat-
ing their care, potentially increasing costs and worsening
outcomes.
What Characteristics and Spending Patterns
Distinguish the Dual-Eligible Population?
Dual-eligible beneficiaries are a varied group, but many
have extensive health care needs, stemming from multiple
illnesses and disabilities. In the case of full duals, for
example, half initially qualified for Medicare because of
disability rather than age, and nearly one-fifth have three
or more chronic conditions (see Figure 1). Consequently,
a sizable share of full duals, more than 40 percent, use
long-term services and supports—a far greater percentage
than for other Medicare or Medicaid beneficiaries.
Although some full duals are fairly healthy and have rela-
tively low health care costs, full duals as a group account
for a disproportionate share of federal and state spending
for Medicare and Medicaid. Full duals make up 13 per-
cent of the combined population of Medicare enrollees
and aged, blind, or disabled Medicaid enrollees (the cate-
gories of Medicaid participants who might also qualify
for Medicare), but they account for 34 percent of the two
programs’ total spending on those enrollees.
2
What Strategies Are States and the Federal
Government Pursuing to Reduce Costs and Improve
the Quality of Care for Dual-Eligible Beneficiaries?
Many states are working to eliminate differences in the
financial incentives that health care providers face under
Medicare and Medicaid and to improve the coordination
and quality of care for dual-eligible beneficiaries within
the scope of current law. States’ efforts include establish-
ing initiatives under which Medicare, Medicaid, and
private insurers pay fees to the same primary care practice
to manage care for patients; contracting with plans in
Medicare’s managed care program (Medicare Advantage)
to provide services covered by Medicaid; coordinating
physical and behavioral health care for dual-eligible
beneficiaries who have chronic mental illnesses; and
developing managed LTSS programs.
3
At the same time,
the federal government, through the Medicare Advantage
program, has encouraged the establishment of special
health plans for full duals that target their particular
needs.
The Affordable Care Act (ACA) created new options for
addressing financing and quality-of-care issues for dual-
eligible beneficiaries.
4
The largest initiative in that area
under the new law is a three-year demonstration project
to integrate Medicare’s and Medicaid’s financing for full
duals, which 26 states applied to participate in. The first
state projects are due to begin this summer.
What Actions Might Federal Lawmakers Take and
How Might They Affect the Budget?
Various restrictions exist under current law that impede
efforts to reduce costs and improve the quality of care for
dual-eligible beneficiaries by more fully integrating that
care. For example, participation in Medicare’s managed
care program is optional for dual-eligible beneficiaries, as
it is for other Medicare beneficiaries. In addition, states
generally have little information about, and limited con-
trol over, the provision of services covered by Medicare.
Moreover, Medicare and Medicaid contract separately
with managed care organizations even if a beneficiary
receives services from both programs through the same
managed care organization.
5
Federal lawmakers might
choose to relax those and other restrictions—or enact
broader program changes—in an effort to more fully
integrate the care provided to full duals.
The impact of such policy changes on the federal budget
would be likely to depend on multiple factors, such as
how payment rates to providers would compare with the
rates under current law, whether certain complex services
(such as behavioral health care) would be included in
2. Age and blindness or disability are two of the eligibility categories
for Medicaid; the dual-eligible population is a subset of those
categories of beneficiaries. (The remaining Medicaid population
consists largely of children and their parents as well as pregnant
women. In addition, a new category of participants—non-
disabled, nonelderly, childless adults—will begin enrolling in
Medicaid in 2014 because eligibility for that group is expanding
under current law. Those other populations tend to have lower
health care costs than the aged, blind, or disabled.)
3. Behavioral health care includes mental health and substance
abuse services.
4. The ACA comprises the Patient Protection and Affordable
Care Act (Public Law 111-148), the health care provisions of
the Health Care and Education Reconciliation Act of 2010
(P.L. 111-152), and, in the case of this report, the effects of subse-
quent related judicial decisions, statutory changes, and adminis-
trative actions.
5. One exception is PACE (Program of All-Inclusive Care for the
Elderly) programs, which can use combined Medicaid and
Medicare funds for the full set of services they provide.

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 3
CBO
Figure 1.
Characteristics of Full Dual-Eligible Beneficiaries, 2009
Source: Congressional Budget Office.
Notes: Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive
benefits from both programs. “Full duals” qualify for full benefits from both programs.
ESRD = end-stage renal disease.
a. Includes federal and state spending for Medicaid but excludes Medicaid payments for Medicare premiums.
b. The Medicare program consists of three parts: Hospital Insurance (Part A), Medical Insurance (Part B), and prescription drug coverage
(Part D). Medicare Part C (known as Medicare Advantage) specifies the rules under which private health care plans can assume
responsibility for, and be compensated for, providing benefits covered under Parts A, B, and D.
Distribution of Full Duals and Spending for Them, by Health Status
(Percent)
0123–45+
0
5
10
15
20
25
30
35
40
45
50
Full-Dual Population
Total Medicare and
Medicaid Spending for
Full-Duals
0 102030405060708090100
Elderly
Originally Enrolled in Medicare
Because of a Disability or ESRD
Receiving Any Long-Term
Services and Supports
Diagnosed With a
Mental Illness
Share of Full Duals With Selected Characteristics
Number of Chronic Conditions Percent
All Full Duals Full Duals in
Top 10 Percent of
Medicaid Spending
per Beneficiary
Full Duals in
Top 10 Percent of
Medicare Spending
per Beneficiary
Full Duals in
Top 10 Percent of
Combined Spending
per Beneficiary
Full Duals in
Bottom 33 Percent of
Combined Spending
per Beneficiary
Full Duals in
Bottom 50 Percent of
Combined Spending
per Beneficiary
0
10,000
20,000
30,000
40,000
50,000
60,000
70,000
80,000
90,000
15,200
14,400
3,800
80,500
17,900
5,300
21,700
75,700
7,400
63,000
60,300
6,900
1,000
1,600
1,500
1,900
3,100
2,000
Medicaid
a
Medicare Parts A and B
b
Medicare Part D
b
Average Spending Per Beneficiary, by Program and Spending Group
(2009 dollars)
*
*
*
[* Value corrected]

4 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
overall payment rates or be paid for separately, and
whether beneficiaries’ participation in new models for
delivering care would be voluntary or mandatory.
Characteristics of Dual-Eligible
Beneficiaries That Affect Health Care
Needs and Spending
Both Medicare and Medicaid serve a broad range of
elderly and disabled beneficiaries. Some of them (full
duals) receive full benefits from both programs. Others
(partial duals) receive full Medicare benefits but limited
assistance from Medicaid, and the remainder (nonduals)
receive benefits only from Medicare or only from Medic-
aid. The need for health care services varies widely both
within and among those groups of beneficiaries, reflect-
ing differences in the prevalence of disabilities and health
conditions. Those differences lead to large variation in
average spending per beneficiary: In 2009, total Medicare
and Medicaid spending per beneficiary (including both
state and federal spending) ranged from an average of
about $8,300 for nondual Medicare beneficiaries to
$33,400* for full duals (see Table 1).
This report focuses on full duals, who are the main target
of recent policy initiatives and who account for a signifi-
cant share of spending by Medicare and Medicaid. Partial
duals share some of the characteristics of full duals, but
they are much less likely to use nursing facilities and
other types of long-term services and supports. That dif-
ference causes average Medicaid spending for them to be
much lower—and average Medicare spending to be
somewhat lower—than for full duals. (More information
about the partial-dual population is presented in Box 1.)
A detailed analysis of the ways in which people become
dual-eligible beneficiaries is beyond the scope of this
report. However, one large group of dual-eligible benefi-
ciaries consists of Medicare enrollees who became eligible
for Medicaid by spending down their resources, in many
cases while they were in nursing facilities. In general, such
beneficiaries have high health care costs. Other dual-
eligible beneficiaries are Medicare enrollees who gained
Medicaid coverage because they had low income and met
Medicaid’s specific eligibility criteria for age, blindness, or
disability; that group may not initially incur large medical
expenses. Still other dual-eligible beneficiaries became
disabled and had low income; they usually qualified for
Medicaid quickly and became eligible for Medicare later
(because a waiting period exists between qualifying for
Social Security’s Disability Insurance program and
qualifying for Medicare coverage).
6
Prevalence of Disabilities and Health Risks
Full duals are much more likely than other Medicare ben-
eficiaries to have initially qualified for Medicare because
of physical or mental disabilities—factors that increase
people’s need for health care, rehabilitation services, and
long-term care and that may reduce their ability to navi-
gate the health care system.
7
Specifically, just over half of
the people who were full duals in 2009 originally became
eligible for Medicare on the basis of disability or end-
stage renal disease (ESRD) rather than age, compared
with just 17 percent of nondual Medicare beneficiaries.
Reflecting that reason for Medicare eligibility, 41 percent
of full duals in 2009 were under age 65, compared with
only 11 percent of nondual Medicare beneficiaries.
Looked at another way, disabled Medicare beneficiaries
were more than three times as likely as elderly Medicare
beneficiaries to be full duals.
In conjunction with higher rates of disability, full duals
were about twice as likely as nondual Medicare beneficia-
ries to have at least three chronic conditions, and they
were nearly three times as likely to have been diagnosed
with a mental illness.
8
Consequently, medical risk
scores—which indicate differences in expected spending
by Parts A and B of Medicare for different beneficiaries
based on diagnosed conditions and demographic charac-
teristics—were about 55 percent higher for full duals, on
average, than for nondual Medicare beneficiaries.
6. People who receive benefits from the Disability Insurance pro-
gram are eligible for Medicare coverage after two years of receiving
disability benefits, regardless of their age. In certain cases, such as
with a diagnosis of end-stage renal disease, the waiting period
depends on the stage of the illness. In addition, some people with
end-stage renal disease are eligible for Medicare without partici-
pating in the Disability Insurance program.
7. See, for example, Linda P. Fried and others, “Untangling the
Concepts of Disability, Frailty, and Comorbidity: Implications for
Improved Targeting and Care,” Journals of Gerontology: Medical
Sciences, vol. 59, no. 3 (March 2004), pp. M255–M263,
http://dx.doi.org/10.1093/gerona/59.3.M255.
8. CBO identified mental illness using risk-adjustment data
(described in the appendix). Medicare enrollees were classified for
this analysis as having a mental illness if they were listed as having
a diagnosis from the previous year of schizophrenia; major depres-
sive, bipolar, and paranoid disorders; or other major psychiatric
disorders.
[* Value corrected]

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 5
CBO
Table 1.
Demographic Characteristics of Dual-Eligible Beneficiaries, Compared With
Those of Certain Other Medicare and Medicaid Beneficiaries, 2009
Source: Congressional Budget Office.
Note: n.a. = not applicable; N.A. = not available; * = between zero and 0.5 percent.
a. Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive benefits
from both programs. “Full duals” qualify for full benefits from both programs; “partial duals” qualify for full benefits from Medicare but
only partial benefits from Medicaid (meaning that Medicaid pays some of the expenses they incur under Medicare, such as premiums,
but does not cover additional health care services, such as long-term services and supports). “Nonduals” qualify for benefits only from
Medicare or only from Medicaid. (For more details, see the glossary.)
b. The Centers for Medicare & Medicaid Services calculates a risk score for each Medicare enrollee on the basis of his or her medical
diagnoses and demographic characteristics. The scores are used to adjust Medicare’s payments to managed care plans to reflect
enrollees’ expected costs for Parts A and B of Medicare. Risk scores are normalized such that the average assigned risk score for enrollees
in fee-for-service Medicare is 1.0. In order to use a common framework for comparing the health status of various beneficiaries, CBO only
reports risk scores from the community version of the CMS-HCC model (see the appendix for details). For that reason and because CBO
includes people enrolled in Medicare Advantage plans (not just fee-for-service Medicare), the average risk score for the whole Medicare
population, as reported above, will not equal 1.0.
c. Includes federal and state spending for Medicaid but excludes Medicaid payments for Medicare premiums.
d. The Medicare program consists of three parts: Hospital Insurance (Part A), Medical Insurance (Part B), and prescription drug coverage
(Part D). Medicare Part C (known as Medicare Advantage) specifies the rules under which private health care plans can assume
responsibility for, and be compensated for, providing benefits covered under Parts A, B, and D.
7.1 2.1 39.6 6.3 **
41 40 11 88 **
59 60 89 12 **
Percentage With Various Characteristics
Female 62 61 54 51
Black 20 22 8 30 **
Hispanic 8 4 1 14 **
Living in a rural area 21 29 20 20
Originally enrolled in Medicare because of a disability
or end-stage renal disease 52 54 17 n.a.
Diagnosed with three or more chronic conditions 19 14 9 N.A.
Institutionalized 15 * 1 4
Receiving any long-term services and supports 44 14 9 18 **
Diagnosed with a mental illness 30 25 11 N.A.
Average Community Medical Risk Score
b
1.5 1.3 1.0 n.a.
15,200 ** 800 n.a. 15,500 **
Medicare
d
14,400 11,800 7,800 n.a.
3,800 3,200 400 n.a.
_
______
_
______
_
_____ ______
Total Average Spending by Medicaid and Medicare
c
33,400 ** 15,700 8,300 15,500
**
Parts A and B
Part D
Nonelderly (Under age 65)
Elderly (Age 65 or older)
Number of Beneficiaries (Millions)
Duals Duals
Beneficiaries
a
Beneficiaries Medicaid Beneficiaries
Medicaid
c
Dual-Eligible
PartialFull Medicare
Nondual
Blind, or Disabled
Nondual Aged,
Average Spending per Beneficiary, by Program (Dollars)
Distribution by Age (Percent)
[** Value corrected]
6 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Among both full duals and nondual Medicare beneficia-
ries, those age 65 or older were much more likely than
younger beneficiaries to have been diagnosed with
three or more chronic conditions, and they had corre-
spondingly higher average medical risk scores (see
Table 2). Those differences between age groups were
larger, however, for the full-dual population. By contrast,
beneficiaries under age 65 in both groups were more
likely than elderly beneficiaries to have been diagnosed
with a mental illness.
Use of Long-Term Care and Related Services
One notable characteristic that distinguishes full duals
from their nondual counterparts in Medicare and Medic-
aid is their high rate of use of both community-based and
institutional long-term services and supports.
9
LTSS
Box 1.
Partial Dual-Eligible Beneficiaries
Partial duals are eligible for complete benefits from
Medicare but only limited benefits from Medicaid.
Those limited benefits consist of having Medicaid
pay some of the expenses they incur under Medicare,
such as premiums and, in many cases, cost sharing for
services covered by Medicare. The extent of the assis-
tance that partial duals receive from Medicaid varies
with their income and assets and, to some extent,
with differences in state policies. (Some states’ Medic-
aid programs have higher ceilings on income and
assets for both full and partial duals than the federal
government requires.)
In certain ways, partial duals are very similar to full
duals: About 40 percent of both populations are
under age 65, roughly 60 percent of both populations
are female, and just over half of both populations
qualified for Medicare because of a disability or
end-stage renal disease (see Table 1 on page 5). On
average, however, partial duals tend to be healthier
and have less need for services than full duals. For
example, fewer of them have at least three chronic
conditions (14 percent of partial duals, compared
with 19 percent of full duals), and their average med-
ical risk score is nearly 15 percent lower than that of
full duals. (Medical risk scores, which the Centers for
Medicare & Medicaid Services calculate to adjust
Medicare’s payments to managed care and prescrip-
tion drug plans, reflect enrollees’ expected costs for
Parts A and B of Medicare.) That difference in aver-
age risk scores, and thus in the predicted use of acute
and postacute care services, is reflected in the fact that
Medicare spent an average of $15,000 per beneficiary
for partial duals in 2009 but $18,200 for full duals.
The key difference in use of services, however,
between those two groups involves long-term services
and supports: Partial duals are 70 percent less likely
to use those services than full duals are.
1
In addition,
less than 0.5 percent of partial duals are institutional-
ized, compared with 15 percent of full duals. To some
extent, differences between the two groups in the use
of nursing facilities reflect the factors that make
someone a full or partial dual-eligible beneficiary.
Partial duals may become eligible for full Medicaid
benefits—and thus become full duals—if they
develop the need for long-term nursing home care,
which is very expensive. Specifically, such beneficia-
ries may gain full Medicaid eligibility because of
spending down their assets or because of higher ceil-
ings on income and assets for people living in nursing
facilities, depending on states’ eligibility rules for
Medicaid.
1. In fact, a comparison of full duals and partial duals who do
not use long-term services and supports shows that those two
populations are similar; the partial duals have slightly more
chronic conditions, somewhat higher medical risk scores, and
somewhat higher Medicare spending, on average. Those dif-
ferences may stem from the fact that partial duals who do not
use long-term services and supports are more likely than their
full-dual counterparts to be elderly.
9. All discussion in this report of use of services refers to services cov-
ered by Medicare or Medicaid; CBO does not have access to data
on beneficiaries’ use of other services. Therefore, this analysis may
underestimate LTSS use by partial duals and nondual Medicare
beneficiaries if those services are paid for by the beneficiary or by
another payer other than Medicare.
JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 7
CBO
Table 2.
Demographic Characteristics of Dual-Eligible Beneficiaries, Compared With
Those of Certain Other Medicare and Medicaid Beneficiaries, 2009, by Age
Source: Congressional Budget Office.
Note: n.a. = not applicable; N.A. = not available; * = between zero and 0.5 percent.
a. Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive benefits
from both programs. “Full duals” qualify for full benefits from both programs; “partial duals” qualify for full benefits from Medicare but
only partial benefits from Medicaid (meaning that Medicaid pays some of the expenses they incur under Medicare, such as premiums,
but does not cover additional health care services, such as long-term services and supports). “Nonduals” qualify for benefits only from
Medicare or only from Medicaid. (For more details, see the glossary.)
b. The Centers for Medicare & Medicaid Services calculates a risk score for each Medicare enrollee on the basis of his or her medical
diagnoses and demographic characteristics. The scores are used to adjust Medicare’s payments to managed care plans to reflect
enrollees’ expected costs for Parts A and B of Medicare. Risk scores are normalized such that the average assigned risk score for enrollees
in fee-for-service Medicare is 1.0. In order to use a common framework for comparing the health status of various beneficiaries, CBO only
reports risk scores from the community version of the CMS-HCC model (see the appendix for details). For that reason and because CBO
includes people enrolled in Medicare Advantage plans (not just fee-for-service Medicare), the average risk score for the whole Medicare
population, as reported above, will not equal 1.0.
c. Includes federal and state spending for Medicaid but excludes Medicaid payments for Medicare premiums.
d. The Medicare program consists of three parts: Hospital Insurance (Part A), Medical Insurance (Part B), and prescription drug coverage
(Part D). Medicare Part C (known as Medicare Advantage) specifies the rules under which private health care plans can assume
responsibility for, and be compensated for, providing benefits covered under Parts A, B, and D.
2.9 4.2 0.8 1.2 4.3 35.3 5.6 0.8 **
Percentage With Various Characteristics
Female 52 69 51 68 44 55 49 66
Black 23 17 26 20 16 7 31 18
Hispanic 69 3 4311322
Living in a rural area 22 20 29 29 22 20 20 14
Originally enrolled in Medicare because of a disability
or end-stage renal disease 100 18 100 23 100 8 n.a. n.a.
Diagnosed with three or more chronic conditions 8 26 10 17 6 10 N.A. N.A.
Institutionalized 4 23 * 1 * 1 2 17
Receiving any long-term services and supports 31 54 10 16 4 9 16 28
Diagnosed with a mental illness 37 25 37 17 19 10 N.A. N.A.
Average Community Medical Risk Score
b
1.2 1.8 1.2 1.4 0.8 1.0 n.a. n.a.
14,600 15,500 1,100 600 n.a. n.a. 16,200 9,900 **
Medicare
d
12,100 16,100 11,100 12,200 6,600 8,000 n.a. n.a.
4,500 3,300 4,200 2,500 800 400 n.a. n.a.
_____
_
____
_
____
_
____
_
____ _____ _____
_
____
Total Average Spending by Medicaid and
Medicare
c
31,100 34,800 16,400 15,300 7,400 8,400 16,200 9,900
**
Nondual Medicare
Nondual Aged,
Blind, or Disabled
Medicaid
or Older
Beneficiaries
Under Age 65 Under Age 65Age 65
Age 65 or Older
Beneficiaries
Age 65
Part D
Number of Beneficiaries (Millions)
Average Spending per Beneficiary, by Program (Dollars)
Medicaid
c
Parts A and B
Age 65 or Older
Full Duals
a
Age 65 or Older
Partial Duals
a
Under Age 65 Under
**
**
**
**
**
**
[** Value corrected]

8 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
includes long-term care provided in nursing homes and
skilled nursing facilities, as well as hospice care, home
health care, and other social support services that enable
beneficiaries to continue living in the community (that is,
outside institutions).
10
In 2009, full duals were about
five times as likely to use LTSS as nondual Medicare
beneficiaries (44 percent versus 9 percent) and more than
twice as likely to use those services as nondual aged,
blind, or disabled (ABD) Medicaid beneficiaries (44 per-
cent versus 18 percent).* Those differences were reflected
in the various groups’ rates of institutionalization: 15 per-
cent for full duals, compared with 1 percent for nondual
Medicare beneficiaries and 4 percent for nondual ABD
Medicaid beneficiaries. Use of LTSS was particularly high
among elderly full duals, more than half of whom used
such services. Likewise, nearly one-quarter of elderly full
duals lived in an institution.
Diversity of Services Needed
Designing cost-effective programs to provide care for full
duals is challenging in part because those beneficiaries
vary widely in their needs for medical treatment, long-
term care, and social services. For example, 85 percent of
full duals lived outside nursing homes in 2009. Of them,
35 percent received community-based long-term services
and supports, 14 percent had multiple chronic conditions
but did not use such services, and the other 51 percent
had no more than one chronic condition and also did not
use any of those services.
11
The need for services can also vary considerably within
such subgroups. For instance, more than half of full duals
who used community-based LTSS in 2009—and one-
third of those in institutions—had no more than one
chronic condition. (However, some disabling conditions
for which beneficiaries may need nursing home care or
community-based services, such as physical, intellectual,
or developmental disabilities, may not be represented in
data on chronic conditions.) In addition, some beneficia-
ries with multiple chronic conditions have behavioral
health problems, cognitive impairments, or developmen-
tal disabilities that compound the effects of other chronic
illnesses and complicate the management of their care.
Given that diversity of needs, using any single approach
to deliver care to all dual-eligible beneficiaries may be
infeasible. An alternative would be to target subgroups
with the particular services they need, using the models of
care that are most appropriate for them.
12
Such targeting
might require more resources and data than a “one size
fits all” approach, however, which would increase the
administrative costs of providing care.
Spending by Medicare and Medicaid for
Dual-Eligible Beneficiaries
Among full duals, Medicare is the primary payer for acute
care services (such as inpatient and outpatient hospital
services, physicians’ services, and prescription drugs) and
for postacute care (such as care in skilled nursing facilities
and home health services).
13
Medicaid is the primary
payer for full duals’ long-term services and supports
(including nursing home care), and it also pays for some
of their acute care costs, such as cost sharing under Medi-
care and some acute care services that Medicare does not
cover (such as dental and vision care). That division of
responsibilities, and the health status and service needs of
full duals, are reflected in the amount that each program
pays per full dual-eligible beneficiary.
In part because full duals have higher-than-average health
risks, they cost Medicare much more, per person, than
other Medicare beneficiaries did in 2009: an average of
about $18,200 (including spending by all parts of the
program), compared with about $8,300 for nondual
Medicare beneficiaries (see Table 1 on page 5). Likewise,
because full duals use long-term services and supports at a
relatively high rate, state and federal Medicaid spending
was almost as high for that population as it was for the
nondual aged, blind, or disabled Medicaid population:
10. Medicare covers care in skilled nursing facilities, hospice care, and
home health services under certain circumstances when a benefi-
ciary meets the requirement for Medicare’s postacute care benefits.
That Medicare coverage is typically short term in nature and is
intended to help beneficiaries recover from acute conditions for
which they are also receiving medical care. Medicaid’s provision of
nursing home, hospice, and home health services could substitute
for those postacute care services for full duals if the Medicare
benefit was not available.
11. That breakdown of beneficiaries follows one used in Randall
Brown and David R. Mann, Best Bets for Reducing Medicare Costs
for Dual Eligible Beneficiaries: Assessing the Evidence (Kaiser Family
Foundation, October 2012), www.kff.org/medicare/8353.cfm.
12. Ibid.
13. The primary payer of a health care bill is the first organization to
pay what it owes for that bill; secondary and other payers make
payments based on any remaining amount owed beyond what the
primary payer covered.
[* Sentence corrected]

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 9
CBO
about $15,200 per beneficiary, on average, versus
$15,500.
14
* That difference is particularly notable
because it means that Medicaid is spending about as
much for only a portion of the health care services that
full duals receive (its share) as for all of the services that
nondual ABD beneficiaries receive.*
Together, Medicare and Medicaid paid an average of
$33,400* per full dual in 2009, with Medicare’s share
being slightly more than half (see Table 3). Of that
amount, 61 percent was for acute care services, 6 percent
was for postacute care, and 33 percent was for long-term
care (including both institutional care and community-
based services).
15
That average for the entire full-dual
population masks wide variation in spending for individ-
uals. For the most costly 10 percent of full duals,
Medicare and Medicaid paid a combined $130,200 per
beneficiary, on average. At the other end of the cost spec-
trum, a substantial share of full duals used relatively few
services: Medicare and Medicaid paid a combined $4,100
per beneficiary, on average, for people in the least costly
33 percent of full duals (see Figure 1 on page 3).
The distribution of spending between the two programs
also varied by beneficiary. In general, dual-eligible benefi-
ciaries for whom Medicaid spent especially large amounts
in 2009 had much lower spending by Medicare, and vice
versa. For example, Medicaid was responsible for nearly
80 percent of the combined spending for full duals who
were in the top 10 percent of Medicaid spending per
beneficiary—people who typically had high long-term
care expenses but close-to-average acute care costs (see
Table 3). Similarly, Medicare covered nearly 80 percent of
total spending for full duals who were in the top 10 per-
cent of Medicare spending—individuals whose average
acute care costs were high but whose long-term care
expenses were relatively low. Spending for full duals who
were in the top 10 percent of combined spending per
beneficiary was more evenly distributed between the two
programs (averaging $63,000 for Medicaid and $67,200
for Medicare in 2009) and among the types of services
paid for. About 54 percent of spending for that costliest
group was for acute care, 38 percent was for long-term
care, and the other 8 percent was for postacute care.
Differences in spending and service use among subgroups
of the full-dual population are partly attributable to dif-
ferences in the prevalence of various chronic conditions.
Among full duals who were in the top 10 percent of Med-
icaid spending in 2009, for instance, 41 percent had
dementia, compared with 14 percent of the overall full-
dual population. Likewise, although full duals in the top
10 percent of Medicare spending or the top 10 percent of
combined spending had much the same set of common
chronic conditions as the total full-dual population, the
prevalence of specific conditions varied substantially
among those groups. Almost half of full duals in the
top 10 percent of Medicare spending had diabetes, and
39 percent had congestive heart failure—roughly twice
the prevalence of those conditions among all full duals.
Other factors drive differences in spending as well. For
example, average spending for elderly and nonelderly full
duals was much closer in 2009 than might be expected,
given how much the two age groups differ in prevalence
of chronic conditions, average medical risk scores, and
use of LTSS (see Table 2 on page 7). Medicaid spending
for the two groups was especially close, partly because
Medicaid spends more on non-LTSS services for the non-
elderly population than for the elderly population, but
also because average Medicaid spending on LTSS among
users of those services is about 40 percent higher for the
nonelderly than for the elderly (not shown in Table 2).
That pattern suggests that chronic conditions may be less
useful predictors of spending for the disabled population
than for the elderly and that other factors also contribute
to disabled beneficiaries’ use of services.
Spending on dual-eligible beneficiaries also varies sub-
stantially among states. That variation may result from
differences in the payment rates, covered services, and eli-
gibility rules of state Medicaid programs as well as from
differences in the share of beneficiaries who have multiple
chronic conditions.
14. All figures for Medicaid spending in this report include both
the state and federal shares of Medicaid spending but exclude
Medicaid payments for Medicare premiums.
15. Spending for long-term care includes only the long-term
care portion of LTSS. Notably, Medicaid’s institutional and
community-based long-term care is included in this category,
but Medicare’s skilled nursing and home health services are
included in the postacute care category. Hospice care—provided
through both Medicare and Medicaid—is included in the acute
care category. See the appendix for more details.
[* Sentence or value corrected]

10 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Table 3.
Spending for Full Dual-Eligible Beneficiaries, by Program and
Type of Service, 2009
Source: Congressional Budget Office.
Notes: Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive
benefits from both programs. “Full duals” qualify for full benefits from both programs.
* = between zero and 0.5 percent; COPD = chronic obstructive pulmonary disease.
a. Includes federal and state spending for Medicaid but excludes Medicaid payments for Medicare premiums.
b. The Medicare program consists of three parts: Hospital Insurance (Part A), Medical Insurance (Part B), and prescription drug coverage
(Part D). Medicare Part C (known as Medicare Advantage) specifies the rules under which private health care plans can assume
responsibility for, and be compensated for, providing benefits covered under Parts A, B, and D.
c. For details about what types of services are included in these categories, see the appendix.
15,200 ** 80,500 21,700 63,000
14,400 17,900 75,700 60,300
3,800 5,300 7,400 6,900
_
____
_
_____
_
_____ ______
Total Average Spending by Medicaid and Medicare
a
33,400 ** 103,700 104,800 130,200
61 33 74 54
1683524
1571913
12676
18 12 13 12
62 13 8
4296
2* 4 2
33 65 13 38
Institutional care 21 45 9 25
Community-based long-term care 12 20 4 13
Most common
Second most common
Third most common
Fourth most common
Fifth most common
Acute care
Postacute care
Long-term care
Five Most Common Chronic Conditions
(Percentage with that condition)
Home health care
Inpatient care
Ambulatory care
Prescription drugs
Other (Includes capitation payments)
Skilled nursing facility care
Average Spending per Beneficiary, by Program (Dollars)
Medicaid
a
Medicare
b
Distribution of Spending by Type of Service (Percent)
c
Parts A and B
Part D
Full Duals in
Top 10 Percent of
Dementia (14)
Osteoporosis (10)
Full Duals inFull Duals in
COPD (17)
Depression (14)
Dementia (24)
Ischemic heart
All Full Duals per Beneficiary
Medicaid Spending
Top 10 Percent of
per Beneficiary
Medicare Spending
Top 10 Percent of
Diabetes (29) Dementia (41) Diabetes (49) Diabetes (42)
per Beneficiary
Combined Spending
COPD (27)
Ischemic heart
Congestive heartCongestive heartDiabetes (31)
Congestive heart COPD (33) Dementia (31)
failure (33)
disease (21) disease (16)
COPD (17)
failure (39)
failure (15) failure (22)
Congestive heart
[** Value corrected]

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 11
CBO
Medicare’s and Medicaid’s Current
Payment Systems for Dual-Eligible
Beneficiaries
The Medicare and Medicaid programs use two types of
payment systems—fee for service (FFS) and risk-based
managed care—to pay for covered benefits for their
enrollees. Under FFS, the programs pay health care
providers a fee for each service performed, whereas under
risk-based managed care, the programs contract with
health plans, most of which are sponsored by private
insurance companies, to provide a set of covered benefits
for a fixed amount per beneficiary. (Those amounts may
be adjusted to reflect the health risks of beneficiaries, as
explained in Box 2.) Both programs have encouraged
managed care systems in an effort to reduce spending and
improve the quality of care by improving beneficiaries’
access to services and increasing the management of their
care.
Managed Care Plans in Medicare and Medicaid
A minority of Medicare beneficiaries and of aged, blind,
or disabled Medicaid beneficiaries are enrolled in risk-
based managed care plans, and the percentages are lower
among dual-eligible beneficiaries.
16
In Medicare, about
25 percent of beneficiaries in 2009 were enrolled in
Medicare Advantage plans—private health plans that
assume the responsibility and financial risk for providing
Medicare benefits. A smaller share of full duals, about
17 percent, were enrolled in Medicare Advantage plans,
and 60 percent of those beneficiaries were enrolled in
special-needs plans (SNPs)—Medicare Advantage plans
that specialize in dual-eligible beneficiaries, people in
institutions, or those with certain chronic conditions.
In Medicaid, enrollment in risk-based managed care
plans has been more common among children and non-
disabled adults than among other beneficiaries; in 2009,
about 35 percent* of nondual aged, blind, or disabled
Medicaid beneficiaries and 15 percent of full duals were
enrolled in such plans. Unlike Medicare’s managed care
plans, which are responsible for providing the full set
of benefits covered by Parts A and B of that program,
Medicaid’s risk-based managed care plans are often not
required to cover certain Medicaid benefits, such as
behavioral health care or long-term care. Medicaid may
cover those “carved-out” services on a fee-for-service basis
or in special managed care arrangements.
Plans that participate in Medicare Advantage submit bids
indicating the per-enrollee payment they are willing to
accept in return for providing all Medicare benefits to an
average Medicare beneficiary enrolling in their plan in
each region where they operate. Medicare makes a
capitated payment to each participating plan (a single
payment that covers all care within a specified set of ben-
efits) on the basis of the plan’s bid and an administratively
determined benchmark that varies geographically with
fee-for-service spending per beneficiary.
17
Payments to
Medicare Advantage plans are adjusted for the risk profile
of a plan’s enrollees, which reflects their expected relative
costs (see Box 2).
18
In addition, since 2012, plans that
reach a certain quality threshold (based on a star rating
system) are eligible for bonuses in the form of higher
benchmarks.
Medicaid’s contracts with risk-based managed care plans
vary considerably by state. In most cases, a state either
sets a payment rate for all plans operating in the state or
negotiates a payment rate with each plan individually.
16. Some states’ Medicaid programs use primary care case manage-
ment or prepaid health plans as an alternative form of managed
care. Enrollment in primary care case management is counted as
part of fee-for-service Medicaid in this analysis because states
continue to pay providers for each claim, in addition to making a
fixed payment for management activities. Enrollment in prepaid
health plans is also counted under fee-for-service Medicaid
because those plans cover only a limited set of services.
17. Before 2012, Medicare Advantage benchmarks were, on average,
roughly 13 percent higher than average FFS spending. The
Affordable Care Act changed how benchmarks are set beginning
in 2012, with those changes phased in until 2017; at that point,
the new benchmarks will range from 95 percent to 115 percent of
average FFS spending. See Medicare Payment Advisory Commis-
sion, Report to the Congress: Medicare Payment Policy (March
2011), http://medpac.gov/documents/Mar11_EntireReport.pdf
(6 MB).
18. That payment system does not apply to two types of Medicare
Advantage plans: PACE (Program of All-Inclusive Care for the
Elderly) and cost plans, neither of which submits bids. PACE
programs are paid on the basis of risk scores, benchmarks, and an
adjustment for the frailty of their enrollees, and cost plans are paid
on the basis of submitted claims (that is, they are reimbursed
according to the costs they incur in delivering covered benefits).
The benchmark revisions enacted in the ACA do not apply to
PACE programs; thus, if those revisions were fully implemented
for Medicare Advantage plans in 2013 (rather than being phased
in until 2017), benchmarks for PACE programs would be about
8 percent to 18 percent higher than benchmarks for Medicare
Advantage plans, depending on the county. (That difference does
not include quality adjustments for Medicare Advantage plans
through the star rating system.)
[* Value corrected]

12 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Continued
Those rates must be certified by the Centers for Medicare
& Medicaid Services (CMS) as being adequate to cover
average expected costs for the covered population
(including administrative expenses).
Dual-Eligible Beneficiaries’ Enrollment in
Different Service-Delivery Systems
The mix of fee-for-service care and risk-based managed
care used in both Medicare and Medicaid means that
full duals receive covered benefits through an array of
fee-for-service and capitated payment systems, with
major differences both within and among states. Those
differences reflect several factors: variation in the avail-
ability of Medicare and Medicaid managed care plans;
state policies governing whether full duals can enroll in
risk-based managed care for Medicaid and, if so, whether
enrollment is mandatory or voluntary; states’ use of mul-
tiple waivers and authority for demonstration projects
Box 2.
Adjusting Medicare’s Payments for the Health Risks of Beneficiaries
Health care costs vary substantially among Medicare
beneficiaries. Some of that variation comes from
unexpected medical problems, and some reflects dif-
ferences in the prevalence of chronic conditions. The
process by which beneficiaries choose health care
plans in Medicare is unlikely to spread costs evenly
among plans—both because some plans may attract
sicker beneficiaries than others do and because unex-
pected health events may not be distributed evenly
among different plans’ enrollees. Thus, to help ensure
that some Medicare Advantage (managed care) and
Medicare Part D (prescription drug) plans do not end
up leaving the market because they had to cover a
more expensive population—and, similarly, to make
sure that plans are not overpaid for a less expensive
population—Medicare adjusts payments to plans
to account for the likely health care costs of their
enrollees.
To do that, the Centers for Medicare & Medicaid
Services (CMS) has developed two models: the Hier-
archical Condition Category (CMS-HCC) model,
which is used for Medicare Advantage plans, and the
Prescription Drug Hierarchical Condition Category
(CMS-RxHCC) model, which is used for Part D
plans. The output of each model is a risk score for
every beneficiary that depends on the person’s set of
diagnoses and demographic characteristics. Payments
to plans are adjusted with those risk scores to account
for differences in expected spending for different
beneficiaries.
CMS calculates the parameters of the models using a
statistical analysis that relates spending by Parts A and
B of Medicare (for the CMS-HCC model) or Part D
(for the CMS-RxHCC model) for a given year to a
set of characteristics of fee-for-service or Part D bene-
ficiaries from the previous year. Those characteristics
include demographic indicators (such as age group
and sex), indicators of chronic conditions, and a set
of interaction terms. The interaction terms involve
either two demographic indicators, two chronic con-
ditions, or a chronic condition and a demographic
indicator. The CMS-HCC model currently includes
70 chronic conditions—called hierarchical condition
categories—and the CMS-RxHCC model includes
78 prescription drug hierarchical condition catego-
ries.
1
As the name implies, some categories include
1. For more information about the two models, see Gregory C.
Pope and others, Evaluation of the CMS-HCC Risk Adjust-
ment Model: Final Report (prepared by RTI International for
the Centers for Medicare & Medicaid Services, March 2011),
http://go.usa.gov/TpRV (pdf, 1 MB); Centers for Medicare
& Medicaid Services, “Advance Notice of Methodological
Changes for Calendar Year (CY) 2014 for Medicare Advan-
tage (MA) Capitation Rates, Part C and Part D Payment
Policies and 2014 Call Letter” (February 15, 2013),
http://go.usa.gov/TuQG (pdf, 1 MB), and “Advance Notice
of Methodological Changes for Calendar Year (CY) 2011
for Medicare Advantage (MA) Capitation Rates, Part C and
Part D Payment Policies and 2011 Call Letter” (February 19,
2010), http://go.usa.gov/TuUR (pdf, 813 KB); John Robst,
Jesse M. Levy, and Melvin J. Ingber, “Diagnosis-Based Risk
Adjustment for Medicare Prescription Drug Plan Payments,”
Health Care Financing Review, vol. 28, no. 4 (Summer 2007),
pp. 15–30, http://go.usa.gov/TpRH (pdf, 483 KB).

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 13
CBO
granted by Medicare and Medicaid to integrate the deliv-
ery of services under the two programs; and the capacity
of local Medicaid managed care plans to manage the ser-
vices needed by full duals in addition to those used by
other subsets of the Medicaid population.
In 2009, nearly three-quarters of full duals received
Medicare and Medicaid services through the FFS delivery
systems in both programs (see Table 4). Only about
5 percent were enrolled in risk-based managed care plans
for both programs (which may have been the same or
separate plans) or in PACE (Program of All-Inclusive
Care for the Elderly) programs, which receive a combined
Medicare and Medicaid payment for full duals who need
the degree of care typically provided in nursing homes.
19
The other 21 percent of full duals were enrolled in either
risk-based Medicaid plans with FFS Medicare, or FFS
Medicaid with Medicare managed care.
Box 2. Continued
Adjusting Medicare’s Payments for the Health Risks of Beneficiaries
a hierarchy of conditions, and only the most severe
condition in the hierarchy that a beneficiary has
is included in the risk score. (For instance, if someone
has been diagnosed with acute myocardial infarction
as well as with unstable angina or other acute
ischemic heart disease, only the more severe condi-
tion, acute myocardial infarction, is included for that
person.) Other conditions are not part of a hierarchy
and are not subject to being overridden by another
condition. The relationships between spending and
the various condition categories, demographic char-
acteristics, and interactions used in the model are
recalibrated periodically as the relationship between
chronic conditions and fee-for-service spending
changes over time.
For Medicare Advantage, CMS maintains two ver-
sions of the CMS-HCC model: the “community”
version described above and an “institutional” version
that is intended to reflect the fact that nursing facili-
ties often take on some of the care delivered by
medical professionals. The institutional CMS-HCC
model includes the same set of hierarchical condition
categories, demographic characteristics, and inter-
actions as the community model, but it uses different
model parameters, which are based on the relation-
ships between those characteristics and spending that
are calculated for institutionalized beneficiaries. In
addition, because CMS does not have diagnostic
information for new Medicare enrollees, it uses “new
enrollee” models to create Medicare Advantage and
Part D risk scores that reflect the relationship
between spending and demographic characteristics
(but not chronic conditions).
Besides their use in adjusting payments, medical risk
scores are also helpful tools for characterizing the
average health status of various groups. For example,
in 2009, the average risk score from the community
version of the CMS-HCC model was 1.534 for full
dual-eligible beneficiaries, compared with 0.985 for
nondual Medicare beneficiaries (see Table 1 on
page 5). That difference suggests that full duals are in
much worse health, on average, than other Medicare
beneficiaries.
1
1. CMS normalizes risk scores such that the average assigned
risk score for the fee-for-service Medicare population is 1.0.
In this analysis, the Congressional Budget Office reports risk
scores only from the community version of the CMS-HCC
model in order to use a common framework for comparing
the health status of various groups. In addition, the average
risk scores reported here include Medicare Advantage enroll-
ees as well as enrollees in fee-for-service Medicare. For those
reasons, the risk scores reported here do not average 1.0.
19. PACE programs receive capitated payments from Medicare and
Medicaid that are combined into a single payment to provide all
services for both programs—including LTSS—to beneficiaries
who are age 55 or older and not living in institutions at the time
of enrollment but who meet the standards of need for institutional
care. PACE programs also receive a frailty adjustment from Medi-
care to account for the additional service needs of their enrollees.
Less than 1 percent of full duals nationwide are enrolled in PACE
programs. For more details, see Dana B. Mukamel and others,
“Program Characteristics and Enrollees’ Outcomes in the Program
of All-Inclusive Care for the Elderly (PACE),” Milbank Quarterly,
vol. 85, no. 3 (September 2007), pp. 499–531, http://dx.doi.org/
10.1111/j.1468-0009.2007.00497.x; and California HealthCare
Foundation, Aging in PACE: The Case for California Expansion
(July 2010), http://tinyurl.com/clbqrm8.

14 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Table 4.
Demographic Characteristics of and Spending for Full Dual-Eligible Beneficiaries,
by Type of Medicare and Medicaid Payment System Enrolled in, 2009
Source: Congressional Budget Office.
Notes: Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive
benefits from both programs. “Full duals” qualify for full benefits from both programs.
PACE = Program of All-Inclusive Care for the Elderly; * = between zero and 0.5 percent; N.A. = not available; LTSS = long-term
services and supports.
a. For Medicaid, includes only people enrolled in comprehensive risk-based managed care plans. Medicaid beneficiaries enrolled in other
types of managed care, such as primary care case management, or enrolled in service-specific managed care plans that are not
comprehensive are counted with the fee-for-service Medicaid population.
b. The Centers for Medicare & Medicaid Services calculates a risk score for each Medicare enrollee on the basis of his or her medical
diagnoses and demographic characteristics. The scores are used to adjust Medicare’s payments to managed care plans to reflect
enrollees’ expected costs for Parts A and B of Medicare.
c. Use of LTSS is based on fee-for-service claims; thus, any use of LTSS within Medicare Advantage or Medicaid managed care (including
PACE programs) is not included in this table.
d. Includes federal and state spending for Medicaid but excludes Medicaid payments for Medicare premiums.
e. The Medicare program consists of three parts: Hospital Insurance (Part A), Medical Insurance (Part B), and prescription drug coverage
(Part D). Medicare Part C (known as Medicare Advantage) specifies the rules under which private health care plans can assume
responsibility for, and be compensated for, providing benefits covered under Parts A, B, and D.
73 9 12 5 *
Distribution by Age (Percent)
Nonelderly (Under age 65) 42 51 29 38 3
Elderly (Age 65 or older) 58 49 71 62 97
38 56 31 42 14
43 32 47 43 46
15 10 18 12 30
32429
** 1*1
1.5 1.3 1.6 1.4 2.1
17 6 15 7 14
49 28 38 23 N.A.
31 20 31 27 42
16,700 9,900 11,200 10,200 30,600
Parts A and B 14,500 11,500 16,700 13,000 20,700
Part D 4,000 3,000 3,300 3,100 3,100
1,800 3,000 6,400 ** 7,400 12,600
18,200 11,700 19,100 17,500 54,400
86,300 61,600 75,100 ** 58,300 97,200
Medicare and
(Medicare
Than PACE
Plans Other
Managed Care
PACE
Medicaid Managed Care
Medicaid
Fee-for-Service
Advantage) and
Managed Care
Medicare
Fee-for-Service
Managed Care
a
Medicaid
Medicare and
Fee-for-Service
Percentage of Full Duals
Medicaid
Medicare and
Distribution by Number of Chronic Conditions (Percent)
None
1–2
Medicaid
d
10th percentile
50th percentile
90th percentile
Medicare
e
Various Points in the Distribution of Spending (Dollars)
Total Medicaid and Medicare Spending per Beneficiary at
Percentage Receiving Any LTSS
c
Percentage With a Mental Illness
3–4
5–6
More than 6
Average Community Medical Risk Score
b
Percentage Who Are Institutionalized
Average Spending per Beneficiary, by Program (Dollars)
[** Value corrected]

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 15
CBO
Considerable diversity exists within those groups as well.
For example, some of the full duals enrolled in FFS
Medicaid have their care managed by a primary care case
manager, a medical home (a team-based care delivery
model, led by a primary care provider, that coordinates
care), or another type of care manager, with those differ-
ent approaches sometimes used in the same state. In other
cases, full duals receive most of their Medicaid-covered
services from FFS providers but are enrolled in managed
care plans for specific services, such as dental care or
behavioral health care. Similarly, states’ Medicaid man-
aged care programs may include carve-outs (separate
payment arrangements) for behavioral health care,
long-term care, or other services—in many cases, when
the Medicaid managed care plans in a state have little
experience with those services. In Medicare, full duals
may be enrolled in managed care through regular Medi-
care Advantage plans or special-needs plans. For full duals
who are enrolled in both Medicare and Medicaid risk-
based plans, the degree of integration between those
plans—administrative, financial, and care-related—also
varies from state to state.
20
Among the many possible combinations of Medicare and
Medicaid payment systems, full duals enrolled in risk-
based managed care for Medicaid—and either FFS or
managed care for Medicare—are less likely than other full
duals to be institutionalized or to receive long-term ser-
vices and supports (see Table 4).
21
Those enrolled in risk-
based Medicaid managed care and FFS Medicare also
have the lowest average risk score, the lowest prevalence
of chronic conditions, and the lowest combined spending
by Medicare and Medicaid among full duals (a median of
$11,700 in 2009). In contrast, spending was highest for
the small share of full duals enrolled in PACE programs
(a median of $54,400). That group, which receives LTSS
by definition, has the highest average risk score, reflecting
a population with a large burden of chronic disease—
40 percent have at least three chronic conditions, and
more than 40 percent have mental illness.
Such variation in spending and health status reflects, at
least in part, the differences between the beneficiary pop-
ulations enrolled in managed care and FFS. Enrollment
in Medicare Advantage is voluntary—as is enrollment in
Medicaid managed care for many dual-eligible beneficia-
ries—and healthier beneficiaries appear to be more likely
to enroll in managed care plans. Recent evidence about
whether risk scores fully adjust for that difference is
mixed.
22
(Special-needs plans and PACE programs are
exceptions, in that their eligibility requirements cause
them to enroll less healthy beneficiaries.) Because differ-
ences in spending are related to differences in health
status that also affect beneficiaries’ enrollment decisions,
it is difficult to tell from the relationship between spend-
ing and health status alone whether one managed care
arrangement would produce lower costs for a given
beneficiary than another arrangement would.
Efforts to Integrate Medicare’s and
Medicaid’s Financing and Coordinate
Care for Dual-Eligible Beneficiaries
To reduce spending on dual-eligible beneficiaries and
improve the quality of their care, federal and state policy-
makers are focusing on two interrelated approaches:
integrating Medicare’s and Medicaid’s financing for those
beneficiaries, and having some entity coordinate the care
that dual-eligible beneficiaries receive from multiple
health care providers. Coordinating care effectively may
be difficult as long as payers and providers face different
financial incentives under the two programs, but aligning
20. See Kaiser Commission on Medicaid and the Uninsured, Medic-
aid and Managed Care: Key Data, Trends, and Issues (Kaiser Family
Foundation, February 2012), www.kff.org/medicaid/8046.cfm.
21. LTSS use is based on fee-for-service claims; thus, any use of LTSS
within Medicare Advantage or Medicaid managed care (including
PACE programs) is not captured in Table 4. However, Medicaid
provides most LTSS, and those services are often carved out of
Medicaid’s managed care contracts (and are usually provided by
fee-for-service Medicaid).
22. See, for example, Sherry Glied and others, Selection, Marketing,
and Medicaid Managed Care, Working Paper 6164 (National
Bureau of Economic Research, September 1997), www.nber.org/
papers/w6164; Jason Brown and others, How Does Risk Selection
Respond to Risk Adjustment? Evidence From the Medicare Advantage
Program, Working Paper 16977 (National Bureau of Economic
Research, April 2011), www.nber.org/papers/w16977; Joseph P.
Newhouse and others, “Steps to Reduce Favorable Risk Selection
in Medicare Advantage Largely Succeeded, Boding Well for
Health Insurance Exchanges,” Health Affairs, vol. 31, no. 12
(December 2012), pp. 2618–2628, http://dx.doi.org/10.1377/
hlthaff.2012.0345; J. Michael McWilliams, John Hsu, and Joseph
P. Newhouse, “New Risk-Adjustment System Was Associated
With Reduced Favorable Selection in Medicare Advantage,”
Health Affairs, vol. 31, no. 12 (December 2012), pp. 2630–2640,
http://dx.doi.org/10.1377/hlthaff.2011.1344; and Gerald F.
Riley, “Impact of Continued Biased Disenrollment from the
Medicare Advantage Program to Fee-For-Service,” Medicare and
Medicaid Research Review, vol. 2, no. 4 (2012), pp. E1–E16,
http://go.usa.gov/b8M4.

16 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
those incentives alone is no guarantee that such coordi-
nation will occur. Successfully implementing both
approaches could improve the quality of care and
decrease spending by reducing duplication of services,
minimizing the extent to which beneficiaries are shifted
between acute and institutional sites of care, and reducing
the provision of conflicting services that may result in
complications and other health problems.
For full duals, although Medicare primarily covers acute
care and Medicaid primarily covers long-term services
and supports, the distinction between the two programs
is not absolute: Some of the services covered by Medicare
and Medicaid overlap, and some may be substituted for
one another. In addition, payment rates for such services
are generally lower in Medicaid than in Medicare. Those
factors—combined with the fact that Medicare is funded
entirely by the federal government whereas Medicaid is
funded partly by the states—create conflicting financial
incentives under the two programs for the federal and
state governments and for health care providers.
23
States, for example, do not have a strong financial
incentive to reduce spending on acute care for full duals
because that spending is largely covered by the federal
government through Medicare (although the states,
through Medicaid, generally contribute to paying dual-
eligible beneficiaries’ cost-sharing amounts for acute
care).
24
Moreover, both programs cover home health care
services, so states may try to maximize the share of such
services paid by Medicare. In addition, Medicare’s pay-
ment rates for postacute care in skilled nursing facilities
(SNFs) are typically higher than Medicaid’s payment
rates to nursing homes. Therefore, nursing homes that
are certified SNFs have a financial incentive for their full-
dual residents to be hospitalized for at least three days,
thereby triggering eligibility for up to 100 days of SNF
benefits provided by Medicare, for which the nursing
home can receive the higher Medicare payment rates. As a
result, nursing home residents may be inappropriately
hospitalized, again shifting financial responsibility from
Medicaid to Medicare.
Recently, both the federal government and state Medicaid
programs have been looking for ways to integrate Medi-
care’s and Medicaid’s financing and service delivery for
dual-eligible beneficiaries to lessen financial incentives
that can lead to inappropriate care—or care in inappro-
priate settings—and thereby reduce unnecessary program
spending. But full duals with multiple chronic or
disabling conditions might continue to be at risk for
lower-quality, fragmented care, stemming from a lack of
communication between health care providers that better
financial integration might not solve. Poor coordination
among providers can cause full duals to receive duplica-
tive services, contradictory advice or procedures for a par-
ticular diagnosis, or poor transitions between settings for
care, all of which reduce the overall quality of their care.
As a result, state Medicaid programs and the federal gov-
ernment are also looking to design care coordination
programs—either in conjunction with or separate from
efforts to align financial incentives—using a variety of
options available under current law.
25
Many care coordi-
nation initiatives include elements to improve the flow of
information among providers, assist patients in making
the transition from one care setting to another (such as
when they are discharged from a hospital to another facil-
ity or to their home), and help patients gain access to
medical and social support services.
26
Spurred in part by new opportunities authorized under
the Affordable Care Act, care and financing arrangements
for full duals are changing rapidly, and more changes are
likely in the next few years. Governments are trying a
variety of approaches, including establishing multipayer
programs, requiring Medicare’s special-needs plans for
dual-eligible beneficiaries to have contracts with state
Medicaid agencies, integrating behavioral and physical
23. See David C. Grabowski, “Medicare and Medicaid: Conflicting
Incentives for Long-Term Care,” Milbank Quarterly, vol. 85, no. 4
(December 2007), pp. 579–610, http://dx.doi.org/10.1111/
j.1468-0009.2007.00502.x.
24. State Medicaid programs are not required to cover the full amount
of Medicare cost sharing for services provided to dual-eligible
beneficiaries if Medicaid’s payment rate is lower than Medicare’s
payment rate. Therefore, in states that do not opt to cover the full
cost-sharing amount, overall payments to providers on behalf of
dual-eligible beneficiaries are lower than payments on behalf of
other Medicare beneficiaries. That difference may make providers
less willing to accept dual-eligible beneficiaries as new patients,
thus limiting those patients’ access to care.
25. See, for example, Michelle Herman and Brianna Ensslin,
Innovations in Integration: State Approaches to Improving Care for
Medicare-Medicaid Enrollees (Center for Health Care Strategies,
February 2013), http://tinyurl.com/d87c5oq.
26. See Lyle Nelson, Lessons From Medicare’s Demonstration
Projects on Disease Management and Care Coordination,
Working Paper 2012-01 (Congressional Budget Office, January
2012), www.cbo.gov/publication/42924.

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 17
CBO
health care, offering managed long-term services and
supports, and taking part in financial alignment
demonstration projects authorized under the ACA.
Multipayer Medical-Home Programs
Various efforts are under way in the Medicaid program at
the federal and state levels to establish so-called medical
homes to improve the quality and coordination of health
care services for Medicaid beneficiaries. (A medical home
is not a facility but a model for delivering health care in
which a team of health care professionals, led by a pri-
mary care provider, coordinates the care given to an
individual or family.) In recent years, nearly half of state
Medicaid programs have launched initiatives to create
patient-centered medical homes.
27
As part of those
efforts, some states and the federal government are devel-
oping multipayer initiatives that include private insurers,
Medicare, and Medicaid.
CMS recently announced a three-year initiative—the
Multi-payer Advanced Primary Care Practice demonstra-
tion—in which Medicare will participate in some states’
multipayer medical-home programs (see Table 5).
28
Eight
states are taking part in that demonstration, under which
Medicare, Medicaid, and private insurers will generally
pay a per-beneficiary care management fee or a bonus to
advanced primary care practices (another name for
patient-centered medical homes). The fee or bonus is
supposed to cover the cost of services, such as coordinat-
ing care among providers, that are intended to improve
the quality and efficiency of care for chronically ill
patients.
Fully Integrated Dual-Eligible Special-Needs Plans
Another approach for coordinating the care received by
full duals and aligning the financial incentives created by
Medicare and Medicaid involves a subset of Medicare
Advantage special-needs plans for dual-eligible beneficia-
ries (or D-SNPs) known as fully integrated dual-eligible
special-needs plans (FIDE-SNPs). As of 2013, regular
D-SNPs are generally required to have risk-based con-
tracts with states to provide, at a minimum, a subset of
services covered by Medicaid, in addition to providing
Medicare services.
29
FIDE-SNPs, by comparison, are gen-
erally required to have risk-based contracts with states to
provide most or all Medicaid services for dual-eligible
beneficiaries—including long-term care—as well as pro-
viding Medicare services.
30
Capitated payments from
Medicare to a FIDE-SNP may be adjusted (beyond the
adjustment for health risks) to reflect the frailty of the
plan’s enrollees, if the average disability level of those
enrollees is similar to that of participants in PACE pro-
grams.
31
Participation in FIDE-SNPs is low thus far: In
January 2013, those integrated plans were operating in
only seven states and enrolled less than 5 percent of the
1.6 million dual-eligible beneficiaries who were enrolled
in SNPs nationwide.
32
Initiatives to Integrate Behavioral and
Physical Health Care
More than half of the dual-eligible beneficiaries who have
chronic physical conditions, many of whom are full
duals, also have diagnoses of mental illness. Those benefi-
ciaries tend to have high health care costs.
33
For example,
CBO found that in 2009, total Medicare and Medicaid
spending was much higher for full duals who had a
mental illness and at least one other chronic condition
than for other full duals ($48,200, on average, versus
$28,600). States are experimenting with a variety of
27. See Mary Takach, “About Half of the States Are Implementing
Patient-Centered Medical Homes for Their Medicaid Popu-
lations,” Health Affairs, vol. 31, no. 11 (November 2012),
pp. 2432–2440, http://dx.doi.org/10.1377/hlthaff.2012.0447.
28. See Centers for Medicare & Medicaid Services, “Multi-payer
Advanced Primary Care Practice (MAPCP) Demonstration Fact
Sheet” (April 5, 2012), http://go.usa.gov/Tw93 (pdf, 22 KB).
29. See Centers for Medicare & Medicaid Services, Announcement of
Calendar Year (CY) 2013 Medicare Advantage Capitation Rates and
Medicare Advantage and Part D Payment Policies and Final Call
Letter (April 2, 2012), p. 114, http://go.usa.gov/TwT3.
30. Originally, FIDE-SNPs were responsible for providing all primary,
acute, and long-term care services for dual-eligible beneficiaries.
CMS modified that requirement in April 2012 to limit the
required coverage of nursing facility services to a minimum of
six months. See Medicare Payment Advisory Commission, Report
to the Congress: Medicare and the Health Care Delivery System
(June 2012), Chapter 3, p. 82, www.medpac.gov/documents/
Jun12_EntireReport.pdf (2 MB).
31. Memorandum from Cheri Rice, Director, Medicare Plan Payment
Group, Centers for Medicare & Medicaid Services, to Medicare
Advantage plans, November 2, 2012, http://tinyurl.com/d9rxuks
(pdf, 96 KB).
32. See Centers for Medicare & Medicaid Services, SNP Compre-
hensive Report (January 2013), http://go.usa.gov/Tw5H.
33. See Richard G. Kronick, Melanie Bella, and Todd P. Gilmer, The
Faces of Medicaid III: Refining the Portrait of People With Multiple
Chronic Conditions (Center for Health Care Strategies, October
2009), p. 8, http://tinyurl.com/n47r9qx.

18 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Table 5.
Selected Federal and State Initiatives to Integrate Medicare’s and Medicaid’s
Financing and Coordinate Care for Dual-Eligible Beneficiaries
Continued
models to address the particularly fragmented care that
those beneficiaries typically receive.
34
Provisions in the ACA promote the coordination of
behavioral and physical health care for Medicaid
beneficiaries, building on the initiatives to establish
patient-centered medical homes that many states have
implemented in recent years. Most providers in those
initiatives receive a monthly per capita payment for coor-
dinating the care of their Medicaid patients.
35
The ACA
created a new state plan option, through which states can
receive a 90 percent federal matching rate for two years
for “health homes”—a type of medical home that serves
Medicaid beneficiaries with a particular set of chronic
Initiative
Financial Alignment
Components Care Coordination Components States Involved
Multi-payer
Advanced Primary
Care Practice
(Three-year
demonstration
launched by CMS)
None Advanced primary care practices are
paid a care management fee by the
relevant payer (Medicare, Medicaid,
or a private health plan) to establish
relationships with beneficiaries and
coordinate their care from a wide
range of providers. Fees and
payments vary among payers, but
some fraction of Medicaid,
Medicare, and private insurers must
participate in the demonstration.
Maine, Michigan, Minnesota,
New York, North Carolina,
Pennsylvania, Rhode Island,
Vermont
Fully Integrated
Dual-Eligible
Special-Needs
Plans (FIDE-SNPs)
in Medicare
Advantage
FIDE-SNPs contract with both
Medicare and Medicaid to provide
an integrated set of services to dual-
eligible beneficiaries
Until 2012, FIDE-SNPs were
required to cover the full range of
acute and long-term care services;
in April 2012, CMS revised the
requirement so that plans must
cover at least six months of nursing
facility services
Arizona, California, Hawaii,
Massachusetts, Minnesota,
New York, Wisconsin
Health Home State
Plan Option
None The initiatives require coordination
between providers of behavioral
health care (such as mental health
and substance abuse services) and
other providers of acute care
Alabama, Idaho, Iowa, Maine,
Missouri, New York, North Carolina,
Ohio, Oregon, Rhode Island,
Wisconsin
Managed Long-
Term Services and
Supports for
Medicaid and
Dual-Eligible
Beneficiaries
Range from none to full integration
with Medicare’s payments
Limited coordination of care in some
states, but many states require
some degree of coordination with
Medicare providers or Medicare
Advantage plans
As of July 2012, Arizona,
California, Delaware, Florida,
Hawaii, Massachusetts, Michigan,
Minnesota, New Mexico, New York,
North Carolina, Pennsylvania,
Tennessee, Texas, Wisconsin,
Washington
34. See Allison Hamblin, James Verdier, and Melanie Au, State
Options for Integrating Physical and Behavioral Health Care,
Technical Assistance Brief (Integrated Care Resource Center,
October 2011), http://tinyurl.com/cbeehyq (pdf, 298 KB).
35. See Mary Takach, “About Half of the States Are Implementing
Patient-Centered Medical Homes for Their Medicaid Popu-
lations,” Health Affairs, vol. 31, no. 11 (November 2012),
pp. 2432–2440, http://dx.doi.org/10.1377/hlthaff.2012.0447.
JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 19
CBO
Table 5. Continued
Selected Federal and State Initiatives to Integrate Medicare’s and Medicaid’s
Financing and Coordinate Care for Dual-Eligible Beneficiaries
Source: Congressional Budget Office.
a. New York, Oklahoma, and Washington proposed testing both models in their demonstration projects. For the purposes of this table, those
states are listed without comment under the model that would be used for the larger population. They are also listed under the other
model with a parenthetical note describing the smaller population to which that model would apply.
conditions and addresses their behavioral and physical
health care needs as well as their needs for institutional
or community-based long-term care. As of May 2013,
11 states had received approval from CMS for their
Health Home State Plan Amendments, and others had
received planning grants.
36
Managed Long-Term Services and Supports
Only a small fraction of full duals who receive long-term
services and supports from Medicaid do so through
managed care programs, but the number of states
with such programs is growing rapidly.
37
In July 2012,
16 states had some kind of managed LTSS program; that
number is expected to rise to 26 states by 2014.
38
That
expansion is accompanied by growth in the number of
health care organizations and plans that are capable of
managing such services. Managed LTSS programs vary
in several ways, including the extent to which they
coordinate with Medicare, the comprehensiveness of the
services they provide, the size of the geographic area they
serve within a state, and whether enrollment is manda-
tory or voluntary for eligible Medicaid beneficiaries.
Initiative
Financial Alignment
Components Care Coordination Components States Involved
Financial
Alignment
Demonstration
Projects
a
Capitation
model
Medicare’s and Medicaid’s payments
to a managed care organization are
combined
Combined payments and limited
service carve-outs are intended to
facilitate coordinated care because
the managed care organization is
responsible for delivering most or all
services
Arizona, California, Hawaii, Idaho,
Illinois, Massachusetts, Michigan,
Minnesota, New Mexico, New York,
Ohio, Oklahoma ( for school of
community medicine and PACE-like
initiatives), Oregon, Rhode Island,
South Carolina, Tennessee, Texas,
Vermont, Virginia, Washington,
Wisconsin
Managed fee-
for-service
model
Medicare’s and Medicaid’s payments
are not combined into a single
stream, but states receive
reimbursements for demonstrated
Medicare savings
States are responsible for ensuring
that beneficiaries receive integrated
access to all acute and long-term
care services covered by Medicare
and Medicaid
Colorado, Connecticut, Iowa,
Missouri, New York (for beneficia-
ries with several chronic condi-
tions), North Carolina, Oklahoma,
Washington (for high-cost and
high-risk beneficiaries)
36. See Centers for Medicare & Medicaid Services, “Approved Health
Home State Plan Amendments” (accessed May 23, 2013),
http://go.usa.gov/bYqm; and Charles Townley and Mary Takach,
Developing and Implementing the Section 2703 Health Home State
Option: State Strategies to Address Key Issues (National Academy for
State Health Policy, July 2012), http://tinyurl.com/c23mzw6.
37. The information in this and the next paragraph is based on Paul
Saucier and others, The Growth of Managed Long-Term Services
and Supports (MLTSS) Programs: A 2012 Update (report prepared
by Truven Health Analytics for the Centers for Medicare & Med-
icaid Services, July 2012), http://go.usa.gov/Tf5B (pdf, 3 MB).
38. Since July 2012, two additional states have implemented managed
LTSS programs, according to CMS. See Centers for Medicare &
Medicaid Services, “Summary—Essential Elements of Managed
Long Term Services and Supports Programs” (accessed June 3,
2013), http://go.usa.gov/bYcx (pdf, 179 KB).

20 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Some managed LTSS programs incorporate both finan-
cial alignment and care coordination components. For
example, 5 of the 16 states that had programs in 2012
require plans to offer options that are fully integrated
with the Medicare program. In those cases, plans are
responsible for covering both Medicaid and Medicare ser-
vices, aligning the financial incentives that exist under the
two programs and providing an incentive to coordinate
care among providers. An additional 7 of those 16 states
require some coordination with Medicare; 2 of the 7
require that a managed LTSS plan also offer an SNP so
the plan can provide Medicare services as well as Medic-
aid services. Such plans may not align financial incentives
because the funding streams for Medicaid and Medicare
are not integrated, but they may promote better coordi-
nation of care among providers. The other 4 states with
managed LTSS programs do not require any coordination
with Medicare. Those programs are also the most likely
to exclude a major service, such as prescription drugs or
primary care, and therefore may have minimal coordina-
tion among providers even within Medicaid. Going for-
ward, most states that are setting up new managed LTSS
programs intend to require full capitation for Medicaid
and Medicare services, as 5 states do now.
Financial Alignment Demonstration Projects
The Affordable Care Act established two organizations
within CMS that have the potential to affect the financ-
ing and quality of care received by full duals. The
Medicare-Medicaid Coordination Office is specifically
responsible for improving the coordination of care for
dual-eligible beneficiaries. The Center for Medicare and
Medicaid Innovation (CMMI) has a broader mission: to
develop innovative payment and service-delivery models
for Medicare and Medicaid. It operates under new
authority created by the ACA to waive the two programs’
rules for the purposes of conducting demonstrations.
Under that authority, CMMI may test and evaluate
methods to modify care and financing—including full
integration of all Medicare and Medicaid funds—for
full duals.
39
In 2011, using the combined authority of those two
organizations, CMS awarded design grants of up to
$1 million each to 15 states to develop approaches to
coordinate care for all of the Medicare and Medicaid
benefits that full duals receive. Later in 2011, CMS
announced a three-year demonstration in which states
can experiment with different ways of integrating Medi-
care’s and Medicaid’s financing for full duals. Twenty-six
states (including the 15 that received the earlier planning
grants) applied to take part in the demonstration, and the
first state projects are scheduled to begin this summer.
The demonstration allows for a notable change to the
regulations that govern Medicare and Medicaid: Benefi-
ciaries may be enrolled automatically in managed care
plans for Medicare benefits (a process known as passive
enrollment), provided that they have the option of
disenrolling or switching plans.
40
The demonstration projects will operate in two phases.
During the first phase, which CMS has stated will last for
three years, CMMI will assess a project’s effects on spend-
ing for Medicare and Medicaid and on the quality of care
that dual-eligible beneficiaries receive.
41
On the basis of
the findings from phase one, a state may be allowed in
phase two to expand its project to cover more or all of its
full-dual population—provided that the Chief Actuary of
CMS certifies that such an expansion would not increase
net spending for Medicare and Medicaid and that the
Secretary of Health and Human Services (HHS) certifies
that the program would provide the same or better qual-
ity of care than beneficiaries receive now.
Most of the states that applied for the financial alignment
demonstration said they wanted to eventually include
all full duals in the geographic areas covered by their
projects, although a few states planned to limit their dem-
onstration projects to subsets of the full-dual population.
39. See MaryBeth Musumeci, State Demonstrations to Integrate Care
and Align Financing for Dual Eligible Beneficiaries: A Review of
the 26 Proposals Submitted to CMS (Kaiser Family Foundation,
October 2012), http://tinyurl.com/a9u9ucr.
40. CMS is encouraging states to allow participating beneficiaries to
choose up front whether to enroll in a managed care plan rather
than enrolling them automatically, particularly in the first year of
the demonstration. See Mindy Yochelson, “CMS Encourages Use
of Opt-In Enrollment by States Involved in Dual Eligibles
Demo,” Health Care Daily Report, Bloomberg BNA (May 8,
2013).
41. See the letter from Cindy Mann, Director, Center for Medicaid,
CHIP, and Survey & Certification, and Melanie Bella, Director,
Medicare-Medicaid Coordination Office, to state Medicaid
directors, July 8, 2011, http://go.usa.gov/Th3F (pdf, 209 KB).

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 21
CBO
A majority of applicants also said that they planned to
implement part or all of their initiatives on a statewide
basis, in some cases using a phased-in approach. If all of
the proposed projects were approved for the populations
included in the applications, the first phase of the dem-
onstration would include about 3 million of the nation’s
7 million full duals. However, CMS has set an enrollment
target of 1 million to 2 million beneficiaries.
42
Capitation Versus Managed Fee for Service. CMS’s dem-
onstration is designed to test two alternative models of
financial alignment: capitation and managed fee-for-
service, which are described below.
43
Of the 26 states that
applied to participate in the demonstration, 18 proposed
capitated models, 5 opted for managed FFS, and
3 proposed testing both approaches.
The capitation model will employ three-way contracts
between CMS, a state, and participating health plans to
cover the full range of Medicare and Medicaid benefits.
44
CMS and the state will jointly set payment rates for the
health plans at levels that are estimated to result in lower
combined Medicare and Medicaid spending for the plans’
enrollees than would occur under current law. CMS has
asserted that payment rates must provide projected up-
front savings for both the federal and state governments
and that without such projected savings, demonstration
projects will not go forward.
Besides allowing full duals to be automatically enrolled in
managed care plans, the demonstration’s guidelines also
suggest that each state establish standards for the quality
of care and for measuring improvement in plans’ perfor-
mance with regard to full duals, rather than try to follow
Medicaid’s and Medicare’s differing guidelines simultane-
ously. Health care plans that take part in the demonstra-
tion (which are distinct from other Medicare Advantage
or Medicaid managed care plans that may be offered by
the same plan sponsors) will be ineligible for quality-
related bonuses under Medicare Advantage’s star rating
system. However, some portion of a plan’s combined
Medicare-Medicaid payment will be withheld during
phase one of the demonstration, and the plan can earn
that portion by meeting certain quality objectives. Many
states’ proposals for the demonstration projects also
include “shared savings” provisions, in which states and
the federal government share the savings if the costs of a
demonstration project are below the agreed-on baseline
of what would have been spent on the demonstration
population in the absence of the project.
Under the managed fee-for-service model, CMS will
allow states to build on their existing FFS delivery
systems. States will be held accountable for ensuring
effective coordination of the services that Medicare and
Medicaid cover for full duals. Specifically, states will be
responsible for ensuring that beneficiaries receive inte-
grated access to all acute care and long-term care services
covered by the two programs, possibly using accountable
care organizations and Medicaid health homes.
45
States
will make the up-front investment in developing
approaches to coordinate care, but CMS will make retro-
active payments to states that can demonstrate savings
to Medicare (net of any increase in federal Medicaid
costs), so long as the care provided meets certain quality
standards.
46
Progress of the Demonstration Projects to Date. The
timing of the financial alignment demonstration projects
is uncertain because the approval process has progressed
more slowly than CMS anticipated. In their applications,
2 states proposed starting their projects in 2012;
13 states, in 2013; and 11 states, in 2014. As of May
2013, however, only 6 states (California, Illinois,
Massachusetts, Ohio, Virginia, and Washington) had
memorandums of understanding from CMS approving
their plans for the demonstration projects, with planned
implementation dates ranging from July 2013 to early
42. Ibid.
43. Ibid.
44. See the memorandum from Melanie Bella, Director, Medicare-
Medicaid Coordination Office, and Jonathan Blum, Director,
Center for Medicare, to organizations interested in offering capi-
tated financial alignment demonstration plans in interested states,
January 25, 2012, http://go.usa.gov/T7Ww (pdf, 333 KB).
45. Accountable care organizations are groups of doctors, hospitals,
and other health care providers who join together to provide
coordinated care to a set of patients and who agree to be held
accountable for the quality and total cost of those patients’ care.
46. See the letter from Cindy Mann, Director, Center for Medicaid,
CHIP, and Survey & Certification, and Melanie Bella, Director,
Medicare-Medicaid Coordination Office, to state Medicaid
directors, July 8, 2011, http://go.usa.gov/Th3F (pdf, 209 KB).

22 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
2014.
47
Furthermore, a recent survey indicates that some
states that have applied for the demonstration but do not
yet have approved memorandums of understanding with
CMS expect to postpone their implementation dates.
48
In addition, as of May 2013, 7 of the 26 applicants
(Arizona, Hawaii, Minnesota, New Mexico, Oregon,
Tennessee, and Wisconsin) had withdrawn from the
financial alignment demonstration or were working on
alternative demonstration projects to coordinate care
for full duals. One of the main reasons that states have
given for dropping out of the financial alignment
demonstration is that they already have a robust market
for Medicare Advantage plans that serve full duals, and
payments to those plans would be likely to decline under
the financial alignment demonstration. Lower payments
could cause plans to drop out of the Medicare Advantage
program, leaving fewer options for beneficiaries.
49
Moreover, New York, one of the states planning to test
both models, has announced that it is dropping the
managed fee-for-service portion of its demonstration
because of the difficulty of trying to manage two new
programs simultaneously. The state is opting instead
to focus its efforts on the capitated portion of the
demonstration.
50
Differences Between Applicant and Nonapplicant States.
States’ decisions about whether to participate in the dem-
onstration—and if so, what model of financial alignment
to adopt—probably depended in part on their experience
with managed care, the characteristics of their full-dual
population, and concerns about making costly changes to
their health care programs that could prove temporary.
Those same factors may also play a role in the success of
the demonstration projects.
Existing managed care programs in Medicare and
Medicaid may be useful building blocks for states that
participate in the demonstration, so the amount and type
of managed care infrastructure in a state probably played
a role in the state’s decision about whether to apply for
the demonstration. For example, states with relatively
high rates of enrollment in Medicare Advantage plans
and Medicaid managed care plans (more than 20 percent
of eligible beneficiaries) were more likely to apply for the
capitated portion of the demonstration than other states
were (see Figure 2). Further differences in managed care
enrollment are also apparent between states that applied
to test a capitation model and those that applied to test a
managed fee-for-service model. For instance, applicants
that proposed a managed FFS model had lower participa-
tion in Medicare managed care plans in 2009 (including
regular Medicare Advantage plans and SNPs) by all
Medicare beneficiaries and by full duals than did appli-
cants proposing capitation or states that did not apply
(see Figure 3). Applicants that proposed a managed FFS
model also had lower enrollment in comprehensive Med-
icaid managed care plans by their full duals—and higher
enrollment in primary care case management programs—
than other states did. Although the three groups of states
(those primarily testing capitation, those primarily testing
managed FFS, and states that did not apply for the dem-
onstration) differed in various ways in 2009, their Medic-
aid programs shared some notable features: considerable
47. The memorandum of understanding with the State of Washing-
ton, one of the three states proposing to test both a managed FFS
and a capitation model, relates only to the managed FFS compo-
nent of its proposal. Washington and Massachusetts initially
planned to begin their demonstration projects in April 2013 but
later agreed to delay implementation until July 2013. See Kaiser
Commission on Medicaid and the Uninsured, Financial Align-
ment Demonstrations for Dual Eligible Beneficiaries Compared:
California, Illinois, Massachusetts, Ohio, and Washington (May
2013), http://tinyurl.com/ldd9fbe (pdf, 739 KB). California ini-
tially planned to begin its demonstration project in October 2013
but has agreed to delay implementation until at least January
2014. See David Gorn, “‘So Many Moving Parts’ to Fit Together,”
California Healthline (May 10, 2013), http://tinyurl.com/
cgpunxl.
48. See Vernon K. Smith and others, Medicaid Today; Preparing
for Tomorrow—A Look at State Medicaid Program Spending,
Enrollment, and Policy Trends (Kaiser Family Foundation,
October 2012), http://tinyurl.com/cmw82pq.
49. Michelle Herman and Brianna Ensslin, Innovations in Integration:
State Approaches to Improving Care for Medicare-Medicaid
Enrollees (Center for Health Care Strategies, February 2013),
http://tinyurl.com/d87c5oq; Michelle Herman and Brianna
Ensslin, personal communications, March 14, 2013; letter from
Janice K. Brewer, Governor of Arizona, and Thomas J. Betlach,
Director, Arizona Health Care Cost Containment System, to
Melanie Bella, Director, Medicare-Medicaid Coordination Office,
April 10, 2013, http://tinyurl.com/bpe8odx (pdf, 24 KB); and
letter from Julie B. Weinberg, Director, New Mexico Human Ser-
vices Department, to Melanie Bella, Director, Medicare-Medicaid
Coordination Office, August 17, 2012, http://tinyurl.com/
qa7pvwt (pdf, 41 KB).
50. See the letter from Gregory S. Allen, Director, Division of
Program Development and Management, New York Office of
Health Insurance Programs, to Melanie Bella, Director,
Medicare-Medicaid Coordination Office, March 21, 2013,
http://go.usa.gov/Thc9 (pdf, 87 KB).
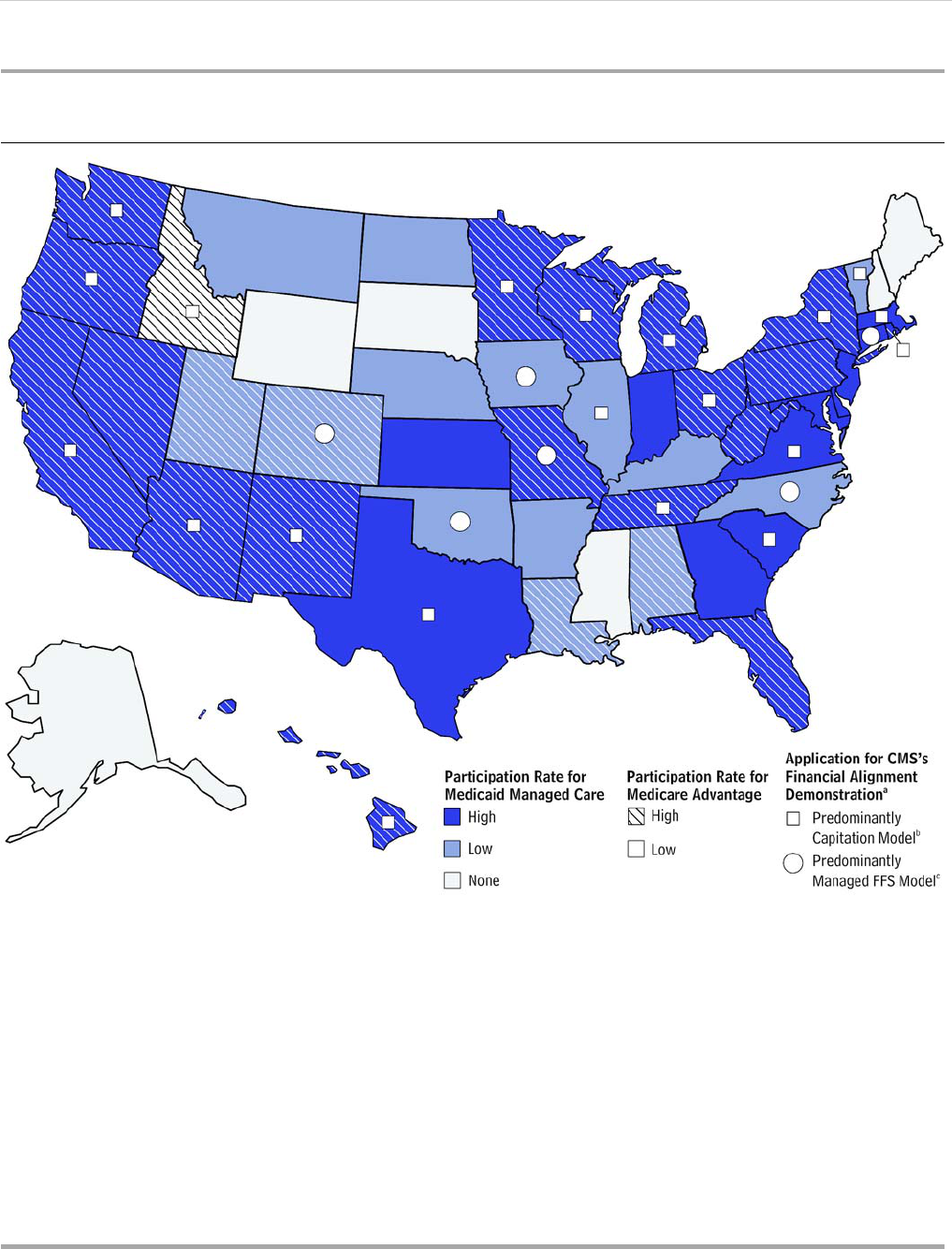
JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 23
CBO
Figure 2.
States’ Participation Rates for Medicare and Medicaid Managed Care and
Application for CMS’s Financial Alignment Demonstration
Source: Congressional Budget Office.
Notes: “High” participation means that more than 20 percent of a state’s eligible beneficiaries were enrolled in Medicare Advantage plans or
Medicaid managed care plans; “low” participation means that 20 percent or fewer eligible beneficiaries were enrolled.
CMS = Centers for Medicare & Medicaid Services; FFS = fee for service.
a. Three states (New York, Oklahoma, and Washington) proposed testing both the capitation model and the managed FFS model in their
demonstration projects. For the purposes of this figure, those states are categorized by whichever model would be used for the larger
population of beneficiaries.
b. Capitation involves making a single payment, generally to a managed care plan, to cover all care that beneficiaries receive within a
specified set of benefits. The capitation model in the demonstration projects will employ three-way contracts between CMS, a state, and
participating health plans to cover the full range of Medicare and Medicaid benefits. CMS and the state will jointly set payment rates for
the health plans at levels that are estimated to result in lower combined Medicare and Medicaid spending for the plans’ enrollees than
would occur under current law.
c. Fee for service involves paying health care providers a fee for each covered service performed for beneficiaries. The managed FFS model
in the demonstration projects will require states to ensure that beneficiaries receive integrated access to all acute care and long-term care
services covered by Medicare and Medicaid, building on the states’ existing FFS delivery systems.

24 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Figure 3.
Enrollment in Medicare and Medicaid Managed Care, 2009, by
States’ Application Status in CMS’s Financial Alignment Demonstration
(Percent)
Source: Congressional Budget Office.
Notes: Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive
benefits from both programs. “Full duals” qualify for full benefits from both programs.
CMS = Centers for Medicare & Medicaid Services; FFS = fee for service; HMO = health maintenance organization.
a. For a list of applicant states, see Table 5. Three states (New York, Oklahoma, and Washington) proposed testing both the capitation model
and the managed FFS model in their demonstration projects. For the purposes of this figure, those states are categorized by whichever
model would be used for the larger population of beneficiaries.
b. Capitation involves making a single payment, generally to a managed care plan, to cover all care that beneficiaries receive within a
specified set of benefits. The capitation model in the demonstration projects will employ three-way contracts between CMS, a state, and
participating health plans to cover the full range of Medicare and Medicaid benefits. CMS and the state will jointly set payment rates for
the health plans at levels that are estimated to result in lower combined Medicare and Medicaid spending for the plans’ enrollees than
would occur under current law.
c. Fee for service involves paying health care providers a fee for each covered service performed for beneficiaries. The managed FFS model
in the demonstration projects will require states to ensure that beneficiaries receive integrated access to all acute care and long-term care
services covered by Medicare and Medicaid, building on the states’ existing FFS delivery systems.
Medicare
Advantage
Special-Needs
Plan
0
10
20
30
Predominantly Capitation Model Predominantly Managed FFS Model States That Have Not Applied
Comprehensive
HMO
Behavioral
Health Care
HMO
Long-Term
Care
HMO
Primary Care
Case
Management
0
10
20
30
Medicare
Advantage
Special-Needs
Plan
0
10
20
30
Comprehensive
HMO
Behavioral
Health Care
HMO
Long-Term
Care
HMO
Primary Care
Case
Management
0
10
20
30
Share of Medicare Beneficiaries in Various Medicare Managed Care Delivery Systems
Share of Medicaid Beneficiaries in Various Medicaid Managed Care Delivery Systems
All Medicare
Beneficiaries
All Aged, Blind, or Disabled
Medicaid Beneficiaries
Full Duals
Full Duals
States That Have Applied for CMS's Financial
Alignment Demonstration, by Model of Alignment Proposed
b
c
a
*
*
*
*
*
*
*
*
*
*
*
*
[* Value corrected]

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 25
CBO
use of managed behavioral health care—indicating that
some states were handling those services separately from
other services and contracting with specialized plans for
them—and almost no managed long-term care.
Full duals’ health status and use of services differ between
applicant and nonapplicant states, which suggests that
differences in health characteristics may also have fac-
tored into states’ decisionmaking process. Although
nonelderly full duals in the three groups of states appear
to be similar in terms of prevalence of chronic conditions,
medical risk scores, and use of long-term services and
supports, more variation exists among the 60 percent of
full duals who are age 65 or older (see Table 6).
51
On
average, elderly full duals in the states that applied to test
a capitation model appear to be somewhat healthier—as
measured by the prevalence of chronic conditions and
dementia and by average risk scores—than those in the
other two groups of states. They also appear less likely to
be using LTSS, both in institutions and overall.
The possibility that the changes allowed under a state’s
financial alignment demonstration project might be
rescinded after three years—if the project is not approved
for phase two—may have discouraged some states from
applying. In particular, some states may have chosen not
to participate because adapting their managed care or care
management infrastructure to fit the demonstration’s
options, or creating new infrastructure altogether, would
require a significant investment that might not generate a
return.
Challenges Facing Efforts to Integrate
Financing and Coordinate Care
The federal government and the states face a host of
obstacles in trying to integrate Medicare’s and Medicaid’s
financing and service delivery for dual-eligible beneficia-
ries, mitigate the current financial incentives that can lead
to inappropriate care, and thereby reduce unnecessary
spending and improve the quality of care. Those chal-
lenges—which are partly reflected in the many different
federal and state efforts that are under way—include the
following:
Because Medicare and Medicaid evolved indepen-
dently over time, they differ in their program rules,
payment rates, appeals procedures, and monitoring
and reporting requirements. Those differences,
combined with the two programs’ complexity, make
integration difficult.
52
Even when fully integrated plans are established, states
lack effective mechanisms to ensure enough enroll-
ment for those plans to operate effectively. Several
analysts have pointed out the difficulties of enrolling
dual-eligible beneficiaries in a single plan for all Medi-
care and Medicaid services as long as enrollment in
Medicare managed care is voluntary.
53
Enrollment is
voluntary because policymakers have decided, at least
to date, that giving Medicare beneficiaries a choice
about whether to participate in a managed care plan is
more important than other considerations.
54
Indeed,
some analysts have noted the importance of choice in
decisions about participation and plan selection to
ensure that frail beneficiaries with multiple needs can
maintain their current care arrangements.
55
As a result,
observers have emphasized the importance of gaining
support and cooperation from stakeholders early in
the process when developing an integrated care initia-
tive that may involve managed LTSS or restrictions on
choice
.
56
51. Although Table 6 shows a total of almost 5 million full duals in
the states that applied to test a capitation model, the demonstra-
tion proposals from all of the applicant states cover only 3 million
full duals in all. That difference occurs because some states are
proposing to target subsets of their full-dual population.
52. See Barbara Coulter Edwards and others, Integrating Medicare and
Medicaid: State Experience With Dual Eligible Medicare Advantage
Special Needs Plans (AARP Public Policy Institute, September
2009), http://tinyurl.com/74cystl (pdf, 716 KB).
53. Ibid.; and Melanie Bella and Lindsay Palmer, Encouraging Inte-
grated Care for Dual Eligibles (Center for Health Care Strategies,
July 2009), http://tinyurl.com/ldzv8mf (pdf, 169 KB).
54. Both beneficiaries and providers may be resistant to the idea of
required enrollment in managed care plans because it might
restrict beneficiaries’ choice of providers or reduce payment rates
or the volume of services provided.
55. See, for example, Patricia Neuman and others, “Dx for a Careful
Approach to Moving Dual-Eligible Beneficiaries Into Managed
Care Plans,” Health Affairs, vol. 31, no. 6 (June 2012), pp. 1186–
1194, http://dx.doi.org/10.1377/hlthaff.2012.0160.
56. See, for example, Harris Meyer, “The Coming Experiments in
Integrating and Coordinating Care for ‘Dual Eligibles,’”
Health Affairs, vol. 31, no. 6 (June 2012), pp. 1151–1155,
http://dx.doi.org/10.1377/hlthaff.2012.0505; Patricia Neuman
and others, “Dx for a Careful Approach to Moving Dual-Eligible
Beneficiaries Into Managed Care Plans,” Health Affairs, vol. 31,
no. 6 (June 2012), pp. 1186–1194, http://dx.doi.org/10.1377/
hlthaff.2012.0160; and Paul Saucier and Wendy Fox-Grage,
Medicaid Managed Long-Term Care (AARP Public Policy
Institute, November 2005), http://assets.aarp.org/rgcenter/il/
ib79_mmltc.pdf (191 KB).

26 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Table 6.
Demographic Characteristics of Full Dual-Eligible Beneficiaries, 2009, in States
That Have Applied or Not Applied for CMS’s Financial Alignment Demonstration
Source: Congressional Budget Office.
Notes: Dual-eligible beneficiaries are people who are enrolled in Medicare and Medicaid at the same time and who are eligible to receive
benefits from both programs. “Full duals” qualify for full benefits from both programs.
CMS = Centers for Medicare & Medicaid Services.
a. For a list of applicant states, see Table 5. Three states (New York, Oklahoma, and Washington) proposed testing both the capitation model
and the managed fee-for-service model in their demonstration projects. For the purposes of this table, those states are categorized by
whichever model would be used for the larger population of beneficiaries.
b. Capitation involves making a single payment, generally to a managed care plan, to cover all care that beneficiaries receive within a
specified set of benefits. The capitation model in the demonstration projects will employ three-way contracts between CMS, a state, and
participating health plans to cover the full range of Medicare and Medicaid benefits. CMS and the state will jointly set payment rates for
the health plans at levels that are estimated to result in lower combined Medicare and Medicaid spending for the plans’ enrollees than
would occur under current law.
c. Fee for service involves paying health care providers a fee for each covered service performed for beneficiaries. The managed fee-for-
service model in the demonstration projects will require states to ensure that beneficiaries receive integrated access to all acute care and
long-term care services covered by Medicare and Medicaid, building on the states’ existing fee-for-service delivery systems.
d. CMS calculates a risk score for each Medicare enrollee on the basis of his or her medical diagnoses and demographic characteristics. The
scores are used to adjust Medicare’s payments to managed care plans to reflect enrollees’ expected costs for Parts A and B of Medicare.
1.7 0.3 0.8
Percentage with various characteristics
Diagnosed with three or more chronic conditions 8 9 8
Institutionalized 4 4 4
Receiving any long-term services and supports 31 36 29
Diagnosed with a mental illness 37 39 36
Diagnosed with dementia 3 3 3
1.2 1.2 1.2
Full Duals Age 65 or Older
Number of beneficiaries (Millions) 2.7 0.4 1.1
Percentage with various characteristics
Diagnosed with three or more chronic conditions 24 27 29
Institutionalized 19 29 30
Receiving any long-term services and supports 51 65 * 56
Diagnosed with a mental illness 23 29 29
Diagnosed with dementia 20 25 26
1.7 1.8 1.9Average community medical risk score
d
Average community medical risk score
d
Number of beneficiaries (Millions)
Capitation Model
b
Fee-for-Service Model
c
Have Not Applied
Model of Alignment Proposed
a
Financial Alignment Demonstration, by
States That Have Applied for CMS's
Predominantly Managed States ThatPredominantly
Full Duals Under Age 65
[* Value corrected]

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 27
CBO
Most managed care plans provide comprehensive
acute and postacute care services. However, many of
those plans lack experience in coordinating care and
bearing financial risk for people who need LTSS or
behavioral health services and in integrating such
services with acute care.
57
Historically, states have not had timely access to the
Medicare data they need to coordinate the services
that dual-eligible beneficiaries receive. In 2011, the
National Association of Medicaid Directors urged that
more efforts be made to minimize the operational
barriers that states faced in getting Medicare data,
standardize practices for obtaining those data, and
highlight successful experiences by states in obtaining
and using the data.
58
CMS’s new Medicare-Medicaid
Coordination Office (MMCO) is working to improve
states’ access to Medicare data for dual-eligible
beneficiaries.
59
Establishing an integrated managed care plan
involves up-front costs, such as expenses to create
new contracts with SNPs or to develop infrastructure
and hire personnel for new PACE programs or other,
similar initiatives.
60
(The Medicare Payment Advisory
Commission recently reported that PACE programs
have estimated start-up costs of $2 million to
$3 million per site.)
Some of those challenges have been evident in the slower-
than-expected pace at which CMS’s financial alignment
demonstration has gotten under way. Participants have
reported various obstacles to implementing their
demonstration projects:
Although creating the MMCO may have improved
some coordination, operational partitions still exist
between Medicare and Medicaid within CMS.
States have continued to experience difficulties and
delays in obtaining and analyzing Medicare data from
CMS.
Uncertainties remain about how shared-savings
arrangements will function in both the capitated and
fee-for-service models.
States have wrestled with how to implement coordi-
nation and integration of care, especially during the
transition to the new system.
61
States have struggled to educate potential enrollees in
their demonstration projects about the new program.
For example, to prepare for full implementation, CMS
conducted field tests in Massachusetts of the first
phases of the passive enrollment process. Those
tests were largely unsuccessful. Beneficiaries reported
that they were confused by the letters they received
explaining the program, which raises questions about
whether many full duals will be able to make an
informed choice about how their care is delivered,
as CMS’s guidelines require.
62
Evaluating the success of the financial alignment demon-
stration projects will also be challenging. Effective
evaluation is a critical component of any demonstration
for Medicare or Medicaid, and evaluating the impact of
the financial alignment demonstration projects on spend-
ing and quality of care may prove difficult, especially if
evaluation is not built into the design. In many partici-
pating states, identifying an appropriate comparison
population in the state will be hard because a large share
57. See Suzanne Gore and Alice Lind, Developing an Integrated Care
Program for Dual Eligibles Using Special Needs Plans (Center for
Health Care Strategies, January 2011), www.chcs.org/usr_doc/
CHCS_SNP_Brief_Jan_2011.pdf (138 KB).
58. National Association of Medicaid Directors, Advancing
Medicare and Medicaid Integration: Policy and Operational
Challenges for State Access to Medicare Data (October 2011),
http://medicaiddirectors.org/node/190.
59. See Medicare-Medicaid Coordination Office, “Medicare Data for
Dual Eligibles for States” (February 20, 2013), http://go.usa.gov/
bxj5.
60. Barbara Coulter Edwards and others, Integrating Medicare and
Medicaid: State Experience With Dual Eligible Medicare Advantage
Special Needs Plans (AARP Public Policy Institute, September
2009), http://tinyurl.com/74cystl (pdf, 716 KB); and Medicare
Payment Advisory Commission, Report to the Congress: Medicare
and the Health Care Delivery System (June 2012), p. 75,
www.medpac.gov/documents/Jun12_EntireReport.pdf (2 MB).
61. See Vernon K. Smith and others, Medicaid Today; Preparing for
Tomorrow—A Look at State Medicaid Program Spending, Enroll-
ment, and Policy Trends (Kaiser Family Foundation, October
2012), http://tinyurl.com/cmw82pq; and Kathleen Gifford and
others, A Focus Group With Medicaid Directors: As FY 2012 Ends,
Looking Toward FY 2013 (Kaiser Family Foundation, June 2012),
http://tinyurl.com/p3e2tg7.
62. See John Reichard, “Bella Says Many States in Giant Duals Demo
Wouldn’t Join Until 2014,” CQ HealthBeat (October 17, 2012).

28 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
of the dual-eligible population will be taking part in the
demonstration. Moreover, if enrollment in the program is
voluntary, or if beneficiaries are permitted to opt out, the
people who participate may differ from the people who
do not in important ways that affect their outcomes.
Using other states as the basis for comparison also
presents problems, given the wide range of initiatives
targeting dual-eligible beneficiaries that both applicant
and nonapplicant states are undertaking.
Individual states may aim to compare spending and
health outcomes for dual-eligible beneficiaries before and
after implementation of the demonstration projects. The
findings from such comparisons may not indicate the
effects of the projects, however, if other changes in the
delivery of health care are occurring at the same time.
Moreover, the findings may not translate to other states
because of the different systems of care that exist among
the states and the potential for other differences between
applicant and nonapplicant states.
Potential Legislative Actions Targeting
Dual-Eligible Beneficiaries and Their
Impact on the Federal Budget
Given the complex and expensive health care needs of
dual-eligible beneficiaries, federal lawmakers may opt to
take further steps to identify and implement strategies
intended to produce savings for the Medicare and
Medicaid programs, improve the quality of care that
dual-eligible beneficiaries receive, or both. Potential legis-
lative actions could range from incremental changes in
Medicare and Medicaid to broader structural reforms that
would combine all benefits for full duals within a single
new program or delivery system. However, if policy
changes that affect dual-eligible beneficiaries are enacted
before the current financial alignment demonstration
projects are well under way, lawmakers may risk missing
the chance to apply any lessons learned from those
efforts.
Anticipating how legislative actions aimed at dual-eligible
beneficiaries would be likely to affect the federal budget is
difficult—in large part because considerable uncertainty
exists about what spending for dual-eligible beneficiaries
will be in coming years even without new legislation. For
example, how many demonstration projects will be con-
ducted under current law, how large will they be, and
how will states and health plans implement specific
features of those projects once negotiations between
CMS and states are finalized? Moreover, how might the
lessons from the demonstration projects be applied to
other beneficiaries and other states under current law? In
particular, the Secretary of HHS and the states have con-
siderable flexibility to experiment with other ways of
delivering health care to full duals, and the Secretary
has the authority to broadly expand any demonstration
projects conducted by CMMI that, on the basis of evalu-
ation, are not expected to compromise the quality of care,
limit the provision of Medicare or Medicaid benefits, or
increase spending.
Potential Legislative Changes
Incremental changes to existing programs might be
intended to make it easier for more states to develop
financial alignment and care coordination initiatives or to
help states that have such initiatives build on them. In
addition, federal lawmakers could encourage new initia-
tives by alleviating some of the impediments that may
have kept states from participating in the financial align-
ment demonstration or from making other changes in
their arrangements for dual-eligible beneficiaries. For
example, legislation could give states funding to create
the infrastructure necessary to restructure their systems
for delivering health care to dual-eligible beneficiaries.
Legislation could also extend the minimum period for
phase one of the financial alignment demonstration, in
case some states see three years as too short an approval
period to justify making the considerable structural
changes needed to improve the delivery of care for dual-
eligible beneficiaries. In addition, if the Secretary of HHS
does not use his or her authority in the future to expand
particular components of CMMI initiatives that law-
makers consider promising, lawmakers could make those
components a requirement for the Medicaid or Medicare
program.
Alternatively, federal lawmakers could enact larger struc-
tural changes that would move full duals into a single,
integrated delivery system that would provide all of the
benefits for which they now qualify under Medicare and
Medicaid. Having one payment system for the care
provided to dual-eligible beneficiaries would eliminate
conflicts between the financial incentives created by
Medicare and Medicaid and would reduce the incentives
for cost shifting that exist under the current, bifurcated
system, which can cause full duals to receive
inappropriate care.

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 29
CBO
Two broad approaches to creating a financially integrated
system could be considered. One approach would be to
continue to involve Medicare and Medicaid but to align
the two programs’ financial incentives by contracting
with a third party—such as a managed care plan,
accountable care organization, or Medicaid health
home—to provide or coordinate care in exchange for a
blended payment rate that covered services from both
programs. Federal lawmakers could specify the amount of
the blended payment rate in statute, or they could allow
CMS to negotiate with the states to determine the
blended payment rate for the set of services covered by
the third party.
A second approach would be for federal lawmakers to
give either Medicaid or Medicare sole financial responsi-
bility for full duals. Several ways of doing that have been
proposed in the past:
63
One alternative would be for the federal government
to give states a block grant to provide all care for full
duals. The block grant could be designed to convert
the federal share of Medicaid and Medicare payments
for full duals into a single payment to each state, as
earlier legislation did with funding for welfare. The
size of the block grant could be adjusted annually for
inflation using various economic indexes. That alter-
native would make federal spending on dual-eligible
beneficiaries more predictable. It would also eliminate
the federal subsidy for each additional dollar that
states spend on care for those beneficiaries, thus giving
states greater incentive to find more cost-effective ways
to care for them. However, the block grant might shift
some of the cost burden and financial risk to states,
which could prompt states to cut optional Medicaid
benefits or other state-funded programs to pay for the
cost of providing care to dual-eligible beneficiaries.
Another alternative would be to construct a “swap”
that would shift responsibility for a portion of the
costs of Medicaid, education, or other programs to the
states in exchange for having Medicare take over all
responsibility for full duals. That alternative might
include creating a single set of federal eligibility crite-
ria for full duals, in contrast to the existing variation in
states’ eligibility requirements for Medicaid. That
approach would also require the Congress or CMS to
set payment rates for Medicare for services that the
program currently does not cover or covers to only a
limited degree, such as long-term care in nursing
facilities and a range of home- and community-based
services. It is unclear whether making the federal gov-
ernment fully responsible for full duals would reduce
overall spending for their care relative to current levels.
On average, Medicare pays higher rates to physicians
for acute care services than Medicaid does, so it is
possible that new Medicare payment rates for services
that the program does not cover now would be higher
than the rates that Medicaid pays for those services.
64
In addition, because state Medicaid programs vary
widely in how they set eligibility criteria for long-term
care and in the tools they use to assess whether people
meet those criteria, an important policy question
would be whether such variation should continue or
whether a single national eligibility standard and a
common assessment tool should apply in all states.
Allowing the variation to continue would raise fairness
issues among the states, but adopting a uniform stan-
dard and common assessment tool could create com-
plex transition issues because some beneficiaries
already receiving long-term care services through
Medicaid might not meet the new criteria.
Although the various approaches described above would
work expressly to align financing for dual-eligible benefi-
ciaries, they would not necessarily improve how medical
care for those beneficiaries is managed or coordinated.
Other explicit care management policies or initiatives
might be required to achieve that goal.
Possible Budgetary Effects of Legislative Changes
To estimate how a proposed change in law would alter
federal spending, analysts must first estimate the path
that spending would be likely to take under current law.
That task, which is often challenging, is especially diffi-
cult now with spending for dual-eligible beneficiaries
63. See Medicare Payment Advisory Commission, Report to the
Congress: Aligning Incentives in Medicare (June 2010), Chapter 5,
p. 142, www.medpac.gov/chapters/Jun10_Ch05.pdf (485 KB);
Brian Bruen and John Holahan, Shifting the Cost of Dual Eligibles:
Implications for States and the Federal Government (Kaiser Family
Foundation, November 2003), http://tinyurl.com/o9x8jzz; and
John Holahan, Dawn M. Miller, and David Rousseau, Rethinking
Medicaid’s Financing Role for Medicare Enrollees, Publication 7862
(Kaiser Family Foundation, February 2009), http://tinyurl.com/
plt6ub6.
64. See Stephen Zuckerman and Dana Goin, How Much Will Medic-
aid Physician Fees for Primary Care Rise in 2013? Evidence From a
2012 Survey of Medicaid Physician Fees (Kaiser Family Foundation,
December 2012), http://tinyurl.com/qbjx62w.

30 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
because of the rapid changes that are going on in many
states. In particular, with the first financial alignment
demonstration projects not yet launched and the features
of many others still being developed, it is difficult to pro-
ject the budgetary effects of new proposals relative to, and
in the midst of, that shifting environment. As the demon-
stration projects begin and progress, further information
about them will allow for improved analysis.
Nevertheless, the fact that the Secretary of HHS has the
ability to make broad changes at his or her discretion will
continue to be a significant source of uncertainty, because
the Secretary may or may not choose to expand demon-
stration projects within or among states. In addition, esti-
mating the federal budgetary effects of the demonstration
projects with any degree of precision would require data
on their spending—including for care management fees
and other costs beyond the provision of medical ser-
vices—which will not be available for some time, as well
as reasonable estimates of what spending for the affected
population would have been without the demonstration.
Despite the many challenges of predicting the budgetary
impact of new proposals aimed at dual-eligible beneficia-
ries, savings might be achieved by combining care
coordination and integration of financing with cuts to
Medicare’s, Medicaid’s, or both programs’ payments for
dual-eligible beneficiaries relative to the amounts paid
for their care under current law. That is, potential federal
savings from policies that would alter payment rates for
health care providers would depend importantly on the
difference between the federal payments made to the
entity in charge of managing care for dual-eligible bene-
ficiaries and projected federal payments for the same
services under current law. Beyond that difference in
payments, whether additional federal savings would
occur would depend on how payments were structured. If
managing entities received a capitated rate, they might be
able to operate efficiently and reduce spending below that
rate—but such efficiencies would not translate into fur-
ther savings for the federal budget unless contracts or the
rate-setting process allowed the government to recoup
some of those additional savings over time. In the case of
block grants to the states, the savings generated from such
grants would depend largely on how much smaller the
block grants were than current-law payments to the states
for the affected population.
The federal savings that could be achieved through new
proposals for dual-eligible beneficiaries would depend on
numerous other factors as well. For example, a number of
programs have tried to reduce Medicare spending by pro-
viding incentives to coordinate care; although many have
succeeded in reducing hospitalizations, the resulting sav-
ings have generally been too small to offset the cost of the
coordination incentives.
65
More recent evidence, how-
ever, suggests that savings from coordinating care may be
greater for the dual-eligible population.
66
Potential sav-
ings from initiatives to better coordinate care could also
be affected if high-cost or complex services, such as LTSS
and behavioral health, were carved out of new programs.
Such carve-outs would limit the ability of managing enti-
ties to fully coordinate the care of higher-cost beneficia-
ries and would reduce the alignment of incentives among
all providers.
Potential savings would also be affected by enrollment
rules. For example, if enrollment in a financial alignment
or coordinated care initiative was voluntary, the potential
for savings would be more limited than if enrollment was
required. Experience with voluntary enrollment in man-
aged care suggests that healthier beneficiaries might be
more likely than others to choose a voluntary managed
care plan (or to remain in a plan in which they had been
automatically enrolled), leaving higher-cost beneficiaries
in a traditional FFS environment. The behavior of pro-
viders could exacerbate that problem if providers had an
incentive to encourage high-cost users to choose FFS
because of differences in payment rates or because the
providers had been excluded from the managed care
network.
The net budgetary impact of a financial alignment or
coordinated care initiative would also depend on any
initial investments required to redesign the health care
delivery system for the full-dual population. In addition,
any spending for outreach to providers and other stake-
holders might limit an initiative’s potential for savings,
particularly in the short run.
65. See Congressional Budget Office, Lessons From Medicare’s Demon-
stration Projects on Disease Management, Care Coordination, and
Value-Based Payment (January 2012), www.cbo.gov/publication/
42860.
66. See Carrie H. Colla and others, “Spending Differences Associated
With the Medicare Physician Group Practice Demonstration,”
Journal of the American Medical Association, vol. 308, no. 10
(September 2012), pp. 1015–1023, http://dx.doi.org/10.1001/
2012.jama.10812.

CBO
Appendix:
Data Used in This Analysis
The Congressional Budget Office (CBO) compiled
information about dual-eligible beneficiaries from multi-
ple sources for this analysis. The primary underlying data
sets are administrative data from the Medicare and Med-
icaid programs that detail beneficiaries’ use of services
and the programs’ payments to health care providers.
CBO merged those data sets to identify beneficiaries
who were enrolled in both programs. Because Medicare’s
administrative data do not cover payments to private
health care plans, CBO combined information from
several of Medicare’s other files of administrative data to
estimate payments to Part C (Medicare Advantage) and
Part D (prescription drug) plans—and thus to calculate
total spending per beneficiary by Medicare or Medicaid.
In addition, CBO used those data to identify the preva-
lence of various chronic conditions among dual-eligible
beneficiaries. CBO chose to focus on 2009 because that
was the most recent year for which all of the relevant
sources of data were available when the analysis began.
Claims-Based Administrative Files
The Beneficiary Annual Summary File (BASF) contains
aggregated beneficiary-level data for everyone who
receives Medicare benefits. Those data include informa-
tion about beneficiaries’ demographic characteristics, the
number of months they have been enrolled in Parts A and
B of Medicare and in Medicare Advantage, and their
diagnoses of chronic conditions. The BASF also contains
data about beneficiaries’ use of services and various par-
ties’ spending for those services, but only for claims
processed by the Centers for Medicare & Medicaid
Services (CMS)—that is, claims covered by fee-for-
service (FFS) Medicare for benefits under Parts A and B
of the program.
1
Payments to providers are reported
separately by the type of service used (such as inpatient
hospital services, outpatient hospital services, and
physicians’ services). Medicare’s payments and bene-
ficiaries’ cost-sharing responsibilities are also included.
(For most dual-eligible beneficiaries, those cost-sharing
responsibilities are covered by Medicaid rather than by
the beneficiary.)
2
The Medicare Part D Prescription Drug Event file con-
tains detailed information about each prescription filled
by someone enrolled in a Part D plan (whether an inde-
pendent Part D plan or a Medicare Advantage drug plan).
Spending on filled prescriptions is broken down by pay-
ment component (ingredient cost, dispensing fee, or sales
tax), by type of payer (plan, low-income cost-sharing sub-
sidy, beneficiary, or third-party payer), and by whether a
beneficiary is in the catastrophic phase of the Part D
benefit (when the person’s out-of-pocket spending for
prescription drugs has exceeded the so-called catastrophic
threshold, meaning that for the rest of the year, the bene-
ficiary is responsible for only 5 percent of his or her drug
costs). The associated denominator file (which provides
demographic and enrollment data) also includes informa-
tion about the number of months that someone was
enrolled in Part D during a given year.
The Medicaid Statistical Information System (MSIS)
file contains detailed information about payments to
providers for all Medicaid-covered services and about
enrollment in managed care plans. MSIS data include
cost-sharing amounts paid to providers for Medicare-
covered services but do not include payments of Medicare
1. CMS also processes a small subset of claims covered by managed
care organizations.
2. State Medicaid programs are required to cover only the amount of
cost sharing that will bring payments up to Medicaid’s payment
rates rather than up to Medicare’s payment rates, which are
generally higher.

32 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
premiums or disproportionate-share payments to hospi-
tals. Unlike the BASF data, the MSIS data include pay-
ments to managed care plans. (Payments to providers by
managed care plans are excluded, however.) The MSIS
data also include information about whether someone is a
full or partial dual-eligible beneficiary.
The two Medicare data sets report information by calen-
dar years, whereas MSIS data are reported on a fiscal year
basis, so there is some mismatch in timing between the
matched Medicare and Medicaid spending. However,
both data sources contain a full year of data and thus
should still accurately represent annual spending patterns.
CBO receives those administrative files from CMS and
Acumen, a company that processes claims for CMS.
Versions of some of the files may be publicly available
through CMS.
Merging Claims-Based Files for
Medicare and Medicaid
Administrative data for Medicare and Medicaid use dif-
ferent identifiers to uniquely (and anonymously) identify
beneficiaries; that difference creates a complication in
matching those data for beneficiaries enrolled in both
programs. CBO acquired a crosswalk from Acumen that
matches the beneficiary identifiers from the Medicare and
Medicaid data sets for each person who received services
from both programs. The crosswalk also includes a
beneficiary’s state of residence.
Dual-eligible beneficiaries were identified by whether a
person showed up in both programs’ data sets. Matches
were counted only if the person’s sex was the same in both
records and if the dates of birth listed in both places were
within 31 days of each other. If a date of birth was invalid
(missing or chronologically impossible) in one of the two
data sets, matches were done by age and were counted if
ages matched within one year. About 0.25 percent of
matches identified through the crosswalk failed to match
on sex, and 1.5 percent failed to match on date of birth
or age. Thus, a total of 1.8 percent of the matched obser-
vations were dropped for failing to meet one or both
criteria.
Of the observations that remained, roughly 1.5 percent of
the observations in the Medicare data matched more than
one observation in the Medicaid data. If the demographic
characteristics matched, CBO assumed that the multiple
Medicaid observations represented the same person and
aggregated them. Multiple Medicaid observations for the
same person may occur when an enrollee moves and
applies for Medicaid coverage in his or her new location.
Determining Medicare’s
Payments to Plans
Administrative data for Medicare do not include the pro-
gram’s payments to Medicare Advantage plans or Part D
plans. CBO estimated those payments using data from
several sources.
Payments to Medicare Advantage Plans
In most cases, Medicare Advantage plans are paid using
a formula that is based on three factors: a benchmark
amount set at the county or regional level, the bid that a
plan submitted to CMS for providing standard Medicare
benefits to the average beneficiary (one with a risk score
of 1.0), and the risk score for a given individual. If a plan’s
bid is below the applicable benchmark, CMS pays a share
of the risk-adjusted difference to the plan as a rebate to
use for supplemental benefits or for reducing premiums.
3
If a plan’s bid is above the benchmark, beneficiaries pay
the difference between the bid and the benchmark, and
CMS pays the plan the risk-adjusted bid minus the
beneficiary payment.
CMS pays Medicare Advantage plans according to their
total enrollment, using the average risk score for their
enrollees. However, to calculate spending figures per ben-
eficiary, CBO estimated the payments made to Medicare
Advantage plans on behalf of each beneficiary each
month the beneficiary was enrolled, using the following
formulas:
If the plan’s submitted bid was no higher than the
benchmark: Payment per enrolled month = [Bid *
RiskScore] + [0.75 * RiskScore * (Benchmark – Bid)]
If the plan’s submitted bid was higher than the
benchmark: Payment per enrolled month = (Bid *
RiskScore) – (Bid – Benchmark)
3. The Affordable Care Act (ACA) changed the Medicare Advantage
benchmarks and introduced a quality-related bonus payment.
Neither change applies here because these data are from 2009,
before the ACA was implemented.

APPENDIX DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 33
CBO
That estimating method could not be used in three cases:
for the Program of All-Inclusive Care for the Elderly
(PACE), for cost plans, and for payments on behalf of
beneficiaries with end-stage renal disease (ESRD). In
2009, PACE programs did not submit bids to CMS, so
they were paid the risk-adjusted benchmark. Those pay-
ments also incorporated a “frailty adjuster,” which
depended on the number of limitations on activities of
daily living that a beneficiary had, but CBO does not
have access to information about that adjuster. Thus, the
estimates of payments to PACE programs used in this
analysis are likely to underestimate actual payments to
some extent.
Cost plans are a type of Medicare Advantage plan that are
paid on the basis of claims for services provided rather
than receiving a capitated payment. The estimates of per
capita payments to cost plans derived from Medicare’s
administrative data suggest that a substantial share of
those claims are not reported. Thus, to approximate pay-
ments to cost plans, CBO started with the formula for
calculating payments to typical Medicare Advantage
plans and modified it to account for the relative differ-
ence between average per capita payments to cost plans
and average per capita payments to typical Medicare
Advantage plans. Of the roughly 20 percent of dual-
eligible beneficiaries enrolled in Medicare Advantage in
2009, fewer than 2 percent were enrolled in cost plans,
and such plans typically do not cover an enrollee’s entire
use of services. (The remaining claims for those enrollees
are covered by traditional fee-for-service Medicare.)
For Medicare Advantage enrollees with end-stage renal
disease, the county or regional benchmark is replaced
with an ESRD-specific benchmark. Plans are paid that
benchmark for each month that a beneficiary with ESRD
is enrolled. The benchmark is not adjusted further for
risk because it is constructed to include the expected costs
of someone with ESRD.
4
CBO used four sets of data to estimate payments to
Medicare Advantage plans:
Intermediate denominator file. This file, which is not
publicly available, includes monthly data on enroll-
ment in all parts of Medicare. It also identifies which
Medicare Advantage or Part D plan a beneficiary is
enrolled in, if applicable.
Plan-submitted bid file. This file, which is not publicly
available, lists the bids that Medicare Advantage and
Part D plans submit to CMS and related information.
For beneficiaries who are listed as being enrolled in
Medicare Advantage but who do not match plan-
specific bid information, CBO calculated a county-
level enrollment-weighted average bid.
County and regional benchmarks. These files are pub-
licly available on CMS’s website.
5
CBO matched bids
from regional preferred provider organizations to
regional benchmarks and matched bids from all other
Medicare Advantage plans to county benchmarks.
Risk-adjustment data. This file, which is not publicly
available, contains the medical and prescription
drug risk scores that CMS calculates for each person
enrolled in Medicare, regardless of Medicare Advan-
tage or Part D enrollment. The data set also contains
the underlying components used to construct those
risk scores, such as age group, sex, disability status, and
chronic conditions (as identified using diagnostic
records from the previous year). New enrollees are
assigned a risk score on the basis of their demographic
characteristics alone, because diagnostic records are
not available for them. Institutionalized beneficiaries
are assigned a medical risk score that is adjusted for
the fact that they receive some care in a nursing facil-
ity. Because the risk-adjustment model uses older data,
CMS calculates a normalization factor each year to
ensure that the average assigned risk score (for new
enrollees, for the community Hierarchical Condition
Category model, and for the institutional Hierarchical
Condition Category model) for fee-for-service benefi-
ciaries equals 1.0 in each year. The normalization fac-
tor for medical risk scores was 1.030 in 2009. CBO
normalized the assigned medical risk scores using that
factor.
Payments to Medicare Part D Plans
Medicare’s payments to prescription drug plans are all
based on the same formula: The plan-submitted bid is
multiplied by a risk score and a frailty adjuster, as
4. Medicare beneficiaries with ESRD are typically not enrolled in
Medicare Advantage plans, unless they enrolled in such a plan
before being diagnosed with ESRD.
5. See Centers for Medicare & Medicaid Services, “Ratebooks &
Supporting Data” (April 25, 2012), http://go.usa.gov/bx8W.

34 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
applicable. The frailty adjuster equals 1.21 for institu-
tionalized beneficiaries under the age of 65; it equals 1.08
for elderly institutionalized beneficiaries and for people
enrolled in the low-income subsidy program who are not
institutionalized. Dual-eligible beneficiaries are automati-
cally enrolled in the low-income subsidy program and
receive a full premium subsidy if their plan’s bid is below
a certain benchmark. Because the majority of dual-
eligible beneficiaries pay no premium, or a very small
premium, for Part D, CBO makes the simplifying
assumption that CMS pays the full Part D premium for
those beneficiaries.
Payments to plans for nondual Medicare beneficiaries
who are not enrolled in the low-income subsidy program
are reduced by the sum of the Part D premium ($30.36
in 2009) and the difference between the chosen plan’s bid
and the national average bid. CBO assumes that CMS
pays the full Part D premium for nondual Medicare ben-
eficiaries who receive full premium assistance under the
low-income subsidy program.
To estimate Medicare’s payments to Part D plans, CBO
used the intermediate denominator file, the plan-
submitted bid file for Part D, and the risk-adjustment
data described above. In the case of the bid file, CBO
calculated a state-level enrollment-weighted average bid
to assign to beneficiaries who were listed as being enrolled
in Medicare Part D but who did not match plan-specific
bid information.
6
In the case of the risk-adjustment data,
CMS calculates a normalization factor for prescription
drug risk scores (as it does for Medicare Advantage risk
scores) to bring the average score to 1.0. For 2009, the
normalization factor for prescription drug risk scores was
1.085, and CBO adjusted those risk scores accordingly.
Calculating Total Spending and
Spending by Type of Service
In this analysis, CBO reports three program-based spend-
ing totals: for Parts A and B of Medicare, for Part D of
Medicare, and for Medicaid. The first total is the sum of
Medicare’s spending for Hospital Insurance and Medical
Insurance (and payments to Medicare Advantage plans,
as applicable). The second is the sum of Medicare’s
payments to prescription drug plans, low-income cost
sharing for prescription drugs (part of the low-income
subsidy benefit in Part D), and 80 percent of spending in
the catastrophic phase of the Part D benefit (which is
included because the federal government covers 80 per-
cent of catastrophic spending as part of its reinsurance to
plans). The third total is the sum of all Medicaid spend-
ing by service type, including payments to plans, in the
Medicaid Statistical Information System file. Types of
services (as shown in Table 3 on page 10) are categorized
as follows:
7
Acute care
• Inpatient care
• Ambulatory care
– In Medicare, outpatient and physicians’ services
– In Medicaid, services provided by physicians,
clinics, nurse midwives, nurse practitioners, and
other practitioners (such as chiropractors, podia-
trists, psychologists, and optometrists), as well as
outpatient hospital services
• Prescription drugs
• Other acute care
– In Medicare, hospice services, purchases of
durable medical equipment, and payments to
Medicare Advantage plans
– In Medicaid, hospice services, transportation,
therapy (speech/language, occupational, and
physical), targeted case management, services
provided by religious nonmedical health care
institutions, rehabilitation, private-duty nursing,
primary care case management, prepaid health
plans, health maintenance organizations, dental
care, laboratory work, abortion services, and
other services (such as prosthetics and eyeglasses)
Postacute care
• Skilled nursing facility care
• Home health care
6. The choice of a county-level or state-level average is related to
plans’ typical service areas, which are county level for Medicare
Advantage and mostly state level for Part D.
7. CBO followed the categorizations designated in Teresa A.
Coughlin, Timothy Waidmann, and Lokendra Phadera, The
Diversity of Dual Eligible Beneficiaries: An Examination of Services
and Spending for People Eligible for Both Medicaid and Medicare
(Kaiser Family Foundation, April 2012), www.kff.org/medicaid/
7895.cfm.

APPENDIX DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 35
CBO
Long-term care
• Institutional care (Medicaid’s payments to nursing
facilities, to intermediate care facilities for people
with mental retardation, and to institutional
mental health facilities)
• Community-based long-term care (Medicaid’s
payments for personal care and for home- and
community-based services)
Identifying Chronic Conditions
Two data sources contain information about the preva-
lence of chronic conditions among Medicare bene-
ficiaries: The Beneficiary Annual Summary File reports
conditions from the CMS Chronic Conditions Data
Warehouse (CCW), and the risk-adjustment files report
conditions that are included in calculating risk scores.
The CCW is one of the standard sources of data about
the chronic conditions of Medicaid and Medicare bene-
ficiaries, but it is constructed only from fee-for-service
claims and therefore is reliable only for beneficiaries who
were in fee-for-service Medicare throughout the period
covered by the data.
CMS created the CCW and the risk-adjustment models
for different purposes and thus had different motivations
for selecting chronic conditions for the two projects. As a
result, the two data sources contain different, but par-
tially overlapping, lists of conditions. In 2009, the CCW
tracked 20 chronic conditions so that researchers could
follow beneficiaries with certain life-altering medical
conditions. The risk-adjustment models are intended to
identify which beneficiaries are expected to have higher
or lower medical and prescription drug costs so that pay-
ments to plans can be adjusted appropriately. Thus, the
models include a much larger number of conditions that
have been found to affect the cost of medical services
(70 conditions) or the cost of prescription drugs
(84 conditions).
8
Another difference between the two sources is the look-
back period (the number of years of diagnoses used to
determine whether a beneficiary has a condition). The
look-back period in the CCW ranges from one year to
three years, depending on the condition. The risk-
adjustment models include diagnoses only from the
previous year. Both sources rely on the diagnostic infor-
mation listed in the claims for payment that physicians
file with CMS, Medicare Advantage plans, or Part D
plans.
CBO used the 20 conditions listed in the CCW as crite-
ria for selecting conditions from the risk-adjustment
models (see Table A-1). For three of the CCW condi-
tions, CBO was unable to find matching risk-adjustment
conditions. In several other cases, the related risk-
adjustment conditions overlap imperfectly with the
CCW conditions. In many cases, a condition is defined
more narrowly for the risk-adjustment models than for
the CCW. That difference is also apparent when compar-
ing the prevalence of chronic conditions in the two data
sets. Among fee-for-service beneficiaries for whom
chronic conditions are listed in both data sets, the vari-
ables used in the risk-adjustment models identify more
beneficiaries with no chronic conditions and fewer bene-
ficiaries with three or more chronic conditions than the
CCW variables do. The same is true when looking only
at conditions that are identified in both data sets. Thus,
the risk-adjustment data for that set of chronic conditions
paint a healthier picture of dual-eligible beneficiaries (and
indeed of all Medicare beneficiaries) than the CCW data
do (see Table A-2).
The two sources produce similar conclusions, however,
when comparing groups of beneficiaries. For example,
both data sets show that dual-eligible beneficiaries are
likely to have a greater number of chronic conditions
than other Medicare beneficiaries and that full duals have
a greater number of chronic conditions than partial duals.
Likewise, both sources of data indicate that institutional-
ized Medicare beneficiaries have more chronic conditions
than noninstitutionalized beneficiaries and that elderly
Medicare beneficiaries have more chronic conditions
than nonelderly beneficiaries.
8. Those numbers of conditions differ from the ones in Box 2 on
page 12 because they are for the 2009 versions of the models,
whereas Box 2 reports values for the 2013 versions of the models.

36 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
Table A-1.
Matching of Chronic Conditions Reported in Two Data Sets, 2009
Source: Congressional Budget Office.
Note: CCW = Centers for Medicare & Medicaid Services’ Chronic Conditions Data Warehouse; MA = Medicare Advantage risk-adjustment
model (CMS-HCC); Rx = prescription drug risk-adjustment model (CMS-RxHCC).
a. The look-back period is the number of years of diagnoses used to determine whether someone has a chronic condition.
b. Although the CCW also lists Alzheimer’s disease separately, CBO does not count it separately as a chronic condition for the purposes of
counting CCW conditions because it is a subset of “Alzheimer’s disease and related disorders or senile dementia.”
c. Listed complications are renal or peripheral circulatory manifestation, neurologic or other specified manifestation, acute complications,
and ophthalmologic or unspecified manifestation.
Condition Reported in the CCW
Look-Back
Period in the CCW
a
Matching Condition Reported in the
Risk-Adjustment Files
Acute myocardial infarction 1 year MA: acute myocardial infarction; Rx: none
Alzheimer’s disease and related
disorders or senile dementia
b
3 years MA: none; Rx: dementia with depression or behavioral
disturbance, dementia/cerebral degeneration
Atrial fibrilation 1 year No match
Cataract 1 year No match
Chronic kidney disease 2 years No match
Chronic obstructive pulmonary disease 1 year MA: chronic obstructive pulmonary disease; Rx: none
Depression 1 year MA: major depressive, bipolar, and paranoid disorders; Rx: none
Diabetes 2 years MA: diabetes with or without complications;
c
Rx: diabetes with or without complications
Glaucoma 1 year MA: none; Rx: open-angle glaucoma, glaucoma and keratoconus
Heart failure 2 years MA: congestive heart failure; Rx: congestive heart failure
Hip/pelvic fracture 1 year MA: hip fracture/dislocation; Rx: pelvic fracture
Ischemic heart disease 2 years MA: acute myocardial infarction, unstable angina and other acute
ischemic heart disease, angina pectoris/old myocardial infarction;
Rx: none
Osteoporosis 1 year MA: none; Rx: osteoporosis and vertebral fractures
Rheumatoid arthritis/osteoarthritis 2 years MA: rheumatoid arthritis and inflammatory connective tissue
disease; Rx: rheumatoid arthritis and other inflammatory
polyarthropathy
Stroke/transient ischemic attack 1 year MA: ischemic or unspecified stroke; RX: none
Colorectal cancer, endometrial cancer,
female breast cancer, lung cancer,
prostate cancer
1 year MA: metastatic cancer and acute leukemia; lung, upper digestive
tract, and other severe cancers; lymphatic, head and neck, brain,
and other major cancers; breast, prostate, colorectal, and other
cancers and tumors; Rx: acute myeloid leukemia; metastatic
cancer, acute leukemia, and severe cancers; lung, upper digestive
tract, and other severe cancers

APPENDIX DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 37
CBO
Table A-2.
Comparison of the Number of Chronic Conditions Among
Medicare Beneficiaries in Two Data Sets, 2009
(Percentage of beneficiaries)
Source: Congressional Budget Office.
Note: CCW = Centers for Medicare & Medicaid Services’ Chronic Conditions Data Warehouse; * =between zero and 0.5 percent.
082181**100
1–2 37 57 5 * * 100
3–4 146321 2 * 100
5–6 7 46 38 8 1 100
More than 6 4 30 44 19 3 100
079201**100
1–2 29 63 7 1 * 100
3–4 105729 4 * 100
5–6 5 37 43 14 1 100
More than 6 3 24 43 25 5 100
Number of Chronic Conditions as
Risk-Adjustment Files
Number of Chronic Conditions as
Reported in the CCW
Number of Chronic Conditions as
Reported in the CCW, Including Only
Conditions Also Reported in the
01–23–45–6More than 6Total
Reported in the Risk-Adjustment Files

38 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID JUNE 2013
CBO
List of Tables and Figures
Tables
1. Demographic Characteristics of Dual-Eligible Beneficiaries, Compared With
Those of Certain Other Medicare and Medicaid Beneficiaries, 2009 5
2. Demographic Characteristics of Dual-Eligible Beneficiaries, Compared With
Those of Certain Other Medicare and Medicaid Beneficiaries, 2009, by Age 7
3. Spending for Full Dual-Eligible Beneficiaries, by Program and Type of Service, 2009 10
4. Demographic Characteristics of and Spending for Full Dual-Eligible Beneficiaries, by
Type of Medicare and Medicaid Payment System Enrolled in, 2009 14
5. Selected Federal and State Initiatives to Integrate Medicare’s and Medicaid’s
Financing and Coordinate Care for Dual-Eligible Beneficiaries 18
6. Demographic Characteristics of Full Dual-Eligible Beneficiaries, 2009, in States That
Have Applied or Not Applied for CMS’s Financial Alignment Demonstration 26
A-1. Matching of Chronic Conditions Reported in Two Data Sets, 2009 36
A-2. Comparison of the Number of Chronic Conditions Among Medicare
Beneficiaries in Two Data Sets, 2009 37
Figures
1. Characteristics of Full Dual-Eligible Beneficiaries, 2009 3
2. States’ Participation Rates for Medicare and Medicaid Managed Care and
Application for CMS’s Financial Alignment Demonstration 23
3. Enrollment in Medicare and Medicaid Managed Care, 2009, by States’ Application
Status in CMS’s Financial Alignment Demonstration 24

JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID 39
CBO
About This Document
This Congressional Budget Office (CBO) report was prepared at the request of the Chairman of the
Senate Committee on Finance. In keeping with CBO’s mandate to provide objective, impartial
analysis, the report makes no recommendations.
The analysis was prepared by Tamara Hayford of CBO’s Health, Retirement, and Long-Term Analysis
Division—in close collaboration with Andrea Noda of CBO’s Budget Analysis Division—with
guidance from Linda Bilheimer and Jean Hearne. Jessica Banthin, Thomas Bradley, Melinda Buntin,
Sheila Campbell, Philip Ellis, Holly Harvey, Paul Jacobs, Michael Levine, Paul Masi, Gordon Mermin,
Jamease Miles, Lyle Nelson, and Lara Robillard provided helpful comments.
Sarah Barth of the Center for Health Care Strategies, Robert Book of American Action Forum, and
Vernon Smith of Health Management Associates reviewed the report. The assistance of external
reviewers implies no responsibility for the final product, which rests solely with CBO.
Christian Howlett edited the report, and Maureen Costantino and Jeanine Rees prepared it for
publication. The report is available on CBO’s website (www.cbo.gov).
Douglas W. Elmendorf
Director
June 2013

CBO
Glossary
accountable care organizations: Groups of doctors,
hospitals, and other health care providers who join
together to provide coordinated care to a set of patients
and who agree to be held accountable for the quality and
total cost of those patients’ care. The Centers for Medi-
care & Medicaid Services is encouraging the development
of accountable care organizations by offering to share
savings with those groups if they can demonstrate that
they have met certain quality standards and savings
benchmarks for their Medicare patients.
acute care: Medical care provided by physicians’ offices,
short-term acute care hospitals, and outpatient care
facilities. Services such as prescription drugs and dental
care are also considered to be acute care.
aged, blind, or disabled (ABD) Medicaid
beneficiaries: People who are eligible for and receive
Medicaid benefits because of age, blindness, or disability
in addition to the amount of their income and assets. The
dual-eligible population is a subset of those beneficiaries.
behavioral health care: Treatment of mental health and
substance abuse problems.
capitated payment: A single payment, made on a per-
enrollee basis, that covers all care within a specified set
of benefits. Medicare and Medicaid make capitated
payments to managed care organizations, which then pay
health care providers for a specific set of benefits for
people enrolled in a managed care plan. The recipient of
a capitated payment keeps the difference between its costs
and the amount of the payment if costs are below the
payment, but it is responsible for paying any costs that
exceed the capitated payment.
cost plan: A type of Medicare Advantage plan in which
payments to plans are based on submitted claims rather
than being capitated. Fewer than 2 percent of dual-
eligible beneficiaries enrolled in a Medicare Advantage
plan are enrolled in a cost plan. Such plans typically do
not cover all of an enrollee’s use of services; the remaining
claims for those enrollees are covered by traditional
fee-for-service Medicare.
dual-eligible beneficiaries: People who are jointly
enrolled in Medicare and Medicaid and who are eligible
to receive benefits from both programs. All dual-eligible
beneficiaries qualify for full Medicare benefits, which
cover their acute and postacute care. Dual-eligible benefi-
ciaries vary, however, in the amount of Medicaid benefits
for which they qualify. The dual-eligible population can
be divided into “full duals” and “partial duals” on the
basis of the Medicaid benefits that people are eligible to
receive. At a minimum, all dual-eligible beneficiaries
qualify to have the Medicaid program pay their premi-
ums for Part B of Medicare (and for Part A, if applicable).
fee for service (FFS): A payment system in which a
health care program or plan pays providers a fee for each
covered service performed for its enrollees.
full duals: Dual-eligible beneficiaries who qualify for full
benefits from Medicaid as well as from Medicare. Thus,
Medicaid pays for their premiums for Part B of Medicare
(and for Part A, if applicable) and covers various health
care services that Medicare does not cover, such as most
types of long-term services and supports (as well as dental
care and other services in some states). In addition, some
states’ Medicaid programs cover the entire cost-sharing
amounts that full duals incur under Medicare, whereas
other states cover only a portion of those amounts.
health home: A type of medical home that serves Medic-
aid beneficiaries who have a particular set of chronic
conditions. Health homes are intended to address those
beneficiaries’ needs for behavioral and physical health
care as well as for institutional or community-based long-
term care. The Affordable Care Act created an optional
program in which states can receive a 90 percent federal
matching rate for up to two years for providing this type
of service.

42 JUNE 2013 DUAL-ELIGIBLE BENEFICIARIES OF MEDICARE AND MEDICAID
CBO
long-term services and supports (LTSS): A category
that encompasses a variety of supportive services provided
to people who have limits on their ability to perform
daily activities, such as bathing or dressing. LTSS typi-
cally excludes medical services that are needed to manage
underlying health conditions. LTSS can be provided in
nursing homes or other institutions, in people’s homes, or
in community-based settings (such as adult day care cen-
ters). Medicaid is the primary government payer for most
of those types of services. The exceptions are skilled
nursing facility services, hospice care, and home health
care services, which are provided by Medicare in some
circumstances.
managed FFS: A model in which providers are paid on a
fee-for-service basis while beneficiaries are enrolled in
care management programs designed to improve the
quality of, and promote the appropriate use of, health
care services.
managed LTSS: Long-term services and supports pro-
vided to Medicaid beneficiaries through managed care
programs. The number of state Medicaid programs
offering managed LTSS is growing rapidly.
medical home: A model for delivering health care—
increasingly being used by state Medicaid programs—
in which a team of health care professionals, led by a
primary care provider, coordinates the care given to an
individual or family.
Medicare Advantage: Medicare’s managed care program,
known formally as Medicare Part C. Most Medicare
Advantage plans receive a capitated payment from Medi-
care in exchange for providing beneficiaries with all of the
services covered by Parts A and B of Medicare. (A small
number of plans, called cost plans, are paid on a claim-
by-claim basis rather than with a capitated payment and
do not necessarily cover all of those services.) Roughly
20 percent of dual-eligible beneficiaries are enrolled in
Medicare Advantage plans.
nondual: A term used to describe Medicare beneficiaries
who are not enrolled in Medicaid or Medicaid beneficia-
ries who are not enrolled in Medicare.
partial duals: Dual-eligible beneficiaries who qualify
to have Medicaid pay some of the expenses they incur
under Medicare. For all partial duals, Medicaid pays the
premiums for Part B of Medicare (and for Part A, if appli-
cable). For some partial duals (depending on the state
they live in and their income and assets), Medicaid also
pays part or all of the cost-sharing amounts they owe
under Medicare.
Parts A, B, C, and D: The Medicare program has three
components: Hospital Insurance (Part A), Medical Insur-
ance (Part B), and prescription drug coverage (Part D).
Medicare Part C (known as Medicare Advantage) speci-
fies the rules under which private health care plans can
assume responsibility for, and be compensated for,
providing benefits covered under Parts A, B, and D.
postacute care: Recuperation and rehabilitation services
provided to patients recovering after a stay in a hospital
for acute care. Postacute care is provided by skilled
nursing facilities, home health agencies, and inpatient
rehabilitation facilities, among others.
Program of All-Inclusive Care for the Elderly (PACE):
A health care program that receives capitated payments in
exchange for offering specialized services to Medicare and
Medicaid beneficiaries who are age 55 or older and who
need the degree of care usually provided in nursing facili-
ties. PACE provides beneficiaries with community-based
long-term services and supports that are intended to help
them remain outside institutions. Notably, PACE pro-
grams may use their Medicare and Medicaid payments
for any services that would enable a beneficiary to con-
tinue to live at home, including physical improvements
to make the home more accessible. In addition, PACE
programs have their own facilities—which provide ser-
vices such as adult day care and visits by physicians—and
offer transportation between a beneficiary’s home and
those facilities.
risk-based managed care: A system in which a health
care program contracts with health plans, most of which
are privately run, to provide a set of covered benefits for a
fixed amount per beneficiary. Those amounts may be
adjusted to reflect the health risks of beneficiaries.
special-needs plan (SNP): A type of Medicare Advan-
tage plan that is designed to provide targeted services to
Medicare beneficiaries who are in institutions, are dual-
eligible beneficiaries, or have a severe or disabling chronic
condition.
