OXFORD MEDICAL PUBLICATIONS
Oxford Handbook of
Emergency
Medicine
Published and forthcoming Oxford Handbooks
Oxford Handbook for the Foundation Programme 3e
Oxford Handbook of Acute Medicine 3e
Oxford Handbook of Anaesthesia 3e
Oxford Handbook of Applied Dental Sciences
Oxford Handbook of Cardiology 2e
Oxford Handbook of Clinical and Laboratory Investigation 3e
Oxford Handbook of Clinical Dentistry 5e
Oxford Handbook of Clinical Diagnosis 2e
Oxford Handbook of Clinical Examination and Practical Skills
Oxford Handbook of Clinical Haematology 3e
Oxford Handbook of Clinical Immunology and Allergy 2e
Oxford Handbook of Clinical Medicine - Mini Edition 8e
Oxford Handbook of Clinical Medicine 8e
Oxford Handbook of Clinical Pharmacy
Oxford Handbook of Clinical Rehabilitation 2e
Oxford Handbook of Clinical Specialties 8e
Oxford Handbook of Clinical Surgery 3e
Oxford Handbook of Complementary Medicine
Oxford Handbook of Critical Care 3e
Oxford Handbook of Dental Patient Care 2e
Oxford Handbook of Dialysis 3e
Oxford Handbook of Emergency Medicine 4e
Oxford Handbook of Endocrinology and Diabetes 2e
Oxford Handbook of ENT and Head and Neck Surgery
Oxford Handbook of Expedition and Wilderness Medicine
Oxford Handbook of Forensic Medicine
Oxford Handbook of Gastroenterology & Hepatology 2e
Oxford Handbook of General Practice 3e
Oxford Handbook of Genetics
Oxford Handbook of Genitourinary Medicine, HIV and AIDS 2e
Oxford Handbook of Geriatric Medicine
Oxford Handbook of Infectious Diseases and Microbiology
Oxford Handbook of Key Clinical Evidence
Oxford Handbook of Medical Dermatology
Oxford Handbook of Medical Sciences
Oxford Handbook of Medical Statistics
Oxford Handbook of Nephrology and Hypertension
Oxford Handbook of Neurology
Oxford Handbook of Nutrition and Dietetics
Oxford Handbook of Obstetrics and Gynaecology 2e
Oxford Handbook of Occupational Health
Oxford Handbook of Oncology 3e
Oxford Handbook of Ophthalmology 2e
Oxford Handbook of Paediatrics
Oxford Handbook of Pain Management
Oxford Handbook of Palliative Care 2e
Oxford Handbook of Practical Drug Therapy 2e
Oxford Handbook of Pre-Hospital Care
Oxford Handbook of Psychiatry 2e
Oxford Handbook of Public Health Practice 2e
Oxford Handbook of Reproductive Medicine & Family Planning
Oxford Handbook of Respiratory Medicine 2e
Oxford Handbook of Rheumatology 3e
Oxford Handbook of Sport and Exercise Medicine
Oxford Handbook of Tropical Medicine 3e
Oxford Handbook of Urology 2e
Oxford Handbook of
Emergency
Medicine
Fourth edition
Jonathan P. Wyatt
Consultant in Emergency Medicine and
Forensic Physician
Royal Cornwall Hospital, Truro, UK
Robin N. Illingworth
Consultant in Emergency Medicine
St James’s University Hospital, Leeds, UK
Colin A. Graham
Professor of Emergency Medicine
Chinese University of Hong Kong,
Hong Kong SAR, China
Kerstin Hogg
Clinical Research Fellow,
The Ottawa Hospital, Ottawa, Canada
with senior international advisors:
Michael J. Clancy
Consultant in Emergency Medicine
Southampton General Hospital,
Southampton, UK
Colin E. Robertson
Professor of Emergency Medicine
Royal Infi rmary, Edinburgh, UK
1
1
Great Clarendon Street, Oxford OX2 6DP
Oxford University Press is a department of the University of Oxford.
It furthers the University’s objective of excellence in research, scholarship,
and education by publishing worldwide in
Oxford New York
Auckland Cape Town Dar es Salaam Hong Kong Karachi
Kuala Lumpur Madrid Melbourne Mexico City Nairobi
New Delhi Shanghai Taipei Toronto
With offi ces in
Argentina Austria Brazil Chile Czech Republic France Greece
Guatemala Hungary Italy Japan Poland Portugal Singapore
South Korea Switzerland Thailand Turkey Ukraine Vietnam
Oxford is a registered trade mark of Oxford University Press
in the UK and in certain other countries
Published in the United States
by Oxford University Press Inc., New York
© Oxford University Press, 2012
The moral rights of the authors have been asserted
Database right Oxford University Press (maker)
First edition published 1999
Second edition published 2005
Third edition published 2006
Fourth edition published 2012
All rights reserved. No part of this publication may be reproduced,
stored in a retrieval system, or transmitted, in any form or by any means,
without the prior permission in writing of Oxford University Press,
or as expressly permitted by law, or under terms agreed with the appropriate
reprographics rights organization. Enquiries concerning reproduction
outside the scope of the above should be sent to the Rights Department,
Oxford University Press, at the address above
You must not circulate this book in any other binding or cover
and you must impose this same condition on any acquirer
British Library Cataloguing in Publication Data
Data available
Library of Congress Cataloging-in-Publication-Data
Data available
Typeset by Cenveo, Bangalore, India
Printed in Italy
on acid-free paper by
L.E.G.O. S.p.A.—Lavis TN
ISBN 978–0–19–958956–2
10 9 8 7 6 5 4 3 2 1
Oxford University Press makes no representation, express or implied, that the
drug dosages in this book are correct. Readers must therefore always check the
product information and clinical procedures with the most up-to-date published
product information and data sheets provided by the manufacturers and the most
recent codes of conduct and safety regulations. The authors and publishers do not
accept responsibility or legal liability for any errors in the text or for the misuse or
misapplication of material in this work. Except where otherwise stated, drug dosages
and recommendations are for the non-pregnant adult who is not breastfeeding.
Dedicated to Dr Robin Mitchell (1964–2010)
Emergency Physician in Christchurch, Edinburgh and Auckland.
Outstanding clinician and teacher, tremendous colleague and friend.
This page intentionally left blank
vii
Abbreviations and symbols
ix
Normal values xvii
Acknowledgements xix
1 General approach
1
2 Life-threatening emergencies
41
3 Medicine
62
4 Toxicology
179
5 Infectious diseases
219
6 Environmental emergencies
253
7 Analgesia and anaesthesia
271
8 Major trauma
319
9 Wounds, fractures, orthopaedics
401
10 Surgery
503
11 Ophthalmology
533
12 Ear, nose and throat
545
13 Obstetrics and gynaecology
563
14 Psychiatry
601
15 Paediatric emergencies
630
Index
737
Contents
This page intentionally left blank

ix
° degrees
8 approximately
+ve positive
–ve negative
± plus or minus
i increase(d)
d decrease(d)
ABC airway, breathing, circulation
ABG arterial blood gas
AC acromio-clavicular
ACE angiotensin-converting enzyme
ACTH adrenocorticotropic hormone
ACS acute coronary syndrome
AF atrial fi brillation
AIDS acquired immune defi ciency syndrome
AIO Ambulance incident offi cer
AIS abbreviated injury scale
ALS advanced life support
ALT alanine aminotransferase
ALTE apparently life-threatening event
AP antero-posterior
APLS Advanced Paediatric Life Support
APTT activated partial thromboplastin time
ARDS adult respiratory distress syndrome
ARF acute renal failure
AST aspartate transaminase
ATLS advanced trauma life support
AV atrio-ventricular
bd twice daily
BKPOP below knee Plaster of Paris
BKWPOP below knee walking Plaster of Paris
BLS basic life support
BMG bedside strip measurement of venous/capillary blood glucose
BNF British National Formulary
BNFC British National Formulary for Children
Abbreviations and symbols

x
ABBREVIATIONS AND SYMBOLS
BP blood pressure
BTS British Thoracic Society
BZP benzylpiperazine
CBRN chemical, biological, radiological, nuclear
CCU critical care unit
CK creatine kinase
cm centimetre(s)
CMV cytomegalovirus
CN chloroacetophenone
CNS central nervous system
CO carbon monoxide
CO
2
carbon dioxide
COHb carboxyhaemoglobin
COPD chronic obstructive pulmonary disease
CPAP continuous positive airways pressure
CPR cardiopulmonary resuscitation
CRF chronic renal failure
CRP C-reactive protein
CSF cerebrospinal fl uid
CT computed tomography
CTPA computed tomography pulmonary angiography
CVP central venous pressure
CVS cardiovascular system
CXR chest X-ray
DIC disseminated intravascular coagulation
DIPJ distal interphalangeal joint
DKA diabetic ketoacidosis
dL decilitre
DPL diagnostic peritoneal lavage
DPT diphtheria, pertussis, and tetanus
DSH deliberate self-harm
DVT deep venous thrombosis
EBV Epstein–Barr virus
ECG electrocardiogram
ECT electroconvulsive therapy
ED emergency department
EEG electroencephalogram
EMLA eutectic mixture of local anaesthetics
ENT ear, nose and throat
EPAP expiratory positive airway pressure

xi
ABBREVIATIONS AND SYMBOLS
ESR erythrocyte sedimentation rate
ET endotracheal
ETCO
2
end-tidal carbon dioxide
FAST focused assessment with sonography for trauma
FB foreign body
FBC full blood count
FFP fresh frozen plasma
FG French Gauge
FiO
2
inspired oxygen concentration
FOB faecal occult blood
G6-PD glucose 6-phosphate dehydrogenase
g gram(s)
G gauge
GA general anaesthetic
GCS Glasgow Coma Score
GFR glomerular fi ltration rate
GI gastrointestinal
GHB gammahydroxybutyrate
GMC General Medical Council
GP general practitioner
GTN glyceryl trinitrate
GU genitourinary
5HT 5-hydroxytryptamine
HATI human anti-tetanus immunoglobulin
Hb haemoglobin
HCG human chorionic gonadotrophin
HCM hypertrophic cardiomyopathy
Hct haematocrit
HDU high dependency unit
HHS hyperosmolar hyperglycaemic state
HIV human immunodefi ciency virus
HONK hyperosmolar non-ketotic hyperglycaemia
hr hour/s
HTLV human T-cell lymphotropic virus
ICP intracranial pressure
ICU intensive care unit
IDDM insulin dependent diabetes mellitus
IHD ischaemic heart disease
IM intramuscular
INR international normalized ratio (of prothrombin time)

xii
ABBREVIATIONS AND SYMBOLS
IO intra-osseous
IPAP inspiratory positive airway pressure
IPg interphalangeal
IPPV intermittent positive pressure ventilation
ISS injury severity score
ITP idiopathic thrombocytopenic purpura
IUCD intrauterine contraceptive device
IV intravenous
IVI intravenous infusion
IVRA intravenous regional anaesthesia
IVU intravenous urography
JVP jugular venous pressure
KE kinetic energy
kPa kiloPascal(s) pressure
KUB X-ray covering the area of kidneys, ureters and bladder
L litre(s)
LA local anaesthetic
LAD left axis deviation
LBBB left bundle branch block
LDH lactate dehydrogenase
LET lidocaine epinephrine tetracaine
LFTs liver function tests
LMA laryngeal mask airway
LMP last menstrual period
LMWH low molecular weight heparin
LP lumbar puncture
LSD lysergic acid diethylamide
LV left ventricular
LVF left ventricular failure
LVH left venticular hypertrophy
m metre(s)
MAOI monoamine oxidase inhibitor
MAST military anti-shock trousers
max maximum
MC metacarpal
MCA Mental Capacity Act
MCPJ metacarpophalangeal joint
MDU Medical Defence Union
MI myocardial infarction
min minute/s

xiii
ABBREVIATIONS AND SYMBOLS
MIO medical incident offi cer
mL millilitre(s)
mmHg millimetres of mercury pressure
mmol millimoles
MMR mumps, measles, and rubella
MRI magnetic resonance imaging
MRSA meticillin resistant Staphylococcus aureus
MS multiple sclerosis
MSU mid-stream specimen of urine
MT metatarsal
MTPJ metatarsophalangeal joint
MUA manipulation under anaesthetic
NAC N -acetyl cysteine
NAI non-accidental injury
ND notifi able disease
NG nasogastric
NHS National Health Service
NIV non-invasive ventilation
NO nitrous oxide
NSAID non-steroidal anti-infl ammatory drug
NSTEMI non-ST segment elevation myocardial infarction
NWBPOP non-weight-bearing Plaster of Paris
O
2
oxygen
OA osteoarthritis
OCP oral contraceptive pill
od once daily
OPG orthopantomogram
ORIF open reduction and internal fi xation
ORT oral replacement therapy
PA postero-anterior
PACS picture archiving and communication system
PAN polyarteritis nodosa
PCI percutaneous coronary intervention
pCO
2
arterial partial pressure of carbon dioxide
PCR polymerase chain reaction
PE pulmonary embolus
PEA pulseless electrical activity
PEEP positive end-expiratory pressure
PEFR peak expiratory fl ow rate
PGL persistent generalized lymphadenopathy

xiv
ABBREVIATIONS AND SYMBOLS
PICU paediatric intensive care unit
PID pelvic infl ammatory disease
PIPJ proximal interphalangeal joint
PO per os (orally/by mouth)
pO
2
arterial partial pressure of oxygen
POP plaster of Paris
PPE personal protective equipment
PPI proton pump inhibitor
PR per rectum
PRF patient report form
PRN pro re nata (as required)
PSP primary spontaneous pneumothorax
PV per vaginam
qds four times a day
RA rheumatoid arthritis
RAD right axis deviation
RBBB right bundle branch block
RBC red blood cells
Rh Rhesus
ROSC restoration of spontaneous circulation
RR respiratory rate
RSI rapid sequence induction/intubation
RSV respiratory syncytial virus
rtPA recombinant tissue plasminogen activator
RTS revised trauma score
RV right ventricular
SA sino-atrial
SARS severe acute respiratory syndrome
SC subcutaneous
SCIWORA spinal cord injury without radiographic abnormality
sec second(s)
SIDS sudden infant death syndrome
SIGN Scottish Intercollegiate Guidelines Network
SIRS systemic infl ammatory response syndrome
SL sublingual
SLE systemic lupus erythematosus
SpO
2
arterial oxygen saturation
SSP secondary spontaneous pneumothorax
SSRI selective serotonin re-uptake inhibitor
STD sexually transmitted disease

xv
ABBREVIATIONS AND SYMBOLS
STEMI ST segment elevation myocardial infarction
SVT supraventricular tachycardia
T ° temperature
T
3
tri-iodothyronine
T
4
thyroxine
TAC tetracaine, adrenaline and cocaine
TB tuberculosis
tds three times a day
TFTs thyroid function tests
TIA transient ischaemic attack
TIMI thrombolysis in myocardial infarction
tPA tissue plasminogen actvator
TSH thyroid stimulating hormone
u/U unit(s)
U&E urea and electrolytes
URTI upper respiratory tract infection
USS ultrasound scan
UTI urinary tract infection
V volts
VA visual acuity
VF ventricular fi brillation
VHF viral hemorrhagic fever
V/Q ventilation/perfusion (scan)
VT ventricular tachycardia
WB weight-bear(ing)
WBC white blood cells
WCC white cell count
WHO World Health Organization
WPW Wolff Parkinson White (syndrome)
This page intentionally left blank

xvii
Note that ‘normal’ values in adults may vary slightly between labs.
Normal values in pregnancy are shown in b The pregnant patient, p.576.
Arterial blood gas analysis
Biochemistry
Normal values
H
+
35–45 nanomol/L
pH 7.35–7.45
pO
2
(on air) >10.6 kPa, 75–100 mmHg
pCO
2
4.5–6.0 kPa, 35–45 mmHg
bicarbonate 24–28 mmol/L
base excess
± 2 mmol/L
alanine aminotransferase (ALT) 5–35 iu/L
albumin 35–50 g/L
alkaline phosphatase 30–300 iu/L
amylase 0–180 Somogyi U/dL
aspartate transaminase (AST) 5–35 iu/L
bicarbonate 24–30 mmol/L
bilirubin 3–17 micromol/L
calcium (total) 2.12–2.65 mmol/L
calcium (ionized) 1–1.25 mmol/L
chloride 95–105 mmol/L
creatine kinase (CK) 25–195 iu/L
creatinine 70–150 micromol/L
C-reactive protein (CRP) <10 mg/L
glucose (fasting) 3.5–5.5 mmol/L
G glutamyl transpeptidase (4)
11–51 IU/L
(5)
7–33 IU/L
magnesium 0.75–1.05 mmol/L
osmolality 278–305 mosmol/kg
potassium 3.5–5.0 mmol/L
sodium 135–145 mmol/L
urea 2.5–6.7 mmol/L
urate (5)
150–390 micromol/L
(4)
210–480 micromol/L

xviii
NORMAL VALUES
Haematology
Metric conversion
Length
Weight
Volume
1 L = 1.76 UK pints = 2.11 US liquid pints
1 UK pint = 20 fl uid ounces = 0.568 L
1 US liquid pint = 16 fl uid ounces = 0.473 L
1 teaspoon 8 5mL
1 tablespoon 8 15mL
Temperature
T ° in °C = ( T ° in Fahrenheit – 32) ×
9
5
–
Pressure
1kPa = 7.5mmHg
RBC (women)
3.9–5.6 × 10
12
/L
(men)
4.5–6.5 × 10
12
/L
Hb (women) 11.5–16.0g/dL
(men) 13.5–18.0g/dL
Hct (women) 0.37–0.47
(men) 0.40–0.54
MCV 76–96 femtoL
WCC
4.0–11.0 × 10
9
/L
neutrophils
2.0–7.5 × 10
9
/L (40–75 % of WCC)
lymphocytes
1.5–4.0 × 10
9
/L (20–40 % of WCC)
monocytes
0.2–0.8 × 10
9
/L (2–10 % of WCC)
eosinophils
0.04–0.40 × 10
9
/L (1–6 % of WCC)
basophils
<0.1 × 10
9
/L (<1 % of WCC)
platelets
150–400 × 10
9
/L
prothrombin time
(factors I, II, VII, X) 12–15sec
APTT (factors VII,
IX, XI, XII) 23–42sec
International Normalized Ratio (INR) therapeutic targets
2.0–3.0 (for treating DVT, pulmonary embolism)
2.5–3.5 (embolism prophylaxis for AF)
3.0–4.5 (recurrent thrombo-embolic disease,
arterial grafts & prosthetic valves)
ESR (women) <
(age in years+10)
/
2
mm/hr
(men) <
(age in years)
/
2
mm/hr
1m = 3 feet 3.4 inches 1 foot = 0.3048m
1cm = 0.394 inch 1 inch = 25.4mm
1kg = 2.20 pounds 1 stone = 6.35kg
1g = 15.4 grains 1 pound = 0.454kg
1 ounce = 28.4g

xix
A number of people provided comments, help and moral support. Special
thanks are due to Dr Phil Munro. We also wish to thank:
Miss Sehlah Abassi, Mr David Alao, Dr Matt Baker, Dr Joan Barber, Dr Ruth
Beach, Mr Dewald Behrens, Dr Ash Bhatia, Dr Angela Bonnar, Dr Rachel
Broadley, Dr Chris Brown, Mrs Debra Clayton, Mr Jon Davies, Dr Kate
Evans, Dr James Falconer, Miss Paula Fitzpatrick, Mrs Jennifer Flemen,
Dr Adrian Flynn, Dr Debbie Galbraith, Mr Blair Graham, Dr Catherine
Guly, Mr Chris Hadfi eld, Dr Steve Halford, Mr Andrew Harrower, Miss
Emily Hotton, Mr Jim Huntley, Mrs Eileen Hutchison, Mr Nicholas Hyatt,
Dr Karen Illingworth, Mr Ian Kelly, Mr Jacques Kerr, Dr Alastair Kidd,
Dr Paul Leonard, Mr Malcolm Lewis, Mr AF Mabrook, Dr Simon Mardel,
Dr Nick Mathiew, Ms Carolyn Meikle, Dr Louisa Mitchell, Dr Claudia
Murton, Dr Louisa Pieterse, Dr Stephanie Prince, Dr Laura Robertson, Miss
Katharine Robinson, Dr Andrew Sampson, Mr Tom Scott, Dr Simon Scott-
Hayward, Ms Karen Sim, Mr Toby Slade, Dr Timothy Squires, Mr Ashleigh
Stone, Dr Luke Summers, Dr Rob Taylor, Dr Ross Vanstone, Ms Fiona
Wardlaw, Dr Mike Wells, Mr Ken Woodburn, Mrs Polly Wyatt.
Acknowledgements
This page intentionally left blank

1
The emergency department 2
Note keeping 4
Radiological requests 6
Triage 7
Discharge, referral, and handover 8
Liaising with GPs 10
Telephone advice 11
Liaising with the ambulance crew 12
Coping as a junior doctor 14
Inappropriate attenders 16
The patient with a label 17
The patient you dislike 18
Special patient groups 19
Discharging the elderly patient 20
The patient with learning diffi culties 21
Patient transfer 22
Breaking bad news 24
What to do after a death 26
Medicolegal aspects: avoiding trouble 28
Medicolegal aspects: the law 30
Infection control and prevention 32
What to carry in your car 34
At the roadside 36
Major incidents 38
General approach
Chapter 1

2 CHAPTER 1 General approach
The emergency department
The role of the emergency department
The emergency department (ED) occupies a key position in terms of the
interface between primary and secondary care. It has a high public profi le.
Many patients attend without referral, but some are referred by NHS
Direct, minor injury units, general practitioners (GPs), and other medical
practitioners. The ED manages patients with a huge variety of medical
problems. Many of the patients who attend have painful and/or distressing
disorders of recent origin.
Priorities are:
• To make life-saving interventions.
• To provide analgesia.
• To identify relevant issues, investigations, and commence treatment.
• To decide upon need for admission or discharge.
ED staff work as a team. Traditional roles are often blurred, with the
important issue being what clinical skills a member of staff is capable of.
ED staff include:
• Nurses (including nurse practitioners, nurse consultants, health care
assistants).
• Doctors (permanent and fi xed-term).
• Reception and administrative staff (receptionists, secretaries,
managers).
• Radiographers, including reporting radiographers.
• Other specialist staff (eg psychiatric liaison nurses, plaster technicians,
physiotherapists, paramedic practitioners, physician assistants,
occupational therapists, clinic/ED ward staff).
• Supporting staff (security, porters, cleaners, police).
Physical resources
A principal focus of the ED is to provide immediate resuscitation for
patients who present with emergency conditions. In terms of sheer
numbers, more patients attend with minor conditions and injuries, often
presenting quite a challenge for them to be seen and treated in a timely
fashion. Different departments have systems to suit their own particular
needs, but most have a resuscitation room, an area for patients on trolleys,
and an area for ambulant patients with less serious problems or injuries.
Paediatric patients are seen in a separate area from adults. In addition,
every ED requires facilities for applying casts, exploring and suturing
wounds, obtaining X-rays, and examining patients with eye problems.
Discharge from the ED
To work effi ciently, the overall hospital system needs to enable easy fl ow
of patients out of the ED. Options available for continuing care of patients
who leave the ED, include:
• Discharge home with no follow-up.
• Discharge home with GP and/or other community support/follow-up.
• Discharge with hospital clinic follow-up arranged.
• Admission to hospital for further investigation and treatment.
• Transfer to another hospital with more specialist facilities.

3
THE EMERGENCY DEPARTMENT
Emergency department staff beyond the emergency
department
In addition to their roles in providing direct clinical care in their
departments, many ED staff provide related clinical care in other settings
and ways:
• Short stay wards (sometimes called clinical decision units) where
emergency care can be continued by ED staff. The intention is for
admissions to these units to be short: most of the patients admitted
to such wards are observed for relatively short periods (<24hr) and
undergo assessments at an early stage to decide about the need for
discharge or longer-term admission.
• Outpatient clinics enable patients with a variety of clinical problems (eg
burns, soft tissue injuries, and infections) to be followed up by ED staff.
• Planned theatre lists run by ED specialists are used by some hospitals to
manage some simple fractures (eg angulated distal radial fractures).
• Telemedicine advice to satellite and minor injury units.
Emergency medicine in other settings
As the delivery of emergency care continues to develop, patients with
emergency problems are now receiving assessment and treatment in a
variety of settings. These include minor injury units, acute medical assessment
units and walk-in centres. Traditional distinctions between emergency
medicine, acute medicine, and primary care have become blurred.

4 CHAPTER 1 General approach
Note keeping
General aspects
It is impossible to over-emphasize the importance of note keeping.
Doctors and nurse practitioners each treat hundreds of patients every
month. With the passage of time, it is impossible to remember all aspects
relating to these cases, yet it may be necessary to give evidence in court
about them years after the event. The only reference will be the notes
made much earlier. Medicolegally, the ED record is the prime source
of evidence in negligence cases. If the notes are defi cient, it may not be
feasible to defend a claim even if negligence has not occurred. A court
may consider that the standard of the notes refl ects the general standard
of care. Sloppy, illegible, or incomplete notes refl ect badly on the
individual. In contrast, if notes are neat, legible, appropriate, and detailed,
those reviewing the case will naturally expect the general standards of
care, in terms of history taking, examination, and level of knowledge, to
be competent.
The Data Protection and Access to Medical Records Acts give patients right
of access to their medical notes. Remember, whenever writing notes, that
the patient may in the future read exactly what has been written. Follow
the basic general rules listed below.
Layout
Follow a standard outline:
Presenting complaint Indicate from whom the history has been obtained
(eg the patient, a relative, or ambulance personnel). Avoid attributing
events to certain individuals (eg patient was struck by ‘Joe Bloggs’).
Previous relevant history Note recent ED attendances. Include family and
social history. An elderly woman with a Colles’ fracture of her dominant
hand may be able to manage at home with routine follow-up provided
she is normally in good health, and has good family or other support, but
if she lives alone in precarious social conditions without such support,
then admission on ‘social grounds’ may be required.
Current medications Remember to ask about non-prescribed drugs
(including recreational, herbal, and homeopathic). Women may not
volunteer the oral contraceptive pill (OCP) as ‘medication’ unless
specifi cally asked. Enquire about allergies to medications and document
the nature of this reaction.
Examination fi ndings As well as + ve features, document relevant –ve
fi ndings (eg the absence of neck stiffness in a patient with headache and
pyrexia). Always document the side of the patient which has been injured.
For upper limb injuries, note whether the patient is left or right handed.
Use ‘left’ and ‘right’, not ‘L’ and ‘R’. Document if a patient is abusive or
aggressive, but avoid non-medical, judgemental terms (eg ‘drunk’).
Investigation fi ndings Record clearly.
Working diagnosis For patients being admitted, this may be a differential
diagnostic list. Sometimes a problem list can help.

5
NOTE KEEPING
Treatment given Document drugs, including dose, time, and route of
administration (see current British National Formulary ( BNF ) for guidance).
Include medications given in the ED, as well as therapy to be continued
(eg course of antibiotics). Note the number and type of sutures or staples
used for wound closure (eg ‘5 × 6/0 nylon sutures’).
Advice and follow-up arrangements Document if the patient and/or
relative is given preprinted instructions (eg ‘POP care’). Indicate when/
if the patient needs to be reviewed (eg ‘see GP in 5 days for suture
removal’) or other arrangement (eg ‘Fracture clinic in one week’).
Record advice about when/why the patient should return for review,
especially if there is a risk of a rare but serious complication (eg for low
back pain ‘see GP if not better in 1 week. Return to the ED at once if
bladder/bowel problem or numb groin/bottom’ that might be features of
cauda equina syndrome).
Basic rules
• Write legibly in ballpoint pen, ideally black, which photocopies well.
• Always date and time the notes.
• Sign the notes, and print your name and status below.
• Make your notes concise and to the point.
• Use simple line drawings or preprinted sheets for wound/injury
descriptions.
• Avoid idiosyncratic abbreviations.
• Never make rude or judgemental comments .
• Always document the name, grade, and specialty of any doctor from
whom you have received advice.
• When referring or handing a patient over, always document the time of
referral/handover, together with the name, grade, and specialty of the
receiving doctor.
• Inform the GP by letter ( b Liaising with GPs, p.10), even if the patient
is admitted. Most EDs have computerized systems that generate such
letters. In complex cases, send also a copy of ED notes, with results of
investigations.
Pro formas
Increasing emphasis on evidence-based guidelines and protocols has
been associated with the introduction of protocols for many patient
presentations and conditions. Bear in mind the fact that, for some patients,
satisfactory completion of a pro forma may not adequately capture all of
the information required.
Electronic records
In an electronic age, there has been an understandable move towards
trying to introduce electronic patient records. The potential advantages
are obvious, particularly in relation to rapidly ascertaining past medical
history. When completing electronic records, practitioners need to follow
the same principles as those outlined above for written records.
Access to old records can make a huge contribution to decision making.
One potential advantage of electronic records is that they can be accessed
rapidly (compared with older systems requiring a porter to search through
the medical records store and retrieve paper-based notes).

6 CHAPTER 1 General approach
Radiological requests
‘I am glad to say that in this country there is no need to carry out
unnecessary tests as a form of insurance. It is not in this country desirable,
or indeed necessary, that over protective and over examination work
should be done, merely and purely and simply as I say to protect oneself
against possible litigation’ — Judge Fallon, quoted by Oscar Craig, Chairman
Cases Committee, Medical Protection Society.
Requesting investigations
The Royal College of Radiologists’ booklet ‘ Making the Best Use of a
Department of Clinical Radiology: Guidelines for Doctors ’ (6th edn, London,
RCR, 2007) contains very useful information and is strongly recommended.
General aspects
• An X-ray is no substitute for careful, thorough clinical examination. It is
usually unnecessary to request X-rays to confi rm the clinical diagnosis
of uncomplicated fractures of the nose, coccyx, a single rib, or toes
(other than the big toe).
• If in doubt about the need for X-rays or the specifi c test required,
consider relevant guidelines (eg Ottawa rules for ankle injuries,
b p.484) and/or discuss with senior ED staff or radiologist.
• When requesting X-rays, describe the indication/mechanism of injury,
clinical fi ndings, including the side involved (right or left — spelt out
in full, not abbreviated) and the suspected clinical diagnosis. This is
important for the radiologist reporting the fi lms without the advantage
of being able to examine the patient.
• Do not worry about specifying exactly which X-ray views are required.
The radiographer will know the standard views that are needed, based
on the information provided (eg AP + simplifi ed apical oblique views for
a patient with suspected anterior shoulder dislocation). In unusual cases,
discuss with senior ED staff, radiographer, or radiologist.
• Always consider the possibility of pregnancy in women of child-bearing
age before requesting an X-ray of the abdomen, pelvis, lumbar spine,
hips, or thighs. If the clinical indication for X-ray is overriding, tell the
radiographer, who will attempt to shield the foetus/gonads. If the risks/
benefi ts of X-rays in pregnant or possibly pregnant women are not
obvious, consult senior ED or radiology staff.
X-ray reporting system
Many hospitals have systems so that all ED X-rays are reported by a
specialist within 24hr. Reports of any missed abnormalities are returned
with the X-rays to the ED for the attention of senior staff, so that
appropriate action can be taken.
System for identifying abnormalities
In addition to the formal reporting system described above, a system is
commonly used whereby the radiographer taking the fi lms applies a sticky
‘red dot’ to hard copy X-ray fi lms and/or request card or to the equivalent
electronic image if they identify an abnormality. This alerts other clinical
staff to the possibility of abnormal fi ndings.
7
TRIAGE
Triage
The nature of ED work means that a sorting system is required to ensure
that patients with the most immediately life-threatening conditions are seen
fi rst. A triage process aims to categorize patients based on their medical
need and the available departmental resources. One most commonly used
process in the UK is the National Triage Scale (Table 1.1 ).
As soon as a patient arrives in the ED he/she should be assessed by a
dedicated triage nurse (a senior, experienced individual with considerable
common sense). This nurse should provide any immediate interventions
needed (eg elevating injured limbs, applying ice packs or splints, and giving
analgesia) and initiate investigations to speed the patient’s journey through
the department (eg ordering appropriate X-rays). Patients should not
have to wait to be triaged. It is a brief assessment which should take no
more than a few minutes.
Three points require emphasis:
• Triage is a dynamic process. The urgency (and hence triage category)
with which a patient requires to be seen may change with time. For
example a middle-aged man who hobbles in with an inversion ankle
injury is likely to be placed in triage category 4 (green). If in the waiting
room he becomes pale, sweaty, and complains of chest discomfort, he
would require prompt re-triage into category 2 (orange).
• Placement in a triage category does not imply a diagnosis, or even the
lethality of a condition (eg an elderly patient with colicky abdominal
discomfort, vomiting, and absolute constipation would normally
be placed in category 3 (yellow) and a possible diagnosis would be
bowel obstruction). The cause may be a neoplasm which has already
metastasized and is hence likely to be ultimately fatal.
• Triage has its own problems. In particular, patients in non-urgent
categories may wait inordinately long periods of time, whilst patients
who have presented later, but with conditions perceived to be more
urgent, are seen before them. Patients need to be aware of this and to
be informed of likely waiting times. Uncomplaining elderly patients can
often be poorly served by the process.
Table 1.1
National Triage Scale Colour Time to be seen by doctor
1 Immediate Red Immediately
2 Very urgent Orange Within 5–10 min
3 Urgent Yellow Within 1 hr
4 Standard Green Within 2 hr
5 Non-urgent Blue Within 4 hr

8 CHAPTER 1 General approach
Discharge, referral, and handover
Most patients seen in the ED are examined, investigated, treated, and
discharged home, either with no follow-up, or advice to see their GP (for
suture removal, wound checks, etc.). Give these patients (and/or attending
relative/friend) clear instructions on when to attend the GP’s surgery and
an indication of the likely course of events, as well as any features that
they should look out for to prompt them to seek medical help prior to
this. Formal written instructions are particularly useful for patients with
minor head injury ( b p.367) and those with limbs in POP or other forms
of cast immobilization ( b Casts and their problems, p.424).
The referral of patients to an inpatient team can cause considerable
anxiety, misunderstanding, and potential confl ict between ED staff and
other disciplines. Before making the referral the following should be
considered.
Is it appropriate to refer this patient to the inpatient team?
Usually, this will be obvious. For example, a middle-aged man with a
history of crushing chest pain and an ECG showing an acute MI clearly
requires urgent management in the ED, and rapid admission for further
investigation and treatment. Similarly, an elderly lady who has fallen, is
unable to weight-bear and has a fractured neck of femur will require
analgesia, inpatient care and surgery.
However, diffi cult situations occur where the clinical situation is less clear;
for example, if a man experienced 4–5min of atypical chest pain, has a
normal ECG and chest X-ray (CXR), and is anxious to go home. Or a lady
has no apparent fracture on X-ray, but cannot weight-bear.
Is there appropriate information to make this decision?
This requires a balance between availability, time, and appropriateness.
In general, simple investigations which rapidly give the diagnosis, or clues
to it, are all that are needed. These include electrocardiogram (ECGs),
arterial blood gas (ABG), and plain X-rays. It is relatively unusual to have
to wait for the results of investigations such as full blood count (FBC), urea
& electrolytes (U&E), and liver function tests (LFTs) before referring a
patient, since these rarely alter the immediate management. Simple trolley-
side investigations are often of great value, for example, stix estimations
of blood glucose (BMG) and urinalysis. If complicated investigations are
needed, then referral for inpatient or outpatient specialist care is often
required.
Has the patient had appropriate treatment pending the admission?
Do not forget, or delay, analgesia. Treat every patient in pain appropriately
as soon as possible. A patient does not have to ‘earn’ analgesia. Never
delay analgesia to allow further examination or investigation. Concern
regarding masking of signs or symptoms (for example, in a patient with an
acute abdomen) is inhumane and incorrect.

9
DISCHARGE, REFERRAL, AND HANDOVER
How to refer patients
Referral is often by telephone, and this can create problems:
• Introduce yourself and ask for the name and grade of the specialist.
• Give a clear, concise summary of the history, investigations, and
treatment that you have already undertaken.
• Early in the discussion say clearly whether you are making a referral for
admission or a request for a specialist opinion. With ever increasing
pressure on hospital beds, inpatient teams can be reluctant to come
and see patients, and may appear to be happier to give advice over
the phone to avoid admission. If, in your view, the patient needs to
be admitted, then clearly indicate this. If, for whatever reason, this is
declined, do not get cross, rude, or aggressive, but contact senior ED
medical staff to speak to the specialist team.
• When the specialist team comes to see the patient, or the patient is
admitted directly to a ward, the ED notes need to be complete and
legible. Make sure that there is a list of the investigations already
performed, together with the available results and crucially, a list of
investigations whose results remain outstanding. The latter is essential
to ensure continuity of care and to prevent an important result ‘falling
through the net’. Similarly, summarize treatment already given and the
response. In an emergency, do not delay referral or treatment merely
to complete the notes, but complete them at the earliest opportunity.
• Encourage inpatient specialists who attend patients to write their
fi ndings and management plan in the notes, adding a signature and the
time/date.
Handing over patients
Dangers of handing over
Handing over a patient to a colleague, because your shift has ended and
you are going home, is fraught with danger. It is easy for patients to be
neglected, or receive sub-optimal or delayed treatment. It is safest
to complete to the point of discharge or referral to an inpatient team
every patient that you are seeing at the end of a shift. Occasionally this
may not be possible (eg if there is a delay in obtaining an X-ray or other
investigation). In these situations, hand over the patient carefully to the
doctor who is taking over and inform the nursing staff of this.
How to hand over
Include in the handover relevant aspects of history and examination
performed, the investigation results, and the treatment undertaken. Sign
and aim to complete records on the patient as soon as possible. Note the
time of hand over, and the name of the doctor or nurse handed over to.
When accepting a ‘handed-over patient’ at the start of a shift, spend time
establishing exactly what has happened so far. Finally, it is courteous (and
will prevent problems) to tell the patient that their further care will be
performed by another doctor or nurse.

10 CHAPTER 1 General approach
Liaising with GPs
Despite changes in the way that care (particularly out of hours) is delivered,
GPs still have a pivotal role in co-ordinating medical care. Often the GP will
know more than anyone about the past history, social and family situation,
and recent events of their patient’s management. Therefore, contact the
GP when these aspects are relevant to the patient’s ED attendance, or
where considerations of admission or discharge are concerned.
Every attendance is followed routinely by a letter to the GP detailing the
reason(s) for presentation, clinical fi ndings and relevant investigations,
treatment given, and follow-up arrangements.
If a patient dies, contact the GP without delay — to provide a medical
contact and assistance to the bereaved family, to prevent embarrassing
experiences (eg letters requesting clinic attendances), and out of courtesy,
because the GP is the patient’s primary medical attendant. Finally, the GP
may be asked to issue a death certifi cate by the Coroner (in Scotland, the
Procurator Fiscal) following further enquiries.
Always contact the GP prior to the discharge of a patient where early
follow-up (ie within the next 24–72hr) is required. This may occur with
elderly patients where there is uncertainty about the home situation and
their ability to manage. A typical example is an elderly lady with a Colles’
fracture of her dominant wrist who lives alone. The ED management of
this patient is relatively simple ( b p.444). However, merely manipulating
a Colles’ fracture into a good position, supporting it in an adequate
cast, and providing analgesia, is only one facet of care. The GP may know
that the lady has supportive relatives or neighbours who will help with
shopping and cooking, and will help her to bath and dress. The GP and
the primary care team may be able to supplement existing support and
check that the patient is coping. Equally, the GP may indicate that with
additional home support (eg home helps, meals, district nurses), the
patient could manage. Alternatively, the GP may indicate that the Colles’
fracture merely represents the fi nal event in an increasingly fragile home
situation and that the patient will require hospital admission, at least in the
short-term.
For the same reasons, a GP who refers a patient to the ED and indicates
that the patient requires admission does so in the full knowledge of that
patient’s circumstances. Always contact the GP if it is contemplated
that the patient is to be discharged — preferably after senior medical
consultation.
Finally, remember that GPs are also under considerable pressure.
Some situations may appear to refl ect the fact that a patient has been
referred inappropriately or the patient may report that they have tried
to contact their GP unsuccessfully. Rather than irately ringing the practice
and antagonizing them, inform the ED consultant who can raise this
constructively and appropriately in a suitable environment.

11
TELEPHONE ADVICE
Telephone advice
Many departments receive calls from patients, parents, and other carers
for advice. Approach these calls in exactly the same way as a face-to-face
consultation. Formally document details of the call, including:
• Date and time of the call.
• The caller’s telephone number.
• The caller’s relationship to the patient.
• The patient’s name, age, and sex.
• The nature of the problem.
• The advice given.
As with all notes, date, time, and sign these notes.
NHS Direct
In England and Wales NHS Direct provides a 24-hr, 7-day a week telephone
service providing information and advice on health matters. It is staffed by
nurses who respond according to protocols.
The telephone number for NHS Direct is 0845 4647.
The equivalent service in Scotland is NHS24 tel. 08454 242424.
These services have internet websites at www.nhsdirect.nhs.uk and
www.nhs24.com
Telephone advice calls from other health professionals
Occasionally, other health professionals request advice regarding the
management of patients in their care. Such advice should be given by
experienced ED staff.
Telemedicine
Increasingly, emergency health care is provided by integrated networks,
which include EDs, minor injuries units, radiology departments, and GP
surgeries connected by telemedicine links. This has advantages in remote
or rural settings, enabling a wide range of injuries and other emergencies
to be diagnosed and treated locally. The combination of video and
teleradiology may allow a decision to be made and explained directly
to the patient. A typical example is whether a patient with an isolated
Colles’ fracture needs to have a manipulation of the fracture. Expertise
is required to undertake telemedicine consultations safely. This specialist
advice should be given by senior ED staff, and careful documentation is
crucial.

12 CHAPTER 1 General approach
Liaising with the ambulance crew
Paramedics and ED staff have a close professional relationship. Paramedics
and ambulance staff are professionals who work in conditions that are
often diffi cult and sometimes dangerous. It is worth taking an off-duty day
to accompany a crew during their shift to see the problems they face.
A benefi t of paramedic training has been to bring ambulance staff into the
ED to work with medical and nursing staff, and to foster the communication
and rapport essential for good patient management.
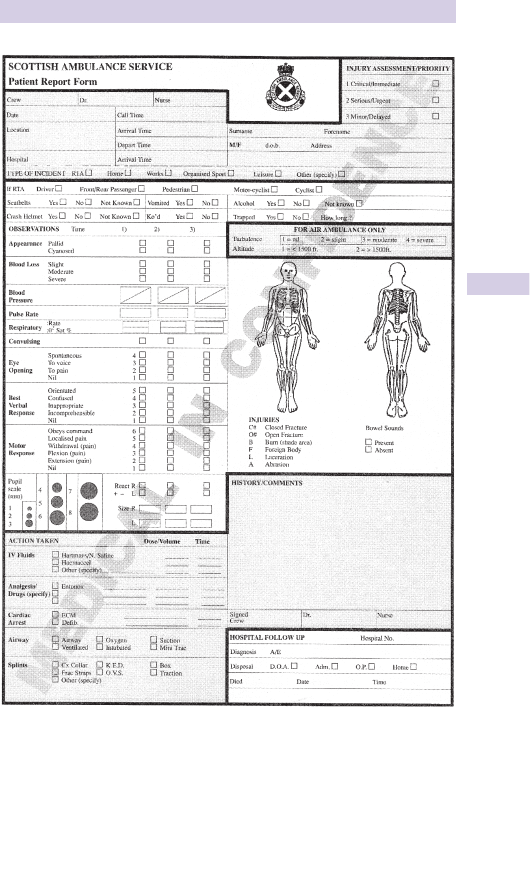
In the UK, a patient brought to an ED by ambulance will routinely have a
patient report form (PRF) (see Fig. 1.1 ). This is completed by the crew at
the scene and in transit, and given to reception or nursing staff on arrival.
The information on these forms can be invaluable. In particular, the time
intervals between the receipt of the 999 call, and arrival at the scene and
at hospital, provide a time framework within which changes in the patient’s
clinical condition can be placed and interpreted.
The initial at-scene assessment will include details of the use of seat belts,
airbags, crash helmets, etc., and is particularly valuable when amplifi ed by
specifi cally asking the crew about their interpretation of the event, likely
speeds involved, types of vehicle, etc.
The clinical features of the Glasgow Coma Score (GCS) , pulse rate, blood
pressure (BP), and respiratory rate form baseline values from which trends
and response to treatment can be judged. Useful aspects in the history/
comments section include previous complaints, current medications, etc.,
which the crew may have obtained from the patient, relatives, or friends.
The PRF will also contain important information about oxygen, drugs, IV
fl uids administered, and the response to these interventions. Before the
crew leave the department, confi rm that they have provided all relevant
information.
Do not be judgemental about the crew’s performance. Remember the
constraints under which they operate. Without the benefi ts of a warm
environment, good lighting, and sophisticated equipment, it can be
exceedingly diffi cult to make accurate assessments of illness or injury
severity, or to perform otherwise simple tasks (eg airway management
and intravenous (IV) cannulation).
Do not dismiss the overall assessment of a patient made by an experienced
crew. While the ultimate diagnosis may not be clear (a situation which
pertains equally in the ED), their evaluation of the potential for life-
threatening events is often extremely perceptive. Equally, take heed of
their description of crash scenes. They will have seen far more than most
ED staff, so accept their greater experience.
Most ambulance staff are keen to obtain feedback, both about specifi c cases
and general aspects of medical care. Like everyone, they are interested
in their patients. A few words as to what happened to Mrs Smith who
was brought in last week and her subsequent clinical course is a friendly
and easy way of providing informal feedback, and helps to cement the
professional relationship between the ambulance service and the ED.
13
LIAISING WITH THE AMBULANCE CREW
Fig. 1.1 An example of a patient reporting form. Reproduced with kind permission
from the Scottish Ambulance Service.

14 CHAPTER 1 General approach
Coping as a junior doctor
Although many junior doctors coming to the ED have completed more
than 12 months of work since qualifi cation, the prospect of working at the
‘sharp end’ can be accompanied by trepidation. As with many potentially
worrying situations in life, reality is not as terrifying as its anticipation. The
number of hours worked may not appear long in comparison with other
posts, but do not assume that this makes an ED job ‘easy’. Being on duty
inevitably involves much time standing, walking, working, thinking, and making
decisions. It is unusual to come off-shift without feeling physically tired.
Active young doctors can usually cope with these physical demands, but a
demanding professional life and demanding social life are rarely compatible.
Make the most of time off and try to relax from the pressures of the job.
One function of relaxation is to enable you to face work refreshed and
invigorated. You are mistaken if you believe that you can stay out all night
and then work unimpaired the next day. Tired doctors make mistakes.
They also tend to have less patience and, as a consequence, interpersonal
confl icts are more likely.
A greater problem is the mental aspect of the job. Doctors often fi nd that
the ED is the fi rst time in their careers when they have to make unequiv-
ocal decisions based on their own assessment and investigations. This is
one of the great challenges and excitements of emergency medicine. It is
also a worry. Decision-making is central to ED practice and, with experi-
ence, the process becomes easier. Developing a structured approach can
pre-empt many problems and simplify your life. After taking an appropriate
history and completing the relevant clinical examination of a patient, ask
yourself a series of questions such as:
• Do I know what is likely to be wrong with this patient?
• What investigations are required to confi rm the diagnosis?
• Do I know what treatment is needed and have I got the skills needed?
• Does this patient require referral to an inpatient team ( b p.8)?
• If not, do they need to be reviewed in the ED or another specialist clinic?
The wide spectrum of problems with which ED patients can present
means that no individual can be expert in every possible condition. It
is therefore as important to recognize and accept when you are out of
your depth as it is to make decisions and treat patients whom you know
you can manage. Seek help appropriately and do not just try to muddle
through. Help may be readily available from senior ED staff, but in some
departments direct contact with a specialist team is required. One of
the most diffi cult situations is where a specialist either refuses to come
to see the patient or gives telephone advice that is clearly inappropriate.
You must always act as the patient’s advocate. If you refer a patient with
a fractured neck of femur, and the telephone message from the inpatient
team is ‘bring him back to the Fracture Clinic in one week’, it is clearly
wrong to carry this out. First, check that the doctor has understood the
details of the patient’s condition and your concerns. More confl ict and
aggravation is caused by communication errors (usually involving second-
hand telephone messages) than by anything else. If the situation remains
unresolved, consult senior ED staff. Whatever happens, never lose your
cool in public and always put your patient’s interests fi rst.

15
COPING AS A JUNIOR DOCTOR
Learning in the ED
Try to learn something new every day. Keep a note of patients with
interesting or unusual problems, and later check what happened to them.
Ask senior staff for advice. Use the ED reference books. Try to note all
new conditions seen during a shift and read about them later.
Staff interaction
The nature of the job, the patients, and the diversity of staff involved
means that a considerable degree of camaraderie exists. For an outsider,
this can initially be daunting. Junior medical staff are likely to work for
4 − 12 months in the department. Other staff may have spent a lifetime
there with long-established friendships (or sometimes animosities).
Respect their position and experience, learn from them.
The nub of this is an understanding that the role of one individual and that
of other individuals in the department are inextricably linked. Any junior
(or senior) doctor who feels that they are the most important individual
in their working environment will have an extremely uncomfortable
professional existence. In the ED, every member of staff has a role. Your
professionalism should dictate that you respect this. Only in this way will
you gain reciprocal respect from other staff members.
Never consider any job ‘beneath you’ or someone else’s responsibility.
Patients come before pride. So, if portering staff are rushed off their
feet and you are unoccupied, wheel a patient to X-ray yourself — it will
improve your standing with your colleagues and help the patient.
Shifts
Rule 1 Never be late for your shift.
Rule 2 If, for whatever reason, you are unable to work a shift, let the
senior staff in the ED know as soon as possible.
Ensure that you take a break. Two or three short breaks in an 8-hr shift
are better than one long one. Remember to eat and maintain your fl uid
intake. Shift working may mean that you will work sometimes with familiar
faces and perhaps occasionally with individuals with whom you fi nd social
contact uncomfortable. Put these considerations aside while you are at
work, for the sake of the patients and your peace of mind.
If you can’t cope
Finally, if you feel that you are unable to manage or that the pressure
of the job is too great — tell someone . Don’t bottle it up, try to ignore it,
or assume that it refl ects inadequacy. It doesn’t. Everyone, at some time,
has feelings of inability to cope. Trying to disguise or deny the situation
is unfair to yourself, your colleagues, and your patients. You need to tell
someone and discuss things. Do it now. Talk to your consultant. If you
cannot face him or her, talk to your GP or another senior member of
staff — but talk to someone who can help you.
The BMA Counselling Service for Doctors (tel: 08459 200169) provides a
confi dential counselling service 24 hr a day, 365 days of the year to discuss
personal, emotional, and work-related problems. The Doctors’ Support
Network ( www.dsn.org.uk ) and Doctors’ Support Line (tel: 0844 395
3010) are also useful resources.

16 CHAPTER 1 General approach
Inappropriate attenders
This is an emotive and ill-defi ned term. Depending upon the department,
such patients could comprise 4–20 % of attendances.
The perception as to whether it is appropriate to go to an ED or attend a
GP will vary between the patient, GP, and ED staff. Appropriateness is not
simply related to the symptoms, diagnosis, or the time interval involved. It
may not necessarily be related to the need for investigation. For example,
not all patients who require an X-ray necessarily have to attend an ED.
Further blurring of ‘appropriate’ and ‘inappropriate’ groups relates to the
geographical location of the ED. In rural areas, GPs frequently perform
procedures such as suturing. In urban areas, these arrangements are less
common. For ill-defi ned reasons, patients often perceive that they should
only contact their GP during ‘offi ce’ hours, and outside these times may
attend an ED with primary care complaints.
It is clearly inappropriate to come to an ED simply because of a real or
perceived diffi culty in accessing primary care. Nevertheless, the term
‘inappropriate attendance’ is a pejorative one — it is better to use the
phrase ‘primary care patients’. It must be recognized that primary care
problems are best dealt with by GPs. Many departments try to prevent
this primary care workload presenting to the ED. Some departments
tackle the problem by having GPs working alongside ED staff.
Managing inappropriate attenders
Only through a continual process of patient education will these problems
be resolved. Initiatives include nurse practitioner minor injury units and
hospital-based primary care services. Evaluations are underway but, to
function effectively, such services require adequate funding and staffi ng.
It can sometimes be diffi cult to deal with primary care problems in the
ED. After an appropriate history and examination, it may be necessary to
explain to patients that they will have to attend their own GP. This may
need direct contact between the ED and the practice to facilitate this.
Inappropriate referrals
Sometimes, it may appear that another health professional (eg GP,
emergency nurse practitioner, nurse at NHS Direct) has referred a patient
to the ED inappropriately. Avoid making such judgements. Treat patients
on their merits, but mention the issue to your consultant. Remember
that the information available to the referring clinician at the time of the
prehospital consultation is likely to have been different to that available at
the time of ED attendance.

17
THE PATIENT WITH A LABEL
The patient with a label
Some patients will have been referred by another medical practitioner,
usually a GP. The accompanying letter may include a presumptive diagnosis.
The details in the letter are often extremely helpful, but do not assume
the diagnosis is necessarily correct. Take particular care with patients who
re-attend following an earlier attendance. The situation may have changed
since the previous doctor saw the patient. Clinical signs may have developed
or regressed. The patient may have not given the referring doctor and
ED staff the same history. Do not pre-judge the problem: start with an
open mind. Apply common sense, however. Keep any previous history in
mind. For example, assume that a patient with a known abdominal aortic
aneurysm who collapses with sudden, severe, abdominal pain, signs of
hypovolaemic shock, and a tender pulsatile mass in the abdomen, to have a
ruptured abdominal aortic aneurysm, rather than intestinal obstruction. The
patient’s
previous ED and hospital case notes are invaluable and will often
give useful information and allow, for example, ECG comparisons, aiding
the diagnostic process. A call to the GP can also provide useful background,
which they may not have had time to include in their referral letter or may
have excluded for confi dentiality or other reasons.
Self-labelled patients
Take care with patients who label themselves. Those with chronic or
unusual diseases often know signifi cantly more about their conditions than
ED staff! In such situations, take special notice of comments and advice
from the patient and/or their relatives. Do not resent this or see it as a
professional affront — rapport with the patient will increase markedly and
management will usually be easier.
Regular attenders
Every ED has a group of ‘regular’ patients who , with time, become physically
and sometimes emotionally attached to the department. Some have
underlying psychiatric illnesses, often with ‘inadequate’ personalities. Some
are homeless. Regular attenders frequently use the ED as a source
of primary care. As outlined above, make attempts to direct them to
appropriate facilities, because the ED is unsuited to the management of
chronic illness, and is unable to provide the continuing medical and nursing
support that these patients require.
Repeated presentations with apparently trivial complaints or with the
same complaint often tax the patience of ED staff. This is heightened if the
presentations are provoked or aggravated by alcohol intake. Remember,
however, that these patients can and do suffer from the same acute events
as everyone else. Keep an open mind, diagnostically and in attitude to the
patient. Just because he/she has returned for the third time in as many
days complaining of chest pain, does not mean that on this occasion he
does not have an acute MI! Maintain adequate documentation for each
attendance. Occasionally, especially with intractable re-attenders, a joint
meeting between the social work team, GP, ED consultant and psychiatric
services is required to provide a defi nitive framework for both the patient
and the medical services. For some patients, it will be possible to follow a
plan of action for ED presentations with a particular complaint.

18 CHAPTER 1 General approach
The patient you dislike
General approach
Accept the patient as he or she is, regardless of behaviour, class, religion,
social lifestyle, or colour. Given human nature, there will inevitably be
some patients whom you immediately dislike or fi nd diffi cult. The feeling
is often mutual. Many factors that cause patients to present to the ED may
aggravate the situation. These include their current medical condition, their
past experiences in hospitals, their social situation, and any concurrent use
of alcohol and/or other drugs. Your approach and state of mind during
the consultation play a major role. This will be infl uenced by whether the
department is busy, how much sleep you have had recently, and when you
last had a break for coffee or food.
Given the nature of ED workload and turnover, confl ict slows down
the process and makes it more likely that you will make clinical errors.
Many potential confl icts can be avoided by an open, pleasant approach.
Introduce yourself politely to the patient. Use body language to reduce a
potentially aggressive response.
The patient’s perspective
Put yourself in the patient’s position. Any patient marched up to by a
doctor who has their hands on hips, a glaring expression, and the demand
‘Well, what’s wrong with you now?’ will retort aggressively.
Defusing a volatile situation
Most complaints and aggression occur when the department is busy and
waiting times are long. Patients understand the pressures medical and
nursing staff have to work under, and a simple, ‘I am sorry you have had to
wait so long, but we have had a number of emergencies elsewhere in the
department’, does much to diffuse potential confl ict and will often mean
that the patient starts to sympathize with you as a young, overworked
practitioner!
There is never any excuse for rude, abusive, or aggressive behaviour
to a patient. If you are rude, complaints will invariably follow and more
importantly, the patient will not have received the appropriate treatment
for their condition. It may be necessary to hand care of a patient to a
colleague if an unresolvable confl ict has arisen.
Management of the violent patient is considered in detail on b p.610.

19
SPECIAL PATIENT GROUPS
Special patient groups
Attending the ED is diffi cult enough, but can be even more so for certain
‘special’ patient groups. It is important that ED staff are sensitive to the
needs of these groups and that there are systems in place to help them
in what may be regarded as an intimidating atmosphere. The following list
is far from exhaustive, but includes some important groups who require
particular consideration:
• Children : they are such an ‘obvious’ and large ‘minority’ group that they
receive special attention to suit their particular needs (see b Paediatric
emergencies, p.630).
• Pregnant women : see b Obstetrics and gynaecology, p.563.
• Those with mental health problems : see b Psychiatry, p.601.
• The elderly : who often have multiple medical problems and live in
socially precarious circumstances.
• Patients with Alzheimer’s disease and other states associated with
chronic confusion.
• Those with learning diffi culties : b p.21.
• Patients with hearing problems.
• The visually impaired.
• Those who do not speak or understand English : arrangements should be in
place to enable the use of interpreters.
• Patients with certain cultural or religious beliefs (particularly amongst
‘minority groups’) : these can impact signifi cantly upon a variety of
situations (eg after unsuccessful resuscitation for cardiac arrest—
b Breaking bad news, p.24).
• Those who are homeless or are away from home, friends, and family
(eg holiday makers).
• Those who have drug/alcohol dependency.
Isn’t everyone special?
Taken at face value, the concept that certain groups of patients are
‘special’ and so require special attention does not meet with universal
approval. There is a good argument that every patient deserves the best
possible care. Whilst this is true, it is also obvious that certain patients
do have additional needs that need to be considered. Many of these
additional needs relate to effective communication. There are some
tremendous resources available that can help practitioners to overcome
communication diffi culties (eg www.communicationpeople.co.uk ).

20 CHAPTER 1 General approach
Discharging the elderly patient
There are no set predisposing factors that determine patients most at risk
following discharge. Those that affect the chance of diffi culties at home
include the current medical problem, underlying functional and social factors.
Risk indicators
Multiple pathologies and atypical symptoms render this group more vulnerable
to the physical, functional, and social effects of acute illness. Past medical
history and pre-admission status are especially important determinants
for patients with dementia or psychiatric illness. There may be evidence of
recently changed circumstances, a recent bereavement, a change in medical or
physical condition, increasing confusion, or unusual behaviour. The patient may
not be able to afford adequate food or heating. Community services may not
be aware that support is needed or help may have been offered, but refused.
Other important indicators are:
• Those living alone.
• Absence of close family support or community services.
• Unsuitable home circumstances (eg external or internal stairs).
• Diffi culty with mobility.
Determining those unable to cope
Look for evidence of self-neglect that suggests that the elderly person
is having diffi culty coping at home (eg poor personal hygiene, unclean or
unsuitable clothing). Evidence of recent weight loss may suggest diffi culties
with food preparation or eating, unavailability of food, or may be due to
serious pathology, such as a malignancy or tuberculosis. Signs of old bruising
or other minor injuries may be consistent with frequent falls. Shortness of
breath and any condition producing impaired mobility are important factors.
Falls are a common problem of old age and require careful analysis, perhaps
at a special ‘Falls’ clinic. Correctable factors include damaged walking aids,
loose rugs, poor lighting, or unsuitable footwear or glasses. Common medical
causes include cerebrovascular disease, arthritis, and side-effects of drugs.
Many elderly people claim that they can cope at home when they are unable
to do so. If in doubt, ask relatives, the GP, and community support agencies.
They may give helpful insight into the patient’s mental state, which can be
investigated/assessed further, whether it be a cognitive or reactive condition.
The decision to discharge
Hospital admission for an elderly person is a frightening experience and
can lead to confusion and disorientation. If circumstances allow, discharge
home is often a more appropriate outcome. If there are concerns regarding
their functional ability and mobility, ask for an occupational therapy and/
or physiotherapy assessment with, if appropriate, a home assessment.
The elderly person is best seen in their home environment with familiar
surroundings, especially if there is evidence of cognitive defi cit. The provision
of equipment and recommendations for adaptations can be made at this
point if required. A wide range of community services including district
nurse, health visitor, home help, crisis care, social work, hospital discharge,
and rapid response therapy teams can be contacted to provide immediate
follow-up and support and play a crucial role in preventing later breakdowns
in home circumstances and unnecessary admissions for social reasons.

21
THE PATIENT WITH LEARNING DIFFICULTIES
The patient with learning diffi culties
Patients with learning diffi culties use the healthcare system more than the
general population. Unfortunately, many healthcare professionals have
little experience with these patients. However, understanding common
illness patterns and using different techniques in communication can result
in a successful consultation. Patients with learning diffi culties often have
complex health needs. There are many barriers to assessing health care,
which may lead to later presentations of illness. Patients may have a high
tolerance of pain — take this into consideration when examining them.
Associated health problems
Patients with learning diffi culties have a higher incidence of certain problems:
• Visual and hearing impairment.
• Poor dental health.
• Swallowing problems.
• Gastro-oesophageal refl ux disease.
• Constipation.
• Urinary tract and other infections.
• Epilepsy.
• Mental health problems ( i incidence of depression, anxiety disorders,
schizophrenia, delirium, and dementia), with specifi c syndromes
having their own particular associations (eg Down’s is associated with
depression and dementia; Prader–Willi with affective psychosis).
• Behavioural problems (eg Prader–Willi, Angelman syndrome).
Leading causes of death
These include pneumonia (relating to refl ux, aspiration, swallowing, and
feeding problems) and congenital heart disease.
The patient’s perspective
Past experiences of hospital are likely to have a big impact on the patient’s
reaction to his/her current situation. Most patients have problems with
expression, comprehension, and social communication. They fi nd it diffi cult
to describe symptoms — behavioural change may the best indication that
something is wrong.
Tips for communication
• Explain the consultation process before starting.
• Speak fi rst to the patient, then to the carer.
• Use open questions, then re-phrase to check again.
• Aim to use language that the patient understands, modifying this
according to comprehension.
• Patients may have diffi culties with time, so try to relate symptoms to
real life temporal events (eg ‘did the pain start before lunch?’)
• They may not make a connection between something that they have
done and feeling ill (eg several questions may be required in order to
establish that they have ingested something).
• Take particular note of what the carer has to say — information from
someone who knows the patient well is invaluable.

22 CHAPTER 1 General approach
Patient transfer
The need to transfer
When patients have problems that exceed the capabilities of a hospital
and/or its personnel, transfer to another hospital may be needed.
Timing the transfer
Do not commence any transfer until life-threatening problems have been
identifi ed and managed, and a secondary survey has been completed.
Once the decision to transfer has been made, do not waste time
performing non-essential diagnostic procedures that do not change the
immediate plan of care. First, secure the airway (with tracheal intubation
if necessary). Ensure that patients with pneumothoraces and chest injuries
likely to be associated with pneumothoraces have intercostal drains
inserted prior to transfer. This is particularly important before sending a
patient by helicopter or fi xed wing transfer. Consider the need to insert a
urinary catheter and a gastric tube.
Arranging the transfer
Speak directly to the doctor at the receiving hospital. Provide the following
details by telephone or telemedicine link:
• Details of the patient (full name, age, and date of birth).
• A brief history of the onset of symptoms/injury.
• The pre-hospital fi ndings and treatment.
• The initial fi ndings, diagnosis, and treatment in the ED and the response
to treatment.
Write down the name of the doctor responsible for the initial reception
of the patient after transfer. Establish precisely where within the receiving
hospital the patient is to be taken. Where possible, prepare the receiving
unit by sending details ahead by fax/email. Pre-printed forms can help in
structuring the relevant details and avoiding omissions.
Preparing for transfer
Transfer team
If the patient to be transferred may require advanced airway care, ensure
they are accompanied by a doctor who can provide this. The accompanying
nurse should be trained in resuscitation with a good knowledge of the
equipment used during transfer.
Equipment
‘Transfer cases’ containing a standardized list of equipment must be
immediately available and regularly checked. Take all the emergency
equipment and drugs that might prove necessary to maintain the ‘Airway’,
‘Breathing’ and ‘Circulation’ (ABC) during transfer. In particular, take at
least twice the amount of O
2
estimated to be necessary (a standard ‘F’
cylinder contains 1360 L of O
2
and will therefore last <3hr running at 10L/
min). Before leaving, ensure that the patient and stretcher are well-secured
within the ambulance. Send all cross-matched blood (in a suitably insulated
container) with the patient.

23
PATIENT TRANSFER
Monitoring during transfer
Minimum monitoring during transfer includes ECG monitoring, pulse
oximetry, and non-invasive BP measurement. If the patient is intubated
and ventilated, end-tidal carbon dioxide (CO
2
) monitoring is mandatory.
An intra-arterial line is recommended, to monitor BP during the journey.
Make allowances for limited battery life on long transfers: spare batteries
may be needed. Plug monitors and other equipment into the mains supply
whenever possible.
Accompanying documentation
Include the following:
• Patient details : name, date of birth, address, next of kin, telephone
numbers, hospital number, GP.
• History, examination fi ndings, and results of investigations (including
X-ray fi lms).
• Type and volume of all fl uids infused (including pre-hospital).
• Management including drugs given (type, route, and time of
administration), practical procedures performed.
• Response to treatment, including serial measurements of vital signs.
• Name of referring and receiving doctors, their hospitals, and telephone
numbers.
Some departments use standard forms to ensure that important
information is complete.
The relatives
Keep the patient’s relatives informed throughout. Explain where and why
the patient is going. Document what they have been told. Arrange transport
for relatives to the receiving hospital.
Before leaving
Prior to transfer, re-examine the patient. Check that the airway is
protected, ventilation is satisfactory, chest drains are working, IV cannulae
patent and well secured, and that the spine is appropriately immobilized,
but pressure areas protected. Ensure that the patient is well-covered to
prevent heat loss. Inform the receiving hospital when the patient has left
and give an estimated time of arrival.
After leaving
Communicate to the receiving hospital the results of any investigations
that become available after the patient has left. Contact the receiving
doctor afterwards to confi rm that the transfer was completed satisfactorily
and to obtain feedback.
Intra-hospital transfers
In many respects, the only difference between intra- and inter-hospital
transfers is the distance. The principles involved in organizing a transfer
are the same, whether the patient is to be conveyed to the computed
tomography (CT) scanner down the corridor, or to the regional
neurosurgical unit miles away.

24 CHAPTER 1 General approach
Breaking bad news
A proportion of patients presenting to the ED have life-threatening
conditions and some will die in the department. Often, the event will be
sudden and unexpected by family and friends. It may already involve other
family members (eg in the context of a road traffi c collision). In contrast to
hospital inpatients or those in general practice, an opportunity to forewarn
relatives as to what has happened or the eventual outcome is unlikely.
The relatives may already be distressed after witnessing the incident or
collapse, and may have been directly involved in providing fi rst aid.
It is inappropriate for junior hospital staff without suitable experience to
speak with distressed or bereaved relatives. The task must be undertaken
by someone with suffi cient seniority and authority, who also has the skills
of communication and empathy. The most important component is time.
Reception
Relatives usually arrive separately and after the patient. Anticipate
this by designating a member of staff to meet them and show them to
a relatives’ room, which should afford privacy, comfortable seating, an
outside telephone line, tea, coffee, and toilet facilities. Paper tissues, some
magazines, and toys for small children are useful.
While the relatives are waiting, a designated nurse should stay with them
to act as a link with the department and the team caring for the patient.
This nurse can pre-warn relatives of the life-threatening nature of the
patient’s condition and assist in building (an albeit short) relationship
between staff and relatives. The link nurse should also check that
important details have been recorded correctly, eg the patient’s name,
address, date of birth, religion (in case last rites are required), next of kin
(name, relationship to patient, address and phone no.), and the patient’s
GP. This information should be collected as soon as possible, since later
the relatives may be too upset to remember all these details or it may be
diffi cult to ask for them.
Breaking the news
Irrespective of who performs this task, remember a number of points. If
you are the person who informs the relatives, ensure the link nurse is with
you. After leaving the resuscitation room or clinical area, allow a minute
or two of preparation to make yourself presentable, checking clothing for
bloodstains, etc. Confi rm that you know the patient’s name. Enter the
room, introduce yourself, and sit or kneel by the relatives so that you are
at their physical level. Ensure that you speak with the correct relatives and
identify who is who. Speak slowly, keep your sentences short and non-
technical. Do not hedge around the subject. In their emotional turmoil,
relatives very often misconstrue information. Therefore, you may need to
re-emphasize the important aspects.
For many critically ill patients, their ultimate prognosis cannot be deter-
mined in the ED. In these situations, do not raise unrealistic expectations
or false hopes, but be honest and direct with the relatives and the patients.

25
BREAKING BAD NEWS
If the patient has died, then use the words ‘death’ or ‘dead’. Do not use
euphemisms such as ‘passed away’, or ‘gone to a better place’.
After giving the news, allow relatives a few minutes to collect their
thoughts and ask questions. In some cases, these may be unanswerable. It is
better to say ‘we don’t yet know’, rather than confuse or give platitudinous
answers.
Common responses to bad news or bereavement include emotional
distress, denial, guilt, and aggression. The feelings of guilt and anger can
be particularly diffi cult to come to terms with, and relatives may torture
themselves with the idea that if only their actions had been different, the
situation would never have arisen, or the clinical outcome would have been
different.
Relatives seeing patients
Many relatives wish to see or touch their loved ones, however briefl y.
Television and cinema have prepared much of the population for the sights
and sounds in the ED. In some departments, relatives are encouraged to
be present in the resuscitation room. In selected situations the stratagem
has benefi ts. If the relatives are present during resuscitation, it is essential
that the link nurse is present with the relatives to provide support, explain
what is happening, and accompany them if they wish to leave.
More frequently, the relatives can see the patient in the resuscitation room
briefl y or while they are leaving the ED (eg to go to CT scan room or
theatre). Even a few seconds, a few words, and a cuddle can be immensely
rewarding for both relative and patient. The link nurse can give guidance
beforehand as to the presence of injuries (especially those involving the
face), monitors, drips, and equipment, to diminish any threatening impact
that these may have.
When death occurs
Even before death has occurred, involvement of religious leaders is valuable.
As early as possible, inform the hospital chaplain, who can provide
invaluable help to relatives and staff.
When a patient has died, offer the relatives the opportunity to see the
body. This contact, which should be in a private quiet room, can greatly
assist in the grieving process. With careful preparation, most patients who
have died from multiple injuries can be seen by relatives in this fashion.
Remember that followers of some faiths, such as Muslims and Hindus,
have important procedures and rituals to be followed after death,
although these may not always be feasible after a sudden death, especially
from trauma. In such situations, discuss the matter with the Coroner’s or
Procurator Fiscal’s offi cer, and obtain help from an appropriate religious
leader to look after the bereaved relatives.

26 CHAPTER 1 General approach
What to do after a death
Who to contact
Any suspicious death must be immediately reported to the Police who
will liaise directly with the Coroner or Procurator Fiscal (in Scotland).
Following all deaths in the ED, a number of important contacts must be
made as soon as possible:
• Informing the next of kin : if the relatives are not already present in ED, it
may be necessary to ask the Police for assistance.
• Notifying the Coroner (Procurator Fiscal in Scotland).
• Informing the patient’s GP.
• Cancelling hospital outpatient appointments.
• Informing social work and health visitor teams as appropriate.
Ensure deceased’s relatives are given information about the process
for death certifi cation and registration, and how to organize funeral
arrangements. Most EDs have useful leafl ets that cover these matters and
can answer many questions. Some departments have formal arrangements
for counselling after bereavement. Often the GP is the best individual
to co-ordinate bereavement care, but in any event, give the relatives a
telephone number for the ED so they can speak to a senior nurse or
doctor if they need further information or help.
Information for the Coroner or Procurator Fiscal
Report sudden deaths as soon as possible to the Coroner (in Scotland
the Procurator Fiscal). It is helpful to give the following information if it
is available:
• Patient’s name, address, date of birth.
• Next of kin (name, relationship, address, phone no.).
• Patient’s GP.
• Date and time of patient’s arrival in the ED.
• Date and time of patient’s death.
• Name and job title of doctor who pronounced death.
• Details of the incident, injuries, or illness.
• Relevant past medical history.
• When the patient last saw a doctor (the Coroner may be happy for a
GP or hospital doctor to write a death certifi cate if they saw the patient
recently for the condition that caused death, eg a patient with known
terminal cancer).
• The patient’s religion : some faiths may wish to arrange burial before the
next sunset, but this may not be feasible after a sudden death.
• Anything else that is important, eg diffi culties in communication with
the next of kin due to language or deafness.

27
WHAT TO DO AFTER A DEATH
Looking after the staff
The death of a patient or the management of patients with critical illness
inevitably affects the ED staff. This is particularly so when some aspect of
the event reminds staff of their own situation or relatives. These episodes
often occur at the busiest times and when everyone in the ED is working
under pressure.
One of the most diffi cult situations is to have to inform parents of the
death of their child and help them in the initial grieving process, and then
return to the busy department where many people are waiting with
increasingly strident demands. It would be easy to respond that such
individuals, with injuries or illnesses that are minor or present for days or
weeks, are time-wasting. However, this approach will lead to confl ict and
is unfair to all concerned. Instead, take 5 − 10min for a break in the staff
room before returning to the fray. Remember that in these circumstances
you too are a patient. Even senior and experienced staff may be distressed
after diffi cult resuscitation situations and may require support.
Organ donation
There is considerable potential to assist with the process of organ/tissue
donation in the ED. However, the possibility of organ donation is sadly
often overlooked in the ED. Many patients who die after unexpected
cardiac arrest are potential donors of corneal tissue and heart valves.
Kidneys may also be retrieved from some patients who have died in the
ED, if a protocol for this has been arranged with the transplant team and
the local Coroner or Procurator Fiscal. Many other patients who are
moribund, intubated and ventilated (eg following massive subarachnoid
haemorrhage) may be identifi ed as potential donors of other tissues
also. Consider the possibility of organ donation in patients who die in the
ED or who are moribund with no hope of survival. Most hospitals have
specialist organ donation nurses (previously known as ‘donor transplant
coordinators’) who will educate, advise and assist with the process of
organ donation. Useful information about organ/tissue transplantation is
available on the website of the British Transplantation Society (www.bts.
org.uk).

28 CHAPTER 1 General approach
Medicolegal aspects: avoiding trouble
Medicolegal problems are relatively common in the ED. Many of these
problems may be avoided by adopting the correct approach.
Attitude
Be polite and open with patients. Try to establish a good rapport. Be as
honest as possible in explaining delays/errors.
Consent (see General Medical Council guidance)
Use the consent form liberally for anything that is complex, risky, or
involves sedation or general anaesthetic (GA). Ensure that the patient
understands what is involved in the procedure, together with its potential
benefi ts and risks. Whenever possible, attempt to obtain consent from
parent/guardian in minors, but do not delay life-saving treatment in order
to obtain consent.
Documentation ( b Note keeping, p.4)
Good notes imply good practice. Keep careful notes, using simple, clear,
unambiguous language. Write your name legibly and document the time
that you saw the patient. Remember that successful defence of a medical
negligence claim may depend upon accurate, legible, comprehensive,
contemporaneous notes. Try to avoid abbreviations, particularly where
there is room for confusion. In particular, name the digits of the hand
(thumb, index, middle, ring, and little fi ngers) and specify right or left by
writing it in full.
Be meticulous in documenting the nature, size, and position of any wounds
( b p.402). Write down a diagnosis, together with a full interpretation
of any investigations. Ensure that all attached documents (nursing
observations, blood results, ECG) are labelled. Document all instructions
and advice given to the patient, together with any follow-up arrangements
made.
Referral ( b Discharge, referral, and handover, p.8)
Always seek senior help or refer those patients with problems beyond
your knowledge or expertise. Record any referral made, together with
the name and grade of the doctor referred to, the time it was made, and
a summary of the facts communicated. After referral, be cautious about
accepting telephone advice alone — an expert cannot usually provide an
accurate opinion without seeing the patient.
Return visits
Take special care with any patient who returns to ED with the same
presenting complaint, because it is no better, has deteriorated, or the
patient is simply dissatisfi ed. Do not automatically rely upon previous
diagnosis and X-ray interpretations as being correct — treat the patient as
if they were attending for the fi rst time. Try to involve the consultant in
these cases.

29
MEDICOLEGAL ASPECTS: AVOIDING TROUBLE
Discharge against advice
Always attempt to persuade the patient to accept the treatment offered,
but if this is refused, or the patient leaves before being seen, ask the patient
to sign an appropriate form. Patients not deemed competent (see Mental
Capacity Act below) to make this decision may need to be held against
their wishes — seek senior help with this. Write full notes explaining what
happened.
Mental Capacity Act (b p.629)
The Mental Capacity Act 2005 outlines how a person is unable to make a
decision for himself if he/she is unable to:
• Understand the information relevant to the decision.
• Retain the information.
• Use or weight that information as part of the process of making the
decision.
• Communicate his/her decision.
A patient lacks capacity if at the time he/she is unable to make a decision
for himself/herself in relation to the matter because of an impairment or a
disturbance in the functioning of the mind or brain.
Access to records
All ED staff should bear in mind that patients may gain access to their
medical records and read what has been written about them. Patients in
the UK have a statutory right of access to information about themselves
(set out in the Data Protection Act 1998) and this includes medical
records. Competent patients may apply for access to, and copies of, their
own records. Applications are usually made in writing via the hospital’s
legal department.
Medical defence organization
Join a medical defence organization. The Medical Defence Union (MDU),
MDDUS, and Medical Protection Society provide professional indemnity
cover for emergencies outside hospital, and advice and support for all
sorts of medicolegal matters that are not necessarily covered by NHS
trusts, eg statements to the Coroner or Procurator Fiscal, support at
inquests or fatal accident inquiries, allegations of negligence, legal actions,
and problems with the GMC. They also provide members with useful
information and booklets about consent, confi dentiality and other issues.
Further information
www.the-mdu.com/hospital
www.mddus.com
www.medicalprotection.org

30 CHAPTER 1 General approach
Medicolegal aspects: the law
Confi dentiality
Medical information about every patient is confi dential and should not
be disclosed without the patient’s consent. In the UK the police do not
have routine access to clinical information, but some information may be
divulged in certain specifi c circumstances:
• The Road Traffi c Act (1972) places a duty on any person to provide
the police, if requested, with information that might lead to the
identifi cation of a vehicle driver who is suspected of an offence under
the Act. The doctor is obliged to supply the person’s name and address,
but not clinical information.
• Suspicion of terrorist activity.
• Gunshot wounds (see www.gmc-uk.org ).
• Disclosure in the public interest. The General Medical Council advises
that this might include situations where someone may be exposed to
death or serious injury (eg murder, rape, armed robbery, child abuse).
Although this may provide ethical permission for the doctor to reveal
details without consent, it does not place him/her under any legal
duty to do so. Discuss these cases with your consultant and/or your
medical defence organization. (General Medical Council (GMC) advice:
www.gmc-uk.org ).
Ability to drive
A patient’s ability to drive may be impaired by injury (especially limb or
eye), by drugs (eg after GA, opiates, alcohol) or medical conditions (eg
TIAs, epilepsy, arrhythmias). In each case, warn the patient not to drive and
ensure that this warning is documented in the notes. It may be prudent to
provide this warning in the presence of a close relative.
For further information on medical aspects of fi tness to drive see:
www.dft.gov.uk/dvla/medical/ataglance.aspx
Police requests for blood alcohol
In the UK, the police may request a blood or urine sample under
Section 5 of the Road Traffi c Act (1988) from a patient they suspect to
have been in charge of a motor vehicle with an illegal blood alcohol level
( > 80mg/100mL). In such circumstances, specimens should only be taken
if they do not prejudice the proper care and treatment of the patient.
The relevant specimens should only be taken by a police surgeon (clinical
forensic physician) and with the patient’s consent.
A change in the law (Police Reform Act 2002) also allows a police surgeon
to take a blood sample from an unconscious patient who is suspected
of having been the driver of a motor vehicle while under the infl uence
of alcohol and/or drugs. The blood sample is retained and tested later,
depending upon the patient later giving consent. Again, only permit the
police surgeon access to the patient if this will not delay or prejudice
proper care and treatment of the patient.

31
MEDICOLEGAL ASPECTS: THE LAW
Reporting deaths to the Coroner (or Procurator Fiscal)
Many deaths that occur in (or in transit to) the ED are sudden and
unexpected, and/or follow trauma. The exact cause of death is seldom
immediately apparent. Accordingly, do not be tempted to sign death
certifi cates. Instead, report all deaths to the Coroner (the Procurator
Fiscal in Scotland). See b p.26 for details of the information required.
Police statements
Do not provide information to the police until patient consent has been
obtained. Writing a police statement requires thought and care. Write
the statement yourself. Keep statements brief and try to avoid hearsay,
conjecture, or opinion on the likely outcome. List injuries using both
medical and non-medical language, explaining terminology in detail as
necessary. State the investigations and treatment provided as accurately
as possible (eg what sutures and how many were used). Having written
the statement, ask your consultant to read it and comment on it. Get
the statement typed (a friendly ED secretary may help if you cannot
type yourself, and will also know how you can claim the relevant fee).
Having checked it, sign and date the statement, and give it to the offi cer
concerned. Always keep a copy of the statement and the ED notes, so
that they are easily available if you are called to court.
Court appearances
In advance Discuss the case with your consultant, and review the notes,
the questions that you might be asked, and the likely court procedures.
Get a good copy of the notes and any investigations. Ask whether you
should take the original records to court.
On the day Dress smartly, arrive early, and behave professionally. Be
prepared for a long wait, so take a book to read. Turn off your mobile
phone. Once in court, you have the option of taking an oath before God
or affi rming without religious connotation. You are equally bound to tell
the truth whichever you choose. Use the same form of address that others
have already used (eg ‘My Lord’, ‘Your Honour’). Answer directly and
simply. Use comprehensible language, free of medical jargon. Remember
that you are a professional witness, not an expert. Therefore, confi ne
the expression of opinion to within the limits of your knowledge and
experience — if asked something outside this, say so!
Inquest/fatal accident inquiry If you are called to give evidence at an inquest
(in Scotland, a fatal accident inquiry), discuss the case with your consultant
and also with your medical defence society.
Further information and advice about reports and appearing in court
The medical defence organizations ( b p.29) have useful advice sheets for
their members about writing reports and appearing in court.

32 CHAPTER 1 General approach
Infection control and prevention
Staff in the ED have an important role in preventing and controlling
infection, which can be a serious risk to patients, relatives, and staff.
Organisms such as Staph. aureus , including MRSA ( b p.235), can readily
be transmitted by contaminated hands or equipment, causing infection of
wounds, fractures, and in-dwelling devices (eg catheters or chest drains).
Infected blood can transmit many infections, including hepatitis B and C
( b p.239) and human immunodefi ciency virus (HIV; b p.242). Viral gas-
troenteritis is usually spread by the faecal-oral route, but vomiting may
cause widespread viral contamination of the surroundings and equipment,
with a risk of transmission to other patients and staff.
Coughing and sneezing produces small droplets of infected secretions,
which could involve viruses such as infl uenza ( b Infl uenza pandemics,
avian fl u, and swine fl u, p.252), severe acute respiratory syndrome (SARS;
b p.251), and respiratory syncytial virus (RSV; b p.682). A nebulizer
used on an infected patient may spread respiratory viruses widely, as
occurred in the outbreak of SARS in Hong Kong in 2003 which involved
many ED staff.
Standard precautions for preventing infection
Standard precautions (also known as ‘universal precautions’) should be
used at all times and with all patients to reduce the risks of infection.
Blood and body fl uids from all patients should be treated as infected.
These standard precautions include:
• Hand hygiene Essential, but often neglected. Decontaminate your hands
before and after every patient contact, and after any activity that might
contaminate hands, including removing gloves. Hands that are visibly
dirty or possibly grossly contaminated must be washed with soap and
water, and dried thoroughly. Alcohol hand gel can be used if the hands
look clean. Cover broken skin with a waterproof dressing.
• Personal protective equipment (PPE) Wear suitable disposable gloves
for any contact with blood, body fl uids, mucous membranes, or non-
intact skin. Latex gloves are widely used, but cause allergic reactions in
some patients and staff, who need special nitrile gloves. Use a disposable
plastic apron if there is a risk of blood or body fl uids contaminating
clothing. After use, dispose of it and wash your hands. Impervious
gowns are needed if there is a high risk of contamination. Use a mask ,
face shield, and eye protection if blood or body fl uids might splash in
your eyes or mouth. Protection against respiratory viruses, eg SARS
or infl uenza requires special masks or respirators (eg FFP3), which must
be fi tted and used properly. Powered air-purifying respirators should be
used for high-risk procedures such as intubating patients with serious
viral infections.
• Safe handling and disposal of sharps Avoid handling needles directly or
using hand-held needles. Never re-sheathe needles. Place used needles
and blades immediately into a ‘sharps bin’. If possible, use safety needles
and cannulae, which reduce the risk of needlestick injury. If, despite
all precautions, a needlestick injury does occur follow local approved

33
INFECTION CONTROL AND PREVENTION
procedures to minimize the risk of infection and look after the people
involved (see b Needlestick injury, p.418).
• Managing blood and bodily fl uids Samples of blood or other body fl uids
must be handled safely, with care not to contaminate request forms
or the outside of the container. Follow local approved procedures
for dealing with spillages of blood or body fl uids: wear suitable PPE
(usually a disposable apron and gloves) and disinfect the spillage with an
appropriate agent such as diluted bleach.
Planning for outbreaks of infectious diseases
Planning to cope with an outbreak of a serious infectious disease such
as SARS or pandemic fl u ( b p.252) is a considerable challenge for ED
staff and for the whole community. The ED must be organized so that
patients can be assessed properly with a minimum risk of infecting staff or
other patients. If possible, patients with serious airborne diseases should
be treated in negative pressure isolation rooms by staff in appropriate PPE
who are fully trained to minimize the risks of spreading and acquiring the
infection. In high risk situations a ‘buddy’ system for staff may be helpful,
with each doctor or nurse being watched closely by another person to
check that full safety precautions are maintained.
Assessment of febrile patients
Hospitals in Hong Kong with experience of SARS use the FTOCC criteria
when assessing febrile patients for potentially serious infectious diseases:
• F — fever ( > 38 ° C).
• T — travel history.
• O — occupational history.
• C — clustering of cases.
• C — contact history (eg someone with SARS or avian fl u).
Similar criteria are used in the UK Health Protection Agency’s algorithm:
www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/AvianInfl uenza/
Further information
Standard precautions
www.rcn.org.uk/downloads/publications/public_pub/002725.pdf
Masks and respirators
www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/SevereAcute
RespiratorySyndrome/Guidelines/sars040Facemasksand respiratorsFAQ/
Pandemic infl uenza/avian fl u
b Infl uenza pandemic, avian fl u, and swine fl u, p.252.
SARS
b SARS, p.251.

34 CHAPTER 1 General approach
What to carry in your car
If you are interested in out of hospital work, join the British Association for
Immediate Care (BASICS: www.basics.org.uk ), which is a valuable source
of information and expertise. It can give advice on clothing, medical and
protective equipment and their suppliers, and Immediate Care courses.
The equipment that could be carried is extensive. In the UK, except in
the most remote situations, it is likely that an ambulance will be on scene
quickly. Emergency ambulances carry many items of equipment, eg for
intubation, volume infusion and splintage, and also some drugs. There is a
risk of carrying too much equipment in your car and getting diverted from
the primary aims of pre-hospital care, which are to perform only relevant
life-saving techniques, and to transfer the patient rapidly and safely to the
nearest appropriate hospital.
The equipment listed below is a personal choice based on experience
attending out-of-hospital calls over the past 20 years:
Personal equipment
• High quality wind/waterproof refl ective jacket and over-trousers. If your
fi nances do not run to this, at least have a refl ective ‘Doctor’ tabard.
• Protective helmet.
• Protective footwear — leather boots with steel toecaps are ideal.
• 2 pairs of latex gloves.
• 1 pair of protective gloves (eg leather gardening gloves).
General equipment
• Refl ective warning triangle.
• Fire extinguisher.
• Heavy-duty waterproof torch.
• Clothes-cutting scissors.
• Mobile phone.

35
WHAT TO CARRY IN YOUR CAR
Medical equipment
The equipment listed is only of value if you know how to use it, it is secure
(ie locked in a case in a locked vehicle), and it is in date:
• Stethoscope.
• Hand-held suction device + Yankauer and soft fl exible suckers.
• Laryngoscope, adult curved blade, spare batteries, and bulb.
• Selection of tracheal tubes of varying sizes + syringe to infl ate cuff.
• Magill’s forceps.
• Selection of oropharyngeal and nasopharyngeal airways.
• Laerdal pocket mask.
• Venous tourniquet.
• Selection of IV cannulae (2 each of 14G and 16G) and syringes.
• 2 × IV-giving sets.
• 2 × 1000mL 0.9 % saline bags.
• 1 roll of 1-inch zinc oxide tape.
• 1 roll of 3-inch Elastoplast.
• Small selection of dressings and bandages.
• Cervical collar.
• Cricothyrotomy kit.
• Intercostal chest drain set.
• 2 × 0/0 silk suture on a hand-held cutting needle.
• Local anaesthetic, eg lidocaine 1 % (for nerve blocks).
• Splints for IV cannulation sites.

36 CHAPTER 1 General approach
At the roadside
Priorities
It is easy in an emergency to forget the simplest, most life-saving
procedures. At worst, an individual trying to help can aggravate the
situation, slow the process of care, and even become a casualty
themselves.
If you arrive fi rst at the scene of a collision, the initial priority is to ensure your
own safety and that of other rescuers.
• Park safely so your car will not obstruct other vehicles (including
emergency vehicles), preferably where its presence will alert other road
users to the collision. Put your hazard warning lights on. If you have a
warning beacon, put it on the roof of the car and switch it on.
• If you have a mobile phone, dial ‘999’ and request ambulance, fi re, and
police to attend. Remember to give the exact location, a brief description
of the incident, and number of casualties. Tell the emergency service
operator who you are, as well as the number of your mobile phone.
• Switch off the engine of your car and of any other vehicles.
• Ensure that no-one is smoking or displays a naked fl ame.
• Events involving electricity or chemicals have specifi c hazards.
Involvement of overhead or underground electric cables poses risks,
compounded if water is involved or sparks produced. The risk from high
tension cables extends for several metres. Phone the power company
to ensure that the source is turned off before approaching. Electrifi ed
rail lines may be short-circuited by a trained individual using a special
bar carried in the guard’s compartment.
Chemical incidents
Do not approach a chemical incident until declared safe by the Fire
Service. Lorries carrying hazardous chemicals must display a ‘Hazchem’
board (see Fig. 1.2 ). This has:
• Information on whether the area should be evacuated, what protective
equipment should be worn, aspects relating to fi re-fi ghting, and if the
chemical can be safely washed down storm drains (top left). A white
plate means that the load is non-toxic.
• A 4-digit UN product identifi cation number (middle left).
• A pictorial hazard diamond warning (top right).
• An emergency contact number (bottom).
The European ‘Kemler’ plate contains only the UN product number
(bottom) and a numerical hazard code (top) — a repeated number means
intensifi ed hazard. Mixed loads <500kg may only be identifi ed by a plain
orange square at the front and rear of the vehicle.
The transport emergency card (TREM card) carried in the driver’s cab
gives information about the chemical for use at the scene of a crash. The
fi re tender may be equipped with CHEMDATA — a direct link with the
National Chemical Information Centre at Harwell. Alternatively, contact
a Poisons Information Centre or the transport company.
Helicopters
If helicopters are used for transport/evacuation, remember:
• Communications in or near helicopters are diffi cult because of the noise.
• Ensure any loose objects are secured to prevent them being blown away.
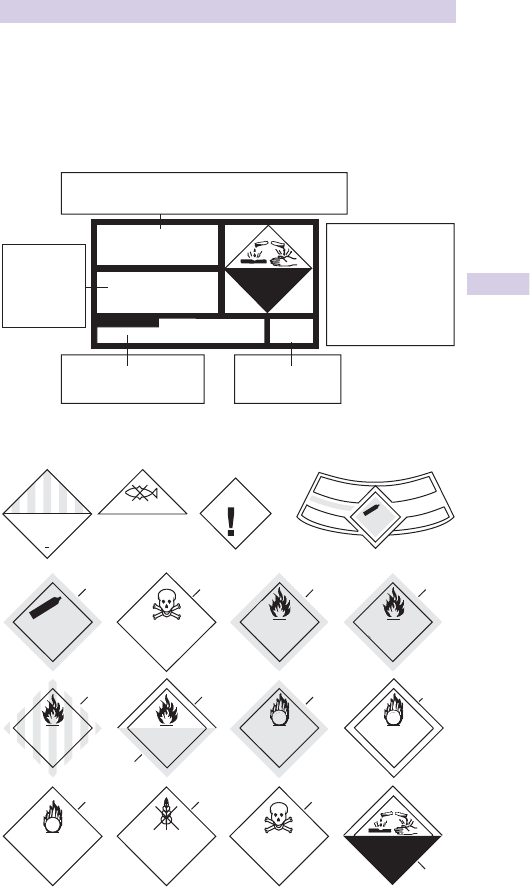
37
AT THE ROADSIDE
• Never enter the landing space area during landing or take-off.
• Never enter or leave the rotor disc area without the pilot’s permission.
• Duck down in the rotor disc area and only approach in full view of the pilot.
• If the helicopter cannot land and the winch is used, do not touch the cable
before it has touched the ground to earth any static electrical charge.
Hazchem advice for the control of the chemical
Specialist advice
and telephone number
Suppliers name
(optional)
0705 826435
Danger labels
Specialist advice
Bromoacetyl bromide
Corrosive
2513
4WE
Pace
transport
Hazard symbol and
description in a
diamond on white
square background
(rest of label is black
lettering on an
orange backround)
Substance
identification
number and
name
Multiload
Marine pollutant
9
Other dangerous
substance
Green
Compressed
gas
2
Red/white
stripes
4.1
Red
Yellow
Organic
peroxide
5.2
6.1
stow a way
from
foodstuffs
Harmful
White White
Toxic
6.1
Corrosive
8
Black
Yellow
5.1
BlueWhite
White Red
Compressed
gas
Red
Flammable
liquid
2
2
2
Poision
gas
Flammable
gas
Oxidising agent
4.1
Spont aneously
combustible
Flammable
solid
O
x
y
g
e
n
O
2
U
.
N
.
1
0
7
2
Fig. 1.2 Hazchem advice and danger labels.

38 CHAPTER 1 General approach
Major incidents
A major incident involves a lot of people. The casualties may have multiple
injuries, minor injuries/burns, or other emergencies such as food poisoning
or chemical inhalation. Every hospital accepting emergencies has a Major
Incident plan to use when the normal resources are unable to cope and
special arrangements are needed. There will be action cards for key staff
detailing their duties. All staff need to familiarize themselves with their
roles in advance.
Call-in lists must be up to date and available at all times.
Major incident practices must be held regularly to check arrangements and
contact details and to remind staff what they should do.
Alert
The ambulance service or the police should warn the hospital of a possible
or defi nite major incident. Initial messages are often inaccurate because
they are based on confused and incomplete information from the scene.
Occasionally, patients arrive without warning from a major incident near
the hospital.
Ensure that the ED consultant on duty is informed immediately of any
suspected major incident, enabling them to participate in the decision
to start the major incident procedure. Senior medical, nursing, and
administrative staff will set up the hospital’s Control Centre and prepare
for action. If the major incident is confi rmed, the full hospital response is
initiated, following the procedures in the plan.
Communications are vital, but switchboards rapidly become overloaded.
Staff should therefore be called in using non-switchboard phones if
possible. All staff should wear their identifi cation badges.
Action in the ED
• Check that the ED consultant and hospital switchboard know about the
incident and that the major incident procedure has been started.
• Inform all ED staff on duty (doctors, nurses, receptionists, porters).
• Call in other ED staff in accordance with the Major Incident plan.
• Clear the ED of any patients who are not seriously ill or injured. Prepare
the department to receive patients from the incident.
• Doctors and nurses arriving to help should be given appropriate action
cards. Staff should have labels or tabards so that ED staff and other
specialties (eg anaesthetists) can be identifi ed easily.
• Prepare a triage point at the ambulance entrance. This should be
staffed by a senior doctor and nurse who direct patients to the most
appropriate area of the department. If possible, a nurse should stay with
each patient until he/she is discharged or admitted to a ward.
• All patients should be labelled immediately with a unique Major Incident
number, which is used on all notes, forms, blood samples, property
bags, and lists of patients. Collect names, addresses, and other details as
soon as possible, but this must not delay triage or emergency treatment.
Keep lists of anyone leaving the ED.
• Ensure that the hospital Control Centre is regularly updated regarding
the situation in the ED.

39
MAJOR INCIDENTS
Wards and theatres
Beds must be cleared to receive patients, preferably on 1 or 2 wards,
rather than many different wards. A senior surgeon should triage patients
needing operations and co-ordinate theatre work.
Relatives and friends
Relatives and friends of casualties should be looked after by social workers
and chaplaincy staff in an area near to, but separate from, the ED, perhaps
in the outpatient department. Keep relatives informed as soon and as
much as possible. Security staff at each entrance to the ED should direct
relatives and friends of casualties to the appropriate area and not allow
them into the ED.
Press
Journalists and television crews will arrive rapidly after a major incident.
Keep them out of the ED — direct them to a pre-arranged room to be
briefed by a press offi cer and senior staff.
Arrangements at the site of a major incident
The police are in overall command. The fi re service take control of the
immediate area if there is a fi re or chemical risk. The police, fi re, and
ambulance services will each have a control vehicle, with an Incident
Offi cer to co-ordinate their staff and the rescue work.
There may be a Medical Incident Offi cer (MIO) and also a Mobile Medical
Team of doctors and nurses, who should if possible be sent from a
supporting hospital, rather than the hospital receiving the fi rst casualties.
These staff must be properly clothed (yellow and green high-visibility
jacket marked ‘Doctor’ or ‘Nurse’, over trousers, green helmet with visor
and chin strap, safety boots, gloves, knee pads, torch, ID badge), and must
be trained and equipped with suitable medical supplies and action cards.
The mobile medical team must report to the MIO, who is in charge of all
medical and nursing staff on site and works closely with the Ambulance
Incident Offi cer (AIO). The MIO should record the names of the mobile
medical team and brief them about their duties and the site hazards and
safety arrangements. The MIO is responsible for supervising the team,
arranging any necessary equipment and supplies, and making sure that the
team are relieved when necessary. The MIO and AIO relay information to
the hospitals and distribute casualties appropriately.
Debriefi ng staff
Debriefi ng is important after a major incident, so that staff can discuss
what happened and express their feelings. Mutual support of the team
is essential. Counselling may be required. Senior staff should prepare a
report on the incident and review the major incident plan.
Further information
NHS Emergency Planning guidance
www.dh.gov.uk/en/Managingyourorganisation/Emergencyplanning/index.htm
CBRN (Chemical, Biological, Radiological and Nuclear) incidents
b Decontamination of patients, p.211.
This page intentionally left blank

41
Anaphylaxis 42
Treatment algorithm for adults with anaphylaxis 44
Choking 45
Cardiac arrest 46
In-hospital resuscitation algorithm 47
Adult basic life support 48
Cardiac arrest management 50
Advanced life support algorithm 52
Notes on using the advanced life support algorithm 53
Post-resuscitation care 54
Central venous access 56
Severe sepsis and septic shock 59
Shock 60
Life-threatening
emergencies
Chapter 2
Life-threatening emergencies in children are considered in
Chapter 15, Paediatric emergencies
631
b Paediatric basic life support 646
b Choking from a foreign body 648
b Anaphylaxis in children 650
b Paediatric advanced life support 652

42 CHAPTER 2 Life-threatening emergencies
Anaphylaxis
( Anaphylaxis in children is covered in b p.650)
Anaphylaxis is a generalized immunological condition of sudden onset,
which develops after exposure to a foreign substance. The mechanism may:
• Involve an IgE-mediated reaction to a foreign protein (stings, foods,
streptokinase), or to a protein–hapten conjugate (antibiotics) to which
the patient has previously been exposed.
• Be complement mediated (human proteins eg G -globulin, blood
products).
• Be unknown (aspirin, ‘idiopathic’).
Irrespective of the mechanism, mast cells and basophils release mediators
(eg histamine, prostaglandins, thromboxanes, platelet activating factors,
leukotrienes) producing clinical manifestations. Angio-oedema caused by
ACE inhibitors and hereditary angio-oedema may present in a similar way
to anaphylaxis. Hereditary angio-oedema is not usually accompanied by
urticaria and is treated with C1 esterase inhibitor.
Common causes
• Drugs and vaccines (eg antibiotics, streptokinase, suxamethonium,
aspirin, non-steroidal anti-infl ammatory drugs (NSAIDs), intravenous
(IV) contrast agents).
• Hymenoptera (bee/wasp) stings.
• Foods (nuts, shellfi sh, strawberries, wheat).
• Latex.
Clinical features
The speed of onset and severity vary with the nature and amount of the
stimulus, but the onset is usually in minutes/hours. A prodromal aura or a
feeling of impending death may be present. Patients on B -blockers or with
a history of ischaemic heart disease (IHD) or asthma may have especially
severe features. Usually two or more systems are involved:
Respiratory Swelling of lips, tongue, pharynx, and epiglottis may lead to
complete upper airway occlusion. Lower airway involvement is similar to
acute severe asthma — dyspnoea, wheeze, chest tightness, hypoxia, and
hypercapnia.
Skin Pruritus, erythema, urticarial, and angio-oedema.
Cardiovascular Peripheral vasodilation and i vascular permeability cause
plasma leakage from the circulation, with d intravascular volume, hypoten-
sion, and shock. Arrhythmias, ischaemic chest pain, and electrocardiogram
(ECG) changes may be present.
GI tract Nausea, vomiting, diarrhoea, abdominal cramps.

43
ANAPHYLAXIS
Treatment
• Discontinue further administration of suspected factor (eg drug).
Remove stings by scraping them carefully away from skin.
• Give 100 % oxygen (O
2
).
• Open and maintain airway. If upper airway oedema is present, get
specialist senior help immediately. Emergency intubation or a surgical
airway and ventilation may be required.
• In patients with shock, airway swelling, or respiratory diffi culty give 0.5mg
(0.5mL of 1:1000 solution) adrenaline intramuscular (IM). Repeat after
5min if there is no improvement. In adults treated with an adrenaline auto-
injector (eg EpiPen
®
) the 300mcg dose is usually suffi cient, but additional
doses may be required. Give only 50 % of the usual dose of adrenaline to
patients taking tricyclic antidepressants, MAOIs, or B –blockers.
• In profound shock or immediately life-threatening situations, give CPR/
ALS as necessary, and consider slow IV adrenaline 1:10,000 or 1:100,000
solution. This is recommended only for experienced clinicians who can
also obtain immediate IV access. Note the different strength of adrenaline
required for IV use. If there is no response to adrenaline, consider glucagon
1–2mg IM/IV every 5min (especially in patients taking B -blockers).
• Give a B
2
-agonist (eg salbutamol 5mg) nebulized with O
2
for
bronchospasm, possibly with the addition of nebulized ipratropium
bromide 500mcg.
• Give IV fl uid if hypotension does not rapidly respond to adrenaline.
Rapid infusion of 1–2L IV 0.9 % saline may be required, with further
infusion according to the clinical state.
• Antihistamine H
1
blockers (eg chlorphenamine 10–20mg slow IV) and
H
2
blockers (eg ranitidine 50mg IV) are commonly given. They are
second line drugs that, with hydrocortisone 100–200mg slow IV, may
reduce the severity/duration of symptoms.
• Admit/observe after initial treatment: prolonged reactions and biphasic
responses may occur. Observe for at least 4–6hr after all symptoms
have settled.
Report anaphylactic reactions related to drugs/vaccines to the Committee
on Safety of Medicines. Further investigation of the cause (and possibly
desensitization) may be indicated. Where identifi ed, the patient and
GP must be informed and the hospital records appropriately labelled.
Medic-Alert bracelets are useful.
Notes on treatment algorithm on b p.44
1 An inhaled B
2
-agonist such as salbutamol may be used as an adjunctive
measure if bronchospasm is severe and does not respond rapidly to
other treatment.
2 If profound shock judged immediately life-threatening give CPR/ALS if
necessary. Consider slow IV adrenaline (epinephrine) 1:10,000 solution.
This is hazardous and is recommended only for an experienced practitioner
who can also obtain IV access without delay. Note the different strength of
adrenaline (epinephrine) that may be required for IV use.
3 If adults are treated with an EpiPen
®
the 300mcg will usually be suffi cient.
A second dose may be required. Half doses of adrenaline (epinephrine)
may be safer for patients on amitriptyline, imipramine, or B -blocker.
4 A crystalloid may be safer than a colloid.
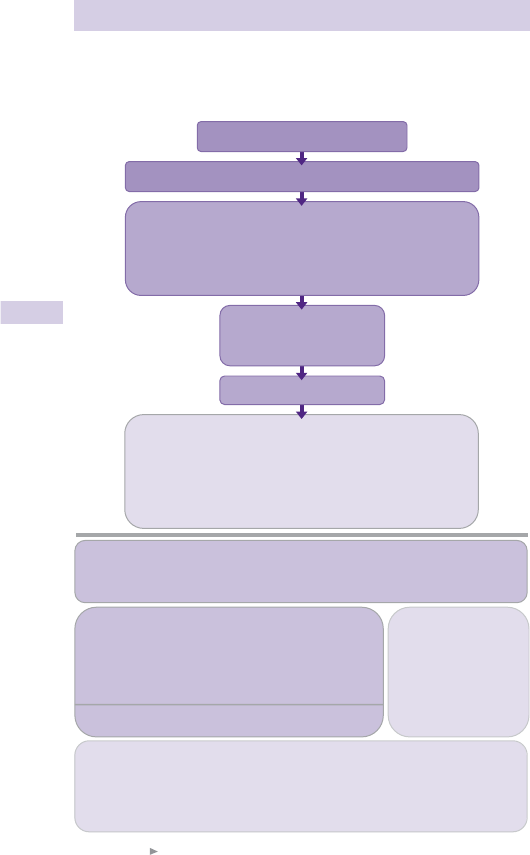
44 CHAPTER 2 Life-threatening emergencies
Treatment algorithm for adults with
anaphylaxis
1
1 Resuscitation Council (UK) guidelines , 2008 . See: www.resus.org.uk
Fig. 2.1 Anaphylaxis algorithm.
When skills and equipment available:
• Establish airway
• High flow oxygen
• IV fluid challenge
3
• Chlorphenamine
4
• Hydrocortisone
5
Monitor:
• Pulse oximetry
• ECG
• Blood pressure
1 Life-threatening problems:
Airway: Swelling, hoarseness, stridor
Breathing: Rapid breathing, wheeze, fatigue, cyanosis, SpO
2
< 92%, confusion
Circulation: Pale, clammy, low blood pressure, faintness, drowsy/coma
3 IV fluid challenge:
Adult - 500–1000 mL
Child - crystalloid 20 mL/kg
Stop IV colloid
if this might be the cause
of anaphylaxis
4 Chlorphenamine 5 Hydrocortisone
200 mg
100 mg
50 mg
10 mg
5 mg
2.5 mg
Child less than 6 months
250 micrograms/kg 25 mg
2 Adrenaline (give IM unless experienced with IV adrenaline)
IM doses of 1:1000 adrenaline (repeat after 5 min if no better)
• Adult: 500 micrograms IM (0.5 mL)
• Child more than 12 years: 500 micrograms IM (0.5 mL)
• Child 6–12 years: 300 micrograms IM (0.3 mL)
• Child less than 6 years: 150 micrograms IM (0.15 mL)
Adrenaline IV to be given only by experienced specialists
Titrate: Adults 50 micrograms; Children 1 microgram/kg
Adrenaline
2
Call for help
• Lie patient flat
• Raise patient’s legs
Diagnosis - look for:
• Acute onset of illness
• Life-threatening airway and/or breathing
and/or circulation problems
1
• And usually skin changes
Airway, Breathing, Circulation, Disability, Exposure
Anaphylactic reaction?
See also: Anaphylactic reactions – Initial treatment
Adult or child more than 12 years
Child 6–12 years
Child 6 months to 6 years
(IM or slow IV) (IM or slow IV)
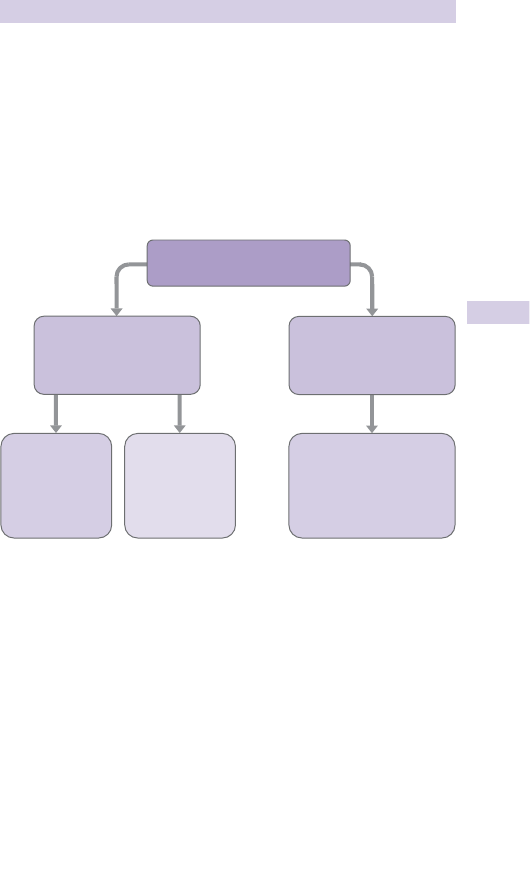
45
CHOKING
Choking
The management of choking is rightly taught as part of fi rst aid. Recognition
of the problem is the key to success. Clues include a person experiencing
a sudden airway problem whilst eating, possibly combined with them
clutching their neck.
Severity of airway obstruction
Victims with severe airway obstruction may be unable to speak or breathe
and become unconscious (see Fig. 2.2 ).
1 Resuscitation Council (UK) guidelines, 2010 ( www.resus.org.uk )
Fig. 2.2 Adult choking algorithm.
1
Unconscious
Start CPR
Conscious
5 back blows
5 abdominal
thrusts
Encourage cough
Continue to check for
deterioration to ineffective
cough or until obstruction
relieved
Assess severity
Mild
Airway obstruction
(effective cough)
Severe
Airway obstruction
(ineffective cough)

46 CHAPTER 2 Life-threatening emergencies
Cardiac arrest
Clinical features and recognition
Follow resuscitation algorithm ( www.resus.org.uk ) shown opposite.
Cardiac arrest is a clinical diagnosis:
• Suspect cardiac arrest in any patient who is unconscious and who
does not have signs of life. If you check a pulse, examine only for a
major (carotid or femoral) one and take no longer than 10sec. Other
‘confi rmatory’ clinical features (eg colour, pupil size/response) waste
time and do not help. Note that some respiratory efforts, such as
gasping, may persist for several minutes after the onset of cardiac arrest.
Occasionally, an arrest may present as a grand mal fi t of short duration.
• Most patients have had a sudden and unexpected out-of-hospital event.
Prior warning to the department is usually relayed by radio or direct
telephone link from the Ambulance Service. While resuscitation is
continued, ensure that accompanying relatives/friends are met and taken
to an appropriate room, which has a telephone, facilities for making tea
and coffee, and where privacy is possible. Arrange for a member of staff to
stay with the relatives to act as a link with the Resuscitation Team.
Information to obtain from ambulance crew/relatives
• Patient details : including age, past medical history, current medication,
chest pain before event
• Times of : collapse (often an approximation), 999 (or 112) call, arrival on
scene, start of cardiopulmonary resuscitation (CPR), fi rst defi brillating
shock (if appropriate), other interventions (eg advanced airway
management, drugs), restoration of spontaneous circulation (ROSC)
• Was there any bystander CPR ?
Where a patient in cardiac arrest is brought to hospital by ambulance, the
cardiac arrest team (ED staff, the hospital team, or a combination of both)
should already be present in the resuscitation room with all equipment
ready to receive the patient.
The team leader
The team leader controls, co-ordinates, organizes the team and makes
treatment decisions. 4–6 team members are optimal. Each should know
their role. Perform resuscitation in a calm, quiet, confi dent manner with
minimal interruption to the performance of basic life support (BLS) or
defi brillation.
Start the following procedures simultaneously:
• Continue BLS.
• Remove/cut clothing from the upper body to allow defi brillation,
ECG monitoring, chest compression, and IV access.
• Obtain the ECG trace (through defi brillator pads or monitor leads).
If already attached to an ECG monitor, note (print out if possible) the
rhythm. Beware movement artefact, disconnected leads, electrical
interference, etc.
• Follow the ALS algorithm ( b p.52).
• Do not interrupt CPR except to perform defi brillation.
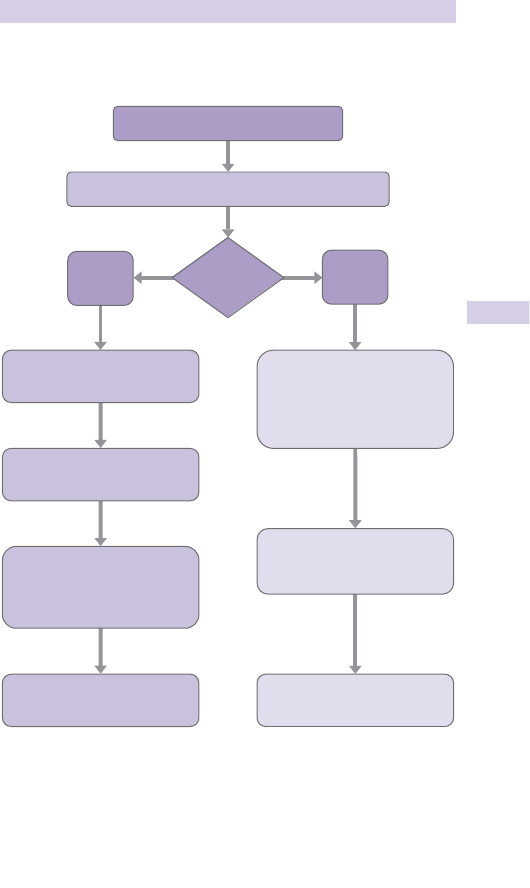
47
IN-HOSPITAL RESUSCITATION ALGORITHM
In-hospital resuscitation algorithm
1
1 Resuscitation Council (UK) guidelines , 2010 ( www.resus.org.uk ).
Fig. 2.3
Advanced life support
when resuscitation team arrives
Shout for HELP and assess patient
Collapsed/sick patient
Handover
to resuscitation team
NO
Signs
of life?
YES
Call resuscitation team
CPR 30:2
with oxygen and airway adjuncts
Apply pads/monitor
Attempt defibrillation
if appropriate
Assess ABCDE
Recognise and treat
Oxygen, monitoring,
IV access
Call resuscitation team
if appropriate
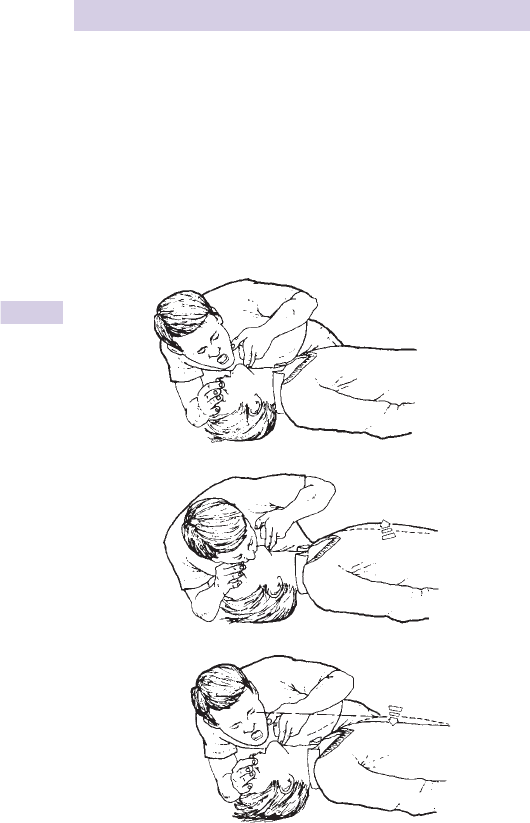
48 CHAPTER 2 Life-threatening emergencies
Adult basic life support
Airway and ventilation
Usually in the ED, advanced airway techniques will be used from the
outset. If basic techniques are used (Fig. 2.4 ):
• With the patient on his/her back, open the airway by tilting the head
and lifting the chin. (Use jaw thrust instead if neck trauma suspected.)
• Remove any visible obstructions from the mouth, but leave well-fi tting
dentures in place.
• Aim for each breath to last 8 1sec and make the chest rise. After each
breath, maintain the head tilt/chin lift, take your mouth away from the
patient’s and watch for the chest to fall as the air comes out.
1 Colquhoun MC et al . (1999). ABC of Resuscitation , 4th edition. BMJ Books, London.
Fig. 2.4 Mouth to mouth ventilation.
1

49
ADULT BASIC LIFE SUPPORT
Technique for chest compression (Fig. 2.5 )
• Place the heel of one hand over the middle of the lower half of the
patient’s sternum, with the other hand on top. Extend or interlock
the fi ngers of both hands and lift them to avoid applying pressure to the
patient’s ribs.
• Positioned above the patient’s chest and with arms straight, press down
to depress the sternum 5–6cm.
• Release all the pressure and repeat at a rate of 100–120/min.
• Compression and release phases should take the same time.
• Use a ratio of 30 chest compressions to 2 ventilations (30:2).
• Aim to change the person providing chest compressions every 2 min,
but ensure that this is achieved without causing signifi cant pauses.
1 Colquhoun MC et al . (1999). ABC of Resuscitation , 4th edition. BMJ Books, London.
Fig. 2.5 Chest compressions.
1

50 CHAPTER 2 Life-threatening emergencies
Cardiac arrest management
Defi brillation
• Most survivors have an initial rhythm of VF/VT. The treatment for this
is defi brillation. With time, the chances of successful defi brillation and
survival d dramatically. Adhesive defi brillator pads have replaced manual
paddles in most hospitals. Place one pad to the right of the upper
sternum below the clavicle, the other in mid-axillary line level with V
6
ECG electrode position. Avoid placement over the female breast. To
avoid problems with pacemakers, keep pads > 15cm away from them.
• With biphasic defi brillators, use shock energy of 150J, for (mostly older)
monophasic defi brillators, select 360J energy.
• Plan for chest compressions to be as continuous as possible, with
minimal delays. Having paused briefl y to assess the rhythm, recommence
compressions until the defi brillator is charged. Pause briefl y to deliver
a shock (removing O
2
sources and transdermal glycerol trinitrate
(GTN) patches), then immediately restart CPR with 30:2 compressions:
ventilation, and continue for 2min before reassessing the rhythm or
feeling for a pulse.
• In monitored patients with pulseless ventricular tachycardia/fi brillation
(VT/VF) where defi brillation is not immediately available, give a single
precordial thump . With a tightly clenched fi st, deliver one direct blow
from a height of 820cm to the lower half of the sternum.
Airway management
Techniques for securing the airway, providing oxygenation and ventilation
are covered in b Airway obstruction: basic measures, p.324. Although
tracheal intubation has long been considered to be the gold standard
defi nitive airway, only attempt this if suitably experienced. Laryngeal
mask airway is a readily available, rapid alternative, which is easy to insert.
Whatever method is used, aim to ventilate (preferably with 100 % O
2
) using
an inspiratory time of 1sec, a volume suffi cient to produce a normal rise of the
chest, at a rate of 10/min. For patients with tracheal tubes or laryngeal mask
airways, ventilate without interrupting chest compressions, which should be
continuous (except for defi brillation or pulse checks as appropriate).
End-tidal CO
2
monitoring is very useful to confi rm correct tracheal tube
placement and indirectly measure cardiac output during CPR.
Drugs
There is little evidence that any drug improves outcome. Central venous
cannulation is diffi cult, has risks and interrupts CPR. Peripheral access
is easy and quick. Having given a peripheral IV drug, give a 20mL saline
bolus and elevate the limb for 10–20sec. If IV access is impossible, consider
intraosseous route ( b p.640). It is no longer recommended for any
drugs to be given by tracheal tube. Similarly, do not attempt intracardiac
injections.
The fi rst drug used in cardiac arrest (after oxygen) is adrenaline. In
the case of VF/VT, administer adrenaline after three shocks, whereas
in asystole/PEA, give it as soon as possible (see b Adult life support
algorithm, p.52).
51
CARDIAC ARREST MANAGEMENT
Non-shockable rhythms: PEA and asystole
Pulseless electrical activity ( PEA ) is the clinical situation of cardiac arrest with
an ECG trace compatible with cardiac output. PEA may be caused by:
• Failure of the normal cardiac pumping mechanism (eg massive MI,
drugs such as B -blockers, Ca
2 +
antagonists or electrolyte disturbance,
eg hypokalaemia, hyperkalaemia).
• Obstruction to cardiac fi lling or output (eg tension pneumothorax,
pericardial tamponade, myocardial rupture, pulmonary embolism (PE),
prosthetic heart valve occlusion, and hypovolaemia).
Prompt and appropriate correction of these can result in survival. Remember
potentially reversible causes as the 4H’s and 4T’s (see Table 2.1 ).
Asystole is the absence of cardiac (particularly ventricular) electrical activity.
If unsure if the rhythm is asystole or fi ne VF, continue chest compressions
and ventilation in an attempt to increase the amplitude and frequency of
VF, and make it more susceptible to defi brillation.
Length of resuscitation
The duration of the resuscitation attempt depends upon the nature of
the event, the time since the onset, and the estimated prospects for a
successful outcome. In general, continue resuscitation while VF/pulseless
VT persists, always provided that it was initially appropriate to commence
resuscitation. If VF persists despite repeated defi brillation, try changing
pad position or defi brillator.
Asystole unresponsive to treatment and arrests which last > 1hr are rarely
associated with survival. However, exceptions occur — particularly in
younger patients, hypothermia, near drowning, and drug overdose.
Mechanical CPR
There are several devices available that can provide mechanical CPR.
These include the ‘AutoPulse’ circumferential load-distributing band chest
compression device (comprising a pneumatically actuated constricting band
and backboard) and the ‘LUCAS’ gas-driven sternal compression device (with
accompanying suction cup to provide active decompression). Widespread
use of these devices may develop if early encouraging results are confi rmed
by larger studies. Mechanical CPR is potentially very useful in situations where
the resuscitation attempt is prolonged (eg cardiac arrest associated with
hypothermia, poisoning or following fi brinolytic treatment for PE), ensuring
consistent CPR over a long period of time and freeing up an additional
member of the team.
Table 2.1
4H’s 4T’s
Hypoxia Tension pneumothorax
Hypovolaemia Tamponade (cardiac)
Hyper/hypokalaemia/metabolic
disorders
Toxic substances (eg overdose)
Hypothermia Thromboembolic/mechanical obstruction
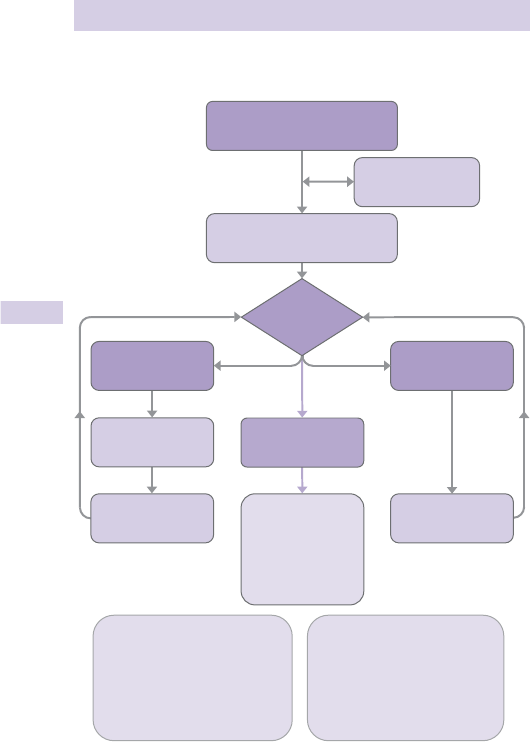
52 CHAPTER 2 Life-threatening emergencies
Advanced life support algorithm
1
1 Resuscitation Council (UK) guidelines , 2010 ( www.resus.org.uk ).
Fig. 2.6
CPR 30:2
Attach defibrillator/monitor
Minimise interruptions
Shockable
(VF/Pulseless VT)
1 Shock
During CPR
• Ensure high-quality CPR: rate, depth, recoil
• Plan actions before interrupting CPR
• Give oxygen
• Consider advanced airway and capnography
• Continuous chest compressions when advanced
airway in place
• Vascular access (intravenous, intraosseous)
• Give adrenaline every 3–5 min
• Correct reversible causes
Reversible causes
• Hypoxia
• Hypovolaemia
• Hypo-/hyperkalaemia/metabolic
• Hypothermia
• Thrombosis - coronary or pulmonary
• Tamponade - cardiac
• Toxins
• Tension pneumothorax
Non-Shockable
(PEA/Asystole)
Call
resuscitation team
Unresponsive?
Not breathing or
only occasional gasps
Return of
spontaneous
circulation
Immediately resume
CPR for 2 min
Minimise interruptions
Immediately resume
CPR for 2 min
Minimise interruptions
Immediate post cardiac
arrest treatment
• Use ABCDE approach
• Controlled oxygenation and
ventilation
• 12-lead ECG
• Treat precipitating cause
• Temperature control/
therapeutic hypothermia
Assess
rhythm

53
NOTES ON USING THE ADVANCED LIFE SUPPORT ALGORITHM
Notes on using the advanced life
support algorithm
• Establish the underlying cardiac rhythm as quickly as possible in order to
determine which ‘loop’ to follow to provide appropriate treatment —
for VF/pulseless VT, the initial focus is defi brillation and good CPR; for
asystole/PEA, the initial focus is good CPR, IV adrenaline, and searching
for potentially reversible causes.
• Do not interrupt CPR except to perform defi brillation.
• Search for and correct potentially reversible causes of the arrest.
• Give IV adrenaline 1mg and amiodarone 300mg for VF/pulseless VT
refractory to three shocks, followed by 1mg adrenaline every 3–5min.
A further dose of 150mg IV amiodarone may be given for recurrent or
refractory VF/VT. Lidocaine (1mg/kg) IV is an alternative to amiodarone,
but do not give it if amiodarone has already been given.
• For torsade de pointes, and refractory VF in patients with suspected
digoxin toxicity or hypomagnesaemia (eg on K
+
losing diuretics), give IV
magnesium sulphate 2g (= 8mmol = 4mL of 50 % solution).
• In asystole and PEA, give IV 1mg adrenaline as soon as possible and
thereafter every 3–5min.
• Exercise caution before using adrenaline in arrests associated with
cocaine or other sympathomimetic drugs.
• Atropine is no longer routinely recommended in asystole or slow PEA.
• In PEA arrests associated with hyperkalaemia, hypocalcaemia, or Ca
2 +
channel blocking drug or magnesium overdose, give 10mL 10 % IV
calcium chloride (6.8mmol).
• With good quality CPR, acidosis develops slowly. Do not ‘routinely’ give
an alkali. Give 50mL of sodium bicarbonate 8.4 % solution (50mmol) if
arrest is associated with tricyclic overdose ( b p.194) or hyperkalaemia
and consider it in patients with severe acidosis (arterial pH<7.1, base
excess less than –10). Allow further administration to be guided by
repeated arterial blood gas (ABG) results.
• Follow loops of the algorithm for as long as it is considered appropriate
for the resuscitation to continue. Provided that the attempt was
commenced appropriately, it should not normally be stopped if the
rhythm is still VF.
Pacing and external cardiac percussion
Pacing may be of value in patients with extreme bradyarrhythmias, but its
value in asystole is unproven (except for rare cases of trifascicular block
with P waves present). If there is a delay before pacing can be performed,
external cardiac percussion can provide a cardiac output and ‘buy time’.
Perform external cardiac percussion using a clenched fi st:
• Over the heart at a rate of 100/min.
• With a blow more gentle than a precordial thump.
• Each blow should generate a QRS complex. If this, and a detectable
output, is not achieved restart conventional CPR.

54 CHAPTER 2 Life-threatening emergencies
Post-resuscitation care
Features such as coma or pupil refl exes are unreliable prognostic
indicators in the early post-resuscitation phase. Accurate prognostication
in an individual patient is rarely possible before 24–72hr. Involve the
intensive care unit/critical care unit (ICU/CCU) team early.
Pending this and following ROSC
• Ensure that the airway is protected ( b p.324).
• Maintain oxygenation and ventilation. Correct hypoxia and prevent
hypercapnoea under ABG guidance (may require IPPV). Use pulse
oximetry to monitor SpO
2
non-invasively, titrating inspired oxygen
concentration to achieve SpO
2
of 94–98 % .
• In intubated patients, insert an oro- or nasogastric tube to decompress
the stomach.
• Obtain a 12-lead ECG and a CXR (check position of tracheal tube,
central lines and presence of pneumothorax etc.).
• Optimize cardiac output: inotropes, vasodilators, fl uids and/or diuretics
may be needed under haemodynamic monitoring guidance. If the arrest
is associated with an acute coronary syndrome, consider immediate
thrombolysis and/or coronary revascularization.
• Cerebral blood fl ow autoregulation is defi cient post-arrest. Maintaining
arterial pressures ‘normal’ for the patient may prevent hypotensive
hypoperfusion. i BP above the normal for the patient may worsen
cerebral oedema.
• Seizures aggravate brain injury by i ICP and cerebral metabolic
requirements. Treat with appropriate anticonvulsants (as b p.149) and
ensure adequate oxygenation and ventilation.
• Measure U&E, Ca
2 +
, Mg
2 +
, and correct abnormalities appropriately.
• Obtain full blood count (FBC) to exclude anaemia contributing to
myocardial ischaemia and to provide an admission baseline.
• Both hypo- and hyperglycaemia compromise neurological outcome.
Monitor plasma glucose concentration regularly and aim to avoid both
hypo- and hyperglycaemia (keep the level d 10mmol/L).
• No drug has been shown to improve cerebral outcome following
cardiac arrest. The routine use of steroids, mannitol, Ca
2 +
channel
blockers, etc., is unwarranted.
• When any drug is used, remember that pharmacokinetic profi les
are often impaired post-resuscitation. Dose adjustment and careful
monitoring are needed.
• Avoid/treat hyperthermia with antipyretic or active cooling.
• There is compelling data to support the early induction of mild
therapeutic hypothermia (32–34 ° C) in patients who are comatose
following out of hospital VF arrest. Mild hypothermia is believed to be
neuroprotective in this situation (and pending more data, may be of
benefi t in other situations as well, eg other arrest rhythms, in-hospital
arrests, paediatric patients). Cooling may be initiated by external
techniques (cooling blankets, water or air circulating blankets) or
internally by an infusion of 30mL/kg of 4 ° C 0.9 % saline — liaise with ICU.
Mild hypothermia is typically maintained for 12–24hr.

55
POST-RESUSCITATION CARE
Training
Theoretical knowledge is important, but many of the skills required during
the management of a cardiac arrest need expert teaching and supervised
practice. Attend an approved Resuscitation Council (UK) Advanced Life
Support course (see www.resus.org.uk ) — preferably before starting in
the ED.

56 CHAPTER 2 Life-threatening emergencies
Central venous access
Indications
Central venous access may be required for:
• Administration of emergency drugs.
• Central venous pressure measurement.
• Administration of IV fl uids, especially when peripheral veins are
collapsed or thrombosed. Note : other routes (eg femoral vein) are
generally preferable for giving large volumes rapidly.
• Transvenous cardiac pacing.
Choice of vein
The external jugular vein is often readily visible and can be cannulated
easily with a standard IV cannula.
The internal jugular and subclavian veins are generally used for central
venous access in the ED. Subclavian vein cannulation has a relatively high
risk of pneumothorax, so the internal jugular vein is usually preferable, via
a ‘high’ approach. When possible, use ultrasound (USS) guidance and the
right side of the neck ( d risk of thoracic duct damage). If, however, a chest
drain is already in situ, use the same side for central venous cannulation.
The femoral vein is useful for temporary access in severe trauma, burns,
and in drug addicts with many thrombosed veins.
Seldinger technique for central venous access
The method of choice, because the relatively fi ne needle d risk of
complications such as pneumothorax. The technique involves inserting
a hollow metal needle into the vein. A fl exible guidewire is threaded
through the needle, which is then removed. A tapered dilator and plastic
cannula are inserted over the guidewire and advanced into the vein. The
guidewire and dilator are removed, and the cannula secured. Once the
cannula is in place, check that venous blood can be freely aspirated and
secure the cannula.
Precautions and problems
Central venous access is a specialized technique with potentially life-
threatening complications, including: pneumothorax, haemothorax, arterial
puncture, thoracic duct damage, air embolism, and infection.
• Expert supervision is essential. Cannulation is particularly diffi cult
and hazardous in hypovolaemic, shocked, or agitated patients. In such
situations, consider whether it is possible to defer the procedure.
• USS has become widely available and is increasingly used by suitably
trained ED specialists. It d complications and failure rates by clarifying
the relative positions of needle, vein, and surrounding structures.
Variant anatomy and vein patency can also be assessed by USS.
• Bleeding dyscrasias and anticoagulant treatment are contraindications
to internal jugular and subclavian vein access.
• Severe pulmonary disease is a relative contraindication to central venous
access, especially by the subclavian route, because a pneumothorax
would be particularly dangerous.

57
CENTRAL VENOUS ACCESS
Methods
Use aseptic technique. If possible, tilt the trolley 10 ° head down to fi ll
the internal jugular and subclavian veins and d risk of air embolus. After
successful or attempted subclavian or internal jugular cannulation, take a
chest X-ray (CXR) to check for pneumothorax and the position of the
cannula.
External jugular vein
The vein can be seen and felt as it crosses superfi cially over the
sternomastoid muscle and runs obliquely towards the clavicle. Gentle
pressure on the lower end of the vein will distend it. A standard IV cannula
can easily be inserted into the external jugular vein, but passing a catheter
centrally may be diffi cult because of valves and the angle at which the vein
joins the subclavian vein.
Internal jugular vein
The internal jugular vein runs antero-laterally in the carotid sheath, parallel
to the carotid artery, and deep to the sternocleidomastoid muscle. The
high approach described has less risk of pneumothorax than lower
approaches (Fig. 2.7 ).
• Turn the patient’s head away from the side to be cannulated.
• Identify the carotid pulse at the level of the thyroid cartilage.
• Insert the needle 0.5cm lateral to the artery, at the medial border of
sternomastoid muscle.
• Advance the needle at an angle of 45 ° parallel to the sagittal plane,
pointing towards the ipsilateral nipple. The vein should be entered at a
depth of 2–4cm and blood aspirated freely. If it is not, try again slightly
more laterally.
Subclavian vein (infraclavicular approach)
• Turn the patient’s head away from the side of cannulation.
• Identify the mid-clavicular point and the sternal notch.
• Insert the needle 1cm below the mid-clavicular point and advance it
horizontally below and behind the clavicle, aiming at a fi nger in the
suprasternal notch. The vein is usually entered at a depth of 4–6cm
(Fig. 2.8 ).
Femoral vein
Insert the needle 81cm medial to the femoral artery and just below the
inguinal ligament, pointing slightly medially and with the needle at 20–30 °
to the skin.
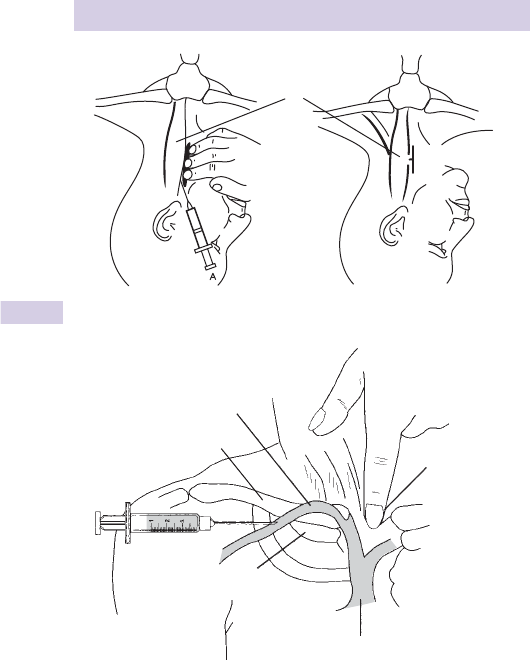
58 CHAPTER 2 Life-threatening emergencies
1 Rosen M et al . Handbook of Percutaneous Central Venous Catheterization. W.B. Saunders,
London.
2 Cosgriff JH. An Atlas of Diagnostic and Therapeutic Procedures for Emergency Personnel .
J.B. Lippincott, Philadelphia.
Fig. 2.7 Internal jugular cannulation.
1
Carotid artery
Sternomastoid
muscle
Fig. 2.8 Subclavian vein cannulation.
2
Clavicle
First rib
Superior vena cava
Finger in
suprasternal
notch
Subclavian vein

59
SEVERE SEPSIS AND SEPTIC SHOCK
Severe sepsis and septic shock
Septic patients have a systemic infl ammatory response syndrome (SIRS)
as a consequence of infection. Severe sepsis refers to septic patients with
evidence of organ hypoperfusion. Septic shock is present when septic
patients exhibit hypotension unresponsive to intravenous fl uid resuscitation.
Systemic infl ammatory response syndrome
This requires 2 or more of:
• Body temperature of > 38 ° C or <36 ° C
• Heart rate > 90/min
• Respiratory rate > 20 breaths/min or PaCO
2
< 4.3kPa
• WCC > 12 × 10
9
/L or <4 × 10
9
/L or > 10 % immature (band) forms
Management
Severely septic patients have SIRS with evidence of hypoperfusion (eg
systolic BP <90mmHg and/or lactate > 3mmol/L). Obtain senior/ICU help
early. Intensive therapy of severely septic patients focuses upon certain
therapeutic goals :
• CVP of 8–12mmHg.
• mean arterial pressure > 65mmHg.
• urine output > 0.5mL/kg/hr.
• central venous saturation > 65 % .
Adopt the following approach:
• Obtain senior/ICU assistance now.
• Assess and manage airway, breathing, circulation (ABC) — in particular,
provide high fl ow oxygen, secure good IV access and give an initial IV
fl uid bolus of 20mL/kg of 0.9 % saline. Some patients may require early
tracheal intubation and IPPV.
• Look for obvious sources of infection.
• Check BMG (and treat if hypoglycaemic).
• Take blood cultures before starting antibiotics (the choice of antibiotics
will depend upon the likely cause and is considered on b p.60).
• Patients who remain hypotensive and/or have a lactate > 3mmol/L
require central venous and arterial catheterization in an intensive care/
resuscitation setting, with IVI noradrenaline to maintain mean arterial
pressure > 65mmHg and IV 0.9 % saline 500mL boluses every 20mins
to achieve CVP 8–12mmHg (12–15mmHg in mechanically ventilated
patients).

60 CHAPTER 2 Life-threatening emergencies
Shock
Shock is a clinical condition characterized by failure to adequately perfuse
and oxygenate vital organs. Clinically, shock is recognized by:
• Hypotension Generally considered to be systolic BP <90mmHg (in
adults), but values may be higher in young, fi t or previously hypertensive
patients. Associated tachycardia ( > 100/min) is common, but may not be
present in patients with cardiac or neurological causes or in those taking
B-blockers. A few patients with haemorrhagic shock have a paradoxical
bradycardia.
• Altered consciousness and/or fainting (especially on standing or sitting
up) may result from d cerebral perfusion.
• Poor peripheral perfusion Cool peripheries, clammy/sweaty skin, pallor,
d capillary return, but note that in the early phase of endotoxic septic
shock there may be vasodilatation with warm peripheries.
• Oliguria d renal perfusion with urine output <50mL/hr (in adults).
• Tachypnoea.
Classifi cation of shock
Traditional classifi cation of types of shock is artifi cial — mixed aetiologies
are common.
Hypovolaemic shock
• Blood loss: trauma, gastrointestinal (GI) bleed (haematemesis, melaena),
ruptured abdominal aortic aneurysm, ruptured ectopic pregnancy.
• Fluid loss/redistribution (‘third spacing’) : burns, GI losses (vomiting,
diarrhoea), pancreatitis, sepsis.
Cardiogenic shock
• Primary : myocardial infarction (MI), arrhythmias, valve dysfunction,
myocarditis.
• Secondary : cardiac tamponade, massive pulmonary embolus, tension
pneumothorax.
Septic shock (see b p.59)
More common at the extremes of age, in patients with diabetes mellitus,
renal/hepatic failure and the immunocompromised (eg HIV infection,
underlying malignancy, post-splenectomy, steroid therapy). Note that
fever, rigors and i white cell count (WCC) may not be present.
• Organisms responsible include Gram + ve and –ve, especially Staph. aureus,
Strep . pneumoniae , N meningitidis , coliforms including enterococci and
Bacteroides (especially in patients with intra-abdominal emergencies,
such as ruptured diverticular abscess). In the immunocompromised,
Pseudomonas, viruses, and fungi may cause septic shock.
Anaphylactic shock: see b p.42.
Neurogenic shock: see b p.382.
Other causes
These include poisoning ( b p.183) and Addison’s disease ( b p.155).

61
SHOCK
Management of shock
Investigation and treatment should occur simultaneously. Get senior help
immediately.
• Address the priorities — ABC.
• Give high fl ow O
2
by mask.
• Secure adequate venous access and take blood for FBC, U&E, glucose,
liver function tests (LFTs), lactate, coagulation screen, and if appropriate,
blood cultures.
• Monitor vital signs, including pulse, BP, SpO
2
, respiratory rate.
• Check ABG.
• Monitor ECG and obtain 12 lead ECG and CXR.
• Insert a urinary catheter and monitor urine output hourly.
• For shock associated with d effective circulating blood volume, give
IV crystalloid (0.9 % saline) 20mL/kg as bolus. Give further IV fl uids
including colloid 9 blood (aim for haematocrit (Hct) > 30 % ) according
to aetiology and clinical response (and in particular, pulse, BP, central
venous pressure (CVP), and urine output). Use caution with IV fl uid
infusion in shock related to cardiogenic causes, and in ruptured or
dissecting aortic aneurysm.
• Look for, and treat specifi cally, the cause(s) of the shock. Echocardiography,
USS, CT, and/or surgical intervention may be required. Specifi c treatments
include:
• Laparotomy : ruptured abdominal aortic aneurysm, splenic and/or
liver trauma, ruptured ectopic pregnancy, intra-abdominal sepsis.
• Thrombolysis/angioplasty : MI.
• Thrombolysis : PE.
• Pericardiocentesis/cardiac surgery : cardiac tamponade, aortic valve
dysfunction.
• Antidotes : for certain poisons.
• Antibiotics : sepsis. The choice of antibiotic will depend upon the
perceived cause and local policies (eg ceftriaxone for meningococcal
disease). Where there is no obvious source, empirical combination
therapy is advised (eg co-amoxiclav + gentamicin + metronidazole).
Obtain specialist microbiological advice early, especially in
neutropaenic/immunocompromised patients.
• Inotropic and vasoactive therapy, assisted ventilation, and invasive
monitoring (including arterial and CVP lines) are often needed as part
of goal directed therapy. Get specialist ICU help early.

Chapter 00
62
Electrocardiogram interpretation 64
Chest pain 66
Angina 67
Acute coronary syndromes 68
ST segment elevation MI 70
Myocardial infarction: electrocardiogram changes 72
STEMI: treatment 76
Pericarditis 78
Bradyarrhythmias 80
Treatment of bradyarrhythmias 82
Tachycardia algorithm–with pulse 84
Tachyarrhythmias 86
Broad complex tachyarrhythmias 87
Narrow complex tachyarrhythmias 88
Atrial fi brillation 89
Hypertensive problems 90
Aortic dissection 92
Haemoptysis 94
Oxygen 95
The dyspnoeic patient 96
Hyperventilation 97
Arterial blood gases 98
Cardiogenic pulmonary oedema 100
Non-cardiogenic pulmonary oedema 102
Pleural effusion 103
Acute asthma: assessment 104
Acute asthma: management 106
COPD 108
Pneumonia 110
Pulmonary aspiration 112
Medicine
Chapter 3

63
Chapter 3
Spontaneous pneumothorax 114
Deep venous thrombosis 118
Pulmonary embolism 120
Upper gastrointestinal bleeding 122
Lower gastrointestinal bleeding 124
Headache 126
Subarachnoid haemorrhage 128
Migraine 130
Other causes of headache 132
Acute confusional state (delirium) 134
Dementia 135
The unconscious patient 136
Collapse and syncope 140
Acute generalized weakness 142
Stroke 144
Transient ischaemic attacks 146
Seizures and status epilepticus 148
Hypoglycaemia 150
Hyperglycaemic crises 152
Sodium derangements 154
Addisonian crisis 155
Thyrotoxic crisis 156
Urinary tract infection 158
Chronic renal failure 160
Hyperkalaemia 162
Hypokalaemia 164
Porphyria 165
Bleeding disorders 166
Patients on anticoagulants 170
Blood transfusion 172
Sickle cell disease 176
Medicine

64 CHAPTER 3 Medicine
Electrocardiogram interpretation
The electrocardiogram (ECG) is normally recorded so that a defl ection
of 10mm = 1mV. The recording rate is 25mm/sec, 1mm = 0.04sec, 1 large
square = 0.2sec. There is an ECG ruler on the inside back cover. Follow a
systematic approach.
Rate Calculate the rate by dividing 300 by the number of large squares in
one R–R interval.
Frontal plane axis Normally lies between –30 * and + 90 * (see Fig. 3.1 ).
With a normal axis, QRS complexes in I and II are both + ve. An axis
more –ve than –30 * (I + ve, aVF and II –ve) is left axis deviation (causes:
left anterior hemiblock, inferior myocardial infarction (MI), ventricular
tachycardia (VT), Wolf Parkinson White (WPW) syndrome). An axis more
+ ve than + 90 * (I –ve, aVF + ve) is right axis deviation (causes: pulmonary
embolism (PE), cor pulmonale, lateral MI, left posterior hemiblock).
P wave Normally <0.12sec wide and <2.5mm tall. They are best seen in
leads II and V
1
which are chosen for rhythm strips or monitoring. A tall
peaked P wave in II may refl ect right atrial hypertrophy; a widened bifi d P
wave left atrial hypertrophy. P waves are absent in atrial fi brillation (AF).
PR interval Normally 0.12–0.2sec (<5 small squares). A short PR interval
(abnormally fast conduction between atria and ventricles) implies an
accessory pathway (eg Wolf Parkinson White syndrome).
A prolonged PR interval occurs in heart block (fi rst, second or third
degree, see b Bradyarrhythmias, p.80).
QRS width Normally 0.05–0.11sec (<3 small squares). Prolonged QRS
complexes may be due to: right bundle branch block (RBBB) (RsR' or
M shape in V
1
), left bundle branch block (LBBB) (QS or W shape
in V
1
with RsR' or M shape in V
6
), tricyclic antidepressant poisoning
( b p.194), hypothermia, ventricular rhythms, and ectopics.
Head
–90°
aVL–30°
aVR–150°
Left
Feet
Right
I 0°
II+60°
+120° III
±180°
aVF
+90°
Fig. 3.1 Diagram of the ECG frontal axis.
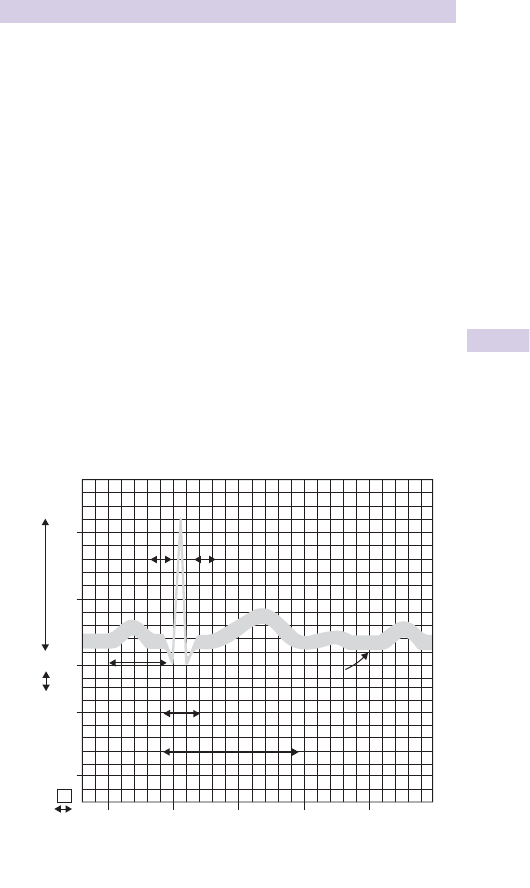
65
ELECTROCARDIOGRAM INTERPRETATION
QRS amplitude The QRS amplitude can indicate left ventricular
hypertrophy (LVH). Signs of LVH are: (S in V
2
+ R in V
5
) > 35mm; R in I >
15mm; R in aV
L
> 11mm.
Q waves May be normal in III, aV
R
, and V
1
, but are abnormal in other
leads if > 0.04sec or > ½ of the height of the subsequent R wave.
ST segment elevation is caused by: acute MI, pericarditis (concave up),
ventricular aneurysm, Prinzmetal’s angina, LVH, Brugada syndrome,
hypertrophic cardiomyopathy, benign early repolarization.
ST segment depression is caused by: ischaemia, digoxin, LVH with strain.
QT interval = start of Q wave to end of T wave.
QT
c
= QT⁄√R–R (Bazett’s formula). Normal QT
c
is <440msec.
At rates of 60–100/min, QT should be <1/2 R–R interval.
A
prolonged QT
c
predisposes to ‘torsades de pointes’ ( b Broad
complex tachyarrhythmias, p.87) and is caused by acute MI, hypothermia,
hypocalcaemia, drugs (quinidine, tricyclic antidepressants), certain
congenital diseases (eg Romano–Ward syndrome).
T waves Abnormal if inverted in V
4–6
. Peaked T waves are seen in early
acute MI and hyperkalaemia ( b p.162). Flattened T waves (sometimes with
prominent U waves) occur in hypokalaemia.
1.0
0.5
0
Q
QRS interval
Isoelectric line
P
U
T
P
PR segment
ST segment
R
S
0.04
0.0
P–R interval
0.2 0.4 0.6 0.8
Seconds
Voltage
(mV)
1 mm 10 mm
Q–T interval
Fig. 3.2
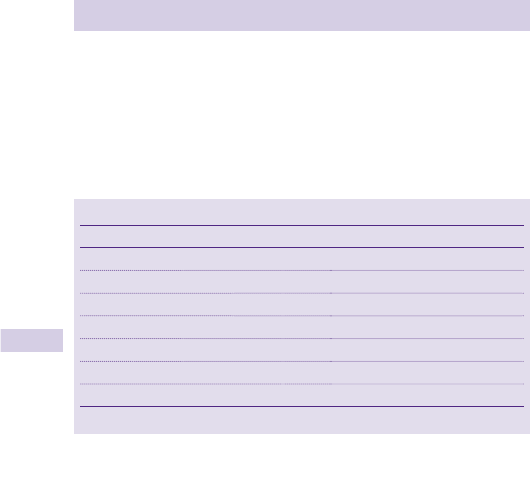
66 CHAPTER 3 Medicine
Chest pain
Always take chest pain seriously. It may refl ect life-threatening illness.
Triage patients with chest pain as ‘urgent’ and ensure that they are seen
within a few minutes. Ischaemic heart disease is understandably the fi rst
diagnosis to spring to mind in the middle-aged or elderly, but chest pain
may have a variety of other disease processes, many of which are also
potentially life-threatening (Table 3.1 ).
Reaching the correct conclusion requires accurate interpretation of the
history, examination and investigations, bearing in mind recognized patterns
of disease presentations.
History
Characterize the pain
• Site (eg central, bilateral or unilateral).
• Severity.
• Time of onset and duration.
• Character (eg ‘stabbing’, ‘tight/gripping’, or ‘dull/aching’).
• Radiation (eg to arms and neck in myocardial ischaemia).
• Precipitating and relieving factors (eg exercise/rest/GTN spray).
• Previous similar pains.
Enquire about associated symptoms Breathlessness, nausea, and vomiting,
sweating, cough, haemoptysis, palpitations, dizziness, loss of consciousness.
Document past history, drug history, and allergies. Old notes and old
ECGs are invaluable — request them at an early stage.
Quickly consider contacting cardiologists if acute coronary syndrome
(ACS) is likely ( b ST segment elevation MI: treatment, p.76).
Examination and resuscitation
Evaluate Airway, Breathing, Circulation (ABC) and resuscitate (O
2
, venous access,
IV analgesia) as appropriate. Listen to both lung fi elds and check for tension pneu-
mothorax and severe left ventricular failure (LVF). Complete full examination.
Investigations
These depend upon the presentation and likely diagnosis, but an ECG and
CXR are usually required. Remember that these may initially be normal
in MI, PE and aortic dissection. Ensure that all patients receive ECG moni-
toring in an area where a defi brillator is readily available.
Table 3.1 The differential diagnosis of chest pain
Common causes Less common causes
Musculoskeletal (eg costochondritis) Aortic dissection
*
Acute coronary syndrome
*
Cholecystitis
Pneumothorax
*
Herpes zoster
Oesophagitis Oesophageal rupture
*
Pneumonia Pancreatitis
*
Pulmonary embolism
*
Vertebral collapse
Obscure origin (eg precordial catch) Tabes dorsalis (very rare)
*
Potentially rapidly fatal.

67
ANGINA
Angina
Angina is defi ned as discomfort in the chest, arm, neck, or adjacent areas
due to myocardial ischaemia. It can be brought on by exertion, cold weather
and emotion. It occurs when coronary artery blood fl ow fails to meet the
O
2
demand of the myocardium (eg during exercise, coronary artery spasm
or anaemia). Ischaemia may produce ST depression or inversion, which
resolves on recovery.
First presentation of angina
Patients may come to the ED with angina as a fi rst presentation of
ischaemic heart disease (IHD). Always consider the possibility of MI. In
particular, suspect myocardial cell death with any pain lasting > 10min (even
if relieved by glyceryl trinitrate (GTN)). A normal examination, normal ECG
and normal baseline cardiac markers do not exclude MI. If in any doubt, admit
the patient . If considering discharge, discuss with senior ED/medical staff.
Atypical cardiac chest pain
Patients with acute MI are occasionally sent home from the ED
inadvertently. Cardiac chest pain may be poorly localized, and may present
with musculoskeletal features or gastrointestinal (GI) upset. In particular,
patients with acute coronary syndromes commonly have chest wall
tenderness. Some patients understandably play down symptoms in order
to avoid admission to hospital. If the clinical history is suspicious of cardiac
pain (especially in a patient with risk factors, such as family history of IHD,
hypertension, smoking), then refer for admission. Do not be fooled by a
normal ECG, normal examination, or the fact that the patient is <30 years
old. Remember that oesophageal pain may improve with GTN and true
cardiac pain may appear to improve with antacids. The decision whether
or not to refer the patient for admission and investigation depends upon
an assessment of the risk of MI. In general, exclude an MI where chest pain
lasting > 15min has some features of IHD. Also refer patients who look
unwell, even if the chest pain lasts <15min.

68 CHAPTER 3 Medicine
Acute coronary syndromes
Coronary artery plaque rupture can result in a variety of ischaemic
conditions which fall under the overall term of ‘acute coronary syndrome’
and include unstable angina, non-ST segment elevation MI (NSTEMI)
and ST segment elevation MI (STEMI). Patients labelled as having acute
coronary syndrome, but without initial ST elevation, comprise a relatively
heterogenous group — some later proving (on the basis of elevated blood
troponin levels) to have suffered an NSTEMI.
The patient presenting with unstable angina or NSTEMI
Unstable angina can occur as worsening angina or a single episode of
‘crescendo’ angina, with a high risk of infarction. Features include angina
at rest, i frequency, i duration, and severity of pain (including response
to GTN). It may be diffi cult to distinguish between unstable angina and
NSTEMI in the ED.
• Provide O
2
to maintain SpO
2
94–98 % and attach cardiac monitor.
• Administer IV opioid analgesia ( ± antiemetic) as required.
• Give aspirin 300mg PO and clopidogrel 300mg PO.
• Start low molecular weight heparin (LMWH), eg dalteparin 120units/
kg SC every 12hr (max 10,000U) or enoxaparin 1mg/kg SC every 12hr.
Synthetic pentasaccharide fondaparinux 2.5mg SC may be used instead.
Follow local guidelines.
• If pain is unrelieved, commence GTN intravenous infusion (IVI; start at
0.6mg/hr and i as necessary), provided systolic BP is > 90mmHg.
• Glycoprotein IIb/IIIa inhibitors (eg eptifi batide and tirofi ban) are going
out of favour for patients at risk of NSTEMI or high TIMI risk score (see
Table 3.2 ).
• If high risk of NSTEMI, haemodynamically stable and no contraindications,
consider atenolol (5mg IV slowly over 5mins repeated once after 15mins),
according to local policy. Contraindications include: hypotension,
bradycardia, second or third degree heart block, heart failure and severe
reactive airways disease.
• Refer for admission, repeat ECGs and blood troponin testing 12hr after
pain onset.
• Discuss with cardiology all patients at high risk of NSTEMI or with TIMI
score > 3. They may benefi t from early revascularization procedures.
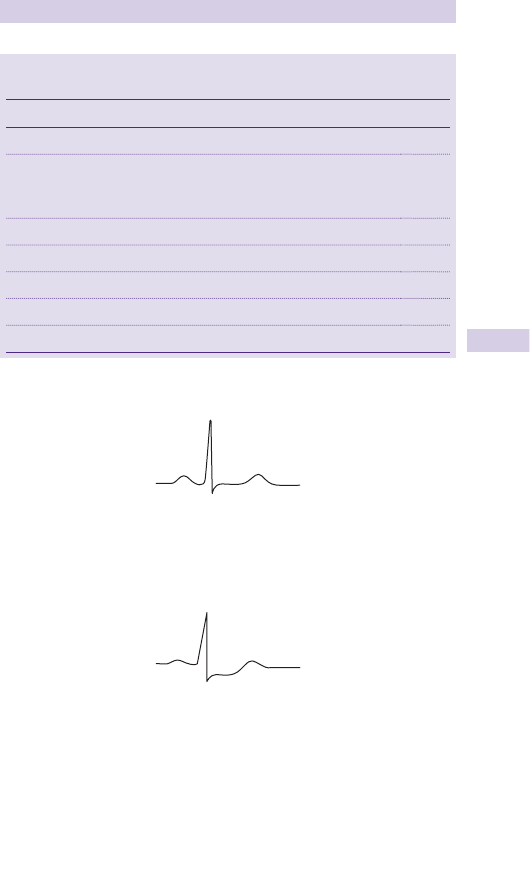
69
ACUTE CORONARY SYNDROMES
Normal lead II (Fig. 3.3 )
Ischaemic changes in lead II (Fig. 3.4 )
Prinzmetal’s or ‘variant’ angina
Angina associated with ST elevation may be due to coronary artery vasos-
pasm. This may occur with or without a fi xed coronary abnormality and
may be indistinguishable from an acute MI until changes resolve rapidly
with GTN as pain is relieved.
Table 3.2 TIMI risk score: increasing score predicts mortality or
adverse event
Risk factor Points
Age > 65 1
3 + risk factors for coronary artery disease
Family history of IHD, hypertension, hypercholesterolemia, diabetes,
or smoker
1
Known coronary artery disease with stenosis ≥50 %
1
Aspirin use in last 7 days 1
Recent episode of angina prior to this event 1
Raised troponin levels (or other cardiac marker) 1
ST segment deviation ≥0.5mm on ECG
1
R
P
T
ST
S
Fig. 3.3
R
P
T
ST
S
Fig. 3.4

70 CHAPTER 3 Medicine
ST segment elevation MI
IHD is the leading cause of death in the Western world. Mortality from
acute MI is believed to be 45 % , with 70 % of these deaths occurring before
reaching medical care. Contributory risk factors for MI include smoking,
hypertension, age, male sex, diabetes, hyperlipidaemia, and family history.
MI pathology
MI mostly affects the left ventricle. It usually results from sudden occlusion
of a coronary artery or one of its branches by thrombosis over a pre-
existing atheromatous plaque. Patients with IHD are at risk of sustaining
an MI if additional stresses are placed upon their already critically impaired
myocardial circulation (eg a high level of carboxyhaemoglobin (COHb)
following smoke inhalation). MI may also occur in vasculitic processes,
eg cranial arteritis ( b p.132) and Kawasaki disease.
MI diagnosis
The diagnosis of acute MI requires 2 out of the following 3 features:
• A history of cardiac-type ischaemic chest pain.
• Evolutionary changes on serial ECGs.
• A rise in serum cardiac markers.
Note that 50–60 % of patients will not have a diagnostic ECG on arrival
and up to 17 % will have an entirely normal initial ECG. Late presentation
does not improve diagnostic accuracy of the ECG.
History
The classic presentation is of sudden onset, severe, constant central
chest pain, which radiates to the arms, neck, or jaw. This may be similar
to previous angina pectoris, but is much more severe and unrelieved
by GTN. The pain is usually accompanied by one or more associated
symptoms: sweating, nausea, vomiting, breathlessness.
Atypical presentation is common. Have a high level of suspicion. Many
patients describe atypical pain, some attributing it to indigestion (be wary
of new onset ‘dyspeptic’ pain). Up to a third of patients with acute MI
do not report any chest pain. These patients tend to be older, are more
likely to be female, have a history of diabetes or heart failure, and have a
higher mortality.
These patients may present with:
• LVF.
• Collapse or syncope (often with associated injuries eg head injury).
• Confusion.
• Stroke.
• An incidental ECG fi nding at a later date.
In a patient who presents with possible MI, enquire about past
medical history (IHD, hypertension, diabetes, hyperlipidaemia) and
contraindications to thrombolysis. Ask about drug history, including drugs
of abuse (particularly cocaine b p.215).

71
ST SEGMENT ELEVATION MI
Examination
Examination and initial resuscitation (maintain SpO
2
in normal range, IV
cannula, analgesia) go hand in hand. The patient may be pale, sweaty, and
distressed. Examination is usually normal unless complications have super-
vened (eg arrhythmias, LVF). Direct initial examination towards searching
for these complications and excluding alternative diagnoses:
• Check pulse, BP and monitor trace (?arrhythmia or cardiogenic shock).
• Listen to the heart (?murmurs or 3rd heart sound).
• Listen to the lung fi elds (?LVF, pneumonia, pneumothorax).
• Check peripheral pulses (?aortic dissection).
• Check legs for evidence of deep vein thrombosis (?PE).
• Palpate for abdominal tenderness or masses (?cholecystitis, pancreatitis,
perforated peptic ulcer, ruptured aortic aneurysm).
Investigations
The diagnosis of ST segment elevation myocardial infarction within the
fi rst few hours is based upon history and ECG changes (serum cardiac
markers may take several hours to rise — see below).
• Record an ECG as soon as possible, ideally within a few minutes of
arrival at hospital. Sometimes patients arrive at hospital with ECGs of
diagnostic quality already recorded by paramedics. If the initial ECG is
normal, but symptoms are suspicious, repeat the ECG every 15min and
re-evaluate.
• Request old notes (these may contain previous ECGs for comparison).
• Ensure continuous cardiac monitoring and pulse oximetry.
• Monitor BP and respiratory rate.
• Obtain venous access and send blood for cardiac markers, U&E, glucose,
FBC, lipids.
• Obtain a CXR if there is suspicion of LVF or aortic dissection.
Cardiac markers
Troponins are now universally used. Troponin T (cTnT) and Troponin
I (cTnI) are proteins virtually exclusive to cardiac myocytes. They are
highly specifi c and sensitive, but are only maximally accurate after 12hr.
Troponin T and I cannot be used to rule out MI in the fi rst few hours. In
addition, cardiac cells may release troponin into the blood when cardiac
muscle is damaged by pericarditis, pulmonary embolism with a large clot
burden, or sepsis. Renal failure reduces excretion of troponin.
Chest pain assessment units
These units are becoming established in some EDs. A combination of
ECGs, ST segment monitoring, cardiac markers, and exercise testing is
used to allow discharge of low to moderate risk patients within 6–12hr.
However, simply excluding an acute coronary syndrome is only part of
the assessment of chest pain.

72 CHAPTER 3 Medicine
Myocardial infarction: ECG changes 1
Infarction of cardiac muscle results in ECG changes that evolve over
hours, days, and weeks in a relatively predictable fashion.
Hyperacute changes
Frequently ignored, although often subtle, some or all of the following
may be observed within minutes of infarction:
• i Ventricular activation time , since the infarcting myocardium is slower to
conduct electrical impulses. The interval between the start of the QRS
and apex of the R wave may be prolonged > 0.045sec.
• i Height of R wave may be seen initially in inferior leads in inferior MI.
• Upward-sloping ST segment — having lost normal upward concavity, the
ST segment straightens, then slopes upwards, before becoming ele-
vated.
• Tall, widened T waves.
Evolving acute changes
In isolation, none of these changes are specifi c to MI. In combination, and
with an appropriate history, they can diagnose MI:
• ST elevation : the most important ECG change. ST segments become
concave down and are signifi cant if elevated > 1mm in 2 limb leads, or
> 2mm in 2 adjacent chest leads.
• Reciprocal ST depression may occur on the ‘opposite side’ of the heart.
• Pathological Q waves (defi ned on b p.65) refl ect electrically inert
necrotic myocardium. ECG leads over a large transmural infarct show
deep QS waves. Leads directed towards the periphery of a large infarct
or over a smaller infarct may show a QR complex or a loss of R wave
amplitude .
• T wave inversion : typically deeply inverted, symmetrical and pointed.
• Conduction problems may develop. LBBB in a patient with acute cardiac
chest pain makes interpretation of the ECG very diffi cult. LBBB does not
have to be new to be signifi cant. Do not delay intervention in patients
with a good clinical history of MI in order to obtain old ECGs.
Sgarbossa criteria for diagnosing ACS in the presence of LBBB
• ST segment elevation > 1mm in leads with positive QRS complexes.
• ST segment depression in leads V1, V2, or V3.
• ST segment elevation > 5mm in lead with negative QRS complexes.
If all 3 are present, MI is likely.
Chronic changes
In the months following an MI, ECG changes resolve to a variable extent.
ST segments become isoelectric, unless a ventricular aneurysm develops.
T waves gradually become + ve again. Q waves usually remain, indicating
MI at some time in the past.
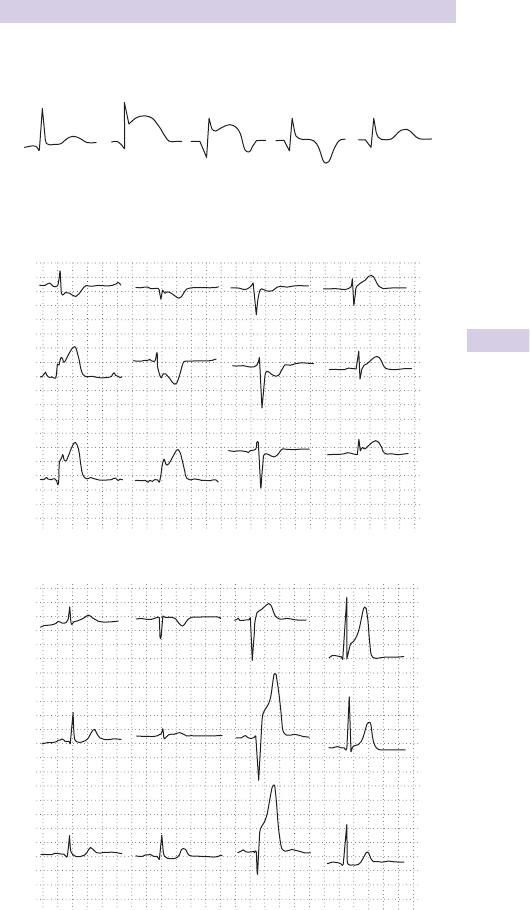
73
MYOCARDIAL INFARCTION: ECG CHANGES 1
Electrocardiogram changes following myocardial infarction
(Fig. 3.5 )
Electrocardiograms after myocardial infarction (Figs 3.6 and 3.7 )
Normal Hours Days Weeks
Months
Fig. 3.5
V
2
V
1
V
4
V
5
II
aVL
V
3
III
aVF
V
6
aVRI
Fig. 3.6 Acute inferolateral infarction with ‘reciprocal’ ST changes in I, aVL, and V
2
–V
3
.
IaVR
V
1
V
4
V
2
V
5
II aVL
V
3
III V
6
aVF
Fig. 3.7 Acute anteroseptal infarction with minimal ‘reciprocal’ STchanges in III and aVF.
74 CHAPTER 3 Medicine
Myocardial infarction: ECG changes 2
Localization of myocardial infarction
MI usually affects the left ventricle (LV), occasionally the right ventricle
(RV), but virtually never the atria. The part of myocardium affected is
implied by which leads show changes (Table 3.3 ).
Posterior myocardial infarction
Posterior MI nearly always occurs as part of inferior (postero-inferior) or
lateral (postero-lateral) MI. No conventional electrode views the poste-
rior heart, since intervening tissues result in an attenuated signal. ECG
diagnosis of true posterior MI may be made from the use of V
7–9
and from
reciprocal changes seen in leads V
1–3
: tall, slightly widened R (reciprocal
of Q), concave up ST depression (reciprocal of ST elevation), upright tall
widened T (reciprocal of inverted T).
Right ventricular infarct
This occurs most often as part of an inferior MI. In the presence of
changes of acute MI in the inferior leads, ST elevation in V
1
suggests right
ventricular involvement. In this case, record an ECG trace from lead V
4
R.
The diagnosis of RV infarct helps determine treatment of ensuing cardiac
failure. Treat RV failure with IV fl uids to maintain adequate fi lling pressure
and exercise caution if considering use of nitrates.
Blood supply to the heart and coronary artery dominance
The left anterior descending artery supplies the anterior and septal cardiac
areas (Fig. 3.9). The circumfl ex branch supplies the anterolateral aspect of
the heart. The right coronary artery supplies the right ventricle. In most
people the right coronary artery also supplies the sino-atrial node, the
inferior wall of the left ventricle and the ventricular septum. In 15 % of
individuals, the inferior wall is supplied by the circumfl ex branch of the left
coronary artery (left dominance).
Table 3.3
ECG leads Location of MI
V
1–3
Anteroseptal
V
5–6
, aV
L
Anterolateral
V
2–4
Anterior
V
1–6
Extensive anterior
I, II, aV
L
, V
6
Lateral
II, III, aV
F
Inferior
V
1
, V
4
R Right ventricle
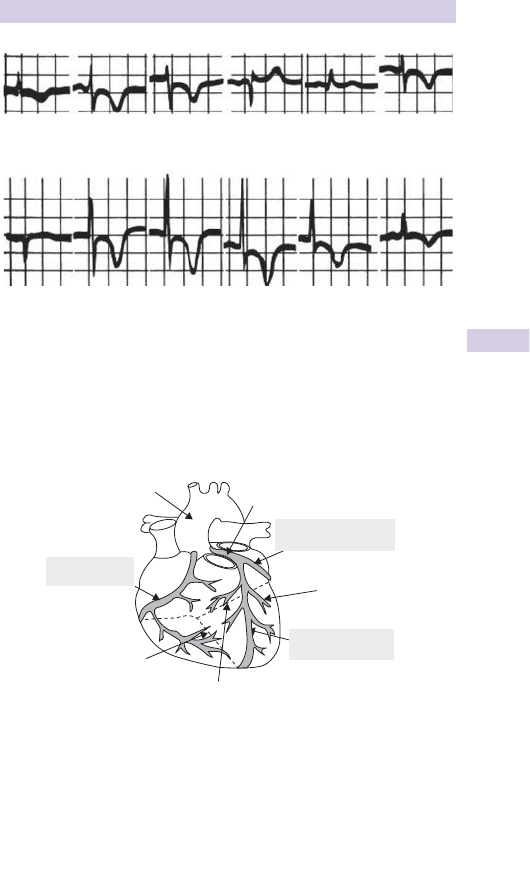
75
MYOCARDIAL INFARCTION: ECG CHANGES 2
V
6
V
5
V
4
aV
R
aV
L
aV
F
V
3
V
2
V
1
IIIIII
Fig. 3.8 ECG of subendocardial infarct.
Ascending aorta
Right coronary
artery
Left main stem
Left anterior
descending artery
Posterior
descending artery
Septal branches
(
of the LAD
)
Circumflex coronary
artery
Diagonal branches
(of the LAD)
Fig. 3.9

76 CHAPTER 3 Medicine
STEMI: treatment
Speed is crucial — time is muscle. Ambulance control may alert the ED in
advance of a patient with cardiac-type chest pain. Work effi ciently as a
team to ensure treatment is not delayed.
• Give O
2
to maintain SpO
2
94–98 % and attach cardiac monitor.
• Obtain IV access and take samples for U&E, glucose, FBC, cardiac
markers.
• Provide small increments of IV opioid analgesia titrated to effect.
• Ensure the patient has had 300mg aspirin and 300mg clopidogrel PO.
• Contact cardiology for primary percutaneous coronary intervention
(PCI). Arrange transport to the cath lab.
• For patients undergoing PCI, consider IV glycoprotein IIb/IIIa receptor
antagonist as an adjuvant. Be guided by local protocol.
• If PCI is not available, consider thrombolysis and monitor carefully. Start
LMWH, heparin, or fondaparinux, according to local protocols.
• If pain continues, give IVI GTN (start at 0.6mg/hr and i as necessary),
provided systolic BP is > 90mmHg.
• Consider atenolol (5mg slowly IV over 5min, repeated once after
15min), or metoprolol, unless contraindicated (eg uncontrolled heart
failure, hypotension, bradyarrhythmias, COPD).
Indications for PCI or thrombolysis
• ST elevation of > 1mm in 2 limb leads, or
• ST elevation of 2mm in 2 or more contiguous chest leads, or
• LBBB in the presence of a typical history of acute MI (NB: LBBB does
not have to be new).
Primary angioplasty for ST segment elevation MI
Primary percutaneous coronary intervention (coronary angioplasty and
stenting) is the treatment of choice for STEMI. Compared with throm-
bolysis, PCI administered within 12hr of symptom onset results in lower
mortality and re-infarction rates. The sooner it is performed, the greater
the benefi ts.
Thrombolysis
If PCI cannot be performed within 90min of diagnosis, thrombolytic
therapy is an alternative. The benefi ts reduce markedly with time delay,
so if PCI is not available, do not delay the administration of a thrombolytic
agent. Rural areas with long hospital transfers may have a protocol for
ambulance administered thrombolysis, aided by telemedicine advice from
the ED or cardiology. Patients presenting > 12hr after symptom onset will
not benefi t from thrombolysis.
Strokes, intracranial haemorrhage and major bleeds are more common
in patients given thrombolysis. Intracranial bleeding is more common in
older patients, those with hypertension on admission and those given tPA.
Prior to administering thrombolysis, always explain the benefi ts and risks
to the patient. Obtain verbal consent to give the medication and record
this in the notes.

77
STEMI: TREATMENT
Contraindications to thrombolysis
Most are relative, but discuss any contraindications with the patient and
cardiology:
• Head injury, recent stroke, previous neurosurgery or cerebral tumour.
• Recent GI or GU bleeding, menstruation, or coagulopathy/warfarin.
• Severe hypertension (eg systolic BP > 200mmHg, diastolic BP > 120mmHg),
aortic dissection or pericarditis.
• Puncture of non-compressible vessel (eg subclavian vein), traumatic
CPR, d GCS post-arrest.
• Major surgery within recent weeks.
• Pregnancy.
Choice of thrombolytic agents
Tissue plasminogen activator (tPA), rather than streptokinase, is the agent
of choice. Always use tPA if streptokinase was given > 5 days ago or in
anterior MI in a patient <75 years old and <4hr of onset of symptoms, or
if hypotensive (systolic BP <90mmHg).
Alteplase (recombinant tPA (rtPA)) is most effective given by an
accelerated regimen, eg 15mg IV bolus, followed by 0.75mg/kg (max 50mg)
IVI for 30min, then 0.5mg/kg (max 35mg) IVI over 60min. Give LMWH (eg
enoxaparin 1mg/kg stat) or heparin concomitantly through a separate IV
line (5000unit IV bolus, then 1000units/hr IV), according to local protocols.
Reteplase (modifi ed tPA) can be given as two IV boluses of 10units each
exactly 30min apart. Give LMWH/heparin as for alteplase.
Tenecteplase (modifi ed tPA) is given as a single IV bolus over 10sec. Dose
according to weight (<60kg = 30mg; 60–69kg = 35mg; 70–79kg = 40mg;
80–89kg = 45mg; > 90kg = 50mg). Give LMWH/heparin as for alteplase.
Streptokinase Given as 1.5mega-units by continuous IVI over 1hr. Strepto-
kinase is allergenic (may require slow IV chlorphenamine 10mg and IV
hydrocortisone 100mg) and frequently causes hypotension ( d IVI rate
and tilt the bed head down — treatment rarely needs to be discontinued).
After a recent streptococcal infection, streptokinase may be ineffective
due to the antibodies produced.
Further management
Arrhythmias Occur commonly after MI. Occasional ventricular ectopics
or transient AF (lasting <30sec) require no treatment. Watch for sudden
VT/VF and treat as in b Cardiac arrest, p.46.
Hypokalaemia Treat if K
+
<4mmol/L.
Pulmonary oedema Treat as described on b p.101.
Cardiogenic shock d cardiac output with tissue hypoxia, which does not
improve with correction of intravascular volume. Mortality is 50–80 % .
Contact ICU and cardiologist. Echocardiography may be required to
exclude conditions requiring urgent surgical repair (mitral regurgitation
from papillary muscle rupture, aortic dissection, ventricular septum rupture,
cardiac tamponade from ventricular wall rupture) or massive PE. If these
are excluded, emergency coronary intervention may i survival.

78 CHAPTER 3 Medicine
Pericarditis
Acute infl ammation of the pericardium characteristically produces chest
pain, low grade fever, and a pericardial friction rub. Pericarditis and
myocarditis commonly co-exist.
Causes
• Myocardial infarction (including Dressler’s syndrome — see b p.79).
• Viral (Coxsackie A9, B1-4, Echo 8, mumps, EBV, CMV, varicella, HIV,
rubella, Parvo B19).
• Bacterial (pneumococcus, meningococcus, Chlamydia , gonorrhoea,
Haemophilus ).
• Tuberculosis (TB; especially in patients with HIV) — see b p.232.
• Locally invasive carcinoma (eg bronchus or breast).
• Rheumatic fever — see b Acute arthritis, p.497.
• Uraemia.
• Collagen vascular disease (SLE, polyarteritis nodosa, rheumatoid
arthritis).
• After cardiac surgery or radiotherapy.
• Drugs (hydralazine, procainamide, methyldopa, minoxidil).
Diagnosis
Classical features of acute pericarditis are pericardial pain, a friction rub
and concordant ST elevation on ECG. The characteristic combination of
clinical presentation and ECG changes often results in a defi nite diagnosis.
Chest pain is typically sharp, central, retrosternal, and worse on deep
inspiration, change in position, exercise, and swallowing. A large pericardial
effusion may cause dysphagia by compressing the oesophagus.
A pericardial friction rub is often intermittent, positional, and elusive. It
tends to be louder during inspiration, and may be heard in both systole
and diastole. Low grade fever is common.
Appropriate investigations include: ECG, chest X-ray, FBC, erythrocyte
sedimentation rate (ESR), C-reactive protein (CRP), U&E, and troponin.
Obtain blood cultures if there is evidence of sepsis or suspicion of a
bacterial cause (eg spread of intrathoracic infection). A pericardial effusion
is most quickly and easily demonstrated by echocardiography or FAST
scanning: clinical evidence of cardiac tamponade is rare.
ECG changes
In acute pericarditis ECG changes result from associated epicardial infl am-
mation (see Fig. 3.10 ). Sinus tachycardia is usual, but AF, atrial fl utter or
atrial ectopics may occur. ST elevation is concave up (unlike MI, b p.72),
and present in at least 2 limb leads and all chest leads (most marked
in V
3–6
). T waves are initially prominent, upright, and peaked, becoming
fl attened or inverted over several days. PR depression (refl ecting atrial
infl ammation) may occur in the same leads as ST elevation (this PR–ST
discordance is characteristic). Pathological Q waves are not present.
Pericardial effusion causes d QRS amplitude in all leads. Electrical alternans
is diagnostic, but rare.
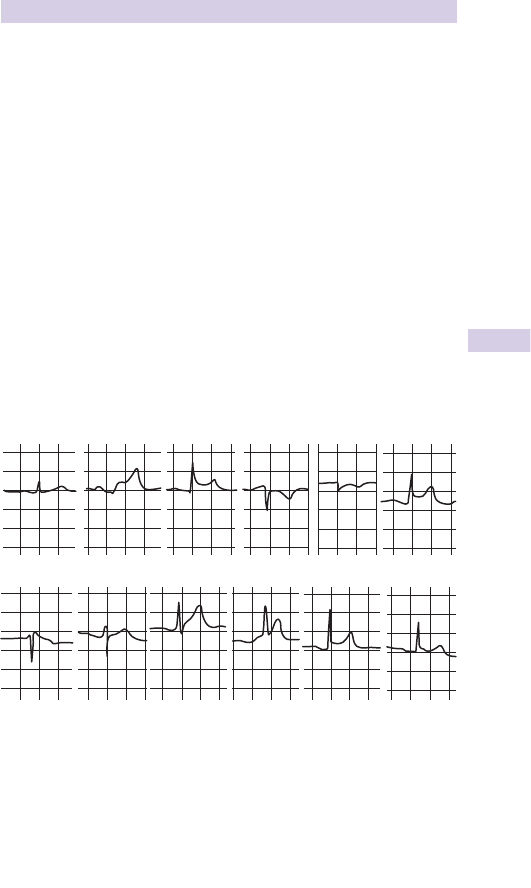
79
PERICARDITIS
Management
Refer to the medical team for echocardiography and treatment.
The appropriate treatment depends on the underlying cause.
Idiopathic pericarditis or viral pericarditis in young patients is usually
benign and self-limiting, responding to symptomatic treatment (high dose
NSAID ± PPI cover). Occasionally, it follows a relapsing course before
‘burning itself out’.
Dressler’s syndrome (autoimmune pericarditis ± effusion 2–14 weeks
after 3 % of MIs) requires cardiology specialist care.
Pericardial effusion may occur with any type of pericarditis. It is relatively
common in acute bacterial, tuberculous, and malignant pericarditis.
Acute tamponade may occur following cardiac rupture with MI, aortic
dissection, or after cardiac surgery. Summon senior help and arrange
immediate echocardiography for patients with signs of tamponade, with
pericardiocentesis under ultrasound guidance, and then a defi nitive
drainage procedure. Emergency ‘blind’ pericardiocentesis is described on
b p.343.
II IIII
V
1
V
2
V
3
V
4
V
5
V
6
aV
F
aV
L
aV
R
Fig. 3.10 ECG of pericarditis.

80 CHAPTER 3 Medicine
Bradyarrhythmias
Bradycardia is a ventricular rate of <60/min in the adult. It usually refl ects
infl uences on or disease of the sino-atrial (SA) node, or atrioventricular
(AV) block. Intraventricular conduction disturbances may progress to AV
block. Sinus bradycardia may be physiological (eg athletes), due to drugs
( B -blockers), or pathological (hypothyroidism, hypothermia, hypoxia, iICP,
sick sinus syndrome, MI, myocardial ischaemia). Bradycardia also occurs in
up to 1/3 of patients with hypovolaemia (eg GI bleed, ectopic pregnancy).
Sick sinus syndrome (or ‘sinus node disease’) is usually the result of
ischaemia or degeneration of SA node. It is characterized by sinus pauses
( > 2sec) or sinus arrest. Junctional or other escape beats may occur and
occasionally a tachyarrhythmia may emerge (‘tachy-brady’ syndrome).
Patients may present with dizziness, collapse, loss of consciousness or
palpitations. A continuous 24hr ECG tape may demonstrate arrhythmias.
AV block may be caused by IHD, drugs (eg excess digoxin) or cardiac
surgery.
First degree AV block Conduction from atria to ventricles occurs every
time, but is delayed. The PR interval is > 0.2sec (5 small squares on
standard ECG) (Fig. 3.11 ).
Second degree AV block Only a proportion of P waves are conducted to
the ventricles. There are two types:
• Mobitz type I block (Wenckebach) : the PR interval becomes increasingly
lengthened until a P wave fails to conduct (Fig. 3.12 ).
• Mobitz type II block : failure to conduct P waves may occur regularly
(eg 3:1) or irregularly, but the PR interval remains constant (Fig. 3.13 ).
Third degree (complete) heart block Atrial activity is not conducted to
ventricles. With a proximal block (eg at the AV node), a proximal escape
pacemaker in the AV node or bundle of His may take over, producing
narrow QRS complexes at a rate of 8 50/min. With distal AV block, a
more distal escape pacemaker results in broad bizarre complexes at a
rate of 8 30/min. Ventricular asystole may occur if the escape pacemaker
stops discharging, unless a subsidiary pacemaker takes over (Fig. 3.14 ).
Intraventricular conduction disturbances
The intraventricular conducting system commences as the bundle of His
and divides into right and left bundle branches — the latter subdivides
further into antero-superior and postero-superior divisions. These two
divisions and the right bundle branch are referred to as the ‘fascicles’.
Blockage of 2 out of 3 fascicles = bifascicular block .
• RBBB + left anterior hemiblock causes left axis deviation and RBBB
pattern on ECG.
• RBBB + left posterior hemiblock causes right axis deviation and RBBB
pattern on ECG.
Trifascicular block is present when bifasciular block is accompanied by
a prolonged PR interval. Note that true blockage of all 3 fascicles would
cause complete heart block, so ‘trifascicular block’ represents impending
progression to complete heart block.
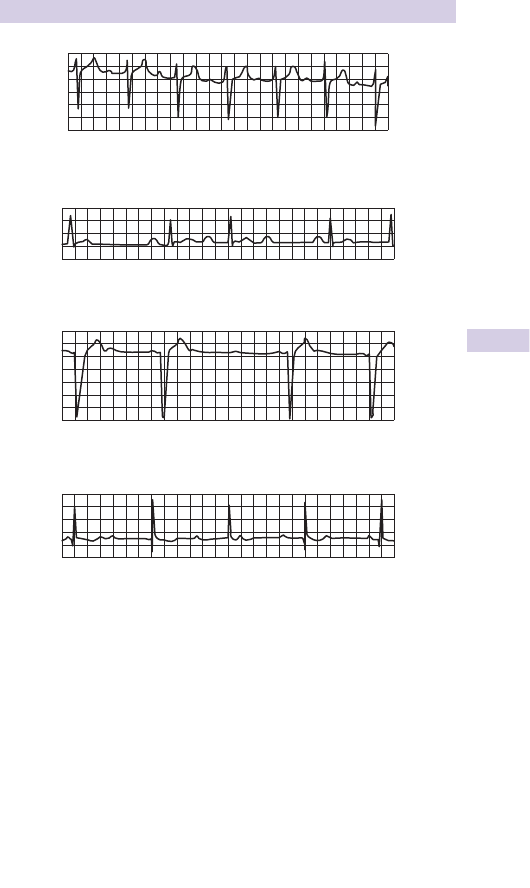
81
BRADYARRHYTHMIAS
Fig. 3.11 ECG of fi rst degree heart block.
Fig. 3.12 ECG of Mobitz type I AV block.
Fig. 3.13 ECG of Mobitz type II AV block.
Fig. 3.14 ECG of complete AV block.
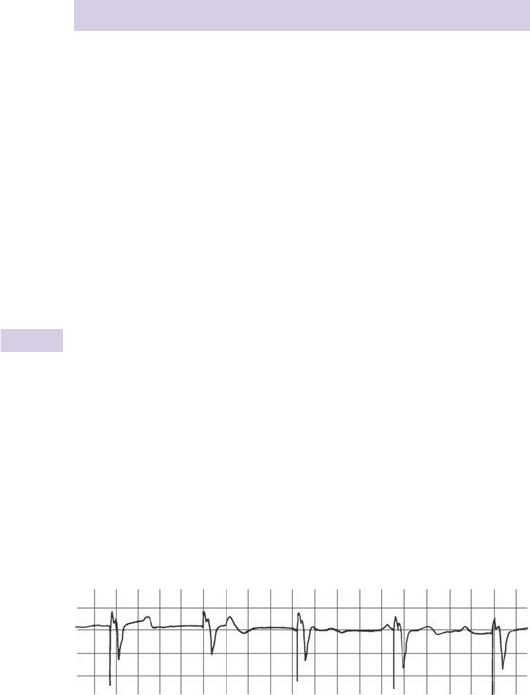
82 CHAPTER 3 Medicine
Treatment of bradyarrhythmias
The emergency treatment of bradycardia depends upon two important
factors: the clinical condition of the patient and the risk of asystole. Give
O
2
, insert an IV cannula and follow the 2010 European Resuscitation
Council Guidelines shown opposite ( www.resus.org.uk ).
Atropine is the fi rst-line drug. The standard dose is 500mcg IV, which may
be repeated to a total of 3mg. Further doses are not effective and may
result in toxic effects (eg psychosis, urinary retention).
Adrenaline (epinephrine) can be used as a temporizing measure prior
to transvenous pacing if an external pacemaker is not available. Give by
controlled infusion at 2–10mcg/min, titrating up according to response
(6mg adrenaline in 500mL 0.9 % saline infused at 10–50mL/hr).
External transcutaneous pacing is available on most defi brillators. It
allows a pacing current to be passed between 2 adhesive electrodes
placed over the front of the chest and the back. Select external demand
pacing mode at a rate of 70/min, then gradually i the pacing current from
zero until capture is shown on the monitor. Clinically, capture results in
a palpable peripheral pulse at the paced rate and clinical improvement in
the patient’s condition. Provide small doses of IV opioid ± sedation if the
patient fi nds external pacing very uncomfortable.
Transvenous cardiac pacing is the treatment of choice for bradycardic
patients who are at risk of asystole. The technique should only be
performed by an experienced doctor. The preferred route of access is the
internal jugular or subclavian vein. However, if thrombolysis has recently
been given or is contemplated, or if the patient is taking anticoagulants,
use the right femoral vein instead. Obtain a CXR to exclude complications.
A correctly functioning ventricular pacemaker results in a pacing spike
followed by a widened and bizarre QRS (Fig. 3.15 ).
Permanent pacemakers and implantable defi brillators
Increasingly sophisticated implantable devices are being used to manage
arrhythmias. Occasionally, a patient will present to the ED with a
malfunctioning pacemaker. Get urgent specialist advice. External trans-
cutaneous pacing will provide temporary support whilst the problem is
resolved. A special magnet may be needed to inactivate an implantable
defi brillator which fi res repeatedly.
Fig. 3.15 Paced rhythm.
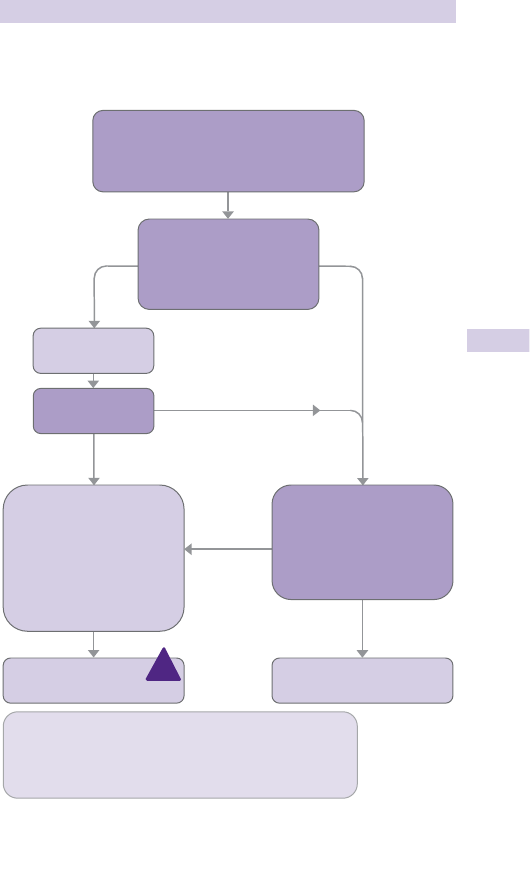
83
TREATMENT OF BRADYARRHYTHMIAS
Algorithm for the management of bradycardia (Fig. 3.16 )
See www.resus.org.uk
Seek expert help
Arrange transvenous pacing
*Alternatives include:
• Aminophylline
• Dopamine
• Glucagon (if beta-blocker or calcium channel blocker overdose)
• Glycopyrronium bromide can be used instead of atropine
YES
NO
Adverse features?
• Shock
• Syncope
• Myocardial ischaemia
• Heart failure
Atropine
500 mcg IV
YES
NO
NO
YES
• Assess using the ABCDE approach
• Give oxygen if appropriate and obtain IV access
• Monitor ECG, BP, SpO
2
, record 12-lead ECG
• Identify and treat reversible causes
(e.g. electrolyte abnormalities)
Observe
Satisfactory
response?
!
Interim measures:
• Atropine 500 mcg IV
repeat to maximum of 3 mg
• Isoprenaline 5 mcg min
–1
IV
• Adrenaline 2–10 mcg min
–1
IV
• Alternative drugs*
OR
• Transcutaneous pacing
Risk of asystole?
• Recent asystole
• Mobitz II AV block
• Complete heart block
with broad QRS
• Ventricular pause >3s
Fig. 3.16 Algorithm for the management of bradycardia.
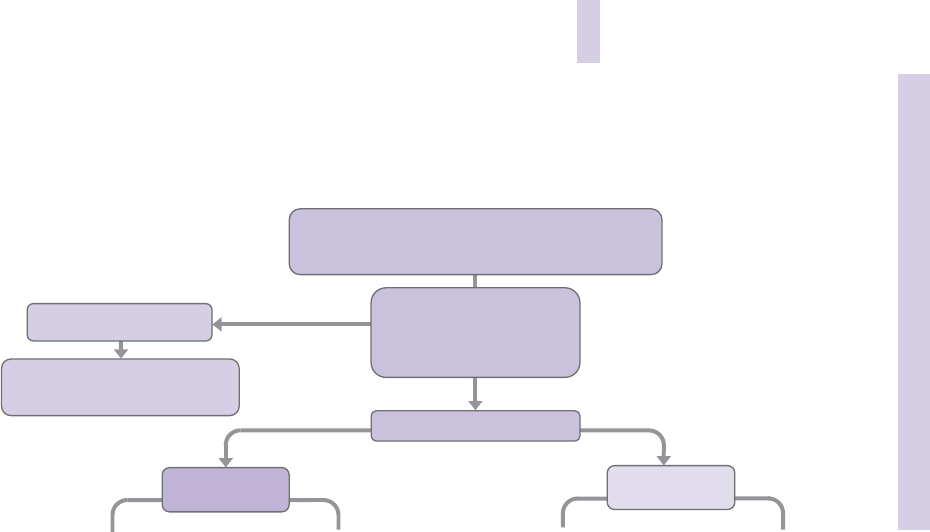
84 CHAPTER 3 Medicine
Tachycardia algorithm–with pulse
Yes/Unstable
• Amiodarone 300 mg IV over 10–20 min
and repeat shock; followed by:
No/Stable
NarrowBroad
Is QRS narrow (< 0.12s)?
Irregula
r
Narrow QRS
Is rhythm regular?
Regular
Irregular Regular
Adverse features?
• Shock
• Syncope
• Myocardial ischaemia
• Heart failure
Synchronised DC Shock
Up to 3 attempts
Broad QRS
Is rhythm regular?
• Assess using the ABCDE approach
• Give oxygen if appropriate and obtain IV access
• Monitor ECG, BP, SpO
2
, record 12-lead ECG
• Identify and treat reversible causes (e.g. electrolyte abnormalities)
• Amiodarone 900 mg over 24 h
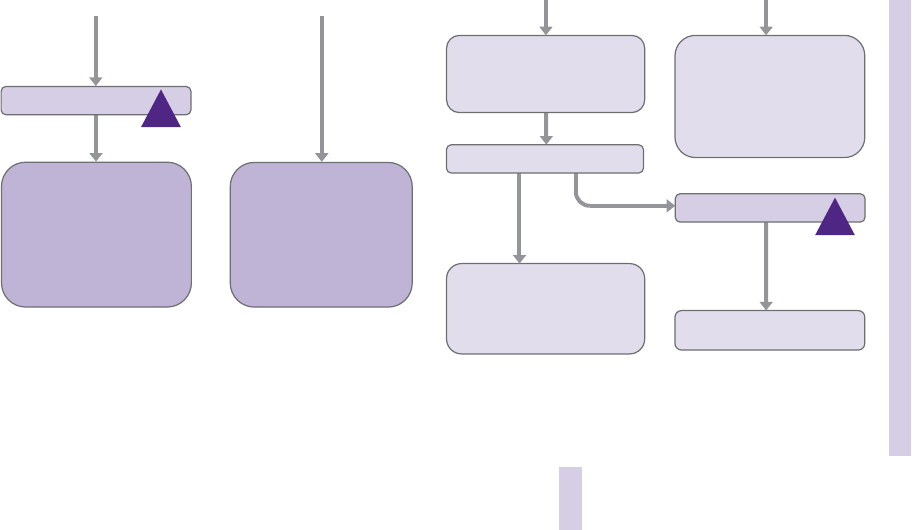
85
TACHYCARDIA ALGORITHM
Irregular narrow complex
tachycardia
Probable atrial fibrillation
Control rate with:
• β-Blocker or diltiazem
• Consider digoxin or amiodarone
if evidence of heart failure
Possibilities include:
• AF with bundle branch block
treat as for narrow complex
• Pre-excited AF
consider amiodarone
• Polymorphic VT
(e.g. torsade de pointes -
give magnesium 2 g over 10 min)
If ventricular tachycardia
(or uncertain rhythm):
• Amiodarone 300 mg IV
over 20–60 min;
then 900 mg over 24 h
If previously confirmed
SVT with bundle branch block:
• Give adenosine as for regular
narrow complex tachycardia
• Use vagal manoeuvres
• Adenosine 6 mg rapid IV bolus;
if unsuccessful give 12 mg;
if unsuccessful give further 12 mg
• Monitor ECG continuously
Probable re-entry paroxysmal SVT:
• Record 12-lead ECG in sinus
rhythm
• If recurs, give adenosine again and
consider choice of anti-arrhythmic
prophylaxis
Yes
Sinus rhythm restored?
No
Possible atrial flutter
• Control rate (e.g. β-Blocker)
Seek expert help
Seek expert help
!
!
Fig. 3.17 Tachycardia algorithm with pulse (www.resus.org.uk).

86 CHAPTER 3 Medicine
Tachyarrhythmias
The single Resuscitation Council 2010 tachycardia algorithm (Fig. 3.17 )
(see www.resus.org.uk ) is based on the fact that, irrespective of the exact
underlying cardiac rhythm, many of the initial management principles in
the peri-arrest setting are the same:
• Rapidly assess ABC.
• Monitor cardiac rhythm and record a 12-lead ECG.
• Provide O
2
.
• Identify and treat reversible causes.
• Assess for evidence of instability (signs of shock, syncope, signs of heart
failure, or myocardial ischaemia) — these indicate the need for urgent
intervention, initially in the form of synchronized cardioversion.
The unstable patient with tachyarrhythmia
Synchronized cardioversion
This requires two doctors — one to perform cardioversion, the other
(experienced in anaesthesia) to provide sedation/anaesthesia and manage
the airway. The patient will not be fasted and is therefore at particular risk
of aspiration. The arrhythmia may d cardiac output and i circulation times,
so IV drugs take much longer to work than usual. If the ‘sedation doctor’
does not appreciate this and gives additional doses of anaesthetic drugs,
hypotension and prolonged anaesthesia may result.
Electrical cardioversion is synchronized to occur with the R wave to
minimize the risk of inducing VF. Synchronized cardioversion is effective
in treating patients who exhibit evidence of instability with underlying
rhythms of SVT, atrial fl utter, atrial fi brillation, and VT — choose an initial
level of energy according to the rhythm:
• For broad complex tachycardia or AF, start with 200J monophasic or
120–150J biphasic. If unsuccessful, i in increments to 360J monophasic
or 150J biphasic.
• Start with a lower energy for atrial fl utter and paroxysmal SVT — use
100J monophasic or 70–120J biphasic. If this is unsuccessful, increase in
increments to 360J monophasic or 150J biphasic.
Amiodarone
If cardioversion is unsuccessful after 3 synchronized shocks, give amio-
darone 300mg IV over 10–20min and repeat shock. Give amiodarone
by central vein when possible as it causes thrombophlebitis when given
peripherally. However, in an emergency, it can be given into a large
peripheral vein.
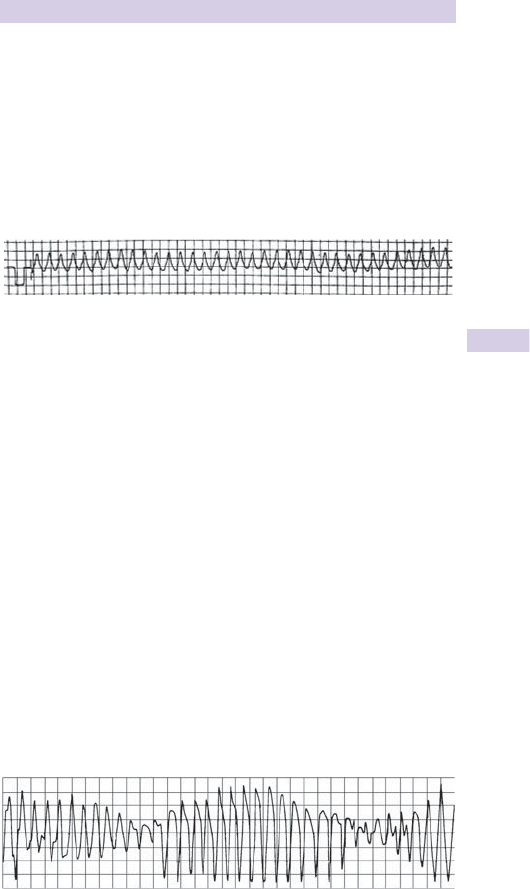
87
BROAD COMPLEX TACHYARRHYTHMIAS
Broad complex tachyarrhythmias
May be caused by VT, or rarely by SVT with aberrant conduction. The
default position should be that broad complex tachycardia is VT. Provide
O
2
as appropriate, insert an IV cannula and follow the Resuscitation
Council guidelines (Fig. 3.17 ) and (www.resus.org.uk ).
The priorities in broad complex arrhythmias associated with tricyclic
overdose are airway management, oxygenation, ventilation and correction
of metabolic disorders: give IV bicarbonate, but avoid anti-arrhythmic
drugs (b Tricyclic antidepressant poisoning, p.194).
Evaluating ECGs: is it VT or SVT with aberrant conduction?
VT is much more likely as a cause of the broad complex tachycardia if:
• The patient is > 60 years.
• The patient has a history of IHD or cardiomyopathy.
• There is clinical evidence of AV dissociation (intermittent cannon ‘a’
waves seen on jugular venous pressure (JVP), fi rst heart sound of vari-
able intensity).
• Inverted P waves in lead II.
• The frontal plane axis is bizarre (–90 ° to –180 ° ).
• The QRS is > 0.13sec.
• There are ‘capture’ or ‘fusion’ beats.
• The QRS is bizarre, not resembling a bundle branch block pattern
• All chest leads (V
1–6
) are concordant (QRS complexes point the same
way).
• R > R´ (or r´) in V
1
.
• There is a deep S wave (either QS, rS or RS) in V
6
.
Torsades de pointes
This is a rare form of polymorphic VT, associated with hypomagnesaemia,
hypokalaemia, long QT interval (congenital or drug related, eg sotalol,
antipsychotics, antihistamines, antidepressants). A constantly changing
electrical axis results in QRS complexes of undulating amplitude. Usually
paroxysmal, it may degenerate to VF. Get expert help and treat with IV
magnesium sulphate (2g over 10min = 8mmol or 4mL 50 % magnesium).
Refractory cases may require overdrive pacing.
Fig. 3.18
Fig. 3.19

88 CHAPTER 3 Medicine
Narrow complex tachyarrhythmias
These are almost always of supraventricular origin. Underlying rhythms
include:
• Sinus tachycardia.
• Paroxysmal AV re-entrant tachycardia (often referred to as ‘SVT’).
• AF with fast ventricular response.
• Atrial fl utter.
• Atrial tachycardia.
• Junctional tachycardia.
Give O
2
, insert an IV cannula, and follow the algorithm in Fig. 3.17 ( www.
resus.org.uk ). Determine if the rhythm is regular. Treat irregular rhythms
(AF) as outlined in Fig. 3.17 . If the ventricular rate is exactly 150/min, atrial
fl utter with 2:1 block is likely (Fig. 3.20 ).
The compromised patient with shock, syncope, acute cardiac failure, or
cardiac ischaemia should be treated with emergency electrical cardioversion.
It is reasonable to give IV adenosine while arranging the cardioversion, as
long as this does not delay the procedure.
For stable patients consider
Vagal stimulation The most effective way is a Valsalva manoeuvre while
supine or tilted head down. Instruct the patient to attempt to blow the
plunger out of a 50mL bladder tip syringe. If unsuccessful, in the young
patient, massage the carotid sinus for 15sec (1 side only), by gently
rubbing in a circular action lateral to the upper border of the thyroid
cartilage. Carotid sinus massage may be dangerous (especially if there is a
carotid bruit or previous stroke/TIA).
Adenosine This temporarily blocks conduction through the AV node. It
has a very short half-life (10–15sec). Adenosine can successfully terminate
re-entrant tachycardias and may ‘unmask’ other conditions (eg atrial
fl utter) by temporarily producing a conduction block. It is contraindicated
in 2 * or 3 * AV block, patients with WPW and asthmatics. The effects
are blocked by theophylline and potentiated markedly (and dangerously)
in the presence of dipyridamole, carbamazepine or in a denervated
heart — seek advice. Warn the patient about transient fl ushing and chest
discomfort. Give adenosine by fast bolus 6mg IV injection into an IV
cannula in the antecubital fossa and fl ush with 0.9 % saline (Fig. 3.17 ) while
recording a rhythm strip. If unsuccessful, repeat with 12mg, then 12mg.
If adenosine is contra-indicated, consider IV verapamil 2.5–5mg over 2min.
Avoid verapamil in patients with cardiac failure, hypotension, concomitant
B -blocker therapy, or WPW.
Fig. 3.20 Narrow complex tachycardia.

89
ATRIAL FIBRILLATION
Atrial fi brillation
Atrial fi brillation is rapid, irregular, uncoordinated atrial activity, and is
associated with an irregular ventricular response.
Causes
Acute AF may be associated with: IHD (33 % ), heart failure (24 % ), hyperten-
sion (26 % ), and valvular heart disease (7 % ). Other cardiac causes are sick
sinus syndrome, pericarditis, infi ltrative heart disease, cardiomyopathy,
myocardititis, congenital heart disease, and post-cardiac surgery.
Non-cardiac causes include: sepsis, PE, thyrotoxicosis, electrocution,
lung or pleural disease, chest trauma, hypokalaemia, hypovolaemia,
hypothermia, drug abuse (eg cocaine). Paroxysmal AF sometimes occurs
in fi t athletes.
Holiday heart: binge drinking or occasionally alcohol withdrawal may
cause acute AF in patients with no other predisposing factors. AF usually
resolves spontaneously within 48hr. The diagnosis of ‘holiday heart’ is one
of exclusion after cardiac disease and other causes have been ruled out.
Clinical features
AF d cardiac output by 10–20 % , irrespective of underlying ventricular
rate. Clinical presentation varies according to the cause and effect of
the AF. Some patients are asymptomatic; others suffer life-threatening
complications (heart failure, angina). Patients with underlying IHD may
develop ischaemia during periods of rapid ventricular rate.
Treatment
Patients in AF can be treated with cardioversion or rate control. If signs of
shock, syncope, acute cardiac failure, or ischaemia are present, consider
electrical cardioversion under sedation. Patients may also be chemically
cardioverted with fl ecainide 50–150mg IV (contraindicated in patients with
cardiac disease) or amiodarone 300mg IV (safer in patients with cardiac
disease). Both drugs may cause hypotension. If the patient has had symp-
toms for longer than 48hr, they are at risk of cardiac thromboembolism
and stroke when cardioverted, so instead, give rate control medications
and commence IV or low molecular weight heparin. Rate control drugs
include metoprolol 5mg IV and diltiazem (IV form not available in UK).
Digoxin 500mcg IV is the drug of choice in patients with CCF. See 2006
NICE guidelines ( www.nice.org.uk ).
Atrial fi brillation in Wolff Parkinson White syndrome
This may result in an irregular, broad complex tachycardia. Impulses are
conducted from the atria via the AV node and an accessory pathway.
Do not give AV-blocking drugs (digoxin, verapamil, or adenosine) as this
can result in acceleration of conduction through the accessory pathway,
leading to cardiovascular collapse or VF. Seek expert help.
Atrial fl utter
The typical atrial rate is 300/min, so a regular 2:1 block will give a QRS
rate of 150/min. Variable block may result in an irregular rate. Consult
with an expert to discuss treatment.

90 CHAPTER 3 Medicine
Hypertensive problems
Bear the following points in mind when managing a hypertensive patient
in the ED:
• Most patients with hypertension are asymptomatic.
• Hypertension is an important risk factor for cardiovascular disease and
stroke.
• Most patients found to be hypertensive in the ED do not require any
immediate intervention or treatment, but do require careful follow-
up — usually by their GP.
• Never intervene on the basis of a single raised BP measurement in the
absence of any associated symptoms and signs.
Approach
Approach patients found to be hypertensive as follows:
• Those with no previous history of hypertension, and no other concerns
or history of other conditions (eg diabetes, peripheral vascular disease,
IHD, or stroke) — arrange follow-up and monitoring with GP.
• Those known to be hypertensive already on treatment — arrange
follow-up and monitoring with GP.
• Those displaying evidence of end organ damage (eg LV hypertrophy,
retinal changes, renal impairment) — refer to the medical team.
• Those with hypertension associated with pain, vasoconstriction (eg acute
pulmonary oedema) or stroke — treat underlying cause where possible.
Do not intervene in stroke associated hypertension except under the
direction of a neurologist or stroke specialist.
• Those with hypertension directly associated with symptoms or
signs — contact the medical team and consider whether intervention
is appropriate (see below).
Mild/moderate hypertension (diastolic 100–125mmHg)
Ascertain if the patient has a past history of hypertension and is taking drug
therapy for this. Examine for retinal changes and evidence of hypertensive
encephalopathy. Investigate as appropriate (U&E, urinalysis, CXR, ECG).
Further management will depend upon the BP and the exact circum-
stances. If the BP is moderately elevated (ie diastolic BP: 110–125mmHg)
and the patient is symptomatic, refer to the medical team. If the patient is
asymptomatic with normal examination and renal function, he/she may be
suitable for GP follow up.

91
HYPERTENSIVE PROBLEMS
Severe hypertension (diastolic > 125mmHg)
Patients with a diastolic BP > 125mmHg require urgent assessment. Search
for evidence of hypertensive encephalopathy : headache, nausea, vomiting,
confusion, retinal changes (haemorrhages, exudates, papilloedema), fi ts,
focal neurological signs, d conscious level. Ask about recent drug ingestion
(eg ecstasy or cocaine — b pp. 214 & 215).
Investigations
Insert an IV cannula and send blood for U&E, creatinine, and glucose. Obtain
a CXR and ECG, and perform urinalysis. If there is d conscious level, focal
signs, or other clinical suspicion that the hypertension may be secondary to
stroke or intracranial haemorrhage, arrange an emergency CT scan.
Management
• Refer patients with a diastolic pressure > 125mmHg or evidence of
hypertensive encephalopathy to the medical team. Resist commencing
emergency treatment until consultation with an expert. There is a sig-
nifi cant risk of complications (stroke or MI) if the BP is reduced rapidly.
It may be appropriate to commence oral antihypertensive therapy using
a B-blocker (eg atenolol or labetalol) or calcium channel blocker (eg
nifedipine).
• If treatment is appropriate, commence an IVI of sodium nitroprusside,
labetalol or GTN with continuous BP monitoring via an arterial line and
admit to high dependency unit (HDU) or ICU. Sodium nitroprusside
has a very short half-life ( 8 1–2min) and acts as a vasodilator of both
arterioles and veins. IV labetolol may be preferred if aortic dissection
( b p.92) or phaeochromocytoma are suspected.
• Beta-blockers are contraindicated in hypertension caused by cocaine,
amphetamine or related sympathomimetic drugs ( b p.215), since
B-blockade may cause unopposed A-adrenergic activity with paradox-
ical hypertension and d coronary blood fl ow.
Hypertension in pregnancy
Hypertension may be part of pre-eclampsia or eclampsia (see b p.592).
Pre-eclampsia is diagnosed with 2 or more of: hypertension ( > 140/90),
proteinuria and oedema. This can be associated with haemolysis,
elevated liver function tests (LFTs), low platelets (HELLP syndrome).
Check urine for protein and check blood for FBC, LFT, platelets, and
coagulation screen. Call for senior obstetric help. Eclampsia is diagnosed
with the onset of grand mal seizures after 20 weeks gestation, and carries
a signifi cant mortality rate.
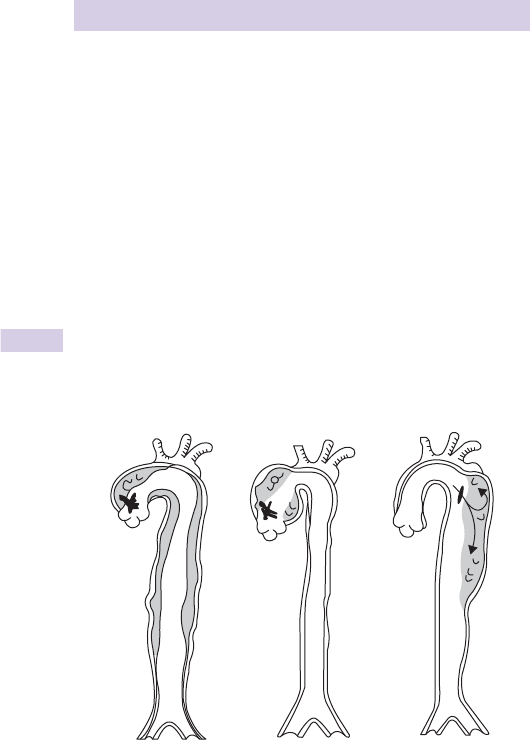
92 CHAPTER 3 Medicine
Aortic dissection
Remember: hypertensive patients with sudden, severe chest, and/or back
pain may have acute aortic dissection.
Pathology
Aortic dissection is longitudinal splitting of the muscular aortic media
by a column of blood. The dissection may spread proximally (possibly
resulting in aortic incompetence, coronary artery blockage, cardiac
tamponade), distally (possibly involving the origin of various arteries), or
rupture internally back into the aortic lumen, or externally (eg into the
mediastinum, resulting in rapid exsanguination).
More than 70 % of patients have a history of hypertension. It occurs
more frequently in those with bicuspid aortic valve, Marfan’s syndrome
or Ehlers–Danlos syndrome. Up to 20 % follow recent cardiac surgery or
recent angiography/angioplasty.
Dissection may be classifi ed Stanford type ‘A’ or ‘B’, according to whether
the ascending aorta is involved or not, respectively. Overall mortality is
30 % (35 % type A and 15 % type B).
Type A Type B
Fig. 3.21

93
AORTIC DISSECTION
History
Aortic dissection may mimic the presentation of an MI, requiring a high
index of suspicion. It typically presents with abrupt onset sharp, tearing or
ripping pain (maximal at onset) in anterior or posterior chest. Migration of
the pain may refl ect extension of the dissection. Syncope occurs in 8 10 %
of patients, sometimes in the absence of any pain. Occasionally, patients
can present with neurological defi cit associated with chest pain.
Examination
The patient is usually apprehensive and distressed, with pain which is dif-
fi cult to alleviate, even using IV opioid. Clues to the diagnosis include:
• An aortic regurgitation murmur (30 % ).
• Asymmetry or absence of peripheral pulses or a pulse defi cit (15–20 % ).
• Hypertension.
• Hypotension with features of tamponade or neurological signs in asso-
ciation with pain (eg secondary to spinal/carotid artery involvement).
Investigations
• Send blood for U&E, glucose, FBC, coagulation, and cross-matching.
• Obtain an ECG and CXR.
Thoracic aortic dissection usually results in an abnormal CXR. One or
more of the following changes may be seen:
• A widened or abnormal mediastinum (present in 875 % ).
• A ‘double knuckle’ aorta.
• Left pleural effusion ( 8 20 % ).
• Deviation of the trachea or nasogastric (NG) tube to the right.
• Separation of two parts of the wall of a calcifi ed aorta by > 5mm (the
‘calcium sign’).
The ECG may demonstrate MI, LVH. or ischaemia.
Note thatu 8 12 % of patients with aortic dissection have a normal CXR
and 8 30 % have a normal ECG.
CT angiography or formal angiography will provide the defi nitive diagnosis.
In a haemodynamically unstable patient, trans-oesophageal echo in theatre
may be the investigation of choice.
Management
On suspicion of aortic dissection:
• Provide O
2
by face mask as appropriate.
• Insert 2 large-bore (14G) IV cannulae and cross-match for 6U (inform
blood bank of suspected diagnosis).
• Give IV morphine and titrate according to response ( ± anti-emetic).
• Call cardiothoracic team and cardiologist at an early stage.
• Insert an arterial line (preferably right radial artery) and discuss with
specialist teams how to control the BP (eg labetalol infusion).
• Arrange further investigation based upon specialist advice and available
resources (eg aortography, echocardiography, CT scan, MRI).
Type A dissections are usually treated surgically; type B lesions are usually
treated medically.
94 CHAPTER 3 Medicine
Haemoptysis
Haemoptysis may be the chief or sole complaint of patients presenting to
the ED. It always warrants investigation.
Causes of haemoptysis
Presentation
Ascertain the exact nature and volume (eg ‘bright red streaks’ or
‘dark brown granules’). Patients sometimes have surprising diffi culty
distinguishing vomited blood from that coughed up. Enquire about weight
loss, and take a drug history and smoking history.
Investigation
• Send blood for FBC, coagulation screen, U&E, LFTs.
• Request Group and Save if evidence of signifi cant haemorrhage.
• If SpO
2
<94 % on air, or the patient has COPD, check ABG.
• Obtain CXR and ECG.
• Perform urinalysis — if shocked, insert catheter and monitor output.
• Collect sputum samples. Send for microscopy, culture, and sensitivity.
• Initiate further investigations according to the likely diagnosis.
Treatment
• Airway : clear and secure (coughing/suction). Put on a face mask and
shield if maintaining the airway or intubating. Ensure nearby high fl ow
suction. Massive haemorrhage may require tracheal intubation. Whilst
preparing for this, tilt trolley so that the patient is head-down.
• Breathing : provide O
2
to maintain saturations at 94–98 % . If ventilation is
inadequate, assist with bag and mask or tracheal tube.
• Circulation : insert a large bore (14G) IV cannula (use 2 if hypovolaemic).
Give IV fl uids/blood/clotting factors as clinically indicated ( b p.172).
Further treatment
Commence specifi c treatment measures aimed at life-threatening
underlying cause (eg LVF, PE, infection, coagulopathy). In cases of large
haemoptysis, it is appropriate to admit for further investigation and treat-
ment. If the patient is stable and has only had a small amount of blood
stained sputum, urgent outpatient investigation may be appropriate.
Respiratory
• Infection (URTI, pneumonia, TB, lung abscess)
• Carcinoma (bronchial or laryngeal)
• Bronchiectasis
Cardiovascular
• Pulmonary oedema
• PE
• Ruptured aortic aneurysm (aorto-bronchial fi stula)
Coagulation
disorder
• Drugs (eg warfarin, heparin)
• Inherited (eg Haemophilia, Christmas disease)
Trauma
• Penetrating or blunt
Other
• Goodpasture’s, Wegener’s granulomatosis

95
OXYGEN
Oxygen
Oxygen is the most commonly administered hospital therapy. In recent
years, high fl ow oxygen was widely used in the treatment of medical
and surgical emergencies, and initial resuscitation. There is now a move
towards safer treatment with controlled oxygen therapy.
Common problems
• Failure to prescribe oxygen.
• Failure to check ABG in patients requiring oxygen therapy.
• Failure to monitor or review patients on oxygen therapy.
• Inadvertent administration of another gas other than oxygen.
• Inadvertent disconnection from the oxygen supply.
• Depletion of an oxygen tank during transfer ( www.nrls.npsa.nhs.uk ).
Oxygen cylinders
When administering oxygen in the ED, always use piped oxygen from the
wall outlet. Only use an oxygen cylinder when transporting the patient
to the radiology department or ward. Oxygen is highly fl ammable. Do
not take a cylinder out of its support cage and never let it fall. In the UK,
oxygen cylinders are colour-coded white. The commonest small cylinder
is B (or M-6), which holds 170L oxygen. The commonest large cylinder is
E (or M-24), holding 680L. Before a patient leaves the ED, always check
that the cylinder is full. If the patient is being transferred to another hos-
pital, check there is enough oxygen for the journey. The formula is:
Volume of cylinder in L/fl ow rate
=
minutes cylinder will last
Oxygen requirements
The aim of oxygen therapy is to optimize tissue oxygen delivery. Use pulse
oximetry to guide whether the patient requires supplemental oxygen. In
previously healthy patients, aim for SpO
2
94–98 % , but in patients with
known COPD or type II respiratory failure, aim for SpO
2
88–92 % . Always
take an ABG in patients with chronic lung disease, to assess their optimal
oxygen treatment (see b p.98 on ABG interpretation). Repeat the ABG
within 30 min after changing the inspired oxygen concentration. When
assessing a critically ill patient, it is appropriate to give high fl ow oxygen
and to titrate the inspired oxygen concentration (FiO
2
) down according
to the ABG results.
Oxygen delivery
• Use a high concentration oxygen reservoir mask (non-rebreathing
mask) in hypoxic patients without chronic lung disease.
• Use a simple face mask for patients with a mild hypoxia, without chronic
lung disease.
• Use a 28 % Venturi mask for patients with COPD or known type II respi-
ratory failure.
• Use a tracheostomy mask for patients with tracheostomy.
Prescribing oxygen
The oxygen prescription should include the target SpO
2
, the oxygen mask
type and oxygen fl ow rate. In an emergency, it is appropriate to administer
oxygen prior to prescribing, but do not forget to prescribe the oxygen
after resuscitation. See www.brit-thoracic.org.uk.

96 CHAPTER 3 Medicine
The dyspnoeic patient
The normal adult respiratory rate is 11–18/min, with a tidal volume of
400–800mL. Acute dyspnoea is a common presenting symptom.
Common causes of acute dyspnoea
Cardiac
• Cardiogenic pulmonary oedema ( b p.100).
• MI ( b p.68).
• PE ( b p.120).
• Arrhythmias ( b p.80).
Respiratory
• Asthma ( b p.104) or exacerbation of COPD ( b p.108).
• Pneumonia ( b p.110).
• Pleural effusion ( b p.103).
• Pneumothorax ( b p.114).
Trauma
• Aspiration of FB or vomit ( b p.112).
• Pneumothorax/haemothorax ( b p.334).
• Flail chest ( b p.332).
• Drowning incident ( b p.258).
Other
• Hypovolaemia or fever from any cause.
• Hyperventilation syndrome ( b p.97).
• Respiratory compensation for metabolic acidosis (DKA, salicylate over-
dose).
Approach
Follow the ABC approach and resuscitate as necessary. The main aim of
treatment is to correct life-threatening hypoxia. Enquire about speed of
onset of dyspnoea, past medical history and associated symptoms (cough,
haemoptysis, fever, wheezing, chest pain). Examine carefully, paying atten-
tion to the respiratory rate, depth, and pattern. Apply a pulse oximeter.
Pulse oximetry
This is simple, rapid, safe, and non-invasive, but it does not provide infor-
mation about ventilation or arterial partial pressure of carbon dioxide
(pCO
2
). A normal oxygen saturation does not exclude signifi cant lung
pathology (eg PE). Pulse oximetry may be inaccurate or misleading in:
• Poor peripheral perfusion/shock.
• Methaemoglobinaemia.
• Hypothermia.
• CO poisoning (see b p.208). SpO
2
values may be falsely high as COHb
reads as oxyhaemoglobin. COHb can be measured on venous blood
gas testing or COHb pulse oximeter.
• Nail varnish/synthetic fi ngernails (if a fi nger probe is used).
• Excessive movement.
Correlate readings with clinical fi ndings: a non-pulsatile trace (or heart
rate different from that on cardiac monitor) suggests the saturation
reading is probably inaccurate.

97
HYPERVENTILATION
Hyperventilation
Hyperventilation is breathing which occurs more deeply and/or more
rapidly than normal. CO
2
is ‘blown off ’, so that pCO
2
d . Hyperventilation
may be primary (‘psychogenic’) or secondary. A classical secondary cause
is DKA — Kussmaul’s respiration represents respiratory compensation for
a metabolic acidosis.
Secondary causes of hyperventilation
• Metabolic acidosis (eg DKA, uraemia, sepsis, hepatic failure).
• Poisoning (eg aspirin, methanol, CO, cyanide, ethylene glycol).
• Pain/hypoxia.
• Hypovolaemia.
• Respiratory disorders (eg PE, asthma, pneumothorax).
Primary (psychogenic or inappropriate) hyperventilation
Typically, the patient is agitated and distressed with a past history of panic
attacks or episodes of hyperventilation. They may complain of dizziness,
circumoral paraesthesia, carpopedal spasm, and occasionally sharp or
stabbing chest pain. Initial examination reveals tachypnoea with equal
air entry over both lung fi elds, and no wheeze or evidence of airway
obstruction. It is important to consider secondary causes (such as PE or
DKA). Therefore, perform the following investigations:
• SpO
2.
• ECG.
• ABG if SpO
2
d , or if symptoms do not completely settle in a few
minutes.
• BMG.
If symptoms do not completely settle in a few minutes, obtain:
• CXR.
• U&E, blood glucose, FBC.
Treatment
Do not sedate a patient who is hyperventilating. Once serious diagnoses
have been excluded, use this information to help reassure the patient with
primary hyperventilation. Often this is all that is required, but it may be
helpful to try simple breathing exercises (breathe in through nose — count
of 8, out through mouth — count of 8, hold for count of 4 and repeat).
Discharge the patient with arrangements for GP follow-up. If these simple
measures fail, reconsider the diagnosis and refer the patient to the medical
team for subsequent observation and treatment.

98 CHAPTER 3 Medicine
Arterial blood gases
Blood gas sampling is useful in assessing breathless patients, septic patients,
diabetic patients in ketoacidosis, those who are critically ill and patients
who have ingested poisons. This enables rapid measurement of blood pH,
bicarbonate, O
2
and CO
2
. Most ED blood gas analysers will also measure
blood glucose, K
+
, Hb, and lactate, so arterial or venous blood gas sampling
will also test for anaemia, hyperkalaemia, and hypoglycaemia.
Assessing respiratory function
Arterial sampling helps in the assessment of a patient with low SpO
2
,
or in patients with known lung disease (especially if they are receiving
supplemental oxygen). If possible (caution required), take the fi rst sample
with the patient breathing room air. If this is not possible, document the
inspired oxygen concentration. Look specifi cally for:
• Hypoxia, (pO
2
<10.6kPa on air).
• Hypercarbia, (pCO
2
> 6.0kPa).
• Bicarbonate retention (HCO
3
–
> 28mmol/L).
• Acidosis (pH <7.35).
Differentiating between type I and type II respiratory failure
In type I failure there is hypoxia with normal or d pCO
2
. In type II failure,
there is hypoxia with i pCO
2
, and frequently an i HCO
3
–
. In type II failure,
the patient may develop life-threatening respiratory failure if administered
high concentrations of oxygen. Aim to maintain SpO
2
at 88–92 % , and
recheck ABGs in 30min.
Differentiating between acute and chronic type II respiratory failure
Patients who normally have a slightly i pCO
2
will also show i HCO
3
–
on ABG. The kidneys adapt over a period of days to retain bicarbonate,
in attempt to buffer the respiratory acidosis (see nomogram inside front
cover). Respiratory acidosis in a patient with chronic type II respira-
tory failure ( i pCO
2
, i HCO
3
–
and pH <7.35) indicates life-threatening
impairment of lung function.
In acute respiratory failure, the lungs are unable to eliminate CO
2
(caused
by d GCS or hypoventilation from any cause), which results in i pCO
2
and
a respiratory acidosis. Patients may require ventilatory support.
A venous blood sample will give accurate readings for K
+
, lactate, glucose,
HCO
3
–
, Hb and COHb. In addition, a normal venous pCO
2
will exclude
hypercarbia.
Other blood gas results
Blood gas analysers calculate the base excess from the HCO
3
–
concentra-
tion and pH. Levels <–2mmol/L indicate that the patient has a metabolic
acidosis. Levels > 2mmol/L indicate a metabolic alkalosis (for example, as a
result of chronic bicarbonate retention in type II respiratory failure).

99
ARTERIAL BLOOD GASES
Metabolic acidosis
The usual pattern of results in metabolic acidosis is pH<7.35, HCO
3
–
<24mmol/L and BE <–2mmol/L. There may be compensatory hypocarbia
(pCO
2
<4.5kPa). Metabolic acidosis has many possible causes:
• i Acid load (lactic acidosis, ketoacidosis, or ingestion of salicylates,
methanol, ethylene glycol, or metformin).
• d Removal of acid (renal failure or renal tubular acidosis types 1 and 4).
• Loss of bicarbonate from the body (diarrhoea, pancreatic, or intestinal
fi stulas, acetazolamide, or renal tubular acidosis type 2).
The anion gap
The anion gap is the quantity of anions not balanced out by cations,
(a measurement of negatively charged plasma proteins). The normal value
is 12–16mmol/L. It is measured by:
(Na
+
+ K
+
) – (Cl
–
+ HCO
3
–
) all measured in mmol/L
Measuring the anion gap helps distinguish the cause of a metabolic acidosis.
A high anion gap indicates that there is excess H
+
in the body. The
commonest cause of a high anion gap metabolic acidosis is lactic acidosis.
Most blood gas analysers will measure lactate (normal <2.0mmol/L).
Causes of a lactic acidosis
• Tissue hypoperfusion (trauma with major haemorrhage, septic shock).
• Tissue hypoxia (hypoxaemia, carbon monoxide or cyanide poisoning).
• Hepatic failure.
• Renal failure.
• Ethylene glycol or methanol poisoning ( b p.203; b p.202).
• Cocaine or amphetamines ( b p.215).
• Salicylate poisoning ( b p.189) or iron poisoning ( b p.201).
• Biguanides (metformin).
• Isoniazid.
• Strenuous exercise.
The other causes of a high anion gap metabolic acidosis are ketoacidosis
(diabetic or alcohol induced) and renal failure.
Causes of a normal anion gap metabolic acidosis are chronic diarrhoea,
pancreatic or intestinal fi stulas, acetazolamide, or renal tubular acidosis.
The osmolal gap
This is the difference between calculated serum osmolarity and laboratory
measured serum osmolality. Serum osmolarity can be calculated by:
(2 × Na
+
) + urea + glucose (all measured in mmol/L)
Subtract the calculated result from the laboratory measured osmolality to
give the osmolal gap. Normally this is <10mOsm/kg.
An elevated osmolal gap can be caused by alcohol, methanol, ethylene
glycol or acetone ingestion, mannitol, or sorbitol.

100 CHAPTER 3 Medicine
Cardiogenic pulmonary oedema
Left heart failure results ine i left ventricular end-diastolic pressure, causing
i pulmonary capillary hydrostatic pressure. Fluid collects in extravascular
pulmonary tissues faster than the lymphatics clear it.
Causes of cardiogenic pulmonary oedema
Often an acute complication of MI and IHD, or exacerbation of pre-ex-
isting cardiac disease (eg hypertension, aortic/mitral valve disease). Other
causes are:
• Arrhythmias.
• Failure of prosthetic heart valve.
• Ventricular septal defect.
• Cardiomyopathy.
• Negatively inotropic drugs (eg B -blockers).
• Acute myocarditis.
• Left atrial (LA) myxoma (may produce syncope, fever, i ESR, but is very
rare).
• Pericardial disease.
The history is frequently dramatic. Dyspnoea and distress may prevent
a full history from being taken. Find out the length of the history and
whether there is any chest pain. Check current drug therapy/allergies and
establish what emergency prehospital treatment has been administered.
Examination usually reveals a tachypnoeic, tachycardic, and anxious
patient. If the pulmonary oedema is severe, the patient may be cyanosed,
coughing up frothy pink sputum and unable to talk. Check pulse and BP,
auscultate the heart for murmurs, and 3rd/4th heart sounds of gallop
rhythm. Look for i JVP (also a feature of PE and cardiac tamponade). Listen
to the lung fi elds — fi ne inspiratory crepitations (crackles) may be limited
to the bases or be widespread. Wheeze may be more prominent than
crepitations. Cardiogenic pulmonary oedema is associated with evidence
of d cardiac output (sweaty, peripherally cool, and pale). Consider other
diagnoses (eg sepsis) in patients with warm, fl ushed extremities.
Investigation
Commence treatment before completing investigations:
• Attach a cardiac monitor and check SpO
2
with pulse oximeter.
• Obtain ECG. Check for arrhythmias, LAD, LVH, LBBB, recent or
evolving MI.
• Send blood for U&E, glucose, FBC, troponin.
• If severely ill or SpO
2
<94 % in air obtain ABG.
• Request old hospital notes/ECGs.
• Obtain a CXR and look for features of cardiogenic pulmonary oedema:
• upper lobe diversion (distension of upper pulmonary veins)
• cardiomegaly (LV and/or LA dilatation)
• Kerley A, B, or C septal lines
• fl uid in interlobar fi ssures
• peribronchial/perivascular cuffi ng and micronodules
• pleural effusions
• bat’s wing hilar shadows.

101
CARDIOGENIC PULMONARY OEDEMA
Treat urgently. Provide the following within the fi rst few minutes:
• Check that the airway is clear.
• Raise the back of the trolley to sit the patient up and support with
pillows if necessary.
• Provide high fl ow O
2
by tight-fi tting face mask.
• If systolic BP > 90mmHg, give 2 puffs of GTN SL (800mcg) and com-
mence GTN IVI, starting at 10mcg/min, i every few minutes according
to clinical response (monitor BP closely; take special care to avoid
hypotension). Alternatively try buccal GTN (3–5mg).
• Give IV furosemide 50mg. Larger doses may be needed in patients
already taking oral furosemide.
• If the patient has chest pain or is distressed, give very small titrated
increments of IV opioid (with anti-emetic). Do not give opioids to
patients who are drowsy, confused. or exhausted as this may precipi-
tate respiratory arrest.
• Consider inserting a urinary catheter and monitor urine output.
• Treat underlying cause and associated problems (arrhythmias, MI,
cardiogenic shock, acute prosthetic valve failure).
Monitor the SpO
2
and the clinical response to this initial treatment. Rapid
improvement may occur, due to venodilatation and reduction of preload.
If the patient does not improve, recheck ABG and consider:
• Non-invasive ventilation (continuous positive airway pressure (CPAP)
or bilevel positive airway pressure (BiPAP). Non-invasive ventilation
(NIV) appears safe in acute cardiogenic pulmonary oedema and may
avoid the need for intubation.
• If hypotensive refer to ICU for treatment of cardiogenic shock ( b
p.77). An intra- arterial line, Swan–Ganz catheter and inotropic support
(dobutamine) are likely to be required. Echocardiography may help to
exclude valve or septal rupture and guide treatment.
• Rapid sequence intubation in the presence of cardiogenic pulmonary
oedema may be associated with cardiovascular collapse. Stop nitrates
prior to administering anaesthesia and be ready to give pressors
± fl uids immediately post-induction.
Prosthetic valve failure
Always consider valve failure in patients with prosthetic valves, of which
a large variety are in common use. All are associated with some risks
(eg embolism, failure, obstruction, infection, haemorrhage from associated
anticoagulation), which vary according to design. Acute failure of a pros-
thetic aortic or mitral valve results in dramatic acute onset pulmonary
oedema with loud murmurs. The patient may deteriorate rapidly and not
respond to standard drug treatment. Resuscitate as described above. CXR
will show a prosthetic heart valve ± pulmonary oedema. Call urgently
for expert help (ICU team, cardiologist, and cardiothoracic surgeon).
Emergency transthoracic or transoesphageal echocardiography confi rms
the diagnosis. Immediate valve replacement is required.

102 CHAPTER 3 Medicine
Non-cardiogenic pulmonary oedema
Pulmonary oedema may occur in the absence of i pulmonary venous
pressure. The following mechanisms may be responsible:
• i Capillary permeability.
• d Plasma oncotic pressure.
• i Lymphatic pressure.
Changes in capillary permeability, secondary to a variety of triggers, is
the mechanism most frequently implicated in non-cardiogenic pulmonary
oedema, when it occurs as the Adult Respiratory Distress Syndrome
(ARDS). Since the mechanisms producing cardiogenic and non-cardiogenic
pulmonary oedema differ, so the approach to treatment differs.
Causes of non-cardiogenic pulmonary oedema
• ARDS (sequel to sepsis, trauma, pancreatitis).
• Intracranial (especially subarachnoid) haemorrhage.
• IV fl uid overload.
• Hypoalbuminaemia (liver failure, nephrotic syndrome).
• Drugs/poisons/chemical inhalation.
• Lymphangitis carcinomatosis.
• Smoke inhalation.
• Near drowning incidents.
• High altitude mountain sickness.
Approach
Distinguishing non-cardiogenic from cardiogenic pulmonary oedema is
usually apparent from the history. Evaluate the patient and resuscitate
according to ABCs. Direct treatment towards the underlying cause and
according to the physiological disturbance. To estimate the latter, invasive
monitoring may be required (urinary, intra-arterial, central venous and
pulmonary artery catheters). Involve ICU early and provide appropriate
IV fl uids, inotropes, tracheal intubation, IPPV and positive end expiratory
pressure (PEEP) as required.

103
PLEURAL EFFUSION
Pleural effusion
Under normal circumstances, each pleural cavity contains <20mL fl uid.
Causes
An exudate is diagnosed if the pleural fl uid:serum protein > 0.5,
fl uid:serum LDH > 0.6, or fl uid LDH > 2/3 the upper limits of laboratory
normal value for serum LDH.
Exudates
• Pneumonia (bacterial, viral, mycoplasma).
• Malignancy (bronchial carcinoma, mesothelioma, lymphoma).
• TB.
• PE with pulmonary infarction.
• Collagen vascular disease (SLE, rheumatoid arthritis).
• Subphrenic abscess.
• Amoebic liver abscess.
• Pancreatitis.
• Chylothorax (thoracic duct injury — rare).
Transudates
• Cardiac failure.
• Nephrotic syndrome.
• Hepatic failure.
• Ovarian hyperstimulation.
• Ovarian fi broma (Meig’s syndrome — rare).
• Peritoneal dialysis.
Clinical presentation
Symptoms are usually due to the underlying disease process. A mild dull
ache and dyspnoea (initially on exercise, later at rest) may occur if the
effusion is large. A history of vomiting followed by chest pain points to a
ruptured oesophagus — a surgical emergency.
Signs of an effusion are not apparent until > 500mL are present. Dyspnoea,
stony dullness to percussion, with absent breath sounds over the effusion are
characteristic. Bronchial breathing may be heard just above the effusion.
Very large unilateral effusions may produce evidence of mediastinal shift
(away from the collection of fl uid).
Investigations
CXR can demonstrate pleural effusions as small as 250mL, as blunting of
the costophrenic angle. Other investigations depend on likely cause.
Treatment
Provide O
2
and resuscitate as necessary, according to the underlying
pathology. Emergency therapeutic pleural aspiration is rarely required in
the ED, except where haemothorax is suspected. Refer to the medical
team for further investigation (including ultrasound guided diagnostic
pleural aspiration).

104 CHAPTER 3 Medicine
Acute asthma: assessment
Follow the British Thoracic Society guidelines ( www.brit-thoracic.org.
uk ) to assess and manage adults presenting with asthma, b p.106. The
guidelines refl ect continuing concern over asthma deaths. Patients with
severe asthma and one or more adverse psychosocial factors (psychiatric
illness, alcohol or drug abuse, unemployment) have i mortality. Measure
the peak expiratory fl ow rate and compare it against that expected (see
Fig. 3.22 ). The peak fl ow acts as an immediate triage tool: remember that
patients with life-threatening asthma may be too dyspnoeic to do this.
Make an initial assessment of the severity of acute asthma based upon
a combination of clinical features, peak fl ow measurement and pulse
oximetry as outlined below.
Moderate exacerbation of asthma
• Increasing symptoms.
• Peak fl ow 50–75 % best or predicted.
• No features of acute severe asthma (below).
Acute severe asthma
Any 1 of:
• Inability to complete sentences in 1 breath.
• Respiratory rate ≥25/min.
• Heart rate ≥110/min.
• Peak fl ow 33–50 % best or predicted.
Life-threatening asthma
A patient with severe asthma with any 1 of:
• Cyanosis.
• Exhaustion, confusion, coma.
• Feeble respiratory effort.
• SpO
2
<92 % .
• Silent chest.
• Bradycardia, arrhythmia, hypotension.
• pO
2
<8kPa.
• Normal pCO
2
(4.6–6.0kPa).
• Peak fl ow <33 % best or predicted.
Near fatal asthma
• i pCO
2
and/or requiring mechanical ventilation with i infl ation
pressures.
Other investigations
Obtain ABG if SpO
2
<92 % or if there are other features of life-threatening
asthma.
Obtain a CXR (without delaying treatment) if there is:
• Suspected pneumomediastinum or pneumothorax.
• Suspected consolidation.
• Life-threatening asthma.
• Failure to respond to treatment satisfactorily.
• Requirement for ventilation.
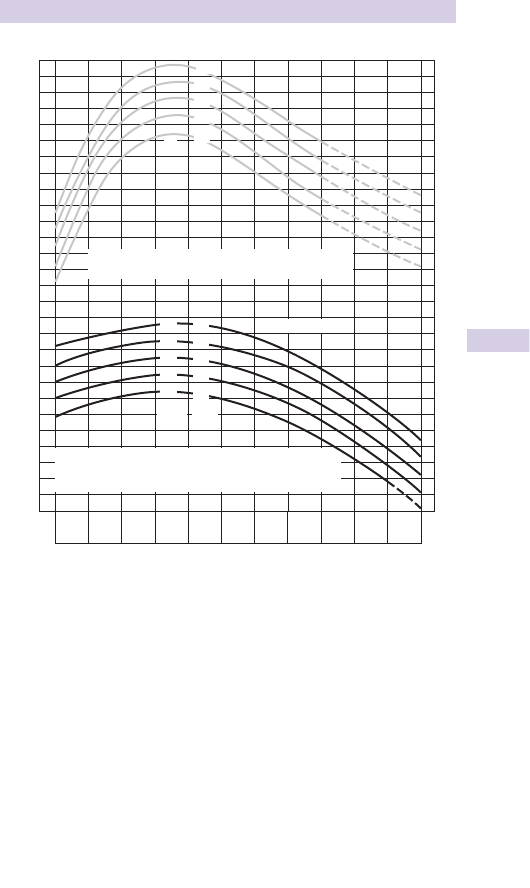
105
ACUTE ASTHMA: ASSESSMENT
PEF L/min
660
650
640
630
620
610
600
590
580
570
560
550
540
530
520
510
500
490
480
470
460
450
440
430
420
410
400
390
380
75
72
69
66
63
Ht.
(ins)
190
Ht.
(cms)
183
175
MEN
167
160
145
152
160
167
175
69
66
63
60
57
Ht.
(cms)
Ht.
(ins)
IN MEN, VALUES OF PEF UP TO 100 LITRES/MIN, LESS THAN
PREDICTED, AND IN WOMEN LESS THAN 85 LITRES/MIN, LESS
THAN PREDICTED, ARE WITHIN NORMAL LIMITS.
15 20 25 30 35 40 45 50 55 60 65
AGE IN YEARS
70
STANDARD DEVIATION MEN
STANDARD DEVIATION WOMEN
48 = litres/min
42 = litres/min
660
650
640
630
620
610
600
590
580
570
560
550
540
530
520
510
500
490
480
470
460
450
440
430
420
410
400
390
380
WOMEN
Fig. 3.22 Peak expiratory fl ow rates in normal adults.
Nunn AJ, Gregg I. (1989). New regression equations for predicting peak expiratory fl ow in adults.
Br Med J 298 : 1068–70.

106 CHAPTER 3 Medicine
Acute asthma: management
Initial treatment
Follow BTS/SIGN guidelines ( www.brit-thoracic.org.uk ) summarized as
follows:
• Provide high fl ow O
2
.
• Put the trolley back and side rails up so the patient is sitting up and
holding on to the side rails (to use pectoral muscles as accessory
muscles of respiration).
• If the patient cannot talk, start treatment, but get senior ED and ICU
help in case intubation and ventilation are required.
• Check trachea and chest signs for pneumothorax.
• Ask about previous admissions to ICU.
• Administer high dose nebulized B
2
agonist (eg salbutamol 5mg or terbu-
taline 10mg), or 10 puffs of salbutamol into spacer device and face mask.
For severe asthma or asthma that reponds poorly to the initial neb-
ulizer, consider continuous nebulization.
• Give a corticosteroid: either prednisolone 40–50mg PO or hydrocorti-
sone (preferably as sodium succinate) 100mg IV.
• Add nebulized ipratropium bromide (500mcg) to B
2
agonist treatment
for patients with acute severe or life-threatening asthma or those with a
poor initial response to B
2
agonist therapy.
• Consider a single dose of IV magnesium sulphate (1.2–2g IVI over 20min)
after consultation with senior medical staff, for patients with acute
severe asthma without a good initial response to inhaled bronchodi-
lator therapy or for those with life-threatening or near-fatal asthma.
• Use IV aminophylline only after consultation with senior medical staff.
Some individual patients with near-fatal or life-threatening asthma with a
poor response to initial therapy may gain additional benefi t. The loading
dose of IVI aminophylline is 5mg/kg over 20min unless on maintenance
therapy, in which case check blood theophylline level and start IVI of
aminophylline at 0.5–0.7mg/kg/hr.
• IV salbutamol is an alternative in severe asthma, after consultation with
senior staff. Draw up 5mg salbutamol into 500mL 5 % dextrose and run
at a rate of 30–60mL/hr.
• A patient who cannot talk will be unable to drink fl uids and may be
dehydrated.
• Avoid ‘routine’ antibiotics.
• Repeat ABG within an hour.
• Hypokalaemia may be caused or exacerbated by B
2
agonist and/or
steroid therapy.

107
ACUTE ASTHMA: MANAGEMENT
Criteria for admission
Admit patients with any features of
• A life-threatening or near-fatal attack.
• Severe attack persisting after initial treatment.
Management of discharge
Consider for discharge those patients whose peak fl ow is > 75 % best or
predicted 1hr after initial treatment. Prescribe a short course of oral pred-
nisolone (eg 40–50mg for 5 days) if initial peak expiratory fl ow rate (PEFR)
<50 % , and ensure adequate supply of inhalers. If possible arrange for
review by an asthma liaison nurse before discharge. At a minimum, inhaler
technique and peak expiratory fl ow monitoring should be reviewed.
Arrange/advise GP/asthma liaison nurse follow-up within 2 days. Fax or email
the discharge summary to GP. Advise to return to hospital if symptoms
worsen/recur.
Referral to intensive care unit
Refer any patient requiring ventilatory support or with acute severe or
life-threatening asthma failing to respond to therapy, evidenced by:
• Drowsiness, confusion.
• Exhaustion, feeble respiration.
• Coma or respiratory arrest.
• Persisting or worsening hypoxia.
• Hypercapnoea.
• ABG showing d pH.
• Deteriorating peak fl ow.
Cardiac arrest in acute asthma
The underlying rhythm is usually PEA. This may refl ect one or more
of the following: prolonged severe hypoxia (secondary to severe
bronchospasm and mucous plugging), hypoxia-related arrhythmias or
tension pneumothorax (may be bilateral). Give advanced life support
according to the guidelines in b Cardiac arrest, p.46 and treat tension
pneumothorax if present ( b p.328). Aim to achieve tracheal intubation
early in view of the higher than normal required lung infl ation pressures
and the attendant risk of gastric infl ation in the absence of a tracheal tube.

108 CHAPTER 3 Medicine
COPD
Chronic obstructive pulmonary disease (COPD) is characterized by
chronic airfl ow limitation due to impedance to expiratory airfl ow, mucosal
oedema, infection, bronchospasm and bronchoconstriction due to d lung
elasticity. Smoking is the main cause, but others are chronic asthma, α-1
antitrypsin defi ciency and chronic infection (eg bronchiectasis).
History
Exertional dyspnoea, cough, and sputum are usual complaints. Ask about:
• Present treatment including inhalers, steroids, antibiotics, theophyllines,
nebulizers, opiate analgesia, and home O
2
treatment.
• Past history: enquire about previous admissions and co-morbidity.
• Exercise tolerance: how far can they walk on the fl at without stopping?
How many stairs can they climb? Do they get out of the house?
• Recent history: ask about wheeze and dyspnoea, sputum volume and
colour. Chest injuries, abdominal problems and other infections may
cause respiratory decompensation.
• Read the hospital notes: have there been prior ICU assessments? Has the
respiratory consultant advised whether ICU would be appropriate?
Examination
Examine for dyspnoea, tachypnoea, accessory muscle use, and lip-pursing.
Look for hyperinfl ation (‘barrel chest’) and listen for wheeze or coarse
crackles (large airway secretions). Cyanosis, plethora (due to secondary
polycythaemia) and right heart failure (cor pulmonale) suggest advanced
disease. Look for evidence of hypercarbia: tremor, bounding pulses,
peripheral vasodilatation, drowsiness, or confusion.
Check for evidence of other causes of acute dyspnoea, particularly: asthma
( b p.104), pulmonary oedema ( b p.100), pneumothorax ( b p.114), PE
( b p.120). Remember that these conditions may co-exist with COPD.
Investigations
• SpO
2
, respiratory rate, pulse rate, BP, T
o
, and peak fl ow (if possible).
• CXR (look for pneumothorax, hyperinfl ation, bullae, and pneumonia).
• ECG.
• ABG (or capillary blood gas), documenting the FiO
2
. Use pCO
2
to guide
O
2
therapy.
• FBC, U&E, glucose, theophylline levels and, if pneumonia is suspected
and/or pyrexial, blood cultures, CRP, and pneumococcal antigen.
• Send sputum for microscopy and culture if purulent.
Treatment
Give O
2
— remember that hypercapnoea with O
2
is multifactorial. The aim
is to maintain SpO
2
88–92 % without precipitating respiratory acidosis or
worsening hypercapnoea (see b Oxygen, p.95 and b Arterial blood
gases, p.98). If the patient is known to have COPD and is drowsy or has
a documented history of previous hypercapnoeic respiratory failure, give
FiO
2
of 28 % via a Venturi mask and obtain ABG. Titrate up the FiO
2
with
serial ABG sampling until the minimum FiO
2
that achieves SpO
2
88–92 % .
Reduce inhaled oxygen concentration if SpO
2
> 92 % .

109
COPD
Give bronchodilators and steroids
• Give nebulized salbutamol 5mg or terbutaline 5–10mg.
• Consider adding nebulized ipratropium 0.5mg.
• Use O
2
driven nebulizers unless the patient has hypercapnoeic, acidotic
COPD, in which case use nebulizers driven by compressed air, supple-
mented by O
2
via nasal prongs at 1–4L/min.
• Give steroids (eg prednisolone 30mg PO stat or IV hydrocortisone
100mg).
Other drug treatments
• Give antibiotics (eg amoxicillin, tetracycline, or clarithromycin) if the
patient reports i purulent sputum, or there is clinical evidence of pneu-
monia and/or consolidation on CXR.
• Consider IV aminophylline or salbutamol if there is an inadequate
response to nebulized bronchodilators.
• Consider naloxone if the patient is taking an opioid analgesic that may
cause respiratory depression.
See NICE guideline on COPD, 2010 ( www.nice.org.uk ).
Non-invasive ventilation (NIV)
NIV is recommended as standard early therapy for hypercapnoeic ventila-
tory failure during exacerbations of COPD. NIV will improve the blood
gas measurements in the ED, d intubation rates, d mortality, and length
of hospital stay.
NIV takes two forms — CPAP and BiPAP, (which may be more suitable for
treating type II respiratory failure in COPD). Both CPAP and BiPAP have
been used to treat acute cardiogenic pulmonary oedema. Patients with
sleep apnoea use CPAP at night. The positive airway pressure is delivered
by a tightly adhered face mask, which is sized to fi t the patient. The patient
is awake, and must be compliant with wearing the mask.
Unlike tracheal intubation, NIV does not protect the airway. Therefore,
contraindications include coma and vomiting. Absolute contraindications
include apnoea and cardiac arrest. A pneumothorax will be converted into
a tension pneuomthorax with NIV. Severe agitation may make effective
NIV impossible.
The patient should always be cared for by staff who are familiar with the
ventilator and mask, in the resuscitation room.
Start BiPAP at 10cmH
2
O inspiratory positive airway pressure (IPAP)/
5cmH
2
O expiratory positive airway pressure (EPAP), and titrate upwards:
• To treat persistent hypercapnoea, increase IPAP by 2cm at a time.
• To treat persistent hypoxia, increase IPAP and EPAP by 2cm at a time.
• The maximum IPAP/EPAP is 25/15cmH
2
O.
• For CPAP, commence treatment at 5–8cmH
2
O.

110 CHAPTER 3 Medicine
Pneumonia
Pneumonia involves symptoms and signs of lower respiratory tract
infection (breathlessness, productive cough, and fever) usually associated
with CXR abnormalities. Pneumocystis pneumonia may occur with minimal
or no CXR changes. Consider pneumonia in patients with septicaemia or
acute confusional states.
Causes
Bacterial (80–90 % ) Streptococcus pneumoniae is the commonest cause of
community-acquired pneumonia. Others include Mycoplasma pneumoniae ,
Haemophilus infl uenzae , Legionella , Chlamydia psittaci , Staphylococcus
aureus (can cause fulminant pneumonia in patients with infl uenza). Gram
–ve and anaerobic infections are rare. Always consider TB, particularly
in chronic alcoholism, poor social circumstances, immigrants and those
travelling to developing countries, or individuals not BCG vaccinated.
Immunosuppressed patients (eg HIV, steroid therapy) are at i risk of TB
and Pneumocystis jirovecii pneumonia.
Viral (10–20 % ) Predominantly infl uenza A&B, respiratory synctal virus
(RSV), rarely varicella and severe acute respiratory syndrome (SARS).
Rickettsial (1 % ) Rarely, Coxiella burnetti .
Signs and symptoms
Fever, cough, and production of sputum are common complaints.
Breathlessness, pleuritic chest pain, myalgia, rigors, or haemoptysis may
occur. Pneumonia can present without obvious chest signs: Mycoplasma
pneumonia may present in children and young adults with sore throat,
headache, nausea, abdominal pain and diarrhoea. Legionella can present
with constitutional upset, diarrhoea or confusion, particularly in the
elderly. Pneumocystis pneumonia in immunosuppressed patients may
present with cough, dyspnoea, and marked hypoxia, with relatively few
other fi ndings.
Examination and investigation
• Check respiratory rate, pulse, and BP.
• Auscultation may reveal a patch of inspiratory crackles, signs of consoli-
dation are present in <25 % .
• Check BMG, SpO
2
(obtain ABG if <94 % , or known to have COPD).
• Assess for signs of SIRS (2 or more of RR > 20, HR > 90, temp > 38.3
o
C
or <36.0
o
C, WCC<4 or > 12 × 10
12
/L, confusion, glucose > 8.3mmol/L),
which in combination with signs of pneumonia signify sepsis.
• Assess for signs of severe sepsis (sepsis + signs of organ dysfunction
b p.59). Oxygen dependence, poor urine output, systolic BP<90mmHg,
blood lactate > 3mmol/L. Commence fl uid resuscitation immediately if
present, take blood cultures and give IV antibiotics.
• Obtain CXR. Look for patchy or lobar opacifi cation, mass lesions, or an
air bronchogram. In early pneumonia the CXR may be normal.
• Obtain blood cultures, sputum cultures, and consider urinary pneumo-
coccal and Legionella antigen testing.
111
PNEUMONIA
Assessment: admit or discharge
Some patients with ‘mild’ illness, good social circumstances, and no signifi -
cant co-morbidity may be safely discharged with appropriate antibiotics
(eg amoxicillin 0.5–1g PO tds), simple analgesia for pleuritic pain to aid
deep breathing/coughing and GP follow-up.
Patients with CURB-65 score ≥3 have severe pneumonia with a high risk of
death; those who score 2 are at i risk of death and should be considered
for inpatient treatment or hospital-supervised outpatient care; patients
with CURB-65 score 0 or 1 are at low risk of death and may be suitable
for home treatment ( www.brit-thoracic.org.uk ; see Table 3.4 ).
Treatment
Patients deemed suitable for discharge
Provide simple analgesia, oral antibiotics, and GP follow-up.
Patients admitted, but not severely unwell
Start either oral or IV antibiotics, as follows:
• Either amoxicillin 0.5–1g PO tds + erythromycin 500mg PO qds (or
clarithromycin 500mg bd).
• Or if IV therapy is needed: ampicillin 500mg IV qds + erythromycin
500mg IV qds (or clarithromycin 500mg bd). Local guidelines will apply.
• Monitor SpO
2
and provide O
2
accordingly.
• Provide simple analgesia.
Patients with sepsis or severe sepsis (see b p.59)
Commence IV crystalloid fl uids, take blood cultures and administer IV
antibiotics (eg co-amoxiclav 1.2g IV tds + clarithromycin 500mg IV bd)
immediately. Contact ICU and make preparations for arterial line, central
line and urinary catheter insertion. Aim for CVP > 8mmHg, MAP > 65mmHg
and urine output > 0.5mg/kg/hr. See severe sepsis guidelines ( www.
surviving sepsis.org ).
Differential diagnosis
Pneumonia-like presentations can occur with pulmonary oedema,
pulmonary infarction, pulmonary vasculitis (eg SLE, PAN, Churg–Strauss
and Wegener’s), aspergillosis, allergic alveolitis, bronchial or alveolar cell
carcinoma, acute pancreatitis, and subphrenic abscess.
Table 3.4
CURB-65 score for pneumonia Score
Confusion 1
Urea > 7mmol/L 1
Respiratory rate ≥30/min
1
Low BP (systolic <90mmHg or diastolic ≤60mmHg)
1
Age ≥65 years
1

112 CHAPTER 3 Medicine
Pulmonary aspiration
Aspiration of solid or liquid material into the upper and lower airways is
likely when one or more of the following features are present:
• d GCS : head injury, stroke, overdose, seizures, sedation, anaesthesia.
• d Cough and/or gag refl exes : related to above factors and/or bulbar
dysfunction, intubation/extubation, Guillain–Barré syndrome, multiple
sclerosis, myasthenia gravis.
• Tendency to regurgitate/vomit: alcohol, full stomach, upper GI tract
pathology (including hiatus hernia, oesophageal obstruction, pregnancy).
• May occur in infi rm or elderly fed via nasogastric tube.
Clinical features
Large food particles suffi cient to cause complete airway obstruction
cause choking, inability to speak, i respiratory effort, cyanosis, loss of
consciousness, and death. Smaller particles may pass through the vocal
cords causing coughing, stridor, tachypnoea, and wheeze. 80 % of patients
are aged <4 years, with peanuts being the classic inhaled objects. Delayed
presentation with cough, wheeze, haemoptysis, unresolved pneumonia,
abscess formation, or empyema occurs in 830 % often days or weeks later.
Vomiting/regurgitation is often witnessed and pulmonary aspiration
confi rmed by seeing gastric contents in the oropharynx or trachea during
intubation or following suction. Gastric content is a mixture of semi-
solid and liquid material — aspiration leads to a sudden onset of severe
dypsnoea, wheeze, and cyanosis. Its acid nature causes severe damage
to the alveolar-capillary membrane, with denaturation of pulmonary
surfactant, i pulmonary permeability with oedema and atelectasis.
Hydrocarbons (eg petrol, paraffi n) cause severe pulmonary toxicity if
aspiration occurs during ingestion or following regurgitation/vomiting.
Investigations
ABG
These show hypoxaemia within minutes of acid aspiration. Initially, patients
may hyperventilate with d pCO
2
until pulmonary compliance i work of
breathing suffi cient to result in hypoventilation.
CXR
Abnormalities develop in > 90 % of patients, but may take hours/days.
Appearances depend on the nature of the aspirated material and the
patient’s position at the time of the episode (right lower lobe is most
frequently and severely affected, followed by left lower lobe and right middle
lobe). In severe aspiration, diffuse bilateral infi ltrates and pulmonary
oedema similar to ARDS appearances are present. Less severe episodes
produce atelectasis followed by alveolar infi ltration.
Intrapulmonary foreign body (including peanuts)
Rarely radio-opaque. Resulting collapse, hyperinfl ation, or consolidation
is usually obvious and depends on whether obstruction is complete or
partial and if supervening infection is present. If the history strongly sug-
gests an inhaled FB, but CXR is normal, consider an expiratory CXR,
which may show evidence of air trapping distal to the obstruction.

113
PULMONARY ASPIRATION
Prevention
Prevention is everything. Pay meticulous attention to airway protection.
This may involve positioning (tilt head down on the right hand side),
suction to the oropharynx (Yankauer catheter avoiding stimulation of the
gag refl ex) and if necessary, tracheal intubation. Tracheal intubation does
not completely protect against aspiration of fl uid into the lungs, but it is
the best preventative measure. In at-risk patients, pass an NG tube to
empty the stomach. However, NG tubes can also predispose to aspiration
by preventing closure of the oesophageal sphincters and interfering with
coughing and clearing the pharynx.
Treatment
Correct hypoxia and give nebulized salbutamol for associated bronchospasm.
If particulate aspiration is present, refer for urgent bronchoscopy. Although
secondary infection is common, the use of antibiotics or steroids is not
routinely indicated.

114 CHAPTER 3 Medicine
Spontaneous pneumothorax
Primary spontaneous pneumothorax (PSP) may occur in previously
healthy individuals. Secondary spontaneous pneumothorax (SSP) occurs
in older patients with pre-existing chronic lung disease (like COPD or TB)
and may also occur with asthma, bronchial carcinoma, Marfan’s syndrome,
infection, cystic fi brosis, and oesophageal rupture.
Presentation
Most patients present with unilateral pleuritic chest pain and dyspnoea.
Classical physical signs may not be present (depending upon the size of
the pneumothorax): tachypnoea, tachycardia, normal/hyper-resonant per-
cussion note withe d air entry on the affected side. Rarely, there may be a
clicking sound at the cardiac apex.
Severe symptoms (inability to speak, gasping, low SpO
2
) should prompt
rapid assessment for tension pneumothorax: tracheal deviation,
tachypnoea, tachycardia, and hypotension. Treat tension with immediate
decompression using a needle in the second intercostal space (just above
the third rib) in the mid-clavicular line ( b p.328). Severe symptoms are
also found in patients with SSP (disproportionate to the pneumothorax
size). In the absence of signs of tension pneumothorax, obtain an
emergency portable CXR and involve an experienced doctor.
Investigation and treatment
• Monitor pulse, SpO
2
, and BP. Ensure IV access.
• Administer high fl ow oxygen (aim SpO
2
90–92 % in patients with
COPD).
• When there are no signs of tension, an ABG will help assess patients
with chronic lung disease, and guide oxygen therapy.
Erect CXR
• When using digital images, always use a picture archiving and communi-
cation system (PACS) workstation. The signs of pneumothorax may be
subtle and diffi cult to spot.
• Look for a displacement of the pleural line.
• Do not mistake the scapular edge for the lung edge.
• Some patients with COPD have emphysematous bullae, which can
mimic pneumothorax. If in doubt, ask for senior review prior to treating
for pneumothorax.
• An air fl uid level at the costophrenic angle may be present.
CT scan
Can be of use in the sub-acute setting for assessing bullous lung disease in
a stable patient. CT is not a primary diagnostic modality.
Intervention
• Should be guided primarily by the patient’s symptoms. If the patient is
breathless, they should undergo an intervention.
• The size of the pneumothorax can be estimated on CXR by measuring
from the chest wall to the lung edge at the level of the hilum. This is

115
SPONTANEOUS PNEUMOTHORAX
only an estimate and assumes symmetrical lung collapse. The cut-off of
2cm is used to determine treatment.
• Intervention for PSP is needle aspiration. If unsuccessful, do not repeat
aspiration. Instead insert a Seldinger chest drain.
• Treatment for symptomatic SSP is chest drain insertion and admission.
• Treatment for SSP without breathlessness is admission. Aspiration
should be performed by an experienced doctor and may require CT.
• Always insert chest drains for bilateral pneumothoraces.
• Always insert a chest drain immediately following emergency needle
decompression.
• Pleural aspiration and drain insertion should be performed by a doctor
who has prior training and experience.
• Ensure the patient has IV access. Perform in a monitored environment
with an assistant and appropriate supervision. Use aseptic technique.
• Always discuss the procedure with the patient and document that they
have given their consent.
• If the patient is on anticoagulation or has a known coagulopathy dis-
order, discuss with a haemotologist fi rst.
Aspiration technique
Confi rm the side of the pneumothorax. Sit the patient upright. Infi ltrate 1 %
lidocaine, then insert a 16G IV cannula just above the 3rd rib (in the 2nd
intercostal space) in the mid-clavicular line. Alternatively, lay the patient on
their side with the pneumothorax side upwards. Insert cannula in the 5
th
intercostal space, in the anterior axillary line. Remove the needle, attach a
three-way tap, then aspirate air with a 50mL syringe. Continue aspiration
until the patient coughs excessively, or until 2.5L of air is removed.
Seldinger chest drain insertion
Confi rm the side of the pneumothorax. Keep the patient comfortable,
ensure adequate analgesia (this may require 1mg increments of morphine IV),
but avoid sedation. Sit the patient upright and rest their hand behind their
head. Infi ltrate 10mL 1 % lidocaine at the anterior axillary line in the 5th inter-
costal space. Aspirate a small amount of pleural air during infi ltration and
note the depth of the pleural space. Locate the pleural space with the intro-
ducer needle (aspirate while advancing through chest wall), then advance the
guidewire through the needle. Remove the introducer needle, make a small
skin incision and gently pass the dilator over the guidewire using a twisting
action. Do not push the dilator more than 1cm past the depth of the pleural
space. Pass the chest drain over the guide wire to a depth of 10–12cm.
Remove the guide wire, connect to an underwater seal drain and suture in
pace. Check the drain is bubbling and swinging, and organize a CXR.
Discharge
Patients without breathlessness, with small PSP may be considered for
discharge. Give the patient verbal and written instructions to return if
their symptoms worsen and warn them not to fl y. Ensure they have an
appointment with a respiratory physician in the next week.
See http://www.brit-thoracic.org.uk
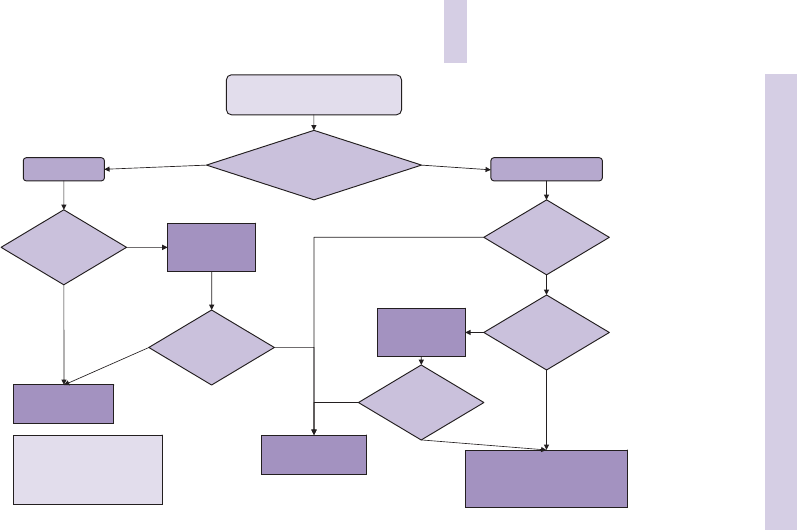
116 CHAPTER 3 Medicine
NO
NO
NO
NO
NO
YES
YES*
YES
YES
YES
YES
NO
Spontaneous pneumothorax
If bilateral/haemodynamically unstable
proceed to chest drain
Age >50 and significant
smoking history
evidence of underlying
lung disease on exam or
CXR?
Secondary
pneumothorax
>2 cm or
breathless
Size
1–2 cm
Admit
high flow oxygen (unless suspected
oxygen sensitive)
observe for 24 hours
Primary
pneumothorax
Size >2 cm
and/or
breathless
Aspirate
16–18G cannula
aspirate <2.5L
Consider discharge
review in OPD in 2–4
weeks
Success
(<2 cm and
breathing
improved)
*In some patients with a large
pneumothorax but minimal
symptoms conservative
management may be
appropriate
Chest drain
Size 8–14Fr
admit
Aspirate
16–18G cannula
aspirate <2.5L
Success
size
now <1 cm
Fig. 3.23 Management of pneumothorax.
1
1 Thorax 2010; 65 (Suppl 2): ii18eii31. doi:10.1136/thx.2010.136986.
This page intentionally left blank

118 CHAPTER 3 Medicine
Deep venous thrombosis
DVT and PE are manifestations of the same disease process whereby
abnormal clotting occurs in the veins of the legs or pelvis. The clots may
break from the vein wall and embolize to the lungs. Untreated DVTs are
associated with a 1–2 % mortality from PE. Around half of those with DVT
will go on to develop post-thrombotic syndrome, with lifelong pain and
swelling of the leg.
Risk factors
• Recent surgery (where a general anaesthetic was administered, espe-
cially orthopaedic, abdominal, spinal and obstetric).
• Recent admission to hospital.
• Current malignancy.
• Being bedbound.
• Sepsis.
• IV drug use (where patient injects in the femoral vein).
• Pregnancy/pelvic masses.
• Immobility such as recent fracture with crutches and plaster cast.
• Previous DVT/PE.
• Thrombophilia or family history of venous thromboembolism.
Clinical features
DVT classically produces leg pain with swelling, warmth, tenderness, and
dilated superfi cial veins in the affected leg. These signs are non-specifi c
and often not present. A small or partially occluding thrombus may be
completely asymptomatic. History and clinical examination alone cannot
safely exclude DVT — if a DVT is suspected, investigate further. Investigate
for PE, rather than DVT if the patient has tachycardia, hypoxia, increased
respiratory rate, or breathlessness ( b Pulmonary embolus, p.120).
Differential diagnosis
• Muscular tear: typically acute onset.
• Rupture of a Baker’s cyst: again, typically acute onset.
• Cellulitis or other infection.
Investigation and management
• Record pulse rate, RR, BP, SpO
2
, and T ° in all patients.
• Take a full history including concurrent illness, past history, recent
operations, travel, and family history.
• Examine the affected leg for signs of plethora, deep vein tenderness,
swelling (measure both legs, 10cm distal to tibial tuberosity), oedema
and dilation of the skin veins.
• Perform full examination checking for signs of PE or occult carcinoma.
• Calculate the clinical probability assessment score. The Wells score
(Table 3.5 ) is the most widely used clinical prediction score.
• Take FBC, U&E, CRP, glucose.
• Take D-dimer if Wells score indicates DVT is ‘unlikely’ (<3 points).
• If D-dimer normal and DVT ‘unlikely’, DVT has been ruled out.
119
DEEP VENOUS THROMBOSIS
The Wells score was not developed with injecting drug users or pregnant
women, both of whom are at higher risk of DVT. These patients should
always undergo ultrasound scanning.
All patients investigated for DVT with a ‘likely’ Wells score ( ≥ 3) or an
elevated D-dimer level require ultrasound scanning. A normal whole leg
ultrasound scan (femoral, popliteal, and calf vein scan) will exclude DVT. If
a thigh scan is performed (the femoral and popliteal veins), DVT can only
be excluded by two normal thigh ultrasound scans, one week apart.
All patients with a ‘likely’ score should be anticoagulated with LMWH
while awaiting an outpatient ultrasound scan.
Patients diagnosed with calf or thigh DVT should be treated with
LMWH and discharged with a week’s supply, an appointment for the
anticoagulation services, and medical outpatient follow-up. Advise them
to return immediately if they become breathless or have chest pain.
Upper limb DVT
Seen almost exclusively in patients with in-dwelling central or long lines,
often for chemotherapy. May be associated with plethora and swelling of
the arm or face. If suspected, request an ultrasound of the arm and neck
veins, or a CT scan with contrast.
Superfi cial thrombophlebitis
Patients present with a painful, tender area of skin. The diagnosis is made
clinically with a fi rm, tender superfi cial vein, and overlying erythema. This
may co-exist with DVT and superfi cial thrombus may propagate into
deep veins. If there is any doubt as to the presence of a DVT, investigate
using the DVT protocol. Otherwise, treat with NSAID. Arrange follow up
either in the ED, a medical clinic or with the GP.
Table 3.5 Wells clinical probability assessment score for DVT
Clinical feature Score
Active cancer (treatment within 6 months or palliative care) 1
Paralysis, paresis, or recent POP immobilization of a leg 1
Recently bedridden for > 3 days or major surgery <12 weeks 1
Localized tenderness along the distribution of the deep venous system 1
Entire leg swelling 1
Calf swelling > 3cm compared with asymptomatic leg 1
Pitting oedema (greater in the symptomatic leg) 1
Dilated superfi cial veins (non-varicose) 1
Previously documented DVT 1
Another diagnosis more likely than DVT -2
Total score < 3 means DVT is ‘unlikely’. Score of 3 or more signifi es DVT is ‘likely’.

120 CHAPTER 3 Medicine
Pulmonary embolism
The mortality of diagnosed and treated pulmonary embolism is 7 % . Many
more people die from undiagnosed PE. Venous thromboembolism develops
in patients already suffering from sepsis, cancer, or COPD or in patients
recovering from stroke, MI, surgery, and joint replacement. Pulmonary
embolic disease can result in a variety of symptoms often misdiagnosed as
asthma, anxiety, pneumonia and ACS.
History
Most patients with PE experience dyspnoea, commonly without other
symptoms. Syncope with cyanosis, cardiac arrest or angina are signs
of massive PE. A minority present with pleuritic chest pain, some with
additional haemoptysis. Always consider PE in patients with unexplained
hypoxia or breathlessness. Take a full history of concurrent illness, surgical
procedures, recent hospital admission, past history including DVT and PE,
travel and family history.
Examination
Examination may be normal.
• Tachycardia and tachypnoea are common.
• Pyrexia following lung infarction is common.
• 30 % of all patients with PE have normal SpO
2
.
• Always record BP. Hypotension indicates massive PE.
• Perform a full respiratory and cardiovascular examination.
• Always examine the legs for signs of DVT.
Any patient scoring 2.0 or more on the Wells score, OR who has an
elevated D-dimer, requires pulmonary imaging. Note that a normal
D-dimer will not exclude PE in a patient with moderate or high probability
of PE. Only a normal D-dimer and a low clinical probability will safely
exclude PE.
Table 3.6 Modifi ed Wells clinical probability assessment score for PE
Clinical feature Score
Signs of DVT (minimum of objective leg swelling and tenderness) 3.0
IV drug use 3.0
PE is the most likely diagnosis 3.0
HR > 100 1.5
Prior PE or DVT diagnosis 1.5
Bed ridden for > 3 days or surgery, within the past 4 weeks 1.5
Cancer (treated actively or with palliation within last 6 months) 1.0
Haemoptysis 1.0
Total score <2.0 = low risk PE, 2.0–6.0 = moderate risk PE, > 6.0 = high risk PE.

121
PULMONARY EMBOLISM
Investigations for suspected pulmonary embolus
• If hypoxic, tachycardic, or hypotensive, insert an IV cannula.
• All patients should have blood taken for FBC and U&Es.
• Take a D-dimer test on any patient who scores <2.0 on the Wells score
(Table 3.6 ). Normal D-dimer in a patient scoring <2.0 excludes PE.
• Arrange ECG (to look for MI or pericarditis) and CXR (to look for
pneumothorax, pneumonia). Many patients with PE have a normal ECG
and CXR.
Diagnostic imaging for pulmonary embolus
There are two forms of imaging for PE: CT pulmonary angiography
(CTPA) and ventilation-perfusion (V/Q) scanning. CTPA uses a higher
dose of radiation (not good for young patients or pregnant patients), but
will give a defi nitive answer, as well as diagnose other conditions often
confused with PE (like aortic dissection).
V/Q scanning uses a low dose of radiation (good for the young and
pregnant), but may not give a defi nitive answer. V/Q scans are reported
as low, intermediate and high probability of PE. The V/Q scan probability
must concord with the clinical probability to diagnose or exclude PE (both
low probability or both high probability). All other combinations are
non-diagnostic and the patient must have a CTPA.
Pitfalls in diagnosis
• Investigating for PE because the patient has an elevated D-dimer. The
D-dimer is irrelevant if there are no clinical symptoms or signs of PE.
• Deciding not to take the D-dimer because the patient is post-surgery,
elderly, or has had recent trauma. If the Wells score is <2.0, a D-dimer
test is rapid and may avoid admission for diagnostic imaging if normal.
Treatment of pulmonary embolus
Anticoagulate with LMWH and arrange to commence the patient on
warfarin therapy. If the patient is ambulant, not hypoxic with a normal
pulse rate and RR, many hospitals commence warfarin and follow-up as
an outpatient. Admit patients who are hypoxic, hypotensive, tachycardic,
tachypnoeic, or elderly for further management.
Suspected massive PE
• In patients with marked hypoxia and/or cardiovascular compromise, call
for urgent ICU expert help.
• If available, an emergency echo will demonstrate a dilated right ventricle
and right heart failure.
• Do not take unstable patients for a CT or V/Q.
• If suspicion of PE is high and the patient is haemodynamically unstable,
administer thrombolytic therapy. Do not delay. Administer alteplase
(rTPA) 100mg over 2 hr or 0.6mg/kg (max 50mg) over 15min as per
European Cardiology guidelines ( www.escardio.org ).

122 CHAPTER 3 Medicine
Upper gastrointestinal bleeding
Causes of upper gastrointestinal bleeding
Common
• Peptic ulceration.
• Mucosal infl ammation (oesophagitis, gastritis, or duodenitis).
• Oesophageal varices.
• Mallory–Weiss tear.
• Gastric carcinoma.
• Coagulation disorders (thrombocytopenia, warfarin).
Rare
• Aorto-enteric fi stula (especially after aortic surgery).
• Benign tumours (eg leiomyomas, carcinoid tumours, angiomas).
• Congenital (eg Ehlers–Danlos, Osler–Weber–Rendu, pseudoxanthoma
elasticum).
History
Take a detailed history, whilst resuscitating as necessary. Upper GI
bleeding usually presents with haematemesis and/or melaena. Major upper
GI bleeding may present with fresh PR bleeding.
Ask about the amount and duration of bleeding, any past history of GI
bleeding or liver problems, and associated symptoms (abdominal pain,
weight loss, anorexia). Syncope usually infers a signifi cant bleed. Take a
full drug history (ask about aspirin, NSAIDs, warfarin, iron) and enquire
about alcohol consumption.
Examination
Check ABCs. Rapidly assess for evidence of hypovolaemic shock (pulse
and respiratory rates, BP, GCS, skin colour/temperature, capillary refi ll).
Look at any available vomit or faeces. Check for abdominal masses,
tenderness or surgical scars (including aortic grafting). Look for stigmata
of liver disease. Perform a PR examination and check for faecal occult
blood (FOB).
Investigation and diagnosis
Request old hospital notes and send blood for FBC, clotting screen, U&E,
blood glucose, Group and Save or cross-matching (according to clinical
features). Urea may be i , but creatinine will be normal unless renal
function is impaired. Check SpO
2
(obtain ABG if <94 % ) and consider CXR
and ECG. Endoscopy is the investigation of choice to identify the source
of the bleeding.
Risk of further bleeding and death
The risk of mortality and further complications increases with increasing age,
co-morbidities (especially cancer and heart failure), liver disease, continued
bleeding, elevated urea, and passage of PR blood.
123
UPPER GASTROINTESTINAL BLEEDING
Only consider patients scoring 0 on the initial Rockall score (Table 3.7 ),
with no further evidence of bleeding, for discharge home from the ED
with follow-up. Any patient scoring > 0 requires urgent endoscopy.
Treatment of moderate/severe haemorrhage
• Check airway and breathing. Provide O
2
to maintain SpO
2
94–98 % .
Insert 2 large (14G) IV cannulae, send FBC, U&E, clotting, cross-match.
• Start IV fl uids followed by blood as necessary.
• Avoid omeprazole acutely unless the patient has known peptic ulcer
disease (give 40mg diluted in 100mL saline as IVI over 30min).
• If the patient is anticoagulated, or has a clotting disorder (eg due to
liver disease), discuss with a haematologist and give vitamin K/clotting
factors/fresh frozen plasma (FFP) accordingly.
• Insert a urinary catheter and monitor the urine output.
• Ensure that patients with severe uncontrolled variceal bleeding, severe
encephalopathy, hypoxia, acute agitation, or evidence of aspiration have
their airways secured, if necessary by tracheal intubation.
Managing severe haemorrhage possibly due to varices
For unstable patients with a past history of varices or clinical features of
hepatic failure, arrange emergency endoscopic treatment:
• Commence fl uid rescucitation.
• Give terlipressin (2mg IV repeated every 4–6hr).
• Check International Normalized Ratio (INR) and give IV vitamin K if
prolonged.
• Give prophylactic antibiotics eg ciprofl oxacin or second/third generation
cephalosporin which may d mortality in severe haemorrhage.
• Consider ballon tamponade as a salvage procedure in a patient with
massive haemorrhage, at risk of death. If experienced in the technique,
insert a 4 lumen Sengstaken/Minnesota tube. Infl ate the gastric balloon
then the oesophageal balloon to a pressure of 30–40mmHg in order to
tamponade the bleeding varices. Regularly aspirate both ports.
See http://www.sign.ac.uk
Table 3.7 Initial Rockall Score for risk of death in upper GI bleeding
Points 0 1 2 3
Age <60 60–79 > 80
Shock HR<100
Systolic
BP > 100mmHg
HR > 100
Systolic
BP > 100mmHg
Systolic
BP<100mmHg
Comorbidity Cardiac failure,
ischaemic heart
disease or
any major
co-morbidity
Renal failure
Liver failure
Disseminated
malignancy
Any score > 0 signifi es increased risk of mortality.

124 CHAPTER 3 Medicine
Lower gastrointestinal bleeding
The commonest cause of apparent lower GI bleeding is upper GI haem-
orrhage. 820 % of acute GI haemorrhage is from the colon or rectum.
Angiodysplasia and bleeding from diverticulae are the most frequent
causes, but infl ammatory bowel disease or, very rarely, aorto-enteric fi stulae
may be responsible. Lower GI haemorrhage often settles spontaneously:
localization of the bleeding source may be diffi cult.
History
Nature of bleeding Melaena may occur following small bowel or proximal
colon bleeding, as well as upper GI haemorrhage. Conversely, large
volumes of fresh or ‘plum-coloured’ rectal bleeding may follow upper GI
haemorrhage. Bloody diarrhoea suggests infl ammatory bowel disease or
infective colitis.
Associated symptoms Weight loss, anorexia, or a change in bowel habit
raise suspicion of colonic carcinoma. Abdominal pain may be a feature
of ischaemic colitis, infl ammatory bowel disease, or carcinoma. Anal pain
commonly occurs with anal fi ssure or complication of haemorrhoids.
Syncope or postural dizziness May indicate signifi cant haemorrhage.
Past medical history Ask about infl ammatory bowel disease, peptic
ulceration, or other illnesses. Previous aortic surgery with graft insertion
can rarely result in formation of an aorto-enteric fi stula (symptoms
include sporadic or fulminant bleeding, often with syncope).
Drug history Ask about salicylates, NSAIDs, corticosteroids, and
anticoagulants.
Family and social history Note any family history of peptic ulcers,
infl ammatory bowel disease. Enquire about alcohol consumption.
Examination
First assess for signs of hypovolaemia and commence resuscitation if nec-
essary. Document pulse, BP (comparing erect and supine, noting any pos-
tural drop), T ° and SpO
2
. Examine the abdomen and PR in all cases.
Investigations
Obtain blood for cross-matching (ask for 4–6U of type specifi c if urgent),
FBC, U&E, glucose, and coagulation studies. Perform an ECG on any
patient > 50 years.
Risk of further bleeding and death
The risk of mortality and further complications increases with increasing
age, co-morbidities, haemodynamic disturbance, and the use of NSAIDs or
aspirin. Only consider discharge if the patient is young, otherwise healthy,
has passed only a small amount of blood PR, and does not take NSAIDs
or anticoagulants. Always arrange follow up for these patients.

125
LOWER GASTROINTESTINAL BLEEDING
Treatment
Patients with signs of hypovolaemia require immediate resuscitation:
• Give O
2
.
• Attach monitoring (cardiac monitor, S pO
2
, BP monitoring).
• Insert two large bore IV cannulae.
• Give 1L of 0.9 % saline or Hartmann’s solution IV stat and give further
fl uids according to response.
• Insert a NG tube.
• Insert a urinary catheter.
• Correct any coagulopathy.
• Consider the need for a central venous line.
• Contact the surgical team and ICU.
See http://www.sign.ac.uk

126 CHAPTER 3 Medicine
Headache
Headaches of non-traumatic origin account for 8 0.5 % of ED attendances;
10–15 % have serious underlying pathology. Patients typically present in
one of three ways:
• Severe headache, unlike any previous one (‘fi rst severe’ or ‘worst
ever’).
• Headache with associated worrying features (altered mental status,
fever, focal neurology).
• Chronic severe headache unresponsive to treatment.
Causes
Primary headaches
• Migraine.
• Tension headaches.
• Cluster headaches.
• Miscellaneous (benign cough headache, benign exertional headache,
headache associated with sexual activity).
Secondary headaches
• Head injury.
• Vascular (stroke, intracranial haematoma, subarachnoid haemorrhage,
unruptured arterio-venous malformation, venous thrombosis, hyper-
tension).
• Non-vascular intracranial disorder ( i cerebrospinal fl uid (CSF) pres-
sure, post-LP, intracranial tumour).
• Substance misuse or withdrawal (including analgesia withdrawal or
rebound).
• Infection (encephalitis or meningitis).
• Metabolic (hypoxia, hypercapnoea, hypoglycaemia, carbon monoxide
(CO) poisoning, dialysis).
• Craniofacial disorder (pathology of skull, neck, eyes, nose, ears, sinuses,
teeth, mouth, temporomandibular joint dysfunction).
• Neuralgias (trigeminal, occipital and other cranial nerves).
Approach
Use a detailed history and examination (including vital signs and neurolog-
ical examination) to search for potentially serious causes. Look particularly
for the following (some typical features in brackets):
• Subarachnoid haemorrhage (sudden, severe onset, syncope) —
b p.128.
• Meningitis or encephalitis (fever, neck rigidity) — b p.224.
• Head injury (history or signs of trauma) — b p.354.
• i intracranial pressure (papilloedema, loss of retinal vein pulsation).
• Stroke (focal neurological signs) — b p.144.
• Acute glaucoma (painful red eye, d VA, irregular semi-dilated pupil) —
b p.542.
• Cranial arteritis (jaw pain, temporal artery tenderness) — b p.132.

127
HEADACHE
History
Features suggesting possible serious pathology are:
• Sudden onset headache.
• Worst headache ever.
• Dramatic change in pattern of headache.
• Known HIV or malignancy.
• The presence of a ventriculo-peritoneal shunt.
• Headache coming on during exertion.
• New onset headache in those aged > 50 years.
Ask about drugs and the possibility of toxins (eg CO).
Examination
Check GCS, pulse rate, respiratory rate, BP, T ° and SpO
2
:
• Feel the head for muscular tenderness, arterial tenderness, trigger
points for neuralgia, and look for evidence of head injury.
• Examine the eyes for VA, pupil reactions, eye movements. Look at the
fundi for papilloedema.
• Palpate the sinuses for tenderness.
• Look in the ears for haemotympanum or infection.
• Check the oral cavity for infection.
• Look for evidence of purpura/rash of meningococcal infection.
• Complete a full neurological examination (include cranial nerves, limb
tone, power, sensation, co-ordination and refl exes).
Check for Kernig’s sign : straightening the knee whilst the hip is fl exed
produces discomfort in the presence of meningeal irritation.
Management
Investigation and emergency treatment will be tailored according to the
presentation of the patient, based upon the likely diagnosis.
• Check FBC, ESR, CRP, U&E, blood glucose.
• If pyrexial and no other obvious source of infection found, take blood
cultures and consider IV cefotaxime 2g. Start IV fl uids and admit.
• Give paracetamol (oral or IV if vomiting) and an NSAID.
• An effective treatment for headache is IV metoclopramide 10mg with IV
fl uids.
• Arrange an emergency CT brain for any patient with an acute severe
headache, or with a history of seizure, or an abnormal neurological
exam. Arrange a CT for any patient with HIV.
• If subarachnoid haemorrhage is suspected and CT normal, admit for
lumbar puncture.
It may be safe to discharge home a patient with slow onset headache that
has resolved following treatment, with normal examination and blood
tests. Arrange GP follow up. Always advise to reattend if symptoms
worsen.

128 CHAPTER 3 Medicine
Subarachnoid haemorrhage
Consider subarachnoid haemorrhage in any ‘worst ever’
or sudden onset headache
Atraumatic subarachnoid haemorrhage can occur at any age and is an
important cause of sudden collapse and death. Most bleeds follow rupture
of saccular (‘berry’) aneurysms in the circle of Willis. Other bleeds may
be due to arteriovenous malformations, tumours, or connective tissue
disorders.
History
Up to 70 % of patients with subarachnoid haemorrhage report rapid onset
or ‘worst ever’ headache. This is classically described as ‘like a blow to the
back of the head’, accompanied by neck pain, photophobia, and vomiting.
In 25 % , exertional activities precede the event. The patient may present
after syncope or fi ts. Drowsiness and confusion are common. ‘Warning
headaches’ may precede subarachnoid haemorrhage. Unilateral eye pain
may occur.
Examination
Document pulse rate, BP, T
o
, and GCS. An unconscious patient with signs
of Cushing’s response signifi es i intracranial pressure. Perform full cranial
and peripheral nerve examination. There may be focal motor and sensory
signs due to intracerebral extension of the haemorrhage or vasospasm,
subhyaloid haemorrhages (blotchy haemorrhages seen in the fundi) or
cranial nerve palsies. Oculomotor nerve palsy is characteristic of a berry
aneurysm involving the posterior communicating artery. Neck stiffness is
often absent in ED presentations, either because meningeal irritation has
not yet occurred or because the patient is deeply unconscious.
Investigation
This may need to proceed alongside resuscitation in seriously ill patients:
• Assess airway and breathing. If the patient is unconscious, open the
airway and contact ICU. Consider urgent RSI, tracheal intubation and
ventilation.
• Obtain venous access and check BMG, FBC, clotting screen, U&E.
• CXR may show changes of neurogenic pulmonary oedema.
• ECG may demonstrate ischaemic changes.
• Arrange emergency CT scan for all suspected cases (maximally sensitive
within 12hr). Admit for lumbar puncture (LP) (done > 12hr after head-
ache onset) even if CT scan is normal.
• Involve the neurosurgical team early. It may be useful to use the Hunt
and Hess score (see Table 3.8 ) when communicating severity by phone.
129
SUBARACHNOID HAEMORRHAGE
Treatment
Tailor this according to the presentation and the need for resuscitation:
• Maintain SpO
2
94–98 % .
• Provide adequate analgesia and antiemetic. Codeine (30–60mg PO),
paracetamol (1g PO) and/or NSAID may suffi ce. Some patients require
more potent analgesics (eg morphine titrated in 1mg increments IV
according to response) — proceed slowly to avoid drowsiness.
• If unconscious (GCS < 8), severely agitated or combative, tracheal intu-
bation (with general anaesthetic (GA)) will allow IPPV and control of
pCO
2
to within normal levels. Insert a urinary catheter and arterial line.
Contact neurosurgical team — further treatment options include:
• Nimodipine (60mg PO every 4hr or 1mg/hr IVI) to prevent and treat
ischaemic neurological defi cits secondary to vasospasm.
• Mannitol IV (eg 200mL of 10 % ) if there is evidence of i ICP.
Table 3.8 Hunt and Hess scale for subarachnoid haemorrahage
Grade
1 Asymptomatic, mild headache, slight nuchal rigidity
2 Moderate to severe headache, nuchal rigidity, no neurologic defi cit
other than cranial nerve palsy
3 Drowsiness/confusion, mild focal neurological defi cit
4 Stupor, moderate-severe hemiparesis
5 Coma, decerebrate posturing

130 CHAPTER 3 Medicine
Migraine
Patients with recurrent migraine rarely attend the ED unless symptoms
are different from usual — take care to avoid missing more serious condi-
tions. The pathogenesis of migraine is not entirely clear, but there is initial
vasoconstriction and subsequent vasodilatation of both intracranial and
extracranial blood vessels.
Presentation
Precipitants include fatigue, alcohol, menstruation, oral contraceptive pill
(OCP), hunger, chocolate, cheese, shellfi sh, and red wine.
A prodrome lasting 5–30min occurs in a third of patients, with blurred
vision, photophobia, or scintillating scotomata (an area of blurred or
absent vision surrounded by moving zig-zag lines), malaise, anorexia, and
vomiting. A few experience hemiparaesthesiae, mild unilateral weakness,
ataxia, or dysphasia. The following headache may last 4–72hr, and is
usually ‘throbbing’ and unilateral, but may be generalized. Photophobia,
nausea, or phonophobia is common.
Rare forms of migraine
Hemiplegic migraine Profound hemiplegia precedes the development of
the headache by 30–60min. The weakness and other focal defi cits usually
resolve quickly. Occasionally, they may be slow or fail to resolve.
Basilar migraine Brainstem disturbances, with impaired consciousness,
vertigo, dysarthria, diplopia, and limb weakness.
Ophthalmoplegic migraine Transient unilateral ophthalmoplegia and
ptosis, which may last several days.
Acephalgic migraine Very occasionally, neurological defects may be
present without headache.
Examination
Look for evidence of other serious diagnoses.
Treatment of acute attacks
• Give simple analgesia (eg paracetamol 1g PO PRN qds or NSAID) in
combination with an anti-emetic (eg metoclopramide 10mg PO, or IV).
• Refer for admission patients who have neurological signs, altered mental
status, or where there is diagnostic uncertainty (including change in
severe headache pattern).
• Acute attacks that fail to respond to simple measures may respond to
other drugs, but these are associated with signifi cant adverse effects.
5HT
1
agonist sumatriptan (6mg SC or 50mg PO or 20mg intranasally) is
effective, but discuss with a senior fi rst.
Sumatriptan causes vasoconstriction and is therefore contraindicated
in IHD, uncontrolled hypertension, basilar, and hemiplegic migraine.
Rebound headache may occur in up to 45 % .
Ergotamine is best avoided (see BNF ). It causes nausea, vomiting,
abdominal pain, and muscular cramps. It is contraindicated in peripheral
vascular disease, IHD, pregnancy, breast feeding, hemiplegic migraine,
Raynaud’s disease, liver and renal impairment, and hypertension.
This page intentionally left blank

132 CHAPTER 3 Medicine
Other causes of headache
Cluster headache
These are more common in men. Often there is a family history. Headache
usually occurs at night, waking the patient. Sometimes alcohol may act as a
precipitant. Headaches are typically ‘clustered’ into up to eight attacks per
day each lasting between 15 and 180min. Pain is usually severe, centred
upon the eye. Associated symptoms, often unilateral, include conjunctival
injection, lacrimation, nasal congestion, rhinorrhoea, forehead, and facial
sweating, miosis, ptosis.
Treatment High fl ow O
2
(12L/min via reservoir mask) for 15min
sometimes provides relief. Otherwise, use paracetamol/NSAID. Consult
before contemplating starting ergotamine or sumatriptan.
Trigeminal neuralgia
Characterized by stabbing unilateral pain within the distribution of the
trigeminal nerves. Stimulation of the ‘trigger area’ (eg by touching, hair
brushing, or even chewing) induces very severe pain. Treat with car-
bamezepine and oral analgesia. Admit if the pain is severe and unrelieved.
Tension headache
The diagnosis is only made after exclusion of more serious pathology.
The history may be described in a dramatic manner. The headache is
usually continuous, pressing, or tight (‘band-like’) in nature. It is usually
bitemporal or occipital. Usual features of migraine are absent and the
headache does not worsen with exertion.
Examination often reveals pericranial muscle tenderness, but is otherwise
normal.
Treat with simple analgesia (eg paracetamol 1g PO qds PRN) and
advise GP follow-up. Reassure the patient that a thorough history and
examination have not revealed any worrying features.
Cranial (‘temporal’ or ‘giant cell’) arteritis (see b p.541)
Consider this in all patients > 50 years with recent onset of headache or
change in headache pattern. There may be weight loss, night sweats, low
grade fever, jaw claudication, ande d vision (up to 10 % present with acute
visual loss), shoulder girdle stiffness, and muscular aches (polymyalgia).
Involvement of carotid or vertebral arteries may lead to TIAs or stroke.
Examination: the temporal arteries may be tender, reddened, pulseless,
or thickened. Fundoscopy is usually normal, but papilloedema can occur
later in the disease.
Investigation: i ESR > > 40mm/hr, often with a low grade anaemia and
leucocytosis. A normal ESR does not exclude temporal arteritis.
Treatment: in view of the serious risk of rapidly progressive visual loss,
if suspected give 200mg IV hydrocortisone (or 40mg prednisolone
PO) immediately. Refer to the neurologist or ophthalmologist as an
emergency — the diagnosis may be confi rmed by temporal artery biopsy.

133
OTHER CAUSES OF HEADACHE
Space-occupying lesions
If the headache is always located on the same side, consider space
occupying lesions and arteriovenous malformations. Headaches that are
dull, aching, and made worse by lying down or straining are typical of
space occupying lesions.
Malignant hypertension
Hypertension is an unusual cause of headaches, but is seen in patients with
malignant hypertension and diastolic BP > 130mmHg ( b p.90).
Ventricular shunts
Assume that any patient who presents with headaches associated with
a ventricular shunt has infection/blockage and refer as an emergency.
Associated drowsiness is a particular pointer to blockage.
Analgesic headache
Chronic use of simple analgesics, sympathomimetics, ergotamine,
or cocaine is associated with headaches. Stopping or starting certain
medications (eg OCP) can also cause headache, as can withdrawal from
caffeine. Exclude serious causes and advise GP follow-up with advice on
medication use.
Cerebral venous thrombosis
This is more common than was previously realized. It presents in similar
fashion to subarachnoid or subdural haemorrhage: sudden onset head-
ache with nausea and vomiting. It may be associated with sinus infections,
pregnancy and the post-partum period. The diagnosis may be missed on
CT, but a clue includes i ICP at LP.
Meningitis (see b p.224)
Encephalitis
Miscellaneous causes
Headaches may also result from:
• Hypoxia and hypercapnoea.
• Poisons: eg CO and solvents ( b p.208).
• Drugs: eg nitrates, sildenafi l.
• Post-traumatic ( b p.368).

134 CHAPTER 3 Medicine
Acute confusional state (delirium)
Defi nition of delirium
Delirium is a form of organic brain syndrome characterized by:
• Disturbed conscious level and mood (overactivity, excitement, drowsi-
ness or stupor).
• Global disturbance of cognition (memory, orientation, attention,
speech, motor function).
• Rapid onset with fl uctuating course (often worse at night, with reversal
of usual sleep–wake cycle) and brief duration.
• Perceptual distortions and hallucinations (especially visual).
Causes of acute confusion
One or more of the following may be the underlying cause of an acute
confusional state (several causes frequently co-exist):
• Prescribed medication: digoxin, cimetidine, steroids, analgesics, diuretics,
anticholinergics, antiparkinsonian drugs.
• Drugs of abuse: opioids, benzodiazepines, ecstasy, amphetamines, hal-
lucinogens.
• Withdrawal: from alcohol, opioids, hypnotics or anxiolytics.
• Infection: pneumonia, UTI, septicaemia, meningitis, encephalitis.
• Metabolic: hypoxia, hypercapnia, hypoglycaemia, acidosis, hyponat-
raemia, hypercalcaemia.
• Cardiac: acute MI, cardiac failure, endocarditis.
• Neurological: head injury, chronic subdural haematoma, meningitis, post-
ictal state.
• Organ failure: respiratory, renal and hepatic failure.
• Endocrine: myxoedema, thyrotoxicosis, diabetes, Addison’s disease.
Differential diagnosis
Delirium can occur at any age, but is much more common in the elderly.
It is often misdiagnosed as schizophrenia, depression, or dementia (see
opposite). Differentiation can be diffi cult, but the following are more
suggestive of physical illness:
• Non-auditory hallucinations.
• Dysarthria.
• Ataxia.
• Gait disturbance.
• Incontinence.
• Focal neurological signs.
Approach
Search systematically for (and exclude) the physical causes of acute confu-
sion outlined above.

135
DEMENTIA
Investigation of acute confusion
Perform a thorough, careful physical and mental state examination (see
b Mental state examination, p.606) on acutely confused patients. It may
be impossible to obtain an accurate history from the patient, so actively
seek other sources of information: relatives, carers, GP, and previous
medical records.
Look carefully for evidence of alcohol/drug intoxication or evidence of
withdrawal states. Examine for focal neurological signs and signs of acute
cardiac, respiratory, or abdominal abnormalities (including acute urinary
retention). Document basic vital signs (GCS, pulse, BP, respiratory rate
and T * ) in all cases.
Mandatory basic investigations
• BMG.
• U&E, FBC, and blood glucose.
• Urinalysis.
• SpO
2
and ABG.
• ECG.
• CXR.
Adopt a low threshold for additional investigations based on clinical
suspicion — blood cultures, serum paracetamol and salicylate, CT brain
scan, and even LP may be indicated.
Be careful not to miss: hypoglycaemia, head injury, Wernicke’s encephalopathy,
opioid intoxication, acute alcohol withdrawal, CO poisoning.
Dementia
Dementia is an acquired, progressive decline in intellect, behaviour, and
personality. It is irreversible and typically occurs with a normal level of
consciousness. Note that patients with dementia are at risk of delirium
resulting from an acute infective or metabolic origin — a clue to this may
be an acute deterioration in mental state.
The commonest causes of dementia are Alzheimer’s disease, vascular
dementia, and Lewy body dementia.

136 CHAPTER 3 Medicine
The unconscious patient: 1
Treatment may be needed before any diagnosis is made. Remember:
• Airway.
• Breathing.
• Circulation.
Initial resuscitation
Airway and cervical spine Whatever the cause of coma, a patient may die
or suffer brain damage due to airway obstruction, respiratory depression.
or circulatory failure. Clear and protect the airway immediately, and
immobilize the cervical spine if trauma is suspected.
Breathing If breathing appears inadequate ventilate with O
2
using a self-
infl ating bag with an O
2
reservoir. An uninjured patient who seems to be
breathing adequately can be examined supine, but nurse him/her in the
recovery position toe d risk of airway obstruction. Record RR.
Circulation Measure pulse and BP. Observe and feel the skin for colour,
sweating and T ° . Obtain reliable venous access. Monitor ECG. Replace IV
fl uid if indicated.
Conscious level Assess level of consciousness using GCS ( b Head injury:
examination, p.360). Check the blood glucose (initially by BMG) and treat
hypoglycaemia immediately ( b p.150). Record pupil size. Give slow IV
thiamine (ie 2 pairs of Pabrinex
®
ampoules in 100mL 5 % glucose over
30min — see BNF ) to patients with a history of alcoholism or who appear
malnourished.
Common causes
• Hypoglycaemia
• Drug overdose
• Head injury
• Stroke
• Subarachnoid haemorrhage
• Convulsions
• Alcohol intoxication
Uncommon causes
• Type 2 respiratory failure
• Cardiac failure
• Arrhythmias
• Hypovolaemic shock
• Anaphylaxis
• Hepatic/renal failure
• Hypothermia/hyperthermia
• Meningitis/encephalitis
• Malaria
• DKA/HHS
• Non-convulsive status epilepticus
• Wernicke’s encephalopathy

137
THE UNCONSCIOUS PATIENT: 1
History
Obtain a history from the ambulance crew and the patient’s relatives and
friends. Ask:
• How was the patient found?
• When was he/she last seen?
• Is there any suggestion of trauma?
• Is there any history of fi ts?
• Has there been recent foreign travel?
• Previous symptoms and medical history (including depression).
• Note any drugs available.
Check previous ED records and hospital notes.
Examination
Examine thoroughly for illness and injury. Check clothes and possessions
for tablets and cards/bracelets warning of pre-existing disease.
i Respiratory rate may refl ect obstructed airway, aspiration, pneumonia,
DKA, liver/renal failure, salicylate poisoning, methanol, or ethylene glycol.
Respiratory depression may be due to poisoning (eg barbiturates, opioids,
tricyclics) or i ICP. Brainstem compression or damage by stroke may
cause rapid, irregular or intermittent (Cheyne–Stokes) breathing.
If bradycardic consider: hypoxia, complete heart block, i ICP, digoxin or
B-blocker poisoning ( b p.198).
If tachycardic consider: airway obstruction, hypoxia, hypovolaemia, SVT,
VT, or anticholinergic overdose.
AF may be associated with cerebral emboli.
Hypotension suggests hypoxia, shock (hypovolaemic, anaphylactic, septic),
or poisoning.
Hypertension may be due to i ICP.
Skin: look for pallor, cyanosis, jaundice, spider naevi, skin crease/scar
pigmentation (Addison’s disease), rashes (eg purpura in meningococcal
infection or DIC), injection marks (drug addiction or medical treatment),
and signs of trauma. Erythema or blistering over pressure points indicate
the patient has been unconscious for some hours.
Measure rectal T° with a low-reading thermometer if the skin feels cold.
Coma is common at <30 ° C ( b Hypothermia: presentation, p.254).

138 CHAPTER 3 Medicine
The unconscious patient: 2
Neurological examination include GCS, limb strength, muscle tone and
refl exes, optic fundi, ear drums, neck stiffness (except in neck injury), and
palpation of the fontanelle in babies. Lateralizing signs, such as facial or
limb weakness, may be caused by a stroke, intracranial bleeding or pre-
existing problems (eg previous stroke or Bell’s palsy). Ocular nerve palsy
or divergent squint with coma can indicate Wernicke’s encephalopathy,
requiring IV thiamine or tricyclic poisoning. Look for subtle signs of
seizure activity (eg twitching of ocular muscles or eyelids, unusual limb
movements), which may indicate non-convulsive status epilepticus. Look
at the fundi — spontaneous central retinal venous pulsations are rare with
i ICP. Subhyaloid haemorrhages (blotchy fundal haemorrhages) suggest
subarachnoid haemorrhage.
Hypoglycaemia can cause localized weakness/coma and mimic stroke.
Coma without lateralizing signs is usually due to poisoning, a post-ictal
state, brainstem stroke, or hepatic failure: extensor plantar refl exes are
common in these conditions.
Tricyclic antidepressants often cause coma with dilated pupils, a divergent
squint, i muscle tone, jerky limb movements, and extensor plantars.
In severe poisoning, there may be muscle fl accidity with respiratory
depression ande d refl exes ( b p.194).
Coma with small pupils and respiratory depression suggests opioid
poisoning ( b p.188). In unexplained coma, give a therapeutic trial
of naloxone (0.4–0.8mg IV), observing for changes in conscious level,
respiratory rate, and pupil size.
Investigations
• BMG and blood glucose. If BMG is low, do not wait for the laboratory
result to confi rm this before starting treatment.
• ABG (record FiO
2
and whether breathing spontaneously or IPPV).
• FBC, prothrombin time, U&E.
• Check paracetamol and salicylate levels if poisoning is suspected: para-
cetamol alone does not cause coma (except in late cases with liver
failure), but a mixture of drugs may have been taken. Drug screening for
sedatives/hypnotics is not needed, but in unexplained coma keep blood
for later analysis if necessary.
• ECG may show arrhythmias ( b Tricyclic antidepressant poisoning,
p.194).
• CXR may show pneumonia, aspiration, trauma, or tumour.
• CT scan may be needed to diagnose subarachnoid haemorrhage, stroke,
or head injury.
Psychogenic coma
Patients sometimes pretend to be unconscious. It can be diffi cult to be
certain of this — exclude other causes fi rst. Suspect psychogenic coma if
serious pathology has been excluded and when the eyes are opened, only
the sclera show as the eyes deviate upwards (Bell’s phenomenon).
This page intentionally left blank

140 CHAPTER 3 Medicine
Collapse and syncope
Syncope is a sudden, transient loss of consciousness, with spontaneous
recovery.
Priorities
• Identify serious or life-threatening problems and institute treatment.
• Decide which patients require admission.
• Decide which patients require follow-up.
History of syncopal episode
Was it a simple faint? Vasovagal or neurally-mediated syncope is a
common response to an overwarm environment or prolonged standing,
and can be precipitated by sudden fright or visual stimuli (eg the sight
of blood). Other contributors are large meals, prolonged starvation
or alcohol. There are usually premonitory symptoms of feeling unwell,
nauseated, dizzy, or tired, with yawning, blurred or ‘tunnel’ vision, or
altered hearing. If the fainter cannot get supine (eg bystanders keeping
them upright), seizure-like twitching may occur ( convulsive syncope ).
Vomiting and incontinence may occur and do not reliably discriminate
seizures from faints.
Was it a seizure? Look at the ambulance records. An eyewitness account
is crucial. Ask what the witnesses actually saw (do not assume they know
what a ‘fi t’ looks like). There should typically be no prodrome, there is
often a cry followed by tonic/clonic movements. Cyanosis, saliva frothing
from the mouth, heavy breathing, tongue biting, or incontinence suggest
a generalized seizure. Post-ictal drowsiness or confusion is normal — very
rapid recovery questions the diagnosis.
Was it a cardiac event? Cardiac syncopal events are also abrupt in
onset (eg collapse due to hypertrophic cardiomyopathy) and may be
accompanied by pallor and sweating. Recovery may be rapid with fl ushing
and deep/sighing respiration in some cases (eg Stokes–Adams attacks).
Nausea and vomiting are not usually associated with syncope from
arrhythmias. Ask about previous episodes and chest pain, palpitations,
history of cardiac disease, and family history of sudden death. Syncope
associated with exertion is a worrying feature: possible causes include
aortic or mitral stenosis, pulmonary hypertension, cardiomyopathy, or
coronary artery disease.
Other causes Carotid sinus syncope is neurally mediated, and often occurs
with shaving or turning the head. Syncope may be secondary to effects of
medication (eg GTN, B-blockers, anti-hypertensive drugs). Syncope may
also be the presenting feature of subarachnoid haemorrhage, ruptured
ectopic pregnancy, aortic or carotid dissection, PE, or GI bleed. Syncope
is rarely caused by a TIA.

141
COLLAPSE AND SYNCOPE
Assessment and treatment
If a patient suddenly loses consciousness in the ED, assess responsiveness
and check for a pulse. Keep the airway clear, give O
2
, and monitor pulse
and ECG. Note any neurological signs during the episode and obtain BP,
SpO
2
, and BMG.
Patients seen following syncope Obtain a detailed account from the patient
and witnesses. Look for signs of tongue biting, incontinence, or other
injuries, examine the CVS for murmurs, arrhythmias or abnormalities.
Perform a neurological examination and look for focal signs. Do postural
tests (supine and standing or sitting pulse and BP). A degree of postural
hypotension is common, but postural symptoms (eg dizziness, weakness,
etc.) are always signifi cant (look for causes of hypovolaemia eg GI bleed,
ectopic pregnancy). Check BMG to exclude hypoglycaemia and an ECG
looking for arrhythmias, LVH, ischaemia, previous or acute MI, and QT
prolongation. An abnormal ECG may be the only clue to an underlying
hypertrophic cardiomyopathy (HCM) or Brugada syndrome.
Disposal
Admit patients for cardiology review within 24 hr if they present with:
• An ECG abnormality.
• Heart failure.
• Loss of consciousness on exertion.
• Family history of sudden death <40 year or inherited cardiac condition.
• Age > 65 year with no prodromal symptoms.
• A heart murmur.
Refer patients for assessment by a specialist in epilepsy if they present
with one or more of:
• A bitten tongue.
• Amnesia, unresponsiveness, unusual posturing, or prolonged limb
jerking, head turning to one side.
• History of a prodrome.
• Post-ictal confusion.
It may be appropriate to discharge patients with full recovery, appropriate
history for vasovagal syncope and a normal examination.
See www.nice.org.uk
Diagnoses not to be missed
• GI bleed: syncope ( ± postural symptoms) indicate signifi cant blood
loss and hypovolaemia. Perform PR examination to check for blood/
melaena.
• Ectopic pregnancy: suspect this in women with syncope and abdominal
pain or gynaecological symptoms. Do a pregnancy test.
• Ruptured abdominal aortic aneurysm.
• PE ( b Pulmonary embolism, p.120). A witness may give a history of
cyanosis. Indicative of massive thrombus.

142 CHAPTER 3 Medicine
Acute generalized weakness
Weakness may be a feature of common neurological problems (eg TIA/
stroke), or accompany many of the causes of collapse (see b Collapse
and syncope, p.140). Less commonly, generalized muscle weakness may
be the presentation of a number of other diseases.
Guillain–Barré syndrome
Guillain–Barré follows a respiratory or GI viral infection and is character-
ized by progressive symmetrical weakness, spreading from distal muscles
to involve proximal muscles. Symptoms and signs include muscle tender-
ness, back pain, loss of muscle refl exes, sensory symptoms (paraesthesiae
of fi ngers and toes) and disturbance of the autonomic nervous system
(hyper- or hypotension, tachy- or bradycardia, bladder atony). Beware
respiratory failure, which can rapidly progress to respiratory arrest. Serial
vital capacity measurements are advised. Refer to the medical team/ICU.
Multiple sclerosis
Multiple sclerosis (MS) is a demylinating disease of the CNS. It is more
common in females and usually presents between ages 20–50. The disease
follows a relapsing and remitting course with sensory loss, stiffness, and
weakness of legs, ataxia, autonomic impairment (bladder dysfunction),
and diplopia. Patients may present with these symptoms during their fi rst
exacerbation or with optic neuritis (pain in one eye with visual blurring).
Arrange admission under neurology. If patient has eye symptoms, arrange
urgent ophthalmology review.
Polymyositis
Polymyositis is an infl ammatory myopathy that presents with symmetrical
proximal muscle weakness, arthritis and sometimes muscular tenderness.
Patients report diffi culty climbing stairs, standing from a low chair, or
lifting arms to brush hair. Creatine kinase (CK) levels are raised. Refer to a
rheumatologist for treatment.
Myasthenia gravis
This is a rare autoimmune disease, which results in painless weakness in
which the muscles are fatiguable, but tendon refl exes and pupil responses
are normal. Ptosis, diplopia, and blurred vision are the commonest pres-
entations. Usually, cranial nerves are involved to a greater extent than
limb muscles and the distribution is asymmetrical. Crises may present with
severe muscle weakness in which the major concern relates to respiratory
compromise — the patient may require emergency temporary ventilatory
support.
If the diagnosis is suspected in a patient not known to have myasthenia
gravis, refer to a specialist who may wish to perform an edrophonium test .
Patients with known myasthenia gravis may present with weakness due
to under-treatment, over-treatment (cholinergic crisis), or an adverse
reaction to an unrelated drug. Refer to the medical team for investigation.

143
ACUTE GENERALIZED WEAKNESS
Periodic paralysis
This encompasses a family of hereditary diseases associated with defects
in muscle ion channels. Episodes of weakness can be associated with
fl uctuations in serum potassium levels lasting a few hours to a week.
Patients may develop myotonia between attacks and fi xed proximal
muscle weakness. Treatment tends only to be required for hypokalaemic
periodic paralysis with oral potassium supplementation.
Wound botulism
Botulism has made a recent come back in the IV drug injecting community.
Botulinum toxin inhibits the release of acetylcholine at neuromuscular
junctions, sympathetic and parasympathetic synapses. Wound infection
with Clostridium botulinum presents with diplopia, blurred vision, ptosis,
and neck weakness, which can progress to respiratory failure. Treatment is
with antitoxin, benzylpenicillin, and metronidazole, along with respiratory
support.
It is worth remembering that generalized weakness may also be caused by:
• Spinal cord compression.
• Tetanus.
• Alcoholic myopathy.
• Diphtheria.
• Lead poisoning.

144 CHAPTER 3 Medicine
Stroke
A stroke is an acute onset of focal neurological defi cit of vascular origin
which lasts > 24hr. The blood supply to the brain has two sources — the
internal carotid and the basilar arteries. The internal carotids supply the
anterior and middle cerebral arteries, known as the anterior circulation.
The basilar artery supplies the posterior cerebral artery in 70 % of people
(the posterior circulation). Anterior and posterior communicating arteries
in the circle of Willis provide collateral circulation in cases of carotid
artery stenosis.
Pathogenesis
70 % of strokes occur in those aged > 70yrs, but they can occur at any age.
Cerebral infarction (80 % )
Results from:
• Thrombosis secondary to atherosclerosis, hypertension and rarely
arteritis.
• Cerebral embolism from AF, valve disease/replacement, post-MI, ven-
tricular aneurysm, myxoma, endocarditis or cardiomyopathy.
• An episode of hypoperfusion.
Cerebral haemorrhage (20 % )
Associated with:
• Hypertension (rupture of small arteries in the brain).
• Subarachnoid haemorrhage (see b p.128).
• Bleeding disorders (including anticoagulants) and intracranial tumours.
Presentation
Stroke preceded by neck pain may indicate carotid/vertebral artery dissec-
tion or subarachnoid haemorrhage. Headache is an unusual presentation
of stroke and may indicate cerebral haemorrhage. Be alert to the possi-
bility of different pathology requiring urgent treatment (eg hypoglycaemia,
Todd’s paresis, hemiplegic migraine, meningitis, encephalitis, brain abscess,
head injury, Bell’s palsy, ‘Saturday night palsy’, tumours).
Undertake a thorough examination including:
• Assessment of mental status/GCS and signs of meningeal irritation.
• Evidence of head or neck injury.
• Examination of pupils, fundi, and cranial nerves.
• Assessment of motor function (tone, power, and refl exes).
• Assessment of sensory function (including speech and comprehension).
• Examination for cerebellar signs (co-ordination, speech).
• Check for sources of embolism (AF, murmurs, carotid bruits).
Localization on clinical grounds alone can be diffi cult, and differentiation
between infarction and haemorrhage requires CT/MRI. NICE recommend
the use of the ROSIER score to identify patients presenting with acute
stroke (see Table 3.9 ). The ROSIER score will pick up the majority of
patients who are having a stroke, but may not identify patients with
posterior circulation infarcts.
145
STROKE
Investigation
Examine and investigate fi rstly to exclude other conditions and secondly
to confi rm the diagnosis of stroke. As a minimum requirement: BMG,
FBC, ESR, U&E, blood glucose, ECG, CXR. Monitor with pulse oximeter
(if SpO
2
<94 % obtain ABG) and cardiac monitor.
Emergency CT
Arrange emergency CT scan where:
• The patient presents with symptoms under 4hr of duration. They may be
eligible for emergency thrombolysis treatment. Time is of the essence.
• The patient is on warfarin, heparin, or other anticoagulant.
• There is a known bleeding disorder.
• GCS <13.
• Unexplained progressive or fl uctuating symptoms.
• Papilloedema, neck stiffness or fever.
• There was a severe headache at onset of symptoms.
Management
• Immediately correct hypoglycaemia if present (see b p.150).
• Hypertension and labile BP are common in the early post-stroke period.
Do not attempt to reduce the BP on presentation.
• Give supplemental oxygen only if SpO
2
<95 % .
• Screen the patient’s ability to swallow (try a teaspoon of water).
• If intracranial haemorrhage has been excluded, all patients should
receive aspirin 300mg as soon as possible. Give this rectally if unable to
swallow. Give PPI if there is a history of dyspepsia. If allergic to aspirin,
give alternative antiplatelet drug such as clopidogrel.
• Wherever possible, admit patients directly to units where they can be
cared for by staff specializing in stroke treatment and rehabilitation.
Thrombolysis
If intracranial haemorrhage has been excluded within 4hr of onset of
symptoms, alteplase may be administered by a trained and supported
emergency physician, only where the patient is managed within a specialist
acute stroke service. See local guidelines and http://www.nice.org.uk
Table 3.9 ROSIER score for stroke recognition
Criteria Points
Facial weakness (asymmetrical) 1
Arm weakness (asymmetrical) 1
Leg weakness (asymmetrical) 1
Speech disturbance 1
Visual fi eld defect 1
Loss of consciousness or syncope –1
Seizure –1
Stroke unlikely if score 0 or less.

146 CHAPTER 3 Medicine
Transient ischaemic attacks
A TIA is an episode of transient focal neurological defi cit of vascular origin
lasting <24hr. A TIA gives major warning for the development of stroke
(5 % within 48hr, up to 50 % in 5 years). Even in patients with resolution of
symptoms/signs, most have evidence of infarction on CT/MRI.
Presentation
Carotid territory involvement produces unilateral weakness or sensory
changes, dysphasia, homonymous hemianopia, or amaurosis fugax.
Vertebrobasilar territory involvement produces blackouts, bilateral motor
or sensory changes, vertigo, and ataxia.
Causes
Most TIAs result from thrombo-embolic disease involving either the
heart (AF, mitral stenosis, artifi cial valves, post-MI) or extracranial vessels
(carotid artery stenosis). Other causes include:
• Hypertension.
• Polycythaemia/anaemia.
• Vasculitis (temporal arteritis, polyarteritis nodosa, SLE).
• Sickle cell disease.
• Hypoglycaemia.
• Any cause of hypoperfusion (eg arrhythmia, hypovolaemia).
• Syphilis.
Assessment
To diagnose a TIA, the symptoms must have resolved within 24hr.
Document vital signs and perform a thorough neurological examination.
Look for possible sources of emboli eg arrhythmias (especially AF), heart
murmurs, carotid bruits, MI (mural thrombus).
Investigations
• Check BMG.
• Send blood for FBC, ESR, U&E, blood glucose, lipids (INR if on anti-
coagulants).
• Record an ECG to search for MI, arrhythmia.
Management
• Calculate the ABCD
2
score (Table 3.10 ).
• Admit to a stroke unit patients scoring 4 or more points, or anyone
with more than one TIA in the previous week.
• Patients scoring 3 or less points, or who present one week after symp-
toms have resolved, may be suitable for discharge with stroke team
follow-up in the next week.
• Start the patient on daily aspirin 300mg immediately.
• Admit patients with continuing symptoms or residual defi cit (by defi ni-
tion, not a TIA).
See http://www.nice.org.uk
147
TRANSIENT ISCHAEMIC ATTACKS
Table 3.10 ABCD
2
score for TIAs
Criteria Points
Age Age 60 or over 1
BP at assessment Systolic > 140mmHg or diastolic > 90mmHg
at assessment
1
Clinical features Speech disturbance 1
Unilateral weakness 2
Duration of symptoms 10–59min 1
60 min or more 2
Diabetes 1
Patients scoring > 4 points are at increased risk.

148 CHAPTER 3 Medicine
Seizures and status epilepticus
First fi t
A fi rst fi t has enormous consequences — do not diagnose without good
evidence
A detailed history from both the patient and any witnesses is crucial to the
diagnosis. The presence of jerking movements or incontinence does not
necessarily refl ect epilepsy. Carefully document what was seen, in order
to avoid confusion with vasovagal syncope or other types of collapse. Full
rapid recovery suggests a syncopal event. Always consider alcohol/drug
use, withdrawal states, hypoglycaemia, arrhythmia, head injury, subarach-
noid haemorrhage, stroke/TIA, infection (including meningitis) or metabolic
disturbance.
As part of the general examination, carefully examine the CNS, documenting:
GCS, confusion, focal abnormalities, fi ndings on fundoscopy. Examine the
cardiovascular system and check for signs of aspiration.
Todd’s paresis may follow seizures — focal defi cit or hemiparesis may
persist for up to 24hr and indicates a high chance of structural lesion.
Investigations BMG, glucose, FBC, U&E, blood cultures if pyrexial, ECG,
and if there are chest signs, a CXR. Check urine pregnancy test if of child-
bearing age. All patients with new onset seizures need brain imaging at
some stage: a signifi cant number have structural CNS abnormalities.
Arrange emergency CT scan for patients with focal signs, head injury,
known HIV, suspected intracranial infection, bleeding disorder (including
anticoagulants), or where conscious level fails to improve as expected.
Disposal A patient presenting with a fi rst seizure may be discharged
home, accompanied by an adult, if they have normal neurological and
cardiovascular examinations, the ECG and electrolytes are normal,
and there is an appointment with an epilepsy specialist in the coming
week. Admit any patient with more than one seizure that day or who
does not fi t the above criteria. Ensure clear documentation of follow-up
arrangements, including booked clinic appointment. Meantime, advise the
patient not to drive or use machinery and to take sensible precautions,
with supervision when performing activities, such as swimming/bathing
until reviewed.
Document this advice in the notes.
Seizures in known epileptics
Ask about any change from the patient’s normal seizure pattern. Possible
causes of poor seizure control include: poor compliance with medica-
tion, intercurrent illness/infection, alcohol, or drug ingestion. Examine to
exclude any injury occurring from the fi t, especially to the head. Occult
dislocations (eg shoulder) may occur. Check vital signs, BMG and anticon-
vulsant levels if toxicity or poor compliance is suspected. Refer patients
with a signifi cant change in seizure pattern to the medical team. Discharge
to the care of a responsible adult those patients who are fully recovered
with no injuries, symptoms or other concerns.

149
SEIZURES AND STATUS EPILEPTICUS
Status epilepticus
This is continuous generalized seizures lasting > 30min or without inter-
vening recovery. Cerebral damage i with duration. Precipitants include
cerebral infection, trauma, cerebrovascular disease, toxic/metabolic dis-
turbances, childhood febrile seizures. Mortality is 8 10 % (due to underlying
pathology). Although seizures typically start as generalized, tonic/clonic,
these features may gradually diminish, making diagnosis diffi cult (coma
with virtually no motor evidence of seizure, eg minimal twitching of ocular
muscles only). Complications include hypoglycaemia, pulmonary hyper-
tension, pulmonary oedema and precipitous i ICP can also occur.
Treatment of status epilepticus
• Establish a clear airway (a nasopharyngeal airway may help).
• Give high fl ow O
2
.
• Monitor ECG, SpO
2
, T ° , pulse rate, and BP.
• Obtain IV access, check BMG and correct hypoglycaemia if present
(50mL of 20 % glucose IV).
• Give IV lorazepam 4mg slowly into a large vein (diazepam 10mg is an
alternative). Repeat IV lorazepam 4mg slowly after 10min if seizures
continue.
• Buccal midazolam 10mg (can be repeated once) or rectal diazepam
solution 10–20mg (can be repeated up to total 30mg) are alternatives if
there is no venous access.
• If alcohol abuse or malnutrition is suspected, give slow IVI thiamine in
the form of Pabrinex
®
2 pairs of ampoules in 100mL of 0.9 % saline (this
occasionally causes anaphylaxis; be prepared to treat — see BNF ).
• Consider the possibility of pregnancy-related fi ts (eclampsia) in women
of childbearing age and treat accordingly (with IV magnesium sulphate—
— as outlined on b p.592).
• Check ABG and save blood for cultures, FBC, U&E, glucose, calcium,
magnesium, LFTs, clotting, drug levels (and toxicology screen if poi-
soning/overdose is suspected).
• Search for features of injury (especially head injury) and infection (look
for a rash).
• If seizures continue despite above therapy, call ICU and consider the
use of phenytoin (18mg/kg IV, 50mg/min) with ECG monitoring, or
fosphenytoin (20mg/kg phenytoin equivalent IV, <150mg/min). A 70kg
patient would require 1400mg phenytoin equivalent of fosphenytoin
(28mL Pro-Epanutin
®
) diluted in 100mL 0.9 % saline or 5 % glucose, given
over 10–15min.
• After 30min, contact ICU and proceed without delay to rapid sequence
induction (ideally with thiopental), tracheal intubation, and continue
anticonvulsant medication.

150 CHAPTER 3 Medicine
Hypoglycaemia
Hypoglycaemia can mimic any neurological presentation including coma,
seizures, acute confusion, or isolated hemiparesis.
Always exclude hypoglycaemia in any patient with coma,
altered behaviour, neurological symptoms, or signs
Plasma glucose is normally maintained at 3.6–5.8mmol/L. Cognitive func-
tion deteriorates at levels <3.0mmol/L, but symptoms are uncommon
> 2.5mmol/L. In diabetics, however, the threshold for symptoms can be
very variable. Hypoglycaemia is potentially fatal, and accounts for 2.4 % of
deaths in diabetics on insulin. Even mild episodes aggravate pre-existing
microvascular complications and lead to cumulative brain damage.
Causes
In diabetics, the commonest cause is a relative imbalance of administered
versus required insulin or oral hypoglycaemic drug. This may result
from undue or unforeseen exertion, insuffi cient or delayed food intake,
excessive insulin administration (due to time, dose or type of insulin).
Other causes are:
• Alcohol (in addition to alcohol directly causing hypoglycaemia, the
features of hypoglycaemia may be mistaken for alcohol intoxication or
withdrawal).
• Addison’s disease.
• Pituitary insuffi ciency.
• Post-gastric surgery.
• Liver failure.
• Malaria.
• Insulinomas.
• Extra-pancreatic tumours.
• Attempted suicide or homicide with large doses of insulin or oral
hypoglycaemic drug.
Symptoms and signs
Common features: sweating, pallor, tachycardia, hunger, trembling, altered
or loss of consciousness, irritability, irrational or violent behaviour, fi tting,
focal neurological defi cit (eg hemiplegia). Look for Medic-Alert bracelet/
chain.
Diagnosis
Check venous or capillary blood with glucose oxidase strip (BMG). If
<3.0mmol/L, take a venous sample for a formal blood glucose level,
but give treatment without waiting for the result. Take appropriate
samples if overdose of insulin, oral hypoglycaemic agent, or other drugs
is suspected.

151
HYPOGLYCAEMIA
Treatment
This depends upon the conscious state and degree of co-operation of the
patient. Choose the appropriate option from the following:
• 5–15g of fast-acting oral carbohydrate (eg Lucozade
®
, sugar lumps,
Dextrosol
®
, followed by biscuits and milk).
• Glucagon 1mg: SC, IM, or IV. Can be administered by relatives, ambu-
lance crew and when venous access is diffi cult. Glucagon is not suitable
for treatment of hypoglycaemia due to sulphonylurea drugs, liver failure
or in chronic alcoholism (as there may be little liver glycogen available
for mobilization).
• Glucose 10 % solution 50mL IV, repeated at 1–2min intervals until the
patient is fully conscious or 250mL (25 g) has been given.
• Glucose 50 % solution (25–50mL IV) is hypertonic, liable to damage
veins and no more effective than glucose 10 % . If glucose 50 % is used,
give it into a large vein and follow with a saline fl ush.
• The time taken for return of consciousness and the incidence of
nausea, vomiting and other adverse effects are similar for IV glucagon
and glucose.
The persistence of an altered conscious level suggests another underlying
pathology (eg stroke), or may refl ect the development of cerebral
oedema due to hypoglycaemia, which has a high mortality. Maintain
plasma glucose at 7–11mmol/L, contact ICU and consider mannitol and/
or dexamethasone. Arrange urgent investigation (eg CT scan) and search
for other causes of altered consciousness.
Overdose Glucose infusions may be needed for 24hr or longer after
poisoning with insulin or oral hypoglycaemic drug, depending upon
exactly what and how much has been taken. Hypokalaemia may be a
problem. Block excision of the injection site has been used as successful
treatment for insulin overdose. Octreotide may be helpful in recurrent
hypoglycaemia due to overdose of a sulphonylurea drug ( b p.197).
Discharge
90 % of patients fully recover in 20min. Provided that the cause for
the episode has been identifi ed and fully corrected, it is reasonable
to discharge the patient after observation in the ED, with appropriate
follow-up.
Arrange follow up having considered the following:
• Why did this episode occur?
• Has there been a recent change of regimen, other drugs, alcohol, etc.?
• Is the patient developing hypoglycaemic unawareness or autonomic
dysfunction?

152 CHAPTER 3 Medicine
Hyperglycaemic crises
Diabetic keto-acidosis (DKA) is caused by absolute or relative d insulin
levels. Plasma glucose i causes an osmotic diuresis, with Na
+
and water
loss (up to 8–10L), hypotension, hypoperfusion, and shock. Normal
compensatory hormonal mechanisms are overwhelmed and lead to
i lipolysis. In the absence of insulin this results in the production of non-
esterifi ed fatty acids, which are oxidized in the liver to ketones.
Younger undiagnosed diabetics often present with DKA developing
over 1–3 days. Plasma glucose levels may not be grossly i ; euglycaemic
ketoacidosis can occur. Urinalysis demonstrates ketonuria.
Hyperosmolar hyperglycaemic state (HHS) is caused by intercurrent
illness, inadequate diabetic therapy and dehydration. It develops over
days/weeks, and is more common in the elderly. HHS is characterized by
i glucose levels ( > 30mmol/L), i blood osmolality, and a lack of urinary
ketones. Mortality is 85–10 % , but may be even higher in the elderly.
Causes
Think of the four ‘I’s separately or (often) in combination:
• Infection: common primary foci are urinary tract, respiratory tract, skin.
• Infarction: myocardial, stroke, GI tract, peripheral vasculature.
• Insuffi cient insulin.
• Intercurrent illness: many underlying conditions precipitate or aggravate
DKA and HHS.
Clinical features
Hyperglycaemic crisis may present in various ways. Some of the following
are usually present:
Signs of dehydration thirst, polydipsia, polyuria, d skin turgor, dry mouth,
hypotension, tachycardia.
GI symptoms are common in DKA with nausea, vomiting, and abdominal
pain. This can be severe and mimic an ‘acute surgical abdomen’.
Hyperventilation (respiratory compensation for the metabolic acidosis)
with deep rapid breathing (Kussmaul respiration) and the smell of acetone
on the breath, is pathognomonic of DKA.
True coma is uncommon, but altered conscious states and/or focal
neurological defi cits (which may correct with treatment) are seen
particularly in older patients with HHS.
Diagnosis and investigations
Aim to confi rm the diagnosis and search for possible underlying cause(s):
• Check BMG and test the urine for glucose and ketones.
• Send blood for U&E, blood glucose, creatinine, osmolality (or calculate
it): mOsm/L= (2 × Na
+
) + glucose (mmol/L) + urea (mmol/L).
• Check ABG (look for metabolic acidosis ± respiratory compensation).
• FBC and CXR (to search for pneumonia).
• ECG and cardiac monitoring (look for evidence of hyper/hypokalaemia).
• Blood cultures and if appropriate, throat or wound swabs.
• Urine/sputum microscopy and culture.

153
HYPERGLYCAEMIC CRISES
Treatment
• If altered consciousness/coma is present, provide and maintain a patent
airway.
• Give high FiO
2
by mask. Consider the possible need for GA and IPPV
for coma ± severe shock.
• Commence IV infusion with 0.9 % saline (if the lab result subsequently
shows initial plasma Na
+
to be > 150mmol/L, give 0.45 % saline). Give
1000mL of 0.9 % saline over 0.5–1hr, then 500mL/hr for next 2–3hr.
Persistent hypotension may require i in infusion rate and/or colloid
administration. Avoid over-rapid infusion with the risks of pulmonary
oedema and ARDS, especially in the elderly and patients with IHD.
• Insulin: start an infusion of soluble insulin using an IV pump or paediatric
burette at 6U/hr. No loading dose is required. Check plasma glucose
levels every hour initially. When plasma glucose <14mmol/L, d insulin
infusion rate to 4U/hr and replace the saline solution with 10 % dextrose
to help ketone clearance and acid-base state.
• Electrolyte balance: although total body K
+
is low, plasma K
+
may be
normal, i or d . With treatment, K
+
enters cells and plasma levels d :
therefore unless initial K
+
levels are > 5.5mmol/L, give 20mmol/hr of
KCl, monitor ECG, and check K
+
levels hourly. Despite the presence of
metabolic acidosis, do not give sodium bicarbonate. Other electrolytes
such as Ca
2 +
, Mg
2 +
, and PO
4
2 –
are commonly disturbed, but rarely need
emergency correction.
• Consider an NG tube to d risk of gastric dilation and aspiration.
• Monitor urine output (most accurate with urinary catheter).
• Consider a central venous catheter to monitor CVP to guide treatment
in the elderly or severe illness.
• Arrange admission to ICU, HDU, or acute medical admissions unit.
Other aspects of treatment
Signs of infection are often masked. T ° is rarely i , and i WCC may only
refl ect ketonaemia. If in doubt, treat with a broad-spectrum antibiotic.
Over-rapid fl uid replacement can cause cardiac failure, cerebral oedema,
and ARDS, especially in patients with underlying cardiac disease or the
elderly. CVP monitoring may be needed.
Clotting Hyperglycaemia causes a hypercoagulable state: DVT or PE may
occur. Administer prophylactic anticoagulation with LMWH in DKA or
hyperosmolar states.

154 CHAPTER 3 Medicine
Sodium derangements
Abnormal sodium states can occur with hypervolaemia, euvolaemia, or
hypovolaemia, depending on the underlying pathophysiological process.
Hypernatraemia
Causes include diabetes insipidus (lack of ADH or lack of renal response
to ADH), diarrhoea, vomiting, diuretics, hypertonic saline, sodium
bicarbonate administration, or Cushing’s syndrome.
Treatment should not correct the Na concentration faster than 1mmol/L/hr.
Use 0.9 % saline to correct hypovolaemia (patients who have tachycardia,
hypotension, or postural hypotension). Once the patient is euvolaemic,
use an infusion of 0.45 % saline, or 5 % dextrose. The free water defi cit can
be calculated using the formula:
Free water defi cit (in litres) = 0.6 × weight (kg) × (serum Na/140–1)
and should be replaced over 48hr (in addition to normal maintenance fl uids).
Check serum Na
+
after 2–3hr to monitor correction rate.
Complications of hypernatraemia include seizures, subdural and intra-
cerebral haemorrhages, ischaemic stroke, and dural sinus thrombosis.
Rapid correction of sodium levels (particularly in chronic hypernatraemia)
can cause cerebral oedema and further neurological complications.
Hyponatraemia
Causes include excessive fl uid loss replaced by hypotonic fl uids (diarrhoea,
burns, prolonged exercise, such as marathon running), polydypsia,
ecstasy ingestion, syndrome of inappropriate ADH secretion, nephrotic
syndrome, renal impairment, hepatic cirrhosis, cardiac failure, and many
prescription drugs (including diuretics, heparin, and ACE inhibitors).
Treatment of acute hyponatraemia (<24hr duration) Those with mild
symptoms can be effectively treated by fl uid restriction. Patients who
present with seizures or signs of raised intracranial pressure are at risk of
death and should be treated more aggressively. Serum Na
+
<120mmol/L
is associated with risk of brain herniation. Give up to 200mL of 2.7 % saline
IV over 30min and recheck serum Na
+
levels.
Treatment of chronic hyponatraemia ( > 24hr duration) is associated with
central pontine myelinolysis, particularly in patients with low K
+
levels or
alcoholic patients. Chronic hyponatraemia should be corrected no faster
than 10mmol/L in 24hr. Treat the underlying cause. This may be as simple
as discontinuing a diuretic. Patients with cardiac failure, cirrhosis, or
nephrotic syndrome (hypervolaemic patients) should be fl uid restricted.
Severe hyponatraemia in association with seizures or d GCS may be
cautiously treated with hypertonic saline (2.7 % saline 200mL over 30min
and recheck serum Na
+
). Aim to increase serum Na
+
by no more than
5mmol/L using this method.
See www.gain-ni.org

155
ADDISONIAN CRISIS
Addisonian crisis
Acute adrenocortical insuffi ciency is rare and easily missed. The most
common cause is sudden withdrawal of chronic steroid therapy (delib-
erately or inadvertently). An Addisonian crisis may also be precipitated
in these patients by intercurrent injury, infection or stress — increasing
steroid requirement. 80 % of Addison’s disease in the UK is idiopathic
(autoimmune), and may be associated with Graves’ disease, Hashimoto’s
thyroiditis, insulin dependent diabetes mellitus (IDDM), pernicious
anaemia, hypoparathyroidism, and ovarian failure. Other causes include
TB, fungal infections, metastatic disease, congenital adrenal hyperplasia,
drugs (eg metyrapone or cytotoxic agents), haemorrhage into the adrenal
glands occurring as a complication of anticoagulation or meningococcal
septicaemia (Waterhouse–Friderichsen syndrome). Look for a Medic–
Alert bracelet indicating that the patient is taking steroids.
Precipitating factors
Infection, trauma, MI, cerebral infarction, asthma, hypothermia, alcohol,
pregnancy, exogenous steroid withdrawal or reduction.
Clinical features
Addison’s disease frequently has an insidious onset with weakness, apathy,
anorexia, weight loss, abdominal pain (which may be severe enough to
mimic an acute abdomen), and oligomenorrhoea. In crisis, the main fea-
tures may be shock (tachycardia, peripheral vasoconstriction, severe pos-
tural hypotension occasionally with syncope, oliguria, profound muscle
weakness, confusion, altered consciousness leading to coma), and hypogly-
caemia. Chronic features of Addison’s disease are: areas of vitiligo and
hyperpigmentation in the palmar creases, buccal mucosa, areolae, scars,
and in the axillae.
Investigations
Hyperkalaemia, hyponatraemia, hypoglycaemia, uraemia, mild acidosis,
hypercalcaemia, and eosinophilia may be present. If Addisonian crisis is
suspected, take appropriate blood samples, but start treatment without
waiting for results.
Management
• Obtain IV access.
• Take blood for cortisol (10mL in a heparinized tube) and ACTH if pos-
sible. Contact the biochemistry lab to warn them that these tests will be
required.
• If features of haemodynamic compromise are present, commence
volume replacement with IV 0.9 % saline if shocked.
• Give hydrocortisone sodium succinate 100mg IV stat.
• Take blood, urine, and sputum for culture and sensitivity.
• Check BMG and blood glucose, and treat hypoglycaemia with 50mL of
10 % glucose IV (repeated if necessary).
• If infection is suspected as a precipitating cause, consider giving broad
spectrum antibiotics.
• Refer for admission.

156 CHAPTER 3 Medicine
Thyrotoxic crisis
A rare condition, occurring in 1–2 % of patients with established
hyperthyroidism (usually toxic diffuse goitre ‘Graves’ disease’). Mortality
is signifi cant (810 % ).
Causes
It is often precipitated by a physiological stressor:
• Premature or inappropriate cessation of anti-thyroid therapy.
• Recent surgery or radio-iodine treatment.
• Intercurrent infection (especially chest infection).
• Trauma.
• Emotional stress.
• DKA, hyperosmolar diabetic crisis, insulin-induced hypoglycaemia.
• Thyroid hormone overdose.
• Pre-eclampsia.
Clinical features
Onset may be sudden with features of hyperthyroidism and adrenergic
overactivity. Fever, cardiovascular, and neurological symptoms are common.
Weight loss, i appetite, tremor, irritability, emotional lability, heat
intolerance, sweating, itch, oligomenorrhoea, agitation, anxiety, confusion,
coma, palpitations, tachycardia, AF (rarely, complete heart block). It may
mimic an ‘acute abdomen’, with abdominal pain, diarrhea, and vomiting.
Differential diagnosis
Includes acute pulmonary oedema, neuroleptic malignant syndrome, septic
shock, anticholinergic or sympathomimetic overdose, drug withdrawal, or
acute anxiety states.
Investigations
• U&E, BMG, and blood glucose, Ca
2 +
(hypercalcaemia occurs in 810 % ).
• FBC, differential WCC, coagulation screen.
• Screen for infection: MSU, blood cultures, sputum.
• T
4
and T
3
(for later analysis), TSH.
• CXR (searching for pulmonary infection or congestive heart failure).
• ECG (looking for arrhythmias).
Treatment
• Manage the airway and give O
2
if indicated.
• Obtain IV access and commence IVI 0.9 % saline (initially 500mL 4-hourly).
• Pass NG tube if vomiting.
• If sedation is required, give small titrated amounts of benzodiazepine
(eg diazepam 5–20mg PO/IV) or haloperidol.
• Commence dexamethasone 4mg 6 hourly PO or give hydrocortisone
100mg IV.
• Give broad spectrum antibiotic if infection is suspected.
• Consider cooling measures in hyperthermia.
• Refer for admission (consider admission to ICU).
• Once admitted, propranolol (or esmolol) and carbimazole will normally
be given together with iodine.
• Do not give aspirin (this can exacerbate the clinical problem by dis-
placing thyroxine from thyroid binding globulin).
This page intentionally left blank

158 CHAPTER 3 Medicine
Urinary tract infection
The urinary tract is normally bacteriologically sterile. Urine infection is
present if > 10
5
colony-forming units are present per mL of urine. Except
at the extremes of age, urinary tract infections (UTIs) are much more
common in females due to the shorter urethral length. Most UTIs occur
because of organisms invading the bladder via the urethra. Proximal
invasion via the ureter may result in acute or chronic pyelonephritis,
particularly if anatomical derangement exists with impaired ureteric
or bladder emptying. In both sexes, underlying structural abnormality i
UTI risk. Blood-borne spread of infection to the urinary tract can occur,
(eg in bacterial endocarditis or systemic Gram –ve infection). UTI is
usually caused by a single organism. The commonest organism (90 % ) at all
ages is E. coli. Proteus, Klebsiella, and saprophytic staphylococci account for
most of the remainder in adults. Other organisms (eg Pseudomonas ) more
commonly cause UTI in hospitalized patients or following instrumentation.
Urinary tract infection: presentation
UTIs usually present to the ED in one of two ways
Lower UTI (cystitis) Dysuria, frequency, haematuria, suprapubic discomfort,
urgency, burning, cloudy urine with an offensive smell. Patients with acute
urethral syndrome have identical symptoms, but –ve urine culture.
Upper UTI (acute pyelonephritis) Often systemically unwell with malaise,
fever, loin and/or back pain, vomiting, rigors and occasionally Gram –ve
septicaemia.
Investigations
Reagent strip (dipstix) urinalysis may show haematuria, proteinuria, + ve
nitrite, and leucocyte esterase tests. A patient with clear urine, –ve on
dipstix testing, is extremely unlikely to have a UTI. False + ve results may
be secondary to urinary tract tumours or excessive exercise. A false –ve
nitrite test may refl ect pathogens that do not convert dietary nitrates to
nitrites.
Urine microscopy may show leucocytes ( > 100/mL correlates well with
infection, but may be due to contamination or other urinary tract
pathology). RBCs are commonly seen on microscopy, but in isolation
have a low degree of sensitivity or specifi city for UTI. Underlying renal
pathology is suggested by fi nding urinary crystals, RBC, or granular casts.
MSU for culture and sensitivity. Transport the sample to the laboratory
without delay to ensure that bacterial overgrowth does not artifi cially i
the count. Dipslides dipped into freshly passed urine and transported in a
plastic container to the laboratory are an alternative.

159
URINARY TRACT INFECTION
Treatment
• It is usually reasonable to discharge female patients with uncomplicated
lower UTIs with antibiotics . Commence a 3–6 day course of trimetho-
prim or nitrofurantoin. Provide advice regarding fl uid intake, no ‘holding
on’, and voiding after intercourse. Drinking barley water is as effective
as attempts at urinary alkalinization with sodium bicarbonate. ( Note:
urinary alkalinization renders nitrofurantoin ineffective). Advise the
patient to see her GP for review, MSU result, and repeat MSU.
• Elderly men and women with asymptomatic bacteriuria should not
receive antibiotic treatment unless they show signs of being unwell.
• In pregnancy, both symptomatic and asymptomatic bacteriuria should
be treated with an antibiotic such as amoxicillin.
• Given the diffi culty in distinguishing prostatitis from simple UTI in men,
they should receive a 2-week course of ciprofl oxacin, trimethoprim, or
co-amoxiclav. Arrange GP follow-up.
• Treat catheterized patients with symptoms or signs of UTI for 7 days
with ciprofl oxacin or co-amoxiclav. Treatment is more effective if the
catheter is changed in the ED prior to commencing antibiotics.
• Do not treat catheterized patients with asymptomatic bacteriuria with
antibiotics.
Refer for investigation and treatment all male patients and females with
recurrent infections, pregnancy, GU malformation, immunosuppression,
or renal impairment.
Patients with acute pyelonephritis usually require admission for parenteral
antibiotics, fl uid replacement, and analgesia. Assess and treat for severe
sepsis ( b Shock, p.60).
See http://www.sign.ac.uk

160 CHAPTER 3 Medicine
Chronic renal failure
Patients with established chronic renal failure (CRF) are likely to be very
well known to the hospital. Obtain old notes and recent blood results,
and liaise early with in-patient specialist teams.
Established chronic renal failure (not on dialysis)
Patients with mild CRF (glomerular infi ltration rate (GFR) > 40mL/min —
100mL/min) are unlikely to have specifi c problems related to their
underlying renal failure. With GFR <40mL/min, and especially if GFR
<10mL/min, complications may infl uence presentation and treatment.
These patients are prone to pathological fractures.
Secondary hyperparathyroidism and osteomalacia (lack of active vitamin D)
occur in moderate GFR. In severe CRF, aluminium bone disease, and B
2
-
microglobulin related amyloidosis may be associated with pathological
fractures.
‘Pseudo-gout’ due to high Ca
2 +
/PO
4
–
production and twitching/tetany due
to hypocalcaemia may occur.
Other problems include:
Defective regulation of extra-cellular fl uid volume There is an i risk of
fl uid depletion in moderate CRF and fl uid retention in severe CRF. High
dose diuretics may be required in severe disease: the combination of
furosemide and metolazone may be effective even with very low GFRs.
Hyperkalaemia Most patients preserve potassium balance, but cannot
deal with sudden K
+
loads (eg dietary, tissue damage/catabolism, GI
bleed). Associated d Ca
2 +
compounds the cardiac effects. Plasma K
+
may
i very quickly, so monitor ECG and check K
+
frequently.
Hypertension Often severe and resistant, with an i incidence of
accelerated phase. Ciclosporin and erythropoietin i BP, and can
precipitate hypertensive encephalopathy.
Drug effects Drugs may accumulate (eg opioids, acyclovir, some
antibiotics), worsen renal failure (eg NSAIDs, ACE inhibitors, which d
renal perfusion), cause hyperkalaemia (eg K
+
sparing diuretics, ACE
inhibitors, NSAIDs).
Infections Impaired WBC function, with i risk of severe infection and
features of infection (eg pain, fever) may be masked by the relative
immuno-compromised state.
Bleeding Platelet function is impaired.
Pericarditis A sign of severe CRF, indicating the need for dialysis.
Neurological dysfunction Usually a sign of severe uraemia — convulsions
and/or altered conscious state indicate a global metabolic disturbance.

161
CHRONIC RENAL FAILURE
Common emergency presentation in haemodialysis patients
Pulmonary oedema Usually occurs shortly before the next dialysis session
and may refl ect fl uid overload due to non-compliance with diet and fl uid
restriction. Most are virtually anuric, so diuretics are ineffective. Get the
patient on dialysis without delay. While this is being arranged give high
fl ow O
2
and SL buccal or IV nitrates.
Pre-dialysis hyperkalaemia May present with neuromuscular symptoms
(eg muscle spasms, weakness, paralysis, paraesthesiae) or arrhythmias,
including cardiac arrest. Standard treatment ( b p.162) can buy time
while emergency dialysis is arranged. When giving glucose/insulin, give
6U of insulin at most (there is a risk of late hypoglycaemia, since insulin
half-life will be i ).
Complications of vascular access Arteriovenous fi stulae are a dialysis
patient’s lifeline — never occlude limb with BP cuffs or tourniquets. Do
not use for vascular access unless life-threatening emergency. Acute
shunt thrombosis (loss of palpable thrill, often local pain/redness) is a
vascular emergency. Arteriovenous fi stulae and central lines are common
infection sources (usually staphylococcal), often with no overt external
abnormality, but presenting with acute ‘viral illness’ symptoms.
Continuous ambulatory peritoneal dialysis
Bacterial peritonitis Occurs every 12–18 patient-months. Features are
cloudy drained dialysate bags, abdominal pain, and peritonism. Systemic
sepsis is usually absent or minimal. Staphylococci are most common
organisms. Suspect underlying surgical cause (most often diverticular
abscess) if Gram –ve organisms or anaerobes present in drainage fl uid,
and particularly if > 1 type of organism is found on microscopy or culture.
Diabetic patients on continuous ambulatory peritoneal dialysis can
develop acute severe (usually non-ketotic) hyperglycaemia , related to high
dialysate glucose concentrations (80–140mmol/L).
Hernias of all types, leakage of dialysate into the abdominal wall or the
pleural cavity, and scrotal swelling (open processus vaginalis) may occur.
Transplant patients
Contact the transplant team whenever any transplant patient presents
to the ED. They will know the patient well and will advise about drug
therapy, intercurrent problems, and help with follow-up.
Acute rejection Signs include pain, tenderness, and swelling over graft,
d urine output, fever, systemic upset, biochemical deterioration. Often
indistinguis\hable from acute bacterial infection: if in doubt treat for both,
pending results of further testing by specialists (renal biopsy, blood, and
urine cultures).
Infections May be opportunist, whilst ‘conventional’ infections are unduly
severe, with response modulated by steroids.
Poor wound healing, avascular necrosis and pathological fractures May
be caused by steroids.

162 CHAPTER 3 Medicine
Hyperkalaemia
Hyperkalaemia is classifi ed as mild (K
+
5.5–6.0mmol/L), moderate (K
+
6.1–6.9mmol/L) or severe (K
+
> 7.0mmol/L).
Causes
Spurious Sample haemolysed or taken from limb with IVI containing K
+
.
d Renal excretion Acute kidney injury, patients with chronic renal failure or
on dialysis with K
+
load, K
+
sparing diuretics (eg spironolactone, amiloride).
Cell injury Crush injury and other causes of rhabdomyolysis, burns,
tumour cell necrosis, massive, or incompatible blood transfusion.
K
+
cellular shifts Acidosis from any cause (eg DKA), drugs (suxamethonium,
B-blockers).
Hypoaldosteronism Addison’s disease, drug-induced (NSAIDs, ACE
inhibitors).
Clinical features
There may be muscle weakness/cramps, paraesthesiae, hypotonia, focal
neurological defi cits. Dangerous hyperkalaemia may be asymptomatic.
ECG changes
ECG changes typically progress as hyperkalaemia worsens as follows:
• Peaked T waves.
• Small, broad, or absent P waves.
• Widening QRS complex.
• Sinusoidal (‘sine wave’ pattern) QRST.
• AV dissociation or VT/VF.
Management of severe hyperkalaemia
Urgent treatment is needed if K
+
> 6.5mmol/L, unless this is a spurious and
incorrect result. If K
+
is reported as > 6.5mmol/L obtain venous access,
monitor and review the ECG. Start treatment immediately (as indicated
below) if there are ECG changes of hyperkalaemia. If there are no ECG signs
of hyperkalaemia take another blood sample for U&E, with care to avoid
haemolysis, and a heparinized sample to measure K
+
on a blood gas machine:
• Give 10mL of 10 % calcium chloride slowly IV (over 5min). This
does not lower K
+
, but antagonizes cardiac membrane excitability.
Hypercalcaemia may possibly potentiate toxicity in patients on digoxin,
so give as an IVI over 30min in these patients.
• Give 10U of short-acting human soluble insulin with 50mL of 50 %
glucose IV. This helps i cellular uptake of K
+
, lowering serum levels by
up to 1mmol/L within 1hr.
• Give 5mg nebulized salbutamol, repeated once as necessary. This will
lower K
+
in most patients, acting in 8 30min.
• Correct volume defi cits/acidosis with IV fl uids and isotonic (1.26 % )
sodium bicarbonate or aliquots (25–50mL) of 8.4 % . Beware fl uid over-
load/osmolar effects, especially in dialysis patients.
• Correct the underlying cause if possible (eg steroid therapy for
Addison’s disease).
• Contact the nephrology team urgently for patients with acute or
chronic renal failure as emergency dialysis may be needed.
Hyperkalaemia in children — see b Renal failure, p.694.

163
HYPERKALAEMIA
Management of hyperkalaemic cardiac arrest
If a patient in cardiac arrest is known to have hyperkalaemia, follow the
standard ALS guidelines ( b p.46), plus one or more of the following:
• Give 10mL of 10 % calcium chloride IV by rapid bolus injection.
• Consider giving 10U of short-acting insulin + 100mL 50 % glucose
rapidly IV.
• If there is severe acidosis, give 50mL 8.4 % sodium bicarbonate rapidly IV.
• Consider haemodialysis for cardiac arrest induced by hyperkalaemia
which is resistant to medical treatment.
Management of moderate hyperkalaemia
Provided that the result is not spurious, a K
+
of 6–6.5mmol/L may be
regarded as ‘moderately’ severe hyperkalaemia.
• Obtain venous access and monitor ECG.
• If there are ECG changes, treat as for severe elevation opposite.
• If there are no ECG changes, give 10U of short-acting human soluble
insulin with 50mL of 50 % glucose IV over 15–30min.
• Look for and treat the underlying cause and consider: diuretics
(eg furosemide 1mg/kg IV slowly) and dialysis.
Management of mild hyperkalaemia
K
+
of 5.5–6mmol/L. Treat the underlying cause and treat any associated
hypovolaemia. Discuss need for specifi c intervention (diuretic, dialysis)
with the medical team.

164 CHAPTER 3 Medicine
Hypokalaemia
Defi ned as K
+
<3.5mmol/L, it is relatively common. Moderate hypoka-
laemia may result in lethargy, weakness, and leg cramps. In severe cases
(K
+
<2.5mmol/L), rhabdomyolysis and respiratory diffi culties may occur.
ECG changes include prominent U waves and fl attened T waves.
Treatment In most instances, aim to replace potassium gradually. The
maximum recommended IV infusion rate of potassium is 20mmol/hr.
Restrict more rapid rates of IV infusion (eg 20mmol in 20–30min) to those
patients who have unstable arrhythmias when cardiac arrest is imminent
(obtain senior/expert advice). Ensure cardiac monitoring occurs during
any potassium IVI.
Associated magnesium defi ciency
Many patients with potassium defi ciency are also magnesium defi cient.
Consider replacing magnesium in those patients who have severe
hypokalaemia.
See also www.resus.org.uk

165
PORPHYRIA
Porphyria
The porphyrias are haem biosynthesis disorders in which enzyme
defi ciencies cause accumulation of porphyrin and porphyrin precursors.
Most cases are hereditary, but abnormal porphyrin metabolism may
develop in iron defi ciency, alcohol excess and lead poisoning. The acute
porphyrias (acute intermittent porphyria, variegate porphyria and heredi-
tary coproporphyria) affect 8 1 in 10,000 people in the UK. The non-acute
porphyrias (eg porphyria cutanea tarda) do not produce acute attacks, but
cause skin photosensitivity sometimes associated with liver disease.
Attacks of acute porphyria are often caused by drugs: barbiturates,
oestrogens, progesterones, sulphonamides, methyldopa, carbamazepine,
phenytoin, sulphonylureas, chloramphenicol, tetracyclines, danazol, some
antihistamines. Other precipitants include: alcohol, smoking, dieting,
emotional and physical stress, infection, substance misuse, pregnancy.
Clinical features of acute porphyria
• Abdominal pain is common and can be severe, with nausea, vomiting
and constipation. Abdominal examination may be normal or there may
be mild generalized tenderness.
• Peripheral neuropathy is usually motor, rather than sensory, and may
progress to paralysis and respiratory failure.
• Tachycardia, hypertension, and postural hypotension.
• Psychiatric manifestations: agitation, depression, mania and hallucina-
tions.
• Hyponatraemia due to inappropriate ADH secretion can cause fi ts or
coma.
Investigation and management of acute porphyria
Look for a Medic-Alert bracelet. Obtain old medical notes.
If an acute attack is suspected, send a fresh urine sample (protected from
light) to test for amino laevulinic acid and porphobilinogen. In an attack,
urine goes dark red or brown, especially if left exposed to light (due to
polymerization of porphobilinogen).
Treat acute attacks supportively (if necessary in ICU). Maintain
carbohydrate intake (PO or IV). Control mild pain with paracetamol or
aspirin; moderate/severe pain with morphine ( ± anti-emetic). Consider
chlorpromazine for agitation; propranolol to control severe hypertension.
Management of status epilepticus is diffi cult as many anticonvulsants are
contraindicated: choose IV diazepam in the fi rst instance. Haem arginate
helps some patients with acute crises (take specialist advice).
Prescribing for patients with porphyria
Many drugs can precipitate attacks, so check with the patient and the
BNF .
However, the safety of many drugs in porphyria is uncertain and effects
vary between patients. If in doubt, obtain specialist advice. In addition to
those mentioned earlier, safe drugs appear to be: ibuprofen, penicillin,
ciprofl oxacin, bupivicaine.
Data is also available on the internet at www.uq.edu.au/porphyria

166 CHAPTER 3 Medicine
Bleeding disorders: 1
Contact a haematologist whenever treating a patient with a
known or suspected bleeding disorder
Haemostasis requires co-ordination between the vascular system, platelets
and coagulation pathways to limit blood loss from the circulation. Platelets
interact with vascular subendothelium, forming a primary platelet plug,
which is strengthened by cross-linked fi brin strands formed via the coagu-
lation cascade to allow restoration of vascular integrity (see Fig. 3.24 ). The
fi brinolytic systems prevent excess clot formation, and inappropriate local
or generalized thrombosis, by promoting lysis of fi brin.
Recognition of bleeding
Bleeding is expected after trauma, but suspect a bleeding disorder if spon-
taneous or excess haemorrhage occurs from multiple or uninjured sites,
into deep tissues, joints or delayed bleeding occurs (hr/day). Bleeding dis-
orders may be congenital or acquired. Ask about previous bleeding after
trauma, dentistry or surgery and the family history.
Congenital disorders Haemophilia A (Factor VIII defi ciency), Haemophilia B
(Factor IX defi ciency), and von Willebrand’s disease. Most adults with a
congenital disorder know the nature of it and carry a National Haemophilia
card or Medic-Alert bracelet giving details. Many haemophiliacs know
more about their required treatment than you! They will be registered
and known at a haemophilia centre.
Acquired disorders May be due to liver disease, uraemia, drug use (ask
specifi cally about aspirin, NSAIDs, warfarin/anticoagulants, alcohol), or
unrecognized conditions such as haematological malignancy.
Hypothermia ( b p.254) from whatever cause aggravates any bleeding
tendency. For example, an INR assay performed at 32 ° C will be prolonged
to the same extent as would occur with a Factor IX level of 2.5 % of
normal. The severity of this may not be recognized merely from standard
tests as these are performed at 37 ° C.
The site of bleeding can give a clue as to the abnormality. Platelet problems
(usually thrombocytopenia) often present with mucocutaneous bleeding
(eg epistaxis, GI, GU, or heavy menstrual bleeding, bruising, purpura,
and petechial haemorrhages). Bleeding into joints or potential spaces (eg
retroperitoneal) and delayed bleeding is more often due to coagulation
factor defi ciencies. Patients with mucocutaneous bleeding and haemorrhage
into deep spaces may have a combined platelet and coagulation factor
abnormality (eg disseminated intravascular coagulation (DIC)).
167
BLEEDING DISORDERS: 1
Investigations
FBC Remember that in acute bleeds, Hb and Hct values fail to demonstrate
the severity of red cell loss as haemodilution takes time. Platelet counts
<100 × 10
9
/L indicate thrombocytopenia, and <20 × 10
9
/L are associated
with a risk of spontaneous bleeding. Bleeding because of platelet problems
can occur with ‘normal’ counts if platelet function is abnormal (eg with
aspirin or clopidogrel).
Prothrombin time (INR) Used to monitor anticoagulant control in patients
on coumarin drugs and may be prolonged in liver disease.
Activated partial thromboplastin time (APTT) Tests components of
intrinsic and common coagulation pathways (essentially all factors except
VII and XIII).
Individual factor levels Can be determined by specifi c assays together
with inhibitor screening tests for antibodies that can prolong normal
plasma clotting.
Collagen exposure
Platelet release
reaction
Platelet aggregation
Platelet fusion
Stable
haemostatic plug
Thrombin
Blood
coagulation
cascade
Tissue
factor
Fibrin
Primary
haemostatic plug
Reduced
blood flow
Vasoconstriction
Serotonin
Thromboxane A
2
, ADP
Platelet
phospholipid
Vessel injury
Fig. 3.24 Reactions involved in haemostasis.

168 CHAPTER 3 Medicine
Bleeding disorders: 2
General aspects of treatment
• Perform routine wound/fracture management of patients with bleeding
disorders, but consider need for prior or simultaneous administration
of factor concentrates/platelets under haematological guidance.
• Spontaneous or traumatic bleeding into the neck or pharynx may cause
rapid airway compromise.
• Always consider intracranial haemorrhage in a patient with headache,
neurological symptoms or minor head trauma. Consult to consider
need for commencing treatment before specifi c investigation (eg CT).
• Never give IM injections.
• Do not attempt central line placement except in extremis, since life-
threatening, uncontrollable bleeding can result.
• Before giving any drug, check whether it may aggravate the condition or
interfere with intercurrent therapy.
Specifi c conditions
Vascular lesions May be inherited (Ehlers–Danlos syndrome, pseudo-
xanthoma elasticum, osteogenesis imperfecta, haemorrhagic telangiectasia)
or acquired (eg due to steroids, infection e.g. meningococcaemia, thrombotic
thrombocytopenic purpura, vasculitis, scurvy).
Platelet disorders Capillary-related mucocutaneous bleeding is common
and may occur immediately after injury/surgery (eg dental extractions).
The platelet count may be normal or d . Acquired thrombocytopenia may
be due to drugs, toxins, infections, autoimmune conditions (eg ITP), DIC,
or to massive blood transfusion. Abnormal platelet function occurs with
uraemia, myeloproliferative disorders, and drugs (eg aspirin).
Coagulation pathway disorders Congenital coagulation pathway disorders
predominate in males. They cause intramuscular or deep soft tissue
haematomas. Bleeding onset after injury/surgery may be delayed 2–3 days.
von Willebrand’s Disease The commonest congenital bleeding disorder,
with VW Factor and Factor VIII defi ciency, and abnormal platelet
function. Clinically, the condition is similar to a platelet disorder, but
milder. Bleeding is commonly mucosal (eg epistaxis) and usually treated
with Factor VIII concentrate (which includes VW Factor).
Haemophilia A Caused by a lack of functional factor VIII which is needed
for clot formation. Often presents with bleeding into deep muscles, large
joints or urinary tract. Intracranial bleeding is a major cause of death at all
ages. Anticipate bleeding up to 3 days after trauma.
In UK, haemophilia A associated with bleeding or potential bleeding is
normally treated by Factor VIII concentrate (some patients have ‘home
supplies’ and may bring them to hospital). The volume (dose) depends
upon the severity of the haemophilia of the individual patient and the
purpose of treatment (ie prophylaxis or therapy for current bleeding).
Haemophilia B (Christmas disease) Involves a defi ciency of Factor IX
activity and is genetically and clinically indistinguishable from haemophilia
A, but much less common. It is normally treated with factor IX
concentrate.
169
BLEEDING DISORDERS: 2
Disseminated intravascular coagulation (DIC)
Patients may present with DIC due to infection (especially Gram –ve
sepsis), trauma, malignancy, pregnancy (amniotic fl uid embolism, placental
abruption, toxaemia, retained products), any cause of shock, incompatible
blood transfusion or massive volume replacement. Following triggering of
the coagulation process, consumption of platelets, and coagulation factors
(particularly fi brinogen, V, VIII, and XIII) occurs with thrombin formation
overwhelming the normal inhibition system, resulting in systemic fi brin dep-
osition (Fig. 3.25 ). Activation of the fi brinolytic system results in dissolution
of fi brin and release of fi brin degradation products.
Investigations Platelet count is usually d , INR i and APTT i , fi brinogen
level d , fi brin degradation products i .
Treatment Is complex and requires control of the primary cause of the
DIC to avoid total depletion of clotting factors. Obtain expert advice
about replacement therapy with platelets, FFP, prothrombin complex
concentrate, heparin and blood (particularly required if the patient is
actively bleeding).
EXTRINSIC SYSTEM
XII (on contact with vascular
endothelium)
INTRINSIC SYSTEM
Tissue factor
+VIII
+Ca
2+
XIIa
XIa
XI
IX
X
Xa
+VIII
+Ca
2+
+Phospholipid
Prothrombin Thrombin
XIIIa
XIII
Cross linking
Fibrin
Fibrinogen
Xa
+V
+Ca
2+
+Phospholipid
Fig. 3.25 Coagulation cascade.

170 CHAPTER 3 Medicine
Patients on anticoagulants
The commonest oral anticoagulant is warfarin sodium, a vitamin K antago-
nist. This inhibits the production of Factors II (prothrombin), VII, IX and
X ande d plasma levels of these factors. Patients, or their relatives, who
are able to give a history will usually know if they are taking warfarin, and
their most recent prothrombin time or INR test result, together with any
changes in treatment.
If this history is not available, suspect patients with prosthetic heart
valves, mitral valve disease, AF, a past history of DVT/PE or TIAs to be
on anticoagulants. Intercurrent illness, liver disease and changes in diet,
and/or alcohol consumption may affect anticoagulant control. Concurrent
drug administration with unrecognized potential for interaction is the
commonest cause for acute changes in anticoagulant control.
These patients usually present with one of three problems.
Acute haemorrhage
Spontaneous bleeding in patients on warfarin most commonly affects
the GI tract, GU tract, joints, or muscles. After injury, expect excessive
or continuing bleeding. Anticipate the i risks of occult or unrecognized
bleeding (eg intraperitoneally or intracranially) after even minor trauma
and maintain a high index of suspicion as to these possibilities.
Check INR and FBC in all patients. Other investigations (eg CT scan of
head/abdomen, USS) will be dictated by the nature of the acute problem.
Patients with life-threatening haemorrhage
For patients with life-threatening haemorrhage, commence volume
replacement and blood transfusion as appropriate (see b Blood trans-
fusion 1, p.172). Contact haematology for specialist advice which may
include phytomenadione (vitamin K
1
) up to 10mg by slow IV injection and
provision of prothrombin complex concentrate.
Patients with less severe haemorrhage
Patients with muscle haematomas, haematuria, or epistaxis also require
hospital admission for observation and specifi c local treatment. Stop war-
farin therapy for one or more days. Phytomenadione 0.5–2mg by slow IV
injection may be advised by the haematologists. Note that vitamin K
1
can
interfere with warfarinization for several days, so take expert advice when
the patient is also at high risk of thrombosis (prosthetic heart valve).
INR levels within the therapeutic range
Patients who develop bleeding with INR levels within the therapeutic
range require investigation of a possible underlying cause (eg GI or GU
tract pathology).
See http://www.bcshguidelines.com

171
PATIENTS ON ANTICOAGULANTS
Check of control of anticoagulation
The therapeutic range for the INR may vary according to the indication for
anticoagulation. An INR of 2.0–3.0 is usually appropriate for DVT prophy-
laxis and 3.0–4.0 for patients with mechanical prosthetic heart valves.
For patients who have INR 4.0–7.0 without haemorrhage, withhold warfarin
therapy for 1 or 2 days, and arrange review by appropriate specialist team
or GP. For patients with INR > 7.0 without haemorrhage, withhold warfarin
and obtain specialist consultation before considering phytomenadione
(vitamin K
1
) 5mg by slow IV injection or orally.
Interactions with other prescribed or proprietary medicines
Many drugs can interfere with anticoagulant control. Before giving or
stopping any drug in a patient taking warfarin or other anticoagulant,
check the potential for interaction — Appendix I in the BNF .
Particular groups of drugs, likely to be prescribed in the ED, which may
cause problems include analgesics (especially NSAIDs), antibacterials and
anti-epileptics. Always LOOK IT UP.
Other oral anticoagulants
Dabigatran (a direct thrombin inhibitor) and rivaroxaban (a Factor Xa
inhibitor) are among a group of new oral anticoagulants which may be
prescribed instead of warfarin or low molecular weight heparin, in certain
conditions. They do not require routine blood monitoring. To date, there
are no guidelines for measuring their effect in patients who are bleeding,
and there is no proven way to reverse their effect. Always discuss bleeding
patients on new oral anticoagulants with a haematologist. Attempts at
reversal may include FFP or prothrombin complex concentrate.

172 CHAPTER 3 Medicine
Blood transfusion 1
It is better to stop bleeding than to have to replace blood loss
General aspects
Correctly documenting and labelling blood tubes and forms, combined
with checking blood products prior to administration, is crucial for safe
patient care. If a patient’s name(s), date of birth, clinical details and address
are unknown or uncertain, identify them for transfusion purposes by a
unique number (usually their unique ED number) and inform the blood
transfusion laboratory.
To avoid confusion, the doctor taking the blood sample must label and
sign the tube at the patient’s bedside, complete the form, and contact
the transfusion service. Only take blood from one patient at a time. Label
tubes immediately to minimize the risk of mislabelling. Blood banks may
refuse to handle incorrectly labelled forms/tubes.
If you knowingly give a blood product (or animal product e.g. gelatin) to
a patient whom you know would not accept this (eg a Jehovah’s Witness)
you are likely to face an indefensible medicolegal claim.
What to send
10mL clotted blood is usually adequate for adults. Where it is obvious
that massive transfusion may be required, send two 10mL samples. On the
request form, indicate how much blood is needed, when and where the
blood is to be sent. Date and sign the form.
What to request
The amount of blood to be delivered and to be kept available at the
transfusion centre for immediate dispatch depends on the patient’s clinical
state and assessment of future blood losses. Assessment of a patient with
hypovolaemic shock is complex and includes recognition of the clinical
situation, the potential blood loss, together with a current assessment
of the patient and investigations. Hb and Hct values may be misleading.
It may take hours for their values to equilibrate to those indicating the
degree of blood loss.
Group and screen The patient’s ABO and Rhesus D group is determined
and the serum tested for unexpected red cell antibodies. Subsequently, if
required, blood can be provided within 10–15min, assuming the antibody
screen is clear. Request ‘Group and screen’ where a patient does not
need transfusion in the ED, but may require it later.
Cross-match Full blood compatibility testing may take up to 1hr. If blood
is required more urgently, ABO and Rh compatible units can usually be
provided within 15min, including an ‘immediate spin cross-match’ as a fi nal
check on ABO compatibility. In exsanguinating haemorrhage, uncross-
matched group O Rhesus –ve blood can be issued immediately.

173
BLOOD TRANSFUSION 1
Blood products
The UK uses blood component therapy. There appears to be no specifi c
advantage in using ‘whole’ blood as opposed to red cells plus a volume
expander.
Red cells (additive solution) Each pack (volume 300mL) is from a single
donor and has a Hct of 0.65–0.75 (0.55–0.65 for RBCs in additive solution).
A transfusion of 4mL/kg will i circulating Hb by 81g/dL.
Whole blood A ‘unit’ contains 530mL (470mL of blood from a single
donor + 63mL preservative solution), with a Hct of 0.35–0.45.
Platelet concentrate either pooled or from a single donor by platelet
pheresis.
Fresh frozen plasma contains clotting factors and fi brinogen.
Cryoprecipitate is derived from FFP when it is thawed. It is rich in factor
VIII, fi brinogen, and von Willebrand Factor.
Prothrombin complex concentrate is a combination of vitamin K
dependent Factors II, VII, IX and X. Use PCC to reverse warfarin.
Transfusion precautions (UK Blood Safety & Quality
Regulations 2005)
• 2 practitioners must confi rm all the following steps before commencing
transfusion. If there is ANY discrepancy, DO NOT transfuse.
• Confi rm the details on the traceability label on the blood component
match the patient’s full name, date of birth, and hospital number (wrist
band if unconscious).
• Check that the traceability label is attached to the blood bag.
• Ensure the donation number, the patient’s blood group/RhD type all
match and that any special requirements are covered.
• Check every component before starting transfusion for signs of discol-
ouration, leaks, clots etc. and the expiry date.
• If all checks are satisfactory, the 2 practitioners should ensure that the
component has been prescribed (prescription form and/or fl uid balance
chart) and sign the front of the traceability label before commencing the
transfusion.
• Infuse all components through a giving set with integral fi lter to trap
large aggregates. Microaggregate fi lters are not routinely required.
• Never add any drug to a blood component infusion.
• Do not use giving-sets which previously contained glucose or gelatin.
• Red cell concentrates may be diluted with 0.9 % saline using a Y giving-
set to improve fl ow rates. Never add any other solution.
• Use a blood warmer, especially for large and/or rapid transfusions.
• Once the transfusion has started, peel off the portion of the signed label
and attach to the appropriate place in the fl uid balance sheet.
• Sign the prescription form to confi rm the patient identity checks.
• Complete and sign the label and return it to the laboratory.
See: www.transfusionguidelines.org.uk

174 CHAPTER 3 Medicine
Blood transfusion 2
Massive transfusion
Loss of 50 % of circulating blood volume within 3hr is perhaps the most
relevant ED defi nition. Resuscitation requires an interdisciplinary team
and clear organization.
In the event of massive blood loss
• Protect the airway and give high fl ow O
2
.
• Get help — two nurses and a senior doctor.
• Insert two large bore cannulae and start IV warm saline 1000mL stat.
• Take FBC, U&E, LFTs, coagulation, and cross-match. Label the blood
tubes and ensure they are sent directly to the laboratory. Do not leave
them unlabelled or lying around in the resusitation room.
• Telephone the haematology laboratory to warn of potential massive
transfusion. Request ABO group-specifi c red cells if the patient is peri-
arrest. This will take only 10min in the laboratory. Otherwise, request
full cross-match and give number of units required.
• Accurate patient ID is essential, even if the patient is unknown.
• Call appropriate senior surgeon — to stop bleeding as soon as possible.
• Start blood transfusion if the patient remains tachycardic and/or hypo-
tensive despite crystalloid resuscitation.
• Repeat all bloods, including FBC, clotting, U&Es, calcium, and magne-
sium levels, every hour.
• Start platelet transfusion if platelet count falls below 75 × 10
9
/L.
• Anticipate the requirement for FFP and consider giving early during
the resuscitation. FFP will replace clotting factors and fi brinogen. Aim
to maintain fi brinogen > 1.0g/L and the INR and APTT <1.5 normal.
Cryoprecipitate may also be used.
• Recombinant Factor VIIa might be used as a ‘last ditch attempt’ to
control bleeding in young patients where surgical control of bleeding
is not possible, and the above has already been corrected. If the drug is
available it is usually ordered by a haematologist.
Massive transfusion complications
Rapid infusion of blood products may lead to:
Hypothermia Blood products are normally stored at 2–6 ° C. Rapid
infusion can cause signifi cant hypothermia. Use blood warmers routinely
for rapid transfusions (eg > 50mL/kg/hr or 15mL/kg/hr in children). Never
warm a blood product by putting a pack into hot water, on a radiator or
any other heat source.
Electrolyte disturbances With massive transfusion, the citrate anticoagulant
may cause signifi cant toxicity, d plasma Ca
2 +
(impairing cardiac function)
and acid–base balance disturbance. This is aggravated in patients with
underlying liver disease, hypotension or hypothermia. Citrate may also
bind Mg
2 +
, causing arrhythmias. Prophylactic or routine administration of
IV calcium salts is not recommended. Monitor ECG and measure ionized
plasma Ca
2 +
levels during massive transfusion. K
+
levels i in stored blood
and hyperkalaemia may follow massive infusion. Routinely monitor the
ECG and check plasma K
+
levels. Transient hypokalaemia may follow 24hr
after large volume transfusion

175
BLOOD TRANSFUSION 2
Blood product administration
Blood transfusion is not a panacea. An improvement in O
2
delivery cannot
be assumed. RBC function deteriorates during storage and changes in O
2
affi nity occur withe d 2,3-DPG levels, while d ATP levels alter RBC mem-
brane deformability causing i cell stiffness and micro-circulatory problems.
UK donations are routinely screened for hepatitis B, HIV, HTLV, syphilis,
and where necessary, CMV. However, blood cannot be sterilized: small
but defi nite risks of infection transmission exist.
Transfusion reactions
Monitor the patient closely for the fi rst 5–10min of the infusion of each
unit of blood to detect early clinical evidence of acute reactions. If the
patient develops a temperature, shortness of breath, chest or abdom-
inal pain or hypotension, suspect a transfusion reaction. Treat allergic
reactions including itching, urticaria, bronchospasm and fever convention-
ally (see b Anaphylaxis treatment, p.43).
Mismatched transfusion By far the commonest cause is a clerical error
when labelling, ordering or administering blood. Transfusion of ABO
incompatible blood causes acute severe haemolysis and circulatory
collapse. In a hypovolaemic, shocked, or anaesthetized patient these
features may be obscured and missed.
If a transfusion reaction is suspected:
ABO incompatability, haemolytic reaction, bacterial infection, severe
allergic reaction, or transfusion-related acute lung injury:
• Stop the transfusion.
• Keep the IV line open with 0.9 % saline.
• Record all observations, give supplemental oxygen.
• Double-check the blood unit label with the patient’s wrist identity band
and other identifi ers.
• Send the unit of blood product and the giving set to the blood bank.
• Take 40mL of blood. Send it as follows:
• 5mL anticoagulated and 5mL clotted blood to blood bank;
• 10mL for U&E;
• 10mL for coagulation screening;
• 10mL for blood cultures.
• Contact the blood bank directly by phone.
• Contact haematologist directly.
• Give broad spectrum antibiotic if infection suspected .
• Monitor fl uid balance and urinary output.

176 CHAPTER 3 Medicine
Sickle cell disease
Sickle cell disease occurs in African, Indian, Middle Eastern, Caribbean,
USA, and Mediterranean populations. It is caused by a genetic mutation in
one of the chains of the Hb molecule. The normal adult Hb genotype AA
produces HbA. In heterozygotes (sickle cell trait) one gene is abnormal
(HbAS) and about 40 % of the patient’s Hb will be HbS. In homozygotes
(sickle cell anaemia), both genes are abnormal (SS) and > 80 % of the Hb
will be HbS. HbS molecules polymerize in deoxygenated or acidotic con-
ditions, causing RBC sickling. Sickle cells are rigid and fragile. They may
haemolyse, or block small vessels leading to tissue ischaemia, infarction
and further sickling (see Fig. 3.26 ). Sickling also occurs with genes coding
other analogous amino acid substitutions (eg HbSC and SD diseases).
Clinical features
Sickle cell trait causes no disability except during conditions of severe
hypoxia (eg sudden depressurization in aircraft, or cardiac arrest).
Patients with sickle cell anaemia have chronic anaemia (Hb 8–10g/dL) with
alternating good health and acute crises. Later, chronic ill health supervenes
with renal failure, bone necrosis (evident in 50 % of patients by age 35
years), osteomyelitis, leg ulcers and iron overload as a consequence of
transfusions. There is predisposition to infection, especially Staphylococcus,
Pneumococcus , and Haemophilus.
Sickle cell crises can occur de novo or follow infection, cold, dehydration,
or any situation where tissue hypoxia/ischaemia occurs. The crisis may
involve thrombosis, haemolysis, marrow aplasia, or acute splenic/liver
sequestration (especially in children aged <5 years). Any acute medical
or surgical emergency may be mimicked (eg acute abdomen, PE, stroke).
Severe aching bony pain and low-grade fever (even in the absence
of infection) is common. Cerebral sickling may present with bizarre
behaviour, psychosis, fi ts, TIAs, stroke, or other focal neurological signs.
Priapism, jaundice, and painful swelling of hands and feet may occur.
Acute chest syndrome
The leading cause of death in sickle cell anaemia. It presents as chest pain,
hypoxia and pulmonary infi ltrates. There may be cough, tachypnoea, and
wheezing. Poorly understood, but infection may be a precipitant.
Acute splenic sequestration
Sudden trapping of large numbers of RBCs in the spleen results in severe
anaemia, an enlarging spleen, hypovolaemia, and thrombocytopenia. It
occurs most commonly in young children — those with sickle cell disease
have a 30 % chance of having acute splenic sequestration by the age of 5
years. It may present with shock and splenomegaly, with a mortality of
> 15 % .
Osteomyelitis and septic arthritis
Osteomyelitis and septic arthritis occur more commonly in sickle cell
disease. Be suspicious if a patient presents with high fever, soft tissue
swelling, or pain in a different pattern to normal. Salmonella is frequently
implicated.
177
SICKLE CELL DISEASE
Investigations
No specifi c tests can detect a sickle cell crisis:
• All patients in the at-risk groups require a sickle test before any anaesthetic
procedure (including regional anaesthesia, Bier’s block).
• Sickle testing (using an oxidizing agent) will detect sickling in homo- and
heterozygote forms. Hb electrophoresis can then distinguish between
HbSS, HbAS and other Hb variants.
• FBC typically shows anaemia (Hb 6–8g/dL, but Hb may be much lower if
acute haemolysis, sequestration or aplasia is present). Post-splenectomy
features may be seen on blood fi lm. WCC may be i (20–60 × 10
9
/L) in
the absence of infection and platelet count is also usually i .
• Infection screen, including blood cultures, midstream specimen of urine
(MSU) and CXR.
• Joint aspiration for culture if septic arthritis is suspected.
• U&E, ABG, ECG.
• Arrange CT brain scan if there are neurological symptoms or signs.
Management of crises
Provide supportive therapy, directed to the patient’s symptoms:
• Get expert help!
• Keep the patient warm, rested and give O
2
if any obvious symptoms or
SpO
2
<94 % .
• Opioids (given IV and titrated to the response) are often required for
pain. Consider morphine IVI or patient analgesia pump.
• Commence rehydration with oral or IV fl uids, but take care not to pre-
cipitate heart failure.
• Transfusion may be required if severe anaemia from acute haemolysis,
sequestration or aplasia occurs, or if there are central nervous system
(CNS) or lung complications.
Empirical antibiotic therapy may be required if infection is thought to be
the trigger for the sickling crisis.
Sickling
Deoxygenation
and acidosis
Sludging
Stasis
Blood viscosity
Fig. 3.26 Sickling cycle.
This page intentionally left blank

179
Poisons: general principles 180
Diagnosis of poisoning 182
Poisons: supportive care 183
Reducing absorption of poison 184
Antidotes for poisons 186
Opioid poisoning 188
Salicylate poisoning 189
Paracetamol poisoning 190
Tricyclic antidepressant poisoning 194
Benzodiazepine poisoning 196
Clomethiazole poisoning 196
Phenothiazine poisoning 196
Barbiturate poisoning 197
Lithium poisoning 197
Sulphonylurea poisoning 197
Beta-blocker poisoning 198
Calcium antagonist poisoning 198
Digoxin poisoning 199
ACE inhibitor poisoning 199
Theophylline poisoning 200
Salbutamol poisoning 200
Iron poisoning 201
Ethanol poisoning 202
Methanol poisoning 202
Ethylene glycol poisoning 203
Paraquat poisoning 204
Petrol and paraffi n poisoning 205
Organophosphate poisoning 206
Cyanide poisoning 207
Carbon monoxide poisoning 208
Chlorine poisoning 209
CS gas (tear gas) 209
Chemical incidents 210
Decontamination of patients 211
Plants, berries and mushrooms 212
Button batteries 213
Illicit drugs 214
Serotonin syndrome 216
Body packers 217
Toxicology
Chapter 4

180 CHAPTER 4 Toxicology
Poisons: general principles
Emergency treatment
Clear and maintain the Airway .
If Breathing appears inadequate ventilate with oxygen using a bag and mask
or ET tube (not mouth-to-mouth in poisoned patients). Give naloxone for
respiratory depression due to opioids ( b p. 188).
Circulation Check pulse. If unconscious and pulseless, start CPR.
Types of poisoning
Unintentional or ‘accidental’ poisoning is most common in inquisitive
small children (1–4 years) who eat tablets, household chemicals, and
plants. Older children and adults may be poisoned by chemicals at school
or work, or by drinking toxic fl uids decanted into drinks bottles. Poisoning
by drugs may result from miscalculation or confusion of doses or by taking
the same drug under different names. Drug smugglers who swallow drugs
wrapped in condoms or polythene, or stuff them in the rectum or vagina,
may suffer poisoning if the packages leak ( b p.217).
Deliberate self-poisoning is the commonest form of poisoning in adults and
may occur in children as young as 6yrs (usually with a family history of self-
poisoning). Drugs or poisons are often taken impulsively, sometimes to
manipulate relatives or friends. Suicidal intent is relatively uncommon, but
assess all patients for this ( b p.612). A few patients leave suicide notes,
and conceal the drugs or poison to evade detection.
Non-accidental poisoning of children is a form of fabricated or induced
illness (previously known as Munchausen’s syndrome by proxy — b
p.733), in which a parent deliberately poisons a child. Homicidal poisoning
is rare and may involve acute or chronic poisoning with chemicals such as
arsenic or thallium.
Chemical plant incidents and terrorism are potential threats to large
numbers of people.
Information about poisons
Tablets may be identifi ed from MIMS Colour Index and descriptions in
the BNF . Drug Information Centres and Poisons Information Services
(see opposite) have access to TICTAC , a computer-aided tablet and capsule
identifi cation system ( www.tictac.org.uk ).
Martindale
1
gives information on many drugs and poisons, and detailed
constituents of non-prescription drugs.
Identifi cation of plants and fungi from reference books may be diffi cult,
especially if only vague descriptions or chewed fragments are available.
The CD-ROM computer software Poisonous Plants and Fungi in Britain
and Ireland
2
helps with identifi cation and details of toxicity. Local botanic
gardens may provide additional help. See also b p.212.
1 Sweetman SC ( ed ). ( 2009 ) Martindale: The Complete Drug Reference , 36
th
edn . Pharmaceutical
Press , London .
2 Dauncey EA et al . ( 2002 ) Poisonous Plants and Fungi in Britain and Ireland ( interactive identifi cation
system on CD-ROM ), 2
nd
edn. Kew Publishing , Kew , www.kewbooks.com.

181
POISONS: GENERAL PRINCIPLES
Poisons Information Centres in the UK
TOXBASE, the UK National Poisons Information Service’s database on
clinical toxicology, is on the internet ( www.toxbase.org ) with a backup
site at www.toxbasebackup.org . It includes information about poisoning
with drugs, household products, plants and fungi, as well as industrial and
agricultural chemicals and agents which might be deliberately released by
terrorists. Access to TOXBASE is password protected and is restricted to
NHS professional staff in the UK and also hospitals in Ireland.
TOXBASE or reference books provide suffi cient information for most
cases of poisoning. More detailed information and specialist advice is
available from Poisons Information Centres and is especially useful for
complex cases or severe poisoning.
The UK National Poisons Information Service has four centres, with a single
telephone number 0844 892 0111 which directs the call to the nearest
centre, or to the on-call centre out of hours. In Ireland advice is available
from the National Poisons Information Centre, Dublin, telephone (01)
809 2566.
Enquiries to Poisons Information Centres are usually answered initially by an
information offi cer using TOXBASE and other reference sources. Medical
staff with specialist toxicology experience are available for advice about
seriously poisoned patients. Poisons Information Centres can also advise
about sources of supply of antidotes that are needed only occasionally, and
about laboratory analyses that may be helpful in managing some patients.
Admission and psychiatric assessment after poisoning
Adults
Patients who are seriously poisoned need admission to a medical ward,
or if appropriate, to ICU. However, most patients who take overdoses
suffer no serious ill effects and may be treated satisfactorily on an ED
observation ward or a Clinical Decisions Unit. Even if there is no risk of
toxicity, admission overnight provides a ‘cooling off’ period for the patient
to get away from the situation that precipitated the overdose. This should
allow a more rational appraisal of the problems and may reduce the risk
of further self-poisoning.
Look for the causes of every episode of deliberate self-harm. A patient
who seems suicidal (see b p.612) must be observed carefully in the ED
and on the ward, because of the risk of further self-harm.
Children with poisoning
Serious poisoning is uncommon in children. Many children appear well
but have been exposed to an unknown amount of a compound which
could be toxic. Admit such children to a paediatric ward for observation:
they can be discharged after a few hours if no toxic effects occur. A child
may be discharged home directly from the ED if the substance taken is
known to be non-toxic. The health visitor may usefully visit the home
to advise about poisoning prevention. In children > 6 years, consider the
possibility of deliberate self-harm and the need for assessment by a child
psychiatrist.

182 CHAPTER 4 Toxicology
Diagnosis of poisoning
The patient or relatives/friends may state what drugs or poison have been
taken, but this information is not always accurate. Self-poisoning is often
an impulsive act whilst under the infl uence of alcohol: the patient may not
know which tablets he/she took. The amount involved is often unclear.
Check any bottles or packets for the names and quantities of drugs or
poisons that were available. If a patient is unconscious or severely poi-
soned, look in hospital notes for details of previous overdoses, and fi nd
out from the GP what drugs had been prescribed. Record the time of
ingestion of the drug or poison. Examine the patient all over for signs of
poisoning, injection marks or self-injury. Exclude other diverse processes
mimicking poisoning (eg head injury, meningitis). In the Far East, and in
EDs where Asian people present with non-specifi c symptoms, hepatitis,
or suspected poisoning, remember that traditional Chinese medicines or
herbs can cause signifi cant toxicity.
Toxidromes: features suggesting a particular poison
• Coma with dilated pupils, divergent squint, tachycardia, i muscle tone,
i refl exes and extensor plantars suggests tricyclic antidepressant or
orphenadrine poisoning ( b p.194).
• Coma with hypotension, respiratory depression and d muscle tone
suggests barbiturates, clomethiazole (b p.196), benzodiazepines with
alcohol, or severe tricyclic antidepressant poisoning ( b p.194).
• Coma with slow respiration and pinpoint pupils is typical of opioid
poisoning (give naloxone, b p.188).
• Tinnitus, deafness, hyperventilation, sweating, nausea and tachycardia
are typical of salicylate poisoning ( b p.189).
• Agitation, tremor, dilated pupils, tachycardia, suggest amphetamines,
ecstasy, cocaine, sympathomimetics ( b p.214), tricyclic antidepressants
( b p.194), or selective serotonin re-uptake inhibitors (b p.216).
Assessment and monitoring
• Assess and record conscious level ( b p.361). Observe frequently.
• Check blood glucose in patients with confusion, coma or fi ts.
• Monitor breathing and record respiratory rate. Use a pulse oximeter,
but note that SpO
2
may be misleadingly high in carbon monoxide (CO)
poisoning — see b p.208).
• Check ABG if patient is deeply unconscious or breathing abnormally.
• Record and monitor the ECG if a patient is unconscious, has tachy- or
bradycardia or has taken drugs or poisons with risk of arrhythmias.
• Record BP and temperature.
Investigations in poisoned patients
The most useful investigations are paracetamol and salicylate levels, blood
glucose, ABG, and urea & electrolytes (U&E). Measure paracetamol if
there is any possibility of paracetamol poisoning (this includes all uncon-
scious patients). Record the time of the sample on the bottle, and in the
notes. Many labs can measure salicylate, iron and lithium and also check
for paraquat if necessary. Comprehensive drug screening is rarely needed
and is only available in specialist centres (ask Poisons Information Service,
b p.181).

183
POISONS: SUPPORTIVE CARE
Poisons: supportive care
Protect the airway
In an unconscious patient use a cuffed ET tube if there is no gag refl ex. If
an oral or nasal airway is used, nurse in the recovery position to minimize
risk of aspiration should vomiting or regurgitation occur.
Monitor breathing and ventilate if necessary
Hypoxia and CO
2
retention are common in deep coma.
Hypotension
This may result from relative hypovolaemia, arrhythmias and cardio-
depressive effects of drugs. Treat according to the cause. Elevate the foot
of the trolley. If BP <90mmHg, consider giving saline or a plasma expander
such as gelatin 500mL IV. Monitor CVP in patients who are elderly or have
cardiac disease. Inotropes such as dopamine (2–5micrograms/kg/min), dob-
utamine (2.5–10micrograms/kg/min), glucagon ( b p.198) or insulin therapy
( b p.187) are occasionally needed, under expert guidance.
Cardiac arrhythmias
Generally rare in poisoned patients. The most likely drugs responsible are
tricyclic antidepressants, beta-blockers, chloral hydrate, digoxin, potassium,
bronchodilators, verapamil, and amphetamines. Look for and correct hypoxia,
respiratory depression, metabolic acidosis and electrolyte abnormalities.
Anti-arrhythmic drugs are very rarely needed: consult a poisons expert fi rst.
Convulsions
Dangerous because they cause hypoxia and acidosis, and may precipi-
tate cardiac arrest. Drugs responsible include tricyclic antidepressants,
mefenamic acid, and theophylline. Check for and correct hypoxia and
hypoglycaemia. Do not give anticonvulsants if fi ts are single and brief, but
if fi ts are repeated or prolonged give IV lorazepam 4mg (or PR diazepam
or buccal midazolam if venous access is not available).
Hypothermia
May occur with any drug causing coma, especially barbiturates,
clomethiazole, and phenothiazines. Check rectal T ° with a low-reading
thermometer. Insulation and passive rewarming are usually adequate.
Hyperthermia ( b p.264)
May occur with amphetamines, cocaine, ecstasy, monoamine oxidase
inhibitors, sympathomimetics, and theophylline. Convulsions and rhab-
domyolysis are common. Active cooling, chlorpromazine and possibly
dantrolene are needed. Get expert help.
Complications of immobility
Prolonged immobility (eg due to tricyclics and barbiturates) risks pressure
areas. Treat blisters like minor burns. Immobility may cause rhabdomyolysis
(leading to renal failure), nerve palsies, and compartment syndrome: if this
is suspected check CK, test urine for myoglobinuria, and get urgent ortho-
paedic advice about measuring compartment pressures.
Urinary retention
Common in coma, especially after tricyclic poisoning. Suprapubic pressure
often stimulates refl ex bladder emptying. Catheterization may be needed
to empty the bladder or to measure urine output.

184 CHAPTER 4 Toxicology
Reducing absorption of poison
Background information
If a poison has been swallowed it is logical to try to remove it and reduce
absorption from the gut. Possible measures include gastric lavage, induced
emesis (eg with ipecacuanha), oral adsorbents (especially activated
charcoal) and whole-bowel irrigation. None of these can be recom-
mended routinely. They may cause signifi cant morbidity and there is very
little evidence that they improve outcomes.
Gastric lavage
This does not empty the stomach of solids and may force gastric contents
through the pylorus into the small bowel. It may cause hypoxia, aspiration
pneumonia and occasionally oesophageal perforation. Gastric lavage
> 1hr after overdose is ineffective in d absorption of poisons. Gastric
lavage does not reduce mortality from poisoning, and it does not deter
patients from taking repeated overdoses.
Practical advice on use of gastric lavage
Only consider this if the patient has taken a life-threatening amount of
poison within the previous 1 hour or is deeply unconscious because of
poisoning. Only consider performing it if there is a strong cough refl ex
or the airway is protected by a cuffed ET tube. Do not use lavage for
poisoning with corrosives (risk of perforation) or with petrol/paraffi n
compounds (risk of pneumonitis), except rarely in severe poisoning on
specialist advice.
• Before starting gastric lavage, check that powerful suction is immedi-
ately available.
• Elevate the foot of the trolley and place the patient in the left lateral
position.
• Give O
2
via nasal cannulae. Monitor ECG.
• Lubricate large disposable stomach tube (36 or 40 French Gauge-FG)
and pass it through the mouth into the stomach. Confi rm position by
aspirating gastric contents or blowing air down the tube while listening
over the stomach.
• Aspirate gastric contents and keep labelled sample for later analysis if
necessary.
• Perform lavage by pouring 300mL aliquots of tepid tap water down
the tube and siphoning it back, while massaging over stomach to help
dislodge tablet debris.
• Continue until the effl uent is clear.
• Consider leaving activated charcoal (50g) in the stomach.
• While withdrawing the tube, occlude it between the fi ngers to prevent
aspiration of fl uid from the tube.

185
REDUCING ABSORPTION OF POISON
Induced emesis
Never use emetics. Ipecacuanha was once used frequently, but it may
cause prolonged vomiting, drowsiness and aspiration pneumonia, and it
does not reduce drug absorption. There is no indication for using ipecac.
Salt solutions may cause fatal hypernatraemia and must never be used as
an emetic.
Activated charcoal
Given within 1hr, this d absorption of therapeutic doses of many drugs,
but there is little evidence of clinical benefi t after overdose. Charcoal d
the half-life of some drugs (eg digoxin), which undergo entero-hepatic
recycling. However, charcoal is messy, unpleasant to take and often causes
vomiting. Aspiration into the lungs can result in fatal pneumonitis. Various
formulations of activated charcoal are available. Actidose Aqua Advance
®
is less unpalatable than some of the other formulations. Carbomix
®
may
cause severe constipation, especially if given in repeated doses.
Do not give activated charcoal for substances which do not bind to it.
These include: iron, lithium, boric acid, cyanide, ethanol, ethylene glycol,
methanol, organophosphates, petroleum distillates and strong acids and
alkalis. Charcoal is most likely to be useful for poisons which are toxic in
small quantities (eg tricyclic antidepressants and theophylline derivatives).
If a dangerous overdose has been taken in the previous 1hr, give charcoal
(PO or via an orogastric tube: adult 50g; child 1g/kg, max 50g). Charcoal
may be effective for > 1hr for sustained release formulations or drugs that
delay gastric emptying (eg tricyclic antidepressants and opioids). Obtain
expert advice before giving charcoal in repeated doses, which are only
helpful in life-threatening poisoning with a few drugs (eg carbamazepine,
dapsone, digoxin, phenobarbital, quinine, theophylline, and salicylate, and
a few other drugs rarely taken in overdose).
Whole-bowel irrigation
Whole-bowel irrigation is rarely needed and should only be used on
expert advice. The aim of whole-bowel irrigation is to empty the bowel
rapidly of solid contents by giving fl uid down a nasogastric (NG) tube
until the rectal effl uent becomes clear. The value of this is uncertain. It
may be useful for poisoning with sustained-release drug formulations or
for poisons such as iron or lithium, which are not absorbed by activated
charcoal. It has also been used to remove packets of cocaine from body
packers and button batteries from children.
Bowel cleansing solutions of polyethylene glycol and electrolytes
(eg Klean-Prep
®
) should be used for whole-bowel irrigation: 2L/hr in
adults (500mL/hr in small children) for 2hr, or occasionally longer. Do not
use normal saline since it may cause fl uid overload and hypokalaemia.
Activated charcoal may be given by NG tube, if appropriate, before whole-
bowel irrigation is started. Continue the irrigation until the rectal effl uent
is clear. Nausea, vomiting, abdominal pain and electrolyte disturbances
may occur. Monitor ECG, U&E and urine output.

186 CHAPTER 4 Toxicology
Antidotes for poisons
The provision of supportive care is essential in all patients. Antidotes are
available for only a few drugs and poisons (Table 4.1 ), and are not always
necessary. More information is available from reference books, TOXBASE
and Poisons Information Centres ( b p.181).
Antidotes are also available for arsenic, lead, mercury, thallium, and other
metals. Specialist advice is essential.
Some antidotes (marked
†
) are very rarely needed: get expert advice
(b p.181) about when and how to use these antidotes and where to
obtain them.
Increasing elimination of poisons
The vast majority of poisoned patients recover with supportive care, plus
appropriate antidotes if necessary. Active removal of absorbed poison is
only needed in special circumstances. Alkalinization of the urine is useful
in salicylate poisoning ( b p.189), but forced alkaline diuresis is no longer
recommended. Haemodialysis is occasionally helpful for severe poisoning
with salicylates, ethylene glycol, methanol, lithium, phenobarbital, and
chlorates. Haemoperfusion is rarely needed, but might be helpful in severe
poisoning with barbiturates, chloral hydrate or theophylline: specialist
advice is essential.
Table 4.1
Poison Antidote Notes
Beta-blockers Glucagon, atropine
b p.198
Carbon monoxide Oxygen
b p.208
Cyanide Sodium nitrite, sodium
thiosulphate, dicobalt edetate,
hydroxocobalamin
b p.207
Digoxin Digoxin antibodies (Digibind)
†
b p.199
Ethylene glycol Ethanol, fomepizole
†
b p.203
Iron salts Desferrioxamine
b p.201
Local anaesthetics Lipid emulsion (Intralipid
®
)
b p.187, b p.284
Methanol Ethanol, fomepizole
†
b p.202
Opioids Naloxone
b p.188
Organophosphates Atropine, pralidoxime
†
b p.206
Paracetamol Acetylcysteine, methionine
b p.190
Sulphonylureas Glucose, octreotide
b p.197
Tricyclic antidepressants Sodium bicarbonate, Intralipid
®
b p.187, b p.194
Warfarin Vitamin K, clotting factors, FFP
b p.170
Adder bites Zagreb antivenom
b p.417
Foreign snakes Antivenoms
†
Expert advice b p.181

187
ANTIDOTES FOR POISONS
Lipid emulsion (Intralipid
®
) therapy for drug toxicity
IV lipid emulsion is rarely needed but can be lifesaving in overdoses
of local anaesthetics such as lidocaine or bupivacaine ( b p.284).
1
,
2
,
3
It may be useful in cardiac arrest caused by some other drugs: the indi-
cations are unclear but case reports record dramatic recovery from
cardiac arrests due to haloperidol, verapamil, and a mixed overdose of
bupropion and lamotrigine.
1
,
2
In animals,
2
lipid emulsion was effective
in poisoning from verapamil (but not nifedipine) and clomipramine (but
not amitriptyline). Consider lipid emulsion in drug-induced cardiac arrest
unresponsive to standard treatment ( b p.50). EDs, theatres, and ICU
should stock lipid emulsion for this emergency.
Lipid emulsion acts as a ‘lipid sink’, binding lipophilic drugs and reducing
the amount of active free drug. It may also affect myocardial metabolism.
Lipid emulsion is not licensed for use in drug overdose and the safety of
rapid infusion is unknown. Lipid interferes with analysis of blood samples,
so if possible take these before starting lipid emulsion, including blood for
later measurement of drug concentrations.
Give Intralipid
®
20 % 1.5mL/kg IV over 1min, then 15mL/kg/hr by intrave-
nous infusion (IVI) (for a 70kg patient give 100mL over 1min, then 500mL
over 30min). Continue CPR. If the circulation is still inadequate after 5min
repeat IV bolus of Intralipid
®
1.5mL/kg twice at 5min intervals and increase
IVI to 30mL/kg/hr (500mL in 15min for 70kg). The maximum recommended
total dose of Intralipid
®
20 % is 12mL/kg (840mL for a 70kg patient).
3
Report cases in which lipid emulsion is used to the Poisons Information
Service ( b p.181) or the Lipid Registry ( http://www.lipidregistry.org ).
Insulin therapy in poisoning
Poisoning with cardiac drugs such as calcium channel blockers (b p.198)
and B -blockers (b p.198) may cause severe hypotension. If standard treat-
ments are ineffective, get expert advice (b p.181) and consider using insulin
therapy, which may improve myocardial carbohydrate metabolism and i BP
and cardiac output. Some case reports and animal studies of severe calcium
channel blocker and B -blocker poisoning have shown benefi ts from high
dose insulin, but the optimum dosage is unclear.
4
,
5
Continuous monitoring is needed, with invasive BP monitoring. Check blood
glucose and potassium at least hourly and give glucose 10 % and potassium
(max 20mmol/hr) as needed. Give an IV bolus of short-acting insulin 1 unit/
kg, then 0.5–2units/kg/hr IVI, titrated to keep systolic BP > 90mmHg and
heart rate > 60/min. In extreme cases, consider increasing insulin dosage to
5–10units/kg/hr, titrated according to response.
1 http://lipidrescue.squarespace.com
2 Jamaty C et al . ( 2010 ) Lipid emulsions in the treatment of acute poisoning: a systematic review
of human and animal studies . Clin Toxicol 48 : 1 – 27 .
3 Association of Anaesthetists of Great Britain and Ireland ( 2010 ) Management of Severe Local
Anaesthetic Toxicity . Available at: http://www.aagbi.org/publications/guidelines.htm
4 Lheureux PER et al . ( 2006 ) Bench-to-bedside review: Hyperinsulinaemia/euglycaemia therapy
in the management of overdose of calcium-channel blockers . Critical Care 10 : 212 . Available at:
http://ccforum.com/content/10/3/212
5 Nickson CP , Little M ( 2009 ) Early use of high-dose insulin euglycaemic therapy for verapamil
toxicity . Med J Aust 191 ( 6 ) : 350 – 2 .

188 CHAPTER 4 Toxicology
Opioid poisoning
The opioids include morphine, diamorphine (heroin), pethidine, codeine,
buprenorphine, nalbuphine, methadone, diphenoxylate, and related drugs.
These are used as analgesics (sometimes combined with paracetamol, as
in co-codamol and co-proxamol), cough suppressants and anti-diarrhoeal
agents. Acute opioid poisoning often occurs in addicts (who may have
needle marks and thrombosed veins and a high risk of HIV and hepatitis).
Clinical features
Opioid poisoning causes coma, d respiratory rate, pinpoint pupils, and
sometimes cyanosis, apnoea, convulsions and hypotension. Hypertension
may occur in pentazocine poisoning. Non-cardiogenic pulmonary oedema
may result from ‘main-lining’ heroin or other opioids.
Respiratory depression may cause death within 1hr of an opioid overdose.
However, delayed respiratory depression can occur in poisoning with
co-phenotrope (diphenoxylate and atropine), in which the opioid effects
usually predominate over atropine toxicity. Delayed toxicity may occur
with slow-release formulations of drugs, and also with methadone, which
has a very long duration of action (half-life 25–50hr).
Treatment
Clear and maintain the airway. If breathing appears inadequate, ventilate
on O
2
with a bag and mask or ET tube. Naloxone is a specifi c antago-
nist for opioids and reverses coma and respiratory depression if given in
suffi cient dosage. Naloxone may be used as a therapeutic trial in sus-
pected opioid poisoning: record coma level, pupil size and respiratory
rate and check for any response. The usual initial dose of naloxone for
adults is 0.8mg IV, repeated at 2–3min intervals if necessary. However, in
known or suspected drug addicts it is best to avoid reversing the opioid
completely, so start with 0.1mg IV (or intranasal, if there is no venous
access) and repeat this at 2–3min intervals until the patient is breathing
adequately, but still drowsy. For children, give 10 micrograms/kg (IV, IM
or IN), repeated as necessary. Intranasal naloxone is given by dripping or
spraying the IV solution into the nose, where it is absorbed rapidly.
Naloxone has a much shorter duration of action than most opioids and
so coma and respiratory depression often recur when naloxone wears
off. The mean half-life of naloxone is 62min, but in some patients the
half-life is > 5hr. Careful observation is essential. More naloxone is often
needed, given IV, by IVI or IM, the dose adjusted depending on the
response (occasionally as much as 75mg in 24hr in methadone poisoning).
Observation is needed for 6hr after the last dose of naloxone. Patients
at risk of respiratory depression should not be allowed to leave hospital:
rather than reversing an opioid fully it is better to keep a patient sedated
but safe by constant observation and titration of naloxone. A patient who
insists on leaving could be given naloxone IM, but will still be at risk of
fatal respiratory depression. In opioid addicts, naloxone may precipitate
a withdrawal syndrome with abdominal cramps, nausea and diarrhoea,
but these usually settle within 2hr. Ventricular tachyarrhythmias occur
occasionally.

189
SALICYLATE POISONING
Salicylate poisoning
Standard aspirin tablets contain 300mg acetylsalicylic acid. Ingestion of
150mg/kg body weight usually produces mild toxicity; 500mg/kg will cause
severe and possibly fatal poisoning. Poisoning can result from absorption
of salicylate ointment through the skin.
Clinical features
Commonly vomiting, tinnitus, deafness, sweating, vasodilatation, hyperven-
tilation, and dehydration. Hypokalaemia may occur.
Severe poisoning may produce confusion, coma, and convulsions.
Children are prone to develop hyperpyrexia and hypoglycaemia.
Rare features include non-cardiogenic pulmonary oedema, cerebral oedema,
and renal failure.
Metabolic and acid-base disturbances
These may be complex: adults usually have a mixed metabolic acidosis
and respiratory alkalosis, but the respiratory effects predominate. In small
children and a few adults, acidosis predominates, and is often associated
with confusion or coma.
Management
Consider gastric lavage if a patient has ingested > 500mg/kg body weight
in the previous 1hr. After ingestion of > 4.5g (or 2g in a child) give 50g
activated charcoal (25g in a child) to d absorption and i elimination of
salicylate. Measure plasma salicylate concentration (and repeat after
a few hours if further symptoms occur, since salicylate level may i due
to continuing absorption). Check U&E, glucose, and ABG if there are
CNS features or signs of severe poisoning. A second dose of charcoal
may be useful if the plasma salicylate increases, suggesting delayed gastric
emptying, or if enteric-coated tablets have been taken.
Mild poisoning Children with plasma salicylate <350mg/L (2.5mmol/L) and
adults with <450mg/L (3.3mmol/L) usually need only i oral fl uids.
Moderate poisoning Children with salicylate > 350mg/L and adults with
> 450mg/L need IV fl uids to correct dehydration and i elimination of
salicylate: sodium bicarbonate 1.26 % (adults 500mL hourly for 3hr)
alkalinizes the urine (which is much more effective than a massive diuresis
in i salicylate excretion). Urine pH should be > 7.5, ideally 8.0–8.5. Repeat
salicylate level, check U&E and add K
+
as necessary.
Severe poisoning CNS features, acidosis or salicylate > 700mg/L (5.1mmol/L)
are associated with signifi cant mortality. Get expert advice ( b p.181)
and consider urgent referral for haemodialysis. Correct acidosis and give
repeated activated charcoal via a NG tube. In life-threatening poisoning
with coma and extreme hyperventilation, paralysis and IPPV may help,
while haemodialysis removes salicylate and corrects the electrolyte
disturbances. Give glucose IV, since brain glucose levels may be low
despite normal blood glucose concentrations. Do not use forced diuresis,
which is ineffective and may cause pulmonary oedema.

190 CHAPTER 4 Toxicology
Paracetamol poisoning
Paracetamol (‘acetaminophen’ in USA) may cause severe liver damage if
12g (24 tablets) or > 150mg paracetamol/kg body weight are taken. Some
patients have risk factors for enhanced toxicity (see below) and may be at
risk if > 75mg/kg has been taken.
In obese patients ( > 110kg) calculate the toxic dose in mg/kg, and the dose
of acetylcysteine, using a weight of 110kg, rather than the patient’s actual
weight.
A metabolite of paracetamol (N-acetyl-p-benzoquinoneimine, NAPQI)
binds glutathione in the liver and causes hepatic necrosis when stores
of glutathione are exhausted. Renal failure from acute tubular necrosis
occurs occasionally, but renal failure without liver failure is rare.
Risk factors for paracetamol toxicity
Alcoholics and patients on drugs that induce hepatic enzymes are at
greater risk of toxicity, because of i production of the toxic metabolite
of paracetamol. The relevant drugs are anticonvulsants, rifampicin, and
St John’s wort.
Patients with malnutrition, anorexia, cachexia, HIV infection or cystic
fi brosis may have d glutathione stores and be at i risk of liver damage.
Clinical features
Nausea, vomiting and abdominal discomfort are common within a few
hours. In untreated patients developing liver damage, vomiting continues
beyond 12hr and there is pain and tenderness over the liver (from 24hr),
jaundice (at 2–4 days), and sometimes coma from hypoglycaemia (at
1–3 days) and hepatic encephalopathy (onset at 3–5 days). Loin pain,
haematuria and proteinuria suggest incipient renal failure. Hepatic failure
causes bleeding from coagulation abnormalities and hyperventilation from
metabolic acidosis. In fatal cases cerebral oedema, septicaemia and DIC
are common. However, many patients survive severe liver damage and
recover completely.
LFTs are normal until > 18hr after the overdose. The most sensitive
lab evidence of liver damage is often a prolonged INR (from 24hr after
overdose). Liver enzymes (ALT and AST) may reach > 10,000units/L at
3–4 days. Bilirubin rises more slowly (max at about 5 days).
Paracetamol antidotes
Acetylcysteine (Parvolex
®
; previously called N-acetylcysteine) is given by
IV infusion in 5 % glucose. Initial dose is 150mg/kg body weight in 200mL
glucose over 15min, 50mg/kg in 500mL over 4hr, then 100mg/kg in 1L
over 16hr. Acetylcysteine can cause side effects (which are more likely
if the plasma paracetamol level is low) — erythema and urticaria around
the infusion site or more generalized rashes, itching, nausea, angioedema,
bronchospasm, and rarely hypotension or hypertension. Side effects are
dose related and usually start in the fi rst hour of treatment. If they occur,
stop the infusion and give an antihistamine (eg chlorphenamine 10mg IV
over 1min). When symptoms have settled, acetylcysteine can usually be
resumed at the lowest infusion rate (100mg/kg body weight over 16hr).

191
PARACETAMOL POISONING
Methionine is rarely needed but may be useful in patients who refuse IV
treatment or if acetylcsteine is not available. Methionine is given orally as
capsules or tablets, 2.5g every 4hr to a total of 10g. Methionine has no
signifi cant adverse effects. It is less effective than acetylcysteine in patients
who are vomiting or who present > 8hr after ingestion. Methionine may
be ineffective in patients treated with activated charcoal.
Children
Serious paracetamol poisoning is rare in children. Young children rarely take
large amounts of paracetamol, and they metabolize it differently from adults
and may have less risk of hepatotoxicity. However, there is no data for assessing
the risk in children, so use the same treatment guidelines as for adults.
If it is certain that <150mg/kg has been taken (or <75mg/kg if there are
risk factors for toxicity: see b p.190, then no investigation or treatment is
needed and the child may be discharged.
Treatment with acetylcysteine is rarely needed in children. Doses are as
for adults (opposite), but with smaller volumes of fl uid for IV infusion.
Pregnancy
Assess the risk of toxicity and treat as for non-pregnant patients.
Acetylcysteine and methionine do not seem to carry any risk to the fetus,
and may protect the fetal liver from damage. Paracetamol overdose does
not appear to cause teratogenic effects.
Staggered overdoses
If the patient took two or more paracetamol overdoses in a day assess
the risk by plotting on the treatment graph the time interval since the fi rst
dose. For overdoses taken over several days the graph cannot be used. If
the patient has symptoms of toxicity or the amount taken was > 150mg/kg
(75mg/kg in high risk groups) take blood for INR, LFTs, U&E and paracetamol
(which may confi rm that some was taken, even if the treatment graph cannot
be used), and treat with acetylcysteine. If in doubt start treatment and get
expert advice.
Outcome of treatment
Treatment with acetylcysteine or methionine within 8hr of an overdose is
very effective in preventing liver and renal damage. Later treatment is less
effective, but still worthwhile.
Late presentation after paracetamol poisoning
Patients who present late are more likely to be severely poisoned than
those who present soon after ingestion. Late presenters often have con-
tinuing vomiting and abdominal pain, which are symptoms of liver damage.
The treatment graph ( b p.193) may be unreliable at > 15hr, because of
insuffi cient data on untreated patients.
Liver transplantation
Liver transplantation is occasionally needed for hepatic failure due to para-
cetamol overdose in patients who presented or were treated late. Appropriate
patients must be identifi ed and referred to a liver transplant unit as soon as
possible. Transplant criteria include arterial pH <7.30 (H
+
> 50nmol/L) after
resuscitation, or PT > 100 seconds (INR > 6.7) and creatinine > 300micromol/L
in patients with grade 3 or 4 hepatic encephalopathy.

192 CHAPTER 4 Toxicology
Management of paracetamol poisoning
The time since ingestion is crucial in interpreting paracetamol concentra-
tions and assessing the need for specifi c treatment. Record the time of
ingestion as accurately as possible. When taking blood for paracetamol
levels record the precise time in the notes and on blood bottles and
forms. Start treatment immediately if the time of ingestion is unknown.
Management within 4 hours of ingestion
Consider activated charcoal ( b p.185) if > 12g or 150mg/kg paracetamol
has been taken in the previous 1hr. Take blood at 4 hr from ingestion
and use graph (Fig. 4.1 ) to assess risk of liver damage: use line A for most
patients; line B for high risk patients. If the result is above the relevant line,
give IV acetylcysteine or oral methionine (see b p.190).
Management at 4–8 hours from ingestion
Measure paracetamol and use the graph to assess risk of liver damage:
for most patients use line A, for high risk patients use line B. If above the
relevant line, or only just below it, give IV acetylcysteine or oral methio-
nine (for doses see b p.190). Treatment is most effective if started before
8 hours: start it at once if paracetamol level is not available by this time
and > 150mg/kg has been taken. Patients treated with acetylcysteine or
methionine within 8 hours of an overdose should be medically fi t for dis-
charge at the end of the treatment course.
Management at 8–15 hours from ingestion
Urgent action is needed: start treatment with IV acetylcysteine immedi-
ately if > 150mg/kg or 12g paracetamol have been taken. Measure plasma
paracetamol and use the graph to assess the risk of liver damage: for most
patients use line A; for high risk patients use line B. If the paracetamol level
is well below the line and patient is asymptomatic, stop acetylcysteine treat-
ment. Continue acetylcysteine if level is above the relevant line, if there is
doubt about the time of ingestion or if the patient has nausea or vomiting. At
the end of acetylcysteine treatment check INR and plasma creatinine: if these
are normal and the patient asymptomatic he/she is medically fi t for discharge.
Management at 15–24 hours from ingestion
Urgent action is needed: give IV acetylcysteine immediately if > 150mg/kg
or > 12g paracetamol have been taken. Measure plasma paracetamol, cre-
atinine and INR. If at 24hr after ingestion a patient is asymptomatic, with
normal INR, normal creatinine, and plasma paracetamol <10mg/L he/she
may be discharged. Other patients need continuing monitoring and possibly
further treatment with acetylcysteine.
Management at > 24 hours from ingestion
Measure paracetamol, LFTs, U&E, creatinine, INR, and ABG. Start treat-
ment with IV acetylcysteine if > 150mg/kg or 12g paracetamol have been
taken, investigations are abnormal or patient is symptomatic. Seek expert
advice from Poisons Information Service ( b p.181) or liver unit.
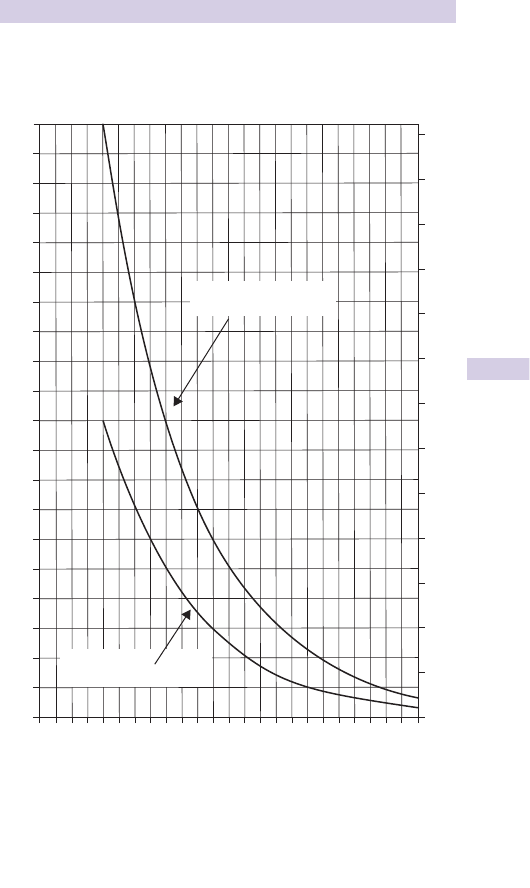
193
PARACETAMOL POISONING
Normal treatment line A for most patients.
High risk treatment line B for patients with chronic alcoholism, malnutrition,
anorexia, cachexia, HIV infection, or cystic fi brosis, or taking anticonvulsants,
rifampicin or St John’s wort.
Note Check whether the laboratory reports paracetamol in mg/L or mmol/L.
Start treatment at once if in doubt about the time of the overdose, or if the
plasma paracetamol is only just below the relevant treatment line.
Fig. 4.1 Paracetamol treatment graph.
200
190
180
170
160
150
140
130
120
110
100
90
80
70
60
50
40
30
20
10
0
0 1 2 3 4 5 6 87 9 10 12 14 16 18 20 22 24
Hours after ingestion
1.3
1.2
1.1
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
Plasma
paracetamol
(mg/L)
Plasma
paracetamol
(mmol/L)
Normal treatment line
A
B
High risk treatment line

194 CHAPTER 4 Toxicology
Tricyclic antidepressant poisoning
Anticholinergic poisoning is usually caused by an overdose of tricyclic anti-
depressants, but may result from other drugs, eg procyclidine or atropine
(present in Atropa belladonna , ‘deadly nightshade’).
Clinical features
Common features are tachycardia, dry skin, dry mouth, dilated pupils,
urinary retention, ataxia, jerky limb movements, and drowsiness leading to
coma. Unconscious patients often have a divergent squint, i muscle tone
and refl exes, myoclonus and extensor plantar responses. The pupils may
be dilated and unreactive. In deep coma there may be muscle fl accidity
with no detectable refl exes and respiratory depression requiring IPPV.
Convulsions occur in 810 % of unconscious patients and may precipitate
cardiac arrest. Patients recovering from coma often suffer delirium and
hallucinations and have jerky limb movements and severe dysarthria.
ECG changes
Sinus tachycardia is usual, but as poisoning worsens PR interval and QRS
duration i . These changes help to confi rm a clinical diagnosis of tricyclic
poisoning in an unconscious patient. The P wave may be superimposed on
the preceding T wave, so the rhythm can look like VT when it is actually
sinus tachycardia with prolonged conduction. In very severe poisoning,
ventricular arrhythmias and bradycardia may occur, especially in hypoxic
patients. Death may follow cardio-respiratory depression and acidosis.
Management
• Clear airway, intubate and ventilate if necessary, and give nursing care.
• Observe continuously, in view of the potential for rapid deterioration.
• Monitor ECG and check ABG in unconscious or post-ictal patients.
• Give activated charcoal by mouth or gastric tube if more than 4mg/kg
has been taken within 1hr and the airway is safe or can be protected.
• Do not give anticonvulsants for single brief fi ts, but give lorazepam or
diazepam IV if fi ts are frequent or prolonged.
• Most arrhythmias occur in unconscious patients within a few hours of
overdose. Treat arrhythmias by correcting hypoxia and acidosis. Sodium
bicarbonate (8.4 % , adult: 50–100mL IV; child: 1mL/kg) may dramatically
improve cardiac rhythm and output (by altering protein binding and
d active free tricyclic drug). Consider further bicarbonate, depending
on the clinical response, ECG and arterial pH. Aim for pH 7.5–7.55,
avoiding excessive alkalosis (pH > 7.65), which may be fatal.
• Avoid anti-arrhythmic drugs. If arrhythmias do not respond to bicarbo-
nate, discuss with a poisons specialist ( b p.181).
• Correct hypotension by elevating the foot of the trolley and giving IV
fl uids. Glucagon may help in severe hypotension ( b p.198). Dopamine
(2–10micrograms/kg/min) is occasionally indicated for unresponsive
hypotension on specialist advice.
• Consider Intralipid
®
( b p.187) for severe arrhythmias or cardiac arrest.
• Do not use physostigmine or fl umazenil (risk of precipitating fi ts).
• Unconscious patients usually improve over about 12hr and regain con-
sciousness within 36hr. Delirium and hallucinations may persist for 2–3
days and require sedation with oral diazepam in large doses (sometimes
20–30mg PO every 2hr initially).
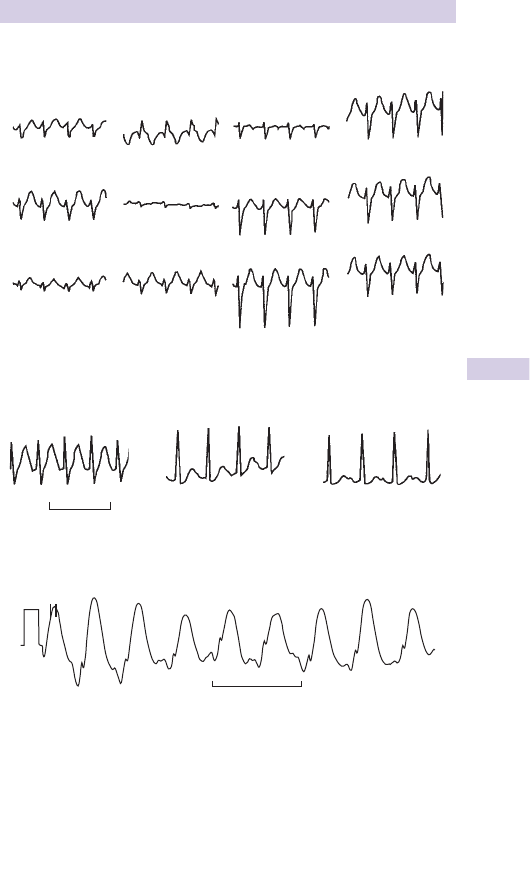
195
TRICYCLIC ANTIDEPRESSANT POISONING
ECG changes in tricyclic antidepressant poisoning
Fig. 4.2 ECG in tricyclic antidepressant poisoning, showing sinus tachycardia with
prolonged conduction, which may be mistaken for VT.
III
II
I
V
2
V
3
V
4
V
5
V
6
aV
L
aV
F
aV
R
V
1
Fig. 4.3 Serial ECG rhythm strips in amitriptyline poisoning, showing spontaneous
recovery with supportive care.
1 second
1 am 4 am
9.30 am
Fig. 4.4 ECG trace in very severe tricyclic antidepressant poisoning. The patient
was unconscious, GCS 3, and was intubated and ventilated, with BP 70/50.
1 second

196 CHAPTER 4 Toxicology
Benzodiazepine poisoning
Benzodiazepine drugs (eg diazepam, nitrazepam, and temazepam) rarely
cause serious poisoning when taken alone in overdose. However, they
potentiate the effects of other CNS depressants, such as alcohol, tricyclic
antidepressants and barbiturates.
Clinical features
Drowsiness, dizziness, ataxia, dysarthria. Rarely, coma, respiratory depres-
sion, mild hypotension. Fatal poisoning is unusual, but may occur from
respiratory depression in elderly patients and those with chronic COPD.
Management
Clear the airway and maintain ventilation if necessary. Provide supportive
care. Gastric lavage and activated charcoal are not indicated if only a
benzodiazepine has been taken.
Many benzodiazepines have long-acting metabolites, which may affect
driving and other motor skills for several days or even weeks after an
overdose. Give appropriate warnings about this.
Flumazenil is a specifi c benzodiazepine antagonist, but is not licensed in
the UK for treating overdosage. It reverses the effects of benzodiazepines
within 1min, but has a short duration of action (<1hr) — as a result,
toxic effects often recur. Flumazenil can cause convulsions and cardiac
arrhythmias and may precipitate a withdrawal syndrome in patients who
are dependent on benzodiazepines. It is particularly dangerous in patients
with combined benzodiazepine and tricyclic antidepressant poisoning,
in whom it may cause convulsions and cardiac arrest. Flumazenil may
occasionally be used by experts managing very severe benzodiazepine
poisoning, but there is no place for its use by the non-specialist.
Clomethiazole poisoning
Clomethiazole overdosage may cause coma, respiratory depression, d
muscle tone, hypotension and hypothermia. Excessive salivation and a
characteristic smell of clomethiazole on the breath are often noticeable.
Treat supportively. IPPV may be necessary.
Phenothiazine poisoning
The phenothiazines (eg chlorpromazine), butyrophenones (eg haloperidol),
and related drugs are used as antipsychotics and anti-emetics. In over-
dosage they may cause drowsiness, coma, hypotension, and hypothermia.
Deep coma and respiratory depression are uncommon. Some conscious
patients suffer dystonic reactions with oculogyric crises and muscle spasms
causing torticollis or opisthotonus. Convulsions may occur. ECG changes
of prolonged PR, QRS, and ST intervals, and arrhythmias are seen particularly
with thioridazine poisoning.
Treat supportively. Activated charcoal may help. If cardiac arrhythmias
occur, correct hypoxia, acidosis and electrolyte abnormalities before
giving any anti-arrhythmic drug. Treat dystonic reactions with procyclidine
(5mg IV or 5–10mg IM), repeated if symptoms recur.

197
SULPHONYLUREA POISONING
Barbiturate poisoning
Now uncommon, except in drug addicts. Overdosage with phenobarbitone
is seen occasionally. Barbiturate poisoning may cause coma, respiratory
depression, hypotension and hypothermia. There are no specifi c neuro-
logical signs. Skin blisters and rhabdomyolysis may result from prolonged
immobility. Treat supportively, with IPPV if necessary. Repeated doses of
activated charcoal may help to remove barbiturates. Very rarely, charcoal
haemoperfusion is indicated in some patients with deep and prolonged
coma and respiratory complications.
Lithium poisoning
Clinical features Often due to therapeutic overdosage or drug interac-
tions (eg with diuretics or NSAIDs), rather than deliberate self-harm.
Symptoms may start up to 24hr after an overdose, especially with slow-
release tablets. Nausea, vomiting and diarrhoea are followed by tremor,
ataxia, confusion, increased muscle tone and clonus. In severe cases there
may be convulsions, coma and renal failure. Lithium-induced nephrogenic
diabetes insipidus may complicate treatment.
Investigations Measure U&E and lithium (plain tube, not lithium heparin).
Therapeutic lithium levels are <1.2mmol/L. Toxic effects are often seen
at > 1.5mmol/L. Soon after a large overdose, higher levels may occur with
little clinical effects, before lithium is distributed to tissues.
Management Activated charcoal does not absorb lithium. Gastric lavage
is indicated within 1hr of a single large overdose, except for slow-
release tablets, which are too large to pass up a gastric tube. Whole-
bowel irrigation ( b p.185) may be considered for slow-release tablets:
discuss this with a poisons specialist ( b p.181). Use standard supportive
measures and control convulsions with diazepam. Observe all patients
for > 24 hours. Give oral fl uids in conscious patients. Forced diuresis is
contraindicated. Haemodialysis is the best treatment in severe poisoning,
but often has to be repeated because of rebound release of lithium from
tissue stores.
Sulphonylurea poisoning
Sulphonylurea drugs are used to treat non-insulin-dependent diabetes.
Accidental or deliberate overdosage causes hypoglycaemia, which may
recur over several days after long-acting drugs, such as chlorpropamide or
glibenclamide. In the Far East, sulphonylurea contamination of illicit drugs
used for erectile dysfunction has caused several cases of hypoglycaemia.
Check blood glucose and U&E. Correct hypoglycaemia with oral or IV
glucose ( b p.150). Observe for at least 24hr (72hr for long-acting drugs)
and check BMG hourly. To prevent recurrent hypoglycaemia give 10 %
glucose IV infusion; in severe cases 20 % glucose may be needed, via
central line because of venous irritation. Hypokalaemia may occur. Check
U&E and add potassium as needed. In severe poisoning, get expert
advice ( b p.181) and consider octreotide (unlicensed indication) which
blocks pancreatic insulin release: initial dose for adults 50micrograms
subcutaneous (SC) or IV.

198 CHAPTER 4 Toxicology
Beta-blocker poisoning
Clinical features
Overdosage with B -blockers (propranolol, oxprenolol, atenolol, labetolol,
sotalol) may cause rapid and severe toxicity with hypotension and cardio-
genic shock. There is usually a sinus bradycardia, but sometimes the heart
rate remains normal. Coma, convulsions, and cardiac arrest may occur. ECG
changes include marked QRS prolongation, and ST and T wave abnormalities.
Propranolol may cause bronchospasm in asthmatics and hypoglycaemia in
children. Sotalol can cause prolonged QTc and VT, with torsades de pointes.
Management
Monitor ECG, heart rate, and BP. Obtain reliable venous access. Check
U&E and blood glucose. Consider activated charcoal ( b p.185).
Bradycardia and hypotension may respond to atropine (1–2mg for adult;
0.02mg/kg for child), but this is often ineffective.
Glucagon is the best treatment for severe cardiotoxicity and seems
to work by activating myocardial adenylcyclase in a way not blocked by
B -blockade. Glucagon 5–10mg IV (50–150micrograms/kg for a child) usually
produces a dramatic improvement in pulse and BP, with return of cardiac
output and consciousness. Glucagon often causes sudden vomiting —
anticipate this and position the patient appropriately. In severe poisoning
glucagon has a transient effect on cardiac output and further doses or an
infusion are needed (4mg/hr, sometimes up to 15mg/hr, reducing gradually).
Some patients need a total of 50–75mg of glucagon, which is reconstituted
from 1mg vials of dry powder. If glucagon is unavailable or ineffective, give
adrenaline (5–10micrograms/min) or dobutamine (2.5–10micrograms/kg/min),
increasing the dose if necessary. Get expert advice ( b p.181) in severe
poisoning.
Cardiac pacing may be tried for bradycardia, but is often ineffective.
Occasionally, circulatory support has to be provided by prolonged chest
compressions or extracorporeal cardiac bypass while more glucagon is
obtained or the B -blocker is metabolized. Consider insulin therapy ( b
p.187) for severe hypotension, and Intralipid
®
( b p.187) in cardiac arrest.
Calcium antagonist poisoning
Poisoning with verapamil, nifedipine, diltiazem or other calcium-channel
blockers is rare, but may be fatal. Nausea, vomiting, dizziness and confusion
may occur. Bradycardia and AV block may lead to AV dissociation, with
hypotension and cardiac arrest (especially in patients taking B -adrenergic
blockers). Metabolic acidosis, hyperkalaemia and hyperglycaemia may occur.
Provide supportive treatment. Monitor ECG and BP. Obtain venous access.
Consider activated charcoal. Check U&E, glucose, calcium. Give atropine
(1–2mg, child 0.02mg/kg) for symptomatic bradycardia. Get expert help.
Pacing may be needed. Calcium gluconate (10–20mL of 10 % slowly IV,
observing ECG) may d prolonged intra-cardiac conduction. Glucagon
may help, as in B -blocker poisoning (see above). Inotropic support with
dobutamine, adrenaline or high dose insulin therapy (b p.187) may be
needed to maintain cardiac output. In severe poisoning or cardiac arrest
consider Intralipid ( b p.187).

199
ACE INHIBITOR POISONING
Digoxin poisoning
Toxicity from the therapeutic use of digoxin is relatively common. Acute
poisoning is rare, but may be fatal. Similar effects occur with digitoxin and
very rarely with plants containing cardiac glycosides (foxglove, oleander
and yew).
Clinical features
Nausea, vomiting, malaise, delirium, xanthopsia (yellow fl ashes or
discolouration of vision). Acute poisoning usually causes bradycardia
with PR and QRS prolongation. There may be AV block, AV disso-
ciation and escape rhythms, sometimes with ventricular ectopics or VT.
Hyperkalaemia occurs, and in severe cases metabolic acidosis due to
hypotension and d tissue perfusion.
Management
Provide supportive treatment. Monitor ECG and BP. Obtain venous
access. Give activated charcoal to d absorption and prevent entero-hepatic
recycling of digoxin ( b p.185). Measure U&E, plasma digoxin, and ABG in
severe poisoning. Get expert help for patients who are severely poisoned.
Correct severe metabolic acidosis with sodium bicarbonate. Treat hyper-
kalaemia > 6mmol/L ( b p.162). Bradycardia and AV block often respond
to atropine IV total 1–2mg (child 0.02mg/kg). Cardiac pacing is not always
effective and a high voltage is often needed for capture. VT may respond
to lidocaine or a B -blocker. Treat severe poisoning with digoxin anti-
bodies (Digibind
®
), which rapidly correct arrhythmias and hyperkalaemia.
Digibind
®
is expensive and rarely needed, so is not stocked in many hospi-
tals: Poisons Information Services (b p.181) can advise about emergency
supplies and the dose required for the patient’s body weight and plasma
digoxin concentration or the quantity taken.
ACE inhibitor poisoning
Overdosage with angiotensin converting enzyme (ACE) inhibitors
(eg captopril, enalapril, lisinopril) may cause drowsiness, hypotension,
hyperkalaemia and rarely, renal failure. Monitor BP and ECG. Give IV 0.9 %
saline if BP is low. Check U&E. Consider activated charcoal ( b p.185).

200 CHAPTER 4 Toxicology
Theophylline poisoning
Theophylline and aminophylline can cause fatal poisoning. Many
preparations are slow-release and may not produce serious toxicity until
12–24 hours after ingestion, so careful observation is essential.
Features
Nausea, vomiting (often severe and not helped by anti-emetics), abdominal
pain, haematemesis, restlessness, i muscle tone, i refl exes, headache,
convulsions. Coma, hyperventilation, hyperpyrexia and rhabdomyolysis
may occur. Sinus tachycardia may be followed by supraventricular and
ventricular arrhythmias and VF. BP may initially i , but later d in severe
poisoning. Complex metabolic disturbances include a respiratory alkalosis
followed by metabolic acidosis, hyperglycaemia, and severe hypokalaemia.
Management
• Treat supportively.
• Monitor ECG, heart rate and BP.
• Obtain venous access and measure U&E, glucose, ABG, plasma theo-
phylline (repeated after a few hours). Repeat K
+
hourly if patient is
symptomatic, since early correction of hypokalaemia may prevent dan-
gerous arrhythmias. Correct hypokalaemia with K
+
(large amounts may
be needed, but no faster than 20mmol/hr).
• Perform gastric lavage if <1hr since ingestion. Give repeated activated
charcoal ( b p.185), by NG tube if necessary.
• Intractable vomiting may respond to ondansetron (8mg slowly IV in adult).
• GI bleeding may require transfusion and ranitidine (but not cimetidine,
which slows metabolism of theophylline).
• Tachycardia with an adequate cardiac output should be observed, but
not treated. Non-selective B -blockers (eg propranolol) may help severe
tachyarrhythmias and hypokalaemia, but cause bronchospasm in asth-
matics. Lidocaine and mexiletine may precipitate fi ts, so disopyramide is
preferable for ventricular arrhythmias.
• Control convulsions with diazepam or lorazepam. Paralyse, intubate,
and provide IPPV if the airway is at risk from coma, fi ts and vomiting.
• Charcoal haemoperfusion may be needed in severe poisoning, especially
if oral or NG activated charcoal is impracticable because of vomiting.
Serious hyperkalaemia may occur during recovery from theophylline
poisoning if large amounts of K
+
were given earlier.
Salbutamol poisoning
Poisoning with B
2
-agonists (eg salbutamol, terbutaline) may cause
vomiting, agitation, tremor, tachycardia, palpitations, hypokalaemia
and hypertension. Rarely, there may be hallucinations, hyperglycaemia,
ventricular tachyarrhythmias, myocardial ischaemia, and convulsions.
Treat supportively:
• Correct hypokalaemia by infusion of K
+
(max 20 mmol/hour).
• Monitor ECG and BP.
• Activated charcoal may d drug absorption.
• Do not treat tachycardia if there is an adequate cardiac output.
Propranolol may help severe tachyarrhythmias and hypokalaemia, but
can precipitate bronchospasm in asthmatics.

201
IRON POISONING
Iron poisoning
Small children often eat iron tablets, many of which resemble sweets.
Serious poisoning is uncommon, but fatalities can occur. Note that iron is
present in some weed/seed preparations.
Different preparations contain the equivalent of 35–110mg of elemental
iron per tablet, sometimes in slow-release form.
Serious toxicity is unlikely unless > 60mg elemental iron/kg body weight
has been taken. The estimated lethal dose is about 150–300mg/kg.
Features
In the fi rst few hours after ingestion nausea, vomiting, diarrhoea and
abdominal pain are common. Vomit and stools are often grey or black and
may contain blood. Hyperglycaemia and i WCC may occur. Most patients
do not develop further features.
In severe poisoning, early effects include haematemesis, drowsiness,
convulsions, coma, metabolic acidosis and shock.
Early symptoms settle after 6–12hr, but a few patients then deteriorate
24–48hr after ingestion, with shock, hypoglycaemia, jaundice, metabolic
acidosis, hepatic encephalopathy, renal failure, and occasionally bowel
infarction. Survivors may develop gastric strictures or pyloric obstruction
2–5 weeks after the overdose.
Management
• Check serum iron, FBC, glucose, and also ABG in severe poisoning.
• Perform gastric lavage if > 20mg elemental iron/kg body weight has
been taken in the previous 1hr. Do not give charcoal, which does not
absorb iron. Iron tablets are radio-opaque and can be counted on a
plain abdominal X-ray fi lm. Whole-bowel irrigation ( b p.185) may be
useful if many tablets remain in the gut, especially with slow-release
formulations.
• Use supportive measures if required.
• Obtain expert advice in serious poisoning. Coma and shock indicate
severe poisoning needing immediate treatment with desferrioxamine
by IV infusion (15mg/kg/hr, max 80mg/kg in 24hr). Desferrioxamine
should also be given if the serum iron exceeds the expected total
iron binding capacity (about 54–75mmol/L): measurement of total
iron binding capacity may give misleading results after iron poisoning.
Desferrioxamine causes hypotension if infused too rapidly and can
produce rashes and rarely, anaphylaxis, pulmonary oedema or ARDS.
The iron-desferrioxamine complex makes the urine orange or red,
which confi rms that free iron has been bound and that desferrioxamine
was required. Reduce desferrioxamine dosage when there is clinical
improvement and serum iron is less than the expected total iron binding
capacity.
• Patients who still have no symptoms 6 hours after an iron overdose
have probably not ingested toxic amounts and may be discharged, with
advice to return if symptoms develop.
• Pregnancy does not alter the treatment needed for iron poisoning;
use desferrioxamine if indicated.

202 CHAPTER 4 Toxicology
Ethanol poisoning
Features
Overdosage of ethanol (ethyl alcohol or ‘alcohol’) is very common.
Alcohol potentiates the CNS depressant effects of many drugs. It initially
causes disinhibition and later ataxia, dizziness, dysarthria and drowsiness.
In severe poisoning there may be coma with respiratory depression,
hypotension, hypothermia and a metabolic acidosis. Hypoglycaemia is a
particular problem in children and may occur after some hours. Death
may result from respiratory failure or aspiration of vomit.
For an adult, the fatal dose of ethanol alone is 8300–500mL of absolute
alcohol: whisky and gin usually contain 40–50 % ethanol. Do not assume
that d GCS is due to alcohol until other causes have been excluded.
Rarely, alcohol causes lactic acidosis (especially in patients with liver disease
or taking biguanide hypoglycaemic drugs) or ketoacidosis (due to dehydration
and hypoglycaemia in alcoholics) — see b p.622.
Treatment
• Maintain a clear airway and adequate ventilation.
• Check blood glucose every 1–2 hours in severe poisoning.
• Correct hypoglycaemia with glucose, not with glucagon.
• Look for signs of injury, especially head injury.
• Emergency measurement of blood ethanol rarely alters management.
• Gastric lavage and activated charcoal are ineffective in ethanol intoxication.
Methanol poisoning
Methanol is used as a solvent and in antifreeze. Ingestion of 10mL of pure
methanol may cause blindness and 30mL can be fatal, the toxic effects
being due to the metabolites formaldehyde and formic acid.
Methylated spirits is a mixture of ethanol and water with about 5 %
methanol: toxicity is almost entirely due to ethanol.
Clinical features
Methanol initially causes only mild transient drowsiness. Serious toxicity
develops after a latent period of 12–24 hours with vomiting, abdominal pain,
headache, dizziness, blurring of vision, and drowsiness leading to coma. There
is a severe metabolic acidosis, hyperglycaemia and i serum amylase. Survivors
may be blind from optic nerve damage and develop Parkinsonian problems.
Management
• Consider gastric lavage if <1hr since ingestion. Do not give charcoal.
• Measure ABG, U&E, Cl
–
, HCO
3
–
, glucose, FBC, LFTs and osmolality,
and plasma methanol if possible. Calculate osmolal gap and anion gap.
• Read Toxbase advice ( b p.181). Discuss with Poisons Information Service.
• Observe for at least 6hr after ingestion, even if asymptomatic.
• Early use of fomepizole or ethanol (as for ethylene glycol, b p.203)
minimizes methanol toxicity and should be started if poisoning is likely,
especially if there is a high anion gap metabolic acidosis.
• Use sodium bicarbonate to correct metabolic acidosis (aim for pH 7.5).
Large amounts may be needed and hypernatraemia may occur.
• Give folinic acid (1mg/kg, max 50mg, IV every 6hr for 48hr).
• In severe poisoning, refer to ICU for haemodialysis and possibly IPPV.

203
ETHYLENE GLYCOL POISONING
Ethylene glycol poisoning
Ethylene glycol is used mainly as antifreeze. Fatal dose for an adult is about
100g (90mL of pure ethylene glycol). Toxic effects are due to metabolites
glycolaldehyde, glycolic acid and oxalic acid. Fomepizole or ethanol block
ethylene glycol metabolism, preventing toxicity.
Clinical features
In the fi rst 12hr after ingestion the patient looks drunk, but does not smell
of alcohol. Ataxia, dysarthria, nausea, vomiting, and sometimes haematem-
esis occur, followed by convulsions, coma and severe metabolic acidosis.
From 12–24hr after ingestion hyperventilation, pulmonary oedema,
tachycardia, cardiac arrhythmias and cardiac failure may develop.
Hypocalcaemia may be severe. Acute tubular necrosis and renal failure
occur at 24–72hr. Cranial nerve palsies may develop.
Urine microscopy shows calcium oxalate monohydrate crystals which are
diagnostic of ethylene glycol poisoning. Some makes of antifreeze contain
fl uorescein, which makes urine fl uoresce in ultraviolet light (eg a Wood’s
lamp from a dermatology department). This helps to confi rm ethylene glycol
poisoning, but the absence of fl uorescence does not exclude poisoning.
Management
• Consider gastric lavage if <1hr since ingestion. Do not give charcoal.
• Measure ABG, U&E, Cl
–
, HCO
3
–
, glucose, FBC, LFTs, osmolality, and
plasma ethylene glycol if possible. Calculate osmolal gap and anion gap.
• Read Toxbase advice (b p.181). Discuss with Poisons Information
Service.
• Observe for at least 6hr after ingestion, even if asymptomatic.
• Monitor ECG, pulse, blood pressure, respiratory rate, and urine output.
• Early use of fomepizole or ethanol minimizes toxicity and should be
started if poisoning is likely.
• High anion gap metabolic acidosis ( b p.99) occurs in ethylene glycol
poisoning (and also methanol poisoning, diabetic ketoacidosis, alcoholic
ketoacidosis, and renal failure), but acidosis only develops after some
ethylene glycol has been metabolized.
• Consider fomepizole: discuss with Poisons Information Service
(b p.181) about indications, dosage, and where to obtain it.
• If fomepizole is not available give ethanol orally as whisky, gin or vodka
(adult 125–150mL, child 2mL/kg) followed by IVI of ethanol, preferably
as 5 % solution in glucose. Initial IV adult dose is 12g ethanol/hr, i for
alcoholics and during haemodialysis and adjusted to maintain blood
ethanol at 81g/L (discuss dose with Poisons Information Service).
• Use sodium bicarbonate to correct metabolic acidosis (aim for pH 7.5).
Large amounts may be needed and hypernatraemia may occur.
• Correct severe hypocalcaemia with calcium gluconate (10mL of 10 %
slowly IV).
• Haemodialysis may be required in severe poisoning, with frequent
measurements of blood ethylene glycol concentrations (and ethanol
if this is used). Intensive care and ventilation may be needed.

204 CHAPTER 4 Toxicology
Paraquat poisoning
Paraquat is an effective weedkiller which is very toxic if ingested: death is
likely after 10mL of liquid paraquat (100 or 200g/L). Paraquat poisoning
is now rare in the UK, where paraquat is no longer approved for sale or
use, but accidental or deliberate poisoning still occurs in many developing
countries.
Inhalation of dilute paraquat spray may cause sore throat and epistaxis,
but not systemic poisoning. No specifi c treatment is needed and
symptoms resolve in a few days. Prolonged contact of paraquat with the
skin causes erythema and sometimes ulceration, but absorption is rarely
suffi cient to cause systemic toxicity. Remove soiled clothing and wash the
skin thoroughly with water.
Splashes in the eyes cause pain and corneal ulceration. Immediately
irrigate with water and refer for ophthalmological review.
Clinical features of paraquat ingestion
Paraquat is corrosive and causes immediate burning pain in the mouth and
throat, nausea and vomiting, followed by abdominal pain and diarrhoea.
Large amounts ( > 6g) of paraquat result in rapid deterioration with shock,
pulmonary oedema, metabolic acidosis, coma, convulsions, and death
within 24hr.
Smaller quantities (3–6g) do not produce shock. After 24hr, chemical
burns of the mouth and throat cause pain and diffi culty in swallowing
and speaking. The burns look white until the surface sloughs after about
3 days, leaving painful raw areas.
Renal failure occurs at 1–2 days and there is mild jaundice.
Paraquat lung usually develops by 5–7 days, with pulmonary oedema and
fi brosis causing breathlessness and cyanosis. Lung shadowing is seen on
CXR. Death from hypoxia occurs 7–14 days after poisoning. 1.5–2g of
paraquat may produce slower respiratory failure, with gradual deteriora-
tion until death up to 6 weeks after ingestion. Survival with lung damage
is uncommon.
Management
• Do not give O
2
, which increases pulmonary toxicity of paraquat.
• Consider gastric lavage if <1hr since ingestion.
• Give oral activated charcoal immediately, with IV analgesia and anti-emetics.
• Send urine (and gastric fl uid if available) for the laboratory to test
for paraquat, which can be done very quickly using sodium dithionite.
A negative test within 4 hours of suspected ingestion excludes signifi -
cant poisoning. If paraquat is present, measure the plasma concentra-
tion if possible, since it helps assessment of the prognosis: the Poisons
Information Services ( b p.181) can advise about paraquat measurement
and the interpretation of results.
• Unfortunately, no treatment improves the outcome of paraquat
poisoning.
• Keep patients who are likely to die as comfortable as possible.

205
PETROL AND PARAFFIN POISONING
Petrol and paraffi n poisoning
Petrol, paraffi n (kerosene), and other petroleum distillates are used as
fuels and solvents. They contain mixtures of hydrocarbons, often with
small quantities of other chemicals. Unintentional poisoning occurs after
liquids have been stored in inappropriate and unlabelled containers. The
major problem is pneumonitis caused by aspiration of hydrocarbons into
the lungs.
Clinical features
In many cases no symptoms occur. There may be nausea, vomiting, and
occasionally diarrhoea. Aspiration into the lungs causes choking, coughing,
wheeze, breathlessness, cyanosis and fever. X-ray changes of pneumonitis
(shadowing in the mid or lower zones) may occur without respiratory
symptoms or signs. Occasionally, pleural effusions or pneumatoceles
develop. In severe cases, there may be pulmonary oedema, drowsiness,
convulsions or coma. Rare problems include renal failure and intravascular
haemolysis.
Management
Many patients remain well and need no treatment.
Avoid gastric lavage unless very large quantities have been taken or there
is serious concern about another poison: in these rare cases lavage may
be done on specialist advice if the patient has a good cough refl ex or the
airway is protected by a cuffed ET tube. Obtain a CXR and observe for
respiratory problems. Patients with a normal initial CXR who have no
symptoms or signs 6 hours after ingestion may be discharged with advice
to return if symptoms develop.
If symptoms occur, treat supportively with O
2
and bronchodilators as
necessary. Steroids and prophylactic antibiotics are unhelpful. IPPV is
occasionally needed because of severe pulmonary oedema.

206 CHAPTER 4 Toxicology
Organophosphate poisoning
Organophosphates are widely used as insecticides. Poisoning with these
chemicals is rare in the UK, but common in many developing countries.
Organophosphates are absorbed through the skin, bronchial mucosa and
gut, and inhibit cholinesterases, causing accumulation of acetylcholine at
nerve endings and neuromuscular junctions. The speed of onset, severity
and duration of toxicity vary between different compounds. Irreversible
binding of cholinesterase (‘ageing’) develops after some minutes or hours.
Pralidoxime reactivates cholinesterase if given promptly, before ageing
occurs.
Organophosphate nerve gas agents such as sarin may be released
deliberately by terrorists. Information is available from Toxbase ( b p.181).
Carbamate insecticides act similarly to organophosphates, but poisoning
with carbamates is generally less severe and pralidoxime is not needed.
Clinical features
Minor exposure to organophosphates may cause subclinical poisoning
with d cholinesterase levels, but no symptoms or signs. Symptoms may be
delayed by 12–24hr after skin exposure.
Early features of toxicity include anxiety, restlessness, insomnia, tiredness,
headache, nausea, vomiting, abdominal colic, diarrhoea, sweating, hyper-
salivation, and miosis. Muscle weakness and fasciculation may develop.
In severe poisoning there is widespread paralysis with respiratory
failure, pulmonary oedema, profuse bronchial secretions, bronchospasm,
convulsions and coma. Hyperglycaemia and cardiac arrhythmias may occur.
Occasionally, delayed effects of poisoning develop 1–4 days after acute
poisoning, with cranial nerve palsies, muscle weakness and respiratory
failure which resolve after 2–3 weeks. A peripheral neuropathy may
develop after 2 weeks, usually involving the legs.
Management
1
• Wear protective clothing and avoid getting contaminated yourself.
• Give supportive treatment as needed.
• Clear the airway and remove secretions. Give O
2
and IPPV if needed.
• Insert two IV cannulae. Take blood for cholinesterase.
• If there are profuse bronchial secretions or bronchospasm, give atro-
pine IV (adult 2mg, child 0.02mg/kg), repeated every 5min with the dose
doubled each time until the chest sounds clear, systolic BP > 80mmHg
and pulse > 80. Some patients need > 100mg of atropine.
• Give diazepam to treat agitation and control convulsions.
• In moderate or severe poisoning give pralidoxime mesylate (also called
P2S). The dose of pralidoxime is 30mg/kg IV over 5–10min, repeated if
necessary every 4hr. Improvement is usually apparent within 30min.
• Poisons Information Services can advise on pralidoxime supply and use:
in the UK the Blood Transfusion Service will supply pralidoxime if there
are multiple casualties with organophosphate poisoning.
1 Eddleston M et al . ( 2008 ) Management of acute organophosphorus pesticide poisoning . Lancet .
371 : 597 – 607 .

207
CYANIDE POISONING
Cyanide poisoning
Cyanide compounds are widely used in industry and may be ingested
or inhaled inadvertently or deliberately. Cyanides produced by burning
polyurethane foam i mortality from smoke inhalation: if there is severe
acidosis consider cyanide toxicity. Cyanide poisoning may be caused by
the drug sodium nitroprusside or ingestion of amygdalin (laetrile) from
the kernels of apricots, cherries and other fruits. Solutions for removing
artifi cial fi ngernails may contain acetonitrile (methyl cyanide).
Cyanides inhibit cytochrome oxidase, blocking the tricarboxylic acid cycle
and stopping cellular respiration. This process is reversible. Inhalation
of hydrogen cyanide often causes death within minutes. Ingestion of
cyanides can produce rapid poisoning, but food in the stomach may delay
absorption and the onset of symptoms. Delayed poisoning may follow
absorption of cyanides through the skin. Ingested cyanide compounds
react with gastric acid to form hydrogen cyanide, which could poison
fi rst-aiders giving mouth to mouth resuscitation.
Clinical features
Acute poisoning causes dizziness, anxiety, headache, palpitations, breath-
lessness, and drowsiness. In severe cases, there may be coma, convulsions,
paralysis, pulmonary oedema, cardiac arrhythmias and cardiorespiratory
failure, with metabolic acidosis. Most of the clinical features result from
severe hypoxia, but cyanosis is uncommon. Classically, there is a smell of
bitter almonds on the breath, but many people cannot detect this.
Management
• Avoid getting contaminated yourself.
• Provide supportive measures: give 100 % O
2
and monitor ECG.
• Remove contaminated clothing and wash exposed skin.
• Consider activated charcoal or gastric lavage within 1hr of ingestion.
• In mild poisoning, reassurance, O
2
and observation may be all that is
required. Exposure to cyanide causes great anxiety and it may be dif-
fi cult to distinguish between fear of poisoning and early symptoms of
toxicity.
• Specifi c antidotes should be available, but are not always needed.
Some specifi c antidotes to cyanide are dangerous in the absence of
cyanide — only give if poisoning is moderate or severe (eg coma). In severe
cyanide poisoning, give dicobalt edetate (Kelocyanor
®
) 300mg IV over 1min,
repeated if there is no improvement after 1min. In the absence of cyanide,
dicobalt edetate may cause cobalt poisoning with facial, laryngeal and
pulmonary oedema, vomiting, tachycardia and hypotension. Alternative
treatment is sodium thiosulphate (adult dose 25mL of 50 % solution IV over
10min; child 400mg/kg) with sodium nitrite (adult dose 10mL of 3 % solution IV
over 5–20min; child dose 0.13–0.33mL of 3 % solution/kg, ie 4–10mg/kg).
Sodium thiosulphate often causes vomiting. Sodium nitrite may cause
hypotension. High doses of hydroxocobalamin (5–10g, Cyanokit
®
) are
useful and relatively safe in cyanide poisoning, especially in victims of
smoke inhalation.

208 CHAPTER 4 Toxicology
Carbon monoxide poisoning
Carbon monoxide (CO) is a tasteless and odourless gas produced by
incomplete combustion. Poisoning may occur from car exhausts, fi res
and faulty gas heaters. CO is also produced by metabolism of methylene
chloride (used in paint strippers and as an industrial solvent). CO d the
O
2
-carrying capacity of the blood by binding haemoglobin (Hb) to form
carboxyhaemoglobin (COHb). This impairs O
2
delivery from blood to
the tissues and also inhibits cytochrome oxidase, blocking O
2
utilization.
These effects combine to cause severe tissue hypoxia.
The elimination half-life of CO is about 4hr on breathing air, 1hr on 100 %
O
2
, and 23min on O
2
at 3 atmospheres pressure.
Clinical features
Early features are headache, malaise, nausea and vomiting (sometimes
misdiagnosed as a viral illness or gastroenteritis, especially if several
members of a family are affected).
In severe poisoning , there is coma with hyperventilation, hypotension,
i muscle tone, i refl exes, extensor plantars and convulsions. Cherry-red
colouring of the skin may be seen in fatal CO poisoning, but is rare in
live patients. Skin blisters and rhabdomyolysis may occur after prolonged
immobility. Pulmonary oedema, MI and cerebral oedema can occur.
Neurological and psychiatric problems sometimes develop some weeks
after CO poisoning, but usually improve over the following year.
Management
• Remove from exposure.
• Clear the airway and maintain ventilation with as high a concentration of
O
2
as possible. For a conscious patient use a tight-fi tting mask with an O
2
reservoir, but if unconscious intubate and provide IPPV on 100 % O
2
.
• Record ECG and monitor heart rhythm: look for arrhythmias and signs
of acute MI.
• Check ABG — SpO
2
measurements are misleading in CO poisoning, as
are p
a
O
2
values, but acidosis indicates tissue hypoxia.
• Check COHb levels (in blood or with a special pulse oximeter):
although these correlate poorly with clinical features, COHb > 15 %
after arrival at hospital suggests serious poisoning. COHb may be up to
8 % in smokers without CO poisoning. A nomogram ( b p.395) can help
to estimate COHb at the time of exposure.
• Correct metabolic acidosis by ventilation and O
2
: try to avoid bicarbo-
nate, which may worsen tissue hypoxia.
• Consider mannitol if cerebral oedema is suspected.
• Hyperbaric O
2
therapy is logical, but of no proven benefi t for CO
poisoning. Transfer to a hyperbaric chamber and pressurization may
take hours and so hyperbaric treatment may be no more effective than
ventilation on 100 % normobaric O
2
. Caring for a critically ill patient in
a small pressure chamber may be impracticable. Discuss with a Poisons
Information Service ( b p.181) and consider hyperbaric treatment if a
patient has been unconscious at any time, has COHb > 20 % , is pregnant,
or has cardiac complications or neurological or psychiatric features. The
Poisons Information Service can advise on the location and telephone
numbers of hyperbaric chambers. Some details are in Table 6.1, b p.261.

209
CS GAS (TEAR GAS)
Chlorine poisoning
Chlorine gas causes lacrimation, conjunctivitis, coughing, wheezing,
breathlessness, and chest pain. Laryngeal and pulmonary oedema may
develop within a few hours.
• Remove from exposure and give O
2
, with bronchodilators if necessary.
If there is laryngeal or pulmonary oedema, consult an expert and give
prednisolone in high dosage (adult 60–80mg/day initially). In severe
cases, IPPV in ICU may be needed.
• If the eyes are painful, irrigate with water or saline, and examine with
fl uorescein for corneal damage.
• Casualties with minor exposure to chlorine but no symptoms may be
allowed home with advice to rest and return if symptoms develop.
• Patients with symptoms when seen in hospital usually need admission
for at least 12 hours for observation. Record serial peak expiratory fl ow
rates, which may warn of deterioration.
CS gas (tear gas)
CS (orthochlorobenzylidene malononitrile) is used for riot control,
police self-protection, and sometimes as a weapon in assaults. It is an
aerosol or smoke, rather than a gas. Exposure to CS causes immediate
blepharospasm and lacrimation, uncontrollable sneezing and coughing,
a burning sensation in the skin and throat, and tightness of the chest.
Vomiting may occur. These symptoms usually disappear within 10min in
fresh air, but conjunctivitis may persist for 30min. Exposure in a confi ned
space may cause symptoms for some hours and is particularly dangerous
in people with pre-existing lung disease. Redness or blistering of the skin
may develop, due to the solvent in the spray.
Treat patients exposed to CS gas in a well-ventilated area. Ensure that
staff wear gloves and close-fi tting goggles. Remove contaminated clothes
and wash affected skin thoroughly. Give O
2
and bronchodilators if
necessary. Reassure the patient that the symptoms will resolve.
If the eyes are painful, blow dry air on them with a fan to vaporize any
remaining CS gas. The irritation should disappear in a few minutes.
Alternatively, irrigate the eyes with saline (although this may cause a
transient worsening of symptoms). When symptoms have settled, record
visual acuity and examine the corneas using fl uorescein. Refer to an
ophthalmologist if symptoms persist.
CN gas (chloroacetophenone) is used in some countries for riot control
and in personal defence devices. CN has similar effects to CS, but is more
toxic.

210 CHAPTER 4 Toxicology
Chemical incidents
Chemical incidents involving single or multiple casualties may result from
accidents (eg release of chlorine gas) or deliberate release of chemicals
(by terrorists or others). CBRN (Chemical, Biological, Radiological and
Nuclear) incidents have many features in common.
If you know or suspect that a patient has been involved in a chemical
incident:
• Inform senior ED staff.
• Avoid contaminating other staff or patients.
• Ensure that you are wearing suitable personal protective equipment
(PPE), unless the patient has already been decontaminated.
• Decontaminate the patient according to departmental guidelines if this
has not been done already (see b p.211).
• Resuscitate as necessary: airway, breathing, and circulation.
• Assess the clinical features and toxic agent.
• Give antidotes if appropriate, and reassess the patient.
• Enquire whether other patients are expected.
• Inform the local Health Protection Team.
• Get expert advice from Toxbase, Poisons Information Service ( b p.181)
or HPA Chemical Hazards and Poisons Division (ChaPD tel. 0870 606
4444).
• If deliberate release is suspected inform the Police and involve other
agencies and the press offi cer.
Chemical agents which might cause a chemical incident include:
• Chlorine — see b p.209.
• CS gas (tear gas) — see b CS gas (tear gas), p.209.
• Cyanide — see b p.207.
• Organophosphates — see b p.206.
Information about chemical incidents
• Health Protection Agency advice on CBRN and chemical incidents:
www.hpa.org.uk/emergency/CBRN.htm
• TOXBASE (see b p.181) section on Deliberate Release gives details
of toxicity and antidotes, with medical, public health and public briefi ng
documents about 60 chemicals that might be deliberately released.
• Home Offi ce guidance on decontamination after CBRN incidents:
http://www.cabinetoffi ce.gov.uk/ukresilience/emergencies/cbrn.aspx
Infection control and prevention: see b p.32.
Major incidents: see b p.38.
Radiation incidents: see b p.268.

211
DECONTAMINATION OF PATIENTS
Decontamination of patients
Decontamination after exposure to a chemical, biological, or radiation
hazard is intended to reduce the risks to the patient and to other people.
Casualties should be decontaminated at the scene after a CBRN inci-
dent, but some contaminated patients are likely to arrive at EDs without
warning. Many people will be worried about contamination, but not
actually at risk. Patients injured by industrial incidents, road traffi c
collisions, bombs, or other incidents may also be contaminated.
Even with advance planning it will be challenging to organize the ED, keep
‘clean’ areas clean, maintain order, and communicate between the ‘decon’
team (in PPE) and other ED staff.
Equipment for decontamination
• Scissors. Buckets. Sponges, soft brushes, wash cloths. Liquid soap.
• Disposable towels. Disposable gowns and slippers. Blankets.
• Plastic bags (large for clothing, small for valuables).
• ID labels and waterproof marking pens (for patients and property bags).
• Plastic bins with polythene liners (for used decontamination equipment).
• Warm or tepid water (hot water might increase chemical absorption).
• 0.9 % saline and drip sets for eye and wound irrigation. LA eye drops.
Decontaminating non-ambulant patients
• Keep contaminated patients outside the ED.
• Clear, prepare, and secure the decontamination area.
• Protect yourself with appropriate PPE and use it properly.
• Work in teams of 2–4 people. Look after each other.
• Tell the team what to look for and what to do.
• In severe poisoning resuscitation, antidote administration, and decon-
tamination may have to be done simultaneously.
• Tell casualties what you are doing.
• Record patient’s name and number on wrist band and property bags.
• Remove or cut off clothing (which removes 80–90 % of contamination).
Do not pull clothing off over the head.
• Fold clothing outside-in and put it in property bags.
• Put valuables in a separate bag. Wash glasses and keep with patient.
• Clean face (protecting airway), open wounds, and sites for IV access,
then from head to toes, front and back (log roll) including skin creases.
• Rinse affected areas with soapy water (saline for wounds and eyes).
• Wipe affected areas gently with a sponge to remove chemicals.
• Rinse with clean water.
• Dry patient. Cover in gown and blanket. Transfer to ‘clean’ trolley.
• Move patient to ‘clean’ area for further assessment and treatment.
• Put contaminated equipment in appropriate containers.
• Contain waste water if possible; if not, inform water/sewage agency.
• Rest and rotate staff as needed.
• Ensure staff are decontaminated before leaving the ‘dirty’ area.
• Record names of staff involved in decontamination.
• Warn staff of possible symptoms and check for signs of poisoning.
• Debrief staff and record events.

212 CHAPTER 4 Toxicology
Plants, berries and mushrooms
Plants and berries
Many children eat plant leaves or brightly-coloured berries, but serious
poisoning from plants is very rare. Identify the plant if possible, using
reference books
1
,
2
,
3
or the CD-ROM computer software Poisonous plants
and fungi in Britain and Ireland ( b p.180). Advice on toxicity and any nec-
essary treatment is available from Poisons Information Services. Many
garden and house plants are non-toxic and no treatment is needed after
ingestion.
Serious poisoning from laburnum is very rare, with only one death
recorded in the UK in 50 years. No treatment needs to be provided for
children who eat laburnum seeds, except for the very few with symptoms
(nausea, salivation, vomiting, headache, rarely convulsions).
Mushroom poisoning
Serious poisoning from mushrooms or fungi is rare. Most deaths are due
to Amanita phalloides (death cap mushroom). Reference books
1
,
4
are
useful, but identifi cation of mushrooms from the description or fragments
available is often uncertain. Advice on toxicity and treatment is available
from Poisons Information Services ( b p.181).
Mushrooms found in gardens are unlikely to produce severe poisoning,
but may cause vomiting and occasionally hallucinations, usually within 2hr
of ingestion. Mushrooms which cause symptoms within 6hr are unlikely
to be seriously toxic. Delayed toxicity occurs with Amanita phalloides and
some other species, which grow throughout the UK.
Amanita phalloides poisoning causes vomiting and profuse watery diarrhoea
after a latent period of 6–12hr, followed by hepatic and renal failure. The
interval between ingestion and the onset of symptoms is crucial in distin-
guishing between non-serious and potentially fatal poisoning.
Try to ascertain if:
• More than one variety of mushroom was eaten (since poisonous and
edible mushrooms often grow together).
• Whether the mushrooms were cooked (since some toxins are inacti-
vated by heat).
• Whether alcohol was taken (since disulfi ram-like effects may occur with
Coprinus species, ink cap mushrooms).
For most toxic mushrooms only symptomatic treatment is required. Activated
charcoal may d absorption if given within 1hr. Get expert advice immediately
if Amanita poisoning is suspected ( b p.181).
1 Cooper MR , Johnson AW , Dauncey EA ( 2003 ) Poisonous Plants and Fungi, An Illustrated Guide ,
2
nd
edn. TSO , London .
2 Dauncey EA ( 2010 ) Poisonous Plants: A Guide for Childcare Providers . Royal Botanic Gardens ,
Kew .
3 Frohne D , Pfänder HJ ( 2004 ) Poisonous Plants , 2
nd
edn. Manson Publishing Ltd , London .
4 Bresinsky A , Besl H ( 1990 ). A Colour Atlas of Poisonous Fungi . CRC Press , London .

213
BUTTON BATTERIES
Button batteries
Small children often swallow button or disc batteries intended for
toys, watches, hearing aids, and other electrical equipment. The larger
batteries may become stuck in the oesophagus, causing perforation or
later stenosis. Most batteries that reach the stomach pass through the
gut without any problem. Corrosive damage could occur from electrical
discharge, but toxicity from battery contents is rare. Mercury poisoning
is very unlikely since mercuric oxide batteries are no longer sold. The
Poisons Information Service may identify the type of battery involved
from the reference number, if this is available on the packet or on a similar
battery to that ingested.
Management
X-ray the chest and abdomen or use a metal detector to fi nd the battery.
A battery stuck in the oesophagus should be removed immediately by
endoscopy (which allows inspection for oesophageal damage and so is
preferable to a magnet or Foley catheter).
An asymptomatic child with a battery in the stomach or bowel can be sent
home with advice to return if any symptoms develop. If the battery has not
been passed after 2 or 3 days, and is causing concern use a metal detector
or repeat X-ray to look for the battery. If it is still in the stomach (which
is rare) consider removal by endoscopy to avoid any risk of perforation or
absorption of battery contents.
Batteries in the small or large bowel almost always pass spontaneously
and should be left to do so, unless they cause symptoms. If abdominal
pain, vomiting, diarrhoea or rectal bleeding occur an abdominal X-ray is
needed to localize the battery, which may require removal by endoscopy
or surgery.
Batteries in the nose
Button batteries lodged in the nose may cause corrosive burns and
bleeding, sometimes with septal perforation after a few weeks. Liaise with
an ENT specialist to remove batteries from the nose as soon as possible.

214 CHAPTER 4 Toxicology
Illicit drugs
Many drugs are used illegally as stimulants or for mood-altering effects.
Toxicity is often seen from heroin ( b p.188), cocaine, ecstasy, and related
drugs. Street names for drugs vary and may be confusing. The Street
Terms database ( http://www.whitehousedrugpolicy.gov/streetterms ) and
Toxbase ( b p.181) have lists of slang names about drugs.
Illicit drugs vary in strength and are often mixed with other drugs or chem-
icals, which may cause unexpected effects. Drugs may be smoked, sniffed
(‘snorted’), swallowed or injected. Injecting drug users are at increased
risk of hepatitis ( b p.239), HIV ( b p.242), necrotizing fasciitis ( b p.234),
botulism ( b p.237), anthrax ( b p.233) and endocarditis ( b p.234).
Ecstasy (MDMA)
‘Ecstasy’ (3,4-methylenedioxymetamphetamine, MDMA) is an amphetamine
derivative used as an illegal stimulant drug. The name ‘ecstasy’ is also used
for benzylpiperazine (BZP), another illegal drug. ‘Liquid ecstasy’ is GHB
( b p.215). MDMA is taken orally as tablets or powder, often at raves or
parties. Some people who have previously tolerated the drug have idiosyn-
cratic reactions, with severe toxicity from a single MDMA tablet.
MDMA causes release of serotonin, catecholamines and other hormones.
Inappropriate ADH secretion, abnormal thirst, and excessive water intake
may result in hyponatraemia and cerebral oedema, especially in women.
Clinical features Euphoria, agitation, sweating, dilated pupils, ataxia, teeth
grinding, headache, tachycardia, hypertension. Severe poisoning can cause
hyperpyrexia, muscle rigidity, rhabdomyolysis, convulsions, coma, cardiac
arrhythmias, renal failure, hepatic failure, cerebral haemorrhage, and DIC.
Metabolic acidosis is common. Features of serotonin syndrome may occur
as may hypoglycaemia, severe hyponatraemia and hyperkalaemia.
Treatment Consider activated charcoal ( b p.185) if <1hr since ingestion.
Observe asymptomatic patients for at least 4hr. Monitor ECG, pulse, BP and
temperature. Record ECG, check U&E, creatinine, glucose, LFTs and CK.
Test urine for blood. In severe cases, check ABG and coagulation.
Supportively treat airway, breathing, and circulation. Get expert advice
( b p.181) and ICU help in severe poisoning. Rapid sequence intubation
may be needed because of trismus and fi ts: use rocuronium, rather than
succinylcholine which may cause hyperkalaemia. Control agitation with
oral or IV diazepam or lorazepam: large doses may be needed. For severe
hypertension, give IV diazepam and GTN. Avoid B -blockers, which may
cause unopposed α-adrenergic stimulation with i BP and d coronary
blood fl ow. Do not treat single short fi ts, but give diazepam or lorazepam
for repeated or prolonged fi ts.
Correct metabolic acidosis (possibly with sodium bicarbonate), checking
ABG and U&E. Treat hyperkalaemia ( b p.162). Treat mild hyponatraemia
by fl uid restriction. IV saline may be needed for severe hyponatraemia:
rapid correction of chronic hyponatraemia can cause brain injury (central
pontine myelinolysis), but this is less likely with acute hyponatraemia caused
by MDMA. Cool as for heat stroke ( b p.264) if hyperpyrexial. If rectal T
> 40 ° C, consider dantrolene 1mg/kg IV (up to 10mg/kg in 24hr). See also
serotonin syndrome — b p.216.

215
ILLICIT DRUGS
Amphetamine
These sympathomimetic stimulants can be swallowed, snorted, smoked
or injected. Body packers may suffer severe poisoning. Toxic features are
euphoria, agitation, psychosis, sweating, dilated pupils, tachycardia, hyper-
tension, vomiting, abdominal pain, fi ts, hyperpyrexia and metabolic acidosis.
Severe poisoning may cause stroke, MI, rhabdomyolysis, renal failure and DIC.
Cardiac arrest can occur in violent agitated patients who need physical
restraint. Treat amphetamine poisoning as for MDMA ( b p.214).
Mephedrone, methedrone, M-cat
Synthetic cathinone compounds, sold as ‘plant food’ (now illegal in the
UK), are snorted or swallowed as stimulants. Toxic effects are similar to
amphetamines: agitation, sweating, tachycardia, palpitations, hypertension.
Some have nausea, hallucinations, fi ts, muscle spasms, nausea, peripheral
vasoconstriction and myocardial ischaemia. Nasal irritation and epistaxis
may occur after snorting these drugs. Treat as for MDMA/amphetamines.
Cocaine
Cocaine base (‘crack’) is usually smoked. Cocaine salt (‘coke’) is
snorted, eaten or injected. Body packers may be poisoned if pack-
ages leak. Toxic effects (due to catecholamines, serotonin and amino
acid stimulation and sodium channel blockade) are euphoria, agitation,
delirium, ataxia, dilated pupils, sweating, vomiting, fi ts, tachycardia,
arrhythmias and hypertension. Chest pain may be due to myocardial
ischaemia or MI (from i catecholamines, i O
2
demand, coronary vaso-
spasm and thrombosis), aortic dissection or pneumothorax. Cerebral
haemorrhage, hyperpyrexia, rhabdomyolysis, renal failure, gut ischaemia
and serotonin syndrome may occur. Cocaine is a local anaesthetic, so
hot air from smoking crack can cause airway burns.
Treat as for MDMA ( b p.214). Give diazepam for agitation (5–10mg
IV, repeated at 5min intervals if needed, sometimes up to 100mg). Treat
chest pain with diazepam, GTN, O
2
and aspirin. GTN, calcium blockers
and phentolamine may d BP and i coronary blood fl ow. Avoid B -blockers,
which may cause paradoxical hypertension and i coronary vasoconstriction.
If ECG suggests acute MI, consider angioplasty or thrombolysis.
Gammahydroxybutyrate (GHB, GBH, ‘liquid ecstasy’)
GHB is used illegally as a body-building agent and psychedelic drug. It is
ingested or injected. Intoxication may cause vomiting, diarrhoea, drowsi-
ness, confusion, ataxia, and agitation. Severe poisoning results in coma,
respiratory depression, fi ts, bradycardia, and hypotension.
Treatment Consider activated charcoal ( b p.185) if <1hr since ingestion.
Observe for at least 4hr and monitor pulse rate, BP and breathing. Provide
supportive treatment as needed. Control agitation and convulsions with
diazepam. Naloxone may reverse some effects of GHB.
LSD (lysergic acid diethylamide)
Causes visual hallucinations, agitation, excitement, tachycardia and dilated
pupils. Hypertension and pyrexia may occur. Paranoid delusions may
require sedation. Massive overdose of LSD is rare, but may cause coma,
respiratory arrest and coagulation disturbances. Treat supportively.

216 CHAPTER 4 Toxicology
Serotonin syndrome
Background
The clinical picture of serotonin syndrome is increasingly recognized
amongst those taking selective serotonin reuptake inhibitors (SSRIs).
The syndrome can occur in patients who have taken therapeutic doses
of SSRIs, and this is especially likely if they have recently started on the
medication or if it is taken in combination with other drugs which increase
production, availability or release of serotonin (eg cocaine, MDMA,
amphetamines) or reduce metabolism (eg MAOIs). Serotonin syndrome
can also occur after an acute overdose. Numerous drugs have been
implicated — in addition to those mentioned above, they include: tricyclic
antidepressants, venlafaxine, tramadol, pethidine, buprenorphine, St John’s
wort, olanzapine and lithium.
Clinical features
Altered mental status
Confusion, hallucinations, and agitation may occur, with drowsiness and
reduced conscious level in severe cases.
Neuromuscular features
Rigidity, shivering/tremor, teeth grinding, ataxia, and hyper-refl exia (especially
affecting the lower limbs) may occur.
Autonomic effects
These include tachycardia, hypertension (or hypotension), fl ushing, diarrhoea,
vomiting and hyperthermia.
Severe cases can result in fi ts, rhabdomyolysis, renal failure and coagulopathy.
Differential diagnosis
This includes neuroleptic malignant syndrome, malignant hyperthermia,
severe infection (eg encephalitis), other direct effects of drug overdose
or withdrawal.
Investigations
Check U&E, glucose, LFTs, CK, FBC, urinalysis, ABG, ECG ± CXR.
Treatment
Provide supportive measures and obtain expert advice (see b p.181).
Agitation, hyperthermia, myoclonic jerking and fi ts may benefi t from diazepam
therapy. Treat rhabdomyolyis with IV fl uids and urine alkalinization.
Cyproheptadine (dose 4–8mg orally) is a serotonin receptor antagonist.
Although data are lacking, there is a good theoretical basis for its use in
serotonin syndrome.

217
BODY PACKERS
Body packers
Body packers try to smuggle drugs such as cocaine or heroin by ingesting
multiple packages of drugs wrapped in condoms or latex. Packages may
also be hidden in the rectum or vagina (individuals who do this are some-
times referred to as ‘ body pushers’ ). Serious or even fatal poisoning may
occur if any packages leak and the drugs are absorbed.
Risk factors
Risk factors for complications occurring when an individual has concealed
drugs include:
• Vomiting, abdominal pain, abnormal vital signs.
• Clinical evidence of poisoning.
• Home made or improvised packaging.
• Large size and/or large number of packets.
• Delayed passage of the packets (beyond 48hr).
• Fragments of packets in the stool.
• Poisoning in a cotransporter.
• Previous abdominal surgery ( i risk of obstruction due to adhesions).
• Concomitant drug use (especially constipating agents).
Management
Suspected body packers need careful assessment and observation. Check
for rectal and vaginal packages if the patient consents: get senior advice if
there is any problem or uncertainty about consent. Try to determine the
drug involved, and the number of packages and type of packaging used.
Observe for at least 8hr for toxic effects, monitoring heart rate, BP, ECG
and SpO
2
. Urine toxicology screening may detect heroin or cocaine.
Give activated charcoal ( b p.185). Consider a naloxone infusion ( b
p.188) for heroin body packers. Abdominal CT or X-ray may show
packets of drugs, which can be removed by whole bowel irrigation ( b
p.185). Surgery may be needed for bowel obstruction or to remove
leaking packages. Avoid endoscopic removal which may damage packaging
and increase drug leakage. Advice is available from Poisons Information
Centres ( b p.181).
Body stuffers
This term is sometimes applied to individuals who swallow drugs imme-
diately prior to being apprehended by the police. The quantity of drugs
ingested in this way may be less than by body packers or pushers.
However, any packaging is likely to be much less robust than that used
by body packers or pushers, thereby increasing the risk of the packages
leaking.
This page intentionally left blank

219
Incubation periods 220
Notifi able infectious diseases 221
Childhood infectious diseases 222
Meningitis 224
Gastroenteritis/food poisoning 226
Fish poisoning 229
Infestations 230
Tuberculosis 232
Anthrax 233
Streptococcal infections 234
Staphylococcal infections 235
Tetanus 236
Gas gangrene 237
Botulism 237
Sexually transmitted diseases 238
Hepatitis 239
Leptospirosis (Weil’s disease) 239
Herpes virus infections 240
Infectious mononucleosis (glandular fever) 241
Human immunodefi ciency virus (HIV) 242
Presentation of HIV +ve patients 244
Imported infectious diseases 246
Malaria 247
Typhoid and paratyphoid (enteric fever) 248
Dengue 248
Poliomyelitis 249
Rabies 249
Viral haemorrhagic fevers 250
Severe acute respiratory syndrome 251
Infl uenza pandemics, avian fl u, and swine fl u 252
Infectious diseases
Chapter 5
220 CHAPTER 5 Infectious diseases
Incubation periods
Incubation period usually <1 week
Incubation period usually 1–3 weeks
Incubation period usually > 3 weeks
Duration of infectivity of infectious diseases
Staphylococcal enteritis 1–6 hours
Salmonella enteritis 6–48 hours (usually 12–24 hours)
Bacillary dysentery ( Shigella ) 1–7 days (usually 1–3 days)
Botulism 12–96 hours (usually 18–36 hours)
Cholera 12 hours–6 days (usually 1–3 days)
Dengue 4–7 days
Diphtheria 2–5 days
Gas gangrene 6 hours–4 days
Legionnaires’ disease 2–10 days (usually 7 days)
Meningococcaemia 1–7 days (usually 3 days)
Scarlet fever 1–4 days
Yellow fever 3–6 days
Brucellosis 7–21 days (occasionally some months)
Chickenpox 10–20 days (usually about 14 days)
Lassa fever 6–21 days
Leptospirosis 2–26 days (usually 7–12 days)
Malaria (falciparum) 7–14 days (occasionally longer)
Malaria (vivax, malariae, ovale) 12–40 days (occasionally > 1 year)
Measles 10–18 days (rash usually 14–18 days)
Mumps 14–18 days
Pertussis (whooping cough) 5–14 days (usually 7–10 days)
Poliomyelitis 3–21 days (usually 7–10 days)
Rubella 14–21 days
Tetanus 1 day–3 months (usually 4–14 days)
Typhoid 3–60 days (usually 7–14 days)
Typhus 7–14 days
Amoebiasis 2 weeks–many months
Hepatitis A 2–6 weeks (usually 4 weeks)
Hepatitis B, hepatitis C 6 weeks–6 months
HIV 2 weeks–3 months (anti-HIV appears)
Infectious mononucleosis 4–7 weeks
Rabies 4 days–2 years (usually 3–12 weeks)
Syphilis 10 days–10 weeks (usually 3 weeks)
Chickenpox 3 days before rash until last vesicle crusts
Hepatitis A 2 weeks before until 1 week after jaundice starts
Measles 4 days before rash until 5 days after rash appears
Mumps 3 days before to 1 week after salivary swelling
Pertussis 3 days before to 3 weeks after start of symptoms
(5 days if on appropriate antibiotic)
Rubella 1 week before to 1 week after onset of rash
Scarlet fever 10–21 days from onset of rash (1 day if on penicillin)

221
NOTIFIABLE INFECTIOUS DISEASES
Notifi able infectious diseases
In Britain certain infectious diseases are ‘notifi able’. A doctor who knows
or suspects that a patient has one of these diseases is obliged to notify the
local Health Protection department. Use the special notifi cation form if
available. Telephone the consultant in Communicable Disease Control if
investigation or control of an outbreak may be needed.
HIV and AIDS are not notifi able diseases, but may be reported in strict
confi dence in the same way.
Notifi able infectious diseases in Britain (ND)
Anthrax
Botulism
Brucellosis
Cholera
Diphtheria
Encephalitis (acute)
*
Erysipelas
* *
Food poisoning
*
Haemolytic uraemic syndrome (HUS)
Haemophilus infl uenzae type b (Hib)
*
*
Infectious bloody diarrhoea ( E. coli O157 infection
*
*
)
Infectious hepatitis (acute)
*
Invasive group A streptococcal disease and scarlet fever
*
Legionnaires’ disease
*
Leprosy
*
Malaria
*
Measles
Meningitis (acute)
*
Meningococcal septicaemia
*
/meningococcal disease
*
*
Mumps
Necrotizing fasciitis
*
*
Paratyphoid
Pertussis (whooping cough)
Plague
Poliomyelitis
Rabies
Rubella
Severe acute respiratory syndrome (SARS)
Smallpox
Tetanus
Tuberculosis
Tularaemia
*
*
Typhoid
Typhus
*
Viral haemorrhagic fever (VHF)
West Nile fever
*
*
Yellow fever
*
Notifi able only in England and Wales.
**
Notifi able only in Scotland.

222 CHAPTER 5 Infectious diseases
Childhood infectious diseases
Children at risk
Unimmunized children are at risk of infections which would be prevented
by the standard immunization schedule. Always ask about vaccination
status in any febrile, unwell child. The common infectious diseases of child-
hood can be very serious in children with immune defi ciency or those on
immunosuppressant drugs . Refer such children for specialist advice if they
develop an infectious disease or have been in contact with one. Children
with cystic fi brosis can become very ill with measles, whooping cough
or chickenpox — refer these also. Neonates rarely develop the common
exanthems of childhood, but require referral if these occur. Chickenpox
can be particularly serious in this age group.
Measles
ND
A virus infection spread by airborne droplets.
Incubation period =10–18 days. Infectious from just before the onset of
symptoms until 5 days after the rash appears.
Initial features (lasting 83 days) are fever, malaise, coryza, conjunctivitis
and cough. Koplik’s spots (small white spots like grains of salt) appear
inside the cheeks. 1–2 days later a red maculopapular rash starts behind
the ears, and spreads to the face and down the body.
Treatment is symptomatic unless there are complications (eg otitis media
or bacterial pneumonia). Febrile convulsions may occur. Encephalitis is
rare, but can be fatal. Hospital admission is rarely needed unless the child
is very ill or has pre-existing disease. In the tropics many malnourished
children die from measles, but in the UK the mortality is very low.
Mumps
ND
Mumps is a virus infection spread by saliva and respiratory droplets.
Infectivity is greatest at the onset of symptoms, but many sub-clinical cases
also spread infection.
Incubation period = 14–18 days.
Typical features are fever with pain and swelling in one or both parotid
glands. Aseptic meningitis may occur. Orchitis affects 10–15 % of post-
pubertal males, but rarely causes sterility. The pain of orchitis may be
relieved by analgesia and a short course of steroids. Orchitis is uncommon
before puberty, so consider torsion of the testis if a child presents with
testicular pain and swelling ( b p.700).

223
CHILDHOOD INFECTIOUS DISEASES
Rubella (German measles)
ND
Rubella is usually a mild disease, but infection during pregnancy may cause
severe congenital disorders, particularly eye defects, heart defects and
deafness. Guidance on the management of, and exposure to, rubella in
pregnancy is available from the Health Protection Agency based in London
( www.hpa.org.uk/infections ). The virus is spread mainly by the airborne
route, with an incubation period of 2–3 weeks and infectivity from 1 week
before symptoms until 1 week after the rash appears. A macular rash
occurs on the face and trunk, with mild fever, occipital lymphadenopathy
and sometimes transient arthralgia. Rare complications are encephalitis
and thrombocytopenia.
Treatment is generally symptomatic. The clinical diagnosis of rubella
is unreliable: similar rashes may occur with enterovirus and parvovirus
infections. If there is concern about rubella infection in pregnancy take
blood for viral antibody levels and arrange urgent follow-up by the GP
or obstetrician.
Whooping cough
see b p.684.

224 CHAPTER 5 Infectious diseases
Meningitis
Causative organisms
Meningitis may be bacterial , viral, or occasionally fungal . Bacterial causes of
meningitis include meningococci, pneumococci, Haemophilus infl uenzae,
Listeria , and tuberculosis (TB). Other bacteria may also cause meningitis in
neonates, the elderly, and immunosuppressed patients.
Clinical features of bacterial meningitis
Some patients with meningitis have the classic features of headache,
neck stiffness, photophobia, fever and drowsiness. However, the clinical
diagnosis of meningitis may be very diffi cult in early cases. Neonates may
present with anorexia, apnoea, or fi ts. Meningitis may start as a ‘fl u-like’
illness, especially in the immunosuppressed or elderly. Consider meningitis
in any febrile patient with headache, neurological signs, neck stiffness, or
d conscious level.
Meningococcal meningitis
ND
is caused by Neisseria meningitidis . It can result
in septicaemia, coma, and death within a few hours of the fi rst symptoms.
Skin rashes occur in 50 % of patients, often starting as a maculopapular
rash before the characteristic petechial rash develops. There may be DIC
and adrenal haemorrhage (Waterhouse–Friderichsen). Meningococcal
septicaemia ( b p.666) may occur without meningitis.
Management
Resuscitate if necessary, give oxygen and obtain venous access.
Start antibiotics immediately (without waiting for investigations) if
the patient is shocked or deteriorating or there is any suspicion of
meningococcal infection (especially a petechial or purpuric rash): give IV
ceftriaxone or cefotaxime (adult 2g; child 80mg/kg). Chloramphenicol is
an alternative if there is a history of anaphylaxis to cephalosporins (see
BNF ). In adults > 55 years add ampicillin 2g qds to cover Listeria . Give
vancomycin ± rifampicin if penicillin-resistant pneumococcal infection is
suspected. Give IV dexamethasone (0.15mg/kg, max 10mg, qds for 4 days)
starting with or just before the fi rst dose of antibiotics, especially if pneu-
mococcal meningitis is suspected.
Initial investigations are FBC, U&E, glucose, clotting screen, ABG, CRP,
blood cultures, EDTA sample for PCR, and clotted blood for serology.
LP is needed if meningitis is suspected, unless there is a coagulopathy
or i ICP: do CT scan if there is suspicion of i ICP (confusion/coma,
hypertension, bradycardia or papilloedema) or focal neurological signs.
Provide supportive treatment including:
• IV fl uids.
• Pressure area care.
• Monitor conscious level, T ° , BP, ECG, SpO
2
, and fl uid balance.
Get expert help promptly and organize ICU care.
For the latest advice and algorithms see www.meningitis.org and
www.nice.org.uk/guidance/CG102/quickrefguide
For meningitis and LP in children see b p.666.

225
MENINGITIS
Prophylaxis of meningococcal infection
While intubating a patient with suspected meningococcal infection wear a
suitable mask (eg FFP3) and a face shield to reduce the risk of infection.
Meningococcal infection is spread by droplets from the nose of an infected
carrier, who may be well. Notify the consultant in Communicable Disease
Control ( b p.221) immediately about any suspected meningococcal
infection and obtain advice about antibiotic prophylaxis. Prophylactic
antibiotics (rifampicin, ciprofl oxacin or ceftriaxone) are needed for the
patient’s family and close contacts. Hospital and ambulance staff do not
need prophylaxis unless they have given mouth to mouth ventilation or
intubated the patient without using protective equipment.
Rifampicin is given 12 hourly for 2 days (5mg/kg for child aged <1 year;
10mg/kg at 1–12 years; 600mg at age > 12 years. It makes the urine orange
or brown, discolours soft contact lenses, and d effectiveness of OCP for
8 4 weeks (see BNF ) — give appropriate warnings and record this in the
notes.
Ciprofl oxacin is given as a single oral dose of 500mg (adults), 250mg (child
5–12 years) or 125mg (child 2–5 years), although it is not licensed for
chemoprophylaxis of meningitis.
Ceftriaxone is given as a single IM dose of 250mg (adults and children
> 12 years) or 125mg (children <12 years).
Tell contacts of meningococcal patients to report to a doctor at once if
they develop symptoms.
TB meningitis
Often gradual onset, with malaise, anorexia, vomiting, headache and even-
tually signs of meningitis. Cranial nerve palsies, spastic paraplegia and coma
can occur. Meningitis may be part of miliary TB ( b p.232), which may be
apparent on chest X-ray. Ophthalmoscopy may show choroidal tubercles
and papilloedema, which is found more commonly than in other forms of
meningitis. Refer for specialist investigation and treatment.
Viral meningitis
Viral causes of meningitis include coxsackie, mumps, and echoviruses.
Viral meningitis produces similar clinical features to bacterial infection, but
the illness is often less severe. The initial management is the same as for
suspected bacterial meningitis. Refer for admission and investigation.
Fungal meningitis
Fungal meningitis is usually part of disseminated infection in immuno-
suppressed patients, (eg those with AIDS ( b p.242), lymphoma, or on
steroid therapy). Cryptococcus neoformans is the commonest organism.
Symptoms usually develop slowly, as with TB meningitis. There may be
papilloedema and focal neurological signs. Admit for specialist investiga-
tion and treatment.

226 CHAPTER 5 Infectious diseases
Gastroenteritis/food poisoning
ND
: 1
Diarrhoea is the usual presenting symptom of gastroenteritis, but it may
also occur in many other conditions as diverse as otitis media, appendicitis
and ulcerative colitis. Antibiotics often cause diarrhoea. Constipation may
present as diarrhoea if there is overfl ow around an obstructing stool.
A rectal tumour may present similarly.
A baby’s parents may seek advice about diarrhoea when in fact the stools
are normal. Breast-fed babies almost always have loose stools, which may
be yellow or green and very frequent, often after every feed. However,
gastroenteritis is very rare in fully breast-fed babies. In children aged
> 6 months, normal stool frequency ranges from 1 stool on alternate days
to 3 stools daily.
Diarrhoea and vomiting may be caused by many types of bacteria and viruses,
and also by some toxins and poisons. Many episodes of gastroenteritis result
from contaminated food, usually meat, milk or egg products, which have
been cooked inadequately or left in warm conditions. The specifi c cause
is often not identifi ed. Some infections are spread by faecal contamination
of water (eg cryptosporidiosis from sheep faeces). Rotavirus infection
(common in children) may be transmitted by the respiratory route. Severe
illness with bloody diarrhoea, haemolysis and renal failure may result from
infection with verocytotoxin producing E. coli (VTEC O157).
Stool microscopy and culture are unnecessary in most cases of gastro-
enteritis, but obtain them if the patient has been abroad, is severely
ill, has prolonged symptoms, comes from an institution or works as a
food-handler.
Food poisoning is a notifi able disease ( b p.221). Immediate notifi cation
by telephone is mandatory if an outbreak is suspected. The food eaten,
symptoms and incubation period may suggest the organism or toxin
involved (see Table 5.1). Carbon monoxide poisoning ( b p.208)
may cause malaise and vomiting in several members of a family and be
misdiagnosed as food poisoning.
History
Record the duration of symptoms and the frequency and description of
stools and vomit. Document other symptoms (eg abdominal pain, fever),
food and fl uid ingested and drugs taken. Enquire about affected contacts,
foreign travel and occupation (especially relevant if a food-handler).
Examination
Look for abdominal tenderness, fever and other signs of infection. Record
the patient’s weight and compare this with any previous records. Assess
the degree of dehydration — this is traditionally classifi ed as mild (<5 % ),
moderate (5–10 % ), or severe ( > 10 % ), as outlined opposite.
227
GASTROENTERITIS/FOOD POISONING
ND
: 1
Clinical evidence of mild dehydration (<5%)
• Thirst.
• d urinary output (in a baby <4 wet nappies in 24hr).
• Dry mouth.
Clinical evidence of moderate dehydration (5–10%)
• Sunken fontanelle in infants.
• Sunken eyes.
• Tachypnoea due to metabolic acidosis.
• Tachycardia.
Clinical evidence of severe dehydration (>10%)
• d skin turgor on pinching the skin.
• Drowsiness/irritability.
Table 5.1 Food poisoning characteristics
Cause Incubation Food Symptoms
*
Staph. aureus 1–6 hours Meat, milk D, V, P, shock
Bacillus cereus 1–16 hours Rice D, V, P
Salmonella 6–48 hours Meat, eggs D, V, P
Escherichia coli 1–2 days Any food D, V, P
E. coli VTEC 0157 1–2 days Meat, milk D, V, P
Campylobacter 1–3 days Meat, milk Fever, P, D
Shigella 1–3 days Any food Bloody D, V, fever
Vibrio parahaem 2–3 days Seafood Watery D
Cholera 12hr–6 days Water, seafood D (watery), shock
Rotavirus 1–7 days D, V, fever, cough
Botulism 12–96 hours Preserved food V, paralysis
Histamine
fi sh poisoning
(scombrotoxin)
<1 hour Fish Flushing, headache,
D, V, P ( b p.229)
Ciguatera fi sh
poisoning
1–6 hours
(rarely
30 hours)
Fish from
tropical
coral reef
D, V, P, paraesthesiae,
muscle weakness ( b p.229)
Paralytic shellfi sh
poisoning
30 min–
10 hours
Shellfi sh Dizziness, paraesthesiae,
weakness, respiratory
failure ( b p.229)
Chemicals <2 hours Food, water Various
Mushrooms <24 hours Mushrooms D, V, P, hallucinations
( b p.212)
*
D = diarrhoea, V = vomiting, P = abdominal pain.

228 CHAPTER 5 Infectious diseases
Gastroenteritis/food poisoning
ND
: 2
Treatment
Most cases are self-limiting, but careful attention is needed to ensure
adequate fl uid replacement and also to prevent cross-infection ( b p.32).
Hospital treatment is needed if the patient looks seriously ill, dehydration
is > 5 % , there is a high fever or the family are unlikely to cope with the
patient at home. Babies aged <3 months may be diffi cult to assess and
can deteriorate rapidly — refer for admission. Severely dehydrated ( > 10 % )
children need immediate IV fl uids, initially 0.9 % saline (10–20mL/kg over
5min, repeated as necessary).
Oral rehydration therapy (ORT) is effective in most patients with gastro-
enteritis (<5 % dehydration). Standard ORT products (eg Dioralyte
®
)
contain glucose, sodium, potassium, chloride and citrate (details in BNF ).
Glucose is important to enhance absorption of sodium and water.
Usual dose of ORT: infant 1–1½ times usual feed volume.
child 200mL after each loose stool.
adults 200–400mL after each loose stool.
Extra ORT can be given if the patient is still thirsty. Frequent small sips
are usually tolerated better than a large drink. Check that the patient (or
parent/carer) can understand the instructions supplied with the ORT
sachets or effervescent tablets and can measure the necessary amounts
of clean water.
Recommence normal feeds and diet after 24hr (or earlier if diarrhoea
has settled or the patient is hungry). Give further ORT if the diarrhoea
continues. A child with acute diarrhoea requires daily review (usually by the
GP), but should be seen earlier if he becomes more ill (especially if drowsy
or pyrexial), or if vomiting and/or diarrhoea worsens. Home-made salt and
sugar mixtures may be dangerously inaccurate for ORT, but if nothing else
is available, one could use salt 2.5mL (half a 5mL spoonful) and sugar 20mL
(4 × 5mL spoonfuls) in 1 pint (500mL) of cooled boiled water.
Drugs other than ORT are rarely needed in gastroenteritis. In adults an
anti-emetic (prochlorperazine 12.5mg IM or 3mg buccal) may be helpful,
but in children prochlorperazine often causes troublesome side effects.
However, oral ondansetron (0.1–0.15mg/kg, max 8mg) reduces vomiting
and the need for IV fl uids and admission. Prolonged vomiting requires
investigation and hospital admission.
Anti-diarrhoeal drugs (eg kaolin, codeine phosphate, loperamide) are
contraindicated in children and rarely needed in adults: they may aggravate
nausea and vomiting and occasionally cause ileus.
Antibiotics are only needed in special circumstances. Most episodes
of gastroenteritis are brief and many are caused by viruses and not helped
by antibiotics. Patients with amoebiasis, giardiasis, Campylobacter or
Shigella infections may need antibiotics: refer to an Infectious Diseases
unit for treatment and follow-up. Antibiotics are occasionally useful in
traveller’s diarrhoea before a long journey or an important meeting:
trimethoprim (200mg bd PO for 5 days) or ciprofl oxacin (500mg bd PO
for 2 days: see the BNF or data sheet about side effects and warnings).

229
FISH POISONING
Fish poisoning
Histamine fi sh poisoning
Also known as scombroid fi sh poisoning or scombrotoxin poisoning, this
is caused by ingesting toxins in fi sh such as tuna, mackerel, and other dark-
meat fi sh, which have been stored improperly. If the fi sh is not cooled
rapidly after it is caught, an enzyme in bacteria converts histidine into his-
tamine and other toxins, which are heat-stable and so are unaffected by
cooking. The patient may notice that the fi sh tastes metallic, bitter, or
peppery and the fl esh looks honeycombed. Symptoms start within a few
minutes to 2 hours, with fl ushing of the face and upper body, headache,
nausea, vomiting, abdominal pain, diarrhoea, dizziness and palpitations.
Urticaria and bronchospasm are less common. The symptoms usually
settle within 6 hours without treatment, but resolve more quickly with
antihistamines (eg chlorphenamine 10mg IV in adults, 250 micrograms/kg
in children). In severe cases cimetidine and, rarely, adrenaline might be
needed, with oxygen, IV fl uids and bronchodilators.
The patient should be told that histamine fi sh poisoning is caused by
improper fi sh handling and storage. It is not an allergic reaction and so the
patient would not have to avoid eating fi sh in future.
Ciguatera fi sh poisoning
This is caused by a neurotoxin called ciguatoxin which is produced by
a dinofl agellate (a unicellular plankton) associated with coral reefs. Fish
imported from the tropics may cause ciguatera poisoning in the UK and
elsewhere. Symptoms usually start 1–6 hours after ingestion with nausea,
vomiting, watery diarrhoea and abdominal pain, followed by neurological
symptoms, including paraesthesiae of the lips, tongue and feet, ataxia and
muscle weakness. A classic feature is paradoxical temperature reversal
(cold objects feel hot and hot objects feel cold). Alcohol makes these
symptoms worse. Bradycardia and hypotension may occur. Treatment is
symptomatic and supportive. Gastro-intestinal symptoms usually settle
within 1 day, but paraesthesiae may persist for weeks or months.
Paralytic shellfi sh poisoning
This can be caused by eating molluscs such as mussels, clams, cockles and
scallops which concentrate a neurotoxin called saxitoxin produced by
dinofl agellate plankton. This plankton proliferates when sea temperatures
rise in summer and may make the sea look red (‘red tide’). Symptoms
start 30 minutes to 10 hours after ingestion, with dizziness, ataxia, paraes-
thesiae and muscle weakness, which may progress to respiratory failure.
Treatment is supportive, with assisted ventilation if necessary. Complete
recovery is usual within 24 hours.

230 CHAPTER 5 Infectious diseases
Infestations
Worms
The most common helminthic infection seen in the UK is the thread-
worm Enterobius vermicularis . This causes anal itching, especially at night.
Sometimes intact worms (length 5–13mm, diameter 0.1–0.5mm) are seen
in the faeces. Unwashed fi ngers transmit ova from the perianal skin to the
mouth. Personal hygiene is important in treatment and in prevention of
reinfection (hand-washing and nail-scrubbing before each meal and after
every visit to the toilet). A bath immediately after getting up removes
ova laid overnight. All members of the family require treatment with
mebendazole or piperazine (see BNF ).
Other helminthic infections include roundworms, hookworms and
tapeworms. Obtain advice from departments of Infectious Diseases or
Tropical Medicine (see b p.246).
Lice
Humans may be infected by the body louse ( Pediculosis humanis corporis ),
head louse ( Pediculosis humanis capitis ), or the ‘crab’/pubic louse ( Phthirus
pubis ).
Head lice are common in school children. Infection is not related to lack
of hygiene or the length of hair. Adult lice are 3–4mm long, vary in colour
from white to grey-black and attach themselves fi rmly to the scalp at the
base of hairs. The egg cases (‘nits’) are white and 1–2mm in diameter,
glued fi rmly to the base of hairs and moving outwards as the hair
grows. Head lice cause intense itching, which may suggest the diagnosis.
Secondary infection may result in impetigo. Head lice are usually treated
with malathion, phenothrin or simeticone, repeated after 7 days (see
BNF ). Drug-resistant lice occur in some areas. Wet combing to remove
head lice takes time and is possibly less effective than drug treatment.
Infection by body lice is related to poor hygiene and infrequent washing
of clothes. Body lice are found in the seams of clothing, and sometimes
in body hair. Treatment is with malathion. Clothes can be disinfected
by boiling or by machine laundering and ironing. Body lice may transmit
ricketsial diseases (louse-borne typhus) and other infections.
Crab lice are usually transmitted sexually. They cause itching in pubic hair
areas. Occasionally, children become infested on eyelashes or eyebrows.
Treat with permethrin or malathion (see BNF ). Sexual partners or other
family members may also need treatment. There may be other co-existing
sexually transmitted diseases.
Fleas
There are many different types of fl ea. They cause itchy bites with linear
erythematous papules. Treat with calamine lotion and an oral antihista-
mine (eg chlorphenamine) if itching is severe. A long-acting insecticide is
needed in the house, especially in cracks in the fl oor and under furniture.
All household cats and dogs must be treated for fl eas. Fleas can transmit
many infections, including plague, typhus and Q fever.

231
INFESTATIONS
Scabies
Scabies is caused by infestation with a mite, Sarcoptes scabiei , which is
about 0.2–0.4mm long and burrows into the skin. It is most often found in
the fi nger webs and on the fl exor aspect of the wrists. After 4–6 weeks,
intense itching occurs, especially at night or after a hot shower. Burrows
(3–15mm long) may be apparent, especially on palpation of affected skin.
Genital lesions are reddish and nodular. Secondary bacterial infection
may occur. Scabies can be confi rmed by microscopy of scrapings from
suspected lesions. Treat with permethrin or malathion (see BNF ). Treat
all members of the household at once. Calamine lotion and an oral
antihistamine may help to relieve itching.
Ticks
Ticks may be acquired from domestic animals or while walking through
undergrowth or exploring caves. Ticks may be removed with tweezers
or curved forceps. They can carry several diseases, including Lyme
disease (see below), tick-borne encephalitis, typhus, and Rocky Mountain
spotted fever. Tick paralysis occurs in North America and Australia,
with progressive paralysis which is often misdiagnosed as poliomyelitis.
However, the risk of infection from tick bites is low in most areas, and so
routine prophylaxis with antibiotics is not recommended.
Lyme disease (Lyme borreliosis) is caused by a tick-borne spirochaete,
Borrelia burgdorferi , and occurs in the UK, most of Europe, the USA, and
parts of Asia and Australia. Most cases occur in the summer and early
autumn, and are transmitted by ticks from deer or sheep. The initial tick
bite may go unnoticed. Clinical illness develops after about 7–14 days
(range 2–30 days) with an expanding red area around the site of the bite
(erythema migrans). The second clinical stage of the disease occurs some
weeks or months later, with fever, muscle and joint pains, and sometimes
facial palsy or other cranial nerve or peripheral nerve palsies. Meningitis,
encephalitis and arthritis may develop. Myocarditis and heart block occur
occasionally. Refer to an Infectious Diseases specialist for confi rmation
and treatment if Lyme disease is suspected.

232 CHAPTER 5 Infectious diseases
Tuberculosis
ND
The Mycobacterium genus is characterized by acid-fast staining (ie it is not
decolourized by acid after staining with hot carbol fuchsin).
Infection with Mycobacterium tuberculosis is common throughout the
world. There is growing concern about the re-emergence of TB in the UK
and other countries. Many cases of TB occur in the lower socio-economic
groups, ethnic minorities and the immunocompromised.
The incidence of TB i with age.
Presentation
TB can involve almost any organ of the body.
Primary infection is usually pulmonary and often asymptomatic.
Post-primary infection may present with malaise, weight loss and night
sweats, with localized symptoms depending on the organs involved.
Pulmonary TB may result in cough, haemoptysis, pneumonia and pleural
effusion ( b p.103).
Miliary TB, with blood-borne infection of many organs, develops over
1–2 weeks with fever, weight loss, malaise and breathlessness: CXR may
show multiple small opacities throughout the lung fi elds, and choroidal
tubercles may be visible in the optic fundi.
TB meningitis causes headaches and vomiting, sometimes with neck
stiffness, cranial nerve palsies and papilloedema (see b p.224).
Tuberculous osteomyelitis usually affects the spine, with collapse of
adjacent vertebrae and a paravertebral abscess.
Patients may present with swollen lymph nodes from tuberculous
lymphadenitis or with sinuses or cold abscesses from bone or soft tissue
infection: microscopy of the discharge will show acid-fast bacilli.
Treatment
Refer patients with suspected TB to an appropriate specialist for
assessment and treatment. Isolation is required for patients with untreated
pulmonary TB. Notify the local Health Protection department ( b p.221).

233
ANTHRAX
ND
Anthrax
ND
Anthrax is caused by the bacterium Bacillus anthracis which affects cows
and other herbivorous animals, especially in warm climates. The bacte-
rium forms spores, which may remain infective for years. Most human
cases of anthrax are cutaneous anthrax caused by direct skin contact with
infected tissues and occur in people working with animal products such as
imported hides. Less common, but more serious, are inhalation anthrax
caused by inhalation of anthrax spores, and intestinal anthrax which is a
rare form of food poisoning caused by under-cooked infected meat.
Anthrax spores released deliberately in terrorist attacks could cause
cutaneous anthrax or inhalation anthrax, which is often fatal.
Cutaneous anthrax starts 2–7 days after infection, with a red papule
which develops into an ulcer with a black leathery eschar, surrounded
by non-pitting oedema. The lesion is painless but may itch. Small satellite
lesions may surround the original lesion. Malaise and fever may occur,
with septicaemia in 10–20 % of cases. Penicillin d risk of complications
from cutaneous anthrax. Clinical diagnosis is confi rmed by microscopy
and culture of the pustule.
Inhalation anthrax starts within 48 hours of exposure (rarely up to 6
weeks) with a fl u-like illness, followed by breathlessness, cyanosis, stridor
and sweating, often with subcutaneous oedema of the chest and neck.
CXR and CT show mediastinal widening from lymphadenopathy and
pleural effusions. Shock, septicaemia and meningitis are common and
usually fatal, despite antibiotics and intensive treatment.
Airborne transmission of anthrax from one person to another does
not occur, but cutaneous anthrax could result from direct contact with
anthrax lesions. Obtain expert advice immediately if anthrax is suspected.
It is a notifi able disease ( b p.221). Post-exposure antibiotics can prevent
anthrax if started early enough. Press enquiries must be anticipated after
any case of anthrax, especially if anthrax has been released deliberately.
Further information is available from: www.hpa.org.uk/infections .
Anthrax in drug users After a serious anthrax outbreak in heroin users
in Scotland in 2010, Health Protection Scotland ( www.hps.scot.nhs.uk )
advised doctors to suspect anthrax in a drug user presenting with any of
the following:
• Severe soft tissue infection and/or signs of severe sepsis/meningitis.
• Clinical features of inhalational anthrax.
• Respiratory symptoms + features of meningitis or intracranial bleeding.
• GI symptoms (eg pain, bleeding, nausea, vomiting, diarrhoea, ascites).
Approach Get expert help early to advise on management (microbiology,
hospital infection control team, Public Health, ICU, surgeons). Start IV
antibiotics according to advice (eg combination of ciprofl oxacin,
clindamycin + penicillin, or if there is soft tissue infection: ciprofl oxacin,
clindamycin, penicillin, fl ucloxacillin + metronidazole). Experts will advise
on whether to use anthrax immune globulin.

234 CHAPTER 5 Infectious diseases
Streptococcal infections
Streptococcus pyogenes and other streptococci may reside in the pharynx
without symptoms, but can cause sore throats ( b p.554), soft tissue
infections ( b pp.413 and 528), scarlet fever, and occasionally endocar-
ditis and septicaemia. Later, non-suppurative sequelae of streptococcal
infections include erythema nodosum, rheumatic fever ( b p.496) and
glomerulonephritis. Streptococci and Staphylococci may cause necrotizing
fasciitis, impetigo, and toxic shock.
Scarlet fever
ND
Some streptococcal infections are associated with scarlet fever. A diffuse
blanching scarlet rash often involves the neck, chest, axillae and groin.
Occlusion of sweat glands makes the skin feel rough, like sandpaper.
During the fi rst 1–2 days of illness there is a ‘white strawberry tongue’,
with red papillae protruding through white furry material. After a few days
the white fur separates, leaving a shiny ‘raspberry tongue’. 10–14 days after
onset of the rash, skin may peel from palms and soles. Treat with penicillin
or erythromycin for 14 days. Complete recovery is usual.
Infective endocarditis
Endocarditis may develop on previously normal heart valves, as well as on
diseased or prosthetic valves. The commonest organism is Strep. viridans , but
many others have been implicated. Many acute cases present with heart failure
and involve Staphylococcus aureus . Injecting drug users are liable to staphyloco-
ccal infection of the tricuspid valve, with fever and pneumonia from septic PE.
Clinical features Fever and changing murmurs suggest endocarditis.
Emboli may cause strokes. Ask about weight loss, malaise, night sweats.
Look for clubbing, splinter haemorrhages, splenomegaly, anaemia,
microscopic haematuria.
Treatment On suspicion of endocarditis, admit immediately for
investigation (blood cultures, echocardiography) and treatment.
Cellulitis and erysipelas
Treat these bacterial skin infections as described in b p.528.
Necrotizing fasciitis
This is a rare and severe bacterial infection of soft tissues. It can occur
with or without obvious trauma and may follow illicit IM heroin injection
(‘muscle popping’). Strep . pyogenes is often involved, sometimes with
Staph. aureus or other bacteria. Often there are both aerobic and
anaerobic organisms. Infection involves fascia and subcutaneous tissues,
with gas formation and development of gangrene. Infection may spread
to adjacent muscles, causing myonecrosis or pyogenic myositis. Similar
infections may involve the abdomen and groin (Fournier’s gangrene).
Initial symptoms and signs may be vague, with very severe pain, but little
to fi nd on examination: the affected area may be tender, sometimes with
slight erythema and swelling. The patient is usually pyrexial. Infection can
spread rapidly and cause marked soft tissue swelling with discolouration,
bruising, haemorrhagic blisters, or overlying skin necrosis. Toxic shock
may develop and the mortality rate is high. X-rays may show gas in the
soft tissues but may be normal.
Treatment involves resuscitation with IV fl uids and antibiotics (penicillin
and clindamycin), urgent surgery to debride the affected area and excise
necrotic tissues, and intensive care.

235
STAPHYLOCOCCAL INFECTIONS
Staphylococcal infections
Staphylococcus aureus is involved in many infections of wounds, soft tissues
( b p.413), joints and bones ( b p.494 and 705). Staphylococci may
also cause impetigo, scalded skin syndrome, food poisoning, toxic shock
syndrome, endocarditis, pneumonia, septicaemia and meningitis.
Impetigo
A highly infectious superfi cial skin infection caused by staphylococci or
streptococci. It may involve normal skin or complicate a pre-existing
condition, such as eczema or scabies. Lesions often start around the
mouth and nose, spreading rapidly on the face and to other parts of the
body. Irregular golden-yellow crusted lesions occur, particularly in strep-
tococcal infections. Staphylococci may cause bullous impetigo, with bullae
containing pus which rupture and dry to form crusts. Treat with topical
fusidic acid or mupirocin (usually for 7 days, max. 10 days) and give oral
fl ucloxacillin or erythromycin if lesions are widespread or there is cellulitis
or pyrexia.
Scalded skin syndrome
Staph . aureus may produce an exotoxin causing separation of the outer
layers of the epidermis, large sections of which slide off with minimal
pressure, leaving large raw areas resembling a severe scald. Drug allergies
can cause similar lesions. Most cases of scalded skin syndrome (toxic
epidermal necrolysis, Lyell’s syndrome) occur in children. Admit for
nursing and medical care.
Toxic shock syndrome
This is caused by exotoxins from Staph. aureus or (less commonly)
Strep . pyogenes . Some cases during menstruation are related to tampons,
other cases occur after surgical operations, burns, other trauma, or local
infections. There is high fever, a generalized erythematous rash, confusion,
diarrhoea, muscle pains, hypotension, and renal failure. Subsequently,
scales of skin separate from hands and feet. Death may occur from multiple
organ failure. Treat for septic shock with IV fl uids and anti-staphylococcal
antibiotics. Remove tampons and send for culture. Refer to ICU. Involve a
surgeon if an associated abscess requires drainage.
Staphylococcal septicaemia
Occurs particularly in debilitated or immune-compromised patients
and in injecting drug users. There may be endocarditis with metastatic
infection of lungs, bone or soft tissues and gangrene due to emboli or
arterial thrombosis. Signs of meningitis and DIC may suggest meningo-
coccal septicaemia ( b p.224) and the rash may be similar.
Meticillin resistant Staphylococcus aureus (MRSA)
MRSA causes particular concern because of antibiotic resistance and is
carried by many asymptomatic people (patients and staff). Transmission
is minimized by hand washing ( b p.32) and other infection control
measures. An information leafl et about MRSA for patients is available at
www.hpa.org.uk/infections/topics_az/staphylo/mrsa_leafl et.htm

236 CHAPTER 5 Infectious diseases
Tetanus
ND
An acute and often fatal disease, common in much of Asia, Africa, and
South America, especially in neonates. Now rare in developed coun-
tries: 30–40 cases/year in UK, many involving the elderly. Injecting drug
users (eg those ‘skin popping’) are also at particular risk. Spores of the
Gram + ve organism Clostridium tetani (common in soil and animal faeces)
contaminate a wound, which may be trivial. The spores germinate in
anaerobic conditions, producing tetanospasmin, an exotoxin which blocks
inhibitory neurones in the CNS and causes muscle spasm and rigidity.
Incubation period is usually 4–14 days, but may be 1 day to 3 months.
In 20 % of cases there is no known wound. Tetanus occasionally occurs
after surgery or IM injections.
Clinical features
Stiffness of masseter muscles causes diffi culty in opening the mouth
(trismus, lockjaw). Muscle stiffness may spread to all facial and skeletal
muscles and muscles of swallowing. Characteristically, the eyes are partly
closed, the lips pursed and stretched (risus sardonicus). Spasm of chest
muscles may restrict breathing. There may be abdominal rigidity, stiff-
ness of limbs and forced extension of the back (opisthotonus). In severe
cases, prolonged muscle spasms affect breathing and swallowing. Pyrexia
is common. Autonomic disturbances cause profuse sweating, tachycardia
and hypertension, alternating with bradycardia and hypotension. Cardiac
arrhythmias and arrest may occur.
Differential diagnoses
Dystonic reaction to metoclopramide or phenothiazines, strychnine
poisoning, quinsy, dental abscess, meningitis, rabies. Procyclidine relieves
muscle spasms from drug-induced dystonia, but will not affect tetanus;
diazepam may relieve dystonia or tetanic spasms.
Management
Obtain senior medical and anaesthetic help. Monitor breathing, ECG and
BP. Refer to ICU. Control spasms with diazepam. Paralyse and ventilate if
breathing becomes inadequate. Clean and debride wounds. Give penicillin
and metronidazole and human tetanus immune globulin.
Prognosis
Depends on severity of disease and quality of care. Short incubation
(<4 days) and rapid progression suggest severe disease with a high mortality.
With expert intensive care, the mortality in adults is <10 % , but neonatal
tetanus is often fatal.
Immunization
Tetanus is eminently preventable by immunization and by proper care of
wounds ( b p.406, b p.410).

237
BOTULISM
ND
Gas gangrene
This is a rapidly spreading infection of muscle caused by toxin-producing
Clostridial bacteria (anaerobic Gram + ve bacilli), usually C. perfringens .
It is fatal if untreated. It may involve wounds of the buttocks, amputa-
tions for vascular disease or severe muscle injuries (eg gunshot wounds).
Occasionally gas gangrene of the perineum occurs without trauma.
Incubation period is usually <4 days (sometimes a few hours). Sudden
severe pain occurs at the wound site. Generalized toxicity develops,
with tachycardia, sweating and fever. Swelling and skin discolouration
occur around the wound, with a serous ooze, marked tenderness and
sometimes haemorrhagic vesicles and crepitus. Shock and renal failure
develop, with death often within 2 days of the fi rst symptoms.
Diagnosis depends on clinical features. Severe pain necessitates wound
inspection (remove or window any plaster of paris (POP). Obtain
immediate senior surgical advice if gas gangrene is suspected. The wound
discharge may contain Gram + ve bacilli. X-rays may show soft tissue gas,
but its absence does not exclude gas gangrene.
Treatment IV antibiotics (penicillin and clindamycin), immediate surgical
removal of all infected tissue, and intensive care. Hyperbaric O
2
and gas
gangrene antitoxin are rarely available and of no proven benefi t.
Botulism
ND
The exotoxin of Clostridium botulinum paralyses autonomic and motor
nerves by blocking acetylcholine release at neuromuscular junctions and
nerve synapses. Infection occurs from eating tinned or preserved food
contaminated with C. botulinum spores: cases have involved sausage,
tinned salmon, hazelnut yoghurt and other foods. Rarely, C. botulinum
infects wounds or colonizes the gut. Injecting drug users may develop
botulism after IM or SC injections of contaminated drugs.
Incubation period is 12–72hr. Initial symptoms may be GI (nausea, vomiting,
abdominal discomfort, dryness of the mouth) or neurological (dizziness,
blurred vision, diplopia). Later problems include dysarthria, dysphagia,
muscle weakness or paralysis, constipation and urinary retention, respiratory
failure, and sudden death. Susceptibility varies: some people who eat
contaminated food develop no symptoms or suffer only mild fatigue.
Clinical signs result from involvement of autonomic and motor nerves:
dry mouth, cranial nerve palsies (ptosis, squint, fi xed pupils, weakness of
tongue), limb weakness with fl acid muscles. Consciousness and sensation
are preserved. Hypotension and ileus may occur. Fever is unusual.
Differential diagnoses are Guillain–Barré syndrome, myasthenia, brainstem
stroke, diphtheria, poisoning (anticholinergics or organophosphates),
paralytic rabies. Botulism may be misdiagnosed as staphylococcal food
poisoning, paralytic shellfi sh poisoning, CO or mushroom poisoning.
Management Get senior help. Assess breathing, ventilate if necessary and
admit to ICU. Botulinum antitoxin reduces mortality and morbidity: see BNF
and TOXBASE ( b p.181). Inform Public Health: others who have eaten
contaminated food may need urgent treatment. Anticipate media enquiries
and the arrival of worried people with tins of suspicious food.

238 CHAPTER 5 Infectious diseases
Sexually transmitted diseases
The commonest sexually transmitted disease (STD) is non-specifi c genital
infection. Other common diseases include chlamydia, gonorrhoea, genital
herpes, trichomoniasis, genital warts, pediculosis pubis, HIV, and syphilis.
Many patients have more than one disease. Suspicion of STD necessi-
tates prompt referral to a genitourinary (GU) medicine clinic for proper
diagnosis, treatment and follow-up of the patient and contacts. Some GU
departments provide an on-call service. Only prescribe antibiotics for
suspected STDs on the advice of a GU specialist.
Genital ulcers and sores
Most genital ulcers/erosions are either multiple and painful or single
and painless. In the UK, multiple genital ulcers are most often due to
herpes simplex; other causes are Behçet’s disease and (rarely) chancroid
or scabies. Multiple painful sores may occur with gonorrhoea, candida,
or other conditions. Painless genital ulceration should suggest syphilis
(primary chancre is a single ulcer, secondary syphilis often multiple:
both are highly infectious and incidence has i recently). Other causes of
painless ulcers include carcinoma and trauma (possibly self-infl icted).
Urethritis
In men, dysuria and urethral discharge are the commonest presenting
symptoms of an STD. However, 5–10 % of men with gonococcal or
non-gonococcal urethritis have no symptoms. Urethritis may result from
physical trauma, foreign bodies or attempts at self-treatment with intra-
urethral chemicals.
Gonorrhoea usually has a shorter incubation period (3–5 days) than non-
gonococcal urethritis (eg chlamydia 7–14 days), but do not rely on a clinical
diagnosis: refer to a GU clinic for diagnosis, management and follow-up.
If no GU advice is available and treatment cannot wait for attendance at
a GU clinic, give doxycycline 200mg PO stat and then 100mg PO daily (or
tetracycline 500mg PO qds). If possible, make a glass slide of the discharge,
dried in air, for the patient to take to the clinic. He should be told not to
pass urine for 4 hours before the appointment, in order to allow serial
urine samples to be taken.
Reiter’s disease is a rare complication of non-gonococcal urethritis. There
is arthritis (mainly of knees, ankles and feet) and sometimes conjunctivitis,
rashes and cardiac and neurological problems.
Gonorrhoea
Gonorrhoea may infect the urethra, cervix, rectum, pharynx or conjunc-
tiva. Men usually have dysuria and urethral discharge, with rectal discharge
and tenesmus in homosexuals. Women are often asymptomatic, but may
have dysuria and vaginal discharge.
Complications include prostatitis, epididymitis, salpingitis, Bartholin’s
abscess; rarely septicaemia with arthritis, fever, rash (maculopapular
initially, then pustular) and endocarditis.

239
HEPATITIS AND LEPTOSPIROSIS
Hepatitis
ND
Hepatitis A (infectious hepatitis)
ND
Hepatitis A occurs throughout the world, but is particularly common in
the tropics and subtropics. It is transmitted by contamination of food or
water with infected faeces or urine. Many infections are asymptomatic.
The incubation period is 2–6 weeks (usually 8 4 weeks). Fever, malaise,
anorexia and nausea may last for 2–7 days before jaundice develops.
Jaundice is more common in adults than in children and is associated with
dark urine, pale stools and tender hepatomegaly.
Treatment is symptomatic, but alcohol should be avoided. Infectivity is
greatest before jaundice develops, so isolation is of little value. Arrange
follow-up by a specialist or GP. Complete recovery is usual. Hepatitis A
vaccine should be considered for close contacts (see BNF ).
Hepatitis B
ND
Hepatitis B is transmitted by infected blood (eg shared needles in drug
abusers, tattooing, needlestick injury) and by sexual intercourse. The incuba-
tion period is 6 weeks to 6 months. The symptoms are similar to hepatitis A,
often with arthralgia and skin rashes. Most patients with hepatitis B recover
completely. A few patients develop liver failure or chronic hepatitis, with a
risk of primary liver cancer. Refer to a specialist for follow-up. Asymptomatic
carriers of hepatitis B virus are common ( 8 0.1 % of the population in the UK,
but 8 20 % in parts of Africa and Asia). Because of the high risk of infection,
all health care workers should be immunized against hepatitis B and use
‘standard precautions’ ( b p.32) when handling all blood samples and
‘sharps’. The management of needlestick injury is described on b p.418.
Hepatitis C, D, and E
ND
Hepatitis C and D are spread in the same way as hepatitis B, and may cause
hepatic failure or chronic liver disease. No immunization is available.
Hepatitis E is similar to hepatitis A, but has a high mortality in pregnancy.
Refer to a specialist for follow-up.
Leptospirosis (Weil’s disease)
ND
Leptospirosis, caused by the spirochaete Leptospira interrogans and other
Leptospira species, is spread by contact with infected rat’s urine, often in
rivers, canals or sewers. The leptospires enter the body through small
breaks in the skin or via mucous membranes of the eyes or nose. About
10 days after exposure (range 2–26 days) the illness starts with fever,
severe muscle pains, headache, sore throat, nausea and vomiting.
Conjunctival reddening is common. A haemorrhagic rash, jaundice, renal
failure and pulmonary haemorrhage may occur (Weil’s disease).
Refer to an Infectious Diseases unit. Treatment is with penicillin or
doxycycline with supportive care and haemodialysis if necessary.
Prophylactic doxycycline is reasonable for people who fall into waterways
likely to be contaminated with leptospires.

240 CHAPTER 5 Infectious diseases
Herpes virus infections
Varicella zoster
Chickenpox results from primary infection with varicella zoster virus, which
then remains dormant in the dorsal root ganglia. Reactivation of the virus
causes shingles . Chickenpox is usually a mild disease of childhood. An itchy
vesicular rash appears, most densely on the trunk and face, but decreasing
peripherally. The lesions appear in crops and crust over in 3–4 days. Fever,
malaise and muscle aches may occur in adults. Infectivity starts 3 days
before the rash appears and lasts until the last lesion has crusted.
Treat symptomatically, eg calamine lotion for itching and paracetamol for
fever. Occasionally, antibiotics are needed for secondary bacterial skin
infection (usually Staph . or Strep .). Pneumonia is rare and in children is
usually staphylococcal, but in adults may be caused by chickenpox virus.
Chickenpox may be severe in neonates and in patients with cystic fi brosis
or immune defi ciency, who need specialist assessment and treatment with
aciclovir and/or varicella-zoster immune globulin. Consider aciclovir also
for adults and older adolescents (see BNF ).
Shingles often occurs in the elderly and may affect any dermatome, most
often thoracic. The pain of shingles may cause diagnostic diffi culty until
the rash appears, usually after 1–4 days. Erythema is followed by vesicles
and then crusting of lesions in a unilateral distribution over 1 dermatome
or 2 adjacent dermatomes. Ophthalmic shingles may affect the eye via
the long ciliary nerves: skin lesions on the side of the tip of the nose
imply a high risk of eye involvement. Oral lesions occur in maxillary and
mandibular shingles. Infection of the geniculate ganglion causes a facial
palsy with lesions in the pinna of the ear and on the side of the tongue
and hard palate (Ramsay–Hunt syndrome ). In severe shingles there may be
weakness of muscles supplied by nerves of the same spinal root.
Antiviral treatment (aciclovir, famciclovir, or valaciclovir) d risk of post-herpetic
pain if given early (within 72hr of start of rash). Dose : aciclovir 800mg 5 times
daily for 7 days. In renal failure antiviral drugs may cause severe toxicity, so
use much smaller or less frequent doses. Patients with immune defi ciency or
ophthalmic zoster need immediate specialist referral and antiviral treatment.
Give analgesia. Antibiotics may be required for secondary infection.
Herpes simplex
Primary herpes simplex infection causes painful vesicles and ulceration of
the mouth or genitalia ( b p.238). The virus may be inoculated into skin
by trauma (herpes gladiatorum, scrumpox) or by contamination of fi ngers
causing herpetic paronychia (whitlow). Infection of the cornea may cause
dendritic ulcers ( b p.543). Herpes simplex meningitis and encephalitis
ND
are uncommon, but may be fatal, especially in immunodefi cient patients.
The herpes simplex virus persists in sensory ganglia and may be reactivated
by stimuli such as sun, cold, trauma, or viral infections. Recurrence of cold
sores of the lips is often preceded by tingling: aciclovir cream or tablets
may prevent the development of vesicles. Secondary bacterial infection
may require antibiotics. Do not incise a suspected whitlow. Cover it with
a dressing and advise care to avoid spreading infection to the lips or eyes.

241
INFECTIOUS MONONUCLEOSIS (GLANDULAR FEVER)
Infectious mononucleosis
(glandular fever)
Infection with the Epstein–Barr virus is common in children and young
adults and is spread by saliva or droplets. Infection often occurs without
clinical disease. In glandular fever there is malaise, fever, a sore throat,
and cervical lymphadenopathy. The throat may be very red and in 25 % of
cases there is also infection with a B -haemolytic streptococcus. In severe
cases there is marked oedema of the throat with tonsillar swelling and a
membranous exudate (‘anginose’ infectious mononucleosis) with diffi culty
in swallowing and breathing. A rash is uncommon unless ampicillin or
amoxicillin are given, causing a widespread erythematous maculopapular
rash (which does not signify allergy to penicillins in general).
Complications of infectious mononucleosis include respiratory obstruction,
ruptured spleen (spontaneously or after minor trauma), thrombocytopenia,
jaundice, meningitis, encephalitis, facial palsy, and acute polyneuritis
(occasionally causing respiratory failure).
Investigations FBC and blood fi lm (for atypical lymphocytes), Monospot
test or Paul–Bunnell test (which may be –ve initially).
Differential diagnosis includes cytomegalovirus and toxoplasmosis.
Treatment is unnecessary in most patients. Severe or complicated cases
need specialist assessment and follow-up. In anginose infectious mono-
nucleosis, a short course of high dose oral steroids gives rapid relief of
symptoms (prednisolone 80mg on day 1; 15mg tds on days 2–3; 10mg tds
on days 4–5; 5mg tds on days 6–7). Steroids are also helpful in patients
with neurological complications. Concurrent B -haemolytic streptococcal
infection requires erythromycin (500mg qds), which would also treat the
rare unrecognized case of diphtheria.

242 CHAPTER 5 Infectious diseases
Human immunodefi ciency virus (HIV)
First reports of acquired immune defi ciency syndrome (AIDS) involved
homosexuals in the USA in 1981. HIV (previously called HTLV-III, LAV, or
ARV) was identifi ed as the causative agent in Paris in 1983.
Structure and pathogenesis
HIV is an RNA retrovirus. Retroviruses are characterized by having the
enzyme reverse transcriptase. This allows viral RNA to be transcribed
(copied) into DNA and incorporated into host cells, which then make a
new virus. This mechanism has proved diffi cult to overcome: no ‘cure’ or
‘vaccine’ is yet available.
Glycoproteins on the surface of HIV bind to specifi c receptors on target
cells. The cellular receptor for HIV is the CD4 molecule. CD4 receptors
are found on a variety of cells, particularly helper/inducer T lymphocytes
(‘CD4 cells’), but also monocytes and macrophages. CD4 cells normally
play a crucial role in co-ordinating the immune response: as HIV infection
progresses and CD4 cell counts d , the patient develops profound cellular
immunodefi ciency. Although other complex mechanisms are also involved,
CD4 cell counts provide a useful index of disease stage and progress.
Transmission
HIV has been found in many body fl uids, but is mostly transmitted via
blood, semen, cervical secretions and, perhaps, breast milk. It may be
acquired by:
• Sexual intercourse (vaginal or anal), with i risk of transmission where
individuals already have a genital mucosal breach (eg co-existent STD).
• Risk of transmission from HIV + ve pregnant mother to baby is 8 15 % .
• Transfusion of unscreened blood/blood products (screening started in
1985 in the UK).
• Contaminated needles shared amongst IV drug abusers. Needlestick
injuries from an HIV positive source carry a risk of 8 0.3 % .
Diagnosis and HIV testing
Antibodies to HIV provide evidence of infection and form the basis of
current blood tests, but these antibodies may not appear until 3 months
after exposure. HIV testing is not appropriate in the ED, but reserved
for clinics where informed consent and counselling are available. Refer
patients requesting HIV tests to local Infectious Diseases/GU clinics or
advisory organizations, eg Terrence Higgins Trust (tel. 0808 802 1221), or
the NHS Sexual Health Helpline (24hr freephone 0800 567 123).
Natural history of HIV infection
HIV infection progresses through phases, which form the basis of the
two commonly used classifi cation systems (World Health Organization
(WHO) and CDC systems).
Acute infection is often sub-clinical, but 2–6 weeks after exposure there
may be a non-specifi c febrile illness with lethargy, myalgia, sore throat,
lymphadenopathy, and often a maculopapular rash on the face and trunk.
This illness usually resolves after 1–2 weeks but sometimes persists for
longer. A long asymptomatic period ( 8 10 years) follows the initial illness.

243
HUMAN IMMUNODEFICIENCY VIRUS (HIV)
Some patients develop persistent generalized lymphadenopathy (PGL),
with lymphadenopathy ( > 1cm) at two non-inguinal sites for 3 months.
Patients become symptomatic as their immunity d , developing unusual
infections and tumours. Many are ‘AIDS-defi ning diseases’ (see below).
The label ‘AIDS’ has signifi cant psychological connotations. Most patients
with AIDS survive > 2 years.
Anti-retroviral drugs (AZT and other drugs) delay the onset of AIDS in
asymptomatic patients and i length of survival. ‘HAART’ (highly active
antiretroviral therapy) is a regime combining 3 or more anti-HIV drugs.
Initial presentation of HIV to the emergency department
Many HIV + ve patients attending the ED are aware of their HIV status.
Some patients, however, present with HIV-related illness, without
knowing (or admitting) that they are HIV + ve. Presentation of any of the
diseases listed below should arouse particular suspicion.
Centers for Disease Control classifi cation of HIV infection
Group I Acute infection
Group II Asymptomatic
Group III Persistent generalized lymphadenopathy
Group IV Symptomatic infection with subgroups:
A — constitutional disease (fever, diarrhoea, weight loss)
B — neurological disease (dementia, peripheral neuropathy)
C — secondary infectious diseases
D — secondary cancers (lymphomas, Kaposi’s sarcoma)
E — other conditions
Some AIDS-defi ning diseases in HIV + ve patients
• Pneumocystis jiroveci pneumonia (previously called P. carinii ).
• Kaposi’s sarcoma.
• Tracheobronchial or oesophageal candidiasis.
• Cerebral toxoplasmosis.
• Pulmonary TB.
• Cytomegalovirus retinitis.
• Cerebral lymphoma.
• Recurrent Salmonella septicaemia.
• Disseminated histoplasmosis.
• Invasive cervical carcinoma.
• Disseminated coccidioidomycosis.
• Cryptococcosis.
• Cryptosporidiosis.
• Progressive multifocal leucoencephalopathy.
• Oesophageal or bronchial herpes simplex.
CD4 counts and AIDS
CD4 counts provide an indication of disease progession: many HIV
+ ve patients know what their last count was. In the USA, CD4 counts
<200/mm
3
may also be used to defi ne AIDS.

244 CHAPTER 5 Infectious diseases
Presentation of HIV + ve patients
Many patients with symptomatic HIV infection bypass the ED and liaise
directly with the specialist unit caring for them. Assessment of HIV + ve
patients is diffi cult in the ED, where advanced infections may present with
relatively few signs and little past history is available. Similarly, interpreta-
tion of investigations is diffi cult without knowledge of previous results.
It is therefore reasonable to have a low threshold for specialist referral.
HIV + ve patients may present with a variety of complications:
Respiratory problems
As CD4 counts d , pneumonia due to Pneumocystis jiroveci (previously
Pneumocystis cariniii ) becomes more likely and it is a common indicator
diagnosis of AIDS. A non-productive cough occurs with dyspnoea and
fever. CXR may show bilateral interstitial mid-zone shadowing, but may
be normal. Obtain blood and sputum cultures, rehydrate with IV fl uids
as necessary and refer urgently for IV co-trimoxazole or pentamidine ±
steroids. Occasionally, Pneumocystis infection may present with fulminant
respiratory failure needing emergency tracheal intubation and IPPV. Other
common infections include Aspergillus , Cryptococcus and TB. Injecting drug
users are at increased risk of bacterial infection, especially Haemophilus
infl uenzae and Strep. pneumoniae .
Neurological problems
Cryptococcus neoformans meningitis may present with headache, fever and
sometimes d conscious level. Neck stiffness and photophobia are rare.
Obtain a CT scan to exclude space-occupying lesions before LP and CSF
examination. Cerebral toxoplasmosis may present similarly, often with
focal signs or fi ts. Neurological problems may also be caused by cerebral
lymphoma, progressive leucoencephalopathy (focal defi cits secondary to
papovaviruses), CMV encephalitis (retinopathy is usually present — see
below) and HIV-associated delirium or dementia.
Eye problems
The most signifi cant eye problem is Cytomegalovirus (CMV) retinitis ,
occurring in 15 % of patients. This presents with blurred vision, blind spots,
‘fl oaters’ or fl ashing lights, and d VA. Characteristic retinal changes are
irregular yellow-white lesions and perivascular haemorrhages that have
been called ‘pizza pie’. Retinal detachment may occur. Refer urgently for
ophthalmological assessment and treatment with ganciclovir or foscarnet.
Mucocutaneous problems
Oral candidiasis, seborrhoeic dermatitis, and oral hairy leukoplakia (white
ridges on lateral border of tongue) are often seen before AIDS develops.
As immunity d , patients may develop herpes simplex, herpes zoster and
molluscum contagiosum. Gum bleeding and dental problems are common:
the former may be due to thrombocytopenia. Kaposi’s sarcoma is seen in
skin and mucous membranes, particularly in homosexuals with AIDS. It is
rarely life-threatening, but requires specialist evaluation and treatment.

245
PRESENTATION OF HIV +VE PATIENTS
Gastrointestinal problems
Nausea, vomiting, diarrhoea and weight loss are common complaints
and can be due to drug therapy. Dysphagia may result from oesopha-
geal candidiasis, herpes simplex, CMV, or Kaposi’s sarcoma, all of which
require specialist investigation and treatment.
CMV colitis can cause a serious illness, characterized by abdominal pain,
diarrhoea and fever. Obtain plain X-rays if the recognized complication
of toxic dilatation is suspected. Other frequently implicated infective
causes of diarrhoea include cryptosporidium, Giardia , microsporidium and
Salmonella . Send stool specimens (including for Clostridium diffi cile ) and
treat severe diarrhoea by IV rehydration and correction of electrolyte
imbalance before referral.
Hepatitis viruses are likely to complicate the picture in injecting drug
users, many of whom are infected with hepatitis B and C.
Drug reactions and side effects
Many patients will present with symptoms due to drug therapy. This may
not be initially apparent: the safest approach is to exclude tumours and
opportunistic infection fi rst.
HIV and emergency department staff
ED staff are often concerned about the possibility of acquiring HIV
from patients. The need to perform invasive emergency procedures on
‘high risk’ patients makes these concerns understandable. Additionally,
apparently ‘low risk’ patients may also pose a threat. Therefore treat
every patient as if he is ‘high risk’. The risk to ED staff is largely in the form
of needlestick injury (although the risk of acquiring HIV following needle-
stick from a HIV + ve source can be d by post-exposure prophylaxis — see
b p.418). Safe practice is refl ected in the recommended standard pre-
cautions (see b p.32) — follow these in all patients. Pregnant staff should
not treat patients with AIDS (because of concern about CMV and herpes
simplex virus).
Handling HIV + ve patients
Despite vigorous attempts to educate the general public, HIV and AIDS
remain taboo subjects amongst many in society. It is imperative to treat
all patients, including those who are HIV + ve, with sensitivity and compas-
sion. Touching and shaking hands with HIV + ve patients is perfectly safe,
and may help to reassure them that the discrimination and irrational treat-
ment they may have received outside hospital does not extend into the
ED. In view of prevailing attitudes towards HIV, patient confi dentiality is of
the utmost importance. Remember that family and friends accompanying
the patient may be unaware of his HIV status.
HIV + ve staff
The risk to patients from ED staff infected with HIV is minimal, but remains
a theoretical possibility. Staff who believe that they may be HIV + ve must
obtain and follow occupational health advice.
Needlestick injury: See b p.418.

246 CHAPTER 5 Infectious diseases
Imported infectious diseases
Patients may present to the ED with infectious diseases acquired abroad.
It is essential to ask where a patient has been, especially in the 6 weeks
before the onset of symptoms. The most common imported diseases
are bowel infections causing diarrhoea ( b p.226). Less common, but
very important diseases include malaria ( b p.247), typhoid ( b p.248),
Legionnaires’ disease ( b p.110) and hepatitis ( b p.239). Rabies ( b
p.249) and viral haemorrhagic fevers, such as Lassa fever ( b p.250) are
very rare in the UK.
Occasionally, tropical diseases are acquired in Britain from bites by
infected insects carried by plane (eg ‘airport malaria’).
Advice about tropical diseases is available from departments of Infectious
Diseases or Tropical Medicine:
• Birmingham (Heartlands Hospital). www.heartofengland.nhs.uk Telephone
0121 424 2000.
• Liverpool (School of Tropical Medicine). www.liv.ac.uk/lstm Telephone
0151 705 3100.
• London (Hospital for Tropical Diseases) www.thehtd.org/Emergencies.
aspx Telephone 0845 155 5000.
• Oxford (Churchill Hospital) Telephone 01865 741 841.
• Glasgow (Brownlee Centre for Infectious and Communicable Diseases,
Gartnavel General Hospital) Telephone 0141 211 3000.
• A public access website provided by the NHS which gives information
for people travelling abroad from the UK is www.fi tfortravel.scot.
nhs.uk
Pyrexia of unknown origin in travellers
Think of and check for malaria ( b p.247) in any febrile patient who has
been in a malarious area. Consider Lassa fever ( b p.250) in someone who
has been in West Africa in the previous 3 weeks. Typhoid ( b p.248) often
presents as a septicaemic illness with constipation, rather than diarrhoea.
TB ( b p.232) and brucellosis may cause fever and sweating at night.
Investigations (warn lab of possible risks)
FBC, thick and thin blood fi lms for malaria, U&E, blood glucose, blood
culture, urine stick testing, microscopy and culture, CXR.
Further investigations may include LFTs and viral titres.
Management Barrier nurse in a cubicle (use a negative pressure room if
available). Wear gown, gloves, goggles and mask. Record vaccination and
prophylaxis history, with countries and areas visited, and dates of travel
and onset of symptoms. Look particularly for confusion, dehydration,
jaundice, rashes, chest signs, liver and spleen enlargement and tenderness,
lymphadenopathy, neck stiffness, photophobia. Seek expert advice at once
if the patient is very ill or there is concern about typhoid or Lassa fever or
other viral haemorrhagic fevers. Refer to an Infectious Diseases specialist.

247
MALARIA
ND
Malaria
ND
Malaria is very common in the tropics and subtropical regions, and is a
parasitic infection transmitted by mosquitoes. The fi ve species which
cause malaria in humans are Plasmodium falciparum, P. vivax, P. malariae,
P. ovale, and P. knowlesi. Falciparum (‘malignant tertian’) malaria is the
most important, since it may be rapidly fatal and drug-resistant strains are
common. Serious complications are unusual in the other types of malaria,
but they may cause febrile convulsions in children.
In the UK malaria occurs in travellers from malarious areas, especially
P. vivax from the Indian subcontinent and P. falciparum from Africa, South-
East Asia, and Central and South America. Malaria often develops despite
antimalarial tablets, because of drug resistance or incorrect dosage. Check
for malaria in any febrile illness within 2 months of visiting a malarious
area. Common misdiagnoses are infl uenza and viral hepatitis.
Clinical features
The incubation period is usually 7–14 days for P. falciparum and 12–40 days for
other types of malaria, but occasionally it is much longer ( > 1 year), especially
in P. malariae and P. vivax infections. There is malaise, fatigue, fever and head-
ache followed by paroxysms lasting 8–12hr of rigors, vomiting and then severe
sweating. The fever may be periodic (classically 48hr in P. ovale or P. vivax,
and 72hr in P. malariae ). Haemolytic anaemia, jaundice and splenomegaly may
occur, but lymphadenopathy is not a feature. P. falciparum may cause cerebral
malaria with coma, fi ts and focal neurological signs. Diarrhoea, cardiac failure,
pulmonary oedema and shock may occur. Deterioration can be rapid.
Investigations
Consider Lassa fever ( b p.250) in recent visitors to West Africa. In any
ill patient who has been in a malarious area send blood for thin and thick
fi lm examination for malaria. Repeated blood fi lms may be needed. Also
arrange FBC (since malaria may cause anaemia, thrombocytopenia and
neutropenia), blood glucose (hypoglycaemia may be severe), U&E (renal
failure is possible), and test the urine for blood (‘black water fever’).
Treatment of falciparum malaria
1
Careful monitoring is needed ± ICU. Obtain expert advice from a tropical
disease specialist ( b p.246), especially if the patient is severely ill or has
come from south-east Asia, where there is widespread drug resistance.
Give quinine, orally or IV depending on the severity of illness: oral quinine
sulphate 600mg (adult) or 10mg/kg (child) every 8hr for 7 days, followed
by doxycycline 200mg od for 7 days, clindamycin 450mg tds for 5 days or
Fansidar
®
3 tablets. Alternative oral drugs are Malarone
®
(proguanil with
atovaquone) or Riamet
®
(artemether with lumefantrine): for details see
BNF. For algorithm
1
see www.britishinfectionsociety.org .
Treatment of benign malarias ( P. vivax, ovale, malariae )
1
The usual treatment is chloroquine (see BNF ). A course of primaquine is
also needed to prevent relapse in vivax and ovale infections, but glucose-
6-phosphate dehydrogenase levels should be checked before primaquine
is used, since it may cause haemolysis in G6PD defi cient patients. In the
UK refer to an Infectious Diseases unit for treatment and follow-up.
1 Lalloo DG et al . ( 2007 ) UK malaria treatment guidelines . Journal of Infection 54 : 111 – 121 .

248 CHAPTER 5 Infectious diseases
Typhoid
ND
and paratyphoid
ND
(enteric fever)
These fevers, caused by Salmonella typhi and S. paratyphi A, B, or C, occur
throughout the world, especially where hygiene is inadequate. They
are spread by contamination of food or water by urine or faeces from
a patient or an asymptomatic carrier. Typhoid may occur despite immu-
nization. Typhoid and malaria are the fi rst diseases to consider if fever
develops soon after a visit to the tropics. The incubation period is usually
7–14 days, but may range from 3–60 days.
Initial symptoms
Headache, fever, and a dry cough, with abdominal discomfort and
anorexia. Constipation is common, but diarrhoea may occur, especially in
children. Confusion and hallucinations may develop.
Physical examination
This may be normal except for fever. There may be a relative brady-
cardia (ie less than the usual 15 beats/min i in pulse rate per ° C of
fever). Splenomegaly and abdominal tenderness occur, but there is no
lymphadenopathy. ‘Rose spots’ are pink macular spots on the lower chest
or upper abdomen which blanch on pressure. There may be signs of
pneumonia or dehydration. Intestinal perforation or haemorrhage occur
occasionally.
Investigations
FBC (mild anaemia is common, WBC usually normal), blood fi lms for
malaria, U&E, LFTs, blood cultures, CXR (for signs of TB or pneumonia).
Treatment
Isolate and barrier nurse. Admit suspected cases to an Infectious Diseases
unit and notify the local consultant in Communicable Disease Control.
The usual drug treatment is with ciprofl oxacin or cefotaxime but other
antibiotics may be needed for drug-resistant infections.
Dengue
Dengue is a mosquito-borne viral infection which is common in southern
Asia, the western Pacifi c, central Africa and central and south America.
Most infections are asymptomatic. Symptoms start after an incubation
period of 4–7 days with fever, malaise, nausea and vomiting, headache,
severe muscle and bone pains (‘break bone fever’). Some patients have
a transient macular rash, petechiae, lymphadenopathy, hepatomegaly,
d WCC and platelets and i liver enzymes.
Most patients recover after 3–7 days with symptomatic treatment. A few
develop dengue shock syndrome (DSS) with hypotension, pleural
effusions, ascites, d plasma protein and bleeding problems. Abdominal
pain may be severe. Treatment is supportive, with careful fl uid balance
management and IV fl uids in DSS. With expert care most patients with
severe dengue eventually make a full recovery.

249
RABIES
ND
Poliomyelitis
ND
Paralytic poliomyelitis is rare in developed countries where vaccination
is routine. Fever is followed by signs of meningitis, pain and spasm in limb
muscles. Respiratory failure may be fatal.
Resuscitate and ventilate if necessary and refer to ICU.
The differential diagnosis includes Guillain–Barré syndrome ( b p.142) and
organophosphate poisoning ( b p.206).
Rabies
ND
Rabies is a viral infection of mammals that occurs in most parts of the
world, including much of the Arctic, as well as tropical and temperate
regions. At present it is not endemic in the UK, Norway, Sweden, Iceland,
Australasia, or Japan. Human and animal rabies is most common in the
Indian subcontinent, China, Thailand, the Philippines, and parts of South
America. Most human infections result from dog bites, but rabies can be
transmitted by many other domesticated or wild animals, such as cats and
foxes. Rabies virus in an animal’s saliva may cause infection by contamina-
tion of a bite or scratch or by absorption through mucous membranes of
the eye, mouth or nose. Rarely, infection occurs from inhalation of the
virus in bat-infested caves.
Prevention of rabies after a bite is described on b p.415.
Advice about post-exposure treatment and suspected cases of rabies is
available in the UK from the Health Protection Agency. For details see
www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Rabies
Clinical features
The incubation period of rabies is usually 3–12 weeks, but can vary from a
few days to > 2 years.
The fi rst symptoms are itching, tingling or pain at the site of the bite
wound. Headache, fever, and malaise occur, with spreading paralysis
and episodes of confusion, hallucination and agitation. Hydrophobia is
characteristic: attempts at drinking cause spasm of muscles involved in
breathing and swallowing and also profound terror. In 8 20 % of cases
there is ‘dumb rabies’ with increasing paralysis but no episodes of spasm
or hyperactivity. Rabies is almost always fatal, even with ICU treatment.
Management
If rabies is suspected, barrier nurse the patient in a quiet room with the
minimum of staff, who must wear gowns, gloves, eye protection and
masks. Obtain advice immediately from a specialist in Infectious Diseases.
Anticipate press enquiries. Record the names of all staff involved, so that
they can be offered rabies immunization.

250 CHAPTER 5 Infectious diseases
Viral haemorrhagic fevers
ND
Lassa fever
Lassa fever occurs in many rural parts of West Africa. It is a viral infection
acquired from infected blood or secretions, transmitted by inadvertent
innoculation (eg needlestick injuries) or contamination of mucous mem-
branes or broken skin. In Africa it is transmitted by multimammate rats.
The incubation period is up to 3 weeks. There is a high mortality.
Early symptoms are non-specifi c with fever, malaise, headache, sore
throat, retrosternal chest pain and backache. Periorbital oedema, swelling
of the neck and conjunctival injection are common. Suspect Lassa fever
in any pyrexial patient who has been in rural West Africa (south of the
Sahara) in the previous 3 weeks. However, malaria and typhoid are much
more common and need urgent diagnosis and treatment.
Management If Lassa fever is possible, barrier nurse the patient in a
cubicle by staff wearing gloves, gowns, goggles and masks. Take special
care to avoid needlestick injuries, which may cause fatal infection. Before
taking any blood samples, discuss the case with a tropical diseases
specialist and the local consultant in Communicable Disease Control.
Start treatment immediately for falciparum malaria ( b p.247). Warn the
laboratory about Lassa fever and send blood for examination for malaria.
The patient will be admitted to an isolation bed, possibly in a high security
Infectious Diseases unit.
Ebola fever and Marburg fever
These are viral haemorrhagic fevers which occur in West and Central
Africa (Zaire, Uganda, Kenya and Sudan), and have similar clinical features
and a high mortality. Transmission is usually by infected blood, but the
viruses may be acquired from monkeys or apes. The incubation period is
usually 4–10 days. Illness starts suddenly with severe headache, high fever,
and generalized pains, especially in the back, followed by severe diarrhoea,
abdominal pain, dry throat, a maculopapular rash, conjunctivitis, and
gastrointestinal bleeding. Isolate and treat as for suspected Lassa fever.
Other viral haemorrhagic fevers
Diseases with similar features (plus in some cases jaundice) include dengue
(see b p.248), Crimean-Congo fever (central Africa, parts of Eastern
Europe, and Asia) and yellow fever (Africa and South America). The initial
management is the same as for Lassa fever.

251
SEVERE ACUTE RESPIRATORY SYNDROME
Severe acute respiratory syndrome
Background
Severe acute respiratory syndrome (SARS) is a viral respiratory illness
caused by a coronavirus. SARS was fi rst recognized in March 2003, but
probably originated in November 2002 in the Guangdong province of
China, where the virus has been found in wild animals. SARS spread to
several countries, causing deaths in south-east Asia and Canada in March to
May 2003. Few cases have occurred since then. No cases are known at the
time of writing, but there is concern that SARS may re-emerge from China.
Spread
SARS is spread by respiratory droplets produced when an infected person
coughs, sneezes, or uses a nebulizer. The virus can also spread when
someone touches an object contaminated by infectious droplets and then
touches his/her mouth, nose, or eyes.
Features
The incubation period of SARS is usually 2–7 days, but may be up to 10 days.
The illness starts with fever ( > 38 ° C), usually associated with rigors, head-
ache, muscle pains and malaise. Diarrhoea may occur. Some patients have
mild respiratory symptoms initially. A dry cough develops after 2–7 days,
with increasing breathlessness from hypoxia caused by pneumonia. Consider
the possibility of SARS in a patient with these symptoms who, within 10 days
of the onset of illness, has visited an area where SARS may occur (especially
China) or worked in a laboratory holding SARS virus samples.
CXR may be normal or may show patchy infi ltrates, and later areas of
consolidation. WCC is usually normal or d initially (lymphopenia).
Management
If SARS is suspected, get expert help (ED consultant, Infectious Diseases
specialist, and infection control staff) and isolate the patient (if possible
in a negative pressure room). Ensure that the minimum number of staff
have contact with the patient. Staff who do have contact must wear masks
or respirators (of FFP3 standard), goggles, gowns and gloves, with strict
handwashing and careful disposal of all items. Provide the patient with an
N95 mask or a surgical mask. Record SpO
2
and give O
2
if necessary, but
avoid fl ow rates of > 6L/min, to minimize virus aerolization. If bronchodila-
tors are needed, use a spacer inhaler rather than a nebulizer. Maintain a
list of all contacts. Expect press enquiries.
An expert will help to assess to decide about admission. Those admitted
should ideally be placed in a negative pressure isolation room with full
infection control measures. Treat as for community-acquired pneumonia
( b p.110).
Further information about SARS is available from:
• www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/
SevereAcuteRespiratorySyndrome/ (Health Protection Agency, UK).
• www.who.int/csr/sars/en/index.html (World Health Organization).

252 CHAPTER 5 Infectious diseases
Infl uenza pandemics, avian fl u, and
swine fl u
Background
Infl uenza is common in the UK and many other countries, particularly
during winter. Most people are ill for only a few days with fever, muscle
aches, coughing and nausea, but there are some deaths, especially in
elderly people.
Pandemic infl uenza occurs when a new subtype of infl uenza A emerges,
which can spread easily from person to person and which is different
from previous strains (so there is no pre-existing immunity). Infl uenza
pandemics occurred in 1918–1919 (with 40–50 million deaths worldwide,
including many children and young adults), and also in 1957 and 1968.
Another pandemic could develop at any time. There was concern about
infl uenza A subtype H5N1, which infected poultry in Hong Kong in
1997 and 2003 and spread to birds across south-east Asia, with carriage
by migrating birds across Asia and to Europe and Africa. This avian fl u
infected many millions of birds and some people in south-east Asia
and Turkey who had been in close contact with infected chickens. The
mortality in these cases was high. In 2009 infl uenza A subtype H1N1
caused a pandemic of swine fl u which started in Mexico and spread to
many other countries. Most patients with swine fl u had only mild illness
but a minority developed severe infection, and some died.
Human-to-human spread of H1N1 or H5N1 fl u is rare, at the time of
writing, but another pandemic could develop if the virus mutates again.
Spread
Like SARS (see b p.251) fl u is spread by droplets coughed or sneezed
into the air, or by direct contact with hands contaminated with the virus.
Features
Consider the possibility of avian fl u or swine fl u in a patient with fever
t 38 ° C and cough or breathlessness, who in the last 7 days has been in
an area affected by H1N1 or H5N1 infl uenza. Laboratory staff and health
care workers in contact with cases of severe unexplained respiratory
illness could also be at risk.
Management
Isolate the patient and treat with precautions against transmission of
the virus, as for SARS ( b p.251). Antiviral treatment with oseltamivir or
zanimivir may be considered, depending on current guidelines.
Further information
Clinical guidelines about the assessment of suspected cases and the man-
agement of infl uenza patients will be updated as the situation changes and
if another pandemic develops. Information is available from the UK Health
Protection Agency: www.hpa.org.uk/infections/topics_az/infl uenza/pandemic

254 CHAPTER 6 Environmental emergencies
Hypothermia: presentation
Defi nitions
Hypothermia exists when the core temperature (T ° )<35 ° C.
Hypothermia may be classifi ed as follows:
Background
Infants and the elderly are at particular risk. In young adults hypothermia
is usually due to environmental exposure (eg hill-walking or cold water
immersion), or to immobility and impaired conscious level from alcohol or
drugs. In the elderly, it is more often a prolonged state of multifactorial origin:
common precipitants include unsatisfactory housing, poverty, immobility,
lack of cold awareness (autonomic neuropathy, dementia), drugs (sedatives,
antidepressants), alcohol, acute confusion, hypothyroidism and infections.
Clinical features
Severe hypothermia may mimic death. Wide variations occur, but as
core T ° d , cerebral and cardiovascular function deteriorate. At 32–35 ° C,
apathy, amnesia, ataxia and dysarthria are common. At <32 ° C, conscious-
ness falls progressively, leading to coma, d BP, arrhythmias (check pulse
for at least 1min before diagnosing cardiac arrest), respiratory depression
and muscular rigidity. Shivering is an unreliable sign. VF may occur sponta-
neously when T ° falls <28 ° C and may be provoked by limb movement or
invasive procedures (especially in the presence of hypoxia).
Diagnosis
Check tympanic T ° (or rectal T ° with an electronic probe or low-reading
thermometer). Tympanic and rectal T ° may lag behind core (cardiac) T °
during rewarming. Oesophageal T ° refl ects core levels more accurately,
but requires special equipment.
Investigations
• U&E.
• FBC, toxicology and clotting screens. Note that hypothermia can cause
or aggravate coagulation disturbances.
• Blood glucose (BMG reading may be falsely d ).
• Amylase ( i levels common, but do not necessarily imply pancreatitis).
• Blood cultures.
• ABG.
• ECG: look for prolongation of elements in the PQRST complex, J-waves,
and arrhythmias (AF and bradycardias are the commonest) (Fig. 6.1 ).
• CXR: look for pneumonia, aspiration, left ventricular failure. Other
X-rays may be required after rewarming (eg for suspected fractured
neck of femur).
• CT scan may be indicated if head injury or stroke is suspected.
Mild hypothermia = 32–35 ° C
Moderate hypothermia = 30–32 ° C
Severe hypothermia = <30 ° C
255
HYPOTHERMIA: PRESENTATION
avR
avL
avF
II
I
III
v
1
v
2
v
3
v
6
v
5
v
4
RHYTHM STRIP II
Fig. 6.1 ECG in hypothermia.
Notes on this ECG
• Rhythm disturbance: atrial fi brillation with slow ventricular response.
• Prolongation of QRS.
• Delayed repolarization ‘J-waves’ (arrowed).
• ST–T wave abnormalities.

256 CHAPTER 6 Environmental emergencies
Hypothermia: management
Principles
• Treat in a warm room ( > 21 ° C).
• Handle the patient gently (to d risk of VF).
• Remove wet clothes and dry the skin.
• Monitor ECG.
• Give warmed, humidifi ed O
2
by mask.
• Intubation, if needed, should be preceded by oxygenation and must be
performed expertly to avoid precipitating arrhythmias.
• Secure IV access. IV fl uid is rarely required unless there is loss of volume
from another cause. If BP d during rewarming, give 300–500mL of
warmed 0.9 % saline or colloid. In unstable patients, consider CVP and
urinary catheter. Warm IV fl uid administration is an ineffi cient rewarming
method and runs the risks of fl uid overload and precipitating arrhythmias.
• Correct hypoglycaemia if present with IV glucose.
• If CPR is required, give chest compressions and ventilations at standard
rates.
• In hypothermic cardiac arrest, the heart may be unresponsive to
defi brillation, pacing and drug therapy. Drug metabolism is d and
unpredictable: avoid drugs until core T ° > 30 ° C.
• Defi brillation is appropriate at normal energy levels if VF/VT occurs.
If 3 shocks are unsuccessful, defer further shocks until core T ° > 30 ° C.
Rewarming methods
The choice depends upon the severity and duration of the condition, available
facilities and the individual patient:
Passive rewarming
Easy, non-invasive, and suitable for mild cases (T ° > 32 ° C). d evaporative
and conductive losses by wrapping in warm blankets (remember to
cover the back and sides of the head) ± polythene sheets. Avoid space
blankets which are noisy and have no advantages over polythene sheets.
Endogenous metabolism and shivering usually generate enough heat to
allow spontaneous rewarming. Aim for a rate of 0.5–2 ° C/hr, but do not
rewarm the elderly with prolonged hypothermia too rapidly ( > 0.6 ° C/hr),
as hypotension or cerebral/pulmonary oedema may develop.
Active rewarming
A water bath at 8 41 ° C is rapid and useful for immersion hypothermia,
but cannot be used in injured patients or if CPR is required. Airway care,
ventilation and monitoring are diffi cult, and hazards include core T ° after-
drop and BP d due to peripheral vasodilation. Hot water bottles and heat
pads are less effi cient and can cause burns. A hot air blanket is more con-
venient than a water bath, provides some heat and reduces heat loss.
Core rewarming
• Airway warming with heated (40–45 ° C) humidifi ed O
2
provides some
additional heat and reduces heat loss. It can be combined with other
rewarming methods. It may reduce the risk of cardiac arrhythmias.
• Peritoneal lavage is simple, and quick to set up. Saline at 45 ° C is run in
via a DPL catheter ( b p.347), left for 10–20mins and replaced with a
fresh warm supply. The fl uid directly heats the liver and retroperitoneal
structures including blood in the IVC.
Extracorporeal rewarming with cardiopulmonary bypass maintains brain
and organ perfusion and, if available, is the method of choice in patients
with severe hypothermia or cardiac arrest. Cardiopulmonary bypass can
result in rapid rewarming with core T ° i at 1 − 2 ° C/5min.

257
FROSTBITE AND NON-FREEZING COLD INJURY
Frostbite and non-freezing cold injury
Frostbite
1, 2
Frostbite occurs when tissues freeze at sub-zero temperatures.
Predisposing factors include inadequate clothing/footwear, hypothermia,
exhaustion, alcohol (which impairs judgement), drugs (eg beta-blockers),
peripheral vascular disease, smoking, and previous cold injury. Frostbite
usually involves extremities, especially fi ngers, toes, nose and ears.
Frostnip may precede frostbite. The skin of the nose, face or fi ngers goes
white and numb, but recovers rapidly on protection from the cold, with
transient paraesthesiae but no tissue loss and no permanent damage.
Superfi cial frostbite involves skin and subcutaneous tissues. The frozen
area is numb, and looks white and waxy. Tissues feel fi rm or hard but are
still pliable. Rewarming is painful. Oedematous hyperaemic skin becomes
mottled or purple, with serum-fi lled blisters. A hard black eschar forms,
and after 8 3 weeks this separates, revealing sensitive red shiny skin.
Deep frostbite involves muscles, nerves and sometimes bone, as well as
skin and superfi cial tissues. The damaged area is hard and remains grey
or white after rewarming. Blood-fi lled blisters develop. The dead tissue
mummifi es and then separates after several weeks or months.
Treatment of frostbite varies with the situation and facilities. Only
frostnip should be treated in the fi eld. Frostbitten tissues need rewarming
as soon as possible but further damage must be avoided: it is better to
walk out on frozen feet than on partially thawed feet. Treat hypothermia
before frostbite. Rewarm frostbitten limbs in water at 37 − 39 ° C until skin
circulation returns (usually 830min). Give analgesia and ibuprofen (which
inhibits prostaglandins). After rewarming let the area dry in warm air (do
not towel dry). Elevate the limb. Expose the area, with a bed cradle to
avoid pressure of bedclothes. Clean the area daily in a whirlpool bath
and encourage movement. If necessary split eschar to relieve stiffness,
but avoid surgical debridement and amputations and allow the eschar to
separate spontaneously: premature surgery causes avoidable tissue loss.
Expert advice is helpful in severe frostbite: the British Mountaineerng
Council ( www.thebmc.co.uk ) has a frostbite advice service. Bone scans or
MRI/MRA may help to defi ne deep tissue injury. In severe frostbite early
thrombolysis with tPA may reduce the risk of eventual amputations.
Non-freezing cold injury
1, 2
Trench foot (immersion foot) is caused by prolonged immersion in cold
water or wet boots at temperatures just above freezing. Vasoconstriction
causes tissue ischaemia and nerve damage. The feet are initially cold,
numb and pale or mottled. On rewarming they become red, swollen and
very painful. Blisters may develop.
Treatment : keep the feet clean, warm and dry, elevated to reduce oedema.
Outcome : most patients recover fully, but some have continued pain,
paraesthesiae and sensitivity to cold.
1 State of Alaska Cold Injury Guidelines . www.chems.alaska.gov/EMS/documents/AKColdInj2005.
pdf
2 Imray C et al . ( 2009 ) Cold damage to the extremities: frostbite and non-freezing cold injuries .
Postgraduate Medical Journal 85 : 481 – 8 .

258 CHAPTER 6 Environmental emergencies
Drowning and near drowning
Defi nitions
Drowning is death by suffocation from submersion in any liquid. Drowning
is a common cause of death in young people. 40 % of drownings occur in
children aged <4 years.
Near drowning is survival (at least temporarily). In adults, the commonest
predisposing factor is alcohol, sometimes with other drugs. A signifi cant
proportion refl ect attempted suicide. In the UK, marine near drowning is
usually associated with hypothermia ( b p.254).
Pathophysiology
Wet drowning Involves signifi cant aspiration of fl uid into the lungs. This
causes pulmonary vasoconstriction and hypertension with ventilation/
perfusion mismatch, aggravated by surfactant destruction and washout,
d lung compliance and atelectasis. Acute respiratory failure is common.
ABG shows hypoxia, hypercarbia, and mixed respiratory/metabolic
acidosis. The onset of symptoms can occur rapidly, but in lesser insults,
symptoms may be delayed.
Contamination Water contaminated with chemical waste, detergents etc.,
may induce further lung injury.
Electrolytes Irrespective of whether aspirated water is salt, fresh, or
swimming pool, changes in serum electrolytes and blood volume are
similar, and are rarely immediately life-threatening.
Gastric fl uid Swallowing of fl uid into the stomach, with gastric dilatation,
vomiting, and aspiration, is common.
Dry drowning In 810–20 % of deaths from drowning, a small amount of
water entering the larynx causes persistent laryngospasm, which results
in asphyxia and an immediate outpouring of thick mucus, froth, and foam,
but without signifi cant aspiration — this is ‘dry drowning’.
Secondary drowning A deterioration in a previously apparently well
patient following successful resuscitation after submersion. It may occur
in 5–10 % of initial survivors.
The mammalian diving refl ex
This is probably seen only in young children, but may explain why
successful resuscitation without neurological defi cit can occur after
prolonged immersion. Cold water stimulates facial nerve afferents, while
hypoxia stimulates the carotid body chemoreceptors. These effects
refl exively d heart rate and vasoconstrict skin, GI tract and skeletal
muscle vessels, redistributing blood to the brain and heart. Associated
hypothermia results in d metabolic demands, delaying cerebral hypoxia.

259
DROWNING AND NEAR DROWNING
Management
• Consider associated injury (eg to the cervical spine from diving into a
shallow pool or surfi ng), and treat appropriately.
• Maintain the airway. Remove regurgitated fl uid/debris by suction of the
upper airway. Ensure adequate ventilation and correction of hypoxia.
If the patient does not have a gag refl ex or is apnoeic, ventilate with
a bag and mask and proceed to early tracheal intubation and IPPV. In
spontaneously breathing patients, give the highest FiO
2
possible. IPPV
will be required if hypoxia and/or hypercapnia are present despite O
2
therapy, or if there are signs of pulmonary oedema. Ventilation with
PEEP may signifi cantly improve oxygenation by i functional residual
capacity, improving V/Q mismatch and enhancing fl uid resorption from
the pulmonary bed. However, PEEP may d venous return to the heart.
• If the patient is in cardiac arrest, commence CPR ( b p.46). Defi brillation
may not be successful until core T ° > 30 ° C ( b p.256). Appropriate rapid
core rewarming techniques are required.
• Remove all wet/cold clothing.
• Monitor core T ° and start rewarming ( b p.256).
• NG tube to relieve gastric dilatation.
• Check U&E, blood glucose, ABG, FBC, CXR, ECG.
• Consider the possibility of alcohol, illegal drugs or drug overdose. Keep
urine and blood samples and test if appropriate, eg paracetamol.
• Do not use ‘prophylactic’ steroids or barbiturates.
• Antibiotics may be warranted if contaminated water (eg sewage) is
involved (see b Leptospirosis, p.239).
• Inhalation of mud/sand etc may require bronchoscopy for clearance.
Outcome
Resuscitation without cerebral defi cit is possible after prolonged submer-
sion (even > 60min), particularly if associated with hypothermia. 50 % of
children recovered apparently lifeless will survive, and even adults with
GCS
3
_
4
/
15
and fi xed dilated pupils can survive unimpaired.
Respiratory effort is a sensitive prognostic sign, but in hypothermic
patients its absence does not necessarily imply poor outcome. Note the
time to the fi rst spontaneous inspiratory gasp.
Poor prognostic factors include extremes of age, severe acidosis,
immersion > 5 min, and coma on admission.
Good prognostic factors include patients who are alert on admission,
hypothermia, older children/adults, brief submersion time, and those
who receive rapid on-scene basic life support and respond to initial
resuscitation measures.
Asymptomatic patients who have no abnormality on repeated clinical
examination, ABG and CXR require observation for at least 4–6 hours
prior to considering discharge. Admit all others to ICU or general ward
as appropriate.

260 CHAPTER 6 Environmental emergencies
Diving emergencies: 1
Consider any symptom developing within 48 hours of a dive as related to
the dive until proven otherwise. On suspicion of a diving-related episode,
seek specialist advice urgently (see Table 6.1 ).
Diving related emergencies fall into four main categories: drowning
( b p.258), barotrauma, decompression illness, and marine bites or stings
( b p.416).
Barotrauma
May occur in any gas-containing body cavity during descent or ascent.
Descent barotrauma (‘squeeze’) results from compression of gas
in enclosed spaces as the ambient pressure i . Commonly, the ears,
sinuses and skin are affected. Middle ear squeeze may be precipitated
by Eustachian tube congestion and leads to erythema, haemorrhage, or
tympanic membrane perforation with conductive hearing loss. Round or
oval window rupture (inner ear squeeze) occurs with sudden pressure
changes between the middle and inner ear and results in acute tinnitus,
vertigo and deafness, and a perilymphatic fi stula. ENT opinion is urgently
required if a perilymphatic fi stula is suspected and for cases of severe or
continuing symptoms. If tympanic membrane rupture has not occurred,
middle ear squeeze can usually be managed with decongestants/simple
analgesics. If it has ruptured, give antibiotics ( b p.551). Instruct the
patient not to dive until the symptoms have resolved and the drum has
completely healed.
Sinus barotrauma has a similar aetiology to middle ear injury and is often
associated with URTI, mucosal polyps and sinusitis. Treat similarly to ear
barotrauma.
Divers who fail to exhale periodically via the nose into their face mask
during descent may develop ‘face mask squeeze’ (skin barotrauma).
Erythema, bruising, and petechial and conjunctival haemorrhages develop
in the enclosed area. Skin tightly enclosed by parts of the diving suit can
have similar appearances. Usually no treatment is required.
Ascent barotrauma is the reverse of squeeze, and particularly affects
the lungs. It may be caused by breath-holding during rapid uncontrolled
ascent or by air trapping in patients with asthma or congenital lung
bullae. Mediastinal emphysema is the commonest event and presents
with i hoarseness, neck swelling, and retrosternal chest discomfort.
Symptoms usually resolve spontaneously with high concentrations of
O
2
. Pneumothorax is a potentially life-threatening complication if it
develops during the dive, as the intrapleural gas cannot be vented and
increasing ascent will precipitate tension. Conventional treatment by
needle decompression, aspiration or chest drain insertion ( b p.336) is
required.
Dental pain may occur on ascent or descent in carious teeth or those
which have had recent fi llings. The affected tooth is tender on tapping.
Treat symptomatically with analgesics and arrange dental referral.
261
DIVING EMERGENCIES: 1
Further information
Diving and Hyperbaric Medicine Division, Institute of Naval Medicine (Gosport, Hampshire,
England) . http://www.royalnavy.mod.uk/training-and-people/rn-life/medical-branch/institute-of-
naval-medicine/diving-and-hyperbaric-medicine-division-dhmd/
Diving Diseases Research Centre (Hyperbaric Medical Centre, Plymouth, England) . www.ddrc.org
British Hyperbaric Association . www.hyperbaric.org.uk/
Scottish Diving Medicine . www.sdm.scot.nhs.uk
Divers Alert Network . www.diversalertnetwork.org
Table 6.1 Sources of advice on diving emergencies and hyperbaric
chambers
England, Wales, Northern Ireland
• Diving Incident Telephone Advice Line,
Institute of Naval Medicine Gosport,
Hampshire
Telephone 07831 151523 (24 hrs)
Ask for Duty Diving Medical Offi cer
• Diving Diseases Research Centre
Plymouth
www.ddrc.org
Telephone 01752 209999 (24 hrs)
Ask for the Duty Diving Doctor
Scotland
• Hyperbaric Medicine Unit
Aberdeen Royal Infi rmary
www.hyperchamber.com
Telephone 0845 408 6008
State ‘diving emergency’. Give your
name and telephone number. Ask for
the Duty Hyperbaric Doctor
In the event of any diffi culties in contacting
these agencies in the UK, telephone 999
and ask for COASTGUARD
Other countries
• Divers Alert Network
www.diversalertnetwork.org
This has links to diving emergency contact
numbers throughout the world
DAN Diving Emergency Hotline
(USA) + 1 919 684 8111

262 CHAPTER 6 Environmental emergencies
Diving emergencies: 2
Decompression illness
There are two forms of decompression illness. The fi rst occurs when
dissolved nitrogen in blood and tissues is not expelled at a suffi cient rate
to prevent bubble formation. The second occurs when air bubbles are
released into the circulation because of pulmonary barotrauma. This
follows if air bubbles enter the pulmonary capillaries from ruptured
alveoli. The bubbles travel via the left side of the heart to the systemic
circulation. Cerebral air embolism usually causes symptoms as the diver
surfaces, with loss of consciousness, fi ts, cardiovascular collapse and chest
pain. Clinically, differentiation between the two forms is diffi cult and initial
management is the same. In general, the sooner the onset of symptoms,
the greater the likely severity. Symptoms may be attributed by the patient
(and the unwary doctor) to musculoskeletal sprains/strains or other minor
injury.
Decompression illness is more likely in divers who have not followed safe
ascent recommendations, the obese, in cold water, and when excessive
exercise has occurred during the dive. It may be precipitated by air travel
if insuffi cient time is left between diving and fl ying for residual nitrogen
to leave the body in a controlled fashion. Bubbles have direct mechanical
and local infl ammatory effects, commonly involving joints, skin, CNS, lungs
and ears.
Joint pain, ‘the bends’, most often affects shoulders and elbows. A dull
aching sensation, i by movement but without localized tenderness
is common. Pruritic rashes, local swelling and a peau d’orange effect
may occur. Back pain, limb weakness, sensory abnormalities or urinary
retention imply spinal cord involvement. Central effects include focal
defi cits, cerebellar disturbance and mood changes.
Treatment for decompression illness is recompression. If delayed, risks
of permanent damage to brain and spinal cord greatly i . The diagnosis of
decompression sickness may only follow the response to recompression.
Pending this, give the highest possible concentration of O
2
. Analgesics and
sedatives can mask recompression responses and should only be used on
specialist advice. Entonox
®
is absolutely contraindicated.
If intubation is required, infl ate the ET tube cuff with sterile water,
since during recompression an air-fi lled cuff will defl ate. IV fl uids (0.9 %
saline or a plasma expander) assist oxygenation of ischaemic tissues and
facilitate discharge of excess tissue nitrogen load into the venous system
by ensuring adequate circulating volume. Some centres may recommend
aspirin and/or dextran solutions to d capillary sludging which accompanies
severe decompression sickness.
Despite dry or wet suits, hypothermia is common. Treat with appropriate
passive or active rewarming ( b p.256).

263
DIVING EMERGENCIES: 2
Air evacuation If, after consultation with the diving medical centre, air
evacuation is necessary, unpressurized aircraft should not fl y above
300m. The diver should breathe 100 % O
2
. On reaching the diving centre,
recompression to a simulated depth of 18m with 100 % O
2
occurs,
interspersed with periods of air breathing to d O
2
toxicity risk. Slow
decompression then follows standard treatment protocols.
Divers usually dive in pairs. If a diver has symptoms of decompression
sickness or pulmonary barotrauma, his ‘buddy’ will be at risk also. Although
recompression may not be required in the buddy, transfer him/her along
with the affected diver and their diving equipment to the recompression
facility.
Obtain the following information before referral, if possible:
• The patient’s current condition, progression since onset, and response
to treatment.
• Time of onset of symptoms related to the dive.
• Dive profi le and history (depth, duration, activity during the dive, speed
of ascent including details of any stoppages, environmental conditions
(water temperature, currents, etc.), pre-dive exercise, alcohol, drugs
and food, type and condition of diving equipment used, clothing worn,
other recent dives). Many divers store much of this information in a
dive computer.
• Previous medical history, previous diving-related episodes, drug history.

264 CHAPTER 6 Environmental emergencies
Heat illness
Body T ° is normally kept at 36–38 ° C by homeostatic mechanisms
which are controlled by the hypothalamus. Hyperthermia occurs when
these mechanisms are overwhelmed by factors acting individually, or
(commonly) together. These conditions can occur even in temperate
climates. At-risk groups include the young and the elderly in conditions
of i temperature and humidity, and patients with unaccustomed or
prolonged muscular activity (eg at ‘raves’, associated with ecstasy or
other drugs), grand mal fi tting, athletes, marathon runners and armed
forces recruits.
Predisposing medical factors include
• Alcohol use or withdrawal (including delirium tremens).
• Cardiac disease.
• Any condition which may cause or aggravate Na
+
/H
2
O loss
(eg gastroenteritis, cystic fi brosis).
• Drugs, including: alcohol, diuretics, salicylates, anticholinergics (antihis-
tamines, tricyclic antidepressants), sympathomimetics (amphetamines,
ecstasy, LSD, cocaine, phencyclidine, appetite suppressants), phenothi-
azines, antipsychotics, MAOI, SSRI.
Heat illness has a spectrum of severity:
Heat cramps ⇔ Heat exhaustion ⇔ Heat stroke
In heat cramps/exhaustion , homeostatic mechanisms still function, but are
overwhelmed.
In heat stroke , all thermoregulatory control is lost, body temperature i
rapidly to very high levels ( > 41 ° C) causing widespread severe tissue and
organ damage. Mortality may exceed 10 % .
Heat cramps
Core T ° of 37–39 ° C. Mental function is normal. Sweating during exercise
and replacement with hypotonic fl uid leads to Na
+
defi ciency. Brief
cramps occur in muscles used in heavy work, usually after exertion.
Heat exhaustion
Core T ° <40 ° C. Mental function is normal. Characterized by mixed
Na
+
/H
2
O depletion. Sweating and tachycardia are usually present.
Symptoms of weakness, fatigue, headache, vertigo, nausea and vomiting,
postural dizziness, syncope. Patients will recover with rest and fl uids.
In mild cases , remove from heat and use simple cooling techniques.
Rehydrate with oral electrolyte solutions.
More severe cases require IV 0.9 % saline or 0.45 % saline/5 % dextrose. Use
clinical assessment, U&E and haematocrit to guide infusion rate. Up to 4L
of fl uid may be required over 6–12hr. Avoid over-rapid infusion which
may cause pulmonary and/or cerebral oedema.
Measurement of core temperature
Tympanic or rectal T ° measurement is appropriate in the ED, but may
underestimate core T ° and respond slowly as this changes. Oesophageal
and intravascular probes give the most accurate readings of core T ° but
require special equipment.

265
HEAT ILLNESS
Heat stroke
Suspect in collapse during or after exercise and in high risk groups. Core
T ° is > 41 ° C (but signifi cant cooling can occur before arrival in the ED).
There is multi-system damage especially to the CNS. Outcome depends
upon the height and duration of i T ° . Mortality is 8 10 % .
• CNS : oedema + petechial haemorrhages cause focal/generalized damage.
• Muscle injury releases enzymes, myoglobin, urate, K
+
, PO
4
3
–
.
• Liver : damaged cells release enzymes. Jaundice commonly develops after
24hr.
• Kidneys : ARF from hypovolaemia, muscle breakdown products, acidosis,
DIC.
• Blood : DIC, thrombocytopenia, leucocytosis.
• Metabolic : i or d K
+
, metabolic acidosis, respiratory alkalosis, hypoglycaemia.
Features
Sweating may be present. The skin surface may feel deceptively cool due
to peripheral vasoconstriction.
• CNS : confusion, delirium, fi tting, coma, oculogyric crisis, dilated pupils,
tremor, muscle rigidity, decerebrate posturing, cerebellar dysfunction.
• CVS : tachycardia, hypotension, arrhythmias.
• Coagulopathy : purpura, conjunctival haemorrhages, melaena, haematuria.
Investigations
ABG, U&E, BMG, CK, clotting screen, LFTs, urate, Ca
2 +
, PO
4
3
–
, ECG, CXR.
Treatment
• Rapid therapy is vital. Do not wait for the results of investigations.
• Remove the patient from the hot environment and remove all clothing.
• Secure the airway (intubation and IPPV if needed). Give high FiO
2
.
• Cooling techniques depend upon facilities available and the clinical state
of the patient. Do not give ‘antipyretics’ such as aspirin/paracetamol.
Evaporative cooling is the most effi cient and applicable treatment. Spray the
naked patient with tepid tap water and blow air over the body with fans.
Ice-packs can be applied to the axillae, groins, neck, and scalp (but avoid
prolonged contact). Consider cold gastric or peritoneal lavage, or cardiopul-
monary bypass if these techniques fail. Aim for cooling rate of at least 0.1 ° C/
min. When core T ° <39 ° C stop active cooling as hypothermia may develop.
• IV fl uids: give 50mL 50 % dextrose IV if BMG <3mmol/litre. Severe hypo-
volaemia is uncommon. If hypotension persists despite d T ° , give IV
0.9 % saline (1–1.5L over 1–2hr). Avoid overloading circulation with risk
of pulmonary/cerebral oedema. CVP monitoring may be needed. CVP
may be initially i due to peripheral vasoconstriction.
• Insert a urinary catheter. If myoglobinuria is present, aim for i urine
output, and consider giving IV bicarbonate and/or mannitol.
• If fi ts occur, give IV lorazepam — but beware of respiratory depression.
Neuroleptic malignant syndrome is an idiosyncratic reaction in patients on
antipsychotics (especially haloperidol, thioridazine, chlorpromazine). Features
are muscle rigidity, extrapyramidal signs, autonomic dysfunction, severe
dyskinesia. Stop the antipsychotic, cool the patient, and give dantrolene.
Malignant hyperpyrexia is a rare autosomal dominant condition related to
use of suxamethonium and volatile anaesthetics. Dantrolene prevents Ca
2 +
release from skeletal muscle and is very effective: initial dose is 2–3mg/kg IV,
then 1 mg/kg as needed, max total dose 10 mg/kg. See guidelines: www.
aagbi.org/publications/guidelines/docs/malignanthyp07amended.pdf

266 CHAPTER 6 Environmental emergencies
Electrical injuries
An electric shock can cause cardiac and respiratory arrest. The heart
often restarts spontaneously, but the respiratory arrest may be prolonged,
causing fatal hypoxia. Thermal injury from the electric current produces
burns and muscle damage. Muscle spasms from a shock may result in
dislocations or fractures or precipitate a fall causing major trauma. Fatal
electrocution can occur from domestic electricity (in the UK 230 volts,
alternating current at 50cycles/sec), but severe injury is more common
with high voltage shocks ( > 1000V).
Lightning causes a direct current (DC) shock at a very high voltage (up to
100,000,000V), but short duration (0.1–1msec).
Electrical fl ash and arc burns
An electrical short-circuit near to a person may cause sudden vaporization
of metal and deposition of a thin layer of hot metal on the skin, without
any electricity passing through the casualty. Electrical fl ash burns may look
dramatic because of discolouration of the skin, but are often superfi cial and
heal uneventfully. In contrast, electrical arcing produces high temperatures,
and may cause deep dermal or full thickness burns, especially if clothing
is set alight.
Contact burns
If electricity has passed through the patient there are usually two or
more entry or exit wounds, which are full thickness burns with white or
charred edges. Tissue damage is more extensive than the visible burns,
especially with high voltage injuries. Deeper layers of skeletal muscle
may be involved and muscle damage can cause myoglobinuria and renal
failure. Myonecrosis and oedema of muscles may produce a compartment
syndrome ( b p.398).
If current passes through the torso, cardiac arrhythmias are more likely
than if only a single limb is involved. Myocardial damage may occur, often
in association with vascular injuries.
Neurological effects of electric shocks include coma, fi ts, headaches,
transient paralysis, peripheral neuropathy, and mood disturbances.
Ophthalmic injuries are common after electrical burns of the head.
Cataracts and glaucoma may develop later.
Electrocution in pregnancy has major risks for the foetus (spontaneous
abortion has been reported). Obtain obstetric advice.
Lightning
The sudden vaporization of sweat and rain water caused by lightning may
explode clothes and shoes off the victim and rupture ear drums. Lightning
burns are superfi cial, often with a characteristic feathered or fern-like
appearance. The limbs are often cold and mottled due to arterial spasm,
which usually resolves over a few hours. Deep muscle damage and myoglob-
inuria are rare. Coma may result from direct brain injury, head injury due to
a fall, or cardiac arrest. CPR, if indicated, may be successful even if required
for prolonged periods. Survivors may be confused and amnesic for several
days and may have fi ts and temporary paralysis. Cataracts are common.

267
ELECTRICAL INJURIES
Management
• At the scene, make sure that the current is turned off before anyone
approaches or touches the casualty. Remember that high voltage elec-
tricity can arc through the air or pass through the ground.
• Check the airway, breathing and circulation. Electrical burns of the
mouth and throat may cause oedema and airway obstruction.
• Perform CPR if necessary, but minimize movement of the spine in case
of trauma.
• Examine thoroughly for head, chest, abdominal and skeletal injuries.
• Examine all over for skin entry/exit burns, and check pulses and
sensation.
• Check the ECG: there may be arrhythmias (eg atrial fi brillation),
conduction defects, ST elevation and T wave changes.
• Check FBC, U&E and creatine kinase (except in minor low-voltage
burns).
• Test the urine for blood. If the stick test is + ve for blood, but there are
no red blood cells on microscopy, treat for myoglobinuria to prevent
renal failure: obtain specialist advice, maintain a high urine output, and
consider using mannitol ± isotonic sodium bicarbonate.
• Fluid loss into muscles results in hypovolaemia: IV fl uids are often
required. After high voltage injuries, widespread fasciotomies may be
needed, with excision or amputation of non-viable tissues and inspec-
tion and further debridement after 48 hours.
Admission
It is reasonable to allow home asymptomatic patients with domestic
and minor low voltage burns, a normal ECG, no history suggestive of
arrhythmia (eg palpitations) and no myoglobinuria, but advise review if any
problem develops.
Admit children who bite electric fl exes for observation, because of the
risk of delayed bleeding from labial blood vessels.
Many patients with electrical injuries will need admission for observation
and monitoring. Admit all patients with high voltage conduction injuries,
cardiac arrhythmias, chest pain or ECG abnormalities, vascular injury or
myoglobinuria.

268 CHAPTER 6 Environmental emergencies
Radiation incidents
In the UK, 24 hour advice and assistance is available via NAIR (National
Arrangements for Incidents involving Radioactivity) on telephone 0800
834153 or via the police. Try to distinguish between external irradia-
tion of a person and contamination with radioactive material. Someone
exposed to X-rays or to gamma rays in a radiation sterilizing unit receives
no further radiation after removal from the source, and there is no risk
of contaminating anyone else. However, a person contaminated with
radioactive material is still exposed to radiation and needs urgent, careful
decontamination to minimize the risks to himself and to other people.
Some hospitals are offi cially designated for the care of casualties contami-
nated with radioactive substances, but in an emergency a patient may be
taken to any ED, where a plan for such events should exist.
Anticipation of a radiation accident
• Inform the ED consultant on duty immediately if a patient from a
radiation incident arrives or is expected.
• Get advice and help from a radiation physicist (from Medical Physics or
radiotherapy department).
• Implement the appropriate Radiation Incident Plan to deal with the patient.
• Expect media enquiries.
Treatment of contaminated casualties
Where possible, treatment should take place in a designated
decontamination room. This room should have a separate entrance,
ventilation arrangements, decontamination facilities with shower, and
contaminated water collection facilities. Cover the fl oor of this room and
entrance/exit corridors with disposable sheeting. All staff must themselves
be decontaminated and checked before leaving this area.
• Turn off air conditioning.
• Pregnant and potentially pregnant staff should not be involved.
• Provide any necessary life-saving treatment, but avoid spreading
contamination.
• ‘Barrier nurse’, as for an infectious disease.
• Assume patients are contaminated until they have been checked by the
radiation physicist.
• Instruct patients and staff not to eat, drink, or smoke.
• Involve the minimum number of staff, who should wear facemasks,
theatre clothing with impermeable gowns or plastic aprons, two pairs of
gloves, and overshoes or rubber boots.
• Restrict and record movements of people in and out of the room.
• Ensure that the ambulance crew waits for monitoring of themselves and
their vehicle.
• Keep everything that may be contaminated for radiation testing.
• Collect the patient’s clothes, dressings, swabs, and any equipment used
in plastic bags, and keep them in the decontamination room.
• All blood/urine samples must be specially labelled and the laboratories
informed of the radiation risk.
• Life-threatening injuries may take precedence over all of the above,
such that patients may need to be managed in the resuscitation room.

269
RADIATION INCIDENTS
Decontamination of the patient
The radiation physicist should determine the sites of contamination and
monitor the effectiveness of treatment. The object is to remove any
contaminating substance and minimize absorption into the body, especially
via the mouth, nose, and wounds.
• Cover any wounds prior to decontamination.
• Avoid splashing.
• Radioactive material can usually be removed from intact skin by washing
with soap and water. Gentle scrubbing may be needed, but it is impor-
tant to avoid damaging the skin. Carefully clean wounds and irrigate
with water or saline.
• Clean the mouth using a mouthwash and a soft toothbrush, with care to
avoid swallowing any fl uid.
• Instruct the patient to blow their nose into paper handkerchiefs. If the
nose is still contaminated irrigate it with small amounts of water.
• Irrigate each eye from the medial side outwards to avoid draining
contaminated water into the nasolacrimal duct.
• Clean the hair by washing with shampoo and by clipping if contamina-
tion persists, but do not shave the scalp.
• If monitoring shows that all contamination has been removed, treat the
patient as for an irradiated, but uncontaminated patient. However, if
contamination persists, or if radioactive material has been ingested or
inhaled, further treatment will be needed after discussion with a radia-
tion specialist.
• Check all staff involved in treating the patient for radioactive contami-
nation before they leave the treatment area.
The irradiated patient
A patient who has been irradiated or contaminated with radiation may be
at risk of radiation sickness or other ill effects. Admit to a designated unit
for assessment and follow-up by a radiotherapist or other specialist.
Initial symptoms of radiation sickness are malaise, nausea, vomiting, and
diarrhoea, starting a few hours after exposure. There is then a latent
period before the main effects of radiation sickness appear. Record any
symptoms and the time of onset. The effects of anxiety and stress may be
similar to the early features of radiation sickness.
Take blood for FBC, U&E, and blood group, recording the time on the
blood tubes and in the notes. Measurement of the lymphocyte count and
analysis of chromosomes at known times after exposure are helpful in
assessing the amount of radiation received and determining the prognosis.
A low (<1.0 × 10
9
/L) or falling lymphocyte count indicates serious
radiation exposure.
Further information
Radiation incidents
http://www.hpa.org.uk/Topics/Radiation/UnderstandingRadiation/
UnderstandingRadiationTopics/RadiationIncidents/incid_Nair/
www.hpa.org.uk (Health Protection Agency).
Deliberate release and CBRN incidents (see also b p.210)
www.hpa.org.uk/emergency/CBRN.htm
This page intentionally left blank

271
Pain relief 272
Analgesics: aspirin and paracetamol 274
Analgesics: NSAIDs 275
Analgesics: opioids 276
Analgesics: Entonox
®
and ketamine 278
Analgesia for trauma 279
Analgesia in specifi c situations 280
Local anaesthesia 282
Local anaesthetic toxicity 284
General principles of local anaesthesia 286
Topical anaesthesia 288
Local anaesthetic administration 289
Bier’s block 290
Local anaesthetic nerve blocks 292
Digital nerve block 294
Nerve blocks at the wrist 296
Nerve blocks of forehead and ear 300
Dental anaesthesia 302
Intercostal nerve block 303
Femoral nerve block 304
Nerve blocks at the ankle 306
Sedation 308
General anaesthesia in the emergency department 310
Emergency anaesthesia and rapid sequence induction 312
Diffi cult intubation 314
General anaesthetic drugs 316
Analgesia and anaesthesia
Chapter 7

272 CHAPTER 7 Analgesia and anaesthesia
Pain relief
Many patients who come to the ED are in pain. Knowledge of the site and
characteristics of the pain is often important in diagnosing the problem.
Relief of pain is an essential and urgent part of treatment. Pain and distress
may prevent patients giving useful details of history and symptoms and
may not allow them to co-operate with investigations or treatment.
Methods of pain relief
Relieving pain often requires analgesic drugs, but other types of treat-
ment are sometimes more important. If an injury is more painful than
expected consider the possibility of infection (eg necrotizing fasciitis,
b p.234) or vascular compromise. Severe pain despite immobilization of
a fracture suggests a vascular injury, compartment syndrome ( b p.398)
or a tight plaster ( b p.424). Refl ex sympathetic dystrophy (Sudeck’s
atrophy) may also cause severe pain starting a few days after relatively
minor trauma.
Splintage
Immobilization of a fracture helps to relieve pain and d requirement for
analgesic drugs. Inhalation analgesia with Entonox
®
( b p.278) is often
helpful while the splint or cast is being applied.
Elevation
Many limb injuries produce considerable swelling, which causes pain
and stiffness. Elevate the limb to d swelling, relieve the pain, and allow
mobilization as soon as possible.
Cold
Cool burns as soon as possible, usually in cold water, to relieve the pain
and stop any continuing thermal injury. Chemical burns from hydrofl uoric
acid ( b p.397) are often extremely painful and need prolonged cooling
in iced water. Pain from recent sprains and muscle injuries may be d by
cooling with ice-packs (or a pack of frozen peas) applied for 10–15min at a
time, with a piece of towelling between the ice-pack and the skin.
Heat
Pain following sprains and strains of the neck, back, and limbs is often
caused by muscle spasm. It may be eased by heat from a hot bath, hot
water bottle, or heat lamp.
Dressings
Pain from minor burns and fi ngertip injuries often resolves after a suitable
dressing is applied.
Local anaesthesia (LA)
LA provides excellent pain relief for fractured shaft of femur ( b p.304,
472) and for some fi nger and hand injuries ( b p.292). Strongly consider
giving analgesia with LA before obtaining X-rays. Check for any possible
nerve injury before injecting LA.

273
PAIN RELIEF
Defi nitive treatment
Reducing a pulled elbow or trephining a subungual haematoma usually
gives immediate relief of pain, so no analgesia is needed.
Psychological aspects of pain relief
Anxiety and distress accompany pain and worsen patients’ suffering.
Psychological support is needed, as well as physical relief from pain.
Patients are helped by caring staff who explain what is happening and
provide support and reassurance. The presence of family members or a
close friend is often helpful.
Analgesics
Many different analgesic drugs are available, but it is best to use only a few
and become familiar with their actions, dosages, side effects, and contrain-
dications. Most hospitals have analgesic policies and limit the choice of
drugs which may be used. Before prescribing any drug, check what treat-
ment has been given. The patient may already be taking analgesia or have
supplies at home. Many drugs interact with others: important drug inter-
actions are listed in the BNF . Ask about drug allergies and record them.
Before giving aspirin or NSAIDs ask and record about indigestion, peptic
ulceration and asthma.

274 CHAPTER 7 Analgesia and anaesthesia
Analgesics: aspirin and paracetamol
Aspirin
Aspirin is a good analgesic for headaches, musculoskeletal pain and
dysmenorrhea, and has antipyretic and mild anti-infl ammatory actions. It
interacts with warfarin, some anticonvulsants and other drugs, and may
exacerbate asthma and cause gastric irritation.
• Do not use aspirin in children <16 years or during breast feeding.
• Adult dose PO is 300–900mg 4–6 hourly (max 4g daily).
Paracetamol (‘acetaminophen’ in USA)
Paracetamol has similar analgesic and antipyretic actions to aspirin, but has
no anti-infl ammatory effects and causes less gastric irritation.
• The therapeutic dose range of paracetamol in children and adults is
10–15 mg/kg. In severe symptoms maximum single dose is 20 mg/kg.
Adults and children who are small for age should be weighed and the
dose calculated. In most patients the dose can safely be based on age.
• The adult dose is 0.5–1g 4–6 hourly (maximum 4g in 24 hours).
• For children aged less than 6 years use paracetamol infant suspension
(120 mg/5 mL).
• 2–3 months (babies with weight > 4 kg, born after 37 weeks):
2.5 mL (60 mg). If necessary a second 2.5 mL dose may be given
after 4–6 hours. Do not give more than two doses in 24 hours.
• 3–6 months: 2.5 mL (60 mg)
• 6–24 months: 5 mL (120 mg)
• 2–4 years: 7.5 mL (180 mg)
• 4–6 years: 10 mL (240 mg).
• For children aged 6 years and over use paracetamol six plus suspension
(250 mg/5 mL):
• 6–8 years: 5 mL (250 mg)
• 8–10 years: 7.5 mL (375 mg)
• 10–12 years: 10 mL (500 mg).
• Paracetamol may be repeated 4–6 hourly. Adults, and children older
than 3 months, may have a maximum of four doses in 24 hours.
• Overdosage can cause liver and renal damage ( b p.190).
Compound analgesics (paracetamol + opioid)
Compound analgesic tablets containing paracetamol and low doses of
opioids are widely used, but have little benefi t over paracetamol alone and
cause more side effects, such as constipation and dizziness, particularly in
elderly people. These compound preparations include:
• Co-codamol 8/500 (codeine phosphate 8mg, paracetamol 500mg).
• Co-dydramol (dihydrocodeine tartrate 10mg, paracetamol 500mg).
Compound preparations of paracetamol and full doses of opioids, eg
co-codamol 30/500 (codeine phosphate 30mg, paracetamol 500mg), are
more potent than paracetamol alone, but may cause opioid side effects,
including nausea, vomiting, constipation, dizziness, drowsiness and respiratory
depression. Opioid dependency can occur with prolonged usage.

275
ANALGESICS: NSAIDs
Analgesics: NSAIDs
Non-steroidal anti-infl ammatory drugs
NSAIDs are often used to treat musculoskeletal pain, with or without
infl ammation, although in many cases non-drug treatment (heat or cold,
elevation) and paracetamol should be tried fi rst. NSAIDs can cause gastric
irritation, diarrhoea, GI bleeding and perforation, with i risk at higher drug
dosage and in patients aged > 60 years and those with a history of peptic
ulcer. NSAIDs may exacerbate asthma and can precipitate renal failure
in patients with heart failure, cirrhosis or renal insuffi ciency. Interactions
occur with diuretics, warfarin, lithium and other drugs (see BNF ). When
possible, advise that NSAIDs be taken after food to d risk of GI side
effects. If NSAID treatment is essential in patients at high risk of GI prob-
lems consider prophylactic treatment with misoprostol (see BNF ).
Many NSAIDs are available and all can cause serious adverse effects,
but ibuprofen, diclofenac and naproxen are relatively safe and cover
most requirements. Ibuprofen has the lowest incidence of side effects,
is the cheapest of these drugs and may be bought without prescription.
Ibuprofen is useful in children as an analgesic and antipyretic, especially
when paracetamol is insuffi cient.
• Ibuprofen dosage 1.2–1.8g daily in 3–4 divided doses (max 2.4g daily).
Child ( > 7kg): 20mg/kg daily in 3–4 divided doses.
• Diclofenac (oral or rectal) 75–150mg daily in 2–3 divided doses.
• Naproxen 500mg initially, then 250mg 6–8-hourly (max 1.25g daily).
Acute gout 750mg initially, then 250mg 8-hourly until pain resolves.
Injectable NSAIDs
Some NSAIDs may be given by injection for musculoskeletal pain (eg acute
low back pain), or for renal or biliary colic. The contra indications and side
effects are the same as for oral treatment. Intramuscular (IM) injections
are painful and can cause sterile abscesses, so oral or rectal treatment is
preferable. NSAIDs provide effective analgesia for renal colic, but the onset
is slower than with IV opioids, which some prefer. A NSAID is particularly
useful in suspected drug addicts who claim to have renal colic.
• Ketorolac may be given IM or slowly IV (initial dose 10mg over at least
15sec: see BNF ). It is useful as an adjunct for MUAs.
• Diclofenac must be given by deep IM injection (not IV, which causes
venous thrombosis). Dose: 75mg, repeated if necessary after 30min
(max 150mg in 24 hours).
Topical NSAIDs
NSAID gels or creams applied to painful areas provide some analgesia, but
are less effective than oral treatment. Systemic absorption may occur and
cause adverse effects as for oral NSAIDs.

276 CHAPTER 7 Analgesia and anaesthesia
Analgesics: opioids
Morphine
Morphine is the standard analgesic for severe pain. As well as providing
analgesia, it is sometimes used for cardiogenic pulmonary oedema ( b p.101)
to relieve distress and to help increase venous capacitance.
Morphine often causes nausea and vomiting in adults, so consider giving an
anti-emetic (cyclizine 50mg IV/IM or prochlorperazine 12.5mg IM). Anti-
emetics are not usually necessary in children aged < 10years.
Other side-effects of opioids include drowsiness and constipation. Respiratory
depression and hypotension may occur, especially with large doses.
Pinpoint pupils can complicate neurological assessment. Naloxone
( b p.188) reverses the effects of opioids.
In acute conditions, give morphine by slow IV injection, which provides
rapid but controlled analgesia. The dose varies with the patient and the
degree of pain. Titrate the dose depending on the response: 2mg may be
adequate in a frail old lady, but sometimes > 20mg is needed in a young fi t
person with severe injuries. Dilute morphine with 0.9 % saline to 1mg/mL
(label the syringe clearly) and give it slowly IV (1–2mg/min in adults) in
1mg increments until pain is relieved. Give further analgesia if pain recurs.
IV morphine dose in children is 100–200micrograms/kg, given in increments,
repeated as necessary. Patient-controlled analgesia using a computerized
syringe pump is very good for post-operative analgesia, but rarely appro-
priate in the ED.
IM injections provide slower and less controlled effects than IV analgesia:
avoid their use, especially in shocked patients. IM morphine could be used
in children needing strong analgesia but not IV fl uids (eg while dressing
superfi cial burns), but oral or nasal analgesia is preferable.
• Morphine may be given orally as Oramorph
®
oral solution:
• child aged 1–5 years: max dose 5mg (2.5mL);
• child aged 6–12 years: max dose 5–10mg (2.5–5mL).
• Codeine is given orally for moderate pain (30–60mg 4hrly, max 240mg
daily) and has side effects similar to morphine. Codeine may also be
given IM (but not IV, because it may cause hypotension).
• Dihydrocodeine is very similar to codeine.
• Diamorphine (heroin) has similar effects to morphine, but is more soluble
and so can be dissolved in a very small volume of diluent. Nasal diamor-
phine provides effective analgesia in children ( b p.281).
• Fentanyl is a short-acting opioid which is often used in anaesthesia.
• Pethidine provides rapid but brief analgesia, but is less potent than mor-
phine. It is sometimes used for renal or biliary colic in preference to
morphine, which occasionally causes smooth muscle spasm ( b p.277).
Pethidine is given slowly IV, titrated as necessary (usual adult dose 50mg
IV), or less effectively IM (50–100mg). Give an anti-emetic with it.

277
ANALGESICS: OPIOIDS
Smooth muscle spasm due to opioid analgesics
In a few patients opioids such as morphine can cause severe pain due to
smooth muscle spasm, especially spasm of the sphincter of Oddi. About
5–20 minutes after morphine has been given, severe colicky abdominal
pain develops. This may be typical of biliary colic but can mimic renal colic,
intestinal perforation or myocardial infarction.
Pain from spasm of the sphincter of Oddi may be relieved by glucagon
(1mg IV, repeated if necessary) although this is liable to cause vomiting.
Naloxone (0.2mg IV, repeated if necessary) is also effective, but may
reverse desired analgesia. GTN can also relieve smooth muscle spasm of
the sphincter of Oddi. Glucagon is probably the treatment of choice for
this rare complication of opioid analgesia.

278 CHAPTER 7 Analgesia and anaesthesia
Analgesics: Entonox
®
and ketamine
Entonox
®
Entonox
®
is a mixture of 50 % N
2
O and 50 % O
2
. It is stored as a compressed
gas in blue cylinders with a blue and white shoulder. It is unsuitable for use
at <–6 ° C, since the gases separate and a hypoxic mixture could be given.
Entonox
®
diffuses more rapidly than nitrogen and so is contra indicated
with the following: undrained pneumothorax (since it may produce a
tension pneumothorax), after diving ( i risk of decompression sickness),
facial injury, base of skull fracture, intestinal obstruction, d conscious level.
Entonox
®
is controlled by a demand valve and inhaled through a mask or
mouthpiece, often held by the patient. It gives rapid and effective analgesia
and is widely used in prehospital care. In the ED, Entonox
®
is useful for
initial analgesia, eg while splinting limb injuries, and for many minor proce-
dures, such as reduction of a dislocated patella or fi nger. Tell the patient
to breathe deeply through the mask or mouthpiece, and warn that he may
feel drowsy or drunk, but that this will wear off within a few minutes.
Ketamine
Ketamine is a dissociative anaesthetic drug which may be given IM or IV by
experts, and which provides strong analgesia in sub-anaesthetic dosage. It
is rarely used in hospital practice for adults, because it may cause severe
hallucinations, but these are less of a problem in children. It is very useful
for sedation of children for procedures such as suturing of minor wounds.
Ketamine is particularly useful in prehospital care and is the most appro-
priate drug in the rare cases when a GA is needed outside hospital for
extrication or emergency amputation.
Airway-protective refl exes are maintained better with ketamine than
with other induction agents, but airway obstruction and aspiration
of gastric contents are still potential hazards. Respiratory depression
is uncommon at normal dosage. Ketamine is a bronchodilator and may
be used in asthmatics. It stimulates the cardiovascular system and often
causes tachycardia and hypertension, so avoid it in severe hypertension.
Hallucinations are less likely if a small dose of midazolam is given and the
patient is not disturbed during recovery from anaesthesia.
Ketamine is available in 3 strengths : 10, 50, and 100mg/mL, which are easily
confused. The IV dose for GA is 1–2mg/kg over 1min, which is effective after
2–7min and provides surgical anaesthesia for 5–10min. The IM dose for GA
is 10mg/kg, which is effective after 4–15min and gives surgical anaesthesia
for 12–25min. Further doses (10–20mg IV or 20–50mg IM) can be given if
major limb movements or i muscle tone prevent extrication of the patient.
For sedation of children undergoing suturing or other minor procedures,
ketamine may be given IM (2.5mg/kg) or IV (1mg/kg over at least 1min).
With this dose of ketamine, LA is needed for cleaning and suturing of
wounds, but little physical restraint should be needed to allow the pro-
cedure to take place. Occasionally, a second dose of ketamine (1mg/kg
IM or 0.5mg/kg IV) is required to achieve adequate sedation. Larger initial
doses provide deeper sedation, but are more likely to cause side effects
(eg vomiting or agitation) during recovery. With low doses of ketamine,
agitation is unlikely and there is no need to add midazolam.

279
ANALGESIA FOR TRAUMA
Analgesia for trauma
Multiple injuries
Entonox
®
may be useful for analgesia during transport and initial resusci-
tation, but only allows administration of 50 % O
2
and should not be used
if there is an undrained pneumothorax. As soon as practicable use other
forms of analgesia, usually IV morphine ( b p.276) and/or nerve blocks
( b p.292), and splint fractures to d pain and d blood loss.
Head injury
Relief of pain is particularly important in head-injured patients, since pain
and restlessness i ICP, which can exacerbate secondary brain injury.
Headache following a head injury can usually be treated with paracetamol,
diclofenac or codeine phosphate (which may cause less central depression
than stronger opioids such as morphine). If the headache is severe or
increasing, arrange a CT scan to look for an intracranial haematoma. Try to
avoid strong opioids, because of concern about sedation and respiratory
depression, but if pain is severe give morphine in small IV increments: the
effects can be reversed if necessary with naloxone. Femoral nerve block
is particularly useful in a patient with a head injury and a fractured femur,
since it d or avoids the need for opioids.
Small children with minor head injuries often deny having headaches, but
look and feel much better if given paracetamol ( b p.274). Give further
doses if necessary over the following 12–24 hours.
Chest injury
Chest injuries are often extremely painful. Good analgesia is essential to
relieve distress and d risk of complications such as pneumonia and res-
piratory failure. Avoid Entonox
®
if a pneumothorax is a possibility, until
this has been excluded or drained. Give high concentration O
2
as soon as
possible and check SpO
2
and ABG. Give morphine in slow IV increments
( b p.276) and monitor for respiratory problems. Intercostal nerve blocks
( b p.303) provide good analgesia for fractured ribs, but may cause a
pneumothorax and should only be used in patients being admitted. In
severe chest injuries get anaesthetic or ICU help: thoracic epidural anaes-
thesia can sometimes avoid the need for IPPV. Before a thoracic epidural
is performed, check X-rays of the thoracic spine for fractures.

280 CHAPTER 7 Analgesia and anaesthesia
Analgesia in specifi c situations
Children
Injured children are distressed by both fear and pain. Parental support
can be very helpful. Sensitive treatment, explanation and reassurance are
important, but give analgesia whenever necessary.
Oral analgesia is usually with paracetamol ( b p.274), but if this is inadequate
add ibuprofen ( b p.275), dihydrocodeine elixir, or Oramorph
®
:
• Ibuprofen dose: 20mg/kg daily in divided doses as ibuprofen suspension
(100mg in 5mL) 1–2 years: 2.5mL; 3–7 years: 5mL; 8–12 years: 10mL; all
3–4 times daily.
• Dihydrocodeine elixir dose: 0.5–1mg/kg PO 4–6-hourly.
• Children in severe pain may benefi t from oral morphine (as Oramorph
®
oral solution — b p.276).
Entonox
®
(b p.278) gives rapid analgesia without the need for an
injection.
IV morphine is appropriate in severe injuries, but take particular care if
there is a head injury, since sedation may occur.
Femoral nerve block ( b p.304) provides good analgesia for femoral
fractures and is usually well tolerated.
Digital nerve block with bupivacaine ( b p.294) is useful for painful fi nger
injuries, especially crush injuries. Provide this before X-ray: when the
child returns from X-ray the fi nger may then be cleaned and dressed
painlessly.
IM morphine could be used to provide analgesia for small burns or
fractured arms, but oral morphine or nasal diamorphine are preferable,
since IM injections are painful and unpleasant.
Nasal diamorphine is not licensed, but is playing an increasing role in the
provision of pain relief in children (see Table 7.1 ).
Acute abdominal pain
It is cruel and unnecessary to withhold analgesia from patients with acute
abdominal pain. Adequate analgesia allows the patient to give a clearer
history, and often facilitates examination and diagnosis: tenderness and
rigidity become more localized, and masses more readily palpable. Good
X-rays cannot be obtained if the patient is distressed and restless because
of renal colic or a perforated ulcer.
Morphine by slow IV injection ( b p.276) is appropriate in severe pain,
unless this is due to renal or biliary colic, in which an NSAID ( b p.275)
may be preferred. Morphine occasionally causes severe abdominal pain due
to smooth muscle spasm of the sphincter of Oddi ( b p.277).
Toothache
Toothache or pain after dental extractions can often be eased by aspirin,
a NSAID or paracetamol. Do not give opioids such as codeine or
dihydrocodeine, which may make the pain worse. Drainage of a dental
abscess may be required to relieve toothache.
281
ANALGESIA IN SPECIFIC SITUATIONS
Nasal diamorphine for analgesia in children
1,2
In the UK, diamorphine is licensed for use IV, IM, SC and PO. Nasal
diamorphine is unlicensed, but clinical studies and experience have shown
that this is an effective and acceptable method of analgesia for children
with limb fractures or small burns who do not need immediate venous
access. It should be given as soon as possible, prior to X-rays.
Contraindications: age <1 year (or weight <10kg), nasal obstruction or
injury, basal skull fracture, opioid sensitivity.
Verbal consent for nasal diamorphine should be obtained from the child’s
parents (and the child if appropriate), since this is an unlicensed route of
administration of this drug. Follow local protocols.
The dose of nasal diamorphine is 0.1mg/kg, given in a syringe in a volume
of 0.2mL. The child is weighed. The appropriate concentration of solution
for the weight of child is achieved by adding a suitable volume of 0.9 %
saline to a 10mg ampoule of diamorphine.
0.2mL of this solution is drawn up into a syringe and given in one or both
nostrils, whilst the child’s head is tilted backwards. Turn the head to each
side, maintaining each position for several secs. A small syringe can be used
to drip the solution into the nose, but if possible use an aerosol device
(eg MAD
®
), allowing for the dead space of the device (0.1mL for MAD,
so draw up 0.3mL). Record the time of administration. Monitor conscious
level for 20min. Respiratory depression is unlikely, but resuscitation facili-
ties and naloxone must be available. Nasal diamorphine provides rapid
analgesia which lasts up to 4 hr.
Fentanyl may also be used nasally (initial dose 2micrograms/kg) as an
alternative to nasal diamorphine.
1 College of Emergency Medicine Clinical Effectiveness Committee ( 2009 ). Guideline for the
management of pain in children . College of Emergency Medicine , London .
2 http://intranasal.net/PainControl/default.htm
Table 7.1 Dosage of nasal diamorphine in children
Weight (kg) Volume of saline (mL) Dose of diamorphine (mg) in 0.2mL
10 2.0 1.0
15 1.3 1.5
20 1.0 2.0
25 0.8 2.5
30 0.7 2.9
35 0.6 3.3
40 0.5 4.0
50 0.4 5.0
60 0.3 6.7

282 CHAPTER 7 Analgesia and anaesthesia
Local anaesthesia (LA)
Indications for LA in the emergency department
LA is indicated in any situation in which it will provide satisfactory
analgesia
or safe and adequate conditions for operations or procedures. These
include the following:
• Insertion of venous cannulae (0.1mL of 1 % lidocaine SC 30 secs prior to
cannulation d pain of cannulation without affecting the success rate).
• Cleaning, exploration and suturing of many wounds.
• Analgesia for some fractures , eg shaft of femur.
• Minor operations/procedures, eg manipulation of some fractures and
dislocations, insertion of chest drain, drainage of paronychia, removal of
corneal FB.
Contraindications to local anaesthetic
• Refusal or poor co-operation by the patient.
• Allergy to local anaesthetic Severe allergic reactions to LA are rare, but
anaphylaxis can occur. If allergy to a LA is alleged, obtain full details of
the circumstances and the drug involved and check with a senior before
giving any LA. It may be possible to use a different drug. Some reactions
are caused by the preservative in multi-dose vials, rather than the drug
itself, so single dose ampoules may not cause a problem. Some alleged
‘allergies’ are actually toxic effects due to overdosage, or faints due to
fear and pain.
• Infection at the proposed injection site Injection into an infl amed area is
painful and could spread infection. High tissue acidity from infl ammation
d effectiveness of LA drugs. Hyperaemia causes rapid removal of the
drug and so a short duration of action and i risk of toxicity. LA nerve
block at a site away from the infected area can provide good anaes-
thesia, eg digital nerve block for paronychia or nerve blocks at the ankle
for an abscess on the sole of the foot.
• Bleeding disorder Anticoagulant therapy and thrombocytopenia are
contraindications for nerve blocks in which there is a risk of inadvertent
arterial puncture.
Special cautions ( i risk of toxicity)
• Small children.
• Elderly or debilitated.
• Heart block.
• Low cardiac output.
• Epilepsy.
• Myasthenia gravis.
• Hepatic impairment.
• Porphyria.
• Anti-arrhythmic or B -blocker therapy (risk of myocardial depression).
• Cimetidine therapy (inhibits metabolism of lidocaine).

283
LOCAL ANAESTHESIA (LA)
Lidocaine (lignocaine)
Lidocaine is the LA used most often for local infi ltration and for nerve
blocks. It is available in 0.5 % , 1 % and 2 % solutions, either ‘plain’ (without
adrenaline) or with adrenaline 1:200,000. For routine use the most suitable
choice is 1 % plain lidocaine.
Duration of action Lidocaine acts rapidly and the effects last from 30–60min
(for plain lidocaine) to 90min (lidocaine with adrenaline). The duration of
action varies with the dosage and the local circulation.
For plain lidocaine the maximum dose is 200mg (20mL of 1 % solution) in a
healthy adult or 3mg/kg in a child.
For lidocaine with adrenaline the maximum dose is 500mg (50mL of 1 %
solution) in a healthy adult or 7mg/kg in a child.
These are the maximum total doses for one or more injections of LA
given together for local infi ltration or nerve block (with care to avoid
intravascular injection). Reduce the dose in debilitated or elderly patients,
or if there is a particular risk of toxicity (see opposite).
Lidocaine can also be used for anaesthesia of the skin (with prilocaine
in EMLA
®
cream, b p.288), urethra and cornea, and also as a spray for
anaesthetizing mucous membranes in the mouth and throat.
Bupivacaine
Bupivacaine is particularly useful for nerve blocks since it has a long
duration of action (3–8hr), although its onset of anaesthesia is slower
than lidocaine. It may also be used for local infi ltration, but not for Bier's
block ( b p.290). Bupivacaine is available in concentrations of 0.25 and
0.5 % with or without adrenaline: the usual choice is 0.5 % bupivacaine
without adrenaline. The maximum dose of bupivacaine (with or without
adrenaline) for a fi t adult is 150mg (30mL of 0.5 % or 60mL of 0.25 % ) and
for a child 2mg/kg.
Prilocaine
Prilocaine has a similar duration of action to lidocaine. It can be used
for local infi ltration or nerve blocks, but is particularly useful for Bier’s
block ( b p.290). High doses (usually > 600mg) may cause methaemoglo-
binaemia. The maximum dose of prilocaine for a healthy adult is 400mg
(40mL of 1 % solution) and for a child 6mg/kg.
Tetracaine (amethocaine)
Tetracaine is used for topical local anaesthesia of the cornea ( b p.535)
and skin ( b p.288).
Proxymetacaine
Proxymetacaine is also used for topical local anaesthesia of the cornea.
It causes less initial stinging than tetracaine and is particularly useful in
children.

284 CHAPTER 7 Analgesia and anaesthesia
Local anaesthetic toxicity
Toxic effects
These result from overdosage of LA or inadvertent intravascular injection.
The fi rst symptoms and signs are usually neurological, with numbness of
the mouth and tongue, slurring of speech, lightheadedness, tinnitus, con-
fusion and drowsiness. Muscle twitching, convulsions and coma can occur.
Cardiovascular toxicity may initially result in tachycardia and hypertension,
but later there is hypotension with a bradycardia and heart block.
Ventricular arrhythmias and cardiac arrest occur occasionally, especially
with bupivacaine.
Early signs of toxicity
These may be detected if the doctor maintains a conversation with
the patient while injecting LA. Toxic effects may start immediately if an
intravascular injection is given. However, peak blood levels usually occur
8 10–25min after injection — so if a relatively large dose has been given, do
not leave the patient alone while anaesthesia develops.
Occasionally, patients initially agree to LA, but become hysterical or faint
(even while lying fl at) when an injection is given. In such circumstances it
may be diffi cult to distinguish immediately between the effects of anxiety
and those of drug toxicity.
Treatment of LA toxicity
• Stop the procedure.
• Call for help.
• Clear and maintain the airway.
• Give 100 % O
2
and ensure adequate lung ventilation.
• Obtain reliable IV access. If possible take blood for U&E.
• Monitor ECG. Record pulse, BP, respiratory rate and conscious level.
• If convulsions occur ensure adequate oxygenation and give lorazepam
(adult dose 2–4mg slowly IV; child: 100micrograms/kg, max 4mg) or
diazepam (adult 5–10mg slowly IV; child 100micrograms/kg).
• Treat hypotension by raising the foot of the trolley. If systolic BP
remains <90mmHg in an adult, give IV fl uids (eg colloid 500mL). In a
child give 20mL/kg if systolic BP <70mmHg.
• Bradycardia usually resolves without treatment. If bradycardia and
hypotension persist give atropine and consider IV lipid emulsion.
• In cardiac arrest due to LA toxicity, give lipid emulsion using Intralipid
®
20 % 1.5mL/kg IV over 1min (bolus of 100mL for 70kg patient) then
15mL/kg/hr (500mL over 30min for 70kg patient). Continue CPR. If
circulation is still inadequate repeat IV bolus of Intralipid twice at 5min
intervals then IVI 30mL/kg/hr (500mL over 15min). Maximum total dose
of 20 % lipid emulsion is 12mL/kg).
• See b p.187 and http://www.aagbi.org/publications/guidelines/docs/
la_toxicity_2010.pdf

285
LOCAL ANAESTHETIC TOXICITY
Adrenaline (epinephrine) in local anaesthesia
Most local anaesthetics cause vasodilatation, so adrenaline is sometimes
added as a vasoconstrictor. This d blood loss, i duration of anaesthesia
and d toxicity by delaying absorption of the LA. Lidocaine with adrenaline
is often useful in scalp wounds, in which bleeding can be profuse but the
bleeding point is not visible.
Bupivacaine with adrenaline is recommended for intercostal nerve block to
d risk of toxicity from rapid absorption in a relatively vascular area.
Lidocaine with adrenaline can be used in some situations (see below for
contraindications) if a relatively large volume of LA is needed, since the
max dose for a healthy adult is 500mg (50mL of 1 % solution) compared to
200mg (20mL of 1 % ) for plain lidocaine. Other possibilities in such circum-
stances include 0.5 % lidocaine, prilocaine (max dose: 40mL of 1 % solution)
or GA.
The maximum concentration of adrenaline in LA is 1 in 200,000, except for
dental anaesthesia in which 1 in 80,000 may be used. The maximum total
dose of adrenaline in a healthy adult is 500micrograms.
Contraindications and cautions
Never use adrenaline for injections in the nose, ears, or penis, nor in Bier's
block ( b p.290). Avoid adrenaline for injections in or near fl ap lacera-
tions, since vasoconstriction could cause ischaemic necrosis. Adrenaline
is traditionally regarded as dangerous in digital nerve blocks of fi ngers and
toes, because of the risk of ischaemia, but some hand surgeons have used
LA with adrenaline uneventfully to reduce bleeding and avoid the need
for a fi nger tourniquet However, LA without adrenaline is advisable for
routine use in fi ngers and toes, to avoid concerns about ischaemia.
Avoid adrenaline in:
• Ischaemic heart disease.
• Hypertension.
• Peripheral vascular disease.
• Thyrotoxicosis.
• Phaeochromocytoma.
• Patients on beta-blockers.
The BNF states that LA with adrenaline appears to be safe in patients on
tricyclic antidepressants.
Storage Keep ampoules and vials of LA with adrenaline in a locked
cupboard separate from those without adrenaline, so that they are
only available by special request and are not used inadvertently or
inappropriately.

286 CHAPTER 7 Analgesia and anaesthesia
General principles of local anaesthesia
Obtain a brief medical history and record drug treatment and allergies.
Think about possible contraindications and cautions for LA ( b p.282).
Obtain expert advice if you have any query.
Consent for local anaesthetic
Explain to the patient what is planned. Verbal consent is adequate for
most LA procedures in the ED.
Written consent is needed:
• If there is a signifi cant risk of a toxic reaction or complication, including
procedures needing large doses of LA.
• Bier's block ( b p.290).
• Intercostal nerve block (risk of pneumothorax).
Safety
Ensure that resuscitation equipment and drugs for toxic reactions are
readily available. Monitoring and IV access are not needed for routine
simple LA, but are essential if there is a risk of complications or toxicity.
Calculate the maximum dose of LA that could be used ( b p.283) and
think how much might be needed. Before drawing up any LA check the
drug label carefully, especially if adrenaline is contraindicated.
Giving local anaesthetic
• Lie the patient down in a comfortable position with the site of injec-
tion accessible and supported. Some patients faint if LA is injected while
they are sitting up.
• Warm the LA to body temperature prior to use.
• Wash your hands, use gloves, and clean the skin.
• Use a fi ne needle if possible. Before inserting the needle warn the
patient and hold the relevant part fi rmly to prevent movement.
• Aspirate and check for blood in the syringe before injecting any LA.
If the needle moves, aspirate again.
• Inject LA slowly to d pain. Do not use force if there is resistance to
injection.
• Maintain a conversation with the patient, to allay anxieties and also to
detect any early signs of toxicity ( b p.284).
Further details of techniques and precautions are listed on other pages:
Topical anaesthesia: b p.288.
Local infi ltration and fi eld blocks : b p.289.
Haematoma block for fractures : b p.289.
Bier’s block (IV regional anaesthesia): b p.290.
Nerve blocks: b pp.292–306.
Recording the local anaesthetic
Write clearly in the notes to record the time and site of injection and the
type and quantity of LA given.

287
GENERAL PRINCIPLES OF LOCAL ANAESTHESIA
Local anaesthesia in children
The general principles are the same as for adults. LA is very useful in chil-
dren, but requires experienced staff. Many children tolerate LA without
any problem, but in some sedation with midazolam ( b p.308) or keta-
mine ( b p.278) can be helpful.
Weigh the child if possible and calculate the maximum dose of LA
( b p.283). In an average size child a simple initial estimate of the maximum
dose of 1 % plain lidocaine is 1mL per year of age (ie 3mL for a 3-year-old
child). If a larger volume may be needed, consider using 0.5 % solution or
lidocaine with adrenaline ( b p.285), or possibly a GA instead.
Prepare everything before bringing the child into the room — rattling
equipment and drawing up LA within sight of a patient causes unnecessary
anxiety. Most parents prefer to stay with their child during the procedure
and this is often helpful. Position the child and parent comfortably. Explain
simply and honestly what is going to happen. Have adequate help to keep
the child still. Use a small needle if possible and inject slowly to minimize
pain from the injection.

288 CHAPTER 7 Analgesia and anaesthesia
Topical anaesthesia
LA applied directly to mucous membranes of the mouth, throat
or urethra will diffuse through and block sensory nerve endings.
Development of anaesthesia may take several minutes and the duration
is relatively short because of the good blood supply. Over-dosage is
dangerously easy because most topical preparations contain high
concentrations of lidocaine (2 % in lidocaine gel, 5 % in ointment, and 4 % or
10 % in lidocaine spray).
Lidocaine gel has been used to allow cleaning of gravel burns, but this is
not advisable: absorption of lidocaine can easily cause toxicity and the
degree of anaesthesia is rarely satisfactory. Scrubbing is often necessary
to remove embedded gravel, so proper anaesthesia is essential. Field
block may be adequate for a small area, but GA is often necessary
for cleaning large or multiple gravel burns, in order to avoid tattooing.
Topical anaesthesia
EMLA
®
cream
‘Eutectic mixture of local anaesthetics’ (EMLA
®
) cream contains lidocaine
2.5 % and prilocaine 2.5 % , and is used for topical anaesthesia of the skin.
EMLA
®
is of limited value in the ED because it must only be applied to
intact skin (not wounds) and the onset of anaesthesia is slow, usually
8 1 hour. EMLA
®
must not be used in children aged <1 year and caution is
needed in patients with anaemia or methaemoglobinaemia.
EMLA
®
can usefully d pain of an injection or cannulation. Apply a thick
layer of EMLA
®
cream to the skin and cover it with an occlusive dressing,
which must be left undisturbed for 1 hour.
Tetracaine (amethocaine) gel (Ametop
®
)
This is similar to EMLA
®
, but acts more quickly and causes vasodilatation,
which aids venous cannulation. It must not be used in wounds because of
the risk of rapid absorption and toxicity.
Other topical LA agents
Topical agents such as TAC (tetracaine, adrenaline, and cocaine) or LET
(lidocaine, epinephrine and tetracaine) are sometimes used to provide
anaesthesia for wound repair. These preparations can provide effective
anaesthesia, but toxic effects may occur from excessive absorption (especially
of cocaine) and they are not licensed in the UK.
Ethyl chloride
Ethyl chloride is a clear fl uid which boils at 12.5 ° C. Spraying the liquid on
the skin causes rapid cooling and freezing of the surface. In the past ethyl
chloride was used for incision of paronychias and small abscesses, but it
rarely provides adequate anaesthesia and it cannot be recommended.
Ethyl chloride is highly infl ammable and is a GA, so it must be handled
with care if it is used at all.

289
LOCAL ANAESTHETIC ADMINISTRATION
Local anaesthetic administration
Local infi ltration anaesthesia
Local infi ltration is the technique used most often in the ED. The LA
injected subcutaneously in the immediate area of the wound acts within
1–2min. Anaesthesia lasts 30–60min with plain lidocaine or 8 90min with
lidocaine and adrenaline.
In clean wounds the pain of injection can often be d by inserting the
needle through the cut surface of the wound. Do not do this in dirty
or old wounds, because of the risk of spreading infection. Less pain is
produced by injecting slowly through a thin needle, injecting in a fan-
shaped area from a single injection site, and by inserting the needle in
an area already numbed by an earlier injection. Rapid injection of LA,
especially in scalp wounds, can cause spraying of solution from the tip
of the needle or from separation of the needle from the syringe. Slow
injection and the use of goggles should d risk of transmission of infection.
Field block
This involves infi ltration of LA subcutaneously around the operative fi eld.
Sometimes it is only necessary to block one side of the area, depending
on the direction of the nerve supply. Field block can be useful for ragged
and dirty wounds, and for cleaning gravel abrasions. Check the max safe
dose before starting a fi eld block. If relatively large volumes of anaesthetic
might be needed, consider 0.5 % lidocaine or lidocaine with adrenaline
( b p.285).
Haematoma block
A Colles’ fracture ( b p.444) can be manipulated after infi ltration of LA
into the fracture haematoma and around the ulnar styloid. This often pro-
vides less effective anaesthesia than Bier’s block ( b p.290) and a poorer
reduction. It converts a closed fracture into an open one and so there is a
theoretical risk of infection, but in practice this is rare.
Contraindications and warnings
• Fractures > 24 hours old (since organization of the haematoma would
prevent spread of the LA).
• Infection of the skin over the fracture.
• Methaemoglobinaemia (avoid prilocaine).
Drug and dosage 15mL of 1 % plain prilocaine. Lidocaine can be used,
but there is a lower margin of safety. Never use solutions containing
adrenaline.
Technique Use a 20mL syringe and 0.6 × 25mm needle. Full asepsis is
essential. Insert the needle into the fracture haematoma and aspirate
blood to confi rm this. Inject slowly to minimize pain and reduce the risk of
high blood levels and toxicity. Anaesthesia develops in 8 5min and lasts for
30–60min. Sometimes anaesthesia is inadequate for proper manipulation
and so an alternative anaesthetic is needed.

290 CHAPTER 7 Analgesia and anaesthesia
Bier’s block
Bier’s block (IV regional anaesthesia) is often used to provide anaesthesia
for reduction of Colles’ fractures or for minor surgery below the elbow.
Bier’s block uses a large dose of LA and so there is a risk of a toxic reaction,
although this is minimized by correct technique. Ensure that the patient
has fasted for 4 hours. Pre-operative assessment is necessary, including
recording of BP and weight. Obtain written consent for the operation.
Bier’s block should only be performed by doctors who are competent
to deal with severe toxic reactions. At least two trained staff must be
present throughout the procedure.
Contraindications
• Severe hypertension or obesity.
• Severe peripheral vascular disease.
• Raynaud’s syndrome.
• Sickle cell disease or trait.
• Methaemoglobinaemia.
• Children aged <7 years.
• Uncooperative or confused patient.
• Procedures needed in both arms.
• Surgery that may last > 30min.
• Surgery that may need the tourniquet to be released.
Proceed with caution in epileptic patients because of the risk of a fi t from
LA toxicity.
Drug and dose
The only drug suitable for Bier’s block is prilocaine, from a single dose
vial without preservative. Never use solutions with adrenaline. Do not
use lidocaine or bupivacaine, which are more likely than prilocaine to
cause toxic effects. The ideal concentration of prilocaine is 0.5 % . If only
1 % prilocaine is available dilute it with an equal volume of 0.9 % saline to
make 0.5 % prilocaine.
The dose of prilocaine is 3mg/kg, which is 42mL of 0.5 % prilocaine for a
70kg adult, or 30mL of 0.5 % prilocaine for a 50kg patient.
Equipment
• Special tourniquet apparatus is essential, with a 15cm wide cuff for
adults.
• Check the tourniquet apparatus and cuff regularly.
• Ordinary BP cuffs and sphygmomanometers are not reliable enough,
and should not be used for Bier’s blocks.
• Check that resuscitation equipment and drugs are available to hand.
• Ensure that the patient is on a tipping trolley.
• Monitor the ECG, BP and SpO
2
throughout.

291
BIER’S BLOCK
Technique for Bier’s block
1
• Insert a small IV cannula in the dorsum of the hand on the side of opera-
tion (ready for injection of prilocaine) and another IV cannula in the
opposite arm (for emergency use if needed).
• Check the radial pulse. Place the tourniquet high on the arm over
padding, but do not infl ate it yet.
• Elevate the arm for 3min while pressing over the brachial artery, to
try to exsanguinate the limb. (Do not use an Esmarch bandage for this
purpose, because of pain).
• While the arm is elevated infl ate the tourniquet to 300mmHg, or at
least 100mmHg above the systolic BP. Lower the arm on to a pillow and
check that the tourniquet is not leaking.
• Record the tourniquet time. A trained person must observe the tourni-
quet pressure constantly during the procedure.
• Slowly inject the correct volume of 0.5 % plain prilocaine into the iso-
lated limb, which will become mottled. If the operation is on the hand,
squeeze the forearm during injection to direct LA peripherally. Test for
anaesthesia after 5min. If anaesthesia is inadequate inject 10–15mL 0.9 %
saline to fl ush the prilocaine into the arm. Occasionally, no adequate
anaesthesia is achieved and GA is needed instead.
• Complete the manipulation or operation. Before applying a POP back
slab remove the cannula from the injured arm.
• The tourniquet cuff must remain infl ated for at least 20min and a
maximum of 45min.
• Obtain a check X-ray while the tourniquet cuff is still infl ated (in case
remanipulation is required).
• If the check X-ray is satisfactory defl ate the tourniquet slowly and
record the time. Maintain a conversation with the patient and watch
carefully for any sign of toxicity. If any toxic effects occur re-infl ate the
tourniquet and give any necessary treatment ( b p.284).
• After release of the tourniquet the arm becomes warm and fl ushed.
Sensation returns after a few minutes.
• Observe the patient carefully for at least 30mins after a Bier’s block in
case of delayed toxicity. Check the circulation of the limb before the
patient is discharged home. Reactive swelling can occur: elevate the
limb in a sling and give POP instructions.
1 College of Emergency Medicine Clinical Effectiveness Committee ( 2010 ) Intravenous regional
anaesthesia for distal forearm fractures (Bier’s block) . College of Emergency Medicine , London .

292 CHAPTER 7 Analgesia and anaesthesia
Local anaesthetic nerve blocks
LA nerve blocks are very useful in the ED for many minor operations
and to provide analgesia. Several nerve blocks are described in the
following sections. Many other nerve blocks and regional blocks are
possible, but are not normally appropriate in the ED. Some should only
be performed by doctors with anaesthetic training, or in a few cases,
dental training.
Equipment for nerve blocks
Ordinary injection needles can be used for most local blocks in the ED.
Anaesthetists sometimes use special pencil-point or short bevel needles
when blocking large nerve trunks and plexuses.
General procedure for nerve blocks
• Follow the general principles of LA ( b p.282).
• Review the relevant anatomy for the block. Determine the site of injec-
tion by feeling for local structures such as arteries or tendons.
• When performing a nerve block hold the needle with the bevel in the
line of the nerve (rather than across it), to reduce the risk of cutting
nerve fi bres.
• Ask the patient about tingling in the area supplied by the nerve. Do not
try to elicit paraesthesiae. If paraesthesiae occur withdraw the needle
2–3mm before injecting.
• Wait for the nerve block to work, but do not leave the patient alone
during this time. Tell the nurse when to call you back, in case you are
busy with other patients. Estimate when a nerve block should be effec-
tive and do not test sensation before then. Small nerves may be blocked
in 5min, but large nerves may take up to 40min.
Failed nerve block
If a nerve block does not work, consider waiting longer or giving another
injection. Before giving any more LA, review relevant anatomy, consider
using ultrasound guidance, and check that the maximum safe dose of the
drug will not be exceeded. Entonox
®
can be helpful as a supplement to
LA for some procedures, such as reduction of dislocations. Alternatively,
sedation ( b p.308) may be useful in some cases. Occasionally, one has to
abandon LA and arrange GA instead.
Ultrasound guidance for nerve blocks
1
Ultrasound guidance can help in identifying nerves and other struc-
tures and allows visualization of the needle position and the spread of
LA. Precise injection of LA adjacent to a nerve gives a faster onset and
longer duration of anaesthesia with a smaller volume of LA, less pain and a
reduced risk of complications. Ultrasound is unnecessary for some nerve
blocks, eg digital nerves and supraorbital nerve block. Ultrasound allows
nerve blockade away from identifying structures, eg medial nerve block in
the forearm.
Successful use of ultrasound for LA requires appropriate equipment,
knowledge of relevant anatomy, and training in ultrasound techniques.
1 Marhofer P ( 2008 ) Ultrasound Guidance for Nerve Blocks . Oxford University Press , Oxford .
This page intentionally left blank

294 CHAPTER 7 Analgesia and anaesthesia
Digital nerve block
Digital nerve block is used frequently for simple operations on the fi ngers
and toes. (The term ‘ring block’ is often used, but is incorrect since it
implies that LA is injected in a ring around the fi nger, which is unnecessary
and might cause ischaemia due to vascular compression).
A dorsal and a palmar digital nerve run along each side of the fi nger and
thumb. Similarly, there are dorsal and plantar nerves in the toes.
1 % plain lidocaine is often used, but bupivacaine (0.5 % plain) is preferable
because it is less painful on injection, and gives prolonged anaesthesia and
analgesia. The traditional advice is never to use adrenaline or any other
vasoconstrictor. In an adult use 1–2mL of LA on each side of the fi nger,
thumb, or big toe. Use smaller volumes in the other toes or in children.
Technique
• Use a 0.6 × 25 mm (23G) needle (0.5 × 16 mm, 25G, in small children).
• Insert the needle from the dorsum on the lateral side of the base of the
digit, angled slightly inwards towards the midline of the digit, until the
needle can be felt under the skin on the fl exor aspect.
• Aspirate to check the needle is not in a blood vessel.
• Slowly inject 0.5–1mL. Continue injecting as the needle is withdrawn.
• Repeat on the medial side of the digit.
• If anaesthesia is needed for the nail bed of the great toe give an addi-
tional injection of LA subcutaneously across the dorsum of the base
of the proximal phalanx, to block the dorsal digital nerves and their
branches. This is also required for anaesthesia of the dorsum of the digit
proximal to the middle phalanx.
Anaesthesia develops after 8 5min. Autonomic nerve fi bres are blocked,
as well as sensory nerve fi bres, so when the block works the skin feels
dry and warm. Occasionally, anaesthesia remains inadequate and another
injection is needed. The maximum volume that can be used in a fi nger,
thumb, or big toe is 5mL. Use less in the other toes or in children.
Single injection digital nerve block
Anaesthesia of the distal phalanx and DIP joint can be achieved by a single
subcutaneous injection in the volar aspect of the base of the fi nger. Pinch
the soft tissues just distal to the proximal skin crease. Insert a 25G needle
just beneath the skin at the midpoint of the skin crease and inject 2–3mL
of 0.5 % bupivacaine. Massage the LA into the soft tissues.
Digital nerve block at metacarpal level
Digital nerves can be blocked where they run in the interspaces between
the metacarpals. Insert a thin needle in the palm through the distal palmar
crease, between the fl exor tendons of adjacent fi ngers. Injection of 3–4mL
of 1 % plain lidocaine will block the adjacent sides of these two fi ngers.
Anaesthesia develops after 5–10min. Alternatively, a dorsal approach can
be used: this is often preferred because it is less painful, but there is an i
risk of inadvertent venepuncture and the digital nerves are further from
the dorsal surface, so a deep injection is needed.
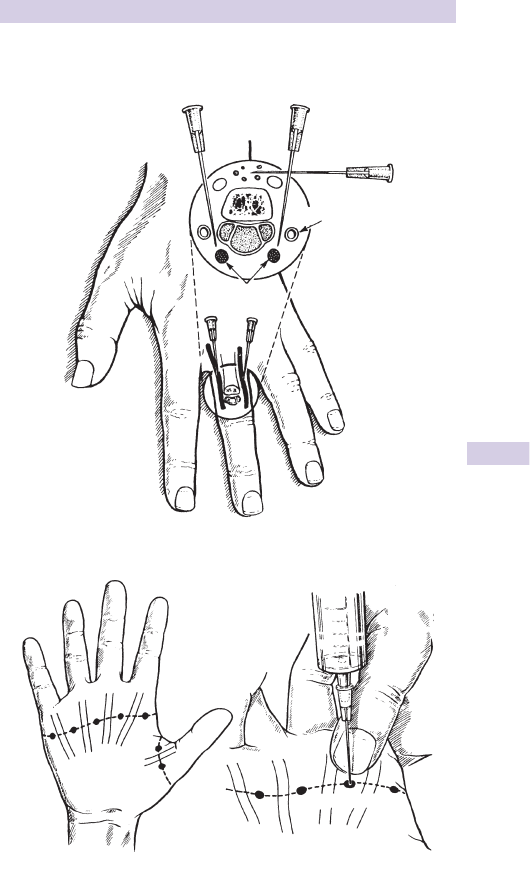
295
DIGITAL NERVE BLOCK
Digital nerve block
Digital artery
Needle position
Digital nerve
Digital nerve block at the base of the finger
Digital nerve block at metacarpal level
Distal palmar
crease
Site of injection
31
3
1
2
Fig. 7.1 Digital nerve block.

296 CHAPTER 7 Analgesia and anaesthesia
Nerve blocks at the wrist: 1
The median nerve supplies sensation to the radial half of the palm, the thumb,
index and middle fi nger, and the radial side of the ring fi nger. The ulnar nerve
supplies the ulnar side of the hand, the little fi nger, and the ulnar side of the
ring fi nger. The radial nerve supplies the dorsum of the radial side of the
hand. The different nerve distributions overlap. In some people, the radial
side of the ring fi nger and the ulnar side of the middle fi nger are supplied by
the ulnar, rather than median nerve. LA block of one or more nerves at the
wrist provides good anaesthesia for minor surgery on the hand and fi ngers.
Median nerve block
At the wrist the median nerve lies under the fl exor retinaculum on the
anterior aspect of the wrist, under or immediately radial to the tendon of
palmaris longus and 5–10mm medial to the tendon of fl exor carpi radialis.
Just proximal to the fl exor retinaculum, the median nerve gives off the
palmar cutaneous branch, which travels superfi cially to supply the skin of
the thenar eminence and the central palm.
Carpal tunnel syndrome is a contraindication to median nerve block.
Technique
• Use a 0. 6mm (23G) needle and 8 5–10mL of 1 % lidocaine.
• Ask the patient to fl ex the wrist slightly and bend the thumb to touch
the little fi nger, in order to identify palmaris longus.
• Insert the needle vertically at the proximal wrist skin crease, between
palmaris longus and fl exor carpi radialis, angled slightly towards palmaris
longus, to a depth of 1 cm. If paraesthesiae occur withdraw the needle
by 2–3 mm.
• Inject 8 5mL of LA slowly.
• Block the palmar cutaneous branch by injecting another 1–2mL SC
while withdrawing the needle.
• Some people do not have a palmaris longus tendon — in this case,
identify fl exor carpi radialis and insert the needle on its ulnar side.
• Ultrasound allows blockade of the median nerve in the forearm.
Ulnar nerve block
In the distal forearm the ulnar nerve divides into a palmar branch (which
travels with the ulnar artery to supply the hypothenar eminence and palm)
and a dorsal branch (which passes under fl exor carpi ulnaris to supply the
ulnar side of the dorsum of the hand).
Technique
• Use a 0.6mm (23G) needle and 5–10mL of 1 % lidocaine. Avoid
adrenaline in peripheral vascular disease.
• Check the radial pulse before blocking the ulnar nerve.
• Feel the ulnar artery and fl exor carpi ulnaris tendon and insert the
needle between them at the level of the ulnar styloid process.
• Aspirate and look for blood in the syringe. Withdraw the needle 2–3mm
if paraesthesiae occur.
• Inject 5mL of LA.
• Block the dorsal branch of the ulnar nerve by SC infi ltration of 3–5mL
of LA from fl exor carpi ulnaris around the ulnar border of the wrist.
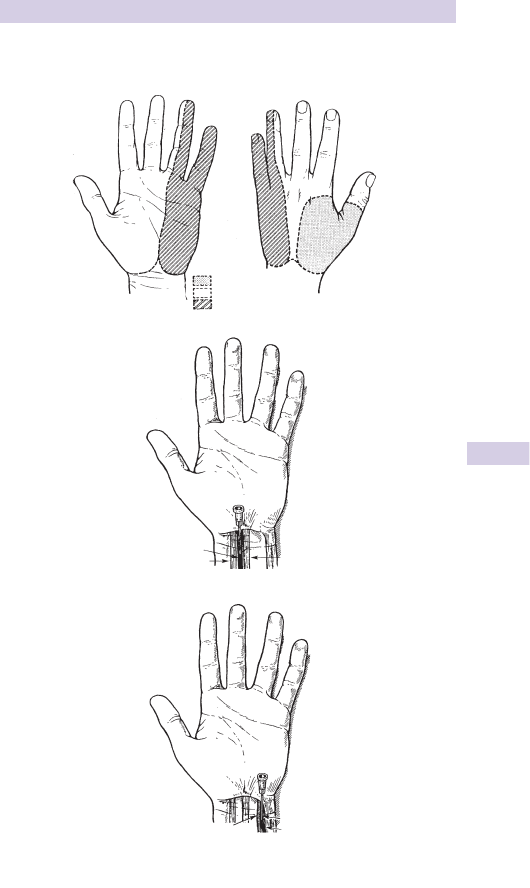
297
NERVE BLOCKS AT THE WRIST: 1
Nerve blocks at the wrist
Radial nerve
Median nerve
Ulnar nerve
Median nerve
Palmaris
longus
Ulnar nerve
Flexor carpi ulnaris
Flexor carpi radialis
Ulnar artery
Fig. 7.2 Nerve blocks at the wrist.

298 CHAPTER 7 Analgesia and anaesthesia
Nerve blocks at the wrist: 2
Radial nerve block
In the distal part of the forearm the radial nerve passes under the tendon
of brachioradialis and lies subcutaneously on the dorsum of the radial side
of the wrist, where it separates into several branches and supplies the
radial side of the dorsum of the hand.
Technique
• Use a 0.6mm (23G) needle and 5mL of 1 % lidocaine, with or without
adrenaline.
• Infi ltrate LA subcutaneously around the radial side and dorsum of the
wrist from the tendon of fl exor carpi radialis to the radio-ulnar joint.
Beware of inadvertent IV injection.
Radial nerve block involves an infi ltration technique and often has a
more rapid onset and shorter duration of action than median nerve and
ulnar nerve blocks. In combined blocks, experts may use lidocaine with
adrenaline in order to prolong the anaesthetic and d the risk of lidocaine
toxicity.
Other nerve blocks in the arm
Nerve blocks at the elbow The median, ulnar, and radial nerves can be
blocked at the level of the elbow, but this is rarely necessary. The onset
of anaesthesia is slower than with blocks at the wrist.
Brachial plexus blocks These should only be used by doctors with
anaesthetic training. Brachial plexus blocks can provide good anaesthesia
for operations on the arm but the onset of anaesthesia is often slow
(30– 45min) and there is a risk of LA toxicity because of the large
dose required. The axillary approach can be used in outpatients. If the
supraclavicular approach is used, admission to hospital is necessary,
because of the risk of a pneumothorax. Ultrasound guidance helps to
allow accurate positioning of the injection, which improves the effective-
ness of the block and reduces the risk of complications.
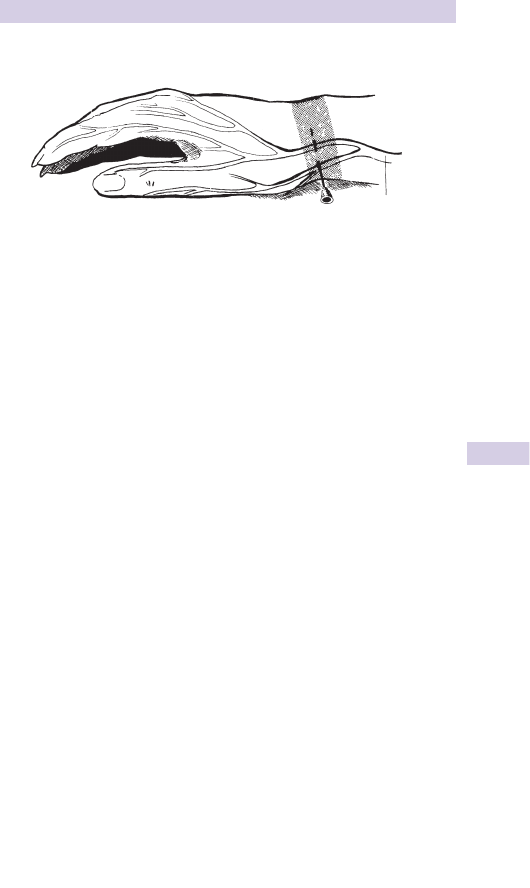
299
NERVE BLOCKS AT THE WRIST: 2
Radial nerve block at the wrist
Radial nerve
Fig. 7.3 Radial nerve block at the wrist.

300 CHAPTER 7 Analgesia and anaesthesia
Nerve blocks of forehead and ear
Nerve blocks of the forehead
Many wounds of the forehead and frontal region of the scalp can be
explored and repaired conveniently under LA block of the supraorbital
and supratrochlear nerves.
The supraorbital nerve divides into medial and lateral branches, and leaves
the orbit through two holes or notches in the superior orbital margin,
8 2.5 cm from the midline. The branches of the supraorbital nerve supply
sensation to most of the forehead and the frontal region of the scalp.
The supratrochlear nerve emerges from the upper medial corner of the
orbit and supplies sensation to the medial part of the forehead.
Technique
• Use 5–10mL of 1 % lidocaine, with or without adrenaline.
• Insert the needle in the midline between the eyebrows and direct it
laterally.
• Inject LA subcutaneously from the point of insertion along the upper
margin of the eyebrow.
• If the wound extends into the lateral part of the forehead SC infi ltration
of LA may be needed lateral to the eyebrow to block the zygomatico-
temporal and auriculotemporal nerves.
Possible complications
• Injury to the eye can occur if the patient moves during the injection.
• It is possible to block the supraorbital nerve at the supraorbital foramen,
but this is not advisable since inadvertent injection into the orbit may
cause temporary blindness if the LA reaches the optic nerve.
Nerve blocks of the ear
The auricle (pinna) of the ear is supplied by branches of the greater
auricular nerve (from inferiorly), lesser occipital nerve (posteriorly), and
the auriculotemporal nerve (anteriorly/superiorly). These nerves can
be blocked by SC infi ltration of up to 10mL of 1 % plain lidocaine in the
appropriate area, or in a ring around the ear.
To block the greater auricular nerve infi ltrate 1cm below the ear lobe from
the posterior border of the sternomastoid muscle to the angle of the
mandible.
Block the lesser occipital nerve by infi ltration just behind the ear.
When blocking the auriculotemporal nerve by infi ltration just anterior
to the external auditory meatus, aspirate carefully to avoid inadvertent
injection into the superfi cial temporal artery.
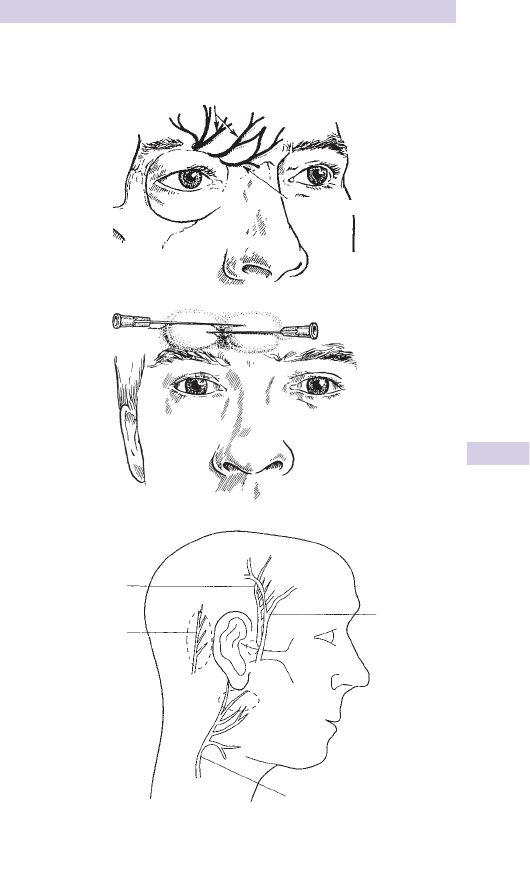
301
NERVE BLOCKS OF FOREHEAD AND EAR
Nerve blocks: forehead and ear
Fig. 7.4 Nerve blocks of the forehead and ear.
Supraorbital nerve
Supratrochlear
nerve
Auriculotemporal
nerve
Superficial
temporal
artery
Greater auricular nerve
Lesser occipital
nerve

302 CHAPTER 7 Analgesia and anaesthesia
Dental anaesthesia
Intraoral injections of local anaesthetic are used frequently for dental pro-
cedures, but can also be useful for cleaning and repair of wounds of the
lips, cheeks, and chin. Instruction by a dentist or oral surgeon is required.
Give dental anaesthetics with dental syringes and cartridges of LA. An
appropriate drug for most purposes is lidocaine 2 % with adrenaline 1 in
80,000. Some dental syringes do not allow aspiration prior to injection.
Disposable dental syringes are preferable to reusable syringes, to d risk of
needlestick injury from resheathing of needles.
Infra-orbital nerve block
The infra-orbital nerve supplies the skin and mucous membrane of the
cheek and upper lip, and also the lower eyelid and the side of the nose.
The nerve emerges from the infra-orbital foramen, which is 0.5cm below
the infra-orbital margin and vertically below the pupil when the eyes are
looking forwards. The nerve can be blocked at the infra-orbital foramen
by injection through the skin, but the intraoral approach is preferable,
because it is less unpleasant for the patient. Insert the needle into the
buccogingival fold between the fi rst and second premolars, and direct it
up towards the infra-orbital foramen.
Mental nerve block
The mental nerve supplies sensation to the lower lip and the chin. It
emerges from the mental foramen, which is palpable on the mandible on
a line between the fi rst and second premolar teeth. The nerve can be
blocked at the mental foramen with 1–2mL of LA, using either an intra- or
extra-oral approach. Avoid injecting into the mental canal, since this may
damage the nerve. If the wound to be repaired extends across the midline
bilateral mental nerve blocks will be needed.
The nerves to a single lower incisor may be blocked by submucous
infi ltration of LA in the buccal sulcus adjacent to the tooth.

303
INTERCOSTAL NERVE BLOCK
Intercostal nerve block
Intercostal nerve blocks can give useful analgesia for patients with rib
fractures who are admitted to hospital, but it is not a routine procedure
and requires training and experience. These blocks must not be used in
outpatients and should not be performed bilaterally because of the risk
of pneumothorax. Patients with obesity or severe obstructive airways
disease have i risk of complications. Alternative procedures used in
ICU are interpleural analgesia and thoracic epidurals, but these are not
appropriate in the ED.

304 CHAPTER 7 Analgesia and anaesthesia
Femoral nerve block
Femoral nerve block is a simple technique and provides good analgesia
within a few minutes for pain from a fractured shaft of femur. It may be
used in children, as well as in adults. Perform femoral block on the clinical
diagnosis of a fractured shaft of femur, before X-ray or the application of
a traction splint.
Femoral nerve block can be used with a block of the lateral cutaneous
nerve of the thigh for anaesthetizing a skin donor site.
Anatomy
The femoral nerve passes under the inguinal ligament, where it lies lateral
to the femoral artery. The femoral nerve supplies the hip and knee joints,
the skin of the medial and anterior aspects of the thigh, and the quadri-
ceps, sartorius and pectineus muscles in the anterior compartment of the
thigh.
Technique
• Use a mixture of lidocaine and bupivacaine to give both rapid onset and
prolonged anaesthesia. In an adult give 5mL of 1 % lidocaine and 5mL of
0.5 % bupivacaine. In a child use 0.1mL/kg of 1 % lidocaine and 0.1mL/kg
of 0.5 % bupivacaine. Check the maximum dose carefully, especially in
children or if bilateral femoral nerve blocks are needed.
• Use a 0.8 × 40 mm (21G) needle in adults and a 0.6 × 25 mm (23G)
needle in children.
• Blocking the right femoral nerve is best performed from the patient’s
left side (and vice versa).
• Using your non-dominant hand palpate the femoral artery just below
the inguinal ligament.
• Clean the skin.
• Insert the needle perpendicular to the skin and 1cm lateral to the
artery to a depth of 8 3cm. If paraesthesiae occurs, withdraw the needle
2–3mm.
• Aspirate and check for blood.
• Inject LA while moving the needle up and down and fanning out later-
ally to 8 3cm from the artery. (The distances quoted refer to adults.)
• If the femoral artery is punctured compress it for 5–10min. If no bleeding
is apparent, continue with the femoral nerve block.
• This ‘blind’ technique for femoral nerve block has a high success rate
and usually provides rapid and effective analgesia. However, ultrasound
( b p.292) can be helpful to delineate the anatomy of the femoral nerve
(which can vary between patients) and to allow precise positioning of
the injection adjacent to the nerve.
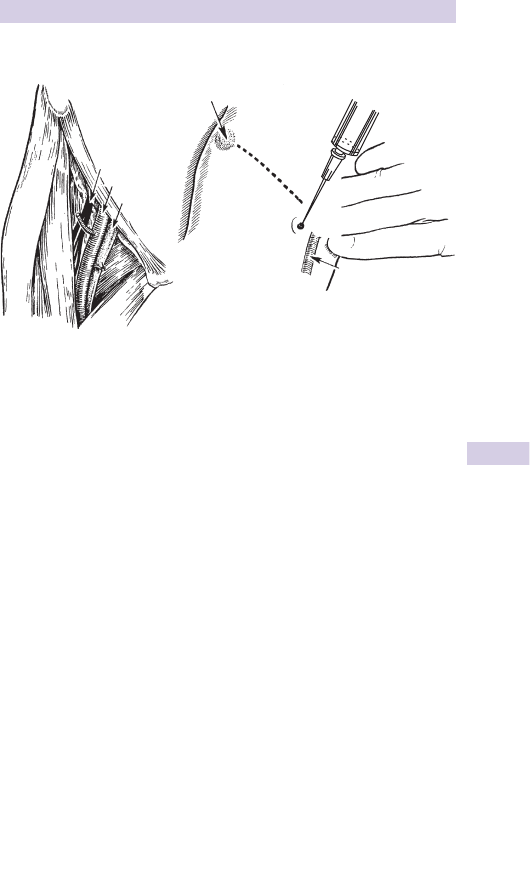
305
FEMORAL NERVE BLOCK
Femoral nerve block
Fig. 7.5 Femoral nerve block.
Anterior superior iliac spine
Femoral nerve
Femoral artery
Femoral vein
Femoral artery

306 CHAPTER 7 Analgesia and anaesthesia
Nerve blocks at the ankle
Indications
• Cleaning, exploration and suturing of wounds of the foot.
• Removal of FB. Drainage of small abscesses on the sole of the foot.
• Analgesia for crush injuries of the forefoot.
• LA blocks at the ankle are particularly useful for anaesthetizing the sole
of the foot, where local infi ltration is very painful and unsatisfactory.
Anatomy
Sensation in the ankle and foot is supplied by 5 main nerves:
• Saphenous nerve (medial side of ankle).
• Superfi cial peroneal nerve (front of ankle and dorsum of foot).
• Deep peroneal nerve (lateral side of big toe and medial side of
2nd toe).
• Sural nerve (heel and lateral side of hind foot).
• Tibial nerve (which forms the medial and lateral plantar nerves,
supplying the anterior half of the sole).
There are individual variations and signifi cant overlap between the areas
supplied by different nerves, especially on the sole of the foot. It is often
necessary to block more than one nerve.
For each of these blocks use a 0.6mm (23G) needle and 5mL of 1 %
lidocaine (with or without adrenaline) or 0.5 % bupivacaine. Check the
maximum dose (b p.283), especially for multiple blocks. Ultrasound can
help to allow accurate injection of LA, so smaller amounts are needed.
Do not use adrenaline in patients with peripheral vascular disease.
Saphenous nerve
Infi ltrate LA subcutaneously around the great saphenous vein, anterior to
and just above the medial malleolus. Aspirate carefully because of the risk
of IV injection.
Superfi cial peroneal nerve
Infi ltrate LA subcutaneously above the ankle joint from the anterior
border of the tibia to the lateral malleolus.
Deep peroneal nerve
Insert the needle above the ankle joint between the tendons of tibialis
anterior and extensor hallucis longus. Inject 5mL of LA.
Sural nerve
Lie the patient prone. Insert the needle lateral to the Achilles tendon and
infi ltrate subcutaneously to the lateral malleolus.
Tibial nerve
Lie the patient prone. Palpate the posterior tibial artery. Insert the needle
medial to the Achilles tendon and level with the upper border of the
medial malleolus, so the needle tip is just lateral to the artery. Withdraw
slightly if paraesthesiae occur. Aspirate. Inject 5–10mL.
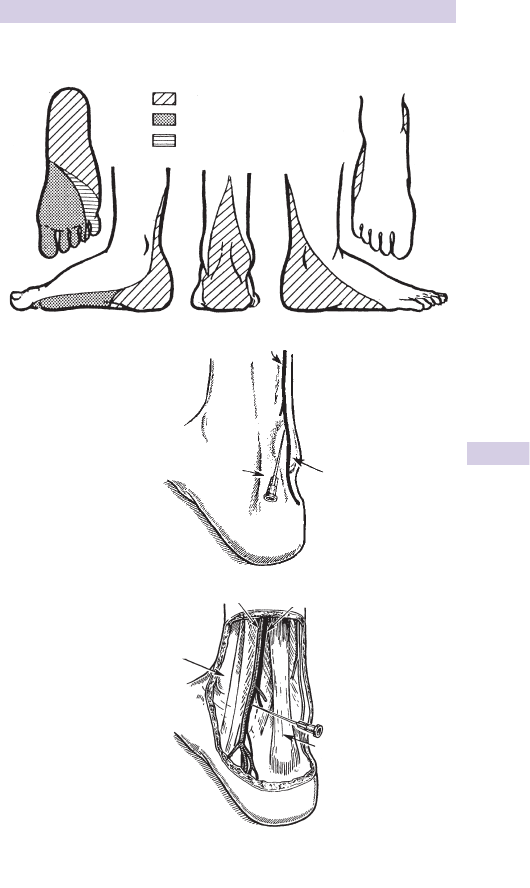
307
NERVE BLOCKS AT THE ANKLE
Nerve blocks at the ankle
Fig. 7.6 Nerve blocks at the ankle.
Sural nerve
Medial plantar nerve
Lateral plantar nerve
Lateral malleolus
Posterior tibial artery
Medial malleolus
Tendo Achilles
Tibial nerve
Sural nerve
Tendo Achilles

308 CHAPTER 7 Analgesia and anaesthesia
Sedation
Sedation is often used in the ED to help patients tolerate distressing
procedures, such as reduction of dislocations. It carries the same risks
and complications as GA. When appropriate, sedation may be used with
an analgesic or LA, but do not use sedation as a substitute for adequate
analgesia or anaesthesia. Sedative drugs may be given PO, IM, IV, or by
inhalation. Oral sedation may be helpful in children. Inhalational sedation
and analgesia with nitrous oxide (Entonox
®
, b p.278) is rapidly revers-
ible, relatively risk-free, and can be used when appropriate in adults and
some children. IV sedation of children is particularly hazardous because of
the narrow margin between sedation and anaesthesia, so it should only be
performed in the ED by staff with specifi c training.
Risk assessment Main risks of sedation are respiratory depression,
d cardiac output and inhalation of gastric contents. Patients at i risk of
respiratory or cardiac complications include elderly, obese and those
with pre-existing heart/lung disease. Patients with renal or hepatic disease
may require d drug dosage. Ideally, patients should be fasted before IV
sedation. Ask about and record pre-existing medical conditions, drug
therapy, allergies, and time of last food and drink. Record pulse and BP. If
there is any uncertainty, postpone the procedure or get expert help.
Equipment Use a trolley which can be tilted head-down. Ensure
suction, resuscitation equipment and drugs are immediately available.
Staff Sedation should only be given by doctors trained in resuscitation.
A second person (doctor or nurse) must be present throughout to assist.
Some sedatives cause amnesia and transient confusion — the presence of a
chaperone may avoid diffi culties if there is any allegation of impropriety.
Drugs for IV sedation All sedative drugs will produce anaesthesia if
given in excessive dosage. Use the minimum dose that will give adequate
sedation and allow the procedure to be completed satisfactorily.
Midazolam is the most suitable benzodiazepine. It has a plasma half-life
of about 2hr in young adults (longer in elderly or obese) and metabolites
are relatively inactive. There are three concentrations (1, 2, and 5mg/mL)
which are easily confused. In fi t adults initial dose of midazolam is 2mg IV
over 1min. If sedation is inadequate after 2min, give incremental doses
of 0.5–1mg (0.25–0.5mL of 10mg/5mL solution). When fully sedated, the
patient will be drowsy with slurred speech, but will obey commands. The
usual dose range is 2.5–7.5mg. Elderly patients are more susceptible to
benzodiazepines — give smaller doses. Give 0.5–1mg as an initial dose: the
total dose needed is usually 1–3mg.
Diazepam is not suitable for IV sedation of outpatients, since it has a prolonged
action and an active metabolite with a plasma half-life of 8 3–5 days.
Opioids such as morphine ( b p.276) may be used IV combined with
midazolam, but there may be a synergistic effect with i risk of respiratory
depression. Give the opioid fi rst in d dosage, followed by careful titration
of midazolam.
Other drugs Propofol ( b p.316) can give excellent sedation for short
procedures, with rapid recovery, but its use requires anaesthetic training.
Ketamine ( b p.278) may be given IV or IM, but requires special training.

309
SEDATION
Monitoring during IV sedation
Ensure patients given IV sedation receive O
2
, pulse oximetry monitoring
and have a venous cannula. Monitor ECG.
Antagonists
The specifi c antagonists fl umazenil (for benzodiazepines) and naloxone
(for opioids) must be available immediately, but should be needed very
rarely. If respiratory depression occurs, standard techniques to maintain
the airway and breathing are more important than giving antagonists.
Flumazenil and naloxone have shorter durations of action than the drugs
they antagonize, so careful observation is essential if either drug is used.
Recovery and discharge after sedation
If IV sedation is used, monitor the patient carefully until recovery is
complete.
Monitoring and resuscitation equipment and drugs must be available.
Minimum criteria for discharging a patient are:
• Stable vital signs.
• Ability to walk without support.
• Toleration of oral fl uids and minimal nausea.
• Adequate analgesia.
• Adequate supervision at home by a responsible adult.
Instruct the patient (both verbally and in writing) not to drive, operate
machinery, make any important decisions or drink alcohol for 24 hours.
Arrange appropriate follow-up. Ensure the adult accompanying the patient
knows who to contact if there is any problem.
Sedation in children
Many children (and their parents and staff) are distressed by proce-
dures such as suturing of minor wounds under LA. Sedation is helpful
to prevent distress and allows procedures to take place with minimal
physical restraint. Sedation may be given by oral or nasal routes, IM or
IV. Paediatric IV sedation requires anaesthetic experience because of the
narrow therapeutic margin between sedation and anaesthesia.
Ketamine given IM in a dose of 2–2.5mg/kg is currently the method of
choice for paediatric sedation in the ED by doctors with appropriate
training ( b p.278). This dose of ketamine does not provide full
anaesthesia and so local anaesthesia is required for cleaning and suturing
of wounds.
Oral midazolam is advocated by some specialists. Oral sedation with
promethazine is not advisable, since it is often ineffective.

310 CHAPTER 7 Analgesia and anaesthesia
General anaesthesia in the emergency
department
GA may be needed in the ED for many different conditions:
• Minor surgery (eg drainage of abscesses, manipulation of fractures).
• Cardioversion.
• Airway problems (eg facial trauma, burns, epiglottitis).
• Respiratory failure (eg asthma, chronic obstructive airways disease,
pulmonary oedema, chest injuries).
• To protect the airway and control ventilation after head injuries and to
keep the patient immobile for a CT scan.
• To protect the airway and maintain ventilation in status epilepticus
unresponsive to standard drug therapy.
• Immediate major surgery (eg thoracotomy or laparotomy for trauma,
ruptured ectopic pregnancy or aortic aneurysm). If at all possible take
the patient to the operating theatre before anaesthesia, as the loss of
sympathetic tone after the onset of anaesthesia can cause catastrophic
hypotension in a hypovolaemic patient. In extreme emergencies, it may
be necessary to operate in the ED.
GA in the ED tends to be stressful for the anaesthetist and potentially
hazardous for the patient, who is usually unprepared for anaesthesia, with
a full stomach and increased risk of aspiration. GA should only be given
by doctors with anaesthetic training, but other staff should know what is
required so they can help when necessary.
Pre-operative assessment
This is essential for safe anaesthesia. If time allows, assess the patient
before contacting the anaesthetist to arrange the anaesthetic. However, if
emergency anaesthesia is needed, call the anaesthetist immediately so that
he/she can come and assess the patient, and get senior help if necessary.
A checklist of questions to ask before GA is shown opposite.
Fitness for GA The American Society of Anaesthesiologists (ASA) classifi -
cation of pre-operative fi tness is widely used by anaesthetists:
1 Healthy patient with no systemic disease.
2 Patient with a mild to moderate disease which does not limit their
activity in any way (eg treated hypertension, mild diabetes, smoker).
3 Patient with a severe systemic disturbance from any cause which limits
activity (eg IHD with d exercise tolerance, severe COPD).
4 Patient with a severe systemic disease which is a constant threat to life
(eg severe chronic bronchitis, advanced liver disease).
5 Moribund patient who is unlikely to survive 24 hours with or without
treatment.
The risk of complications from GA correlates well with ASA group. Only
patients in ASA groups 1 and 2 should be given an elective anaesthetic
by a junior anaesthetist in the ED. Children aged <7 years should not
usually have a GA in the ED, except in an emergency.

311
GENERAL ANAESTHESIA IN THE EMERGENCY DEPARTMENT
Pre-operative investigations
No investigation except ‘dipstick’ urinalysis is needed, unless pre-operative
assessment reveals a problem. Measure Hb in any patient who appears
anaemic. Check for sickle cell disease in any patient of Afro-Caribbean,
Cypriot or Indian origin. Measure U&E in patients on diuretics, and blood
glucose in diabetics. ECG and CXR are not needed, unless clinically
indicated. Perform a pregnancy test if pregnancy is possible.
Checklist for pre-operative assessment in the ED
• Is the patient expected to go home after recovery from anaesthetic?
• Is there a responsible adult who can look after the patient at home?
Preparation for GA
Ideally, the patient should have nothing to drink for 4 hours and no food
for 6 hours before anaesthesia. Explain why this is necessary. Fasting does
not guarantee an empty stomach. Trauma, pregnancy and opioids delay
gastric emptying.
If the patient is in pain, give analgesia and an antiemetic. Discuss with
the anaesthetist any other drug treatment that is required. Patients with
a hiatus hernia or gastro-oesophageal refl ux need antacid prophylaxis
(eg ranitidine 50mg IV and an antacid).
Explain the proposed operation and anaesthetic to the patient (and
relatives if appropriate) and ensure valid consent is obtained. The patient
must be clearly labelled with a wrist-band. Remove contact lenses, false
teeth and dental plates.
Recovery and discharge after anaesthesia
When the operation has fi nished, place the patient in the recovery posi-
tion and ensure continuous observation by trained staff until recovery is
complete. The anaesthetist should stay with the patient until conscious-
ness is regained and the airway is controlled. Monitoring and resuscitation
equipment and drugs must be available. The minimum criteria for dis-
charging a patient are the same as following sedation ( b p.309).
Importantly, tell the patient (both verbally and in writing) not to drive,
operate machinery, make any important decisions or drink alcohol for
24 hours. Arrange appropriate follow-up and make sure that the adult
accompanying the patient knows who to contact if there is a problem.
• Age.
• Weight.
• Time of last drink.
• Time of last food.
• Drugs.
• Drugs given in the ED.
• Time of last analgesia.
• Allergies.
• Sickle cell risk?
• Infection risk?
• Family history of GA problems?
• Airway problem?
• Dentures/crowns/loose teeth?
• Chest disease?
• Smoker?
• Cardiac disease?
• Blood pressure.
• GI problem?
• Other illness?
• Possibility of pregnancy?
• Previous GA? (problems?)
• Consent form signed?

312 CHAPTER 7 Analgesia and anaesthesia
Emergency anaesthesia and rapid
sequence induction
Emergency anaesthesia and intubation are often needed to protect the
airway and provide adequate ventilation in a patient with a head injury or
multiple trauma. There is a high risk of aspiration of gastric contents into
the lungs, so use a cuffed ET tube (uncuffed in small children). In a patient
with a gag refl ex any attempt to intubate without anaesthesia may cause
vomiting and aspiration. Anaesthesia before intubation is essential in head-
injured patients to minimize the i in ICP.
Rapid sequence induction (RSI)
RSI involves administration of a sedative or induction agent virtually
simultaneously with a neuromuscular blocking agent to allow rapid
tracheal intubation. RSI should only be performed by staff who have had
specifi c training and experience in the techniques and the drugs used, and the
recognition and management of possible problems . However, it is useful if
ED staff who have not had such training understand the principles of RSI,
so that they can assist as needed.
• Call for senior ED/anaesthetic/ICU help.
• Check all drugs and equipment, including suction, bag and masks,
laryngoscope (and spare with large blade), tracheal tubes and introducers,
syringe and valve or clamp for ET tube cuff, connectors.
• Check that the trolley can be tilted head-down easily.
• Check monitoring equipment (ECG, BP, pulse oximeter, end-tidal CO
2
monitor).
• Explain the procedure to the patient if possible.
• Assess the risks and any conditions which might cause problems with
intubation (eg trauma to the face or neck, d mouth opening, receding
chin). Identify a back-up plan ( b p.314) and communicate this to the
team.
• Establish monitoring (ECG and pulse oximetry) and secure IV access.
• Protect the cervical spine in all trauma patients: an assistant should
provide in-line immobilization during intubation. In other patients, use a
pillow and position the head and neck to aid intubation.
• If possible, pre-oxygenate for 3min with 100 % O
2
via a tight-fi tting mask,
with the patient breathing spontaneously. If breathing is inadequate,
ventilate for 2min on 100 % O
2
with a bag and mask, with an assistant
applying cricoid pressure by pressing fi rmly downwards with a thumb
and index fi nger on the cricoid cartilage, while supporting the patient’s
neck with the other hand.
• Give an induction agent (eg thiopental or etomidate) quickly to provide
rapid anaesthesia. Cricoid pressure must be maintained continuously
until the airway is secure.
• Follow the induction agent immediately with a muscle relaxant (usually
suxamethonium).
• Keep the face mask tightly applied until the anaesthetic and relaxant are
effective. Then intubate and infl ate the cuff quickly.

313
EMERGENCY ANAESTHESIA AND RAPID SEQUENCE INDUCTION
• Try to confi rm tracheal placement of the tube: ideally it will have
been seen passing through the cords, but this may not be possible in an
emergency intubation. Check air entry in both sides of the chest. Check
end-tidal CO
2
(but this may be misleading if oesophageal intubation
occurs in a patient who has recently consumed antacids or fi zzy drinks).
If CO
2
is not detected, oesophageal intubation has occurred.
• Cricoid pressure can be released when the ET tube is correctly
positioned, the cuff has been infl ated and ventilation is satisfactory.
• Secure the tracheal tube.
• Continue observation and monitoring.

314 CHAPTER 7 Analgesia and anaesthesia
Diffi cult intubation
Diffi culties with intubation may result from problems with the equipment,
the patient, the circumstances of intubation, and from lack of experience
or skill.
Equipment
Proper working equipment must be available where intubation may be
needed — pillow, suction, laryngoscope (and spare) with interchange-
able blades, ET tubes of different diameters (cut to suitable lengths,
but with uncut tubes available), syringe and clamp for cuff, connectors,
fl exible stylet, gum-elastic bougie, lubricating jelly, Magill’s forceps, tape for
securing ET tube. A face mask and ventilating bag, and oral/nasal airways
must be immediately available. Laryngeal masks and cricothyroidotomy
equipment must be accessible. Fibre-optic laryngoscopes are useful in
skilled hands, but are not routinely kept in EDs.
The patient
Patients may be diffi cult to intubate because of facial deformity or
swelling, protruding teeth, d mouth opening from trismus or trauma, d
neck movement or instability of the cervical spine, epiglottitis or laryngeal
problems, tracheal narrowing or deviation, blood, vomit or FB in the
airway.
Circumstances and skills
Intubation is much easier in the controlled environment of an operating
theatre than in an emergency in the ED or in pre-hospital care. Skilled help
is vital — in-line immobilization of the neck, cricoid pressure, and assistance
with equipment and cuff infl ation are needed. Practice intubating manikins
regularly.
Practical points
Before attempting intubation, oxygenate by bag and mask ventilation.
Take a deep breath as you start intubation — if the patient is not intubated
successfully when you have to breathe again, remove the ET tube and
laryngoscope, and ventilate with O
2
for 1–2min using a bag and mask
before making another attempt. Consider adjusting the patient’s position,
using a different size of laryngoscope blade or ET tube or a stylet or
bougie. Cricoid pressure can help by pushing the larynx backwards into
view. The BURP manoeuvre (Backwards Upwards Rightwards Pressure
on the thyroid cartilage) may be useful in a diffi cult intubation.
Oesophageal intubation
Fatal if unrecognized. The best way of confi rming tracheal intubation is to
see the ET tube pass between the vocal cords. Inadvertent oesophageal
intubation can produce misleadingly normal chest movements and breath
sounds. End-tidal CO
2
measurement helps to confi rm tracheal intubation,
but end-tidal CO
2
can be misleadingly i in patients who have taken
antacids or fi zzy drinks. If in doubt, remove the ET tube and ventilate with
bag and mask.

315
DIFFICULT INTUBATION
Failed intubation drill
Persistent unsuccessful attempts at intubation cause hypoxia and i risk of
aspiration and damage to teeth and other structures. If three attempts at
intubation are unsuccessful, follow a failed intubation drill:
• Inform all staff that intubation attempts have ceased and get senior
help.
• Ventilate the patient on 100 % O
2
using bag and mask, and an oral or
nasal airway, while an assistant maintains cricoid pressure.
• If ventilation is impossible, turn the patient onto the left side and tilt the
trolley head down, while maintaining cricoid pressure. If ventilation is
still impossible release cricoid pressure slowly and attempt to ventilate
again.
• A laryngeal mask airway (LMA) can be very useful in this situation but
requires training. Practice the technique of LMA insertion on manikins
and on patients in the operating theatre whenever possible.
• Cricothyroidotomy ( b p.326) is rarely needed, but must be performed
promptly if necessary.
• In non-emergency cases, the patient can be allowed to wake up, but this
is not an option in a life-threatening emergency. Discuss the problem
with a senior anaesthetist.
• Warn the patient and GP if the diffi culty with intubation is liable to
recur.
Laryngospasm
Laryngospasm occurs when the laryngeal muscles contract and occlude
the airway, preventing ventilation and causing hypoxia.
Causes
• Stimulation of the patient during light anaesthesia.
• Irritation of the airway by secretions, vomit, blood or an oropharyngeal
airway.
• Irritant anaesthetic vapours.
• Extubation of a lightly anaesthetized patient.
Treatment
• Give 100 % O
2
.
• Clear the airway of secretions, using gentle suction.
• Gently ventilate the patient using a bag and mask. Over-infl ation is liable
to fi ll the stomach and cause regurgitation.
• Monitor the ECG for bradycardia or arrhythmias.
In severe laryngospasm, an experienced anaesthetist may consider
deepening anaesthesia or giving suxamethonium to allow intubation, or
ventilation with a bag and mask. In a hypoxic patient, suxamethonium may
cause bradycardia requiring treatment with atropine.

316 CHAPTER 7 Analgesia and anaesthesia
General anaesthetic drugs
GA should only be given after anaesthetic training.
IV anaesthetic induction agents are used for induction of anaesthesia,
as the sole drug for short procedures (eg cardioversion), for treatment
of status epilepticus unresponsive to other anticonvulsants ( b p.149),
for total IV anaesthesia and for sedation of a ventilated patient. They are
particularly hazardous in patients with upper airway obstruction or severe
hypovolaemia. Thiopental, etomidate and many other drugs are unsafe in
acute porphyria (see b p.165 and BNF ).
Propofol is particularly useful in day-case surgery, and for manipulation of
fractures and dislocations, because recovery is rapid. The injection may
be painful. Hypotension is common and severe bradycardia may occur.
Induction dose is 1.5–2.5mg/kg.
Etomidate causes less hypotension than propofol or thiopental (and so
may be useful in patients who are already hypotensive), and recovery
is rapid. However, the injection is painful, and uncontrolled muscle
movements and adrenocortical suppression may occur. Induction dose
is up to 0.3mg/kg.
Ketamine ( b p.278) is used mainly in prehospital care, but may be useful
for rapid sequence intubation in hypotensive patients and in acute asthma.
Induction dose is 1–2mg/kg IV.
Thiopental (thiopentone) is a barbiturate drug. Thiopentone solution is
unstable and has to be prepared from powder to form a 2.5 % solution
(25mg/mL). Care is needed with injections because extravasation causes
irritation, and arterial injection is particularly dangerous. Hypotension may
occur, especially with overdosage. The induction dose in a fi t adult is up
to 4mg/kg (child: 2–7mg/kg).
Muscle relaxants
Suxamethonium is a short-acting depolarizing muscle relaxant, which is
often used to allow intubation, especially in rapid sequence induction of
anaesthesia ( b p.312). In a dose of 1mg/kg it causes muscle fasciculation
followed rapidly by fl accid paralysis. Suxamethonium is contra-indicated
in hyperkalaemia and also in burns, paraplegia or crush injuries, where
dangerous hyperkalaemia may develop if suxamethonium is used 5–120 days
after injury. Suxamethonium causes i ICP and i intraocular pressure. Usual
duration of action is 8 5min, but prolonged paralysis occurs in patients with
abnormal pseudo-cholinesterase enzymes.
Rocuronium is a muscle relaxant that may be used for intubation if
suxamethonium is contraindicated.
Atracurium and vecuronium are non-depolarizing muscle relaxants,
which act for 8 20–30min. They cause fewer adverse effects than older
relaxants (eg pancuronium). Paralysis from these drugs can be reversed
with neostigmine, which is given with atropine or glycopyrronium to
prevent bradycardia.

317
GENERAL ANAESTHETIC DRUGS
Inhalational anaesthetics
These can be used for analgesia (especially Entonox
®
), induction of
anaesthesia (particularly in upper airway obstruction, when IV induction of
anaesthesia is hazardous), and for maintenance of anaesthesia.
Nitrous oxide (N
2
O) is widely used for analgesia as Entonox
®
, a 50:50
mixture with O
2
( b p.278). It is also used frequently in GA in a
concentration of 50–70 % in O
2
, in combination with other inhaled or
IV anaesthetics. N
2
O is contraindicated in certain circumstances (eg
undrained pneumothorax) — see b p.278.
Halothane, enfl urane, isofl urane, and sevofl urane are inhalational
anaesthetic agents that are given using specially calibrated vaporizers in
O
2
, or a mixture of N
2
O and O
2
. Sevofl urane is particularly useful for
gas induction of anaesthesia in upper airway obstruction. Halothane is
also effective for gas induction, but now rarely used because of the risk
of hepatotoxicity, especially after repeated use. Halothane sensitizes the
heart to catecholamines, so adrenaline must not be used with halothane.
These inhalational anaesthetic drugs can cause malignant hyperpyrexia
( b p.265) in susceptible patients.
This page intentionally left blank

319
Major trauma: treatment principles 320
Investigations in major trauma 322
Airway obstruction: basic measures 324
Airway obstruction: surgical airway 326
Tension pneumothorax 328
Chest wall injury 330
Traumatic pneumothorax 334
Haemothorax 335
Chest drain insertion 336
Pulmonary contusions and aspiration 338
Penetrating chest injury 340
Aortic injury 344
Focused assessment with sonography for trauma
(FAST) scan 346
Diagnostic peritoneal lavage (DPL) 347
Blunt abdominal trauma 348
Penetrating abdominal trauma 350
Renal trauma 351
Bladder, urethral, and testicular trauma 352
Head injury: introduction 354
Head injury: triage and monitoring 356
Head injury: history 358
Head injury: examination 360
Head injury: imaging 362
Management of serious head injury 364
Minor head injury 366
Post-concussion symptoms 368
Maxillofacial injuries: introduction 370
Middle third facial fractures 372
Zygomatic, orbital and frontal sinus fractures 374
Mandibular injuries 376
Penetrating neck trauma 378
Spine and spinal cord injury 380
Dermatomes 386
Gunshot injuries 388
Blast injuries 389
Burns: assessment 390
Major burns: resuscitation 392
Inhalation injury 394
Management of smaller burns 396
Crush syndrome 398
Major trauma
Chapter 8

320 CHAPTER 8 Major trauma
Major trauma: treatment principles
Patients who present with serious (or apparently serious) injuries require
immediate assessment and resuscitation. The fi ner points of history taking
may have to wait until later. However, suspect major trauma in:
• High speed road collisions, vehicle ejection, rollover, prolonged extrication.
• Death of another individual in the same collision.
• Pedestrians thrown up or run over by a vehicle.
• Falls of more than 2m.
Management of specifi c injuries is outlined in subsequent pages. Although
treatment should be tailored to the needs of each individual patient, many
therapeutic interventions are common to all patients:
Airway control
Use basic manoeuvres (suction, chin lift, oropharyngeal airway) to open
the airway and apply O
2
by face mask ( b p.324). Avoid tilting the head or
moving the neck if there is a chance of neck injury. If the airway remains
obstructed despite these measures, get ED and ICU and/or anaesthesia
help and consider advanced manoeuvres ( b p.326).
O
2
Provide high fl ow O
2
to all. Patients who are apnoeic or hypoventilating
require assistance by bag and mask ventilation prior to tracheal intubation
and IPPV.
Cervical spine control
This is the fi rst priority in any patient who presents with possible spine injury
(eg neck pain, loss of consciousness). Provide immediate in-line manual
cervical immobilization by placing one hand on each side of the patient’s
head and holding it steady (without traction) and in line with the remainder
of the spine. Whilst maintaining manual immobilization, ask an assistant to
apply an appropriately sized hard cervical collar. Adhesive tape and sandbags
may be applied, but may cause problems in certain patients (eg patients who
are vomiting or uncooperative patients who have consumed alcohol).
IV fl uids
Insert 2 large cannulae into forearm or antecubital fossae veins. If initial
attempts fail, consider a femoral venous line or an intra-osseous line. If these
fail or are inappropriate, consider a central line or a cut-down onto the long
saphenous vein. However, bear in mind the diffi culties and potential hazards
of attempting central venous access in hypovolaemic patients.
Commence IV fl uids for patients with hypovolaemic shock with 1L of 0.9 %
saline (or Hartmann’s solution) in adults (20mL/kg in children). Consider
urgent blood transfusion if > 2L (in an adult) have been given ( b p.174)
and look for sources of bleeding — chest, abdomen, and pelvis.
Analgesia
Adequate pain relief is often forgotten or deferred. Give morphine IV
(diluted in saline to 1mg/mL) titrated in small increments according to
response. Provide an antiemetic (eg cyclizine 50mg IV) at the same time.
Consider other forms of analgesia (eg regional nerve blocks, immobilization,
and splintage of fractures).

321
MAJOR TRAUMA: TREATMENT PRINCIPLES
Antibiotics
Give prophylactic IV antibiotics for compound fractures and penetrating
wounds of the head, chest or abdomen. Antibiotic choice follows local
policy — a broad spectrum antibiotic (eg cefuroxime) is useful.
Tetanus
Ensure tetanus prophylaxis in all patients ( b p.410).
Advanced trauma life support (ATLS
®
)
The ATLS concept was introduced by the American College of Surgeons
in an attempt to improve the immediate treatment of patients with serious
injury. The ATLS
®
approach has enabled some standardization of trauma
resuscitation. According to ATLS
®
, treatment of all patients with major
trauma passes through the same phases:
• Primary survey.
• Resuscitation phase.
• Secondary survey.
• Defi nitive care phase.
A key feature of ATLS
®
is frequent re-evaluation of the patient’s problems
and the response to treatment. Any deterioration necessitates a return to
evaluate the ‘ABC’ (airway, breathing, and circulation).
Primary survey
On initial reception of a seriously injured patient, life-threatening prob-
lems should be identifi ed and addressed as rapidly as possible. An ‘ABC’
approach is adopted, with each of the following aspects being quickly
evaluated and treated:
A — airway maintenance with cervical spine control.
B — breathing and ventilation.
C — circulation and haemorrhage control.
D — disability (rapid assessment of neurological status).
E — exposure (the patient is completely undressed to allow full examination).
With optimum staffi ng and direction, instead of considering each of these
aspects sequentially (from ‘A’ to ‘E’), aim to address them simultaneously.
Resuscitation phase
During this period, treatment continues for the problems identifi ed
during the primary survey. Further practical procedures (eg insertion of
oro/nasogastric tube, chest drain and urinary catheter) are performed.
Occasionally, immediate surgery (damage control surgery) is required for
haemorrhage control before the secondary survey.
Secondary survey
This is a head to toe examination to identify other injuries. This should be
accompanied by relevant imaging and other investigations. Monitor the
patient closely — any deterioration requires a repeat ABC assessment.
A high index of suspicion is essential to avoid missing occult injuries —
particularly in the severely injured and those with d conscious level.
Defi nitive care phase
The early management of all injuries is addressed, including fracture
stabilization and emergency operative intervention.

322 CHAPTER 8 Major trauma
Investigations in major trauma
Select specifi c investigations according to the presentation, but bear in
mind that all patients with major trauma require: group and save/X-match,
BMG, X-rays, ABG. Consider measuring lactate levels.
BMG
This is mandatory for all patients with major trauma and particularly
important on any patient with GCS<15/15.
SpO
2
Attach a pulse oximeter on ED arrival, then monitor continuously.
Blood tests
Check U&E, FBC, and glucose in all patients. If there is any possibility of
signifi cant haemorrhage, request a group and save, or cross-match. Request
a baseline clotting screen in patients with major haemorrhage or those at
special risk (eg alcoholics or those on anticoagulants). Request fresh frozen
plasma and platelets early for patients with major haemorrhage.
X-rays
Multiply injured patients often require multiple X-rays. Obtain CXR and
pelvic X-rays as a minimum. Cervical spine X-rays do not change the initial
management in the resuscitation room and can be deferred to the secondary
survey. Don lead aprons and gloves, and remain with the patient whilst
X-rays are taken — in particular, ensure satisfactory immobilization of the
cervical spine throughout. Accompany the patient if he needs to be taken
to the radiology department for further imaging.
Urinalysis
Test the urine for blood if there is suspicion of abdominal injury.
Microscopic haematuria is a useful marker of intra-abdominal injury.
Arterial blood gas
Provides useful information about the degree of hypoxia, hypoventilation
and acidosis. In critically ill patients (especially those requiring ventilatory
support or those destined for neurosurgery/ICU) repeat as necessary and
consider inserting an intra-arterial line to continuously monitor BP.
Electrocardiogram
Monitor all patients; record an ECG if > 50 years or signifi cant chest trauma.
Computed tomography scan
CT is increasingly used to evaluate head, neck and truncal injuries. An
appropriately trained doctor should accompany the patient to the CT
scanner and monitoring must continue. Local protocols will dictate which
patients have a total body ‘pan scan’ rather than selective imaging. Patients
with haemodynamic instability should not go to the CT scanner.
USS (FAST) and DPL
Focused assessment with sonography for trauma (FAST; b p.346) is a USS
technique to identify free fl uid in the peritoneal or pericardial cavities. It can
be performed by a trained ED doctor, surgeon, or radiologist. Local policy
and expertise will determine individual ED practice. DPL ( b p.347) is rarely
used now in developed countries given the availability of FAST and CT. DPL
still plays an important role if FAST and CT are not available.
Other investigations
Angiography is indicated in certain specifi c circumstances (major pelvic
fracture, aortic injury). Occasionally, other tests requiring specialist expertise
(eg echocardiography) may prove to be useful.
323
INVESTIGATIONS IN MAJOR TRAUMA
Trauma scoring
Trauma scoring is often used in research on the epidemiology and man-
agement of trauma. A basic understanding of the accepted system of
trauma scoring may be of benefi t to those treating injured patients.
Injury Severity Score (ISS)
The ISS is widely used to retrospectively score the anatomical injuries of
an individual patient. The score is obtained by fi rst scoring each individual
injury using the Abbreviated Injury Scale (AIS), which attributes a score
between 1 and 6 to each individual injury, as follows:
AIS 1 = minor injury AIS 4 = severe injury
AIS 2 = moderate injury AIS 5 = critical injury
AIS 3 = serious injury AIS 6 = inevitably fatal injury
To calculate the ISS from an array of AIS scores for a patient, the 3 highest
AIS scores in different body regions are squared then added together.
ISS considers the body to comprise 6 regions: head/neck; face; chest;
abdomen; extremities; external (skin). Possible ISS scores range from 1 to
75. Any patient with an AIS = 6 is automatically given an ISS of 75. See
www.aast.org/Library/TraumaTools/InjuryScoringScales.aspx
For example, see Table 8.1 .
The Revised Trauma Score
The Revised Trauma Score (RTS) is used to assess the physiological
disturbance of a trauma patient. The score is calculated from the respira-
tory rate, systolic BP and GCS. Each of these parameters are assigned a
code (value) to which a weighting factor is applied. The 3 resultant scores
are then added together to give the RTS. The RTS ranges from 0 (worst
possible) to 7.84 (best).
TRISS methodology
Combining the ISS with the RTS and adding a weighting factor according to
the age of the patient, it is possible to calculate a ‘Probability of Survival’ (Ps)
for each patient, based upon the national norm. Patients who survive with
Ps<0.5 are regarded as ‘unexpected survivors’; patients who die with Ps > 0.5
as ‘unexpected deaths’. By analysing the results of treating a large number of
patients, TRISS methodology may be used to compare ‘performances’ (eg of
one hospital against the national norm).
Table 8.1
Injuries AIS (body region)
Closed linear temporal skull fracture AIS = 2 (head/neck)
Major aortic arch rupture at its root AIS = 5 (chest)
Bilateral pulmonary contusions AIS = 4 (chest)
Massive splenic rupture with hilar disruption AIS = 5 (abdomen)
Multiple widespread superfi cial abrasions AIS = 1 (external)
ISS=(5)
2
+ (5)
2
+ (2)
2
= 54. The ISS is non-linear and some scores (eg 15) are impossible.
One accepted defi nition of ‘major trauma’ is an ISS > 15.

324 CHAPTER 8 Major trauma
Airway obstruction: basic measures
Severely injured patients die rapidly unless oxygenated blood reaches
the brain and other vital organs. Clear, maintain, and protect the airway,
ensure that ventilation is adequate and give O
2
in as high a concentra-
tion as possible. The most urgent priority is to clear an obstructed airway,
but avoid causing or exacerbating any neck injury: instruct someone to
hold the head and neck in a neutral position until the neck is satisfactorily
immobilized. Ensure you always wear personal protective equipment.
When treating any seriously injured patient, always ensure that O
2
, suction
and airway equipment are readily available. Get senior ED ICU/anaesthetic
help early if a patient with a serious airway problem arrives or is expected.
Causes of airway obstruction
• Coma from any cause can result in airway obstruction and loss of
protective airway refl exes.
• Blood or vomit may block the airway.
• The airway may be disrupted by trauma of the face or larynx, or may be
occluded by a haematoma or by oedema following burns.
Assessment of airway obstruction
Talk to the patient and see if he responds. A lucid reply shows that the
airway is patent, that he is breathing and that some blood is reaching the
brain, at least for the moment. Ensure that the neck does not move until it
has been checked and cleared of injury ( b p.320).
Look and listen to check how the patient is breathing. Complete airway
obstruction in someone who is still trying to breathe results in paradoxical
movements of the chest and abdomen, but no breath sounds. Gurgling,
snoring and stridor are signs of partial obstruction.
Management of airway obstruction
• Look in the mouth and pharynx for FBs, blood, and vomit. The tip of a
laryngoscope may be useful as an illuminated tongue depressor.
• Remove any FB with Magill’s forceps and suck out any liquid with a large
rigid suction catheter. See if the patient responds and has a gag refl ex,
but beware of precipitating coughing or vomiting.
• If vomiting occurs, tilt the trolley head down and suck out any vomit.
• Lift the chin and use the jaw thrust manoeuvre (see opposite) to open
the airway, but do not fl ex or extend the neck.
• After any airway intervention, look, listen, and feel to reassess airway
patency and effi cacy of breathing.
• If the gag refl ex is absent or poor, insert an oropharyngeal airway
(see opposite). This helps to hold the tongue forwards, but can cause
vomiting or coughing if there is a gag refl ex. If the gag refl ex is present
or the patient’s jaws are clenched, consider a nasopharyngeal airway .
Although a nasopharyngeal airway is useful in some situations, avoid its
use if there is evidence of severe facial or head injury.
• If the airway is now patent and the patient is breathing, give high
concentration O
2
(15L/min via a non-rebreathing reservoir mask).
• If the airway is patent, but breathing inadequate, ventilate the patient with
O
2
bag and mask device and prepare for tracheal intubation. If possible,
one person should hold the mask on the face with both hands to ensure a
good seal, whilst a second person squeezes the ventilation bag.

325
AIRWAY OBSTRUCTION: BASIC MEASURES
Insertion of oropharyngeal airway
• Select the appropriate size of airway.
• Hold an airway against the patient’s face. A correctly sized airway
reaches from the corner of the mouth to the external auditory canal.
A large adult usually needs a size 4 airway, most men require size 3,
some women need a size 2. An incorrectly sized airway may make the
obstruction worse, rather than better.
• Open the patient’s mouth and use a rigid suction catheter with high
power suction to suck out any fl uid or blood from the oropharynx.
• Insert the oropharyngeal airway ‘upside down’ for 4–5cm (half way),
then rotate it 180 ° and insert it until the fl ange is at the teeth.
• In children, use a laryngoscope as a tongue depressor and insert the
airway the ‘correct way up’ to avoid trauma to the palate.
• Re-check the airway and breathing and give high fl ow O
2
.
• Ventilate the patient if breathing is inadequate.
Insertion of nasopharyngeal airway
• Select an appropriate airway, usually a 7.0mm for adult males and
a 6.0mm for adult females. A safety pin through the fl ange end will
prevent displacement into the nose or nasopharynx.
• Lubricate the airway with water or a water-soluble lubricant.
• Insert the tip of the airway into one nostril and direct the airway
posteriorly, aiming the tip at the tragus of the ear.
• The airway should slide easily into the nose until the fl ange abuts
the nostril and the tip is just visible in the pharynx. Never force a
nasopharyngeal airway into the nostril — any bleeding produced will
markedly aggravate the airway problem.
• Re-check the airway and breathing and give high fl ow O
2
.
Jaw thrust manoeuvre
The aim of this is to open the upper airway with minimum movement of
the cervical spine. Place the forefi ngers of both hands immediately behind the
angles of the mandible and push the mandible anteriorly. This will lift the
tongue anteriorly and thus away from the posterior pharyngeal wall.
Tracheal intubation in trauma
An injured patient who has no gag refl ex needs tracheal intubation to
maintain the airway and protect it against blood and vomit. Intubation
may also be needed because of: apnoea (after initial ventilation with a
bag-valve-mask), respiratory inadequacy, to prevent potential obstruction
from facial burns or to allow manipulation of ventilation in patients with
i ICP). Intubation in such circumstances requires emergency anaesthesia:
suitable expertise, appropriate equipment and assistance are essential
( b p.312). An assistant must hold the head to prevent movement of the
neck during intubation, while another assistant provides cricoid pressure.
Confi rm correct tracheal tube placement by:
• Seeing the tube pass through the cords.
• Observing symmetrical chest movement.
• Listening over both axillae for symmetrical breath sounds.
• Confi rming placement with end-tidal carbon dioxide (CO
2
) monitoring.
If airway obstruction is complete, the obstruction cannot be relieved and
intubation is impossible, an urgent surgical airway is needed ( b p.326).

326 CHAPTER 8 Major trauma
Airway obstruction: surgical airway
Surgical cricothyroidotomy or jet insuffl ation of the airway via a needle
cricothyroidotomy is needed if the airway is obstructed by trauma,
oedema or infection, and the trachea cannot be intubated. Emergency
tracheostomy is not indicated in this situation because it is too time-
consuming to perform and the necessary expertise may not be available.
Needle cricothyroidotomy
This is a rapid temporizing measure whilst preparation is made for a defi n-
itive airway (eg surgical cricothyroidotomy). Jet insuffl ation via a cannula
placed through the cricothyroid membrane can provide up to 45min of
oxygenation of a patient with partial airway obstruction (Fig. 8.1 ).
• Use a large IV cannula-over-needle (adults: 12 or 14G; children: 16 or
18G), attached to a syringe. If right-handed, stand on the patient’s left.
• Palpate the cricothyroid membrane between the thyroid and cricoid
cartilages. Hold the cricoid cartilage fi rmly with the left hand.
• Pass the needle and cannula at a 45 ° angle to the skin in the midline
through the lower half of the cricothyroid membrane into the trachea.
• Aspirate whilst advancing the needle. Aspiration of air confi rms entry
into the trachea. Withdraw the needle whilst advancing the cannula
down into position in the trachea.
• Connect the cannula via a Y connector or O
2
tubing with a side hole to
wall O
2
at 15L/min (in a child the rate should initially be set in L/min at
the child’s age in years, increasing if necessary until capable of causing
chest movement). Hold the cannula fi rmly in position. Occlude the side
hole or the end of the Y connector with a thumb for 1 in 5sec to give
intermittent insuffl ation of O
2
.
Spontaneous breathing through the small airway of a cannula is very
diffi cult, but the patient should be able to exhale partially in the 4sec
between jets of O
2
. However, CO
2
retention occurs and limits the time
that jet insuffl ation can be tolerated. Proceed immediately to a defi nitive
airway (call a senior ENT or maxillofacial surgeon).
Surgical cricothyroidotomy
This technique is not appropriate in children aged <12 years.
• Stand on the patient’s right. Feel the thyroid and cricoid cartilages and
the cricothyroid membrane between them.
• Clean the area and give LA (if the patient is conscious and time allows).
• Hold the thyroid cartilage with the left hand and make a transverse
incision through the skin and the cricothyroid membrane.
• Use a tracheal dilator or curved artery forceps to open the hole into
the trachea. Do not worry about any bleeding at this time.
• Insert a lubricated tracheostomy tube (5–7mm diameter) through the
cricothyroid membrane into the trachea.
• Remove the introducer from the tracheostomy tube, infl ate the cuff
and connect the tube to a catheter mount and ventilation bag.
• Confi rm correct placement with end-tidal CO
2
monitoring.
• Ventilate the patient with O
2
and secure the tracheal tube.
• Examine the chest and check for adequacy of ventilation.
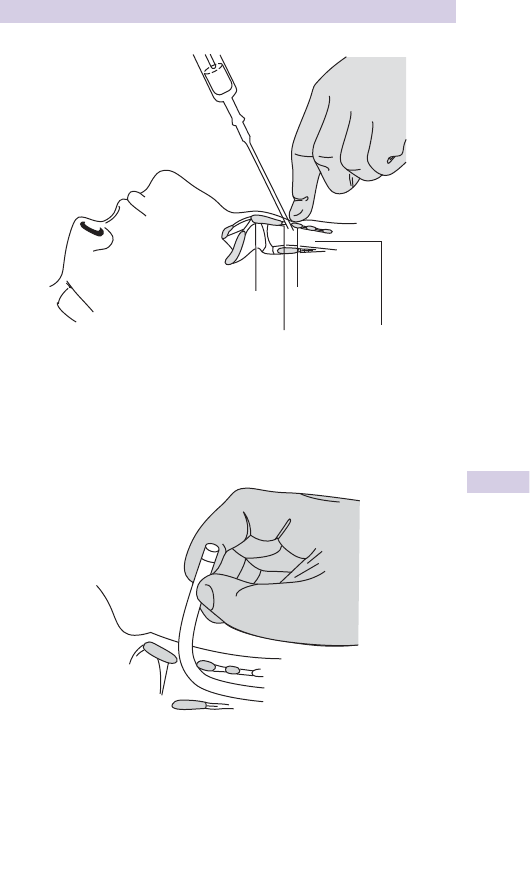
327
AIRWAY OBSTRUCTION: SURGICAL AIRWAY
Cricoid
cartilage
Thyroid
cartilage
Cricothyroid
membrane
Trachea
Fig. 8.1 Needle cricothyroidotomy.
Fig. 8.2 Surgical cricothyroidotomy.

328 CHAPTER 8 Major trauma
Tension pneumothorax
Tension pneumothorax is a life-threatening emergency and requires
prompt recognition and treatment. It occurs when gas progressively
enters the pleural space, but is unable to leave. Increasing pressure causes
complete lung collapse on the affected side and ultimately pushes the
mediastinum to the other side. Movement of the mediastinum leads to
kinking of the great vessels, thereby d venous return and cardiac output.
Additional compromise results from compression of the lung on the
other side, particularly in patients undergoing IPPV. The process leading
to tension pneumothorax may occur very rapidly, culminating in cardiac
arrest within minutes.
Causes
Tension pneumothorax is seen most frequently following trauma, but it
may also occur iatrogenically after attempted insertion of a central venous
line ( b p.56). A small (perhaps unsuspected) simple pneumothorax
is particularly likely to become a tension pneumothorax when IPPV is
commenced.
Features
• Dyspnoea, tachypnoea, and acute respiratory distress.
• Absent breath sounds on the affected side.
• Hyper-resonance over the affected lung (diffi cult to demonstrate in a
noisy environment).
• Distended neck veins (unless hypovolaemic), tachycardia, hypotension,
and ultimately, loss of consciousness.
• Tracheal deviation away from the affected side (this is rarely clinically
apparent).
• i Airway pressure in a patient receiving IPPV.
Diagnosis
This is entirely clinical : do not waste time obtaining X-rays.
Treatment
• Apply high fl ow O
2
by face mask.
• Perform immediate decompression by inserting an IV cannula (16G
or larger) into the second intercostal space in the mid-clavicular line,
just above the third rib (to avoid the neurovascular bundle; Fig. 8.3 ).
Withdraw the needle and listen for a hiss of gas.
• Tape the cannula to the chest wall.
• Insert an axillary chest drain on the affected side immediately
( b p.336).
• Remove the cannula and apply an adhesive fi lm dressing.
• Check the patient and obtain a CXR.
Note : the risk of causing a pneumothorax by needle decompression in a
patient who did not have one is approximately 10 % . If the patient is very
muscular or obese, consider using a longer cannula than normal (e.g. central
venous line) to ensure that the pleural cavity is reached.
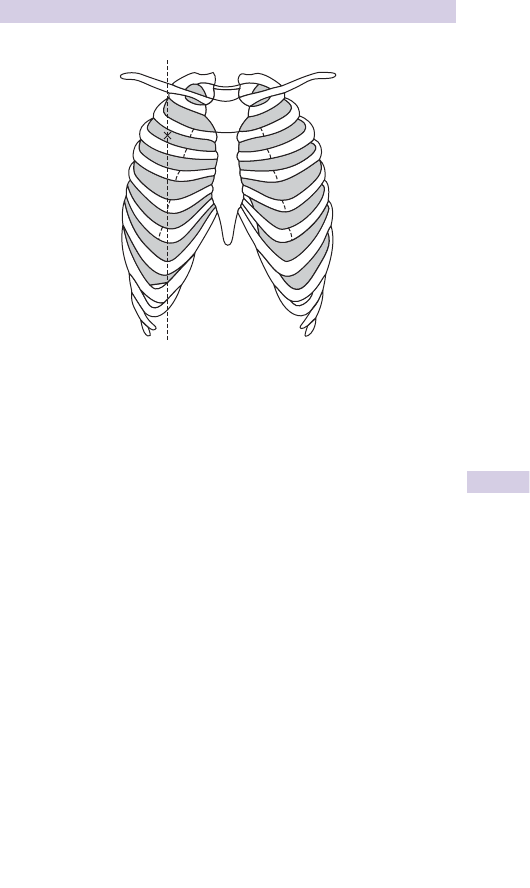
329
TENSION PNEUMOTHORAX
Mid-clavicular line
Fig. 8.3 Site for needle decompression of right tension pneumothorax.

330 CHAPTER 8 Major trauma
Chest wall injury 1
Background
Blunt chest wall trauma is extremely common — both as an isolated injury
and as part of multiple injuries. It can cause great morbidity in the elderly.
Isolated rib fracture
A history of trauma with subsequent musculoskeletal pain suggests rib
fracture. The diagnosis is confi rmed by localized chest wall tenderness —
the diagnosis of a single rib fracture is a clinical one. Check for features
which are suggestive of pneumothorax (dyspnoea, d air entry, see b
p.334), secondary pneumonia or multiple rib fractures, and if any are
present, obtain a CXR.
Treat uncomplicated isolated rib fracture with oral analgesia (eg
co-codamol ± NSAID). Warn the patient that the rib may remain painful
for ≥ 3 weeks and to seek medical advice if additional symptoms develop.
Multiple rib fractures
Observe the chest wall carefully for possible fl ail segment, and look for
clinical evidence of pneumothorax or, in late presentations, secondary
pneumonia.
Check SpO
2
, ABG, and obtain a CXR. Note that up to 50 % of rib fractures
may not be apparent on CXR.
Treat Flail segment and pneumothorax ( b p.332). Treat patients with
uncomplicated multiple rib fractures according to the presence of other
injuries and pre-existing medical problems as follows:
In patients with other injuries requiring IPPV, discuss the potential need
for chest drains with the ICU team ( i risk of pneumothorax).
Patients with pre-existing pulmonary disease and limited respiratory
reserve require admission for analgesia and physiotherapy.
Patients with chest infection often require admission for analgesia,
antibiotics and physiotherapy, depending upon past medical history,
clinical, and radiological fi ndings.

331
CHEST WALL INJURY 1
Sternal fracture
Sternal fracture frequently occurs during road traffi c collisions, either
due to impact against the steering wheel or seat belt. The injury may be
associated with myocardial contusion, great vessel injury and spinal injury
(see below).
Features Anterior chest pain with localized tenderness over the sternum.
Investigations
• Place on a cardiac monitor.
• Record an ECG to exclude arrhythmias, MI ( b p.70) or myocardial
contusion (look for ST changes, particularly elevation). Consider further
investigation with echocardiography.
• Check cardiac specifi c enzymes (troponins) if there are ECG changes.
• Request CXR and lateral sternal X-ray: the latter will demonstrate the
fracture (which is usually transverse), the former, associated injuries.
Treatment Provide O
2
and analgesia. Admit patients who have evidence
of myocardial contusion or injuries elsewhere. Only consider discharging
those patients who have an isolated sternal fracture, with a normal ECG,
no associated injuries and normal pre-existing cardiopulmonary function.
Patients who are discharged require oral analgesia (eg co-codamol
± N SAID) and GP follow-up.
Note Rarely, forced fl exion of the chest causes a displaced sternal
fracture with wedge fractures of upper thoracic vertebrae. Check the
spine carefully, ask about pain, and look for kyphosis and tenderness
(which may not be apparent). Lateral thoracic X-rays often fail to show
the upper thoracic vertebrae, so if injury is suspected there, consider
requesting a CT scan.
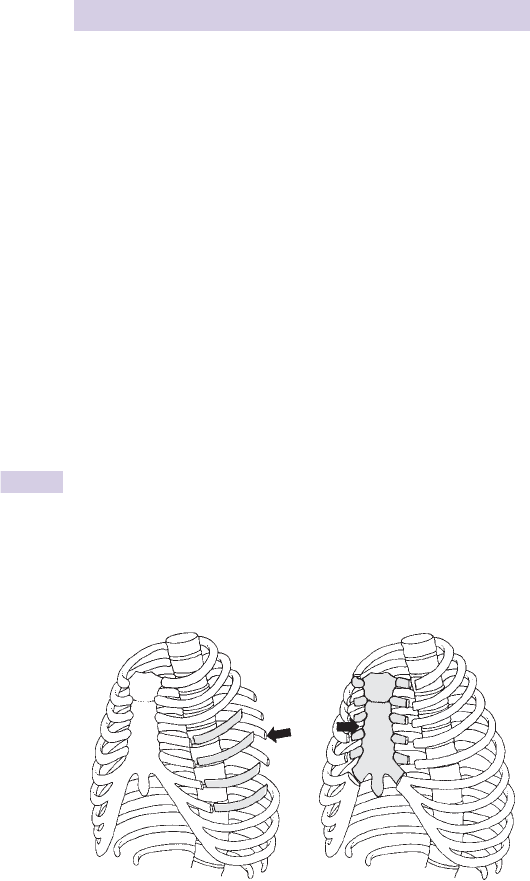
332 CHAPTER 8 Major trauma
Chest wall injury 2
Flail segment
Fractures of ≥3 ribs in 2 places allows part of the chest wall to move
independently. This fl ail segment usually indicates signifi cant injury to the
underlying lung (typically pulmonary contusions). Large fl ail segments occur
laterally when several ribs on one side fracture anteriorly and posteriorly.
Similarly, an anterior fl ail segment is produced by bilateral fractures of all
ribs anteriorly — in this case, the free portion comprises the sternum, costal
cartilages, and the medial parts of the fractured ribs (see Fig. 8.4 ).
Presentation The fl ail segment causes pain and moves paradoxically
compared with the rest of the chest wall, limiting the effectiveness of
respiration. The diagnosis is a clinical one, but it can be diffi cult to make.
Look tangentially at the chest for areas which move paradoxically (ie
inwards during inspiration and outwards during expiration). There may be
associated features of respiratory distress (cyanosis, tachypnoea). Check for
pneumothorax or haemothorax ( b p.334).
Investigations Assessment of the extent of respiratory compromise is
largely clinical, aided by a few simple investigations:
• SpO
2
on pulse oximetry.
• ABG — the combination of hypoxia and respiratory acidosis ( i p CO
2
,
i H
+
) indicates severe respiratory compromise.
• CXR will demonstrate fractures and associated injuries (eg pulmonary
contusions, pneumothorax, haemothorax).
Treatment
• Provide high fl ow O
2
and treat associated life-threatening problems.
• Contact the ICU/anaesthesia team and carefully consider the need for
immediate or urgent tracheal intubation with IPPV.
• Careful observation and monitoring in an high dependency unit (HDU)
or ICU is required.
• Consider inserting an intra-arterial line for frequent ABG analyses.
• Selected patients may benefi t from epidural analgesia in ICU.
Lateral flail segment Anterior flail segment
Fig. 8.4 Lateral (left) and anterior (right) fl ail segments.

333
CHEST WALL INJURY 2
Ruptured diaphragm
Left-sided ruptures predominate (75 % ).
Major rupture of the diaphragm, with associated herniation of abdominal
contents into the chest, is a severe injury resulting from a signifi cant
traumatic insult (often massive abdominal crushing). Depending upon the
extent of the injuries, the patient may present with hypovolaemic shock
and respiratory compromise. Note that a ruptured diaphragm may have
some clinical features similar to a tension pneumothorax. Call a surgeon
and anaesthetist : the patient will require urgent intubation and IPPV.
Minor rupture, with less dramatic herniation, may present in more subtle
fashion and result from penetrating injury. The diagnosis is diffi cult to
identify on CT scanning and is frequently missed initially — it is important
because:
• It is often associated with injury to both abdominal and thoracic contents.
• There are possible late complications (eg bowel herniation/obstruction).
• It does not heal spontaneously.
Suspect a ruptured diaphragm from the mechanism of injury, and an
abnormal or high hemi-diaphragm contour on erect CXR. Look for
stomach or bowel loops in the chest: the gastric tube may be seen coiled
in the intra-thoracic stomach. If a ruptured diaphragm is suspected,
resuscitate the patient and refer to a surgeon.
Oesophageal rupture
Traumatic (non-iatrogenic) rupture of the oesophagus is uncommon, but
may follow blunt or penetrating injury. Suspect it if the patient complains of
chest and back/neck pain in the presence of a normal ECG. Look for surgical
emphysema in the neck. CXR may demonstrate pneumomediastinum
(a layer of gas around the heart/mediastinum), a left sided pleural
effusion or pneumothorax. Provide O
2
, IV analgesia, and start IV antibi-
otics (eg cefuroxime 1.5g). Resuscitate, treat other injuries, and refer to a
cardiothoracic surgeon.
Boerhaave’s syndrome is ‘spontaneous’ rupture of the oesophagus
associated with overindulgence and vomiting. Patients are classically
middle-aged and present with severe chest pain, signs of shock, and
subcutaneous emphysema. If this condition is suspected, treat as outlined
above for traumatic oesophageal rupture.

334 CHAPTER 8 Major trauma
Traumatic pneumothorax
Background
Pneumothorax frequently results from blunt injury with associated rib
fractures or from penetrating injury (knife stabbing or gunshot wound).
It may also be iatrogenic, secondary to attempted insertion of a central
venous line.
Clinical features
Patients are likely to complain of symptoms relating to the associated
injuries (eg rib fractures, b p.330). The degree of breathlessness resulting
from a pneumothorax depends largely upon its size. Other features may
be present, including surgical emphysema, cyanosis, d air entry over the
affected lung. Severe dyspnoea and distended neck veins/hypotension
suggest tension pneumothorax ( b p.328).
CXR demonstrates the pneumothorax. Both inspiratory and expiratory
X-rays are not required. Wherever possible, obtain an erect CXR. X-rays
taken with the patient lying supine may not show a free lung edge, despite
a considerable pneumothorax, because in this position air tends to lie
anteriorly in the pleural space. If there is no defi nite pneumothorax visible
on a supine CXR, features which are suggestive of a pneumothorax are:
• Hyperinfl ation of the affected hemithorax with depressed hemidiaphragm.
• Double contour of a hemidiaphragm.
• Basal hyperlucency of the affected lung.
• Visualization of apical pericardial fat tags.
CT scan obtained to assess other injuries will easily demonstrate a
pneumothorax. SpO
2
and ABG may reveal hypoxia.
Treatment
Tension pneumothorax is an emergency requiring immediate needle
decompression ( b p.328). Provide O
2
and drain other traumatic
pneumothoraces using a chest drain and open technique, as described on
b p.336.
Note: although not currently considered to be ‘standard practice’, there
is increasing experience with initially managing some patients who have
isolated chest injury and small traumatic pneumothoraces in a conservative
fashion, using close observation and no chest drain. Further experience
will be needed before this approach can be widely recommended. Patients
who have multiple injuries and/or other injuries (particularly those
requiring GA and IPPV) certainly require chest drain insertion in the ED.

335
HAEMOTHORAX
Haemothorax
Blood may collect in the pleural cavity in association with a pneumothorax
(haemopneumothorax) or without (haemothorax). A large amount of
bleeding into the pleural space suffi cient to produce hypovolaemic shock
is termed massive haemothorax .
Clinical features
The clinical presentation is similar to that seen in traumatic pneumo-
thorax, except that there may be dullness to percussion over the affected
lung and, with massive haemothorax, evidence of hypovolaemia.
CXR Blood from a haemothorax collects under the affected lung, showing
up as i shadowing on a supine X-ray, with no visible fl uid level. It may be
very diffi cult to distinguish haemothorax from pulmonary contusions on
supine X-ray, but haemothorax may produce blurring of a hemidiaphragm
contour or of the costophrenic angles.
Treatment
Give O
2
and insert 2 large venous cannulae (sending blood for X-matching).
If hypovolaemic, start IV fl uids before inserting a large ( ≥ 32FG) chest
drain. Although it is common practice to try to direct the chest drain
towards the diaphragm, this seldom makes a difference in practice — it is
more important to use a chest tube of suffi cient calibre in order to minimize
blockages due to blood clots.

336 CHAPTER 8 Major trauma
Chest drain insertion
Use the ‘open’ technique, as described below. Explain the procedure,
obtain consent and confi rm that the patient has venous access, is breathing
O
2
, and is fully monitored. Ensure that all equipment is ready and a good
light and assistance are available. Give adequate IV opioid analgesia to
conscious patients as this procedure can be painful.
• Abduct the ipsilateral arm fully.
• Don a sterile gown and gloves, and use a face shield to protect against
blood splashes.
• Clean the skin with antiseptic and cover with sterile drapes.
• Identify the 5th intercostal space just anterior to the mid-axillary line
(count down and across from the angle of Louis at the level of the 2nd
rib) (Fig. 8.5 , top).
• Generously infi ltrate LA (1 % lidocaine ± adrenaline) under the skin and
down to the periosteum at the upper edge of the 6th rib.
• Prepare the chest drain; remove and discard the trocar (in adults, use a
size 28–32FG; in children, use the largest size that will comfortably pass
between the ribs).
• Make a 2–3cm skin incision in the line of the ribs (Fig. 8.5 ).
• Use blunt dissection with artery forceps to open the tissues down to
the pleural space, just above the 6th rib.
• Puncture the pleura with the artery forceps.
• Insert a gloved index fi nger into the pleural cavity to ensure there are
no adhesions and that you are within the thoracic cavity (Fig. 8.5 ).
• Insert the chest drain ensuring that all drainage holes are inside the
chest (typically ≈ 15–20cm in adults).
• Connect the drain to an underwater seal and look for ‘swinging’.
• Suture the drain securely in place (eg with heavy silk) and cover with
an adhesive fi lm dressing and adhesive tape (Fig. 8.5 ). Whilst securing
it, get an assistant to hold the drain so that it does not inadvertently
fall out. It is useful to insert two untied sutures at the site of exit of the
chest drain, so that these can be later tied to close the exit site when
the drain is removed.
• Check the underwater seal is ‘swinging’ in the tube with respiration.
• Listen for air entry and check the patient.
• Obtain a CXR to confi rm placement: if the tube has been inserted too
far (eg so that it is touching the mediastinum), pull it back slightly and
re-suture and secure in place.
• Afterwards, keep the water seal drainage bottle below the level of the
patient. Avoid clamping the tube.
Referral to a thoracic surgeon If the chest drain initially yields > 1500mL
of blood, or subsequently drains > 200mL/hr for 2hr, refer urgently to a
thoracic surgeon for possible urgent thoracotomy.
Ruptured bronchus Persistent, continuing bubbling of gas through the
underwater drain may refl ect a major rupture of the tracheobronchial
tree, especially if the lung fails to re-expand. Bronchial rupture may also
present with haemoptysis or tension pneumothorax. Involve a thoracic
surgeon at an early stage.
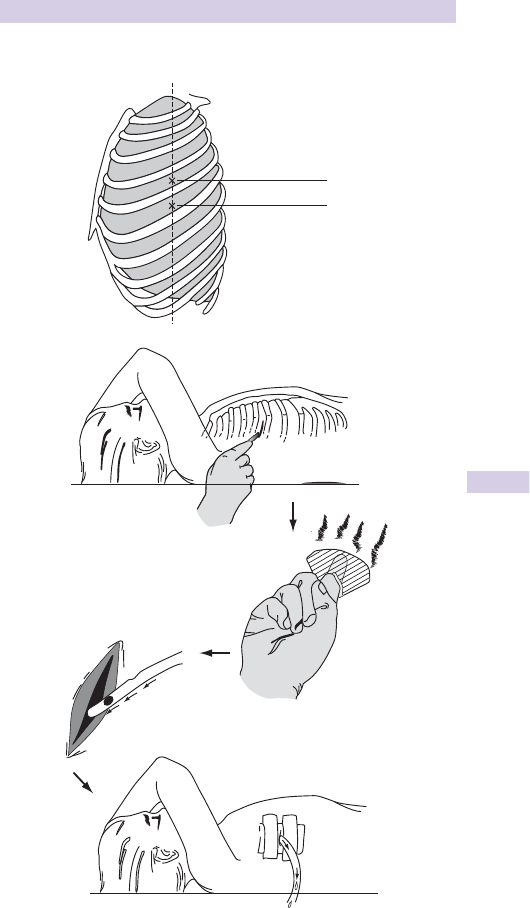
337
CHEST DRAIN INSERTION
Mid-axillary line
4
th
ICS
5
th
ICS
Fig. 8.5 Chest drain insertion.

338 CHAPTER 8 Major trauma
Pulmonary contusions and aspiration
Pulmonary contusions
High energy transfer during blunt injury (eg road traffi c collisions or high
falls) often causes pulmonary contusions. Suspect these in all patients with
fl ail segments ( b p.332).
Clinical features
Pulmonary contusions produce ventilation-perfusion mismatch which may
lead to hypoxia and respiratory distress, and i the likelihood of ARDS.
Radiological appearances
Pulmonary contusions may be visible on initial CXR as patchy opacifi cation.
However, initial radiological appearances are non-specifi c and may be
confused with those seen after pulmonary aspiration or haemothorax
( b p.335). X-ray changes resulting from pulmonary contusions tend to be
progressive and become more prominent with time.
Management
Provide high fl ow O
2
and check ABG to help assess the need for GA,
tracheal intubation and IPPV. Involve ICU specialists early.
Pulmonary aspiration ( b see p.112)
Inhalation of vomit and other foreign material may add considerably to
the damage resulting from the initial injury.
Common associations
• Inhalation of vomit after head injury with d conscious level and impaired
protective laryngeal refl exes: gastric contents are particularly irritant to
the respiratory tract.
• Inhalation of blood and teeth after facial trauma.
• Inhalation of water and foreign matter in near drowning ( b p.258).
Presentation
Suspect pulmonary aspiration from the history, associated respiratory
signs and X-ray appearance. The CXR may show diffuse opacifi cation
affecting one or both lungs — the distribution depends upon the position
at the time of aspiration.
Management
• Check SpO
2
, ABG, and obtain a CXR.
• Provide high fl ow O
2
.
• Treat other injuries.
• Consider the need for GA, tracheal intubation, and IPPV. Bronchoscopy
may be needed to remove large FBs from within the bronchial tree.
• Even if there is no urgent requirement for IPPV, remember that the
respiratory problem is likely to worsen (with development of infection/
ARDS), so involve the ICU team early.
• Do not give routine antibiotics, unless there is a specifi c indication,
such as immersion in sewage or in rat-infested water with the risk of
developing leptospirosis (see b p.239).
This page intentionally left blank

340 CHAPTER 8 Major trauma
Penetrating chest injury 1
In the UK, unlike the USA, chest ‘stabbing’ is far more frequent than
‘shooting’. Both types of injury can pose a serious threat to life.
Initial assessment and resuscitation
Do not be misled by seemingly innocuous wounds. The size of the external
wound has no correlation with the potential for internal injury. All patients
need O
2
, venous access (send blood for cross-matching, or group and
save) and resuscitation according to an evaluation of the airway/ cervical
spine, breathing, and circulation. Remove all of the patient’s clothes and
log roll to check for wounds to the back of the trunk and perineum.
Particularly in gunshot injuries, make a quick early check for evidence
of spinal cord injury. Remember also that penetrating chest injury often
involves the abdomen (and vice-versa). During initial assessment aim to
exclude or identify and treat the following:
• Tension pneumothorax ( b p.328).
• Sucking chest wound ( b p.342).
• Cardiac tamponade ( b p.342).
• Massive haemothorax ( b p.334 and 335).
Further management depends partially upon haemodynamic status.
The stable patient
Many patients present without overt evidence of signifi cant injury:
• Provide O
2
, secure venous access, and send blood for group and save.
• Monitor SpO
2
, pulse, BP, and respiratory rate.
• Administer minimal or no intravenous fl uids.
• Perform a FAST scan if possible to look for cardiac tamponade
( b p.346).
• Obtain a CXR (ideally postero-anterior (PA) erect).
• Record an ECG.
• Provide IV analgesia as required (see b p.320).
• Consider tetanus status and the need for prophylactic antibiotics
(eg 1.5g IV cefuroxime — according to local policy).
• Cover the chest wound with a sterile dressing (for sucking chest
wound — see b p.342).
• Drain any pneumothorax with a chest drain (having decompressed any
tension pneumothorax — b p.328). Do not insert the drain through the
wound (this i the risk of infection).
• Refer all patients for admission, observation, formal wound cleaning,
exploration, and closure. If the patient remains stable overnight, with
no clinical or radiological abnormalities (on repeat CXR ≥ 6hr after the
fi rst), they may be safely discharged with arrangements for review.
• Carefully document the size, position and other features of the
chest wound, remembering the potential medicolegal signifi cance
( b p.402).

341
PENETRATING CHEST INJURY 1
The unstable patient
Haemodynamic instability may be due to tension pneumothorax, massive
haemothorax, sucking chest wound, or cardiac tamponade. Treat each of
these as outlined on b p.342 involving a senior surgeon at an early stage.
Indications for thoracotomy
Thoracotomy in theatre will be required for signifi cant haemorrhage,
which typically means:
• > 1.5 L of free blood obtained by initial chest drainage, or.
• > 200mL of blood draining per hr, via the chest drain.

342 CHAPTER 8 Major trauma
Penetrating chest injury 2
Open chest injury
An open wound between the pleural cavity and the outside may cause
respiratory insuffi ciency. When the chest expands on inspiration there is
less resistance to air movement through the open chest wound than down
the tracheobronchial tree. Air fl ow into the lungs is reduced and the lung
collapses as air enters the pleural space and produces a pneumothorax.
Hypoxia develops rapidly.
Features
Look for respiratory distress, tachypnea, and cyanosis.
Management
• Provide high fl ow O
2
.
• Cover the chest wound with a square of polythene or sterile dressing.
• Secure 3 sides of the dressing to the chest wall with adhesive tape,
leaving one side free. This will allow air to exit through the chest
wall during expiration, but prevent air entry into the chest cavity.
• Insert a chest drain (not through the wound) to drain the pneumothorax.
• Provide further resuscitation as necessary.
• Call a thoracic surgeon to arrange formal wound closure.
Cardiac tamponade
Haemorrhage into the pericardial sac may compromise cardiac output.
Continuing bleeding leads to cardiac tamponade, culminating in cardiac
arrest. Cardiac tamponade usually results from penetrating trauma but
may occur after blunt trauma.
Features
Clinical diagnosis requires a high index of suspicion. The oft-quoted Beck’s
triad comprises distended neck veins, hypotension, and muffl ed heart
sounds. Identifying muffl ed heart sounds is rarely easy in a noisy ED and
neck veins may not be distended in a hypovolaemic patient. Kussmaul’s
sign and pulsus paradoxus are classical, but rarely helpful.
Investigation
The investigation of choice is a FAST scan ( b p.346) in the ED resuscitation
room to identify the presence of pericardial fl uid. USS signs of cardiac
tamponade include right ventricular collapse. Formal echocardiography
is rarely available immediately. CXR and ECG are rarely helpful, but may
exclude co-existent conditions (eg pneumothorax).
Treatment
• Provide O
2
, insert 2 IV lines, commence IV fl uid infusion if severely
shocked and monitor ECG.
• Request that the thoracotomy tray be made ready.
• Contact the most senior available cardiothoracic/general/trauma
surgeon and anaesthetist and alert the operating theatre.
• If the patient’s condition permits, arrange immediate transfer for
thoracotomy in theatre. Theatre thoracotomies have better outcomes
than those done in the ED.

343
PENETRATING CHEST INJURY 2
• If the patient deteriorates to a peri-arrest state, consider pericardiocen-
tesis using a long 18G needle connected to a 20mL syringe and 3-way
tap. Puncture the skin 1–2cm below the xiphisternum at 45 ° to the skin.
Aspirate while advancing the needle cephalad, aiming towards the tip of
the left scapula. ST and T wave changes, widened QRS or arrhythmias
imply that the needle has been advanced too far.
• Aspiration of a small amount of blood (eg 20–40mL) may improve
cardiac output temporarily and ‘buy time’ to organize thoracotomy.
• Pericardiocentesis is often unsuccessful due to clots which have formed
in the pericardial sac and which cannot be aspirated.
• Perform immediate thoracotomy in the ED for cardiac arrest from
penetrating trauma. Do not waste time on pericardiocentesis.
Thoracotomy for cardiac tamponade
Thoracotomy in the ED may be required in certain life-threatening
emergencies, including cardiac arrest due to penetrating chest injury: the
principal aim is to decompress the pericardium and relieve tamponade.
First exclude and treat other reversible causes of cardiac arrest (upper
airway obstruction, b p.324; tension pneumothorax, b p.328).
Thoracotomy is not indicated for cardiac arrest following blunt injury.
Procedure
• Summon expert help (ED consultant; cardiothoracic, general or trauma
surgeon; anaesthetist) and proceed immediately. Do not wait.
• Whilst the thoracotomy tray is being opened, don gloves, a face shield and
an apron, ensure that the patient is being ventilated with O
2
via a tracheal
tube, and start external chest compressions ( b p.49). Continue rapid IV
infusion via multiple lines and obtain blood for transfusion.
• Standing on the patient’s left side, abduct the left arm, stop chest com-
pressions and open the left chest wall. Start the incision at the medial
end of the 5th intercostal space and cut laterally just above the 6th
rib into the axilla. Use a rib retractor to access the thoracic cavity. If
necessary, improve access further by continuing the incision medially
using strong scissors to cut through the sternum and into the right 5th
intercostal space (clamshell thoracotomy). Speed is of the essence.
• Identify the heart: carefully incise vertically through the bulging pericar-
dium over its anterior surface, avoiding the left phrenic nerve.
• Evacuate blood from the pericardial sac and identify the damage.
• Place a fi nger over the cardiac defect and perform internal cardiac
massage by compressing the heart between 2 fl at hands, with fi ngers
placed over defects. Close myocardial wounds using interrupted 4/0
prolene sutures, using tefl on or pericardial buttresses if necessary.
Once sutures are in place, stop internal cardiac massage and check
cardiac rhythm and output. If the heart is fi brillating, defi brillate using
internal defi brillation paddles, by placing a paddle over each side of the
heart. Start with 5J energy initially, i as necessary to max of 50J. Use an
external defi brillator if no internal paddles are available.
• Once a pulse has been restored, ensure that hypovolaemia is corrected.
Give cefuroxime 1.5g IV, insert an arterial line and urinary catheter,
recheck U&E, glucose, FBC, and clotting.
• The cardiothoracic surgeon will direct further surgical management.

344 CHAPTER 8 Major trauma
Aortic injury
The vast majority of aortic injuries ( ≈ 90 % ) are sustained during high energy
blunt trauma (eg road traffi c collisions, high falls). Only a small proportion
of these patients reach hospital with signs of life. The usual site of rupture
is just distal to the origin of the left subclavian artery, possibly caused
by differential shearing forces between the mobile arch and the fi xed
descending thoracic aorta. An alternative proposed mechanism is that
during rapid deceleration the fi rst rib and clavicle swing down and directly
‘nip’ the aorta (‘osseous pinch’ theory). The injury is relatively unusual in
children, who are perhaps protected by having more elastic tissues.
Features
Patients who reach hospital alive are most likely to have a partial or
contained rupture, with a haematoma confi ned by aortic adventitia. They
may complain of chest and back pain and there may be a harsh systolic
murmur, absent or d pulses (with differential BP between arms and legs),
and evidence of hypovolaemic shock: features of other signifi cant non-
aortic injuries may predominate.
Diagnosis
The diagnosis of aortic injury can be diffi cult: adopt a high index of
suspicion. An erect CXR is invaluable provided that the patient’s condition
permits it.
CXR features suggesting aortic injury include:
• Widened mediastinum ( > 8cm on PA fi lm).
• Abnormal aortic arch contour.
• Deviation of the trachea to the right side.
• Deviation of an orogastric/NG tube to the right side (such that it lies to
the right of the T4 spinous process).
• Depression of the left main bronchus > 40 ° below the horizontal.
• Left pleural cap or fractured fi rst/second ribs are often quoted, but are
of little diagnostic value.
• The CXR may be normal!
Management
Resuscitate and treat other injuries. Aortic injuries are associated with
other severe chest injuries, eg fl ail segments, pulmonary contusions. As
a minimum, provide O
2
, insert two IV cannulae, start IV fl uids, provide
analgesia, monitor vital signs and SpO
2
. Check U&E, glucose, FBC, clotting,
ABG, and cross-match. Insert urinary catheter and arterial line.
Involve a cardiothoracic surgeon or a vascular surgeon with expertise in
aortic injury. Refer urgently for specialist investigation (CT scan and/or
aortography). Involve anaesthetist/ICU. Control BP (avoid over-infusion
of IV fl uids; use glyceryl trinitrate (GTN) infusion IV to maintain systolic
BP ≈ 90mmHg) prior to treatment. This usually involves open surgical
repair, but some centres have reported good short-term results using
endovascular stents.
This page intentionally left blank

346 CHAPTER 8 Major trauma
Focused assessment with sonography
for trauma (FAST) scan
Increasingly used in the ED resuscitation room to assess the chest and
abdomen of acutely injured patients, especially those with shock.
Can be performed by a trained ED doctor, surgeon, or radiologist.
Advantages
• Can be done in ED.
• Quick: takes 2 − 3min.
• Non-invasive.
• Repeatable if concerns persist or the patient’s condition changes.
Disadvantages
• Operator dependent.
• Does not defi ne injured organ, only presence of blood or fl uid in
abdomen or pericardium.
Ideally performed with a portable or hand-held USS scanner.
Looks at four areas for the presence of free fl uid only:
• Hepatorenal recess (Morrison’s pouch).
• Splenorenal recess.
• Pelvis (Pouch of Douglas).
• Pericardium.
The scan is usually done in that order, as the hepatorenal recess is the
fi rst to fi ll with fl uid in the supine position, and is most easily identifi ed.
If the indication for FAST scanning is to identify cardiac tamponade, the
fi rst view should be the pericardial view.
Free fl uid appears as a black echo-free area:
• Between the liver and the right kidney.
• Between the spleen and the left kidney.
• Behind the bladder in the pelvis.
• Around the heart in the pericardium.
A positive FAST scan is one which identifi es any free fl uid in the
abdomen or in the pericardium.
Visible free fl uid in the abdomen implies a minimum volume of ≈ 500mL.
The fi nding of blood in the pericardium after trauma is an indication
for emergency thoracotomy, ideally in the operating theatre; however,
thoracotomy should be performed in the ED if the patient arrests.
FAST scanning requires training prior to use on trauma patients; there is a
signifi cant false-negative rate in inexperienced hands.
1
1 See http://www.trauma.org/index.php/main/article/214/

347
DIAGNOSTIC PERITONEAL LAVAGE (DPL)
Diagnostic peritoneal lavage (DPL)
DPL is helpful in situations where clinical evidence of intra-abdominal
injury is equivocal and neither CT nor USS is available. DPL may also be
useful to search for intra-abdominal bleeding in shocked head-injured
patients, or those whose massive pelvic fracture is being externally fi xed
(see b p.466). DPL is used less often now that FAST scanning and CT
have become more readily available. Also, some injuries are treated
conservatively (eg ‘minor’ splenic injury in children) and so a + ve DPL is
of less value than a specifi c diagnosis made by CT. The open technique
of DPL is shown below. Ideally, DPL is done by the surgeon who will
perform the laparotomy if the DPL is + ve.
How to perform diagnostic peritoneal lavage
• Explain the procedure and obtain consent if conscious.
• Ensure that the bladder has been decompressed by a urinary catheter.
• Ensure that an orogastric/NG tube has been passed.
• Enlist an assistant and bright light.
• Clean the skin with antiseptic and drape with sterile towels.
• Infi ltrate LA (1 % lidocaine with adrenaline) around the proposed site of
incision.
• Make a vertical midline skin incision ≈ 3cm long at a point one-third
of the distance from the umbilicus to the symphysis pubis. However,
use a supra-umbilical site if the patient has lower abdominal scars, is
pregnant, or has a pelvic fracture. Request that the assistant exerts gentle
pressure on the wound edges, in order to minimize bleeding.
• Divide the linea alba, identify the peritoneum and grasp it between
2 surgical clips.
• Gently bring the peritoneum into the wound and feel its edge between
fi nger and thumb to ensure that no bowel has been caught in the clips.
• Make a tiny peritoneal incision, insert a peritoneal dialysis catheter
(without the needle) and direct it downwards into the pelvis.
• Gently twist the peritoneal clip to obtain a good seal around the
catheter. Attempt to aspirate any free fl uid.
• If obvious enteric contents or > 5mL blood is aspirated — stop, the DPL
is + ve and the patient requires a laparotomy.
• Infuse 1L of warmed 0.9 % saline. Keep the catheter and seal in place and
allow 5min for the fl uid to mix. Agitate the abdomen gently.
• Place the empty bag on the fl oor and allow the fl uid to siphon out.
• Send fl uid for laboratory analysis. Since a + ve DPL commits the surgeon
to a laparotomy, an objective measurement is helpful.
• Close the abdomen in layers.
Criteria for + ve DPL
• Aspiration of > 5mL free blood or obvious enteric contents.
• RBC count > 100,000/mm
3.
• WBC count > 500/mm
3.
• Food debris or other enteric contents (eg vegetable fi bres).
Note: air enters the peritoneal cavity during DPL and may be visible on
subsequent CXR or abdominal X-rays.

348 CHAPTER 8 Major trauma
Blunt abdominal trauma
Blunt injury to the abdomen may be isolated or associated with injuries
elsewhere. Evaluation of the abdomen may be particularly diffi cult in the
latter situation. The mechanisms of injury responsible are diverse and
include road traffi c collisions, crushing injuries, high falls, and direct blows
(eg kicks and punches). Remember that lower chest injury may be associated
with splenic or liver injuries.
Examination
• Assess for hypovolaemia. Check pulse, BP, and capillary refi ll.
• Look for bruising (eg ‘lap belt’ imprint). (Measurements of abdominal
girth are unhelpful and unreliable as a means of assessing intra-abdominal
haemorrhage).
• Feel for tenderness and evidence of peritonism. Listening for bowel sounds
is not helpful: their presence or absence is not a discriminating feature.
• Check for femoral pulses.
• Log roll to check for loin tenderness and back injury.
• Examine the perineum and perform a rectal examination , checking
perineal sensation, anal tone, rectal integrity/blood and in the male, the
position of the prostate. A high-riding, ‘boggy’ or impalpable prostate
may indicate urethral injury (see b p.352).
Investigations
The need for and choice of investigation depend upon individual
circumstances, local policy, facilities, and expertise. Patients who are
haemodynamically unstable or who have peritonism require immediate
referral for laparotomy.
Perform urinalysis in all patients. A positive urinalysis is a marker for intra-
abdominal solid organ injury, not just renal tract injury. Insert a urinary
catheter in patients who present with haemodynamic disturbance or who
are critically ill (unless there is evidence of urethral injury, see b p.352).
Perform a pregnancy test in all women of child bearing age.
Serum amylase does not discriminate between those with signifi cant
intra-abdominal injury and those without; it is unhelpful in the early stages
of trauma resuscitation.
Plain abdominal X-ray is rarely useful, unless associated bony injury
or bowel perforation is suspected: free intraperitoneal gas may be
demonstrated on an erect CXR.
FAST (USS) provides a rapid, repeatable, non-invasive bedside test. It
is operator-dependent. Haemoperitoneum is identifi ed by scanning the
hepatorenal and splenorenal recesses, and the pelvis. The pericardium
can also be scanned to look for tamponade. See b p.346.
CT scans are extensively used to evaluate abdominal injuries as well as
identifying injuries in other regions (eg retroperitoneum, brain, chest).
The major advantage of CT is the ability to diagnose the injured organ(s)
within the abdomen and to quantify injuries (minor laceration of liver or
spleen vs. multiple deep lacerations with signifi cant haemoperitoneum).

349
BLUNT ABDOMINAL TRAUMA
Initial stabilization (see b p.320)
• Provide O
2
.
• Treat airway and breathing problems.
• Insert 2 wide bore ( > 16G) IV lines.
• Send blood for U&E, glucose, FBC, clotting screen, and cross-matching.
• Give IV fl uids according to initial evidence of hypovolaemia and
response to treatment. Give blood ± blood products early if unstable.
• Provide IV analgesia as necessary (contrary to popular opinion, this
does not compromise clinical abdominal evaluation).
• Consider the need for orogastric/NG tube and urinary catheter.
• Involve a surgeon at an early stage.
• Inform the senior surgeon, duty anaesthetist and theatre staff if an
urgent laparotomy is needed.
Further evaluation and treatment
Once resuscitation is under way, further evaluation and treatment will
depend largely upon the clinical situation:
Haemodynamically unstable Refer urgently to a senior surgeon for laparotomy.
Inform the operating theatre and the duty anaesthetist immediately. There is
no need (or time) to attempt to defi ne the intra-abdominal injury. Damage
control surgery should be considered in unstable, acidotic or cold patients.
Clinical peritonism Resuscitate as above, provide IV antibiotics (eg cefuroxime
1.5g) and refer urgently to a surgeon for laparotomy.
Haemodynamically stable, no peritonism Refer to a surgeon for further
investigation and observation. FAST (USS) and abdominal CT scans are
very useful in further assessment of these patients. Depending on local
policy, others may be appropriately managed with regular observations
and clinical re-examination.
Possible abdominal injury in the multiply injured These patients provide a
diagnostic challenge: tailor investigations and management to individual
circumstances. FAST (USS) and DPL are rapid, simple, and useful tools
to help to identify signifi cant intra-abdominal haemorrhage in the
multiply injured patient. CT has superior diagnostic accuracy, but it is
time-consuming and requires transfer and IV contrast. If the patient
is haemodynamically stable, abdominal CT is conveniently performed
simultaneously with head CT. A patient who is haemodynamically unstable
should be transferred to theatre, never to the CT scanner.
Abdominal trauma in pregnancy
Involve a senior obstetrician and gynaecologist at an early stage. USS can
demonstrate fetal viability and look for signs of abruption and uterine
rupture. Remember to check Rhesus/antibody status — b p.594.

350 CHAPTER 8 Major trauma
Penetrating abdominal trauma
Most penetrating abdominal injuries are caused by knives or guns. The
size of the external wound bears no relationship to the severity of intra-
abdominal injuries. These injuries have medicolegal implications ( b p.403).
Initial approach
On receiving the patient, provide O
2
, secure venous access and resuscitate
according to an initial assessment of:
• Airway and cervical spine.
• Breathing.
• Circulation.
Obtain complete exposure at an early stage in order to check for
additional wounds to the chest, back, loins, buttocks, and perineum.
Evaluation of abdominal injury
Unless the patient presents with hypovolaemic shock, it may be diffi cult to
decide the extent and severity of the abdominal injury on clinical grounds.
In addition to standard monitoring and palpation of the abdomen, perform
a digital rectal examination and (especially in gunshot injuries) check carefully
for spinal cord/cauda equina injury ( b p.380).
Investigations
Urinalysis Check the urine for blood.
Blood Check BMG, U&E, glucose, FBC, clotting, group and save/cross-match.
X-rays Obtain an erect CXR if possible to check for free gas under the
diaphragm and a supine abdominal X-ray to identify bullet fragments, etc.
FAST (USS) FAST scanning will rapidly identify the presence of free intra-
abdominal fl uid which would mandate a laparotomy ( b p.346).
DPL This is rarely helpful in penetrating injuries.
Management
• Give O
2
; insert two IV cannulas and send blood as outlined above.
• In the unstable patient, give IV fl uid as necessary, but do not give
excessive IV fl uids — aggressive infusion worsens outcome. A systolic BP
≈ 90mmHg in a conscious patient is enough until the start of surgery.
• Provide IV analgesia (eg titrated increments of morphine) as required.
• Give IV antibiotics (eg cefuroxime 1.5g + metronidazole 500mg).
• Consider the need for tetanus prophylaxis ( b p.410).
• Cover the wound with a sterile dressing. Never probe or explore
the wound in the ED to try and defi ne depth and possible peritoneal
penetration. Involve the surgeon early to decide further management.
• Patients who are haemodynamically unstable, have gunshot wounds, or
have obvious protruding bowel contents require urgent resuscitation
and immediate laparotomy. Cover protruding omentum or bowel with
saline soaked sterile swabs and do not push it back into the abdomen.
• Investigation and treatment of other patients varies according to local
policy. Some patients may be managed conservatively with monitoring
and close observation.

351
RENAL TRAUMA
Renal trauma
Most renal injuries result from direct blunt abdominal trauma, the kidney
being crushed against the paravertebral muscles or between the 12th
rib and the spine. Indirect trauma (eg a fall from a height) can tear the
major blood vessels at the renal pedicle or rupture the ureter at the pelvi-
ureteric junction. Penetrating injuries are relatively rare. Many patients
with renal trauma also have other important injuries, which may obscure
the diagnosis of the renal injury.
Children are particularly prone to renal injuries. Trauma may uncover
congenital abnormalities, hydronephrosis, or occasionally incidental tumours.
Clinical features
Most patients give a history of a blow to the loin or fl ank and have loin
pain followed by haematuria (which may be delayed). The loin is tender and
there may be visible bruising or abrasions. Worsening renal pain may indicate
progressive renal ischaemia. Perinephric bleeding can cause loin swelling and
a palpable mass. Haematuria may be absent in severe injuries in which there
are renal vascular tears, thrombosis or complete ureteric avulsion.
Investigations
Look for and record visible haematuria and test for microscopic
haematuria. Get venous access, send blood for FBC, U&E, glucose, clotting
screen, and group and save.
IVU was the standard investigation for suspected renal injuries, but this has
been largely replaced by abdominal CT. If CT is not available, IVU can be
used to elucidate the form and function of an injured kidney and confi rm a
functioning contra-lateral kidney. An unstable patient requiring immediate
laparotomy may need an intra-operative IVU to diagnose a renal injury
and to check that the other kidney is functioning.
CT Urgent abdominal CT is needed if there is frank haematuria or if the
patient was shocked (but is now stable) and has frank or microscopic
haematuria. The surgical team should be involved before CT is arranged.
Patients should be haemodynamically stable for transfer to CT. IVU is
unnecessary if contrast enhanced CT is planned or has been done.
FAST (USS) shows renal morphology and confi rms the presence of two
kidneys, but does not demonstrate function.
Selective angiography is occasionally helpful.
Stable patients with isolated microscopic haematuria do not need urgent
IVU or CT, but require review and appropriate follow-up.
Management
Most blunt renal injuries settle with bed rest and analgesia. Give prophylactic
antibiotics after consulting the surgical team and according to local policy.
Repeat and record pulse, BP, and T ° .
Patients with penetrating renal injuries and severe blunt renal trauma need
urgent expert urological assessment ± emergency surgery: the warm
ischaemic time of a kidney is only ≈ 2hr. Resuscitate with IV fl uids and give
IV analgesia and antibiotics.

352 CHAPTER 8 Major trauma
Bladder, urethral, and testicular
trauma
Bladder injury
Most bladder ruptures are into the peritoneal cavity, caused by direct
blows to the lower abdomen. These injuries often occur in people with
distended bladders. Bone fragments from a fractured pelvis may also
penetrate the bladder ( b p.466).
Clinical features
Lower abdominal pain ± peritonism may be associated with haematuria
or an inability to pass urine. Look for perineal bruising and blood at the
external urethral meatus. Perform a rectal examination to check for the
position of the prostate and the integrity of the rectum.
Investigations and management
X-ray the pelvis to check for fractures. If there is no sign of urethral injury,
pass a catheter to check for haematuria. Refer to the urology team. A
cystogram will show extravasation from a bladder injury. Intra-peritoneal
ruptures need laparotomy and repair. Extraperitoneal ruptures may heal
with catheter drainage and antibiotics.
Urethral injuries
Posterior urethral tears are often associated with pelvic fractures.
Urethral injury may also result from blows to the perineum (especially
falling astride).
Look for perineal bruising and blood at the external urethral meatus
and perform a rectal examination (an abnormally high-riding prostate or
inability to palpate the prostate imply urethral injury).
If urethral injury is suspected, do not attempt urethral catheterization, but
refer urgently to the urology team. Some urologists perform a retrograde
urethrogram to assess urethral injury, but many prefer suprapubic
catheterization and subsequent imaging.
Penile injuries
See b p.523.
Testicular trauma
Injury to the scrotum/testis may result in a scrotal haematoma or testicular
rupture. Both conditions require good analgesia. Further treatment depends
upon the exact diagnosis. USS may help to distinguish between scrotal
haematoma and testicular rupture. Scrotal haematoma may respond
to conservative measures. Testicular rupture requires urgent surgical
exploration and repair.
Scrotal injuries
Wounds involving the scrotal skin may need to be sutured (preferably
with absorbable sutures) — most heal rapidly. Refer for investigation if
there is complete scrotal penetration with the attendant risk of damage
to the testis, epididymis or vas deferens. If the testis is visible through the
wound, refer for surgical exploration and repair in theatre.
This page intentionally left blank

354 CHAPTER 8 Major trauma
Head injury: introduction
The size of the problem
Many patients with serious or fatal trauma have suffered a head injury.
Additionally, minor head injuries are a frequent reason for attendance at
an ED. Blunt injury is far more common than penetrating injury.
Common causes of head injury
• Road traffi c collisions of all types.
• Falls.
• Assaults.
• Sporting and leisure injuries.
• Workplace injuries.
• Other mishaps.
Pathophysiology
Brain injury may be primary or secondary.
Primary injury occurs at the time of the head injury. This takes the form
of axonal shearing and disruption, with associated areas of haemorrhage.
This primary damage may be widespread (‘diffuse axonal injury’) or
localized (eg ‘contre-coup’ frontal contusions in a fall hitting the occiput).
Secondary injury occurs later, due to various problems that commonly
co-exist. Many of these are preventable or treatable, and should thus be
the focus during resuscitation:
• Hypoxia.
• Hypovolaemia and cerebral hypoperfusion.
• Intracranial haematoma with localized pressure effects and i ICP.
• Other causes of i ICP, including cerebral oedema and hypercapnia.
• Epileptic fi ts.
• Infection.
The role of intracranial pressure
Once the skull sutures have fused, the cranium is a closed box. Thus, a
small i in volume (eg from swelling or haematoma) results in a large i in
ICP (see Fig. 8.6 ). As ICP i , cerebral perfusion pressure d , since:
Cerebral perfusion pressure = Mean arterial pressure – ICP
Once cerebral perfusion pressure falls <70mmHg, signifi cant secondary
brain injury may occur. Control of ICP and BP (including avoiding wild
swings in BP) is an important treatment goal, especially as the normal
cerebrovascular auto-regulatory mechanisms are impaired after head
injury. Cerebral arterioles remain sensitive to p CO
2
, however, with an
i p CO
2
resulting in marked arterial vasodilatation and unwanted i ICP.
Controlling p CO
2
to within normal levels is therefore important.
i ICP produces a diminishing conscious level and causes herniation
of the temporal lobe through the tentorial hiatus, compressing the
oculomotor nerve, resulting in ipsilateral pupillary dilatation. This may
progress to contralateral hemiparesis and brainstem compression with
cardiorespiratory arrest. i ICP leads to a refl ex i in systemic arterial BP
together with bradycardia: this combination is the Cushing response .
355
HEAD INJURY: INTRODUCTION
Indications for referral to hospital
Any one of the following criteria indicates the need for hospital assessment:
• Impaired conscious level at any time.
• Amnesia for the incident or subsequent events.
• Neurological symptoms (vomiting, severe and persistent headache,
seizures).
• Clinical evidence of a skull fracture (cerebrospinal fl uid leak, peri-orbital
haematoma).
• Signifi cant extracranial injuries.
• Worrying mechanism (high energy, possible non-accidental injury,
possible penetrating injury).
• Continuing uncertainty about the diagnosis after fi rst assessment.
• Medical co-morbidity (anticoagulant use, alcohol abuse).
• Adverse social factors (eg alone at home).
The following are highly recommended:
• The SIGN (Scottish Intercollegiate Guidelines Network) guideline on
head injury is accessible at www.sign.ac.uk
• The NICE (National Institute for Health and Clinical Excellence) clinical
guidelines on head injury published in 2007 and accessible at www.nice.
org.uk
Intracranial pressure
Intracranial blood volume
Fig. 8.6 ICP according to intracranial blood volume.

356 CHAPTER 8 Major trauma
Head injury: triage and monitoring
Triage
Every ED requires a system for the rapid initial assessment of head-injured
patients. The exact system will depend upon local policy, expertise
and facilities. It must enable patients with signifi cant injuries to receive
immediate resuscitation and ensure urgent treatment of those patients
liable to complications. Experienced nursing staff can quickly identify those
patients in need of urgent attention, based upon:
• The mechanism of injury.
• History from the ambulance crew.
• An assessment of vital signs.
• Conscious level according to the Glasgow Coma Scale ( b p.361).
• Limb power.
• Pupil responses.
• BMG.
For patients who are haemodynamically stable, alert and orientated , with no
neurological defi cit and an apparently minor head injury, it is appropriate
to proceed to obtaining a full history, as outlined on b p.358.
For patients with multiple injuries and/or a serious head injury , there will be
no time initially to obtain a full history. Instead, proceed rapidly to initial
assessment and resuscitation. During the fi rst few seconds, it is useful to
obtain an impression of the severity of the head injury. One simple method
(AVPU) classifi es patients according to their response to stimulation:
• A lert.
• Responsive to V oice.
• Responsive only to P ain.
• U nresponsive.
If a patient is unresponsive or responds only to pain, call for senior
ED help and an ICU specialist or anaesthetist, since expert airway care
(RSI, tracheal intubation and IPPV) will be needed.
Monitoring
Every head-injured patient requires regular neurological observations.
These should include measurements of GCS, pupil response, limb power,
pulse, BP and respiratory rate on a standard chart, such as the one shown
in Fig. 8.7 . This monitoring is critical if complications such as intracranial
haematomas, fi ts and hypovolaemia from other injuries are to be detected
and treated at an early stage. Any deterioration in GCS is an emergency:
re-examine the patient and correct identifi able problems promptly whilst
obtaining urgent senior help.
357
HEAD INJURY: TRIAGE AND MONITORING
NAME
TIME
UNIT No
D. of B.
WARD
NEUROLOGICAL OBSERVATION CHART
DATE
C
O
M
A
S
C
A
L
E
Eyes
Open
Spontaneously
Eyes closed
by swelling
=C
Endotracheal
tube or
Tracheostomy
=T
Usually
records the
best arm
response
40
39
38
37
36
35
34
33
32
31
30
+ reacts
– no reaction
c. eye closed
Record
right (R)
and left (L)
separately if
there is a
difference
between the
two sides.
Temperature °C
Oriented
Confused
Sounds
None
None
Obey commends
Localise pain
Normal Flexion
Abnormal Flexion
Extension to pain
Inappropriate Words
Incomprehensible
To speech
To pain
None
4
3
2
1
3
2
1
1
2
3
4
5
6
7
8
Pupil
scale
(m.m.)
240
230
220
210
200
190
90
80
70
60
50
40
30
Respiration
PUPILS
L
I
M
M
O
V
E
M
E
N
T
B
A
R
M
S
L
E
G
S
right
left
Normal power
Normal power
Mild weakness
Mild weakness
Severe weakness
Severe weakness
Spastic flexion
Extension
Extension
No response
No response
Size
Reaction
Size
Reaction
Blood
pressure
and Pulse
rate
26
22
18
14
10
6
180
170
160
150
140
130
120
110
100
4
5
3
2
1
4
5
6
Best
verbal
response
Best
motor
response
Fig. 8.7 An example of a neurological observation chart.

358 CHAPTER 8 Major trauma
Head injury: history
It may be impossible to obtain a complete history from the patient,
particularly if there was loss of consciousness and/or amnesia. Use all
available sources of information, including friends and family, other
witnesses, and the ambulance crew. Cover the following areas:
Mechanism of injury
Eliciting the exact mechanism of injury will provide an impression of the
nature of the forces involved and the risk of subsequent complications.
Consider the possibility that the head injury may have been preceded and
caused by another medical problem (eg arrhythmia, epilepsy, diabetes).
Time of injury
This information is useful, but may not be known.
Loss of consciousness/amnesia
A period of unconsciousness implies a head injury of at least moderate
severity. It can be diffi cult to establish exactly how long unconsciousness
lasted, particularly if there is associated amnesia. Document the length of
amnesia (both before and after injury), but remember that the full extent
of the amnesia may not become apparent until much later.
Subsequent symptoms
Some symptoms are relatively common after head injury (eg headache
and vomiting) — many patients will complain of these without being
directly asked. There are a number of other symptoms, however, which
the patient may not mention unless specifi cally asked. Enquire about the
following symptoms:
• Headache.
• Nausea and vomiting.
• Limb weakness.
• Paraesthesiae.
• Diplopia.
• Rhinorrhoea.
• Otorrhoea.
Past medical history
Document pre-existing illnesses and symptoms, particularly those that may
have caused the head injury (eg cardiac arrhythmias, epilepsy, diabetes),
or might make the consequences more severe (eg bleeding tendency).
Enquire about previous head injury (an old skull fracture visible on new
X-rays may otherwise be confusing).
Drug history
Ask particularly about recent alcohol and other drug ingestion and
whether or not the patient is taking anticoagulant drugs (eg warfarin).
This is very important, since patients with bleeding disorders and/or on
anticoagulants have a much higher risk of intracranial problems after head
injury, often require CT and must be admitted to hospital ( b p.366).

359
HEAD INJURY: HISTORY
Social history
Before contemplating discharge of any head-injured patient, fi nd out if
there is a responsible adult at home, or if there is someone else with
whom the patient could go and stay.
Tetanus status
If there are any wounds, consider the need for tetanus prophylaxis.

360 CHAPTER 8 Major trauma
Head injury: examination
Resuscitation proceeds with examination, according to problems identi-
fi ed in the primary survey. Follow initial brief neurological examination
(GCS, pupil reactions, limb weakness) by defi nitive complete examination:
Cervical spine injury
Consider this possibility in all cases (see b p.320).
Glasgow Coma Scale
Determining the conscious level is a crucial part of the neurological examin-
ation. The adult score ranges from a minimum of 3 to a maximum of 15 and
is calculated as shown in Table 8.2 . Repeated GCS recordings are a crucial
part of monitoring the head injured patient. A fall in GCS indicates a poten-
tially serious deterioration and mandates a search for correctable conditions.
Vital signs
Record pulse, BP, and respiratory rate.
BMG
This is essential in all patients with altered conscious level.
Alcohol
Record if the patient smells of alcoholic drinks but never assume d GCS is
due to alcohol.
Eye signs
Document pupil size (in mm) and reaction to light. Unilateral pupillary
dilatation may refl ect orbital injury or oculomotor nerve compression
due to i ICP ( b p.354). Check for a full range of eye movements and
the presence of diplopia or nystagmus. Look in the fundi, although
papilloedema is a late sign of i ICP. If there is any suspicion of eye injury,
measure VA ( b p.534). In infants, check for retinal haemorrhages
( b p.731).
Scalp, face, and head
Examine the cranial nerves and search for abnormal cerebellar signs
(nystagmus, hypotonia, intention tremor, dysdiadochokinesia). Carefully
record scalp, ear or facial injury. Examination of facial injuries is on
b p.370.
The limbs
Check limb tone, power, sensation and refl exes. Abnormalities (eg
hemiparesis) may result from the primary brain insult or be a consequence
of a developing intracranial haematoma requiring urgent intervention.
A stroke can cause a fall resulting in a head injury.
Other injuries
The presence of a head injury can render identifi cation of non-cranial
injuries diffi cult. Intra-abdominal injuries often co-exist with serious head
injuries and are diffi cult to detect; have a low threshold for FAST ± CT.
In particular, relatively minor non-life-threatening orthopaedic injuries
(eg fi nger dislocations, wrist fractures) are easily missed. Ensure full
examination, including palpation of all limbs for possible injury.
361
HEAD INJURY: EXAMINATION
Signs of base of skull fracture
This is often a clinical diagnosis. One or more of the following may be seen:
• Bilateral orbital bruising confi ned to the orbital margin (‘panda eyes’).
• Subconjunctival haemorrhage (no posterior margin of bleeding seen).
• Haemotympanum or bleeding from the auditory meatus.
• CSF otorrhoea or rhinorrhoea ( ± anosmia). Fluid mixtures containing
relatively similar quantities of blood and CSF will separate into a ‘double
ring’ when dropped onto blotting paper.
• Battle’s sign: bruising over the mastoid process without local direct trauma
follows petrous temporal bone fracture, but takes several days to appear.
Glasgow Coma Scale (adults)
The GCS assesses the level of consciousness by scoring three aspects of
the patient’s response and adding up the scores to reach a fi nal score.
Notes
• Record GCS in shorthand showing its component parts (for example,
GCS 10/15 (E3, V2, M5) means that the patient opens eyes to verbal
commands, speaks incomprehensible sounds, localizes a painful stimulus).
Similarly, when communicating with other health professionals describe
the total score (GCS) and list its components.
• Unconsciousness is generally taken to mean no eye response and GCS ≤8.
• ‘Abnormal fl exion’ implies decorticate rigidity; and ‘abnormal extension’
implies decerebrate rigidity.
• The GCS is diffi cult to apply to small children, but may be modifi ed as
outlined on b p.717.
Table 8.2 Glasgow Coma Scale
Eye response open spontaneously 4
open to verbal command 3
open to pain 2
no response 1
Verbal response talking and orientated 5
confused/disorientated 4
inappropriate words 3
incomprehensible sounds 2
no response 1
Motor response obeys commands 6
localizes pain 5
fl exion/withdrawal 4
abnormal fl exion 3
extension 2
no response 1
Total (GCS) Range 3–15

362 CHAPTER 8 Major trauma
Head injury: imaging
Traditional use of X-rays has largely been replaced by CT scanning; EDs
in some countries have abandoned skull X-rays altogether, so be aware of
local policies and protocols. In the UK, Scottish Intercollegiate Guidelines
Network (SIGN) guidelines on the early management of patients with a
head injury ( www.sign.ac.uk ) were updated in 2009. In England and Wales,
National Institute for Health and Clinical Excellence (NICE) guidance,
published in 2007, is available at www.nice.org.uk
The role of CT scanning
CT scanning is used to identify and defi ne the brain injury, especially
intracranial haematomas amenable to surgical treatment. Ensure adequate
resuscitation before transferring for CT scan. In many cases, this will
include RSI, tracheal intubation, and IPPV. Always arrange for appropri-
ately trained staff to accompany the patient to the CT scanner. When
clinical features point strongly to an intracranial haematoma (eg the
emergence of focal signs or a deteriorating GCS), discuss promptly with a
neurosurgeon the benefi ts of transferring the patient to a centre that has
both CT scanning facilities and an emergency neurosurgical service.
Indications for CT scan
Request CT scan for any of the following (see www.nice.org.uk ):
• GCS <
13
/
15
at any point since injury.
• GCS
13–14
/
15
at 2hr post-injury.
• Suspected open or depressed skull fracture.
• Any sign of basal skull fracture.
• Post-traumatic seizure.
• Focal neurological defi cit.
• > 1 episode of vomiting (except in children <12 years, where clinical
judgement is required).
• Amnesia for > 30min of events before impact
*
.
• Loss of consciousness and/or amnesia combined with one of: age > 65
years, coagulopathy (including clotting disorder, anticoagulant drug
treatment) or dangerous mechanism
*
(eg pedestrian hit by car, fall > 1m
or 5 steps).
Most requests will be urgent (scan performed and interpreted within an
hour), except for the two indications marked with an asterisk
*
, which if
isolated, may allow CT scan to be obtained less urgently (within 8hr),
depending upon locally agreed policy.
Interpretation of CT scan
CT scans must be assessed by someone with appropriate expertise.
• Skull fractures are obvious, as is the degree of depression of fragments.
• Intracranial haematomas may cause midline shift and take several forms:
extradural haematomas ( b p.365) appears as a high density (white)
lens-shaped lesions. Subdurals conform more to the surface of the brain
( b p.365). Extradural and subdural haematomas can co-exist.
• Cerebral contusions appear as patches of low or mixed attenuation.
• Cerebral swelling may take some time to develop, causing the ventricles
to appear smaller than normal.
363
HEAD INJURY: IMAGING
Skull X-rays: rationale
Skull X-rays are quick, cheap, and easy to obtain but they should only be
used when CT scanning is not available in adult patients with minor head
injury who do not need an immediate CT scan. Standard views are: antero-
posterior (AP), lateral and Towne’s. They are useful to detect skull vault
fractures, but do not defi ne any intracranial lesion. Identifi cation of skull
fractures has been traditionally held to be important because of the i risk
of intracranial haematoma, particularly if the conscious level is impaired
(see Table 8.3 ). If CT is planned, do not waste time doing skull X-rays.
Indications for skull X-rays
Skull X-rays should no longer be used when CT scanning is immediately
available. If CT is not available, it can be used to identify adult patients
with skull vault fractures, who will then require transfer for CT scanning.
They have virtually no role now in the assessment of head injuries.
Interpretation of skull X-rays
It can be diffi cult to distinguish fractures from vascular markings and
suture lines. If in doubt, examine the relevant part of the head for sign of
injury and seek a senior opinion. Linear fractures appear as sharp-edged
lucent lines, which have a different appearance from vascular markings.
Depressed fractures take various forms, but tangential views may demon-
strate the depressed bone. Base of skull fractures are often not visible, but
there may be indirect evidence in the form of an intracranial aerocoele or
fl uid (air/blood) level in a sinus. Check each of the main sinuses (frontal,
sphenoidal, maxillary) in turn, remembering that the lateral skull X-ray is
usually obtained with the patient lying supine (‘horizontal beam’, ie occiput
downwards). This will affect the orientation of the fl uid level.
Table 8.3 Risks of operable intracranial haematoma after head injury
GCS
15
/
15
Overall 1 in 6000
GCS
15
/
15
With no other features 1 in 31,300
GCS
15
/
15
With post traumatic amnesia 1 in 6,700
GCS
15
/
15
With skull fracture 1 in 81
GCS
15
/
15
With skull fracture and amnesia 1 in 29
GCS
9–14
/
15
Overall 1 in 51
GCS
9–14
/
15
With no skull fracture 1 in 180
GCS
9–14
/
15
With skull fracture 1 in 5
GCS
3–8
/
15
Overall 1 in 7
GCS
3–8
/
15
With no skull fracture 1 in 27
GCS
3–8
/
15
With skull fracture 1 in 4
Adapted from Teasdale et al .

364 CHAPTER 8 Major trauma
Management of serious head injury
Tailor management according to the needs of each individual patient.
Initial management
• Clear, establish and maintain the airway, provide O
2
and protect the
cervical spine ( b p.320).
• Check breathing — provide support with bag/valve/mask device as
necessary. Examine for and treat any serious chest injury.
• Check BMG and treat hypoglycaemia if present ( b p.322).
• Insert two large IV cannulae and send blood for X-matching, FBC,
clotting screen, U&E, and glucose.
• Correct hypovolaemia, resuscitate, and treat other injuries.
• If GCS ≤
8
/
15
, the patient will require urgent airway protection with RSI,
tracheal intubation and IPPV (see b p.312). Call for senior ED help and
request help from ICU and/or anaesthesia. Check ABG and ventilate to
p CO
2
of ≈ 4.5kPa.
• Liaise early with an anaesthetist, ICU and a neurosurgeon (see below).
• Contact a radiologist early to arrange a CT scan with minimum delay.
• In the multiply or seriously injured patient who will require a CT
scan, concerns of opioid drugs masking pupillary signs are less important
than ensuring adequate analgesia. Give titrated IV opioid analgesia
( b p.320), after recording GCS, pupil reactions, and basic neurological
examination.
• Give IV antibiotics for patients with compound skull fractures.
Cefuroxime 1.5g IV is a suitable choice, but be guided by local policy.
Regional neurosurgical centres vary as to whether or not they advise
prophylactic antibiotics for clinical base of skull fracture (there is no
compelling evidence that they prevent meningitis): follow local policy.
• Clean and close scalp wounds to control scalp bleeding (use simple
interrupted silk sutures for rapid closure), but do not allow this to
unduly delay CT scan or neurosurgical transfer.
• Insert a urinary catheter.
• Consider the need for an orogastric tube. Avoid using NG tubes in
facial injury or any possibility of base of skull fracture.
• Consider the need for tetanus immunization.
Indications for neurosurgical referral
• CT shows a recent intracranial lesion.
• Patient fulfi ls the criteria for CT scan, but this cannot be done within an
appropriate period of time.
• Persisting coma (GCS <
9
/
15
) after initial resuscitation.
• Confusion which persists > 4hrs.
• Deterioration in conscious level after admission (a sustained drop of
one point on the motor or verbal subscales, or two points on the eye
opening subscale of the GCS).
• Progressive focal neurological signs.
• Seizure without full recovery.
• Depressed skull fracture.
• Defi nite or suspected penetrating injury.
• CSF leak or other sign of a basal fracture.

365
MANAGEMENT OF SERIOUS HEAD INJURY
Treating complications
Early recognition and treatment of complications is essential to prevent
secondary brain damage. It is crucially important to prevent hypoxia and
hypovolaemia adding to the primary cerebral insult.
Seizures
Check BMG, glucose, and ABG. Treat with IV lorazepam 4mg. Repeat
this once if not initially effective. Start an IV phenytoin infusion (loading
dose 10–15mg/kg IV over 30min with ECG monitoring) to prevent further
fi ts. Fits which continue for ≥ 10 − 15min or recur despite this treatment
require senior ED and ICU help, RSI, tracheal intubation, and IPPV.
Deteriorating conscious level
Having corrected hypoxia, hypercapnia and hypovolaemia, a diminishing
conscious level is likely to refl ect intracranial pathology, leading to i ICP,
requiring urgent investigation and treatment. Bradycardia, hypertension,
and a dilating pupil are very late signs of i ICP. Speed is of the essence.
Liaise with a neurosurgeon who will advise on use of agents to d ICP
(eg a bolus of 0.5g/kg IV mannitol — typically 200mL of 20 % for an adult).
Mannitol is an osmotic diuretic which may temporarily d ICP and ‘buy time’
to get the patient to theatre for drainage of an intracranial haematoma.
Other examples of deterioration requiring urgent reassessment
• The development of agitation or abnormal behaviour.
• The development of severe or increasing headache or persistent vomiting.
• New or evolving neurological symptoms/signs (eg limb weakness).
Intracranial haematoma
Causes of neurological deterioration after head injury include hypoxia,
hypovolaemia, seizures, cerebral swelling, and intracranial haematomas.
Intracranial haematomas are important, as prompt surgery may save lives.
Patients with bleeding disorders or on anticoagulants have a greatly i risk
of developing an intracranial haematoma after head injury.
Extradural haematoma
Classically, extradural haematoma follows bleeding from the middle
meningeal artery’s anterior branch after temporal bone fracture. Texts
describe head injury with initial loss of consciousness, then return to full
consciousness, before neurological deterioration as intracranial bleeding
continues and ICP i . However, many patients deviate from classical ‘talk
and die’ descriptions: extradural haemorrhage may occur in non-temporal
areas, with no skull fracture and no initial loss of consciousness.
Subdural haematoma
Bridging vein bleeding between brain and dura causes subdural
haematoma. Unlike extradural haematoma (which is separated from brain
surface by the dura), subdural haematoma conforms to the brain surface.
This helps distinguish extradural from subdural haematoma on CT.
Subdural haematoma may be acute or chronic. Acute subdural haematoma
is associated with a severe brain insult. Chronic subdural haematoma often
occurs in elderly and alcoholics ( i risk perhaps due to cerebral atrophy).
Chronic subdural haematoma develops over several days, often presenting
with fl uctuating conscious level, sometimes with an obscure (or even no)
history of head injury.

366 CHAPTER 8 Major trauma
Minor head injury
Introduction
Assessment and management of patients who have sustained relatively
minor primary brain insults can be diffi cult. This is especially true when
assessment is rendered awkward by virtue of age, epilepsy, drug, or
alcohol ingestion. In these circumstances, adopt a cautious approach and
admit the patient for observation until the picture becomes clearer.
Golden rules for managing head injury are :
• Never attribute a d GCS to alcohol alone.
• Never discharge a head-injured patient to go home alone.
• Admit patients with head injury and coexisting bleeding tendency
(including those taking anticoagulant drugs).
Differential diagnosis
Consider whether another condition could be principally responsible for
the patient’s symptoms. For example, small children who vomit after head
injury may be suffering from otitis media or a throat infection. Otitis media
may be responsible for both the vomiting (with fever) and for the head
injury (by causing unsteadiness of gait, resulting in a fall).
Indications for admission
• d GCS (ie <
15
/
15
), neurological defi cit or post-traumatic seizure.
• Signifi cant neurological symptoms (severe headache, vomiting, irrita-
bility or abnormal behaviour, continuing amnesia > 5min after injury).
• Signifi cant medical problems, particularly bleeding tendency (including
inherited diseases and anticoagulant drugs).
• Inability to assess due to epilepsy, consumption of alcohol or drugs.
• Clinical or radiological evidence of skull fracture.
• No one available at home or no safe home to go to (including suspected
NAI and domestic violence).
Observation of those admitted
All patients require regular neurological observations (see b p.356). Act
promptly if conscious level d or neurological defi cit develops. Remember
that one of the principal reasons for admitting patients with apparently
minor head injuries is to monitor for the development of intracranial
problems. In these cases, resuscitate, liaise with a neurosurgeon and
obtain an urgent CT scan.
If after 12–24hr of observation, the patient is symptom-free, haemo-
dynamically stable and is GCS
15
/
15
with no neurological defi cit, it is
reasonable to consider discharge. Patients who do not fall into this category
(ie symptomatic, d GCS or neurological defi cit) require a CT scan.

367
MINOR HEAD INJURY
Discharging patients
Most of the patients who present with minor head injury can be safely
discharged directly from the ED. Ensure that there is a responsible adult
available to accompany them home and someone to stay with them for
24hr once they get home. Warn the patient and the accompanying adult
of the potential problems following a head injury (Box 8.1 ) — and what
to do if any of these problems are experienced. Give advice regarding
analgesia. Most EDs have standard written instructions which are given
to the patient and accompanying adult. Examples of head injury warning
instructions are shown below.
Box 8.1 An example of head injury warning instructions
Adults
• Ensure a responsible person is available to keep an eye on you for the
next 24hr and show them this card.
• Rest for the next 24hr.
• Do take painkillers such as paracetamol to relieve pain and headache.
• DO N OT drink alcohol for the next 24hr.
• DO take your normal medication, but DO NOT take sleeping tablets
or tranquilizers without consulting your doctor fi rst.
• If any of the following symptoms occur then you should return or be
brought back to the hospital or telephone the hospital immediately.
Tel (01
* * * ) * * * * * *
(24hr):
• headache not relieved by painkillers such as paracetamol;
• vomiting;
• disturbance of vision;
• problems with balance;
• fi ts;
• patient becomes unrousable.
Children
• Your child has sustained a head injury and following a thorough
examination we are satisfi ed that the injury is not serious.
• Your child may be more tired than normal.
• Allow him/her to sleep if he/she wants to.
• Give Calpol
®
or Disprol
®
(paediatric paracetamol) for any pain or
headache.
• Try to keep your child resting for 24hr.
• If your child should develop any of the following:
• headache not relieved by paediatric paracetamol;
• vomiting;
• altered vision;
• irritability;
• fi ts;
• becomes unrousable.
• Bring him/her back to the hospital or telephone for advice
immediately: Tel (01
* * * ) * * * * * *
(24hr).
Alternative suggested written advice is available from the National Institute for Clinical
Excellence ( www.nice.org.uk ).

368 CHAPTER 8 Major trauma
Post-concussion symptoms
Presentation
Post-concussion symptoms are common after head injury and cause much
anxiety in patients and their relatives. The most frequent complaints are:
• Headache.
• Dizziness.
• Lethargy.
• Depression.
• Inability to concentrate.
Headaches occur in most patients admitted to hospital after head injuries:
in ≈ 30 % the headaches persist for > 2 months. The headaches are usually
intermittent and become worse during the day or on exertion. Some
appear to be ‘tension headaches’ and are often not signifi cantly helped by
analgesics. Migraine attacks may become more frequent or severe after a
head injury. Headaches that do not fi t these patterns may refl ect serious
intracranial pathology.
Non-specifi c dizziness is common after concussion. Detailed questioning
may distinguish dizziness from vertigo due to disturbance of the vestibular
mechanisms. Dizziness may be caused by postural hypotension or by
drugs (eg co-codamol and other analgesics) or alcohol (to which patients
are often more sensitive after a head injury).
Diagnosis
Post-concussion symptoms are diagnosed by exclusion of other problems
or complications following head injury. Take a careful history, including
questions about drowsiness, intellectual function, neck pain, photophobia,
vomiting, and rhinorrhoea.
Examine the patient for any specifi c cause of the symptoms and for any
neurological defi cit. Look particularly for evidence of meningitis or an
intracranial haematoma. Check for papilloedema.
Elderly or alcoholic patients or those with a bleeding tendency are prone
to develop chronic subdural haematomas, which may cause confusion or
intellectual deterioration, often without localizing signs. Obtain a CT.
Treatment
After a careful history and examination, with appropriate investigations
to exclude other problems, reassure the patient and explain that the
symptoms are likely to resolve gradually. Reduced short-term memory
and impaired concentration may make it diffi cult for a patient to return
to work and cause additional stress and anxiety: give suitable explanations
and discuss the provision of a sick note with the GP.
Follow-up
Since symptoms may last for some time, arrange appropriate follow-up.
This usually involves the GP, who needs to be kept fully informed of the
clinical fi ndings and diagnosis.
This page intentionally left blank

370 CHAPTER 8 Major trauma
Maxillofacial injuries: introduction
These injuries often look dramatic and can be life-threatening as well as
causing signifi cant long-term morbidity.
Common causes are road traffi c collisions, assaults, and sport.
Emergency resuscitative measures
• Perform a rapid initial assessment to look for and treat airway obstruc-
tion or major bleeding ( b p.320). Remember the possibility of an
associated neck injury. Blood may rapidly accumulate in the pharynx
requiring anterior ± posterior nasal packing for control ( b p.552).
• Management of airway obstruction is complex, intubation often diffi cult
and occasionally a surgical airway is required: obtain experienced ED
and anaesthetic assistance early. Use jaw thrust, chin lift, and suction to
establish a patent airway.
• With bilateral mandibular fractures, the tongue may fall backwards.
Restore airway patency by pulling the fractured segment anteriorly or
by inserting a large (0 silk) suture in the tongue and pulling anteriorly.
• Maxillary fractures may be displaced far enough backwards to compromise
the airway by contact of the soft palate against the posterior pharyngeal
wall. This can be relieved by hooking two fi ngers behind the hard palate,
and pulling forwards and upwards, but this can produce considerable
bleeding.
History
Important clues may be obtained from knowing the causative events both
in relation to the facial injury itself and also of injury to the head, spine etc.
Drug history (eg anticoagulants or bleeding tendency) may be important.
Examination
Inspect the face from the front, side and above (by standing above and
behind the patient). Look for:
• Asymmetry.
• Flattening of the cheek (depressed zygomatic fracture).
• ‘Dish face’ deformity (fl attened elongated face due to posterior and
downward displacement of the maxilla).
• Nasal deviation or saddle deformity. Measure the intercanthal distance:
if > 3.5cm suspect naso-ethmoidal fracture — see below.
• Uneven pupillary levels (due to orbital fl oor fracture).
• CSF rhinorrhoea (causes ‘tramline’ effect with central CSF and blood
either side).
• Subconjunctival haemorrhage without a posterior border (suggests an
orbital wall or anterior cranial fossa fracture).
Palpate the facial bones systematically. Start over the superior orbital
margins. Work down feeling both sides at the same time checking for
pain, deformity, crepitus and movement. Feel specifi cally for steps in the
inferior orbital margin and zygoma. Subcutaneous emphysema implies a
compound fracture — often of the maxillary sinus.

371
MAXILLOFACIAL INJURIES: INTRODUCTION
Check for hypo/anaesthesia of the cheek, side of the nose and upper lip
(infra-orbital nerve injury), and for numbness of the upper teeth (anterior
superior alveolar nerve in the infra-orbital canal), and lower teeth and lip
(inferior dental nerve damage due to mandibular fracture).
Examine inside the mouth, checking for dental malocclusion (ie the teeth
do not meet together properly when the mouth is closed), loose, or lost
teeth (this may need CXR), bruising and bleeding.
Examine the eyes carefully ( b p.536): assume any laceration below the
medial canthus involves the lacrimal duct until proven otherwise.
Investigations
In patients with multiple injuries, imaging of the chest, pelvis and cervical
spine will take precedence. Even with ‘isolated’ facial injuries, perform
imaging of the cervical spine and head, where indicated, before facial
X-rays or CT scanning.
Facial X-rays are often both diffi cult to perform (because of poor patient
cooperation) and diffi cult to interpret. Get maxillofacial specialist advice
regarding the views required and their interpretation. CT scanning is often
required prior to defi nitive maxillofacial surgery.
The commonly required views include:
• Occipitomental 10 ° , 30 ° , and 45 ° .
• Lateral.
• Orthopantomogram (for mandible).
Treatment
Treatment of specifi c facial fractures is considered in b p.372, b
p.374, b p.376. Remember that even in the absence of a visible fracture
on X-ray, patients in whom there is clinical suspicion of facial fracture
(swelling, tenderness, asymmetry, numbness, etc.) require expert attention
and/or follow-up.

372 CHAPTER 8 Major trauma
Middle third facial fractures
Dento-alveolar fractures
These injuries involve only the teeth and their bony support. Look for
deranged occlusion and stepped malalignment of teeth, bruising of gums,
and palpable fracture in the buccal sulcus.
Le Fort facial fractures (Fig. 8.8 )
These lie between the frontal bone, the skull base and mandible. They
involve the upper jaw, teeth, nose, maxillary, and ethmoid air sinuses
• Le Fort I involves the tooth-bearing portion of the maxilla. Look for
lengthening of the face due to the dropped maxillary segment. There
may be movement or a split of the hard palate, a haematoma of the soft
palate/buccal sulcus, and malocclusion.
• Le Fort II involves the maxilla, nasal bones and the medial aspects of
the orbits. Look for a ‘dished-in’ face, a step in the infra-orbital margin,
infra-orbital nerve damage, malocclusion and surgical emphysema.
The maxilla may be fl oating — if the upper teeth are pulled (gently!)
the maxilla may move forward. Check for epistaxis, CSF rhinorrhoea,
diplopia, and subconjunctival haematoma. Facial swelling occurs rapidly
and is often severe. Later, bilateral peri-orbital bruising may be evident.
• Le Fort III involves the maxilla, zygoma, nasal bones, ethmoid and the
small bones of the base of the skull. The entire midface is fractured from
the base of the skull. Features include those of type II plus: fl attened
zygomatic bones (which may be mobile and tender), steps over the
fronto-zygomatic sutures, movement and deformity of the zygomatic
arch, and different pupillary levels. There is usually severe facial swelling
and bruising. Pharyngeal bleeding may severely compromise the airway
and cause hypovolaemic shock.
Le Fort fractures may be asymmetrical (eg Le Fort II on the right and III on
the left).
Naso-ethmoidal fractures
These produce a fl attened nasal bridge with splaying of the nasal complex,
saddle-shaped deformity of the nose, traumatic telecanthus, periorbital
bruising, subconjunctival haematoma, epistaxis, CSF rhinorrhea, and
supraorbital or supratrochlear nerve paraesthesia.
Management of middle third facial fractures
• Resuscitate and establish a clear airway as described on b p.324.
• Refer dentoalveolar fractures for repositioning and immobilization with
acrylic/metal splints ± wiring.
• Refer all patients with middle third or naso-ethmoidal fractures to the
maxillofacial surgeons for admission. Any continuing haemorrhage
requires packing — leave this to the specialist. Tell the patient not to blow
the nose ( i subcutaneous emphysema and may drive bacteria into fracture
sites and intracranially). Prophylactic antibiotics are often advised by
maxillofacial surgeons. Ensure tetanus prophylaxis ( b p.410).
• Discuss patients with CSF leaks with the neurosurgeons.
• Clean and dress compound facial lacerations, but do not close them
(unless actively bleeding); they may need formal debridement and they
provide access to fractures for open reduction and internal fi xation.
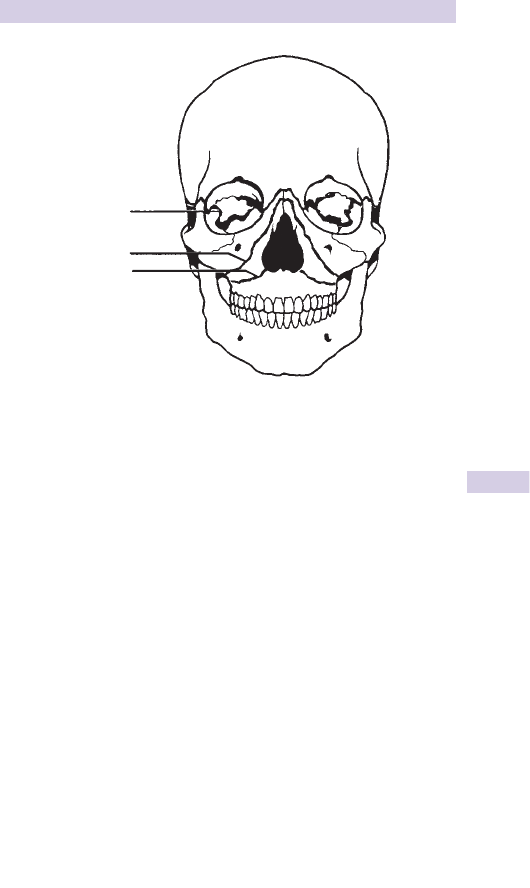
373
MIDDLE THIRD FACIAL FRACTURES
Le Fort III
Le Fort II
Le Fort I
Fig. 8.8 Le Fort classifi cation of facial fractures.

374 CHAPTER 8 Major trauma
Zygomatic, orbital and frontal
sinus fractures
Zygomatic (malar) fractures
These injuries are usually due to a direct blow and are frequently
associated with severe eye injuries. ‘Tripod fractures’ involve fractures
through the zygomatico-temporal and zygomatico-frontal sutures, and the
infra-orbital foramen.
Examination Look for fl attening of the cheek (often obscured later by
swelling), a palpable defect in the infra-orbital margin, infra-orbital nerve
damage, diplopia, and subconjunctival haemorrhage (especially if no
posterior margin is seen). Isolated fractures of the zygomatic arch may be
accompanied by a palpable defect over the arch and limited or painful jaw
movement resulting from interference with the normal movement of the
coronoid process of the mandible.
Orbital ‘blow-out’ fractures
Caused by a direct blow to the globe of the eye (commonly from a squash
ball or shuttlecock) resulting in a fracture of the orbital fl oor and prolapse
of contents into the maxillary sinus.
Examination Check for diplopia due to inferior rectus entrapment
(the patient cannot look up and medially), enophthalmos, and surgical
emphysema. Carefully check the eye itself for injury (hyphaema, retinal
detachment, glaucoma, blindness). Record the visual acuity. Test infra-
orbital nerve function. Fractures of the fl oor of the orbit may not be
easily visible on X-ray, but can often be inferred by the soft tissue mass in
the roof of the maxillary sinus (‘tear drop’ sign), clouding of the sinus and
surgical emphysema.
Management of zygomatic and orbital fractures
• Tell the patient not to blow his/her nose.
• Refer all patients (including those in whom a fracture is clinically
suspected but not evident on X-ray) to maxillofacial specialists who
will advise regarding prophylactic antibiotics and will arrange further
investigation (usually CT scanning) and treatment.
• Involve the ophthalmologists if the eye is also injured.
Note: Patients with orbital emphysema who complain of sudden d in
vision may be suffering from a build-up of air under pressure which is
compromising retinal blood fl ow. These patients need emergency
decompression.
Frontal sinus fractures
Presenting features include supraorbital swelling, tenderness and
crepitus, occasionally with supraorbital nerve anaesthesia. CT scanning
will determine whether or not there are fractures of simply the anterior
wall or of both anterior and posterior sinus walls ( ± depressed fragments).
Give IV antibiotics and refer for admission and observation, which in the
case of depressed fragments, should be to the neurosurgical team.
This page intentionally left blank

376 CHAPTER 8 Major trauma
Mandibular injuries
Considerable force is required to fracture the mandible, so look for
concurrent head or other injuries. The mandible may be fractured at a site
distant from the point of impact (eg a fall on the chin may cause condylar
fractures). There are often fractures at two or more sites (Fig. 8.9). The
temporomandibular joint may be dislocated or the condyle driven through
the temporal bone causing a skull base fracture.
Symptoms and signs
The patient usually presents with pain (aggravated by jaw movement
or biting). Check for swelling, tenderness, or steps on palpation of the
mandible. Look for malocclusion, loose or missing teeth, and intra-oral
bruising. Numbness of the lower lip indicates injury to the inferior dental
nerve where it passes through the ramus of the mandible.
X-rays
Request an orthopantomogram (OPG). Temporomandibular joint
dislocation and condylar fractures are best shown by condylar views.
Management
Simple undisplaced single fractures not involving the teeth can be treated
with analgesia, soft diet, prophylactic antibiotics (eg penicillin or co-amoxiclav),
tetanus cover, and referral to the maxillofacial outpatient department. Refer
displaced or multiple fractures to the on-call specialist.
Refer to the on-call specialist patients with bilateral condyle fractures or
single fractures with mal occlusion or deviation of the jaw on opening.
Advise patients with unilateral asymptomatic fractures to take a soft diet
and arrange outpatient follow-up.
Temporomandibular joint dislocation
This is almost invariably anterior, but can be uni- or bilateral. It may be
caused by a direct blow to the (often open) jaw, or in patients with lax
joint capsule/ligaments by yawning, eating, dystonic reactions or intubation.
The patient cannot close the mouth, the jaw protrudes anteriorly and
diffi culty in swallowing leads to drooling of saliva. The pain is often over
the temporal fossa, rather than the temporomandibular joint itself. Obtain
X-rays only if there is a history of direct trauma.
Treatment If seen shortly after dislocation, reduction can usually be achieved
simply and without anaesthesia or sedation (Fig. 8.10 ). Explain the process to
the patient. Sit in front of him/her and with your gloved thumb(s) protected
by a gauze swab press down and backwards on the lower molar teeth,
while gently cupping and lifting the chin with the fi ngers. After reduction
advise the patient to take a soft diet, and not to yawn (diffi cult!) or open
the mouth widely for 24hr. Delayed presentations can be associated with
muscle spasm requiring anaesthesia and muscle relaxants.
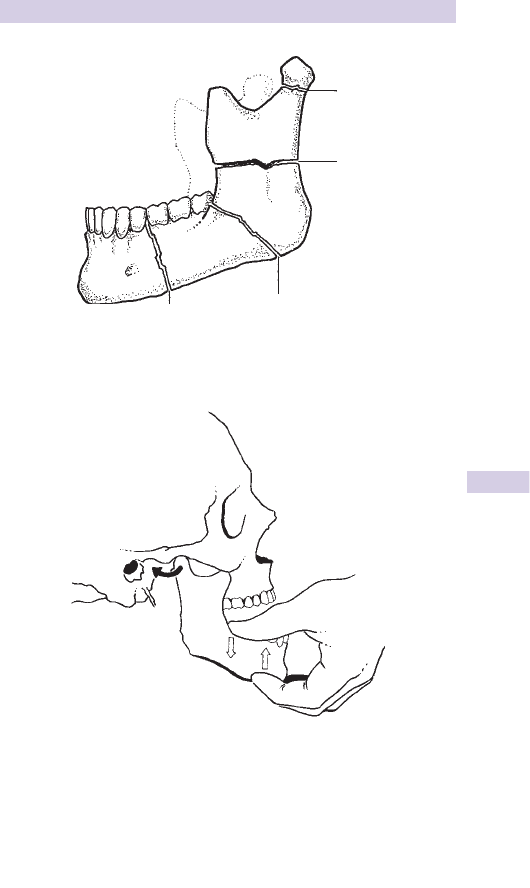
377
MANDIBULAR INJURIES
Fig. 8.10 Reduction of dislocated temporomandibular joint.
Neck
Ramus
Angle
Bod
y
Fig. 8.9 Common fracture sites of the mandible.

378 CHAPTER 8 Major trauma
Penetrating neck trauma
In the UK, neck ‘stabbings’ and ‘slashings’ are not uncommon, but gunshot
wounds to the neck are rare. The neck is divided into ‘zones’ when classifying
wounds.
• Zone 1 extends from the clavicles to the cricoid cartilage.
• Zone 2 extends from the cricoid to the angle of the mandible.
• Zone 3 is the area from the angle of the mandible to the skull base.
Initial assessment and resuscitation
Every patient requires high fl ow O
2
, wide bore venous access (send blood
for X-matching) and resuscitation according to an evaluation of the airway
and cervical spine, breathing and circulation. Quickly check for evidence
of spinal cord injury. Do not aim to raise the BP too high; a systolic of
≈ 90mmHg is suffi cient if the patient is conscious. Look for and rapidly
treat the following:
• Direct airway injury — may need emergency surgical airway ( b p.326).
• Tension pneumothorax ( b p.328).
• Major external haemorrhage — apply pressure to the wound.
• Massive haemothorax ( b p.335).
Occasionally the open end of a cut trachea will be seen in extensive neck
wounds; secure the airway temporarily by passing an ET or tracheostomy
tube into the lumen and securing the tube carefully. Further management
depends partially upon haemodynamic status:
The unstable patient
Haemodynamic instability may be due to tension pneumothorax or
massive haemothorax. Persistent major bleeding from a neck wound
(usually Zone 2) associated with haemodynamic instability is an indication
for emergency surgical exploration in theatre. Other indications for
exploration include:
• Breach of platysma (do not probe or explore the wound in the ED).
• Evidence of vascular injury (haemorrhage, expanding haematoma).
• Evidence of surgical emphysema (indicates laryngeal or oesophageal
disruption which requires repair).
The stable patient
Many patients are stable and have little evidence of signifi cant injury.
• Provide O
2
, secure venous access, and send blood for group and save.
• Monitor SpO
2
, pulse, BP, and respiratory rate.
• Obtain a CXR (to exclude pneumothorax/haemothorax).
• Provide IV analgesia as required (see b p.320).
• Consider tetanus status and the need for prophylactic antibiotics
(eg 1.5g IV cefuroxime — according to local policy).
• Investigations may include cervical spine X-rays and/or CT neck.
• Occasionally 4-vessel angiography or duplex ultrasound scanning (to
exclude vascular injury) and a contrast swallow/oesophagoscopy (to
exclude oesophageal injury) are required (usually Zone 1 or 3 injuries).
• Refer all patients to ENT or maxillofacial surgeons for admission, obser-
vation, formal wound cleaning, exploration and closure.
• Carefully document the size, position and other features of the neck
wound, in view of the high medicolegal signifi cance ( b p.403).
This page intentionally left blank

380 CHAPTER 8 Major trauma
Spine and spinal cord injury: 1
Consider the possibility of spinal injury when managing every injured
patient. Careless manipulation or movement can cause additional spinal
injury. Maintain a particularly high index of suspicion and provide spinal
immobilization in patients with:
• Major trauma.
• ‘Minor’ trauma with spinal pain and/or neurological symptoms/signs.
• Altered consciousness after injury.
• A mechanism of injury with a possibility of spinal injury (eg road traffi c
collision, high fall, diving, and rugby injuries).
• Pre-existing spinal disease (eg rheumatoid arthritis, ankylosing spond-
ylitis, severe osteoarthritis, osteoporosis, steroid therapy), as serious
fractures or dislocations may follow apparently minor trauma.
The commonest sites of spinal injury are the cervical spine and the
thoracolumbar junction.
Airway management and spinal immobilization
These two aspects demand immediate attention in any patient with
possible spinal injury — manage them together. The neck is the commonest
site of cord injury. If immobilization is not achieved with unstable injuries,
it is the site at which most additional cord or nerve root damage can be
produced.
• Perform manual immobilization rapidly (without traction), keeping the
head and neck in the neutral position, by placing both hands around the
neck and interlocking them behind, with the forearms preventing head
movement (see Fig. 8.11 ).
• Apply a hard collar with continued manual stabilization or support with
sand bags placed on either side of the head and tape applied to the
forehead to prevent rotation. The collar should fi t securely, but not
occlude the airway or impair venous return from the head. Take care
in patients with pre-existing neck deformity (eg ankylosing spondylitis —
b p.497) not to manipulate the neck or to force the collar into place.
• Ensure airway patency and adequate ventilation — hypoxia compromises
an injured cord. Initially in an unconscious patient, jaw thrust and suction
to the upper airway can be used. Remember that oropharyngeal stimu-
lation can provoke severe bradyarrhythmias. Simple airway adjuncts
such as oro- and nasopharyngeal airways often maintain upper airway
patency, but sometimes tracheal intubation is required. This must be
performed by an individual experienced in advanced anaesthetic tech-
niques (usually RSI, rarely fi bre-optic) with an assistant controlling the
head/neck to limit cervical spine movement.
• Ventilation can deteriorate due to cord oedema/ischaemia, so look
regularly for diaphragmatic breathing (diaphragm is supplied by C3/4/5)
and the use of accessory muscles of respiration. Use pulse oximetry and
regular ABG analysis to confi rm adequate oxygenation and ventilation.
Tracheal intubation and controlled ventilation may be required.
• Usually, patients will have been transported on a spinal board, which
should be removed as soon as the primary survey is completed and
resuscitation commenced (Fig. 8.12 ). Remove the board before imaging
if possible.
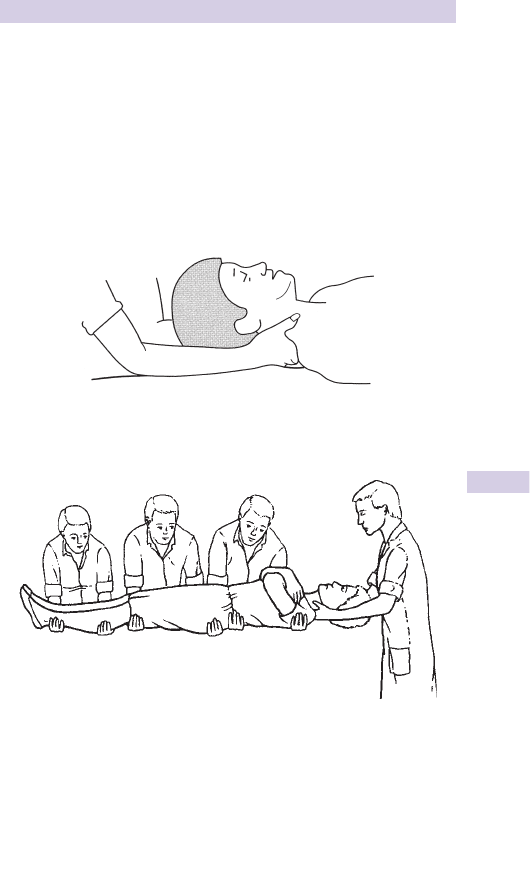
381
SPINE AND SPINAL CORD INJURY: 1
Suspect spinal injury in patients with d consciousness if there is:
• Flaccid arrefl exia.
• d Anal tone on PR examination.
• Diaphragmatic breathing.
• An ability to fl ex (C5/6), but not to extend (C6/7) the elbow.
• Response to painful stimulus above, but not below the clavicle.
• Hypotension with associated bradycardia.
• Priapism.
Fig. 8.12 Co-ordinated 4 person lift.
Fig. 8.11 Manual immobilization of the neck.

382 CHAPTER 8 Major trauma
Spine and spinal cord injury: 2
Managing the circulation
Monitor ECG and BP. Interruption of the sympathetic system in the cord
causes loss of vasomotor tone, with vasodilatation, i venous pooling,
and d BP. Flaccidity and arrefl exia, together with the absence of a refl ex
tachycardia or an associated (inappropriate) bradycardia are pointers to
this, but before diagnosing ‘neurogenic shock’ exclude and treat other
causes of hypotension (eg blood loss, tension pneumothorax). IV fl uids
( b p.320) usually correct any relative hypovolaemia, but inotropes may be
needed if d cardiac output persists despite adequate volume replacement
and correction of bradyarrhythmias by atropine. Use CVP monitoring of
patients in neurogenic shock to prevent fl uid overload.
Other considerations
Insert a urinary catheter (strict aseptic technique) to monitor urine output
and prevent bladder distension. If there is no craniofacial injury, an NG
tube will prevent gastric distension (ileus commonly develops after cord
injury), and d risk of aspiration and respiratory embarrassment.
With blunt injury mechanisms, up to two-thirds of individuals with spinal
cord injury have major injuries at other sites. Conscious patients can
usually describe a sensory level and paralysis, with pain at the level of
the vertebral injury. Have a high index of suspicion for thoracic/abdominal
injury — clinical features may be obscured by sensory or motor defi cits
from the cord injury itself. Abdominal distension may occur and there may
be no signs of peritonism. FAST (USS), CT, or DPL may be required.
Neurological examination
Carefully perform and document the neurological examination, including
light touch and pinprick sensation, proprioception, muscle power, tone,
co-ordination, and deep tendon refl exes. Evidence of distal, motor, or
sensory function implies an incomplete lesion and hence the possibility
of recovery. The accuracy of this baseline examination is important,
since cephalad progression of abnormalities is a sensitive marker of
deterioration, and in the cervical region, may lead to respiratory failure.
Document muscle group strength in upper and lower limbs using the 0–5
grading system (see Table 8.4 ). It is standard practice to record the most
caudal location which has intact (normal) motor and sensory function.
Examine the perineum and perform a PR examination; look for voluntary
contraction and anal tone. An intact bulbocavernosus refl ex (squeezing
glans penis l contraction of bulbocavernosus muscle — S2,3,4) and anal
cutaneous refl ex (scratching peri-anal skin l anal contraction — S4,5)
imply sacral sparing.
Spinal examination
Log-roll the patient. The person controlling the head and neck directs
movement. Carefully examine for tenderness, step-deformity, gibbus,
widening of interspinous gaps and prominence of spinous processes. There
may not be overlying tenderness with vertebral body fractures. Remove
any debris from under the patient. Keep the patient covered and warm, as
d sympathetic vasomotor tone l i risk of hypothermia. To d risk of pressure
sores, remove the patient rapidly from the spinal board.
383
SPINE AND SPINAL CORD INJURY: 2
Incomplete cord injury patterns
There are several recognized patterns of incomplete spinal cord injury.
Although the resultant physical signs can be predicted from a detailed
knowledge of neuroanatomy, bear in mind that some patients present
with an atypical injury and therefore an atypical pattern of injury.
Anterior cord syndrome Loss of power and pain sensation below the
injury, with preservation of touch and proprioception.
Posterior cord syndrome Loss of sensation, but power preserved.
Brown-Séquard syndrome Hemisection of the cord producing ipsilateral
paralysis and sensory loss below the injury, with contralateral loss of pain
and temperature. This syndrome occurs more frequently after penetrating
injury than after closed injury.
Central cervical cord syndrome Typically seen in elderly patients following
extension injuries to the neck, with degenerative changes being the only
X-ray abnormality. It is characterized by incomplete tetraparesis, which
affects the upper limbs more than the lower limbs (as nerves supplying the
upper limbs lie more centrally within the cord). Sensory defi cits are variable.
Spinal cord injury without radiographic abnormality
A signifi cant proportion of children with spinal cord injury have no
radiographic abnormality. The extent of both the neurological defi cit and
recovery is variable. Adults may similarly have spinal cord injury due to
traumatic herniation of an intervertebral disc, epidural haematoma or
ligamentous instability, yet plain radiographs may appear normal.
Table 8.4 Grading muscle strength
Grading of muscle power
0 Total paralysis
1 Palpable or visible contraction
2 Movement with gravity eliminated
3 Movement against gravity
4 Weaker than usual
5 Normal strength
Muscles supplied by various nerve roots
C5 Shoulder abductor (deltoid)
C6 Wrist extensors (extensor carpi radialis)
C7 Elbow extensor (triceps)
C8 Middle fi nger fl exor (fl exor digitorum profundus)
T1 Little fi nger abductor (abductor digiti minimi)
L2 Hip fl exors (iliopsoas)
L3 Knee extensors (quadriceps)
L4 Ankle dorsifl exors (tibialis anterior)
L5 Big toe extensor (extensor hallucis longus)
S1 Ankle plantar fl exors (soleus, gastrocnemius)

384 CHAPTER 8 Major trauma
Spine and spinal cord injury: 3
Imaging (for indications for cervical spine X-rays see b p.462) X-rays
are readily available, but interpretation can be diffi cult. Whenever possible
get senior expert help. Cord injury can occur without X-ray abnormality.
This may be due to i soft tissue elasticity allowing excessive movement
(children), or cord compression from disc prolapse (younger patients), or
vascular involvement, or spondylosis (older patients).
Cervical spine Request AP, lateral (must show C7/T1 junction) and open-
mouth odontoid peg views if CT of the cervical spine is not indicated.
Displacement (subluxation/dislocation) and fractures of vertebral bodies,
spinous processes, and peg are best seen on lateral view. Unifacet
dislocation causes anterior displacement ≤ 50 % of AP diameter of
vertebral body. Displacement > 50 % suggests bilateral facet dislocation.
Look for swelling of prevertebral soft tissues.
AP views show injuries to the pedicles, facets, and lateral masses.
Open-mouth odontoid view usually demonstrates peg fractures.
Flexion/extension views to assess neck stability are rarely indicated soon
after injury, as muscle spasm may inhibit movement and there is potential
to aggravate cord damage. Obtain senior advice before requesting these
views. CT is usually a more appropriate investigation.
Thoracolumbar spine Standard views are AP and lateral. In the thoracic
region overlapping structures may make interpretation diffi cult and
necessitate other imaging. If X-rays are of diagnostic quality, visualization
of compression or burst fractures, and displacement is not diffi cult, but
these have little relation to the degree of cord injury.
CT and MRI CT delineates bony abnormalities and the extent of spinal
canal encroachment. CT of the cervical spine (base of skull to T4 level) is
indicated for patients requiring CT brain for signifi cant head injury or as
part of a 'pan-scan' for multiple trauma (see SIGN and NICE guidelines).
CT or magnetic resonance imaging (MRI) are useful for patients in whom
there is clinical suspicion of injury (persistent pain, positive neurology)
despite normal X-rays.
Further treatment
Immobilize cervical injuries using a fi rm, well-fi tting cervical collar (eg
Philadelphia), pending a decision to undertake skeletal traction. Skeletal
traction using Gardner–Wells calipers, or halo devices and pulley/weight
systems may be undertaken by orthopaedic/neurosurgical staff to reduce
fracture-dislocations, improve spinal alignment and decompress the cord.
Thoracolumbar fracture-dislocations are normally treated by bed rest
with lumbar support. In specialist units, unstable injuries may be surgically
fi xed. High dose steroid therapy is no longer widely recommended as part
of the treatment for blunt spinal cord injury — follow local protocols.
With penetrating injuries, if the object is still in place, arrange removal in
theatre where the spinal cord/canal injury can be directly seen.
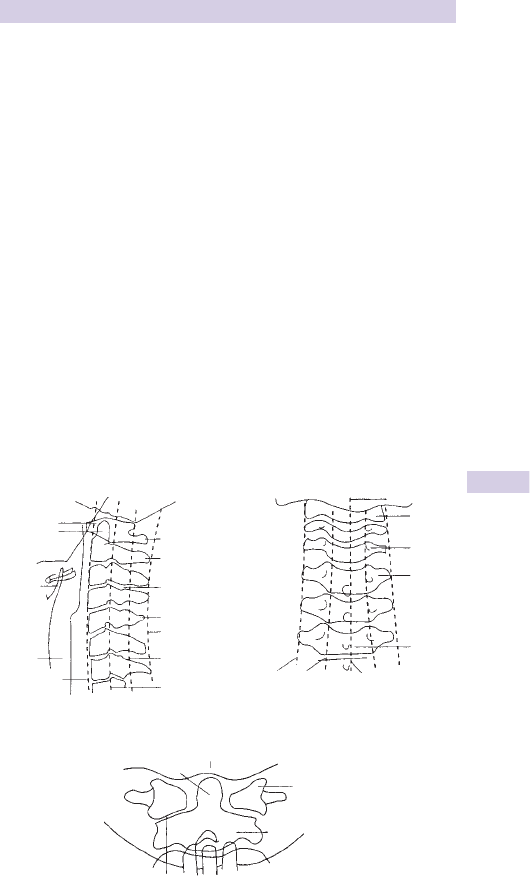
385
SPINE AND SPINAL CORD INJURY: 3
Assessment of spinal X-rays
Interpreting spinal X-rays can be diffi cult. If in any doubt, get senior expert
help. A systematic approach helps to prevent injuries from being missed:
• Check alignment of the vertebrae. The spine should be straight or
follow gentle curves and should not exhibit any ‘steps’. On the lateral
X-ray assess the alignment by checking in turn: anterior vertebral
border, posterior vertebral border, posterior facets, anterior border
of spinous processes, and posterior border of spinous processes. Look
also at interspinal distances.
• Check alignment on the AP fi lm by following the spinous processes
and the tips of the transverse processes (Fig. 8.13 ). Look for rotational
deformity and asymmetry.
• Assess the integrity of each spinal vertebra, including the vertebral
bodies, laminae, and pedicles.
• Be vigilant in assessing the odontoid peg view (Fig. 8.13 ), looking for
asymmetry/displacement of the lateral masses of C1. Distinguish frac-
tures (limited to bone area) from overlying soft tissue shadows (extend
beyond area of bone). Note that the atlanto-odontoid distance should
be ≤3mm in adults and ≤ 5mm in children.
• Look for indirect evidence of signifi cant spinal injury ( i prevertebral
space). The normal soft tissue prevertebral thickness at the antero-
inferior border of C3 (ie distance between pharynx and vertebral body)
is <0.5cm.
Lateral cervical spine
Atlas
Axis
Facet joint
Spinous
processes
Line of posterior
spinous
processes
Line of posterior
wall of canal
Line of posterior
edge of vertebral
bodies
Base of skull
Dens
Axis
Lateral mass
Articular surface
Line of
transverse
process
Line of
pedicles
Line of spinous
processes
Spinous
process
Transverse
process
Pedicle
Axis
Mandible
Atlas-dens gap
Odontoid
Epiglottis
Line of anterior
edge of vertebral
bodies
Trachea
Odontoid peg view
AP cervical spine
Fig. 8.13 Interpretation of spinal X-rays.
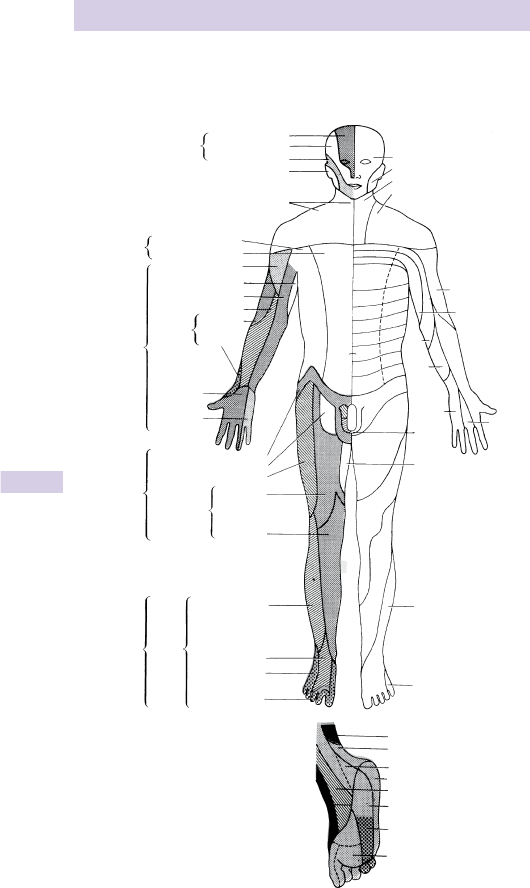
386 CHAPTER 8 Major trauma
Dermatomes
Dermatomes front (Fig. 8.14 )
Ophthalmic division
Maxillary division
Trigeminal
V
C.2
C.3
C.4
C.5
T.3
T.5
T.6
T.7
T.8
T.9
T.2
T.1
C.6
C.8
C.7
S.2,3
Obturator
T.10
T.11
T.12
L.1
L.2
L.3
L.4
L.5
S.1
Lateral cutaneous br.
Anterior cutaneous br.
Axillary
Radial
Median
Brachial
plexus
Ulnar
Ilioinguinal
Femoral
Lumbar
plexus
Saphenous
Sciatic
Sural
Medial plantar
Sural
Lateral plantar
Lateral plantar
Lateral plantar
Tibial
Saphenous
Medial cutaneous
Medial plantar
Superficial and
deep peroneal
Sacral
plexus
Lateral cutaneous
nerve of calf
Anterior
cutaneous
rami
Genitofemoral
Lateral cutaneous
Posterior
cutaneous
Superficial
branch
Intercostobrachial
Medial cutaneous
Musculocutaneous
Intercostal
nerves
T.2-T.11
Mandibular division
Cervical plexus,
superficial branches
Great auricular, C.2,C.3
Fig. 8.14
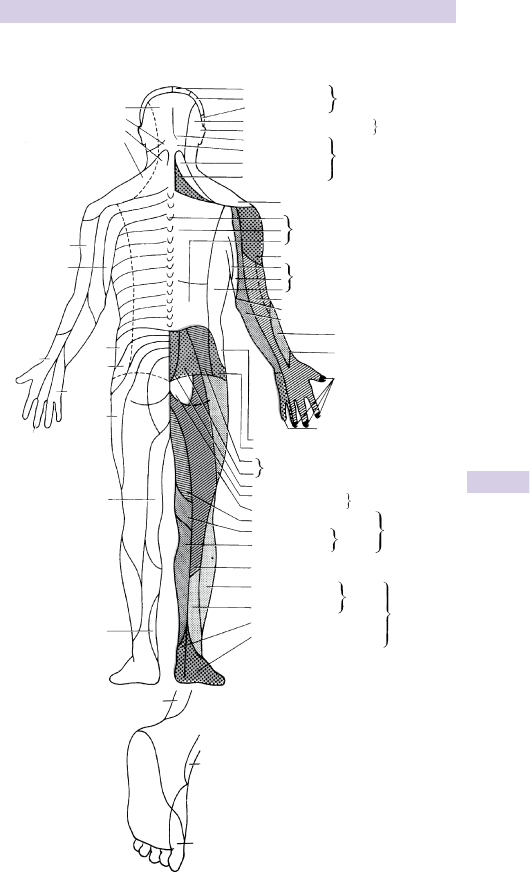
387
DERMATOMES
Dermatomes back (Fig. 8.15 )
C.2
C.3
C.2
C.4
Ophthalmic division
Maxillary division
Mandibular division
Great auricular branch, C.2, C.3
Trigeminal
Dorsal
branches
Dorsal rami of thoracic nerves
Occipital, C.2
Occipital, C.3
Supraclavicular, C.3, C.4
Occipital, C.4
Occipital, C.5–C.8
Mastoid branch, C.2, C.3
C.5
T.3
T.5
T.4
T.6
T.7
T.8
T.9
T.2
T.1
C.6
C.8
C.7
T.10
T.11
T.12
L.1
L.2
L.3
S.3
S.2
L.3
L.5
L.4
L.5
L.5
L.4
S.1
S.1
Femoral
Lumbar plexus
Pudendal plexus
Perforating branch of
posterior cutaneous
Sural
Superficial peroneal
Posterior cutaneous
Saphenous
Obturator
Lateral cutaneous
Medial cutaneous
Tibial
Lateral plantar
Median
Dorsal cutaneous branch of ulnar
Gluteal branch of 12th intercostal
Lateral cutaneous br. of iliohypogastric
Lateral branches of dorsal
rami of lumbar and sacral
Medial cutaneous
Intercostobrachial
Musculocutaneous
Medial and lateral cutaneous br. of radial
Posterior aspect
Sacral plexus
Common
peroneal
Anterior branch of radial
Lateral cutaneous branches
of intercostal nerves
Cutaneous branch of axillary
Superfical
cervical plexus
Medial branches of dorsal rami, L.1–S.6
Fig. 8.15

388 CHAPTER 8 Major trauma
Gunshot injuries
In the UK, inform the police as soon as possible whenever a patient
presents with a gunshot wound. Wounds produced by bullets/missiles are
determined by kinetic energy (KE) transfer, missile fl ight characteristics,
and the tissue injured.
Kinetic energy transfer
The KE of a missile is directly proportional to its mass and to the square
of its velocity (KE = ½mv
2
). Thus, tissue injury depends more upon the
bullet’s velocity than its mass. At velocities > speed of sound, the rate of
dissipation of KE becomes proportional to the velocity
3
or even higher
powers. Bullets travelling at > 1,000ft/sec (300m/sec) are ‘high velocity’.
The tissue itself
Tissue density affects a missile, and the energy dissipation and tissue
destruction. Bone involvement may cause additional retardation, while
bony fragments cause secondary injuries.
Cavitation
High velocity bullets transmit energy to the tissues, compressing and
accelerating them at right angles away from the track. This leads to cavity
formation around the track. Over a few micro-seconds the cavity enlarges
and then collapses. Tissue elasticity perpetuates a process of cavity refor-
mation and collapse, with rapidly d amplitude of oscillations until all KE is
expended. This causes highly destructive stretching, tearing and shearing
of tissues, causing injury many times the size of the bullet. Since the pres-
sure in the cavity is sub-atmospheric, debris and organisms are sucked in.
Clinical aspects
The principles of resuscitation of a patient with gunshot injury are identical
to those for any major trauma case. Specifi c aspects are:
• Consider staff safety: involve police and check the patient for weapons.
• The magnitude of the external wounds may bear little relationship to
the severity of internal injury. Remove the patient’s clothes (police
evidence) and examine the entire body for entrance/exit wounds that
are often missed in hairy areas (eg scalp, axillae, and perineum).
• Patients are often young and fi t: signs of hypovolaemia may be delayed.
• Chest injuries are commonly associated with pneumothorax ( b
p.334). PEA cardiac arrest should prompt rapid exclusion of tension
pneumothorax then immediate thoracotomy to relieve cardiac
tamponade ( b p.343).
• Abdominal wounds are associated with a high incidence of internal
injury and require laparotomy and antibiotic cover.
• Gunshot wounds are prone to anaerobic infection (especially tetanus
and gas gangrene): clothing/fragments spread widely through tissues
distant from the wound track. Extensive surgical debridement (wide
excision/fasciotomy) is often required to remove devitalized tissue and
foreign material. All high velocity injuries need delayed primary closure
with grafting or suture at 3–5 days.
• Ensure tetanus cover and give prophylactic antibiotics.
• X-ray (AP + lateral) one body region above and one body region below
any wound, as well as the region involved, to look for metallic FBs.

389
BLAST INJURIES
Blast injuries
Blast injuries may be due to explosions involving domestic gas, industrial
sites (eg mines/mills), or bombs. Often several mechanisms co-exist to
cause injury.
Blast wave (primary blast injury) This is an extremely short-lived
pressure wave (lasting a few milliseconds only) which expands outwards
from the explosive focus. It is produced by intense compression of air
at the interface of the rapidly expanding hot gases. The effects can be
dramatically aggravated and reinforced by refl ection from solid surfaces,
such as buildings. Blast wave injuries are caused by 3 mechanisms:
• Disruption at air/tissue interfaces (especially lungs and ears, producing
blast lung and tympanic membrane rupture, respectively).
• Shearing injuries at tissue/tissue interfaces causing subserous and
submucosal haemorrhage.
• Implosion of gas-fi lled organs leading to perforation of the GI tract and
cerebral or coronary air embolism.
Blast winds These are fast moving columns of air that follow the initial
blast wave. Their destructive force can be immense, leading to traumatic
amputation or even complete dismemberment. Blast winds also carry
debris (masonry, glass, etc.), which act as secondary missiles causing
fragmentation injuries.
Fragmentation injuries Objects from a bomb (eg nails, casing, nuts,
and bolts) or fl ying debris (masonry, wood, glass) cause lacerations or
penetrating injuries. This is classifi ed as secondary blast injury .
Flash burns These are usually superfi cial, affecting exposed skin in those
close to the explosion. Smoke inhalation may also occur.
Tertiary blast injuries result from individuals being thrown by the blast
wind, often causing severe multiple injuries.
Quaternary blast injuries include all explosion related injuries or illnesses
not due to primary, secondary, or tertiary mechanisms listed above.
Psychological The psychological effects of blast injury are often severe,
comprising acute fear, anxiety, and the potential for chronic sequelae.
General aspects of treatment
The principles of blast injury treatment are identical to those for patients
with other causes of major trauma ( b p.320).
Clinical features in blast injuries may be delayed, both in terms of onset
and development of clinical signs. This particularly relates to lung and intra-
abdominal complications; therefore, observe all patients for at least 48hr.
Search for pneumothorax (may be tension), respiratory failure/ARDS,
peritonitis, abnormal neurological signs (suggesting air embolism),
eardrum perforation, anosmia (direct olfactory nerve damage). Note that
ventilation of patients with blast injuries is a highly specialized area, with
potential risks of producing tension pneumothoraces and air embolism.
Other aspects For forensic reasons, ensure that all the patient’s clothes,
belongings, and any missile fragments are carefully retained, bagged,
labelled, and kept secure until given to police offi cers.

390 CHAPTER 8 Major trauma
Burns: assessment
Types of burns
• Thermal.
• Chemical.
• Electrical ( b p.266).
• Radiation ( b p.268).
History
Determination of the circumstances resulting in the patient being burned
is essential to appreciate the nature of the insult and potential associated
risks. Do not, however, delay resuscitation in an attempt to obtain a full
history. Consider the following questions:
• Was there an explosion? (risk of blast injuries).
• Was the fi re in an enclosed space? (CO poisoning, smoke inhalation).
• What was the burning material? (burning plastics release cyanide).
• When was the patient removed from the fi re?
• How long was the patient exposed to fi re and smoke?
• Was there a history of loss of consciousness?
• Did the patient fall or jump to escape the fi re? (look for other injuries).
• What is the patient’s past medical history and tetanus status?
Initial assessment
This proceeds with resuscitation. Check : Airway, Breathing and Circulation.
Particular problems associated with burns are:
• Airway burns : suggested by hoarseness, stridor, dysphagia, facial and
mouth burns, singeing of nasal hair, soot in nostrils, or on palate
• Spinal injury : particularly seen with blast injuries and in those who have
jumped from buildings to escape fi re
• Breathing problems : contracting full thickness circumferential burns
(‘eschar’) of the chest wall may restrict chest movement
• Circulatory problems : hypovolaemic shock is a feature of severe burns
and may also result from other associated injuries.
Assessing extent
Estimation of the percentage of body surface area burnt is diffi cult for
non-experts. Use Lund and Browder charts appropriate for the age of the
patient (see Table 8.5 , Fig. 8.16 ). The palmar surface of the patient’s palm
(not including the fi ngers) represents ≈ 0.75 % body surface area.
Assessing depth
Burn depth varies with the temperature and duration of heat applied.
Superfi cial (fi rst and second degree) burns range from minor erythema
(fi rst degree) through painful erythema with blistering, to deep partial
thickness (second degree) burns, which do not blanch on pressure.
Full thickness (third degree) burns may be white, brown, or black and
look ‘leathery’. They do not blister and have no sensation.
On the day of injury it may be diffi cult to distinguish deep superfi cial
(second degree) burns from full thickness (third degree) burns, but
correctly making this distinction does not alter the initial management.
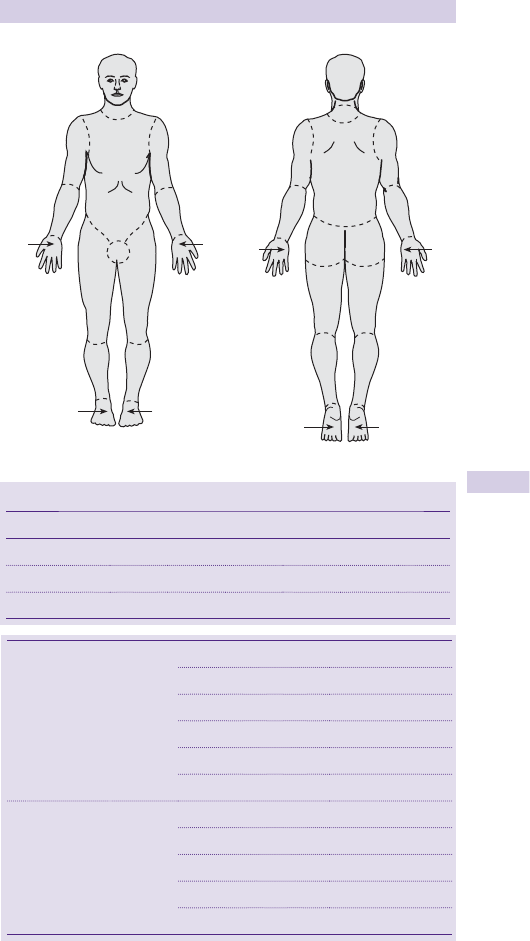
391
BURNS: ASSESSMENT
A
B
C
1
2
13
C
B
2
1
A
1
2
13
2
BB
C
C
2
1
/
2
2
1
/
2
1
1
/
2
1
1
/
2
1
1
/
2
1
1
/
2
1
1
/
2
1
1
/
2
1
1
/
2
1
1
/
2
1
3
/
4
1
3
/
4
1
3
/
4
1
3
/
4
Fig. 8.16 Assessing extent of burns — Lund and Browder charts.
Table 8.5 Relative percentage of area affected by growth (age in years)
0 1 5 10 15 Adult
A: half of head 9
1
/
2
8
1
/
2
6
1
/
2
5
1
/
2
4
1
/
2
3
1
/
2
B: half of thigh 2
3
/
4
3
1
/
4
4 4
1
/
2
4
1
/
2
4
3
/
4
C: half of leg 2
1
/
2
2
1
/
2
2
3
/
4
3 3
1
/
4
3
1
/
2
Adults rule of 9’s: head = 9 %
each arm = 9 %
each leg = 18 %
front of trunk = 18 %
back of trunk = 18 %
perineum = 1 %
Infants rule of 5’s: head = 20 %
each arm = 10 %
each leg = 20 %
front of trunk = 10 %
back of trunk = 10 %

392 CHAPTER 8 Major trauma
Major burns: resuscitation
Prehospital fi rst aid measures
• Ensure rescuer safety fi rst — be guided by the fi re crew.
• Remove the patient from the burning environment. If clothes are smoul-
dering, apply cold water and remove them, unless adherent.
• Provide high fl ow O
2
. Cover burns in clean sheets.
Airway and cervical spine protection
• Treat airway obstruction ( b p.320).
• Continue O
2
and apply a hard cervical collar if there is any possibility of
spinal injury — cervical spine imaging will be required subsequently.
• If there is any evidence of impending airway obstruction (stridor,
oropharyngeal swelling — see b p.394), call immediately for senior ED
help and a senior anaesthetist. Urgent GA and tracheal intubation may
be life-saving. Use uncut endotracheal (ET) tubes to allow for swelling
of lips and face.
Analgesia
• Obtain IV access with two large peripheral cannulae.
• Send blood: X-matching, FBC, COHb, U&E, glucose, and coagulation.
• Provide analgesia (IV morphine titrated according to response).
• Provide an antiemetic (eg IV cyclizine 50mg).
Fluid resuscitation
• Give IV fl uids. Start with isotonic crystalloid (eg 0.9 % saline) at 2–4mL of
crystalloid per kg body weight per % body surface area burned, over the
fi rst 24hr following injury. Give half of this volume in the fi rst 8hr.
• Check pulse, BP, and respiratory rate every 10–15min initially.
• Insert a urinary catheter and test the urine. Patients with myoglobinuria
are at particularly high risk of acute renal failure — reduce this risk by
adequate fl uid resuscitation. Use urine output to guide fl uid therapy.
• Review the rate of IV volume replacement frequently and adjust it
according to haemodynamic parameters, in order to maintain a satisfac-
tory urine output ( > 50mL/hr in adults; 1 − 2mL/kg/hr in children).
• Some burns units prefer a colloid (eg Gelofusine
®
or albumin) to form a
component of the initial volume replacement: follow local policy.
• Patients with full thickness burns of body surface area > 10 % may require
red cell transfusion in addition to the above measures.
Breathing
• Check COHb and ABG.
• Circumferential full thickness chest burns restricting chest movement
require escharotomy. Cut the burnt areas down to viable tissue to
release the constriction. Cutting diathermy can be helpful to reduce the
signifi cant blood loss involved in extensive escharotomy.
• Obtain a CXR.

393
MAJOR BURNS: RESUSCITATION
The burn
• Measure the area of the burn as a % of body surface area.
• Irrigate chemical burns with warmed water (see b p.396).
• Cover the burn with cling fi lm or dry sterile sheets. Do not apply
extensive burns dressings before assessment by a burns specialist.
• Involve a burn specialist at an early stage — in the UK, the National Burn
Bed Bureau will help to locate a suitable bed (tel. 01384 215576).
• Ensure tetanus prophylaxis, but avoid ‘routine’ prophylactic antibiotics.
The burnt patient in cardiac arrest
• Follow standard guidelines.
• Give a large bolus of IV fl uid.
• If there is a strong possibility of cyanide poisoning (eg burnt plastic
furniture in a house fi re), give appropriate antidote, eg dicobalt edetate
(see b p.207).
Vascular impairment to limbs and digits
Consider the need for longitudinal escharotomies. These are occasionally
needed if ischaemia causes severe pain: get advice from a burns specialist.

394 CHAPTER 8 Major trauma
Inhalation injury
The commonest inhalation injury is smoke inhalation accompanying burns
in house fi res. Inhalation injury alone may be fatal and it i mortality for a
given body surface area of burn. Smoke is a complex and unpredictably
variable mixture of solid, liquid and gas constituents.
Common components of inhalation injury include:
• Direct thermal injury.
• Soot particles cause local injury to the cilia of the respiratory tract and
obstruct small airways.
• ≈ 85 % of fi re deaths are caused by CO ( b p.208).
• Gas products of combustion : oxides of sulphur, nitrogen, ammonia,
chlorine, hydrogen cyanide, phosgene, isocyanates, ketones, and
aldehydes are highly irritative and cause laryngospasm. Some react
with water in the respiratory tract producing strong acids which cause
bronchospasm, mucosal injury and oedema.
The nature of the inhaled insult determines the site, severity, and systemic
features. The upper respiratory tract can dissipate heat effi ciently, so that
direct thermal injury to the lower respiratory tract is rare unless steam or
other hot vapours are inhaled. In the lower airway, toxic components such
as CO, oxides of sulphur, nitrogen, hydrogen cyanide, hydrogen chloride
cause direct injury, and may act as systemic poisons.
Clinical features
Suspect smoke inhalation if any of the following features are present:
exposure to smoke or fi re in an enclosed space, confusion or altered/loss
of consciousness, oropharyngeal burns, hoarseness/loss of voice, singed
nasal hairs, soot in nostrils or sputum, wheeze, dysphagia, drooling or
dribbling, stridor.
Investigations
Peak fl ow rate Determine this in all patients.
ABG Detection of hypoxia, hypercapnia, and acidosis may be helpful, but
does not correlate well with the severity of inhalation injury. Note that
pulse oximetry has limited value because of the diffi culty in distinguishing
between oxyhaemoglobin and COHb.
CXR Usually normal initially, later features of ARDS may develop.
Carboxyhaemoglobin (COHb) CO poisoning cannot be detected by
physical examination, SpO
2,
or pO
2
. Either arterial or venous COHB
can be measured. Clinical features correlate poorly with COHb levels.
Use the nomogram opposite to estimate COHb levels at the time of
exposure. The management of CO poisoning is covered on b p.208.
ECG CO binds to myoglobin 3 × more avidly than to Hb and by affecting
the myocardium may produce arrhythmias, ischaemia, or even MI.
Fibre optic bronchoscopy, xenon lung scanning, ventilation-perfusion
scans, or lung function testing may subsequently be required to assess
lung problems due to inhalational injury.
395
INHALATION INJURY
Management
Signs of upper airway problems (facial burns, stridor, dysphagia, drooling,
d consciousness) indicate the need for early tracheal intubation by an
experienced doctor (ED/ICU/anaesthesia) with appropriate training.
Mucosal swelling in the oropharynx and epiglottis can progress rapidly and
necessitate a surgical airway ( b p.326). A surgical airway in these circum-
stances can be diffi cult due to burned skin and loss of landmarks. Meticulous
preparation and planning for the airway are essential. Flexible bronchoscopy
may help to assess thermal injury to the upper airway and help intubation.
Assisted ventilation with PEEP may be indicated.
Give the highest possible concentration of humidifi ed O
2
. Hyperbaric O
2
may be indicated for CO poisoning, but remains controversial ( b p.208).
If bronchospasm occurs, give nebulized B
2
agonist (salbutamol 5mg) via an
O
2
powered nebulizer. i in microvascular permeability leads to pulmonary
oedema 2–3 days after injury and pneumonia after 7–14 days. Pulmonary
fi brosis is common among survivors.
Inadequate IV fl uid resuscitation is associated with greater pulmonary
oedema. Burned patients who have smoke inhalation need larger amounts
of IV fl uids to maintain cardiac and urine output.
Inhalation of HCN from smouldering plastics (eg polyurethane) results in
rapid systemic absorption. Measurement of blood CN concentration is
diffi cult and takes several hours. Cyanide poisoning may be suggested by a
severe metabolic acidosis, a high lactate and i anion gap. Consider cyanide
antidotes ( b p.207), but they are potentially toxic so do not use blindly.
There is no proven benefi t from steroid therapy.
Nomogram of decay of COHb with time
This nomogram (Fig. 8.17 ) allows back-calculation estimation of the likely
peak COHb level. It will considerably under-read for children and patients
who received a high prehospital FiO
2
.
Fig. 8.17 Adapted from Clark et al . (1981).
1
2
3
4
5
TIME SINCE
EXPOSURE
Hours
Measured
concentration
100%
80
60
50
40
30
20
10
8
6
4
10
20
30
40
50
60
70
80
90
100%
Original
exposure
concentration

396 CHAPTER 8 Major trauma
Management of smaller burns
Assessment ( b p.390)
First aid measures
Separate the patient and burning agent. Cool affected area with copious
quantities of cold water, but beware of hypothermia in infants and young
children.
Need for admission
Admit patients with large burns or signifi cant smoke inhalation for IV
fl uids, resuscitation and analgesia. In the UK, the National Burn Bed Bureau
will search for an appropriate bed (Tel: 01384 215576) after discussion
with the local burns unit. Also refer for admission burns of suspected NAI
origin and patients who would be unable to cope at home (eg an elderly
person or if living in diffi cult social circumstances).
Referral to a burns specialist
Refer patients with the following:
• Airway burns.
• Signifi cant full thickness burns, especially over joints.
• Burns > 10 % .
• Signifi cant burns of special areas (hands, face, perineum, feet).
The burn wound
• Leave full thickness burns uncovered and refer to a specialist.
• Do not de-roof partial thickness burns with blistering — consider simple
aspiration. Most can be cleaned and covered with an appropriate
dressing (see below).
Hand burns Consider covering with soft paraffi n inside a polythene bag
or glove sealed at the wrist, changed after 24hr. Simple paraffi n/tulle
dressings are an alternative — follow local policy. Elevate to minimize
swelling. Avoid silver sulphadiazine cream except on specialist advice.
Facial burns Leave uncovered, or consider application of soft paraffi n.
Eye burns Check VA and refer to a specialist with prior irrigation if
chemical burns ( b p.538).
Perineal and foot burns Burns in these areas should be referred for burns
unit admission as they require specialist nursing and wound care.
Burns dressings
The ideal burns dressing is sterile, non-adherent, and encourages wound
healing in a moist environment. The diversity of dressings available refl ects
the fact that this ideal dressing remains elusive. Senior ED nursing staff will
advise on local preference and policy. Accumulation of fl uid means that
many dressings need to be changed at ≈ 48hr — often this is appropriately
done at a GP surgery.

397
MANAGEMENT OF SMALLER BURNS
Analgesia and tetanus
Unless there is a contraindication and/or if the patient is elderly, NSAID is
appropriate and effective analgesia for many burns, which do not require
admission. Ensure prophylaxis against tetanus.
Burns in children and non-accidental injury
Unintentional burns are common in children — use the opportunity to
offer advice regarding injury prevention. A minority of burns may result
from NAI. Suspect NAI ( b p.730) and seek senior help in the following
situations:
• When the explanation does not fi t the burn.
• Late presentation.
• Other suspicious injuries.
• Stocking and glove distribution scalds ( ± sparing of the buttocks) — this
implies forced immersion in hot water.
• Circular full thickness burns ≈ 0.75cm diameter may represent cigarette
burns.
Chemical burns
Initial assessment is notoriously diffi cult. Alkalis tend to produce more
severe burns and can continue to penetrate even after initial irrigation.
Treat chemical burns with copious irrigation with water, continued for at
least 20min in alkali burns.
Hydrofl uoric acid burns
Hydrofl uoric acid is used industrially in a number of processes. Contact
with the skin causes particularly severe burns, often with signifi cant tissue
damage and severe pain. This is because hydrofl uoric acid rapidly crosses
lipid membranes and penetrates the tissues deeply, where it releases the
highly toxic fl uoride ion. Fluoride ions may gain access to the circulation
and produce a variety of systemic problems by a variety of mechanisms,
including interfering with enzyme systems and producing hypocalcaemia
by binding to calcium.
Manage hydrofl uoric acid burns as follows:
• Provide copious lavage to the affected skin then apply iced water (this
provides better pain relief than calcium gluconate gel).
• Call a plastic surgeon at an early stage.
• Check serum Ca
2 +
and Mg
2 +
, and U&E.
• Record an ECG and place on a cardiac monitor.
• Treat hypocalcaemia.
Cement burns
Wet cement or concrete can cause chemical burns due to the alkali
contact. These are usually partial thickness, but may be full thickness. They
often occur when wet cement falls into a work boot, but the burn is not
initially noticed. Involve a specialist at an early stage.
Phenol burns
Phenol may be absorbed through the skin, resulting in systemic toxicity
and renal failure. Get advice from Poisons Information Service ( b p.181).

398 CHAPTER 8 Major trauma
Crush syndrome
A spectrum of conditions characterized by skeletal muscle injury
(rhabdomyolysis). Causes include :
• Direct injuries and severe burns causing muscle damage.
• Compartment syndromes: ‘true’ crush injuries produced by entrapment,
or ‘self-crushing’ (eg an unconscious individual from drug overdose or
alcohol excess lying on a hard surface). A vicious cycle is established
where i muscle compartment pressure obstructs blood fl ow, the
muscles become ischaemic and oedematous, further i compartment
pressure and d blood fl ow leading to more ischaemia and muscle cell
death.
• Non-traumatic causes: metabolic disorders (diabetic states, d K
+
,
d PO
4
3–
), myxoedema, neuroleptic malignant syndrome, myositis due to
infection, or immunological disease.
• Exertional: from undue exertion, grand mal fi tting, rave dancing
(particularly associated with ecstasy or cocaine use), often complicated
by hyperthermia.
Clinical features
Adopt a high index of suspicion. Symptoms depend on the underlying
cause, but muscle pain, tenderness and swelling may not be present at the
time of admission. In the lower limbs, the condition is commonly confused
with DVT. The classic compartment syndrome with pain on passive
muscle stretching and sensory defi cits may take several days to develop
and can pass unnoticed. The presence of distal pulses does not rule out a
compartment syndrome.
Investigations
i CPK levels refl ect muscle damage. Check U&E, PO
4
3–
, Ca
2 +
and urate.
70 % have myoglobinuria and pigmented granular casts (urinary stix tests
do not differentiate between Hb and myoglobin). However, absence of
myoglobinuria does not exclude rhabdomyolysis, as myoglobin clears
rapidly from plasma and its presence in urine depends upon the release
rate, the degree of protein binding, GFR, and urine fl ow. If DIC is suspected,
check a coagulation screen.

399
CRUSH SYNDROME
Treatment
Local problems Urgent orthopaedic referral is needed for compartment
syndromes. If the difference between intra-compartmental and diastolic
pressures is <30mmHg, fasciotomy, excision of dead muscle and even
distal amputation may be required. These procedures may induce
life-threatening electrolyte shifts, bleeding, local infection, and later
generalized sepsis.
Systemic complications Severe metabolic complications start after
revascularization. Hyperkalaemia may be life-threatening ( b p.162).
Hypocalcaemia is common initially, but rarely symptomatic.
Acute renal failure can be produced by pre-renal, renal, and obstructive
elements. Following restoration of circulation or release from entrapment,
fl uid leaks into damaged areas d circulating plasma volume. Intracellular
muscle contents enter the circulation and myoglobin and urate crystals can
block the renal tubules. This process is aggravated by the d intravascular
volume and associated metabolic acidosis. DIC and drugs which inhibit
intra-renal homeostatic mechanisms (eg NSAIDs and B -blockers) may
also contribute.
Prompt correction of fl uid defi cits and acidosis (often with CVP
monitoring) and establishing a good urinary fl ow is essential. Alkalinization
of the urine may be required: early use of mannitol has been advocated,
but can cause pulmonary oedema if renal impairment is already present.
If renal failure occurs, dialysis may be needed, but prospects for renal
recovery are good.
This page intentionally left blank

401
The approach to wounds 402
Further assessment of skin
wounds 404
Wound management 406
Tetanus prophylaxis 410
Antibiotic prophylaxis 411
Wound aftercare 412
Infected wounds and
cellulitis 413
Bite wounds 414
Specifi c bites and stings 416
Needlestick injury 418
Puncture wounds 419
How to describe a
fracture 420
Compound fractures 422
Dislocations 423
Casts and their problems 424
Soft tissue injuries 426
Other soft tissue
problems 427
Physiotherapy in the ED 428
Approach to hand injuries 430
Clinical signs of hand
injury 432
Hand wounds and
associated injuries 434
Hand fractures and
dislocations 436
Thumb fractures and
dislocations 438
Soft tissue hand injuries 440
Other soft tissue hand
problems 441
Carpal bone fractures and
dislocations 442
Colles’ fracture 444
Other wrist fractures 446
Soft tissue wrist injuries/
problems 447
Forearm fractures and related
injury 448
Elbow injuries 450
Soft tissue elbow
problems 452
Anterior shoulder
dislocation 454
Other types of shoulder
dislocation 456
Other shoulder injuries 458
Soft tissue shoulder
problems 460
Soft tissue neck injuries 462
Facial wounds 464
Pelvic fractures 466
Hip dislocations and
acetabular fractures 468
Sacral and coccygeal
fractures 469
Hip fractures 470
Shaft of femur fractures 472
Approach to knee injuries 474
Knee fractures and
dislocations 476
Soft tissue knee injuries 478
Other knee problems 479
Tibial and fi bular shaft
fractures 480
Pretibial lacerations 481
Calf and Achilles tendon
injuries 482
Approach to ankle
injuries 484
Ankle fractures and
dislocations 486
Ankle sprains 487
Foot fractures and
dislocations 488
Toe injuries 490
Soft tissue foot problems 491
Low back pain 492
Acute arthritis 494
Eponymous fractures 498
Wounds, fractures,
orthopaedics
Chapter 9

402 CHAPTER 9 Wounds, fractures, orthopaedics
The approach to wounds
Wounds often have medicolegal implications — therefore record notes
thoroughly, legibly, and accurately ( b Note keeping, p.4). Resuscitation
is the initial priority for the seriously wounded patient. Stop bleeding by
applying direct pressure.
History
Key questions are:
• What caused the wound? (knives/glass may injure deep structures).
• Was there a crush component? (considerable swelling may ensue).
• Where did it occur? (contaminated or clean environment).
• Was broken glass (or china) involved? (if so, obtain an X-ray).
• When did it occur? (old wounds may need delayed closure + antibiotics).
• Who caused it? (has the patient a safe home to go to?).
• Is tetanus cover required? (see b p.410).
Examination
Consider and record the following:
• Length : preferably measure. If not, use the term ‘approximately’ in the
notes.
• Site : use diagrams whenever possible (rubber stamps are recom-
mended). Consider taking digital photographs, particularly for com-
pound fractures, in order to minimize the risk of infection by disturbing
the wound as little as possible prior to surgery.
• Orientation : vertical, horizontal or oblique.
• Contamination : by dirt or other FBs may be obvious.
• Infection : either localized or spreading, is a feature of delayed presen-
tations and is associated in particular with certain specifi c injuries (eg
‘reverse fi ght bites’ — see Bite wounds).
• Neurological injury : test and record motor and sensory components of
relevant nerves. Be aware that complete nerve transection does not
automatically result in complete loss of sensation — some feeling is likely
to be preserved (particularly in the hand). Assume that any altered sen-
sation refl ects nerve injury.
• Tendons : complete division is usually apparent on testing. Partial tendon
division is easily missed unless the wound is carefully examined — the
tendon may still be capable of performing its usual function. Look in
the wound whilst moving the relevant joint, and attempt to re-create the
position of the injured part at the time of injury (eg clenched fi st) to
bring the injured structures into view.
• Vascular injury : check for distal pulses.
• Depth : wounds not fully penetrating the skin are ‘superfi cial’. Do not try to
judge depth of other wounds before exploration. In some circumstances
(eg neck wounds), exploration is not appropriate in the ED.
• Type of wound : inspection often allows wounds to be described, helping
to determine the mechanism of trauma (blunt or sharp injury) and
hence the risk of associated injuries. The crucial distinction is whether a
wound was caused by a sharp or blunt instrument. If in doubt, avoid any
descriptive term and simply call it a ‘wound’. This avoids inaccuracy and
courtroom embarrassment! Use the terms as described opposite.

403
THE APPROACH TO WOUNDS
Forensic classifi cation of wounds and injury
The expert forensic evaluation of injury is outside the remit of the ED
specialist, but a simple understanding helps to avoid incorrect use of
terminology with associated confusion (and sometimes embarrassment).
Incised wounds May also be referred to as ‘cuts’. Caused by sharp injury
(eg knives or broken glass) and characterized by clean-cut edges. These
typically include
‘stab’ wounds (which are deeper than they are wide) and
‘slash’ wounds (which are longer than they are deep).
Lacerations Caused by blunt injury (eg impact of scalp against pavement
or intact glass bottle), the skin is torn, resulting in irregular wound edges.
Unlike most incised wounds, tissues adjacent to laceration wound edges
are also injured by crushing and will exhibit evidence of bruising.
Puncture wounds Most result from injury with sharp objects, although a
blunt object with suffi cient force will also penetrate the skin.
Abrasions Commonly known as ‘grazes’, these result from blunt injury
applied tangentially. Abrasions are often ingrained with dirt, with the
risk of infection and in the longer term, unwanted, and unsightly skin
‘tattooing’. Skin tags visible at one end of the abrasion indicate the edge
of skin last in contact with the abrading surface and imply the direction in
which the skin was abraded.
Burns See b p.390.
Bruises Bruising refl ects blunt force (crush) injury to the blood vessels
within the tissues, resulting in tender swelling with discoloration:
sometimes localized bleeding collects to form a haematoma. The term
‘contusion’ is sometimes used as an alternative for bruise — it has no
particular special meaning (or value). Record the site, size, colour, and
characteristic features of any bruising. It is impossible to determine the
exact age of a bruise from its colour. However, yellow colour within a
bruise implies (except in the neonate) that it is > 18hr old.
Scratches These may comprise either a ‘very superfi cial incision’ or a
‘long, thin abrasion’ — leave the distinction to an expert.
Interpersonal violence — medicolegal implications
Victims of violence frequently attend ED for treatment of their injuries.
Some patients (particularly those who have suffered domestic violence)
may not provide an accurate account of how the injuries occurred and may
not seek involvement of the police. Classical defence wounds include:
• Isolated ulna shaft fracture as the arm is raised to protect against blunt
injury.
• Incised wounds on the palmar aspects of the palms and fi ngers sustained
in attempts to protect against knife attack.
In cases where the police are involved and where injuries are serious or
extensive, the police may arrange to obtain photographs and a forensic
physician (police surgeon) may be involved in the role of documenting
injuries. Most ED patients who have suffered violence do not see a
forensic physician (police surgeon). Therefore, ED staff have a dual role of
treating injuries and recording them accurately for medicolegal purposes.

404 CHAPTER 9 Wounds, fractures, orthopaedics
Further assessment of skin wounds
Investigation
X-ray if there is suspicion of fracture, involvement of joint, penetration of
body cavity or FB. Specify on request forms that a FB is being sought, to
allow appropriate views and exposure. Most metal (except aluminium)
and glass objects > 1mm in diameter will show up on X-ray. Some objects
(eg wood) may not: USS may demonstrate these. CT or MRI are also
occasionally helpful.
Note: X-ray all wounds from glass that fully penetrate the skin
During X-ray, use radio-opaque markers (eg paper clip) taped to the skin
to identify the area of concern.
Wound swabs for bacteriology are unhelpful in fresh wounds, but obtain
them from older wounds showing signs of infection.
By far the most important investigation is:
Wound exploration under appropriate anaesthesia
Allows full assessment and thorough cleaning of wounds that extend fully
through the skin. Do not explore the following wounds in the ED:
• Stab wounds to the neck, chest, abdomen, or perineum.
• Compound fracture wounds requiring surgery in theatre.
• Wounds over suspected septic joints or infected tendon sheaths.
• Most wounds with obvious neurovascular/tendon injury needing repair.
• Other wounds requiring special expertise (eg eyelids).
Obtain relevant X-rays beforehand. Adequate anaesthesia is essential —
in adults LA (eg 1 % plain lidocaine) is often suitable ( b p.282), but
document any sensory loss fi rst (if there is altered sensation, presume
nerve injury and refer for formal exploration in theatre). Do not inject
LA into the edges of an infected wound: it will not work in that acidic
environment and it may spread the infection. GA may be the preferred
option for treating some wounds in young children.
Inspect wounds for FBs and damage to underlying structures. Most
problems with wound exploration relate to bleeding. If it proves diffi cult
to obtain a good view:
• Obtain a good light and an assistant. The assistant retracting on a stitch
placed on either side of the middle of the wound allows full exposure.
• Press on any bleeding point for ≥ 1min, then look again. Lidocaine with
adrenaline ( b p.283) is useful in scalp wounds which are bleeding
profusely.
• If bleeding continues, consider a tourniquet for up to 15min. Consider
a sphygmomanometer BP cuff infl ated above systolic pressure (after
limb elevation for 1min) on the limbs, or a ‘fi nger’ of a sterile rubber
glove may be used on fi ngers or toes. Never leave a patient alone with
a tourniquet on, lest it is forgotten. Ensure removal of the tourniquet
afterwards. Record the time of application and removal.
If these measures fail, refer for specialist exploration in theatre. Do
not blindly ‘clip’ bleeding points with artery forceps, for fear of causing
iatrogenic neurovascular injury. Sometimes, small blood vessels in the
subcutaneous tissues can be safely ligated using an appropriate absorbable
suture (eg 4/0 or 6/0 Vicryl (braided polyglactin) or Dexon).

405
FURTHER ASSESSMENT OF SKIN WOUNDS
The approach to foreign bodies
FBs within soft tissues can cause pain, act as a focus for infection, or
migrate and cause problems elsewhere. Therefore, remove FBs from
recent wounds where possible, particularly if lying near a joint (but if FB
is within a joint, refer to the orthopaedic team for formal exploration and
removal). FBs which can be seen or felt or are causing infection are usually
best removed. Finding FBs is frequently diffi cult without a bloodless fi eld
and good light. It may be appropriate to leave some FBs, such as gunshot
deeply embedded in buttock soft tissues (antibiotic cover advised).
However, most FBs of any size not removed in the ED warrant specialist
consideration.
Patients not infrequently present with symptoms relating to (suspected)
FBs under old healed wounds. In these circumstances, refer to an expert
for exploration under appropriate conditions.
Fishhooks
The barbs on some fi shhooks can make removal diffi cult. In some cases,
it may be necessary to push a fi shhook onwards (under LA) and thus out
through the skin — wire cutters can then cut through the hook below the
barb and allow release. Wear eye protection when doing this.
There are alternative methods for removing fi shhooks. Smaller fi shhooks
that are relatively superfi cially embedded can sometimes be pulled back
and removed through the entry wound once a hollow needle has been
advanced alongside the hook to cover the barb.

406 CHAPTER 9 Wounds, fractures, orthopaedics
Wound management
Wound cleaning
Thoroughly clean all wounds irrespective of whether closure is
contemplated, to d risk of infection. The standard agent used for wound
cleaning is 0.9 % (normal) saline, possibly preceded by washing using tap
water. Aqueous chlorhexidine or 1 % cetrimide solutions are sometimes
used. Do not use hydrogen peroxide or strong povidone iodine solutions.
Wounds ingrained with dirt may respond to pressure saline irrigation
(19G needle attached to 20mL syringe), or may require to be scrubbed
with a toothbrush (use goggles to d chance of conjunctival ‘splashback’).
Devitalized or grossly contaminated wound edges usually need to be
trimmed back (debrided), except on the hand or face. If dirt or other
foreign material is visible despite these measures, refer to a specialist, who
may choose to leave the wound open.
Wound closure
There are three recognized types of wound closure:
Primary closure Surgical closure (by whatever physical means) soon after
injury.
Secondary closure No intervention: heals by granulation (secondary
intention).
Delayed primary closure Surgical closure 3–5 days after injury.
If there is no underlying injury or FB, treat fresh wounds by primary
closure as soon as possible. Accurate opposition of wound edges and
obliteration of dead space provides the best cosmetic outcome with least
infection risk.
Wounds not usually suitable for primary closure in the ED include:
• Stab wounds to the trunk and neck.
• Wounds with associated tendon, joint or neurovascular involvement.
• Wounds with associated crush injury or signifi cant devitalized tissue/
skin loss.
• Other heavily contaminated or infected wounds.
• Most wounds > 12hr old (except clean facial wounds).
Methods of closure
If in doubt, sutures are usually the best option (see opposite).
Steri-Strips™ Adhesive skin closure strips allow skin edges to be opposed
with even distribution of forces. They are inappropriate over joints, but
useful for pretibial lacerations, where skin is notoriously thin and sutures
are likely to ‘cut out’. Before application, make Steri-Strips™ stickier by
applying tincture of benzoin to dry skin around the wound. Leave 3–5mm
gaps between Steri-Strips™. See also b Pretibial lacerations, p.481.
Skin tissue glue Particularly useful in children with superfi cial wounds and
scalp wounds. After securing haemostasis, oppose the dried skin edges before
applying glue to the wound. Hold the skin edges together for 30–60sec to
allow the glue to set. Ensure that glue does not enter the wound. Do not
use tissue glue near the eyes or to close wounds over joints.
407
WOUND MANAGEMENT
Staples Quick and easy to apply, particularly suited to scalp wounds.
Staple-removers are required for removal.
Sutures (‘stitches’ or ‘ties’) Traditional and most commonly used method
to achieve primary closure. Oppose the skin aiming for slight eversion
of wound edges, using strong non-absorbable inert monofi lament suture
material attached to curved cutting needles (eg prolene, polypropylene
or nylon) with knots tied on the outside. Interrupted simple surgical
knots tied using instruments are relatively easy, economical of thread
and have a low risk of needlestick injuries. Specialized continuous sutures
(eg subcuticular) are not appropriate for wounds in the ED. The size of
thread used and time to removal vary according to the site. Use absorbable
sutures (eg Vicryl) on the lips and inside the mouth. Absorbable sutures
may also be used to close subcutaneous tissues to d chance of haematoma
and infection. Suture choice and time to removal are given in Table 9.1 .
Key points when suturing
The technique of a basic instrument tie is shown in Figs 9.1 – 9.6 .
• Tie sutures just tight enough for the edges to meet.
• Do not close a wound under tension.
• Handle the skin edges with toothed forceps only.
• Avoid too many deep absorbable sutures.
• Mattress sutures are useful on some deep wounds, but avoid on hands
and face.
• Dispose of sharps as you use them — do not make a collection.
• Use strategic initial sutures to match up obvious points in irregular
wounds.
• If a suture does not look right — take it out and try again.
• If it still does not look right — get help!
Table 9.1 Suture choice and time to removal
Part of body Suture and size Time to
removal
Scalp 2/0 or 3/0 non-absorbable
†
glue
or staples
7 days
Trunk 3/0 non-absorbable
†
10 days
Limbs 4/0 non-absorbable
†
10 days
Hands 5/0 non-absorbable 10 days
Face 5/0 or 6/0 non-absorbable 3–5 days *
Lips, tongue, mouth Absorbable eg 6/0 Vicryl/Dexon –
†
One size smaller may be appropriate for children.
*
Sutures may be replaced with Steristrips at 3 days.
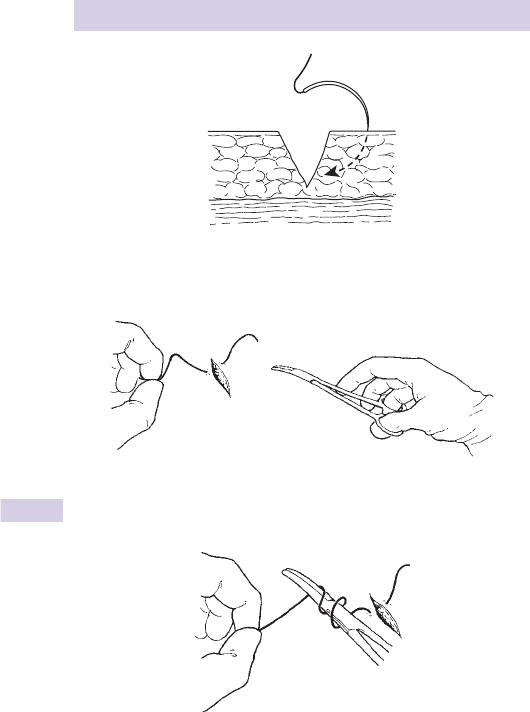
408 CHAPTER 9 Wounds, fractures, orthopaedics
Fig. 9.1
Fig. 9.2
Fig. 9.3
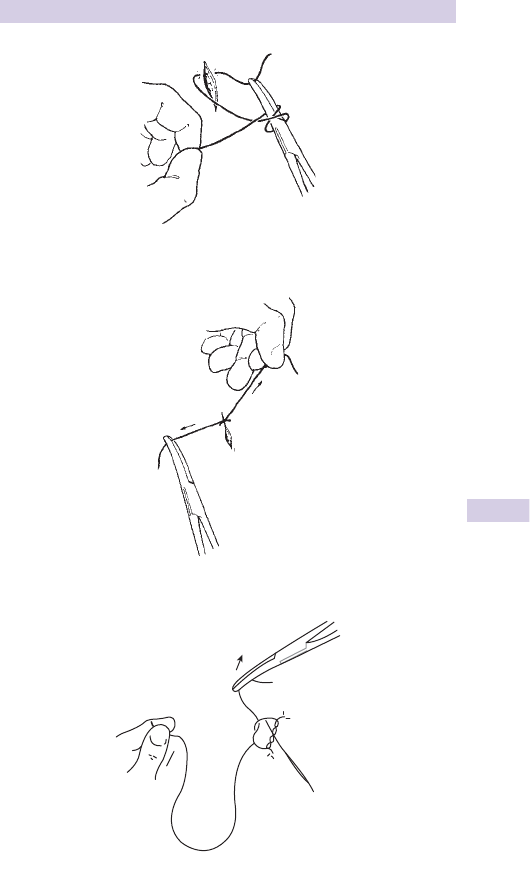
409
WOUND MANAGEMENT
Fig. 9.4
Fig. 9.5
Fig. 9.6

410 CHAPTER 9 Wounds, fractures, orthopaedics
Tetanus prophylaxis
Tetanus causes many deaths in the developing world. Occasional cases
still occur in the UK. Injecting drug users are at risk (particularly if using
SC or IM routes). The exotoxin tetanospasmin produced by the anaerobic,
spore-forming Gram + ve bacillus Clostridium tetani interferes with neuro-
transmission ( b p.236). Spore proliferation and toxin production is likely in
heavily contaminated wounds with devitalized tissue. However, any wound
(including a burn) is a potential risk: always ensure tetanus prevention.
Tetanus immunization programme
Standard active immunization involves an initial course of 3 IM or deep SC
doses of 0.5mL tetanus toxoid (formalin inactivated toxin) given at monthly
intervals starting at 2months of age, followed by booster doses at 4 and
14years. A full course of 5 doses is considered to result in lifelong immu-
nity. From 2006 in the UK, combined tetanus/diphtheria/inactivated polio
vaccine replaced previous tetanus/diphtheria vaccine for adults and adoles-
cents. Immunization required after injury depends upon immunization status
of the patient and the injury. Inadequate immunity against tetanus is particu-
larly likely in immigrants, the elderly, patients with d immunity and those who
have refused vaccination.
Anti-tetanus prophylaxis
The need for tetanus immunization after injury depends upon a patient’s
tetanus immunity status and whether the wound is ‘clean’ or ‘tetanus prone.’
The following are regarded as ‘tetanus prone’:
• Heavy contamination (especially with soil or faeces).
• Devitalized tissue.
• Infection or wounds > 6hr old.
• Puncture wounds and animal bites.
Follow Department of Health guidelines. See www.dh.gov.uk
Do not give tetanus vaccine if there is a past history of a severe reaction:
give HATI. Pregnancy is not a contraindication to giving tetanus prophylaxis.
Patient is already fully immunized
If the patient has received a full 5-dose course of tetanus vaccines,
do not give further vaccines. Consider human anti-tetanus immunoglob-
ulin (‘HATI’ 250–500units IM) only if the risk is especially high (eg wound
contaminated with stable manure).
Initial course complete, boosters up-to-date, but not yet complete
Vaccine is not required, but do give it if the next dose is due soon and it
is convenient to give it now. Consider human anti-tetanus immunoglob-
ulin (‘HATI’ 250–500units IM) in tetanus prone wounds only if the risk is
especially high (eg wound contaminated with stable manure).
Initial course incomplete or boosters not up-to-date
Give a reinforcing dose of combined tetanus/diphtheria/polio vaccine and refer
to the GP for further doses as required to complete the schedule. For tetanus-
prone wounds, also give one dose of HATI at a different site. The dose of
HATI is 250units IM for most tetanus prone wounds, but give 500units if > 24hr
have elapsed since injury or if there is heavy contamination or following burns.
Not immunized or immunization status unknown or uncertain
Give a dose of combined tetanus/diphtheria/polio vaccine and refer to
the GP for further doses as required. For tetanus-prone wounds, also give
one dose of HATI (250–500units IM) at a different site.

411
ANTIBIOTIC PROPHYLAXIS
Antibiotic prophylaxis
Antibiotics are not required for most wounds. Thorough cleaning is the
best way of preventing infection. After cleaning and closure, consider
oral antibiotic prophylaxis (eg penicillin + fl ucloxacillin) for certain
wounds: compound fi ngertip fractures and wounds in those at extra risk
(eg valvular heart disease, post-splenectomy). Co-amoxiclav has activity
against anaerobes, and is appropriate for bites and heavily contaminated
or infected wounds: leave these wounds open. Antibiotics are indicated
for penetrating injuries which cannot be properly cleaned ( b Puncture
wounds, p.419). Although a scientifi c basis is lacking, antibiotics are
frequently used for wounds > 6hr old, complex intra-oral wounds and in
workers at high risk (gardeners, farmers, fi shermen).

412 CHAPTER 9 Wounds, fractures, orthopaedics
Wound aftercare
Dressings
A large variety of dressings are available, with little scientifi c evidence to
help choose between them: choice depends upon personal preference/
prejudice and local departmental policy. A dry non-adherent dressing
will protect most wounds from inadvertent contamination in the fi rst
few days. Dressings are not usually necessary for facial and scalp wounds.
Beware circulatory problems resulting from encircling dressings/bandages
applied too tightly to digits or other parts of limbs. Burns dressings are
considered in b p.396.
General advice
Advise to keep wounds clean and dry for the fi rst few days. Limb wounds
require rest and elevation for the fi rst 24hr. After this, restrict movements
to avoid undue stress causing the suture line to open up (especially where
the wound is over a joint). Warn all patients to return if features of infec-
tion develop (redness, i pain, swelling, fever, red streaks up the limb).
Approximate times to suture removal are shown on Table 9.1 — these need
to be adjusted to meet the occasion. For example, sutures over joints are
sensibly left 14 days to avoid dehiscence. Similarly, sutures may need to be
left in for longer where wound healing may be delayed (eg DM, the elderly,
malnourished, and those on steroids). Local policy will dictate where suture
removal occurs (GP surgery or ED). If available, discharge with illustrated
instructions about wound care and suture removal. This may particularly
help patients with memory impairment or under the infl uence of alcohol.
Specifi c advice
Patients often ask when to return to work. If a question of personal safety
or safety of the public or work colleagues is involved, advise to return to
usual duties only once the wound has healed and sutures are out. This
particularly applies to food handlers and some workers with machinery.
Provide a sickness certifi cate for the patient’s employer as appropriate.
Review and delayed primary closure
Arrange review of heavily contaminated wounds, infected wounds not
requiring admission, and other wounds at particular risk of infection at
≈ 36hr. Check T
*
and look for wound discharge and erythema, ascending
lymphangitis, and regional lymphadenopathy. Systemic symptoms or evi-
dence of spreading infection despite oral antibiotics are indications for
admission for wound toilet, rest, elevation, and IV antibiotics.
Treat other wounds deemed initially to be at less risk of infection, but
not suitable for primary closure, with cleaning, light packing/dressing, and
review at 3–5 days. Ideal dressings keep wounds moist, so consider the
need for dressing changes prior to closure. If the wound is clean, employ
delayed primary closure after wound cleaning and debridement under
appropriate anaesthesia. If despite further cleaning and debridement,
foreign material remains ingrained, consider if the patient requires admis-
sion. If there is much exudate and evidence of local infection, take wound
swabs for culture, consider removing the sutures, clean and redress the
wound, give oral antibiotics, and arrange further review.
Do not use ‘loose closure’ in contaminated wounds. The technique has all
the risks of infection combined with a poor cosmetic result.

413
INFECTED WOUNDS AND CELLULITIS
Infected wounds and cellulitis
Wound infection after injury
Although prompt treatment with cleaning and primary closure will d risk,
any wound may become infected. The risk of infection is i by:
• Contamination (eg bites) and foreign material (including excess sutures).
• Haematoma.
• Devitalized tissue.
• Poor nutrition and d immunity (eg steroid therapy).
Pain is usually the fi rst clue to wound infection. Note that many soft tissue
infections (cellulitis, erysipelas) occur in the absence of an obvious wound
(see b Cellulitis and erysipelas, p.528).
Examination Indicates the extent of the infection. Erythema and tenderness
limited to the area around the wound suggest localized infection. Swelling
and fl uctuation are evidence of a collection of pus. Remove all sutures,
together with pus and devitalized tissue, under appropriate anaesthetic.
Send wound swabs for culture. Consider the possibility of a retained FB —
X-ray/explore as appropriate. After thorough cleaning, leave the wound
open, cover with a dressing and arrange review with a dressing change in
36hr. Consider the need for antibiotics (eg co-amoxiclav) particularly for
cellulitis, for the immunocompromised and for patients at particular risk
(eg those with prostheses and valvular heart disease).
Consider admission (for rest, elevation, analgesia, wound/blood cultures,
and IV antibiotics) in patients with one or more of the following:
• A red line spreading proximally (ascending lymphangitis).
• Regional (sometimes tender) lymphadenopathy.
• Pyrexia > 38 * C.
• Systemic upset.
Soft tissue crepitus is ominous, suggesting gas-forming organisms ( b p.237).
Infected hand wounds
A particularly common problem is an infected wound on the dorsum of
the hand over a MCPJ after a punch injury. These are often bite wounds,
presenting late with infection in the region of the joint. Refer for explora-
tion/washout in theatre and antibiotics ( b p.416).
Infected facial wounds
Take infected wounds of the cheek very seriously. They pose a signifi cant
threat of sepsis spreading intracranially, resulting in papilloedema and
ophthalmoplegia due to cavernous sinus thrombosis. Adopt a low
threshold for referring for admission and IV antibiotics.
Infected surgical wounds
Infection of a recent surgical wound after a planned procedure is a rel-
atively common complication. In addition to the possible threat to life,
wound infection can have disastrous implications as far as the success of
the preceding operation is concerned (eg hernias may recur). Contact
the team which performed the surgery as soon as possible, to allow the
surgeon to treat the complication.

414 CHAPTER 9 Wounds, fractures, orthopaedics
Bite wounds
Bites and infection
Bites cause contaminated puncture wounds, contaminated crush injuries,
or both. All carry a high risk of bacterial infection, some also a risk of viral
or other infections (eg rabies).
Bacterial infection is particularly likely in:
• Puncture wounds (cat/human bites).
• Hand wounds, wounds > 24hr old.
• Wounds in alcoholics, diabetics, or the immunocompromised.
Bacteria responsible include: streptococci, Staphylococcus aureus , Clostridium
tetani , Pasteurella multocida (cat bites/scratches), Bacteroides , Eikenella
corrodens (human bites).
Approach
Establish what the biting animal was, how long ago and where the bite
occurred. Obtain X-rays if fracture, joint involvement (look for air) or
radio-opaque foreign body (FB) (tooth) is suspected.
Management of bite wounds
Cleaning
Explore fresh bite wounds under appropriate anaesthetic, debride and clean
thoroughly with ‘normal’ saline (or by washing using tap water). Refer sig-
nifi cant facial wounds and wounds involving tendons or joints to a specialist.
Closure
Cosmetic considerations usually outweigh risks of infection for most facial
wounds, so aim for primary closure. Elsewhere, choose between primary
or delayed primary closure — the latter is usually preferred in bite wounds
affecting limbs, due to the increased risk of infection. Do not close
puncture bite wounds that cannot be satisfactorily irrigated.
Antibiotic prophylaxis
Deciding whether or not to employ prophylactic antibiotics for bite
wounds can be diffi cult and is controversial. Many departments advocate
prophylactic antibiotics for all bite wounds. One approach is to give
antibiotics for patients with any of the following:
• Puncture bites.
• Crush injuries with devitalized tissues.
• Bites to the hand, wrist, or genitals.
• Bites that are primarily closed.
• Bites from humans, cats, and rats.
• Bitten individuals who are immunocompromised (eg immunosuppressed,
diabetes, post-splenectomy, rheumatoid arthritis, those with prosthetic
joints).
Co-amoxiclav is an appropriate broad spectrum agent, effective against
Strep , Staph , Pasteurella , and Eikenella . Alternatives for patients allergic to
penicillin/amoxicillin include doxycycline + metronidazole or (especially if
pregnant) ceftriaxone alone.
Do not use erythromycin or fl ucloxacillin alone as prophylaxis.

415
BITE WOUNDS
Tetanus
Bite wounds are tetanus-prone. Give prophylaxis accordingly (b p.410).
Rabies (covered fully in b p.249)
Rabies results after the ‘bullet-shaped’ RNA rhabdovirus present in saliva
of infected animals is transmitted to humans via a mucous membrane or
skin break. After thorough cleaning, refer all patients who might have
been in contact with a rabid animal to an Infectious Diseases specialist.
Obtain further help from the Virus Reference Laboratory, London (020
8200 4400). The long incubation period of the rabies virus (14–90 days)
allows successful post-exposure prophylaxis at even a relatively late stage,
according to agreed guidelines.
Hepatitis, HIV
Consider possible risks of hepatitis B, C, and HIV in anyone who presents
following a human bite and treat accordingly (see under b Needlestick
injury, p.418). Quantifying risks can be diffi cult, particularly for example, in
‘reverse fi ght bites’ ( b p.416) where the other person involved may be
unknown. If in doubt, take a baseline blood sample for storage (to allow
later testing if necessary) and provide cover against hepatitis B.
Treatment of infected bites
Most bacterial infections occur > 24hr after injury and are due to
staphylococci or anaerobes. Pain, infl ammation, swelling ± regional
lymphadenopathy within 24hr suggests P. multocida infection. Take wound
swabs of all infected wounds, then treat with cleaning, elevation, analgesia,
and antibiotics. Oral co-amoxiclav and outpatient review at ≈ 36hr is
appropriate for localized wound infection with no systemic symptoms and
no suspected underlying joint involvement. Refer patients with spreading
infection for IV antibiotics and admission.
Septicaemia is uncommon after bite injury, but has been reported with
the Gram –ve bacillus Capnocytophaga canimorsus , previously known as
Dysgonic Fermenter 2 (DF-2). Infection produces a severe illness with
septicaemia and DIC, often in immunocompromised (splenectomized
individuals, diabetics, or alcoholics). Take wound swabs and blood
cultures, then give IV antibiotics and refer.
Prevention of dog bites
Injury prevention measures aimed at preventing children from being bitten
includes legislation relating to ‘dangerous dogs’ and education. Children
may be taught the following:
• To treat dogs with respect.
• To avoid disturbing a dog that is sleeping, eating, or feeding puppies.
• To avoid shouting or running in the presence of a dog.
• Not to approach or play with unfamiliar dogs.

416 CHAPTER 9 Wounds, fractures, orthopaedics
Specifi c bites and stings
Human bites and ‘fi ght bites’
Many human bites occur ‘in reverse’, when an individual punches another
in the mouth, causing wounds on the dorsum of the hand over the MCPJs.
Underlying joint involvement is common and may progress to septic
arthritis unless treated aggressively with exploration, irrigation and anti-
biotics. Refer all patients for this. Consider hepatitis B, C, and HIV, give
appropriate prophylaxis ( b Needlestick injuries, p.418) and arrange
counselling.
Tick bites
Ticks are recognized vectors of a number of exotic diseases worldwide.
In the UK, patients often present with embedded sheep ticks. Remove
ticks by gentle traction with blunt forceps applied as close to the skin as
possible. Avoid traditional folklore methods of removal, which may cause
the tick to regurgitate, promoting infection. In areas where Lyme disease
is endemic (see b p.231), some physicians provide antibiotic prophylaxis
with amoxicillin.
Insect bites
Minor local reactions are common. Treat with ice packs, rest, elevation,
analgesia and antihistamines (eg chlorphenamine PO 4mg tds or a non-
sedating alternative such as loratadine PO 10mg od). Occasionally, insect
bites may be complicated by cellulitis and ascending lymphangitis requiring
antibiotics ( b Infected wounds and cellulitis, p.413).
Wasps and honey bee stings
May cause local reactions or anaphylaxis—treat promptly (b p.42). Flick
out bee stings left in the skin. Treat local reactions as for insect bites.
Jellyfi sh stings and fi sh spines
Most jellyfi sh in UK coastal waters are harmless. Wash the bitten part in sea
water then pour vinegar (5 % acetic acid) over it to neutralize the toxin.
Fish spines (typically Weever fi sh) produce a heat labile toxin, which
may be neutralized by immersion in hot water for 30min. Occasionally,
tiny parts of the fi sh spines become embedded and cause long-term
irritation. Localizing and removing these tiny FBs is diffi cult, so refer to an
appropriate expert.
Contact with other wild animals
Contact with rats’ urine may cause leptospirosis (Weil’s disease) — see
b p.239. Provide prophylactic doxycycline to anyone who presents
following an episode of signifi cant exposure (eg immersion in river water
or sewage). Unusual bites may pose specifi c threats, which infectious
disease specialists will advise about (eg monkey bites may cause herpes
simplex infection: give prophylactic oral aciclovir). Bats may carry rabies
( b p.249).

417
SPECIFIC BITES AND STINGS
Snake bites
The European adder is the only native venomous snake in the UK. It is
grey/brown, with a V-shaped marking behind the head and dark zig-zag
markings on the back. Most bites occur in summer. Venom is injected by
a pair of fangs. The venom contains enzymes, polypeptides, and other low
molecular weight substances. Only 50 % of bites cause envenomation.
Features
Envenomation causes pain and swelling: look for 2 puncture marks 1cm
apart. Vomiting, abdominal pain, diarrhoea, and hypotension may follow.
Investigation
Check urine, perform an ECG, and take blood for: FBC, U&E, LFTs,
coagulation screen, and D-dimer.
Treatment
• Prehospital : rest (and avoid interference with) the bitten part.
• Clean and expose wound, give analgesia and IV fl uids for hypotension.
• Treat anaphylaxis urgently according to standard guidelines
( b Anaphylaxis, p.42).
• Give prophylactic antibiotics (eg co-amoxiclav) and ensure tetanus
cover.
• Antivenom has its own risk of anaphylaxis, but may be given for signs of
systemic envenoming, hypotension, WCC > 20 × 10
9
/L, ECG changes,
elevated cardiac enzymes, metabolic acidosis or signifi cant limb swelling
(eg past the wrist for bites on the hand, or past the ankle for bites on
the foot, within 4 hr).
• Obtain specifi c advice from a Poisons Information Centre ( b p.181).
• Observe for least 24hr, all patients who have any symptoms after snake
bite.

418 CHAPTER 9 Wounds, fractures, orthopaedics
Needlestick injury
A needlestick injury is a specialized puncture wound. In a clinical setting, it
may represent failure to follow universal precautions ( b p.32) and should
provoke a review of policy and procedure.
Many infective agents have been transferred by needlestick: Blastomycosis,
Brucellosis, Cryptococcosis, Diphtheria, Ebola fever, Gonorrhoea, Hepatitis B,
Hepatitis C, Herpes zoster, HIV, Leptospirosis, Malaria, Mycobacteriosis,
Mycoplasmosis, Rocky Mountain spotted fever, Scrub typhus, Sporotrichosis,
Staph aureus , Strep pyogenes , Syphilis, Toxoplasmosis, TB.
In practice, the principal risks are hepatitis B and C and HIV. The risk of
acquiring hepatitis B following a needlestick from a carrier has been estimated
at 2–40 % . All hospital workers should be immunized against hepatitis B and
have regular checks of their antibody status. The risk of hepatitis C is believed
to be 3–10 % . In contrast, the risk of acquiring HIV after needlestick with HIV
+ ve source is much less (estimated at 0.2–0.5 % , but may be higher if signifi -
cant volumes are injected). There is a small ( ≈ 0.03 % ) risk of HIV transmis-
sion after mucocutaneous exposure (ie exposure of cuts, abrasions, mucous
membranes including the eye). The (small) risk of acquiring HIV following
needlestick injury from a person with known HIV may be reduced further
by post-exposure prophylaxis, but time is of the essence (see below). No
proven post-exposure prophylaxis currently exists for hepatitis C. Preventing
needlestick injuries and exposure to these viruses is therefore crucial.
Management
• Wash the wound with soap and water.
• Ensure tetanus cover.
• Ensure hepatitis B cover: if not previously immunized, give hepatitis B
immunoglobulin and start an active immunization course (give fi rst vaccine
in the ED and arrange subsequent doses). If previously immunized, check
antibody titres. If satisfactory, take no further action. If low, give booster
vaccine. If very low give both immunoglobulin and start vaccine course.
Many local needlestick policies advise obtaining informed consent from
the source patient, prior to taking blood to check hepatitis and HIV status.
In practice, the identity of the source patient is not always clear: do not
withhold hepatitis B prophylaxis if there is any doubt.
• If the source patient is known to be (or suspected of being) HIV + ve,
follow local guidelines and/or refer immediately to an infectious dis-
eases specialist to discuss post-exposure prophylaxis and follow-up.
Follow Department of Health guidance on www.dh.gov.uk Combined
prophylaxis therapy (eg 1 Truvada
®
tablet od and 2 Kaletra
®
tablets bd –
ie 245mg tenofovir od + 200mg emtricitabine od + 400mg lopinavir bd +
100mg ritonavir bd) is most effective if started within an hour of exposure,
but may be worth considering up to 72hr. However, prophylaxis has side
effects, especially diarrhoea. Involve both healthcare worker and a local
expert in deciding whether or not to start prophylaxis. Either way, advise
the patient to use barrier contraception and not to give blood as a donor
until subsequent HIV seroconversion has been ruled out.
• Take baseline blood for storing (serology for possible future testing),
and in the case of a possible HIV source patient, also take FBC, U&E,
LFTs, and amylase).
• If the incident occurred in hospital, report it to Occupational Health.

419
PUNCTURE WOUNDS
Puncture wounds
Puncture wounds are small skin wounds with possible deep penetration.
Stab wounds to the trunk and neck are considered elsewhere
( b Penetrating chest injury, p.340).
Puncture wounds often involve the sole of the foot, patients having
trodden on a nail. Examine to exclude neurovascular injury, then obtain an
X-ray looking for FB. If signifi cant foreign material is present radiologically,
or the patient has associated fracture, tendon injury, or neurovascular
defi cit, refer for formal exploration and cleaning in theatre under a
bloodless fi eld. Otherwise:
• Irrigate and clean other wounds under local anaesthetic (LA) where
possible (consider nerve blocks). For wounds to the sole of the foot
this may be impractical. As a compromise, immerse foot in warm anti-
septic (eg povidone iodine solution) for 15min.
• Apply a dressing and advise review/follow-up with GP as appropriate.
• Ensure adequate tetanus cover ( b Tetanus prophylaxis, p.410).
• Prescribe simple analgesia.
• Strongly consider prophylactic oral antibiotic cover (eg co-amoxiclav).
Some puncture wounds may become infected despite treatment. This may
be due to retained foreign material in the wound. Pseudomonas osteitis is
an uncommon, but recognized complication of puncture wounds to the
foot, particularly where a nail has gone through training shoes to cause
the wound. Refer infected wounds for formal exploration and irrigation.

420 CHAPTER 9 Wounds, fractures, orthopaedics
How to describe a fracture
Clear, precise, complete descriptions of fractures aid accuracy and save
time when referring patients.
System for describing fractures
• State the age of the patient and how the injury occurred.
• If the fracture is compound, state this fi rst (and Gustilo type —
b p.422).
• Name the bone (specify right or left, and for the hand, whether dominant).
• Describe the position of the fracture (eg proximal, supracondylar).
• Name the type of fracture (eg simple, spiral, comminuted, crush).
• Mention any intra-articular involvement.
• Describe deformity (eg displacement, angulation) from anatomical
position.
• State grade or classifi cation of fracture (eg Garden IV).
• State presence of any complications (eg pulse absent, paraesthesia,
tissue loss).
• Other injuries and medical problems.
Example using this system
‘29 year old male motorcyclist with a compound fracture of the left
humerus. It is a transverse fracture of the humeral shaft and is Gustilo type I
compound and minimally displaced with no neurovascular compromise … ’
Type of fracture
Simple Single transverse fracture of bone with only 2 main fragments.
Oblique Single oblique fracture with only 2 main fragments.
Spiral Seen in long bones as a result of twisting injuries, only 2 main
fragments.
Comminuted Complex fracture resulting in > 2 fragments.
Crush Loss of bone volume due to compression.
Wedge Compression to one area of bone resulting in wedge shape
(eg vertebra).
Burst Comminuted compression fracture with scattering of fragments.
Impacted Bone ends driven into each other.
Avulsion Bony attachment of ligament or muscle is pulled off.
Hairline Barely visible lucency with no discernible displacement.
Greenstick Incomplete fracture of immature bone follows angulatory force,
with one side of the bone failing in compression, the other side in tension.
Torus/buckle Kinking of the metaphyseal cortex follows axial
compression.
Plastic deformation Deformation beyond the elastic limit but below the
fracture point results in bending of bone ± microfractures (not apparent
on X-ray).
Pathological Fracture due to underlying disease (eg osteoporosis,
metastasis, Paget’s disease).

421
HOW TO DESCRIBE A FRACTURE
Stress Certain bones are prone to fracture after repetitive minor injury.
Fracture-dislocation Fracture adjacent to or in combination with a
dislocated joint.
Deformity Describe deformity using the terms displacement, angulation
and rotation.
Displacement (‘translation’) Describe the relative position of two bone
ends to each other. Further describe the direction that the distal fragment
is displaced from the anatomical position (eg volar, lateral). Also estimate
the degree of apposition of the bone ends (eg 50 % ).
Angulation This is usually described in terms of the position of the point
of the angle (eg posterior angulation means that the distal fragment is
pointing anteriorly). This can sometimes be confusing. Although a little
long-winded, one way to avoid confusion is to describe the direction
in which the distal part points, relative to the anatomical position (eg a
Colles’ fracture may be described as a ‘fracture of the distal radius in
which the distal fragment points dorsally’). Try to measure the angle on
X-ray.
Rotation Describe the degree of rotation from the anatomical position, in
terms of the direction (eg external or internal rotation) in which the distal
part has moved.
Fractures — the role of osteoporosis
Osteoporosis is an important factor in a signifi cant proportion of fractures
seen in the ED. The following fractures are frequently (but by no means
exclusively) associated with osteoporosis:
• Colles’ fracture ( b p.444).
• Fracture of surgical neck of humerus ( b p.459).
• Lumbar spine vertebral fracture.
• Fracture of neck of femur ( b p.470).
• Pubic rami fracture ( b p.466).
Patients with post-menopausal osteoporosis may be treated with
a biphosphonate in an attempt to d risk of future fractures, but do not
commence this treatment in the ED.
Long bone anatomy
Each long bone has a shaft or diaphysis with an epiphysis at each end.
While the bone is growing these are separated by an epiphyseal growth
plate and this narrows down into the bone shaft. The transitional area
of bone is the metaphysis. In addition to these landmarks, the femur and
humerus have a ball-shaped head, a narrower neck, and at the lower ends
a widened area consisting of the medial and lateral condyles of the femur,
and the medial and lateral epicondyles of the humerus. Fractures prox-
imal to these areas of the femur and humerus are termed supracondylar.
Intercondylar fractures involve the central, distal, and juxta-articular
portion. Fractures of the proximal femur between the greater and lesser
trochanters are termed intertrochanteric.

422 CHAPTER 9 Wounds, fractures, orthopaedics
Compound fractures
Compound (or open) fractures occur when a fracture is open to the air
through a skin wound. They incur a risk of infection and can be associated
with gross soft tissue damage, severe haemorrhage, or vascular injury. Treat
as orthopaedic emergencies requiring rapid assessment and treatment.
Classifi cation of compound injuries
Gustilo classifi cation of compound injuries:
Type I Compound fracture where wound is <1cm long and appears clean.
Type II Compound fracture where wound > 1cm, but is not associated
with extensive soft tissue damage, tissue loss, or fl ap lacerations.
Type IIIA Either: compound fracture with adequate soft tissue coverage of
bone despite extensive soft tissue damage or fl ap laceration or any fracture
involving high energy trauma or bone shattering regardless of wound size.
Type IIIB Compound fracture with extensive soft tissue loss, periosteal
stripping, and exposure of bone.
Type IIIC Compound fracture associated with vascular injury needing repair.
Management
Provide adequate fl uid replacement, analgesia, splintage, antibiotics, and
tetanus prophylaxis prior to surgical treatment. Rapidly complete the
following steps while contacting orthopaedic service:
• Treat life-threatening injuries before limb threatening injuries. Do not
be distracted from initial priorities by dramatic distal limb injuries.
• Control obvious haemorrhage by direct manual pressure whilst
commencing IV fl uids and/or blood replacement.
• Give analgesia in the form of incremental IV opioids ( b p.276).
• Once analgesia is adequate, correct obvious severe deformities with
gentle traction and splint. Certain dislocations may require immediate
correction. Remove obvious contaminants if possible (eg large lumps of
debris or plant matter).
• ‘Routine’ wound swabs for bacteriological culture are no longer recom-
mended. They do not alter management and are poor predictors of
deep infection.
• If available, take digital photographs of the wound (this helps to avoid
the need for repeated inspection by different clinicians).
• Irrigate with saline, then cover the wound with a sterile moist dressing
(eg saline soaked pads). Immobilize the limb in a POP backslab. Do not
repeatedly inspect the wound as this greatly i risk of infection. Once
dressed and in POP, leave injuries covered until surgery.
• Give IV antibiotics (eg co-amoxiclav (1.2g) or cefuroxime (1.5g)
according to local policy). Consider adding gentamicin or metronida-
zole if the wound is grossly contaminated.
• Give tetanus toxoid if indicated, and give HATI if gross wound
contamination present (b p.410).
Record presence/absence of distal pulses/sensation and recheck frequently.
Limb salvage or amputation
Orthopaedic surgeons often face a diffi cult decision as to whether or not
a limb can be salvaged. Gustilo type IIIC injuries are associated with a
high rate of amputation. The Gustilo classifi cation alone is not always an
accurate predictor of outcome: other tools have been developed to assist.
For example, the Mangled Extremity Severity Score takes into account the
extent of skeletal and soft tissue damage, the extent and severity of limb
ischaemia, associated shock, and age.

423
DISLOCATIONS
Dislocations
A dislocation involves complete loss of congruity between articular
surfaces, whereas a subluxation implies movement of the bones of the
joint, but with some parts of the articular surface still in contact. Describe
dislocations in terms of the displacement of the distal bone. For example,
the most common shoulder dislocation is described as ‘anterior’, with the
humeral head lying in front of the glenoid. Aim to reduce dislocations as
soon as possible in order to prevent neurovascular complications, d risk
of recurrence and d pain. However, in general, aim to X-ray (to identify
the exact dislocation ± associated fracture) before attempting a reduction.
Exceptions to this principle are:
• Dislocations associated with considerable neurovascular compromise
requiring urgent intervention (this includes some ankle fracture-
dislocations).
• Uncomplicated patellar dislocations (see b Knee fractures and
dislocations, p.476).
• Uncomplicated mandibular dislocations (see b Mandibular injuries,
p.376).
• Some patients with (very) recurrent shoulder dislocations, where there
may be longer-term concerns regarding radiation exposure.
• Some patients with collagen disorders resulting in hypermobility
(eg Ehlers–Danlos syndrome) and unusual/recurrent dislocations
without signifi cant trauma.
• ‘Pulled elbow’ in young children (see b Paediatric upper limb injuries,
p.724).
Use analgesia/sedation/anaesthesia appropriate to the dislocation and
the individual circumstances. For example, patellar dislocations often
reduce under Entonox
®
, fi nger proximal interphalangeal joint (PIPJ)
dislocations with LA digital nerve blocks, shoulder dislocations with IV
analgesia ± sedation, whereas posterior hip dislocations typically require
manipulation under GA. Except in very exceptional circumstances, X-ray
after manipulation to confi rm adequate reduction and also to check for
fractures which may not have been apparent on initial X-rays.

424 CHAPTER 9 Wounds, fractures, orthopaedics
Casts and their problems
Plaster of Paris (POP)
POP is cheap, easy to use and can be moulded. Usually applied in the form
of a bandage or multiply folded as a supporting slab (see Figs 9.7 and 9.8 ).
Disadvantages are susceptibility to damage (POP rapidly disintegrates if wet)
and that it takes up to 48hr for larger casts to dry fully after application. Cut
slabs to shape prior to use and apply over wool roll and stockinette. Mould
with palms (not fi ngertips) to avoid point indentation of plaster.
Resin casts
More costly, but lighter and stronger than POP and more resistant to
water or other damage. Made of cotton or fi breglass impregnated with
resin that hardens after contact with water. Sets in 5–10min, maximally
strong after 30min. Resin casts are more diffi cult to apply and remove.
Being more rigid and harder to mould, there is i risk of problems from
swelling or pressure necrosis. Remove/cover any sharp edges on the cast.
Complications of casts
Give all patients discharged with casts clear written instructions (including
a contact phone number) to return if they develop pain or other symp-
toms in the immobilized limb. Formal cast checks within 24hr are only
required if there is particular concern about swelling. Simple swelling or
discolouration of fi ngers or toes usually responds to elevation and simple
exercises.
Is the cast too tight?
Act immediately upon suspicion of circulatory compromise from a cast.
Look for the ‘fi ve p’s: pain, pallor, paraesthesia, paralysis, and ‘perishing
cold’. If any of these are present:
• Elevate limb.
• Cut wool and bandages of backslab until skin is visible along the whole
length of limb.
• Split full casts and cut through all layers until skin is visible along the
whole length of limb.
Any undivided layers will continue to obstruct the circulation until
released. If this action fails to completely relieve the symptoms, contact
orthopaedic and vascular surgery staff immediately, as angiography and
urgent surgical intervention may be required. Note that compartment
syndrome may occur in the presence of normal pulses.
Is the cast too loose?
Test by trying to move the plaster longitudinally along the limb. Replace
excessively loose or damaged casts, unless there is an outweighing risk of
fracture slippage.
Local discomfort
If there is local pressure discomfort (eg over a malleolus), cut a window
in the cast to allow direct inspection of the skin. Trim or replace plasters,
which restrict movement unduly.
Cast removal
Standard POP and selected resin casts may be removed with plaster
shears. Use a plaster saw only after instruction in its proper use. In both
cases, be careful to avoid skin damage.
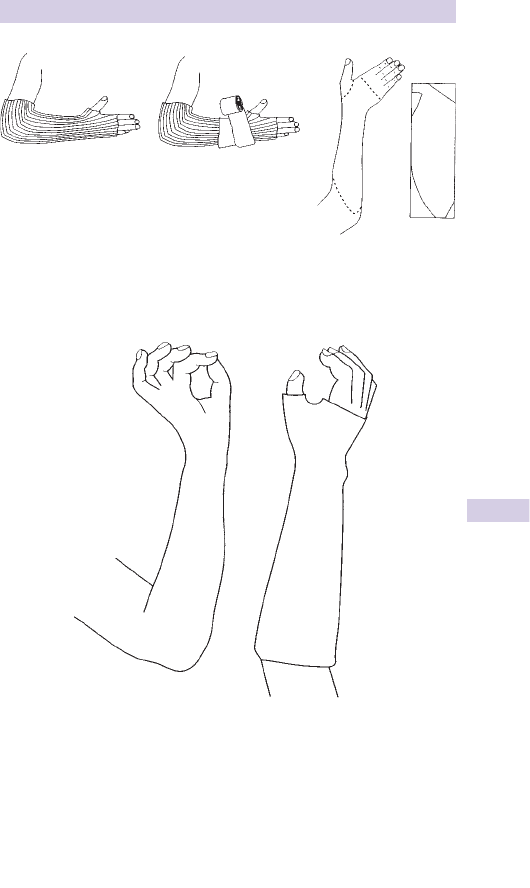
425
CASTS AND THEIR PROBLEMS
Application of
stockinette
Application of
wool roll
Limb positional POP
shape
Fig. 9.7 Application of a Colles’ backslab POP.
Limb position
Sca
p
hoid POP sha
p
e
Fig. 9.8 Application of a scaphoid POP.

426 CHAPTER 9 Wounds, fractures, orthopaedics
Soft tissue injuries
Sprains
These occur from overstretching and tearing of ligaments. Sprains vary
from sparse fi brous tears to complete disruption of a ligament complex.
The results are pain, tenderness, and soft tissue swelling. Ligament sprains
are traditionally graded into three types, although distinguishing clinically
between them may be diffi cult:
• First degree sprains involve minor tearing of ligament fi bres and are
entirely stable.
• Second degree sprains are more severe partial sprains — there may be some
resultant slight ligamentous laxity, but with a defi nite end-point on stressing.
• Third degree sprains refl ect completely torn ligaments causing signifi cant
laxity: patients sometimes report hearing a ‘snap’ at the time of injury.
Ligament sprains are very common, but there is a lack of reliable evidence
about treatment. Prolonged immobilization seems to be detrimental
to recovery, due to muscle wasting and loss of proprioception. Painful
minor sprains respond well to traditional measures: ice, compression
with elastic support/strapping, elevation and progressive mobilization as
soon as symptoms allow. Simple analgesics such as paracetamol or NSAID
(eg ibuprofen) may help. Complete ligament rupture can be relatively
painless, but if associated with gross joint instability may require surgical
repair. Associated haemarthroses require orthopaedic appraisal, aspiration,
and often initially, protection and immobilization in POP.
Strains
Indirect injury involving muscle-tendon units may be classifi ed in a similar
fashion to ligament sprains. Pain on palpation over the site of injury is also
reproduced by passive stress or active contraction of the affected muscle
unit. Sometimes, a palpable defect may be apparent in complete ruptures
(which typically occur at the musculotendinous junction). However, asso-
ciated swelling may prevent any defect from being easily palpable. Treat
minor strains similarly to sprains; consider specialist review for complete
ruptures, some of which may require surgical repair.
Direct muscle injuries
These result from direct impact causing local pain, bruising, and soft
tissue swelling. Note that associated bone contusions can occur, such as
in the perimeniscal areas of the knee (these are visible on MRI). Treat
minor injuries with ice, analgesia, and early mobilization within the limits
of symptoms. For more signifi cant injuries, consider and treat according
to possible risks of compartment and crush syndromes (with rhabdomy-
olysis) and large haematomas (see next section).
Haematomas
Blood can accumulate as a result of traumatic disruption of the vascular struc-
tures in bone, muscle, or soft tissues. Deceptively large volumes of blood can
be accommodated within the soft tissue planes of the chest wall or thigh.
In the presence of massive visible bruising of the torso or a limb, check for
shock and measure Hb and Hct. Perform a coagulation screen. Blood trans-
fusion may be necessary. Treat minor haematomas with compression dress-
ings, ice and consider ultrasound therapy. Large haematomas or supervening
infection requires selective surgical drainage, haemostasis and antibiotics.

427
OTHER SOFT TISSUE PROBLEMS
Other soft tissue problems
Myositis ossifi cans
After some muscle or joint injuries, calcifi cation can occur within a hae-
matoma leading to restriction of movement and loss of function. Frequent
sites include calcifi cation within a quadriceps haematoma (eg following a
rugby injury) where inability to fl ex the knee > 90 * at 48hr after injury
indicates an i risk of myositis ossifi cans. Other sites include the elbow
and femur. Passive stretching movements of joints may be implicated
in the development of myositis ossifi cans. This particularly applies at
the shoulder, hip, and knee, where passive exercises are performed for
spasticity following paraplegia or head injury.
Treatment involves immobilizing the limb or joint for a period of weeks,
under specialist supervision. Early excision is contraindicated, as it is
invariably followed by massive recurrence, but delayed excision (after
6–12 months) can improve function.
Tendonitis/tenosynovitis
This includes a wide range of conditions, some of which may have medico-
legal implications (‘overuse’ or ‘repetitive strain’ injury). Examples include:
• Classic tenosynovitis : swelling along a tendon sheath, with pain on passive
stretching or upon attempted active movement against resistance.
• Chronic paratendonitis (eg affecting Achilles tendon): swelling around the
tendon with localized pain and tenderness.
• Tendon insertion infl ammation causes epicondylitis in adults (see b
p.452) and traction apophysitis in children ( b Osteochondritis, p.708).
Appropriate initial treatment usually includes rest, immobilization,
and NSAID. Later, consider involving an appropriate specialist (eg
physiotherapist or hand therapist).
Bursitis
Infl ammation of bursae most frequently affects the subacromial,
olecranon, and prepatellar bursae. There is localized swelling and
tenderness: generalized joint effusion and/or tenderness along the whole
joint line suggests an alternative diagnosis. In many instances, bursitis is
non-infective, and responds to rest and NSAID. Signifi cant warmth
and erythema raise the possibility of an infective origin. In this case,
consider aspiration for bacteriological culture and provide antibiotics (eg
co-amoxiclav or penicillin + fl ucloxacillin).
Other problems
Other causes of joint or limb pain with no specifi c history of trauma in
the adult patient include stress fractures, cellulitis, and other infections,
osteoarthritis and other forms of acute arthritis, and nerve compression
(eg carpal tunnel syndrome). Apparently atraumatic limb pain in children
may present with limping — likely underlying causes vary according to the
age ( b The limping child, p.704).

428 CHAPTER 9 Wounds, fractures, orthopaedics
Physiotherapy in the ED
At its simplest, the term ‘physiotherapy’ in the ED includes the advice
given to each patient following minor injury. At the other extreme, it
encompasses the assessment and treatment of selected patients by skilled,
experienced physiotherapists. It is valuable for a department to have close
links with a physiotherapy unit, preferably with designated physiotherapy
staff responsible for ED referrals. Find out local arrangements for access
to and use of physiotherapy services.
‘Everyday’ physiotherapy
Minor soft tissue injuries are amongst the most commonly seen problems
in EDs. Once bony injury has been excluded (clinically and/or radiologi-
cally) ensure that patients are discharged with clear, consistent advice on
how to manage their own injuries in every case:
• Be clear and specifi c about what the patient is to do.
• Set a realistic time limit after which the patient should seek further
attention if their symptoms are not improving.
• Give additional written instructions for reinforcement (eg ankle sprains,
minor knee injuries) as patients forget much verbal advice.
Protection/rest/ice/compression/elevation (PRICE)
This forms the traditional basic framework for treatment of most acute
soft tissue injuries.
Protection
Protect the injured part (eg using crutches or a walking stick).
Rest
With most acute injuries, advise a period of 24–48hr rest after an injury.
Ice
Ice is often advocated both in immediate fi rst aid of soft tissue injuries,
and in subsequent treatment. Crushed ice cubes wrapped in a damp cloth
(to avoid direct contact with the skin) placed against an injured joint may
d swelling and pain. Do not apply for more than 10–15min at a time.
Repeat every few hours initially. A cold pack or bag of frozen vegetables
can be used (do not refreeze if for consumption!).
Compression
Despite a distinct lack of evidence, injured joints (particularly the ankle)
are often treated in some support. The easiest to use is an elasticated
tubular bandage (eg Tubigrip
®
), either single or doubled over. If provided,
advise not to wear it in bed and to discard as soon as convenient. If not
provided, explain why, or the patient may feel inadequately treated. Avoid
providing support bandages to patients with elbow and knee injuries — the
bandage tends to be uncomfortable and ‘dig in’ and in the case of the
knee, may affect venous return and i chance of DVT.
Elevation
Initially, advise elevation of injured limbs above horizontal to d swelling
and discomfort. This is particularly important in hand or foot injuries.
Exercise
Start gentle, controlled exercises for any injured joint as soon as symp-
toms allow. Demonstrate what is expected and confi rm that the patient
understands what to do.

429
PHYSIOTHERAPY IN THE ED
Formal physiotherapy
Physiotherapists are trained in the rehabilitation and treatment of injury,
based on a detailed knowledge of relevant limb and joint anatomy, bio-
mechanics, and physiology. In the ED, physiotherapy staff are valuable in
assessment and treatment of acute soft tissue injuries, patient education
and advice, and in the provision of appropriate mobility aids after injury
(particularly in the elderly). In order to make the best use of physiotherapy
services, follow these guidelines:
• Refer early if required for acute injury. Aim for the patient to be seen
for initial assessment the same day, so treatment needs can be properly
assessed.
• Discuss the problem and treatment options with the physiotherapy staff
prior to referral.
• Use the physiotherapy service for selected cases, not as a general rule.
• Never use the physiotherapy department to simply offl oad diffi cult or
problematic patients.
Physiotherapists have a range of different treatments at their disposal,
which typically focus upon regaining range of movement and mobility,
improving strength and proprioception.
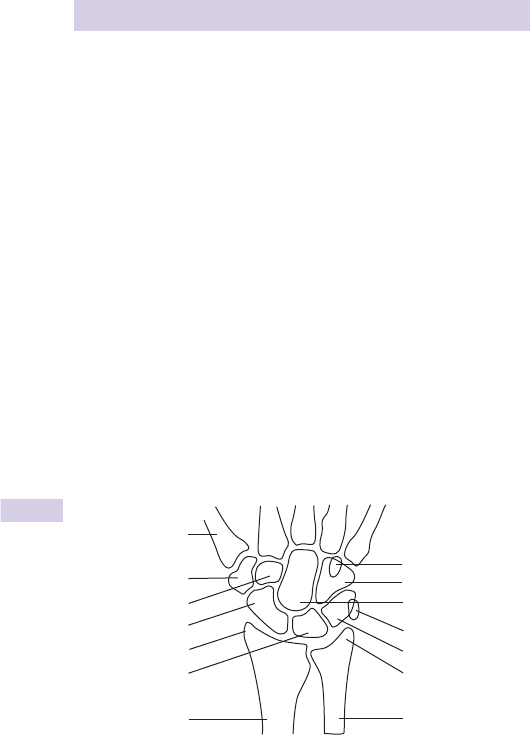
430 CHAPTER 9 Wounds, fractures, orthopaedics
Approach to hand injuries
The history
Determine and record whether the patient is right- or left-handed, their
occupation, and social situation. These points may have treatment implica-
tions, (eg an elderly person living alone with little social support may not
cope at home after a dominant hand injury).
Suspect patients presenting with wounds on the dorsum of the hand over
the index, middle, ring, or little fi nger MC heads of having sustained a
human bite (‘fi ght bite’) whatever history is given ( b p.416).
Terminology
To avoid confusion always refer to fi ngers by name not number (index,
middle, ring, little).
Use: palmar (or volar), dorsal, radial, ulnar (not anterior, posterior, lateral,
medial).
Bones of the hand and wrist
There are 14 phalanges and 5 metacarpals (MCs). Name the metacarpals
according to the corresponding fi ngers (ie thumb, index, middle, ring,
and little) — this avoids confusion. There are 8 carpal bones arranged in
2 rows. The proximal row (radial to ulnar) is comprised of scaphoid, lunate,
triquetral, and pisiform (Fig. 9.9 ). The distal row (radial to ulnar) are trape-
zium, trapezoid, capitate, and hamate.
1st metacarpal
Trapezium
Trapezoid
Scaphoid
Radial styloid
Lunate
Ulna
Ulnar styloid
Triquetral
Pisiform
Capitate
Hamate
Hook of hamate
Radius
Fig. 9.9 AP view of normal wrist.
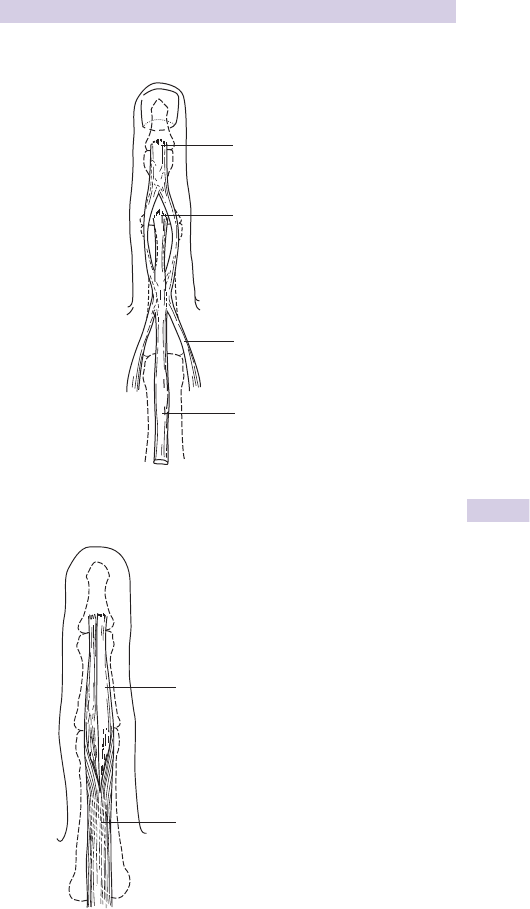
431
APPROACH TO HAND INJURIES
Anatomy of fi nger extensor tendon (Fig. 9.10 )
Lateral bands insert
into distal phalanx
Proximal phalanx
Middle phalanx
Distal phalanx
Middle slip of extensor expansion
inserts to middle phalanx
Tendons of intrinsic hand muscles
join extensor expansion
Insertion of extensor
tendon to proximal phalanx
Fig. 9.10 Anatomy
of fi nger extensor
tendon.
Anatomy of fi nger fl exor tendon (Fig. 9.11 )
Flexor digitorum profundus
insertion to distal phalanx
Flexor digitorum superficialis dividing
Fig. 9.11 Anatomy of fi nger fl exor tendon.

432 CHAPTER 9 Wounds, fractures, orthopaedics
Clinical signs of hand injury
Examination of hand injuries
Injury to the hand’s rich collection of nerves, blood vessels, and tendons
results in considerable functional defi cit. Assess carefully, taking into
account hand anatomy and clinical patterns of injury (Figs 9.12 and 9.13 ).
Specifi c signs of injury
Table 9.2 Specifi c signs of injury
Median nerve
d sensation in the palm over radial 3½ digits
unable to abduct thumb against resistance
Ulnar nerve
d sensation palmar and dorsal 1½ fi ngers,
little fi nger fl exed (non-functioning lumbrical)
unable to cross index and middle fi ngers
d abduction/adduction
Radial nerve
d sensation dorsum fi rst web space
(no motor branches in hand, but proximal injury
results in inability to extend wrist)
Digital nerve
d sensation along radial or ulnar half of digit distally:
note that some sensation is usually preserved,
even with signifi cant nerve injuries
Superfi cial fl exor hold other fi ngers straight (immobilizing all deep
fl exors), then unable to fl ex PIPJ (unreliable for
index fi nger). Also, 8 10 % of individuals do not
have a fl exor superfi cialis tendon to the little fi nger
Deep fl exor unable to fl ex DIPJ
Extensors complete division prevents extension (at DIPJ
causes mallet deformity)
central slip division causes Boutonnière deformity
in recent trauma, hold PIPJ at 90 * over table
edge, and try to extend versus resistance —
DIPJ hyperextends in central slip division
(Elson’s test)
Deformity a small amount of rotational deformity of a digit
(typically associated with a spiral/oblique MC or
fi nger fracture) can have a dramatic effect upon
long-term hand function (see Fig. 9.14): check
carefully to ensure that there is no abnormal
overlapping of fi ngertips in the palm on
making a fi st
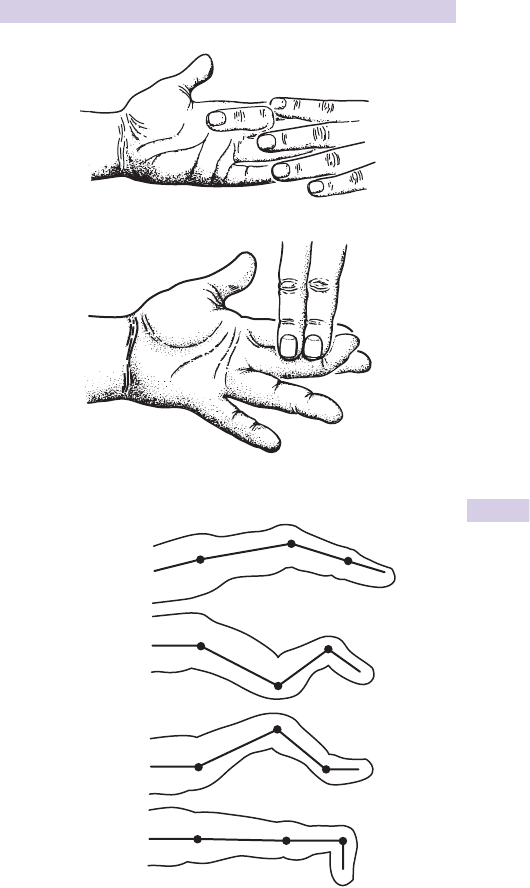
433
CLINICAL SIGNS OF HAND INJURY
Fig. 9.12 Testing superfi cial fl exor fi nger tendon.
Fig. 9.13 Testing deep fl exor fi nger tendon.
MCPJ
Normal
Swan neck
Boutonnière
Mallet
PIPJ
DIPJ
Fig. 9.14 Finger deformities.

434 CHAPTER 9 Wounds, fractures, orthopaedics
Hand wounds and associated injuries
General principles of treating hand wounds
• Remove rings as soon as possible after any hand or arm injury as swelling
can develop relatively rapidly. Try soap or water-based lubricant before
using ring-cutters. Alternatively, pass string or 0/0 silk under the ring and
wrap it fi rmly around the fi nger distally, allowing the ring to come off
over the compressed tissues.
• Elevate to diminish swelling and pain.
• Avoid subcutaneous sutures.
• For patients who are uncooperative due to excess alcohol consumption,
consider admission for a few hours to allow suturing with better
co-operation later.
• X-ray any hand injury caused by glass.
• Remember to consider tetanus cover.
Exploration under anaesthesia
If it is obvious that surgical intervention by a hand surgeon is required, do
not explore the wound in the ED. This particularly applies to suspected
nerve injuries, where the use of LA renders subsequent assessment diffi -
cult. Conversely, clinical assessment of tendon injuries can be misleading if
the patient is reluctant to move due to pain. Exploration under anaesthesia
is necessary in this situation and to exclude division of > 50 % of a tendon
(where clinical examination may be normal, but repair is required). Use an
appropriate LA nerve block (as outlined on b Nerve blocks at the wrist,
pp.296–299).
During exploration, consider the position of the hand at the time of injury:
reproducing this may reveal injuries otherwise hidden. Therefore, put all
mobile structures through their full range of movement.
Extensor tendon injuries
> 50 % or complete division needs repair (eg 4/0 or 5/0 non-absorbable
monofi lament using Bunnell or Kessler stitch) by an experienced surgeon.
This may be achieved under LA in the ED, depending on facilities and
expertise. Follow extensor tendon repair with appropriate immobi-
lization (eg volar slab type POP with fi nger joints in full extension and
slight fl exion at the MCPJs). Treat <50 % division by splintage in extension
(eg POP slab as above) under the care of the hand surgeon.
Flexor tendon injuries
Refer immediately for specialist repair.
Nerve injuries
Complete division of a nerve may cause surprisingly little sensory loss,
so take complaints of any altered sensation very seriously. Refer patients
with suspected nerve injuries. Digital nerves can be repaired up to the
level of the distal phalangeal joint (DIPJ), although it may be decided not to
attempt to repair injuries which are distal to the PIPJ. Remember that it is
functionally important to have intact sensation over the ‘edges’ of the hand
(the thumb, the radial aspect of the index fi nger or ulnar aspect of the little
fi nger). Patients sometimes present late after digital nerve injuries — repair
can still be quite successful up to 2 weeks after injury.

435
HAND WOUNDS AND ASSOCIATED INJURIES
Reverse fi ght bites
Treat and refer as outlined in b Specifi c bites and stings, p.416. Consider
transfer of blood-borne infection as discussed in b Needlestick injury,
p.418.
Amputations
Refer patients with partial or complete digital amputation with bony loss.
Recent proximal amputations without crush injury in fi t young patients
may be suitable for re-implantation: others may be treated with ‘termi-
nalization’ or advancement fl ap. Let the hand surgeon decide. Meanwhile,
dress, bandage and elevate, give IV analgesia, tetanus cover, broad spec-
trum antibiotics (eg cephalosporin), and keep fasted. Wrap the amputated
part in moist saline swabs and place in a sealed plastic bag, surrounded by
ice/water mix at 4 * C.
Note: Do not freeze or place the amputated part directly in solution.
Finger pad amputations
Skin loss less than 1cm
2
without bony exposure may be allowed to heal
with non-adherent dressings. Larger areas of tissue loss (particularly in
adults) may require skin grafting or advancement fl ap, but some do heal
satisfactorily with simple dressings.
Ring avulsions
Refer all circumferential and signifi cant degloving injuries.
Compound injuries
Wounds over dislocations or fractures usually require specialist atten-
tion. Distal compound phalangeal fractures may be treated in the ED with
wound cleaning, closure, review, and prophylactic antibiotics.
Crush injuries
Frequently cause ‘burst’ injury fi ngertip wounds. Clean the wounds and
take into account the likely swelling when considering closure. Elevate,
dress, give analgesia, and arrange review.
Nail bed lacerations
Accurate repair (eg 6/0 Vicryl) may prevent nail deformity. Nailfold-lacerations
extending towards the nail bed require removal of the nail to allow suture.
Consider replacing the nail after to act as a temporary dressing.
Foreign bodies under nail
Splinters and other FBs under fi ngernails are relatively common. Apply a
digital block and remove with fi ne forceps. If the FB cannot be reached
easily, cut away an appropriate piece of nail.
Subungual haematomas
Blood frequently collects under the nail after a crush injury, causing pain
by pressure. If > 50 % of the nail is affected, trephine the nail distal to the
lunula, using a red hot paper clip or battery operated drill.
High pressure injection injuries
Industrial grease or paint guns may cause small skin wounds, which initially
appear trivial, disguising a devastating injury with risk of permanent stiff-
ness and signifi cant tissue loss. X-rays may help to identify the extent of
foreign material. Refer all such patients to a hand surgeon for immediate
exploration and debridement.

436 CHAPTER 9 Wounds, fractures, orthopaedics
Hand fractures and dislocations
Distal phalangeal fractures
Treat closed fractures of the distal portion (tuft) of the distal phalanx with
analgesia and elevation. Treat compound burst injuries (from crushing
injuries or hammer blows) with meticulous exploration, wound toilet/
repair under LA and arrange follow-up. Give antibiotics (not a substitute
for primary surgical treatment).
Mallet fi nger with fracture
‘Mallet fi nger’ injury may be associated with a small fracture at the base
of the distal phalanx at the point of attachment of the extensor tendon.
Treat as for (the more usual) mallet fi nger injury without fracture by
plastic mallet splint for ≈ 6weeks, advice and follow-up (see details on
b Soft tissue hand injuries, p.440). Refer larger bony fragments ( >
1
/
3
articular surface) with mallet deformity or those with subluxation for pos-
sible K-wire internal fi xation.
Proximal and middle phalangeal fractures
Treat undisplaced fractures with elevation, neighbour strapping (Fig. 9.17 ),
and analgesia. Manipulate angulated proximal and middle phalangeal frac-
tures under digital or wrist blocks. A useful tip for proximal phalangeal
fractures is to use a needle-holder or pencil placed adjacent to the web
space as a fulcrum. Maintain reduction using neighbour strapping and a
volar slab POP or fl exible padded aluminium (Zimmer) splint, although
the latter can be diffi cult to secure. If reduction is unsatisfactory or cannot
be maintained, refer for surgical fi xation.
Index, middle, and ring metacarpal fractures
Check for displacement or rotational deformity and refer if present. Treat
with analgesia, elevation, and protect in a volar slab POP. Internal fi xation
may be considered for midshaft MC fractures with marked angulation, but
can be complicated by marked post-operative stiffness.
Phalangeal dislocations
X-ray all dislocations prior to reduction for presence of associated
fractures. Reduce under digital or metacarpal nerve block ( b p.294) or
Entonox
®
by traction and gentle manipulation, then check integrity of
the collateral ligaments. Confi rm reduction on X-ray and immobilize the
fi nger by neighbour strapping. Elevate the hand, provide oral analgesia and
arrange follow-up.
Fig. 9.15 Mallet fi nger deformity.
Fig. 9.16 Mallet fi nger with avulsion fracture.
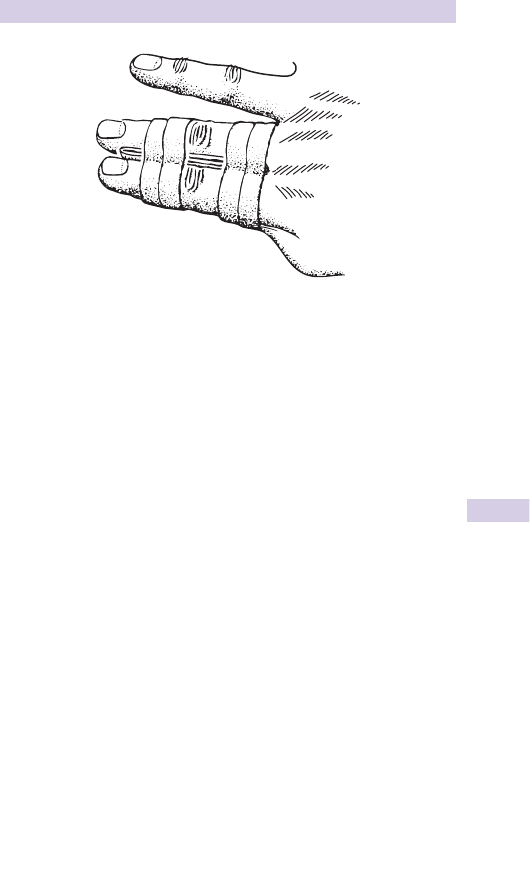
437
HAND FRACTURES AND DISLOCATIONS
Little (5th) metacarpal fractures
Common result of punching. Check for rotational deformity by gently
fl exing fi ngers into the palm (they should point roughly to the thenar emi-
nence and touch, but not overlap adjacent fi ngers on fl exion). Angulation
is common with neck fractures and rarely requires correction, with even
up to 40 * being accepted. Apply neighbour strapping, elevate and give
analgesia. A volar slab POP for 2weeks is sometimes advocated — follow
local protocols. Warn the patient that the 5th knuckle will be shorter than
before. Arrange follow-up and advise hand exercises as soon as possible.
Refer to orthopaedic team if there is rotational deformity or signifi cant
angulation, particularly with base and shaft fractures, which may need
surgery. Also refer patients with associated wounds, remembering that
these may be compound human bites (‘reverse fi ght-bites’ — b Specifi c
bites and stings, p.416).
Little (5th) metacarpal dislocations
Dislocations at the base of the 5th MC may be associated with a fracture.
Refer for reduction and internal fi xation.
Fig. 9.17 Neighbour (buddy) strapping.
438 CHAPTER 9 Wounds, fractures, orthopaedics
Thumb fractures and dislocations
Dislocation at metacarpophalangeal joint
After X-rays and LA block, attempt reduction. If successful, assess and
document the integrity of the collateral ligaments (see b Soft tissue
hand injuries, p.440), then immobilize in slight ( ≈ 15 * ) fl exion in a POP and
arrange follow-up in fracture clinic. Reduction may be unsuccessful due to
‘button-holing’ — in this case, refer for open reduction.
Gamekeeper’s thumb with associated avulsion fracture
Most abduction injuries result in ulnar collateral ligament injury without
fracture, but occasionally an avulsion fracture occurs at the point of
ligament attachment instead. Treat this in a scaphoid POP and refer to
fracture clinic, unless the bony fragment is displaced by more than 2mm,
in which case internal fi xation will probably be required.
If undisplaced, treat in scaphoid POP, and refer to fracture clinic, but if
displaced, refer for internal fi xation.
Thumb dislocations
Dislocations usually follow falls onto the thumb or hyperextension
injuries. They can occur at any level, including at the interpahalangeal
joint (IPJ), MCPJ, and at the carpometacarpal joint. Reduce dislocations
by traction and local pressure under combined median and radial nerve
blocks ( b Nerve blocks at the wrist, p.296). Confi rm reduction by X-ray,
immobilize in a scaphoid POP, and arrange follow-up.
MC
Fig. 9.18
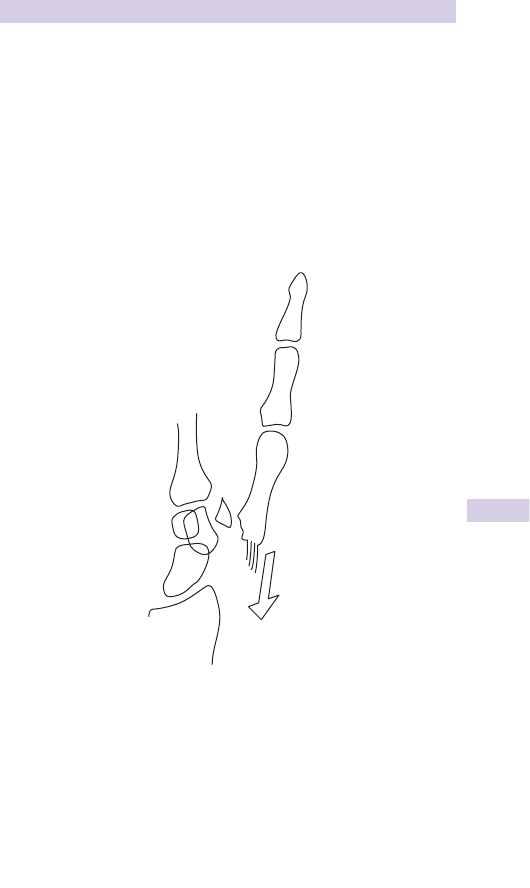
439
THUMB FRACTURES AND DISLOCATIONS
Bennett’s fracture-dislocation ( b p.498)
This is a fracture through the base of the thumb (1st) MC with radial
subluxation of the MC, leaving a small proximal fragment still joined to
the trapezium (Fig. 9.19 ). The injury results from a fall onto the thumb
or from a fall/blow onto a fi st closed around the thumb. Deformity and
swelling occur over the base of the thumb and may be mistaken clinically
for a scaphoid injury. This is an unstable injury requiring expert attention.
If undisplaced, apply a Bennett’s type POP (similar to a scaphoid POP, but
with the thumb abducted). If there is any displacement, refer for manipu-
lation under anaesthetic (MUA)/fi xation. Maintaining reduction often
requires the use of screw or Kirschner wire fi xation.
Fig. 9.19 Bennett’s fracture-dislocation.

440 CHAPTER 9 Wounds, fractures, orthopaedics
Soft tissue hand injuries
Gamekeeper’s thumb
The thumb’s ulnar collateral ligament is crucial for stability and function.
It is typically injured in hyperabduction injuries (eg falls while skiing).
Complete rupture usually results in the two parts of the ligament being
separated by the adductor aponeurosis (the ‘Stener lesion’), so satisfac-
tory healing cannot occur. If tender over the ulnar collateral ligament of
the thumb MCPJ, obtain X-rays: if these demonstrate a fracture, do not
stress the joint, but treat appropriately instead ( b Thumb fractures and
dislocations, p.438). If no fracture, assess stability of the ulnar collateral
ligament by gentle abduction of the MCPJ (compare with the other hand).
Examine the ulnar collateral ligament with the thumb slightly (15 * ) fl exed.
If pain precludes adequate examination, consider Entonox
®
(and/or LA
injection) and repeat the examination. Signifi cant ( > 30 * ) laxity implies
complete rupture and need for operative repair.
Treat uncomplicated sprains with analgesia, elevation, and either criss-
cross adhesive strapping (‘thumb spica’) or a scaphoid POP if symptoms
are severe, and arrange follow-up. Refer suspected or demonstrable
ulnar collateral ligament rupture to the orthopaedic surgeon, to consider
primary surgical repair.
Mallet fi nger
Injury to the extensor mechanism at the DIPJ is relatively common and
results from forced fl exion of the DIPJ or from a blow/fall directly onto
the fi ngertip. In the elderly it can follow minimal trauma. There is loss of
full active extension at the DIP joint. Normal fl exion is preserved.
X-ray to exclude associated fracture — treated as outlined on b p.436.
In the absence of a large fragment, treat in a plastic (mallet) splint secured
with tape for ≈ 6weeks (see b p.436). Ensure that the patient understands
the importance of wearing the splint at all times and to keep the fi nger
straight if the splint is removed for washing (eg hold fi nger against a fl at
surface until splint replaced). Warn that there may be a small degree of
permanent fl exion deformity. Arrange initial follow-up at ≈ 7–10 days, to
ensure compliance with treatment and to reassess in case swelling has
d and a smaller splint is required.
Volar plate injury
These are signifi cant injuries, often with prolonged morbidity. Hyperextension
at the PIPJ injures the volar plate at the base of the middle phalanx with or
without evidence of bony involvement. Examination shows fusiform swelling
of the PIPJ with tenderness over the volar aspect. Treat with ‘buddy strapping’
to adjacent fi ngers (or ‘Bedford splint’), elevate, provide analgesia, and begin
mobilization immediately. Arrange review to ensure full mobility is regained.
A2 pulley injury
The fi nger fl exor tendon sheath at the PIPJ is thickened and known as the A2
pulley. Occasionally (especially in rock climbers), the tendon cuts through
the A2 pulley, causing characteristic bowstringing on fl exion. There may
be associated tendon injury. Treat conservatively with buddy strapping (or
Bedford splint) and elevation. Arrange hand specialist follow-up.
Boutonnière deformity ( b Eponymous fractures, p.498)
Characteristic deformity from untreated rupture/division of central slip
fi nger extensor tendon may follow blunt or penetrating trauma.

441
OTHER SOFT TISSUE HAND PROBLEMS
Other soft tissue hand problems
Pulp infections
Infection of the pulp space at the fi ngertip may refl ect underlying FB or
osteomyelitis, so X-ray to search for these and treat accordingly. If X-rays
are normal, incise the pointing area under LA digital block. Send pus for
bacteriology, apply a dressing, commence oral antibiotics (eg fl ucloxacillin
250–500mg PO qds), and arrange follow-up.
Paronychia
Infection of the nailfold adjacent to the nail is common. In the early stages,
oral antibiotics (eg co-amoxiclav or fl ucloxacillin) may cure.
Once pus has developed, drain this under LA digital block by an incision
over the fl uctuance (usually a small longitudinally-orientated incision
adjacent to the proximal nailfold suffi ces, but pus under the nail may
require removal of a segment of nail). Antibiotics are then unnecessary,
unless there is spreading infection (in which case, consider co-amoxiclav).
Pyogenic fl exor tenosynovitis
Infection of a fi nger fl exor tendon sheath may follow penetrating injury.
Classical signs (Kanavel’s signs) are:
• Tenderness over the fl exor tendon.
• Symmetrical swelling of the fi nger.
• Finger held in fl exion.
• Extreme pain on passive extension.
Ensure tetanus prophylaxis, then refer urgently for exploration, irrigation,
and IV antibiotics.
Other infections
These include palmar space infections and septic arthritis — refer
immediately for specialist treatment.
Locked fi nger
Elderly patients with underlying osteoarthritis (OA) sometimes present
with locking at a fi nger MCPJ. A fi xed fl exion deformity is present, such
that the patient can fl ex, but not fully extend at the MCPJ. There is usually
no particular history of trauma — the underlying cause is entrapment of the
palmar plate on an osteophyte. Refer for an early hand surgeon opinion:
surgery may be required.
Trigger fi nger/thumb
This is relatively common, but not particularly related to trauma. Most
cases are satisfactorily treated by steroid injection into the fl exor tendon
sheath, but leave this to a specialist.

442 CHAPTER 9 Wounds, fractures, orthopaedics
Carpal bone fractures and dislocations
Scaphoid fractures
Assess and document whether there is tenderness over the scaphoid in all
wrist injuries. Scaphoid fractures occur from falling onto an outstretched
hand or from ‘kick-back’ injuries (eg from a steering wheel in a car crash
or football goalkeeper making a save). Pain and swelling over the wrist’s
radial aspect may be accompanied by diffi culty gripping.
Look for
• Tenderness in anatomical snuffbox: compare both sides.
• Tenderness over palmar aspect of scaphoid (scaphoid tubercle).
• Scaphoid pain on compressing the thumb longitudinally.
• Scaphoid pain on gentle fl exion and ulnar deviation of the wrist.
• Tenderness over dorsum of scaphoid.
X-rays Request specialized scaphoid (not wrist) views. Four views
are usually taken (AP, lateral, right, and left obliques). Remember that
scaphoid fractures may not be visible on initial X-rays. The scaphoid
mostly fractures through the waist, but sometimes through the tubercle
(the latter does not give rise to signifi cant complications).
Treatment If there is clinical or radiological evidence of fracture, apply a
scaphoid POP or splint, and arrange review in 10–14 days. Treat minimal
snuffbox tenderness without radiologically visible fracture with analgesia,
and a wrist splint and arrange review as above.
Complications Include non-union, avascular necrosis, and OA.
Follow-up of clinically suspected scaphoid fractures (but normal X-rays)
is often undertaken in ED clinic. Review at 10–14 days after injury, when
if there is no clinical evidence of fracture, patients may be discharged. If,
however, there is continuing pain and/or scaphoid tenderness, repeat
the X-rays: treat visible fractures in POP; but if X-rays are still normal,
treat in splint or POP, and arrange MRI (or bone scan for those with
claustrophobia or other contraindication to MRI) to defi nitively answer
whether there is a fracture or signifi cant carpal ligament injury.
Lunate dislocations
These injuries are rare, but often missed (Fig. 9.22 ). They follow falls onto
the outstretched wrist, and result in pain and swelling anteriorly over the
wrist. Median nerve paraesthesia may be a clue to the diagnosis. X-ray
shows dislocation and rotation of the lunate so that it is shifted in front
of the carpus and its concave surface faces towards the palm instead of
distally. The AP view may look relatively normal, so carefully scrutinize
lateral views. Refer for immediate MUA.
Complications Median nerve injury, avascular necrosis, Sudeck’s atrophy.
Other carpal dislocations
Isolated dislocations of other carpal bones occur, but often injuries are more
complicated and involve dislocations (and fractures) of one row of carpal
bones (eg trans-scaphoid perilunate dislocation; Fig. 9.21 ). Surprisingly,
perhaps, given almost inevitable signifi cant swelling, these injuries can be
missed. Give analgesia and refer for reduction by the orthopaedic team.
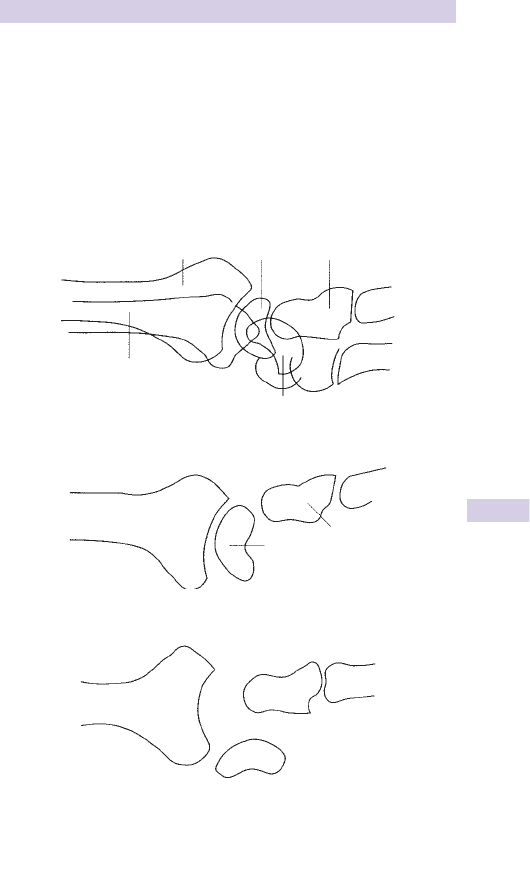
443
CARPAL BONE FRACTURES AND DISLOCATIONS
Flake avulsion carpal fractures
Small avulsions from the dorsum of the carpus are often from the
triquetrum. Treat with immobilization in a POP backslab or wrist support
splint, analgesia, and refer to fracture clinic.
Fractured hook of hamate
Local palmar tenderness may give rise to suspicion of a fracture of the
hook of the hamate. Diagnosis can be diffi cult: specialized X-rays or CT
may be required to demonstrate the fracture. Immobilize in POP and
refer to fracture clinic.
Radius
Ulna
Scaphoid
Lunate Capitate
Fig. 9.20 Wrist: normal lateral.
Lunate
Capitate
Fig. 9.21 Perilunate dislocation.
Fig. 9.22 Lunate dislocation.
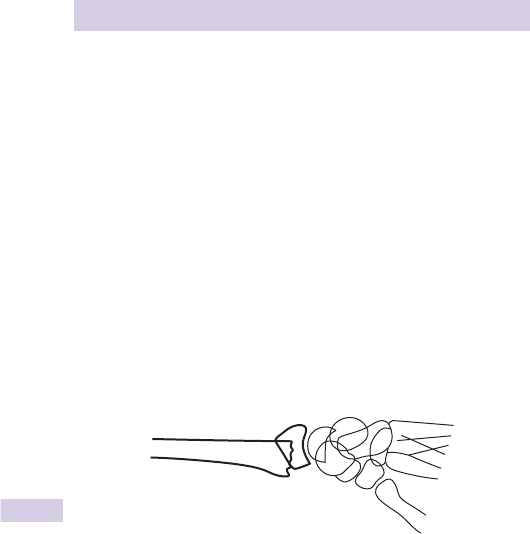
444 CHAPTER 9 Wounds, fractures, orthopaedics
Colles’ fracture
Presentation
This fracture affects the radius within 2.5cm of the wrist, such that the
distal fragment is angulated to point dorsally. It usually results from a fall
onto an outstretched hand. Osteoporosis contributes to i frequency in
post-menopausal women. Colles’ fractures produce characteristic clinical
deformity (sometimes likened to a ‘dinnerfork’). Check for scaphoid
tenderness, distal sensation, and pulses in all cases.
Radiological features
X-ray appearances include one or more of the following:
• Posterior and radial displacement (translation) of the distal fragment.
• Angulation of the distal fragment to point dorsally (the articular surface
of the distal radius normally has a 5 * forward tilt on the lateral wrist
X-ray).
• Angulation of the distal fragment to point more radially (the articular
surface of the distal radius is normally tilted 22 * towards the ulnar side
on AP wrist X-ray).
• Impaction, leading to shortening of the radius in relation to the ulna.
Treatment
Provide analgesia, immobilize in a backslab POP, and elevate with a sling.
Discharge those with undisplaced fractures (if they will manage at home)
and arrange fracture clinic follow-up. Advise the patient to keep moving
fi ngers, thumb, elbow, and shoulder.
Deciding if MUA is indicated
MUA is required for:
• Grossly displaced fractures.
• Loss of normal forward radial articular surface tilt on lateral wrist X-ray.
Neutral or minimal tilt may be acceptable in the very young or very old
(particularly in the non-dominant limb). Seek senior advice if unsure.
Timing of MUA
Patients with compound fractures and/or symptoms of nerve compression
require urgent MUA. For many other patients, the timing of the procedure
is less important. Many EDs undertake closed manipulation of Colles’
fractures in adult patients at the time of initial presentation, whilst others
arrange for the patient to return for the procedure within 1–2days to a
specifi c theatre list as a day case.
Fig. 9.23 Colles' fracture

445
COLLES’ FRACTURE
MUA procedure for Colles’ fractures
Consent
Discuss the risks and benefi ts of the procedure. In particular, explain that, if
left untreated, an angulated Colles’ fracture may result in long-term stiffness
and a signifi cantly weaker grip. The principal risks of manipulation are:
• Tears to the skin on the dorsum of the wrist (especially in those with
thin skin (eg on steroids) and/or signifi cant swelling (eg on warfarin).
• Late slippage of the bones requiring a further procedure.
• Risks of the anaesthetic employed.
Choice of anaesthetic
The anaesthetic options available include: haematoma block ( b p.289),
intravenous regional anaesthesia ( b Bier’s block, p.290), IV sedation ( b
p.308), GA ( b p.310). The choice of anaesthetic will depend upon local
protocols, as well as patient related factors, such as the type of fracture
and extent of fasting. For example, a minimally angulated fracture in an
elderly individual may be satisfactorily managed using a haematoma block,
whereas a more dramatically angulated and displaced fracture may not.
Evidence suggests that Bier’s block is superior to haematoma block (see
www.bestbets.org ).
Technique
Different individuals may employ different techniques, but the aim is to
attempt to return the anatomy to its previous position. In particular, it is
important to correct the dorsal angulation (‘restore the volar cortex’).
Many descriptions of reduction techniques involve initial traction and ‘dis-
impaction’ of the fragments, followed by wrist fl exion and pronation with
pressure over the distal radial fragment(s). Some operators focus more
upon gentle direct manipulation of the distal fragment, rather than indirect
measures (traction, wrist fl exion, etc.).
Following manipulation, apply a backslab POP, whilst maintaining the
reduction, with the wrist slightly fl exed and pronated (avoid excessive
fl exion as this can cause additional long-term problems). Satisfactory
reduction can be confi rmed by image intensifi er/X-ray. If the reduction is
not satisfactory, repeat the manipulation procedure.
Medium and long-term complications of Colles’ fracture
Patients may present to the ED with later complications following Colles’
fracture (and the treatment provided for it), including the following:
• Stiffness of wrist and adjacent limb joints : refer for physiotherapy.
• Malununion and cosmetic problems : refer to GP/orthopaedic team.
• Refl ex sympathetic dystrophy (Sudeck’s atrophy) : refer for physiotherapy
and GP/orthopaedic follow-up.
• Carpal tunnel syndrome may occur after Colles’ fracture, but also refl ect
other problems (eg lunate dislocation): check original X-rays.
• Extensor pollicis longus rupture may occur some weeks after fractures
with minimal displacement: see b Soft tissue wrist injuries/problems,
p.447.
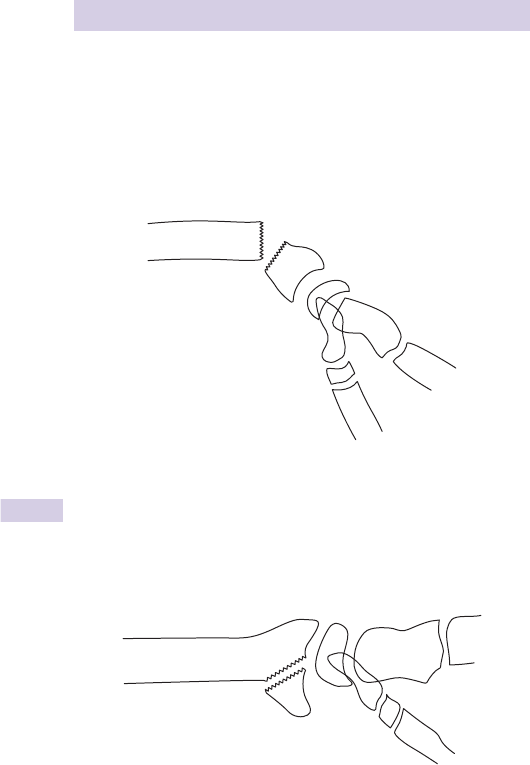
446 CHAPTER 9 Wounds, fractures, orthopaedics
Other wrist fractures
Smith’s fracture
This is an unstable distal radius fracture (sometimes referred to as a
‘reverse Colles’ fracture’) where the distal fragment is impacted, tilted to
point anteriorly and often displaced anteriorly (Fig. 9.24 ). It usually follows
a fall onto a fl exed wrist. Give analgesia, immobilize in a backslab POP and
refer for MUA (often diffi cult to hold in position after reduction) or ORIF
using a buttress plate (preferred in some orthopaedic centres).
Barton’s and reverse Barton’s fracture ( b p.498)
An intra-articular fracture involving only the dorsal or volar portion of
the distal radius is called a Barton’s fracture and reverse Barton’s fracture
(Fig. 9.25 ), respectively. The resultant fragment tends to slip, so the fracture
is inherently unstable. Provide analgesia, immobilize in a POP backslab and
refer. Most patients require ORIF and plating.
Isolated radial styloid fracture
Caused by similar mechanisms of injury as scaphoid fractures (ie falls onto
an outstretched hand or kickback injuries). It is sometimes referred to as
a Hutchinson fracture ( b Eponymous fractures, p.500). Treat with anal-
gesia, backslab POP, elevation sling and fracture clinic. Internal fi xation is
occasionally required.
Fig. 9.24 Smith’s fracture (lateral view).
Fig. 9.25 Lateral view of a reverse Barton’s fracture.

447
SOFT TISSUE WRIST INJURIES/PROBLEMS
Soft tissue wrist injuries/problems
Wrist sprain
Exclude scaphoid or other fracture (or dislocation) before considering the
diagnosis of a ‘simple wrist sprain’. Relatively minor damage to ligaments
around the wrist can occur following hyperextension or fl exion of the
wrist, causing swelling and tenderness around the joint. Treat with a wrist
splint or tubigrip support, analgesia, or NSAIDs, and progressive exercise.
Continuing pain and problems arouse suspicions of more signifi cant injury
(possibly involving other structures, such as the scapholunate ligament or
triangular fi brocartilage complex). Refer for specialist investigation.
TFCC injury
The triangular fi brocartilage complex at the distal end of the ulna may
be injured with associated structures. Often, these injuries only become
apparent later, when what was diagnosed as a ‘simple wrist sprain’ fails to
settle — pain and tenderness persists over the TFCC. Arrange specialist
follow-up for further investigation (eg MRI) and treatment.
Rupture of wrist/hand tendons
Rupture of tendons may occur without penetrating trauma. The most
common rupture involves extensor pollicis longus a few weeks after
(usually undisplaced) fracture of the distal radius. Rupture of other
extensor (and occasionally fl exor) tendons occurs in association with
OA, rheumatoid arthritis (RA), scaphoid non-union, chronic renal failure
(CRF), systemic lupus erythromatosus (SLE). Refer to a hand surgeon.
Radial tenosynovitis (‘intersection syndrome’)
Typically follows unaccustomed repetitive activity, such as gardening, DIY,
or decorating. Over hours to days, a painful fusiform swelling develops
over the radial aspect of the distal forearm. Movement of the wrist pro-
duces pain and palpable (occasionally audible) crepitus. Immobilize in a
simple adjustable wrist splint and unless contraindicated, prescribe NSAID
for 7–10days. After this, allow gradual mobilization of the wrist and
educate about eliminating the cause. Immobilize severe cases in a forearm
POP for 2 weeks before beginning mobilization.
De Quervain’s tenosynovitis
Affects the tendon sheaths of abductor pollicis longus and extensor pol-
licis brevis. Pain, swelling, and crepitus occur over the lateral (dorso-radial)
aspect of the radial styloid. Symptoms can be reproduced by thumb or
wrist movement. Finkelstein described grasping the patient’s thumb and
rapidly ‘abducting the hand ulnarward’, but probably more useful is pain
on ulnar movement of the wrist with the thumb clenched in a fi st. Treat
with NSAID and splintage for 7–10 days. A removable fabric wrist splint
(including the thumb) may suffi ce, but consider a scaphoid type POP for
severe pain. Persistent symptoms may respond to steroid injection of the
tendon sheath using an aseptic technique.

448 CHAPTER 9 Wounds, fractures, orthopaedics
Dislocation of radio-ulnar joint
Fracture of radius
Fig. 9.26
Forearm fractures and related injury
If one forearm bone is fractured, look for a fracture or dislocation of the other.
Obvious deformity in an adult forearm indicates fracture of the radial and
ulna shafts. Initially treat with:
• Analgesia (eg increments of IV morphine + anti-emetic until pain
relieved).
• Immobilization in backslab POP.
• If one or both fractures are compound, give IV antibiotics ( b p.422),
tetanus cover, and dress the wound.
Always check distal pulses and sensation, and examine for associated
injuries at the wrist and elbow. Only once this has been done and the
patient is comfortable, can he/she be sent for X-ray. Ensure X-rays
demonstrate the whole lengths of the radius and ulna, including separate
views of both the elbow and wrist joints.
Fractures of both radius and ulna shafts
Adult fractures, unlike those in children, may be markedly displaced with
little or no bony contact between the fragments. Rotational deformity is
common. Check carefully for clinical evidence of neurovascular injury.
Closed reduction is diffi cult, and often fails or is complicated by late
slippage. Treat fractures with analgesia/immobilization as above and refer
for ORIF.
Isolated ulna shaft fracture
These usually occur from a direct blow to the outer edge of the forearm
(it is typically seen as a defence injury) or from a fall striking the ulna shaft.
X-ray the whole ulna and radius to exclude associated fracture or disloca-
tion of the radial head (see below). If undisplaced, treat in an above elbow
POP with the elbow fl exed to 90 * and the forearm in mid-supination.
Refer all displaced or angulated fractures for ORIF.
Galeazzi fracture-dislocation (see b p.499)
Defi ned as a fracture of the radius associated with dislocation of the distal
radio-ulnar joint at the wrist (Fig. 9.26 ). Always look for subluxation of
the ulna in radial fractures. Treat with analgesia and immobilization in a
temporary POP backslab. Refer for ORIF.
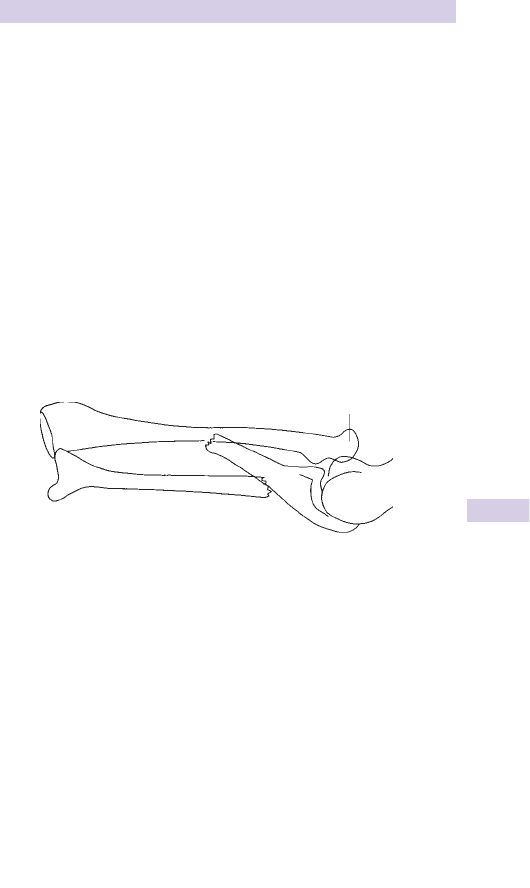
449
FOREARM FRACTURES AND RELATED INJURY
Monteggia fracture-dislocation (see b p.501)
Defi ned as a fracture of the ulna associated with dislocation of the radial
head. Occurs from forced pronation of the forearm (eg fall onto an out-
stretched, fully pronated forearm). Can also occur by a direct blow or
fall onto the proximal ulna, displacing the head of the radius. Treat with
analgesia and immobilization in a temporary above-elbow POP backslab.
Refer to the orthopaedic team for ORIF (or sometimes in children, for
treatment with MUA and POP).
A related injury is the Hume fracture ( b Eponymous fractures, p.500)
in which anterior dislocation of the radial head is combined with an
olecranon fracture. Refer for ORIF.
Note: Monteggia fracture-dislocations are not infrequently missed at
initial presentation, due to attention being distracted by the ulna fracture
(Fig. 9.27 ). To avoid this:
• Request elbow and wrist X-rays in any patient with forearm shaft
fracture.
• Check all elbow X-rays carefully to ensure that the radial shaft is
normally aligned and that the radial head abuts the capitellum.
Isolated radial shaft fracture
These are very uncommon. Always treat and assume that there is some
associated damage to the distal radio-ulnar joint at the wrist.
Dislocated radial head
Fracture of the ulna
Fig. 9.27 Monteggia fracture-dislocation.

450 CHAPTER 9 Wounds, fractures, orthopaedics
Elbow injuries
In any injured elbow look specifi cally for:
• Elbow effusion (felt as a tense, bulging swelling halfway between the
lateral epicondyle and the point of the olecranon).
• The normal relationship between the olecranon and the lateral and
medial epicondyles: all should form an equilateral triangle with the
elbow fl exed.
• Range of movement: X-ray patients who cannot fully extend the elbow
and fl ex to touch the shoulder tip.
Olecranon fractures
Follow falls onto the point of the elbow. The olecranon fragment may dis-
place proximally due to pull of triceps. Swelling, tenderness, or crepitus are
present on examination. In the young, the olecranon epiphysis may cause con-
fusion on X-rays. Treat undisplaced or hairline fractures in an above elbow
backslab POP at 90 * , provide analgesia and arrange fracture clinic follow-up.
Refer fractures that are displaced or involve the elbow joint for ORIF.
Radial head/neck fractures
Follow falls onto outstretched wrist (the radial head impacts against the
capitellum) or direct trauma to the elbow. They sometimes occur in
combination with a wrist fracture. Examine movements — extension and
fl exion are usually limited, but supination and pronation may be relatively
normal. Look for an elbow effusion and palpate for tenderness over the
radial head while supinating/pronating the elbow. X-ray confi rms elbow
effusion, but fractures may be diffi cult to see. Treat undisplaced fractures
with analgesia, and a collar and cuff sling. If very painful, immobilize in an
above elbow POP backslab at 90 * . Arrange fracture clinic review. Refer
comminuted or displaced fractures as they may require MUA, internal
fi xation or occasionally excision/replacement of the radial head.
Elbow effusion, no visible fracture
Always assume that a radial head/neck fracture is present: provide
analgesia, a collar and cuff sling, and arrange review to ensure that full
movement is regained. Extra symptomatic relief may be achieved by
aspiration of the elbow joint (via a point midway between the olecranon
and lateral epicondyle) under aseptic conditions.
Elbow fat pad sign
Elevated anterior fat pad
Fractured radial head
Posterior
fat pad
Fig. 9.28 Elbow fat pad sign.

451
ELBOW INJURIES
Dislocated elbow
Examination reveals loss of the normal triangular relationship between the
olecranon and epicondyles. Check distal pulses and sensation as brachial
artery, median and ulnar nerves may be damaged. Elbow dislocations may
be classifi ed according to the direction of dislocation and the presence of
associated fractures (eg fractured coronoid). The most frequent injury is
postero-lateral dislocation (ie movement of the distal part in a postero-
lateral direction).
After analgesia and X-ray, most dislocations may be reduced in the ED
under IV sedation with full monitoring ( b Sedation, p.308). However, GA
is sometimes required.
Reduction Choose between the following techniques for reduction of
postero-lateral dislocations:
• Flex the elbow to 60 * with countertraction on the upper arm. Pull on
the fully pronated forearm at this angle. Slight fl exion at the elbow may
be necessary.
• Alternatively, lever the olecranon forward with both thumbs while
holding the elbow fl exed and while an assistant provides traction on the
forearm.
Reduction is confi rmed by a ‘clunk’ and restoration of the normal
triangular relationship of the elbow landmarks. Once reduced, recheck
pulses and sensation, immobilize in an above elbow POP backslab at 90 *
and X-ray again (looking for associated fractures). Consider admission for
analgesia and observation for possible signifi cant limb swelling. If unable to
reduce, refer for reduction under GA.
Supracondylar fractures (see b p.722)
Fractures of the distal third of the humerus usually occur from falls onto
the outstretched hand. They are most common in children (b p.722),
but also occur in adults. The elbow may be grossly swollen and deformed,
but the normal triangular relationship of the olecranon and epicondyles is
characteristically preserved. Check distal pulses and sensation carefully as
the brachial artery, ulnar, median, and radial nerves can all be damaged.
Immobilize in an above elbow backslab POP and give analgesia. Refer to
the orthopaedic surgeon as MUA/ORIF are usually required.
Fractures of the capitellum occasionally occur in isolation. If undisplaced,
treat conservatively with analgesia and POP. Refer those with displaced
fractures for specialist treatment (possibly ORIF).
Medial collateral ligament injury
Instability on stress testing of the medial (ulnar collateral) ligament implies
a signifi cant injury. Treat in backslab POP with the elbow fl exed to 90 *
and supported in a sling. Arrange fracture clinic follow-up.
Other elbow injuries
Elbow injuries are relatively common in children. Specifi c injuries in children
are considered as follows:
• Supracondylar fracture ( b Paediatric upper limb injuries, p.722).
• Lateral and medial condylar injury — ( b p.724).
• Pulled elbow — ( b Paediatric upper limb injuries, p.724).

452 CHAPTER 9 Wounds, fractures, orthopaedics
Soft tissue elbow problems
Injuries to biceps and brachialis
Infl ammation of biceps and/or brachialis at the site of attachment at the
elbow can cause persistent symptoms: treat with rest and NSAID. Biceps
brachii can rupture either at its long head in the bicipital groove or near
the elbow insertion. Long head ruptures typically affect the elderly and
result in a characteristic abnormal shape and low biceps position on
attempted elbow fl exion against resistance: unless the patient is young,
fi t, and active, surgical repair is rarely indicated. Distal ruptures are some-
times treated conservatively, but some may benefi t from repair: arrange
orthopaedic review to consider this.
Lateral epicondylitis
This is commonly called ‘tennis elbow’. It follows repetitive or exces-
sive stress to the origin of the forearm and hand extensor muscles at
the lateral epicondyle. It can occur spontaneously, but usually follows
repetitive lifting, pulling, or sports (eg as a result of an incorrect backhand
technique in tennis). Infl ammation, oedema, and microtears occur within
the extensor insertion.
Look for localized swelling, warmth or tenderness over the lateral epicondyle
and immediately distal to it.
Examine movements: dorsifl exion of the pronated wrist against resistance
will reproduce symptoms.
X-ray if the problem follows acute injury. Refer to the orthopaedic
surgeon if there is an avulsion fracture.
Treat with analgesia (preferably NSAID) and ice application. Support the
arm in a broad arm sling and advise rest, followed by progressive exercise
and avoidance of aggravating movements. If symptoms are recurrent
or prolonged, refer as steroid injection, forearm clasp, physiotherapy,
and occasionally surgery may help. Current evidence suggests that
corticosteroid injection may provide short-term relief, but long-term
benefi t remains unproven.
Medial epicondylitis
Often called ‘golfer’s elbow’, this condition has a similar pathophysiology
to lateral epicondylitis: it is frequently seen in racket sports and golf.
Examine for localized tenderness and swelling over the forearm fl exor
insertion at the medial epicondyle. Flexion of the supinated wrist against
resistance will reproduce symptoms. There may be d grip strength and
≈ 60 % of patients have some symptoms of associated ulnar neuritis.
Treat as for lateral epicondylitis.
Osteochondritis dissecans
This can affect the elbow and cause locking of the elbow joint. X-rays may
reveal a defect and/or loose body. Refer to the orthopaedic team.

453
SOFT TISSUE ELBOW PROBLEMS
Olecranon bursitis
Infl ammation, swelling and pain in the olecranon bursa may follow minor
trauma or occur spontaneously. Other causes include bacterial infection
(sometimes following penetrating injury) and gout. Elbow movements
are usually not limited. Look for overlying cellulitis, wounds, and systemic
symptoms and check for i T * (these suggest infection). Gout or bacterial
infection can be confi rmed by aspiration of the bursa under aseptic
conditions and immediate microscopy for crystals or bacteria. Aspirate
using a small needle at a shallow angle and try to aspirate the bursa
completely.
Non-infective bursitis Provide analgesia, NSAID, and rest the arm in
a broad arm sling. Symptoms should resolve with rest over a period
of weeks. Rarely, persistent symptoms require surgical excision of the
olecranon bursa.
Gout bursitis Treat as above. Arrange follow-up through the patient’s GP.
Infective bursitis If there is evidence of underlying infection, treat with
rest, NSAID and start antibiotics (eg co-amoxiclav or fl ucloxacillin +
penicillin). Occasionally, infection requires referral to the orthopaedic
surgeon for surgical drainage.
Olecranon bursa haematoma A history of blunt trauma to the olecranon
followed rapidly by ‘golf ball-sized’ swelling over the olecranon, but with
a full range of elbow movement (and no evidence of fracture), implies
a haematoma in the olecranon bursa. Treat conservatively: attempts at
drainage may result in secondary infection.
Nerve compression
Ulnar nerve entrapment at the elbow (‘cubital tunnel syndrome’) is the
second most common upper limb nerve entrapment (median nerve
compression in carpal tunnel syndrome is the commonest. Refer these
chronic conditions back to the GP.
Acute radial nerve palsy above the elbow presents with sudden wrist drop
following a history of compression (eg crutch use, falling asleep with arm
over the back of a chair). The underlying injury is usually a neurapraxia,
which has the potential to recover completely given time with conservative
measures. It is crucial to ensure that fl exion contractures do not develop
in the meantime: provide a removable wrist splint, advise regular passive
wrist exercises, and refer for physiotherapy and follow-up to ensure
recovery.

454 CHAPTER 9 Wounds, fractures, orthopaedics
Anterior shoulder dislocation
This is a common injury, which typically results from forced external
rotation/abduction of the shoulder. The humeral head usually dislocates
to lie anterior and slightly inferior to the glenoid. Patients often present
supporting the affected arm with the uninjured arm.
The diagnosis is usually obvious on examination. Look for:
• Step-off deformity at the acromion with palpable gap below the
acromion.
• Humeral head palpable antero-inferiorly to the glenoid.
• Evidence of complications: check especially for distal pulses and
d sensation over the lateral aspect of the shoulder (the ‘badge’ area)
supplied by the axillary nerve.
Give analgesia and support in a temporary sling. X-ray before reduction
to exclude associated fractures. X-rays show loss of congruity between
humeral head and the glenoid. The humeral head is displaced medially and
inferiorly on an antero-posterior (AP) shoulder X-ray.
Treatment
Reduce under sedation/analgesia with full monitoring, using one of the
methods described below/opposite. The choice of technique is personal
and depends partly upon familiarity. Apply minimal force to prevent
humeral fracture or further soft tissue damage. In patients with habitual
recurrent dislocation (and in a signifi cant proportion of other patients
as well), reduction may be easily achievable with minimal use of drugs
(eg Entonox
®
alone). Take time and perform the manoeuvre slowly.
Note that in situations where IV sedation cannot be used or needs to be
avoided, intra-articular lidocaine is an option.
External rotation method
This simple technique has a good rate of success. With the patient reclining
at 45 * , slowly and gently (without force) externally rotate the shoulder
to 90 * . If the dislocation has not yet reduced, forward fl ex (elevate) the
shoulder slowly.
Kocher’s method
Lie the patient back almost fl at, and once sedation and analgesia are
adequate:
• With the elbow fl exed to 90 * , slowly externally rotate the shoulder.
Pause if there is any resistance and continue only when muscles relax.
• Slowly adduct the upper arm across the chest with the shoulder still
held in external rotation.
• Once adducted as far as possible, internally rotate the shoulder by
fl ipping the forearm towards the opposite shoulder.
Reduction may occur at any time during the manoeuvre: success is more
likely if the patient is relaxed (avoid traction) and if initial external rotation
reaches 90 * . A ‘clunk’ or return of normal glenoid contour confi rms
success.
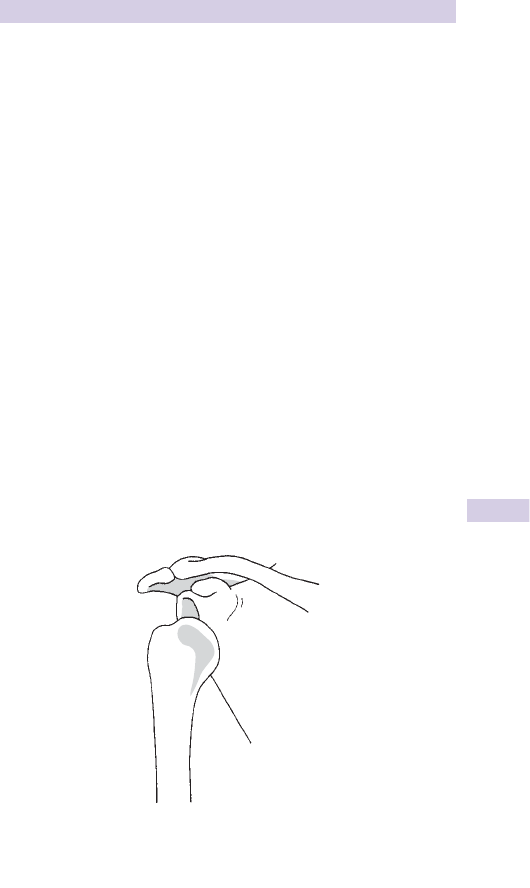
455
ANTERIOR SHOULDER DISLOCATION
Modifi ed Milch method
Slowly abduct the straight arm to 110 * . With the elbow extended, apply
gentle steady traction to the arm, while an assistant controls movement of
the humeral head back into the glenoid.
Other techniques
Scapular manipulation With the patient lying prone, ‘manipulate’ the
scapula onto the glenoid by pushing the inferior tip of the scapula medially
and the superior part laterally.
Stimson’s technique A more traditional method with the patient prone.
Apply a weight strapped to the forearm/wrist of the affected side as it
hangs down and await reduction.
Hippocratic methods Many techniques have been described over many
centuries, but are probably of historical interest only.
Post-reduction After reduction, recheck pulses and sensation (including
axillary and radial nerves), and obtain a check X-ray. Immobilize in a
collar and cuff, and body bandage. Local policy sometimes includes
shoulder immobilization webbing or braces as standard. Provide analgesia
(eg co-dydramol) and arrange follow-up. If unsuccessful, diffi cult or if
shoulder has been dislocated > 24hr, refer for reduction under GA.
Fracture-dislocation of the shoulder
Most involve fractures of the greater tuberosity associated with ante-
rior dislocation of the shoulder (Fig. 9.29 ). Reduce under sedation as
with uncomplicated dislocations — in most cases the fracture will reduce
satisfactorily along with the dislocation. However, refer large or complex
fracture-dislocations involving the humeral head, neck or shaft.
Fig. 9.29 Anterior dislocation of the right shoulder.

456 CHAPTER 9 Wounds, fractures, orthopaedics
Other types of shoulder dislocation
Posterior dislocation
This uncommon injury is easy to miss. It results from a blow onto the
anterior shoulder or a fall onto the internally rotated arm. It may also
occur during seizures or after an electric shock (when other injuries and
medical problems may be partly responsible for it being initially over-
looked). The patient presents with the shoulder internally rotated. AP
shoulder X-ray may appear normal, but careful inspection reveals an
abnormally symmetrical appearance of the humeral head (‘light bulb sign’)
and loss of congruity between the humeral head and the glenoid (Figs 9.30
and 9.31 ). A modifi ed axial shoulder X-ray (from above) or a translateral
view will confi rm posterior dislocation of the humeral head. Manipulate
under sedation by applying traction and external rotation to the upper
limb at 90 * to the body. If diffi cult, refer for reduction under GA. Treat
and follow-up as for anterior dislocation.
Fig. 9.31 Modifi ed axial view of posterior shoulder dislocation.
Fig. 9.30 AP view of posterior shoulder dislocation: light bulb sign.

457
OTHER TYPES OF SHOULDER DISLOCATION
Luxatio erecta
This is a rare inferior dislocation of the humeral head. The patient presents
with arm held abducted above head. Check carefully for neurovascular
complications. Reduce under sedation by traction in line with the abducted
upper arm, followed by adduction of the shoulder. May require reduction
under GA. Treat and follow-up as for anterior dislocation.
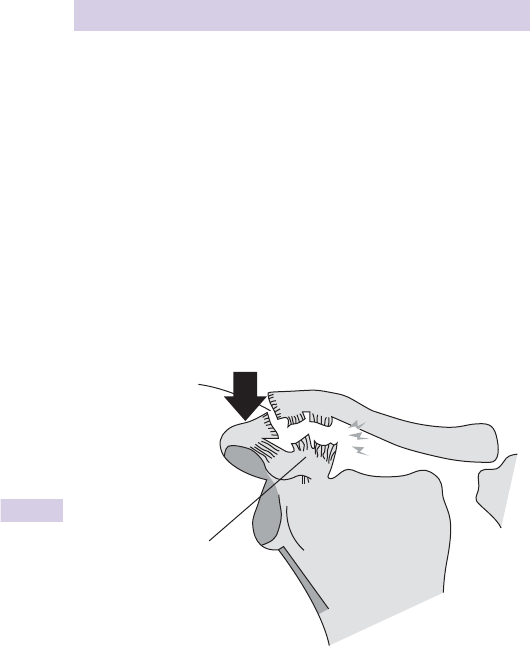
458 CHAPTER 9 Wounds, fractures, orthopaedics
Other shoulder injuries
Acromio-clavicular (AC) joint injury
Common injuries which usually follow falls onto the shoulder or violent
sudden movements of the upper limb. Look for local pain, swelling, or
a palpable step over the AC joint. X-rays show fractures or AC joint
disruption (vertical subluxation of the AC joint > 1–2mm) (Fig. 9.32 ). The
diagnosis may be made more obvious by asking the patient to hold a heavy
object while the X-ray is taken. AC joint injuries are classifi ed:
• Grade I : minimal separation. Only acromio-clavicular ligaments involved.
• Grade II : obvious subluxation, but still some apposition of bony ends.
• Grade III : complete dislocation of AC joint, indicating rupture of the
conoid and trapezoid ligaments, in addition to the acromio-clavicular
ligaments.
Treat with analgesia, support in a broad arm sling, and arrange follow-up
for grades II and III injuries. These measures allow complete recovery in
most cases. Occasionally, selected patients benefi t from internal fi xation.
Clavicle fracture
This common injury results from direct trauma or from falls onto the out-
stretched hand or point of the shoulder. Check carefully for neurovascular
complications (these are rare, but potentially life-threatening).
Treat with analgesia, a broad arm sling and arrange fracture clinic follow-
up. The vast majority of fractures unite satisfactorily with conservative
treatment. Rarely, grossly displaced fractures are internally fi xed.
Scapular fracture
Usually results from direct trauma and implies a forceful mechanism of
injury. Check carefully for associated injuries to the thorax, such as rib
fractures or haemo-pneumothorax.
Treat isolated fractures with a broad arm sling, analgesia, and arrange
follow-up.
Grade III
Acromio-clavicular
ligament
Conoid and
trapezoid ligaments
Fig. 9.32

459
OTHER SHOULDER INJURIES
Humeral neck/head fracture
These result from direct trauma to the upper arm or from falls onto an
outstretched hand. Examine for tenderness or swelling over the proximal
humerus. Shoulder movements are usually limited by pain. X-rays typically
reveal impacted or oblique fractures, with or without associated fractures
of the greater and lesser tuberosities. Fractures may be classifi ed as 2, 3,
or 4-part fractures according to the number of fragments resulting (eg a
fractured humeral neck combined with a fractured greater tuberosity will
be a ‘3 part fracture’).
Treat with a collar and cuff support, analgesia, and follow-up. Warn the
patient to expect signifi cant visible bruising to appear, extending down
the arm towards the elbow (for this reason, it is helpful to document the
lack of any clinical evidence of elbow injury at fi rst presentation). Refer all
comminuted, displaced, or markedly angulated humeral neck fractures as
MUA and, occasionally, internal fi xation/hemi-arthroplasty are indicated.
Shaft of humerus fracture
Results from a fall onto an outstretched hand or onto the elbow. The
fracture may be obvious and palpable. Check distal pulses, radial nerve
and elbow joint. X-ray reveals a transverse, comminuted, or spiral humeral
shaft fracture.
Provide analgesia and support the fracture in a POP U-slab (slab of plaster
from the axilla down to and around the olecranon and up the outside of
the upper arm). Apply with the elbow fl exed to 90 ° and hold in place
with a bandage. Alternative treatment includes a ‘hanging cast’ POP
(above elbow POP at 90 ° — the weight of POP and arm hold the fracture
in a satisfactory position). Refer if displaced, comminuted, or angulated, or
if neurovascular complications are suspected. MUA and internal fi xation
are required in these cases.
Rotator cuff tears
Tears (supraspinatus rupture most commonly) usually follow chronic
rotator cuff disease in patients > 40years. May follow trauma (eg falls with
hyperabduction or hyperextension of the shoulder). Examine for d range
of movement, weakness, crepitus, and tenderness over the cuff insertions
and subacromial area. Examine supraspinatus strength by testing resistance
to abduction. Look for bony avulsions on X-ray (tensile strength of the
cuff exceeds adjacent bone). Treat conservatively initially with analgesia
and support in a broad arm sling, followed by exercises/physiotherapy
at ≈ 10days. Arrange follow-up for patients with signifi cantly d range of
movement — complete tears (particularly in younger patients) may require
surgical repair.
Ruptured biceps
The long head of biceps can rupture at its proximal insertion on lifting or
pulling (see b Soft tissue elbow problems, p.452). This may follow little
force (and with little pain) in the elderly. Look for the ruptured biceps
muscle as a bulge above the elbow. Treat with initial analgesia and support
in a sling, followed by later exercises. Surgical repair is rarely indicated.

460 CHAPTER 9 Wounds, fractures, orthopaedics
Soft tissue shoulder problems
The shoulder is vulnerable to degenerative disease and injury, due to its
extreme mobility and hence, relative instability. Stability relies mainly on
the rotator cuff, a muscle sheath, which wraps around and inserts into the
humeral head under the deltoid. The rotator cuff comprises supraspinatus
(initiates abduction), infraspinatus and teres minor (externally rotate), and
subscapularis (internally rotates). The rotator cuff may be injured acutely
or due to a chronic degenerative process (eg impingement syndromes or
rheumatoid arthritis).
Impingement syndromes
The acromion process may compress or ‘impinge’ on the underlying sub-
acromial bursa and rotator cuff during repetitive or strenuous shoulder
use. Supraspinatus and its tendon are most commonly affected. Minor
impingement is associated with infl ammation, pain, and loss of function
and is reversible with treatment. Rotator cuff tendonitis is more chronic
and can lead to degeneration or tearing of the cuff. Although rotator cuff
tendonitis and degenerative tears usually occur in later life, acute tears can
occur in younger patients.
Examination of the shoulder
Examine both shoulders for comparison with the patient sitting relaxed.
Look for deformity of the clavicle or sternoclavicular joint, AC joint
deformity (eg OA or injury), wasting of the deltoid muscle (axillary nerve
damage), a step in the deltoid contour, or a gap below the acromion
(subluxation or dislocation).
Feel for tenderness over sternoclavicular joint, clavicle, AC joint,
subacromial area, rotator cuff insertion, biceps tendon insertion.
Move the shoulder gently in all directions to test passive movements. Test
strength of active movements. Test abduction (normal range 0–170 ° ),
forward fl exion (0–160 ° ), backward extension (0–60 ° ), external rotation
(put hand on back of head), internal rotation (put hand behind back to
touch shoulder blade).
Examine for crepitus on movement, restriction, pain (note any painful
arc) and weakness of particular movements.
Test sensation over the badge area (upper outer arm) supplied by axillary
nerve. Examine the cervical spine when shoulder examination does not
reveal a cause for symptoms.
In suspected impingement syndromes consider the following:
Neer’s impingement test Fully abducting the straight arm will re-create
symptoms.
Hawkin’s impingement test Hold the arm at 90 ° abduction and 90 ° elbow
fl exion. Rotating the arm across the body will recreate symptoms.
LA injection of 10mL 1 % plain lidocaine into the subacromial bursa
(approach just under acromion process from behind) should help pain, but
will not affect strength or range of movement, aiding assessment. Adding
hydrocortisone, methylprednisolone or triamcinolone to LA injection is
useful for fi rst presentation of acute impingement. Warn that symptoms
may i briefl y after steroid injection. Avoid repeated injection as it can
precipitate tendon rupture.

461
SOFT TISSUE SHOULDER PROBLEMS
Differential diagnosis of shoulder pain
Includes referred pain from a degenerative cervical spine, C5/6 disc pro-
lapse, brachial plexus neuritis, axillary vein thrombosis, suprascapular
nerve compression, Pancoast’s syndrome, or cervical rib.
Subacromial bursitis
Early form of impingement in younger patients. Follows unaccustomed
activity or exercise. Look for a painful arc of 60–100 ° abduction with
dull, aching pain, worse on activity. Differential diagnosis includes gout,
sepsis, or RA. Treat with analgesia, NSAID, and ice. Demonstrate simple
exercises (eg gentle pendulum swings and circling movements of the arm,
crawling fi ngers up a wall). LA injection will improve pain, movement, and
help confi rm diagnosis. Consider steroid injection if fi rst presentation.
Rotator cuff tendonitis
Usually a longer history, chronic pain ( ± sleep disturbance), in patients aged
25–40years. Examine for tenderness and crepitus over humeral insertions
of the rotator cuff and d active and passive shoulder movements. X-ray
may show osteophytes or subacromial calcifi cation. LA injection may
d pain, but usually does not i strength or range of movement. Treat as for
subacromial bursitis. In more severe cases, consider formal physiotherapy
and orthopaedic referral.
Calcifi c tendonitis
A poorly understood process of calcium deposition and resorption
within the rotator cuff tendon. Commoner in women. May be related to
degenerative change or follow minor trauma. Most common site is within
supraspinatus 1–2cm proximal to humeral insertion. Acute pain (occurs
during periods of calcium resorption, granulation, and healing) often starts
at rest, worsens on movement and at night. Examine for tenderness at the
rotator cuff insertion. There may be crepitus, painful limitation of move-
ment or a painful arc. The calcium deposits may be evident on X-ray.
Most episodes spontaneously resolve in 1–2weeks. Treat with analgesia,
NSAID, and ice. Immobilize briefl y in a broad arm sling, but start gentle
exercises (as above) once symptoms allow. Arrange orthopaedic
follow-up; steroid injection and/or physiotherapy and, rarely, surgical
treatment, may be required.
Adhesive capsulitis
A misleading term, since it is caused by a generalized contracture of the
shoulder capsule, not adhesions. Causes include immobilization, injury, or
diabetes. Commoner in women and rare <40 or > 70years old. Insidious
onset results in diffuse, aching pain (worse at night) and restricted active
and passive shoulder movements. The cuff is usually not tender. X-rays
exclude posterior dislocation ( b p.456). Refer to orthopaedics for MUA,
arthroscopy, and capsulotomy.

462 CHAPTER 9 Wounds, fractures, orthopaedics
Soft tissue neck injuries
Neck sprains
Neck injuries that do not involve fractures, dislocations, ligamentous laxity,
or spinal cord damage are common. Most follow car crashes involving
neck hyperextension. These injuries have been referred to as: ‘whiplash’
or ‘whiplash-type’ injuries, ‘hyperextension’ or ‘acceleration fl exion —
hyperextension’ injuries or most simply, ‘neck sprains’. Patients with con-
tinuing symptoms are often referred to as having a ‘whiplash-associated
disorder’. MRI (which rarely changes management) reveals many to have
signifi cant soft tissue injuries.
History
Neck pain and stiffness may not appear until 12hr after injury — symptoms
are typically maximal at ≈ 48hr. Ask about other symptoms (some are
relatively common), which include: headache, shoulder pain, backache,
altered limb sensation. A range of other symptoms may also occur,
including: dizziness, tinnitus, vertigo, and visual disturbance.
Examination
Perform a neurological examination. In fully alert, neurologically intact
patients examine for any midline or paravertebral tenderness, muscle
spasm or deformity. If there is no midline tenderness, assess active neck
movements. If there is localized bony tenderness, pain on active move-
ments or any neurological symptoms, immobilize fully and X-ray.
X-ray
1
Arrange cervical X-rays (AP, lateral and odontoid peg views) in the pres-
ence of high energy trauma, neurological symptoms or signs, d conscious
level or serious injury elsewhere. In the absence of these, do not routinely
X-ray if the patient is fully conscious, has no midline neck tenderness, and
can rotate the neck by 45 ° to right and left.
Check for evidence of fracture or dislocation. The most common
abnormality is loss of the normal cervical lordosis (neck ‘straightening’) —
this implies neck muscle spasm and does not necessarily indicate cervical
spine injury. If the patient has severe pain or any abnormal neurology, but
the initial plain X-rays are normal, consider requesting a CT scan.
Treatment
If there is any clinical or radiological suspicion of vertebral or spinal cord
injury, refer urgently, maintaining cervical spine immobilization.
Treat patients in whom there is no suspicion of spinal cord or vertebral
injury with initial analgesia (eg co-dydramol and/or ibuprofen) and advise
GP follow-up. Leave referral to a physiotherapist for the GP to decide,
based upon progression of symptoms. Avoid the use of a soft collar (the
evidence is against it), but instead encourage early mobilization.
Prognosis
The rate of resolution of symptoms after neck sprains is highly variable.
Many patients ( > 40 % ) continue to complain of pain, stiffness, and other
symptoms for many months. It is often diffi cult to make a long-term
prognosis within 12 months of the injury.
1 Available at : www.ohri.ca/emerg/cdr/cspine.html

463
SOFT TISSUE NECK INJURIES
Non-traumatic neck pain
Neck pain without injury may result from a variety of causes:
• Cervical disc herniations : present with neck pain, sensory and motor
signs. Even if X-rays are normal, refer for further investigation (such as
MRI) and treatment.
• Acute torticollis (‘wry neck’) refl ects painful sternocleidomastoid spasm,
which may occur on waking or after sudden neck movement. It responds
to NSAID, local heat (eg heat pad or hot water bottle), and (in severe
cases), physiotherapy.
• Referred pain : eg tonsillitis/quinsy (especially in children).
• Dystonic reactions : eg drug-induced (see b Complications of psychiatric
drugs, p.619).
• Cervical arthritis : including both OA and RA.

464 CHAPTER 9 Wounds, fractures, orthopaedics
Facial wounds
See also the sections on bony facial injuries ( b pp. 370–376).
Cosmetic considerations
These are very important. The fi nal appearance of a scar depends partly upon
the orientation of the wound and its relation to natural skin lines (modifi ed
from Langer’s description), but also upon initial management. Cleaning is
crucial, but do not debride with tissue excision in the ED. Consider suturing
facial dog bites ( b p.414) and non-contaminated facial wounds up to 24hr
after injury (get senior advice fi rst). Close facial wounds in layers, using 5/0
Dexon or Vicryl for deeper layers, with knots tied on the deep aspect. Aim
to remove skin sutures (interrupted 6/0 non-absorbable monofi lament) at
3 days and replace with Steri-Strips™ to minimize scarring. Consider GA
to treat facial wounds in children.
Damage to parotid duct/gland and facial nerve
This is particularly likely with incised wounds in the pre-auricular area.
The facial nerve emerges through the parotid gland to supply the muscles
of facial expression: unrepaired injury results in permanent disfi gurement.
The parotid duct runs transversely forwards from the anterior portion
of the gland, parallel and inferior to the zygomatic arch, before entering
the mouth opposite the second upper molar (look for blood here, as this
implies proximal duct injury). Refer for exploration in theatre if there is
clinical suspicion of involvement of any of these structures.
Associated head injury
Consider the possibility of signifi cant head or neck injury in all patients
with a facial wound.
Specifi c wounds
Lip wounds Oppose the vermilion border accurately (it is often easiest
to do this fi rst). Remember that even a 1mm mismatch will result in a
permanent visible abnormality. Close in layers if the wound extends into
subcutaneous or muscle layers.
Tongue and oral wounds Check the teeth: if any are broken or missing,
consider obtaining soft tissue lateral X-rays of the lips in a search for
embedded fragments. Small superfi cial lacerations need not be closed, but
close deeper ones in layers, using absorbable sutures (eg 4/0 or 5/0 Vicryl/
Dexon for mucosal surfaces). Close through and through oral lacerations
in layers (mucosa, muscle, and subcutaneous tissue, skin).
Eyebrow wounds Do not shave the eyebrows. Exclude an underlying
fracture by palpation (and X-rays, as appropriate).
Eyelid wounds Many may be sutured with 6/0 non-absorbable monofi la-
ment. Full eye examination, excluding a FB, is necessary. Refer wounds if
there is involvement of lid margin, loss of tissue, or if lacrimal duct (medial
canthus) or gland (superolateral) injury is suspected.
Ears Involvement of cartilage requires suture with fi ne absorbable
material (by an Ear, Nose and Throat (ENT) specialist) prior to skin
closure. Give prophylactic antibiotic cover (eg co-amoxiclav) if there is
any contamination.

465
FACIAL WOUNDS
Langer’s lines (Fig. 9.33 )
Fig. 9.33 Langer’s lines.

466 CHAPTER 9 Wounds, fractures, orthopaedics
Pelvic fractures
Major pelvic fractures result from very high energy trauma and are true
orthopaedic emergencies. Associated thoracic or abdominal injuries
occur in 10–20 % — the principal immediate risk is massive haemorrhage
and exsanguination. Compound fractures of the pelvis have a mortality
of > 50 % . Associated bladder or urethral damage is common. Rectal and
vaginal injuries occur occasionally.
Assessment
• Resuscitate as for any severely traumatized patient ( b Major trauma:
treatment principles, p.320).
• Obtain a pelvic X-ray on all patients with multisystem injury
( b p.322).
• Look carefully for evidence of hypovolaemia and treat appropriately.
• Examine pubis, iliac bones, hips, and sacrum for tenderness, bruising,
swelling, or crepitus. Do not try to ‘spring the pelvis’ to assess
stability — this is unreliable, unnecessary, and may cause additional
haemorrhage/damage. Similarly, avoid log rolling patients with obvious
pelvis fractures — enlist a number of helpers and perform a straight lift.
• Look carefully for wounds especially in the perineum.
• Perform a rectal examination for anal tone, palpable fractures and to
detect bleeding, rectal tears, and urethral damage (high riding, boggy
prostate).
• Test urine for blood, but do not catheterize if urethral injury is
suspected.
• Look at X-rays carefully for disruption of normal pelvic contours
(Shenton’s lines), asymmetry and widening of the pubic symphysis or
sacroiliac joints.
Classifi cation of pelvic fractures (Table 9.3 )
Table 9.3 Tile classifi cation of pelvic injuries (see Fig. 9.34)
Type A (Stable injuries) include avulsion fractures, isolated pubic ramus
fractures, iliac wing fractures, or single stable fractures elsewhere in
pelvic ring
Type B Rotationally unstable but vertically stable
B1 ‘Open book’ antero-posterior compression fractures, causing
separation of the pubic symphysis and widening of one or both
sacroiliac joints
B2 Ipsilateral compression causing the pubic bones to fracture and
override
B3 Contralateral compression injury resulting in pubic rami fractures on
one side and compression sacroiliac injury on the other
Type C (Rotationally unstable and vertically unstable) The pelvic ring is
completely disrupted or displaced at 2 or more points. Associated
with massive blood loss and very high mortality. Subdivided into C1
(unilateral), C2 (bilateral) and C3 (involving acetabular fracture)
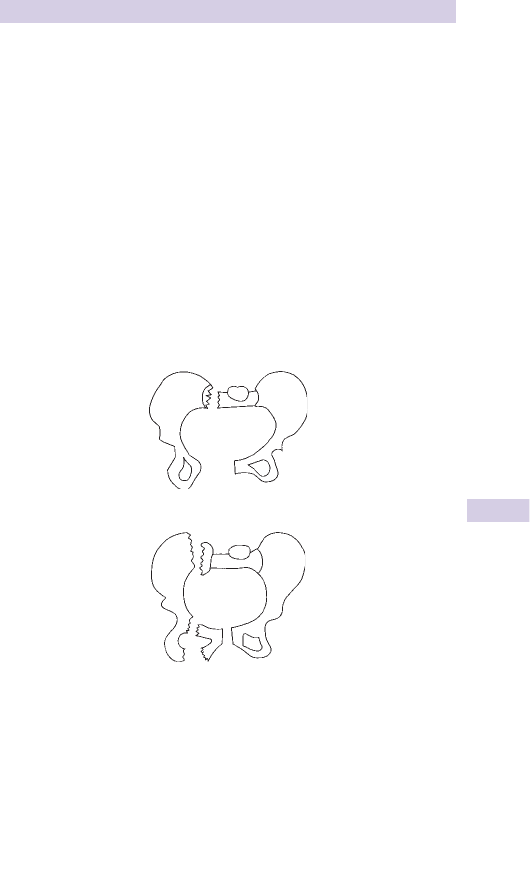
467
PELVIC FRACTURES
Treatment
Stable type A injuries require analgesia and bed rest until able to mobi-
lize (usually 3–6weeks). Isolated pubic ramus fractures are common and
often missed in the elderly (particularly when the focus is on a potential
fractured neck of femur). Refer to orthopaedics for analgesia, initial bed
rest, then mobilization.
Unstable type B and C fractures are an orthopaedic emergency
Resuscitate as for any major trauma ( b p.320). Correct hypovolaemia,
anticipate coagulopathy and ensure blood is rapidly available as massive
transfusion may be required. If DPL ( b p.347) is employed, use a supra-
umbilical approach, as pelvic haematoma may track up the abdominal
wall. Minimize movement, but support an obviously unstable pelvis frac-
ture associated with severe haemorrhage using a pelvic binder or splint
(eg SAM sling). Consider reduction and immobilization using an external
fi xator applied either in the resuscitation room or operating theatre to
halt haemorrhage. If this fails, angiography and selective embolization are
indicated.
Avulsion fractures around the pelvis
Avulsion fractures occur at attachments of various muscles as follows:
• Anterior inferior iliac spine — rectus femoris (typically results from a
miskick into the turf).
• Anterior superior iliac spine — sartorius.
• Ischial tuberosity — hamstrings.
In most instances, symptomatic treatment based upon rest (consider
crutches) and analgesia suffi ces. Larger avulsions (particularly of the ischial
tuberosity) may require internal fi xation (to avoid complications such as
non-union).
Type B1 fracture
Type C1 fracture
Fig. 9.34 Examples of pelvic fractures.

468 CHAPTER 9 Wounds, fractures, orthopaedics
Hip dislocations and acetabular fractures
Acetabular fractures
Often accompany traumatic hip dislocation following violent injury such
as falls or blows to the hip. Posterior rim fractures are the most common.
Complications include massive haemorrhage, sciatic nerve damage,
myositis ossifi cans, and secondary OA. Resuscitate, give analgesia and deal
with priorities fi rst. Additional X-rays (eg 45 ° oblique ‘Judet’ views) or CT
are often required to make an exact diagnosis. Refer to orthopaedics for
traction, protected weight-bearing, or in some cases internal fi xation.
Central dislocation of the hip
This injury is essentially a serious pelvic fracture, which involves the
head of the femur being driven through the (fractured) acetabular fl oor
following a fall or force directed along the length of the femur (eg car
dashboard). The diagnosis is usually obvious on an AP pelvis X-ray. Treat
associated injuries and for shock, and give analgesia. Contact the ortho-
paedic surgeon immediately.
Traumatic posterior dislocation of the hip
Implies major trauma, often with other critical injuries (eg dashboard knee
injury in a car crash) or fractured posterior acetabulum. Limb is short-
ened, internally rotated with hip fl exed and adducted. This appearance
may be absent if there is also a femoral shaft fracture. Check for sciatic
nerve damage — examine foot dorsifl exion and below knee sensation.
Complications: sciatic nerve injury, avascular necrosis of femoral head (risk
i the longer the hip is dislocated), and secondary OA. Diagnosis is usually
obvious on AP X-ray, but lateral views may be needed to exclude dislocation.
Treat as follows:
• Resuscitate the patient and deal with A, B, C priorities fi rst.
• Give analgesia — posterior dislocation causes severe pain.
• Refer for reduction under GA. In unconscious, multiply injured patients,
consider an early attempt to reduce the dislocation.
Reduction technique for posterior dislocation (‘Allis technique’)
• It is easiest and safest to reduce the dislocation if the anaesthetized
patient is placed on the fl oor. If this is not possible, stand on the trolley.
An assistant presses down on the patient’s anterior superior iliac spines
to hold down the pelvis.
• Flex hip and knee both to 90 ° , and correct adduction and internal
rotation deformities.
• Grip the patient’s lower leg between your knees and grasp patient’s
knee with both hands.
• Lean back and lever the knee up pulling the patients hip upwards.
A ‘clunk’ confi rms successful reduction. X-ray to confi rm reduction.
Dislocated hip prostheses
Relatively common, follows minor trauma. Confi rm posterior dislocation
of hip prosthesis by X-ray. Treat with IV opioid and refer to orthopaedics
for MUA (and assessment of prosthesis stability) under GA.
Anterior dislocation of the hip
Less common. The leg is held abducted and externally rotated. Complications
include damage to the femoral nerve, artery, and vein. Give analgesia and
refer for reduction under GA.

469
SACRAL AND COCCYGEAL FRACTURES
Sacral and coccygeal fractures
Fractures of the sacrum
Usually occur from violent direct trauma such as falls. Damage to sacral
nerve roots may occur. Check carefully for saddle anaesthesia, d anal tone,
lower limb weakness, or bladder dysfunction. Refer to the orthopaedic
team.
Fracture of the coccyx
Follows a fall onto the bottom. Do not X-ray routinely — the diagnosis
is clinical. Perform a rectal examination and check for local coccygeal
tenderness, palpable fractures, or evidence of rectal damage. Refer patients
with rectal tears to the general surgeon. Refer to the orthopaedic team if
the coccyx is grossly displaced, as it may require manipulation under LA
or even excision. Treat the remainder symptomatically (eg suggest a ring
cushion and provide analgesia).

470 CHAPTER 9 Wounds, fractures, orthopaedics
Hip fractures
Intracapsular fractures of the neck of femur
Can follow relatively minor trauma. Risk i in the elderly, because of
osteoporosis, osteomalacia, and i rate of falls. These fractures can disrupt
the blood supply to the femoral head, causing avascular necrosis.
Fractures around the hip in younger patients imply high energy injury: the
incidence of non-union or avascular necrosis may be as high as 20 % .
Diagnosis
Usually follows a fall onto the hip or bottom. Pain may radiate down
towards the knee. The affected leg may be shortened and externally
rotated. Check for hypothermia and dehydration (the patient may have
been lying for hours). Look for tenderness over the hip or greater
trochanter, particularly on rotation. Suspect hip fracture in an elderly
person who:
• Exhibits sudden inability to WB. There may be no history of injury,
particularly in the presence of confusion or dementia.
• Is unable to WB and has pain in the knee (the hip may not be painful).
• Has ‘Gone off her feet’.
X-rays
Look closely for disrupted trabeculae/cortices and abnormal pelvic
contours (Shenton’s lines). Fractures of the femoral neck are not always
visible on initial X-rays. Repeat X-rays, bone scanning, or MRI may be
required if symptoms continue. Intracapsular femoral neck fractures may
be graded according to the Garden classifi cation.
Treatment
• Obtain IV access and draw blood for U&E, glucose, FBC, and
cross-match.
• Start IV infusion if indicated (eg dehydration or shock).
• Give IV analgesia plus an anti-emetic. Provide all analgesia IV in small
increments every few minutes until pain is controlled.
• Obtain an ECG to look for arrhythmias/MI and consider need for CXR.
• Arrange other investigations as indicated by history/examination.
• Admit to orthopaedic ward.
Intertrochanteric fracture
These affect the base of the femoral neck and the intertrochanteric region.
Initial management is identical to neck of femur fractures outlined above.
Isolated trochanteric avulsion fracture
Sudden force may avulse insertions of gluteus medius (greater trochanter)
or iliopsoas (lesser trochanter). Give analgesia and refer for follow-up for
gradual mobilization and symptomatic treatment.
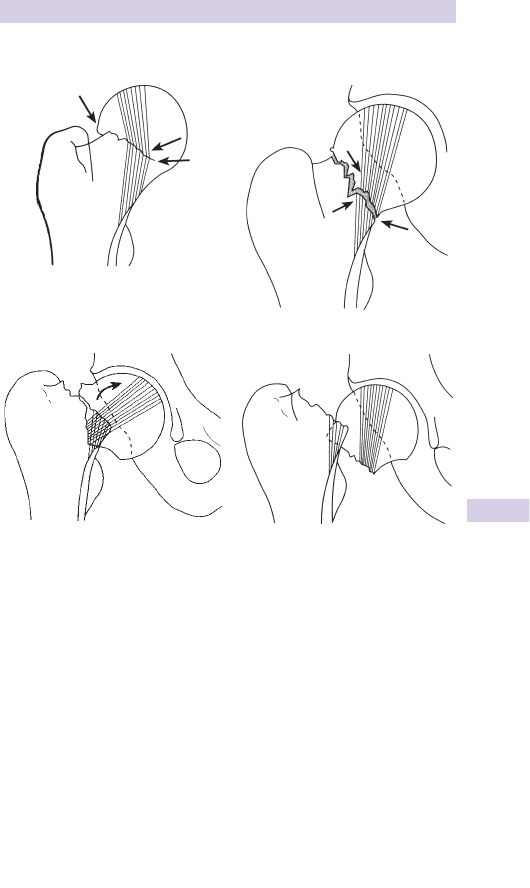
471
HIP FRACTURES
The Garden classifi cation (Fig. 9.35 )
Hip pain after injury, but no fracture
Elderly patients who report hip pain and struggle to walk after a fall, but
yet have no fracture of hip or pubic rami on X-ray may need assessment
by an occupational therapist or physiotherapist before deciding if they
can be safely discharged home with analgesia and appropriate walking aid.
A small, but signifi cant, proportion of such patients will turn out to have
a hip fracture. Therefore, arrange for all patients to return for further
imaging (eg MRI or CT) if pain continues for more than 1 week. In some
patients with very signifi cant symptoms, consider requesting MRI or CT
scan at the time of initial presentation to show up a hip fracture not
identifi ed on plain X-rays.
Garden I
Garden II
Garden III
Garden IV
Fig. 9.35 The Garden classifi cation.
Garden I: trabeculae angulated, but inferior cortex intact. No signifi cant displacement.
Garden II: trabeculae in line, but a fracture line visible from superior to inferior
cortex. No signifi cant displacement.
Garden III: obvious complete fracture line with slight displacement and/or rotation
of the femoral head.
Garden IV: gross, often complete, displacement of the femoral head.

472 CHAPTER 9 Wounds, fractures, orthopaedics
Shaft of femur fractures
Enormous force is required to break an undiseased adult femoral shaft.
Fractures are frequently associated with multisystem trauma. Treatment
of immediately life-threatening injuries takes priority. Transverse, spiral,
or segmental shaft fractures usually result from falls, crushing injuries, or
high-speed road traffi c collisions. There is often associated dislocation of
the hip or other serious injury to the pelvis, hip, and knee.
Complications
Closed fractures of the femoral shaft, even without obvious vascular
injury, may be associated with marked blood loss. Up to 1.5L of blood
may be lost without visible thigh swelling. Rarely, gross blood loss may
occur from compound femoral fractures. Later complications include fat
embolism/ARDS. The incidence of complications is d by early splintage
and early defi nitive treatment (usually closed intramedullary nailing).
Diagnosis
The diagnosis is usually clear on examination with deformity, shortening,
external rotation and abduction at the hip on the affected side. The frac-
ture may be felt or even heard on movement of the lower limb. Carefully
check for associated pelvic, knee, or distal limb injuries or for the presence
of associated wounds. Document sensation and pulses in the limb and
re-check frequently.
Treatment
Before X-rays, resuscitate, exclude life-threatening injuries, replace IV
fl uids, give adequate analgesia, and splint fractures as follows:
• Assess ABCs, establish priorities, and resuscitate.
• Start fl uid replacement via 2 large-bore IV cannulae.
• Obtain blood for cross-matching.
• Administer IV analgesia — give small increments of opioid (with an
anti-emetic) until pain is controlled,
• Strongly consider femoral nerve block (b p.304). As this starts to take
effect ( ≈ 5–10min), prepare splintage and immobilize in Thomas or other
traction splint.
• Arrange X-rays of the femur and contact the orthopaedic team.
Subtrochanteric fractures
Involve the most proximal part of the femoral shaft, at or just distal to the
trochanters. Typically involve high-energy trauma in younger patients and
are often associated with other serious injuries. They can also occur as iso-
lated injuries following relatively minor trauma in those with osteoporosis
or metastatic disease. Treat as for femoral shaft fractures.
Supracondylar fractures
Fractures of the distal third of the femur usually follow violent direct force.
They are frequently comminuted and often intra-articular with associated
damage to the knee joint. In adults, the distal femoral fragment tends to
rotate due to pull from gastrocnemius. Treat as for femoral shaft frac-
tures, but note that femoral nerve block may not be as effective.

473
SHAFT OF FEMUR FRACTURES
Splints for fractured femoral shaft
The Thomas splint is traditional, but other forms of telescopic, metal, or
pneumatic traction splints are increasingly being used. These are conven-
ient, and particularly suitable for temporary immobilization in patients
going directly to theatre or in transit to hospital. Ensure adequate padding
around the groin and the ankle to avoid pressure necrosis of the skin.
Application of a Thomas splint
• Measure circumference of the uppermost part of the uninjured thigh
in cm.
• Select splint of appropriate ring size (also have sizes above and below
ready).
• Prepare splintage — wrap ring in wool roll.
• Slide sleeve of tubigrip over splint to support leg from ring to distal calf.
Secure tubigrip by tying to ring or taping along sides of splint. If the ring
has a buckle this should be on the upper half of the ring.
• Prepare the limb for skin traction — gently. If time permits, shave hair
from medial and lateral aspects of limb.
• Apply splint (if using femoral nerve block wait until this is effective).
Start with adhesive skin traction, making sure the foam part adequately
covers the malleoli. Remove backing and apply adhesive tape along sides
up limb, extending as far up the limb as possible. Trim off the remaining
tape.
• Wrap the leg from ankle to mid-thigh with gauze bandage.
• Apply traction to the leg. Gently pull the ankle with one hand and
support the knee with the other. Correct the abduction and external
rotation while pulling steadily.
• Slide the Thomas splint over the leg until it is against the perineum.
Take care not to snag the skin or genitalia. If the splint does not fi t,
replace it while maintaining traction.
• Tie the cords from the heel end of the skin traction to the end of the
splint while maintaining traction. Insert 2 tongue depressors between
the cords and twist them until the cords are reasonably taut.
• Place wool roll padding under the thigh and if necessary, add more
padding around the groin.
• Bandage around the whole splint from thigh to lower calf with a broad
bandage.
• Support and elevate the leg on a pillow.
• Check distal pulses.
• Arrange X-rays.

474 CHAPTER 9 Wounds, fractures, orthopaedics
Approach to knee injuries
History
Many knee injuries seen in the ED result from sports, particularly foot-
ball and rugby. Carefully document the exact mechanism of injury as it
provides clues to the diagnosis. Valgus or varus stresses can damage the
medial and lateral collateral ligaments, respectively. Flexed, twisting knee
injuries are frequently associated with meniscal injuries. The anterior cru-
ciate ligament (isolated or associated with medial collateral and/or medial
meniscal injuries) may tear during forced fl exion or hyperextension.
Posterior cruciate ligament injuries may follow falls or dashboard impact
where the tibia is forced backwards violently (often associated with medial
or lateral ligament injuries).
Rapid onset tense swelling in a knee is usually an acute haemarthrosis .
Swelling developing more gradually over several days is more likely to
represent a reactive effusion. Ask about previous knee problems: swelling,
clicking, locking, or giving way (the last two suggest underlying meniscal
pathology). Document any previous knee surgery or the presence of
other joint problems. In a hot, swollen, painful, and stiff knee without a
history of signifi cant trauma consider and exclude septic arthritis.
Examination
Always examine both legs with the patient suitably undressed and lying
supine. If there is much discomfort, consider giving oral analgesia and
re-examine in 10–15min. Reassure him/her that you will not suddenly pull
or move the leg without warning.
Look for bruising, swelling, redness, abrasions, or other wounds.
Feel for warmth, crepitation, or the presence of a knee effusion (patellar
tap or ballottable fl uid).
Ask the patient to straight leg raise The ability to do this against resistance
virtually excludes quadriceps, patellar tendon rupture, or transverse
patellar fractures. If unable (possibly due to pain), ask the patient to kick
forwards whilst sitting with the affected leg dangling free.
Assess tone and bulk of quadriceps muscle and compare with the other
side.
Assess knee movement Gentle encouragement or supporting the limb
may be required, but do not use any force.
Assess the cruciate ligaments Try to bring the knee to 90 ° fl exion, sit on
the patient’s foot and hold the leg with both hands around the upper tibia.
Ensure the quadriceps and hamstring muscles are relaxed. Using body
weight, gently rock backwards and forwards looking for anterior glide
(draw) of the tibia (indicating rupture of the anterior cruciate ligament)
or posterior glide of the tibia (indicating rupture of the posterior cruciate
ligament). Up to 5mm movement is normal — always compare both
legs. If unable to fl ex to 90 ° , assess with slight fl exion ≈ 10 ° . Repeat the
procedure with the tibia slightly internally rotated.

475
APPROACH TO KNEE INJURIES
Assess the collateral ligaments With the leg straight, gently apply a valgus
stress to the knee joint (ie move the lower leg laterally) examining for
laxity or pain in the medial collateral ligament. Next apply a varus stress
(ie move the lower leg medially) examining for laxity or pain in the lateral
collateral ligament complex. Repeat the procedure with the knee in ≈ 20 °
fl exion as this will relax the cruciate ligaments. Compare both sides.
Palpate around the knee joint examining all the structures around the
knee for tenderness, swelling, warmth, or crepitus (eg bony landmarks,
ligament insertions, and over the joint line medially and laterally).
X-rays for knee injuries
X-rays form the mainstay of initial imaging for knee trauma: other imaging
(eg CT, MRI) may be indicated after specialist consultation. Obtain X-rays
following knee injuries where there is suspected fracture or other signifi -
cant injury. Use the Ottawa knee rules to assist the decision (in those
aged between 18 and 55 years) as to whether or not to X-ray:
X-rays are only required if any of the following are present:
• There is isolated bony tenderness of the patella.
• There is bony tenderness over the fi bula head.
• The patient cannot fl ex the knee to 90 ° .
• The patient could not weight-bear (take at least 4 steps) both immedi-
ately after the injury and at the time of examination.
Adopt a lower threshold for obtaining X-rays in those aged <18 or
> 55years, patients intoxicated with alcohol, those suffering from bone
disease (eg RA, documented osteoporosis), and for those who reattend
the ED with the same injury (having not been X-rayed initially).

476 CHAPTER 9 Wounds, fractures, orthopaedics
Knee fractures and dislocations
Patellar fracture
This may follow a direct blow or fall onto the patella or sudden violent
knee fl exion or contraction of the quadriceps muscle. Look for pain,
swelling, crepitus, and diffi culty extending the knee. Displaced, transverse
fractures result in an inability to straight leg raise (this is also a feature of
rupture of the quadriceps tendon or patellar tendon — b Soft tissue knee
injuries, p.478). There may be an associated haemarthrosis.
X-rays may be diffi cult to interpret as the patella overlies the distal femur
on the AP view and can obscure subtle fractures. Do not routinely order
‘skyline’ views of the patella. Take care not to mistake a bipartite patella
for a fracture (the accessory bone is typically in the upper, lateral part of
the patella).
Treatment
• Treat vertical fractures with analgesia, immobilize in a non-weight-
bearing cylinder POP, supply crutches, and arrange orthopaedic
follow-up.
• Transverse fractures tend to displace due to the pull of quadriceps.
Treat with analgesia, immobilization in a POP backslab, and refer to
the orthopaedic team for probable ORIF (occasionally, the orthopaedic
team may decide to treat an undisplaced transverse fracture conserva-
tively).
Dislocation of the patella
The patella typically dislocates laterally. This often follows medial stress
to the knee — the dislocation may reduce spontaneously. There may be
a history of recurrent dislocation. The patient has a painful knee, held in
fl exion with obvious lateral displacement of the patella. X-rays are not
generally required prior to reduction of the dislocation. Reduction can
usually be achieved using Entonox
®
— IV analgesia is seldom required.
Stand on the lateral side of the affected limb and hold the affected knee
gently. Using a thumb, lever the patella medially in one smooth, fi rm
movement whilst gently extending the knee at the same time. Successful
reduction is obvious and should rapidly relieve symptoms. Once reduced,
obtain X-rays, immobilize in a canvas (‘cricket pad’) back-splint or cylinder
cast POP, provide analgesia and arrange orthopaedic follow-up. Surgery is
not usually indicated for fi rst time dislocations.
Spontaneous reduction/patella subluxation The patient who has
experienced spontaneous reduction and/or subluxation prior to arrival at
hospital will typically have maximal tenderness over the medial aspect of
the upper patella refl ecting damage to the attachment of vastus medialis.
There may be ‘apprehension’ when gentle lateral pressure is applied to the
patella. If clinical features are dramatic, rest in a splint (occasionally cylinder
POP may be needed), otherwise refer for physiotherapy and orthopaedic
follow-up.

477
KNEE FRACTURES AND DISLOCATIONS
Dislocation of the knee
Although rare, this injury indicates severe disruption of the ligamentous
structures and soft tissues of the knee. Look carefully for associated
injuries (eg femur or lower limb), and document distal pulses and
sensation — the popliteal artery or nerve are often injured. Reduction
requires adequate (IV opioid) analgesia, and usually GA or sedation with
full precautions. Reduce by simple traction on the limb and correcting
deformity. Check distal pulses and sensation after reduction, immobilize
in a long leg POP backslab, and arrange orthopaedic admission. Check
the circulation repeatedly, since popliteal artery damage may not become
apparent for some hours — angiography is usually required. Compartment
syndrome is another recognized complication.
Tibial plateau fractures
Falls onto an extended leg can cause compression fractures of the
proximal tibia. Valgus stresses crush or fracture the lateral tibial plateau.
These injuries are commonly seen in pedestrians injured following
impact with car bumpers. Varus injuries result in crushing or fracture of
the medial tibial plateau and are usually associated with rupture of the
opposite collateral ligaments. Examine for tenderness over the medial
or lateral margins of the proximal tibia. Look for swelling, haemarthrosis,
or ligamentous instability (also try to assess the cruciate ligaments — b
Approach to knee injuries, p.474). Look carefully on X-rays for breaks in
the articular surfaces of the proximal tibia, avulsions from the ligamentous
attachments, or loss of height from the medial and lateral tibial plateaux,
but beware, this may be subtle.
Treat with immobilization in a long leg POP backslab following adequate
analgesia and refer to orthopaedic staff. Fractures of the tibial plateau often
require elevation ± ORIF with bone grafting. Admit all patients with an
acute haemarthrosis. Treat small, isolated avulsions without haemarthro-
sis with immobilization, crutches, and analgesia, and arrange orthopaedic
follow-up.
Posterolateral corner injuries
The posterolateral corner of the knee is comprised of a group of ligaments
and muscles/tendons that add to the stability of the joint. Postero-lateral
corner injuries often occur in association with other signifi cant knee
trauma (eg dislocations, rupture of anterior or posterior cruciate liga-
ments, but isolated injuries can occur. Suspect this injury when signifi cant
symptoms follow the application of varus force to the anteromedial aspect
of the extended knee. Chronic instability can result. X-rays may be normal
or show subtle avulsions or widening of the lateral joint space. Urgent
MRI and orthopaedic referral will enable prompt treatment.

478 CHAPTER 9 Wounds, fractures, orthopaedics
Soft tissue knee injuries
Acute haemarthrosis
Rapid onset swelling following a knee injury, often warm, tense, and
painful. Common causes include cruciate ligament rupture, tibial avulsion,
tibial plateau, or other fractures. An acute haemarthrosis indicates serious
injury. Refer for orthopaedic appraisal following splintage, analgesia and
appropriate X-rays. Aspiration of a haemarthrosis (advocated by some
experts to provide analgesia) requires strict aseptic technique.
Cruciate ligament rupture
The combination of considerable pain and swelling can make it diffi cult to
elicit classical physical signs of a fresh cruciate tear. A history of an audible
‘pop’ at the time of injury is highly suggestive of anterior cruciate rupture.
Anterior cruciate tears often occur in association with tears of the medial
collateral ligament and/or medial meniscus. Examine for the presence of
haemarthrosis, abnormal i anterior glide of the tibia (‘ + ve anterior draw
test’) and injuries to the medial collateral ligament or other structures.
Look carefully at X-rays for avulsion of the anterior tibial spine (anterior
cruciate insertion). Give analgesia and refer to the orthopaedic surgeon.
In posterior cruciate ligament tears , the tibia may appear to sag back
when the knee is fl exed, so the tibia can be pulled into a more normal
position causing a ‘false + ve’ anterior draw. X-rays may reveal the relevant
posterior tibial spine to be avulsed. Provide analgesia and refer.
Collateral ligament injuries
Tenderness over the medial or lateral collateral ligament, with pain at this
site on stress testing, indicates collateral ligament injury. Most injuries are
isolated, and have no associated haemarthrosis and no abnormality on
X-ray. Compare the injured knee with the uninjured one. The degree of
laxity on stress testing will help to guide treatment:
• Local tenderness with no laxity (or very slight laxity) implies a grade I
injury. Treat with analgesia, physiotherapy ( ± crutches) in the expecta-
tion of full recovery in 2–4weeks.
• Local tenderness with minor/moderate laxity, but with a defi nite end-
point implies a grade II injury. Provide analgesia, crutches, instruction on
quadriceps exercises and refer for orthopaedic follow-up.
• Major laxity (ie the joint opening up > 1cm) with no end-point implies
complete rupture. Consider a POP cylinder (or splint), and provide
crutches, analgesia, quadriceps exercises, and orthopaedic follow-up.
Ruptured quadriceps
Complete rupture of the distal quadriceps insertion can result from a
direct injury or from sudden, violent contraction of the quadriceps muscle.
Examination reveals complete inability to straight leg raise — never assume
this is just due to pain. There may be a palpable defect in the muscle inser-
tion. Refer to the orthopaedic surgeon for repair.
Ruptured patellar tendon
Examine for complete inability to straight leg raise, a high-riding patella, a
palpable defect in the patellar tendon. There is frequently an associated
avulsion of the tibial tuberosity. Refer to orthopaedics for repair.

479
OTHER KNEE PROBLEMS
Other knee problems
Acutely locked knee
A springy block to full extension (which varies from just a few degrees to
much more) in the knee indicates an underlying meniscal injury or other
loose body in the knee joint. Obtain knee X-rays (including a tunnel view),
which may show a loose body. Do not attempt to unlock the knee by
manipulation as this is usually painful and futile. Give analgesia and refer
for arthroscopy.
Prepatellar and infrapatellar bursitis
This results from infl ammation of the fl uid-fi lled bursa in front of or just
below the patella, respectively, typically from unaccustomed kneeling.
Treat with rest (which may involve the use of crutches), a short course of
NSAID, and avoidance of the causative activity. Persistent symptoms may
necessitate elective excision of the bursa. Infective bursitis may occur ( i T °
and cellulitis are clues to this): aspirate fl uid for culture and sensitivity, and
start antibiotics (eg co-amoxiclav).
Other causes of knee pain
Patients present not infrequently with knee pain of variable duration and
no history of trauma.
In adults, causes include Baker’s cyst, osteoarthritis (especially in the
elderly), and acute arthritic conditions, including septic arthritis (rare but
important). Also rare, but worthy of consideration is osteosarcoma, which
typically affects teenagers or young adults, producing pain and swelling.
In children, causes include sepsis (including both septic arthritis
and osteomyelitis ( b The limping child, p.704), Osgood–Schlatter’s
disease, osteochondritis dissecans, Johansson–Larsen’s disease (all in b
Osteochondritis, p.708), chondromalacia patellae, referred pain from the
hip, malignancy (eg leukaemic deposits).

480 CHAPTER 9 Wounds, fractures, orthopaedics
Tibial and fi bular shaft fractures
Adult tibial fractures are usually a result of direct blows or falls onto the
tibial shaft. Spiral fractures of the tibia or fi bula follow violent twisting
injuries, usually from sports (eg soccer, rugby, skiing). Displaced fractures
typically involve both the tibia and the fi bula. A large portion of the tibia
has relatively little soft tissue covering — compound injuries are common.
Displaced tibial shaft fractures may be complicated by injury to the popliteal
artery and compartment syndromes ( b Crush syndrome, p.398). Fractures
of the proximal fi bula may be associated with injury to the common pero-
neal nerve. Check (repeatedly) for distal pulses and sensation.
Diagnosis is usually easy. Look for deformity, localized swelling, or tenderness.
Regard all wounds near the fracture site as potential compound injuries.
X-rays Ensure X-rays show the whole length of tibia and fi bula. Examine
closely for the presence of other injuries (eg around the knee or ankle).
Undisplaced stress fractures can occur, particularly in adults involved in
sports, and may not be visible on initial plain X-rays. Persisting symptoms
suggestive of stress fracture require orthopaedic follow-up (and may
eventually require specifi c coned X-rays or even bone scanning).
Tibial shaft fractures
Treat undisplaced transverse tibial shaft fractures with analgesia and long leg
POP backslab. Spiral and oblique fractures also need immobilization, but are
potentially unstable, so refer to orthopaedic team for admission. Immobilize
displaced fractures in a long leg POP backslab following IV analgesia
and refer (to consider MUA or closed intramedullary nailing). Badly com-
minuted or segmental fractures may require ORIF. Contact orthopaedics
immediately if suspected vascular injury, sensory defi cit or gross swelling.
Treat compound fractures initially as on b p.422 and refer to the
orthopaedic surgeon for urgent wound toilet, debridement, and
fi xation—see www.boa.ac.uk/en/publications/boast
Fibular shaft fractures
These can occur in combination with a tibial fracture, as a result of a direct
blow (eg from a car bumper) or from twisting injuries. The common
peroneal nerve may be damaged in proximal fi bular injuries. Examine
specifi cally for weakness of ankle dorsifl exion and d sensation of the lateral
aspect of the forefoot.
Treat undisplaced proximal or fi bular shaft fractures with analgesia and
elevation. Support in a tubigrip or padded bandage. If unable to WB, use a
below knee POP for comfort with crutches until WB is possible. Arrange
follow-up in all cases. Refer displaced or comminuted fractures to the
orthopaedic team.
Stress fractures of the fi bula are relatively common, typically affecting the
fi bular neck of military recruits and athletes following vigorous training.
Treat symptomatically with rest and analgesia.
Maisonneuve fracture ( b p.501)
Transmitted forces may fracture the proximal fi bula following an ankle
injury. This usually involves fracture of the medial malleolus, fracture of
the proximal fi bula or fi bular shaft, and implies damage to the distal tibio-
fi bular syndesmosis. Examine the proximal fi bula in all ankle injuries and
X-ray if locally tender.
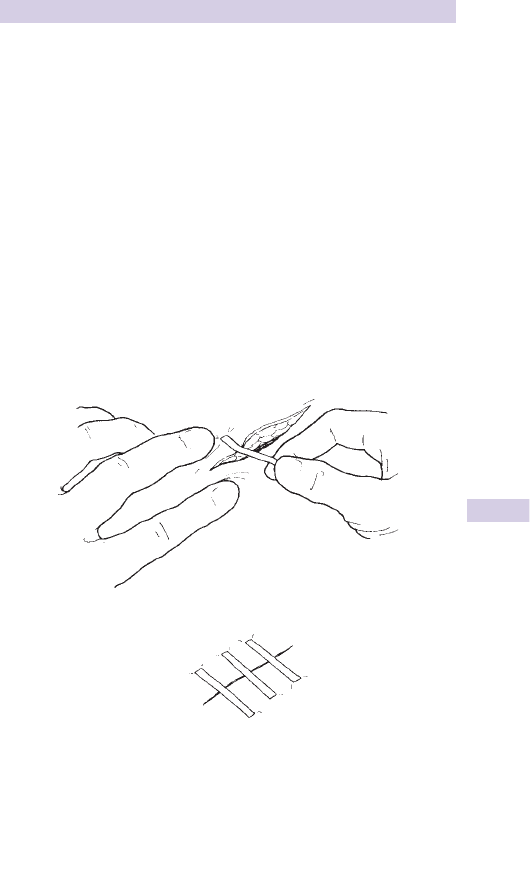
481
PRETIBIAL LACERATIONS
Pretibial lacerations
Common in the elderly following relatively minor trauma. Most pretibial
lacerations can be satisfactorily treated in the ED with adhesive strips
(‘Steri-Strips™’). Clean and irrigate to remove clot, and close using
Steri-Strips™ under appropriate anaesthesia. Aim to leave gaps of ≈ 0.5cm
between the Steri-Strips™. Apply a non-adherent dressing and light
compression bandage. Instruct the patient to elevate the limb whenever
possible (Fig. 9.36 ). Arrange follow-up (ED or GP) for 5 days’ time for
wound inspection and dressing change (but leave underlying Steri-Strips™
until the wound is healed). Consider admission for patients with poor
social support.
Note Suturing pretibial wounds is not usually recommended as the
pretibial skin is friable and undue tension compromises wound healing.
Complications are likely in patients with large, distally based and poorly
viable skin fl aps, and patients on steroids or anticoagulants (check clotting
control). Refer to plastic surgeons large lacerations where skin edges
cannot be opposed, or where complications are likely.
Fig. 9.36 Application of Steristrips.

482 CHAPTER 9 Wounds, fractures, orthopaedics
Calf and Achilles tendon injuries
Calf muscle tears
Acute tears of the gastrocnemius muscle often occur during sports. They can
also occur simply from stepping from a bus or kerb, or from a sudden jump.
Sharp or burning pain in the calf is followed by i stiffness or pain on weight-
bearing. Examine for localized tenderness and/or swelling over the calf muscle
bellies. The medial head of gastrocnemius is more commonly injured.
Carefully check the Achilles tendon for signs of rupture (see below).
Differential diagnosis includes DVT ( b p.118) or rupture of a Baker’s cyst.
Treat with analgesia, NSAID, and initial ice application. Raising the heel with a
pad may also help. Advise elevation of the leg and progressive weight-bearing
as guided by symptoms. Use of crutches may be required if symptoms are
severe (in this case, arrange follow-up and early physiotherapy).
Calf muscle bruising
Direct blunt calf trauma can result in haematoma formation and considerable
swelling. Be alert to the possibility of compartment syndrome, particularly
where there is a signifi cant mechanism of injury (eg b p.398).
Achilles tendon rupture
Achilles tendon rupture can occur without prior symptoms during sudden
forceful contraction of the calf. Usually this occurs during sports (notori-
ously badminton). It also occurs in other situations (eg running for a bus
or missing a step and landing heavily). Patients on ciprofl oxacin, oral ster-
oids or with a history of steroid injection of the Achilles tendon area are
at i risk. The patient often describes a sudden sharp pain behind the ankle
like a ‘bang’ or similar description. Patients often mistakenly initially believe
that they have sustained a blow to the back of the ankle. Examination
may reveal swelling, pain, bruising, and often a (diagnostic) palpable defect
(gap) in the tendon ≈ 5cm above the calcaneal insertion. Plantar fl exion
against resistance will be weaker than on the normal (uninjured) side, but
do not rely on this when making a diagnosis.
Beware plantar fl exion (even standing on tip-toes) may still be possible
due to action of the tibialis posterior, peroneal, and toe fl exor muscles.
Calf squeeze test (Simmonds/Thompson’s test) Kneel patient on a chair,
facing the back, with feet hanging free over the edge. Alternatively,
position the patient to lie prone on a trolley with ankles over the end.
Gently squeeze mid-calf and look for normal plantar fl exion of the ankle
(Fig. 9.37 ). To avoid confusion do not describe the result as + ve or –ve,
just state ‘calf squeeze test normal’ or ‘abnormal’.
Treatment Remains controversial, so follow local policy. Treatment
options are:
• Conservative management : many ruptures are managed with crutches,
analgesia, and immobilization for 6weeks in a long leg plaster with the
ankle in plantar fl exion and knee fl exed to ≈ 45 ° . This is followed by
careful rehabilitation under the care of the orthopaedic team and physi-
otherapist.
• Primary surgical repair is often employed in young patients and athletes.
Refer to the orthopaedic team to consider this.
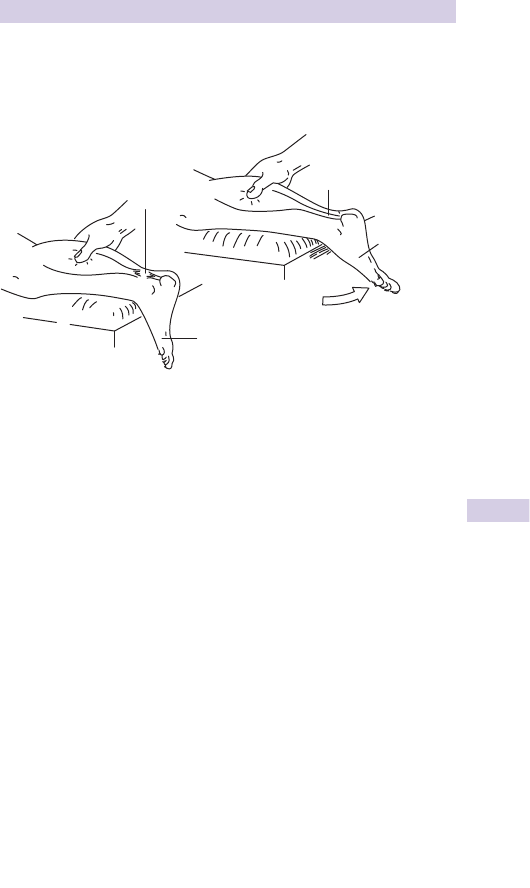
483
CALF AND ACHILLES TENDON INJURIES
Note Sometimes a ‘partial’ Achilles tendon rupture is suspected. In this
instance, the safest initial treatment is immobilization in a non-weight-bearing
BKPOP with ankle fl exion, crutches, and orthopaedic follow-up. USS can
help to determine the state of the tendon.
Achilles tendonitis/paratendonitis
This frequently follows unaccustomed activity or overuse (eg dancing,
jumping, running, or even walking) and may be associated with familial
hypercholesterolaemia. There is usually a history of i pain, aggravated by
ankle movements. Examine for localized pain, swelling, and palpable crep-
itus over the Achilles tendon (the most common site is ≈ 5cm from its
insertion). The calf squeeze (Simmonds) test is normal. Check lipid profi le.
Treat with analgesia, NSAID, and a brief period of rest (eg 1–2 days) before
gradually returning to normal activities as guided by symptoms. Occasionally,
1–2 weeks in a BKWPOP may be useful. A heel pad inserted into footwear
may help. Athletes may benefi t from removal of heel tabs from training shoes
if implicated. Avoid local steroid injection, which may i risk of tendon rupture
by impeding healing or by allowing premature resumption of activity.
Calf/leg pain with no history of trauma
A variety of conditions may be implicated, including:
• Shin splints : a variety of pathophysiological processes have been sug-
gested, including tibial periostitis. This condition is characterized by pain
over the anterior distal tibial shaft after running on hard surfaces. Advise
rest and NSAID.
• Stress fractures : can affect the tibia (as well as the fi bula — see b p.480).
Treat with analgesia and POP with orthopaedic follow-up.
• Bursitis : infl ammation of the bursae around the insertion of the Achilles
tendon responds to conservative measures.
• DVT: see b p.118.
• Cellulitis : see b p.413.
• Ischaemia : see b p.531.
• Ruptured Baker’s cyst.
Tendon
rupture
Tendon intact
Foot planta
r
flexes
No/reduced movement
Fig. 9.37 Calf squeeze test to check integrity of Achilles tendon.

484 CHAPTER 9 Wounds, fractures, orthopaedics
Approach to ankle injuries
Ankle injuries are among the most common problems presenting to the
ED. Adopt a logical, consistent approach to identify which patients are
likely to have a fracture and to avoid unnecessary X-rays in patients with
uncomplicated sprains.
History
Establish the exact mechanism of injury. Most are inversion injuries
(where the sole of the foot turns to face medially as the ankle is plantar
fl exed) causing damage to structures around the lateral malleolus (most
notably, the anterior talofi bular ligament). Eversion injuries occur less com-
monly and damage the structures around the medial malleolus. Hyper-
dorsifl exion and plantar fl exion injuries occur less frequently.
The following are relevant in the initial assessment of ankle injuries:
• A fracture is more likely in patients who are unable to weight bear
(WB) immediately following the injury.
• A ‘crack’ or ‘snap’ may be heard and is not indicative by itself of a
fracture.
• Ice, analgesia, and elevation may infl uence the appearance of an ankle
injury.
Examination
Examine from the knee down for tenderness over:
• Proximal fi bula.
• Lateral malleolus and ligaments.
• Medial malleolus and ligaments.
• Navicular.
• Calcaneum.
• Achilles tendon.
• Base of 5th metatarsal (MT).
Is an X-ray required
1
?
Follow the Ottawa ankle rules (Fig. 9.38 ) for adults and X-ray ankles if
patients:
• Were unable to WB for 4 steps both immediately after the injury and at
the time of examination.
• Have tenderness over the posterior surface of the distal 6cm (or tip) of
the lateral or medial malleolus.
Note that tenderness over the navicular, calcaneum, base of 5th MT or
proximal fi bula require specifi c X-rays to exclude fractures.
Adopt a lower threshold for X-ray in the very young, the elderly, and in
patients who are diffi cult to assess (eg intoxicated).
1 Adapted from Stiell IG ( 1993 ) Decision rules for the use of radiography in acute ankle injuries.
Refi nement and prospective validation . J Am Med Ass 269 : 1127 – 32 .
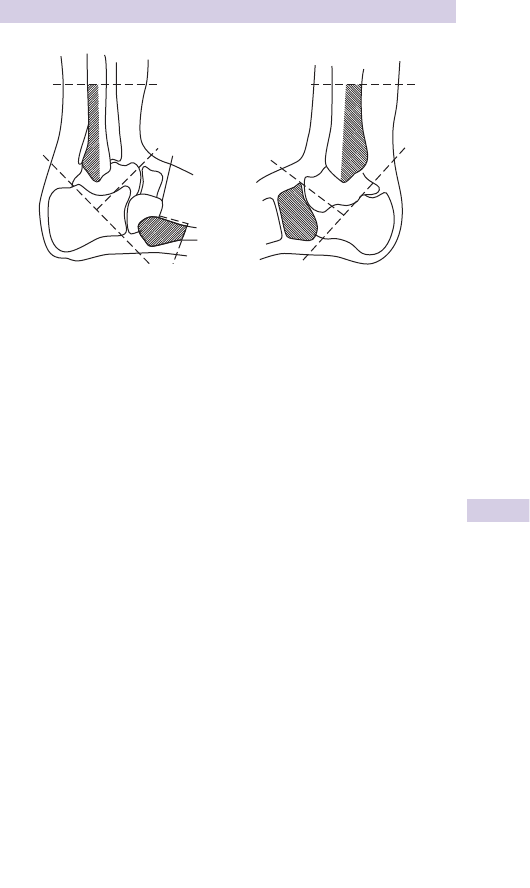
485
APPROACH TO ANKLE INJURIES
Fig. 9.38 The Ottawa ankle rules.
Guidelines for X-ray in a simple ankle injury. Bony tenderness over the points indicated requires
an X-ray. X-ray is also required if the patient is unable to weight-bear immediately after the injury
or to walk 4 steps in the ED.
X-ray the ankle for malleolar tenderness and the foot for metatarsal/tarsal tenderness. If the patient
is not X-rayed then they are given instructions to return after 5 days if they have trouble weight-
bearing.
Adapted from Stiell IG (1993) Decision rules for the use of radiography in acute ankle injuries.
Refi nement and prospective validation. J Am Med Ass 269: 1127–32.

486 CHAPTER 9 Wounds, fractures, orthopaedics
Ankle fractures and dislocations
Clinical assessment and imaging after ankle injury is outlined in b p.484.
Ankle fractures
Fractures around the ankle most commonly involve the malleoli — medial,
lateral, and what is commonly referred to as the ‘posterior malleolus’
(the posterior part of the distal tibia). The mortice joint formed by the
talus and the distal tibia, fi bula, ligaments, and the distal tibio-fi bular
syndesmosis allows very little rotation or angulation at the ankle joint.
As a consequence, forced twisting or angulation of the ankle joint causes
fractures associated with ligamentous injuries and in severe cases, disruption
of the distal tibio-fi bular syndesmosis.
Treatment depends upon a combination of clinical fi ndings and X-ray
appearances. Look carefully for talar shift.
• Small avulsion fractures essentially refl ect ligament/joint capsule damage.
Treat with rest, elevation, analgesia, and early mobilization as for sprains.
• Larger avulsion fractures may require initial immobilization in BKPOP
with crutches and orthopaedic follow-up.
• Undisplaced, isolated medial or lateral malleolar fractures are usually
stable and do well with conservative measures. Provide analgesia,
crutches, and immobilize in a well-padded BKPOP cast. Advise limb
elevation and arrange orthopaedic follow-up. Note that an isolated
‘high’ lateral malleolus fracture may only be apparent on the lateral
X-ray and may be associated with deltoid (medial) ligament injury with
instability — some require ORIF.
• Displaced fractures of the medial or lateral malleolus require ORIF. Give
analgesia and, as appropriate, IV sedation to allow reduction of talar shift.
Immobilize the limb in a BKPOP slab and refer to the orthopaedic team.
• Bimalleolar or trimalleolar fractures are unstable. Having attempted to
reduce any signifi cant talar shift (with appropriate sedation), place in a
BKPOP, obtain fresh X-rays, and refer to the orthopaedic team.
Ankle dislocation
Dislocation of the ankle is an orthopaedic emergency. Treat promptly
on diagnosis. Examination shows gross deformity of the ankle, severe
stretching of the skin (resulting in fracture blisters, skin necrosis, or
even converting the injury to a compound fracture), and often defi cits in
peripheral pulses or sensation. The ankle can dislocate in the absence of
associated fractures, but this is uncommon.
Treatment Prompt closed reduction and immobilization in POP usually
has to precede X-ray (unless available immediately). ‘Prompt treatment’
does not justify reduction without considering analgesia or sedation.
• Give Entonox
®
, IV analgesia, or sedation as appropriate with full
precautions.
• Warn the patient there may be a brief i in discomfort as the ankle
reduces.
• With the knee fl exed and supported, gently grasp the heel with one
hand and support the patient’s calf with the other.
• Pull smoothly on the heel — it may be necessary to slightly exag-
gerate the deformity in order to obtain reduction. Success is indicated
by return of normal ankle contours, relief of skin tension, and often
dramatic relief of pain.
• Once reduced, re-check pulses and sensation, immobilize in a POP slab,
and arrange check X-rays.
• Refer the patient to the orthopaedic team immediately.

487
ANKLE SPRAINS
Ankle sprains
Clinical assessment and imaging after ankle injury is outlined in b p.484.
The structures most frequently injured in inversion injuries are the lateral
joint capsule and the anterior talofi bular ligament. Increasing injury causes
additional damage to the calcaneofi bular ligament and posterior talofi bular
ligament.
Treatment
Historically, treatment of sprained ankles has been based upon ‘RICE’
(rest, ice, compression, elevation), but the scientifi c basis for all the
elements of this is distinctly lacking!
Advise initial rest, elevating the ankle above hip level, and to consider
applying ice intermittently during the fi rst 2 days for periods of 10–15min.
Begin to WB as soon as symptoms allow, but elevate at all other times.
An elastic support from toes to knee is traditional, but of no proven value
(and may be harmful by i pain without speeding recovery). If used, ensure
that it is not worn in bed. Advise the patient to gently exercise the ankle
in all directions and to use simple analgesia regularly until symptoms
improve. Most patients with minor sprains can expect full recovery in
≈ 4weeks. It may be possible to resume sports gradually within 2weeks,
depending on progress.
The inability to WB implies more severe injury. Provide crutches to those
completely unable to WB despite analgesia, with advice to elevate the
ankle. Arrange review at 2–4days — if still unable to WB, consider
10days’ immobilization in a below-knee cast, with subsequent outpatient
follow-up. Other approaches include the use of adhesive strapping or pre-
formed ankle braces. These may be useful in selected cases. Patients can
usually expect good functional recovery and should not regard the ankle
as ‘weak’. Long-term problems (eg weakness/instability whilst walking
over rough ground) are often related to d ankle proprioception following
immobilization, so aim to mobilize as soon as possible.
Long-term complications
Do not regard ankle sprains simply as trivial injuries: patients may suffer
long-term morbidity (which often causes them to return to the ED):
• Instability often manifests itself by recurrent ankle sprains. Refer to
physiotherapy (to include isometric exercises).
• Peroneal tendon subluxation refl ects a torn peroneal retinaculum,
allowing the peroneal tendons to slip anteriorly. The clinical presenta-
tion includes clicking and a sensation of something slipping. Movement
of the foot/ankle (especially eversion) reproduces the subluxation.
Refer for orthopaedic follow-up — surgery is an option.
• Peroneal nerve injury is relatively common, but not frequently sought
for. Neurapraxia results from stretching of branches of the peroneal
nerve at the time of injury, with subsequent d sensation over part of the
dorsum of the foot and d proprioception at the ankle joint (refl ecting
injury to the articular branches).

488 CHAPTER 9 Wounds, fractures, orthopaedics
Foot fractures and dislocations
Crushing or other violent injuries to the foot can result in signifi cant
long-term disability. Multiple fractures or dislocation of the tarsals
or MTs are often overlooked in the presence of other severe injuries.
Delayed or inadequate treatment result in high rates of post-traumatic
OA. Compartment syndromes ( b p.398) or vascular injuries may occur.
Amputations or severe mangling injuries of the foot are rarely suitable for
reconstruction/re-implantation due to poor long-term functional results.
Talar injuries
Falls onto the feet or violent dorsifl exion of the ankle (eg against car
pedals in a crash) can result in fractures to the anterior body or articular
dome of the talus. Displaced fractures and dislocations frequently result in
avascular necrosis.
Treat with analgesia, immobilization in a backslab POP, and refer promptly
for orthopaedic treatment (may require MUA and/or ORIF). Dislocations
of the talus require prompt reduction under GA.
Upper/midfoot dislocations
These injuries follow violent twisting, inverting or everting injuries of the
foot. Peritalar/subtalar dislocations involve the articulation between the
talus and the calcaneum. Give adequate analgesia and refer to ortho-
paedics for prompt reduction under GA. Mid-tarsal dislocations involve
the mid-tarsal joint (comprising the calcaneum and talus posteriorly and
the navicular and cuboid anteriorly) and are treated similarly. Isolated
dislocation of the talus is rare and requires prompt reduction under GA.
Calcaneal fracture
Calcaneal fractures most often follow a fall from height directly onto the
heels. Always exclude associated injuries of the cervical and lumbar spine,
pelvis, hips, or knees. Examine for swelling, bruising, and tenderness over
the calcaneum, particularly over the sides. Examine both calcanei for com-
parison, remembering that fractures are commonly bilateral. Examine the
Achilles tendon for injury ( b p.482). Request specifi c calcaneal X-rays and
scrutinize carefully breaks in the cortices, trabeculae or subtle signs of com-
pression (reduction in Bohler’s angle — see Fig. 9.39 ). Refer all fractures to
orthopaedic staff. The majority will require admission for elevation, analgesia
and in selected cases, ORIF following CT scanning.
Tibia
Talus
Calcaneum
35°–40°
Fig. 9.39 Bohler’s angle (normally 35–45 ° ).

489
FOOT FRACTURES AND DISLOCATIONS
Clinically suspected calcaneal fracture, but X-rays normal
Sometimes, clinical suspicion of a calcaneal fracture is not confi rmed by
X-rays at the time of initial presentation. It is possible that X-rays may
initially fail to identify a calcaneal fracture. Therefore, treat clinically
with analgesia, rest, elevation, crutches and arrange review at 7–10days,
when consideration can be given to further imaging if symptoms persist
(eg more X-rays and/or CT scan).
Metatarsal fractures and dislocations
Multiple MT fractures may follow heavy objects falling onto the feet or
more commonly, after being run over by a vehicle tyre or wheel. In all
such cases, consider the possibility of tarso-metatarsal (Lisfranc) dislo-
cation. This can be easily missed on standard foot X-rays, which do not
usually include a true lateral view — look to check that the medial side
of the second MT is correctly aligned with the medial side of the middle
cuneiform. Check for presence of the dorsalis pedis pulse. Multiple, dis-
placed, or dislocated MT fractures require urgent orthopaedic treatment.
Support in a POP backslab following analgesia and refer for MUA, K-wire
fi xation, or occasionally, ORIF. MT stress fractures are discussed below.
Isolated avulsion fractures of the 5th MT base
These follow inversion injuries of the ankle, the base of the 5th MT being
avulsed by the tendon of peroneus brevis. Always examine this area in
ankle injuries and request foot X-rays if tender. Do not mistake accessory
bones or the epiphysis (which runs parallel, not transverse to the 5th
MT base). Treat with analgesia, elevation, and support in a padded crepe
bandage or temporarily, in a BKPOP if symptoms are severe. Arrange
orthopaedic follow-up.
Jones fracture (of the 5th MT)
This is a transverse fracture of the 5th MT just distal to the intermetatarsal
joint. It is a signifi cant fracture as it is prone to non-union. Treat with
analgesia, crutches, BKPOP, and orthopaedic follow-up.
Stress fractures of the MTs
Fatigue fractures of the MTs are common. They typically follow prolonged
or unusual exercise (hence the term ‘march fracture’), but often occur
without an obvious cause. The commonest site is the 2nd MT shaft, but
the 3rd MT or rarely the navicular or other MTs may be affected. Examine
for swelling over the forefoot (there may be none) and localized tender-
ness over the MT shaft or on longitudinal compression of the MT shaft
(do this by pressing on the MT head below the toe — pain will be felt along
the MT shaft). X-rays are usually normal initially. Callus or periosteal reac-
tion seen at ≈ 2–3weeks on X-ray will confi rm the diagnosis, but this is not
required for treatment.
Treat symptomatically with analgesia, elevation, rest, and modifi ed daily
activity as required. A padded insole may help. Firm shoes or boots
may be more comfortable than fl exible trainers. Expect full recovery in
6–8 weeks. If unable to WB, consider a brief period in a BKPOP (or
‘Aircast’ boot) until symptoms improve.

490 CHAPTER 9 Wounds, fractures, orthopaedics
Toe injuries
Most toe injuries do not require X-ray
The treatment of isolated closed fractures of the toe phalanges without
clinical deformity or other complicating factors is not altered by X-rays.
X-ray the following:
• Obvious deformity, gross swelling or suspected dislocation.
• Suspected compound injuries.
• If any tenderness over the MT head or MTPJ.
• Suspected FB.
Toe fractures
Treat uncomplicated phalangeal fractures with simple analgesia, elevation,
and support with padded buddy strapping. Advise the patient to resume
normal activities as soon as possible, but explain that some discomfort
may be present for up to 4–6weeks. Hospital follow-up is not normally
required. Manipulate displaced fractures under LA digital block (as des-
cribed for fi ngers on b p.294). Angulated toe phalangeal fractures can be
diffi cult to manipulate — a useful trick is to use a pen (or needle holder)
placed between the toes as a fulcrum. Once satisfactorily reduced, buddy
strap and confi rm the position with X-rays.
Dislocated toes
Untreated, toe dislocations may cause troublesome, persistent symptoms.
Reduce promptly under LA digital block and splint by buddy strapping.
Always confi rm reduction by X-ray, and discharge with analgesia and
advice on elevation and gradual mobilization.
Compound toe injuries
Careful wound toilet, debridement, and repair is essential to ensure rapid
healing and avoid infective complications. Ensure that there is adequate
tetanus prophylaxis. Always clean wounds thoroughly under adequate
anaesthesia (usually LA digital block), provide antibiotics and analgesia.
Advise the patient to elevate the injured foot and arrange follow-up
according to local practice. More severe injuries will require exploration
and repair under GA. Refer these cases to the orthopaedic team.
Mangled or amputated toes
Functional results of attempted re-implantation of amputated toes or
repair of badly mangled toes are often poor. Provide analgesia and refer
to the orthopaedic surgeon for wound management and amputation of
unsalvageable toes.

491
SOFT TISSUE FOOT PROBLEMS
Soft tissue foot problems
Puncture wounds to the foot
• ‘Simple’ puncture wounds : see b p.419.
• Weever fi sh injuries : see b p.416.
FBs embedded in the foot
Searching for small FBs in the sole of the foot has been likened to search -
ing for a needle in a haystack. Follow the principles set out in b Further
assessment of skin wounds, p.428. Nerve blocks ( b p.306) can be useful
to allow exploration of foot wounds.
Morton’s metatarsalgia
A burning discomfort radiating to the toes may result from an interdigital
nerve neuroma at the level of the MT heads. The nerve between the 2nd
and 3rd MT heads is frequently affected. There is localized tenderness,
which is also reproduced on compression of MT heads together. Advise
simple analgesia and GP follow-up to consider referral to a foot surgeon.
Plantar fasciitis
Plantar fasciitis can occur spontaneously or as a chronic overuse injury.
Infl ammation develops in the plantar fascia, typically at its calcaneal
insertion. This results in gradually increasing, burning pain in the sole of
the foot and heel, which is worse on WB. Examine for localized tender-
ness over the calcaneal insertion of the plantar fascia and heel pad. X-ray
may reveal a calcaneal spur, but this is not a useful diagnostic feature.
Advise NSAID, rest and elevation for 1–2 days, with GP follow-up. A padded
shoe insole or sorbothane heel pad may help. Severe, persistent cases are
occasionally treated with local steroid injection or even surgical division of
the plantar fascia.
Osteochondritis dissecans ( b p.708)
Osteochondritis of a MT head (usually the 2nd — Freiberg’s disease) causes
gradual onset pain on WB. The cause is often unclear, but it may follow
minor injury. Examination may reveal local tenderness but little else. X-ray
for evidence of fl attening, widening, or fragmentation of the MT head or
narrowing of the MTPJ.
Treat initially with simple analgesia. Refer persistent cases to orthopaedics
to consider excision of the MT head or osteotomy.
In-growing toenails
Refer back to the GP for elective treatment, unless there is evidence
of infection. In this case, consider oral antibiotics (eg fl ucloxacillin or
co-amoxiclav), or if there is an acute paronychia, incision, and drainage
under LA. On occasion, it may be appropriate to excise a wedge of nail
under LA.

492 CHAPTER 9 Wounds, fractures, orthopaedics
Low back pain
Low back pain is the commonest cause of lost work days in the UK. The
initial ED approach is to identify any patients who may have immediately life-
threatening problems (eg leaking aortic aneurysm) and sort the rest into:
• Simple (‘mechanical’) back pain : no investigations or referral required.
• Nerve root pain : referral and investigation needed if symptoms persistent
or progressive.
• Possible serious spinal pathology : referral and investigation required.
• Suspected cord compression : immediate neurosurgical/orthopaedic
referral mandatory.
Psychogenic back pain is not an ED diagnosis. If in doubt, refer.
History
General Document patient’s age, sex and employment. Note onset
and duration of symptoms, character, position and radiation of pain,
exacerbating or relieving factors. Precipitants include injuries, falls, heavy
lifting, or unaccustomed activity.
Past history Detail any previous back problems or surgery, other medical
conditions (eg rheumatoid arthritis, OA, osteoporosis).
Drug history Is the patient using analgesia (and has it helped?). Ask about
corticosteroids and contraindications to NSAIDs.
Social history Ask about home circumstances, work, and stress.
Systemic enquiry Weakness, altered sensation, weight loss, anorexia,
fever, rigors, cough, sputum, haemoptysis, bowel, or urinary symptoms.
Examination
‘Unwell’ patient Immediately assess airway, breathing, and circulation.
Look for shock and a pulsatile abdominal mass, peritonism, evidence of
blood loss, radial-femoral pulse discrepancies or asymmetry.
‘Well’ patient Look for signs of weight loss, cachexia, anaemia, clubbing,
or muscle wasting. Inspect the back for muscle spasm, scars, scoliosis, or
other deformity. If possible, watch the patient walk, looking for spasm,
abnormal posture or limping. Palpate for tenderness over the spine, lower
ribs and renal angles. With the patient supine on a trolley, look for muscle
wasting in the legs. Examining both sides:
• Straight leg raise : note the angle which reproduces pain (lumbar nerve
root irritation).
• Crossed straight leg raise : nerve root symptoms reproduced by lifting
contralateral leg strongly suggests lumbar disc prolapse and nerve root
entrapment.
Perform a neurological examination Check tone, power, sensation, and
refl exes in the lower limbs:
• L4 covers sensation of medial lower leg; quadriceps power; knee jerk.
• L5 covers sensation of lateral lower leg and great toe; extensor hallucis
longus power; hamstrings jerk.
• S1 covers sensation of little toe and lateral foot; foot plantar fl exors
power; ankle jerk. Always check perineal and perianal sensation.
Perform a rectal examination for anal tone, masses, or blood. Examine the
abdomen for masses. Document peripheral pulses and perfusion.

493
LOW BACK PAIN
Investigation
Check T ° and urinalysis. X-ray is indicated for some patients aged
> 55years, or those who are systemically unwell, with a history of trauma
(except clinical coccyx fracture), or where malignancy, infection, or HIV is
suspected. In the latter cases, also check C-reactive protein (CRP), FBC,
U&E.
Treatment
Refer urgently patients with lower limb weakness, altered perineal or
perianal sensation, sphincter disturbance (this is strongly suggestive of
cauda equina syndrome due to central lumbar disc prolapse). An MRI scan
will confi rm this diagnosis — in which case, urgent consultation with a
neurosurgeon will allow emergency surgical decompression to be planned
as appropriate.
Refer patients with the following: aged <20 or > 55years, unremitting or
increasing symptoms, widespread neurological signs, weight loss, systemic
illness, pyrexia, chronic corticosteroids, osteoporosis, or HIV + ve patients
with thoracic pain.
Treat simple ‘mechanical’ back pain with regular simple analgesia and/or
NSAID. Avoid the routine use of opioids. Small doses of benzodiazepines
(eg diazepam 2–5mg tds) may be useful, but tend to cause drowsiness.
Advise the patient to aim to return to normal activity, even if some
discomfort persists. Avoid bed rest. Expect recovery in 4–6weeks. Nerve
root symptoms mostly resolve over weeks to months with the above
treatment, physiotherapy or manipulation. In all cases, give written and
verbal advice for immediate return if limb weakness, numbness, bladder,
or bowel problems occur. Advise follow-up with the GP.

494 CHAPTER 9 Wounds, fractures, orthopaedics
Acute arthritis 1
Approach
Whenever a patient presents with a painful joint, try to distinguish
whether the source of pain is articular or peri-articular. Painful joints of
articular origin produce warmth, tenderness, and swelling about the entire
joint, with painful movement in all directions. Pain of peri-articular origin
(outside joint capsule), such as bursitis/tendinitis tends to result in tender-
ness and swelling localized to a small area, with pain on passive movement
only felt in limited planes.
Consider a septic cause in every patient who presents with acute arthritis.
Useful investigations include white blood cells (WBC), erythrocyte
sedimentation rate (ESR), or CRP, and joint aspiration.
Joint aspiration
The most important diagnostic test in patients presenting with acute
arthritis is examination of the synovial fl uid. When joint aspiration is per-
formed, ensure that an aseptic technique is employed. Avoid joint aspira-
tion through an area of cellulitis. Send fl uid for Gram stain, culture, crystal
examination, and cell count (Table 9.4 ). Remember that the absence of
bacteria on Gram staining does not exclude septic arthritis.
Causes of polyarthritis
• Rheumatoid arthritis.
• Ankylosing spondylitis.
• Reiter’s disease.
• Psoriatic arthritis.
• Arthritis associated with infl ammatory bowel disease.
• Viral arthritis.
• Rheumatic fever.
• Gonococcal arthritis.
• Gout.
Table 9.4
Normal Reactive Infectious
Colour Colourless/pale yellow Yellow Yellow
Turbidity Clear, slightly turbid Turbid Turbid, purulent
Cell count/mm 200–1000 3000–10,000 > 10,000
Predominant cell
type
Mononuclear Neutrophil Neutrophil
Gram stain None None + ve
Culture –ve –ve + ve

495
ACUTE ARTHRITIS 1
Septic arthritis
Pyogenic infection usually reaches a joint via the bloodstream, but may
also develop from adjacent osteomyelitis or external skin puncture
wounds. Sepsis may progress to complete joint destruction within 24hr.
Infective agents Staph aureus, Gonococcus, Strep, TB, Salmonella. Haemophilus
was the commonest organism in babies before Haemophilus immunization,
but is now rare. There is an i incidence in patients with rheumatoid
arthritis, those taking steroids, the immunosuppressed and at the extremes
of age. Do not overlook septic arthritis superimposed on a non-infectious
joint (eg gout, rheumatoid joints).
Presentation Typically only 1 joint is affected and is red, painful, and
swollen. No movement is usually tolerated (but steroids and analgesics
can mask many of the common features of septic arthritis). The joint is
held in position of most comfort, usually slight fl exion. There may be
fever, shaking, and rigors. Note that hip joint infection may not produce
obvious external fi ndings due to its deep location. Do not overlook a
septic joint with signs obscured by concomitant antibiotic use. IV drug
abusers may have involvement of uncommon joints of the axial skeleton
(eg sacroiliac, vertebral, and sterno-clavicular joints).
Investigation FBC, ESR, or CRP, blood cultures, joint aspiration (see Table
9.4 ). X-rays may be initially normal or show only soft tissue swelling with
displacement of capsular fat planes. Later, features of bone destruction
occur.
Treatment Commence IV antibiotics (eg fl ucloxacillin + benzylpenicillin).
Refer urgently to the orthopaedic team for joint irrigation/drainage,
analgesia, splintage of the joint.
Note: Prosthetic joint infection can be diffi cult to detect, but pain is
typically constant and present at rest. Early infection (within 3 months
of surgery) may cause obvious wound infl ammation. This is less likely to
be apparent in delayed or later infections. There may be little in the way
of systemic symptoms. Suggestive radiological features include widening
and lucency of the bone-cement interface by > 2mm, movement of the
prosthesis, periosteal reaction and fractures through the cement, although
X-rays may be normal. Adopt a low threshold for suspecting prosthetic
joint infections and referral to the orthopaedic team.
Traumatic arthritis
Joint pain, tenderness, d range of movement and haemarthrosis after
injury implies intra-articular fracture. Note, however, that septic arthritis
may occur in association with trauma, even in the absence of penetrating
injury.
Osteoarthritis
Elderly patients with known OA may suffer acute ‘fl are ups’. Constitutional
symptoms are not a feature. X-rays may show asymmetrical joint space
narrowing, osteophytes and subchondral cyst formation. Advise NSAID
and/or paracetamol, plus graduated exercises.

496 CHAPTER 9 Wounds, fractures, orthopaedics
Acute arthritis 2
Acute gout
Most often affects 1st MTPJ or knee. Precipitated by trauma, diet, diuretics,
renal failure, myeloproliferative disease and cytotoxics. Ask about previous
renal stones. Look for tophi. Joint aspiration reveals negatively birefringent
crystals. Septic arthritis can occur with gout — ensure aspirates are Gram
stained and cultured. X-rays initially show soft tissue swelling, later punched
out lesions in peri-articular bone. Serum uric acid may be i , but can be
normal in an attack. Treat with rest and NSAID (eg diclofenac 75mg bd)
or if NSAID is contra-indicated, consider colchicine (500mcg bd initially,
slowly i to qds as needed to control symptoms, preferably with GP review).
Do not alter treatment of patients already on long-term gout therapy.
Note: oral steroids (eg prednisolone 30mg od for 5 days) may help patients
who are unable to tolerate NSAIDs or who are resistant to other treatments.
Acute pseudogout
Typically affects the knees, wrists, or hips of an elderly person with history
of arthritic attacks precipitated by illness, surgery, or trauma. Associated
with: hyperparathyroidism, haemochromatosis, Wilson’s disease, hypothy-
roidism, diabetes, hypophosphatemia. X-ray shows calcifi cation in joint,
menisci, tendon insertions, ligaments, bursae. Aspiration reveals weakly
+ ve birefringent crystals on polarizing microscopy. Treat symptomatically
(with NSAID) and refer.
Rheumatoid arthritis
Presentation Persistent symmetrical deforming peripheral arthropathy
typically starts with swollen, painful, stiff hands and feet, which gradually
get worse, with larger joints becoming involved. Other modes of presen-
tation are: persistent or relapsing monoarthritis of different large joints,
systemic illness with minimal joint problems, sudden onset widespread
arthritis, vague limb girdle aches.
Hand signs include MCPJ and PIPJ swelling, ulnar deviation and volar
subluxation at MCPJs, boutonnière, and ‘swan-neck’ fi nger deformities.
Extensor tendon rupture may occur.
Neck problems Degeneration of the transverse ligament of the dens
carries the risk of subluxation and cord damage.
Extra-articular features SC nodules, vasculitis, pulmonary fi brosis,
splenomegaly, anaemia, pleurisy, pericarditis, scleritis, kerato-conjunctivitis.
Rhematoid factor is + ve in 70 % of cases.
X-rays show soft tissue swelling, peri-articular osteoporosis, joint space
narrowing, bony erosions/subluxation.
Treatment Refer patients who are systemically unwell. Others may
benefi t from NSAID, splintage, and rheumatology clinic referral.
Viral arthritis
Rubella, hepatitis B, mumps, Epstein–Barr virus, and enteroviruses may
cause arthritis. In hepatitis B, arthritis usually affects PIPJ, MCPJ or knee
and precedes the onset of jaundice. Rubella is associated with an acute
symmetrical arthritis and tenosynovitis.

497
ACUTE ARTHRITIS 2
Rheumatic fever (see b p.672)
This is a non-infectious immune disease which follows infection with
Group A β -haemolytic streptococci. Typically, a migratory or additive
symmetrical polyarthritis affects the knees, ankles, elbows, and wrists.
Diagnosis is based on revised Jones criteria: evidence of previous
streptococcal infection (ie recent scarlet fever, + ve throat swab, or anti-
streptolysin titre > 200U/mL) plus 2 major or 1 major plus 2 minor criteria.
Major criteria: carditis (pericarditis, myocarditis or endocarditis), migratory
polyarthritis, chorea, SC nodules, rash (erythema marginatum).
Minor criteria: i ESR/CRP, arthralgia, fever, history of previous rheumatic
fever (or rheumatic heart disease), i PR interval on ECG.
Investigations: Throat swab, ESR, CRP, and anti-streptolysin titre.
Treatment Refer for admission, rest, aspirin, benzyl penicillin, and splintage.
Sero-negative spondyloarthropathies
These have the following common features: involvement of the spine and
sacroiliac joints, infl ammation then calcifi cation of bony tendon insertions,
peripheral infl ammatory arthropathy, and extra-articular manifestations
such as uveitis, aortic regurgitation, and pulmonary fi brosis.
Ankylosing spondylitis
Usually presents with chronic low back pain in men aged 15–30 years.
Progressive spinal fusion ultimately results in a fi xed kyphotic spine
(which is particularly prone to fracture after injury), hyperfl exed neck,
and restricted respiration. Hips, shoulders, and knees may be involved.
Other features are: iritis, apical lung fi brosis, plantar fasciitis, and Achilles
tendonitis. There may be normochromic anaemia and i ESR. X-rays
show ‘bamboo spine’ (squared vertebrae), eroded apophyseal joints and
obliterated sacro-iliac joints.
Reiter’s syndrome
Triad of urethritis, conjunctivitis and sero-negative arthritis may follow
infection (urethritis, cervicitis, or dysentery). May cause large joint
monoarthritis of a WB leg joint. Other features: iritis, keratoderma
blenorrhagicum, circinate balanitis, plantar fasciitis, Achilles tendonitis,
aortic incompetence.
Joint aspirate yields infl ammatory cells, with –ve culture. WCC and ESR
are i .
Psoriatic arthritis
Arthritis rarely precedes skin involvement.
Enteropathic arthropathies
Infl ammatory bowel disease is associated with spondyloarthritis and large
joint mono-arthropathy. There may also be a migratory polyarthritis.
Gonococcal arthritis
May present with fever, migratory tenosynovitis and polyarthralgia,
arthritis (knee, ankle or wrist) and skin rash. Genital infection may be
silent, especially in women. Take swabs with special culture media and
refer for investigation.

498 CHAPTER 9 Wounds, fractures, orthopaedics
Eponymous fractures
Correctly applied, the one or two words that comprise an eponymous injury
convey succinctly an otherwise involved description of a complex fracture.
Aviator’s astragalus
Fractures of the neck of the talus, previously commonly observed amongst
World War II pilots who crash-landed their damaged planes on returning
from bombing raids. The injuries resulted from the upward thrust of the
rudder bar, causing dorsifl exion forcing the talus against the anterior tibia.
Bankart lesion
Avulsion of the joint capsule and glenoid labrum resulting from anterior
dislocation of the shoulder joint. It is implicated as a causative factor for
recurrent dislocations.
Barton’s fracture
First described by Barton in 1839, this complex distal radial fracture is
intra-articular. Displacement of the distal radial fragment allows subluxa-
tion of the carpal bones. A rare variety is called a Lentenneur’s fracture.
Bennett’s fracture dislocation
These intra-articular fractures of the base of the fi rst MC are notorious
for allowing the main MC fragment to slip into a poor position. If conserv-
ative treatment (POP) is preferred to internal fi xation, careful follow-up
will be needed to ensure a satisfactory outcome.
Boutonnière deformity
Rupture of the central slip of the extensor tendon at the PIPJ allows the
base of the middle phalanx to ‘button-hole’ through. The remaining two
parts of the extensor expansion slip along the side of the fi nger and act
as fl exors at the PIPJ, whilst still extending the DIPJ. This produces the
characteristic deformity.
Boxer’s fracture
Fracture of the neck of the little fi nger MC rarely occurs during formal
boxing when gloves are worn. It is much more commonly seen following
impromptu street or bar-room brawls: innocuous-looking overlying
wounds are often compound human (‘reverse fi ght’) bites ( b Specifi c
bites and stings, p.416).
Bumper fracture
The height of the average car bumper renders the adult pedestrian (who
is unfortunate enough to be knocked down) particularly vulnerable to a
fracture through the lateral tibial condyle into the tibial plateau. There is
often an associated tear to the medial collateral knee ligament.
Chance fracture
A horizontal fracture through a vertebral body, associated arch, and
spinous process may result from an injury involving distraction and fl exion.
It typically involves the lumbar spine of car passengers restrained only by a
lap belt in a road traffi c collision.

499
EPONYMOUS FRACTURES
Clay-shoveller’s fracture
Resistance against neck fl exion may produce an avulsion of the tip of a
spinous process of the lower cervical or upper thoracic spine. The lesion
typically affects C7.
Colles’ fracture
Abraham Colles, Professor of Surgery in Dublin, described this common
distal radial fracture in 1814. The classic dinner fork deformity results from
posterior displacement and angulation of the distal fragment ( b p.444).
Dashboard dislocation
A high speed head-on road traffi c collision causing the dashboard to
impact upon the fl exed knee often results in posterior dislocation of the
hip.
Dupuytren’s fracture-dislocation
A highly unstable ankle injury in which there is a fracture of the distal
fi bula shaft, disruption of the medial ankle ligament and posterior tibio-
fi bular ligament. The result is gross diastasis and dislocation of the talus
laterally.
Essex–Lopresti fracture-dislocation
A heavy fall on the outstretched hand may cause a comminuted fracture of
the radial head. It is associated with tearing of the interosseous membrane
(diastasis), allowing subluxation of the distal ulna.
Galeazzi fracture-dislocation
Describes the combination of a fracture of the distal radial shaft with dis-
location of the distal radio-ulnar joint ( b Forearm fractures and related
injury, p.448). A Moore’s fracture dislocation is a similar injury, except that
the radial fracture involves the distal radius, not the shaft.
Gamekeeper’s thumb
Rupture of the ulnar collateral ligament of the 1st MCPJ was originally
described as an occupational injury amongst gamekeepers, sustained whilst
breaking the necks of wounded rabbits. It is now most commonly seen as
a result of skiing injuries, particularly on artifi cial slopes, when the thumb
is caught in the diamond latticework matting. The injury requires prompt
diagnosis and treatment in order to avoid the long-term complication of
a weak pinch-grip.
Hangman’s fracture
Although no longer a part of modern life in the UK, executions were pre-
viously achieved by hanging. The victim was allowed to fall several feet
before being arrested by a noose. This produced rapid death from sever-
ance of the cervical spinal cord. The mechanism of injury is a combina-
tion of distraction and extension, causing an unstable (hangman’s) fracture
of the pedicles of the axis (C2), and disrupting the intervertebral disc
between C2 and C3. The fracture may also result from extension and
axial compression and may occur without neurological damage.

500 CHAPTER 9 Wounds, fractures, orthopaedics
Hill–Sachs lesion
This is an impacted compression fracture of the humeral head, which
occurs during anterior shoulder dislocation. It is produced by the recoil
impaction of the humeral head against the rim of the glenoid as the former
dislocates. It is believed by some to be an important causative factor for
recurrent dislocation.
Horse rider’s knee
Frontal impact at the level of the proximal tibio-fi bular joint may result in pos-
terior dislocation of the fi bular head. Reduction usually requires an MUA.
Hume fracture-dislocation
This refers to the combination of an olecranon fracture with dislocation
of the radial head.
Hutchinson fracture
Also referred to as a ‘chauffeur’ fracture, this is the name sometimes given
to a fracture of the radial styloid. It is classically caused by forced radial
deviation of the wrist when the starting handle of an old-fashioned motor
car ‘kicks back’.
Ice skater’s fracture
Children aged 2–8years are susceptible to stress fractures of the distal
fi bula.
Jefferson fracture
An unstable ‘blowout’ fracture of C1 follows an axial load. One third are
associated with a C2 fracture.
Jones fracture
This is a transverse fracture of the base of the 5th MT just distal to
the intermetatarsal joint. It is a more signifi cant injury than an avulsion
fracture at the insertion of peroneus brevis, as it is prone to non-union
( b Foot fractures and dislocations, p.489).
Le Fort facial fractures
Experiments by Le Fort in 1901 were followed by descriptions of facial
fractures and classifi cation into three anatomical types ( b Middle third
facial fractures, p.372), including the Guérin fracture (Le Fort I).
Lisfranc fracture-dislocation
Fracture dislocation at the tarso-metatarsal joint is a signifi cant injury. It is
named after the surgeon who described the surgical operation of partial
amputation of the foot at the level of the tarso-metatarsal joint.
Luxatio erecta
First described in 1859, this is an uncommon shoulder dislocation (inferior
glenohumeral dislocation). The term is derived from Latin and describes
the erect hyperabducted position of the arm after dislocation. The injury
follows a hyperabduction force, most often after a fall. Axillary nerve
damage occurs in 60 % . Reduction of the dislocation may follow overhead
traction or conversion to an anterior dislocation to which conventional
techniques can be applied.

501
EPONYMOUS FRACTURES
Maisonneuve injury
An unstable injury in which rupture of the medial ankle ligament is associ-
ated with a diastasis and proximal fi bula fracture.
Malgaigne’s fracture
An unstable injury in which the pelvic ring is disrupted in two places:
anteriorly (through both pubic rami) and posteriorly (sacroiliac joint
disruption, or fracture of ilium or sacrum).
Mallet injury
Stubbing a fi nger may rupture the extensor tendon (or avulse its phalan-
geal attachment) at the DIPJ, causing a ‘mallet deformity’, in which the DIPJ
is held fl exed. The mechanism of injury is forced fl exion of the extended
DIPJ.
March fracture
This refers to a stress fracture of the (usually 2nd) MT shaft after stren-
uous and unaccustomed exercise. Traditionally, it was observed after
heavy marching in new army recruits.
Monteggia fracture-dislocation
Fracture of the proximal ulna shaft is associated with dislocation of the
radial head. The latter is relatively easy to miss. Never accept an ulna
fracture as an isolated injury without obtaining complete views of both
forearm bones, including the elbow and wrist joints.
Nursemaid’s elbow
Alternative name for a ‘pulled elbow’ in a pre-school child ( b p.724).
Nutcracker fracture
Lateral force applied to the forefoot may cause the cuboid to be fractured
as it is compressed between the calcaneum and the base of the 4th and
5th MTs.
O’Donahue’s triad
A torn medial meniscus, ruptured anterior cruciate ligament and ruptured
medial collateral ligament combine to produce a signifi cant knee injury.
Pelligrini–Stieda’s disease
Ossifi cation of the medial collateral knee ligament may follow avulsion of
the superfi cial part from its attachment to the medial femoral condyle.
Pilon fracture
These intra-articular fractures of the distal tibia are uncommon, but may
also be subdivided into three types.
Pipkin fracture-dislocation
This refers to a posterior hip dislocation in which part of the femoral
head is avulsed by the ligamentum teres and remains attached to it
within the acetabulum. The avulsed fragment is rarely large enough to be
reattached.

502 CHAPTER 9 Wounds, fractures, orthopaedics
Pott’s fracture
This term has come to be applied indiscriminately to any ankle fracture,
which may be simply subdivided into ‘uni-’, ‘bi-’, or ‘tri-malleolar’.
Rolando fracture
Essentially a comminuted Bennett’s fracture, the classic description is of
Y shaped intra-articular fractures at the base of the 1st MC. Treatment
is diffi cult.
Runner’s fracture
Stress fractures of the tibia are particularly common amongst runners who
chalk up many miles of running on roads each week.
Smith’s fracture
The so-called ‘reversed Colles’ fracture’ was fi rst described by Smith in
1847.
Straddle fracture
Falls astride classically produce bilateral vertical pubic rami fractures.
Tillaux fracture
An avulsion fracture of the distal lateral tibia may occur due to the pull of
the anterior tibio-fi bular ligament.
Toddler’s fracture
Undisplaced spiral fractures of the tibial shaft in children <7 years
often follow minimal trauma and not be visible on initial X-ray.
Subperiosteal bone formation is usually apparent radiologically by 2 weeks
(see b Paediatric lower limb injuries, p.727).

503
Approach to abdominal pain 504
Causes of acute abdominal pain 506
Acute appendicitis 507
Acute pancreatitis 508
Biliary tract problems 510
Peptic ulcer disease 511
Intestinal obstruction 512
Mesenteric ischaemia/infarction 514
Large bowel emergencies 516
Anorectal problems 518
Retention of urine 520
Testicular problems 522
Penile problems and prostatitis 523
Ureteric colic 524
Abscesses 526
Cellulitis and erysipelas 528
Complications of varicose veins 529
Ruptured abdominal aortic aneurysm 530
Acute limb ischaemia 531
Surgery
Chapter 10

504 CHAPTER 10 Surgery
Approach to abdominal pain
First aim to identify patients requiring resuscitation or urgent treatment.
The need for resuscitation is apparent in emergencies with associated
hypovolaemic and/or septic shock. Less obvious, but equally important,
is recognition of patients requiring urgent treatment with no clinical
evidence of shock (especially ruptured abdominal aortic aneurysm).
History
The pain Determine details of site, radiation, shift, character, timing,
precipitating, and relieving factors.
Vomiting Record anorexia, nausea, and vomiting. Ask about the nature
of vomit (blood, bile, etc.). Vomiting that follows the onset of abdominal
pain tends to imply a surgical cause, whereas vomiting preceding pain is
often non-surgical.
Bowel disturbance Enquire about recent change of bowel habit,
particularly any rectal bleeding.
Other symptoms Do not forget that abdominal pain may be due to
urological, respiratory, cardiovascular or gynaecological disorders.
Past history Determine the nature of previous surgery, preferably by
obtaining old notes.
Examination
Vital signs Pulse, BP, respiratory rate, GCS, and T ° may indicate the need
for immediate intervention.
Abdomen Note distension and scars from previous surgery. Check the
hernial orifi ces. Palpate gently for areas of tenderness. It is unnecessary
and unkind to attempt to elicit rebound tenderness — tenderness on
percussion is ample evidence of peritonitis. Perform PR/PV examination.
General Look for evidence of dehydration and jaundice. Examine the
respiratory and cardiovascular systems.
Investigations
Assessment of patients with abdominal pain in the ED usually depends
upon history and examination rather than sophisticated tests. However,
the following investigations may prove useful:
• BMG: DKA may present with abdominal pain ( b Hyperglycaemic
crises, p.152).
• Urinalysis : abdominal pain may result from urinary stones or infection.
Perform a urine pregnancy test on all women of childbearing age.
• Blood tests : consider the need for FBC, U&E, amylase, coagulation
screen, and cross-matching. If clearly unwell, check ABG, and lactate.
Although FBC is frequently requested in patients with abdominal pain,
the awaited WCC rarely alters initial patient management.
• ECG : especially in patients aged > 55 years, who may be suffering from
an atypical presentation of an acute medical problem, most notably
acute myocardial infarction (MI).

505
APPROACH TO ABDOMINAL PAIN
• Chest X-ray : a CXR is useful to exclude conditions above the diaphragm,
which may mimic abdominal conditions (eg congestive heart failure,
basal pneumonia).
• Abdominal X-ray : Specifi c indications for abdominal X-ray include
suspicion of intestinal obstruction, toxic megacolon, sigmoid volvulus, GI
perforation and urinary calculi ( b Ureteric colic, p.524). X-rays are not
indicated in patients with suspected uncomplicated appendicitis, UTI,
‘simple’ constipation, gastroenteritis, GI bleeding, acute pancreatitis.
They are not ‘routinely indicated’ in the investigation of abdominal pain.
In severely ill patients requiring imaging, CT or USS is usually more
appropriate than plain abdominal X-rays.
• USS : reveals gallstones, free peritoneal fl uid, urinary stones and aortic
aneurysms. It is increasingly used in the ED, but needs specifi c training.
• CT scan may have a role in assisting with the diagnosis of certain
conditions (eg acute appendicitis).
Treatment
Prompt resuscitation and provision of analgesia are integral components
of the management of serious abdominal conditions. Ensure that patients
who are very sick and/or hypotensive receive early IV fl uids and full
monitoring (this includes measuring urinary output via a urinary catheter).
Follow the guidelines outlined in b Severe sepsis and shock for patients
with suspected sepsis, p.59.
The traditional belief that analgesia should not be given because it
might mask a serious diagnosis is incorrect and cruel. Diagnosis is often
easier when pain is relieved and the patient can give a better history and
co-operate with examination. The most appropriate form of analgesia is
usually IV opioid (eg morphine).
It can be diffi cult to decide if admission is needed for a patient with
abdominal pain. Adopt a low threshold for seeking senior help. In general,
if doubt exists, refer to the surgeon, who may decide that it is prudent to
admit the patient for observation and investigation.
Pitfalls
• Steroids, NSAIDs, or obesity may render physical signs less obvious.
• B -blockade may mask signs of shock.
• Absence of fever does not exclude infection, especially in the very old,
the very ill, and the immunosuppressed.
• When severe abdominal pain is out of all proportion to the physical
fi ndings, consider mesenteric infarction, aortic rupture/dissection, acute
pancreatitis, torsion of ovarian cyst.
• Splenic rupture may occur after relatively trivial trauma in patients with
glandular fever or haematological disorders.
• Consider gynaecological causes of abdominal pain in any woman of
child-bearing age — always perform a pregnancy test.
• WCC may be normal in established peritonitis/sepsis.
• Amylase may be normal in acute pancreatitis. Conversely, moderate
amylase i may occur in acute cholecystitis, perforated peptic ulcer, and
mesenteric infarction.

506 CHAPTER 10 Surgery
Causes of acute abdominal pain
The cause of abdominal pain is often unclear initially. Indeed, many patients
get better without any defi nite cause being identifi ed (‘non-specifi c’
abdominal pain). Remember also that a patient is much more likely to
have a common condition (perhaps with an atypical presentation), rather
than a very rare condition. Thus, a patient presenting with atypical abdom-
inal pain is more likely to have acute appendicitis than tabes dorsalis, lead
poisoning, or acute intermittent porphyria. The following conditions are
seen relatively frequently:
Surgical
• Non-specifi c abdominal pain.
• Acute appendicitis.
• Cholecystitis and biliary colic.
• Pancreatitis.
• Peptic ulcer disease (including perforation).
• Ruptured abdominal aortic aneurysm.
• Mesenteric infarction.
• Diverticulitis.
• Large bowel perforation.
• Intestinal obstruction from various causes.
• Ureteric calculi.
• Urinary retention.
• Testicular torsion.
• Intussusception.
• Cancer (especially of the colon: see below).
Gynaecological
• Ectopic pregnancy.
• Pelvic infl ammatory disease (PID).
• Rupture/torsion of ovarian cyst.
• Endometriosis.
• Mittelschmertz.
Medical
• MI.
• Pneumonia.
• Pulmonary embolus (PE).
• Aortic dissection.
• Acute hepatitis.
• DKA.
• Urinary tract infection (UTI).
• Herpes zoster.
• Irritable bowel syndrome.
• Gastroenteritis.
Cancer causing abdominal pain
Unexplained abdominal pain in patients > 50 years may be caused by
cancer, especially of the large bowel. The pain may result from transient
or partial bowel obstruction. Ask about previous episodes of pain, weight
loss and change of bowel habit. If there is no indication for admission,
consider referral to a surgical clinic for investigation.

507
ACUTE APPENDICITIS
Acute appendicitis
This common cause of abdominal pain in all ages is particularly diffi cult to
diagnose in the extremes of age and in pregnancy. However, the diagnosis
of acute appendicitis is often missed initially at all ages.
History
The classic presentation is of central colicky abdominal pain, followed by
vomiting, then shift of the pain to the right iliac fossa. Many presentations
are atypical, with a variety of other symptoms (eg altered bowel habit,
urinary frequency) partly depending upon the position of the tip of the
infl amed appendix (retrocaecal 74 % ; pelvic 21 % ; paracaecal 2 % ; other 3 % ).
Examination (see also Table 10.1 )
In the early stages, there may be little abnormal; in the late stages the patient
may be moribund with septic shock and generalized peritonitis. Between
these extremes, there may be a variety of fi ndings, including i T ° , tachy-
cardia, distress, foetor oris. There is usually a degree of tenderness in the
right iliac fossa ( ± peritonitis). Rovsing’s sign (pain felt in the right iliac fossa on
pressing over the left iliac fossa) may be present. PR examination may reveal
tenderness high up on the right with infl ammation of a pelvic appendix.
Investigations
The diagnosis of acute appendicitis is essentially clinical. CT and X-rays are
not routinely indicated, but perform urinalysis ± pregnancy test. Although
FBC may reveal an i WCC, this is not invariable.
Differential diagnosis
Depending upon the presentation, the potential differential diagnosis is very
wide — remember to consider urinary, chest, and gynaecological causes.
Treatment
• Obtain IV access and resuscitate if necessary. Commence IV fl uids if
there is evidence of dehydration.
• Give IV opioid and antiemetic (eg slow IV metoclopramide 10mg).
• If acute appendicitis is likely, or even possible, keep ‘nil by mouth’ and
refer to the surgeon. If appendicectomy is required, pre-operative antibi-
otics (eg cefuroxime + metronidazole) d risk of infective complications.
Appendix mass
Untreated, acute appendicitis may proceed to perforation with general-
ized peritonitis, or may become ‘walled off’ to produce a localized right
iliac fossa infl ammatory mass. There are many causes of such a mass. Refer
to the surgeon for further investigation and management.
Table 10.1 Causes of a right iliac fossa mass
• Appendix mass
• Caecal carcinoma
• Crohn’s disease
• Ovarian mass
• Pelvic kidney
• Enlarged gall bladder
• Iliocaecal TB
• Iliac lymphadenitis
• Psoas abscess
• Retroperitoneal tumour
• Actinomycosis
• Common iliac artery aneurysm
• Spigelian hernia

508 CHAPTER 10 Surgery
Acute pancreatitis
This is a relatively common serious cause of abdominal pain in the middle
aged and elderly, with an incidence of ≈ 5 per 100,000/year.
Causes
Often due to gallstones and alcohol. Many are idiopathic. Other causes:
hypothermia, trauma, infection (glandular fever, mumps, Coxsackie, and
infectious hepatitis), hyperlipidaemia, hyperparathyroidism, drugs (steroids,
azathioprine, thiazides, and statins), polyarteritis nodosa, pancreatic
cancer.
Symptoms
Typically, the complaint is of severe constant epigastric pain radiating to
the centre of the back, with associated nausea and vomiting.
Signs
The patient may be distressed, sweating and mildly pyrexial. Look for evi-
dence of shock — there may be a need for urgent resuscitation. Abdominal
tenderness is likely to be maximal in the epigastrium ± guarding. The oft-
quoted, but uncommon bluish discolouration in the loins (Grey Turner’s
sign) only develops after several days.
Investigations
• Check BMG and SpO
2.
• Serum amylase is likely to be grossly i to > 5 × upper limit of normal
range (but if not diagnostically i , consider urinary amylase level).
• FBC may reveal i WCC.
• U&E, Ca
2 +
, LFTs, glucose — hypocalcaemia is relatively common.
• Coagulation screen.
• CXR, ECG, ABG; consider lactate if unwell.
Treatment
• Provide oxygen (O
2).
• Obtain IV access and resuscitate with IV fl uids as necessary.
• Give IV analgesia (eg morphine titrated according to response —
b Approach to abdominal pain, p.504).
• Give an anti-emetic (eg cyclizine 50mg or metoclopramide 10mg
slow IV).
• Insert an nasogastric (NG) tube.
• Insert a urinary catheter and monitor urine output.
• Consider early insertion of a central venous line to monitor the central
venous pressure (CVP) and guide IV fl uid therapy in the seriously ill,
particularly the elderly.
• Contact the appropriate specialist(s) and transfer to HDU/ICU.

509
ACUTE PANCREATITIS
Complications of acute pancreatitis
Acute pancreatitis has a signifi cant mortality. Early complications
include acute renal failure, disseminated intravascular coagulation (DIC),
hypocalcaemia, adult respiratory distress syndrome (ARDS). Later,
pancreatic abscess or pseudo-cyst may occur. The risk of death may
be predicted according to the number of prognostic indicators present
(Glasgow scoring system).
3 or more of the following on admission and subsequent repeat tests over
48hr constitutes severe disease:
Age > 55yrs; WCC > 15 × 10
9
/L; fasting glucose > 10mmol/L; urea
> 16mmol/L; arterial partial pressure of oxygen ( p O
2
) <7.9kPa; Ca
2 +
<2mmol/L; albumin <32g/L; serum LDH > 600U/L; AST > 100U/L.
Chronic pancreatitis
The term chronic pancreatitis implies permanent pancreatic damage. The
condition often results from alcohol excess. Some patients with chronic
pancreatitis present frequently to the ED requesting opioid analgesia. This
can pose a diffi cult problem for the doctor who has not treated them
previously. Follow the approach shown opposite and request previous
hospital case notes early.

510 CHAPTER 10 Surgery
Biliary tract problems
The majority of emergency biliary tract problems relate to gallstones.
Both solitary cholesterol and multiple mixed gallstones are common
amongst the middle aged and elderly. Pigment stones comprise a small
proportion — they occur in hereditary spherocytosis, malaria, and
haemolytic anaemia.
Complications of gallstones Acute and chronic cholecystitis, biliary colic,
obstructive jaundice, ascending cholangitis, mucocoele, empyema, acute
pancreatitis, gallstone ileus, carcinoma of the gallbladder.
Acute cholecystitis
History Impaction of gallstones with acute infl ammation of the gallbladder
usually manifests itself by right hypochondrial pain radiating to the right
side of the back ± vomiting.
Examination Look for features of an acute infl ammatory process. Fever
is frequently present, combined with right hypochondrial tenderness
(particularly felt on inspiration — Murphy’s sign). There may be a palpable
mass — this is also a feature of mucocoele and empyema (the latter causing
high fever, extreme tenderness and septic shock).
Management
• Provide IV analgesia and anti-emetic (see b Analgesics: opioids, p.276).
• Check FBC (WCC often i ), U&E, glucose, amylase, LFTs.
• CXR, ECG (in case pain is due to atypical presentation of MI).
• USS will confi rm the diagnosis (tenderness on pressing the USS
transducer over the area where the thickened gallbladder containing
stones is located is called the ultrasonic Murphy’s sign).
• Commence antibiotics (eg cefotaxime 1g IV) and refer to the surgeon.
Biliary colic/chronic cholecystitis
Patients (sometimes with known gallstones) may present with short-lived
recurrent episodes of epigastric/right hypochondrial pain ± radiation to
the back. This pain of biliary colic/chronic cholecystitis may be diffi cult to
distinguish from other causes, including peptic ulcer disease. If the pain has
subsided and there are no residual abnormal physical signs, discharge the
patient with arrangements for GP or surgical outpatient follow-up.
Common bile duct stones
Stones within the common bile duct can cause several problems:
• Acute pancreatitis ( b p.508).
• Obstructive jaundice.
• Ascending infection.
Obstructive jaundice
Biliary obstruction results in i jaundice with pale stools and dark urine
( ± pain). Acute hepatitis and cholangio-/pancreatic carcinoma may present
in a similar fashion. A palpable gallbladder implicates pancreatic carcinoma
as the more likely diagnosis (Courvoisier’s law: ‘In the presence of jaun-
dice, if the gallbladder is palpable, the cause is unlikely to be a stone’).
Ascending cholangitis
Biliary stasis predisposes to infection, characterized by Charcot’s triad
(abdominal pain, jaundice, and fever). The patient may be very ill and require
resuscitation for septic shock ( b p.59).

511
PEPTIC ULCER DISEASE
Peptic ulcer disease
Perforated peptic ulcer
History Perforation of a gastric or duodenal ulcer is usually a severely
painful sudden event. It may occur in those without known peptic ulcer
disease, as well as those with previously diagnosed problems. However,
close questioning may reveal recent symptoms attributed to ‘indigestion’.
Sudden localized epigastric pain spreads to the remainder of the
abdomen — the pain is worse on coughing or moving and may radiate to
the shoulder tip.
Examination Although distressed, the patient often prefers to lie still,
rather than roll about. However, some patients in extreme pain writhe or
roll in agony and are unable to keep still for examination or X-rays until
analgesia is given. Absent bowel sounds, shock, generalized peritonitis and
fever develop as time passes.
Investigations An erect CXR will demonstrate free gas under the
diaphragm in ≈ 75 % of patients with perforated peptic ulceration (if the
patient is not fi t enough for an erect CXR, obtain a left lateral decubitus
X-ray). In those cases where the diagnosis is suspected, but not proven by
X-ray, a contrast CT scan may help.
Other relevant investigations are: U&E, glucose, amylase (may be slightly i ),
FBC (WCC typically i ), SpO
2
, ABG, ECG/troponin (ensure symptoms do
not refl ect MI rather than peptic ulcer disease).
Treatment
• Give O
2.
• Provide IV analgesia (eg morphine titrated according to response).
• Give an antiemetic (eg slow IV metoclopramide 10mg).
• Resuscitate with IV 0.9 % saline.
• Refer to the surgeon and give IV antibiotics (eg cefotaxime 1g and in
late presentations, metronidazole 500mg as well).
Other GI perforations
Perforations may affect any part of the GI tract, but the chief causes are
peptic ulceration, trauma, diverticular disease, and colonic carcinoma. The
emergency treatment principles are similar to those of perforated peptic
ulcer (described above). Bowel perforation usually results in gas under the
diaphragm on an erect CXR, but remember that there are other possible
causes, including: recent surgery, peritoneal dialysis, gas-forming infections,
and occasionally, vaginal gas insuffl ation during waterskiing, or oral sex.
Other presentations of peptic ulcer disease
In addition to perforation, peptic ulcer disease may also present with
upper or lower GI haemorrhage ( b p.122), or pain from oesophagitis,
gastritis or duodenitis. If the patient’s presentation suggests infl ammation
of the upper GI tract, consider discharging the patient with a supply of
antacid and GP follow-up. This course of action is not appropriate if there
is any possibility of serious complication. Similarly, it is not usually appro-
priate to initiate therapy with H
2
blockers or proton pump inhibitors in
the ED without an accurate diagnosis.

512 CHAPTER 10 Surgery
Intestinal obstruction
Intestinal obstruction may be mechanical or paralytic in nature.
Paralytic intestinal obstruction is relatively rare in the ED. Causes include
postoperative ileus, electrolyte disturbance (eg hypokalaemia) and
pseudo-obstruction (see opposite).
Causes of mechanical intestinal obstruction
• Adhesions after previous surgery.
• Obstructed hernia (commonly: inguinal, femoral, para-umbilical,
incisional; rarely: obturator, Spigelian, lumbar).
• Tumours (gastric, pancreatic or large bowel carcinoma).
• Volvulus (gastric, caecal or most commonly, sigmoid) — see b p.516.
• Infl ammatory mass (eg diverticular, Crohn’s).
• Peptic ulcer disease.
• Gallstone ileus.
• Intussusception.
History
Classic symptoms of intestinal obstruction are: abdominal pain, distension,
vomiting, and constipation. The exact presentation depends upon the
site of obstruction and the underlying cause. Ask about previous surgery.
A history of severe pain suggests strangulation and developing ischaemia
in a closed loop. The nature of the vomit (eg faeculent) may give a clue to
the site of obstruction.
Examination
Check T ° . Look for evidence of dehydration or shock. Carefully examine
the hernial orifi ces (an obstructed femoral hernia is otherwise easily
missed). Inspect for scars from old surgery. Note any distension and
areas of tenderness (peritonism implies the surgical problem is advanced).
Bowel sounds may be tinkling or absent. PR examination may reveal an
‘empty’ rectum.
Investigations
Blood tests Check U&E, glucose, amylase, FBC, LFTs, clotting, group, and
save.
X-rays Request CXR and supine abdominal X-rays. If there is no con-
vincing evidence of obstruction on the supine view, but still a high index of
clinical suspicion, consider requesting an erect abdominal fi lm. X-rays may
demonstrate distended loops of bowel (with multiple fl uid levels visible
on an erect abdominal view). The site and nature of the distended bowel
loops may suggest the site of obstruction. Note that although gallstone
ileus is rare, X-rays may be diagnostic — the fi stula between the bowel and
gallbladder allows gas into the biliary tree, which shows up as an abnormal
Y-shaped gas shadow in the right hypochondrium).
ECG Obtain this if the patient is middle-aged or elderly.
ABG If the patient is shocked, check SpO
2
, ABG and lactate.
Old notes Request previous hospital case notes as soon as possible.

513
INTESTINAL OBSTRUCTION
Management of mechanical obstruction
• Insert an IV cannula and start IVI 0.9 % saline.
• If the patient is shocked, resuscitate with O
2
and IV fl uids and insert a
urinary catheter. Consider the need to insert a central venous line to
guide resuscitation and involve ICU specialists at an early stage.
• Provide analgesia (eg IV morphine titrated according to response —
b Analgesics: opioids, p.276).
• Give an anti-emetic (eg cyclizine 50mg).
• Insert a NG tube.
• Refer to the surgical team for ongoing care.
Intestinal pseudo-obstruction
This condition results from chronic impairment of GI motility. Many of
the patients affected are elderly and taking tricyclic antidepressants or
other drugs with anticholinergic actions. Although pseudo-obstruction
may involve any part of the GI tract, it typically presents with colonic
distension. On rare occasions, this may be suffi ciently severe to rupture
the caecum or cause hypotension by compressing the inferior vena cava
and blocking venous return. There may be a diagnostic X-ray appearance
showing gas in the bowel all the way to the rectum, whereas in a classical,
more proximal obstruction, gas will be absent from the rectum. Treatment
of acute colonic distension from pseudo-obstruction is by decompression
using a colonoscope.

514 CHAPTER 10 Surgery
Mesenteric ischaemia/infarction
Acute mesenteric infarction
Abrupt cessation of the blood supply to a large portion of the gut results
in irreversible gangrene of the bowel within a relatively short space of
time. This is associated with a very high mortality. Unfortunately, however,
the diagnosis can be very diffi cult to make — the challenge therefore lies
with making an early diagnosis.
Pathophysiology
One or more of the following processes may be responsible:
• Mesenteric arterial embolism (often associated with AF).
• Mesenteric arterial thrombosis.
• d Mesenteric arterial blood fl ow (eg hypotension secondary to MI).
• Mesenteric venous thrombosis.
Most cases involve either arterial embolism or thrombosis.
History
Acute mesenteric infarction usually occurs in middle-aged or elderly
patients. It is often heralded by severe, sudden onset, diffuse abdominal
pain. Typically, the severity of the pain initially far exceeds the associated
physical signs. The pain may radiate to the back.
Some patients have a preceding history of chronic mesenteric ischaemia,
with pain after meals and weight loss. There is often an associated history
of vascular disease elsewhere (eg intermittent claudication).
Examination
Shock, absent bowel sounds, abdominal distension, and tenderness are
late signs. Initially, there may be little more than diffuse mild abdominal
tenderness. If the diagnosis is suspected, search carefully for evidence of
an embolic source (eg AF, recent MI with high risk of mural thrombus,
aortic valve disease or valve prosthesis, recent cardiac catheter).
Investigations
• U&E, BMG, and laboratory blood glucose.
• Amylase may be moderately i
• FBC may demonstrate i WCC.
• Coagulation screen.
• Group and save.
• ABG typically reveals a severe metabolic acidosis and lactate may be i .
• X-rays may show non-specifi c dilatation of bowel loops and, in advanced
cases, gas within the hepatic portal venous system.
• ECG may demonstrate AF.
• Other specialist investigations (USS, CT, angiography) may be helpful,
but let the surgeon decide about this.
Management
If the diagnosis is suspected:
• Resuscitate with O
2
and IV fl uids.
• Provide analgesia (eg IV morphine titrated according to response).
• Consider broad spectrum IV antibiotics.
• Refer urgently to the surgeon.

515
MESENTERIC ISCHAEMIA/INFARCTION
Ischaemic colitis
Chronic arterial insuffi ciency to the bowel usually affects the mucosa and
submucosa, typically in the region of the splenic fl exure (junction of territory
supplied by the superior and inferior mesenteric arteries).
The patient presents with abdominal pain, starting in the left iliac fossa.
Loose stools with blood may be passed. The patient may have had
previous similar episodes and exhibit evidence of cardiovascular disease.
Examination may reveal a low grade pyrexia, tachycardia, and colonic
tenderness with blood PR.
Check FBC, U&E, group and save, ECG, CXR. Plain abdominal X-rays
may show ‘thumb printing’ (submucosal colonic oedema), typically at the
splenic fl exure. Provide analgesia, IV fl uids, and refer to the surgical team.

516 CHAPTER 10 Surgery
Large bowel emergencies
Volvulus (see bowel obstruction — b p.512)
Responsible for ≈ 10 % of large bowel obstruction. Occurs at the caecum
or, more commonly, the sigmoid, due to poor fi xation in their respective
iliac fossae.
Sigmoid volvulus usually occurs in the elderly with initially intermittent
cramping lower abdominal pain and progressive abdominal distension,
which may be spontaneously relieved by passage of large amounts of
fl atus/faeces. Some patient’s progress to complete obstruction: marked
distension progressing to fever and peritonitis suggests strangulation.
Plain abdominal X-ray typically shows a large single dilated loop of colon
(a ‘bent inner tube’) on the left side with both ends down in the pelvis.
Refer to the inpatient surgical team for sigmoidoscopy (if not strangulated)
or surgery if strangulated.
Caecal volvulus is most common between the ages of 25–35yr. Patients
have symptoms of acute onset small bowel obstruction.
Plain abdominal fi lms usually show one large dilated segment of the colon
in the mid-abdomen with distended small bowel loops and empty distal
large bowel. Refer to the surgical team.
Diverticular disease
Diverticulosis is common in the middle-aged and elderly, particularly
affecting the sigmoid colon. Without signifi cant complications, there may
be a change in bowel habit with passage of mucus.
Acute diverticulitis
Results from infl ammation/perforation of a diverticulum and may be con-
fi ned to colonic wall by the serosa. If this perforates, then infl ammation may
remain localized (pericolic abscess) or spread (frank peritonitis). Symptoms
and signs refl ect the extent of the infection — there may be lower abdom-
inal dull constant pain, low grade fever with tenderness, rigidity and occa-
sionally a mass in the left lower quadrant. The elderly (the group most at
risk of diverticulitis and its complications), and those on immunosuppres-
sants may not manifest the expected pyrexia and signs of peritonitis.
Investigations Check FBC, U&E, CRP, group and save, and blood cultures.
Plain abdominal X-rays may show non-specifi c changes and help to
exclude perforation/large bowel obstruction. An erect CXR often shows
copious subdiaphragmatic gas in free perforations.
Treatment Give analgesia, IV fl uids, keep fasted, and refer to the surgeon.
Start broad spectrum antibiotics (eg cefuroxime + metronidazole).
Complications
• Perforation: may be localized and walled off (forming an abscess), or
generalized.
• Intestinal obstruction: both large and small (due to adherent loops).
• Massive PR bleeding.
• Fistulae to adjacent structures: small bowel, uterus, vagina, bladder.
• Post-infective strictures.

517
LARGE BOWEL EMERGENCIES
Ulcerative colitis
Severe acute colitis is characterized by the passage of > 6 loose bloody
motions per day, together with systemic signs (tachycardia, fever) and
hypoalbuminaemia. There is a risk of haemorrhage, perforation and toxic
megacolon. The crucial points in management are early recognition and
prompt referral to the inpatient gastroenterology service, for aggressive
medical therapy (IV and PR steroids, IV fl uids) and joint review by medical
and surgical teams. Surgery may be required for complications, especially
toxic megacolon. Suspect toxic megacolon if the colonic width is > 5.5cm
on abdominal X-ray (this sign is associated with a 75 % risk of requiring
colectomy). Refer any patient who presents with suspected new onset
ulcerative colitis for investigation and control of the disease.
Mesenteric ischaemia/infarction
See b p.514.
Crohn’s disease
Colonic Crohn’s disease may present as colitis with bloody diarrhoea,
urgency and frequency, similar to ulcerative colitis.
Fibrosis may cause diarrhoea or obstructive symptoms.
Peri-anal disease with chronic anal fi ssure may be the fi rst presenting
symptom. Emergency surgery is indicated in acute fulminating Crohn’s
colitis with bleeding, toxic dilatation, or perforation.
Epiploic appendagitis
Primary infl ammation of one of the hundreds of appendices epiploicae on
the antimesenteric colonic border may present in similar fashion to acute
diverticulitis or appendicitis. However, T ° and WCC are usually normal.
Although often diagnosed at laparotomy, CT scan may be characteristic,
allowing conservative treatment (including IV analgesia).
Irritable bowel syndrome
Patients are usually aged 20–40 years with a prolonged history of inter-
mittent symptoms — altered bowel function (diarrhoea, constipation, or
diarrhoea alternating with constipation). Typically, the abdominal pain
is crampy/aching and localized in the lower abdomen over the sigmoid
colon. Pain may be eased by the passage of stool or fl atus. Examination
fails to reveal any worrying features. The diagnosis is one of exclusion — be
vigilant for clues that may point to other organic disease.

518 CHAPTER 10 Surgery
Anorectal problems
Any PR bleeding requires surgical follow-up to exclude malignancy.
Complications of haemorrhoids (‘piles’)
• Bleeding: haemorrhoids typically cause painless, bright red PR bleeding,
associated with defaecation, but blood is not mixed with the stools.
Check the abdomen and inspect the anus — if there is no prolapsed or
external haemorrhoid, perform PR and arrange surgical follow-up.
• Prolapsed piles are acutely painful — treat conservatively with adequate
analgesia (may need admission), bed rest, and stool softeners.
• Thrombosed external pile is due to rupture of a tributary of the inferior
haemorrhoidal vein, producing a peri-anal haematoma . One or more
dark blue nodules covered with squamous epithelium may be visible at
the anus and a clot palpable. Refer to the surgeon to decide between
incision and drainage under LA or conservative management.
Anal fi ssure
Typically causes severe pain on defaecation and for 1–2hr afterwards.
There may be blood on the toilet paper, but usually bleeding is minimal. The
fi ssure is located just inside the anal orifi ce and is usually associated with
the passage of hard stools. Most are located posteriorly in the midline. PR
examination may be impossible due to pain, but the fi ssure is often visible
with traction of anal skin.
Treatment Prescribe analgesia and stool softeners. Most heal spon-
taneously, but the presence of signifi cant ulceration, hypertrophied
tissue, or a skin tag suggests chronicity and need for surgical follow-up. Be
suspicious of those fi ssures not in the midline and those that are multiple
(the differential diagnosis includes chronic infl ammatory bowel disease,
anal cancer and adenocarcinoma of the rectum invading the anal canal).
Pruritus ani
Not strictly an emergency problem. There are numerous possible causes:
• Poor hygiene.
• Fissure, prolapsing piles, fi stulae, rectal prolapse, anal cancer.
• Contact dermatitis due to local applications (especially local anaes-
thetics).
• Threadworms.
• Part of a general condition (eg obstructive jaundice, lymphoma, severe
iron defi cency anaemia, uraemia, diabetes).
• Lichen sclerosis.
• Sexually transmitted disease (herpes, anal warts, HIV).
Treatment requires identifi cation of the underlying problem–refer to the
GP. In the meantime, advise avoidance of ointments and creams.
Pilonidal abscess
An infected pit in the natal cleft causes pain and/or offensive discharge.
Treatment Refer to the surgical team. Treatment may involve initial incision
and drainage, followed by healing, then elective excision of the sinus.
Note: Fissures, tears or bruising around the anus of a child arouses
suspicion of abuse in the fi rst instance. Refer to a specialist and avoid
rectal examination.
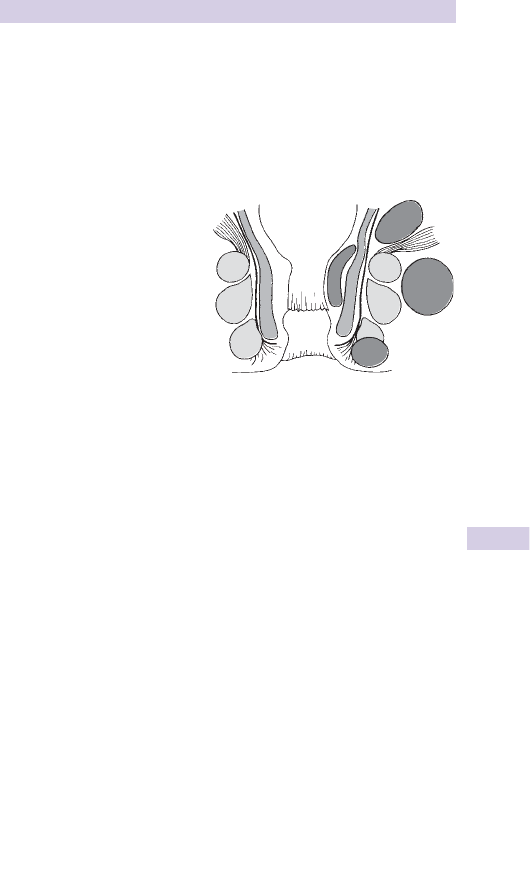
519
ANORECTAL PROBLEMS
Anorectal abscesses
Most begin with infection involving an anal crypt and its gland, from which
it can spread between the external and internal sphincters to a variety of
sites — these determine its symptomatology and mode of presentation.
Peri-anal and ischiorectal abscesses account for ≈ 80 % of cases. In 20 % ,
there is a clear predisposing cause, such as infl ammatory bowel disease,
anorectal cancer, or anal fi ssure (Fig. 10.1 ).
Clinical features Pain is a prominent initial feature of peri-anal and
superfi cial ischiorectal abscesses, followed by local signs of infl ammation.
Patients complain of persistent dull throbbing pain, made worse by walking
and sitting, and prior to defaecation. Such symptoms are less evident with
deep infections, which tend to develop slowly with pyrexia and systemic
upset. Peri-anal abscesses produce localized fl uctuant red tender swellings
close to the anus. With ischiorectal sepsis, the fi ndings are more diffuse
and fl uctuance is a late fi nding. Deeper infections are less obvious — PR
examination may reveal a mass or tender area of induration.
Treatment Provide analgesia and refer to the surgical team for incision
and drainage under GA.
Venereal proctitis
The organisms are similar to those transmitted by vaginal intercourse:
assume more than one type of organism is present. Patients complain of
pain, irritation, discharge, and bleeding. Consider gonococcus, chlamydia,
syphilis, herpes simplex. Refer urgently to a genitourinary specialist.
Rectal foreign bodies
X-rays may demonstrate the position and shape of FBs. More especially,
look for the presence of any free air — perforation of the rectum or colon
is the most frequent and most serious complication, in which case give
IV antibiotics (eg cephalosporin + metronidazole). Refer the patient for
removal of the FB by the surgical team.
A
B
C
The four types of anorectal
abscess—(A) Perianal.
(B) Ischio-rectal. (C) Submucous.
(D) Pelvi-rectal.
(After W.F.W. Southwood, F.R.C.S., Bath).
D
Fig. 10.1 Types of anorectal abscesses.

520 CHAPTER 10 Surgery
Retention of urine
Causes of acute urinary retention
This more commonly presents in the male:
Common causes in males
• Prostatic hyperplasia/cancer.
• Urethral stricture.
• Post-operative.
Common causes in females
• Retroverted gravid uterus.
• Atrophic urethritis.
• Multiple sclerosis.
Other causes include: acute urethritis, prostatitis, phimosis, urethral
rupture following trauma, bladder blood clot, urethral calculus, prolapsed
intervertebral disc, drugs (alcohol, antihistamines, anticholinergics,
antihypertensives, tricyclics), faecal impaction, anal pain.
Presentation
In most cases, the diagnosis is obvious: the patient complains of inability
to pass urine combined with bladder discomfort. Remember, however,
to consider the diagnosis in those patients unable to describe their symp-
toms (eg those unconscious after trauma).
Examination will reveal a tender enlarged bladder, with dullness to
percussion well above the symphysis pubis. Search for the causes
listed above. In particular, search for evidence of prolapsed disc/cord
compression by checking the lower limb power/refl exes and perineal
sensation. Perform PR examination to assess anal tone and the prostate.
Initial management
The patient requires urgent bladder decompression. Provided there is
no contraindication (eg urinary retention following trauma or as a result
of urethral stenosis), achieve this by urethral catheterization. Use an
aseptic technique (male catheterization is described opposite). If urethral
catheterization is impossible or contraindicated, consider the need for
a suprapubic catheter, but this should only be performed by a doctor
experienced in the technique.
Further management
After bladder drainage, record the volume of urine obtained, then
re-examine the abdomen for pathology that might have been previously
masked.
Test the urine for the presence of blood and send a mid-stream specimen
of urine (MSU) for culture and sensitivity. Perform investigations
appropriate to the likely underlying cause, and then refer to the urology
team.

521
RETENTION OF URINE
Chronic urinary retention
Patients with chronic retention often have massive, almost painless
bladder distension. They are at risk of pressure damage to the upper
urinary tract. Following drainage, they may develop haematuria or
post-obstructive diuresis, with attendant problems of signifi cant fl uid and
electrolyte derangements.
Male catheterization
• Prepare the equipment — a Foley catheter size 14G is appropriate for an
adult. Ensure that the patient does not have an allergy to latex.
• Check the volume required for the catheter balloon.
• Wash hands and don sterile gloves.
• Clean the external genitalia with antiseptic solution and surround with a
sterile fi eld.
• Slowly insert local anaesthetic into the urethra.
• Gently massage the local anaesthetic down the urethra and wait for a
few minutes for the LA to take effect.
• Holding the penis at right angles to the body, insert the lubricated
catheter. The catheter should pass easily into the bladder with drainage
of urine. If any resistance or diffi culty is encountered, stop and seek
senior assistance.
• Once urine appears, advance the catheter a few centimeters further
before infl ating the balloon.
• Connect the catheter to a closed drainage system and tape the tubing
to the upper thigh.
• Ensure that the foreskin is not left retracted — this could result in
paraphimosis.

522 CHAPTER 10 Surgery
Testicular problems
Remember that any pain of testicular origin may be initially referred to
the abdomen.
Testicular torsion
Testicular torsion is most frequently seen in children and young adults.
Any suspicion of testicular torsion should prompt immediate referral. The
condition is covered fully on b Inguinal and scrotal swellings, p.700.
Acute epididymitis
Causes
For those aged <35 years, infection with chlamydia or gonococcus is com-
monly responsible. Acute epididymitis in those aged > 35 years is usually
secondary to UTI and associated with underlying urinary tract pathology.
Clinical features
There is typically a gradual onset of progressive testicular ache, with sub-
sequent swelling of the epididymis and testis. There may be a history of
dysuria or urethral discharge. The patient may be pyrexial. The epididymis
is acutely tender, with the testis lying low in the scrotum. Advanced, late
cases may have progressed to abscess formation.
Investigations
Send an MSU and take a urethral swab (take lab advice regarding the
correct media for chlamydia).
Management
The chief initial concern is to ensure that testicular torsion is not being
missed: if there is any possibility of this ( b Inguinal and scrotal swellings,
p.700), refer urgently. Treatment of acute epididymitis comprises antibi-
otics (eg ciprofl oxacin for 2 weeks), analgesia, and rest. Some patients
require admission; others may be managed on an outpatient basis. Urology
investigation and follow-up will be required, so involve the urologist early.
Patients with suspected chlamydia or gonococcus require appropriate
advice and contact tracing of sexual partners.
Orchitis
Orchitis may present as epididymo-orchitis, an extension of bacterial
epididymitis (see above). Orchitis of viral origin may also occur — typically
mumps, following ≈ 5days after parotitis. Mumps orchitis may be unilateral
or bilateral and can occur in the absence of overt parotitis. Rarely, orchitis
is secondary to tuberculosis (TB) or syphilis.
Treatment
All patients with orchitis require analgesia and follow-up. If there is any
possibility of bacterial infection, antibiotics are indicated (see above).
Testicular lumps
Patients may present to the ED with scrotal/testicular lumps. Causes are
varied and include: hydrocoele, inguinal hernia, epididymal cyst, epidi-
dymitis, orchitis, and testicular tumour. Many patients will be managed
appropriately by referral back to GP or to an outpatient clinic. Be particu-
larly wary of an apparent epididymo-orchitis which has failed to respond
to antibiotics — it could be an atypical presentation of a testicular tumour.
Testicular trauma—See b p.352.

523
PENILE PROBLEMS AND PROSTATITIS
Penile problems and prostatitis
Paraphimosis
Paraphimosis occurs when the foreskin is left retracted, thereby causing
swelling of the glans, which results in diffi culty replacing the foreskin to
its proper position. Untreated, tissue necrosis may develop. Paraphimosis
may be iatrogenic, occurring after urethral catheterization.
Treatment Initially attempt reduction by manual decompression, which
may require the use of Entonox
®
, IV sedation, or LA (a small amount
of topical 1–2 % lidocaine gel or injection of 10mL plain 1 % lidocaine
around the base of the penis). Digital pressure may allow the glans to
d in size, prior to the foreskin being delivered back into its usual position.
If unsuccessful, refer to the surgical team for reduction under GA or
dorsal slit of the prepuce followed by later circumcision.
Priapism
Priapism is persistent (and usually painful) penile erection.
Causes
• Iatrogenic (following intra-cavernosal injection of one or more of:
papaverine, alprostadil, vasoactive intestinal polypeptide, phentolamine
for impotence).
• Others: leukaemia, myeloma, sickle cell disease, spinal injury, drugs
(eg sildenafi l [Viagra], phenothiazines, cannabis, cocaine), renal dialysis.
Management Priapism is a urological emergency. Refer urgently to the
urology team. Initial emergency treatment of a prolonged ( > 6hr) artifi cial
erection (ie following an intra-cavernosal drug injection or oral sildenafi l)
is to aspirate 50mL of blood from each corpus cavernosum through a
19G butterfl y needle into a 50mL syringe with a Luer lock.
Urethritis
This usually presents with dysuria/urinary frequency, refl ecting underlying
STD. Refer for appropriate investigation, treatment, and follow-up.
Prostatitis
Infl ammation of the prostate may be acute or chronic and present in a
variety of ways (fever, urgency, frequency, perineal pain, urethral dis-
charge). PR examination reveals a tender prostate. Urinalysis demonstrates
protein. Refer for further investigation and treatment.
Penile trauma
Minor superfi cial tears
These are relatively common. Most involve the frenulum. The patient
complains of pain and bleeding following sexual intercourse. Bleeding
usually responds to local pressure (if this is not successful, consider tissue
glue or refer to the surgical team). Once bleeding has stopped, advise a
period of abstinence from sexual activity ( ≈ 10 days) to allow healing to
occur and prevent recurrence.
Fracture of the penis
This occurs infrequently. It involves injury to the tunica albuginea of the
erect penis. The result is penile tenderness and swelling. Refer to the urolo-
gist for urgent surgical exploration, evacuation of haematoma and repair.

524 CHAPTER 10 Surgery
Ureteric colic
New onset fl ank/back pain in the elderly may represent a leaking
aortic aneurysm (even if haematuria is present).
Causes
Calculi or blood clots may cause ureteric (or ‘renal’) colic. Colicky pain
is produced by ureteric obstruction, i intraluminal pressure, and muscle
spasm. Calculi most commonly consist of calcium oxalate and/or calcium
phosphate. Less common are magnesium ammonium phosphate (associated
with UTIs and urea-splitting organisms, such as Proteus ), urate, and cystine
stones.
Calculi are associated with hypercalcaemia, hyperoxaluria and
hyperuricaemia. ‘Staghorn’ calculi in the collecting system predispose to
infections.
Calculi may form throughout the length of the renal tract. They vary in size
from tiny particles to large ‘stones’ in the bladder. They cause symptoms
from local obstruction, infection, and rarely may ulcerate through the wall
of the structure in which they are present.
Clinical features
The most common presenting symptoms are pain from obstruction or
UTI and/or haematuria. Constant dull, severe, loin discomfort is associ-
ated with excruciating colicky pain, spreading to the respective iliac fossa,
testis, tip of penis or labia. The pain may cause the patient to move or walk
about. Nausea, vomiting, pallor, sweating are common. There is frequently
a previous history of stone disease — ask about this and whether there is
any past history of renal disease. Ask about urinary and GI symptoms.
Apart from loin tenderness, abdominal examination is usually normal,
but check the haemodynamic status, pulses, bruits and the abdominal
aorta, as a ruptured aortic aneurysm can present in a similar fashion
( b p.530). Pyrexia or rigors suggest associated infection. Microscopic
(sometimes frank) haematuria is common. Symptoms are usually relieved
when the stone passes into the bladder, but larger calculi may then cause
obstruction at the bladder neck or the urethra producing acute urinary
retention. Bladder calculi may present with symptoms of UTI and/or
bladder irritation (frequency, dysuria, strangury, and haematuria).

525
URETERIC COLIC
Investigations
• Urinalysis and MSU: blood on stix testing is present in > 80 % of patients
with proven stones. A pH > 7.6 implies associated infection with urea
splitting organisms.
• U&E, creatinine, glucose, Ca
2 +
, PO
4
2–
, urate levels.
• ‘KUB’ X-ray: 90 % of urinary calculi are radio-opaque. X-ray is ≈ 50 %
sensitive and ≈ 70 % specifi c for the diagnosis of ureteric calculi and is
a very useful follow-up of patients with known stones. Common sites
for calculi include the pelvi-ureteric and vesico-ureteric junctions.
Remember that the ureters lie adjacent to the tips of the spinal trans-
verse processes.
• Use USS/Doppler instead in pregnant patients or those with renal
disease.
• CT without contrast is ≈ 95 % sensitive and ≈ 95 % specifi c and has the
advantage of assisting diagnosis of other causes of abdominal and/or loin
pain.
• Intravenous urography (IVU) is the most accurate investigation when
CT is not available or where endoscopic or surgical treatment is
contemplated. A delayed nephrogram on the affected side at 5min is
common. As contrast enters the collecting system, the site and degree
of the obstruction can be assessed.
Treatment
Give IV opioid titrated to effect, together with an NSAID (either IV keto-
ralac, or oral/rectal diclofenac). Do not use antispasmodics, anticholinergics
and ‘pushing fl uids’.
• Aim to discharge patients (with arrangements for appropriate outpa-
tient investigation) when symptoms have completely resolved, and in
whom the CT/IVU shows no obstruction. Note that in some patients
the process of becoming pain-free merely represents complete obstruc-
tion.
• Admit (for further investigation and treatment) patients whose pain
persists, or in whom investigation confi rms continued obstruction,
infection, sepsis or renal impairment.

526 CHAPTER 10 Surgery
Abscesses
An abscess is a localized collection of pus resulting in a painful soft tissue
mass that is often fl uctuant, but surrounded by fi rm granulation tissue and
erythema. The cause is usually bacterial, resulting from minor trauma to
the epithelium/mucosa or blockage of apocrine glands. A history of a pre-
vious lump at the site suggests infection of a sebaceous cyst. Check BMG
in all patients.
For patients with recurrent abscesses, check for signs of hidradenitis
suppurativa, diabetes, infl ammatory bowel disease, and malignancy. Ask
about steroid use.
Treatment
Incision and drainage A general surgical principle is that a collection of
pus requires drainage. On occasions, depending upon local policy, it may
be appropriate to do this in the ED. Some abscesses (eg face, breast,
perineum, paediatric) require specialist attention. Regional, parenteral,
or GA may be needed to supplement LA which works poorly in this
situation.
Technique Incise along the length of the fl uctuance and deep enough
to enter the cavity. An elliptical incision will prevent premature closure
and re-accumulation of pus. Send pus for culture. Ensure that loculi in
the cavity are gently broken by the use of a curette. Consider inserting
a loose antiseptic wick in the cavity to ensure drainage and prevent
premature closure.
Antibiotics are not indicated in patients with normal host defences as long
as the abscess is localized. Evidence of surrounding or spreading infection
may warrant antibiotics (eg co-amoxiclav or penicillin + fl ucloxacillin) and
on occasions, admission (see below).
Refer the following:
• Those who are systemically unwell (pyrexial, tachycardic, rigors),
immuno-compromised and those not responding to treatment.
• Abscesses secondary to IV drug misuse.
• Those with infection in certain anatomical sites: face ( i risk of cavernous
sinus thrombosis), those potentially involving the airway (sublingual
abscesses, Ludwig’s angina), axillary, groin, retropharyngeal, perineal,
and breast abscesses.
• Those with extensive or progressing cellulitis/lymphangitis.
These patients may require IV antibiotics (eg co-amoxiclav or fl ucloxacillin
+ penicillin), analgesia and surgical drainage. Take blood for FBC,
clotting studies and blood culture. Treat sepsis/septic shock where
necessary ( b p.59).

527
ABSCESSES
Breast infection
Lactational breast abscess These are usually peripherally located and due
to Staph. aureus . Local discomfort proceeds to painful swelling. Overlying
skin may be red. Extreme cases may undergo necrosis and spontaneous
discharge.
Treatment If seen prior to frank abscess formation, consider antibiotic
treatment alone — prescribe a penicillinase-resistant antibiotic. If there
is any suspicion of an abscess, refer for needle aspiration — if pus is
found, drainage will be needed. Encourage the infant to feed from the
contralateral breast whilst the affected side is emptied of milk manually
or by breast pump.
Non-lactational breast abscess Typically affects the 30–60-year age
group, usually peri-areolar, recurrent, and related to duct ectasia/
periductal mastitis. Refer for needle aspiration, culture, and antibiotics
(metronidazole and fl ucloxacillin). Note that infl ammatory breast cancer
may mimic septic mastitis and breast abscess. Incision of neoplastic lesions
may have disastrous results.
Perineal abscesses See b Anorectal problems, p.518.

528 CHAPTER 10 Surgery
Cellulitis and erysipelas
Cellulitis (see b Infected wounds and cellulitis, p.413)
Cellulitis refl ects bacterial skin infection (usually streptococcal, occasion-
ally staphylococcal). It can occur in association with a skin wound acting
as a portal of entry for infection (eg athlete’s foot), but it may also occur
without any obvious breach in the skin. Ascertain whether or not there is
evidence of systemic upset or any background problems, such as immuno-
defi ciency, diabetes, or steroid therapy.
The area of affected skin is red, warm to the touch with poorly defi ned
margins. Check T ° and look for lymphangitis and/or lymphadenopathy.
Treatment depends upon the nature and extent of clinical fi ndings as
follows:
• Treat patients who have localized limb infection and no evidence of
systemic upset with oral antibiotics (either phenoxymethylpenicillin +
fl ucloxacillin or co-amoxiclav or erythromycin) and arrange follow-up
in 24–48hr.
• Admit patients who are systemically unwell or have spreading infection
(eg lymphangitis extending above the knee from an area of cellulitis on
the foot). Obtain venous access, take blood cultures and start IV antibi-
otics (either benzylpenicillin + fl ucloxacillin or co-amoxiclav).
Patients with cellulitis of the face (particularly around the eye) are
at risk of signifi cant intracranial complications (notably cavernous
sinus thrombosis) — start IV antibiotics and refer for admission to the
ophthalmology team.
Erysipelas
This streptococcal infection is limited to the more superfi cial parts of
the skin, resulting in an area of redness and heat with clearly defi ned
margins. Treat with antibiotics as outlined for cellulitis above, except that
phenoxymethylpenicillin alone (500mg PO qds for 7 days) suffi ces in most
cases.
Necrotizing fasciitis
See b Streptococcal infections, p.234.

529
COMPLICATIONS OF VARICOSE VEINS
Complications of varicose veins
Occasionally, patients may attend the ED with complications of their
varicose veins.
Bleeding from varicose veins
Patients with chronic venous hypertension associated with varicose veins
have a signifi cant risk of haemorrhage from the dilated thin-walled veins
which commonly surround the area of lipodermatosclerosis at the ankle.
Haemorrhages may be profuse and suffi cient to cause hypovolemic shock.
In extreme cases, this may even cause death.
Treatment
Control bleeding by elevating the leg, applying a non-adherent dressing
and pressing fi rmly. Follow this with appropriate bandaging; unless there
is evidence of occlusive arterial disease (varicose veins and arterial disease
frequently co-exist in the elderly). Some patients may require resuscita-
tion with IV fl uids.
Refer for admission those who were shocked at presentation, those
who have subsequently bled through the bandaging, those with occlusive
arterial disease, and those who live alone. All patients will require surgical
outpatient follow-up — advise patients who are discharged about fi rst aid
measures in the event of a rebleed.
Superfi cial thrombophlebitis
This occurs most frequently in patients with varicose veins or prothrom-
botic states (eg underlying infl ammatory and malignant conditions). It
usually manifests itself with redness, tenderness and induration along the
course of the involved vein.
Treatment
Bed rest, elevation, and analgesia (NSAID). Pain typically d over 1–2 weeks
and the patient is left with a hard thrombotic cord. Superfi cial throm-
bophlebitis is only rarely associated with DVT, but occasionally thrombosis
spreads from the long saphenous vein to involve the femoral vein. If there
is any question of deep vein involvement, request an USS. If the thrombotic
process involves the sapheno-femoral junction or the ilio-femoral system,
refer for anticoagulation ( b p.170).
Venous ulcers
Venous (varicose) ulcers tend to be chronic and recurrent. They are typi-
cally found on the medial side of the ankle. There is often associated derma-
titis with surrounding brown discolouration, thickening of the skin and leg
oedema. There is often mixed venous and arterial disease, especially in the
elderly. Although ischaemic ulcers tend to lie on the lateral aspect of the
ankle, exclude ischaemic ulceration by checking the peripheral pulses (request
Doppler in patients with oedematous legs). Look for areas suspicious of
malignant change, which may rarely occur in chronic ulcers (Marjolin’s ulcer).
Treatment
Clean the ulcer with normal saline and dress it with either paraffi n gauze
or colloidal dressing. Follow this with fi rm bandaging (unless there is co-
existing arterial disease) and advise leg elevation when the patient rests.
Avoid dressings with topical antibiotics and indiscriminate use of oral anti-
biotics. Prescribe oral antibiotics (eg co-amoxiclav) only if there is cellulitis.
Liaise with the GP about the need for surgical outpatient follow-up and to
arrange for redressing by the district nurse.

530 CHAPTER 10 Surgery
Ruptured abdominal aortic aneurysm
Middle-aged and elderly people frequently develop abdominal aortic aneu-
rysms. Rupture is relatively common and responsible for a large number
of deaths, many of which occur suddenly out of hospital. Even when the
patient reaches hospital alive, there is a signifi cant mortality. The patient’s
best chance of survival lies with early diagnosis, prompt resuscitation and
rapid transfer to theatre. Most aneurysms are saccular and found in the
infrarenal portion of the aorta — haemorrhage after rupture is usually into
the retroperitoneum. Aneurysm extension to involve the renal arteries
renders surgery more diffi cult and i risk of post-operative complications.
History
Presentation is highly variable, ranging from PEA cardiac arrest to painless
sudden collapse of obscure origin, through to a classical history of central
abdominal and lower back pain in a patient with a known aneurysm. Pain is
usually a feature: typically sudden in onset and severe in nature.
Examination
The seriously ill patient may present a characteristic picture: distressed,
pale, sweating, tachycardic, and hypotensive, with mottled skin of the
lower body and a tender pulsatile abdominal mass. One or both femoral
pulses may be absent.
Diagnosis
Ruptured aortic aneurysm is not infrequently misdiagnosed as ureteric colic.
Adopt a low threshold of suspicion in any middle aged or elderly patient
who presents with back pain, abdominal pain or collapse. In some patients
(eg the obese), it may be diffi cult to be certain about the presence of a pul-
satile abdominal mass. In such cases, assume that the problem is a ruptured
abdominal aortic aneurysm and commence resuscitative measures, whilst
appropriate experts are summoned and relevant emergency confi rmatory
investigations (eg USS or CT scan) are performed. It may be safer and quicker
to perform USS in the ED, rather than transfer the patient for CT scan.
Management
• Provide high fl ow O
2
.
• Obtain venous access with 2 large bore venous cannulae.
• Send blood for FBC, U&E, glucose, baseline coagulation screen, LFTs
and emergency X-matching (10U red cells + 8U platelets + 8U fresh
frozen plasma).
• Provide IV analgesia (eg morphine titrated according to response).
• Provide IV anti-emetic (eg cyclizine 50mg).
• Give IV fl uids as necessary, but avoid excessive fl uid resuscitation. Treat
major hypovolaemia, but accept moderate degrees of hypotension
(systolic BP > 90mmHg). In general, patients who are conscious and
passing urine require minimal IV fl uid therapy until they reach theatre.
• Obtain a CXR.
• Insert a urinary catheter and a radial arterial line and record an ECG.
• Call the vascular surgeon and anaesthetist at an early stage: aortic cross-
clamping is the mainstay of resuscitation in the unstable patient.
• Ensure that other relevant staff (eg emergency theatre staff) are
informed.

531
ACUTE LIMB ISCHAEMIA
Acute limb ischaemia
Clinical features
Irrespective of the cause, the cardinal features of acute limb ischaemia are
summarized by the 6 P’s:
• Pain.
• Paraesthesia (later anaesthesia).
• Pallor (later mottled, cyanosed).
• Pulselessness.
• Paralysis (due to muscle damage — this may be irreversible after 4–6hr).
• Perishing cold.
Where an acute arterial occlusion occurs in a previously normal limb,
the features of ischaemia will be i because of the absence of a developed
collateral circulation. In the absence of a traumatic cause (either direct
arterial injury, or indirect injury such as compartment syndrome — b Crush
syndrome, p.398) the commonest causes are embolism or thrombosis.
Embolic
Cardiac sources account for > 80 % (AF, post MI, prosthetic valves, atrial
myxoma, vegetations, and rheumatic heart disease). Acute embolic events
affect the legs much more often than the arms (ratio 5:1). Artery bifurca-
tions are affected most commonly.
Risk factors Diabetes, smoking, hypertension, hypercholesterolaemia.
Past history Ask about previous transient ischaemic attack (TIA), stroke, MI.
Examination A clear demarcation between normal and ischaemic skin
suggests an embolic cause of an acutely ischaemic limb. Look for potential
sources of emboli (irregular pulse, abnormal heart sounds, murmurs,
valve clicks, etc.). Check all pulses in both the affected and contralateral
limbs. The presence of normal pulses in the contralateral limb suggests
an embolic cause, whereas absent contralateral pulses makes thrombosis
more likely (even if a potential embolic source exists).
Investigations ECG, CXR, U&E, CK, FBC, coagulation screen, ABG,
urinalysis (checking for myoglobin), cross-match. Cardiac and/or abdominal
USS may be required and if thrombosis in situ is suspected, angiography
indicated.
Thrombotic
Thrombosis may develop acutely at the site of atheromatous disease.
A previous history of intermittent claudication/vascular impairment is
likely. The other limb is also likely to have features of chronic vascular
insuffi ciency (muscle wasting, hair loss, ulceration).
Treatment
• Give appropriate pain relief (usually IV opioid).
• Correct hypovolaemia and other causes of low fl ow states as necessary.
• Re-vascularization is required within 6hr to avoid permanent muscle
necrosis (and subsequent need for amputation) and metabolic effects (such
as rhabdomyolysis and renal failure). If the cause is embolic, embolectomy
is required. If thrombotic, angiography will defi ne the site and extent of the
lesion: thrombolysis ± reconstructive surgery is then undertaken.
This page intentionally left blank
534 CHAPTER 11 Ophthalmology
Approach to eye problems
History
Always take a full ophthalmic history. Which eye is affected (are both)?
What is the disturbance? Are there fl ashing lights or fl oaters? How quickly
did the symptoms come on? How does it affect the patient’s lifestyle (job,
reading, watching TV)? Ask about prior ophthalmic/optician treatment
and take a full medical and drug history. Family history of glaucoma may
also be relevant.
Always measure visual acuity of patients presenting with eye problems.
Patients with potentially serious pathology include those with:
• Sudden visual loss.
• Signifi cantly d VA.
• Penetrating eye injuries.
• Chemical burns of the eye (these require immediate treatment and
specialist referral).
Have a low threshold for involving an ophthalmologist if a patient who is
already blind in one eye, presents with a problem with the ‘good eye’.
Examination
Visual acuity (VA) is the key to eye examination: measure this fi rst.
Failure to document VA may constitute negligence
Use a Snellen chart, read at 6m, for each eye separately. Allow patients
to use glasses if available, if not employ a pinhole (made using a needle
through a piece of card). Use of a pinhole eliminates refractive error.
VA is expressed as:
Distance from chart in m/no. of line on chart (normal vision is 6/6)
For example, a patient whose VA is recorded as Right eye 6/5; Left eye
6/60 can read the bottom line with the right eye, but only the top line with
the left eye. If patients read additional letters of the line below, record
using + number of extra letters (eg 6/12 + 2).
Bring patients unable to read chart at 6m forward until they can read the
chart (eg 3/60 = top line read at 3m). Very poor vision: try counting fi ngers
or detecting hand movement at 1m, or light perception.
A hand-held chart at 30cm is an alternative if a full Snellen chart is
unavailable — ability to read small print implies normal VA for that eye.
For patients who are illiterate, there is an alternative chart with various
different versions of the letter ‘E’ — ask the patient to state which
directions the 3 limbs of the letter point.

535
APPROACH TO EYE PROBLEMS
Pupils Record pupil size, shape, direct, and consensual responses to light
and accommodation.
Eye movements Check full range and ask about diplopia. Look for
nystagmus.
Visual fi elds Check carefully in patients with visual loss.
Fundoscopy In a darkened room, fi rst note the presence of a red refl ex.
A lost or d red refl ex is an abnormal fi nding, typically caused by vitreous
haemorrhage, cataracts, or major corneal abrasions. Assess the optic
discs, look for retinal haemorrhages and vessel abnormalities.
Direct assessment Under a bright light look for infl ammation or FBs.
Subtarsal examination If there is a possibility of FB, evert the upper eyelid
by pressing down lightly over the upper lid with a cotton bud or orange
stick and rotating the lid upwards over it. Ask the patient to look down
throughout.
Slit lamp examination Learn how to use a slit lamp. It allows a detailed
view of conjunctiva, cornea, and anterior chamber. Fluorescein staining
reveals corneal abnormalities, particularly when viewed under blue light,
when abrasions appear green. Fluorescein is available either in drop form
or dried onto a strip. Remember that fl uorescein can permanently stain
clothes and contact lenses.
Intraocular pressure Digital assessment is unreliable. Formal measurement
of intra-ocular pressure is useful, but requires training and is left to the
eye specialist in many departments.
Temporal arteries Palpate for tenderness if temporal arteritis is a
possibility.
LA drops to aid examination
Sometimes, blepharospasm prevents satisfactory examination. Consider
LA drops (1 or 2 drops of 1 % amethocaine/tetracaine or 0.4 % oxybupro-
caine. 0.5 % proxymetacaine causes less stinging and is useful in children).
Never discharge patients with a supply of local anaesthetic drops .
Notes on ophthalmological treatments
Antibiotic ointment and drops Apply to the lower fornix (between
lower eyelid and sclera) then ask the patient to keep the eye shut for
1–2min. Ointment has the advantage over drops in that it lasts longer:
for example, chloramphenicol ointment needs to be given 4 times a day,
whereas drops need to be given every 2hr initially. Theoretical concerns
about aplastic anaemia are not well-founded (see the BNF ).
Eye pads Previously recommended following the administration of LA
drops and for patients with corneal abrasions, they tend not to be useful
unless the pad seals the eyelid shut.
Driving Advise patients not to drive until their vision has returned to
normal (this particularly applies after use of mydriatic agents). In addition,
advise patients not to drive whilst wearing an eye pad. Document the
advice given in the notes.
536 CHAPTER 11 Ophthalmology
Ophthalmological trauma
Blunt eye injuries
Blunt injury to the face may result in injury to the orbit or its bony margins.
Compression of the eye in an antero-posterior direction (eg squash ball
or fi st) can cause a ‘blow-out’ fracture of the fl oor of the orbit.
Orbital compartment syndrome and blindness can arise from a retrobulbar
haematoma . Unless diagnosed and treated as an emergency, optic nerve
ischaemia develops and the patient can lose sight in the affected eye
within a few hours. Proptosis, reduced eye movements, reduced visual
acuity and pain all point to a retrobulbar haematoma. There may be an
afferent pupillary defect.
Assessment
• Look for proptosis.
• Check visual acuity.
• Check pupillary refl exes.
• Check for enophthalmos and d infra-orbital nerve sensation, both found
in a blowout fracture.
• Document range of eye movements, looking in particular for entrapment
of the extra-ocular muscles.
• Look for a hyphaema (a horizontal fl uid level in the anterior chamber
when the patient is upright). It can cause pain, photophobia, blurred
vision and can i intra-ocular pressure, causing nausea and vomiting.
• Stain the cornea and examine using slit lamp for corneal abrasions.
• Ophthalmoscopic examination may reveal lens dislocation, hyphaema,
vitreous, subhyaloid, or retinal haemorrhage. Sometimes retinal oedema
(‘commotio retinae’) may be seen as white patches with diffuse margins
on the posterior pole of the eye.
X-ray if there is bony tenderness or clinical evidence of orbital or facial
bone fracture.
Treatment
Any patient suspected of a retrobulbar haematoma requires an emergency
lateral canthotomy. This should be performed by an ophthalmologist or
a trained emergency physician, under local anaesthetic in the ED, and
reduces the retro-orbital pressure.
Nurse patients with obvious globe injury head up at 45 ° . Refer urgently.
Provide prophylactic oral antibiotics (eg co-amoxiclav) for uncomplicated
facial or orbital fractures, and arrange for maxillofacial follow-up, with
advice to avoid nose-blowing in the meantime.

537
OPHTHALMOLOGICAL TRAUMA
Penetrating eye injuries
Suspect intraocular foreign body if there is a history of hammering or
work involving metal on metal. Find out if protective glasses were worn.
Ascertain whether a small foreign body travelling at speed may have pen-
etrated the orbit (eg during grinding, hammering, chiselling). Failure to
suspect and diagnose these injuries can have serious consequences.
Assessment
• Check visual acuity.
• Look for pupil irregularity.
• Look for puncture/entry wounds on both aspects of the eyelids, the
cornea and sclera. Corneoscleral wounds are often situated inferiorly,
due to upturning of the eyeball as the patient blinks.
• Examine the anterior chamber. There may be a shallow anterior
chamber, air bubbles, a fl at cornea, defl ated globe and a positive Seidel’s
test (dilution of fl uorescein by aqueous humour leaking from the ante-
rior chamber).
• Look for a hyphaema.
• Look for vitreous haemorrhage on fundoscopy.
X-ray all patients with possible globe penetration (consider also CT or USS)
Give analgesia, tetanus prophylaxis, IV antibiotics (eg 1.5g cefuroxime),
and refer all patients with penetrating eye injuries immediately to an
ophthalmologist, even if there are other major injuries needing attention
at the same time.
Never manipulate or try to remove embedded objects (eg darts).
538 CHAPTER 11 Ophthalmology
Corneal trauma
Conjunctival FB
The typical history is of dust or grit blown into an eye by the wind. The FB
usually gravitates into the lower fornix — remove with a cotton bud.
Subtarsal FB
FBs may not gravitate into the lower fornix, but may remain stuck under
the upper eyelid. The patient reports pain on blinking. Fluorescein staining
reveals characteristic vertical corneal abrasions (the cornea has been
likened to an ‘ice rink’). Evert the upper eyelid and remove the FB with
a cotton bud. Discharge with topical antibiotic (eg chloramphenicol oint-
ment qds or fusidic acid eye drops).
Corneal abrasions
Often result from a newspaper or fi ngernail in the eye. Irritation, photo-
phobia, and lacrimation occur. Use LA drops and fl uorescein staining to
examine the cornea. Exclude FB or penetrating injury. Prescribe regular
antibiotic ointment (eg chloramphenicol) and oral analgesia. An eye patch
which seals eyelids closed will aid the symptoms and recovery. If the patient
is very uncomfortable, consider instilling a drop of 1 % cyclopentolate to
dilate the pupil (this reduces iris spasm) or a drop of 0.1 % diclofenac.
Advise the patient not to drive until vision has returned to normal. Advise
also to return for review if symptoms continue beyond 36hr.
Corneal foreign body
Instill LA and attempt removal with a cotton bud. If unsuccessful, remove
with a blue (23G) needle introduced from the side (ideally using a slit
lamp). Ensure that the patient’s head is fi rmly fi xed and cannot move for-
wards onto the needle: it can help for the operator’s hand to rest lightly
on the patient’s cheek. After complete removal of the FB, check that the
anterior chamber is intact, instill and prescribe antibiotic ointment, and
advise the patient to return if symptomatic at 36hr. Refer patients with
large, deep or incompletely removed FB, or if a rust ring remains.
Arc (welder’s) eye/‘snowblindness’
Exposure to ultraviolet light can cause superfi cial keratitis. Climbers/skiers,
welders, and sunbed users who have not used protective goggles develop
pain, watering, and blepharospasm several hours later. LA drops allow
examination with fl uorescein staining, revealing multiple punctate corneal
lesions. Consider instilling a drop of 1 % cyclopentolate or 0.1 % diclofenac
into both eyes. Discharge with an eye pad, oral analgesia, and advice
not to drive until recovered. Anticipate resolution within 24hr. Do not
discharge with LA drops.
Chemical eye burns
Chemical burns from alkali or acid are serious. Triage urgently ahead,
check Toxbase and provide immediate eye irrigation with lukewarm
normal saline for at least 20min, or until the pH of tears has returned to
normal (7.4). A 1L bag of 0.9 % saline with standard IV tubing is ideal. LA
may be needed to enable full irrigation. Identify the substance involved
and contact Poisons Unit. Refer alkali and acid burns immediately.
Superglued eyelids
Wash with warm water. The eye will open within 4 days. If the patient
reports a FB sensation, this may represent a lump of glue, which may
cause an abrasion if left untreated: refer to the ophthalmologist.

539
CONTACT LENS PROBLEMS
Contact lens problems
Contact lenses are of two basic types: hard or soft. Soft lenses, composed
of hydrogels, are more comfortable to wear. Avoid using fl uorescein with
contact lenses, as permanent staining may occur.
‘Stuck lens’
Most contact lens users are adept at removing their contact lenses. New
users, however, not infrequently experience diffi culty in their removal.
Moisten soft lenses with saline, then remove by pinching between fi nger
and thumb. Special suction devices are available to help remove hard
lenses.
‘Lost lens’
Patients may present concerned that they are unable to fi nd their contact
lens and cannot remember it falling out. Check under both eyelids
carefully (evert the upper lid if the lens is not immediately apparent) and
remove the offending lens, if present.
Hypersensitivity and overuse
Preservatives in lens cleaning fl uid cause itching and may evoke a reaction.
Advise to stop using the lenses, give local antibiotic ointment and arrange
ophthalmological follow-up.
Acanthamoeba keratitis
This is a protozoal infection of the cornea which occurs in contact lens
users, associated with poor lens hygiene or swimming whilst wearing
contact lenses. The eye becomes painful and red. Corneal oedema
and ulceration develops. If acanthamoeba infection is suspected, refer
immediately for ophthalmological care.
Other problems
Treat and refer conjunctivitis, corneal abrasions, or ulcers apparently
related to contact lenses as outlined opposite. Advise avoidance of use of
both contact lenses until the problem has resolved.
540 CHAPTER 11 Ophthalmology
Sudden visual loss
Sudden visual loss requires emergency assessment and treatment.
Amaurosis fugax
The patient describes temporary loss of vision in one eye, like a ‘curtain
coming down’, with complete recovery after a few seconds to minutes.
The cause is usually a thrombotic embolus in the retinal, ophthalmic,
or ciliary artery, originating from a carotid atheromatous plaque. Refer
urgently to the ophthalmology team.
Central retinal artery occlusion
The central retinal artery is an end artery. Occlusion is usually embolic
(check for atrial fi brillation and listen for carotid bruits), causing sudden
painless d VA to counting fi ngers or no light perception. The patient may
have a history of amaurosis fugax. Direct pupil reaction is sluggish or
absent in the affected eye, but it reacts to consensual stimulation (afferent
pupillary defect). Fundoscopy reveals a pale retina, with a swollen pale
optic disc and ‘cherry red macula spot’ (the retina is thinnest here and
the underlying choroidal circulation is normal). Retinal blood vessels are
attenuated and irregular: there may be ‘cattle-trucking’ in arteries.
Treat by digitally massaging the globe for 5–15sec then release and
repeat to dislodge the embolus, whilst awaiting the urgent arrival of an
ophthalmologist.
If there is any delay in the patient being seen by the ophthalmologist,
consider (and discuss) the following options:
• Giving sublingual glyceryl trinitrate (GTN).
• Giving IV 500mg acetazolamide (to d intra-ocular pressure).
• Reconsider the diagnosis. In particular, consider whether or not tempo-
ral arteritis is a possibility: ask about jaw claudication, headaches, scalp
tenderness.
Central retinal vein occlusion
This is a more frequent cause of sudden painless visual loss than arterial
occlusion. Predisposing factors include: old age, chronic glaucoma, arte-
riosclerosis, hypertension, polycythaemia. Examination reveals d VA, often
with an afferent pupillary defect. Fundoscopy reveals a ‘stormy sunset’
appearance: hyperaemia with engorged veins and adjacent fl ame-shaped
haemorrhages. The disc may be obscured by haemorrhages and oedema.
Cotton wool spots may be seen. Although the outcome is variable and
there is no specifi c treatment, refer urgently as the underlying cause may
be treatable, thus protecting the other eye.

541
SUDDEN VISUAL LOSS
Temporal (giant cell) arteritis
Infl ammation of the posterior ciliary arteries causes ischaemic optic neu-
ritis and visual loss. It is relatively common in those aged > 50 years and
is associated with polymyalgia rheumatica. The other eye remains at risk
until treatment is commenced. Rapid and profound visual loss may be pre-
ceded by headaches, jaw claudication, general malaise, and muscular pains.
The temporal arteries are characteristically tender to palpation. Retinal
appearances have been termed ‘pale papilloedema’: the ischaemic disc is
pale, waxy, elevated and has splinter haemorrhages on it. If suspected, give
200mg IV hydrocortisone immediately, check erythrocyte sedimentation
rate (ESR) (typically > > 40mm/hr, but can be normal) and refer urgently.
Vitreous haemorrhage
Occurs in diabetics with new vessel formation, in bleeding disorders and
in retinal detachment. Small bleeds may produce vitreous fl oaters with
little visual loss. Large bleeds result in painless d d VA, an absent red refl ex
and diffi culty visualizing the retina. Refer urgently. Meanwhile, elevate the
head of the bed to allow blood to collect inferiorly.
Retinal detachment
Occurs in myopes, diabetics, the elderly and following trauma. The rate
of onset is variable: patients may report premonitory fl ashing lights or a
‘snow-storm’, before developing cloudy vision. There may be a visual fi eld
defect. Macular involvement causes d VA. The affected retina is dark and
opalescent, but may be diffi cult to visualize by standard ophthalmoscopy.
Refer urgently for surgery and re-attachment.
Optic neuritis
Usually presents in a young woman. Optic nerve infl ammation causes
visual loss over a few days. Pain on eye movement may occur. An afferent
pupillary defect is associated with d VA, d colour vision (colour red looks
faded) and normal/swollen optic disc. Most recover untreated, later some
develop multiple sclerosis. Refer to the ophthalmologist.
Other causes
Patients with chronic visual loss due to a variety of conditions may present
acutely (senile macular degeneration, glaucoma, optic atrophy, cataract,
choroidoretinitis). Drugs which can cause painless visual loss include
methanol ( b p.202) and quinine (in overdose). Refer immediately all
patients in whom an acute visual loss cannot be excluded.
542 CHAPTER 11 Ophthalmology
The red eye
Patients commonly present with a red eye with no history of trauma, but
it is critical not to miss certain diagnoses. Refer all patients with new fi nd-
ings of d VA, abnormal pupil reactions, or corneal abnormalities.
Orbital and preseptal cellulitis
This is a major infection of the orbital tissues. The infection is most fre-
quently spread from the paranasal sinuses (ethmoid sinusitis), facial skin or
lacrimal sac. Occasionally, the infection follows direct trauma to the orbit
or from haematogenous spread. Patients present with fever, eyelid swelling,
erythema, and proptosis. Always assess patient for signs of severe sepsis
( b Severe sepsis and shock, p.59) and resuscitate as necessary. Obtain
venous access, take blood for cultures, commence intravenous antibi-
otics (eg co-amoxiclav) and fl uids. Refer urgently to the ophthalmologist.
Some aggressive infections may require surgical treatment. Cavernous
sinus thrombosis and meningitis are potential complications.
Acute iritis (acute uveitis)
A relapsing condition of the young and middle-aged associated with anky-
losing spondylitis, ulcerative colitis, sarcoid, AIDS, and Behçet’s syndrome.
Symptoms include Acute onset pain, photophobia, ‘fl oaters’, blurred
vision and watering.
Signs d VA, tender eye felt through the upper eyelid, circumcorneal
erythema, small pupil (may be irregular due to previous adhesions).
Shining a light into the ‘good’ eye causes pain in the other. Pain i as eyes
converge and pupils react to accommodation (Talbot’s test). Slit lamp
may reveal hypopyon and white precipitates on the posterior cornea.
Refer urgently to the ophthalmologist for steroid eye drops, pupil
dilatation, analgesia, investigation, and follow-up.
Acute closed angle glaucoma
Long-sighted middle-aged or elderly with shallow anterior chambers
are at risk. Sudden blocked drainage of aqueous humor into the canal of
Schlemm causes intra-ocular pressure to increase from 10–20mmHg up to
70mmHg. This may be caused by anticholinergic drugs or pupil dilatation
at night (reading in dim light).
Symptoms include preceding episodes of blurred vision or haloes around
lights due to corneal oedema. Acute blockage causes severe eye pain,
nausea/vomiting.
Signs d VA, hazy oedematous cornea with circumcorneal erythema and a
fi xed semi-dilated ovoid pupil. The eye feels tender and hard through the
upper eyelid. Measure intraocular pressure if this facility is available.
Treatment Instill a 4 % pilocarpine drop every 15min to produce ciliary
muscle contraction and aqueous humor drainage. Apply prophylactic 1 %
pilocarpine drops into the other eye also. Give analgesia (eg morphine IV
with anti-emetic). Arrange an emergency ophthalmology opinion: consider
giving acetazolamide 500mg IV (to d intra-ocular pressure) meantime and/
or mannitol 20 % up to 500mL intravenous infusion over 1hr.

543
THE RED EYE
Conjunctivitis
Caused by bacteria ( Strep. pneumoniae or H. infl uenza ), viruses (adeno-
virus), or allergy. The sensation of a FB may involve both eyes. The con-
junctiva is red and infl amed, sometimes with eyelid swelling. VA and pupils
are normal. Bacterial infection classically produces sticky mucopurulent
tears, viral infection copious watery tears (associated with photophobia
and pre-auricular lymphadenopathy in the highly contagious adenoviral
‘epidemic keratoconjunctivitis’). Prescribe antibiotic eye drops or oint-
ment (eg fusidic acid, chloramphenicol, or gentamicin) regularly for 5 days.
Advise not to share towels or pillows. Most cases settle relatively quickly:
advise patients to return if symptoms do not improve within 4 days.
Ulcerative keratitis
Corneal ulceration causes pain with photophobia. It is apparent on
fl uorescein staining under a slit lamp.
• Hypopyon (pus in the anterior chamber) implies bacterial infection.
• Vesicles in the ophthalmic division of the trigeminal nerve occur with
herpes zoster infection.
• A dendritic branching ulcerative pattern suggests herpes simplex.
If this is misdiagnosed and steroid eye drops given, ulceration can
be disastrous. As a non-specialist, do not prescribe steroid eye
drops — leave this to the ophthalmologist.
Whatever the infective agent, refer corneal ulceration immediately.
Episcleritis
Infl ammation beneath one area of the conjunctiva is usually associated
with a nodule and a dull aching discomfort. VA, pupils, and anterior
chamber are normal. Prescribe oral NSAIDs and advise outpatient follow-
up to consider steroid eye drops if there is no resolution.
Blepharitis
This chronic problem is quite common. Eyelashes are matted together
and itchy. Ensure that there is no associated corneal ulceration, provide
topical antibiotics (eg chloramphenicol) and refer for GP follow-up.
External hordeolum (stye)
Treat staphylococcal infections of eyelash roots with antibiotics drops.
Internal hordeolum (chalazion)
A chalazion is an infl ammatory reaction in a blocked meibomian gland,
which may become secondarily infected. Treat infected tarsal
(meibomian)
glands with topical antibiotics (eg chloramphenicol) together with oral
antibiotics (eg co-amoxiclav). Refer patients who develop an abscess or
nodule affecting vision.
Dacrocystitis
Acute infection of the lacrimal sac may follow nasolacrimal duct
obstruction. Treat early infections with oral antibiotics (co-amoxiclav);
later, refer for drainage.
Subconjunctival haemorrhage
This usually presents as a painless, well-defi ned area of haemorrhage
over the sclera. May result from vomiting or sneezing. Following trauma,
consider orbital or base of skull fracture and treat accordingly.
This page intentionally left blank

546 CHAPTER 12 Ear, nose and throat
Ear, nose, and throat foreign bodies
Ear foreign bodies
All sorts of FBs may become lodged in the external auditory canal,
including insects, vegetable matter, and various inert objects. The patient
may present with pain, deafness, discharge or, in the case of live insects, an
irritating buzzing in one ear.
Diagnosis depends upon direct visualization with the auriscope. In children,
remember that, as with FBs elsewhere, there may be no history of FB
available.
Removal
• Many FBs can be removed under direct vision with hooks. Manipulate
gently to avoid causing damage or further impaction.
• Drown live insects in 2 % lidocaine fi rst.
• Do not try to syringe out vegetable matter with water, as this may cause
swelling and pain.
• If there is some diffi culty (eg ball bearing or bead in an uncooperative
child), refer to ear, nose, and throat (ENT) department to consider
removal under GA. Removal of beads using an orange stick with a tiny
amount of superglue on the end has been described, but carries some
obvious dangers and requires complete patient co-operation.
Embedded ear-rings The ‘butterfl y’ piece of an ear ring may become
embedded in the posterior part of the ear lobe, causing infl ammation or
infection. The ear-rings are usually easily removed once adequate analgesia
has been established: render the ear anaesthetized with a greater auricular
nerve block ( b Nerve blocks of forehead and ear, p.300), or directly
infi ltrate local anaesthetic into the lobe, remembering that this is a highly
sensitive area. The butterfl y is released by applying pressure in a posterior
direction. Occasionally, forceps and a small posterior skin incision may be
required to open up the track. If there is evidence of infection, prescribe
antibiotics (eg co-amoxiclav) and arrange GP follow-up. Advise the patient
not to wear ear-rings until the symptoms have settled.
Nasal foreign bodies
Usually affects children, who present with offensive unilateral nasal discharge.
Also occurs in adults with psychotic illness or learning disabilities.
Removal Remove easily accessible, anterior nasal FBs in ED. However,
there is a risk of aspiration with any nasal FB, particularly in uncooperative
patients. Refer such patients to an ENT surgeon for removal with airway
protection. Instruct the patient to blow their nose whilst occluding the
unaffected nostril. If unsuccessful, consider attempting removal with a
nasal speculum, hook, and forceps, as appropriate. A fi ne bore tracheal
suction catheter attached to wall suction can also work. One technique
which has been reported in cooperative children is to ask a parent to
blow into the child’s mouth (‘parent’s kiss’), having fi rst ensured a good
seal and also occluded the normal nostril.
Nasal button, batteries, or magnets ( b p.213) can cause signifi cant damage,
so refer to ENT.

547
EAR, NOSE, AND THROAT FOREIGN BODIES
Inhaled foreign bodies
Aspiration causing complete upper airway obstruction is an emergency,
requiring immediate intervention ( b p.324). FBs lodged in the larynx or
tracheobronchial tree cause persistent coughing. There may not be a clear
history — a coughing/spluttering episode in a child should arouse suspicion
of an inhaled FB. Auscultation of the chest is often normal, but may reveal
wheezes or localized absence of breath sounds.
CXR may be normal or show a radio-opaque FB with distal consolidation
or hyperinfl ation (FB acting as a ball valve). A CXR in expiration may
show this more clearly. Refer to a cardiothoracic surgeon.
Ingested foreign bodies
Various FBs, both radio-opaque (eg coins, rings) and non-radio-opaque
(eg plastic pen tops, aluminium ring pulls) are frequently swallowed by
children and by adults with psychiatric disorders. Provided the FB reaches
the stomach, it is likely to pass through the remainder of the gastroin-
testinal tract without incident. An exception is button battery ingestion
( b p.213). For radio-opaque FBs, confi rm with lateral neck X-ray and
CXR that it is not impacted in the oesophagus. A metal detector may
confi rm a swallowed coin has reached the stomach. Refer patients who
are symptomatic, have impacted FBs, or who have swallowed potentially
dangerous items (button batteries, razor blades, open safety pins). Note
that magnets can be dangerous if two or more are ingested, since they can
attract each other through tissues and cause pressure necrosis/perforation
of bowel. Only discharge patients who are asymptomatic (with advice
to return if they develop abdominal pain and/or vomiting), and arrange
suitable follow-up. Unless the ingested FB is valuable or of great sentimental
value, examination of the stools by the patient for the FB is unnecessary.
It may take weeks to pass.
Impacted fi sh bones
Fish bones often become stuck in the pharynx or oesophagus. Direct visu-
alization with a good light (a head torch can be useful) and wooden spatula
acting as tongue depressor may reveal fi sh bones lodged in the tonsils or
base of the tongue — remove with Tilley’s forceps. If no FB is seen, obtain
soft-tissue lateral neck X-rays (look for prevertebral soft tissue swelling
and fi sh bone, bearing in mind not all are radio-opaque), then refer to
ENT for endoscopy. Depending on local policy, the ENT team may decide
to see the patient immediately, or (provided the patient can swallow) the
following day (in which case discuss the need for prophylactic antibiotics).
A fi sh bone can scratch the pharynx causing sensation of a FB to persist
after it has gone.
Oesophageal food bolus obstruction
Usually involves a lump of meat. Patients with complete obstruction
present unable to swallow solids or liquids (including their own saliva).
There may be retrosternal discomfort. Refer to the surgical team for
endoscopy. Glucagon (1mg IV) relieves some episodes of food bolus
obstruction, but endoscopy is still advisable to look for oesophageal
stenosis or malignancy.

548 CHAPTER 12 Ear, nose and throat
Ear examination
Scope of the examination
Full ear examination includes assessment of the vestibulocochlear nerve
and auroscope examination. Check for mastoid or pinna tenderness.
Look at the external ear canal for discharge, or swelling and examine
the tympanic membrane for colour, translucency, bulging, and the cone
of light.
Assessing hearing
Hearing can be assessed by asking the patient to place one fi nger in their
ear. Stand a foot behind the patient’s unoccluded ear and whisper a two
syllable word. Ask the patient to repeat the word.
Weber’s and Rinne’s tests
Weber’s test — strike a 512Hz tuning fork and place in the centre of the
forehead. In conductive deafness, the sound localizes to the deaf ear, with
sensorineural deafness, the sound localizes to the good ear.
Rinne’s test — strike a 512Hz tuning fork and place it on the mastoid
process. Ask the patient to tell you when they no longer hear the sound,
then immediately place in front of the auditory meatus. In a normal ear, air
conduction is heard for twice as long as bone conduction. In conductive
deafness, bone conduction is heard for longer than air conduction.
In sensorineural deafness, air conduction is heard longer than bone
conduction.
Nystagmus
To complete assessment of the vestibulocochlear nerve, examine for
nystagmus. All forms of nystagmus can be associated with intracranial
lesions, as well as peripheral causes; however, downbeat and upbeat nys-
tagmus in particular, signify a central cause. Tinnitus or deafness tends to
suggest a peripheral cause. Peripheral nystagmus is exacerbated by gazing
towards the side of the fast phase (Alexander’s Law). Central nystagmus
may change direction, depending on the side of gaze.

549
COCHLEAR IMPLANTS
Vertigo
Vertigo is the impression or illusion of movement when there is none.
Take care to distinguish vertigo from the more general term of ‘dizziness’,
which is often used to describe a feeling of light-headedness.
Causes
• Benign positional vertigo. Diagnosed with Hallpike’s test which induces
positional vertigo. Mostly caused by posterior semicircular canal cana-
lithiasis. Medications are ineffective.
• Menière’s disease: a disorder of the inner ear. Patients have recurrent
vertigo, tinnitus and deafness and should be managed by ENT.
• Acute labyrinthitis: Caused by reactivation of herpes simplex virus.
Some have an upper respiratory tract prodrome. Some individuals are
unable to work or perform normal daily duties because of vertigo and
vomiting.
• Otitis media.
• Acoustic neuroma (or vestibular schwannoma). This presents with slow
onset deafness and tinnitus. Dizziness is less common.
• Cholesteatoma.
• Stroke or transient ischaemic attack.
• Trauma.
• Wax or FB in the ear.
Take a careful history and examine for causes of vertigo. Manage patients
who present with vertigo according to the underlying cause. The
cause may be unclear, in which case refer to the medical/ENT team as
appropriate.
Cochlear implants
Cochlear implants consist of an implanted radio receiver and decoder
package containing a magnet (above and behind the ear), together with a
removable external microphone/radio transmitter. X-rays and CT do not
damage this device, provided that the external microphone/transmitter is
fi rst removed and switched off. MRI can cause signifi cant damage to the
device and the patient. If there are concerns relating to a cochlear implant,
refer to ENT. In particular, refer patients with:
• Signifi cant direct trauma, including exposure by a scalp wound.
• Suspected otitis media of the implanted ear.

550 CHAPTER 12 Ear, nose and throat
Earache
Otitis externa
Often caused by Pseudomonas, Staph. aureus, Strep. pneumoniae, E. coli.
Common in swimmers/surfers and after minor trauma. This causes intense
itching and pain, which gradually increases. Discharge and hearing loss may
be present (profuse discharge implies middle ear disease). On examina-
tion, the external canal is infl amed and oedematous. Oedema and debris
may obscure the tympanic membrane. Pain is induced by pressing on the
tragus or pulling the pinna.
Management Prescribe topical antibiotics and topical steroids, advise
against swimming, and arrange GP follow-up. In severe cases (eg if the
drum is not visible), refer to an ENT surgeon for aural toilet to remove
debris from the auditory canal.
Cellulitis or furunculosis of the ear canal
Cellulitis of the ear canal may be caused by scratching or by infection of
hair follicles (furunculosis). Staph. aureus is the usual organism. Itching
and a feeling of pressure are followed by pain in the ear, with deafness
if the ear canal is occluded by swelling. Examination shows swelling and
infl ammation of the ear canal, with tenderness over the tragus and pain on
movement of the ear.
Treat with analgesia (eg NSAID) and antibiotics (eg fl ucloxacillin 500mg
PO qds for 5 days). Arrange follow-up by a GP (or ENT in severe cases).
Acute otitis media
Most common in children aged 3–6 years and may follow an upper respi-
ratory tract infection. Commonest pathogens are Strep. pneumoniae and
H. infl uenzae.
Presentation Earache may be accompanied by fever, deafness, irritability
and lethargy. Typically, hearing loss precedes pain. Examination of the
tympanic membrane shows evidence of infl ammation with loss of the light
refl ex and bulging of the drum. Eventual perforation results in purulent
discharge with some relief of pain. Look for associated swelling/tenderness
over the mastoid — this implies secondary mastoiditis (see below).
Treatment Prescribe oral analgesia. The use of antibiotics remains
very controversial. Oral antibiotics (eg 5-day course of amoxicillin or
clarithromycin) are of questionable value, but are frequently given.
Consider oral antibiotics if no improvement within 72hr, or earlier if
there is deterioration or perforation. If perforation has occurred (often
heralded by a sudden i pain), arrange ENT follow-up and advise not to
swim. Otherwise, arrange GP follow-up.
Acute mastoiditis
This is an uncommon, but important diagnosis to make, because of the
risk of intracranial spread of infection. Mastoiditis follows an episode of
acute otitis media — consider it if there is no response to therapy (eg dis-
charging ear for > 10 days). Suspect it if there is pain, redness, swelling or
tenderness over the mastoid process. The pinna may be pushed forwards/
outwards — swelling may mean that the drum is not visible. Refer urgently
to the ENT surgeon for admission and IV antibiotics.

551
EARACHE
Cholesteatoma
This erosive condition affects the middle ear and mastoid. A cholest-
eatoma can result in life-threatening intracranial infection. There may be
an offensive discharge, with conductive hearing loss, vertigo or facial nerve
palsy. Tympanic membrane examination shows granulation tissue and/or
perforation with white debris. Refer to the ENT surgeon.
Traumatic tympanic membrane rupture
This may result from direct penetrating injury, blast injury ( b p.389)
or basal skull fracture ( b p.361). Pain is associated with d hearing.
Perforation is visible on examination.
Treatment Most heal spontaneously with conservative measures and advice
to keep out of water. Arrange ENT follow-up and give prophylactic oral
antibiotics according to local policy. Note that gentamicin or neomycin
eardrops may cause sensorineural deafness because of ototoxicity when
the tympanic membrane is ruptured.
Barotrauma
Sudden changes in atmospheric pressure with a blocked Eustachian tube
can result in pain and hearing loss. This usually affects aircraft passengers
and divers, especially if they have a cold (viral upper respiratory tract
infection). Pain is often relieved by the Valsalva manoeuvre (breathing out
with the mouth closed, while pinching the nose). Decongestant nasal spray
may help if the problem does not resolve spontaneously. Give analgesia
(NSAID). Arrange ENT follow-up if the pain persists.

552 CHAPTER 12 Ear, nose and throat
Epistaxis
Nasal bleeding may be idiopathic or follow minor trauma (eg nose picking).
When it occurs in patients with hypertension and coagulation disorders
haemorrhage can be severe with signifi cant mortality. Epistaxis may follow
isolated nasal fracture and more major facial injury.
Site of bleeding
Most nasal bleeding is from the anterior nasal septum in or close to Little’s
area. A few patients have posterior nasal bleeding, which may be brisk.
Equipment
Direct visualization of the anterior nasal cavity is aided by a headlamp
(eg battery-operated head torch), fi ne soft suction catheter, and nasal
speculum. Wear goggles to avoid blood splashes in the eyes.
Initial approach
Associated facial injury Assess ABC (especially pulse and BP) and resuscitate
as necessary. Treat hypovolaemia vigorously.
No associated injury Check airway patency, pulse, and BP. Treat
hypovolaemia aggressively. Check coagulation status of patients on
anticoagulants and treat appropriately ( b p.170). Sit the patient up and
instruct them to compress the fl eshy part of their nose between fi nger
and thumb for 10min. If this stops the bleeding, the patient may be
discharged after 30min observation.
Continuing bleeding after pressure
Adults Apply a cotton wool pledget soaked in 4 % lidocaine with 1 in 1000
adrenaline. Then, with a headlamp and nasal speculum, try to identify the
bleeding point. Treat small anterior bleeding points with cautious cautery
by applying a silver nitrate stick for 10–15sec. Avoid excessive cautery and
never cauterize both sides of the septum — this may cause septal necrosis. If
cautery stops the bleeding, observe for 15min, and discharge with GP follow-
up. Advise avoidance of sniffi ng, picking or blowing the nose meantime.
Children Applying nasal antiseptic cream (eg Naseptin
®
) is as effective as
cautery in stopping bleeding. The cream is relatively easy to apply.
Continuing bleeding despite cautery
Insert a nasal pack. A specialized compressed surgical sponge nasal tampon
(eg Merocel
®
or Rapid Rhino) is ideal: gently insert a lubricated tampon
(horizontally) and ‘infl ate’ with a 10mL syringe of saline. Alternatively, pack
the nose in a traditional way with 1.25cm wide ribbon gauze soaked in oily
paste (eg bismuth iodoform paraffi n paste). Once packing has stopped the
bleeding, refer to ENT for admission: observation is advisable (especially
in the elderly). The pack may dislodge and obstruct the airway.
Continuing bleeding despite packing
Refer to the ENT surgeon. The bleeding site is likely to be posterior and can
cause hypovolaemic shock. In this situation, insert 2 large bore venous cannulae,
send blood for FBC, coagulation screen, cross-matching, and commence an IVI.
Posterior nasal bleeding usually responds to tamponade with a Foley
catheter. Remove the nasal tampon and insert a lubricated, uninfl ated
Foley catheter through the bleeding nostril into the nasopharynx. Infl ate
the balloon with air and gently withdraw the catheter, thus tamponading
the bleeding site. Secure the catheter to the cheek with tape, and then
re-insert the anterior nasal tampon.

553
NASAL FRACTURE
Nasal fracture
The prominent exposed position of the nose, combined with the delicacy
of its bones, render it relatively prone to injury.
Remember that the nose is part of the head, so nose injury = head injury
(and potentially cervical spine injury also).
History
The nose is commonly broken by a direct blow (eg from a punch) or
following a fall onto the face. Nasal fracture is usually accompanied by
bleeding. Search for a history of associated facial/head injury (diplopia, loss
of consciousness, etc.).
Examination
This is a clinical diagnosis based upon a history of injury with nasal swelling
and tenderness. Having made the diagnosis, assess whether there is nasal
deviation: it is useful to ask the patient to look in a mirror. Check and
record whether the patient can breathe through each nostril. Look for
an associated septal haematoma — this will appear as a smooth bulging
swelling, which may obstruct the nasal passage. Children are at particular
risk of septal haematoma, which predisposes to secondary infection and
septal necrosis.
Assess for additional injuries to the head or face (eg tender mandible,
diplopia, tender maxilla). Injury to the bridge of the nose may result in
persistent epistaxis and/or cerebrospinal fl uid rhinorrhoea.
Investigation
Do not X-ray to diagnose a nasal fracture — the diagnosis is a clinical one.
Obtain appropriate X-rays (eg orthopantomogram (OPG) or facial views)
if there is clinical suspicion of other bony injuries. Nasal fractures are often
apparent on facial X-rays or CT scans.
Treatment
• Resuscitate and treat for associated head injury.
• Continuing nasal haemorrhage is uncommon — refer to an ENT surgeon
to consider urgent manipulation under anaesthetic (MUA) to stop the
bleeding: meanwhile, insert a nasal tampon.
• Refer urgently to an ENT surgeon if there is a septal haematoma — this
will require incision and drainage in order to prevent septal necrosis.
• Clean and close overlying skin wounds: steristrips often allow good skin
apposition. If there is signifi cant contamination of the wound, start a
course of prophylactic oral antibiotics (eg co-amoxiclav: one tablet PO
tds for 5 days).
• Provide oral analgesia (eg ibuprofen 400mg PO tds).
• If the nose is deviated/distorted, or if there is too much swelling to
judge, arrange for ENT follow-up at 5–7 days, so that MUA may be
performed within 10 days. It is particularly important to ensure accurate
reduction of fractures in children.
• Discharge with head injury instructions to the care of a relative.

554 CHAPTER 12 Ear, nose and throat
Sore throat
Tonsillitis
Causes Acute pharyngo-tonsillitis may result from infection with a variety
of viruses or bacteria:
• Viral: Epstein–Barr virus (EBV), herpes simplex virus, adenoviruses.
• Bacterial: group A
B
-haemolytic streptococcus (most common bacterial
cause), mycoplasma , Corynebacterium diphtheriae .
Features Sore throat is frequently accompanied by fever, headache,
and mild dysphagia. Inspection of the tonsils reveals infl ammation — the
presence of pus on the tonsils suggests bacterial infection. Enlarged
cervical lymph nodes are found in a variety of infections, but generalized
lymphadenopathy (sometimes also with splenomegaly) is indicative of
glandular fever (infectious mononucleosis — see b p.241).
Diagnosis Despite the clinical pointers described above, it is usually
impossible to distinguish clinically bacterial from viral causes.
Investigation Consider throat swabs and anti-streptolysin titre in severe
cases. If glandular fever is suspected, send blood for FBC and Paul–Bunnell
(or Monospot) test.
Treatment Unless contraindicated, give paracetamol (1g PO qds PRN) or
ibuprofen (400mg PO tds PRN) and discharge to GP. Although frequently
prescribed, oral antibiotics are rarely of benefi t: a sensible approach is to
limit their use for patients with any of the following: a history of valvular
heart disease, immunosupression, diabetes, marked systemic upset,
peritonsillar cellulitis, known B –haemolytic streptococci. In this case,
prescribe penicillin 500mg PO qds for 5 days (or clarithromycin 500mg PO
bd for 5 days if allergic). Avoid ampicillin, amoxicillin, and co-amoxiclav,
which cause a rash in patients infected with EBV.
Occasionally, patients with acute tonsillitis may be unable to swallow
fl uids (this is more commonly a feature of peritonsillar or retropharyngeal
abscess). In this case, refer for IV antibiotics and IV fl uids.
Complications Otitis media, sinusitis, retropharyngeal abscess, peritonsillar
abscess.
Peritonsillar abscess (quinsy)
Typically, preceded by a sore throat for several days, the development of
a peritonsillar abscess is heralded by high fever, pain localized to one side
of the throat, and pain on swallowing. Diffi culty swallowing can result in
drooling. Trismus may make inspection diffi cult, but if visualized there is
tense bulging tonsil, pushing the uvula away from the affected side. Group
A B -haemolytic streptococci are frequently implicated.
Treatment Insert an IV cannula and give IV benzyl penicillin 1.2g
(clarithromycin 500mg if allergic to penicillin), and refer immediately to an
ENT surgeon for aspiration or formal drainage.

555
SORE THROAT
Retropharyngeal abscess
Spread of infection from adjacent lymph nodes may occasionally cause a
retropharyngeal abscess, particularly in children aged <3 years.
It is characterized by a sore throat, diffi culty swallowing, fever, and
dehydration. In children, cough is typically absent from the history (unlike
in croup and other viral causes of upper airway obstruction). There
may be evidence of airway compromise (stridor, neck hyperextension,
signs of hypoxia). The differential diagnosis includes acute epiglottitis
( b p.677). Lateral X-rays of the neck show soft tissue swelling (obtain
these in the resuscitation room, rather than moving the patient to the
X-ray department).
Treatment Get senior ED, ENT, and anaesthetic help. If the patient is a
child with evidence of respiratory distress, do not upset them further.
Airway obstruction may be precipitated by examination of the throat, so
avoid this until appropriate staff and equipment are ready to cope with
airway problems. The child can sit on mum’s knee in the resuscitation
room. On suspicion of a retropharyngeal abscess in an adult, insert an IV
cannula, take bloods and blood cultures, give IV fl uids and IV co-amoxiclav
1.2g, and refer immediately to an ENT surgeon.
Pharyngeal burns after cocaine use
Smoking cocaine can result in dangerous burns of the throat, since the
drug acts as a local anaesthetic. Swelling of the epiglottis may result in
airway obstruction.
Paranasal sinusitis
Bacterial infection may result from direct spread from infected tooth roots
or (more usually) be secondary to viral upper respiratory tract infection
(URTI).
Clinical features
• Clear nasal discharge becoming purulent.
• Pain in (and often also tenderness over) the affected sinus.
• Fever.
• Headache and/or toothache.
Management
Provide analgesia. Despite a lack of convincing evidence, oral antibiotics
(eg amoxicillin, doxycycline or erythromycin) and nasal decongestant
(eg 1 % ephedrine) are commonly given. Advise GP follow-up. In severe
cases, refer to ENT.

556 CHAPTER 12 Ear, nose and throat
Facial nerve palsy
The facial (VII) nerve supplies the muscles of facial expression. Clinical
examination reveals whether facial nerve palsy is of upper motor neurone
or lower motor neurone type.
Upper motor neurone paralysis is usually due to a stroke ( b p.144),
resulting in unilateral facial muscle weakness, but with sparing of the
muscles of the forehead. If stroke is the cause, there may be additional
evidence elsewhere (eg hemiparesis affecting the limbs).
Lower motor neurone paralysis of the facial nerve results in weakness
of the muscles of one side of the face. The facial nerve arises from its
nucleus in the pons, emerges from the pons to travel past the cerebello-
pontine angle, through the petrous part of the temporal bone, to emerge
from the stylomastoid foramen and thence into the parotid gland, where
it divides into branches. During its passage through the petrous temporal
bone, the facial nerve is accompanied by the chorda tympani (carrying
taste fi bres from the anterior 2/3 of one half of the tongue) and gives off
the nerve to stapedius . Lesions of the facial nerve in the temporal bone
therefore produce loss of taste and hyperacusis (noise is distorted and
sounds loud) on the affected side.
Causes of lower motor neurone facial palsy
• Bell’s palsy: the commonest cause (see below).
• Pontine tumours and vascular events: usually associated with other signs.
• Acoustic neuroma: usually with evidence of other nerve involvement
(V, VI, VIII nerves) at the cerebello-pontine angle.
• Ramsay–Hunt syndrome (herpes zoster infection — see below).
• Trauma.
• Middle ear infection and cholesteatoma (see b Earache, p.550).
• Sarcoidosis.
• Parotid gland tumours, trauma and infection.
• Human immunodefi ciency virus (HIV).
Bell’s palsy
Bell’s palsy is the commonest cause of sudden onset isolated lower motor
neurone facial nerve palsy. It is believed to result from viral infection, pro-
ducing swelling of the facial nerve within the temporal bone: there may be
associated hyperacusis and loss of taste of the anterior two-thirds of one
half of the tongue. The absence of involvement of other cranial nerves is a
reassuring feature, helping to secure this clinical diagnosis.
Treatment Most patients recover completely over several months
without treatment — a small percentage are left with permanent weakness.
Recovery is quicker if prednisolone is started within 72hr of the onset of
symptoms (prednisolone 60mg daily for 5 days, then 10mg less each day;
total of 10 days of treatment). Antiviral drugs do not seem to be helpful.
Advise the use of artifi cial tears and an eye patch at night, to prevent
corneal drying, and refer for ENT follow up.
Ramsay–Hunt syndrome
This is due to herpes zoster infection of the geniculate ganglion. Clinical
features of Bell’s palsy are present, together with (painful) herpetic vesi-
cles present in the external auditory meatus and occasionally also, the soft
palate. Refer to an ENT specialist for aciclovir and follow up.

557
SALIVARY GLAND PROBLEMS
Salivary gland problems
Saliva is a mixture containing water, various ions, mucin, and amylase, pro-
duced by the parotid, submandibular, and sublingual salivary glands. The
problems most commonly affecting the salivary glands are infection and
calculous disease.
Acute bilateral parotitis
Painful swelling of both parotid glands in children is most frequently
due to mumps infection ( b p.222). In adults, painless bilateral parotid
swelling may be due to Sjögren’s syndrome, sarcoidosis, hypothyroidism,
lymphoma, drugs (eg oral contraceptive). In each of these cases, there are
often other features, which will help in diagnosis.
Acute unilateral parotitis
Painful unilateral parotid swelling may occur as part of mumps infection,
but also in other circumstances (eg poor oral hygiene, post-operatively).
Refer to an ENT surgeon for admission and IV antibiotics. Chronic pain-
less unilateral parotitis is often neoplastic (mostly benign) in origin.
Calculous disease
Mechanical obstruction of the fl ow of saliva is most commonly due to
salivary gland stones, affecting the submandibular gland. Obstruction may
also occur from neoplasms or strictures.
Features Blockage of a salivary duct causes pain and swelling of the
affected gland on eating. Bimanual palpation of the fl oor of the mouth
may reveal a stone — occasionally this may be visible intra-orally at the
duct orifi ce. If there is superimposed infection, it may be possible to
express pus from the duct.
Investigation Obtain X-rays of the fl oor of the mouth. If the patient
presses down with the tongue when the X-ray is taken the stone may be
seen more easily below the mandible on a lateral view or OPG.
Treatment Refer to an oral or ENT surgeon. If an immediate consultation
is not available, discuss the use of antibiotics in the meantime (these are
often reserved for situations where there is evidence of salivary gland
infection).
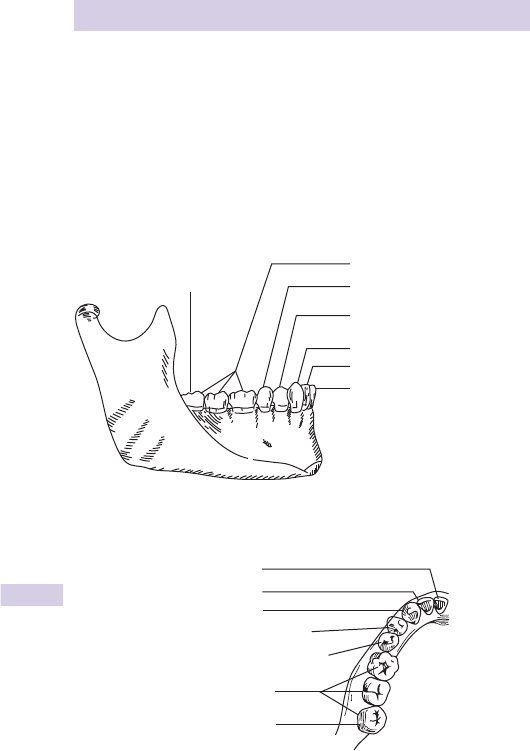
558 CHAPTER 12 Ear, nose and throat
Dental emergencies: 1
Dental anatomy (Figs. 12.1 & 12.2)
The primary teeth erupt between 6 months and 2 years — they are replaced
by permanent teeth which fi rst start to appear at | 6 years (Table 12.1 ).
There are 20 primary and 32 permanent teeth. The permanent teeth are
made up of 4 quadrants of 8 teeth: right upper, left upper, right lower, left
lower. Each quadrant comprises (from medial to lateral): central incisor,
lateral incisor, canine, fi rst premolar, second premolar, fi rst molar, second
molar, and third molar (‘wisdom tooth’).
Wisdom tooth
3rd 2nd 1st
Permanent molars
Central incisor
Lateral incisor
Canine (cuspid)
First premolar (biscuspid)
Second premolar (biscuspid)
Fig. 12.1 Dental anatomy: lower jaw lateral view.
Central incisor
Lateral incisor
Permanent molars
W
isdom tooth
Second premolar (bicuspid)
First premolar (bicuspid)
Canine (cuspid)
Fig. 12.2 Dental anatomy: upper jaw — view from below.
559
DENTAL EMERGENCIES: 1
Table 12.1 Tooth eruption
Deciduous Permanent
Incisors 6–10 months 7–8 years
Canine 16–20 months 11 years
Premolars 11–13 years
Molars 10–24 months 6–25 years
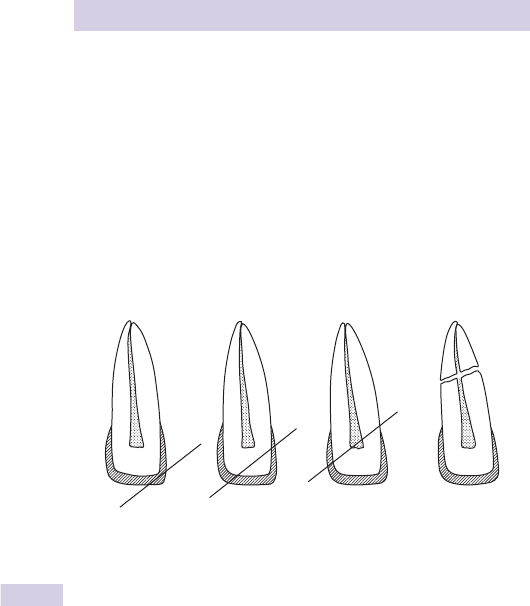
560 CHAPTER 12 Ear, nose and throat
Dental emergencies: 2
Damaged teeth
Chipped teeth and crowns which have become dislodged do not require
immediate attention: redirect the patient instead to their dentist. Specialist
‘sensitive teeth’ toothpaste rubbed over the broken area of tooth may
d pain.
Tooth fractures which involve the pulp present with a small area of bleeding
and are exquisitely tender to the touch. Refer to the on-call dentist.
Mobile teeth after trauma need to be stabilized as soon as possible — advise
the patient to avoid manipulating the tooth and to refer to the dentist.
Simple classifi cation of tooth fractures
Avulsed teeth
Missing teeth need to be accounted for (especially in the unconscious
patient) in order to exclude the possibility of aspiration. Obtain a
postero-anterior (PA) and lateral CXR to search for both the tooth and
secondary problems, such as pulmonary collapse and air trapping distal to
the obstruction. Ensure that there is adequate tetanus prophylaxis.
Avulsed permanent teeth brought to the ED may be suitable for
re-implantation. Avulsed primary teeth are usually not suitable.
A history of rheumatic fever, valvular heart disease, or immunosuppressive
treatment are contraindications to re-implantation. Milk is the best easily
available transport medium to advise a patient to bring a tooth in. The
best chance of success lies with early re-implantation (within the fi rst few
hours). Handle the tooth as little as possible. Hold it by the crown to
clean it gently with 0.9 % saline. Orientate the tooth, and then replace it
within the socket using fi rm pressure (this may be easiest after LA — see
Dental anaesthesia b p.302). Refer immediately to the on-call dentist
for stabilization and prophylactic antibiotics (eg clarithromycin). Ensure
tetanus prophylaxis.
(a) (b) (c) (d)
Fig. 12.3 Simple classifi cation of tooth fractures (a) enamel only; (b) enamel and
dentine; (c) enamel, dentine, and pulp; and (d) root fracture.
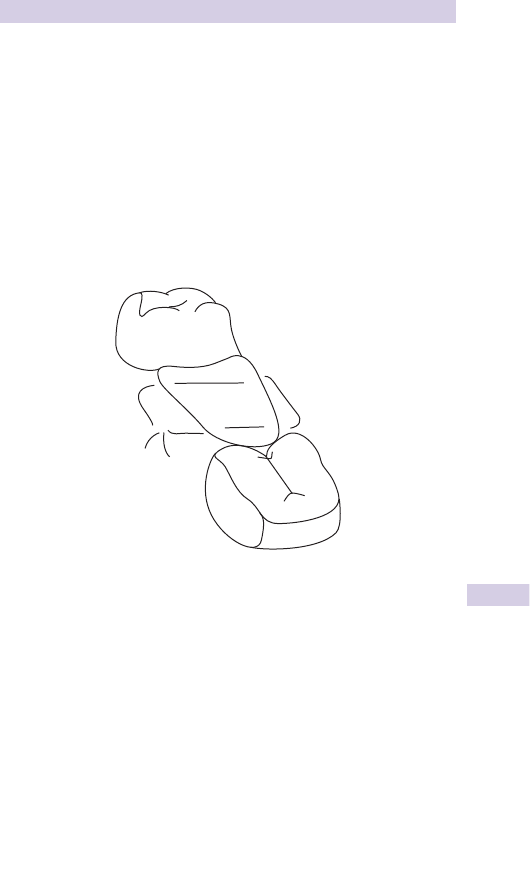
561
DENTAL EMERGENCIES: 2
Post-extraction problems
Haemorrhage after tooth extraction may respond to simple measures.
Ask the patient to bite on a rolled up piece of gauze placed over the
socket for 10min. If this is unsuccessful, consider stopping the bleeding by
inserting a horizontal mattress suture (eg using ‘Vicryl’), placed under LA
using lidocaine with adrenaline (Fig. 12.4 ). If bleeding continues despite
these measures, apply direct pressure, send a coagulation screen and
refer to the on-call dentist.
Dry socket pain may follow tooth extraction (typically 3–8 days later)
when bone is exposed in the empty socket. Gently irrigate the socket
with warm saline. Prescribe oral antibiotics (eg penicillin or erythromycin)
and analgesia and refer to the dentist.
Dental infection
Toothache without associated local or systemic symptoms/signs usually
responds to analgesia (eg ibuprofen 400mg PO tds with food). Add antibi-
otics (eg penicillin or clarithromycin) if there is a suspicion of local infection.
Advise follow-up with a dentist.
Toothache with associated swelling, trismus, dysphagia, or systemic evidence
of infection requires immediate referral to a maxillofacial surgeon for IV
antibiotics and surgical drainage.
Fig. 12.4 Horizontal mattress suture in tooth socket.
This page intentionally left blank

563
Gynaecological problems 564
Vaginal discharge 566
Contraceptive problems 568
Genital injury and assault 570
Gynaecological pain 572
Vaginal bleeding 574
The pregnant patient 576
Emergency normal delivery 578
Diffi culties in normal delivery 580
Vaginal bleeding in pregnancy 582
Spontaneous abortion 584
Ectopic pregnancy 586
Vaginal bleeding in later pregnancy 588
Abdominal pain in pregnancy 590
Medical complications of pregnancy 592
Trauma in pregnancy 594
Cardiac arrest in pregnancy 596
Post-partum problems 598
Obstetrics and
gynaecology
Chapter 13

564 CHAPTER 13 Obstetrics and gynaecology
Gynaecological problems
The history
For gynaecological problems, always take a proper gynaecological history.
This involves asking personal and sometimes sensitive questions so
privacy and confi dentiality are of utmost importance. Interview the patient
without other family members being present:
• Ask about the presenting problem. Always ask about abdominal pain,
dyspareunia, and vaginal discharge.
• Take a detailed menstrual history including the date of the last menstrual
period, length of cycle, and description of the bleeding.
• Obtain a full obstetric history asking about children, pregnancies,
miscarriages, terminations, and infertility treatment.
• Do not forget to ask about sexual activity, type and number of partners
in past year. Also establish what form of contraception has been used.
• Has she ever been treated for a sexually transmitted disease (STD)?
• When was the last smear test and what was the result?
Examination procedure
Prior to performing a vaginal examination, explain the procedure to the
patient and ensure you are in a private room. Allow the patient privacy
to undress. Wearing gloves, examine the patient in an unhurried manner,
in the presence of a chaperone, who might usefully ‘guard’ the door to
prevent sudden inadvertent interruption. Use a chaperone even when
the patient is being examined by female member of staff. Document the
name of the chaperone in the medical record. Full examination includes
digital and speculum vaginal examination to inspect the vagina and cervix,
and taking swabs. This is followed by digital bimanual palpation. In certain
circumstances (eg patients with painful vulval ulcers), this may not be
appropriate in the ED. Vaginal examination in young children may require
GA and should be undertaken by an expert. Adopt a low threshold for
referring such patients.

565
GYNAECOLOGICAL PROBLEMS
Vulvovaginal pain
Distinguish between dysuria, dyspareunia (pain on vaginal penetration),
and constant vulvovaginal pain/irritation. The latter is often associated
with infection or ulceration. Enquire about other symptoms (abdominal
pain, vaginal discharge and bleeding).
Vulval ulcers
• Herpes simplex virus is sexually transmitted and usually due to type
II, but is increasingly due to type I virus (responsible for cold sores).
Primary infection is extremely painful, lasting up to 3 weeks and
sometimes causing urinary retention. Look for shallow yellow
vulvovaginal or perineal ulcers with red edges. Cervical ulcers may also
be present, although pain may prevent speculum examination. Refer
primary infections immediately for aciclovir, analgesia and to exclude
co-existing infection. Recurrent infections are less severe, but may
last up to a week. Treat with topical and oral aciclovir (200mg fi ve
times a day for 1 week) and arrange genitourinary (GU) follow-up,
with advice to avoid sexual contact meantime. Do not prescribe
aciclovir in pregnancy, but arrange for an obstetric opinion.
• Other sexually transmitted diseases may cause ulceration: syphilis
(non-tender indurated ulcers (‘chancres’) and lymphadenopathy),
chancroid, lymphogranuloma venereum, and granuloma inguinale
( b p.238). Refer to GU clinic and advise to abstain from sexual contact
until treated.
• Squamous carcinoma causes indurated ulcers with everted edges
especially in the elderly. Refer.
• Consider also : Behçet’s syndrome (arthritis, iritis, genital/oral ulceration),
tuberculosis (TB), Crohn’s disease.
Painful lumps
• Bartholin’s abscess : infection of vestibular (Bartholin’s) cyst/gland at the
posterior part of the labium majus is usually due to Staph. , Strep ., or
E. coli , but may be due to N. gonorrhoea . Refer for incision and drainage
(under GA) and a full GU screen.
• Infected sebaceous cysts may also require incision and drainage.
• Urethral carbuncle : this small, red, painful swelling at the external urethral
meatus is due to urethral mucosal prolapse. It may cause dysuria. Refer
to an appropriate clinic to consider excision or diathermy.
Pruritis vulvae
Vulval irritation may be caused by a generalized pruritic skin disorder
(eg eczema), infection (particularly candidiasis) and other causes of
vaginal discharge ( b p.566), urinary incontinence, threadworms, and vulval
warts. Genital warts (including condylomata accuminata) are usually
sexually transmitted and caused by human papillomavirus 6. Other STDs
may coexist. Refer to GU clinic.

566 CHAPTER 13 Obstetrics and gynaecology
Vaginal discharge
May be physiological or due to atrophic vaginitis, infections including
STDs, cervical and endometrial carcinoma, a variety of fi stulae, and FBs.
Physiological
A creamy/white discharge is normal. Variation in its consistency and
amount occurs with puberty, pregnancy, oral contraceptive pill (OCP)
use, ovulation, and immediately prior to menstruation.
Atrophic vaginitis
A profuse, sometimes bloody, yellow discharge may result from vaginal
epithelial thinning due to d oestrogen levels associated with the meno-
pause. This responds well to local topical or oral oestrogens, most appro-
priately prescribed by the patient’s GP.
‘Thrush’
Candida albicans is the commonest vaginal infection. A white discharge
accompanies a red painful vulvovaginitis. Occurs in pregnancy, after oral
antibiotics, and with HIV and diabetes: check for glycosuria. Treatment
options include clotrimazole pessaries, oral fl uconazole, and topical
application of live yoghurt. Advise GP for follow-up of any continuing
symptoms.
Other infections
Refer patients suspected of the following STDs to GU clinic and advise
abstinence from sexual contact in the meantime:
• Neisseria gonorrhoea may be asymptomatic, cause urethritis (dysuria),
cervicitis (vaginal discharge), or pelvic infl ammatory disease (PID;
b Gynaecological pain, p.573).
• Trichomonas vaginalis infection results in a smelly profuse yellow
discharge.
• Chlamydia trachomatis causes chronic cervicitis, Reiter’s syndrome, and
PID. It may be present asymptomatically.
• Gardnerella vaginalis produces a brown offensive discharge.
Cervical and endometrial carcinoma
Classically presenting with bleeding between periods, these may cause
discharge. Refer to a gynaecologist.
Fistulae
Colovaginal fi stulae may follow diverticulitis or locally invasive colorectal
carcinoma. Other fi stulae (including vesicovaginal and ureterovaginal) may
occur after pelvic surgery. Refer for admission and investigation.

567
VAGINAL DISCHARGE
Foreign bodies
Tampons, condoms, and various other items may be ‘lost’ or forgotten
about in the vagina. Removal with forceps under direct vision should cure
the offensive vaginal discharge. If a condom has been removed, ascertain
whether or not post-coital contraception is required ( b Contraceptive
problems, p.568). Consider hepatitis B/HIV prophylaxis and GU referral
for STD screen, depending upon the circumstances. Vaginal tampons
(particularly highly-absorbent ones which have been left in situ for many
hours) are associated with ‘toxic shock syndrome’.
Toxic shock syndrome
Tampons used during menstruation have been implicated in many cases
of the ‘toxic shock syndrome’. First described in 1978, it is caused by exo-
toxin produced by Staph. aureus (usually TSS toxin 1), or occasionally,
Strep . Multi-organ failure may follow.
Features High fever, headache, vomiting, diarrhoea, myalgia, altered
conscious level, hypotension, and a widespread erythematous macular
rash (with subsequent desquamation one week later, especially of palms
and soles).
Diagnosis Based upon clinical fi ndings. Recent menstruation and the above
features should prompt suspicion.
Investigation Includes vaginal examination. U&E, LFTs, clotting screen, FBC,
blood lactate, blood and vaginal cultures, ECG, CXR.
Treatment Manage the patient in the resuscitation room. If due to a tampon:
remove it. Follow guidelines for severe sepsis ( b p.59). Obtain venous
access, give intravenous antibiotics and start crystalloid. If hypotension is
refractory, consider measuring central venous pressure, placing an arterial
line, and starting inotropic support. The patient may require intensive care
treatment.

568 CHAPTER 13 Obstetrics and gynaecology
Contraceptive problems
Missed pill
Advice will depend on the type of OCP the patient takes (combined, com-
bined low dose oestrogen, or progesterone only). However, as a general
rule, if the combined pill is delayed for more than 12hr, the patient should
be advised to take the forgotten pill and use barrier contraception for
7 days. If there are less than 7 days of pills left in the pack, she should run
two packs together. The same applies if they have diarrhoea. If the patient
has had unprotected sexual intercourse and may require emergency con-
traception, it is worth referring to the NHS website ( http://www.nhs.uk ),
which gives specifi c advice for each type of pill. This provides comprehensive
patient advice that could also be printed and given to the patient.
Post-coital contraception
Women may attend the ED requesting post-coital contraception after:
• Isolated unprotected sexual intercourse.
• Burst or lost condom.
• Missed OCP.
• Complete or partial expulsion of intrauterine contraceptive device
(IUCD).
• Rape.
The risk of pregnancy following unprotected intercourse is greatest during
5 days around ovulation, but exists at other times also. Patients given
post-coital contraception require assessment and treatment including
counselling and follow-up: usually this will be with the GP and/or family
planning clinic. Options include levonorgestrel and insertion of IUCD.
Levonorgestrel must be given within 72hr of intercourse (95 % effective
if taken <24hr, 58 % effective at 72hr). An IUCD must be inserted within
5 days of intercourse. Both levonorgestrel and IUCD act principally to
render the endometrium hostile to implantation.
Levonorgestrel (previously called ‘the morning after pill’)
In the UK, pharmacists can sell this without prescription to women
aged over 16 years. It is usually the preferred option if patient presents
within 72hr of unprotected intercourse. Exclude contraindications (acute
porphyria, pregnancy, focal migraine), then give levonorgestrel 1.5mg
(Levonelle
®
1500) as soon as possible. Advise the patient to return if
she vomits shortly after taking the medication: give a replacement dose if
vomiting occurs within 3hr of taking it. Explain that there is a chance of
failure. Arrange follow-up (usually with the GP) in 3 weeks to confi rm
that menstruation has occurred. Advise alternative contraception (eg
condoms) meantime and discuss future contraception plans. Advise also
about the theoretical risk of ectopic pregnancy: instruct her to return if
she develops abdominal pain. Document that this advice has been given.
Note: hormonal emergency contraception is less effective if the patient
is already taking enzyme-inducing drugs: take specialist advice. Options
include an IUCD or i dose of levonorgestrel to 3mg (see BNF) .

569
CONTRACEPTIVE PROBLEMS
IUCD
This may be useful for patients unable to take the OCP (eg previous pul-
monary embolus), patients who wish to use IUCD long-term and for those
presenting between 3 and 5 days after unprotected intercourse. Failure is
very rare. Insertion is uncomfortable and requires appropriate training:
refer to the gynaecology team. Note that IUCD should not be used with
a history of recent PID.
Prescribing to patients on OCP
Both progestogen-only oral contraceptives and (combined) OCP may fail
if enzyme inducing drugs are prescribed. These include: rifampicin, rifab-
utin, carbamazepine, phenytoin, topiramate, griseofulvin, phenobarbital,
and primidone. Patients need alternative or additional contraception if
these drugs are started. Rifampicin and rifabutin are such potent enzyme-
inducing drugs that contraceptive precautions should continue for at least
4 weeks, even after a short course of rifabutin or rifampicin (as used for
prophylaxis of meningococcal infection).
Antibiotics and the OCP (refer to BNF)
Broad spectrum antibiotics commonly prescribed in the ED may inter-
fere with oestrogen absorption and cause contraceptive failure. Before
prescribing antibiotics to a female of childbearing age, ask whether she
is taking the OCP. Advise additional contraceptive precautions (eg
condoms), whilst taking the antibiotics and for 7 days after. If these 7 days
run beyond the end of a packet, start the next packet immediately without
a break. Document in the notes that this advice has been given.

570 CHAPTER 13 Obstetrics and gynaecology
Genital injury and assault
The history may be misleading. Combine a high index of suspicion with a
full examination to exclude signifi cant injury.
Blunt genital injury may result from falls astride. Most resultant vulval
haematomas settle with rest and ice packs. Refer very large haematomas
for evacuation in theatre.
Penetrating injury may follow assault, FB insertion, or migration/
perforation of an IUCD (particularly during insertion). Abdominal pain
associated with a vaginal wound may be due to peritonitis. Obtain venous
access, erect chest X-ray (for free gas), abdominal X-ray (for FB), group
and save, give antibiotics, and refer. Refer other vaginal tears without
peritonitis for exploration and repair.
Rape and sexual assault
Rape is defi ned in the UK as vulval penetration by the penis without
consent. Rape and other forms of sexual assault are believed to be grossly
under-reported. Those who do report it have special requirements. Privacy
is essential: ideally, a specially equipped room will be devoted to assess-
ment of women who have been sexually assaulted. Ensure that a female
member of staff is present throughout. Documentation must be legible
and meticulous. An established protocol will allow prompt and thorough
investigation and treatment. Usually, ED staff provide emergency treat-
ment and resuscitation, but most of the other aspects, including collection
of forensic evidence are dealt with by a forensic physician (police surgeon),
ideally in a specialized Sexual Assault Referral Centre. Sometimes, women
initially decline police involvement: full assessment and documentation
may prove useful if there is a change of mind.
First exclude life-threatening or serious injuries.
History
Establish the type, date, time, and place of the assault. Ask what occurred
(vaginal/anal penetration, oral sexual activity, other injuries). Ask about
contraception use and enquire about LMP. Find out what is known about
the assailant(s), and their risk of HIV and hepatitis B. In particular are they
injecting drug users, do they originate from sub-Saharan Africa, are they
homosexual?
Examination
Look for evidence of vaginal, oral or anal injury (the forensic physician
will take swabs). Record any other injuries, such as bites, bruising, or skin
wounds (photographs of non-genital injuries may be useful — taken by the
police with the patient’s consent).
Investigation
Obtain written informed consent. The police will be keen to retain
clothing, loose hairs, fi ngernail clippings, and tampons for evidence.
Similarly, the forensic physician will take appropriate swabs (vaginal, oral,
anal). Perform a pregnancy test. Take and store blood for future DNA and
viral testing.

571
GENITAL INJURY AND ASSAULT
Treatment
• Resuscitate as necessary. Refer urgently the 1 % of patients who have
sig nifi cant genital injuries (eg vaginal tears) requiring surgical intervention.
• Consider the need for post-coital contraception (see b p.568).
• If the patient is not immunized, give hepatitis B immunoglobulin and
start an active immunization course.
• Assess the risk of HIV. If the assailant is known to have HIV or is from
an at risk group, discuss the risk of disease transmission with the patient.
Involve a local expert such as a virologist or infectious disease specialist
prior to offering HIV prophylaxis ( b Needlestick injury, p.418).
• Assess tetanus vaccine requirements.
• Arrange follow-up to exclude STD. Consider antibiotic prophylaxis
against STD if the patient is unlikely to attend follow-up: liaise with the
GU team.
• Provide initial counselling and ensure a safe place to stay (a social
worker may arrange this).
• Arrange future counselling. Inform the patient about independent local
advice available (eg Rape Crisis Centre).
• Ascertain from the patient if she wishes her GP to be informed.
Telephone advice
Women may telephone the ED for advice after being raped. Advise them
to inform the police immediately, and then attend the police station or
the ED. Discourage them from washing, changing clothes, using a toilet or
brushing teeth before being examined.

572 CHAPTER 13 Obstetrics and gynaecology
Gynaecological pain
Gynaecological disorders presenting to the ED with abdominal pain may
be diffi cult to distinguish from other disorders. Obtain a full history of
the pain: sudden onset of severe colicky pain follows ovarian torsion and
acute vascular events; more insidious onset and continuous pain occur in
infection and infl ammation. Radiation of the pain into the back or legs sug-
gests gynaecological origin. Other clues in the history include co-existing
symptoms of vaginal discharge, vaginal bleeding, or missed last menstrual
period (LMP).
Abdominal and pelvic pain in early pregnancy may be due to ectopic
pregnancy or threatened abortion ( b p.584): both occur in patients
who do not realize that they are pregnant or who deny the possibility of
pregnancy due to embarrassment.
Pain related to the menstrual cycle
Consider fi rst: could any associated vaginal bleeding be from ectopic
pregnancy or threatened abortion?
Physiological dysmenorrhoea Pain regularly preceding menstruation and
peaking on the fi rst day of a period may be physiological. Suggest NSAID
and refer to the GP.
Endometriosis Growth of functional endometrial tissue in the pelvis
outside the uterus may produce cysts and adhesions. Patients often
present age 8 30 years with dysmenorrhoea and menstrual problems,
infertility and dyspareunia. Symptoms are usually chronic and recurrent
in a cyclical fashion, and are appropriately followed up by the GP.
Occasionally, an endometrial cyst may rupture and bleed severely into
the pelvis, presenting in similar fashion to ruptured ectopic pregnancy.
Resuscitate for hypovolaemia and refer urgently.
Rupture of a corpus luteum cyst Occurs premenstrually, but may also
cause signifi cant haemorrhage, requiring resuscitation.
Mittelschmerz Mid-cycle extrusion of an ovum from a follicular cyst can
cause abdominal pain, which seldom requires admission or investigation.
Uterine problems
Perforation is seen especially in the presence of IUCD.
Leiomyomas (‘fi broids’) may undergo torsion (sudden severe colicky pain
with tender uterus), or may infarct (‘red degeneration’) particularly during
pregnancy. Refer such suspected problems for specialist investigation.
Ovarian problems
Torsion causes sudden onset sharp unilateral pain and usually involves an
already enlarged ovary (cyst, neoplasm). Abdominal and per vagina (PV)
tenderness may be present. Clinical diagnosis is diffi cult: if suspected,
refer for USS and/or laparoscopy.
Bleeding into an ovarian cyst may present similarly and require investigation.

573
GYNAECOLOGICAL PAIN
Pelvic infl ammatory disease
This term includes infection which has spread from the cervix to the
uterus (endometritis), Fallopian tubes (salpingitis), ovaries (oophoritis), or
adjacent peritoneum (peritonitis). Severity ranges from chronic low grade
infection (with relatively mild symptoms) to acute infection (with severe
symptoms) which may result in abscess formation.
Causes 90 % are sexually transmitted: sexually active women aged
15–20 years are at particular risk. Most of the remaining 10 % follow
pregnancy terminations or dilatation and curettage.
Organisms Chlamydia trachomatis commonest. Also: Neisseria gonorrhoea,
Mycoplasma hominis, Ureaplasma urealyticum .
Features Bilateral lower abdominal tenderness, vaginal discharge, fever
> 38
o
C, abnormal vaginal bleeding, deep dyspareunia, cervical motion
tenderness, and adnexal tenderness all point to PID.
Management Resuscitate with IV fl uids if shocked. Check urinalysis and
send high vaginal swab and cervical swab, FBC, ESR. Refer all suspected
cases to the gynaecologist: even though not all will require admission,
they will require antibiotics (eg oral ofl oxacin 400 mg twice daily plus oral
metronidazole 400mg twice daily for 14 days) and follow-up.
Sequelae Ectopic pregnancy (5 × i risk) or infertility, therefore have a low
threshold for empirical treatment. (See http://www.rcog.org.uk ).
574 CHAPTER 13 Obstetrics and gynaecology
Vaginal bleeding
See b Vaginal bleeding in pregnancy, p.582.
Triage ahead patients with severe bleeding or evidence of hypovolaemic
shock. Resuscitate fi rst (O
2
, cross-match and obtain Rhesus status, start
IV fl uids) and ask questions later. Most patients with vaginal bleeding,
however, do not require resuscitation. Take a careful menstrual history and
ask about associated symptoms. Attempt to assess the amount of bleeding.
Interpretation of a patient’s description is notoriously diffi cult, but useful
pointers are the presence of clots and the rate of tampon use. Always
consider the possibility of pregnancy: remember that ruptured ectopic
pregnancy can present before a period is missed ( b p.586). Examine for
evidence of hypovolaemia and abdominal masses/tenderness. Depending
upon the circumstances, speculum and bimanual vaginal examinations may
be required: local policy will determine who should perform this.
Menorrhagia
Dysfunctional uterine bleeding Heavy and/or irregular periods without
obvious pelvic pathology may result from hormonal imbalance. It is
particularly common at menarche. Most settle without treatment or with
simple measures (eg mefenamic acid 500mg PO tds after food). Refer to
the GP, unless the bleeding is very heavy.
Uterine leiomyomas (fi broids) Often cause menorrhagia. May present
with a painful complication, such as torsion or infarction.
Other causes Endometriosis, PID, IUCD, polyps, vaginal carcinoma,
hypothyroidism.
Bleeding unrelated to pregnancy or periods
Trauma The history may be elusive.
Post-operative Signifi cant bleeding is a risk of any gynaecological operation.
Resuscitate and refer.
OCP problems Breakthrough bleeding on the OCP may be due to
endometrial hyperplasia. Exclude treatable vaginal/cervical lesions, arrange
a cervical smear and refer to GP.
Cervical erosion Replacement of stratifi ed squamous epithelium by
columnar epithelium may produce a mucoid discharge with a small
amount of post-coital or intermenstrual bleeding. The cervix appears red.
Obtain a cervical smear and arrange follow-up.
Cervical polyp Causes post-coital bleeding. Refer to the gynaecologist.
Cervical cancer 90 % are squamous carcinoma. Strongly associated with
human papilloma virus, some consider it an STD. Suspect in anyone
presenting with post-coital or intermenstrual bleeding. Speculum
examination reveals nodules, ulcers, or erosions, which may bleed to
touch. Advanced disease may present with pyometra, ureteric obstruction,
rectovaginal fi stula. Arrange urgent gynaecology follow-up for any patient
with an abnormal looking cervix.

575
VAGINAL BLEEDING
Uterine carcinoma Mostly adenocarcinoma. Classically presents with
heavy and frequent post-menopausal bleeding, but normal examination.
Arrange assessment and diagnostic curettage with the gynaecologist.
Other causes Thrombocytopenia, other coagulation disorders and anti-
coagulant drugs.

576 CHAPTER 13 Obstetrics and gynaecology
The pregnant patient
Pregnant patients presenting with emergency problems create under-
standable anxiety. There are two patients: one may be suffering unseen.
Maintaining foetal oxygenation is crucial: call the obstetrician early.
Terminology
The 40 weeks of pregnancy are divided into 3 trimesters. Traditionally, prob-
lems in the fi rst trimester are considered ‘gynaecological’.
• Gravidity = total number of pregnancies (eg a woman in fi rst pregnancy is
a ‘primigravida’).
• Parity = number of pregnancies after 24 weeks + number before (eg a
woman who has had 1 child and 2 spontaneous abortions is described as 1
+ 2; gravidity = 3).
• Abortion is foetal death before 24 wks; stillbirth is foetal death after 24 wks.
Progression of pregnancy (see also Fig. 13.1 )
Peristalsis and ciliary action carries the fertilized ovum to the uterus,
which it reaches as a blastocyst 8 5 days after ovulation. The blastocyst
implants in the endometrium: the inner part forms the embryo, the outer
part membranes and placenta. Trophoblastic tissue produces human cho-
rionic gonadotrophin (HCG), (peaks in fi rst trimester) acting on the
corpus luteum, (essential until the placenta produces oestrogen and
progesterone). HCG then d , whereas oestrogen and progesterone i .
Symptoms of pregnancy Amenorrhoea, breast tenderness and fullness,
polyuria, tiredness, nausea (appear by 8 6 weeks). Vomiting is common,
occasionally severe enough to cause dehydration and weight loss
(‘hyperemesis gravidarum’). Refer for admission and rehydration.
Signs of pregnancy Not obvious in early pregnancy: uterine enlargement (see
opposite), breast changes.
Pregnancy testing see b p.582.
Maternal physiological changes
Cardiac output i by 30 % , peripheral vascular resistance d : BP (especially
diastolic) d slightly. Blood vol i by 30 % , plasma vol i by 45 % , Hb d slightly.
Systolic fl ow murmurs are common. Water retention occurs, causing
ankle oedema and carpal tunnel syndrome. Ventilation i : the patient may feel
dyspnoeic. Backache is common.
d Lower oesophageal pressure causes heartburn; d gut motility causes
constipation; i venous pressure in pelvis may cause varicose veins and
haemorrhoids. Platelets, ESR, cholesterol, fi brinogen i ; albumin d .
See Table 13.1 for normal values in pregnant and non-pregnant women.
Diagnostic imaging in pregnancy
Try to avoid X-rays and CT scans. Excessive radiation exposure risks con-
genital malformation, growth retardation, and neoplasia. However, do not
withhold necessary X-rays in life-threatening illness. Most head, neck, and
extremity X-rays can be obtained without foetal risk by appropriate lead
screening. When requesting X-rays, ensure the radiographer is aware the
patient is pregnant. USS has not been shown to have adverse effects. If in
doubt, discuss imaging requests with a radiologist.
Prescribing in pregnancy and during breast-feeding
Consult the BNF before prescribing drugs in pregnancy or during breast
feeding. The following are generally considered safe in pregnancy: penicillin,
cephalosporins, nystatin, paracetamol, chlorphenamine, cimetidine.
Avoid the following: trimethoprim, tetracyclines, streptomycin, warfarin,
thiazides.
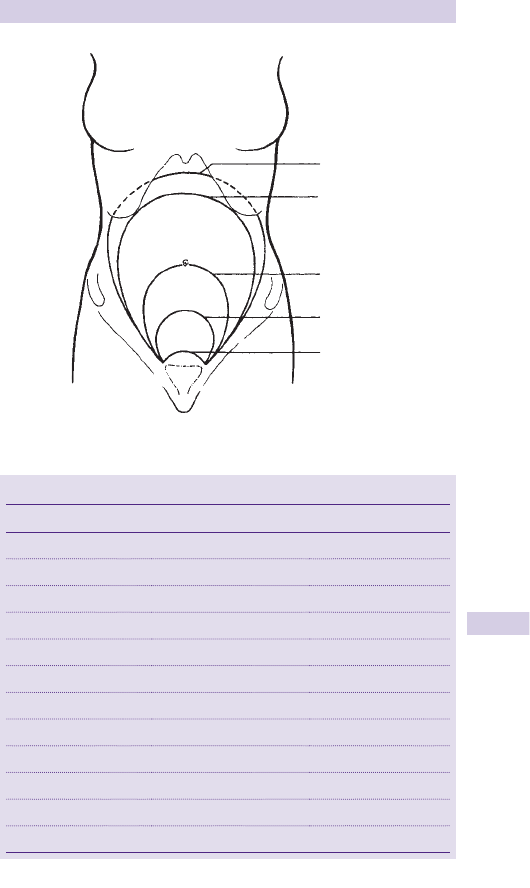
577
THE PREGNANT PATIENT
36 weeks
40 weeks
22 weeks
16 weeks
12 week
Fig. 13.1 Uterine size in pregnancy.
Table 13.1 Normal values in pregnant and non-pregnant women
Value Non-pregnant Pregnant
Haematocrit 0.37–0.47 0.32–0.41
Haemoglobin (g/dL) 11.5–16.0 11.0–15.0
White cell count (/L) 4.0–11.0 × 10
9
5.0–16.0 × 10
9
Platelets (/L) 150–400 × 10
9
134–400 × 10
9
ESR (mm/hr) (age in years + 10)/2 44–114
Fibrinogen (g/L) 2–4 4–6
Albumin (g/L) 35–50 28–40
Urea (mmol/L) 2.5–6.7 1.6–6.0
Creatinine (mmol/L) <110 38–90
p CO
2
(kPa) 4.5–6.0 (34–46mmHg) 3.6–4.2 (27–32mmHg)
p O
2
(kPa) > 10.6 ( > 80.6mmHg) > 10.6 ( > 80.6mmHg)
HCO
3
–
(mmol/L) 24–28 18–23
‘All pregnant women attending (accident and) emergency departments with
anything other than minor complaints should be seen quickly and in conjunction with
an obstetrician or senior midwife.’ (See http://www.cmace.org.uk/ ).

578 CHAPTER 13 Obstetrics and gynaecology
Emergency normal delivery
Sometimes even the best laid plans for controlled delivery in the labour
ward go awry and patients present in an advanced stage of labour and
deliver in the ED. This is particularly likely in a very rapid (‘precipitate’)
labour. ED staff therefore need to know about normal delivery.
Labour
At onset of labour, painless and irregular (Braxton Hicks) contractions are
replaced by painful uterine contractions with cervical dilatation ( > 3cm) ±
‘show’ (mucus/blood discharge). There may be rupture of membranes.
Presentation
In the ED only ‘OA’ (occiput anterior) vertex presentations are likely to
proceed so fast that delivery occurs before specialist help arrives.
Stages of labour
First Onset of labour until cervix is fully dilated (10cm). Usually lasts > 6hr.
The upper part or ‘segment’ of the uterus contracts, the lower segment
(including the cervix) dilates. Contractions i in frequency (every 2min)
and duration (last 1min). The head starts to descend.
Second Full dilatation until baby is born. Lasts 8 40min in primigravida,
8 20min in multigravida. Contraction of upper segment, abdominal muscles
and diaphragm cause head to descend then rotate (usually to lie occiput
anterior). An overwhelming desire to push helps expel the baby.
Third Placenta and membranes deliver and uterus retracts ( 8 15min).
Assessment of a patient in labour
Check pulse, BP, and palpate the abdomen. Listen for foetal heart sounds
with fetal stethoscope or Doppler probe (rate should be 120–160/min).
Gently examine the perineum. Do not fully examine the vagina unless the
head is crowning and birth is imminent. Instead, transfer to labour ward.
Management of delivery (see Fig. 13.2)
• Call obstetric/paediatric/anaesthetic help and encourage partner to stay.
• Offer Entonox
®
(50:50 mixture of nitrous oxide and O
2
).
• Don sterile gloves and stand on the patient’s right.
• As head crowns discourage bearing down: advise rapid shallow breaths.
• Use left hand to control escape of head (to prevent perineal tearing).
• Press gently forwards with right thumb and fi ngers either side of anus.
• Once head is delivered, allow it to extend.
• Feel for cord around neck: slip it over head, or if impossible, clamp, and
divide.
• Allow anterior shoulder to deliver fi rst (mother pushing if necessary).
• Give 5U oxytocin and 500mcg ergometrine IM (Syntometrine
®
).
• Deliver the baby, wrap him/her up and resuscitate as necessary
( b p.642).
Management of the cord
Once baby cries and cord pulsation ceases, hold baby level with mother
and clamp the cord twice (15cm from umbilicus). Divide between clamps.
Place a plastic Hollister crushing clamp 1–2cm from umbilicus and cut 1cm
distally. Check that 2 normal arteries are present in the cord.
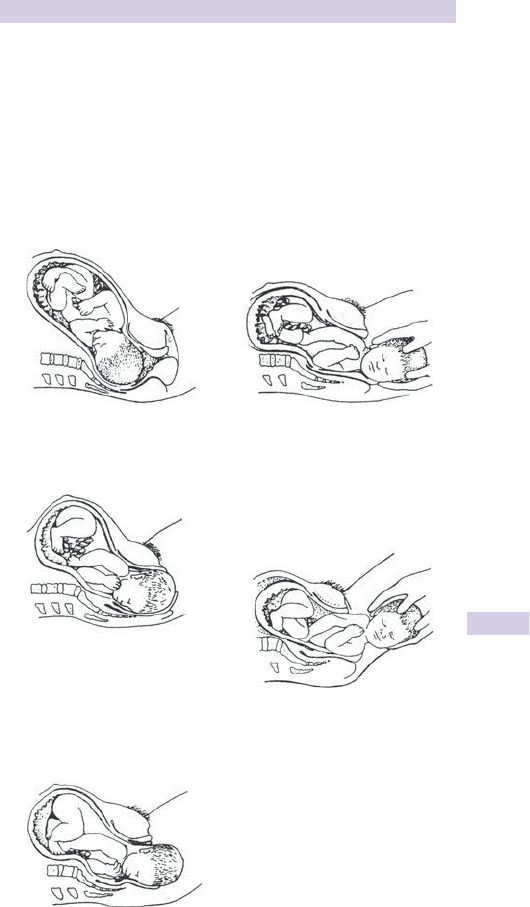
579
EMERGENCY NORMAL DELIVERY
Management of the third stage
A few minutes after delivery, regular contractions begin again, causing the
placenta to detach. The cord may be seen to move down accompanied by
a small gush of blood. The placenta may be felt in the vagina. The Brandt–
Andrews technique helps removal: apply gentle downwards traction on
the cord whilst exerting upward pressure on uterus (preventing inversion).
Examine placenta carefully. Give Rhesus anti-D immunoglobulin if Rh –ve
( b p.582). Immediate post-partum problems are the domain of the
specialist and include: post-partum haemorrhage, amniotic fl uid embolism,
uterine rupture, or inversion.
(1)
1st stage of labour. The cervix
dilates. After full dilatation
the head flexes further and
descends further into the pelvis.
(2)
During the early second
stage the head rotates at
t
he level of the ischial spine
so the occiput lies in the
anterior part of pelvis.
In late second stage the
head broaches the vulval ring
(crowning) and the perineum
stretches over the head.
(5)
Birth of the posterior
shoulder is aided by lifting
the head upwards whilst
maintaining traction.
(3)
The head is born. The shoulders still lie
transversely in the midpelvis.
(4)
Birth of the anterior shoulder.
The shoulders rotate to lie in the
anteroposterior diameter of the
pelvic outlet. The head rotates
externally. Downward and
backward traction of the head by
the birth attendant aids delivery
of the anterior shoulder.
Fig. 13.2 Management of pregnancy.
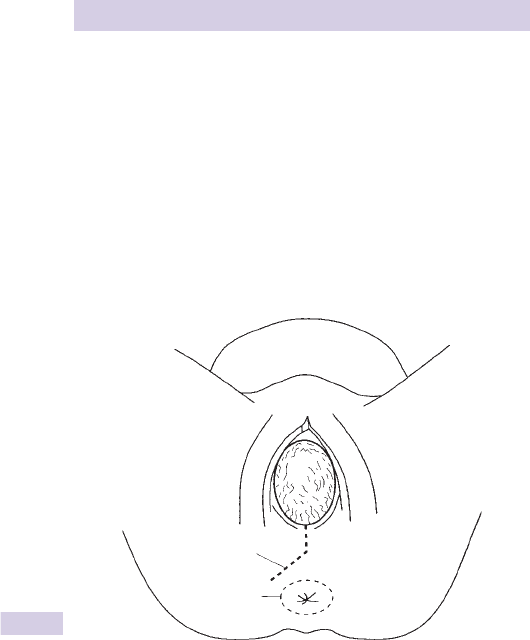
580 CHAPTER 13 Obstetrics and gynaecology
Diffi culties in normal delivery
Meconium-stained liquor
See b Cardiopulmonary resuscitation of the newborn, p.644.
Imminent perineal tear
The risk of perineal tearing may be minimized by controlled delivery. An
extensive tear risks the integrity of the external anal sphincter. If a tear
is imminent, perform an episiotomy (Fig. 13.3 ). Infi ltrate 5–10mL of 1 %
lidocaine postero-laterally from the posterior fourchette. Cut the perineal
tissues postero-laterally using straight scissors with blunt points (see
diagram below), avoiding large veins. After delivery, carefully examine the
episiotomy wound which needs to be closed in layers using absorbable
sutures.
Diffi culty in delivering the shoulders (shoulder dystocia)
After delivery of the head, the shoulders usually rotate to lie in an antero-
posterior (AP) direction, so the fi rst one can be delivered anteriorly. If
this does not occur, apply gentle digital pressure to obtain rotation. Try
to help delivery of the anterior shoulder by gently bending the baby’s
neck towards the mother’s anus. The reverse action may then deliver the
posterior shoulder. If these manoeuvres are unsuccessful, hook a fi nger
into the axilla of the anterior shoulder to bring it down.
Line of incision
Anal sphincter
Fig. 13.3 Performing an episiotomy.
This page intentionally left blank

582 CHAPTER 13 Obstetrics and gynaecology
Vaginal bleeding in pregnancy
Vaginal bleeding in pregnancy produces understandable maternal distress.
It may indicate serious illness that is a threat to the life of both the foetus
and mother.
Causes
An indication of possible causes of vaginal bleeding related to pregnancy
is apparent from gestation (see opposite). Bleeding may, of course, be
unrelated to pregnancy.
Pregnancy testing
Even if the patient denies pregnancy and there is no history of
amenorrhoea, consider pregnancy. Most pregnancy tests look for B -HCG
produced by the developing trophoblast. Serum B -HCG levels rapidly
i so that pregnancy may be confi rmed by serum tests within days of
implantation and remain + ve until 20 weeks. Urine tests have improved
considerably in recent years, but do not rely upon them to defi nitely
exclude pregnancy.
USS easily demonstrates most pregnancies by 5 weeks after LMP.
Principles of treating blood loss in pregnancy
• Give O
2
.
• Obtain venous access with large bore cannulae and replace fl uids
aggressively.
• Consider coagulopathy: obtain FBC and clotting screen.
• Consider prophylaxis against Rhesus haemolytic disease of the
newborn.
Anti-D immunoglobulin
A Rhesus –ve mother exposed to Rh + ve foetal blood during pregnancy
may develop antibodies. These IgG antibodies may cross the placenta
during subsequent pregnancies and cause Rhesus haemolytic disease of
the (Rh + ve) newborn. The production of maternal antibodies may be
prevented by appropriate use of anti-D Ig. Consider this every time that
there is possible foeto-maternal bleeding (ruptured ectopic pregnancy,
spontaneous abortion, trauma, antepartum haemorrhage, labour, and
delivery). Guidelines have been produced for the use of anti-D Ig (see
www.rcog.org.uk ). Check the Rhesus and antibody status of all women
with bleeding in early pregnancy and give 250U anti-D Ig IM to those that
are Rh –ve and non-immune. After delivery or bleeding occurring in later
pregnancy, Rh –ve mothers are likely to require larger doses of anti-D
Ig (see BNF ). Therefore, check the Rhesus and antibody status and also
perform a Kleihauer test. This will give an indication of the extent of any
foeto-maternal haemorrhage: Blood Transfusion Service will advise.
583
VAGINAL BLEEDING IN PREGNANCY
Causes of vaginal bleeding in pregnancy
Table 13.2 Causes of vaginal bleeding in pregnancy
Pregnancy related Non-pregnancy related
1st trimester Spontaneous abortion At any stage Infection
Ectopic pregnancy Vaginal ulcers
Trophoblastic disease Vaginal infl ammation
Cervical erosions
Cervical polyps
Coagulation disorders
Trauma
2nd trimester Spontaneous abortion
Trophoblastic disease
Abruptio placentae
Placenta praevia
3rd trimester Abruptio placentae
Placenta praevia
‘Show’ of pregnancy
Vasa praevia

584 CHAPTER 13 Obstetrics and gynaecology
Spontaneous abortion
Terminology
Use the term ‘miscarriage’ (not ‘abortion’) with patients. Both refer to foetal
loss before 24 weeks. Spontaneous abortion affects > 20 % pregnancies.
Threatened abortion refers to vaginal bleeding through a closed cervical
os. 50 % proceed to miscarry. If the cervix dilates or products of conception
are passed, abortion is inevitable. Inevitable abortion becomes complete
abortion if all products are passed. Retained products of conception
in an incomplete abortion may become infected, causing a septic abortion .
Alternatively, products may be retained as a missed abortion , which carries
a risk of disseminated intravascular coagulation (DIC).
Aetiology
Mothers may feel guilty, but the causes are largely beyond their control.
Risk factors include:
• Chromosomal anomalies ( > 50 % ).
• First pregnancy, maternal disease, and age > 30 years.
• Uterine abnormalities.
• Drugs (especially isotretinoin).
• Cervical incompetence, immunological factors, and trauma.
Approach
Establish the gestation. Think: is this a ruptured ectopic pregnancy? Vaginal
bleeding in spontaneous abortion ranges from light to severe. Severe
bleeding with hypovolaemia may occur in inevitable abortion. Abdominal
pain is associated with a lower chance of fetal survival. Any pain with
threatened abortion tends to be light and crampy. Severe pain and
bleeding with hypotension and bradycardia implies ‘cervical shock’, where
products of conception are stuck in the cervical os. Abdominal or cervical
tenderness suggests an alternative diagnosis (ectopic pregnancy or septic
abortion). Vaginal examination provides other important clues: look for
cervical dilatation (remember that the external os of a multigravida usually
accepts a fi ngertip) and products in the os.
Investigation
USS may exclude ectopic pregnancy and indicate foetal viability: local
policy will determine who performs this. Urine pregnancy tests remain
+ ve for several days after foetal death. Check Rhesus status and baseline
serum B-HCG. Cross-match and obtain FBC if shocked.
Treatment
Resuscitate if signifi cant pain or haemorrhage and refer urgently. If cervical
shock is present, remove products of conception from the cervical os using
sponge forceps. If severe bleeding continues, give 500mcg ergometrine IM.
Unfortunately, no intervention appears to alter foetal survival in threatened
abortion. Patients with light bleeding, no abdominal pain, and a closed os
(threatened abortion) may be allowed home after USS and gynaecology
review. Reassure, emphasize that it is not her fault, advise bed rest and
abstinence from sexual intercourse until gynaecology follow-up in 2 days.
Provide Rhesus anti-D Ig 250u IM if Rh –ve and non-immune.

585
SPONTANEOUS ABORTION
Septic abortion
Sepsis may follow spontaneous, surgically induced or ‘backstreet’ abortion.
Organisms S. aureus, C. welchii, Bacteroides, E. coli, streptococci, Clostridium
sordelli .
Features vaginal bleeding, offensive discharge, i T ° , d BP, uterine
tenderness, peritonitis. Note that pyrexia is not invariable — particularly
with Clostridium sordelli which can result in a severe infection with high
mortality.
Obtain FBC, clotting screen, blood cultures, blood lactate, vaginal swabs,
X-match, Rhesus status, erect CXR (to look for free gas).
Resuscitate with IV fl uids, give co-amoxiclav 1.2g IV, follow the severe
sepsis guidelines ( b p.59) and refer urgently. Monitor urine output and
consider central and arterial lines.
Missed abortion
Very occasionally presents several weeks or months after foetal death
with no expected features of pregnancy, a –ve pregnancy test and DIC.
Resuscitate, and involve senior obstetrician and haematologist.

586 CHAPTER 13 Obstetrics and gynaecology
Ectopic pregnancy
Gestational sac implantation outside the uterus has i and now occurs in
8 1 in 100 pregnancies in the UK. 96 % implant in the Fallopian tube, 2 %
in the interstitial part of uterus, 1.5 % intra-abdominally. The risk of
heterotopic pregnancy (combined intrauterine and ectopic pregnancy) is
8 1 in 4000.
Importance
Ectopic pregnancy is the commonest cause of maternal mortality in the
fi rst trimester. The diagnosis is frequently missed. Consider it in any young
woman presenting with abdominal pain or vaginal bleeding, especially
when combined with an episode of syncope.
Risk factors
These include anything which delays or limits normal transit of the ferti-
lized ovum to the uterus: PID, pelvic surgery/adhesions, previous ectopic,
endometriosis, assisted fertilization, IUCD, progesterone only pill, con-
genital anatomical variants, ovarian and uterine cysts/tumours. Note that
although pregnancy is unusual after tubal ligation, when it does occur
there is a relatively high chance ( 8 1 in 6) of it being an ectopic pregnancy.
Pathology
Implantation of the gestational sac in the Fallopian tube may have three
results:
• Extrusion (tubal abortion) into the peritoneal cavity.
• Spontaneous involution of pregnancy.
• Rupture through the tube causing pain and bleeding.
Implantation in a uterine horn is particularly dangerous: pregnancy
may reach 10–14 weeks before rupture. Exceptionally, intraperitoneal
pregnancies may proceed almost to term.
Symptoms
Ectopic pregnancy may present with sudden severe lower abdominal pain
with collapse or fainting, and vaginal bleeding. There is usually (but not
always) a history of amenorrhoea (often 8 weeks). Haemorrhage may
cause shoulder tip pain (from blood irritating the diaphragm) and features
of hypovolaemia. Nausea and vomiting are common.
Many patients have more chronic symptoms, with recurrent abdominal
pain and slight irregular vaginal bleeding, which may be fresh or dark (like
‘prune juice’). Pain may have continued for > 1week before presentation,
occasionally as long as 4 weeks. The pain may be worse on defecation.
Some patients have no vaginal bleeding.
Enquire about symptoms of pregnancy (eg breast tenderness) and possible
risk factors for ectopic pregnancy.

587
ECTOPIC PREGNANCY
Signs
Look for hypovolaemic shock. If present, volume replacement must
accompany full assessment. Abdominal tenderness is variable, ranging
from mild to severe with peritonism. Cullen’s sign (discolouration around
the umbilicus) is of historical interest only. Bimanual vaginal examination
reveals tender adnexa and sometimes a mass, but may be better deferred
to a specialist (risk of i bleeding). Speculum inspection usually shows
vaginal blood.
Investigation
Must not delay resuscitation and referral.
Pregnancy test is almost always + ve, but serum B-HCG levels are lower
than expected for normal pregnancy.
Transabdominal USS is useful if it demonstrates an intrauterine pregnancy,
free fl uid in the pouch of Douglas and/or an adnexal mass. Frequently it is
inconclusive. Transvaginal USS may be better.
Differential diagnosis
• Threatened abortion : bleeding is usually more severe ( b p.584).
• Ruptured corpus luteum cyst : the corpus luteum supports pregnancy for
the fi rst 6–8 weeks. Rupture causes sudden peritoneal irritation, but
rarely bleeds signifi cantly.
• PID ( b p.573): Note that ectopic pregnancy can cause mild pyrexia
and a raised WCC, which may easily be misinterpreted as evidence of
pelvic infection.
• Trophoblastic disease ( b Vaginal bleeding in later pregnancy, p.588).
Treatment
Give O
2
, insert two large (12 or 14G) cannulae, cross-match 6U of blood,
request Rhesus status. Resuscitate initially with crystalloid IV fl uids as
necessary. If suspected, refer urgently to the gynaecology team since
sudden deterioration may occur. Signifi cant haemorrhage requires urgent
surgery. Alert the anaesthetist and theatre team early. Check Rhesus and
antibody status: anti-D immunoglobulin may be needed ( b p.582).

588 CHAPTER 13 Obstetrics and gynaecology
Vaginal bleeding in later pregnancy
Gestational trophoblastic disease
Occasionally, a fertilized ovum may form abnormal trophoblastic tissue,
but no fetus. The pathological spectrum ranges from benign hydatidiform
mole to invasive choriocarcinoma. Choriocarcinoma is relatively rare,
affecting 8 1 in 40,000 pregnancies.
Presentation Usually vaginal bleeding at 12–16 weeks, with passage of
tissue, which may resemble frogspawn. Often accompanying abdominal
pain and sometimes pre-eclampsia or eclampsia. The uterus may be much
larger than expected for dates. DIC may occur.
Investigations USS shows ‘snowstorm’ and no foetus. Serum HCG is
grossly i .
Management Obtain venous access, serum HCG, FBC, group and save, IV
fl uids/resuscitation, and refer.
Antepartum haemorrhage
Bleeding after 20 weeks occurs in 2.5 % of pregnancies. Abruptio placentae
and placenta praevia are most likely causes, although other cervical or
vaginal lesions may be responsible.
Abruptio placentae
Premature separation of the normally situated placenta affects 8 1 % of
pregnancies. It causes haemorrhage which may risk the foetus, depending
on the extent of placental involvement, and rapidity of separation.
Risk factors Pre-eclampsia, previous abruption, trauma ( b p.594), smoking,
i parity, cocaine.
Presentation There is usually some vaginal bleeding (‘revealed haemorrhage’),
but occasionally bleeding is limited to the confi nes of the uterus (‘concealed
haemorrhage’). In either case, there may be much more utero-placental
bleeding than is immediately apparent. There may be abdominal pain
and tenderness or back pain. Abruptio placentae may precipitate labour.
A large bleed can cause DIC or absent foetal heart sounds.
Placenta praevia
The placenta is situated wholly or partly over the lower uterine segment
and cervical os.
Risk factors Mother aged > 35 years, high parity, previous placenta praevia,
twins, uterine abnormalities (including previous Caesarian section).
Presentation Most present with bright red painless vaginal bleeding in the
third trimester. 15 % present in labour.
If placenta praevia is a possibility, do not perform digital or speculum
vaginal examination.
Vasa praevia
Rarely, an abnormal foetal blood vessel may be attached to the membranes
over the internal os. Haemorrhage may cause foetal exsanguination, usually
during labour.

589
VAGINAL BLEEDING IN LATER PREGNANCY
Management of antepartum haemorrhage
• Call an obstetrician immediately.
• Give O
2
.
• Obtain venous access (2 large bore cannulae) and resuscitate with IV
fl uids as necessary.
• Send U&E, FBC, blood glucose, cross-match, Rhesus and antibody
status, Kleihauer test, clotting screen.
• Monitor the foetus (cardiotocography).
• USS locates the placenta, demonstrates the foetus and may show
concealed haemorrhage.
• Give anti-D immunoglobulin as advised by Blood Transfusion Service if
Rh –ve ( b p.582).

590 CHAPTER 13 Obstetrics and gynaecology
Abdominal pain in pregnancy
Approach
Attempting to deduce the cause of abdominal pain can ordinarily be
quite diffi cult: in pregnancy it is even more so. Some possible underlying
diseases may be causing unseen foetal distress and can produce rapid
maternal deterioration. Therefore, triage ahead, contact the obstetrician,
and resuscitate vigorously. Initial investigations usually include BMG, uri-
nalysis, blood tests, and USS. Vaginal bleeding accompanying abdominal
pain implies a gynaecological or obstetric problem. Remember, however,
that the reverse is not necessarily true: ruptured ectopic pregnancy and
concealed haemorrhage in abruptio placentae may present without
vaginal bleeding. In later pregnancy, even if there is doubt as to whether
the principal problem is obstetric or not, involve the obstetrician at an
early stage.
Pregnancy related causes of abdominal pain
The following are considered elsewhere:
• Ectopic pregnancy ( b p.586).
• ‘Red degeneration’ of a fi broid ( b Uterine problems, p.572).
• Gestational trophoblastic disease ( b Vaginal bleeding in later preg-
nancy, p.588).
• Abruptio placentae ( b p.588).
• Onset of labour ( b Emergency normal delivery, p.578).
Torsion, rupture, or haemorrhage into an ovarian cyst
This may involve the corpus luteum of pregnancy. Sudden onset lower
abdominal pain results. USS may demonstrate the problem.
Acute polyhydramnios
Excessive amniotic fl uid may complicate pregnancy involving uni-ovular
twins. Pain and vomiting is accompanied by a large abdomen for gestation
and an unusually mobile foetus.
Pre-eclampsia
Abdominal pain (particularly right upper quadrant pain) in pregnancy may
refl ect pre-eclampsia (see b p.592). Check BP and urinalysis and refer
urgently.

591
ABDOMINAL PAIN IN PREGNANCY
Non-obstetric causes of abdominal pain
Urinary tract infection
UTI is relatively common in pregnancy due to urinary stasis. Women
are at particular risk if they have had previous UTI. Abdominal/loin pain
and pyrexia with rigors indicate acute pyelonephritis. Send MSU, FBC,
and blood cultures, and refer for IV antibiotics. Treat patients with
asymptomatic UTI or cystitis without evidence of pyelonephritis with oral
antibiotics (eg amoxicillin 250mg PO tds or a cephalosporin) and arrange
GP follow-up when the MSU result will be available. When prescribing
antibiotics in pregnancy, take care to avoid those drugs which are contra-
indicated (eg trimethoprim, tetracyclines — see BNF ).
Acute appendicitis
Presentation in early pregnancy may be as classically described, but can
be confused with ectopic pregnancy or rupture/torsion of an ovarian cyst.
In later pregnancy, the point of maximal tenderness in acute appendicitis
rises towards the right hypochondrium. Check BMG, serum amylase, and
urinalysis. Give analgesia and refer if suspected.
Gallstones
Pain from gallstones not infrequently presents for the fi rst time in preg-
nancy. The presentation of biliary colic and cholecystitis is similar to that
in the non-pregnant patient ( b Biliary tract problems, p.510). USS reveals
stones and associated pathology. Give analgesia and refer: if possible, the
patient will be treated conservatively.
Acute pancreatitis
This is usually related to gallstones. There is a signifi cant risk to mother
and fetus. Presentation and treatment are as described in b p.508.
Perforated peptic ulcer
If suspected, obtain erect CXR with lead shield for the fetus. Resuscitate
and refer ( b p.511).
Intestinal obstruction
Often follows adhesions from previous surgery. The diagnosis may not
be immediately obvious: pain, vomiting, and constipation may be initially
attributed to pregnancy. These symptoms, together with abdominal
tenderness and high pitched bowel sounds suggest the diagnosis. An erect
abdominal X-ray will confi rm it, but this should only be requested by a
specialist.

592 CHAPTER 13 Obstetrics and gynaecology
Medical complications of pregnancy
Pre-eclampsia and eclampsia
This poorly understood vasospastic uteroplacental disorder affects 7 % of
pregnancies. It results in widespread systemic disturbance involving the
liver, kidneys, coagulation, and cardiovascular systems. Placental infarcts
may occur and compromise the foetus.
Pre-eclampsia 2 or more of: hypertension ( > 140/90), proteinuria and
oedema. Variant presentation: haemolysis, elevated LFTs, low platelets
(HELLP syndrome) particularly affects multigravida.
Progression to eclampsia is heralded by: confusion, headache, tremor,
twitching, i refl exes. Visual disturbance and/or abdominal pain may occur.
Eclampsia The onset of fi ts after 20 weeks (or fi ts in association with
pre-eclampsia). Maternal mortality is 2 % , perinatal mortality 15 % .
Management
See www.rcog.org.uk
• Refer all patients with BP > 140/90, or proteinuria and oedema.
• Obtain FBC, uric acid, U&E, LFTs, clotting screen, ECG, foetal
monitoring.
• Restrict fl uids to a total of 80mL/hr or 1mL/kg/hr (because of the risk of
pulmonary oedema).
• If there is evidence of impending eclampsia or the patient starts to
fi t: call the obstetrician and anaesthetist, check BMG, control airway,
consider left lateral position, give O
2
and 4g magnesium sulphate slowly
IV over 10min, followed by a maintenance magnesium sulphate 1g/h
IVI. Treat recurrent fi ts with a further 2g magnesium sulphate IV over
10min.
• Follow local advice regarding control of hypertension (eg labetalol 10mg
slow IV bolus, followed by an IVI starting at 1–2mg/min, i as required).
• Urgent delivery is a priority in eclampsia, both for mother and foetus.
Disseminated intravascular coagulation
DIC may complicate a variety of obstetric problems: abruptio placentae,
intrauterine death, missed abortion, amniotic fl uid embolism, eclampsia,
sepsis, trophoblastic disease.
Clinical picture Widespread haemorrhage and microvascular occlusion.
Obtain FBC, cross-match, clotting screen, fi brin degradation products,
fi brinogen, U&E, and LFTs.
Treatment Resuscitate with O
2
, IV fl uids (according to CVP), blood
transfusion, and FFP. Refer urgently and consider urgent delivery and
treatment of underlying disease.

593
MEDICAL COMPLICATIONS OF PREGNANCY
Diabetes mellitus
Pregnancy encourages hyperglycaemia. IDDM in pregnancy may be more
diffi cult to control and is associated with an i insulin requirement. DKA
occurs relatively easily ( b Hyperglycaemic crises, p.152).
Thromboembolic disease
Pregnancy carries an i risk and is a signifi cant cause of maternal mortality.
The exact risk in each trimester is as yet unclear, as little research has
involved pregnant women. However, it would seem that the more gravid
the woman, the greater the risk of DVT and PE. Caesarian section, pre-
vious DVT/PE, a family history and bed rest all increase the risk.
Clinical probability scoring for DVT or PE is diffi cult as all derived scores
excluded pregnant women. Therefore, pregnant women should have
imaging, rather than D-dimer and clinical probability assessment.
USS is the safest initial investigation for DVT. Remember that to exclude
DVT with ultrasound requires either one normal complete scan (calf,
popliteal fossa and thigh) or two normal thigh and popliteal scans, one
week apart ( b p.118).
Pulmonary embolism presents with pain or dyspnoea ( b p.120).
Unfortunately, these are not infrequent symptoms during pregnancy. A
normal SpO
2
in air will not exclude PE. Always request a CXR as this
will reveal other life threatening causes (pneumothorax) and is required
for VQ reporting. Investigation for PE starts with bilateral leg ultrasound
scans (no risk to foetus). If these are normal, the patient should have a VQ
scan (b Pulmonary embolism, p.120). If the VQ scan cannot diagnose or
exclude PE, arrange a CT scan .
During investigation for DVT or PE it is standard practice to commence
thrombosis treatment with low molecular weight heparin (LMWH).
Thrombolysis has been used successfully in peri-arrest pregnant women
with a clear clinical picture of PE. If the patient is not peri-arrest, always
endeavour to obtain diagnostic imaging.
Warfarin is teratogenic in the fi rst trimester and may cause fetal or
placental bleeding in later pregnancy, so avoid it in pregnancy.
Other problems
Thyrotoxicosis presents not infrequently in pregnancy.
Pre-existing heart disease worsens as blood volume and cardiac output i :
involve a specialist early.
Although rare, consider aortic dissection in any pregnant patient with
unexplained, severe chest, back or neck pain ( b p.92).

594 CHAPTER 13 Obstetrics and gynaecology
Trauma in pregnancy
Background
Principal causes are similar to those in the non-pregnant: road traffi c colli-
sions, falls and assaults. Contrary to popular opinion, the use of seat belts
does d risk of serious injury in pregnancy. The ‘lap’ belt should lie over the
anterior superior iliac spines.
Anatomical considerations
The following are worthy of consideration:
• As the uterus enlarges it rises out of the pelvis with the bladder — both
are at i risk of injury.
• The size of the uterus and stretching of the peritoneum make abdomi-
nal assessment diffi cult.
• The bony pelvis is less prone to fracture, but retroperitoneal haemor-
rhage may be torrential due to i vascularity.
• The pregnant uterus may obstruct the inferior vena cava, causing supine
hypotension and increased bleeding from lower limb wounds.
• The diaphragm is higher in pregnancy.
• The pituitary doubles in size and is at risk of infarction in untreated
hypovolaemic shock.
Physiological considerations
Pregnancy is associated with dramatic changes in physiology:
• Pregnant patients may tolerate up to 35 % loss of blood volume before
manifesting classic signs of hypovolaemic shock, largely at the risk of
uteroplacental circulation.
• The d functional residual capacity and i O
2
requirement result in
hypoxia developing more quickly.
• There is an i risk of regurgitation of gastric contents.
• Coagulation may be deranged or rapidly become so.
Injuries to the uterus, placenta, and foetus
Foetal injury Both blunt and penetrating trauma may damage the foetus. It
is, however, more likely to suffer as a result of maternal hypoxia/hypovol-
aemia or placental abruption.
Placental abruption Deceleration forces in blunt trauma may shear the
inelastic placenta from the elastic uterus. Haemorrhage (maternal and
foetal) may be signifi cant and result in DIC. This may present with vaginal
bleeding (much may be concealed internally), uterine tenderness, or foetal
distress.
Uterine rupture This is relatively uncommon. Major rupture causes severe
bleeding. The uterus and foetus may be felt separately.
Amniotic fl uid embolism Rare and carries a poor prognosis. Presents with
sudden collapse, dyspnoea, d BP, fi tting, and bleeding (from DIC).

595
TRAUMA IN PREGNANCY
Approach to the injured pregnant patient
Follow that outlined in b Major trauma, p.319, with the additional specifi c
points.
History
Determine gestation and any problems in this and previous pregnancies.
Examination
• Involve an obstetrician early: examine vagina for bleeding or rupture of
membranes.
• Palpate for fundal height (mark skin), abdominal tenderness, uterine
contractions.
• Listen for foetal heart sounds and rate using a foetal stethoscope
(Pinard) or Doppler probe.
• Remember that head injury may mimic eclampsia and vice-versa.
Investigation
• Check BMG, coagulation screen, Rhesus/antibody status, and Kleihauer
test.
• Consider CVP monitoring (remembering the CVP is lower in preg-
nancy).
• Monitor foetal heart (cardiotocograph) — the rate should be 120–160/
min.
• USS investigates foetal viability, placental injury, gestational age, and free
peritoneal fl uid.
• Do not withold essential X-rays, but do consider early USS to look
for free intra-abdominal fl uid and foetal viability. Seek senior advice.
Remember that the greatest risks from X-rays to the foetus are in early
pregnancy. In later pregnancy, risks to the foetus may be outweighed by
failure to identify injuries by not obtaining X-rays.
• DPL has been largely superceded by USS (FAST scan) — but if indicated,
use a supra-umbilical open approach (see b p.347).
Treatment
• Give O
2
and summon senior obstetric, ICU, and surgical help early.
• If chest drains are required insert 1–2 intercostal spaces higher than
usual.
• Decompress the inferior vena cava by manually displacing the uterus to
the left or by using a 15 ° right lateral (Cardiff) wedge, or if neck injury
has been excluded, by nursing in left lateral position.
• Treat fl uid losses with aggressive IV fl uid replacement.
• An NG tube d risk of regurgitation and aspiration.
• Remember tetanus prophylaxis ( b p.410).
• Consider anti-D immunoglobulin if the patient is Rh –ve.
• Even if there is no overt maternal injury refer for foetal monitoring for
4hr.
• Abdominal tenderness, hypovolaemia or foetal distress may require
urgent laparotomy.
• If the patient has a cardiac arrest, perform emergency Caesarian section
if the patient is > 24wks pregnant and 5mins has elapsed without output
(see b p.596).

596 CHAPTER 13 Obstetrics and gynaecology
Cardiac arrest in pregnancy
Rate Estimated in late pregnancy at 7 1 in 30,000.
Causes stroke, PE, uteroplacental haemorrhage, amniotic fl uid embolism,
eclamptic fi ts and haemorrhage, anaesthetic problems, and drug reactions,
underlying heart disease. Ischaemic heart disease is rarely implicated:
the underlying rhythm is more commonly pulseless electrical activity
than ventricular fi brillation. Unfortunately, this is refl ected in the poor
prognosis.
Remember the following physiological factors
• The airway is diffi cult to control (large breasts, full dentition, neck
oedema and obesity). Ventilation may be diffi cult and intubation
technically challenging.
• i aspiration risk ( d lower oesophageal pressure, i intragastric pressure)
therefore securing defi nitive airway early is essential.
• i O
2
requirements in pregnancy, yet harder to ventilate ( d chest
compliance).
• Chest compression is awkward (fl ared ribs, raised diaphragm, obesity,
breast hypertrophy).
• Gravid uterus compresses inferior vena cava diminishing venous return.
• There are 2 patients: mother and foetus.
Approach to resuscitation
Follow Resuscitation guidelines for managing adult cardiac arrest ( b p.46).
The special situation of pregnancy means some additional points apply.
If there is advanced warning, think ahead. In addition to the usual team
needed for airway control, IV access and chest compressions, organize:
• An anaesthetist for the airway, an obstetrician to perform a Caesarian
section and a paediatrician to resuscitate the baby.
• The neonatal resuscitation equipment (overhead warmer, suction,
airway equipment and oxygen).
• A member of staff to apply cricoid pressure at the beginning of
resuscitation and until the airway is secured.
• A member of staff to manually displace the uterus to the left until a left
lateral tilt has been established with a Cardiff wedge.
It may take time for help to arrive and there may be no warning prior to
patient arrival. In the meantime, proceed as follows:
• Call the obstetrician, paediatrician, and ED consultant immediately.
• Apply cricoid pressure (Sellick manoeuvre) at the beginning of
resuscitation and until the airway is secured.
• Aim to secure the airway with a cuffed tracheal tube at an early stage.
• Decompress the inferior vena cava by either manual displacement of
the uterus to the left, or the use of sandbags or a special 15 ° right lateral
(‘Cardiff ’) wedge.
• Consider and treat the cause (eg remember that hypovolaemic shock
from unseen haemorrhage may respond to a large IV fl uid challenge).
• If there is no return of spontaneous circulation within 5min perform a
Caesarian section (providing the patient is > 24 weeks pregnant).

597
CARDIAC ARREST IN PREGNANCY
Emergency Caesarian section
Rationale After several minutes of maternal cardiac arrest the best chance
of survival for the foetus is to be removed from the now hostile hypoxic
environment of the uterus. Caesarian section also benefi ts the mother by
decompressing the inferior vena cava, resulting in i venous return.
Procedure Continue closed chest compression and ventilation. Make
a midline skin incision from pubic symphysis to epigastrium. Incise the
underlying uterus vertically, starting 6cm above the bladder peritoneal
refl ection. Continue the uterine incision upwards to the fundus, through
an anteriorly placed placenta if necessary. Speed is essential. Deliver the
baby, holding it head down and below the level of the mother’s abdomen.
Clamp and cut the umbilical cord. Resuscitate the baby ( b p.642).

598 CHAPTER 13 Obstetrics and gynaecology
Post-partum problems
Physiology of the puerperium
Within 24hr of delivery uterine involution results in the fundus being
level with the umbilicus. By 2 weeks the uterus should be impalpable.
Uterine discharge (‘lochia’) gradually d , but may last up to 6 weeks. An
initially bloody discharge becomes yellow within 2 weeks. The external
cervical os gradually closes so that after 1 week it no longer accepts
a fi nger. Speculum examination will now reveal the typical parous os
(see Fig. 13.4 ).
Post-partum haemorrhage
Primary Haemorrhage > 500mL in the fi rst 24hr is often related to
retained placenta/clots. This, together with uterine inversion and amniotic
fl uid embolism are principally problems of the labour ward.
Secondary Excessive fresh vaginal bleeding between 1 day and 6 weeks
after a delivery affects 8 1 % pregnancies. The most common cause is
retained products of conception: uterine involution may be incomplete
and USS may reveal the retained products. Other causes include
intrauterine infection (see below), genital tract trauma, trophoblastic
disease. Resuscitate appropriately for blood loss and refer. Severe
bleeding may respond to IV oxytocin.
Pyrexia
Treat according to the underlying cause, which include the following:
• Pelvic infection (see below).
• UTI.
• Mastitis.
• Chest infection.
• DVT or PE.
• Illness apparently unrelated to pregnancy/delivery.
Pelvic infection
Involves a signifi cant threat: may be complicated by septicaemia, necro-
tizing fasciitis, DIC or septic PE. There is an i risk with: surgical proce-
dures in labour, prolonged membrane rupture, internal foetal monitoring,
and repeated examinations.
Features Uterine tenderness and subinvolution, pyrexia, offensive lochia,
peritonitis.
Send Vaginal swabs for culture, FBC, group and save, clotting screen and
blood cultures.
Resuscitate with O
2
and IV fl uids and refer. For septic shock, follow
severe sepsis guidelines, give IV co-amoxiclav (1.2g) and IV metronidazole
(500mg), monitor CVP, consider inotropes and ventilation.
Infected episiotomy wound
Refer to obstetrician.
599
POST-PARTUM PROBLEMS
Mastitis and breast abscess
Mastitis is commonly due to Staph . or Strep . Send milk for culture and
commence oral antibiotics (eg co-amoxiclav). Instruct patient to express
and discard milk from the affected breast, but to continue breast-feeding
from the other. Arrange GP follow-up.
Refer patients with abscesses for surgical drainage by incision or the now
preferred aspiration.
Psychiatric illness
Rapid hormonal swings are responsible for elation being frequently
replaced by tearfulness and anxiety (‘fourth day blues’). Less commonly
(0.5 % pregnancies) puerperal psychosis occurs. Those with a previous psy-
chotic illness are at particular risk. Exclude sepsis and refer for psychiatric
help. The patient may need to be compulsorily detained ( b Compulsory
hospitalization, p.628).
Thromboembolic disease
A major cause of maternal mortality throughout pregnancy and the
puerperium. Adopt a high index of suspicion and refer for investigation
( b Pulmonary embolus, p.120).
Nulliparous Multiparous
Fig. 13.4 Appearance of the cervical os.
This page intentionally left blank

601
Approach to psychiatric problems 602
Glossary of psychiatric terms 603
The psychiatric interview 604
Mental state examination 606
The aggressive patient: background 608
Safe consultations with potentially violent patients 609
Managing aggression 610
Emergency sedation of a violent patient 611
Deliberate self-harm 612
Assessment of suicide risk 614
Mental health assessment issues 615
Depression 616
Mania 617
Schizophrenia 618
Complications of psychiatric drugs 619
Munchausen’s syndrome 620
Medically unexplained symptoms 621
Alcohol abuse 622
Acute alcohol intoxication 623
Alcohol withdrawal 624
Alcohol-related brain injury 625
Help for alcoholics 625
Drug and substance abuse 626
Compulsory hospitalization 628
Mental Capacity Act 629
Psychiatry
Chapter 14

602 CHAPTER 14 Psychiatry
Approach to psychiatric problems
Psychiatric presentations comprise 8 1–2 % of ED new attendances. These
patients are sometimes considered unwelcome because they are seen as
complex, heavy consumers of staff time and energy, and not infrequently
exhibit aggressive and/or disturbed behaviour. A careful systematic
approach to patients presenting with psychiatric emergencies produces
an accurate diagnosis in most cases. If this is not possible, the informa-
tion gained will at least assist referral to the appropriate service, allowing
management of the problem.
Liaison psychiatry service
Many EDs have close links with liaison psychiatrists and specialist psychi-
atric nurses. These individuals are used to managing a variety of psychiatric
problems, including overdose and deliberate self-harm. In an emergency
situation, they can act as an important source of advice.
Potential points of confl ict
The ED is not an ideal environment for the assessment of potential
psychiatric illness. Remember the following:
• The vast majority of aggressive, violent or bizarrely behaving patients in
the ED are not suffering from a formal psychiatric illness. Many require
the police, rather than psychiatric services.
• Admission is not mandatory simply because a psychiatric illness has
been diagnosed.
• The presence of alcohol or drug intoxication makes any assessment of
mental state very diffi cult and in many cases impossible — do not assume
that this in itself refl ects an acute psychiatric problem.
• Acute alcohol withdrawal is a medical emergency with a signifi cant
mortality — refers to the medical team, not acutely to the psychiatric
service.
• Acute confusional states are usually organic rather than psychiatric in
origin – investigate with this in mind.
• An emergency Section form must be signed by the examining doctor,
but this does not have to be a psychiatrist.
Similarly, psychiatric staff within the ED need to consider the following:
• EDs are under pressure to manage large numbers of patients in a timely
fashion, so it may be diffi cult for ED staff to spend large amounts of time
with any single patient.
• Lack of appropriate interview facilities may make it necessary to
compromise patient privacy rather than the safety of staff.
• A psychiatric referral can be appropriate in a patient who has
consumed alcohol, if there is a signifi cant psychiatric history
(‘Dual Diagnosis’).
General approach to psychiatric problems
Adopt the same approach of history taking and examination as with other
general medical problems. Do not dismiss psychiatric patients as ‘mad,
therefore the psychiatrist can sort them out’ — this can result in misdiagnosis
and inappropriate referral.

603
GLOSSARY OF PSYCHIATRIC TERMS
Glossary of psychiatric terms
Concrete thinking Impairment of abstract, or symbolic thinking
(eg interpretation of proverbs, explanation of similarities).
Delirium An organic syndrome characterized by rapid onset global
disturbance of cognition, and disturbed consciousness.
Delusion A fi rm, usually false, belief unshakeable by logical argument or
contrary experiences and which is out of keeping with the patient’s social
or cultural norms.
Flight of ideas Thoughts rapidly cycle linked by chains of ideas or
verbal associations or sounds resulting in disjointed, or in extreme cases,
incomprehensible speech.
Hallucination A false perception not due to a sensory distortion or
misinterpretation, but which occurs at the same time as real perceptions.
Hallucinations can occur in each of the sensory modalities. Auditory
hallucinations are most commonly associated with psychiatric illness.
Visual and other hallucinatory phenomena suggest organic aetiology.
Ideas of reference A feeling that others are talking about or looking
at the patient for some reason. Insight is usually retained, which is not the
case in delusions of reference.
Obsession Recurrent, persistent, and intrusive thoughts, impulses or
mental images that the individual usually tries to resist, fi nds unpleasant
and recognizes as senseless.
Passivity An experience of being under external control either
physically, emotionally or intellectually. Suggests schizophrenia.
Perseveration Repetition of an idea, thought, speech or an action
beyond the point of relevance (eg giving the answer of an initial question
in response to subsequent unrelated questions). Pathognomonic of
organic brain disease.
Pressure of speech Rapid or hurried speech, often occurs with fl ight
of ideas.
Psychosis Extreme disorders of thinking and perception, often involving
delusions and hallucinations, with loss of insight.
Thought blocking A feature of schizophrenia in which a train of
thought stops abruptly and, following a pause, a new line of conversation
begins.
Thought broadcasting More than simply feeling others can read
personal thoughts. An experience of thoughts spilling out beyond personal
control or that, thoughts are being relayed from external sources.
Thought insertion Thoughts that are not the patient’s own are put in
his mind from outside.
Thought withdrawal The feeling that thoughts have been removed or
stolen by an external infl uence.

604 CHAPTER 14 Psychiatry
The psychiatric interview
Setting and safety
Conduct the interview in a quiet, relatively private and preferably less
clinical setting. Many EDs have specifi c facilities designed for this purpose
(following specifi c joint guidance from the Royal College of Psychiatrists
and British Association for Emergency Medicine – Council Report CR118,
2004). Irrespective of this, do not under any circumstances allow the need
for privacy to compromise your safety! Ensure that other staff are easily
available and can be summoned immediately if necessary. If this is not
possible, either conduct the interview within the main ED (in a cubicle
or side-room) and/or ensure that other staff are present during the
interview. Position yourself between the patient and the exit.
Approach
In the initial interview, focus upon the following:
• Listen in supportive fashion and obtain an accurate history of the
presenting problem.
• Assess the mental state, emotions, and attitudes of the patient.
• Make a formulation (identify the key factors of the present illness, list
probable causes, explain why the patient became ill, and plan treat-
ment).
Initial history
Take a rapid, thorough history, concentrating upon the following
questions:
• What is the presenting complaint?
• What factors have caused the patient to present here and now?
• Is there a past history of psychiatric illness or medication?
• What does the patient want (advice, treatment or admission)?
• Are the patient’s wishes appropriate?
Ethnic minorities
Be aware of the different communities living within the vicinity and take
special care to remain sensitive to their needs. Assessment of mental
health problems needs to take into account the relevant cultural and
religious issues.
Language
It can be particularly challenging to assess the mental health of patients
who do not speak English. The following solutions may be explored:
• Assessment may be performed by an ED or mental health professional
who speaks the patient’s language (the ideal result).
• A health professional from another discipline acts as an interpreter.
• An interpreter who is not a health professional, but who is trained in
mental health issues may be used.
Note that children should not be used as interpreters. Similarly, it is not
good practice to rely upon family members to interpret.

605
THE PSYCHIATRIC INTERVIEW
Taking a full psychiatric history
The extent to which a detailed psychiatric history is required in the ED
varies according to the circumstances. The key features of a psychiatric
history are:
Presenting complaint List the principal complaints and try to detail the
course and severity of each. Ask about the effect of each problem on the
person’s life and work. Carefully determine how he came to be referred
or why he presented here and now. When was he last well?
Past psychiatric history Ask about previous psychiatric or physical illness,
hospital admissions (particularly if compulsory) and any outpatient
contact (eg community psychiatric nurse), day hospital, day centres, or
crisis intervention groups. Record psychiatric or other medications as
accurately as possible.
Personal and family history Obtain an outline of the patient’s life
history: birth, childhood, circumstances of upbringing (including parental
relationships — marital disharmony, separation, violence, adoption, single
parent, brought up by a grandparent, etc.). Ask about education, academic
achievements, and relationships with family or friends. Ask if there has
been any recent bereavement and what effect this has had.
Work history Is the patient employed? If not, ask about any previous
jobs. Ask about the impact of any loss, change, or failure in work on the
patient’s life or mental status, and conversely determine if psychiatric or
other illness has had any effect on employment.
Sexual/marital history Gently enquire about relationships and sexual
experiences only where relevant. This may reveal important information
about the patient’s personality and relationships to others. It may form
a major part of the presenting complaint (eg recent ending or change in
a relationship or a history of sexual abuse). A more detailed account of
sexual aberration or fantasy may be required in a forensic examination.
Substance misuse Try to estimate alcohol, tobacco, drug, or other
substance misuse by the patient. Although it may be diffi cult to obtain
accurate information, do not assume that patients always underestimate
their consumption of such substances.
Forensic history Record any previous criminal charges, convictions or
contact with the police, including the dates on which they occurred.
Ask if the patient has any present charges or court actions pending
against him.
Social circumstances Determine where the patient lives and if he shares
accommodation with others. Enquire about income and how he is coping
fi nancially. Ask if there are any dependents, any outstanding debts, and if
he is receiving any form of social support or monetary assistance.
Personality Try to describe the patient’s usual and present mood. How
does he feel about himself and about other people? How does he enjoy
himself and how does he react to good, bad or stressful events?
Corroboration Extremely important information can be gathered from
close relatives, GPs, community, or social services, and should be sought
to verify or enhance information obtained directly from the patient.

606 CHAPTER 14 Psychiatry
Mental state examination
Having taken an appropriately thorough history, make an assessment of
the patient’s mental state. If the patient is violent, disturbed, or for some
other reason unable to provide background history, the information or
observations gathered, whilst assessing mental state become even more
crucial to diagnosis.
Appearance and behaviour
Gather information from the moment the interview begins. Is the patient
appropriately dressed; is he clean and tidy, or neglected? Does his general
posture, body movement, and facial expression suggest fear, anxiety,
aggression, withdrawal, detachment, or low mood? Does he maintain
eye contact? Does he respond appropriately to external stimuli or is he
easily distracted? Does he appear to be hallucinating or responding to no
obvious stimuli? Are there any abnormal movements, tics, grimaces, or
dystonic movements? Note whether behaviour is steady and consistent,
or labile and unpredictable.
Speech
Describe the rate, volume, intonation, and spontaneity of speech. Note
the presence of dysarthria or dysphasia. Record any examples of invented
new words (neologisms), unusual phrases, perseveration, or garbled
speech verbatim. Note vagueness, over-preciseness, or sudden switching
to new themes or subjects (fl ight of ideas).
Mood
Taking cues from appearance and behaviour, enquire about the patient’s
prevailing mood, opinion of himself, and view of the future. Enquire about
suicidal thoughts and thoughts of harm to others. Ask about disturbances
in sleep, appetite, libido, concentration, and mood variations during a
typical day. Ask about irritability or memory disturbance (particularly of
short-term memory).
Thought abnormalities
These are best recorded as they are found during the interview
(eg thought blocking or fl ight of ideas). Test for concrete thinking by asking
the patient to interpret a simple proverb. Ideas of reference or perse-
cutory delusions may require direct enquiry to be revealed (eg asking
about neighbours, electrical devices). Similarly, passivity phenomena may
require specifi c questioning to be elicited (eg Is anyone making you think
or move without you wanting to?)
Hallucinations
Record the presence of any hallucinations including their nature and spe-
cifi c content. Visual, olfactory, gustatory and tactile hallucinations should
prompt suspicion of organic, rather than psychiatric disease.
Insight and mental capacity
Does he believe he is ill, does he think he requires treatment and would
he be willing to accept it? Does he have mental capacity ( b p.615)?

607
MENTAL STATE EXAMINATION
Assessment of risk
Consider whether the patient and/or others are at any risk of harm. Ask if
the patient has any thoughts of self-harm and/or harm to other individuals.
Establish if there is any past history of self-harm or violence. Try to decide
if the patient is at risk of abuse/neglect and consider whether he may be a
‘vulnerable adult’ — such concerns should trigger a Safeguarding Alert.
Children at risk
Find out if there are any children in the patient’s household and, if so,
whether or not there are satisfactory arrangements in place to care for
them. Concerns should prompt consideration of involvement of Social
Services and/or Child Protection referral.
Physical examination
A physical examination completes any psychiatric evaluation. Specifi cally
check for evidence of those physical illnesses which can be associated with
psychiatric disturbance (eg thyroid disease, substance withdrawal, head
injury, epilepsy, cerebrovascular disease, or other intracranial pathology).
Carefully examine for focal neurological signs, meningism, organic confu-
sional states, intoxication, and injury. In acute psychological disturbance,
perform and record the following basic observations and investigations
(this may prove to be very diffi cult in violent or aggressive individuals):
• Baseline pulse, respiratory rate, BP and SpO
2.
• Temperature (T) ° .
• BMG/blood glucose.
• Urinalysis.
• Breath alcohol.
Undertake other investigations such as U&E, FBC, CXR, or CT scanning
if clinically relevant. Urine drug screening, TFTs or electroencephalogram
may be indicated in some situations, but are rarely available acutely.
Cognitive assessment
Although the psychiatric interview will, in general, reveal information
about a patient’s cognitive abilities, a formal evaluation of higher mental
function is essential. Failure to do this can lead to organic brain disease
being falsely labelled as a ‘functional’ or purely psychiatric illness, resulting
in inappropriate treatment. Assess the following:
• Level of consciousness (eg alert, hyperalert, withdrawn, or comatose).
• Orientation.
• Attention and concentration.
• Registration of new information.
• Recall of recent and distant memories.
• Ability to interpret instructions and carry out tasks.
The Mini-Mental State Examination
The Mini-Mental State Examination was designed as a screening tool for
the assessment of cognitive function in the elderly. It is in widespread use,
but note that as with many psychological tests, it is subject to copyright.

608 CHAPTER 14 Psychiatry
The aggressive patient: background
A signifi cant (albeit small) proportion of patients exhibit aggressive
behaviour towards staff (and others) who are attempting to help them.
Sometimes this amounts to physical violence. It is vital that all ED staff
receive appropriate training in this area, bearing in mind that recogni-
tion and prevention of aggression is just as important as knowing how to
manage it when it occurs.
Underlying causes
Medical illness
Recognize that a patient’s agitation or aggression may be because of an
underlying treatable acute medical condition. Such conditions may be
compounded (as well as being potentially caused) by the use of alcohol
and/or illicit drugs :
• Hypoglycaemia ( b p.150).
• Head injury.
• Hypoxia (any cause).
• Distended bladder.
• Post-ictal confusional states (epilepsy or drug overdose).
• Organic brain syndromes (eg acute confusional states— b p.134).
Psychiatric illness
Most violent, aggressive, or bizarre patients in the ED are not mentally
ill. Violence resulting directly from psychiatric illness, which needs urgent
treatment is relatively uncommon. It is restricted to a small number of
patients and tends to be associated with the following:
• A past history of violent behaviour.
• Schizophrenia and other psychoses (eg mania or paranoid disorders),
especially when there are delusions or hallucinations that focus upon
one particular individual.
• Personality disorder, particularly sociopathic, impulsive, or explosive
disorders.
• Learning disability.
Warning signs of impending violence
Violent episodes can frequently be predicted and often prevented. The
experienced practitioner may be able to spot the signs of approaching
trouble at an earlier stage. Warning signs include the following:
• Angry facial expressions, gestures, and posture (aggressive body
language).
• Restlessness, overt irritation, discontentment, pacing about,
over-arousal (dilated pupils, tachycardia, increased respiratory rate).
• Prolonged eye contact.
• Loud speech and changes in tone of voice.
• Verbally threatening and/or reporting feelings of anger/violence.
• Repeating behaviour, which has previously preceded violent episodes.
• Blocking escape routes.

609
SAFE CONSULTATIONS WITH POTENTIALLY VIOLENT PATIENTS
Safe consultations with potentially
violent patients
Planning before the consultation
Physical design issues
Many departments have specially designed facilities with the interview
room door designed to open outwards in order to allow rapid, easy exit.
It is important to regard any loose items as potential weapons
(eg telephones, chairs, lamps).
Safety fi rst
Safety comes fi rst — ensure that patients are not allowed to harm them-
selves, other patients, or staff. Aim to conduct the consultation in a quiet,
comfortable and, preferably, non-clinical area. However, compromise
privacy, rather than safety, so if there are concerns, it may be necessary to
undertake the consultation in a standard cubicle. Consider having another
member of staff present during the consultation. Before consulting with
any potentially violent patient ensure the following:
• Other staff know where you are and who you are with.
• You know how to get help (a ‘panic button’ or other personal alarm).
• Staff know to respond immediately.
• Staff know what to do if there is a problem.
Information gathering
Obtain as much information as possible beforehand. Useful sources of
information may include relatives, police, social services, GP, and other
health professionals.
The consultation
The outcome of the consultation depends heavily upon how it is conducted:
• Ensure that your own body language does not provoke the situation.
• Remain calm and sympathetic, maintaining a reassuring and non-
judgmental manner.
• Listen to any immediate complaint or grievance with a minimum of
interruption.
• Engage in conversation, with continuing reassurances that you are there
to help.
• Adopt an attentive, but relaxed posture.
• Speak slowly and clearly, keeping your voice low.
• Avoid excessive eye contact.
• Sit between the patient and the door and not directly facing the patient
(as this may appear confrontational and will provide a larger target for
attack).
• Never turn your back on the patient, particularly when leaving the
room.

610 CHAPTER 14 Psychiatry
Managing aggression
Violent behaviour is unusual if a calm, sensible approach is followed. If vio-
lence does occur, focus upon preventing the patient from harming other
patients/relatives, staff, or themselves. See www.nice.org.uk
Approach to the aggressive patient
Get immediate help from police/security offi cers and other staff. Avoid
physical confrontation, and ensure that you position yourself within the
examination room or cubicle with no block to your escape. Take note of
where the alarm buttons are situated. Continue de-escalation techniques.
• Find out what the problem is, establish a rapport and encourage
reasoning.
• Show concern and stay attentive.
• Avoid patronizing comments. Never insult the patient, or make
promises or commitments that cannot be kept.
• Direct body contact can be misinterpreted.
• Do not engage in prolonged eye contact.
• Remember that psychotic patients have different perceptions of
personal space and may feel threatened by staff coming into what would
otherwise be a normal and non-threatening distance.
• Try to maintain a calm atmosphere with a non-critical, non-domineering
approach.
Management of physical violence
If physical violence occurs, safety of staff, other patients, and relatives
takes priority. Concern for property is secondary — it can be replaced.
Even during a violent act, a calm approach with talking and listening often
prevents escalation of the event and the need for physical confrontation.
Physical restraint Avoid physical intervention if at all possible. Where
physical restraint is required, use the minimum degree of force, applied for
the minimum length of time in order to control the episode. Apply it in a
manner that attempts to calm, rather than provoke, further aggression.
This will require suffi cient members of staff to control the event without
injury to anyone involved.
Restrain the patient by holding clothing rather than limbs. If limbs have to
be grasped, hold near a major joint to reduce leverage and the possibility
of fracture or dislocation. Remove the patient’s shoes or boots. In
exceptional circumstances (eg when a patient is biting) the hair may have
to be held fi rmly. Never apply pressure to the neck, throat, chest, back,
pelvis or abdomen. Do not deliberately infl ict pain.
Do not attempt restraint unless suffi cient staff/expertise is available. Put
one person in charge to ensure airway and breathing are not compromised
and vital signs are monitored. Only d restraint once it is certain that the
risk has d — this may mean use of medication.
Weapons Ask for any weapon to be placed in a ‘neutral’ position,
rather than handed over. Do not attempt to remove a weapon from an
aggressor.

611
EMERGENCY SEDATION OF A VIOLENT PATIENT
Emergency sedation of a violent patient
Pharmacological restraint using sedative drugs is a last resort, and should
only be given on the advice of senior and experienced staff. Emergency
sedation carries signifi cant dangers. Sedative drugs may mask important
signs of underlying illness, eg an intracranial haematoma requiring urgent
treatment. The normal protective refl exes (including airway refl exes, such
as gag and cough response) will be suppressed. Respiratory depression
and the need for tracheal intubation and IPPV may develop. Adverse car-
diovascular events (eg hypotension and arrhythmias) may be provoked,
particularly in a struggling, hypoxic individual. Finally, staff need to be
aware of medicolegal implications of carrying out any restraint.
Oral tranquillization
If possible sedative drugs should be given orally, rather than by injection,
but oral treatment may not be feasible in a violent and disturbed patient.
• Give lorazepam (1–2 mg PO) if there is no psychotic context.
• Give lorazepam (1–2 mg PO) + antipsychotic (eg haloperidol 1.5–3mg
PO) if there is a psychotic context.
• Allow suffi cient time for response before considering a second dose.
IM tranquillization
If oral therapy inappropriate (refused, failed or not indicated).
• Give lorazepam (2–4 mg intramuscular (IM) in non-psychotic context).
• Give lorazepam (2–4 mg IM) + antipsychotic (eg haloperidol 5–10mg IM)
if there is a psychotic context. When using haloperidol ensure
procyclidine is immediately available to treat acute dystonia or other
extrapyramidal side-effects.
• Allow suffi cient time for response before considering a second dose.
• Avoid IM diazepam, chlorpromazine or thioridazine.
IV tranquillization
Only in truly exceptional circumstances, when immediate tranquillization
is essential, IV drugs may be used (ideally after senior consultation):
Consider IV benzodiazepine or IV haloperidol.
Avoid parenteral clomethiazole, barbiturates, and paraldehyde, as they
are associated with a signifi cant risk of respiratory depression.
See NICE Clinical Guideline 25 on ‘Violence’
http://guidance.nice.org.uk/CG25/QuickRefGuide/pdf/English
After the violent episode
Following any episode of verbal aggression or physical violence, ensure
that the staff involved record full detailed notes and that standard local
incident forms are completed. Report the episode to the senior member
of staff and to the police (as appropriate), if they are not already involved.
Subsequently, when dealing with the violent patient, do not purposely
avoid the patient or treat him obviously differently, since this will merely
emphasize concepts of his own unacceptability and may lead to further
aggression.

612 CHAPTER 14 Psychiatry
Deliberate self-harm
Deliberate self-harm (DSH) accounts for 8 20 % of acute medical admissions
in the UK. Psychiatric symptoms are often associated with DSH, but tend
to be transient and predominantly related to social or emotional factors.
Psychiatric illness is relatively uncommon ( 8 5–8 % of cases, mostly depres-
sion). 8 90 % of DSH involve self-poisoning, the remainder physical self-
injury (eg cutting). Most DSH episodes are impulsive (considered for <1hr
beforehand). Associated alcohol consumption is common and may have
precipitated the event. However, assess carefully — 1 % of DSH patients do
commit suicide within a year. Some hospitals admit DSH patients to an ED
observation ward, allowing alcohol to wear off until the situation can be
properly assessed. Useful guidance on the treatment and management of
self-harm in EDs has been published by NICE ( www.nice.org.uk ).
Triage
Patients who present following an episode of physical self-harm and/or
overdose require rapid initial assessment (triage) in order to establish the
degree of urgency of the situation, mental capacity, and willingness to stay,
distress levels, and presence of mental illness. Factors that may render the
situation more urgent include:
• Need for urgent treatment for physical injury and/or overdose.
• Immediate risk of violence to others.
• Immediate risk of further self-harm.
• Need for treatment, but patient threatening to leave.
Australian Mental Health Triage Scale
This combined physical and mental health triage scale is recommended
by NICE and can be adapted for easy use (see www.rcpsych.ac.uk ). Some
features are summarized in the Table 14.1 .
There should be a system in place so that self-harm patients are checked
upon at least every hour — a change in triage category may require more
urgent assessment.
Table 14.1 The Australian Mental Health Triage Scale
Triage
category
Features
1 Extremely
urgent
Violent, possessing a weapon, or further self-harm in the ED
2 Very
urgent
Extremely agitated/restless, aggressive, confused/unable to
cooperate, or requiring restraint
3 Urgent Agitated/restless, bizarre behaviour, psychotic symptoms, severe
depression and/or anxiety
4 Less urgent Symptoms of anxiety and/or depression without suicidal ideation
5 Least urgent Compliant, cooperative and communicative

613
DELIBERATE SELF-HARM
Management plan
All patients who present to the ED after self-harm should be offered a
psychosocial assessment of needs and risk by an appropriately trained indi-
vidual. Some units continue to admit all patients with DSH for psychiatric
appraisal once medically fi t, but sheer numbers can make this diffi cult.
A selective approach distinguishes patients with underlying psychiatric
pathology and/or true suicidal intent — both requiring formal psychiatric
evaluation. Many centres have developed psychiatric liaison services with
medical and nursing mental health specialists who can offer timely and
expert input.
Assessment
Involve family/carers whenever possible, with the patient’s consent.
Focus upon:
• Events and circumstances leading up to the episode of self-harm.
• Preparation, concealment, and true intention of a DSH act.
• Outcome of DSH act (eg unintended danger or accidental discovery).
• Current stresses, fi nancial, legal, or interpersonal problems.
• Alcohol or substance misuse.
• Previous self-harm or psychiatric illness.
Decide about psychiatric referral using this information. If in doubt, refer.
Also refer immediately any child or adolescent who presents with DSH.
Many EDs have a system whereby patients who are not deemed to be
at immediate risk can return the following day for an appointment with
a psychiatric liaison nurse/specialist for psychosocial assessment. In the
absence of such a system, ensure that the patient’s GP receives written
communication about the patient’s ED attendance and discharge.
Factors suggesting suicidal intent
• Careful preparation (eg saving tablets) and/or signifi cant premeditation.
• Final acts (eg organizing fi nances, insurance or a will).
• Carrying out DSH alone, secretly or when unlikely to be discovered.
• Not seeking help following DSH.
• A defi nite, sustained wish to die.
Suicide notes can be important, but are sometimes left for dramatic effect
and so are not always reliable indicators.
Consider all self-harm acts by individuals aged > 65 years to be evidence of
suicidal intent until proved otherwise.
Risk of further self-harm
Recurrence is most likely if there have been repeated previous episodes
(eg habitual self-cutters or recurrent overdoses).
Socio-demographic predictors include being single or separated, aged 25–
54 years, being unemployed or social class V.
Other factors include drug or alcohol dependence, a history of criminal
behaviour, previous psychiatric treatment, or the presence of a personality
disorder.
614 CHAPTER 14 Psychiatry
Assessment of suicide risk
Prevention of suicide is a primary aim in assessing DSH. Certain factors
are common among completed suicides and are signifi cant if found in a
DSH patient:
• Male.
• Elderly (particularly female).
• Living alone.
• Separated, divorced, or widowed.
• Unemployed or retired.
• Physical illness (eg painful, debilitating, or terminal conditions).
• Psychiatric illness (especially schizophrenia and depression).
• Alcoholism.
• Sociopathic personality disorder.
• Violent method of DSH (eg hanging, shooting, drowning, or high fall).
Modifi ed Sad Persons Scale
It can be diffi cult for clinicians without a psychiatric background to make an
assessment of the suicide risk. The modifi ed ‘Sad Persons Scale’ attempts
to assist non-psychiatrists with this task. It may serve as a guide regarding
the need for referral or admission (Table 14.2 ).
Table 14.2 Modifi ed Sad Persons Scale
Score
Sex male 1
Age <19 or > 45 years. 1
Depression or hopelessness 2
Previous suicide attempts or psychiatric care 1
Excessive alcohol or drug use 1
Rational thinking loss (psychotic or organic illness) 2
Separated, widowed, or divorced 1
Organized or serious attempt 2
No social support 1
Stated future intent (determined to repeat or ambivalent) 2
Interpretation of total score
Score <6 may be safe to discharge (depending upon circumstances).
Score 6–8 probably requires psychiatric consultation.
Score > 8 probably requires hospital admission.

615
MENTAL HEALTH ASSESSMENT ISSUES
Mental health assessment issues
Patients who present with deliberate self-harm can present diffi cult prob-
lems that are not often a feature of patients who do not have mental
health problems. The management of some of these issues is addressed by
NICE ( www.nice.org.uk ) and summarized below.
Timing of psychosocial assessment
The ideal is to offer psychosocial assessment of patients with DSH as
soon as possible. There are occasions when this assessment needs to be
delayed, including the following:
• Life-saving treatment for physical injuries is needed.
• The patient is unconscious and/or signifi cantly under infl uence of
alcohol/drugs and, therefore, not capable of being properly assessed.
Patient threatening to leave the department
Not infrequently, patients state that they wish to leave the department
before psychosocial assessment. Very often, it is possible to persuade
them to stay. Perform an assessment of the patient’s mental capacity and
mental illness to decide whether it is necessary to detain him/her under
the Mental Capacity Act or Mental Health Act if he/she attempts to leave.
Diminished mental capacity and/or signifi cant mental illness
If there is diminished mental capacity and/or signifi cant mental illness,
refer for urgent mental health assessment and prevent the patient from
leaving the department. If the patient does manage to leave the depart-
ment despite best efforts, contact the police in order to try to bring him/
her back.
No reduction in mental capacity and no signifi cant mental illness
If there is no reduction in mental capacity and no signifi cant mental illness
and the patient leaves the department, pass information on to his/her GP
and to the relevant mental health services as soon as possible, to enable
rapid follow up.
Physical treatments
Management of poisoning is the focus of Chapter 4. Note that it is
sensible to measure paracetamol levels in any patient who presents with a
history of overdose of paracetamol and/or other drugs.
Superfi cial skin wounds <5cm long are often managed satisfactorily with
tissue adhesive strips. Deeper skin wounds, or those > 5cm in length
require standard assessment and treatment ( b Wound management,
p.406).
Repeat self-harmers
There may be local organizations to help self-harmers, as well as national
organizations, such as the Samaritans (a listening service). Specifi c advice
for people who repeatedly self-injure includes advice and instruction on
harm minimization issues, self-management of superfi cial injuries, and
dealing with scar tissue.
616 CHAPTER 14 Psychiatry
Depression
Everyone experiences low mood at times. It needs treatment when pro-
longed, unrelenting, inappropriate or disabling. Lifetime risk of depression
is 8 10 % for men and 8 20 % for women. General population prevalence is
3–6 % ( i with age). Co-existing psychiatric or physical illness can make the
diagnosis of depression diffi cult. Conversely, depression may be the pre-
senting feature of physical illness (eg hypothyroidism, Cushing’s syndrome,
or malignancy). 8 15 % of those with recurrent affective disorder eventually
commit suicide. Persisting suicidal ideation or recent DSH, even if trivial, is
highly signifi cant in the presence of a diagnosis of depression.
Aetiology
Complex, with genetic, social, environmental, and neurochemical factors.
Mood disorders are more common in relatives of depressives. Life events
involving loss (partner, friend, health, job, status) can precipitate depres-
sion (risk i to 6 × normal in 6 months after such an event). Loss of a
parent in childhood, unemployment, and lack of confi ding relationship
with a partner i vulnerability. Neurochemical mechanisms are involved
(‘amine theory’). Effective antidepressants i brain availability of serotonin
and noradrenaline.
Presentation and symptoms
Depressed patients almost always have persistent low mood, loss of
interest and enjoyment (anhedonia) and lack of energy. Mood is unaffected
by circumstances. Look for common features (Table 14.3 ).
Look for self-neglect. Does the patient exhibit psychomotor retardation
(slow movements and speech) or is he agitated? Is eye contact maintained?
Are there defi cits of short-term memory and cognition that improve with
i effort? Psychotic symptoms occur in very severe cases (eg hallucinations
or delusions). These are mood congruent: derogatory voices, ideas of
poverty, guilt, nihilism (patient believes he has no bowel, no clothes, no
life, etc.). Anxiety can be a feature of depression.
Atypical depression can involve reversal of usual somatic symptoms leading
to i appetite, i weight, hypersomnia, and reversed diurnal mood variation.
Treatment
Arrange psychiatric assessment for patients with severe depression , suicidal
ideation, or psychotic features. Most respond to antidepressants, but do
not start these in the ED. Some patients also require antipsychotics or
ECT. In cases with psychotic features or where there is a high risk of death
from suicide or profound self-neglect, ECT is effective.
Mild/moderate cases may respond to psychological therapy. Counselling
can help specifi c problems (eg bereavement or marital diffi culties).
Table 14.3 Common features indicating a person’s mood
Common symptoms Somatic or vegetative symptoms
d Self-esteem and self-confi dence
Sleep disturbance
d Concentration and attention d Appetite
Memory disturbance (esp short-term) Weight loss
Bleak and pessimistic views of the future Constipation
Ideas of self-harm or suicide Amenorrhoea
Feelings of guilt or worthlessness Loss of interest or enjoyment
617
MANIA
Mania
Mania and hypomania are less common than other mood disorders, but
more often require compulsory hospital admission. Pathologically elevated
mood combines with over-activity, irrationality, poor judgement and lack of
insight (see Table 14.4 for primary and other features). This leads to severe
disruption of relationships, employment or fi nances. Untreated, high rates
of divorce, debt, violence, or suicide occur. Onset may be acute or insidious.
Manic disorders can arise spontaneously or follow depressive illness, stress,
surgery, infection, or childbirth. Antidepressant medication, ECT, steroids,
and amphetamines can all precipitate mania, as can lithium withdrawal.
Hypomania denotes an intermediate state without delusions,
hallucinations or complete disruption of normal activities.
Differential diagnosis
Schizophrenia can present with disorganized behaviour, violent
excitement, delusions, and incomprehensible speech. The content of
delusions (ie bizarre, rather than mood-congruent), will help distinguish
this from mania.
Approach to the patient
Stay calm and non-confrontational. Beware infectious optimism, which can
easily lead to underestimating the severity of illness or the requirement
for admission. Seek additional information from relatives. Irritability can be
the dominant symptom of mania and may be expressed as a savage, highly
detailed catalogue of the interviewer’s shortcomings. Irritable patients can
become angry or violent in the face of even minor frustrations.
Treatment
Overt manic illness is best managed in hospital to avoid behaviour harmful
to the patient or others. Insight is often d or absent, so compulsory
admission may be required. Liaise with the psychiatrist before commencing
defi nitive drug treatment as this may adversely affect assessment. Lithium
carbonate is traditional and effective in most cases, both to treat the
acute episode and as prophylaxis against recurrent mania. However, it
usually takes some days to work, so an antipsychotic (eg olanzapine) or
benzodiazepine may be needed initially.
Table 14.4 Primary and other features of mania
Primary features Other features
Over-cheerfulness Irritability
Over-talkativeness Flight of ideas
Over-activity Distractibility
Grandiosity
d Requirement for sleep
Delusions (mood-congruent)
Hallucinations
Impaired judgement
Irresponsibility and impetuousness
Gambling and promiscuity

618 CHAPTER 14 Psychiatry
Schizophrenia
This affects all areas of personal function, including thought content and
process, perception, speech, mood, motivation and behaviour. A common
pattern is acute exacerbation with i residual handicap between episodes.
30 % of those who suffer a fi rst episode never have another. Another 30 %
develop chronic symptoms requiring frequent admission or long-term
care. The lifetime risk is 1/100.
Clinical features
No single symptom is pathognomonic: hallucinations or delusions simply
confi rm psychosis.
Schneider’s First Rank Symptoms originally suggested schizophrenia in the
absence of organic disorder. It is now acknowledged that they can occur
in mania and other conditions:
• Auditory hallucinations ≥ 2 voices discussing the subject in the third
person or giving a running commentary on his/her thoughts/behaviour.
• Thought withdrawal, insertion, or broadcasting.
• Somatic passivity sensations, emotions, or actions are externally imposed
or controlled.
• Delusional perception a genuine perception takes on abnormal signifi -
cance for the subject and is the basis of their delusional system.
• Gedankenlautwerden voices repeating the subject’s thoughts out loud or
anticipating the subject’s thoughts.
Diagnosis
Mental state examination will help to exclude organic and affective
disorders, remembering:
• Non-auditory hallucinations are more common in organic conditions.
• Delusions in depression and mania are mood-congruent.
Differential diagnoses
Organic causes: temporal lobe epilepsy, drug-induced states, alcoholic
hallucinosis, cerebral tumour, encephalitis, head injury.
Psychiatric: affective psychoses, schizo-affective disorder, psychogenic
psychosis, delusional disorder (eg infestation), personality disorder.
Management
Patients not known to have schizophrenia
Refer to the psychiatric team who will advise about the need for urgent
antipsychotic treatment.
Patients known to have schizophrenia
Schizophrenics frequently present to the ED with mental health issues
and problems. It can be diffi cult to formulate a management plan
unless relevant background information is available. Liaise with relevant
individuals (including community psychiatric nurse and psychiatrist) to
decide whether to treat in hospital or in the community and what form
any treatment should take.

619
COMPLICATIONS OF PSYCHIATRIC DRUGS
Complications of psychiatric drugs
Antipsychotic drugs
Acute dystonic reactions (grimacing, facial, and masseter spasm, deviated
gaze, torticollis, limb rigidity, and behavioural disturbances) frequently
present to EDs. They follow ingestion of antipsychotics (eg phenothiazines
or haloperidol) and/or other drugs (eg metoclopramide), even in
therapeutic dosages. Reactions can occur up to 1 week after ingestion.
Acute dystonia can dislocate the mandible. Dystonia can be mistaken for
malingering, as symptoms can be briefl y interrupted by voluntary actions.
Once diagnosed, treat with :
Procyclidine 5 mg IV bolus, repeated as necessary after a few minutes.
Dramatic resolution of symptoms occurs within minutes, confi rming the
diagnosis. Symptoms may recur — treat with oral procyclidine 5mg every
8hr. Large doses of procyclidine cause euphoria and fi xed dilated pupils,
hence, its abuse by some patients. Diazepam also works, but is less specifi c
and carries risks of excessive drowsiness or respiratory depression.
Clozapine
An atypical antipsychotic used in treatment-resistant schizophrenia.
Agranulocytosis occurs in 3 % of patients. For this reason, all patients are
enrolled with the Clozaril Patient Monitoring Service (telephone 0845 769
8269) who supervise regular blood screening. Check FBC for neutropenia
in any patient presenting with fever, sore throat, or other infection.
Monoamine oxidase inhibitors (MAOIs)
MAOIs (eg phenelzine, tranylcypromine), irreversibly block enzymes
responsible for oxidative metabolism of 5HT, noradrenaline, tyramine,
and other amines. Once discontinued, enzyme inhibition continues
for up to 2 weeks, during which time other drugs should not be intro-
duced. Newer, reversible MAOIs (‘RIMAs’ — eg moclobemide) cease to
have effects after 24–48hr. MAOIs cause postural hypotension, but acute
hypertensive reactions follow ingestion of amine rich foods (eg Bovril
TM
,
Marmite
TM
, cheese, red wine). Noradrenaline release causes vasocon-
striction, tachycardia, and hypertension that can, in severe cases, lead to
intracerebral or subarachnoid haemorrhage. Similar hypertensive crises
can be caused by concurrent use of L-dopa, sympathomimetics, ampheta-
mine, or drinking certain low-alcohol beers or wines.
Lithium
Lithium toxicity presents with severe nausea, vomiting, cerebellar signs, or
confusion. SSRIs (eg fl uoxetine), anticonvulsants, antipsychotics, diuretics,
methyldopa, and calcium channel blockers can all precipitate toxicity.
Look for tremor, cerebellar ataxia, muscular twitching (myoclonus), spasti -
city, choreiform movements, up-going plantar responses, incoordina tion,
slurred speech, impaired concentration, drowsiness, coma.
Check serum lithium (plain, not lithium heparin tube!) and U&E
immediately. Serum lithium levels correspond poorly with clinical signs
(toxicity can occur within therapeutic range), so diagnosis of toxicity is
based on clinical observations. Stop lithium and treat according to severity
of toxicity ( b p.197).

620 CHAPTER 14 Psychiatry
Munchausen’s syndrome
Also known as ‘hospital hopper’, this is characterized by recurrent hospital
admissions with factitious symptoms and signs of physical illness. Other basic
components are a morbid attraction to the sick role, pathological lying and
pleasure from deceiving medical staff. The incidence is unknown, but it is prob-
ably underestimated. It is believed to be commoner in men with peak onset at
30–40 years. There may be an underlying personality disorder, but true psy-
chiatric illness is rare. Origins are uncertain: excessive dependency, inability to
form trusting relationships, attention-seeking, childhood hospitalization, and
resentment of doctors for previous treatment have all been suggested.
Presentation
Common presentations involve detailed and convincing descriptions of
cardiac chest pain, abdominal pain (especially pancreatitis), haematemesis,
haemoptysis, rectal bleeding, haematuria, or pyrexia. More rarely, patients
present with artefactual dermatitis or with a dramatic history of trauma
(eg fall or pedestrian knockdown). Distinguish Munchausen’s from:
• Malingering: fabricating illness for defi nite gain (eg stealing drugs, avoid-
ing court appearance, faking symptoms to obtain opioids).
• Somatoform disorders: physical symptoms or signs without organic cause,
but not under voluntary control.
• Fabricated and induced illness: see b p.733.
Suspicious features
• Incomplete or inconsistent disclosure of personal details and past history.
• Patient a long way from home area for unclear reasons.
• Recent dramatic history of myocardial infarction (MI), surgery, or
complications elsewhere.
• Excellent knowledge of fi ner details of past treatment and/or complications.
• Multiple scars : laparotomies, sternotomy, venous cutdowns.
• Elaborate history of allergy (eg allergic to all painkillers except pethidine).
• Unconvincing claims of medical or paramedical occupation.
• Unusual/demanding behaviour and/or avoidance of eye contact.
• No ascertainable organic cause for the symptoms.
Management
Early recognition is important, but fi rst exclude genuine illness. There may
be no alternative to admission and observation to make the diagnosis, even
though this achieves the patient’s aim. If suspicions are aroused, discreetly
check past history. Once discovered, most patients self-discharge, often
noisily, but rarely violently.
Avoid a ‘showdown’ Simply state that deception is at an end, that no
retribution is planned and offer to help the patient with their problem.
Do not use placebos to uncover fabricated illness — they can work equally
well on genuine symptoms!
Once discovered, record events carefully, particularly the medical history
given, background details, appearance, scars. Circulate details to other EDs.
Factitious disorder in health care workers
The Clothier report (Department of Health, 1994) advised that
patients with severe personality disorder (by inference, factitious disorder)
should be prevented from working in health-related disciplines. Detection
of factitious disorder in health care workers has serious implications. If
suspected, discuss immediately with the ED consultant.

621
MEDICALLY UNEXPLAINED SYMPTOMS
Medically unexplained symptoms
Background
A signifi cant proportion of patients who attend the ED have symptoms
for which no cause is found. Some of these patients manage to build up a
signifi cant volume (or volumes!) of medical records.
Terminology
There is a potentially confusing range of terms in use.
Somatization
Physical symptoms with presumed psychological origin.
Somatoform pain disorder
Persistent, severe unexplained pain, which is attributed to psychological
disorders.
Conversion (dissociative) disorders
Loss or disturbance of normal motor or sensory function, which is attrib-
uted to a psychological origin (thoughts/memories to the conscious mind
are ‘converted’ into physical symptoms (eg amnesia).
Factitious symptoms
Symptoms which are intentionally produced, with the aim of receiving a
medical diagnosis—when there is secondary gain (eg legal compensation,
obtaining opioid drugs), it is known as malingering .
Medically unexplained symptoms
This is an umbrella term, which makes no assumptions about the cause of
the symptoms.
Differential diagnosis
Patients who present acutely with medically unexplained symptoms
may be suffering from a range of problems, including: anxiety, depres-
sion, psychosis, ‘functional somatic illness’, conversion disorders, factitious
disorders, malingering, and uncommon medical syndromes that have not
yet been diagnosed.
Approach to patients with medically unexplained symptoms
The Royal College of Psychiatrists ( www.rcpsych.ac.uk ) has published
some useful recommendations. Consider the following:
• Try to obtain past medical and psychiatric records/summaries
(computerized records may assist in this process) and/or speak to
the GP.
• If the patient’s medical complaints are known to be unexplained (or
part of a psychiatric illness), then further investigations may be inappro-
priate.
• Investigate judiciously — do not underestimate the ability to cause iatro-
genic harm.

622 CHAPTER 14 Psychiatry
Alcohol abuse
Alcohol-related problems account for up to 15 % of the ED workload in
the UK. Alcoholics have i rates of heart disease, malignancy, and stroke,
but often succumb to injuries. Excessive alcohol consumption is a feature
of 30 % of road traffi c fatalities, 25 % of fatal work injuries, 30 % of drown-
ings and 50 % of burn deaths. Alcohol is involved in 8 30 % of suicides, 8 60 %
of homicides and most assaults. Suspicion is the key to detecting alcohol
problems.
Units
The number of ‘units’ (10mL of pure alcohol) is included on packaging.
A bottle of wine contains 8 10U and a bottle of spirits 8 30U. Current
advice is a ‘safe’ limit of 21U/week (males) and 14U/week (females).
Alcohol absorption, metabolism, and elimination
Alcohol is absorbed from the small intestine and to a lesser extent, the
stomach. The rate of absorption depends on the nature of the drink and
any associated food consumed. Alcohol is absorbed more slowly from
dilute drinks (eg wine) compared with more concentrated fortifi ed sherry
or port. Alcohol is water soluble, so distributes throughout the body. It is
mostly metabolized in the liver by an enzymatic process involving alcohol
dehydrogenase, which converts it to acetaldehyde and then acetic acid. A
relatively small amount of alcohol is excreted unchanged in the urine (and
to a lesser extent, in breath and sweat).
Clearance of alcohol The rate of clearance of alcohol from the blood
varies enormously between individuals, with typical quoted values of
10–20mg/dL/hr in most adults, although higher values occur in some
chronic alcoholics.
Assessing alcohol problems
A history of alcohol consumption is notoriously unreliable when taken
from heavy drinkers and chronic alcoholics, who may signifi cantly under-
report the extent of their drinking and its effect upon their lives. The actual
amount of alcohol consumed is less important than the consequences of
drinking to the patient. Cover the following areas:
Biological GI upset/bleeding, withdrawal fi ts, blackouts, peripheral
neuropathy.
Psychological Low mood, hallucinations, delusions, memory problems.
Social Marital, work, driving, debt, criminality.
Signifi cant features include compulsion to drink and loss of control.
The CAGE questionnaire
• Have you ever felt you should Cut down your drinking?
• Have people Annoyed you by criticizing your drinking?
• Have you ever felt Guilty about your drinking?
• Have you ever had a drink fi rst-thing in the morning to steady your
nerves or to get rid of a hangover (Eye-opener)?
Any single, + ve answer is signifi cant and > 1 + ve answer is probably
diagnostic of chronic alcohol dependence.

623
ACUTE ALCOHOL INTOXICATION
Acute alcohol intoxication
Effects of intoxication
Alcohol depresses the nervous system — initial euphoric effects are due to
suppression of inhibition by the cerebral cortex. Effects vary between indi-
viduals and Table 14.5 is a very rough guide. Behaviour, including propen-
sity to violence, is infl uenced by environment and social setting. Although
death may occur at levels > 350mg/100mL, the risk of a harmful or fatal
event increases at any level: especially road traffi c collisions, work and
home accidents and assaults (including sexual assault). The current UK
blood alcohol legal limit for driving is 80mg/mL.
Alcohol intoxication is characterized by slurred speech, incoordination,
unsteady gait, nystagmus, lethargy, and facial fl ushing. The differential diagnosis
is extensive: head injury, hypoglycaemia, post-ictal confusional states, hepatic
encephalopathy, meningitis, encephalitis, or intoxication with other drugs. In
most patients these conditions can be excluded by examination and simple
investigations (although some not infrequently coexist with acute alcohol
intoxication — especially head injury and hypoglycaemia).
Management
Aim to discharge conscious, ambulant patients who exhibit uncomplicated
acute alcohol intoxication if accompanied by a responsible adult.
Violent patients who appear intoxicated require examination prior to
escort from the ED by police. As a minimum, perform a brief neurological
examination, simple observations and BMG.
Comatose patients are a medical emergency. Protect the airway
and anticipate vomiting (recovery position may be useful). Exclude
hypoglycaemia and other metabolic causes of coma. Exclude head or
neck injury, and adopt a low threshold for X-ray and/or CT scanning.
Close observation is mandatory.
Alcohol-induced hypoglycaemia particularly affects chronic alcoholics
and children. It also occurs in binge drinkers who present with alcoholic
ketoacidosis. Hypoglycaemia can occur during intoxication and up to 24hr
after. In children, fi ts may result.
Coagulation disorders often occur in chronic alcoholics with liver damage.
Consider this in patients presenting with GI haemorrhage or head injury.
Table 14.5 Effects of various concentrations of alcohol
Blood alcohol concentration
(mg/100mL = mg/dL)
Effects
30–50 Measurable impairment of motor skills
50–100 Reduced inhibitions, ‘excitant effect’
100–150 Loss of co-ordination and control
150–200 ‘Drunkenness’, nausea, ataxia
200–350 Vomiting, stupor, possible coma
350 + Respiratory paralysis, possible death

624 CHAPTER 14 Psychiatry
Alcohol withdrawal
‘Simple’ alcohol withdrawal
Uncomplicated alcohol withdrawal is common, usually starting within 12hr
of stopping (or reducing) alcohol intake. Withdrawal symptoms often
commence before alcohol is completely cleared from the blood. Features
include anxiety, restlessness, tremor, insomnia, sweating, tachycardia,
and ataxia. Simple withdrawal can be managed on an outpatient or day
patient basis. It may be appropriate to commence treatment in the ED for
uncomplicated withdrawal (eg diazepam 5–10mg PO or chlordiazepoxide
10–30mg), but continuing treatment should not be prescribed by ED staff.
Inpatient detoxifi cation is indicated for those with a history of withdrawal
seizures, delirium tremens or with withdrawal symptoms who are being
admitted for other problems. The revised Clinical Institute Withdrawal
Assessment for Alcohol (CIWA-Ar) Score assesses 10 clinical signs of
withdrawal and may help to guide treatment ( www.agingincanada.ca/
CIWA.HTM ). Note: alcoholics admitted with ‘simple’ withdrawal may be
thiamine defi cient, and need parenteral and/or oral thiamine.
Delirium tremens
Occurs in a small minority of alcoholics who undergo withdrawal and
carries a signifi cant mortality. It typically starts > 48hr after stopping
drinking. As well as ‘simple’ withdrawal, there may be signifi cant auto-
nomic hyperactivity, with tachycardia, hyper-refl exia, hypertension, fever,
visual or tactile hallucinations, sinister delusions, disorientation, and confu-
sion. Deaths occur from arrhythmias (secondary to acidosis, electrolyte
disturbance, or alcohol-related cardiomyopathy), infection, fi ts or cardio-
vascular collapse. Monitor closely, check BMG, give IV diazepam as appro-
priate (especially for fi ts) and refer to the medical team/HDU.
Alcohol withdrawal fi ts
These typically comprise self-limiting grand mal seizures which occur
hours or days after the last alcoholic drink. Check BMG and treat fi ts in
a standard fashion ( b Seizures and status epilepticus, p.149). Examine
carefully for possible head injury.
Alcoholic ketoacidosis
This can occur when an alcoholic stops drinking, vomits repeatedly and
does not eat. Ketoacidosis develops from fatty acid breakdown, compli-
cated by dehydration from vomiting. The patient usually presents 1–2 days
after the last binge with vomiting, signs of chronic alcohol abuse and a
high anion gap metabolic acidosis. Arterial blood gas (ABG) may reveal
d p CO
2
, d HCO
3
–
, normal p O
2
. pH is variable because metabolic acidosis
may be altered by metabolic alkalosis from vomiting and possibly respi-
ratory alkalosis. Plasma ethanol is low or absent. Differential diagnosis
includes salicylate, methanol and ethylene glycol poisoning ( b p.203).
Give IV 0.9 % saline with 5 % glucose and thiamine supplementation,
whilst monitoring U&E, glucose. Refer to the medical team and consider
HDU/ICU.

625
HELP FOR ALCOHOLICS
Alcohol-related brain injury
Wernicke Korsakoff syndrome develops in problem drinkers who are
thiamine defi cient. Autopsy analysis suggests that the syndrome may occur
in as many as 12.5 % of chronic alcohol misusers. A presumptive diagnosis
of the Wernicke Korsakoff syndrome may be made in patients with a
history of alcohol misuse and one or more of the following unexplained
symptoms: ataxia, ophthalmoplegia, nystagmus, confusion, memory distur-
bance, reduced conscious level, hypotension, and/or hypothermia.
Wernicke’s encephalopathy
This is characterized by degenerative changes surrounding the third
ventricle and aqueduct, particularly the mammillary bodies. It presents
with an acute confusional state, nystagmus, ophthalmoplegia, ataxia, and
polyneuropathy. Ataxia typically affects the trunk and lower extremities.
Clinical abnormalities may develop acutely or evolve over several days.
Initial treatment involves parenteral thiamine (eg Pabrinex
®
10mL as an IV
infusion in 100mL 0.9 % saline over 30min). Note that this may occasionally
cause anaphylaxis, so ensure that resuscitation facilities are available.
Subsequent treatment involves oral thiamine.
Korsakoff’s psychosis
This is an amnesic state with profound retrograde and anterograde
amnesia, but relative preservation of other intellectual abilities. It typically
develops after Wernicke’s encephalopathy, but some patients develop
a combined syndrome from the outset with memory loss, eye signs and
unsteadiness but without confusion.
Treat with parenteral thiamine and admission as for Wernicke’s
encephalopathy.
Help for alcoholics
The relatively regular contact between those with alcohol problems and
EDs may be viewed as an opportunity to offer intervention. There is good
evidence to suggest that brief interventions may reduce alcohol consump-
tion and the risk of physical harm. Consider the 1min Paddington Alcohol
Test to help patients who present with alcohol-related problems ( http://
alcalc.oxfordjournals.org/cgi/reprint/44/3/284 ).
The following organizations may help:
Alcoholics Anonymous ( www.alcoholics-anonymous.org.uk ), plus local
networks and telephone numbers.
Al-Anon for relatives telephone number 020 7403 0888 (and websites
www.al-anonuk.org.uk and www.al-anon.alateen.org ).

626 CHAPTER 14 Psychiatry
Drug and substance abuse
Drug users present to the ED at times of crisis (eg acute intoxication,
overdose, withdrawal or other medical complications of drug use). Do
not assume all drug users present to the ED simply to obtain drugs. Find
out about local addiction services and how referrals are made. Direct
those seeking help with a drug problem to the appropriate services. Know
local preferred drugs of abuse and the preferred methods of taking them.
Find out what terminology is used locally for each substance.
Do not supply drugs of dependence to addicts. Prescriptions are carefully
controlled by addiction services and pharmacists. Elaborate tales of lost
or stolen drugs/prescriptions are invariably false.
Manage painful conditions in drug addicts as for other patients. Do
not withhold analgesia if in obvious pain. For minor complaints, simple
analgesia is as effective as in non-drug users. Do not dismiss symptoms
simply because the patient is a drug user. Even drug abusers get acute
appendicitis and other common acute illnesses.
Intoxication
As with alcohol, mild cases require little intervention. Observation by a
responsible adult or briefl y in a ward usually suffi ces. Discharge patients
when ambulant and fully orientated, having excluded serious problems.
Glue and solvents Users may smell of substances or have them on their
clothes or skin. There may be a perioral rash. Intoxication produces
euphoria, agitation or drowsiness, slurred speech, and unsteady gait.
Benzodiazepines and CNS depressants Mild intoxication is similar to that
with alcohol. i intoxication produces nystagmus, diplopia, strabismus,
hypotonia, clumsiness, and moderately dilated pupils.
Amphetamines, ecstasy, cocaine and mephedrone Produce hyperstim-
ulation, restlessness, pyrexia and sympathomimetic effects. Cocaine
effects occur more rapidly. Severe cases exhibit paranoia, violent
behaviour or seizures. Cocaine may also cause chest pain, arrhythmias or
even MI. Ecstasy can cause an idiosyncratic reaction similar to malignant
hyperthermia (see b Illicit drugs, p.214).
Overdose
Protect the airway, provide oxygen (O
2)
as required and exclude hypogly-
caemia or serious injury in all cases.
Opioid overdose is often inadvertent, either from use of unusually pure
drugs or after a period of abstinence (tolerance is d ). Characteristic signs
are coma with pinpoint pupils and respiratory depression (see b p.188).
Pulmonary oedema, hypothermia and rhabdomyolysis can occur. Hypoxia
may cause dilated pupils. If opioid overdose is suspected, give naloxone
0.4–0.8mg IV, repeated according to response. See b Antidotes to poisons
(b p.186) for further detail regarding treatment. Remember to ensure that
the patient is observed for at least 6h after the last dose of naloxone.
Intentional overdose requires assessment of suicide risk ( b p.614) and
mental capacity in case the patient threatens to leave against advice.

627
DRUG AND SUBSTANCE ABUSE
Skin complications
SC drug injection (‘skin popping’) can cause cellulitis, abscesses, extensive
skin necrosis, necrotizing fasciitis, tetanus, botulism and anthrax. Refer for
formal exploration, drainage and follow-up by the surgical team for all
but the most minor infections. Apparently ‘simple’ abscesses may extend
deeply into muscle or form part of a false aneurysm! Needle fragments
rarely require removal unless they embolize (eg to the lungs).
Anthrax in drug users
After an outbreak of anthrax in heroin users in Scotland in 2010, Health
Protection Scotland ( www.hps.scot.nhs.uk ) advised doctors to suspect
anthrax in a drug user presenting with any of the following:
• Severe soft tissue infection and/or signs of severe sepsis/meningitis.
• Clinical features of inhalational anthrax ( b p.233).
• Respiratory symptoms + features of meningitis or intracranial bleeding.
• GI symptoms (eg pain, bleeding, nausea, vomiting, diarrhoea, ascites).
Approach
Get expert help early to advise on management (ICU, surgeons, micro-
biology, Public Health, hospital infection team). Start IV antibiotics
according to advice (eg combination of ciprofl oxacin, clindamycin + peni-
cillin or if there is soft tissue infection: ciprofl oxacin, clindamycin, peni-
cillin, fl ucloxacillin + metronidazole). Experts will advise on whether to
use anthrax immune globulin intravenous (human) antitoxin.
Vascular complications
IV injection (‘mainlining’) of drugs causes phlebitis, DVT, and bacterial
endocarditis. Chronic injectors may resort to neck or groin vessels (the
femoral artery being commonly damaged). Arterial injection can cause
false aneurysms, fi stulae, or peripheral emboli. Occasionally, IV drug users
present with massive and devastating blood loss from an injection site
(particularly the groin): apply fi rm pressure, resuscitate with IV fl uids ±
blood and call for the surgical team.
Inadvertent arterial injection of poorly soluble preparations causes severe
limb pain, skin pallor and mottling with paraesthesiae in the presence of
palpable (often bounding) peripheral pulses. Diffuse soft tissue damage
may result in compartment syndromes, rhabdomyolysis, renal failure, and
irreversible limb damage necessitating amputation.
Orthopaedic complications
Injecting drug users who present with acutely painful joints (especially hip
joints) may have septic arthritis. Clinical and radiological evidence may be
minimal, so adopt a high index of suspicion. Provide analgesia, take blood
cultures, and FBC, and admit for joint aspiration and IV antibiotics.
Drug withdrawal states
Sometimes drug users present to hospital with overt evidence of drug
( ± alcohol) withdrawal. It can be diffi cult to judge whether the problem
is due to drug intoxication, drug-related (eg stimulant induced psychosis,
‘panic reaction’), drug withdrawal, or to coexistent disease. Observe
and monitor closely — treat symptomatically (eg with small doses of oral
benzodiazepines as necessary) and refer to the medical team.

628 CHAPTER 14 Psychiatry
Compulsory hospitalization
Compulsory detention of patients in the UK requires the patient to be both:
• Suffering from a mental disorder (mental illness or handicap).
• Requiring emergency hospital admission to protect the health or safety
of the patient or for the protection of others.
Emergency detention under mental health legislation does not allow
treatment for psychiatric illness. Emergency treatment of psychiatric or
physical illness is carried out under common law . In this situation, there
must be an immediate threat to life or serious danger to the patient or
others, if treatment is not given. For this reason, mental health legislation
cannot be used to impose emergency treatment without patient consent.
Note that ED patients are not legally inpatients until they go to a ward.
Detention of psychiatric emergencies in the ED
England and Wales
Section 2 is used most commonly in the ED. It requires recommendations
from 2 doctors to be accepted by an approved social worker and allows
detention for up to 28 days for assessment and treatment.
Scotland
The Mental Health (Care and Treatment) (Scotland) Act 2003 came into
effect in 2005 — see www.nes-mha.scot.nhs.uk/ . Part 5 of the Act enables
a fully registered medical practitioner to grant an emergency detention
certifi cate that authorizes managers of a hospital to detain someone for
72hr. Before granting an emergency detention certifi cate, the medical
practitioner also needs to consult and gain the consent of a mental health
offi cer, unless impracticable. The patient is then examined by an approved
medical practitioner (psychiatrist), who if not satisfi ed that the relevant
criteria are met, cancels the certifi cate.
Northern Ireland
Mental Health (Northern Ireland) Order 1986, Part II.
Article 4 — Admission for assessment of mental disorder.
• Requires 2 or 3 doctors including the responsible medical offi cer (RMO)
— in charge of patient’s treatment.
• Application by nearest relative or an approved social worker.
• Lasts 7 days, renewable up to 14 days.
• Lasts until discharge by RMO board or nearest relative or until detained
under article 12.
Section 136 (England)
This allows a police offi cer to detain someone in a public place when he/
she appears to be mentally disordered and is causing a disturbance. The
police offi cer’s responsibility is to take the detained person to a ‘place
of safety’ (usually a police station or psychiatric ward) where he/she is
assessed by a psychiatrist and approved social worker.
The Mental Health Act (Scotland) 2003 provides police offi cers in Scotland
with similar powers: a police constable may remove a person to a place of
safety from a public place, if a mental disorder is suspected and it is also
suspected that the person needs immediate care and treatment.

629
MENTAL CAPACITY ACT
Mental Capacity Act
The Mental Capacity Act 2005 (MCA) offers a comprehensive framework
for decision-making on behalf of adults aged > 16 years lacking capacity to
make decisions on their own behalf. It only applies in England and Wales.
Defi ning capacity
A person lacks capacity if, when a decision needs to be made, they are
unable to make or communicate the decision because of an ‘impairment
or disturbance of the mind or brain’. There is a 2-stage test of capacity:
• Is there an impairment of, or disturbance in the functioning of, the
person’s mind or brain? If so,
• Is the impairment or disturbance suffi cient that the person lacks the
capacity to make that particular decision?
Five statutory principles
• Capacity must be assumed unless it is established to be lacking.
• A person is not being treated as unable to make a decision unless all
practicable steps to help him do so have been taken without success.
• A person should not be treated as unable to make a decision merely
because he makes an unwise decision.
• A decision made, or action performed, for or on behalf of a person who
lacks capacity must be taken in his/her best interests.
• Before a decision is made or an action performed, consideration must
be given to whether the purpose for which it is needed can be as effec-
tively achieved in a way that is less restrictive of the person’s rights and
freedom of action.
Assessment of capacity
A person lacks capacity if he/she fails:
• To understand the information relevant to the decision.
• To retain the information relevant to the decision.
• To use or weigh the information.
• To communicate the decision (by any means).
Admission and treatment
Patients can be admitted and treated under the Mental Capacity Act 2005
only if 6 qualifying safeguards are met:
• The person is at least 18 years old.
• The person has a mental disorder.
• The person lacks capacity to decide whether to be in hospital or care
home for the proposed treatment or care.
• The proposed deprivation of liberty is in the person’s best interests and
it is necessary and proportionate response to the risk of harm.
• The person is not subject, or potentially subject, to specifi ed provisions
of the Mental Health Act in a way that makes them ineligible.
• There is no advance decision, or decision of an attorney or deputy
which makes the proposed deprivation of liberty impossible.
In other circumstances, consider using the Mental Health Act 1983 to
admit mentally disordered patient who lack capacity to consent.

Chapter 00
630
The paediatric environment 632
Primary assessment and resuscitation of the sick child 634
Standard immunization schedule 636
Venous access and venepuncture 638
Intra-osseous infusion 640
Resuscitation of the newborn 642
Cardiopulmonary resuscitation of the newborn 644
Paediatric basic life support 646
Choking from a foreign body 648
Anaphylaxis in children 650
Paediatric advanced life support 652
Paediatric advanced life support notes 654
Children with abnormal heart rates or rhythms 656
Sudden infant death syndrome (SIDS) 658
Problems of neonates and infants 660
Skin problems in infants 662
The febrile child 663
Purpuric rashes 664
Paediatric emergencies
Chapter 15
Paediatric problems also covered elsewhere in this book:
b Consent
28
b Poisoning 179
b Incubation periods of infectious diseases 220
b Childhood infectious diseases 222
b Meningitis 224
b Gastroenteritis/food poisoning 226
b Infestations 230
b Analgesia in specifi c situations 280
b Nasal diamorphine 281
b Local anaesthesia in children 287
b Sedation 309
b Instructions after minor head injury 367
b Tetanus prophylaxis 410
b Earache 550
b Sore throat 554

631
Meningococcal disease 666
How to perform a lumbar puncture 670
Skin lesions in multisystem disease 672
Paediatric ENT problems 674
Stridor: upper respiratory infections 676
Severe acute asthma in children 678
Acute bronchiolitis 682
Whooping cough
ND
684
TB
ND
and cystic fi brosis 685
Pneumonia 686
Fits, febrile convulsions, and funny turns 688
Status epilepticus 690
Diabetic ketoacidosis 691
Urinary tract infection (UTI) 692
Renal failure 694
Haematuria 695
Poisoning in children 696
Prevention of paediatric poisoning 697
Abdominal pain in children 698
Inguinal and scrotal swellings 700
Foreskin problems and zip entrapment 702
The limping child 704
The painful hip 706
Osteochondritis 708
Major paediatric trauma 710
Injury prevention 711
Resuscitation of the injured child 712
Considerations in paediatric trauma 714
Head injuries in children 716
Paediatric fractures and dislocations 718
Approach to limb injuries in children 720
Paediatric upper limb injuries 722
Paediatric lower limb injuries 726
Child abuse 728
Presentation of child abuse 730
Management of child abuse 734
Paediatric emergencies
Chapter 15

632 CHAPTER 15 Paediatric emergencies
The paediatric environment
Dealing with children
Children are not little adults. They differ from adults anatomically, physi-
ologically, emotionally, and in the spectrum of pathological conditions
to which they are susceptible. It is natural for those hospital staff who
have not previously dealt with children to be slightly apprehensive about
treating them, particularly when they are distressed or seriously unwell.
Be guided by more experienced staff, who are often adept at dealing
with children as patients (and very often as parents as well). Such staff
are particularly good at recognizing children who are seriously unwell —
listen carefully to what they have to say. There is no substitute for expe-
rience, but practical courses aimed at managing emergencies in children
(eg Advanced Paediatric Life Support (APLS)) are highly recommended.
These courses deservedly devote much time to the recognition of seriously
ill or injured children, according to whether or not they are physiologically
deranged. Consider each child according to expected ‘normal’ physiological
values (see Table 15.1 ).
Children do not always respond in the same way to illness as adults. They
are particularly likely to be frightened of doctors, nurses, and hospitals.
Do not waste the opportunity to make important observations (respi-
ratory rate, pattern, and effort, behaviour, conscious level, colour, and
parental interaction). Spend time talking to children to reassure them
and win their confi dence before starting any examination or performing
any procedure (unless, of course, they require emergency resuscitation).
Lowering yourself to their physical level will make you less intimidating.
Involve the parents from the start (see below). Where appropriate, allow
children to relax and play with toys. Play therapists can be particularly
helpful providing distraction during procedures.
Dealing with parents
Parents are patients too. They are likely to be understandably upset and
worried. Take time to explain to the parents exactly what is happening
to their children at all stages. Obtain appropriate consent, but do not
delay life-saving measures. For the sake of both parents and children, try
to allow parents to remain with their children as much as possible. This is
especially important during resuscitation where an experienced member
of the nursing staff should be allocated to look after and explain to parents
what is happening. If the presence of the parents is impeding the progress
of the resuscitation, gently ask them to leave.
Analgesia
Differences between adults and children do not diminish the need to
provide adequate analgesia for children. Reassurance is often an important
component, but be honest and do not be tempted to tell to a child that a
painful procedure (eg emergency insertion of an intravenous (IV) cannula)
will not produce any pain or discomfort — this will simply cause the child
to lose confi dence.

633
THE PAEDIATRIC ENVIRONMENT
Weight estimation
All children should be weighed when they require treatment in the ED.
This is as important as the vital signs in children. In an emergency, use a
Broselow tape or one of the formulae for estimating children’s weight.
The following formula estimates a child’s weight based upon age (between
1 and 10 years):
weight in kg = (age in years + 4) × 2
so a 6-year old child will weigh:
(6 + 4) × 2 = 20kg
This formula often underestimates the weight of many children in the
UK or other developed countries but it may overestimate the weight of
children from other regions. A formula using mid-arm circumference
(MAC) has been developed in Asia
1
and is:
weight in kg = (mid-arm circumference in cm – 10) × 3
so a child with a 15cm MAC will weigh: (15 – 10) × 3 = 15kg.
Drug doses
Do not estimate ‘rough doses’ of drugs for children based on knowledge
of adult doses. Instead, use the weight and age of a child, together with a
reference source (eg BNF for Children http://bnfc.org/bnfc ) to determine
the appropriate dose.
Preparation for resuscitation
Find out where the paediatric resuscitation equipment is kept and how it
works. Learn the paediatric resuscitation guidelines and practice basic life
support (BLS) and other procedures on manikins. Ask your local resuscitation
offi cer for help with training. Knowledge of normal (expected) physiology at
various ages will help you to evaluate sick children in the ED.
1 Cattermole GN et al . Mid-arm circumference can be used to estimate children's weights .
Resuscitation . 2010 . Available at: http://dx.doi.org/10.1016/j.resuscitation.2010.05.015 .
PMID: 20619953 .
Table 15.1 Normal (expected) physiological values at different ages
*
Age (years) Respiratory rate Heart rate Systolic BP
<1 30–40 110–160 70–90
1–2 25–35 100–150 80–95
2–5 25–30 95–140 80–100
5–12 20–25 80120 90–110
> 12 15–20 60–100 100–120
Expected systolic BP = 80 + (age in years × 2) mmHg.
*
Adapted from APLS.

634 CHAPTER 15 Paediatric emergencies
Primary assessment and resuscitation
of the sick child
Caring for a sick child is a daunting task. Get experienced help early; call
for senior ED, paediatric, and ICU/PICU help if you are alerted that a sick
or injured child is being brought to the ED.
Perform a primary assessment of Airway, Breathing, Circulation, and
Disability to identify and treat life-threatening problems as they are found
in order to maintain vital functions before disease specifi c therapies
are started. Early recognition and treatment is essential to avoid cardio-
respiratory arrest with its poor outcome.
Airway
Assess patency by looking, feeling, and listening.
Resuscitate: if there is no air movement, perform chin lift or jaw thrust.
If there is still no evidence of air movement, give rescue breaths using an
appropriately-sized bag-valve-mask device. If the child is breathing, listen
for stridor, and look for recession.
Breathing
Assess the effort of breathing by measuring the respiratory rate, looking
for intercostal recession and accessory muscle use, and listen for gasping,
stridor, wheeze, and grunting.
Assess the effi cacy of breathing by looking for chest expansion, auscultation
of the chest, and measuring SpO
2
.
Assess the effects of respiratory failure by assessing mental status and
by measuring the heart rate (increases with hypoxia, but bradycardia is
a pre-terminal sign) and examining skin colour (hypoxia causes pallor,
cyanosis is a late sign). Reduced breathing effort may indicate exhaustion
(a pre-terminal sign), cerebral depression, or neuromuscular disease.
Resuscitate : give high fl ow O
2
to any child with respiratory diffi culty or
hypoxia. If respiration is inadequate, support with basic airway care and
bag valve mask ventilation and get senior ED/ICU/PICU help to provide a
defi nitive airway (tracheal intubation and IPPV).
Circulation
Assess heart rate (bradycardia is a late sign of cardiovascular failure) pulse
volume, capillary refi ll, BP (hypotension is a pre-terminal sign), skin tem-
perature. Look for the effects of circulatory failure: tachypnoea, mottled
cold skin, poor urine output, agitation, and drowsiness.
Resuscitate: give high fl ow oxygen (O
2
) to all shocked patients. Gain IV/IO
access, take blood samples and give 20mL/kg of crystalloid. Re-assess and
repeat if necessary.

635
PRIMARY ASSESSMENT AND RESUSCITATION OF THE SICK CHILD
Disability
Any problem with ‘ABC’ can affect ‘D’.
Assess conscious level. Initially, categorize according to AVPU scale:
A — Alert
V — responds to Voice
P — responds to Pain
U — Unresponsive
Check pupil size, reaction and equality.
Assess GCS (or children’s equivalent — see b Head injuries in children,
p.716) and posture (fl oppy, decerebrate, decorticate, etc.). Check BMG.
Resuscitate: a child who does not respond to voice has an urgent need
to secure the airway. Treat hypoglycaemia and fi ts, and get senior help
urgently.
After initial evaluation and intervention, a more detailed approach to iden-
tify specifi c problems should follow. Re-assess ABCD frequently to assess
progress and detect deterioration. Undertake a secondary assessment by
obtaining a full history (from parents, paramedics, teachers and witnesses)
and undertaking a detailed physical examination.
636 CHAPTER 15 Paediatric emergencies
Standard immunization schedule
The UK Department of Health actively encourages immunization for
children according to the standard schedule shown below.
1
The recom-
mended timing of the early immunizations is a compromise between
trying to protect children whilst they are at most risk and delaying it until
immunization is likely to be most effective. Children who have completed
a course of immunization against a particular disease are obviously less
likely to present with that disease. Unfortunately, a signifi cant proportion
of children are still not receiving standard vaccines (Table 15.2 ). Carefully
enquire exactly which immunizations the child has received (information
is often available from the child’s GP or health visitor). Failure to follow
the recommended schedule may result in the child presenting with an
otherwise unusual disease.
The Hib vaccine
Haemophilus infl uenzae , a small Gram –ve bacillus, has been responsible
for the deaths of many young children. Type b has been implicated most
frequently in serious paediatric disease, causing meningitis, pneumonia,
cellulitis, and most, particularly, acute epiglottitis. The Haemophilus B
(‘Hib’) vaccine has dramatically reduced the incidence of epiglottitis.
Pneumococcal vaccine
This was introduced as routine in the UK in 2006.
1 Department of Health . Immunization against infectious disease - 'The Green Book' . HMSO,
London , 2007 . Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/
PublicationsPolicyAndGuidance/DH_079917 . See also: BNFC .
Table 15.2 Standard childhood vaccines
Age Vaccine
2 months Diphtheria, tetanus, pertussis, polio, Hib, pneumococcal
3 months Diphtheria, tetanus, pertussis, polio, Hib, meningitis C
4 months Diphtheria, tetanus, pertussis, polio, Hib, pneumococcal, meningitis C
12 months Hib, meningitis C
13 months Measles, mumps, rubella, (MMR), pneumococcal
3–5 years Diphtheria, tetanus, pertussis, polio, MMR
13–18 years Tetanus, diphtheria, polio
* May also be given in infancy, if appropriate.
637
STANDARD IMMUNIZATION SCHEDULE
Reactions to immunizations
Vaccination is frequently wrongly blamed for symptoms caused by
incidental viral illness. However, mild reactions, such as swelling and ery-
thema at the injection site, are relatively common following administration
of a variety of immunizations. These respond to symptomatic treatment
and an expectant approach. Severe anaphylactic reactions, involving
airway obstruction or circulatory collapse are uncommon, but require
prompt and aggressive treatment ( b Anaphylaxis, p.42).
Immunization in other countries
If a child who normally lives outside the UK attends the ED, enquire
carefully about their vaccination history. Likewise, if you are working
outside the UK, make sure you know the local immunization schedule as this
can have a signifi cant impact on the type of communicable disease seen,
particularly in children.
Immunization in the ED
If a child attending the ED has not been immunized against diphtheria,
tetanus, and pertussis and needs tetanus immunization, give the ‘triple
vaccine’ (DPT) to avoid repeated injections. Inform the GP about any
immunizations given.
1 See: Illingworth RS. The Normal Child . 10th edn. Churchill Livingstone, Edinburgh, 1991.
Table 15.3 Paediatric milestones
1
(after allowance for preterm delivery)
2 months Eyes follow movement. Smiles and makes noises when talked to
3 months Holds object placed in hand
3–4 months Turns head to sound
6 months Sits on fl oor with hands forwards for support
Transfers object from one hand to the other
9–10 months Crawls
12 months Walks with one hand held; says 2 or 3 words with meaning
13 months Walks unaided
18 months Makes tower of 2 or 3 bricks
21–24 months Joins 2 or 3 words together to make sentence
2 years Can build a tower of 6 or 7 bricks
2½ years Knows full name and gender; can stand on tiptoes

638 CHAPTER 15 Paediatric emergencies
Venous access and venepuncture
Venepuncture
Needles frighten children. Topical anaesthetic cream (eg tetracaine —
b p.288) is useful whenever the need for blood sampling is not urgent. 4 %
tetracaine (Ametop
®
, amethocaine) anaesthetizes the skin and d pain, but
should be applied for 30min before venepuncture and for 45min before can-
nulation. Identify prominent veins at 2 separate sites, apply cream and cover
with an adhesive fi lm dressing, then let the child play.
As in adults, if an IV cannula is inserted, it should be possible to obtain
samples of blood via this: even if aspiration fails, blood will often drip out.
The amount of blood sampled depends upon the size of the child and
laboratory requirements, remembering that total blood volume is only
80mL/kg. Check requirements and obtain the appropriate bottles before
attempting venepuncture.
Neonates FBC and U&E can be performed on capillary samples obtained
from heel pricks. Ask an assistant to hold the foot and ankle fi rmly to
encourage venous engorgement, then smear white soft paraffi n on the
heel and prick it with a lancet. Collect drops of blood into prepared
capillary sample tubes.
Toddlers and infants Aspirate via a 23G butterfl y needle in the hand or
forearm. This allows the needle to stay in the vein, despite the child
moving. Samples of 1mL are usually required.
Older children Use a 21G butterfl y needle.
IV cannulae
The route chosen to obtain venous access will depend upon the available
veins and urgency of the problem. First attempt to insert an IV cannula
percutaneously into an upper limb vein. Once inserted, fl ush the cannula,
then secure it with adhesive tape, a splint, and bandage. In general, the fol-
lowing sizes of cannulae are appropriate:
• 24G (orange/yellow) : neonates and infants.
• 22G (blue) : toddlers and small children.
• 20G (pink) or 18G (green) : older children.
Smaller cannulae are designed so the needle does not protrude much
beyond the end of the cannula. This means that once a ‘fl ashback’ is
obtained, the tip of the cannula may already be within the vein: advancing
the needle further may puncture the other side of the vein and exit it. If
attempts to insert a cannula into the hand or arm fail, it may be possible
to use veins in the feet, ankle, or in the scalp (useful in neonates, but fi rst
ensure that the intended target is not the superfi cial temporal artery). In
an emergency, allow a maximum of 90sec and if still unsuccessful then gain
intra-osseous access ( b p.640), which is quick, easy, and reliable. Other
venous access routes (eg central, femoral) require specialist training, are
time-consuming and are associated with signifi cant complications (see
opposite). Give fl uids by infusion pump or paediatric infusion set to avoid
over-transfusion.

639
VENOUS ACCESS AND VENEPUNCTURE
Other routes of venous access
Femoral lines The femoral vein lies medial to the artery in the groin.
It allows rapid venous access to be obtained and is particularly useful in
cardiac arrest where physical constraints (eg several resuscitating staff)
restrict access to the neck. Complications include sepsis (use strict aseptic
technique), i risk of thrombosis and damage to other structures including
the hip joint.
External jugular vein cannulation is an option in children in whom spinal
injury is not a concern. Place the child 15–30 ° head down and turn
the neck to one side. The vein runs superfi cially and caudally over the
sternocleidomastoid at the junction of its middle and lower third. Ask an
assistant to compress the vein distally to distend and immobilize it.
Central venous access The techniques (and complications) are similar to
those in adults ( b p.56), except that smaller equipment is needed. The
safe insertion of central lines in children requires considerable experience
and training, and often requires ultrasound guidance, which is sometimes
unavailable in a resuscitation situation. Other routes are usually more
appropriate during resuscitation.
‘Cut downs’ (eg long saphenous vein at the ankle) may be performed during
resuscitation, but can be time-consuming. In infants, the long saphenous
vein is located half a fi nger breadth superior and anterior to the medial
malleolus. For children it is one fi nger breadth superior and anterior to
the medial malleolus.
Umbilical venous access can useful in newborn resuscitation ( b p.645).

640 CHAPTER 15 Paediatric emergencies
Intra-osseous infusion
If urgent venous access is required, but not obtained within 90sec by per-
cutaneous venous puncture, strongly consider using the intra-osseous
route. Fluid and drugs given into the medullary cavity of long bones
rapidly reach the central venous circulation. Gaining intra-osseous access
is reasonably easy and can be performed quickly. It is particularly useful in
young children, but may be used in all ages, including adults.
Indications include major burns and trauma, cardiac arrest, and septic
shock.
Contraindications include infection or fracture at (or proximal to) the
insertion site, ipsilateral vascular injuries, multiple unsuccessful attempts,
osteogenesis imperfecta, osteopetrosis.
Equipment Intra-osseous needles are usually of 16–18G and have a central
metal stylet attached to a handle. A battery powered mechanical driver
(EZ-IO) with paediatric or adult intra-osseous needles is available and
can be used to insert the needle to a specifi c depth, possibly reducing
complications such as compartment syndrome. It can be used in children
weighing more than 3kg.
Site of insertion First choice is the proximal tibia 2.5cm below the tibial
tuberosity on the fl at anteromedial surface (thus avoiding the epiphyseal
growth plate). If this route is not available, because of local infection
or trauma, use the distal tibia (proximal to the medial malleolus), distal
femur (3cm above the lateral lower femoral condyle on the anterolateral
surface), or the anterolateral proximal humerus at the greater tuberosity
(Fig. 15.1 ).
Manual intra-osseous needle insertion technique
• Support the limb on a pad or blanket.
• Sterilize the skin and use an aseptic technique. A small skin incision may
be needed.
• Firmly grasp the handle and use a twisting motion to advance the needle
and stylet through the cortex of the bone. (Note that some intra-
osseous needles are designed with a thread and so require a rotatory,
not an oscillatory, action).
• Aim at 90 ° to the bone surface, or slightly away from the epiphyseal
growth plate. Stop when the slight ‘give’ of the medullary cavity is felt.
• Remove the stylet and try to confi rm correct placement by aspirating
bone marrow (use this to check BMG or cross-match).
• If aspiration is not possible, the needle may still be correctly positioned:
attach a primed 3-way tap with extension set and fl ush the needle and
3-way tap with 10mL of 0.9 % saline, and ensure that there is no swelling
of the surrounding soft tissues.
• Although connecting it to IV tubing and a pressurized infusion bag may
work, it is often much more effective in children to give drugs and fl uid
by boluses using 20mL syringes and the 3-way tap).
• If necessary, immobilize with a plaster of Paris (POP) backslab applied
carefully to the posterior leg (eg for transport to a PICU).
641
INTRA-OSSEOUS INFUSION
Mechanical intra-osseous needle insertion technique
• Support the limb on a pad or blanket.
• Use a 15mm needle for patients weighing 3–39kg; a 25mm needle for
patients more than 39kg; and a 45mm needle for obese adult patients.
• Identify the insertion point and place the needle, loaded into the
mechanical driver (drill), at the insertion point.
• Insert the needle, perpendicular to the skin, up to the 5mm line.
• Remove the driver and stylet, attach a primed 3-way tap with extension
set and fl ush the needle and 3-way tap with 10mL of 0.9 % saline.
• Attach the giving set and secure as for manually inserted intra-osseous
needles.
Use the blood taken from an intra-osseous needle for BMG or cross
matching, but not for FBC (automated blood counters may give spurious
results). If using an intra-osseous needle in responsive patients, infi ltrate
1 % lidocaine into the skin before insertion, and consider administering
1–2mL of 2 % lidocaine slowly into the needle before beginning the infusion
to minimize pain (maximum 3mg/kg lidocaine in children).
Complications of intra-osseous access
• Extravasation of fl uid and compartment syndrome.
• Infection (cellulitis or osteomyelitis).
• Iatrogenic fracture.
• Fat or bone micro-emboli.
• Fractures and/or epiphyseal growth plate injury.
Intra-osseous needles must be removed within 24hr to minimize the risk
of infection and other complications. Conventional IV access should be
secured as soon as possible after intra-osseous needle insertion.
Fig. 15.1 Tibial intra-osseous access.

642 CHAPTER 15 Paediatric emergencies
Resuscitation of the newborn
Neonatal resuscitation is usually undertaken by paediatricians, but
unexpected deliveries require other personnel to initiate resuscitation.
Fortunately, most newborn babies do not need resuscitation. The
discomfort of being born into a hostile environment provides the major
initial stimulus to breathe. Ideally, any baby requiring resuscitation should
be treated in a warm room with an overhead heater. Call urgently for
experienced help.
Approach (see Fig. 15.2 )
Make sure the cord is securely clamped and then dry the baby, remove
the wet towels and wrap the baby in dry towels. Very preterm babies
(<28 weeks) should be wrapped in food grade plastic as rapidly as
possible without drying. Assess colour, tone, breathing by chest movement
(auscultation at birth is unreliable), and heart rate (best assessed by steth-
oscope placed over the apex). Repeat assessments every 30sec during
resuscitation. Traditionally, an Apgar score (ranging from 0–10, based
upon assessment of heart rate, respirations, muscle tone, refl ex irrita-
bility, and colour) at 1 and 5min is calculated, and used to assess newborn
babies. However, do not delay resuscitation to calculate the score.
A healthy baby will have good tone, will cry within a few seconds of
delivery and have a heart rate of 120–150/min, and will become rapidly
pink during the fi rst 90sec.
Less healthy babies will have poorer tone, slower heart rates, and may not
establish adequate respiration by 90–120sec. The most sick will be pale,
fl oppy, apneic, and bradycardic.
Airway
Open the airway by placing the baby’s head in the neutral position (with
the neck neither fl exed nor extended). Because of the large occiput,
this will require a towel under the shoulders of the baby. Avoid hyper-
extension of the neck as this can occlude the pharyngeal airway. Very
fl oppy babies may also need either chin lift or jaw thrust. Remove visible
meconium or secretions using a paediatric Yankauer sucker.
Breathing
If the baby is not breathing adequately by 90sec, give 5 infl ation breaths
(pressures of 30cm water for 2–3sec). Ventilate a term baby with air,
but use oxygen for premature and/or hypoxic neonates. If the heart rate
increases, this indicates successful ventilation of the lungs. If the baby is
apnoeic, continue ventilation at 30–40 breaths/min until self-ventilating. If
the heart rate does not increase, then the most likely cause is that the
lungs have not been infl ated. Recheck head position and consider a jaw
thrust and longer infl ation time. If the airway is obstructed, consider an
oropharyngeal airway, laryngoscopy and suction. Repeat the 5 infl ation
breaths. If the heart rate remains <60/min or absent despite good chest
movement, start chest compressions.

643
RESUSCITATION OF THE NEWBORN
Dry the baby
Remove any wet towels and cover
Start the clock or note the time
Reassess heart rate every 30s
If heart rate is not detectable
or slow (<60 min
–1
)
consider venous access and drugs
Assess (tone), breathing and heart rate
If gasping or not breathing:
Open the airway
Give 5 inflation breaths
Consider SpO
2
monitoring
Re-assess
If no increase in heart rate
look for chest movement
When the chest is moving:
If heart rate is not detectable
or slow (<60 min
–1
)
Start chest compressions
3 compressions to each breath
Birth
30 s
60 s
AT
ALL
STAGES
ASK:
DO
YOU
NEED
HELP?
Acceptable*
pre-ductal SpO
2
2 min 60%
3 min 70%
4 min 80%
5 min 85%
10 min 90%
If chest not moving:
Recheck head position
Consider 2-person airway control
and other airway manoeuvres
Repeat inflation breaths
Consider SpO
2
monitoring
Look for a response
If no increase in heart rate
look for chest movement
Fig. 15.2 Algorithm for newborn life support. From Resuscitation Council (UK).
Newborn Life Support , 2010. See www.resus.org.uk
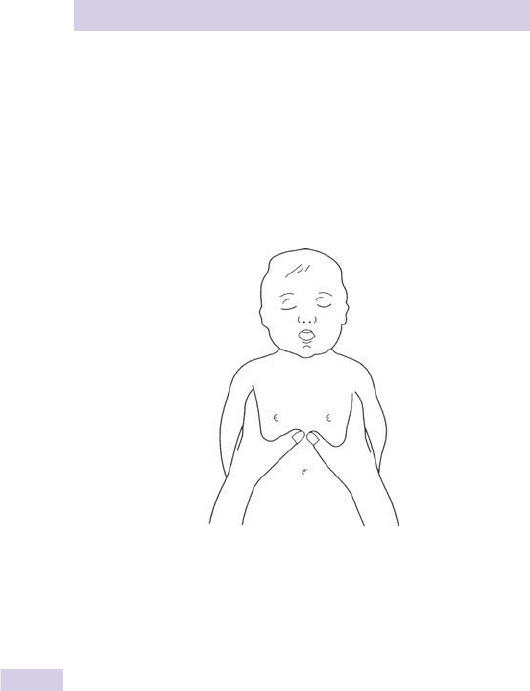
644 CHAPTER 15 Paediatric emergencies
Cardiopulmonary resuscitation of the
newborn
Chest compression (only to be started after successful lung infl ation).
Grip the chest in both hands in such a way that two thumbs can press on
the lower third of the sternum, (just below the intermammary line) with
the fi ngers over the spine at the back (Fig. 15.3 ). Aim for a rate of 100/min,
and to depress the antero-posterior (AP) diameter of the chest by a third.
Use a chest compression to infl ation ratio of 3:1 .
Tracheal intubation
Treat continuing apnoea with tracheal intubation using a 3mm tube
(2.5mm in premature babies). Precede intubation by pre-oxygenation with
bag valve mask ventilation for 30sec.
Drugs
Only use drugs if there is no signifi cant cardiac output despite effective
lung infl ation and chest compression. Give drugs intravenously via an
umbilical vein catheter or intra-osseous needle.
• Give adrenaline 10mcg/kg (0.1mL/kg of 1 in 10 000 if there is no initial
response. If this is ineffective the dose may be increased to 30 mcg/kg
(0.3mL/kg of 1 in 10 000).
• Give sodium bicarbonate 1–2mmol/kg (2–4mL of 4.2 % solution/kg) when
there is no cardiac output despite all resuscitative efforts or in profound
or unresponsive bradycardia.
• Hypoglycaemia is a potential problem for all newborns and BMG is
unreliable when reading <5mmol/L. Take blood sample to confi rm and
treat immediately with a bolus of 2.5mL/kg of 10 % glucose.
Usin
g
encirclin
g
fin
g
ers
Fig. 15.3 Method of CPR in the newborn.
645
CARDIOPULMONARY RESUSCITATION OF THE NEWBORN
• Suspect hypovolaemia if : very pale baby, pulseless electrical activity
(PEA), history of antepartum haemorrhage, placenta praevia, or vasa
praevia, or unclamped cord. Give 10mL/kg 0.9 % saline followed by
O –ve blood, repeated as necessary.
• Atropine and calcium have no role in newborn resuscitation.
Venous access — the umbilical vein
The easiest and fastest method of obtaining venous access in the newborn
is to cannulate the umbilical vein. Identify the umbilical vein in the cut
umbilical stump: it is the single large dilated vessel adjacent to the two
constricted arteries (Fig. 15.4 ). Prepare a 5F gauge catheter with 0.9 %
saline and insert it 5cm into the umbilical vein. Suture and secure in place.
If there are no signs of life after 10min of continuous and adequate
resuscitation efforts, then discontinuation of resuscitation may be justifi ed;
involve senior ED and neonatal staff in this decision.
Meconium aspiration
In the presence of meconium, do not attempt to aspirate the nose and
mouth of meconium as the head presents. If a baby is delivered with thick
meconium and is unresponsive at birth (absent or inadequate respiration,
heart rate <100/min or hypotonia), perform laryngoscopy and clear meco-
nium under direct vision using a wide bore catheter. Aim to intubate the
larynx and apply suction to the tracheal tube which is then withdrawn.
However, if intubation cannot be achieved immediately, clear the
orophyarynx and start bag-valve-mask infl ation. If while attempting to
clear the airway the heart rate falls <60/min, stop airway clearance, give
infl ation breaths and start ventilating the baby with a bag-valve-mask
device.
If meconium staining is present, but the infant is vigorous at birth, no
special treatment is required immediately, but the infant should be closely
observed.
Vein
Arteries
Fig. 15.4 Diagram of a cross-section of the umbilicus.

646 CHAPTER 15 Paediatric emergencies
Paediatric basic life support
Follow the algorithm (Fig. 15.5 ). Note that the approach to choking is
considered on b p.648.
Evaluate responsiveness
Check the child’s responsiveness — gently stimulate and ask loudly ‘are you
alright?’ Do not shake if you suspect cervical spine injury. If the child does
not respond, shout for help ± get someone to go for assistance.
Open airway
Open the airway by head tilt and chin lift. Desirable degrees of tilt are
neutral <1 year and ‘sniffi ng the morning air’ > 1 year. Do not press on the
soft tissues under the chin as this may block the airway. If it is still diffi cult
to open the airway, try a jaw thrust. If there is any suspicion that there
may have been a neck injury, instruct a second rescuer to manually immo-
bilize it, and use either chin lift or jaw thrust alone. If this is unsuccessful,
add the smallest amount of head tilt needed to open the airway.
Check breathing
Whilst keeping the airway open, look listen and feel for breathing for
10sec. If the child is not breathing or is making infrequent irregular breaths,
carefully remove any obvious obstruction, give 5 initial rescue breaths
(with the rescuer taking a breath between each rescue breath).
Rescue breaths
For children > 1 year , whilst maintaining head tilt and chin lift, give breaths
mouth to mouth, pinching off the nose. Blow steadily for 1–1.5sec
watching for the chest to rise. Take your mouth away, watch the chest fall
and repeat this sequence 5 times.
For the infant (<1 year) ensure the neutral position of the head and apply
chin lift. Give mouth to mouth and nose breaths, ensuring a good seal.
Blow steadily for 1–1.5sec watching for chest rise. Take your mouth away,
watch the chest fall and repeat this sequence 5 times.
Diffi culty achieving an effective breath suggests airway obstruction. Open
the mouth and remove visible obstruction (no blind fi nger sweep), ensure
appropriate head tilt/chin lift and neck position. Try a jaw thrust if head
tilt/chin lift has not worked. Try up to 5 times to give effective breaths. If
still unsuccessful, move to chest compression.
Check pulse
Over the next 10sec check for signs of life: any movement, coughing or
normal breathing and check for a pulse (use carotid for > 1yr and brachial
for those <1 year). If there are no signs of life and/or no pulse or pulse
<60/min with poor perfusion or you are unsure: start chest compression.
Chest compression
For infants , perform chest compressions (100–120/min) by placing both
thumbs fl at side by side on the lower third of the sternum with the tips
pointing towards the infant’s head. Encircle the rib cage with tips of fi ngers
supporting the infant’s back. Press down with thumbs at least one third of
the depth of the chest.
In children > 1 year using the heel of one hand, compress the lower half
of the sternum by at least one-third of the depth of the chest at a rate of
100–120/min. Use two hands if necessary to achieve the depth required.
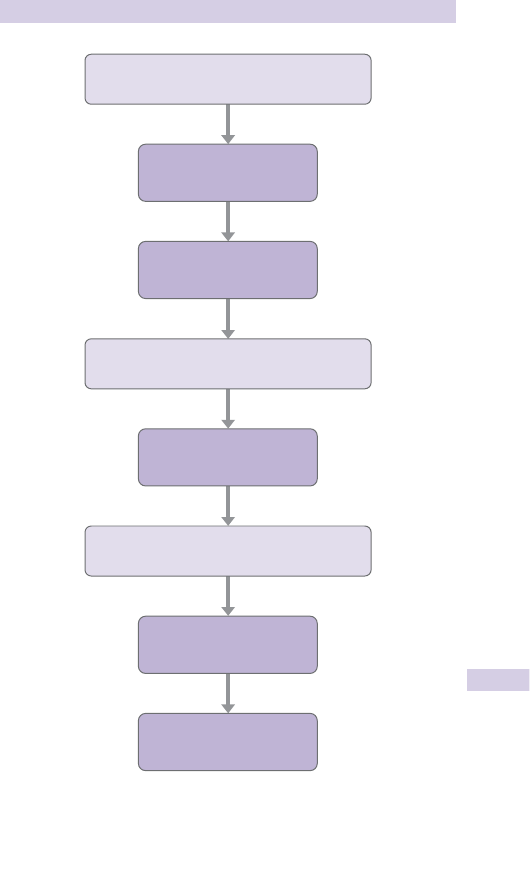
647
PAEDIATRIC BASIC LIFE SUPPORT
Unresponsive?
Shout for help
Open airway
5 rescue breaths
Call resuscitation team
No signs of life?
Not breathing normally?
15 chest compressions
2 rescue breaths
15 compressions
Fig. 15.5 Paediatric basic life support (healthcare professionals with a duty
to respond). Resuscitation Council (UK). Paediatric basic life support , 2010.
See www.resus.org.uk

648 CHAPTER 15 Paediatric emergencies
Choking from a foreign body
Despite preventative measures (eg making pen tops with holes in them),
children continue to die each year from airway obstruction due to FB
impaction. FB aspiration produces a sudden onset airway problem and
must be distinguished from other causes of airway obstruction (epiglot-
titis, bacterial tracheitis see b Stridor: upper respiratory tract infections,
p.677), which may be worsened by the basic measures described below.
The majority of choking events in children are witnessed and occur during
play or whilst eating. FB airway obstruction is characterized by sudden
onset of respiratory distress associated with coughing, gagging or stridor
with no other signs of illness. If the child is coughing effectively (fully
responsive, loud cough, able to take a breath before coughing, crying or
verbal response to questions), encourage coughing and observe for the
cough becoming ineffective.
Conscious, but ineffective cough
If conscious with an ineffective cough, give 5 back blows. In the infant,
support in a head downwards prone position and in the child aim for a
head down or forward leaning position. Deliver 5 sharp back blows with
the heel of one hand centrally between the shoulder blades. If ineffective,
turn to supine position and give 5 chest thrusts to infants (using the same
landmarks as for cardiopulmonary resuscitation (CPR), but thrusts are
sharper and delivered at a slower rate) and abdominal thrusts to children
> 1 year. Perform abdominal thrusts from behind the child, placing your fi st
between the umbilicus and xiphisternum, and grasping it with your other
hand, then pulling sharply inwards and upwards — repeat up to 5 times.
Following chest or abdominal thrusts, if the object has not been expelled
and the victim is still conscious then repeat the sequence of back blows
and chest (for infant) or abdominal (for children) thrusts.
Do not use abdominal thrusts for infants.
Unconscious from foreign body airway obstruction
If a child with FB airway obstruction is or becomes unconscious, place him
on a fl at surface, then open the mouth and look for any obvious object. If
one is seen, use a single fi nger sweep to remove it. It may be possible to
remove the FB with Magill’s forceps under direct laryngoscopy. Do not
attempt blind or repeated fi nger sweeps. Open the airway and attempt
5 rescue breaths. If a breath does not make the chest rise, reposition
the head before making the next attempt. If there is no response whilst
attempting the 5 rescue breaths, proceed to chest compression with
ventilation using a ratio of 15:2. Each time the airway is opened, check for
a foreign body and if visible, try to remove it (Fig. 15.6 ).
If it appears that the obstruction has been relieved, open and check
the airway. If the child is not breathing, deliver rescue breaths. If initial
measures prove unsuccessful and the child is hypoxic, oxygenate via a
surgical airway until senior help arrives. Perform needle cricothyroidotomy
in children aged <12 years, surgical cricothyroidotomy in older children
( b Airway obstruction: surgical airway, p.326).
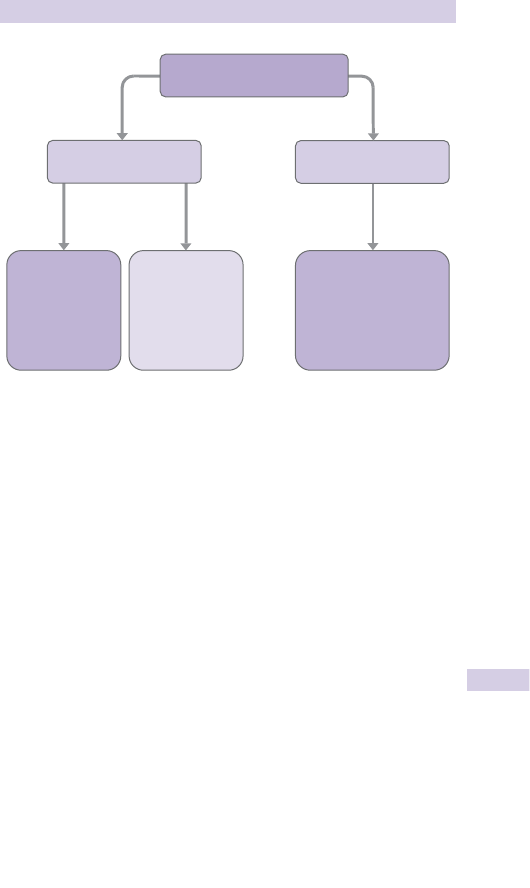
649
CHOKING FROM A FOREIGN BODY
Unconscious
Open airway
5 breaths
Start CPR
Conscious
5 back blows
5 thrusts
(chest for infant)
(abdominal for
child >1 year)
Encourage cough
Continue to check for
deterioration to ineffective
cough or until obstruction
relieved
Effective cough
Ineffective cough
Assess severity
Fig. 15.6 Paediatric foreign body airway obstruction treatment. Resuscitation
Council (UK). Paediatric FB airway obstruction , 2010. See www.resus.org.uk
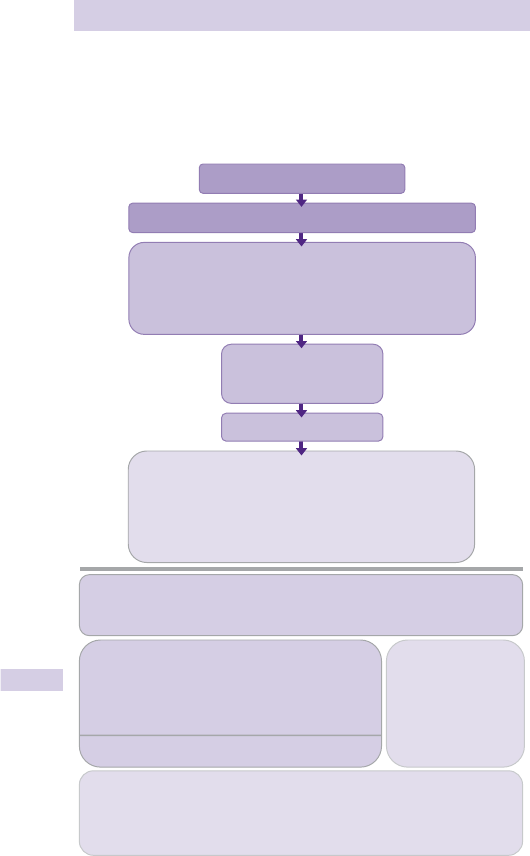
650 CHAPTER 15 Paediatric emergencies
Anaphylaxis in children
The background, causes and pathophysiology of anaphylaxis in children
is similar to that in adults — see b p.42. Treat according to the 2008 UK
Resuscitation Council algorithm, shown in Fig. 15.7 . After initial treatment,
admit the child for observation in case of a delayed or biphasic reaction.
1 See http://www.resus.org.uk/pages/reaction.pdf for details. Notes are shown opposite .
When skills and equipment available:
• Establish airway
• High flow oxygen
Monitor:
• IV fluid challenge
3
• Pulse oximetry
• Chlorphenamine
4
• ECG
• Hydrocortisone
5
• Blood pressure
1 Life-threatening problems:
Airway: Swelling, hoarseness, stridor
Breathing: Rapid breathing, wheeze, fatigue, cyanosis, SpO
2
< 92%, confusion
Circulation: Pale, clammy, low blood pressure, faintness, drowsy/coma
3 IV fluid challenge:
Adult - 500–1000 mL
Child - crystalloid 20 mL/kg
Stop IV colloid
if this might be the cause
of anaphylaxis
4 Chlorphenamine 5 Hydrocortisone
200 mg
100 mg
50 mg
10 mg
5 mg
2.5 mg
Child less than 6months
250 micrograms/kg 25 mg
2 Adrenaline (give IM unless experienced with IV adrenaline)
IM doses of 1:1000 adrenaline (repeat after 5 min if no better)
• Adult: 500 micrograms IM (0.5 mL)
• Child more than 12 years: 500 micrograms IM (0.5 mL)
• Child 6–12 years: 300 micrograms IM (0.3 mL)
• Child less than 6 years: 150 micrograms IM (0.15 mL)
Adrenaline IV to be given only by experienced specialists
Titrate: Adults 50 micrograms; Children 1 microgram/kg
Adrenaline
2
Call for help
• Lie patient flat
• Raise patient’s legs
Diagnosis - look for:
• Acute onset of illness
• Life-threatening airway and/or breathing
and/or circulation problems
1
• And usually skin changes
Airway, Breathing, Circulation, Disability, Exposure
Anaphylactic reaction?
Adult or child more than 12 years
Child 6–12 years
Child 6 months to 6 years
(IM or slow IV)
(IM or slow IV)
Fig. 15.7 UK Resuscitation Council algorithm 2008.

651
ANAPHYLAXIS IN CHILDREN
Notes for anaphylaxis algorithm opposite
1 Intramuscular (IM) adrenaline is the agent of choice in anaphylaxis and
should be administered without delay.
2 If profound shock is judged immediately life-threatening, consider giving
a slow bolus of 1mcg/kg of intravenous (IV) adrenaline as a 1 in 100,000
solution (= 10micrograms/mL solution). This is hazardous and is recom-
mended only for experienced specialists who can also obtain IV access
without delay. Note that a different dilution of adrenaline is required
for IM compared to IV use. Adrenaline can also be given via the IO
route in the same dose as the IV route.
3 An inhaled B
2
-agonist such as salbutamol may be used as an adjunctive
measure if bronchospasm is severe and does not respond rapidly to
other treatment.
4 For children who have been prescribed an EpiPen
®
, 150 mcg can be
given instead of 120 mcg, and 300 mcg can be given instead of 250 mcg
or 500 mcg.
5 Crystalloid may be safer than a colloid.
6 Do not use the subcutaneous route for adrenaline. It has no role in
anaphylaxis because its absorption is appreciably slower than IM
adrenaline.
Consider taking blood samples for mast cell tryptase testing as soon as
possible after starting treatment if the cause is thought to be venom-
related, drug-related or idiopathic (see www.nice.org.uk/cg134):
• A sample as soon as possible after emergency treatment has started.
• A second sample ideally within 1–2 hours (but no later than 4 hours)
from the onset of symptoms.

652 CHAPTER 15 Paediatric emergencies
Paediatric advanced life support
Overall, cardiac arrest in children has a worse outcome than in adults,
because the underlying causes are different. However, the situation is
likely to be far from hopeless if a child arrests within the ED or other
areas of the hospital. Effective immediate resuscitation is important to
minimize hypoxic organ damage. Early recognition of the child presenting
with impending cardio-respiratory arrest may allow prompt intervention
and prevent secondary cardiac arrest (Fig. 15.8 ).
Follow the guidelines shown opposite. Establish BLS ( b p.646) and use
a ratio of 15:2 while ventilating with a bag-valve-mask. Aim for tracheal
intubation by a highly skilled operator as soon as possible, then ventilate
at a rate of 10–12/min with compressions uninterrupted at 100–120/min.
Non-shockable rhythm: PEA and asystole
Give BLS with high concentration O
2
. Give adrenaline IV/IO 10mcg/kg
(0.1mL/kg of 1 in 10,000). If no other access is present, consider giving
100mcg/kg adrenaline via the trachea, but this is the least satisfactory
route. Give IV/IO adrenaline every 3–5min (every other loop). As in adults
( b p.51), PEA may refl ect a correctable underlying cause.
In particular, exclude tension pneumothorax and consider hypovolaemia.
Haemorrhage, septic shock, and dehydration are implicated relatively
frequently, so consider an initial IV fl uid bolus of 20mL/kg 0.9 % saline
early in the resuscitation. Follow this with further IV fl uid/blood if
hypovolaemia is still present or suspected. If circulation returns, ventilate
at 12–20breaths/min to achieve a normal pCO
2
and monitor ETCO
2
to
confi rm correct tracheal tube placement.
Shockable rhythm: VF/pulseless VT
VF is uncommon in children, but is more likely in witnessed and sudden
collapse. It occasionally occurs in children with congenital heart disease,
hypothermia or electrolyte disturbance. Follow the ‘VF/VT’ treatment
algorithm shown opposite. Give one shock of 4J/kg if using a manual
defi brillator. These energy levels are appropriate for both monophasic
and biphasic defi brillators. When selecting the energy level to use during
defi brillation, if the defi brillator can only deliver certain predetermined
‘stepped’ shocks, choose the nearest higher ‘step’ to that required. Pads
or paddles for children should be 8–12cm in size and 4.5cm for infants.
Resume CPR immediately without reassessing rhythm or feeling for a
pulse. Continue CPR for 2min and if still in VF/VT, give a second shock
and resume CPR immediately for 2min. Consider reversible causes. If still
in VF/VT at this time, give a third shock. Give adrenaline 10 mcg/kg and
amiodarone 5mg/kg (diluted in 5 % glucose) once chest compressions have
restarted and give a fourth shock after 2min CPR. Continue giving shocks
every 2min and adrenaline immediately before every other shock (ie every
3–5min), until a return of spontaneous circulation. Amiodarone 5mg/kg
can be repeated once after the fi fth shock. Uninterrupted good quality
CPR is vital — only interrupt chest compressions and ventilation for
defi brillation.
See b Paediatric advanced life support notes, p.654.
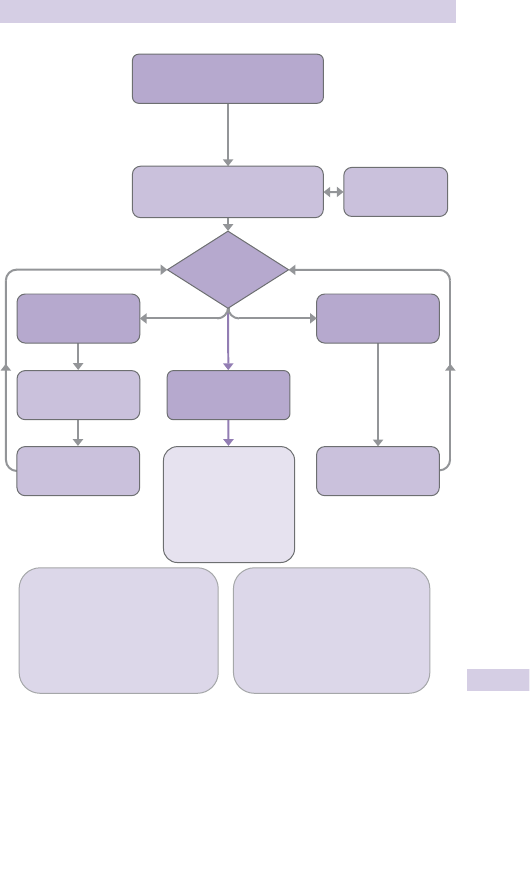
653
PAEDIATRIC ADVANCED LIFE SUPPORT
CPR
(5 initial breaths then 15:2)
Attach defibrillator/monitor
Minimise interruptions
Shockable
(VF/Pulseless VT)
1 Shock
4J/kg
During CPR
• Ensure high-quality CPR: rate, depth, recoil
• Plan actions before interrupting CPR
• Give oxygen
• Consider advanced airway and capnography
• Continuous chest compressions when advanced
airway in place
• Vascular access (intravenous, intraosseous)
• Give adrenaline every 3–5 min
• Correct reversible causes
Reversible causes
• Hypoxia
• Hypovolaemia
• Hypo-/hyperkalaemia/metabolic
• Hypothermia
• Tamponade - cardiac
• Thromboembolism
• Toxins
• Tension pneumothorax
Non-Shockable
(PEA/Asystole)
Call
resuscitation team
(1 min CPR first,
if alone)
Unresponsive?
Not breathing or
only occasional gasps
Return of
spontaneous
circulation
Immediately resume
CPR for 2 min
Minimise interruptions
Immediately resume
CPR for 2 min
Minimise interruptions
Immediate post cardiac
arrest treatment
• Use ABCDE approach
• Controlled oxygenation and
ventilation
• Investigations
• Treat precipitating cause
• Temperature control
Assess
rhythm
• Therapeutic hypothermia?
Fig. 15.8 Paediatric advanced life support. Resuscitation Council (UK). Paediatric
advanced life support guidelines , 2010. Available at: www.resus.org.uk

654 CHAPTER 15 Paediatric emergencies
Paediatric advanced life support notes
Airway
O
2
Give high fl ow oxygen (use a well-fi tting mask with a reservoir).
Suction Use a rigid suction catheter to aspirate pharyngeal contents.
Oropharyngeal airway An airway may help when ventilating with a bag
valve mask device while personnel and equipment are prepared for
tracheal intubation. Size the airway by matching its length to the distance
between the central incisor teeth and the angle of the mandible. Use a
tongue depressor or laryngoscope to displace the large tongue and insert
the airway the ‘right way up’ in order to avoid trauma to the palate.
Bag-valve-mask ventilation Attach high fl ow O
2
to a self-infl ating bag-valve-
mask device. Use a 500mL (up to age 1 year) or 1600mL bag ( > 1 year).
Tracheal intubation This method of securing the airway requires experience
and practice. Call for senior help. Always use a capnograph. Follow the
same technique as that described for adults ( b p.324), except:
• Use a straight-bladed laryngoscope in infants (<1 year).
• Use correct size of endotracheal (ET) tubes in children, either cuffed or
uncuffed.
• Correct size of ET tube: internal diameter (mm) = (age in years/4) + 4
If intubation is not achieved within 30sec, ventilate with high fl ow O
2
via
bag-valve-mask. Consider a rescue airway, such as a laryngeal mask.
Equipment sizes, drugs, and doses
Become familiar with and use the Broselow tape. See Box 15.1 for key
formulae
Venous access First attempt to secure peripheral venous access. If this is
not obtained within 90sec, attempt intra-osseous access ( b p.640).
High dose adrenaline is not recommended and may be harmful. Consider it
only in exceptional circumstances.
Atropine 20mcg/kg (minimum dose 100mcg, max 600 mcg) may be used
for patients with bradycardia related to increased vagal tone. There is no
evidence of effi cacy for atropine.
Magnesium is indicated for polymorphic VT or documented
hypomagnesaemia — give 25–50mg/kg over several min to a max of 2g.
Calcium chloride (0.2mL/kg of 10 % solution) is given for hypocalcaemia,
hyperkalaemia and clinically severe overdose of calcium channel blocking
drugs. Do not give in the same IV/IO line as bicarbonate.
Sodium bicarbonate is not recommended routinely, but consider it in
prolonged arrest, hyperkalaemia, and arrhythmias associated with tricyclic
antidepressant overdose. The dose is 1–2mL/kg of 8.4 % solution IV/IO.
Ensure adequate fl ushing after giving it. Avoid mixing with other agents
(it inactivates adrenaline and precipitates out calcium).
Glucose Treat hypoglycaemia with IV glucose (0.5g/kg).
IV fl uids Give a 20mL/kg IV normal saline bolus where cardiac arrest is
secondary to hypovolaemia or sepsis.
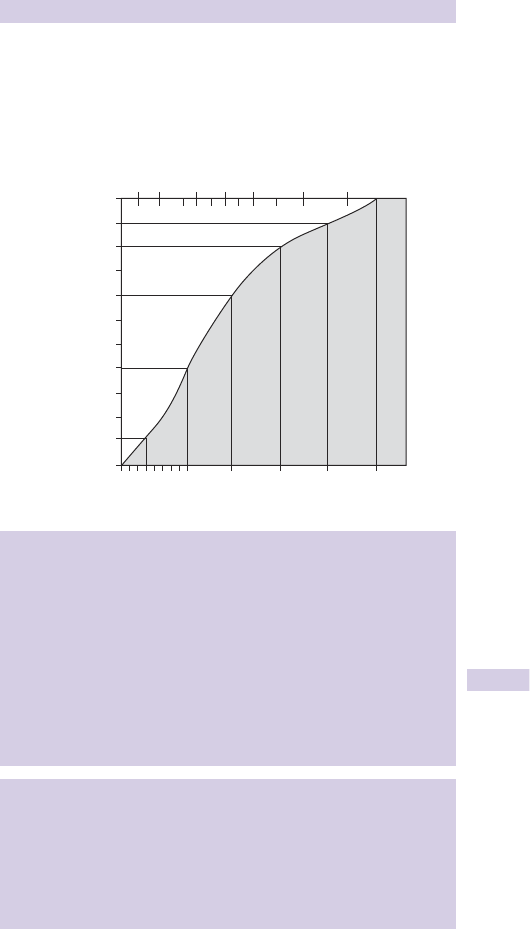
655
PAEDIATRIC ADVANCED LIFE SUPPORT NOTES
Discontinuing resuscitation
Resuscitation efforts are unlikely to be successful if there is no return
of spontaneous circulation at any time after 30min of life support and in
the absence of recurring or refractory VF/VT. Prolong resuscitation for
patients who are hypothermic or who may have been poisoned.
Paediatric resuscitation chart (Fig. 15.9 )
14
50 60
Length
80 100 120 140 150
cm
12
10
8
Age (years)
6
4
2
1
9 months
6 months
3 months
Wei
g
ht 5 10 20 30 40 50 k
g
Fig. 15.9
Box 15.1 Key resuscitation formulae
Assume birth weight of 3.5kg, reaching 10kg by the end of the fi rst year
Weight in kg = (age in years + 4) x 2 {works for ages 1–10 years}
Tracheal tube internal diameter in mm = (age/4) + 4
Tracheal tube length (oral) in cm = (age/2) + 12
Laryngeal mask sizes for children:
• Size 1 for weight up to 5kg.
• Size 1.5 for weight 5–10kg.
• Size 2 for weight 10–20kg.
• Size 2.5 for weight > 20kg.
IV fl uid challenge 20mL/kg
Defi brillation for VF/pulseless VT = 4J/kg
Drug doses
• Glucose in hypoglycaemia : 5mL/kg of 10 % (2.5mL in neonates).
• Adrenaline IV in cardiac arrest : 0.1mL/kg of 1 in 10,000.
• Lorazepam IV for seizures : 0.1mg/kg.
• Diazepam PR for seizures : 0.5mg/kg.
• Midazolam buccal for seizures : 0.5mg/kg.
• Phenytoin IVI for continuing seizures : 18mg/kg IVI over 30min.
• Morphine for pain : IV 0.1–0.2mg/kg (titrated according to pain).

656 CHAPTER 15 Paediatric emergencies
Children with abnormal heart rates or
rhythms
Background
Arrhythmias are uncommon: obtain expert advice at an early stage.
Children may present with poor feeding, heart failure, shock or palpita-
tions. Sinus tachycardia may be as fast as 220/min in infants and 180/min in
children. Consider undiagnosed congenital heart disease in infants.
Bradycardia
Heart rates of <60/min are usually pre-terminal events in response to pro-
found hypoxia and ischaemia, but can be due to i ICP or poisoning. Treat
the underlying cause and if the child is shocked and <60/min start CPR,
give O
2
and ventilate as necessary. Give IV 20mL/kg fl uid bolus. If this is
ineffective, give adrenaline 10mcg/kg IV.
If the bradycardia is due to vagal stimulation (eg tracheal intubation or
tracheal suctioning), give atropine 20mcg/kg (minimum dose 100mcg, max
600mcg).
Ventricular tachycardia in children
Until proved otherwise, initially consider wide complex tachycardia in
children to be VT.
• Causes of VT: hyperkalaemia, long QT syndrome. Tricyclic poisoning
(p192) often produces a tachycardia and wide QRS resembling VT.
• Children with VT and who are clinically shocked but conscious require
urgent anaesthesia followed by synchronized shocks starting at 1J/kg
(followed if necessary by 2J/kg).
• If the child is not clinically shocked , involve a (paediatric) cardiologist and
consider amiodarone 5mg/kg IVI over 60 min.
• Torsades de pointes is treated with magnesium sulphate IVI 25–50mg/kg
(up to a maximum of 2g); seek expert guidance.
SVT in children
Distinguish SVT from sinus tachycardia (where heart rate is <200/min,
P waves are upright in ECG leads I and AVF, there is beat to beat variation
in rate, and history consistent with shock).
If clinically shocked , but responsive, obtain expert help to give
synchronized shocks (starting at 1J/kg, increasing if unsuccessful to 2J/kg)
under anaesthesia. If there is any delay, try adenosine IV as outlined for
haemodynamically stable patients.
In the absence of clinical evidence of shock , try vagal stimulation : immersion
of the face in iced water, or Valsalva manoeuvre or unilateral carotid
massage. If this is unsuccessful, give adenosine 100mcg/kg rapid IV
followed by a saline fl ush, followed if still unsuccessful by further dose(s)
at 200mcg/kg, then 300mcg/kg. If this fails, seek expert help and consider
IV amiodarone.
This page intentionally left blank

658 CHAPTER 15 Paediatric emergencies
Sudden infant death syndrome (SIDS)
SIDS (also called SUDI—sudden unexplained death in infancy; previously
known as ‘cot death’ or ‘crib death’) is decreasing in incidence, but
each death is a tragedy. A senior doctor (consultant) should manage
distressed parents (and staff). It remains a leading cause of infant death
(1 in 2000 live births), 90 % occurring between 1 and 6 months of age. Most
hospitals now have detailed SUDIC (Sudden Unexpected Death in Infancy
and Childhood) protocols, which should be followed in this situation.
Defi nition Sudden death in infancy with no cause identifi ed after autopsy.
Aetiology Although the aetiology is unknown, a variety of theories have
been proposed, including prone sleeping position, airway obstruction,
apnoea, viral illness, and overheating.
Risk factors Passive smoking, males, winter months, sleeping prone,
premature babies, twins, apnoeic spells in fi rst week of life, lower
socio-economic groups, maternal illicit drug abuse in pregnancy, sibling
with SIDS.
Prevention
• Avoid overheating (aim for ambient T ° of 16–20 ° C).
• Avoid duvets and excess bedding in infancy.
• Place infant’s feet at cot end to prevent migration under blankets.
• Sleep supine (unless Pierre–Robin, scoliosis, or oesophageal refl ux).
• Consider apnoea alarm.
• Avoid infant sharing bed with parent.
Approach
• Take the infant into the resuscitation room and continue resuscitation
as for cardiac arrest unless there is post-mortem staining or rigidity.
• Call the ED consultant and consultant paediatrician.
• Ensure that a named senior nurse stays with the parents.
• Immediately death is declared, prepare yourself, then inform the parents
in the presence of the senior nurse. Use the techniques described in
b Breaking bad news, p.24. Refer to the child throughout by their fi rst
name.
• Some hospitals have dedicated bereavement counsellors — involve them
early.
• Allow the parents to see and hold the baby, and suggest that they keep
a lock of their hair.
• Take digital or polaroid photographs of the baby: give them to the
parents and fi le copies in the notes.
• Explain further procedures (eg autopsy) to the parents and provide
written information eg ‘A guide to the post mortem examination proce-
dure involving a baby or child’ (DoH ref 29768/A).
• Offer to request a minister of religion and involve a social worker.
• Careful documentation including general appearance, state of nutrition,
weight, rectal temperature (T ° ), marks from procedures, rashes, any
visible injuries, and appearance of the retinae.
• Inform GP to arrange to visit parents and discuss whether to suppress
lactation with bromocriptine if mother is breast-feeding.

659
SUDDEN INFANT DEATH SYNDROME (SIDS)
• Retain clothes and bedding (stored in a paper bag, not polythene) and
inform police and coroner (Procurator Fiscal in Scotland) in all cases.
• Ensure blood, urine, and skin specimens will be obtained (looking for
infection and inborn errors of metabolism).
• Arrange a further appointment for the parents with the same consultant
paediatrician.
• Suggest the Foundation for the Study of Infant Deaths, which has various
leafl ets and a ‘Cot Death Helpline’ (Telephone 0870 787 0554).
• Advise about preventative measures for siblings. If the baby was a
twin, recommend admission of the surviving twin with the mother for
monitoring and investigation.
• Cancel any hospital outpatient appointments and vaccination
appointments for the child.
• Inform the parents that the police will visit them as a matter of course.
• Finally, consider yourself and your colleagues.
Staff have feelings too
All staff involved with the child and family (ambulance staff, police,
GP, nurses and doctors — including you) will be traumatized by the
experience. Those who are themselves parents with young children may
be particularly distressed. At the very least, a debriefi ng session over a
cup of coffee will be required.
‘Near miss sudden infant death syndrome’ (apparently life-
threatening event)
Refer to the paediatrician for admission and monitoring any infant whose
parents report an apparently life-threatening event (‘ALTE’): apnoea,
colour change, tone change, cyanosis, choking, gagging. The patient may
appear well at the time of presentation. Liaise with the paediatric team
and take blood (to include FBC, U&E, glucose, calcium, magnesium,
phosphate) and admit for apnoea monitoring.
The differential diagnosis includes arrhythmias and congenital heart disease,
child abuse, gastro-oesophageal refl ux, meningitis and sepsis, seizures and
metabolic disorders. In 50 % of cases, no cause is found. Despite parental
anxiety, short apnoeic episodes (<15sec) may, in fact, be entirely normal.
Theophylline, home monitoring devices, and counselling have all been
used for infants believed to be at risk.

660 CHAPTER 15 Paediatric emergencies
Problems of neonates and infants
Neonatal cephalhaematoma
This haematoma results from birth trauma and overlies a single skull bone
(usually parietal). It resolves spontaneously: do not attempt to aspirate.
Umbilical cord sepsis
The dried cord separates at 1 week. If the stump develops signs of
infection (becoming moist and red), refer to the paediatrician.
Breast swelling
Neonatal breasts commonly swell, due to exposure to maternal
hormones. Occasionally, these breasts lactate (‘witch’s milk’) and very
occasionally become infected, requiring parenteral antibiotics.
Neonatal jaundice
Jaundice within 24hr of birth is highly abnormal. Neonates who develop
jaundice after 24hr mostly have ‘physiological jaundice’ (typically in the
fi rst week, especially premature babies) or ‘breast milk jaundice’ (typically
in second week: self-limiting, breast feeding can usually continue). Refer
all patients to exclude serious underlying disorders: Rhesus haemolytic
disease; ABO incompatibility; congenital spherocytosis; glucose-6-
phosphate dehydrogenase (G-6-PD) defi ciency; CMV infection; hypothy-
roidism; biliary atresia. The paediatrician will check: serum bilirubin
(including ratio of conjugated: unconjugated), FBC; blood fi lm; U&E; LFTs;
direct antiglobulin test; TFTs; and infection screen.
Neonatal conjunctivitis
A watery/sticky eye in the fi rst few days of life may be due to an unopened
tear duct, or occasionally to gonococcal or chlamydial infection acquired
from the mother’s genital tract. Therefore, take a swab for Gram staining
for gonococci and culture for chlamydia. Refer the baby and mother if
organisms are demonstrated, otherwise arrange GP follow-up.
Sepsis
Potentially life-threatening sepsis (eg meningitis) may present in a non-
specifi c manner in infants (this is especially true of neonates). Classic presen-
tations are replaced by: feeding problems, irritability, drowsiness, jaundice,
hypotonia, poor weight gain, petechiae or skin rash, apnoea, bradycardia,
and cyanotic episodes. Neonates at i risk are those with low birth weight,
those previously ventilated and those with congenital abnormalities.
Treatment Give O
2
and IV fl uids (20mL/kg). Refer for admission and
urgent investigation: BMG, urine culture, FBC, blood cultures, TORCH
screen (Toxoplasma, Rubella, CMV, Herpes), CXR, abdominal X-ray (if
necrotizing enterocolitis suspected), LP. Commence ‘blind’ antibiotics
(see BNFC ).

661
PROBLEMS OF NEONATES AND INFANTS
Crying babies
It is quite normal for babies to cry. The amount of crying varies
enormously, as does the ability of parents to cope with it. With more
acute onset of irritability and crying exclude an acute cause (eg otitis
media, incarcerated hernia, testicular torsion, intussusception, fractured
limb), before reassuring and counselling the parents. Parents who are
driven to despair may benefi t from a self-help group (eg CRY-SIS 020
7404 5011 www.cry-sis.com ) or follow-up with a paediatrician.
Feeding diffi culties
Parents bring their babies to the ED with a variety of feeding problems.
The underlying causes vary widely and range from acute life-threatening
sepsis to chronic parental anxiety or overfeeding. Obtain a careful feeding
history and watch the baby feed. Babies normally require at least 15mL of
milk/kg/day at day 1, increasing to | 150mL/kg/day by day 7. Plot weight,
height, and head circumference on centile charts. Take weight loss or
failure to satisfactorily gain weight seriously — it may be due to a signifi cant
underlying disorder (eg pyloric stenosis). Remember that newborn babies
lose up to 10 % of their birth weight in the fi rst week, but should regain it
by 2 weeks. Arrange for the health visitor to advise. Refer chronic feeding
problems to GP or paediatrician.
Bilious vomiting
Occasionally neonates and infants present with bilious vomiting, a
sign of serious pathology. The most important differential diagnosis is
intestinal malrotation (volvulus) secondary to peritoneal bands, which
requires emergency laparotomy to avoid total small bowel infarction
( b Abdominal pain in children, p.698). Consult a paediatric surgeon
urgently. Other differential diagnoses include an obstructed hernia,
Hirschsprung’s disease or sepsis.
Metabolic diseases (inborn errors of metabolism)
Occasionally neonates present to the ED days after birth with coma or
seizures with no obvious cause (infection, trauma, hypoglycaemia, etc.).
These infants may have an inborn error of metabolism (e.g. maple syrup
urine disease, urea cycle disorders, and hyperammonaemia) and they
require urgent specialist paediatric care, often at a tertiary children’s
hospital. If an older child presents to the ED with a previously diagnosed
metabolic disease, seek expert advice by referring to the paediatricians
early. Remember the parents will know more about the disease than you.
Treatment Give O
2
and IV fl uids (20mL/kg) and treat hypoglycaemia, and
sepsis. Refer for admission and urgent investigation by a paediatrician.
Emergency treatment protocols for this challenging group of patients are
available at the British Inherited Metabolic Disease Group website ( http://
www.bimdg.org.uk/protocols/documents.asp?o=1&tid=1 ).
662 CHAPTER 15 Paediatric emergencies
Skin problems in infants
Minor skin problems are common in infants. The combination of a
skin rash and an ill infant should arouse suspicion of serious illness (eg
b Meningococcal disease, p.666) and prompt urgent referral. Do not
discharge an infant with an undiagnosed rash — obtain an expert opinion.
Neonates
Multiple tiny white papules ( milia ) seen on the face of neonates are super-
fi cial epidermal inclusion cysts. Erythematous lesions with central white
vesicles are common in the fi rst days of life — erythema toxicum (‘neonatal
urticaria’). Both are harmless and disappear spontaneously within days.
Peeling skin
Peeling skin is a common feature of post-mature babies and should be dis-
tinguished from scalded skin syndrome and Kawasaki disease ( b p.672).
Scalded skin syndrome (‘toxic epidermal necrolysis’)
This staphylococcal infection results in red peeling skin, sometimes with
blistering. Refer for admission and IV antibiotics.
Eczema
Usually managed most appropriately by GP and outpatient department
with emollients ± topical corticosteroids, but if very severe, refer for a
period of inpatient treatment. Sometimes the scratched skin becomes
secondarily infected, requiring admission for IV antibiotics.
Impetigo
Any breach in the skin (eg eczema, nappy rash, scabies) may develop
impetigo. Staphylococcal or streptococcal infection results in an ulcera-
tive erythematous area, which forms a golden brown crust that spreads
rapidly. If the infection is localized and the child is well, treat with topical
fucidic acid (if extensive — oral penicillin and fl ucloxacillin), arrange GP
follow-up and advise the parents to isolate the child from other children
until it has resolved. If the child is unwell, refer for IV antibiotics.
Nappy rash (‘ammoniacal dermatitis’)
Erythema with some ulceration in the nappy area, but sparing the fl exures,
is usually the result of excessive moisture contact with the skin. Treat
by exposure to fresh air as much as practicable and frequent changing of
nappies. Consider barrier creams (see BNFC).
Monilial infection
Nappy rash may become infected with Candida albicans , leading to erythema
of the fl exures. Give nystatin cream and advise regular changing.
Seborrhoeic dermatitis
This erythematous greasy rash commonly involves the nappy area, the
occipital region and behind the ears. It may become infected with Candida
albicans — treat with nystatin and refer to GP.

663
THE FEBRILE CHILD
The febrile child
Febrile illness is extremely common in childhood and many parents will
bring their child to the emergency department, rather than to a primary
care team for assessment, particularly when they feel the child is very
unwell. Primary care teams will also refer febrile children to hospital for
assessment when the child is seriously ill or the diagnosis is in doubt.
Approach
• Assess the airway, breathing and circulation of the child to identify and
treat life-threatening problems as they are found in order to maintain
vital functions before disease specifi c therapies are started ( b Primary
assessment and resuscitation of the sick child, p.634).
• Involve senior ED staff, PICU, and senior paediatric staff as soon as you
suspect the child is critically unwell.
• Measure and record the temperature (electronic thermometer in
axilla if <4 weeks old, can also use tympanic thermometer if older
than 4 weeks).
• Specifi cally look for an impaired conscious level and lack of recognition
of parents/carers. Check BMG in all sick children.
• Early recognition and treatment of respiratory failure and shock is
essential to avoid cardiorespiratory arrest.
• Administer oxygen to maintain SpO
2
> 94 % .
• Give a bolus of IV/IO 0.9 % saline 20mL/kg if any signs of shock (tachy-
cardia, CRT > 2sec, mottled skin, purpuric rash, d conscious level).
• If there is any suspicion or sign of meningococcal disease, administer
parenteral benzylpenicillin or cefotaxime as soon as possible.
• If the child is <3 months old, check FBC, blood cultures, CRP and
urine; if unwell, or WCC <5 or > 15 × 10
9
/L, or <1 month old, perform
lumbar puncture (LP) and give parenteral antibiotics. If <1 month old,
add ampicillin to cover Listeria .
• If the child is > 3 months old, check FBC, blood cultures, CRP and urine;
get CXR if T ° > 39 ° C or WCC > 20 × 10
9
/L or clinically unwell.
• Check U&E, ABG, and lactate if clinically unwell or drowsy.
• Consider LP if clinically unwell and febrile at any age, especially <1 year.
• If drowsy or d conscious level, consider adding IV acyclovir to cover
possibility of herpes simplex encephalitis.
• Resuscitate aggressively with repeated IV fl uid boluses, inotropes and
early ventilation for children with d conscious level.
• In older children, do not forget rarer causes of fever and impaired
conscious level, including illicit drugs such as MDMA (‘Ecstasy’) or other
amphetamines, or ketamine.
• Get a detailed history of the illness from parents and carers at the
earliest opportunity; remember the vaccination history and any recent
travel, or recent illness in the child’s family or school.
1 See the ‘ NICE Guidance on Feverish Illness in Children ’. Available at: http://www.nice.org.uk/
nicemedia/live/11010/30524/30524.pdf

664 CHAPTER 15 Paediatric emergencies
Purpuric rashes
The development of a purpuric rash in a child is often greeted with
considerable and understandable parental alarm, due to the well-
publicized association with meningococcal disease. History, examination,
and FBC will help to identify the cause.
Causes of purpuric lesions
• Meningococcal disease.
• Henoch–Schönlein purpura.
• Thrombocytopenia.
• Idiopathic thrombocytopenic purpura;
• Leukaemia;
• Septic shock;
• Aplastic anaemia.
• Some viral illnesses.
• Trauma.
• Forceful coughing or vomiting may cause petechiae of the face.
Meningococcal disease (see b p.666)
Presume that an ill child (particularly an infant) who develops a purpuric
rash has meningococcal meningitis/septicaemia and treat urgently for this.
Henoch–Schönlein purpura
This vasculitic process affects small arteries in the kidneys, skin, and GI
tract. It is relatively common in 4–11-year olds and appears to follow a
viral or bacterial infection. Erythematous macules develop into palpable
purpuric lesions, which are characteristically concentrated over the
buttocks and extensor surfaces of the lower limbs, although the distribution
can be atypical in younger children. Associated symptoms include
abdominal pain, testicular pain and joint pains (arthritis in ankles and
knees). Nephritis may occur, producing micro- or macroscopic haematuria,
proteinuria. Very occasionally, this progresses to renal failure.
Check BP, urinalysis, urine microscopy, FBC (platelets are normal), U&E.
Refer to the paediatrician.
Idiopathic thrombocytopenic purpura
Probably results from autoimmune reaction to preceding viral infection.
Presents with a purpuric rash, mucous membrane bleeding, conjunctival
haemorrhage and occasionally, GI bleeding. Check FBC (platelets are
<30 × 10
9
/L). Refer for investigation and follow-up. In the presence of
lymphadenopathy or splenomegaly, consider alternative diagnoses.
Treatment is usually expectant, since the natural course is for most cases
to resolve spontaneously over 3 months. Occasionally, life-threatening
haemorrhage occurs: obtain expert help, resuscitate with O
2
and IV fl uids
and give platelets.
Acute leukaemia
This may present acutely to the ED with purpura associated with throm-
bocytopenia. Look for hepatomegaly, splenomegaly and lymphadenopathy.
FBC/blood fi lm reveals anaemia with blast cells, d platelets, and i WBC).
Refer for admission.
This page intentionally left blank

666 CHAPTER 15 Paediatric emergencies
Meningococcal disease
See algorithm Fig. 15.10 b p.668–9.
Meningococcal disease is unpredictable. Most children present acutely
febrile and may not have a rash in the early stages.
Septicaemia
Children presenting with septicaemia may have:
• A history of fever/rigors but be afebrile at the time of presentation.
• Isolated severe limb pain in the absence of any other physical signs.
• Abdominal pain, diarrhoea and vomiting are common in septicaemia.
• Alertness until late in the illness.
Patients presenting in septic shock without meningitis have the worst
prognosis.
Meningitis
Young children may present with fever, vomiting, irritability and confusion.
Those aged <2 years are less likely to have neck stiffness or photophobia.
Take parental concerns about a child’s responsiveness and alertness
seriously. Older children typically present more classically with fever,
vomiting, headache, stiff neck and photophobia. Teenagers may present
with a change of behaviour (eg confusion, aggression), which may be
falsely attributed to alcohol or drugs.
Rash
Underlying meningococcal disease may be very advanced by the time a
rash appears. This may initially be blanching, macular, or maculopapular.
Children without a rash or with a blanching rash can still have meningo-
coccal disease. The classic rapidly evolving petechial or purpuric rash may
be a very late sign and can carry a poor prognosis.
Urgent treatment and experienced help are essential. CT scanning of the
brain should be undertaken if there is impaired conscious level or focal
neurological signs or signs of i ICP. CT scans must not delay treatment.
LP has no immediate role in the ED care of the critically ill child and can
be fatal. LP is contraindicated if there is extensive purpura, shock, impaired
consciousness, coagulopathy, local infection or i ICP on CT or clinically.
Give antibiotics (IV ceftriaxone or cefotaxime) immediately to:
• All children with a fever and petechial/purpuric rash.
• Children in shock with or without a rash.
• Children with clinical meningitis, but LP contraindicated.
Take any haemorrhagic rash in a febrile child very seriously. Although
many children with fever and petechiae have viral illnesses, there is no
room for complacency. Ensure that all have their vital signs measured, and
are carefully checked for signs of meningitis or septicaemia.

667
MENINGOCOCCAL DISEASE
Airway and ventilation
Intubate and ventilate:
• If impaired conscious level or i ICP clinically.
• Prior to CT scanning if critically ill.
• If fl uid resuscitation requirement is > 40mL/kg.
Seek expert help for rapid sequence induction/intubation (RSI)—
haemodynamic collapse is common. Consider using IV ketamine for
induction if experienced in its use.
Fluid resuscitation
Vast quantities of IV fl uids are required in meningococcal septicaemia—
often up to 100mL/kg. Many UK authorities recommend 4.5 % human
albumin solution (HAS) for fl uid resuscitation, but give crystalloid (0.9 %
saline) if HAS is not immediately available.
Inotropes
• Dopamine or dobutamine at 10–20mcg/kg/min. Make up 3 × weight (kg)
mg in 50mL 5 % glucose and run at 10mL/hr = 10mcg/kg/min.
• These dilute solutions can be used via a peripheral vein.
• Start adrenaline via a central line only (seek expert help) at 0.1mcg/kg/min.
Make up 300mcg/kg in 50mL of saline at 1mL/hour = 0.1mcg/kg/min.
Hypoglycaemia (glucose <3mmol/L)
5mL/kg 10 % glucose bolus IV and then glucose infusion at 80 % of
maintenance requirements over 24 hrs.
Correction of metabolic acidosis (pH <7.2)
1mmol/kg NaHCO
3
IV = 1mL/kg 8.4 % NaHCO
3
over 20min or 2mL/kg
4.2 % NaHCO
3
in neonates.
If K
+
<3.5mmol\L
Give 0.25mmol/kg KCl diluted in saline or glucose over 30min IV with
ECG monitoring. Caution if anuric.
If total calcium <2mmol/L or ionized Ca
2 +
<1.0mmol/L
Give 0.1mL/kg 10 % calcium chloride (0.7mmol/mL) over 30min IV (max
10mL) or 0.3mL/kg 10 % calcium gluconate (0.22mmol/mL) over 30min
(max 20mL).
If Mg
2 +
<0.75 mmmol/L
Give 0.2mL/kg of 50 % MgSO
4
over 30min IV (max 10mL).
See: Meningitis Research Foundation ( www.meningitis.org ) and ‘NICE Guidance on Bacterial
meningitis and meningococcal septicaemia’ . Available at: http://www.nice.org.uk/nicemedia/
live/13027/49341/49341.pdf

RECOGNITION
May present with predominant SEPTICAEMIA (with shock), MENINGITIS (with raised ICP) or both. Purpuric/petechial non-blanching rash is typical.
Some may have neither shock nor meningitis. Rash may be atypical or absent in some cases.
SIGNS OF SHOCK?
Tachycardia
Capillary refill time >2 seconds
Cold hands/feet; pale or blue skin
Respiratory distress/ oxygen saturation <95% in air
Altered mental state/decreased conscious level
Decreased urine output (<1ml/kg/hr)
Hypotension (late sign)
Hypoxia on arterial blood gas
Base deficit (worse than -5 mmol/l)
Increased lactate (>2 mmol/l)
Bacterial meningitis
algorithm
www.meningitis.org
CLINICAL FEATURES OF
MENINGITIS?
Do not perform Lumbar Puncture; nil by mouth
Do not perform Lumbar Puncture; Nil by mouth
ABC & High flow Oxygen (minimum 10 l/min) by face mask
Measure glucose.
Insert 2 large i.v. cannulae (or intraosseous); Take bloods, see
VOLUME RESUSCITATION
Immediate bolus of 20ml/kg of 0.9% Sodium Chloride over 5–10 minutes and reassess
immediately
If shock persists immediately give second bolus of 20ml/kg of 0.9% Sodium Chloride
or of 4.5% human Albumin over 5–10 minutes and reassess immediately
Observe closely for response/deterioration
Consider urinary catheter to monitor output
ABC and Oxygen (minimum 10 l/min) by face mask
Measure glucose.
Give Mannitol (0.25g/kg) bolus or 3% Saline (3 ml/kg) over 5 minutes
Treat shock if present
Call anaesthetist and contact PICU
Intubate and ventilate to control PaCO
2
(4–4.5 kPa)
Urinary catheter and monitor output, NG tube
RAISED INTRACRANIAL PRESSURE?
Reduced (GCS ≤8) or fluctuating level of consciousness
Relative Bradycardia and Hypertension
Focal neurological signs
Abnormal posture or posturing
Seizures
Unequal, dilated or poorly responsive pupils
Papilloedema (late sign)
Abnormal ‘doll’s eye’ movements
YES
NO
NO
NO
YES
YES
Call consultant in Emergency Medicine, Paediatrics, Anaesthesia or Intensive Care
Initial assessment looking for shock/raised ICP
Do not perform Lumbar Puncture
Give IV ceftriaxone (80 mg/kg od) without delay
Do not use ceftriaxone at the same time as calcium-containing solutions:
in this situation use cefotaxime (50 mg/kg qds)
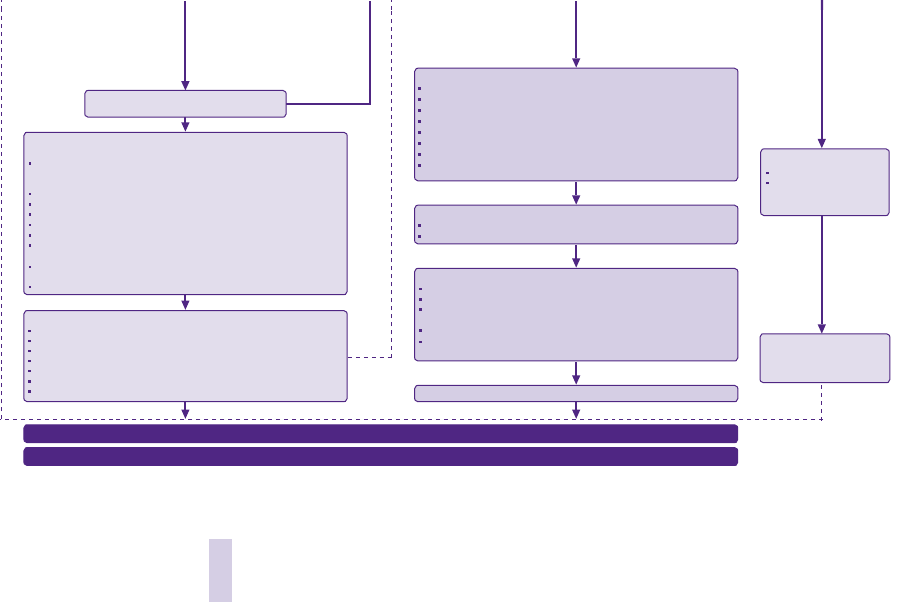
Fig. 15.10 Management of meningococcal disease in children and young people. Reproduced with kind permission from the Meningitis Research Foundation
www.meningitis.org
Take blood for glucose, FBC, coagulation screen, U&E, Ca
2 +
, Mg
2 +
, PO
4
3 –
, blood cultures, ABG, lactate, cross-match, and PCR for N. meningitidis.
Close monitoring for signs of
Raised ICP
Shock
Perform LP if no contraindication
DO NOT DELAY ANTIBIOTICS
Repeated Review
Children with MD can
deteriorate rapidly.
Deterioration detected?
Anticipate, monitor and correct:
Hypoglycaemia
Acidosis
Hypokalaemia
Hypocalcaemia
Hypomagnesaemia
Anaemia
Coagulopathy (Fresh Frozen Plasma 10ml/kg)
After 40ml/kg fluid resuscitation
STILL SIGNS OF SHOCK?
Transfer to Intensive Care by Paediatric Intensive Care Retrieval Team
Notify public health
NEUROINTENSIVE CARE
30˚ head elevation, midline position
Avoid internal jugular lines
Repeat Mannitol or 3% Saline if indicated
Sedate (muscle relax for transport)
Cautious fluid resuscitation (but correct coexisting shock)
Monitor pupillary size and reaction
Avoid hyperthermia
Once patient is stabilised, consider CT scan to detect other intracranial pathology if
GCS ≤8, fluctuating conscious level or focal neurological signs
STEPWISE TREATMENT OF SEIZURES
i.v. Lorazepam (0.1 mg/kg) or Midazolam (0.1 mg/kg) bolus
Consider Paraldehyde (0.4 ml/kg PR)
Phenytoin (18mg/kg over 30 min i.v. with ECG monitoring)
If persistent seizures:
Thiopental (thiopentone) 4mg/kg in intubated patients (beware of hypotension)
Midazolam/Thiopental infusion
Perform delayed LP when stable and no contraindications
Do not restrict fluids unless there is evidence of:
Raised intracranial pressure, or
Increased antidiuretic hormone secretion
GO TO BACTERIAL MENINGITIS ALGORITHM
WILL REQUIRE URGENT ELECTIVE INTUBATION AND VENTILATION
Call anaesthetist and contact PICU
Immediate bolus of 20ml/kg of 0.9% Sodium Chloride or 4.5% Human Albumin over
5–10 minutes and reassess immediately; Continue boluses if necessary with repeated
clinical and laboratory assessments including blood gas measurements.
Start peripheral inotropes (Dopamine); if IO access start Adrenaline
ET Tube (Cuffed if possible) and CXR
Anticipate pulmonary oedema (ensure PEEP)
Central venous access
Urinary catheter to monitor output, Nasogastric tube
Start Adrenaline infusion (central) if continuing need for Volume resuscitation and
Inotropes
For warm shock (warm peripheries, bounding pulses and low diastolic pressure) give
Noradrenaline (central) or Dopamine (peripheral)
If fluid and inotrope resistant shock discuss with paediatric intensivist.
YES
NO
Repeated review
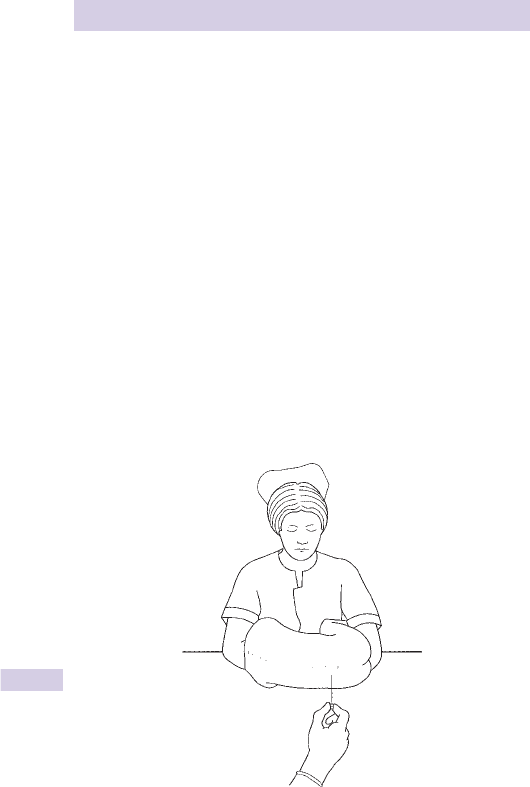
670 CHAPTER 15 Paediatric emergencies
How to perform a lumbar puncture
• Take senior advice before performing a LP.
• Confi rm that there is no contra-indication to LP (eg prolonged
or focal seizure, focal neurological signs, purpuric rash, GCS<13,
pupillary dilatation, impaired oculocephalic refl exes, abnormal posture,
hypertension, bradycardia, coagulopathy, papillodema).
• Prepare parents, set up equipment, and enlist help from an experienced
nurse.
• Position the child on their side, curled up into a ball (Fig. 15.11 ).
• Mark the skin with a pen in the midline at level of iliac crests.
• Scrub and don sterile gown and gloves.
• Clean the skin with antiseptic solution and cover with sterile drapes.
• Consider LA for the skin with 1 % lidocaine solution.
• Slowly insert the 21G lumbar puncture needle aiming towards the
umbilicus.
• If this causes much pain, withdraw needle and use more lidocaine LA
(but <3mg/kg — b Analgesia in specifi c situations, p.280).
• If no CSF is obtained, withdraw needle and reassess its direction, then
try again.
• Collect 4 drops of CSF in each of 3 bottles and send for: microscopy
and Gram stain, culture and sensitivity; cell counts; glucose and protein.
• If bloody tap is obtained, send the clearest sample for cell counts.
Fig. 15.11 Positioning for a lumbar puncture.
This page intentionally left blank

672 CHAPTER 15 Paediatric emergencies
Skin lesions in multisystem disease
The appearance of the skin may provide a valuable clue to an under-
lying disease process. If suspected, refer all of the following diseases to a
paediatrician.
Kawasaki disease (mucocutaneous lymph node syndrome)
This disease, believed to be related to a viral infection, was fi rst reported
in Japan in 1967 and has now spread worldwide. Most cases affect chil-
dren <5 years. Extensive skin and mucosal changes occur, including an
erythematous rash, which may affect palms and soles and desquamate.
Conjunctivitis, uveitis, fi ssured lips, and a strawberry tongue may be seen.
Other features: fever, acute cervical lymphadenopathy, arthritis, and
diarrhoea. Coronary artery aneurysm (and subsequent thrombosis) is a
signifi cant complication.
If Kawasaki disease is suspected check FBC, erythrocyte sedimentation
rate (ESR), and viral titres, and refer to a paediatrician.
Dermatitis herpetiformis
This is the skin manifestation of coeliac disease. Vesicles and papules occur
over the knees, elbows and buttocks. The lesions are very itchy and produce
much scratching. Dapsone is effective treatment: refer to a paediatrician.
Erythema multiforme
Target lesions often with pale blistered centres are symmetrically distributed,
particularly over the extensor surfaces of the limbs, sometimes including the
hands and feet. The skin lesions combined with fever, systemic illness, oral
and genital ulceration comprise the Stevens–Johnson syndrome.
Causes include infection (herpes, mycoplasma, tuberculosis TB) and drugs
(sulphonamides, barbiturates).
Erythema nodosum
Painful red skin nodules or plaques on the anterior surfaces of both shins
with associated fever, lethargy and arthralgia. It may be due to strepto-
coccal infection, TB, sulphonamides, ulcerative colitis, or sarcoid.
Erythema marginatum
A transient erythematous rash with raised edges occurs in 20 % of cases
of rheumatic fever ( b p.496). Rheumatic fever is an autoimmune disease
which follows infection with group A streptococci. Once common, it is
now unusual in the UK.
Diagnose using the revised Duckett–Jones criteria (2 or more major; or
1 major and 2 minor, plus evidence of preceding streptococcal infection
eg throat swab, i ASO titre):
Major criteria Erythema marginatum, carditis, polyarthritis, Sydenham’s
chorea, subcutaneous nodules.
Minor criteria Fever, arthralgia, i ESR, i WBC, previous rheumatic fever,
prolonged PR interval.

673
SKIN LESIONS IN MULTISYSTEM DISEASE
Erythema chronicum migrans (see b Infestations, p.230)
The characteristic skin rash of Lyme disease begins as a red papule, which
spreads to produce erythematous lesions with pale centres and bright
edges. Lyme disease is a multisystem disorder resulting from tick-borne
infection. It initially manifests with one or more of a variety of symptoms,
including fever, headache, malaise, arthralgia, myalgia. The rash is present in
most cases. The diagnosis can be elusive, but consider it if there has been
any history of travel to an affected area.
Identifying skin lesions (Table 15.4 )
Description
• Impalpable coloured lesion <1cm diameter = macule.
• Impalpable coloured lesion > 1cm diameter = patch.
• Palpable lump <0.5cm diameter = papule.
• Palpable lump > 0.5cm diameter = nodule.
• Palpable fl uid-fi lled lesion <0.5cm diameter = vesicle.
• Palpable fl uid-fi lled lesion > 0.5cm diameter = bulla
Table 15.4 Skin lesions and possible causes
Feature Causes
Peeling skin Toxic epidermal necrolysis (‘scalded skin syndrome’), Kawasaki
disease.
Streptococcal infection
Blistering
lesions
Staphylococcus (impetigo and toxic epidermal necrolysis), scabies,
chickenpox, herpes zoster, herpes simplex, Stevens–Johnson,
pompholyx, coxsackie A16 (hand, foot and mouth disease),
dermatitis herpetiformis, epidermolysis bullosa, drugs
Lesions on
palms and
soles
Coxsackie A16, Kawasaki disease, erythema multiforme, scables,
pompholyx
Pruritis Eczema, urticaria, psoriasis, chickenpox, scabies, lice, insect bites,
dermatitis herpetiformis

674 CHAPTER 15 Paediatric emergencies
Paediatric ENT problems
Background
Due to frequent infections and large concentrations of active lymphoid
tissue, certain ear, nose, and throat (ENT) problems are very common
in paediatric practice. For example, acute suppurative otitis media
( b Earache, p.550) has an incidence of 20 % amongst pre-school children;
secretory otitis media (‘glue ear’) has a prevalence of 5 % amongst all
children. Rhinorrhoea from coryza and rhinitis is even more common.
Approach
Although many ENT diseases are usually considered as primary care
problems, children often present to the ED suffering from them. It is
obviously important to examine the ears and throat of any child presenting
with a fever. Remember, however, that the ill, septic child with large red
tonsils may also have a signifi cant septic focus elsewhere (eg meningitis or
pneumonia).
Examination
Examination of the ears and throat is generally disliked by children and as
a result, can prove to be rather a struggle. It is therefore sensible to leave
this part of the full examination of a child until last. Parental help can be
invaluable in allowing examination of the slightly uncooperative toddler or
younger child. Sit the child on a parent’s lap for examination of the ears
and throat, as shown in Fig. 15.12 .
The diffi cult examination
Despite various manoeuvres, it can be very diffi cult to adequately
visualize the throat of a child who adamantly refuses to open their mouth.
A useful trick is to draw the face of a ‘Smiley Man’ on the end of a wooden
spatula. The child may then consent to the ‘Smiley Man’ having a look at
their throat (preferably with the ink side up!).
Presentation and treatment
The presentation, diagnosis and treatment of specifi c ENT diseases in
both children and adults are described in Chapter 12.
• b Ear, nose, and throat foreign bodies, p.546.
• b Earache, p.550.
• b Epistaxis, p.552.
• b Nasal fracture, p.553.
• b Sore throat, p.554.
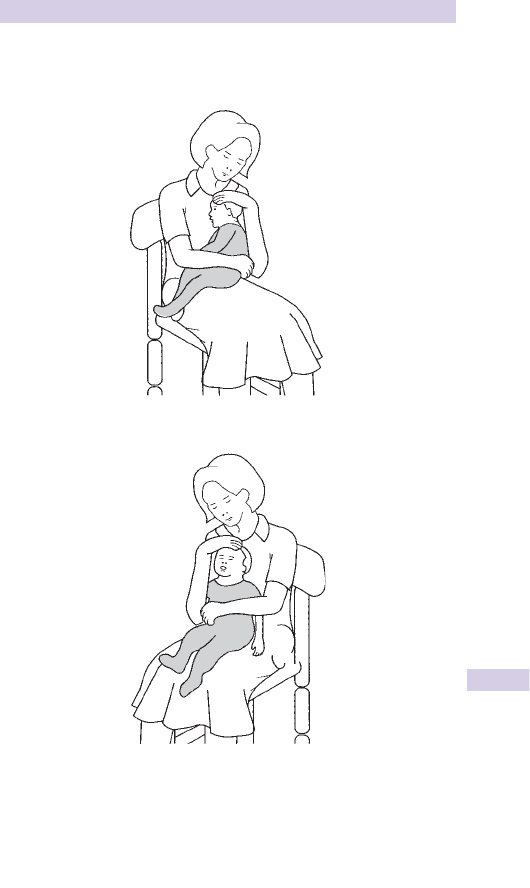
675
PAEDIATRIC ENT PROBLEMS
Examining a child’s ear In an infant pull the pinna back and down
(rather than up) for the best view.
Fig. 15.12 Examining a child’s throat.

676 CHAPTER 15 Paediatric emergencies
Stridor: upper respiratory infections
The upper airway is a tube which may be blocked by: distortion (eg tongue
falling back in coma), extrinsic compression (eg haematoma), swelling of
its wall (eg burns, croup, epiglottitis, diphtheria), or FB within.
Signs of upper airway obstruction Stridor, marked dyspnoea, drowsiness,
subcostal/suprasternal recession, drooling of saliva, diffi culty speaking, and
cyanosis. Any of these warn of impending obstruction.
Stridor is a high pitched inspiratory noise. It occurs in croup, acute
epiglottitis, inhaled FB, laryngeal trauma, laryngomalacia (‘congenital
laryngeal stridor’), angioneurotic oedema. See Table 15.5 .
Acute croup (laryngotracheobronchitis)
Viral in origin (para-infl uenza virus in > 80 % ). Common between 6 months,
and 5 years of age. Spring and autumn epidemics occur. Illness lasts 8 3–5
days. Coryzal symptoms usually precede harsh stridor, a barking cough
(‘seal’s bark’) with hoarseness i over several days. Temperature (T) * is only
mildly i . Leave the child in a comfortable position preferably in the arms
of the parent, who can hold an O
2
mask near the child. Look for signs of
signifi cant airway obstruction, but do not examine the pharynx as this may
precipitate laryngospasm or obstruction. If any of these signs are present,
or if SpO
2
<92 % in air refer urgently — intubation may be required. Use the
modifi ed Westley croup score by adding individual values as follows:
• Stridor : none = 0, only when upset or agitated = 1, at rest = 2.
• Retractions : mild = 1, moderate = 2, severe = 3.
• Air entry : normal = 0, mild decrease = 1, marked decrease = 2.
• SpO
2
<92 % on air : none = 0, with agitation = 4, at rest = 5.
• Level of consciousness : normal = 0, altered conscious level = 5.
Children with moderate (score 3–5) or severe croup (score 6–11) and
impending respiratory failure (score > 11) require admission to hospital.
Give oral dexamethasone 0.15mg/kg or nebulized budesonide (1–2mg in
5mL 0.9 % saline) if vomiting or severe respiratory distress and refer to
the paediatric team. If severe (score > 5), consider nebulized adrenaline
driven by O
2
at 8L/min (0.5mL/kg of 1:1000, max 5mL; repeat as required).
Refer severe cases to PICU (<1 % of croup is severe). Many children with
mild croup (score 0–2) can be safely discharged from the ED after a brief
period of observation. This decision should be taken by an experienced
emergency physician or paediatrician. Discharge in the evening may be
inadvisable, since croup can worsen overnight.
Diphtheria
Although rare in the UK, the exotoxin of Corynebacterium diphtheriae
may produce serious organ damage (especially myocarditis) and upper
respiratory tract obstruction. The non-immunized child may present
with pyrexia, sore throat, and dysphagia due to an adherent pharyngeal
exudate. Cervical lymphadenopathy causes a ‘bull neck’ appearance.
(Note that infectious mononucleosis may present similarly — b p.241).
Treat with O
2
, obtain ECG and venous access, send blood for FBC, blood
culture, and obtain a throat swab. Refer for antitoxin (20,000U IM after a
test dose) and IV erythromycin.

677
STRIDOR: UPPER RESPIRATORY INFECTIONS
Acute epiglottitis
Increasingly uncommon, due to widespread Hib vaccination. Rapidly
progressive airway obstruction may result. Children aged 2–7 years are
most usually involved, although it does occur in older children and adults.
Unlike croup, stridor is usually soft and may even be absent. Onset is
typically acute. The child is systemically unwell with pyrexia > 38.5 * C,
but little or no cough. In severe cases, the child may be ominously quiet,
unable to speak, sitting upright drooling saliva in a ‘sniffi ng position’.
Management Do not attempt to visualize the throat as this may precipitate
total airway obstruction. Let the child adopt the most comfortable
position, give humidifi ed O
2
and call urgently for anaesthetic, ICU and
ENT help. Nebulized adrenaline (0.5mL/kg of 1:1000, max 5mL) may ‘buy
time’. Defer doing blood tests (FBC, blood cultures) and treatment with
IV cefotaxime until an anaesthetist has assessed the child. Lateral neck
X-rays are unnecessary and potentially hazardous. Intubation, if required,
may be very diffi cult to perform. A safe approach is for an experienced
anaesthetist to use a gaseous induction in the presence of a surgeon who
is prepared for a surgical airway. Airway swelling may require a smaller
than expected diameter (and thus uncut) ET tube. Let the anaesthetist
know the number of adrenaline nebulizers given, as halothane induction
could precipitate arrhythmias. If visualization of the tracheal orifi ce is
diffi cult at laryngoscopy due to oedema, ask an assistant to squeeze the
chest and look for an air bubble emerging from the trachea.
Loss of the airway — if this happens, summon help and attempt to
ventilate with O
2
using bag and mask. If ventilation proves impossible,
obtain a surgical airway (needle cricothyroidotomy if <12 years, surgical
cricothyroidotomy if ≥ 12 years) — see b p.326.
Bacterial tracheitis
May be due to Staph. aureus, Strep. , or H. infl uenzae . The presentation
of ‘croup’, plus moderate/severe pyrexia, and production of copious
secretions suggests the diagnosis. If suspected, refer and treat as for acute
epiglottitis (intubation is often required). Bacterial tracheitis can cause
rapid onset of septic shock.
Table 15.5 Clinical presentations of upper airway obstruction
Croup Epiglottitis Bacterial
tracheitis
Foreign
body
Age 1–2 years 2–6 years Throughout
childhood
Throughout
childhood
Onset 1–2 days <24hr <24hr <24hr
History Coryza, barking
cough
Sore throat,
dysphagia
Rattling cough,
sore throat
Signs T ° <38.5 non-toxic,
harsh stridor,
hoarseness
T ° > 38.5
toxic, upright
position
T ° > 38.5 toxic,
mucopurulent
secretions, soft/
absent stridor
Afebrile,
non-toxic
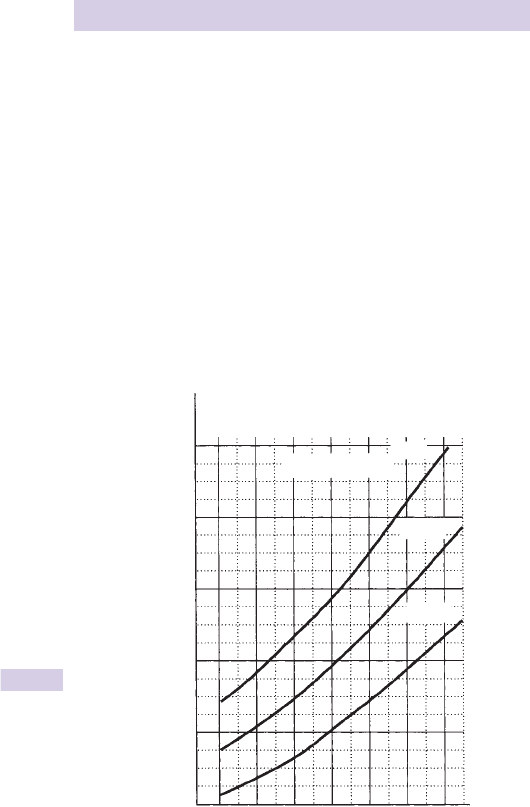
678 CHAPTER 15 Paediatric emergencies
Severe acute asthma in children
Assess conscious level, degree of breathlessness, degree of agitation, use
of accessory muscles, amount of wheezing, pulse rate and respiratory
rate. Attempt to measure peak fl ow if age > 5 years (See Fig. 15.13 for
normal peak fl ow).
Follow the 2011 British Thoracic Society/Scottish Intercollegiate Guidelines
Network (BTS/SIGN) Guidelines based on age and severity ( http://www.
sign.ac.uk/pdf/sign101.pdf ). Investigations, including blood gas estimations,
rarely alter immediate management.
Cautions Children with severe asthma attacks may not appear distressed.
Wheeze and respiratory rate correlate poorly with severity of airway
obstruction. Increasing tachycardia denotes worsening asthma, a fall in
heart rate in life-threatening asthma is pre-terminal.
Assessment in the very young (<2 years) may be diffi cult — get expert
help.
Normal peak expiratory fl ow in children aged 5–18 years.
Fig. 15.13
100
200
300
400
Peak expiratory flow (litres/min)
500
600
Height (cm)
–2SD
Mean
Boys and girls
2SD
110 120 130 140 150 160 170

679
SEVERE ACUTE ASTHMA IN CHILDREN
Management of acute asthma in children aged > 2 years
(Figs 15.14 and 15.15 )
• Summon senior ED/PICU/paediatric help if asthma is severe.
• Provide high fl ow O
2
via face mask (or nasal cannulae).
• Give an inhaled B-agonist. In mild or moderate asthma use a metered
dose inhaler with a spacer, and 2–4 puffs of 100mcg salbutamol every
10–20min.
• In severe or life threatening asthma use an O
2
-powered nebulizer with
salbutamol 2.5–5mg or terbutaline 5–10mg.
• Give oral prednisolone (20mg for children aged 2–5 years; 30–40mg if
aged > 5 years). If already taking maintenance steroids, give 2mg/kg (max
60mg). In children who vomit, repeat the dose of prednisolone and
consider IV hydrocortisone 4mg/kg.
• Add ipratropium bromide 0.25mg every 20–30 min if there is poor initial
response to nebulized B-agonist.
• Consider salbutamol (15mcg/kg) given IV over 10min in severe cases
with a poor response to initial nebulized salbutamol and ipratropium
bromide. Refer to PICU urgently and check K
+
levels.
• Aminophylline is not recommended in children with mild to moderate
asthma. In severe or life-threatening asthma unresponsive to maximal
doses of bronchodilators and systemic steroids, take specialist advice
and consider IV aminophylline (5mg/kg over 20min; maintenance IV
infusion at 1mg/kg/hr; omit loading dose if already receiving oral theo-
phyllines).
• Consider an IVI of magnesium sulphate 40mg/kg over 20min, but
evidence of benefi t is limited.
• Do not give ‘routine’ antibiotics.
Notes If possible, repeat and record peak fl ow 15–30min after starting
treatment. If the patient is not improving, give further nebulized B-agonist.
Pulse oximetry is helpful in assessing response to treatment. An SpO
2
≤ 92 % in air after initial bronchodilator therapy usually indicates the need
for more intensive in-patient care usually in PICU. CXR is indicated for
severe dyspnoea, focal chest signs, or signs of severe infection.
Consider need for anaesthesia/intubation/IPPV and PICU transfer
• Deteriorating peak fl ow or worsening or persistent hypoxia or normal/
increased pCO
2
levels on ABG.
• Exhaustion, feeble respiratory effort, confusion, or drowsiness.
• Coma or respiratory arrest.
Management of acute asthma in children aged <2 years
Assessing acute asthma in early childhood is diffi cult: get specialist help
(see www.sign.ac.uk ). Intermittent wheezing attacks are usually due to viral
infection. Differential diagnosis includes: aspiration and other pneumonias,
bronchiolitis, tracheomalacia, complications of underlying conditions (eg
congenital abnormalities, cystic fi brosis). If there is no response to inhaled
bronchodilators, review the diagnosis:
• Use a metered dose inhaler with spacer to give B-agonist therapy.
• Consider systemic steroids early in the management of moderate to
severe asthma in infants (10mg of soluble prednisolone).
• Consider adding inhaled ipratropium bromide (0.25mg) to inhaled
B-agonists for more severe symptoms.
680 CHAPTER 15 Paediatric emergencies
Fig. 15.14 Management of acute asthma in 2–5-year-olds.
See: www.brit-thoracic.org.uk and www.sign.ac.uk
ASSESS ASTHMA SEVERITY
Moderate asthma
SpO
2
≥92%
No clinical features of
severe asthma
NB: If a patient has signs and
symptoms across categories,
always treat according to
their most severe features
Severe asthma
SpO
2
<92%
Too breathless to talk or eat
Heart rate >140/min
Respiratory rate >40/min
Use of accessory neck
muscles
Life threatening asthma
SpO
2
<92% plus any of:
Silent chest
Poor respiratory effort
Agitation
Altered consciousness
Cyanosis
Age 2–5 years
Reassess within 1 hour
ASSESS RESPONSE TO TREATMENT
Record respiratory rate, heart rate and oxygen saturation every 1–4 hours
RESPONDING
Continue bronchodilators 1–4 hours prn
Discharge when stable on 4 hourly
treatment
Continue oral prednisolone for up to 3 days
At discharge
Ensure stable on 4 hourly inhaled treatment
Review the need for regular treatment and the use
of inhaled steroids
Review inhaler technique
Provide a written asthma action plan for treating
future attacks
Arrange follow up according to local policy
NOT RESPONDING
Arrange HDU/PICU transfer
Consider:
Chest X-ray and blood gases
IV salbutamol 15 mcg/kg bolus over
10 minutes followed by continuous
infusion 1–5 mcg/kg/min (dilute to
200 mcg/ml)
IV aminophylline 5 mg/kg loading
dose over 20 minutes (omit in those
receiving oral theophyllines)
followed by continuous infusion
1 mg/kg/hour
β
2
agonist 2–10 puffs via
spacer ± facemask [given
one at a time single puffs,
tidal breathing and inhaled
separately]
Increase β
2
agonist dose
by 2 puffs every 2 minutes
up to 10 puffs according to
response
Consider soluble oral
prednisolone 20 mg
β
2
agonist 10 puffs via
spacer ± facemask or
nebulized salbutamol
2.5 mg or terbutaline 5 mg
Soluble prednisolone 20 mg
or IV hydrocortisone
4 mg/kg
Repeat β
2
agonist up to
every 20–30 minutes
according to response
If poor response add
0.25 mg nebulized
ipratropium bromide
Nebulized β
2
agonist:
salbutamol 2.5 mg or
terbutaline 5 mg plus
ipratropium bromide
0.25 mg nebulized
Oral prednisolone 20 mg or
IV hydrocortisone 4mg/kg
if vomiting
Discuss with senior clinician,
PICU team or paediatrician
Repeat bronchodilators
every 20–30 minutes
Oxygen via face mask/nasal prongs to achieve SpO
2
94–98%
681
SEVERE ACUTE ASTHMA IN CHILDREN
Fig. 15.15 Management of acute asthma in children aged less than 2 years.
See: www.brit-thoracic.org.uk and www.sign.ac.uk
ASSESS ASTHMA SEVERITY
Moderate asthma
SpO
2
≥92%
PEF >50% best or predicted
No clinical features of
severe asthma
NB: If a patient has signs and
symptoms across categories,
always treat according to
their most severe features
Severe asthma
SpO
2
<92%
PEF 33–50% best or
predicted
Heart rate >125/min
Respiratory rate >30/min
Use of accessory neck
muscles
Life threatening asthma
SpO
2
<92% plus any of:
PEF <33% best or predicted
Silent chest
Poor respiratory effort
Altered consciousness
Cyanosis
Age >5 years
Reassess within 1 hour
ASSESS RESPONSE TO TREATMENT
Record respiratory rate, heart rate, oxygen saturation and PEF/FEV every 1–4 hours
RESPONDING
Continue bronchodilators 1–4 hours prn
Discharge when stable on 4 hourly
treatment
Continue oral prednisolone 30–40 mg
for up to 3 days
At discharge
Ensure stable on 4 hourly inhaled treatment
Review the need for regular treatment and the use
of inhaled steroids
Review inhaler technique
Provide a written asthma action plan for treating
future attacks
Arrange follow up according to local policy
NOT RESPONDING
Continue 20–30 minute nebulizers and
arrange HDU/PICU transfer
Consider: Chest X-ray and blood gases
Consider risks and benefits of:
Bolus
IV salbutamol 15 mcg/kg if not
already given
Continuous IV salbutamol infusion
1–5 mcg/kg/min (200 mcg/ml solution)
IV aminophylline 5 mg/kg loading
dose over 20 minutes (omit in those
receiving oral theophyllines) followed by
continuous infusion 1 mg/kg/hour
Bolus IV infusion of magnesium sulphate
40 mg/kg (max 2 g) over 20 minutes
β
2
agonist 2–10 puffs via
spacer
Increase β
2
agonist dose
by 2 puffs every 2 minutes
up to 10 puffs according to
response
Oral prednisolone
30–40 mg
β
2
agonist 10 puffs via
spacer or nebulized
salbutamol 2.5–5 mg
or terbutaline 5–10 mg
Oral prednisolone 30–40 mg
or IV hydrocortisone
4 mg/kg if vomiting
If poor response nebulized
ipratropium bromide 0.25 mg
Repeat β
2
agonist and
ipratropium up to every
20–30 minutes according to
response
Nebulized β
2
agonist:
salbutamol 5 mg or
terbutaline 10 mg plus
ipratropium bromide
0.25 mg nebulized
Oral prednisolone 30–40 mg
or IV hydrocortisone
4mg/kg if vomiting
Discuss with senior clinician,
PICU team or paediatrician
Repeat bronchodilators
every 20–30 minutes
Oxygen via face mask/nasal prongs to achieve SpO
2
94–98%

682 CHAPTER 15 Paediatric emergencies
Acute bronchiolitis
1
Viral infection of the small airways results in infl ammation, oedema, and
excessive secretions, presenting with signs of obstructive airways disease.
Acute bronchiolitis is common, particularly in the winter months and pre-
dominantly involves infants (typically 3–6 months). Those at particular risk
are the very young (aged <6 weeks), the premature (born <35 weeks)
and those with chronic respiratory, congenital heart disease, immunode-
fi ciency, or neurological problems. Parental smoking increases the risk of
bronchiolitis. Breast feeding for more than two months appears to have a
protective effect. Most infants recover completely within 2 weeks.
Agents responsible
75 % are caused by respiratory syncytial virus (RSV). Other causes include
infl uenza, para-infl uenza, adeno-, and enteroviruses.
Presentation
Coryza, rhinorrhoea, and mild fever progress to respiratory distress
with dyspnoea, dry cough, feeding diffi culties, and wheeze (variable).
Some children may present with apnoea. Inspection may reveal cyanosis,
dehydration, tachypnoea ( > 50/min), nasal fl aring, grunting, subcostal and
intercostal recession. The chest is usually visibly hyperinfl ated in bronchi-
olitis. There may be tachycardia and prolonged expiration ( ± wheeze) with
fi ne end-inspiratory crepitations.
Complications
Feeding diffi culties, apnoeic spells, and respiratory failure (hence, adopt
a low threshold for admission). Secondary bacterial infection can occur,
but is uncommon. Long-term airway damage may occasionally occur
(obliterative bronchiolitis).
Investigations
• Apply a pulse oximeter, and check the pulse and CRT.
• Do not do routine blood tests unless the infant is febrile or an
alternative diagnosis, such as pneumonia or sepsis is more likely.
• Consider CXR and ABG/capillary gas only for those with progressive,
atypical or severe illness. Do not do CXR routinely.
• Fluorescent antibody tests on nasopharyngeal aspirate to demonstrate
the presence of RSV are recommended; these help with cohorting and
isolation arrangements on the wards (see opposite), particularly during
the annual epidemic season in winter.
• Assess feeding diffi culties by offering a bottle feed.
CXR shows hyperinfl ation with downward displacement of the diaphragm
due to small airway obstruction and gas trapping. There may also be
collapse or consolidation (usually upper lobe) or perihilar infi ltrates hard
to distinguish from pneumonia.
Differential diagnoses for bronchiolitis include congenital heart disease,
asthma, pneumonia, cystic fi brosis, inhaled foreign body and septicaemia.

683
ACUTE BRONCHIOLITIS
Treatment
Refer all infants with respiratory distress, feeding diffi culties (<50 % usual
fl uid intake in previous 24 hr), SpO
2
<94 % on air, apnoeic episodes, or
dehydration. Emergency treatment is largely supportive, comprising
humidifi ed O
2
(aiming to keep SpO
2
> 92 % ), NG or IV fl uids and some-
times CPAP or IPPV. Dehydration may be severe enough to warrant an
IV fl uid bolus of 20mL/kg. Treatment with inhaled bronchodilators may
achieve short-term (30–60min) clinical improvement in a minority, but
there is no convincing evidence of effi cacy. Nasal suction may help those
in respiratory distress. Ribavirin is of no value and should not be used.
Do not give antibiotics for bronchiolitis, but consider for severe illness
suggestive of co-existing pneumonia or septicaemia. There is no benefi t
from using ipratropium, oral or inhaled steroids, or nebulized adrenaline.
Do not use these therapies in acute bronchiolitis.
PICU referral and ventilatory support is indicated for those with recurrent
apnoea, persistent acidosis pH <7.25, infants with d conscious level, poor
chest wall movement, and low SaO
2
(<92 % ) despite FiO
2
> 60 % , and
those with hypercapnoea.
Cross infection is a serious problem during epidemics. Ensure all persons
entering a cubicle containing a child with bronchiolitis clean their hands
before and after seeing the patient, and use gloves and plastic aprons.
Prevention
Palivizumab is a humanized monoclonal RSV antibody, which is used as a
prophylactic agent to reduce the severity of RSV disease in at risk infants.
It can be considered for use on a case-by-case basis in infants who:
• Were born prematurely (<35 weeks gestation).
• Have acyanotic congenital heart disease.
• Have chronic lung disease.
• Have severe congenital immunodefi ciency.
Infants should be selected for this treatment by a local lead paediatric
specialist.
1 See the SIGN Guideline on Bronchiolitis in Children . Available at: http://www.sign.ac.uk/pdf/
sign91.pdf

684 CHAPTER 15 Paediatric emergencies
Whooping cough
ND
Caused by Bordetella pertussis , whooping cough is a notifi able disease with
an incubation period of 5–14 days ( b p.220). It is common (particularly
in the autumn) in children not immunized against it. A similar disease
may also occur with other viral infections ( Bordetella parapertussis and
adenoviruses).
Presentation
Coryza is followed by increasing cough (typically worse at night, and
tending to occur in bouts, often culminating in vomiting). Severe coughing
bouts may result in conjunctival haemorrhages. The characteristic ‘whoop’
is an inspiratory noise produced after a coughing bout. It is not present in
all infants with whooping cough. The cough may persist for several weeks.
Complications
Illness is often prolonged. There is a risk of neurological damage and bron-
chiectasis. Infants are at particular risk of death from apnoeic episodes.
Investigations
Send blood for viral titres, mycoplasma antibodies and FBC (usually
reveals markedly i lymphocytes). CXR may be normal or show ‘shaggy’
right heart border.
Treatment
Refer infants aged <6 months (risk of apnoea) and any acutely unwell child.
Discharge others (having informed the Infectious Diseases consultant)
with PO erythromycin (12.5mg/kg qds) and advice to avoid contact with
other children for 5 days. Arrange GP follow-up and give PO erythromycin
(12.5mg/kg qds) as prophylaxis to unimmunized infant siblings.
Prevention
Encourage immunization.

685
TB
ND
AND CYSTIC FIBROSIS
TB
ND
and cystic fi brosis
Pulmonary TB
TB is being seen increasingly again ( b p.232). It is more common in
visitors from overseas or HIV + ve children. TB may present in a variety
of ways in children: persistent cough and fever, growth retardation,
meningitis, pleural effusion, monoarticular arthritis, lymphadeno pathy,
back pain, hepatosplenomegaly.
Investigation CXR.
Treatment Refer suspected cases for specialist evaluation, including
Mantoux (0.1mL intradermal tuberculin) and treatment.
Cystic fi brosis
Recurrent respiratory infections in neonates and infants raise the possibility
of cystic fi brosis, tracheo-oesophageal fi stula, cleft palate, or a defect in
immunity. Cystic fi brosis is an autosomal recessive disorder affecting 1 in
2000 children. It may present neonatally with meconium ileus or later with
respiratory infections ( ± fi nger clubbing), failure to thrive, rectal prolapse
and steatorrhoea. Once diagnosed, a child will remain closely monitored
and treated by both GP and a specialist CF respiratory team. Involve this
team at an early stage if a child with cystic fi brosis presents with respira-
tory infection.
686 CHAPTER 15 Paediatric emergencies
Pneumonia
Pneumonia is relatively common at all ages, but the infective agents
responsible vary (Table 15.6 ). Viruses are most commonly found as a
cause in younger children. In older children, when a bacterial cause is
found, it is most commonly Strep. pneumoniae.
Symptoms
Often an URTI is followed by i fever, cough, dyspnoea, lethargy, feeding
diffi culties, and dehydration. Pleuritic chest pain, abdominal pain, and
neck stiffness may occur. The presence of headache, abdominal pain,
maculopapular rash, and joint pains suggests Mycoplasma infection.
Signs
The child is usually dyspnoeic, pyrexial, and unwell. Classic signs of
consolidation ( b p.114) are often absent, especially in infants and younger
children. Look for evidence of infection elsewhere (ears, throat) and
dehydration. If wheeze is present in a pre-school child, bacterial pneumonia
is unlikely, although it does occur occasionally with mycobacteria in older
children.
Investigations
• Take throat swabs.
• Obtain blood for FBC, cultures, viral titres, and mycoplasma antibodies.
• Check SpO
2
.
• Obtain urine for culture.
• CXR may demonstrate widespread bronchopneumonia or lobar
consolidation. Cavitation suggests Staphyloccocal pneumonia or TB.
Treatment
If SpO
2
<92 % , give O
2
. Treat dehydration with IV fl uids. Refer for admission
and antibiotics. IPPV is rarely required.
The choice of antibiotic will depend upon the likely infective agent and
local/national protocols (see British Thoracic Society guidelines: www.
brit-thoracic.org.uk and see Box 15.2 ).
Refer to ICU those unable to maintain SpO
2
> 92 % with 60 % O
2
, those
with signs of shock, increasing respiratory rate/pulse rate with respiratory
distress and exhaustion, those with slow irregular breathing or recurrent
apnoea.
Table 15.6 Infective agents responsible for pneumonia
Age Common causes
Neonates
E. coli , B -haemolytic Strep., Chlamydia trachomatis , Listeria
monocytogenes , CMV
Infants and
toddlers
RSV, para-infl uenza viruses, Strep pneumoniae , H. infl uenzae ,
Mycoplasma
Older children Strep pneumoniae , H. infl uenzae , Mycoplasma

687
PNEUMONIA
Box 15.2 Antibiotic treatment for suspected bacterial
pneumonia
Uncomplicated community acquired pneumonia
• Neonate : benzylpenicillin and gentamicin.
• Neonate and child under 6 months : cefuroxime or co-amoxiclav (or
benzylpenicillin if lobar pneumonia or S. pneumoniae suspected).
• Child 6 months to 5 years : oral amoxicillin or oral erythromycin.
• Child 5–18 years : oral erythromycin (or oral amoxicillin if
S. pneumoniae suspected).
Add fl ucloxacillin if staph suspected eg in infl uenza or measles
Use erythromycin if atypical pathogens suspected or penicillin allergic
Severe community acquired pneumonia of unknown aetiology
• Neonate : benzylpenicillin and gentamicin.
• 1 month to 18 years : cefuroxime or co-amoxiclav (or benzylpenicillin
if lobar pneumonia or S. pneumoniae suspected).
Use erythromycin if atypical pathogens such as mycoplasma (more
common in children over 5 years) or Chlamydia suspected or penicillin
allergic. Add fl ucloxacillin if Staphylococcus suspected.

688 CHAPTER 15 Paediatric emergencies
Fits, febrile convulsions, and
funny turns
A careful history is crucial. Epileptic fi ts may take many forms:
Grand mal (tonic/clonic) Loss of consciousness and shaking of all limbs.
Petit mal (‘absences’) Child pauses in speech or other activity and is
unaware of episode.
Focal fi t Involves 1 part of body (progression to grand mal = Jacksonian
march).
Myoclonic fi t May be violent and includes drop attacks.
Infantile spasm (Salaam attack) May involve truncal fl exion and cause a fall.
Temporal lobe epilepsy Numerous bizarre presentations.
The fi tting patient
The child who is still fi tting on arrival to hospital is likely to have had a
prolonged seizure and needs urgent attention.
• Give O
2
.
• Secure the airway. If teeth are clenched, do not try to prise them
open to insert an airway. Instead, if the airway is obstructed, try a
nasopharyngeal airway ( b p.325).
• Give IV lorazepam (0.1mg/kg) or if venous access is unsuccessful, per
rectum (PR) diazepam (0.5mg/kg) or buccal midazolam (0.5mg/kg).
• Check bedside strip measurement of venous/capillary blood glucose
(BMG) and treat hypoglycaemia with IV 0.5g/kg dextrose (5mL/kg of
10 % ).
• Treat fever > 38 * C with rectal paracetamol.
• If fi ts continue, follow the algorithm for status epilepticus ( b p.690).
After the fi t has fi nished
Reassess Airway, Breathing, Circulation. Continue O
2
and place in the
recovery position. Check for injuries and perform regular observations.
First fi t Refer for investigation of possible causes. U&E, blood glucose,
Ca
2 +
, Mg
2 +
, FBC, and urinalysis will be required.
Subsequent fi t If appropriate, check serum anticonvulsant level and
arrange for GP/outpatient clinic to receive the results and adjust dose
appropriately. Allow home patients with known epilepsy who have
fully recovered and have no obvious cause for the fi t (eg meningitis,
hypoglycaemia).
Febrile convulsions
These are grand mal seizures lasting <5min and secondary to pyrexia of
febrile illness. Commonest cause of fi ts between 6 months and 5 years,
affecting 3 % of children. Although 30 % recur, only 1 % go on to develop
epilepsy in adult life. By defi nition, children already diagnosed as epileptic,
do not have febrile convulsions, but ‘further fi ts’. Treat patients who arrive

689
FITS, FEBRILE CONVULSIONS, AND FUNNY TURNS
fi tting with O
2
, airway care and IV lorazepam, PR diazepam or buccal
midazolam as described opposite. Check BMG and T * . Give PR (or if
conscious, oral) paracetamol (15mg/kg). Examine thoroughly for a source
of infection (particularly meningitis) and perform an infection screen: U&E,
FBC, blood cultures, MSU, CXR and LP. Consider discharging children
aged > 2 years with second or subsequent febrile convulsion, and obvious
benign and treatable cause for pyrexia, with appropriate treatment. Liaise
with GP to consider arranging for parents to administer rectal diazepam
or buccal midazolam to terminate future febrile fi ts. Admit children aged
<2 years, those with fi rst febrile fi ts, and those with serious infections or
an unknown cause of pyrexia.
Approach to the febrile child aged <3 years
Usually symptoms and signs of illness are non-specifi c. General aspects of
behaviour and appearance provide the best guide as to whether a serious
illness is likely. The degree of fever and response to antipyretics is not
helpful. Up to 5 % of those who present with fever will have bacteraemia.
Admit any febrile child <3 years who appears unwell/ miserable.
Febrile infants ( > 38 * C) aged <3 months are especially diffi cult to assess
and require admission for a ‘septic screen’ (FBC, serology, blood cultures,
urine culture ± CXR, lumbar puncture (LP). Discuss with a neonatologist
the need for IV antibiotics in babies aged <28 days.
Young children aged 3 months–3 years who have a clear focus of infection
and appear well should be treated as indicated. If there is no clear focus of
infection, consider short-term admission in a paediatric facility.
Funny turns
Only a minority of reported ‘funny turns’ are epileptic fi ts. Most require
referral and investigation. The history is crucial.
Infants Irregular and varying depth of respiration during sleep is normal,
but can cause parental alarm. Self-limiting apnoeic or cyanotic episodes
may be due to: fi ts, inhaled FBs, near-miss cot death, gastro-oesophageal
refl ux and laryngeal spasm, or arrhythmias (eg SVT).
Toddlers Breath-holding attacks commonly accompany frustration. They
may cause the toddler to turn blue, lose consciousness, and even have
a brief fi t. Refl ex anoxic episodes (‘pallid syncope’) are due to excess
vagal stimulation in illness or after injury. Bradycardia, pallor and loss of
consciousness is occasionally accompanied by a short fi t.
Older children Syncope on exertion should prompt consideration of aortic
stenosis, SVT, coarctation or hypertrophic cardiomyopathy. Vasovagal
episodes and hyperventilation also cause ‘collapse’. Atypical or unheralded
collapse or seizures may be a feature of inherited long QT syndrome, and
is associated with torsades de pointes. Obtain an ECG in any child who
presents with collapse or ‘fi rst fi t’.

690 CHAPTER 15 Paediatric emergencies
Status epilepticus
Defi nition a fi t (or consecutive fi ts without complete recovery between)
lasting > 30min. The duration of the seizures is often underestimated
because the intensity of the jerking diminishes with time and small
amplitude twitching may be easily missed.
Status epilepticus usually involves tonic-clonic fi ts and as in adults, is
associated with signifi cant mortality ( 8 4 % ) and morbidity (up to 30 % have
long-term neurological damage). Prompt treatment with termination of
the fi t is crucial to d these risks.
Causes meningitis, head injury, altered drug therapy, or non-compliance in
known epileptic child, metabolic disturbances, encephalopathy (including
Reye’s syndrome), ‘febrile status’, poisoning.
Treatment algorithm for the fi tting child
1
• Open and maintain airway and give O
2
.
• Do not prise open clenched teeth — consider nasopharyngeal airway.
• Rapidly obtain venous access and check BMG.
• Give lorazepam 0.1mg/kg IV over 30–60sec * (if no venous access: give
0.5mg/kg diazepam PR or buccal midazolam 0.5mg/kg).
• Treat hypoglycaemia with 0.5g/kg dextrose (5mL/kg of 10 % ) IV.
• Apply pulse oximeter and send blood for investigations (see below).
• Check T * : if > 38 * C give paracetamol 15mg/kg PR.
If seizure continuing at 10min
• Repeat lorazepam 0.1mg/kg IV over 30–60sec
*
(or if vascular access still
not obtained, give paraldehyde 0.4mL/kg PR in the same volume of olive
oil or 0.9 % saline).
• Get senior help and call for senior ED/anaesthetic/PICU help.
If seizure continuing after a further 10min
• If not known to be taking phenytoin: start phenytoin infusion 18mg/kg
IV * over 20min (monitor BP and ECG) or if already on phenytoin, give
phenobarbital 20mg/kg IV * over 10min.
If seizure continuing after a further 20min
• Paralyse, intubate and ventilate using IV thiopental (induction dose 4mg/
kg) and consider a thiopental infusion.
• Transfer to ICU/PICU for ventilation and EEG monitoring.
Investigations : BMG and blood glucose, U&E, Ca
2 +
, Mg
2 +
, PO
4
3 –
, LFTs, FBC,
ABG/capillary gas, blood cultures, coagulation screen, CXR. If taking anti-
convulsant(s): check serum level(s). Obtain CT scan of head if intracranial
disease is suspected (unless clinically meningitis), in which case treat
immediately — b Meningococcal disease, p.666).
1 See APLS Manual 4th edn, 2005 .
* Intraosseous route is an alternative.

691
DIABETIC KETOACIDOSIS
Diabetic ketoacidosis
Diabetic ketoacidosis will usually present to the ED in a child who is known
to be diabetic, but occasionally it can be the fi rst presentation of DKA.
The child will present with features including altered conscious level,
polyuria, polydipsia, nausea, vomiting, and abdominal pain. Children with
DKA can die from cerebral oedema (unpredictable and has 25 % mortality),
aspiration pneumonia, or hypokalaemia. All of these are avoidable with
appropriate treatment.
Be very careful not to misdiagnose the abdominal pain of DKA as a ‘surgical
abdomen’ or to dismiss the child as ‘hyperventilating’ (the i respiratory
rate is due to profound metabolic acidosis). Call senior ED and paediatric
staff when DKA is suspected.
Causes First episode of DKA in a previously well child. In a child with
known diabetes, lack of insulin, change of therapy, and intercurrent viral
illness can cause DKA. Fever suggests sepsis (fever is not part of DKA).
Treatment algorithm for the child with DKA
1
• Open and maintain airway if not fully conscious and give high fl ow O
2
.
• Attach cardiac monitor (look for tall T-waves) and record CRT/BP.
• Rapidly obtain venous access and check BMG (remember BMG often
underestimates blood glucose in DKA) and estimate weight.
• Take blood for glucose, U&E, FBC, VBG (and ketones if available).
• If evidence of shock (tachycardia, prolonged CRT, hypotension), give
10mL/kg 0.9 % saline as a bolus; repeat as required up to 30mL/kg.
Confi rm the diagnosis of DKA
• Check history with child and parents: polyuria, polydipsia; vomiting,
abdominal pain, drowsiness, and i respiratory rate.
• Biochemical : high glucose ( > 11mmol/L; acidosis (pH<7.3, bicarbonate
<15mmol/L); glycosuria and ketonuria.
Involve senior paediatric ± PICU staff
• Assess level of dehydration (mild <3 % ; moderate 5 % (dry mucous
membranes/ d skin turgor); severe 8 % (sunken eyes, i CRT, shocked and
needed fl uid bolus) and record in ED notes.
• Involve PICU if very young (<2 years), severe acidosis (pH<7.1), severe
dehydration or d conscious level (cerebral oedema, i risk of aspiration).
Further care
• Do not start insulin until IV fl uids have been running for at least 1hr —
earlier insulin therapy is associated with i cerebral oedema.
• Do not administer bicarbonate except on specialist PICU advice.
• Follow local protocols for continuing fl uid replacement, but remember
that over-infusion of fl uid is associated with cerebral oedema.
•
Aim for replacement of fl uids and potassium over 48hr or longer.
1 See http://www.bsped.org.uk/professional/guidelines/docs/DKAGuideline.pdf for full details.

692 CHAPTER 15 Paediatric emergencies
Urinary tract infection (UTI)
UTI in children requires prompt investigation, since progressive
renal failure and hypertension may occur insidiously. 35 % have proven
vesico-ureteric refl ux: early treatment may help to prevent renal failure.
UTI may present in a variable and non-specifi c fashion. Consider and
exclude UTI as part of the initial approach to any ill child presenting
to the ED.
Presentations
Older children typically present with lower abdominal pain, dysuria,
frequency, offensive urine, haematuria or fever. However, dysuria and
frequency do not always refl ect UTI. Children <3 years old often present
unwell with fever and irritability, but no specifi c signs. Infants may present
with poor feeding, vomiting, and failure to thrive.
Examination
Always check the BP and feel for loin tenderness (pyelonephritis) and
abdominal masses (polycystic kidneys).
Investigation
Obtain a clean catch specimen of urine for urinalysis, microscopy, culture
and sensitivity. This can prove to be quite diffi cult, depending upon the
age of the child. Try one of the following approaches:
Neonates and infants
• Clean the perineum with sterile water, then tap with 2 fi ngers just
above the symphysis pubis (ideally 1hr post-feed) and catch the urine
which is forthcoming, trying to avoid the fi rst few millilitres.
• Clean the perineum as above and use a urine collection pad according
to the manufacturer’s instructions.
• Suprapubic aspiration is useful if the baby is seriously ill. Clean the
skin with antiseptic solution, then using sterile gloves and an aseptic
technique, insert a 21G needle in the midline 2.5cm above the pubic
crest and aspirate urine.
Toddlers and older children
• Co-operation will enable an MSU to be obtained (in the male, gently
retract the foreskin (if possible) and clean the glans fi rst; in the female,
separate the labia and clean the perineum front to back, fi rst).
• If the child is uncooperative, try a urine collection pad or bag.
Dipstick urinalysis at the bedside will reveal the presence of blood, protein,
sugar, bilirubin, ketones or nitrite. A positive nitrite test is accepted as
good evidence of UTI. Urine pH is not usually helpful, for although pH
<4.6 or > 8.0 may refl ect infection, it may also be due to various acid-base
disorders. Urinalysis may be normal, despite bacteriuria. Urine microscopy
allows a search for pyuria and bacteriuria (highly suggestive of UTI) and an
accurate assessment of other constituents (see Table 15.7 ). Perform FBC,
U&E, blood glucose, and blood cultures if septicaemic, loin pain or i T ° .
693
URINARY TRACT INFECTION (UTI)
Treatment
• Children with suspected pyelonephritis or who appear toxic : resuscitate
as necessary with IV fl uids ( b p.663) and refer for admission and
IV antibiotics (eg cefotaxime). Infection with beta lactamase producing
E. coli is said to be increasing, and some recommend at least one dose
of gentamicin, pending sensitivities. Give antibiotics for 10 days.
• Symptomatic children with abnormal urinalysis (proteinuria or haematuria) :
start a 3-day course of antibiotics PO (trimethoprim or cefalexin —
dose according to age, refer to BNFC ). Encourage plenty of oral fl uids
and complete voiding of urine. Offer advice to the child and parents
(eg avoid tight underwear, use toilet paper wiping from front to back).
• Organize paediatric follow-up to receive results of MSU and to arrange
subsequent investigations : this may include U&E, blood glucose, ultra-
sound scan (USS) and a variety of other tests (eg isotope renography
and micturating cysto-urethrography), according to local policy.
• Recurrent UTIs with anogenital signs may be due to sexual abuse.
Table 15.7 Urine microscopy fi ndings and their signifi cance
Red cells Normally <3/mm
3
White cells Normally <3/mm
3
Epithelial
cells
Present normally: shed from urinary epithelium
Bacteria
or fungi
Always abnormal, refl ecting infection or specimen contamination
Casts Hyaline casts — comprise Tamm–Horsfall protein: may be normal,
but i in fever, exercise, heart failure, after diuretics
Fine granular casts — may be present normally, eg after exercise
Coarse granular casts — abnormal, seen in various renal disorders
Red cell casts — imply glomerular disease and glomerular bleeding
White cell casts–occur in glomerulonephritis and pyelonephritis
Epithelial casts — usually refl ect tubular damage
Crystals Phosphate, urate, and oxalate crystals may not be pathological, but
are also seen in Proteus UTI and hyperuricaemia.
See the ‘NICE Guidance on UTI in Children’. Available at: http://www.nice.org.uk/nicemedia/
pdf/CG54quickrefguide.pdf
694 CHAPTER 15 Paediatric emergencies
Renal failure
Causes of acute renal failure
Pre-renal Hypovolaemia (bleeding, dehydration, sepsis), heart failure,
nephrotic syndrome.
Renal Haemolytic uraemic syndrome, glomerulonephritis, acute tubular
necrosis, drugs.
Post-renal Obstruction following trauma or calculi.
Presentation and investigation
Presentation varies according to the cause. Emergency investigations include
MSU for microscopy, culture and sensitivity, urine and plasma osmolality, U&E,
blood glucose, FBC, albumin, LFTs, clotting screen, and ECG monitoring.
Treatment
Get expert help early. Pre-renal failure from hypovolaemia (urine: plasma
osmolality ratio usually > 5) should respond to treatment of the underlying
condition and an IV fl uid challenge (20mL/kg of 0.9 % saline, ± colloid/blood
products, depending on cause). Urinary catheter and CVP monitoring may
help to assess fl uid status. Urgent ultrasound can assess for obstruction
of the urinary tract, the presence of stones and vascular fi lling status. ED
treatment of renal failure focuses on hyperkalaemia and hypertension.
Hyperkalaemia Children presenting with hyperkalaemia (K
+
> 7) in
advanced renal failure may require emergency measures prior to dialysis.
Obtain expert help. Give 0.5mL/kg of 10 % calcium gluconate over 5min
to stabilize the myocardium if there are ECG changes (widened QRS
complexes or tall T waves). Give sodium bicarbonate 1mmol/kg IV
and commence an IVI of glucose (0.5g/kg/hr) with insulin (0.05U/kg/hr).
Consider nebulized salbutamol (2.5mg if <3 years; 5mg if 3–7 years; 10mg
if > 7years) or Calcium Resonium
®
1g/kg PO or PR. Nebulized salbutamol,
IV sodium bicarbonate, glucose/insulin all temporarily d serum K
+
by
shifting it into cells: defi nitive treatment (dialysis) will still be required.
Hypertension Hypertension related to volume overload in renal failure
may require IV nitrate therapy in the ED (as for pulmonary oedema), but
otherwise seek expert help for further intervention.
Nephrotic syndrome Most cases of oedema, heavy proteinuria and
hypoalbuminaemia ( ± hypercholesterolaemia) are idiopathic (‘minimal change
nephropathy’). Presentation is diverse and includes: anorexia, lethargy, frothy
urine, mild diarrhoea, abdominal pain, ascites, oliguria, peri-orbital, or genital
oedema. The prognosis is generally good, but peritonitis, renal or cerebral
venous thrombosis may occur. Check U&E, albumin, LFTs, FBC, complement,
cholesterol and lipids. Refer for further investigation/treatment.
Haemolytic uraemic syndrome Micro-angiopathic haemolytic
anaemia, thrombocytopenia and renal failure of haemolytic uraemic
syndrome typically affect infants/toddlers following a diarrhoeal illness
( E. coli 0157 , verocytotoxin, or shigella). The disease is also associated
with SLE, HIV and various tumours. The child may present oliguric or
anuric with d conscious level due to encephalopathy. Mortality is > 5 % .
FBC reveals anaemia with visible RBC fragments, thrombocytopenia,
and leucocytosis. Coombs test is –ve. Urea and creatinine are usually
i and there may be electrolyte disturbances. Treat life-threatening
hyperkalaemia as above and refer for possible dialysis and transfusion.
695
HAEMATURIA
Haematuria
Dark or discoloured urine is frightening for both the child and parents.
Although it may refl ect haematuria, it may refl ect other causes: very
concentrated urine, beetroot, porphyria, conjugated hyperbilirubinaemia,
free Hb or myoglobin (usually black, as seen in rhabdomyolysis and
malaria), or drugs (Table 15.8 ).
If haematuria is confi rmed by urinalysis, obtain a full history, remembering
to ask about preceding illnesses and trauma, foreign travel, drug history,
and family history of renal or bleeding disorders. Full examination includes
BP and a careful check for abdominal masses and oedema.
Causes of macroscopic haematuria
• UTI (including schistosomiasis).
• Glomerulonephritis.
• Trauma.
• Wilm’s tumour.
• Bleeding disorder.
• Urinary tract stones.
• Drugs (warfarin, cyclophosphamide).
• Factitious.
Microscopic haematuria may be associated with: exercise, hypercalciuria
or be familial.
Glomerulonephritis is often an immune reaction following an URTI due
to B-haemolytic Strep infection 2–3 weeks previously. It may present with
haematuria, oliguria ± hypertension and uraemia. A similar presentation
can occur with Henloch–Schönlein purpura ( b Purpuric rashes, p.664),
SLE or Berger’s disease (mesangial IgA nephropathy).
Investigation
Send MSU and obtain plain X-rays of the urinary tract if there is
abdominal pain suggesting stones (relatively rare). Check U&E, blood
glucose, FBC, clotting screen, and if signifi cant bleeding (or if haematuria
follows trauma) X-match. Further tests may be required (throat swab,
urine, and serum osmolalities, viral titres, antistreptolysin-O, antinuclear
antibodies, complement levels), but do not assist emergency treatment.
Management
Severe haematuria with clots requires resuscitation with IV fl uids ( ± blood),
but is uncommon in children, except after trauma. Treat associated severe
hypertension or hyperkalaemia associated with renal failure as described
opposite. Refer children with haematuria of non-traumatic origin to the
paediatrician.
Table 15.8 Possible alternative causes of discoloured urine
Drug/food Colour
Rifampicin Orange/pink
Desferrioxamine, senna, rhubarb Brown
Methylene blue Green

696 CHAPTER 15 Paediatric emergencies
Poisoning in children
Paediatric poisoning may take many forms:
• Neonatal poisoning from drugs taken by mother prior to birth
(eg opioids, benzodiazepines).
• ‘Accidental’ (unintentional) poisoning is the most common form
of poisoning. It largely involves toddlers and pre-school children
(boys > girls), who are at particular risk because of their innate
curiosity and considerable indiscretion in putting things in their
mouths. Children may be poisoned by any drugs that they can get
their hands on, but also mushrooms, berries, plants, household items
(eg disinfectant) and other objects misinterpreted as drink, food or
sweets (eg button batteries).
• Inadvertent self-poisoning with recreational drugs (including alcohol and
volatile agents).
• Iatrogenic poisoning by administration of the wrong dose ± wrong
drug can happen with frightening ease. Paediatric dosage charts,
calculators, obsessional checking, attention to detail and restriction of
junior doctors’ hours should help to prevent this in the ED.
• Deliberate self-poisoning in an apparent suicide attempt occurs in older
children.
• Intentional poisoning by a parent, guardian, or carer is a sinister aspect
of child abuse, which includes fabricated or induced illness ( b p.772).
The child may present in a bizarre fashion, with a non-specifi c illness, for
which the diagnosis is not immediately apparent.
Approach
Follow the general guidelines described in b pp.180–7 to treat poisoned
patients, with initial attention to oxygenation (airway), ventilation
(breathing) and circulation. Links to the National Poisons Information
Service ( www.toxbase.org Telephone 0844 892 0111) will provide
advice for specifi c poisonings ( b p.180). With notable exceptions (eg
paracetamol, opioids, iron, and digoxin) there are few ‘antidotes’ available:
treatment is often largely supportive.
Try to elicit the substance(s) ingested, the amount involved and the time
since ingestion. The majority of ingestions are unintentional and the time
to presentation is often short. Gastric emptying procedures are rarely
performed, and should be considered only if a life-threatening amount
of a drug has been ingested in the previous hour and the airway can be
protected ( b p.184). Avoid ipecac (ipecacuanha), which is ineffective in
d drug absorption and can be dangerous.
Never try to empty the stomach
following ingestion of petrol or corrosives ( b p.205).
Charcoal
The role of charcoal (dose 1g/kg PO in infants; 15–30g in older children) in
paediatric poisoning is limited by its lack of palatability. Attempts are cur-
rently being made to make charcoal more palatable, yet remain effective.

697
PREVENTION OF PAEDIATRIC POISONING
Prevention of paediatric poisoning
Background
Poisoning in children is very common. More than 40,000 children
present to hospital in the UK each year, many of whom are admitted for
observation. Thankfully, relatively few (10–15 per year) die. More than
75 % of paediatric unintentional ingestions involve drugs and poisons in
the home that are plainly visible to the child. Poisoning is particularly likely
to occur at times of ‘stress’ (eg arrival of new baby, disturbed parental
relationships, moving house) when there may be d supervision and
disruption of the usual routine. Perhaps partly for this reason, children
who present with a fi rst episode of poisoning are at i risk of further
episodes. It is therefore important to advise the parents of ways of
preventing poisoning in children (see list below).
Offi cial measures: packaging of drugs
Legislation has been introduced to try to tackle the problem of poisoning
in children. Perhaps the most successful has been the widespread adoption
of child-resistant drug containers. Unfortunately, it is not yet mandatory
for these containers to be used for liquid drugs or potentially dangerous
household items, such as bleach. Some drugs are presented in ‘strip
packaging’, in the hope that an impulsive child would lose interest before
gaining access to a signifi cant quantity.
Advice for parents (consider providing a leafl et)
• Provide adequate supervision for toddlers and young children,
particularly when visiting friends and relatives.
• Keep all medicines locked out of reach in a cupboard.
• Only purchase those drugs presented in child-resistant containers.
• Dispose of out-of-date drugs and those no longer required.
• Never refer to drugs as ‘sweets’ in an attempt to encourage the child to
take them.
• Take medicines out of sight of the child to help prevent imitation.
• Keep all alcohol, perfumes, cosmetics, detergents, and bleaches out of
reach.
• Ensure that all turpentine, paints, and weed killers are securely locked
and inaccessible.
• Give away all toxic plants.
• Keep ashtrays and waste baskets empty.

698 CHAPTER 15 Paediatric emergencies
Abdominal pain in children
The approach to the initial assessment and management of children
presenting with abdominal pain is similar in many ways to that in adults
( b p.504). Beware underlying ‘medical’ causes (eg DKA, pneumonia).
Remember that disease processes may progress with great rapidity in
children, therefore adopt a low threshold for referring children with
abdominal pain to the surgical team. Whilst many of the common causes
of abdominal pain are the same in children as in adults (eg b Acute
appendicitis, p.507), be aware of causes that are typically paediatric
(eg intussusception). Likewise, certain causes of intestinal obstruction are
seen almost exclusively in children.
Paediatric causes of intestinal obstruction
• Congenital (eg oesophageal/duodenal atresia, Hirschsprung’s disease).
• Meconium ileus.
• Hypertrophic pyloric stenosis.
• Intussusception.
• Hernia (inguinal, umbilical).
Hypertrophic pyloric stenosis
Features
This condition is relatively common, typically presenting with effortless
vomiting at between 2–10 weeks. It occurs more frequently in boys than
girls and in fi rst-born children. Vomiting becomes projectile in nature, with
progressive dehydration and constipation. The vomit is not bile-stained.
After vomiting, the baby appears hungry and keen to feed again. In
advanced cases, there may be a profound hypochloraemic alkalosis, with
associated hypokalaemia.
Diagnosis
Look for visible peristalsis. Abdominal palpation confi rms the diagnosis if
an olive-sized lump is felt in the epigastrium (most prominent during a test
feed). If the diagnosis is suspected, but not proven clinically, resuscitate
(as below) and arrange USS.
Management
Once diagnosed, keep the infant nil by mouth. Insert an IV cannula and
send blood for U&E, glucose, and FBC. Commence fl uid resuscitation
under senior guidance and refer to the surgeon — operative treatment
needs to be delayed until dehydration and electrolyte abnormalities have
been corrected (this may take > 24hr). Defer insertion of a NG tube for
appropriately experienced staff.
Volvulus
This is associated with congenital malrotations, but may occur in other
circumstances also (eg Meckel’s diverticulum, adhesions from previous
surgery). It can present with abdominal pain and other features of intestinal
obstruction (vomiting, distension), sometimes with a palpable mass.
Obtain an abdominal X-ray and refer promptly to the surgical team in
order to maximize the chance of intervening to preserve bowel.

699
ABDOMINAL PAIN IN CHILDREN
Intussusception
Telescoping of one segment of bowel into another may affect the small
or large bowel, but most cases are ileocolic. Typically affects children
aged between 6 months and 4 years. The child may suddenly become
distressed, roll up into a ball, and appear unwell. Vomiting may develop
and the child may pass a ‘redcurrant jelly’ stool. These features, however,
together with pyrexia and a palpable mass, are not invariably present:
sometimes the presentation is shock without obvious cause. X-rays may
be normal or reveal an absent caecal shadow.
If intussusception is suspected, refer urgently to the surgical team.
The diagnosis may be confi rmed by air or barium enema, which may
also be curative, by reducing the intussusception. A barium enema
characteristically reveals a ‘coiled spring’ sign or sudden termination of the
barium, but is contra-indicated if there is evidence of perforation.
Acute appendicitis (see b p.507)
Consider this diagnosis in any child presenting with abdominal pain. Acute
appendicitis can occur in children of all ages. It can be a diffi cult diag-
nosis to make, especially in the very young. ‘Atypical’ clinical presentation
(eg diarrhoeal illness) is often associated with delayed diagnosis and an i
rate of perforation. Do not perform a rectal examination — in the unlikely
event of this being considered essential, leave it to the surgical team.
Abdominal mass
There are many causes of abdominal masses in children, many of which
may be relatively benign and asymptomatic:
• Full bladder.
• Full colon.
• Enlarged liver and/or spleen.
• Pregnancy in older children.
• Hydronephrosis.
• Hypertrophic pyloric stenosis (see opposite).
• Appendix mass.
• Intussusception.
• Volvulus.
• Neuroblastoma.
• Nephroblastoma (Wilm’s tumour).
Intra-abdominal malignancy
Neuroblastoma and nephroblastoma may reach a large size before causing
symptoms (eg haemorrhage into the tumour).
Neuroblastomas arise most commonly from the adrenal glands, but may
occur at any point along the sympathetic chain.
Nephroblastomas (Wilm’s tumours) arise from the kidneys and may present
with haematuria.
All children with suspected malignant abdominal masses require CT scan
and/or USS investigation — refer urgently to the surgical team.

700 CHAPTER 15 Paediatric emergencies
Inguinal and scrotal swellings
Painless groin and scrotal lumps
The parents or child who discovers a lump may become very concerned.
The absence of pain is to some extent reassuring, in that an acute surgical
problem is unlikely. Ascertain when the swelling appeared, whether it
changes in size or disappears, or whether there are any other symptoms.
Reducible inguinal hernia
Inguinal herniae in childhood result from a persistent patent processus
vaginalis and are therefore indirect in nature. They are commoner in boys
than girls and often bilateral. The history is typically of an intermittent
swelling, which appears with coughing or straining. If the swelling can be
demonstrated, it will be impossible to get above it. If it cannot be demon-
strated, a thickened spermatic cord may be palpated (sometimes known
as the ‘silk sign’). Refer neonatal herniae for admission and surgery, refer
infants and older children to a surgical clinic for elective surgery.
Painless irreducible inguinal hernia
Refer all irreducible inguinal hernias for admission and surgery (preceded
by gallows traction in the infant).
Hydrocoele
This transilluminable painless scrotal swelling has similar aetiology to
inguinal hernia. It appears gradually, rather than suddenly, and does not
empty or reduce on palpation. Refer to a surgical clinic. An encysted
hydrocoele of the cord may be impossible to distinguish from an irreduc-
ible inguinal hernia and therefore requires surgical exploration.
Undescended, retractile, or ectopic testis
Complete descent of the testis has yet to occur in 3 % of term infants and
30 % of premature infants. Arrange surgical follow-up if the testis cannot
be brought down to the fundus of the scrotal sac: orchidopexy will be
required if the testis fails to descend by 4 years.
Inguinal lymphadenopathy
This is on the list of differential diagnoses of painless inguinal swellings.
Look for a potential source of infection in the leg and for involvement of
any other lymph node groups.
Idiopathic scrotal oedema
An obscure allergic condition of the scrotal skin is possibly a variant of
angioneurotic oedema. Redness, mild tenderness and oedema are not
limited to one hemiscrotum. The testis is normal. The condition settles
spontaneously, a process helped by antihistamines (eg chlorphenamine
PO, doses: child 1–2 years require 1mg bd; 2–5 years require 1mg qds;
6–12 years require 2mg qds). If in doubt — refer.

701
INGUINAL AND SCROTAL SWELLINGS
Painful groin and scrotal lumps
Painful irreducible inguinal hernia
Likely to contain obstructed or strangulated small bowel. Confi rm
clinical suspicion of intestinal obstruction (pain, vomiting and abdominal
distension) by X-ray. Resuscitate as necessary with IV fl uids, give analgesia
and refer for surgery.
Testicular torsion
Commonest in the neonatal period and around puberty. In the neonatal
period the torsion is extravaginal in nature and often diagnosed late. Later
in childhood, torsion of a completely descended testis is intravaginal
due to a high insertion of tunica vaginalis. Undescended testes are also
at particular risk of torsion. Classical presentation is with sudden onset
severe pain and vomiting. Occasionally, the pain is entirely abdominal.
Examination reveals a red, tender swollen testis. The opposite testis may
be seen to lie horizontally, rather than vertically (Angell’s sign). Fast and
refer all suspected torsions for urgent surgery: exploration, untwisting and
bilateral orchidopexy.
Torsion of the hydatid of Morgagni
This remnant of the paramesonephric duct on the superior aspect of the
testis is prone to undergo torsion, causing pain and vomiting. A discrete
tender nodule may be palpable. Refer, as surgical exploration and excision
of the hydatid provides more rapid relief than the alternative conservative
treatment (analgesia and rest).
Epididymo-orchitis
Unusual in paediatric age group, but may be associated with UTI. A painful
swollen red testis and epididymis usually develops over a longer period of
time, but may be diffi cult to distinguish from testicular torsion. Refer for
an urgent surgical opinion.
Mumps orchitis
The diagnosis is usually apparent because of parotitis ( b Childhood infec-
tious diseases, p.222). Refer if there is doubt or symptoms are severe.
Henoch-Schönlein purpura
Occasionally, testicular pain may be one of the initial presenting complaints
of Henoch-Schönlein purpura (see b p.664).

702 CHAPTER 15 Paediatric emergencies
Foreskin problems and zip entrapment
Phimosis
The foreskin may normally remain non-retractile up to age 5 years.
Foreskin that remains non-retractile after this, which ‘balloons’ on
micturition, or is associated with recurrent balanitis may benefi t from
surgery (preputial stretch or circumcision). Advise the parents to see their
GP to discuss referral to a paediatric surgeon.
Balanitis
Balanitis produces redness, swelling, and even pus. Take a swab, check
for glucose in urine and send an MSU. Treat with amoxicillin (10mg/kg
PO qds) or erythromycin (10mg/kg PO qds). If redness and swelling involve
the whole penis: refer for IV antibiotics.
Paraphimosis
Irreducible, retracted foreskin results in pain and swelling of the glans.
As in the adult, cold compresses and lubricating jelly may allow reduction.
If not, refer for reduction under GA.
Penile zip entrapment
Unfortunately, underpants do not completely protect boys (and
sometimes men) from catching their foreskins in trouser zips. On many
occasions the entrapment will be released quickly by the child or parent.
On others, the child will present to the ED.
The optimal method to achieve release depends upon the entrapment
• 15 % zip foreskin through the moveable part of the zip, so that it is simply
caught between the teeth of the zip alone. In this case, achieve easy
release by cutting transversely through the zip below the entrapment.
• 85 % of entrapments involve the foreskin being caught between the
teeth and the moveable part of the zip. Local anaesthetic (either
injection using plain lidocaine or topical gel) may allow manipulation and
release. If this fails, the least traumatic option is to divide the moveable
part of the zip into 2 parts by dividing the central section (‘median bar’
or ‘bridge’) using bone cutters or wire cutters (use gauze to protect
against parts of the zip fl ying off; Fig. 15.16 ). Older children and adults
may tolerate this in the ED, but in younger boys referral for release
under GA is sensible. Circumcision is rarely required.
703
FORESKIN PROBLEMS AND ZIP ENTRAPMENT
Fig. 15.16 Method to achieve release from zip entrapment.
Strong wire
cutters
Zip slider
Zip bridge
Zip bridge
Zip slider
Zip slider
Zip bridge
Top view
Side view

704 CHAPTER 15 Paediatric emergencies
The limping child
This common problem can cause diagnostic diffi culty, particularly in the
young child who cannot provide a history and is diffi cult to examine. It is
important to try to exclude some causes of a limp that will require urgent
treatment.
Consider the following
• Trauma (fractures, soft tissue injury, FB in foot, NAI).
• Specifi c hip problems (Perthes’, slipped epiphysis, irritable hip —
b p.706).
• Infection (osteomyelitis, septic arthritis).
• Arthritis (Still’s disease, juvenile ankylosing spondylitis).
• Osteochondritis ( b p.708).
• Referred pain from infl ammatory process elsewhere.
• Malignant disease (Ewing’s sarcoma, leukaemia).
• Sickle cell crisis ( b p.176).
Adopt the following approach:
History
Ascertain whether the problem developed suddenly (eg after trauma) or
gradually. Enquire about recent illness and other symptoms, including joint
pains elsewhere.
Examination
Check T * . If the child is walking, assess the gait. Carefully inspect all of
the painful leg for erythema, swelling, deformity, and note the position
adopted. Exclude a relatively simple problem, such as a FB embedded
in the foot. Note any skin rashes. Palpate the limb for tenderness, joint
effusions, and range of movement (compare with the other side). If the
child will not walk, but can crawl without any apparent discomfort, this
localizes the problem to below the knee (thereby avoiding the need to
request ‘routine’ X-rays of the hips).
Investigation
If the child can walk, looks well, and there is no abnormality apparent on
examination, consider providing analgesia and arranging to review after
a few days, rather than undertaking all of the following investigations
immediately. Ensure the parents are told that they should return earlier
if the limp gets worse.
X-ray the tender or swollen part, particularly if there is a history of injury.
If there is no obvious tenderness, X-ray the pelvis to include both hips.
If the X-rays do not reveal a fracture, check WCC and CRP (or plasma
viscosity/ESR). If the hip is implicated, but X-rays are normal, request USS
of the hip (some experts prefer to use USS as the initial investigation). MRI
is emerging as having a potentially useful role. Follow local ED protocols
where available.
Management
Treat according to the cause (see opposite and b pp.706–9).

705
THE LIMPING CHILD
Trauma
Treat according to cause, which may include a FB in the soft tissues. There
may not always be a clear history of injury — this particularly applies to
toddler’s fracture (see b Paediatric lower limb injuries, p.726).
Osteomyelitis
Acute osteomyelitis usually results from blood-borne spread of a
distant pathogen (eg from the respiratory tract). Staph. aureus is usually
responsible, with almost invariable involvement of the metaphysis of a
long bone (most commonly proximal or distal femur, or distal tibia).
Features i T * , lethargy, localized tenderness (which may be misdiagnosed
as trauma). Septic shock may occur (especially in infants).
Investigations i WCC, i CRP, i ESR > 50mm/hr (but all may be normal
initially). X-ray changes occur after 8 10days.
Treatment If suspected, refer for admission, IV antibiotics 9 surgical
drilling/drainage.
Septic arthritis
Most commonly, Staph. aureus infection in the hip or knee. Occasionally
secondary to penetrating injury but usually haematogenous spread from a
distant site. Constitutional symptoms, fever and joint pain occur. A joint
effusion may be clinically evident. Joint movement is likely to be severely
impaired. Investigations may reveal i WCC, i CRP and i ESR. Refer for
urgent confi rmatory joint aspiration and treatment.
Non-septic arthritis
Multiple painful joints are more likely to be due to a juvenile arthritic
process (eg RA or ankylosing spondylitis) than septic arthritis. Pain felt
in several joints frequently accompanies a variety of infections and other
diseases, eg rubella, rheumatic fever, Henoch–Schönlein purpura. Refer to
the paediatrician for further investigation.

706 CHAPTER 15 Paediatric emergencies
The painful hip
The limping child may be able to localize pain to the hip, but hip pain may
be referred to the knee. Hip problems causing a limp include trauma,
infection and other disorders as in b The limping child, p.704. Specifi c hip
problems include:
Perthes’ disease (Legg–Calvé–Perthes’ disease)
Aseptic necrosis of the upper femoral (capital) epiphysis presents with a
painful limp in children aged 3–10 years. Boys are affected more than girls
(M:F = 4:1). 15 % are bilateral. Aetiology is unclear, but Perthes’ disease is
often grouped with the osteochondritides ( b p.708). Often d range of hip
movement due to pain. FBC, CRP, ESR, and blood cultures are normal.
X-ray changes refl ect stage of disease and are progressive (as opposite):
1 i joint space on medial aspect of capital epiphysis (compare sides)
2 i bone density in affected epiphysis (appears sclerotic)
3 Fragmentation, distortion (fl attening) and lateral subluxation of upper
femoral epiphysis (leaving part of the femoral head ‘uncovered’)
4 Rarefaction of the adjacent metaphysis in which cysts may appear
Treatment Refer for specialist assessment and treatment. Most cases
respond satisfactorily to conservative therapy.
Slipped upper femoral (capital) epiphysis (Fig. 15.18 )
This sometimes occurs during puberty and has been attributed to
hormonal imbalance. It occurs in children (particularly boys: M:F = 3:1)
who have one of 2 body types: obese with underdeveloped genitalia or
tall, thin rapidly growing adolescent with normal sexual development.
Presentation A child aged 10–16 years may develop a painful limp suddenly
or gradually. Often there is a history of trauma. The leg may be slightly
adducted, externally rotated, and shortened. Movement of affected hip is
d compared with the other side (esp. abduction and internal rotation).
X-ray Obtain AP pelvis and lateral hip views ± ‘frog-leg’ views. Subtle slips
may only be seen on lateral view. Larger slips will be obvious on all views.
Look for Trethowan’s sign: a line drawn along the superior border of the
femoral neck normally cuts through the epiphysis (see Fig. 15.18 ).
Treatment Refer to orthopaedics for internal fi xation ± manipulation.
Complications Avascular necrosis, chondrolysis, and osteoarthritis.
Irritable hip (‘transient synovitis’)
Common cause of sudden painful hip and limp in children of all ages.
Aetiology is unclear, but many cases appear to follow a viral illness.
Presentation varies from a slight limp to great diffi culty WB. X-rays are
normal. USS may show a hip effusion and allow aspiration for microscopy
and culture. (Apply tetracaine cream over the hip before USS).
Pyrexia, i WCC, i CRP (and/or i ESR/plasma viscosity) suggest infection.
Treatment If signifi cant physical signs (signifi cant pain, d movement,
diffi culty weight-bearing) or there is evidence suggesting infection, refer
to the orthopaedic team for admission for rest, traction and further
investigation. If physical signs are not dramatic and X-rays and blood tests
normal, discharge with NSAID, advise rest and review within a few days.
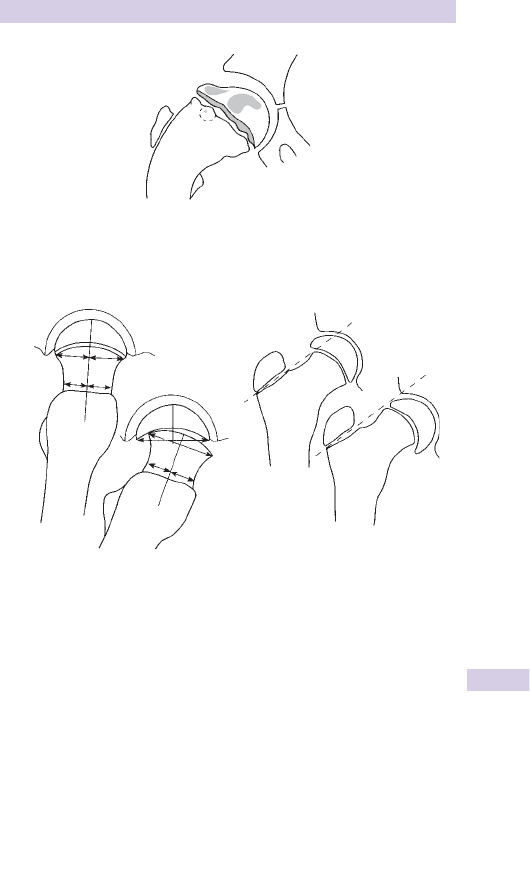
707
THE PAINFUL HIP
Fig. 15.17 Changes in the hip in Perthes’ disease.
Fig. 15.18 Slipped upper femoral epiphysis.
Lateral view showing normal (left)
and abnormal
(
ri
g
ht
)
AP view: Trethowan's sign; 1 normal,
2 abnormal hi
p
P
A
N
1
2

708 CHAPTER 15 Paediatric emergencies
Osteochondritis
This term is applied to a heterogeneous array of non-infectious disorders
affecting various epiphyses. They may be divided into 3 groups, according
to the proposed aetiology (see Table 15.9 ).
Crushing osteochondritis
Apparently spontaneous necrosis of an ossifi cation centre occurs at a time
of rapid growth. This is followed by new bone formation.
Perthes’ disease — see b The painful hip, p.706.
Scheuermann’s disease Fragmentation of low thoracic/upper lumbar
vertebral epiphyseal plates of adolescents results in chronic back pain and
a ‘round-shouldered’ kyphotic appearance. X-rays show anterior wedging
of vertebral bodies, with sclerotic notches (Schmorl’s nodes) on inferior
or superior vertebral borders. Diagnostic criteria are > 50 * of kyphosis
and wedging in 3 adjacent vertebrae. Treat symptomatically with NSAID
and refer for orthopaedic follow-up.
Kohler’s disease Avascular necrosis of the navicular affects children
(particularly boys) aged 3–5 years. A painful limp develops, with tenderness
on the dorsum of the foot over the navicular. The sclerotic fragmented
navicular seen on X-ray is also seen in many asymptomatic children. Treat
symptoms with rest, NSAID and orthopaedic follow-up. If symptoms are
severe, consider BKPOP.
Kienbock’s and Freiberg’s disease — usually affect young adults
Traction apophysitis
The pull of a strong tendon causes damage to the unfused apophysis to
which it is attached.
Osgood-Schlatter’s disease Traction apophysitis of the tibial attachment of
the patellar tendon is especially seen in boys aged 10–15 years. Anterior
knee pain after exercise is characteristic. The tibial tuberosity is prominent
and tender. The pain may be reproduced by attempted extension against
resistance.
X-rays are not always needed, but show an enlarged and sometimes
fragmented tibial tuberosity. Treat symptomatically with rest, NSAID and
orthopaedic follow-up. Most settle with conservative measures.
Johansson–Larsen’s disease (Sinding Larsen’s disease) Traction apophysitis
of the lower pole of the patella in young adolescents results in local
tenderness. Treat with rest, NSAID and orthopaedic follow-up.
Sever’s disease Traction apophysitis of the calcaneal attachment of the
Achilles tendon occurs in 8–14-year-olds. The resulting limp is associated
with local calcaneal tenderness. X-rays may reveal a fragmented sclerotic
calcaneal apophysis. Treat with rest, NSAID, a heel raise and orthopaedic
follow-up.

709
OSTEOCHONDRITIS
Osteochondritis dissecans
A piece of articular cartilage and adjacent bone become partially or
completely separated as an avascular fragment. The cause is believed to
be an osteochondral fracture from repeated minor trauma. The lateral
aspect of the medial condyle of distal femur is the most commonly affected
site. Intermittent pain, swelling and joint effusion result. If the fragment
becomes detached as a loose body, locking or giving way may occur.
X-ray Demonstrates the fragment or defect.
Treatment Refer the locked knee immediately. Treat the remainder with
rest, consider crutches, and arrange orthopaedic follow-up.
Table 15.9 Classifi cation of osteochondritis
Type of
osteochondritis
Bone affected Eponym
Crushing
osteochondritis
Femoral head
Perthes’ disease (
b p.706)
Vertebrae Scheuermann’s disease
2nd metatarsal head Freiberg’s disease
Navicular Kohler’s disease
Lunate Kienbock’s disease
Capitulum Panner’s disease
Osteochondritis
dissecans
Medial femoral
condyle
Talus
Elbow
Metatarsal
Traction apophysitis Tibial tuberosity Osgood–Schlatter’s disease
Lower pole of patella Johansson–Larsen’s disease
Calcaneum Sever’s disease
710 CHAPTER 15 Paediatric emergencies
Major paediatric trauma
The background
Trauma is the largest single cause of death in children: 8 500 deaths/ year
in the UK (Table 15.10 ). As in adults, blunt injury in children is far more
common than penetrating injury. The number of deaths in children after
trauma is dwarfed by the number who sustain serious injuries. Most
serious injuries result from road traffi c collisions and falls.
> 70 % of paediatric trauma deaths occur in the pre-hospital setting.
Most of these children are either dead when found or have sustained
overwhelming injuries. The greatest potential for reducing trauma
deaths clearly lies with injury prevention. However, there is enormous
potential to reduce the number of permanently disabled children by early
identifi cation of injuries and expert treatment. The best outcome results
from involvement of senior and experienced staff at an early stage. Prompt
recognition of the seriously injured child is crucial to this.
Pattern of injuries
Anatomical and physiological differences mean that the pattern of injuries
in children differ considerably from those in adults. Compared with
adults, children have: smaller physical size, a relatively larger head, more
compliant bones, a higher ratio of surface area to body weight, epiphyses.
Experience and an awareness of the patterns of paediatric injury will
assist resuscitation efforts. The smaller size and physical proximity of
internal organs frequently results in the dissipated forces causing injuries
to multiple structures (multiple injuries). The compliance of the bony
thoracic cage in children allows signifi cant underlying organ injury without
rib fractures. Similarly, certain injuries not uncommon in adults (eg rupture
of thoracic aorta), rarely occur in children.
Table 15.10 Causes of trauma deaths in children
Road traffi c collisions 48 %
Fires 15 %
Drowning 12 %
Hanging 8 %
Falls 8 %
Non-accidental injury 5 %
Other 4 %

711
INJURY PREVENTION
Injury prevention
Terminology
The term ‘accident’ implies an unforeseen unintentional event, one which
occurs by chance. The implication is that ‘accidents’ cannot be prevented.
However, there is considerable evidence to suggest that ‘accidents’ are
far from random events, but are relatively predictable and amenable to
prevention. For this reason, medical experts now prefer to avoid use
of the terms ‘accidents’ and ‘accident prevention’ and refer to ‘injury
prevention’ instead.
Background
Injuries to children tend to occur more frequently in certain groups and
at certain times:
• Boys sustain more injuries than girls.
• Injuries are associated with social deprivation.
• Injuries often occur at times of family stress and change (including
marital disharmony, moving house and holidays).
Prevention theory
Prevention of injury does not simply refer to physical injuries, but
poisonings also. Injuries and/or the effects of injuries may be prevented in
a number of different ways:
Primary prevention measures stop injuries occurring. For example, the
installation of fences around domestic swimming pools may reduce
drowning, locked medicine cabinets might prevent inadvertent poisoning.
Secondary prevention measures reduce the extent of harm caused by an
injurious event. The most obvious examples are helmets, seat belts, and
air bags in the context of road traffi c collisions.
Tertiary ‘prevention’ includes most forms of fi rst aid and hospital treatment,
and aims to limit the effect of an injury after it has already happened
(eg surgery to stop intra-abdominal haemorrhage, antidotes for certain
poisons).
Prevention strategies and the role of ED staff
The focus of hospital staff treating injured patients has understandably
always been the injuries themselves (‘tertiary prevention’). In addition
to any possible issues of NAI, ED staff need to consider how future
injuries to children might be prevented (eg by discussing with parents the
benefi ts of bicycle helmets). In the context of an individual child, it may
sometimes be appropriate to contact the GP/health visitor with a view to
seeing if interventions might prevent future injuries to a particular child
and siblings.
More general interventions include:
• Leafl ets and posters in the waiting room to target a captive audience
• Media involvement on certain issues, such as minimizing the risks of
fi reworks and sparklers
Further details of children’s injuries and injury prevention are available
from the Royal Society for the Prevention of Accidents ( www.rospa.org.uk )
and the Child Accident Prevention Trust ( www.capt.org.uk ).

712 CHAPTER 15 Paediatric emergencies
Resuscitation of the injured child
The priorities in managing major paediatric trauma (Airway, Breathing,
Circulation) are the same as in adults ( b p.320). Staff accustomed to
treating adults may have diffi culty with equipment sizes and drug doses.
Estimate the child’s weight ( b p.633). Call for help as soon as a seriously
injured child arrives (or is expected) in the ED — senior ED doctor, ICU/
PICU doctor and surgeon (preferably paediatric). It is often very helpful
to seek the help of a paediatrician to assist with vascular access and,
calculation of drug doses, particularly for pre-school children.
Airway with cervical spine control
Clear and secure the airway (suction and adjuncts) and provide O
2
.
If the airway is obstructed, use jaw thrust (not head tilt/chin lift) and call
for expert help (senior ED/PICU/ICU) as intubation may be required.
Ensure that manual immobilization of the cervical spine is maintained,
whilst a patient airway is being obtained. When the airway is secure, an
appropriately-sized hard collar with tape and sandbags should be used
until injury to the cervical spine has been excluded.
Breathing
Quickly exclude and treat life-threatening chest injuries. Children are
prone to swallow air, placing them at risk of massive gastric dilatation (can
cause d BP and subsequent aspiration): consider an orogastric tube.
Circulation with haemorrhage control
As in adults, hypotension is a late sign of hypovolaemia. Look carefully for
other evidence: tachycardia, tachypnoea, agitation, lethargy, pale cold skin
with d capillary refi ll time (best elicited on the sternum). Obtain venous
access (consider the intra-osseous route) as described on b p.640. Treat
hypovolaemia by stopping haemorrhage (splinting fractures, applying
pressure to wounds, prompt surgery for internal haemorrhage) and
giving IV fl uid/blood resuscitation. Give a 10mL/kg IV 0.9 % saline bolus
rapidly and reassess. If there is no clinical improvement, give a further
10mL/kg crystalloid IV fl uid bolus and repeat if necessary up to 40mL/kg.
Remember that over-aggressive fl uid replacement may worsen the
situation if the patient is suffering from internal haemorrhage. If further
fl uid is required, give blood products (whole blood 20mL/kg or 10mL/kg
packed cells) and request fresh frozen plasma (FFP) and platelets from the
laboratory for massive transfusion.
Disability
Make a rapid assessment of the child’s neurological status ( b p.356).
Exposure
Early complete inspection is mandatory, but subsequently cover the child
as much as possible in order to d anxiety and prevent excessive heat loss.

713
RESUSCITATION OF THE INJURED CHILD
Analgesia ( b Analgesia in specifi c situations, p.280)
Analgesia is often forgotten or not considered early enough, even with
major injuries. Prompt and adequate analgesia given to injured children
will gain their confi dence, enhancing assessment and treatment. Give IV
analgesia titrated according to response. Do not use IM or SC analgesia.
In severe pain give morphine IV
• Up to 100 mcg/kg over 5min if 6–12 months.
• Up to 200 mcg/kg over 5min if > 12 months.
Certain fractures are amenable to LA nerve block techniques (eg femoral
nerve block for femoral shaft fractures — b p.304). Nasal diamorphine
( b Analgesia in specifi c situations, p.280) and Entonox
®
( b Analgesics:
Entonox
®
and ketamine, p.278) may also be useful for analgesia before IV
access is available.
Parents
Remember the parents’ needs: allocate a member of staff to this task
( b p.278). Children who have suffered a traumatic event are at risk of
developing post-traumatic stress disorder — inform the parents or guardians
about this. Briefl y describe possible symptoms (sleep disturbance, night-
mares, diffi culty concentrating, and irritability). Suggest to the parents/
guardians that they contact the child’s GP if symptoms persist beyond one
month (NICE Clinical Practice Guideline 2005 (see http://www.nice.org.uk/
nicemedia/pdf/CG026fullguideline.pdf ).

714 CHAPTER 15 Paediatric emergencies
Considerations in paediatric trauma
Spinal injury
Cervical spine injury is relatively uncommon in children, but keep the
whole spine immobilized until history, examination ± X-rays exclude
injury. Injuries in children tend to involve upper (C1–3 level), rather than
lower cervical spine. Remember that rotatory subluxation may cause
signifi cant cervical spine injury without fracture: the clue is combination of
injury, neck pain and torticollis. Interpretation of cervical spine X-rays in
younger children is frequently complicated by pseudo-subluxation of C2
on C3 and of C3 on C4. If in doubt, continue immobilization and obtain
an expert opinion.
The paediatric spine is inherently more elastic so momentary inter-
segmental displacement may endanger the cord without disrupting bones
or ligaments. This can result in spinal cord injury without radiological
abnormality (SCIWORA). Usually there are objective signs of injury,
but these can be delayed. Therefore, if children present with transient
neurological symptoms after neck injury, make sure you assess them
carefully. Exclusion of signifi cant injury requires an alert child with normal
spinal and neurological examination with no painful distracting injuries and
normal radiology (rarely the case for the seriously injured child).
Head injury
Of those children who die from trauma, most succumb to head
injuries. Anatomical differences should be borne in mind. In infants, unfused
sutures allow the intracranial volume to i with intracranial haemorrhage,
causing relatively large bleeds and even shock. Similarly, scalp wounds
in infants and young children may bleed profusely and result in signifi cant
hypovolaemia. Assessment of children may prove diffi cult. An isolated
episode of vomiting after minor head injury is a frequent occurrence. To
assess level of consciousness, use the standard GCS ( b p.361) for children
aged ≥ 4 years; children aged <4 years require an adapted scale ( b p.717,
which contains further details about head injuries in children).
Chest injury
Signifi cant thoracic visceral injuries may occur without rib fractures. There
is a relatively high incidence of pulmonary contusion. Children have little
respiratory reserve and can desaturate quickly. If a chest drain is required
to treat a pneumothorax or haemothorax, use a size appropriate for the
size of the child (as indicated by Broselow tape).
Abdominal and pelvic injury
Look for hypovolaemia. Abdominal palpation cannot yield useful infor-
mation until child’s cooperation and confi dence are gained. Restrict any
PR and PV examinations to the senior surgeon. USS and/or CT scan has
replaced DPL. Gastric tubes are useful to treat the air swallowing and
gastric dilatation prevalent in injured children. Insert an appropriately-sized
urinary catheter if urine cannot be passed spontaneously or if accurate
output measurement is required (eg after severe burns).

715
CONSIDERATIONS IN PAEDIATRIC TRAUMA
Burns
Burns and smoke inhalation from house fi res still cause death in many chil-
dren each year. Even more frequently, children present with scalds from
hot or boiling liquids. The majority of these results from simple incidents
in the home: ensure that treatment includes injury prevention advice for
parents ( b p.711). Remember that some (occasionally characteristic)
burns may refl ect NAI. Assessment and treatment of the burned child
follows similar lines to those in adults; urgent priorities include securing
the airway (with an uncut ET tube) and adequate analgesia ( b p.320). IV
fl uid requirements in major burns depend upon the extent of the burn (use
Lund–Browder charts, b p.391) and clinical response (see b p.390).
Drowning and submersion incidents
Children continue to die from drowning each year despite improved
swimming education. Their high surface area to body weight ratio makes
them prone to hypothermia. Cardiac arrest after immersion warrants
prolonged resuscitation ( b p.259). Presume cervical spine injury and
immobilize the neck. Prolonged submersion ( > 8min), no respiratory effort
after 40min of CPR, persistent coma, persistent pH<7.0, persistent PaO
2
<8kPa imply a poor prognosis. Hypothermia favours a better prognosis.
Of those who survive after hospital CPR, 70 % make a complete recovery.
Wounds in children
Older children may allow wounds to be explored, cleaned, and sutured
under LA, providing they are given appropriate explanation (sometimes
it is worth demonstrating on teddy fi rst) and a parent is allowed to stay
with them. Injection of LA is least painful if a fi ne needle is employed and
the LA is warmed, buffered and injected slowly. Some children, however,
do not tolerate LA. Whilst some superfi cial wounds may be cleaned and
closed (steristrips or tissue glue) without anaesthesia, often sedation
or GA is needed. Anaesthesia is needed to allow adequate exploration
and cleaning of the wound and to d risks of infection and tattooing from
embedded dirt. Never allow the lack of co-operation to compromise
treatment, particularly with facial wounds, where wound closure under
GA may produce the best cosmetic result.
Ketamine
Ketamine can be used in the ED as an alternative to GA and provides
excellent analgesia for undertaking minor procedures in children ( b p.278;
see http://www.collemergencymed.ac.uk/CEM/Clinical % 20Effectiveness
% 20Committee/Guidelines/Clinical % 20Guidelines/default.asp ). Ketamine
should only be used by clinicians experienced in its use and capable of
managing any airway complications. Ketamine is
contraindicated if:
• The child has had a full meal within 3hr.
• There is a high risk of laryngospasm (active respiratory infection, active
asthma, age <12 months).
• There are severe psychological problems (cognitive or motor delay or
severe behavioural problems).
• Cardiovascular disease (congenital heart disease, cardiomyopathy, i BP).
• Signifi cant head injury or neurological disease, porphyria, hyperthyroidism.

716 CHAPTER 15 Paediatric emergencies
Head injuries in children
The principles of head injury management in children are the same as in
adults ( b pp.362–7), but there are some important differences (including
the assessment of conscious level in small children).
Causes of head injury
Most head injuries in children are due to falls, but few of these cause
serious injury. Severe head injury is often the result of a child running out
in front of a vehicle. Some deaths are caused by NAI ( b p.731), especially
in babies who have been shaken violently, dropped, or thrown.
Assessment of a head-injured child
History
Record details of the injurious event, the time it occurred and the
condition of the child before and after injury. Ascertain if the child was
previously well. In particular, elicit any history of fi ts or bleeding disorder.
An infection can render a child prone to falls and also cause subsequent
symptoms: a small child who vomits after a fall may be suffering from otitis
media rather than the effects of a head injury.
Determine the condition of the child immediately after injury: if he cried
at once, he did not lose consciousness. Record if he was unconscious,
confused or drowsy (and for how long) and whether he vomited or was
unsteady or dizzy. Ask about headache. Remember to take into account
the fact that a child might normally be asleep at the time he is examined.
Examination
Do not use the standard adult GCS ( b p.361) in children aged <4 years —
instead use the adapted scale opposite. Exclude hypoglycaemia. Note
whether the child looks well and is behaving normally. Measure pupil size
and check reactivity. Examine the head for signs of injury, but also look for
injuries elsewhere. Check T * and consider co-existing illness, such as ear,
throat, or urinary infections, or occasionally meningitis.
Management of head injury in children
When faced with a child with severe injuries summon senior help and
follow standard resuscitation guidelines ( b p.364). If there is any suspicion
of NAI, involve the paediatrician at an early stage ( b p.734).
Indications for immediate CT scan (see www.nice.org.uk)
Any 1 of: witnessed loss of consciousness for >5mins, any amnesia
lasting >5mins, abnormal drowsiness, >2 discrete episodes of vomiting,
clinically suspected NAI, post-traumatic epilepsy, GCS <14/15 or for an
infant <15/15 on ED assessment, suspected open or depressed skull injury
or tense fontanelle, any sign of basal skull fracture, focal neurological
defi cit, infants with bruising, swelling or laceration >5cm, dangerous
mechanism of injury.
Admission or discharge
Admit and observe children with continuing symptoms or signs, skull
fracture or if mechanism of injury suggests serious trauma (eg fall from
upstairs window). When contemplating discharge, ensure that adequate
supervision from a responsible adult is available. Provide the parent/guardian
with a verbal explanation and a written advice sheet ( b p.367, or see www.sign.
ac.uk or http://guidance.nice.org.uk/index.jsp?action=download&o=36265 ).
717
HEAD INJURIES IN CHILDREN
Glasgow Coma Scale (children)
The ‘Eye’ and ‘Motor’ components of the GCS are similar as for adults
( b p.361), but a modifi ed ‘Verbal score’ is used in small children. The
paediatric version of the GCS is shown in Table 15.11 (see www.nice.org.uk ).
Assessment of the best verbal response is likely to require assistance from
parent/guardian/carer.
In pre-verbal or intubated patients, the ‘best grimace response’ may be
used in place of the ‘best verbal response’, as shown in Table 15.12 .
Transient cortical blindness after head injury
Occasionally, children present with blindness immediately or soon after
an apparently minor head injury. The mechanism is unclear, but in most
cases blindness resolves spontaneously within a few hrs. In the meantime,
arrange a CT scan to exclude intracranial haematoma.
Table 15.11 Paediatric version of the Glasgow Coma Scale.
Best eye response Score
Eyes open spontaneously 4
Eye opening to verbal command 3
Eye opening to pain 2
No eye opening 1
Best verbal response
Alert, babbles, coos, words, or sentences to usual ability 5
Less than usual ability and/or spontaneous irritable cry 4
Cries inappropriately 3
Occasionally whimpers and/or moans 2
No vocal response 1
Best motor response
Obeys commands or has normal spontaneous movements 6
Localizes to painful stimuli or withdraws to touch 5
Withdrawal to painful stimuli 4
Abnormal fl exion to pain (decorticate) 3
Abnormal extension to pain (decerebrate) 2
No motor response to pain 1
Total 3–15
Table 15.12 ‘Best grimace response’
Score
Spontaneous normal facial/oro-motor activity 5
Less than usual spontaneous ability and/or only responds to touch 4
Vigorous grimace to pain 3
Mild grimace to pain 2
No response to pain 1
718 CHAPTER 15 Paediatric emergencies
Paediatric fractures and dislocations
Many paediatric fractures are similar to those in adults and prone to
similar complications. Bones in children differ from those in adults in two
important respects: they have epiphyses and are softer (hence fractures
are more common than signifi cant ligament injuries). Certain types of
paediatric fractures refl ect these differences:
Greenstick fracture An incomplete fracture in which one cortical surface of
a bone breaks, whilst the other side bends.
Torus (‘buckle’) fracture Another form of incomplete fracture characterized
by a buckling of the cortex.
Plastic deformation (‘bowing deformation’) Traumatic bending of long bone
shaft without visible fracture occasionally occurs in young children.
Epiphyseal injuries
Injuries to the traction epiphyses are avulsion injuries (eg peroneus brevis
insertion into the base of the 5th MT).
Injuries to the pressure epiphyses at the end of long bones adjacent to
the articular surface have been classifi ed into 5 types — the Salter-Harris
classifi cation (see Fig. 15.19 ):
• Type I : the epiphysis separates or slips on the metaphysis.
• Type II : a small piece of metaphysis separates with the epiphysis
(commonest type).
• Type III : a vertical fracture through the epiphysis joins that through the
epiphyseal plate.
• Type IV : a fracture passes from articular surface through the epiphyseal
plate into metaphysis.
• Type V : a crush injury to the epiphyseal plate (X-rays may be normal).
Note that Salter–Harris types I and V may not be apparent on the initial
X-ray. Undisplaced type I fractures often affect distal tibia and fi bula and
may present with circumferential tenderness around the growth plate.
Treat with POP and immobilization according to clinical fi ndings.
Epiphyseal growth plate injury
A concern specifi c to any epiphyseal injury is that premature fusion of a
growth plate may result, with resultant limb shortening and deformity. The
risk correlates to some extent with the mechanism of injury and amount
of force involved. The different Salter–Harris fractures carry a different
level of risk of long-term growth plate problems. The risk is low for types I
and II (particularly if undisplaced), moderate for type III and highest for
types IV and V. Problems are usually averted if Salter–Harris type III and IV
injuries are accurately reduced and held (eg by internal fi xation). Type V
fractures are notoriously diffi cult to diagnose and often complicated by
premature fusion: fortunately they are relatively rare.
Dislocations
Dislocated joints are relatively unusual in children. Most commonly
involved are the patella ( b p.726) or the radial head (‘pulled elbow’ —
b p.724). Similarly, due to relative strengths of bone and ligament,
injuries to ligaments are much less common in children than in adults.
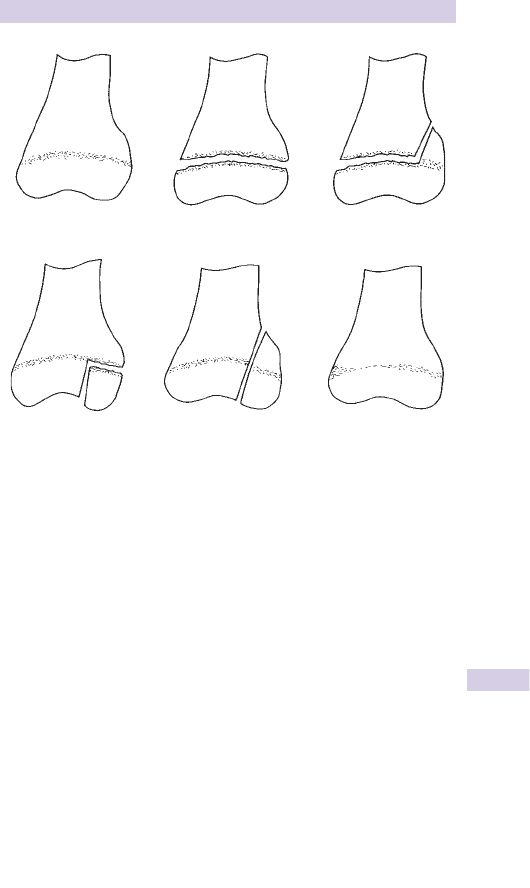
719
PAEDIATRIC FRACTURES AND DISLOCATIONS
Fig. 15.19 Salter–Harris classifi cation of epiphyseal injuries.
Normal Type I Type II
T
yp
e III T
yp
e IV T
yp
e V

720 CHAPTER 15 Paediatric emergencies
Approach to limb injuries in children
Limb injuries are very common in children. Whilst most of the points
outlined in the general approach to trauma in adults may be successfully
applied, certain modifi cations may be required.
History
Carefully elicit the mechanism of injury. The history may be confused or
not forthcoming: try to establish a rapport with the child (and parents)
nevertheless, in order to gain the child’s confi dence for the examination.
Examination
Search for evidence of a fracture (swelling, deformity, bony tenderness)
and any associated neurovascular injury. Remember the adage that the
most easily missed fracture is the second fracture: examine also for
additional injuries to adjacent bones and joints.
Is an X-ray required?
If in doubt, obtain an X-ray. The ease with which children’s bones fracture
and the diffi culties with history and examination mean that it is sensible
to adopt a low threshold for requesting X-rays. Ensure that two views at
right angles are taken (eg AP and lateral), including associated joints.
Interpreting X-rays
Many fractures are subtle and easily missed. To minimize the chance of
this occurring, visually trace around the cortex of each bone, looking for
any irregularities. Interpretation of paediatric X-rays is complicated by
the presence of various ossifi cation centres and accessory ossicles. Both
are commonly mistaken for fractures (eg the olecranon epiphysis, the os
trigonum and bipartite patella). Ossifi cation centres appear and fuse in a
relatively predictable fashion, although the rate at which this occurs varies
slightly from child to child (see Table 15.13 ). Knowledge of this process,
combined with experience of seeing many paediatric X-rays, greatly assists
interpretation. If in doubt about an X-ray, obtain a second opinion (there
is no justifi cation for X-raying the uninjured side to see what ‘normal’ is).
As an additional safeguard, most EDs now operate a policy of all X-rays
being reported by a radiologist within 24hr.
Treatment
Give prompt, appropriate analgesia ( b p.713). Follow the treatment
suggested for specifi c fractures ( b pp.722–7). Many undisplaced fractures
will unite satisfactorily with a period of immobilization in POP (eg fractured
distal radius), collar and cuff (eg fractured radial head) or broad arm sling
(eg fractured clavicle). Minor angulation at the fracture site can be accepted,
particularly in young children. Often, however, angulated fractures
require MUA.
Compound fractures and dislocations
Give analgesia and give IV antibiotics (eg cefuroxime 25mg/kg slow IV
bolus) and ensure tetanus cover. Take a digital photograph of the wound
and keep it covered to minimize the risk of infection. Apply a dressing,
splint the injured limb and refer the patient to the orthopaedic surgeon.
721
APPROACH TO LIMB INJURIES IN CHILDREN
Table 15.13 Ossifi cation centres
Centre First appears Fuses
Humeral head 0–6 months 18–21 years
Capitulum 3–6 months 14–16 years
Medial epicondyle 4–7 years 18–21 years
Lateral epicondyle 9–13 years 14–16 years
Trochlea 9–10 years 14–16 years
Radial head 4–5 years 14–17 years
Distal radius 6–12 months 17–19 years
Olecranon 9–11 years 13–16 years
Distal ulna 4–5 years 16–18 years
Capitate birth–3 months —
Hamate birth–4 months —
Triquetral 1–3 years —
Lunate 2–4 years —
Trapezium 2–4 years —
Trapezoid 3–5 years —
Scaphoid 3–5 years —
Pisiform 9–12 years —
1st MC base 1–3 years 14–17 years
Femoral head birth–6 months 15–19 years
Greater trochanter
3–4 years 17–19 years
Lesser trochanter 11–14 years 15–18 years
Distal femur birth 17–20 years
Patella 2–6 years 4–8 years
Proximal tibia birth 15–18 years
Distal tibia birth–6 months 14–17 years
Proximal fi bula 2–4 years 16–19 years
Distal fi bula birth–1 year 14–17 years
Posterior calcaneum 5–8 years 13–16 years
Central calcaneum birth 13–16 years
Talus birth —
Navicular 2–3 years —
Cuneiform bones 1–3 years —
These dates are subject to individual variation. In general, epiphyses in girls fuse before those in boys.

722 CHAPTER 15 Paediatric emergencies
Paediatric upper limb injuries: 1
Some fractures and dislocations are common in both adults and children
and are treated similarly. Certain injuries are either specifi c to children
or are treated differently in children: these are described in the next six
pages. Paediatric fractures are painful and need appropriate immobilization
and analgesia ( b p.713).
Clavicle fracture
Common in children and adults alike. Treatment is similar: oral analgesia,
broad arm sling and fracture clinic follow-up. Even if X-rays do not appear to
show a fracture, treat as for a fracture. Warn parents about a developing
lump (callus).
Shoulder injuries
Shoulder dislocations are relatively rare in children. Salter-Harris types I
and II epiphyseal fractures may occur in the proximal humerus: refer
to the orthopaedic team if signifi cant displacement or > 20 * angulation.
Otherwise, give analgesia, collar and cuff, and fracture clinic follow-up.
Humeral shaft fracture
Check particularly for radial nerve injury. Remember to consider
NAI especially if <3 years old or fracture is spiral. Treat as for adults
( b p.459).
Supracondylar humeral fracture
Follows a fall on an outstretched hand. Swelling may be considerable.
Check for associated neurovascular defi cit (particularly brachial artery,
median and radial nerves). 25 % of supracondylar fractures are undisplaced
and may not be obvious on X-ray, although a joint effusion will be seen.
Most fractures are displaced, angulated or rotated. The extent of angulation
(both in sagittal and coronal planes) is easy to underestimate. Viewed
from laterally, the capitulum normally makes an angle of 45 * with the
humeral shaft (see Fig. 15.20 ). The anterior humeral line (drawn along
the front of humeral shaft on the lateral view) normally passes through the
middle of the ossifi cation centre of the capitulum in the distal humerus.
Also, the normal carrying angle (seen in AP view) is 10 * . Record radial
pulse frequently and consider compartment syndrome.
Treatment provide analgesia and refer for manipulation under GA if:
• Neurovascular defi cit: operation is urgent if circulation is compromised.
• > 50 % displacement.
• > 20 * angulation of the distal part posteriorly (see Fig. 15.21 ).
• > 10 * medial or lateral angulation.
Refer others for observation and admission if there is much swelling. If no
signifi cant angulation, displacement or swelling, discharge with analgesia, a
collar and cuff under a body bandage (elbow at 90 * with confi rmed radial
pulse present) and fracture clinic follow-up. Consider using a padded back
slab POP if signifi cant pain is present.
Complications malunion with persistent deformity, stiffness (including
myositis ossifi cans), neurovascular defi cit (eg Volkmann’s contracture).
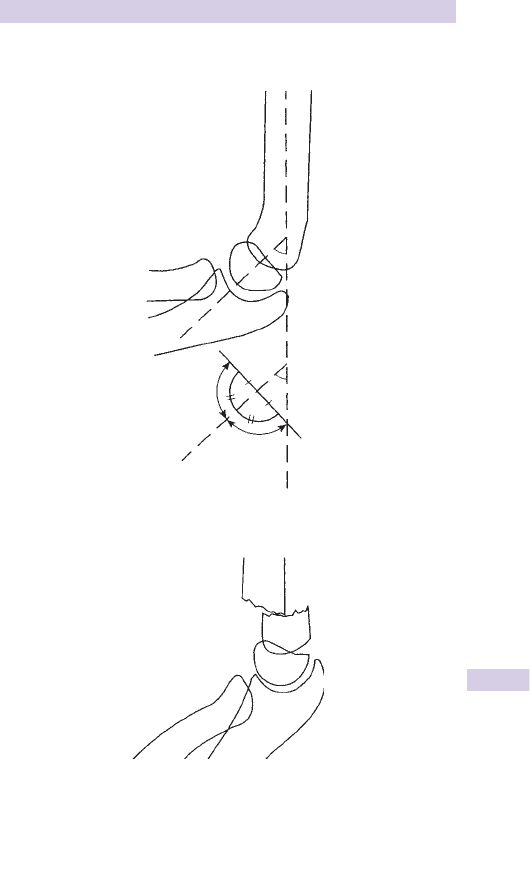
723
PAEDIATRIC UPPER LIMB INJURIES: 1
Supracondylar humeral fractures
Fig. 15.20 Normal lateral view — the capitulum makes an angle of 45 * with the
humeral shaft.
45°
Fig. 15.21 Supracondylar fracture with > 20 * angulation and 750 % displacement.

724 CHAPTER 15 Paediatric emergencies
Paediatric upper limb injuries: 2
Lateral epicondylar epiphyseal injury
Salter–Harris type II injury may follow a fall on outstretched hand. The
elbow is swollen, with d movement and maximum tenderness on the
lateral aspect. X-rays demonstrate the fracture, which may be displaced
by the pull of the forearm extensors, requiring surgical reduction. Treat
undisplaced fractures with a long arm back slab POP, collar and cuff at
90 * , analgesia and fracture clinic follow-up.
Medial epicondylar epiphyseal injury
Maximal tenderness is apparent on the medial side of the elbow. Check
carefully for ulnar nerve damage. Refer immediately if the ulnar nerve is
involved, or if the fracture is displaced. Treat undisplaced fractures with
analgesia, collar and cuff at 90 * under clothes (confi rm radial pulse is
present) and fracture clinic follow-up.
Radial head/neck fracture
The radiocapitellar line is drawn down the axis of the proximal radius on
the lateral view of the elbow and should bisect the capitellum. Failure to do
so suggests occult radial neck fracture or radial head dislocation. Most of
these fractures can be managed satisfactorily with analgesia, collar and cuff
(some prefer a broad arm sling) and fracture clinic follow-up ( b p.450).
Refer to the orthopaedic surgeon if there is signifi cant angulation.
Elbow injury without obvious fracture
Treat elbow injuries where there is clinical suspicion of fracture, but
none seen on X- ray, along the same lines as for an undisplaced fracture
(analgesia, collar and cuff, and fracture clinic follow-up). This includes
children who have d range of movement and whose X-rays show an
elbow effusion (‘fat pad sign’) — see b p. 450.
Subluxation of the radial head (‘pulled elbow’)
A direct pull on the arm of a child aged 1–5 years may result in the radial
head being pulled out of the annular ligament (‘nursemaid’s elbow’). The
child then refuses to use the arm. If there is a characteristic history, there
is no need to X-ray. The traditional reduction technique involves fl exing
the elbow to 90 * , then supinating the elbow fully. However, manipulating
the elbow into full pronation may give a better reduction rate ( www.
bestbets.org.uk ). A click is sometimes felt or heard during reduction.
If full pronation fails, try full supination and leave for 10min. Allow the
child to play and watch: he will usually use the arm again soon. If he does
not, obtain X-rays and senior help. Repeat manipulation can be done
once, but if that does not lead to a rapid improvement in function then
place the arm in a sling, give analgesia and plan to review in 1–2 days.
The elbow may reduce spontaneously or may need further manipulation.
Rarely, repeated manipulation is unsuccessful until sedation is given. After
successful manipulation advise the parents to avoid pulling the arm
forcefully. A pulled elbow may recur up to about age 5 if the arm is pulled,
but after that the child should have no long term problems with the
elbow.

725
PAEDIATRIC UPPER LIMB INJURIES: 2
Radius/ulna shaft fractures
Radius and ulna shaft fractures often cause signifi cant displacement or
angulation: provide IV analgesia, immobilize in a broad arm sling, obtain
X-rays and refer for manipulation under GA. Never accept an isolated
forearm shaft fracture without X-rays demonstrating the entire radius
and ulna, otherwise a Monteggia or Galeazzi fracture-dislocation may be
missed ( b Forearm fractures and related injury, p.448).
Distal radial fracture (including Salter–Harris type II injuries)
A common fracture in all ages of children (and adults) after a fall on an
outstretched hand. The fracture results in localized tenderness and
variable swelling. Check carefully for a second injury (eg involving the
thumb or scaphoid). X-rays will demonstrate the fracture and allow
assessment of the need for MUA.
Moderate displacement or slight angulation may be accepted (particularly in
younger children): if in doubt, obtain a senior opinion.
Minimally displaced or undisplaced greenstick, buckle or torus fractures
commonly occur just proximal to the distal radial epiphysis. Treat with
analgesia, elevation, a backslab forearm POP (extend this above the elbow
in children <2 years or it will fall off) and arrange review and plaster
completion at 24hr. Children who present with discrete tenderness over
the distal radial growth plate, but without a fracture apparent on X-ray
should be treated identically to those with a radiological proven fracture—
presume a growth plate injury (sometimes a subperiosteal haematoma
can be seen on ultrasound). Beware osteomyelitis ( b The limping child,
p.704), which can cause tenderness over the distal radius and be mistaken
for trauma.
Removable splints For co-operative children (usually > 4 years old) with
torus/buckle fractures of the distal radius, an alternative option is to use
removable splints. Parents and children report better functioning and
fewer days off school. Splints should be retained until pain wears off (usually
<3 weeks) and follow-up is not required if pain settles as expected.
Scaphoid fracture
Despite being uncommon, particularly in younger children, seek clinical
evidence of scaphoid fracture in any child with wrist/forearm injury and
obtain scaphoid views if appropriate ( b p.442). Treat radiologically
evident and suspected fractures as for adults as described in b Carpal
bone fractures and dislocations, p.442.
Metacarpal and phalangeal injuries
Treat these injuries along similar lines to those described for adults
( b Hand fractures and dislocations, p.436). Remember, however, that
children may not tolerate manipulation under LA: anaesthetic help may
be required.

726 CHAPTER 15 Paediatric emergencies
Paediatric lower limb injuries
Hip fracture
Children rarely sustain neck of femur fractures similar to those seen in
adults. In the pre-adolescent child, trauma may precipitate a slipped upper
femoral epiphysis ( b The painful hip, p.706). Younger children who have
been subjected to considerable violence may suffer a Salter–Harris type I
injury to the proximal femoral epiphysis — carefully exclude other injuries
and refer to the orthopaedic surgeon.
Femoral shaft fracture
May be spiral (the majority) or transverse, depending upon the mechanism
of injury. Considerable energy is required to produce a femoral fracture:
check for other injuries. Resuscitate as necessary with IV fl uids and
provide nasal diamorphine ( b p.281) or IV opioid analgesia ( b p.280).
Perform a femoral nerve block (as described on b p.304) to provide
additional analgesia, using 0.2mL/kg of 0.5 % plain bupivicaine (1mg/kg).
Allow 20min for this to work, then apply skin traction. Gallows traction
may be used on infants and children <2 years, but is best erected on the
ward. A spiral fracture in a non-ambulatory child suggests child abuse —
swelling is often not dramatic.
Knee injuries
Knee ligament injuries are rare in children compared with adults: suspect
a fracture or epiphyseal injury instead. This is a refl ection of the relative
strengths of ligament and bone in the child. So, for example, an injury
which might cause anterior cruciate ligament rupture in the adult will often
produce avulsion of its tibial attachment in the child. This tibial plateau
fracture will produce a haemarthrosis and will be apparent on the lateral
X-ray. Provide analgesia and refer to the orthopaedic surgeon.
Patella fractures
Do not confuse a congenitally bipartite patella for a fracture. The small
bony fragment in a bipartite patella lies superolaterally and has rounded
edges.
Patellar sleeve fractures are not uncommon in children and adolescents.
These osteochondral fractures typically result from high impact jumping
activities or sports. Suspect clinically if there is local pain and tenderness
and an inability to actively extend the knee. Radiographs can be misleading
as only a small bony fragment is avulsed, usually from the inferior pole, but
a large part of the articular surface is removed with it, but is impossible
to see on plain X-ray. Provide analgesia and splintage and refer to the
orthopaedic team for MRI to confi rm the diagnosis ± ORIF.
Patella dislocation
This is seen relatively frequently in children and is treated in a similar way
to that in adults (see b p.476). Examine the X-rays carefully as associated
osteochondral ‘chip’ fractures of the undersurface of the patella occur
relatively frequently in children.

727
PAEDIATRIC LOWER LIMB INJURIES
Tibial shaft fracture
Treat most fractures as for adults: splintage, IV analgesia, and referral for
elevation and admission. Compound fractures require IV antibiotics and
wound surgery. Displaced or angulated fractures require MUA and POP;
undisplaced fractures respond to treatment with above knee non-WB
POP and subsequent mobilization using crutches.
Toddler’s fracture
Minor trauma in 1–4-year-olds may result in characteristic spiral undis-
placed distal tibial fractures. These may not be apparent on the initial
X-rays: localized warmth and tenderness with a history of trauma may
suggest the diagnosis in the otherwise wide differential of the limping
child ( b p.704). If a fracture is visible on initial X-rays treat by rest in a
POP and arrange fracture clinic follow-up. If the diagnosis is made without
a visible fracture, treat in POP and review clinically and radiologically at
10 days: further X-rays may then demonstrate a long strip of periosteal
tibial new bone formation. Continue to treat according to symptoms.
Ankle injuries
Ankle ligament injuries are less common than in adults, but are treated
similarly (as are ankle fractures — b p.486). If there is no fracture apparent
on X-ray, but there is much tenderness over the distal tibial or fi bular
epiphysis, treat as a growth plate injury (undisplaced Salter–Harris type I
fracture) with BKPOP, crutches, elevation, analgesia and fracture clinic
follow-up.
Calcaneal and other foot injuries
See b Foot fractures and dislocations, p.488.

728 CHAPTER 15 Paediatric emergencies
Child abuse
The boundaries of what defi nes acceptable behaviour and what constitutes
child abuse are open to some debate and are certainly affected by historical
and cultural factors. For example, corporal punishment, once considered
normal and usual, is now unacceptable. The extremes of child abuse,
however, are easily defi ned.
Types of child abuse
• Physical abuse (NAI) — including bruises, fractures, wounds, and burns.
• Sexual abuse.
• Poisoning.
• Suffocation.
• Neglect or emotional abuse.
• Fabricated and induced illness (previously known as ‘Munchausen
syndrome by proxy’).
Prevalence
It is impossible to be sure how common child abuse is. It is generally
agreed that it is much more prevalent than was previously believed.
4 % of children are brought to the attention of professional agencies for
suspected abuse. It is believed that 8 0.1 % of UK children suffer severe
physical abuse each year and it has been estimated that 100–150 child
deaths occur each year as a result of abuse by parents or carers.
Aetiology
Child abuse affects both boys and girls. The fi rst-born child is most
frequently affected. Infants and young children are at most risk of serious
injury or death, partly refl ecting their physical vulnerability. The abuser is
often a parent or cohabitant of a parent, more commonly male and may
have suffered abuse themselves as a child. Sometimes the child may be
targeted because they are unwanted (eg ‘she should have been a boy’).
Whilst the abuser may be a young parent with unrealistic expectations and
living in diffi cult social circumstances (unemployment, drug abuse), often
they do not conform to this standard description. Child abuse affects all
levels of society. Clear links between domestic violence and physical abuse
of children have been identifi ed. Children whose parents have mental
health problems may be more vulnerable to abuse and neglect.
Role of the junior emergency department doctor
Managing the child and family where there is suspected child abuse is an
extremely delicate skill, requiring considerable tact and experience. The
role of the junior doctor is to consider the possibility of child abuse and
to involve a senior doctor at an early stage. Recent NICE guidance is avail-
able at http://www.nice.org.uk/nicemedia/live/12183/44872/44872.pdf

729
CHILD ABUSE
The suspicious history
Certain features should alert the doctor to the possibility of child abuse:
• Injuries inconsistent with the history given.
• Injuries inappropriate for developmental age (eg a baby aged <3 months
‘rolled off a bed’).
• Changing history of injury, or vague history, lacking vivid details.
• Delay in seeking medical attention.
• Abnormal parental attitudes (eg apparent lack of concern for child).
• Frequent ED attendances.
• Occasionally, children provide an account of abuse.

730 CHAPTER 15 Paediatric emergencies
Presentation of child abuse: 1
Physical child abuse is commonly referred to as NAI. Children may present
with a variety of injuries, which may occur singly or in combination.
Bruising
Children naturally sustain bruises during minor incidents as part of
‘growing up’. Bruising over the knees and shins is a normal fi nding in chil-
dren, particularly toddlers, who are also prone to sustaining injuries to
their foreheads and chins as a result of falls. Older children frequently
sustain bruises over the lateral aspect of their elbows and hips, during
normal play and sport activities. As well as considering the possibility
of NAI, remember that bruising may occur as part of an unusual patho-
logical disease process (eg Henoch–Schönlein purpura, haemophilia, ITP,
leukaemia, and other causes of thrombocytopenia). A Mongolian blue spot
is an innocuous congenital fi nding on the lower back of some young chil-
dren (especially non-Caucasians), which may be confused with bruising.
The following features should prompt consideration of NAI:
• Bruising in unusual sites (eg medial aspect of upper arms or thighs).
• Multiple bruising of different ages (very diffi cult for the non-expert to
judge) at less common sites.
• Uncommon injuries bilaterally.
• Finger ‘imprinting’ (eg grip complexes around upper limbs or slap
marks).
• Imprints or marks from other objects (eg belt, stick).
• Human bite marks (probably adult if canines > 3cm apart: ensure
photographs next to a ruler are planned after admission).
• Petechiae on the face may refl ect smothering and asphyxiation (it
has been previously suggested that 2–10 % of SIDS may have been
smothered), but remember that petechiae also occur with forceful
coughing or vomiting.
Wounds and burns
Children commonly sustain wounds and burns unintentionally. However,
deliberately infl icted burns are found in a signifi cant proportion of physically
abused children.
The following suggest the possibility of NAI:
• Torn frenulum of upper lip (can also refl ect a ‘normal’ toddler injury).
• Perineal wounds and burns (see sexual abuse b p.732).
• Small, deep circular burns with raised edges suggest cigarette burns.
• Hand, lower limb, and buttock burns may follow forced immersion in
bath water that is too hot. These burns tend to be of the ‘stocking and
glove’ type, without higher splash burns. Parts of the buttocks may be
spared, where skin has been in contact with the bath, not the water.

731
PRESENTATION OF CHILD ABUSE: 1
Head injuries
Most head injuries result from unintentional incidents (‘accidents’). In
infants, they often result from the parent or carer dropping the child. The
fractures caused by this tend to be single, linear, and involve the parietal
bone.
Consider NAI if the following occur:
• Retinal haemorrhages (characteristic, but not diagnostic of shaking —
they may also rarely be seen in CO poisoning, for example). In the
context of NAI, retinal haemorrhages are often associated with subdural
haematomas.
• Occipital skull fracture.
• Multiple, wide or comminuted fractures.
• Subdural haematoma in an infant or toddler.
Natural progression of bruises
Swelling and tenderness of bruising suggests relatively recent origin,
but this is not very reliable. Accurate assessment of the age of bruising
according to its colour is not possible, except that a yellow bruise is
almost certainly > 18hr old. Oft-quoted natural temporal progression of
colour changes of bruising allows only a guess at the age of a bruise —
avoid being drawn on this issue, which may have considerable legal
implications. Instead, record the fi ndings as accurately as possible: describe
the colour, size, and distribution of the bruising. Usually a child suspected
of having suffered physical abuse will also be examined by a relevant
expert, such as a paediatrician and/or police surgeon (clinical forensic
physician).

732 CHAPTER 15 Paediatric emergencies
Presentation of child abuse: 2
Fractures
Certain fractures are very common in children. Pay attention to the
history of injury and whether or not it appears to be consistent with the
fracture(s) sustained. Multiple fractures of different ages (especially if
previously undiagnosed and/or not brought to medical attention) should
arouse suspicion of NAI. To help assess the approximate age of a bony
injury, see Table 15.14 .
Remember that times vary according to the age of the child.
Consider NAI in the following fractures
• Multiple fractures of different ages.
• Rib and spinal fractures.
• Fractures in infants who are not independently mobile.
• Long bone fractures in children <3 years old.
• Epiphyseal separation and metaphyseal ‘chip’ fractures of the knee, wrist,
elbow, and ankle. These Salter–Harris I and II injuries are associated
with traction, rotation, and shaking.
A few rare bone diseases may mimic NAI
• Osteogenesis imperfecta (blue sclerae, dental abnormalities and brittle
bones — autosomal dominant).
• Pathological fractures (through multiple cystic bone lesions).
• Rickets (enlarged, cupped epiphyses, craniotabes, ‘bow legs’).
• Copper defi ciency (eg Menkes’ kinky hair syndrome).
Neglect and emotional abuse
There will be an element of emotional abuse as part of other forms of
abuse, which may be manifest in the child in a variety of ways: behavioural
problems, sleep disturbance, soiling, nocturnal enuresis. The neglected
child may be dirty and unkempt, fail to thrive, and/or fall below the 3rd
centile for height and weight. Occasionally, nutritional defi ciencies may
be extreme (eg rickets). Developmental milestones are often delayed
(and may even regress).
Note the apparent attitudes of the parents/carers towards their child
(eg critical and hostile or remote and unconcerned) and the child’s attitude
to the parents/carers (if in doubt as to whether this seems appropriate,
ask an experienced nurse).
Table 15.14 Natural progression of fractures
Presence of soft tissue swelling 0–10 days
Periosteal new bone formation 10–14 days
Loss of defi nition of the fracture line 14–21 days
Callus formaton 14–42 days
Remodelling
8 1 year

733
PRESENTATION OF CHILD ABUSE: 2
Sexual abuse
This may affect boys or girls and takes many forms, ranging from exposure
to indecent acts through to rape. The abuser is often a male relative or
carer who is well known to the child. The child may present in a variety
of ways:
• Injury to the genitalia or anus.
• Perineal pain, discharge, or bleeding.
• Behavioural disturbance, enuresis, encopresis.
• Inappropriate sexual behaviour.
• The child may allege sexual abuse.
• Sexually transmitted disease (including anogenital warts).
• Pregnancy.
Accurately record statements made by the child ‘word for word’ using
quotation marks. Do not pursue a genital examination, but involve a
senior doctor at an early stage, who may wish to examine the genitalia
using a colposcope, in collaboration with a police surgeon (clinical forensic
physician). In the context of an allegation of recent sexual assault, the
collection of forensic samples for DNA analysis is likely to be required.
Fabricated or induced illness (previously known as Munchausen
syndrome by proxy)
A parent/carer may invent a history of illness in a child and fabricate
physical signs to substantiate it. The history often involves one or more of
the following: apnoeic episodes, fi ts, bowel disturbances, rashes, allergies,
or fevers. Classically, the deceiver is the mother. The child may be made
ill by administering drugs or poisons. If suspected, do not confront the
deceiver, but take blood and urine samples for a toxicology screen and
refer to the paediatric team.
Bear in mind that some parents may be naturally very anxious and may
exaggerate symptoms, rather than deliberately fabricate them.

734 CHAPTER 15 Paediatric emergencies
Management of child abuse
Role of the junior emergency department doctor
The junior ED doctor needs to be vigilant in considering abuse when
initially assessing and treating children. Any suspicion of child abuse should
prompt involvement of an expert senior doctor (paediatrician or ED
consultant). In every hospital system there will be a designated doctor
for child protection who should be available for advice. He or she will
examine the child and arrange hospital admission for further investigations
(eg skeletal survey) as necessary. Social Services and the police may need
to be involved. The child may require examination by a police surgeon
(clinical forensic physician) and samples/photographs obtained. Follow
local procedures.
The chief consideration is the treatment and protection of the child, so
do not delay treatment of painful or apparently life-threatening problems,
whilst awaiting an ‘expert’. Ensure that all documentation is legible and
meticulous. Remember that if child abuse is considered likely, siblings may
also be at risk.
UK law: The Children Act 1989
This act replaced previous statutes. Central to the Act is the concept that
the welfare of the child is paramount. In the short term, the 1989 Children
Act may be used to obtain orders to protect children. A variety of orders
may be obtained:
Police Protection Order
A police offi cer has legal powers to take any child into ‘police protection’
for up to 72hr if deemed necessary for his/her own protection. This order
may be used to prevent a child being taken away from the ED by a parent
or guardian against medical advice.
Emergency Protection Order
This has replaced the ‘Place of Safety Order’. A court order valid for up
to 8 days may be obtained if the child is believed to be at signifi cant risk of
harm. Such an order would normally be requested by a social worker.
Child Assessment Order
This court order may be obtained in order to allow an assessment to be
performed of a child who appears to be at risk of injury.
Care Order
This transfers the care of a child from the parent(s) to the local authority
Social Services department. If a care order is in force, matters requiring
parental consent should be referred to the social worker (not the foster
carer).
Residence Order
This court order defi nes where a child should live and who has parental
responsibility.

735
MANAGEMENT OF CHILD ABUSE
Child Protection Plan (replaces the ‘Child Protection
Register’)
This register is kept by the social services. It contains a list of names of
those children considered to be at current risk of harm. ED staff should be
aware of how to access Child Protection Register information. Previous
hospital case notes are also very useful in this respect. When searching for
previous records, remember that many children may be known by several
surnames.
Child protection conferences
A conference may be called by Social Services if it is suspected that a child
has been abused. Child protection conferences should be held promptly
and aim to defi ne a protection plan for the future protection of the child
and family. Unlike the criminal courts, where the onus is on the prosecution
to prove abuse ‘beyond reasonable doubt’, child protection conferences
will determine whether a child is deemed to be at risk of signifi cant harm
and whether a protection plan is required. Case conferences consist of a
number of individuals, including: chairman (usually a senior member of the
Social Services department), hospital consultant, GP, social worker, police,
health visitor, teacher, education welfare offi cer, child abuse advisor, local
authority solicitor. Parents are always invited and older children may also
attend.
This page intentionally left blank

737
Index
A
A2 pulley injury 440
abbreviations ix–xv
abdominal aortic aneurysm,
ruptured 530
abdominal injury,
children 714
abdominal mass,
children 699
abdominal pain 504
analgesia 280
in cancer 506
in children 698
in pregnancy 590
abdominal trauma 348 , 350
abortion 584
abruptio placentae 588 , 594
abscess 526
anorectal 519
Bartholin’s 565
breast 599
peritonsillar 554
pilonidal 518
retropharyngeal 555
Acanthamoeba keratitis 539
ACE inhibitor poisoning 199
acetabular fractures 468
acetaminophen see
paracetamol
acetylcysteine 190–2
Achilles tendon injuries 482
acid-base nomogram
inside front cover
acidosis
lactic 99
metabolic 99
acromio-clavicular joint
injury 458
activated charcoal 185
activated partial
thromboplastin
time xviii , 167
acute confusional state 134
Addisonian crisis 155
adenosine, supraventricular
tachycardia 88
adhesive capsulitis 461
adrenaline (epinephrine)
anaphylaxis 44
bradycardia 82–3
cardiac arrest 53
children 650–2
local anaesthesia 285
newborn 644
advanced life support
adult 52–3
newborn 642–5
paediatric 652–5
advanced trauma life
support (ATLS) 321
aggression 608 , 610
AIDS and HIV 242–5
airway management 48
burns 390 , 392 , 394–5
cardiac arrest 50
children 646 , 654
foreign body 648
nasopharyngeal
airway 325
newborn 642
spinal injury 380
surgical 326–7
airway obstruction 45 ,
112 , 324
children 677
alcohol (ethanol)
absorption, metabolism,
and elimination 622
abuse 622
intoxication 202 , 623
and police 30
withdrawal 624
alcohol-related brain
injury 625
alteplase 77
Amanita phalloides 212
amaurosis fugax 540
ambulance crew 12
Ambulance Incident
Offi cer 39
aminophylline 106
in children 679
amiodarone 86
amniotic fl uid
embolism 594
amphetamine 215 , 626
amputation 422 , 435
toes 490
anaesthesia
general 310 , 316
local 282
topical 288
see also local anaesthesia
anal fi ssure 518
analgesia 274–281
children 275–6 , 280–1 ,
632 , 713
anaphylaxis 42 , 44
in children 650–1
angina 67
Prinzmetal’s (variant) 69
unstable 68
angio-oedema 42
angioplasty for MI 76
anion gap 99
ankle
fractures 486
injuries 484
in children 727
nerve blocks 306–7
Ottawa rules 484–5
sprains 487
ankylosing spondylitis 497
anorectal problems 518
anthrax 233 , 627
anti-D immunoglobulin 582
antibiotics
abscess 526
bites 411 , 414
in compound fractures 422
and oral contraception 569
pneumonia 111 , 687
prophylaxis 411
anticoagulants 170
antidotes 186–7
antipsychotic drugs 619
aortic aneurysm, abdominal,
ruptured 530
aortic dissection 92
aortic injury 344
apophysitis, traction 708
appendicitis 507
children 699
epiploic 517
pregnancy 591
arc (welder’s) eye 538
arterial blood gases 98
diagram inside front cover
arthritis 494
in children 705
septic 495 , 705
aspiration, pulmonary 112 ,
338
aspirin (salicylate) 274
poisoning 189
asthma
acute 104–7
cardiac arrest 107
children 678–81
asystole 51
atracurium 316
atrial fi brillation 89
atrial fl utter 89
atrioventricular block 80
atropine 82 , 654
as antidote 186
poisoning 194
attenders
inappropriate 16
regular 17

738
INDEX
Australian Mental Health
Triage Scale 612
Autopulse 51
avian fl u 33 , 252
aviator’s astragalus 498
B
back pain 492
bacterial tracheitis,
children 677
bad news, breaking 24
balanitis 702
Bankart lesion 498
barbiturate poisoning 197
barotrauma 260–3 , 551
Bartholin’s abscess 565
Barton’s fracture 446
basic life support 48
newborn 642–4
paediatric 646–7
BASICS 34
batteries, button 213
Bazett’s formula (QTc) 65
Beck’s triad 342
bee stings 416
Bell’s palsy 556
Bennett’s fracture 439
benzodiazepine poisoning 196
bereavement 24
berry poisoning 212
beta-blocker poisoning 198
biceps injury 452 , 459
Bier’s block 290
biliary tract problems 510
bilious vomiting 661
birth, emergency
delivery 578
bites 414–7
dogs 415
human 416
infection 413–5
insects 416
reverse fi ght bites
415–16 , 435
snake bites 417
and stings 416
tetanus 410
ticks 231 , 416
bladder injury 352
blast injuries 389
bleeding disorders 166
blepharitis 543
blindness, sudden 540
blood pressure, normal,
children 633
blood transfusion 172
reactions 175
blow-out fracture 374
BMA Counselling Service
for Doctors 15
body packers 217
Boerhaave’s syndrome 333
Bohler’s angle 488
bombs (blast injuries) 389
bone anatomy 421
Bordetella pertussis , whooping
cough 684
botulism 143 , 237
boutonnière deformity 433 ,
440 , 498
bowel problems 511–7
boxer’s fracture 498
brachial plexus blocks 298
bradycardia 80
algorithm 83
children 656
brain injury,
alcohol-related 625
breast
abscess 527 , 599
swelling, babies 660
breastfeeding and
drugs 576
breathlessness
(dyspnoea) 96
British Association for
Immediate Care
(BASICS) 34
bronchiolitis 682
bronchus, ruptured 336
Brown-Séquard
syndrome 383
Brugada syndrome 65
bruises 403
child abuse 728–31
bumper fractures 498
bupivacaine 283
burns 390–3 , 396–7
airway, from cocaine 555
and child abuse 397
children 715
inhalation injury 394
BURP manoeuvre 314
bursitis 427
infrapatellar 479
button batteries 213
C
Caesarian section 597
CAGE questionnaire 622
calcaneal fracture 488
calcifi c tendonitis 461
calcium antagonist
poisoning 198
calculous disease 557
calf
injuries 482
squeeze test 482–3
cancer and abdominal
pain 506
capacity, defi ning 629
carbamate insecticides 206
carbon monoxide
poisoning 208 , 394–5
carboxyhaemoglobin 70 ,
208 , 394–5
cardiac arrest 46–55
algorithms 47 , 52
asthma 107
children 646–7 , 652–5
drugs 50 , 644 , 654
hyperkalaemic 163
newborn 644
pregnancy 596
reversible causes 51
cardiac arrhythmias 80–89
in children 656
in poisoning 183
cardiac markers 71
cardiac pacing 53 , 82
cardiac tamponade 342
cardiogenic pulmonary
oedema 100
cardiogenic shock 60 , 77
cardiopulmonary
resuscitation
adult 46–53
children 646–7 , 652–5
mechanical 51
newborn 644
cardioversion,
synchronised
86
carpal tunnel syndrome 445
casts 424
catheterization, male 521
cauda equina syndrome 493
CBRN incidents (chemical/
biological/radiological/
nuclear) 39 , 210
cellulitis 234 , 413 , 453 , 528
ear canal 550
orbital 542
cement burns 397
central cord syndrome 383
central retinal artery
occlusion 540
central retinal vein
occlusion 540
central venous access 56
cephalhaematoma 660
cerebral haemorrhage 144
cerebral infarction 144
cerebral venous
thrombosis 133
cervical cancer
566 , 574
cervical cord syndrome,
central 383
cervical disc herniation 463
cervical erosion 574
cervical spine control 320 ,
712
chalazion 543
chance fracture 498
charcoal, activated 185

739
INDEX
CHEMDATA 36
chemical burns 397
of eyes 538
chemical incidents 36 ,
37 , 210
decontamination 211
roadside 36
chest compression 49
children 646
newborn 644
chest drain insertion 115 ,
336–7
chest injury 328–344
analgesia 279
children 714
penetrating 340 , 342
chest pain 66
assessment units 71
atypical 67
differential diagnosis 66
pericarditis 78
sickle cell disease 176
chickenpox 240
child abuse 728–35
fractures 732
child protection
plan 735
Children Act (1989) 734
chlorine poisoning 209
choking 45 , 648
cholangitis, ascending 510
cholecystitis 510
cholesteatoma 551
Christmas disease 169
chronic obstructive
pulmonary disease 108
chronic renal failure 160
ciguatera fi sh poisoning 229
clavicle fracture 458
children 722
clay-shoveller’s
fracture 499
clomethiazole
poisoning 196
Clothier report 620
clozapine 619
CN gas 209
co-codamol 274
co-dydramol 274
coagulation cascade 169
coagulation disorders 166
cocaine 215 , 626
pharyngeal burns 555
coccyx fractures 469
cochlear implants 549
codeine 276
cognitive assessment 607
cold injury 257
colitis
ischaemic 515
ulcerative 517
collapse 140
collateral ligament injuries
knee 475 , 478
thumb 438 , 440
Colles fracture 444 , 499
colovaginal fi stulae 566
coma 136 , 138
alcohol overdose 623
Glasgow Coma
Scale 360–1
children 717
hypoglycaemia 151
compartment
syndrome 398
compound fractures 422
compulsory
hospitalisation 628
concussion 368
confusional state 134
conjunctival FB 538
conjunctivitis 543
neonatal 660
consent 28
contact lens problems 539
contraceptive problems 568
convulsions 148–9
children 688
poisoning 183
COPD 108
coping as a junior
doctor 14
corneal trauma 538
coronary syndromes,
acute 68
Coroner 26 , 31
corpus luteum cyst 572 , 587
cortical blindness 717
cot death 658
counselling service 15
court, going to 31
cranial arteritis 132 , 541
cricoid pressure 312–5
cricothyroidotomy 326–7
Crohn’s disease 517
croup 676
cruciate ligaments 474 , 478
crush syndrome 398
crushed fi ngers 435
crying babies 661
CS gas 209
CT scan
coma 138
headache 127–8
head injury 362
stroke 145
trauma 322 , 348
ureteric colic 525
CURB-65 score 111
Cushing response 354
cut down, venous 639
cyanide poisoning 207 , 395
cystic fi brosis 685
cystitis 158
D
dacrocystitis 543
dantrolene 183 , 214 , 265
dashboard dislocation 499
De Quervain’s
tenosynovitis 447
death 24–27
decompression illness 260
decontamination
chemical 211
radiation incidents 211 , 268
deep venous
thrombosis 118
in IV drug users 627
in pregnancy 593
defi brillation 50
children 652–3
defi brillator, implantable 82
dehydration 152 , 227 , 681
deliberate self-harm 612
delirium 134 , 603
delirium tremens 624
delivery, emergency 578
delusion 603
dementia 135
dengue fever 248
dental anaesthesia 302
dental anatomy 558
dental emergencies 558
see also teeth
dento-alveolar
fractures 372
depression 616
dermatitis
herpetiformis 672
dermatomes 386–7
detention, compulsory 628
diabetes mellitus 152
hypoglycaemia 150
pregnancy 593
diabetic ketoacidosis 152
children 691
diagnostic peritoneal
lavage 347
dialysis problems 160–1
diamorphine 276
nasal 281
diaphragm, ruptured 333
diarrhoea 226
diazepam
overdose 196
status epilepticus 149
children 690
diclofenac 275
digital nerve block 294–5
digital nerve injury 432 , 434
digoxin poisoning 199
diphtheria 676
discharge from ED 2 , 8
against advice 29
elderly patient 20

740
INDEX
disclosure in public
interest 30
dislike of a patient 18
dislocations 423
ankle 486
children 718
elbow 449 , 451
fi nger 436
hip 468
knee 477
patella 476
children 726
shoulder 454–7
thumb 438
toes 490
wrist 442 , 448
disseminated intravascular
coagulation 169 , 592
diverticular disease 516
diving emergencies 260–3
documentation see
notes
dog bites 415
dressings 412
burns 396
Dressler’s syndrome 79
driving 30 , 535
drowning 258
children 715
drug abuse
complications 627
illicit drugs 214
withdrawal 627
drugs
anaesthetic 316
doses in children 633 , 644
interactions with
OCP 569
newborn doses 644 , 655
psychiatric, complications
of 619
see also poisoning
dry socket pain 561
Dupuytren’s fracture 499
dyspnoea 96
dystonic reaction 619
E
ear
examination 548 , 674
nerve blocks 300–1
problems 546–551
wounds 464
earache 550
Ebola fever 250
ECG 64
bradyarrhythmias 81
diagram inside back cover
hyperkalaemia 162
hypothermia 255
myocardial infarction
72–5
pericarditis 78
tachyarrythmias 87–9
tricyclic antidepressant
poisoning 194–5
eclampsia 592
ecstasy 214 , 626
liquid 215
ectopic pregnancy 586
eczema 662
edrophonium test 142
elbow
fat-pad sign 450
injuries 450
children 724
problems, soft
tissue 452–3
pulled 724
elderly patient,
discharge 20
electrical injuries 266
emesis, induced 185
EMLA cream 288
emotional abuse 732
endocarditis 740
endometriosis 572
enfl urane 317
enteric fever 248
Entonox
®
278–9
environmental
emergencies 253
epicondylitis 452
epididymitis 522
epididymo-orchitis 701
epiglottitis 677
epilepsy 148 , 688
see also seizures
epinephrine see adrenaline
epiphyseal injury
children 718
Salter-Harris
classifi cation 719
epiphysis, slipped upper
femoral 706
epiploic appendagitis 517
episcleritis 543
episiotomy 580
epistaxis 552
ergotamine 130
erysipelas 528
erythema
chronicum migrans
673
marginatum 672
multiforme 672
nodosum 672
toxicum, infants 662
ESR xviii
Essex Lopresti fracture 499
ethanol see alcohol
ethyl chloride 288
ethylene glycol
poisoning 203
etomidate 316
extensor tendon
injury 432 , 434
external jugular vein 57
eye 533
burns 538
examination 534
foreign bodies 537
injury 536
problems and HIV 244
eye signs
head injury 360
in poisoning 182
eyebrow wounds 464
eyelid wounds 464
eyelids, superglued 538
F
fabricated illness 620 , 733
facial burns 394–6
facial fractures 370–7
facial injury 370 , 464
facial nerve palsy 556
facial wounds 464
factitious disorder 621
in health care
workers 620
fainting 140
FAST scan (focused
assessment with
sonography for
trauma) 346
fatal accident inquiry 31
febrile child 663
febrile convulsions 688
feeding diffi culties,
babies 661
femoral neck, fracture 470
femoral nerve block 304–5
femoral shaft
fracture 472
children 726
femoral vein
children 639
venous access
56–7
fentanyl 276 , 281
fetal injury 594
fi bula, fractures 480
fi eld block 289
fi ght bites, reverse 415–6
fi nger pad amputations 435
fi ngers
crushed fi ngers 435
digital nerve block 294–5
dislocations 436
fractures 456–7 , 725
fi shhooks, removal of 406
fi sh bones in pharynx 547
fi sh poisoning 229
fi sh spine stings 416
fi ts see convulsions; seizures
fl ail segment 332
fl eas 230
fl exor tendon injury 432–4

741
INDEX
fl umazenil 196 , 309
follow-up arrangements 5
food poisoning 226–9
foot
dislocations 488
fractures 488
soft tissue problems 491
forearm injuries 448 , 725
forehead, nerve blocks 300
foreign bodies
ear 546
eye 537–8
foot 491
ingested 213 , 547
inhaled 112 , 547 , 648 , 677
nose 213 , 546
rectal 519
under fi ngernail 435
vaginal 567
wounds 405
foreskin problems 523 , 702
fractures
and child abuse 732
eponymous 498–502
see also specifi c fractures
fragmentation injuries 389
frontal sinus, fractures 374
frostbite 257
fundoscopy 535
funny turns 689
furunculosis of ear 550
G
Galeazzi fracture 448 , 499
gallstones 510
in pregnancy 591
gamekeeper’s thumb 438 ,
440 , 499
gammahydroxybutyrate
(GHB, GBH) 215
Garden classifi cation 471
gas gangrene 237
gastric lavage 184
gastroenteritis 226 , 228
gastrointestinal bleeding
lower 124
upper 122
General Medical Council 30
generalized weakness 142
genital injury 570 , 733
genital ulcers/sores 238
german measles 223
gestational trophoblastic
disease 588
GHB 215
giant cell arteritis 132 , 541
glandular fever (infectious
mononucleosis) 241
Glasgow Coma Scale 360–1
children 717
glaucoma 542
glue (for wounds) 406
glue sniffi ng 626
golfer’s elbow 452
gonorrhoea 238
gout, acute 496
gout bursitis 453
GPs, liaising with 5 , 10
Graves’ disease 156
gravidity 576
grease gun injuries 435
groin lumps 700
GTN intravenous
infusion 68
Guillain-Barré
syndrome 142
gunshot injuries 30 , 388
gynaecological
problems 564 – 575
H
haemarthrosis, knee 478
haematemesis 122
haematoma
block 289
extradural 365
intracranial 365
risks, after head injury 363
soft tissue 426
subdural 365
subungual 435
haematuria, children 695
haemodialysis problems
161
haemolytic uraemic
syndrome 694
haemophilia 166 , 168
Haemophilus infl uenzae 636
haemoptysis 94
haemorrhage
antepartum 588
and anticoagulants 170
cerebral 144
lower GI 124
post-partum 598
subarachnoid 128
tooth extraction 561
upper GI 122
vitreous 541
haemorrhoids 518
haemostasis 167
haemothorax 335
hallucinations 603
haloperidol 611
halothane 317
hamate fracture 443
hand
anatomy 430
arthritis 496
crushed fi ngers 435
infections 413 , 441
injuries 430 , 432
wounds 413 , 434
hand hygiene 32
handover of patients 9
hangman’s fracture 499
Hawkin’s impingement
test 460
Hazchem board 36 , 37
head injury 354–368
analgesia 279
and child abuse 731
children 714 , 716
examination 360
Glasgow Coma
Scale 360–1
history 358
imaging 362–3
management 364
minor 366
monitoring 356–7
risks of haematoma 363
triage 356
headache 126–133
analgesic
133
cluster 132
sudden severe 128
tension 132
hearing 548
heart block 80–81
heart rates
inside back cover
normal, children 633
heat illness 264
heat stroke 265
helicopters 36
Henoch-Schönlein
purpura 664
hepatitis 220 , 239 , 415
hernia 161 , 512 , 698 , 700–1
heroin 188 , 217 , 233 ,
276 , 627
herpes simplex 240 , 565
herpes zoster 240
Hib vaccine 636
high pressure injection
injuries 435
Hill-Sachs lesion 500
hip
dislocations 468
fractures 468 , 470
in children 726
hip pain in children 706
HIV 242–5
horse rider’s knee 500
hospitalization,
compulsory 628
Hume fractures 449 , 500
humerus
fractures 459
children 722
Hunt and Hess scale,
subarachnoid
haemorrhage 129
Hutchinson fracture 500
hydatid of Morgagni, torsion
of 701

742
INDEX
hydrocarbons 112 , 205
hydrocoele 700
hydrofl uoric acid
burns 397
hyperbaric
chambers 261
oxygen 208 , 395
hyperglycaemic crises 152
hyperkalaemia 162
renal failure 160 , 694
hypernatraemia 154
hyperosmolar
hyperglycaemic state 152
hypertension 90
malignant 133
in pregnancy 91 , 592
in renal failure 160 , 694
hyperthermia 183 , 264
hypertrophic
cardiomyopathy 141
ECG 141
hyperventilation 97
hypoglycaemia 150–1
alcohol-induced 623
coma 136 , 138
newborn 644
sulphonylurea
poisoning 197
hypokalaemia 164
hyponatraemia 154
hypotension
poisoning 183
see shock 60–1
hypothermia 254–6
bleeding disorders 166
blood transfusion 174
and drowning 258
ECG 255
in poisoning 183
rewarming methods 256
hypovolaemic shock 60
aortic aneurysm 530
burns
390
GI bleed 122 , 124
pregnancy 582–9
transfusion 172
trauma 320
I
ice 428
ice skater’s fracture 500
idiopathic thrombocytopenic
purpura 664
iliac fossa mass 507
imaging
children 720
head injury 362–3
spine and spinal
cord 384 , 482
see also CT; X-ray
immersion foot 257
immobilization,
spinal 380–1
immunization 636
immunoglobulin,
anti-D 582 , 595
impetigo 235 , 662
impingement syndromes
in shoulder 460
impingement test 460
inappropriate attenders 16
incubation periods of
infectious diseases 220
induced illness 620
, 733
infantile spasm 688
infection
bites 413–15
cellulitis 528
control and prevention 32
dental 561
pelvic 566 , 573
wounds 235 , 413
see also abscess
infections
staphylococcal 235
streptococcal 234 , 528
infectious diseases 33 , 219
childhood 222
duration of infectivity 220
imported 246
incubation periods 220
notifi able 221
tropical diseases 246
infectious
mononucleosis 241
infestations 230
infl uenza
pandemic 33 , 252
infraorbital nerve block 302
infrapatellar bursitis 479
inguinal swellings
children 700
inhalation injury 394
children 715
inhalational
anaesthetics 317
injury prevention 711
injury severity
score (ISS) 323
inquest 31
INR xviii , 167 , 170
insect bites 416
insecticide poisoning 206
insulin overdose 151
insulin therapy in
poisoning 187
intercostal (chest) drain
insertion 115 , 336–7
intercostal nerve block 303
internal jugular vein 57–8
interview, psychiatric 604
intestinal obstruction 512 ,
591
in pregnancy 591
intra-hospital transfers 22
intracranial haematoma 365
intracranial pressure 354–5
Intralipid in
poisoning 187 , 284
LA toxicity 284
intraocular pressure 535
intraosseous infusion 640–1
intrauterine contraceptive
device 569
intravenous fl uids
children 640
trauma 340
intubation 312–5
diffi cult 314
failed intubation drill 315
intussusception 699
ipratropium bromide, in
asthma 679 , 680
iritis, acute 542
iron poisoning 201
irradiated patient 268–9
irritable bowel
syndrome 517
irritable hip, children 706
ischaemic colitis 515
ischaemic limb 531
isofl urane 317
ISS (injury severity
score) 323
IUCD 569
IVU in renal trauma 351
J
jaundice
hepatitis 239
neonatal 660
obstructive 510
jaw thrust manoeuvre 325
Jefferson fracture 500
jellyfi sh stings 416
Johansson-Larsen’s
disease 708
joint aspiration 494
Jones fracture 489 , 500
jugular vein 56–8
children 639
junior doctor, coping as 14
K
Kawasaki disease 672
Kemler plate 36
Kernig’s sign 127
ketamine 278 , 316
children 715
ketoacidosis
alcoholic 624
children 691
diabetic 152
ketorolac 275

743
INDEX
knee
children 726
injuries 474–8
problems 479
Kocher’s method, shoulder
dislocation 454
Kohler’s disease 708
Korsakoff’s psychosis 625
L
labour 578
lactic acidosis 99
Langer’s lines 464–5
laryngospasm 315
laryngotracheobron chitis 676
Lassa fever 250
Le Fort fractures 372–3 , 500
learning diffi culties 21
legal aspects 28–31
Legg-Calvé-Perthes’
disease 706–7
leptospirosis 239
leukaemia, acute 664
levonorgestrel 568
lice 230
lidocaine 283
lidocaine gel 288
life support, advanced 52–3
newborn 642–5
paediatric 652–5
trauma (ATLS)
321
life support, basic 46–9
newborn 643
paediatric 646–7
lightning 266
lignocaine see lidocaine
limb injuries
acute ischaemia 531
paediatric 720
salvage 422
limping child 704
lip wounds 464
lipid emulsion in
poisoning 187 , 284
LA toxicity 284
Lisfranc fracture 500
lithium 617
complications of 619
lithium
poisoning 197 , 619
liver transplantation,
paracetamol
poisoning 191
local anaesthesia 272 , 282
children 287
consent 286
contraindications 282
indications 282
infi ltration 289
toxicity 284
see also nerve blocks
locked fi nger 441
locked knee 479
long bone anatomy 421
lorazepam 611
low back pain 492
lower GI tract bleeding 124
LSD 215
Lucas CPR device 51
lumbar puncture,
children 670
lunate dislocation 442
Lund and Browder charts
(for burns) 391
luxatio erecta 457 , 500
Lyme disease 231
M
magnesium
arrhythmias 53 , 85 , 87
children 654 , 656
asthma 106
children 679 , 680
defi ciency 164
eclampsia 149 , 592
normal range xvii
Maisonneuve injury 480 , 501
major incidents 38
chemical 36, 37 , 210
radiation 268
malar fractures 374
malaria 247
Malgaigne’s fracture 501
malingering 620
mallet fi nger 433 , 436 ,
440 , 501
mandibular injuries 376–7
mania 617
mannitol 129 , 365 , 542
MAOIs 619
Marburg fever 250
march fracture 501
mastitis 599
mastoiditis 550
maxillofacial injuries 370
measles 222
meconium aspiration 645
median nerve block 296–7
median nerve
injury 432 , 442
medical defence
organisation 29
Medical Incident Offi cer 39
medically unexplained
symptoms 621
medicolegal aspects 28 , 30
melaena 124
meningitis 224–5 , 666–9
fungal 225
tuberculous 225
viral 225
meningococcal
infection 224 , 664 , 666–9
menorrhagia 574
menstrual cycle and
pain 572
Mental Capacity Act 29 ,
615 , 629
mental health, triage 612
mental health
legislation 615 , 628–9
mental nerve block 302
mental state
examination 606
mephedrone 215 , 626
mesenteric ischaemia 514
metabolic acidosis 99
metabolic diseases 661
metacarpal fractures
436–7
children 725
metacarpophalangeal
joint 438
metatarsal fractures 489
methanol poisoning 202
methedrone 215
methicillin resistant Staph.
aureus 235
methionine 191–2
midazolam
sedation 308
status epilepticus 149 ,
655 , 688 , 690
migraine 130
Milch method, shoulder
dislocation 455
milestones, paediatric 637
milia 662
Mini-Mental State
Examination 607
miscarriage (abortion) 584
mittelschmerz 572
Mobile Medical Team 39
monilial infection 662
monoamine oxidase
inhibitors 619
Monteggia fracture 449 , 501
mood, affect 616
“morning after pill” 568
morphine 276
children 280
overdose 188
smooth muscle spasm 277
trauma 279
Morton’s metatarsalgia 491
mouth to mouth
ventilation 48 , 646
MRSA 235
MSU 158
multiple sclerosis 142
mumps 222
orchitis 222 , 701
Munchausen’s
syndrome 620
by proxy 733
muscle injuries 426
muscle relaxants 316
mushroom poisoning 212

744
INDEX
myasthenia gravis 142
myocardial infarction 68–77
ECG changes 72–5
localization 74
NSTEMI 68
STEMI 70 , 76–7
myoclonic fi t 688
myositis ossifi cans 427
N
N-acetylcysteine 190
nailbed lacerations 435
naloxone 188
nappy rash 662
narrow complex
tachycardia 88
nasal bleeding 552
nasal diamorphine 281
nasal foreign bodies 546
nasal fracture 553
nasoethmoidal fracture 372
nasopharyngeal airway 325
near drowning 258
neck
cervical spine
injury 380–5
pain 463
penetrating injury 378
soft tissue injury 462
wounds 378
necrotizing fasciitis 234
needle cricothyroidotomy
326–7
needlestick injury 418
Neer’s impingement
test 460
neglect 732
nephroblastoma 699
nephrotic syndrome 694
nerve blocks 292
ankle 306–7
digital 294–5
ear 300–1
femoral 304–5
forehead 300–1
infraorbital 302
intercostal 303
median 296–7
mental 302
radial 297–9
supraorbital 300–1
sural 306–7
tibial 306–7
ulnar 296–7
nerve injuries, hand 432 , 434
neuroblastoma 699
neuroleptic malignant
syndrome 265
neurological examination
coma 138
head injury 360
spinal injury 382
newborn resuscitation 642
NHS Direct 11
NHS 24 , 11
nimodipine 129
nitrous oxide 278 , 317
non-accidental
injury 728–33
non-cardiogenic pulmonary
oedema 102
non-shockable rhythms 51
non-steroidal anti-
infl ammatory
drugs 275
normal values
blood tests xvii–xviii
physiological, children 633
pregnancy 577
note keeping 4–5 , 28
notifi able infectious
diseases 221
NSAIDs 275
nursemaid’s elbow 501
nutcracker fracture 501
nystagmus 548
O
obsession 603
obstetrics and
gynaecology 563
obstructive jaundice 510
OCP 4 , 569
O’Donahue’s triad 501
oesophageal intubation 314
oesophageal obstruction
(food bolus) 547
oesophageal rupture 333
olecranon bursitis 453
olecranon fracture 450
ophthalmology 533
opioids 276
poisoning 188
sedation 308
optic neuritis 142 , 541
oral contraceptive pill 4
drug interactions 569
oral rehydration
therapy 228
oral wounds 464
orbital blow-out
fractures 374
orchitis 522 , 701
mumps 222
organ donation 27
organophosphate
poisoning 206
oropharyngeal airway 325
children 654
Osgood-Schlatter’s
disease 708
osmolal gap 99
ossifi cation centres 721
osteoarthritis 495
osteochondritis 708–9
osteochondritis
dissecans 452 , 479 ,
491 , 709
osteomyelitis 705
fi nger infection 441
sickle cell disease 176
tuberculosis 232
otitis externa 550
otitis media 550
Ottawa ankle rules 484–5
Ottawa knee rules 475
ovarian problems 572
oxygen therapy 95
hyperbaric oxygen 208 ,
261 , 395
P
P wave 64
pacemakers 82
pacing (in ALS) 53
paediatric emergencies 630
paediatric fractures 718
paediatric milestones 637
paediatric resuscitation
chart 655
pain relief 272
palivizumab,
RSV disease 683
pancreatitis 508
in pregnancy 591
paracetamol 274
poisoning 190–3
paraffi n poisoning 205
paralysis, periodic 143
paranasal sinusitis 555
paraphimosis 523 , 702
paraquat poisoning 204
paratyphoid 248
parity 576
paronychia 441
parotid gland injury 464
parotitis 557
Parvolex (acetylcysteine)
190
patella fracture 476 , 726
patellar tendon rupture 478
pathological fractures 420
patients
discharge from ED 2 , 8
discharge of elderly
patient 20
dislike of specifi c 18
inappropriate
attenders 16
regular attenders 17
‘special’ patient groups 19
transfer of patient 22
with a label 17
with learning
diffi culties 21
PEA 51

745
INDEX
peak expiratory fl ow
rates 105
children 678
Pelligrini-Stieda’s
disease 501
pelvic fractures 466–7
pelvic infection 598
pelvic infl ammatory
disease 573
pelvic injury, children 714
penile problems 523 , 702
peptic ulcer disease 511
pregnancy 591
pericardial effusion 78–9
pericardiocentesis 79 , 343
pericarditis 78
perineal tear, imminent 580
periodic paralysis 143
peritoneal dialysis 161
peritoneal lavage 347
peritonitis 161 , 504 , 507 ,
516
peritonsillar abscess 554
peroneal nerve block 306–7
peroneal nerve injury 487
peroneal tendon
subluxation 487
perseveration 603
personal protective
equipment 32 , 34
Perthes disease 706–7
pertussis, whooping
cough 684
pethidine 276
petit mal 688
petrol poisoning 205
phalangeal fractures 436
pharyngeal burns
(cocaine) 555
phenol burns 397
phenothiazine
poisoning 196
phimosis 702
physiological values in
children 633
physiotherapy 428
Pilon fractures 501
pilonidal abscess 518
Pipkin fracture 501
placenta praevia 588
placental abruption 588 , 594
plant poisoning 212
plantar fasciitis 491
plaster of Paris 424–5
platelet disorders 168
pleural effusion 103
Pneumocystis
infection 110 , 244
pneumonia 110
children 686
differential diagnosis 111
pneumothorax
spontaneous 114–6
tension 328–9
traumatic 334
poisoning 179
chemical incidents 38 , 211
deliberate 180 , 753
diagnosis 182
fi sh 229
food 226–8
general principles 180
in children 181 , 696–7
reducing
absorption 184–5
supportive care 183
poisons information 180–1
police requests for blood
alcohol 30
police statements 31
poliomyelitis 249
polyhydramnios 590
polymyositis 142
porphyria 165
post-coital
contraception 568
post-concussion
symptoms 368
post-partum problems 598
post-resuscitation care 54
Pott’s fracture 502
PR interval 64
pre-eclampsia 590 , 592
pregnancy 563 , 576 – 599
abdominal pain 590
bleeding in 582–3 , 588
cardiac arrest 596
ectopic 586
electric shock 266
hypertension 91 , 592
psychiatric problems 599
thrombosis 593
trauma 594
pregnancy tests 582
prepatellar bursitis 479
pretibial lacerations 481
priapism 523
prilocaine
283
Prinzmetal’s angina 69
Procurator Fiscal 10 , 26 , 31
propofol 308 , 316
prostatitis 523
prostheses, hip 468
prosthetic joint infection 495
prosthetic valve failure 101
protective equipment 32 , 34
prothrombin time
(INR) xviii , 167 , 170
proxymetacaine 283
pruritus ani 518
pruritus vulvae 565
pseudo-gout 496
psychiatric assessment 604
after deliberate self
harm 612–4
history 605
psychiatric drugs,
complications of 619
psychiatric interview 604
psychiatry 601
psychogenic coma 138
psychosis 603
pulmonary aspiration 112 ,
338
pulmonary contusion 332 ,
338
pulmonary embolus 120
in pregnancy 593
pulmonary oedema
cardiogenic 100–1
non-cardiogenic 102
pulp infections 441
pulse oximetry 95 , 96
CO poisoning 208
pulseless electrical
activity (PEA) 51 , 107
puncture wounds 419
purpuric rash 664
pyelonephritis 158 , 159
children 692–3
pregnancy 591
pyloric stenosis 698
pyogenic tenosynovitis 441
pyrexia of unknown
origin 246
Q
Q waves 65 , 72
QRS amplitude 65
QRS width 64
QT interval 65
quadriceps rupture 478
quinsy 554
R
rabies 249 , 415
radial fractures 444–6 ,
448–9 , 724–5
radial head fracture 450 ,
724
radial head subluxation
(pulled elbow) 724
radial nerve block 297–9
radial nerve injury 432 , 453
radial styloid fracture 446
radial tenosynovitis 447
radiation incidents 268
decontamination 211 , 269
radiological requests 6
radius, fractures 444–6 ,
448–9
children 724–5
Ramsay Hunt
syndrome 556
rape 570
rapid sequence induction
(intubation, RSI) 312–5

746
INDEX
rashes 664 , 666 , 672
records see note keeping
recuronium 316
red cell transfusion 173
red dot system 6
red eye 542
referral 8 , 28
inappropriate 16
patient with a label 17
regular attenders 17
Reiter’s disease 238 , 497
rejection, transplant 161
relatives
bereaved 24–5
in cardiac arrest 46
in major incidents 39
renal failure 160 , 694
renal trauma 351
rescue breaths 48
children 646
resin casts 424
respiratory depression
coma 137
opioids 188 , 276
respiratory failure,
type I II 98
respiratory rate
coma 137
normal, children 633
respiratory syncytial
virus 682–3
resuscitation
burns 392
cardiac arrest 46–53
pregnancy 596
children 634–5 , 646–7 ,
652–5
formulae 655
discontinuing 51 , 655
mechanical 51
newborn 642–5
paediatric trauma 712
post-resuscitation care 54
trauma 320–1
unconscious patient 136
resuscitation chart
paediatrics 655
reteplase 77
retinal artery occlusion 540
retinal detachment 541
retinal vein occlusion 540
retropharyngeal
abscess 555
return visits 28
reverse fi ght bites 415–16 ,
435
Revised Trauma Score 323
rewarming methods 256
rhabdomyolysis 214–6 ,
265 , 398
rheumatic fever 497
rheumatoid arthritis 496
rib fracture 330–2
rifampicin
190 , 225 , 569
ring avulsions 435
Rinne’s test 548
Road Traffi c Act 30
roadside procedures 36
Rockall score 123
Rolando fracture 502
Romano–Ward
syndrome 65
Rosier score, stroke 145
rotator cuff tears 459
rotator cuff tendonitis 461
Rovsing’s sign 507
RSV 682–3
rubella 223
runner’s fracture 502
S
sacrum fracture 469
Sad Persons Scale 614
safety, personal 609
salaam attack 688
salbutamol
anaphylaxis 43 , 651
asthma 106 , 679–681
COPD 109
hyperkalaemia 162 , 694
inhalation injury 395
poisoning 200
salicylate poisoning 189
salivary gland problems 557
Salter-Harris classifi cation,
epiphyseal injury 718–9
saphenous nerve
block 306–7
SARS 33 , 251
scabies 231
scalded skin
syndrome 235 , 662
scaphoid fracture 442
children 725
scapula fracture 458
scarlet fever 234
Scheuermann’s disease 708
schizophrenia 618
thought blocking 603
SCIWORA 714
scrotal injuries 352
scrotal swellings,
children 700
seborrhoeic dermatitis 662
sedation, of violent
patient 611
sedation for
procedures 308
children 309
seizures 148– 9 , 688
Seldinger technique 44 ,
56 , 115
self-harm
deliberate 612 , 614
risk of 607
self-labelled patients 17
sepsis 59
in babies 660
septic arthritis 495
septic shock 59–61
septicaemia,
meningococcal 666–9
sero-negative spondylo-
arthropathies 497
serotonin syndrome 216
severe acute
respiratory syndrome
(SARS) 33 , 251
Sever’s disease 708
sevofl urane 317
sexual abuse 733
sexual assault 570
sexually transmitted
diseases 238
Sgarbossa criteria,
ACS in LBBB 72
sharps, safe handling
disposal 32
shellfi sh poisoning 229
shifts 15
shin splints 483
shingles 240
shock 60
anaphylactic 42–4
cardiogenic 60 , 77
hypovolaemic 60 , 172–4
in poisoning 183
neurogenic 382
septic 59
shockable rhythm 52 , 652–3
shoulder
dislocation 454–7
injuries 458–9
children 722
pain diagnosis 461
soft tissue problems 460–1
shoulder dystocia 580
sick sinus syndrome 80
sickle cell disease 176–7
Sinding Larsen’s disease 708
sinusitis 555
SIRS (systemic infl ammatory
response syndrome) 59
skin lesions
causes 673
children 672
popping (drugs) 627
problems, infants 662
skin tissue glue 406
skull fracture 355 , 361–4
basal fracture 361 , 364
child abuse 731
compound (open) 364
depressed 362 , 364
slit lamp examination 535
Smith’s fracture 446 , 502
snake bites 417
Snellen chart 534

747
INDEX
snowblindness 538
sodium bicarbonate
cardiac arrest
children 654
newborn 644
hyperkalaemia 162 , 694
tricyclic antidepressant
poisoning 194–5
sodium derangements
154
soft tissue injuries 426
solvent abuse 626
somatoform pain
disorder 621
sonography, trauma
scan 346
space-occupying
lesions 133
sphincter of Oddi,
spasm 277
spinal cord injury 380–5
airway management
380
children 714
circulation 382
examination 382
imaging
384–5 , 462
incomplete injury
patterns 383
muscle power
grading 383
neurological
examination 382
without radiographic
abnormality
(SCIWORA) 383 , 714
spinal
immobilization 380–1
spine
control 320
injury 380–5
children 714
Xrays 384–5 , 462
sprains 426
ankle 487
neck 462
wrist 447
ST segment 65 , 70–5
staff 2
care after death of
patient 27
debriefi ng after major
incident 39
interaction 15
sudden infant death
syndrome 659
staphylococcal
infections 235 , 662
staples 407
status epilepticus 148–9
children 690
Steristrips 406 , 481
sternum fracture 331
stillbirth 576
Stimson’s technique 455
stings, bites 416
stool culture 226
straddle fracture 502
strains 426
streptococcal
infections 234 , 528
streptokinase 77
stress fractures, MTs 489
stridor 676
stroke 144
Rosier score 145
stye 543
subacromial bursitis 461
subarachnoid
haemorrhage 128
subclavian vein 56
venous access 57–8
subconjunctival
haemorrhage 543
substance misuse 626
subtarsal examination 535
subtrochanteric
fractures 472
subungual haematoma 435
sudden infant death
syndrome 658
suicide, risk of 614
sulphonylurea
poisoning 197
sumatriptan 130
superglued eyelids 538
supracondylar fracture 451 ,
742
supraorbital nerve
block 300–1
supratrochlear nerve 300–1
supraventricular tachycardia
(SVT) 86–8
children 656
sural nerve block 306–7
surgery 503
surgical airway 326–7
sutures 407–9
suxamethonium 316
swine fl u 33 , 252
symbols ix
synchronized
cardioversion 86
syncope 140
funny turns in,
children 689
synovitis, transient 706
systemic infl ammatory
response syndrome 59
T
T waves 65 , 72
tachyarrythmias 86–9
tachycardia
algorithm 84–5
talar injuries 488
team leader 46
tear gas 209
teeth
eruption 559
extraction,
haemorrhage 561
fractures 560
toothache 280 , 561
see also dental
emergencies
telemedicine 11
telephone advice 11
temperature, core,
measurement of 254 ,
264
temporal arteritis 132 , 541
temporal lobe epilepsy 688
tendon injury
Achilles
482
fi nger 432–4 , 440
hand 447
in wounds 404
patella 478
quadriceps 478
tendonitis 427
tenecteplase 77
tennis elbow 452
tenosynovitis 427 , 441
terrorism, poisoning 181
testis problems 522
children 700
torsion 522 , 701
trauma 352
undescended 700
tetanus 236
prophylaxis 410
tetracaine 283 , 288 , 535
TFCC injury 447
theophylline poisoning 200
thiopentone 316
Thomas splint 473
thoracolumbar spine 384
throat 554 , 674–7
examination,
children 674–5
foreign bodies 547
infection 554 , 676–7
sore 554
thrombocytopenic purpura,
idiopathic 664
thromboembolic disease, in
pregnancy 593 , 599
thrombolysis
myocardial
infarction 76–7
pulmonary embolus 121
stroke 145
thrombophlebitis,
superfi cial 119 , 529
thrombosis, deep vein 118
pregnancy 593
thrush 566, 662

748
INDEX
thumb, collateral ligament
injuries 438 , 440
thyrotoxic crisis 156
TIA 146–7
tibia
fractures 477 , 480
children 727
tibial nerve block 306–7
ticks, bites 231 , 416
TICTAC 180
Tillaux fracture 502
TIMI risk score 69
toddler’s fracture 502 , 727
Todd’s paresis 144 , 148
toe fractures 490
toe injuries 490
toenails, ingrowing 491
tongue wounds 464
tonsillitis 554
torsades de pointes
87
torticollis 463
TOXBASE 181
toxic shock syndrome 235 ,
567
tracheal intubation 312–5
children 654
newborn 644
trauma 325
tracheal tube size for
children 654–5
tracheitis, bacterial 677
traction apophysitis 708
tranquillization,
emergency 611
transcutaneous pacing 82
transfer of patient 22
transfusion
blood 172
massive 174
transfusion reactions 175
transient ischaemic
attacks 146
transplant patients 161
transplantation of
liver, paracetamol
poisoning 191
transport emergency card
(TREM) 36
transvenous pacing 82
trauma
injury prevention 711
injury severity score
(ISS) 323
in pregnancy 594
major 319–99
paediatric 710
paediatric
resucitation 712
Revised Trauma
Score 323
trench foot 257
triage 7
mental health 612
tricyclic antidepressant
poisoning 194–5
trigeminal neuralgia 132
trigger fi nger/thumb 441
TRISS methodology 323
tropical diseases 246
troponins 71
trouble
aggressive patient 608
avoidance of 28 , 608
violence/violent
patients 608–611
tuberculosis 232 , 685
tuberculous meningitis 225
tympanic membrane
rupture 551
typhoid 248
U
ulcerative colitis 517
ulcerative keratitis 543
ulna, fractures 448 , 725
ulnar nerve block 296–7
ulnar nerve injury 432 , 453
ultrasound
diagnosis of DVT 119 , 593
for nerve blocks 292
in pregnancy 576 , 584 ,
587 , 589
in trauma (FAST) 346 ,
595
for venous access 56 , 639
umbilical cord sepsis 660
umbilical vein
cannulation 645
unconscious patient 136
upper gastrointestinal tract
bleeding 122
upper respiratory tract
infections, children 676
ureteric colic 524
urethral carbuncle 565
urethral injuries 352
urethritis 238 , 497
urinary retention 520
urinary tract infections
(UTIs) 158 , 591
children 692
urine microscopy 158 , 693
urticaria, neonatal 662
USS see ultrasound
uterine bleeding 574
uterine problems 572
uterine rupture 594
uterine size, pregnancy 577
uveitis 542
V
vaccines, immunization 636
vaginal bleeding 574
in pregnancy 582–3 , 588
vaginal infection 566
Valsalva manoeuvre 88
varicella zoster 240
varices 123
varicose veins 529
vecuronium 316
venereal proctitis 519
venous access
central 56
children 638
choice of vein 56
cut down 639
intraosseous 640–1
umbilical vein 645
venous thrombosis 118
cerebral 133
in pregnancy 593
venous ulcers 529
ventilation
in asthma 107 , 679
in children 654
in COPD 108
hyperventilation 97
mouth to mouth 48 , 646
in newborn 642
non-invasive 109
ventricular activation
time 72
ventricular shunts 133
ventricular
tachycardia 86–7
children 652 , 656
vertigo 549
violence/violent
patients 608–11
intoxication 623
viral arthritis 496
viral haemorrhagic
fevers 250
visual acuity 534
visual loss, sudden 540
vitreous haemorrhage 541
volar plate injury 440
volvulus 516 , 698
vomiting, bilious vomiting in
babies 661
von Willebrand’s
disease 166 , 168
vulval ulcers 565
vulvovaginal problems 565
W
wasp stings 416
weakness, generalised 142
Weber’s test 548
weight estimation,
children 633
Weil’s disease 239
Wells criteria 119–20
Wernicke’s
encephalopathy 625
whole-bowel irrigation 185

749
INDEX
whooping cough 684
Wilm’s tumour 699
Wolff-Parkinson-White
syndrome 89
worms 230
wounds 401–19
of abdomen 350
antibiotics 411 , 422
bites/stings 414
of chest 340–3
child abuse 730
classifi cation 403
cleaning 406
closure 406
delayed primary
closure 412
ear 464
exploration 404
foreign bodies in 405
of hand 434
infection 413 , 415
in children 715
lip 464
of neck 378
oral 464
puncture 419
tendon injury 434
of tongue 464
X-rays 404
wrist
anatomy 430
dislocations 442–3
fractures 442– 6
nerve blocks 296–9
X
X-rays
children 720
in pregnancy 576
reporting system 6
requests 6
Z
zip entrapment of
foreskin 702
zygomatic (malar)
fractures 374



