1
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
Association between person- centred
care and healthcare providers’ job
satisfaction and work- related health: a
scoping review
Cornelia van Diepen ,
1,2,3
Andreas Fors ,
1,2
Inger Ekman,
1,2
Gunnel Hensing
4
To cite: van DiepenC, ForsA,
EkmanI, etal. Association
between person- centred
care and healthcare
providers’ job satisfaction
and work- related health: a
scoping review. BMJ Open
2020;10:e042658. doi:10.1136/
bmjopen-2020-042658
► Prepublication history and
additional material for this paper
is available online. To view these
les, please visit the journal
online (http:// dx. doi. org/ 10.
1136/ bmjopen- 2020- 042658).
Received 10 July 2020
Revised 20 November 2020
Accepted 24 November 2020
1
Institute of Health and Care
Sciences, Sahlgrenska Academy,
University of Gothenburg,
Goteborg, Sweden
2
Centre for Person- Centred
Care (GPCC), University of
Gothenburg, Gothenburg,
Sweden
3
Erasmus School of Health
Policy & Management,
Erasmus University Rotterdam,
Rotterdam, The Netherlands
4
School of Public Health
and Community Medicine,
Sahlgrenska Academy,
University of Gothenburg,
Gothenburg, Sweden
Correspondence to
Dr Cornelia van Diepen;
cornelia. van. diepen@ gu. se
Original research
© Author(s) (or their
employer(s)) 2020. Re- use
permitted under CC BY- NC. No
commercial re- use. See rights
and permissions. Published by
BMJ.
ABSTRACT
Objective This scoping review aimed to explore and
describe the research on associations between person-
centred care (PCC) and healthcare provider outcomes, for
example, job satisfaction and work- related health.
Design Scoping review.
Eligibility criteria Studies were included if they were
empirical studies that analysed associations between PCC
measurement tools and healthcare providers outcomes.
Search strategy Searches in PubMed, CINAHL, Psychinfo
and SCOPUS databases were conducted to identify
relevant studies published between 2001 and 2019. Two
authors independently screened studies for inclusion.
Results Eighteen studies fullled the inclusion criteria.
Twelve studies were cross- sectional, four quasi-
experimental, one longitudinal and one randomised
controlled trial. The studies were carried out in Sweden,
The Netherlands, the USA, Australia, Norway and Germany
in residential care, nursing homes, safety net clinics, a
hospital and community care. The healthcare provider
outcomes consisted of job satisfaction, burnout, stress of
conscience, psychosocial work environment, job strain
and intent to leave. The cross- sectional studies found
signicant associations, whereas the longitudinal studies
revealed no signicant effects of PCC on healthcare
provider outcomes over time.
Conclusion Most studies established a positive
association between PCC and healthcare provider
outcomes. However, due to the methodological variation, a
robust conclusion could not be generated. Further research
is required to establish the viability of implementing PCC
for the improvement of job satisfaction and work- related
health outcomes through rigorous and consistent research.
INTRODUCTION
Healthcare providers play a key role in the
development of a sustainable population
health. The WHO has repeatedly high-
lighted the importance of well- educated
and trained healthcare workers at a relevant
level of density and distribution geographi-
cally and over professional specialities. The
WHO emphasise the recruitment and reten-
tion of healthcare workers as particularly
important in low- income and middle- income
countries, and countries where competing
labour markets have led to both recruitment
and retention challenges.
1
It is noteworthy
that the United Nations has pointed out
healthcare workers as essential to reaching
the sustainable development goal three to
‘ensure healthy lives and promote well- being
for all at all ages’.
2
The quality of the provided care is influ-
enced by the attraction and retention of
qualified and committed healthcare staff.
3
However, the work environment for health-
care staff is currently characterised by high
demands, low control, ethical stress, sched-
uled working hours, low salary and for most
groups, limited possibilities for career devel-
opment.
4–6
The healthcare providers experi-
ence increased stress and dissatisfaction due
to high expectations and job pride coupled
with insufficient time, skills and social support
at work.
3 6
According to two systematic reviews, inter-
ventions containing changes in working
conditions, organising support, changing
care, increasing communication skills and
changing work schedules are most effective
for improving the work environment.
6 7
In a
recent review, a good work environment was
found a defining factor for higher patient satis-
faction with the provided care.
5
Therefore,
Strengths and limitations of this study
► A transparent and rigorous search strategy was
employed.
► The person- centred care measurement tool un-
derwent scrutinisation for applicability in affecting
healthcare provider outcomes.
► We applied a range of healthcare provider outcome
possibilities.
► The included studies were only written in English.
► We did not assess the quality of the outcome
measures.
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

2
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
interventions focused on improving patient safety and
satisfaction should first consider improving employees’
health and creating safer work environments.
8 9
The Model of Care (MoC) provided by the healthcare
staff can largely influence the work environment for
healthcare personnel.
10
An MoC can be defined most
broadly as ‘the way health services are delivered as it aims
to ensure people get the right care, at the right time, by
the right team and in the right place’ (p3).
11
Improved
patient outcomes and cost- effectiveness are the general
objectives in implementing MoCs, according to a recent
review of systematic reviews on MoC interventions.
12
This same review revealed that only 13% of the included
reviews had healthcare provider outcomes (eg, well-
being, fatigue, stress and satisfaction). However, health-
care professionals should be considered defining factors
in the effects of implementing an MoC as the model
governs how healthcare personnel execute their work,
which directly affects patients’ treatment and health.
There is a growing interest in the model of person-
centred care (PCC) since authorities, such as the WHO,
have called for enabling patients to engage in their
healthcare.
13
PCC has also been endorsed by professional
and patient organisations.
14 15
The concept of PCC is
based on ethical principles and has its roots in the holistic
paradigm, which highlight the importance of knowing
the patient also as a capable human being with needs and
resources.
16–19
PCC is an approach to care in which rela-
tionships are formed and fostered with healthcare profes-
sionals, care providers and patients (often with relatives)
and is supported by values of respect for the person, indi-
vidual right to self- determination, mutual respect and
understanding.
20
Application of PCC in practice contains
core components such as: inclusion of patients narra-
tives, cocreating a health plan, and documentation and
follow- up of the health plan.
19 21
PCC can form a critical
component for effective change in the work environmet
of healthcare professionals.
22
The work environment
often suffers under ethical conflicts and lack of support
and control in daily tasks,
4 5 23
which could be abated
by working in a person- centred manner. Thus, there is
reason to look closer into how implementing PCC influ-
ences the work environment for healthcare professionals.
Although person- centred and patient- centred care
differ, they are often used interchangeably in the liter-
ature.
18 24
Patient- centred care is more focused on the
need of care patients have in common regarding their
disease and treatment while PCC, besides needs, empha-
sises the capabilities and strengths that each person
possess as valuable resources in a collaborative partner-
ship between the patient (often including relatives) and
healthcare professionals.
17
A concept review of the differ-
ence has highlighted how PCC differed to patient- centred
care on a deeper level of a meaningful (person) versus
a functional (patient) life.
25
Certain contexts require
specific types of ‘centredness’ such as family- centred,
relationship- centred, client- centred, patient- focused and
person- focused care.
26
Therefore, this scoping review
accepted all concepts when they followed the PCC prop-
erties highlighted earlier.
Most studies of PCC analysed patients’ point of view
and showed positive results such as shorter hospital stay,
reduced symptoms, improved care experiences and
increased self- efficacy.
27–30
Three reviews have focused
on PCC and healthcare provider outcomes.
31–33
The
reviews found limited indications of a positive associa-
tion between PCC and healthcare provider outcomes.
However, these reviews only focused on the association in
nursing homes and among elderly care.
31–33
There have
been PCC implementations across healthcare sectors,
and there is a need for an overview of how PCC and staff
outcomes are connected.
Aim
This scoping review aimed to explore and describe the
research on associations between PCC and healthcare
provider outcomes.
METHODS
A scoping review methodology was applied to allow for
mapping of the main concepts and a way to give an idea
of what evidence is available for the research area.
34
This
methodology was chosen over a systematic review as the
study aimed to clarify the PCC concept and identify its
relation to key characteristics within healthcare provider
outcomes rather than answer a clinically meaningful
question.
35
Search strategy
The search engines PubMed, CINAHL, Psychinfo and
SCOPUS were accessed in February 2020 for studies
published in academic journals between 2001 and 2019.
The search terms included “person centred” OR
“person centredness” OR “client centred” OR “patient
centred” OR “relationship centred” OR “family centred”
“patient focused” OR “person focused”. AND “Job Satis-
faction” OR “Absenteeism” OR “presentism” OR “Occu-
pational Stress” OR “Personnel Turnover” OR “Sick
Leave” OR “Stress, Psychological” OR “Dyssomnias” OR
“sleep disorder” OR “sleep disturbances” OR “occupa-
tional health” OR “moral stress”. Most terms were overar-
ching concepts (MESH terms), and the search captured
both British and American spellings. See online supple-
mental appendix 1 for the entire search strategy.
Selection of studies
There is no established consensus on the operationali-
sation of PCC.
16 36
To prevent an array of related terms
and to increase the possibility to compare, we applied
a more narrow definition than those used in earlier
reviews. The eligibility criteria in this scoping review were
guided by the six PCC dimensions created in 2001 by the
Institute of Medicine, now called National Academy of
Medicine. These six dimensions are respect for patients’
values, preferences and expressed needs; coordination
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from
3
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
and integration of care; information, communication
and education; physical comfort; emotional support—
relieving fear and anxiety; involvement of family and
friends.
37
The relevant studies needed to display a connec-
tion to these dimensions of PCC.
Types of participants included all healthcare personnel
in contact with patients such as registered nurses (RNs),
licenced practical nurses and physicians.
Types of outcomes included healthcare provider
outcomes such as job satisfaction and work- related health
outcomes.
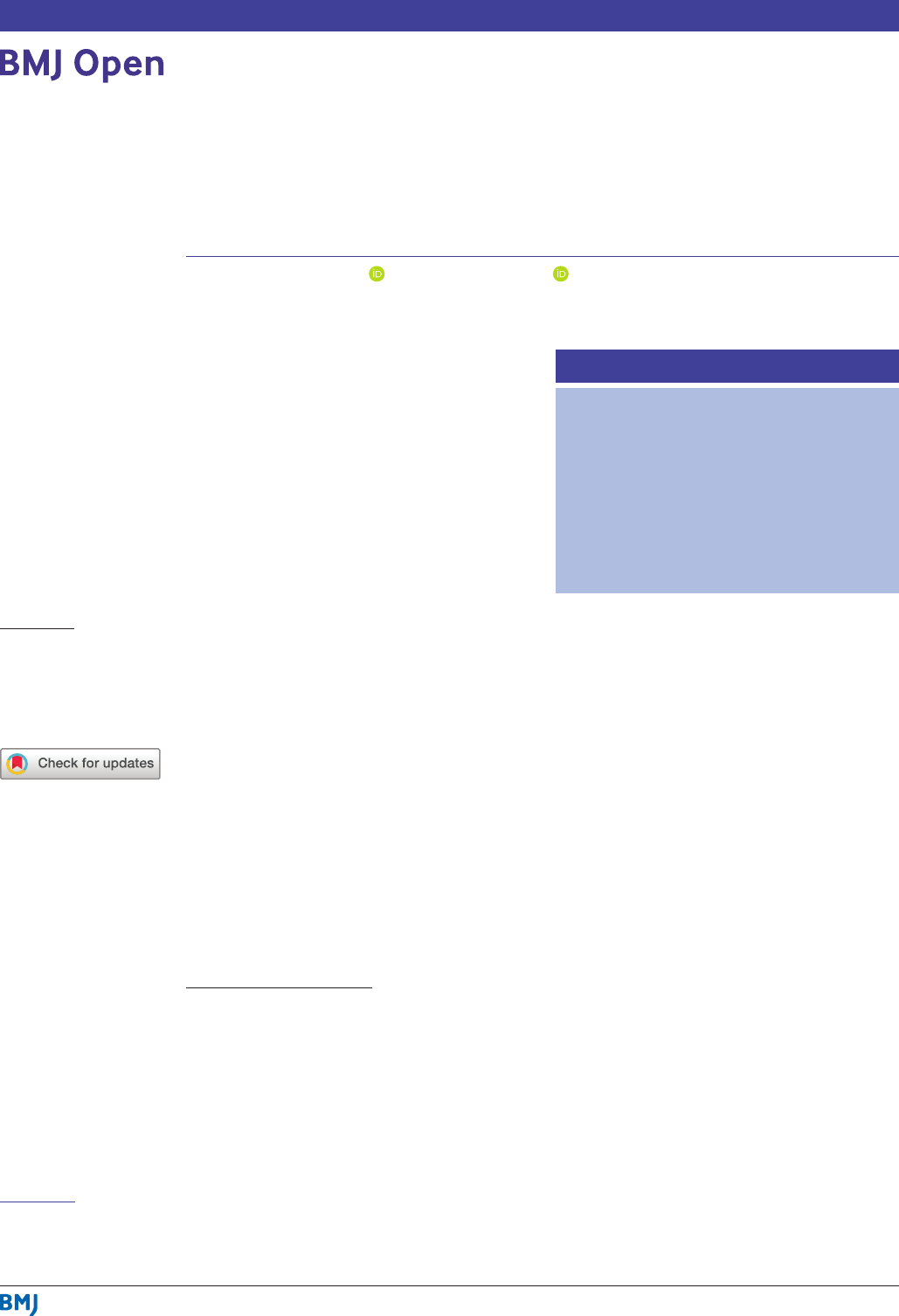
Data extraction and synthesis of results
The data extraction and synthesis of results are presented
in the flowchart (figure 1). The results obtained from
the online search engines were collected and duplicates
removed by the first author (CvD). The search and collec-
tion yielded 1263 titles and abstracts, which were subse-
quently screened for relevance by two authors (CvD and
AF) through the research software program for systematic
reviews ‘Rayyan’.
38
All studies with one author deeming
possible relevance were discussed, and a selection of 45
studies for full- text review was created in agreement by
both authors.
The full text of the potentially relevant studies was
obtained and first reviewed based on the PCC measure-
ment tool to be associated with any healthcare provider
outcome in the results. Disagreements were resolved by
consensus between the two authors. Second, the six dimen-
sions of PCC were compared with the PCC measurement
tool used in the studies. The first dimension ‘respect for
patients’ values, preferences and expressed needs’ is the
core of PCC and needed to be addressed in the tool. PCC
is a broad concept affecting different elements to care,
39
and that needed to be reflected in the PCC measurement
tool. Therefore, the authors decided that at least two of
the other five dimensions needed to be present in order
for the tool to be considered to measure a model of PCC
that could affect healthcare provider outcomes. The two
authors did this inclusion process together. When a PCC
dimension was present in the PCC measurement tool, a ‘+’
sign was inserted, and a ‘−’ was inserted when that partic-
ular dimension was absent. As a result, table 1 shows the
included studies and their reference to the six dimensions.
Figure 1 Flow chart for study inclusion.
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

4
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
Table 1 The presence of the six dimensions of person- centred care
37
within the person- centred care measurement tools in the included studies
Dimensions*
Person- centred care
measurement tool Tool subscales Authors
Respect for
patients’ values,
preferences and
expressed needs
Coordination
and
integration of
care
Information,
communication
and education
Physical
comfort
Emotional
support—
relieving fear and
anxiety
Involvement
of family
and friends
Person- centred Care
Assessment Tool (P-
CAT)
13 items
► Personalising care.
► Organisational
support.
► Environmental
accessibility.
Edvardsson et al,
53
Wallin et al,
44
Røen et
al,
55
Schaap et al,
48
Silén et al,
42
Sjögren et al,
43
Vassbø et al
57
+ + + + + –
Person- entred Climate
Questionnaire- Staff
version (PCQ- S)
14 items
► Safety.
► Everydayness.
► Hospitality.
Edvardsson et al,
40
Lehuluante et al,
41
Wallin et al,
44
Sjögren et al,
43
Vassbø et al,
57
Åhlin et al
45
+ – + + + +
Patient Centred
Medical Homes
(PCMH) rating
24 items
► Access to care and
communication
with patients.
► Communication
with other
providers.
► Tracking data.
► Care management.
► Quality
improvement.
► Work environment.
Lewis et al,
51
Nocon et al
52
+ + + – – –
The subscale
‘recognition of
personhood’ of the
Approach to Dementia
Questionnaire (ADQ)
11- items
Dichter et al,
56
Willemse et al
50
+ – + + + –
Continued
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

5
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
Dimensions*
Person- centred care
measurement tool Tool subscales Authors
Respect for
patients’ values,
preferences and
expressed needs
Coordination
and
integration of
care
Information,
communication
and education
Physical
comfort
Emotional
support—
relieving fear and
anxiety
Involvement
of family
and friends
8 dimensions
Person- Centred Care
Questionnaire
35 items
► Respect for clients’
values, preferences
and expressed
needs.
► Provision of
information and
education.
► Access to care.
► Emotional support.
► Involvement of
family and friends.
► Continuity and
secure transition of
care.
► Physical comfort.
► Coordination of
care.
van der Meer et al
49
+ + + + + +
Patient- Centred Care
Questionnaire
35 items
► Taking patients’
preferences into
account.
► Coordination of
care.
► Information and
education provided
to patients.
► Level of patient’s
physical comfort.
► Emotional support
for patients.
► Involvement of
patient’s family and
friends.
► Continuity and
transition.
► Access to care.
den Boer et al
47
+ + + + + +
Table 1 Continued
Continued
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

6
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
After scrutinising the full- text of 45 studies for relevance,
five studies did not have a healthcare provider outcome
connected to a PCC measurement tool. Seventeen studies
were excluded for not following our set criteria for PCC.
Three studies were reviews, and two were excluded due to
language. Finally, all four authors confirmed the decision
to include or exclude a study.
The following details of the included studies were
extracted and summarised: authors, year of publication,
country, study design, setting and participants, PCC
measurement tool, staff outcome measures, and main
results (see table 2). Given the variability of the study
designs that are included in this scoping review, a qual-
itative analysis was used to synthesise the results, and the
results are presented in a narrative form.
Patient and public involvement statement
This research was designed without patient involvement.
However, patient care and healthcare organisations were
involved in the interpretation of the results through a
workshop.
RESULTS
This scoping review aimed to explore and describe the
research on associations between PCC and healthcare
provider outcomes. Eighteen studies fulfilled the inclu-
sion criteria (table 2).
Characteristics of the included studies
Seven studies were conducted in Sweden,
40–46
four in the
Netherlands,
47–50
two in the USA,
51 52
two in Australia,
53 54
one in Norway,
55
one in Germany
56
and one study was
conducted in three countries (ie, Sweden, Norway and
Australia).
57
The included studies consisted of twelve cross- sectional
studies,
41–44 46 47 49–51 53 55 57
four quasi- experiments,
40 48 52 56
one longitudinal study
45
and one randomised controlled
trial (RCT).
54
The six studies with a longitudinal design
had a follow- up duration between 8 months in the RCT
54
and 4 years in a quasi- experimental study.
52
The setting for the studies was residential care (homes
with care availability) for eight studies,
40 43–45 48 49 53 54
nursing homes (homes with 24 hours medical care) for
six studies,
42 46 50 55–57
safety net clinics (primary care for
uninsured persons) for two studies,
51 52
hospital for one
study
41
and community care (care for independent living
persons) for the last study.
47
In 12 studies, the participants were all healthcare
staff.
40 42 43 46 48–54 57
In the other studies, participants were
specified as RNs,
41 47
managers, unit head nurses, and
staff,
55
caregivers,
56
nurse assistants and nurse’s aides,
44
and RNs and nurse assistants.
45
Measurement for PCC
The rationale for measuring PCC and healthcare
provider outcomes was for 13 studies to examine the
extent to which staff members rated their provided care
Dimensions*
Person- centred care
measurement tool Tool subscales Authors
Respect for
patients’ values,
preferences and
expressed needs
Coordination
and
integration of
care
Information,
communication
and education
Physical
comfort
Emotional
support—
relieving fear and
anxiety
Involvement
of family
and friends
Individualized Care
Inventory (ICI)
43 items
► Knowing the
person.
► Resident autonomy.
► Staff- to- resident
communication.
► Staff- to- staff
communication.
Elfstrand Corlin and
Kazemi
46
+ + + + + +
The Bradford
University’s Dementia
Care Mapping and
Person- Centred Care
training manual
Jeon et al
54
+ + + – + –
*‘+’ indicates the presence and ‘−’ indicates the absence of this person- centred care (PCC) dimension within the PCC measurement tool.
Table 1 Continued
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from
7
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
Table 2 Characteristics and results of included studies
Authors (country) Study design Setting, participants Person- centred care measure
Staff outcomes: measurement
tool Results
den Boer et al
47
(Netherlands)
Cross- sectional Community care,
registered nurses (RNs)
n=153
Adapted version of the Patient-
Centred Care Questionnaire 35
items
Job satisfaction: a 38- item job
satisfaction questionnaire
Job satisfaction:
signicant positive
association with PCC
Dichter et al
56
(Germany) Quasi-
experimental
6- month and
18- month follow-
up
Nursing home,
caregivers
n=201
The subscale ‘recognition of
personhood’ of the Approach to
Dementia Questionnaire (ADQ) 11
items
Job satisfaction: Copenhagen
Psychosocial Questionnaire
4- items
Burnout: Copenhagen Burnout
Inventory (CBI) 6- items
Job satisfaction:
signicant positive
effect of PCC
intervention
Burnout: no signicant
effect of PCC
intervention
Edvardsson et al
53
(Australia)
Cross- sectional Residential aged care,
all staff
n=297
Person- Centred Care Assessment
Tool (P- CAT), 13 items
Job satisfaction: measure of job
satisfaction (MJS)
22 items
Job satisfaction:
signicant positive
association with PCC
Edvardsson et al
40
(Sweden)
Quasi-
experimental
12 months follow-
up
Residential aged care,
all staff
n=171 (baseline)
n=143 (follow- up)
P- CAT 13 items
Person- Centred Climate
Questionnaire- Staff version (PCQ- S)
14 items
Stress of conscience: Stress of
Conscience questionnaire (SCQ)
9 items
Job strain: Demand- Control-
Support Questionnaire (DCSQ)
11 items
Stress of conscience:
signicant negative
effect of PCC
intervention
Job strain: no
signicant effect of
PCC intervention
Elfstrand Corlin and
Kazemi
46
(Sweden)
Cross- sectional Nursing homes,
all staff
n=322
Individualized Care Inventory (ICI)
43 items
Job satisfaction: a single
question
Job satisfaction:
signicant association
to subscales of PCC
Jeon et al
54
(Australia) Cluster
randomised
controlled trial
8 months follow-
up
Residential aged care,
all staff
n=194
Burnout: Maslach Burnout
Inventory (MBI) 22 items
Burnout: signicant
effect of DCM
intervention but not the
PCC intervention
Lehuluante et al
41
(Sweden)
Cross- sectional Hospital,
RNs
n=206
PCQ- S 14 items Job satisfaction: satisfaction with
nursing care and work scale 34
items
Job satisfaction:
signicant association
to subscales of PCC
Lewis et al
51
(USA) Cross- sectional Safety net clinic,
all staff
n=603
5 PCMH subscales 22 items Job satisfaction: a single
question
Burnout: a single question
Job satisfaction:
signicant association
to subscales of PCC
Burnout: signicant
association to
subscales of PCC
Continued
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

8
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
Authors (country) Study design Setting, participants Person- centred care measure
Staff outcomes: measurement
tool Results
Nocon et al
52
(USA) Quasi-
experimental
4- year follow- up
Safety net clinic,
all staff
n=536 (baseline)
n=589 (postintervention)
5 PCMH subscales 24 items Job satisfaction: a single
question
Burnout: a single question
Job Satisfaction: no
signicant effect of
PCC intervention
Burnout: no signicant
effect of PCC
intervention
Wallin et al
44
(Sweden) Cross- sectional Residential aged care,
nurse assistants and
nurse’s aides
n=225
P- CAT 13 items, PCQ- S 14 items Job satisfaction: Job Satisfaction
Questionnaire
20 items
Job satisfaction:
signicant positive
association with PCC
Røen et al
55
(Norway) Cross- sectional Nursing homes,
managers, unit head
nurses and staff
n=175
P- CAT 13 items Job satisfaction: a single
question
work- related psychosocial
factors: the General Nordic
Questionnaire for Psychosocial
and Social Factors at Work
32 items
Job satisfaction:
signicant association
to PCC
Work- related
psychosocial factors:
signicant association
to PCC
Schaap et al
48
(Netherlands)
Quasi-
experimental
14 months follow-
up
Residential aged care,
all staff
n=227
P- CAT 13 items Job satisfaction: the Maastricht
Work Satisfaction Scale in Health
Care 21 items
Burnout: MBI 6 items
Job satisfaction: no
signicant effect of
PCC intervention
Burnout: no signicant
effect of PCC
intervention
Silén et al
42
(Sweden) Cross- sectional Nursing home,
all staff
n=212
P- CAT 13 items, PCQ- S 14 items Work- related psychosocial
factors: Swedish version of the
Conditions of Work Effectiveness
Questionnaire 19 items
Work- related
psychosocial factors:
signicant association
with PCC
Sjögren et al
43
(Sweden) Cross- sectional Residential aged care,
all staff
n=1169
P- CAT 13 items, PCQ- S 14 items Job satisfaction: Satisfaction with
Nursing Care and Work Scale 34
items
Stress of Conscience: SCQ 9
items
Job strain: DCSQ 11 items
Job satisfaction:
signicant positive
association with PCC
Stress of conscience:
signicant negative
association with PCC
Job stress: signicant
negative association
with PCC
Van der Meer et al
49
(Netherlands)
Cross- sectional Residential aged care,
all staff
n=466
8 dimensions Person- Centred Care
Questionnaire 35 items
Job satisfaction: MJS 38 items Job satisfaction:
signicant positive
association with PCC
Table 2 Continued
Continued
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

9
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
as person- centred.
41–47 49–51 53 55 57
The other four quasi-
experimental studies and the RCT analysed the effect of
specific interventions designed to increase the level of
PCC.
40 48 52 54 56
Three out of these five invention studies
measured the effect of the Dementia Care Mapping
(DCM) intervention.
48 54 56
DCM is an internationally
recognised complex intervention in dementia research
and care containing a developmental evaluation cycle
to monitor and revise action plans.
48
The RCT
54
applied
the Bradford University’s PCC training manual in addi-
tion to the DCM training manual as the intervention
model. The study from the USA
52
measured PCC after the
Patient- Centred Medical Home (PCMH) intervention.
Core components of the PCMH include comprehensive
primary care, quality improvement, care management
and enhanced access.
51
Finally, the implementation of
the Swedish national guidelines was tested for PCC prop-
erties in combination with the effect of the implementa-
tion on staff.
40
The PCC measurement tool differed, as there were seven
questionnaires and one intervention. The most applied
tool in the included studies was the Person- centred Care
Assessment Tool (P- CAT), which was used on its own in
two quasi- experimental studies
40 48
and two cross- sectional
studies.
53 55
Four studies combined the P- CAT with the
Person- centred Climate Questionnaire–Staff version
(PCQ- S).
42–44 57
The PCQ- S was used by itself in one cross-
sectional
41
and one longitudinal study.
45
The other seven
studies applied different PCC measurement tools: PCMH
subscales questionnaire,
51 52
the subscale ‘recognition of
personhood’ of the Approach to Dementia Question-
naire,
50 56
eight dimensions of PCC measure,
49
an adapted
version of the Patient- Centred Care Questionnaire
47
and
Individualized Care Inventory (ICI).
46
The Bradford
University’s DCM and PCC training manual was applied
as the PCC measurement tool in the RCT.
54
Six PCC measurement tools were constructed of
subscales. The eight dimensions PCC questionnaire
and Patient- Centred Care Questionnaire had subscales
that followed the Picker Institute dimensions of PCC,
58
but with different subscale titles. The other four tools
followed their own subscales, which varied in number and
concepts. All tools with the subscales and reference to the
six dimensions of PCC are presented in table 1.
Measurement of staff outcomes
The included studies contained six healthcare provider
outcomes: job satisfaction, burnout, psychosocial work
environment, stress of conscience, job strain and intent
to leave.
Job satisfaction was estimated in 14 studies with 10
different measurement tools. Three out of these used
the Measure of Job Satisfaction.
49 53 57
In two studies,
job satisfaction was measured with the Satisfaction with
Nursing Care and Work Scale.
41 43
Four studies applied
a single question approach: ‘Overall, I am satisfied with
my current job’,
51 52
‘How will you describe your general
experience of your job satisfaction?’
55
or ‘I am happy at
Authors (country) Study design Setting, participants Person- centred care measure
Staff outcomes: measurement
tool Results
Vassbø et al
57
(Sweden,
Norway, Australia)
Cross- sectional Nursing homes,
all staff
n=341
P- CAT 13 items, PCQ- S 14 items Job satisfaction: MJS 37 items Job satisfaction:
signicant positive
association with PCC
Willemse et al
50
(Netherlands)
Cross- sectional Nursing homes,
all staff
n=1147
The subscale ‘recognition of
personhood’ of ADQ 11 items
Job satisfaction: 3- item scale
derived from the Leiden Quality
of Work Questionnaire.
Burnout: MBI 8 items.
Intent to leave: Subscale Leiden
Quality of Work Questionnaire 3
items
Job satisfaction:
signicant association
to PCC
Burnout: signicant
association to PCC
Intent to leave:
signicant association
to PCC
Åhlin et al
45
(Sweden) Longitudinal
cohort study
1- year follow- up
Residential aged care,
RNs and nurse assistants
n=488
PCQ- S 14 items Stress of conscience: SCQ 9
items
Stress of conscience:
no signicant
association to PCC
PCC, person- centred care.
Table 2 Continued
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

10
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
work’.
46
Five studies used different job satisfaction ques-
tionnaires: Copenhagen Psychosocial Questionnaire,
56
a
38- item job satisfaction questionnaire,
47
the Maastricht
Work Satisfaction Scale in Health Care.
48
3- item scale
derived from the Leiden Quality of Work Questionnaire
(LQWQ)
50
and Job Satisfaction Questionnaire.
44
Six studies estimated burnout. Three studies applied
the Maslach Burnout Inventory or a setting- appropriate
version.
48 50 54
The two studies from the USA had their
measure stated as ‘Using your own definition of burnout,
please check one’ with a 5- option scale.
51 52
The German
study used the Copenhagen Burnout Inventory.
56
Three studies
40 43 45
assessed stress of conscience. All
these studies were set in Sweden and applied the Stress of
Conscience Questionnaire.
Psychosocial work environment was measured in two
studies, which applied different constructs: the General
Nordic Questionnaire for Psychosocial and Social Factors
at Work
55
and a Swedish version of the Conditions of
Work Effectiveness Questionnaire.
42
Job strain was estimated in two studies and measured
in both through the Demand- Control- Support Question-
naire.
40 43
Finally, intent to leave was assessed in one study
50
by a
3- item scale that was derived from the LQWQ.
Results from the included studies
This section presents the results based on the six health-
care provider outcomes and their association with PCC
and is a synthesis of the results presented in table 2.
Job satisfaction was positively associated with PCC in
eight studies.
41 43 44 47 49 50 55 57
Three cross- sectional studies
by Edvardsson et al,
53
Elfstrand Corlin and Kazami
46
and
Lewis et al
51
showed an association between job satisfac-
tion and only subscales of PCC, that is, ‘personalising
care’ and ‘organisational support’,
53
‘knowing the person’
and ‘resident autonomy’
46
and ‘quality improvement
subscale’ and ‘work environment covariate’.
51
Three
quasi- experiment studies by Dichter et al
56
, Nocon et al
52
and Schaap et al
48
found no significant improvement in
job satisfaction after the PCC implementation.
There were mixed results in the association between
burnout and PCC. Two cross- sectional studies by Lewis
et al
51
and Willemse et al
50
found negative associations
between PCC and burnout levels. The quasi- experimental
studies by Nocon et al
52
and Schaap et al
48
found no signif-
icant results. The quasi- experimental study by Dichter et
al,
56
the longitudinal study by Åhlin et al
45
and the RCT by
Jeon et al
54
found non- significant results but nonetheless
an increase in burnout levels over time.
The stress of conscience was negatively associated with
PCC in the cross- sectional study by Sjögren et al.
43
In the
quasi- experimental study by Edvardsson et al,
40
the PCC
intervention significantly reduced stress of conscience.
However, the longitudinal study by Åhlin et al
45
found no
significant results.
The association between PCC and the psychosocial
work environment was analysed in two cross- sectional
studies. Røen et al
55
found that PCC was positively asso-
ciated with most psychosocial and social factors included
in the study, except for the subscale of decision demands.
Silén et al
42
found that PCC mediated the association
between higher access to structural empowerment and
higher psychological empowerment, which improved the
psychosocial work environment significantly.
Job strain was not affected by the intervention in the
quasi- experimental study by Edvardsson et al.
40
The cross-
sectional study by Sjögren et al
43
did find a negative asso-
ciation between job strain and PCC.
The one study that measured intent to leave by Willemse
et al
50
showed a negative association with PCC, meaning
that staff were less likely to leave with higher perceived
PCC.
DISCUSSION
This scoping review explored and described the research
performed to assess the associations between PCC and
healthcare provider outcomes. Eighteen studies fulfilled
the inclusion criteria. The healthcare provider outcomes
measured in the studies were job satisfaction, burnout,
stress of conscience, psychosocial work environment,
job strain and intent to leave. The main findings of this
review support an association between PCC and health-
care provider outcomes as the cross- sectional studies
had mostly significant results. However, the longitu-
dinal studies showed, with two exceptions, no significant
improvement in the healthcare provider outcomes.
The review identified eight PCC measurement tools
that were scrutinised through the six PCC dimensions
and only included if they addressed the first and at least
two other dimensions. The quality assessment of the PCC
tools was applied to capture PCC as a multifaceted frame-
work, which is necessary when there is the expectation of
an improvement in the work environment.
6 7
A strength in this study is the approach applied here,
which might have restricted the number of included
studies, but created a quality assessment of the tools that
ensured the results could be compared within the health-
care provider outcomes. To confirm the occurrence
of the PCC dimensions in the tools and interventions,
additional research needed to be performed to find the
complete questionnaires or details on the interventions,
as the included studies did not disclose more on the PCC
measurement tool beyond the subscales.
This scoping review did not exclude studies based on
the healthcare facility. Many healthcare facilities, partic-
ularly nursing homes and residential care, have incorpo-
rated elements of PCC.
22 59
Thus far, there is no golden
standard for PCC, and previous studies have stressed the
importance of being aware of the normative relations
and cultural aspects as well as practical hinders such as
routines for documentation and suitable premises when
implementing more PCC.
60 61
This review provided an
overview of the research done across healthcare settings,
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from
11
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
and interestingly, similar results were found across the
incorporated healthcare facilities and type of participants.
A limitation of the included studies was the occurrence
of a ‘ceiling effect’. A ‘ceiling effect’ occurs when only
well- functioning healthcare facilities want to implement
PCC and participate in research.
62
The baseline measure-
ments in the included intervention studies were already
considerably high, which made a substantial improve-
ment unachievable. Moreover, the cross- sectional studies
were, with one exception,
51
performed in healthcare
facilities that did not undergo an intervention.
Additionally, all PCC measurement questionnaires
were self- reported, and the included studies revealed a
‘perceived’ occurrence of PCC. This occurrence could be
overestimated as with the growing interest in PCC health-
care providers might want to appear more person- centred
in their work than they are, which was also considered a
possibility in other PCC studies.
19 40 49
PCC is based on
ethics that can be summarised as ‘aiming at the good life
with and for others in just institutions’.
63
This implies
that also managers in their leadership form a partnership
with their staff and listen to their narratives and formu-
late a plan, aiming at good working conditions for them.
Operationalisation of person- centred ethics in health-
care is not a quick fix, but rather a process of developing
the professional role and changing the clinical mind set
through reflection on theory and practice.
19
Healthcare providers experience job pride and high
expectations of being a healthcare professional.
3 6
This
makes it likely that there is an overestimation of PCC and
job satisfaction, and an underestimation of job strain,
ethical stress and burnout. These overestimations have
the consequence that in the cross- sectional studies, the
PCC and healthcare provider outcomes were signifi-
cant and, for the quasi- experimental studies, with high
baseline measurements, a significant improvement was
unattainable.
The scoping review approach allowed for all possible
job satisfaction and occupational health- related outcomes
to be included. Still, the results only provided a limited
range of six healthcare provider outcomes. Moreover, the
lack of quality assessment of these outcomes formed a
limitation to the review. The six outcomes with different
measurement tools among them impeded the compar-
ison of the importance of the results of the included
studies. For example, 14 studies had job satisfaction as a
measure in their studies, and 10 different measures were
used. This variation suggests that the healthcare provider
outcomes do not have an established measurement tool
which makes the relative importance of one measure
compared with another unclear in this context.
7 33
The variation in measures caused difficulty in asserting
if PCC could be an MoC that can attract and retain
qualified healthcare professionals, as was suggested by
McCormack and McCance.
22
Similar to the results of the
scoping review by Jessup et al,
12
most research focused on
the patients and financial gain rather than the health-
care provider outcomes. This is despite the healthcare
providers being a defining factor in ensuring patient
safety and hospital care quality.
4
Interventions should
aim at improving both patient and healthcare provider
outcomes,
5 8
which can be achieved with PCC as one
of its cornerstones is the collaboration between profes-
sionals and staff and respect for each other’s knowledge
and experiences.
19
Other reviews on the improvement
of healthcare provider outcomes emphasised that the
intervention needs to be well- defined and continue for
an extended period.
6 7
When research into healthcare
providers becomes more established in the area of MoC
interventions, more consistent scrutinisation can be
achieved, and a better prediction can be made into the
benefits of implementing an MoC, such as PCC, on the
entire healthcare system.
CONCLUSION
This scoping review showed, to a limited extent, a posi-
tive association between PCC and healthcare provider
outcomes. With a significant variation of measurement
tools and conflicting findings across the studies, it is diffi-
cult to provide an overall conclusion.
The implications for future research is the necessity for
increasing the focus on healthcare providers in analysing
the effect of implementing PCC. More specifically, a better
understanding of the impact of the different dimensions
of PCC on staff and how PCC can contribute to improving
the healthcare work environment.
Twitter Cornelia van Diepen @kim24501
Contributors The authors developed and conceived the review together. CvD
and AF completed screening and extraction of data. CvD drafted rst version of
the manuscript including design of the tables with feedback from all authors. The
manuscript was then revised in different steps by AF, GH and IE with CvD taking the
main responsibility for writing. All authors approved the nal version of the review.
Funding The Centre for Person- Centred Care at the University of Gothenburg
(GPCC), Sweden. GPCC is funded by the Swedish Government's grant for Strategic
Research Areas, Care Sciences (Application to Swedish Research Council no.
2009-1088).
Disclaimer All authors had access to the data (literature identied and tables) in
the study and can take responsibility for the integrity of the data and the accuracy
of the data analysis. The lead author afrms that this manuscript is an honest,
accurate and transparent account of the study being reported; that no important
aspects of the study have been omitted; and that any discrepancies from the study
as planned (and, if relevant, registered) have been explained.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data sharing not applicable as no datasets were
generated and/or analysed for this study.
Supplemental material This content has been supplied by the author(s). It has
not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been
peer- reviewed. Any opinions or recommendations discussed are solely those
of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and
responsibility arising from any reliance placed on the content. Where the content
includes any translated material, BMJ does not warrant the accuracy and reliability
of the translations (including but not limited to local regulations, clinical guidelines,
terminology, drug names and drug dosages), and is not responsible for any error
and/or omissions arising from translation and adaptation or otherwise.
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

12
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
Open access This is an open access article distributed in accordance with the
Creative Commons Attribution Non Commercial (CC BY- NC 4.0) license, which
permits others to distribute, remix, adapt, build upon this work non- commercially,
and license their derivative works on different terms, provided the original work is
properly cited, appropriate credit is given, any changes made indicated, and the use
is non- commercial. See:http:// creativecommons. org/ licenses/ by- nc/ 4. 0/.
ORCID iDs
Corneliavan Diepen http:// orcid. org/ 0000- 0001- 6991- 9443
AndreasFors http:// orcid. org/ 0000- 0001- 8980- 0538
REFERENCES
1 World Health Organization. Working for health and growth: investing
in the health workforce. Report of the high- level Commission on
health employment and economic growth.; 2016. 978 92 4 151130 8.
2 United Nations. Sustainable development goals. Available: https://
sust aina bled evel opment. un. org/ sdg3 [Accessed 01-12-2020].
3 Castle NG, Engberg J. Organizational characteristics associated with
staff turnover in nursing homes. Gerontologist 2006;46:62–73.
4 Aiken LH, Sloane DM, Bruyneel L, etal. Nurses’ reports of working
conditions and hospital quality of care in 12 countries in Europe. Int J
Nurs Stud 2013;50:143–53.
5 Copanitsanou P, Fotos N, Brokalaki H. Effects of work environment
on patient and nurse outcomes. Br J Nurs 2017;26:172–6.
6 Marine A, Ruotsalainen J, Serra C, etal. Preventing occupational
stress in healthcare workers. Cochrane Database Syst Rev
2006:CD002892.
7 Ruotsalainen JH, Verbeek JH, Mariné A, etal. Preventing
occupational stress in healthcare workers. Cochrane Database Syst
Rev 2015;184.
8 Hall LH, Johnson J, Watt I, etal. Healthcare staff wellbeing,
burnout, and patient safety: a systematic review. PLoS One
2016;11:e0159015–12.
9 Aiken LH, Sermeus W, Van den Heede K, etal. Patient safety,
satisfaction, and quality of hospital care: cross sectional surveys of
nurses and patients in 12 countries in Europe and the United States.
BMJ 2012;344:e1717.
10 Davidson P, Halcomb E, Hickman L, etal. Beyond the rhetoric: what
do we mean by a 'model of care'? Aust J Adv Nurs 2006;23:47–55.
11 ACI. Understanding the process to develop a model of care: an ACI
framework. Chatswood NSW Agency for Clinical Innovation; 2013.
www. aci. health. nsw. gov. au. 978 1 74187 862 2.
12 Jessup R, Putrik P, Buchbinder R, etal. Identifying alternative models
of healthcare service delivery to inform health system improvement:
Scoping review of systematic reviews. BMJ Open 2020;10:e036112.
13 WHO. Who global strategy on people- centred and integrated health
services: interim report, 2015. Available: http://www. who. int/ serv iced
eliv erys afety/ areas/ people- centred- care/ global- strategy/ en/
14 EPF. Manifesto 2019: putting what matters to patients at the heart of
EU health policy, 2019. Available: https://www. epp. eu/ les/ uploads/
2019/ 05/ EPP- MANIFESTO- 2019. pdf
15 Bartz CC. International council of nurses and person- centered care.
Int J Integr Care 2010;10 Suppl:29–31.
16 Olsson L- E, Jakobsson Ung E, Swedberg K, etal. Efcacy of person-
centred care as an intervention in controlled trials - a systematic
review. J Clin Nurs 2013;22:456–65.
17 Ekman I, Swedberg K, Taft C, etal. Person- centered care- ready for
prime time. Eur J Cardiovasc Nurs 2011;10:248–51.
18 Leplege A, Gzil F, Cammelli M, etal. Person- centredness: conceptual
and historical perspectives. Disabil Rehabil 2007;29:1555–65.
19 Britten N, Moore L, Lydahl D, etal. Elaboration of the Gothenburg
model of person- centred care. Health Expect 2017;20:407–18.
20 McCance T, McCormack B, Dewing J. An exploration of person-
centredness in practice. Online J Issues Nurs 2011;16:1.
21 Coulter A, Entwistle VA, Eccles A, etal. Personalised care planning
for adults with chronic or long- term health conditions. Cochrane
Database Syst Rev 2015;85.
22 McCormack B, McCance TV. Development of a framework for
person- centred nursing. J Adv Nurs 2006;56:472–9.
23 Bégat I, Ellefsen B, Severinsson E. Nurses' satisfaction with their
work environment and the outcomes of clinical nursing supervision
on nurses' experiences of well- being -- a Norwegian study. J Nurs
Manag 2005;13:221–30.
24 Edvardsson D, Innes A. Measuring person- centered care: a
critical comparative review of published tools. Gerontologist
2010;50:834–46.
25 Håkansson Eklund J, Holmström IK, Kumlin T, etal. Patient
Education and Counseling “ Same same or different ? ” A review of
reviews of person- centered and patient- centered care. Patient Educ
Couns 2018;102:3–11.
26 Hughes JC, Bamford C, May C. Types of centredness in health care:
themes and concepts. Med Health Care Philos 2008;11:455–63.
27 Ekman I, Wolf A, Olsson L- E, etal. Effects of person- centred care
in patients with chronic heart failure: the PCC- HF study. Eur Heart J
2012;33:1112–9.
28 Brännström M, Boman K. Effects of person- centred and integrated
chronic heart failure and palliative home care. prefer: a randomized
controlled study. Eur J Heart Fail 2014;16:1142–51.
29 Fors A, Ekman I, Taft C, etal. Person- centred care after acute
coronary syndrome, from hospital to primary care - A randomised
controlled trial. Int J Cardiol 2015;187:693–9.
30 Wolf A, Vella R, Fors A. The impact of person- centred care
on patients' care experiences in relation to educational level
after acute coronary syndrome: secondary outcome analysis
of a randomised controlled trial. Eur J Cardiovasc Nurs
2019;18:299–308.
31 Barbosa A, Sousa L, Nolan M, etal. Effects of person- centered care
approaches to dementia care on staff: a systematic review. Am J
Alzheimers Dis Other Demen 2015;30:713–22.
32 Rajamohan S, Porock D, Chang Y- P. Understanding the relationship
between staff and job satisfaction, stress, turnover, and staff
outcomes in the Person- Centered care nursing home arena. J Nurs
Scholarsh 2019;51:560–8.
33 van den Pol- Grevelink A, Jukema JS, Smits CHM. Person-
centred care and job satisfaction of caregivers in nursing homes:
a systematic review of the impact of different forms of person-
centred care on various dimensions of job satisfaction. Int J Geriatr
Psychiatry 2012;27:219–29.
34 Arksey H, O'Malley L. Scoping studies: towards a methodological
framework. Int J Soc Res Methodol 2005;8:19–32.
35 Munn Z, Peters MDJ, Stern C, etal. Systematic review or scoping
review? guidance for authors when choosing between a systematic
or scoping review approach. BMC Med Res Methodol 2018;18:1–7.
36 Harding E, Wait S, Scutton J. Report summary: the state of play in
person- centred care. London, United Kingdom The Health Policy
Partnership; 2015. http://www. heal thpo licy part nership. com/ person-
centred- care/
37 Institute of Medicine. Crossing the quality chasm: a new health
system for the 21th century. Washington, DC: National Academies
Press, 2001.
38 Ouzzani M, Hammady H, Fedorowicz Z, etal. Rayyan—a web and
mobile APP for systematic reviews. Syst Rev 2016;5:1–10.
39 McCormack B, McCance T. Person- Centred nursing theory and
practice. Oxford: Wiley- Blackwell, 2010.
40 Edvardsson D, Sandman PO, Borell L. Implementing national
guidelines for person- centered care of people with dementia in
residential aged care: effects on perceived person- centeredness,
staff strain, and stress of conscience. Int Psychogeriatr
2014;26:1171–9.
41 Lehuluante A, Nilsson A, Edvardsson D. The inuence of a person-
centred psychosocial unit climate on satisfaction with care and work.
J Nurs Manag 2012;20:319–25.
42 Silén M, Skytt B, Engström M. Relationships between structural
and psychological empowerment, mediated by person- centred
processes and thriving for nursing home staff. Geriatr Nurs
2019;40:67–71.
43 Sjögren K, Lindkvist M, Sandman P- O, etal. To what extent is the
work environment of staff related to person- centred care? A cross-
sectional study of residential aged care. J Clin Nurs 2015;24:1310–9.
44 Wallin AO, Jakobsson U, Edberg A- K. Job satisfaction and
associated variables among nurse assistants working in residential
care. Int Psychogeriatr 2012;24:1904–18.
45 Åhlin J, Ericson- Lidman E, Eriksson S, etal. Longitudinal
relationships between stress of conscience and concepts of
importance. Nurs Ethics 2013;20:927–42.
46 Elfstrand Corlin T, Kazemi A. Accounting for job satisfaction:
examining the interplay of person and situation. Scand J Psychol
2017;58:436–42.
47 den Boer J, Nieboer AP, Cramm JM. A cross- sectional study
investigating patient- centred care, co- creation of care, well- being
and job satisfaction among nurses. J Nurs Manag 2017;25:577–84.
48 Schaap FD, Finnema EJ, Stewart RE, etal. Effects of dementia care
mapping on job satisfaction and caring skills of staff caring for older
people with intellectual disabilities: a quasi- experimental study. J
Appl Res Intellect Disabil 2019;32:1228–40.
49 van der Meer L, Nieboer AP, Finkenügel H, etal. The importance of
person- centred care and co- creation of care for the well- being and
job satisfaction of professionals working with people with intellectual
disabilities. Scand J Caring Sci 2018;32:76–81.
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from

13
van DiepenC, etal. BMJ Open 2020;10:e042658. doi:10.1136/bmjopen-2020-042658
Open access
50 Willemse BM, De Jonge J, Smit D, etal. Staff's person- centredness
in dementia care in relation to job characteristics and job- related
well- being: a cross- sectional survey in nursing homes. J Adv Nurs
2015;71:404–16.
51 Lewis SE, Nocon RS, Tang H, etal. Patient- Centered medical home
characteristics and staff morale in safety net clinics. Arch Intern Med
2012;172:23–31.
52 Nocon RS, Fairchild PC, Gao Y, etal. Provider and staff morale, job
satisfaction, and burnout over a 4- year medical home intervention. J
Gen Intern Med 2019;34:952–9.
53 Edvardsson D, Fetherstonhaugh D, McAuliffe L, etal. Job
satisfaction amongst aged care staff: exploring the inuence
of person- centered care provision. Int Psychogeriatr
2011;23:1205–12.
54 Jeon Y- H, Luscombe G, Chenoweth L, etal. Staff outcomes from the
caring for aged dementia care resident study (CADRES): a cluster
randomised trial. Int J Nurs Stud 2012;49:508–18.
55 Røen I, Kirkevold Øyvind, Testad I, etal. Person- centered care in
Norwegian nursing homes and its relation to organizational factors
and staff characteristics: a cross- sectional survey. Int Psychogeriatr
2018;30:1279–90.
56 Dichter MN, Trutschel D, Schwab CGG, etal. Dementia care
mapping in nursing homes: effects on caregiver attitudes,
job satisfaction, and burnout. A quasi- experimental trial. Int
Psychogeriatr 2017;29:1993–2006.
57 Vassbø TK, Kirkevold M, Edvardsson D, etal. Associations between
job satisfaction, person- centredness, and ethically difcult situations in
nursing homes- A cross- sectional study. J Adv Nurs 2019;75:979–88.
58 Picker Institute. Principles of patient- centered care, 1987. Available:
http:// pickerinstitute. org/ about/ picker- principles/
59 Sjögren K, Lindkvist M, Sandman P- O, etal. Organisational and
environmental characteristics of residential aged care units providing
highly person- centred care: a cross sectional study. BMC Nurs
2017;16:1–9.
60 Moore L, Britten N, Lydahl D, etal. Barriers and facilitators to the
implementation of person- centred care in different healthcare
contexts. Scand J Caring Sci 2017;31:662–73.
61 Dellenborg L, Wikström E, Andersson Erichsen A. Factors that may
promote the learning of person- centred care: an ethnographic
study of an implementation programme for healthcare
professionals in a medical emergency ward in Sweden. Adv in
Health Sci Educ 2019;24:353–81.
62 Cramer D, Howitt DL. The SAGE dictionary of statistics: a practical
resource for students in the social sciences. 3rd ed. New Delhi: Sage,
2005.
63 Ricoeur P. Oneself as another (originally published in French under
the title soi- meme comme un autre, 1990). London: The University of
Chicago Press, 1992.
44147171. Protected by copyright.
on December 7, 2020 at Swets Subscription Service REF:http://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2020-042658 on 7 December 2020. Downloaded from
