E
NDOCRINOLOGY
U
PDATE
E
NDOCRINOLOGY NEWS FROM
M
AYO
C
LINIC
volume 1
number 4
2006
Adrenal Incidentalomas: An Approach to Uncertainty
Adrenal incidentaloma is defined as an adrenal
mass 1 cm or more in diameter that is discovered
serendipitously by radiologic examination, in the
absence of symptoms or clinical findings sug-
gestive of adrenal disease. As imaging techniques
have improved and computed imaging has become
accepted practice in medicine, the identification of
adrenal incidentalomas has become more
frequent.
William F. Young, Jr, MD, of the Division of
Endocrinology, Diabetes, Metabolism, and
Nutrition at Mayo Clinic in Rochester, says:
“Adrenal incidentalomas are not new. Instead of
finding them at autopsy, we are now finding them
during life with computed imaging. There is an
age-dependent occurrence of adrenal cortical
adenomas found at autopsy. Thus, the probability
of finding an unsuspected adrenal adenoma on
computed abdominal imaging in a 20- to 29-year-
old person is approximately 0.2%, compared with
7% in a person older than 70 years.” The majority
of adrenal incidentalomas are clinically nonhyper-
secretory benign adrenal cortical adenomas.
However, more than 45 different diagnoses have
been reported in patients with incidentally
discovered adrenal masses (Table on page 2).
An adrenal incidentaloma should be charac-
terized with respect to both functional status, with
a medical history, physical examination, and
hormonal assessment, and malignant potential,
with an assessment of the imaging phenotype and
mass size.
Hormonal Evaluation
The term “subclinical Cushing’s syndrome”
describes adrenal incidentaloma with autonomous
cortisol-secreting cortical adenomas in patients
who lack the typical signs and symptoms of
hypercortisolism. Subclinical Cushing’s syndrome
affects 8% of all adrenal incidentaloma patients.
Although these patients lack the usual obvious
signs of Cushing’s syndrome, they may have the
adverse effects of continuous endogenous cortisol
secretion, including hypertension, obesity,
diabetes, and osteoporosis. Because their 24-hour
urinary cortisol secretion may be normal, all
adrenal incidentaloma patients should undergo a
1-mg overnight dexamethasone suppression test.
Of all patients with adrenal incidentalomas,
approximately 5% prove to have pheochromo-
cytomas. Even though clinically silent, pheochro-
mocytomas can be lethal. In evaluation of an
adrenal incidentaloma patient, the clinician has a
powerful predictor of pheochromocytoma, the
“imaging phenotype.” Dr Young says: “The imaging
phenotype is so powerful that, even when
biochemical testing for pheochromocytoma is
normal but the imaging phenotype is typical of
pheochromocytoma, these patients should be
treated with Ȋ-adrenergic and ȋ-adrenergic
blockade and tumor resection. At Mayo Clinic, the
most reliable biochemical method for identifying
adrenal pheochromocytoma is measuring
fractionated metanephrines and catecholamines in
a 24-hour urine collection, the sensitivity and
specificity of which are both 98%.”
All patients with adrenal incidentalomas who
have hypertension should be evaluated for
primary aldosteronism. A reasonable screening
test is determination of the ambulatory morning
plasma aldosterone concentration–to–plasma
renin activity ratio (PAC/PRA ratio, where PAC is
reported in ng/dL and PRA is reported in ng/mL
per hour). The PAC/PRA ratio can be obtained
while the patient is treated with any antihy-
pertensive drug except spironolactone, epleren-
one, or high-dose amiloride. A PAC/PRA ratio of
20 or higher and a PAC of 15 ng/dL or higher
Geoffrey B. Thompson, MD, and William F. Young, Jr, MD
Inside This Issue
A Clinical Conundrum: The
Diagnosis and Treatment of
Androgen Deficiency in
Older Men . . . . . . . . . . . . . . . 3
Bariatric Surgery: Important
Considerations for the
Clinician and Patient . . . . . 4
A Practical Approach to
the Patient With Subclinical
Hypothyroidism . . . . . . . . . . 6
constitute a positive screening test
result; however, the cutoff for
a positive test is laboratory
dependent.
Assessment of
Malignant Potential
Computed imaging is the most
powerful tool available to the
clinician to guide the management
of patients with adrenal inci-
dentaloma. Geoffrey B. Thompson,
MD, of the Department of Surgery
at Mayo Clinic in Rochester, notes:
“The lipid-rich nature of cortical
adenomas is helpful in dis-
tinguishing these benign neo-
plasms from malignancy.” Imaging
characteristics consistent with
a benign cortical adenoma
include round and homogeneous
density, smooth contour and
sharp margination, diameter
usually less than 4 cm; unilateral
location, low unenhanced CT
attenuation values, and marked
CT contrast medium washout
(Figure 1). The imaging pheno-
type consistent with pheochromo-
cytoma includes delayed contrast
medium washout on CT, high
signal intensity on T2-weighted
MRI, cystic and hemorrhagic
changes, and variable size (Figure
2). Adrenocortical carcinoma
imaging characteristics include
irregular shape, inhomogeneous
density because of central areas
of low attenuation due to tumor
necrosis, tumor calcification,
diameter usually more than 4 cm,
unilateral location, high
unenhanced CT atten-
uation values, and inhomo-
geneous enhancement on
CT with intravenous con-
trast medium. The imaging
phenotype of metastases
includes irregular shape
and inhomogeneous nature,
tendency to be bilateral,
high unenhanced CT atten-
uation values, and delayed
intravenous contrast med-
ium washout on CT.
The greatest lesion
diameter of the adrenal mass is predictive of
malignancy. In 1 study, a 4-cm cutoff was 90%
sensitive for detecting adreno-cortical carcinoma,
even though 76% of lesions more than 4 cm in
diameter were benign. Dr Thompson cautions:
“Clearly, adrenal mass size should not be used as
the only variable to guide treatment. The primary
role of fine-needle aspiration (FNA) biopsy is to
differentiate adrenal from nonadrenal tissues
(eg, metastases or infection); FNA biopsy cannot
distinguish between primary adrenal benign and
malignant lesions. Pheochromocytoma should
always be excluded with normal biochemistry
before attempting FNA biopsy of an adrenal
mass.”
Frequency and Duration of Follow-up
An area of uncertainty in the management of a
patient with adrenal incidentaloma is the
frequency and duration of follow-up evaluations.
Autonomous function (glucocorticoid and
catecholamine) not present at baseline can be
detected with longer-term follow-up (eg, 4 years).
Repeat imaging at 3 months, 1 year, and 2 years
may be helpful in excluding primary and
metastatic malignancy.
Endocrinology Consultation 800-313-5077 www.mayoclinic.org
MAYO CLINIC ENDOCRINOLOGY UPDATE 2
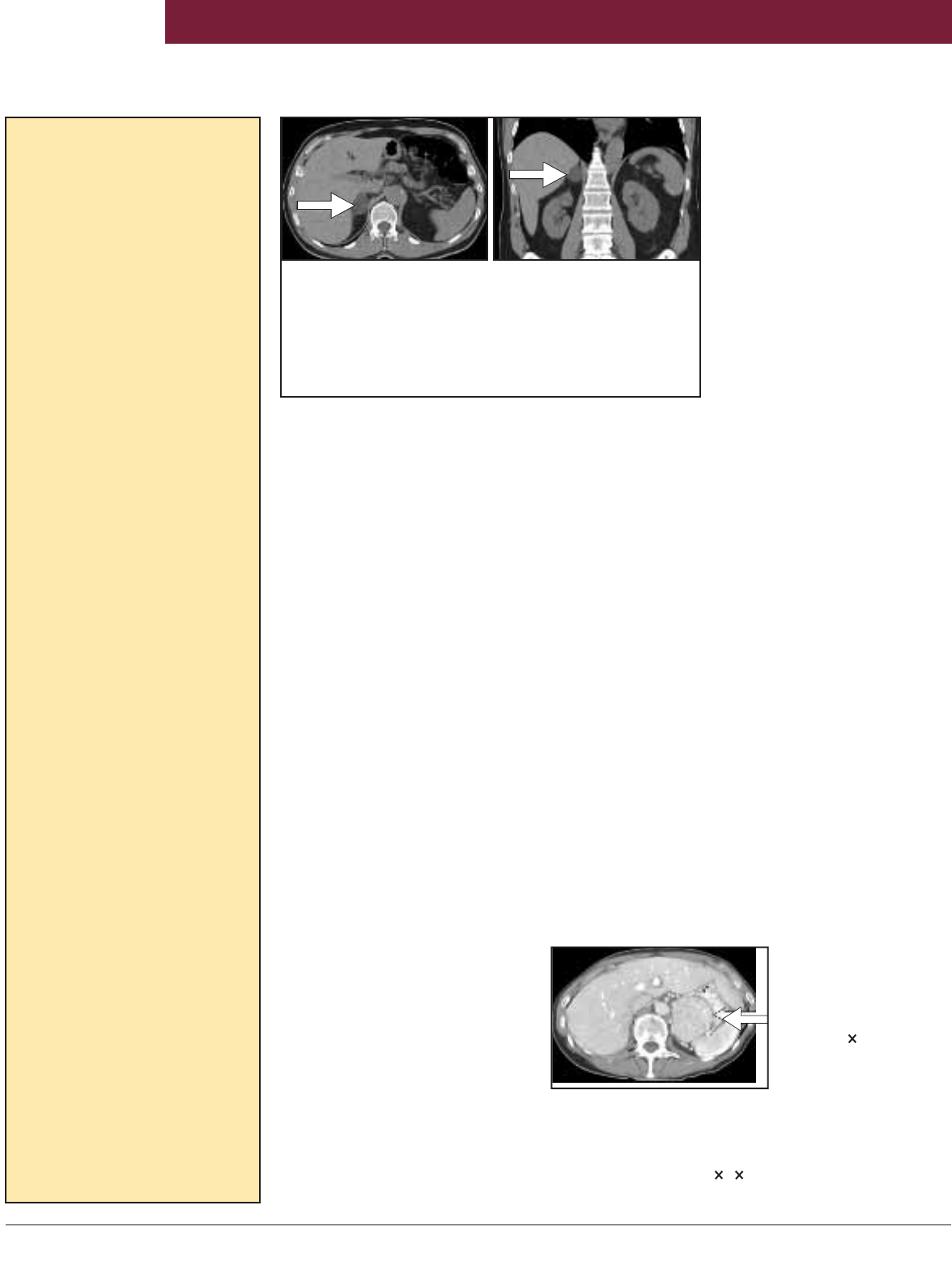
Figure 2. An ab-
dominal CT scan
obtained to eval-
uate bilateral leg
swelling shows a
dense 6.5 5.4-cm,
heterogeneously en-
hancing mass in
the left adrenal
gland (arrow). Results of hormonal testing in this 61-
year-old normotensive woman were positive for
pheochromocytoma. The patient was treated with
Ȋ-
and ȋ-adrenergic blockade followed by laparoscopic
adrenalectomy where a 7 5 5-cm pheochromocytoma
was removed.
Table. Differential Diagnosis
of Asymptomatic Adrenal
Incidentalomas
Benign nonfunctioning mass
Adenoma
Adenomatoid tumor
Adrenolipoma
Amyloidosis
Cyst
Ganglioneuroma
Granuloma
Hamartoma
Hematoma
Hemangioma
Infection (fungal, tuberculosis,
echinococcosis, cryptococcosis,
nocardiosis)
Leiomyoma
Lipoma
Lymphangioma
Myelolipoma
Neurofibroma
Oncocytoma
Pseudocyst
Teratoma
Malignant nonfunctioning mass
Adrenocortical carcinoma
Angiosarcoma
Ganglioneuroblastoma
Leiomyosarcoma
Liposarcoma
Malignant peripheral nerve sheath
tumor
Metastatic carcinoma (eg, breast,
lung, kidney, stomach, pancreas,
ovary, colon, esophagus)
Primary malignancy
Primary malignant melanoma
Primitive neuroectodermal tumor
Subclinical hyperfunctioning mass
Composite pheochromocytoma
Congenital adrenal hyperplasia
Androgen- and estrogen-secreting
neoplasms
Massive macronodular hyperplasia
Nodular hyperplasia
Pheochromocytoma
Primary aldosteronism
Primary malignancy
Sex cord-stromal tumor
Subclinical Cushing’s syndrome
Pseudoadrenal mass
Mistaken vasculature
Liver
Lymph nodes
Pancreatic mass
Renal mass
Spleen
Stomach mass
Technical artifact
Adapted from Young WF Jr. Management
approaches to adrenal incidentalomas: a
view from Rochester, Minnesota. Endocrinol
Metab Clin North Am. 2000;29:159-85.
Figure 1. An abdominal CT scan (A, axial image; B, coronal
image) obtained to evaluate nonspecific abdominal pain shows
a round, uniform, low-density 2-cm right adrenal mass (arrows).
Results of hormonal testing in this 66-year-old hypertensive
man for subclinical Cushing’s syndrome, primary aldosteronism,
and pheochromocytoma were normal. The patient is being
followed with repeat imaging and hormonal testing.
A
B
Testosterone replacement in young men with hypo-
gonadism maintains or improves bone mineral
density, body composition, virilization, libido, sexual
function, and sense of well-being. As men age,
however, it is difficult to differentiate true hypo-
gonadism from the changes of normal aging. There
is uncertainty if the physiologic changes of aging
are due to testosterone deficiency and if treating
normal older men with testosterone is beneficial.
Because testosterone-dependent diseases such as
benign and malignant prostate growth become
very common as men age, the risk/benefit ratio for
testosterone replacement in older men is more
difficult to define than it is in young men.
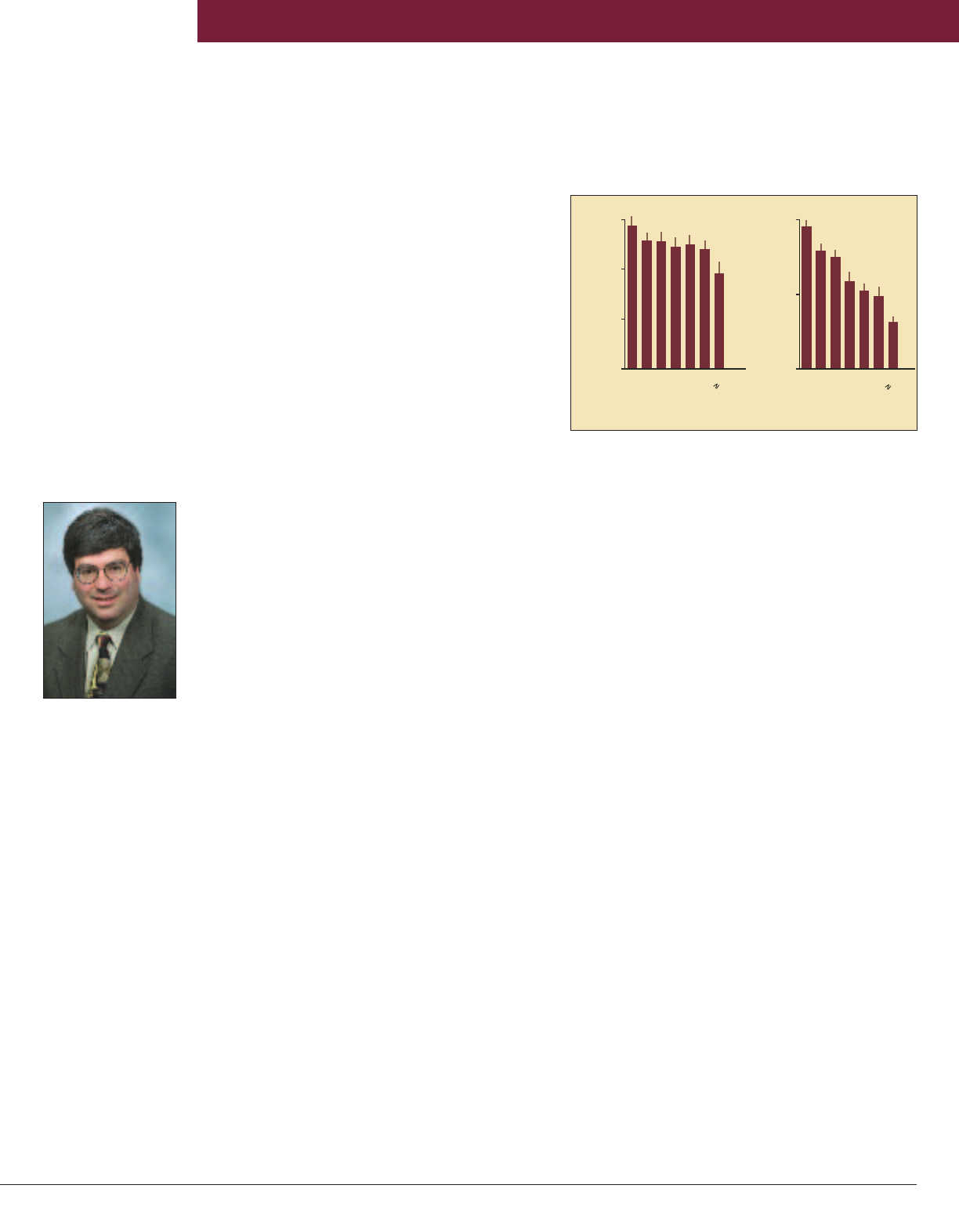
Large epidemiologic studies document a decline
in testosterone production and an increase in sex
hormone–binding globulin (SHBG) as men age,
resulting in a much greater decline in the active
fraction, measured as free or bioavailable
testosterone (Figure). Most studies testing the
effects of testosterone administration in normal
elderly men included men older than 60 years
whose baseline total testosterone levels were in the
low-normal to mildly low range (eg, <350 ng/dL)
or had bioavailable testosterone levels less than 70
ng/dL. These studies, most of which were
published between 1990 and 2002, have been of
short duration and included relatively small
numbers of subjects. Although the results from the
various studies are not entirely consistent, a
composite of the changes seen with testosterone
treatment in older men is shown in the Table on
page 4. Todd B. Nippoldt, MD, of the Division
of Endocrinology, Diabetes, Metabolism, and
Nutrition at Mayo Clinic in Rochester, cautions: “It
is important to emphasize that there are no data on
clinically important end points, such as bone
fracture risk, cardiovascular events, development
of malignancy, or mortality, for testosterone
treatment in normal elderly men.”
Men with gynecomastia, osteoporosis,
diminished libido, erectile dysfunction, loss of
muscle mass, beard, or body hair, or hot flashes
warrant an evaluation for hypogonadism. Because
of the increased level of SHBG with aging, the
laboratory evaluation in older men should start
with a measurement of total testosterone along
with free or bioavailable testosterone. Dr Nippoldt
notes: “It is important to determine the etiology of
a low testosterone level before starting replace-
ment therapy. Blood levels of luteinizing hormone
(LH), follicle-stimulating hormone (FSH), and
prolactin should be measured in all men with low
testosterone levels. Elevated serum LH and FSH
concentrations indicate primary testicular failure,
and no further studies are needed. Elevated serum
prolactin levels, in the absence of prolactin-
increasing drugs, should dictate computed
imaging of the sellar region.”
Low (or “inappropriately normal”) LH and FSH
imply a central cause for hypogonadism, which
may be functional or structural. A functional
abnormality in the hypothalamic-pituitary axis is
more common. This functional abnormality may
be idiopathic or due to “normal aging,” but several
medical conditions should be considered as well:
obstructive sleep apnea, recent illness or surgery
(eugonadal sick syndrome), extreme emotional
distress, or adverse effects of medications (eg,
high-dose glucocorticoids, narcotic pain relievers,
or drugs that increase prolactin). The only way to
definitively exclude a structural lesion is by sellar
computed imaging. The decision to obtain sellar
MRI depends on the severity of the deficiency, the
patient’s age, and the potential presence of other
pituitary dysfunction or mass effect (eg, headaches
or vision disturbance).
The decision on whether to begin testosterone
replacement in an elderly man may be difficult.
There are no definitive data regarding the level of
testosterone required to prevent osteopenia and
maintain muscle mass. However, values of total
testosterone less than 200 ng/dL or bioavailable
testosterone less than 70 ng/dL are probably
Endocrine Surgery Consultation 507-284-2166 www.mayoclinic.org
MAYO CLINIC ENDOCRINOLOGY UPDATE 3
Todd B. Nippoldt, MD
A Clinical Conundrum: The Diagnosis and
Treatment of Androgen Deficiency in Older Men
Figure. Total and bioavailable testosterone (T) levels
from 346 men in Rochester, Minnesota, stratified by
age. (Data from Khosla S, et al. Relationship of serum
sex steroid levels and bone turnover markers with bone
mineral density in men and women: a key role for
bioavailable estrogen. J Clin Endocrinol Metab.
1998;83:2266-74. Copyright 1998, The Endocrine
Society. Reprinted with permission.)
0
200
400
600
0
100
200
<
3
0
30
-
39
40
-
49
50
-
59
60
-
69
70
-
79
80
<30
30
-
39
40
-
49
50
-
59
60
-
69
70
-
79
80
Total T, ng/dL
Bioavailable T, ng/dL
Age, y
Age, y
inadequate, and patients
with these levels should be
considered for replacement,
even in the absence of hypo-
gonadal symptoms. Many
men have symptoms compat-
ible with hypogonadism with
testosterone values at the
lower end of the normal range
or just mildly diminished, and
it is difficult to know if this is
the cause for these symp-
toms. Dr Nippoldt says: “In
this situation, a therapeutic
trial of testosterone replace-
ment is warranted. Replacing
testosterone in doses ade-
quate to bring the total testos-
terone level to the mid-normal
range and bioavailable testos-
terone level higher than 80
ng/dL for at least 3 months is
usually an adequate trial.
Elderly men metabolize testos-
terone at a slower rate than
younger men and usually require lower doses than
those typically used for young hypogonadal men.
If the testosterone replacement trial has no impact
on the symptoms, testosterone replacement should
be discontinued.”
Potential risks for parenteral testosterone
replacement include exacerbating or unmasking
benign prostatic hypertrophy, prostate cancer,
obstructive sleep apnea, and polycythemia. No
studies have defined the incidence of these
potential risks or the cost-effectiveness of pre-
treatment screening or monitoring. Dr Nippoldt
advises: “In the absence of these data, it is
reasonable to obtain baseline digital rectal
examination, prostate-specific antigen level,
complete blood cell count, and a history regarding
the potential for obstructive sleep apnea. The
frequency of rechecking these studies during
therapy depends on the patient’s age, family
history, and baseline values. Any new symptom
should be investigated. If polycythemia develops,
overnight polysomnography should be considered
to exclude obstructive sleep apnea.”
Table. Changes Seen With Testosterone Treatment in Older Men
Lean body mass No change or increases (0%-5%)
Fat mass No change or decreases (0%-25%)
Strength No change or modest increase
Physical functioning No change
Sense of well-being Improves
Libido Increases
Erectile dysfunction No change (improves in those with very low T)
Spatial cognition Improves
Memory No effect
Bone resorption/
formation markers Improves or no change
Bone mineral density No change (increases in those with very low T)
Total cholesterol Declines (9%-12%)
HDL cholesterol No change
LDL cholesterol Declines (11%)
Insulin sensitivity No change or improves (equivocal)
IGF-1 level Increases
PSA No change or increases (remains in normal range)
Prostate volume Minimal increase
Hematocrit Increases (0%-7%), more if sleep apnea is present
MAYO CLINIC ENDOCRINOLOGY UPDATE 4
Endocrinology Consultation 800-313-5077 www.mayoclinic.org
Bariatric Surgery: Important Considerations
for the Clinician and Patient
The number of bariatric operations per-
formed in the United States is increasing
each year. Several factors have contributed
to this trend: the continued rise in the
prevalence of severe obesity, the lack of
effective medical therapies for obesity, and
a growing body of literature reporting
multiple health benefits in patients who
have undergone bariatric procedures. As a
result, patients, physicians, and third-party
payers have become more receptive to this
therapy.
Counseling the patient interested in
bariatric surgery presents many challenges.
Maria L. Collazo-Clavell, MD, of the Division
of Endocrinology, Diabetes, Metabolism, and
Nutrition at Mayo Clinic in Rochester,
comments: “Several bariatric operations are
offered that vary in their mechanisms of weight
loss, effects on medical comorbidities, and
perioperative and long-term risks. Adding to the
complexity, institution-specific outcomes may
not always reflect the published results achieved
by more established and experienced centers.”
Bariatric operations are categorized by their
mechanism of weight loss, restriction of dietary
Maria L. Collazo-Clavell, MD, and
Michael L. Kendrick, MD
intake, and induction of maldigestion/malab-
sorption of calories. The restrictive procedures
available are the vertical banded gastroplasty
(VBG) and the laparoscopic adjustable gastric
band (LAGB). The VGB consists of a stapled
proximal gastric pouch with a fixed (nonadjustable)
outlet created by a mesh band or silicone rubber
ring. Lower perioperative morbidity and an
acceptable early weight loss compared with
Roux-en-Y gastric bypass (RYGB) were
encouraging, but several randomized trials have
demonstrated inferior weight loss compared with
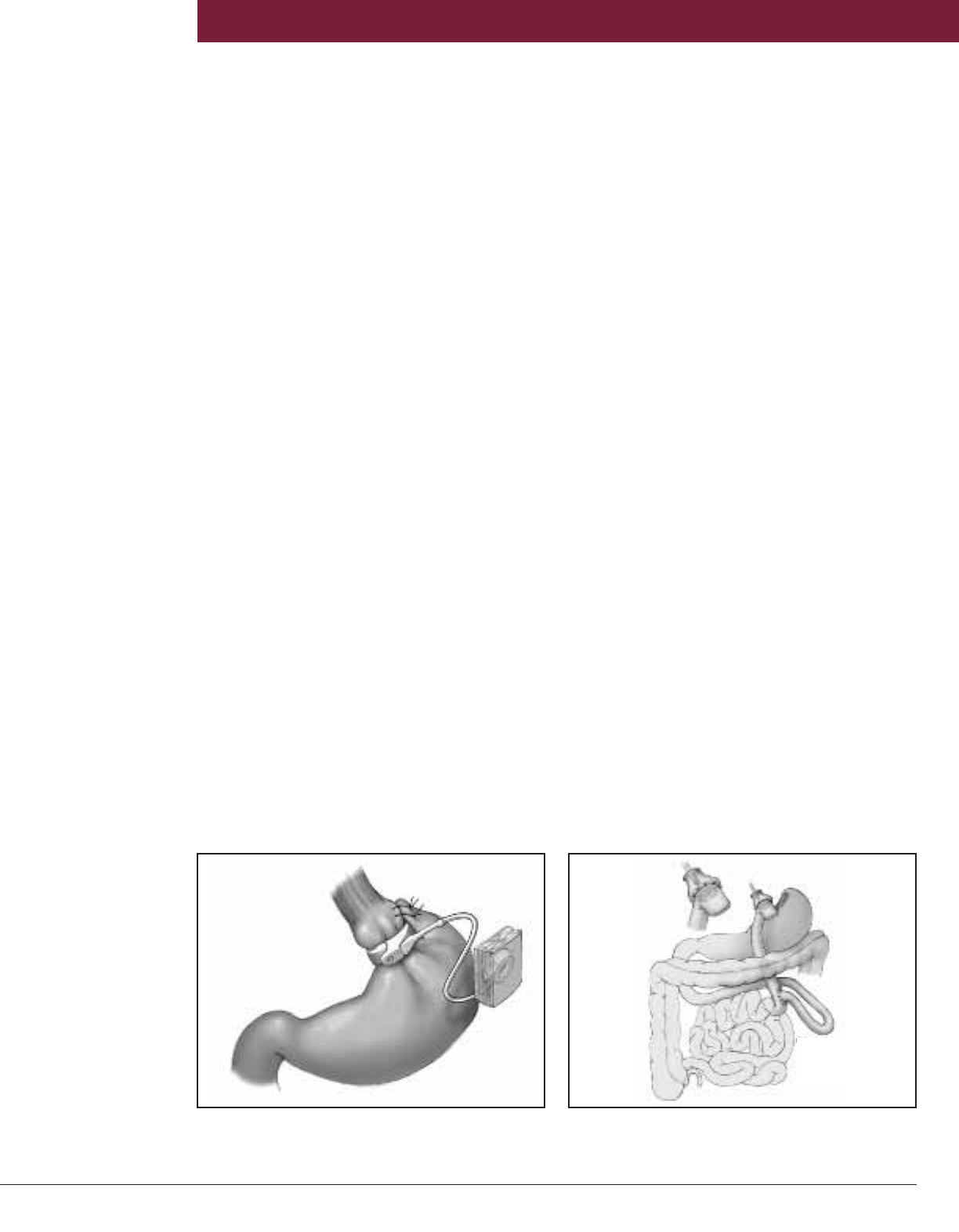
RYGB. The LAGB procedure has 2 components—
a silicone band with an inner inflatable cuff and a
reservoir connected by tubing (Figure 1). The
band is placed around the gastric cardia to create
a small (15 mL) proximal gastric pouch
with an adjustable restrictive outlet that
limits the amount of food that can be consumed.
The reservoir is implanted in the subcutaneous
tissue of the abdominal wall where it can be
accessed percutaneously to either add or remove
saline to adjust the inflatable cuff (Figure 1).
Michael L. Kendrick, MD, of the Department of
Surgery at Mayo Clinic in Rochester, comments:
“This adjustable feature provides the ability to
fine-tune the desired effect of restriction. The
absence of any bowel transection or anastomosis
leads to lower perioperative risks. Disadvantages
include less weight loss and lower resolution of
weight-related comorbid conditions compared
with RYGB and lack of long-term outcome
data. Intermediate and long-term complications
can be substantial, with reoperation required in
up to 20% of patients. At Mayo Clinic Rochester,
we no longer offer the VBG and offer the LAGB
only in limited clinical circumstances.”
Dr Kendrick explains: “RYGB is the most
common bariatric surgery performed at our
institution and nationwide. The current
procedure consists of a small proximal cardia
pouch (10-30 mL) and a 75- to 150-cm Roux limb
(Figure 2). The length of the Roux limb can vary,
influencing the weight loss observed and risk
for nutritional sequelae. In several series, RYGB
has provided greater initial and sustained weight
loss than purely restrictive operations and has
demonstrated long-term effectiveness with
reduction of comorbidities and minimal risk for
long-term nutritional complications.”
Several malabsorptive procedures are
available. Modifications to the RYGB, with
lengthening of the Roux limb and shortening of
the common channel, promote a malabsorptive
rather than maldigestive physiology (long-limb
RYGB, the very, very long-limb RYGB [VVLL-
RYGB], and the distal RYGB). Biliopancreatic
diversion (BPD) is a short common channel
procedure combined with a distal gastrectomy,
capable of achieving marked and sustained
weight loss. The increased incidence of stomal
ulceration, severe protein-calorie malnutrition,
diarrhea, and dumping has limited its broad
acceptance. The duodenal switch (DS) involves
transection of the first portion of the duodenum
with resection of the greater curvature of the
stomach leaving a 100- to 150-mL lesser
curvature-based gastric sleeve with an intact
antrum and pylorus. The proximal ileum is
divided 250 cm from the ileocecal junction,
and the biliopancreatic limb is anastomosed to
the distal ileum, creating a short (100 cm)
common channel. A duodenoileostomy is then
constructed, bringing the Roux limb up to the
gastric sleeve. Advantages of the DS include
reduced stomal complications, absence of
MAYO CLINIC ENDOCRINOLOGY UPDATE 5
Endocrine Surgery Consultation 507-284-2166 www.mayoclinic.org
Figure 1. The LAGB bariatric operation. The LAGB
consists of a silicone band with an inner inflatable cuff
and a reservoir connected by tubing.
Figure 2. The RYGB procedure consists of a small
proximal cardia pouch (10-30 mL) and a 75- to 150-cm
Roux limb.
Roux limb =
150 cm

MAYO CLINIC ENDOCRINOLOGY UPDATE 6
Endocrinology Consultation 800-313-5077 www.mayoclinic.org
Subclinical hypothyroidism occurs when the
serum thyroid-stimulating hormone (TSH) level
rises above the upper limit of normal (ULN)
despite a normal serum free thyroxine (FT4)
concentration. Subclinical hypothyroidism or mild
thyroid failure is a common problem with a
prevalence of 4% to 8.5% in the adult population.
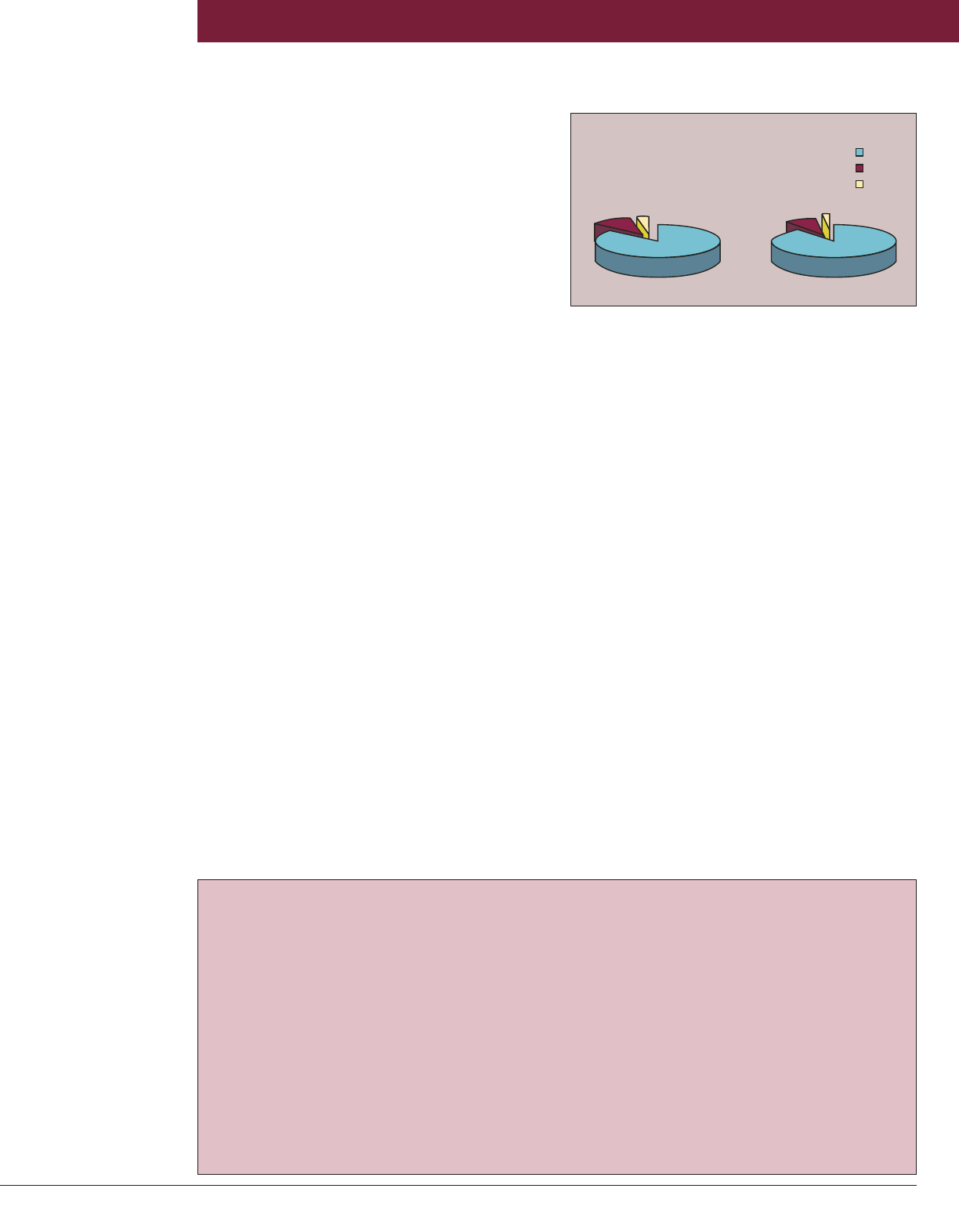
The prevalence of subclinical hypothyroidism
increases with advancing age and is higher in
women (Figure on page 7).
Because serum TSH has a log-linear relation-
ship with circulating thyroid hormone levels (eg, a
2-fold change in FT4 produces a 100-fold change
in TSH), it is the key test for the diagnosis of
subclinical hypothyroidism. Vahab Fatourechi,
MD, of the Division of Endocrinology, Diabetes,
Metabolism, and Nutrition at Mayo Clinic in
Rochester, notes: “The laboratory reference ranges
for TSH and FT4 may not be representative of a
given individual’s personal normal range. That is,
the laboratory reference ranges are wider than the
ranges of thyroid hormones that are typically
observed in an individual over time. For the
diagnosis of subclinical hypothyroidism, other
causes of elevated serum TSH, such as recovery
from nonthyroidal illness, assay variability,
heterophil antibodies, central hypothyroidism with
biologically inactive TSH, and thyroid hormone
resistance, should be excluded. However, the most
common cause of elevated serum TSH is auto-
immune thyroid disease.”
What Is the Upper Limit of Normal for TSH?
The ULN for serum TSH is the subject of hot
debate. The reference range used by Mayo
Medical Laboratories is 0.3 to 5.0 mIU/L. However,
data that support a move to lower the ULN of
TSH to 3.0 mIU/L
and possibly 2.5
mIU/L have been
published. These lower
ULN cutoffs are ob-
tained if individuals
at risk of thyroid
disease are excluded
from the reference
range population. The
strongest argument
for lowering the ULN
of TSH is the higher
rate of positive antithyroid antibodies (reflecting
underlying autoimmune thyroid disease) for
individuals with TSH concentrations between 3
and 5 mIU/L and the higher rate of progression to
clinical thyroid disease for this subgroup. The
argument against lowering the ULN for serum
TSH is that 22 million to 28 million additional
individuals in the United States would be
considered hypothyroid if the ULN of the TSH
range were decreased to 2.5 to 3.0 mIU/L. Dr
Fatourechi cautions: “Our own data show that
decreasing the ULN of the TSH reference range to
3.0 mIU/L results in a 3-fold increase in the diag-
nosis of hypothyroidism in patients without a history
of thyroid disease. Yet there is no evidence that
intervention at these levels of TSH is beneficial. In
fact, some evidence shows that lowering serum
TSH to the proposed new normal range by adjust-
ment of the thyroxine dose does not improve
patients’ well-being or their nonspecific complaints.”
Dr Fatourechi continues: “Obviously for patients
with TSH levels between 3 and 5 mIU/L, follow-
up and possibly measurement of thyroperoxidase
(TPO) antibody may be considered.”
A Practical Approach to the
Patient With Subclinical Hypothyroidism
dumping, excellent long-term maintenance of
weight loss, and decreased incidence of severe
protein-calorie malnutrition with the DS
compared with BPD. At Mayo Clinic Rochester,
the VVLL-RYGB and the DS are offered to
individuals with body mass index (calculated as
weight in kilograms divided by the square of
height in meters) greater than 55 in whom
malabsorptive procedures are associated with
superior weight loss.
Dr Collazo-Clavell notes: “A patient’s decision
to consider bariatric surgery is not an easy one.
Which bariatric procedure is best for an
individual depends on multiple factors—amount
of weight loss desired, preexisting medical
comorbidities, and preference, to name a few.”
Each year, more than 300 bariatric procedures are
performed at Mayo Clinic Rochester and Mayo
Clinic Arizona. Multidisciplinary teams of
nutritionists and specialists from the fields of
surgery, internal medicine, psychology, and
psychiatry work in an integrated fashion to
evaluate, educate, and prepare patients in hopes
of maximizing success and minimizing short-
and long-term complications of bariatric surgery
for weight loss.
Vahab Fatourechi, MD
Should All Patients With Subclinical
Hypothyroidism Be Treated With Thyroid
Hormone Replacement?
There is consensus for initiating thyroxine
replacement therapy for all patients with elevated
TSH higher than 10 mIU/L, even if FT4 is within
the normal laboratory range. However, con-
troversy continues concerning whether patients
with serum TSH levels between 5 and 10 mIU/L
should be treated. The argument in favor of
replacement therapy is based on numerous
proposed consequences of untreated subclinical
hypothyroidism: progression to clinical hypo-
thyroidism, subtle systemic symptoms of hypo-
thyroidism, lipid abnormalities, adverse cardiac
end points, cardiac dysfunction, adverse fetal
effects and pregnancy outcomes, possible contri-
bution to infertility, neuromuscular dysfunction,
psychiatric dysfunction, and cognitive dysfunction.
Dr Fatourechi explains: “If studies show that
mildly elevated serum TSH has adverse cardiac
effects, then therapy of all cases of subclinical
hypothyroidism will make sense. Several
investigators have demonstrated subtle cardio-
vascular dysfunction in subclinical hypo-
thyroidism, but clinical significance is ques-
tionable. However, to date, most studies have
shown a lack of association of subclinical hypo-
thyroidism with cardiac events and cardiovascular
mortality. Surprisingly, the results of an epidem-
iologic study suggested that for individuals older
than 80 years a slightly higher-than-normal TSH
had survival benefit. Because of the large number
of individuals potentially impacted, there is an
urgent need for settling this controversy. Until
guidance from carefully designed randomized
trials becomes available, individuals with serum
TSH levels between 5 and 10 mIU/L should be
treated selectively. Thyroxine replacement therapy
should be reserved for patients who have goiter,
women who are anticipating pregnancy or are
pregnant, or patients with depression or bipolar
disorder. Patient preference, clinical circumstance,
age, presence of symptoms of hypothyroidism,
TPO antibody positivity, and level of and
progression of TSH over time should also be
considered. We also suggest that subclinical hypo-
thyroidism associated with autoimmune thyroid-
itis of children and adolescents should be treated.
Our data show that patients with serum TSH levels
above 8 mIU/L have a high likelihood of progres-
sion to TSH above 10 mIU/L in 4 years and may be
considered for thyroxine replacement therapy.
“Improvement in serum lipid levels with
thyroxine replacement therapy is more likely for
patients who have baseline TSH levels higher than
10 mIU/L. If hyperlipidemia is encountered in a
patient with a serum TSH between 5 and 10
mIU/L, specific lipid-directed therapy or lifestyle
changes are needed. Some of these recom-
mendations do not have definitive evidence-based
support; however, we believe a practical approach
is needed until more evidence becomes available.”
MAYO CLINIC ENDOCRINOLOGY UPDATE 7
Endocrine Surgery Consultation 507-284-2166 www.mayoclinic.org
8%
2%
<5.0
5.1- 10
>10
0
Female
11%
3%
TSH, mIU/L
Male
90%86%
Figure. Serum TSH levels in 123,958 patients aged 50
years or older seen at Mayo Clinic, 1995-1997.
Endocrinology Update
Produced by
Mayo Clinic
200 1st Street SW
Rochester, MN 55905
Medical Editor
William F. Young, Jr, MD
Editorial Board
M. Regina Castro, MD
Bart L. Clarke, MD
Maria L. Collazo-Clavell, MD
Clive S. Grant, MD
Publication Manager
Elizabeth M. Rice
Art Director
Ron O. Stucki
Production Designer
Connie S. Lindstrom
Manuscript Editor
Jane C. Wiggs
Media Support Services
Contributing Artists
Joseph M. Kane
Siddiqi Ray
Endocrinology Update is written for
physicians and should be relied upon
for medical education purposes only.
It does not provide a complete
overview of the topics covered and
should not replace the independent
judgment of a physician about the
appropriateness or risks of a
procedure for a given patient.
Endocrinology Update
Education Opportunities
Please call 800-323-2688 or visit www.mayo.edu
/cme/endocrinology.html for more information
about these courses or to register.
10th Mayo Clinic Endocrine Course
The 10th Mayo Clinic Endocrine Course will be
held March 18-23, 2007, on the Big Island of
Hawaii. This course, created for endocrinologists
and interested internists and surgeons, will
present the latest material on the diagnosis and
treatment of endocrine disorders. This 5-day
course (7:30 AM to 12:30 PM daily) will span the
full spectrum of endocrinology through short
lectures, case-based debates, clinicopathologic
sessions, clinical pearls sessions, and small group
discussions with experts. The digital audience
response system will be used extensively, and
there will be many opportunities for interaction
with the course faculty. Optional sessions on
thyroid ultrasonography and technology in
diabetes will be offered.
Mayo Clinic Nutrition in Health and Disease
Mayo Clinic Nutrition in Health and Disease will
be held November 8-9, 2007, at the Hilton San
Francisco Financial District in San Francisco,
California. This course, designed for physicians,
dietitians, nurses, and pharmacists, will provide
an in-depth overview of challenging nutritional
issues that clinicians encounter in the ambulatory
and hospital settings.
MAYO CLINIC ENDOCRINOLOGY UPDATE 8
NON-PROFIT
ORGANIZATION
U.S. POSTAGE PAID
ROCHESTER, MN
PERMIT NO. 259
To make an
appointment for
a patient through
the Referring
Physicians
Service, use
these toll-free
numbers:
Mayo Clinic
Rochester
800-533-1564
Mayo Clinic
Arizona
866-629-6362
Mayo Clinic
Jacksonville
800-634-1417
MC5810-1206
200 First Street SW
Rochester, Minnesota 55905
www.mayoclinic.org
© 2006, Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.
MAYO, MAYO CLINIC and the tri
p
le-shield Mayo logo are trademarks and service marks of MFMER.
Geoffrey B. Thompson, MD, David R. Farley, MD, Melanie L. Richards, MD, and Clive S. Grant, MD
Mayo Clinic Rochester Endocrine Surgeons
If you would like to be removed from the Mayo Clinic Endocrinology Update mailing list, please send an e-mail with your request
to [email protected]. However, please note this opt-out only applies to Mayo Clinic Endocrinology Update. You may
continue to receive other mailings from Mayo Clinic in the future. Thank you.
