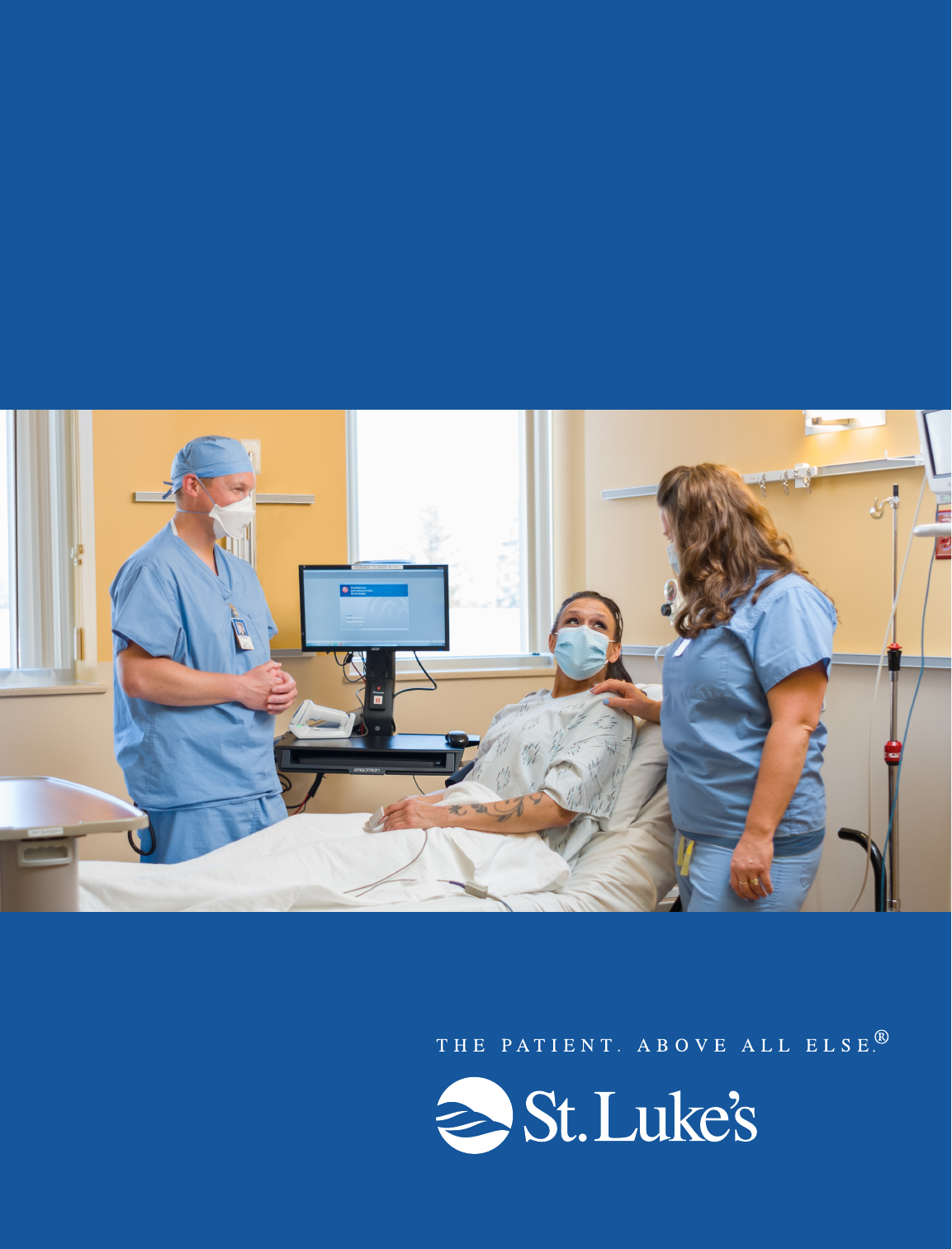
Surgical &
Procedural Care
Patient Handbook
St. Luke’s Information
3 Important Phone Numbers
3 Visitors
3 Parking and Directions
3 Finding Your Way at St. Luke’s
How to Prepare
4 Before your Procedure
4 Preoperative Physical Checklist
Pre-Procedure
5 Food, Drink and Medications
5 Getting Ready
5 What to Bring to the Hospital
5 Coping with Anxiety
Procedure
6 At the Hospial Before Your Procedure
7 Anesthesia
7 In the Operating Room (OR)
Post-Procedure
8 After Your Surgery
Discharge
9 Pain Management
9 Nausea/Vomiting Management
10 Signs of Bleeding
10 Signs of Infection
10 Discharge Instructions
11 Leaving the Hospital
12 Notes
Table of Contents
Your procedure is at St. Luke’s Surgical & Procedural Care, 1015 E. 1st Street, Duluth, MN. This guide
will help you prepare for your procedure and know what to expect during your stay.
Appointment Date:
Surgeon’s Name and Phone Number:
A day or two before your surgery, a nurse will call you. They will give you an arrival time for your procedure
and any additional instructions you need to prepare for your procedure. If you have not been called by
7 pm one business day before your procedure, call 218.249.5244.
The information provided
is a general overview for all
surgical procedures. Your
surgeon may also give you
more detailed information
related to the specific
procedure you are having.
2 | St. Luke’s
St. Luke’s Information
IMPORTANT PHONE NUMBERS
St. Luke’s Hospital
Available 24/7
218.249.5555
Pre-Admissions Testing
Monday – Friday, 8 am – 4:30 pm
218.249.5644
St. Luke’s Surgical & Procedural Care
Monday – Friday, 5:30 am – 8 pm
218.249.5244
St. Luke’s Financial Specialists
218.249.5340
St. Luke’s Facility Assistants
Available 24/7
218.249.4940
Northland Pharmacy
Monday – Friday, 8 am – 6 pm
218.249.2460
VISITORS
Generally, you may have one adult visitor accompany
you the day of your procedure. This person should be
your support person.
• Check St. Luke’s website (slhduluth.com/visitors)
or call your surgeon’s office for the most up-
to-date visitor policy.
• Once you go into the operating room (OR),
your visitor may need to return to the
Surgical & Procedural Care waiting room.
• For refreshments, there is a coffee shop located
on the 2nd floor of Building A. Also, Blue Waves
Café is located on the 3rd floor of the hospital.
PARKING AND DIRECTIONS
• Park for free in the covered lot in front of
Building A (1015 E. 1st Street).
• Enter Building A. There will be an information
desk staff member or volunteer to help direct
you, and wheelchairs for patient use.
• Take elevators to 3rd floor, to the Surgical &
Procedural Care waiting room and check in at
the desk.
• For more information, visit slhduluth.com/surgery.
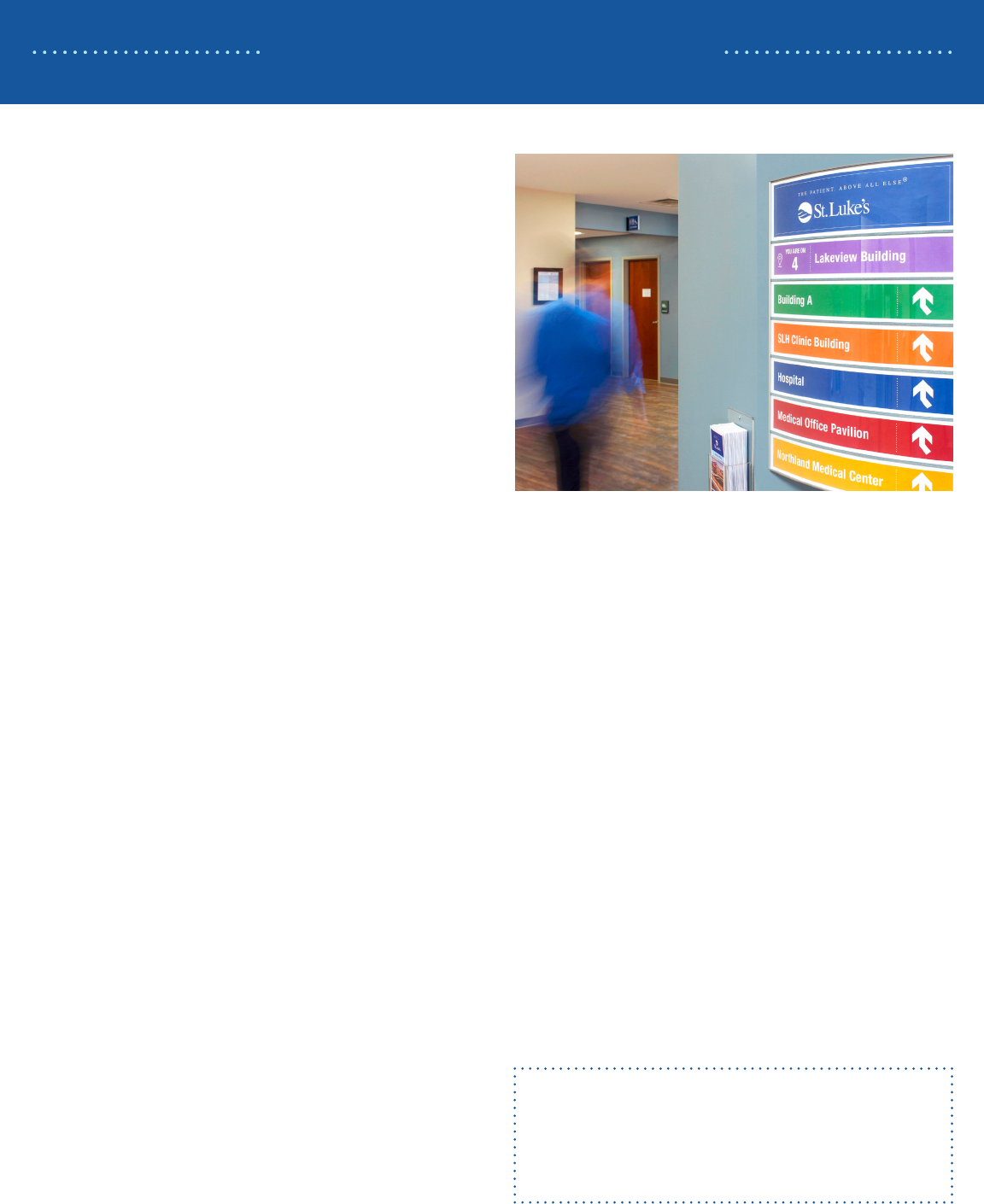
FINDING YOUR WAY AT ST. LUKE’S
To help make St. Luke’s as easy to navigate as
possible, all building and parking lot signs and
maps are color coded.
• Building A – GREEN
• Hospital – BLUE
• Medical Office Pavilion – RED
• Lakeview Building – PURPLE
• Northland Medical Center – GOLD
• SLH Clinic Building – ORANGE
There are campus maps located near all
entrance points, as well as courtesy phones and
digital directories. Once you are in a St. Luke’s
building there will be color-coded signage to direct
you to services in that building and to other
St. Luke’s buildings.
For a detailed map of St. Luke’s Campus,
visit slhduluth.com/map.
Need Help?
If you ever need assistance finding your way
at St. Luke’s or a wheelchair escort, call
St. Luke’s Facility Assistants at 218.249.4940.
Surgical & Procedural Care | 3
How to Prepare
BEFORE YOUR PROCEDURE
Here are several important things you will need to do
before your procedure.
• See your primary care provider. Schedule
a preoperative physical with your primary care
provider within 30 days of your procedure.
(If you do not have a primary care provider, reach
out to your surgeon’s office.) To help you and
your provider make sure you are ready for your
procedure, bring this booklet and talk through all of
the items in the Preoperative Physical Checklist
(next column) at your preoperative
physical appointment.
• Call your insurance provider. To see if a prior
authorization is required by your insurance policy,
call your insurance provider. If this is not completed
by the time of surgery, your procedure may be
delayed.
• Stop smoking. Since non-smokers have fewer
infections and faster healing, it is recommended
that you stop smoking 4 weeks prior to surgery.
• Stop drinking alcohol. All patients are required
to abstain from alcohol for 2 weeks prior to
surgery. This prevents complications such as
bleeding, infection, heart problems, and a longer
hospital stay.
• Receive a nurse phone call. A day or two
before your surgery, a nurse will call you. They will
give you an arrival time for your procedure and any
additional instructions you need to prepare for your
procedure. If you have not been called by 7 pm
one business day before your procedure,
call 218.249.5244.
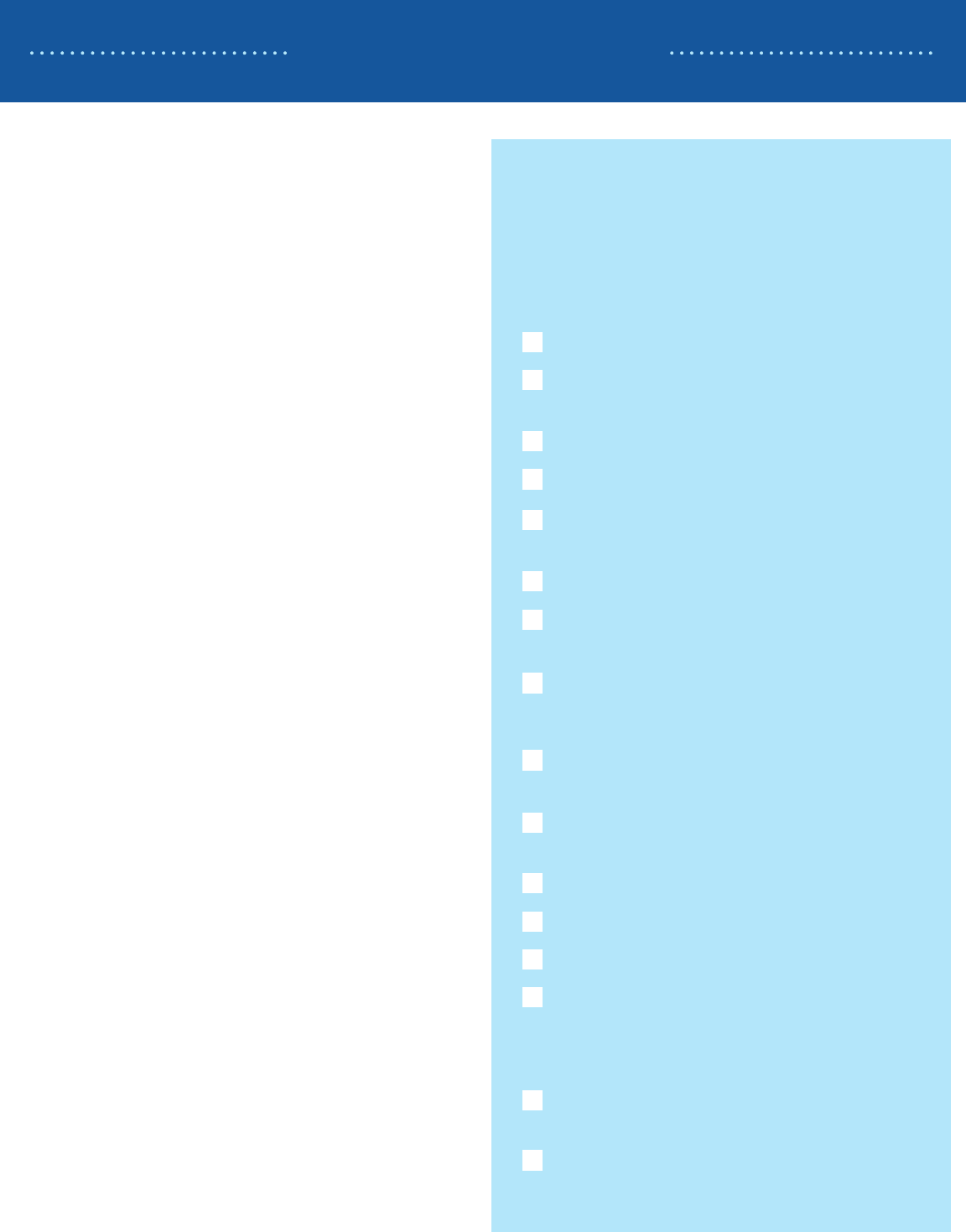
PREOPERATIVE PHYSICAL CHECKLIST
Bring this checklist to your preoperative physical with
your primary care provider. Review the items on this
list to help avoid complications and delays in care.
Discuss if you are ready to have the procedure
by reviewing:
How well your blood sugar is controlled
If your Body Mass Index (BMI) is within a
safe range
Smoking cessation difficulties
Alcohol cessation difficulties
Whether insurance preauthorization is
needed and who to contact
Whether preoperative lab work is needed
Whether any diagnostic work is needed
(e.g., EKG)
Your health care directive (optional)
Discuss medication instructions if you take:
Blood thinners or anticoagulants
(e.g., Coumadin or Plavix)
Blood thinning medications (e.g., NSAIDs
or aspirin)
Diabetic medications or insulin
Scheduled pain medications
Blood pressure medication
Vitamins
Discuss your plan for recovering, specifically
regarding:
Ordering adaptive equipment
(e.g., crutches or a walker)
Arranging discharge to a long-term care or
rehabilitation facility
4 | St. Luke’s
Pre-Procedure
GETTING READY
• Arrange for a responsible adult to drive you home
after your procedure.
• If a wristband is placed at your lab appointment
(generally 2 to 3 days before your surgery), you
must leave it on.
• Before you arrive, please remove:
• All makeup and nail polish
• All body piercings and jewelry, including
wedding rings
• Bathe/shower the night before or morning of
surgery. Do not apply lotions, deodorants, oils
or powders.
• Do not shave the operative site.
• Notify your surgeon immediately if you develop
cold, flu or other symptoms of illness.
WHAT TO BRING TO THE HOSPITAL
• Wear loose, comfortable clothing
• DO bring:
• Your insurance card and picture ID
• An updated list of medications
• A container for your hearing aids, glasses,
contacts and/or dentures
• Your CPAP machine and mask, if you use one
• Emergency inhalers, if you are prescribed them
• DO NOT bring:
• Money or credit cards
• Medications
• Anything of value that you do not want lost
or damaged
COPING WITH ANXIETY
You may experience feelings of fear and anxiety
leading up to your procedure. Talk with your primary
care provider if you are unable to cope with anxiety.
The day of your procedure, inform surgical staff
immediately upon arrival. We will listen carefully and
do everything we can to make sure you are
comfortable. We will also notify your anesthesiologist
who will decide whether medication to help your
anxiety is appropriate.
To prevent complications or delays in your care, you
must follow these instructions.
FOOD, DRINK AND MEDICATIONS
• You may have clear liquids or water up to 6 hours
prior to your procedure.
• After midnight prior to your procedure, do not eat
any food or use tobacco products. This includes
hard candy, chewing gum, cigarettes and
chewing tobacco.
• For children less than 36 months old, breast
milk may be given up to 4 hours prior to
procedure or formula up to 6 hours prior to
procedure. However, follow the same guidelines
for solids and other liquids.
• Follow instructions from your primary care
provider regarding medications taken before
your surgery. You can continue to take
prescribed pain medication until the morning
of surgery. Acetaminophen (Tylenol) is ok to
take prior to surgery. Do not take NSAIDS
(Ibuprofen, Advil, Motrin, Aleve) without
discussing with your surgeon.

Surgical & Procedural Care | 5
Procedure
• Room Assignment: After you check in at the
front desk of Surgical & Procedural Care, the
staff will let your surgical team know you have
arrived. As soon as your room is available, you
will be brought back to your private preoperative
room. Your support person may accompany you,
if you wish.
• Vitals Check: Staff will weigh you and take
your vitals (temperature, heart rate, blood
pressure, etc.).
• Clothing Prep: You will be asked to remove
all clothing, including your undergarments, and
change into a hospital gown and socks.
• Medication Verification: Your nurse will verify
your medications along with the last date and
time taken. They will complete an assessment
and place an IV. An IV is a soft flexible tube
placed inside a vein, in which medications can be
administered through. There are several options
available to increase the comfort of your
IV placement.
• Additional Testing: Labs or diagnostic testing,
such as an EKG, may be completed.
• Meet and Greet: You will meet your
anesthesiologist and surgeon to discuss your care
and sign consent forms.
• Skin Prep: Depending on the type of procedure
you are having, you may require a skin prep. This
may require staff to clip hair and cleanse around
the operative site. Do not shave the operative site
before coming to the hospital.
• Specialized Clothing: You may be given
compressive stockings to wear and/or have
special sleeves applied to your lower legs that
provide intermittent pressure cycles. These will
help your blood circulation during and after
surgery, helping to prevent the formation of blood
clots.
• Specialized Protection: A foam dressing may
be placed to prevent skin injuries on areas that
your nurse has identified as high risk for skin
breakdown during your procedure.
• Keeping You Informed: Sometimes there are
unforeseen or emergent circumstances that may
require a delay in your procedure start time. We
will communicate updates or possible delays to
the best of our abilities.
AT THE HOSPITAL BEFORE
YOUR PROCEDURE
6 | St. Luke’s
Procedure
ANESTHESIA
Your anesthesiologist provider will meet with you, and
together you will decide which type of anesthesia
is best for you. You may be asked to provide a
urine sample for pregnancy testing prior to receiving
anesthesia. You may not drive for 24 hours after
receiving any type of anesthesia, sedation or
narcotic medication.
There are several forms of anesthesia. Below is
an overview of each one.
General Anesthesia
This form of anesthesia is inhaled through a
mask and/or given through your IV. Once you
are completely asleep from the anesthesia, the
anesthesia provider will gently place a breathing tube
into your airway. Your anesthesia team, which may
consist of an anesthesiologist and a certified nurse
anesthetist, will monitor you very closely. They will
be watching your vital signs and comfort level. With
general anesthesia, you will not move, feel pain, or
have any memory of the procedure.
Sedation
This form of anesthesia is provided through your IV
and allows you to be comfortable while still breathing
on your own. Your levels of sedation and awareness
will depend on the type of procedure you are having.
Your anesthesia team will monitor you closely by
watching your vital signs and comfort level.
Spinal and Epidural Anesthesia
These forms of anesthesia numb parts of your body
to block pain. They are given through injection(s)
in or around the spine. Additional medication is
provided through your IV to relax and sedate you.
This additional medication often induces sleep and
most patients have no memory of the procedure.
Depending on several factors, your anesthesiologist
will determine if you are a candidate for spinal or
epidural anesthesia.
Peripheral Nerve Blocks
Medication can be injected near the nerves of the
surgery site to help alleviate post-operative pain.
Your anesthesiologist will discuss whether a nerve
block is a good option for you.
IN THE OPERATING ROOM (OR)
Before you leave your preoperative room there will be
a safety check. This will include verifying your name,
date of birth, and type of procedure. This will be
repeated when you arrive in the OR.
• You will be taken to the OR on the bed from your
preoperative room. Once you reach the OR, you
will be transferred to another bed.
• Your anesthesia team will place monitoring
equipment. This will include a blood pressure
cuff on your arm, a pulse oximeter on your finger,
and electrode stickers on your chest to monitor
your heart.
• For your safety and comfort, you will be
continuously monitored by your anesthesia team.
• The OR is a sterile environment. Everyone in the
room will wear protective coverings to reduce risk
of contamination. You may receive an antibiotic
through your IV to help prevent infection.
• The OR room temperature is cool. Keeping the
temperature low may be helpful in reducing
bacteria in the environment, as well as keeping
your surgical team cool. You will be given warm
blankets for your comfort.
Surgical & Procedural Care | 7
Post-Procedure
AFTER YOUR SURGERY
• Recovery Unit: Depending on the kind
of anesthesia you received, you may go to
the recovery unit as you wake up after
your procedure.
• Postoperative Update: You may not remember
speaking to your surgeon while you are in the
recovery unit. Usually, your surgeon will update
your support person while you are still waking up.
• Postoperative Care Location: After the
recovery unit, you will return to Surgical &
Procedural Care (unless you are admitted to the
hospital to stay overnight). A nurse will monitor
your vital signs, assess your comfort, nausea and
wakefulness.
• Ensuring Your Comfort: Your nurse will make
you as comfortable as possible by dimming the
lights, providing warm blankets, and making sure
you are positioned comfortably. They will also
offer you fluids and a light snack.
• Postoperative Instructions: The nurse will
review your postoperative medications and
instructions with you and your support person
before discharge. You may still feel sleepy when
you leave, so it is advised that you spend the
remainder of the day resting at home, with your
support person.
• Recovery Support – Movement: Your nurse
will encourage movement following your
procedure. Movement is proven to help prevent
complications such as pneumonia, blood clots,
constipation, skin breakdown and inability to
urinate. Continue to move as directed during your
recovery at home.
• Recovery Support – Breathing Exercises:
Your nurse will encourage you to cough and take
deep breaths after your procedure. This helps
to prevent pneumonia. You are encouraged to
continue coughing and deep breathing often
during your recovery at home.
• IV Removal: Before you leave the hospital,
your IV will be removed. Firm pressure should
be applied to the IV area for several minutes to
minimize bleeding and bruising.

8 | St. Luke’s
Discharge
PAIN MANAGEMENT
Pain control is very important for your recovery. After
your procedure, you will be asked to rate your pain
on a scale from zero to 10, zero being no pain and
10 being the worst pain possible. It is important to
communicate to your care team what level of pain is
tolerable.
Depending on your procedure, pain may be expected
and you may not be pain-free when you leave.
However, there are several options available to help
lessen pain. Some pain management techniques
frequently used are pain medication and non-
medication pain relief. It is helpful to have a plan to
use a combination of these during your recovery.
Pain Medication
It is encouraged that you keep a log of when you
take pain medications to prevent accidental overdose.
Narcotics. Narcotics may be prescribed
following your procedure. These are used for
moderate to severe pain. It is important to take
these medications as prescribed. Oftentimes they
are prescribed “as needed,” and should only
be taken if you’re in pain. These should be taken
only when pain cannot be managed by
over-the-counter medications and non-medicated
pain relief methods.
Risks of narcotics can include constipation,
nausea, sleepiness and decreased tolerance
to pain. To prevent constipation, drink plenty
of liquids, move frequently, and take over-the-
counter stool softeners. Discuss with your
surgeon or pharmacist which stool softener they
recommend for you.
Over-the-Counter (OTC)/Non-narcotics
Many narcotic medications already contain Tylenol
(acetaminophen). You should not exceed 4,000
milligrams (mg) of acetaminophen in a 24-hour
period. Nonsteroidal anti-inflammatories such as
Ibuprofen, Motrin, Advil, Aleve and Naproxen may
be taken as directed.
For children, follow packaging instructions for the
maximum amount of medication your child can
have in a single day. Call your child’s provider if
you are unsure of the instructions. Consult your
provider before giving aspirin to your child.
Non-Medication Pain Relief
Ice. Double-bagged ice cubes or commercially
made ice packs can be used. Be sure to place
a towel between the ice and skin to prevent
frostbite or damage to the skin. Use ice as
directed by your surgeon.
Elevation. Elevate the affected area above the
level of the heart as able. This decreases swelling,
which helps alleviate pain.
Alternative pain management techniques.
Alternative techniques include guided imagery,
meditation, music, acupuncture, massage,
essential oils, or other techniques suggested by
your surgeon.
NAUSEA/VOMITING MANAGEMENT
Nausea is not uncommon following anesthesia,
especially following abdominal and gynecological
surgeries. If you’ve experienced post-operative
nausea or vomiting in the past, please let your
anesthesia team know before surgery.
If you become nauseous, here are some things that
can help:
• Chew on ice chips and drink clear liquids, slowly
progressing to bland foods as you’re able.
• Take pain medications with food.
• Aromatherapy, such as peppermint oil,
may help.
• Ask your care providers if medication to treat
nausea is appropriate for you.
Surgical & Procedural Care | 9
Discharge
DISCHARGE INSTRUCTIONS
A nurse will review discharge instructions regarding your post-operative care with you. Make sure your questions
and concerns are addressed by either your nurse or surgeon.
SIGNS OF BLEEDING
Bleeding may happen inside of the body or outside of the body. Depending on the type of procedure you
had, some bleeding could be normal and expected. Ask your surgeon what normal bleeding is for the type of
procedure you had. If you are unsure as to whether your bleeding is normal, call your surgeon’s office. If you are
experiencing heavy bleeding call 911.
SIGNS OF INFECTION
Most surgical infections appear at the incision site within 30 days after surgery. Surgical wound infections may
have pus draining from them, and can be red, painful, or hot to touch. You may have a fever and feel sick. Call
your surgeon immediately if you are experiencing any signs of infection.
10 | St. Luke’s
Leaving the Hospital
LEAVING THE HOSPITAL
Many procedures do not require a hospital stay. If
your procedure does require a stay, it will be our goal
to help you transition to the next phase of your care
as quickly as possible. When you are discharged, it
allows a bed to be available for someone else who
needs the high level of care that our inpatient setting
provides.
• Inform your care providers of your preferred
pharmacy. Northland Pharmacy, located on
St. Luke’s campus, is available to fill your
prescriptions Monday through Friday, 8 am
to 6 pm. They accept most insurance plans.
• If you are planning to go to a skilled nursing
or rehab facility after your procedure, tell your
surgeon and nurse.
• If you are planning to go home after your
procedure, you will need to have a responsible
adult available to drive you home. You should not
drive for 24 hours following your procedure or
while you are taking narcotic medications.
• A nurse may call you following your procedure to
see how you are doing. If you have any concerns
or questions, contact your surgeon’s office.
LEARN MORE
If you’d like to learn more about your procedure or
health condition, visit slhduluth.com/HealthLibrary
Surgical & Procedural Care | 11
Notes
12 | St. Luke’s
Notes
Surgical & Procedural Care | 13
Notes

915 E. 1st Street
Duluth, MN 55805
218.249.5555
06/22
