
Medicare Benefit Policy Manual
Chapter 8 - Coverage of Extended Care (SNF) Services
Under Hospital Insurance
Table of Contents
(Rev. 12283; Issued: 10-05-23)
Transmittals Issued for this Chapter
10 - Requirements - General
10.1 - Medicare SNF PPS Overview
10.2 - Medicare SNF Coverage Guidelines Under PPS
10.3 - Hospital Providers of Extended Care Services
20 - Prior Hospitalization and Transfer Requirements
20.1 - Three-Day Prior Hospitalization
20.1.1 - Three-Day Prior Hospitalization - Foreign Hospital
20.2 - Thirty-Day Transfer
20.2.1 - General
20.2.2 - Medical Appropriateness Exception
20.2.2.1 - Medical Needs Are Predictable
20.2.2.2 - Medical Needs Are Not Predictable
20.2.2.3 - SNF Stay Prior to Beginning of Deferred Covered
Treatment
20.2.2.4 - Effect of Delay in Initiation of Deferred Care
20.2.2.5 - Effect on Spell of Illness
20.2.3 - Readmission to a SNF
20.3 – Payment Bans
20.3.1 - Payment Bans on New Admissions
20.3.1.1 - Beneficiary Notification
20.3.1.2 - Readmissions and Transfers
20.3.1.3 - Sanctions Lifted: Procedures for Beneficiaries Admitted
During the Sanction Period
20.3.1.4 - Payment Under Part B During a Payment Ban on New
Admissions

20.3.1.5 - Impact of Consolidated Billing Requirements
20.3.1.6 - Impact on Spell of Illness
30 - Skilled Nursing Facility Level of Care - General
30.1 – Administrative Level of Care Presumption
30.2 - Skilled Nursing and Skilled Rehabilitation Services
30.2.1 - Skilled Services Defined
30.2.2 - Principles for Determining Whether a Service is Skilled
30.2.2.1 – Documentation to Support Skilled Care Determinations
30.2.3 - Specific Examples of Some Skilled Nursing or Skilled
Rehabilitation Services
30.2.3.1 - Management and Evaluation of a Patient Care Plan
30.2.3.2 - Observation and Assessment of Patient’s Condition
30.2.3.3 - Teaching and Training Activities
30.2.4 - Questionable Situations
30.3 - Direct Skilled Nursing Services to Patients
30.4. - Direct Skilled Therapy Services to Patients
30.4.1 – Skilled Physical Therapy
30.4.1.1 - General
30.4.1.2 - Application of Guidelines
30.4.2 - Speech-Language Pathology
30.4.3 - Occupational Therapy
30.5 - Nonskilled Supportive or Personal Care Services
30.6 - Daily Skilled Services Defined
30.7 - Services Provided on an Inpatient Basis as a “Practical Matter”
30.7.1 - The Availability of Alternative Facilities or Services
30.7.2 - Whether Available Alternatives Are More Economical in the
Individual Case
30.7.3 - Whether the Patient’s Physical Condition Would Permit
Utilization of an Available, More Economical Care Alternative
40 - Physician Certification and Recertification for Extended Care Services
40.1 - Who May Sign the Certification or Recertification for Extended Care
Services
50 - Covered Extended Care Services
50.1 - Nursing Care Provided by or Under the Supervision of a Registered
Professional Nurse
50.2 - Bed and Board in Semi-Private Accommodations Furnished in Connection
With Nursing Care
50.3 - Physical, Therapy, Speech-Language Pathology and Occupational Therapy
Furnished by the Skilled Nursing Facility or by Others Under
Arrangements With the Facility and Under Its Supervision
50.4 - Medical Social Services to Meet the Patient’s Medically Related Social
Needs
50.5 - Drugs and Biologicals
50.6 - Supplies, Appliances, and Equipment
50.7 - Medical Service of an Intern or Resident-in-Training
50.8 - Other Services
50.8.1 - General
50.8.2 - Respiratory Therapy
60 - Covered Extended Care Days
70 - Medical and Other Health Services Furnished to SNF Patients
70.1 - Diagnostic Services and Radiological Therapy
70.2 - Ambulance Service
70.3 - Inpatient Physical Therapy, Occupational Therapy, and Speech-Language
Pathology Services
70.4 - Services Furnished Under Arrangements With Providers
10 - Requirements - General
(Rev. 228, Issued: 10-13-16, Effective: 10-18-16, Implementation: 10-18-16)
The term “extended care services” means the following items and services furnished to
an inpatient of a skilled nursing facility (SNF) either directly or under arrangements as
noted in the list below:
• Nursing care provided by or under the supervision of a registered professional
nurse;
• Bed and board in connection with furnishing of such nursing care;
• Physical or occupational therapy and/or speech-language pathology services
furnished by the skilled nursing facility or by others under arrangements with
them made by the facility;
• Medical social services;
• Such drugs, biologicals, supplies, appliances, and equipment, furnished for use in
the skilled nursing facility, as are ordinarily furnished by such facility for the care
and treatment of inpatients;
• Medical services provided by an intern or resident-in-training of a hospital with
which the facility has in effect a transfer agreement (see §50.7) under an approved
teaching program of the hospital, and other diagnostic or therapeutic services
provided by a hospital with which the facility has such an agreement in effect, and
• Other services necessary to the health of the patients as are generally provided by
skilled nursing facilities, or by others under arrangements.
Post-hospital extended care services furnished to inpatients of a SNF or a swing bed
hospital are covered under the hospital insurance program. The beneficiary must have
been an inpatient of a hospital for a medically necessary stay of at least 3 consecutive
calendar days. Time spent in observation or in the emergency room prior to (or in lieu
of) an inpatient admission to the hospital does not count toward the 3-day qualifying
inpatient hospital stay, as a person who appears at a hospital’s emergency room seeking
examination or treatment or is placed on observation has not been admitted to the hospital
as an inpatient; instead, the person receives outpatient services. For purposes of the SNF
benefit’s qualifying hospital stay requirement, inpatient status commences with the
calendar day of hospital admission. See 31 Fed. Reg. 10116, 10118-19 (July 27, 1966).
The beneficiary must also have been transferred to a participating SNF within 30 days
after discharge from the hospital, unless the exception in §20.2.2 applies. In addition, the
beneficiary must require SNF care for a condition that was treated during the qualifying
hospital stay, or for a condition that arose while in the SNF for treatment of a condition
for which the beneficiary was previously treated in the hospital.

Extended care services include SNF care for beneficiaries involuntarily disenrolling from
Medicare Advantage plans as a result of a Medicare Advantage plan termination when
they do not have a 3-day hospital stay before SNF admission, if admitted to the SNF
before the effective date of disenrollment (see Pub. 100-04, Medicare Claims Processing
Manual, chapter 6, section 90.1).
10.1 - Medicare SNF PPS Overview
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
Section 1888(e) of the Social Security Act provides the basis for the establishment of the
per diem federal payment rates applied under the PPS to SNFs that received their first
payment from Medicare on or after October 1, 1995. A transition period applied for those
SNFs that first accepted payment under the Medicare program prior to October 1, 1995.
The Balanced Budget Act (BBA) of 1997 sets forth the formula for establishing the rates
as well as the data on which they are based. See also Pub. 15-1, Provider Reimbursement
Manual, Part I, chapter 28, section 2836 for background information on the SNF PPS;
Pub. 100-04, Medicare Claims Processing Manual, chapter 6, sections 30ff. for SNF PPS
billing instructions; and Pub. 100-08, Medicare Program Integrity Manual, chapter 6,
sections 6.1ff. regarding medical review of SNF PPS claims.
10.2 - Medicare SNF Coverage Guidelines Under PPS
(Rev. 12283, Issued:10-05-23, Effective:01-08-24, Implementation:01-08-24)
Under SNF PPS, covered SNF services include post-hospital SNF services for which
benefits are provided under Part A (the hospital insurance program) and all items and
services which, prior to July 1, 1998, had been paid under Part B (the supplementary
medical insurance program) but furnished to SNF residents during a Part A covered
stay other than the following:
• Physician services, physician assistant services, nurse practitioner and
clinical nurse specialist services, certified mid-wife services, qualified
psychologist services, marriage and family therapist services, mental health
counselor services, certified registered nurse anesthetist services, certain
dialysis-related services, erythropoietin (EPO) for certain dialysis patients,
hospice care related to a terminal condition, ambulance trips that convey a
beneficiary to the SNF for admission or from the SNF following discharge,
ambulance transportation related to dialysis services, certain services
involving chemotherapy and its administration, radioisotope services, certain
customized prosthetic devices, certain blood clotting factors and, for services
furnished during 1998 only, the transportation costs of electrocardiogram
equipment for electrocardiogram test services.
Certain additional outpatient hospital services (along with ambulance transportation
that conveys a beneficiary to a hospital or CAH to receive the additional services) are

excluded from coverage under SNF PPS and are billed separately. The additional
services are:
• Cardiac catheterization services;
• Computerized axial tomography (CT scans);
• Magnetic resonance imaging (MRIs);
• Radiation therapy;
• Ambulatory surgery involving the use of a hospital operating room;
• Emergency services;
• Angiography services; and
• Lymphatic and venous procedures.
The CMS identifies the above services using HCPCS codes that are periodically
updated.
The CMS publishes the HCPCS coding changes in each year via a Recurring Update
Notification. Other updates for the remaining quarters of the FY will occur as needed
due to the creation of new temporary codes representing services included in SNF
PPS prior to the next annual update. To view the online code list of exclusions from
consolidated billing (CB, the SNF “bundling” requirement), go to the CB Overview
page at www.cms.gov/Medicare/Billing/SNFConsolidatedBilling/index.html and
proceed as follows:
• In the left-hand column of the CB Overview page, scroll down to the
applicable Part A MAC (Medicare Administrative Contractor) Update to
access the list of excluded codes that are billable by institutional providers
(similar information is available for practitioners and other noninstitutional
suppliers on the applicable Part B MAC Update). To view the most current
update (the one that displays the most recent set of revisions to the code list),
click on the “Part A MAC Update” link for the current year. This directs to a
page that lists by Major Category (indicating the type of service) the specific
changes in coding for this year.
• To see a complete list of the CB exclusions (along with the ambulatory
surgery and Part B therapy inclusions), scroll down the Part A MAC Update
page to the “Downloads” section. Then, click on the link to the zipped file
entitled “Annual SNF Consolidated Billing HCPCS Updates” for the current
year. Once this file is unzipped, the complete exclusion list can be selected in

either Microsoft Excel or Text formats, and can then be searched for
individual codes.
• For a general explanation of the types of services encompassed by each of
the Major Categories, scroll down the Part A MAC Update page to the
“Downloads” section, and click on the link to the “General Explanation of the
Major Categories.” (For example, Major Category III.A lists the excluded
chemotherapy codes, and Major Category III.B lists the excluded
chemotherapy administration codes.)
For further information on the SNF CB provision, see Pub. 100-04, Medicare Claims
Processing Manual, chapter 6, sections 10 through 20.6.
10.3 - Hospital Providers of Extended Care Services
(Rev. 228, Issued: 10-13-16, Effective: 10-18-16, Implementation: 10-18-16)
In order to address the shortage of rural SNF beds for Medicare patients, rural hospitals
with fewer than 100 beds may be reimbursed under Medicare for furnishing post-hospital
extended care services to Medicare beneficiaries. Such a hospital, known as a swing bed
facility, can “swing” its beds between the hospital and SNF levels of care, on an as-
needed basis, if it has obtained a swing bed approval from the Department of Health and
Human Services. See Pub. 100-01, Medicare General Information, Eligibility, and
Entitlement Manual, Chapter 5, Section 30.3 (“Hospital Providers of Extended Care
Services”) for a description of general rules applicable to SNF-level services furnished in
hospital swing beds; also, see Pub. 100-04, Medicare Claims Processing Manual, chapter
6, sections 100ff regarding SNF PPS billing procedures for SNF-level services furnished
in rural (non-CAH) swing-bed hospitals.
When a hospital is providing extended care services, it will be treated as a SNF for
purposes of applying coverage rules. This means that services provided in the swing bed
are subject to the same Part A coverage, deductible, coinsurance and physician
certification/recertification provisions that are applicable to SNF extended care services.
The SNF coverage provisions are set forth in 42 CFR 409 Subpart D and are more fully
explained in this chapter. A patient in a swing bed cannot simultaneously receive
coverage for both SNF-level services under Part A and inpatient hospital ancillary
services under Part B.
Swing bed patients who no longer qualify for Part A coverage of SNF-level services
under the Medicare program (due to exhaustion of Part A SNF benefits, dropping below a
SNF level of care, etc.) revert to receipt of a hospital level of care in the swing bed (see
the Medicare Benefit Policy Manual, Chapter 6, “Hospital Services Covered Under Part
B,” §10). Thus, any further Medicare coverage in the swing bed would be for inpatient
hospital ancillary services under Part B, notwithstanding a patient’s eligibility for
Medicaid NF coverage.
A dually-eligible patient who continues to receive a SNF level of care or who has
dropped below the SNF level may nonetheless still qualify for Medicaid coverage of
nursing facility (NF) services, if the hospital has a Medicaid swing bed agreement that
has been approved by the State in which the facility is located. Such agreements permit
Medicaid-participating rural hospitals to use their beds interchangeably to furnish both
acute hospital care and NF care to Medicaid recipients, when no beds are available in
area nursing facilities (see Pub. 45, State Medicaid Manual, chapter 4, section 4560).
20 - Prior Hospitalization and Transfer Requirements
(Rev. 1, 10-01-03)
A3-3131, SNF-212
In order to qualify for post-hospital extended care services, the individual must have been
an inpatient of a hospital for a medically necessary stay of at least three consecutive
calendar days. In addition, effective December 5, 1980, the individual must have been
transferred to a participating SNF within 30 days after discharge from the hospital, unless
the exception in §20.2 applies.
20.1 - Three-Day Prior Hospitalization
(Rev. 10880, Issued: 08-06-21, Effective: 11-08-21, Implementation: 11-08-21)
In accordance with section 226(c)(1)(B) of the Social Security Act and the implementing
regulations at 42 CFR 409.30(a)(2), the hospital discharge must have occurred on or after
the first day of the month in which the individual attained age 65 or, effective July 1,
1973, became entitled to health insurance benefits under the disability or chronic renal
disease provisions of the law. The 3 consecutive calendar day stay requirement can be
met by stays totaling 3 consecutive days in one or more hospitals. In determining
whether the requirement has been met, the day of admission, but not the day of discharge,
is counted as a hospital inpatient day.
Time spent in observation or in the emergency room prior to (or in lieu of) an inpatient
admission to the hospital does not count toward the 3-day qualifying inpatient hospital
stay, as a person who appears at a hospital’s emergency room seeking examination or
treatment or is placed on observation has not been admitted to the hospital as an
inpatient; instead, the person receives outpatient services. For purposes of the SNF
benefit’s qualifying hospital stay requirement, inpatient status commences with the
calendar day of hospital admission. See 31 Fed. Reg. 10116, 10118-19 (July 27, 1966).
To be covered, the extended care services must have been for the treatment of a condition
for which the beneficiary was receiving inpatient hospital services (including services of
an emergency hospital) or a condition which arose while in the SNF for treatment of a
condition for which the beneficiary was previously hospitalized. In this context, the
applicable hospital condition need not have been the principal diagnosis that actually
precipitated the beneficiary’s admission to the hospital, but could be any one of the
conditions present during the qualifying hospital stay.
In addition, the qualifying hospital stay must have been medically necessary. Medical
necessity will generally be presumed to exist. When the facts that come to the A/B
MACs (A) attention during the course of its normal claims review process indicate that
the hospitalization may not have been medically necessary, it will fully develop the case,
checking with the attending physician and the hospital, as appropriate. The A/B MAC
will rule the stay unnecessary only when hospitalization for 3 days represents a
substantial departure from normal medical practice. However, in accordance with Pub.
100-04, Medicare Claims Processing Manual, Chapter 30, §130.2.A, when a beneficiary
qualifies for limitation on liability in connection with the hospital stay (or a portion
thereof), this conclusively establishes that the hospital stay (or portion thereof) was not
medically necessary.
Even if a beneficiary’s care during a qualifying hospital stay becomes less intensive
during the latter part of the stay, the date of hospital “discharge” in this context is still
considered to be the day that the beneficiary physically leaves the hospital, and the level
of care being furnished at that particular point is not a determining factor as long as some
portion of the stay included at least 3 consecutive days of medically necessary inpatient
hospital services. In addition, when a hospital inpatient’s care needs drop from acute- to
SNF-level but no SNF bed is available, the regulations at 42 CFR 424.13(c) permit a
physician to certify that the beneficiary’s continued inpatient stay in the hospital is, in
fact, medically necessary under this particular set of circumstances (see also Pub. 100-01,
Medicare General Information, Eligibility, and Entitlement Manual, Chapter 4, §10.6).
Accordingly, such additional, “alternate placement” days spent in the hospital can be
included in the 3-day count toward meeting the SNF benefit’s qualifying hospital stay
requirement.
The 3-day hospital stay need not be in a hospital with which the SNF has a transfer
agreement (see Pub. 100-01, Medicare General Information, Eligibility, and Entitlement
Manual, Chapter 5, §30.2 for a discussion of the SNF’s required transfer agreement with
a hospital). However, the hospital must be either a Medicare-participating hospital or an
institution that meets at least the conditions of participation for an emergency services
hospital (see Pub. 100-01, Medicare General Information, Eligibility, and Entitlement
Manual, Chapter 5, §20.2, for the definition of an emergency services hospital). A
nonparticipating psychiatric hospital need not meet the special requirements applicable to
psychiatric hospitals (see Pub. 100-01, Medicare General Information, Eligibility, and
Entitlement Manual, Chapter 5, §20.3). Stays in Religious Nonmedical Health Care
Institutions (see Pub. 100-01, Medicare General Information, Eligibility, and Entitlement
Manual, Chapter 5, §40, for definition of RNHCIs) are excluded for the purpose of
satisfying the 3-day period of hospitalization. See Pub. 100-02, Medicare Benefit Policy
Manual, Chapter 9, §40.1.5, regarding a qualifying stay that consists of “general inpatient
care” furnished in a hospital under the hospice benefit.
NOTE: While a 3-day stay in a psychiatric hospital satisfies the prior hospital stay
requirement, institutions that primarily provide psychiatric treatment cannot participate in
the program as SNFs. Therefore, a patient with only a psychiatric condition who is
transferred from a psychiatric hospital to a participating SNF is likely to receive only
non-covered care. In the SNF setting, the term “non-covered care” refers to any level of
care less intensive than the SNF level of care that is covered under the program. (See
§§30ff.).
20.1.1 - Three-Day Prior Hospitalization - Foreign Hospital
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
Regardless of whether a foreign hospital stay is itself coverable under the heading of
“foreign hospital services” (see Pub. 100-04, Medicare Claims Processing Manual,
chapter 32, §§350ff. for a description of the foreign hospital services that are payable by
Medicare), an inpatient stay of 3 or more days in a hospital outside the United States may
nevertheless satisfy the prior inpatient stay requirement for post-hospital extended care
services within the United States as long as the foreign hospital can qualify as an
“emergency hospital” (see Pub. 100-01, Medicare General Information, Eligibility, and
Entitlement Manual, chapter 5, §20.2, for the definition of an emergency services
hospital). If a stay of 3 or more days in a hospital outside the United States is being
considered to satisfy the prior inpatient stay requirement, the SNF will submit
documentation to the A/B MAC (A). This evidence will be either:
A. An itemized bill or hospital form prepared by the foreign hospital showing dates
of admission and discharge and a description of the illness or injury treated
(obtained from the beneficiary); or
B. A medical report prepared by the foreign hospital and sent to the patient’s U.S.
physician showing dates of admission and discharge and a description of the
illness or injury treated (obtained from the physician).
If neither type of evidence can be obtained, the SNF will secure whatever information is
available for submission to the A/B MAC (A). When the A/B MAC (A) receives a bill
involving a prior inpatient stay in a foreign hospital, it contacts the regional office for a
determination as to whether the prior stay requirement is met. If the regional office states
the hospital does not qualify as an “emergency hospital,” the A/B MAC (A) advises the
provider that the prior inpatient stay requirement is not met.
If the regional office states the hospital qualifies as an “emergency hospital” and
documentation is submitted as outlined in either §§20.2.1 or 20.2.2 which otherwise
meets the prior-stay requirement, the A/B MAC (A) processes the SNF claim.
20.2 - Thirty-Day Transfer
(Rev. 1, 10-01-03)
A3-3131.3, SNF-212.3

20.2.1 - General
(Rev. 161, Issued: 10-26-12, Effective: 04-01-13, Implementation: 04-01-13)
A3-3131.3.A, SNF-212.3.A
Post-hospital extended care services represent an extension of care for a condition for
which the individual received inpatient hospital services. Extended care services are
“post-hospital” if initiated within 30 days after discharge from a hospital stay that
included at least three consecutive days of medically necessary inpatient hospital
services. In certain circumstances the 30-day period may be extended, as described in
§20.2.2 below. Even if a beneficiary’s care during a qualifying hospital stay becomes
less intensive during the latter part of the stay, the date of hospital “discharge” in this
context is still considered to be the day that the beneficiary physically leaves the hospital,
and the level of care being furnished at that particular point is not a determining factor as
long as some portion of the stay included at least 3 consecutive days of medically
necessary inpatient hospital services.
In determining the 30-day transfer period, the day of discharge from the hospital is not
counted in the 30 days. For example, a patient discharged from a hospital on August 1
and admitted to a SNF on August 31 was admitted within 30 days. The 30-day period
begins on the day following actual discharge from the hospital and continues until the
individual is admitted to a participating SNF, and requires and receives a covered level of
care. Thus, an individual who is admitted to a SNF within 30 days after discharge from a
hospital, but does not require a covered level of care until more than 30 days after such
discharge, does not meet the 30-day requirement. (See §20.2.2 below for an exception
under which such services may be covered.) Conversely, as long as a covered level of
care is needed and initiated in the SNF within the specified timeframe, the timely transfer
requirement is considered to be met even if actual Medicare payment does not
commence until later (for example, in a situation where another payment source that is
primary to Medicare has assumed financial responsibility for the initial portion of the
SNF stay).
If an individual whose SNF stay was covered upon admission is thereafter determined not
to require a covered level of care for a period of more than 30 days, payment could not be
resumed for any extended care services he or she may subsequently require, even though
he or she has remained in the facility, until the occurrence of a new qualifying hospital
stay. In the absence of a new qualifying hospital stay, such services could not be deemed
to be “post-hospital” extended care services. (For exception, see §20.2.2 below.)
20.2.2 - Medical Appropriateness Exception
(Rev. 1, 10-01-03)
A3-3131.3.B, SNF-212.3.B
An elapsed period of more than 30 days is permitted for SNF admissions where the
patient’s condition makes it medically inappropriate to begin an active course of
treatment in a SNF immediately after hospital discharge, and it is medically predictable at
the time of the hospital discharge that he or she will require covered care within a
predeterminable time period. The fact that a patient enters a SNF immediately upon
discharge from a hospital, for either covered or noncovered care, does not necessarily
negate coverage at a later date, assuming the subsequent covered care was medically
predictable.
20.2.2.1 - Medical Needs Are Predictable
(Rev. 1, 10-01-03)
A3-3131.3.B.1, SNF-212.3.B.1
In determining the type of case that this exception is designed to address, it is necessary
to recognize the intent of the extended care benefit. The extended care benefit covers
relatively short-term care when a patient requires skilled nursing or skilled rehabilitation
services as a continuation of treatment begun in the hospital. The requirement that
covered extended care services be provided in a SNF within 30 days after hospital
discharge is one of the means of assuring that the SNF care is related to the prior hospital
care.
This exception to the 30-day requirement recognizes that for certain conditions, SNF care
can serve as a necessary and proper continuation of treatment initiated during the hospital
stay, although it would be inappropriate from a medical standpoint to begin such
treatment within 30 days after hospital discharge. Since the exception is intended to
apply only where the SNF care constitutes a continuation of care provided in the hospital,
it is applicable only where, under accepted medical practice, the established pattern of
treatment for a particular condition indicates that a covered level of SNF care will be
required within a predeterminable time frame. Accordingly, to qualify for this exception
it must be medically predictable at the time of hospital discharge that a covered level of
SNF care will be required within a predictable period of time for the treatment of a
condition for which hospital care was received and the patient must begin receiving such
care within that time frame.
An example of the type of care for which this provision was designed is care for a person
with a hip fracture. Under the established pattern of treatment of hip fractures it is known
that skilled therapy services will be required subsequent to hospital care, and that they
can normally begin within four to six weeks after hospital discharge, when weight
bearing can be tolerated. Under the exception to the 30-day rule, the admission of a
patient with a hip fracture to a SNF within 4 to 6 weeks after hospital discharge for
skilled care, which as a practical matter can only be provided on an inpatient basis by a
SNF, would be considered a timely admission.
20.2.2.2 - Medical Needs Are Not Predictable
(Rev. 1, 10-01-03)
A3-3131.3.B.2, SNF-212.3.B.2
When a patient’s medical needs and the course of treatment are not predictable at the
time of hospital discharge because the exact pattern of care required and the time frame
in which it will be required is dependent on the developing nature of the patient’s
condition, an admission to a SNF more than 30 days after discharge from the hospital is
not justified under this exception to the 30-day rule. For example, in some situations the
prognosis for a patient diagnosed as having cancer is such that it can reasonably be
expected that additional care will be required at some time in the future. However, at the
time of discharge from the hospital it is difficult to predict the actual services that will be
required, or the time frame in which the care will be needed. Similarly, it is not known in
what setting any future necessary services will be required; i.e., whether the patient will
require the life-supporting services found only in the hospital setting, the type of care
covered in a SNF, the intermittent type of care which can be provided by a home health
agency, or custodial care which may be provided either in a nursing home or the patient’s
place of residence. In some instances such patients may require care immediately and
continuously; others may not require any skilled care for much longer periods, perhaps
measured in years. Therefore, since in such cases it is not medically predictable at the
time of the hospital discharge that the individual will require covered SNF care within a
predeterminable time frame, such cases do not fall within the 30-day exception.
20.2.2.3 - SNF Stay Prior to Beginning of Deferred Covered Treatment
(Rev. 1, 10-01-03)
A3-3131.3.B.3, SNF-212.3.B.3
In some cases where it is medically predictable that a patient will require a covered level
of SNF care within a predeterminable time frame, the individual may also have a need for
a covered level of SNF care within 30 days of hospital discharge. In such situations, this
need for covered SNF care does not negate further coverage at a future date even if there
is a noncovered interval of more than 30 days between the two stays, provided all other
requirements are met. (See example 1 below.) However, this rule applies only where
part of the care required involves deferred care, which was medically predictable at the
time of hospital discharge. If the deferred care is not medically predictable at the time of
hospital discharge, then coverage may not be extended to include SNF care following an
interval of more than 30 days of noncovered care (see example 2). Where it is medically
predictable that a patient will require a covered level of SNF care within a specific time
frame, the fact that an individual enters a SNF immediately upon discharge from the
hospital for noncovered care does not negate coverage at a later date, assuming the
requirements of the law are met (see example 3).
EXAMPLE 1:
A patient who has had an open reduction of a fracture of the femoral neck and has a
history of diabetes mellitus and angina pectoris is discharged from the hospital on
January 30, 1991 and admitted immediately to a SNF. He requires, among other services,
careful skin care, appropriate oral medications, a diabetic diet, a therapeutic exercise
program to preserve muscle tone and body condition, and observation to detect signs of
deterioration in his condition or complications resulting from his restricted mobility,
which necessitates skilled management of his care to ensure his safety and recovery. It is
medically predictable that when he is medically allowed to bear weight on the affected
limb, skilled rehabilitative services will be required. After he is in the SNF for two days,
he becomes unhappy and at his request is released to his home in the care of a full time
private duty nurse. Five weeks later, when he reaches weight bearing, he is readmitted to
the SNF for the needed rehabilitative care. The patient would be eligible for coverage
under the program for the care furnished him during both of these stays.
EXAMPLE 2:
An individual is admitted to a SNF for daily skilled rehabilitative care that, as a practical
matter, can be provided only on an inpatient basis in a SNF. After three weeks, the
therapy is discontinued because the patient’s condition has stabilized and daily skilled
services are no longer required. Six weeks later, however, as a result of an unexpected
change in the patient’s condition, daily skilled services are again required. Since the
second period of treatment did not constitute care which was predictable at the time of
hospital discharge and thus could not be considered as care which was deferred until
medically appropriate, it would not represent an exception to the 30-day exception rule.
Therefore, since more than 30 days of noncovered care had elapsed between the last
period of covered care and the reinstitution of skilled services, payment could not be
made under the extended care benefit for the latter services.
EXAMPLE 3:
A patient whose right leg was amputated was discharged from the hospital and admitted
directly to a SNF on January 30, 1991. Although upon admission to the SNF the patient
required help with meeting his activities of daily living, he did not require daily skilled
care. Subsequently, however, after the stump had healed, daily skilled rehabilitative
services designed to enable him to use a prosthesis were required. Since at the time of
the patient’s discharge from the hospital it was medically predictable that covered SNF
care would be required at a predeterminable time interval, and since such care was
initiated when appropriate, the patient would be entitled to extended care benefits for the
period during which such care was provided.
20.2.2.4 - Effect of Delay in Initiation of Deferred Care
(Rev. 1, 10-01-03)
A3-3131.3.B.4, SNF-212.3.B.4
As indicated, where the required care commences within the anticipated time frame, the
transfer requirement would be considered met even though more than 30 days have
elapsed. However, situations may occur where complications necessitate delayed

initiation of the required care and treatment beyond the usual anticipated time frame (e.g.,
skilled rehabilitative services which will enable an amputee patient to use a prosthetic
device must be deferred due to an infection in the stump). In such situations, the 30-day
transfer requirement may still be met even though care is not started within the usual
anticipated time frame, if the care is begun as soon as medically possible and the care at
that time is still reasonable and necessary for the treatment of a condition for which the
patient received inpatient hospital care.
20.2.2.5 - Effect on Spell of Illness
(Rev. 228, Issued: 10-13-16, Effective: 10-18-16, Implementation: 10-18-16)
In the infrequent situation where the patient has been discharged from the hospital to his
or her home more than 60 days before he or she is ready to begin a course of deferred
care in a SNF, a new spell of illness begins with the day the beneficiary enters the SNF
thereby generating another 100 days of extended care benefits (see Pub. 100-01,
Medicare General Information, Eligibility, and Entitlement Manual, Chapter 3, section
10.4.1). Another qualifying hospital stay would not be required, providing the care
furnished is clearly related to a hospital stay in the previous spell of illness and represents
care for which the need was predicted at the time of discharge from such hospital stay.
20.2.3 - Readmission to a SNF
(Rev. 242, Issued: 03-16-18, Effective: 06-19-18; Implementation: 06-19-18)
If an individual who is receiving covered post-hospital extended care, leaves a SNF and
is readmitted to the same or any other participating SNF for further covered care within
30 days after the day of discharge, the 30-day transfer requirement is considered to be
met. The same is true if the beneficiary remains in the SNF to receive custodial care
following a covered stay, and subsequently develops a renewed need for covered care
there within 30 consecutive days after the first day of noncoverage. Thus, the period of
extended care services may be interrupted briefly and then resumed, if necessary, without
hospitalization preceding the resumption of SNF coverage. (See §§20.2.2 and 20.2.2.3
above for situations where a period of more than 30 days between SNF discharge and
readmission, or more than 30 days of noncovered care in a SNF, is followed by later
covered care.)
20.3 – Payment Bans
(Rev. 1, 10-01-03)
A-01-131
20.3.1 - Payment Bans on New Admissions
(Rev. 1, 10-01-03)
Under the Social Security Act at §§1819(h) and 1919(h) and CMS’ regulations at 42 CFR
488.417, CMS may impose a denial of payment for new admissions (DPNA) against a
SNF when CMS finds that a facility is not in substantial compliance with requirements of

participation. Further, the regulations require CMS to impose a DPNA when a SNF (1)
fails to be in substantial compliance for three months after the last day of the survey
identifying the noncompliance, or (2) is found to have provided substandard quality of
care on the last three consecutive standard surveys. A/B MACs (A) are responsible for
applying these payment sanctions to new SNF admissions resulting from adverse survey
findings.
The SNFs under a denial of payment sanction are still considered Medicare-participating
providers.
Imposition of a payment ban on SNF new admissions is described in 42 CFR 488.401. In
applying payment bans, refer to the following definition of “new admission” to a SNF
contained in 42 CFR 488.401.
[a] resident who is admitted to the facility on or after the effective date of a denial
of payment remedy and, if previously admitted, has been discharged before that
effective date. Residents admitted before the effective date of the denial of
payment, and taking temporary leave, are not considered new admissions, nor
subject to the denial of payment.
“Temporary leave” is defined as residents who leave temporarily for any reason. This
definition would include both beneficiaries who are out of the SNF at midnight but who
later return to the SNF and beneficiaries who require inpatient hospitalization and return
to the SNF directly upon hospital discharge. If residents were not subject to a denial of
payment when they went on temporary leave, they are not, upon their return, considered
new admissions for the purposes of the denial of payment. A beneficiary is considered
discharged when he/she leaves the facility with no expectation of return, e.g., a
beneficiary transferred to another SNF or discharged to home, etc.
Beneficiaries admitted before the effective date of the denial of payment and taking
temporary leave, whether to receive inpatient hospital care, outpatient services, or as
therapeutic leave, are not considered new admissions, and are not subject to the denial of
payment upon return. This policy applies even if there are multiple hospitalizations and
returns to the SNF during the period sanctions are in effect. However, a resident who is
discharged to a different SNF and is later readmitted to the original SNF, currently under
a payment ban, will be subject to the denial of payment sanction. Similarly, a beneficiary
who is discharged from an acute care hospital to a long-term rehabilitation hospital, a
wing bed, or a hospice would be considered a new admission upon return to the original
SNF.
Beneficiaries enrolled through cost-based HMOs are subject to the same requirements as
fee-for-service beneficiaries.
Hospices contract with SNFs for services related to the beneficiary’s terminal condition.
These bills are not processed by the A/B MAC (A) or (HHH). However, there will be
situations where a beneficiary is admitted as a hospice patient, but later requires daily
skilled care unrelated to the terminal condition. If the beneficiary was initially admitted
as a hospice patient prior to the date sanctions were imposed, and meets the requirements
for Part A coverage; sanctions will not be applicable. Benefits will be paid under SNF
PPS from the first date the beneficiary qualifies for Medicare Part A for care unrelated to
the terminal condition. The facility must complete the Medicare-required assessments
from the start of care for the unrelated condition.
20.3.1.1 - Beneficiary Notification
(Rev. 1, 10-01-03)
Before admitting a beneficiary, the SNF must notify the beneficiary or responsible family
member that sanctions have been imposed, and explain how the sanctions will affect the
beneficiary’s benefits. This Notice of Non-Coverage also applies to former residents that
had been discharged with no expectation of return and are being readmitted after the
imposition of the payment ban. SNFs failing to provide this notification will be held
liable for all Part A services covered under SNF PPS. The beneficiary notice must meet
the following criteria:
a. It must be in writing.
b. It must explain the reason sanctions were imposed.
c. It must explain the beneficiary’s liability for the cost of SNF services during the
period the payment ban is in effect.
d. It must explain that Medicare Part A benefits may be available if the beneficiary
chooses a different Medicare-participating SNF that is not under sanction.
20.3.1.2 - Readmissions and Transfers
(Rev. 1, 10-01-03)
When determining if the beneficiary was admitted prior to the imposition of the ban, the
actual status of the beneficiary rather than the primary payor is the determining factor.
Therefore, there may be situations where the beneficiary is a private pay patient or a dual
eligible who was receiving Medicaid benefits prior to the imposition of the payment ban.
If this private pay patient or dual eligible goes to the hospital for needed care, and meets
the Medicare Part A criteria upon return to the SNF, the readmission is exempt from the
denial of payment sanction.
20.3.1.3 - Sanctions Lifted: Procedures for Beneficiaries Admitted
During the Sanction Period
(Rev. 1, 10-01-03)
For new admissions to certified beds, Medicare payments for eligible beneficiaries should
begin on the date the sanction is lifted. The beneficiary must meet technical eligibility
requirements (e.g., a 3-day hospital stay, etc.), services must be reasonable and necessary

and the beneficiary must be receiving skilled care. The date the sanction is lifted is
considered the first day of the Part A stay.
For SNF PPS payment purposes, the period between the actual date of admission and the
last day the sanction was in effect should be billed as non-covered days.
20.3.1.4 - Payment Under Part B During a Payment Ban on New
Admissions
(Rev. 1, 10-01-03)
Facilities subject to a payment ban may continue to bill services for beneficiaries who are
not in a Part A stay in the same way as any other SNF. However, services that would
have been payable to the SNF as Part A benefits in the absence of a payment sanction
must not be billed to either the A/B MAC (A) or the A/B MAC (B) as Part B services.
20.3.1.5 - Impact of Consolidated Billing Requirements
(Rev. 1, 10-01-03)
The SNF may not charge the beneficiary or family members for any services that, in the
absence of a payment sanction, would have been covered under the SNF PPS.
However, the beneficiary is entitled to reimbursement for those services excluded from
the SNF PPS rate. Services excluded from consolidated billing such as outpatient
hospital emergency care and related ambulance service should be billed by the
provider/supplier actually furnishing services, and not by the SNF.
20.3.1.6 - Impact on Spell of Illness
(Rev. 1, 10-01-03)
The SNF days during the sanction period will be used to track breaks in the spell of
illness. A beneficiary’s care in an SNF met the skilled level of care standards if a
Medicare SNF claim for the services provided in the SNF was denied on grounds other
than that the services were not at a skilled level of care. If the patient is receiving a
skilled level of care the benefit period cannot end.
30 - Skilled Nursing Facility Level of Care - General
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132, SNF-214
Care in a SNF is covered if all of the following four factors are met:
• The patient requires skilled nursing services or skilled rehabilitation services, i.e.,
services that must be performed by or under the supervision of professional or
technical personnel (see §§30.2 - 30.4); are ordered by a physician and the
services are rendered for a condition for which the patient received inpatient

hospital services or for a condition that arose while receiving care in a SNF for a
condition for which he received inpatient hospital services;
• The patient requires these skilled services on a daily basis (see §30.6); and
• As a practical matter, considering economy and efficiency, the daily skilled
services can be provided only on an inpatient basis in a SNF. (See §30.7.)
• The services delivered are reasonable and necessary for the treatment of a
patient’s illness or injury, i.e., are consistent with the nature and severity of the
individual’s illness or injury, the individual’s particular medical needs, and
accepted standards of medical practice. The services must also be reasonable in
terms of duration and quantity.
If any one of these four factors is not met, a stay in a SNF, even though it might include
the delivery of some skilled services, is not covered. For example, payment for a SNF
level of care could not be made if a patient needs an intermittent rather than daily skilled
service.
In reviewing claims for SNF services to determine whether the level of care requirements
are met, the A/B MAC (A) first considers whether a patient needs skilled care. If a need
for a skilled service does not exist, then the “daily” and “practical matter” requirements
are not addressed. See section 30.2.2.1 for a discussion of the role of appropriate
documentation in facilitating accurate coverage determinations for claims involving
skilled care. Additional material on documentation appears in the various clinical
scenarios that are presented throughout these level of care guidelines.
Coverage of nursing care and/or therapy to perform a maintenance program does not turn
on the presence or absence of an individual’s potential for improvement from the nursing
care and/or therapy, but rather on the beneficiary’s need for skilled care.
Eligibility for SNF Medicare A coverage has not changed with the inception of PPS.
However, the skilled criteria and the medical review process have changed slightly. For
Medicare to render payment for skilled services provided to a beneficiary during a SNF
Part A stay, the facility must complete an MDS.
EXAMPLE: Even though the irrigation of a suprapubic catheter may be a skilled
nursing service, daily irrigation may not be “reasonable and necessary” for the treatment
of a patient’s illness or injury.
30.1 – Administrative Level of Care Presumption
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
Under the SNF PPS, beneficiaries who are admitted (or readmitted) directly to a SNF
after a qualifying hospital stay are considered to meet the level of care requirements of 42
CFR 409.31 up to and including the assessment reference date (ARD) for the initial
Medicare assessment prescribed in 42 CFR 413.343(b), when correctly assigned one of
the case-mix classifiers that CMS designates for this purpose as representing the required
level of care. While this assessment is commonly referred to as the “5-day” assessment
(reflecting its original 5-day assessment window), an additional 3 grace days have always
been available beyond that window for actually setting the ARD; further, as of October 1,
2019, those additional 3 grace days are directly incorporated into the assessment window
itself, thus resulting in an overall 8-day assessment window. The current set of case-mix
classifier designations appears in the paragraph entitled “Case Mix Adjustment” on the
SNF PPS web site, at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-
Payment/SNFPPS/index.html. If the beneficiary is not admitted (or readmitted) directly
to a SNF after a qualifying hospital stay, the administrative level of care presumption
does not apply.
For purposes of this presumption, the assessment reference date is defined in accordance
with 42 CFR 483.315(d), and must be set for no later than the eighth day of posthospital
SNF care. Consequently, if the ARD for the initial Medicare assessment prescribed in 42
CFR 413.343(b) is set for day 9, or later, the administrative level of care presumption
does not apply. The coverage that arises from this presumption remains in effect only for
as long thereafter as it continues to be supported by the facts of the beneficiary’s
condition and care needs. Accordingly, the SNF is expected to monitor carefully for and
document any changes in the patient’s condition, in order to determine the continuing
need for Part A SNF benefits after the ARD. Moreover, this administrative presumption
does not apply to any subsequent assessments.
To be correctly assigned, the data coded on the Resident Assessment Instrument (RAI)
must be accurate and meet the definitions described in the Long Term Care Facility RAI
User’s Manual. The beneficiary must receive services in the SNF that are reasonable and
necessary. Services provided to the beneficiary during the hospital stay are reviewed to
ensure proper coding of the most recent version of the RAI. The two examples illustrated
below demonstrate a correct assignment and an incorrect assignment.
Incorrect Assignment: IV med provided in hospital coded on MDS, but IV was for a
surgical procedure only – as a consequence, the MDS is not
accurate and the presumption does not apply (see Chapter 3,
Section P of the RAI).
Correct Assignment: Beneficiary is receiving oxygen therapy as well as rehab service.
The respiratory therapy services are found reasonable and
necessary; however, the rehab services are found not reasonable
and necessary, resulting in a revised case-mix classification.
Beneficiary was and is now correctly assigned – presumption
applies.
A beneficiary who is not assigned one of the case-mix classifiers designated as
representing the required level of care on the initial Medicare assessment prescribed in 42
CFR 413.343(b) is not automatically classified as meeting or not meeting the SNF level
of care definition. Instead, the beneficiary must receive an individual level of care
determination using existing administrative criteria and procedures.
The following scenarios further clarify that a beneficiary’s correct assignment of one of
the case-mix classifiers that CMS designates for this purpose as representing the required
level of care would serve to trigger the coverage presumption under the initial Medicare
assessment only when that assessment occurs directly following the beneficiary’s
discharge from the qualifying hospital stay (i.e., the hospital discharge and subsequent
SNF admission both occur on the same day).
1. Routine SNF Admission Directly From Qualifying Hospital Stay
If the beneficiary is admitted to the SNF immediately following a 3-day qualifying
hospital stay, there is a presumption that he or she meets the Medicare level of care
criteria when correctly assigned one of the case-mix classifiers that CMS designates for
this purpose as representing the required level of care. The presumption lasts through the
assessment reference date of the initial Medicare assessment, which must be set for no
later than the eighth day of the stay.
2. Admission to SNF does not immediately follow discharge from the qualifying hospital
stay, but occurs within 30 days (as required under the “30 day transfer” rule)
If the beneficiary is discharged from the hospital to a setting other than the SNF, the
presumption of coverage does not apply, even if the beneficiary’s SNF admission occurs
within 30 days of discharge from the qualifying hospital stay. Accordingly, coverage
would be determined based on a review of the medical evidence in the file.
3. SNF Resident is Re-Hospitalized and Then Returns Directly to the SNF
If a beneficiary who has been in a covered Part A stay requires readmission to a hospital,
and subsequently returns directly to the SNF for continuing care, a new initial Medicare
assessment under the regulations at 42 CFR 413.343(b) would be required if the
beneficiary’s absence from the SNF exceeds the 3-day interruption window specified
under the SNF PPS’s interrupted stay policy (see Pub. 100-04, Medicare Claims
Processing Manual, Chapter 6, §120.2). In this scenario, there is a presumption that he or
she meets the level of care criteria upon direct readmission from the hospital to the SNF
when correctly assigned one of the case-mix classifiers that CMS designates for this
purpose as representing the required level of care. The resulting presumption of coverage
lasts through the assessment reference date (ARD) of that assessment, which must be set
for no later than the eighth day of the stay. Alternatively, if the absence from the SNF
does not exceed the 3-day interruption window, the beneficiary’s return to the same SNF
would represent a continuation of the previous SNF stay; as such, there would be no new
initial Medicare assessment and no new presumption of coverage; however, any days
remaining from the previous presumption would continue to apply through the ARD of
the original assessment.
4. Routine SNF Admission Directly From Qualifying Hospital Stay, but Initial Portion of
SNF Stay Covered by Another Insurer (Medicare as Secondary Payer)
When a beneficiary goes directly from a qualifying hospital stay to the SNF, but the
initial portion of the SNF stay is covered by another insurer that is primary to Medicare,
Medicare coverage would not start until coverage by the primary insurer ends.
Accordingly, the Medicare required assessment schedule would not begin until the first
day of Medicare coverage. If a beneficiary met the level of care criteria for Medicare
coverage during the first 8 days of the stay following a qualifying hospital stay, and the
other insurer covered this part of the stay, there is no presumption. If Medicare becomes
primary before the eighth day of the stay following a qualifying hospital stay, the
presumption would apply through the assessment reference date on the initial Medicare
assessment or, if earlier, the eighth day of the stay.
5. Readmission to SNF Within 30 Days After Discharge From Initial SNF Stay – No
Intervening Hospitalization
As noted in scenario 1, if a beneficiary is initially admitted to the SNF directly from the
qualifying hospital stay for a covered Part A SNF stay, the presumption for that stay is
applicable when the beneficiary is correctly assigned one of the case-mix classifiers that
CMS designates for this purpose as representing the required level of care. However, if
that beneficiary is discharged to a non-hospital setting and then subsequently readmitted
to the SNF beyond the 3-day interruption window as described in scenario 3 above, there
is no presumption applicable to the second SNF admission. (If the beneficiary is
transferred to a hospital, and returns directly to the SNF, see scenario 3 above).
Alternatively, if the absence from the SNF does not exceed the 3-day interruption
window, the beneficiary’s return to the same SNF would represent a continuation of the
previous SNF stay; as such, any days remaining from the previous presumption would
continue to apply through the ARD of the original assessment.
6. Initial, Non-Medicare SNF Stay Followed by Qualifying Hospitalization and
Readmission to SNF for Medicare Stay
Dually eligible (Medicare/Medicaid) beneficiaries whose initial stay in the SNF is either
Medicaid-covered or private pay, are eligible for the Medicare presumption of coverage
when readmitted directly to the SNF following a qualifying hospitalization, when
correctly assigned one of the case-mix classifiers that CMS designates for this purpose as
representing the required level of care. (Of course, in order to qualify for Medicare
coverage upon readmission, the beneficiary must be placed in the portion of the
institution that is actually certified by Medicare as a SNF.) No presumption of coverage
applies when Medicare is the secondary payer for days 1 through 8 of the covered stay
where Medicare becomes primary after day 8 due to a reversal or denial by the secondary
insurer.
7. Transfer From One SNF to Another
There is no presumption of coverage in cases involving the transfer of a beneficiary from
one SNF to another or from SNF-level care in a hospital swing bed to a SNF. The
presumption only applies to the SNF stay that immediately follows the qualifying
hospital stay when the beneficiary is correctly assigned one of the case-mix classifiers
that CMS designates for this purpose as representing the required level of care.
Therefore, in cases involving transfer of a beneficiary from a swing-bed hospital to a
SNF, the presumption only applies if the beneficiary was receiving acute care (rather than
SNF-level care) immediately prior to discharge from the swing-bed hospital.
30.2 - Skilled Nursing and Skilled Rehabilitation Services
(Rev. 1, 10-01-03)
A3-3132.1, SNF-214.1
30.2.1 - Skilled Services Defined
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
Skilled nursing and/or skilled rehabilitation services are those services, furnished
pursuant to physician orders, that:
• Require the skills of qualified technical or professional health personnel such as
registered nurses, licensed practical (vocational) nurses, physical therapists,
occupational therapists, and speech-language pathologists or audiologists; and
• Must be provided directly by or under the general supervision of these skilled
nursing or skilled rehabilitation personnel to assure the safety of the patient and to
achieve the medically desired result.
NOTE: “General supervision” requires initial direction and periodic inspection of the
actual activity. However, the supervisor need not always be physically present or on the
premises when the assistant is performing services.
Skilled care may be necessary to improve a patient’s current condition, to maintain the
patient’s current condition, or to prevent or slow further deterioration of the patient’s
condition.
30.2.2 - Principles for Determining Whether a Service is Skilled
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.1.B, SNF-214.1.B
• If the inherent complexity of a service prescribed for a patient is such that it can
be performed safely and/or effectively only by or under the general supervision of
skilled nursing or skilled rehabilitation personnel, the service is a skilled service;
e.g., the administration of intravenous feedings and intramuscular injections; the
insertion of suprapubic catheters; and ultrasound, shortwave, and microwave
therapy treatments.

• The A/B MAC (A) considers the nature of the service and the skills required for
safe and effective delivery of that service in deciding whether a service is a skilled
service. While a patient’s particular medical condition is a valid factor in
deciding if skilled services are needed, a patient’s diagnosis or prognosis should
never be the sole factor in deciding that a service is not skilled.
EXAMPLE: When rehabilitation services are the primary services, the key issue is
whether the skills of a therapist are needed. The deciding factor is not the patient’s
potential for recovery, but whether the services needed require the skills of a therapist
or whether they can be provided by nonskilled personnel. (See §30.5.)
• A service that is ordinarily considered nonskilled could be considered a skilled
service in cases in which, because of special medical complications, skilled
nursing or skilled rehabilitation personnel are required to perform or supervise it
or to observe the patient. In these cases, the complications and special services
involved must be documented by physicians' orders and notes as well as nursing
or therapy notes.
EXAMPLE:
Whirlpool baths do not ordinarily require the skills of a qualified physical therapist.
However, the skills, knowledge, and judgment of a qualified physical therapist might be
required where the patient’s condition is complicated by circulatory deficiency, areas of
desensitization, or open wounds. The documentation needs to support the severity of the
circulatory condition that requires skilled care (see section 30.2.2.1).
• In determining whether services rendered in a SNF constitute covered care, it is
necessary to determine whether individual services are skilled, and whether, in
light of the patient’s total condition, skilled management of the services provided
is needed even though many or all of the specific services were unskilled.
EXAMPLE:
An 81-year-old woman who is aphasic and confused, suffers from hemiplegia, congestive
heart failure, and atrial fibrillation, has suffered a cerebrovascular accident, is
incontinent, has a Stage 1 decubitus ulcer, and is unable to communicate and make her
needs known. Even though no specific service provided is skilled, the patient’s condition
requires daily skilled nursing involvement to manage a plan for the total care needed, to
observe the patient’s progress, and to evaluate the need for changes in the treatment plan.
As discussed in section 30.2.2.1 below, the medical condition of the patient must be
described and documented to support the goals for the patient and the need for skilled
nursing services.
• The importance of a particular service to an individual patient, or the frequency
with which it must be performed, does not, by itself, make it a skilled service.
EXAMPLE:
A primary need of a nonambulatory patient may be frequent changes of position in order
to avoid development of decubitus ulcers. However, since such changing of position
does not ordinarily require skilled nursing or skilled rehabilitation personnel, it would not
constitute a skilled service, even though such services are obviously necessary.
• The possibility of adverse effects from the improper performance of an otherwise
unskilled service does not make it a skilled service unless there is documentation
to support the need for skilled nursing or skilled rehabilitation personnel.
Although the act of turning a patient normally is not a skilled service, for some
patients the skills of a nurse may be necessary to assure proper body alignment in
order to avoid contractures and deformities. In all such cases, the reasons why
skilled nursing or skilled rehabilitation personnel are essential must be
documented in the patient’s record.
30.2.2.1 – Documentation to Support Skilled Care Determinations
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
Claims for skilled care coverage need to include sufficient documentation to enable a
reviewer to determine whether—
• Skilled involvement is required in order for the services in question to be
furnished safely and effectively; and
• The services themselves are, in fact, reasonable and necessary for the treatment of
a patient’s illness or injury, i.e., are consistent with the nature and severity of the
individual’s illness or injury, the individual’s particular medical needs, and
accepted standards of medical practice. The documentation must also show that
the services are appropriate in terms of duration and quantity, and that the services
promote the documented therapeutic goals.
Such determinations would be made from the perspective of the patient’s condition when
the services were ordered and what was, at that time, reasonably expected to be
appropriate treatment for the illness or injury. Thus, when a service appears reasonable
and necessary from that perspective, it would not then be appropriate to deny the service
retrospectively merely because the goals of treatment have not yet been achieved.
However, if it becomes apparent at some point that the goal set for the patient is no
longer a reasonable one, then the treatment goal itself should be promptly and
appropriately modified to reflect this, and the patient should then be reassessed to
determine whether the treatment goal as revised continues to require the provision of
skilled services. By the same token, the treatment goal itself cannot be modified
retrospectively, e.g., when it becomes apparent that the initial treatment goal of
restoration is no longer a reasonable one, the provider cannot retroactively alter the initial
goal of treatment from restoration to maintenance. Instead, it would make such a change
on a prospective basis only.
Although the presence of appropriate documentation is not, in and of itself, an element of
the definition of a “skilled” service, such documentation serves as the means by which a
provider would be able to establish and an A/B MAC (A) would be able to confirm that
skilled care is, in fact, needed and received in a given case.
It is expected that the documentation in the patient’s medical record will reflect the need
for the skilled services provided. The patient’s medical record is also expected to provide
important communication among all members of the care team regarding the
development, course, and outcomes of the skilled observations, assessments, treatment,
and training performed. Taken as a whole, then, the documentation in the patient’s
medical record should illustrate the degree to which the patient is accomplishing the
goals as outlined in the care plan. In this way, the documentation will serve to
demonstrate why a skilled service is needed.
Thorough and timely documentation with respect to treatment goals can help clearly
demonstrate a beneficiary’s need for skilled care in situations where such need might not
otherwise be readily apparent, as when the treatment’s purpose changes (for example,
from restoration to maintenance), as well as in establishing the efficacy of care that
serves to prevent or slow decline—where, by definition, there would be no
“improvement” to evaluate. For example, when skilled services are necessary to
maintain the patient’s current condition, the documentation would need to substantiate
that the services of skilled personnel are, in fact, required to achieve this goal. Similarly,
establishing that a maintenance program’s services are reasonable and necessary would
involve regularly documenting the degree to which the program’s treatment goals are
being accomplished. In situations where the maintenance program is performed to
maintain the patient’s current condition, such documentation would serve to demonstrate
the program’s effectiveness in achieving this goal. When the maintenance program is
intended to slow further deterioration of the patient’s condition, the efficacy of the
services could be established by documenting that the natural progression of the patient’s
medical or functional decline has been interrupted. Assessments of all goals must be
performed in a frequent and regular manner so that the resulting documentation provides
a sufficient basis for determining the appropriateness of coverage.
Therefore the patient’s medical record must document as appropriate:
• The history and physical exam pertinent to the patient’s care, (including the
response or changes in behavior to previously administered skilled services);
• The skilled services provided;
• The patient’s response to the skilled services provided during the current visit;
• The plan for future care based on the rationale of prior results.
• A detailed rationale that explains the need for the skilled service in light of the
patient’s overall medical condition and experiences;
• The complexity of the service to be performed;
• Any other pertinent characteristics of the beneficiary.
The documentation in the patient’s medical record must be accurate, and avoid vague or
subjective descriptions of the patient’s care that would not be sufficient to indicate the
need for skilled care. For example, the following terminology does not sufficiently
describe the reaction of the patient to his/her skilled care:
• Patient tolerated treatment well
• Continue with POC
• Patient remains stable
Such phraseology does not provide a clear picture of the results of the treatment, nor the
“next steps” that are planned. Objective measurements of physical outcomes of treatment
should be provided and/or a clear description of the changed behaviors due to education
programs should be recorded so that all concerned can follow the results of the provided
services.
30.2.3 - Specific Examples of Some Skilled Nursing or Skilled
Rehabilitation Services
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.1.C, SNF-214.1.C
The following sections describe specific examples of skilled nursing or skilled
rehabilitation services.
30.2.3.1 - Management and Evaluation of a Patient Care Plan
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.1.C.1, SNF-214.1.C.1
The development, management, and evaluation of a patient care plan, based on the
physician’s orders and supporting documentation, constitute skilled nursing services
when, in terms of the patient’s physical or mental condition, these services require the
involvement of skilled nursing personnel to meet the patient’s medical needs, promote
recovery, and ensure medical safety. However, the planning and management of a
treatment plan that does not involve the furnishing of skilled services may not require
skilled nursing personnel; e.g., a care plan for a patient with organic brain syndrome who
requires only oral medication and a protective environment. The sum total of nonskilled
services would only add up to the need for skilled management and evaluation when the
condition of the beneficiary is such that there is an expectation that a change in condition
is likely without that intervention.
The patient’s clinical record may not always specifically identify “skilled planning and
management activities” as such. Therefore, in this limited context, if the documentation
of the patient’s overall condition substantiates a finding that the patient’s medical needs
and safety can be addressed only if the total care, skilled or not, is planned and managed
by skilled nursing personnel, it is appropriate to infer that skilled management is being
provided, but only if the record as a whole clearly establishes that there was a likely
potential for serious complications without skilled management, as illustrated in the
following Examples.
EXAMPLE 1:
An aged patient with a history of diabetes mellitus and angina pectoris is recovering from
an open reduction of the neck of the femur. He requires, among other services, careful
skin care, appropriate oral medications, a diabetic diet, a therapeutic exercise program to
preserve muscle tone and body condition, and observation to notice signs of deterioration
in his condition or complications resulting from his restricted (but increasing) mobility.
Although any of the required services could be performed by a properly instructed
person, that person would not have the capability to understand the relationship among
the services and their effect on each other. Since the nature of the patient’s condition, his
age and his immobility create a high potential for serious complications, such an
understanding is essential to assure the patient’s recovery and safety. The management
of this plan of care requires skilled nursing personnel until such time as skilled care is no
longer required in coordinating the patient’s treatment regimen, even though the
individual services involved are supportive in nature and do not require skilled nursing
personnel. The documentation in the medical record as a whole is essential for this
determination and must illustrate the complexity of the unskilled services that are a
necessary part of the medical treatment and which require the involvement of skilled
nursing personnel to promote the stabilization of the patient's medical condition and
safety.
EXAMPLE 2:
An aged patient is recovering from pneumonia, is lethargic, is disoriented, has residual
chest congestion, is confined to bed as a result of his debilitated condition, and requires
restraints at times. To decrease the chest congestion, the physician has prescribed
frequent changes in position, coughing, and deep breathing. While the residual chest
congestion alone would not represent a high risk factor, the patient’s immobility and
confusion represent complicating factors which, when coupled with the chest congestion,
could create high probability of a relapse. In this situation, skilled overseeing of the
nonskilled services would be reasonable and necessary, pending the elimination of the
chest congestion, to assure the patient’s medical safety. The documentation in the
medical record as a whole is essential for this determination and must illustrate the
complexity of the unskilled services that are a necessary part of the medical treatment and
which require the involvement of skilled nursing personnel to promote the patient's
recovery and medical safety in view of the patient's overall condition.
30.2.3.2 - Observation and Assessment of Patient’s Condition
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.1.C.2, SNF-214.1.C.2
Observation and assessment are skilled services when the likelihood of change in a
patient’s condition requires skilled nursing or skilled rehabilitation personnel to identify
and evaluate the patient’s need for possible modification of treatment or initiation of
additional medical procedures, until the patient’s condition is essentially stabilized.
EXAMPLE 1:
A patient with arteriosclerotic heart disease with congestive heart failure requires close
observation by skilled nursing personnel for signs of decompensation, abnormal fluid
balance, or adverse effects resulting from prescribed medication. Skilled observation is
needed to determine whether the digitalis dosage should be reviewed or whether other
therapeutic measures should be considered, until the patient’s treatment regimen is
essentially stabilized. The medical documentation must describe the skilled services that
require the involvement of nursing personnel to promote the stabilization of the patient's
medical condition and safety.
EXAMPLE 2:
A patient has undergone peripheral vascular disease treatment including revascularization
procedures (bypass) with open or necrotic areas of skin on the involved extremity.
Skilled observation and monitoring of the vascular supply of the legs is required. The
medical documentation must describe the skilled services that require the involvement of
nursing personnel to promote the patient's recovery and medical safety in view of the
patient's overall condition.
EXAMPLE 3:
A patient has undergone hip surgery and has been transferred to a SNF. Skilled
observation and monitoring of the patient for possible adverse reaction to the operative
procedure, development of phlebitis, or skin breakdown, is both reasonable and
necessary. The medical documentation must describe the skilled services that require the
involvement of nursing personnel to promote the patient's recovery and medical safety in
view of the patient's overall condition.
EXAMPLE 4:
A patient has been hospitalized following a heart attack, and following treatment but
before mobilization, is transferred to the SNF. Because it is unknown whether exertion
will exacerbate the heart disease, skilled observation is reasonable and necessary as
mobilization is initiated, until the patient’s treatment regimen is essentially stabilized.
The medical documentation must describe the skilled services that require the
involvement of nursing personnel to promote the stabilization of the patient's medical
condition and safety.
EXAMPLE 5:
A frail 85-year-old man was hospitalized for pneumonia. The infection was resolved, but
the patient, who had previously maintained adequate nutrition, will not eat or eats poorly.
The patient is transferred to a SNF for monitoring of fluid and nutrient intake, assessment
of the need for tube feeding and forced feeding if required. Observation and monitoring
by skilled nursing personnel of the patient’s oral intake is required to prevent
dehydration. The medical documentation must describe the skilled services that require
the involvement of nursing personnel to promote the patient's recovery and medical
safety in view of the patient's overall condition.
EXAMPLE 6:
A patient with congestive heart failure may require continuous close observation to detect
signs of decompensation, abnormal fluid balance, or adverse effects resulting from
prescribed medication(s) that serve as indicators for adjusting therapeutic measures. The
medical documentation must describe the skilled services that require the involvement of
nursing personnel to promote the patient’s recovery and medical safety in view of the
patient’s overall condition, to maintain the patient’s current condition, or to prevent or
slow further deterioration in the patient’s condition.
If a patient was admitted for skilled observation but did not develop a further acute
episode or complication, the skilled observation services still are covered so long as there
was a reasonable probability for such a complication or further acute episode.
“Reasonable probability” means that a potential complication or further acute episode
was a likely possibility.
Information from the patient's medical record must document that there is a reasonable
potential for a future complication or acute episode sufficient to justify the need for
continued skilled observation and assessment.
Such signs and symptoms as abnormal/fluctuating vital signs, weight changes, edema,
symptoms of drug toxicity, abnormal/fluctuating lab values, and respiratory changes on
auscultation may justify skilled observation and assessment. Where these signs and
symptoms are such that there is a reasonable potential that skilled observation and
assessment by a licensed nurse will result in changes to the treatment of the patient, then
the services are reasonable and necessary. However, observation and assessment by a
nurse is not reasonable and necessary to the treatment of the illness or injury where these
characteristics are part of a longstanding pattern of the patient's waxing and waning
condition which by themselves do not require skilled services and there is no attempt to
change the treatment to resolve them.
Skilled observation and assessment may also be required for patients whose primary
condition and needs are psychiatric in nature or for patients who, in addition to their
physical problems, have a secondary psychiatric diagnosis. These patients may exhibit
acute psychological symptoms such as depression, anxiety or agitation, which require
skilled observation and assessment such as observing for indications of suicidal or hostile
behavior. However, these conditions often require considerably more specialized,
sophisticated nursing techniques and physician attention than is available in most
participating SNFs. (SNFs that are primarily engaged in treating psychiatric disorders are
precluded by law from participating in Medicare.) Therefore, these cases must be
carefully documented.
30.2.3.3 - Teaching and Training Activities
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.1.C.3, SNF-214.1.C.3
Teaching and training activities, which require skilled nursing or skilled rehabilitation
personnel to teach a patient how to manage their treatment regimen, would constitute
skilled services. Some examples are:
• Teaching self-administration of injectable medications or a complex range of
medications;
• Teaching a newly diagnosed diabetic to administer insulin injections, to prepare
and follow a diabetic diet, and to observe foot-care precautions;
• Teaching self-administration of medical gases to a patient;
• Gait training and teaching of prosthesis care for a patient who has had a recent leg
amputation;
• Teaching patients how to care for a recent colostomy or ileostomy;
• Teaching patients how to perform self-catheterization and self-administration of
gastrostomy feedings;
• Teaching patients how to care for and maintain central venous lines, such as
Hickman catheters;
• Teaching patients the use and care of braces, splints and orthotics, and any
associated skin care; and
• Teaching patients the proper care of any specialized dressings or skin treatments.
The documentation must thoroughly describe all efforts that have been made to educate
the patient/caregiver, and their responses to the training. The medical record should also
describe the reason for the failure of any educational attempts, if applicable.
EXAMPLE:
A newly diagnosed diabetic patient is seen in order to learn to self-administer insulin
injections, to prepare and follow a diabetic diet, and to observe foot-care precautions.
Even though the patient voices understanding of the nutritional principles of his diabetic
diet, he expresses dissatisfaction with his food choices and refuses to comply with the
education he is receiving. This refusal continues, notwithstanding efforts to counsel the
patient on the potentially adverse consequences of the refusal and to suggest alternative
dietary choices that could help to avoid or alleviate those consequences. The patient’s
response to the recommended treatment plan as well as to all educational attempts is
documented in the medical record.
30.2.4 - Questionable Situations
(Rev. 1, 10-01-03)
A3-3132.1.D, SNF-214.1.D
There must be specific evidence that daily skilled nursing or skilled rehabilitation
services are required and received if:
• The primary service needed is oral medication; or
• The patient is capable of independent ambulation, dressing, feeding, and hygiene.
30.3 - Direct Skilled Nursing Services to Patients
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.2, SNF-214.2
Nursing services are considered skilled when they are so inherently complex that they
can be safely and effectively performed only by, or under the supervision of, a registered
nurse or, when provided by regulation, a licensed practical (vocational) nurse. (See
42CFR §409.32) If all other requirements for coverage under the SNF benefit are met,
skilled nursing services are covered when an individualized assessment of the patient’s
clinical condition demonstrates that the specialized judgment, knowledge, and skills of a
registered nurse or, when provided by regulation, a licensed practical (vocational) nurse
are necessary. Skilled nursing services would be covered where such skilled nursing
services are necessary to maintain the patient’s current condition or prevent or slow
further deterioration so long as the beneficiary requires skilled care for the services to be
safely and effectively provided, and all other requirements for coverage under the SNF
benefit are met. Coverage does not turn on the presence or absence of an individual’s
potential for improvement from nursing care, but rather on the beneficiary’s need for
skilled care.
A condition that would not ordinarily require skilled nursing services may nevertheless
require them under certain circumstances. In such instances, skilled nursing care is
necessary only when (a) the particular patient’s special medical complications require the
skills of a registered nurse or, when provided by regulation, a licensed practical nurse to
perform a type of service that would otherwise be considered non-skilled; or (b) the
needed services are of such complexity that the skills of a registered nurse or, when
provided by regulation, a licensed practical nurse are required to furnish the services.
A service is not considered a skilled nursing service merely because it is performed by or
under the direct supervision of a nurse. If a service can be safely and effectively
performed (or self-administered) by an unskilled person, the service cannot be regarded
as a skilled nursing service although a nurse actually provides the service. Similarly, the
unavailability of a competent person to provide a nonskilled service, regardless of the
importance of the service to the patient, does not make it a skilled service when a nurse
provides the service.
Some examples of direct skilled nursing services are:
• Intravenous or intramuscular injections and intravenous feeding;
• Enteral feeding that comprises at least 26 percent of daily calorie requirements
and provides at least 501 milliliters of fluid per day;
• Naso-pharyngeal and tracheotomy aspiration;
• Insertion, sterile irrigation, and replacement of suprapubic catheters;
• Application of dressings involving prescription medications and aseptic
techniques (see §30.5 for exception);
• Treatment of decubitus ulcers, of a severity rated at Stage 3 or worse, or a
widespread skin disorder (see §30.5 for exception);
• Heat treatments which have been specifically ordered by a physician as part of
active treatment and which require observation by skilled nursing personnel to
evaluate the patient’s progress adequately (see §30.5 for exception);
• Rehabilitation nursing procedures, including the related teaching and adaptive
aspects of nursing, that are part of active treatment and require the presence of
skilled nursing personnel; e.g., the institution and supervision of bowel and
bladder training programs;
• Initial phases of a regimen involving administration of medical gases such as
bronchodilator therapy; and
• Care of a colostomy during the early post-operative period in the presence of
associated complications. The need for skilled nursing care during this period
must be justified and documented in the patient’s medical record.
30.4 - Direct Skilled Therapy Services to Patients
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.1.C, SNF-214.1.C
The following sections contain examples and guidelines concerning direct skilled therapy
services to patients, including skilled physical therapy, occupational therapy, and
speech/language pathology therapy.
Coverage for such skilled therapy services does not turn on the presence or absence of a
beneficiary’s potential for improvement from therapy services, but rather on the
beneficiary’s need for skilled care. Therapy services are considered skilled when they are
so inherently complex that they can be safely and effectively performed only by, or under
the supervision of, a qualified therapist. (See 42CFR §409.32) These skilled services
may be necessary to improve the patient’s current condition, to maintain the patient’s
current condition, or to prevent or slow further deterioration of the patient’s condition.
If all other requirements for coverage under the SNF benefit are met, such skilled therapy
services are covered when an individualized assessment of the patient’s clinical condition
demonstrates that the specialized judgment, knowledge, and skills of a qualified therapist
are necessary for the performance of the rehabilitation services.
30.4.1 – Skilled Physical Therapy
(Rev. 1, 10-01-03)
A3-3132.3A, SNF-214.3.A
30.4.1.1 - General
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
Skilled physical therapy services must meet all of the following conditions:
• The services must be directly and specifically related to an active written
treatment plan that is based upon an initial evaluation performed by a qualified
physical therapist after admission to the SNF and prior to the start of physical
therapy services in the SNF that is approved by the physician after any needed
consultation with the qualified physical therapist. In those cases where a
beneficiary is discharged during the SNF stay and later readmitted, an initial
evaluation must be performed upon readmission to the SNF, prior to the start of
physical therapy services in the SNF;
• The services must be of a level of complexity and sophistication, or the condition
of the patient must be of a nature that requires the judgment, knowledge, and
skills of a qualified physical therapist;
• The services must be provided with the expectation, based on the assessment
made by the physician of the patient’s restoration potential, that the condition of
the patient will improve materially in a reasonable and generally predictable
period of time; or, the services must be necessary for the establishment of a safe
and effective maintenance program; or, the services must require the skills of a
qualified therapist for the performance of a safe and effective maintenance
program. NOTE: See Section E. Maintenance Therapy for more guidance
regarding when skilled therapy services are necessary for the performance of a
safe and effective maintenance program.
• The services must be considered under accepted standards of medical practice to
be specific and effective treatment for the patient’s condition; and,
• The services must be reasonable and necessary for the treatment of the patient’s
condition; this includes the requirement that the amount, frequency, and duration
of the services must be reasonable.
EXAMPLE 1:
An 80-year old, previously ambulatory, post-surgical patient has been bed-bound for 1
week, and, as a result, had developed muscle atrophy, orthostatic hypotension, joint
stiffness and lower extremity edema. To the extent that the patient requires a brief period
of daily skilled physical therapy to restore lost functions, those services are reasonable
and necessary and must be documented in the medical record (see §30.2.2.1).
EXAMPLE 2:
A patient with congestive heart failure also has diabetes and previously had both legs
amputated above the knees. Consequently, the patient does not have a reasonable
potential to achieve ambulation, but still requires daily skilled physical therapy to learn
bed mobility and transferring skills, as well as functional activities at the wheelchair
level. If the patient has a reasonable potential for achieving those functions in a
reasonable period of time in view of the patient’s total condition, the physical therapy
services are reasonable and necessary and must be documented in the medical record (see
§30.2.2.1).
Physical therapy services are not reasonable and necessary and would not be covered if
the expected results are insignificant in relation to the extent and duration of physical
therapy services that would be required to achieve those results.
Some SNF inpatients do not require skilled physical therapy services but do require
services, which are routine in nature. When services can be safely and effectively
performed by supportive personnel, such as aides or nursing personnel, without the
supervision of a physical therapist, they do not constitute skilled physical therapy.
Additionally, services involving activities for the general good and welfare of the patient
(e.g., general exercises to promote overall fitness and flexibility and activities to provide
diversion or general motivation) do not constitute skilled physical therapy.
30.4.1.2 - Application of Guidelines
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.3.A.2, SNF-214.3.A.2
Some of the more common skilled physical therapy modalities and procedures are:
A. Assessment
The skills of a physical therapist are required for the ongoing assessment of a patient’s
rehabilitation needs and potential. Skilled rehabilitation services concurrent with the
management of a patient’s care plan include tests and measurements of range of motion,
strength, balance, coordination, endurance, and functional ability.
B. Therapeutic Exercises
Therapeutic exercises, which must be performed by or under the supervision of the
qualified physical therapist, due either to the type of exercise employed or to the
condition of the patient.
C. Gait Training
Gait evaluation and training furnished to a patient whose ability to walk has been
impaired by neurological, muscular, or skeletal abnormality often require the skills of a
qualified physical therapist.
Repetitious exercises to improve gait, or to maintain strength and endurance, and
assistive walking can be appropriately provided by supportive personnel, e.g., aides or
nursing personnel, and would not necessarily require the skills of a physical therapist.
Thus, such services are not inherently skilled. However, see §30.2.2. for the specific
circumstances in which an ordinarily nonskilled service can nevertheless be considered
skilled. Documentation of the patient’s condition in the medical record must describe the
circumstances which delineate the need for skilled rather than unskilled services during
gait training.
D. Range of Motion
Only the qualified physical therapist may perform range of motion tests and, therefore,
such tests are skilled physical therapy. Range of motion exercises constitute skilled
physical therapy only if they are part of active treatment for a specific disease state which
has resulted in a loss or restriction of mobility (as evidenced by physical therapy notes
showing the degree of motion lost, the degree to be restored and the impact on mobility
and/or function).
Generally, range of motion exercises which are not related to the restoration of a specific
loss of function may be provided safely by supportive personnel, such as aides or nursing
personnel, and as such would not necessarily require the skills of a physical therapist.
Passive exercises to maintain range of motion in paralyzed extremities that can be carried
out by aides or nursing personnel would not be considered skilled care. However, see
§30.2.2. for the specific circumstances in which an ordinarily nonskilled service can
nevertheless be considered skilled. Documentation of the patient’s condition in the
medical record must describe the circumstances which delineate the need for skilled
rather than unskilled services during range of motion training.
E. Maintenance Therapy
Therapy services in connection with a maintenance program are considered skilled when
they are so inherently complex that they can be safely and effectively performed only by,
or under the supervision of, a qualified therapist. (See 42CFR §409.32) If all other
requirements for coverage under the SNF benefit are met, skilled therapy services are
covered when an individualized assessment of the patient’s clinical condition
demonstrates that the specialized judgment, knowledge, and skills of a qualified therapist
are necessary for the performance of a safe and effective maintenance program. Such a
maintenance program to maintain the patient’s current condition or to prevent or slow
further deterioration is covered so long as the beneficiary requires skilled care for the safe
and effective performance of the program. When, however, the individualized
assessment does not demonstrate such a necessity for skilled care, including when the
performance of a maintenance program does not require the skills of a therapist because it
could safely and effectively be accomplished by the patient or with the assistance of non-
therapists, including unskilled caregivers, such maintenance services do not constitute a
covered level of care.
A service is not considered a skilled therapy service merely because it is furnished by a
therapist or by a therapist/therapy assistant under the direct supervision of a therapist. If
a service can be self-administered or safely and effectively furnished by an unskilled
person, without the direct supervision of a therapist, the service cannot be regarded as a
skilled therapy service even when a therapist actually furnishes the service. Similarly,
the unavailability of a competent person to provide a non-skilled service, regardless of
the importance of the service to the patient, does not make it a skilled service when a
therapist furnishes the service.
However, even though it would not otherwise require the skills of a therapist, the
performance of a maintenance program may nevertheless require such skills under certain
circumstances. Specifically, skilled therapy services are necessary for the performance of
a safe and effective maintenance program only when (a) the particular patient’s special
medical complications require the skills of a qualified therapist to perform a therapy
service that would otherwise be considered non-skilled; or (b) the needed therapy
procedures are of such complexity that the skills of a qualified therapist are required to
perform the procedure.
If the specialized knowledge and judgment of a qualified therapist are required, the
establishment or design of a maintenance program by a qualified therapist, the instruction
of the beneficiary or appropriate caregiver by a qualified therapist regarding a
maintenance program, and the necessary periodic reevaluations by a qualified therapist of
the beneficiary and maintenance program are considered skilled therapy services, to the
extent provided by regulation.
EXAMPLE: A patient with Parkinson’s disease may require the services of a physical
therapist to determine the type of exercises that are required to maintain his present level
of function. The initial evaluation of the patient’s needs, the designing of a maintenance
program which is appropriate to the capacity and tolerance of the patient and the
treatment objectives of the physician, the instruction of the patient or supportive
personnel (e.g., aides or nursing personnel) in the carrying out of the program, would
constitute skilled physical therapy and must be documented in the medical record (see
§30.2.2.1).
While a patient is receiving a skilled physical therapy program, the physical therapist
should regularly reevaluate the patient’s condition and adjust any exercise program the
patient is expected to carry out independently or with the aid of supportive personnel to
maintain the function being restored. Consequently, by the time it is determined that no
further skilled therapy services are needed, i.e., by the end of the last skilled session, the
physical therapist will have already designed any maintenance program required and
instructed the patient or supportive personnel in the carrying out of the program.
F. Ultrasound, Shortwave, and Microwave Diathermy Treatments
These modalities must always be performed by or under the supervision of a qualified
physical therapist.
G. Hot Packs, Infra-Red Treatments, Paraffin Baths, and Whirlpool Baths
Heat treatments and baths of this type ordinarily do not require the skills of a qualified
physical therapist. However, the skills, knowledge, and judgment of a qualified physical
therapist might be required in the giving of such treatments or baths in a particular case,
e.g., where the patient’s condition is complicated by circulatory deficiency, areas of
desensitization, open wounds, fractures, or other complications. There must be clear
documentation in the medical record of the special medical complications that describe
the need for the skilled therapy provided by the therapist.
30.4.2 - Speech -Language Pathology
(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
See Pub. 100-02, Medicare Benefit Policy Manual, Chapter 1, “Inpatient Hospital
Services.”
See §30.4.1.2.E. Maintenance Therapy for the specific circumstances in which speech-
language pathology therapy is appropriate in connection with a maintenance program.
30.4.3 - Occupational Therapy

(Rev. 179, Issued: 01-14-14, Effective: 01-07-14, Implementation: 01-07-14)
A3-3132.3.C, SNF-214.3.C
See Pub. 100-02, Medicare Benefit Policy Manual, Chapter 1, “Inpatient Hospital
Services.”
See §30.4.1.2.E. Maintenance Therapy for the specific circumstances in which
occupational therapy is appropriate in connection with a maintenance program.
30.5 - Nonskilled Supportive or Personal Care Services
(Rev. 1, 10-01-03)
A3-3132.4, SNF-214.4
The following services are not skilled services unless rendered under circumstances
detailed in §§30.2:
• Administration of routine oral medications, eye drops, and ointments (the fact that
patients cannot be relied upon to take such medications themselves or that State
law requires all medications to be dispensed by a nurse to institutional patients
would not change this service to a skilled service);
• General maintenance care of colostomy and ileostomy;
• Routine services to maintain satisfactory functioning of indwelling bladder
catheters (this would include emptying and cleaning containers and clamping the
tubing);
• Changes of dressings for uninfected post-operative or chronic conditions;
• Prophylactic and palliative skin care, including bathing and application of creams,
or treatment of minor skin problems;
• Routine care of the incontinent patient, including use of diapers and protective
sheets;
• General maintenance care in connection with a plaster cast (skilled supervision or
observation may be required where the patient has a preexisting skin or
circulatory condition or requires adjustment of traction);
• Routine care in connection with braces and similar devices;
• Use of heat as a palliative and comfort measure, such as whirlpool or steam pack;
• Routine administration of medical gases after a regimen of therapy has been
established (i.e., administration of medical gases after the patient has been taught
how to institute therapy);
• Assistance in dressing, eating, and going to the toilet;
• Periodic turning and positioning in bed; and
• General supervision of exercises, which have been taught to the patient and the
performance of repetitious exercises that do not require skilled rehabilitation
personnel for their performance. (This includes the actual carrying out of
maintenance programs where the performances of repetitive exercises that may be
required to maintain function do not necessitate a need for the involvement and
services of skilled rehabilitation personnel. It also includes the carrying out of
repetitive exercises to improve gait, maintain strength or endurance; passive
exercises to maintain range of motion in paralyzed extremities which are not
related to a specific loss of function; and assistive walking.) (See Medicare
Benefit Policy Manual, Chapter 1, “Inpatient Hospital Services.”)
30.6 - Daily Skilled Services Defined
(Rev. 249, Issued: 11-02-18, Effective: 12-04-18, Implementation: 12-04-18)
Skilled nursing services or skilled rehabilitation services (or a combination of these
services) must be needed and provided on a “daily basis,” i.e., on essentially a 7-days-a-
week basis. A patient whose inpatient stay is based solely on the need for skilled
rehabilitation services would meet the “daily basis” requirement when they need and
receive those services on at least 5 days a week. (If therapy services are provided less
than 5 days a week, the “daily” requirement would not be met.)
This requirement should not be applied so strictly that it would not be met merely
because there is an isolated break of a day or two during which no skilled rehabilitation
services are furnished and discharge from the facility would not be practical.
EXAMPLE:
A patient who normally requires skilled rehabilitation services on a daily basis may
exhibit extreme fatigue, which results in suspending therapy sessions for a day or two.
Coverage may continue for these days since discharge in such a case would not be
practical.
In instances when a patient requires a skilled restorative nursing program to positively
affect his functional well-being, the expectation is that the program be rendered at least 6
days a week. (Note that when a patient’s skilled status is based on a restorative program,
medical evidence must be documented to justify the services. In most instances, it is
expected that a skilled restorative program will be, at most, only a few weeks in
duration.)
The daily basis requirement can be met by furnishing a single type of skilled service
every day, or by furnishing various types of skilled services on different days of the week
that collectively add up to “daily” skilled services. However, arbitrarily staggering the
timing of various therapy modalities through the week, merely in order to have some type
of therapy session occur each day, would not satisfy the SNF coverage requirement for
skilled care to be needed on a “daily basis.” To meet this requirement, the patient must
actually need skilled rehabilitation services to be furnished on each of the days that the
facility makes such services available.
It is not sufficient for the scheduling of therapy sessions to be arranged so that some
therapy is furnished each day, unless the patient's medical needs indicate that daily
therapy is required. For example, if physical therapy is furnished on 3 days each week
and occupational therapy is furnished on 2 other days each week, the “daily basis”
requirement would be satisfied only if there is a valid medical reason why both cannot be
furnished on the same day. The basic issue here is not whether the services are needed,
but when they are needed. Unless there is a legitimate medical need for scheduling a
therapy session each day, the “daily basis” requirement for SNF coverage would not be
met.
30.7 - Services Provided on an Inpatient Basis as a “Practical Matter”
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
A3-3132.6, SNF-214.6
In determining whether the daily skilled care needed by an individual can, as a “practical
matter,” only be provided in a SNF on an inpatient basis, the A/B MAC (A) considers the
individual’s physical condition and the availability and feasibility of using more
economical alternative facilities or services.
As a “practical matter,” daily skilled services can be provided only in a SNF if they are
not available on an outpatient basis in the area in which the individual resides or
transportation to the closest facility would be:
• An excessive physical hardship;
• Less economical; or
• Less efficient or effective than an inpatient institutional setting.
The availability of capable and willing family or the feasibility of obtaining other
assistance for the patient at home should be considered. Even though needed daily
skilled services might be available on an outpatient or home care basis, as a practical
matter, the care can be furnished only in the SNF if home care would be ineffective
because the patient would have insufficient assistance at home to reside there safely.
EXAMPLE: A patient undergoing skilled physical therapy can walk only with
supervision but has a reasonable potential to learn to walk independently with further
training. Further daily skilled therapy is available on an outpatient or home care basis,
but the patient would be at risk for further injury from falling, because sufficient
supervision and assistance could not be arranged for the patient in his home. In these
circumstances, the physical therapy services as a practical matter can be provided
effectively only in the inpatient setting.
30.7.1 - The Availability of Alternative Facilities or Services
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
A3-3132.6.A, SNF-214.6.A
Alternative facilities or services may be available to a patient when health care providers
such as home health agencies are utilized. These alternatives are not always available in
all communities and even where they exist they may not be available when needed.
EXAMPLE: Where the residents of a rural community generally utilize the outpatient
facilities of a hospital located some distance from the area, the hospital outpatient
department constitutes an alternative source of care that is available to the community.
Roads in winter, however, may be impassable for some periods of time and in special
situations institutionalization might be needed.
In determining the availability of more economical care alternatives, the coverage or
noncoverage of that alternative care is not a factor to be considered. Home health care
for a patient who is not homebound, for example, may be an appropriate alternative in
some cases. The fact that Medicare cannot cover such care is irrelevant.
The issue is feasibility and not whether coverage is provided in one setting and not
provided in another. For instance, an individual in need of daily skilled physical therapy
might be able to receive the services needed on a more economical basis from an
independently practicing physical therapist. However, the fact that Medicare payment
could not be made for the services because an expense limitation (if applicable) to the
services of an independent physical therapist had been exceeded or because the patient
was not enrolled in Part B, would not be a basis for determining that, as a practical
matter, the needed care could only be provided in a SNF.
In determining the availability of alternate facilities or services, whether the patient or
another resource can pay for the alternate services is not a factor to be considered.
30.7.2 - Whether Available Alternatives Are More Economical in the
Individual Case
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
A3-3132.6.B, SNF-214.6.B
If the A/B MAC (A) determines that an alternative setting is available to provide the
needed care, it considers whether the use of the alternative setting would actually be more
economical in the individual case.
EXAMPLE 1:
If a patient's condition requires daily transportation to the alternative source of care (e.g.,
a hospital outpatient department) by ambulance, it might be more economical from a
health care delivery viewpoint to provide the needed care in the SNF setting.
EXAMPLE 2:
If needed care could be provided in the home, but the patient’s residence is so isolated
that daily visits would entail inordinate travel costs, care in a SNF might be a more
economical alternative.
30.7.3 - Whether the Patient’s Physical Condition Would Permit
Utilization of an Available, More Economical Care Alternative
(Rev. 1, 10-01-03)
A3-3132.6.C, SNF-214.6.C
In determining the practicality of using more economical care alternatives, the A/B MAC
(A) considers the patient’s medical condition. If the use of those alternatives would
adversely affect the patient’s medical condition, the A/B MAC (A) concludes that as a
practical matter the daily skilled services can only be provided by a SNF on an inpatient
basis.
If the use of a care alternative involves transportation of the individual on a daily basis,
the A/B MAC (A) considers whether daily transportation would cause excessive physical
hardship. Determinations on whether a patient’s condition would be adversely affected if
an available, more economical care alternative were utilized should not be based solely
on the fact that the patient is nonambulatory. There are individuals confined to
wheelchairs who, though nonambulatory, could be transported daily by automobile from
their homes to alternative care sources without any adverse impact. Conversely, there are
instances where an individual’s condition would be adversely affected by daily
transportation to a care facility, even though the individual is able to ambulate to some
extent.
EXAMPLE: A 75-year-old woman has suffered a cerebrovascular accident and cannot
climb stairs safely. The patient lives alone in a second-floor apartment accessible only by
climbing a flight of stairs. She requires physical therapy and occupational therapy on
alternate days, and they are available in a CORF one mile away from her apartment.
However, because of her inability to negotiate the stairs, the daily skilled services she
requires cannot, as a practical matter, be provided to the patient outside the SNF.
The “practical matter” criterion should never be interpreted so strictly that it results in the
automatic denial of coverage for patients who have been meeting all of the SNF level of
care requirements, but who have occasion to be away from the SNF for a brief period of
time. While most beneficiaries requiring a SNF level of care find that they are unable to
leave the facility, the fact that a patient is granted an outside pass or short leave of
absence for the purpose of attending a special religious service, holiday meal, family
occasion, going on a car ride, or for a trial visit home, is not, by itself evidence that the
individual no longer needs to be in a SNF for the receipt of required skilled care. Where
frequent or prolonged periods away from the SNF become possible, the A/B MAC (A)
may question whether the patient’s care can, as a practical matter, only be furnished on
an inpatient basis in a SNF. Decisions in these cases should be based on information
reflecting the care needed and received by the patient while in the SNF and on the
arrangements needed for the provision, if any, of this care during any absences. (See the
Medicare Benefit Policy Manual, Chapter 3, “Duration of Covered Inpatient Services,”
§20.1.2, for counting inpatient days during a leave of absence.)
A conservative approach to retain the presumption for limitation of liability may lead a
facility to notify patients that leaving the facility will result in denial of coverage. Such a
notice is not appropriate. If a SNF determines that covered care is no longer needed, the
situation does not change whether the patient actually leaves the facility or not.
40 - Physician Certification and Recertification of Extended Care
Services
(Rev. 10880, Issued: 08-06-21, Effective: 11-08-21, Implementation: 11-08-21)
Payment for covered posthospital extended care services may be made only if a physician
(or, as discussed in §40.1 of this chapter, a physician extender) makes the required
certification, and where services are furnished over a period of time, the required
recertification regarding the services furnished.
The SNF must obtain and retain the required certification and recertification statements.
The A/B MAC (A) may request them to assist in determining medical necessity when
necessary. The SNF will determine how to obtain the required certification and
recertification statements. There is no requirement for a specific procedure or form as
long as the approach adopted by the facility permits verification that the certification and
recertification requirement is met. Certification or recertification statements may be
entered on or included in forms, notes, or other records that would normally be signed in
caring for a patient, or on a separate form. Except as otherwise specified, each
certification and recertification is to be separately signed.
If the SNF’s failure to obtain a certification or recertification is not due to a question of
the necessity for the services, but to the physician’s or physician extender’s refusal to
certify on other grounds (e.g., an objection in principle to the concept of certification and
recertification), the SNF cannot charge the beneficiary for covered items or services. Its
provider agreement precludes it from doing so.
If a physician or physician extender refuses to certify, because, in his/her opinion, the
patient does not, as a practical matter, require daily skilled care for an ongoing condition
for which he/she was receiving inpatient hospital services (or for a new condition that
arose while in the SNF for treatment of that ongoing condition), the services are not
covered and the facility can bill the patient directly. The reason for the refusal to make
the certification must be documented in the SNF’s records.
Certifications must be obtained at the time of admission, or as soon thereafter as is
reasonable and practicable (see Pub.100-04, Medicare Claims Processing Manual,
Chapter 6, §120.2, regarding the circumstances under which a resumption of SNF care
following a temporary break in SNF coverage would be considered a new “admission”
under the SNF PPS’s interrupted stay policy). The routine admission order established
by a physician is not a certification of the necessity for post-hospital extended care
services for purposes of the program. There must be a separate signed statement
indicating that the patient will require on a daily basis SNF covered care.
In addition, only physicians may certify outpatient physical therapy and outpatient
speech-language pathology services.
40.1 - Who May Sign the Certification or Recertification for Extended
Care Services
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
A certification or recertification statement must be signed by the attending physician or a
physician on the staff of the skilled nursing facility who has knowledge of the case, or by
a physician extender (that is, a nurse practitioner (NP), a clinical nurse specialist (CNS)
or, effective with items and services furnished on or after January 1, 2011, a physician
assistant (PA)) who does not have a direct or indirect employment relationship with the
facility, but who is working in collaboration with the physician.
In this context, the definition of a “direct employment relationship” is set forth in the
regulations at 20 CFR 404.1005, 404.1007, and 404.1009. Under the regulations at 42
CFR 424.20(e)(2)(ii), when a physician extender has a direct employment relationship
with an entity other than the facility, and the employing entity has an agreement with the
facility that includes the provision of general nursing services under the regulations at 42
CFR 409.21, an “indirect employment relationship” exists between the physician
extender and the facility. By contrast, such an indirect employment relationship does not
exist if the agreement between the facility and the physician extender’s employer solely
involves the performance of delegated physician tasks under the regulations at 42 CFR
483.30(e).
Further information regarding certification and recertification of extended care services,
including details on the content of the certification or recertification, timing of
recertifications and the impact of delays on certifications and recertifications, appears in

Pub. 100-01, Medicare General Information, Eligibility, and Entitlement Manual, Chapter
4, “Physician Certification and Recertification of Services,” §§40 - 40.6.
50 - Covered Extended Care Services
(Rev. 1, 10-01-03)
A3-3133, SNF-230
Patients covered under hospital insurance are entitled to have payment made on their
behalf for covered extended care services. Payment may be based on reasonable cost or
be under the SNF Prospective Payment System (see §10). The facility may charge the
beneficiary for services they request that are not included in the PPS rate or otherwise
covered by Medicare (i.e. extra meals for family members).
An inpatient is a person who has been admitted to a skilled nursing facility or swing bed
hospital for bed occupancy for purposes of receiving inpatient services. A person is
considered an inpatient if formally admitted as an inpatient with the expectation that they
will remain at least overnight and occupy a bed even though it later develops that they
can be discharged and do not actually use a bed overnight.
NOTES:
1. Custodial care (see Medicare Benefit Policy Manual, Chapter 16, “General Exclusions
from Coverage,” §110) is not a covered extended care service.
2. When patients requiring inpatient hospital services occupy beds in a SNF, they are
considered inpatients of the SNF. In such cases, the services furnished in the SNF
may not be considered inpatient hospital services, and payment may not be made
under the program for such services. Such a situation may arise where the SNF is a
distinct part of an institution the remainder of which is a hospital, and either there is
no bed available in the hospital, or for any other reason the institution fails to place
the patient in the appropriate bed. The same rule applies where the SNF is a separate
institution. For the same reason, where patients who require extended care services
occupy beds in a hospital, payment cannot be made on their behalf for the services
furnished to them in the hospital, unless the services are extended care services
furnished pursuant to a swing bed approval. (See Medicare Benefit Policy Manual,
Chapter 1, “Inpatient Hospital Services,” §10.)
3. When patients who require SNF services are placed in a noncertified part of an
institution which contains a participating “distinct part” SNF, the services may be
paid under certain conditions, based on the limitation of liability provisions. (See
Medicare Claims Processing Manual, Chapter 30, “Limitation of Liability,” §10.4.)
The extended care services in §§50.1 - 50.9, below, are covered under hospital insurance.
50.1 - Nursing Care Provided by or Under the Supervision of a
Registered Professional Nurse
(Rev. 1, 10-01-03)
A3-3133.1, SNF-230.1
Nursing care provided by or under the supervision of a registered professional nurse is
covered.
However, the services of a private-duty nurse or other private-duty attendant are not
covered. Private-duty nurses or private-duty attendants are registered professional
nurses, licensed practical nurses, or any other trained attendant whose services ordinarily
are rendered to, and restricted to, a particular patient by arrangement between the patient
and the private-duty nurse or attendant. Such persons are engaged or paid by an
individual patient or by someone acting on their behalf, including a SNF that initially
incurs the cost and looks to the patient for payment for such noncovered services.
Where the SNF acts on behalf of a patient, the services of the private-duty nurse or other
attendant under such an arrangement are not extended care services regardless of the
control which the SNF may exercise with respect to the services rendered by such
private-duty nurse or attendant.
50.2 - Bed and Board in Semi-Private Accommodations Furnished in
Connection With Nursing Care
(Rev. 1, 10-01-03)
A3-3133.2, SNF-230.2
(See Medicare Benefit Policy Manual, Chapter 1, “Inpatient Hospital Services,” §10.1,
for provisions relating to inpatient accommodations.)
50.3 - Physical Therapy, Speech-Language Pathology, and Occupational
Therapy Furnished by the Skilled Nursing Facility or by Others Under
Arrangements With the Facility and Under Its Supervision
(Rev. 242, Issued: 03-16-18, Effective: 06-19-18, Implementation: 06-19-18)
Physical therapy (PT), speech-language pathology (SLP), and occupational therapy (OT)
services must be provided by the SNF or by others under arrangements with the SNF for
beneficiaries in either a covered Part A stay or a non-covered stay in the SNF (see Pub.
100-04, Medicare Claims Processing Manual, Chapter 6, §20.5, for a more detailed
discussion of therapy services under consolidated billing, the SNF “bundling”
requirement). Bundling of therapy services to the SNF is not required for beneficiaries
residing in a non-certified portion of the same institution that also includes a participating
distinct part SNF. See Chapter 7, SNF Part B Billing, §10 in the Medicare Claims
Processing Manual, for a clarification of bill types used to make this distinction clear in
billing. For a discussion of skilled therapy (that is, PT, SLP, and OT) services in the
context of the SNF level of care criteria, see §§30.4ff. of this chapter.
50.4 - Medical Social Services to Meet the Patient’s Medically Related
Social Needs
(Rev. 1, 10-01-03)
A3-3133.4, SNF-230.4
Medical social services are those social services, which contribute meaningfully to the
treatment of a patient’s condition. Such services include, but are not limited to:
a. Assessment of the social and emotional factors related to the patient’s illness, his
or her need for care, response to treatment, and adjustment to care in the facility;
b. Appropriate action to obtain case work services to assist in resolving problems in
these areas; and
c. Assessment of the relationship of the patient’s medical and nursing requirements
to his or her home situation, financial resources, and the community resources
available to him or her in making the decision regarding their discharge.
50.5 - Drugs and Biologicals
(Rev. 1, 10-01-03)
A3-3133.5, SNF-230.5, Rev. A3-1838 dated 06/01, A3-3133.5.A, SNF-230.5.A, A3-
3133.5.B, SNF-230.5.B, A3-3133.5.C, SNF-230.5.C, A3-3133.5.D, SNF-230.5.D
Drugs and biologicals for use in the facility, which are ordinarily furnished by the facility
for the care and treatment of inpatients, are covered. Such drugs and biologicals are not
limited to those routinely stocked by the skilled nursing facility but include those
obtained for the patient from an outside source, such as a pharmacy in the community.
Drugs and biologicals are included in the SNF PPS except for those Part B drugs
specifically excluded. Since the provision of drugs and biologicals is considered an
essential part of skilled nursing care, a facility must assure their availability to inpatients
in order to be found capable of furnishing the level of care required for participation in
the program. When a facility secures drugs and biologicals from an outside source, their
availability is assured only if the facility assumes financial responsibility for the
necessary drugs and biologicals, i.e., the supplier looks to the facility, not the patient, for
payment.
Payment may not be made for particular uses of drugs that the FDA has expressly
disapproved or that are designated as not covered in the Medicare National Coverage
Determinations Manual, chapter 2.
If the A/B MAC (A) has reason to question whether the FDA has approved a drug or
biological for marketing, it will obtain satisfactory evidence of FDA’s approval.
Acceptable evidence includes a copy of the FDA’s letter to the drug’s manufacturer
approving the new drug application (NDA); or listing of the drug or biological in the
FDA’s “Approved Drug Products” or “FDA Drug and Device Product Approvals”; or a
copy of the manufacturer’s package insert, approved by the FDA as part of the labeling of
the drug, containing its recommended uses and dosage, as well as possible adverse
reactions and recommended precautions in using it. When necessary, the Medicare
regional office may be able to help in obtaining information.
See instruction in the Medicare Benefit Policy Manual, Chapter 1, “Inpatient Hospital
Services,” §30.1, “Drugs Included in the Drug Compendia,” which also apply to drugs
furnished to SNF inpatients.
However, drugs not included, or approved for inclusion, in the drug compendia are
nevertheless covered in a SNF if such drug:
1. Was furnished the patient during their prior hospitalization;
2. Was approved for use in the hospital by the hospital’s pharmacy and drug
therapeutics (or equivalent) committee;
3. Is required for the continuing treatment of the patient in the skilled nursing
facility; and
4. Is reasonable and necessary.
Under the limited circumstances mentioned in items 1 through 4 above, a combination
drug approved by a hospital pharmacy and drug therapeutics committee may also be
covered as an extended care service.
Rules for drugs and biologicals applicable to hospital inpatients found in the Medicare
Benefit Policy Manual, Chapter 1, “Inpatient Hospital Services,” §§30, 30.3, and 30.5,
also apply to inpatients of SNFs. They are:
• General information concerning drugs and biologicals furnished to inpatients;
• Combination drugs; and
• Drugs for use outside the SNF.
50.6 - Supplies, Appliances, and Equipment
(Rev. 1, 10-01-03)
A3-3133.6, SNF-230.7

Instructions in the Medicare Benefit Policy Manual, Chapter 1, “Hospital Inpatient
Services,” §40 - “Supplies, Appliances, and Equipment,” also apply to SNF inpatients.
50.7 - Medical Service of an Intern or Resident-in-Training
(Rev. 228, Issued: 10-13-16, Effective: 10-18-16, Implementation: 10-18-16)
The medical services of an intern or resident-in-training under an approved teaching
program of a hospital with which the facility has in effect the required transfer agreement
are covered under hospital insurance (see Pub. 100-01, Medicare General Information,
Eligibility, and Entitlement Manual, chapter 5, section 30.2 for a discussion of the SNF’s
required transfer agreement with a hospital).
An “approved teaching program” means a program approved by the Council on Medical
Education of the American Medical Association or, in the case of an osteopathic hospital,
approved by the Committee on Hospitals of the Bureau of Professional Education of the
American Osteopathic Association. In the case of services of an intern or resident-in-
training in the field of dentistry in a hospital or osteopathic hospital, the teaching program
must have the approval of the Council on Dental Education of the American Dental
Association.
The medical and surgical services furnished to the facility’s patients by interns and
residents-in-training of a hospital with which the facility has a transfer agreement are
covered under medical insurance if the services are not covered under hospital insurance.
50.8 - Other Services
(Rev. 1, 10-01-03)
A3-3133.9, SNF-230.10
50.8.1 - General
(Rev. 1, 10-01-03)
A3-3133.9.A, SNF-230.10.A
Other services that are necessary to the health of the patients are covered if the services
are generally provided by, or under arrangements made by, skilled nursing facilities. The
medical and other health services described in the Medicare Benefit Policy Manual,
Chapter 6, “Hospital Services Covered Under Part B,” §§10 - 10.2.4, are generally
provided by, or under arrangements made by, skilled nursing facilities and are therefore
extended care services. For coverage of diagnostic services and radiological therapy
under Part A, the conditions described in §70.1 must be met.
Items or services that would not be included as inpatient hospital services if furnished to
an inpatient of a hospital are also excluded from coverage as extended care services. For
instance, the provision of personal laundry services by skilled nursing facilities is not a
covered service under Medicare, since it would not be covered if provided to an inpatient
of an acute care hospital. See the Medicare Benefit Policy Manual, Chapter 6, “Hospital
Services Covered Under Part B,” §10, for covered inpatient hospital services.
The use of an operating room and any special equipment, supplies, or services would not
constitute covered extended care services except when furnished to the facility by a
hospital with which the facility has a transfer agreement, since operating rooms are not
generally maintained by skilled nursing facilities. However, supplies and nursing
services connected with minor surgery performed in a skilled nursing facility that does
not require the use of an operating room or any special equipment or supplies associated
with such a room would be covered extended care services and paid as part of inpatient
SNF PPS.
50.8.2 - Respiratory Therapy
(Rev. 242, Issued: 03-16-18, Effective: 06-19-18, Implementation: 06-19-18)
Prior to BBA 1997, respiratory therapy could be provided by a SNF either under an
arrangement with a hospital with which the SNF had a transfer agreement or through the
SNF’s nursing staff. Section 4432(b)(5)(D) of the BBA amended section 1861(h)(7) of
the Act to cover the full range of services that SNFs generally provide, either directly or
under arrangements with any qualified outside source. As a result, the services of
respiratory therapists are now covered under Part A when provided under arrangements
made directly between the SNF and any qualified respiratory therapist, regardless of
whether the therapist is employed by the SNF’s transfer agreement hospital (see the
regulations at 42 CFR 409.27(b)).
60 - Covered Extended Care Days
(Rev. 1, 10-01-03)
Not Applicable
See the Medicare Benefit Policy Manual, Chapter 3, “Duration of Covered Inpatient
Services,” for the following topics:
• Post-hospital extended care benefit days available in a benefit period;
• Definition of an inpatient benefit day;
• Late discharge;
• Leave of absence;
• Discharge or death on first day of entitlement or participation; and
• Inpatient service days counting toward benefit maximums.
70 - Medical and Other Health Services Furnished to SNF Patients
(Rev. 228, Issued: 10-13-16, Effective: 10-18-16, Implementation: 10-18-16)
The medical and other health services listed below are covered under Part B when
furnished by a participating SNF either directly or under arrangements to inpatients who
are not entitled to have payment made under Part A (e.g., benefits exhausted or 3-day
prior-stay requirement not met).
Services payable under Part B are:
• Diagnostic x-ray tests, diagnostic laboratory tests, and other diagnostic tests;
• X-ray, radium, and radioactive isotope therapy, including materials and services
of technicians;
• Surgical dressings, and splints, casts, and other devices used for reduction of
fractures and dislocations;
• Prosthetic devices (other than dental) which replace all or part of an internal body
organ (including contiguous tissue), or all or part of the function of a permanently
inoperative or malfunctioning internal body organ, including replacement or
repairs of such devices;
• Leg, arm, back, and neck braces, trusses, and artificial legs, arms, and eyes
including adjustments, repairs, and replacements required because of breakage,
wear, loss, or a change in the patient’s physical condition;
• Outpatient physical therapy, outpatient speech language pathology services, and
outpatient occupational therapy (see Pub. 100-02, Medicare Benefit Policy
Manual, Chapter 10, “Covered Medical and Other Health Services,” §220.1.4);
• Screening mammography services;
• Screening pap smears and pelvic exams;
• Influenza, pneumococcal pneumonia, and hepatitis B vaccines;
• Some colorectal screening;
• Prostate screening;
• Ambulance services;
• Hemophilia clotting factors.
• Epoetin Alfa (EPO) for ESRD beneficiaries when given in conjunction with
dialysis.
See Pub. 100-04, Medicare Claims Processing Manual chapter 6, for information on
billing for these services. See §70.1 of this chapter for the conditions under which
diagnostic services and radiological therapy furnished by SNFs are covered. For
coverage of total parenteral nutrition (TPN) and enteral nutrition (EN) as a prosthetic
device, see Pub. 100-02, Medicare Benefit Policy Manual, Chapter 6, “Hospital Services
Covered Under Part B,” and the Medicare National Coverage Determinations Manual,
chapter 1, Part 3, §180.2.
Rental or purchase of durable medical equipment from SNFs for use in the patient’s
home (other than a hospital or SNF, as discussed in Pub. 100-02, Medicare Benefit Policy
Manual, chapter 15, §110.1.D) is covered under Part B in accordance with the provisions
of Pub. 100-02, Medicare Benefit Policy Manual, Chapter 6, “Hospital Services Covered
Under Part B,” §80 (also see Pub. 100-04, Medicare Claims Processing Manual, chapter
7, §60, for the related SNF billing instructions). DME rendered to Part A inpatients of a
SNF is covered as part of the prospective payment system and is not separately payable.
For coverage of provider ambulance services, see Pub. 100-02, Medicare Benefit Policy
Manual, Chapter 6, “Hospital Services Covered Under Part B".
Drugs, biologicals, and blood are not covered under Part B when furnished by a SNF.
70.1 - Diagnostic Services and Radiological Therapy
(Rev. 1, 10-01-03)
A3-3137.1, SNF-260.1
Diagnostic x-ray and radiological therapy may be provided directly by a SNF if, as part
of its compliance with the conditions of participation, the SNF has a radiological
department, which meets the same standards required of a hospital furnishing such
services under the program, or if the SNF meets the portable x-ray supplier standards.
Portable x-ray services provided by a SNF under arrangements are covered only if
furnished by an approved supplier. When a SNF furnishes laboratory services directly, it
must have a Clinical Laboratory Improvement Act (CLIA) number or a CLIA certificate
of waiver. SNFs may bill for laboratory services rendered under arrangement for tests
NOT on the CLIA waived list.
70.2 - Ambulance Service
(Rev. 1, 10-01-03)
A3-3138, SNF-260.C
For requirements relating to provider ambulance service, see the Medicare Benefit Policy
Manual, Chapter 10, “Ambulance Services.”
70.3 - Inpatient Physical Therapy, Occupational Therapy, and Speech-
Language Pathology Services
(Rev. 37, Issued: 08-12-05; Effective/Implementation: 09-12-05)
Under Part A, physical therapy, occupational therapy, and speech pathology services are
included in the SNF PPS rate for cost reporting periods beginning on or after July 1,
1998. For inpatient Part B residents and outpatient services, payment for such services is
under a fee schedule. The SNF must bill for physical therapy, occupational therapy, or
speech-language pathology services for Part A residents beginning with its first cost
reporting period that starts on or after July 1, 1998, and for Part B for services furnished
on or after July 1, 1998. The SNF (rather than an outside provider/supplier such as an
approved clinic or rehabilitation agency, or a participating hospital) bills Medicare.
Payment is made directly to the SNF. The patient is responsible only for applicable Part
A coinsurance or the Part B deductible and coinsurance amounts.
See also the Medicare Benefit Policy Manual, Chapter 1, “Inpatient Hospital Services.”
70.4 - Services Furnished Under Arrangements With Providers
(Rev. 261, Issued: 10-04-19, Effective: 11-05-19, Implementation: 11-05-19)
The SNF may arrange with others to furnish covered services such as physical therapy,
occupational therapy, or speech-language pathology services. The SNF (rather than an
outside provider/supplier, another SNF or a HHA) bills Medicare, and payment is made
directly to the SNF. When such arrangements are made, SNF receipt of payment for the
arranged services (as with services provided directly) relieves the beneficiary or any other
person of further liability to pay for them. See Pub. 100-01, Medicare General
Information, Eligibility, and Entitlement Manual, chapter 5, section 10.3, for a general
discussion of services furnished “under arrangements.”
The specific details of the ensuing payment arrangement between the SNF and the
outside supplier (such as the actual payment amount and timeframe) represent a private,
“marketplace” transaction that is negotiated between the parties themselves and falls
outside the purview of CMS. This means, for example, that payments by the SNF to an
outside supplier for bundled services furnished to the SNF’s Part A resident under an
arrangement made with the outside supplier are not governed by the specific Medicare
fee schedule amounts or claims processing timeframes that would apply to services billed
to Medicare separately under Part B; however, in order for the arrangement itself to be
valid, the SNF must, in fact, make payment to its supplier for services rendered. See Pub.
100-04, Medicare Claims Processing Manual, chapter 6, sections 10.4ff. for additional
information on arrangements between SNFs and their suppliers.
The arrangement must also comply with the fraud and abuse laws (see Pub. 100-01,
Medicare General Information, Eligibility, and Entitlement Manual, chapter 1, section
20.3, and Pub. 100-04, Medicare Claims Processing Manual, chapter 6, section 80.5).
Questions about the interpretation and enforcement of the statutory anti-kickback

provisions in section 1128B(b) of the Social Security Act should be directed to the
attention of the Industry Guidance Branch in HHS’s Office of the Inspector General
(OIG); see the regulations at 42 CFR Part 1008 and the OIG website at
https://oig.hhs.gov/compliance/advisory-opinions/index.asp.
Transmittals Issued for this Chapter
Rev # Issue Date Subject Impl Date CR#
R12283BP
10/05/2023
Internet Only Manual Updates to Pub. 100-02
and 100-04 to Implement Consolidated
Appropriations Act 2023 Changes for Skilled
Nursing Facility (SNF)
01/08/2024
13271
R10880BP
08/06/2021
Internet Only Manual Updates to Pub. 100-
01,
100-02, and 100-04 to Implement
Consolidated Appropriations Act Changes and
Correct Errors and Omissions (SNF)
11/08/2021
12009
R261BP 10/04/2019
Manual Updates for CR11152 Implementation
of the Skilled Nursing Facility (SNF) Patient
Driven Payment Model (PDPM)
11/05/2019
11454
R249BP 11/02/2018
Internet Only Manual Updates to Pub. 100-
01,
100-02 and 100-04 to Correct Errors and
Omissions (SNF) (2018 Q4)
12/04/2018
11004
R242BP 03/16/2018
Internet Only Manual Updates to Pub. 100-
01,
100-02 and 100-04 to Correct Errors and
Omissions (SNF) (2018)
06/19/2018
10512
R228BP 10/13/2016
Internet Only Manual Updates to Pub. 100-
01,
100-02 and 100-04 to Correct Errors and
Omissions (SNF)
10/18/2016
9748
R227BP 09/16/2016
Internet Only Manual Updates to Pub. 100-
01,
100-02 and 100-04 to Correct Errors and
Omissions (SNF) –
Rescinded and replaced by
Transmittal 228
10/18/2016
9748
R211BP 10/16/2015
Internet Only Manual Updates to Pub. 100-
01,
100-02 and 100-04 to Correct Errors and
Omissions (2015)
11/16/2015
9336
R204BP 03/13/2015
Updates to the Medicare Internet-Only
Manual Chapters for Skilled Nursing Facility
(SNF) Providers
06/15/2015
8997
R183BP 04/04/2014
Internet Only Manual Updates to Pub. 100-
01,
100-02 and 100-04 to Correct Errors and
Omissions
05/05/2014
8669
R182BP 03/21/1014
Implementing the Part B Inpatient Payment
Policies from CMS-1599-F
04/21/2014
8666
R179BP 01/14/2014
Manual Updates to Clarify Skilled Nursing
Facility (SNF), Inpatient Rehabilitation
Facility (IRF), Home Health (HH), and
Outpatient (OPT) Coverage Pursuant to
Jimmo vs. Sebelius
01/07/2014
8458
R176BP 12/13/2013
Manual Updates to Clarify Skilled Nursing
Facility (SNF), Inpatient Rehabilitation
Facility (IRF), Home Health (HH), and
Outpatient (OPT) Coverage Pursuant to
Jimmo vs. Sebelius – Rescinded and replaced
by Transmittal 179
01/07/2014
8458
R161BP 10/26/2012
Manual Updates to Clarify SNF Claims
Processing
04/01/2013
8044
R155BP 04/20/2012
Allowing Physician Assistants to Perform
Skilled Nursing Facility (SNF) Level of Care
Certifications and Recertifications
02/13/2012
7701
R153BP 1/13/2012 Allowing Physician Assistants to Perform
Skilled Nursing Facility (SNF) Level of Care
Certifications and Recertifications –
Rescinded and replaced by Transmittal 155
02/13/2012
7701
R89BP 05/16/2008
Medical and Other Health Services Furnished
to SNF Patients
06/16/2008
5991
R73BP 06/29/2007
Coverage Requirements for Therapy Services
Provided in a Skilled Nursing Facility
10/01/2007
5532
R58BP 11/09/2006
Swing Bed Hospital Updates 12/11/2006
5114
R57BP 11/08/2006
Clarification/Update to Chapter 8, Pub. 100-
02
12/14/2006
4220
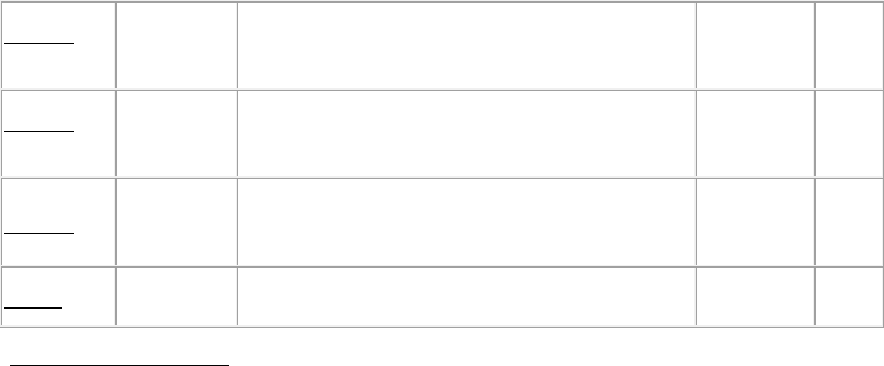
R54BP 09/15/2006
Clarification/Update to Chapter 8, Pub. 100-
02
12/14/2006
4220
R40BP 11/18/2005
Skilled Nursing Facility Prospective Payment
System
02/16/2006
4079
R37BP
08/12/2005
Conforming Changes for Change Request
3648 to Pub. 100-02
09/12/2005
3912
R1BP 10/01/2003
Introduction to the Benefit Policy Manual N/A N/A
Back to top of Chapter
