
1
DOH 530-129 January 2019
State of Washington
Emergency Care Systems
Air Ambulance Service Plan
Initial Development and Implementation January 16, 2007
Revised October 2010
Revised January 2019
Office of Community Health Systems
2
DOH 530-129 January 2019
State of Washington
Emergency Care Systems
Air Ambulance Service Plan
Revised January 2019
For more information or additional copies of this document contact:
Washington State Department of Health
Office of Community Health Systems
Emergency Care Systems
111 Israel Road S.E.
Olympia, WA98504-7424
360-236-2840
3
DOH 530-129 January 2019
Preface
RCW 70.168.010 states “It is in the best interest of the citizens of Washington State to establish
an efficient and well-coordinated statewide emergency medical services and trauma care system
to reduce costs and incidence of inappropriate and inadequate trauma care and emergency
medical service and minimize the human suffering and costs associated with preventable
mortality and morbidity.”
The Department of Health (department) recognizes air ambulance services as having a distinctive
role within the emergency care system. Aircraft have statewide flight range capabilities and
logistical considerations that differ from ground services that require a strategic approach in
managing resources and a coordinating a system of medical response.
This approach enables citizen access to the best patient care and transport capabilities. It works
to mitigate an unsafe prehospital transport environment to the extent possible.
Air ambulances can provide a high level of out-of-hospital care, and rapid, expedient transport
for critically sick and injured patients.
Strategic coordination, deployment, and quality assurance strategies for air ambulance services
can improve outcomes in patient care.
For these reasons, our EMS and Trauma Care Steering Committee (EMSTC-SC) recommended
the development of a statewide Air Ambulance Plan (plan). With oversight from the department,
the air ambulance services workgroup (workgroup) and Prehospital Technical Advisory
Committee (PHTAC) were tasked to develop and manage the plan.
4
DOH 530-129 January 2019
Special acknowledgements to:
Chris Martin, RN, Airlift Northwest
Brenda Nelson, RN, Airlift Northwest
Jacob Dalstra, FP-C, Life Flight Network
Dwight Brown, BSN, RN, CEN, CFRN, Clinical Leader, Island Air Ambulance
Jackie Hamilton, President and Director of Operations, Island Air Ambulance
Bob Berschauer, Washington Ambulance Association
Catie Holstein, Washington State Department of Health
Jason Norris, Washington State Department of Health
Dr. Lynn Wittwer, Medical Program Director Chair, Clark County
Dr. Jim Nania, EMS Medical Program Director, Spokane County
Dr. Michael Sullivan, EMS Medical Program Director, San Juan County
Dr. Rich Utarnachitt, Medical Director, Airlift Northwest
Dr. Jim Bryan, Medical Director, Life Flight Network
Dr. Marvin Wayne, EMS Medical Program Director, Whatcom County
Department of Health Office of Community Health Systems
Washington State EMS and Trauma Care Steering Committee
Local and Regional EMS and Trauma Care Councils
Northwest Association of Aeromedical Responders
National Association of State EMS Officers
Aeromedical Accreditation Organizations
National Organization of State Offices of Rural Health
5
DOH 530-129 January 2019
Page Contents
3
Preface
4
Special Acknowledgements
5
Table of Contents
6
Purpose
7
Executive Summary
7
Washington State EMS and Trauma Steering Committee Vision, Mission,
Priorities
8
Introduction
8
Regulatory framework
9
Who We Are
9
How We Work
10
Why We Have a Statewide Air Ambulance Plan
10
Who We Reach
11
Statewide Analysis of Air Ambulance Services
12
o Air ambulance assets
13
o Distribution of resources
14
o Geographical coverage
20
o Response time to prehospital scene
20
o Response time to trauma, cardiac and stroke facilities
21
o Review of operational guidance for use of air ambulance
21
o Data collection, analysis and quality assurance
22
o Summary of Statewide Analysis of Air Ambulance Services
23
o Measures of success and outcomes – Historical Snapshot 2010-2017
21
Recommended Goals and Strategies for 2018 – 2021 Plan Period
25
Statewide Recommendations for EMS Use of Air Ambulance
26
Determination of medical necessity for air ambulance transport
28
Relative potential contraindications to air ambulance transport
29
Standards for EMS activation for air ambulance services
30
Early activation of an air ambulance service
32
Communication standards for EMS and air ambulance services
33
Safety of ground crews around aircraft
34
Landing zone considerations
35
Hospital destination decision for patients transported by air ambulance
36
Inter-facility transports
37
Use of fixed-wing service in the pre-hospital setting
39
Appendix
40
Appendix A - Projected response times from buffer zones to trauma facilities
45
Appendix B - Projected response times from buffer zones to cardiac facilities
48
Appendix C - Projected response times from buffer zones to stroke facilities
53
Appendix D - Definition of terms
56
Bibliography
6
DOH 530-129 January 2019
Purpose
The purpose of this plan is:
• To assess and analyze statewide air ambulance use in order to generate a strategic
approach for coordinating and improving emergency care in the out-of-hospital setting.
• To provide peer-reviewed guidance about air ambulance asset use for emergency care
system partners.
• To serve as both a planning resource for each EMS and trauma care region’s (regional
EMSTC) biennial plan for prehospital resources, and as a guideline for developing
regional EMS patient care procedures (PCP) about air ambulance service use.
7
DOH 530-129 January 2019
Executive Summary
The Washington State EMS and Trauma Care Steering Committee (EMSTC-SC) establishes the
vision, mission and priorities of the emergency care system to support state strategic planning.
Below are the vision, mission, and priorities for the 2018-2021 strategic planning period.
Vision
Washington has an emergency care system that reduces death, disability, human suffering, and
costs from injury and medical emergencies.
Mission
We work to maintain and strengthen an accessible, efficient, high-quality, well-coordinated,
statewide emergency care system.
Challenges
Rapidly changing healthcare environment, limited and declining resources, increasing demand,
workforce shortages, barriers to quality assurance and improvement, unequal access, rapidly
changing technology, drivers of public expectations, and sustainability of community
collaboration.
Priorities
Quality, cost, access, data-driven decision making, education and outreach, improving
integration and collaboration, resource and workforce development, regulatory adjustment.
The overarching goals of the Washington state emergency care system as reflected in the state
strategic plan are to:
1. Increase access to quality, affordable, and integrated emergency care for everyone in
Washington.
2. Prepare for, respond to, and recover from public health threats.
3. Promote programs and policies to reduce the incidence and effect of injuries, violence,
and illness.
4. Promote and enhance continuous quality improvement of emergency care systems for
Washington.
5. Work toward sustainable emergency care funding, enhance workforce development, and
demonstrate impact on patient outcomes.
Strategies and objectives in the plan align with the vision, mission, and priorities established by
the EMSTC-SC, and are designed to evaluate, advance and develop air ambulance service use
across the state.

8
DOH 530-129 January 2019
Introduction
This plan was developed and initially implemented in January of 2006 through the collaborative
work and dedication of EMS and trauma care stakeholders. The department provided oversight,
technical guidance, and support as needed. The first revision and current version of the Air
Medical Plan occurred in October of 2010. This is the second revision. The need for future
revisions will be evaluated biennially.
The plan provides a broad overview of air ambulance services planning and use in Washington
state.
The plan includes a clear purpose and an analysis of air ambulance use for the planning period.
That supports the development of goals to improve the air ambulance component of the EMS
system as aligned with the state EMS plan. Measurable outcomes and achievable strategies for
improving air ambulance use and out-of-hospital medical care are included.
The plan includes a historical snapshot of goals, strategies, and outcomes from previous planning
cycles, and a review of the regulatory framework for air ambulance services.
The plan provides peer-reviewed recommendations for EMS use of air ambulance services that
local and regional EMS councils use to develop operational guidance for EMS about air
ambulance services use.
Regulatory Framework
This section provides a broad overview of Washington state regulations. It is not intended to be
an all-inclusive list of the regulations that may apply to air ambulance services operating in the
state.
RCW 18.73 requires the department to establish minimum standards for air ambulance services
and equipment, and requires the department to issue an air ambulance license.
The goal of the statute is to:
• Ensure safe emergency medical care and transport by ambulance is provided to
Washington state citizens.
The specific objectives of the statute are to:
• Establish minimum medical and clinical standards for air ambulance services to provide
medical care to ill and injured citizens, and;
• Ensure consistent, high-quality, medical care can be delivered by air ambulance services
in Washington State.
WAC 246-976-320 identifies the regulatory standards for air ambulance services.
9
DOH 530-129 January 2019
The rule implements the goals and specific objectives of the statute by proposing minimum
standards for:
• Completing a department-approved application for licensure and verification;
• Documentation to validate aircraft registration, operations specification, and
airworthiness of fixed-wing and aeromedical helicopters;
• Documentation required to determine proof of insurance;
• Physician medical director oversight including quality management and a review of
patient care data, and patient care protocols for medical treatment and care;
• Staffing by qualified medical personnel for all air ambulance services;
• Training and administration requirements for medical personnel for all air ambulance
services;
• Aircraft configuration serving medical purposes under state purview that is specific to
providing adequate medical care;
• Administration requirements, and minimum lists of medical equipment and medications
that must be available for patient care.
Who We Are
We recognize that the air ambulance component of our EMS system needs an evidence-based,
peer-reviewed, stakeholder-supported, and consistent approach to developing, monitoring, and
evolving air ambulance services using specialized subject matter experts in the field.
Air ambulance subject matter experts from our state air ambulance services comprise the bulk of
the statewide air ambulance workgroup. This includes department-appointed and certified EMS
physician medical program directors (MPD) and their appointed physician delegates (MPDD).
They provide physician oversight as needed to air ambulance services, nurses, paramedics, and
other licensed air ambulance professionals, pilots, EMS regional executive directors, Department
of Health EMS staff members, other first responders, and invested partners.
The workgroup is a subgroup of the Pre-Hospital Technical Advisory (PHTAC) Committee,
whose role is to advise the Washington State EMS and Trauma Care Steering Committee
(EMSTC-SC) on the provisions of EMS care.
How We Work
The workgroup led by the department meets regularly to develop, manage, and monitor success
of this plan. Workgroup members collaborate to identify and analyze challenges, and to develop,
prioritize, design, and implement goals, strategies and solutions. The group seeks relevant
evidence-based guidance, peer-reviewed research, and best practices to update guidance for the
use of air ambulance services. Yearly, the workgroup reports accomplishments to the PHTAC
and EMS and Trauma Care Steering Committee (EMSTC-SC).
10
DOH 530-129 January 2019
Why We Have a Statewide Air Ambulance Plan?
The Trauma Care Systems Act requires the department to implement mechanisms to determine
distribution of pre-hospital resources to:
• Provide citizens access to high-quality EMS care.
• Prevent inefficient duplication of resources.
• Promote a healthy and experienced pre-hospital workforce.
The methods to determine distribution of ground EMS services are managed through the regional
EMS and Trauma Care (regional EMSTC) planning process. The minimum and maximum
number of services needed are identified and memorialized in the EMSTC regional plans.
The difference between the regional EMSTC plans and the air ambulance service plan is about
the distinctive differences between air and ground vehicles. Those include time and distance
capabilities, the overlay of federal aviation regulations, and state limitations in regulation of air
ambulance services.
Unique critical influences affecting the distribution of air ambulance services in comparison to
ground services include the market and capital cost of helicopters, airplanes, and specially
trained clinical staff members.
The department evaluates and monitors statewide need and distribution of air ambulance services,
and works collaboratively with air ambulance services to determine where air ambulance bases
should be established.
To promote consistency in statewide EMS planning processes, this work is memorialized in this
plan. It serves as the primary document that reflects the evaluation, monitoring, and outcomes of
air ambulance use. This plan is managed biennially. Every two years the plan is reviewed,
revised, and approved through the same process as the regional EMSTC plans.
Who We Reach
Although not exclusive, the primary audience for this plan includes the EMSTC-SC, regional
EMSTCs, MPDs and delegates, designated and categorized medical facilities, licensed and
verified EMS services, certified EMS personnel, and other emergency care system partners.
Secondary audiences include other state offices and professional associations such as the
Northwest Association of Aeromedical Responders, National Organization of State Offices of
Rural Health, National Association of State EMS Officers, federal agencies with air transport
capabilities, and others.
11
DOH 530-129 January 2019
Statewide Analysis of Air Ambulance Services
Air ambulance utility is apparent in remote wilderness and rural areas of the state.
Similarly, urban areas may be as close as 20 minutes from a major medical facility but are
isolated due by large bodies of water. While ground ambulance transport is feasible using the
state’s ferry system, such transports result in significant delays. Traffic patterns and congestion
in major urban areas must also be considered when discussing use of air ambulance services.
Without the availability of air ambulances, the clinical outcome of many patients in these areas
would be negatively affected.
Principles of air ambulance asset use are incumbent on the multi-regional and statewide flight
range capabilities, along with logistical considerations for aircraft. Air ambulances can provide
an advanced level of out-of-hospital care and rapid, expedient transport for critically sick and
injured patients.
Safety must always remain at the forefront of any discussion about the use of air ambulance
services in the state. Inclusion of safety-related concepts and the peer-reviewed
recommendations identified in this plan must be reflected in all local, regional and state
operational guidance documents (triage and destination tools, guidelines, patient care procedures,
county operating procedures, MPD protocols, etc.) about the use of air ambulance services.
Limitations to our current analysis are primarily about challenges with data. Data about air
ambulance use is collected from the state trauma registry, and is limited to patients treated and
transported for trauma care. Trauma-designated facilities are mandated by law to report data to
the trauma registry. Unlike trauma-designated facilities, EMS is not mandated to report data to
our state EMS data registry (WEMSIS). This makes collecting and analyzing data about other
aspects of our system challenging. The department and many other system partners are
strategically addressing challenges with WEMSIS. Because of these challenges with data, there
was limited review and use of patient and transport-related data in this current analysis.
For the purposes of this revision, our statewide analysis of air ambulance services includes an
evaluation of the following components:
• Air ambulance assets
• Distribution of air ambulance resources
• Geographical coverage
• Response time to prehospital scene
• Response time to trauma, cardiac, and stroke-designated and categorized facilities
• Available data to review on air ambulance use
• Review of operational guidance documents about use of air ambulance
12
DOH 530-129 January 2019
Air ambulance assets in Washington State as of the date of implementation of this plan are
reflected in the Table 1.
Washington state and federal government air ambulance resources are listed in Table 2 on page
13.
Each service uses aircraft of differing type, make and model. These aircraft have unique
performance capabilities. All are configured to comply with state and national standards for
patient transportation.
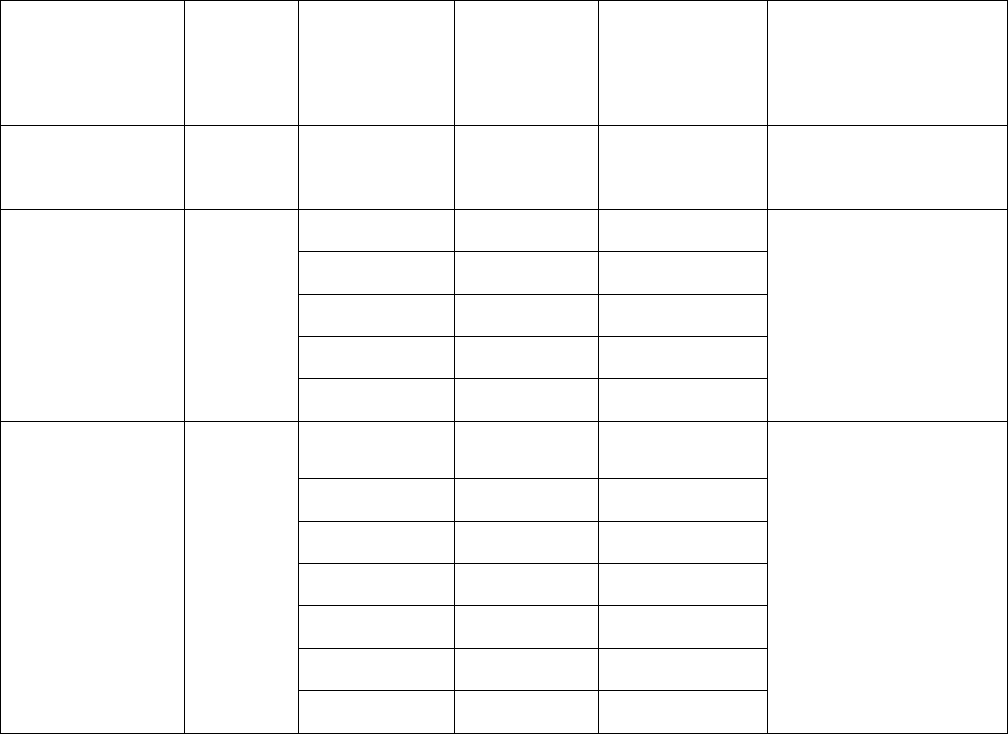
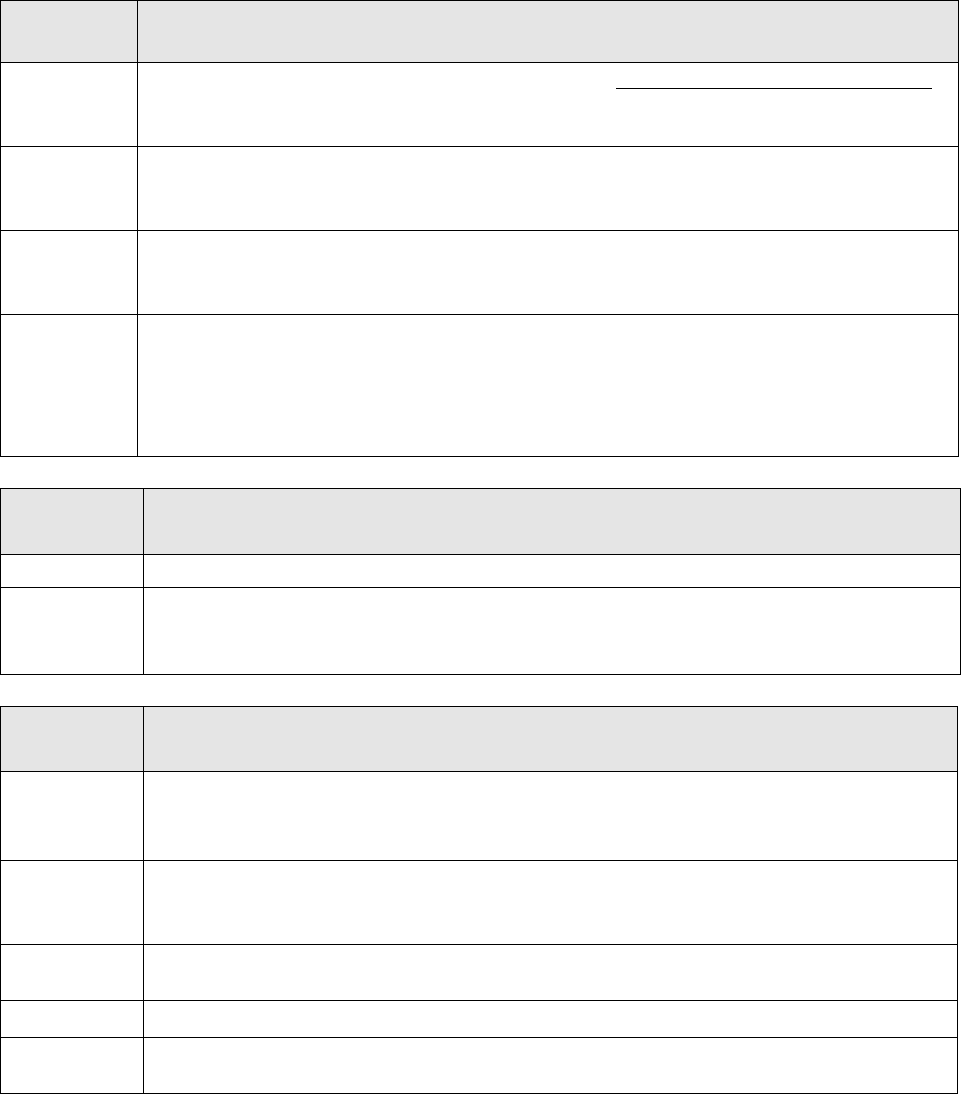
Table 1: Licensed and Verified Air Ambulance Services in Washington State as of date of
publication.
Air Ambulance
Service
License
Type
Base
Location
Region
Base
Location
County
Base Location
City / Town
Base Location(s)
Border State(s)
Island Air
Ambulance
AIRV North San Juan Friday Harbor None
Airlift
Northwest
AIRV
Central
King
Seattle
None
North
Whatcom
Bellingham
North
Snohomish
Arlington
West
Thurston
Tumwater
South Central
Yakima
Yakima
Life Flight
Network
AIRV
North Central Okanogan Brewster
Aurora, Oregon
Pendleton, Oregon
Warrenton, Oregon
Lewiston, Idaho
Sandpoint, Idaho
South West
Clark
Kelso
East
Whitman
Pullman
North Central
Grant
Moses Lake
South Central
Benton
Richland
South Central
Klickitat
Dallesport
East
Spokane
Spokane
Air ambulance services holding accreditation by a department-recognized accreditation body
may provide specialized services such as neonatal care, transport of cardiac assist devices, and
other such specialties. Local and regional EMSTCs are encouraged to work with air medical
services within their region to identify specialized services available, and to coordinate
accordingly.
13
DOH 530-129 January 2019
Federal government air ambulance resources are exempt from state licensure in accordance with
RCW 18.73.130. Federal services located in Washington state may provide limited services
outside of the provisions of declared emergencies. During state emergency declarations,
coordination with federal resources will occur through appropriate state and federal agencies.
This list is current as of September 1, 2017.
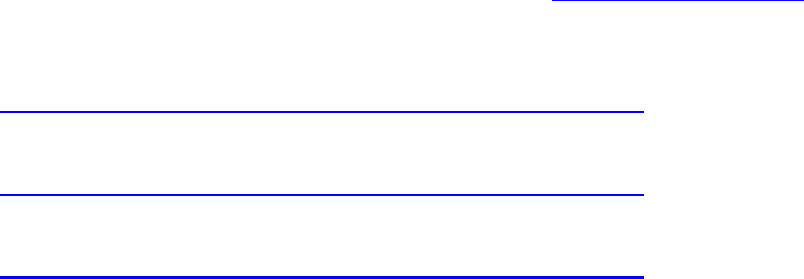
Table 2: Federal government air ambulance resources
Government
Branch
Name
Region
County
Federal
Air Force
Fairchild Air Force Base
East
Spokane
Army
Joint Base Lewis-McChord
West
Pierce
Coast
Guard
13th Coast Guard District Northwest Clallam
Coast
Guard
Columbia Sector Southwest Pacific
Navy
Naval Air Station - Whidbey
North
Island
Navy Naval Station – Everett North
Snohomi
sh
Navy
Naval Base – Bremerton / Bangor
Northwest
Kitsap
National
Guard
Air
96
th
Aviation Troop Command –
JBLM
West Pierce
Army
141
st
Fairchild Airforce Base - JBLM
West
Pierce
Army
141
st
Fairchild Airforce Base –
Spokane
East Spokane
Distribution of resources is an important consideration in establishing, assessing, and
monitoring citizen access to emergency medical care and transport services.
Factors and influences about distribution of air ambulances include: time and distance
capabilities, the overlay of federal aviation regulations, and state limitations in regulation of air
ambulance services. Critical influences for distributing air ambulance services include the
market and capital cost of helicopters, airplanes, and specially trained clinical staff.
The department evaluates and monitors statewide need and distribution of air ambulance services
in conjunction with the services in determining where air ambulance bases should be established.
The principles that guide distribution discussions are to:
• Provide citizens access to high-quality EMS care.
• Prevent inefficient duplication of resources.
• Promote a healthy and experienced pre-hospital workforce.
14
DOH 530-129 January 2019
• Provide transport by the highest level of service, in the most expedient fashion to the
highest level facility that can manage the patient’s condition.
The following method will determine distribution of air ambulance services. During this
planning cycle this information will be used to identify unserved and underserved areas.
1) Identify and update the Emergency Care System GIS Map with the current number and
locations of air ambulance bases in Washington state.
2) Update the projected response time model using a central point (air ambulance base)
within a 360-degree buffer zone for 15-, 20-, 30-, 45-, and 60-minute intervals.
3) Develop a mechanism to estimate the percent of geography and population covered by
each buffer zone.
4) Identify the designated and categorized facilities within each buffer zone.
5) Identify gaps, unserved and underserved areas.
Additionally during this plan period, the workgroup will:
1) Develop a strategy to identify baseline performance standards about access and
response times.
2) Develop a strategy to assess performance about access and response times.
3) Evaluate the feasibility of establishing a minimum number of recommended air
ambulance services needed to achieve access and response time performance standards.
Based on our current evaluation of air ambulance assets and base locations, current number of
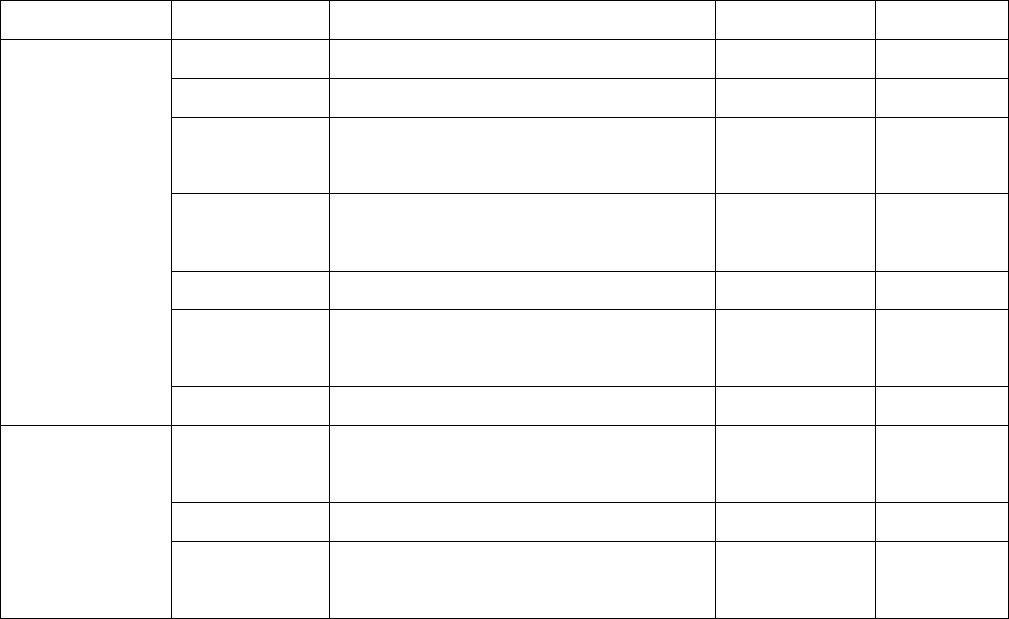
air ambulance bases by EMS region is identified below in Table 4.
Table 4. Number of verified air ambulance service bases with helicopters by EMSTC region at
publication date.
EMSTC
Region
Current number of AIRV Bases with Helicopters by
Region
North
2
Northwest
0
Central
1
West
1
Southwest
1
North Central
2
South Central
3
East
2
Total statewide
12
Geographical Coverage
The measures of success and outcomes – historical snapshot for 2010-2016 section on page 23,
shows the standards and outcomes of geographical coverage for the latest planning cycle.
15
DOH 530-129 January 2019
Because of improvements in aircraft flying speed capabilities, we’ve updated the projected
response time models using an air ambulance base at a central fixed point within a 360-degree
buffer zone. The buffer zone calculations are based on how many nautical miles (1.15 miles = 1
nautical mile) are flown at average helicopter speed of 150 mph. Projected flight time and
distance calculations in intervals of 15, 20, 30, 45, and 60 minutes are shown in Table 5.
Table 5. Projected flight time and distance calculations
15 Min
20 Min
30 Min
45 Min
60 Min
37.5 miles
50 miles
75 miles
112.5 Miles
150 Miles
32.61 NM
43.48 NM
65.17 NM
97.83 NM
43.48 NM
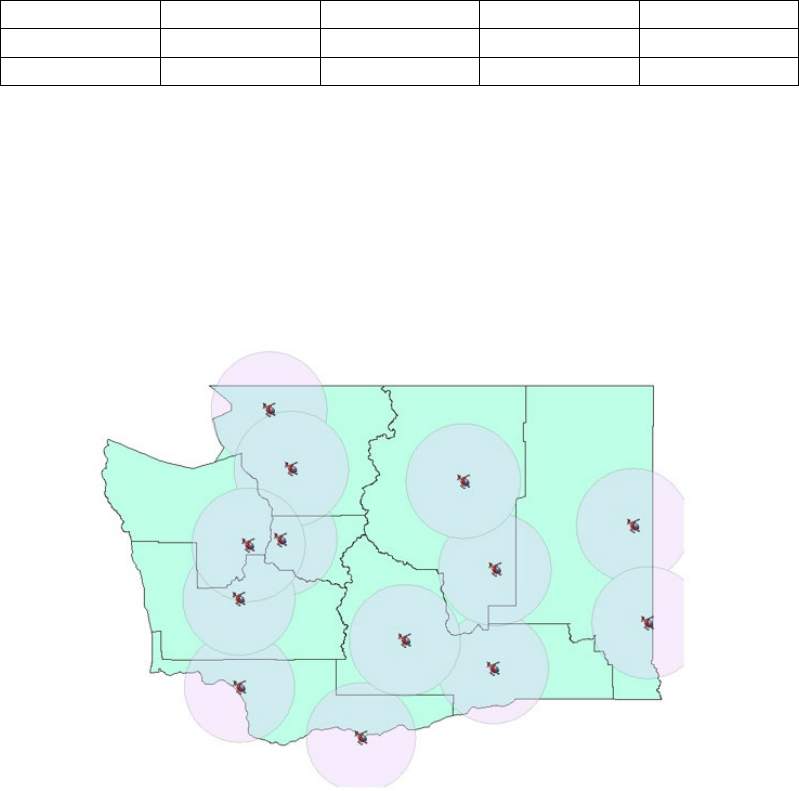
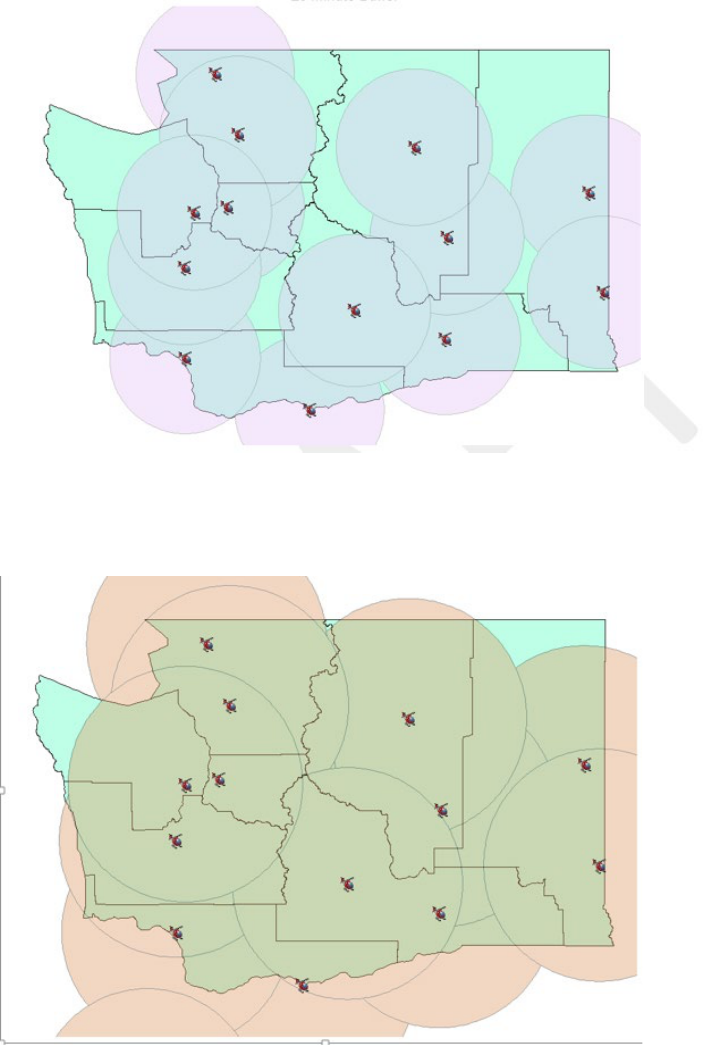
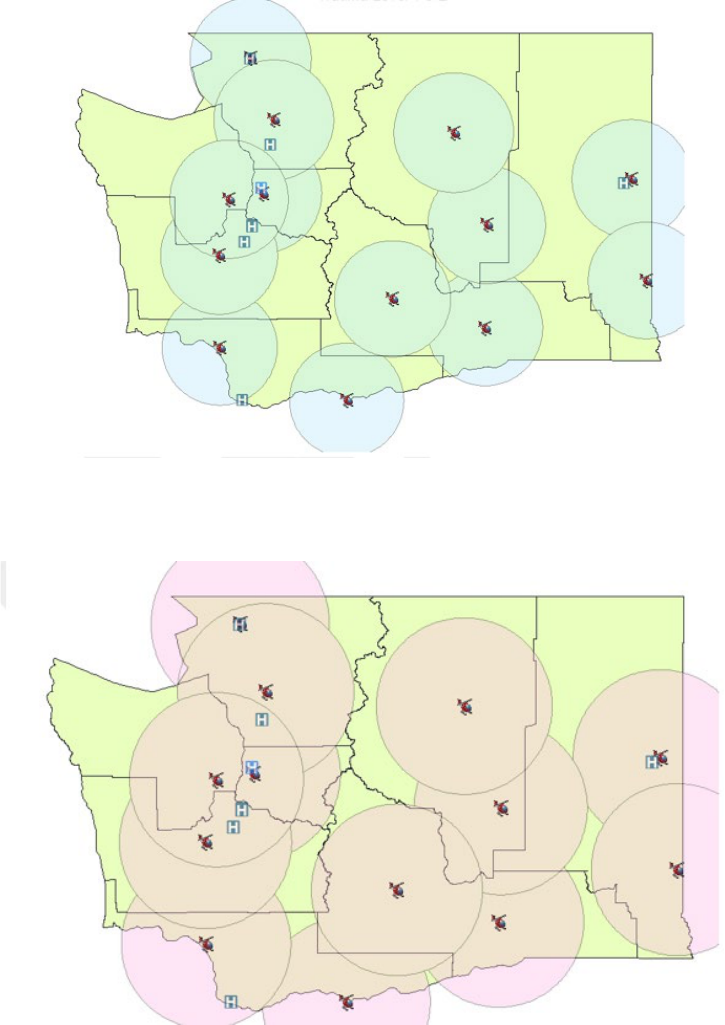
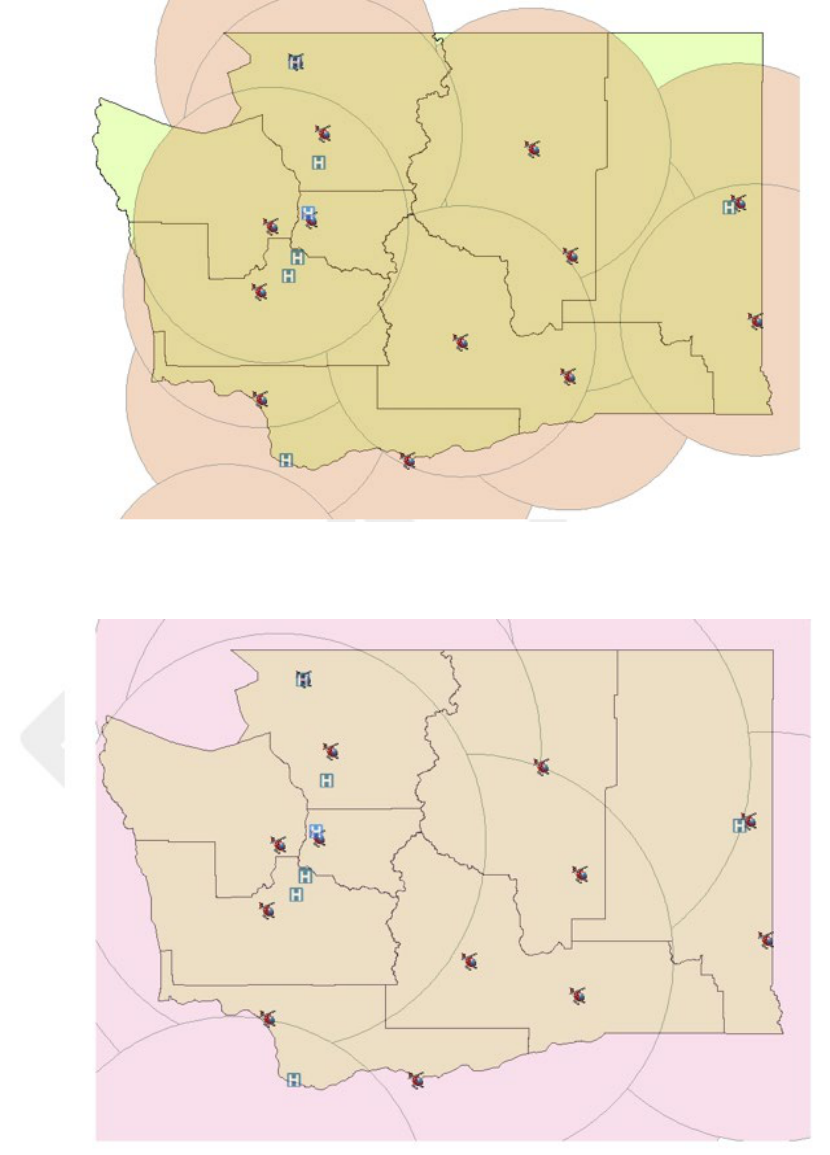
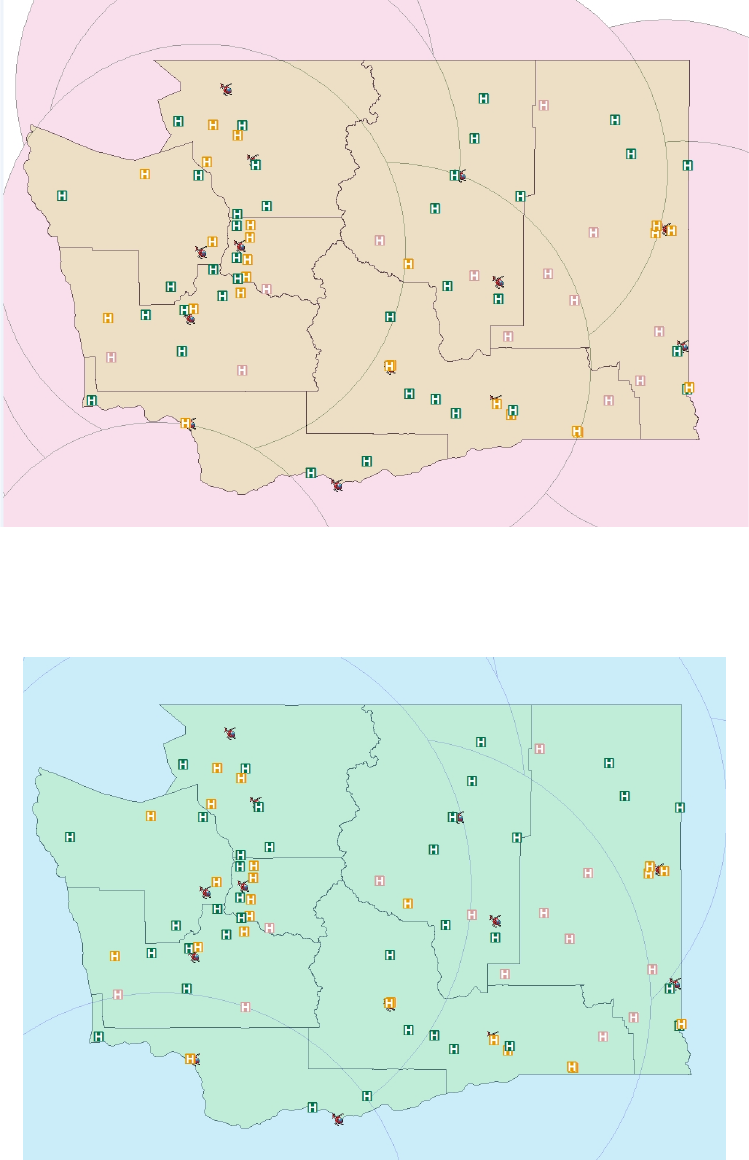
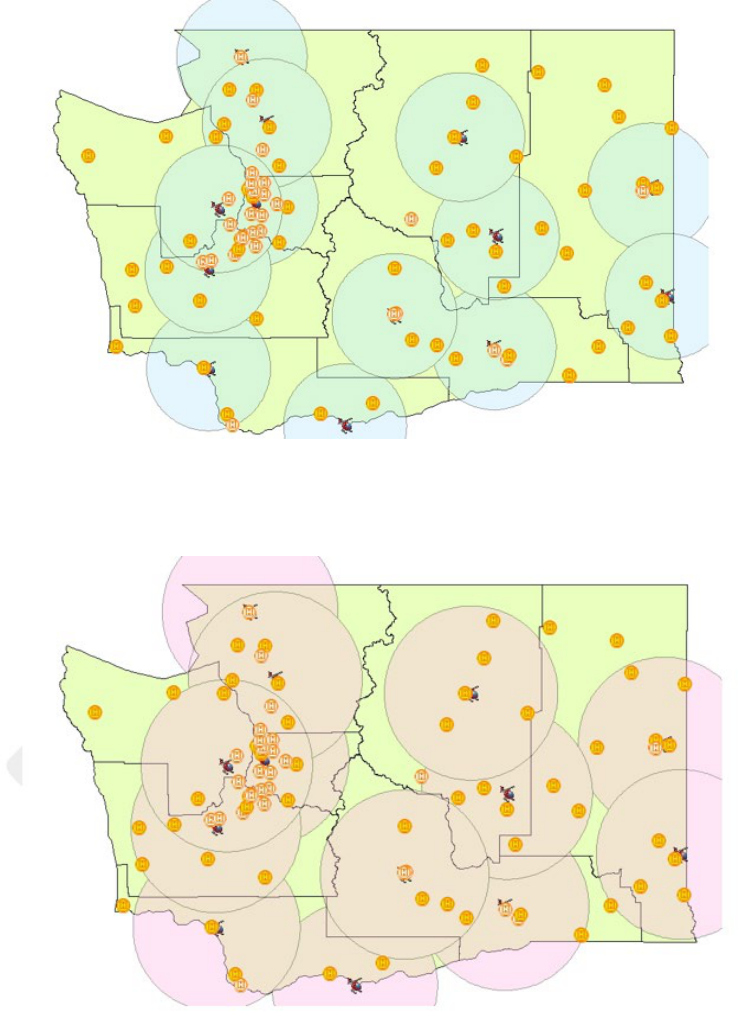
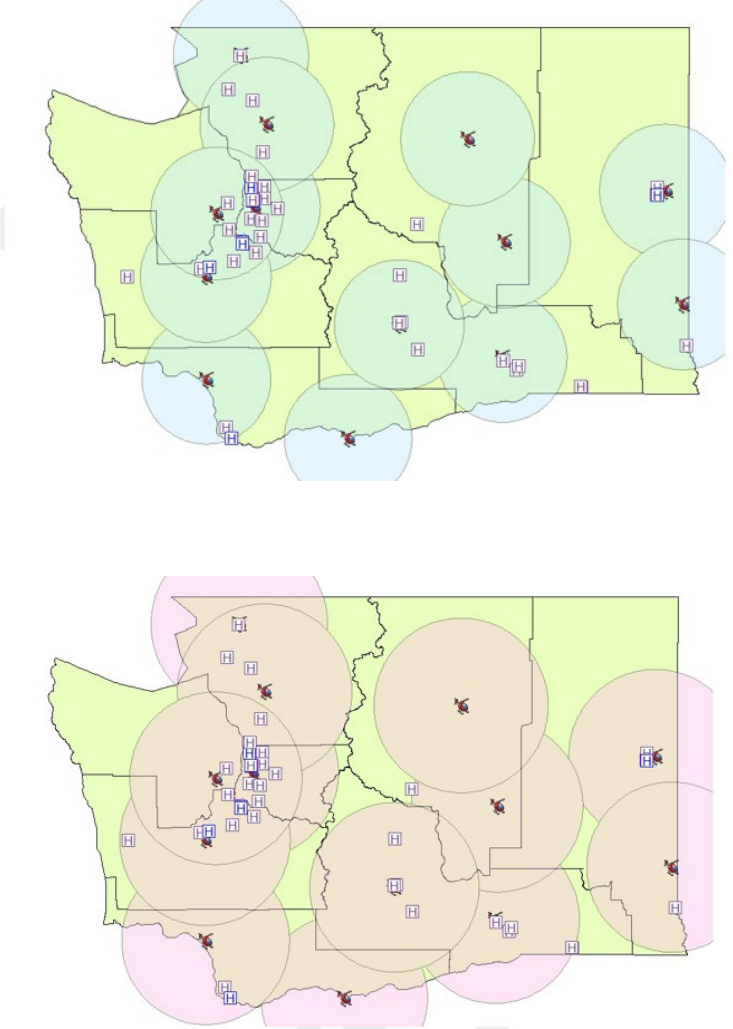
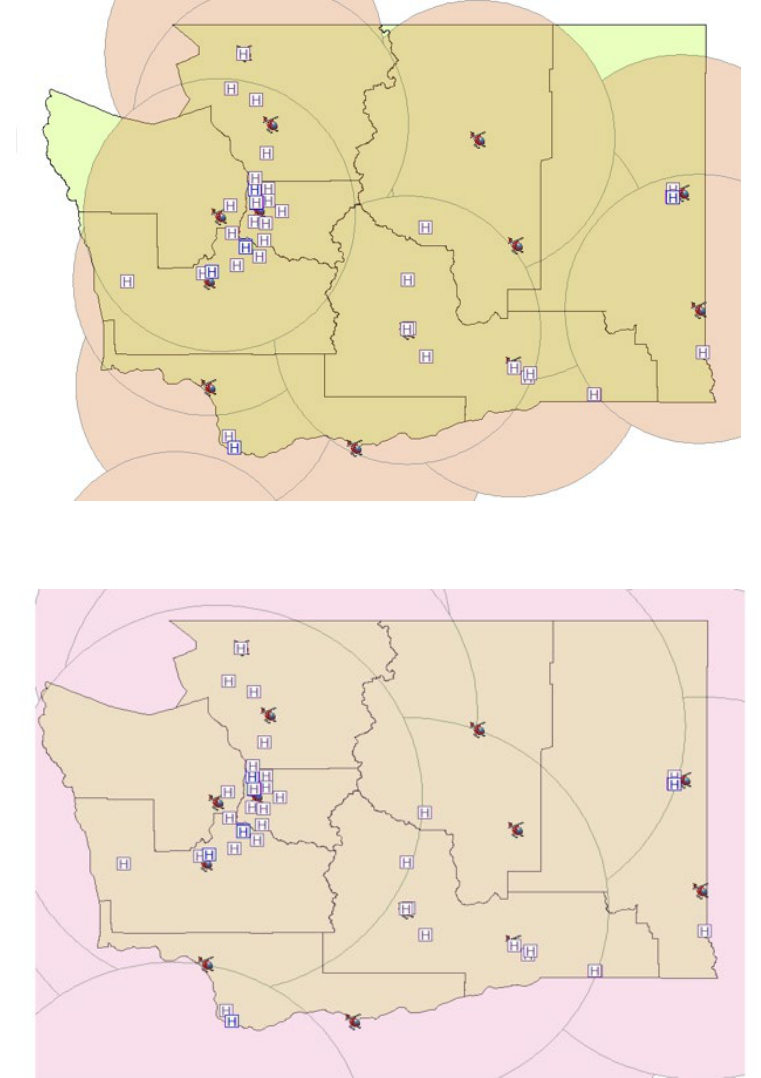
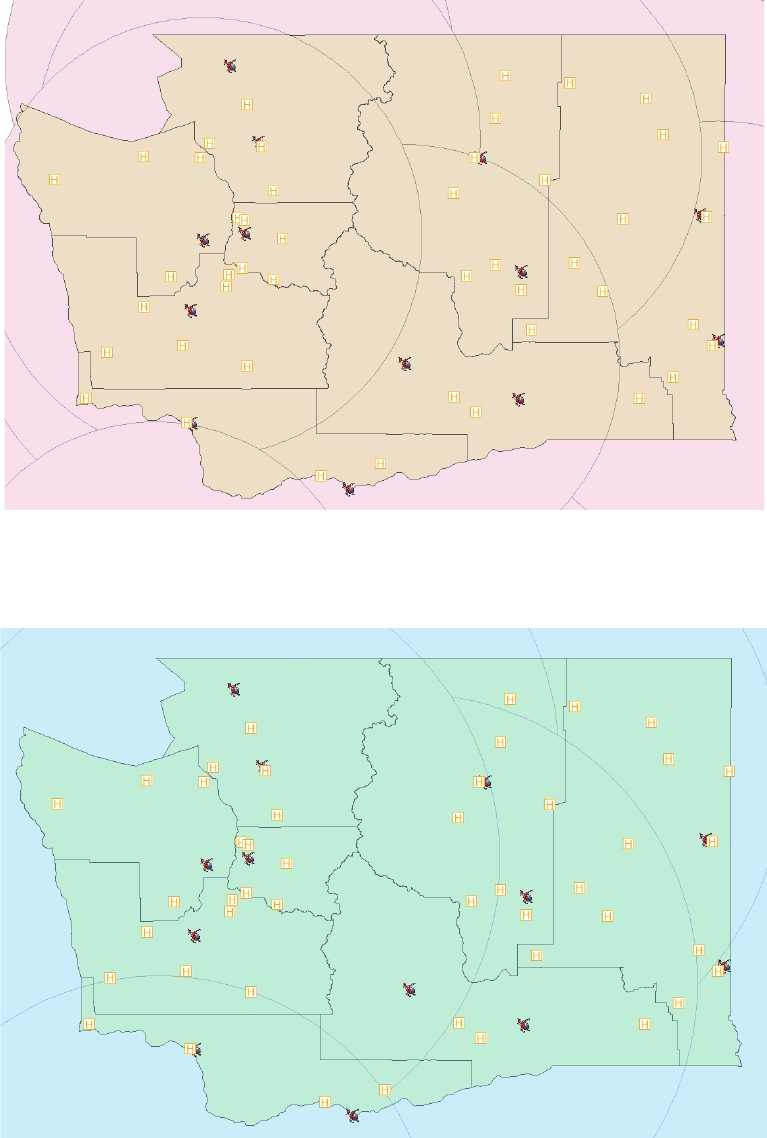
The updated maps in Figures 1 through 5 shows the location of air medical service bases with
the projected response times to the geographical area within the buffer zones for intervals of 15,
20, 30, 45, and 60 minutes.
Helicopter/Rotor Wing
Figure 1. Geographical Coverage from Air Ambulance Base 15 Minute Response Time
16
DOH 530-129 January 2019
Figure 2. Geographical Coverage from Air Ambulance Base 20 Minute Response Time
Figure 3. Geographical Coverage from Air Ambulance Base 30 Minute
Response Time
17
DOH 530-129 January 2019
Figure 4. Geographical Coverage from Air Ambulance Base 45 Minute
Response Time
Figure 5. Geographical Coverage from Air Ambulance Base 60 Minute
Response Time
18
DOH 530-129 January 2019
Airplane / Fixed-wing
Washington state has historically used helicopters only for prehospital transport from an
emergency scene. However, some air ambulance services also have fixed-wing aircraft that
are used for inter-facility transports. Between 2010 and 2017, the use of fixed-wing aircraft
for prehospital transport from an emergency scene was prohibited because of concerns
about patient safety, including the following:
• Fixed-wing aircraft landing zones (runways) have limited and fixed locations. Rotor-
wing aircraft can land at the scene of an emergency and directly at a hospital landing
pad.
• Fixed-wing transports require rendezvous with a ground ambulance service to transfer the
patient from the aircraft landing area to and from the scene and treatment facility.
These and other factors were believed to increase the total out-of-hospital time for the patient.
Changes in federal regulations during the previous plan cycle limited state authority over some
aspects of air services.
During this plan revision process, a review of published literature and other state regulations
provided little evidence to support the limitation of fixed-wing services based on the above
concerns. Additionally, the use of established fixed-wing services in the islands and in rural
areas of our state may have some benefit.
Washington has one fixed-wing service that applied and was granted verified trauma status in
2017 serving the San Juan Islands.
The use of fixed-wing aircraft for prehospital transport from an emergency scene is a new
standard. Therefore, performance measures must be established to monitor fixed-wing use and
performance for prehospital emergency incidents during this planning cycle.
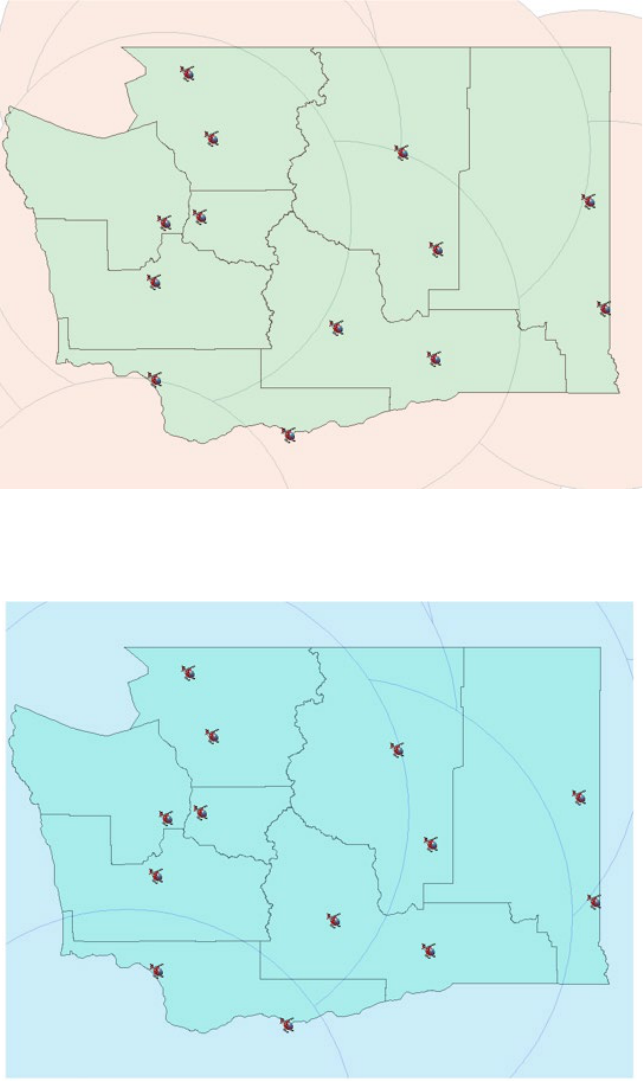
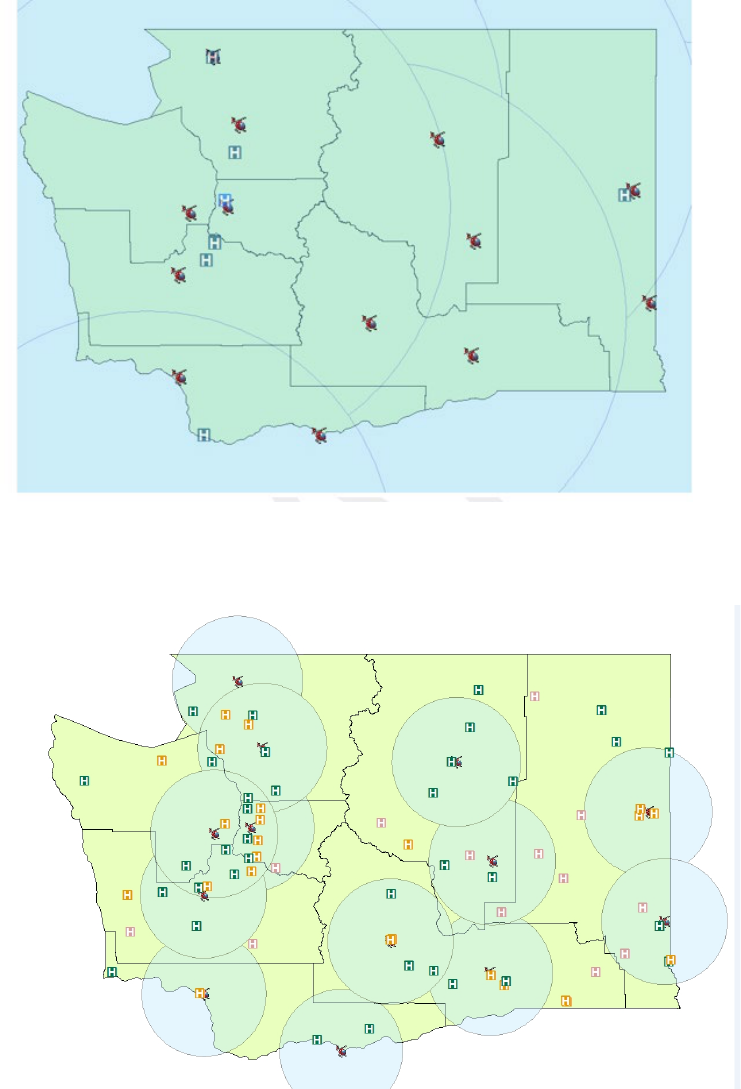
Because fixed-wing aircraft are rarely used for transport from an emergency scene in a
prehospital environment, our goals for geographical coverage of fixed-wing services in this
plan, were limited to identifying the location of existing fixed-wing bases and possible
airports with landing capabilities, which are depicted in Figures 6 and 7.
19
DOH 530-129 January 2019
Figure 6. Fixed-wing Air Ambulance Bases
Figure 7. Washington State Airports
(Reflects only the possibility of use by fixed-wing air ambulance services and may not be an all-inclusive
list).
20
DOH 530-129 January 2019
Response Time to Prehospital Scene
WAC 246-976-390(12) states: “Verified air ambulance services must meet minimum agency
response times as identified in the State Plan.”
The measures of success and outcomes – historical snapshot for 2010-2016 section on page 23,
shows the standards and outcomes for response time to prehospital scene for the latest planning
cycle.
Limitations in data, as discussed on page 11, inhibited a comprehensive statewide analysis of air
ambulance response times to prehospital scene. Improving data is a primary goal for the air
ambulance workgroup.
Historically, the standards prescribed in previous plan cycles for response times to scene were
calculated from the time the air ambulance service receives a request for service to when the
helicopter arrives on scene. Because of our current work around improving data collection and
analysis, this standard may be updated as our capabilities with data evolve.
Safety of patients, ground EMS personnel and air ambulance personnel are of primary concern.
Therefore, exceptions to response time standards will include those times when weather or other
factors preclude the air ambulance from safely flying to an EMS scene.
The updated maps in Figures 1 through 5 (page 15-17) show the location of air medical service
bases with the projected response times to the geographical area within the buffer zones for
intervals of 15, 20, 30, 45, and 60 minutes.
Response Time Standards to Trauma, Cardiac and Stroke Facilities
Air ambulance services are subject to requirements of the Washington State Pre-hospital
Triage Destination Procedures for trauma, cardiac and stroke related care.
The measures of success and outcomes – historical snapshot for 2010-2017 section on page 23,
depicts the standards and outcomes of response time standards to trauma facilities for the latest
planning cycle.
Limitations in data, as discussed on page 11, inhibited a comprehensive statewide analysis of air
ambulance response times to prehospital scene. Improving data is a primary goal for the air
ambulance workgroup.
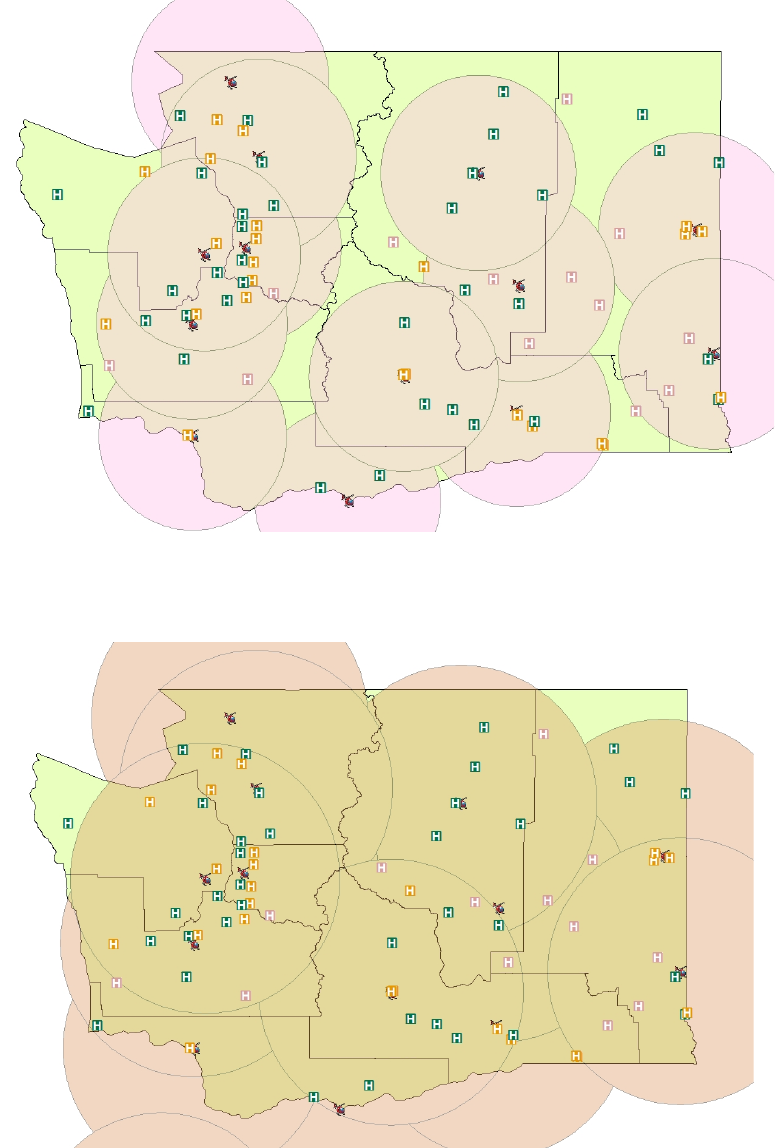
However, updated maps that show projected response times from air ambulance buffer zones to
trauma, cardiac and stroke facilities are in the appendices of this plan (pages 40 through 52,
Figures 8 through 32)
21
DOH 530-129 January 2019
Review of Operational Guidance for Use of Air Ambulances
RCW 70.168.060 authorizes and directs the DOH to establish minimum standards and guidance
for developing facility and prehospital EMS patient care protocols, and regional EMS patient
care procedures. State guidance for protocols and procedures are almost always developed
through collaborative work with stakeholders in ad hoc committees, or existing technical
advisory committees (TAC).
Four major categories of operational and clinical guidance documents exist and influence
treating and transporting patients in the emergency care system. Each document is defined in
statute and rule, and has a prescribed purpose. They are:
• Washington State Prehospital Trauma, Cardiac, and Stroke Triage Destination
Procedures (state triage tools)
• Regional EMS Patient Care Procedures (PCP)
• County Operational Procedures (COP); and
• DOH-approved Medical Program Director EMS Patient Care Protocols (Protocols)
In the 2010-2017 plan cycle, a goal was established and achieved to develop regional PCPs for
using air ambulance resources. However, no statewide standard or guidance was developed.
That resulted in developing inconsistent standards about use of air ambulance services across the
EMS regions.
During this plan cycle, the air ambulance workgroup will evaluate regional patient care
procedures, and will establish peer reviewed statewide recommendations for air ambulance use
for future revisions of regional EMS PCPs. These recommendations will be included as a part of
this plan.
Data Collection and Analysis, and Quality Assurance
Because of challenges in data collection and analysis in the previous plan period, our ability
to analyze air ambulance use and patient outcomes has been difficult.
In 2013, the department reviewed air ambulance service data in the trauma registry, Our trauma
epidemiologist provided a report to the EMSTC-SC about statewide use. In summary the data
revealed the following:
1. During 1995-2011, the number of ground EMS transports from the scene had a four-fold
increase and the inter-hospital ground transports had a 12-fold increase, while there was
no appreciable increase in the number of air transports.
2. The overall EMS volume stayed stable during 2006-2011.
3. People with motor-vehicle related injuries are likely to be transported by air. Any decline
in motor vehicle trauma is likely to negatively affect the use of air ambulance services.
To some extent, the recent decline in air ambulance transports could be attributed to
declining motor vehicle trauma, and to rising elderly falls.
4. The central and east regions attract most air transports from the scene and transferring
hospitals. This is because Harborview Medical Center, the state’s only level I trauma

22
DOH 530-129 January 2019
center, is in the Central Region, and Providence Sacred Heart Medical Center is the only
level II trauma center in the East Region.
5. Data from 2007 through 2011 clearly illustrate that demand for air ambulance services has
remained consistent. There has been no appreciable increase in demand during this period.
During this plan revision process, the department trauma epidemiologist evaluated available data
about air ambulance services, provided a summary, and made recommendations on how to
improve air ambulance data collection and quality. This summary and any completed work was
reported to the EMSTC-SC in September of 2018.
Summary of Statewide Analysis of Air Ambulance Services
The intent of our analysis is to assess if Washington has adequate air ambulance services that are
accessible to our citizens, and are used appropriately to transport patients to definitive care and
improve patient outcomes.
The assessment should help identify gaps such as unserved or underserved areas, and provide
information for the workgroup to develop recommendations for goals, standards and outcomes
for the next plan cycle.
The following summary and recommendations are based on the information presented in the
previous sections.
The assessment of distribution of resources and geographical coverage – during this plan revision,
air ambulance service locations were updated and added to the Emergency Care Services GIS
map. We are able to identify the air ambulance assets available statewide; however, there is
insufficient information, data, and evidence based methodology available to determine what the
minimum recommended air ambulance services for Washington should be. Additionally, states
are limited in regulating air ambulance services about distribution of resources. No requirement or
formal mechanism is in place for air ambulance services to notify the department of changes or
additions in air ambulance bases and assets across the state. Often, air ambulance services will
add or change a base without consulting with the department.
The assessment of response times to prehospital scene and trauma, cardiac and stroke facilities
revealed that there is insufficient data collection, preparation, and analysis to evaluate air
ambulance services’ response time performance. During the plan revision, we updated the
calculation used to project response times to the scene and to trauma facilities. We revised the
maps showing projected response times within a buffer zone to designated trauma facilities within
that buffer zone, and added maps for cardiac and stroke facilities.
The assessment of available data for analyzing air ambulance use revealed that there is
insufficient data, information, and quality assurance processes in place at a local, regional and
statewide level to evaluate the effectiveness of air ambulance service use and care statewide.
The assessment of review of operational guidance documents about air ambulance use
revealed that operational guidance does exist, and is inconsistent across the state.
23
DOH 530-129 January 2019
Measures of Success and Outcomes
Historical Snapshot 2010-2017
The goals, standards and outcomes for the air ambulance component of the EMS and trauma
care system from 2010-2016 included:
Goal One
To support a system of air ambulance response providing safe and expeditious
transport of critically ill patients to the appropriate designated trauma service.
Standard
To provide 70 percent of the state population access to air ambulance service
within 30 minutes or less and 100 percent of the state population access to air
ambulance service within 60 minutes or less.
Outcome
When assessing access of air ambulance services, the amount of geographical
coverage air ambulances provided increased to 93 percent of the land area of the
state and 99 percent of the residential population.
Standard
To provide 70 percent of the state population access to designated services within
30 minutes or less and 100 percent of the state population access to air ambulance
service within 60 minutes or less.
Outcome
Distribution of level I and II trauma, cardiac, and stroke designated and
categorized services affect the ability to deliver patients in a timely manner to
the higher-level trauma services, even by air. Geographic gaps in the 30-
minute response time buffer zones are consistent with the lack of level I or II
trauma, cardiac, and stroke designated and categorized services.
Goal Two
Regional EMS Patient Care Procedures (PCPs) for the use of air ambulance
resources are included in approved regional EMSTC plans.
Standard
No standards for PCPs were established.
Outcome Regional EMSTCs developed and adopted patient care procedures for the
response of air ambulance resources in most regions; however, inconsistent
standards about air ambulance use in patient care procedures exist statewide.
Goal
Three
Air ambulance resources throughout Washington state provide optimal coverage
while avoiding costly and inefficient duplication of resources.
Standard
To provide 70 percent of the state population access to air ambulance service
within 30 minutes or less and 100 percent of the state population access to air
ambulance service within 60 minutes or less.
Outcome
Distribution of resources provides coverage for 68 percent of the state’s land area
and more than 90 percent of the residential population within a 30-minute
response time from air ambulance bases to scene.
Outcome
100 percent of the state’s population can receive air ambulance service in 60
minutes or less.
Standard
Arrival within 30 minutes of receiving a request for service, 80 percent of the time.
Outcome
There is insufficient statewide data to accurately measure and report on this
standard.

24
DOH 530-129 January 2019
Other accomplishments during this plan cycle included:
• Revision of the air ambulance rules WAC 246-976-320 to modernize standards.
• Updates to the department’s Emergency Care Services GIS Map to include air bases,
their assets and updated buffer zones.
Recommended Goals and Strategies for 2018-2021 Plan Period
Recommended goals within the scope of this workgroup for this plan cycle include:
• Assess and improve air ambulance data submission and quality to the trauma and
EMS (WEMSIS) data registries.
• Identify and implement a methodology to better assess and monitor citizen access to
air ambulances, response time to prehospital scene and definitive care.
• Identify baseline performance standards about access and response times.
• Evaluate the feasibility of establishing a minimum number of recommended air
ambulance services needed to achieve response time performance standards.
• Assess performance and outcomes.
• Identify and improve quality assurance activities at local, regional, and state levels to
monitor patient outcomes and the effectiveness of using of fixed-wing ambulances to
prehospital events.
• Improve local, regional, and statewide guidance for air medical use.
Specific suggested strategies to achieve these goals that are reflected in the PHTAC EMS
strategic plan.

25
DOH 530-129 January 2019
Statewide Recommendations for EMS Use of Air Ambulance
Purpose
The purpose of this section is to establish minimum standards and guidance in accordance with
RCW 70.168.060 for developing facility and prehospital EMS patient care procedures and
protocols about use of air ambulances.
Background
The department recognizes air ambulance services as having a distinctive role in the emergency
care system. The multi-regional and statewide flight range capabilities along with logistical
considerations for aircraft are factors that require a coordinated system of medical response and a
statewide strategic approach in managing emergency medical services (EMS) resources. This
approach enables citizen access to the best patient care and transport capabilities, and works to
mitigate an unsafe prehospital transport environment to the extent possible. Air ambulances can
provide the highest level of out-of-hospital care, and rapid, expedient transport for critically sick
and injured patients. Strategic development, deployment, and quality assurance strategies for air
ambulance services can improve outcomes in patient care.
For these reasons, our EMS and Trauma Care Steering Committee (EMSTC-SC) recommended
the development of a statewide Air Ambulance Strategic Plan (plan). With oversight from the
department, the Air Ambulance Services Workgroup (workgroup) and Prehospital Technical
Advisory Committee (PHTAC) were tasked to develop and manage the plan.
In 2000, the statewide aeromedical workgroup identified strategic initiatives that were
memorialized in the 2010 Washington State Air Ambulance Plan, to develop, adopt, and
implement guidance for air ambulance response using evidence-based practices to ensure high-
quality patient care, as well as the safety of the public, flight and ground response teams. The
intent of this guidance is for local and regional EMS and trauma care councils (EMSTC) to adopt
evidence based recommendations for the activation and use of air ambulance services into
regional EMS and trauma care plans, regional patient care procedures, and local county
operating procedures across the state.
The following pages provide statewide peer-reviewed guidance for activating and using air
ambulance services.
26
DOH 530-129 January 2019
Determination of Medical Necessity for Air Ambulance Transport
Goal
To promote the development of consistent guidance for determining the medical necessity for air
ambulance transport.
Background
General principles for making a determination for the mode of transport include:
• Patients requiring clinical interventions should be provided those interventions in the
most expeditious manner possible.
• Patients who are stable should be transported in a manner that best addresses the needs
of the patient and the system.
• Patients with critical injuries or illnesses resulting in unstable vital signs require transport
by the fastest available means, and with a transport team that has the appropriate level of
care capabilities, to a center capable of providing definitive care.
• Patients with critical injuries or illnesses should be transported by a team that can provide
intra-transport critical care services.
• Patients who require high-level care during transport, but who do not have time-critical
illness or injury, may be candidates for ground critical care transport (i.e., by a specialized
ground critical care transport vehicle with the level of care exceeding that of local EMS)
if such service is available and logistically feasible.
Recommendations
The use of air ambulance transport should be considered when:
• The patient’s clinical condition requires minimization of time spent out of the hospital
environment during the transport.
• The patient is located in an area that is inaccessible to ground transport.
• The patient requires critical care life support (e.g., monitoring personnel, specific
medications, and specific equipment) during transport, which is not available with ground
transport options.
• The use of local ground transport would leave the local area without adequate emergency
medical services coverage.
27
DOH 530-129 January 2019
• If local ground transport is not an option, explore whether the patient’s and system’s
needs can be met by an available regional ground critical care transport service.
• Patient meets trauma, cardiac, or stroke triage criteria and the scene time plus ground
transport time to the closest designated trauma hospital exceeds the estimated time of
arrival (ETA) of air ambulance service or ground ALS intercept.
• The scene time, plus ground transport time to local hospital, is less than air ambulance
service or ALS intercept arrival time to the scene. Consider initiating ground
transportation and diverting the air ambulance service or ALS intercept to the destination
hospital for continued patient care or if transport to a definitive care hospital will be
necessary and applicable.
• Transport time to the appropriate facility may be reduced by more than 15 minutes.
28
DOH 530-129 January 2019
Relative Contraindications to Air Ambulance Transport
Goal
To identify potential contraindications to air ambulance transport to minimize time spent on
determining the most appropriate transport resource for patients.
Recommendation
In general, potential contraindications to air ambulance transport will fall within the following
categories:
• Hazardous materials
• Highly infectious disease (such as Ebola)
• Weather
• Patient weight (aircraft dependent)
Air ambulance services should be contacted to assist in determining whether they can transport
should a situation that falls within one of the above categories be present at the scene of an
emergency.
If any of the four conditions listed above are present, consider initiating ground transport and
identifying a rendezvous location if air ambulance confirms the ability to transport.
29
DOH 530-129 January 2019
Standards for EMS Activation of an Air Ambulance Service
Goal
To provide guidance to EMS and trauma care councils and medical program directors for
developing patient care procedures, county operating procedures, and patient care protocols
about who may activate and cancel air ambulance services.
Recommendations
Any public safety personnel, medical or nonmedical, may call to request on-scene air transport
when it appears necessary.
The highest level of certified pre-hospital personnel on scene may cancel the air ambulance
response if they determine the patient condition does not warrant air transport.
Procedures
1. The call should be initiated through dispatch services. The caller should:
a. Provide the location using latitude and then longitude
b. Identify the frequency for operation
c. Identify the point of contact on ground
2. The air ambulance communication staff will provide an approximate launch time and
flight time, and will advise “when lifted” to the dispatchers requesting air ambulance
service.
3. The dispatching agency will provide the air ambulance service with the correct radio
frequency to use for contacting EMS ground units.
30
DOH 530-129 January 2019
Early Activation of an Air Ambulance Service
Goal
To encourage early activation procedures that could minimize time to definitive care.
Background
Before arrival of first responders, an air ambulance service provider may be launched based on
information from dispatch indicating a high likelihood that an air ambulance will be necessary.
This will expedite arrival should first responders confirm the need for air transport.
Recommendations
Medical program directors, and local and regional councils, should identify in their procedures
who may initiate early activation or cancel air ambulances. Consider the following:
• Any public safety personnel, medical or nonmedical, may call to request on-scene air
transport when it appears necessary. This may include law enforcement, EMS providers,
fire personnel or other first responders. Medical facilities can call air ambulance services
as needed.
• The first arriving on-scene personnel with the highest level of EMS certification should
determine whether air ambulance should continue or be canceled.
First responders will identify if there a high index of suspicion that air ambulance services will
be required. The local dispatch center should notify responding ground crews that an air
ambulance has been activated. Criteria to consider include:
Transport considerations:
• Prolonged pre-hospital time (i.e. prolonged extrication, transport time, and/or extraction
from wilderness environment).
• Distance to a designated trauma center or categorized facility is greater than 30 minutes
away.
Mechanism of injury - considerations:
• Death in the same vehicle
• Ejected from vehicle
• Anticipated prolonged extrication: greater than 20 minutes with significant injury.
• Long fall: greater than 30 feet for adults, 15 feet for children.
• Sudden or severe deceleration
• Multiple casualty incidents
31
DOH 530-129 January 2019
Patient characteristics – considerations:
• Glasgow Coma Scale (GCS) less than or equal to 13
• Patient was unconscious and not yet returned to GCS of 15
• Respiratory rate less than 10 or greater than 29 breaths per minute
• BP less than 90 mmHg or clinical signs of shock
• Penetrating injury to the chest, neck, head, abdomen, groin or proximal extremity (above
the knee or elbow)
• Flail chest / unstable chest wall fractures
• Major amputation of extremity
• Burns second-degree > 20 percent
• Burns third-degree >10 percent
• Facial or airway burns with or without inhalation injury
• Third-degree burns involving the eyes, neck, hands, feet or groin
• High voltage electrical burns
• Paralysis / spinal cord injury with deficits
• Suspected pelvic fracture
• Multi-system trauma (three or more anatomic body regions injured)
32
DOH 530-129 January 2019
Communication Standards for EMS and Air Ambulance Services
Goal
To promote consistent practices, and to improve communication between air and ground
ambulance services.
Recommendation
Regional EMS and trauma care councils are encouraged to establish a pre-coordinated
communication procedure to identify the correct, compatible frequencies, and applicable
collaborative communication processes between air and ground EMS services and E911 centers.
The procedure should encourage terminology that promotes understanding and safety between
air and ground EMS services, and consider the following:
• Do not use 10 codes when communicating with air ambulance services.
• The standardized method of providing GPS coordinates is to provide the latitude and then
the longitude.
• The procedure should describe and direct how ground EMS services should wave a
helicopter off or advise the aircraft to abort landing.
• Nationally recognized incident management language and procedures such as an incident
command system (ICS) should be used.
• Air ambulance personnel will contact the receiving hospital as soon as possible after
liftoff from the scene.
33
DOH 530-129 January 2019
Safety of Ground Crews around Aircraft
Goal
To promote safety of all personnel around aircraft.
Recommendations
Local and regional EMSTCs should encourage and advocate training between EMS, and air and
ground ambulance services.
Written procedures should direct ground EMS crews:
• Not to approach the aircraft until directed to do so by flight crews.
• Not to approach the tail of the aircraft.
• To use situational awareness while operating around aircraft.
34
DOH 530-129 January 2019
Landing Zone Considerations for Helicopters
Goal
To promote safe consistent practices for EMS and air ambulances for managing landing zones
for helicopters.
Recommendations
Written procedures should direct ground EMS crews to:
1. Select a location for the landing zone that is at least 100 feet by 100 feet (generally the
length of a basketball court and double the width). The pilot of the aircraft is the decision-
maker about landing zones.
2. Assure that the landing zone location is free of loose debris.
3. Assure that the approach and departure paths are free of obstructions, and identify to the
pilot hazards such as wires, poles, antennae, trees, etc.
4. Provide air medical services with the latitude and longitude of the landing zone. Avoid
using nomenclature such as “Zone 1.”
5. Mark night landing zone with lights. Cones may be used if secured or held down. Do
not use flares.
6. Establish security for the landing zone for safety and privacy.
7. Avoid pointing spotlights and high beams toward the aircraft. Bright lights (such as scene
lights) should be dimmed as helicopter approaches.
8. Not approach a helicopter unless escorted by an aircrew member.
9. Consult with aircrew members before loading and unloading. Loading and unloading
procedures will be conducted under the direction of flight personnel.
35
DOH 530-129 January 2019
Hospital Destination Decisions for Patients Transported by Air ambulance Services
Goal
To direct to EMS services to use state-approved triage destination procedures for trauma, cardiac,
and stroke patients.
Procedure
Air ambulance services must adhere to and comply with the State of Washington Prehospital
Trauma Triage and Destination Procedures when identifying the most appropriate receiving
facility for trauma, cardiac, or stroke patients.
These procedures are at the links below or you can email HSQA.EMS@doh.wa.gov to request a
copy be sent to you.
Prehospital Trauma Triage Destination Procedure
https://www.doh.wa.gov/Portals/1/Documents/Pubs/530143.pdf
Prehospital Cardiac Triage Destination Procedure
https://www.doh.wa.gov/Portals/1/Documents/Pubs/346050.pdf
Prehospital Stroke Triage Destination Procedure
https://www.doh.wa.gov/Portals/1/Documents/Pubs/530182.pdf
36
DOH 530-129 January 2019
Inter-facility Transports
Goal(s)
To promote efficient coordination for inter-facility transports using air ambulances.
To encourage local and regional familiarity with air ambulance services and their specialized
capabilities.
To promote standardization in information provided to air ambulances when requesting inter-
facility transport of patients.
Background
Air ambulances transport patients in a pre-hospital and inter-facility setting. Air ambulances
may provide care to special populations such as neonates, or patients with specialized equipment
such as intra-aortic balloon pumps.
Becoming familiar with capability of local and regional air ambulance resources and establishing
standardized request processes for inter-facility transports could decrease inefficiencies and
improve time to definitive care.
Recommendations
Regional EMS and trauma care councils and medical program directors should work with air
ambulance services in their region to identify what specialized care air medical services can
provide.
Patient care procedures about inter-facility transport should include a provision for the minimum
information air ambulance services will need to make arrangements or referrals for inter-facility
transports. Consider the following information as a minimum standard:
• Physician to physician referral and destination
• Patient weight
• Special equipment (intra-aortic balloon pump, isolette, cardiac assist devices, etc.)
• Additional rider (at the discretion of the pilot)
37
DOH 530-129 January 2019
Use of Fixed-wing Service in the Pre-Hospital Setting
Goal
To assist in determination of which mode of air transport is best suited to meet the patient’s needs
in the pre-hospital setting.
Recommendations
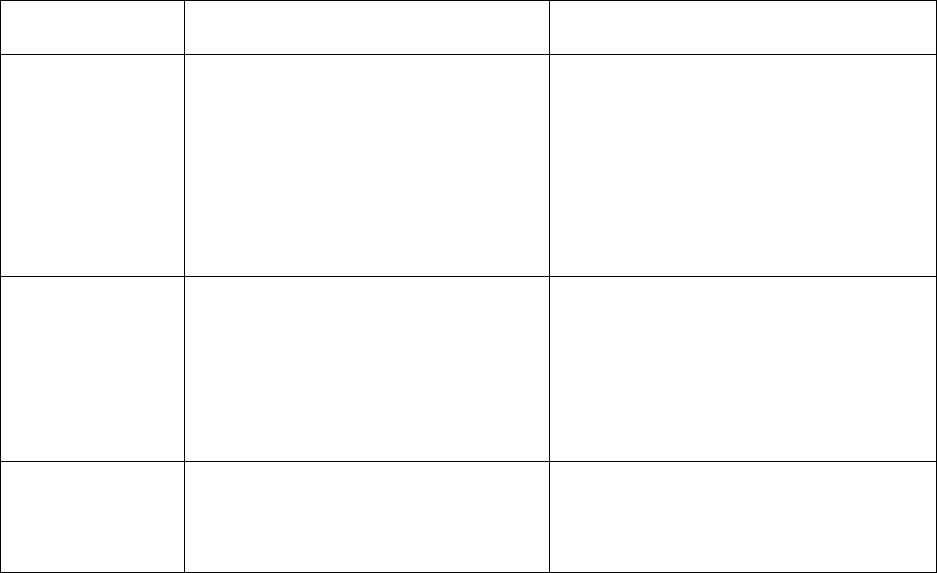
Relative comparative considerations for air transport modes:
Characteristic
Rotor-wing (Helicopter)
Fixed-wing (Airplane)
Response time
Decreased response time to the
patient (up to about 100 miles
depending on logistics such as
duration of ground transfer leg).
Decreased response time to patients
when transport distances exceed
about 100 miles.
Requires landing at airport, with two
extra legs between airports and the
patient origin and destination.
Out-of-hospital
transport time
Decreased out-of-hospital transport
time.
In comparison with ground transport,
decreased out-of-hospital transport time.
Requires landing at airport, with two
extra legs between airports and the
patient origin and destination.
Weather
In comparison with fixed-wing,
more susceptible to weather
constraints (e.g. icing conditions,
weather minimums).
In comparison with rotor-wing, less
susceptibility to weather constraints.
Factors that department-approved medical program directors may use to determine what mode
of air transport to use may include:
• Is it time critical
• Medical necessity
• Service availability
• Membership
Other factors to consider include:
• When the closest most appropriate rotor-wing service has been contacted and reports that
it is unavailable.
38
DOH 530-129 January 2019
• When weather prohibits rotor-wing to fly.
• In remote location where rotor-wing cannot safely fly or land
• If transport will require a distance of greater than 100 nautical miles (o nautical mile
equals about 1.15077945 miles on land).
• If using rotor-wing service for BLS transport will leave the 30-minute air ambulance
response buffer zone without adequate rotor-wing coverage for critical patients.
• If the expected arrival of a rotor-wing ambulance will take 60 minutes or greater.
39
DOH 530-129 January 2019
Appendices
A
Projected response times from buffer zones to trauma facilities
B
Projected response times from buffer zones to cardiac facilities
C
Projected response times from buffer zones to stroke facilities
D
Definition of Terms Used
40
DOH 530-129 January 2019
Appendix A
Projected response time from air ambulance base to trauma designated facilities within buffer
zone.
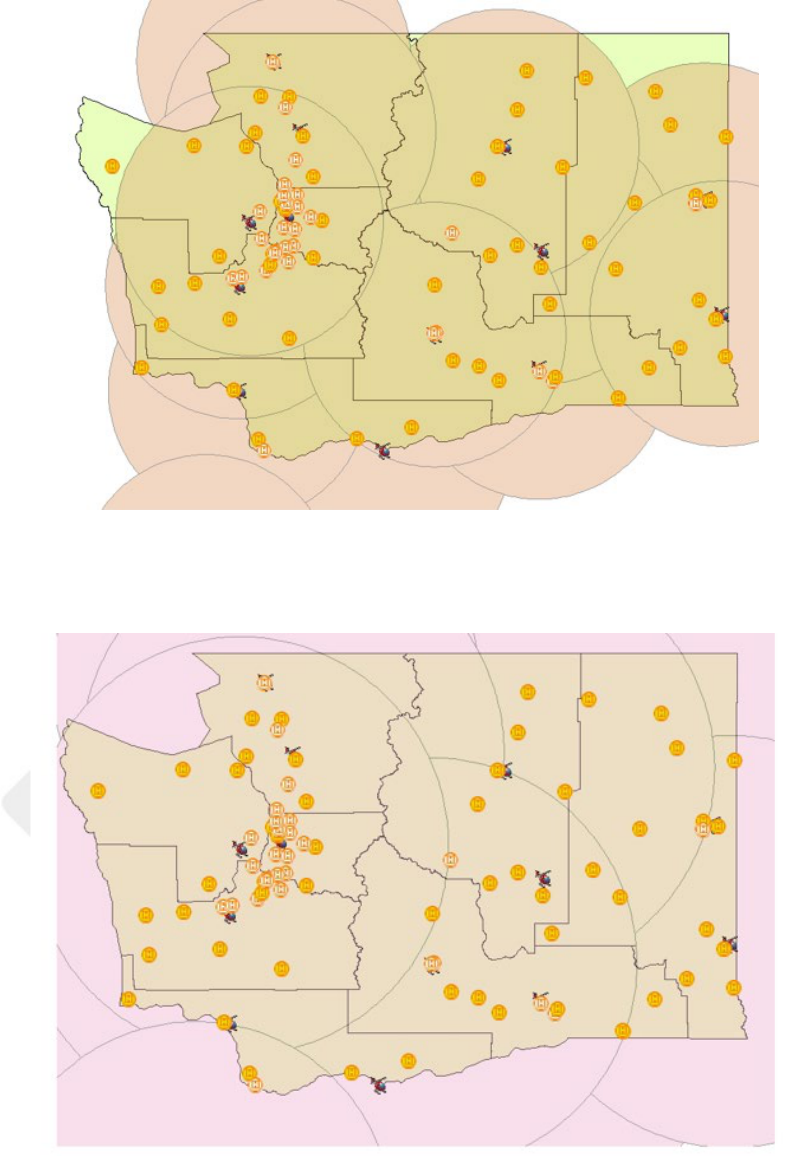
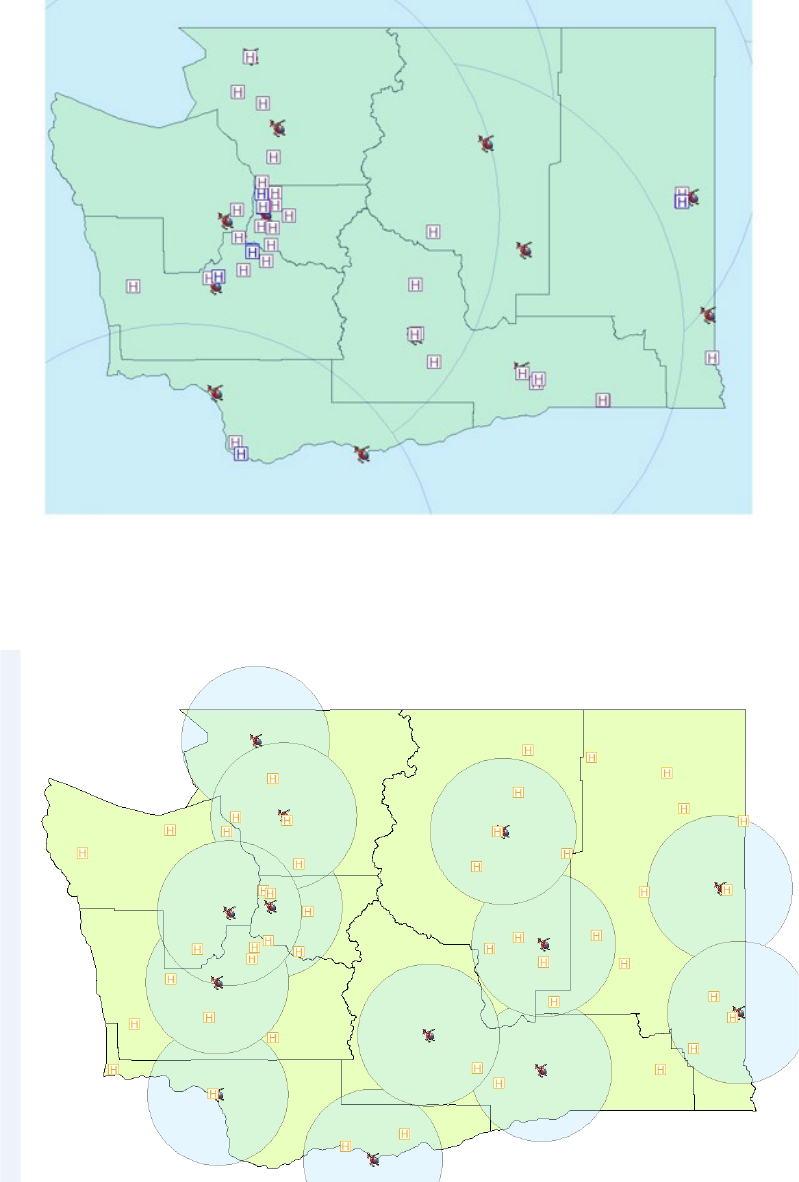
Figure 8. Projected 15-minute response time from air ambulance base to level I and II designated trauma facilities
within the buffer zone.
Figure 9. Projected 20-minute response time from air ambulance base to level I and II designated trauma facilities
within the buffer zone.
41
DOH 530-129 January 2019
Figure 10. Projected 30-minute response time from air ambulance base to level I and II designated trauma
facilities within the buffer zone
Figure 11. Projected 45- minute response time from air ambulance base to level I and II designated trauma
facilities within the buffer zone
42
DOH 530-129 January 2019
Figure 12. Projected 60-minute response time from air ambulance base to level I and II designated trauma facilities
within the buffer zone
Figure 13. Projected 15-minute response time from air ambulance base to level III, IV, V designed trauma facilities
within the buffer zone
43
DOH 530-129 January 2019
Figure 14. Projected 20-minute response time from air ambulance base to level III, IV, V designed trauma facilities
within the buffer zone
Figure 15. Projected 30-minute response time from air ambulance base to level III, IV, V designed trauma facilities
within the buffer zone
44
DOH 530-129 January 2019
Figure 16. Projected 45-minute response time from air ambulance base to level III, IV, V designed trauma facilities
within the buffer zone
Figure 17. Projected 30-minute response time from air ambulance base to level III, IV, V designed trauma facilities
within the buffer zone
45
DOH 530-129 January 2019
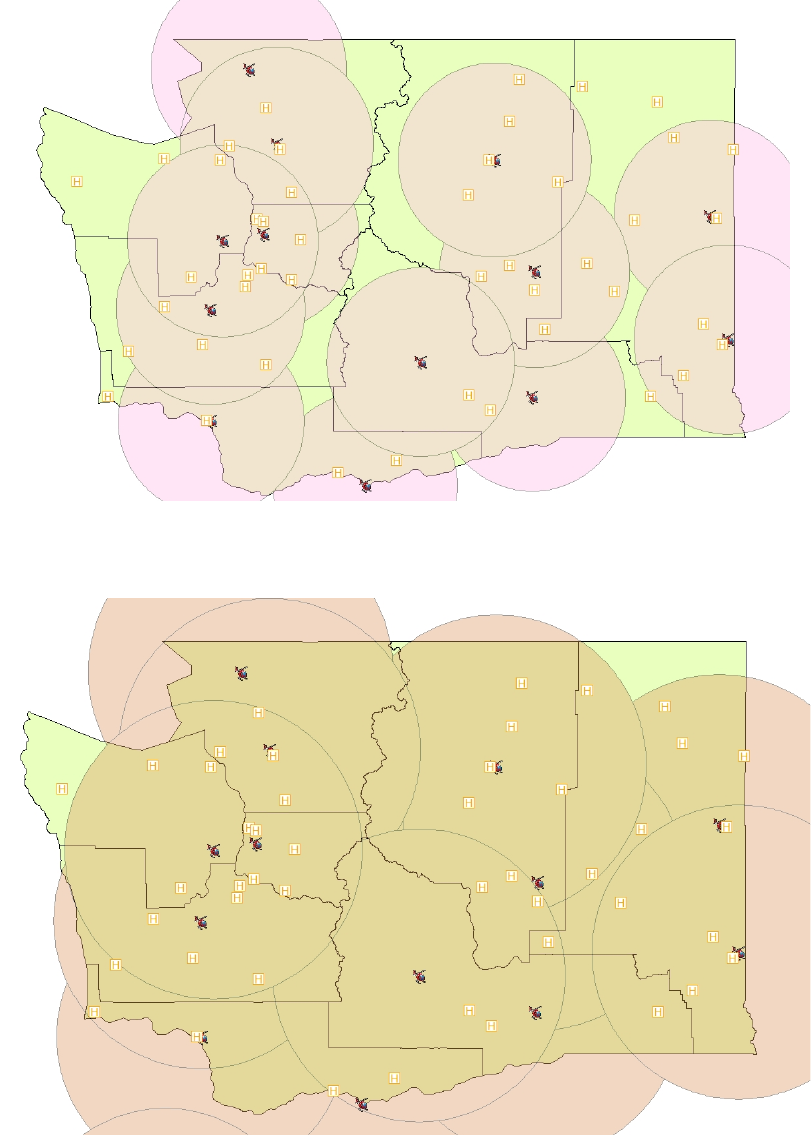
Appendix B
Projected response time from air ambulance base to cardiac categorized facilities within buffer
zone.
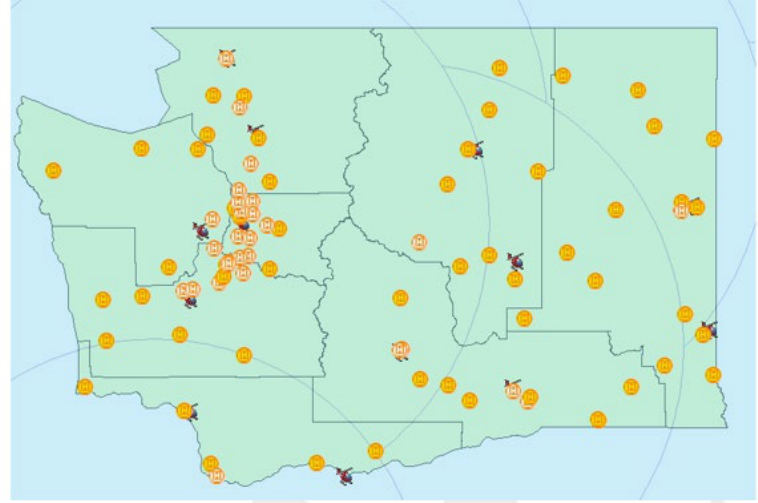
Figure 18. Projected 15-minute response time from air ambulance base to level I and II categorized cardiac facilities
within the buffer zone.
Figure 19. Projected 20-minute response time from air ambulance base to level I and II categorized cardiac facilities
within the buffer zone
46
DOH 530-129 January 2019
Figure 20. Projected 30-minute response time from air ambulance base to level I and II categorized cardiac facilities
within the buffer zone
Figure 21. Projected 45- minute response time from air ambulance base to level I and II categorized cardiac facilities
within the buffer zone
47
DOH 530-129 January 2019
Figure 22. Projected 60-minute response time from air ambulance base to level I and II categorized cardiac facilities
within the buffer zone
48
DOH 530-129 January 2019
Appendix C
Projected response time from air ambulance base to stroke categorized facilities within buffer
zone.
Figure 23. Projected 15-minute response time from air ambulance base to level I and II categorized stroke facilities
within the buffer zone
Figure 24. Projected 20-minute response time from air ambulance base to level I and II categorized stroke facilities
within the buffer zone
49
DOH 530-129 January 2019
Figure 25. Projected 30 minute response time from air ambulance base to Level I and II categorized stroke facilities
within the buffer zone
Figure 26. Projected 45-minute response time from air ambulance base to level I and II categorized stroke facilities
within the buffer zone
50
DOH 530-129 January 2019
Figure 27. Projected 60-minute response time from air ambulance base to level I and II categorized stroke facilities
within the buffer zone
Figure 28. Projected 15-minute response time from air ambulance base to level III categorized stroke facilities within
the buffer zone
51
DOH 530-129 January 2019
Figure 29. Projected 20-minute response time from air ambulance base to level III categorized stroke facilities within
the buffer zone
Figure 30. Projected 30-minute response time from air ambulance base to level III categorized stroke facilities within
the buffer zone
52
DOH 530-129 January 2019
Figure 31. Projected 45-minute response time from air ambulance base to level III categorized stroke facilities within
the buffer zone
Figure 32. Projected 60-minute response time from air ambulance base to level III categorized stroke facilities within
the buffer zone
53
DOH 530-129 January 2019
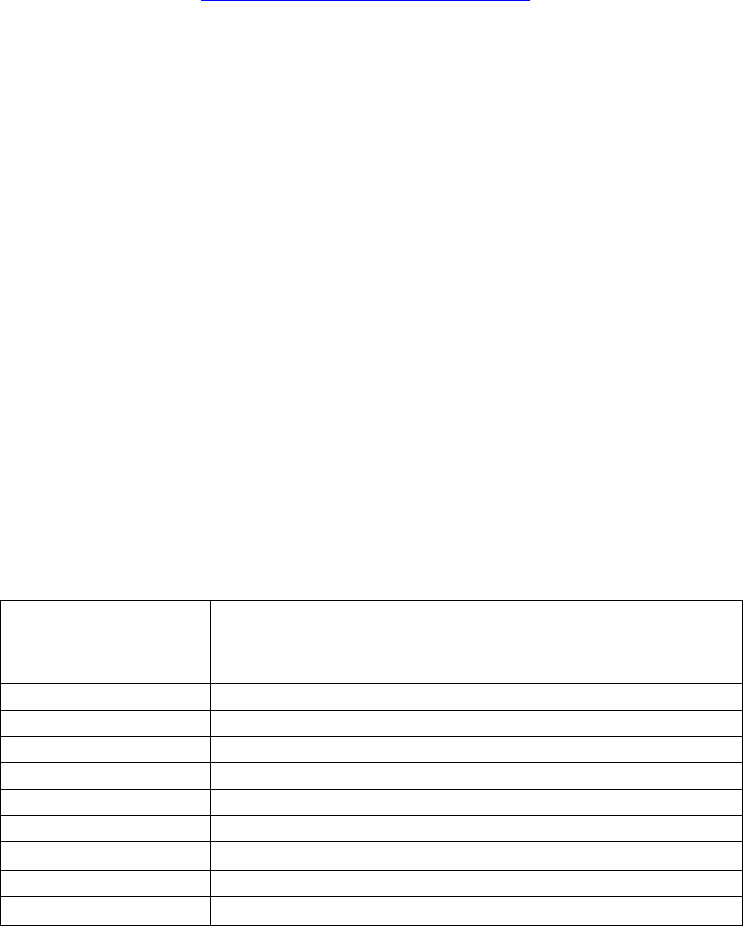
Appendix D
Definition of Terms Used
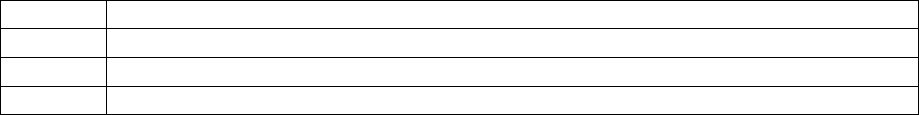
Term
Definition(s)
Activation
A request for service.
Ambulance
Means a ground or air vehicle designed and used to transport the ill and
injured, and to provide personnel, facilities, and equipment to treat
patients before and during transportation. (RCW 18.73.030)
Ambulance service
Means an organization that operates one or more ambulances. (RCW
18.73.030)
Aircraft
Means a vehicle designed for flight that is powered by liquid petroleum
fuel. (NAAMTA Standards Manual Glossary)
Aircraft type
The FAA lists three main aircraft types: fixed-wing (airplane), rotorcraft
(helicopter), and experimental aircraft. Within these categories are
specific designations for aircraft based on a number of variables. When
referencing the aircraft you may be asked for a specific make and model.
(NAAMTA Standards Manual Glossary)
Arrival at
Destination
The date and time the vehicle arrived at the destination landing area.
(NEMSIS)
Arrived at Patient
The date and time the responding unit arrived at the patient’s side.
Arrived on Scene
(1) Means the date and time the vehicle arrived at the destination landing
area. (NEMSIS)
(2) The point at which a vehicle is stopped on the scene of a response
destination or address. (NAAMTA Standards Manual Glossary)
Auto Launch
Based on pre-determined criteria an algorithm is built into a computer-
aided dispatch (CAD) system that automatically activates an air
ambulance as a primary response unit to a call in addition to other
primary responders.
Cancellation
Air ambulance services are no longer needed and the request for service
is canceled.
54
DOH 530-129 January 2019
Departure
(1) The date and time the responding unit left the scene with a patient
(started moving).
(2) An aircraft taking off from an airport. (NAAMTA Standards Manual
Glossary)
Destination Patient
Transferred
The date and time that patient care was transferred to the destination
healthcare facilities staff.
Dispatch
Acknowledged
Date/Time
The date and time the dispatch was acknowledged by the EMS unit.
(NEMSIS)
Dispatch Notified
Date/Time
The date and time dispatch was notified by the 911 call taker (if a
separate entity).
Early Activation
An air ambulance service provider is requested to respond and is
launched to a scene before arrival of first responders, based on the high
index of suspicion that specialty services or rapid transport will be
necessary. (Discussed 10.24.2017, discussed differentiation between auto
launch, early activation, simultaneous activation, etc.)
En Route Date /
Time
The date and time the unit responded; that is, the time the vehicle started
moving.
En Route Interval
A measurement that begins at the time a response unit starts to move
toward an incident, and the time the unit comes to a complete stop at the
location of the incident. (NAAMTA Standards Manual Glossary)
Fixed-wing
aircraft
Means airplane
Flight time
The estimated time from launch to the aircraft landing at the scene.
Landing zone
The physical landing location for the aircraft. . A landing zone should be
a flat area, free from obstructions, a minimum of 100 by 100 feet.
Landing zone
hazard assessment
The assessment of the landing zone. A landing zone should be a flat
area, free from obstructions, a minimum of 100 by 100. Landing zone
assessment should include evaluation of overhead wires, rocks, uneven
55
DOH 530-129 January 2019
surfaces, loose debris, trees, vehicles, foot traffic, and high winds. Such
hazards should be reported to the pilot.
Launch
An air ambulance service provider is requested to respond to the scene
After the arrival and patient assessment by first responders, based on the
ground medic’s determination that specialty services are necessary.
Launch time
The time at which the helicopter lifts from the launch location and is en
route to the scene.
Patient Arrived at
Destination
The date and time the responding unit arrived with the patient at the
destination or transfer point.
PSAP Call
Date/Time
The date and time the phone rings (911 call to public safety answering
point or other designated entity) requesting EMS services. (NEMSIS)
Rendezvous
To meet up with. An alternate site for patient transfer from ground
ambulance to air ambulance.
Rotor-wing
aircraft
Means helicopter (Merriam-Webster)
Trauma response
area
Means a service coverage zone identified in an approved regional plan.
(WAC 246-976-010)
Unit Notified
Dispatch
(1) The date and time the responding unit was notified by dispatch.
(NEMSIS)
(2) To send out emergency resources promptly to an address or incident
location for a specific purpose. (NAAMTA Standards Manual
Glossary).
Standby
A state of heightened alertness and preparation for an air ambulance
service provider about a possible mission. While on standby status, the
aircraft will remain available to respond to another request for service.
The next course of action would be for EMS to request launch or to
cancel the standby.
56
DOH 530-129 January 2019
Resources
Below are some resources air ambulance workgroup members presented and reviewed during the
development of this plan.
1. 2012 Air Medical Transport Conference Abstracts Scientific Assembly, Monday, October
22, 2012. Air Medical Journal 31.5 (2012): 225-30. Web.
2. Wish, John R, and Daniel P Davis. Auto Launch/early Activation: A Survey of AAMS
Members and Literature Review. Air Medical Journal 24.2 (2005): 83-8. Web.
3. McQueen, Carl, Mike Smyth, Gavin Perkins, and Joanne Fisher. Does the Use of Dedicated
Dispatch Criteria by Emergency Medical Services Optimise Appropriate Allocation of
Advanced Care Resources in Cases of High Severity Trauma? A Systematic Review. Injury
46.7 (2015): 1197-206. Web.
4. Kehoe, Sheehan, Davies, and David. 13: Reliability of Dispatch Criteria for Activation of
a Helicopter-Based Out-of-Hospital EMS System. Annals of Emergency Medicine 51.4
(2008): 474-75. Web.
5. Hirshon, Galvagno, Comer, Millin, Floccare, Alcorta, Lawner, Margolis, Nable, and Bass.
Maryland’s Helicopter Emergency Medical Services Experience From 2001 to 2011:
System Improvements and Patients’ Outcomes. Annals of Emergency Medicine 67.3
(2016): 332-40.e3. Web.
6. L'Heureux Randy, Bell Nathaniel J, Schuurman Nadine, and Hameed Syed M. Modelling
Optimal Location for Pre-hospital Helicopter Emergency Medical Services. BMC
Emergency Medicine 9.1 (2009): 6. Web.
7. Early Activation of an Air Medical Helicopter and Auto Launch Recommendations.
AAMS,aams.org/publications/early-activation-air-medical-helicopter-auto-launch-
recommendations/.
8. Goldstein, Doig, Bates, Rink, and Kortbeek. Adopting the Pre-hospital Index for
Interfacility Helicopter Transport: A Proposal. Injury 34.1 (2003): 3-11. Web.
9. Brändström, Helge, Ola Winsö, Lars Lindholm, and Michael Haney. Regional Intensive
Care Transports: A Prospective Analysis of Distance, Time and Cost for Road, Helicopter
and Fixed-wing Ambulances. Scandinavian Journal of Trauma, Resuscitation and
Emergency Medicine 22.1 (2014): 36. Web.
10. Milligan, Jones, Helm, and Munford. The Principles of Aeromedical Retrieval of the
Critically Ill. Current Anaesthesia & Critical Care 1.1 (2010): 22-26. Web.
57
DOH 530-129 January 2019
