August 2022
ISSUE BRIEF
1
HP-2022-20
Unwinding the Medicaid Continuous Enrollment Provision:
Projected Enrollment Effects and Policy Approaches
KEY POINTS
• After expiration of the COVID-19 public health emergency (PHE), Medicaid’s continuous
enrollment provision will come to an end. Using longitudinal survey data and 2021 enrollment
information, we currently project that 17.4 percent of Medicaid and Children’s Health
Insurance Program (CHIP) enrollees (approximately 15 million individuals) will leave the
program based on historical patterns of coverage loss.
• Approximately 9.5 percent of Medicaid enrollees (8.2 million) will leave Medicaid due to loss of
eligibility and will need to transition to another source of coverage. Based on historical
patterns, 7.9 percent (6.8 million) will lose Medicaid coverage despite still being eligible
(“administrative churning”), although HHS is taking steps to reduce this outcome.
• Children and young adults will be impacted disproportionately, with 5.3 million children and 4.7
million adults ages 18-34 predicted to lose Medicaid/CHIP coverage. Nearly one-third of those
predicted to lose coverage are Latino (4.6 million) and 15 percent (2.2 million) are Black.
• Almost one-third (2.7 million) of those predicted to lose eligibility are expected to qualify for
Marketplace premium tax credits. Among these individuals, over 60 percent (1.7 million) are
expected to be eligible for zero-premium Marketplace plans under the provisions of the
American Rescue Plan (ARP). Another 5 million would be expected to obtain other coverage,
primarily employer-sponsored insurance.
• An estimated 383,000 individuals projected to lose eligibility for Medicaid would fall in the
coverage gap in the remaining 12 non-expansion states – with incomes too high for Medicaid,
but too low to receive Marketplace tax credits. State adoption of Medicaid expansion in these
states is a key tool to mitigate potential coverage loss at the end of the PHE.
• States are directly responsible for eligibility redeterminations, while CMS provides technical
assistance and oversight of compliance with Medicaid regulations. Eligibility and renewal
systems, staffing capacity, and investment in end-of-PHE preparedness vary across states. HHS
is working with states to facilitate enrollment in alternative sources of health coverage and
minimize administrative churning. These efforts could reduce the number of eligible people
losing Medicaid compared to the estimates above.
• The Inflation Reduction Act of 2022 extends the ARP’s enhanced and expanded Marketplace
premium tax credit provisions until 2025, providing a key source of alternative coverage for
those losing Medicaid eligibility.
August 19, 2022

August 2022
ISSUE BRIEF
2
INTRODUCTION
The Families First Coronavirus Response Act (FFCRA) mandated continuous Medicaid enrollment throughout
the federal COVID-19 public health emergency (PHE) period for nearly all of those enrolled in Medicaid on or
after the date of enactment on March 18, 2020, through the end of the month in which the PHE declaration
ends. In exchange for meeting these and other provisions, the FFCRA temporarily increased the federal
medical assistance percentage (FMAP) by 6.2 percentage points, which all states received. The continuous
enrollment provision suspended Medicaid’s regular eligibility renewal and redetermination process by
prohibiting termination of ineligible individuals as a condition of receiving the temporary increased FMAP
except for those who voluntarily disenroll or are no longer a state resident.
*
A temporary increase in federal
matching also applies to the Children’s Health Insurance Program (CHIP) during the PHE, and the continuous
enrollment provision applied to states running CHIP as part of combined Medicaid/CHIP programs.
†
At the end
of the PHE states will have 12 months to initiate redeterminations of Medicaid and CHIP eligibility for all
enrollees and two additional months (14 months total) to complete all pending actions. State Medicaid
programs vary with respect to their staffing, administrative capacity, and sophistication of enrollment and
renewal systems.
The nation’s uninsured rate declined to a historic low of 8.0% in the first quarter of 2022, due in part to the
continuous enrollment provision in Medicaid as well as strong enrollment outreach efforts and expanded
Marketplace subsidies under the American Rescue Plan (ARP).
1
Between February 2020 and December 2021,
Medicaid enrollment grew by approximately 15.5 million individuals, from 71.2 million to 86.7 million (a 21.8
percent increase).
2
Many of these individuals gained Medicaid eligibility due to pandemic-related changes in
income and employment, while others may have enrolled in Medicaid during this time due to a change in
family composition (e.g., the addition of a child), disability, or pregnancy status. Research indicates that
Medicaid enrollment growth during the pandemic was primarily driven by increased retention of existing
enrollees rather than new applications.
3
,
4
Coverage changes in Medicaid are common, and even short gaps in insurance can have negative effects on
access to care.
5
,
6
A recent analysis found that 21 percent of Medicaid enrollees changed coverage within one
year, with 8 percent disenrolling and reenrolling in Medicaid within the year.
7
Changes in Medicaid coverage
occur for several reasons, including loss of Medicaid eligibility due to income fluctuations or changes in family
circumstances, becoming eligible for a different source of coverage (e.g., through an employer ), or
administrative churning. Administrative churning refers to the loss of Medicaid coverage despite ongoing
eligibility, which can occur if enrollees have difficulty navigating the renewal process, states are unable to
contact enrollees due to a change of address, or other administrative hurdles.
Based on typical coverage changes in Medicaid that would have occurred without the continuous enrollment
provision, and the economic and labor market fluctuations that occurred during the PHE, many current
enrollees will no longer be eligible for Medicaid after the PHE ends and will need to transition to a different
source of coverage (sometimes referred to as “unwinding” the coverage protections of the COVID-19 PHE).
Additionally, some enrollees may be at risk of Medicaid coverage loss due to administrative reasons. The risk
of administrative churning may be particularly high after the PHE due to the volume of redeterminations states
must conduct and the time since Medicaid agencies last communicated with many beneficiaries. Previous
_______________________
*
States are required to review eligibility only once every 12 months for beneficiaries whose eligibility is based on Modified Adjusted
Gross Income (MAGI) methodologies and at least once every 12 months for non-MAGI beneficiaries.
†
The enhanced federal match rate for CHIP is the result of the standard calculation of CHIP’s FMAP, which is based on Medicaid’s
FMAP. The continuous enrollment provision does not apply to people enrolled in separate CHIP programs. See:
https://www.medicaid.gov/state-resource-center/downloads/covid-19-faqs.pdf

August 2022
ISSUE BRIEF
3
analyses have projected the estimated number of individuals likely to lose Medicaid coverage at the end of the
PHE, with one study predicting a range of 5 to 14 million individuals and another predicting 12.9 to 15.8 million
individuals leaving Medicaid.
8
,
9
The U.S. Department of Health and Human Services (HHS) is leveraging all of
its programs and divisions in a robust stakeholder engagement strategy to ensure individuals remain
connected to coverage. The Centers for Medicare and Medicaid Services (CMS) is working closely with state
Medicaid agencies, Marketplaces, navigators, health plans, and many others. These efforts are outlined later
in the Discussion section.
This issue brief presents current HHS projections of transitions in coverage due to the sunset of the continuous
enrollment provision at the end of the PHE; describes administrative actions underway to mitigate coverage
losses; and highlights legislative approaches including the Inflation Reduction Act of 2022 that could help
promote seamless coverage transitions at the end of the PHE.
METHODS
The objectives of this analysis were to predict the range of estimates for how many Medicaid enrollees are
likely to lose coverage when the PHE ends, assess whether coverage loss is likely to be due to loss of eligibility
or due to administrative churning, and identify alternative coverage options available to those who lose
Medicaid.
This analysis used the Survey for Income and Program Participation (SIPP), based on data from March 2015 to
November 2016. The SIPP is a nationally representative, longitudinal panel survey in which respondents are
followed across multiple years (4 years in total for each panel) and income and health insurance enrollment
information is collected monthly. In our analysis, the 21-month timespan from March 2015 to November 2016
was treated as an analogous period to the PHE lasting March 2020 through December 2021. Based on the
2015-2016 data, we estimated Medicaid eligibility and enrollment in December 2016 (analogous to December
2021, the projected end of the PHE) among those enrolled in Medicaid for at least one month between March
2015 and November 2016, the 21-month PHE simulation period. Once someone enrolled in Medicaid during
the PHE, we treated them as enrolled until the end of the PHE.
We classified our study sample of those “ever in Medicaid” during the 21-month period from March 2015
through November 2016 into three categories at the end of the PHE: (1) those still eligible and enrolled in
Medicaid; (2) those eligible for Medicaid but no longer enrolled (i.e., not enrolled due to administrative
churning); and (3) those no longer eligible for Medicaid (i.e., not eligible due to income or a change in
categorical status).
‡
In addition to enrollment, we also estimated eligibility for Medicaid and CHIP based on
January 2021 modified adjusted gross income (MAGI) percent-of-poverty limit rules, which captures variation
by state and eligibility group (infants, children 1-5, children 6-18, pregnant beneficiaries, adult
parents/caregivers, other adults, and beneficiaries 65 or older). We assume individuals receiving
Supplemental Security Income (SSI) remained automatically enrolled in Medicaid.
§
For all SIPP estimates,
references to Medicaid include CHIP except where otherwise noted.
Among those ineligible for Medicaid at the end of the PHE, we assessed enrollment and eligibility for
subsidized Marketplace coverage, employer-sponsored insurance (ESI), and other coverage based on 2021 ARP
eligibility criteria. Individuals were deemed eligible for subsidized Marketplace coverage if they were not
_______________________
‡
In this brief, the term “eligible” refers to individuals that could obtain Medicaid coverage based on the Medicaid eligibility
requirements in their state but does not mean that an individual is enrolled in Medicaid coverage.
§
Eligibility predictions do not account for medically needy pathways or other optional pathways for seniors or those with disabilities.
Those who reported being enrolled in Medicaid in December 2016 were classified as eligible for Medicaid regardless of whether they
were predicted to be eligible based on these rules.

August 2022
ISSUE BRIEF
4
eligible for Medicaid, had incomes above 100% of the federal poverty level (FPL), and did not have access to
minimum essential coverage (MEC).
**
To calculate zero-premium Marketplace coverage options under the
ARP among subsidy-eligible individuals, we applied estimates of the proportion of the uninsured population
eligible for zero-premium plans based on American Community Survey data and county-level premium rates.
10
Medicaid coverage enrollment and eligibility estimates were calculated by Medicaid expansion status, age,
race and ethnicity, income, and sex.
We consider several alternative scenarios and time frames for coverage changes, depending on the rate of
administrative churning compared to historical rates, and how quickly states choose to conduct their
redeterminations after the expiration of the PHE.
All estimates presented in this brief have been projected forward to account for the difference in Medicaid
enrollment between December 2016 and December 2021. The primary limitation of this analysis is that the
data are based on historical data. Although differences in Medicaid enrollment are accounted for, differences
in population changes or economic conditions between 2014-2016 and now are not. Therefore, estimates may
not reflect the present-day distribution of income or rates of administrative churning. Also, due to the
unknown expiration date of the PHE, our analysis, which is based on an end date of the PHE of December
2021, will slightly underestimate the total population affected by the end of the continuous enrollment
provision. In addition, while the SIPP data shows actual insurance enrollment in December 2016, in the post-
PHE period, it is likely to take recently-disenrolled people time to identify and enroll in other available
coverage options. Estimates of zero-dollar premium availability were based on population-level averages for
the subsidy-eligible uninsured population as a whole, rather than based on individual income and premiums;
accordingly, these projections are not precise estimates and should be interpreted with caution. Finally, all
references to Medicaid eligibility or enrollment in the SIPP analysis include CHIP. However, while many
children continue to be eligible for CHIP after losing Medicaid, our analysis did not separately estimate
eligibility for CHIP versus Medicaid at the end of the PHE, or distinguish between states with separate CHIP
programs and those that are combined with Medicaid, since the SIPP did not have adequate sample size for
reliable state estimates.
RESULTS
An estimated 80.1 million individuals were enrolled in Medicaid at some point during the 21-month study
period (2015-2016). This estimate is lower than actual December 2021 Medicaid/CHIP enrollment of 86.7
million, but all remaining estimates in this report were adjusted to account for this difference in enrollment.
Total Medicaid Disenrollment
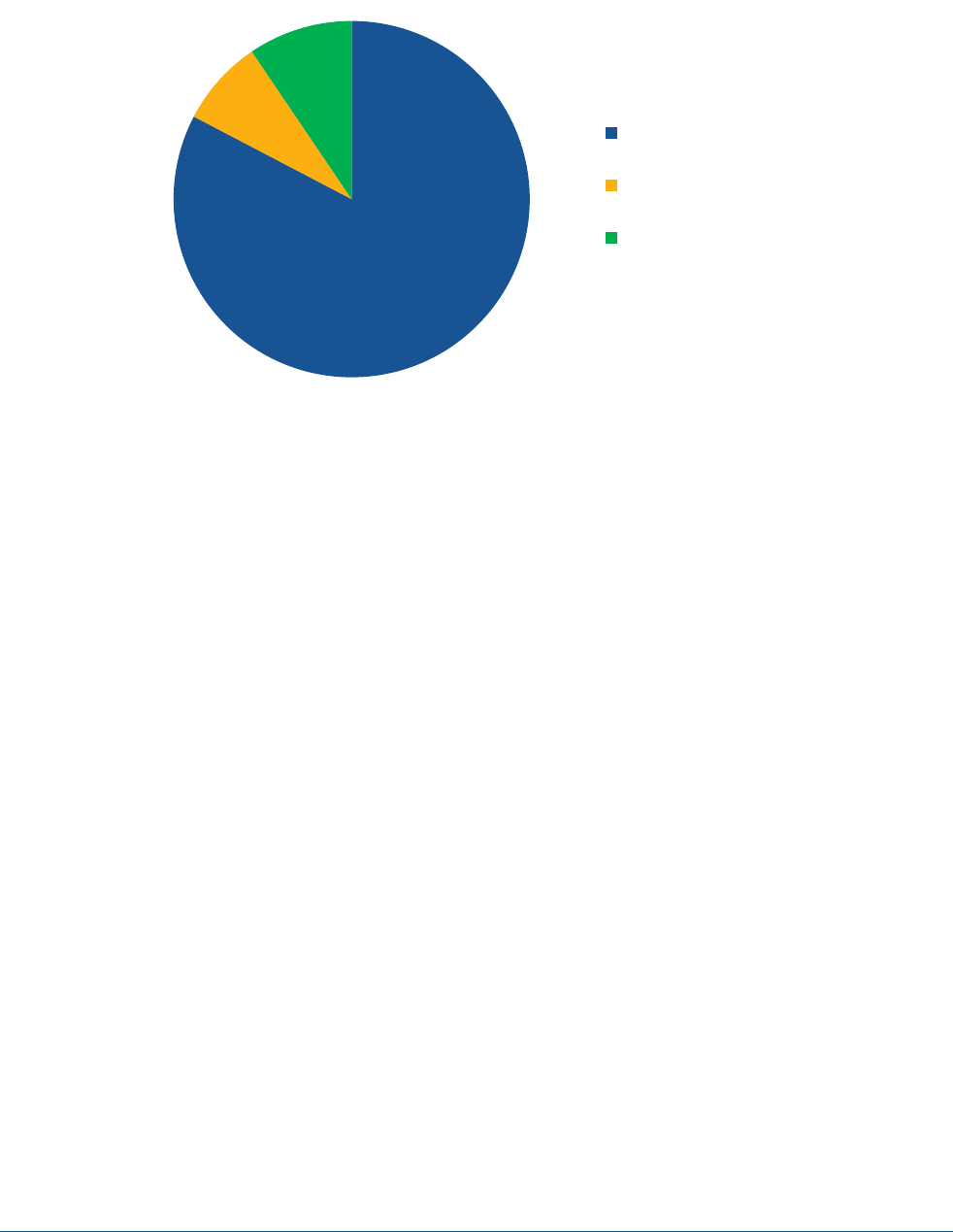
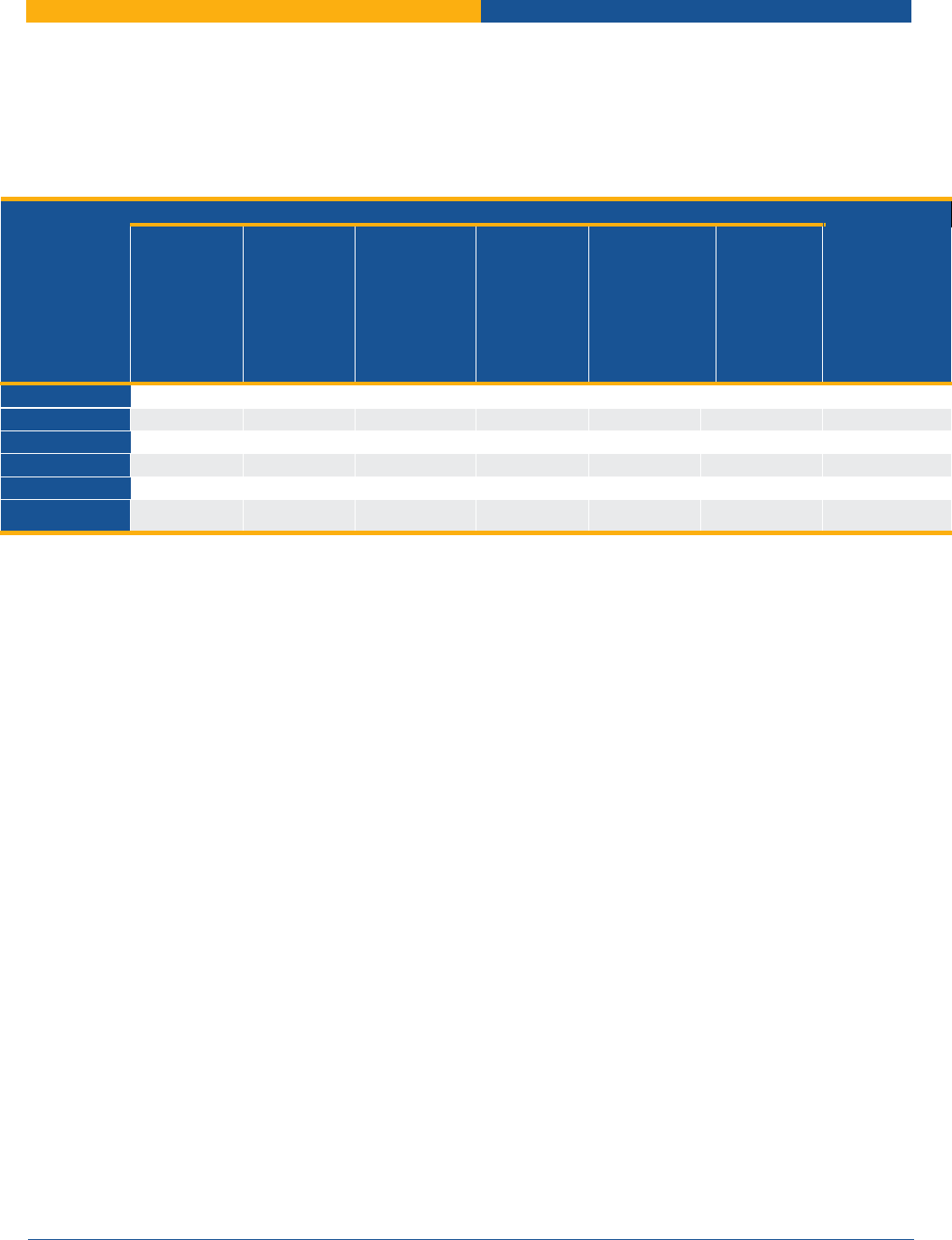
Figure 1 shows the predicted proportion of Medicaid enrollees that maintained Medicaid enrollment, were
ineligible for Medicaid, or experienced administrative churning (i.e., were eligible for Medicaid but not
enrolled) based on 2015/2016 SIPP data. Approximately 9.5 percent of enrollees (8.2 million of 86.7 million)
were predicted to be ineligible for Medicaid after the PHE, while 7.9 percent (6.8 million of 86.7 million) were
predicted to lose coverage despite being eligible for Medicaid. Combined, this leaves 82.7 percent (or 71.7
million people) predicted to be eligible and maintain enrollment in Medicaid post-PHE, and 15 million total
_______________________
**
MEC was defined as coverage as of December 2016 in Medicare, CHAMPUS, VA, TRICARE, or health insurance provided by someone
outside of the household. Coverage provided through “other” insurance or the Indian Health Service were not classified as MEC.
Income determinations were based on December 2015 MAGI rules.
August 2022
ISSUE BRIEF
5
predicted to leave the program from loss of eligibility or administrative churning. The primary reasons for
Medicaid eligibility loss were changes in income, changes in family composition, or moving to another state.
Figure 1. Predicted Eligibility, Ineligibility, and Administrative Churn Among Medicaid Enrollees at End of PHE
Source: Analysis of SIPP treating March 2015-Nov. 2016 as analogous to March 2020-Dec. 2021 PHE, among enrollees ever-
enrolled in Medicaid during the 21-month period.
Potential Trajectories of Administrative Churning
We estimated five different scenarios based on varying degrees of administrative churning and
redetermination time frames to estimate how disenrollment will be impacted. Scenarios 1-4 assume an even
rate of redeterminations processed over the 12 months of 2021, while scenario 5 assumes states process
redeterminations over a six-month timeframe. The scenarios were:
1. A “no churning” scenario in which only those who are no longer eligible for Medicaid are disenrolled.
While this scenario is not realistic since it assumes zero percent administrative churning among still-
eligible individuals, it provides a sense of how many people are likely to lose Medicaid even if renewal
were fully optimized and no eligible individuals left the program. In this scenario, a total of 8.2 million
individuals will lose Medicaid coverage at the end of the PHE due to a change in Medicaid eligibility
and 684,000 individuals would leave Medicaid each month during the first year after the PHE
expiration.
2. A “low churning” scenario in which those who are no longer eligible for Medicaid are disenrolled (8.2
million), and administrative churning is half of the 2016 historical rate. This scenario would result in
total disenrollment (administrative churning plus eligibility loss) of 11.6 million individuals and monthly
disenrollment of 968,000 individuals over 12 months.
3. A “typical churning” scenario in which the 8.2 million individuals who are no longer eligible for
Medicaid are disenrolled and churning rates match the historical average in 2016 SIPP data. This
scenario reflects the primary estimates (“Base Case”) presented throughout this brief. Under this
scenario, a total of 15 million individuals are predicted to leave Medicaid, with monthly disenrollment
of 1.3 million individuals over 12 months.
4. A “high churning” scenario in which we assume those who are no longer eligible for Medicaid are
disenrolled, as well as 50 percent excess administrative churning above historical rates. This scenario
could occur if there is substantial beneficiary confusion, high rates of moving or changes in residence,
and/or overloaded state Medicaid eligibility systems. This scenario would result in total disenrollment
of 18.4 million individuals, with monthly disenrollment of 1.5 million individuals over 12 months.
71.7M
(82.7%)
8.2M
(9.5%)
6.8M
(7.9%)
Still Enrolled in Medicaid
Not Eligible for Medicaid
Administrative Churning
August 2022
ISSUE BRIEF
6
5. A “high churning” six-month redetermination scenario in which we assume those who are no longer
eligible are disenrolled as well as 50 percent excess administrative churning processed over a six-
month timeframe. This would result in the same total disenrollment as in scenario 4 (18.4 million
individuals) but monthly disenrollment of 3.1 million individuals over six months.
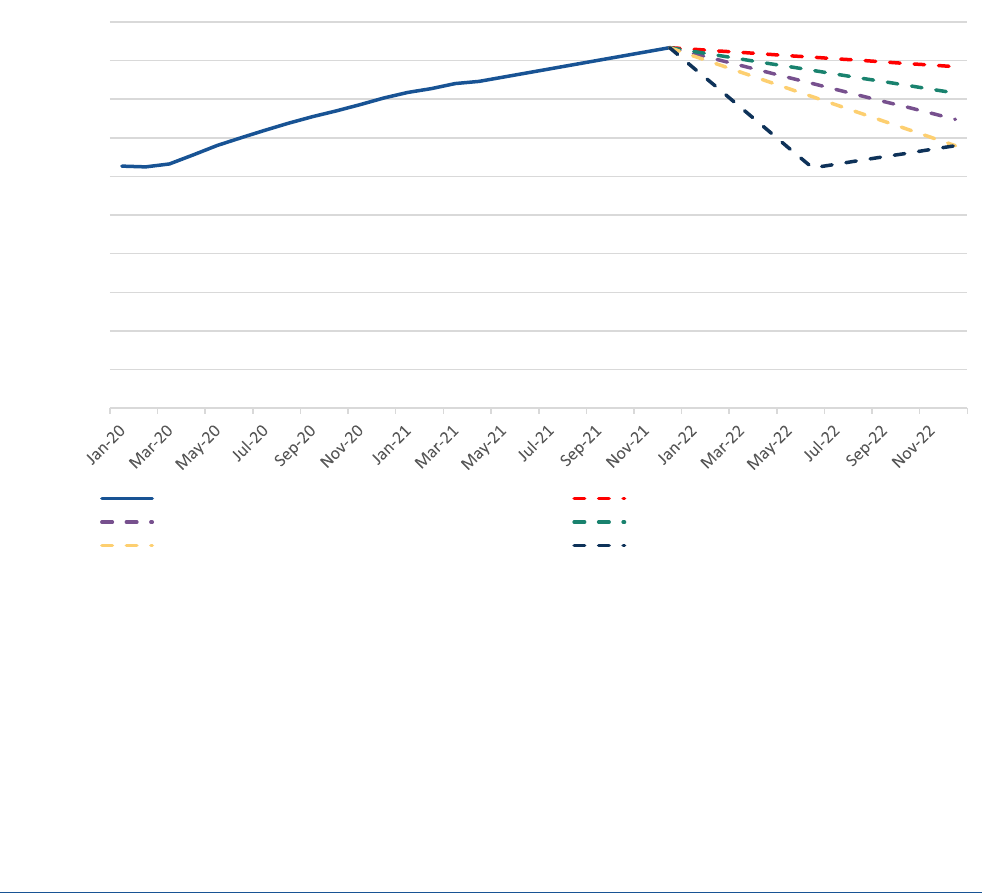
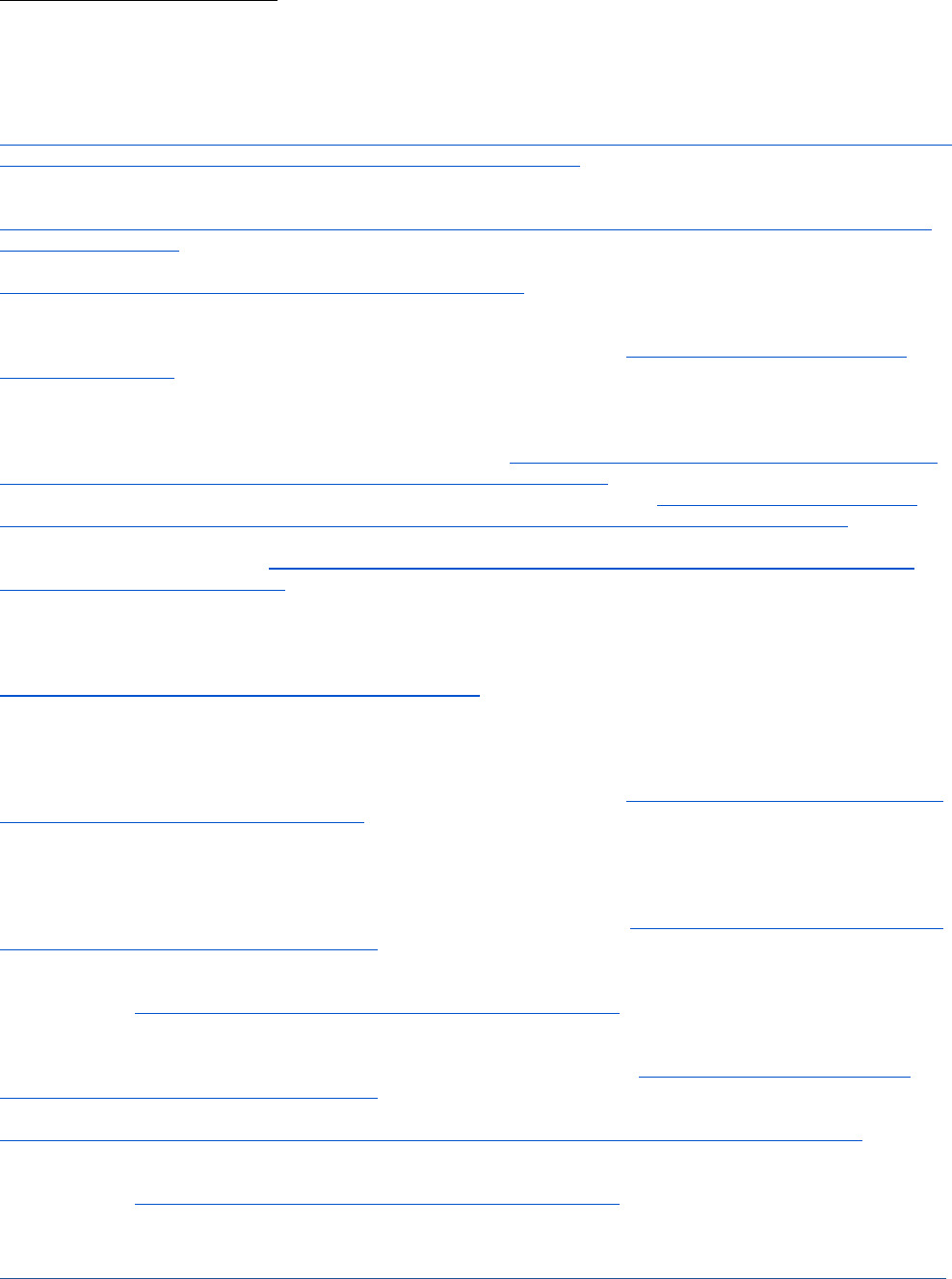
Figure 2 plots actual monthly Medicaid enrollment from January 2020 – December 2021 and projects total
Medicaid eligibility loss during 2022 under the above five scenarios. The projections in Figure 2 account for
new monthly enrollment (based on January-April 2021 enrollment rates), but do not account for individuals
who were disenrolled from Medicaid at the end of the PHE who may re-enroll over the course of 2022. The
scenarios shown in Figure 2 result in a range of total Medicaid enrollment estimates by December 2022, from
74 million under a high churning scenario to 84 million under a scenario with a zero rate of churning.
Accounting for new enrollment, we predict that net totals of 5.8 million, 9.3 million, and 12.7 million would
leave the program from loss of eligibility or administrative churning across low, medium, and high levels of
historical churning, respectively.
Figure 2. Projected Medicaid Coverage Loss During 12 Months of 2022 Under Alternative Assumptions About
Rates of Administrative Churning
Demographics
Demographics and State Patterns of Individuals Leaving Medicaid
Among the 8.2 million individuals predicted to be ineligible for Medicaid in the post-PHE period, 5.4 million (66
percent) resided in states that expanded Medicaid under the Affordable Care Act (ACA) as of 2021, while 2.8
million (34 percent) resided in non-expansion states (Table 1). Among the 6.8 million individuals predicted to
be disenrolled despite being eligible for Medicaid, 4.7 million (69%) resided in expansion states and 2.1 million
(31%) resided in non-expansion states (Table 1).
84M
77M
81M
74M
71M
40,000,000
45,000,000
50,000,000
55,000,000
60,000,000
65,000,000
70,000,000
75,000,000
80,000,000
85,000,000
90,000,000
Actual Enrollment No churning - only loss of eligibility
Typical churning Low churning
High churning High churning - 6 months
Source: Analysis of SIPP treating March 2015-Nov. 2016 as analogous to March 2020-Dec. 2021 PHE, among enrollees
ever-enrolled in Medicaid during the 21-month period. New monthly Medicaid enrollment in 2021 based on monthly
enrollment January-April 2021.

August 2022
ISSUE BRIEF
7
Table 1. Predicted Medicaid Coverage Loss at the end of the PHE by Medicaid Expansion Status
Characteristic
Loss of Medicaid Eligibility
Disenrolled Despite Being Eligible
for Medicaid
(Administrative Churning)
State Expansion Status
N
%
N
%
Expansion
5,400,000
66%
4,700,000
69%
Non-Expansion
2,800,000
34%
2,100,000
31%
Children and young adults, as well as Latino and Black individuals, are predicted to be impacted
disproportionately. Children ages 0-17 make up nearly one in five of the individuals predicted to be ineligible
for Medicaid and over half of the 6.8 eligible but disenrolled individuals (i.e., administrative churning), while
young adults ages 18-34 comprise more than one in three of those predicted to lose Medicaid eligibility and
nearly one-quarter of those predicted to experience administrative churning (Table 2). Further, Latino
individuals comprise over one quarter of those predicted to be ineligible for Medicaid and over one-third of
those predicted to experience churning, while Black individuals comprise fourteen percent of those predicted
to lose Medicaid eligibility and 15 percent of those predicted to experience churning (Table 2). Those with
incomes 138-250% FPL comprise nearly 40% of those predicted to be ineligible for Medicaid, while those with
incomes less than 100% FPL comprise over half of those predicted to experience administrative churning.
Table 2. Predicted Medicaid Coverage Loss at the end of the PHE by Age, Race, Sex, and Income
Characteristic
Loss of Medicaid Eligibility
Disenrolled Despite Being Eligible
for Medicaid
(Administrative Churning)
Age
N
%
N
%
0-17
1,399,000
17.1%
3,896,000
57.1%
18-24
1,387,000
16.9%
823,000
12.1%
25-34
1,763,000
21.5%
737,000
10.8%
35-44
1,120,000
13.7%
511,000
7.5%
45-54
967,000
11.8%
390,000
5.7%
55-64
777,000
9.5%
288,000
4.2%
65+
791,000
9.6%
173,000
2.5%
Race/Ethnicity
Latino
2,190,000
26.7%
2,409,000
35.3%
White non-Latino
3,967,000
48.4%
2,648,000
38.8%
Black non-Latino
1,125,000
13.7%
1,027,000
15.1%
Asian/Native
Hawaiian/Pacific Isl.
501,000
6.1%
394,000
5.8%
Multi-racial, other
420,000
5.1%
342,000
5.0%
Sex
Male
4,298,000
52.4%
2,880,000
42.2%
Female
3,906,000
47.6%
3,937,000
57.8%
Income*
<100% FPL
691,000
8.4%
3,761,000
55.2%
>100-138% FPL
555,000
6.8%
1,077,000
15.8%
>138-250% FPL
3,038,000
37.0%
1,714,000
25.1%
>250-400% FPL
2,032,000
24.8%
264,000
3.9%
>400% FPL
1,889,000
23.0%
2,000
0.0%
*Modified Adjusted Gross Income (MAGI) in December 2016 as a percentage of the federal poverty level (FPL).
August 2022
ISSUE BRIEF
8
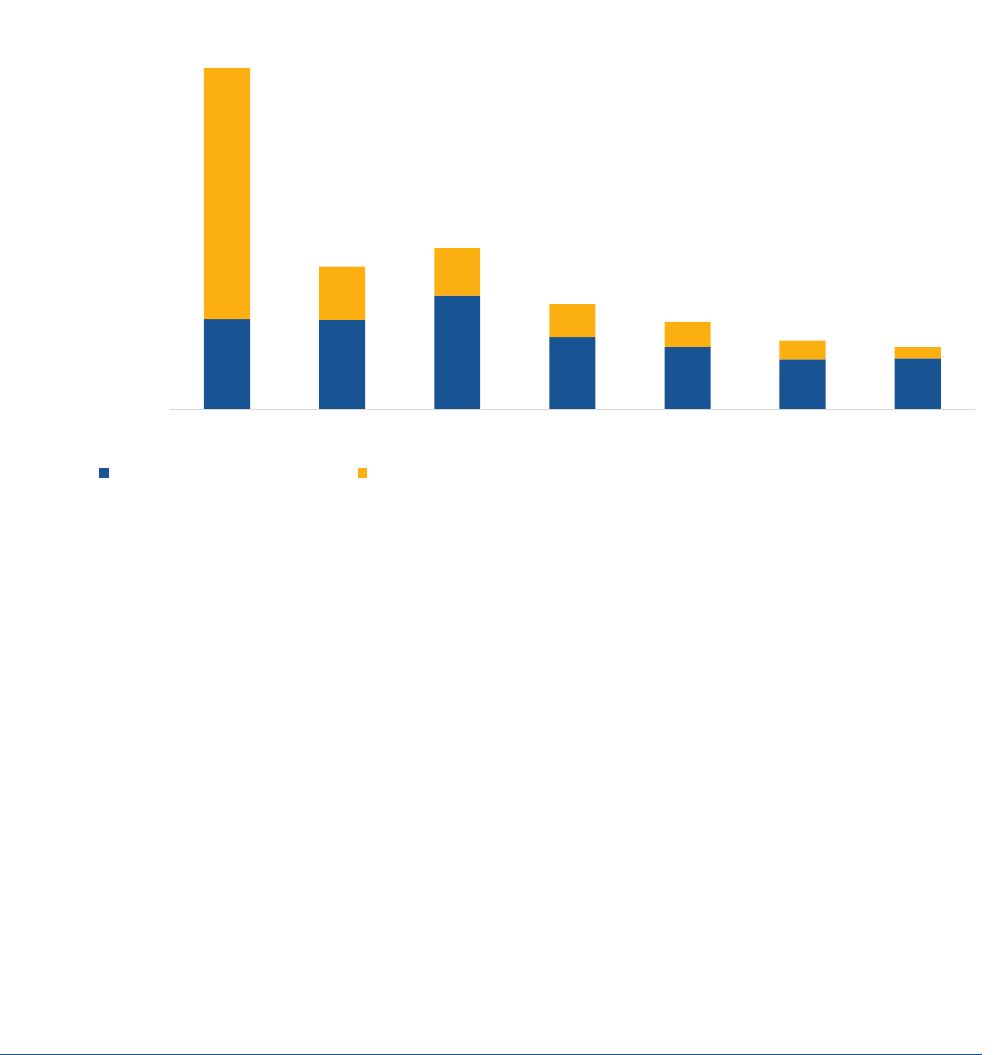
Figures 3 and 4 show rates of Medicaid eligibility loss and administrative churning within each age, income,
and racial and ethnic group. As evident in Figure 3, the majority of children losing coverage are likely still
eligible for Medicaid or CHIP. State-level CHIP policies may play a role in how many children lose Medicaid
coverage at the end of the PHE. Fewer children will become ineligible for Medicaid or CHIP at the end of the
PHE in states with more generous CHIP eligibility limits. Additionally, more children are likely to experience
churning in states where there are greater administrative barriers to transitioning from Medicaid to CHIP. For
example, thirteen states have a separate CHIP, and 26 states charge an enrollment fee or premiums in CHIP. In
these states, children are less likely to be automatically enrolled in CHIP compared to states that operate joint
programs or don’t charge premiums or fees, increasing the risk of administrative churning among children. In
states with combined Medicaid/CHIP programs, coverage transitions should be more seamless.
Figure 3. Predicted Medicaid Coverage Loss Due to Eligibility Loss versus Administrative Churning, by Age
Note: Each bar adds to 100%, showing the breakdown of predicted Medicaid coverage loss due to administrative churning versus loss
of eligibility.
Source: Analysis of SIPP treating March 2015-Nov. 2016 as analogous to March 2020-Dec. 2021 PHE, among enrollees ever-enrolled in
Medicaid during the 21-month period. Projections are from the Base Case scenario.
27.8%
60.0%
72.6%
69.5%
69.6%
67.3%
78.6
72.2%
40.0%
27.4%
30.5%
30.4%
32.7%
21.4%
0
1,000,000
2,000,000
3,000,000
4,000,000
5,000,000
6,000,000
0-17 18-24 25-34 35-44 45-54 55-64 65+
Number of Individuals Predicted to Lose
Medicaid
Loss of Medicaid Eligibility Disenrolled Despite Being Eligible for Medicaid (Administrative Churning)

August 2022
ISSUE BRIEF
9
Figure 4. Predicted Medicaid Coverage Loss Due to Eligibility Loss versus Administrative Churning, by Race
and Ethnicity
Note: Each bar adds to 100%, showing the breakdown of predicted Medicaid coverage loss due to administrative churning
versus loss of eligibility.
Source: Analysis of SIPP treating March 2015-Nov. 2016 as analogous to March 2020-Dec. 2021 PHE, among enrollees ever-
enrolled in Medicaid during the 21-month period. Projections are from the Base Case scenario.
Loss of Medicaid Eligibility and Alternative Coverage Options
Alternative health insurance options are available for the majority of individuals who become ineligible for
Medicaid or CHIP after the end of the PHE (Figure 5). In our study population, approximately 3.6 million of the
individuals predicted to be ineligible for Medicaid at the end of the PHE were enrolled in ESI and 1.4 million
individuals were enrolled in other insurance, including Marketplace coverage without Advanced Premium Tax
Credits (APTCs), Medicare, military health insurance, non-Marketplace nongroup coverage, and insurance
classified as “other” in SIPP after losing Medicaid. Another one-third of the individuals ineligible for Medicaid
at the end of the PHE (2.7 million of 8.2 million) were potentially eligible for post-ARP premium tax credits
(Table 3).
††
Of this group, 1.6 million were eligible for APTCs and cost-sharing reductions (incomes 100-250%
FPL), and 1.7 million were eligible for APTCs and also likely eligible for a zero-premium Marketplace plan.
An estimated 383,000 individuals ineligible for Medicaid at the end of the PHE fell in the coverage gap and
were not enrolled in or eligible for any insurance (Figure 5 and Appendix Table 1). These individuals earned less
than 100% FPL and resided in the 12 non-expansion states, meaning that their incomes were too high for their
state’s Medicaid program but too low (<100% FPL) to qualify for subsidized Marketplace coverage. Under the
_______________________
††
Under the ARP, ACA marketplace premium subsidies are substantially enhanced for people at every income level and offered to
those with income above 400% FPL for the first time. These enhanced and expanded premium tax credits will expire at the end of
2022.
36.0%
82.8%
60.4%
49.5%
51.9%
64.0%
17.2%
39.6%
50.5%
48.1%
0
1,000,000
2,000,000
3,000,000
4,000,000
5,000,000
6,000,000
7,000,000
Latino White non-Latino Black non-Latino Asian/Native
Hawaiian/Pacific Isl.
Multi-racial, other
Number of Individuals Predicted to Lose
Medicaid
Loss of Medicaid Eligibility Disenrolled Despite Being Eligible for Medicaid (Administrative Churning)

August 2022
ISSUE BRIEF
10
ARP the only individuals not potentially eligible for some type of subsidized coverage are generally those in the
Medicaid coverage gap.
‡‡
Figure 5. Predicted Health Coverage Enrollment and Eligibility among those Predicted to Lose Medicaid
Eligibility after the PHE
Source: Analysis of SIPP treating March 2015-Nov. 2016 as analogous to March 202-Dec. 2021 PHE, among enrollees ever enrolled in
Medicaid during the 21-month period. Projections are from the Base Case scenario.
Table 3. Marketplace Eligibility among those Predicted to Lose Medicaid Eligibility after the PHE
Income
Potentially Eligible for
APTCs*
Eligible for Zero-Premium
Marketplace Plan**
Eligible for APTCs and
CSRs
<100%
0
0
0
100 - 138%
259,000
259,000
259,000
>138 - 250%
1,306,000
1,156,000
1,306,000
>250 - 400%
552,000
219,000
0
>400% FPL
573,000
22,000
0
TOTAL
2,689,000
1,656,000
1,565,000
APTCs = Advanced Premium Tax Credits. CSRs = Cost Sharing Reductions.
* Under the ARP, there is no upper income limit on APTC availability, though in practice some higher income individuals may
not receive any APTCs because their premiums are below the required income share under the ACA even without an APTC.
**Based on applying the zero-premium eligibility proportion among uninsured non-elderly adults using CPS data in ASPE brief
“Access to Marketplace Plans with Low Premiums on the Federal Platform Part II: Availability Among Uninsured Non-Elderly
Adults Under the American Rescue Plan” to the number of individuals predicted to lose Medicaid eligibility but be eligible for
Marketplace premiums within each income band. This group overlaps with those eligible for cost-sharing reductions (CSRs)
and both groups are a subset of those potentially eligible for APTCs.
_______________________
‡‡
Under the ARP, there is no upper income limit on APTC availability, though in practice some higher income individuals may not
receive any APTCs because their premiums are below the required income share under the ACA even without an APTC
229,000
383,000
1,418,000
2,689,000
3,595,000
Affordable ESI Offer but Not Enrolled
Medicaid Coverage Gap
Changed to Non-Marketplace Coverage that Precludes APTCs
Eligible for APTCs
Changed to ESI

August 2022
ISSUE BRIEF
11
DISCUSSION
Using pre-pandemic Medicaid enrollment from national survey data as an approximation for the PHE, we
currently project that 9.5 percent (8.2 million) of individuals enrolled in Medicaid as of December 2021 will
lose Medicaid eligibility at the end of the PHE and need to transition to another source of coverage. An
additional 7.9 percent (6.8 million) are projected to lose Medicaid coverage despite still being eligible, due to
administrative churning. In our analysis, two-thirds of those predicted to lose Medicaid eligibility (5.0 million
of the 8.2 million) were projected to enroll in ESI or other non-Marketplace coverage. Among those without
ESI, the majority would be eligible for low or no-cost coverage through the Marketplace, with the exception of
those who fall in the Medicaid coverage gap in states that have not expanded Medicaid. Children and young
adults, as well as Latino and non-Latino Black populations, are expected to be disproportionately affected by
Medicaid coverage loss once the PHE ends, and seamless transitions to CHIP will play an important role for
many in maintaining coverage.
Overall, this means that while our model projects that as many as 15 million individuals could leave Medicaid
after the PHE, approximately one third (5 million) are likely to obtain other coverage outside the Marketplace
(primarily ESI) and nearly 3 million (20 percent) would have a subsidized Marketplace option. Additionally,
some individuals who lose Medicaid eligibility at the end of the PHE may regain it during the unwinding period
and some individuals who lose coverage despite being eligible (i.e., experience churning) may re-enroll.
These findings highlight the importance of administrative and legislative actions to reduce the risk of coverage
losses after the continuous enrollment provision ends. Successful policy approaches must address the
different reasons for coverage loss. Broadly speaking, one set of strategies is needed to increase the likelihood
that those losing Medicaid eligibility acquire other coverage, and a second set of strategies is needed to
minimize administrative churning among those still eligible for coverage. Importantly, some administrative
churning is expected under all scenarios, though reducing the typical churning rate by half would result in the
retention of 3.4 million additional enrollees. The next section discusses some of the administrative actions the
CMS is currently taking, as well as opportunities for legislation that can reduce the risk of coverage loss after
the PHE.
Administrative Actions
CMS is working closely with state Medicaid agencies, Marketplaces, navigators and assisters, beneficiary and
consumer advocates, health plans, agents and brokers, departments of insurance, and many others as part of a
robust stakeholder engagement strategy to ensure individuals remain connected to coverage.
Working with State Medicaid Agencies to Reduce Churning: States are directly responsible for eligibility
redeterminations for Medicaid beneficiaries, while CMS provides oversight of compliance with Medicaid
regulations and technical assistance. For over a year, CMS has coordinated with state Medicaid and CHIP
agencies to develop state unwinding plans that will minimize churning and maximize coverage retention. CMS
has hosted regular workgroups, bi-weekly and individual calls with states, and developed a variety of guidance
documents, tools, and resources for state use in planning efforts. In March 2022, CMS released a new suite of
guidance and planning and communications tools that offer states a roadmap to restore routine eligibility and
enrollment operations after the PHE ends and promote continuity of coverage.
11
This guidance includes
outlining strategies for working with managed care plans such as working with plans to obtain and update
beneficiary contact information; sharing renewal files with plans to conduct outreach and provide support to
individuals enrolled in Medicaid during their renewal period; enabling plans to conduct outreach to individuals
who have recently lost coverage for procedural reasons; and permitting plans to assist individuals to transition
to and enroll in ACA Marketplace coverage if ineligible for Medicaid or CHIP.

August 2022
ISSUE BRIEF
12
When the PHE ends, states will have a 12-month unwinding period to initiate renewals of eligibility for all
individuals enrolled in Medicaid and CHIP. The Administration has committed to providing states with 60 days
advanced notice before the expiration of the PHE to support state planning. States are expected to prioritize
eligibility and enrollment work in a manner that prevents inappropriate terminations and promotes smooth
transitions to other coverage for individuals no longer eligible for Medicaid, CHIP, or a Basic Health Program
(BHP).
§§
CMS has also strongly encouraged states to spread their eligibility redeterminations over the full 12-
month unwinding period to help achieve manageable workloads, reduce the risk of administrative churning,
and achieve a renewal schedule that is sustainable in future years.
There are many actions states can take to minimize churning during unwinding, including adopting strategies
to streamline enrollment and renewal processes, investing in resources and staff to process the volume of
eligibility determinations, and implementing additional efforts to update enrollee contact information. States
can expand the number of data sources used at redetermination to increase the number of individuals
renewed based on available information. For example, Medicaid enrollees who also receive Supplemental
Nutrition Assistance Program (SNAP) benefits often have recent verified information on file that could assist in
approving and renewing Medicaid coverage. State Medicaid agencies could use SNAP data to expedite
application processing. For non-MAGI beneficiaries who must complete a renewal form, states can use pre-
populated renewal forms to reduce the burden on enrollees. States can also extend the period for enrollees to
provide information needed to redetermine their eligibility and provide beneficiaries with the same minimum
of 30 days to return the form that is required for MAGI beneficiaries. For the unwinding period, states may
seek time-limited authority under section 1902(e)(14)(A) of the Social Security Act to pursue strategies to
streamline the renewal process, reduce churning, and ease the administrative burden states may experience in
light of challenges including that many enrollees have moved during the pandemic and a significant time has
passed since agencies last communicated with many of them. This will not only support state efforts to
promote continuity of coverage in Medicaid/CHIP but also facilitate seamless coverage transitions, particularly
for Medicaid-enrolled children who become eligible for coverage in a separate CHIP.
Finally, among the 12 states that have not yet expanded Medicaid, Medicaid expansion to low-income adults is
another critical tool to reducing the risk of coverage losses after the PHE. A recent ASPE report documented
the coverage gains in states that recently expanded Medicaid since 2019,
1
and if the remaining non-expansion
states were to follow suit, this would provide a needed alternative form of coverage for the estimated 383,000
individuals in the coverage gap who are projected to lose insurance after the PHE. More broadly, 3.8 million
uninsured nonelderly adults with incomes below 138% FPL would become newly eligible for Medicaid if their
states were to expand the program.
12
Outreach to Those Losing Medicaid Eligibility: CMS, in partnership with state Medicaid agencies and state-
based Marketplaces, is deploying a multifaceted strategy to facilitate continuity of coverage for consumers
who are no longer eligible for Medicaid/CHIP coverage. CMS is examining a variety of improvements to federal
Marketplace policies and systems to streamline the consumer experience in transitioning from Medicaid/CHIP
coverage to private insurance, such as improving the notices consumers receive in the mail and streamlining
verification processes to limit the number of people required to provide additional paper documentation
during the application process.
_______________________
§§
Section 1331 of the Affordable Care Act gives states the option of creating a Basic Health Program (BHP), a health benefits coverage
program for low-income residents who do not qualify for Medicaid, CHIP, or other minimum essential coverage and have income
between 133 percent and 200 percent of the federal poverty level (FPL). Two states, New York and Minnesota, have implemented
BHPs which together cover approximately 1 million individuals.
August 2022
ISSUE BRIEF
13
Medicaid and CHIP agencies can also help people who are no longer eligible start the process of transitioning
to other health insurance by providing information about coverage options and linking people to enrollment
assistance. CMS is working with state Medicaid agencies to ensure states that use the federal platform are
securely sending the Marketplace accurate and complete contact information to allow CMS to effectively
increase outreach to individuals no longer eligible for Medicaid/CHIP coverage.
Additionally, navigators and other assistance personnel will maintain a critical physical and virtual presence in
communities across the U.S. to help consumers understand basic concepts and rights related to health
coverage, provide enrollment assistance, and work with individuals to link coverage to care. CMS is
broadening pathways for enrollment assistance and increasing funding to navigator grantees to support new
requirements during unwinding. Specifically, CMS allocated a total of $100M to federal Marketplace navigator
grantee organizations for the 2022-2023 budget period, including $12.5M in support of additional direct
outreach, education, and enrollment activities for unwinding.
CMS is also providing information to people with Medicaid coverage to prepare for the restart of yearly
Medicaid/CHIP eligibility reviews, including on the importance of updating contact information and checking
the mail for renewal forms, and coverage options in the event a beneficiary is no longer eligible for
Medicaid/CHIP.
More broadly, HHS is leveraging all of its programs and divisions – including the Indian Health Service, the
Community Health Center Program, regional offices, and public affairs – to inform and engage external
stakeholders. This includes creating a website (Medicaid.gov/unwinding) where stakeholders can access an
unwinding toolkit printed in multiple languages and template social media graphics to use in outreach to
beneficiaries, among other resources; a website (Medicaid.gov/renewals) where beneficiaries can get
connected to their state’s eligibility website in order to update their contact information; and hosting monthly
information calls for beneficiaries, consumer advocates, providers, state officials, and other stakeholders
where they can learn about new resources related to the unwinding process.
Legislative Opportunities
In addition to administrative actions, there are also legislative opportunities to help mitigate coverage loss at
the end of the PHE:
Extend the ARP’s Marketplace subsidies past 2022: The Inflation Reduction Act of 2022 extends the ARP’s
enhanced and expanded subsidies to individuals obtaining Marketplace coverage. These subsidies were
previously scheduled to expire at the end of 2022. The law is projected to save 13 million Marketplace
enrollees an average of $800 per year on health insurance costs.
13
Prior ASPE analyses have shown the impacts
of the ARP on lowering Marketplace premiums and improving plan affordability. The ARP subsidy provisions
enable three in five uninsured consumers and four in five current Marketplace enrollees to find a zero-
premium plan (after premium tax credits) on HealthCare.gov.
14
The 2022 Open Enrollment Period resulted in
the highest-ever Marketplace enrollment of 14.5 million,
15
and surveys indicate that an additional 2 million
adults reported Marketplace enrollment in early 2022 compared to 2020, accounting for approximately half of
the 4 million total adults who gained health coverage during this period.
1
This extension of the ARP’s premium
tax credit in the Inflation Reduction Act will allow millions of people, including newly disenrolled Medicaid
beneficiaries, to continue to benefit from the enhanced and expanded premium subsidies and maintain access
to zero- and low-premium Marketplace plans.
16
Expand Twelve-Month Continuous Eligibility Provisions in Medicaid: Continuous eligibility policies can
mitigate both Medicaid coverage loss and administrative churning by guaranteeing continued eligibility for
Medicaid over a 12-month period regardless of changes in income or circumstances. States currently have the

August 2022
ISSUE BRIEF
14
option of providing 12-months of continuous eligibility for children enrolled in Medicaid or CHIP, and over half
of states have done so.
17
Currently, 12 months of continuous eligibility for Medicaid-enrolled adults is only
available via section 1115 demonstrations, and only two states have done so to date (New York, which still
maintains the policy, and Montana, which no longer has this policy in effect). The process for states to provide
12 months of continuous eligibility for adults could be streamlined through new legislation creating a state
plan option. Alternatively, legislation could mandate that states provide 12-month continuous Medicaid/CHIP
eligibility for adults and children. To promote continuous eligibility for the pregnant population enrolled in
Medicaid, the American Rescue Plan (ARP) included a temporary option for states to use federal matching
funds to extend continuous Medicaid and CHIP eligibility for pregnant beneficiaries from 60 days up to 12
months postpartum. This option became available to states on April 1, 2022, and will last five years.
CONCLUSION
Unwinding the PHE’s continuous enrollment provision in Medicaid will lead to millions of current enrollees no
longer being eligible for the program, and administrative churning could put millions of additional people at
risk for losing Medicaid coverage even though they are still eligible. HHS is taking a wide range of proactive
steps to reduce the number of individuals who are at risk of becoming uninsured due to the unwinding of the
PHE. Facilitating enrollment in alternative health insurance coverage among those determined ineligible for
Medicaid through coordination with state and federal Marketplaces and enhanced outreach and education
efforts will help minimize potentially harmful gaps in health insurance coverage. Efforts by states and
community groups, in collaboration with CMS, can reduce the risk of administrative churning among those still
eligible for Medicaid coverage. Finally, the extension of the enhanced ARP premium subsidies in the Inflation
Reduction Act will increase affordability and access to alternative health insurance at the end of the PHE,
helping preserve the historic coverage gains in ACA-related coverage in 2021 and 2022.
1,
18
In the post-PHE
period, tracking enrollment will be critical to monitoring progress and directing resources to minimize
interruptions in coverage.
August 2022
ISSUE BRIEF
15
APPENDIX
Appendix Table 1. Enrollment and Eligibility in Alternative Health Insurance among Those Predicted to Lose
Medicaid Eligibility after the PHE
Income (%
FPL)
Not APTC Eligible
APTC Eligible
Ineligible for
Medicaid or
Marketplace
APTCs
(Coverage
Gap) ***
Affordable
ESI Offer
but not
enrolled
Enrolled in
ESI
Enrolled in
other non-
Marketplace
coverage
that
precludes
APTCs
Potentially
Eligible for
APTCs*
Eligible for
Zero Premium
Marketplace
Plan**
Eligible for
APTCs and
CSRs
<100%
78,000
164,000
177,000
0
0
0
383,000
100 - 138%
0
82,000
214,000
259,000
259,000
259,000
>138 - 250%
85,000
1,105,000
540,000
1,306,000
1,156,000
1,306,000
>250 - 400%
37,000
1,156,000
288,000
551,000
219,000
0
>400% FPL
29,000
1,088,000
199,000
573,000
22,000
0
TOTAL
229,000
3,595,000
1,418,000
2,689,000
1,656,000
1,565,000
383,000
Notes:
** Under the ARP, there is no upper income limit on APTC availability, though in practice some higher income individuals may not
receive any APTCs because their premiums are below the required income share under the ACA even without an APTC.
**Based on applying the zero-premium eligibility proportion among uninsured non-elderly adults using CPS data in ASPE brief
“Access to Marketplace Plans with Low Premiums on the Federal Platform Part II: Availability Among Uninsured Non-Elderly Adults
Under the American Rescue Plan” to the number of individuals predicted to lose Medicaid eligibility but be eligible for Marketplace
premiums within each income band. This group overlaps with those eligible for cost-sharing reductions (CSRs).
*** Some of these categories are partially overlapping and therefore sum to greater than the total.
HP-2022-20
August 2022
ISSUE BRIEF
16
REFERENCES
1
Lee A, Ruhter J, Peters C, De Lew N, Sommers BD. National Uninsured Rate Reaches All-Time Low in Early 2022. (Issue Brief No. HP-
2022-23). Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. August 2022.
2
Monthly Medicaid & CHIP Application, Eligibility Determination, and Enrollment Reports & Data. Accessed at:
https://www.medicaid.gov/medicaid/national-medicaid-chip-program-information/medicaid-chip-enrollment-data/monthly-medicaid-
chip-application-eligibility-determination-and-enrollment-reports-data/index.html
3
Centers for Medicare & Medicaid Services. CMS Releases August Medicaid and CHIP Enrollment Trends Snapshot Showing Continued
Enrollment Growth. June 21, 2021. Accessed at:
https://www.cms.gov/newsroom/press-releases/new-medicaid-and-chip-enrollment-snapshot-shows-almost-10-million-americans-
enrolled-coverage-during
4
Khorrami P and Sommers BD. Changes in US Medicaid Enrollment During the COVID-19 Pandemic. May 5, 2021. Accessed at:
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2779458
5
Sugar S, Peters C, DeLew N, Sommers BD. Medicaid Churning and Continuity of Care: Evidence and Policy Considerations Before and
After the COVID-19 Pandemic (Issue Brief No. HP-2021-10). Washington, DC: Office of the Assistant Secretary for Planning and
Evaluation, U.S. Department of Health and Human Services. April 12, 2021. Accessed at: https://aspe.hhs.gov/reports/medicaid-
churning-continuity-care
6
Abdus, S. Part-year Coverage and Access to Care for Nonelderly Adults https://journals.lww.com/lww-
medicalcare/Fulltext/2014/08000/Part_year_Coverage_and_Access_to_Care_for.6.aspx
7
Medicaid and CHIP Payment and Access Commission. An Updated Look at Rates of Churn and
Continuous Coverage in Medicaid and CHIP. October 2021. Accessed at: https://www.macpac.gov/wp-content/uploads/2021/10/An-
Updated-Look-at-Rates-of-Churn-and-Continuous-Coverage-in-Medicaid-and-CHIP.pdf
8
Williams E, Rudowitz R and Corallo B. Kaiser Family Foundation. May 10, 2022. Accessed at: https://www.kff.org/medicaid/issue-
brief/fiscal-and-enrollment-implications-of-medicaid-continuous-coverage-requirement-during-and-after-the-phe-ends/
9
Buettgens M and Green A. What Will Happen to Medicaid Enrollees’ Health Coverage after the Public Health Emergency? Urban
Institute. March 9, 2022. Accessed at: https://www.urban.org/research/publication/what-will-happen-medicaid-enrollees-health-
coverage-after-public-health-emergency
10
Branham, D.K, Conmy, A.B., DeLeire, T., Musen, J., Xiao, X., Chu, R.C., Peters, C., and Sommers, B.D. (March 29, 2021). Access to
Marketplace Plans with Low Premiums on the Federal Platform, Part I: Availability Among Uninsured Non-Elderly Adults and
HealthCare.gov Enrollees Prior to the American Rescue Plan (Issue Brief No. HP-2021-07). Washington, DC: Office of the Assistant
Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Accessed at:
https://aspe.hhs.gov/pdfreport/access-to-low-premiums-issue-brief.
11
Medicaid.gov. Unwinding and Returning to Regular Operations after COVID-19. https://www.medicaid.gov/resources-for-
states/coronavirus-disease-2019-covid-19/unwinding-and-returning-regular-operations-after-covid-19/index.html.
12
Rudich J, Branham DK, Peters C, and Sommers BD. Estimates of Uninsured Adults Newly Eligible for Medicaid If Remaining 12 Non-
Expansion States Expand Medicaid: 2022 Update (Data Point No. HP-2022-06). Office of the Assistant Secretary for Planning and
Evaluation, U.S. Department of Health and Human Services. February 2022. Accessed at: https://www.aspe.hhs.gov/reports/updated-
estimates-medicaid-eligibility-non-expansion-states
13
Executive Office of the President, Office of Management and Budget. Statement of Administrative Policy H.R. 5376 – Inflation
Reduction Act of 2022. August 6, 2022. https://www.whitehouse.gov/wp-content/uploads/2022/08/SAP-H.R.-5376.pdf.
14
Branham DK, Eibner C, Girosi F, Liu J, Finegold K, Peters C, and Sommers BD. Projected Coverage and Subsidy Impacts If the American
Rescue Plan’s Marketplace Provisions Sunset in 2023 (Data Point No. HP-2022-10). Office of the Assistant Secretary for Planning and
Evaluation, U.S. Department of Health and Human Services. March 23, 2022 Accessed at: https://www.aspe.hhs.gov/reports/impacts-
ending-american-rescue-plan-marketplace-provisions
15
Lee A, Chu RC, Peters C, and Sommers BD. Health Coverage Changes Under the Affordable Care Act: End of 2021 Update. (Issue Brief
No. HP-2022-17). Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. April
2022. Accessed at: https://aspe.hhs.gov/reports/health-coverage-changes-2021-update
16
Branham DK, Eibner C, Girosi F, Liu J, Finegold K, Peters C, and Sommers BD. Projected Coverage and Subsidy Impacts If the American
Rescue Plan’s Marketplace Provisions Sunset in 2023 (Data Point No. HP-2022-10). Office of the Assistant Secretary for Planning and
Evaluation, U.S. Department of Health and Human Services. March 23, 2022. Accessed at: https://aspe.hhs.gov/reports/impacts-
ending-american-rescue-plan-marketplace-provisions
17
Medicaid.gov. Continuous Eligibility for Medicaid and CHIP Coverage. September 2021. Accessed at:
https://www.medicaid.gov/medicaid/enrollment-strategies/continuous-eligibility-medicaid-and-chip-coverage/index.html.
18
Lee A, Chu RC, Peters C, and Sommers BD. Health Coverage Changes Under the Affordable Care Act: End of 2021 Update. (Issue Brief
No. HP-2022-17). Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. April
2022. Accessed at: https://aspe.hhs.gov/reports/health-coverage-changes-2021-update
August 2022
ISSUE BRIEF
17
HP-2022-20
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Office of the Assistant Secretary for Planning and Evaluation
200 Independence Avenue SW, Mailstop 447D
Washington, D.C. 20201
For more ASPE briefs and other publications, visit:
aspe.hhs.gov/reports
SUGGESTED CITATION
Unwinding the Medicaid Continuous Enrollment Provision:
Projected Enrollment Effects and Policy Approaches (Issue Brief
HP-2022-20) Washington, DC: Office of the Assistant Secretary
for Planning and Evaluation, U.S. Department of Health and
Human Services. August 19, 2022
COPYRIGHT INFORMATION
All material appearing in this report is in the public domain and
may be reproduced or copied without permission; citation as to
source, however, is appreciated.
___________________________________
Subscribe to ASPE mailing list to receive
email updates on new publications:
aspe.hhs.gov/join-mailing-list
For general questions or general
information about ASPE:
aspe.hhs.gov/about
