18 Journal of Nursing Regulation
Nurse Practice Acts Guide and Govern:
Update 2017
Kathleen A. Russell, JD, MN, RN
The state’s duty to protect those who receive nursing care is the basis for a nursing license. That license is an authorization
or permission from state government to practice nursing. The guidelines within the state nurse practice act and the state
nursing regulations provide the framework for safe, competent nursing practice. All nurses have a duty to understand their
nurse practice act and regulations, and to keep up with ongoing changes as this dynamic document evolves and the scope
of practice expands.
Keywords: Board of nursing, education standards, licensure, nurse practice act, nursing regulation, public protection, scope of practice
Learning Objectives
⦁
Recall the history of nurse practice acts (NPAs).
⦁
Describe the eight elements of an NPA.
⦁
Discuss disciplinary action, including grounds and possible
actions.
⦁
Name the ways that licensure status and board of nursing
(BON) actions are communicated to the public.
⦁
Identify the purpose of state involvement in the regulation of
nursing practice.
P
ermitting a new driver to get behind the wheel of a car
requires the driver to know the laws governing driving;
however, the laws do not tell the whole story. For example,
what is a driver to do when entering an unprotected intersection?
What governs the driver’s movement into the intersection? How
does the driver account for the weather, vehicle, and road condi
-
tions? What is the driver’s knowledge and experience level? Any
new driver needs guidance or rules to manage the inherent risks.
Inherent risks are also a part of nursing. Patients are ill;
medications and treatments have benefits and adverse effects; clini
-
cal situations are undetermined, open ended, and highly variable
(Benner, Malloch, & Sheets, 2010, p. 6). Providing nursing care
sometimes feels like the new driver navigating that unprotected
intersection. As with the new driver, education and standards pro
-
vided by laws and regulations designed to protect the public pro-
vide guidance in nursing practice.
Nursing requires specialized knowledge, skill, and indepen
-
dent decision making:
The practice of nursing involves behavior, attitude and judg
-
ment, and physical and sensory capabilities in the applica-
tion of knowledge, skills, and abilities for the benefit of the
client. Nursing careers take widely divergent paths—prac
-
tice focus varies by setting, by types of clients, by differ-
ent disease, therapeutic approach or level of rehabilitation.
Nurses work at all points of service in the health care system
(Sheets, 1996).
A layperson does not necessarily have access to health profes
-
sional credentials and he or she does not ordinarily judge whether
the care received is delivered according to standards of care.
Because health care poses a risk of harm to the public if practiced
by professionals who are unprepared or incompetent, licensed pro
-
fessionals are governed by laws and regulations designed to mini-
mize the risk.
Additionally, nurses are mobile and sophisticated, and they
work in a society that is changing and asymmetrical for consum
-
ers. The result is that the risk of harm is inherent in the intimate
nature of nursing care. Thus, the state is required to protect its
citizens from harm (Sheets, 1996). That protection comes in the
form of reasonable laws to regulate occupations such as nursing.
Consequently, these laws include standards for education, scope of
practice, and discipline of professionals.
History of Nurse Practice Acts
Before the Industrial Revolution, individuals could evaluate the
quality of services they received. Many communities were small,
and everyone knew everyone. Basic needs were met mostly by each
family, and when people turned to others, they knew the reputa
-
tions of those who provided services. At that time, anyone could
call themselves a nurse. However, as technology and knowledge
advanced, a variety of people and groups began to provide services
(Sheets, 1996). Individuals were no longer good arbiters of the
quality of a provider or a service:
The Progressive Era (1890–1920) in the United States was
a wellspring of innovative ideas and industrialization. The
era saw advancements in science, urbanization, education,
Continuing Education
www.journalofnursingregulation.com 19Volume 8/Issue 3 October 2017
and law, which in turn led to remarkable social, economic,
and political reform; however, it was the confluence of these
factors that led to the modernization of the professions and
the idea of professional regulation and licensing (Alexander,
2017).
Regulation implies government intervention to accom
-
plish an end beneficial to its citizens. Because the United States
Constitution does not include provisions to regulate nursing, the
responsibility falls to the states. Under a state’s police powers, it
has the authority to make laws to maintain public order, health,
safety, and welfare (Guido, 2010, p. 34). In addition to the state’s
need to protect the public, nursing leaders wanted to:
legitimize the profession in the eyes of the public, limit the
number of people who hired out as nurses, raise the quality
of professional nurses, and improve educational standards in
schools of nursing (Penn Nursing Science, 2012).
The first nurse registration law was enacted in 1903 in
North Carolina, and it was written to do just that—protect the
title of nurse and improve the practice of nursing. Developing
nursing examinations and issuing licenses was entrusted to the
North Carolina Board of Nursing (North Carolina Nursing
History, 2017). New Jersey, New York, and Virginia passed regis
-
tration laws later that same year. These early acts did not define the
practice of nursing; however, in 1938, New York defined a scope
of practice for nursing (NCSBN, 2010). By the 1970s, all states
required licensure for registered and practical nurses.
Advanced practice nurses can be traced to the Civil War,
when nurses assisted with anesthesia services during surgery
(Hamric, Spross, & Hanson, 2005, p. 4). Advanced practice reg
-
istered nurse (APRN) roles and specialization have continued to
this day, as has the evolution of formal scope of practice language
within legislative statutes.
Nurse’s Guide to Action
How could a law function as a guide to action if almost no one
knows it (Howard, 2011, p. 30)? The laws and regulations for
the nursing profession can only function properly if nurses know
the current laws and regulations governing practice in their state.
Laws governing individual health care providers are enacted
through state legislative action. Regulatory authority is derived
from legislative action. Whereas a state constitution forms the
framework for state governments, legislatures enact laws that grant
specific authority to regulatory agencies. For example, a state leg
-
islature enacts an NPA to regulate nursing and delegates author-
ity to the state boards of nursing (BONs) to enforce the NPA.
The mission or purpose of the BON is to protect the public. State
legislatures delegate many enforcement activities to state admin
-
istrative agencies. This delegation of regulatory authority allows
the legislature to use the expertise of the administrative agencies
in the implementation of statutes.
All states and U.S. territories have an NPA and a set of
regulations or rules that must be considered together. The broad
nature of the NPA is insufficient to provide the complete guidance
for the nursing profession. Therefore, each state develops rules or
regulations that seek to clarify or make the NPA more specific.
Regulations and rules must be consistent with the NPA and can
-
not extend beyond it. These regulations and rules undergo a pro-
cess of public review before enactment (NCSBN, 2011a; Ridenour
& Santa Anna, 2012, p. 504). Once enacted, regulations and rules
have the full force and effect of law.
Although the specificity of NPAs varies among states, all
NPAs include:
⦁
definitions
⦁
authority, power, and composition of a BON
⦁
educational program standards
⦁
standards and scope of nursing practice
⦁
types of titles and licenses
⦁
protection of titles
⦁
requirements for licensure
⦁
grounds for disciplinary action, other violations, and possible
remedies.
Specific NPA and regulations may be located on the BON
website. Additionally, the NCSBN Nurse Practice Act Toolkit
(NCSBN, 2017a) includes a Find Your Nurse Practice Act tool that
provides links to each state’s NPA and regulations. The NPA is
found as chapters in the state law or state statute. Regulations are
found in the state administrative code. Additionally, at least 18
BONs have created Nurse Practice Acts/Jurisprudence online, self-
paced continuing education courses (NCSBN Learning Extension,
2017).
Definitions
Terms or phrases used in statutes must be clear and unambiguous
for the intent of a law to be useful to legislators and citizens. A law
does not need to define terms that are commonly understood; how
-
ever, definitions are often included to avoid ambiguity about word
meanings. For example, encumbered, reinstatement, and reactivation are
often defined in NPAs. An encumbered license is defined as a license
with current discipline, conditions, or restrictions. Reinstatement is
different from reactivation in that reinstatement refers to reissuance
of a license following disciplinary action, whereas reactivation is
a reissuance not related to disciplinary action (NCSBN, 2012a).
Authority, Power, and Composition of a BON
The NPA grants authority to regulate the practice of nursing
and the enforcement of law to an administrative agency or BON,
which is charged with maintaining the balance between the rights
of the nurse to practice nursing and the responsibility to protect
the public health, safety, and welfare of its citizens (Brous, 2012,
p. 508). The membership and qualifications of the BON, terms of
office, meetings, and election of officers are specified in the NPA.
The BON is usually composed of registered nurses (RNs), licensed

20 Journal of Nursing Regulation
practical/vocational nurses (LPN/VNs), advanced practice nurses,
and members representing the public.
How BON membership is constituted depends on state
statute. Some states give the governor authority to appoint mem
-
bers to the BON after reviewing suggestions from professional
nursing organizations. Other states require nominations from pro
-
fessional organizations with appointment by the director or head of
the regulatory agency. Only in North Carolina are BON members
elected by the general public. In still other states, the legislature
appoints public members (Brent, 2012, p. 2). The BON typically
hires an executive officer, who has the authority to staff the office
with nurses, attorneys, investigators, and administrative staff.
Typically, the powers and duties of BONs include:
⦁
making, adopting, amending, repealing, and enforcing rules
⦁
setting nursing education standards
⦁
setting fees for licensure
⦁
performing criminal background checks
⦁
licensing qualified applicants
⦁
maintaining database of licensees
⦁
ensuring continuing competence
⦁
developing nursing standards of practice
⦁
collecting and analyzing data
⦁
implementing discipline process
⦁
regulating registered nurses
⦁
regulating unlicensed assistive personnel
⦁
hiring BON employees.
Educational Program Standards
Most U.S. BONs set standards for prelicensure nursing educational
programs and clinical learning experiences and approve such pro
-
grams that meet requirements of the NPA. These standards are
reflected in the rules that accompany the NPA. The prelicensure
program standards include accreditation, curriculum specifics,
administrator and faculty qualifications, continuing approval,
and approval of new, or withdrawal of approved, nursing educa
-
tion programs.
Specific curriculum rules often include necessary standards
of evidence-based clinical judgment; skill in clinical management;
biological, physical, social, and behavioral science requirements;
professional responsibilities; legal and ethical issues; patient safety;
and best practices of nursing.
Standards and Scope of Nursing Practice
Nursing care is both directed and evaluated by the NPA and regu-
lations/rules. The standards and scope of nursing practice within
an NPA are aligned with the nursing process. For example, com
-
prehensive nursing assessment based on biological, psychological,
and social aspects of the patient’s condition; collaboration with the
health care team; and patient-centered health care plans, includ
-
ing goals and nursing interventions, can all be language within
the NPA. Further standards include decision making and critical
thinking in the execution of independent nursing strategies, provi
-
sion of care as ordered or prescribed by authorized health care pro-
viders, evaluation of interventions, development of teaching plans,
delegation of nursing intervention, and advocacy for the patient.
Rules are often more specific and inclusive than the act. The
NPA may require safe practice, whereas the rules may specify a plan
for safe practice, requiring orientation and training for competence
when encountering new equipment and technology or unfamiliar
care situations; communication and consultation with other health
team members regarding patient concerns and special needs, sta
-
tus, or changes; response or lack of response to interventions; and
significant changes in patient condition (NCSBN, 2012a, 2012b).
The NPA typically identifies delegating and assigning nursing
interventions to implement the plan of care as within an RN’s scope of
practice (NCSBN, 2012a). The rules, however, spell out the RN’s
responsibility to organize, manage, and supervise the practice of
nursing. Indeed, the rules can delineate the specific steps for effec
-
tive delegation by an RN as ensuring:
⦁
unlicensed assistive personnel have the education, legal author-
ity, and demonstrated competency to perform the delegated
task
⦁
tasks are consistent with unlicensed assistive personnel’s job
description
⦁
tasks can be safely performed according to clear, exact, and
unchanging directions
⦁
results of the task are reasonably predictable
⦁
tasks do not require assessment, interpretation, or independent
decision making
⦁
patient and circumstance are such that delegation of the task
poses minimal risk to the patient
⦁
consequences of performing the task improperly are not life
threatening
⦁
RNs provide clear directions and guidelines regarding the task
(NCSBN, 2012b).
Title and Licensure
NPA language generally includes a statement regarding the title of
RN and LPN/VN. By specifying that the title of RN is “given to
an individual intended to practice nursing” and LPN/VN is “given
to an individual licensed to practice practical/vocational nursing,”
the NPA protects these titles from being used by unauthorized
persons and thereby protects the public (NCSBN, 2012a).
Each state’s NPA also includes statements regarding exami
-
nation for licensure as RNs and LPN/VNs, including frequency
and requisite education before examination and reexamination.
Additional requirements of licensure by examination typically
include:
⦁
application and fee
⦁
graduation from an approved prelicensure program or a pro-
gram that meets criteria comparable to those established by
the state
⦁
passage of the professional examination
⦁
attestation of no report of substance abuse in the last 5 years
www.journalofnursingregulation.com 21Volume 8/Issue 3 October 2017
⦁
verification of no report of actions taken or initiated against a
professional license, registration, or certification
⦁
attestation of no report of acts or omissions that are grounds for
disciplinary action as specified in the NPA.
The majority of jurisdictions include criminal background
checks as an additional requirement for licensure (NCSBN,
2012c).
Further requirements are also included in NPAs for licen
-
sure by examination of internationally educated applicants, licen-
sure by endorsement, as well as licensure renewals, reactivation,
and continuing education. Endorsement is an approval process for
a nurse who is licensed in another state. Obtaining licensure by
endorsement often includes prelicensure requirements and verifi
-
cation of licensure status from the state where the nurse obtained
licensure by examination (NCSBN, 2012a).
Although statutory language varies from state to state
regarding the licensure of APRNs, most states recognize clini
-
cal nurse specialist, nurse midwife, nurse practitioner, and regis-
tered nurse anesthetist as APRN roles and require certification by
a national nurse certification organization. Education and specific
scope of practice for APRNs varies from state to state.
Grounds for Disciplinary Action, Violations, Statute of
Limitations, Possible Remedies, and Reciprocal Discipline
The majority of nurses are competent and caring individuals who
provide a satisfactory level of care; however, when a nurse deviates
from the standard of care or commits an error, a complaint may
be filed with the BON. The BON, through its statutory author
-
ity specified in the NPA, is responsible for reviewing and acting
on complaints. A BON can take formal action only if it finds suf
-
ficient basis that the nurse violated the NPA or regulations. Each
case varies and needs to be considered on its own merits (Brous,
2012, pp. 510–511; NCSBN, 2012d). Since BONs take dis
-
ciplinary action in order to protect the public by ensuring that
only properly qualified and ethical individuals practice nursing,
this public safety objective is not time-limited. Therefore, in the
absence of a specific statute to the contrary, statutes of limitations
are inapplicable to BON license revocation and other disciplinary
proceedings (NCSBN, 2017b).
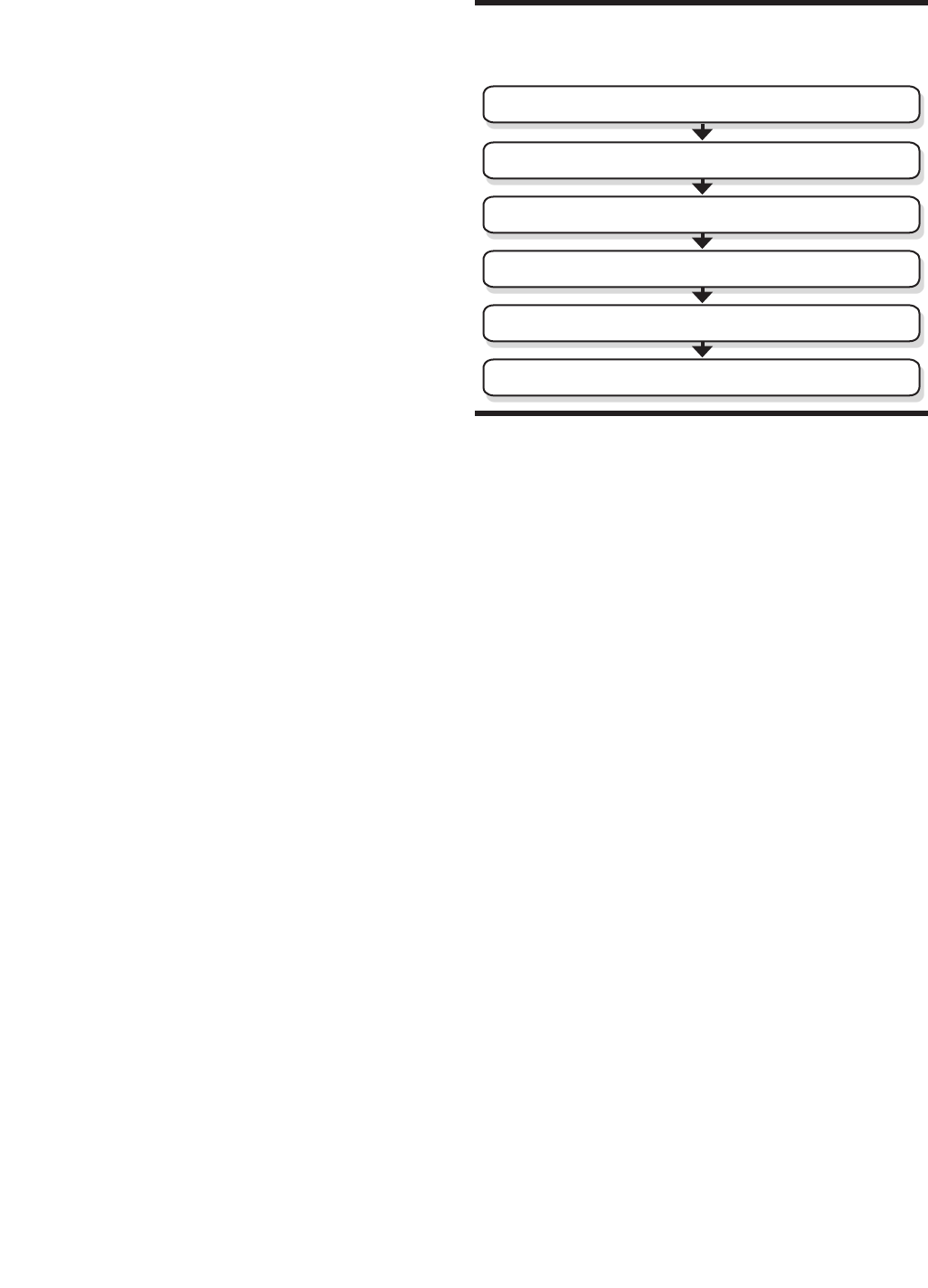
For an overview of the disciplinary process from receipt of
complaint to resolution, see Figure 1. Complaints about nursing
care are often grouped into the following categories:
⦁
Practice-related: breakdowns or errors during aspects of the nurs-
ing process (Wade, 2015)
⦁
Drug-related: mishandling, misappropriation, or misuse of con-
trolled substances
⦁
Boundary violations: nontherapeutic relationships formed
between a nurse and a client in which the nurse derives a ben
-
efit at the client’s expense (NCSBN, 2009)
⦁
Sexual misconduct: inappropriate physical or sexual contact with
a client
⦁
Abuse: maltreatment of clients that is physically, mentally, or
emotionally harmful (Russell & Wade, 2015)
⦁
Fraud: misrepresentation of the truth for gain or profit (usually
related to credentials, time, or payment)
⦁
Positive criminal background checks: detection of reportable crim-
inal conduct as defined by statute (NCSBN, 2011b, 2012e;
Russell & Beaver, 2013; Russell, 2016).
If a substance use disorder is suspected from the evidence,
some BONs may offer the nurse a nondisciplinary alternative-to-
discipline program. These programs are monitoring programs, not
treatment programs. The possibility of avoiding the public noto
-
riety of discipline can be a driving factor in breaking through the
nurse’s denial of substance use disorder and movement to a pro
-
gram that will assist in retaining her or his license. These programs
refer nurses for evaluation and treatment, monitor the nurse’s com
-
pliance with treatment and recovery recommendations, monitor
abstinence from drug or alcohol use, and monitor their practice
upon return to work. Alternative-to-discipline programs aim to
return nurses to practice while protecting the public. Various mod
-
els of alternative-to-discipline programs exist, and their use varies
among BONs (NCSBN, 2017c). Some programs provide services
via the BON, a contracting agency, a BON special committee,
a peer-assistance program of a professional association, or a peer-
assistance employee program (NCSBN, 2012f).
Some states have incorporated an alternative-to-discipline
program for practice-related complaints (NCSBN, 2016). These
programs seek to provide patient safety through timely education
and oversight (Holm & Emrich, 2015). This type of program shifts
the focus to improving practice and professional responsibility. To
participate in a practice-related alternative-to-discipline program,
the practice by the nurse must not pose a threat to patient safety.
These programs vary by state.
FIGURE 1
Board of Nursing Complaint Process
Filing a complaint
Initial review of complaint
Investigation
Board proceedings
Board actions
Reporting and enforcement

22 Journal of Nursing Regulation
For all other grounds, the final decision reached by the BON
is based on the findings of an investigation and the results of the
board proceedings. The language used to describe the types of
actions available to BONs varies according to each state’s statute.
Although terminology may differ, board action affects the
nurse’s licensure status and ability to practice nursing in the state
taking action. BON actions may include the following:
⦁
fine or civil penalty
⦁
referral to an alternative-to-discipline program for prac-
tice monitoring and recovery support for those with drug- or
alcohol-dependence or some other mental or physical condition
⦁
public reprimand or censure for minor violation of the NPA,
often with no restrictions on license
⦁
imposition of requirements for monitoring, remediation, edu-
cation, or other provision tailored to the particular situation
⦁
limitation or restriction of one or more aspects of practice, such
as probation with limits on role, setting, activities, or hours
worked
⦁
separation from practice for a period (suspension) or loss of
license (revocation or voluntary surrender)
⦁
other state-specific remedies (NCSBN, 2012g).
An attempt to evade disciplinary action merely by flee
-
ing the state does not protect the public. Therefore, a state board
of nursing is well within its legitimate authority to take action
against a licensee on the basis of another state’s disciplinary action
that implicates the individual’s ongoing ability and likelihood to
practice professionally and safely. This reciprocal or retained juris
-
diction action serves to assist the BON to fulfill the legislature’s
charge to protect the public (NCSBN, 2017b).
Public Access to Licensure Status and Board Actions
Licensure status and BON actions are public information, and
BONs use a variety of methods to communicate this information,
including newsletters, database and websites. Licensure infor
-
mation and board action for most states are also available to the
public via Nursys QuickConfirm License Verification
©
(Nursys
QuickConfirm
©
, 2017). Any individual or entity may use this ser-
vice free of charge.
Federal law requires that state adverse actions taken against
a health care professional’s license be reported to the federal data
bank. The National Practitioner Data Bank (NPDB) was estab
-
lished in 1986 by Congress as a workforce tool to “prevent prac-
titioners from moving from state-to-state without disclosure or
discovery of previous damaging performance” (U.S. Department of
Health & Human Services, 2017a). As such, the NPDB is a reposi
-
tory of reports containing information on certain adverse actions
related to health care practitioners, providers, and suppliers. The
data bank also includes information on medical malpractice pay
-
ments. Information housed within NPDB is not available to the
general public. Only authorized eligible entities may query the
NPBD. The NPDB Guidebook (U.S. Department of Health and
Human Services & Health Resources and Services Administration,
2015) contains specific information regarding authorized queri
-
ers, which generally includes hospitals, other health care entities,
professional societies, licensing boards, attorneys, and the licensee.
There is a nominal charge for an authorized individual or entity to
query the NPDB (U.S. Department of Health & Human Services,
2017b).
Being Informed About Your NPA
Ignorance of the law is never an excuse! The NPA and state regu-
lations are not resources one can study in a prelicensure nursing
education program and then put aside. The act and the regulations
are dynamic documents that evolve and are updated or amended as
changes in law or rules are made:
Inherent in our current healthcare system are changes which
relate to demographic changes (such as the aging of the
“baby boomers”); advances in technology; decreasing health
-
care dollars; advances in evidence-based healthcare proce-
dures, practices and techniques; and many other societal and
environmental factors (NCSBN, 2012h).
State BONs are resources for the NPA and regulations.
Links to NPAs are available on most state BON websites. Some
BONs attempt to provide new information to nurses via their web
-
site or newsletter (Tedford, 2011). For example, the Virginia BON
posts a list of frequently asked questions to help nurses navigate
the various aspects of licensure and posts announcements regard
-
ing practice or licensing changes on their homepage (Virginia
Board of Nursing, 2017). Use the Find Your Nurse Practice Act
tool (NCSBN, 2017a) or take your jurisdiction’s Nurse Practice
Act/Jurisprudence online, self-paced continuing education course
(NCSBN Learning Extension, 2017).
The state’s duty to protect those who receive nursing care is
the basis for a nursing license. That license is an authorization or
permission from state government to practice nursing. The guide
-
lines within the state NPA and the state nursing regulations pro-
vide the framework for safe, competent nursing practice. All nurses
have a duty to understand their NPA and regulations and to keep
up with ongoing changes as this dynamic document evolves and
the scope of practice expands. The guidelines of the NPA and the
regulations provide safe parameters within which to work and
protect patients from unprofessional and unsafe nursing practice
(Brent, 2012, p. 5; Mathes & Reifsnyder, 2014). More than 100
years ago, state governments established BONs to protect the pub
-
lic’s health and welfare by overseeing and ensuring the safe practice
of nursing. Today, BONs continue their duty, but the law cannot
function as a guide to action if almost no one knows about it. “To
maintain one’s license in good standing and continue practicing,
nurses must understand that rights are always accompanied by
responsibilities” (Brous, 2012, p. 506). It is your responsibility to
know your state’s NPA and rules before you enter that unprotected
intersection of nursing care.

www.journalofnursingregulation.com 23Volume 8/Issue 3 October 2017
References
Alexander, M. (2017). The evolution of professional regulation. Journal of
Nursing Regulation, 8(2), 3.
Benner, P. E., Malloch, K., & Sheets, V. (Eds.). (2010). Nursing pathways for
patient safety. Chicago, IL: National Council of State Boards of Nurs
-
ing.
Brent, N. J. (2012). Protect yourself: Know your nurse practice act [Online CE].
Retrieved from https://www.nurse.com/ce/protect-yourself-know-
your-nurse-practice-act
Brous, E. (2012). Nursing licensure and regulation. In D. J. Mason, J. K.
Leavitt, & M. W. Chaffee (Eds.). Policy & politics in nursing and health
care (6th ed.). St. Louis, MO: Saunders.
Guido, G. W. (2010). Legal & ethical issues in nursing (5th ed.). Boston, MA:
Pearson.
Hamric, A. B, Spross, J. A., & Hanson, C. M. (2005). Advanced practice nurs
-
ing: An integrative approach. St. Louis, MO: Elsevier Saunders.
Holm, M., & Emrich, L. (2015). Justice with dignity alternative to discipline for
nurses with practice errors. Retrieved from https://www.ncsbn.org/2015_
DCM_Holm_Emrich.pdf
Howard, P. K. (2011). The death of common sense: How law is suffocating Amer
-
ica. New York, NY: Random House.
Mathes, M., & Reifsnyder, J. (2014). Nurse’s law: Legal questions & answers for
the practicing nurse. Indianapolis, IN: Sigma Theta Tau International,
Center for Nursing.
National Council of State Boards of Nursing. (2009). Professional boundaries:
A nurse’s guide to the importance of appropriate professional boundaries [Bro
-
chure]. Chicago, IL: Author.
National Council of State Boards of Nursing. (2010). Nurse practice act—
Arkansas v4 [Online course]. Retrieved from http://learningext.com/
hives/c3ce5f555a/summary
National Council of State Boards of Nursing. (2011a). What you need to know
about nursing licensure and boards of nursing [Brochure] Chicago, IL:
Author.
National Council of State Boards of Nursing. (2011b). State and territorial
boards of nursing: What every nurse needs to know [Brochure]. Chicago, IL:
Author.
National Council of State Boards of Nursing. (2012a). Model act. Chicago,
IL: Author.
National Council of State Boards of Nursing. (2012b). Model rules. Chicago,
IL: Author.
National Council of State Boards of Nursing. (2012c). The 2011 Uniform
Licensure requirements. Retrieved from https://www.ncsbn.org/
12_ULR_table_adopted.pdf
National Council of State Boards of Nursing. (2012d). Filing a complaint.
Retrieved from www.ncsbn.org/163.htm
National Council of State Boards of Nursing. (2012e). Initial review of a com
-
plaint. Retrieved from https://www.ncsbn.org/1616.htm
National Council of State Boards of Nursing. (2012f). Board proceedings.
Retrieved from https://www.ncsbn.org/672.htm
National Council of State Boards of Nursing. (2012g). Board action.
Retrieved from https://www.ncsbn.org/673.htm
National Council of State Boards of Nursing. (2012h). Changes in healthcare
professions’ scope of practice: Legislative considerations [Brochure]. Retrieved
from www.ncsbn.org/Scope_of_Practice_2012.pdf
National Council of State Boards of Nursing. (2016). Member board profile -
discipline, delegation, telenursing mbp 2016. Retrieved from https://www.
ncsbn.org/MBPD_D_TelehealthLinks.pdf
National Council of State Boards of Nursing. (2017a). Nurse practice act tool
-
kit. Retrieved from https://www.ncsbn.org/npa-toolkit.htm
National Council of State Boards of Nursing. (2017b). Statute of Limitations
and Retained Jurisdiction. Retrieved from https://www.ncsbn.org/
Statute_of_Limitations_and_Retained_Jurisdiction.pdf
National Council of State Boards of Nursing. (2017c). Alternative to disci
-
pline programs for substance use disorder. Retrieved from https://www.
ncsbn.org/alternative-to-discipline.htm
NCSBN Learning Extension. (2017). Nurse practice acts/jurisprudence.
Retrieved from https://learningext.com/nurses/p/nurse_practice_acts
North Carolina Nursing History. (2017). A century of caring video. Retrieved
from https://nursinghistory.appstate.edu/century-caring-video
Nursys QuickConfirm
©
. (2017). QuickConfirm License Verification
©
.
Retrieved from https://www.nursys.com/LQC/LQCSearch.aspx
Penn Nursing Science. (2012). History of nursing timeline. Retrieved from
www.nursing.upenn.edu/nhhc/Pages/timeline_1900-1929.
aspx?slider1=1#chrome
Ridenour, N., & Santa Anna, Y. (2012). An overview of legislation and reg
-
ulation. In D. J. Mason, J. K. Leavitt, & M. W. Chaffee (Eds.). Policy
& politics in nursing and health care (6th ed.). St. Louis, MO: Saunders.
Russell, K. A. (2012). Nurse practice acts guide and govern nursing prac
-
tice. Journal of Nursing Regulation, 3(3), 36–42.
Russell, K. A. (2016). Due process and right-touch regulation strengthen
regulatory decision making. Journal of Nursing Regulation, 7(2), 39–42.
Russell, K. A. & Beaver, L. K. (2013). Professionalism extends beyond the
workplace. Journal of Nursing Regulation, 3(4), 15–18.
Russell, K. A. & Wade, A. (2015). When the court interprets legislative
intent: mandatory reporting of child abuse. Journal of Nursing Regula
-
tion, 6(1), 39–42.
Sheets, V. (1996). Public protection or professional self-preservation?
Unpublished manuscript, National Council of State Boards of Nursing.
Tedford, S. A. (2011, October). When was the last time you read the nurse
practice act? ASHN update. Retrieved from http://epubs.
democratprinting.com/publication/index.php?i=83957&m=&l=&
p=4&pre=&ver=swf
U.S. Department of Health and Human Services, & Health Resources and
Services Administration. (2015). National practitioner data bank guide
-
book. Rockville, MD: U.S. Department of Health and Human Ser-
vices. Retrieved from https://www.npdb.hrsa.gov/resources/
aboutGuidebooks.jsp?page=DOverview.jsp
U.S. Department of Health & Human Services. (2017a). NPDB national
practitioner data bank - about us. Retreived from https://www.npdb.
hrsa.gov/topNavigation/aboutUs.jsp
U.S. Department of Health & Human Services. (2017b). NPDB national
practitioner data bank - Querying the NPDB. https://www.npdb.hrsa.
gov/hcorg/aboutQuerying.jsp
Virginia Board of Nursing. (2017). Board home. Retrieved from https://
www.dhp.virginia.gov/nursing/default.htm
Wade, A. (2015). The BON’s authority to interpret regulations, negli
-
gence, and nurse practice act statutes. Journal of Nursing Regulation,
6(3), 25–28.
Kathleen A. Russell, JD, MN, RN, is a Senior Policy Advisor,
Nursing Regulation, National Council of State Boards of Nursing,
Chicago, Illinois.
This continuing education article is an important update of the reasons for
and the significance of state nurse practice acts and associated regulations
originally published in 2012 (Russell, K. A. [2012]. Nurse practice acts
guide and govern nursing practice. Journal of Nursing Regulation,
3(3), 36–42).
