
Protecting Health, Improving Lives
Alzheimer’s Disease State Plan
Pursuant to Alzheimer’s Disease Assistance Act (410 ILCS 405)
2020 – 2023 Report and Recommendations
September 2020
State of Illinois
Illinois Department of Public Health

2
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Table of Contents
Overview ......................................................................................................................................... 3
2020-2023 Short-Term Recommendations ................................................................................... 5
Introduction .................................................................................................................................... 8
Legislative History .......................................................................................................................... 9
Alzheimer’s Disease and Related Disorders: Conventions ....................................................... 10
Opportunities and Challenges ..................................................................................................... 12
Impact and Trends of Alzheimer’s Disease ................................................................................. 15
Behavioral Risk Factor Surveillance System ................................................................................ 16
Cognitive Impairment ................................................................................................................ 16
Caregiver Activities .................................................................................................................... 17
Economics of Alzheimer’s Disease ............................................................................................... 18
Effects of Caregiving on Employees and Employers .................................................................. 19
Costs to Illinois Citizens ............................................................................................................. 20
Services to Address the Needs of Persons with Alzheimer’s Disease, Their Families, and
Caregivers ..................................................................................................................................... 21
Illinois’ Alzheimer’s Disease Network ........................................................................................ 21
Regional Alzheimer’s Disease Assistance Centers ................................................................. 21
ADA Center Primary Provider Sites ....................................................................................... 24
State Supported Alzheimer’s Disease Research ........................................................................ 24
Illinois Alzheimer’s Disease Advisory Committee ...................................................................... 25
Illinois State Agencies Programs and Support .......................................................................... 26
Illinois Department of Public Health ...................................................................................... 26
Illinois Department on Aging ................................................................................................. 26
Illinois Guardianship and Advocacy Commission .................................................................. 27
Dementia Care Services ............................................................................................................. 27
Dementia-Specific Training Requirements ................................................................................ 28
Quality Care Measures .............................................................................................................. 28
Skilled Nursing Facilities (SNFs) ............................................................................................. 28
Assisted Living Facilities (ALF) ................................................................................................ 29
Supportive Living Programs (SLP) .......................................................................................... 29
Geriatric-Psychiatric Services .................................................................................................... 29
Home and Community-Based Resources .................................................................................. 31
Residential Options for Persons with Dementia ........................................................................ 32
Public Safety and Law Enforcement .......................................................................................... 33
Acknowledgements ...................................................................................................................... 35
References .................................................................................................................................... 37
Appendix B: 2020-2023 Long-Term Recommendations…………………………………………………………38

3
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Overview
What is the Alzheimer’s Disease Illinois State Plan?
The Alzheimer’s Disease Illinois State Plan was established in January 2014 and is required to be
revised every three years in accordance with the Alzheimer’s Disease Assistance Act. The
current plan is a revision of the original plan and reflects new initiatives implemented over the
last three years. Although Alzheimer’s disease is the most common form of dementia, the plan
is intended to include all dementias, such as vascular, Lewy-Body, and frontotemporal, within
the progress, prioritization, and recommendations. In addition, the plan integrates
improvements made within the Healthy Brain Initiative, Illinois Cognitive Resources Network,
and state requirements for staff training and health care facilities advertising.
The plan is produced by the Illinois Department of Public Health (IDPH) in conjunction with the
Alzheimer’s Disease Advisory Committee (ADAC) and relevant Alzheimer’s disease stakeholders.
The intent of the plan is to guide research, diagnosis, referral, support, and treatment services
within each of the following areas:
• Illinois’ Alzheimer’s Disease Network (Regional Alzheimer’s Disease Assistance Centers and
Primary Provider Sites)
• State Supported Alzheimer’s Disease Research
• Illinois Alzheimer’s Disease Advisory Committee
• Illinois State Agencies’ Alzheimer’s Programs and Support (Illinois Department of Public
Health, Illinois Department on Aging, Illinois Department of Human Services, and Illinois
Department of Healthcare and Family Services)
• Dementia Care Services
• Dementia Specific Training Requirements
• Quality Care Measures (Skilled Nursing Facilities, Assisted Living Facilities/Supportive Living
Facilities, and Other Settings)
• Geriatric-Psychiatric Services
• Home and Community-Based Resources
• Residential Options for Persons with Dementia
• Public Safety and Law Enforcement
Who is the Plan for?
The Alzheimer’s Disease Illinois State Plan is for any person, community, agency, institution, or
organization that has the means to and interest in helping implement recommendations
outlined in the plan. The goal is to help serve patients and caregivers impacted by Alzheimer’s
disease and related dementias (AD/ADRD). This plan can also be useful for policy and decision
makers to gauge what is happening in Illinois around AD/ADRD and what still needs to be done.

4
2020 – 2023 Alzheimer’s Disease Illinois State Plan
How to Use this Plan?
This plan is meant “to guide” AD/ADRD-related efforts within the State of Illinois. This plan is
not a substitute for individualized work or action plans developed by organizations or persons
interested in addressing the needs of people impacted by AD/ADRD. It should be viewed as a
compass shared by all the stakeholders that will give a unifying direction to their programs. The
recommendations can be used to formulate specific goals, objectives, and strategies that can
be pursued by individual stakeholders. Collaboration is encouraged among stakeholders to
increase the effectiveness of their individual efforts.
5
2020 – 2023 Alzheimer’s Disease Illinois State Plan
2020 – 2023 Recommendations to Address the
Needs of People with Alzheimer’s Disease and related dementias, Their Families,
and Caregivers
SHORT-TERM RECOMMENDATIONS
The Alzheimer’s Disease Advisory Committee identified the following recommendations as
feasible to accomplish during the three-year reporting time.
Illinois’ Alzheimer’s Disease Network
• Short-term recommendation (ST) 1 - Maintain and grow new state funding for the regional
Alzheimer’s Disease Assistance Centers (RADAC) to assure funding is sustainable for collaborative
efforts among the ADA centers and other academic institutions throughout the state. The ADA
centers are described on pages 21-24. (Assign to the regional ADA Centers.)
• ST 2 - Improve the quality of local care available for people with AD/ADRD by providing training for
primary provider sites (PPS) staff, families, and stakeholders. Because PPS sites are multidisciplinary
in nature, it is necessary to expand the number and knowledge base of providers by building
linkages with organizations representing primary care physicians and internists, midlevel advanced
practice nurses, and social workers. Organizations include, but not limited to the Geriatric
Workforce Enhancement Program funded by the Health Resources and Services Administration
(HRSA), the Illinois Academy of Family Physicians, the Illinois Chapter of the American College of
Physicians, the Illinois Primary Health Care Association, local health departments, Illinois Society of
Advanced Practice Nursing, Association of Nurse Practitioners – Illinois Region 5, and the National
Association of Social Workers, Illinois Chapter. The PPS program is described on page 24. (Assign to
the ADA Center PPS.)
State Supported Alzheimer’s Disease Research
• ST 3 - ADA center staff should continue facilitating meetings with other research entities (institutes
of higher education and care providers) within the state to encourage an exchange of ideas and to
foster research collaborations. Federal and foundation research grants could be developed to
address ways to impact the public health burden and health disparities, and to develop a roadmap
to increase a diverse research workforce interested in careers to address the issues faced by people
at risk or living with AD/ADRD.
• ST 4 - Continue increasing local participation in and awareness of clinical trials and studies on
cognitive health and impairment.
• ST 5 - Improve research, care, and support funding in Illinois by expanded promotion of the state
income tax check-off fund.
Illinois State Agencies Programs and Support
• ST 6 - Provide links from IDPH’s website to the state’s ADA centers and to the Alzheimer’s
Association (www.alz.org) to improve the access to and dissemination of information and resources
on the IDPH website. (Assign to IDPH.)
• ST 7 – Develop additional state data collection reports related to AD/ADRD. Provide up-to-date
information on the resources need for caregivers and families. (Assign to IDPH.)
• ST 8 - Integrate Healthy People objectives on “Older Adults” and “Dementias, including Alzheimer’s
disease” into topic areas in the State Health Improvement Plan. (Assign to IDPH.)
• ST 9 - Seek federal grant opportunities to promote the development of a dementia-capable state
and dementia-friendly communities to ensure a competent workforce and communities that are not
6
2020 – 2023 Alzheimer’s Disease Illinois State Plan
only safe for and accessible to people with AD/ADRD, but also support and empower people with
AD/ADRD and their family members to continue living high-quality lives. Illinois Department on
Aging (IDoA) programs are described on page 22. (Assign to IDoA.)
• ST 10 - Support the expansion and availability of supportive living program (SLP) dementia
care units in the state as initiated by the Illinois Department of Healthcare and Family
Services (HFS). (Assign to HFS.)
• ST 11 - Support the expansion and growth of the final home and community-based services (HCBS)
regulations so that individuals have the opportunity to receive these services in a manner that
protects individual choice and promotes community integration. Support programs that will further
this recommendation even if it is not covered by Medicaid or Medicare. (Assign to HFS.)
• ST 12 - With suitable funding, identify and promote culturally appropriate strategies designed to
increase public awareness about AD/ADRD, to reduce conflicting messages, to decrease stigma, and
to promote early diagnosis. (IDPH)
• ST 13 Continue to administer the Behavioral Risk Factor Surveillance System (BRFSS) cognitive
impairment and caregiver modules in Illinois on a frequency based on Centers for Disease Control
and Prevention (CDC) guidelines and use this and other surveillance data to enhance awareness of
public health programming (e.g., link between BRFSS questions on cognition to health-related
quality of life or falls prevention). Approximately $68,000 is needed to implement both modules.
• ST 14 Train ombudsman, Care Coordination Units (CCU) and Area Agencies on Aging (AAA) service
providers, adult protective services staff, and managed care organizations to be knowledgeable
about Alzheimer's disease and related dementias. (IDoA)
• ST 15 Ensure the same public benefits are accessible for all persons with Alzheimer’s disease
regardless of age. Persons eligible to receive services must be able to do so whether funding is
provided by the Illinois Department of Human Services (DHS) Division of Rehabilitation Services (for
those in the program before age 60, including persons with younger-onset Alzheimer’s), IDoA, the
Medicaid program, or some other source
Implement structural changes that will improve access to Medicaid-funded home and community-
based long-term services and supports (LTSS), and streamline program eligibility and service delivery
to consumers between state agency programs. Structural changes should include:
i. a. A uniform assessment process for access and eligibility to services.
ii. b. A “no-wrong-door” entry into state services across HFS, IDoA, and IDPH.
iii. c. Conflict-free case management. (IDoA)
Achieve a re-balancing of long-term services and supports (LTSS) by shifting individuals into home
and community-based services and away from long-term institutional care when that option is safe
for the individual.
• ST16 Enhance IDoA’s website to include information about specific resources available to individuals
with Alzheimer’s disease and related dementias, such as the Illinois ADA centers, Alzheimer’s
Association, and alz.gov. (IDoA).
7
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Dementia Care Services
• ST 17 - Continue to strengthen health care practices at the point of diagnosis by encouraging
dedicated staff support or by providing referrals to appropriate entities such as ADA centers, the
Alzheimer’s Association, or the state’s aging and disability resource centers. Assist in planning care
or providing case management and developing formal mechanisms for education and referral to
health care institutions and community-based agencies that offer specialized expertise, social
supports, and mental health services.
• ST 18 - Work with stakeholders to preserve the elements of Medicaid essential to those living
with AD/ADRD and their families. Evaluate the use of Medicaid and Medicare waivers that would
strengthen care coordination and management to reduce the use of more expensive facility-
based long-term care services when cost efficient home- and community-based services are
appropriate.
• ST 19 - Provide physical, emotional, educational, and financial assistance to unpaid caregivers of
people with dementia, including respite and support services.
Dementia-Specific Training Requirements. The following recommendations are intended to
maintain core competency of the profession and
to improve access to care and consumer
knowledge of care options, to
equalize benefits for people with young onset Alzheimer’s
disease, and to improve care coordination across health settings.
• ST 20 – In order to provide better models of AD/ADRD education and training, develop incentives for
partnerships between and among various providers. This may include centers of excellence,
educational and vocational programs, and community colleges and universities. The intent of these
partnerships is to have individuals pursue careers in dementia care, geriatrics, or neurology.
Providers should include every discipline that comes into contact with a person with the AD/ADRD
and their family.
• ST 21 - Develop an AD/ADRD training certificate that allows students the opportunity to receive
certification as they receive college credit. Certification can take place for medical, nurse
practitioner, and physician assistant students within their geriatric or long-term care rotation.
Physicians and nurse practitioners already certified in geriatrics in Illinois are encouraged to offer
mentorship opportunities to these students.
Accountability and Staffing to Provide Quality Care in Residential Care Settings/Improve
Residential Care
• ST 22 - Develop and mandate effective training in behavioral interventions (using evidence-based
practices) for personnel working with people with AD/ADRD in residential care settings.
• ST 23 - Require residential care facilities, as a condition of licensure, to institute an approved protocol
for dealing with behavioral issues of individuals with AD/ADRD and to ensure all staff members are
trained in implementing protocol.
• ST 24 - Advocate for the appropriate use and referral for comfort care/palliative and hospice
services within licensed nursing facilities. (Skilled Nursing Facilities)
• ST 25 - Convene a panel of experts to replace the basic AD/ADRD care provisions in the assisted
living facility (ALF) and supportive living programs (SLP) regulations with comprehensive provisions
that reflect current best practices and evidence-based research in dementia care, like those found in
Subpart U. (ALF/SLP)
• ST 26 - Create a tiered structure of Medicaid reimbursement for residential care facilities to
compensate for the higher cost of caring for individuals with AD/ADRD, both early onset and
diagnoses after 65 years of age.
8
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Geriatric-Psychiatric Services
• ST 27 - Explore the concept of linking hospital diagnostic codes with reimbursement and level of
training.
Other
• ST 28 - Strengthen the laws and penalties that make it a criminal offense for an individual to
financially exploit a cognitively impaired individual.
Introduction
In 2019, there were 230,000 people with AD/ADRD living in Illinois.
This figure is projected to
reach 260,000 in 2025, a 13 percent increase. If all the people with Alzheimer’s disease in
Illinois lived in one city, it would be the state’s second largest. Alzheimer’s disease is not a
disease that limits itself to a particular race, marital status, country of origin, religion, or sexual
preference.
Nationally, the cost of caring for those with AD/ADRD is estimated to total $290 billion in 2019,
increasing to $1.1 trillion (in today’s dollars) by mid-century. Medicare and Medicaid cover
about 67% of the total health care and long-term payments.
In 2019, the Medicaid cost of
caring for people with Alzheimer’s disease in Illinois was $1.7 million and is projected to
increase to $2.2 in 2025, a 27% increase.
Throughout this plan, recommendations are provided for new policies to address Illinois’
response to AD/ADRD. These recommendations can be achieved through close collaboration
among partner and public input to advocate for appropriate legislative action and regulatory
change and facilitate public-private partnerships. These action steps are designed to ensure
Illinois becomes a “dementia-capable state,” as defined in the Alzheimer’s Disease Assistance
Act (410 ILCS 405), meaning Illinois and its long-term care services, community-based services,
and dementia-support systems have:
• the ability to identify people with dementia and their caregivers;
• information, referral, and service coordination systems that provide person-centered
services to people with dementia and their caregivers;
• eligibility criteria for public programs that are equitable for people with dementia;
• coverage of services that people with dementia and their caregivers are likely to use;
• a professional caregiving workforce that knows about Alzheimer's disease and other
dementias and how to serve that population and their caregivers; and
• quality assurance systems that take into account the unique needs of people with
dementia and their caregivers.
The Illinois Alzheimer’s Legislators Alliance, comprised of 66 members of the General Assembly,
has recognized the importance of ensuring Illinois is dementia-capable and stands ready to
9
2020 – 2023 Alzheimer’s Disease Illinois State Plan
move the state forward in crafting a better response to the growing public health crisis of
AD/ADRD. The alliance was instrumental in coordinating three public hearings to gain broad
input into the content of this plan. The public hearings were held in southern, central, and
northern areas of Illinois. Community members and staff of agencies providing programs and
services to people with AD/ADRD, their families, and caregivers offered suggestions for the
plan.
Legislative History
Illinois has been involved in addressing Alzheimer’s disease and related dementias for many
years. In 1984, the House Appropriations Committee and the Legislative Research Unit
collaborated on a major conference that generated an 11-bill legislative package, which became
known as the “Alzheimer’s Initiative” and was approved unanimously in 1985. A key
component of the legislative initiative was the Alzheimer’s Disease Assistance Act
(410 ILCS 405). The legislation required that by January 1, 1987, and every three years
thereafter, IDPH prepare an Illinois Alzheimer's Disease Assistance Plan in consultation with the
Illinois Alzheimer’s Disease Advisory Committee (ADAC) to guide research, diagnosis, referral,
and treatment services within each service area described by IDPH; provide oversight of three
regional Alzheimer’s disease assistance centers (ADA centers), including their primary provider
sites (PPS); and coordinate Alzheimer’s Disease Research Fund (ADRF) grants.
In 2003, a legislative task force on Alzheimer’s disease was created (HJR 14) to obtain a
snapshot of the current status of Alzheimer’s disease activities and to receive updated
information and recommendations for ensuring Illinois would be able to respond to the rise in
the number of people affected by the disease.
In 2007, the General Assembly passed Senate Joint Resolution 43 (SJR 43), recommending IDPH,
in partnership with the ADAC, prepare a report addressing the impact of Alzheimer’s disease
and related dementias in Illinois and the resources and services needed to improve the state’s
capacity to address the disease.
In 2012, the Alzheimer’s Disease Assistance Act was amended (P.A. 97-0768) to include revised
state plan requirements to reflect a more dementia capable state. The plan was submitted to
the Office of the Governor and the General Assembly by January 1, 2014, as required by the act.
Other legislation addressing living arrangements for people with Alzheimer’s disease,
information gathering and autopsies, quality incentives, and respite programs have been
enacted. The State Adult Protective Services Act was amended (P.A. 99-143) to include people
with Alzheimer’s disease and Illinois created specialty license plates for Alzheimer’s disease
awareness (P.A. 98-0259).
10
2020 – 2023 Alzheimer’s Disease Illinois State Plan
In 2015, the Illinois General Assembly passed legislation (P.A. 99-0322) to create the Silver
Search program, as part of the Endangered Missing Persons Advisory statutes. The program,
which began in 2016, is a coordinated effort to bring awareness, education, and resources to
help find and safely return people with Alzheimer’s or dementia that go missing. The Silver
Search program strives to bring awareness to the increasing incidences of people with
Alzheimer’s or dementia that get lost and ways in which the public can help law enforcement
return them home safely.
In 2016, the General Assembly passed the Alzheimer’s Disease and Related Dementia Services
Act (P.A. 99-0822) that established minimum training requirements for employees of
organizations and facilities that provide Alzheimer’s and dementia-related services.
The 2018 hospital assessment legislation (P.A. 100-0581) approximately tripled funding
available for Alzheimer’s research at the three Illinois regional ADA centers.
In 2019, the General Assembly passed legislation (P.A. 101-0588) authorizing the creation of a
dementia coordinator within IDPH. This position will be responsible for implementation of this
Alzheimer’s Disease State Plan and will coordinate resources for Alzheimer’s and other
dementias across state agencies. The act also changed the membership structure for the
Alzheimer’s Disease Advisory Committee from 16 to 17 members by adding an individual with
medical or academic experience with early onset Alzheimer’s disease or related disorders.
Alzheimer’s Disease and Related Disorders: Conventions
In this plan, Alzheimer’s disease is often used as shorthand for the term “Alzheimer’s disease
and related disorders” (AD/ADRD). Alzheimer’s disease also includes mild cognitive impairment.
As the field is rapidly advancing the definitions are evolving because of scientific learning. For
consistency with the intent of the General Assembly through the implementation of the
Alzheimer’s Disease Assistance Act and for the greatest impact on the residents in Illinois, the
recommendations in this Alzheimer’s Disease State Plan are for AD/ADRD and not just
Alzheimer’s disease.
AD/ADRD are the conditions leading to the constellation of signs and symptoms described by
the term, dementia. As defined in the Alzheimer’s Disease Assistance Act, dementia is a
“general term for cognitive decline caused by various diseases and conditions that result in
damaged brain cells or connections between brain cells.” There is a decline in cognitive
function along with physical function and behavior from a previous level of functioning.
Dementia represents the transition to when cognitive function prevents an individual from
carrying out customary activities at work or home.
Alzheimer’s disease is one of many conditions that can result in dementia. It happens to be the
most common dementia seen in old age. It is an irreversible, progressive brain disease and is

11
2020 – 2023 Alzheimer’s Disease Illinois State Plan
fatal.
It slowly destroys brain function and leads to dementia. It is characterized by cognitive
decline (e.g., memory loss, confusion, and poor reasoning), behavioral and psychiatric disorders
(e.g., depression, delusions, agitation), and declines in functional status (e.g., ability to perform
activities of daily living and self-care).
Alzheimer’s disease is a specific disease of the brain that was identified more than 100 years
ago, but research into its causes, risk factors, and potential treatments has gained momentum
only in the last 30 years. The hallmarks of Alzheimer’s disease are the accumulation of
abnormal proteins in the brain: clumps of beta-amyloid (called amyloid plaques) and tangled
bundles of tau fibers (called neurofibrillary tangles). Most experts now agree the accumulation
of plaques and tangles in the brain may begin 20 or more years before the symptoms of
dementia appear. Many current studies are investigating the benefits of exercise, diet, and
other lifestyle modifications that may prevent or delay the onset of Alzheimer’s disease.
The causes of Alzheimer’s disease are not completely understood, but researchers believe they
include a combination of genetic, environmental, and lifestyle factors.
The importance of any
one of these factors in increasing or decreasing the risk of developing Alzheimer’s disease may
differ from person-to-person. In rare cases, known as early or younger-onset Alzheimer’s
disease, people develop symptoms in their 30s, 40s, or 50s. In more than 90% of people with
Alzheimer’s disease, symptoms do not appear until after age 60 and the incidence of the
disease increases with age.
The first symptom of Alzheimer’s disease is often memory impairment. As the disease
progresses, memory continues to decline and other functions, like language skills and decision-
making, become more difficult. Personality and behavior changes also may occur. A person with
the disease may no longer recognize family and friends.
Eventually, the person with Alzheimer’s disease is completely reliant on others for assistance
with the most basic activities of daily living, such as eating.
Dementia also is caused by other known and yet undefined diseases and conditions in the
brain. Three common neurodegenerative causes are vascular disease, Lewy Body disease, and
frontotemporal. Some of these, such as frontotemporal, start at a much younger age when a
person is in their 50s and early 60s, and can impair language or behavior, while leaving memory
intact. Defining the contribution of Alzheimer’s disease and related disorders to dementia, in
terms of clinical presentation and diagnosis, is challenging. Researchers now recognize many of
these diseases and conditions can co-occur in the brain and work together to influence the
onset of dementia.

12
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Opportunities and Challenges
Illinois has opportunities to improve its ability to meet the needs of persons with AD/ADRD
because of an increased focus at the federal level. Since the last state plan, there has been
much advanced at the national level as far as funding for AD/ADRD research. There is a
competitive space for states and others to attract those funds. It is an opportunity and a
challenge on how to organize most effectively to compete for federal grants. Some of the state
plan recommendations lay the groundwork to support ideas to help Illinois be more
competitive to apply for federal funding. A $425 million increase, the largest ever funding
increase for Alzheimer’s and dementia research from the National Institutes of Health (NIH),
was advocated for by the Alzheimer’s Association, the Alzheimer’s Impact Movement (AIM). For
2019, The total annual funding for Alzheimer’s and other dementias is now $2.3 billion. Billions
of dollars are also being spent by the United States and biotech companies. Recent interest has
focused on a variety of factors including retinal changes, cerebral spinal changes, and stringent
blood pressure ranges.
NIH provides funding for Alzheimer’s disease research and significant dollars have been
awarded to Illinois research institutions. From 2017-2019, there were 411 Alzheimer’s disease
related projects in the state totaling $242 million, with an additional 94 sub-projects totaling
$35 million, which demonstrates Illinois’ research capacity. Increased partnerships between the
state and research institutions may lead to increased federal funding.
With the passage of the National Alzheimer’s Project Act of 2011 (NAPA), the federal
government has become more invested in AD/ADRD research and the optimal treatment and
care of both AD/ADRD patients and their caregivers. The National Plan to Address Alzheimer’s
Disease was published in May 2012. The goals of the plan are to prevent and effectively treat
AD/ADRD by 2025, enhance care quality and efficiency, expand support for people with the
disease and their families, enhance public awareness and engagement, track progress, and
drive improvement. The federal government has committed more than $50 million to achieve
these goals. The national plan was updated in 2013 to include new federally supported
programs available to states and organizations to foster research and to improve the care of
patients and caregivers. The following research milestones were achieved by federal
leadership:
o To shorten the time to treatment and prevention, the NIH launched the Accelerating
Medicines Partnership – Alzheimer’s Disease (AMP-AD) efforts to stimulate clinical
trial biomarker collection and drug target identification for the field. These include
the AMP-AD Knowledge Portal and Global Alzheimer’s Association Interactive
Network (GAAIN), big data hubs that allow for cloud-based analysis on a larger scale
than would be possible by any individual research team.
o The NIH is modernizing and transforming the Alzheimer’s Disease Research
Centers (ADRC) program. By integrating transformative recommendations from an
expert panel, ADRCs will be better able to achieve the objectives of the national

13
2020 – 2023 Alzheimer’s Disease Illinois State Plan
plan. The next generation of ADRCs will increase flexibility and collaboration by
leveraging expanded resources, capabilities, and research participants across the
network.
o NIH launched the Alzheimer’s Disease Preclinical Efficacy Database (AlzPED), a
knowledge platform to disseminate data and analysis to scientists from academic
centers, industry, and disease-focused foundations to promote efficiency,
transparency, reproducibility, and accuracy of research aimed at preclinical therapy
development for Alzheimer’s. AlzPED is designed to help identify critical data, design
elements, and methodology missing from studies.
o The National Institute on Aging (NIA), in partnership with the Alzheimer’s
Association, provided an update on the National Strategy for Recruitment and
Participation in Alzheimer’s Disease Clinical Research in July 2018. The new
national strategy identifies actions to increase recruitment and participation among
diverse audiences.
o The NIH launched the All of Us research program, a historic effort to gather data
from at least 1 million Americans to accelerate research, improve health, and enable
precision medicine for diseases including Alzheimer’s.
o The NIA, in collaboration with the Alzheimer’s Association, launched the
International Alzheimer’s Disease Research Portfolio (IADRP), a public database
capturing the full spectrum of current global Alzheimer’s and dementia research
investments and resources. For the first time, the dementia research community,
government, organizations, and potential donors can see which areas are receiving
the most and least funding, allowing these groups to better invest resources.
The national Alzheimer’s disease plan identified challenges the nation faces, as well as some
specific to Illinois. These include:
• Lack of full-time state coordinator.
• Lack of quality care memory support facilities funded by Medicaid.
• Racial disparities in terms of prevalence and supportive resources.
• Difficulty in attracting and maintaining nurses and nursing assistants in long-term
care/memory care.
• Growing number of unpaid family caregivers.
• High out-of-pocket costs and limited state oversight for memory care services in assisted
living.
• While research on AD/ADRD has made steady progress, there are no pharmacological or
other interventions to definitively prevent, treat, or cure the disease. There has been
more focus on understanding life-style risk factors as it relates to dementia.
• Seamless coordination among acute care, community and long-term care, and
community care.
• Ability to pay for memory care facilities for individuals’ dollars above Medicaid funding.
• Recognition of all health care professions as a resource for care.
• Creating dementia friendly communities.

14
2020 – 2023 Alzheimer’s Disease Illinois State Plan
• Awareness and recognition of lesbian, gay, bisexual, transgender, and queer (LGBTQ)
older adults with respect to dementia care.
• While many groups have taken steps to develop quality measures to assess AD/ADRD
and to improve training of the health and long-term care workforce, there is room for
improvement.
• Family members and other informal caregivers who take on the responsibility of caring
for a loved one with AD/ADRD need support. The majority of people with AD/ADRD live
in the community and their families provide most of their care. The toll of caregiving can
have major implications for caregivers and families; about one-third of caregivers report
symptoms of depression.
• Stigmas and misconceptions associated with AD/ADRD are widespread and profoundly
impact the care provided to, and the isolation felt by, people with AD/ADRD and their
families.
• Public and private sector progress is significant, but coordination and tracking are
limited; as is data to assess the incidence, prevalence, trends, and costs.
• Illinois has no state-funded office designated to oversee and coordinate state-based
programming of AD/ADRD. While many state agencies support a specific aspect of
AD/ADRD service or care, better understanding of programs and coordination of efforts
through one lead agency is needed.
• Illinois’ fiscal limitations affect the ability to improve AD/ADRD programs and services.
Strong partnerships could lead to increased federal funding to the state.
Building Our Largest Dementia (BOLD) Infrastructure for Alzheimer's Act (P.L. 115-406) is
intended to create an Alzheimer's public health infrastructure across the country to implement
effective Alzheimer's interventions focused on public health issues, such as increasing early
detection and diagnosis, reducing risk, and preventing avoidable hospitalizations. The act will
establish this by creating Alzheimer's and Related Dementias Public Health Centers of
Excellence; providing funding to state, local and tribal public health departments; and
increasing data analysis and timely reporting. As of this date, the BOLD Act has passed but
funds have not been allocated. With state investment and organization, Illinois can be
competitive to become a Center of Excellence.
Opportunities exist, including:
• A $425 million increase was advocated for by the Alzheimer’s Association known as the
Alzheimer’s Impact Movement. This was the largest NIH funding increase ever for dementia
research. For 2019, total annual funding is now $2.3 billion.
• Billions of dollars are also being spent on dementia research from biotech companies. Areas
of interest and opportunity for improved understanding include retinal changes, cerebral
spinal changes, impact of stringent blood pressure parameters, and lifestyle changes.
• The state’s Regional Alzheimer’s Disease Assistance Centers (RADAC) are uniquely
placed to provide guidance regarding improvements to respond to AD/ADRD and
15
2020 – 2023 Alzheimer’s Disease Illinois State Plan
support for those dealing with Alzheimer’s disease. The ADACs are described on page
21.
• The state’s regional ADACs address clinical needs and enhance the awareness of the
disease through research activities.
• Organizations, such as the Alzheimer’s Association, provide information, resources,
support, and other services to people with AD/ADRD, to their families, to caregivers, and
to professionals. The organizations also advocate for the needs of people with
Alzheimer’s disease.
• Public/private partnerships, such as that of IDPH and the Alzheimer’s Association, are
beneficial to assess the needs of people with cognitive impairment and caregivers using
Illinois BRFSS data.
• The Alliance is comprised of members of the General Assembly who are supportive of
making Illinois a dementia-capable state.
• IDoA received two grants from the Administration on Community. 1) Funding for the
Alzheimer’s Disease Initiative - Specialized Supportive Services Program to offer
evidence-based programs for persons with dementia and their caregivers and webinars.
2) Funding for the Alzheimer’s Disease Supportive Services Program – Part B to offer
Savvy Caregiver, Stress Busting for Caregivers, Dementia Friendly America Initiative, and
Supportive Gap Filling Services for persons with dementia and their caregivers. IDoA also
piloted the Dementia Care Specialist Program in the ADRCs. This training program is
based on the core competencies developed by IDPH for individuals in the aging network
working directly with persons with dementia and their caregivers in a non-clinical
capacity.
Impact and Trends of Alzheimer’s Disease
Today, approximately 5.8 million Americans are living with AD/ADRD, including 230,000 in
Illinois (projected to reach 260,000 in 2025, a 13% increase), the sixth leading cause of death in
the country, and the fifth leading cause of death for those older than age 65. It is projected
that the number of people with this disease may double or even triple by 2050, barring a major
medical breakthrough.
Approximately 500,000 people develop AD/ADRD each year in the United States. By 2050, that
number could reach 1 million a year. AD/ADRD is not a disease that limits itself to a particular
race, marital status, country of origin, religion, or sexual preference.
This disease leaves no survivors. While the number of deaths attributed to most major diseases
declined between 2000 and 2017 – prostate cancer (by 1.9%), heart disease (by 8.9%), stroke
(by 12.7%), and HIV (by 60.6%) – AD/ADRD deaths climbed, increasing 145%. In 2017, there
were 4,021 deaths from AD/ADRD in Illinois.
16
2020 – 2023 Alzheimer’s Disease Illinois State Plan
With appropriate resources, researchers believe they will be able to develop treatments that
slow the progression of AD/ADRD and, as a result, improve the quality of life for people with
AD/ADRD, their families, and their caregivers. Of course, the ultimate goal is a cure for the
disease.
The need to diagnose AD/ADRD earlier, even before patients have symptoms, has spawned
research interest into "biomarkers"— tests such as a brain scan or blood test that would
conclusively prove someone has AD/ADRD, independent of the patient's cognitive functioning.
Such a biomarker could be a more reliable indicator of a treatment response in drug studies
and not subject to the inherent variability of cognitive testing.
Another profound development in the care of AD/ADRD patients is the realization that
compared to all diseases, AD/ADRD incurs the highest societal cost. Patients often require
placement in nursing homes or assisted living facilities and their family members may have to
leave the work force to provide care. Although most AD/ADRD patients are of retirement age,
some are younger than 65; diagnosis often necessitates dropping out of the work force as well.
There also is a greater emphasis on the health and well-being of the caregivers of persons with
AD/ADRD. AD/ADRD often claims two individuals: the patient and his/her caregiver,
particularly if the caregiver is the spouse. And it is often the spouse/partner that suffers the
most, dealing with the behavioral and caregiving requirements of the patient who may be
unaware of his/her impairment and resistant to caregiving. The Alzheimer’s disease research
community is making greater investments into methods to identify and to address caregiver
stress, and to improve the quality of caregiving for the benefit of both the patient and the
caregiver.
Behavioral Risk Factor Surveillance System
BRFSS is a data system that provides information on behaviors and conditions related to the
leading causes of death, injury, and disability. BRFSS is a joint effort of the CDC and state health
departments. In Illinois, BRFSS surveys are conducted as random-dialed telephone interviews
of adult residents throughout the State. BRFSS questions are scripted and conducted by trained
interviewers. BRFSS data are used to identify the need for services, target populations at
greatest risk, evaluate past efforts, and guide health policy decisions.
A unique feature of BRFSS is the ability to generate specific data related to particular question
responses. Two “optional” BRFSS modules are related to cognitive impairment and caregiver
activity for persons with Alzheimer’s disease.
Cognitive Impairment
In 2015, BRFSS cognitive impairment module questions were included on the Illinois survey.
17
2020 – 2023 Alzheimer’s Disease Illinois State Plan
• 9.6% of Illinois adults aged 60 or older self-reported confusion or memory loss that is
happening more often or getting worse over the past 12 months; 53.5% of them have
not talked to a health care professional about it.
Among Illinois adults aged 60 or older with confusion or memory loss:
• 43% reported always, usually, or sometimes given up day-to-day household activities or
chores they use to do.
• 30.2% reported always, usually, or sometimes interfered with their social lives.
• 34.7% reported always, usually, or sometimes needing help with day-to-day activities.
• 7.2% reported they never received help with day-to-day activities from a family
member or friend.
As a result of the Healthy Brain Initiative efforts, IDPH and partners used BRFSS state and
county data to develop two Burden Updates, one focusing on increased confusion or memory
loss and the challenges faced by caregivers (for the state and regionally for 13 Planning and
Service Areas [PSAs]); and a second specific to caregiver demographic and socioeconomic
characteristics, time spent providing care, and health problems of both individuals who receive
care and caregivers. A statewide webinar to showcase the Burden Updates was conducted
March 25, 2015 for area agencies on aging, local health departments, and other groups to
increase awareness of cognitive health issues and to offer tips for using the data in local
planning to address the needs of persons with cognitive impairment and caregivers.
Caregiver Activities
The 2015 Illinois BRFSS caregiver data demonstrate that 131,800 persons reported providing
care to a family, friend, or neighbor with dementia and other cognitive disorders. The majority
of caregivers have been providing care for two to five years (37.2%) or more than five years
(27%). An additional 22.5% have been providing care for six months to less than two years and
only 13.2% are relatively new caregivers providing care less than six months. Half (49.9%)
provide up to eight hours of care each week on average. About 15% provide nine to 19 hours
per week, about 17% provide 20 to 39 hours a week and another 17% provide 40 hours of more
a week. In calculating the economic value of care provided by unpaid caregivers, the
Alzheimer’s Association used a methodology that, in 2012, valued care at $12.33 per hour.
However, it is much more expensive if families must hire care in the marketplace. The most
recent data showed the national average cost of a non-medical home health aide was $21 per
hour (or $168 for an eight-hour day). The Illinois average was the same, although the average
was slightly higher in Chicago and in the Highland Park area at an average of $22 per hour.
The surveillance data denote the extent of self-reported confusion or memory loss among non-
institutionalized adults aged 60 or older who may require services and support now or in the
future. This underscores the need for increased awareness about changes in memory and
confusion that may warrant discussions with health care and service providers so patients can
18
2020 – 2023 Alzheimer’s Disease Illinois State Plan
be provided with accurate information and linked to needed services. In addition, caregiver
services must be more accessible and comprehensive in all areas of Illinois to address the needs
of persons with AD/ADRD and their family, friends, and neighbors serving as caregivers.
The cognitive impairment module and the caregiving module were included in the 2013 and
2015 survey.
Economics of Alzheimer’s Disease
AD/ADRD poses a substantial financial burden on society. As the number of people with
AD/ADRD and other dementias grow, spending for their care will increase dramatically. The
total aggregate payments for AD/ADRD health care, long-term care, and hospice in the United
States are projected to jump from $290 billion in 2019 to $1.1 trillion in 2050 (in 2019 dollars).
This rise includes a four-fold increase in both government spending under Medicare and
Medicaid and out-of-pocket spending.
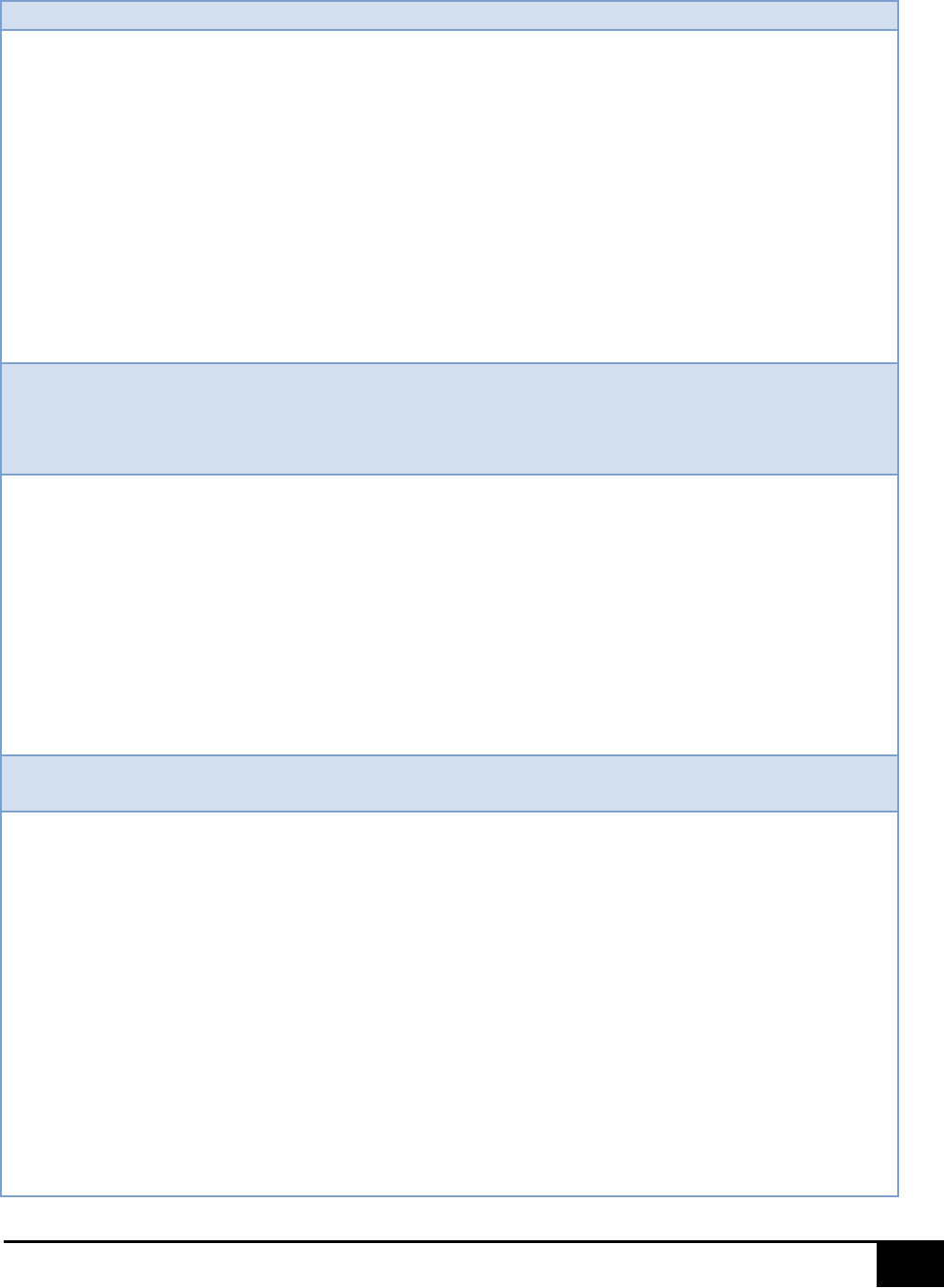
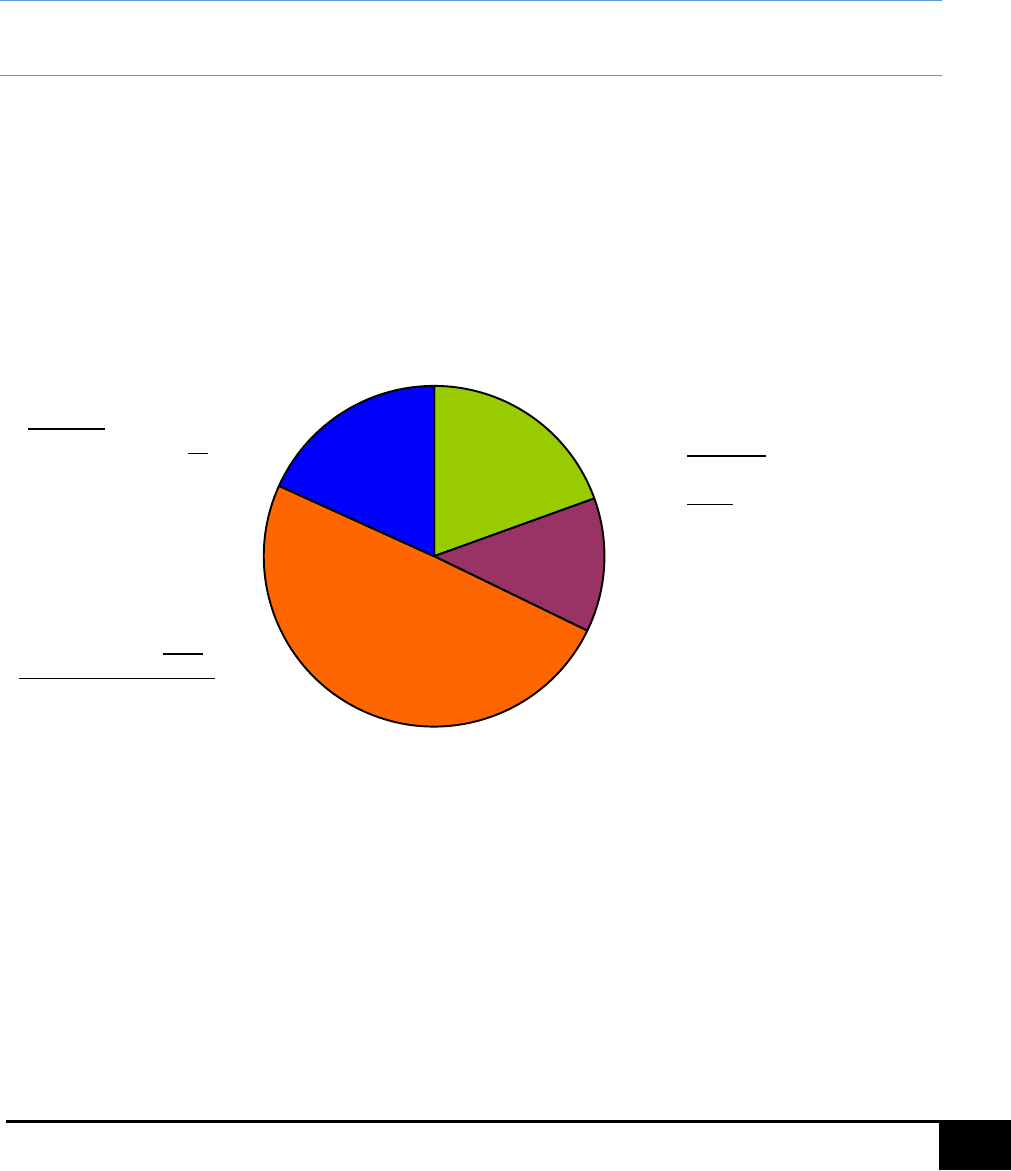
2019 Costs of Alzheimer's = $290 Billion in the U.S.
Source: Alzheimer’s Association, 2019 Alzheimer’s Disease Facts and Figures, Alzheimer’s Dement 2019;15(3):321-87.
The table below describes the average annual per-person payments for health care and long-
term care services for Medicare beneficiaries age 65 and older with and without Alzheimer’s or
other dementias.
Out-of-Pocket $34B
Other $27B
Medicare $107B
Medicaid $35B
The average per person
Medicare costs for those with
AD/ADRD are more than
three times higher than for
those without these
conditions.
The average per person
Medicaid costs for those
with AD/ADRD are 23
times higher than for
those without these
conditions.
3
Nearly 30% of people with
AD/ADRD are on both
Medicare and Medicaid,
compared to 11% of those
without these conditions.
19
2020 – 2023 Alzheimer’s Disease Illinois State Plan
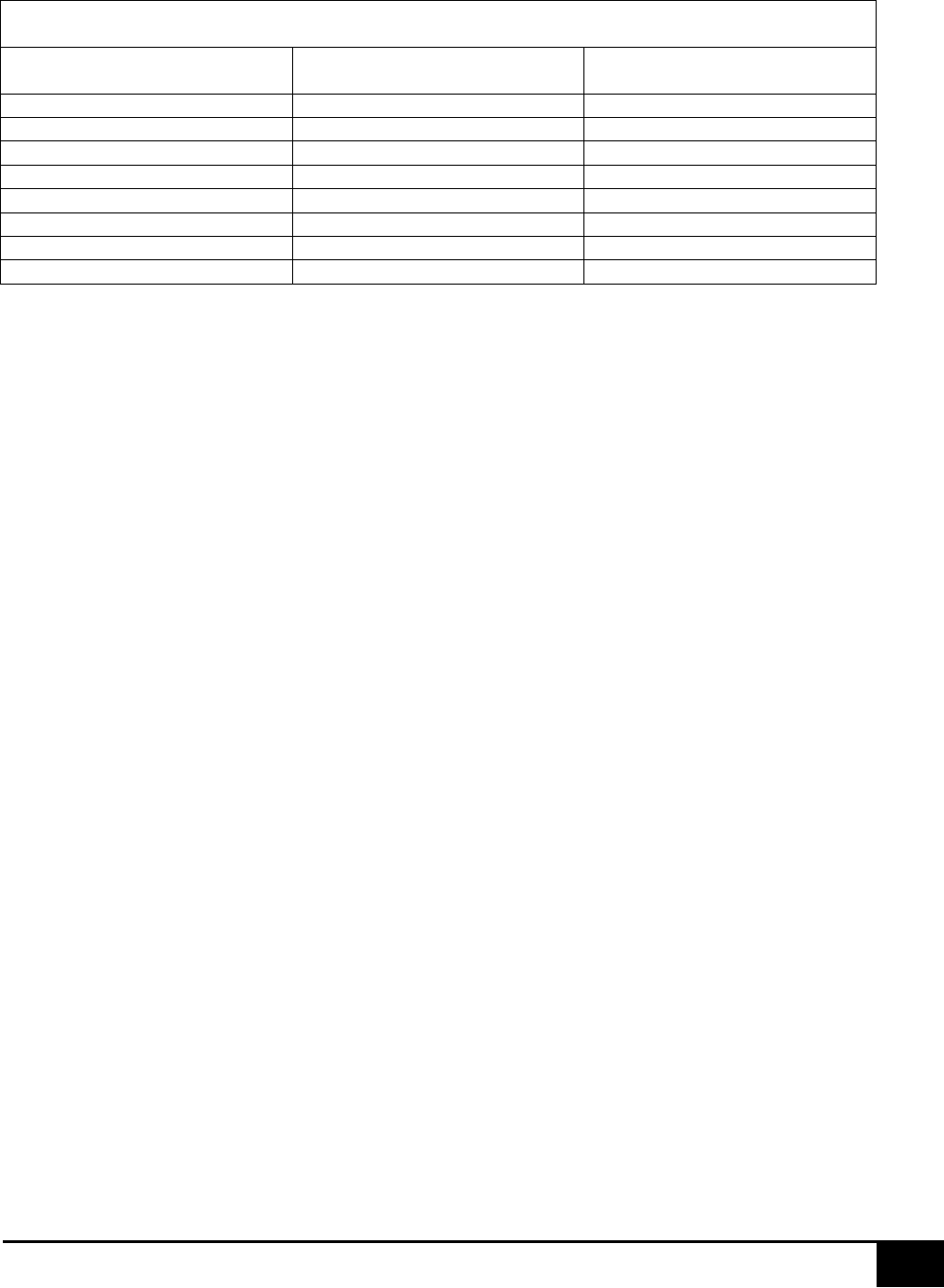
Average Annual Per-person Payments for Health Care and Long-Term Care Services, Medicare Beneficiaries
Age 65 and Older, With and Without Alzheimer’s Disease and Other Dementias, in 2018 Dollars.
Payment Source
Beneficiaries with Alzheimer’s
Disease and Other Dementias
Beneficiaries without Alzheimer’s
Disease and Other Dementias
Medicare
$24,598
$7,561
Medicaid
$8,565
$365
Uncompensated
$381
$382
HMO
$1,261
$1,544
Private Insurance
$2,253
$1,422
Other Payer
$937
$242
Out of Pocket
$10,798
$2,336
Total*
$48,977
$13,976
Source: Unpublished data from the Medicare Current Beneficiary Survey for 2011. *Payments from sources do not equal total payments
exactly due to the effect of population weighting. Payments for all beneficiaries with Alzheimer’s disease or other dementias include payments
for community-dwelling and facility-dwelling beneficiaries.
Caring for people with AD/ADRD also strains health and long-term care systems. Individuals
with AD/ADRD use a disproportionate number of health care resources; for instance, they are
hospitalized twice as often as people the same age who do not have the disease.
Similarly,
while people living in nursing homes are a small percentage of the older population 50% of
nursing home residents have AD/ADRD.
As the number of people with AD/ADRD grows over
the next two decades, the disease will place a major strain on these care systems, as well as on
Medicare and Medicaid, the major funders of this care.
In addition to strain on health care and long-term care systems, Alzheimer’s disease requires
significant caregiving resources. More than 16 million Americans provide unpaid care for
people with Alzheimer’s disease and other dementias. Eighty-three percent of the help
provided to older adults in the United States comes from family members, friends, or other
unpaid caregivers. In 2018, caregivers of people with AD/ADRD provided an estimated 18.5
billion hours of informal (i.e., unpaid) assistance, a contribution to the nation valued at $233.9
billion. The total lifetime cost of care for someone with dementia was estimated at $350,174 in
2018 dollars. The costs associated with family care make up 70% of lifetime dementia care
costs.
In 2018 there were 588,000 caregivers in Illinois who provided 670 million hours of unpaid care,
with a total value of unpaid care estimated at $8.5 billion.
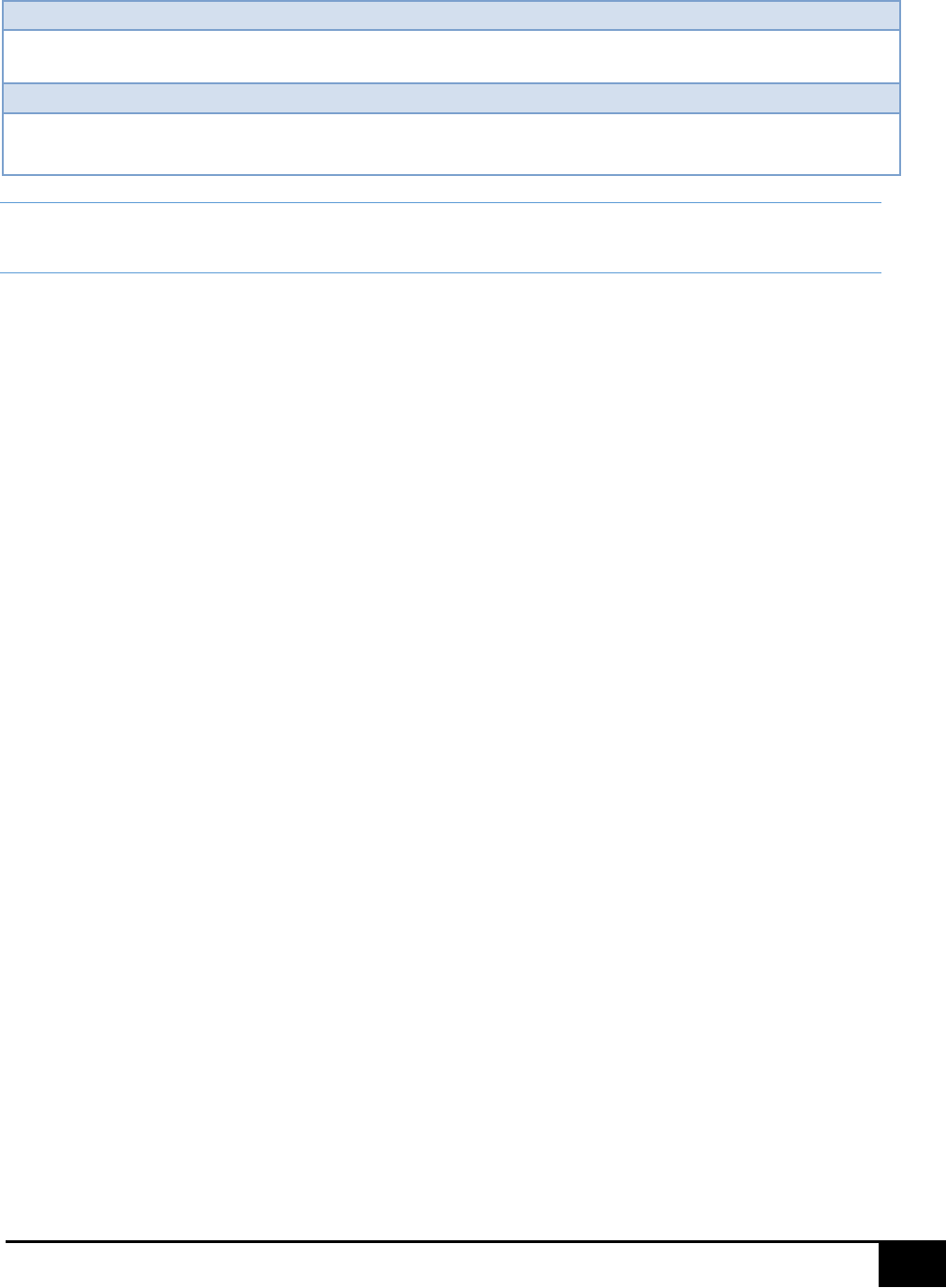
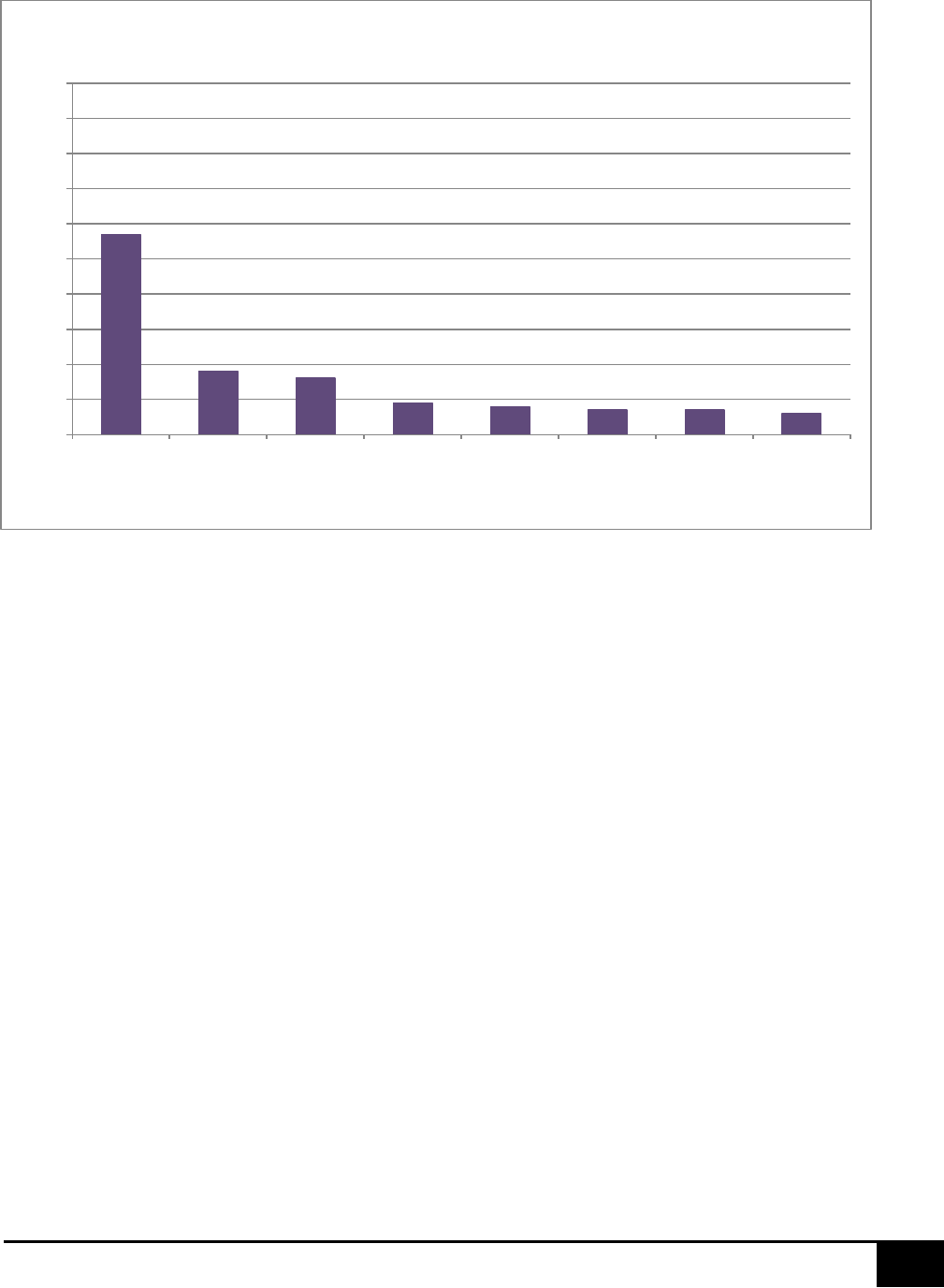
Effects of Caregiving on Employees and Employers
Many care contributors for people with AD/ADRD experience disruptions to employment
because of the demands of caregiving. Among people employed at any time since they became
caregivers of someone with AD/ADRD, 9% ultimately quit their jobs to continue providing care,
57% had to go in late to work or leave early, and 16%had to take a leave of absence. Other
work-related challenges for dementia caregivers who had been employed at any time since
they began caregiving are summarized in the chart below.
20
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Source: Alzheimer’s Association, 2019 Alzheimer’s Disease Facts and Figures, Alzheimer’s Dement 2019;15(3):321-87.
In addition to employment disruptions, dementia caregivers face significant financial impact of
caregiving. In 2018, caregivers reported nearly twice the average out-of-pocket costs (e.g.,
medical, personal care, and household expenses for the person with dementia; personal
expenses and respite services for the caregiver) of non-dementia caregivers ($11,233 versus
$6,075). Survey data from 2016 indicates 48% of caregivers cut back on spending and 43% cut
back on saving due to the out-of-pocket costs of providing help to someone with dementia.
Costs to Illinois Citizens
High out-of-pocket costs are a reality for individuals with AD/ADRD and their caregivers despite
other sources of financial assistance. In 2011, Medicare beneficiaries age 65 and older with
Alzheimer’s disease paid $10,798 out-of-pocket on average for health care and long-term care
services not covered by other sources.
Average out-of-pocket payments were $3,548 per
person for community-dwelling individuals. For individuals living in nursing homes and other
residential facilities, per-person out-of-pocket expenses were almost six times higher –
averaging $20,207.
57%
18%
16%
9%
8%
7% 7%
6%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Went in late,
left early or
took time off
Went from full-
to part-time
or cut back
hours
Took a leave
of absence
Gave up
working
entirely
Turned down
a promotion
Received a
warning about
performance/
attendance
Lost any
benefits
Retired early
Work-Related Changes Among Caregivers of People
with Alzhiemer's Disease or Other Dementias
21
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Services to Address the Needs of Persons with Alzheimer’s Disease and
related dementias, Their Families, and Caregivers
Illinois’ Alzheimer’s Disease Network
Regional Alzheimer’s Disease Assistance Centers
A regional Alzheimer's disease assistance center (ADAC) is considered the top tier of dementia
care providing diagnostic evaluation, treatment, referral, and research. An ADAC must be a
postsecondary higher educational institution having a medical school affiliated with a medical
center and having a NIH and NIA sponsored Alzheimer's Disease Core Center. Any regional
ADAC that previously was designated as having a National Alzheimer's Disease Core Center but
no longer carries such designation can continue to serve as a regional ADAC. ADACs are staffed
by a network of physicians, medical specialists, social workers, nurses, educational specialists,
and research scientists with expertise in dementia care and research. ADACs provide
comprehensive diagnosis and treatment facilities and services; consultation and referral service
for individuals with AD/ADRD and their families; research programs and facilities; training,
consultation, and continuing education for caregivers; centralized data collection, processing,
and storage; and AD/ADRD scientific and medical research programs.
In 2012, funding levels for states with senior populations similar to Illinois to support their
ADAC programs were much larger than that of Illinois with Florida at $16.6 million, California at
$5.9 million, and Arizona at $4 million. In fiscal 2003, Illinois provided $3.3 million in state
funds. In fiscal 2004 this annual amount was reduced to $1.7 million when the funding
mechanism was changed to include a federal match, while in fiscal 2013 and 2014, funds were
cut by an additional 1.75%. If the original $3.3 million per year had been left intact and matched
with federal dollars, Illinois would be on par with other states.
The regional ADACs, funded by HFS, in Illinois are:
• Northwestern Alzheimer’s Disease Assistance Center (NADAC) for Northern Illinois,
Northwestern University Feinberg School of Medicine, Chicago
NADAC serves the Chicago metropolitan area, Cook County and eight collar counties. The
Neurobehavior and Memory Clinic, an essential component of NADAC, attracts patients
throughout Illinois, the Midwest region, nationally, and internationally.
NADAC has an affiliated faculty of approximately 50 clinicians and basic scientists from 13
departments at Northwestern University who engage in research and clinical practice
related to brain aging, cognitive function, and dementia. The mission of NADAC is to
investigate the causes and clinical characteristics of neurodegenerative diseases, to ensure
patients and families are the beneficiaries of the latest advances, and to explore the neural
foundations of behavior and cognition in health and disease. Areas of clinical emphasis

22
2020 – 2023 Alzheimer’s Disease Illinois State Plan
include Alzheimer’s disease, primary progressive aphasia, frontotemporal degeneration,
and mild cognitive impairment.
The Northwestern Neurobehavior and Memory Clinic environment is multidisciplinary and
includes behavioral neurologists, neuropsychologists, neuropsychiatrists, social workers,
and a geriatric physician. In fiscal 2019, there were 505 new and 383 unique return
patients seen in the Neurobehavior and Memory Clinic for a total of 888 unique patient
visits. The clinic provides state-of-the-art diagnostic and treatment services and ongoing
care for patients and families. The clinic treats the whole patient and offers education,
counseling, and support services for both patients and their families. Since patients are
seen multiple times as needed over the course of the year by different multidisciplinary
providers, the total number of patient visits to the Neurobehavior and Memory Clinic was
1,643.
NADAC provides dementia education to clinicians, research scientists, persons living with
dementia, family caregivers, and the general community through a variety of modalities.
Bi-monthly Alzheimer’s disease seminars reach more than 600 clinicians, scientists, and
students per year. The annual Alzheimer Day consistently reaches more than 400 people.
While NADAC searches for new and better treatments for dementia disorders, a primary
aim is to provide persons living with dementia and their families opportunities for
education, support, and social engagement. These are primarily offered through the Miller
Family Alzheimer Support Services and include support and education programs for newly
diagnosed patients and families, a mentorship program for persons with dementia paired
with first-year medical students, in addition to several creative arts-based interventions,
including improvisational theatre, music, and art.
Over the past year NADAC contributed to the advancement of scientific research and
published 46 peer reviewed papers, four book chapters/invited papers, delivered 11
extramural presentations, and obtained seven new grants. An annual newsletter is
distributed to more than 8,500 persons living with dementia, family caregivers, clinicians,
scientists, and other professionals, in addition to the general community. NADAC
maintains a website (www.brain.northwestern.edu) directed to professionals as well as the
public. The site contains pages for caregivers, health care providers, investigators, and
patients.
NADAC is focused on raising awareness on Alzheimer’s disease and related dementias
through brochures, newsletters, the Northwestern Center website, community lectures,
and town hall meetings. NADAC community engagement includes partnering with African-
American community leaders to promote access to education and awareness, to family
support services, and to research opportunities. NADAC is a leader within the Illinois
Cognitive Resources Network, in collaboration with all Illinois ADACs; Alzheimer’s
Association; and aging, disability and public health networks with a focus on the
development of dementia friendly Illinois communities.

23
2020 – 2023 Alzheimer’s Disease Illinois State Plan
• Rush Alzheimer’s Disease Assistance Center (RADAC) for Northern Illinois, Rush University
Medical Center, Chicago
The overall goal of RADAC is to provide an infrastructure to support high-quality clinical
care, community-wide education, and research into the causes, prevention, and treatment
of Alzheimer’s disease. These activities foster the independence and wellbeing of Illinois
citizens and reduce disability and other common chronic age–related conditions. The
RADAC has four cores carefully designed to provide this infrastructure: 1) administrative,
2) clinical and patient-oriented research, 3) population research and laboratory studies,
and 4) education.
In fiscal 2019, the RADAC conducted 2,294 clinical evaluations, including new and return
patients at the RADAC clinic and evaluations as part of an ongoing study funded by sources
other than State funds; produced more than 100 manuscript publications; 1,381 telephone
contacts were made with Data Repository participants to request study participation,
schedule study visits, collect study data, and provide study information; more than 23,000
persons participated in 501 educational activities, including community leadership
networking, community engagement, community research presentations, community
giving, and media presentations, including 58% White, 39% African American, 27%
Latinx/Hispanic, and 3% other.
• Southern Illinois University (SIU), School of Medicine, Center for Alzheimer's Disease and
Related Disorders (CADRD), Springfield
CADRD is a state-supported center with seven aims:
• Provide diagnostic services, treatment, and case management to patients and
families throughout Illinois, excluding the Chicago area (special attention is directed
to rural areas).
• Provide training, consultation, and continuing education to the public, students,
residents, practicing physicians, and other health care professionals.
• Maintain a centralized patient database for monitoring patients and controls
evaluated at CADRD and the primary provider sites (PPS). See the paragraph below
for further explanation and recommendations relevant to PPS.
• Support clinical and basic research in the fields of dementia and associated
locomotor disorders of older people, through the provision of research support staff,
carefully diagnosed patients, and non-patient controls.
• Provide legislators, the public, and news media information pertaining to the latest
developments and services in the field of aging.
• Enhance the recruitment of neurologically healthy older people and persons with
very early dementia for participation in aging research, including the brain bank
program.
• Enlist the participation of PPSs into one or more areas of research.

24
2020 – 2023 Alzheimer’s Disease Illinois State Plan
In fiscal 2017-2018, CADRD completed 1,265 initial and 5,658 follow-up assessments of
individuals with cognitive problems. CADRD provided 365 educational and training sessions in
21 different communities with 11,085 attendees. Ninety-four publications were produced.
The PPS system organized by SIU consists of 32 sites located in 27 different counties to serve
the primarily rural portion of Illinois and is addressed in this plan.
ADA Center Primary Provider Sites (PPS)
PPS are community-based medical programs that work directly with ADAC staff who have the
expertise to diagnose, to treat, and to make referrals for patients with dementia symptoms,
and to provide supportive services to their families. The concept of PPSs evolved because of
the need for accessible diagnostic and treatment centers throughout the state, in addition to
the three regional ADACs. Rush and Northwestern serve the Chicago metropolitan area that
includes Cook, DuPage, Grundy, Kane, Kankakee, Lake, McHenry, Kendall, and Will counties.
The SIU Center for Alzheimer’s Disease and Related Disorders serves the remaining 93 counties.
In populous areas, PPSs may include dementia specialists, social workers, psychologists, nurse
practitioners, and educational specialists. In rural areas, a minimal staff of a nurse, a social
worker, and a supervising physician may comprise the PPS.
The 32 PPSs follow SIU assessment guidelines and coordinators attend training biannually in
Springfield. As each community has different needs, some examples of additional services
offered by PPS are transportation, respite care, support groups; and Tai Chi, exercise, art
appreciation, and other non-pharmacological interventions for those with dementia. In fiscal
2017-2018, these sites completed 768 initial and 1,094 follow-up assessments of individuals
with cognitive problems and provided 344 education programs in 44 different communities
with 8,801 people in attendance.
State Supported Alzheimer’s Disease Research
State law requires the Illinois Alzheimer’s Disease State Plan to address the “level of state
support of Alzheimer's research through Illinois universities or other institutions and the results
of such investments reflected both in research outcomes and subsequent federal investment in
research.” However, it is difficult to provide specific, quantifiable data.
The most direct state source of research dollars is provided through the Alzheimer’s Disease
Research Act (410 ILCS 410). The act gave IDPH the responsibility of establishing a program that
awarded grants to encourage research on Alzheimer’s disease. The state income tax check-off
donation is the source of this funding. IDPH has promulgated rules to establish criteria for the
determination of awards and distribution of grants. Under the Alzheimer’s Disease Research
Act, additional donations to this fund received by the State of Illinois also can be used for grant
awards.

25
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Illinois Alzheimer’s Disease Advisory Committee
The Alzheimer's Disease Advisory Committee (ADAC) was established through the Alzheimer’s
Disease Assistance Act and consists of 17 voting members and five non-voting members
appointed by the IDPH director. The directors of the following state agencies, or their
designees, serve as nonvoting members: Department on Aging, Department of Healthcare and
Family Services, Department of Public Health, Department of Human Services, and
Guardianship and Advocacy Commission.
Appointed members include persons experienced in research and the delivery of services to
individuals with Alzheimer's disease or a related disorder and their families. Per the act, the
membership structure shall include:
(1) one individual from a statewide association dedicated to Alzheimer's care, support,
and research;
(2) one individual from a non-governmental statewide organization that advocates for
seniors;
(3) the dementia coordinator of the Illinois Department of Public Health, or the dementia
coordinator's designee;
(4) one individual representing the Community Care Program's Home and Community
Services Division;
(5) one individual representing the Adult Protective Services Unit;
(6) three individuals from Alzheimer's Disease Assistance Centers;
(7) one individual from a statewide association representing an adult day service
organization;
(8) one individual from a statewide association representing home care providers;
(9) one individual from a statewide trade organization representing the interests of
physicians licensed to practice medicine in all of its branches in Illinois;
(10) one individual representing long-term care facilities licensed under the Nursing Home
Care Act, an assisted living establishment licensed under the Assisted Living and
Shared Housing Act, or supportive living facilities;
(11) one individual from a statewide association representing the interests of social
workers;
(12) one individual representing Area Agencies on Aging;
(13) the Medicaid director of the Department of Healthcare and Family Services, or the
Medicaid director's designee;
(14) one individual from a statewide association representing health education and
promotion and public health advocacy; and
(15) one individual with medical or academic experience with early onset Alzheimer's
disease or related disorders.
The ADAC reviews programs and services provided by state agencies directed toward persons
with AD/ADRD, and, by consensus, recommends changes to improve the state's response.
ADAC’s recommendations are reflected throughout this state plan.

26
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Illinois State Agencies Programs and Support
Illinois Department of Public Health
IDPH is responsible for implementing activities of the Alzheimer’s Disease Assistance Act (410
ILCS 405) and the Alzheimer’s Disease Research Act (410 ILCS 407).
Illinois Department on Aging
An important factor in Illinois’ response to Alzheimer’s disease has been the efforts of the IDoA
to develop an infrastructure to aid persons with dementia and their caregivers.
The Senior Help Line connects caregivers and professionals to information and to services,
including community-based services, caregiver resources, and information about how to access
important services.
Adult Protective Services addresses questions of alleged abuse in domestic (non-institutional)
settings, including physical abuse, sexual abuse, emotional abuse, confinement, passive neglect,
willful deprivation, and financial exploitation. Changes to the Adult Protective Services Act in
2013 ensure adults with Alzheimer’s disease are included in the protections afforded by this
law.
The Long-Term Care Ombudsman Program protects and promotes the rights and quality of life
for people who reside in long-term care facilities (nursing homes). This program advocates for
residents by informing residents and their families of their rights; resolving complaints;
providing information on residents needs/concerns to their families, program staff, and their
community; and advocating for improved standards of care.
The Senior Health Insurance Program is a free counseling service that answers questions
regarding Medicare, Medicare supplemental insurance, Medicare advantage plans, prescription
drug coverage through Medicare and other resources, prescription costs from Social Security,
long-term care insurance, Medicare claims and appeals, and Medicare beneficiary rights and
guarantees.
Area Agencies on Aging (AAA) serve as a gatekeeper for federal funds from Title III of the Older
Americans Act. These programs are distributed throughout Illinois in 13 planning and service
areas (PSAs). Each AAA is responsible for planning, coordinating, and advocating for the
development of a comprehensive and coordinated system of services for the elderly and
caregivers within the boundaries of each PSA. These services include legal services, congregate
meals, home modification, home-delivered meals, options counseling, family caregiver services,
senior health assistance, and supportive services. This local expertise is important due to the
considerable heterogeneity in services available in the various regions.
Care Coordination Units (CCUs) function as gatekeepers to the state long-term care system by
coordinating and integrating community-based long-term care services available throughout
the entire aging network for and on behalf of frail and vulnerable older persons. Care

27
2020 – 2023 Alzheimer’s Disease Illinois State Plan
coordinators employed by CCUs assess older individuals’ needs, determine eligibility for
specified services, develop care plans with the consent of the older person and/or their family,
coordinate service delivery, and generally manage service needs on a regular basis. The CCUs
are supported through a combination of State general revenue funds and Title III federal funds.
Illinois Guardianship and Advocacy Commission
The Illinois Guardianship and Advocacy Commission safeguards the rights of persons with
disabilities through the work of three distinct programs: the Office of State Guardian (OSG), the
Legal Advocacy Service, and the Human Rights Authority. The commission is governed by a
board of 11 commissioners who are appointed by the governor and confirmed by the Senate.
The OSG serves as guardian for adults with disabilities as appointed by courts and when there is
no one else available to serves as guardian. The Legal Advocacy Service provides legal advice
and representation for both children and adults with disabilities most often providing
representation for individuals facing involuntary mental health admission or treatment. The
Human Rights Authority investigates allegations of disability rights violations committed against
persons with disabilities by disability service providers.
The commission works with individuals with Alzheimer’s Disease and Related Disorders through
its OSG when the OSG is court-appointed to serve as guardian of last resort, when individuals
have encounters with the mental health service system and may need legal advice or
representation from the commission’s Legal Advocacy Service, or when individuals experience
rights violations by a service provider, such as a nursing home, hospital, or home health agency,
that may warrant an investigation by the Human Rights Authority.
The commission maintains an intake unit that provides referrals to commission services as well
as information about adult guardianship, advanced directives, and advocacy resources for
persons with disabilities. The commission is also mandated to provide guardianship training for
newly appointed guardians; the on-line guardianship training along with other commission and
resource information is available through the commission’s website (http://gac.state.il.us). The
commission’s toll-free intake number is (866) 274-8023 (TTY: ([866] 333-3362)
Dementia Care Services
Access to, and coordination of, dementia care resources are critical to ensure people with
Alzheimer’s disease can experience the highest quality of life possible, to support caregivers,
and to control health care costs. Often those just diagnosed are not presented with
information of available care options. Those with a diagnosis under the age of 65 experience an
especially acute need for resources. People with dementia who receive care from a multitude
of providers often suffer from the lack of coordination between providers, or the lack of
dementia knowledge in the people treating them. This lack of knowledge leads to unnecessary
emergency department visits, and overuse of antipsychotic and other sedative medications.
28
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Dementia-Specific Training Requirements
In Illinois, there are specific dementia training requirements for skilled nursing facilities (SNFs)
and assisted living facilities (ALFs) with dementia care programs (77 IL Adm. Code 300.7000-
7080 and 77 IL Adm. Code 295.4060). There are also training requirements listed for supportive
living programs (SLPs) with dementia care pilots (89 IL Adm. Code 146.600-710).
In Illinois, certified nursing assistants (CNA) receive 120 hours of initial instruction. Of those 120
hours, 12 hours at minimum are required to be dementia-specific (IL Adm. Code, 77, 395.300, r
- z). The statute includes a thorough list of topics to be covered as part of the training. CNAs
working in special care units (SCU) are required to have an additional 12 hours of dementia
specific continuing education training each year (IL Adm. Code, 77, 300.7050 (e), 1 - 10).
In Illinois, Senate Bill 2301, enacted August 15, 2016, created the Alzheimer's Disease and
Related Dementias Services Act requiring Alzheimer's disease and related dementias services
programs to provide materials defining the philosophy of the program, specific services offered,
and behavior management tactics employed at admission, enrollment, or earlier upon request.
The act specifies training requirements for staff with direct access to clients with Alzheimer's
disease or a related dementia and requires employers to maintain records of such training and
the curriculum used. IDPH must provide information about AD/ADRD training on its website
and must promulgate rules to implement the act.
It is recommended that the State should ensure adequate funding and other incentives to
guarantee dementia care training is available for, and accessible to, family/friends of those with
dementia and other unpaid caregivers; staff of State agencies; the health care workforce
providing caregiver respite and support services; in-home and community-based services; and
staff in licensed residential care settings.
Quality Care Measures
Illinois has an Alzheimer's Disease and Related Dementias Special Care Disclosure Act that
requires licensed residential care settings that provide specialized care to individuals with
dementia to disclose information about their program to the state agency responsible for
licensing of that setting, as outlined in the act.
In addition, SCU regulations exist for skilled nursing and intermediate care facilities (77 IL Adm.
Code 300.7000-7080; “Subpart U”). There are basic dementia provisions in the regulations for
ALFs (77 IL Adm. Code 295.4060). For SLPs, there are basic special regulations that apply to the
dementia care pilot that HFS is implementing (89 IL Adm. Code 146.600-710).
Skilled Nursing Facilities
These facilities provide skilled nursing care, continuous observations, restorative services, and
other services with frequent medical supervision. Skilled nursing and rehabilitation staff
manage, observe, and evaluate care. These facilities also provide for residents who need care
and treatment required in the post-acute phase of illness or during reoccurrences of symptoms
29
2020 – 2023 Alzheimer’s Disease Illinois State Plan
in long-term illness. Medicare certifies these facilities to ensure they have the staff and
equipment to give skilled nursing care, rehabilitation services, and other related health services.
These facilities are Medicare, Medicaid, and private pay.
Assisted Living Facilities
The IDPH Division of Assisted Living oversees 504 licensed establishments regulated under the
Assisted Living and Shared Housing Establishment Code (77 Illinois Administrative Code
295). This division is responsible for conducting and processing annual and complaint survey
investigations, incident report investigations, and follow-up surveys, when applicable. This is a
state licensure program with no federal oversight as the residents in both assisted living and
memory care areas are private pay through an establishment contract. Renewal applications
and licensure fees are required yearly.
Supportive Living Programs
Illinois developed the Supportive Living Program as an alternative to nursing home care for low-
income older people and people with physical disabilities ages 22-64.
By combining personal care and other services, residents can live independently and take part
in decision-making. Personal choice, dignity, privacy, and individuality are emphasized.
HFS has obtained a "waiver" to allow payment for services not routinely covered by Medicaid.
These include personal care, homemaking, laundry, medication supervision, social activities,
recreation, and 24-hour staff to meet residents' scheduled and unscheduled needs. The
resident is responsible for paying the cost of room and board to the SLP provider.
Currently, there are 152 certified SLP providers with 12,777 apartments. Another 11 projects
with 1,130 apartments are in various stages of development. There are five dementia sites with
119 apartments.
Geriatric-Psychiatric Services
Due to the sometimes-challenging behaviors associated with Alzheimer’s disease and other
dementias, individuals or program staff caring for someone with memory loss may seek
assistance through psychiatric hospitalization. Admission to in-patient psychiatric units should
be limited to extreme cases and implemented only after all behavioral interventions are
explored. With optimal management methods, many individuals can be effectively treated and
stabilized through medication management and observation within the safe and secure
environment of the facility in which they reside.
For psychiatric hospitalization to occur, an individual must meet basic mental health code
criteria of being deemed harmful to him or herself or others. Common behaviors that may be
associated with Alzheimer’s disease and related dementias can include delusions,
hallucinations, paranoia, agitation or aggression, depression, anxiety, sexual inappropriateness,
and self-harming behaviors.

30
2020 – 2023 Alzheimer’s Disease Illinois State Plan
The current system for admission to behavioral care relies on the hospital emergency
department as the access point for evaluation and admission to the psychiatric unit for
behavioral treatment. The system is inadequate, inefficient, and inappropriate, because many
emergency departments do not have the expertise, staff, time, and stabilizing environment to
deal with a dementia patient whose behavior may be out of control.
Also, the availability of hospital geriatric-psychiatric beds is low, particularly outside Cook
County, resulting in many individuals spending two- to three-days receiving inadequate or even
counterproductive care in the emergency department waiting for beds to become available.
Furthermore, emergency departments are not able to provide the long-term holistic nursing
support that is an important component of dementia care.
While some psychiatric hospitals have begun to address the challenge of caring for individuals
with memory loss in their facilities by creating geriatric units, what defines such a unit is not
addressed on a state level to ensure consistency.
Staff in the geriatric psychiatric units of hospitals are not currently receiving standardized
training to ensure the best evidence-based care practices are utilized when treating individuals
with cognitive challenges associated with dementia. These care practices differ from those
implemented in the treatment of individuals without the cognitive challenges.
Additionally, after receiving psychiatric treatment and stabilization, facilities are often reluctant
to accept or re-admit individuals with a behavioral history. Such denial creates challenges in
placement of individuals with Alzheimer’s disease or other dementia into appropriate care
facilities at time of discharge.
The current model is not capable of meeting the current or future needs of people with
AD/ADRD who exhibit advanced behavioral issues. Assuming that the current model could be
improved, it is necessary to design incentives to encourage changes to meet the needs of
persons with AD/ADRD with behavioral issues requiring intervention.
The concerns discussed above highlight the complexity of the issue. It is recommended, over
the three-year period of this strategic plan, to set a priority to review the scope of the problem
and identify solutions to gain a better understanding of the type of care needed to improve the
model. During the writing of this plan, initial discussions were held to begin thinking about an
improved model of care. Preliminary ideas included the following, but it is imperative further
conversations be held to discuss these ideas and identify additional recommendations:
• Provide higher level of hospital reimbursement for patients with AD/ADRD because it
requires a higher level of care than other patients. Though there are standards to address
reimbursement for patients with dementia, the standards are not high enough that facilities
are willing to accept the patient. There would be a cost to implement this approach, so it
would be valuable to implement a model or a Medicaid waiver as a pilot. A pilot may take
the form of additional financial incentives and more training.

31
2020 – 2023 Alzheimer’s Disease Illinois State Plan
• Train all direct care workforce in hospital settings as an avenue to keep costs down. If
emergency department staff were better trained, then patients may not need to go to
psychiatric units. Conversely, if staff in psychiatric units were better trained, patient care
would be better and there would be less chance of them being readmitted to a hospital
emergency system. It is beneficial to raise the level of training in both settings.
• Increase awareness of legal aspects which may inhibit appropriate care being provided.
Identify how family members, caregivers, and providers can support appropriate care while
upholding the dignity and rights (e.g., Mental Health Declaration, Power of Attorney) of
people with AD/ADRD who may not have the insight to know they need assistance.
• Gain a better understanding of the decision-making process long-term care facilities use
to determine when to send a patient to a psychiatric unit. Establish a workgroup to
identify a systematic way to research the scope of the problem, identify the factors facilities
consider when making their decision, and identify what facilities need to provide care in
these situations and what the state regulatory agencies feels is feasible.
• Identify strategies to decrease the number of patients with AD/ADRD who are dropped
off in emergency departments because they present unsafe behavior – some are left just
to sit there - also known as hospital dumping. Identify if other workgroups have reviewed
this practice and determined recommendations. Research what the Centers for Medicare
and Medicaid Services covers. Increase the ability for emergency department staff to
recognize patients with AD/ADRD and assist with facilities to accept them back. Learn what
makes facilities who do not have patients coming into the emergency department different
than those who do.
Home and Community-Based Resources
Home and community-based services for people with AD/ADRD are essential for a number of
reasons:
• These are the services preferred by most persons with AD/ADRD and their families.
• The federal government is encouraging states to focus on home and community-based
care rather than on institutional care; this has been a priority in Illinois.
• In most cases, home and community-based care has been shown to be more
economical than institutional care.
• In Illinois, there are growing numbers of memory café’s intended to provide social
support of individuals with early stage dementia within their local community.
• Adult day care services that allow respite for caregivers during the week.
• Palliative and hospice care programs are becoming more sensitive and skilled at
providing care for individuals in late and final stages of dementia.
To allow a person with Alzheimer’s disease to reside in a home or community-based living
situation for as long as possible, services must be available to:
• enable individuals diagnosed in the early stages to function safely and independently
for as long as possible, and
• support caregivers – functionally, financially, educationally, and emotionally – with the
provision of in-home care.
32
2020 – 2023 Alzheimer’s Disease Illinois State Plan
In order to provide sufficient home and community-based services that achieve these goals, it is
recommended that services be standardized across human services agencies, and better-
coordinated between publicly- and privately-funded entities. Furthermore, the evaluation,
development, and expansion of both established and unique service models (e.g., early stage
adult day services, volunteer respite models) should be encouraged.
• Governor JB Pritzker has proposed $24 million dollars to fund the Community Care
Program in 2020. This program helps direct person-centered care plans to keep
individuals aging in place and to avoid nursing home placement.
IDPH’s role includes:
• Provide communications regarding education requirements for Home Health, Home
Services and Home Nursing agencies regarding requirements to meet the provisions of
Part 973 “Alzheimer’s Disease and Related Dementias Services Code.”
• Through survey visits, monitor progress and implementation of the educational
standards for supervisory, nursing, CN., and home service workers.
• Monitor agencies who advertise and provide contractual services to clients with
Alzheimer’s or dementia-related disease for compliance with part 973 of the
administrative code.
In addition, in 2017, the Community Care Program (CCP) Task Force reviewed data suggesting
that nearly 20% of non-Medicaid CCP participants were eligible for Medicaid but not enrolled in
Medicaid. The source of funding for these participants was 100% State general revenue dollars,
rather than Medicaid funding, which is 50% federal and 50% State dollars. Thus, the State
could achieve significant cost savings if it were able to enroll this group of Medicaid-eligible CCP
participants on Medicaid. One identified barrier to enrollment was the low reimbursement rate
paid to care coordination units (CCUs) to assist with completing the paperwork to enroll on
Medicaid, which is often a lengthy process requiring significant staff time. In 2018, legislation
was enacted to increase the rates paid to providers to complete Medicaid enrollment
paperwork for CCP clients. This legislation also created a sub-committee of the Older Adult
Services Advisory Committee (OASAC) to monitor the progress of the Medicaid enrollment
initiative. An initial group of more than 8,000 CCP clients who appear to be eligible for
Medicaid but are not enrolled are being analyzed by the committee and steps are being taken
to ensure these individuals, if eligible, are enrolled. Additionally, the new reimbursement rate
for providers went into effect July 1, 2019. The success of this Medicaid enrollment initiative
will support the financial sustainability of the CCP program, which provides critical services that
allow people living with Alzheimer's and dementia to remain in their homes while receiving
necessary services.
Residential Options for Persons with Dementia
The need for quality residential care for people with dementia greatly exceeds the current
capacity for such care in Illinois. There are an estimated 210,000 people living with Alzheimer’s
disease in Illinois. However, Illinois only has approximately 1,200 long-term care facilities
serving more than 100,000 residents and few facilities have dementia units.

33
2020 – 2023 Alzheimer’s Disease Illinois State Plan
People living in independent sections of a continuing care facility who later develop dementia
and their family are often reluctant to transfer to higher levels of care because of the stigma
and costs involved.
The need for affordable SLPs appropriate for people with dementia is especially acute and the
availability of even costly ALFs with dementia care does not meet the demand. There are only
55 ALFs with freestanding dementia care buildings and 78 with dementia units.
Evidence suggests people with dementia do best in the least restrictive environment that is
appropriate for them. However, because most people cannot afford or obtain assisted living,
they may be forced to receive care within a skilled nursing facility.
Public Safety and Law Enforcement
In considering public safety and law enforcement as they pertain to individuals living with
Alzheimer’s disease or related dementia, the State considers the safety of the individual and
the safety of the public. People with AD/ADRD comprise a growing portion of the population
and the number of individuals living in the community (versus long-term care facilities) who are
experiencing cognitive decline is also increasing. As a result, the likelihood of public safety
officials who serve the community interacting with persons with cognitive decline or dementia
will continue to grow.
While not required by statute, dementia training for law enforcement officers is now part of
police academy training because of a recommendation by the Silver Search Advisory Committee
and adoption by the training board. Existing officers who have completed the academy are
trained by mobile units throughout the state, so eventually all police officers will be trained
with basic information about Alzheimer’s and dementia.
However, standardized, statewide dementia training is not currently part of the curriculum for
new or existing firefighters, paramedics, or other ambulance personnel. These first responders
and other public safety personnel do not learn best practices for identifying individuals with
dementia, communication techniques, or strategies for diffusing challenging behaviors. Being
knowledgeable about dementia and how it may affect the memory, communication abilities,
and judgment of those with varying degrees of dementia will greatly benefit both the service
provider and the person with dementia. Ignorance of how dementia may impair the functioning
of the person may lead to ineffective or even counterproductive interactions and results.
Evidence-based research has shown that driving ability declines with age and declining
cognitive ability. Not only does the cognitively impaired driver place himself/herself at risk, but
the impaired driver places others at risk as well. Consistent with the recommendations of the
Alzheimer’s Association, an “evaluation by an objective third party” is an avenue to assess
whether a driver is cognitively impaired. The Secretary of State’s Driver Vehicle Services
already includes an objective test of drivers’ abilities by requiring drivers 75 years of age and
older to pass a driving exam when they present for license renewal. Although valuable, this on-
34
2020 – 2023 Alzheimer’s Disease Illinois State Plan
the-road test is only a shallow measure of many critical higher-level cognitive functions., such
as decision-making and situation interpretation. Thus, to improve the assessment of an older
adult, this 2020-2023 State Plan recommends the addition of the standard written exam to the
current driver’s license renewal process for those 75 years of age and older. This would add
another cognitive dimension and increases the likelihood that those who may have Alzheimer’s
disease or another dementia will be recognized. All drivers in Illinois 75 years of age and older
are already tested for behind the wheel, so adding the standard written exam as a routine
requirement is a logical, reasonably low-cost method to screen for drivers who may be
impaired. This will strengthen the State’s ability to ensure its drivers are driving safely.
Additionally, motor vehicle service facility personnel should be trained not to assist any person
completing any part of the renewal process, including vision screening, the written exam, and
the driving exam. To do so may allow an otherwise unqualified person to receive a license.
About 3 million Americans with AD/ADRD go missing each year. If an elderly person is not found
within 24 hours, there is a 50% chance he/she will suffer serious injury or die. Additionally, it is
estimated that 60% of people living with Alzheimer’s or dementia will wander at some point
during the diagnosis. Several years ago, Illinois passed legislation
1
adding “missing endangered
seniors” to the list of individuals who require the Illinois State Police to initiate immediate
action through the statewide Law Enforcement Agencies Data System (LEADS). In 2015, the
General Assembly passed legislation to create Silver Search in Illinois, a coordinated effort to
bring awareness, education, and resources to help find and safely return people with
Alzheimer’s and dementia who go missing. Silver Search focuses on providing proactive
training, and reactive technology to locate quickly and efficiently someone who has Alzheimer’s
or dementia that goes missing.
The Silver Search law, which went into effect in 2016, created an Endangered Missing Person
Advisory to notify the public about a missing and endangered person when they wander. An
Endangered Missing Person Advisory is a voluntary partnership with law enforcement, local
broadcasters, and other partners to notify the public about a missing and endangered person.
The advisory is initiated by the local law enforcement agency. The purpose of the advisory is to
get as many people looking for the missing person as possible. Emails, faxes, radio and
television broadcasts, text messages, and law enforcement bulletins are all means to
disseminate the information about the missing person. Because of the partnership with the
Illinois Department of Transportation and the Illinois Tollway Authority, the dynamic message
signs on the interstates and tollways are now utilized during advisories when a person is
missing while driving in a vehicle. The Illinois Lottery also utilizes digital lottery terminals in
lottery retail outlets to display advisories as another way to spread information about an
endangered person.

35
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Acknowledgements
The Illinois Alzheimer’s Disease State Plan was prepared by the Alzheimer’s Disease Advisory
Committee, partners from public health and aging service organizations, and academic
institutions.
Illinois Alzheimer’s Disease Advisory Committee (appointed and nominated members)
Tom Ala Physician - Southern Illinois University, School of Medicine
(SIU/SOM) Center for Alzheimer's Disease & Related Disorders
Raj Shah Physician - Rush Alzheimer’s Disease Center
Jeff Christiansen Representative of law enforcement - DuPage County Sheriff’s
Office
Jen Belkov Representative from leading advocacy organization serving
persons with Alzheimer’s Disease - Alzheimer's Association, Illinois
Chapter
Evan Davis Representative of a licensed hospital - Memorial Health System
Cindy DeGroot Registered Nurse
Nancy Flowers Representative of hospice with palliative care for dementia -
Rainbow Hospice and Palliative Care
Susan Fonfa Illinois Department of Healthcare and Family Services
Jeannine Forrest Representative of Home Car Agency Serving Persons with
Dementia - Through the Forrest, LLC
Susan Helm Family member/representative
Samuel Hill Person with early stage Alzheimer’s disease
Colette Jordan Representative of Area Agency on Aging - Northeastern Illinois
Area Agency on Aging
Kathleen Knope Person with early stage Alzheimer’s disease
Lori Kerns Representative of skilled nursing facilities serving persons with
dementia - Heritage Enterprises
Shana Lister Representative of a long-term care facility under Assisted Living
and Shared Housing Act - Regency Nursing Care
Jennifer Martin Illinois Department of Public Health, Office of Health Promotion
Carol Mauck General public (over age 65)
M.-Marsel Mesulam Physician - Northwestern University Cognitive Neurology &
Alzheimer’s Disease Center
Mary Milano Illinois Guardianship and Advocacy Commission
Conny Moody Illinois Department of Public Health, Office of Health Promotion
Darby Morhardt General public/ Northwestern University Alzheimer’s Disease
Center
Beth Phelps Family member/representative
Geunyeong Pyo Illinois Department of Human Services

36
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Phyllis Roate Illinois Department on Aging
Melvin Siegel Representative of a long-term care facility - Mavin Enterprises Ltd.
Sarah Smith Illinois Guardianship and Advocacy Commission
Orlinda Speckhart Licensed social worker - SIU/SOM
Robert Thieman General public (over age 65)
Additional Partners:
Debra Bryars Illinois Department of Public Health, Office of Health Care
Regulation
Ross Carey-Walden Illinois Department of Public Health, Office of Health Care
Regulation
Jack Fleeharty Illinois Department of Public Health, Office of Health Care
Regulation
Kara Helton Illinois Department of Healthcare and Family Services
Aimee Isham Illinois Department of Public Health, Office of Health Care
Regulation
Lynda Kovarik Illinois Department of Public Health, Office of Health Care
Regulation
Greg Kyrouac SIU/SOM Center for Alzheimer's Disease & Related Disorders
Michelle Millard Illinois Department of Public Health, Office of Health Care
Regulation
Teresa Parks Illinois Guardianship and Advocacy Commission
Karen Senger Illinois Department of Public Health, Office of Health Care
Regulation
37
2020 – 2023 Alzheimer’s Disease Illinois State Plan
References
1 Alzheimer’s Association, 2019 Alzheimer’s Disease Facts and Figures, Alzheimer’s &
Dementia.
2 Hebert LE, Beckett LA, Scherr PA, Evans DA. Annual Incidence of Alzheimer Disease in the
United States Projected to the Years 2000 through 2050. Alzheimer Disease & Associated
Disorders. 2001;15(4):169-173.
3 The 2015 Illinois Behavioral Risk Factor Surveillance System, Cognitive Impairment Module
Data, Caregiver Module, Illinois Department of Public Health
4 Market Survey of Long-Term Care Costs: The 2012 MetLife Market Survey of Nursing Home,
Assisted Living, Adult Day Services, and Home Care Costs, November 2012,
https://www.metlife.com/mmi/research/2012-market-survey-long-term-care-
costs.html#keyfindings
5 Unpublished tabulations based on data from the Medicare Current Beneficiary Survey for
2011.
6 Hurd Martorell P, Delavande A, Mullen K, Langa K., Monetary Costs of Dementia in the
United States. New England Journal of Medicine. 2013; 368:1326-1334. Available
at: http://www.nejm.org/toc/nejm/368/14/.
7 Maslow K. How many hospital patients have dementia? In Silverstein N and Maslow K,
eds. Improving Hospital Care for People with Dementia. New York, NY: Springer; 2006.
8 Magaziner J, German P, Zimmerman SI, Hebel JR, Burton L, Gruber-Baldini AL, May C, Kittner
S. The prevalence of dementia in a statewide sample of new nursing home admissions aged
65 and older. Gerontology. 2000; 43(4): 514-520.
9 National Alliance for Caregiving and AARP. Caregiving in the U.S. Unpublished data analyzed
under contract for the Alzheimer’s Association; 2009.
10 Gallup Healthways Wellbeing Survey, In U.S., Caregivers Suffer From Poor Physical Health,
February 2011.
11 Gallup Healthways Wellbeing Survey, More Than One in Six American Workers Also Act as
Caregivers, July, 2011.
12 Couglin, J., (2010). Estimating the Impact of Caregiving and Employment on Well-Being:
Outcomes and Insights in Health Management, Vol 2; Issue 1.
13 Gallup Healthways Wellbeing Survey, Caregiving Costs U.S. Economy $25.5 Billion in Lost
Productivity, July, 2011.
14 Metlife Study of Working Caregivers and Employer Health Costs: National Alliance for
Caregiving. 2010.
15 United States Census Bureau, State and County Quickfacts,
http://quickfacts.census.gov/qfd/states/17000.html
16 National Institute of Health. Research Portfolio Online Reporting Tools. Available at
https://projectreporter.nih.gov/reporter.cfm . Accessed July 5, 2019.
17 National Institute of Health. Driving Safety and Alzheimer’s Disease. Available at
https://www.nia.nih.gov/health/driving-safety-and-alzheimers-disease. Accessed July 8,
2019.
38
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Appendix A
2017 – 2020 Recommendations to Address the Needs of Persons with Alzheimer’s
Disease and related dementias, Their Families and Caregivers
LONG-TERM RECOMMENDATIONS
Illinois’ Alzheimer’s Disease Network
• LT 2 - Continue to utilize the strengths of each of the three Alzheimer’s Disease Assistance Centers
(ADAC), including epidemiology studies (Rush), non-AD related dementias (Northwestern), and
rural outreach (SIU) to collaborate with the Illinois Department of Healthcare and Family Services
and other State agencies; seek federal or private matches to leverage State funding for projects
that capitalize on ADAC strengths; and foster partnerships among the Aging and Disability Resource
Network, the Alzheimer's Association and members of the Illinois Cognitive Resource Network.
(Regional Alzheimer’s Disease Assistance Centers)
• LT 3 - Promote sharing of databases with information relevant to ADRD and/or the caregivers of
persons with ADRD to advance research in Illinois. State of Illinois agencies who provide reports to
the Alzheimer’s Disease Advisory Committee should share relevant databases on data.illinois.gov.
(Illinois Department of Public Health). Research databases developed and maintained by the
regional ADACs should enable submission of requests for data, specimens, or potential participants
via web-based platform(s). (Regional Alzheimer’s Disease Assistance Centers)
• LT 5 - Integrate and expand the coordination between ADACs, PPS, and other stakeholders to
support persons living with AD/ADRD and their families by providing access to ongoing education,
community based long-term care services, counseling, and support throughout the course of the
disease. (Regional Alzheimer’s Disease Assistance Centers)
State Supported Alzheimer’s Disease Research
• LT 7 Evaluate strategies to improve partnerships with private entities and identify strategies used
by other states to leverage additional research dollars.
• LT 9 - Promote Illinois as a competitive location for conducting research associated with
Alzheimer’s disease.
Illinois State Agencies
• LT 11 - Include Alzheimer’s disease as a data point in IPLAN and urge inclusion of Alzheimer’s
disease in local health needs assessments, as well as integration of Alzheimer’s disease awareness
and education into local health department’s community health plans. (Illinois Department of
Public Health)
• LT 12 - Promote strategies to help ensure the State and local public health department have
awareness of, and develops expertise in, cognitive health and impairment. (Illinois Department of
Public Health)
• LT 16 - Provide grants to eligible Illinois organizations and institutions to improve service delivery,
to develop evidence-based programs, and to address unmet needs for individuals with Alzheimer’s
and related dementias. (Illinois Department on Aging)
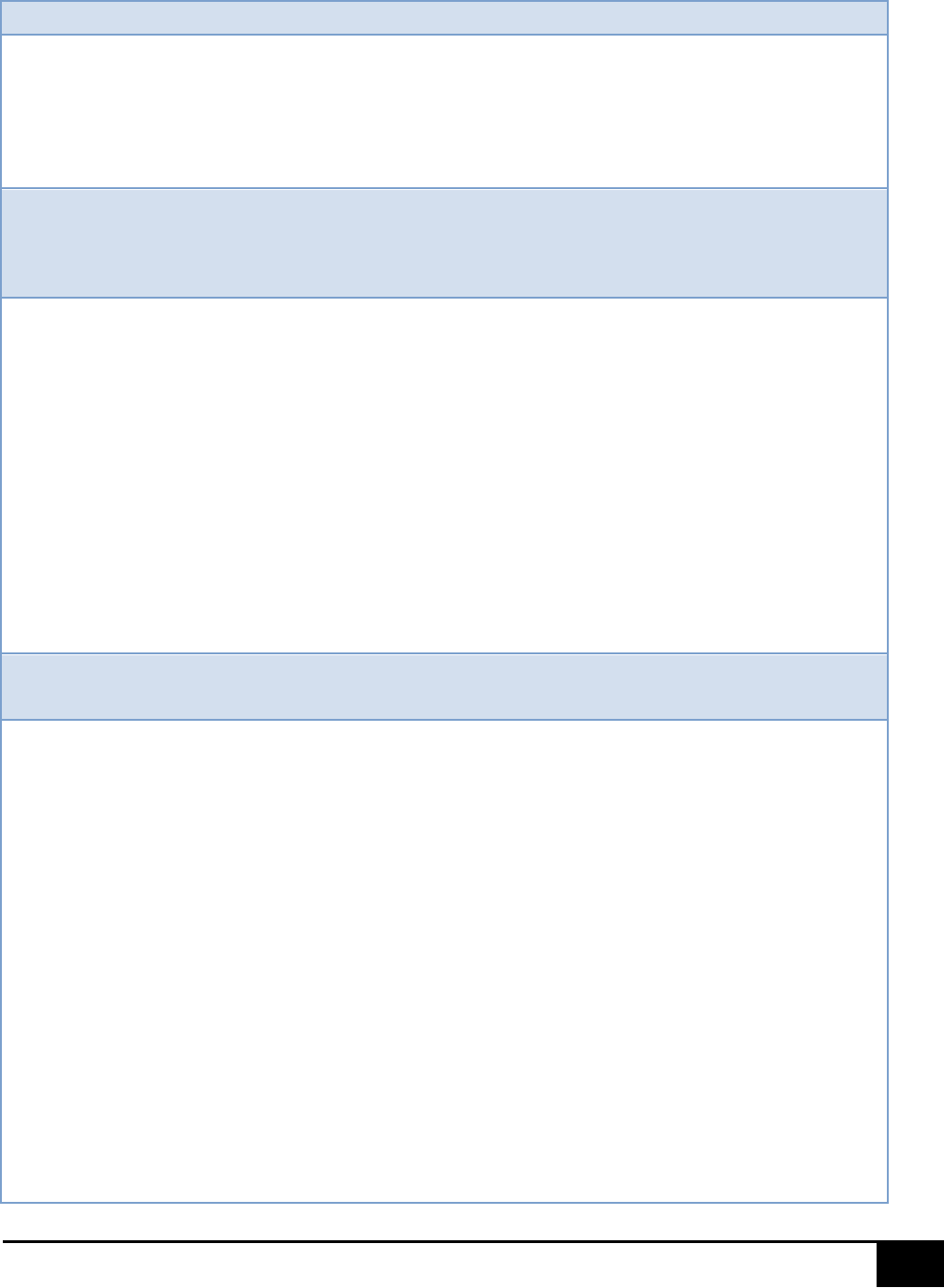
39
2020 – 2023 Alzheimer’s Disease Illinois State Plan
Dementia Care Coordination
• LT 19 - Enhance the ability of Aging and Disability Resource Centers (in partnership with local public
health departments) to reduce social isolation and to promote the efficient assessment, referral
and care coordination for people with dementia and their caregivers through implementation of
Dementia Capable State procedures and through more Illinois communities being recognized as
members of Dementia Friendly America. (Illinois Department on Aging, Illinois Department of
Public Health)
Dementia-Specific Training Requirements -
The following recommendations are intended
to maintain core competency of the profession and to improve access to care and consumer
knowledge of care options, to equalize benefits for people with young onset Alzheimer’s disease,
and to improve care coordination across health settings.
• LT 20 - Require periodic training for those employed in settings in which they are highly likely to
encounter persons with dementia. This includes State agencies and departments (e.g., Illinois
Department of Human Services, Illinois Department on Aging), programs, and subcontractors.
Settings may include but are not limited to emergency department and hospital personnel, senior
centers, primary care physician offices, and first responders.
• LT 22 - In order to assure consistency in training, dementia-specific curricula should be developed,
adapted ,or recommended for various professional caregiving audiences, taking into account the
cultural background and literacy level of the trainee(s), and should include an assessment to
learning and outcomes measures (including how the training impacts the quality of care) should be
identified and tracked. Dementia specific care expectations should be integrated into agencies
policies and procedures and performance reviews. The curricula should be reviewed periodically
to assure it is up to date and reflects current research and practice. Training should be accessible
through a variety of formats, including, but not limited to, classroom, webinars, online, video
conferencing, and audio conferencing.
Accountability and Staffing to Provide Quality Care Measures in Residential
Care Settings/Improve Residential Care
• LT 23 - Convene a panel of experts to review and update the SNF special care unit regulations,
assuring they reflect current best practices and evidence-based research in dementia care.
(Skilled Nursing Facilities)
• LT 26 - Form a task force to examine the possibility of establishing standards for dementia SCUs
specializing in serving those with severe behavioral issues. The task force would consist of experts
in the field of dementia care, particularly experts in frontotemporal dementia (FTD) and other
atypical dementias; experts in medical and non-pharmaceutical behavior management; family
members of those with FTD or other atypical dementias; and care providers who currently have
programs in place and are able to provide care for the most challenging dementia residents. Note:
A subset of individuals with dementia experience severe behavior changes that can be difficult to
care for in traditional long-term care settings. This is especially true for people with atypical
dementias, such as FTD. Families of these individuals are often challenged with finding appropriate
placement, and even then, may find themselves needing to find another placement if their family
member acts out. Staff may not receive adequate training and may not understand how to best
work with these individuals. (Other residential settings)
• LT 27 - Form a task force to examine current services offered across State agencies. This task force
will make recommendations as to how these various agencies may be able to work together to
provide appropriate services for those with younger-onset dementia. Those with younger-onset
dementias (diagnosed prior to age 65) find a lack of appropriate programs and services. Adult day
40
2020 – 2023 Alzheimer’s Disease Illinois State Plan
programs and residential care are generally focused at persons 65 years of age or older. (Other
residential settings)
Geriatric-Psychiatric Services
• LT 28 - Create a standardized definition of a geriatric psychiatric unit, including acceptable and
appropriate admission criteria to be followed by admitting facilities.
Home- and Community-Based Resources -
The following efforts are recommended to
facilitate increased availability and informed utilization of home- and community-based services.
• LT 29 - Increase access to respite services and gap filling for those with Alzheimer’s and other
dementias who are not eligible for Medicare or Medicaid (including those under 65).
• LT 30 - Coordinate efforts between public and social service transportation providers to improve
community mobility, regardless of age, including expansion and reimbursement of transportation
services for people with Alzheimer’s disease. Support should be included for an “arm to arm”
model (driver walks the individual to the door and waits for a caregiver to answer and guide the
individual inside) and implement dementia training for transportation providers.
• LT 31 - Encourage development and implementation strategies for recruitment of volunteer respite
providers through a variety of sources, including nursing and other allied medical science schools’
intern programs, volunteer organizations, AARP, school volunteer placement offices, and religious
groups, and expand resources for caregivers of individuals with dementia.
Residential Options for Persons with Dementia -
To improve quality, quantity, and
access to care, the following should be addressed: disparities in care, consumer education and
empowerment, innovations in care, and the well-being of people with dementia in residential
facilities.
• LT 32 - Within the state’s aging and disability resource centers, inform the public on how to plan for
the financing, insuring, and legal issues associated with meeting long-term care needs. Develop
and promote educational resources for better understanding of long-term care financing options.
Create a network of patient navigators to assist with long-term care planning and placement.
• LT 33 - Test new models and expand evidence-based best practices in alternative care facilities
caring for individuals with dementia. Explore the option of developing a pilot program of small
group homes for those with a diagnosis of dementia. Many states have licensed small group
homes as a care option for individuals with dementia. These settings, which are similar to the
center for independent living model, are small, homelike and community based. Given that most
individuals with dementia require custodial care, this may be a better and more cost-effective
option than large, institutional-based settings.
Public Safety and Law Enforcement
• LT 34 - Ensure financial assistance through the Illinois Department on Aging and the Illinois
Department of Human Services Division of Rehabilitation Services to family caregivers for
programs, such as Medic Alert/Safe Return and Comfort Zone, through the Alzheimer’s Association
or other safety locator programs to help lower the incidences of wandering/missing person reports
for those with dementia. Lower reports of wandering and lost individuals will also result in lower
costs to first responder agencies, as there will be less need for response to missing and endangered
person calls. Emergency home response systems are inappropriate for this population.
• LT 35 – Review and identify evidence-based practices on promoting safe driving among persons
with AD/ADRD. Strategies may range from safety measures for those still driving, screening when
driving becomes unsafe, and finding other transportation options. Resources should include
educational materials on signs that driving has become unsafe; strategies for discussing driving
concerns with the person, family, and physician; driving simulation testing sites; and the process
41
2020 – 2023 Alzheimer’s Disease Illinois State Plan
for canceling driving privileges. Collaborate with the Illinois Secretary of State’s Office to research
the strategy to add the standard written test to the existing renewal process for those 75 years of
age and older.
• LT 36 - Ensure those who practice law in Illinois and serve the elderly are knowledgeable in
recognizing and interacting with persons with Alzheimer’s disease or related dementias. The Illinois
State Bar Association should develop appropriate accreditation and continuing legal education
requirements in this regard.
Printed by Authority of the State of Illinois
P.O.#46196095 100 6/19
