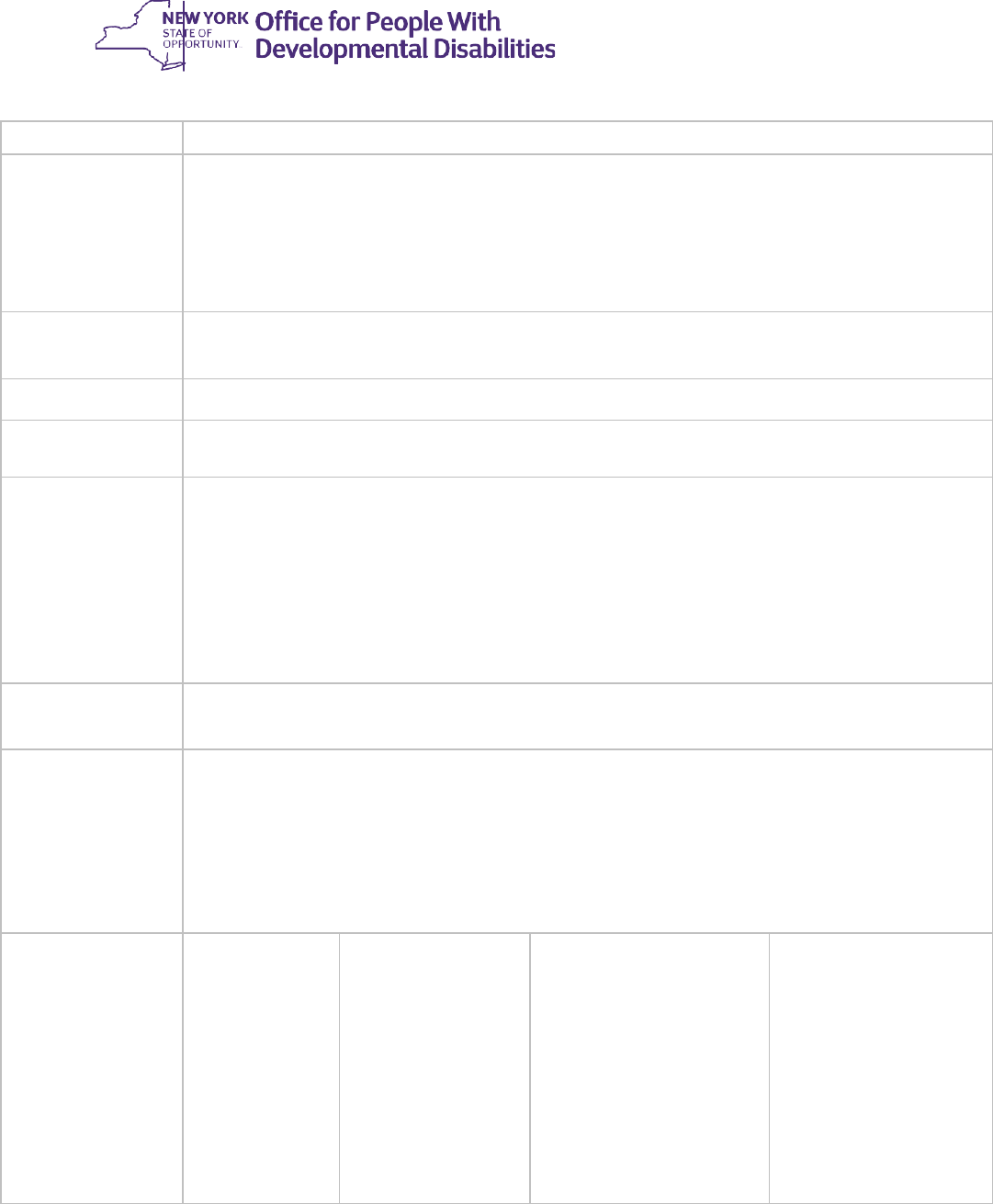
Transmittal:
22-ADM-04
To:
Executive Directors of Voluntary Provider Agencies
Developmental Disabilities Regional Office (DDRO) Directors
Care Coordination Organizations (CCOs)
Issuing
OPWDD Office:
OPWDD Division of Service Delivery-Statewide Services
Date:
May 6, 2022
Subject:
Intensive Behavioral (IB) Services Requirements
Suggested
Distribution:
OPWDD Regional Office Front Door Staff & IB Services Liaisons
Intensive Behavioral (IB) Services Administrative & Clinical Staff
Quality Improvement Staff
Executive Directors of Care Coordination Organizations (CCOs)
Care Managers and Supervisors
FIDA-IDD Care Managers
IB Service Providers
Contact:
opwdd.behavioral.intervention.regulation@opwdd.ny.gov
Attachments:
Attachment A: IB Services Application
Related
ADMs/INFs
Releases
Cancelled
Regulatory
Authority
MHL & Other
Statutory Authority
Records
Retention
ADM #2017-01 ADM #2013-03
14 NYCRR
633.16; 624
MHL §§ 13.07; 13.09;
13.15
18 NYCRR §504.3(a)
18 NYCRR §517.3
14 NYCRR §635-4.5
New York False
Claims Act (State
Finance Law §192)
Page 1 of 14
Page 2 of 14
Purpose:
This Administrative Directive Memorandum (ADM) defines the scope of Intensive Behavioral
(IB) Services, the required credentials of staff members who deliver and/or supervise the
delivery of IB Services, the role of the Service Access, Program Implementation and
Stakeholder Support Regional Field Offices (SPS-RO) in the authorization of IB Services,
additional requirements to become an IB Services Provider agency, and the billing,
documentation and reporting requirements of provider agencies authorized to deliver IB
Services. This ADM supersedes ADM #2013-03, and specifically outlines changes to the
allocation of authorized billable hours and changes to the assessment criteria for inclusion in IB
Services.
Applicability:
This ADM applies to:
• Provider agencies authorized by the Office for People With Developmental Disabilities
(OPWDD) to deliver IB Services;
• Care Coordination Organizations (CCOs) and FIDA-IDD Care Managers
regarding Life Plan documentation and planning; and
• Individuals requesting service authorization of IB services.
Discussion:
1. Background and Scope of Intensive Behavioral (IB) Services
Intensive Behavioral (IB) Services is a Home and Community Based Waiver Service (HCBS)
that provides focused clinical and behavioral treatment and intervention to prevent an
individual’s behaviors from reaching a crisis level. IB Services are not a crisis intervention
service. Intensive Behavioral Services may be provided to individuals who live in non-certified
settings or OPWDD certified Family Care Homes (FCHs)and who present with substantial
challenging behaviors that put them at imminent risk of placement into a more restrictive living
environment. IB Services cannot be provided to individuals residing in certified settings other
than Family Care.
When an individual is authorized to receive IB Services, the service is time-limited and is
capped at 12 months (i.e., 365 calendar days) from enrollment into the service. During this time,
IB Services Providers deliver behavioral supports to authorized individuals. IB Service
Providers will not be reimbursed for IB Services provided beyond the amount of authorized IB
Services per individual.
Intensive Behavioral Services include the completion of a Functional Behavior Assessment
(FBA) and development of an individualized Behavior Support Plan (BSP) for individuals
authorized to receive IB Services. Completion of the FBA and BSP may include the adaptation
or transition of existing FBA or BSPs to a new environment (for example, an FBA or BSP
developed for an inpatient or other treatment setting may be adapted, transitioned, and/or
updated for a home environment). This service also includes training the family/caregiver on
the BSP, evaluating the effectiveness of the BSP, and working with the individual with the goal
of maintaining the individual in a less-restrictive setting.
Page 3 of 14
All interventions designed to manage challenging behaviors must conform with the sections of
person-centered behavioral intervention regulations (14 NYCRR § 633.16), as well as in
conformance with any other applicable laws, regulations and agency specific policies and
procedures.
2. Individual Authorization Requirements and Applications for IB Services
A. Individual Authorization Requirements
SPS-RO designated staff will review individuals on a case-by-case basis to determine their
appropriateness for IB Services. To be authorized for IB Services, an individual must:
(1) Have a complete application submitted for service authorization;
(2) Be determined OPWDD-eligible;
(3) Be enrolled in the HCBS Waiver;
(4) Reside in a non-certified setting (except for an OPWDD-certified Family Care Homes);
(5) Have documentation substantiating that the individual is at imminent risk of being placed
in a more restrictive living environment due to challenging behaviors;
(6) Have a clear need for the type of services provided under the IB Services model, as
clinically determined by OPWDD (e.g., not psychiatric);
(7) Likely be able to benefit from the provision of IB Services; and
(8) Not have received IB services in the last three (3) years.
Additionally, the SPS-RO will review the application and information from the Coordinated
Assessment System (CAS) or Child and Adolescent Needs and Strengths (CANS-NY)
Comprehensive Assessment in making service authorization decisions for IB Services.
B. Applications for IB Services
For authorization of IB Services to be considered, a complete IB Services application (see
Attachment A) must be submitted by the referring entity to the appropriate SPS-RO for review. A
complete application includes:
• The IB Services application form;
• A current Life Plan;
• Additional documentation that supports the individual’s need for IB services;
• Documentation requested by the DDRO; and
• Relevant assessments, including:
o For individuals under 18 years old, a recent summary report of the Child and
Adolescent Needs and Strengths (CANS)-NY, which must reflect the individual’s
current functioning and indicate appropriateness for IB Services; or
o For individuals 18 years and older, a completed Coordinated Assessment
System (CAS).

Page 4 of 14
3. Authorization, Reauthorization, and Discontinuance of IB Services
A. Circumstances Impacting the Authorization or Continuation of IB Services
Authorization for enrollment into IB Services is valid for up to one year from the initial
authorization date. After 365 calendar days, the authorization for IB Services will expire. If an
individual is authorized and enrolled in IB Services within the one-year window, all IB Services
(i.e., the Plan Fee services and Hourly Fee services) must conclude within 365 days from the
date of enrollment. Individuals who do not enroll in IB Services within their one year of
authorization must be re-reviewed to ensure appropriateness for services continue to apply, and
therefore must submit a new application for authorization.
The SPS-RO may initiate a review of an individual’s IB services authorization at any time. If an
individual no longer meets the authorization criteria for IB Services (e.g., they move to a
certified setting), they must be discharged from IB Services immediately.
B. Reauthorization of IB Services
If the implementation of IB Services needs to be extended beyond the initial authorization
service limits that includes the Plan Fee services and Hourly Fee services of 50 hours/200 units,
a referral can be made to the SPS-RO for additional re-authorized IB Services hours. Re-
authorization for the additional IB Service hours is available in limited exceptions for cases
where substantial changes in the individual’s clinical and behavioral presentation have occurred
since the initial authorization for IB Services, and the significant changes are resulting in a need
to complete a new FBA and new or substantially modified BSP within the service period (one
calendar year from initial authorization). An individual must demonstrate clinical and behavioral
changes so significant that the initial FBA and BSP produced under IB Services cannot simply
be updated to reflect current issues. This referral must include a rationale explaining why there’s
a significant need to authorize additional IB service hours. This rationale must explain:
• Why the additional service hours are needed to address the clinical and behavioral
needs of the individual;
• Changes in the individual’s caregiver supports requiring additional training or changes to
the BSP; or
• Any other significant clinical need requiring an authorization of more IB Service hours.
The SPS-RO may re-authorize an individual for up to an additional 25 hours, for a maximum of
75/300 total implementation hours/units in a service period to be used within twelve months
from initial enrollment. The additional 25 hours for reauthorization must be used in completing a
new FBA and developing a new or substantially modified BSP, which is then implemented in
accordance with the Hourly Fee requirements using the remaining hours of the 25 hours
allocated during that reauthorization period.
4. Written Agreement Acknowledging Cooperation Regarding Services
Because IB Services require the cooperation of the IB Services Provider, individual,
family/caregiver or Family Care Provider, and other service providers, it is important that all
Page 5 of 14
parties understand the purpose of IB Services and the commitment that is required of all parties
for the service to be successful. Therefore, the IB Services Provider must develop a Written
Agreement between the IB Services Provider, individual, and/or the parent/caregiver or Family
Care Provider regarding the nature, time-limited duration, and scope of IB Services to be
provided. The agreement must be signed by the provider and individual or parent/caregiver or
Family Care Provider and Family Care Sponsoring Agency. IB Services must not begin until
this Written Agreement is signed by all parties.
5. Requirements of the Functional Behavior Assessment and Behavior Support Plan
The Functional Behavior Assessment (FBA) and Behavior Support Plan (BSP) must be
developed by a Licensed Psychologist, Licensed Clinical Social Worker (LCSW), or a Behavior
Intervention Specialist (BIS) as defined in paragraph 633.16(b). For the purposes of delivering
IB Services, a staff member who is a BIS must always operate under the clinical supervision of
a Licensed Psychologist or an LCSW.
The IB Services clinician must develop the FBA and BSP in consultation with the individual to
the greatest extent appropriate, the individual’s parent(s) and/or caregiver(s), other service
providers or supporting parties, and other clinical experts as needed.
A) Functional Behavior Assessment: The IB Services clinician must develop the FBA in
accordance with the requirements of paragraph 633.16(d)(1) except as otherwise noted
in this ADM.
B) Behavior Support Plan: The IB Services clinician must develop the BSP in
accordance with the requirements of paragraphs 633.16(e)(2) and (e)(3) except as
otherwise noted in this ADM.
C) BSPs to be Used in Multiple Service Settings: When a BSP is being utilized in more than
one service setting, the IB Services Provider must consult and coordinate with these
other service settings in order to develop an appropriately integrated plan and prevent
conflicting or inappropriate strategies. Intensive Behavioral Services Providers must
ensure the plan can be implemented by caregivers and support staff across settings,
without IB Services Provider support, in anticipation of the conclusion of IB Services as
a time-limited service.
D) Schedule of Review: For IB Services, the BSP must be reviewed every 60 days or more
frequently as needed. This review schedule must start at the BSP’s implementation and
continue until the last day of the approved service delivery or hourly fee limits have been
reached, whichever is sooner.
E) Prohibition of Restrictive Physical Interventions and Exclusionary Time Out: Behavior
Support Plans developed through IB Services must not incorporate the use of a
restrictive physical intervention (see 14 NYCRR 633.16(j)(1)), or time-out rooms (also
known as exclusionary time-out; see 14 NYCRR 633.16(j)(3)(iv) for description).
Note, some individuals who receive IB Services may require specific interventions prescribed by
a physician for their treatment or protection due to self-injurious behavior (SIB), aggression,
agitation, hyperactivity, depression, anxiety, and other concerns. These health and safety
interventions may include medication(s) and/or mechanical devices (e.g., helmets, arm
Page 6 of 14
sleeves/splints, Posey mitts). Restrictive interventions may be utilized by the family or caregivers
if they are prescribed by a physician, but these prescribed interventions are not to be
incorporated into the Behavior Support Plan developed under IB Services. In these cases, the
use of such interventions by the individual and their caregiver does not prohibit the individual from
receiving IB Services. However, these IB Services-prohibited interventions can only be used as
directed in a physician’s order and must not be incorporated for use into a Behavior Support Plan
developed under IB Services.
F) Required Plan Monitoring Post Provision of IB Services: Behavior Support Plans
developed through IB Services should be created with an understanding of available
resources, natural supports, and the ability of caregivers and service providers to
implement any behavior techniques and strategies proposed. Behavior Support Plans
should avoid utilizing strategies that cannot be successfully implemented by the
individual’s primary caregivers or cannot continue to be used after IB Services have
concluded.
G) Written Informed Consent: Prior to implementing a BSP, written informed consent must
be obtained as specified in subdivision 633.16(g). The requirement for written informed
consent is not limited to plans containing restrictive/intrusive interventions. The consent-
giver must have the right to revoke approval of the BSP at any time, and request that a
revised BSP be developed in accordance with the requirements of this ADM and within
the limitations of available hours and/or one-year limited time span per authorization
period, whichever is sooner.
H) Review of Restrictive Interventions, Intrusive Interventions, and Rights Limitations: A
schedule to review and analyze the frequency, duration and/or intensity of use of the
restrictive/intrusive intervention(s) and/or limitation on an individual’s rights if included in
the Behavior Support Plan is required. The results of this review must be documented
and used to determine if and when revisions to the BSP are needed. For the purposes of
IB Services, the schedule of reviews conducted by the IB Services Provider must be no
less frequently than every 60 days
6. Trainings Related to the Individual’s BSP
Parents/caregivers, Community Habilitation staff, and Family Care Providers responsible for
the support and supervision of an individual who has a BSP must be trained by the IB Services
provider in the implementation of the individual’s plan to ensure interventions are utilized and
implemented as intended and as written. IB Services Providers may only teach
parents/caregivers, Community Habilitation staff, and Family Care Providers the specific
protective interventions identified in the BSP created for the individual for whom they provide
care. Respite staff may only be trained, as clinically necessary, in those positive behavioral
approaches, strategies and supports detailed in an individual’s BSP that are expected to
improve the respite staff’s ability to support that individual during delivery of respite services.
Depending on the needs of the individual or setting, Intensive Respite for High Behavioral
Needs staff may receive training consistent with the requirements of the OPWDD-approved
training course on the use of positive behavioral approaches, strategies and/or supports and
physical intervention techniques as described in 633.16(i)(3)(i) and (ii).
Page 7 of 14
IB Service Providers must only educate parents/caregivers on the specific interventions
identified in the BSP created by the IB Services Provider. This training by the IB
Services Provider is not equivalent to the comprehensive OPWDD training curriculum
outlined in 633.16(i) and does not result in certification of any kind.
7. Additional FBA & BSP Practices and Considerations
A. Training Documentation
All training of parties responsible for implementation of the plan, and any retraining when a BSP
is modified, must be documented by the IB Services Provider (see “Documenting Intensive
Behavioral Services, page 9).
B. Examination After Physical and/or Emergency Interventions
Immediately after the use of any physical intervention or emergency intervention by Community
Habilitation staff, respite staff, or the Family Care Provider, the individual must be visually
examined for possible injury, the individual must be asked if they experience pain or discomfort,
and any findings from such examinations must be documented. Community Habilitation staff
and respite staff must report the results of their examination to their supervisor as soon as
reasonably possible and have the parents/caregivers co-sign the documentation completed by
staff indicating their agreement with the results of the examination. The Family Care Provider
must document the results of the examination and report the occurrence to their agency Family
Care Provider liaison as soon as reasonably possible. If an injury is suspected, appropriate
medical care must be provided or arranged for by staff or the Family Care Provider. Any injury
that meets the criteria in 14 NYCRR Section 624.4 (generally that the injury requires treatment
more than first aid) must be reported in accordance with Part 624.
8. Emergency Interventions
Nothing in this ADM shall prevent the use of an emergency intervention by Community
Habilitation staff, Respite staff, or Family Care Providers to prevent an individual, who is
undergoing acute behavioral or emotional disturbance, from seriously injuring themself or
others. Emergency techniques to prevent or minimize injury must only be used for no longer
than the duration of the incident, with the least restrictive intervention being utilized. These
emergency techniques may constitute a reportable incident under 14 NYCRR Part 624 and if
so, are to be reported in accordance with the requirements of that Part.
9. Reimbursable Services
IB Services Providers can bill at either the Plan Fee or Hourly Fee, whichever is appropriate.
The Plan Fee is a one-time fee that covers the initial development of the individual’s FBA and
BSP, whereas the Hourly Fee may only be billed for services provided after the initial FBA and
BSP is developed. Providers cannot receive an hourly fee until the plan fee is billed.
If an individual is receiving services through a clinic, clinic services must be separate and
distinct from the IB Services being delivered.
Page 8 of 14
A. Plan Fee
IB Services Providers may receive a one-time Plan Fee to develop the individual’s
Functional Behavior Assessment (FBA) and the individualized Behavior Support Plan (BSP).
Services related to the development of the FBA and BSP include:
• Reviewing records and evaluations regarding the individual’s challenging
behaviors;
• Conducting relevant assessments and collecting data pertinent to the challenging
behaviors and replacement behaviors;
• Communicating with other professionals or service providers, including review of
written reports, telephone contact, or electronic contact about the individual;
• Communicating with the individual, the family, or others through written reports,
telephone contact, electronic contact or face-to-face encounters; and
• Writing the FBA and BSP.
B. Hourly Fee
(i)
Allowable Services Generally
Following the completion of the services covered by the Plan Fee, an IB Services
Provider may begin providing and billing for implementation services under the
Hourly Fee. IB Services face-to-face services generally cannot be billed when the
individual is receiving another Medicaid-funded service, except in unique
circumstances (see subsection (8)(B)(ii) below). Hourly Fee services include:
• Training of the primary caregiver(s) and/or direct support professionals who
provide services to the individual, on how to use the behavioral supports,
interventions, and strategies that are specified in the BSP;
• Training the individual on using the behavioral supports, interventions and
strategies that are specified in the BSP; and
• Monitoring the implementation of the BSP through activities including:
o Observing the individual, family and/or staff as they utilize the supports,
interventions and strategies that are specified in the BSP, and/or
o Following up with the individual, family and/or staff as to the effectiveness of
the supports, interventions, and strategies (either via face-to-face contact,
telephone calls, or electronic contacts),
• Updating the BSP after monitoring to remove supports, strategies and
interventions that are not effective, to introduce less restrictive interventions (i.e.,
fading), and/or to include new supports, strategies and interventions,
• Transition planning with the individual, family, collaterals, and other agencies to
refer the individual to appropriate services, to maintain continuity of care through
longer-term implementation of behavior strategies specified in the BSP, and
progress related to the plan,

Page 9 of 14
• Completing a new FBA or updating the FBA when it no longer reflects the
individual’s current presentation and/or needs and therefore cannot adequately
inform the formulation of the BSP, and
• Completing a new BSP when a new FBA has been completed due to the initial
BSP no longer reflecting the individual’s current presentation and/or needs.
(ii)
Allowable Services Simultaneous with Other Medicaid Service Billing
For IB Services implementation hours (i.e., Hourly Fee), delivery of face-to-face
services with the individual while the individual is at another/receiving another
Medicaid service cannot be billed for the IB Services Hourly Fee, except in certain
circumstances. These circumstances include when:
• The individual is receiving Family Care or Community Habilitation services and IB
Services are being provided for the purpose of training Family Care and
Community Habilitation staff with the implementation and/or monitoring of the
BSP created under IB Services, and the BSP indicates that the individual will
benefit from the training of these support services staff;
• The individual is receiving respite services and IB Services are being provided for
the purposes of training respite staff, and the BSP created under IB Services
indicates that the individual will benefit from the training of these support services
staff; and
• When Care Managers are conducting face-to-face visits with the individual as
long as the IB Services staff person is present, and the coordination of services
is promoted.
10. Documenting Intensive Behavioral Services
A. Plan Fee Service Documentation
For the Plan Fee, staff must have completed both a Functional Behavior Assessment
(FBA) and a Behavior Support Plan (BSP), both of which should be fully compliant with
the criteria described in this ADM. The following documentation must be maintained to
support payment of the Plan Fee:
(i)
Life Plan Requirements
Individuals must have a Life Plan developed by the Care Coordination Care
Manager (CM) that covers the time period of the payment claim for the Plan Fee
and Hourly Fee. The Care Manager must include the following elements:
(a)
Category of waiver service provided (e.g., Intensive Behavioral Services or IB
Services);
(b)
Identification of the agency delivering the IB Services as the provider of
service;

Page 10 of 14
(c)
Specification of the frequency of IB Services as “Plan/Hourly” as there are
two components to this service, and it is important to list components
accurately;
(d)
Specification of the duration as “time limited”; and
(e)
Effective date for IB Services (the date the individual was enrolled in IB
Services); this date must be on or before the first date of service that the
provider bills for completion of the FBA and BSP.
(ii)
Functional Behavior Assessment Requirements
The IB Services Provider must develop an FBA for every individual they serve.
At minimum, the following elements must also be included in the FBA:
(a)
The individual’s name;
(b)
The individual’s Medicaid Client Identification Number (CIN);
(c)
The category of waiver service provided (e.g., Intensive Behavioral Services or
IB Services);
(d)
Identification of the agency providing IB Services as the provider of the service;
(e)
Date on which the assessment was completed;
(f)
Name, signature, and title of the IB Services clinician completing the FBA, and
the date the FBA was completed (i.e., the date of signature); and
(g)
Co-signature of the licensed supervisor (if applicable) and corresponding date of
signature.
(iii)
Behavior Support Plan Requirements
The IB Services Provider must complete and maintain the individual’s Behavior
Support Plan developed under IB Services. The billing date of service for the Plan Fee
must be the date that the BSP is signed by the Licensed Psychologist or LCSW
responsible for oversight of the BSP. In addition, the BSP must be in effect for the
period of time the IB Services claim is submitted. The following elements must be
included in the BSP:
(a)
The individual’s name;
(b)
The individual’s Medicaid Client Identification Number (CIN);
(c)
The category of waiver service provided (e.g., Intensive Behavioral Services or
IB Services);
(d)
Identification of the agency providing IB Services as the provider of the service;
(e)
Name, signature, and title of the IB Services clinical staff person writing the BSP
and the date the BSP was completed (i.e., the date of signature);
(f)
Co-signature of the licensed supervisor (if applicable) and corresponding date of
signature; and
(g)
Evidence (e.g., documentation) of when the BSP was last reviewed, which must
occur at minimum every 60 days following implementation. If a re-authorization
of IB Services is requested and authorized for an additional 25 hours to be used
with the calendar year, it is required that a review will occur immediately, and
then subsequent reviews will occur again no less frequently than every 60 days.
Page 11 of 14
All reviews must be documented by the provider clinician with the name,
signature, and title of the IB Services clinical staff person who conducted the
review, the date of the review, and a summary of any changes made to the
BSP.
B. Hourly Fee Service Documentation
(iv)
Life Plan Requirements
Individuals must have a Life Plan developed by the Care Coordination Care
Manager (CM) that covers the time period of the payment claim for the Plan Fee
and Hourly Fee. The Care Manager must include the following elements:
(f)
Category of waiver service provided (e.g., Intensive Behavioral Services or IB
Services);
(g)
Identification of the agency delivering the IB Services as the provider of
service;
(h)
Specification of the frequency of IB Services as “Plan/Hourly” as there are
two components to this service, and it is important to list components
accurately;
(i)
Specification of the duration as “time limited”; and
(j)
Effective date for IB Services (the date the individual was enrolled in IB
Services); this date must be on or before the first date of service that the
provider bills for completion of the FBA and BSP.
(v)
Behavior Support Plan
The IB Services Provider must maintain a current, signed version of the individual’s IB
Services- developed BSP to support all hourly-fee services billed.
(vi)
Daily Narrative Notes
For the implementation hours (Hourly Fee), staff must complete a narrative note for each
day of service that the hourly fee is billed. The Daily Narrative Note must include:
(a)
The individual’s name;
(b)
Identification of category of waiver service provided (e.g., Intensive
Behavioral Services or IB Services);
(c)
A daily description of the IB Services provided for the day, allowable services
are described in the “Reimbursable Services” section described above;
services are individualized based on the individual’s BSP, (e.g., the staff
person documents that they “taught the individual to use a relaxation
technique”);
(d)
Documentation of start and stop times for each “session”. As this is an hourly
service, the provider must document the service start time and service stop
time for each continuous period of Intensive Behavioral service provision or
“session”;
Page 12 of 14
(e)
The individual’s response to the service (e.g., the staff person documents that
“the individual was able to use the relaxation technique twice”);
(f)
The date the service was provided;
(g)
The primary service location (e.g., the individual’s residence);
(h)
The name, signature, and title of the IB Services staff person providing the
service;
(i)
The date the service was documented (Note: date the note was written must
be contemporaneous to the date the IB Services was provided;
“contemporaneous” is defined as “at the time the service was delivered or
shortly after”).
11. Provider Requirements
In order to be authorized by OPWDD to deliver IB Services, a provider must demonstrate that
they are authorized to provide HCBS waiver services to individuals with developmental
disabilities and must demonstrate that they employ or have access to the necessary clinical staff
to deliver, and, as necessary, supervise the delivery of IB Services. An agency that does not
have clinical staff that meets the educational, experiential, and/or licensure criteria referenced in
this ADM will not be authorized to become a provider of IB Services.
A. Educational, Licensure and Supervision Requirements
At a minimum, staff delivering IB Services must meet at least one of the following
requirements:
• NYS Licensed Psychologist;
• NYS Licensed Clinical Social Worker (LCSW);
• NYS Licensed Behavior Analyst (LBA);
• Board Certified-Behavior Analyst (BC-BA); or
• Behavior Intervention Specialist (BIS) meeting the criteria in 14 NYCRR
633.16(b)
If the staff delivering IB Services is a BIS or Board Certified-Behavior Analyst (though
not an LBA) they must also be clinically supervised by a NYS licensed psychologist
or an LCSW that meet criteria as outlined in 14 NYCRR 633.16.
With respect to claim submissions to Medicaid, the National Provider Identification (NPI)
of either the NYS licensed psychologist, LBA, or the LCSW is a required claim element
and must be included in both the Attending NPI and Referring/Ordering NPI field whether
the service is provided directly by these licensed staff or by BIS staff under their
supervision.
B. Clinician Enrollment
Federal regulations at 42 CFR 455.410 specify that the state Medicaid agency require all
ordering or referring physicians or other professionals providing services under the State
plan or under a waiver of the plan be enrolled as participating providers. As a result,
Licensed Psychologists and LCSWs either providing or supervising provision of IB
Services must enroll. Licensed Behavior Analysts providing IB Services must enroll.
Additionally, New York State Medicaid requires that LCSWs first enroll in Medicare

Page 13 of 14
before Medicaid enrollment is allowable.
C. Oversight and Supervision
Provider agencies must have an adequate plan of oversight and supervision for delivery
of IB Services. The oversight and supervision plan must effectively demonstrate the
systems and controls in place that address the following:
• The number of supervisees assigned to each clinical supervisor (Licensed
Psychologist and/or LCSW); the type of supervision to be provided (in-person
individual or group);
• The required frequency of supervision;
• The provision of a contingent emergency supervisor if the assigned supervisor is
not immediately available (the emergency supervisor must still meet the
qualifications of a regular supervisor);
• Requirements for the supervisor’s record or log of supervision including:
o Name and title of the supervisee;
o Date, length and location of supervision;
o Type of supervision; and
o Signature and title of the supervisor in supervision notes;
• The nature of supervision (e.g., review of treatment/interventions, observations,
in-service training); and
• A method for evaluating the effectiveness of supervision.
12. Payment Standards
A. Billing Units
Once an individual is authorized and enrolled, the IB Services Provider will be reimbursed a
one-time Plan Fee at the completion of the Functional Behavior Assessment (FBA) and
Behavior Support Plan (BSP). Thereafter, time spent implementing the BSP, as described in
this ADM, will be reimbursed with an hourly regional fee (i.e., Hourly Fee), which is billed in
quarter hour units.
The Hourly Fee is billed in quarter hour countable service units. For each 15 minutes of service,
the agency may bill one quarter-hour unit. There is no “rounding-up,” i.e., a full 15 minutes of
service must be provided to bill one unit. An agency may only be paid a maximum of 8 hours a
day per individual for the Hourly Fee. This is an intensive service and all implementation hours
(Hourly Fee), including the re-authorization of an additional 25 hours/100 units when it occurs,
must be utilized within one calendar year from date of enrollment.
B. Caps on Implementation Service Billing Hours (Hourly Fees)
Per initial authorization, providers may only be reimbursed up to 50 hours for implementation
services provided over the course of 12 months. Implementation hours (i.e., Hourly Fee) may
only be billed after the FBA and BSP have been completed, and the Plan Fee has been billed
and paid by Medicaid.

Page 14 of 14
For individuals who have been re-authorized for IB Services, the IB Service Provider may
only be reimbursed up to 25 hours for implementation services.
C. When Allowable IB Services Can Be Billed
For each continuous period of service delivery (or “session”), the provider must document the
delivery of at least one service described in the “Reimbursable Services” section of this ADM for
each continuous period of IB Services provision. Countable service time is the time that “counts”
toward billing. This includes direct face-to-face service time and other indirect time when IB
Services staff is delivering the IB Services, but the individual is not present (e.g., training
caregivers). Staff members do not need to perform a face-to-face service during every service
delivery session but must provide at least one of the services as described in the “Reimbursable
Services” section and appropriately document the delivery of service(s).
13. Documentation Retention
All documentation specified above, including the Life Plan and service documentation, must be
retained for a period of at least ten (10) years from the date the service was completed to
protect against potential false or fraudulent Medicaid claims under the New York False Claims
Act. The date of issuance of the final payment through the State Financial System (SFS) to the
provider/agency is the date used to establish the start of the ten (10) year retention period.
