My career goal is to build on my emerging presence as a clinical research scientist in the sickle cell disease
(SCD) multicenter clinical trial community to become skilled at designing effective trials for the discovery of
novel approaches to preventing end-organ damage in children with SCD. As a new faculty member, I have led
the implementation of clinical trials designed by others; as I move towards independence, it is my long term
goal to design, implement, and lead a research team in the conduct of multicenter randomized clinical trials,
particularly in the understudied area of hypertension and progressive kidney disease in pediatric SCD. During
my training, I recognized that a major unmet need in the SCD field is research that evaluates therapies to
prevent the well established cardiovascular risk associated with untreated hypertension and progressive
kidney. This K23 will provide a mentored environment in which I will learn to design, conduct, and analyze
multicenter clinical trials, when they are appropriate and when other measures can be used. To accomplish
this training, I will 1) develop a longitudinal cohort of pediatric patients with SCD to evaluate the incidence of
hypertension and kidney disease and 2) conduct a feasibility trial of losartan for cohort participants with
abnormal nocturnal dipping. At the end of this mentored grant, I will have the experience, preliminary data,
and multidisciplinary team required to lead a definitive trial of antihypertensive therapy to prevent
cardiovascular complications of SCD in pediatric populations.
2. Candidate Background. I selected St. Jude Children’s Research Hospital for my pediatric hematology
oncology fellowship, receiving mentoring by Drs. Russell Ware and Winfred Wang, two national leaders in SCD
clinical trials. I published six SCD manuscripts with these mentors, two articles focused on the analysis of a
clinical trial.(1-6) I selected a laboratory research track during fellowship for two reasons. First, I firmly believe
that a fundamental understanding of laboratory science is essential to the success of translating bench
research into clinical trials. Second, I believe that education (MSPH) in clinical research can be maximized by
delaying matriculation until after gaining practical experience participating in clinical trials. I selected a gene
therapy lab under the mentorship of Dr. Derek Persons, (co-mentor, Dr. Arthur Neinhuis), exploring differences
between hydroxyurea and gene therapy for the correction of organ damage, including kidney pathology, in the
SCD murine model.(3, 5) After fellowship, I selected an academic appointment at the University of Alabama at
Birmingham, a program known for its strong participation in pediatric SCD clinical trials. Under the mentorship
of Dr. Thomas Howard, I was able to design a junior investigator career trajectory focused on my goal to lead
future clinical trials by participating in current SCD trials (Table 1) and evaluating barriers to successful trial
design and enrollment.(7) I worked to establish an identity within the small SCD trial community through
publications and presentations at annual meetings. In the last five years, I published 14 manuscripts on SCD,
11 manuscripts as first author, and presented 6 abstracts on SCD at the American Society of Hematology
Annual Meetings and co-author on an additional 4 abstracts.(1-20) The co-authors on my manuscripts include
investigators from 15 different institutions that participate in multicenter SCD clinical trials. I developed
relationships with investigators through publication, executive conference calls, and national trial meetings.
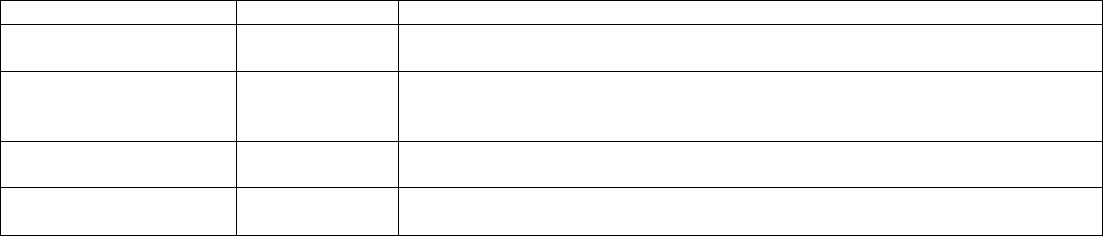
Table 1. Current Efforts as Site PI
Trial
Year
Experience
Pneumococcal Vaccine
Trial (NCT00918580)
2009-2011
Lead the local research team in an international, industry sponsored trial.
Abstract presented at American Society of Hematology Annual Meeting.
BABY HUG Trial
(NCT00006400)
2010-present
Lead a secondary data analysis of BABY HUG, resulting in presented
abstract and published results for this analysis.(5) Served on additional
BABY HUG writing committees Site PI for BABY HUG Follow UP II.(6)
SIT Trial
(NCT00072761)
2010-present
Oversaw an ancillary study to explore barriers and facilitators to enrollment
in a clinical trial of hydroxyurea to prevent SCI.(7)
HU Prevent Trial
NCT01389024
2012-present
Analyzed barriers to enrollment in this feasibility trial
Serve as Site PI/active member in executive meeting conference calls
With this background of SCD clinical trial participation, I sought out additional relevant educational experiences
and mentored training to enhance my understanding of epidemiology, and biostatistics. I completed the UAB
Clinical and Translational Science Training Program (5UL1RR025777) and I am currently enrolled in the UAB
MSPH Program in Clinical and Translational Science. To complement my local coursework and mentoring, I
received two scholar awards to attend national summer institutes. The American Society of Hematology
awarded me as a 2010 Scholar, Clinical Research Training Institute, working with national hematology mentors
on therapeutic trial design. The NHLBI/Office of Behavioral and Social Science Research awarded me as a
2013 scholar, Summer Institute on Randomized Behavioral Trials, working with leaders to better comprehend
interventions and strategies to enhance enrollment in randomized clinical trials.

Despite my participation in SCD trials and early MSPH coursework, I understand that initiating and leading a
multi-center clinical trial for a rare disease requires additional mentoring from national experts in the
design, conduct, and analysis of clinical trials. This K23 will provide me a unique skill set to become a leader in
SCD trials, skilled at conducting efficient and effective clinical trials to prevent end-organ disease.
3. Career Goals and Objectives. My short term goal is to develop expertise in feasibility, conduct and
analysis of clinical trials that elicits vital background information necessary to plan future multicenter trials. My
long term goal is to become an independent, extramurally funded clinical investigator with expertise in
designing efficient multicenter clinical trials that test novel strategies to prevent end-organ damage in SCD.
To meet my short term goals, I will develop the protocol for a feasibility trial, have it reviewed and revised. I will
conduct this single site feasibility trial of a novel approach to treating in adolescent patients with SCD. I have
developed a mentoring team skilled in the design, conduct, and analysis of multicenter clinical trials and trials
of anti-hypertensive therapy for children. I will also conduct a prospective cohort study to determine the
incidence of hypertension and role for biomarkers. My short term goals include:
1) Didactic Coursework to Develop Expertise in Design, Conduct and Analysis of Trials
- Complete a MSPH program for Clinical and Translational Science (42 hours)
- Complete graduate level coursework in Biostatistics and Epidemiology (Table 3)
2) Practical Training in Design, Conduct, and Analysis of Feasibility Trials and Prospective Cohort Studies
- Prepare and conduct a feasibility trial of Losartan for adolescent patients with SCD and abnormal
nocturnal dipping (Aims 1 and 2)
- Identify barriers and facilitators to acceptance of a SCD clinical trial of hypertension (Aim 1a)
- Develop strategies to monitor adherence to study medication and procedures (Aim 1b)
- Develop and implement a data safety monitoring plan during a clinical trial (Aim 2)
- Develop a data management plan and analytic strategies applied to prospective trials (Aim 2)
- Establish and follow a pediatric SCD cohort for hypertension and kidney injury (Aim 3)
- Identify risk factors or markers associated with impending kidney injury (Aim 3)
3) Mentored Training in the Conduct of Multicenter Clinical Trials and Trials of Rare Disease
- Participate in the Maternal Fetal Hypertension Program and Neurofibromatosis Clinical Trials
Consortium (Mentors: Dr. Cutter & Korf)
Long term goals: At the end of this K23, I will have the background data and skill set necessary to submit an
independent investigator proposal to conduct a multicenter SCD hypertension trial using losartan, including the
appropriate research infrastructure. If the feasibility trial demonstrates that a definitive trial can be performed
using a small sample size, I would plan to submit a R01 application to perform that trial. If the feasibility trial
demonstrates that a definitive trial requires a large sample size, as is likely, I plan to submit a R34 application
to perform a feasibility trial to establish a multi-center trial network. If losartan has no effect on restoring
normal blood pressure dipping, I will utilize the mentored training in the design and conduct of a feasibility trial
to submit a R34 application for the evaluation of an alternative therapeutic target for hypertension.
Hypertension and renal disease are risk factors for increased morbidity and mortality in sickle cell disease
(SCD). Young SCD patients may develop microalbuminuria and hyposthenuria while hypertension increases
risk for stroke, a significant problem in pediatric SCD. Among 79 adolescent SCD patients at UAB, 31% have
hypertension as defined by NHLBI tables for age and height and 25% have microalbuminuria (>30mcg/mg).
Persistent untreated hypertension may contribute to the early prevalence of chronic kidney disease (CKD) in
SCD. The mortality rate in young adults with CKD on dialysis is high; 26% of young adults with SCD die within
one year of starting dialysis. Mean blood pressure (BP) should decrease while sleeping, but 90% of
adolescent SCD patients tested in our clinic have abnormal nocturnal dipping, a known pediatric risk
factor for adverse cardiovascular outcomes. Abnormal nocturnal dipping will be defined as <10% dip in BP
(mean daytime BP-mean nocturnal BP)/mean daytime BP x 100.) This high prevalence mandates a search for
evidence of benefit to normalization of nocturnal BP and the optimal BP treatment strategy in pediatric SCD.
This K23 proposal focuses on didactic and practical mentored training in the development of treatments for
SCD and in the conduct of SCD clinical trials. My long term goal is to initiate a phase III, multicenter trial to
define the role of antihypertensive therapy for SCD patients. My short term goals to be accomplished during
this K23 proposal focuses on developing expertise in trial design, conduct, and analysis. A mentorship team
with unique areas of expertise in clinical trials will mentor me in the conduct of 1) a prospective pediatric SCD
cohort study to evaluate changes in BP and blood/urine biomarkers of kidney injury over three years and 2) a
single site randomized feasibility trial of losartan in cohort patients identified with abnormal nocturnal dipping.
The three year prospective cohort will be used to define the incidence of hypertension (in-clinic and 24 hour)
and kidney injury among 200 SCD patients (6-19yrs). From this cohort, we expect to enroll 40 SCD patients
(11-19yrs) with abnormal circadian blood pressure in a six month feasibility trial to systematically evaluate the
acceptance and eligibility rates, adherence, dosing and safety for a losartan trial, and develop background data
on the effect of losartan in patients with abnormal nocturnal dipping.
Specific Aim 1: To conduct a randomized feasibility trial in adolescent SCD patients with abnormal
nocturnal dipping. Prior to conducting a definitive multicenter trial of losartan to prevent target organ damage
from abnormal nocturnal dipping, a feasibility trial is required to 1) determine the estimated rates of eligibility
and acceptability of enrollment into an adolescent SCD hypertension trial, 2) demonstrate participant
adherence to study medication (daily oral losartan), 3) estimate compliance with study procedures including 24
hour Ambulatory Blood Pressure Monitoring (ABPM) at 0, 3, and 6 months. We anticipate that 30% of cohort
participants (HbSS/SB
0
thalassemia and ages 11-19 years) will have both abnormal nocturnal dipping by
ABPM and hypertension in clinic. We hypothesize that we will need to approach 60 of the 200 cohort
participants to enroll 40 participants in this 6 month feasibility trial of losartan.
Specific Aim 2: To demonstrate in a feasibility trial the optimal dose of losartan and effect size
necessary to conduct a trial of losartan in participants with abnormal nocturnal dipping. To
determine the optimal losartan dose, participants will receive losartan (0.7mg/kg) and randomized to monthly
titration to achieve a clinic BP <95th percentile (standard dosing strategy) or BP <75th percentile (intensive
dosing strategy). A strict data safety plan and monitoring board will evaluate the safety of both dosing
strategies. We hypothesize that intensive losartan dosing is safe to utilize in a clinical trial, will be adhered to
by participants and can be maintained in an open label fashion. To determine the effect size needed to power
a definitive trial of losartan for participants with abnormal nocturnal dipping, ABPM will be performed at
baseline, 3 and 6 months to determine the differences in BP and standard deviation from baseline to exit.
Specific Aim 3: To prospectively evaluate the incidence of hypertension in patients with SCD and the
potential role of biomarkers of disease. Two hundred patients with HbSS or SB0 thalassemia (6-20 yrs) will
enroll in a three year prospective cohort study (At this time: 109 participants consented. Expect 200 enrolled by
2015). Participants will undergo annual 24 hr ABPM and urine/blood biomarkers of kidney injury. Over three
years, we will describe the incidence of hypertension and its association to biomarkers. Additional analysis will
explore the role of SCD therapies (hydroxyurea, transfusion) or laboratory values on these outcomes.
The proposed research will offer insight into the previously unexplored area of antihypertensive therapy in
pediatric SCD. The K23 will provide mentored training in design, conduct, and analysis of clinical trials for a
rare disease, with an emphasis on feasibility and safety monitoring. The results of this proposal will be
incorporated into an R34 application to conduct a multi-center pilot study to demonstrate feasibility of this trial
prior to submission of a R01 application for a definitive trial. This K23 application represents the first step in
developing the expertise and data required to lead the small SCD trialist community in efforts to reduce the
long term, severe complications resulting from untreated hypertension and kidney disease in pediatric SCD.
