
Employee
Handbook

www.commhealthcare.com
Page 1 of 89
Contents
WELCOME! ................................................................. 3
WHAT IS HOME CARE? ...................................... 3
OFFICE HOURS AND LOCATIONS ........................ 4
JOB ASSIGNMENTS .................................................. 5
STARTING A NEW CASE ................................ 5
CASE TYPES ....................................................... 7
PROBATIONARY PERIOD ............................. 7
REPORTING AND RECORDING .................... 7
GRIEVANCE PROCEDURES .................. Error!
Bookmark not defined.
WHILE WORKING WITH CLIENTS ...................... 8
AIDS ..................................................................... 8
LOITERING/VISITING .................................... 8
TIPPING, SOLICITING & GIFTS .................... 8
ALCOHOL, DRUGS, & SMOKING .................. 8
ARGUMENTS ..................................................... 8
TRANSPORTING CLIENTS ............................ 9
HIPAA .................................................................. 9
CULTURAL DIVERSITY ............................... 11
ADMINISTRATION OF MEDICATION ..... 12
DEALING WITH CONFLICT ........................ 12
SAFETY GUIDELINES FOR WORKING IN
THE HOME ...................................................... 13
HANDLING MONEY ...................................... 14
UNIVERSAL PRECAUTIONS ....................... 14
USE OF GLOVES ............................................. 14
USE OF OTHER PROTECTIVE GEAR ....... 14
PREVENTION FROM NEEDLE STICK
INJURIES: ........................................................ 14
INFECTIOUS DISEASE ................................. 15
ON-THE-JOB INJURIES ................................ 15
DISASTER (EMERGENCY
PREPAREDNESS) .......................................... 15
EMERGENCY PLAN: ...................................... 16
INCLEMENT WEATHER .............................. 16
FIRE: .................................................................. 16
POWER FAILURE: ......................................... 16
MEDICAL EMERGENCY: .............................. 16
HEALTHCARE PROXY .................................. 17
GENERAL EMPLOYMENT RULES ...................... 18
IMMIGRATION COMPLIANCE ................... 18
CODE OF CONDUCT ...................................... 18
APPEARANCE AND DRESS CODE ............. 19
PHOTO IDENTIFICATION CARD ............... 20
CONFLICT OF INTEREST ............................ 20
WORKPLACE ADMINISTRATIVE
SEARCHES ....................................................... 20
FINANCIAL REPORTING ............................. 20
PROTECTION OF ASSETS ........................... 21
ANTI-COMPETITIVE CONDUCT ............... 21
FINANCIAL INDUCEMENTS ....................... 21
PERSONNEL FILES ........................................ 22
PERFORMANCE EVALUATIONS ............... 22
PLAN OF CARE ............................................... 22
REPORTING EMERGENCIES, ACCIDENTS,
AND CHANGES ............................................... 23
TELEPHONE CALLS ...................................... 23
STEALING ........................................................ 24
CRIMINAL ACTIVITY ................................... 24
CONFIDENTIALITY AND PRIVACY .......... 24
EQUAL EMPLOYMENT OPPORTUNITY .. 26
AMERICANS WITH DISABILITIES POLICY
............................................................................ 26
RELIGIOUS ACCOMMODATIONS .............. 27
ANTI-RETALIATION POLICY ..................... 28
SEXUAL HARASSMENT ............................... 29
SOLICITATION AND DISTRIBUTIONS .... 34
ELECTRONIC MAIL, SOCIAL MEDIA AND
INTERNET ....................................................... 34

www.commhealthcare.com
Page 2 of 89
PHOTO WAIVER AND RELEASE ............... 34
DRUG AND ALCOHOL POLICY .................. 35
COMPLAINT PROCEDURES ....................... 36
TIME AND ATTENDANCE – TIME OFF ............ 38
TIME AND ATTENDANCE: ......................... 38
TARDINESS: ................................................... 38
FAMILY AND MEDICAL LEAVE ................. 38
SICK DAYS ....................................................... 48
PAID SICK TIME POLICY FOR NYC AIDES
............................................................................ 49
LEAVE OF ABSENCE: .................................... 51
TAKING OFF/UNPAID VACATION: ......... 52
NURSING MOTHERS .................................... 52
JURY DUTY: .................................................... 52
MILITARY LEAVE ......................................... 53
TIME OFF TO VOTE ...................................... 53
LEAVE FOR BONE MARROW DONATION
............................................................................ 53
LEAVE FOR BLOOD DONATION ............... 53
RESIGNATION ................................................ 54
WAGE AND PAYROLL INFORMATION ............ 55
WAGES ............................................................. 55
OVERTIME ...................................................... 55
PAYROLL ERRORS ....................................... 56
MEAL PERIODS ............................................. 56
TIMESHEETS .................................................. 56
USE OF THE ELECTRONIC ATTENDANCE
VERIFICATION SYSTEM (EAVS) .............. 59
USE OF PHONE CLOCK IN .......................... 60
USE OF MOBILE APP ................................... 60
WAGE PARITY ............................................... 63
INSTRUCTIONS TO VIEW YOUR ONLINE
PAY STUB ........................................................ 64
LIVE-IN CASE RULES ............................................ 66
BENEFITS ................................................................. 71
HOLIDAY PAY: ............................................... 71
WORKER’S COMPENSATION .................... 71
DISABILITY INSURANCE ............................ 71
YEARLY COMPLIANCE REQUIREMENTS ........ 72
IN-SERVICE: .................................................... 72
PHYSICALS: ..................................................... 72
PPD/QUANTIFERON .................................... 73
INFLUENZA: .................................................... 73
FALSE CLAIMS PREVENTION ............................. 74
ABUSE AND NEGLECT REPORTING POLICY . 79
FACT-FINDING AND ISSUE RESOLUTION
(“FAIR”) PROGRAM .............................................. 81
ACKNOWLEDGMENT OF RECEIPT ................... 88
www.commhealthcare.com
Page 3 of 89
WELCOME!
We want to welcome you as an employee of Community Health Care. You are
joining an agency whose principle goal is to assist our clients in the time of need. We
are proud to say that our agency enjoys a fine reputation for the highest standards
of care for our client’s. The elevated quality of our services is due in a great part to
the concerned dedication of our employees. We believe that by working as a team,
and maintaining strong communications amongst ourselves, is the reason for our
success. We are pleased to have you join our family. We hope your experience working
here will be a positive and rewarding one.
To help you become familiar with our agency, we have prepared this handbook. We
believe that it is vital that you understand all of our policies and expectations and this
handbook will familiarize you with the responsibilities of being an employee. This
handbook is just a summation of our policies and is in no way meant to be a
comprehensive description of every policy and procedure. Should you need
clarification on anything, please contact your supervisor. If you have any questions,
comments or suggestions, please do not hesitate to contact us.
Once again, welcome to
Community Health Care.
49 North Airmont Rd
Montebello, NY 10901
Office 845-425-6555
Fax 845-425-9035
WHAT IS HOME CARE?
Home Care are services to the disabled, chronically ill, or recovering person(s) providing for
treatment and or effective functioning in a home environment? Home care can assist in the
provision of services to adults and children in danger of abuse or neglect. Home care is
appropriate when a person needs assistance that cannot easily be effectively provided by
family members or friends for a short or long period of time.
www.commhealthcare.com
Page 4 of 89
OFFICE HOURS AND LOCATIONS
Main Office
49 North Airmont Rd
Montebello NY 10901
Hours: Monday thru Thursday 9:00am-5:00pm, Friday 9:00am-1:00pm
845-425-6555
Please note: The below offices are Recruiting Offices only.
Rockland County
Address: 1 Hillcrest Center, Suite 101
Spring Valley NY 10977
Hours: Monday thru Thursday 9:00-5:00,
Friday 9:00-1:00
Putnam county
Address: 73 Gelenia Avenue #4
Carmel NY 10512
Hours: Monday thru Thursday 9:00-1:00,
Friday – Closed
Orange County
1. Address: 90 North Street, Suite 202
Middletown NY 10940
Hours: Monday thru Thursday 9:00am-5:00pm,
Friday 9:00am-1:00pm
2. Address: 562 RT 17M Suit 10 (2ndFloor)
Monroe, NY 10950
Hours: Monday thru Thursday 9:00-2:00,
Friday – Closed
3. Address: 290 Broadway Suite #6
Newburgh, NY 12550
Hours: Monday thru Thursday 9:00-5:00
Friday 9:00-1:00 pm
Westchester County
1. Address: 435 South Broadway suite 5
Yonkers NY 10705
Hours: Monday thru Thursday 9:00-5:00,
Friday 9:00-1:00
2. Address: 910 Main St.
Peekskill NY 10566
Hours: Monday thru Thursday 9:00-5:00,
Friday 9:00-1:00
3. Address: 99 Mamaroneck Ave #6, 2
nd
floor
White Plains NY 10601
Hours: Monday thru Thursday 9:00-5:00,
Friday 9:00-1:00
Sullivan County
Address: 20 Mountain Mall Plaza, 121 Broadway
Monticello NY 12701
Hours: Monday thru Thursday 9:00-5:00,
Friday 9:00-1:00 pm
Dutchess County
Address: 25 Market Street, 4
th
Floor
Poughkeepsie NY 12601
Hours: Monday thru Thursday 9:00-5:00,
Friday – 9:00-1:00
Ulster County
Address: 22 Dederick Street 2
nd
floor
Kingston NY 12601
Hours: Monday thru Thursday 9:00-5:00,
Friday 9:00-1:00 pm
www.commhealthcare.com
Page 5 of 89
JOB ASSIGNMENTS
In accordance with Department of Health requirements, you are only qualified and authorized to
accept a job assignment after attending and completing orientation.
All job assignments are made by our Coordinator. In making case assignments, which are solely in
our discretion, we take into account various factors, including, but not limited to:
• Special language requirements of a Client;
• Contract entity and/or Client requests;
• Constant Care determines that a particular Aide does not fit in with the Client’s needs or
attitudes;
• Another Aide is better qualified for the position, hours or geographic location;
• Assignment determined by geographic location; and
• Such other factors as Constant Care deems appropriate for that assignment.
Nonetheless, the Coordinator will make every effort to assign cases most suited to you with
regards to your location, availability, and type of case or other stated preference. You are expected
to be cooperative and be flexible in accepting assignments. If, however, if you cannot accept a
particular case, you should tell the Coordinator your reasons for declining the case so that future
assignments will be more suitable for you.
We now have a mobile app which is used to instantly broadcast many of our available cases.
To sign up download the MEDFLYT app available thru the Appstore or Google Play
Use code 7689 to sign up.
Once you have accepted an assignment, we expect you to fulfill your obligation. Do not ask the
client to change her hours for your convenience. If this case does not work into your schedule,
you must notify the Coordinator. She/he will then make any necessary changes, even if it means
replacing you.
STARTING A NEW CASE
The Coordinator will contact you with all relevant information about the client This includes dates,
times and location. She/he will give you as much information as the agency has on each client. The
Coordinator will also review the clients plan of care with you.
All schedule changes must be done through the designated Coordinator. If the client wishes to
change their time or date of services, they must contact the office. Do not take it upon
yourself to make any changes without authorization. This could result in your removal from
the case.

www.commhealthcare.com
Page 6 of 89
You will not be paid for working any days or hours that were not scheduled through the Agency
and which we did not authorize. Therefore, it is extremely important that you notify the Agency
and coordinate any work through the Agency so that we can know when you are working and
pay you accordingly. Unauthorized hours/visits will not be paid for.
When given an assignment by the agency you are the only person who should be working.
Any employee who has an unauthorized individual covering their case will not be paid and
will be dismissed from the agency.
❖
If you arrive at your client’s home and they are not there, or you are turned away, contact your
coordinator immediately. We will attempt to find you a new case that is in close proximity to your
location. You are required to accept such a case if offered by the Coordinator.
If your client does not answer the door, do not assume they are not home. Your patient may have
fallen and cannot get up. Stay there, call the coordinator either with your cell phone or from a
neighbor’s home, but do not leave until the office has authorized for you to leave.
Never use your car to drive your client anywhere. This is extremely dangerous and could result
in you being personally sued. You may go out with the client, and escort them to an
appointment in either a cab, or in the family car, but you cannot drive under any condition.
You are to bring you own meals unless there have been other arrangements made. Most clients
have very limited income, so please be considerate, and refuse their offerings. You must be aware
of different cultures and adhere to them i.e. kosher homes.
If you are working a 6-hour shift or less there is no break time allowed. Please eat before or after
your shift. If you are working anything longer than that, please call the Coordinator so that she/he
can make arrangements for you with the client and family for breaks/lunch/dinner time.
If break time will be allotted by the coordinator you are not be allowed to leave the patients home.
The break will need to be taken at the patient’s home.
You may never be in the client’s home if the client is not present. If the client leaves his/her home,
you must contact your coordinator immediately and leave at the same time. You must remember
to clock out BEFORE you leave the client’s home and get your timesheet signed.
While assigned to a shift you may not leave the client’s home until your shift time is over, unless
you are doing errands for the client. If you need to leave for an emergency, you may only do so
with authorization from the coordinator.
Make sure that you have your ID badge on you at all times.
Dress appropriately, according to office regulations
Stay professional at all times.
Should you find difficultly with your client and wish to be removed from the case, you
must provide 2 weeks written notice along with a reasonable explanation.
www.commhealthcare.com
Page 7 of 89
CASE TYPES
Mutual Patients: A Visit in which Caregivers provide service to two Patient’s at once.
Linked with: A Visit in which a Caregivers provide service to two Patient’s that are typically
scheduled as back-to-back Visits.
Live-in: A 24-hour Visit in which the Caregiver remains at the Patient’s residence overnight
but where the Aide works 13 hours (subject to some exceptions)
PROBATIONARY PERIOD
All Aides are considered probationary for the first 90 days of employment. During the
probationary period, the Agency evaluates if you are able to perform your job competently.
The probationary period also provides you with an opportunity to decide if you would like to
become a regular Aide with Constant Care. Constant Care may extend the probationary period
should circumstances warrant it, in its sole discretion. Neither being in, nor completion of,
the probationary period will change the “at-will” nature of your employment in any way.
REPORTING AND RECORDING
Any changes in your client’s must be reported to the Coordinator immediately. If you
notice any bruising, discomfort, personality changes, lethargic behavior etc…contact the office
immediately.
❖
If the patient was taken to the Emergency room or was hospitalized, you must report this to
your coordinator immediately. You are not allowed or expected to go to the Client’s home if
you know they are not there. You can never work for a client while he/she is hospitalized or
in rehab or otherwise not home. Please be advised that attempting to report work time when
you know that the Client was not home and you were not required or expected to work for the
Client is tantamount to Medicaid fraud and will be investigated. You may be immediately
terminated if it is determined that you attempted to report work time for such situations.

www.commhealthcare.com
Page 8 of 89
WHILE WORKING WITH CLIENTS
AIDS
New York State regulations forbid the release of confidential information. This includes
AIDS related information. Only the appropriate designated person has the rights to such
information and is not required to disclose such information. Therefore, you should always
use universal precautions on every client since you may not know whether the Client has
AIDS.
LOITERING/VISITING
Aides are requested to leave the premises of the client’s home or facility upon completion
of scheduled shift.
Never bring children, family, friends or pets to your client’s location, and under no
circumstances should anybody visit you while you are working. This is a DOH violation
and will result in termination.
TIPPING, SOLICITING & GIFTS
Aides are forbidden to engage in unauthorized solicitations such as subscriptions,
catalogs, fund-raisers, petitions, etc…
Aides are not to accept gifts, money, clothing, food, etc. This includes borrowing money
from a client’s family. We also forbid the solicitation of money/gifts from fellow employees.
ALCOHOL, DRUGS, & SMOKING
To ensure a safe and productive work environment, The Agency prohibits the use,
purchase, sale, possession, or transfer of any alcoholic beverage or nonmedical prescribed
controlled drug while on agency property, client property or scheduled working hours.
Community Health Care has a zero-tolerance policy regarding Alcohol, drugs, and
smoking. Arriving to work under the influence of drugs and/or alcohol will result in
immediate termination.
The Agency also prohibits employees from reporting for or being at work while under
the influence of alcohol or drugs. Employees who are using a prescribed drug which might
in any way affect job performance should report this to the Coordinator.
The full drug and alcohol policy can be found at the end of this handbook.
You are not allowed to smoke in the client’s home, even if they are a smoker.
ARGUMENTS
In the event that a client or family member communicates in an argumentative manner,
do not argue back, and do not abandon the client. Call the office Immediately, either
from their home phone or walk outside, and use your cell Phone. If you feel threatened
by the client or any visitor in their home, please call the Coordinator immediately. The
www.commhealthcare.com
Page 9 of 89
Agency is committed to providing a safe workplace for you and you will not be allowed to
stay in a home if you have reasonable concerns about your safety.
In a calm manner, describe to the Coordinator what is taking place or what has occurred.
The office will direct you as to what actions must be taken.
Be prepared to come into the office directly after your shift. A written report explaining
the incident must be prepared and documented. Your signature and wording will be
required at this time. It is important that this is done as soon as possible so that the report
is accurate (within 24 hours).
TRANSPORTING CLIENTS
Aides are not permitted to use any motor vehicle to drive their client while on assignment.
HIPAA
HIPAA stands for Health Insurance Portability and Accountability Act. It is a new federal
law whose purpose is to protect the privacy of personal medical information that is shared
with doctors, nurses, hospitals, insurance companies and other health care providers.
HIPAA’s Privacy Rule puts new limits on how personal medical information is used and
shared, gives patient the right to access their medical records and puts greater protection
on those medical records. In the past personal health information was sold or shared to
make decisions regarding employment, for marketing purposes, to coordinate care for
disease management and to help determine drug costs. This was done without notice to or
consent of the patient. The Privacy Rule applies to all forms of personal health information
– written, electronic or oral.
Who has to follow the HIPAA Rules?
All health care providers – doctors, nurses, aides, insurance companies, health care
agencies, hospitals, laboratories and business associates of these persons must follow the
HIPAA rules.
What is personal health information?
Personal Health information includes any information regarding the past, present or
future physical or mental health or condition of a person that is used for treatment or
payment of healthcare. The HIPAA rules include additional information that is protected by
the privacy rule – any information that can be used to identify individuals. This might be
the name, social security number, address, health insurance numbers, doctor’s name,
diagnosis, etc. This information can connect a person to specific health information.
Protected Health Information (PHI) is that personal health information that is transmitted
or stored electronically or in any form other than hard copy.
What does The Agency have to do to meet the new regulations?
The Agency must do several things in order to fulfill its legal obligations. We must
provide patient and employee education about the privacy rights and how patient
information can be used. Policies and procedures must be developed for the patient and
employee to follow. All employees must be trained about the policies and procedures. Most
important of all, employees must be aware of the way that they contribute to the

www.commhealthcare.com
Page 10 of 89
maintenance of patient confidentiality – not discussing cases with people who are not
involved in the patient’s care, keeping records secure and out of the sight of people who do
not work for the agency, properly destroying patient documents that are no longer needed
or pieces of paper that have patient information written on them, disclosing only the
minimum amount of information that is needed, taking other measures to protect patient
confidentiality such as learning about practices.
What information does the patient need to know?
Patients will be informed of the new privacy rule and their rights under this rule,
through a “Notice of Privacy Rights”. The nurse will give this document to the patient at the
time of the first nursing visit and will ask the patient to sign a consent form to use and share
the PHI for treatment, payment and health care operations. This consent form must be kept
on file for six years.
How can PHI be used and disclosed legally?
In order for patient to receive treatment, have the treatment paid for by their insurance
company and for the health care agency to operate, protected health information (PHI)
must be used and disclosed by the people involved in the care of the patient. PHI is used
when it is shared, examined, applied and analyzed. PHI is disclosed when it is released,
transferred or accessed in any way by outside the health care agency. PHI maybe used or
disclosed in the following instances: for treatment, payment or health care operations; with
authorization or agreement from the patient; for disclosure to the patient; for incidental
uses such as doctors talking to patients in a hospital room or on the phone or a nurse who is
taking care of the patient. For other uses or disclosures, the patient must sign a special
authorization form.
What requirements are related to the special authorization form?
This form must be signed by the patient when information must be used or shared with
a third party for purpose not related to treatment, payment or health care operations. The
authorization may be revoked by the patient at any time. Each authorization must give a
specific description of the information to be used or shared, the name of the person who is
getting the information, the purpose of the disclosure, date of expiration of authorization
and must be written in plain English. The information that is share must be minimum
necessary.
Are there other times when PHI can be disclosed without obtaining a special
authorization?
Yes, PHI may be legally disclosed without obtaining a special authorization from the
patient for the purpose of audits, civil and criminal investigations, law enforcement, judicial
and administrative proceedings, reporting public health and safety and suspected/known
cases of abuse, neglect or domestic violence and other legal requirements. In emergency
circumstances PHI may be disclosed. PHI may also be shared with relatives, coroners and
medical examiners.
Can I tell if the patient says I can?
Disclosure may be made to family members, friends or other people that patients
indicate is involved in their care or payment of health care unless the patient objects in

www.commhealthcare.com
Page 11 of 89
whole or part. In any other situation not described previously, you need to get the patient’s
written authorization to disclose any PHI.
What if “they” are listening?
An incidental use or disclosure is a secondary use of disclosure that cannot reasonably
be prevented, is limited in nature and occurs as a result of an otherwise permitted use or
disclose. They are permitted only to the extent that reasonable safeguards have been
applied and do not disclose any more of the PHI than is necessary to accomplish the
permitted use or disclosure – this is known as the Minimum Necessary Standard. An
example might be the disclosure about a patient by a home health aide in the patient’s home
that might be overheard by the other family members not involved in the patient’s care.
What is “minimum necessary rule”?
Use or disclosure of PHI must be limited to the smallest amount that is needed to get a
job done. This means that not all employees may have the same amount of formation about
a patient. Each employee should have only the information that is necessary for them to
carry out their job. This rule does not apply to use or disclosure of medical records for
treatment purposes since the health care provider needs access to the entire record to
provide quality care.
What happens if an individual or agency fails to follow these laws?
Failure to comply may result in civil and/or criminal penalties.
Does HIPAA take precedence over other existing confidentiality laws?
In cases where state laws are stricter than the HIPAA rules, the state laws take
precedence. An example is the HIV confidentiality laws.
Does HIPAA have any other part beside the Privacy Rule?
Yes, there are three parts to the HIPAA regulations. You have already heard about the
Privacy Rule. HIPAA also sets standards for the electronic transmission of PHI if order to
standardize how this is done throughout the country. There will also be a Security Rule
which will create standards governing the security of protected health information (PHI);
these regulations have not been written yet.
CULTURAL DIVERSITY
The aide will have many clients with cultural backgrounds and traditions different from
his/her own. You have to remember to respect and value each client as an individual.
Cultural background can influence a variety of situations, for example:
• How friendly your client is toward strangers.
• How they feel about having you or anyone else in their home.
• How close they want you to stand to them when talking to them.
The religion of a client and his/her family can also affect the way they behave. Religion can
be very important to the client who is very ill or dying. As an aide, you have to respect these
differences, even if they are very different from your own. Never question the client’s religion,
and refrain from discussing your own religious beliefs. Be aware of and honor any dietary
restrictions your client may have based on religious beliefs. Discuss with the nurse, client and
www.commhealthcare.com
Page 12 of 89
family any meal planning and food preparation adjustment as needed. Keep physical contact
to a minimum for those clients whose cultural or religious backgrounds make them less
comfortable to being touched. You still need to care for the client but talk to the nurse about
ways to reduce unnecessary touching. Be sensitive to your client’s cultural and religious
background. Treat all clients with dignity and respect. Expect your clients to treat you
respectfully as well.
ADMINISTRATION OF MEDICATION
Constant Care Aides are allowed to only dispense medication out of pill containers which are
pre-filled by a family member or licensed healthcare professional. No other methods are
tolerated under any circumstance.
Aides may not administer non-prescription medication directly to a client. They can only
assist. Assisting is defined as bringing the prescription (bottle or container), opening the
prescription, and allowing the client to take the prescription out of the container and take the
prescription without the assistance of the Aide. This includes putting the pill in the client’s
mouth.
DEALING WITH CONFLICT
Everyone has had to deal with difficult people or situations at one time or another. Learning
to deal with the conflict through better listening and communications skills can be the key to
solving the problem at hand.
Conflict Resolution
• Stay calm
• Assess the situation
• Identify the problem
• Describe the problem briefly and accurately to your designated contract person, i.e.,
family/supervisor/coordinator.
• Confirm that you heard and understood.
• Remember that you need to keep your patient, patient’s family or co-worker happy. You
are the peacekeeper.
• Listen to the person presenting the conflict. He/she should feel that you are interested
and willing to help.
• Interpersonal relationships are very important.
• Do not escalate the situation. It is not important to feel like you have to when a verbal
argument. If a situation develops, please contact your agency for support.
Interpersonal Relationships
Supportive Relationships
The relationship between the aide and the client is one of the most important elements in a
successful home care situation. There are certain behaviors that will promote communication
and covey caring to a client. Everyone wants to be listened to, care about, accepted, liked,
respected, understood and regarded as capable or competent.
Clients must feel Supported

www.commhealthcare.com
Page 13 of 89
When a patient feels respected and understood, he/she is less likely to be destructive or angry
or uncooperative. When there is a mutual respect between the client and the aide, the tasks in
the care plan will be more easily accomplished.
Supportive Communication
Communicating respect and support can be done both by what is said and how it is said. There
are some phrases that will upset almost anybody such as “that’s silly” or “do this or else”. Equally
important is the tone of voice in which the words are said. A simple phrase can be said in an
angry tone that contradicts the words.
Non-verbal behavior such as good listening habits or body language is also important. Good
listening includes nodding, repeating back what the client says and leaning forward. Facial
expressions convey respect with a smile and attentive behaviors. It helps to sit someone who is
sitting rather than standing over him/her. Touch especially with the elderly, help to convey
warmth and interest. Some people do not like to be touched and their feelings should be
respected.
You must keep communication open and positive through your tone of voice facial
expressions and body posture.
SAFETY GUIDELINES FOR WORKING IN THE HOME
Aides shall not be required to work in any situation that would threaten or endanger his/her
health or safety. The Aide shall immediately report to their Coordinator any working
conditions that threaten or endanger the health or safety of the Aide or Client. No Aide shall
suffer any discipline or negative job consequences as a result of reporting an unsafe work
situation. Aides shall contact their Coordinator in the event of an emergency.
No Aide shall be required to provide at his/her own expense, protective garments to perform
any task for a Client. The Employer maintains an adequate supply of protective garments at
the branch location. Aides are responsible for securing these items prior to servicing their
Client. If such a situation arises where there are insufficient protective garments, the Aide
will report the situation immediately to his/her Coordinator.
When going to into a home for the first time, take a few minutes to think about the kind of
home it is, and what problems you are likely to run into while there. You must expect the
unexpected and be prepared for it.
Some, but not all, precautions and factors you should consider include:
1. Side rails on the bed should be up.
2. Your patient should be safely positioned at all times I bed or chair.
3. When getting your patient up, watch for signs of dizziness and wait until they pass
before letting them stand.
4. Wheelchair brakes should be locked when standing still.
5. Smoking in bed should be discouraged or, if necessary, must be supervised.
6. The room should be kept clear of extra equipment especially at night.
7. Make sure shoes are kept well tied and worn for household activities.
8. Make sure hazardous tools are kept locked.
9. Prepare an escape plan in case of fire, with alternate routes to safety and make sure
everyone in the home knows what to do.
10. Above all use common sense when approaching all job and tasks
www.commhealthcare.com
Page 14 of 89
HANDLING MONEY
When shopping for the client remember to write down the amount of money your client
gives you and return with a register receipt and the exact change. Have the client sign
everything. The document indicating how much money they gave you, the receipt, and how
much change they received. All of this should total up and equal the amount originally
received. You will be responsible for any lost or unaccountable money.
You many not accept access to the patient’s bank account (this includes the debit card and pin
number) without authorization from the Coordinator.
UNIVERSAL PRECAUTIONS
You must wash your hands:
o Upon entering a client’s home
o When hands are soiled
o Between handling individuals client’s
o Before contact with the face and mouth of the client
o After personal use of the bathroom
o After changing or assisting with client’s personal needs/bathroom
o Before preparing meals and after preparing meals
o After housekeeping duties are preformed
USE OF GLOVES
you should wear gloves for touching blood and body fluid (urine, feces, saliva etc), mucous
membranes or non-intact (broken) skin of all clients, handling items or surfaces soiled with
blood or body fluids (this includes used bed linen and used towels, wash clothes)
GLOVES SHOULD BE DISCARDED, AND HANDS WASHED, AFTER CONTACT WITH CLIENT.
GLOVES SHOULD BE DISCARDED IF THEY ARE TORN OR HANDS BECOME MOIST.
Gloves are available to be picked up in all satellite offices. You can also call your coordinator to
mail you a box of gloves. When assigned to a case, the agency will provide you with 1 box of
gloves per month. You are expected to take the gloves with you when you leave the case. Don’t
leave it at the client’s home.
USE OF OTHER PROTECTIVE GEAR
All home care workers must carefully follow the instructions of the nurse regarding use of
masks and/or gowns or other gear, such as face masks. Home care workers should not put
on special gear unless instructed to by the nurse.
PREVENTION FROM NEEDLE STICK INJURIES:
If your client uses any injectable medication they should be disposed of in a puncture
proof container with a tight-fitting screw top. Please notify the agency if you notice syringes
being disposed of improperly.
If your client uses any injectable medication, please shake out any bed linens/laundry
carefully to avoid accidental needle stick from careless handling by client/family/nurse.

www.commhealthcare.com
Page 15 of 89
If you get stuck by a needle stick it must be reported to your coordinator or Human Resources
Representative immediately, latest before the end of the shift, to ensure proper medical
intervention is provided to you.
INFECTIOUS DISEASE
If you believe or know you were exposed to disease carrying organisms, immediately and
thoroughly wash your hands or other exposed area for two (2) minutes using warm soapy
water. If eyes were splashed, rinse thoroughly with clear water only. Call the Agency right
after the incident.
You must notify the agency if you have any open, draining wounds (sores) or rash or any
other potentially contagious condition. Until this condition improves, you cannot perform
direct personal care or handle client’s equipment.
If you contact any contagious illnesses (like the flu), call your coordinator to discuss your
assignment.
ON-THE-JOB INJURIES
If you are injured on the job, you are required to call your Coordinator immediately and
explain that you have to complete report related to a workplace injury. You must then
complete the report and submit it in a timely fashion. These requirements apply no matter
how slight or minor the injury might seem. If you have questions about whether the injury
is reportable, still call your Coordinator and ask – do not make these decisions on your own.
Your failure to follow this procedure may result in the appropriate workers’ compensation
report not being filed in accordance with the law, which may consequently jeopardize your
right to benefits. In addition, if we learn that you did not timely report an injury that was
sustained or aggravated on the job, you may be terminated for violating this policy which
requires timely filing of a claim.
DISASTER (EMERGENCY PREPAREDNESS)
Occurrence/Situation can impact our ability to provide services and care to our Clients.
Examples of an emergency may be a snowstorm, power failure, hurricane and transit strike.
In the event of an emergency, Aide cooperation and understanding is needed. We may need
to change your case assignment (re-assign you to a case closer to your residence location or
to a case of greater risk status- based on the classification system defined in the policy). We
may need to ask you to work more hours for which you will be paid or to ask you to work
different days, etc.
We expect that all our Aides will understand the strong need to be available during an
emergency. We request that all Aides will call in to their Coordinator to offer help even when
you are not scheduled to work. Your Coordinator will inform you when the emergency is over.
The following procedure will be followed: the Field Nurse assigns a status to each Client based
on Agency criteria (nature of illness, family backup, etc.). When an emergency arises:
www.commhealthcare.com
Page 16 of 89
• Constant Care Coordinators inform Clients that we will be implementing
our Emergency Disaster Plan.
• Coordinators begin calling Aides to rearrange assignments in an effort to
provide care according to Client Constant Care status.
• Calls are placed to Aides in an effort to ascertain who is available. Aides
are expected to call Constant Care as well.
• Your Coordinator will inform you when the emergency is over.
EMERGENCY PLAN:
In the event of certain kinds of emergencies, the following instructions must be followed:
• If you are unable, for any reason, to work all of your assigned hours, you must call the
agency as soon as possible.
• If there is a natural disaster (hurricane, flood, snowstorm, etc..) you should make
every effort to get to you assigned client. Once you are with your client, listen to
instructions from a local emergency radio or television station. You must notify the
agency if you are unable to reach the client.
• Make sure you call the office and let them know exactly what you are doing. We might
redirect you to a case for that day closer to your home.
INCLEMENT WEATHER
The Agency provides client services even in the event of inclement weather. In the event
Aides have difficulty with transportation due to the weather, they must contact a supervisor
to discuss their options as soon as possible before the beginning of their shift.
FIRE:
If you are with a client and a fire occurs, you should, at the first sign of smoke, go immediately
to the safest exit with the client. Once away from danger, call the fire department. If the
client cannot be moved, close the door of the client’s room and go to the nearest safe
telephone. Dial 911 give them the exact address and name of yourself and the client. Do not
attempt to put out the fire yourself. Do not return to the house until the fire department has
given you permission to do so. Notify the agency as soon as you and your client are out of
danger.
POWER FAILURE:
If you are with a client and there is a power failure, try to keep the client as warm and
comfortable as possible. Inform the agency as soon as possible. If the client is on life-support
equipment be certain to switch to the generator back up. Notify the utility company and
contact the agency as soon as possible. If your client is in a life-threatening situation, call 911
immediately.
MEDICAL EMERGENCY:
If a medical emergency occurs while you are with a client, these are the general rules which
you should follow.
o Seek emergency help by dialing the number provided on the emergency sheet
on the emergency list.
o Keep client as comfortable as possible.
o Observe the client and report all symptoms to emergency personnel.
o Notify the agency of situation and outcome.
www.commhealthcare.com
Page 17 of 89
You are responsible for the safety and wellbeing of your client during the assigned hours. If
for any reason you cannot provide all the hours of service required, you must notify the
agency at once.
HEALTHCARE PROXY
Advanced directives protect the Client’s rights to make his/her own choices; legal, valid
decisions concerning future medical care and treatment. Aides must abide by client advanced
directives.
Types of advanced directives include:
• Do Not Resuscitate (DNR): This is a written instruction to hospital/home
personnel concerning what actions to take if a terminally ill Client suffers a
cardiopulmonary arrest (heart and breathing stops).
• Living Will: This specifies written instructions regarding what health care is to
be given to a Client if the Client becomes incapable of making his/her own
decisions.
• Health Care Proxy: This is an individual who is selected or appointed by a Client
to make decisions if the Client becomes unable to do so for himself/herself. The
person must be eighteen (18) years of age, mentally competent and need not be a
member of the family.
As a health care provider, Constant Care reviews and provides a packet of information on
advanced directives to its Clients. Clients who have indicated in writing their wish not to
be resuscitated once they have expired have this instruction documented in a Living Will.
This document is usually posted by a Client’s bedside or in an area convenient for anyone
to see within the Client’s home. If your Client has this document, clarify with the family or
your Nurse Supervisor if this document is in place for both the home and hospital or the
hospital only. You need not call 911 if your Client has a DNR (Do Not Resuscitate) order.
Report directly to your Client’s Hospice Nurse or Constant Care for changes in the Client’s
condition.
If you report to work and your client is not home, does not answer, or refuses care, please
call the office immediately. The office staff will see if a reassignment is available for you
that day.
If you report to work or become ill or have an emergency that requires you to leave early,
call the office immediately. You will be required to stay with the client until relief staff
arrives.
www.commhealthcare.com
Page 18 of 89
GENERAL EMPLOYMENT RULES
You are the direct provider of care to our clients and represent our agency to the client, family
and friends. Because you work in the client’s home we expect you to adhere to our high standards
of personal conduct at all times. We expect you to use good judgment, common sense, and a high
regard for the rights of the clients in your care.
In your client’s home, you are not a guest. You are there to provide services for the client. Here are
some important rules to know when working at Community Home Health Care.
EMPLOYMENT AT WILL
We are happy to welcome you to The Agency. We sincerely hope that your employment
here will be a positive and rewarding experience. However, we cannot make any
guarantees about your continued employment. Your employment here is at will. This
means that you are free to quit at any time, for any reason. We are also free to
terminate your employment at any time, for any reason with or without notice, with or
without cause. No employee or The Agency’s representative, other than the CEO or
Administrator has the authority to change the at will employment relationship or to
contract with any employee for different terms of employment. Nothing in this Handbook
constitutes a contract or promise of continued employment.
IMMIGRATION COMPLIANCE
In compliance with the federal Immigration Reform and Control Act of 1986, as amended, the
Agency is committed to employing only individuals who are authorized to work in the United
States. Accordingly, each new Aide, as a condition of employment, must complete the
Employment Eligibility Verification Form I-9 and present acceptable documentation
establishing identity and employment eligibility.
If an Aide is authorized to work in this country for a limited time, the individual will be
required to submit proof of renewed employment eligibility prior to expiration of that period
to remain employed by the Agency.
CODE OF CONDUCT
To function effectively, every organization must develop policies and procedures to protect
its clients and to ensure that co-workers’ and the business’s rights are respected. Constant
Care is no exception. Generally, conduct that violates our policies, including those outlined in
this Handbook, or that may be unethical and/or illegal will not be tolerated.
While this Handbook cannot describe every possible situation or instance, below is a non-
exhaustive list of the types of conduct for which the Agency would impose strong disciplinary
action or even immediate termination:
• Client abuse/neglect or failure to report suspected abuse/neglect.
• Client abandonment.

www.commhealthcare.com
Page 19 of 89
• Violation of Constant Care’s policies prohibiting discrimination, harassment, and
retaliation.
• Violation of our No Smoking Policy, Drug and Alcohol Policy, Confidentiality Policy,
Code of Ethics, or other policies outlined in this Handbook.
• Violation of HIPAA or state law regarding disclosure of confidential Client
information.
• Insubordination or failure to obey reasonable instructions from a client or from
Constant Care.
• Falsifying employment, legal, or other records, including time sheets and records of
care, or other forms of dishonesty
• Stealing or attempting to steal employer, Aide, or client property.
• Excessive absenteeism or tardiness.
• No-call, no-show.
• Neglecting job duties during working time.
• Physical fighting or violence (actual or threatened) on employer or client property
at any time.
• Using offensive or profane language, especially towards or in the presence of clients
or clients’ family members.
• Bringing dangerous or unauthorized weapons onto client or Agency premises.
• Refusing to work required overtime.
• Bringing friends or family into the client’s home.
• Demonstrating incompetence or poor or sloppy work quality.
The above list is not-exhaustive, and the Agency may discipline or terminate a Aide for any
reason. In addition, the Agency may choose to impose any form of discipline it deems
appropriate under the circumstances, including termination for even a first violation.
Aides who are terminated by the Agency for disciplinary reasons or poor performance are
not eligible for rehire.
APPEARANCE AND DRESS CODE
Your appearance reflects the kind of person you are and the quality of work you do.
Appropriate, neat, clean clothing must be worn. The following are examples of DO’S and
DON’TS:
DO DON’T
Slacks/Capri’s Shorts
Skirts knee length or longer Mini Shirts
Scrubs
Tank Tops
Hair neatly tied back Do Rags
Solid Shoes/Sneakers Flip-flops, high-heels, sandals Short
sleeve shirts Halter tops
Tattered Jeans or cut off shorts
Your body should be clean and free of odor, please use deodorant. No strong perfume or
aftershave should be used. Hair must be clean and neatly combed. Long hair should be
fastened back and off the shoulders. Fingernails should be clean and reasonably short.
www.commhealthcare.com
Page 20 of 89
Excessive jewelry is not permitted. Identification badges are provided by the agency and
must be worn at all times. If you require modifications of our dress code standards due to
religious reasons, please speak to your Coordinator and inform them of the precise reason that
you are requesting the modification. If reasonable, such requests may be granted by the
Agency.
You will be sent home if you are not properly attired.
PHOTO IDENTIFICATION CARD
In accordance with New York State Health Department regulations, Community Home Health
Care is providing you with a Photo Identification card. This identification card must be
worn on your clothing at all times while you are working.
Lost or stolen cards must be reported to HR immediately. Failure to wear your ID badge or
excessive loss or damage to cards can lead to disciplinary action up to and including
termination.
Your identification card must be returned to this agency upon termination of your
employment.
CONFLICT OF INTEREST
In order to perform their duties with honesty and fairness and in the best interest of the Agency
and Aides must avoid conflicts of interest in their employment. Conflicts of interest may arise
from having a position or interest in or furnishing managerial or consultative services to any
concern or business from which the Agency obtains goods or services or with which it competes
or does business, from soliciting or accepting gifts, excessive entertainment or gratuities from any
person or entity that does or is seeking to do business with the Agency and from using Agency
property for personal or private purposes. Conflicts also may arise in other ways. If an Aide has
any doubt or any question about any of his or her proposed activities, guidance or advice should
be obtained from the Director of Human Resources.
WORKPLACE ADMINISTRATIVE SEARCHES
To assist in providing a reliable, efficient and productive work force for the proper care of Clients,
to assist in providing Aides with a safe working environment, to assist in the effective operation
of the Compliance Program and to supplement the Drug and Alcohol Policy, supervisors may
conduct unannounced administrative searches of Agency premises, offices, work areas, property
and equipment and the contents of such property and equipment. No Aide should have any
expectation of privacy on the Agency property or in their offices or work areas including lockers,
desks, cabinets, drawers, shelves or trash cans or in folders, envelopes or packages located on
Agency premises. In addition, searches of temporary space of live in aides at clients of the Agency
may be subject to search at the discretion of the Agency as a result of a complaint of a Client
whose property is occupied. Personal possessions or materials should not be brought to work if
they are of a sensitive or confidential nature. The Agency policy on Workplace Administrative
Searches may be obtained from the Department of Human Resources or designee. Other policies
permit monitoring of and access to computers by supervisors. The use of computers, e-mail and
access to the Internet must be reasonable and responsible.
FINANCIAL REPORTING
www.commhealthcare.com
Page 21 of 89
All financial reports, accounting records, research reports, expense accounts, time sheets and
other documents must accurately and clearly represent the relevant facts or the true nature of a
transaction. Improper or fraudulent accounting, documentation or financial reporting is not only
contrary to Agency policy, it may be in violation of applicable laws. Sufficient and competent
evidential matter or documentation shall support all cost reports.
PROTECTION OF ASSETS
The Agency will make available to Aides assets and equipment necessary to conduct Agency
business including such items as computer hardware and software, billing and medical records,
both hardcopy and in electronic format, fax machines, office supplies and various types of medical
equipment. Aides should strive to use Agency assets in a prudent and effective manner. The
Agency property should not be used for personal reasons or be removed from the Agency without
approval from a departmental manager. An Aide who believes that any medical equipment is not
operating properly nor has an inaccurate calibration should immediately report the problem to
his or her supervisor.
ANTI-COMPETITIVE CONDUCT
The Agency will not engage in anticompetitive conduct that could produce an unreasonable
restraint of trade or a substantial lessening of competition. Evaluation of anti-competitive
conduct requires legal guidance. Communication by Aides with competitors about matters that
could be perceived to have the effect of lessening competition or could be considered as collusion
or an attempt to fix prices should take place only after consultation with legal counsel.
FINANCIAL INDUCEMENTS
No Aide shall offer any financial inducement, gift, payoff, kickback, or bribe intended to directly
or indirectly induce, influence or reward favorable decisions of any government personnel or
representative, any customer, contractor or vendor in a commercial transaction or any person in
a position to benefit the Agency or the Aide in any way. Aides are strictly prohibited from
engaging in any corrupt business practice either directly or indirectly. No Aide shall make or offer
to make any payment or provide any other thing of value to another person with the
understanding or intention that such payment or other thing of value is to be used for an unlawful
or improper purpose. Appropriate commissions, rebates, discounts and allowances are
customary and acceptable business inducements provided that they are approved by
Administration and that they do not constitute illegal or unethical payments. Any such payments
must be reasonable in value, competitively justified, properly documented, and made to the
business entity to which the original agreement or invoice was made or issued. Such payments
should not be made to individual Aides or agents of business entities.
www.commhealthcare.com
Page 22 of 89
PERSONNEL FILES
Constant Care maintains an official personnel file for all Aides. The personnel file includes such
information such as the Aide’s job application, record of training, performance appraisals, salary
increases and other employment records.
Constant Care needs your help in keeping your personnel file accurate and up-to-date. Promptly
notify your Coordinator of any changes to your name, home address, telephone number and
emergency contact(s).
Personnel files are the property of Constant Care and access to this information is restricted.
Generally, only supervisors and management personnel who have a legitimate reason to view
information in a file are allowed to do so.
Under no circumstances will Constant Care permit reproduction of a personnel file (either
particular pages or the entire contents) or removal of a personnel file from the premises.
If you are applying for a mortgage or other credit, or have another reason to allow outsiders to
obtain information from your personnel record, you must provide Constant Care with written
authorization for release of information.
PERFORMANCE EVALUATIONS
Performance reviews are an ongoing communication between Aides and supervisors to provide
a clear understanding of what is expected in the job. A performance review provides an
opportunity for Aides to communicate any concerns they may have about their job or their future.
HHA’s are expected to have a working knowledge of permissible activities involved in their work.
If there is a question regarding an activity that may be beyond the scope of employment, please
call your Coordinator for help.
Annual Review
Aides’ performance will be reviewed at least once annually, on or around their anniversary date.
Other periodic reviews may be scheduled as an ongoing form of communication between Aides
and supervisors.
Performance Problems
In the event that an Aide demonstrates unacceptable behavior or has difficulty performing all of
the duties as assigned, the Administrator will work with the Aide to correct job performance.
PLAN OF CARE
You are under the direct supervision of a registered nurse on all cases. Prior to your arrival
on a case, a professional nurse will visit the client to evaluate the physical and emotional
needs of your client. Once the evaluation is complete, the nurse will develop a plan of care
with the client. The plan of care will explain exactly what your client’s needs are and what
your duties will be under that plan of care. It is very important that you perform only the
duties authorized by that plan of care. You are not permitted to change the plan of care or the
duties. If you do, you may be disciplined, including terminated.
If you observe any changes in your client’s condition, you must report such a change to your
nursing supervisor so amendments can be made. If you are asked to do something that is not
specified on the nurse’s care plan by the Client or their family, please call your Coordinator.
www.commhealthcare.com
Page 23 of 89
The duties on the plan of care should be reflected on your time slip. You cannot falsify the
duties performed on a shift.
The Nurse is available for you to discuss any problems as they arise regarding the plan of
care, and to help find solutions to those problems. Home visits are made by the nurse on a
regular basis to assure that client’s needs are being met. Also, the nurse will be coming out
to evaluate you and ensure that you are following the plan of care in a safe and efficient
manner.
REPORTING EMERGENCIES, ACCIDENTS, AND CHANGES
Reporting emergencies, accidents, and changes in Client condition is a key part of a
Aide’s duties.
For life-threatening emergencies, call “911” immediately. In the event of a client’s death,
expected or unexpected, please record accurately all data regarding the death. Aides shall
record the exact time and the events that happened. After calling 911, contact the office
for further directions.
If there is an accident, you (or the client) must call the office immediately. Following the
telephone call, you must document what took place and what was done on an Incident
Report Form and send your documentation to the office within 24 hours so that the Agency
can comply with New York State reporting requirements. You must also contact the office
as soon as possible to report on changes in client condition.
Some examples of accidents or changes that you must report to the office are:
• Client injury or illness
• Theft or Illegal activities in the home
• Injury or illness to yourself
• Unusual or dangerous client/family behavior
• Any occurrence requiring police or emergency service
• Change in client condition
• Client Hospitalization
• Client admitted to a Nursing Home/Rehab
• Out of Home Respite/Care
• Structural damage to the client’s home
• Client Non-compliance with medical care
• Unsanitary conditions in the client’s home (insect, rodent, etc.)
• Failure of Universal Precautions or an incident of exposure to blood, bodily
fluids or other infectious waste
• Your client has left their home
When you call the office, answer all questions thoroughly and follow instructions carefully.
The office staff will also need to fill out our special incident report form in addition to your
form and documentation. Accordingly, your cooperation with the office staff is essential!
Please see the Health & Safety section of this Handbook for more information.
TELEPHONE CALLS
www.commhealthcare.com
Page 24 of 89
No personal calls are to be made from the client’s phone unless for patient related business.
For example, reporting to your coordinator changes in patient’s condition, patient care
questions, 911, calls to M.D. office, etc.. If there is an emergency call to be made, please
reverse the charges to the person you are calling. If your family needs to reach you please
give them the office phone number and a message will be passed on to you.
o DO NOT give you home phone number to the client or client’s family.
o You can answer the client’s phone if you are working.
Cell phones should be turned off before you enter your client’s home. Do not answer your
cell phone while caring for a client. You may check you cell phone during break time or
when your shift is over.
STEALING
We will not tolerate theft from the agency, client or family. We will make every effort to
support any employee who is unjustly accused of stealing.
If you are accused of stealing property from the client, we will conduct a fair investigation.
Aides are expected to cooperate in such investigations and answer any questions. Refusal to
participate in such investigation or lying to a supervisor in the course of the investigation will
be grounds for termination.
If it is established through our investigation that an Aide is guilty of stealing, we will refer the
case to law enforcement. You may also be reported for theft by the client and their family.
Likewise, we reserve the right to report you to the home care aide registry for any egregious
misconduct, such as theft.
CRIMINAL ACTIVITY
All of our employees are required to go through the CHRC program- which requires a detailed
background check via the Department of Health. If an Aide is arrested, we may be required to
put you on administrative leave pending our review of the circumstances related to the
arrest. We will consider various factors, such as the nature of the alleged offense, and/or the
Aide’s explanation of the circumstances and their job responsibilities, when determining how
the arrest affects your employment, if at all.
CONFIDENTIALITY AND PRIVACY
You are never allowed to discuss any information about your client with any other person,
including your family, friends or co-workers. All information about your client is confidential
and the law prohibits you from disclosing this information to any third-party. Any issue or
information related to your cases and clients should be discussed only with your nursing
supervisor and/or the Coordinator.
If any person other than the client wishes to discuss the client’s condition, you must direct
them to your Coordinator. Do not give out names, phone numbers or address of any family
member of a Client, and do not discuss the medical or physical condition of the client or family
member with any third-party.

www.commhealthcare.com
Page 25 of 89
If you are experiencing a personal issue while working on a case or are being mistreated by
a Client, this should be addressed with your Human Resources Representative. Again this is
not to be discussed with anyone but the correct contact person. If you are not sure which
individual you should be reaching out to, simply ask for direction from the Human Resource
Representative. She will direct your call to that individual.
Aides may also learn Agency business information during their employment. The Agency
requires Aides to agree, as a condition of their employment with the Agency, to preserve the
Agency’s Confidential Information. This means that Aides cannot, directly or indirectly,
disclose, reveal, publish, or otherwise make available to any person or entity the Agency’s
Confidential Information. Whenever referred to in this Handbook, “the Agency’s Confidential
Information” will mean all trade secrets and other information not generally known to the
public, in whatever format, whether presently existing or developed in the future, relating
directly or indirectly to the Agency’s business, including the Agency’s intellectual property,
products and services of the Agency, the manner in which services are provided, advertised,
delivered, or designed, Client lists and Client data, referral lists, business strategies,
techniques, plans, contracts, terms of agreements, transactions, potential transactions, work-
in-progress, financial information, accounting information, pricing information, credit
information, market studies, sales information, revenue, costs, communications, research and
development, inventions, designs, studies, plans, specifications, patents, applications for
particular technologies, designs, business relationships of the Agency (including proposed
relationships with clients or referral sources, suppliers, distributors, licensees and licensors),
management systems, sales and marketing plans and strategies, terms of contracts with
clients or managed care plans and any other payor of services, referral history of a particular
referral source, contacts and information about contacts at payors or referral sources,
information regarding pending applications to payors, methods and processes, service
delivery information, information concerning the condition, treatment or financial history of
a client, and any protected health information. This list is not exhaustive, and the Agency’s
Confidential Information also includes other information that is marked or otherwise
identified or treated as confidential or proprietary, or that would otherwise appear to a
reasonable person to be confidential or proprietary in the context and circumstances in
which the information is known or used.
Aides may disclose the Agency’s Confidential Information in connection with the Aide’s work
at the Agency, as required by law, or if an owner of the Agency expressly authorizes such
disclosure in writing. Further, as a condition of being employed by the Agency, the Aide
agrees to take all reasonable precautions to safeguard the confidential nature of the Agency’s
Confidential Information and any other precautions with respect thereto which the Agency
may reasonably request. Aides will not reproduce or otherwise copy any of the Agency’s
Confidential Information other than as required in discharging their duties while employed
by the Agency. Aides agrees that all of the Agency’s Confidential Information shall be the sole
and exclusive property of the Agency and its assigns at all times, and Aides assign to the
Agency any rights Aides may have or somehow acquire in the Agency’s Confidential
Information.
After a Aide’s employment with the Agency ends, the Aide will not disseminate any of the
Agency’s Confidential Information unless such information is generally known in the trade or
industry, and such general knowledge is not the result of the Aide’s dissemination of the

www.commhealthcare.com
Page 26 of 89
Agency’s Confidential Information and the Aide provides the Agency with reasonable advance
notice of such dissemination. Aides agree to provide the Agency with written notice of any
and all attempts to compel dissemination of the Agency’s Confidential Information at least
five (5) working days before complying with any subpoena, order, or any other directive
seeking such Dissemination. In situations where it is not possible to provide five (5) working
days’ notice, Aides will notify the Agency of any attempt to compel dissemination of the
Agency’s Confidential Information as soon as possible.
EQUAL EMPLOYMENT OPPORTUNITY
The Agency is an equal opportunity employer and complies with all applicable federal, state,
and local fair employment practices laws. As such, the Agency strictly prohibits and does not
tolerate discrimination against Aides, applicants, contractors, subcontractors, vendors,
consultants, or any other person working for the Agency because of race, color, religion,
creed, national origin or ancestry, ethnicity, sex (including pregnancy), gender, age, physical
or mental disability, citizenship, past, current, or prospective service in the uniformed
services, genetic information, or any other characteristic protected under applicable federal,
state, or local law. All Agency Aides, other workers, and representatives are prohibited from
engaging in unlawful discrimination. This policy applies to all terms and conditions of
employment, including, but not limited to, hiring, training, promotion, discipline,
compensation, benefits, and termination of employment. This policy applies at the Agency’s
offices, at your work site(s), while performing work for the Agency off-site, and at Agency-
sponsored or work-related events or activities.
If you are subjected to or observe any conduct that you believe violates this policy, you must
promptly speak to, write, or otherwise contact your supervisor, the Administrator, or a
Human Resources Aide. These individuals will ensure that a prompt investigation is
conducted. Your complaint should be as timely as possible. While you can report at any time,
the Agency prefers that you submit your complaint within 30 days of the offending conduct
to allow for the most effective investigation possible. Your complaint should also be as
detailed as possible, including the names of all individuals involved and any witnesses. You
may be asked to confirm your complaint in writing. The Agency will investigate the facts and
circumstances of all claims of perceived harassment and will take prompt corrective action,
if appropriate. All complaints will be kept confidential to the maximum extent possible and,
where appropriate, Aide making the complaint will be advised of the final disposition of the
matter.
Any Aide or other worker, regardless of position or title, whom the Agency determines has
subjected an individual to discrimination or retaliation in violation of this Policy will be
subject to discipline, up to and including termination of employment.
AMERICANS WITH DISABILITIES POLICY
The Agency complies with the Americans with Disabilities Act (ADA), as amended, and all
applicable state and local fair employment practices laws, and is committed to providing
equal employment opportunities to qualified individuals with disabilities.
If you believe you need an accommodation because of your disability, you are responsible for
requesting a reasonable accommodation from the Human Resources Department. You may
make the request orally or in writing, but in the event of an oral request you may be asked to

www.commhealthcare.com
Page 27 of 89
confirm your request in writing. Requests for accommodations should include all relevant
information, such as:
• A description of the accommodation you are requesting.
• The reason you need an accommodation.
• How the accommodation will help you perform the essential functions of your job.
The Agency may ask you to provide supporting documents showing that you have a disability
within the meaning of the ADA and applicable state or local laws, and that your disability
necessitates a reasonable accommodation. If the information provided in response to this
request is insufficient, the Agency may require that you see a health care professional of its
choosing, at its expense. If you fail to provide the requested information or see the designated
health care professional, your request for a reasonable accommodation may be denied. The
Agency will keep confidential any medical information that it obtains in connection with your
request for a reasonable accommodation.
After receiving your request (and medical documentation where appropriate), the Agency
will engage in an interactive dialogue with you to determine the precise limitations of your
disability and explore potential reasonable accommodations that could overcome those
limitations. It may also be necessary to consult with your client(s) to determine the feasibility
and effectiveness of potential accommodations.
The Agency makes determinations about reasonable accommodations on a case-by-case
basis considering various factors and based on an individualized assessment in each
situation. The Agency strives to make determinations on reasonable accommodation
requests expeditiously, and will inform the individual once a determination has been made.
For New York City Aides, the Agency will make a written final determination to you
identifying any accommodation that is granted or denied.
RELIGIOUS ACCOMMODATIONS
The Agency complies with Title VII of the Civil Rights Act of 1964, and all applicable state and
local fair employment practices laws, and is committed to providing equal employment
opportunities to all individuals, regardless of their religious beliefs and practices or lack
thereof. Consistent with this commitment, the Agency will provide a reasonable
accommodation of an applicant’s or Aide’s sincerely held religious belief if the
accommodation would resolve a conflict between the individual’s religious beliefs or
practices and a work requirement, unless doing so would create an undue hardship for the
Agency.
If you believe you need an accommodation because of your religious beliefs or practices or
lack thereof, you should request an accommodation from the Human Resources Department.
You may make the request orally or in writing, but in the event of an oral request you may be
asked to confirm your request in writing. Requests for accommodations should include all
relevant information, such as:
• A description of the accommodation you are requesting.
• The reason you need an accommodation.
• How the accommodation will help resolve the conflict between your religious
beliefs or practices or lack thereof and one or more of your work requirements.

www.commhealthcare.com
Page 28 of 89
After receiving your request, the Agency will engage in an interactive dialogue with you to
explore potential accommodations that could resolve the conflict between your religious
beliefs and practices and one or more of your work requirements. The Agency may ask you
to provide additional information about your religious practices or beliefs and the
accommodation requested. If you fail to provide the requested information, your request for
an accommodation may be denied.
The Agency makes determinations about religious accommodations on a case-by-case basis
considering various factors and based on an individualized assessment in each situation.
The Agency strives to make determinations on religious accommodation requests
expeditiously, and will inform the individual once a determination has been made.
ANTI-RETALIATION POLICY
No one will be subject to, and the Agency prohibits, any form of discipline, reprisal,
intimidation, or retaliation for good faith reports or complaints of incidents of harassment of
any kind, pursuing any discrimination claim, or cooperating in related investigations. For
more information, please refer to the Anti-Retaliation Policy below.
A. Anti-Retaliation Statement
The Agency strictly prohibits and does not tolerate unlawful retaliation against any Aide or
other covered persons by any Aide. All forms of unlawful retaliation are prohibited, including
any form of discipline, reprisal, intimidation, or other form of retaliation for participating in
any activity protected by law. Protected activities include:
• Lodging a good faith internal complaint (written or oral) opposing unlawful
discrimination or harassment or complaining about violations of wage and hour law.
• Filing a good faith complaint of unlawful discrimination or harassment with the US
Equal Employment Opportunity Commission (EEOC) or a state or local Fair
Employment Practices Agency or in court.
• Participating in the Agency’s internal investigation into allegations of sexual
harassment.
• Supporting another Aide’s internal or administrative complaint of unlawful
discrimination.
• Filing a good faith complaint with the US Department of Labor, state wage and hour
Agency, or in court about wage and hour or pay practice concerns or participating in a
wage and hour investigation or audit.
• Requesting an accommodation under the Americans with Disabilities Act or applicable
state law.
• Requesting or taking leave under the Family and Medical Leave Act or applicable state
law.
The examples above are illustrative only, and not exhaustive. No form of retaliation for any
protected activity will be tolerated.
Any Aide, regardless of position or title, whom the Agency determines has subjected an
individual to retaliation in violation of this Policy will be subject to discipline, up to and
including termination of employment.
B. Complaint Procedure
www.commhealthcare.com
Page 29 of 89
If you are subjected to or observe any conduct that you believe violates this policy, you must
promptly speak to, write, or otherwise contact your supervisor, the Administrator, or a
Human Resources Aide. These individuals will ensure that a prompt investigation is
conducted.
Your complaint should be as timely as possible. While you can report at any time, the
Agency prefers that you submit your complaint within 30 days of the offending conduct to
allow for the most effective investigation possible.
Your complaint should also be as detailed as possible, including the names of all individuals
involved and any witnesses. You may be asked to confirm your complaint in writing. The
Agency will investigate the facts and circumstances of all claims of perceived retaliation and
will take prompt corrective action, if appropriate. All complaints will be kept confidential to
the maximum extent possible and, where appropriate, Aide making the complaint will be
advised of the final disposition of the matter.
SEXUAL HARASSMENT
The Agency is committed to maintaining a workplace free from all unlawful harassment. One
form of harassment prohibited by this Policy is sexual harassment. Sexual harassment is
unlawful, violates Agency policy, and will not be tolerated. The law prohibits coworkers and
third parties, as well as supervisors and managers, with whom Aides come into contact with,
from engaging in harassment.
Appropriate sanctions and/or disciplinary action, up to and including termination, will be
enforced against individuals engaging in sexual harassment and against supervisory and
managerial personnel who knowingly allow such behavior to continue.
While this specific policy addresses sexual harassment, harassment and discrimination
against persons of all protected classes is prohibited. In New York State, such classes include
age, race, religious denomination, color, national origin, sexual orientation, military status,
sex, disability, marital status, domestic violence victim status, gender identity and criminal
history.
A. Sexual Harassment Definition
Sexual harassment is a form of sex discrimination and includes harassment on the basis of
sex, sexual orientation, self-identified or perceived sex, gender expression, gender identity
and the status of being transgender. Sexual harassment includes unwelcome conduct which
is either of a sexual nature, or which is directed toward an individual because of that
individual’s sex, when:
1. Such conduct has the purpose or effect of unreasonably interfering with an individual’s
work performance or creating an intimidating, hostile or offensive work environment,
even if the complaining individual is not the intended target of the sexual harassment;
2. Such conduct is made either explicitly or implicitly a term or condition of employment;
or
3. Submission to or rejection of such conduct is used as the basis for employment decisions
affecting an individual’s employment.

www.commhealthcare.com
Page 30 of 89
Sexual harassment known as “hostile environment” consists of words, signs, jokes, pranks,
intimidation or physical violence which are of a sexual nature, or which are directed at an
individual because of that individual’s sex. Hostile environment harassment also consists of
unwanted verbal or physical advances, sexually explicit derogatory statements or sexually
discriminatory remarks made by someone in the workplace which are offensive or
objectionable to the recipient, which cause the recipient discomfort or humiliation, or which
interfere with the recipient’s job performance.
Sexual harassment known as “quid pro quo” harassment occurs when a person in authority
tries to trade job benefits for sexual favors. This can include hiring, promotion, continued
employment or any other term, condition or privilege of employment.
Sexual harassment can occur between males and females, or between persons of the same
sex. Sexual harassment that occurs because the target is transgender is also unlawful.
B. Sexual Harassment Examples
The following describes some of the types of acts that may be unlawful sexual harassment:
• Physical acts of a sexual nature, such as:
• Touching, pinching, patting, kissing, hugging, grabbing, brushing against another
Aide’s body or poking another Aide’s body;
• Rape, sexual battery, molestation or attempts to commit these acts.
• Unwanted sexual advances, propositions, or other sexual comments, such as:
• Requests for sexual favors accompanied by implied or overt threats concerning
the target’s job performance evaluation, a promotion or other job benefits or
detriments;
• Subtle or obvious pressure for unwelcome sexual activities;
• Sexually oriented gestures, noises, remarks, jokes or comments about a person’s
sexuality or sexual experience, which are sufficiently severe or pervasive to create
a hostile work environment.
• Sexual or discriminatory displays or publications anywhere in the workplace, such as:
• Displaying pictures, posters, calendars, graffiti, objects, promotional material,
reading materials or other materials that are sexually demeaning or
pornographic. This includes such sexual displays on workplace computers or cell
phones and sharing such displays while in the workplace.
• Hostile actions taken against an individual because of that individual’s sex, sexual
orientation, gender identity or status of being transgender, such as:
• Interfering with, destroying or damaging a person’s workstation, tools or equipment,
or otherwise interfering with the individual’s ability to perform the job;
• Sabotaging an individual’s work;
• Bullying, yelling, name-calling.
• Sex stereotyping – When conduct or personality traits are considered inappropriate
simply because they may not conform to other people’s ideas or perceptions about
how individuals of a particular sex should act or look.

www.commhealthcare.com
Page 31 of 89
The Agency’s policy also applies to harassment based on race, color, religion, national origin,
ancestry, ethnicity, creed, age, disability, citizenship, veteran and military status, marital
status, domestic violence victim status, genetic information, or any other characteristic
protected by law. Such harassment often takes a similar form to sexual harassment and
includes harassment that is:
• Verbal (e.g. epithets, derogatory statements, slurs, derogatory comments or jokes, or
obscene language).
• Physical (e.g. assault or inappropriate physical contact).
• Visual (e.g. displaying derogatory posters, cartoons, drawings or making derogatory
gestures).
• Online (e.g. derogatory statements in an e-mail or through any social media platform).
This list is illustrative only, and not exhaustive. No form of harassment will be tolerated.
C. Complaint and Investigation Procedure
Preventing sexual harassment is everyone’s responsibility. The Agency cannot prevent or
remedy harassment unless it knows about it. Anyone who witnesses, becomes aware of, or is
subjected to behavior that may constitute harassment or otherwise violates this Policy is
strongly encouraged to immediately report such behavior to their Coordinator. If an
individual is not comfortable reporting to their Coordinator, they should then report it to
Human Resources.
Reports of harassment or any other violation of this Policy should be made in writing, though
verbal reports will be accepted. A Complaint Form for the submission of reports of unlawful
harassment or any other violation of this Policy may be found in Human Resources. Any
report should be as detailed as possible and include the names of all individuals involved, a
description of the incident(s) complained of, the names of all witnesses, and any
documentation or other evidence that supports the allegations. If the report is verbal, the
complainant will be asked to complete a written Complaint Form. If he or she declines, the
Agency may prepare a Complaint Form based on the verbal report.
All supervisors and managers who receive a report or information about, observe, or suspect
any potential harassment or other violation of this Policy must immediately report it to
Human Resources. A supervisor or manager who fails to make such a report or otherwise
knowingly allows harassing or retaliatory behavior to continue will be subject to disciplinary
action, up to an including termination of employment.
The Agency will conduct an investigation of any report or complaint of harassment or any
other violation of this Policy that it receives. Investigations will be conducted in a prompt,
thorough, and timely manner, and will be confidential to the extent possible. The Agency will
take prompt and appropriate corrective action whenever it determines that harassment or
another violation of this Policy has occurred.
All persons involved in the Agency’s investigation will be accorded due process, as outlined
below. While the process may vary from case to case depending on the circumstances, an
investigation of a report of harassment or other violation of this Policy will generally include
the following steps:
www.commhealthcare.com
Page 32 of 89
o Upon receipt of a report of harassment or other violation of this Policy, the Agency
will conduct an immediate review of the allegations, and take any appropriate interim
action.
o Relevant information will be collected.
o Interview the complainant, witnesses, and the accused.
o Where appropriate, depending on the facts of each case, notify appropriate and/or
involved parties about the investigation, its outcome, and/or relevant information.
o Implement any remedial measures.
Aides are required to participate and answer truthfully any questions posed in an
investigation by the Agency.
D. Retaliation Prohibited
The Agency strictly prohibits and does not tolerate any retaliation against an individual
because he or she has in good faith made a complaint of harassment or testified or assisted
in a legal proceeding. Any Aide who believes that he or she has been subjected to retaliation
must immediately make a report to Human Resources.
E. Redress Rights and Adjudication Forums for Sexual Harassment
Sexual harassment is misconduct and will be grounds for discipline, including termination.
Sex harassment is unlawful under the New York Human Rights Law, the New York City
Human Rights Law, and the federal Civil Rights Act of 1964, Title VII. In addition, there may
be applicable local laws that prohibit harassment and sex discrimination.
A complaint alleging a violation of the Human Rights Law may be filed with either the Division
of Human Rights (DHR) or in New York State Supreme Court. DHR’s main office contact
information is: NYS Division of Human Rights, One Fordham Plaza, Fourth Floor, Bronx, New
York 10458. You may call (718) 741-8400 or visit: www.dhr.ny.gov
. Contact DHR at (888)
392-3644 or visit dhr.ny.gov/complaint for more information. A complaint alleging a
violation of Title VII may be filed with the Equal Employment Opportunity Commission
(EEOC) within three hundred days of the alleged harassment. Contact the EEOC by calling 1-
800-669-4000 (TTY: 1-800-669-6820), visiting their website at www.eeoc.gov or via email
at
info@eeoc.gov if you wish to file a complaint with the EEOC. Aides who work in New York
City may file a complaint of sexual harassment with the New York City Commission of Human
Rights (CHR), at 40 Rector Street, 10th Floor, New York, New York, by calling 311 or (212)
306-7450 or visiting
www.nyc.gov/html/cchr/html/home/home.shtml.
The remedies available to victims of sexual harassment vary depending on the circumstances
and the forum involved, but may include requiring the defendant(s) to take action to stop the
harassment, or redress the damage caused, including reinstatement/instatement to a job,
payment of monetary damages (e.g. back pay, out-of-pocket expenses), compensatory
damages, punitive damages in certain circumstances, reasonable attorneys’ fees, and civil
fines.
If the sexual harassment involves unwanted physical touching, coerced physical
confinement or coerced sex acts, the conduct may constitute a crime. Redress can be sought
by contacting the local police department.
www.commhealthcare.com
Page 33 of 89
SEXUAL HARASSMENT COMPLAINT FORM
If you believe that you have been subject to unlawful harassment or retaliation, you are strongly
encouraged to complete this form and submit it to Human Resources. Please complete all aspects of
this form in as much detail as possible. In particular, you are encouraged to include your name and
contact information, as anonymous complaints may be very difficult to investigate.
The Agency prohibits retaliation of any kind against an individual for making a complaint in
good faith.
Please use additional sheets of paper if necessary.
Your Name: _______________________________________ Your Title/Position: _____________________________
Your Phone Number: ____________________________ Your Coordinator’s Name:________________________
COMPLAINT INFORMATION
1. Name and title of any alleged harasser or retaliator:
Name: ________________________________________________ Title: ___________________
2. Details of the harassment or retaliation. Please include as much detail as possible, including what
happened, how it is affecting you and your work, and your reasons for believing that the conduct is
sexual or other harassment or retaliation.
__________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________
3. Date(s) of harassment or retaliation:
__________________________________________________________________________________________________________________
4. Please list the names and contact information of each witness or individual who may have
information related to your complaint:
__________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________
__________________________________________________________________________________________________________________
5. Identify any documents or other evidence that you believe substantiates your complaint of
harassment or retaliation. Attach any relevant documents and evidence.
__________________________________________________________________________________________________________________
I certify that I have read (or have had read to me) the foregoing complaint and know the contents of
this complaint; and that the foregoing is true and correct, based on my current knowledge,
information, and belief.
Signature: __________________________ Date: __________________

www.commhealthcare.com
Page 34 of 89
SOLICITATION AND DISTRIBUTIONS
In the interest of maintaining a proper business environment and preventing interference
with work and inconvenience to others, Aides may not solicit other Aides during working
time, or distribute literature during working time or at any time in working areas. Persons
not employed by Constant Care are prohibited from soliciting or distributing literature on
Agency and client property.
For purposes of this policy:
• Solicitation includes, but is not limited to, approaching someone in person or
through employer-owned property such as computers, smartphones, e-mail
systems, and intranets for any of the following purposes: offering anything for sale,
asking for donations, collecting funds or pledges, seeking to promote, encourage or
discourage participation in or support for any organization, activity or event, or
membership in any organization, or distributing or delivering membership cards or
applications for any organization.
• Distribution includes, but is not limited to, disseminating or delivering in person
or through employer-owned property such as bulletin boards, computers,
smartphones, e-mails, and intranets any literature or other materials including
circulars, notices, papers, leaflets, or other printed, written, or electronic matter
(except that distributing or delivering membership cards or applications for any
organization is considered solicitation and not distribution).
• Working time includes any time in which either the person doing the solicitation
(or distribution) or the person being solicited (or to whom non-business literature
is being distributed) is engaged in or required to be performing work tasks.
Working time excludes times when Aides are properly not engaged in performing
work tasks, including break periods and meal times.
• Working areas include areas where Aides are performing work, including Clients’
homes or premises.
ELECTRONIC MAIL, SOCIAL MEDIA AND INTERNET
Some Aides may use social media websites e.g. Face Book, Linked In, etc. as a medium of self-
expression and the Agency respects the right of Aides to use such sites. However, if an Aide
chooses to identify him or herself on such Internet venues, the following code of conduct is
expected:
• Aides must be professional, truthful and respectful in all communications and blogs. Aides
must not use obscenities, profanity, or vulgar language. Aides must not use blogs or
personal Web sites to disparage the Agency or share any confidential information or
information that is considered PHI under HIPAA. Aides may not use blogs or personal
Web sites to harass or intimidate other Aides, Clients, or Clients’ families.
• Aides may not use blogs or personal Web sites to discuss engaging in behavior that is
prohibited by Agency policies, including, but not limited to, the use of alcohol and drugs,
sexual activity, sexual harassment.
PHOTO WAIVER AND RELEASE
By acknowledging this Handbook you hereby consent to and authorize the Agency (a) taking
at any time, in the Agency’s discretion, my photograph, whether alone or with other people,
(b) using and re-using each such photograph in print, electronic or other media, or copies of

www.commhealthcare.com
Page 35 of 89
same for the Agency’s publications, advertising, marketing (including social media
marketing), publicity, promotions, public relations, and news media business activities,
including, but not limited to, the Agency’s website and in the Agency’s business development
or other promotional materials, including print, broadcast, and electronic media, including
social media. I can withdraw this consent at any time by notifying the corporate office. By
accepting employment with the Agency, I, and my successors and assigns, release and
discharge the Agency from each claim or cause of action arising out of or in connection with
its use of my photograph or name pursuant to this consent (including, without limitation,
each claim or cause of action arising under Section 50 of the New York Civil Rights Law).
DRUG AND ALCOHOL POLICY
To help insure a safe, healthy and productive work environment for all Aides, Clients and their
families and others, the Agency has adopted a policy maintaining a workplace free of drugs
and alcohol. This policy restricts certain items and substances from being brought to the
workplace and prohibits Aides from reporting to work or working under the influence of
illegal drugs, alcohol and other controlled substances which may affect their ability perform
work safely. An Aide who feels that he/she has a substance abuse problem is encouraged to
seek professional help. The Agency will also offer referral service to any Aide who voluntarily
requests help.
This policy includes pre-employment, post-incident, reasonable suspicion and annual testing
as well as searches and investigations to the extent permissible by law.
Rules
1. Processing, manufacturing, distribution, dispensing and/or the use of illegal drugs, drug
paraphernalia, unauthorized controlled substances, illegal use of legal drugs and other
intoxicants during work hours or in work areas is prohibited.
2. Reporting to or being at work under the influence of illegal drugs or unauthorized controlled
substances a prohibited. Reporting to and being under the influence of alcohol or other legal
intoxicant that can adversely affect an Aide’s performance or the safety of the Aide, those
surrounding the Aide is also prohibited.
3. Legally prescribed drugs may be permitted provided that the drugs are prescribed to the
Aide by an authorized medical practitioner for current use by the employer. Reporting to and
being at work under the influence of prescribed or over-the-counter drugs, where such use
prevents an Aide from performing the duties of the job, or poses a safety risk to other
persons or property is prohibited. Aides taking a prescription over-the- counter drug are
personally responsible for confirming with their physician that they may safely perform any
job duties while taking such items. Aides taking a legal substance that could impair their safe
work must advise their immediate supervisor, who may assign the Aide to non-hazardous
duties or send them home. An Aide’s failure to notify their supervisor at the start of their
work shift will result in disciplinary action up to and possible termination of employment.
4. The possession or use of alcohol during work hours or in a client’s home is prohibited.
5. Nothing set forth in this policy shall be construed as limitation upon the right to terminate
an Aide at any time and upon any reason and the right of the Aide to resign at any time for any
reason.
6. Any Aide who is found to be in violation of this policy will be subject to discipline up to and
including termination.

www.commhealthcare.com
Page 36 of 89
An Aide, to the extent consistent with applicable federal, state and local laws, will be required
to undergo a screening test for the use of illegal and non-prescription drugs, alcohol or other
substances under any of the following or other circumstances which may be determined by
The Agency under this policy:
1. Post Incident – If you involved in a work place incident resulting in personal injury to the
you, the client, or others, or damage to property or workplace, or circumstances which could
have resulted in personal injury to either the Aide or others, or damage to property when
there is a reasonable suspicion to believe that the incident has occurred due to drug or alcohol
use.
2. Reasonable Suspicion – When there is reasonable suspicion, satisfactory to the Agency’s
management, to believe that an Aide is under the influence of illegal drugs, unauthorized
controlled substance, alcohol or other intoxicants during work hours or while in the
workplace or that the Aide has reported to work under the influence of illegal drugs,
unauthorized controlled substances, alcohol or other intoxicants which could affect the safety
of the Aide and/or others.
3. Annual – When the Agency, upon its discretion, requires screenings on a yearly basis in
addition to any other screen that was given in that year.
Any Aide who tests positive for drugs or alcohol and who believe the test results are incorrect,
nay request a retest of the original specimen at his/her cost.
The Agency reserves the right to search any Aide or property for illegal drugs, drug
paraphernalia, unauthorized controlled substance, alcohol or other intoxicants. Agency may
have a third party complete the search (s). This shall include, but is not limited to, clothing,
personal effects, vehicles, buildings, offices, parking lots, desks, cabinets, locker, closets, lunch
boxes and equipment.
Aides who refuse to submit to testing as required by the Agency or who fail to complete the
test will be subject to discipline, up to and including immediate termination of employment.
Job applicants who refuse to submit to drug and alcohol testing will be deemed to have
withdrawn themselves from the application process and will no longer be considered for
employment.
COMPLAINT PROCEDURES
Questions or problems concerning your job should be brought up with your Coordinator. It
is expected that most difficulties will be satisfactorily resolved in this way. If for some reason,
a matter you discussed with the Agency staff is not resolved to your satisfaction, we have an
open door policy, which means that you can discuss any issues with the next level, a director.
If at this time you are still not satisfied with the decision, you may file a complaint with your
Coordinator and request that it be submitted to the Board of Directors. This review will take
place, and answered within a reasonable amount of time (not to exceed 30 days). The decision
rendered by the Board of Directors will be final.
You will find a complaint form at the end of this Handbook. You may also submit a
complaint on any piece of paper you have available. Please send all complaints to the
Quality Assurance Department.

www.commhealthcare.com
Page 37 of 89
For complaints that allege a violation of the law, you are required to follow the FAIR
program if you are not satisfied with the Board of Directors’ response. Thus, where your
complaint alleges a violation of the law, and the Board has rejected your complaint, you
are required to follow the FAIR Program if you wish to pursue your complaint and the
complaint alleges a violation of some law.
www.commhealthcare.com
Page 38 of 89
TIME AND ATTENDANCE – TIME OFF
The agency is open 24 hours a day, 7 days a week.
Call 845-425-6555 anytime.
TIME AND ATTENDANCE:
All personnel are expected to show up at their assignments on time, with proper identification
and dressed appropriately.
It is your responsibility to arrive at your assignment promptly at the start of the shift. If you
ae unable to cover your case for any reason, you must notify The Agency as early as possible
so that we can arrange for coverage.
You can call our office at any time, 24hours, and 7 days per week. Office hours are from 9.00
a.m. to 5.00 p.m. Monday through Thursday; Friday 9.00 a.m. to 1.00 p.m. In addition, The
Agency’s supervisor is on-call whenever the office is closed and can be reached by calling the
regular office number.
Failure to notify The Agency that you will be out sick, late, on vacation, etc. may be grounds to
terminate your employment. While we understand that situations arise which may stop or
delay you from working on a particular day, it is extremely important that such information
be known to The Agency.
TARDINESS:
Tardiness or failing to report to work as scheduled can be problematic for the clients. If an
Aide is sick or is going to be late, he /she must call the office main phone number at 845- 425-
6555. When calling, be sure to identify the reason for calling off or reporting to work late. If
you are working in New York City and you are calling off or reporting late due to one of the
reasons protected by the New York City Safe and Sick Time Law, please follow our policy in
this Handbook, which requires you to notify your Coordinator that you are absent or late due
to one of the reasons covered by the Law.
Do not call your Client directly. You are employed by the Agency not the Client.
You MUST NOT arrive late or leave early unless approved by the Agency.
Excessive and repeated tardiness without proper reasons will lead to termination.
FAMILY AND MEDICAL LEAVE
The Company provides leave according to the Family and Medical Leave Act of 1993 (FMLA) and the
New York Paid Family Leave (NYPFL) Law to covered employees in certain circumstances and as
more fully described in this policy.
Eligibility
To qualify for FMLA leave, you must: (1) have worked for the Company for at least 12 months; (2)
have worked at least 1,250 hours in the last 12 months; and (3) be employed at a work site where the
Company has 50 or more employees within 75 miles. If you have any questions about your eligibility
for FMLA leave, please contact the Human Resources Department.
www.commhealthcare.com
Page 39 of 89
To qualify for NYPFL, a New York employee whose regular schedule is 20 or more hours per week
must have worked for the Company for at least 26 consecutive weeks preceding the first full day
leave begins. A New York employee whose regular schedule is less than 20 hours per week must have
worked in the Company’s employment for 175 days to qualify for NYPFL. If you have any questions
about your eligibility for NYPFL, please contact the Human Resources Department.
Leave Entitlement
FMLA. You may take up to 12 weeks of unpaid FMLA leave in a 12-month period, which is
measured using a “rolling” method that is measured backward from the date you use any FMLA
leave, for any of the following reasons:
1. the birth of a son or daughter and in order to care for such son or daughter (leave to be
completed within one year of the child's birth);
2. the placement of a son or daughter with you for adoption or foster care and in order to care
for the newly placed son or daughter (leave to be completed within one year of the child's
placement);
3. to care for a spouse, son, daughter, or parent with a serious health condition;
4. for your own serious health condition which renders you unable to perform any of the
essential functions of your position; or
5. a qualifying exigency of a spouse, son, daughter, or parent who is a military member on
covered active duty or called to covered active duty status (or has been notified of an impending
call or order to covered active duty).
You may take up to 26 weeks of unpaid FMLA leave in a single 12-month period, beginning on the
first day that you take FMLA leave to care for a spouse, son, daughter, or next of kin who is a Covered
Service member and who has a serious injury or illness related to active duty service, as defined by
the FMLA's regulations (see Definitions section, Military Caregiver Leave subsection below).
NYPFL. You may take up to the following amounts of NYPFL, for the reasons listed below, in a 52
consecutive week period:
• Starting January 1, 2018: 8 weeks of leave;
• Starting January 1, 2019: 10 weeks of leave; and
• Starting January 1, 2021: 12 weeks of leave.
The 52 consecutive week period is measured using a “rolling” method that is measured backward
from the date you use any NYPFL.
NYPFL may be taken for the following reasons:
1. To care for a spouse, domestic partner, child, parent (including in-laws), grandparent, or
grandchild with serious health condition;
2. To bond with a child during the first 12 months after the child’s birth or placement for
adoption or foster care or to meet adoption or foster care obligations (leave to be completed
within one year of the child’s birth or placement); or
3. To meet qualifying exigencies arising from the fact that your spouse, domestic partner, child,
or parent is on active duty or “has been notified of an impending call to active duty” in the U.S.
Armed Forces.
Note that NYPFL is not available for the employee’s own serious health condition.
During NYPFL, paid benefits will be provided by the Company’s NYPFL insurance carrier, at the
following levels provided by law:
• January 1, 2018: 50% of the employee’s Average Weekly Wage (AWW), up to 50% of the NYS
Average Weekly Wage (NYS AWW).
• January 1, 2019: 55% of the employee’s AWW, up to 55% of the NYS AWW.
• January 1, 2020: 60% of the employee’s AWW, up to 60% of the NYS AWW.
• January 1, 2021: 67% of the employee’s AWW, up to 67% of the NYS AWW.
www.commhealthcare.com
Page 40 of 89
The NYS Average Weekly Wage is the average weekly wage paid across New York State during the
previous calendar year and is determined and published by the New York State Department of Labor
each year.
Pay under NYPFL is available from the first day of the leave (no waiting period). The insurance
carrier, not the Company, is responsible for approving and paying benefits under the NYPFL Law. To
receive such benefits, you will be required to file a claim with the carrier and to follow the carrier’s
requirements with respect to claim filing, certification, and supporting documentation (see NYPFL
Claim and Certification Procedure section below).
If you are eligible for leave under both the FMLA and the NYPFL, your leaves under both of
these laws will run concurrently to the maximum extent permitted by law.
Family Members Working for the Company
FMLA. Where eligible spouses both work for the Company, they will be limited to a combined total of
12 weeks of FMLA leave in a 12-month period for the birth/placement of and bonding with a child
and the care of a parent with a serious health condition. The spouses will also be limited to a
combined total of 26 weeks of FMLA leave in a 12-month period to care for a Covered Servicemember
with a serious injury or illness (see Definitions section, Military Caregiver Leave subsection below).
NYPFL. The Company will not permit more than one employee to take NYPFL at the same time to
care for the same family member (e.g., where both spouses or other qualifying relatives work for the
Company).
Definitions
Serious Health Condition – FMLA. For FMLA purposes, “serious health condition” means an illness,
injury, impairment, or physical or mental condition that involves: (a) inpatient care; or (b) continuing
treatment by a health care provider.”
Inpatient care means an overnight stay in a hospital, hospice, or residential medical care facility,
including any period of incapacity, as defined by the law, or any subsequent treatment in connection
with such inpatient care.
A serious health condition involving continuing treatment by a health care provider requires any one
or more of the following:
• A period of incapacity of more than three consecutive, full calendar days, and any
subsequent treatment or period of incapacity relating to the same condition, that also
involves: (a) treatment two or more times, within 30 days of the first day of incapacity,
unless extenuating circumstances exist, by a health care provider, a nurse under direct
supervision of a health care provider, or a provider of health care services (e.g., physical
therapist) under orders of, or on referral by, a health care provider; or (b) treatment by a
health care provider on at least one occasion which results in a regimen of continuing
treatment under the supervision of the health care provider;
• Any period of incapacity due to pregnancy or for prenatal care;
• Any period of incapacity or treatment for such incapacity due to a chronic serious health
condition;
• A period of incapacity which is permanent or long-term due to a condition for which
treatment may not be effective; and
• Any period of absence to receive multiple treatments (including any period of recovery
therefrom) by a health care provider or a provider of health care services under orders of, or
on referral by, a health care provider.
Serious Health Condition – NYPFL. For NYPFL purposes, “serious health condition” means illness,
injury, impairment, or physical or mental condition that involves: (a) inpatient care in a hospital,

www.commhealthcare.com
Page 41 of 89
hospice, or residential health care facility; or (b) continuing treatment or continuing supervision by a
health care provider.
A serious health condition involving continuing treatment or continuing supervision by a health care
provider requires any one or more of the following:
• More than 3 consecutive full days of inability to work, attend school, perform regular
activities, or other incapacity due to a condition, plus any subsequent treatment or period of
incapacity that involves treatment two or more times, or treatment at least once that results
in a regimen of continuing treatment under the supervision of a health care provider.
• Any period of inability to work, attend school, perform regular activities, or other incapacity
due to a chronic serious health condition that requires periodic visits for treatment by a
health care provider, continues over an extended period of time (including recurring
episodes of an underlying condition), and may cause episodic rather than a continuing
period of incapacity (e.g., asthma, diabetes, epilepsy).
• A long-term or permanent period of inability to work, attend school, perform regular
activities, or other incapacity due to a condition for which treatment may not be effective
(e.g., Alzheimer’s, severe stroke, or terminal disease). The family member must be under the
continuing supervision of, but need not be receiving active treatment by, a health care
provider.
• A period of inability to work, attend school, perform regular activities, or other incapacity
due to treatment (including any period of recovery therefrom) by a health care provider for
restorative surgery, or for a condition that would likely result in more than 3 consecutive full
days of incapacity without treatment (e.g., cancer, severe arthritis, kidney disease).
Qualifying Exigency. For purposes of both FMLA and NYPFL, “qualifying exigency” means a situation
arising out of the fact that the employee's spouse, child, or parent is a military member in the United
States Armed Forces, Reserves, or National Guard on covered active duty or who has been notified of
an impending call or order to covered active duty status (“Military Member”).
“Covered active duty,” for members of the Regular Armed Forces, means duty during deployment of
the Military Member with the Armed Forces to a foreign country. “Covered active duty,” for members
of National Guard or Reserves, means duty during the deployment of the Military Member with the
Armed Forces to a foreign country under a call or order to active duty in support of a “contingency
operation,” as defined by law.
A “qualifying exigency” exists where one of the following events occurs:
• Short-notice deployment. To address any issue that arises from the fact that the Military
Member is notified of an impending call or order to covered active duty, for a period of seven
(7) or less calendar days from the date of notification;
• Military events and related activities. To attend any official ceremony, program, or event
sponsored by the military that is related to the covered active duty or call to covered active
duty status of the Military Member, or family support or assistance programs and
informational briefings sponsored or promoted by the military, military service
organizations, or the American Red Cross that are related to the covered active duty or call
to covered active duty status of the Military Member;
• Childcare and school activities. To attend to certain childcare and school activities that are
necessitated by the Military Member’s active duty or call to active duty status, such as: (i)
arranging for alternative childcare; (ii) providing childcare on an urgent, immediate need
basis (but not on a routine, regular, or everyday basis); (iii) enrolling in or transferring to a
new school or daycare facility; and (iv) attending meetings with employees at a school or
daycare facility;

www.commhealthcare.com
Page 42 of 89
• Financial and legal arrangements. To make or update financial and legal arrangements to
address the Military Member’s absence while on covered active duty or call to covered active
duty status;
• Counseling. To attend counseling provided by someone other than a health care provider, for
oneself, for the Military Member, or for the biological, adopted, or foster child, a stepchild, or
a legal ward of the Military Member, or a child for whom the Military Member stands in loco
parentis, who is either under age 18, or age 18 or older and incapable of self-care because of
a mental or physical disability at the time that FMLA leave is to commence, provided that the
need for counseling arises from the covered active duty or call to covered active duty status
of the Military Member;
• Rest and recuperation. To spend time with a Military Member who is on short-term,
temporary, rest and recuperation leave during deployment for up to fifteen (15) calendar
days;
• Post-deployment activities. To attend arrival ceremonies, reintegration briefings and events,
and any other official ceremony or program sponsored by the military for a period of 90
days following the termination of the Military Member's covered active duty status; and to
address issues that arise from the death of a Military Member while on covered active duty
status;
• Parental care. To provide certain care to a Military Member’s parent who is incapable of self-
care, and where each instance of the care provided is necessitated by the Military Member’s
covered active duty. Covered activities provided to the parent of a Military Member under
this provision include: (1) arranging for alternative care for a parent of the Military Member;
(2) providing care for a parent of the Military Member on an urgent, immediate need basis;
(3) admitting or transferring the parent of a Military Member to a care facility; and (4)
attending meetings with employees at a care facility where the parent of a Military Member
resides or stays; or
• Additional activities. To address other events which arise out of the Military Member’s
covered active duty or call to covered active duty status, provided that Multisorb and
employee agree that such leave shall qualify as an exigency, and both agree to the timing and
duration of such leave.
FMLA Military Caregiver Leave. For purposes of Military Caregiver Leave under the FMLA, “Covered
Servicemember” means:
• A current member of the Armed Forces (including a member of the National Guard or
Reserves) who is undergoing medical treatment, recuperation, or therapy, is otherwise in
outpatient status, or is otherwise on the temporary disability retired list, for a serious injury
or illness (“Current Servicemember”);” or
• A veteran who: (1) is undergoing medical treatment, recuperation, or therapy for a serious
injury or illness; (2) was a member of the Armed Forces (including a member of the National
Guard or Reserves); (3) was discharged within the five-year period before the eligible
employee first takes FMLA leave to care for him or her; and (4) was discharged or released
from the Armed Forces under conditions other than dishonorable (“Covered Veteran”). An
eligible employee must commence leave to care for a Covered Veteran within five years of
the Covered Veteran’s active duty service.
For purposes of Military Caregiver Leave under the FMLA “serious injury or illness” means:
• In the case of a Current Servicemember, an injury or illness that was incurred by him or her
in the line of duty on active duty in the Armed Forces (or that existed before the beginning of
his or her active duty and was aggravated by service in the line of duty on active duty in the
Armed Forces) and that may render the Covered Servicemember medically unfit to perform
the duties of his or her office, grade, rank, or rating; and

www.commhealthcare.com
Page 43 of 89
• In the case of a Covered Veteran, an injury or illness that was incurred or aggravated by him
or her in the line of duty, while on active duty in the Armed Forces, and which manifested
itself before or after he or she became a veteran, and is:
1. A continuation of a serious injury or illness that was incurred or aggravated when
the Covered Veteran was a member of the Armed Forces and rendered him or her
unable to perform the duties of his or her office, grade, rank, or rating;
2. A physical or mental condition for which the Covered Veteran has received a VA
Service Related Disability Rating (“VASRD”) of 50 percent or greater and such
VASRD rating is based, in whole or in part, on the condition precipitating the need
for leave;
3. A physical or mental condition that substantially impairs the Covered Veteran’s
ability to secure or follow a substantially gainful occupation by reason of a disability
or disabilities related to military service or would do so absent treatment; or
4. An injury, including a psychological injury, on the basis of which the Covered
Veteran has been enrolled in the Department of Veterans Affairs Program of
Comprehensive Assistance for Family Caregivers.
Important limitation: If an employee does not take all of his or her 26 workweeks of leave entitlement
to care for a Covered Servicemember during the 12-month period, the remaining part of his or her 26
workweeks of leave is forfeited.
Maximum duration of leave in any 12-month period: The Military Caregiver Leave is applied on a per-
Covered-Servicemember, per-injury, basis such that an employee may be entitled to take more than
one period of 26 workweeks of leave if the leave is to care for different Covered Servicemembers or
to care for the same Covered Servicemember with a subsequent serious injury or illness, except that
no more than 26 workweeks of leave my be taken within any single 12-month period.
“Next of kin”: An employee is “next of kin” of a Covered Servicemember if he or she is the nearest
blood relative of the Covered Servicemember (other than the Covered Servicemember’s spouse,
parent, or child). Unless the Covered Servicemember has specifically designated in writing a
particular blood relative as his or her nearest blood relative for the purposes of the Military
Caregiver Leave, the following is the order of priority used to identify the nearest blood relatives of
the Covered Servicemember: (a) blood relatives who have been granted legal custody of the Covered
Servicemember; (b) siblings; (c) grandparents; (d) aunts and uncles; and (e) first cousins. When no
such designation is made, and there are multiple family members with the same level of relationship
to the Covered Servicemember, all such family members shall be considered the Covered
Servicemember’s next of kin and may take FMLA leave to provide care to the Covered
Servicemember, either consecutively or simultaneously. When such designation has been made, the
designated individual shall be deemed to be the Covered Servicemember’s only next of kin.
Intermittent and Reduced Schedule Leave
FMLA. If medically necessary, FMLA leave occasioned by a serious health condition may be taken
intermittently (in separate blocks of time due to a serious health condition) or on a reduced leave
schedule (reducing the usual number of hours you work per workweek or workday). Medically
necessary means that there must be a medical need for the leave and the leave can best be
accomplished through an intermittent schedule. FMLA leave may also be taken intermittently or on a
reduced leave schedule for a qualifying exigency relating to covered military service.
If FMLA leave taken intermittently is unpaid, the Company will reduce the employee’s salary based
on the amount of time actually worked. In addition, while an employee is on an intermittent or
reduced schedule leave, the Company may temporarily transfer him or her to an available alternative
position that better accommodates his or her leave schedule and has equivalent pay and benefits.
www.commhealthcare.com
Page 44 of 89
When intermittent FMLA leave is needed to care for an immediate family member or the employee’s
own illness, and is for planned medical treatment, the employee must attempt to schedule treatment
so as to minimize disruption to the Company’s operations. Employees should consult with the
Company prior to scheduling the treatment in order to arrange a schedule that best suits the needs of
the employee and the Company.
NYPFL. Eligible employees may take NYPFL intermittently in no less than daily increments. The
maximum number of days of NYPFL available to an employee is calculated based on the average
number of days the employee works per week. For example, aa worker with a schedule of 5+ days
per week can take up to the then-applicable maximum weeks of leave multiplied by 5 days (in 2018,
the maximum is 8 weeks, so the worker would be eligible for up to 40 days of leave in a 52-week
period). For an employee who works 3 days per week (60% of the work week) can receive only 60%
of the then-applicable maximum leave (in 2018, this would be 60% of 40 days, so the employee
would be eligible for up to 24 days of leave in a 52-week period).
Concurrent Leave. Where FMLA and NYPFL run concurrently, intermittent leave will be immediately
deducted from the employee’s FMLA entitlement. Because intermittent NYPFL is measured in daily
increments, intermittent leave will be deducted from the employee’s NYPFL entitlement each time
the hours taken under FMLA add up to the number of hours in an employee’s usual work day.
NYPFL Contributions and Waivers
Consistent with the NYPFL Law, the Company will fund the NYPFL insurance policy through
deductions from the pay of all employees, except those who have filed valid waivers in accordance
with this policy. The Company will make the maximum deductions permitted by law.
Employees whose regular schedule is 20 or more hours per week but who will not work 26
consecutive weeks, and employees whose regular schedule is less than 20 hours per week and who
will not work 175 days in a 52-consecutive-week period, may file a waiver of NYPFL benefits. Upon
filing a waiver, the employee will be exempt from making contributions to NYPFL and thus will not
be subject to payroll deductions. However, the employee will be ineligible for NYPFL benefits.
If the work schedule of an employee who has filed a waiver changes so that he or she will work 26
consecutive weeks, or 175 days in a 52-consecutive-week period, the waiver will be automatically
revoked within 8 weeks of the change. The employee will then be obligated to make contributions,
including any retroactive amounts due from date of hire.
Application for FMLA Leave and/or NYPFL
To take FMLA leave or NYPFL, an employee must provide the Company with advance notice of the
need for leave as follows:
• Foreseeable Leave. Where the need for leave is foreseeable (e.g., planned medical treatment,
expected birth or placement of a child, planned medical treatment for a serious injury or
illness of a family member, etc.), an employee must provide the Company with at least 30
days advance notice of the need for leave.
o If 30 days advance notice is not possible (e.g., because of lack of knowledge of
approximately when the leave will be required to begin, a change in circumstances,
or a medical emergency), the employee must at least provide notice as soon as
practicable under the circumstances. Normally, it should be practicable for the
employee to provide notice of the need for leave either the same day he or she
becomes aware of a qualifying event or the next business day.
o Whether FMLA leave is to be continuous or is to be taken intermittently or on a
reduced schedule basis, notice need only be given one time, but the employee shall
advise the Company as soon as practicable if dates of scheduled leave change or are
extended, or were initially unknown. To qualify for NYPFL, employees must provide
www.commhealthcare.com
Page 45 of 89
the Company with notice as soon as practicable before each day of intermittent
leave.
• Unforeseeable Leave. When the approximate timing of the qualifying event and the need for
leave is not foreseeable, the employee must provide notice as soon as practicable under the
facts and circumstances of the qualifying event. Absent unusual circumstances, it generally
should be practicable for the employee to provide notice 2 hours before a scheduled shift as
required by the Company’s policy. it should generally be practicable for the employee to
provide notice within two business days after learning of the need for leave.
An employee who fails to provide advance notice in compliance with these policies must explain
to the Company why he or she was unable to do so. Absent unusual circumstances, an
employee’s failure to follow these policies will result in FMLA leave and/or NYPFL being denied
or delayed.
The notice rules apply to each day of intermittent leave under the NYPFL. If an employee is planning
a medical treatment or a series of treatments under FMLA or NYPFL or is taking Military Caregiver
Leave under the FMLA, he or she must consult with the Company first regarding the dates of such
treatment to work out a schedule that best suits the needs of both the employee or the Covered
Military Member, if applicable, and the Company.
Applications for leave under FMLA and/or NYPFL should be submitted in writing to the Benefits
Administrator. Application forms are available in the Human Resources Department. In addition,
employees seeking NYPFL will be required to file a claim with the Company’s NYPFL insurance
carrier (see NYPFL Claim and Certification Procedure section, below).
Failure to provide proper notice of your need for FMLA leave and/or NYPFL may result in the denial
or delay of protected leave, depending on the particular facts and circumstances.
FMLA Certification Procedure
If an employee is requesting FMLA leave because of his or her own or a covered relation’s serious
health condition, the employee and the relevant health care provider must supply appropriate
medical certification. Employees may obtain Medical Certification forms from the Human Resources
Department. When an employee requests leave, the Company will notify him or her of the
requirement for medical certification and when it is due (at least 15 days after leave is requested). If
the employee provides at least 30 days' notice of medical leave, he or she should also provide the
medical certification before leave begins. Failure to provide requested medical certification in a
timely manner may result in denial of FMLA-covered leave until it is provided.
The Company, at its expense, may require an examination by a second health care provider
designated by the Company. If the second health care provider’s opinion conflicts with the original
medical certification, the Company, at its expense, may require a third, mutually agreeable, health
care provider to conduct an examination and provide a final and binding opinion. The Company may
require subsequent medical recertification. Failure to provide requested certification within the
required timeframe may result in delay of further leave until it is provided.
The Company also reserves the right to require certification from a covered military member's health
care provider if an employee is requesting military caregiver leave and certification in connection
with military exigency leave.
NYPFL Claim and Certification Procedure
To obtain NYPFL benefits, you must file a claim with the Company’s NYPFL insurance carrier on the
carrier’s prescribed form(s). The employee will also be required to provide the NYPFL insurance
carrier with sufficient certification of the need for leave and supporting documentation as provided
by the NYPFL Law, the relevant insurance policy, and the carrier’s own requirements. For example,
the employee may be required to provide:
www.commhealthcare.com
Page 46 of 89
• Certification from a health care provider regarding the serious health condition for which
the employee needs leave:
• Documentation such as a birth certificate establishing the birth of a child;
• Documentation such as court documents or placement letters establishing that the employee
is in the process of adopting or has adopted a child or is fostering a child; or
• Certification of military exigencies and supporting military orders.
When you inform the Company of the need for NYPFL, the Company will provide you with a copy of
the relevant claim form(s) and complete any employer portion(s). You can also obtain and file the
claim form(s) directly through our NYPFL insurance carrier, Standard Security, via phone: 800-
477-0087, website: sslicny.com. Contact the carrier if you have any questions about the forms and
documents you must submit in support of your claim for benefits.
Reporting While on Leave
While you are on NYPFL, you should notify the Company and/or the NYPFL insurance carrier as soon
as practicable (within two business days, if feasible) if there is any change in your circumstances or if
your dates of leave change or were initially unknown and become known or estimated.
Conditions of FMLA Leave and NYPFL
The following conditions apply to leave taken under FMLA and/or NYPFL pursuant to this policy,
except where otherwise required by applicable law:
An employee taking an approved leave of absence may not engage in other work or employment
during the leave of absence. If an employee engages in other work or employment during the leave of
absence, the employee will be considered to have violated the terms of the leave of absence, and to
have voluntarily terminated his or her employment with the Company.
An employee on approved leave who fails to return to work at the end of his or her leave will be
required to reimburse the Company for all health insurance premium payments expended by the
Company on the employee’s behalf during the leave, unless the reason the employee does not return
to work is due to: (a) the continuation, recurrence, or onset of a serious health condition of the
employee or the employee’s spouse, son, daughter, or parent; (b) the serious injury or illness of a
spouse, son, daughter, or parent, or next of kin, who is a Covered Servicemember; or (c) other
circumstances beyond the employee’s control.
Employees will not receive holiday pay during leave except as required by applicable law.
An employee may be subject to termination during a leave for reasons including but not limited to
falsification of reason for or status of the circumstances surrounding the leave of absence.
If business conditions require a reduction in force, employees on an approved leave of absence will
be considered for lay-off and treated in the same manner as active employees.
Employee Compensation and Benefits during FMLA and/or NYPFL
Compensation during FMLA. As noted above, FMLA leave is unpaid. However:
Nothing in this policy prevents an employee from applying for worker’s compensation or NYS
Disability benefits. Leave which is covered by workers’ compensation or disability benefits will be
designated as FMLA leave to the maximum extent permitted by law.
www.commhealthcare.com
Page 47 of 89
Employees not receiving workers’ compensation, disability (including NYS short term disability), or
NYPFL benefits will be required to use their accrued PTO and Sick hours during FMLA leave, and
such leaves will run concurrently with the employee’s FMLA leave. Employees will also be required
to use any accrued PTO and sick hours during any waiting periods for disability benefits or workers’
compensation benefits.
Compensation during NYPFL. As noted above, NYPFL is paid by the Company’s NYPFL insurance
carrier in accordance with the insurance policy, the maximum benefits set forth in the law, and the
carrier’s own rules and procedures.
Where leave is taken under NYPFL, the employee may but is not required to use accrued PTO or sick
hours during the leave. Use of accrued PTO or sick hours will allow the employee to receive full pay
during the leave until paid time off is exhausted.
Where an employee is paid for accrued PTO or sick hours during NYPFL (whether concurrent with
FMLA or not), the Company will be entitled to receive the NYPFL payment from the NYPFL carrier as
reimbursement for the NYPFL portion of the amount paid to the employee. In no event shall an
employee’s use of accrued PTO or sick hours during NYPFL result in the employee’s receipt of more
than 100% his or her average weekly wage.
Health Insurance during FMLA and/or NYPFL. To the extent required by law, the Company will
maintain group health insurance benefits for employees on FMLA leave and/or NYPFL on the same
basis as coverage would have been provided if the employee had been actively working during the
leave period. Any share of group health plan premiums which had been paid by the employee prior to
leave must continue to be paid by the employee during the leave period. Where the employee is
receiving pay directly from the Company (i.e., using sick, personal, or vacation time), deductions for
group health insurance will continue to be made on the same basis as if the employee was actively
working. Where the employee is not receiving pay from the Company, arrangements will be made for
employees to pay their share of the group health insurance premiums while on leave. If the Company
pays the employee’s share of any premium payments, the Company reserves the right to recover the
full value of those payments made in any manner permitted by law.
An employee whose health insurance coverage is maintained pursuant to this policy during an
approved FMLA and/or NYPFL leave will be subject to any changes in the Company’s group health
plan that occur while he or she is on leave (e.g., changes in coverage, premiums, deductibles).
If an employee’s premium payment is more than thirty (30) days late while the employee is on FMLA
leave and/or NYPFL, his or her group health insurance benefits may be terminated and the employee
will be extended continuing coverage opportunities in accordance with COBRA. However, if coverage
is terminated for this reason and the employee returns to work from FMLA leave, the employee’s
group health insurance benefits will be reinstated, to the same extent the employee would have been
entitled to those benefits had he or she not taken leave.
If an employee gives unequivocal notice of his or her intent not to return to work, the Company’s
obligation to continue group health insurance benefits will cease, subject to COBRA.
Other Benefits. An approved FMLA leave and/or NYPFL pursuant to this policy will not result in the
loss of any employment benefit that may have accrued before the date the leave of absence started.
For all periods when an employee uses accrued PTO or sick hours concurrently with FMLA or NYPFL,
benefits that are accumulated on an accrual basis will continue to accrue to the extent they would
have otherwise, and deductions for group health insurance will continue to be made on the same
basis as if the employee was not on leave. Employees will not accrue or receive any benefits (other
www.commhealthcare.com
Page 48 of 89
than group health insurance benefits as noted above) for periods where FMLA and/or NYPFL is not
run concurrently with use of the employee’s accrued PTO or sick hours
Return from an Approved FMLA Leave and/or NYPFL
Unless the employee’s employment was or would have been terminated for reasons unrelated to the
leave (e.g., reorganization, lay off, reduction in force, etc.), the Company will restore an employee
who returns from approved FMLA and/or NYPFL leave to the same position that the employee held
prior to the leave or to an equivalent position with substantially similar duties, conditions,
responsibilities, privileges, and status as the original position, subject to the terms, limitations, and
exceptions provided by law.
Before returning from an approved FMLA leave granted as a result of an employee’s own serious
health condition, an employee must present a written fitness-for-duty certification from his or her
medical care provider. An employee’s failure to provide such certification at the time the employee
attempts to return to work may result in a delay or denial of job restoration.
Employees are expected to return to work when the FMLA leave and/or NYPFL ends, unless an
employee requests and is granted an extension of leave as an accommodation or pursuant to another
Company policy. If an employee does not return to work on the agreed upon date after expiration of
FMLA leave and/or NYPFL, and an extension of leave was not granted to the employee, the employee
will be considered to have voluntarily terminated his or her employment.
With respect to certain “highly paid” or “key” employees, there may be specified and limited
circumstances under which the Company may refuse to reinstate such individuals following FMLA
leave. This determination will be made in accordance with applicable law.
Further Information
Employees wanting further information regarding this policy should consult with the Human
Resources Department.
The Company will not interfere with, restrain, or deny an employee the exercise of any right
provided under the FMLA or discriminate against any person for opposing any practice made
unlawful by the FMLA or for being involved in any proceeding under or relating to the FMLA. If a
prohibited act has occurred, or the FMLA was not followed, a complaint may be filed with the United
States department of labor or a private action instituted.
The Company will not discriminate or retaliate against an employee because he or she claimed
NYPFL benefits, attempted to claim NYPFL benefits, or testified or is about to testify in a proceeding
under the NYPFL Law.
This policy is intended to implement the FMLA and the NYPFL and their accompanying regulations.
To the extent this policy is inconsistent therewith, the law and regulations will govern. Further, to the
extent any state or local law provides for additional leave benefits, the Company will comply with any
such requirements.
SICK DAYS
If you are sick, it is imperative that you call the office directly. If you need to get in touch with
the on-call supervisor after hours, call the office number 845-425-6555 and the answering
service will get in touch with us. When leaving a message with the answering service you must
wait for a call back. if you did not receive a call back, we did not receive your message.

www.commhealthcare.com
Page 49 of 89
If you are out sick, you must inform The Agency if you will be returning to work the next day.
This contact is to be made by 5.00 p.m. of each day that you are out. If you do not have contact
with The Agency office personnel before 5.00 p.m. we will automatically assume that you are
(take out not) going to work the next day. Should you report to work without contacting the
office, you will not be paid. You will be expected to leave the patient’s home and immediately
contact the agency for further instructions.
- If an employee is out for 3 or more days, a doctor’s note must be provided upon return to
work, explaining the reason for the absence.
- An employee must provide an indication of when he/she will be able to work when calling
off from work.
- Employees will not be paid for time not worked with the exception of approved and
documented leave time as defined under the Benefits Section of this handbook.
- Aides who need additional leave beyond 3 days are expected to make the request for such
leave affirmatively to their Coordinator and discuss their need for additional leave. The
Agency may request additional information from you at that point. You are expected to work
with your Coordinator and/or other Agency representative who is requesting the information
in order to evaluate your leave request. To the extent leave from work is granted, Aides must
keep their Coordinator apprised of their circumstances and ongoing leave from work at least
weekly (unless a different arrangement is made pursuant to FMLA or other laws). Failure to
provide timely updates will lead to termination based on job abandonment.
PAID SICK TIME POLICY FOR NYC AIDES
All Aides begin to accrue sick leave on their first day of work, but are not eligible to begin
using sick leave until 120 days after the start of their employment. In addition, an Aide must
work at least 80 hours in New York City in a calendar year to be eligible to use sick time.
Aides accrue sick leave at a rate of 1 hour for every 30 hours worked, up to 40 hours in a year,
and may use sick leave as it is accrued (after 120 days after the start of employment, and
completion of at least 80 hours). The Employer uses a calendar year basis for all accrual.
Aides will be paid the same rate for sick pay as they would have earned had they worked
those hours, for the scheduled hours that day. Sick time may be requested in ½ day
increments (4-hour minimum and, beyond the 4-hours, increments of 30 minutes or more as
needed); an Aide scheduled for up to 8 hours of work may use 8 hours of accrued sick pay (if
he or she has accrued that much); an Aide scheduled for up to 12 hours of work may use 12
hours of accrued sick pay (if he or she has accrued that much).
Aide will be paid for sick time used no later than the payday for the next regular payroll period
beginning after the sick time was used by the Aide.
A maximum of 40 hours may be used in any calendar year.
Aides may use sick leave only for authorized uses under the Law and the Rules, including:
a. The Aide’s mental or physical illness, injury, or health condition;
b. The Aide’s need for medical diagnosis, care, or treatment of a mental or physical
illness, injury, or health condition;
c. The Aide’s need for preventive medical care;
d. The Aide's elective surgery, including organ donations;

www.commhealthcare.com
Page 50 of 89
e. Care of a family member who needs medical diagnosis, care, or treatment of an
illness, injury, or health condition, or who needs preventive medical care;
f. Care of a family member who has elective surgery, including organ donations;
g. Closure of Aide’s workplace due to a public health emergency (as declared by the
Commissioner of the New York City Department of Health and Mental Hygiene or the
Mayor);
h. The Aide’s need to care for a child whose school or child care provider is closed due
to a public health emergency; or
i. “Safe time.” For purposes of this policy, “safe time” means time that Aide may take
off from work: (a) To obtain services from a domestic violence shelter, rape crisis
center, or other shelter or services program; (b) to participate in safety planning,
temporarily or permanently relocate, or take other actions to increase the safety of
the Aide or Aide’s family members from future harm; (c) to meet with an attorney or
other social service provider to obtain information and advice on, and prepare for or
participate in, any criminal or civil proceeding, including matters related to a family
offense matter, sexual offense, stalking, human trafficking, custody, visitation,
matrimonial issues, orders of protection, immigration, housing, discrimination in
employment, housing or consumer credit; (d) to file a complaint with law
enforcement; (e) to meet with a district attorney’s office; (f) to enroll children in a
new school; or (g) to take other actions necessary to maintain, improve, or restore
the physical, psychological, or economic health or safety of the Aide or the Aide’s
family member.
For purposes of this policy, a family member means a child (biological, adopted, or foster
child; legal ward; child of an Aide standing in loco parentis), grandchild, spouse, domestic
partner, parent, grandparent, child or parent of an Aide’s spouse or domestic partner, and
sibling (including a half, adopted, or step sibling).
Aides must give as much notice as practical in the circumstances for use of sick leave, but not
less than 7 calendar days’ notice for foreseeable or pre-scheduled absence. However, where
it is not feasible to give significant advance notice, such as emergencies or sudden unexpected
conditions, the Aide must notify their Coordinator as soon as practicable in the
circumstances. Failure to give proper notice, where notice is possible, may result in denial of
the leave or disciplinary action.
An employer may be asked to confirm, in writing or otherwise, that sick time was taken
pursuant to the NY Sick Leave law. Use of sick time for reasons not covered by the NY Sick
Leave law will be subject to disciplinary action.
Aides may be required to submit documentation signed by a licensed health care professional
for an absence of more than three consecutive work days.
Up to 40 hours of unused accrued time will be carried over to the next calendar year, and will
be available to use as of January 1, subject to the limit of 40 hours use in any calendar year.
If an Aide leaves the Agency, and returns within 6 months, any accrued unused time will be
retained. Sick time will not be paid out upon voluntary or involuntary termination of
employment.

www.commhealthcare.com
Page 51 of 89
Excessive absenteeism (apart from proper use of Sick Leave), failure to properly call in
advance of leave (except where not possible in circumstances like emergencies), or patterned
absences may be subject to disciplinary action.
Please feel free to contact Human Resources with any questions you may have about Paid
Sick Leave, or to find out how many hours you have accrued or used.
LEAVE OF ABSENCE:
An employee wishing to take a leave of absence is required to do so in writing. The agency
requires a minimum of two (2) weeks’ notice, and will allow you a three (3) month
absence. If you require an extension, it must be done in writing. If the absence is covered by
the Family and Medical Leave Act, the NYS Paid Family Leave, or other types of leave and you
are eligible under those laws for leave, the Agency will designate the leave as such leave and
you will receive the proper paperwork. To the extent you are not covered by any law, such
as FMLA, or you have exhausted your leave entitlement under applicable laws (such as
FMLA), the Agency will provide you with up to six (6) months of unpaid leave, provided that
(a) there is not an effective alternative accommodation that allows the Aide to remain at
work, and (b) such leave does not pose an undue hardship.
If requesting a leave for medical reasons, the Agency may request appropriate medical
information to verify the Aide’s medical condition and need for leave. Failure to provide the
information requested by Agency may result in the delay or denial of the requested leave.
Consistent with applicable law, the Agency also reserves the right to require Aides to submit
to an examination by a medical professional it selects.
A leave of absence granted pursuant to this policy will be unpaid, but an Aide may use any or
all of his or her accrued paid time off during such leave. While on a leave of absence under
this policy, Aides may be eligible for short-term disability and/or long-term disability
insurance benefits, subject to and in accordance with the plan documents governing such
benefits [confirm]. Group health benefits (e.g., medical insurance) will be available to Aides
at their own expense, subject to and in accordance with COBRA. All benefits that operate on
an accrual basis (e.g., paid time off) will cease to accrue during any portion of leave that is
unpaid.
Where an Aide’s request for leave does not specify an exact or fairly specific return date (e.g.,
October 4 or around the second week of November), or where the Aide requires additional
leave beyond what was originally granted, the Agency may require the Aide to provide
periodic updates on his or her condition and possible date of return.
The Agency may require Aides seeking to return to work following a leave to provide
appropriate medical information and/or require the Aide to submit to a medical examination,
consistent with applicable law.
After your absence and before returning to work all missed in-services must be made up, and
all compliance issues rectified. You cannot return to work until the human resources
specialist has approved that you are in compliance with all the legal requirements for taking
on a case (e.g., immunization requirements). Failure to comply with these requirements will
result in termination.
www.commhealthcare.com
Page 52 of 89
Upon your return to work, the Agency will make every effort to provide you with as close to
or similar work as you had before your leave. There is no guarantee that you will return to
your previous client.
If you are away or out of the county, you are still responsible to contact the office. Not
returning to work when scheduled to return will result in termination. If Aide does return at
a future date, the Aide will be considered a new hire, and all documentation, benefits and
wages will be granted as a new Aide.
If an Aide is unable to return to work following the exhaustion of the leave provided under
this policy, the Aide will be deemed to have abandoned his or her job, with the exception of
Aides who were under a leave of absence due to a disability. For such Aides, the Aide must
request and receive an accommodation under the Agency’s Americans with Disabilities Act
policy. Each request for such an accommodation under the ADA policy will be evaluated on
a case-by-case basis, and the Agency may request appropriate medical information to verify
the Aide’s medical condition and need for additional leave. Failure to provide the information
requested may result in the delay or denial of the requested leave.
TAKING OFF/UNPAID VACATION:
Vacation requests must be approved by the Coordinator and done at least two (2) weeks
in advance. Your request may be declined if there is not adequate coverage. Therefore,
you can request time off as soon as you make your plans but must remind the Client Service
Specialist two (2) weeks prior to your leave.
NURSING MOTHERS
In consideration of working mothers who may be lactating, the Agency will provide a
reasonable amount of break time to accommodate an Aide desiring to express breast milk for
her child (infancy up to three years of age). If possible, lactation breaks should be taken
during the breaks already provided to the staff member. Any additional breaks taken to
express milk may be unpaid.
An Aide who needs lactation breaks should speak to the Coordinator and the client to arrange
for break time and so that reasonable efforts can be made to provide a room or other location
for the staff member to express milk in private. The Agency prohibits discrimination on the
basis of the need to express breast milk.
Aides may be able to begin work before the regularly scheduled start of their shift or continue
working past the regularly scheduled end of their shift to make up any time used for unpaid
lactation breaks. Aides who wish to do so should speak with the office administrator in
advance to make appropriate arrangements.
JURY DUTY:
If an employee is called to jury duty, he/she must notify the coordinator and submit a copy of
the Notice to Serve. If an employee reports for jury duty and is excused, The Agency requests
that he/she return to work to complete his/her regular workday.
www.commhealthcare.com
Page 53 of 89
If an employee does indeed serve as a juror he/she should submit proof of service. The agency
will then reimburse the first forty dollars of such juror`s daily wages during the first three days
of jury service.
MILITARY LEAVE
Aides who are required to fulfill military obligations in any branch of the Armed Forces of the
United States or in State military service will be given the necessary time off and reinstated in
accordance with federal and state law. The time off will be unpaid, except where state or federal
law dictates otherwise. Accrued paid time off may be used for this leave.
Military orders should be presented to the Coordinator and arrangements for leave made as early
as possible before departure.
You must notify your Coordinator of your intent to return to employment based on requirements
of the law. Your benefits may continue to accrue during the period of leave in accordance with
state and federal law.
TIME OFF TO VOTE
If an Aide is qualified to vote and desires to do so but his or her normal work hours make voting
impossible, the Aide should notify his or her Coordinator in writing not more than ten, nor fewer
than two, working days before the day of the election. The written statement should include the
reasons why the Aide finds it impossible to vote before or after his or her normal work hours.
The Coordinator will review the statement and inform the Aide of what alternate arrangements
can be made to allow him or her to vote and whether the Aide is entitled to time off with pay, up
to two hours, to vote.
Exempt Aides may be provided additional time off with pay when necessary to comply with state
and federal wage and hour laws..
LEAVE FOR BONE MARROW DONATION
Unless otherwise required by applicable law, upon request, eligible Aides will be given unpaid
leaves of absence to undergo a medical procedure to donate bone marrow. The combined length
of the leaves will be as determined by the physician conducting the procedure, but may not
exceed twenty-four work hours, unless otherwise agreed by the Agency.
Aides will be required to provide documentation from the physician conducting the procedure to
verify the need for and length of bone marrow donation leave. Retaliation for requesting a leave
of absence for purposes of donating bone marrow is prohibited
LEAVE FOR BLOOD DONATION
Unless otherwise required by applicable law, upon request, Aides working 20 or more hours per
week on average will be given three (3) hours of unpaid time off in each 12 month period to
donate blood. Aides must obtain approval from their Coordinator prior to scheduling an
appointment to donate blood. The Agency may, due to business necessity, deny a request for a
particular leave time and require that the leave be taken at a more appropriate time.
Aides will be required to provide documentation to verify blood donation leave. Retaliation for
requesting a leave of absence for purposes of donating blood is prohibited.

www.commhealthcare.com
Page 54 of 89
RESIGNATION
If you resign from your employment with the agency, you are expected to give a minimum
of two (2) weeks’ notice.
You are expected to work a minimum of one (1) day per 12 month period. If you do not work
at least 1 day, in-service is not considered working, it will be considered as you voluntarily
resigned.
www.commhealthcare.com
Page 55 of 89
WAGE AND PAYROLL INFORMATION
The Agency and you are required to keep accurate records of time worked in order to calculate Aides’
pay. You will be paid on a weekly basis. You must submit a written timesheet AND the clock-in
verification system must be used.
The week starts on Saturday 12am and ends on Friday 11:59pm. Timesheets should be filled out
accordingly and hours should be accounted for based on a Saturday to Friday week schedule.
As a general matter, Aides are only permitted to work those hours that were authorized for the Client
to receive care from the Agency. Of course, the Agency understands that exceptions and
circumstances beyond the Aides’ control will arise from time to time. For example, if a Aides is
required to stay longer than their scheduled shift because the relief Aides has not arrived, the Aide
will be paid for the additional time that he/she renders services to the Client. However, Aides can
never approve additional hours for themselves, and the Clients cannot extend Aides’ hours of work.
The Coordinator should be immediately contacted before the Aides undertakes performing any
additional work beyond your scheduled shift time.
Unless otherwise instructed, staff is not permitted to work or provide services to Clients while the
Client is admitted into a hospital.
As noted above, depending on the client’s needs, an Aide may need to wait for replacement staff
before you can leave at the end of your shift. If the replacement staff is more than 15 minutes late,
the Aide should call the office. The Agency will make every effort to locate the replacement staff and
call the Aide back with an explanation and/or substitute. Aides are required to remain with the client
until arrangements can be made to meet the client’s needs.
You are not permitted to work anywhere else at the same time you are working for your client. You
may not work for the client more than the allotted hours as set forth by the Coordinator.
WAGES
Your hourly rate shall be initially determined at the time of employment. You will be notified at the
time of hire of your basis of pay (salary, hourly) and your pay rate. Salaries and/or wages may be
changed from time to time at the Agency’s determination.
In addition, Aides will receive, for all Wage Parity cases, a Wage Parity benefit and/or cash in lieu of
a benefit for the first 40 hours of work. Any work performed beyond 40 hours in a workweek will be
paid at one and one-half times the regular rate of pay. Wage Parity will not be paid for hours worked
above 40 per week. The Agency will also comply with any applicable local living wage and wage parity
laws.
If you have any questions regarding your compensation, please contact your HR Representative.
OVERTIME
Non-exempt Aides will receive overtime pay in accordance with applicable federal and state law at a
rate of one and one-half times their regular rate of pay for all hours worked over 40 hours in any
www.commhealthcare.com
Page 56 of 89
workweek. Overtime pay is based on hours actually worked. Any overtime work must be approved
by your Coordinator before the overtime hours are worked. Failure to comply with this requirement
may subject you to discipline.
Overtime will be paid based on the Aides’ “regular rate of pay.” The regular rate of pay may vary
from week to week if the Aide works jobs that have different or multiple rates of pay. If you ever
have questions about how your overtime rate was computed, please come and speak with us.
PAYROLL ERRORS
You should review your payroll checks for errors. If you believe there are errors in your pay,
including that you have been overpaid or underpaid, that improper deductions have been taken from
your pay, or that your pay does not accurately reflect all hours worked, including overtime, you must
report your concerns to the Human Resources Representative immediately. The Agency will
promptly investigate all reported complaints and, if appropriate, take corrective action.
The Agency prohibits and will not tolerate retaliation against any Aide because that Aide filed a good
faith complaint under this policy. Specifically, no one will be denied employment, promotion or any
other benefit of employment or be subjected to any adverse employment action based on that
person’s good faith complaint. In addition, no one will be disciplined, intimidated or otherwise
retaliated against because that person exercised rights under this policy or applicable law.
MEAL PERIODS
If you work for more than 6 consecutive hours, you are entitled to a meal period during your shift.
However, the nature of home care necessitates that only one Aide be on duty at any given time. Thus,
it is customary for Aides to eat on the job without being relieved as they cannot abandon the Client.
Given the requirements that an Aide remain with the Client, you voluntarily consent to taking your
meal period without being fully relieved of your duties and you understand and agree that this means
that your meal period may be interrupted by a call to duty. However, your meal period will be paid.
If you do not want to voluntarily consent to this arrangement, and instead desire a meal period
completely relieved from duties, you must submit a written request to the Coordinator. In that case,
the Agency may remove you from the case to which you are assigned and undertake reasonable
efforts to find a replacement case that allows you to take such meal periods. Such meal periods may
be unpaid as permitted by applicable law.
TIMESHEETS
TIMESHEETS MUST BE SUBMITTED BY MONDAY AT 12PM, EVEN ON A HOLIDAY.
If your time slip is late, you will not be paid that week. You will receive your pay the
following week. We strongly encourage your timesheets to be submitted on time so that we
can ensure timely pay.
Timesheets can be sent to:
FAX
845-352-2808
Mail

www.commhealthcare.com
Page 57 of 89
It is your responsibility to confirm that the hours on the timesheets are entirely accurate. Time
worked is considered time spent on the job performing duties assigned by the Coordinator within
the allotted number of hours per week.
Please be advised that all time sheets must be signed by yourself and the client at the end of each
day. Do not hold off until the end of the week to obtain all signatures. Do get a signature each
and every day before you leave the clients home. Dates, times, personal information, signatures
and patient information must be filled out correctly. You are required to enter the time that you
actually start work and the time that you finish working.
Here is a step by step guide on how to a timesheet should be filled out:
48 Bakertown Road #205 Monroe NY 10950
Timesheets@commhealthcare.com
If you mail your time slips they may not reach us by Monday 12:00pm, If you
do mail your time slips, please understand that if the mail is delayed, we are
not responsible.
Drop it off in the designated box at the closest satellite office.
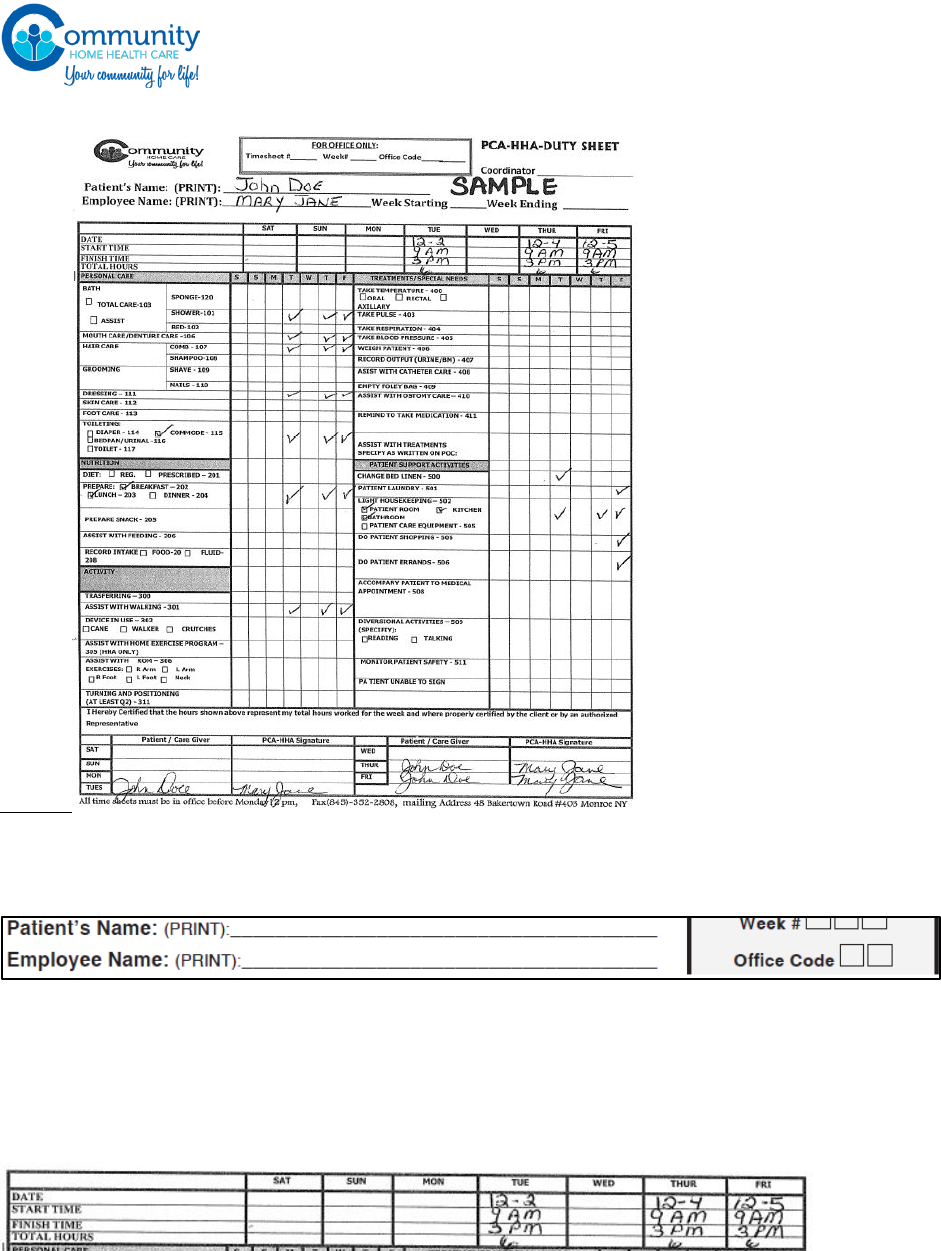
www.commhealthcare.com
Page 58 of 89
Patient’s Name: write the full name of your patient CLEARLY
Employee’s Name: write your name CLEARLY.
- Don’t scribble! If the name is not clear we may not know to whom the timesheet belongs
and it may delay your pay.
Date: enter a clear date for each day you worked. For ex: if you word Sunday, enter the date for
Sunday in the Sunday field.)
Start time: enter the time you arrived to the patient’s house
Finish time: enter the time you left the patient’s house
- If you are doing a live in case, you should write the words “live in” in this field.
Total time: enter the total amount of hours you worked for each day.
In the next section you must check off all the duties you performed at the patient’s home, per day.
Each shift you must have performed a minimum of 5 duties which should include at least 1
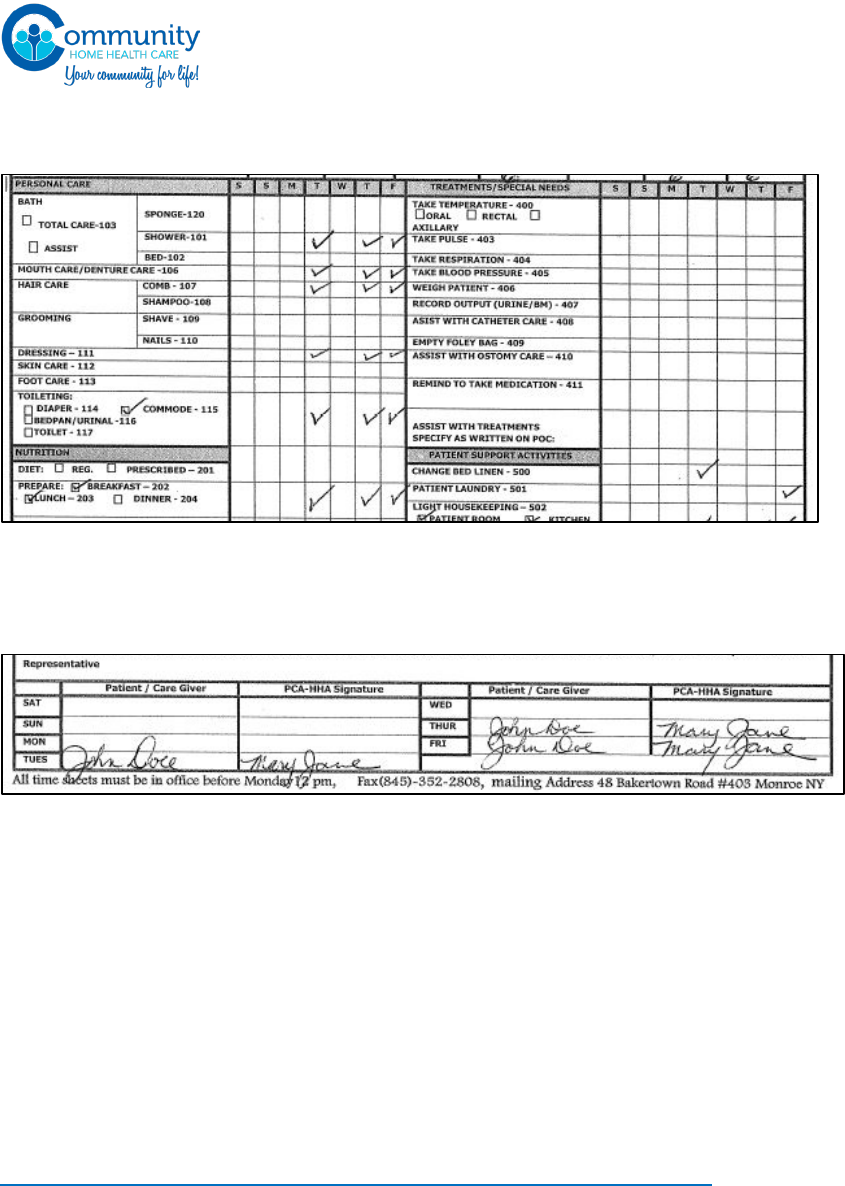
www.commhealthcare.com
Page 59 of 89
“personal Care Duty”. Take your time in filling this section out correctly. If you forget to fill it out, or
you did duties out of your plan of care, it may delay your pay.
In the signature section, the patient will need to sign for each day that you worked. For ex: if you
worded on Tuesday, the patient will need to sign the ‘patient/caregiver’ field for Tuesday. You will
also need to sign in the ‘PCA-HHA Signature’ field for each day you worked. If any of the signatures
are missing, it WILL delay payment.
.
If after reviewing the above details on how a timesheet should be filled out you still have
questions, feel free to reach out to your coordinator or HR Representative who will be more than
happy to assist you with your questions. We want to be sure you understand how to complete it.
Each timesheet consists of 3 slips. the white copy comes into the office, the yellow copy is for the
client and the pink copy is for your records.
The agency has a standard PCA/HHA timesheet. In Some Circumstances, specific vendors may
require a caregiver to fill out a different timesheet. Before going to a new case for the first time,
it is your responsibility to confirm with the coordinator which timesheet should be used for that
client. Be s ure to use the correct time slip for your client.
USE OF THE ELECTRONIC ATTENDANCE VERIFICATION SYSTEM (EAVS)
Community Home Health Care requires the use of an EAVS when working with a client. You are
required to use the EAVS system when you report to work for the client, and when you have
completed your shift. Clock in and out must be done from the client’s home phone or thru the
designated mobile app. On those occasions when calling from the client’s home phone is not possible,
and the mobile app is not available to you, it must be discussed with your Coordinator.
www.commhealthcare.com
Page 60 of 89
On your ID badge, you will be provided with a designated ID number to use for clocking in. It is
prohibited to allow anyone else to use your ID number. You must clock in and out for each shift that is
worked. Failure to use the call-in system properly may cause a delay in your pay.
A Clock in/out is IN ADDITION to timesheets. A clock in does not replace the need to submit a
timesheet. Clock ins can only be done using the Consumer’s phone. You may not use your personal
phones to clock in or out.
USE OF PHONE CLOCK IN
Phone Numbers:
English
845-533-9033
Toll
877-833-4935
French/creole
845-531-5990
Spanish
914-401-0025
Russian
845-678-8394
CALL IN:
1. Dial the number
2. Press 1 for CALL IN
3. Enter your Assignment ID
4. The system will repeat the
assignment you entered. Press 1
to confirm or 0 to re-enter & call
is complete.
CALL OUT:
1. Dial the number
2. Press 2 for CALL OUT
3. Enter your assignment ID
4. The system will repeat the assignment you entered.
Press 1 to confirm or 0 to re-enter & call is complete.
5. Enter all the duty IDs that you did for the
patient. This can be found on the timesheet
near each duty (small 3 digit number)
6. Press 000 to complete the call
Rules:
Call in/Call out: can only be done from the patients home phone. Calling in from
personal cell phone will not be allowed.
A call out for a shift without a call in will NOT be accepted.
Live in: when working on a live in case, you should call in reguraly when you to the case.
The following 1pm the aide should clock out and immediately clock back in. This should be
done every day at 1pm.
Shabbat observant: Notify the agency if the patient is Shabbat observant and therefore you
cannot use the patients phone.
No direct phone number: Patients may not always have a direct phone number. In such a
case notify the agency of the situtation.
Rotary phone: The time attendence system will not work a rotary phone.
Payroll is generated through the call in and call out system.
If you are experiencing problems with calling in or calling out, please notify the
agency immediately.
Calling in and out is NOT instead of the timesheet, timesheets must also be submitted.
USE OF MOBILE APP
Community Home Health Care now has a mobile app to make the process of calling in and out
easier for you.
Setup guide
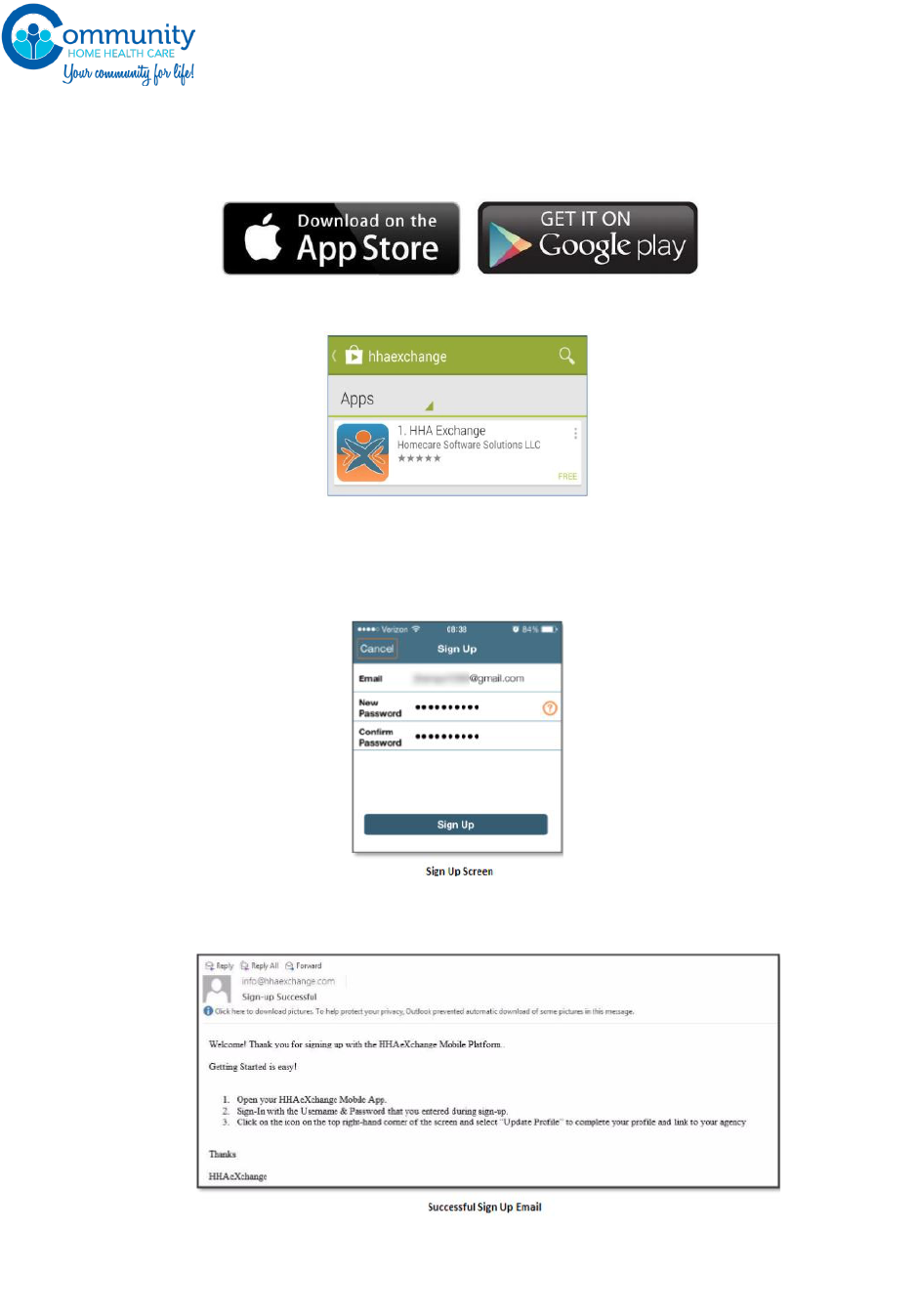
www.commhealthcare.com
Page 61 of 89
The HHA Mobile App is free and is available for download on iTunes and Google Play stores.
The
Caregiver is responsible for downloading and installing the application then reporting
the required
Credentials to the agencies they are working for in order to use the application.
To download the HHA Mobile App, go to either the iTunes App store or Google Play and
search on the
keywords HHA Exchange. The app will appear on the search results screen:
Install the HHA Mobile App and Sign Up
Once you have downloaded the App, press Sign Up on the bottom left of the main screen.
The App will prompt you for:
o Your Email Address
o A Password (minimum of 8 letters, 1 capital, and 1 numeric value
Select [Sign Up] once you have entered your email and confirmed your password. These will
serve as your log in credentials going forward. When you successfully created an account,
you will receive a verification email.
Register: After receiving the verification email, log into the App. Review the Terms of User
Agreement, and after selecting the Agree button, you will be brought to the Main Screen,
which will display a message prompting you to click the 3 dot icon in the upper right hand
corner. Click the icon and select Update Profile
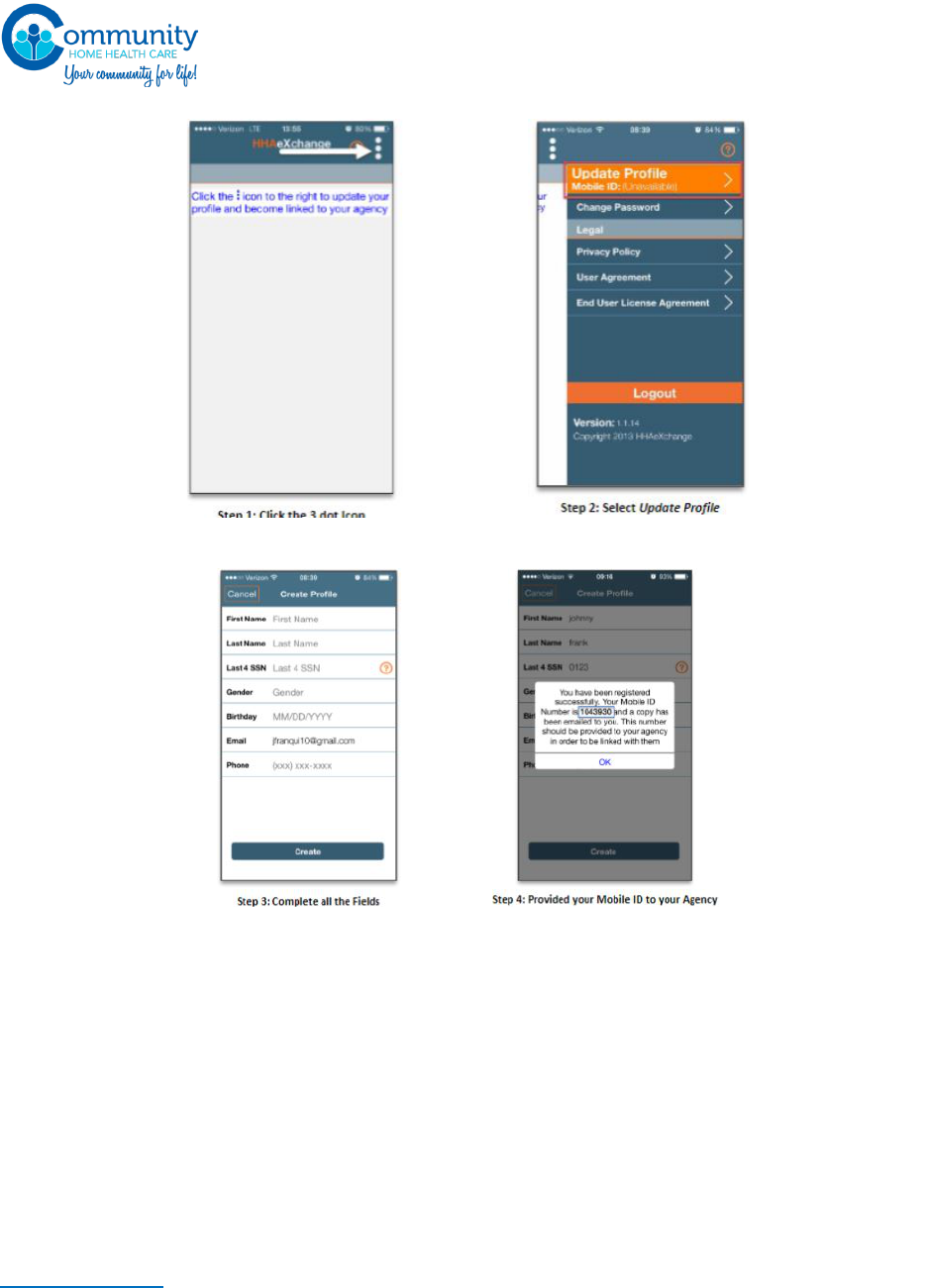
www.commhealthcare.com
Page 62 of 89
Complete all fields on the Create Profile page and click the [Create] button. If all the
information has been entered correctly, a message will appear containing your Mobile ID:
Note: the values for Last Name, Last 4 SSN, Gender, and Birthday must match the
information on record with the agency. If one of the values does not match, the Mobile App
will not link correctly
The HHAexchange system will send a second email after successful registration. This one
will contain your Mobile ID as well as instructions on how to log in and begin using the
Mobile App
Call your HR representative to provide them with your mobile ID number. Your
HR representative will link your account.
Once the setup is complete you will be able to clock in and out using this app. Please
note: this app works with GPS. You must be in the client’s home when you clock
in/out for us to accept the clock in/out as valid.
COMPENSATION
www.commhealthcare.com
Page 63 of 89
Payroll checks will be mailed out to your home weekly on Thursday. You can also choose to
receive your pay via direct deposit. Community Home Health Care highly recommends you
choose the direct deposit benefit to avoid disruptions in check distribution due to weather
or failed delivery methods.
If you wish to receive direct deposit, please submit the direct deposit form found on the next
page. Once signed up, your pay will be in your bank account Friday morning at 6am (this may
vary depending on your bank). Your paystubs will be available to view online. If you decide
to opt out of the online paystub viewing, your paystub will be mailed to your home.
If you are working for an eligible client, you will receive Wage parity benefits in addition to
your pay. Below you will find more detailed information on our Wage Parity Program.
WAGE PARITY
Aides who work on cases that are reimbursed by Medicaid in whole or in part and in certain regions
of the State are eligible to receive “wage parity” benefits in addition to minimum wage. The wage
parity amounts vary from region to region and year to year. Information about wage parity will be
distributed during orientation or can be requested from the Human Resources Representative.
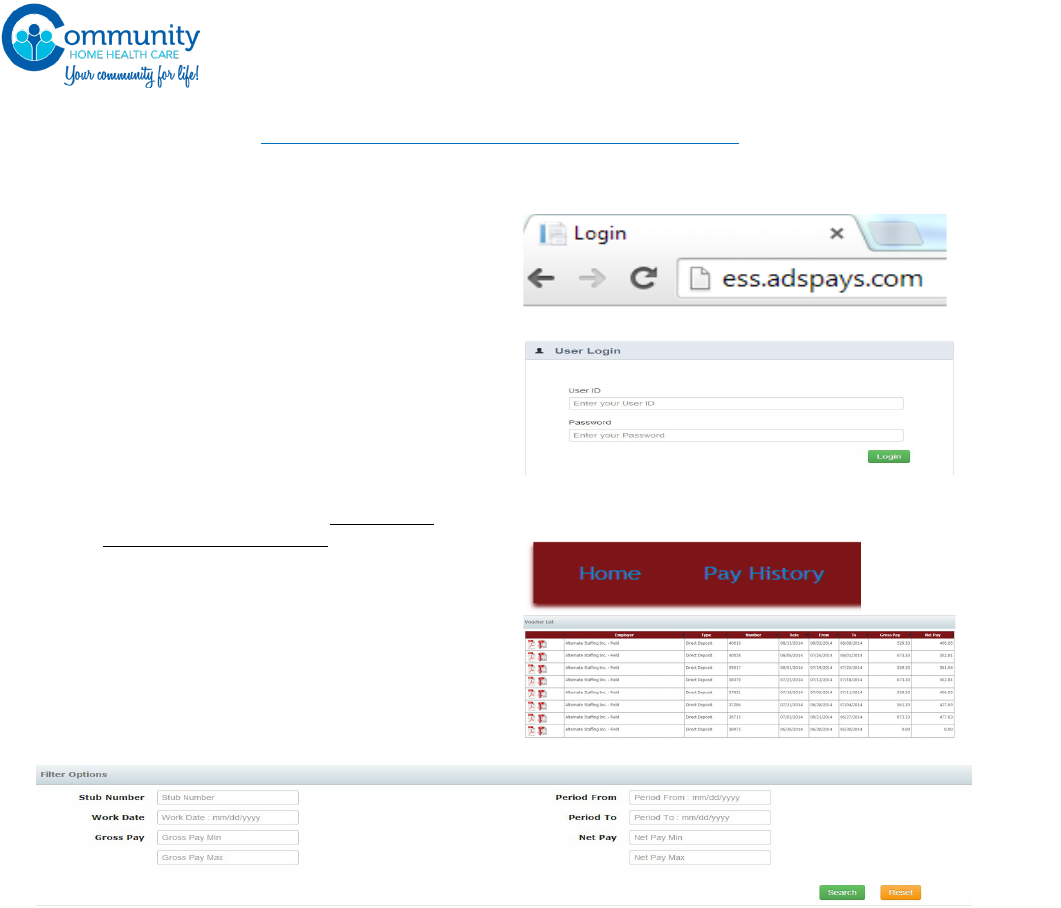
www.commhealthcare.com
Page 64 of 89
INSTRUCTIONS TO VIEW YOUR ONLINE PAY STUB
AVAILABLE FILTER OPTIONS
• Search for specific Voucher Number
• Looking for a specific visit? enter the date in question to search
• Search for range of Gross Pay $ amounts
• Search Paystubs within Pay Period Begin and End dates
• Search for range of Net $ amounts
1) In order to view or download paystubs, popups on your browser will need to be unblocked
2) If attempting to view a paystub on a mobile device the “desktop feature” may need to be
activated.
3) Paystubs will be available to view for 12 months
4) If you forget your password please contact your payroll dept. to reset.
Login instructions;
• OPEN THE BROWSER
• GO TO: ess.adspays.com
• ENTER USERNAME: Your first name, first
initial of your last name followed by the
last for digits of your social security
number (Ex for John Due – johnd1234)
• ENTER TEMPORARY PASSWORD: Your
entire social security number (without
dashes ex, 123456789) upon your first
login attempt the system will prompt
you to change the password, enter
your new password twice and be sure
to save it for your records.
NAVGITATION
• click on “Pay History” on the top left of
the page
• scroll down the page to view payroll
history summery information
click on the red icon on the left to view/print or
download your paystub.
www.commhealthcare.com
Page 65 of 89
Direct Deposit Form
Community Home Health Care offers DIRECT DEPOSIT to all our employees. This option, if you decide to choose
it, allows Community Home Health Care to deposit your weekly pay into your own personal savings or checking
accounts. Instead of receiving a check every week, your money will be available to
you every Friday Morning.
All who choose DIRECT DEPOSIT will have their paystubs available online to view and print. Paystubs will not
be mailed.
If you still wish to receive your weekly pay stub in the mail from us, in the form of a non-negotiable check that
cannot be cashed, please check the box below. If no box is on this form is checked, your paystubs will be
accessible online and will not be mailed. If you receive the weekly pay stub in the mail it will not be available
online
We ask anyone who would like to participate in DIRECT DEPOSIT to fill in their account information below and
return this page to your local Community Home Health Care Office. Attach either a blank voided check or a
savings deposit slip or BOTH if splitting deposit. You cannot have DIRECT DEPOSIT and receive a pay check.
---------------------------------------------------------------------------------------------------------------------------------------------
PRINT ALL INFORMATION
Direct Deposit Request (Don’t forget to staple your voided check or filled in deposit slip for savings) I authorize
my employer/payer to initiate electronic credit entries and, if necessary, debit entries and adjustments for any
credit entries made in error, to my financial institution list below:
FIRST NAME:_________________________ LAST NAME:________ _________________ SS#________________________
HOME ADDRESS:________________________________________________ APT.#_________
CITY:__________________________________ STATE:__________ ZIP CODE:________________
BANK NAME: ______________________________________________________________________________________
BANK ADDRESS_____________________________________________________________________________________
CITY____________________________________ STATE___________ ZIP CODE__________________
ROUTING NUMBER_____________________ CHECKING ACCT#_____________________ DEPOSIT% ________
ROUTING NUMBER_____________________ SAVINGS ACCT# ______________________ DEPOSIT% ________
[ ] I agree to have my paystubs available online
[ ] I wish to receive my weekly pay stub by mail. I am aware the paystubs will not be available to view
and print online.
EMPLOYEE SIGNATURE: ___________________________________ DATE:____________________
www.commhealthcare.com
Page 66 of 89
LIVE-IN CASE RULES
You will be paid for all hours worked on a 24-hour/live-in shift. During each full 24-hour period during
which you are required to be on duty, you agree that you will receive Bona Fide Meal Periods of up to 3
hours total and a Bona Fide Sleep Period of up to 8 hours, and that these hours (total of 11) will not count
as hours worked. All other hours during the course of such 24-hour period will be considered hours
worked and you will be paid at the applicable rates for such work.
“Bona Fide Meal Periods” are meal periods (e.g., one each for breakfast, lunch, and dinner) that are
uninterrupted, duty free, and at least 30 minutes in duration. While you may not leave the premises, you
shall leave your work area during each of your Bona Fide Meal Periods. You are not required to eat with
the Client during your meal period or take your meal period during the same time that the Client eats
his/her meal.
“Bona Fide Sleep Periods” are regularly scheduled sleep periods, which include at least 5 consecutive
hours that are not interrupted by a call to duty, in adequate sleeping facilities.
It is expected that you will only be required to work for 13 hours of the entire 24-hour shift you are
assigned to be with the Client. It is expected that you will enjoy a total of at least 3 hours of Bona Fide
Meal Periods as well as an 8-hour Bona Fide Sleep Period for each full 24-hour shift. Where you
receive a total of at least 3 hours of Bona Fide Meal Periods as well as an 8-hour Bona Fide Sleep
Period, you will be credited with 13 hours of work for the 24-hour shift.
“Adequate sleeping facilities” means that you have access to basic sleeping amenities (e.g., a bed and
linens); enjoy reasonable standards of comfort (e.g., heat); and have access to basic bathroom and
kitchen facilities, which may be shared (e.g., bathing and toilet facilities, refrigerator, stove, sink,
utensils).
If you “live-in”1 the home of the Client, “adequate sleeping facilities” means private quarters (i.e., a
living and sleeping space that is separate from the Client or other Aides) in a homelike environment
(i.e., a space that includes facilities for cooking and eating, a bathroom, and a space for recreation
(these additional facilities may be shared by you and the Client and/or other household members).
To ensure that you are paid for all hours you work, you will be asked to certify on each timesheet
whether or not you have received at least a total of at least 3 hours of Bona Fide Meal Periods and/or
at least an 8-hour Bona Fide Sleep Period for each full 24-hour shift. If you do not receive a Bona Fide
Meal Period or a Bona Fide Sleep Period on any one shift, you must (1) contact your Coordinator as soon
as possible following the conclusion of the shift at issue (generally, not later than within 24 hours
following the end of the shift); and (b) complete a “Sleep and Meal Period Exception Certification Form”
and return the form to your Coordinator as soon as possible (generally, within 72 hours of the shift). A
blank Sleep and Meal Period Exception Certification Form is set forth in the Appendix to this Handbook
and additional forms are available from any Coordinator.
1
You “live in” if you reside at your worksite on a “permanent basis” (i.e., you stay there seven nights a
week and have no other home of your own), or for “extended periods of time” (i.e., you work and sleep
there five days a week (120 hours or more) or five consecutive days or nights (regardless of the total
number of hours).

www.commhealthcare.com
Page 67 of 89
If you believe that you were not paid for all hours worked that you identified on a Sleep and Meal
Period Exception Certification Form or otherwise, you must contact the Human Resources
Department immediately and report the actual hours that you worked so that you can be
compensated for all of your hours worked.
No Aide will be subject to any reprisal or other adverse action for reporting missed or interrupted
meal or sleep periods or for submitting a Sleep and Meal Period Exception Certification Form. But
any Aide who knowingly submits a false report or Sleep and Meal Period Exception Certification Form
will be subject to disciplinary action, up to and including termination of employment.
www.commhealthcare.com
Page 68 of 89
Sleep and Meal Period Exception Certification Form
Employee Name (Print): _______________________________
Date of Shift: ________________
I attest that during my shift on the date noted above:
□ I did not have access to adequate sleeping facilities. Explain: ________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
□ I did not receive a duty-free, uninterrupted sleep period of at least 5 consecutive
hours. Explain: ___________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
□ I received a duty-free, uninterrupted sleep period of at least 5 consecutive hours,
but did not receive a duty-free, uninterrupted 8-hour sleep period. Specifically,
my sleep period was interrupted by a call to duty for a total of _____ hours.
Explain: ___________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
□ I did not receive a total of at least 3 hours of Bona Fide Meal Periods. Instead, I
only received a total of ___ hours of Bona Fide Meal Periods (do not include in this
figure any duty-free, uninterrupted meal periods you were able to take that were
less than 30 minutes in duration). Explain: ____________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
I certify, under penalty of perjury, that the information contained in this Sleep and Meal
Period Exception Certification Form is true, accurate, and complete.
____________________________________________ _____________
Signature Date

www.commhealthcare.com
Page 69 of 89
Keep in mind
Take your
food, clothes
and
toiletries to
last your
schedule.
(pack your
things in a
clean
luggage)
Shower daily
and do not
forget your
deodorants.
(presentation
is very
important)
Change into
your
pajamas at
night
(Pajamas is
only for
night time
not during
the day)
Make sure
you are
appropriately
dressed
during
working
hours
Do not talk
too loud on
the phone,
Avoid
chatting on
the phone
when your
patient is
awake
Always
address
your
patient
and
family
members
as Ms,
Mrs., or
Mr.
Do not eat
the patient
food or use
your
patient
phones to
make long
distance
calls
Scheduling
All live-in case are priority one (These patients
must never be left alone even for 5 minutes
unless authorized by your supervisor only. For
every errands and shopping, you must also call
your coordinator for notification and approval)
Make sure to write down
the dates and times of
your patient medical
appointments, that way
you do not miss any
appointments.
Be prepared to stay
longer than expected
in case of an
emergency
Nutrition
Make sure your patient eats breakfast, lunch and
dinner every day. Also make sure your patient drink
enough fluids. If your patient is not eating well, you
must call your coordinator and inform her.
Make sure your
patient is sitting
up for all meals.
If you think your patient is
losing weight, you must call
your coordinator and inform
her.
Skin Care and Hygiene
Please bath or assist
your patient in
bathing or
showering. If your
patient refuses
shower or does not
cooperate during
showers, please call
and inform your
coordinator.
You must check
your patient skin
and report any
sores, ulcers,
bruises, cuts,
swelling and black
and blue marks
If your patient
uses diaper, make
sure you change
the diapers
frequently as
needed. Always
apply Vaseline on
the diaper area to
prevent diaper
rash.
If your patient is
chair or bed bound,
you must turn and
position patient
every 2-3 hours or
as indicated in the
plan of care to
prevent skin break
down.
Please change
patient into a
pajamas for
bedtime and
change in day
clothes during
the day.
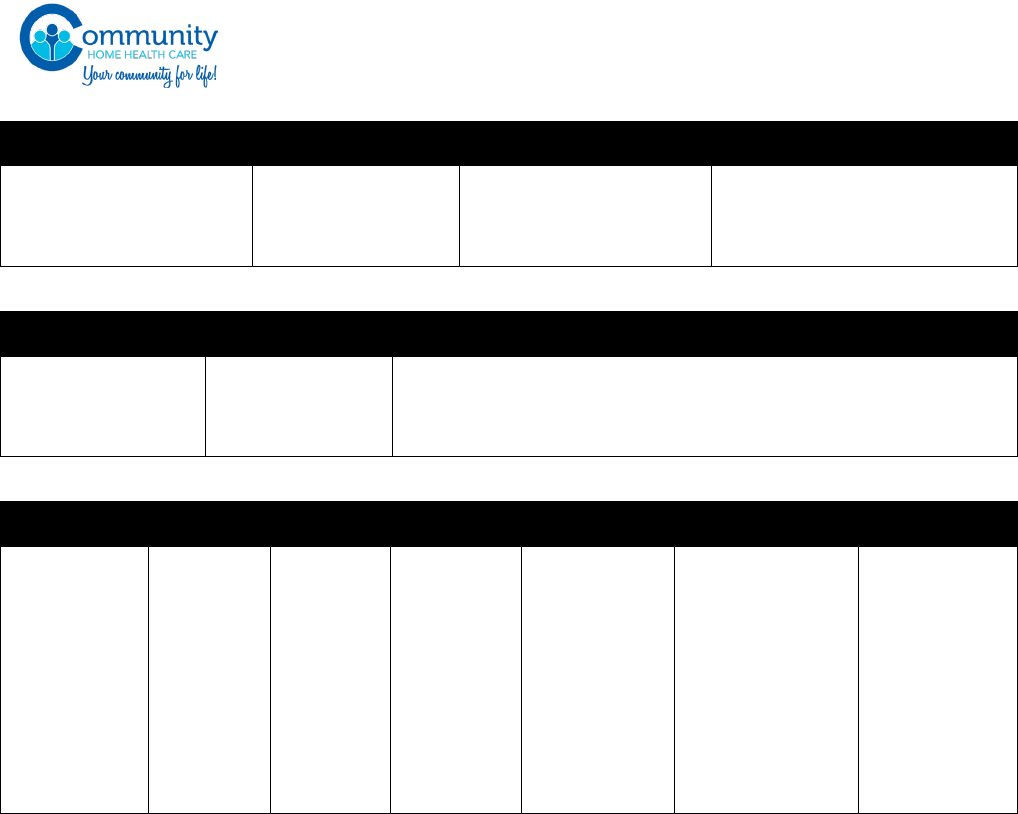
www.commhealthcare.com
Page 70 of 89
Housekeeping
Please sweep the house
daily and mop and
vacuum as needed .
Change linens as
needed but at the
minimum weekly.
Keep bathroom, kitchen
and all living areas tidy
and clean at all times.
Laundry should be done as
needed but at the minimum
weekly.
Activities
Do you know how
to safely operate
the Hoyer lift?
Do you know
how to safely use
the wheel chair?
Do you know how to safely transfer your patient from the bed
to the wheelchair, from the bed to the commode, from the wheel
chair to the commode?
Aide’s Change Over
Introduction-
Say your
name, Show
your ID
badge
POC-
Review
the POC
with the
other aide
and with
the
patient.
Routine-
Review
the
patient’s
routine
with the
other aide
at the
case.
Meals-
Review the
patients
preferred
meal time,
diet, with
the other
aide.
Equipment-
Review with
the other aide
how to use
the patients
Hoyer lift,
Wheel chair,
Walker and
etc...
Personal Care-
Review with the
other aide the
showing/bathing
and dressing
routine, Any
specific
preferences
Family
member’s
information-
Ask the other
aide for family
members
information in
case needed.
www.commhealthcare.com
Page 71 of 89
BENEFITS
A comprehensive benefits pamphlet is available in all of our satellite offices, and it will be provided
to you for review during orientation. You many also request from your HR representative to have a
pamphlet mailed to you. This section generally describes some of the benefits we provide to all Aides.
Because the terms and conditions of various plans change over time, a summary of the benefits being
offered by the Agency will be given at orientation.
HOLIDAY PAY:
The following days are considered holidays and you will be given an additional $1.00 per hour
if you work these days:
• New Years Day
• July 4
th
• Thanksgiving Day
• Christmas Day
WORKER’S COMPENSATION
If you are injured while on the job, you may be covered for the medical expenses you incur for the
work-related injury and salary lost during the period that you are disabled from working. All Aides
are required to report injuries prior to leaving their assignment. Aides may forfeit any right to care
by not promptly reporting to this agency.
DISABILITY INSURANCE
You are entitled to New York State Disability benefits if you have a non-job related illness and are
unable to work for more than seven (7) days, and are receiving medical care. If you are ill or require
hospitalization, notify the office immediately. New York State Disability will pay up to 50% of you
average/weekly salary, after the first seven (7) days of illness, and for up to 26 weeks. Aides on
disability leave are still required to notify their Coordinator of their status and periodically check in
with the Agency. Information about your condition and circumstances may be required before you
are reinstated to work.
MEDICAL INSURANCE:
Eligible employees may enroll in a single, a single plus one dependent, or a family contract health
insurance plan offered by the Agency. Eligibility will be defined by the specific insurance contract in
effect. Information and enrollment forms may be obtained from Human Resources.
www.commhealthcare.com
Page 72 of 89
YEARLY COMPLIANCE REQUIREMENTS
Below is a list of annual compliance requirements that must be met by each Aide as a condition of them
continuing to work a case. If the requirements expire and are not renewed, the aide is not authorized to
service the case. To be clear, service rendered on the first day that the aide is out of compliance with any
of the below requirements will not be paid. Aides should not report to work on the first day that they are
out of compliance with these requirements.
It is the Aide’s obligation to make sure their credentials are updated and in compliance with the law before
they render any services. The Agency will make every attempt to contact an Aide on the phone number
and email address provided to obtain updated compliance paperwork before the date that the
compliance paperwork is scheduled to expire. But if an Aide fails to hand in updated Compliance
paperwork on time, the Agency will consider it as a voluntary resignation and/or the Aide will not be
allowed to work the case until the paperwork is updated and in compliance with all requirements.
IN-SERVICE:
In-service is held every quarter according to the DOH regulations. Twelve (12) hours of in service
education is required each year for Home Health Aides and six (6) hours is required each year for
Personal Care Aides. In-service is completed online. To start your in-service go to
www.commhealthcare.showdme.net. Upon hire, you will be assigned a username (usually your
email) and password. If you do not know what your username is, feel free to call your designated HR
Representative for assistance.
You will be paid for attending the in-service. Please be sure to report your in-service on the
timesheet/EVV for the week in which the in-service is taken. You are not allowed to do any work in
addition to the 6 or 12 hours of in-service. This means that any work related to the in-service must
be completed within the 6 or 12-hour sitting. You cannot complete tests or similar written
assignments beyond the 6 or 12-hour sitting. Should there be extenuating circumstances and you are
required to spend more than 6 or 12 hours in the in-service, you need to accurately report such
additional time on your EVV or paper timesheet.
All Aides must complete the yearly in-services in order to stay in compliance with the Agency’s
Policies and Procedures. Failure to comply will result in an in-active status, and you will be replaced
on your case. If you have skipped any of the in- service hours, you will have to reapply to the Agency
as a new hire.
In-service payment will only be issued after a full “learning path” was completed. You are required
to complete each learning path in one single sitting of (each learning path is 6 hours).
PHYSICALS:
Each employee must have a physical examination within the past year by a physician prior to
the beginning of the client contact. Physical Examinations must include evidence of freedom
from condition, which may prove hazardous to you or your patient’s health. A yearly self-
assessment is required.

www.commhealthcare.com
Page 73 of 89
PPD/QUANTIFERON
PPD’s are required prior to employment and on an annual basis for employees with a negative
initial PPD. An employee may also choose to submit a Quantiferon TB gold test instead of the
PPD.
Employees who convert from a negative to a positive reading must be seen by a physician for
medical evaluation. Documentation of chest x-ray showing no evidence of active tuberculosis
or documentation of prophylactic treatment, and which should be sent directly to the agency
and maintained in the employee’s personnel file.
TB SCREEN
A yearly self-assessment is required or all employees with a history of a positive PPD or
Quantiferon TB Gold Test
INFLUENZA:
The Agency requires all Aides to have documented influenza vaccination status on file each year and
require unvaccinated personnel to wear a surgical mask at all times while in areas where Clients or
residents may be present during periods that the Commissioner of Health determines that the
influenza season is underway.

www.commhealthcare.com
Page 74 of 89
FALSE CLAIMS PREVENTION
Community Home Health Care has a longstanding practice of fair and truthful dealing with its
participants, their families, the government, health professionals and others. No individual
associated with Community Home Health Care shall engage in any act of fraud, abuse or waste, such
as knowingly making false statements of material fact, in the preparation or submission of any claim
for reimbursement under the Medicaid program. This policy applies to all Community Home Health
Care employees, contractors or other agents. Compliance with this Policy is a condition of
employment or business relationship with Community Home Health Care. Violation of this policy is
grounds for immediate termination of employment or agency relationship.
This policy outlines Community Home Health Care’s anti-fraud policy, and the specific federal and
New York State laws relating to fraud, abuse and waste.
A. Definitions of Fraud, Abuse and Waste
Fraud is an intentional misrepresentation that, when relied on by a payer or other person, deceives
that person to his or her detriment. Abusive tactics are broader than fraud, and may include
submitting deceptive or misleading claims to a government program like Medicaid, or using a false
statement to support a claim. Waste may include other deceptive tactics, such as over-utilization of
otherwise necessary services.
Types of fraud, abuse, or waste which may lead to liability are:
• Knowingly filing a false or fraudulent claim for payments to Medicaid or another governmentally
funded health care program, such as billing for services not actually provided;
• Knowingly making or using a false record or statement to obtain payment on a false or
fraudulent claim from Medicaid or other governmental program, such as documenting clinical
care not actually provided;
• Conspiring to defraud Medicaid or other governmentally funded health care program by
attempting to have a false or fraudulent claim paid; or
• Knowingly making or using, or causing to be made or used, a false record to statement to conceal,
avoid or decrease an obligation to pay or transmit money or property to the government.
Examples of the above include but are not limited to:
• Completing timesheets for services not actually provided;
• Paying an invoice known to be false;
• Accepting or soliciting kickbacks or illegal inducements from vendors of services, or offering or
paying kickbacks or illegal inducements to vendors of services;
• Paying, offering gifts, money, remuneration or free services to entice a Medicaid recipient to use
Community Home Health Care services;
• Using Medicaid reimbursement to pay a personal expense;
• Embezzling; and
• Ordering and charging for medical services not necessary for the participant.
B. Mandatory Reporting Requirement.
www.commhealthcare.com
Page 75 of 89
If any individual subject to this policy has reason to believe that anyone associated with Community
Home Health Care has engaged in any fraud, abuse or waste, the individual has a duty to report any
such observations and concerns immediately to Chaya Rubin. Community Home Health Care shall
not retaliate against anyone submitting a timely report pursuant to this policy.
All reports shall be investigated under the supervision of Chaya Rubin. All employees and
contractors have a duty to cooperate with any investigation conducted by Community Home Health
Care.
Community Home Health Care will take any necessary action to respond appropriately to any
substantiated offense and to prevent any further offenses, including but not limited to terminating
employees or contractors. Offenses will be evaluated for voluntary self-disclosure under applicable
laws, and when warranted, they will be referred to federal and state authorities. Community Home
Health Care will cooperate with government officials investigating or prosecuting any individual
referred by Community Home Health Care.
C. Federal and State False Claims Act Statutes
Federal False Claims Act
The Federal False Claims Act is a law that prohibits a person or entity, such as the Agency, from:
• Knowingly presenting to a Government agency a false claim for payment or approval;
• Knowingly using a false record or statement, such as work orders and invoices for work never
performed, to receive payment or approval of a false claim;
• Knowingly using a false record or statement to avoid an obligation to pay the Government;
• Knowingly conspiring to defraud the Government by getting a false claim paid; or
• Committing any other fraudulent acts detailed in the False Claims Act.
These prohibitions include claims submitted to federal health care programs like Medicare or
Medicaid. The False Claims Act broadly defines the terms “knowing” and “knowingly.” Specifically,
knowledge will have been proven for purposes of the False Claims Act if the person or entity: (1) has
actual knowledge of the information; (2) acts in deliberate ignorance of the truth or falsity of the
information; or (3) acts in reckless disregard of the truth or falsity of the information. Reckless
disregard is a term that means a conscious indifference to the consequences of one’s actions. The
law specifically provides that a specific intent to defraud is not required in order to prove that the
law has been violated.
A person or entity found guilty of violating the False Claims Act is required to repay all of the
fraudulently obtained money. In addition, the civil penalty for filing a false claim is between $5,000
and $10,000 per false claim and the damages recoverable by the Government can be up to three
times the value of the amount falsely received. In addition to being liable for damages and civil-
penalties, violating the False Claims Act can subject a person or entity to exclusion from participation
in federal health care programs, such as Medicare and Medicaid.
Private persons are permitted to bring civil actions for violations of the False Claims Act on behalf
of the United States (also known as “qui tam” actions). If the suit is successful, the private person is
entitled to receive a percentage of the recovery, depending on the level of government intervention,
www.commhealthcare.com
Page 76 of 89
as well as reasonable attorneys’ fees. Persons bringing these claims (also known as “relators” or
“whistleblowers”) are granted whistleblower protection under the law.
Program Fraud Civil Remedies Act
The Program Fraud Civil Remedies Act authorizes the Department of Health and Human Services
and other Government agencies to impose civil penalties upon persons making false claims or
statements. The conduct prohibited by the Act is similar to that prohibited by the Federal False
Claims Act. A violation of the Program Fraud Civil Remedies Act is punishable by a $5,000 civil
penalty for each wrongfully filed claim, plus damages up to twice the amount of value received by
the individual or entity that committed the fraud. The Act imposes liability on people or entities that
file a claim that they know or have reason to know:
• Is false, fictitious, or fraudulent;
• Includes or is supported by any written statement that contains false, fictitious, or fraudulent
information;
• Includes or is supported by a written statement that omits a material fact, which causes the
statement to be false, fictitious, or fraudulent, and the person or entity submitting the statement
has a duty to include the omitted fact; or
• is for payment for property or services not provided as claimed.
New York False Claims Act
The New York False Claims Act is modeled after the Federal False Claims Act and operates in a very
similar manner. The grounds for liability are the same in that the prohibited conduct involves
intentional or reckless falsity in obtaining payment from, or avoiding payment to the New York State
government. The New York State Attorney General and local government bodies have the authority
to investigate violations under the New York False Claims Act. The civil penalties for filing a false
claim are between $6,000 and $12,000 per claim. In addition, the government (state or local) can
collect damages of up to three times the amount of the value received by the individual or entity that
committed the fraud.
There are also criminal penalties for intentionally making a false statement or intentionally
submitting a false claim to the New York State or local government. Any person who submits false
statements or deliberately conceals material information in order to receive public assistance, such
as Medicaid, is guilty of a misdemeanor under the New York Social Services Law. The person may
also be subject to more serious criminal penalties under the New York Penal Law depending on the
severity of the fraud. Committing a fraudulent insurance act or engaging in health care fraud also
may subject the person to criminal liability.
Like the Federal False Claims Act; a private person may bring a “qui tam” civil action against a person
or entity on behalf of the Government. Qui tam plaintiffs are entitled to a percentage of the proceeds
collected from the defendant. This percentage depends on whether or not the Attorney General or
local government elects to intervene in the action. Persons bringing these claims (also known as
relators or whistleblowers) are granted whistleblower protection under the law.
In addition to the New York False Claims Act, the New York Social Services Law imposes a civil
penalty on a person or entity who knowingly obtains or attempts to obtain payment for items or

www.commhealthcare.com
Page 77 of 89
services furnished under any Social Services program, including Medicaid, by the, use of a false
statement, deliberate concealment, or other fraudulent scheme. The law gives the New York State
Department of Health the authority to impose a civil penalty of no more than $2,000 per violation
on any person who causes Medicaid payments to be made if the person knew or had reason to know
that:
• The payment involved the providing or ordering of care, services, or supplies that were
medically improper, unnecessary or in excess of the documented medical needs of the person
to whom they were furnished;
• The care, services, or supplies were not provided as claimed;
• The person who ordered or prescribed care, services, or supplies which were medically
improper, unnecessary, or in excess of the documented medical need of the person to whom
they were furnished was suspended or excluded from the medical assistance program at the
time the care, services, or supplies were furnished; or
• The services or supplies for which payment was received were not, in fact, provided.
Whistleblower Protections
Whistleblowing employees are protected from retaliation by their employers for reporting fraud,
waste, and abuse. Both the Federal and New York False Claims Acts provide protection to private
individuals who bring “qui tam” actions and who are later discharged, demoted, suspended,
threatened, harassed, or in any other manner discriminated against in the terms and conditions of
their employment as a result of the action. Federal law remedies include reinstatement with
comparable seniority, back pay, interest on any back pay, and compensation for any special damages
including litigation costs and reasonable attorneys’ fees. New York law remedies include an
injunction to restrain continued discrimination, reinstatement with comparable seniority and full
fringe benefits, back pay, interest on the back pay, and compensation for any special damages
including litigation costs and reasonable attorneys’ fees.

www.commhealthcare.com
Page 78 of 89
COMPLAINT FORM
Name: ________________________________________ Today’s Date:_________________________
Complaint:
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
__________________________________________________________________________________________________________
Fax form to 845-738-1761 Email: Qualityassurance@commhealthcare.com

www.commhealthcare.com
Page 79 of 89
ABUSE AND NEGLECT REPORTING POLICY
The Agency is committed to the safety and well-being of all its clients. Observing, screening and
reporting abuse and neglect is included at orientation for all new Aides. In addition, an in- service
program, “Abuse and Neglect”, is presented as part of the ongoing in-service schedule.
The following operation definitions are used to assist in determining if clients are victims of abuse or
neglect:
Child Abuse
The physical, sexual or emotional maltreatment of a child, it may be overt or covert
Child Neglect
The failure by parents or guardians to provide for the basic needs of a child by physical or emotional
deprivation that interferes with normal growth and development or that places the child in jeopardy
Elder Abuse
Non-accidental acts of physical or mental mistreatment (including that of a sexual nature) of an
elderly or vulnerable adult
Elder Neglect
A pattern of conduct or inaction by a person entrusted with caring for an elderly or vulnerable adult
that results in deprivation of care necessary to maintain that person’s physical or mental health
As part of the initial and ongoing client assessments, the Director of Nursing observes for signs of
abuse and neglect. Care givers are encouraged to report observable changes in family dynamics,
changes in client status and any bruising or injury the client sustains. The client’s support system is
identified at time of admission and encouraged to discuss concerns related to the client. Identification
and use of community resources is also discussed to help individuals in the client’s support system
in coping with caring for an ill or elderly person.
If there is a reasonable suspicion of abuse or neglect, an incident report is completed and the situation
is discussed with the Administrator. Mandated reporters, i.e., health care professionals are required
to report cases of suspected child abuse or neglect by calling 1-800-635-1522 in New York State.
Non-mandated reporters are to call the New York State Central Registry in Albany at 1-800-342-
3720. Reporting is necessary to protect the child and obtain services for the Client(s) to assist in
dealing with the actions leading to abuse or neglect. In conjunction with the physician, Adult
Protective Services(APS) is contacted if there is concern for the safety and welfare of an adult client.
All actions taken by the Agency’s staff regarding reporting and follow-up of suspected or actual abuse
and/or neglect are documented in the client record.
The Agency maintains a list of community resources as well as the telephone number for APS. The
Agency is committed to the safety of:
1. All Agency personnel who come in direct contact with Clients receive a complete
orientation and participate in on-going training to recognize potentially hazardous
conditions related to the service they provide.

www.commhealthcare.com
Page 80 of 89
2. Initial and ongoing Client or care giver instruction on home safety management is
appropriate to the provider’s level of responsibility, as it relates to the client’s needs.
3. Home safety management includes the following areas:
• Basic home and bathroom safety
• Fire response and means of emergency exit from home
• Storage of supplies, drugs, controlled substances, solutions and
sharp/needles
• Transfers and ambulation with assistive devices
• Use of medical equipment and electrical incidents
• Waste disposal (double boxing, bagging and use of non-penetrable
container)
4. Clients and care givers receive written instructions whenever possible.
5. Client/care giver knowledge and performance of safety procedures are evaluated
and documented in an ongoing basis.
6. Agency personnel use a safety checklist to document existing or potential safety
hazards.
7. All personnel are knowledgeable of the system for reporting accidents, injuries and
safety hazards.
8. The staff’s use of the safety management program is evaluated periodically and in-
service education is based on the findings of those evaluations.
www.commhealthcare.com
Page 81 of 89
FACT-FINDING AND ISSUE RESOLUTION
(“FAIR”) PROGRAM
1. Overview of the FAIR Program. Community Home Care values each employee and looks forward
to good relations with and among all of its employees. Occasionally, however, disagreements may
arise between you and Community Home Care or between employees in a context that involves
Community Home Care We believe that the resolution of such disagreements will be best
accomplished by internal dispute resolution and, where that fails, by binding arbitration that is
conducted by an arbitrator. For these reasons, Inc. has adopted this Fact-finding and Issue Resolution
Program (the “FAIR Program”).
2. Effect of This Document. By singing this agreement, you agree that all “Claims” (as defined below
in paragraph 3) between “You” and the “Agency” (as defined below in paragraph 3) shall be resolved
exclusively by the internal dispute resolution procedures and the binding arbitration procedures
described in this document.
The FAIR Program is an essential element of your employment and, for current employees, continued
employment with the Agency. Although the FAIR Program is a binding agreement between you and
the Agency, it does not create a contract of employment or otherwise affect the at-will nature of your
employment. You indicate your agreement to be bound by the FAIR Program’s terms and conditions
by signing this document.
3. What Does The FAIR Program Cover?
A. The FAIR Program applies to any and all Claims, regardless of when
those claims arose or accrued. For avoidance of doubt, the provisions
of this agreement apply to claims that accrued or arose before
execution of this agreement and to claims that accrued or arose after
execution of this agreement. The provisions of this agreement also
apply to Claims that arose after your employment with the Agency
ends.
C. For purposes of the FAIR Program and this document, the “Agency”
and/or “Community Home Care” means Community Health Aide
Services and its parents, subsidiaries, affiliates, predecessors, and
successors, as well each of their current and former owners,
members, managers, shareholders, partners, directors, officers,
employees, and agents.
D. “You” and “Your” refers to you and any other person who may assert
your rights.
E. “Claim” includes any claim, dispute, allegation, controversy, or
action between You and the Agency that in any way arises from, or
relates to, your employment with the Agency or the termination of
your employment with the Agency, regardless of that Claim accrued

www.commhealthcare.com
Page 82 of 89
or arose. A Claim encompasses, for example, any employment, labor,
wage-and-hour, overtime, and compensation claims, including,
without limitation, any Claim that may arise under the following laws:
o Title VII of the Civil Rights Act of 1964
o the Civil Rights Act of 1991
o the Age Discrimination in Employment
Act of 1967
o the Americans with Disabilities Act of
1990
o the Fair Labor Standards Act of 1938
or any state wage and hour laws, such
as the New York Labor Law
o New York Public Health Law Section
3614-c, also known as the Wage Parity
Law
o the Rehabilitation Act of 1973
o the Older Workers Benefit Protection
Act
o the Family and Medical Leave Act of
1993
o the Occupational Safety and Health Act
of 1970
o the Worker Adjustment and
Retraining Notification Act of 1988
o any state anti-discrimination, anti-
retaliation, or whistleblower laws
(including, without limitation, the New
York State Human Rights Law and the
New York State Whistleblower Law)
o any other federal, state, or local
statute, regulation, or common-law
doctrine regarding employment,
employment discrimination,
harassment, terms and conditions of
employment, termination of
employment, compensation, breach of
contract, or defamation.
o disputes about the validity,
enforceability, coverage or scope of
the FAIR Program or any part thereof.
The above list is not exclusive, and is only provided to illustrate examples of Claims.
Are any Claims excluded from this FAIR Program? The term “Claim” does not include the following,
which are for a court or an agency and not an arbitrator to decide:
controversies, claims or other disputes
for injunctive relief for unfair
competition or unauthorized use or
disclosure of confidential information
or trade secrets
claims for workers’ compensation
(except that claims for interference
with or retaliation for filing a workers’
compensation claim will be
considered a Claim subject to
arbitration under the FAIR Program)
claims for unemployment
compensation benefits
claims for employee welfare benefits
(e.g., medical, health, dental)
claims for retirement benefits under
the Employee Retirement Income
Security Act (“ERISA”) (except that
claims for interference with or
retaliation for exercising protected
rights under ERISA shall be considered
Claims subject to arbitration under the
FAIR Program)
unfair labor practice charges under
the National Labor Relations Act
www.commhealthcare.com
Page 83 of 89
The FAIR Program does not prevent You from filing a charge, testifying, assisting, or otherwise
participating in any investigation or proceeding conducted by the equal employment opportunity
commission, or another government agency to the extent that You have a protected right to do so.
But if You take such action in relation to a claim, controversy, or other dispute that would constitute
a Claim and you have not fully pursued such dispute through the FAIR Program, the Agency may
request the agency in question to defer its processing or investigation of such charge until the FAIR
Program has been completed. Notwithstanding Your rights under this subsection, You agree that, to
the maximum extent permitted by law, You may recover monetary relief with respect to a Claim only
through the FAIR Program.
Further, the FAIR Program does not require the Agency to begin arbitration proceedings or initiate
any other procedure before taking any action regarding your employment with which you might
disagree, such as coaching, counseling, warning, reprimand, suspension, investigation, discipline,
demotion, changing your days or hours of work, or termination.
4. Can A Claim Be Resolved in Court? No. Under the FAIR Program, You and the Agency each waive
your respective rights to have a Claim decided by a court, judge, jury and, where permitted by law,
an administrative agency. Instead, You and the Agency hereby agree that the internal dispute
resolution and arbitration procedures set forth below are the sole and exclusive methods for
resolving any and all Claims.
5. Submitting a Claim Under the FAIR Program? If You believe that You have a Claim against the
Agency, You should first give the Agency a chance to investigate and resolve the Claim before You file
a demand for arbitration (the arbitration process is explained further below). You do not need to use
any specific form to submit a Claim. Simply write a letter explaining your Claim and the relief sought,
and submit the Claim letter to the Human Resources Manager. If You do not receive a response
from the Agency within 30 days of the date that you submitted Your letter to Human
Resources, or you disagree with the response from the Agency, and you wish to pursue the
Claim further, You must submit your Claim exclusively to binding arbitration with the
American Arbitration Association (“AAA”) in accordance with the AAA’s Employment
Arbitration Rules and Mediation Procedures.
6. How Much Time do You Have to File a Claim? An arbitration proceeding must be commenced
within the time period prescribed by the statutes of limitations applicable to the Claim being
asserted. For purposes of statute of limitations, an arbitration proceeding is deemed commenced
when a demand for arbitration is filed with the AAA.
7. How Does The Arbitration Process Begin? To start the arbitration process, the party wishing to
file a Claim must file a written demand in accordance with the rules of the AAA for starting the
arbitration process. More information about the AAA may be obtained at www.adr.org or by calling
1.800.778.7879.
8. How Is the Arbitrator Selected? Arbitrators will be selected by the parties in accordance with
the AAA’s Employment Arbitration Rules and Mediation Procedures. The arbitrator must be a
licensed attorney or a retired judge selected from the AAA’s Employment Arbitration Rules and
Mediation Procedures Employment Dispute Resolution Roster, or a similar list if such list is
www.commhealthcare.com
Page 84 of 89
unavailable. Unless the parties agree otherwise, the arbitrator must be a retired or former judge or
a lawyer who has at least 5 years of experience with employment-related claims.
9. Can An Attorney Represent You? Yes. Any party may be represented by an attorney. If you
need assistance finding an attorney, there may be resources available to you, such as the American
Bar Association (
www.americanbar.org and 800-285-2221 or 202-662-1000) or the Legal Aid
Society (www.legal-aide.org or 212-577-3300 or 718-722-3100).
10. When And Where Will The Arbitration Hearing Take Place? The arbitration hearing will be
conducted by the arbitrator in whatever manner will most expeditiously permit full presentation of
evidence and arguments of the parties. The arbitrator will set the time, date, and place of the hearing,
notice of which must be given to the parties at least 30 calendar days in advance, unless the parties
agree otherwise. Any arbitration hearing will take place within Rockland County, State of New York,
unless the parties agree otherwise.
11. What Rules And Law Apply To The Arbitration? Arbitration under the FAIR Program will be
conducted pursuant to the AAA’s Employment Arbitration Rules and Mediation Procedures, except
that under no circumstances will an arbitrator have the authority to hear or decide any Claim on a
class, collective, or other group or representative basis. The arbitrator must apply the substantive
law, including the applicable burdens of proof and persuasion, that would be applied by a court
hearing the Claim in the venue of the arbitration. The arbitrator may grant relief that could be
granted by a court hearing the Claim, including an award of attorneys’ fees and costs.
12. Can Claims Be Heard On A Class, Representative, Or Collective Basis? No. Notwithstanding
anything to the contrary: (a) no arbitrator is permitted to hear or decide any Claim on a class,
collective, or other group or representative basis; (b) all Claims between You and the Agency must
be decided individually; and (c) the AAA’s Supplementary Rules for Class Action Arbitration (and any
similar rules) will not have any applicability to any Claim. This means that if You have a Claim, neither
You nor the Agency will have the right, with respect to that Claim, to do any of the following in court
or before an arbitrator: (a) pursue or obtain any relief from a class, collective, or other group or
representative action; (b) act as a private attorney general; or (c) join or consolidate a Claim with the
Claim of any other person. Thus, the arbitrator shall have no authority or jurisdiction to process,
conduct, or rule upon any class, collective, private attorney general, or other representative or group
proceeding under any circumstances. If there is more than one Claim between You and the Agency,
those Claims may be heard in a single arbitration.
13. Who Pays For The Arbitration? The party claiming to be aggrieved is responsible for paying
the applicable filing fee in effect and established by the AAA at the time the demand for arbitration is
made. If You file the demand for arbitration and cannot obtain a waiver of the filing fee, You can ask
the Agency to pay the filing fee. The Agency will review every such request in good faith and consider
whether to cover all or part of such filing fee.
The arbitrator will charge a fee for his/her services and his/her costs. The parties will equally share
the arbitrator’s fees and other costs of the arbitration. However, if sharing equally in the cost of the
arbitrator’s fees would cause you financial hardship, You can ask the Agency to pay, in full, the
arbitrator’s fees and other costs. The Agency will pay all of the arbitrator’s costs and fees as necessary
to implement this FAIR Program.
Each party will be responsible for its own attorneys’ fees and costs, but the arbitrator may award
either party reasonable attorneys’ fees and costs in accordance with the applicable law.
www.commhealthcare.com
Page 85 of 89
14. Are The Parties Entitled to Discovery Or Depositions? Yes. All discovery will be governed
by the AAA rules.
15. Can You have Witnesses Testify At The Arbitration? Yes. At the hearing, the parties will have
the right to present proof through testimony and documentary evidence, and to cross-examine
witnesses who testify at the hearing. The arbitrator will require all witnesses to testify under oath.
The arbitrator(s) will also have the authority to decide whether any person who is not a witness may
attend the hearing.
16. The Arbitrator’s Decision/Award. The Arbitrator will issue his or her award promptly after
the arbitration hearing concludes or post-hearing briefs are received. The arbitrator’s award will set
forth the factual and legal basis for the award, including his or her legal reasoning, and contain a
summary of the facts, the issues, the governing law applied, and the relief requested and awarded. It
must also identify any other issues resolved and the disposition of any statutory claims. The
arbitrator’s award will be final and binding on the parties.
17. How Long Does the FAIR Program Apply to You? The FAIR Program will remain in effect and
survive the cessation of Your employment relationship or affiliation with the Agency, regardless of
the reason for such cessation.
18. Miscellaneous Provisions Regarding the Fair Program:
Choice of Law. The FAIR Program and the terms of this agreement shall be governed by the
Federal Arbitration Act (“FAA”). The parties acknowledge and agree that the FAIR Program
evidences a transaction involving interstate commerce.
Severability. If any part or provision of the FAIR Program or this agreement is held to be
invalid, illegal, or unenforceable, such holding will not affect the legality, validity, or
enforceability of the remaining parts, and each provision of the FAIR Program and this
agreement will be valid, legal, and enforceable to the fullest extent permitted by law.
However, in the event the provision prohibiting class, collective, or representative actions is
found to be unlawful or unenforceable, then the entire FAIR Program and this agreement will
be considered null and void.
Notices. Any notice required to be given to You will be directed to Your last known address
as reflected in the records of the Agency. Any notice required to be given to the Agency will
be directed to the Administrator at [INSERT ADDRESS].
Amendment. The Agency reserves the right to amend or terminate the FAIR Program. Such
amendments may be made by providing notice to You, electronically or in writing, of such
amendment or termination.
Waiver. No waiver may be granted by either party, except in writing. No waiver of any
provision of the FAIR Program will constitute a waiver of any other provision of the FAIR
Program (whether or not similar), nor will such waiver constitute a continuing waiver unless
otherwise expressly provided in such writing.
By signing the Handbook Acknowledgment of Receipt, You confirm that You have read and
understand the terms and conditions of the FAIR Program, which require You to submit all
Claims to binding arbitration on an individual basis. No provision of any other document You
may receive from the Agency will be construed as a waiver of the provision prohibiting class,
collective, or representative actions.
www.commhealthcare.com
Page 86 of 89
Time-Off Request
Please present to the office 2 weeks prior to request
Aide's Name: ____________________ Coordinators Name:____________________
Days off/Vacation
Dates: from____________ to______________
Partial Day [ ] Full Day [ ]
Permanently off case
Today’s date: ____________
Last date of work: ___________ (two weeks from today’s date)
Reason: ____________________________________________________________
Your Patients Name(s):_______________________________
_______________________________
_______________________________
_______________________________
Your Signature: _______________________________ Date: _________________
PLEASE CONTACT YOUR COORDINATOR TO VERIFY APPROVAL
000161.01368 Business 17288486v1

www.commhealthcare.com
Page 87 of 89
www.commhealthcare.com
Page 88 of 89
ACKNOWLEDGMENT OF RECEIPT
I hereby acknowledge receiving a copy of the Agency’s Handbook. I have had the
opportunity to ask questions about the policies. As a condition of my employment with
the Agency, I agree to comply with all the rules and procedures of the Agency, as
stated in this Handbook and any other document that may be issued to me during
my employment, including the FAIR AGREEMENT.
I understand that the Agency has the maximum discretion permitted by law to interpret,
administer, add to, change, or delete provisions in this Manual and Handbook at any time.
Additionally, I acknowledge that no promise of job security has heretofore been given to
me and that there are no such promises contained in the Handbook since I am employed
AT WILL and may resign at any time or be fired from my job at any time, with or without
notice and with or without cause.
Aide Name (PRINT)
Aide Signature
Date:

www.commhealthcare.com
Page 89 of 89
Orientation Verification
I, _________________________________________________ , have attended orientation today with
Community Home Health Care. I hereby agree that as an employee with Community Home
Health care, I am responsible for understanding and abiding by the policies and procedures
set forth in the orientation and in the provided employee handbook.
Provided to me was the following, not limited to:
Employee handbook released august 2018
HIPAA regulations
HIV Confidentiality
Infection Control review
Advance Directives/Living Will/DNR
Client abuse reporting law& caring for the sensory impaired client
Emergency/disaster preparedness
Aide and home safety review
General company policies, procedures and forms
Payroll guidelines
o Training on the use of timesheets
o Training on the use of electronic clock in/clock out system
Photo Waiver and Release
Drug and alcohol policy
Sleep & Meal period policy for employees on duty for 24 hours or more
FMLA and PFL policy
Fact-finding and issue resolution (“Fair”) Program policy
False claims act
NYC Earned sick time act
Health Insurance Information
Wage Parity Benefits
I Agree to the above.
Employee Signature: __________________________________________________ date:____________________
Agency Rep Signature: _________________________________________________ date:___________________
