
The BACPR Standards and Core Components for
Cardiovascular Disease Prevention
and Rehabilitation 2017
(3rd Edition)
The Six Core Components
for Cardiovascular Disease
Prevention and Rehabilitation
Supported by
The British Association for Cardiovascular Prevention and Rehabilitation is an affi liated group of the
The
Six Core Components
for Cardiovascular Disease
Prevention and Rehabilitation
Supported by
A
U
D
I
T
A
N
D
E
V
A
L
U
A
T
I
O
N
L
O
N
G
-
T
E
R
M
S
T
R
A
T
E
G
I
E
S
Health
behaviour
change and
education
P
s
y
c
h
o
s
o
c
i
a
l
h
e
a
l
t
h
L
i
f
e
s
t
y
l
e
r
i
s
k
f
a
c
t
o
r
m
a
n
a
g
e
m
e
n
t
m
a
n
a
g
e
m
e
n
t
M
e
d
i
c
a
l
r
i
s
k

Foreword
All health care professionals are motivated to provide the best care and achieve the optimal
outcomes for their patients. This has been a recurrent ambition I have heard from colleagues
working in the front line of the NHS. The 3rd edition of the BACPR Standards & Core
Components provide an excellent and essential guide to support cardiac rehabilitation and
prevention programmes across the UK.
Taking the findings of research and translating these into day to day practice is the starting point
of a chain of events that will achieve this ambition. The evidence-based standards allow us to
drive quality improvement and the National Audit of Cardiac Rehabilitation allows us to know how
well we are doing. None of this however would be possible without the efforts of the healthcare
professionals providing cardiac rehabilitation across the UK.
Cardiovascular disease is a long term condition. Saving someone’s life following a heart condition
is vital, but giving them a fulfilling life that is worth living is equally important. The aims of cardiac
rehabilitation and prevention is to provide the patient and family with the skills and knowledge to
self-manage, facilitate recovery both physically and psychologically and educate to reduce the risk
of further CVD events, as well as achieving an absolute risk reduction in cardiovascular mortality.
The NHS should provide and fund evidence-based care, but the reduction in hospital admissions
for patients who receive comprehensive cardiac rehabilitation, there exists an added financial
motive to invest in these essential services.
Leo was 47 when he had a heart attack followed by triple bypass surgery. While he was in
hospital he was offered a place on a cardiac rehabilitation programme. Following cardiac
rehabilitation, as he says, it is about being in control – “I definitely feel much better in myself. I’m
more in control of my own health than I ever was before.”
The BHF is delighted to be able to support the publication of these updated Standards and
Core Components, but more importantly work with the BACPR team and members, to promote
excellence in cardiovascular disease prevention and rehabilitation.
Dr Mike Knapton, Associate Medical Director, BHF
Supported by
Contents
1
Introduction
1
1.1
Definition
1
1.2
Evidence
2
1.3
National and local factors for assuring quality
3
1.4
Cardiac rehabilitation pathway of care
3
1.5
Funding
4
2
The Standards
5
2.1
The delivery of six core components by a qualified and
competent multidisciplinary team, led by a clinical coordinator
6
2.2
Prompt identification, referral and recruitment of eligible
patient populations
7
2.3
Early initial assessment of individual patient needs, which
informs agreed personalised goals that are reviewed regularly
8
2.4
Early provision of a structured cardiovascular prevention
and rehabilitation programme (CPRP), with a defined
pathway of care, which meets the individual’s goals and is
aligned with patient preference and choice
9
2.5
Upon programme completion, a final assessment of
individual patient needs and demonstration of sustainable
health outcomes
10
2.6
Registration and submission of data to the National Audit
for Cardiac Rehabilitation (NACR) and participation in the
National Certification Programme is desirable
10
3
The Core Components
11
3.1
Health behaviour change and education
12
3.1.1
Health behaviour change
12
3.1.2
Education
12
3.2
Lifestyle risk factor management
13
3.2.1
Physical activity and exercise
13
3.2.2
Healthy eating and body composition
14
3.2.3
Tobacco cessation and relapse prevention
14
3.3 Psychosocial health
15
3.4
Medical risk management
16
3.5
Long-term strategies
17
3.6
Audit and evaluation
18
4
Appendices
20
Appendix 1
References
20
Appendix 2
Acknowledgements
24
Standards and Core Components 2017 (3rd Edition) 1
1. Introduction
This is an update (third edition) of the BACPR Standards & Core Components and represents
current evidence-based best practice and a pragmatic overview of the structure and function
of Cardiovascular Prevention and Rehabilitation Programmes (CPRPs) in the UK.
The previously described seven standards have now been reduced to six but without sacrificing any
of the key elements and with a greater emphasis placed on measurable clinical outcomes, audit and
certification. Similarly, the second edition provided an overview of seven core components felt to be
essential for the delivery of quality prevention and rehabilitation, and this too has been reduced to six.
The interplay between cardio-protective therapies and medical risk factors is almost impossible to
disentangle for the vast majority of patients and even if specific drug therapies are deployed exclusively
for risk factor modulation, the indirect effect will also be cardio-protective. Thus, these have been
combined into a single core component – medical risk management.
This updated and revised third edition is designed to build upon the success of the earlier publications
and to refocus the attention of commissioners, health-care professionals, politicians and the public
on the critical importance of robust, quality markers of service structure and content. However, the
overarching aim of these standards and core components remains unchanged – to provide a blueprint
upon which all effective prevention and rehabilitation services are designed and a template through
which any variation in quality of service delivery can be assessed.
It is recognised that cardiac rehabilitation (CR) has an established evidence-base and existing services
are in a strong position to evolve in order to provide care to include an ever-broadening spectrum of
in-scope patients, from those with established atherothrombotic vascular disease right through to those
asymptomatic individuals who have been deemed at high risk for the future development of adverse
cardiovascular events.
1-3
In addition, there is enormous overlap in terms of profile and potential benefits
for patients with other non-communicable diseases, particularly individuals with chronic respiratory
disease and certain forms of cancer.
4-5
Therefore, an opportunity exists to further expand the influence
of prevention and rehabilitation services which may, in turn, allow financial resources to be released and
a more cost-effective deployment of staff and facilities to take place.
All such potential developments will require innovative practice and close working between providers
and commissioners whilst also adhering to the principles set out within this BACPR Standards & Core
Components document.
1.1 Definition
There are many definitions of cardiac rehabilitation.
6-8
The following definition presents their combined
key elements:
“The coordinated sum of activities* required to influence favourably the
underlying cause of cardiovascular disease, as well as to provide the best possible
physical, mental and social conditions, so that the patients may, by their own
efforts, preserve or resume optimal functioning in their community and through
improved health behaviour, slow or reverse progression of disease”.
*The BACPR’s six core components for cardiovascular disease prevention and rehabilitation
constitute the coordinated sum of activities.
2 British Association for Cardiovascular Prevention and Rehabilitation
In meeting these defined goals, all CPRPs should aim to offer a service that takes a multidisciplinary
biopsychosocial approach in order to best influence uptake, adherence and long-term healthier living.
The involvement of partners, other family members and carers is also important.
9-11
1.2 Evidence
The evidence base that supports the merits of comprehensive CR is robust and consistently
demonstrates a favourable impact on cardiovascular mortality and hospital re-admissions in patients
with coronary heart disease
12
although there remains some uncertainty regarding the effect of CR on
all-cause mortality.
13-14
For patients who have experienced myocardial infarction (MI) and/or coronary
revascularisation, attending and completing a course of exercise-based CR is associated with an
absolute risk reduction in cardiovascular mortality from 10.4% to 7.6% when compared to those who
do not receive CR, with a number needed to treat (NNT) of 37. In terms of recurrent MI and repeat
revascularisation, the effect of CR would appear to be neutral, however, there is a significant reduction
in acute hospital admissions (reduced from 30.7% to 26.1%, NNT 22) which is a key determinant of the
intervention’s overall cost-efficacy.
13
For individuals with a diagnosis of heart failure, CR may not reduce total mortality but does impact
favourably on hospitalisation, with a 25% relative risk reduction in overall hospital admissions and
a 39% reduction (NNT 18) in acute heart failure related episodes.
15
The consequences of relapse
and readmission are enormous in terms of quality of life, associated morbidity and financial impact
thus the more recent emphasis on the importance of CR for heart failure patients within national and
international guidelines. In terms of direct measures of anxiety, depression and quality of life, CR
demonstrates consistently favourable outcomes for all patient groups and for those with heart failure,
a clinically relevant (and highly statistically significant) change in the Minnesota Living with Heart Failure
questionnaire point score of 5.8.
15
Finally, there is persuasive data supporting the benefits of different modes of CR delivery with no
apparent difference in either clinical or quality of life outcomes when comparing supervised centre-based
CR with that undertaken in a domestic environment, nor any major variation in healthcare costs.
16
This
should allow CPRPs to be more flexible in their CR offer and to be more innovative when attempting to
attract either new or hitherto hard to reach “in-scope” groups.
In summary, CR reduces both cardiovascular mortality and episodes of acute hospitalisation whilst also
improving functional capacity and perceived quality of life. CPRPs support an early return to work and
the development of self-management skills,
17
and can be delivered effectively in a variety of formats,
including traditional supervised centres as well as domestic settings. Given that CR remains one of the
most clinically and cost-effective therapeutic interventions in cardiovascular disease management,
13 18
it is vital that systems are in place to maximise uptake and adherence. There is continued emphasis
(supported by these updated standards) placed upon the importance of early CR, commencing
within two weeks of either hospital discharge or confirmed diagnosis in the case of stable angina or
heart failure. Starting within this timeframe has been shown to be both safe and feasible, as well as
improving patient uptake and adherence.
19-22
In addition, there is evidence to suggest that if a member
of the CPRP to which a patient has been referred is able to make contact with the patient during the
in-hospital stay and begin the process of personalised goal-setting, then this may lead to greater uptake
of prevention/rehabilitation services.
23-24
1. Introduction
Standards and Core Components 2017 (3rd Edition) 3
1.3 National and local factors for assuring quality
Quality assurance is facilitated through an alliance at both local (e.g. commissioners, service providers
and service users) and national level, together with participation in the National Audit for Cardiac
Rehabilitation (NACR) and ultimately attainment of national certification (Figure 1).
Figure 1: NCP_CR certification logo
The aim of this “alliance” is to deliver evidence-based and consistently high-quality CPRPs across all four
nations which can be accessed by all individuals deemed eligible. The National Certification Programme
(NCP_CR) has been designed in order to demonstrate that this is indeed the case and that programmes
are meeting (or working towards) a set of minimum quality standards adapted from those described
within this document, and which are reflective of the aggregated data submitted to the NACR.
25
The
NCP_CR is delivered via a BACPR/NACR collaborative and it is envisaged that all CPRPs will submit
complete data sets to NACR and register for certification.
1.4 Cardiac rehabilitation pathway of care
The Department of Health Commissioning Guide for Cardiac Rehabilitation
18
summarises a
recommended six-stage pathway of care from patient presentation (e.g. diagnosis or cardiac event),
identification for eligibility, referral, and assessment through to long-term management (Figure 2). Whilst
intended for England, this pathway of care is relevant to all four nations. Each of these stages within
this process are vital for programme uptake and adherence, the achievement of meaningful clinical
outcomes and ensuring longer-term behaviour change and desired health outcomes. The assessed
information must also be managed in a manner to fulfil the need for audit and evaluation.
Figure 2: Department of Health Commissioning Guide Six-Stage Patient Pathway of Care
1. Introduction
4 British Association for Cardiovascular Prevention and Rehabilitation
1.5 Funding of CPRPs
Previously published guidance has suggested a minimum cost per patient for CR.
18 26-28
However,
the 2010 Department of Health Commissioning Pack has now been reviewed in 2016 by Monitor (an
organisational part of NHS Improvement) which recommends the CR costing tool.
29 30
This tool allows
CPRPs to work out the costs as per staff profile required to meet the needs of the population they serve.
This model only takes account of staff costs over 16 one-hour sessions which means that individual
CPRPs would need to add other capital and services costs and adjust in respect of the number of
sessions they run.
These revised standards and core components place equal emphasis on lifestyle risk factor
management, psychosocial health and medical risk factor management whilst placing health behaviour
change and education at the very centre of this model of care. Therefore, costings developed within
business cases and/or funding (commissioning) determined by local clinical commissioning groups or
health boards would need to reflect the corresponding mix of expertise and time allocation required for
qualified and competent practitioners to employ an evidence-based approach across the six stages of
CR (Figure 2).
1. Introduction

Standards and Core Components 2017 (3rd Edition) 5
2. The Standards
The six standards for cardiovascular prevention and rehabilitation are:
Standard One The delivery of six core components by a qualified and competent multidisciplinary
team, led by a clinical coordinator.
Standard Two Prompt identification, referral and recruitment of eligible patient populations.
Standard Three
Early initial assessment of individual patient needs which informs the agreed
personalised goals that are reviewed regularly.
Standard Four Early provision of a structured cardiovascular prevention and rehabilitation programme
(CPRP), with a defined pathway of care, which meets the individual’s goals and is
aligned with patient preference and choice.
Standard Five Upon programme completion, a final assessment of individual patient needs and
demonstration of sustainable health outcomes.
Standard Six Registration and submission of data to the National Audit for Cardiac Rehabilitation
(NACR) and participation in the National Certification Programme (NCP_CR).
Important notes:
• Within the standards criteria the word shall is used to express a requirement that all programmes
are expected to comply with (Grade A/B recommendations based on the highest quality
evidence available and recognised as best practice). The word should is used to express a
recommendation that is recognised as desirable (Grade C/D recommendation).
• In some cases these recommendations may exceed the current minimum standards required for
the National Certification Programme, which sets annual targets based on national averages.
Performance indicators associated with meeting the minimum standards required for
programme certification can be found at: www.bacpr.com
6 British Association for Cardiovascular Prevention and Rehabilitation
STANDARD 1
The delivery of six core components by a qualified and competent
multidisciplinary team, led by a clinical coordinator
• Each programme shall deliver the six essential core components to ensure clinically effective care
and achieve sustainable health outcomes (as presented in Section 3).
• The team shall include a senior clinician who has responsibility for coordinating, managing and
evaluating the service. This also includes: resource and financial management for the service;
collaboration with NHS data analysts to successfully draw on all available funding and identify
any savings arising from reduced hospital admissions; and engagement with funding and
commissioning bodies.
• There shall be an appropriately qualified and competent named lead for each of the core
components. These practitioners who lead each of the core components should be able to
demonstrate that either they or their delivery team have appropriate training, professional
development, qualifications, skills and competency for the component(s) for which they are
responsible. Practitioners should use the BACPR Competences Frameworks, where available.
• The team shall include a physician who has sustained interest, commitment and knowledge in
cardiovascular disease prevention and rehabilitation.
• The delivery of the core components requires expertise from a range of different professionals
working within their scope of practice. The composition of each team may differ but collectively
the team shall have the necessary knowledge, skills and competencies to meet the standards
and deliver all the core components. Patients benefit from access to a wide range of specialists,
which most typically may include:
• Dietitian
• Exercise specialist
• Nurse specialist
• Occupational therapist
• Pharmacist
• Physician with special interest in prevention and rehabilitation
• Physiotherapist
• Practitioner Psychologist
• There shall be dedicated administrative support.
• The cardiovascular prevention and rehabilitation team shall actively engage and collaborate with
the patient’s/client’s wider care team (e.g. general practitioners, practice nurses, cardiovascular
disease specialist nurses, sports and leisure instructors, social workers and educationalists) to
create a truly comprehensive approach to long-term management.
• When designing, evaluating and developing programmes, service users should also be included
in this process.
2. The Standards
Standards and Core Components 2017 (3rd Edition) 7
STANDARD 2
Prompt identification, referral and recruitment of eligible patient populations
a. Patient Identification:
• The following priority patient groups shall be offered a CPRP irrespective of age, sex, ethnic
group and clinical condition:
• acute coronary syndrome
• coronary revascularisation
• heart failure
• Programmes should also aim to offer this service to other patient groups known to benefit:
• stable angina, peripheral arterial disease, post-cerebrovascular event
• post-implantation of cardiac defibrillators and resynchronisation devices
• post-heart valve repair/replacement
• post-heart transplantation and ventricular assist devices
• Adult Congenital Heart Disease (ACHD)
• It is recognised that asymptomatic individuals who have been identified as high cardiovascular
risk for CVD events are likely to benefit from the same professional lifestyle interventions and
risk factor management as those that currently qualify for CPRPs. In addition, risk factors
for cardiovascular disease are largely shared with the wider spectrum of non-communicable
diseases such as cancer, chronic obstructive pulmonary disease and atrial fibrillation.
4-5
Existing
cardiovascular prevention and rehabilitation services, if appropriately resourced, are in a strong
position to provide high quality, cost-effective interventions to individuals both with and without
established CVD. CPRPs should demonstrate an ambition to broaden their offer and initiate
discussions with commissioners locally.
• It is recognised that local policy may be required to address priority groups in the first instance to
reduce variation, ensuring consistency and equity of access. These standards however advocate
investment in cardiovascular prevention and rehabilitation services as to ensure all patient groups
ultimately benefit.
b. Patient Referral:
• An agreed and coordinated patient referral and/or recruitment process shall be in place so that
all eligible patients are identified and invited to participate.
•
CPRPs shall receive the referral of an eligible patient either during the in-patient stay or within 24 hrs
of discharge. Referrals sent within a community setting or following a day case intervention shall be
received by the CPRP within 72 hrs of the individual being identified as eligible.
• Prior to discharge, all eligible hospitalised patients should be encouraged by healthcare
professionals to attend and complete a CPRP
c. Recruitment:
• Upon receipt of referral, all patients deemed eligible shall be contacted within 3 working days to
review their progress and discuss enrolment.
• A mechanism of re-offer and re-entry should be put in place for patients who initially decline.
2. The Standards
8 British Association for Cardiovascular Prevention and Rehabilitation
STANDARD 3
Early initial assessment of individual patient needs, which informs the
agreed personalised goals that are reviewed regularly
• The initial assessment shall commence within 10 working days of receipt of referral.
•
The initial assessment is deemed complete when documentation of all the following has taken place:
• Demographic information and social determinants of health;
• Medical history, current health status and symptoms, together with a review of any relevant
investigations;
• Lifestyle risk factors (exposure to tobacco, adherence to a cardioprotective diet, body
composition, physical activity status and exercise capacity);
• Psychosocial health (anxiety, depression, illness perception, social support, psychological
stress, sexual wellbeing and quality of life);
• Medical risk management (control of blood pressure, lipids and glucose, use of
cardioprotective therapies and adherence to pharmacotherapies).
• Additional parameters should be assessed on an individual basis and may include psychosocial
factors such as anger, hostility, substance misuse, and occupational distress.
• Even if the initial assessment cannot be completed in its entirety (e.g. exercise capacity
assessment temporarily contraindicated) this shall not delay the assessment of the remaining
elements or the commencement of a formal CPRP.
• The initial assessment shall identify each individual’s needs using validated measures that are
culturally sensitive and also take account of associated co-morbidities.
• The assessment shall identify any physical, psychological or behavioural issues that have the
potential to impact on the patient’s ability to make the desired lifestyle changes.
• The assessment shall include formal risk stratification for exercise utilising all relevant patient
information (e.g. left ventricular ejection fraction, history of arrhythmia, symptoms, functional capacity).
• The written care plan should include a defined pathway of care which meets the individual patient
needs, participation preferences and choices.
• Patients shall receive on-going assessment throughout their CPRP and a regular review of their
goals with adjustments agreed and documented where required.
2. The Standards

Standards and Core Components 2017 (3rd Edition) 9
STANDARD 4
Early provision of a structured Cardiovascular Prevention and
Rehabilitation Programme (CPRP) with a defined pathway of
care which meets the individual’s goals and is aligned with
patient preference and choice
• A CPRP shall be deemed underway once patient goal(s) have been identified and appropriate
interventions have begun. This should occur immediately following completion of the initial
assessment (Standard 3) and shall occur within 10 working days of receipt of referral.
• In instances where commencement of group-based exercise has to be postponed, such as a
patient presenting with a contraindication to exercise, this shall not delay initiating management
strategies in other relevant core components.
• In order to maximise uptake, completion and outcomes, CPRPs shall deliver a menu-based
approach to meet a patient’s individual needs. This should include choice in terms of venue (e.g.
home, community, hospital) and scheduling of sessions (e.g. early mornings, evening & weekends).
• CPRPs can be delivered using a variety of modes (e.g. centre-based, home-based, manual-
based, web-based etc.). Irrespective of mode of programme delivery:
• Interventions provided are evidence-based and address the individual’s needs across all the
relevant core components.
• Patients shall have access to the multidisciplinary team as required.
• Patients shall be supported to participate in a personalised structured exercise programme
at least two to three times a week, designed specifically to increase physical fitness. This
requires documented evidence of regular review, goal setting and exercise progression.
• There shall be documented interaction between the patient and the multidisciplinary team
lasting a minimum of 8 weeks.
2. The Standards

10 British Association for Cardiovascular Prevention and Rehabilitation
STANDARD 5
Upon programme completion, a final assessment of individual
patient needs and demonstration of sustainable health outcomes
• In order to demonstrate effective health outcomes and ascertain the extent to which a patient’s
goals have been achieved, a formal assessment shall be performed at programme completion
which includes all the initially assessed components:
• Lifestyle related risk factors (exposure to tobacco, adherence to a cardioprotective diet, body
composition, physical activity status and exercise capacity);
• Psychosocial health (anxiety, depression, illness perception, social support, psychological
stress, sexual wellbeing and quality of life);
• Medical risk management (control of blood pressure, lipids and glucose, use of
cardioprotective therapies and adherence to pharmacotherapies).
• Any additional parameters assessed initially should be re-assessed formally upon programme
completion. For example, additional psychosocial factors such as anger, hostility, substance
misuse, and occupational distress.
• Data from the final assessment shall be formally recorded for evaluation of outcome measures
and audit.
• Final assessment shall be used to identify any unmet goals as well as any newly developed or
evolving clinical issues. This shall assist the formulation of long-term strategies.
• Within 10 working days of programme completion, the primary care provider (and the referral
source where relevant) shall be provided with a pre/post comparison of the patient’s risk factor
profile together with current medications and a summary of the long-term strategies proposed. A
copy shall also be provided to the patient.
STANDARD 6
Registration and submission of data to the National Audit for
Cardiac Rehabilitation (NACR) and participation in the National
Certification Programme
• Formal audit and evaluation shall include service level and patient level data at baseline and
following CR on clinical outcomes, patient experience and satisfaction.
• In order to monitor the quality of service delivery and to clearly demonstrate clinical outcomes
every service shall routinely submit the required audit data to NACR each year.
• Every cardiovascular prevention and rehabilitation service should strive to meet requirements
for the National Certification Programme and submit their data to the certification panel. Once
achieved, CPRPs should maintain their certification status.
2. The Standards

Standards and Core Components 2017 (3rd Edition) 11
3. The Core Components
A key aim of a CPRP, through the core components, is not only to improve physical health and quality
of life but also to equip and support people to develop the necessary skills to successfully self-manage.
Delivery should adopt a biopsychosocial evidence-based approach which is culturally appropriate and
sensitive to individual needs and preferences.
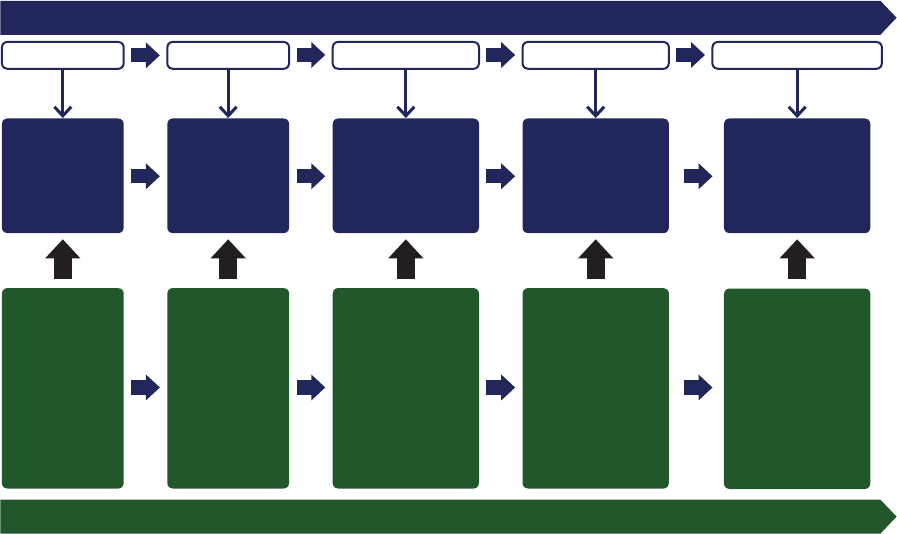
Figure 3 illustrates the six core components which include:
• Health behaviour change and education
• Lifestyle risk factor management
- Physical activity and exercise
- Healthy eating and body composition
- Tobacco cessation and relapse prevention
• Psychosocial health
• Medical risk management
• Long-term strategies
• Audit and evaluation
Practitioners who lead each of the core components must be able to demonstrate that they (or their
delivery team) have appropriate training, professional development, qualifi cations, skills and competency
for the component(s) for which they are responsible (Standard 1). BACPR aims to be a resource for
providing guidance on the knowledge, skills and competences required for each of the components.
Figure 3: The BACPR model for Cardiovascular Disease Prevention and Rehabilitation
A
U
D
I
T
A
N
D
E
V
A
L
U
A
T
I
O
N
L
O
N
G
-
T
E
R
M
S
T
R
A
T
E
G
I
E
S
Health
behaviour
change and
education
P
s
y
c
h
o
s
o
c
i
a
l
h
e
a
l
t
h
L
i
f
e
s
t
y
l
e
r
i
s
k
f
a
c
t
o
r
m
a
n
a
g
e
m
e
n
t
m
a
n
a
g
e
m
e
n
t
M
e
d
i
c
a
l
r
i
s
k
The Six Core Components
for Cardiovascular Disease Prevention and Rehabilitation
12 British Association for Cardiovascular Prevention and Rehabilitation
3.1. Health behaviour change and education
In meeting individual needs, health behaviour change and education are integral to all the other
components of cardiovascular prevention and rehabilitation. Adopting healthy behaviours is the
cornerstone of prevention and control of cardiovascular disease.
3.1.1 Health behaviour change
To facilitate effective behaviour change, cardiovascular prevention and rehabilitation services should ensure:
• The use of health behaviour change interventions and key behavior change techniques underpinned
by an up-to-date psychological evidence-base.
31
• The provision of or access to, training in communication skills for all staff which may include
motivational interviewing techniques and relapse prevention strategies.
• The provision of information and education to support fully informed choice from a menu of evidence-
based locally available programme components. Offering choice may improve uptake and adherence
to cardiovascular prevention and rehabilitation.
16-32
• They address any cardiac or other misconceptions (including any about cardiovascular prevention
and rehabilitation) and illness perceptions that lead to increased disability and distress.
33-35
• Support for patients (and significant supporting others) including goal-setting and pacing skills, and
exploring problem-solving skills in order to improve long-term self-management.
• Regular follow up to assess feedback and advise on further goal setting.
36
• Where possible, the patient identifies someone best placed to support him/her (e.g. a partner,
relative, close friend). The accompanying person should be encouraged to actively participate in
CPRP activities whenever possible, to maximise patient recovery and health behaviour change whilst
also addressing their own health behaviours.
37-39
3.1.2 Education
Education should be delivered not only to increase knowledge but importantly to restore confidence and
foster a greater sense of perceived personal control. As far as possible, education should be delivered
in a discursive rather than a didactic fashion. It is not enough to simply deliver information in designated
education sessions; health behaviour change needs to be achieved simultaneously and fully integrated
into the whole service.
Attention should be paid to establishing existing levels of knowledge and to assessing learning needs (of
individuals and groups), and subsequently tailoring information to suit assessed needs.
• Patients (and significant supporting others) should be encouraged to play an active role in the
educative process, sharing information in order to maximise uptake of knowledge.
• Education should be culturally sensitive and achieve two key aims:
- To increase knowledge and understanding of risk factor reduction
- To utilise evidence-based health behaviour change theory in its delivery. Incorporation of both
aspects of education increases the probability of successful long-term maintenance of change.
3. The Core Components
Standards and Core Components 2017 (3rd Edition) 13
• The educational component should be delivered using high quality and varied teaching methods
which take account of different learning styles and uses the best available resources to enable
individuals to learn about their condition and management. Information should be presented in
different formats using plain language and clear design, and tailored to the learning needs identified
during initial assessment.
40
• The education component of cardiovascular prevention and rehabilitation should empower individuals
to better manage their condition. Topics may include:
• Pathophysiology and symptoms
• Physical activity, healthy eating and weight management
• Tobacco cessation and relapse prevention
• Self-management and behavioural management of other risk factors including blood pressure,
lipids and glucose
• Medical and pharmaceutical management of blood pressure, lipids and glucose
• Psychological and emotional self-management
• Social support and other contextual factors
• Activities of daily living
• Occupational/vocational factors
• Resuming and maintaining sexual relations and dealing with sexual dysfunction
• Surgical interventions and devices
• Cardiopulmonary resuscitation
• Additional information, as specified in other components.
3.2 Lifestyle risk factor management
Physical activity and exercise, together with a healthy diet and avoidance of obesity and exposure to all
forms of tobacco, represents a lifestyle that is strongly associated with good cardiovascular health. All
patients should have the opportunity to discuss their concerns across all of these lifestyle risk factors as
relevant. Achievement of the lifestyle targets, as defined by the most up to date Joint British Societies
Guidelines, should utilise evidence-based health behaviour change approaches led by specialists in
collaboration with the multidisciplinary team. Supporting individuals in developing self-management skills
is the cornerstone of long-term cardiovascular prevention and rehabilitation.
3.2.1 Physical activity and exercise
• Staff leading the exercise component of cardiovascular prevention and rehabilitation should be
appropriately qualified, skilled and competent.
41
• Baseline assessment of physical fitness shall be carried out to inform risk assessment, tailor the
exercise prescription and aid goal setting.
42-45
• Best practice standards and guidelines for physical activity and exercise prescription shall be used.
42-44
3. The Core Components
14 British Association for Cardiovascular Prevention and Rehabilitation
• Risk stratification, based upon clinical features and baseline exercise capacity shall be undertaken.
42
This will then determine the appropriate:
- Exercise prescription, activities of daily living (ADL) guidance and support
- Staffing levels and skills
41
- Resuscitation support and provision in line with current Resuscitation Council UK / BACPR
guidance
46
- Choice of venue (home/community/hospital).
• Patients should receive individual guidance and advice on ADLs together with a tailored activity
and exercise plan with the collective aim to increase physical fitness as well as overall daily energy
expenditure and decrease sedentary behaviour. The activity and exercise plan should be identified
with the patient, take account of their co-morbidities and should be sensitive to their physical,
psychosocial (cognitive and behavioural) capabilities and needs.
3.2.2 Healthy eating and body composition
• Staff leading the dietary component of cardiovascular prevention and rehabilitation should be
appropriately qualified, skilled and competent.
• All patients shall have a baseline assessment of their dietary habits, including adherence with a
cardioprotective diet and measurement of their weight, body mass index and waist circumference.
• The focus of advice should be on making healthy dietary choices to reduce total cardiovascular risk
and improve body composition.
• Misconceptions about nutrition, dieting and weight cycling should be addressed and corrected.
47-48
• Patients should receive personalised dietary advice that is sensitive to their culture, needs and
capabilities coupled with support to help them achieve and adhere to the components of a
cardioprotective diet as defined by the most up to date Joint British Societies and NICE guidelines.
49-51
• Patients with additional co-morbidities leading to more complex dietary requirements should be
assessed and managed individually by a registered dietitian.
• Weight management may form an important component in cardiovascular prevention and
rehabilitation and could include:
• weight gain (e.g. in debilitated patients)
• weight loss, which where appropriate and in relation to excess fat, is best achieved through a
combination of increased physical activity and reduced caloric intake
52
• weight maintenance (e.g. in those who have recently quit smoking
53
or those with heart failure).
• It may be appropriate to refer to the appropriate specialists for pharmacotherapy and/or bariatric
surgery in order to co-manage weight loss.
54
3.2.3 Tobacco cessation and relapse prevention
Staff delivering the tobacco cessation and relapse prevention component of cardiovascular prevention
and rehabilitation should be appropriately qualified, skilled and competent in keeping with the NHS
Centre for Smoking Cessation and Training Standard which is available for download from their website
– www.ncsct.co.uk.
55
3. The Core Components
Standards and Core Components 2017 (3rd Edition) 15
• Current and past tobacco use should be assessed in all patients including whether they are a current user
or recent quitter, their history of tobacco use, past quit attempts and exposure to second hand smoke.
• In patients who are currently using tobacco, frequency and quantity of use should be quantified. In
addition, motivation to quit and a measure of nicotine dependence should be assessed, together with
identifying psychological co-morbidities like depression and tobacco use by others at home.
• At the first assessment, medical advice to quit should be reinforced and a quit plan discussed which
proposes the use of pharmacological support and follow up counselling within the prevention and
rehabilitation service. Every effort should be made to assist individuals to achieve complete cessation
of all forms of tobacco use, with repeat assessment of progress with cessation at every visit.
56-58
• Patient preference is a priority regarding the choice of aids to use in tobacco cessation. The use of
evidence-based therapies like Varenicline (Champix) and combination long- and short-acting nicotine
replacement therapy is considered the gold standard, however non-medical nicotine delivery devices
like e-cigarettes should also be considered as evidence is building for their efficacy. Guidance for
cessation advisers can be found in the NCSCT e-cigarette briefing.
59
• Preventing relapse is vital and may include prolonging the use of NRT and Varenicline (Champix)
beyond the usual duration, and/or e-cigarettes in cases where cessation has been problematic. Risk
of relapse is higher when an individual lives, socialises or works closely with others who use tobacco,
therefore encouraging quit attempts in partners/spouses/friends/children may be helpful.
3.3 Psychosocial health
People taking part in cardiovascular prevention and rehabilitation may have many different emotional
issues, and a comprehensive, holistic assessment is crucial to achieving the desired outcomes.
Every patient should be screened for psychological, psychosocial and sexual health and wellbeing as
ineffective management can lead to poor health outcomes.
60-62
•
Staff leading the psychosocial health component should be appropriately qualified, skilled, and competent.
• All patients should undergo a valid assessment of:
- Psychological distress, for example, anxiety and depression (using an appropriate tool – Hospital
Anxiety and Depression Scale (HADS) is available through the NACR)
-
Quality of life (using an appropriate tool - Dartmouth Primary Care Cooperative (COOP) and Minnesota
Living With Heart Failure (MLWHF) are available through the NACR)
- Psychological stressors
- Illness perceptions and self-efficacy for health behaviour change
- Adequacy of social support (covered in Dartmouth COOP – available through NACR)
- Alcohol and substance misuse
• Services should help patients to increase awareness of ways in which psychological development,
including illness perceptions, stress awareness and improved stress management skills can affect
subsequent physical and emotional health.
• Attention should be paid to social support, as social isolation or lack of perceived social support
is associated with increased cardiac mortality.
63
Whereas appropriate social support is helpful,
overprotection may adversely affect quality of life.
64
3. The Core Components
16 British Association for Cardiovascular Prevention and Rehabilitation
• Levels of psychological intervention (for psychological distress):
- Cardiovascular prevention and rehabilitation teams are best placed to deal with the normal range of
emotional distress associated with a patient’s precipitating cardiac event.
- Where appropriately trained psychological practitioners exist within the cardiovascular prevention
and rehabilitation team, individuals with clinical levels of anxiety or depression related to their
cardiac event can be managed within the service.
• In the absence of dedicated psychological practitioners in the team, individuals with clinical signs of
anxiety and depression, unrelated to their cardiac event, or with signs of severe and enduring mental
health problems, should have access to appropriately trained psychological practitioners and their GP
should be informed.
65-67
• Services should be aware of patients with problems related to alcohol misuse or substance misuse
and offer referral to an appropriate resource.
• It is also important to consider vocational advice and rehabilitation/financial implications and to
establish an agreed referral pathway to appropriate support and advice.
• Sexual health issues are also common with cardiovascular disease, and can negatively impact quality
of life and psychological wellbeing.
68-69
• Every patient should be provided with the opportunity to raise any concerns they may have
in relation to sexual activity and/or function. Assessment of patients’ sexual concerns can be
beneficial.
70
• Concerns or issues raised on assessment should be addressed through sexual counselling and
medical management where indicated.
70-72
• Patients dealing with longstanding or complex sexual health issues should be offered referral to an
appropriate resource.
70-72
3.4 Medical risk management
• Staff leading the medical risk management component of cardiovascular prevention and rehabilitation
services should be appropriately qualified, skilled and competent. Ideally an independent prescriber
should be part of the multidisciplinary team.
• Best practice standards and guidelines for medical risk factor management (blood pressure, lipids
and glucose),
49-51 73-75
optimisation of cardioprotective therapies and management of patients with
implantable devices
42 76-77
should be used.
• Assessment should include:
- Measurement of blood pressure, lipids, glucose, heart rate and rhythm.
- Current medication use (dose and adherence).
- Patients’ beliefs about medication as this affects adherence to drug regimens.
78
- A discussion regarding sexual activity / function (pending patient’s willingness to discuss).
- Implantable device settings where applicable.
• During the CPRP, blood pressure and glucose should be regularly monitored with the aim of helping
the individual to reach the targets defined in national guidelines by programme completion.
49-51 73-75
3. The Core Components
Standards and Core Components 2017 (3rd Edition) 17
• Key cardioprotective medications are prescribed according to current guidance.
• Cardioprotective medications should be up-titrated during the programme so that evidence-based
dosages are achieved.
• Cardiovascular prevention and rehabilitation staff should be involved with initiation and/or titration
of appropriate pharmacotherapy either directly through independent prescribing by a member of
the multidisciplinary team or agreed protocols / patient group directives or through liaison with an
appropriate healthcare professional (e.g. cardiologist, primary care physician).
•
Erectile dysfunction in cardiovascular patients is typically multifactorial with vascular disease, psychogenic
factors and medication all acting as potential contributors. Individuals with erectile dysfunction should be
considered for medication review and appropriate referral made where indicated.
• In people with Implantable devices, such as implantable cardiac defibrillators and/or cardiac
resynchronisation therapy:
• Devices can have an impact on psychological and physical function, exercise ability, which should
be considered within the individualised programme and may require additional expertise.
42 79-80
• Liaison with specialist cardiac services is important (e.g. arrhythmia nurse specialist,
electrophysiologist and cardiac physiologist).
• Cardiovascular prevention and rehabilitation services also provide an opportunity to identify patients
who may benefit from an implantable device.
76
3.5 Long-term strategies
By the end of the CPRP the patient should have:
• undergone assessment and reassessment as identified in Standards 3 and 5
• participated in a tailored programme that encompasses the Core Components
• identified their long-term management goals.
3.5.1 Patient responsibilities
• By the end of the programme patients will have been encouraged to develop full biopsychosocial
self-management skills and so be empowered and prepared to take ownership of their own
responsibility to pursue a healthy lifestyle. Carers, spouses and family should also be equipped to
contribute to long-term adherence by helping and encouraging the individual to achieve their goals.
• Patients and their families should be signposted and encouraged, where appropriate, to join:
- local heart support groups
- community exercise and activity groups
- community dietetic and weight management services
- tobacco and smoking cessation services.
• Promoting ongoing self-management strategies could also include online applications or tools and
self-monitoring resources.
3. The Core Components
18 British Association for Cardiovascular Prevention and Rehabilitation
3.5.2 Service responsibilities
•
Patients should be supported to plan and implement self-management strategies to help them transition
from the CPRP and continue to work towards minimising their risk of cardiovascular disease progression
following programme completion.
•
Upon programme completion there should be a formal assessment of lifestyle risk factors (physical
activity, diet and tobacco use as relevant), psychological and psychosocial health status, medical risk
factors (blood pressure, lipids and glucose) and use of cardioprotective therapies together with long-term
management goals. This should be communicated by discharge letter to the referrer and the patient as
well as those directly involved in the continuation of healthcare provision.
•
There should be communication and collaboration between primary and secondary care services to
achieve the long-term management plan.
•
Patients should be registered onto GP Practice CHD/CVD registers.
3.6 Audit and Evaluation
The NHS and its services are required, through NICE Guidance, to offer CR to all eligible patients and
in doing so they are duty bound to audit their performance locally and supply data to ensure equity of
service delivery nationally. Although uptake to CR is improving the quality of the services delivered is not
unified across the UK.
81
The BACPR recommends that every CPRP should formally audit and evaluate their service which can
be achieved through using the NACR directly or through upload of data if collected on local provider
software. The BACPR include the contribution of data to the National Audit for Cardiac Rehabilitation
(NACR) as a standard as this plays a key role in monitoring the quality of service delivery and influencing
and informing national policy. Data entered directly or uploaded to NHS Digital (the organisation that
hosts NACR data) should include both individual and service level data based on assessment and
including outcomes.
Service level audit should therefore include the collection of data to meet the following aims:
• Monitor and manage patient progress
• Monitor cardiovascular prevention and rehabilitation service resources
• Evaluate programmes in terms of clinical and patient-reported outcomes
• Benchmarking against local, regional and national standards
• Provide measures of performance and quality for commissioners and providers of cardiovascular
prevention and rehabilitation services
• Contribute to the national audit functions
• Present and share cardiovascular prevention and rehabilitation outcomes in both clinical and
patient formats
Where service resources and service design permits, the BACPR encourages cardiovascular prevention
and rehabilitation teams to provide one-year follow-up data as part of audit. NHS Digital-NACR has
the capability and capacity to capture this data within their online software. The ability to report at 12
months requires a high level of integration and communication between secondary and primary care
which can be achieved without duplication of work if carried out within the NHS Digital-NACR software
which is integrated along the patient journey.
3. The Core Components
Standards and Core Components 2017 (3rd Edition) 19
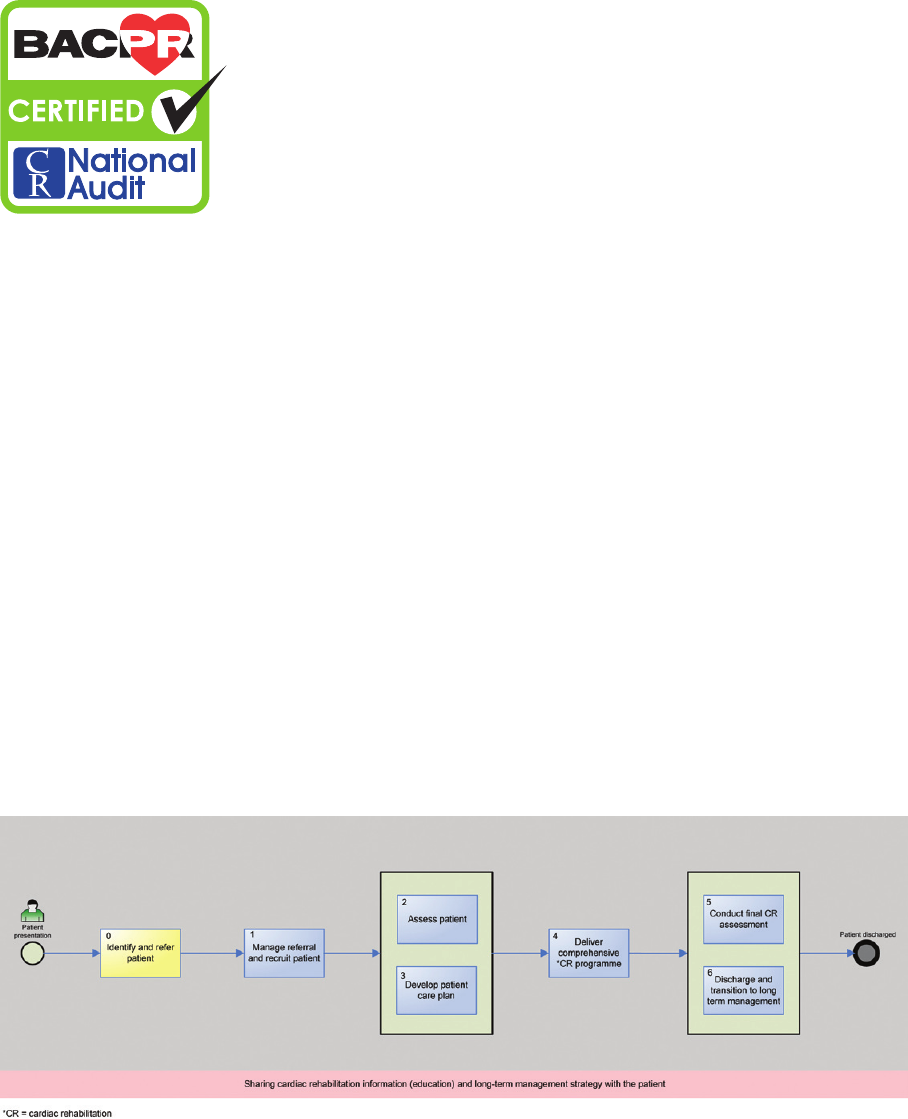
Figure 4. CR patient journey aligned with NACR data entry pathway
3.6.1 National Certification Programme for Cardiac Rehabilitation (NCP_CR)
The BACPR and the NACR launched a joint National Certification Programme for Cardiac Rehabilitation
(NCP_CR) in 2016 with an aim to ensure that all programmes are working to agreed clinical standards.
The new 2017 Standards and Core Components are aligned with data requirements for the NCP_CR.
25
The BACPR encourages all programmes to submit data and register for the NCP_CR so that patients,
wherever they live, can be confident that the services on offer meet agreed minimum standards.
The ultimate goal is for all CR programmes to deliver services in line with the Standards and Core
Components in this document, however at present most programmes are working towards the minimum
standards as outlined in the NCP_CR.
81
Future NACR reports will incorporate the extent by which
programmes are meeting NCP_CR criteria.
3. The Core Components
CR patient journey aligned with NACR data entry pathway
National Audit of Cardiac Rehabilitation
GP / Acute
Identify and refer
patient
Reason for referral
recorded in Initiating
Event. Source of
referral, and referral
date recorded
Referral dates and
start dates for all
early and core rehab
Risk Assessment
Previous events and
comorbidities
Manage referral
and recruit patient
Acute / Outpatient
Assessment 1, baseline
before core rehab
delivery:
From patient
self assessment
questionnaire, and clinical
appointment
Measures physical /
activity / fitness / anxiety
and depression / drugs
Tailored rehab based on
assessment
Assess Patient
Develop patient care
plan
Outpatient / Community
Duration and number
of sessions measured:
type of rehab delivered
recorded. Core
components listed
Deliver
comprehensive
CR Programme
Outpatient / Community
Assessment 2 end
of rehab. Repeat of
measurements at Ass 1
for outcomes
Onward referral
recorded
Ass 3 at 12 month follow
up if resourced to do so
Conduct final CR
Assessment
Discharge and
transition to long term
management
Outpatient / Community / GP
20 British Association for Cardiovascular Prevention and Rehabilitation
4. Appendices
Appendix 1: References
1. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Vascular protection in people with
diabetes. Canadian Journal of Diabetes. 2013;37(Suppl 1):S100-4.
2. Dasgupta K, Quinn RR, Zarnke KB, et. al. for the Canadian Hypertension Education Program. The 2014 Canadian
Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk,
prevention, and treatment of hypertension. Canadian Journal of Cardiology. 2014;30:485-501.
3. Schuler G, Adams V, Goto Y. Role of exercise in the prevention of cardiovascular disease: results, mechanisms, and
new perspectives. European Heart Journal. 2013;34:1790-9.
4. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation.
2016;133(11):1104-14.
5. Lim SS, Vos T, Flaxman AD, colleagues. A comparative risk assessment of burden of disease and injury attributable
to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of
Disease Study 2010. The Lancet. 2012;380(9859):2224-60. Available at: http://www.sciencedirect.com/science/
article/pii/S0140673612617668
6. The World Health Organisation (WHO). Cardiac rehabilitation and secondary prevention: long term care for patients
with ischaemic heart disease. Briefing letter. Copenhagen, Denmark: WHO Regional office for Europe, 1993.
7. Feigenbaum E. Cardiac rehabilitation services [microform] / [E. Feigenbaum, E. Carter]. Rockville, MD U.S. Dept. of
Health and Human Services, Public Health Service, National Center for Health Services Research and Health Care
Technology Assessment; Available from National Technical Information Service, 1987.
8. Goble AJ, Worcester MU. Best practice guidelines for cardiac rehabilitation and secondary prevention. Melbourne,
Australia: The Heart Research Centre, on behalf of Department of Human Services Victoria, 1999.
9. DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: a meta-analysis.
Medical Care. 2007;45(6):521-8.
10. Gatchel RJ, Oordt MS. Clinical health psychology and primary care: Practical advice and clinical guidance for
successful collaboration. Washington, DC: American Psychological Association, 2003.
11. Carlson JJ, Norman GJ, Feltz DL, Franklin BA, Johnson JA, Locke SK. Self-efficacy, psychosocial factors, and
exercise behavior in traditional versus modified cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation.
2001;21(6):363-73.
12. Anderson L, Thompson DR, Oldridge N, Zwisler A, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation
of coronary heart disease. Cochrane Database of Systematic Reviews. 2016;Issue 1(Art. No.: CD001800.) Available at:
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001800.pub3/abstract
13. Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ. 2015;351 Available at: http://www.bmj.com/content/
bmj/351/bmj.h5000.full.pdf
14. Rauch B, Davos CH, Doherty P, Saure D, Metzendorf M-I, Salzwedel A, Voller H, Jensen K, Schmid J-P, on
behalf of the Cardiac Section of the European Association of Preventive Cardiology (EAPC). The prognostic
effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: A systematic review and
meta-analysis of randomized and non-randomized studies – The Cardiac Rehabilitation Outcome Study (CROS).
European Journal of Preventive Cardiology. 2016;23(18):1914-39. Available at: http://journals.sagepub.com/doi/
abs/10.1177/2047487316671181
15. Sagar VA, Davies EJ, Briscoe S, Coats AJS, Dalal HM, Lough F, Rees K, Singh S, Taylor RS. Exercise-based
rehabilitation for heart failure: systematic review and meta-analysis. Open Heart. 2015;2(1) Available at:
http://openheart.bmj.com/content/2/1/e000163
16. Taylor RS, Dalal H, Jolly K, Zawada A, Dean SG, Cowie A, Norton RJ. Home-based versus centre-based cardiac
rehabilitation. Cochrane Database of Systematic Reviews. 2015(8) Available at: http://dx.doi.org/10.1002/14651858.
CD007130.pub3
17. Yohannes AM, Doherty P, Bundy C, Yalfani A. The long-term benefits of cardiac rehabilitation on depression, anxiety,
physical activity and quality of life. Journal of Clinical Nursing. 2010;19(19-20):2806-13.
18. National Institute for Health and Care Excellence. Cardiac rehabilitation services: commissioning guide. London: NICE,
2013. Available at: https://www.nice.org.uk/guidance/qs9/resources/cardiac-rehabilitation-services-commissioning-
guide-304110253
19. Eder B, Hofmann P, von Duvillard SP, Brandt D, Schmid J, Pokan R, Wonisch M. Early 4-Week cardiac rehabilitation
exercise training in elderly patients after heart surgery. Journal of Cardiopulmary Rehabilitation and Prevention.
2010;30(2):85-92.
20. Maachi C, Fattirolli F, Molino Lova R, Conti AA, Luisi MLE, Intini R, Zipoli R, Burgisser C, Guarducci L, Masotti G,
Gensini GF. Early and late rehabilitation and physical training in elderly patients after cardiac surgery. American Journal
of Physical and Medical Rehabilitation. 2007;86:826-34.
Standards and Core Components 2017 (3rd Edition) 21
21. Aamot I, Moholdt T, Amundsen B, Solberg HS, Mørkved S, Støylen A. Onset of exercise training 14 days after
uncomplicated MI: a randomized controlled trial. European Journal of Cardiovascular Prevention and Rehabilitation.
2010;17(14):387-92.
22. Haykowsky M, Scott J, Esch B, Schopflocher D, Myers J, Paterson I, Warburton D, Jones L, Clark AM. A meta-
analysis of the effects of exercise training on left ventricular remodeling following myocardial infarction: start early and
go longer for greatest exercise benefits on remodeling. Trials. 2011;12(92): DOI: 10.1186/745-6215-12-92.
23. Davies P, Taylor F, Beswick A, Wise F, Moxham T, Rees K, Ebrahim S. Promoting patient uptake and adherence
in cardiac rehabilitation. Cochrane Database of Systematic Reviews. 2010; Issue 7.(Art. No.: CD007131.):
DOI:10.1002/14651858.CD007131.pub2.
24. Cossette S, Frasure-Smith N, Dupuis J, Juneau M, Guertin M. Randomized controlled trial of tailored nursing
interventions to improve cardiac rehabilitation enrolment. Nursing Research. 2012;61(2):111-20.
25. Furze G, Doherty P, Grant-Pearce C. Development of a UK National Certification Programme for Cardiac Rehabilitation
(NCP_CR). British Journal of Cardiology. 2016;23:102-5.
26. National Audit of Cardiac Rehabilitation. Annual reports 2007 to 2016. University of York: British Heart Foundation
Available at: http://www.cardiacrehabilitation.org.uk/reports.htm
27. National Institute for Health and Care Excellence. Chronic heart failure: Costing report for CG 108. Implementing NICE
Guidance. London: NICE, 2010. Available at: https://www.nice.org.uk/guidance/cg108/resources
28. Department of Health. Commissioning pack for cardiac rehabilitation. London: Department of Health, 2010.
Available at: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/
PublicationsPolicyAndGuidance/Browsable/DH_117504
29. Monitor. 2016/2017 National tariff payment system. London: NHS England Publications, 2016. Available at: https://
www.gov.uk/government/uploads/system/uploads/attachment_data/file/509697/2016-17_National_Tariff_Payment_
System.pdf
30. Department of Health. Cardiac rehabilitation: Costing tool guidance. London: Department of Health, 2010. Available at:
http://www.cardiacrehabilitation.org.uk/docs/Cardiac%20Rehabilitation%20Costing%20Tool%20Guidance.pdf
31. National Institute for Health and Care Excellence. Behaviour change: Individual approaches. PH49. London: NICE,
2014. Available at: https://www.nice.org.uk/guidance/ph49
32. Dalal HM, Wingham J, Evans P, Taylor R, Campbell J. Home based cardiac rehabilitation could improve outcomes.
BMJ. 2009;338(12, 1):1921.
33. Stafford L, Berk M, Jackson HJ. Are illness perceptions about coronary artery disease predictive of depression and
quality of life outcomes? Journal of Psychosomatic Research. 2009;66(3):211-20.
34. French DP, Cooper A, Weinman J. Illness perceptions predict attendance at cardiac rehabilitation following acute
myocardial infarction: A systematic review with meta-analysis. Journal of Psychosomatic Research. 2006;61:757-67.
35. Furze G, Lewin R, Murberg TA, Bull P, Thompson D. Does it matter what patients think? The relationship between
changes in patients’ beliefs about angina and their psychological and functional status. Journal of Psychosomatic
Research. 2005;59:323-9.
36. Institute of Medicine. Priority areas for national action: Transforming healthcare quality. Washington, DC: National
Academies Press, 2003:52.
37. Moser DK, Dracup K. Role of spousal anxiety and depression in patients’ psychosocial recovery after a cardiac event.
Psychosomatic Medicine. 2004;66:527-32.
38. Franks M, Stephens MAP, Rook KS, Franklin BA, Keteyian SJ, Artinian NT. Spouses’ provision of health-related
support and control to patients participating in cardiac rehabilitation. Journal of Family Psychology. 2006;20(2):311-8.
39. Wood DA, Kotseva K, Connolly S, Jennings C, Mead A, Jones J, Holden A, De Bacquer D, Collier T, De Backer
G, Faergeman O, on behalf of EUROACTION Study Group. Nurse-coordinated multidisciplinary, family-based
cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and
asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet.
2008;371:1999-2012.
40. Knowles MS, Holton EF, Swanson RA. The Adult Learner: The definitive classic in adult education and human
resource development (8th ed.). Burlington, MA: Elsevier, 2015.
41. British Association for Cardiovascular Prevention and Rehabilitation Exercise Professionals Group (BACPR-EPG).
Position statement: Essential competences and minimum qualifications required to lead the exercise component in
early cardiac rehabilitation. 2011. Available at http://www.bacpr.com.
42. Association of Chartered Physiotherapists in Cardiac Rehabilitation (ACPICR). ACPICR standards for physical activity
and exercise in the cardiac population. 2015. Available at: http://acpicr.com/publications
43. American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). Guidelines for Cardiac Rehabilitation
and Secondary Prevention Programs. 5th ed. Champaign, IL: Human Kinetics, 2013.
4. Appendices
22 British Association for Cardiovascular Prevention and Rehabilitation
44. Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, Franklin B, Sanderson B, Southard D. Core
components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the
American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical
Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity,
and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation.
2007;115(20):2675-82.
45. Piepoli MF, Corrà U, Adamopoulos S, et al., on behalf of the Cardiac Rehabilitation Section of the European
Association for Cardiovascular Prevention and Rehabilitation (EACPR). Secondary prevention in the clinical
management of patients with cardiovascular diseases. Core components, standards and outcome measures for
referral and delivery: A Policy Statement from the Cardiac Rehabilitation Section of the EACPR. Endorsed by the
Committee for Practice Guidelines of the European Society of Cardiology. European Journal of Preventive Cardiology.
2014;21(6):664-81.
46. Resuscitation Council (UK). Requirements for resuscitation training and facilities for supervised cardiac rehabilitation
programmes. 2013. Available at: https://www.resus.org.uk/cpr/requirements-for-resuscitation-training/
47. British Nutrition Foundation. Obesity: The report of the British Nutrition Foundation Task Force. London: Blackwell
Science, 1999.
48. Tylka TL, Annunziato RA, Burgard D, Daníelsdóttir S, Shuman E, Davis C, Caolgero RM. Weight-inclusive versus
weight-normative approach to health: evaluation the evidence for prioritizing well-being over weight loss. Journal of
Obesity. 2014;Article ID 983495. Available at: http://dx.doi.org/10.1155/2014/983495
49. National Institute for Health and Care Excellence. Myocardial infarction: cardiac rehabilitation and prevention of further
cardiovascular disease. CG172. London: NICE, 2013. Available at: https://www.nice.org.uk/guidance/cg172
50. National Institute for Health and Care Excellence. Unstable Angina and NSTEMI: the early management of unstable
angina and non-ST-segment-elevation myocardial infarction. CG94, Updated 2013. London: NICE, 2010. Available at:
www.nice.org.uk/CG94
51. JBS3 Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3).
Heart. 2014;100(Suppl 2):ii1-ii67. Available at: http://heart.bmj.com/content/100/Suppl_2/ii1.short
52. Shaw K, Gennat H, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database of Systematic
Reviews. 2006;Oct 18(4):CD003817.
53. Aubin H-J, Farley A, Lycett D, Lahmek P, Aveyard P. Weight gain in smokers after quitting cigarettes: meta-analysis.
BMJ. 2012;345:e4439. Available from: https://doi.org/10.1136/bmj.e4439
54. National Institute for Health and Care Excellence. Obesity guidance on the prevention, identification, assessment and
management of overweight and obesity in adults and children. CG43. London: NICE, 2006, updated 2013. Available
at: http://www.nice.org.uk/CG43NICE
55. NHS Centre for Smoking Cessation and Training (NCSCT). NCSCT training. Available at: http://www.ncsct.co.uk/
training
56. Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews.
2008(1):Art. No.: CD001188. DOI: 10.1002/14651858.CD001188.pub3
57. National Institute for Health and Clinical Excellence. Brief interventions and referral for smoking cessation: guidance.
PH1. London: NICE, 2006. Available at: http://guidance.nice.org.uk/PH1
58. National Institute for Health and Care Excellence. Smoking cessation services in primary care, pharmacies, local
authorities and workplaces, particularly for manual working groups, pregnant women and hard to reach communities.
PH10. London: NICE, 2008, Updated 2013. Available at: http://guidance.nice.org.uk/PH10
59. McEwen A, McRobbie H, on behalf of the National Centre for Smoking Cessation and Training (NCSCT) and Public
Health England. Electronic cigarettes: A briefing for stop smoking services. Dorchester: NCSCT, 2016. Available at:
http://www.ncsct.co.uk/publication_electronic_cigarette_briefing.php
60. Shibeshi WA, Young-Xu Y, Blatt CM. Anxiety worsens prognosis in patients with coronary artery disease. Journal of
the American College of Cardiology. 2007;49:2021-7.
61. Dickens C, McGowan L, Percival C, Tomenson B, Cotter L, Heagerty A, Creed F. New onset depression following
myocardial infarction predicts cardiac mortality. Psychosomatic Medicine. 2008;70:450-5.
62. Kronish IM. Persistent depression affects adherence to secondary prevention behaviors after acute coronary
syndromes. Journal of General Internal Medicine. 2006;21:1178-83.
63. Mookadam F, Arthur H. Systematic overview: social support and its relationship to morbidity and mortality after acute
myocardial infarction. Archives of Internal Medicine. 2004;164(14):1514-8.
64. Joekes K, Maes S, Warrens M. Predicting quality of life and self-management from dyadic support and overprotection
after myocardial infarction. British Journal of Health Psychology. 2007;12:473-89.
65. National Institute for Health and Care Excellence. Depression in adults with a chronic condition. CG 91. London: NICE,
2009. Available at: https://www.nice.org.uk/guidance/CG91
4. Appendices
66. National Institute for Health and Care Excellence. Common mental health problems: Identification and pathways to
care. CG123. London: NICE, 2011. Available at: https://www.nice.org.uk/guidance/cg123
67. Whalley B, Rees K, Davies P, Bennett P, Ebrahim S, Lui Z, West R, Moxham T, Thompson DR, Taylor
RS. Psychological interventions for coronary heart disease. Cochrane Database of Systematic Reviews.
2011;10(8):CD002902. Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002902.pub3/full
68. Træen B, Olsen S. Sexual dysfunction and sexual well-being in people with heart disease. Sexual and Relationship
Therapy. 2007;22:193-208.
69. Günzler C, Kriston L, Harms A, Berner MM. Association of sexual functioning and quality of partnership in patients in
cardiovascular rehabilitation-a gender perspective. The Journal of Sexual Medicine. 2009;6(1):164-74.
70. Steinke EE, Jaarsma T, Barnason SA, Byrne M, Doherty S, Dougherty CM, Bengt F, Kautz DD, Mårtensson J,
Mosack V, Moser DK, 2013;128:2075–96 C. Sexual counselling for individuals with cardiovascular disease and their
partners: a consensus document from the American Heart Association and the ESC Council on Cardiovascular
Nursing and Allied Professions (CCNAP). Circulation. 2013;128(18):2075-96. Available at: https://doi.org/10.1161/
CIR.0b013e31829c2e53
71. Tra Levine GN, Steinke EE, Bakaeen FG, Bozkurt B, Cheitlin MD, Conti JB, Foster E, Jaarsma T, Kloner RA, Lange
RA, Lindau ST, Maron BJ, Moser DK, Ohman EM, Seftel AD, Stewart WJ. Sexual activity and cardiovascular disease:
a scientific statement from the American Heart Association. Circulation. 2012;125(8):1058-72. Available at: https://doi.
org/10.1161/CIR.0b013e3182447787
72. Steinke EE, Swan JH. Effectiveness of a videotape for sexual counseling after myocardial infarction. Research in
Nursing and Health. 2004;27:269-80.
73. National Institute for Health and Care Excellence. Hypertension. CG127. London: NICE, 2011, Updated 2016.
Available at: http://guidance.nice.org.uk/CG127
74. National Institute for Health and Care Excellence. Cardiovascular disease: risk assessment and reduction, including
lipid modification: CG181. London: NICE, 2014, Updated 2016. Available at: https://www.nice.org.uk/guidance/cg181
75. National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. NG28. London: NICE,
2015, Updated 2016. Available at: https://www.nice.org.uk/guidance/ng28
76. National Institute for Health and Care Excellence. Implantable cardioverter defibrillators and cardiac resynchronisation
therapy for arrythmias and heart failure: TA314. London: NICE, 2014. Available at: https://www.nice.org.uk/guidance/
ta314
77. National Institute for Health and Care Excellence. Chronic heart failure: management of chronic heart failure in adults in
primary and secondary care. CG108. London: NICE, 2010. Available at: http://www.nice.org.uk/CG108
78. Byrne M, Walsh J, Murphy AW. Secondary prevention of coronary heart disease: Patient beliefs and health-related
behaviour. Journal of Psychosomatic Research. 2005;58:403-15.
79. Fitchet A, Doherty PJ, Bundy C, Bell W, Fitzpatrick AP, Garratt CJ. Comprehensive cardiac rehabilitation programme
for implantable cardioverter-defibrillator patients: a randomised controlled trial. Heart. 2003;89(2):155-60.
80. Lewin RJ, Frizelle DJ, Kaye GC. A rehabilitative approach to patients with internal cardioverter-defibrillators. Heart.
2001;85(4):371-2.
81. Doherty P, Salman A, Furze G, Dalal H, Harrison A. Does cardiac rehabilitation meet minimum standards: an
observational study using UK national audit? Open Heart. 2017;3(e0005) Available at: http://openheart.bmj.com/
content/4/1/e000519
4. Appendices
24 British Association for Cardiovascular Prevention and Rehabilitation
4. Appendices
Appendix 2: Acknowledgements
The membership of the BACPR Standards & Core Components development groups is representative of many UK
professional associations and institutions with all members working within the cardiovascular rehabilitation field. The
individual members of the development group, working under the auspices of the BACPR, expressed no conflict of
interests regarding the material contained in this document.
We are also grateful to our affiliated colleagues in cardiovascular care, who have participated in the consultation
process and provided important feedback.
The BACPR Standards and Core Components (3rd Edition) Primary Writing Group
Prof. John Buckley (Exercise Physiologist; BACPR Past President), Prof. Patrick Doherty (Physiotherapist; BACPR
Past President), Prof. Gill Furze (Nurse; BACPR Past President), Dr Jenni Jones (Physiotherapist; BACPR Past
President), Sally Hinton (Physiotherapist; BACPR Executive Director), Jo Hayward (Nurse; BACPR Council Member),
Dr Joe Mills (Consultant Cardiologist, BACPR President), Dr Linda Speck (Consultant Clinical Health Psychologist).
The BACPR Standards and Core Components (3rd Edition) Development Group
Dr Alison Atrey Dietitian, England
Dr Molly Byrne Senior Lecturer, Ireland
Prof John Buckley Exercise Physiologist, England
Jacqueline Cliff Nurse, Wales
Dr Aynsley Cowie Physiotherapist, Scotland
Prof Patrick Doherty Physiotherapist, England
Prof Gill Furze Nurse, England
Sally Hinton Physiotherapist, England
Jo Hayward Nurse, England
Dr Catriona Jennings Nurse, England
Dr Jenni Jones Physiotherapist, England
Louise Jopling Nurse, England
Dr Joe Mills Consultant Cardiologist, England
Dr Linda Speck Consultant Clinical Health Psychologist, Wales
The BACPR Standards and Core Components (2nd Edition) Development Group
Prof John Buckley Exercise Physiologist, England
Kathryn Carver Nurse, England
Wendy Churchouse Nurse, Wales
Dr Susan Connolly Consultant Cardiologist, England
Prof Patrick Doherty Physiotherapist, England
Prof Gill Furze Nurse, England
Sally Hinton Physiotherapist, England
Dr Jenni Jones Physiotherapist, England
Prof Bob Lewin Clinical Psychologist, England
Alison Mead Dietitian, England
Paul Smith Nurse, Wales
Dr Linda Speck Consultant Clinical Health Psychologist, Wales
Dr Iain Todd Consultant Medical Rehabilitation Physician, Scotland
Charlotte-Anne Wells Occupational Therapist, Northern Ireland
Standards and Core Components 2017 (3rd Edition) 25
The original 2007 Development Group
Chetali Agrawal Dietitian, England
Linda Binder Nurse, NHS Heart Improvement Programme, England
Prof Patrick Doherty Physiotherapist, England
Geoffrey Dorrie BACR Phase IV and service user representative, England
Bernie Downey Nurse, Northern Ireland
Linda Edmunds Nurse, Wales
Judith Edwards Nurse, England
Gillian Fitnum Nurse, England
Dr Dorothy Frizelle Clinical Psychologist, England
Shirley Hall Nurse, British Heart Foundation
Sally Hinton Physiotherapist, England
Prof Bob Lewin Clinical Psychologist, England
Carol Over Occupation Therapist, Wales
Ann Ross Physiotherapist, Scotland
Dr Malcolm Walker Consultant Cardiologist, England
Prof David Wood Consultant Cardiologist, England
Anticipated review
These standards replace the previously published standards of 2012. We anticipate a further review of these
standards in 2021.
4. Appendices
26 British Association for Cardiovascular Prevention and Rehabilitation
Notes:
Standards and Core Components 2017 (3rd Edition) 27

“Promoting excellence in cardiovascular disease
prevention and rehabilitation”
Our Mission statement is:
To support health professionals in the development,
delivery and assessment of evidence-based, individualised
programmes of prevention and rehabilitation, which have
been appropriately funded and which are accessed both by
individuals with established Cardiovascular Disease (CVD)
and those with signifi cant CVD risk factors.
The British Association for Cardiovascular Prevention and Rehabilitation
British Cardiovascular Society
9 Fitzroy Square, London, W1T 5HW
Email: [email protected]
Direct Line: +44 (0)20 7380 1919
Fax: +44 (0)20 7388 0903
Website: www.bacpr.com
Registered Charity Number 1135639
Company limited by guarantee. Registered in England 5086964
Follow us on Twitter
@bacpr
Like our
Facebook page
