1
ALLEGHENY COLLEGE
Summary Plan Description
For the
Allegheny College Health & Welfare Employee Benefit Plan
Amended and Restated Effective
July 1, 2018
This document with the attached documents listed on the final page, constitute the
Summary Plan Description required by ERISA §102.
2
TABLE OF CONTENTS
1. DEFINITIONS................................................................................................................... 3
2. INTRODUCTION ............................................................................................................. 5
3. GENERAL INFORMATION ABOUT THE PLAN ................................................. 6
4. ELIGIBILITY AND PARTICIPATION REQUIREMENTS ................................... 7
5. SUMMARY OF PLAN BENEFITS .......................................................................... 15
6. OTHER LAWS THAT MAY AFFECT YOUR BENEFITS ............................... 16
7. HOW THE PLAN IS ADMINISTERED .................................................................. 19
8. CIRCUMSTANCES WHICH MAY AFFECT BENEFITS ................................. 20
9. AMENDMENT OF TERMINATION OF THE PLAN ........................................ 211
10. NO CONTRACT OF EMPLOYMENT .................................................................... 21
11. CLAIMS PROCEDURES........................................................................................... 21
12. STATEMENT OF ERISA RIGHTS ....................................................................... 233
APPENDIX ................................................................................................................................ 26

3
1. Definitions
Capitalized terms used in the Plan have the following meanings:
“Administrator” means Allegheny College or such other person or committee
as may be appointed from time to time by Allegheny College to supervise the
operation and administration of the Plan. The Administrator shall be the “named
fiduciary” under the “Plan”.
“Benefit Program” means an arrangement providing Employee benefits
established by Allegheny College which is a part of this Plan.
“COBRA” means the Consolidated Omnibus Budget Reconciliation Act of 1985,
as amended.
“Dental” means a Benefit Program under the Plan which is a group dental plan
that provides dental benefits (directly or otherwise) to Employees, former
Employees, and their families, as provided under the terms of such group Dental
insurance contract.
“Employee” means any common-law Employee of Allegheny College, who in
order to participate in Benefit Programs under the Plan, must satisfy the eligibility
provisions for each applicable Benefit Program under the Plan.
“Enrollment Period” means such period of time prior to the beginning of the
Plan year, established at the discretion of the Administrator. This Enrollment
Period, as specified by the Administrator and communicated to eligible
Employees, is the period of time during which eligible Employees and
Participants may elect, or reject, to participate in the Plan.
“ERISA” means the Employee Retirement Income Security Act of 1974, as
amended.
“GINA” means the Genetic Information Nondiscrimination Act of 2008.
“HSA Benefits” means a Health Savings Account (HSA) established outside the
Section 125 Plan with the Employee’s HSA trustee/custodian that may be funded
by the Employer and/or Eligible Employee with pre-tax contributions.
“HIPAA” means the Health Insurance Portability and Accountability Act of 1996,
as amended.
“Life and Accidental Death & Dismemberment Benefits” means a Benefit
Program under the Plan which provides group life and accidental death &
dismemberment benefits to Employees under the terms of such Group Term Life
and Accidental Death & Dismemberment insurance contract.
"Long Term Disability" means a group Benefit Program under the Plan that
provides long term income protection for disabled Employees under the terms of
such Long Term Disability insurance.
4
“Medical” (or “Health Plan”) means a Benefit Program under the Plan which is a
group health plan and which provides benefits for medical to Employees, former
Employees, and their families, as provided under the terms of such Medical Plan.
“NMHPA” means the Newborns’ and Mothers’ Health Protection Act of 1996, as
amended.
“Named Fiduciary” means Allegheny College.
“Plan Sponsor” means Allegheny College.
“Plan Year” means the 12-month period beginning each July 1.
“Prescription Drug” means a Benefit Program offered to participants enrolled in
Medical and which provides prescription drug benefits to Employees, former
Employees, and their families, as provided under the terms of such Prescription
Drug Plan.
“Spouse” means a partner in a legal marriage.
“Participant” means an eligible Employee who has met the requirements of
component benefit in the Plan and participates in the Plan.
“Plan” means this Allegheny College Welfare Employee Benefits Plan.
“Plan Administrator” means Allegheny College.” refers only to a person of the
opposite sex who is a husband or wife.
“USERRA” means the Uniformed Services Employment and Reemployment
Rights Act of 1994.
"Vision" means a Benefit Program under the Plan which is a group vision plan
and which provides benefits for vision to Employees, former Employees, and
their families, as provided under the terms of such Vision Plan.
"WHRCA” means the Women’s Health and Cancer Rights Act of 1998, as
amended.

5
2. Introduction
The College established and maintains the Plan for the exclusive benefit of its
eligible Employees and their spouses and dependents. This Plan includes
component Benefit Programs that are subject to ERISA and programs that are
not subject to ERISA. Descriptions of component Benefit Programs that are not
subject to ERISA are included in this Summary Plan Description for purposes of
convenience.
The Plan provides benefits through the following component Benefit Programs:
• PPO Medical with Prescription Drug (Attachment 1)
• High Deductible Health Plan with Prescription Drug and HSA Benefits
(Attachment 2)
• Dental (Attachment 3)
• Vision (Attachment 4)
• Life & Accidental Death & Dismemberment (Attachment 5)
• Long Term Disability (Attachment 6)
• Voluntary employee pay-all individual insurance coverage (no attachment)
Some of these component Benefit Programs require completion of application
forms, annual elections, and/or other administrative forms. These component
Benefit Programs require you to make an annual election to enroll for coverage.
Each of these component Benefit Programs is summarized in a certificate of
insurance, benefit booklet or a description of benefits issued by an insurance
company. A copy of each booklet or other document is attached to this document
in Attachments #1 through #6 as noted above. These documents, together,
make up the “summary plan description” or “SPD” for the Plan.
Electronic Forms
To facilitate efficient operation of the Plan, the Plan may allow forms (including,
for example, election forms and notices), whether required or permissive, to be
sent and/or made by electronic means. Copies of these documents may be
made available to you in electronic format as well.
Purpose of This Wrap SPD Document
You are being provided this document to give you an overview of the Plan and to
address certain information that may not be addressed in the Attachments. This
document, together with the Attachments, is the SPD required by ERISA. This
document is not intended to give you any substantive rights to benefits that are
not already provided by the Attachments. If you have not received a copy of the
Attachments, contact the Office of Human Resources of Allegheny College. You
must read the Attachments and this Wrap SPD to understand your benefits.

6
3. General Information about the Plan
Facts
Plan Name: Allegheny College Health & Welfare Employee Benefits Plan
Type of Plan: Welfare plan providing medical, prescription drug, dental,
vision, life, accidental death and dismemberment benefits,
long term disability benefits and voluntary employee pay-all
individual insurance coverage
Plan Year: July 1 to June 30.
Plan Number: 501
Effective Date: August 1, 1978. The Plan has been amended several times
since its original effective date, most recently as of July 1,
2018.
Funding Medium and Type of Plan Administration:
Some benefits under the Plan are self-funded, some are fully insured. As
discussed below under the heading “How the Plan Is Administered”, the
Company and the insurance companies share responsibility for administering the
majority of the component Benefit Programs under the Plan.
The PPO Medical and the High Deductible Medical Plan (w/ HSA Benefits)
are self-funded by the Company.
Other Benefit Programs, including Dental, Vision, Life & Accidental Death &
Dismemberment, Long Term Disability and voluntary employee pay-all individual
insurance coverage are fully insured.
The Company is responsible for paying claims with respect to the self-insured
benefits. The insurance companies, not the Company, are responsible for paying
claims with respect to the insured benefits.
Plan Sponsor: Allegheny College
520 North Main Street
Meadville, PA 16335-3903
814-332-3100
Plan Sponsor’s EIN: 25-0965212
Plan Administrator: Allegheny College
Attn: Office of Human Resources
520 North Main Street

7
Meadville, PA 16335-3903
814-332-2312
Named Fiduciary: Allegheny College
520 North Main Street
Meadville, PA 16335-3903
814-332-3100
For each of the insured component Benefit Programs, the Insurance Company is
a Named Fiduciary with respect to decisions regarding whether a claim for
benefits will be paid under the insurance contract.
Agent for Service of Legal Process:
Allegheny College
Attn: Patricia Ferrey
Director of Human Resources
520 North Main Street
Meadville, PA 16335-3903
814-332-2312
Service for legal process may also be served on the Plan
Administrator.
Plan Document: The Plan and its attachments constitute the written plan
document required by ERISA §402.
Important Disclaimer: Benefits hereunder are provided pursuant to insurance
contracts or pursuant to a governing plan document adopted by the College. If
the terms of this document conflict with the terms of such insurance contracts or
governing plan document, then the terms of the insurance contracts or governing
plan document will control, rather than this document, unless otherwise required
by law.
4. Eligibility and Participation Requirements
Eligibility and Participation
An eligible Employee with respect to the Plan will be any common law employee
of the College who is eligible to participate in and receive benefits under one or
more of the component Benefit Programs. To determine whether you or your
Spouse and dependents are eligible to participate in a component benefit
program, please read the eligibility information contained behind the Attachments
for the applicable component Benefit Programs. A summary of this information is
set forth below.
8
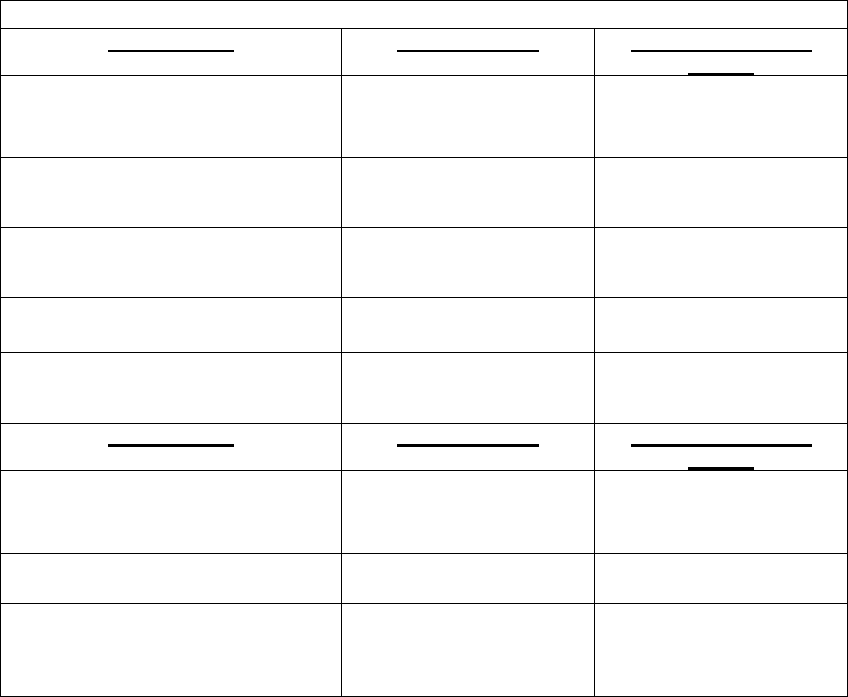
Eligibility and Entry Date:
Summary of Eligibility and Participation Provisions
Benefit Plans
Who is Eligible
When Participation
Begins
PPO Medical with Prescription Drug
Employee and
Dependents
First day of the month
following date of hire
High Deductible Medical with
Prescription Drug and HSA
Benefits
Employee and
Dependents
First day of the month
following date of hire
*Retiree Medical
(includes retirees on Phased
Retirement)
Retiree and Dependents
First day of the month
following date of
retirement
Dental
Employee and
Dependents
First day of the month
following date of hire
Vision
Employee and
Dependents
First day of the month
following date of hire
Benefit Plans
Who is Eligible
When Participation
Begins
Life and
Accidental Death &
Dismemberment
Employee
First day of the month
following date of hire
Long Term
Disability
Employee
First day of the month
following date of hire
Voluntary employee pay-all
insurance coverage.
Note: These benefits are not
subject to ERISA
Employee
First day of the month
following date of hire
*”Retiree Medical” applies to any employee who retires at age 58 and with 10
years of continuous full-time employment immediately upon retirement date.
If an Employee satisfies both conditions, the College considers the Employee
a “retiree.” The same medical coverage provided to active Employees will
continue for the retiree until the age of 65. If a spouse is under age 65 at the
time the retired Employee turns age 65, the spouse would be offered
continued medical coverage under COBRA for 36 months, or until age 65,
whichever occurs first.
Additional Information Regarding Eligibility Requirements and Participation
• An eligible dependent means any son or daughter who is tax dependent of a
participant as defined in the Internal Revenue Code section 152, but who has not
exceeded the maximum age as defined in the applicable Benefit Program. For
purposes of the Medical, Dental and Vision benefits, effective July 1, 2012, an
Eligible Dependent includes any child of the Participant who is under age twenty-
six (26). Please refer to Attachments in Appendix A for specific information
regarding dependent eligibility for other Benefit Programs.
If both you and your Spouse are eligible employees of Allegheny College you
may be covered under the Plan as an eligible employee or as a dependent of
9
your Spouse (if the eligible employee is considered a full-time employee). Your
dependent children may be covered under the Plan either by you or your
Spouse, but not both.
Benefits for Adopted Children / Guardianship Agreements
With respect to component Benefit Programs that are group health plans, the
Plan will extend benefits to dependent children placed with you for adoption or a
child under guardianship under the same terms and conditions as apply in the
case of dependent children who are natural children of other participants.
Employee Participants who currently cover eligible dependents under a
Guardianship Agreement will be required, upon enrollment and subsequent
requests, to show proof of continued guardianship in order to continue coverage
in the Plan for dependent child(ren).
Qualified Medical Child Support Orders
With respect to component benefit plans that are group health plans, the
Allegheny College Welfare Benefit Plan will also provide benefits as required by
any qualified medical child support order, or “QMCSO” (defined in ERISA Section
609(a)). The Plan will provide benefits to dependent children placed with
participants or beneficiaries for adoption under the same terms and conditions as
apply in the case of dependent children who are natural children of participants
or beneficiaries, in accordance with ERISA Section 609(c).
In order for this Plan to recognize a Qualified Medical Child Support Order it must
satisfy the following criteria:
It must be a judgment, decree or other court order relating to health benefits
coverage for a dependent child of a covered Employee; and the order must
specify:
a. the name and address of the Employee or their designee;
b. the name and mailing address of each dependent child covered by the
order;
c. a reasonable description of the type of coverage offered by the Plan;
d. a beginning period for which the order applies; and
e. the name and address of each alternate payee, which means the
Spouse, former Spouse, legal guardian of the dependent child or the child
of an Employee.
Upon receipt of a medical child support order, the Plan Administrator shall
promptly notify the Employee and Alternate Payee. The Plan Administrator shall
determine whether an order received meets the criteria and promptly notify the
Employee and each alternate payee. In the event of a dispute regarding any
medical child support order furnished to the Plan Administrator, the Employee or
alternate payee shall promptly notify the Plan Administrator in writing.
Coverage shall commence upon either the date specified in the order or the date
the Employee becomes eligible for coverage, if later.
10
Any order that requires the Allegheny College Health & Welfare Employee
Benefit Plan to provide any type of benefit or increased benefits not otherwise
provided by this Plan, other than under COBRA, will not be recognized as a
Qualified Medical Child Support Order.
Please see the Plan Administrator for questions regarding Qualified Medical
Child Support Orders.
Children’s Health Insurance Program Reauthorization Act – 2009.
If you and your Dependents are eligible but not enrolled for coverage under your
employer’s group health plan you may enroll in two circumstances: 1) you or your
dependent’s Medicaid or CHIP coverage is terminated as a result of loss of
eligibility; and 2) you or your dependent becomes eligible for a Subsidy under
Medicaid or CHIP (if offered by your state). You or your dependent(s) must
request coverage within 60 days after you or your dependent is terminated from,
or determined to be eligible for such assistance.
Initial Enrollment
Information regarding the enrollment process is available through the Office of
Human Resources of Allegheny College. New Employees must generally enroll
within certain time periods after being hired, as described in the chart on page 7.
For those Benefit Programs that require the Employee to make a benefit election,
new Employees must make an election to participate no later than 30 days after
becoming eligible to participate.
The benefit election process requires the Employee to make a salary reduction
election which authorizes Allegheny College to reduce your pay by the amount of
your required contribution. This salary reduction election must be completed,
specifying what benefits you want before your benefit elections and deductions
will take effect. If you do not complete the benefit election process, including the
salary reduction election, within the 30-day period, you will be deemed to have
elected not to receive any benefits under the Benefit Programs and must wait
until the next annual enrollment period to elect coverage.
Annual (Open) Enrollment
During the later part of each Plan year, at the discretion of the Plan
Administrator, Employees will be given the opportunity to elect to participate in
the Benefit Programs that require elections. These benefit elections will be
effective on the following July 1st and will continue up through the last day of the
Plan year, which is June 30th. Elections will be made by Employees according
to the procedures determined and communicated by the Plan Administrator.
You must specify your elections in accordance with those procedures for any
benefits you want to receive during the Plan Year.
Mid-Year Election Changes
11
You may not change your benefit elections during the Plan Year except in
certain, specific circumstances, such as if you experience a Change in Status
Event. Examples include a change in legal marital status, change in number of
dependents, change in employment status, and change in dependent status.
You must make your election change request within 30 days of the Change in
Status Event. Please refer to the Allegheny College Flexible Benefit Plan SPD
for more information regarding mid-year election changes.
Employees that participate in the HSA Benefits will be permitted to change their
HSA Benefits election at any time during the Plan year.
HIPAA Special Enrollment Rights
In certain circumstances and with respect to particular component Benefit
Programs, enrollment may occur at times outside the open enrollment period
(this is referred to as “special enrollment”). The Plan’s separate Special
Enrollment Notice also contains important information about your potential
special enrollment rights.
The mid-year election change rules and the HIPAA Special Enrollment Rights are
intended to comply with the Internal Revenue Code “cafeteria plan” requirement.
Termination of Participation
Your participation and the participation of your eligible family members in the
Plan will end based on the date upon which you terminate employment with the
College. Coverage may also terminate if you fail to pay your share of an
applicable premium, if your hours drop below any required hourly threshold, if
you submit false claims or for any other reason as set forth in the certificate of
insurance, benefit booklets, benefit summaries, or other governing documents for
the component benefit program. You should consult the applicable Attachments
for specific termination information, including reasons your benefits will terminate
and when coverage under each Benefit Program will end. A summary of when
coverage for each Benefit Program will terminate can be found below.
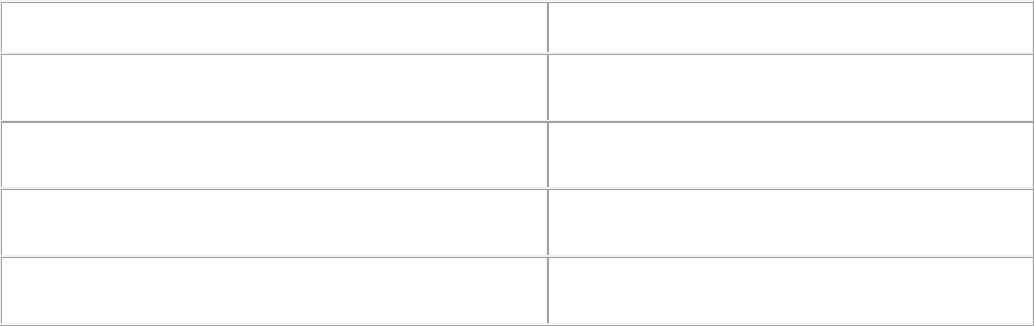
Your coverage under each component Benefit Program will be terminated in
accordance with the following schedule:
Benefit Programs
When Benefits Terminate
PPO Medical w/ Prescription Drug and
High Deductible Medical Plan w/ Prescription Drug
Benefits are terminated on last day of the month in
which employment ends
Retiree PPO Medical w/ Prescription Drug and
High Deductible Medical w/ Prescription Drug
Benefits are terminated on the last day of the month in
which retiree attains age 65
Dental
Benefits are terminated on the last day of the month in
which employment ends
Vision
Benefits are terminated on the last day of the month in
which employment ends
12
Group Term Life and
Accidental Death & Dismemberment
Benefits are terminated on the last day of employment
Long Term Disability
Benefits are terminated on last day of employment
Voluntary employee pay-all insurance coverage
Post-tax payroll deductions cease immediately when
employment ends. Employees must arrange for
premiums to be billed on a direct pay basis if they
intend to continue coverage beyond last day of
employment.
Pre-tax payroll contributions for component Benefit Programs will cease
immediately on the date the Employee ceases to meet the eligibility requirements
for participation in the Flexible Benefits Plan (Cafeteria plan). Post-tax payroll
contributions cease immediately when employment ends.
Coverage for your spouse and dependents stops when your coverage stops and
for other reasons specified in the Attachments (for example, divorce or a
dependent's attaining age limit). Coverage also ceases for Employees, Spouses,
and dependents upon termination of the Plan.
Continuation Provision for Disabled Employees
Six Month Continuation of Health & Welfare Benefits
Disabled Employees who remain absent from work due to an approved Short Term
Disability or approved Workers Compensation claim are entitled to continue coverage
under the Allegheny College Health & Welfare Employee Benefit Plan on the same basis
as active employees up to a maximum period of six months from the initial date of
disability. Disabled Employees will be required to contribute their share of the premium
cost during this continuation period or coverage will be terminated. COBRA coverage
will be offered in accordance with COBRA regulations following the end of the
continuation period.
Extended Continuation of Medical Benefits
Employees who are absent from work, approved for and considered disabled under the
Company's Short Term Disability program or Workers Compensation benefits are
required to file for Long Term Disability coverage during the fifth month of
disability. Employees deemed disabled in accordance with the Allegheny College Long
Term Disability insurance policy will be eligible to continue their medical benefits under
the same basis as active employees beginning on the first day of the seventh month
following the initial date of disability, for a period no greater than 12 months. Disabled
employees will be required to contribute premiums for the medical benefits provided
during the period of disability in accordance with a schedule provided by Human
Resources or medical coverage will be terminated.
Upon expiration of this continuation period, employees will be entitled to remain enrolled
in medical coverage in accordance with COBRA law, however, will be required to pay
the full COBRA premium cost for medical benefits until their COBRA coverage period
expires
13
Continuation Coverage under COBRA and USERRA
COBRA Rights
As the Employee ("covered Employee"), you have a right to choose COBRA
coverage if you lose medical, dental or vision coverage because of a reduction in
your hours of employment or the termination of your employment (for reasons
other than gross misconduct on your part). The spouse of a covered Employee
has the right to choose COBRA coverage if group health coverage is lost as a
result of any of the following four reasons:
• A termination of the covered Employee’s employment (for reasons other
than gross misconduct) or reduction in the covered Employee's hours of
employment;
• The death of the covered Employee;
• Divorce or legal separation from the covered Employee; or
• The covered Employee becomes entitled to Medicare.
A dependent child of the covered Employee has the right to choose COBRA
coverage if group health coverage is lost as a result of any of the following five
reasons:
• A termination of the covered Employee’s employment (for reasons other
than gross misconduct) or reduction in the covered Employee's hours of
employment;
• The death of the covered Employee;
• The divorce or legal separation of the covered Employee;
• The covered Employee becomes entitled to Medicare; or
• Loss of dependent child status under the plan rules.
In addition, a dependent child born to or adopted by the covered Employee
during a period of COBRA coverage has the right to continuation coverage.
Such a child may be added to COBRA coverage upon notification to Human
Resources.
Each person who is eligible for COBRA coverage is entitled to make a separate
election of COBRA coverage. Thus, a spouse or dependent child is entitled to
elect COBRA coverage even if the covered Employee does not make that
election.
Under the law, the covered Employee, spouse or a family member has the
responsibility of informing the Plan Administrator of a divorce, legal
separation, or a child's loss of dependent status under the group health
plan. This notice to the Plan Administrator must be given within 60 days of
the date of any such event. If notice is not given within the 60-day period,

14
the spouse or dependent (as applicable) will not be entitled to COBRA
coverage.
The Employer is responsible for notifying the Plan Administrator of the covered
Employee's death, termination of employment or reduction in hours, or Medicare
entitlement within 30 days of the date coverage will end as a result of the event.
When the Plan Administrator is notified that a qualifying event described above
has happened, the Plan Administrator will in turn notify you that you have the
right to choose COBRA coverage. Under the law, you have at least 60 days from
the date you would lose coverage because of one of the events described above
to inform the Plan Administrator that you want COBRA coverage.
If you do not choose COBRA coverage, your group health coverage will end.
If you choose COBRA coverage and pay the required premiums, the Plan is
required to give you coverage which, as of the time coverage is being provided,
is identical to the coverage provided by the Employer to similarly situated active
Employees, spouses or family members. This means that if the coverage for
similarly situated Employees, spouses or family members change, your
coverage will change.
Duration of COBRA Coverage
COBRA coverage under a Health Care Spending Account may be maintained for
the remainder of the Plan Year in which the qualifying event occurs. If you have
any questions about COBRA, please contact the Plan Administrator. The law
provides that COBRA coverage may end earlier than explained above for any of
the following reasons:
• The Employer no longer provides the group health coverage to any
Employees;
• The premium for COBRA coverage is not paid on time;
• After the date of the COBRA election, you become covered under
another group health plan which does not contain any preexisting
condition exclusion or limitation that applies to you; or after the date of
the COBRA election, you become covered under a group health plan
that does have a preexisting condition exclusion or limitation that
applies to you if the exclusion or limitation should not apply as a result
of application of the requirements of the Health Insurance Portability
and Accountability Act of 1996;
• After the date of the COBRA election, you become entitled to Medicare;
or
• You cancel COBRA coverage.
Moved from other section -- If you have any questions about your COBRA rights,
please read the COBRA Notification Form, a copy of which has been previously
furnished to you and your spouse (if covered). Please contact the Plan
Administrator if you need another copy.
Continuation Coverage Rights While on Military Leave (USERRA)

15
The Uniformed Services Employment and Reemployment Rights Act of 1994
(USERRA) is a federal law intended to ensure that persons who serve or have
served in the Armed Forces, Reserves, National Guard or other “uniformed
services” will be considered on a leave of absence and will be entitled to the
rights and benefits, not determined by seniority, as are generally provided to
similarly situated Employees on a leave of absence or on other types of leave.
While on military leave you will be entitled to continue your group health
coverage, including any dependent coverage, for the lesser of the length of the
leave or 24 months. This entitlement will end if you provide written notice of your
intent not to return to work following the completion of the military leave. If the
military leave is for a period of 31 days or more, the Allegheny College can
require you to pay 102% of the total premium (determined in the same manner
as a COBRA continuation coverage premium). If coverage is not continued
during the entire period of the military leave because you decline to pay the
premium or the leave extends beyond 24 months, the coverage will be reinstated
upon reemployment with no exclusions (other than for service-related illnesses or
injuries) or waiting periods (other than those applicable to all eligible Employees).
Contact the Plan Administrator for more information regarding your rights while
on Military Leave.
5. Summary of Plan Benefits
Available Benefits and Contributions
The cost of the benefits provided through the component Benefit Programs may
be funded in part by College contributions and in part by Employee pre-tax
contributions. Please contact the Office of Human Resources for specific
contribution rates required for each benefit plan. The College will determine and
periodically communicate your share of the cost of the benefits provided through
each component benefit, and it may change that determination at any time.
The College will pay its contributions and your contributions to an insurance
carrier(s) to pay benefits directly to or on behalf of you or your eligible family
members from the College’s general assets.
The Plan will provide benefits in accordance with the requirements of all
applicable laws, such as COBRA, HIPAA, NMHPA, WHCRA, USERRA and the
Patient Protection and Affordable Care Act.
Administrative Requirements and Timelines
As described in the Attachments, there may be other reasons that a claim for
benefits is not paid, or is not paid in full. For example, claims must generally be
submitted for payment within a certain period of time, and failure to submit within
that time period may result in the claim being denied. In this regard, please
consult the Attachments.

16
6. Other Laws that May Affect Your Benefits
Genetic Information Nondiscrimination Act (GINA)
GINA prohibits employer-sponsored group health plans and health insurers
providing group insurance from:
• Increasing premium or contribution amounts based on genetic information:
• Requesting or requiring an individual or family member to undergo a
genetic test: and
• Requesting, requiring or purchasing genetic information prior to or in
connection with enrollment, or at any time for underwriting purposes.
Genetic information means:
• The individual’s genetic tests;
• The genetic tests of family members;
• The manifestation of a disease or disorder in family members; or
• Any request for, or receipt of, genetic services or participation in clinical
research that includes genetic services, by the individual or family
member.
Genetic information does not include information about the sex or age of any
individual, it does include, with respect to a pregnant woman, an individual who is
utilizing an assisted reproductive technology, or a family member, genetic
information of any fetus carried by the pregnant woman or of any embryo legally
held by the individual or family member.
Nondiscrimination in Benefits
Benefits provided under this Plan or any Benefit Program will not discriminate in
any of the following ways:
• On the basis of any health factor including evidence of insurability;
• As to eligibility for benefits on the basis of a health factor; or
• On the basis of premiums or contributions for similarly situated individuals.
Newborn’s and Mother’s Health Protection Act
Group health plans and health insurance issuers generally may not, under Federal
law, restrict benefits for any hospital length of stay in connection with childbirth for
the mother or newborn child to less than 48 hours following a vaginal delivery, or
less than 96 hours following a cesarean section. However, Federal law generally
does not prohibit the mother’s or newborn’s attending providers, after consulting
with the mother, from discharging the mother or her newborn earlier than 48 hours
(or 96 hours as applicable). In any case, plans and issuers may not, under Federal
law, require that a provider obtain authorization from the Plan or the insurance
issuer for prescribing a length of stay not in excess of 48 hours (or 96 hours as
applicable).
17
Rights under the Women’s Health and Cancer Rights Act
Under Federal law, group health plans and health insurance issuers that provide
medical and surgical benefits with respect to a mastectomy must provide certain
benefits to a participant or beneficiary who is receiving benefits in connection with
mastectomy and who elects breast reconstruction.
Specifically, the group health plan and issuer must provide coverage in a manner
determined in consultation with the attending physician and the patient, for (i)
reconstruction of the breast on which the mastectomy has been performed; (ii)
surgery and reconstruction of the other breast to produce a symmetrical
appearance; and (iii) prostheses and physical complications during all stages of
mastectomy, including lymphedemas. This coverage may be subject to annual
deductibles and coinsurance provisions, consistent with other benefits under the
medical coverage option.
Special Rights on Childbirth
Group health plans and health insurance issuers offering group insurance
coverage generally may not, under federal law, restrict benefits for any hospital
length of stay in connection with childbirth for the mother or newborn child to less
than 48 hours following a normal vaginal delivery, or less than 96 hours following
a cesarean section. However, federal law generally does not prohibit the
mother’s or newborn’s attending provider, after consulting with the mother, form
discharging the mother or her newborn earlier than the above periods. In any
case, such plans and issuers may not, under federal law, require that a provider
obtain authorization from the plan or the insurance issuer for prescribing a length
of stay not in excess of the above periods.
Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA)
To the extent any applicable Benefit Program provides benefit coverage for
mental health services and substance abuse services, the Benefit Program will
comply with the rules beginning on or after July 1, 2010 and will include:
- Offer the same access to care and patient costs for mental health and
substance use disorder benefits as those that apply to general medical or
surgical benefits;
- Treat mental health/substance use disorder coverage and
medical/surgical coverage equally in terms of out-of-pocket costs, benefit
limits and practices such as prior authorization and utilization review used
by the insurer;
- Contain a single combined deductible for mental health/substance use
disorder coverage and medical/surgical coverage; and
This mental health and substance abuse coverage is subject, however, to any
applicable deductibles and coinsurance, as well as any limits on the number of
covered hospital days and/or outpatient visits.
18
HIPAA Privacy
The Plan will comply with the privacy regulations under HIPAA. These regulations
set national standards for the protection of certain personal health
information. This information, referred to as “protected health information,” is
information that: (i) could identify a participant (or to which there is a reasonable
basis to determine the identity of the participant) and (ii) relates to the participant’s
past, present, or future physical or mental condition.
As required under HIPAA, the Plan will not use or disclose your protected health
information for purposes other than treatment, payment or healthcare operations,
without your written authorization or as required by law.
➢ “Treatment” includes the provision, coordination, or management of health
care providers.
➢ “Payment” includes activities by the Plan to obtain premiums or determine
or fulfill the Plan’s obligation for coverage, including determinations of
eligibility or coverage, adjudication or subrogation of claims, billing, claims
management, collection activities, health care data processing, review of
medical necessity, review of appropriateness of care or justification of
charges, and utilization review activities.
➢ “Healthcare Operations” include conducting quality assessment and
improvement activities, case management and care coordination, reviewing
and evaluating Plan performance, securing contracts, conducting or
arrangement for medical review or auditing functions and business planning
and development.
Unless a participant gives the Plan written authorization, the Plan may disclose
protected health information to the Plan Administrator only for Plan administration
and enrollment purposes and only if there is adequate separation between the
Company as Plan Administrator and as Employer. In addition, “Summary Health
Information” may be disclosed by the Plan to the Company as the Employer for
purposes of obtaining premium bids for health insurance coverage under the Plan
or modifying, amending, or terminating the Plan. Prior to receiving any protected
health information, the Company must certify to the Plan that adequate separation
exists.
All protected health information used, requested or disclosed is limited to the
minimum amount necessary to accomplish the intended purpose(s) of the
disclosure.
As a participant in the Plan, you have certain rights with respect to your protected
health information, including the right to inspect and copy your medical records,
request amendment or correction to your records, restrict the use or disclosure of
your protected health information, and request an accounting of the uses and
disclosures of your protected health information.

19
The Plan has included policies and procedures specifically designed to safeguard
your protected health information when it is in electronic format. This includes
administrative, physical and technical safeguards to ensure your protected health
information cannot be inappropriately accessed while it is stored and transmitted
to insurers and others that administer the Plan. This includes:
➢ Ensuring that adequate separation exists between your protected health
information maintained by the Plan and your Employer and this separation
is supported by appropriate security measures.
➢ Ensuring that insurance carriers and claims administrators agree to an
appropriate level of information security when handling your electronic
protected health information.
The Plan reserves the right to change privacy and security practices and to make
the new provisions effective for all protected health information
maintained. Should the privacy and/or security practices change, a revised notice
will either be mailed or electronically transmitted to you.
A Notice of Privacy Practices containing a description of these uses and
disclosures of protected health information, your rights, the Plan’s duties and
complaint procedures has been sent by the Company to all Plan participants. A
copy of the notice is available upon request from the Company. For more
information regarding your privacy rights under HIPAA, please contact the Plan
Manager.
7. How the Plan Is Administered
Plan Administration
The administration of the Plan is under the supervision of the Plan Administrator.
The Director of Human Resources is the person who has been designated to act
on behalf of the Plan Administrator.
The principal duty of the Plan Administrator is to see that the Plan is carried out,
in accordance with its terms, for the exclusive benefit of persons entitled to
participate in the Plan. The administrative duties of the Plan Administrator
include, but are not limited to, interpreting the Plan, prescribing applicable
procedures, determining eligibility for and the amount of benefits, and authorizing
benefit payments and gathering information necessary for administering the Plan.
The Plan Administrator may delegate any of these administrative duties among
one or more persons or entities, provided that such delegation is in writing,
expressly identifies the delegate(s) and expressly describes the nature and
scope of the delegated responsibility.
The Plan Administrator has the discretionary authority to interpret the Plan in
order to make eligibility and benefit determinations as it may determine in its sole
discretion. The Plan Administrator also has the discretionary authority to make
factual determinations as to whether any individual is entitled to receive benefits
under the Plan.

20
The College will bear its incidental costs of administering the Plan.
Power and Authority of Insurance Companies
Benefits under the Plan are fully insured. Benefits are provided under a group
insurance contract entered into between Allegheny College and the Insurance
Companies. Claims for benefits are sent to the Insurance Companies. The
Insurance Companies are responsible for determining and paying claims, not
Allegheny College.
The Insurance Companies are responsible for (a) determining eligibility for a
benefit and the amount of any benefits payable under the Plan; and (b) providing
the claims procedures to be followed and the claims forms to be used by eligible
individuals pursuant to the Plan.
As the Named Fiduciary for benefit determinations, the Insurance Companies
have the discretionary authority to interpret the Plan in order to make benefit
determinations. The Insurance Companies also have the authority to require
eligible individuals to furnish them with such information as they determine
necessary for the proper administration of the Plan.
Your Questions
If you have any general questions regarding the Plan, please contact the Director
of Human Resources, who acts on behalf of the Plan Administrator.
If you have any questions regarding your eligibility for, or the amount of, any
benefit payable under the plan, please contact the appropriate insurance
company.
8. Circumstances Which May Affect Benefits
Denial, Recovery, or Loss of Benefits
Your benefits (and the benefits of your eligible family members) will cease when
your participation in the Plan terminates. See Section 4.
Your benefits will also cease upon termination of the Plan.
Other circumstances can result in the termination, reduction, recovery (through
subrogation or reimbursement), or denial of benefits. For example, benefits may
be denied under the medical or dental Benefit Programs if you have a preexisting
condition and incur costs within the exclusionary period. See the Attachments for
additional information.
21
9. Amendment of Termination of the Plan
Amendment or Termination
Allegheny College, as the sponsor of the Plan, has the general right to amend or
terminate the Plan at any time. The Plan may be amended or terminated by a
written instrument signed by the Vice President of Finance and Planning of the
College. The Vice President of Finance and Planning of the College is
authorized to amend or terminate the Plan and to sign insurance contracts with
the insurance companies, including amendments to those contracts. Note, for
this purpose, that an insurance contract is not necessarily the same as the Plan.
(An insurance contract is how benefits under a particular component program
offered through the Plan are provided.) Consequently, termination of an
insurance contract does not necessarily terminate the Plan.
The Company, as Plan Sponsor, has the right to amend or terminate the Plan at
any time. The Plan may be amended or terminated by a written instrument duly
adopted by the Company or any of its delegates.
10. No Contract of Employment
No Contract of Employment
The Plan is not intended to be, and may not be construed as constituting, a
contract or other arrangement between you and the College to the effect that you
will be employed for any specific period of time.
11. Claims Procedures
Claims for Fully Insured Benefits
For purposes of determining the amount of, and entitlement to, benefits of the
component Benefit Programs provided under insurance or contracts,
the
respective insurer is the named fiduciary under the Plan, with the full power to
interpret and apply the terms of the Plan as they relate to the benefits provided
under the applicable insurance contract.
To obtain benefits from the insurer of a component benefit program, you must
follow the claims procedures under the applicable insurance contract, which may
require you to complete, sign, and submit a written claim on the insurer's form.
(See the Attachments for more information.)
The insurer will decide your claim in accordance with its reasonable claims
procedures, as required by ERISA (if ERISA applies) and other applicable law.
The insurer has the right to secure independent medical advice and to require
such other evidence as it deems necessary in order to decide your claim. If the
insurer denies your claim in whole or in part, you will receive a written notification
setting forth the reason(s) for the denial.
22
If your claim is denied, you may appeal to the insurer for a review of the denied
claim. The insurer will decide your appeal in accordance with its reasonable
claims procedures, as required by ERISA (if ERISA applies) and other applicable
law. If you do not appeal on time, you will lose your right to file suit in a state or
federal court, because you will not have exhausted your internal administrative
appeal rights (which generally is a prerequisite to bringing suit in state or federal
court). Note that under certain circumstances, you may also have the right to
obtain external review (that is, review outside of the Plan). (See the Attachments
for more information.)
Claims for Self-Funded Benefits
For purposes of determining the amount of, and entitlement to, benefits under the
component Benefit Programs provided through Allegheny College’s general
assets, the Plan Administrator is the named fiduciary under the Plan, with the full
power to make factual determinations and to interpret and apply the terms of the
Plan as they relate to the benefits provided through a self-funded arrangement.
The Plan Administrator has delegated certain administrative duties to a third
party claims administrator. To obtain benefits from a self-funded arrangement,
you must complete, execute, and submit to the third party claims administrator a
written claim on the form.
In accordance with HIPAA, the third party claims administrator has the right to
secure independent medical advice and to require such other evidence as it
deems necessary to decide your claim.
The third party claims administrator will decide your claim in accordance with
reasonable claims procedures, as required by ERISA. If the claims administrator
denies your claim in whole or in part, then you will receive a written notification
setting forth the reason(s) for the denial. (See the Attachments for more
information.)
If your claim is denied, you may appeal to the third party claims administrator for
a review of the denied claim. The claims administrator, operating on behalf of the
Plan Administrator, will decide your appeal in accordance with reasonable claims
procedures, as required by ERISA. If you do not appeal on time, you will lose
your right to file suit in a state or federal court, because you will not have
exhausted your internal administrative appeal rights (which generally is a
prerequisite to bringing a suit in state or federal court).
External Review Process for Medical and Prescription Drug Claims –
Upon exhaustion of the internal claims and appeal procedures, an Employee
may request that the Claim be reviewed under the Medical Plan’s external review
process. The Medical and Prescription Drug Plan shall comply with the
applicable State external review process, if any, and if none, the federal external
review process. Please refer to the Attachments for more information in the
Medical and Prescription Drug Plan booklets.

23
12. Statement of ERISA Rights
Your Rights
As a participant in the Plan,
you are entitled to certain rights and protections
under the Employee Retirement Income Security Act of 1974 (ERISA). ERISA
provides that all plan participants shall be entitled to:
Receive Information about Your Plan and Benefits
Examine, without charge, at the Plan Administrator's office and at other specified
locations, such as worksites, all documents governing the Plan, including
insurance contracts, and a copy of the latest annual report (Form 5500 Series), if
any, filed by the Plan with the U.S. Department of Labor and available at the
Public Disclosure Room of the Employee Benefits Security Administration.
Obtain, upon written request to the Plan Administrator, copies of documents
governing the operation of the Plan, including insurance contracts and copies of
the latest annual report (Form 5500 Series) and updated summary plan
description (SPD). The Plan Administrator may make a reasonable charge for the
copies.
Receive a summary of the Plan's annual Form 5500, if any is required by ERISA
to be prepared, in which case Allegheny College, as Plan Administrator, is
required by law to furnish each participant with a copy of this summary annual
report.
Third Party
Claims Administrator: Highmark Blue Cross Blue Shield (Active and Retiree
PPO Blue Medical & High Deductible Medical)
One Fifth Avenue Place
Pittsburgh, PA 15222
1-800-235-4999
CVS Caremark (Prescription Drug)
P.O. Box 6590
Lee’s Summit, MO 6406
1-800-552-8159
Insurers: United Concordia Companies, Inc. (Dental)
100 Senate Avenue
Senate Plaza
Camp Hill, PA 17011
1-412-544-2346
Vision Benefits of America (Vision)
300 Weyman Plaza
Pittsburgh, PA 15236-4900
1-412-881-4900
24
Metlife (Group Life, AD&D and Long Term Disability)
Metropolitan life Insurance Company
200 Park Avenue
New York, NY 10166
1-800-275-4638
AFLAC (this coverage is not subject to ERISA)
American Family Life Assurance Company of Columbus
1932 Wynnton Road
Columbus, GA 31999
800-992-3522
COBRA Rights
As identified in this SPD, you may continue medical, dental and/or vision benefits
for yourself, your spouse, or your dependents if there is a loss of coverage under
the Plan as a result of a qualifying event. You or your dependents may have to
pay for such coverage. Review this SPD and the documents governing the Plan
on the rules governing your COBRA continuation coverage rights.
Prudent Actions by Plan Fiduciaries
In addition to creating rights for Plan participants, ERISA imposes duties upon
the people who are responsible for the operation of the Employee benefit plan.
The people who operate your Plan, called “fiduciaries” of the Plan, have a duty to
do so prudently and in the interest of you and other Plan participants and
beneficiaries. No one, including your employer or any other person, may fire you
or otherwise discriminate against you in any way to prevent you from obtaining a
Plan benefit or exercising your rights under ERISA.
Enforce Your Rights
If your claim for a welfare benefit is denied or ignored, in whole or in part, you
have a right to know why this was done, to obtain copies of documents relating to
the decision without charge, and to appeal any denial, all within certain time
schedules. Under ERISA, there are steps that you can take to enforce the above
rights. For instance, if you request a copy of Plan documents or the latest annual
report (Form 5500), if any, from the Plan and do not receive them within 30 days,
you may file suit in a federal court. In such a case, the court may require
Allegheny College as Plan Administrator, to provide the materials and pay you up
to $110 per day until you receive the materials, unless the materials were not
sent because of reasons beyond the control of the administrator. If you have a
claim for benefits which is denied or ignored in whole or in part, and if you have
exhausted the claims procedures available to you under the Plan (discussed in
Section 10), you may file suit in a state or federal court.
If it should happen that Plan fiduciaries misuse the Plan's money, or if you are
discriminated against for asserting your rights, you may seek assistance from the
25
U.S. Department of Labor, or you may file suit in a federal court. The court will
decide who should pay court costs and legal fees. If you are successful, the court
may order the person you have sued to pay these costs and fees. If you lose, the
court may order you to pay these costs and fees, for example, if it finds your
claim is frivolous.
Assistance with Your Questions
If you have any questions about your Plan, you should contact the Plan
Administrator. If you have any questions about this statement or about your rights
under ERISA,
or if you need assistance in obtaining documents from the Plan
Administrator, you should contact the nearest office of the Employee Benefits
Security Administration, U.S. Department of Labor (listed in your telephone
directory) or contact the Division of Technical Assistance and Inquiries,
Employee Benefits Security Administration, U.S. Department of Labor, 200
Constitution Avenue N.W., Washington, D.C. 20210. You may also obtain certain
publications about your rights and responsibilities under ERISA by calling the
publications hotline of the Employee Benefits Security Administration.

26
Appendix
ATTACHMENTS:
Attachment #1 Highmark Blue Cross Blue PPO Shield (Medical)
with CVS Prescription Drug
Attachment #2 Highmark Blue Cross Blue Shield High Deductible
(Medical) with CVS Prescription Drug
Attachment #2 United Concordia (Dental)
Attachment #3 Vision Benefits of America (Vision)
Attachment #4 Metlife Life and Accidental Death Dismemberment
Attachment #5 Metlife Long Term Disability
Attachment #6 AFLAC product summary (contact Human Resources)
