
KELLEY LYNCH FOR USAID
USAID BANGLADESH HEALTH STRATEGY
2022-2027
I. Goal
USAID/Bangladesh’s Office of Population, Health and Nutrition (OPHN) will support resilient
health systems that deliver quality, equitable health services with the purpose of
improving the health status of Bangladeshis.
II. Introduction/Strategy Development Process
This strategy considers the health system holistically, and articulates where, within that system,
OPHN will focus interventions in order to have the greatest impact on our goal above. This
strategy does not include everything OPHN will do; rather it outlines major areas of strategic
interest. OPHN will have additional sub-strategies, for example in nutrition, or in tuberculosis (TB),
which will flow from this strategy.
While developing the strategy, OPHN considered: 1) areas where health system performance is
weakest, 2) opportunities to improve health systems performance, and divisional or national level
population health outcomes, through USAID programming, 3) coordination with other USAID offices,
donors, and Government of the People’s Republic of Bangladesh (GOB) interventions, 4) whether the
proposed area of intervention is within USAID’s manageable interest and comparative advantage, 5)
innovative opportunities to leverage other funding (Development Partners (DP), Private Sector
Engagement, and Domestic Resource Mobilization).
III. Strategy
Bangladesh has significantly improved health status over the past two decades, but some indicators
lag behind, and systemic gaps remain. Bangladesh has sustained strong economic growth over the
past decade. The country aims to graduate from Least Developed Country (LDC) status in 2026, and
become an upper-middle-income country by 2031. DPs contribute only 7-8% of the health budget. In
this context, OPHN will 1) focus on catalytic interventions, and 2) further shift programming
away from direct service delivery and towards health systems strengthening, in order to
build resilient health systems that will sustainably deliver affordable, accessible, accountable and
reliable health services. This will generate measurable improvement in national level health
outcomes.
Within the overall framework of health systems strengthening, OPHN will work to enhance
resilience. Resilient health systems are better able to absorb and recover from natural and
manmade shocks such as pandemics, floods, and earthquakes, while sustaining quality, equitable health
services. OPHN will support flexible health systems for rapid and appropriate responses to short and
long-term shocks and their secondary impacts. Shocks and stressors often have disproportionate
impacts on vulnerable populations. OPHN will work to ensure that health systems maintain equity
during shocks. Interventions in this area may include integrated programming with other USAID
Offices.
2

________________
i. Overarching Themes/Principles:
OPHN identified the following five overarching principles which are cross-cutting and which will apply
to all of the priority intervention areas described below.
Equity - Despite Bangladesh’s successes in public health, some people have been left behind. An
equitable health system affords every individual a fair opportunity to attain their highest level of
health regardless of social or demographic factors, with particular emphasis on underserved, socially
excluded, and vulnerable populations.
1
OPHN will identify equity gaps, both in access to quality health
services, and in health outcomes, and will work to close those gaps. Equity can be measured in many
different ways, including economic status, educational status, ethnicity, gender, religion, geography,
and other methods. OPHN will use high-quality evidence to assess equity and to measure progress
towards closing equity gaps.
Quality - Despite Bangladesh’s success in scaling up the availability of health services, the quality of
those services is sometimes not as high as desired, which negatively impacts health outcomes. A quality
health system is responsive to patient and population needs and uses data-informed, continuous
process improvement to consistently provide safe, effective, trusted, and equitable healthcare to
improve and maintain health outcomes for all people.
2
OPHN programming will work to strengthen
systems to improve the quality of healthcare and health services provided from all sources in the
country - public, private, and NGO.
Resource Optimization - OPHN will support the adoption of sustainable approaches to
mobilize and use resources efficiently, effectively, and transparently to improve health outcomes.
3
This
includes financial and non-financial resources both from within and from outside the health sector.
This intervention area includes work related to the cost-effectiveness of programs and interventions,
governance and evidence-based decision making, budgeting, budget execution, and other areas.
Evidence-Based Decision Making - OPHN will use high-quality evidence, data, and research
to inform strategic decisions and project management. OPHN will also support the use of high quality
evidence at all levels of the health system.
Flexibility and Adaptive Management - OPHN will endeavor to use procurement
mechanisms which allow for flexibility. OPHN will adaptively manage projects to ensure that we can
take advantage of unexpected opportunities and contextual changes, ensure agile responses to
emergencies, and ensure that implementation continues during shocks. Contrary to OPHN’s approach
of focusing on systems strengthening, short-term direct service delivery may be required during
emergencies (e.g., surge staff to mitigate cholera outbreaks, deliver health services during cyclone
response, etc.).
1
USAID’s Vision for Health Systems Strengthening 2030.
2
Ibid.
3
Ibid.
3

ii. Areas of Strategic Focus:
OPHN will focus on the areas of the health system outlined below as high-priority interventions
under this strategy.
A. Out of the six health systems pillars, OPHN will address one - commodities -
comprehensively, from the top to the bottom of the health system pyramid. OPHN will work to
improve systems for commodity security, logistics, and regulation at all levels to
ensure that quality, affordable medicines and other health commodities are consistently available to
healthcare providers and patients when and where they are needed. Interventions will focus on
establishing and strengthening efficient, transparent, accountable systems. Under this intervention
area, the Directorate General of Health Services (DGHS) will be a key counterpart. Areas of
intervention may include support for:
● Transparent and well-regulated procurement processes that promote resource
optimization,
reduce opportunities for corruption, and ensure the procurement of quality, affordable
commodities, in the right quantities, and in a timely manner to avoid stock-outs. This will be
implemented from the national level down to the district/upazila level.
● Strong regulatory systems with effective and transparent enforcement mechanisms to
ensure that medicines and other commodities are safe and effective, including those
available in the private sector.
● Strong logistics systems that effectively and efficiently deliver commodities to points of
service throughout the country, and that accurately record and monitor stock status to
enable effective decision-making.
USAID has successfully supported the Directorate General of Family Planning (DGFP) in this area, and
will build upon those learnings to support the more complex DGHS systems. This is an area in which
few other donors are working, and in which USAID has a strong comparative advantage based on in-
depth technical knowledge and previous programming.
B. Governance and Policy Reforms - At the national level, in both the rural and urban health
systems, OPHN will engage in strategic advocacy and targeted technical assistance
(TA) for catalytic policy reforms, especially related to health sector governance.
USAID will focus on specific, catalytic opportunities to improve health system governance; and
equity, quality, and resource optimization. These may include, for example:
● regulatory functions;
● workforce planning;
● certification and licensing for public and private facilities, laboratories, and providers;
● facility accreditation;
● data reporting and use (including from private sector facilities);
● adopting emerging technical best-practices in service delivery; and
● other opportunities identified during the strategy period.
4
Interventions in this area will lay the groundwork for, and reinforce, USAID’s systems strengthening
work in other areas of this strategy (e.g. commodities, urban health, etc.). Therefore, work in this
area may include any of OPHN’s technical areas (e.g. maternal mortality, nutrition, social and behavior
change, etc.). USAID efforts in this area will be coordinated with other donors working on policy
reform.
C. Integrated Local-Level Health Systems Strengthening (Rural) - OPHN will support
integrated health systems strengthening in the public sector at the district and upazila levels.
Strengthened health systems at this level will ensure that high-quality, affordable health care is available
to all equitably, which will result in improved health outcomes. Integrated health system strengthening
interventions recognize that local level health systems are intertwined, and improving health outcomes
depends on holistically strengthening integrated systems (e.g., in order to deliver services at a local
service delivery point, all health systems must be functioning. The failure of any one system impacts
overall facility functioning and ability to deliver services). Programming in this area will include
interventions to strengthen all six health systems, with tailoring to address the systems with the most
critical gaps in each geographic area. Interventions may include:
● Information: Strengthen information/data systems to accurately collect and report data from
the public and private sectors. Build a culture of data use. Support local officials and health
managers to understand the epidemiological data from their geographic area and use it effectively
for decision making as well as for the design and management of health programs that will
address their communities’ most pressing needs. Advance policies and enforcement to ensure
private sector data feeds into the public system to improve overall stewardship of the sector,
which links to policy efforts in section B.
● Governance: Strengthen systems for responsive, transparent, accountable management at
the local level. Centralized systems can constrain the ability of local leaders and managers to
respond to local needs, ensure equitable health service access, and identify and remedy quality
issues. This intervention area includes both assistance to improve government systems, and
community activation and organization to enhance accountability.
● Commodities: This intervention will draw on and complement intervention area “A”,
commodities. This intervention will work closely with vertical commodities interventions on
their implementation at the local level of the health system. Additionally, this intervention
may enhance the work of vertical commodities interventions through additional support to
local governments in areas where commodity logistics is particularly weak.
● Human Resources: Support rational, long-term workforce planning and management to
ensure that facilities are adequately staffed with the right mix of employees and expertise to
effectively deliver high-quality, equitable services; strengthen GOB systems for pre- and in-service
training and skill development (transition out of USAID training health workers); and improve
regulation of health (medical, nursing, midwifery, etc.) education.
● Financing: Work with local and central governments to enhance resource optimization
through evidence-based decision making and improved governance (including increased
accountability); improve equity through social protection schemes and other means.
● Service Delivery: Strengthen systems to improve the quality of public and private
service delivery as well as facility readiness for services that impact key indicators.
5
While these efforts will focus on integrated health systems strengthening, interventions will be
targeted to advance lagging indicators through those systems (e.g., maternal and newborn mortality).
Health systems interventions may include a wide range of technical areas in order to be responsive to
the conditions in each geographic area. These may include maternal and child health, reproductive
health, nutrition, infectious disease, and other areas.
D. Urban Health - Forty percent of Bangladesh’s population lives in urban areas. Providing quality,
equitable health care to urbanites is key to achieving universal health coverage. The national
government does not comprehensively provide urban primary healthcare, leaving the responsibility to
local governments (Municipalities and City Corporations). This has resulted in a significant gap in health
coverage. Urban health is dominated by a proliferation of private, for-profit providers. The urban slum
population is growing twice as fast (7%) as the population in the rest of urban areas (3.3%). Private
healthcare is relatively expensive, which heightens disparities for the 28% of urban dwellers who live in
poverty. Quality varies significantly and the private sector is not effectively regulated. OPHN will work
with the public (national and municipal) and private sectors to systematically improve access to quality,
affordable primary healthcare for urbanites, with a focus on closing equity gaps. This may include the
introduction of new partnership, financing, and service procurement models. Interventions may
include:
● Governance: Support public sector stewardship of the private sector as part of the GOB’s
mandate to provide quality, equitable healthcare in urban areas. This includes both public
sector provision of healthcare, and support for the GOB’s regulatory and enforcement
roles. Support effective coordination and responsibility sharing between national and
local/municipal governments.
● Financing: Support the GOB to efficiently finance urban primary health care (e.g.,
costing, budget advocacy, TA on budget execution, TA on public financial management, TA
on strategic purchasing); stimulate private sector investment in urban healthcare (e.g.,
improve access to finance); and catalyze innovative approaches to improve equity and
promote affordable healthcare for urbanites (e.g., health protection and social insurance
schemes, other models to reduce out-of-pocket expenses including rationalization of
prescriptions and diagnostics).
● Information: As new health systems are introduced and strengthened in urban areas,
ensure the inclusion of data systems to collect and use data from the public and private
sectors; support evidence based decision making.
● Commodities: As new health systems are introduced and strengthened in urban areas,
ensure that commodity logistics and supply chain systems are integrated, so that public
facilities have access to medical equipment and medicines; support effective regulation
and enforcement of drug quality, and rational use of pharmaceuticals within the private
sector.
● Human Resources: Support rational workforce planning and management to ensure
that facilities are adequately staffed with the right mix of employees and expertise to
effectively deliver high-quality, equitable services.
● Service Delivery: Support systems for the public and private delivery of quality,
equitable healthcare in urban areas as USAID discontinues direct service delivery
6

and focuses on strengthening health systems.
E. While this strategy focuses on integrated interventions, OPHN will also implement
selected disease specific health systems interventions in the public and private sectors at
different levels of the health system. These interventions will strengthen health systems to
make them more resilient and ensure that they are able to deliver quality, equitable health services,
while optimizing resources, with the purpose of improving outcomes in specific disease
areas. These may include: family planning; nutrition; TB; and preventing, detecting, and controlling
infectious disease outbreaks. Diseases addressed through vertical interventions may also be included
in integrated programming, through both intra- and inter-office integration, when integrated methods
will yield more impactful programming. Sub-strategies will be developed for some technical areas,
including multi-sector nutrition and TB.
F. Bangladesh’s private health sector has expanded significantly over the past decade.
Although many Bangladeshis face financial barriers to accessing private healthcare (including high out
of pocket expenses that often lead to catastrophic health expenditure and exacerbate equity issues),
many others now have the financial means to do so. This relieves some of the burden on the public
sector, ultimately optimizing financial resources in the sector, expanding coverage, and moving
Bangladesh closer to universal health coverage. Still, quality and regulation remain a concern
throughout the private sector. OPHN will identify and leverage private sector
opportunities to improve quality, equity, and resource optimization across our
portfolio.
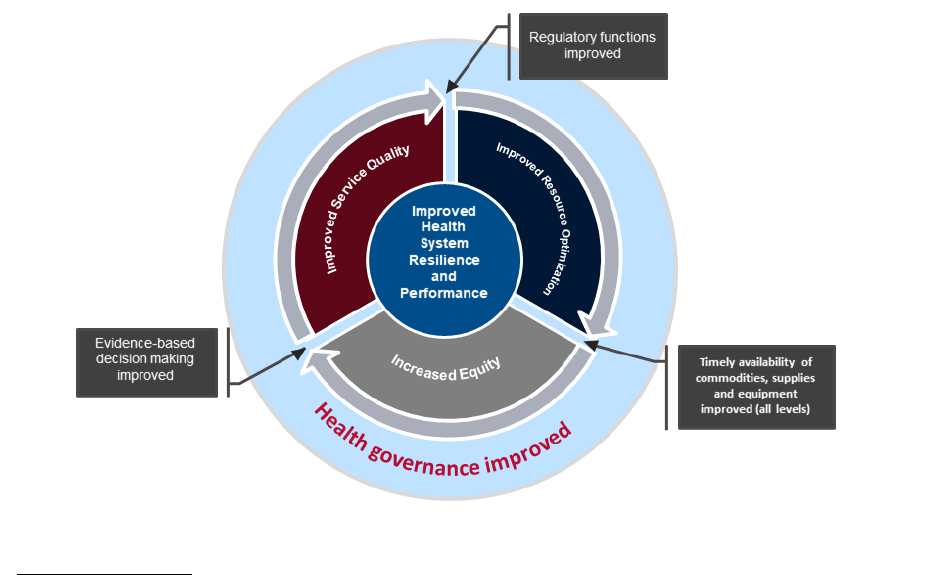
iii. Conceptual Framework:
The areas of strategic focus outlined above will improve resource optimization, service quality, and
equity of health service provision, thereby improving health system resilience and performance,
leading to improved health status/outcomes. Specific efforts to improve data for decision making,
commodity security and regulatory functions will contribute to resource optimization, quality, and
equity. This will strengthen health system governance, which will also reinforce resource
optimization, quality, and equity in a virtuous cycle of quality improvement and health sector
management. This is depicted in the figure below.
7
iv. Stakeholders:
OPHN has identified a number of stakeholders relevant to successfully implementing this strategy.
These include the Ministries of Health and Family Welfare; Local Government, Rural
Development and Cooperatives; Planning; Livestock; Agriculture; Women and Children’s Affairs;
and Social Welfare. Development partners include the United Kingdom’s Foreign Commonwealth
and Development Office, Global Affairs Canada, World Bank, Asian Development Bank, Deutsche
Gesellschaft für Internationale Zusammenarbeit, Japanese International Cooperation Agency,
Sweden International Development Cooperation Agency, UNICEF, UNFPA, WHO, and other
members of the Health, Population and Nutrition DP Consortium. Private sector entities,
including providers, pharmacies, product manufacturers, and insurance companies are also among
OPHN stakeholders.
8
