
1
Evaluation and Management Services Reference Guide
Updated February 2024
(Adjusted per CMS 2024 and 2023 changes)
Contents
Section One: Introduction ............................................................................................................................................................. 1
Summary of Revisions to E/M CPT Codes .................................................................................................................................. 1
Section Two: Descriptions, Definitions and Elements of Medical Decision Table ......................................................................... 3
Description of Total Time ............................................................................................................................................ 10
Prolonged Service Time ........................................................................................................................................................... 11
Add-On Complexity Code ........................................................................................................................................................ 12
Section Three: Clinical Examples of Code Level Selection ........................................................................................................... 16
Outpatient Visits ...................................................................................................................................................................... 16
Inpatient Visits......................................................................................................................................................................... 26
Section Four: Split or Shared Visits: ............................................................................................................................................ 34
Section Five: Additional Resources ............................................................................................................................................. 34
E/M Coding and Documentation Resources ........................................................................................................................... 34
Used with permission of the American Medical Association. AMA CPT Professional 2024, Page 10: “Table 1: Levels of
Medical Decision Making (MDM)” - Pages 7-9: “Number and Complexity of Problems Addressed at the Encounter,”
“Risk of Complications and/or Morbidity or Mortality of Patient Management,” and “Guidelines for Selecting Level
of Service Based on Time” - Page 31-33: “Prolonged Services With or Without Direct Patient Contact on the Date of
an Evaluation and Management Service” - Pages 13-14: “Guidelines for Selecting Level of Service Based on Time” -
Page 6: Split or Shared Visits . ©Copyright American Medical Association 2023. All rights reserved.
Section One: Introduction
Over the past years, the Centers for Medicare & Medicaid Services has made significant revisions to evaluation and
management services, allowing physicians to select the E/M visit level to bill based on either total time spent on the date of
patient encounter or the medical decision making used in the provision in the visit. In 2022, changes were established for
the office and outpatient setting. In 2023, reforms extended across all health care settings including hospitals, emergency
departments, nursing facilities and patients’ homes. 2024 brings an add on complexity code G2211 and split or shared visits.
Summary of Revisions to E/M CPT Codes
Two new changes in 2024:
• Add-On Complexity Code: G2211: Visit complexity inherent to evaluation and management associated with medical
care services that serve as the continuing focal point for all needed health care services and/or with medical care
services that are part of ongoing care related to a patient’s single, serious condition or a complex condition.
2
• AMA has defined split or shared visits when an E/M service is performed by a physician and non-physician
practitioner from the same group practice. Billing is based on provider who performed the substantive portion of
the visit as determined by MDM or by which professional spent the majority of time performing services.
Previous revisions to be aware of:
• The history and physical exam elements are no longer required to choose code level for a service; however, when an
appropriate history and physical examination is performed, it should be documented.
• The level of code selection is based on medical decision making or total time on the date of the encounter.
• Medical decision making is based on three elements:
o Number and complexity of problems addressed
o Amount or complexity of data to be reviewed and interpreted
o Level of risk of complications and morbidity/mortality
• The definition of total time includes face-to-face and non-face-to-face time on the date of encounter spent by the
provider, including time reviewing medical records; reviewing tests; reviewing or obtaining a medical history;
ordering medications, tests and procedures; providing documentation in the electronic health record; and
communicating with the patient, family members or caregivers and any other health care professional involved in
the care of the patient on the date of the encounter.
• Documentation of time spent is only required when time is used to choose the code level.
CPT codes deleted include: 99201, 99217-99220, 99224-99226, 99241, 99251, 99318, 99324-99228, 99334-99337,
99339- 99340, 99343 and 99354-99357.
Revisions to the codes most often used by ID physicians include E/M office visit codes (99201-99215), hospital inpatient and
observation care services (99221-99223 and 99231-99239), consultation codes (99242-99245 and 99252-99255) and
prolonged services (99358-99259, 99415-99416 and 99417), plus the establishment of a new prolonged services (99418).
The changes will provide continuity across all E/M coding and documentation.
About This Guide
This Evaluation & Management Services Reference Guide is designed to educate ID physicians on these important changes
and to assist them in choosing a CPT® code that best reflects the E/M services provided to a patient. The initial version of
this guide was created in 2021 to address changes in outpatient E/M codes that were implemented in 2022, and later 2023
revisions. This updated version of the guide expands on the initial version by addressing new inpatient E/M coding changes
for 2024.
The guide provides real-world clinical examples of how to select the most appropriate CPT codes for inpatient and
outpatient visit encounters (codes 99202-99215). Definitions of the various elements of medical decision making and time,
along with other coding conventions, are covered. The clinical examples follow a single patient case, from a minor problem
with a low level of medical decision making (MDM) as it then progresses to the highest level of MDM, indicating the
elements that led to the code that was chosen.
The updated guide was developed under the leadership of IDSA’s Coding and Payment Subcommittee. IDSA wishes to thank
the following IDSA members who contributed time and expertise to the development of this guide: Catherine M. Berjohn,
CDR, MC, USN; Ronald Devine, MD; Amy Beth Kressel, MD, MS, FIDSA, FSHEA; Asher Schranz, MD; Timothy Sullivan, MD; Casi
Wyatt, DO, FIDSA; John Fangman, MD; Nilesh H. Hingarh, MS, MD, MBA; Alice Kim, MD, MBA; Prashant Malhotra, MBBS,
MD; and Matt Shoemaker, MD. IDSA also wishes to acknowledge Kay Moyer from CRD Associates LLC for her contributions.
3
Section Two: Descriptions, Definitions and Elements of Medical Decision Table
Risk of Complications and Morbidity or Mortality of Patient Management Problems
Risk of complications and/or morbidity or mortality of patient management decisions made at the visit, associated with the patient’s problem(s) and
treatment(s):
• Includes possible management options selected and those considered, but not selected
• Addresses risks associated with social determinants of health
Two of the three elements must be met or exceeded when selecting the code level. For example, for a new patient encounter involving moderate problems
addressed, a limited review of data and a low level of risk, then the MDM would be low, and the code selected should be 99203.
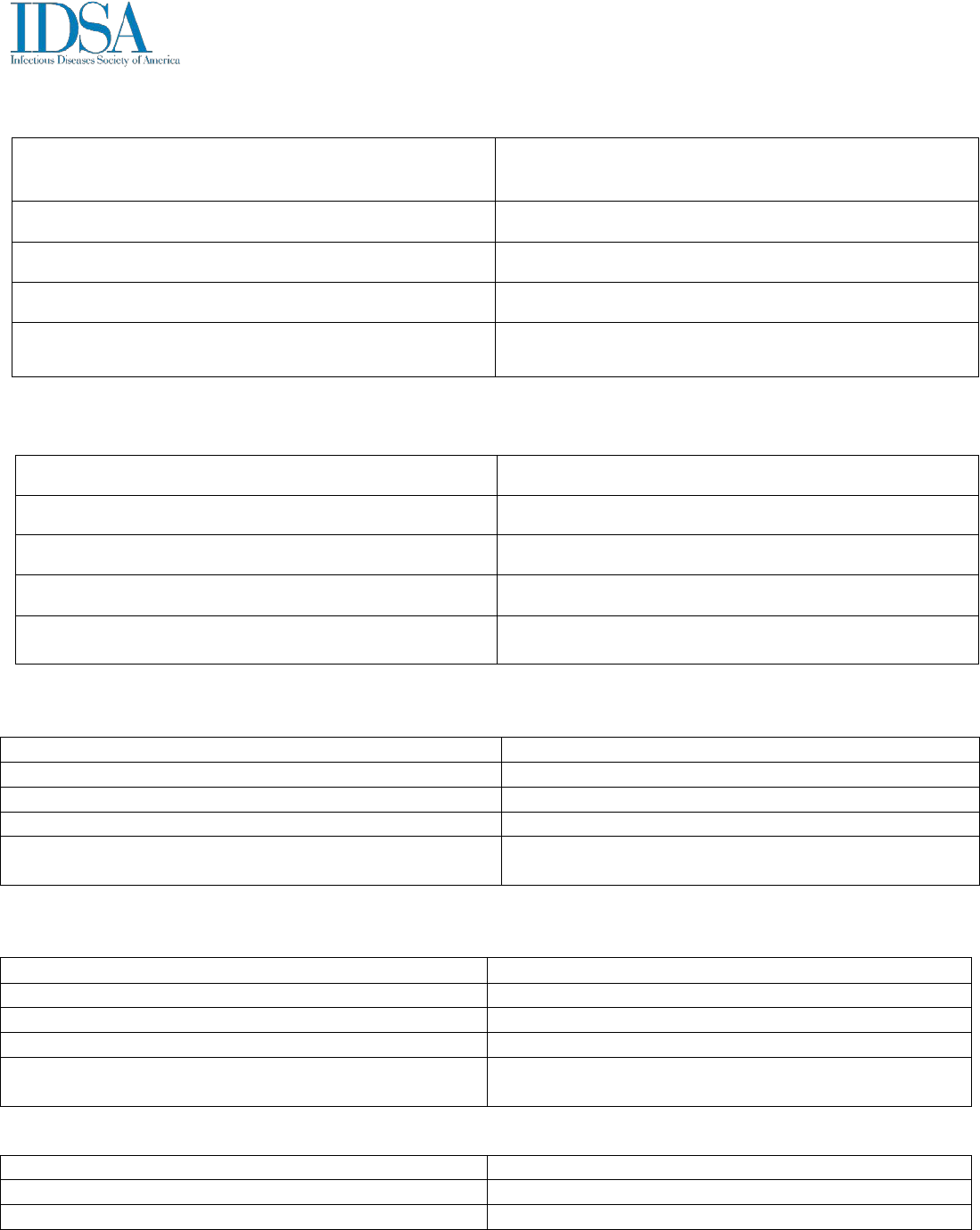
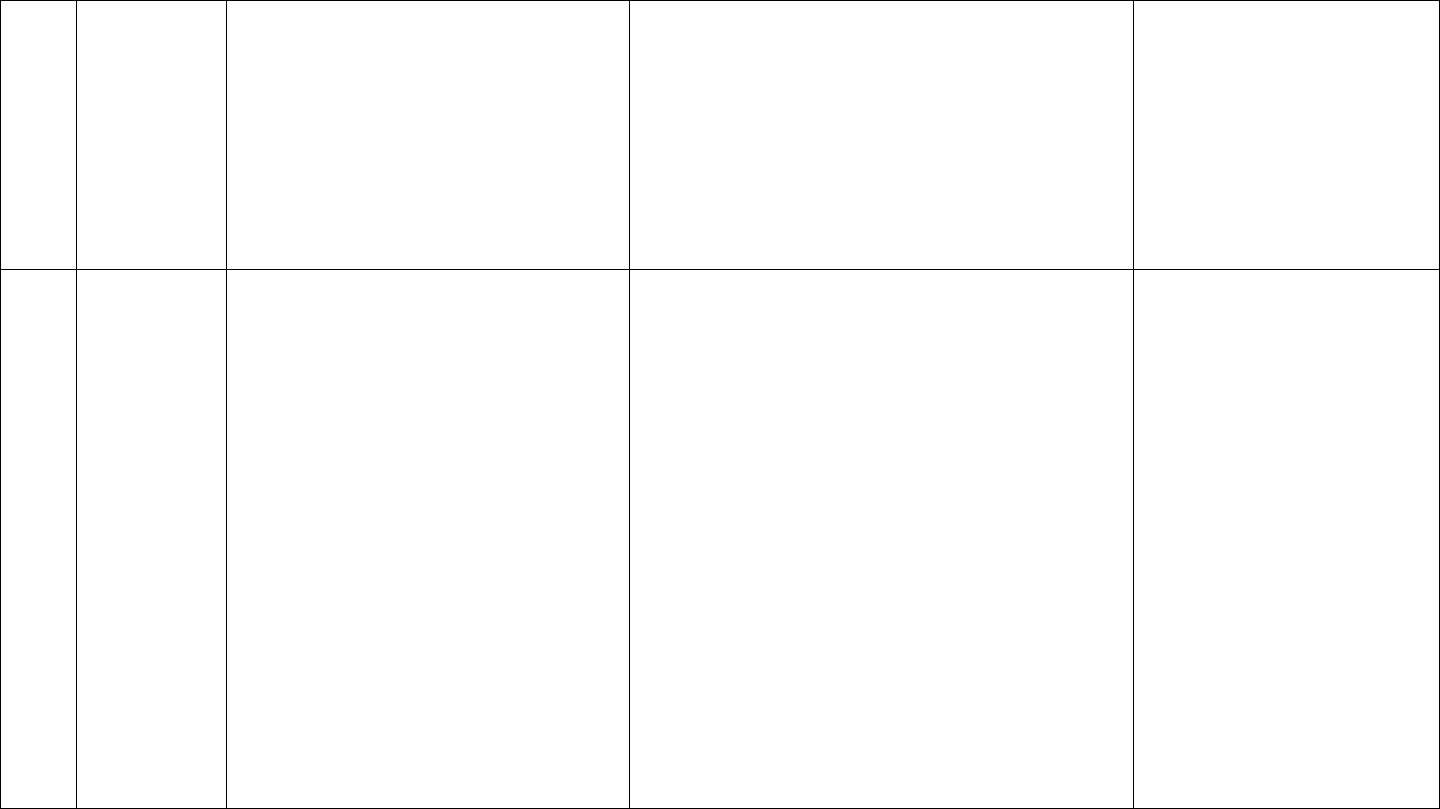
Table 1 below provides information on these elements for some of the more commonly used CPT® codes.
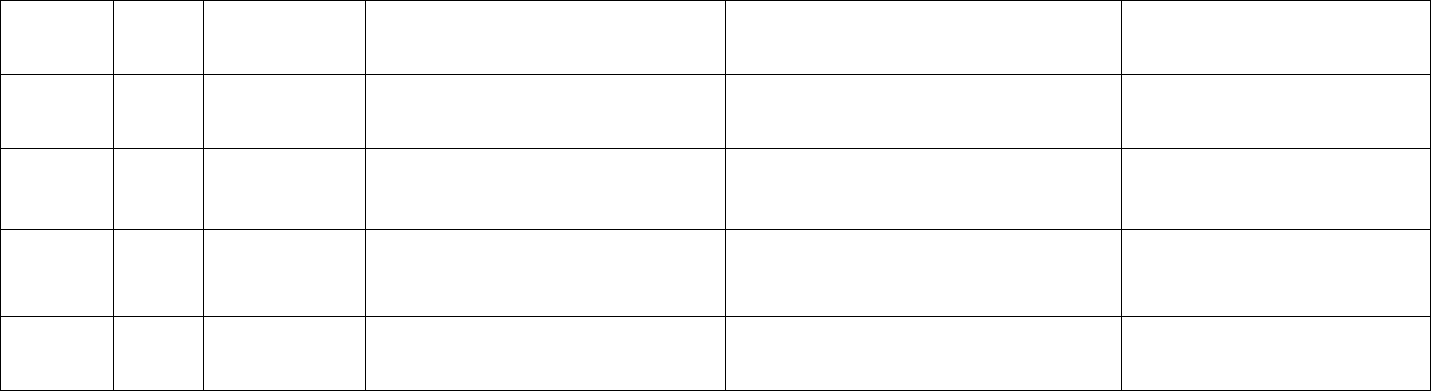
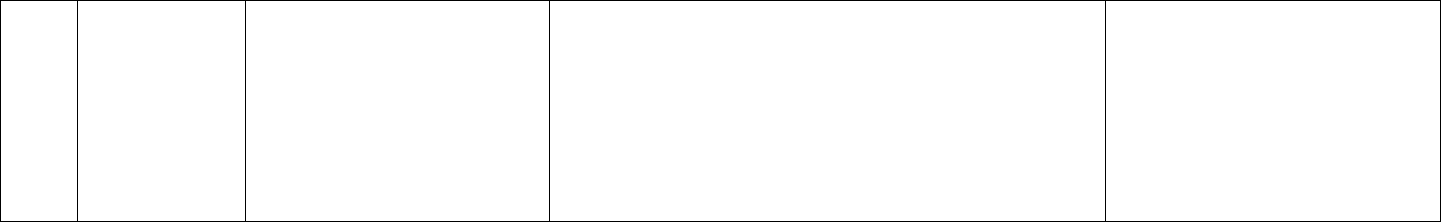
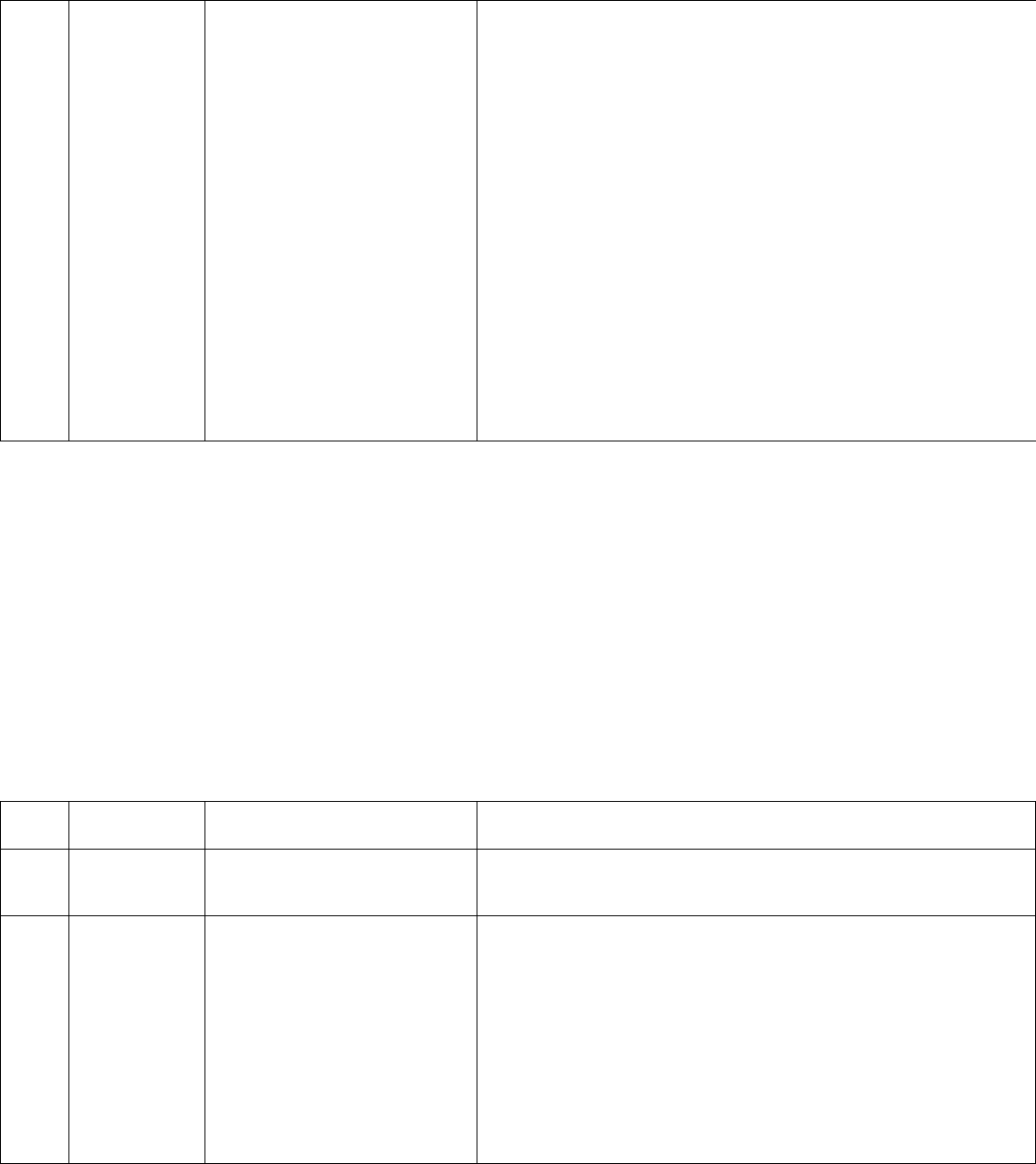
Table 1: Abbreviated Table of Code Level Selection
Outpatient
Code
Inpatient
Code
MDM Level
(Based on 2 of 3
MDM Elements)
Problems (Number and Complexity)
Amount and/or Complexity Data Reviewed/
Analyzed
Level of Risk
99202
99212
99242
99221
99231
99252
Straightforward
Minimal
Minimal or none
Minimal
99203
99213
99243
99221
99231
99253
Low
Low
Limited
Low
99204
99214
99244
99222
99232
99254
Moderate
Moderate
Moderate
Moderate
99205
99215
99245
99223
99233
99255
High
High
Extensive
High
* Each unique test, order or document contributes to the combination of 2 or combination of 3 in Category 1
4
Medical Decision Making
MDM is composed of three elements:
•
Number and complexity of problems addressed at encounter
•
Amount and/or complexity of data reviewed/analyzed
•
Level of risk associated with care of the patient
Some additional hints for meeting requirements for “Amount and/or Complexity Data Reviewed/Analyzed”:
• If a note(s) is reviewed from another service line, specifically state the date and author or clinical service of EACH note reviewed.
• If used, document that an independent historian is used and the reason why they are required.
• Document discussions with other providers or appropriate sources (i.e., lawyer, case manager, teacher) regarding the patient that are used in
medical decision making. Asynchronous (not in person) discussion can be used for MDM if initiated and completed within 1-2 days of date of
encounter.
• State specific risk of complications, including morbidity and/or mortality of patient management decisions, and document if risk is high or moderate,
which can affect MDM. This includes those patient management decisions considered, but not done.
• Document if surgery or intervention is needed to manage the infection and risk of such intervention in common language terms of high, medium,
low or minimal risk.
• Document if social determinants of health are present and impact your decision making. Some examples include lack of reliable transportation for
appointments, homeless, person who uses drugs, etc.
• Document if an infection is limb or life threatening.
Some considerations that can support “high risk of morbidity from additional diagnostic testing or treatment”:
• Specifically state if a patient is receiving an antimicrobial that carries high risk of morbidity or has significant medication interactions, and clearly
document in the note the risks and possible adverse effects and how frequently monitoring needs to be done. Some examples of this include:
1. High-risk medications that require intensive monitoring: aminoglycosides, amphotericin, IV acyclovir, vancomycin, linezolid, colistin, rifampin,
etc.
2. High-risk medication interactions: azoles, antibiotics that can cause QT prolongation, especially if patient is already on other medications that
also do this (e.g., antibiotic interaction with warfarin, HIV medications, rifampin, etc.).
• Note of clarification that the level of risk notes that it is the risk from the condition and not from the risk of the management.
There are four types of MDM (straightforward, low, moderate and high). The level of MDM is chosen based on meeting or exceeding two of the three
MDM elements: number and complexity of problems addressed at encounter, amount and/or complexity of data reviewed/analyzed, and level of risk
associated with care of the patient.
5
Number and Complexity of Problems Addressed at the Encounter
Per the AMA CPT code book, “A problem is a disease, condition, illness, injury, symptom, sign, finding, complaint or other matter which is addressed at the
encounter.” A problem may or may not have an established diagnosis at the time of the encounter. A problem is considered addressed if it is evaluated or
treated during the encounter. Consideration for further testing or treatment that is not elected to do is considered addressing a problem. A problem is not
addressed merely by noting it in the medical record when no evaluation or treatment is considered during that encounter. A problem during a hospital
inpatient or observation encounter is determined by the problem status on the date of encounter, which may be different than that on admission or other
previous encounters. Comorbidities and underlying diseases are not considered in the selection of the E/M service unless they are addressed by the provider
and their presence increases the amount and/or complexity of data to be reviewed and analyzed or the risk of complications and/or morbidity or mortality of
patient management. The final diagnosis for a condition does not determine the complexity or risk. An extensive evaluation of signs or symptoms may be
required for the evaluation to determine a diagnosis that may not represent a highly morbid condition. Multiple problems of lower severity may cause a higher
risk due to their interaction, and this interaction and increased risk should be documented. These definitions have been adapted from American Medical
Association CPT® Professional 2024 edition.
Types of Problems That Affect Level Selection
The following definitions have been adapted from the American Medical Association CPT® Professional 2024 edition.
A minimal problem is a problem that may not require the presence of a physician or other qualified health care professional, but a service is still provided by a
physician or other QHCP. An example is a patient who is receiving a routine injection (i.e., testosterone injection, vaccine), and the patient is seen by the
provider to answer questions about the injection being received.
A self-limited or minor problem has a definite and prescribed course, is transient in nature, and is likely not to permanently alter the patient’s health status.
• A patient is evaluated for upper respiratory symptoms and diagnosed with a viral upper respiratory tract infection. No further evaluation, treatment or
monitoring is indicated.
• A patient is hospitalized for a non-ID problem and is noted to have a rash. You see the patient and determine it is tinea corporis and recommend topical
treatment.
A stable, chronic illness has an expected duration of at least one year or until the death of the patient (e.g., diabetes, hypertension, HIV). The term “chronic”
does not relate to the stage or severity of the illness. The term “stable” means the patient has reached their treatment goal.
• A patient with well-controlled HIV on ART who is admitted for a non-ID problem. The physician will confirm the patient’s ART regimen and assess for
drug interactions.
A chronic illness with exacerbation, progression or side effects of treatment is a chronic illness that has acutely worsened, is partially controlled or is progressing
6
with the treatment intent of controlling progression through additional care and treatment of side effects.
• A patient with known HIV is hospitalized for a non-ID issue. They disclose that they have been nonadherent to ART and their CD4 count has declined. The
physician is consulted to evaluate ART options with the patient and plan for treatment, monitoring and follow-up.
A chronic illness with severe exacerbation, progression or side effects of treatment has a significant risk of morbidity and may require escalation in the level of
care.
• An HIV patient previously well controlled is now with falling CD4+ cell count and now has an opportunistic infection.
• A hospitalized patient with pneumonia, urinary tract infection or other infection with hypotension is now requiring ICU level of care.
• A diabetic foot infection not improved and worsening and may require surgical intervention for debridement.
• Chronic prosthetic joint infection on long-term oral suppression > 1 year presents with acute prosthetic joint infection.
An acute, uncomplicated illness or injury is a recent or new short-term problem with low risk of morbidity with considered treatment and little risk of mortality
with treatment with expected full recovery without functional impairment. A problem that is normally self-limited or minor but is not resolving with the
prescribed course can be considered an acute, uncomplicated illness.
• A patient is hospitalized with a non-ID problem and, while inpatient, complains of dysuria and is found to have a urinary tract infection. The physician
evaluates the patient to recommend treatment for uncomplicated acute cystitis.
An acute, uncomplicated illness or injury requiring hospital inpatient or observation level of care is a recent or short-term problem with low risk of morbidity
with considered treatment and little risk of mortality with treatment with expected full recovery without functional impairment and requires hospital inpatient
or observation level setting.
• A patient is hospitalized with an uncomplicated cellulitis. Due to a history of antibiotic allergies and intolerances, she is hospitalized for intravenous
vancomycin. The physician is consulted to confirm the plan of care and assess antibiotic monitoring needs.
A stable, acute illness is a problem that is new or recent for which treatment has been initiated and the patient has improved even though it has not yet
resolved.
• A patient is admitted with acute pyelonephritis and treated with intravenous antibiotics with good response. The consult is needed to provide comment
on an oral antibiotic to complete the patient’s course of therapy upon discharge.
An undiagnosed new problem with uncertain prognosis indicates there is a problem in the differential diagnosis that may represent in condition likely to result
in a high risk of morbidity without treatment.
• An otherwise healthy patient is hospitalized with fever of unknown origin. Evaluation is needed by the ID physician.
• A patient hospitalized for a non-ID problem is found to have a marked leukocytosis. Evaluation is needed by the ID physician.
An acute illness with systemic symptoms is an illness that causes systemic symptoms and has a high risk of morbidity without treatment. Systemic symptoms
may not be general and may affect only a single system.
7
• A patient is hospitalized with cellulitis, found to be febrile and tachycardic.
• A patient with acute pyelonephritis with fever and nausea and vomiting.
• A patient with community acquired bacterial pneumonia, with associated leukocytosis.
• An ICU patient develops a ventilator-associated pneumonia and has fever.
An acute, complicated injury is an injury that requires treatment that includes evaluation of body systems that are not directly part of the injured organ, the
injury is extensive, or the treatment options are multiple or associated with risk of morbidity.
• A trauma patient who develops postoperative or other infection from their injuries.
An acute or chronic illness or injury that poses a threat to life or bodily function is an acute illness with systemic symptoms, an acute complicated injury or
chronic illness or injury with exacerbation or progression or side effects of treatment that poses a threat to life or bodily function in the near term without
treatment. This can include some symptoms that may represent a condition that that is significantly probable and could pose a potential threat to life or bodily
function.
• A patient is hospitalized with septic shock
• A patient with bacterial meningitis
• Necrotizing fasciitis
• Infective endocarditis with systemic symptoms
• COVID-19 pneumonia requiring invasive mechanical ventilation
• A foot infection that requires amputation for control/cure
• Multifocal Staphylococcus aureus infection until source control achieved
Amount and/or Complexity of Data to Be Reviewed and Analyzed
Data are considered analyzed when the practitioner reviews medical data in determining the level of MDM. Tests ordered are presumed to be analyzed when
the results are reported and are counted toward level selection during the encounter in which the tests were ordered and are not counted during subsequent
encounters. Results that are auto populated in the medical record can be considered as analyzed or as being reviewed if they are indeed analyzed or reviewed
at that encounter and have not previously been reviewed. If a test is ordered outside of the encounter, then it may be counted during the visit in which it was
analyzed and therefore used for MDM. Recurring orders that have previously been ordered may be counted during the encounter in which they were analyzed.
If the data are a service for which a professional component is separately reported by the physician or other QHCP, such as an ECG performed in the office and
the ECG with interpretation were separately billed, this cannot be used twice. Those data are not considered ordered, analyzed, reviewed or independently
interpreted for the determination of level of MDM.
Tests reviewed may include imaging, laboratory, psychometric or physiologic data. Evaluating pulse oximetry using a pulse oximeter is not considered a test.
A unique test is defined by the CPT code set (e.g., basic metabolic panel [80047]) and is considered a single test despite possibly having multiple laboratory

8
values included. Reviewing multiple results of the same unique test when compared during an E/M service counts as one unique test. Tests that have
overlapping elements are not considered unique even if those tests are identified by distinct CPT codes. Some examples include if both a CMP and BMP are
reviewed, this only counts as a single test due to overlapping values of the BMP being encompassed in the CMP. Review of a molecular panel counts as a single
test even though multiple targets are reported.
A unique source is a physician or other QHCP who is in a distinct group or different specialty or subspecialty or a unique entity. All medical record notes from a
unique source count as one element toward MDM.
External physician or other QHCP is a physician or other QHCP who is not in the same group practice or is in a different specialty or subspecialty.
Discussion requires an interactive exchange that must be direct and not through intermediaries such as clinical staff or trainees, nor does it involve sending
chart notes or written exchanges that are within progress notes. The discussion does not need to be on the date of the encounter but is counted only once and
only when it is used in decision making of the encounter. It may be asynchronous, but follow-up must be initiated and completed within a short period of time
such as within one to two days. Two-way virtual discussions using the electronic health record messaging and chat functions on the day of the encounter would
meet the criteria for a discussion regarding a patient through an interactive exchange if that interaction is used in medical decision making on the day of
encounter. Simply routing a chart note through the electronic health record would not meet the necessary criteria for “discussion.”
An independent historian is an individual such as a parent, guardian, surrogate, spouse or witness who provides additional history to the history provided by
the patient who is unable to provide a complete or reliable history or because a confirmatory history is judged to be necessary. The independent history does
not need to be obtained in person but does need to be obtained directly from the historian who is providing the information. Some examples of independent
historians include a spouse, parent or adult caregiver for a developmentally disabled patient or patient with a traumatic brain injury or dementia. Using a
medical interpreter would not qualify as an “independent historian.” If an independent historian is used, it is important to clearly document the historian and
why they were specifically needed to provide history (i.e., why the patient is unable to provide his/her own history).
Independent interpretation involves the interpretation of a test for which there is a CPT code, and an interpretation or report is customary. When a review and
interpretation of a test is performed and documented by the provider, but not separately reported (billed), then this would represent an independent
interpretation. This report does not need to conform to the usual standards of a complete report of the test. This does not include interpretation of tests that
do not have formal reports such as a complete blood count with differential and blood cultures. Examples would include reviewing a chest radiograph and
documenting in the medical record an interpretation, but not separately reporting (billing) the interpretation of the chest radiograph.
An appropriate source includes professionals who are not health care professionals but may be involved in the management of the patient, such as a lawyer,
upper officer, case manager or teacher, and does not include discussion with family or informal caregivers.
Risk of Complications and/or Morbidity or Mortality of Patient Management
Risk is the probability and/or consequence of an event to occur when the addressed problem is treated appropriately. The level of risk is determined by the
9
nature of the considered event, such that a low probability of death to occur with treatment may be a high risk, whereas a high chance of a minor, self-limited
adverse effect of treatment may be a low risk. Risk is based on the problems addressed at the encounter and includes diagnostics and disposition considered
during the encounter. Diagnostics, therapeutics and decisions regarding hospitalization, escalation of care or surgery considered during the encounter
contribute to the risk and include those considered, but not done.
Social determinants of health are economic and social conditions that influence the health of people in communities. Common SDOHs include insecurity in
realms such as food, housing, and transportation; patients living in group homes; and persons who use drugs. For information on how and when to use ICD-10
diagnosis codes to report SDOH, visit cms.gov/files/document/zcodes-infographic.pdf.
Drug therapy requiring intensive monitoring for toxicity involves monitoring of a therapeutic agent that has the potential to cause serious morbidity or death
and requires intensive monitoring for potential adverse effects and not primarily for assessment of therapeutic efficacy. Per AMA’s 2024 CPT guidelines, drug
therapy monitoring should be done with generally accepted practice standards for the agent but may be patient specific. Monitoring may be long term or short
term, and if long term, it must be performed no less than quarterly. Monitoring can include laboratory tests, physiologic tests or imaging, but it does not
include history or examination. The drug therapy monitoring can be included in the MDM of the encounter if it is considered in the management of the patient
during that encounter. Providers should explicitly document the need for intensive drug monitoring in the medical record. Documentation could be,
“[medication name] requires intensive drug monitoring due to concerns for possible adverse effects of [medication name] including [list adverse effects] and
will be monitored with [list tests or images] to be done [list frequency].” An example would be, “Telavancin requires intensive drug monitoring due to concerns
for possible adverse effects of telavancin, including acute kidney injury, and will be monitored with basic metabolic panel to be done twice weekly while on
therapy.”
10
Description of Total Time
The element of coding by time includes the total time of all activities related to the patient visit on the date of the
encounter including face-to-face time with the patient and/or family/caregiver and non-face-to-face time personally
spent by the physician and/or other QHCP on date of encounter, including but not limited to:
•
Preparing to see patient (e.g., review tests, medical records)
•
Obtaining history
•
Performing a medically appropriate physical examination
•
Counseling and education (patient, family member, caregiver)
•
Ordering medications, tests and procedures
•
Referring and communicating to other health care professionals
•
Documenting the encounter
•
Independent interpretation of tests (when not separately reported)
•
Care coordination (when not separately reported)
Total time involves the above activities regardless of location such as on or off an inpatient unit or in the office. Total
time does not include time involved with any activities that are separately reported nor travel time. Total time does not
include any activities or time spent other than on the date of the encounter. To bill by time, the total time spent on
patient care activities on the date of the encounter should be documented correctly and not guessed or rounded, and
activities performed should be documented for that time (e.g., reviewing medical records, reviewing labs or tests,
obtaining history, discussion of plan of care with patient), but it is not necessary to document time for each activity
individually – rather, just the total time with all activities. Time spent with normal activities by ancillary clinical staff
(such as check-ins, obtaining vital signs, wound dressing changes, arranging home health care, obtaining medical
records, etc.) should not be used to calculate total time.
For shared or split visits between a physician and other QHCP, such as advanced practice providers, only distinct time
spent separately on the date of the encounter may be summed to equal total time. If a physician and QHCP perform the
same activity together, then time can only be counted for one of the providers in the sum of the total time.
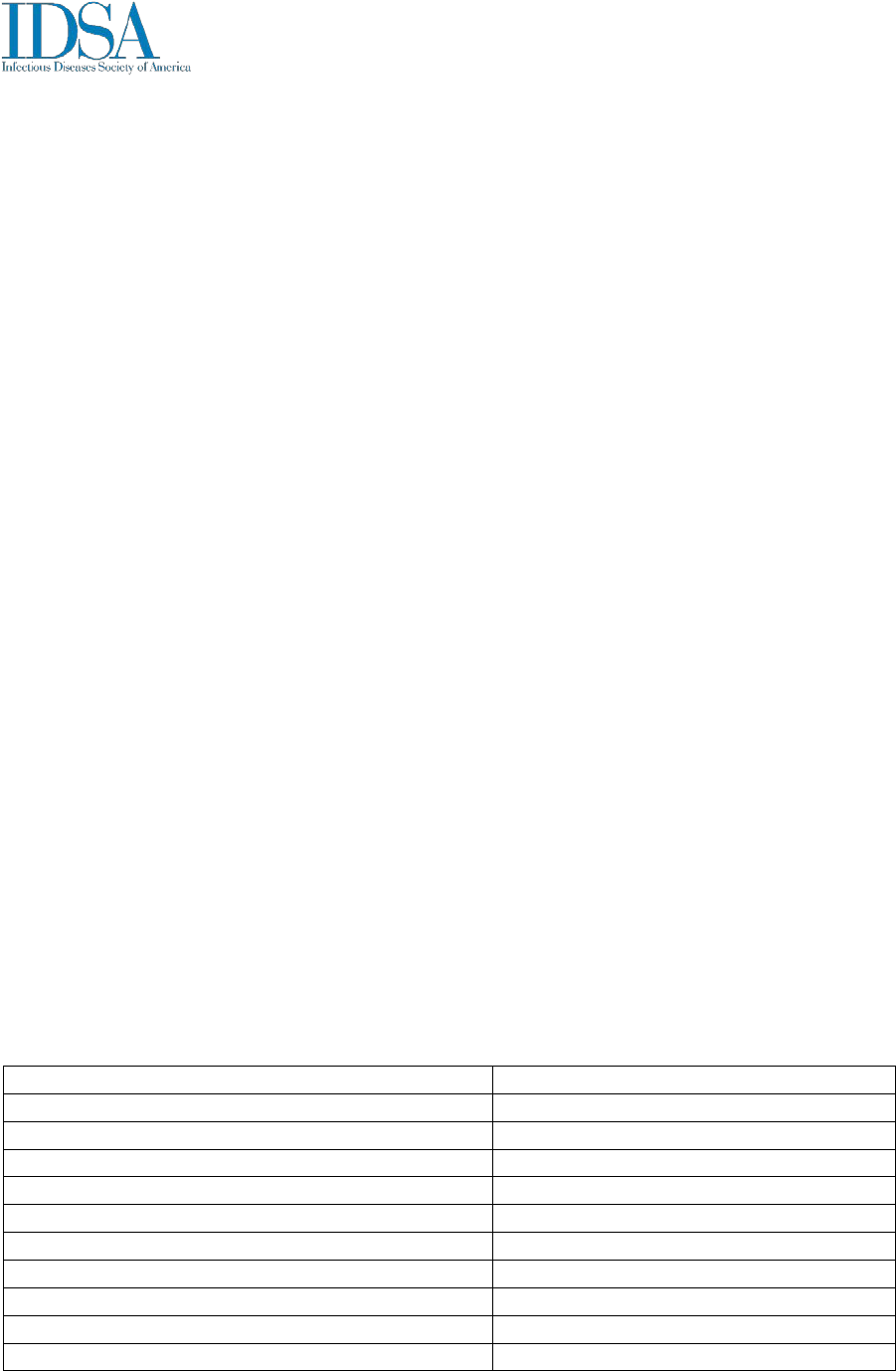
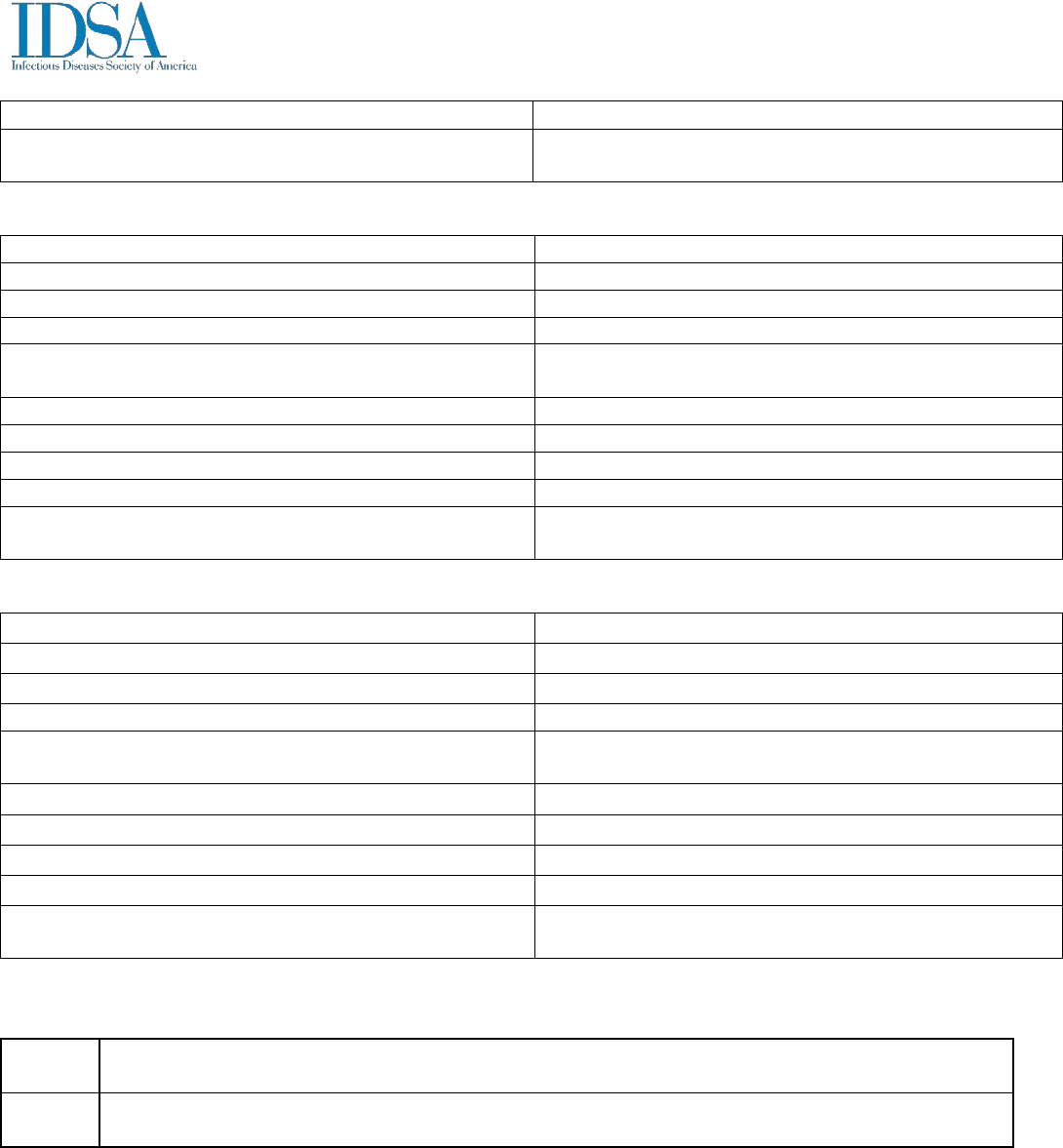
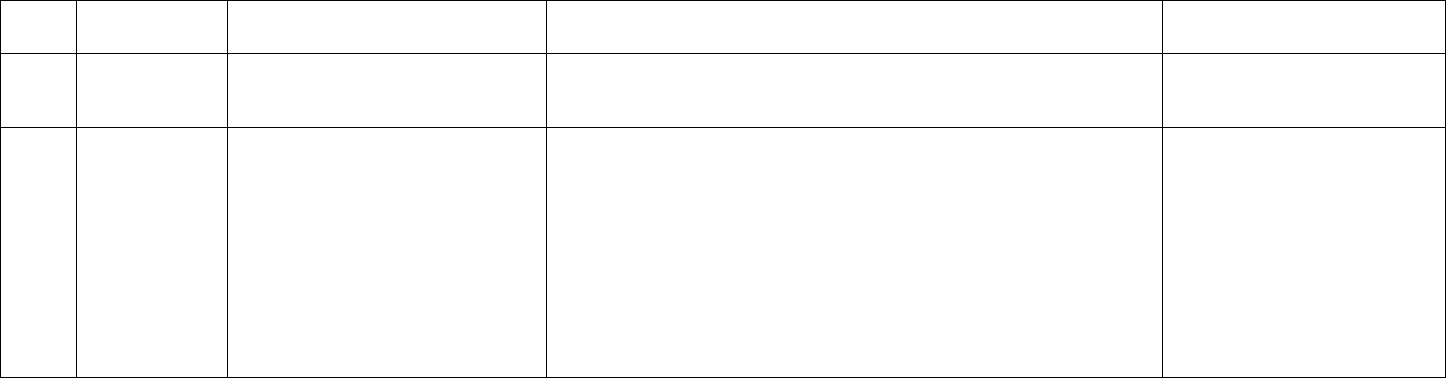
Table 2 provides information on which code should be selected based on total time spent on the date of the encounter for
new and established patients.
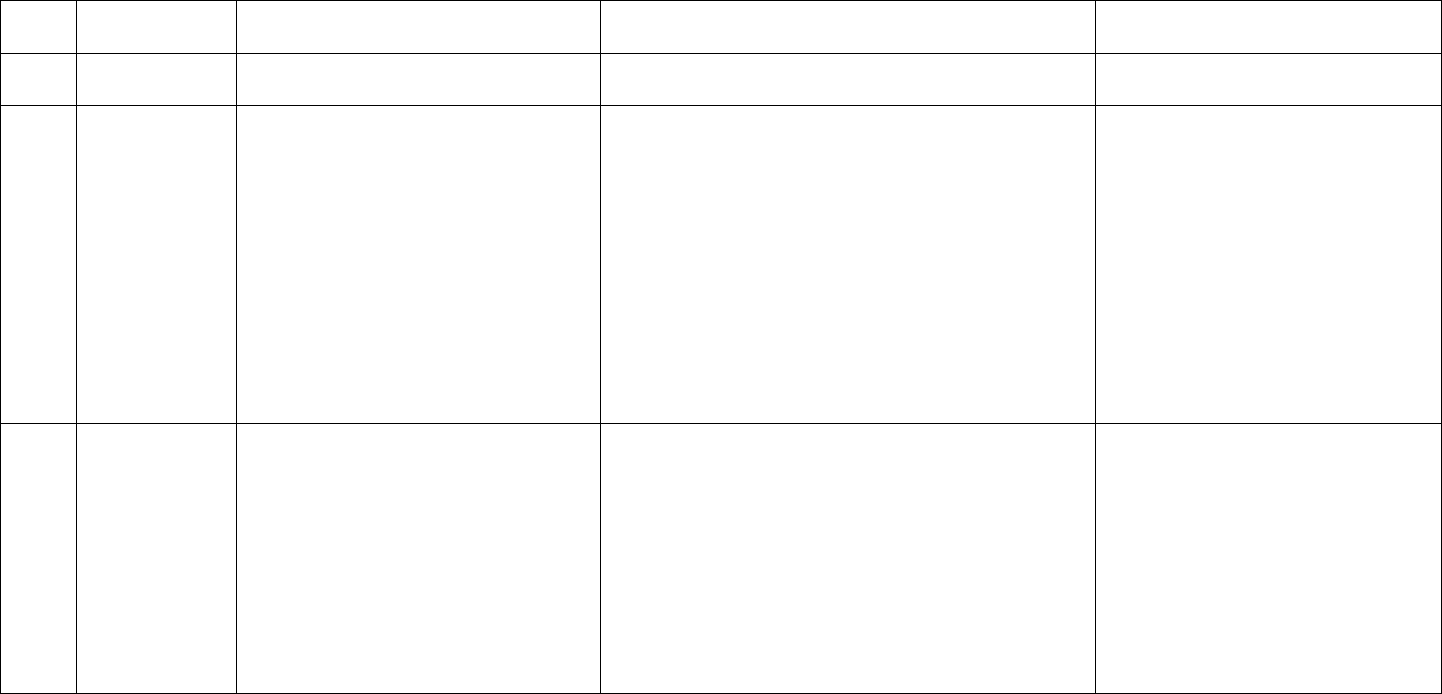
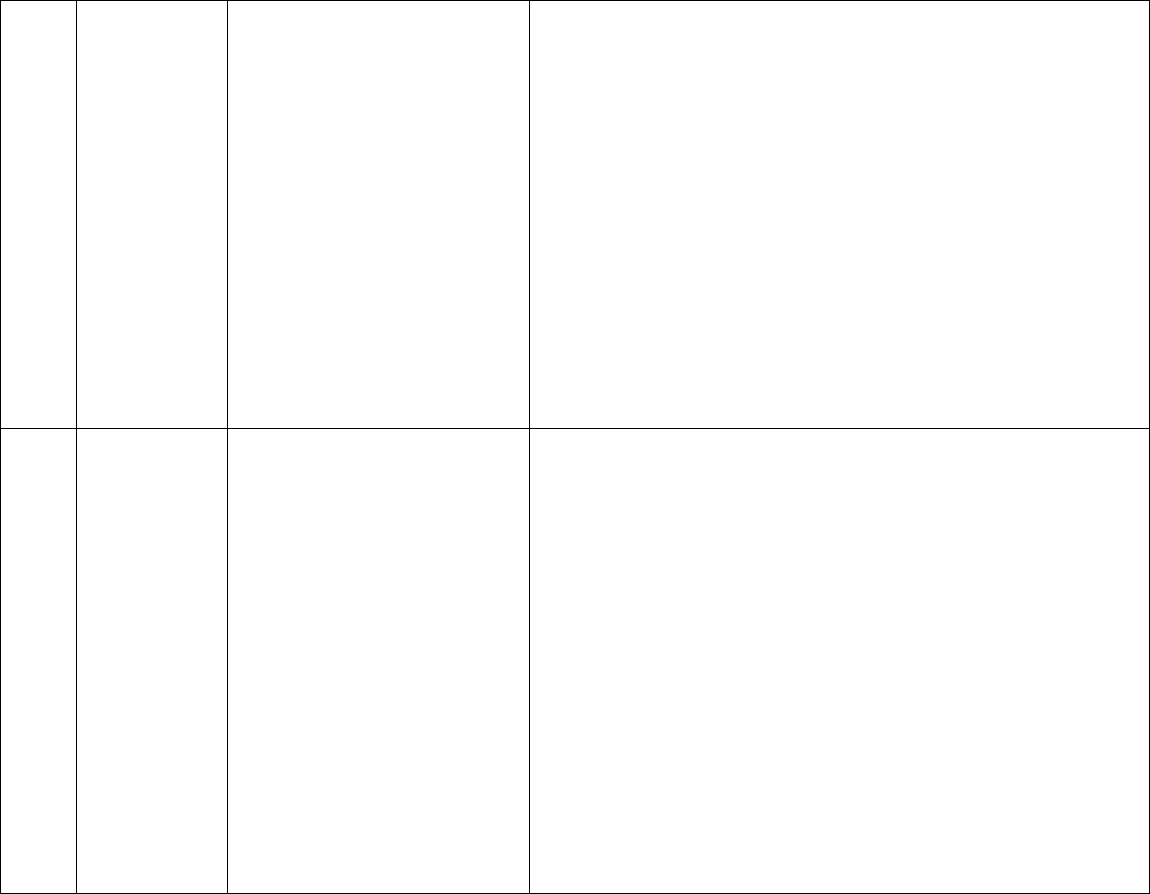
Table 2: Total Time Spent on the Date of the Encounter for E/M Codes
New Outpatient E/M CPT® Code
Total Time*
99202
15 minutes
99203
30 minutes
99204
45 minutes
99205
60 minutes
Established Outpatient E/M CPT® Code
Total Time*
99211
Time component removed
99212
10 minutes
99213
20 minutes
99214
30 minutes
11
99215
40 minutes
Initial Hospital Inpatient E/M CPT® Code
Total Time*
99221
40 minutes
99222
55 minutes
99223
75 minutes
Subsequent Hospital Inpatient E/M CPT® Code
Total Time*
99231
25 minutes
99232
35 minutes
99233
50 minutes
Office or Outpatient Consultations E/M CPT® Code
Total Time*
99242
20 minutes
99243
30 minutes
99244
40 minutes
99245
55 minutes
Inpatient Consultations E/M CPT® Code
Total Time*
99252
35 minutes
99253
45 minutes
99254
60 minutes
99255
80 minutes
*Total Time is time that must be met or exceeded to report the code.
Prolonged Service Time
Prolonged services CPT codes have been changed to include total time on date of encounter, regardless of time spent
face-to-face/on the unit or non-face-to-face/off the unit.
CPT code 99417 is used to report prolonged services when the total time on the date of encounter of an outpatient
service (99205, 99215, 99245) exceeds 15 minutes beyond the time required to report the highest-level service. CPT
code 99418 is used to report prolonged services when the total time on the date of encounter during an inpatient or
observation service (99223, 99233, 99255) exceeds 15 minutes beyond the time required to report the highest-level
service. CPT codes 99417 and 99418 are to be reported only when the primary E/M service has been selected based on
time and the highest level of E/M service has been achieved and the total time has exceeded 15 minutes beyond the
time requirement for that selected E/M code. CPT codes 99417 and 99418 can be billed in subsequent 15-minute
increments to account for all total time spent in patient care activities on the date of encounter. Do not report a unit of
99417 or 99418 of less than 15 minutes (i.e., all 15 minutes must be achieved to be able to report 99417 or 99418).
Total time for prolonged services includes the same activities able to be used to select the initial E/M code based on
time. Medicare does not recognize CPT codes 99417 and 99418 and has developed two G codes to report prolonged
services on the date of encounter. Code G2212 is used in association with an office or other outpatient E/M visit
(99202-99215) and requires that the highest E/M level be selected by time. More than 15 minutes beyond the maximum
time for that level must be exceeded before the G code may billed. G2212 should be billed in 15-minute increments.
Code G0316 may be used to report prolonged services in association with an initial hospital or subsequent hospital

12
E/M visit of the highest level only (99223 and 99233) and is also billed in 15-minute increments, with time thresholds
to report G0316 being 90 minutes for 99223 and 65 minutes for 99233.
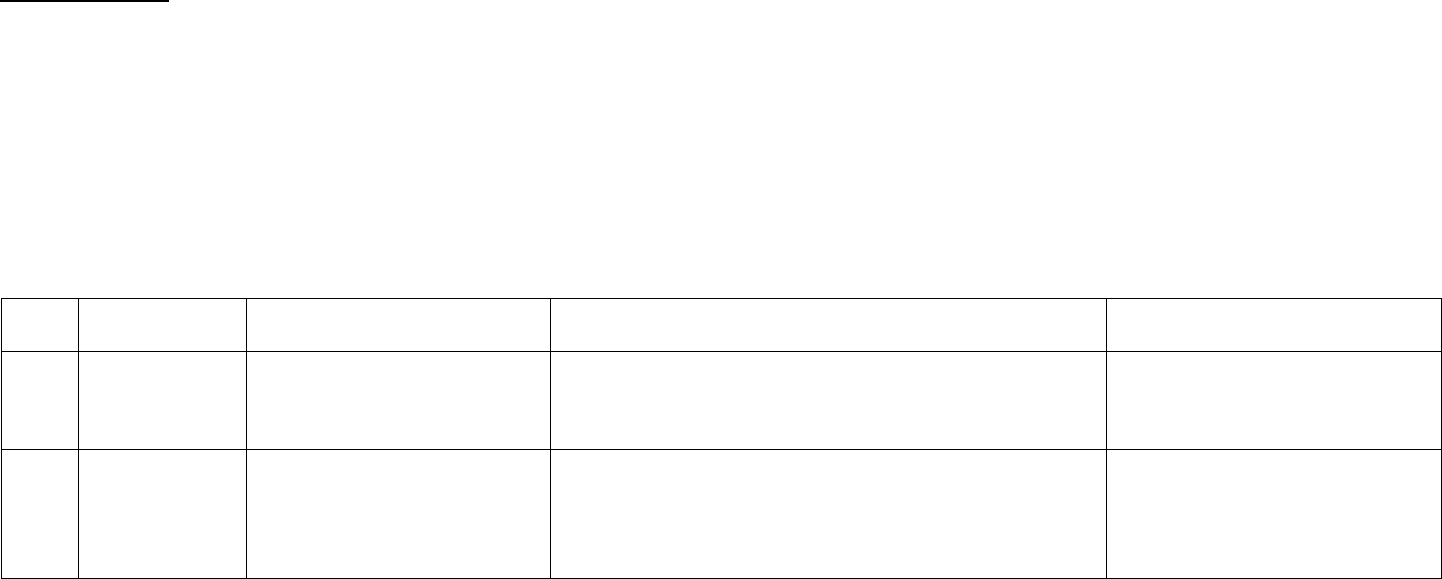
Examples
A provider spends a total time of 83 minutes with a new patient. The time limit for a new outpatient visit, E/M visit 99205,
is 60-74 minutes. The 83-minute visit is 23 minutes beyond the minimal time limit of 99205 of 60 minutes, and therefore
the provider may bill CPT code 99417. For each additional 15 minutes, code 99417 may be reported. Tables 3 through 10
illustrate reporting prolonged service codes on date of encounter (99417 and 993X0). Tables 3, 4 and 5 were adapted from
the American Medical Association CPT® Professional 2024 edition.
Add-On Complexity Code
• CMS proposes a separate add-on payment for healthcare common procedure coding system (HCPCS) code G2211.
The add-on code is designed to capture resource costs associated with E/M visits for primary care and longitudinal
care of complex patients
• G2211: Visit complexity inherent to evaluation and management associated with medical care services that serve as
the continuing focal point for all needed health care services and/or with medical care services that are part of
ongoing care related to a patient’s single, serious condition or a complex condition.
o Billed with office/outpatient evaluation and management (E/M) services.
o Cannot be billed when modifier 25 is appended to the E/M code.
o Code is used to report services for longitudinal care
o CMS clarified that the provider/patient relationship is the focal point of when deciding whether to bill the
complex care code.
o
“The most important information used to determine whether the add-on code could be billed is the
relationship between the practitioner and the patient. If the practitioner is the focal point for all needed
services, such as a primary care practitioner, the HCPCS G2211 add-on code could be billed. Or, if the
practitioner is part of ongoing care for a single, serious and complex condition, e.g., sickle cell disease, then
the add-on code could be billed. The add-on code captures the inherent complexity of the visit that is
derived from the longitudinal nature of the practitioner and patient relationship.”
[1]
• For ID physicians, use of this code may be appropriate for HIV primary care visits, and for the longitudinal care of
some chronic infections, for example mycobacterial infections or osteomyelitis. It should not be used for a one-time
consultation or the short-term management of an acute infection.
[1]
CRD Associates via CMS Manual System, Pub 100-04 Medicare Claims Processing Manual, Transmittal 12372;
https://www.cms.gov/files/document/r12372cp.pdf Accessed by CRD Associates on December 14, 2023.
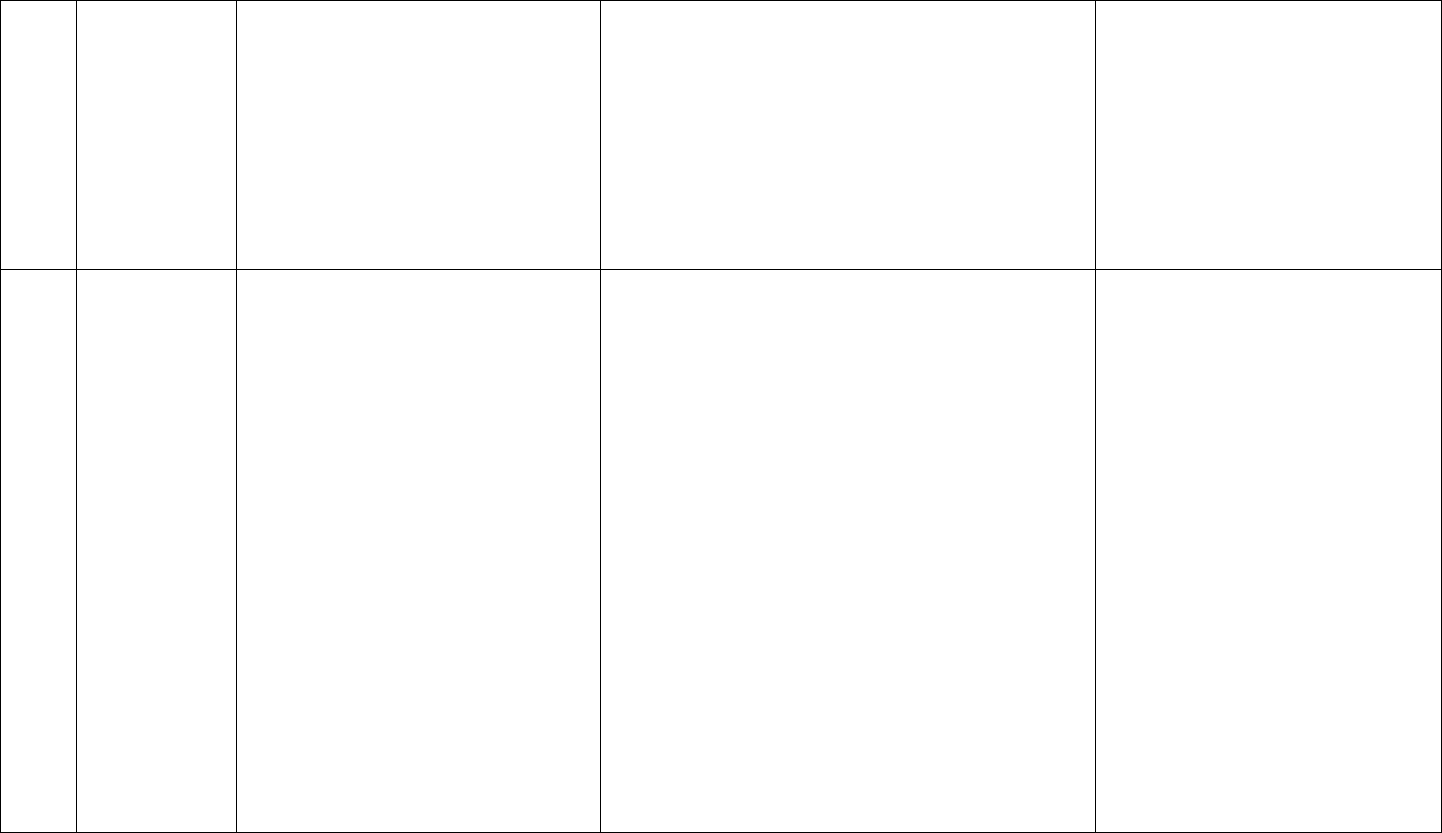
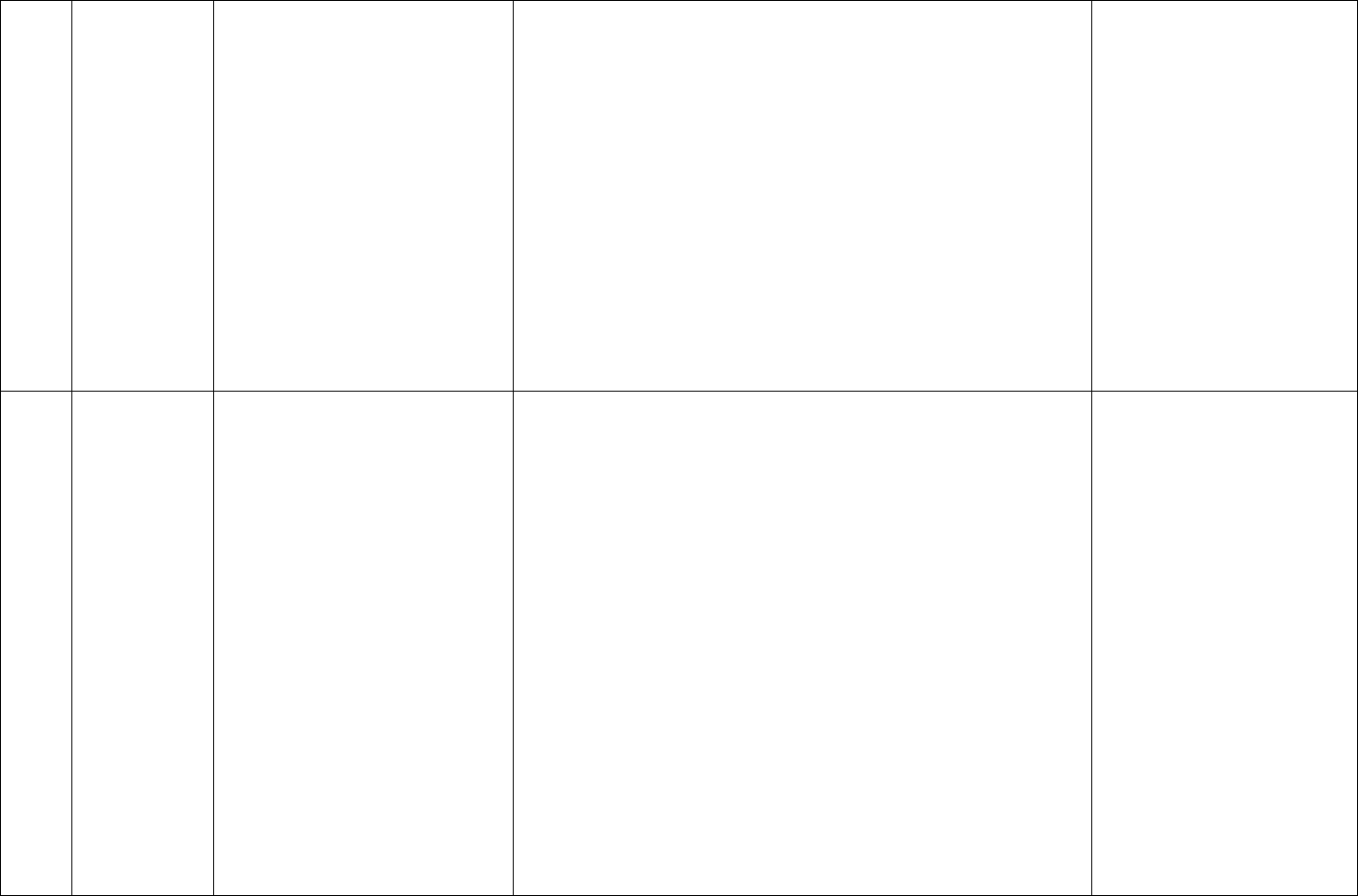
Table 3: Using Code 99417 With New Patient Office or Other Outpatient Services E/M
Use With 99205 (New Patient)
Code(s) Reported
Less than 75 minutes
Use appropriate E/M code
75-89 minutes
99205 x1 AND 99417 x1
90-104 minutes
99205 x1 AND 99417 x2
105 minutes or more
99205 x1 AND 99417 x3 or more for each additional 15
minutes
13
Table 4: Using Code 99417 With Established Patient Office or Other Outpatient Services E/M
Use With 99215
(Established Patient)
Code(s) Reported
Less than 55 minutes
Use appropriate E/M code
55-69 minutes
99215 x1 AND 99417 x1
70-84 minutes
992015 x1 AND 99417 x2
85 minutes or more
992015 x1 AND 99417 x3 or more for each additional 15
minutes
Table 5: Using Code 99417 With Office or Other Outpatient Consultation Services E/M
Table 6: Using Code 99418 With Initial Hospital Care Services E/M
Use With 99223 (Outpatient Consult)
Code(s) Reported
Less than 75 minutes
Use appropriate E/M code
90-104 minutes
99223 x1 AND 99418 x1
105-119 minutes
99223 x1 AND 99418 x2
120 minutes or more
99223 x1 AND 99418 x3 or more for each additional 15
minutes
Table 7: Using Code 99418 With Subsequent Hospital Inpatient or Observation Care Services E/M
Use With 99233 (Outpatient Consult)
Code(s) Reported
Less than 50 minutes
Use appropriate E/M code
65-79 minutes
99233 x1 AND 99418 x1
80-94 minutes
99233 x1 AND 99418 x2
95 minutes or more
99233 x1 AND 99418 x3 or more for each additional 15
minutes
Table 8: Using Code 99418 With Inpatient or Observation Consultations E/M
Use With 99255 (Outpatient Consult)
Code(s) Reported
Less than 80 minutes
Use appropriate E/M code
95-109 minutes
99255 x1 AND 99418 x1
Use With 99245 (Outpatient Consult)
Code(s) Reported
Less than 70 minutes
Use appropriate E/M code
70-84 minutes
99245 x1 AND 99417 x1
80-99 minutes
99245 x1 AND 99417 x2
100 minutes or more
99245 x1 AND 99417 x3 or more for each additional 15
minutes
14
110-124 minutes
99255 x1 AND 99418 x2
125 minutes or more
99255 x1 AND 99418 x3 or more for each additional 15
minutes
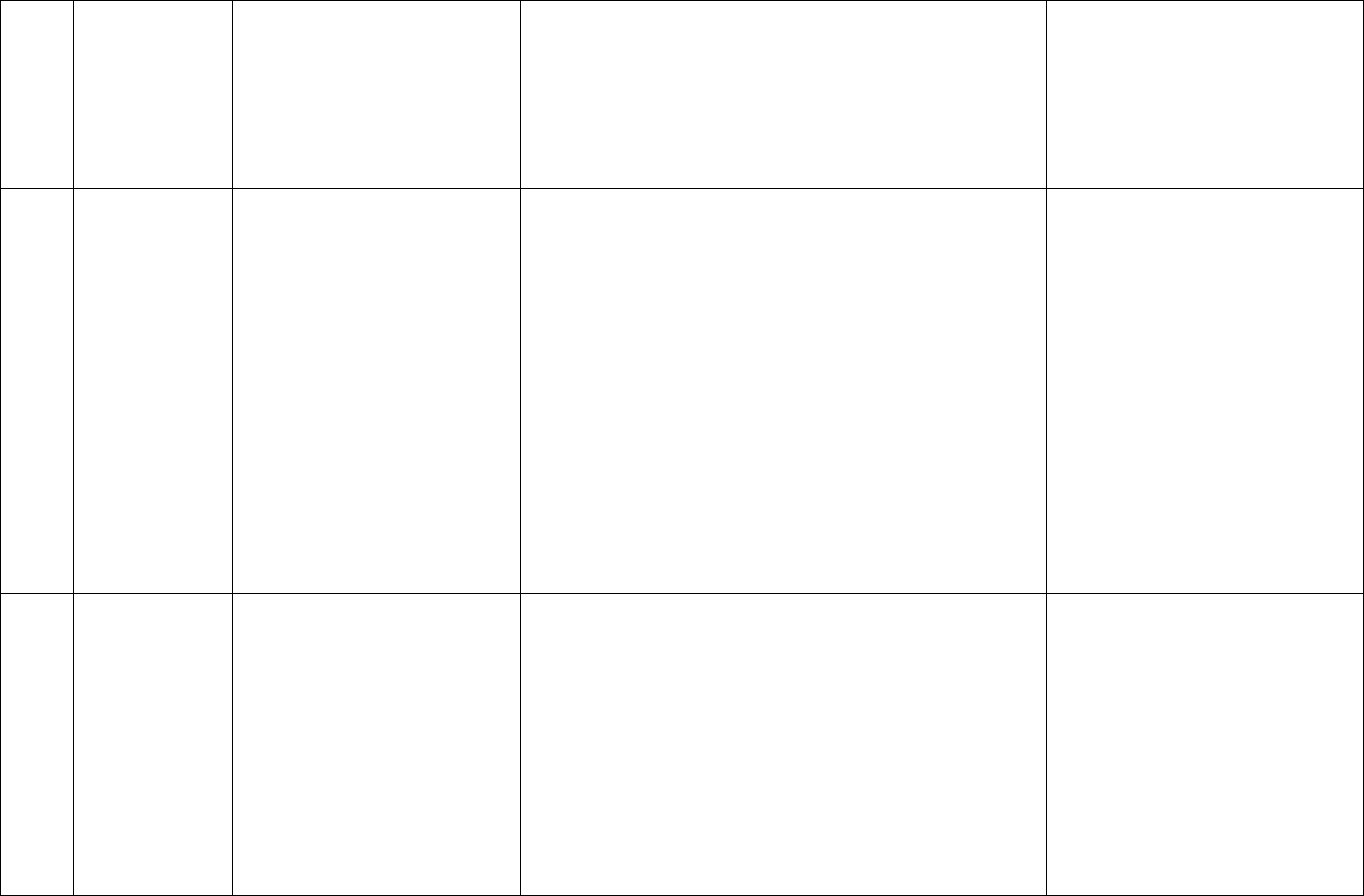
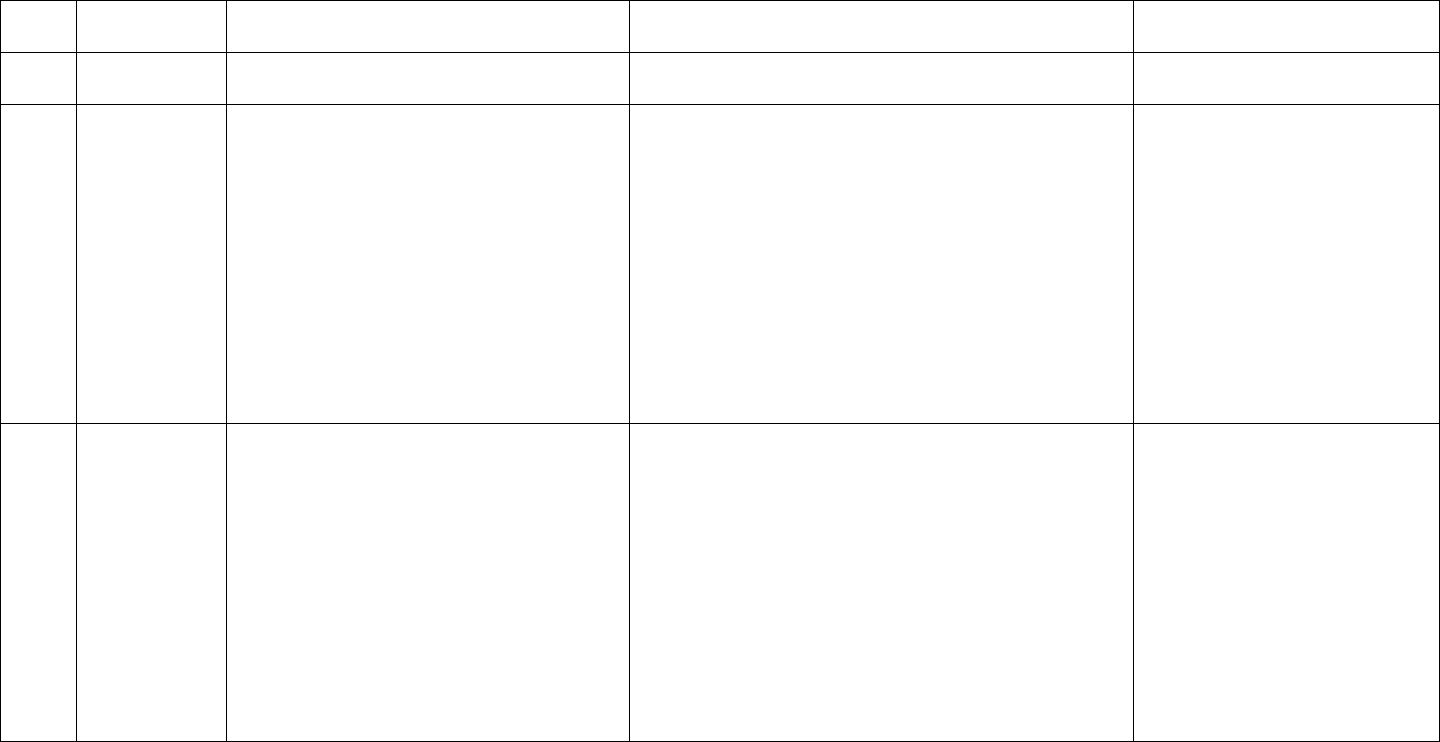
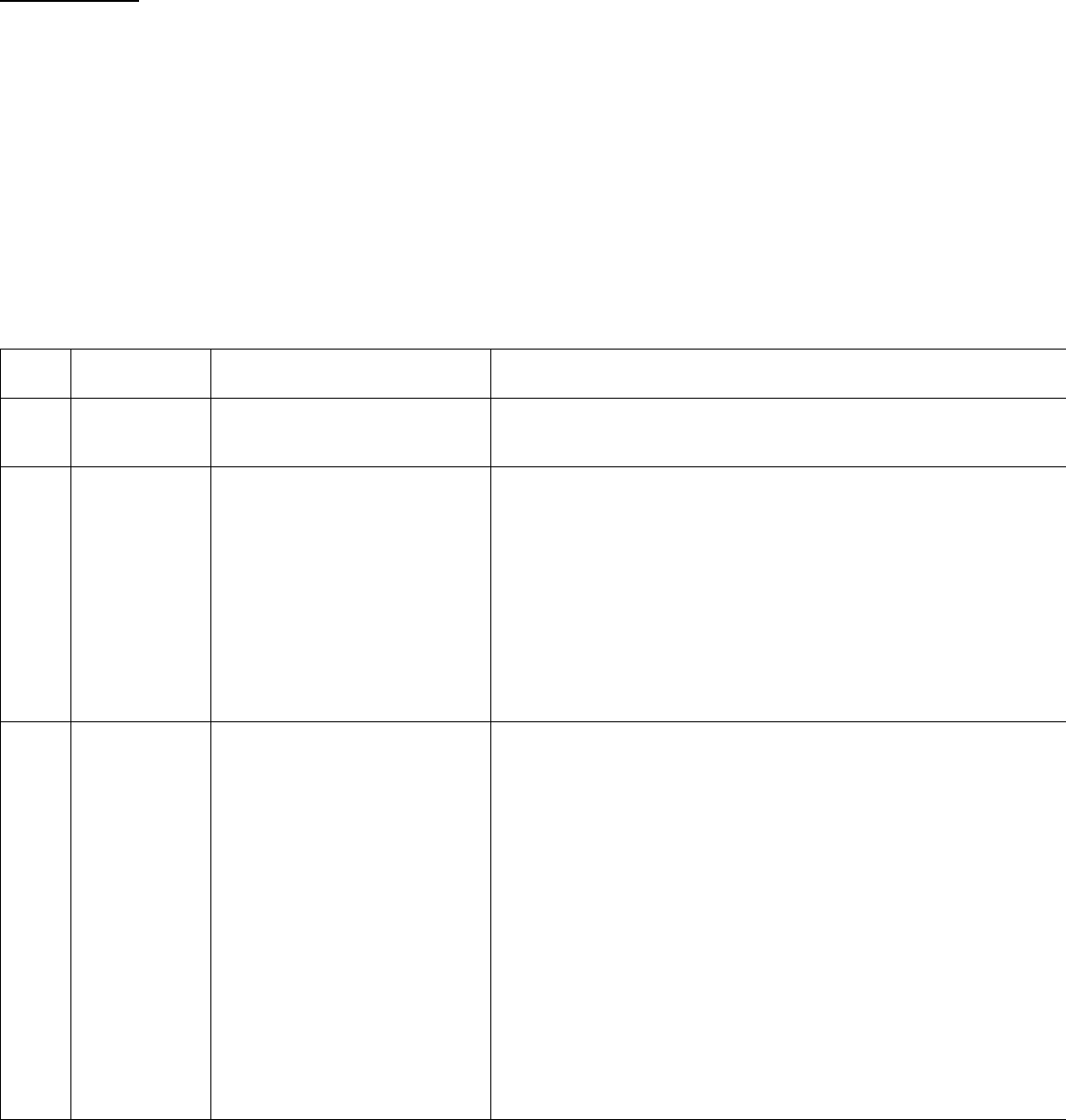
Table 9: Using Code G2212 With Office or Other Outpatient Consultation Services E/M
Use With 99205 (New Patient)
Code(s) Reported
60-74 minutes
99205
89-103 minutes
99205 x1 AND G2212 x1
104-118 minutes
99205 x1 AND G2212 x2
119 minutes or more
99205 x1 AND G2212 x3 or more for each additional 15
minutes
Use With 99215 (Established Patient)
40-54 minutes
99215
69-83 minutes
99215 x1 AND G2212 x1
84-98 minutes
99215 x1 AND G2212 x2
99 minutes or more
99215 x1 AND G2212 x3 or more for each additional 15
minutes
Table 10: Using Code G0316 With Hospital Inpatient or Observation Care Services E/M
Use With 99223 (New Patient)
Code(s) Reported
Less than 89 minutes
Use appropriate E/M code
90-104
99223 x1 AND G0316 x1
105-119 minutes
99223 x1 AND G0316 x2
120 minutes or more
99223 x1 AND G0316 x3 or more for each additional 15
minutes
Use With 99233 (Established Patient)
Less than 64 minutes
Use appropriate E/M code
65-79 minutes
99233 x1 AND G0316 x1
80-94 minutes
99233 x1 AND G0316 x2
95 minutes or more
99233 x1 AND G0316 x3 or more for each additional 15
minutes
Critical Care Service Codes
99291
Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74
minutes
99292
Each additional 30 minutes of critical care provided beyond the first 74 minutes (billed in addition to
99291)
Critical care codes are reimbursed at a higher rate than traditional E/M codes and may be used by physicians in any
specialty, including infectious diseases. Many ID physicians already use these codes. Critical care codes are typically used for
care provided in an intensive care unit, but they may be used for the care of critically ill patients outside of an ICU as long as
the visit meets the time requirements and definition of critical care.
Critical care codes may be used when all of the following criteria are met:

15
1. The patient has a critical illness.
• A critical illness is a life-threatening condition that impairs one or more organ systems.
2. Care provided meets the definition of “critical care.”
• Critical care is defined in AMA’s CPT Book 2024 as “high complexity decision making to assess, manipulate and
support vital system function(s) to treat single or multiple vital organ system failures and/or to prevent further
life-threatening deterioration of the patient’s condition.”
3. Care does not duplicate care provided by another billing physician.
• Physicians from more than one specialty may use critical care codes when billing for the care of the same
patient on the same day, if care is not provided concurrently (i.e., at the exact same time) and the care is not
duplicative.
4. Time requirements are met.
• Critical care time is defined as time spent either at the bedside or in the patient’s hospital unit directly engaged
in care for that patient.
• It may include time spent reviewing records, discussing management and documenting in the medical record.
• Time is the total time spent in one day and does not need to be continuous.
16
Section Three: Clinical Examples of Code Level Selection
The following clinical examples build on a base level patient; with each subsequent example, the severity of the patient’s problem progresses, therefore
indicating a higher level of MDM. MDM includes an increase in the number or complexity of problems to be assessed, along with review of increasing amounts of
complex data and risk.
The notes of the case are presented first, followed by the MDM table highlighting (in red) the elements that were considered when choosing the code
level. As noted previously, E/M code level selection is now based on medical decision making or time. In the clinical examples that follow, there are
examples that include medical decision making or time used to justify code selection.
Outpatient Visits
Outpatient Clinical Example #1: CPT Code Level 99202 (New Patient)/99212 (Established Patient)
Patient is 65-year-old with congestive heart failure, diabetes mellitus type 2 and hypertension who presents with leg swelling and erythema, and no tenderness.
Exam indicates signs of venous stasis, but no cellulitis. Advised leg elevation and follow-up visit with primary care physician for management of congestive heart
failure medication. No antimicrobials were prescribed. Follow-up as needed.
Medical decision making for this case is a straightforward review of a single self-limiting problem with review of minimal data and a minimal level of risk;
therefore, code level 99202 or 99212 is indicated, as shown in red below:
CPT
Code
MDM Level
Problems (Number and
Complexity)
Data Reviewed
Level of Risk
99202
99212
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
Minimal
99203
99213
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique
Low
Low risk of morbidity from additional
diagnostic testing or treatment
17
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital
inpatient or observation level of
care
source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
99204
99214
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated
injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not
separately reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
Moderate
Moderate risk of morbidity from
additional diagnostic testing or
treatment
Examples only:
• Prescription drug management
• Decision regarding minor surgery
with identified patient or procedure
risk factors
• Decision regarding elective major
surgery without identified patient or
procedure risk factors
• Diagnosis or treatment significantly
limited by social determinants of
health
99205
99215
High
High
• 1 or more chronic illness with
severe
progression/exacerbation/adve
rse effects or treatment
• 1 acute or chronic illness or
injury that poses threat to life
or body function
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not
separately reported)
High
High risk of morbidity from additional
diagnostic testing or treatment
Examples only:
• Drug therapy requiring intensive
monitoring for toxicity
• Decision regarding elective major
surgery with identified patient or
procedure risk factors
• Decision regarding emergency major
surgery
• Decision regarding hospitalization or
escalation of hospital-level care
18
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with
external physician/other qualified health care
professional/appropriate source (not separately reported)
• Decision not to resuscitate or to de-
escalate care because of poor
prognosis
• Parenteral controlled substances
19
Outpatient Clinical Example #2: CPT Code Level 99203 (New Patient)/99213 (Established Patient)
Patient is 65-year-old with congestive heart failure, diabetes mellitus type 2 and hypertension who presents with leg swelling and erythema that began four
days ago. Patient indicates there is some pain in the leg and is feeling warm; however, vital signs show no systemic fever. Exam suggestive of nonpurulent
cellulitis. Review of prior PCP patient medical records show no history of methicillin-resistant Staphylococcus aureus. Cultures not available for review. Patient
indicates no allergies. Prescribed five-day course of cephalexin with follow-up with ID physician in seven days.
Medical decision making for this case is low level for a single, acute, uncomplicated problem that involved the review of a prior external note. Even though
moderate risk level could be met, since two of the three elements of MDM are needed, code level 99203 or 99213 is indicated, as shown in red below:
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data Reviewed
Level of Risk
99202
99212
Straightforward
Minimal
• 1 self-limited problem or minor problem
Minimal or none
Minimal
99203
99213
Low
Low
• 2 or more self-limited/minor
problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or injury
requiring hospital inpatient or
observation level of care
Limited
(Must meet the requirements of at least 1 of the 2
categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each
unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent
historian(s)
Low
Low risk of morbidity from additional
diagnostic testing or treatment
99204
99214
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/adverse
effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new problem
with uncertain prognosis
• 1 new problem or acute illness
with systemic symptoms
• 1 acute complicated injury
Moderate
(Must meet the requirements of at least 1 out of 3
categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique
source*
• Review of the result(s) of each unique test*
• Ordering of each unique test*
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
Moderate
Moderate risk of morbidity from
additional diagnostic testing or treatment
Examples only:
• Prescription drug management
• Decision regarding minor surgery with
identified patient or procedure risk
factors
• Decision regarding elective major
surgery without identified patient or
procedure risk factors
20
• Independent interpretation of a test performed by
another physician/other qualified health care
professional (not separately reported)
or
Category 3: Discussion of management or test
interpretation
• Discussion of management or test interpretation with
external physician/other qualified health care
professional/appropriate source (not separately
reported)
• Diagnosis or treatment significantly
limited by social determinants of
health
99205
99215
High
High
• 1 or more chronic illness with severe
progression/exacerbation/adverse
effects or treatment
• 1 acute or chronic illness or injury that
poses threat to life or body function
Extensive
(Must meet the requirements of at least 2 out of 3
categories)
Category 1: Tests, documents or independent
historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique
source*
• Review of the result(s) of each unique test*
• Ordering of each unique test*
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by
another physician/other qualified health care
professional (not separately reported)
or
Category 3: Discussion of management or test
interpretation
Discussion of management or test interpretation
with external physician/other qualified health care
professional/appropriate source (not separately
reported)
High
High risk of morbidity from additional
diagnostic testing or treatment
Examples only:
• Drug therapy requiring intensive
monitoring for toxicity
• Decision regarding elective major
surgery with identified patient or
procedure risk factors
• Decision regarding emergency major
surgery
• Decision regarding hospitalization or
escalation of hospital-level care
• Decision not to resuscitate or to de-
escalate care because of poor
prognosis
• Parenteral controlled substances
Outpatient Clinical Example #3: CPT Code Level 99204 (New Patient)/99214 (Established Patient)
Patient is 65-year-old with congestive heart failure, diabetes mellitus type 2 and hypertension who presents with leg swelling and erythema that began four
days ago. Patient indicates some pain in leg and is feeling warm with temperature reading of 101.2°F. Exam is suggestive of purulent cellulitis. Discussion with
21
patient’s primary care provider notes history of soft tissue infection with methicillin-resistant Staphylococcus aureus. Patient indicates no allergies. Complete
blood count, comprehensive metabolic panel and wound culture ordered. Five days of oral doxycycline prescribed with discussion of adverse effects. Patient is
instructed to follow up in one week, or sooner if the problem worsens.
Medical decision making for this case has now progressed to a moderate level since the problem is now a single new problem with systemic symptoms, and
data reviewed involves ordering three unique tests, discussion with another provider and review of external records, and the patient was given a prescription;
therefore, code level 99204 or 99214 is indicated, as shown in red below:
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data Reviewed
Level of Risk
99202
99212
Straightforward
Minimal
• 1 self-limited problem or minor problem
Minimal or none
Minimal
99203
99213
Low
Low
• 2 or more self-limited/minor
problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or injury
requiring hospital inpatient or observation
level of care
Limited
(Must meet the requirements of at least 1 of the 2
categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each
unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent
historian(s)
Low
Low risk of morbidity from
additional diagnostic testing or
treatment
99204
99214
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/adverse effects
of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new problem with
uncertain prognosis
• 1 new problem or acute illness with
systemic symptoms
• 1 acute complicated injury
Moderate
(Must meet the requirements of at least 1 out of 3
categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique
source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by
another physician/other qualified health care professional
Moderate
Moderate risk of morbidity from
additional diagnostic testing or
treatment
Examples only:
• Prescription drug management
• Decision regarding minor surgery
with identified patient or
procedure risk factors
• Decision regarding elective major
surgery without identified patient
or procedure risk factors
• Diagnosis or treatment
22
(not separately reported)
or
Category 3: Discussion of management or test
interpretation
• Discussion of management or test interpretation with
external physician/other qualified health care
professional/appropriate source (not separately reported)
significantly limited by social
determinants of health
99205
99215
High
High
• 1 or more chronic illness with severe
progression/exacerbation/adverse effects
or treatment
• 1 acute or chronic illness or injury that poses
threat to life or body function
Extensive
(Must meet the requirements of at least 2 out of 3
categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique
source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by
another physician/other qualified health care
professional (not separately reported)
or
Category 3: Discussion of management or test
interpretation
• Discussion of management or test interpretation
with external physician/other qualified health care
professional/appropriate source (not separately
reported)
High
High risk of morbidity from additional
diagnostic testing or treatment
Examples only:
• Drug therapy requiring intensive
monitoring for toxicity
• Decision regarding elective major
surgery with identified patient or
procedure risk factors
• Decision regarding emergency
major surgery
• Decision regarding hospitalization
or escalation of hospital-level care
• Decision not to resuscitate or to
de-escalate care because of poor
prognosis
• Parenteral controlled substances
23
Outpatient Clinical Example #4: CPT Code Level 99205 (New Patient)/99215 (Established Patient)
Patient is 65-year-old with congestive heart failure, diabetes mellitus type 2 and hypertension who presents with leg swelling and erythema that began four days
ago. Patient is ill with some confusion and unable to provide history. Patient’s daughter is called to obtain history, and patient’s daughter mentions patient has
had fever, malaise and severe leg pain. Exam indicates patient is very sick with leg erythema and severe tenderness. Patient has no allergies. Vital signs reveal
hypotension and tachycardia. Decision is made to send patient to emergency room for hospitalization and emergent surgical evaluation for possible necrotizing
fasciitis. Complete blood count, comprehensive metabolic panel and blood cultures are ordered. Recommendation that patient be started on IV vancomycin
with therapeutic drug monitoring and IV piperacillin-tazobactam, and daily labs are ordered to monitor creatinine while on IV vancomycin and piperacillin-
tazobactam. Case discussed with ER and surgical attending physicians. Patient transported to ED for admission.
Medical decision making for this case is at the highest level, given that the patient has an acute illness that poses threat to life or body function. The data
reviewed are now more complicated in nature and involve speaking with an independent historian (the patient’s daughter), ordering tests (more than three)
and discussions with other providers. The risk has now increased to the high level, given the patient needs to be hospitalized and started on IV antibiotics, with
consideration for emergency surgery. Therefore, code level 99205 or 99215 is indicated, as shown in red below:
CPT
Code
MDM Level
Problems (Number
and Complexity)
Data
Reviewed
Level of Risk
99202
99212
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
Minimal
99203
99213
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital inpatient
or observation level of care
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
Low
Low risk of morbidity from
additional diagnostic testing or
treatment
24
99204
99214
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate source
(not separately reported)
Moderate
Moderate risk of morbidity from
additional diagnostic testing or
treatment
Examples only:
• Prescription drug
management
• Decision regarding minor
surgery with identified patient
or procedure risk factors
• Decision regarding elective
major surgery without
identified patient or
procedure risk factors
• Diagnosis or treatment
significantly limited by social
determinants of health
99205
99215
High
High
• 1 or more chronic illness with
severe progression/exacerbation/
adverse effects or treatment
• 1 acute or chronic illness or injury
that poses threat to life or body
function
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
High
High risk of morbidity from
additional diagnostic testing or
treatment
Examples only:
• Drug therapy requiring
intensive monitoring for
toxicity
• Decision regarding elective
major surgery with identified
patient or procedure risk
factors
• Decision regarding emergency
major surgery
• Decision regarding
hospitalization or escalation of
hospital-level care
• Decision not to resuscitate or
to de-escalate care because of
poor prognosis
• Parenteral controlled
substances
25
Outpatient Clinical Example #5: Using Time to Select Code Level
58-year-old male established patient with venous insufficiency and chronic edema of both legs presents with complaint of redness and pain in the right lower
leg. Examination notes cellulitis of right lower leg with no open wounds, ulcers, abscesses or purulence. Patient prescribed cephalexin. Discussion with patient
on facilitating resolution of cellulitis through elevating leg to decrease edema. Instructions on use, wear and care of compression stockings. Total time for
patient care on date of encounter was 34 minutes.
As total time of visit on date of encounter is 34 minutes, this meets the time requirement of CPT 99214, which ranges from 30 to 39 minutes. The code to report is
99214. In this case, while the MDM was low and would have met criteria for 99213, the actual time devoted to the patient exceeded time for 99213; therefore,
using time to select the code level is a more accurate description and more appropriate way to value the physician’s services.
26
Inpatient Visits
Inpatient Clinical Example #1
Patient is 65-year-old with congestive heart failure and diabetes mellitus type 2 with right foot plantar diabetic ulcer
and has been admitted to hospital for exacerbation of congestive heart failure. Patient is seen regarding right foot
diabetic ulcer present for four months without healing. On examination, there is a Wagner grade 1 ulcer on plantar
aspect of right foot over first metatarsophalangeal joint and no presentation of purulent drainage or surrounding
erythema. Recommendations for offloading and wound care are given. No antibiotics or further evaluation is needed.
Medical decision making for this case does not involve any data review or ordering of tests or prescription medications.
There is minimal risk of morbidity regarding recommendations for offloading and wound care. This is not a chronic
problem as it has not been present for at least one year and therefore would be an acute problem. This would be a
straightforward level MDM, as shown in red below. Note: “Chronic” or “acute” may have different meanings in the clinical
realm than in the coding/billing realm.
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data Reviewed
99221
99231
99252
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
99221
99231
99253
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital
inpatient or observation level of
care
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
99222
99232
99254
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated
injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate source (not
separately reported)
27
99223
99233
99255
High
High
• 1 or more chronic illness with
severe
progression/exacerbation/
adverse effects or treatment
• 1 acute or chronic illness or
injury that poses threat to life
or body function
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
Inpatient Clinical Example #2
Patient is 65-year-old with congestive heart failure and diabetes mellitus type 2 with a right foot plantar diabetic ulcer
admitted to hospital for exacerbation of congestive heart failure. Patient seen regarding right diabetic foot ulcer, which
has been present for four months without healing. On examination, ulcer located on the plantar aspect of right foot
over the first metatarsophalangeal joint. There appears to be bone exposed, no purulence or surrounding erythema.
Order placed for c-reactive protein and MRI of right foot performed with recommendations to follow up in outpatient
office.
Medical decision making for this case involves ordering of two unique tests. No treatment was recommended and risk of
ordered tests is low. This would be a low level MDM, as shown in red below:
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data
Reviewed
Level of Risk
99221
99231
99252
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
Minimal
99221
99231
99253
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital
inpatient or observation level of
care
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
Low
Low risk of morbidity from
additional diagnostic testing or
treatment
28
99222
99232
99254
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated
injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate source
(not separately reported)
Moderate
Moderate risk of morbidity from
additional diagnostic testing or
treatment
Examples only:
• Prescription drug management
• Decision regarding minor
surgery with identified patient
or procedure risk factors
• Decision regarding elective
major surgery without identified
patient or procedure risk factors
• Diagnosis or treatment
significantly limited by social
determinants of health
99223
99233
99255
High
High
• 1 or more chronic illness with
severe
progression/exacerbation/
adverse effects or treatment
• 1 acute or chronic illness or
injury that poses threat to life
or body function
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
High
High risk of morbidity from
additional diagnostic testing or
treatment
Examples only:
• Drug therapy requiring intensive
monitoring for toxicity
• Decision regarding elective major
surgery with identified patient or
procedure risk factors
• Decision regarding emergency
major surgery
• Decision regarding
hospitalization or escalation of
hospital-level care
• Decision not to resuscitate or to
de-escalate care because of poor
prognosis
• Parenteral controlled substances
Inpatient Clinical Example #3
65-year-old patient with congestive heart failure and diabetes mellitus type 2 with right foot plantar diabetic ulcer,
which has been present for four months, has been admitted to hospital for right diabetic foot infection. Patient notes
right foot ulcer redness and drainage over past two days.
Patient is afebrile with normal heart rate and blood pressure. Patient is experiencing malaise. Exam significant for ulcer
on plantar aspect of right foot over first metatarsophalangeal joint with purulent drainage, but no frank bone exposed.
Redness of right forefoot is present. Review of podiatrist notes documented from that same day note possible plans
for debridement of infected ulcer. Laboratory review shows that nasal swab PCR was positive for methicillin-resistant
Staphylococcus aureus. C-reactive protein and CT of right foot is ordered. Treatment is started with piperacillin-
tazobactam and vancomycin IV.
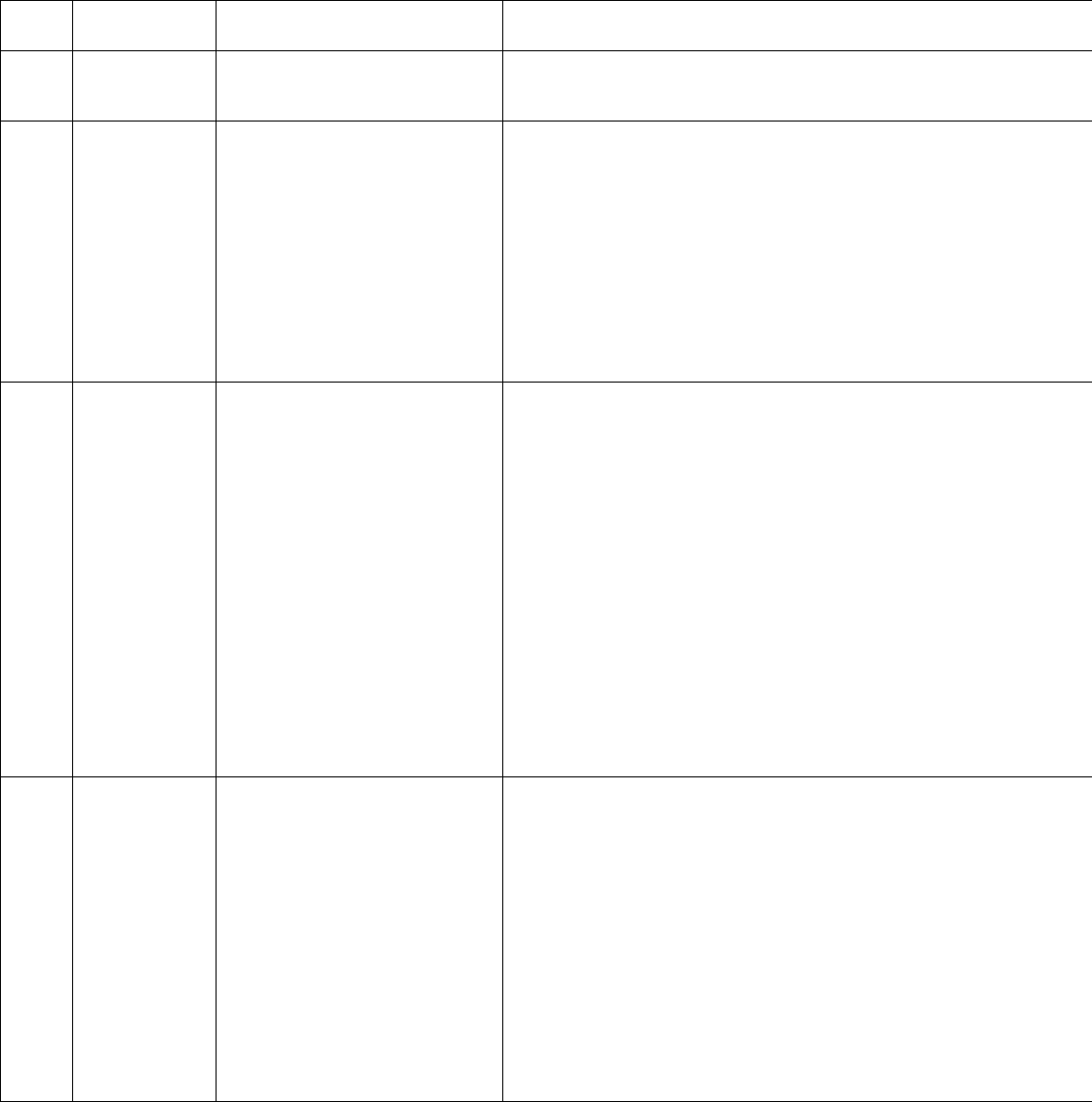
29
Medical decision making for this case involves review of one unique test, ordering of two unique tests and review of one
external note. Risk is moderate, as a prescription medication was ordered. This is an acute problem with systemic
symptoms. Systemic symptoms do not have to be general and may affect only a single system. This would be a moderate
level MDM, as shown in red below:
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data Reviewed
99221
99231
99252
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
99221
99231
99253
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital
inpatient or observation level of
care
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
99222
99232
99254
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated
injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate source (not
separately reported)
99223
99233
99255
High
High
• 1 or more chronic illness with
severe
progression/exacerbation/
adverse effects or treatment
• 1 acute or chronic illness or
injury that poses threat to life
or body function
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
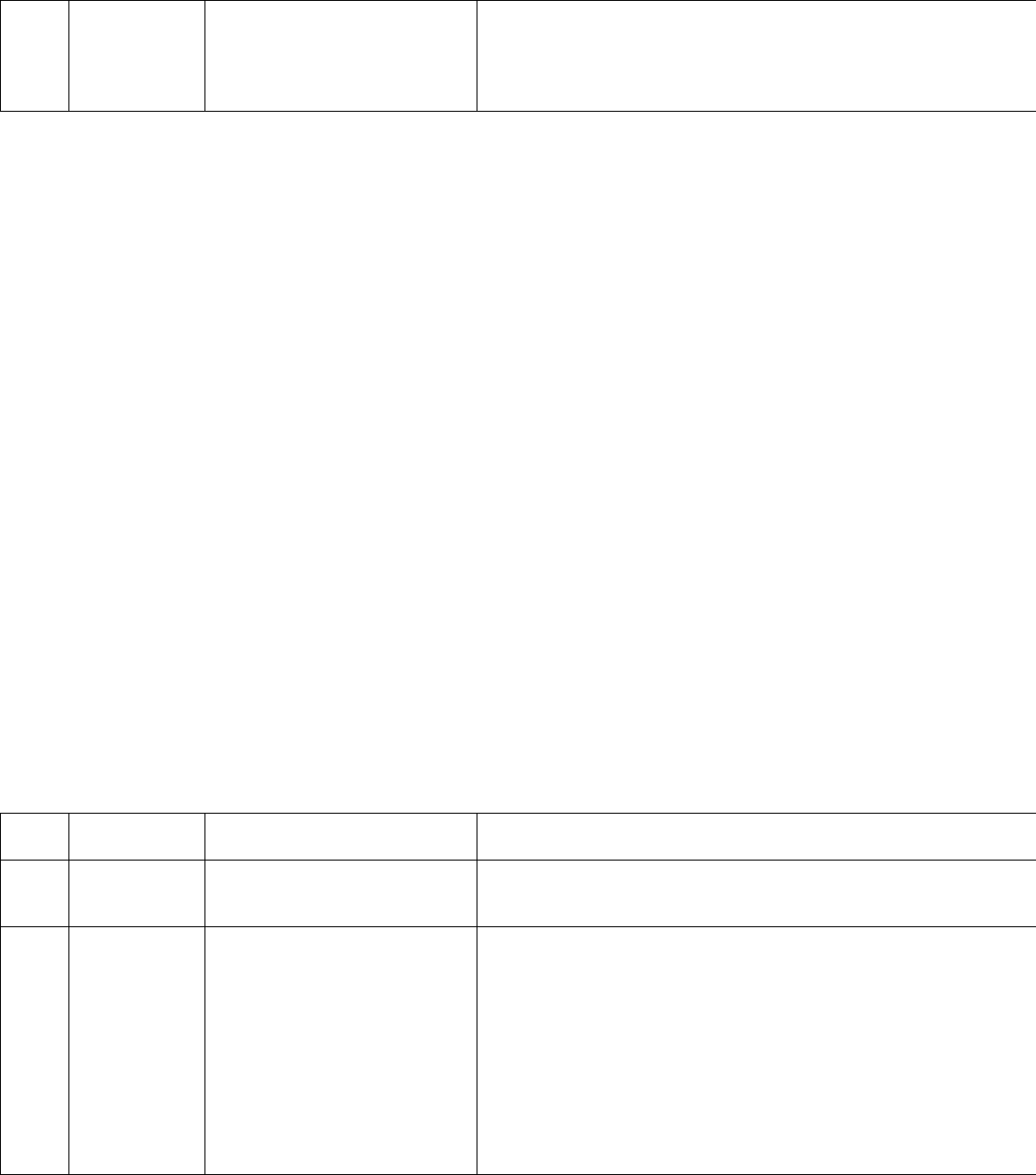
30
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
Inpatient Clinical Example #4
65-year-old with congestive heart failure and diabetes mellitus type 2 with right foot plantar diabetic ulcer admitted to
hospital concerning a right-sided diabetic foot infection. Patient seen one day ago for initial consultation with
recommendations and start of treatment with piperacillin-tazobactam and vancomycin IV. The c-reactive protein that
was ordered on initial consultation was noted to be elevated. Right foot CT scan, which was also previously ordered on
initial consultation, was noted to show an abscess in right forefoot area with possible osteomyelitis present. Patient is
now hypotensive and tachycardic. The right foot erythema has progressed to involve entire right foot with blackened
discoloration of some right toes. Two sets of blood cultures and a complete blood count are ordered. Communication
with patient’s attending physician regarding worsening clinical status and infection, with recommendation to transfer
to ICU with podiatry re-evaluation for surgical intervention, including possible need for amputation with
documentation, in medical record. Escalation of antibiotics to provide broader spectrum coverage, including MDROs, is
ordered
Medical decision making for this case involves an acute illness that poses threat to life or body function and a need to
escalate level of care in the hospital. Data reviewed only meet moderate level because the two sets of blood cultures
ordered only count as one test since they are not unique tests, and the complete blood count will add to a combination of
two data elements ordered. Although the previously ordered c-reactive protein and CT of the right foot were reviewed
during this encounter, they cannot be used in the MDM for the current encounter since they are from a previous order
from a previous encounter and therefore would not be used to determine the MDM for this encounter. The ordering of
the test includes the review of that test result. The only new tests that could count for this encounter would be blood
cultures and complete blood count that were ordered. Although the data reviewed MDM element is only moderate since
there was discussion with a physician affecting the MDM, the problem and risk MDM elements are used in the MDM level
decision since they are higher than the data reviewed MDM element. This would be a high-level MDM as shown in red
below:
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data Reviewed
99221
99231
99252
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
99221
99231
99253
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital
inpatient or observation level of
care
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
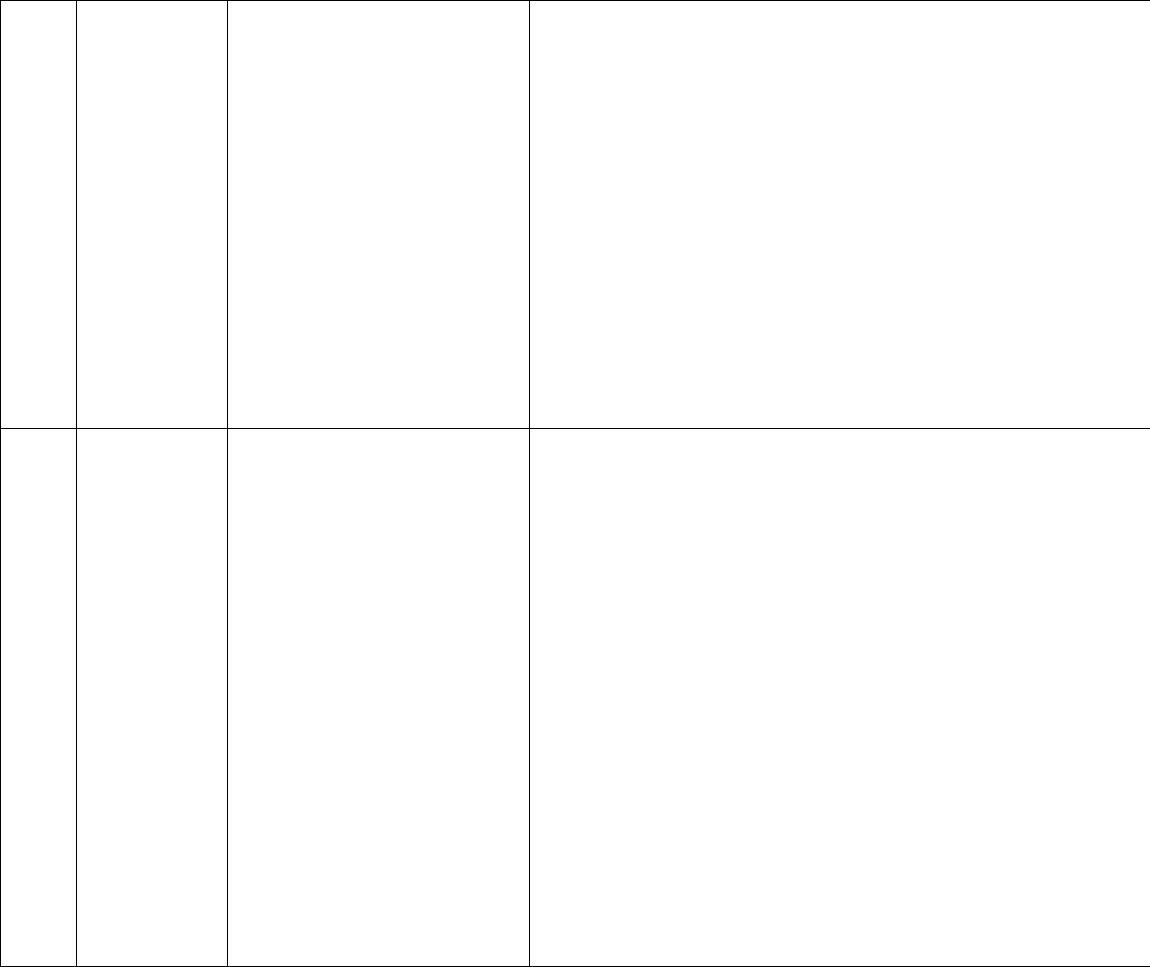
31
99222
99232
99254
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated
injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate source (not
separately reported)
99223
99233
99255
High
High
• 1 or more chronic illness with
severe
progression/exacerbation/
• adverse effects or treatment
• 1 acute or chronic illness or
injury that poses threat to life
or body function
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
Inpatient Clinical Example #5
65-year-old with congestive heart failure and diabetes mellitus type 2 with right foot plantar diabetic ulcer admitted to
hospital for right-sided diabetic foot infection. Patient seen for recommendations regarding further evaluation and
treatment. Review of medical record is conducted since admission. Patient provides reliable history. Patient’s spouse is
in room and adds to history. (Note that history obtained from patient’s spouse may be included in total time but would
not qualify as independent historian because patient is able to provide reliable history so no need for additional or
confirmatory history.)
Laboratory results reviewed include blood cultures without growth at day 2, complete blood count with leukocytosis
and normal creatinine on chemistry. Examination of patient shows right foot diabetic ulcer present with surrounding
cellulitis. Discussion with patient regarding recommendations of right foot MRI and antibiotic treatment. Patient’s
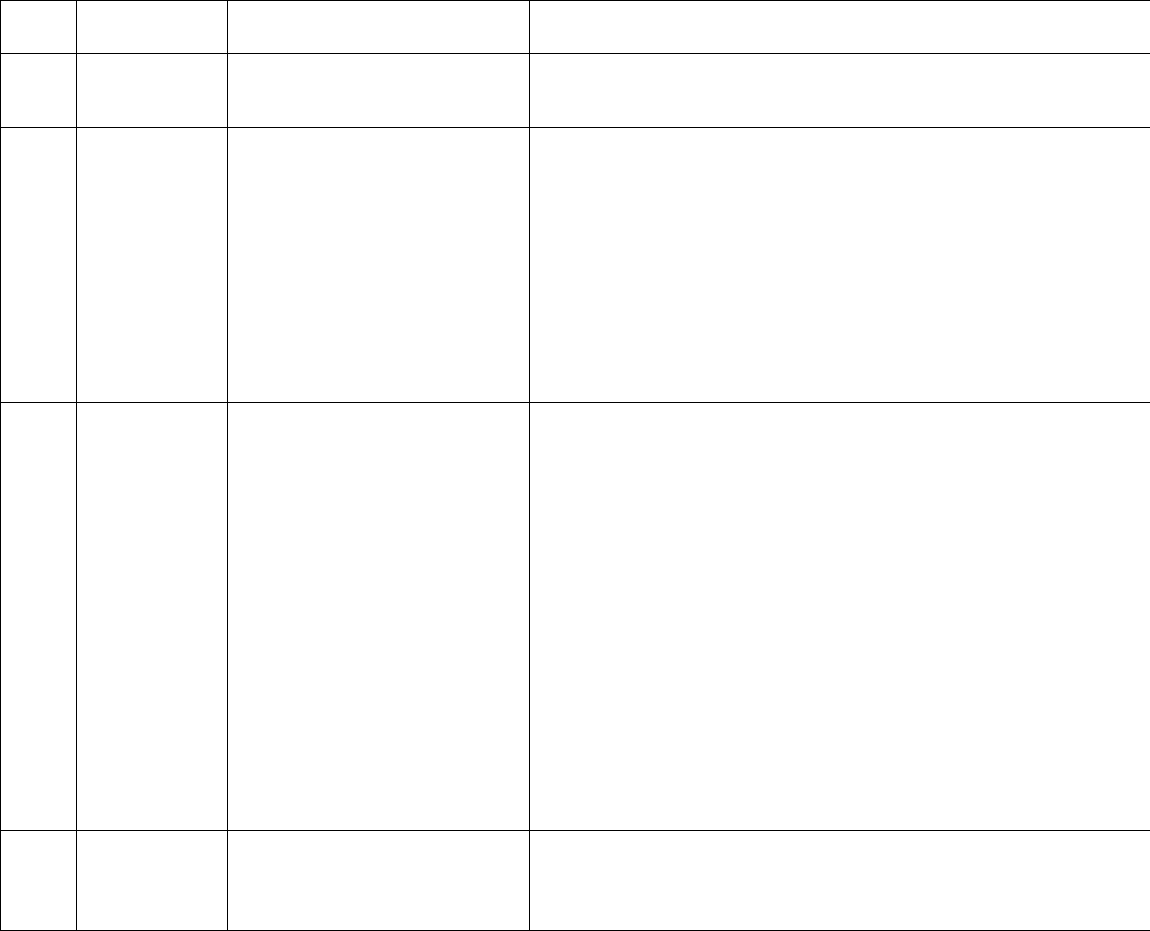
32
hospital attending is called regarding recommendations from the outpatient office. Patient’s hospital case manager is
also notified regarding need to arrange outpatient IV antibiotics from the outpatient office.
Documentation of notes are completed, spending a total time of 78 minutes on the day of encounter for an initial
hospital E/M visit. Documentation shows that 78 minutes were spent on date of encounter with review of medical
records, obtaining history, performing a physical examination, reviewing laboratory studies, discussing with the
patient’s attending physician and case manager and completing documentation. (Travel time between the hospital and
office cannot be included.)
This would be a moderate MDM (99223) based on the MDM elements but because the total time was 78 minutes,
which exceeds the time threshold of 75 minutes for 99223, then the appropriate code would be 99223 based on total
time, as shown in red below:
CPT
Code
MDM Level
Problems
(Number and Complexity)
Data Reviewed
99221
99231
99252
Straightforward
Minimal
• 1 self-limited problem or minor
problem
Minimal or none
99221
99231
99253
Low
Low
• 2 or more self-
limited/minor problems
• 1 stable chronic illness
• 1 acute, uncomplicated illness or
injury
• 1 stable acute illness
• 1 acute, uncomplicated illness or
injury requiring hospital
inpatient or observation level of
care
Limited
(Must meet the requirements of at least 1 of the 2 categories)
Category 1: Tests and documents
• Any combination of 2 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
or
Category 2: Assessment requiring an independent historian(s)
99222
99232
99254
Moderate
Moderate
• 1 or more chronic problem with
progression/exacerbation/
adverse effects of treatment
• 2 or more stable chronic illnesses
• 1 undiagnosed new
problem with uncertain
prognosis
• 1 new problem or acute
illness with systemic
symptoms
• 1 acute complicated
injury
Moderate
(Must meet the requirements of at least 1 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate source (not
separately reported)
99223
99233
99255
High
High
• 1 or more chronic illness with
severe
progression/exacerbation/
Extensive
(Must meet the requirements of at least 2 out of 3 categories)
Category 1: Tests, documents or independent historian(s)
• Any combination of 3 from the following:
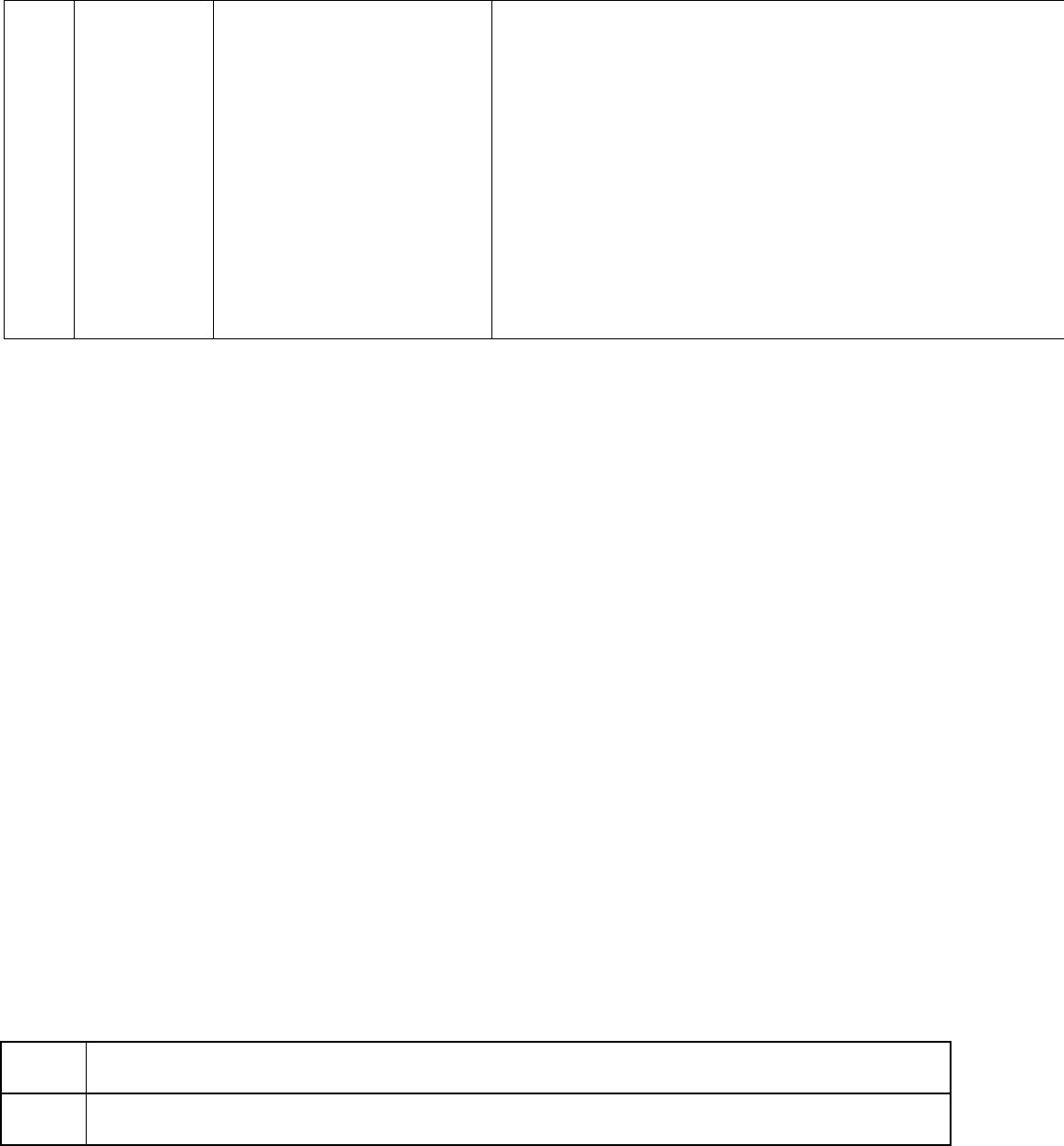
33
adverse effects or treatment
• 1 acute or chronic illness or
injury that poses threat to life
or body function
• Review of prior external note(s) from each unique source
• Review of the result(s) of each unique test
• Ordering of each unique test
• Assessment requiring an independent historian(s)
or
Category 2: Independent interpretation of tests
• Independent interpretation of a test performed by another
physician/other qualified health care professional (not separately
reported)
or
Category 3: Discussion of management or test interpretation
• Discussion of management or test interpretation with external
physician/other qualified health care professional/appropriate
source (not separately reported)
Inpatient Clinical Example #6
45-year-old man with history of heart transplantation seven months ago presents with fever, confusion, hemoptysis and
hypotension. Initiation of intubation in emergency room, with vasopressors and admission to ICU. Chest imaging reveals
large cavitary lung lesion suspicious for invasive pulmonary aspergillosis. Initiation of empiric voriconazole and
antibiotics. Total time spent on evaluating patient, reviewing lab results, imaging, coordinating management with
patient’s other physicians and documenting visit in electronic medical record resulted in 40 minutes.
While this visit meets criteria for a high level of MDM and could be billed as 99233, it also meets the definition of a
critical care service. If time spent, presence of a life-threatening illness and critical care services provided are
appropriately documented in the medical record, then this visit should be billed as 99291.
99291
Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74
minutes
99292
Each additional 30 minutes of critical care provided beyond the first 74 minutes (billed in addition to
99291)
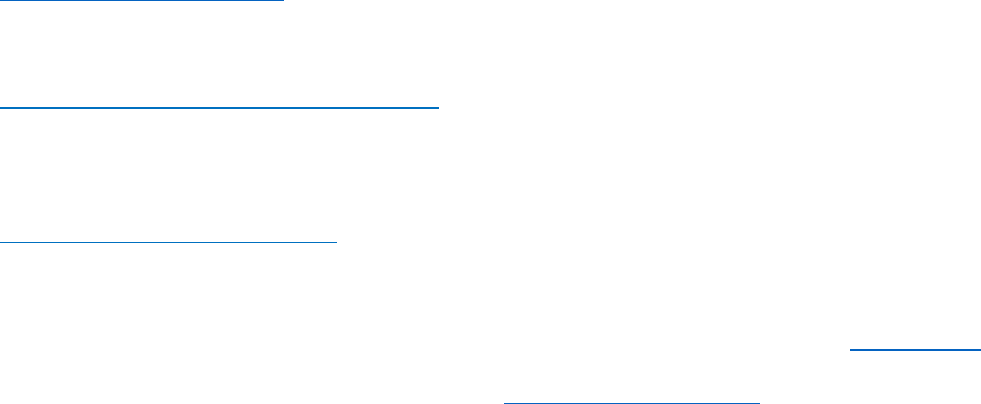
34
Section Four: Split or Shared Visits:
• A split/shared visit is an E/M service performed by a physician and a nonphysician practitioner belonging to the
same group practice. Determination of the billing provider for the split/shared E/M service is based on the
provider that spent either more than half of the total time performing the service or provided a substantive
portion of the medical decision making as defined by CPT®.
• It’s key to understand and develop a potential strategy to bill the highest level based on MDM under physician or
highest level based on time under NPP at a reduced rate. There may be difference in payment to a NPP than to a
physician such as with Medicare.
• For shared or split visits between a physician and other NPP, such as advanced practice providers, only distinct
time spent separately on the date of the encounter may be summed to equal total time. If a physician and
QHCP perform the same activity together, then time can only be counted for one of the providers in the sum of
the total time.
• CMS’s Level II Modifier FS can be used for split or shared evaluation and management visits. For E/M services
split or shared between a physician and a non-physician practitioner (NPP) in a facility setting where both
physician and NPP are in the same group. This modifier may not be used in an office or other setting outside of
a facility setting defined as hospital or skilled nursing facility.
• Substantive portion of the MDM requires that the physician or non-physician practitioner make or approve the
management plan for the number of complexity or problems addressed at the encounter and takes
responsibility of plan including the risk of patient management. This results in the physician or non-physician
practitioner performing two of three elements of MDM used to select the code level based.
Section Five: Additional Resources
E/M Coding and Documentation Resources
AMA E/M CPT® Code Resources
AMA is the official source of CPT® code information and guidelines. This website provides information on the revised E/M
codes and provides a learning module to assist physicians and their staff in navigating those changes.
CMS Evaluation and Management Services Guide
This guide from the Centers for Medicare & Medicaid Services is a comprehensive guide issued by CMS to educate
providers on the appropriate use of E/M codes and the associated documentation. The guide has been updated to
include the revisions to the office visit E/M codes.
CMS Evaluation & Management Visits
CMS has provided several resources for documentation and payment for E/M visits under the Medicare Physician Fee
Schedule.
To assist with questions regarding CPT® coding or other reimbursement issues, IDSA offers Ask the Coder. This
service is available to IDSA members to aid in understanding and resolving medical coding issues. For more
information and general inquiries, contact IDSA staff via clinicalaffairs@idsociety.org.
